Making Addiction Treatment More Realistic and Pragmatic: The Perfect Should Not be the Enemy of the Good

This essay was also published by Health Affairs on January 3, 2022.
Last year saw drug overdose deaths in the U.S. surpass an unthinkable milestone: 100,000 deaths in a year. This is the highest number of drug overdoses in our country’s history, and the numbers are climbing every month.
There is an urgent need for a nationwide, coordinated response that a tragedy of this magnitude demands. Recent data from 2020 shows that only 13 percent of people with drug use disorders receive any treatment. Only 11 percent of people with opioid use disorder receive one of the three safe and effective medications that could help them quit and stay in recovery.
The magnitude of this crisis demands out-of-the-box thinking and willingness to jettison old, unhelpful, and unsupported assumptions about what treatment and recovery need to look like. Among them is the traditional view that abstinence is the sole aim and only valid outcome of addiction treatment.
While not using any drugs or alcohol poses the fewest health risks and is often necessary for sustained recovery, different people may need different options. Temporary returns to use after periods of abstinence are part of many recovery journeys, and it shouldn’t be ruled out that some substance use or ongoing use of other substances even during treatment and recovery might be a way forward for some subset of individuals.
Reduced number of heavy drinking days is already recognized as a meaningful clinical outcome in research and medication development for alcohol addiction. Clinical endpoints other than abstinence , such as reduced use, are now being considered in medication trials for drug use disorders. This could facilitate the approval of a wider range of medications to treat addiction, as well as open the door to medications that address symptoms associated with it, such as sleep disorders and anxiety. The existing medications methadone, buprenorphine, and naltrexone have proven to be effective at reducing relapse risk and improving other outcomes in patients with opioid use disorder, but more options could benefit more patients. And medications to treat other drug use disorders are needed.
Temporary returns to drug use are so common and expected during treatment and recovery that addiction is described as a chronic relapsing condition, like some autoimmune diseases. Yet these setbacks may still be regarded by family, friends, communities, and even physicians as failures, resetting the clock of recovery to zero. Patients in some drug addiction treatment programs are even expelled if they produce positive urine samples.
Healthcare and society must move beyond this dichotomous, moralistic view of drug use and abstinence and the judgmental attitudes and practices that go with it.
There are still many unknowns about the different trajectories that recovery may take, but stereotypes should not guide us in the absence of knowledge. Research in the field of nicotine addiction shows that a person’s first cigarette after a period of abstinence raises the risk of returning to their pre-treatment use pattern but does not always have that outcome. Research on the consequences of returning to opioid, stimulant, or cannabis use after a period of non-use is still needed, but there is little evidence to support the assumption—reinforced in movies and TV shows—that a single return to drug use following on a one-time loss of resolve will automatically lead the individual straight back to their former compulsive consumption.
Medicine can perhaps learn from the recovery world, where a distinction is increasingly made between a one-time return to drug use, a “slip” or “lapse,” and a return to the heavy and compulsive use pattern of an individual’s active addiction—the more stereotypical understanding of relapse. The distinction is meant to acknowledge that a person’s resolve to recover may even be strengthened by such lapses and that they need not be catastrophic for the individual’s recovery.
A return to substance use after a period of abstinence may also, in some cases, lead to less frequent use than before treatment. Such a trajectory has been identified in research on drug and alcohol treatment outcomes in adolescents . For some drugs, any reduced use is likely beneficial : Less frequent illicit substance use means less frequent need to obtain an illicit substance and fewer opportunities for infectious disease transmission or fatal overdose. It may also increase the likelihood that a person can be a supportive family member, hold a job, and make other healthy choices in their life.
But as long as treatment is only regarded as successful if it produces abstinence, then even one-time lapses can trigger unnecessary guilt, shame, and hopelessness. If an individual feels like they are bad, weak, or wrong for taking a drink or drug after a period in recovery, it could potentially make it more likely for those slips to become more serious relapses. As it now stands, even a slip can produce a positive urine sample or force the honest patient to self-report a return to drug use, which can then trigger the judgment and punitive policies of their treatment program or the law as well as trigger the personal sense that they have failed again and there is no hope for their recovery.
Another deleterious effect of equating treatment success with abstinence and drug use with treatment failure is that some people with SUDs are unready to give up substances completely. In fact, this is one of the main reasons people who could benefit from addiction treatment do not seek it. Although it may not be ideal or optimal, treating an opioid or methamphetamine use disorder even while a person continues to use cannabis or alcohol would be a net individual and public health benefit.
Realistically and pragmatically addressing addiction requires that we not let the perfect be the enemy of the good. Right now, we need all the good we can get. It also means offering supports for people with SUD that protect against the worst consequences of drug use. Syringe-services programs reduce HIV transmission and offer people an entry point into treatment; naloxone distribution to people who use opioids and their families reduces overdose fatalities. Neither of these measures increase drug use in communities that implement them, as critics often worry.
Other harm-reduction modalities being studied include personal drug-testing equipment like fentanyl test strips, as well as overdose prevention centers—places where people can use drugs under medical supervision, which are in operation in other countries and, as of late November, are available in New York City. Such services could potentially help mitigate some of the risks associated with lapses and relapses, such as heightened risk of overdose due to lost tolerance. The latter currently accounts for many fatal overdoses after people with an untreated opioid use disorder are released from prison, for example.
Drug addiction is a chronic but treatable disorder with well-understood genetic and social contributors. It is not a sign of a person’s weakness or bad character. Continued or intermittent use of drugs, even by people who know they have a disorder and are trying hard to recover from it, must be acknowledged as part of the reality of the disorder for many who struggle with it. Just as we must stop stigmatizing addiction, we must also stop stigmatizing people who use drugs as being bad or weak, and instead offer them support to help prevent addiction’s most adverse consequences.


Dr. Nora Volkow, Director
Here I highlight important work being done at NIDA and other news related to the science of drug use and addiction.
Recent Blog Posts
50 years after founding, NIDA urges following science to move beyond stigma

The power of protective layers: Employers advancing whole-person health

Innovative projects answer NIDA’s challenge to implement substance use prevention in primary care
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 181, NO. 4 CURRENT ISSUE pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Substance Use Disorders and Addiction: Mechanisms, Trends, and Treatment Implications
- Ned H. Kalin , M.D.
Search for more papers by this author
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health ( 1 ) suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol. When considering other substances, the report estimated that 4.4 million individuals had a marijuana use disorder and that 2 million people suffered from an opiate use disorder. It is well known that stress is associated with an increase in the use of alcohol and other substances, and this is particularly relevant today in relation to the chronic uncertainty and distress associated with the COVID-19 pandemic along with the traumatic effects of racism and social injustice. In part related to stress, substance use disorders are highly comorbid with other psychiatric illnesses: 9.2 million adults were estimated to have a 1-year prevalence of both a mental illness and at least one substance use disorder. Although they may not necessarily meet criteria for a substance use disorder, it is well known that psychiatric patients have increased usage of alcohol, cigarettes, and other illicit substances. As an example, the survey estimated that over the preceding month, 37.2% of individuals with serious mental illnesses were cigarette smokers, compared with 16.3% of individuals without mental illnesses. Substance use frequently accompanies suicide and suicide attempts, and substance use disorders are associated with a long-term increased risk of suicide.
Addiction is the key process that underlies substance use disorders, and research using animal models and humans has revealed important insights into the neural circuits and molecules that mediate addiction. More specifically, research has shed light onto mechanisms underlying the critical components of addiction and relapse: reinforcement and reward, tolerance, withdrawal, negative affect, craving, and stress sensitization. In addition, clinical research has been instrumental in developing an evidence base for the use of pharmacological agents in the treatment of substance use disorders, which, in combination with psychosocial approaches, can provide effective treatments. However, despite the existence of therapeutic tools, relapse is common, and substance use disorders remain grossly undertreated. For example, whether at an inpatient hospital treatment facility or at a drug or alcohol rehabilitation program, it was estimated that only 11% of individuals needing treatment for substance use received appropriate care in 2018. Additionally, it is worth emphasizing that current practice frequently does not effectively integrate dual diagnosis treatment approaches, which is important because psychiatric and substance use disorders are highly comorbid. The barriers to receiving treatment are numerous and directly interact with existing health care inequities. It is imperative that as a field we overcome the obstacles to treatment, including the lack of resources at the individual level, a dearth of trained providers and appropriate treatment facilities, racial biases, and the marked stigmatization that is focused on individuals with addictions.
This issue of the Journal is focused on understanding factors contributing to substance use disorders and their comorbidity with psychiatric disorders, the effects of prenatal alcohol use on preadolescents, and brain mechanisms that are associated with addiction and relapse. An important theme that emerges from this issue is the necessity for understanding maladaptive substance use and its treatment in relation to health care inequities. This highlights the imperative to focus resources and treatment efforts on underprivileged and marginalized populations. The centerpiece of this issue is an overview on addiction written by Dr. George Koob, the director of the National Institute on Alcohol Abuse and Alcoholism (NIAAA), and coauthors Drs. Patricia Powell (NIAAA deputy director) and Aaron White ( 2 ). This outstanding article will serve as a foundational knowledge base for those interested in understanding the complex factors that mediate drug addiction. Of particular interest to the practice of psychiatry is the emphasis on the negative affect state “hyperkatifeia” as a major driver of addictive behavior and relapse. This places the dysphoria and psychological distress that are associated with prolonged withdrawal at the heart of treatment and underscores the importance of treating not only maladaptive drug-related behaviors but also the prolonged dysphoria and negative affect associated with addiction. It also speaks to why it is crucial to concurrently treat psychiatric comorbidities that commonly accompany substance use disorders.
Insights Into Mechanisms Related to Cocaine Addiction Using a Novel Imaging Method for Dopamine Neurons
Cassidy et al. ( 3 ) introduce a relatively new imaging technique that allows for an estimation of dopamine integrity and function in the substantia nigra, the site of origin of dopamine neurons that project to the striatum. Capitalizing on the high levels of neuromelanin that are found in substantia nigra dopamine neurons and the interaction between neuromelanin and intracellular iron, this MRI technique, termed neuromelanin-sensitive MRI (NM-MRI), shows promise in studying the involvement of substantia nigra dopamine neurons in neurodegenerative diseases and psychiatric illnesses. The authors used this technique to assess dopamine function in active cocaine users with the aim of exploring the hypothesis that cocaine use disorder is associated with blunted presynaptic striatal dopamine function that would be reflected in decreased “integrity” of the substantia nigra dopamine system. Surprisingly, NM-MRI revealed evidence for increased dopamine in the substantia nigra of individuals using cocaine. The authors suggest that this finding, in conjunction with prior work suggesting a blunted dopamine response, points to the possibility that cocaine use is associated with an altered intracellular distribution of dopamine. Specifically, the idea is that dopamine is shifted from being concentrated in releasable, functional vesicles at the synapse to a nonreleasable cytosolic pool. In addition to providing an intriguing alternative hypothesis underlying the cocaine-related alterations observed in substantia nigra dopamine function, this article highlights an innovative imaging method that can be used in further investigations involving the role of substantia nigra dopamine systems in neuropsychiatric disorders. Dr. Charles Bradberry, chief of the Preclinical Pharmacology Section at the National Institute on Drug Abuse, contributes an editorial that further explains the use of NM-MRI and discusses the theoretical implications of these unexpected findings in relation to cocaine use ( 4 ).
Treatment Implications of Understanding Brain Function During Early Abstinence in Patients With Alcohol Use Disorder
Developing a better understanding of the neural processes that are associated with substance use disorders is critical for conceptualizing improved treatment approaches. Blaine et al. ( 5 ) present neuroimaging data collected during early abstinence in patients with alcohol use disorder and link these data to relapses occurring during treatment. Of note, the findings from this study dovetail with the neural circuit schema Koob et al. provide in this issue’s overview on addiction ( 2 ). The first study in the Blaine et al. article uses 44 patients and 43 control subjects to demonstrate that patients with alcohol use disorder have a blunted neural response to the presentation of stress- and alcohol-related cues. This blunting was observed mainly in the ventromedial prefrontal cortex, a key prefrontal regulatory region, as well as in subcortical regions associated with reward processing, specifically the ventral striatum. Importantly, this finding was replicated in a second study in which 69 patients were studied in relation to their length of abstinence prior to treatment and treatment outcomes. The results demonstrated that individuals with the shortest abstinence times had greater alterations in neural responses to stress and alcohol cues. The authors also found that an individual’s length of abstinence prior to treatment, independent of the number of days of abstinence, was a predictor of relapse and that the magnitude of an individual’s neural alterations predicted the amount of heavy drinking occurring early in treatment. Although relapse is an all too common outcome in patients with substance use disorders, this study highlights an approach that has the potential to refine and develop new treatments that are based on addiction- and abstinence-related brain changes. In her thoughtful editorial, Dr. Edith Sullivan from Stanford University comments on the details of the study, the value of studying patients during early abstinence, and the implications of these findings for new treatment development ( 6 ).
Relatively Low Amounts of Alcohol Intake During Pregnancy Are Associated With Subtle Neurodevelopmental Effects in Preadolescent Offspring
Excessive substance use not only affects the user and their immediate family but also has transgenerational effects that can be mediated in utero. Lees et al. ( 7 ) present data suggesting that even the consumption of relatively low amounts of alcohol by expectant mothers can affect brain development, cognition, and emotion in their offspring. The researchers used data from the Adolescent Brain Cognitive Development Study, a large national community-based study, which allowed them to assess brain structure and function as well as behavioral, cognitive, and psychological outcomes in 9,719 preadolescents. The mothers of 2,518 of the subjects in this study reported some alcohol use during pregnancy, albeit at relatively low levels (0 to 80 drinks throughout pregnancy). Interestingly, and opposite of that expected in relation to data from individuals with fetal alcohol spectrum disorders, increases in brain volume and surface area were found in offspring of mothers who consumed the relatively low amounts of alcohol. Notably, any prenatal alcohol exposure was associated with small but significant increases in psychological problems that included increases in separation anxiety disorder and oppositional defiant disorder. Additionally, a dose-response effect was found for internalizing psychopathology, somatic complaints, and attentional deficits. While subtle, these findings point to neurodevelopmental alterations that may be mediated by even small amounts of prenatal alcohol consumption. Drs. Clare McCormack and Catherine Monk from Columbia University contribute an editorial that provides an in-depth assessment of these findings in relation to other studies, including those assessing severe deficits in individuals with fetal alcohol syndrome ( 8 ). McCormack and Monk emphasize that the behavioral and psychological effects reported in the Lees et al. article would not be clinically meaningful. However, it is feasible that the influences of these low amounts of alcohol could interact with other predisposing factors that might lead to more substantial negative outcomes.
Increased Comorbidity Between Substance Use and Psychiatric Disorders in Sexual Identity Minorities
There is no question that victims of societal marginalization experience disproportionate adversity and stress. Evans-Polce et al. ( 9 ) focus on this concern in relation to individuals who identify as sexual minorities by comparing their incidence of comorbid substance use and psychiatric disorders with that of individuals who identify as heterosexual. By using 2012−2013 data from 36,309 participants in the National Epidemiologic Study on Alcohol and Related Conditions–III, the authors examine the incidence of comorbid alcohol and tobacco use disorders with anxiety, mood disorders, and posttraumatic stress disorder (PTSD). The findings demonstrate increased incidences of substance use and psychiatric disorders in individuals who identified as bisexual or as gay or lesbian compared with those who identified as heterosexual. For example, a fourfold increase in the prevalence of PTSD was found in bisexual individuals compared with heterosexual individuals. In addition, the authors found an increased prevalence of substance use and psychiatric comorbidities in individuals who identified as bisexual and as gay or lesbian compared with individuals who identified as heterosexual. This was most prominent in women who identified as bisexual. For example, of the bisexual women who had an alcohol use disorder, 60.5% also had a psychiatric comorbidity, compared with 44.6% of heterosexual women. Additionally, the amount of reported sexual orientation discrimination and number of lifetime stressful events were associated with a greater likelihood of having comorbid substance use and psychiatric disorders. These findings are important but not surprising, as sexual minority individuals have a history of increased early-life trauma and throughout their lives may experience the painful and unwarranted consequences of bias and denigration. Nonetheless, these findings underscore the strong negative societal impacts experienced by minority groups and should sensitize providers to the additional needs of these individuals.
Trends in Nicotine Use and Dependence From 2001–2002 to 2012–2013
Although considerable efforts over earlier years have curbed the use of tobacco and nicotine, the use of these substances continues to be a significant public health problem. As noted above, individuals with psychiatric disorders are particularly vulnerable. Grant et al. ( 10 ) use data from the National Epidemiologic Survey on Alcohol and Related Conditions collected from a very large cohort to characterize trends in nicotine use and dependence over time. Results from their analysis support the so-called hardening hypothesis, which posits that although intervention-related reductions in nicotine use may have occurred over time, the impact of these interventions is less potent in individuals with more severe addictive behavior (i.e., nicotine dependence). When adjusted for sociodemographic factors, the results demonstrated a small but significant increase in nicotine use from 2001–2002 to 2012–2013. However, a much greater increase in nicotine dependence (46.1% to 52%) was observed over this time frame in individuals who had used nicotine during the preceding 12 months. The increases in nicotine use and dependence were associated with factors related to socioeconomic status, such as lower income and lower educational attainment. The authors interpret these findings as evidence for the hardening hypothesis, suggesting that despite the impression that nicotine use has plateaued, there is a growing number of highly dependent nicotine users who would benefit from nicotine dependence intervention programs. Dr. Kathleen Brady, from the Medical University of South Carolina, provides an editorial ( 11 ) that reviews the consequences of tobacco use and the history of the public measures that were initially taken to combat its use. Importantly, her editorial emphasizes the need to address health care inequity issues that affect individuals of lower socioeconomic status by devoting resources to develop and deploy effective smoking cessation interventions for at-risk and underresourced populations.
Conclusions
Maladaptive substance use and substance use disorders are highly prevalent and are among the most significant public health problems. Substance use is commonly comorbid with psychiatric disorders, and treatment efforts need to concurrently address both. The papers in this issue highlight new findings that are directly relevant to understanding, treating, and developing policies to better serve those afflicted with addictions. While treatments exist, the need for more effective treatments is clear, especially those focused on decreasing relapse rates. The negative affective state, hyperkatifeia, that accompanies longer-term abstinence is an important treatment target that should be emphasized in current practice as well as in new treatment development. In addition to developing a better understanding of the neurobiology of addictions and abstinence, it is necessary to ensure that there is equitable access to currently available treatments and treatment programs. Additional resources must be allocated to this cause. This depends on the recognition that health care inequities and societal barriers are major contributors to the continued high prevalence of substance use disorders, the individual suffering they inflict, and the huge toll that they incur at a societal level.
Disclosures of Editors’ financial relationships appear in the April 2020 issue of the Journal .
1 US Department of Health and Human Services: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality: National Survey on Drug Use and Health 2018. Rockville, Md, SAMHSA, 2019 ( https://www.samhsa.gov/data/nsduh/reports-detailed-tables-2018-NSDUH ) Google Scholar
2 Koob GF, Powell P, White A : Addiction as a coping response: hyperkatifeia, deaths of despair, and COVID-19 . Am J Psychiatry 2020 ; 177:1031–1037 Link , Google Scholar
3 Cassidy CM, Carpenter KM, Konova AB, et al. : Evidence for dopamine abnormalities in the substantia nigra in cocaine addiction revealed by neuromelanin-sensitive MRI . Am J Psychiatry 2020 ; 177:1038–1047 Link , Google Scholar
4 Bradberry CW : Neuromelanin MRI: dark substance shines a light on dopamine dysfunction and cocaine use (editorial). Am J Psychiatry 2020 ; 177:1019–1021 Abstract , Google Scholar
5 Blaine SK, Wemm S, Fogelman N, et al. : Association of prefrontal-striatal functional pathology with alcohol abstinence days at treatment initiation and heavy drinking after treatment initiation . Am J Psychiatry 2020 ; 177:1048–1059 Abstract , Google Scholar
6 Sullivan EV : Why timing matters in alcohol use disorder recovery (editorial). Am J Psychiatry 2020 ; 177:1022–1024 Abstract , Google Scholar
7 Lees B, Mewton L, Jacobus J, et al. : Association of prenatal alcohol exposure with psychological, behavioral, and neurodevelopmental outcomes in children from the Adolescent Brain Cognitive Development Study . Am J Psychiatry 2020 ; 177:1060–1072 Link , Google Scholar
8 McCormack C, Monk C : Considering prenatal alcohol exposure in a developmental origins of health and disease framework (editorial). Am J Psychiatry 2020 ; 177:1025–1028 Abstract , Google Scholar
9 Evans-Polce RJ, Kcomt L, Veliz PT, et al. : Alcohol, tobacco, and comorbid psychiatric disorders and associations with sexual identity and stress-related correlates . Am J Psychiatry 2020 ; 177:1073–1081 Abstract , Google Scholar
10 Grant BF, Shmulewitz D, Compton WM : Nicotine use and DSM-IV nicotine dependence in the United States, 2001–2002 and 2012–2013 . Am J Psychiatry 2020 ; 177:1082–1090 Link , Google Scholar
11 Brady KT : Social determinants of health and smoking cessation: a challenge (editorial). Am J Psychiatry 2020 ; 177:1029–1030 Abstract , Google Scholar
- Cited by None
- Substance-Related and Addictive Disorders
- Addiction Psychiatry
- Transgender (LGBT) Issues
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Open access
- Published: 22 February 2021
Addiction as a brain disease revised: why it still matters, and the need for consilience
- Markus Heilig 1 ,
- James MacKillop ORCID: orcid.org/0000-0003-4118-9500 2 , 3 ,
- Diana Martinez 4 ,
- Jürgen Rehm ORCID: orcid.org/0000-0001-5665-0385 5 , 6 , 7 , 8 ,
- Lorenzo Leggio ORCID: orcid.org/0000-0001-7284-8754 9 &
- Louk J. M. J. Vanderschuren ORCID: orcid.org/0000-0002-5379-0363 10
Neuropsychopharmacology volume 46 , pages 1715–1723 ( 2021 ) Cite this article
84k Accesses
95 Citations
321 Altmetric
Metrics details
The view that substance addiction is a brain disease, although widely accepted in the neuroscience community, has become subject to acerbic criticism in recent years. These criticisms state that the brain disease view is deterministic, fails to account for heterogeneity in remission and recovery, places too much emphasis on a compulsive dimension of addiction, and that a specific neural signature of addiction has not been identified. We acknowledge that some of these criticisms have merit, but assert that the foundational premise that addiction has a neurobiological basis is fundamentally sound. We also emphasize that denying that addiction is a brain disease is a harmful standpoint since it contributes to reducing access to healthcare and treatment, the consequences of which are catastrophic. Here, we therefore address these criticisms, and in doing so provide a contemporary update of the brain disease view of addiction. We provide arguments to support this view, discuss why apparently spontaneous remission does not negate it, and how seemingly compulsive behaviors can co-exist with the sensitivity to alternative reinforcement in addiction. Most importantly, we argue that the brain is the biological substrate from which both addiction and the capacity for behavior change arise, arguing for an intensified neuroscientific study of recovery. More broadly, we propose that these disagreements reveal the need for multidisciplinary research that integrates neuroscientific, behavioral, clinical, and sociocultural perspectives.
Similar content being viewed by others
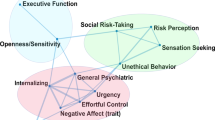
Subtypes in addiction and their neurobehavioral profiles across three functional domains
Gunner Drossel, Leyla R. Brucar, … Anna Zilverstand

