Connection denied by Geolocation Setting.
Reason: Blocked country:
The connection was denied because this country is blocked in the Geolocation settings.
Please contact your administrator for assistance.

Point-of-care testing
Point-of-care product device testing is critical to ensuring that medical devices are effective and safe for use by patients. We support your studies that assess the safety, accuracy, and effectiveness of medical devices at the point of care.
We offer a wide range of testing services, including clinical performance testing, usability testing, and comparative testing, among others.

Human factor studies
Comparator studies.
When you’re ready to assess the safety and efficacy of your product in comparison to other devices or instruments, we can help design and conduct comparator studies, ensuring that they are conducted to the highest quality standards and regulatory guidelines.
- Head-to-head studies
- Non-inferiority studies
- Superiority studies
Let's discuss your project
Contact our pharma solutions experts to design a custom program to accommodate the needs of your study.
Let's discuss your next project
Connect with our team of experts today.
Remnant samples
R&D consulting
Regulatory strategy
Research & discovery
Commercialization
Clinical trial lab services
Companion diagnostics
Sponsored testing
Data licensing
Patient recruitment
Patient engagement
Mobile services
Rare diseases
Cell & gene therapy
Cardiometabolic
More therapeutic areas
Life Sciences

Our company
- How we operate
- Corporate responsibility
- Inclusion and diversity
- Actions and insights
- Specialty labs

- Site map •
- Privacy Notices •
- Terms •
- Contact us •
- Language assistance / non-discrimination •
- Asistencia de idiomas / Aviso de no discriminación •
- 語言協助 / 不歧視通知 •
- Accessibility •
- Your Privacy Choices •
Quest® is the brand name used for services offered by Quest Diagnostics Incorporated and its affiliated companies. Quest Diagnostics Incorporated and certain affiliates are CLIA certified laboratories that provide HIPAA covered services. Other affiliates operated under the Quest® brand, such as Quest Consumer Inc., do not provide HIPAA covered services.
Quest®, Quest Diagnostics®, any associated logos, and all associated Quest Diagnostics registered or unregistered trademarks are the property of Quest Diagnostics. All third-party marks—® and ™—are the property of their respective owners. © 2024 Quest Diagnostics Incorporated. All rights reserved. Image content features models and is intended for illustrative purposes only.
www.QuestDiagnostics.com says
You are now leaving the Quest Diagnostics web site. Quest Diagnostics does not control the site you are about to enter and accepts no responsibility for its content.
We'll redirect you to MyDocBill.com, the website of Quest’s billing services provider. Here, Quest patients have secure access to pay their bill, update insurance, edit their profile and view their account history.
Employer Health and Wellness
To schedule an appointment for your employer health and wellness screening (biometric screening), we need to redirect you to the Health & Wellness website.
- Your doctor must have ordered your COVID-19 antibody testing or you must have purchased a test through QuestDirect. COVID-19 is highly contagious. If you are currently experiencing COVID-19 symptoms, you must first contact your doctor for next steps..
- We can only accept patients in our Patient Service Centers who have been confirmed to be COVID-19 symptoms-free for at least 10 days.
Purchased Tests
Please visit our appointment scheduling page to make your appointment.

The Ultimate Guide to Marketing Your Pharmacy’s Point of Care Testing Services
Share on social media, point of care testing (poct) is a powerful tool for independent pharmacies, offering an opportunity to expand revenue streams and provide essential healthcare services to your community. .
This comprehensive guide will explore effective marketing strategies to make your POCT services successful. From understanding your target market to leveraging online reviews, we’ve got you covered.
Understanding Your Target Market
Before diving into marketing strategies, it’s crucial to understand your target market thoroughly. This knowledge can differentiate between a successful campaign and one that falls flat. Here are some ways to get to know your customers better:
- Ask Your Patients: Conduct formal Q&A surveys or have your staff engage in conversations with patients. Get insights into their needs and preferences.
- Know Your Demographics: Determine whether your pharmacy caters to an elderly population, busy executives, or families with children. Tailor your tests and messaging accordingly.
- Competitor Analysis: Research what urgent care centers or same-day clinics in your area offer, their pricing, and accessibility. Identify gaps in services and focus on filling them.
Marketing to Your Current Patients
Dr. Lisa Faast often teaches that retaining and expanding business with current customers is easier than acquiring new ones. Here are some high-converting, low-cost in-store marketing strategies:
- Signage, Flyers, and Posters: Use vibrant colors and clear messaging throughout your store. Place posters strategically in areas where patients spend time, like waiting areas and drive-through lanes.
- Bag Stuffers: Change these monthly, promoting different POCT Services. Offer discounts or special promotions to incentivize purchases.
- Staff Training: Ensure your staff is knowledgeable and comfortable discussing point-of-care testing with patients. Regular training sessions improve their ability to upsell and cross-sell related products.
Leverage Social Media Marketing for POCT
Utilize social media to reach a broader audience, create awareness about your services, and remove barriers from your patients’ minds by addressing potential questions and concerns about new services like POCT. Provide answers to common queries such as appointment requirements, walk-in availability, duration, costs, required documentation, and operating hours. By eliminating uncertainty, you make it easier for individuals to take action.
In addition to addressing questions, incorporate the following types of posts:
- Educational Posts: Share infographics, video clips, or live Q&A sessions with healthcare experts to educate your audience. Include local infection rates and common health issues in your town.
- Testimonials: Capture video testimonials from satisfied customers, showcasing authentic and engaging recommendations.
- Promotions and Discounts: Create flash sales and countdown timers for special offers. Consider offering multiple-test discounts to encourage family or group testing.
Partner with Local Businesses and Healthcare Providers
Form strategic alliances in your community to increase visibility and credibility. Identify partners that share your target audience. Potential collaborators include local gyms, health food stores, chiropractors, dentists, optometrists, and healthcare providers. Consider collaborations like reciprocal promotions or discounted services for partner customers. Establish relationships with healthcare providers without point-of-care testing but with substantial patient databases. Engage with local employers by offering bulk testing discounts, on-site testing, or infection control programs like supplements.
Email Marketing to Grow P OCT
Email marketing enables direct communication with patients, fostering engagement and trust. Consistency is key. Provide value, education, and entertainment in your emails. Increase promotional email frequency to ensure you’re top-of-mind when patients require testing services. If you have a weekly email or newsletter, consider having a section for point-of-care testing.
Participate In Community Health Events
Position your pharmacy as a healthcare hub by participating in wellness and health events. Offer free or discounted tests during local health events in collaboration with organizations. Present educational material to establish expertise and offer recorded videos for those unable to attend in person.
Utilize Local Media
Local media outlets like community papers, TV, or radio stations can effectively spread the word. Distribute press releases when launching services, even if they aren’t entirely new. Sponsor health segments on local radio shows to subtly promote your POCT services.
Build relationships with local media personnel and keep them updated on your pharmacy’s clinical products and services through regular emails.
Leverage Online Reviews
Online reviews play a crucial role in attracting new customers. Encourage satisfied customers to leave positive reviews in exchange for discounts on future services. Respond thoughtfully to all reviews, demonstrating your commitment to customer feedback.
Simplify the review process with QR codes and include review links in follow-up emails.
Grow Through Referrals
Implement a robust referral program for your POCT services by following these steps:
- Determine Reward Amount
- Establish Guidelines and Logistics
- Track Performance
- Train Your Team
- Promote to the World!
Leverage Thank You Cards for Your POCT Referral Program
Implement a thank-you card program to enhance referrals. After a patient undergoes testing, send them a handwritten thank-you card. Express well wishes and politely request referrals.
Monitor and Adapt
Regularly evaluate your marketing efforts by tracking key performance indicators (KPIs). Select 3-4 essential KPIs to focus on, such as the total number of tests performed, gross sales, referrals, and customer feedback. Be open-minded and flexible, ready to adjust your strategies based on performance metrics and customer feedback.
By implementing these strategies, you can create a comprehensive marketing campaign that drives awareness, engagement, and trust in your pharmacy’s POCT services. Solidify your trusted community healthcare provider position, ensuring your success in a competitive market. If you’re ready to start or grow your point-of-care testing program, consider joining Pharmacy Badass University for comprehensive support and resources. Become a Pharmacy Badass and lead the way in Point of Care Testing in your community!
HHS Gives Pharmacists Expanded Vaccine Authority For COVID
September 15, 2020

Holy Moly! Audits Galore – What You Need To Know
October 26, 2020
What’s The Scoop With Test Claims?
September 27, 2020
3 Easy Strategies to Increase Your Clinical Revenue for Independent Pharmacies
October 9, 2020
October Is The New January
October 2, 2020

How To Attract New Patients With An Exclusive Club
October 20, 2020
High-End Pharmacy Marketing Graphics On A Low-End Budget
September 8, 2020

The One Marketing Mistake You Are Probably Making
November 5, 2020

5 OTCs You Should Be Selling
November 6, 2020

The Perfect Fall Marketing Plan
About DiversifyRx DiversifyRx is dedicated to helping pharmacy owners kick ass and create profitable, thriving pharmacies. We strongly believe the key to success is diversifying your revenue streams and maximizing each opportunity that is right for you. DiversifyRx was created by a pharmacy owner for pharmacy owners. We offer tons of free information and our Pharmacy Badass University membership. This site contains affiliate links to products or services. We may receive a commission for purchases made through these links. Trending Now Semaglutide and Tirzepatide Resources for Independent Pharmacies
First steps for cash-based functional medicine pharmacy revenue.

The Case for Targeted Marketing for Independent Pharmacy Owners

Pharmacy Profit Boost: Travel Medications

4 Ways To Diversify Your Pharmacy’s Revenue
Follow us on social media.
- Chat with NCPA
What’s the point of POCT?
NCPA April 9, 2024
For your patients, pharmacy-based point-of-care testing is a convenient, accessible way to get the care they need. For pharmacies, it’s a way to connect with those in your community and generate revenue. We’ve got two resources to get you started with POCT or expand your existing program.
The NCPA Innovation Center will be offering the NASPA Pharmacy-Based Point-of-Care Test and Treat National Certificate Program on May 16 in a virtual format. Enroll for the chance to gain the skills and information necessary to develop a testing program such as influenza, Group A Streptococcus, HIV, Hepatitis C, coronaviruses, and chronic diseases.
You can also download the comprehensive Guide to Implementing Point-of-Care Testing Services in Community Pharmacy , sponsored by QuidelOrtho and brought to you by the NCPA Innovation Center and NASPA. It too can help with setting up and providing these services, marketing them in your community, and navigating reimbursement.

WesternU COP names classroom in honor of Ken Thai, NCPA officer
Cms expands mtm, addresses plan steering in cy 2025 ma and part d final rule, today: webinar with dea on pharmacy security, new ncpa core program aims to grow skills in financials, operations, marketing, and leadership.

- December 21, 2023 | How Healthcare Providers are Shifting Toward Home Care
- August 8, 2023 | Sustainability in Medical Manufacturing
- February 22, 2023 | Understanding the evolving Laboratory Supply Chain
- January 26, 2023 | Mergers, Acquisitions, and Respiratory season with Quidel
- November 16, 2022 | Driving Value Through Clinical Education
How to leverage point-of-care testing to help improve patient care & generate revenue
Sponsored – McKesson

With the rising demand for point-of-care testing (POCT), health systems and physician practices are finding new ways to improve patient care and outcomes, strengthen operational efficiencies with in-office laboratories and access new revenue sources.
In 2020, there were upwards of 266,000 laboratories in the United States laboratory market. More than 120,000 of those facilities were physician office labs (POLs), including independent practices and hospital-affiliated physician offices with point-of-care lab testing, according to the 2021 HIDA Laboratory Market Report. 1
If your health system or physician practice is seeking ways to increase patient satisfaction and build revenue-generating services that set you apart from the competition, adding or upgrading an in-office lab and point-of-care testing could be a profitable solution.
Meeting the demand for point-of-care testing
The COVID-19 pandemic has increased the demand for point-of-care testing and diagnostics in the United States and globally, boosting revenues in the laboratory testing market by 9.1% year-over-year since 2020. 1
At the same time, lab testing for a lengthy list of other acute and chronic conditions and diseases is always in demand. To keep up with patient expectations for quality care, services and convenience, your physician office or health system must be supported with the right lab operations for better health systems management.
“It’s extremely important for health systems to have a well-defined and streamlined laboratory solution for their network,” says John Harris, vice president of strategic accounts, laboratory, at McKesson Medical-Surgical.
“Having the right mix of central lab and point-of-care testing can ensure that healthcare providers are able to diagnose and treat patients in the most efficient way possible.”
Point-of-care testing can help generate revenue for your health system
When your health system or physician practice implements and establishes point-of-care testing, your business becomes more appealing to patients. At the same time, you’re taking steps toward generating additional revenue and controlling costs.
Leveraging your health system’s in-house lab for revenue generation offers the ability to:
- Reduce or eliminate payments to other labs
- Exert greater control over setting lab fees
- Provide direct oversight of lab-testing quality
- Eliminate or reduce delays in send-out testing
- Receive direct reimbursement by insurance and Medicare to create more efficient healthcare revenue-cycle management
- Maintain a competitive advantage by providing lab services unavailable at other healthcare provider offices
- Schedule fewer follow-up appointments, creating openings for new patients and reducing staff time spent contacting patients who don’t follow through with off-site lab testing
Point-of-care testing can help increase patient satisfaction
Providing in-office lab services to patients sets your practice or health system apart from competitors. Most patients welcome the convenience of not having to drive to a separate lab for diagnostic testing or schedule a follow-up appointment for results.
Faster turnaround times for lab results can also lead to a speedier diagnosis, which means treatment can begin sooner and patient outcomes can be improved.
“Point-of-care testing is critical to the success of a patient’s overall wellness,” says Harris. “Whether you’re confirming strep before providing antibiotics or monitoring a patient’s A1C levels to adjust treatment, having testing results at the point of interaction can dramatically affect the patient’s treatment and overall health.”
Considering the cost of an in-house lab
Providing point-of-care testing for your patients can pay off by generating revenue in the long run. However, your practice or health system must consider and plan for some initial and recurring costs that may accompany the implementation of POCT.
These expenses can include:
- Renovation and downtime costs. You may need to upgrade electricity, add water lines and lighting, and do other renovations that could create downtime
- Equipment purchase or rental costs. These can include a lab-only (no food allowed) refrigerator, centrifuges, rocker, and supplies such as urine collection cups and phlebotomy consumables
- Lab manager salary and other lab staff wages
- Regulatory fees, including federal CLIA fees for a moderately complex point-of-care lab, inspection fees, and state inspection or other fees
With point-of-care testing at more than one location, it’s important to standardize products and processes to ensure that all point-of-care labs are using the most appropriate and cost-effective products to generate higher revenue and minimize loss.
Many health systems evaluate their product and supplies with a full value-analysis team. The team may include clinicians, nurses, quality management and supply chain experts. The analysis team may also create patient-education and infection-prevention resources and guidelines.
“When thinking through the clinical, operational and financial outcomes of a lab strategy, several departments should be involved in the process,” says Harris. “There are many elements to a laboratory decision. Having a diverse team of experts can ensure that the right decisions for the entire system are being made.”
Work with your distributor to plan & prepare
When developing the best point-of-care testing strategy for your health system, your distributor can help you design and prepare your business plan.
McKesson Medical-Surgical specializes in laboratory testing, products and services, offering expertise and guidance on many aspects of implementing an expanded lab and point-of-care testing, including:
- Analysis of patient population and payer mix
- Equipment setup and purchasing vs. rental costs
- Knowledge and assessment of testing demand
- Creation of a value-based care analysis
- Standardization of supply chain operations
“It’s important to understand the goals of the health system and build lab solutions around them,” says Harris.
“We take a holistic approach when it comes to lab strategy and planning, because success looks different from system to system. We’re diligent in understanding those needs and have a robust team of lab specialists who can partner with our customers to ensure maximum success.”
We’re here to help
McKesson Medical-Surgical specializes in laboratory testing, products and services across the non-acute continuum. We offer specialized implementation teams, equipment setup, lab consulting and a wide array of other laboratory system solutions to help seamlessly integrate your lab operations.
Customer Service
Point-of-Care Testing
Get reimbursed for covid-19, flu, strep & more.

GROW YOUR BUSINESS THROUGH POINT-OF-CARE TESTING
Pharmacists now are authorized to order, administer and bill for point-of-care testing (POCT). Leverage an end-to-end solution that manages the entire process for you. From identifying point-of-care testing opportunities that make sense for your pharmacy to streamlining documentation, billing and reporting, learn how OmniSYS can help effectively manage point-of-care testing for your pharmacy.
Reimbursable tests vary by state and payer but commonly include:
- Blood glucose
- COVID-19
GET REIMBURSED FOR COVID-19 TESTING

The CARES Act authorizes all US pharmacists to administer COVID-19 testing and Medicare has provided a pathway to reimbursement . Talk to an expert to learn how you can quickly take advantage of this opportunity.
AN END-TO-END SOLUTION FOR POINT-OF-CARE TESTING
Understand the opportunity.
Learn which point-of-care tests your state allows pharmacists to perform, and which payers are reimbursing for pharmacy-administered tests.

Prepare to be a provider of care
Leverage online training to get credentialed for the tests you want to perform and contracted with the payers you want to bill.
Get credentialed and enrolled
Shifting payer mixes and staffing changes make keeping track of each practitioner’s credentials and enrollment status an unavoidable challenge. Take advantage of credentialing and payer enrollment services so that you can focus on delivering care.

Document the encounter
Take advantage of guided documentation driven by payer requirements for quick, easy and effective documentation of the encounter.
Optimize your reimbursement
Get the reimbursement you’ve earned with real-time verification for eligibility, coverage and payer requirements.

Share results electronically
Share the results with your patient’s primary care provider or other healthcare team members as well as any public health organizations. * For COVID-19 testing, results will be automatically reported to the required public health organization(s).
Help Medicare patients select the right plan
Leverage a plan comparison tool to help Medicare eligible patients select an in-network plan at your pharmacy based on their unique prescription needs.

