
- My presentations

Auth with social network:
Download presentation
We think you have liked this presentation. If you wish to download it, please recommend it to your friends in any social system. Share buttons are a little bit lower. Thank you!
Presentation is loading. Please wait.
To view this video please enable JavaScript, and consider upgrading to a web browser that supports HTML5 video
HEALTH CARE DELIVERY SYSTEM IN INDIA
Published by Abner Powers Modified over 8 years ago
Similar presentations
Presentation on theme: "HEALTH CARE DELIVERY SYSTEM IN INDIA"— Presentation transcript:
Pregnancy, Child Tracking & Health Services Management System Challenges in rolling out J. P. Jat Demographer & Evaluation officer Directorate of Medical,
Health planning in India and National Rural Health Mission
Reproductive and Child Health Programme (RCH). ▪ Programme launched on 15 th October 1997 ▪ ‘People have the ability to reproduce and regulate their fertility,
St Christopher and Nevis

WELCOME HEALTH PROFILE BANGLADESH. MINISTRY OF HEALTH & FAMILY WELFARE (MOHFW)-BANGLADESH MOHFW is responsible to ensure basic health care to the people.
Key Recommendations Role of DaiMas in NRHM The Role of Traditional Birth Attendants in The National Rural Health Mission National Consultation May 2, Delhi.

Presentation to Select Committee On Social Services District Health System Jeanette R Hunter 30 July2013.
Dr. P. Saxena, Director, Central Bureau of Health Intelligence (CBHI), Dte. GHS, Ministry of Health & FW, Govt. of India & Head - WHO C.C. on FIC in India.

FIRST REFERRAL UNIT.

Health Planning & Managment.
NRHM DISTRICT ACTION PLANS PARTICIPATORY & EVIDENCE BASED PLANNING PROCESS.
Management structure of the Integrated Disease Surveillance Project
Dr. Rakesh Kumar, Dr. Kapil Yadav, Dr. Chandrakant S Pandav, Professor & Head, Centre for Community Medicine, All India Institute of Medical Sciences,

Health System in India Tej Ram Jat Centre for Health Equity

Health Care Delivery and Referral System in Thailand
Hospital administration. The definitions given by various authors can be explained as follows: As a hospital administrator, he has to carry out management.

General people’s Committee for Health & Environement
Government of India Policy Reform in Family Welfare Program of India : Community Mobilization & Community Participation under Reproductive & Child Health.

NATIONAL AND COMMUNITY MENTAL HEALTH PROGRAMME. AIMS OF NCMHP To ensure treatment and prevention of mental and neurological disorder. To ensure treatment.
National Mental Health Programme. Govt of India integrated mental health with other health services at rural level. It is being implemented since 1982.
About project
© 2024 SlidePlayer.com Inc. All rights reserved.
Health System in India
Mar 18, 2019
571 likes | 1.74k Views
Health System in India. Tej Ram Jat Centre for Health Equity & Jan Swasthya Abhiyan, India [email protected]. Introduction. The political economy context The organisational structure and delivery mechanism Health financing mechanisms Coverage patterns
Share Presentation
- health system
- health care
- government spending
- male health worker
- indian health system development