Drug addiction: from bench to bedside
Julian Cheron & Alban de Kerchove d’Exaerde

The neurobiology of drug addiction: cross-species insights into the dysfunction and recovery of the prefrontal cortex
Ahmet O. Ceceli, Charles W. Bradberry & Rita Z. Goldstein
Introduction
Close to a quarter of a century ago, then director of the US National Institute on Drug Abuse Alan Leshner famously asserted that “addiction is a brain disease”, articulated a set of implications of this position, and outlined an agenda for realizing its promise [ 1 ]. The paper, now cited almost 2000 times, put forward a position that has been highly influential in guiding the efforts of researchers, and resource allocation by funding agencies. A subsequent 2000 paper by McLellan et al. [ 2 ] examined whether data justify distinguishing addiction from other conditions for which a disease label is rarely questioned, such as diabetes, hypertension or asthma. It concluded that neither genetic risk, the role of personal choices, nor the influence of environmental factors differentiated addiction in a manner that would warrant viewing it differently; neither did relapse rates, nor compliance with treatment. The authors outlined an agenda closely related to that put forward by Leshner, but with a more clinical focus. Their conclusion was that addiction should be insured, treated, and evaluated like other diseases. This paper, too, has been exceptionally influential by academic standards, as witnessed by its ~3000 citations to date. What may be less appreciated among scientists is that its impact in the real world of addiction treatment has remained more limited, with large numbers of patients still not receiving evidence-based treatments.
In recent years, the conceptualization of addiction as a brain disease has come under increasing criticism. When first put forward, the brain disease view was mainly an attempt to articulate an effective response to prevailing nonscientific, moralizing, and stigmatizing attitudes to addiction. According to these attitudes, addiction was simply the result of a person’s moral failing or weakness of character, rather than a “real” disease [ 3 ]. These attitudes created barriers for people with substance use problems to access evidence-based treatments, both those available at the time, such as opioid agonist maintenance, cognitive behavioral therapy-based relapse prevention, community reinforcement or contingency management, and those that could result from research. To promote patient access to treatments, scientists needed to argue that there is a biological basis beneath the challenging behaviors of individuals suffering from addiction. This argument was particularly targeted to the public, policymakers and health care professionals, many of whom held that since addiction was a misery people brought upon themselves, it fell beyond the scope of medicine, and was neither amenable to treatment, nor warranted the use of taxpayer money.
Present-day criticism directed at the conceptualization of addiction as a brain disease is of a very different nature. It originates from within the scientific community itself, and asserts that this conceptualization is neither supported by data, nor helpful for people with substance use problems [ 4 , 5 , 6 , 7 , 8 ]. Addressing these critiques requires a very different perspective, and is the objective of our paper. We readily acknowledge that in some cases, recent critiques of the notion of addiction as a brain disease as postulated originally have merit, and that those critiques require the postulates to be re-assessed and refined. In other cases, we believe the arguments have less validity, but still provide an opportunity to update the position of addiction as a brain disease. Our overarching concern is that questionable arguments against the notion of addiction as a brain disease may harm patients, by impeding access to care, and slowing development of novel treatments.
A premise of our argument is that any useful conceptualization of addiction requires an understanding both of the brains involved, and of environmental factors that interact with those brains [ 9 ]. These environmental factors critically include availability of drugs, but also of healthy alternative rewards and opportunities. As we will show, stating that brain mechanisms are critical for understanding and treating addiction in no way negates the role of psychological, social and socioeconomic processes as both causes and consequences of substance use. To reflect this complex nature of addiction, we have assembled a team with expertise that spans from molecular neuroscience, through animal models of addiction, human brain imaging, clinical addiction medicine, to epidemiology. What brings us together is a passionate commitment to improving the lives of people with substance use problems through science and science-based treatments, with empirical evidence as the guiding principle.
To achieve this goal, we first discuss the nature of the disease concept itself, and why we believe it is important for the science and treatment of addiction. This is followed by a discussion of the main points raised when the notion of addiction as a brain disease has come under criticism. Key among those are claims that spontaneous remission rates are high; that a specific brain pathology is lacking; and that people suffering from addiction, rather than behaving “compulsively”, in fact show a preserved ability to make informed and advantageous choices. In the process of discussing these issues, we also address the common criticism that viewing addiction as a brain disease is a fully deterministic theory of addiction. For our argument, we use the term “addiction” as originally used by Leshner [ 1 ]; in Box 1 , we map out and discuss how this construct may relate to the current diagnostic categories, such as Substance Use Disorder (SUD) and its different levels of severity (Fig. 1) .
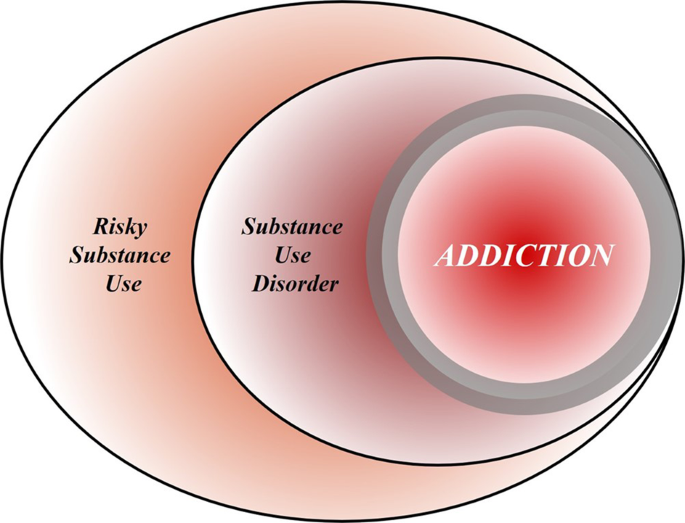
Risky (hazardous) substance use refers to quantity/frequency indicators of consumption; SUD refers to individuals who meet criteria for a DSM-5 diagnosis (mild, moderate, or severe); and addiction refers to individuals who exhibit persistent difficulties with self-regulation of drug consumption. Among high-risk individuals, a subgroup will meet criteria for SUD and, among those who have an SUD, a further subgroup would be considered to be addicted to the drug. However, the boundary for addiction is intentionally blurred to reflect that the dividing line for defining addiction within the category of SUD remains an open empirical question.
Box 1 What’s in a name? Differentiating hazardous use, substance use disorder, and addiction
Although our principal focus is on the brain disease model of addiction, the definition of addiction itself is a source of ambiguity. Here, we provide a perspective on the major forms of terminology in the field.
Hazardous Substance Use
Hazardous (risky) substance use refers to quantitative levels of consumption that increase an individual’s risk for adverse health consequences. In practice, this pertains to alcohol use [ 110 , 111 ]. Clinically, alcohol consumption that exceeds guidelines for moderate drinking has been used to prompt brief interventions or referral for specialist care [ 112 ]. More recently, a reduction in these quantitative levels has been validated as treatment endpoints [ 113 ].
Substance Use Disorder
SUD refers to the DSM-5 diagnosis category that encompasses significant impairment or distress resulting from specific categories of psychoactive drug use. The diagnosis of SUD is operationalized as 2 or more of 11 symptoms over the past year. As a result, the diagnosis is heterogenous, with more than 1100 symptom permutations possible. The diagnosis in DSM-5 is the result of combining two diagnoses from the DSM-IV, abuse and dependence, which proved to be less valid than a single dimensional approach [ 114 ]. Critically, SUD includes three levels of severity: mild (2–3 symptoms), moderate (4–5 symptoms), and severe (6+ symptoms). The International Classification of Diseases (ICD) system retains two diagnoses, harmful use (lower severity) and substance dependence (higher severity).
Addiction is a natural language concept, etymologically meaning enslavement, with the contemporary meaning traceable to the Middle and Late Roman Republic periods [ 115 ]. As a scientific construct, drug addiction can be defined as a state in which an individual exhibits an inability to self-regulate consumption of a substance, although it does not have an operational definition. Regarding clinical diagnosis, as it is typically used in scientific and clinical parlance, addiction is not synonymous with the simple presence of SUD. Nowhere in DSM-5 is it articulated that the diagnostic threshold (or any specific number/type of symptoms) should be interpreted as reflecting addiction, which inherently connotes a high degree of severity. Indeed, concerns were raised about setting the diagnostic standard too low because of the issue of potentially conflating a low-severity SUD with addiction [ 116 ]. In scientific and clinical usage, addiction typically refers to individuals at a moderate or high severity of SUD. This is consistent with the fact that moderate-to-severe SUD has the closest correspondence with the more severe diagnosis in ICD [ 117 , 118 , 119 ]. Nonetheless, akin to the undefined overlap between hazardous use and SUD, the field has not identified the exact thresholds of SUD symptoms above which addiction would be definitively present.
Integration
The ambiguous relationships among these terms contribute to misunderstandings and disagreements. Figure 1 provides a simple working model of how these terms overlap. Fundamentally, we consider that these terms represent successive dimensions of severity, clinical “nesting dolls”. Not all individuals consuming substances at hazardous levels have an SUD, but a subgroup do. Not all individuals with a SUD are addicted to the drug in question, but a subgroup are. At the severe end of the spectrum, these domains converge (heavy consumption, numerous symptoms, the unambiguous presence of addiction), but at low severity, the overlap is more modest. The exact mapping of addiction onto SUD is an open empirical question, warranting systematic study among scientists, clinicians, and patients with lived experience. No less important will be future research situating our definition of SUD using more objective indicators (e.g., [ 55 , 120 ]), brain-based and otherwise, and more precisely in relation to clinical needs [ 121 ]. Finally, such work should ultimately be codified in both the DSM and ICD systems to demarcate clearly where the attribution of addiction belongs within the clinical nosology, and to foster greater clarity and specificity in scientific discourse.
What is a disease?
In his classic 1960 book “The Disease Concept of Alcoholism”, Jellinek noted that in the alcohol field, the debate over the disease concept was plagued by too many definitions of “alcoholism” and too few definitions of “disease” [ 10 ]. He suggested that the addiction field needed to follow the rest of medicine in moving away from viewing disease as an “entity”, i.e., something that has “its own independent existence, apart from other things” [ 11 ]. To modern medicine, he pointed out, a disease is simply a label that is agreed upon to describe a cluster of substantial, deteriorating changes in the structure or function of the human body, and the accompanying deterioration in biopsychosocial functioning. Thus, he concluded that alcoholism can simply be defined as changes in structure or function of the body due to drinking that cause disability or death. A disease label is useful to identify groups of people with commonly co-occurring constellations of problems—syndromes—that significantly impair function, and that lead to clinically significant distress, harm, or both. This convention allows a systematic study of the condition, and of whether group members benefit from a specific intervention.
It is not trivial to delineate the exact category of harmful substance use for which a label such as addiction is warranted (See Box 1 ). Challenges to diagnostic categorization are not unique to addiction, however. Throughout clinical medicine, diagnostic cut-offs are set by consensus, commonly based on an evolving understanding of thresholds above which people tend to benefit from available interventions. Because assessing benefits in large patient groups over time is difficult, diagnostic thresholds are always subject to debate and adjustments. It can be debated whether diagnostic thresholds “merely” capture the extreme of a single underlying population, or actually identify a subpopulation that is at some level distinct. Resolving this issue remains challenging in addiction, but once again, this is not different from other areas of medicine [see e.g., [ 12 ] for type 2 diabetes]. Longitudinal studies that track patient trajectories over time may have a better ability to identify subpopulations than cross-sectional assessments [ 13 ].
By this pragmatic, clinical understanding of the disease concept, it is difficult to argue that “addiction” is unjustified as a disease label. Among people who use drugs or alcohol, some progress to using with a quantity and frequency that results in impaired function and often death, making substance use a major cause of global disease burden [ 14 ]. In these people, use occurs with a pattern that in milder forms may be challenging to capture by current diagnostic criteria (See Box 1 ), but is readily recognized by patients, their families and treatment providers when it reaches a severity that is clinically significant [see [ 15 ] for a classical discussion]. In some cases, such as opioid addiction, those who receive the diagnosis stand to obtain some of the greatest benefits from medical treatments in all of clinical medicine [ 16 , 17 ]. Although effect sizes of available treatments are more modest in nicotine [ 18 ] and alcohol addiction [ 19 ], the evidence supporting their efficacy is also indisputable. A view of addiction as a disease is justified, because it is beneficial: a failure to diagnose addiction drastically increases the risk of a failure to treat it [ 20 ].
Of course, establishing a diagnosis is not a requirement for interventions to be meaningful. People with hazardous or harmful substance use who have not (yet) developed addiction should also be identified, and interventions should be initiated to address their substance-related risks. This is particularly relevant for alcohol, where even in the absence of addiction, use is frequently associated with risks or harm to self, e.g., through cardiovascular disease, liver disease or cancer, and to others, e.g., through accidents or violence [ 21 ]. Interventions to reduce hazardous or harmful substance use in people who have not developed addiction are in fact particularly appealing. In these individuals, limited interventions are able to achieve robust and meaningful benefits [ 22 ], presumably because patterns of misuse have not yet become entrenched.
Thus, as originally pointed out by McLellan and colleagues, most of the criticisms of addiction as a disease could equally be applied to other medical conditions [ 2 ]. This type of criticism could also be applied to other psychiatric disorders, and that has indeed been the case historically [ 23 , 24 ]. Today, there is broad consensus that those criticisms were misguided. Few, if any healthcare professionals continue to maintain that schizophrenia, rather than being a disease, is a normal response to societal conditions. Why, then, do people continue to question if addiction is a disease, but not whether schizophrenia, major depressive disorder or post-traumatic stress disorder are diseases? This is particularly troubling given the decades of data showing high co-morbidity of addiction with these conditions [ 25 , 26 ]. We argue that it comes down to stigma. Dysregulated substance use continues to be perceived as a self-inflicted condition characterized by a lack of willpower, thus falling outside the scope of medicine and into that of morality [ 3 ].
Chronic and relapsing, developmentally-limited, or spontaneously remitting?
Much of the critique targeted at the conceptualization of addiction as a brain disease focuses on its original assertion that addiction is a chronic and relapsing condition. Epidemiological data are cited in support of the notion that large proportions of individuals achieve remission [ 27 ], frequently without any formal treatment [ 28 , 29 ] and in some cases resuming low risk substance use [ 30 ]. For instance, based on data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) study [ 27 ], it has been pointed out that a significant proportion of people with an addictive disorder quit each year, and that most afflicted individuals ultimately remit. These spontaneous remission rates are argued to invalidate the concept of a chronic, relapsing disease [ 4 ].
Interpreting these and similar data is complicated by several methodological and conceptual issues. First, people may appear to remit spontaneously because they actually do, but also because of limited test–retest reliability of the diagnosis [ 31 ]. For instance, using a validated diagnostic interview and trained interviewers, the Collaborative Studies on Genetics of Alcoholism examined the likelihood that an individual diagnosed with a lifetime history of substance dependence would retain this classification after 5 years. This is obviously a diagnosis that, once met, by definition cannot truly remit. Lifetime alcohol dependence was indeed stable in individuals recruited from addiction treatment units, ~90% for women, and 95% for men. In contrast, in a community-based sample similar to that used in the NESARC [ 27 ], stability was only ~30% and 65% for women and men, respectively. The most important characteristic that determined diagnostic stability was severity. Diagnosis was stable in severe, treatment-seeking cases, but not in general population cases of alcohol dependence.
These data suggest that commonly used diagnostic criteria alone are simply over-inclusive for a reliable, clinically meaningful diagnosis of addiction. They do identify a core group of treatment seeking individuals with a reliable diagnosis, but, if applied to nonclinical populations, also flag as “cases” a considerable halo of individuals for whom the diagnostic categorization is unreliable. Any meaningful discussion of remission rates needs to take this into account, and specify which of these two populations that is being discussed. Unfortunately, the DSM-5 has not made this task easier. With only 2 out of 11 symptoms being sufficient for a diagnosis of SUD, it captures under a single diagnostic label individuals in a “mild” category, whose diagnosis is likely to have very low test–retest reliability, and who are unlikely to exhibit a chronic relapsing course, together with people at the severe end of the spectrum, whose diagnosis is reliable, many of whom do show a chronic relapsing course.
The NESARC data nevertheless show that close to 10% of people in the general population who are diagnosed with alcohol addiction (here equated with DSM-IV “dependence” used in the NESARC study) never remitted throughout their participation in the survey. The base life-time prevalence of alcohol dependence in NESARC was 12.5% [ 32 ]. Thus, the data cited against the concept of addiction as a chronic relapsing disease in fact indicate that over 1% of the US population develops an alcohol-related condition that is associated with high morbidity and mortality, and whose chronic and/or relapsing nature cannot be disputed, since it does not remit.
Secondly, the analysis of NESARC data [ 4 , 27 ] omits opioid addiction, which, together with alcohol and tobacco, is the largest addiction-related public health problem in the US [ 33 ]. This is probably the addictive condition where an analysis of cumulative evidence most strikingly supports the notion of a chronic disorder with frequent relapses in a large proportion of people affected [ 34 ]. Of course, a large number of people with opioid addiction are unable to express the chronic, relapsing course of their disease, because over the long term, their mortality rate is about 15 times greater than that of the general population [ 35 ]. However, even among those who remain alive, the prevalence of stable abstinence from opioid use after 10–30 years of observation is <30%. Remission may not always require abstinence, for instance in the case of alcohol addiction, but is a reasonable proxy for remission with opioids, where return to controlled use is rare. Embedded in these data is a message of literally vital importance: when opioid addiction is diagnosed and treated as a chronic relapsing disease, outcomes are markedly improved, and retention in treatment is associated with a greater likelihood of abstinence.
The fact that significant numbers of individuals exhibit a chronic relapsing course does not negate that even larger numbers of individuals with SUD according to current diagnostic criteria do not. For instance, in many countries, the highest prevalence of substance use problems is found among young adults, aged 18–25 [ 36 ], and a majority of these ‘age out’ of excessive substance use [ 37 ]. It is also well documented that many individuals with SUD achieve longstanding remission, in many cases without any formal treatment (see e.g., [ 27 , 30 , 38 ]).
Collectively, the data show that the course of SUD, as defined by current diagnostic criteria, is highly heterogeneous. Accordingly, we do not maintain that a chronic relapsing course is a defining feature of SUD. When present in a patient, however, such as course is of clinical significance, because it identifies a need for long-term disease management [ 2 ], rather than expectations of a recovery that may not be within the individual’s reach [ 39 ]. From a conceptual standpoint, however, a chronic relapsing course is neither necessary nor implied in a view that addiction is a brain disease. This view also does not mean that it is irreversible and hopeless. Human neuroscience documents restoration of functioning after abstinence [ 40 , 41 ] and reveals predictors of clinical success [ 42 ]. If anything, this evidence suggests a need to increase efforts devoted to neuroscientific research on addiction recovery [ 40 , 43 ].
Lessons from genetics
For alcohol addiction, meta-analysis of twin and adoption studies has estimated heritability at ~50%, while estimates for opioid addiction are even higher [ 44 , 45 ]. Genetic risk factors are to a large extent shared across substances [ 46 ]. It has been argued that a genetic contribution cannot support a disease view of a behavior, because most behavioral traits, including religious and political inclinations, have a genetic contribution [ 4 ]. This statement, while correct in pointing out broad heritability of behavioral traits, misses a fundamental point. Genetic architecture is much like organ structure. The fact that normal anatomy shapes healthy organ function does not negate that an altered structure can contribute to pathophysiology of disease. The structure of the genetic landscape is no different. Critics further state that a “genetic predisposition is not a recipe for compulsion”, but no neuroscientist or geneticist would claim that genetic risk is “a recipe for compulsion”. Genetic risk is probabilistic, not deterministic. However, as we will see below, in the case of addiction, it contributes to large, consistent probability shifts towards maladaptive behavior.