Providing point-of-care testing doesn’t have to be hard. Where do you want to start?
Credentialing, paperless documentation, reimbursement, talk to a point-of-care testing expert.
Tell us a little about your pharmacy business so we can match you with the right technology expert for your needs.
Copyright 2024 XiFin, Inc. All rights reserved.
Fill in the form to download our whitepaper.
- First Name *
- Last Name *
- Pharmacy Name *
- State/Province * State/Province AB AK AL AR AZ BC CA CO CT DC DE FL GA HI ID IL IN IA KS KY LA MA MB MD ME MI MN MO MS MT NB NC ND NE NH NJ NL NM NV NS NT NU NY OH OK ON OR PA PE PR QC RI SD SC SK TN TX UT VT VA WA WI WV WY YT
- Country * Country United States Canada
- Phone Number *
- Which describes your pharmacy? * Which describes your pharmacy? Independent Retail Chain Hospital Outpatient Mail Order Specialty Pharmacy
- Hidden utm_source
- Hidden utm_medium
- Hidden utm_campaign
- Hidden utm_term
- Hidden utm_content
- Hidden gclid_field
- Hidden li_fat_id
- Name This field is for validation purposes and should be left unchanged.
Point-of-Care Testing
- What is point-of-care testing?
In the early days of medicine, few medical tests existed that were done at the patient’s bedside. By the 1950s, automated technologies meant centralized clinical laboratories could run large numbers of tests at low cost. It became common to send samples away to laboratories and then wait days to weeks for results.
As the need for faster test results has grown and certain testing devices have become portable and easy to use, medical testing has evolved once again. Today, results from clinical laboratories remain a crucial component of your health care, but they are now complemented by tests performed outside of the laboratory, wherever you are.
Point-of-care testing spans so many areas of medicine that it is best defined by where it’s done – anywhere outside the centralized laboratory – rather than by the kinds of tests that are performed. It may be referred to by many different names, such as near-patient testing, remote testing, satellite testing, and rapid diagnostics. In general, point-of-care testing encompasses any tests that are performed at or near a patient and at the site where care or treatment is provided. Results are typically available relatively quickly so that they can be acted upon without delay.
Point-of-care tests can happen in a wide variety of locations: in your home, at a health care practitioner’s office, in the emergency department, in an infectious disease containment unit, in ambulances, at an accident scene, in the military, in the radiology department, on a cruise ship, or even on the space shuttle. And a wide variety of people can perform point-of-care tests, including laboratory professionals, emergency first responders, radiologists, doctors, nurses, physician assistants, or other health care practitioners. They may even be done by yourself, sometimes called “self-tests” or “home tests.”
Devices for point-of-care tests come in an array of forms. They may use basic dipsticks as with urinalysis , handheld devices like glucose meters, or sophisticated molecular analyzers to detect infectious diseases. A health care practitioner may use a handheld device to perform a test at a patient’s bedside. Alternatively, that health care practitioner may collect a blood sample from the patient and walk the sample down the hallway to a satellite lab, where the sample is processed and tested on instrumentation. Both examples are considered point-of-care testing.
And the same type of point-of-care device may be used by a health care practitioner and a “lay person” such as yourself. For example, glucose meters are used by health care practitioners in hospitals to monitor patients in intensive care units. Glucose meters can also be used by diabetics at home to monitor levels and to adjust their insulin if necessary. Though the regulation and oversight of the use of these devices may differ when health care practitioners use them as opposed to the general public, they are more or less comparable devices.
The most common point-of-care tests are blood glucose monitoring and home pregnancy tests . Other common tests are for hemoglobin , fecal occult blood , rapid strep , as well as prothrombin time/international normalized ratio (PT/INR) for people on the anticoagulant warfarin. As medical care evolves to become more consumer-focused, point-of-care testing will continue to be an important way to perform medical testing. However, for you to receive the highest quality care by using these tests, it’s important that point-of-care tests are part of a testing continuum that includes centralized clinical laboratories and a team of health care practitioners.
- About Point-of-Care Testing

Why is Point-of-Care Testing Growing?
As health care becomes more consumer-focused, the need for convenient diagnosis, monitoring, and screening tests is expanding worldwide. In some cases, technology has caught up; testing devices that are smaller, more portable, and easier to operate have been developed.
The market for point-of-care testing is estimated to grow 9.3% between 2013 and 2018. There are a number of reasons for this trend. Point-of-care tests provide results in real time, rather than in hours or days, so they can help you and your providers make faster, and hopefully better, decisions about your medical care. With results in hand during your consultation, you can receive immediate follow-up testing or treatments without returning for another office visit.
For example, if you are given a point-of-care test and diagnosed with influenza right away, your health care practitioner can explain why you don’t need antibiotics and instead treat you with an antiviral medication if it’s appropriate.
Point-of-care testing is useful as medical care shifts to a focus on prevention, early detection, and managing chronic conditions. In the emergency room, early detection can help determine if people with flu-like symptoms have influenza or if they have a higher-risk infection like Middle Eastern Respiratory Syndrome (MERS). In the health care practitioner’s office, the rapid strep test allows for earlier treatment of strep throat and reduces the risk of complications from not treating it. At home, glucose meters allow people with diabetes to tailor their insulin therapy. It makes up the largest segment of the point-of-care testing market.
There is also a growing need for rapid screening for infectious diseases like HIV , dengue fever , malaria, and influenza. Infectious disease tests are useful in community clinics and remote or resource-limited areas where there may not be access to a central lab or where infrastructure is limited for transporting samples. Infectious disease tests at the point of care can also lead to prompter treatment, which can prevent infections from spreading.
When time is of the essence, such as in emergency departments or at accident scenes, point-of-care tests provide immediate information about blood gases , electrolytes , or troponin .
When used as part of a larger health care strategy, point-of-care testing can make diagnosis and treatment a smoother and more efficient process. Point-of-care tests are most beneficial when they are viewed as one step in a testing continuum that may begin at the point-of-care, but eventually leads to coordinated testing with a central laboratory.
When used properly, point-of-care testing can lead to more efficient, effective medical treatments and improved quality of medical care.
At home, point-of-care tests allow for more frequent and more consistent testing and can empower you to take control of your medical care. Ideally, the end result is higher quality care. For example, clinical trials have shown that individuals monitoring blood thinners (anticoagulants) like warfarin at home had fewer major complications from the treatment.
Point-of-care testing is also crucial in emergency situations and in the operating room. If someone is having a stroke, a first responder or other healthcare practitioner needs to measure prothrombin time/international normalized ratio (PT/INR) to test blood coagulation before he or she can give stroke medications. Point-of-care tests are also used to measure coagulation during open-heart surgery and organ transplants.
Point-of-care tests can also help alleviate emergency room overcrowding by reducing the time it takes to treat people and thus shortening their stays. They are also useful in disaster situations like Hurricane Katrina or any scenario that prevents access to power, water, and laboratory infrastructure.
When used in a healthcare practitioner’s office, point-of-care testing can reduce follow-up visits or calls. In one study, delivering the routine tests hemoglobin A1c , hemoglobin , and lipids at the point-of-care decreased tests ordered for each patient by 21%, reduced follow-up calls by 89%, and reduced patient follow-up visits by 61%.
One concern with conventional laboratory testing is that people may not return for treatment if they have to go home and wait for results. This has been the case for HIV viral load and tuberculosis testing. In one study at a clinic in Ghana, point-of-care testing helped remedy this problem. When people seeking care at a tuberculosis clinic were offered HIV tests on the spot, they were more likely to also return for HIV care.
Point-of-care testing can also provide test results in locations where clinical laboratories don’t exist or are too far away, like in the developing world, rural regions, or on cruise ships or even the space shuttle.
While many point-of-care tests are designed to be relatively simple and low risk to use, they are not error-proof. Individuals using point-of-care tests, even healthcare practitioners, must carefully follow test directions and be familiar with the test system. Some point of care tests, such as those used to adjust doses of medications, have the potential to lead to serious health consequences if not performed properly. Many large hospitals have point-of-care coordination teams to ensure that testing procedures are properly followed.
It’s important that the convenience of point-of-care testing does not tempt users to apply them beyond their intended purpose or misinterpret results. For example, glucose meters and point-of-care hemoglobin A1c tests are designed only for monitoring diabetes and should not be used for diagnosis or screening.
You and your health care practitioner also need to be cautious when comparing test results from different sources. Just as test results may not be consistent from laboratory to laboratory, they may vary between point-of-care testing techniques, or between laboratory results and point-of-care results.
One major challenge is managing the data generated by point-of-care tests. When tests are performed at the point-of-care, it is important that the results are incorporated into your health record.
If you are performing point-of-care tests at home, it’s best to seek professional guidance. For example, if you are monitoring a medicine like warfarin for anticoagulation , a testing mistake could lead to a blood clot or internal bleeding. That’s why it’s recommended that you learn to perform the test with professional supervision and have the result verified by a clinician before performing it at home and periodically to ensure consistent technique.
Getting a follow-up diagnosis from a healthcare practitioner is also important if you use home screening tests. For example, the U.S. Food and Drug Administration (FDA) approved HIV testing for home use in 2012. While home tests are less sensitive and home users can make more mistakes than professionals, the FDA thought the benefit of increased HIV testing outweighed the risks.
Home tests and some point-of-care HIV tests used in clinics, for example, detect only HIV antibody and not the HIV antigen, so they may miss some early infections with HIV. All HIV screening tests that are positive should be followed by a second, different antibody test for diagnosis, and should not stand alone to make a diagnosis. Though HIV home tests and point-of-care tests can offer speed, convenience and privacy, it is important for individuals using these tests to seek follow-up care and diagnosis.
While speed is often one of the advantages of point-of-care tests, the results may not be as specific or sensitive as centralized laboratory test results. For example, there are several types of rapid influenza diagnostic tests (RIDTs) available to help differentiate influenza (flu) from other infections with similar symptoms that must be treated differently. Depending on the method, RIDTs may be done in less than 15 minutes in a health care practitioner’s office or may be sent to a laboratory, with the results available the same day.
But not all RIDTs have the same ability to detect influenza. Some tests can only detect influenza A while others can detect both influenza A and influenza B but not distinguish between the two. Still others can detect and distinguish between influenza A and B but may not detect the latest strain of influenza circulating that year due to antigenic changes in the virus. Moreover, point-of-care flu tests are not designed to identify the subtype of influenza the patient has, i.e. H3N2 or the pandemic H1N1 strain.
Point-of-care tests may also deliver a more limited range of results compared to full laboratory workups. So, following up with a laboratory test will likely be necessary after an initial test at the point of care.
In general, point-of-care tests should be viewed as a valuable tool for medical testing, but not the only tool. Since you benefit most when point-of-care tests and central laboratory tests are coordinated, it’s important that point-of-care tests are not used in isolation.
For some conditions, like diabetes, point-of-care testing has already drastically altered how care is delivered and managed. With the market for point-of-care testing only expected to expand, it will continue to change the way healthcare is delivered, making care more patient-driven and focused, providing more data to support evidence-based medicine .
New point-of-care tests that may emerge in the future include new technologies intended to manage critically ill patients in the emergency room, in the hospital, or undergoing surgery, such as complete blood count or tests for drug overdoses. And new tests may be developed for earlier cancer detection, such as cervical cancer. Point-of-care tests will also continue to be important for managing chronic conditions.
Infectious disease testing is the fastest growing area of point-of-care testing. These tests are intended to diagnose infections quickly, to allow timely treatment, limit their spread, and slow or prevent outbreaks. These may include point-of-care tests for Lyme disease , avian influenza (bird flu), chikungunya virus, and drug-resistant bacteria such as methicillin-resistant Staphylococcus aureus (MRSA) .
In the developing world and remote rural regions, the use of point-of-care tests is motivated by the need for better options to make diagnosis and treatment of diseases like malaria, HIV, and tuberculosis more accessible and affordable. In the developed world, respiratory and sexually transmitted infections are areas where new point-of-care tests could help.
For the last two decades, efforts have been underway to develop new technologies to bring more tests to the point-of-care and to make the tests more sensitive and specific. Molecular techniques such as polymerase chain reaction (PCR) will likely be used to deliver new infectious disease tests at the point-of-care. Another big focus area has been lab-on-a-chip systems. These miniature devices are designed to rapidly automate every step of a laboratory test using very small sample sizes, without the need for manual handling of the sample.
Point-of-care testing is never likely to replace clinical laboratory testing. However, as technology evolves to meet the demand for more streamlined, higher quality healthcare, point-of-care testing will continue to be a growing part of your healthcare experience.
There are many point-of-care tests available in a variety of settings. Here are some that you may encounter:
St. John, A. and Price, C. P. (2014 August) Existing and Emerging Technologies for Point-of-Care Testing. Clinical Biochemistry Review . Available online at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4204237/. Accessed 11/10/2015.
Henry’s Clinical Diagnosis and Management by Laboratory Methods. 22nd ed. McPherson R, Pincus M, eds. Philadelphia, PA: Saunders Elsevier: 2011.
Tietz Textbook of Clinical Chemistry and Molecular Diagnostics. Burtis CA, Ashwood ER, Bruns DE, eds. 5th edition, St. Louis: Elsevier Saunders; 2012.
Santrach, P. J. Mayo Clinic. Current and Future Applications of Point-of-care Testing, Available online at https://wwwn.cdc.gov/cliac/pdf/addenda/cliac0207/addendumf.pdf. Accessed 10/12/2015.
(2013 March 29, Updated) Point-of-care Diagnostic Testing. National Institutes of Health. Available online at https://report.nih.gov/nihfactsheets/ViewFactSheet.aspx?csid=112. Accessed 10/12/2015.
(2010) Lab Medicine. Point-of-Care Testing Guideline. Published by CLSI. Available online at https://labmed.ascpjournals.org/content/41/8/499.full. Accessed 10/12/2015.
Gubbin, P.O., et al. (2014) Point-of-Care Testing for Diseases: Opportunities, Barriers, and Considerations in Community Pharmacy. Journal of the American Pharmacists Association . Available online at https://www.medscape.com/viewarticle/827464_5. Accessed 10/12/2015.
(2012 September) Burns, E. TechTarget. Clinicians discuss pros and cons of point-of-care testing devices. Available online at https://searchhealthit.techtarget.com/feature/Clinicians-discuss-pros-and-cons-of-point-of-care-testing-devices. Accessed 10/12/2015.
Ritzi-Lehnert, M. (2012) Development of chip-compatible sample preparation for diagnosis of infectious diseases. Expert Review of Molecular Diagnostics . Available online at https://www.medscape.com/viewarticle/759549_5. Accessed 11/10/2015.
Ansell, J. (2014 November 7) Home Monitoring for Warfarin Therapy. National Blood Clot Alliance. Available online at https://www.stoptheclot.org:home-monitoring-for-warfarin-therapy.htm. Accessed 11/10/2015.
Rooney, K.D. and Schilling, U.M. (2014) Point-of-care testing in the overcrowded emergency department – can it make a difference? Critical Care . Available online at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4331380/. Accessed 11/10/2015.
Crocker, J.B. et al. (2014) Implementation of point-of-care testing in an ambulatory practice of an academic medical center. American Journal of Clinical Pathology . Available online at https://www.ncbi.nlm.nih.gov/pubmed/25319979. Accessed 11/10/2015.
Kost, G.J., et al. (2006) Katrina, the tsunami, and point-of-care testing. American Journal of Clinical Pathology . Available online at https://ajcp.ascpjournals.org/content/126/4/513.long. Accessed 11/10/2015.
Appiah, L. T. et al. (2009) Efficacy and Acceptability of Rapid, Point-of-Care HIV Testing in Two Clinical Settings in Ghana. AIDS Patient Care and STDs . Available online at https://online.liebertpub.com/doi/abs/10.1089/apc.2008.0224. Accessed 11/10/2015.
Howick, J., et al. (2014) Current and future use of point-of-care tests in primary care: an international survey in Australia, Belgium, The Netherlands, the UK and the USA. BMJ Open . Available online at https://bmjopen.bmj.com/content/4/8/e005611.full. Accessed 11/10/2015.
(2014 September) Point-Of-Care Diagnostic Market worth $27.5 Billion by 2018. Markets and Markets . Available online at https://www.marketsandmarkets.com/PressReleases/point-of-care-diagnostic.asp. Accessed 11/10/2015.
(Reviewed, 16 March 2015). Clinical Laboratory Improvement Amendments (CLIA). Centers for Disease Control and Prevention. Available online at https://wwwn.cdc.gov/clia/Resources/WaivedTests/. Accessed 11/23/2015.
(Modified 10 August 2015). Clinical Laboratory Improvement Act. Centers for Medicare and Medicaid Services. Available online at https://www.cms.gov/Regulations-and-Guidance/Legislation/CLIA/. Accessed 11/23/2015.
(September 28, 2015) Silas Grossman, The “Tricorder” of Patient Care, Part 1: From glucometers to genetics and the future of testing. Advance for Administrators of the Laboratory . Available online at https://laboratory-manager.advanceweb.com/Features/Articles/The-Tricorder-of-Patient-Care-Part-1.aspx. Accessed 11/30/2015.
(October 26, 2015) Grossman, Silas. The “Tricorder” of Patient Care, Part 2: From glucometers to genetics and the future of testing. Advance for Administrators of the Laboratory. Available online at https://laboratory-manager.advanceweb.com/Features/Articles/The-Tricorder-of-Patient-Care-Part-2-2.aspx. Accessed 11/30/2015.
(April 2014) Paxton, Anne. How POC testing is pushing the envelope. CAP Today . Available at https://www.captodayonline.com/how-poc-testing-is-pushing-the-envelope/. Accessed 11/30/2015.
- Sign-up for Our Newsletter
Ask a Laboratory Scientist