Presentation Transcript
Health System in India Tej Ram Jat Centre for Health Equity & Jan Swasthya Abhiyan, India [email protected]
Introduction • The political economy context • The organisational structure and delivery mechanism • Health financing mechanisms • Coverage patterns • Current status of health and health care
The Political Economy Context • A democratic federal system which is subdivided into 28 States, 7 union territories and 593 districts • In most of the states three local levels of government (Panchayati-raj) • Per capita income US $440 • 435 million Indians are estimated to live on less than US $ 1 a day • 36% of the total number of the worlds’ poor are in India • Tax based health finance system with health insurance • 80% health care expenditure born by patients and their families as out-of -pocket payment (fee for service and drugs) • Expenditure on health care is second major cause of indebtedness among rural poor
Characteristics of Indian Health System • Complex mixed health system - Publicly financed government health system - Fee-levying private health sector
Different Phases of Indian Health System Development • Pre-independence phase • Development centred phase • Comprehensive Primary Health Care phase • Neoliberal economic and health sector reform phase • Health systems phase
Main Systems of Medicine • Western allopathic • Ayurveda • Unani • Siddha • Homeopathy
Government Health System • Three levels of responsibilities- • First- • health is primarily a state responsibility • Second- - the central government is responsible for developing and monitoring national standards and regulations - sponsoring various schemes for implementation by state governments - providing health services in union territories • Third- • both the centre and the states have a joint responsibility for programmes listed under the concurrent list.
Administrative Structure 1. Central Ministries of Health and Family Welfare – - Responsible for all health related programmes - Regulatory role for private sector 2. State Ministries of Health and Family Welfare 3. District Health Teams headed by Chief Medical and Health Officer
Service Delivery Structure • Sub Health Centres- staffed by a trained female health worker and/or a male health worker for a population of 5000 in the plains and a population of 3000 in hilly and tribal areas. • Primary Health Centres- staffed by a medical officer and other paramedical staff for a population of 30,000 in the plains and a population of 20,000 in hilly, tribal and backward areas. A PHC centre supervises six to eight sub centres.
Service Delivery Structure • Community health centres- with 30-50 beds and basic specialities covering a population of 80,000 to 120,000. The CHC acts as a referral centre for four to six PHCs. • District/General hospitals- at district level with multi speciality facilities (City dispensaries) • Medical colleges, All India institute of Medical Sciences and quasi government institutes (NIHFW and SIHFWs)
Health Financing Mechanisms.. • Revenue generation by tax • Out of pocket payments or direct payments • Private insurance • Social insurance • External Aid supported schemes
Spending on Health • Annually over 150,000 crores or US$34 billion, which is 6% of GDP (Government spending on health Is only 0.9% of GDP) • Out of this only 15 % is publicly financed 4% from social insurance, 1% by private insurance remaining 80% is out of pocket spending ( 85% of which goes in private sector) • Only 15% of the population is in organised sector and has some sort of social security the rest is left to the mercy of the market
The Aspects of Neoliberal Economic Reforms Affecting Public Health • Increasing unregulated privatisation of the health care sector with little accountability to patients • Cutting down government Health care expenditure • Systematic deregulation of drug prices resulting in skyrocketing prices of drugs and rising cost of health services • Selective intervention approach instead comprehensive primary health care • Measure diseases in terms of cost effectiveness • Techno centric approach( emphasis on content instead processes)
Contradictions • India has the largest numbers of medical colleges in the world • It produces the largest numbers of doctors among developing countries • It gets “medical Tourists” from developed countries • This country is fourth largest producer of drugs by volume in the world
But... the current situation…. • Only 43.5% children are fully immunised. • 79.1% of children from 6 months to 5 years of age are anaemic. • 56.1% ever married women aged 15-49 are anemic. • Infant Mortality Rate is 58/1000 live births for the country with a low of 12 for Kerala and a high of 79 for Madhya Pradesh. • Maternal Mortality Rate is 301 for the country with a low of 110 for Kerala and a high of 517 for UP and Uttaranchal in the 2001-03 period. • Two thirds of the population lack access to essential drugs. • 80% health care expenditure born by patients and their families as out-of -pocket payment (fee for service and drugs) • Health inequalities across states, between urban and rural areas, and across the economic and gender divides have become worse • Health, far from being accepted as a basic right of the people, is now being shaped into a saleable commodity
Contd…. • poor are being excluded from health services • Increased indebtedness among poor (Expenditure on health care is second major cause of Indebtedness among rural poor) • Difference across the economic class spectrum and by gender in the untreated illness has significantly increased • Cutbacks by poor on food and other consumptions resulting increased illnesses and increasing malnutrition
Health Inequities • The infant mortality Rate in the poorest 20% of the population is 2.5 times higher than that in the richest 20% of the population • A child in the ‘Low standard of living’ economic group is almost four times more likely to die in childhood than a child in a better of high standard living group • A person from the poorest quintile of the population, despite more health problems, is six times less likely to access hospitlisation than a person from richest quintile.
Health Inequities • A girl is 1.5 times more likely to die before reaching her fifth birthday • The ratio of doctors to population in rural areas is almost six times lower than that for urban areas. • Per person, government spending on public health is seven times lower in rural areas compared to government spending urban areas
- More by User
Newborn Health in India
Newborn Health in India. Newborn health in India . 25 million (2.5 crore) births per year - Accounts for 20% of global births 0.9 million (9 lakh) die in neonatal period - Accounts for about 25% of global deaths. India accounts for highest births & neonatal deaths globally.
272 views • 14 slides
HEALTH CARE DELIVERY SYSTEM IN INDIA
MODEL OF HEALTHCARE DELIVERY. RESOURCES. CURATIVEPREVENTIVEPROMOTIVE. PUBLICPRIVATEVOLUNTARYINDIGENOUS. CHANGE IN HEALTH STATUS. HEALTH STATUS OR HEALTH PROBLEM . . . . . . . HEALTH STATUS AND HEALTH PROBLEMS. An assessment of the
5k views • 35 slides
Public Health in India
Aalok Ranjan Chaurasia. Public Health in India. Outline. Health and Public Health Public Health in India Before the Colonial period During the Colonial period After the colonial period Essential Public Health Functions Mortality transition in India. Health.
1.14k views • 41 slides

Health Education in India
Well gathered information that are described in great detail about the insights of health education in india.
204 views • 10 slides

Health care delivery system in India
Health care delivery system in India. Framework. Introduction Evolution of health care services in India Role of different committees Organizational structure in India Health care delivery system in India Gaps in structure Finance allocation Integrated approach of health care delivery
20.37k views • 46 slides
Child Health in India
Child Health in India. By Vikash Moderator: Dr. Chetna Maliye. Introduction & History: History of Child health services in India. Major Milestones for child health in India. Child Health Statistics: Indicators of Survival Mortality Statistics:
1.97k views • 52 slides