In dismissing the relevance of genetic risk for addiction, Hall writes that “a large number of alleles are involved in the genetic susceptibility to addiction and individually these alleles might very weakly predict a risk of addiction”. He goes on to conclude that “generally, genetic prediction of the risk of disease (even with whole-genome sequencing data) is unlikely to be informative for most people who have a so-called average risk of developing an addiction disorder” [ 7 ]. This reflects a fundamental misunderstanding of polygenic risk. It is true that a large number of risk alleles are involved, and that the explanatory power of currently available polygenic risk scores for addictive disorders lags behind those for e.g., schizophrenia or major depression [ 47 , 48 ]. The only implication of this, however, is that low average effect sizes of risk alleles in addiction necessitate larger study samples to construct polygenic scores that account for a large proportion of the known heritability.
However, a heritability of addiction of ~50% indicates that DNA sequence variation accounts for 50% of the risk for this condition. Once whole genome sequencing is readily available, it is likely that it will be possible to identify most of that DNA variation. For clinical purposes, those polygenic scores will of course not replace an understanding of the intricate web of biological and social factors that promote or prevent expression of addiction in an individual case; rather, they will add to it [ 49 ]. Meanwhile, however, genome-wide association studies in addiction have already provided important information. For instance, they have established that the genetic underpinnings of alcohol addiction only partially overlap with those for alcohol consumption, underscoring the genetic distinction between pathological and nonpathological drinking behaviors [ 50 ].
It thus seems that, rather than negating a rationale for a disease view of addiction, the important implication of the polygenic nature of addiction risk is a very different one. Genome-wide association studies of complex traits have largely confirmed the century old “infinitisemal model” in which Fisher reconciled Mendelian and polygenic traits [ 51 ]. A key implication of this model is that genetic susceptibility for a complex, polygenic trait is continuously distributed in the population. This may seem antithetical to a view of addiction as a distinct disease category, but the contradiction is only apparent, and one that has long been familiar to quantitative genetics. Viewing addiction susceptibility as a polygenic quantitative trait, and addiction as a disease category is entirely in line with Falconer’s theorem, according to which, in a given set of environmental conditions, a certain level of genetic susceptibility will determine a threshold above which disease will arise.
A brain disease? Then show me the brain lesion!
The notion of addiction as a brain disease is commonly criticized with the argument that a specific pathognomonic brain lesion has not been identified. Indeed, brain imaging findings in addiction (perhaps with the exception of extensive neurotoxic gray matter loss in advanced alcohol addiction) are nowhere near the level of specificity and sensitivity required of clinical diagnostic tests. However, this criticism neglects the fact that neuroimaging is not used to diagnose many neurologic and psychiatric disorders, including epilepsy, ALS, migraine, Huntington’s disease, bipolar disorder, or schizophrenia. Even among conditions where signs of disease can be detected using brain imaging, such as Alzheimer’s and Parkinson’s disease, a scan is best used in conjunction with clinical acumen when making the diagnosis. Thus, the requirement that addiction be detectable with a brain scan in order to be classified as a disease does not recognize the role of neuroimaging in the clinic.
For the foreseeable future, the main objective of imaging in addiction research is not to diagnose addiction, but rather to improve our understanding of mechanisms that underlie it. The hope is that mechanistic insights will help bring forward new treatments, by identifying candidate targets for them, by pointing to treatment-responsive biomarkers, or both [ 52 ]. Developing innovative treatments is essential to address unmet treatment needs, in particular in stimulant and cannabis addiction, where no approved medications are currently available. Although the task to develop novel treatments is challenging, promising candidates await evaluation [ 53 ]. A particular opportunity for imaging-based research is related to the complex and heterogeneous nature of addictive disorders. Imaging-based biomarkers hold the promise of allowing this complexity to be deconstructed into specific functional domains, as proposed by the RDoC initiative [ 54 ] and its application to addiction [ 55 , 56 ]. This can ultimately guide the development of personalized medicine strategies to addiction treatment.
Countless imaging studies have reported differences in brain structure and function between people with addictive disorders and those without them. Meta-analyses of structural data show that alcohol addiction is associated with gray matter losses in the prefrontal cortex, dorsal striatum, insula, and posterior cingulate cortex [ 57 ], and similar results have been obtained in stimulant-addicted individuals [ 58 ]. Meta-analysis of functional imaging studies has demonstrated common alterations in dorsal striatal, and frontal circuits engaged in reward and salience processing, habit formation, and executive control, across different substances and task-paradigms [ 59 ]. Molecular imaging studies have shown that large and fast increases in dopamine are associated with the reinforcing effects of drugs of abuse, but that after chronic drug use and during withdrawal, brain dopamine function is markedly decreased and that these decreases are associated with dysfunction of prefrontal regions [ 60 ]. Collectively, these findings have given rise to a widely held view of addiction as a disorder of fronto-striatal circuitry that mediates top-down regulation of behavior [ 61 ].
Critics reply that none of the brain imaging findings are sufficiently specific to distinguish between addiction and its absence, and that they are typically obtained in cross-sectional studies that can at best establish correlative rather than causal links. In this, they are largely right, and an updated version of a conceptualization of addiction as a brain disease needs to acknowledge this. Many of the structural brain findings reported are not specific for addiction, but rather shared across psychiatric disorders [ 62 ]. Also, for now, the most sophisticated tools of human brain imaging remain crude in face of complex neural circuit function. Importantly however, a vast literature from animal studies also documents functional changes in fronto-striatal circuits, as well their limbic and midbrain inputs, associated with addictive behaviors [ 63 , 64 , 65 , 66 , 67 , 68 ]. These are circuits akin to those identified by neuroimaging studies in humans, implicated in positive and negative emotions, learning processes and executive functions, altered function of which is thought to underlie addiction. These animal studies, by virtue of their cellular and molecular level resolution, and their ability to establish causality under experimental control, are therefore an important complement to human neuroimaging work.
Nevertheless, factors that seem remote from the activity of brain circuits, such as policies, substance availability and cost, as well as socioeconomic factors, also are critically important determinants of substance use. In this complex landscape, is the brain really a defensible focal point for research and treatment? The answer is “yes”. As powerfully articulated by Francis Crick [ 69 ], “You, your joys and your sorrows, your memories and your ambitions, your sense of personal identity and free will, are in fact no more than the behavior of a vast assembly of nerve cells and their associated molecules”. Social and interpersonal factors are critically important in addiction, but they can only exert their influences by impacting neural processes. They must be encoded as sensory data, represented together with memories of the past and predictions about the future, and combined with representations of interoceptive and other influences to provide inputs to the valuation machinery of the brain. Collectively, these inputs drive action selection and execution of behavior—say, to drink or not to drink, and then, within an episode, to stop drinking or keep drinking. Stating that the pathophysiology of addiction is largely about the brain does not ignore the role of other influences. It is just the opposite: it is attempting to understand how those important influences contribute to drug seeking and taking in the context of the brain, and vice versa.
But if the criticism is one of emphasis rather than of principle—i.e., too much brain, too little social and environmental factors – then neuroscientists need to acknowledge that they are in part guilty as charged. Brain-centric accounts of addiction have for a long time failed to pay enough attention to the inputs that social factors provide to neural processing behind drug seeking and taking [ 9 ]. This landscape is, however, rapidly changing. For instance, using animal models, scientists are finding that lack of social play early in life increases the motivation to take addictive substances in adulthood [ 70 ]. Others find that the opportunity to interact with a fellow rat is protective against addiction-like behaviors [ 71 ]. In humans, a relationship has been found between perceived social support, socioeconomic status, and the availability of dopamine D2 receptors [ 72 , 73 ], a biological marker of addiction vulnerability. Those findings in turn provided translation of data from nonhuman primates, which showed that D2 receptor availability can be altered by changes in social hierarchy, and that these changes are associated with the motivation to obtain cocaine [ 74 ].
Epidemiologically, it is well established that social determinants of health, including major racial and ethnic disparities, play a significant role in the risk for addiction [ 75 , 76 ]. Contemporary neuroscience is illuminating how those factors penetrate the brain [ 77 ] and, in some cases, reveals pathways of resilience [ 78 ] and how evidence-based prevention can interrupt those adverse consequences [ 79 , 80 ]. In other words, from our perspective, viewing addiction as a brain disease in no way negates the importance of social determinants of health or societal inequalities as critical influences. In fact, as shown by the studies correlating dopamine receptors with social experience, imaging is capable of capturing the impact of the social environment on brain function. This provides a platform for understanding how those influences become embedded in the biology of the brain, which provides a biological roadmap for prevention and intervention.
We therefore argue that a contemporary view of addiction as a brain disease does not deny the influence of social, environmental, developmental, or socioeconomic processes, but rather proposes that the brain is the underlying material substrate upon which those factors impinge and from which the responses originate. Because of this, neurobiology is a critical level of analysis for understanding addiction, although certainly not the only one. It is recognized throughout modern medicine that a host of biological and non-biological factors give rise to disease; understanding the biological pathophysiology is critical for understanding etiology and informing treatment.
Is a view of addiction as a brain disease deterministic?
A common criticism of the notion that addiction is a brain disease is that it is reductionist and in the end therefore deterministic [ 81 , 82 ]. This is a fundamental misrepresentation. As indicated above, viewing addiction as a brain disease simply states that neurobiology is an undeniable component of addiction. A reason for deterministic interpretations may be that modern neuroscience emphasizes an understanding of proximal causality within research designs (e.g., whether an observed link between biological processes is mediated by a specific mechanism). That does not in any way reflect a superordinate assumption that neuroscience will achieve global causality. On the contrary, since we realize that addiction involves interactions between biology, environment and society, ultimate (complete) prediction of behavior based on an understanding of neural processes alone is neither expected, nor a goal.
A fairer representation of a contemporary neuroscience view is that it believes insights from neurobiology allow useful probabilistic models to be developed of the inherently stochastic processes involved in behavior [see [ 83 ] for an elegant recent example]. Changes in brain function and structure in addiction exert a powerful probabilistic influence over a person’s behavior, but one that is highly multifactorial, variable, and thus stochastic. Philosophically, this is best understood as being aligned with indeterminism, a perspective that has a deep history in philosophy and psychology [ 84 ]. In modern neuroscience, it refers to the position that the dynamic complexity of the brain, given the probabilistic threshold-gated nature of its biology (e.g., action potential depolarization, ion channel gating), means that behavior cannot be definitively predicted in any individual instance [ 85 , 86 ].
Driven by compulsion, or free to choose?
A major criticism of the brain disease view of addiction, and one that is related to the issue of determinism vs indeterminism, centers around the term “compulsivity” [ 6 , 87 , 88 , 89 , 90 ] and the different meanings it is given. Prominent addiction theories state that addiction is characterized by a transition from controlled to “compulsive” drug seeking and taking [ 91 , 92 , 93 , 94 , 95 ], but allocate somewhat different meanings to “compulsivity”. By some accounts, compulsive substance use is habitual and insensitive to its outcomes [ 92 , 94 , 96 ]. Others refer to compulsive use as a result of increasing incentive value of drug associated cues [ 97 ], while others view it as driven by a recruitment of systems that encode negative affective states [ 95 , 98 ].
The prototype for compulsive behavior is provided by obsessive-compulsive disorder (OCD), where compulsion refers to repeatedly and stereotypically carrying out actions that in themselves may be meaningful, but lose their purpose and become harmful when performed in excess, such as persistent handwashing until skin injuries result. Crucially, this happens despite a conscious desire to do otherwise. Attempts to resist these compulsions result in increasing and ultimately intractable anxiety [ 99 ]. This is in important ways different from the meaning of compulsivity as commonly used in addiction theories. In the addiction field, compulsive drug use typically refers to inflexible, drug-centered behavior in which substance use is insensitive to adverse consequences [ 100 ]. Although this phenomenon is not necessarily present in every patient, it reflects important symptoms of clinical addiction, and is captured by several DSM-5 criteria for SUD [ 101 ]. Examples are needle-sharing despite knowledge of a risk to contract HIV or Hepatitis C, drinking despite a knowledge of having liver cirrhosis, but also the neglect of social and professional activities that previously were more important than substance use. While these behaviors do show similarities with the compulsions of OCD, there are also important differences. For example, “compulsive” substance use is not necessarily accompanied by a conscious desire to withhold the behavior, nor is addictive behavior consistently impervious to change.
Critics question the existence of compulsivity in addiction altogether [ 5 , 6 , 7 , 89 ], typically using a literal interpretation, i.e., that a person who uses alcohol or drugs simply can not do otherwise. Were that the intended meaning in theories of addiction—which it is not—it would clearly be invalidated by observations of preserved sensitivity of behavior to contingencies in addiction. Indeed, substance use is influenced both by the availability of alternative reinforcers, and the state of the organism. The roots of this insight date back to 1940, when Spragg found that chimpanzees would normally choose a banana over morphine. However, when physically dependent and in a state of withdrawal, their choice preference would reverse [ 102 ]. The critical role of alternative reinforcers was elegantly brought into modern neuroscience by Ahmed et al., who showed that rats extensively trained to self-administer cocaine would readily forego the drug if offered a sweet solution as an alternative [ 103 ]. This was later also found to be the case for heroin [ 103 ], methamphetamine [ 104 ] and alcohol [ 105 ]. Early residential laboratory studies on alcohol use disorder indeed revealed orderly operant control over alcohol consumption [ 106 ]. Furthermore, efficacy of treatment approaches such as contingency management, which provides systematic incentives for abstinence [ 107 ], supports the notion that behavioral choices in patients with addictions remain sensitive to reward contingencies.
Evidence that a capacity for choosing advantageously is preserved in addiction provides a valid argument against a narrow concept of “compulsivity” as rigid, immutable behavior that applies to all patients. It does not, however, provide an argument against addiction as a brain disease. If not from the brain, from where do the healthy and unhealthy choices people make originate? The critical question is whether addictive behaviors—for the most part—result from healthy brains responding normally to externally determined contingencies; or rather from a pathology of brain circuits that, through probabilistic shifts, promotes the likelihood of maladaptive choices even when reward contingencies are within a normal range. To resolve this question, it is critical to understand that the ability to choose advantageously is not an all-or-nothing phenomenon, but rather is about probabilities and their shifts, multiple faculties within human cognition, and their interaction. Yes, it is clear that most people whom we would consider to suffer from addiction remain able to choose advantageously much, if not most, of the time. However, it is also clear that the probability of them choosing to their own disadvantage, even when more salutary options are available and sometimes at the expense of losing their life, is systematically and quantifiably increased. There is a freedom of choice, yet there is a shift of prevailing choices that nevertheless can kill.
Synthesized, the notion of addiction as a disease of choice and addiction as a brain disease can be understood as two sides of the same coin. Both of these perspectives are informative, and they are complementary. Viewed this way, addiction is a brain disease in which a person’s choice faculties become profoundly compromised. To articulate it more specifically, embedded in and principally executed by the central nervous system, addiction can be understood as a disorder of choice preferences, preferences that overvalue immediate reinforcement (both positive and negative), preferences for drug-reinforcement in spite of costs, and preferences that are unstable ( “I’ll never drink like that again;” “this will be my last cigarette” ), prone to reversals in the form of lapses and relapse. From a contemporary neuroscience perspective, pre-existing vulnerabilities and persistent drug use lead to a vicious circle of substantive disruptions in the brain that impair and undermine choice capacities for adaptive behavior, but do not annihilate them. Evidence of generally intact decision making does not fundamentally contradict addiction as a brain disease.
Conclusions
The present paper is a response to the increasing number of criticisms of the view that addiction is a chronic relapsing brain disease. In many cases, we show that those criticisms target tenets that are neither needed nor held by a contemporary version of this view. Common themes are that viewing addiction as a brain disease is criticized for being both too narrow (addiction is only a brain disease; no other perspectives or factors are important) or too far reaching (it purports to discover the final causes of addiction). With regard to disease course, we propose that viewing addiction as a chronic relapsing disease is appropriate for some populations, and much less so for others, simply necessitating better ways of delineating the populations being discussed. We argue that when considering addiction as a disease, the lens of neurobiology is valuable to use. It is not the only lens, and it does not have supremacy over other scientific approaches. We agree that critiques of neuroscience are warranted [ 108 ] and that critical thinking is essential to avoid deterministic language and scientific overreach.
Beyond making the case for a view of addiction as a brain disease, perhaps the more important question is when a specific level of analysis is most useful. For understanding the biology of addiction and designing biological interventions, a neurobiological view is almost certainly the most appropriate level of analysis, in particular when informed by an understanding of the behavioral manifestations. In contrast, for understanding the psychology of addiction and designing psychological interventions, behavioral science is the natural realm, but one that can often benefit from an understanding of the underlying neurobiology. For designing policies, such as taxation and regulation of access, economics and public administration provide the most pertinent perspectives, but these also benefit from biological and behavioral science insights.
Finally, we argue that progress would come from integration of these scientific perspectives and traditions. E.O. Wilson has argued more broadly for greater consilience [ 109 ], unity of knowledge, in science. We believe that addiction is among the areas where consilience is most needed. A plurality of disciplines brings important and trenchant insights to bear on this condition; it is the exclusive remit of no single perspective or field. Addiction inherently and necessarily requires multidisciplinary examination. Moreover, those who suffer from addiction will benefit most from the application of the full armamentarium of scientific perspectives.
Funding and disclosures