This form enables patients to ask specific questions about lab tests. Your questions will be answered by a laboratory scientist as part of a voluntary service provided by one of our partners, American Society for Clinical Laboratory Science. Please allow 2-3 business days for an email response from one of the volunteers on the Consumer Information Response Team.
Send Us Your Question
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Point-of-care testing.
Michael C. Larkins ; Aparna Thombare .
Affiliations
Last Update: May 29, 2023 .
- Continuing Education Activity
Point-of-Care Testing (POCT) is clinical laboratory testing conducted close to the site of patient care where care or treatment is provided.POCT provides rapid turnaround of test results with the potential to generate a result quickly so that appropriate treatment can be implemented, leading to improved clinical or economic outcomes compared to laboratory testing. Technological advances, such as miniaturization of electronics and improved instrumentation, have revolutionized POCT, enabling the development of smaller and more accurate devices. POCT can be performed by various healthcare professionals and, in some cases, even by patients themselves. This review explores the methodology, benefits, utilization, and factors that can interfere with POCT, highlighting the importance of an interprofessional team in evaluating and treating patients using POCT. By leveraging the expertise of different healthcare professionals, POCT can be effectively integrated into patient care, leading to improved outcomes and patient satisfaction.
- Identify appropriate indications for point-of-care testing based on patient presentation and clinical scenario.
- Apply quality control measures and perform regular maintenance and calibration of point-of-care testing equipment to ensure accurate and reliable results.
- Implement point-of-care testing procedures following established protocols, including proper specimen collection, handling, and storage.
- Collaborate with other healthcare professionals in the interpretation and integration of point-of-care test results into patient management plans.
- Introduction
Point-of-Care Testing (POCT) is clinical laboratory testing conducted close to the site of patient care where care or treatment is provided. [1] POCT provides rapid turnaround of test results with the potential to generate a result quickly so that appropriate treatment can be implemented, leading to improved clinical or economic outcomes compared to laboratory testing. [2]
Traditional laboratory testing typically involves a multiple-step process that includes collecting samples from the patient at the bedside or the clinic, transporting them to a centralized laboratory (often located far away), and then subjecting the samples to several processing steps. [3] The delay in treatment caused by the time-consuming traditional laboratory testing can hinder timely clinical decision-making. POCT addresses this challenge by bringing the laboratory to the patient. Portable and handheld testing devices enable healthcare workers to perform rapid testing on samples, significantly reducing the time needed for medical decision-making.
The concept of on-site or near-patient testing for blood analysis was initially explored in England during the 1950s and was referred to as "near-patient testing." [4] In the early 1980s, Dr. Gerald J. Kost introduced the term "point-of-care testing" after extensive research on the application of biosensors for monitoring ionized calcium levels in whole blood. [5] The term "point-of-care testing" was subsequently codified with the definition of "testing at or near the site of patient care." [3]
Technological advances, including the miniaturization of electronics and improved instrumentation, have facilitated the development of increasingly smaller and more accurate POCT devices. [6] Cutting-edge POCT integrates microneedles and microfluidics for improved comfort, speed, and accuracy. [7] [8]
The following features of POCT are ubiquitous: [9]
- POCT should be simple to use.
- Reagents and consumables should have durable resistance during storage and use.
- POCT results should align with established laboratory methods.
- POCT should ensure safety during testing.
Various guidelines, such as the ASSURED Guidelines by the World Health Organization (WHO), exist for specific subsets of POCT, such as sexually transmitted infections (STI). [9] The ASSURED acronym stands for Affordable, Sensitive, Specific, User-friendly, Rapid, Robust, Equipment-free, and Delivered (to the end user), which are key criteria for effective POCT, as proposed by the World Health Organization (WHO). Affordable is for patients at risk of infection, and equipment-free means no complex equipment is required.
The National Academy of Clinical Biochemistry (NACB) has developed evidence-based guidelines for POCT, providing grading and recommendations to optimize the use of POCT based on scientific research and clinical evidence. [10]
POCT guidelines generally emphasize the rapid results and cost-effectiveness of POCT, along with the importance of high sensitivities and specificities to support informed clinical decision-making.
- Specimen Requirements and Procedure
There are 3 primary stages in the POCT process: pre-analytical, analytical, and post-analytical. The pre-analytical phase occurs before running the POCT on a sample and involves collection, transport, preparation, and loading. The analytical phase is the stage in which the actual testing sequence of a POCT is conducted. The post-analytical phase begins when testing is complete, and an obtained result is available. During this phase, the obtained result from the test is communicated for treatment through the electronic medical record (EMR) or written or verbal instructions directly to the treatment team. The post-analytical step is also when "so-called" critical values, which are values that deviate significantly from normal reference values and indicate a pathological process. The resultant values are interpreted during this step to guide appropriate actions and interventions.
Specimen collection and handling are critical components of POCT since testing is performed directly on the collected specimen. [11] The pre-analytical phase of specimen collection and handling is crucial and represents the most critical controllable variable in POCT. Adhering to personnel regulations, appropriately preparing patient and specimen collection containers (including fixatives or special media), and ensuring compliance with patient and specimen identification requirements are essential for effective collection and handling. Additionally, accurate clinical documentation and proper specimen storage are necessary to maintain the integrity, accuracy, and safety of the testing process.
Adhering to the manufacturer's instructions for use (MIFU) or package insert is crucial in ensuring accurate testing in POCT. This is particularly important regarding sample preparation, including factors like centrifugation time, and may vary between manufacturers and sample types. Professionals performing POCT should carefully follow the specific instructions provided by the manufacturer for each apparatus used. Professionals prefer some POCT methods that utilize whole blood as they eliminate the need for additional processing steps or centrifugation. Additionally, sample collection containers must be within the manufacturer's date stamp to maintain the quality and reliability of the testing process.
POCTs are more susceptible to interfering substances and have a narrow margin of error due to smaller sample sizes compared to conventional laboratory tests.
Proper technique is crucial when drawing samples, particularly when accessing a central line. [12] This involves flushing the line with heparin and discarding at least twice the volume of the line (2 to 5 mL) before sample collection. It is recommended to wait at least 15 minutes after a blood transfusion before drawing a sample for POCT.
Samples collected for blood gas analysis are susceptible to changes in oxygen partial pressure. Therefore, it is crucial to maintain anaerobic conditions during sample collection to ensure accurate laboratory values. [13] Controlling factors such as removing all air bubbles from a sample, using a plastic syringe for collection, and the time and temperature of sample storage (if storage is required) before analysis are crucial for accurate blood gas analysis.
- Diagnostic Tests
POCT testing devices are classified based on the testing modality and the test size. [9] Test size in POCT spans a wide range, and ongoing research focuses on miniaturization. Handheld POCT devices, including dipsticks and meters like glucometers, represent smaller-scale options within this spectrum.
The most recent iterations of these devices feature cartridges that enable multiple tests, including whole blood analysis for cardiac markers, blood gases, and various hematologic and endocrine analytes. On the larger end of this spectrum, there are larger benchtop POCT units that require dedicated space near a patient to qualify as POC.
Many of these benchtop POCT units are equipped with multiple testing types and modalities, allowing for a wide range of diagnostic tests to be performed within a single device. Common examples of tests performed on benchtop POCT units include hemoglobin A1c, C-reactive protein (CRP), and general chemistry analytes. The demand for smaller and more precise benchtop POCT devices has been a significant catalyst for innovation in reducing the size of these instruments. Advancements in technology and engineering have enabled the development of compact and highly accurate benchtop POCT units.
Testing Strips and Lateral-flow Testing
POCT encompasses a wide range of testing modalities tailored to specific applications. The most basic POCT takes advantage of an interaction between an analyte and a substance, usually impregnated or contained, so that a sample can be added or mixed in a controlled manner. [14] An example is using test strips (eg, urine test strips). These strips are generally dried, porous matrices with impregnated carrier elements that interact with the analyte(s) when exposed. The interaction between the analyte and the testing reagents often involves a chemical reaction that produces a color change. This color change can be interpreted as a binary value indicating the presence or absence of the analyte or as an indication of the analyte concentration using a scale (eg, trace protein, 1+, 2+, 3+).
A more complex approach to POCT is lateral-flow testing. This type of diagnostic testing utilizes a layer of supporting material, such as porous paper of cellulose fiber filters or woven meshes. The supporting material contains capillary beds to whisk fluid samples to location(s) on the support material with substances that react with measured analytes in the sample. A well-known example is the at-home pregnancy test, which commonly utilizes an immunoassay to detect the presence of human chorionic gonadotropin (hCG, specifically beta-hCG) in urine.
Urine is exposed to one end of the supporting material in the test device; capillary beds then move the urine through the supporting material to specific sites that react with beta-hCG. This configuration commonly has 2 lines of reactive material, one that serves as the control and another that indicates a binary yes or no indication. The test is positive if both lines (also known as stripes) appear or change color and negative if only the control line is visible. Failure of the control line to appear indicates an invalid or faulty test, which could result from a manufacturing defect, damage, or expired test.
In many instances, POCTs that utilize simple test strips or lateral-flow testing provide qualitative or semiquantitative results and do not provide precise information regarding the specific concentration of the measured analyte.
Immunoassays
POCT testing that utilizes immunoassays relies on antibodies to bind to a specific target when the concentration exceeds a certain threshold. [14] Targets in immunoassays for POCT can encompass a wide range of substances, including proteins, drugs, and pathogens. POCTs are available in various formats, including both individual tests and platforms with multiple built-in tests. In general, testing platforms require more space and greater expertise and training; this generally scales with the number of tests offered.
Deciding between using a testing platform versus an individual test or even utilizing an array of individual tests depends on the workflow and throughput required. Higher sample volume can often be accommodated more effectively using a POCT testing platform. However, the suitability of a specific platform depends on the testing type and the platform's capabilities.
One subset of immunoassays is the direct assay, which provides a straightforward method for detecting an analyte. In a direct immunoassay, the analyte of interest is directly bound by an antibody that specifically recognizes and binds to it. This binding event is then detected, typically through fluorescence, by an optical sensor. The fluorescence signal indicates the presence and quantity of the analyte in the sample.
In situations where a direct assay is not feasible, competitive immunoassays can be employed. These assays utilize the principle of competitive binding between a measurable, secondary analyte and the target analyte. As the test antibodies bind to more of the primary analyte, the level of bound, measurable analyte decreases due to competitive binding; this allows for the determination of the primary analyte's concentration. Unlike simple test strip-based POCT, immunoassay POCT provides quantitative information for specific analytes. [15] [16]
Antigen-based Testing
POCT, which involves the detection of known antigens or antibodies specific to a particular disease or disease state, has been widely employed as a common practice in healthcare. [17] Immunoassay-based POCT is commonly used to rapidly detect group A Streptococcus , mononucleosis, and influenza A and B. These tests utilize immunoassays that bind specific antigens or antibodies. Immunosay-based POCT offers a fast turnaround time (TAT) but may have lower sensitivities and specificities compared to traditional laboratory and molecular testing methods.
Molecular POCT
The demand for molecular POCT with high sensitivity and specificity and a relatively short turnaround time (although longer than antigen-based testing) spurred its development. [17] This form of testing detects DNA or RNA sequences indicative of the presence of disease. Nucleic acid amplification testing (NAAT) is used to identify DNA or RNA in small test samples. The nucleic acids of interest are replicated to increase their concentration (ie, amplify them) so they are easier to detect. [18]
There are various forms of this testing, including reverse transcription polymerase chain reaction (RT-PCR) and isothermal amplification methods such as nicking endonuclease amplification reaction (NEAR) and transcription-mediated amplification (TMA).
It is important to note that while molecular POCTs often have higher sensitivities and specificities compared to antigen-based POCTs, this is not always the case. Additionally, the increased sensitivity and specificity provided by this POCT modality may not always be clinically beneficial, as the detection of an analyte does not necessarily correlate with a specific disease state or the need for treatment (eg, the presence of a small amount of Clostridium difficile in a patient's stool does not always indicate the need for treatment of a C difficile infection. [19]
- Testing Procedures
Testing procedures for POCT vary based on the specific manufacturer, test, and sample type. For accurate results in most POCT units, setting up and calibrating the specific test before use properly is essential. Following the manufacturer's instructions for use (MIFU) or package insert for each POCT apparatus is crucial in achieving accurate testing.
General POCT Testing Procedures
- A sample is obtained for analysis. This could be a drop of blood for blood glucose concentration via a glucometer or urine for beta-hCG. Various requirements regarding the patient's state, the specimen's state, and the preparation needed for accurate testing exist. This is discussed in further detail in both the "Specimen Requirements and Procedures" and "Quality Control and Lab Safety" sections. [20]
- The sample is applied to the POCT device. Immediately before this step, a reagent may facilitate accurate testing. For example, some POCT units for COVID-19 require samples obtained via nasopharyngeal or oropharyngeal swabs to be placed in a reagent solution to facilitate the transfer of antigen into the solution. [21] This allows for the distribution of the antigen throughout the solution and increases test accuracy. In some types of POCT, the sample can be directly applied to the device, which typically includes a disposable cartridge for analyzing the analyte. This disposable cartridge can be disposed of after use, reducing the risk of cross-contamination.
- Once the test is performed, the result is obtained and can be directly transferred to the patient's electronic medical records (EMR) if the POCT device is integrated or interfaced with the EMR system.
- Interfering Factors
Due to the portable nature of POCT, the reagents, tests, and samples are often exposed to conditions that may differ from those in a traditional laboratory setting. Humidity, temperature, time to testing, and oxygen content can fluctuate more in the POCT setting than in the conventional laboratory environment. Most interfering factors with POCT occur before the test is run (pre-analytical phase). [22]
Errors in the pre-analytical phase can occur during patient identification and in the specimen's identification, collection, handling, processing, transport, and storage. These errors may include hemolysis, clotting, underfilling or overfilling a specimen container, improperly securing specimen containers before transport, prolonged tourniquet time, and changes in the sample concentration (eg, during aliquoting).
Notably, the detection of hemolysis in POCT using whole blood samples (including fingerstick tests) is challenging. [23] Errors during specimen transfer and loading, such as bubbles, microclots, and gross clotting, can occur, especially if the procedure is not followed appropriately or lacks oversight. Increased time to testing can interfere with POCT, as observed in the case of blood glucose testing in whole blood. Adequate training is a critical component of POCT, as pre-analytical errors have an inverse association with test operator experience.
Other interfering factors may be directly related to the patient's physical state. For instance, elevated biotin intake (eg, from vitamin supplementation) can interfere with certain immunoassays, such as human immunodeficiency virus (HIV) POCT. [24] This stems from the interaction between biotin and streptavidin in the assay. Affected assays include but are not limited to pancreatic, prostate, and ovarian cancer POCT and pituitary and thyroid function tests. Reading the MIFU or package insert is essential for POCT, as certain drugs can interfere with the test and affect accuracy. Some POC glucose monitoring systems may report erroneously elevated glucose levels in patients treated with maltose, icodextrin, galactose, or xylose. [25]
Hemolysis, icterus, and lipemia may result in inaccurate or incalculable results. Potassium measurements are susceptible to this error. Testing in conventional laboratories often includes a step to determine the serum index in addition to testing for a specific analyte. [13]
Collectively, these indices are often referred to as hemoglobin (H), lipemia (L), and icterus (I), or HIL, indices. [26] These are obtained most typically via spectrophotometric assessment. However, in POCT, hemolysis, icterus, and lipemia can only be detected by visual inspection of a centrifuged aliquot of the sample. High turbidity or an excess of an untested component in a sample, such as in whole blood samples with high concentrations of lipids, may also skew test results or result in an error. [27]
Ways to resolve these errors vary based on the devices used and MIFU; in some cases, dilution can resolve sample errors related to excess bilirubin, and ultracentrifugation can help fix errors related to excess lipids. Patients with reduced or compromised peripheral circulation, as seen in patients with sepsis, shock, or diabetic ketoacidosis, may have inadequate capillary blood samples. [28]
- Results, Reporting, and Critical Findings
POCT results that yield critical values are typically acted upon promptly, leading to potential changes in clinical management. [29] This could be as benign as a reflexive beta-hCG taken after a positive urine pregnancy test in the emergency department. Therefore it is essential to record the result and action taken whenever a critical value result is obtained.
Critical values, unlike urgent or STAT tests, are defined as test results that significantly deviate from the established normal range, irrespective of the patient's condition. STAT or urgent tests are designated as such by the individual ordering the test, and therefore prior knowledge of the patient's status is generally needed.
Reporting Critical Findings
Critical values should be treated as reportable events, even if previous critical values are already known for a particular patient. [29] The critical value reporting policy should be consistently followed for each instance of obtaining a critical value. Deviation from this policy should only be considered in exceptional cases supported by sufficient evidence, such as obvious testing errors or pre-analytical errors, justifying the decision to ignore the critical value.