Health Insurance In India
Health Insurance In India. 1. COURSE OBJECTIVES. To understand the health insurance industry in India To know about the health insurance companies. To learn about various health insurance product features. 2. PART I Health Insurance in India: Needs Assessment and Overview
1.37k views • 78 slides
INFRASTRUCTURE OF HEALTH SYSTEM IN INDIA
INFRASTRUCTURE OF HEALTH SYSTEM IN INDIA. By Dr. Snehal Kasare. INTRODUCTION.
425 views • 25 slides
Education System in India
Education System in India. Nalanda University (450 -1150 AD).
596 views • 21 slides
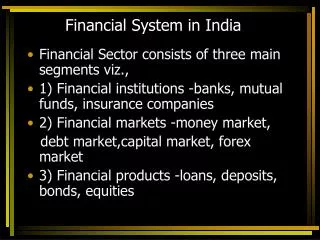
Financial System in India
Financial System in India. Financial Sector consists of three main segments viz., 1) Financial institutions -banks, mutual funds, insurance companies 2) Financial markets -money market, debt market,capital market, forex market 3) Financial products -loans, deposits, bonds, equities.
1.09k views • 62 slides
Banking System in India
Banking System in India. Indigenous bankers. Individual bankers like Shroffs, Seths, Sahukars, Mahajans, etc. combine trading and other business with money lending. Vary in size from petty lenders to substantial shroffs
9.32k views • 28 slides
Banking System in India. BANKING SYSTEM IN INDIA. Commercial Banks by Ownership. BANKS BY INCLUSION IN SECOND SCHEDULE OF RBI ACT, 1934 AS ON MARCH 31, 2003. Classification Continued. Public Sector Banks Nationalized Banks (19) State Bank of India and its assosciates Private Sector Banks
1.16k views • 9 slides
EDUCATION SYSTEM IN INDIA
EDUCATION SYSTEM IN INDIA. Fourfold Emphasis Quality Education Attention to science & technology Moral values Relating education to life. Education policy of 1968. Big country and big population 72% of population is in rural areas Lack of infrastructure Lack of transportation
564 views • 7 slides
BANKRUPTCY SYSTEM IN INDIA
BANKRUPTCY SYSTEM IN INDIA. Bankruptcy is a legally declared inability of an individual or organization to pay their creditors. Filing bankruptcy can make it possible to eliminate the legal obligation to pay most of debts. PURPOSE OF BANKRUPTCY :
394 views • 13 slides

Health Specialist in India
Sukhjinder Singh Yogi is renowned health specialist in india.Basically he is offering his services in Chandigarh,Ludhiana,Jalandhar and Amritsar.Here you will get solution of all types of health problems like Skin ,hair,digestion,weight related issues, Sexual problems.For more enlightenment, feel free to contact at 9914000365,9357000019
160 views • 8 slides
health centre in india
The yogshala provide a platform to each person who want to live a healthy life hence with our different types of yoga techniques you can wait in good physical figure and even can instruct others that how to do yoga by joining our yoga teacher program. Join us today at - http://www.theyogshala.com
387 views • 23 slides

Health insurance in India
Bajaj Allianz offers individual Health insurance in India, family floater health insurance, senior citizen, critical illness and top up health insurance policies.
146 views • 5 slides

SMAS Health Emergency Alert System Services in India
SMAS company give you best option to safe your health by Health emergency alert system services. The Vehicle tracking system specially designed for vehicles. A sos button that alerts the emergency contacts with the click of a button.
58 views • 5 slides

Health Sector in India
The PPT is all about the health sector in India.
99 views • 8 slides

HEALTH CARE DELIVERY SYSTEM IN INDIA. Health system It is designed to meet the health needs of the community, through the use of available knowledge and resources . Two major themes: It should meet the needs of entire population and not merely selected group. Primary health care.
6.16k views • 49 slides

Newborn Health in India. Newborn health in India. 25 million (2.5 crore) births per year - Accounts for 20% of global births 0.9 million (9 lakh) die in neonatal period - Accounts for about 25% of global deaths. India accounts for highest births & neonatal deaths globally.
162 views • 14 slides
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.8(10); 2022 Oct

Health care delivery model in India with relevance to diabetes care
Ashok kumar das.
a Department of Endocrinology, Pondicherry Institute of Medical Sciences, Pondicherry, Tamil Nadu, India
Banshi Saboo
b Diacare, Diabetes Care & Hormone Clinic, Ahmedabad, India
Anuj Maheshwari
c Shri Hari Kamal Diabetes & Heart Clinic, Lucknow, India