Supported by the Swedish Research Council grants 2013-07434, 2019-01138 (MH); Netherlands Organisation for Health Research and Development (ZonMw) under project number 912.14.093 (LJMJV); NIDA and NIAAA intramural research programs (LL; the content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health); the Peter Boris Chair in Addictions Research, Homewood Research Institute, and the National Institute on Alcohol Abuse and Alcoholism grants AA025911, AA024930, AA025849, AA027679 (JM; the content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health).
MH has received consulting fees, research support or other compensation from Indivior, Camurus, BrainsWay, Aelis Farma, and Janssen Pharmaceuticals. JM is a Principal and Senior Scientist at BEAM Diagnostics, Inc. DM, JR, LL, and LJMJV declare no conflict of interest.
Leshner AI. Addiction is a brain disease, and it matters. Science. 1997;278:45–7.
Article CAS PubMed Google Scholar
McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–95.
Schomerus G, Lucht M, Holzinger A, Matschinger H, Carta MG, Angermeyer MC. The stigma of alcohol dependence compared with other mental disorders: a review of population studies. Alcohol Alcohol. 2011;46:105–12.
Heyman GM. Addiction and choice: theory and new data. Front Psychiatry. 2013;4:31.
Article PubMed PubMed Central Google Scholar
Heather N, Best D, Kawalek A, Field M, Lewis M, Rotgers F, et al. Challenging the brain disease model of addiction: European launch of the addiction theory network. Addict Res Theory. 2018;26:249–55.
Article Google Scholar
Pickard H, Ahmed SH, Foddy B. Alternative models of addiction. Front Psychiatr.y 2015;6:20.
Google Scholar
Hall W, Carter A, Forlini C. The brain disease model of addiction: is it supported by the evidence and has it delivered on its promises? Lancet Psychiatr. 2015;2:105–10.
Hart CL. Viewing addiction as a brain disease promotes social injustice. Nat Hum Behav. 2017;1:0055.
Heilig M, Epstein DH, Nader MA, Shaham Y. Time to connect: bringing social context into addiction neuroscience. Nat Rev Neurosc.i 2016;17:592–9.
Article CAS Google Scholar
Jellinek EM. The disease concept of alcoholism. Hillhouse Press on behalf of the Christopher J. Smithers Foundation: New Haven, CT; 1960.
Stevenson A. Oxford dictionary of English. 3 ed. New York, NY: Oxford University Press; 2010.
Fan J, May SJ, Zhou Y, Barrett-Connor E. Bimodality of 2-h plasma glucose distributions in whites: the Rancho Bernardo study. Diabetes Care 2005;28:1451–6.
King AC, Vena A, Hasin D, De Wit D, O’Connor CJ, Cao D. Subjective responses to alcohol in the development and maintenance of alcohol use disorder (AUD). Am J Psychiatry. 2021. https://doi.org/10.1176/appi.ajp.2020.20030247 .
GBD. 2016 Alcohol and Drug Use Collaborators. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry. 2018;5:987–1012.
Edwards G, Gross MM. Alcohol dependence: provisional description of a clinical syndrome. Br Med J. 1976;1:1058–61.
Article CAS PubMed PubMed Central Google Scholar
Epstein DH, Heilig M, Shaham Y. Science-based actions can help address the opioid crisis. Trends Pharm Sci. 2018;39:911–16.
Amato L, Davoli M, Perucci CA, Ferri M, Faggiano F, Mattick RP. An overview of systematic reviews of the effectiveness of opiate maintenance therapies: available evidence to inform clinical practice and research. J Subst Abus Treat. 2005;28:321–9.
Cahill K, Stevens S, Perera R, Lancaster T. Pharmacological interventions for smoking cessation: an overview and network meta-analysis. Cochrane Datab System Rev. 2013;5:CD009329.
Jonas DE, Amick HR, Feltner C, Bobashev G, Thomas K, Wines R, et al. Pharmacotherapy for adults with alcohol use disorders in outpatient settings a systematic review and meta-analysis. JAMA. 2014;311:1889–900.
Article PubMed CAS Google Scholar
Mark TL, Kranzler HR, Song X. Understanding US addiction physicians’ low rate of naltrexone prescription. Drug Alcohol Depend. 2003;71:219–28.
Article PubMed Google Scholar
Nutt DJ, King LA, Phillips LD. Drug harms in the UK: a multicriteria decision analysis. Lancet. 2010;376:1558–65.
Wilk AI, Jensen NM, Havighurst TC. Meta-analysis of randomized control trials addressing brief interventions in heavy alcohol drinkers. J Gen Intern Med. 1997;12:274–83.
Laing RD. The divided self; a study of sanity and madness. London: Tavistock Publications; 1960.
Foucault M, Khalfa J. History of madness. New York: Routledge; 2006.
Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL. et al.Comorbidity of mental disorders with alcohol and other drug abuse. Results Epidemiologic Catchment Area (ECA) study.JAMA. 1990;264:2511–8.
Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–16.
Lopez-Quintero C, Hasin DS, de Los Cobos JP, Pines A, Wang S, Grant BF, et al. Probability and predictors of remission from life-time nicotine, alcohol, cannabis or cocaine dependence: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Addiction. 2011;106:657–69.
Humphreys K. Addiction treatment professionals are not the gatekeepers of recovery. Subst Use Misuse. 2015;50:1024–7.
Cohen E, Feinn R, Arias A, Kranzler HR. Alcohol treatment utilization: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2007;86:214–21.
Sobell LC, Cunningham JA, Sobell MB. Recovery from alcohol problems with and without treatment: prevalence in two population surveys. Am J Public Health. 1996;86:966–72.
Culverhouse R, Bucholz KK, Crowe RR, Hesselbrock V, Nurnberger JI Jr, Porjesz B, et al. Long-term stability of alcohol and other substance dependence diagnoses and habitual smoking: an evaluation after 5 years. Arch Gen Psychiatry. 2005;62:753–60.
Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830–42.
Skolnick P. The opioid epidemic: crisis and solutions. Annu Rev Pharm Toxicol. 2018;58:143–59.
Hser YI, Evans E, Grella C, Ling W, Anglin D. Long-term course of opioid addiction. Harv Rev Psychiatry. 2015;23:76–89.
Mathers BM, Degenhardt L, Bucello C, Lemon J, Wiessing L, Hickman M. Mortality among people who inject drugs: a systematic review and meta-analysis. Bull World Health Organ. 2013;91:102–23.
Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, et al. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72:757–66.
Article PubMed PubMed Central CAS Google Scholar
Lee MR, Sher KJ. “Maturing Out” of binge and problem drinking. Alcohol Res: Curr Rev. 2018;39:31–42.
Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ. Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction. 2005;100:281–92.
Berridge V. The rise, fall, and revival of recovery in drug policy. Lancet. 2012;379:22–23.
Parvaz MA, Moeller SJ, d’Oleire Uquillas F, Pflumm A, Maloney T, Alia-Klein N, et al. Prefrontal gray matter volume recovery in treatment-seeking cocaine-addicted individuals: a longitudinal study. Addict Biol. 2017;22:1391–401.
Korponay C, Kosson DS, Decety J, Kiehl KA, Koenigs M. Brain volume correlates with duration of abstinence from substance abuse in a region-specific and substance-specific manner. Biol Psychiatry Cogn Neurosci Neuroimaging. 2017;2:626–35.
PubMed PubMed Central Google Scholar
Janes AC, Datko M, Roy A, Barton B, Druker S, Neal C, et al. Quitting starts in the brain: a randomized controlled trial of app-based mindfulness shows decreases in neural responses to smoking cues that predict reductions in smoking. Neuropsychopharmacology. 2019;44:1631–38.
Humphreys K, Bickel WK. Toward a neuroscience of long-term recovery from addiction. JAMA Psychiatry. 2018;75:875–76.
Verhulst B, Neale MC, Kendler KS. The heritability of alcohol use disorders: a meta-analysis of twin and adoption studies. Psychol Med. 2015;45:1061–72.
Goldman D, Oroszi G, Ducci F. The genetics of addictions: uncovering the genes. Nat Rev Genet. 2005;6:521–32.
Kendler KS, Jacobson KC, Prescott CA, Neale MC. Specificity of genetic and environmental risk factors for use and abuse/dependence of cannabis, cocaine, hallucinogens, sedatives, stimulants, and opiates in male twins. AJ Psychiatry. 2003;160:687–95.
Schizophrenia Working Group of the Psychiatric Genomics C. Biological insights from 108 schizophrenia-associated genetic loci. Nature. 2014;511:421–7.
Wray NR, Ripke S, Mattheisen M, Trzaskowski M, Byrne EM, Abdellaoui A, et al. Genome-wide association analyses identify 44 risk variants and refine the genetic architecture of major depression. Nat Genet. 2018;50:668–81.
Wray NR, Lin T, Austin J, McGrath JJ, Hickie IB, Murray GK, et al. From basic science to clinical application of polygenic risk scores: a primer. JAMA Psychiatry. 2021;78:101–9.
Walters RK, Polimanti R, Johnson EC, McClintick JN, Adams MJ, Adkins AE, et al. Transancestral GWAS of alcohol dependence reveals common genetic underpinnings with psychiatric disorders. Nat Neurosci. 2018;21:1656–69.
Visscher PM, Wray NR. Concepts and misconceptions about the polygenic additive model applied to disease. Hum Hered. 2015;80:165–70.
Heilig M, Leggio L. What the alcohol doctor ordered from the neuroscientist: theragnostic biomarkers for personalized treatments. Prog Brain Res. 2016;224:401–18.
Rasmussen K, White DA, Acri JB. NIDA’s medication development priorities in response to the Opioid Crisis: ten most wanted. Neuropsychopharmacology. 2019;44:657–59.
Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. AJ Psychiatry. 2010;167:748–51.
Kwako LE, Schwandt ML, Ramchandani VA, Diazgranados N, Koob GF, Volkow ND, et al. Neurofunctional domains derived from deep behavioral phenotyping in alcohol use disorder. AJ Psychiatry. 2019;176:744–53.
Kwako LE, Bickel WK, Goldman D. Addiction biomarkers: dimensional approaches to understanding addiction. Trends Mol Med. 2018;24:121–28.
Xiao P, Dai Z, Zhong J, Zhu Y, Shi H, Pan P. Regional gray matter deficits in alcohol dependence: a meta-analysis of voxel-based morphometry studies. Drug Alcohol Depend. 2015;153:22–8.
Ersche KD, Williams GB, Robbins TW, Bullmore ET. Meta-analysis of structural brain abnormalities associated with stimulant drug dependence and neuroimaging of addiction vulnerability and resilience. Curr Opin Neurobiol. 2013;23:615–24.
Klugah-Brown B, Di X, Zweerings J, Mathiak K, Becker B, Biswal B. Common and separable neural alterations in substance use disorders: a coordinate-based meta-analyses of functional neuroimaging studies in humans. Hum Brain Mapp. 2020;41:4459–77.
Volkow ND, Fowler JS, Wang GJ. The addicted human brain: insights from imaging studies. J Clin Investig. 2003;111:1444–51.
Goldstein RZ, Volkow ND. Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications. Nat Rev Neurosci. 2011;12:652–69.
Goodkind M, Eickhoff SB, Oathes DJ, Jiang Y, Chang A, Jones-Hagata LB, et al. Identification of a common neurobiological substrate for mental illness. JAMA Psychiatry. 2015;72:305–15.
Scofield MD, Heinsbroek JA, Gipson CD, Kupchik YM, Spencer S, Smith AC, et al. The nucleus accumbens: mechanisms of addiction across drug classes reflect the importance of glutamate homeostasis. Pharm Rev. 2016;68:816–71.
Korpi ER, den Hollander B, Farooq U, Vashchinkina E, Rajkumar R, Nutt DJ, et al. Mechanisms of action and persistent neuroplasticity by drugs of abuse. Pharm Rev. 2015;67:872–1004.
Luscher C, Malenka RC. Drug-evoked synaptic plasticity in addiction: from molecular changes to circuit remodeling. Neuron. 2011;69:650–63.
Everitt BJ. Neural and psychological mechanisms underlying compulsive drug seeking habits and drug memories–indications for novel treatments of addiction. Eur J Neurosci. 2014;40:2163–82.
Lesscher HM, Vanderschuren LJ. Compulsive drug use and its neural substrates. Rev Neurosci. 2012;23:731–45.
Cruz FC, Koya E, Guez-Barber DH, Bossert JM, Lupica CR, Shaham Y, et al. New technologies for examining the role of neuronal ensembles in drug addiction and fear. Nat Rev Neurosci. 2013;14:743–54.
Crick F. The astonishing hypothesis: the scientific search for the soul. Scribner; Maxwell Macmillan International: New York, NY; 1994.
Vanderschuren LJ, Achterberg EJ, Trezza V. The neurobiology of social play and its rewarding value in rats. Neurosci Biobehav Rev. 2016;70:86–105.
Venniro M, Zhang M, Caprioli D, Hoots JK, Golden SA, Heins C, et al. Volitional social interaction prevents drug addiction in rat models. Nat Neurosci. 2018;21:1520–29.
Martinez D, Orlowska D, Narendran R, Slifstein M, Liu F, Kumar D, et al. Dopamine type 2/3 receptor availability in the striatum and social status in human volunteers. Biol Psychiatry. 2010;67:275–8.
Wiers CE, Shokri-Kojori E, Cabrera E, Cunningham S, Wong C, Tomasi D, et al. Socioeconomic status is associated with striatal dopamine D2/D3 receptors in healthy volunteers but not in cocaine abusers. Neurosci Lett. 2016;617:27–31.
Morgan D, Grant KA, Gage HD, Mach RH, Kaplan JR, Prioleau O, et al. Social dominance in monkeys: dopamine D2 receptors and cocaine self-administration. Nat Neurosci. 2002;5:169–74.
Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017;2:e356–e66.
Gilbert PA, Zemore SE. Discrimination and drinking: a systematic review of the evidence. Soc Sci Med 2016;161:178–94.
Oshri A, Gray JC, Owens MM, Liu S, Duprey EB, Sweet LH, et al. Adverse childhood experiences and amygdalar reduction: high-resolution segmentation reveals associations with subnuclei and psychiatric outcomes. Child Maltreat. 2019;24:400–10.
Holmes CJ, Barton AW, MacKillop J, Galván A, Owens MM, McCormick MJ, et al. Parenting and salience network connectivity among African Americans: a protective pathway for health-risk behaviors. Biol Psychiatry. 2018;84:365–71.
Brody GH, Gray JC, Yu T, Barton AW, Beach SR, Galván A, et al. Protective prevention effects on the association of poverty with brain development. JAMA Pediatr. 2017;171:46–52.
Hanson JL, Gillmore AD, Yu T, Holmes CJ, Hallowell ES, Barton AW, et al. A family focused intervention influences hippocampal-prefrontal connectivity through gains in self-regulation. Child Dev. 2019;90:1389–401.
Borsboom D, Cramer A, Kalis A. Brain disorders? Not really… why network structures block reductionism in psychopathology research. Behav Brain Sci. 2018;42:1–54.
Field M, Heather N, Wiers RW. Indeed, not really a brain disorder: Implications for reductionist accounts of addiction. Behav Brain Sci. 2019;42:e9.
Pascoli V, Hiver A, Van Zessen R, Loureiro M, Achargui R, Harada M, et al. Stochastic synaptic plasticity underlying compulsion in a model of addiction. Nature. 2018;564:366–71.
James W. The dilemma of determinism. Whitefish, MT: Kessinger Publishing; 2005.
Gessell B. Indeterminism in the brain. Biol Philos. 2017;32:1205–23.
Jedlicka P. Revisiting the quantum brain hypothesis: toward quantum (neuro)biology? Front Mol Neurosci. 2017;10:366.
Heyman GM. Addiction: a disorder of choice. Cambridge, MA: Harvard University Press; 2010.
Heather NQ. Is addiction a brain disease or a moral failing? A: Neither. Neuroethics. 2017;10:115–24.
Ahmed SH, Lenoir M, Guillem K. Neurobiology of addiction versus drug use driven by lack of choice. Curr Opin Neurobiol. 2013;23:581–7.
Hogarth L, Lam-Cassettari C, Pacitti H, Currah T, Mahlberg J, Hartley L, et al. Intact goal-directed control in treatment-seeking drug users indexed by outcome-devaluation and Pavlovian to instrumental transfer: critique of habit theory. Eur J Neurosci. 2019;50:2513–25.
Mathis V, Kenny PJ. From controlled to compulsive drug-taking: the role of the habenula in addiction. Neurosci Biobehav Rev. 2019;106:102–11.
Luscher C, Robbins TW, Everitt BJ. The transition to compulsion in addiction. Nat Rev Neurosci. 2020;21:247–63.
Robinson TE, Berridge KC. Addiction. Annu Rev Psychol. 2003;54:25–53.
Everitt BJ, Robbins TW. Neural systems of reinforcement for drug addiction: from actions to habits to compulsion. Nat Neurosci. 2005;8:1481–89.
Koob GF, Volkow ND. Neurocircuitry of addiction. Neuropsychopharmacology. 2010;35:217–38.
Tiffany ST. A cognitive model of drug urges and drug-use behavior: role of automatic and nonautomatic processes. Psychol Rev. 1990;97:147–68.
Robinson TE, Berridge KC. The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Res Rev. 1993;18:247–91.
Koob GF, Le Moal M. Plasticity of reward neurocircuitry and the ‘dark side’ of drug addiction. Nat Neurosci. 2005;8:1442–4.
Stein DJ, Costa DLC, Lochner C, Miguel EC, Reddy YCJ, Shavitt RG, et al. Obsessive-compulsive disorder. Nat Rev Dis Prim. 2019;5:52.
Vanderschuren LJ, Everitt BJ. Drug seeking becomes compulsive after prolonged cocaine self-administration. Science 2004;305:1017–9.
American_Psychiatric_Association. Diagnostic and statistical manual of mental disorders: DSM-5™. 5th ed. Arlington, VA, US: American Psychiatric Publishing, Inc; 2013.
Book Google Scholar
Spragg SDS. Morphine addiction in chimpanzees. Comp Psychol Monogr. 1940;15:132–32.
Lenoir M, Cantin L, Vanhille N, Serre F, Ahmed SH. Extended heroin access increases heroin choices over a potent nondrug alternative. Neuropsychopharmacology. 2013;38:1209–20.
Caprioli D, Venniro M, Zeric T, Li X, Adhikary S, Madangopal R, et al. Effect of the novel positive allosteric modulator of metabotropic glutamate receptor 2 AZD8529 on incubation of methamphetamine craving after prolonged voluntary abstinence in a rat model. Biol Psychiatry. 2015;78:463–73.
Augier E, Barbier E, Dulman RS, Licheri V, Augier G, Domi E, et al. A molecular mechanism for choosing alcohol over an alternative reward. Science. 2018;360:1321–26.
Bigelow GE. An operant behavioral perspective on alcohol abuse and dependence. In: Heather N, Peters TJ, Stockwell T, editors. International handbook of alcohol dependence and problems. John Wiley & Sons Ltd; 2001. p. 299–315.
Higgins ST, Heil SH, Lussier JP. Clinical implications of reinforcement as a determinant of substance use disorders. Annu Rev Psychol. 2004;55:431–61.
Satel S, Lilienfeld SO. Brainwashed: the seductive appeal of mindless neuroscience. New York, NY: Basic Books; 2015.
Wilson EO. Consilience: the unity of knowledge. New York, NY: Vintage Books; 1999.
Saunders JB, Degenhardt L, Reed GM, Poznyak V. Alcohol use disorders in ICD-11: past, present, and future. Alcohol Clin Exp Res 2019;43:1617–31.
Organization. WH. ICD-11 for mortality and morbidity statistics. 2018. https://icd.who.int/browse11/l-m/en . Accessed 21 Oct 2020.
Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, brief intervention, and referral to treatment (SBIRT): toward a public health approach to the management of substance abuse. Subst Abus. 2007;28:7–30.
Witkiewitz K, Hallgren KA, Kranzler HR, Mann KF, Hasin DS, Falk DE, et al. Clinical validation of reduced alcohol consumption after treatment for alcohol dependence using the World Health Organization risk drinking levels. Alcohol Clin Exp Res 2017;41:179–86.
Hasin DS, O’Brien CP, Auriacombe M, Borges G, Bucholz K, Budney A, et al. DSM-5 criteria for substance use disorders: recommendations and rationale. AJ Psychiatry. 2013;170:834–51.
Rosenthal RJ, Faris SB. The etymology and early history of ‘addiction’. Addict Res Theory. 2019;27:437–49.
Martin CS, Steinley DL, Verges A, Sher KJ. The proposed 2/11 symptom algorithm for DSM-5 substance-use disorders is too lenient. Psychol Med. 2011;41:2008–10.
Degenhardt L, Bharat C, Bruno R, Glantz MD, Sampson NA, Lago L, et al. Concordance between the diagnostic guidelines for alcohol and cannabis use disorders in the draft ICD-11 and other classification systems: analysis of data from the WHO’s World Mental Health Surveys. Addiction. 2019;114:534–52.
PubMed Google Scholar
Lago L, Bruno R, Degenhardt L. Concordance of ICD-11 and DSM-5 definitions of alcohol and cannabis use disorders: a population survey. Lancet Psychiatry. 2016;3:673–84.
Lundin A, Hallgren M, Forsman M, Forsell Y. Comparison of DSM-5 classifications of alcohol use disorders with those of DSM-IV, DSM-III-R, and ICD-10 in a general population sample in Sweden. J Stud Alcohol Drugs. 2015;76:773–80.
Kwako LE, Momenan R, Litten RZ, Koob GF, Goldman D. Addictions neuroclinical assessment: a neuroscience-based framework for addictive disorders. Biol Psychiatry. 2016;80:179–89.
Rehm J, Heilig M, Gual A. ICD-11 for alcohol use disorders: not a convincing answer to the challenges. Alcohol Clin Exp Res. 2019;43:2296–300.
Download references
Acknowledgements
The authors want to acknowledge comments by Drs. David Epstein, Kenneth Kendler and Naomi Wray.
Author information
Authors and affiliations.
Center for Social and Affective Neuroscience, Department of Biomedical and Clinical Sciences, Linköping University, Linköping, Sweden
Markus Heilig
Peter Boris Centre for Addictions Research, McMaster University and St. Joseph’s Healthcare Hamilton, Hamilton, ON, Canada
- James MacKillop
Homewood Research Institute, Guelph, ON, Canada
New York State Psychiatric Institute and Columbia University Irving Medical Center, New York, NY, USA
Diana Martinez
Institute for Mental Health Policy Research & Campbell Family Mental Health Research Institute, Centre for Addiction and Mental Health (CAMH), Toronto, ON, Canada
Jürgen Rehm
Dalla Lana School of Public Health and Department of Psychiatry, University of Toronto (UofT), Toronto, ON, Canada
Klinische Psychologie & Psychotherapie, Technische Universität Dresden, Dresden, Germany
Department of International Health Projects, Institute for Leadership and Health Management, I.M. Sechenov First Moscow State Medical University, Moscow, Russia
Clinical Psychoneuroendocrinology and Neuropsychopharmacology Section, Translational Addiction Medicine Branch, National Institute on Drug Abuse Intramural Research Program and National Institute on Alcohol Abuse and Alcoholism Division of Intramural Clinical and Biological Research, National Institutes of Health, Baltimore and Bethesda, MD, USA
Lorenzo Leggio
Department of Population Health Sciences, Unit Animals in Science and Society, Faculty of Veterinary Medicine, Utrecht University, Utrecht, the Netherlands
Louk J. M. J. Vanderschuren
You can also search for this author in PubMed Google Scholar
Contributions
All authors jointly drafted the paper.
Corresponding author
Correspondence to Markus Heilig .
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Heilig, M., MacKillop, J., Martinez, D. et al. Addiction as a brain disease revised: why it still matters, and the need for consilience. Neuropsychopharmacol. 46 , 1715–1723 (2021). https://doi.org/10.1038/s41386-020-00950-y
Download citation
Received : 10 November 2020
Revised : 11 December 2020
Accepted : 14 December 2020
Published : 22 February 2021
Issue Date : September 2021
DOI : https://doi.org/10.1038/s41386-020-00950-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Persistent impacts of smoking on resting-state eeg in male chronic smokers and past-smokers with 20 years of abstinence.
- Yoonji Jeon
- Dongil Chung
Scientific Reports (2023)
A contextualized reinforcer pathology approach to addiction
- Samuel F. Acuff
- James G. Murphy
Nature Reviews Psychology (2023)
Functional genomic mechanisms of opioid action and opioid use disorder: a systematic review of animal models and human studies
- Camille Falconnier
- Alba Caparros-Roissard
- Pierre-Eric Lutz
Molecular Psychiatry (2023)
A neuromarker for drug and food craving distinguishes drug users from non-users
- Leonie Koban
- Tor D. Wager
Nature Neuroscience (2023)
Does a Survivorship Model of Opioid Use Disorder Improve Public Stigma or Policy Support? A General Population Randomized Experiment
- Jarratt D. Pytell
- Geetanjali Chander
- Emma E. McGinty
Journal of General Internal Medicine (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Engineering
- Write For Us
- Privacy Policy