- Clinical Significance
Because of its quick turnaround time and place in various workflows, POCT has great clinical significance; the information gleaned from POCT is used routinely to guide patient treatment and management. POCT offers several advantages compared to conventional lab testing, with benefits that vary depending on the specific setting in which the testing is conducted. [20] [30]
POCT, performed near patients, typically enhances patient satisfaction and experience by eliminating the need for sample transport, reducing turnaround time (TAT), and avoiding procedure delays. POCT enables patient counseling, prevents unnecessary treatment escalation, and provides rapid results outside the hospital setting, such as in outpatient testing, to avoid hospitalization or confirm viral illness, thereby reducing antibiotic use.
POCT offers advantages in different test types. For example, fingerstick blood glucose measurements can replace venipuncture for serum testing, requiring less training and posing lower risks of complications and infection, thereby improving patient experience and safety. [31] In specific patient populations like neonates or those prone to increased blood loss from phlebotomy, the smaller sample volume required for POCT is advantageous.
POCT has some drawbacks, primarily related to the potential for less accurate results than traditional laboratory testing. This can be attributed to variable personnel training and control over pre-analytical, analytical, and post-analytical variables, which can be better managed in a laboratory setting. POCT can be more costly on a per-test basis compared to traditional laboratory testing, primarily due to the single-use nature of most POCT devices, which adds to the overall expenses. [32] Documentation challenges and potential errors in recording or documenting POCT results can occur due to varying personnel practices and workflow processes within a clinical setting.
- Quality Control and Lab Safety
All facilities or sites in the US that conduct diagnostic testing or medical treatment using human specimens are subject to regulation under the Clinical Laboratory Improvement Amendments of 1988 (CLIA 88). [33] CLIA designates tests that are simple to perform and have a low risk of producing incorrect results as waived tests. Most point-of-care tests are waived; however, some are non-waived and are subcategorized as moderately complex tests. Waived tests are excluded from competency assessment requirements per the Centers for Medicare & Medicaid (CMS), though various state and accrediting bodies may still keep this requirement in place. Non-waived tests are subject to specific quality standards, including proficiency testing, quality control (QC), and personnel requirements.
The successful development of effective quality control for laboratory testing requires using verified controls to ensure that a POCT is functioning as expected and will yield accurate results. [34] QC material contains the analytes of known concentrations. The frequency of quality control testing should be determined based on the complexity and risks associated with the test in question. For high-throughput devices, QC should be run at least once daily. New lots of reagents are tested with these controls before being used to run patient samples. Additionally, such controls allow for troubleshooting among different individual tests and operators. The internal QC documentation, which includes the date and time of testing, lot number, and user identification, is essential for effective QC.
Patient testing must be associated with the specific lot numbers for all products used for POCT, including the device, reagents, and sample collection materials. Many POCTs contain electronic records of such information, though historically, this information has been recorded in a logbook. Significant variables to ensure ongoing quality assurance include expiration dates for reagents, controls, and sample collection materials, proper storage and management of all materials involved in POCT, and proper establishment of acceptable ranges for test values. [34]
Due to the decentralized nature of POCT, effective personnel management on an individual level is critical. Ideally, every person that runs POCT would be competent with the safe and accurate operation of each POCT. Many larger institutions implement electronic training modules and regularly track individual competency for POCT, in line with the requirements set by accreditation bodies such as CLIA. Accreditation bodies, including CLIA, require 6 main competency elements: 1) direct observation of test operation, 2) monitoring of both recording and reporting of test results, 3) review of intermediate steps of POCT (test results, QC records), 4) direct observation of preventative maintenance and function check performance, 5) assessment of test performance using specimens previously analyzed, and 6) assessment of personnel problem-solving skills. [35]
Lab safety is a critical component of effective POCT for the patient, the sample collector, and the person that runs the POCT. One unique aspect of POCT is that the same person often carries the collection and test execution. Because of this, care must be taken so that task overload and errors in collection, transport, and analysis do not occur. Contamination of a POCT can impact multiple patients and operators, especially if the POCT in question is frequently used. The proper use of personal protective equipment (PPE) and corresponding protocols are critical for the protection of personnel and the accuracy of testing. [36]
The rules of universal precaution should be applied to POCT, and protective measures such as splash shields and biosafety cabinets should be employed based on manufacturer and government agency guidelines. Recommendations for competency elements in POCT vary depending on the type of test and the samples collected. For example, POC molecular testing for nasal swabs, such as in the case of COVID-19 testing, generally requires specific personal protective equipment (PPE) to prevent exposure to airborne pathogens during testing. [37] [38]
Lab safety also applies to adequately disposing of samples and waste after completing POCT. [39] All laws, regulations, and accreditation requirements for medical waste disposal must be followed. After sample collection via venipuncture, the needle must be covered; fingerstick lancets must be single-use. All needles and lancets must be appropriately disposed of in a hazardous waste container designated for needles (a sharps container).
Proper disposal of POCT swabs depends on local and facility waste disposal procedures. However, a general guideline is that swabs used for POCT that remove the sample from the swab (for example, POCT that wash or require swirling of the swab in fluid) do not require disposal in a designated biohazard receptacle. [8] Swabs contaminated with biological material must be disposed of in a proper biohazard bag. Finally, when appropriate, the proper removal or covering of protected health information (PHI) must be considered on all samples and sample containers. This applies to both physical and electronic information.
- Enhancing Healthcare Team Outcomes
POCT occurs in a wide range of clinical settings, including inpatient, outpatient, and non-clinical settings, such as homes, airports, and cruise ships. The COVID-19 pandemic significantly increased the use of POCT, with billions of tests rapidly developed and distributed worldwide to help control the spread of the virus and facilitate the timely identification of infected individuals.
Various healthcare professionals, including physicians, nurses, medical technologists, and trained personnel, perform point-of-care testing to obtain immediate results that inform and guide clinical patient management decisions. Due to the diverse range of healthcare professionals and workflows involved in POCT, providing adequate training, facilitating interprofessional communication, and establishing clear guidance to ensure accurate testing and effective relay of test results to the treatment team is crucial.
Interprofessional committees dedicated to the implementation, execution, and continuous quality management of POCT have been recommended as they play a crucial role in enhancing the quality of healthcare delivery within entire health systems. These committees promote collaboration, standardization, and effective oversight of POCT practices, ultimately benefiting patient care. [40] [Level 1] Various randomized clinical trials using POCT demonstrate improved patient outcomes compared to conventional laboratory testing. [41] [42] [43] [Level 1]
One of the advantages of point-of-care testing (POCT) is the ability to update the patient's electronic medical record (EMR) with real-time test results. This enables the interprofessional team to access the most accurate and updated data, leading to a more comprehensive and functional clinical picture. As a result, healthcare professionals, such as pharmacists, can make more efficient and informed decisions regarding medication dosing, such as adjusting warfarin or aminoglycoside dosages, based on the patient's current status.
Using POCT facilitates closer monitoring of a patient's condition by nurses. With real-time access to test results through the EMR, nurses can promptly detect any significant changes and alert the attending physician or appropriate healthcare professionals for clinical intervention. Interprofessional coordination and collaboration among physicians, advanced practice practitioners, specialists, pharmacists, lab technicians, and nurses are crucial in utilizing POCT effectively and ultimately enhancing patient outcomes. By working together, the healthcare team can make well-informed decisions and provide timely and targeted care based on the POCT results [Level 5]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Michael Larkins declares no relevant financial relationships with ineligible companies.
Disclosure: Aparna Thombare declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Larkins MC, Thombare A. Point-of-Care Testing. [Updated 2023 May 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Implementation of point-of-care testing in a pediatric healthcare setting. [Crit Rev Clin Lab Sci. 2019] Review Implementation of point-of-care testing in a pediatric healthcare setting. Patel K, Suh-Lailam BB. Crit Rev Clin Lab Sci. 2019 Jun; 56(4):239-246. Epub 2019 Apr 11.
- Review Point-of-care testing (POCT) and evidence-based laboratory medicine (EBLM) - does it leverage any advantage in clinical decision making? [Crit Rev Clin Lab Sci. 2017] Review Point-of-care testing (POCT) and evidence-based laboratory medicine (EBLM) - does it leverage any advantage in clinical decision making? Florkowski C, Don-Wauchope A, Gimenez N, Rodriguez-Capote K, Wils J, Zemlin A. Crit Rev Clin Lab Sci. 2017 Nov-Dec; 54(7-8):471-494. Epub 2017 Nov 23.
- Perceptions of an ideal point-of-care test for sexually transmitted infections--a qualitative study of focus group discussions with medical providers. [PLoS One. 2010] Perceptions of an ideal point-of-care test for sexually transmitted infections--a qualitative study of focus group discussions with medical providers. Hsieh YH, Hogan MT, Barnes M, Jett-Goheen M, Huppert J, Rompalo AM, Gaydos CA. PLoS One. 2010 Nov 30; 5(11):e14144. Epub 2010 Nov 30.
- The future of Cochrane Neonatal. [Early Hum Dev. 2020] The future of Cochrane Neonatal. Soll RF, Ovelman C, McGuire W. Early Hum Dev. 2020 Nov; 150:105191. Epub 2020 Sep 12.
- Executive summary. The National Academy of Clinical Biochemistry Laboratory Medicine Practice Guideline: evidence-based practice for point-of-care testing. [Clin Chim Acta. 2007] Executive summary. The National Academy of Clinical Biochemistry Laboratory Medicine Practice Guideline: evidence-based practice for point-of-care testing. Nichols JH, Christenson RH, Clarke W, Gronowski A, Hammett-Stabler CA, Jacobs E, Kazmierczak S, Lewandrowski K, Price C, Sacks DB, et al. Clin Chim Acta. 2007 Apr; 379(1-2):14-28; discussion 29-30. Epub 2007 Jan 12.
Recent Activity
- Point-of-Care Testing - StatPearls Point-of-Care Testing - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Point of Care Testing (POCT)
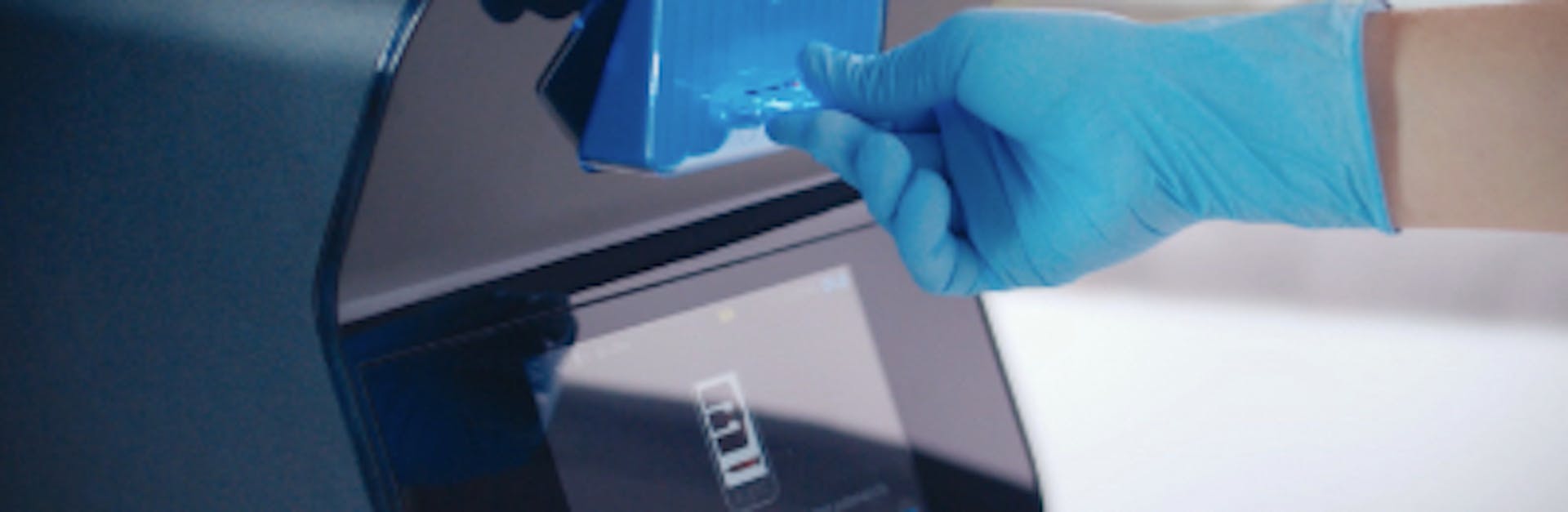
Providers of healthcare make efforts to treat patients quickly and to achieve the best possible outcome. Quick and accurate test results can help to provide the best quality patient care and allow a health professional to make better and more effective decisions with their patient. Point-of-care testing , also known as near-patient testing , typically means carrying out a test using a device or test kit in the presence of the patient and without the need to send a sample to a laboratory. Many new point-of-care devices utilize technological advancement to improve the quality of care.
What is point-of-care testing?
Point-of-care testing , often abbreviated to POC testing, is medical testing done at or near the point of care . In this context, POC refers to the location of the patient. Sending all samples and specimens away to be processed at medical laboratories means waiting a long time for results. This can lead to wasted time in critical contexts or patients being treated without their care team having full information about their needs. Instead, POC testing makes it far easier for results to be obtained quickly and reliably. With these results available, medical staff can more easily make informed decisions about a patient’s treatment and care.
POC testing vs. laboratory testing: Pros and cons
The main advantage of point-of-care testing is the shorter time it takes to obtain a result. Typically, results may also be presented in a way that is easier to understand, but this is not always the case and results may still require a healthcare professional to interpret them safely. POC testing can also be performed by people who have not had formal laboratory training. This includes nurses, doctors, paramedics and testing by patients themselves. There are many kinds of near-patient testing , including malaria antigen testing, pregnancy tests, blood glucose monitoring, urinalysis and many more. These tests often require relatively easy sample collection such as body fluids (e.g. saliva or urine) or finger-prick blood. Together with other portable medical equipment, such as thermometers or blood pressure devices, they can facilitate rapid and convenient medical assessment. However, POC testing can have disadvantages. For example, based on the available technology used in the device, studies have shown that errors may be more frequent with POC testing than with laboratory testing. This can arise because the POC testing environment is generally less controlled than laboratory conditions and the results can be at higher risk of external interference than laboratory processes, which can lead to inaccuracy. POC approaches can also be more costly than laboratory based testing. A study from 1995 demonstrated that the cost of POC testing for glucose was anywhere from 1.1 to 4.6 times higher than the same test in the laboratory. There are hidden costs that may often be overlooked, such as those associated with a quality control program or equipment upkeep. However, other kinds of hidden costs such as buildings, staff and overheads can apply to laboratory testing as well. Nonetheless, the immediacy and convenience of POC testing can balance the increased costs. Rapid results can allow a treatment plan to be put into effect quickly, and where time is critical for better care, this can make a big difference. Even where time is not critical and is more a matter of convenience, being able to move on with diagnosis and treatment is almost always of benefit to the patient. In some circumstances, a rapid result can help to allow a safe medical discharge from hospital, shortening the length of stay and helping to reduce costs of care. There are also examples of wearable monitoring and testing devices, which can decrease the rate of readmittance to hospital, by providing telemetry results to the clinic or information that patients themselves can use. As technology continues to develop and point-of-care testing devices continue to improve, the issues of accuracy associated with POC testing are likely to resolve. As more experience and understanding is gained with using point-of-care devices, the benefits of quick results and ease of testing are likely to come to be seen as significant and desirable as well as routine.
Hematology point-of-care devices
Point-of-care testing has become popular in many medical subfields, including hematology. In recent years, continued progress in medical device engineering has resulted in more advanced POC testing devices. Over the past several decades, the POC hemoglobin meter has been a popular and useful device. However, when compared with a laboratory complete blood count, this indicates only a small part of the useful or important information available from a full analysis of the blood cells. More recently, the use of a range of techniques in combination with advanced digital technology has allowed the development of a point-of-care complete blood count analyzer. Among other approaches to achieve this, engineers have employed digital microscopy and machine vision using near‐infrared spectroscopy and multiple wavelength light absorption. This means that the complete blood count can now be carried out as a point-of-care test with the same accuracy as traditional laboratory reports, with less invasive sample collection, greater speed and more convenience. Complete blood counts are just one of many tests that POC testing devices are capable of. Other common hematology point-of-care testing devices include:
- Prothrombin time analyzers, for evaluating blood clots.
- aPTT testing, for hemostatic assessment.
- D-dimer testing, to rule out pulmonary embolism or DVT.
- Viscoelastic assays, for trauma and obstetrics.
- Activated clotting time testing, for monitoring heparin levels.
- Malarial antigen testing, for screening for malaria.
Today, the most commonly used and modern point-of-care testing devices have been shown to produce accurate and reliable hematology results, promoting better quality medical care across a wide range of conditions.
POCT for clinical trials and research
In recent years, researchers have integrated more advanced POCT devices in clinical trials to provide results faster than local laboratories. Clinical trials often require that participants have specific characteristics. Some examples of clinical trial POCT include pregnancy, glucose, oxygen concentration, and flu tests. Researchers can verify the status of participants at the site of the clinical trial. POCT screening can rule out participants who do not fulfill the requirements of the study. One major application of POCT testing in clinical trials is rapid CBC testing. Researchers can obtain quantitative CBC results in just a few minutes. Applications of rapid CBC testing in clinical trials include: 1. Identifying participants with anemia A rapid CBC test typically includes red blood cell, hemoglobin, and hematocrit counts. If any of these are low, it could indicate that an individual has anemia. In clinical trials involving subjects with anemia, a rapid CBC test can quickly confirm the presence of the disorder. 2. Identifying participants with blood disorders Just as in the case of anemia, other blood disorders can also be identified quickly using a rapid CBC test. Some disorders that can be discovered include autoimmune disorders, bone marrow disorders, leukemia, lymphoma, myeloproliferative neoplasms, myelodysplastic syndrome, sickle cell disease, thalassemia, and cancer that has spread to the bone marrow.
3. Screening for infections In clinical trials to develop better treatment for immune disorders, a rapid CBC test can quickly identify participants with infections (high or low WBC count). This means that patients with infections can receive life-saving treatment quickly. If researchers discover infections at a rapid rate, then they can also find the root cause faster. 4. Monitoring patients’ reactions to clinical trial drugs (companion diagnostics) Rapid CBC testing post-treatment can help monitor patients’ reactions to clinical trial drugs. With frequent CBC testing, researchers can quickly halt therapy if patients are experiencing extreme adverse effects. Frequent CBC testing can also improve patient adherence as it can uncover patients who are not correctly following the prescribed therapy. A publication in Applied Clinical Trials highlighted three case studies of POCT for clinical trials and research: 1. Screen and enroll in a single visit In an influenza study, researchers used a POCT device to test participants for influenza, get rapid results, and enroll them right away. The alternative would have been to let patients go home and wait for results from a lab before enrolling. Several of these patients may have fallen sick and not returned for enrollment. 2. Reduce screen failure rates In a global chronic kidney disease clinical trial, researchers used a POCT device to pre-screen participants. They tested for estimated glomerular filtration rate (eGFR) and urine albumin-to-creatinine ratio (UACR). 3. Obtain faster results In a rare disease study, scientists used a POCT device to measure C-Reactive Protein (CRP). The test enabled them to identify patients who were having “heart-attack-like” symptoms.
Discover Sight OLO - Near-patient Testing
Disclaimer: The content of this knowledge post intends to provide general information related to topics that are relevant to blood diagnostics and may not be used in relation to the operation of Sight OLO. For detailed information on the diagnostic parameters and specifications of Sight OLO, please refer to the official Operator's Manual.
Related posts
Complete Blood Count