Mohanan Nair V
d Kandala Cooperative Hospital, Trivandrum, Kerala, India
Samar Banerjee
e Dept. of Medicine, Vivekananda Institute of Medical Sciences, Kolkata, West Bengal, India
Jayakumar C
f Department of General Medicine, Sree Gokulam Medical College and Research Foundation, Trivandrum, Kerala, India
g Department of Community Medicine, Sree Gokulam Medical College and Research Foundation, Trivandrum, Kerala, India
Sunil Prasobh P
h Department of Internal Medicine, Government Medical College, Kollam, Kerala, India
Anjana Ranjit Mohan
i Department of Diabetology, Dr. Mohan's Diabetes Specialities Centre, Chennai, India
Vasudevan Sambu Potty
j Department of Urology, Government Medical College, Trivandrum, Kerala, India
Jothydev Kesavadev
k Department of Diabetology, Jothydev's Diabetes Research Centers, Trivandrum, Kerala, India
Associated Data
No data was used for the research described in the article.
The Indian healthcare scenario presents a spectrum of contrasting landscapes. Socioeconomic factors, problems with medical infrastructure, insufficiency in the supply of medical requisites, economic disparities due to major differences in diabetes care delivery in the government and private sectors and difficulty in accessing quality health care facilities challenges effective diabetes care in India. The article gives insights into the practical solutions and the proposed White paper model to resolve major challenges faced by the Indian diabetes care sector for effective diabetes care delivered at Jothydev's Diabetes Educational Forum Global Diabetes Convention 2019.
- • The prevalence of diabetes in India is on its rise.
- • Socioeconomic factors, lack of diagnosis etc challenges Indian diabetes care system.
- • Health care models appropriate for Indian scenario should be developed.
- • Public-Private partnership is required for effective health care delivery.
Diabetes; Health care model; Patient adherence; India; Health care policies.
1. Introduction
Diabetes is a health-related global concern that threatens the economy of developing nations, especially India. India's large population and socio-economic transitions have made it an epicenter of diabetes. In 2017, diabetes alone exhausted about 5–25% share of an average Indian household earnings by spending about 31 billion US dollars on diabetes management [ 1 ]. Several challenges contribute to diabetes among Indians, including unawareness about diabetes and its complications, inadequate healthcare facilities and lack of access, healthcare expenditure, non-adherence to treatment, and lack of accountability.
Collective and active involvement of healthcare professionals (HCPs) and stakeholders involved in diabetes care is required to build a focused multidisciplinary approach. Some of the government and/or private organizations have tried to implement effective educational programs for increasing awareness about the proper management of diabetes [ 2 ]. Despite these promising approaches, attention and improvisation of efforts are essential for developing a healthcare system that delivers quality diabetes care. Delivering accessible, affordable, and high-quality care are some of the major challenges it faces and therefore healthcare delivery systems must identify more proactive ways to manage patients in the community and in their homes.
Jothydev's Professional Education Forum (JPEF) Annual Diabetes Convention is an international diabetes convention with the global participation of diabetes care professionals from all streams. JPEF Global Convention 2019 organized a discussion forum including diabetes experts from India who are actively involved in patient care either in clinical practice or in diabetes administration. The experts proposed a “White paper model” to sort out the challenges faced during diabetes management in India.
The article aims to emphasize how various aspects of diabetes care delivery can be congregated to develop a “White paper model” which will harmonize the development of the most appropriate health care delivery model for India.
2. Diabetes burden in India
According to the International Diabetes Federation (IDF), about 77 million of Indians aged 20–79 years are currently living with diabetes, and the number is expected to increase to 134.2 million by 2045. It is estimated that more than 1 million deaths are attributed to diabetes and diabetes-related complications in India alone. These huge numbers rank India as the first in the world with the highest socio-economic diabetes burden. It is estimated that in low-income families, the cost of diabetes treatment for an adult with diabetes is up to 25 per cent of the family income. A study conducted by Anjana et al in 15 states of India reported that the mean prevalence of prediabetes in India is 10.3% (state-wise range, 6.0–14.7%) [ 3 , 4 ] Survey studies revealed that about 10–16% of the urban and 5–8% of the rural populations have diabetes [ 5 , 6 ].
According to the data published by IDF in 2019, 43.9 million people with diabetes are undiagnosed in India because of the poorly developed healthcare systems ( https://www.diabetesatlas.org/upload/resources/material/20200302_133351_IDFATLAS9e-final-web.pdf ). The number is quite alarming from an Indian perspective as the progression from pre-diabetes to diabetes occurs much faster in the Asian population than in any other ethnic population [ 7 , 8 ]. The worrisome fact is that the prevalence is increasing in children and young adults.
3. Poor outcome and type 2 diabetes mellitus (T2DM) complications as an indicator of insufficient care and monitoring