Essay on Drug Abuse

Here we have shared the Essay on Drug Abuse in detail so you can use it in your exam or assignment of 150, 250, 400, 500, or 1000 words.
You can use this Essay on Drug Abuse in any assignment or project whether you are in school (class 10th or 12th), college, or preparing for answer writing in competitive exams.
Topics covered in this article.
Essay on Drug Abuse in 150 words
Essay on drug abuse in 250-300 words, essay on drug abuse in 500-1000 words.
Drug abuse is a global issue that poses serious risks to individuals and society. It involves the harmful and excessive use of drugs, leading to physical and mental health problems. Drug abuse can result in addiction, organ damage, cognitive impairment, and social and economic difficulties. Prevention efforts should focus on education, raising awareness about the dangers of drug abuse, and promoting healthy lifestyles. Access to quality healthcare and addiction treatment services is crucial for recovery. Strengthening law enforcement measures against drug trafficking is necessary to address the supply side of the problem. Creating supportive environments and opportunities for positive engagement can help prevent drug abuse. By taking collective action, we can combat drug abuse and build healthier communities.
Drug abuse is a growing global concern that poses significant risks to individuals, families, and communities. It refers to the excessive and harmful use of drugs, both legal and illegal, that have negative effects on physical and mental health.
Drug abuse has severe consequences for individuals and society. Physically, drug abuse can lead to addiction, damage vital organs, and increase the risk of overdose. Mentally, it can cause cognitive impairment, and psychological disorders, and deteriorate overall well-being. Additionally, drug abuse often leads to social and economic problems, such as strained relationships, loss of employment, and criminal activities.
Preventing drug abuse requires a multi-faceted approach. Education and awareness programs play a crucial role in informing individuals about the dangers of drug abuse and promoting healthy lifestyle choices. Access to quality healthcare and addiction treatment services is vital to help individuals recover from substance abuse. Strengthening law enforcement efforts to curb drug trafficking and promoting international cooperation is also essential to address the supply side of the issue.
Community support and a nurturing environment are critical in preventing drug abuse. Creating opportunities for individuals, especially young people, to engage in positive activities and providing social support systems can serve as protective factors against drug abuse.
In conclusion, drug abuse is a significant societal problem with detrimental effects on individuals and communities. It requires a comprehensive approach involving education, prevention, treatment, and enforcement. By addressing the root causes, raising awareness, and providing support to those affected, we can combat drug abuse and create a healthier and safer society for all.
Title: Drug Abuse – A Global Crisis Demanding Urgent Action
Introduction :
Drug abuse is a pressing global issue that poses significant risks to individuals, families, and communities. It refers to the excessive and harmful use of drugs, both legal and illegal, that have detrimental effects on physical and mental health. This essay explores the causes and consequences of drug abuse, the social and economic impact, prevention and treatment strategies, and the importance of raising awareness and fostering supportive communities in addressing this crisis.
Causes and Factors Contributing to Drug Abuse
Several factors contribute to drug abuse. Genetic predisposition, peer pressure, stress, trauma, and environmental influences play a role in initiating substance use. The availability and accessibility of drugs, as well as societal norms and cultural acceptance, also influence drug abuse patterns. Additionally, underlying mental health issues and co-occurring disorders can drive individuals to self-medicate with drugs.
Consequences of Drug Abuse
Drug abuse has devastating consequences on individuals and society. Physically, drug abuse can lead to addiction, tolerance, and withdrawal symptoms. Substance abuse affects vital organs, impairs cognitive function, and increases the risk of accidents and injuries. Mental health disorders, such as depression, anxiety, and psychosis, are often associated with drug abuse. Substance abuse also takes a toll on relationships, leading to strained family dynamics, social isolation, and financial instability. The social and economic costs of drug abuse include increased healthcare expenses, decreased productivity, and the burden on criminal justice systems.
Prevention and Education
Preventing drug abuse requires a comprehensive and multi-faceted approach. Education and awareness programs are essential in schools, communities, and the media to inform individuals about the risks and consequences of drug abuse. Promoting healthy coping mechanisms, stress management skills, and decision-making abilities can empower individuals to resist peer pressure and make informed choices. Early intervention programs that identify at-risk individuals and provide support and resources are crucial in preventing substance abuse.
Treatment and Recovery
Access to quality healthcare and evidence-based addiction treatment is vital in addressing drug abuse. Treatment options include detoxification, counseling, behavioral therapies, and medication-assisted treatments. Rehabilitation centers, support groups, and outpatient programs provide a continuum of care for individuals seeking recovery. Holistic approaches, such as addressing co-occurring mental health disorders and promoting healthy lifestyles, contribute to successful long-term recovery. Support from family, friends, and communities plays a significant role in sustaining recovery and preventing relapse.
Law Enforcement and Drug Policies
Effective law enforcement efforts are necessary to disrupt drug trafficking and dismantle illicit drug networks. International cooperation and collaboration are crucial in combating the global drug trade. Additionally, drug policies should focus on a balanced approach that combines law enforcement with prevention, treatment, and harm reduction strategies. Shifting the emphasis from punitive measures toward prevention and rehabilitation can lead to more effective outcomes.
Creating Supportive Communities:
Fostering supportive communities is vital in addressing drug abuse. Communities should provide resources, social support networks, and opportunities for positive engagement. This includes promoting healthy recreational activities, providing vocational training, and creating safe spaces for individuals in recovery. Reducing the stigma associated with drug abuse and encouraging empathy and understanding are crucial to building a compassionate and supportive environment.
Conclusion :
Drug abuse remains a complex and multifaceted issue with far-reaching consequences. By addressing the causes, raising awareness, implementing preventive measures, providing quality treatment and support services, and fostering supportive communities, we can combat drug abuse and alleviate its impact. It requires collaboration and a collective effort from individuals, communities, governments, and organizations to build a society that is resilient against the scourge of drug abuse. Through education, prevention, treatment, and compassion, we can pave the way toward a healthier and drug-free future.
Essay on Drug addiction for Students and Children in 1500 Words
It is an informative essay on drug addiction for students and children. This article includes signs, causes, consequences,
Table of Contents
Introduction (Essay on Drug addiction)
Drug addiction is an expanding issue in all over the world. People often use drugs as a way for their difficulties, although drug creates its effects. Drug addiction affects not only health and relationships but also society and the environment . Many treatments option lead people to a sober and healthy life.
Drug addiction is a chronic disorder of the brain. Insidiously, the brain thinks drugs are necessary despite the negative consequences. Addiction forces people to do their best to get drugs.
As per the National Institute on Drug Abuse, in 2013, more than half of new illegal drug users were below the age of 18. While initial drug use is voluntary and usually begins with experiments, repeated use can affect a person’s self-control, causing appetite. These desires often fuel continuous addiction.
Signs of drug addiction
The symptoms of drug addiction vary from drug to drug. Some medications need more time to cause noticeable symptoms. Sometimes, the symptoms combined with routine behavior, making it difficult to determine that the person is addicted.
Typical symptoms of drug addiction include needle marks on the arms of injector drug users and continuous nasal pressure ulcers for drug users.
Identifying a drug issue is often the initial step toward recovery. However, because of the severe withdrawal symptoms of some medications, people should seek professional help to regain health.
Causes of drug addiction
People use drugs for many reasons, but they do not start taking drugs to become addicted to them. Although the first use is voluntary, continual use is often the result of physical changes in the brain.
Drugs affect the brain’s reward system, producing excess “dopamine,” the chemical responsible for pleasant feelings. Our mind intends to repeat satisfying activities, including those related to drug use. The sense of pleasure of using drugs causes the brain to associate drugs with rewards, which causes appetite.
1. Surrounding factors
Drugs provide a momentary sense of accomplishment, euphoric feelings, and a general sense of confidence and satisfaction. Many factors in life can promote drug abuse.
Parental behavior plays a vital role in whether a child tries with drugs later in life. An unstable family with a lack of parental supervision often leads to child neglect. Quality of life can also affect drug addiction. Living in a deprived society can increase the risk of drug abuse.
2. Stress and anxiety
People struggling with stress and anxiety may feel the need to self-medicate with cannabis, stimulants, or other drugs to reduce their fears.
They assume that regular consumption of drugs will ease their problems. Similarly, some students and athletes use performance-enhancing drugs to keep up with the intention of consistently excellent play.
It exposes adolescents to social pressure from peers who use the substance. Teens are sensitive and spend much time with their peers. Those who use drugs often force their peers to experiment. According to NIDA, most first-time drug users are teenagers.
3. Biological reasons
Studies show that a person’s predisposition to addiction positively correlates with genetic similarity to a relative who was addicted to drugs in the past. Mental disorders and diseases are also risked factors.
The consequences of drug abuse
Substance abuse has adverse effects that affect not only the individual. Illegal drugs cost the United States around $194 billion a year because of loss of productivity, health care costs, and crime costs.
The most immediate effect of drug abuse is the deterioration of health. Death results from a drug abuse use disorder. According to a report from the National Drug Control Office in 2014, drug-related deaths occur every 14 minutes in the United States.
One of the major health problems associated with drug use is the lack of hygiene practices that can lead to HIV spasm, AIDS, hepatitis, or other fatal diseases like:
- Cardiovascular disease
- Heart attack
- Cancer
- Pulmonary disease
- Mental disorders
- Neonatal abstinence syndrome (withdrawal symptoms in addicted children)
In 2011, over 1.4 million patients visited the emergency department because of a drug-related incident. Cocaine has been involved in over half a million visits.
Illegal drug production and use harm to society and the environment.
- Chemical toxicity hazard to those living nearby
- Risk of fire or explosion for houses in the immediate vicinity
- Long-term environmental impact of toxic waste
Cleaning a methamphetamine lab is expensive. The rehabilitation of children exposed to the chemicals used to make metamorphosis requires specialized training and resources. This requires time and work that officials can devote to other issues.
Drug users rarely take into account the dangers of improper disposal of drugs or accessories. The removal of needles and drug-related materials contributes to environmental pollution.
Illegal drug users require intensive treatment after long-term drug use. In 2012, 23.2 million users of the substance treatment, as agreed by the National Drug Control Office. Treatment of drug addiction can affect the cost of social services and government resources, increasing the burden on taxpayers.
3. Relation
New behavioral patterns resulting from drug use can damage relationships. The purchase of their drugs is becoming the primary concern of the drug user. This often leads them to steal from friends, family, or the workplace to afford more drugs, which damages trust among their peers.
Parents who use drugs, neglect, or abuse their children. Adverse family conditions are harmful to children and can pave the way for future drug use.
Teen drug addicts leave school because of poor academic performance. Their academic and social skills suffer, causing family tensions. They often distance themselves from friends and attract peers.
Drug addiction may predispose people to commit crimes. The possession or purchase of illegal drugs is illegal, and people often resort to theft or other crime to pay for it.
Studies show that drug use is more common among those arrested than in the general population. The National Drug Control Policy Authority reported that between 62 and 84 percent of those arrested in five major metropolitan areas in 2013 were positive for at least one illegal drug.
The three most common drugs present during testing are marijuana, cocaine, and opiates, and many people have been positive for many drugs.
Also, a survey was done by the Justice Statistics Bureau in 2004. Among prisoners in prison showed that 35 percent of state prisoners and 28 percent of federal prisoners revealed they were under the influence of drugs when they committed the crime for which they were arrested.
Treatments of Drug addiction
1. meditation for drug addiction.
Here are a few of the best home solutions for drug addiction. Meditative research has examined the effects of meditation and has shown that it measures relief of addiction.
Meditation can improve mindfulness and awareness of thoughts and feelings. You can direct this positive energy to control emotions and preventing negative experiences or stress that lead to drug use.
2. Art therapy for drug addiction
Many researchers suggest changes in behavior as the most effective means for drug addiction, and art therapy has gained considerable popularity.
Art therapy enables addicts to build self-esteem and confidence, avoid adverse reactions to typical triggers, and exit from a destructive lifestyle to create and appreciate beauty. This therapy is associated with lower levels of depression and anxiety, which often cause addiction.
3. Apple cider vinegar
Apple cider vinegar (ACV) is commonly used to reduce the appetite for smoking cigarettes and other drugs. This can attribute to the chemical composition of vinegar, including acetic acid and malic acid.
While the full impact of ACV is still underway. Its ability to stop appetite and improve the body’s immune system is significant.
4. Caffeine
Some think, caffeine as a drug (and in some respects, this is the case), it also can eliminate addictive habits. Caffeine is used as a substitute for addiction to energy substances such as alcohol, ecstasy, or cocaine.
An increase in adrenaline and cognitive energy can almost be mistaken for these tides of drugs and can allow real addiction to fade out without severe withdrawal symptoms. However, you can become addicted to caffeine, so use it very less and carefully!
5. Skullcap
Skullcap is a strong nervous agent that is commonly recommended to people in the first days of withdrawal symptoms.
If you suffer from insomnia, headache, nausea, and depression, you will go through drug withdrawal and that’s when you need this herb the most. It is by no entails a therapy for addiction, but it can ease the method and make it less painful.
Government Policy to control drug addiction
Drug abuse policies address issues such as driving under the influence of drugs, prescription drug abuse, prevention methods, and the impact of drugs on specific populations. Drug policy in the United States works to prevent drug addiction and educate the public about the risks of using and selling drugs.
The Indian government solves the drug problem through its strategy of two main approaches – reduction of supply and reduction of demand. Restricting supply is the responsibility of law enforcement authorities.
The demand reduction strategy belongs to the social sector. The Ministry of Social Justice and the Government of India Government implements measures to reduce demand.
The primary strategy is to enable society the community to deal with drug addiction. The approach is to regard drug abuse as a psychosocial, medical problem social interventions can solve that at three different levels.
Leave a comment Cancel reply

Smarts Side
Essay on drug addiction
Essay on drug addiction: Today drug addiction is spreading very fast not only in our country but in the whole world. Most of the young people are coming under its influence. In such a situation, the government is making a lot of efforts on its part so that people can get rid of drugs. For this reason, children are specially explained about the evils of drugs in schools so that they can stay away from drugs. Many times in the examination and in any competition, essays are written on de-addiction or on the harm caused by drugs. If you are also looking for information about de-addiction essay , then read our today’s article completely and learn how to write essay on de-addiction in 100, 150, 250, 500 words.
Table of Contents
Essay on drug addiction in 100 words
Drug addiction has become a very serious problem for our society today. Due to this the lives of many youths are being ruined. Once a person gets addicted to drugs, then he cannot leave it even if he wants to. In such a situation, there is a lot of damage to the social and personal life of a person due to intoxication. Intoxication is not of one type but of many types such as alcohol, cannabis, opium, beer, beedi, cigarette, drugs etc.
But the question is, why do people take drugs? There are different reasons behind every person getting intoxicated. Some people take intoxication as a hobby and some to forget some sorrow. But if the government bans the sale of narcotics, then it can be got rid of to a great extent. Along with the government, the people of the whole country should also cooperate in this.
Essay on drug addiction in 150 words
The progress and future of every country depends on the youth of that country. But if the young generation of the country starts taking drugs, then no one can save that country from destruction. But some youths do not understand this and consider it very good to take drugs. This is the reason why today most of the youth get intoxicated with drugs like gutkha, cigarette, beedi, tobacco and alcohol.
Although the government of our country is also running many anti-drug campaigns, but still drug addiction is increasing. This is the reason that many types of terrible diseases such as mouth cancer, lung cancer etc. are being seen in people today. In such a situation, all the people should make efforts to free the people of the country from drugs. People have to be made aware by giving them information about the harm caused by drugs.
Essay on drug addiction in 250 words
For any country, the people there means the public is very important. But if the people start walking on the wrong path, then the country can never progress again. Today, the way many young people of our country India have become addicted to drugs, due to this their future is going into darkness. Intoxicants like alcohol, cigarette, beedi, opium, heroin make a person hollow from inside. To consume drugs means to invite death.
harm caused by intoxication
No one in the society respects the person who is intoxicated. An intoxicated person fights with his family members after getting intoxicated, due to which the atmosphere of the house deteriorates. Apart from this, those who do drugs can never bring happiness in their life, nor do they have money. When a person becomes addicted to drugs, then he also starts stealing and doing other illegal things.
Some ways to get rid of addiction
To get rid of a dangerous habit like addiction, not one but many efforts will have to be made, such as –
- People should be told about the disadvantages of drugs and awareness should be brought in them.
- Drugs should be completely banned by the government and if ever a person is caught drinking or selling drugs, then he should be punished severely.
- In order to get rid of drug addiction, the government has opened many de-addiction centers. That’s why it is the responsibility of all of us that if someone around our house is addicted to drugs, then he should be encouraged to quit drugs and should be sent to the de-addiction center for treatment.
Essay on drug addiction in 500 words
Today in our country the habit of intoxication is increasing among most of the people. It is a matter of concern that the youth especially are falling prey to drugs. Young people have become so addicted to drugs that they cannot suggest any other work other than drugs. This is the reason why the Government of India has made a lot of efforts to save the youth and adults of the country from drugs. But the government will be successful in its efforts only when the people also cooperate in it.
harm caused by addiction
The disadvantages of intoxication are not one but many, the information about which is given below –
- Intoxication harms the external and internal body of a person.
- After getting intoxicated, a person is not able to differentiate between right and wrong, due to which he sometimes harms himself as well as other people.
- People who are intoxicated always quarrel in their house. In such a situation, due to mutual estrangement and quarrels, many times the family life of the people becomes hell.
- Due to intoxication, a person gets many types of diseases and many times he has to lose his life.
- No one in the society respects the people who are intoxicated and such people do not get work anywhere.
why do people do drugs
Nowadays drug addiction has become like a fashion which is practiced openly by young generation and adults. Many times people do drugs only because they want to get rid of their mind from sorrows. But they do not know that if intoxication had so much power that it could end the sorrows of a person, then there would be no unhappy person in the whole world. Many times people consume alcohol or opium at the behest of their friends and gradually they become addicted to it again. But they do not know that intoxication gives rise to many evils and makes a person’s life unbalanced.