Lymphocytes
We'd love to hear from you..
How to run a laboratory: Determining point-of-care testing options
One of the most important aspects of implementing a new laboratory is determining which tests to offer. Start by using your practice data and demographics to select the first set of tests to implement.
For primary care practices with a well-established patient base, you'll have a clear grasp of the types of illnesses that present most commonly. You could also base your testing decisions on which tests you have sent out most frequently in the recent past. However, you might end up with a broad range of tests, including esoteric, rarely ordered tests.
Instead, to capture the most commonly needed tests, consider using the 80/20 rule. According to the 80/20 rule, a small number of common conditions will account for most of the tests you'll order.1
Here's a theoretical example: If your practice sees 1,000 patients per month and 70% of the patient visits require a lab result to initiate or modify a treatment plan, then this means that 700 treatment plans per month use lab data. If you stack-rank the tests that influence 80% of your treatment plans, about 500-550 treatment plans per month would benefit from physician office lab testing. These are the tests you'll want to offer first.
The list of tests below covers many of the patient conditions that present in a typical primary care practice.
General screening
Tests used for general screening:, testing options for general screening*:.
*Sysmex offers the XW TM -100 CLIA-waived CBC automated hematology analyzer. Contact your McKesson Medical-Surgical account manager for more information.
Risk-based screening
Tests used for risk-based screening (based on individual, gender, age, prior history or other risk element):.
- Pediatric lead testing
- Fecal occult blood for patients over 50
- Lipid screening for patients with a family or personal history of heart disease
- Medicare preventive services (CMS) 2
- CDC recommends HIV screening for adults aged 13-64 years 3
- CDC recommends HCV screening for baby boomers 4
- CDC recommends HPV screening in combination with Pap tests 5
- PT/INR for patients on anticoagulant therapy
- Complete blood count for anemia ad infection
Testing options for risk-based screening**:
Follow-up screening, tests used to follow up a positive screening result or medication follow-up:.
- PT/INR for anticoagulant therapy
- Lipids/glucose/ALT and AST for elevated lipids and statin therapy
Testing options for follow-up screening**:
Acute onset symptom disorder testing, tests used to manage acute onset symptom disorders (respiratory, fever, pain/discomfort):.
- CBC for anemia, appendicitis, infection, others
- Amylase for GI pain and appendicitis
- Influenza for respiratory symptoms
- Group A strep for respiratory symptoms
- RSV for respiratory symptoms
- GI pain/gastric blood
- Urinalysis for dehydration, UTI, others
- Glucose for ketone breath, disorientation, loss of consciousness
Testing options for acute onset symptoms:
Physician office laboratory testing supports initiatives in improved patient outcomes and better patient satisfaction, a broader range of practice services, enhanced revenue opportunities and MACRA compliance. While first steps to initiate testing may seem daunting, the future is bright in many ways for practices that choose in-office testing and the patients that count on them for their healthcare needs.
For more tips and guidance, continue reading McKesson's six-part series, The primary care physician's guide to expanding your practice with point-of-care testing .
**Both the list of tests and product examples described herein are a representative subset of options and are not a comprehensive list of all testing options.
***Most listed manufacturers offer more than one testing method or technology option
1: https://www.forbes.com/sites/kevinkruse/2016/03/07/80-20-rule/?sh=6e6036f53814 2: https://www.cms.gov/Medicare/Prevention/PrevntionGenInfo/medicare-preventive- services/MPS-QuickReferenceChart-1.html 3: https://www.cdc.gov/hiv/testing/ 4: https://www.cdc.gov/hepatitis/hcv/guidelinesc.htm 5: https://www.cdc.gov/vaccines/pubs/surv-manual/chpt05-hpv.pdf
Be advised that information contained herein is intended to serve as a useful reference for informational purposes only and is not complete clinical information. This information is intended for use only by competent healthcare professionals exercising judgment in providing care. McKesson cannot be held responsible for the continued currency of or for any errors or omissions in the information.
© 2021 McKesson Medical-Surgical Inc.