Mounting evidence from studies conducted in India highlighted the fact that the percentage of people with diabetes with poor glycemic control (HbA1c >8%), uncontrolled hypertension, dyslipidemia, and vascular complications related to diabetes is greater than 50% [ 9 , 10 ]. that vary across regions. The ICMR-INDIAB study had shown that the prevalence of undiagnosed hypertension, and dyslipidemia is high and the level of glycemic control among subjects with self-reported diabetes in India is poor [ 11 , 12 , 13 ]. A study from Maharashtra showed that even with the use of pharmacological agents HbA1c was found to be >7% in 72.7% of patients tested. being on pharmacological agents. Equivalently, studies conducted among PWD from Madhya Pradesh (n = 540) reported that 72% still had an HbA1c ≥ 7% while on oral antidiabetic agents (OAD), on insulin and both OAD and insulin [ 14 ]. The Delhi Diabetes Community (DEDICOM) survey including adults with diabetes (n = 819) from middle and upper socioeconomic backgrounds showed a very low percentage of PWD (13%) had monitored their previous year's HbA1c. The mean frequency of self-monitoring of blood glucose (SMBG) was estimated as 3.1/month with approximately >40% with HbA1c> 8% [ 9 ]. Further studies revealed that poor diabetes management leads to various micro and macrovascular complications, which largely contributes to the increased risk of mortality and morbidity rates among PWD. Mohan et al in their study reported that the prevalence of Coronary Artery Disease (CAD) was 21.4% among PWD compared to 9.1% in subjects with normal glucose tolerance in the scenario where the chances of occurrence of CAD even before the onset of diabetes' [ 15 ].
4. Challenges in health care delivery for diabetes in India
In India, diabetes management becomes arduous due to various reasons such as diabetes unawareness among the community, poor access to quality care, scarcity of trained staff, monitoring facility, and the unavailability of antidiabetic drugs.
4.1. Low awareness and diagnosis of diabetes
Awareness of diabetes and its complications plays a vital role in successful disease management. Several studies analyzed the relationship between diabetes awareness and undiagnosed diabetes levels among the Indian population. The ICMR-INDIAB (Phase I) reported that only 43.2% of the population were aware of diabetes, and the level of awareness was significantly low among rural residents compared to urban residents (36.8% vs. 58.4%, p < 0.001) [ 16 ]. A study from Western India (n = 400) reported that 9.4% of the population had good awareness, 71.3% had moderate and 18.2% patients had low awareness of diabetes [ 17 ]. Another study from South India revealed good awareness and positive attitude in 55.6% and 52.8% people respectively. Among 25.4% of the people known to have diabetes, only 40.7% had good knowledge, 53.8% had a positive attitude, and 57.6% had good practice patterns [ 18 ]. A study by Deepa et al which assessed the awareness rate of complications among PWD, reported that 51.5% of the general population and 72.7% of population with diabetes knew that diabetes could affect other organs [ 19 ]. Also, low socio-economic position (SEP) measured by educational level, occupation and income increases the risk of diabetes especially T2D [ 20 , 21 ] These studies highlight the importance of enhancing the awareness level about diabetes, associated comorbidities, and management among PWD and the general population.
4.2. Lack of diagnosis and access to quality care
In India, the number of undiagnosed cases is high and the diagnosis is often made incidentally through abnormal urine or blood glucose tests or from other associated complications. It is estimated that >50% of diabetes cases in rural areas, and about 30% in urban areas remain undiagnosed. A cross-sectional house-to-house survey from the Gwalior-Chambal region of India involving 7608 subjects aged 20–79 years reported that about 50% of the PWD among the rural population were diagnosed for the first time [ 22 ]. In India, the unknown-to- known diabetes ratio is higher (3.3:1) for rural areas compared to urban areas (about 1.8:1) [ 23 ]. Treatment expenditure burden, logistic issues for patients living in rural settings, underdeveloped public health-care infrastructure, and unavailability of antidiabetic medications may contribute to the higher rate of unknown-to-known diabetes ratio and mortality rate in rural areas [ 24 ]. Despite including insulin in the National List of Essential Medicines, the most common cause of death in type 1 diabetes in India is lack of access to insulin [ 25 ]. The uncertainty in the availability of medicines and the lack of price control over the private sector, also adds to the poor diabetes treatment outcomes. For the prevention and control of major non communicable diseases (NCDs), the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS) was launched in 2010 with focus on strengthening infrastructure, human resource development, health promotion, early diagnosis, management and referral. Under NPCDCS, NCD Cells are being established at National, State and District levels for programme management, and NCD Clinics are being set up at District and CHC levels, to provide services for early diagnosis, treatment and follow-up for common NCDs. Provision has been made under the programme to provide free diagnostic facilities and drugs for patients attending the NCD clinics ( https://www.nhm.gov.in/index1.php?lang=1&level=2&sublinkid=1048&lid=604 ). Similar to NPCDCS is the National Diabetes Control Programme initiated by the Government of India on pilot basis during the seventh five-year plan in 1987 in some districts of Tamil Nadu, Jammu & Kashmir and Karnataka, but due to paucity of funds in subsequent years this programme could not be expanded further in remaining states ( http://pib.nic.in/release/release.asp?relid=34389 ). The National Programme for Health Care of the Elderly (NPHCE) is an articulation of the International and national commitments of the Government as envisaged under the UN Convention on the Rights of Persons with Disabilities (UNCRPD), National Policy on Older Persons (NPOP) adopted by the Government of India in 1999 and has envisaged providing promotional, preventive, curative and rehabilitative services in an integrated manner for the elderly (nhp.gov.in).
4.3. Medication adherence and patient issues