drug addiction efforts
Although many efforts are being made by our government to get rid of drug addiction, but those efforts will be successful only when the public will also give their full contribution. The government should make strict laws to make the country drug free and they should be strictly followed. The law should not forgive people who are caught doing drugs or those who do drug business. For this, there are many government and non-government organizations in our country, which can make people aware by running drug free campaign.
It should always be kept in mind that people who are addicted to drugs cannot be completely free from addiction, but such people can be brought slowly on the right path only through understanding and love. It takes time to change the state of mind of drug addicts and for this they should be treated in de-addiction centers.
vikashkumarpanvari
You might also like, my country essay, winter season essay in english, spring season essay, essay on guru gobind singh, 10 sentences on winter season, student life essay, essay on online education, my india great essay, women empowerment essay, essay on teacher, 10 lines on lion, essay on ideal student, 10 lines on papaya, essay on discipline, swami vivekananda essay, horse essay, dowry system essay, unemployment essay, essay on bhagat singh, essay on tree plantation, leave a reply cancel reply.
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Patient Care & Health Information
- Diseases & Conditions
- Drug addiction (substance use disorder)
Drug addiction, also called substance use disorder, is a disease that affects a person's brain and behavior and leads to an inability to control the use of a legal or illegal drug or medicine. Substances such as alcohol, marijuana and nicotine also are considered drugs. When you're addicted, you may continue using the drug despite the harm it causes.
Drug addiction can start with experimental use of a recreational drug in social situations, and, for some people, the drug use becomes more frequent. For others, particularly with opioids, drug addiction begins when they take prescribed medicines or receive them from others who have prescriptions.
The risk of addiction and how fast you become addicted varies by drug. Some drugs, such as opioid painkillers, have a higher risk and cause addiction more quickly than others.
As time passes, you may need larger doses of the drug to get high. Soon you may need the drug just to feel good. As your drug use increases, you may find that it's increasingly difficult to go without the drug. Attempts to stop drug use may cause intense cravings and make you feel physically ill. These are called withdrawal symptoms.
Help from your health care provider, family, friends, support groups or an organized treatment program can help you overcome your drug addiction and stay drug-free.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Drug addiction symptoms or behaviors include, among others:
- Feeling that you have to use the drug regularly — daily or even several times a day
- Having intense urges for the drug that block out any other thoughts
- Over time, needing more of the drug to get the same effect
- Taking larger amounts of the drug over a longer period of time than you intended
- Making certain that you maintain a supply of the drug
- Spending money on the drug, even though you can't afford it
- Not meeting obligations and work responsibilities, or cutting back on social or recreational activities because of drug use
- Continuing to use the drug, even though you know it's causing problems in your life or causing you physical or psychological harm
- Doing things to get the drug that you normally wouldn't do, such as stealing
- Driving or doing other risky activities when you're under the influence of the drug
- Spending a good deal of time getting the drug, using the drug or recovering from the effects of the drug
- Failing in your attempts to stop using the drug
- Experiencing withdrawal symptoms when you attempt to stop taking the drug
Recognizing unhealthy drug use in family members
Sometimes it's difficult to distinguish normal teenage moodiness or anxiety from signs of drug use. Possible signs that your teenager or other family member is using drugs include:
- Problems at school or work — frequently missing school or work, a sudden disinterest in school activities or work, or a drop in grades or work performance
- Physical health issues — lack of energy and motivation, weight loss or gain, or red eyes
- Neglected appearance — lack of interest in clothing, grooming or looks
- Changes in behavior — major efforts to bar family members from entering the teenager's room or being secretive about going out with friends; or drastic changes in behavior and in relationships with family and friends
- Money issues — sudden requests for money without a reasonable explanation; or your discovery that money is missing or has been stolen or that items have disappeared from your home, indicating maybe they're being sold to support drug use
Recognizing signs of drug use or intoxication
Signs and symptoms of drug use or intoxication may vary, depending on the type of drug. Below you'll find several examples.
Marijuana, hashish and other cannabis-containing substances
People use cannabis by smoking, eating or inhaling a vaporized form of the drug. Cannabis often precedes or is used along with other substances, such as alcohol or illegal drugs, and is often the first drug tried.
Signs and symptoms of recent use can include:
- A sense of euphoria or feeling "high"
- A heightened sense of visual, auditory and taste perception
- Increased blood pressure and heart rate
- Decreased coordination
- Difficulty concentrating or remembering
- Slowed reaction time
- Anxiety or paranoid thinking
- Cannabis odor on clothes or yellow fingertips
- Major cravings for certain foods at unusual times
Long-term use is often associated with:
- Decreased mental sharpness
- Poor performance at school or at work
- Ongoing cough and frequent lung infections
K2, Spice and bath salts
Two groups of synthetic drugs — synthetic cannabinoids and substituted or synthetic cathinones — are illegal in most states. The effects of these drugs can be dangerous and unpredictable, as there is no quality control and some ingredients may not be known.
Synthetic cannabinoids, also called K2 or Spice, are sprayed on dried herbs and then smoked, but can be prepared as an herbal tea. A liquid form can be vaporized in electronic cigarettes. Despite manufacturer claims, these are chemical compounds rather than "natural" or harmless products. These drugs can produce a "high" similar to marijuana and have become a popular but dangerous alternative.
- Elevated mood
- An altered sense of visual, auditory and taste perception
- Extreme anxiety or agitation
- Hallucinations
- Increased heart rate and blood pressure or heart attack
- Violent behavior
Substituted cathinones, also called "bath salts," are mind-altering (psychoactive) substances similar to amphetamines such as ecstasy (MDMA) and cocaine. Packages are often labeled as other products to avoid detection.
Despite the name, these are not bath products such as Epsom salts. Substituted cathinones can be eaten, snorted, inhaled or injected and are highly addictive. These drugs can cause severe intoxication, which results in dangerous health effects or even death.
- Feeling "high"
- Increased sociability
- Increased energy and agitation
- Increased sex drive
- Increased heart rate and blood pressure
- Problems thinking clearly
- Loss of muscle control
- Panic attacks
- Psychotic and violent behavior
Barbiturates, benzodiazepines and hypnotics
Barbiturates, benzodiazepines and hypnotics are prescription central nervous system depressants. They're often used and misused in search for a sense of relaxation or a desire to "switch off" or forget stress-related thoughts or feelings.
- Barbiturates. An example is phenobarbital.
- Benzodiazepines. Examples include sedatives, such as diazepam (Valium), alprazolam (Xanax), lorazepam (Ativan), clonazepam (Klonopin) and chlordiazepoxide (Librium).
- Hypnotics. Examples include prescription sleeping medicines such as zolpidem (Ambien) and zaleplon (Sonata).
- Slurred speech
- Lack of coordination
- Irritability or changes in mood
- Problems concentrating or thinking clearly
- Memory problems
- Involuntary eye movements
- Lack of inhibition
- Slowed breathing and reduced blood pressure
- Falls or accidents
Meth, cocaine and other stimulants
Stimulants include amphetamines, meth (methamphetamine), cocaine, methylphenidate (Ritalin, Concerta, others) and amphetamine-dextroamphetamine (Adderall XR, Mydayis). They're often used and misused in search of a "high," or to boost energy, to improve performance at work or school, or to lose weight or control appetite.
- Feeling of happy excitement and too much confidence
- Increased alertness
- Increased energy and restlessness
- Behavior changes or aggression
- Rapid or rambling speech
- Larger than usual pupils, the black circles in the middle of the eyes
- Confusion, delusions and hallucinations
- Irritability, anxiety or paranoia
- Changes in heart rate, blood pressure and body temperature
- Nausea or vomiting with weight loss
- Poor judgment
- Nasal congestion and damage to the mucous membrane of the nose (if snorting drugs)
- Mouth sores, gum disease and tooth decay from smoking drugs ("meth mouth")
- Depression as the drug wears off
Club drugs are commonly used at clubs, concerts and parties. Examples include methylenedioxymethamphetamine, also called MDMA, ecstasy or molly, and gamma-hydroxybutyric acid, known as GHB. Other examples include ketamine and flunitrazepam or Rohypnol — a brand used outside the U.S. — also called roofie. These drugs are not all in the same category, but they share some similar effects and dangers, including long-term harmful effects.
Because GHB and flunitrazepam can cause sedation, muscle relaxation, confusion and memory loss, the potential for sexual misconduct or sexual assault is associated with the use of these drugs.
Signs and symptoms of use of club drugs can include:
- Larger than usual pupils
- Chills and sweating
- Involuntary shaking (tremors)
- Behavior changes
- Muscle cramping and teeth clenching
- Muscle relaxation, poor coordination or problems moving
- Reduced inhibitions
- Heightened or altered sense of sight, sound and taste
- Memory problems or loss of memory
- Reduced consciousness
- Increased or decreased heart rate and blood pressure
Hallucinogens
Use of hallucinogens can produce different signs and symptoms, depending on the drug. The most common hallucinogens are lysergic acid diethylamide (LSD) and phencyclidine (PCP).
LSD use may cause:
- Greatly reduced perception of reality, for example, interpreting input from one of your senses as another, such as hearing colors
- Impulsive behavior
- Rapid shifts in emotions
- Permanent mental changes in perception
- Rapid heart rate and high blood pressure
- Flashbacks, a reexperience of the hallucinations — even years later
PCP use may cause:
- A feeling of being separated from your body and surroundings
- Problems with coordination and movement
- Aggressive, possibly violent behavior
- Lack of pain sensation
- Increase in blood pressure and heart rate
- Problems with thinking and memory
- Problems speaking
- Intolerance to loud noise
- Sometimes seizures or coma
Signs and symptoms of inhalant use vary, depending on the substance. Some commonly inhaled substances include glue, paint thinners, correction fluid, felt tip marker fluid, gasoline, cleaning fluids and household aerosol products. Due to the toxic nature of these substances, users may develop brain damage or sudden death.
Signs and symptoms of use can include:
- Possessing an inhalant substance without a reasonable explanation
- Brief happy excitement
- Behaving as if drunk
- Reduced ability to keep impulses under control
- Aggressive behavior or eagerness to fight
- Nausea or vomiting
- Appearing under the influence of drugs, with slurred speech, slow movements and poor coordination
- Irregular heartbeats
- Lingering odor of inhalant material
- Rash around the nose and mouth
Opioid painkillers
Opioids are narcotic, painkilling drugs produced from opium or made synthetically. This class of drugs includes, among others, heroin, morphine, codeine, methadone, fentanyl and oxycodone.
Sometimes called the "opioid epidemic," addiction to opioid prescription pain medicines has reached an alarming rate across the United States. Some people who've been using opioids over a long period of time may need physician-prescribed temporary or long-term drug substitution during treatment.
Signs and symptoms of narcotic use and dependence can include:
- A sense of feeling "high"
- Reduced sense of pain
- Agitation, drowsiness or sedation
- Problems with attention and memory
- Pupils that are smaller than usual
- Lack of awareness or inattention to surrounding people and things
- Problems with coordination
- Constipation
- Runny nose or nose sores (if snorting drugs)
- Needle marks (if injecting drugs)
When to see a doctor
If your drug use is out of control or causing problems, get help. The sooner you seek help, the greater your chances for a long-term recovery. Talk with your health care provider or see a mental health provider, such as a doctor who specializes in addiction medicine or addiction psychiatry, or a licensed alcohol and drug counselor.
Make an appointment to see a provider if:
- You can't stop using a drug
- You continue using the drug despite the harm it causes
- Your drug use has led to unsafe behavior, such as sharing needles or unprotected sex
- You think you may be having withdrawal symptoms after stopping drug use
If you're not ready to approach a health care provider or mental health professional, help lines or hotlines may be a good place to learn about treatment. You can find these lines listed on the internet or in the phone book.
When to seek emergency help
Seek emergency help if you or someone you know has taken a drug and:
- May have overdosed
- Shows changes in consciousness
- Has trouble breathing
- Has seizures or convulsions
- Has signs of a possible heart attack, such as chest pain or pressure
- Has any other troublesome physical or psychological reaction to use of the drug
Staging an intervention
People struggling with addiction usually deny they have a problem and hesitate to seek treatment. An intervention presents a loved one with a structured opportunity to make changes before things get even worse and can motivate someone to seek or accept help.
It's important to plan an intervention carefully. It may be done by family and friends in consultation with a health care provider or mental health professional such as a licensed alcohol and drug counselor, or directed by an intervention professional. It involves family and friends and sometimes co-workers, clergy or others who care about the person struggling with addiction.
During the intervention, these people gather together to have a direct, heart-to-heart conversation with the person about the consequences of addiction. Then they ask the person to accept treatment.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Like many mental health disorders, several factors may contribute to development of drug addiction. The main factors are:
- Environment. Environmental factors, including your family's beliefs and attitudes and exposure to a peer group that encourages drug use, seem to play a role in initial drug use.
- Genetics. Once you've started using a drug, the development into addiction may be influenced by inherited (genetic) traits, which may delay or speed up the disease progression.
Changes in the brain
Physical addiction appears to occur when repeated use of a drug changes the way your brain feels pleasure. The addicting drug causes physical changes to some nerve cells (neurons) in your brain. Neurons use chemicals called neurotransmitters to communicate. These changes can remain long after you stop using the drug.
Risk factors
People of any age, sex or economic status can become addicted to a drug. Certain factors can affect the likelihood and speed of developing an addiction:
- Family history of addiction. Drug addiction is more common in some families and likely involves an increased risk based on genes. If you have a blood relative, such as a parent or sibling, with alcohol or drug addiction, you're at greater risk of developing a drug addiction.
- Mental health disorder. If you have a mental health disorder such as depression, attention-deficit/hyperactivity disorder (ADHD) or post-traumatic stress disorder, you're more likely to become addicted to drugs. Using drugs can become a way of coping with painful feelings, such as anxiety, depression and loneliness, and can make these problems even worse.
- Peer pressure. Peer pressure is a strong factor in starting to use and misuse drugs, particularly for young people.
- Lack of family involvement. Difficult family situations or lack of a bond with your parents or siblings may increase the risk of addiction, as can a lack of parental supervision.
- Early use. Using drugs at an early age can cause changes in the developing brain and increase the likelihood of progressing to drug addiction.
- Taking a highly addictive drug. Some drugs, such as stimulants, cocaine or opioid painkillers, may result in faster development of addiction than other drugs. Smoking or injecting drugs can increase the potential for addiction. Taking drugs considered less addicting — so-called "light drugs" — can start you on a pathway of drug use and addiction.
Complications
Drug use can have significant and damaging short-term and long-term effects. Taking some drugs can be particularly risky, especially if you take high doses or combine them with other drugs or alcohol. Here are some examples.
- Methamphetamine, opiates and cocaine are highly addictive and cause multiple short-term and long-term health consequences, including psychotic behavior, seizures or death due to overdose. Opioid drugs affect the part of the brain that controls breathing, and overdose can result in death. Taking opioids with alcohol increases this risk.
- GHB and flunitrazepam may cause sedation, confusion and memory loss. These so-called "date rape drugs" are known to impair the ability to resist unwanted contact and recollection of the event. At high doses, they can cause seizures, coma and death. The danger increases when these drugs are taken with alcohol.
- MDMA — also known as molly or ecstasy — can interfere with the body's ability to regulate temperature. A severe spike in body temperature can result in liver, kidney or heart failure and death. Other complications can include severe dehydration, leading to seizures. Long-term, MDMA can damage the brain.
- One particular danger of club drugs is that the liquid, pill or powder forms of these drugs available on the street often contain unknown substances that can be harmful, including other illegally manufactured or pharmaceutical drugs.
- Due to the toxic nature of inhalants, users may develop brain damage of different levels of severity. Sudden death can occur even after a single exposure.
Other life-changing complications
Dependence on drugs can create a number of dangerous and damaging complications, including:
- Getting an infectious disease. People who are addicted to a drug are more likely to get an infectious disease, such as HIV , either through unsafe sex or by sharing needles with others.
- Other health problems. Drug addiction can lead to a range of both short-term and long-term mental and physical health problems. These depend on what drug is taken.
- Accidents. People who are addicted to drugs are more likely to drive or do other dangerous activities while under the influence.
- Suicide. People who are addicted to drugs die by suicide more often than people who aren't addicted.
- Family problems. Behavioral changes may cause relationship or family conflict and custody issues.
- Work issues. Drug use can cause declining performance at work, absenteeism and eventual loss of employment.
- Problems at school. Drug use can negatively affect academic performance and motivation to excel in school.
- Legal issues. Legal problems are common for drug users and can stem from buying or possessing illegal drugs, stealing to support the drug addiction, driving while under the influence of drugs or alcohol, or disputes over child custody.
- Financial problems. Spending money to support drug use takes away money from other needs, could lead to debt, and can lead to illegal or unethical behaviors.
The best way to prevent an addiction to a drug is not to take the drug at all. If your health care provider prescribes a drug with the potential for addiction, use care when taking the drug and follow instructions.
Health care providers should prescribe these medicines at safe doses and amounts and monitor their use so that you're not given too great a dose or for too long a time. If you feel you need to take more than the prescribed dose of a medicine, talk to your health care provider.
Preventing drug misuse in children and teenagers
Take these steps to help prevent drug misuse in your children and teenagers:
- Communicate. Talk to your children about the risks of drug use and misuse.
- Listen. Be a good listener when your children talk about peer pressure and be supportive of their efforts to resist it.
- Set a good example. Don't misuse alcohol or addictive drugs. Children of parents who misuse drugs are at greater risk of drug addiction.
- Strengthen the bond. Work on your relationship with your children. A strong, stable bond between you and your child will reduce your child's risk of using or misusing drugs.
Preventing a relapse
Once you've been addicted to a drug, you're at high risk of falling back into a pattern of addiction. If you do start using the drug, it's likely you'll lose control over its use again — even if you've had treatment and you haven't used the drug for some time.
- Follow your treatment plan. Monitor your cravings. It may seem like you've recovered and you don't need to keep taking steps to stay drug-free. But your chances of staying drug-free will be much higher if you continue seeing your therapist or counselor, going to support group meetings and taking prescribed medicine.
- Avoid high-risk situations. Don't go back to the neighborhood where you used to get your drugs. And stay away from your old drug crowd.
- Get help immediately if you use the drug again. If you start using the drug again, talk to your health care provider, your mental health provider or someone else who can help you right away.
Drug addiction (substance use disorder) care at Mayo Clinic
- Substance-related and addictive disorders. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5th ed. American Psychiatric Association; 2013. https://dsm.psychiatryonline.org. Accessed Aug. 15, 2022.
- Brown AY. Allscripts EPSi. Mayo Clinic. April 13, 2021.
- DrugFacts: Understanding drug use and addiction. National Institute on Drug Abuse. https://www.drugabuse.gov/publications/drugfacts/understanding-drug-use-addiction. Accessed Aug. 15, 2022.
- American Psychiatric Association. What is a substance use disorder? https://psychiatry.org/patients-families/addiction-substance-use-disorders/what-is-a-substance-use-disorder. Accessed Sept. 2, 2022.
- Eddie D, et al. Lived experience in new models of care for substance use disorder: A systematic review of peer recovery support services and recovery coaching. Frontiers in Psychology. 2019; doi:10.3389/fpsyg.2019.01052.
- Commonly used drugs charts. National Institute on Drug Abuse. https://www.drugabuse.gov/drug-topics/commonly-used-drugs-charts. Accessed Aug. 16, 2022.
- Drugs, brains, and behavior: The science of addiction. National Institute on Drug Abuse. https://www.drugabuse.gov/publications/drugs-brains-behavior-science-addiction/drug-misuse-addiction. Accessed Aug. 16, 2022.
- Drugs of abuse: A DEA resource guide/2020 edition. United States Drug Enforcement Administration. https://admin.dea.gov/documents/2020/2020-04/2020-04-13/drugs-abuse. Accessed Aug. 31, 2022.
- Misuse of prescription drugs research report. National Institute on Drug Abuse. https://www.drugabuse.gov/publications/research-reports/misuse-prescription-drugs/overview. Accessed Aug. 17, 2022.
- Principles of drug addiction treatment: A research-based guide. 3rd ed. National Institute on Drug Abuse. https://www.drugabuse.gov/publications/principles-drug-addiction-treatment-research-based-guide-third-edition/preface. Accessed Aug. 17, 2022.
- The science of drug use: A resource for the justice sector. National Institute on Drug Abuse. https://nida.nih.gov/drug-topics/criminal-justice/science-drug-use-resource-justice-sector. Accessed Sept. 2, 2022.
- Naloxone DrugFacts. National Institute on Drug Abuse. https://nida.nih.gov/publications/drugfacts/naloxone. Accessed Aug. 31, 2022.
- Drug and substance use in adolescents. Merck Manual Professional Version. https://www.merckmanuals.com/professional/pediatrics/problems-in-adolescents/drug-and-substance-use-in-adolescents. Accessed Sept. 2, 2022.
- DrugFacts: Synthetic cannabinoids (K2/Spice). National Institute on Drug Abuse. https://www.drugabuse.gov/publications/drugfacts/synthetic-cannabinoids-k2spice. Accessed Aug. 18, 2022.
- Hall-Flavin DK (expert opinion). Mayo Clinic. March 5, 2021.
- Poppy seed tea: Beneficial or dangerous?
Associated Procedures
- Cognitive behavioral therapy
News from Mayo Clinic
- Science Saturday: Preclinical research identifies brain circuit connected to addictive behaviors July 22, 2023, 11:00 a.m. CDT
- What is naloxone and should everyone have access to it? Feb. 16, 2023, 05:06 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

25,000+ students realised their study abroad dream with us. Take the first step today
Meet top uk universities from the comfort of your home, here’s your new year gift, one app for all your, study abroad needs, start your journey, track your progress, grow with the community and so much more.

Verification Code
An OTP has been sent to your registered mobile no. Please verify

Thanks for your comment !
Our team will review it before it's shown to our readers.