- Blood gases/acid-base
- Cardiac markers
- Coagulation/fibrinolysis
- Infection/sepsis
- Information management
- Kidneys/fluids
- Neonatology
- Point-of-care testing
- Process optimization
- Quality assurance
- Preanalytical phase
- Creatinine/urea
- Electrolytes
- Hemoglobins
- Natriuretic peptide
- About this site
- Journal scanner Explore selected articles curated by biochemist and journalist Chris Higgins
Sign up for our quarterly newsletter and get the newest articles from acutecaretesting.org

- Articles >
Management of point-of-care testing
Printed from acutecaretesting.org
December 1999

Point-of-care testing (POCT) is a delivery option for performing laboratory testing closer to the patient. Due to increasing healthcare pressures for faster turnaround of laboratory results and the development of a broader menu of testing devices, POCT is growing in popularity. Devices today are more portable, require less blood, and have computerized information management.
Despite its popularity, point-of-care-testing does not necessarily yield laboratory-comparable results. Delivery of laboratory testing outside the laboratory exposes a device to a variety of environmental, technique and patient factors that can adversely affect the analysis. Quality assurance of POCT requires an appreciation of the technical and operational factors that can influence the testing process.
The potential of point-of-care testing for faster test results does not necessarily guarantee improved patient outcomes. Only through participation of the laboratory on interdisciplinary management teams can the utilization of POCT be optimized for patient benefit. Future expansion of POCT will highlight the importance of the laboratory and develop new, evolving roles for the laboratory consultant in direct patient care.
Point-of-care testing - introduction
Point-of-care testing (POCT) is an alternative to central or core laboratory testing. POCT can be defined as “diagnostic testing conducted close to the site where clinical care is delivered”. Other names for POCT include: near-patient, decentralized, ancillary, alternate site, patient-focused, bedside, satellite, and peripheral testing.
These terms describe the considerable variation in which POCT is delivered. POCT devices can be brought directly to the patient’s bedside for analysis, or specimens can be collected and carried to stationary POCT equipment in the patient’s bathroom, in a spare utility room on the ward or even on a mobile cart.
Point-of-care testing can meet critical therapeutic needs for selective inpatient populations, like the emergency room, operating rooms, or intensive care units, as well as outpatient clinic, physician’s office, and home healthcare nursing. POCT devices are more portable than central laboratory instrumentation and have therefore found application in medical transport vehicles like helicopters, airplanes, and ambulances.
Despite its portability and apparent simplicity, POCT is comparable to other laboratory tests and faces similar preanalytical, analytical, and postanalytical issues [1]. Poor phlebotomy, fingerstick, or collection technique [2-5], lack of patient preparation [6-8], use of anticoagulants, transportation delays, and collection from intravenous lines [9-12] can affect the quality of the specimen.
Inappropriate reagent storage and analysis in hot or humid conditions [13-17], patient hematocrit [18], medications [19-21], and other metabolic conditions [22-25] can affect the accuracy and precision of test results. After analysis, the handling of test results can further create transcription and interpretation errors [26-30]. Overall, as with any laboratory test, considerations for the cost effectiveness and patient benefit impact the utility of POCT [31].
A recent survey of U.S. hospitals illustrates these issues [32]. When asked, “What are the advantages and disadvantages of POCT?” hospitals responded that the greatest advantage is the potential of POCT to impact turnaround time (92 %), patient satisfaction (34 %), and length of stay (21 %). Since POCT provides faster results, there is the potential for more rapid institution of therapy and beneficial patient outcomes.
On the other hand, the disadvantage of POCT is inaccuracy (73 %), difficulty performing/documenting controls and calibrations (58 %), training requirements for multiple staff (58 %), device precision (57 %), and cost (46 %). Although POCT is faster, the technical performance may not be equivalent to traditional laboratory tests conducted in a central laboratory. Yet, despite these potential benefits and concerns, only 2 % of hospitals have actually analyzed the impact of POCT on length of stay or performed cost studies (7 %).
Point-of-care testing, thus, presents the opportunity for improved care, but whether beneficial outcomes are realized depends on the balance of quality and clinical need. The convenience of POCT too often results in poor quality and over-utilization that raise the cost of care. Stringent monitoring is required not only of POCT quality but also of utilization and clinical outcomes.
The number of devices and operators complicates the oversight and practical management of POCT. Institutions can have dozens of devices and hundreds of operators. Testing personnel come from all areas of patient care with various educational levels, from medical technologists to nursing and clinical support staff [26,29].
Maintaining equivalent levels of device accuracy [11,33] as well as operator technical competency is a challenge facing those in charge of POCT. Establishment of a POCT quality assurance program requires an appreciation of clinical need, expertise in the technical aspects of POCT devices, and above all an ability to work on an interdisciplinary healthcare team [1,34-36].
Point-of-care testing - quality concerns
Although POCT devices are widely marketed and even available to the general public for personal testing purposes, the devices are not necessarily innocuous. Glucose meters are involved in the largest number of complaints filed with the U.S. Food and Drug Administration for any medical device [37]. As of 1993, over 3,200 incidents have been recorded from patient self-management, including at least 16 deaths.
Poorly maintained blood gas analyzers [38] and urinometers [39-40] on inpatient medical units can act as an infectious reservoir for antibiotic-resistant organisms. Even desktop cholesterol analyzers can generate misleading results [41]. In a survey of British outpatient clinics, 21 % of proficiency survey samples were >1 mmol/L (39 mg/dL) from the target mean, leading to a misclassification of as many as 16 % of patients [41].
POCT devices as a remote extension of the laboratory generate medical information that leads to clinical action. When the device is used inappropriately and incorrect results are produced, further diagnostic intervention can result in increased healthcare costs and risk to the patient.
Point-of-care testing devices are deceptively simple to operate, but simplicity does not guarantee quality. The particular application of the POCT must consider the peculiarities of the patient population (Fig. 1). In home use for patient self-monitoring, POCT devices are utilized by a single operator to serially monitor one patient.
POCT in the home employs capillary samples on ambulant, generally well patients. In contrast, hospital use of POCT devices are utilized by many operators on multiple acutely ill patients. Since many of these patients already have intravenous lines, samples other than fingerstick capillary blood are possible [1].
FIG. 1: Comparison of clinical applications for point-of-care glucose testing. Home testing presents different demands on the testing device than hospital testing.
Precision is more important in home use, while accuracy is paramount to inpatient use. For home use, a device may be biased from truth, but the device is functional provided that the patients know how to trend and treat themselves off the results generated on that particular device.
The absolute accuracy of that device versus a laboratory reference is not as important as the precision and day-to-day consistency. In a hospital, however, patients may enter through the emergency room, have surgery in an operating room, spend time in an intensive care unit and a general medical unit, and, after discharge, have home nursing or outpatient visits where POCT results are intermixed with laboratory values.
POCT results in a health system must correlate to the laboratory value or else the clinician must mentally correct the value to the laboratory reference for treatment. Standardization of POCT is particularly difficult given the lack of stable, whole-blood-based international standards and the inability of many POCT devices to accept samples other than whole blood. POCT, therefore, must indirectly standardize to other analyzers that can be made traceable to the International System of units.
Comparability is the goal of POCT quality assurance and the motivation behind regulations that govern laboratory testing in the United States. Federal regulations from the Clinical Laboratory Improvement Amendments of 1988 (CLIA ’88) [42-45] and private laboratory accrediting agencies like the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) [46-47], College of American Pathologists (CAP) [48], and Commission on Office Laboratory Accreditation (COLA) [49] regulate the performance standards of laboratory testing not only in central laboratories but also at the point of care.
Specifically, these agencies ensure that written procedures for POCT exist, appropriate quality control is performed, operators have specific training on the devices, ongoing operator competency is documented, and a result trail can be reconstructed linking the test result to the operator (and their training) and the device (and quality control performed on that device).
Additional guidelines for more complex POCT require on-site laboratory supervision, validation of devices and reagents, daily sign-off of patient results, and incorporation into institutional policies for performance improvement, leadership, human resources, management of information, and infection control.
Overall, point-of-care testing is treated the same as other laboratory tests by ensuring that proper controls have been instituted over variables that can affect test performance.
Management of point-of-care testing
Managing the quality of POCT requires an interdisciplinary team approach. Since the testing is performed on the medical unit by clinical staff with immediate interpretation, the laboratory must ensure test quality through the clinicians. Many institutions have formed interdisciplinary committees to set policies and direct performance improvement of POCT.
These committees represent every discipline that has a stake in the testing process with members from the laboratory, nursing, physicians, purchasing, infection control, and administration. Each discipline brings its expertise to the table to discuss and resolve issues. These committees function best when the members look beyond the personal goals of their discipline (multidisciplinary teams) towards the common goal of premier patient care (interdisciplinary teams).
A major function of an interdisciplinary committee is the selection of appropriate POCT technologies to match the needs of various patient populations. While use of a single device may be the easiest means of managing POCT, technical limitations do not always allow equivalent application to all patients. Home-use devices are frequently calibrated to function in the range of normal hematocrits, but hospitalized patients do not have normal hematocrits.
Trauma, postsurgical, and oncology patients frequently have hematocrits of 25-35 %. Neonates and polycythemic patients, on the other hand, may have hematocrits of 50 % and higher. POCT devices, like glucose meters, can be adversely affected by extremes in hematocrit [2,18]. Consideration of patient effects should also include patient medications [19-21], lipemia [8], and other metabolic conditions like uremia [18].
Oxygen tension can affect device performance such that the difference between arterial, capillary and venous blood may be unacceptable [9-10, 24-25]. Collection of inpatient specimens from lines and the effect of those specimens on POCT should be analyzed.
The environment may also preclude use of some devices. Extremes of temperature, light, and humidity can degrade POCT reagents [13-14, 16-17]. Use of POCT in home health-care nursing practices where the devices may be exposed to freezing temperatures in the winter and hot temperatures in the summer may require the staff to store the devices in their home rather than the trunk of a car.
Vibrations as experienced in a moving vehicle can also affect POCT results. Further, consider the effects of altitude when measuring blood gases in a helicopter or pressurized airplane [16,50]. A quality assurance program for POCT must therefore consider factors that can affect the testing process [51] that may not be an issue for plasma/serum analysis in the well-controlled conditions of a central, non-mobile laboratory (Fig. 2).
FIG. 2: Factors affecting point-of-care testing results. A host of preanalytical, analytical, and postanalytical variables can impact the quality of a point-of-care result.
Since point-of-care testing is meant for rapid analysis, most POCT devices utilize whole blood or other types of specimens that do not require extensive processing. The use of whole blood for POCT creates technical biases when compared to the central laboratory. Whole blood to plasma/serum correlations are offset depending on the patient’s hematocrit.
For glucose in a patient with a hematocrit of 45 %, the whole blood value is approximately 11 % lower than in plasma/serum due to the lower concentration of water inside erythrocytes [1] (Fig. 3). Consensus recommendations for POCT glucose to laboratory result differences should be less than 15 % and POCT device precision should be less than 5 % of the coefficient of variation, which yield a total, medically acceptable tolerance of 20-25 % for comparison of POCT and central laboratory results [52-56].
This leaves little room for a whole blood to plasma bias. Glucose meter manufacturers have therefore created “plasma” calibrated devices and mathematical offsets to improve laboratory correlation. By calibrating to a plasma “reference” method, POCT glucose results can better match the central laboratory that predominantly analyzes plasma or serum samples.
FIG. 3: Whole blood to plasma conversion of glucose levels. RBC = Red blood cell, erythrocyte, Hct = hematocrit.
The use of whole blood by POCT also creates difficulty with the evaluation and control of POCT devices. While plasma/serum is more homogeneous, whole blood has cells that tend to settle, creating sample discontinuities. Analytes like glucose are stable once separated from erythrocytes in plasma/serum, but glycolysis continues in whole blood, decreasing glucose levels over time. Hemolysis can also occur in whole-blood and result in analytical interferences and increases in intracellular analytes like potassium.
Whole blood controls are manufactured with cell stabilizers that can further create biases with some devices. Use of these artificial specimens can affect results as evidenced on whole-blood proficiency surveys [57-58]. Devices like the HemoCue hemoglobin analyzer that requires cell lysis for hemoglobin to contact reagents during analysis, may show continuously increasing values over time as the cells slowly lyse. Use of stabilized whole-blood products with such devices require longer incubation periods than fresh patient specimens. These factors must be built into quality control procedures.
Point-of-care training and continuing education
Quality assurance of POCT must not only consider analytical effects on the device, but must also ensure that operators interact with the devices in a consistent manner. Since POCT is widely marketed, both patients and clinical operators must demonstrate acceptable levels of competency.
Initial training should be standardized so that the same information is delivered in an identical fashion. This can be accomplished through the use of training check lists, written procedures, demonstrations, and even videotapes.
Nothing, however, compares to a validation of the actual performance of the operator both before initial use and at frequent ongoing intervals to ensure the same level of performance over time. In a recent survey by the College of American Pathologists, standardized training and frequent measurement of ongoing operator competency were aspects of glucose programs that demonstrated the most significant levels of performance improvement [34].
For POCT, operator performance is dependent on motivation, technical competency, and the complexity of the testing device (Fig. 4). On a busy medical inpatient unit, performance of quality control and maintenance/cleaning of POCT devices frequently take a secondary place to direct patient care. This can lead to more frequent problems with POCT on intensive care units.
Use of POCT by patients or clinical staff who do not appreciate the technical factors affecting POCT analysis may further result in inaccuracies solely because the operator unknowingly introduced biases. Simpler devices with internal checks that prevent result reporting when controls fail are thus easier to manage at the point of care than more complex devices that require elaborate maintenance.
While an advanced degree with a laboratory training background is more important for such complex devices, studies have shown that for simpler devices the performance of operators is independent of their educational level, provided that the operators complete a standardized training program [27-29].
Patients and clinical staff who appreciate the necessity of POCT in disease management are more likely to take better care of the devices and show an interest in performance improvement. The interdisciplinary committee is often a good place to resolve issues of staff motivation and quality assurance compliance, since its members represent a variety of both laboratory and clinically focused opinions.
This committee must consider motivational factors and weigh clinical necessity when deciding whether to utilize POCT at a particular site and how operators should be trained.
Information management The addition of information management capabilities to devices assists the practical management of point-of-care testing. Instruments that require operator and patient identification, reagent lots and date/time in order to perform a test enhance compliance and the ability to track and trend data automatically through a computer. Compliance with manual documentation is one of the flaws of POCT.
Even with the best quality assurance program, there are tests that are conducted whose results do not get recorded. Unfortunately, these tests are difficult to trace, and only counts of reagent utilization can offer clues to missing tests and lost billing opportunities. Where and when those tests were conducted is virtually impossible to trace. Currently, over half of POCT is manually or visually interpreted.
These include occult blood, urine dipsticks, pregnancy tests, pH, drugs of abuse, urine microscopy, and infectious disease. However, for instrumentation-based POCT like blood gases, coagulation, glucose, electrolytes and hemoglobin, the acquisition of pertinent information at the time the test is conducted assists documentation.
POCT information management involves three components: data capture, connectivity, and data management. Each device collects information during testing. Data from many devices are then transmitted via connection to a common, remote database or collection site where it can be reduced and managed. Currently, there are a variety of ways to transmit data; internet, radio, infrared, and direct serial connections.
The immediacy of POCT, however, presents a dilemma for information management. Since treatment optimally occurs at the time the test is conducted, data collected by a POCT device for later transmission are irrelevant to clinical treatment. POCT results are generally recorded manually to the patient’s medical record along with clinical action at the time the test is conducted. If the POCT device only intermittently transfers data, then one record of the test exists in manual, written form and another in electronic format, increasing the chance for transcription errors and duplicating the documentation effort.
This “immediacy” dilemma is a challenging aspect of POCT information management. Direct connection devices are currently the most widely marketed means of reliably connecting POCT devices to laboratory information systems and hospital information systems. However, by attaching a cable, the POCT device is no longer portable and loses its functional advantages.
On the other hand, portable devices only transmit data intermittently, whenever they are brought into connectivity or docking stations. In order to get around this problem, some manufacturers have incorporated battery rechargers into the docking stations, requiring the device to eventually get back to its station in order to continue working. Still others lock out further testing until the device is connected after each test.
Once collected in a central database, by whichever connectivity means, the information can be utilized to document regulatory compliance, monitor trends for performance improvement, and determine clinical outcomes. In troubleshooting discrepancies between POCT and the laboratory, data linking the operator and individual device to the test result are fundamental to determining the nature of the problem.
The electronic database provides this documentation by containing records of quality control performed on the device as well as operator competency. These records also serve to document routine performance of quality control as required by regulatory agencies.
FIG. 5: The Johns Hopkins Medical Institutions' Quality Assurance Program. Five databases in our program monitor aspects of quality assurance and offer quantitative parameters for continuous performance improvement.
In our institution, we have set up a custom database (Fig. 5) that contains five components. The first documents initial performance of the device and reagent/control lots for later reference in troubleshooting. The second utilizes operator quality control to document operator competency.
Each month, the means and standard deviation for each control are calculated for the entire hospital and compared to the mean and standard deviation for each operator (Table I). Those operators having a mean outside two group standard deviations from the group mean are targeted for reeducation.
By utilizing quality control conducted during routine use, we avoid having to visually inspect operators on a regular basis and prevent the additional testing (and cost) involved in those inspections. The objective, quantitative measures of quality control replace the subjectivity of visually monitoring operator performance and set a standard performance goal for operators to achieve.
These algorithms are automatically performed by the computerized database and allow only problem reports to be generated. Only reports that actually require technologist or nursing intervention are printed. This reduces paperwork and the task of manual review, saving labor and cost while maintaining quality.
A third component of our database stores proficiency and patient correlation results, allowing us to continuously verify the accuracy of individual devices against the laboratory. A fourth component trends performance monitors on the medical unit. Deficiencies in policy compliance and problems occurring on the units can be targeted for continuing education.
The effect of those education efforts can also be quantitatively determined. A final component is patient outcome. Since the POCT database interacts with the electronic patient medical record and the laboratory information system, the effects of POCT can be determined on selective patient populations.
Information management thus has unlimited potential not just for POCT but also for other laboratory tests, since the cost and labor-saving computer algorithms developed to ensure the quality of POCT can be applied to other modes of more traditional testing.
TABLE Ia and b: Johns Hopkins Medical Institutions' POCT data management report summarizing operator statistics for glucose. This report allows quantitative comparisons of operator performance and can indicate operators whose performance differs from other operators, Jean Nurse high control, or who are not compliant with quality control testing, like Jane Doe. Control = optical check or electronic control, SD = standard deviation, CV = coefficient of variation, Group = entire institution.
z-score= Mean(operator) – Mean(group) SD(group) The advantage of our custom database allows us to connect and manage information from any device in the same manner. With almost 1 million tests conducted yearly at the point of care, we would not be able to manage the data in a cost-effective way without automatic computer algorithms. We chose to create a custom database because of limitations with currently marketed POCT software.
The primary limitation of current POCT is its exclusivity to a single device. For institutions with different types of device, a separate computer database must be maintained, with different software and reports. Current software also does not allow institutions to customize reports or data reductions. Since our database resides in a common format, standard queries can be constructed by our point-of-care testing coordinators as our needs change.
Finally, current software does not generate management reports. While individual operator or meter statistics can be calculated, no comparative statistics are utilized. These current limitations prevent the small institution from realizing the potentials that can be gained from POCT data in an electronic format.
Thus, manufacturers of POCT devices need to coordinate and standardize the industry to a common electronic format in order to allow future advancements in the area of POCT data management. Collection and manipulation of manual POCT will also be an area for future development.
Clinical outcomes
Turnaround time is frequently the driving force for point-of-care testing. However, in a recent survey of British physicians who utilized blood glucose and urine dipstick testing, 85 % of the clinicians trusted central laboratory results, 38 % did not trust bedside results, and 35 % would not accept responsibility for results obtained at the bedside [30].