Poor medication adherence is a well-documented challenge in patients with diabetes. Poor adherence not only compromise clinical outcomes in PWD, but also increases healthcare costs, complications, hospitalizations, and mortality rates. Specific factors identified as key contributors to poor medication adherence were medication costs, regimen complexity, lack of transportation, long wait times at the pharmacy, patient's emotional well-being, and patient beliefs and fears (due to the fact of fear of insulin and dependence on medications or insulin etc.) [ 26 , 27 ]. Basu et al in their study conducted in a tertiary care government hospital in Central Delhi (n = 375) reported non-compliance to medications in 17.6% of PWD, and suboptimal glycemic control in 69% of patients (n = 259) on insulin therapy. The authors also reported missed clinic appointments and suboptimal refill adherence in 71.2% of patients due to out of pocket expenditure on medications and travel [ 28 ]. Studies from a rural hospital of Western India (n = 307) and Southern India (n = 162) had reported 23.7% and 95.6% compliance rate respectively in patients with diabetes [ 17 , 29 ]. Indeed, the poor clinical outcomes experienced by patients with diabetes may be due, at least in part, to poor medication adherence.
4.4. Time constraints and suboptimal knowledge among physicians
Suboptimal knowledge of or improper adherence to the recommended guidelines, constraints of time and facilities, and attitude are the major issues observed in India, which lead to improper management of blood glucose levels and other complications. However, a survey of clinical diabetologists showed that low awareness among physicians (22.7%), non-applicability of Western guidelines in Indian patients (22.7%), and treatment cost (18.2%) are the existing barriers to the practice of evidence-based diabetes management. Poor referrals to endocrinologists, and other specialists, lack of counseling, and lack of practice of evidence-based medicine impede the efficiency of patient care in India. These factors may also lead to poor patient compliance which in turn compromises safety and treatment effectiveness and hence may contribute to increase in morbidity and mortality rates. Also, general practitioners (GPs) getting certified as diabetologists from low-level universities and colleges and lack of requirement of national qualification for practice affect the regulation of quality diabetes care.
4.5. Lack of trained diabetes educators and disparity in funding
According to the American Diabetes Association (ADA) recommendations, measurement and monitoring of the key outcomes of Diabetes Self-Management Education and Support (DMSE/S) including self-management, clinical outcomes, health status, and quality of life are essentially required for appropriate diabetes management [ 30 ]. The lack of trained diabetes educators in India not only increases the burden on physicians to educate patients but also leads to an increase in the incidence and prevalence of T2DM. It is also documented that dietitians in India were generally unfamiliar with the details of the process used to identify, evaluate, and synthesize the research into the guidelines [ 31 ].
In India, the wide disparity in funding for diabetes and healthcare facilities exist due to variable levels of awareness of diabetes and the economic impact of diabetes care on the people and government.
5. Suggested measures to improve health care delivery in India
A concerted and multidisciplinary approach in treating diabetes has been recognized as a beneficial strategy to prevent the rising prevalence of diabetes-associated complications in India. Government initiatives are essentially required to deliver quality care to the maximum number of PWD. Various health care models, focusing on reorganizing the health care services with better-designed delivery systems, have been tested to improve clinical outcomes in patients with diabetes [ 32 ]. Specific interventions for provider education, patient education, financial incentives, feedback, and reminders have also been found useful in some studies [ 33 ].
5.1. Education and training
Primary care is the first point of contact between patients and health system which delivers whole-person care for health needs. In India, lack of trained and experienced physicians at primary level health facilities is a major limitation. Trained healthcare staff is a prerequisite to deliver quality care and establish a referral linkage system with the secondary/tertiary level [ 34 ]. Ethiopia has tested one of the models for health delivery to patients with chronic illness, which provides specialized support of once a month to nurse-led primary health centers [ 35 ]. The patient-centered approach reduces long-term diabetes complications with the timely involvement of trained diabetes educators, community involvement, and maintenance of treatment registers. The Indian National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS) recommends training of nurses as diabetes educators. The ten principles of care for people with diabetes or at risk for diabetes framed by the National Diabetes Education Program (NDEP) simplify the approach to diabetes. The first seven of the guiding principles highlight the steps to be implemented in the primary care physician level to alleviate the diabetes burden. The ten guiding principles of NDEP ( https://www.aafp.org/news/health-of-the-public/20180905ndepprinciples.html ) are listed as follows:
- Principle 1: Identify People with Undiagnosed Diabetes and Prediabetes
- Principle 2: Manage Prediabetes to Prevent or Delay the Onset of Type 2 Diabetes
- Principle 3: Provide Comprehensive, Patient-centered Diabetes Care
- Principle 4: Provide Ongoing Self-management Education and Support for People with Diabetes
- Principle 5: Encourage Lifestyle Modification for People with Diabetes
- Principle 6: Address Overweight and Obesity in the Management of Diabetes
- Principle 7: Individualize Blood Glucose Management for People with Diabetes
- Principle 8: Provide Multifactorial Cardiovascular Disease Risk Reduction
- Principle 9: Detect and Monitor Diabetes Microvascular Complications and Provide Treatment to Slow Their Progression
- Principle 10: Consider the Needs of Special Populations with Diabetes
5.2. Strengthening the health care systems