- School Education /
Essay on Drug Abuse in 250 and 500 Words in English for Students
- Updated on
- Apr 2, 2024

Drug abuse refers to the excessive and frequent consumption of drugs. Drug abuse can have several harmful effects on our mental and physical health. Ronald Reagan, the 40th President of the USA, passed the Anti-Drug Abuse Act of 1986 and initiated the War on Drugs . He said, ‘Let us not forget who we are. Drug abuse is a repudiation of everything America is.’
Consuming drugs not only harms the individual himself but also affects society as a whole. Studies have shown that people who consume drugs become addicted to it. This addiction turns into substance abuse, resulting in self-damage, behaviour changes, mood swings, unnecessary weight loss, and several other health problems. Let’s understand what drug abuse is and how to fight it.
This Blog Includes:
Essay on drug abuse in 250 words, why do people consume drugs, why is drug abuse bad, laws in india against drug consumption, steps to prevent drug addiction, 10 lines essay on drug abuse.
Quick Read: Essay on CAA (Citizenship Amendment Act)
‘When people consume drugs regularly and become addicted to it, it is known as drug abuse. In medical terminology, drugs means medicines. However, the consumption of drugs is for non-medical purposes. It involves the consumption of substances in illegal and harmful ways, such as swallowing, inhaling, or injecting. When drugs are consumed, they are mixed into our bloodstream, affecting our neural system and brain functioning.
The Indian government has taken significant steps to help reduce the consumption of drugs. In 1985, the Narcotics Drugs and Psychotropic Substances Act came into force. This act replaced the Opium Act of 1857, the Opium Act of 1878, and the Dangerous Drugs Act of 1930.
Drug abuse can lead to addiction, where a person becomes physically or psychologically dependent on the substance and experiences withdrawal symptoms when attempting to stop using it.
Drug abuse can have serious consequences for the individual and society as a whole. On an individual level, drugs can damage physical health, including organ damage, infectious diseases, and overdose fatalities. Not only this, a person already suffering from mental health disorders will face more harmful aftereffects. Addiction disrupts our cognitive functioning and impairs our decision-making abilities.
To fight drug abuse, we need collective action from all sections of society. Medical professionals say that early intervention and screening programmes can identify individuals at risk of substance misuse and provide them with the necessary support services. Educating people, especially those who are at-risk, about drug abuse and its harmful effects can significantly help reduce their consumption.
Drug abuse is serious and it must be addressed. Drug abuse is killing youth and society. Therefore, it is an urgent topic to address, and only through sustainable and collective efforts can we address this problem.
Quick Read: Success in Life Speech
Essay on Drug Abuse in 500 Words
Drug abuse is known as frequent consumption. In time, these people become dependent on drugs for several reasons. Curiosity drives adolescents and teenagers, who are among the most susceptible groups in our society. Cocaine, marijuana, methamphetamine, heroin, etc. are some of the popular drugs consumed.
The very first question about drugs is: why do people consume drugs? Studies have shown that more than 50% of drug addicts consider drugs as a coping mechanism to alleviate emotional or psychological distress. In the beginning, drugs temporarily relieve feelings of anxiety, depression, or trauma, providing a temporary escape from difficult emotions or life circumstances.
Some consume drugs out of curiosity, some under peer pressure, and some want to escape the painful experiences. Some people enjoy the effects drugs produce, such as euphoria, relaxation, and altered perceptions. Recreational drug use may occur in social settings or as a form of self-medication for stress relief or relaxation.
The National Institute on Drug Abuse states that drugs can worsen our eyesight and body movement, our physical growth, etc. Marijuana, one of the most popular drugs, can slow down our reaction time, affecting our time and distance judgement and decreasing coordination. Cocaine and Methamphetamine can make the consumer aggressive and careless.
Our brain is the first victim of drugs. Drugs can disorder our body in several ways, from damaging organs to messing with our brains. Drugs easily get mixed into our bloodstream, and affect our neural system. Prolonged and excessive consumption of drugs significantly harms our brain functioning.
The next target of drug abuse is our physical health and relationships. Drugs can damage our vital organs, such as the liver, heart, lungs, and brain. For example, heavy alcohol use can lead to cirrhosis of the liver, while cocaine use can increase the risk of heart attack and stroke.
Here is an interesting thing; the USA has the highest number of drug addicts and also has strict laws against drug consumption. According to a report by the Narcotics Control Bureau, around 9 million people in India consume different types of drugs. The Indian government has implemented certain laws against drug consumption and production.
The Narcotic Drugs and Psychotropic Substances Act, 1985 (NDPS), prohibits the production, sale, purchase, and consumption of narcotics and other illegal substances, except for scientific and medical purposes.
Also, Article 47 of the Indian Constitution states that ‘ The State shall endeavour to bring about prohibition of the consumption, except for medicinal purposes, of intoxicating drinks and drugs which are injurious to health.’
Quick Read: Essay on Indian Festivals in 500 Words
Several steps can be taken to prevent drug addiction. But before we start our ‘War on Drugs’ , it is crucial to understand the trigger point. Our social environment, mental health issues and sometimes genetic factors can play a role in drug abuse.
- Education and awareness are the primary weapons in the fight against drugs.
- Keeping distance from people and places addicted to drugs.
- Encourage a healthy and active lifestyle and indulge in physical workouts.
- Watch motivating videos and listen to sound music.
- Self-motivate yourself to stop consuming drugs.
- Talk to a medical professional or a psychiatrist, who will guide you to the right path.
Drug abuse is a serious problem. The excessive and frequent consumption of drugs not only harms the individual but also affects society as a whole. Only a collective approach from lawmakers, healthcare professionals, educators, community leaders, and individuals themselves can combat drug abuse effectively.
Quick Read: Speech About Life
Here is a 10-line essay on drug abuse.
- Drug abuse can significantly affect our physical growth
- Drug abuse can affect our mental functioning.
- Drug abuse may provide instant pleasure, but inside, it weakens our willpower and physical strength.
- Educating people, especially those who are at-risk, about drug abuse and its harmful effects can significantly help reduce their consumption.
- Drugs easily get mixed into our bloodstream, and affect our neural system.
- Prolonged and excessive consumption of drugs significantly harms our brain functioning.
- In 1985, the Narcotics Drugs and Psychotropic Substances Act came into force.
- The USA has the highest number of drug addicts and also has strict laws against drug consumption.
- Drug addicts consider drugs as a coping mechanism to alleviate emotional or psychological distress.
- Adolescents and teenagers are the most vulnerable section of our society and are driven by curiosity.
Ans: Drug abuse refers to the excessive and frequent consumption of drugs. Drug abuse can have several harmful effects on our mental and physical health.
Ans: ‘When people consume drugs regularly and become addicted to it, it is known as drug abuse. In medical terminology, drugs means medicines. However, the consumption of drugs is for non-medical purposes. It involves the consumption of substances in illegal and harmful ways, such as swallowing, inhaling, or injecting. When drugs are consumed, they are mixed into our bloodstream, affecting our neural system and brain functioning.
Ans: Drug abuse is known as frequent consumption. In time, these people become dependent on drugs for several reasons. Adolescents and teenagers are the most vulnerable section of our society who are driven by curiosity. Cocaine, marijuana, methamphetamine, heroin, etc. are some of the popular drugs consumed. The Narcotic Drugs and Psychotropic Substances Act, 1985 (NDPS), prohibits the production, sale, purchase, and consumption of narcotics and other illegal substances, except for scientific and medical purposes.
Popular Essay Topics for Students
For more information on such interesting topics, visit our essay writing page and follow Leverage Edu.
Shiva Tyagi
With an experience of over a year, I've developed a passion for writing blogs on wide range of topics. I am mostly inspired from topics related to social and environmental fields, where you come up with a positive outcome.
Leave a Reply Cancel reply
Save my name, email, and website in this browser for the next time I comment.
Contact no. *

Connect With Us
25,000+ students realised their study abroad dream with us. Take the first step today.

Resend OTP in

Need help with?
Study abroad.
UK, Canada, US & More
IELTS, GRE, GMAT & More
Scholarship, Loans & Forex
Country Preference
New Zealand
Which English test are you planning to take?
Which academic test are you planning to take.
Not Sure yet
When are you planning to take the exam?
Already booked my exam slot
Within 2 Months
Want to learn about the test
Which Degree do you wish to pursue?
When do you want to start studying abroad.
January 2024
September 2024
What is your budget to study abroad?
How would you describe this article ?
Please rate this article
We would like to hear more.
Have something on your mind?

Make your study abroad dream a reality in January 2022 with
India's Biggest Virtual University Fair

Essex Direct Admission Day
Why attend .

Don't Miss Out

Essay on Addiction
Students are often asked to write an essay on Addiction in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Addiction
Understanding addiction.
Addiction is a strong desire to do something repeatedly, even if it’s harmful. It’s like a brain disease. People can get addicted to different things like drugs, alcohol, or even activities like gambling.
Why People Get Addicted
People can get addicted for many reasons. Some may feel good when they do something, so they repeat it. Others may want to escape from problems or stress. Sometimes, it’s because of peer pressure or trying to fit in.
Effects of Addiction
Addiction can harm a person’s health. It can lead to diseases, mental problems, and even death. It can also ruin relationships and cause problems at work or school.
Overcoming Addiction
Overcoming addiction is hard, but possible. It needs strong willpower and often help from doctors or therapists. Support from family and friends is also important. Remember, it’s okay to ask for help.
Preventing Addiction
To avoid addiction, we should learn about its dangers. It’s also important to make good friends and have healthy habits. Always remember, it’s okay to say no if something doesn’t feel right.
250 Words Essay on Addiction
What is addiction.
Addiction is when a person can’t stop doing something, even if it’s harmful. It can be about drugs, alcohol, games, or even food. The person knows it’s bad but can’t stop. It’s like a strong pull that keeps them going back.
How Does it Start?
Addiction often starts with trying something new. This could be a friend offering a cigarette, or playing a new video game. At first, it seems fun and exciting. But over time, the person starts needing it more and more. It becomes a need, not just a want.
The Impact of Addiction
Addiction can hurt a person in many ways. It can make them sick, or cause problems at school or work. It can also hurt their relationships with family and friends. They may lie or steal to keep doing what they’re addicted to. This can lead to feelings of guilt and shame.
Fighting Addiction
Fighting addiction is hard, but not impossible. It starts with admitting there’s a problem. Then, the person needs help from professionals like doctors or counselors. They can give advice, medicine, or therapy to help the person quit. Support from family and friends is also important.
Remember, it’s okay to ask for help. Everyone struggles with something at some point. With the right help and support, anyone can overcome addiction.
Addiction is a serious problem that can harm a person’s health, work, and relationships. But with help and support, it can be overcome. It’s important to understand addiction so we can help others or ourselves if needed.
500 Words Essay on Addiction
Addiction is a serious issue that affects many people around the world. It is a state where a person cannot stop using a substance or engaging in a behavior, even if it is harmful. The person becomes dependent on the substance or the activity to feel good or normal.
Types of Addiction
Addiction can be of two types: substance addiction and behavioral addiction. Substance addiction involves drugs, alcohol, nicotine, or other substances. Behavioral addiction involves activities like gambling, eating, or using the internet.
Causes of Addiction
There is no single reason why someone becomes addicted. It can be due to a mix of genetic, environmental, and psychological factors. Some people may be more prone to addiction because of their genes. Others may turn to addictive substances or behaviors to cope with stress or emotional issues.
Addiction has a negative impact on a person’s health, relationships, and daily life. It can lead to physical health problems like heart disease or mental health issues like depression. Addiction can also strain relationships with family and friends and make it hard for the person to perform well at school or work.
Overcoming addiction is not easy, but it is possible with the right help and support. This can include professional treatment like therapy or medication, as well as support from loved ones. It is important for the person to learn healthy ways to cope with stress and other triggers that may lead to addictive behavior.
Prevention is key in the fight against addiction. This can involve teaching young people about the dangers of substance use and addictive behaviors. It also means creating supportive environments where people can talk about their struggles and seek help if they need it.
In conclusion, addiction is a complex issue that requires understanding, support, and prevention efforts. It is important for everyone to be aware of the signs of addiction and to seek help if they or someone they know is struggling. Remember, overcoming addiction is possible with the right help and support.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on Actual Self
- Essay on Things To Argue
- Essay on Things That Matter
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Essay on Addiction for Students and Children
500 words essay on addiction.
As we all know that excess of anything can be very dangerous, the same way, addiction of any kind can hamper the life quality of an individual. The phrase states that addiction is a family disease as one person uses and the whole family suffers. The above statement stands true in all its essence as the addict does not merely suffer but the people around him suffer greatly too. However, that does not mean they can’t be helped. Addiction is curable and we must not give up on the person who is addicted, rather help them out for a better life.

Cost of Addiction
Addiction comes at a great cost and we need to be able to recognize its harmful consequences to not let ourselves or anyone become an addict. Firstly, addiction has major health hazards. Intake of anything is bad for our body , and it does not matter what type of addiction it is, it will always impact the mental and physical health of a person.
For instance, if you are addicted to drugs or food, you will get various diseases and illnesses. Similarly, if you are addicted to video games, your mental health will also suffer along with physical health.
Moreover, people who are addicts usually face monetary issues. As they use that thing in excess, they spend loads of money on it. People become obsessed with spending all their fortunes on that one thing to satisfy their addiction. Thus, all these addictions of drugs , alcohol , gambling, and more drain the finances of a person and they usually end up in debt or even worse.
Furthermore, the personal and professional relationships of addicts suffer the most. They end up doing things or making decisions that do not work in their favor. This constraint the relationships of people and they drift apart.
Moreover, it also hampers their studies or work life. When you are spending all your money and time on your addiction, naturally your concentration levels in other things will drop. However, all this is not impossible to beat. There are many ways through which one can beat their addiction.
Get the huge list of more than 500 Essay Topics and Ideas
Beat Your Addiction
It is best to work towards beating your addiction rather than getting beat by it. One can try many ways to do so. Firstly, recognize and identify that you have an addiction problem. That is the first step to getting cured. You need to take some time and understand the symptoms in order to treat them. Motivate yourself to do better.
After that, understand that the journey will be long but worthwhile. Identify the triggers in your life and try to stay away from them as far as possible. There is no shame in asking for professional help. Always remember that professionals can always help you get better. Enroll yourself in rehabilitation programs and try to make the most out of them.
Most importantly, do not be hesitant in talking to your loved ones. Approach them and talk it out as they care most about you. They will surely help you get on the right path and help you in beating addiction for better health and life.
Q.1 What are the consequences of addiction?
A.1 Addiction has very severe consequences. Some of them are health hazards, monetary issues, relationship problems, adverse problems on studies and work of a person. It seriously hampers the quality of life of a person.
Q.2 How can one get rid of addiction?
A.2 A little help can go a long way. One can get rid of addiction by enrolling in rehabilitation programs and opening up about their struggle. Try to take professional help and talk with your close ones to become better.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App

- All Publications
- Priorities Magazine Spring 2018
- The Next Plague and How Science Will Stop It
- Priorities Magazine Winter 2018
- Priorities Magazine Fall 2017
- Little Black Book of Junk Science
- Priorities Magazine Winter 2017
- Should You Worry About Artificial Flavors Or Colors?
- Should You Worry About Artificial Sweeteners?
- Summer Health and Safety Tips
- How Toxic Terrorists Scare You With Science Terms
- Adult Immunization: The Need for Enhanced Utilization
- Should You Worry About Salt?
- Priorities Magazine Spring 2016
- IARC Diesel Exhaust & Lung Cancer: An Analysis
- Teflon and Human Health: Do the Charges Stick?
- Helping Smokers Quit: The Science Behind Tobacco Harm Reduction
- Irradiated Foods
- Foods Are Not Cigarettes: Why Tobacco Lawsuits Are Not a Model for Obesity Lawsuits
- The Prevention and Treatment of Osteoporosis: A Review
- Are "Low Dose" Health Effects of Chemicals Real?
- The Effects of Nicotine on Human Health
- Traditional Holiday Dinner Replete with Natural Carcinogens - Even Organic Thanksgiving Dinners
- A Primer On Dental Care: Quality and Quackery
- Nuclear Energy and Health And the Benefits of Low-Dose Radiation Hormesis
- Priorities in Caring for Your Children: A Primer for Parents
- Endocrine Disrupters: A Scientific Perspective
- Good Stories, Bad Science: A Guide for Journalists to the Health Claims of "Consumer Activist" Groups
- A Comparison of the Health Effects of Alcohol Consumption and Tobacco Use in America
- Moderate Alcohol Consumption and Health
- Irradiated Foods Fifth Edition
- Media/Contact
- Write For Us
The War on Drugs is Also a War on Pain Patients
Related articles.
In a recent New York Times essay, a professor of anesthesia and pain management recently protested the Drug Enforcement Administration's opioid manufacturing quotas and micromanagement of doctors treating their patients' pain. At a time when DEA S.W.A.T. teams frequently raid doctors' offices for "inappropriate" prescribing, the professor's essay demonstrated boldness. Unfortunately, the professor's reform proposals were much less bold.

In a March 22 opinion column in the New York Times entitled “The DEA Needs to Stay Out of Medicine,” Vanderbilt University Medical Center associate professor of anesthesiology and pain management Shravani Durbhakula, MD, documents powerfully how patients suffering from severe pain—many of them terminal cancer patients—have become collateral casualties in the government’s war on drugs.
Decrying the Drug Enforcement Administration’s progressive tightening of opioid manufacturing quotas, Dr. Durbhakula writes:
In theory, fewer opioids sold means fewer inappropriate scripts filled, which should curb the diversion of prescription opioids for illicit purposes and decrease overdose deaths — right? I can tell you from the front lines that that’s not quite right. Prescription opioids once drove the opioid crisis. But in recent years opioid prescriptions have significantly fallen, while overdose deaths have been at a record high. America’s new wave of fatalities is largely a result of the illicit market, specifically illicit fentanyl . And as production cuts contribute to the reduction of the already strained supply of legal, regulated prescription opioids, drug shortages stand to affect the more than 50 million people suffering from chronic pain in more ways than at the pharmacy counter.
Dr. Durbhakula provides stories of patients having to travel long distances to see their doctors in person due to DEA requirements about opioid prescriptions. However, despite their efforts, they find that many of the pharmacies do not have the opioids they require because of quotas. She writes:
Health care professionals and pharmacies in this country are chained by the Drug Enforcement Administration. Our patients’ stress is the result not of an orchestrated set of practice guidelines or a comprehensive clinical policy but rather of one government agency’s crude, broad‐stroke technique to mitigate a public health crisis through manufacturing limits — the gradual and repeated rationing of how much opioids can be produced by legitimate entities.
In the essay, Dr.Durbhakula does not question or challenge the false narrative that the overdose crisis originated with doctors “overprescribing” opioids to their pain patients.
Unfortunately, Dr. Durbhakula’s proposed policy recommendations would do little to advance patient and physician autonomy. She would merely transfer control over doctors treating pain from the cops to federal health bureaucracies and let those agencies set opioid production quotas. For instance, she claims, “It’s incumbent on us [doctors] to hand the reins of authority over to public health institutions better suited to the task.”
No. The “reins of authority” belong in the hands of patients and doctors.
Dr. Durbhakula suggests that “instead of defining medical aptness, the DEA should pass the baton to our nation’s public health agencies” and proposes that the Centers for Disease Control and Prevention and the Food and Drug Administration “collaborate” to “place controls on individual prescribing and respond to inappropriate prescribing.” She elides the fact that these public health agencies will “respond” to doctors or patients who don’t comply with their regulations by calling the cops.
To be sure, Dr. Durbhakula has good intentions. But replacing actual cops—the DEA—with federal health agencies that can order those cops to arrest non‐compliant doctors and patients is like rearranging the deck chairs on the Titanic. True, her proposed new pain management overlords would have greater medical expertise, but they would still reign over doctors and patients and assault their autonomy. And, as we learned during the COVID-19 pandemic, they will not be immune to political pressures and groupthink .
While her policy prescriptions may be flawed, Dr. Durbhakula deserves praise for having the courage to point out that the war on drugs is also a war on pain patients. Alas, courageous doctors are in short supply these days. Most doctors keep their heads down and follow the cops’ instructions.
After I read her essay, I wrote the following (unpublished) letter to the editor of the New York Times :
Dear Editor— Kudos to Dr. Durhakula for speaking out against the Drug Enforcement Administration’s intruding on doctors’ pain treatment (“ The DEA Needs to Stay Out of Medicine ,” March 22, 2024). As my colleague and I explained in our 2022 Cato Institute white paper, “ Cops Practicing Medicine ,” for more than 100 years, law enforcement has been increasingly surveilling and regulating pain management. The DEA maintains a schedule of substances it controls, and it categorizes them based on what the agency determines to be their safety and addictive potential. The DEA even presumes to know how many and what kind of controlled substances—from stimulants like Adderall to narcotics like oxycodone—the entire US population will need in future years, setting quotas on how many each pharmaceutical manufacturer may annually produce. The DEA restricts pain management based on the flawed assumption that what they consider to be “overtreatment” caused the overdose crisis. However, as my colleagues and I showed, there is no correlation between the opioid prescription rate and the rate of non‐medical opioid use or opioid addiction. And, of course, as fear of DEA reprisal has caused the prescription rate to drop precipitously in the last dozen years, overdose deaths have soared as the black market provided non‐medical users of “diverted” prescription pain pills first with more dangerous heroin and later with fentanyl. Researchers at the University of Pittsburgh School of Public Health found that overdose fatalities have been rising exponentially since at least the late 1970s, with different drugs predominating during various periods. Complex sociocultural, psychosocial, and socioeconomic forces are at the root of the overdose crisis, requiring serious investigation. Yet policymakers have chosen the lazy answer by blaming the overdose crisis on doctors treating pain. When cops practice medicine, overdoses increase, drug cartels get richer, and patients suffer. Sincerely, Jeffrey A. Singer, MD, FACS Senior Fellow, Cato Institute
When cops practice medicine, overdoses increase, drug cartels get richer, and patients suffer.
Reprinted with permission. Dr. Singer's original piece can be found here on the Cato Institute website
View the discussion thread.