Quality is thus a major concern, and there is a considerable effort expended in ensuring the quality of POCT. Managing technical interferences, assuring operator competency, and management of POCT data cost an institution in labor, oversight, and reagents. Without documentation of patient benefit, there is little reason to choose POCT over central laboratory testing.
The cost of POCT is often misleading due to the interdisciplinary nature of the testing process and the hidden costs of supervising the test quality. In general, POCT is characterized by low to moderate device cost and high individual test cost when compared to centralized laboratory instruments that can cost hundreds of thousands of dollars but pennies per test in reagents [31].
Ways to minimize the cost of POCT include increasing the testing volume on each device, decreasing non-patient quality control testing, minimizing the number of trained operators, utilizing lower paid operators, and limiting POCT to medically necessary populations [11,59-62]. POCT too often tends to be an additional service in an institution rather than a replacement for central laboratory testing.
While there are numerous cost comparisons published, there are few well-controlled studies of POCT patient outcome. In one study, the use of coagulation testing was examined in cardiac surgery patients diagnosed with microvascular bleeding (N=66) [63]. The control group received standard aPTT and PT testing from the central laboratory (N=36), while the experimental group had access to POCT and utilized a simple treatment algorithm (N=30).
Those patients with access to coagulation POCT had fewer transfusions (fresh frozen plasma, platelets, and packed cells), decreased operative times, fewer reoperative admissions for bleeding, and less mediastinal chest tube drainage. The overall savings was estimated at USD 1,200 per patient or USD 215,000 annually.
Although coagulation POCT has the potential for patient benefit, the manner in which the POCT device is integrated into treatment and diagnosis will determine the utility of POCT. When utilizing POCT-activated partial thromboplastin for femoral sheath removal, over 93 % of bedside values agree with central laboratory result based on a single decision point [64].
However, agreement of only 53–78 % with the central laboratory was found for the same device when utilized for more complex therapies (heparin dosage adjustment or heparinization after thrombolysis) based on two to five decision points. Clinicians must therefore understand the limitations of the POCT device as a diagnostic tool and rely on the laboratory for more complex therapeutic interpretations.
POCT is too often over-utilized with little patient benefit. In an Australian study, a retrospective chart review was conducted on 2,294 hospitalized patients [65]. The hospital had a policy of obtaining a bedside dipstick urinalysis on admission. The charts indicated that no result was recorded in 12 % of patients, a normal result in 75 %, an expected abnormal result in 9 %, and an unexpected abnormal result in 4 %.
Physicians were questioned in the 101 cases where an unexpected abnormal result was recorded. Of these, the physician was aware of the abnormality only a third of the time (N=30), ordered additional investigations in only half of those cases (N=15), and altered treatment in none of the cases. Thus, the expense of conducting routine admission urine dipsticks did not lead to any change in treatment or beneficial outcome. One has to ask why this test was conducted in the first place.
In the urine dipstick POCT study, physician acknowledgment of the POCT result was an issue. If POCT is meant to improve laboratory turnaround time then acknowledgment of the result and therapeutic action should take place concurrently. Delays in physician acknowledgment and therapeutic action from POCT have been examined at the University of Southern California Medical Center, Los Angeles [66].
The components of laboratory turnaround time were examined to justify the construction of a satellite laboratory in the emergency room. While minor improvements could be made to those steps of the testing process under laboratory control; namely transportation, processing, analysis, and result reporting, a delay of 45 minutes was noted before clinicians became aware of test results and instituted therapy.
Due to this delay, the construction of a satellite laboratory was not justified. Thus, laboratory testing, whether conducted at the point of care or in a central laboratory is only one component of patient therapeutic management. In order to optimize patient benefit, all steps of the patient’s pathway must be examined and optimized.
Point-of-care testing offers the potential for immediate test results and therapeutic action. However, merely offering POCT on a medical unit does not guarantee beneficial patient outcome. Delays in physician acknowledgment, overutilization of POCT, and inconsistencies in quality can actually increase healthcare costs and risk to the patient.
POCT is a remote extension of the laboratory and has the same preanalytical, analytical, and postanalytical concerns that face central, core laboratory testing. The portable nature of POCT adds environmental, patient, and operator factors that are unique to its application outside of the well-controlled environment of a formal laboratory.
As inpatient populations become more acute, the demands for a wider menu of tests, with faster results, on smaller volume specimens will only increase the pressure for POCT and find new applications for POCT in the future.
As POCT expands, the traditional laboratorian’s role will need to change as they take on a more direct, active participation on the patient care team. In this role, the laboratorian will bring expertise in laboratory analysis into the manufacturing realm, improving the design of POCT devices, and onto the medical unit, improving the quality and laboratory comparability of POCT results.
References Nichols JH. Management of near-patient glucose testing. Endocrinology and metabolism. In: Service training and continuing education 1994; 12: 325-34. Atkin SH, Dasmahapatra A, Jaker MA, Chorost MI, Reddy S. Fingerstick glucose determination in shock. Ann Intern Med 1991; 114: 1020-24. Kilpatrick ES, Rumley AG, Rumley CN. The effect of haemolysis on blood glucose meter measurement. Diabet Med 1995; 12: 341-43. Wiedermann BL, Schwartz JS, McCoy P. Experience with rapid latex agglutination testing for group A streptococcal pharyngitis in a pediatric group office laboratory. J Am Board Fam Pract 1991; 4: 79-82. Mackenzie AM, Li MM, Chan FT. Evaluation of a kit for rapid detection of group A streptococci in a pediatric emergency department. Can Med Assoc J. 1988; 138: 917-19. Macrae FA, St John JB, Caligiore P, Taylor LS, Legge JW. Optimal dietary conditions for hemoccult testing. Gastroenterology 1982; 82: 899-903. Bassett ML, Goulston KJ. False positive and negative hemoccult reactions on a normal diet and effect of diet restriction. Aust NZ J Med 1980; 10: 1-4. Vallera DA, Bissell MG, Barron W. Accuracy of portable blood glucose monitoring: Effect of glucose level and prandial state. Am J Clin Pathol 1991; 95: 247-52. Chaisson KM. Comparison of arterial and capillary blood glucose with the use of the Accu-chek III. Prog Cardiovasc Nurs 1995; 10: 27-30. Larsson-Conn U. Differences between capillary and venous blood glucose during oral glucose tolerance tests. Scand J Clin Lab Invest 1976; 36: 805-08. Cohen FE, Sater B, Feingold KR. Potential danger of extending SMBG techniques to hospital wards. Diabet Care 1986; 9: 320-22. Bennett BD. Blood glucose determination: point-of-care testing. Sout Med J. 1997; 90: 687-80. King JM, Eigenmann CA, Colagiuri S. Effect of ambient temperature and humidity on performance of blood glucose meters. Diabet Med 1995; 12: 337-40. Ridgewell P, Holmes J. Effect of temperature on results obtained with the Reflolux II. Clin Chem 1990; 36: 1705-06. Gautier JF, Bigard AX, Douce P, Duvallet A, Cathelineau G. Influence of simulated altitude on the performance of five blood glucose meters. Diabet Care 1996; 19: 1430-33. Gregory M, Ryan R, Barnett JC, Youtz T. Altitude and relative humidity influence results produced by glucose meters using dry reagent strips. Clin Chem 1988; 34: 1312. Lewis K, Joyce-Nagata B, Fite EG. The effect of time and temperature on blood glucose measurements. Home Healthcare Nurse 1992; 10: 56-61. Jacobs E, Vadasdi E, Roman S, Coman N. The influence of hematocrit, uremia and hemodialysis on whole blood glucose analysis. Lab Med 1993; 24: 295-300. Anderson GD, Yuellig TR, Krone RE. An investigation into the effects of oral iron supplementation on in vivo hemoccult stool testing. Am J Gastroenterology 1990; 85: 558-61. Blebea J, McPherson RA. False-positive guiac testing with iodine. Arch Pathol Lab Med 1985 ; 109: 437-40. Demise JJ, Nelson LA, Lawson LA, Walker MM. Effect of drug products containing blue dye on hemoccult and gastroccult tests. Am J Hosp Pharm 1987; 44: 356-57. Sylvester ECJ, Price CP, Burrin JH. Investigation of the potential for interference with whole blood glucose strips. Ann Clin Biochem 1994; 31: 94-96. Kilpatrick ES, Rumley AG, Smith EA. Variations in sample pH and p O 2 affect ExacTech meter glucose measurements. Diabet Med 1994; 11: 506-09. Halloran SP. Influence of blood oxygen tension on dipstick glucose determinations. Clin Chem 1989; 35: 1268-69. Kost GJ, Vu HT, Lee JH, et al . Multicenter study of oxygen-insensitive handheld glucose point-of-care testing in critical care/hospital/ambulatory patients in the United States and Canada. Crit Care Med 1998; 26: 581-90. Nanji AA, Poon R, Hinberg I. Comparison of hospital staff performance when using desk top analyzers for “near patient” testing. J Clin Pathol 1988; 41: 223-25. Lamb LS, Parrish RS, Goran SF, Biel MH. Current nursing practice of point-of-care laboratory diagnostic testing in critical care units. Am J Crit Care 1995; 4: 429-34. Hilton S, Rink E, Fletcher J, et al . Near patient testing in general practice: attitudes of general practitioners and practice nurses, and quality assurance procedures carried out. Brit J Gen Pract 1994; 44: 577-80. Nanji AA, Poon R, Hinberg I. Near-patient testing: Quality of laboratory test results obtained by non-technical personnel in a decentralized setting. Am J Clin Pathol 1988; 89: 797-801. Gray TA, Freedman DB, Burnett D, Szczepura A, Price CP. Evidence based practice: clinician’s use and attitudes to near patient testing in hospitals. J Clin Pathol 1996; 49: 903-08. Nichols JH. Cost analysis of point-of-care laboratory testing. In: Advances in pathology. New York: Mosby-Year Book, Inc, 1996; 9: 121-34. Bickford G. Decentralized testing in the 1990s: a survey of United States hospitals. Clin Lab Med 1994; 14: 623-45. Carr SR, Slocum J, Tefft L, Haydon B, Carpenter M. Precision of office-based blood glucose meters in screening for gestational diabetes. Am J Obstet Gynecol 1996; 173: 1267-72. Jones BA, Howanitz PJ. Bedside glucose monitoring quality control practices: a college of American Pathologists Q-probes study of program quality control, documentation, program characteristics, and accuracy performance in 544 institutions. Arch Pathol Lab Med 1996; 120: 339-45. Lewandrowski K, Cheek R, Nathan DM, et al. Implementation of capillary blood glucose monitoring in a teaching hospital and determination of program requirements to maintain quality testing. Am J Med 1992; 93: 419-26. Nichols JH, Dyer K, Liszewski CA, et al. Standardizing the quality assurance of near-patient testing. In: Proceedings of the 17th International Symposium of the Electrolyte/Blood Gas Intercontinental Working Group of the International Federation of Clinical Chemistry. The confluence of critical care analysis and near-patient testing. Madison, WI: Omnipress, 1998: 164-80. Greyson J. Quality control in patient self-monitoring of blood glucose. Diabet Care 1993; 16: 1306-08. Acolet D, Ahmet Z, Houang E, Hurley R, Kaufman ME. Enterobacter cloacae in a neonatal intensive care unit: account of an outbreak and its relationship to use of third generation cephalosporins. J Hosp Infect 1994; 28: 273-86. Rutala WA, Kennedy VA, Loflin HB, Sarrubbi FA. Serratia marcescens nosocomial infection of the urinary tract associated with urine measuring containers and urinometers. Am J Med 1981; 70: 659-63. Kocka FE, Roemisch E, Causey WA, O’Dell A. The urinometer as a reservoir of infectious organisms. Am J Clin Pathol 1977; 67: 106-07. Summerton AM, Summerton N. The use of desk-top cholesterol analyzers in general practice. Pub Health 1995; 109: 363-67. Department of Health and Human Services, Health Care Finance Administration. Clinical Laboratory Improvement Amendments of 1988. Final rule. Fed Regist 1992: 57: 7001-288. Department of Health and Human Services, Health Care Finance Administration. Medicare, Medicaid and CLIA programs: CLIA program fee collection: Correction and final rule. Fed Regist 1993, 58: 5211-37. Department of Health and Human Services, Health Care Finance Administration. CLIA program: Categorization of tests and personnel modifications. Fed Regist 1995, 60: 20035-51. Department of Health and Human Services, Health Care Finance Administration. CLIA program: Categorization of waived tests. Fed Regist 1995, 60: 47534-43. JCAHO. Accreditation Manual for Pathology and Laboratory Services. Oakbrook Terrace, IL: Joint Commission on Accreditation of Healthcare Organizations, 1996. JCAHO. CAMH Comprehensive Accreditation Manual for Hospitals. Oakbrook Terrace, IL: Joint Commission on Accreditation of Healthcare Organizations, 1998. CAP Laboratory Accreditation Program. Point-of-care testing. In: Inspection checklist. Northfield, IL: College of American Pathologists, 1996. COLA. Laboratory Accreditation Manual. Columbia, MD: Commission on Office Laboratory Accreditation, 1997. Burritt MF, Santrach PJ, Hankins DG, Herr D, Newton NC. Evaluation of the i-STAT portable clinical analyzer for use in a helicopter. Scand J Clin Lab Invest 1996; 56: 121-28. Dybkaer R, Martin DV, Rowan RM (eds.) Good practice in decentralized analytical clinical measurement. Scand J Clin Lab Invest 1992; Suppl 209: 1-116. American Diabetes Association. Consensus statement of self-monitoring of blood glucose. Diabet Care 1987; 10: 95-99. American Diabetes Association. Consensus statement of self-monitoring of blood glucose. Diabet Care 1994; 17: 81-86. American Diabetes Association. Consensus statement of self-monitoring of blood glucose. Diabet Care 1996; 19: S62-66. Price CP, Burrin JM, Nattrass M. Extra-laboratory blood glucose measurement: A policy statement. Diabet Med 1988; 5: 705-09. Skendzel LP, Barnett RN, Platt R. Medically useful criteria for analytic performance of laboratory tests. Am J Clin Pathol 1985; 83: 200-05. AAB. Whole blood glucose survey. Brownsville, TX: American Association of Bioanalysts, 1998. CAP. EXCEL, Whole blood glucose survey. Northfield, IL.: College of American Pathologists, 1998. Lee-Lewandrowski E, Laposata M, Eschenbach K, et al. Utilization and cost analysis of bedside capillary glucose testing in a large teaching hospital: Implications for managing point-of-care testing. Am J Med 1994; 97: 222-30. Winkelman JW, Wybenga DR, Tanasijevic MJ. The fiscal consequences of central vs distributed testing of glucose. Clin Chem 1994; 40: 1628-30. Greendyke RM. Cost analysis of bedside glucose testing. Am J Clin Pathol 1992; 97: 106-07. Bell DSH. Hazards of inaccurate readings obtained by self-monitoring of blood glucose. Diabet Care 1990; 13: 1131-32. Despotis G., et al. Prospective evaluation and clinical utility of on-site monitoring of coagulation in patients undergoing cardiac operation. J Thorac Cardiovasc Surg 1994; 107: 271. Werner M, et al. Effect of analytic uncertainty of conventional and point-of-care assays of activated partial thromboplastin time on clinical decisions in heparin therapy. Am J Clin Pathol 1994; 102: 237. Del Mar C, Badger P. The place of routine urine testing on admission to hospital. Med J Aust 1989; 151: 151-53. Saxena S, Wong ET. Does the emergency department need a dedicated STAT laboratory? Continuous quality improvement as a management tool for the clinical laboratory. Am J Clin Pathol 1993; 100: 606-10. + View more - View less
References Nichols JH. Management of near-patient glucose testing. Endocrinology and metabolism. In: Service training and continuing education 1994; 12: 325-34. Atkin SH, Dasmahapatra A, Jaker MA, Chorost MI, Reddy S. Fingerstick glucose determination in shock. Ann Intern Med 1991; 114: 1020-24. Kilpatrick ES, Rumley AG, Rumley CN. The effect of haemolysis on blood glucose meter measurement. Diabet Med 1995; 12: 341-43. Wiedermann BL, Schwartz JS, McCoy P. Experience with rapid latex agglutination testing for group A streptococcal pharyngitis in a pediatric group office laboratory. J Am Board Fam Pract 1991; 4: 79-82. Mackenzie AM, Li MM, Chan FT. Evaluation of a kit for rapid detection of group A streptococci in a pediatric emergency department. Can Med Assoc J. 1988; 138: 917-19. Macrae FA, St John JB, Caligiore P, Taylor LS, Legge JW. Optimal dietary conditions for hemoccult testing. Gastroenterology 1982; 82: 899-903. Bassett ML, Goulston KJ. False positive and negative hemoccult reactions on a normal diet and effect of diet restriction. Aust NZ J Med 1980; 10: 1-4. Vallera DA, Bissell MG, Barron W. Accuracy of portable blood glucose monitoring: Effect of glucose level and prandial state. Am J Clin Pathol 1991; 95: 247-52. Chaisson KM. Comparison of arterial and capillary blood glucose with the use of the Accu-chek III. Prog Cardiovasc Nurs 1995; 10: 27-30. Larsson-Conn U. Differences between capillary and venous blood glucose during oral glucose tolerance tests. Scand J Clin Lab Invest 1976; 36: 805-08. Cohen FE, Sater B, Feingold KR. Potential danger of extending SMBG techniques to hospital wards. Diabet Care 1986; 9: 320-22. Bennett BD. Blood glucose determination: point-of-care testing. Sout Med J. 1997; 90: 687-80. King JM, Eigenmann CA, Colagiuri S. Effect of ambient temperature and humidity on performance of blood glucose meters. Diabet Med 1995; 12: 337-40. Ridgewell P, Holmes J. Effect of temperature on results obtained with the Reflolux II. Clin Chem 1990; 36: 1705-06. Gautier JF, Bigard AX, Douce P, Duvallet A, Cathelineau G. Influence of simulated altitude on the performance of five blood glucose meters. Diabet Care 1996; 19: 1430-33. Gregory M, Ryan R, Barnett JC, Youtz T. Altitude and relative humidity influence results produced by glucose meters using dry reagent strips. Clin Chem 1988; 34: 1312. Lewis K, Joyce-Nagata B, Fite EG. The effect of time and temperature on blood glucose measurements. Home Healthcare Nurse 1992; 10: 56-61. Jacobs E, Vadasdi E, Roman S, Coman N. The influence of hematocrit, uremia and hemodialysis on whole blood glucose analysis. Lab Med 1993; 24: 295-300. Anderson GD, Yuellig TR, Krone RE. An investigation into the effects of oral iron supplementation on in vivo hemoccult stool testing. Am J Gastroenterology 1990; 85: 558-61. Blebea J, McPherson RA. False-positive guiac testing with iodine. Arch Pathol Lab Med 1985 ; 109: 437-40. Demise JJ, Nelson LA, Lawson LA, Walker MM. Effect of drug products containing blue dye on hemoccult and gastroccult tests. Am J Hosp Pharm 1987; 44: 356-57. Sylvester ECJ, Price CP, Burrin JH. Investigation of the potential for interference with whole blood glucose strips. Ann Clin Biochem 1994; 31: 94-96. Kilpatrick ES, Rumley AG, Smith EA. Variations in sample pH and p O 2 affect ExacTech meter glucose measurements. Diabet Med 1994; 11: 506-09. Halloran SP. Influence of blood oxygen tension on dipstick glucose determinations. Clin Chem 1989; 35: 1268-69. Kost GJ, Vu HT, Lee JH, et al . Multicenter study of oxygen-insensitive handheld glucose point-of-care testing in critical care/hospital/ambulatory patients in the United States and Canada. Crit Care Med 1998; 26: 581-90. Nanji AA, Poon R, Hinberg I. Comparison of hospital staff performance when using desk top analyzers for “near patient” testing. J Clin Pathol 1988; 41: 223-25. Lamb LS, Parrish RS, Goran SF, Biel MH. Current nursing practice of point-of-care laboratory diagnostic testing in critical care units. Am J Crit Care 1995; 4: 429-34. Hilton S, Rink E, Fletcher J, et al . Near patient testing in general practice: attitudes of general practitioners and practice nurses, and quality assurance procedures carried out. Brit J Gen Pract 1994; 44: 577-80. Nanji AA, Poon R, Hinberg I. Near-patient testing: Quality of laboratory test results obtained by non-technical personnel in a decentralized setting. Am J Clin Pathol 1988; 89: 797-801. Gray TA, Freedman DB, Burnett D, Szczepura A, Price CP. Evidence based practice: clinician’s use and attitudes to near patient testing in hospitals. J Clin Pathol 1996; 49: 903-08. Nichols JH. Cost analysis of point-of-care laboratory testing. In: Advances in pathology. New York: Mosby-Year Book, Inc, 1996; 9: 121-34. Bickford G. Decentralized testing in the 1990s: a survey of United States hospitals. Clin Lab Med 1994; 14: 623-45. Carr SR, Slocum J, Tefft L, Haydon B, Carpenter M. Precision of office-based blood glucose meters in screening for gestational diabetes. Am J Obstet Gynecol 1996; 173: 1267-72. Jones BA, Howanitz PJ. Bedside glucose monitoring quality control practices: a college of American Pathologists Q-probes study of program quality control, documentation, program characteristics, and accuracy performance in 544 institutions. Arch Pathol Lab Med 1996; 120: 339-45. Lewandrowski K, Cheek R, Nathan DM, et al. Implementation of capillary blood glucose monitoring in a teaching hospital and determination of program requirements to maintain quality testing. Am J Med 1992; 93: 419-26. Nichols JH, Dyer K, Liszewski CA, et al. Standardizing the quality assurance of near-patient testing. In: Proceedings of the 17th International Symposium of the Electrolyte/Blood Gas Intercontinental Working Group of the International Federation of Clinical Chemistry. The confluence of critical care analysis and near-patient testing. Madison, WI: Omnipress, 1998: 164-80. Greyson J. Quality control in patient self-monitoring of blood glucose. Diabet Care 1993; 16: 1306-08. Acolet D, Ahmet Z, Houang E, Hurley R, Kaufman ME. Enterobacter cloacae in a neonatal intensive care unit: account of an outbreak and its relationship to use of third generation cephalosporins. J Hosp Infect 1994; 28: 273-86. Rutala WA, Kennedy VA, Loflin HB, Sarrubbi FA. Serratia marcescens nosocomial infection of the urinary tract associated with urine measuring containers and urinometers. Am J Med 1981; 70: 659-63. Kocka FE, Roemisch E, Causey WA, O’Dell A. The urinometer as a reservoir of infectious organisms. Am J Clin Pathol 1977; 67: 106-07. Summerton AM, Summerton N. The use of desk-top cholesterol analyzers in general practice. Pub Health 1995; 109: 363-67. Department of Health and Human Services, Health Care Finance Administration. Clinical Laboratory Improvement Amendments of 1988. Final rule. Fed Regist 1992: 57: 7001-288. Department of Health and Human Services, Health Care Finance Administration. Medicare, Medicaid and CLIA programs: CLIA program fee collection: Correction and final rule. Fed Regist 1993, 58: 5211-37. Department of Health and Human Services, Health Care Finance Administration. CLIA program: Categorization of tests and personnel modifications. Fed Regist 1995, 60: 20035-51. Department of Health and Human Services, Health Care Finance Administration. CLIA program: Categorization of waived tests. Fed Regist 1995, 60: 47534-43. JCAHO. Accreditation Manual for Pathology and Laboratory Services. Oakbrook Terrace, IL: Joint Commission on Accreditation of Healthcare Organizations, 1996. JCAHO. CAMH Comprehensive Accreditation Manual for Hospitals. Oakbrook Terrace, IL: Joint Commission on Accreditation of Healthcare Organizations, 1998. CAP Laboratory Accreditation Program. Point-of-care testing. In: Inspection checklist. Northfield, IL: College of American Pathologists, 1996. COLA. Laboratory Accreditation Manual. Columbia, MD: Commission on Office Laboratory Accreditation, 1997. Burritt MF, Santrach PJ, Hankins DG, Herr D, Newton NC. Evaluation of the i-STAT portable clinical analyzer for use in a helicopter. Scand J Clin Lab Invest 1996; 56: 121-28. Dybkaer R, Martin DV, Rowan RM (eds.) Good practice in decentralized analytical clinical measurement. Scand J Clin Lab Invest 1992; Suppl 209: 1-116. American Diabetes Association. Consensus statement of self-monitoring of blood glucose. Diabet Care 1987; 10: 95-99. American Diabetes Association. Consensus statement of self-monitoring of blood glucose. Diabet Care 1994; 17: 81-86. American Diabetes Association. Consensus statement of self-monitoring of blood glucose. Diabet Care 1996; 19: S62-66. Price CP, Burrin JM, Nattrass M. Extra-laboratory blood glucose measurement: A policy statement. Diabet Med 1988; 5: 705-09. Skendzel LP, Barnett RN, Platt R. Medically useful criteria for analytic performance of laboratory tests. Am J Clin Pathol 1985; 83: 200-05. AAB. Whole blood glucose survey. Brownsville, TX: American Association of Bioanalysts, 1998. CAP. EXCEL, Whole blood glucose survey. Northfield, IL.: College of American Pathologists, 1998. Lee-Lewandrowski E, Laposata M, Eschenbach K, et al. Utilization and cost analysis of bedside capillary glucose testing in a large teaching hospital: Implications for managing point-of-care testing. Am J Med 1994; 97: 222-30. Winkelman JW, Wybenga DR, Tanasijevic MJ. The fiscal consequences of central vs distributed testing of glucose. Clin Chem 1994; 40: 1628-30. Greendyke RM. Cost analysis of bedside glucose testing. Am J Clin Pathol 1992; 97: 106-07. Bell DSH. Hazards of inaccurate readings obtained by self-monitoring of blood glucose. Diabet Care 1990; 13: 1131-32. Despotis G., et al. Prospective evaluation and clinical utility of on-site monitoring of coagulation in patients undergoing cardiac operation. J Thorac Cardiovasc Surg 1994; 107: 271. Werner M, et al. Effect of analytic uncertainty of conventional and point-of-care assays of activated partial thromboplastin time on clinical decisions in heparin therapy. Am J Clin Pathol 1994; 102: 237. Del Mar C, Badger P. The place of routine urine testing on admission to hospital. Med J Aust 1989; 151: 151-53. Saxena S, Wong ET. Does the emergency department need a dedicated STAT laboratory? Continuous quality improvement as a management tool for the clinical laboratory. Am J Clin Pathol 1993; 100: 606-10.
May contain information that is not supported by performance and intended use claims of Radiometer's products. See also Legal info .