The quality crisis of the Indian health care sector is well recognized. The required public health facilities in India count to about 74,150 health centers per million population, but the existing number comes to only half of the original requirement. Many Indian states lack laboratories for testing and more than half of existing laboratories are not properly equipped or staffed. Hence, there is an urgent need to build a well organized infrastructure and make existing healthcare facilities healthier to improve quality of diabetes care and outcomes.
5.3. Use of affordable technologies
In India, several care-delivery models for a range of chronic illnesses have been developed to achieve quality care. Some approaches include Cardiovascular Risk Reduction in South Asia (CARRS) diabetes care delivery model for tertiary care facilities, which had been designed as the quality improvement strategy by the All India Institute of Medical Sciences (AIIMS), New Delhi the New Delhi-based Centre for Chronic Disease Control (CCDC) and Public Health Foundation of India (PHFI), and Atlanta-based Emory University. In 2016, Ali et al. compared with usual care in a poorly-controlled diabetes setting (1146 PWD [575 intervention; 571 usual care]) for 28-months and found that 18.2% of intervention participants achieved an HbA1c <7.0% and BP < 130/80mmHg compared to usual care participants [ 36 ]. The CARRS model demonstrated the importance of low-cost strategies to achieve diabetes care goals and to improve the quality of life in patients with poorly controlled diabetes.
The AIIMS and CCDC have developed mHealth based digital clinical decision support software (DSS) tools for improving healthcare delivery in various clinical settings. A mobile health-based electronic decision support system, known as mPower Heart mHealth System comprising of DSS integrated Electronic Health Record (EHR), was used primarily by trained nurse care coordinators in the out-patient clinics. mHealth/e-Health based digital clinical DSS model was adopted for state-wide implementation in 56 health facilities throughout the Indian states of Tripura and Mizoram and more than 45,000 individuals with hypertension/diabetes have been treated using DSS.
Diabetes Tele Management System® (DTMS®) originally developed and practiced at Jothydev's Diabetes Research Centre since 1997 has been found to be advantageous in many aspects of diabetes management such as in frequently titrating the doses of medications, drastically reducing the frequency of hospital visits, providing cost-effective treatment, and advices on diet and lifestyle to achieve the customized treatment goals. A study which analyzed the impact of DTMS® in glycemic control had reported that frequent telemedicine follow-ups based on self-monitoring of blood glucose (SMBG) aids in slow and steady titration of drug dose and reducing the risk of serious hypoglycemia [ 37 ]. A retrospective study, which evaluated the cost-effectiveness of the telemedicine program, DTMS® in T2DM patients with a six month follow-up data revealed that telemedicine for diabetes management is cost-effective and safe [ 37 ]. DTMS® had also found to be effective in preventing microvascular and macrovascular complications in 93.5% of the type 2 diabetes subjects [ 38 ]. All these studies emphasize the potential benefits of implementing and practicing affordable technologies such as telemedicine especially in treating the low economic category.
International guidelines recommend diabetes technologies to maintain quality of life and prevent the future cost of treating diabetes. Hence, the government should take necessary steps to avail effective use of diabetes technologies to reduce the diabetes treatment burden.
5.4. Public-private partnership
Public-Private partnership is one of the proven strategies to improve access to healthcare, especially in remote areas. Several reasons stress the establishment of private-public partnerships in diabetes care. Firstly, more than 80–90% of the qualified doctors involved in the treatment of diabetes and associated disorders work in the private sector and is one of the reasons why patients prefer private sector, especially affordable patients. Secondly, it is very much essential that a public-private partnership is required for both clinical care and for research as most of the original research publications in diabetes from India come from the private institutions involved in original research. So a public-private partnership for diabetes care and research will have numerous beneficial effects. Some projects such as “Changing Diabetes Barometer and Changing Diabetes in Children” are running successfully in India. The Public Health Foundation of India has tied up with West Bengal and Madhya Pradesh governments to train public sector doctors in diabetes care. These models should be encouraged in resource-constrained areas.
5.5. Health care governance
Government initiatives are encouraged to create guidelines on diabetes management, provide funds for public awareness programs, and to ensure an uninterrupted supply of medicines and diagnostic services to PWD. Around the world, various governments have conducted different types of patient education programs and have also achieved positive health outcomes among PWD. In India, similar efforts and services are required at the grass-root level to set quality standards, underpin clinical governance, and to contain the new-age diabetes pandemic. Regular programs should be organized wherein senior doctors from secondary/tertiary level health facilities and medical colleges should mandatorily visit rural areas to help peripheral health workers improve their knowledge and skills.
5.6. Universal screening for gestational diabetes mellitus (GDM)
Wide variability in reported prevalence estimates for GDM in India, varying from less than 4% to nearly 18% which refers to the variable screening procedures [ 39 ]. The treatment of GDM is suboptimal in India since the patients are not getting treated by the speciality team which is quite essential to prevent the progression to type 2 diabetes. Although the Government of India endorses Diabetes in Pregnancy Study Group India (DIPSI) criteria for GDM diagnosis, real success depends on the commitment level and knowledge of healthcare providers [ 40 , 41 ].
The barriers to the health care delivery model for diabetes management and its suggestive measures are summarized in Figure 1 .

HCD Model for effective diabetes management.
6. Conclusion
Focus on diabetes education, proactive physician participation, extensive research and a well-planned healthcare system oriented towards diabetes care, form the main areas of desired intervention. Universal screening of diabetes and primary health care possible through public-private partnership may be appropriate in the Indian context. Healthcare professionals should update themselves with recent advances in diabetes diagnosis and treatment and engage in educating patients and the general population. Another welcome initiative on the part of the government will be to subsidize the treatment and care of PWD. Thus a combined effort from patients, healthcare professionals, government, and NGOs can only help to tide over the situation.
Declarations
Author contribution statement.
All authors listed have significantly contributed to the development and the writing of this article.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Declaration of interests statement.
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.

IMAGES
VIDEO
COMMENTS
The National Rural Health Mission (NRHM) was launched on 12th April 2005, to provide accessible, affordable and quality health care to the rural population, especially the vulnerable groups. On 1st May 2013,Cabinet has approved the launch of National Urban Health Mission (NUHM) as a Sub-mission of an over-arching National Health Mission (NHM ...
Presentation Transcript. HEALTH CARE DELIVERY SYSTEM IN INDIA. Health system It is designed to meet the health needs of the community, through the use of available knowledge and resources. Two major themes: It should meet the needs of entire population and not merely selected group. Primary health care.
Health Care Delivery System in India - Free download as Powerpoint Presentation (.ppt / .pptx), PDF File (.pdf), Text File (.txt) or view presentation slides online. The health care delivery system in India has 3 main levels - central, state, and local. [1] At the central level, the main organizations are the Ministry of Health and Family Welfare, Directorate General of Health Services, and ...
India has made significant improvements in the health outcomes of its people. However progress is uneven across states, and demographic and epidemiological changes means the country faces a double burden of disease and an ageing population - presenting challenges and opportunities, as it seeks to transform its health sector. India has a mixed health-care delivery system. Policy ...
INTRODUCTION. Health care delivery system is the organization of people, institutions & resources that deliver health care services to meet the health needs of the country. India is a Union of 29 states & 7 Union territories. Apart from central Government each state has developed it's own system of health care delivery.
The health care delivery system in India has three main levels - central, state, and local/peripheral. At the central level, the key organizations are the Ministry of Health and Family Welfare, which is responsible for policymaking, planning, and coordination; the Directorate General of Health Services, which handles functions like surveys, planning, and programming; and the Central Council of ...
system of medicine in the health delivery system of the country. 18.2EVOLUTION OF HEALTH CARE DELIVERY SYSTEM 18.2.1 History of Evolution of Health Services Health is a positive state of well-being and not a mere absence of diseases. Health, further implies complete adjustment of the individual to his total environment, physical and social.
hcds - Free download as Powerpoint Presentation (.ppt / .pptx), PDF File (.pdf), Text File (.txt) or view presentation slides online. The health care delivery system in India has both public and private sectors. The public sector focuses on primary health care and includes community health centers, rural hospitals, and specialist hospitals. It also oversees health insurance schemes and programs.
Health care delivery system in India At the block level • Objective - to provide primary health care to all the sections of the society. • 80% of the population is scattered in villages • 20% of rural population have health care facilities. Community health Centre's • Established and maintained by the State Government under MNP/BMS ...
22 Primary Health Care Delivery system. In 1977-Rural health scheme on principle of placing people's health in people's hands Three tier system of health care delivery system Basic tenet of primary health care is universal coverage village level 1)Anganwadi worker 2)ASHA worker. 23 Under ICDS prog. 1 AWW for 1000 population.
The public healthcare system in India is primarily managed and funded by the government, while private healthcare providers, including hospitals, clinics, and diagnostic labs, operate on a profit basis. According to the Economic Survey 2022, the government expenditure on healthcare was 2.1% of GDP in 2021-22 compared to 1.8% in 2020-21.
HEALTH CARE DELIVERY SYSTEM IN INDIA. HEALTH CARE DELIVERY SYSTEM IN INDIA. Health system It is designed to meet the health needs of the community, through the use of available knowledge and resources . Two major themes: It should meet the needs of entire population and not merely selected group. Primary health care. 5.53k views • 49 slides
Health Care Delivery System in India - Free download as Powerpoint Presentation (.ppt), PDF File (.pdf), Text File (.txt) or view presentation slides online. 454
that health care organizations can become more resilient, agile, and innovative through digitally-enabled business models with data at the core. The pandemic added urgency and accelerated the process of change for healthcare to become more digitally enabled. Healthcare delivery is moving outside the four walls of traditional health system.
Presentation Transcript. Health System in India Tej Ram Jat Centre for Health Equity & Jan Swasthya Abhiyan, India [email protected]. Introduction • The political economy context • The organisational structure and delivery mechanism • Health financing mechanisms • Coverage patterns • Current status of health and health care. The ...
The Indian healthcare scenario presents a spectrum of contrasting landscapes. Socioeconomic factors, problems with medical infrastructure, insufficiency in the supply of medical requisites, economic disparities due to major differences in diabetes care delivery in the government and private sectors and difficulty in accessing quality health care facilities challenges effective diabetes care in ...