PhD, DABCC, FACB Associate Professor of Pathology Tufts University School of Medicine Director, Clinical Chemistry Baystate Health System 759 Chestnut Street Springfield, MA 01199 USA

Acute care testing handbook
Get the acute care testing handbook.
Your practical guide to critical parameters in acute care testing.

Scientific webinars
Check out the list of webinars.
Radiometer and acutecaretesting.org present free educational webinars on topics surrounding acute care testing presented by international experts.
Related Articles
Laboratory supervision of point-of-care blood gas, sign up for the acute care testing newsletter.
Disclaimer: This translation was last updated on August 2, 2022. For up-to-date content, please visit the English version of this page.
Disclaimer: The Spanish COVID-19 site is currently undergoing significant updates which may lead to a delay in translated content. We apologize for any inconvenience.
Guidance for SARS-CoV-2 Rapid Testing Performed in Point-of-Care Settings
Summary of recent changes.
- HHS and CDC’s new guidance [288 KB, 9 pages] no longer requires reporting of negative results for non-NAAT tests (rapid or antigen test results).
- This update also no longer requires reporting of antibody test results, positive or negative.
View Previous Updates
- This guidance provides information on the regulatory requirements for SARS-CoV-2 rapid testing performed in point-of-care settings, collecting specimens and performing rapid tests safely and correctly, and information on reporting test results.
- This guidance is intended for individuals and facilities who are setting up and performing rapid testing in point-of-care settings and is not intended for use or reporting of self-tests performed by the individual being tested.
Regulatory Requirements for Rapid Testing in Point-of-Care Settings
- Reporting Requirements for Rapid Testing in Point-Of-Care Settings
Specimen Collection & Handling of Rapid Tests in Point-of-Care Settings
Learn more about performing rapid tests in point-of-care settings.
- More Point-Of-Care Resources
Point-of-care testing uses rapid diagnostic tests performed or interpreted by someone other than the individual being tested or their parent or guardian and can be performed in a variety of settings. Rapid tests used in point-of-care settings can be NAAT , antigen , or antibody tests.
These tests can be used to diagnose current or detect past SARS-CoV-2 infections in various point-of-care settings, including but not limited to:
- Physician offices
- Urgent care facilities
- School health clinics
- Long-term care facilities and nursing homes
- Temporary locations, such as drive-through sites managed by local organizations
There are four different types of CLIA certificates [47 KB, 1 page] , any one of which is appropriate for point-of-care testing. A CLIA certificate is required to perform point-of-care testing. A CLIA Certificate of Waiver is appropriate if SARS-CoV-2 point-of-care testing is the only testing being performed. It can be obtained as follows:
- Complete an application ( Form CMS-116 [311 KB, 10 pages] ), available on the CMS CLIA website or from a local State Agency.
- Send the completed application to the address of the local State Agency for the state where testing will be performed.
- Pay the CLIA Certificate of Waiver fee, following instructions provided by the State Agency.
See How to Obtain a CLIA Certificate of Waiver [1.4 MB, 9 pages] for more information. Laboratories or point-of-care testing sites that have applied for a CLIA Certificate of Waiver to perform SARS-CoV-2 point-of-care testing can begin testing and reporting SARS-CoV-2 results as soon as they have submitted their application to the State Agency, as long as they meet any additional state licensure requirements that apply. A non-certified point-of-care testing site will be treated as operating under a Certificate of Waiver while their application is being processed. The point-of-care testing site must keep its certificate information current. The State Agency should be notified of any changes to the laboratory or testing site ownership, name, address, or director within 30 days.
During the COVID-19 public health emergency, CMS allows a laboratory or testing site to use its existing Certificate of Waiver to operate a temporary COVID-19 testing site in an off-site location, such as a nursing home or drive-through location. A temporary COVID-19 testing site can only perform CLIA-waived or FDA-authorized point-of-care tests for SARS-CoV-2 and must be under the direction of the existing laboratory or testing site director.
CMS has provided specific guidance for the use of FDA authorized OTC self-tests when these tests are either performed or the results are interpreted by someone other than the individual being tested or their parent or guardian. In these circumstances, the tests are not considered self-tests and the point-of-care testing site that performs the testing or interprets the test results needs a CLIA certificate and must report results as described below. See Over The Counter (OTC) Home Testing and CLIA Applicability [187 KB, 5 pages] for more information from CMS.
Tests That Can Be Used in Point-of-Care Settings
Refer to the U.S. Food and Drug Administration (FDA) website for a list of the SARS-CoV-2 point-of-care and rapid tests that have received Emergency Use Authorization (EUA) . Tests that have been authorized for use in a point-of-care setting will have a W, for Waived, in the Authorized Settings column of the FDA table. The laboratory or testing site must use a test authorized for point-of-care use by the FDA and must follow the manufacturer’s instructions for each test. The instructions for use provide specific information on how to perform the test, which specimens can be used, and the people who may be tested.
OTC tests can be purchased and used in a point-of-care setting. However, when these tests are either performed or the results are interpreted by someone other than the individual being tested or their parent or guardian, then the CLIA reporting requirements for waived tests must be followed.
Reporting Requirements for Rapid Testing in Point-of-Care Settings
A CLIA-certified laboratory or testing site must report all positive SARS-CoV-2 diagnostic and screening test results to the person who was tested or that person’s healthcare provider. CLIA-certified laboratories or testing sites are no longer required to report negative results for non-NAAT tests (rapid or antigen test results) or antibody tests, positive or negative. Depending on the test manufacturer’s instructions for use, which can be found on FDA’s EUA website , the laboratory or testing site may be required to report a negative test result as a “presumptive negative.”
A CLIA-certified laboratory or testing site must also report all positive SARS-CoV-2 test results to their respective state , tribal , local , and territorial health department’s website in accordance with the Coronavirus Aid, Relief, and Economic Security (CARES) Act; refer to the CMS interim final rule for regulatory reporting requirements [596 KB, 55 pages] . In addition, laboratories and testing sites can find out more about How to Report COVID-19 Laboratory Data . CLIA-certified laboratories or testing sites are no longer required to report negative results for non-NAAT tests (rapid or antigen test results) or antibody tests, positive or negative.
CMS-certified long-term care (LTC) facilities can submit point-of-care SARS-CoV-2 testing data, including antigen, antibody, and nucleic acid amplification test (NAAT) testing data, to CDC’s National Healthcare Safety Network (NHSN). This CDC- and CMS-preferred pathway to submit data to CDC’s NHSN applies only to CMS-certified LTC facilities. Test data submitted to NHSN will be reported to appropriate state, tribal, local, and territorial health departments using standard electronic laboratory messages. Other types of LTC facilities can also report testing data in NHSN for self-tracking or to fulfill state or local reporting requirements, if any. While NHSN is the CDC- and CMS-preferred pathway, Medicare and Medicaid-certified LTC facilities can submit data through the other mechanisms described in the Current Methods of Submission section of HHS Laboratory Reporting Guidance [287 KB, 9 pages] to meet the reporting requirements.
Each point-of-care test has been authorized for use with certain specimen types and should only be used with those specimen types. Proper specimen collection and handling are critical for all COVID-19 testing, including those tests performed in point-of-care settings. A specimen that is not collected or handled correctly can lead to an inaccurate or unreliable test result.
Personnel collecting specimens or working within 6 feet of patients suspected to be infected with SARS-CoV-2 should maintain proper infection control and use recommended personal protective equipment (PPE), which could include an N95 or higher-level respirator (or face mask if a respirator is not available), eye protection, gloves, and a lab coat or gown.
Personnel handling specimens but not directly involved in the collection (e.g., self-collection) and not working within 6 feet of the patient should follow Standard Precautions . It is recommended that personnel wear well-fitting cloth masks , facemasks, or respirators at all times while at the point-of-care site where the testing is being performed.
For additional information about the proper collection and handling of each of the specimen types, please refer to CDC’s Interim Guidelines for Collecting and Handling of Clinical Specimens for COVID-19 Testing.
Disinfect surfaces within 6 feet of the specimen collection and handling area at these times:
- Before testing begins each day
- Between each specimen collection
- At least hourly during testing
- When visibly soiled
- In the event of a specimen spill or splash
- At the end of every testing day
CDC recommends the following practices when performing tests in point-of-care settings:
Before the Test
- Implement appropriate control measures to prevent these potentially negative outcomes from happening.
- Find more information at CDC’s Biological Risk Management for Point-of-Care Testing Sites .
- Find more information on Risk Assessment Best Practices and Risk Assessment templates [2.2 MB, 69 pages] .
- Learn more about CDC’s Guidelines for Handling and Processing Specimens Associated with COVID-19 .
- Use a new pair of gloves each time a specimen is collected from a different person. If specimens are tested in batches, also change gloves before putting a new specimen into a testing device. Doing so will help to avoid cross-contamination.
- Do not reuse used test devices, reagent tubes, solutions, swabs, lancets, or fingerstick collection devices.
- Store reagents, specimens, kit contents, and test devices according to the manufacturer’s instructions found in the package insert.
- Discard tests and test components that have exceeded the expiration date or show signs of damage or discoloration (such as reagents showing any signs of alteration).
- Do not open reagents, test devices, and cassettes until the test process is about to occur. Refer to the manufacturer’s instructions to see how long a reagent, test device, or cassette can be used after opening.
- Label each specimen with appropriate information to definitively connect that specimen to the correct person being tested.
- When transferring specimens from a collection area to a testing area, follow the instructions for the point-of-care test used.
During the Test
- Follow all the manufacturer’s instructions for performing the test in the exact order specified.
- Perform regular quality control and instrument calibration, as applicable, according to the manufacturer’s instructions. If quality control or calibration fails, identify and correct issues before proceeding with patient testing.
- When processing multiple specimens successively in batches, ensure proper timing for each specimen and each step of the testing process, as specified by the test manufacturer. To avoid cross-contamination, change gloves before putting a new specimen into a testing device.
After the Test
- Read and record results only within the amount of time specified in the manufacturer’s instructions. Do not record results from tests that have not been read within the manufacturer’s specified timeframe.
- Decontaminate the instrument after each use. Follow the manufacturer’s recommendations for using an approved disinfectant, including proper dilution, contact time, and safe handling.
- Always discuss used and unused COVID-19 test kit waste with your facility leadership, facility waste management contractor, your State Department of Public Health, and the test manufacturer’s technical support. All waste disposal must comply with your local, tribal, regional, state, national, and/or international regulations. Waste disposal regulations may vary at the state and local levels; see Environmental Protection Agency Regulations and State Universal Waste Programs in the United States for more information.
CDC has free training and tools to help you learn the basics about performing point-of-care testing. The companies that make the tests and testing systems also have free training resources designed to help you use the tests. Find links in this section to resources and training that will help you get ready to test.
CDC Educational Materials for Rapid Testing in Point-of-Care Settings
Many COVID-19 point-of-care and rapid tests fall into a category called waived tests , which are tests performed in a laboratory or at a testing site under a CLIA Certificate of Waiver. CDC has free educational and training resources for waived point-of-care testing, including:
Ready? Set? Test! is an online training course that explains the waived testing process and how to help ensure that test results are accurate and reliable.
A Ready? Set? Test! booklet [9 MB, 56 pages] that contains tips, reminders, and resources along with forms and examples for use in your testing site (also available in Spanish [6.9 MB, 56 pages] ).
A Self-Assessment Checklist [372 KB, 4 pages] you can use to help ensure good testing practices and provide reliable, high-quality test results.
The COVID-19 Point-of-Care Batch Testing Tips Infographic [2 MB, 2 Pages] gives advice for performing batch testing.
Visit CDC’s Waived Tests page for more information and resources.
Laboratories and testing sites can find additional free, online training courses relevant to working with SARS-CoV-2 specimens on CDC’s Preparing and Supporting Laboratories Responding to COVID-19 web page.
More Point-of-Care Resources
- Performing Facility-wide SARS-CoV-2 Testing in Nursing Homes
- SARS-CoV-2 (COVID-19) Fact Sheet: Guidance – Proposed Use of Point-of-Care Testing Platforms for SARS-CoV-2 (COVID-19) [63 KB, 3 pages]
- Frequently Asked Questions about Coronavirus (COVID-19) for Laboratories
- CDC Isolation Precautions
- Using Personal Protective Equipment (PPE)
- Core Infection Prevention and Control Practices for Safe Healthcare Delivery in All Settings
- CMS COVID-19 FAQs on Medicare Fee-for-Service Billing [1.5 MB, 181 pages]
- CMS Guidance on SARS-CoV-2 Laboratory Testing
- CMS FAQs on SARS-CoV-2 Surveillance Testing [78 KB, 1 page]
- U.S. Food and Drug Administration (FDA) FAQs on Testing for SARS-CoV-2
- FDA COVID-19 Emergency Use Authorizations (EUAs) for Medical Devices
- FDA Medical Device Reporting (MDR) Information
As of January 19, 2022
- Added language about reporting results of over-the-counter (OTC) tests when used in a point-of-care setting.
As of December 31, 2021
- Updated waste management guidance.
As of March 8, 2021
- Edited “Regulatory Requirements for Point-of-Care and Rapid Testing” section to add updated Centers for Medicare & Medicaid Services (CMS) guidance for SARS-CoV-2 point-of-care tests and Clinical Laboratory Improvement Amendments (CLIA) Certificates of Waiver.
- Added new training resources from manufacturers of SARS-CoV-2 point-of-care and rapid tests.
- Added a link to CDC’s Biological Risk Management for Point-of-Care Testing Sites.
As of January 28 , 2021
- Edited to add language about antibody testing.
As of December 30 , 2020
- Edited “Specimen Collection and Handling Point-of-Care Tests” section to add language which clarifies the personal protective equipment (PPE) recommended for personnel collecting point-of-care (POC) specimens versus the PPE recommended for personnel handling POC specimens but not directly involved in collection and not working within 6 feet of patients.
As of December 26, 2020
- Added to whom staff at long-term care facilities (LCTFs) should report point-of-care antigen testing data under “Reporting Requirements for Point-of-Care Testing” section
As of December 10, 2020
- Added a new “Help with Performing Point-of-Care Tests” section, which includes training resources for performing POC tests.
As of December 2, 2020
- Modified page to include Frequently Asked Questions about Point-of-Care Testing
To receive email updates about COVID-19, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
Apologies; the page you are requesting is currently unavailable. The request resembles an abusive automated request. If you believe this an error, please contact us and we will assist in resolving the issue.
Thank you for visiting!

IMAGES
VIDEO
COMMENTS
Even if the shift in public perception is a long way off, there's already demand for point-of-care testing at pharmacies. Lackie Drug, an independent pharmacy in Roanoke, Arkansas, gives up to 1,000 flu and strep tests every year. Tarrytown Pharmacy in Austin, Texas, gives up to 1,500 per year. Notably, patients are paying cash for these ...
As with any new pharmacy service, developing a business plan can help with anticipating challenges, evaluating business readiness to implement POCT, and leveraging strengths to effectively introduce and sustain POCT ... The optimal space for point-of-care testing in a pharmacy depends on several factors, including the number of tests offered ...
The value of point of care testing in planning for future health threats. In addition to being able to provide better access and cost-efficiency to healthcare, point of care testing will also be valuable in order to plan for future health threats. Emerging infectious diseases are seemingly on the rise due to increased globalization and climate ...
The COVID-19 pandemic has increased the demand for point-of-care testing and diagnostics in the United States and globally, boosting revenues in the laboratory testing market by 9.1% year-over-year since 2020. 1. At the same time, lab testing for a lengthy list of other acute and chronic conditions and diseases is always in demand.
What is Point-of-care Testing? Point-of-care tests produce rapid, reliable results that aid in identification and monitoring of acute infections or chronic disease. POCT involves screenings and tests at or near the point of care, which produce actionable results within minutes. There are 4 primary goals of POCT. 1.
BACKGROUND. Driven by quicker diagnostic paybacks, point of care testing (POCT), also known as bedside testing, near-patient testing, alternate-site testing, and ancillary testing, has modernized patient care ().The College of American Pathologists (CAP) describes POCT as 'testing that does not require permanent dedicated space and it refers to those analytical patient-testing activities ...
May 9, 2022. Point-of-care (POC) testing within retail clinics and pharmacies can play a significant role in helping reduce the spread of infectious diseases. This reality was perhaps best illustrated during the height of the pandemic when healthcare clinics located within local pharmacies provided some of the quickest and easiest options for ...
Point-of-care testing. Point-of-care product device testing is critical to ensuring that medical devices are effective and safe for use by patients. We support your studies that assess the safety, accuracy, and effectiveness of medical devices at the point of care. We offer a wide range of testing services, including clinical performance ...
The Clinical Laboratory Improvement Amendments (CLIA), a set of federal regulatory standards introduced in 1988, governs every lab that performs human testing in the United States. 1. Before you can test any patient samples, you must first have a CLIA license. Your POCT lab is likely to qualify for a Certificate of Waiver.
Point of Care Testing (POCT) is a powerful tool for independent pharmacies, offering an opportunity to expand revenue streams and provide essential healthcare services to your community. This comprehensive guide will explore effective marketing strategies to make your POCT services successful. From understanding your target market to leveraging online reviews, we've got you covered. Understanding
Point-of-care testing enables Test and Treat algorithms for targeted clinical scenarios. Centralized diagnostics play a critical role for more complex—and less time constrained—diagnosis. Understanding the Clinical Impact for the patient at the point of access is essential.
The NCPA Innovation Center will be offering the NASPA Pharmacy-Based Point-of-Care Test and Treat National Certificate Program on May 16 in a virtual format. Enroll for the chance to gain the skills and information necessary to develop a testing program such as influenza, Group A Streptococcus, HIV, Hepatitis C, coronaviruses, and chronic diseases.
The POCT viability conclusion shows the four automating the processing of POCT test results by Mobihealth are all viable, whereas the business models without the back synchronisation pose less risks and are viable as well. Point-Of-Care Testing enables clinical tests at or near the patient with the assumption that test results will be available instantly or in a very short time frame to assist ...
Meeting the demand for point-of-care testing. The COVID-19 pandemic has increased the demand for point-of-care testing and diagnostics in the United States and globally, boosting revenues in the laboratory testing market by 9.1% year-over-year since 2020. 1
From identifying point-of-care testing opportunities that make sense for your pharmacy to streamlining documentation, billing and reporting, learn how OmniSYS can help effectively manage point-of-care testing for your pharmacy. Reimbursable tests vary by state and payer but commonly include: A1C. Flu. Strep.
Point-of-Care Testing. Learn about point-of-care testing (POCT), which encompasses any laboratory tests that are performed at or near a patient and at the site where care or treatment is provided. Point-of-care test results are typically available relatively quickly so that they can be acted upon without delay.
Point-of-Care Testing (POCT) is clinical laboratory testing conducted close to the site of patient care where care or treatment is provided.[1] POCT provides rapid turnaround of test results with the potential to generate a result quickly so that appropriate treatment can be implemented, leading to improved clinical or economic outcomes compared to laboratory testing.[2]
Point of Care Testing Kee, Sarah., Adams, Lynsey., Whyte, Carla J., McVicker, Louise. Background Point of care testing (POCT) refers to testing that is performed near or at the site of a patient with the result leading to a possible change in the care of the patient. Over the past few years, the popularity and demand of POCT has been
Point-of-care testing, often abbreviated to POC testing, is medical testing done at or near the point of care. In this context, POC refers to the location of the patient. Sending all samples and specimens away to be processed at medical laboratories means waiting a long time for results. This can lead to wasted time in critical contexts or ...
Tests used for risk-based screening (based on individual, gender, age, prior history or other risk element): Glucose. Pediatric lead testing. Fecal occult blood for patients over 50. Lipid screening for patients with a family or personal history of heart disease. Medicare preventive services (CMS) 2. HIV/HCV/HPV.
Point-of-care testing (POCT) is a delivery option for performing laboratory testing closer to the patient. Due to increasing healthcare pressures for faster turnaround of laboratory results and the development of a broader menu of testing devices, POCT is growing in popularity. Devices today are more portable, require less blood, and have ...
Training Goal and Objectives. After completing this training, participants will be able to: Describe basic safety procedures and the importance of quality in point-of-care (POC) settings performing CLIA-waived testing. Identify the major considerations that impact workspace setup, testing workflow, and hazardous waste management at POC sites.
Key Points. This guidance provides information on the regulatory requirements for SARS-CoV-2 rapid testing performed in point-of-care settings, collecting specimens and performing rapid tests safely and correctly, and information on reporting test results. This guidance is intended for individuals and facilities who are setting up and ...
POINT-CARE TESTING GUIDELINES. The following guideline is a step-by-step outline that can be used in the development of a point-of-care program. Although the outline is directed to a hospital or large institution point-of-care program, it may also be adjusted to smaller sites, such as a physician's office laboratory (POL).
U.S. Food and Drug Administration
The global market for Point of Care (POC) Molecular Diagnostics estimated at US$3.7 Billion in the year 2023, is projected to reach a revised size of US$8.8 Billion by 2030, growing at a CAGR of ...