By Jeffrey Singer
Jeffrey A. Singer, MD received his BA from Brooklyn College and his MD from New York Medical College. After completing his surgical residency and receiving Board Certification he began a private practice as a general surgeon in Phoenix, Arizona and became a Fellow of the American College of Surgeons. He is a Senior Fellow at the Cato Institute in Washington, DC, serving in the Department of Health Policy Studies. He is also a Visiting Fellow at the Goldwater Institute in Phoenix, AZ. His principal areas of scholarship are health care policy, drug policy, drug prohibition, and harm reduction. Dr. Singer has been practicing medicine for more than 30 years.
Latest from Jeffrey Singer :
The Disease and Harm Minimization Models of Addiction Essay
Introduction, the disease model of addiction, the harm minimization model of addiction, discussion & conclusion.
In the present day, addictions remain a global problem, with citizens of every country suffering from them. To deal with the problem and to create a universal concept for it, several models of addiction have been created. The (brain) disease model of addiction and the harm minimization (reduction) model of addiction are the most recognized now; they are, however, fundamentally different. The aim of the present paper is to conduct analysis on the two models, and demonstrate the better one based on a comparison. While the disease model is older and is, therefore, more tried and tested, it is now outdated, with its basic theory dehumanizing those addicted.
As mentioned above, the disease model of addiction has been firmly established in medical knowledge. The nurses are educated on it (Kaye et al., 2014, p. 231), including the matter of the lack of Vitamin B as a result of alcohol usage (Kaye et al., 2014, p. 237). In this case, Vitamin B is given in tablets to compensate (Kaye et al., 2014, p. 85). According to the theory, drug users are pathologic and consume drug excessively. While the brain disease model admits the importance of social and environmental studies, it does not include intention to analyse them (Tekin 2018). After a study with the model in conjunction with neuroscience, health care practitioners claimed that addiction took away drug users’ ability to choose, making medical intervention necessary (Szott, 2014). This was caused by drugs affecting the brain’s mesolimbic dopamine system (Tekin 2018). The mesolimbic dopamine system controls individual reactions to food, sex, and sociality.
Studies written in line with the disease model of addiction are numerous and touch upon different types of addiction. For example, Gainsbury et al. (2018) analyse gambling addiction; while their study includes behavioural assistance and increasing awareness, it includes legislation on interventions as well, making the state an actor in the case. Thus, according to the theory, drug users have no responsibility over their actions, and their actions are de-stigmatized; they are represented as a passive category.
The model now tends to attract more and more criticism. Kuorikoski & Uusitalo (2018) claim that the model should not position agency as a property of brain. They state that the decision are not solely made by brain, but by one’s commitments to those around them, changes in environment, and that an impression of medications making a brain healthy is flawed. The authors claim that addiction remains a social phenomenon as well, and understanding it simply as a brain disease creates an opportunity for harmful administrative or medical usage. Another point of their criticism is that the disease model of addiction tends to brand too many drug users as beyond help, denying medications for those could still receive help. Therefore, the disease model faces a lot of criticism, and even those who still use it, such as Gainsbury et al., do it in a combination with the different theory.
The other model is the harm minimization model of addiction. It pictures drug user as people who are currently at risk, but can improve by themselves if provided with the necessary instruments and information. An American organization called the Harm Reduction Coalition has created eight principles on the matter. Notably, one of them is to accept that drug usage is a part of one’s life and that the task at hand is not to condemn it, but to limit its harmful effects (Szott, 2014). To achieve this, it is advised to encourage people to save funds, including usage of augmented reality for it (Gainsbury et al., 2018). Kaye et al. state the main purposes of the harm minimization model as to “decrease consumption, decrease the hazards of consumption, increase social functioning, increase the potential for abstinence” (Kaye et al., 2014, p. 253). Thus, the model focuses on preventing the harmful effects of drug use through communication instead of judging and forbidding it.
Like the previous model, the harm minimization model is already widely used, despite being newer. For example, a Portuguese project called Kosmicare has gone through many difficulties to earn recognition, but has been functioning since 2000 (Soares 2017). Kosmicare is a harm reduction festival area, and its team is made of medical professionals. It is based on human rights and includes creating drug consumption facilities, education, and methadone maintenance (Soares 2017). While risk evaluation is not compatible with the project’s activity and the harm minimization model in general, the drug users are expected to conduct risk evaluation by themselves. Another case of usage of the harm minimization model deals is smoking. According to Abrams et al. (2018b), the model is effective in that area as it helps to move smokers to less dangerous ways of smoking such as e-cigarettes. The purpose is, therefore, to make tobacco cigarettes completely obsolete (Abrams et al., 2018a). The means to it are to inform people on the comparative influence of different ways of smoking, rather just the fact of smoking.
The models, as evident, are notably different from each other. In the disease model, the addiction is characterised as removing autonomy from the drug users, placing responsibility on medical personnel and authorities. In the harm reduction model, the drug takers maintain their autonomy and make their own decisions, with the medical professionals simply providing the options (Szott, 2014). Therefore, they most notably differ in their consideration of the patients.
Many medical scholars do not accept any one of the models, instead utilizing them both in one way or another. For example, Wakefield (2020) points out that, while the harsher forms of the disease model, such as the perception of drug users having brain damage, should be omitted, drug use is still a mental disorder. Barnett et al. (2018) argues for it as well, even outright stating that a ‘hybrid approach’ is necessary. A questionnaire by Szott (2014) and a different study by Barnett et al. (2017) demonstrate that many practicing doctors already tend to follow a ‘hybrid approach’, using harm minimizing practices. The latter even included allowing their patients to continue taking the drug in the case of a relapse. However, the same analysis has proved that, while doctors use harm minimizing practices, their purpose and perception of the problem remain in line with the disease model.
The ‘hybrid approach’ can be considered to only be temporary. As the models are fundamentally different, they may not be used in conjunction forever. For example, the disease model considers relapse a failure of treatment, while the harm minimization model allows for it on the condition of a safer manner (Bayles, 2014). In addition, the disease model requires significant funding, as the most treatment programs have failed, and new ones need to be invented (Hall et al., 2015). The depiction of drug use as a brain disease creates a negative image as well, provoking hostility and fear. Finally, the disease model fails to acknowledge that multiple factors cause drug use, and can be treated not just with medication, but with behavioural interventions as well (Tekin 2018). All of these factors prove that the disease model is outdated, and its fundamental incompatibility will stop its usage in the future altogether.
Abrams, D. B., Glasser, A. M., Pearson, J. L., Villanti, A. C., Collins, L. K., & Niaura, R. S. (2018a). Harm minimization and tobacco control: Reframing societal views of nicotine use to rapidly save lives . Annual Review of Public Health , 39 (1), 193–213. Web.
Abrams, D. B., Glasser, A. M., Villanti, A. C., Pearson, J. L., Rose, S., & Niaura, R. S. (2018b). Managing nicotine without smoke to save lives now: Evidence for harm minimization . Preventive Medicine , 117 , 88–97. Web.
Barnett, A. I., Hall, W., Fry, C. L., Dilkes-Frayne, E., & Carter, A. (2017). Drug and alcohol treatment providers’ views about the disease model of addiction and its impact on clinical practice: A systematic review . Drug and Alcohol Review , 37 (6), 697–720. Web.
Barnett, A. I., Hall, W., Fry, C. L., Dilkes-Frayne, E., & Carter, A. (2018). Implications of treatment providers’ varying conceptions of the disease model of addiction: A response . Drug and Alcohol Review , 37 (6), 729–730. Web.
Bayles, C. (2014). Using mindfulness in a harm reduction approach to substance abuse treatment: A literature review . International Journal of Behavioral Consultation and Therapy , 9 (2), 22–25. Web.
Gainsbury, S. M., Tobias-Webb, J., & Slonim, R. (2018). Behavioral Economics and gambling: A new paradigm for approaching harm-minimization . Gaming Law Review , 22 (10), 608–617. Web.
Hall, W., Carter, A., & Forlini, C. (2015). Brain disease model of addiction: Misplaced priorities? The Lancet Psychiatry , 2 (10), 867. Web.
Kaye, A. D., Vadivelu, N., & Urman, R. D. (Eds.). (2014). Substance Abuse: Inpatient and Outpatient Management for Every Clinician (2015th ed.). Springer.
Kuorikoski, J., & Uusitalo, S. (2018). Re-socializing the vulnerable brain: Building an ethically Sustainable brain disease model of addiction . Frontiers in Sociology , 3 . Web.
Soares, M., Carvalho, M. C., Valbom, M., & Rodrigues, T. (2017). Tackling harm reduction, human rights and drug uses on recreational environments: Tensions, potentialities and learnings from the KOSMICARE Project (Portugal). Revista Crítica De Ciências Sociais , (112), 3–24. Web.
Szott, K. (2014). Contingencies of the will: Uses of harm reduction and the disease model of addiction among Health Care Practitioners . Health: An Interdisciplinary Journal for the Social Study of Health, Illness and Medicine , 19 (5), 507–522. Web.
Tekin, S. (2018). Brain mechanisms and the disease model of addiction: is it the whole story of the addicted self? A philosophical-skeptical perspective. In H. Pickard & S. H. Ahmed (Eds.), The Routledge Handbook of Philosophy and Science of Addiction (pp. 401-410). Taylor & Francis.
Wakefield, J. C. (2020). Addiction from the Harmful Dysfunction Perspective: How there can be a mental disorder in a normal brain . Behavioural Brain Research , 389 , 112665. Web.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, April 1). The Disease and Harm Minimization Models of Addiction. https://ivypanda.com/essays/the-disease-and-harm-minimization-models-of-addiction/
"The Disease and Harm Minimization Models of Addiction." IvyPanda , 1 Apr. 2024, ivypanda.com/essays/the-disease-and-harm-minimization-models-of-addiction/.
IvyPanda . (2024) 'The Disease and Harm Minimization Models of Addiction'. 1 April.
IvyPanda . 2024. "The Disease and Harm Minimization Models of Addiction." April 1, 2024. https://ivypanda.com/essays/the-disease-and-harm-minimization-models-of-addiction/.
1. IvyPanda . "The Disease and Harm Minimization Models of Addiction." April 1, 2024. https://ivypanda.com/essays/the-disease-and-harm-minimization-models-of-addiction/.
Bibliography
IvyPanda . "The Disease and Harm Minimization Models of Addiction." April 1, 2024. https://ivypanda.com/essays/the-disease-and-harm-minimization-models-of-addiction/.
- Colorblind Racism and Its Minimization
- Trinity Health Organization's Challenges Minimization
- Waste Minimization at the Nowra Chemical Manufacturers
- Cost Minimization vs. Cost-Effectiveness Analyses
- American Estate Tax, Laws and Ways of Minimization
- Energy Consumption and Minimization Methods
- Minimization of New Building Carbon Footprint
- Terrorist Acts Prevention and Aftermaths Minimization
- Cost Minimization for a Firm's Production
- Minimization of Nurse Burnout: Outcomes, Approach, and Budget
- Cognitive Behavioral Group Therapy for Drug Addiction
- Combating Drug Addiction Through Integrated Treatment Solutions
- High Rates of Opioid Abuse in Low-Income Individuals
- Drug Abuse and Chip Technology
- The Importance of Alcoholics Anonymous Meetings
Home — Essay Samples — Nursing & Health — Drug Addiction — Drug Addiction – The Scourge Of Modern Society
Socio-cultural Context of Drug Addiction and Ways to Deal with It
- Categories: Drug Addiction Drugs
About this sample

Words: 1347 |
Published: Jul 15, 2020
Words: 1347 | Pages: 2 | 7 min read

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr Jacklynne
Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
2 pages / 799 words
4 pages / 1991 words
4 pages / 2018 words
1 pages / 536 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Drug Addiction
Drug addiction is a widely misunderstood condition. The timeless nature versus nurture debate is often brought up when discussing drug dependence. Is addiction a mental illness or a consequence of poor lifestyle choices? Are [...]
The Drug Enforcement Commission (DEC) has expressed concern about the increasing number of children who are engaged in alcohol and substance abuse. How can guidance counselors assist DEC to curb the problem of drug abuse?Use and [...]
A drug is any substance other than food that provides nutritional support that, when inhaled, injected, smoked, consumed, absorbed via a patch on the skin, or dissolved under the tongue causes a temporary physiological and often [...]
He lowers his hand to reach down, and curves a strong grip around her small wrist, abruptly stopping her in her tracks. “What is it, what's troubling you?” he asked in an anxious voice once again. “It's...I'm pregnant!” Finally [...]
Louse-borne typhus is one of the oldest pernicious diseases, that has been haunting mankind since ages. Known by the many names such as “camp fever”, “war fever”, “jail fever” and “tabarillo” and confused with many other fevers [...]
In 1946 the World HealthOrganisation (WHO) defined health as a ‘state of complete physical, mental and social well-being. This definition integrates the main concepts of health and identifies that health can be viewed [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Serial Season 4

“Serial” returns with a history of Guantánamo told by people who lived through key moments in Guantánamo’s evolution, who know things the rest of us don’t about what it’s like to be caught inside an improvised justice system.
Published March 21, 2024
Listen to and follow Serial Season 4
- Apple Podcasts

Listen to the trailer for Serial Season 4: Guantánamo.
Your browser doesn't support HTML5 audio. Try listening here.

“So, it felt very like college-like… Without it being… Obviously the next day wasn’t classes, it was Gitmo… ”
Poor baby raul, episode 1 — poor baby raul.

“I wanted to create a persona, a thing that was not human.”
The special project, episode 2 — the special project.
- Episode 3 arrives April 4
About Serial Season 4
Right after Sept. 11, the United States created a brand-new criminal justice system at Guantánamo Bay. It was a prison and a court designed to deal with the people we had captured whom we suspected of being members of the Taliban or al Qaeda.
But to do what we wanted to do at Guantánamo — to interrogate detainees the way we wanted, to hold them indefinitely without charging them with a crime — we had to push aside the old, time-tested rules for detaining prisoners of war. And the consequences of that fell on ordinary people: thousands of military personnel, hundreds of prisoners, everybody scrambling through the same experiment.
There has been great journalism about the legal maneuvering to justify Guantánamo, and about the detainee abuse and the politics and policy. But “Serial” reporters Sarah Koenig and Dana Chivvis were after the inside stories, a picture of Guantánamo you could get only from the people who went through it. For years, though, all the best stories they heard about Guantánamo were off the record. But they stuck with it, figuring maybe once enough people were back in civilian life they’d be willing to tell those stories on the record. A couple of years ago, the “Serial” team started contacting people again: guards, interrogators, commanders, lawyers, chaplains, translators and former prisoners. More than a hundred people. And a remarkable number of them said: Okay, I’m ready. Here’s what happened.
“Serial” Season 4 is a history of Guantánamo told by people who lived through key moments in its evolution, who know things the rest of us don’t about what it’s like to be caught inside an improvised justice system.

- Sofia degli Alessandri is an Italian composer based in London. Her music combines field recordings, synths, chamber instruments and electronic beats. She composes for film, television, dance and other media.
- Hosts Sarah Koenig and Dana Chivvis Producer Jessica Weisberg Editor Julie Snyder Additional Reporting Cora Currier Fact Checking and Research Ben Phelan Additional Fact Checking Jessica Suriano Music supervision, sound design, and mixing Phoebe Wang Original score Sofia degli Alessandri Additional Editing David Kestenbaum, Jen Guerra, Alvin Melathe, Ellen Weiss and Ira Glass Contributing Editors Rozina Ali and Carol Rosenberg Assistant Producer Emma Grillo Translators and Interpreters Raza Sayibzada, Nael Hijjo, Atiq Rahin, Dana El-Issa, Bachar Alhalabi, and Omama Osman Art Direction Pablo Delcan Art Max Guther Standards Editor Susan Wessling Legal Review Al-Amyn Sumar and Maya Gandhi Reporting and Research Amir Khafagy and Sami Yousafazai Additional Production Daniel Guillemette and Katie Mingle Executive Assistant Mack Miller Supervising Producer Ndeye Thioubou Deputy Managing Editor Sam Dolnick
- At the New York Times, thanks to Elizabeth Davis-Moorer, Nina Lassam, Susan Beachy, Kitty Bennett, Alain Delaquérière, Sheelagh McNeill, Kirsten Noyes, Jack Begg, Jeffrey Miranda, Colleen Wormsley, Peter Rentz, John-Michael Murphy, Jordan Cohen, Zoe Murphy, Pierre-Antoine Louis, Mahima Chablani, Kelly Doe, Anisha Muni, Kimmy Tsai, Victoria Kim, Ashka Gami, Brad Fisher, Maddy Masiello, Daniel Powell, Marion Lozano, Tug Wilson and Aisha Khan
- Special thanks Katie Mingle, Jenelle Pifer, Alissa Shipp, Nadia Reiman, Anita Badejo, Katie Fuchs, Alison Beckman at the Center for Victims of Torture, Clive Stafford Smith, Alisa Dogramadzieva, Shuaib Almosawa, Mohamed Elfaki, Freshta Taeb, Edgar August, Esther Whitfield, Lauren Myerscough-Mueller, Mark Fallon, Pardiss Kebriaei, Steve Vladeck, Charlie Savage, Michelle Shephard, Bastian Berbner, John Goetz, Sarah Mirk and everyone involved in “Guantánamo Voices,” Peter Jan Honigsberg, Tim Golden, John Ryan, Stuart Couch, Shayana Kadidal, Ray Rivera, Steven Kleinman, Steve Wood and Lee Riffaterre

Serial is a podcast from the creators of This American Life, hosted by Sarah Koenig. Serial tells one story — a true story — over the course of a season.
A high-school senior named Hae Min Lee disappeared one day after school in 1999, in Baltimore County, Maryland. A month later, her body was found in a city park. She'd been strangled. Her 17-year-old ex-boyfriend, Adnan Syed, was arrested for the crime, and within a year, he was sentenced to life in prison.
In May 2014, a U.S. Special Operations team in a Black Hawk helicopter landed in the hills of Afghanistan. Waiting for them were more than a dozen Taliban fighters and a tall American, who looked pale and out of sorts: Bowe Bergdahl. Bergdahl, a U.S. soldier, had been a prisoner of the Taliban for nearly five years, and now he was going home. Learn more
“Serial” is heading back to court. This time, in Cleveland. Not for one extraordinary case; instead, Serial wanted to tackle the whole criminal justice system. To do that we figured we’d need to look at something different: ordinary cases. So we did. Inside these ordinary cases we found the troubling machinery of the criminal justice system on full display. Learn more

Serial Productions makes narrative podcasts that have transformed the medium. From the powerful forces shaping our public schools to a mystery at the heart of a scandal that rocked Britain, Serial expands the boundaries of audio investigative storytelling. Learn more
Further Reading From The Times
The guantánamo docket, a closer look at what the u.s. lets you see of its war court at guantánamo bay, conditions at guantánamo are cruel and inhuman, u.n. investigation finds.
- Share full article
Podcasts From The New York Times
The Daily: The biggest stories, five days a week, including the indictment of Donald Trump , the implosion of Silicon Valley Bank and the threat to abortion pills .
The Run-Up: Astead W. Herndon grapples with the big ideas already animating the 2024 election by reporting from inside the political establishment .
Hard Fork: Kevin Roose and Casey Newton make sense of the world of tech, including Google's Place in the A.I. Arms Race and the arrival of GPT-4 .
Modern Love: Anna Martin unpacks the complicated love lives of real people, exploring topics like getting ghosted and how to stop searching for the perfect partner .
Popcast: A weekly conversation from Jon Caramanica and The Times’s music team, with roundtables on artists like Ice Spice , Taylor Swift and SZA .
From Opinion
The Ezra Klein Show: Real conversations on the forces shaping the world, such as the increasing pace of A.I. development and China's global influence .
First Person: Lulu Garcia-Navarro explores intimate conversations about big ideas, like the experiences of a war reporter and treating obesity as a disease.
Advertisement

IMAGES
COMMENTS
Drug addiction, also known as substance-use disorder, refers to the dangerous and excessive intake of legal and illegal drugs. This leads to many behavioral changes in the person as well as affects brain functions. Drug addiction includes abusing alcohol, cocaine, heroin, opioid, painkillers, and nicotine, among others.
Conclusion. Drug addiction is a multifaceted issue that requires a nuanced and comprehensive approach. By understanding the underlying causes of addiction, acknowledging the impact on individuals, families, and communities, and implementing effective prevention and treatment strategies, societies can work towards reducing the prevalence of drug addiction.
Impact of Drug Addiction on Society. Drug addiction has been a significant issue worldwide for many decades, impacting not only individuals addicted to illegal substances but also the society surrounding them. This essay aims to explore the influence of drug addiction on society at the local, national, and global scale.
4 pages / 1929 words. Introduction The allure of escaping reality often propels individuals towards the perilous path of drug and alcohol addiction. This essay endeavors to scrutinize the pervasive theme of substance abuse, as depicted in various literary and cinematic works.
Introduction. Drug and substance abuse is an issue that affects entirely all societies in the world. It has both social and economic consequences, which affect directly and indirectly our everyday live. Drug addiction is "a complex disorder characterized by compulsive drug use" (National Institute on Drug Abuse, 2010).
Drug addiction is a chronic disease characterized by drug seeking and use that is compulsive, or difficult to control, despite harmful consequences. Brain changes that occur over time with drug use challenge an addicted person's self-control and interfere with their ability to resist intense urges to take drugs.
One of the consequences of using drugs is, eventually, an individual becoming addicted. Addiction refers to a neuropsychological disorder that involves persistently feeling an urge to engage in particular behaviors despite the significant harm or negative effects. The psychology that explains addiction covers many areas, such as an illness or ...
The Mechanism of Addiction. The path to drug addiction commences with the voluntary act of taking drugs. Over time, a person's ability to choose not to consume becomes compromised; seeking and consuming the drug becomes compulsive. This behavior largely results from the effects of prolonged drug exposure on brain functioning.
Ms. Holimon explains that her father's conduct made her a very unhappy child and caused her to take drugs at a very early age. By the age of fifteen, she was a serious drug addict; however, she succeeded to graduate from high school and find a job as a secretary. Nonetheless, Ms. Holimon did not manage to preserve her working place on the ...
This essay was also published by Health Affairs on January 3, 2022. ... Drug addiction is a chronic but treatable disorder with well-understood genetic and social contributors. It is not a sign of a person's weakness or bad character. Continued or intermittent use of drugs, even by people who know they have a disorder and are trying hard to ...
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol.When considering other substances, the report estimated that 4.4 million individuals ...
Risky (hazardous) substance use refers to quantity/frequency indicators of consumption; SUD refers to individuals who meet criteria for a DSM-5 diagnosis (mild, moderate, or severe); and addiction ...
Essay on Drug Abuse in 250-300 words. Drug abuse is a growing global concern that poses significant risks to individuals, families, and communities. It refers to the excessive and harmful use of drugs, both legal and illegal, that have negative effects on physical and mental health. Drug abuse has severe consequences for individuals and society.
Its ability to stop appetite and improve the body's immune system is significant. 4. Caffeine. Some think, caffeine as a drug (and in some respects, this is the case), it also can eliminate addictive habits. Caffeine is used as a substitute for addiction to energy substances such as alcohol, ecstasy, or cocaine.
A drug is a natural or synthetic substance which when taken into a living body affects the normal functioning or structure and it is used in the diagnosis, mitigation, treatment or prevention of a disease. Drug misuse is using a [...] Drug addiction is a complex and contentious issue that has sparked debates for decades.
Many times in the examination and in any competition, essays are written on de-addiction or on the harm caused by drugs. If you are also looking for information about de-addiction essay, then read our today's article completely and learn how to write essay on de-addiction in 100, 150, 250, 500 words.
Cannabis often precedes or is used along with other substances, such as alcohol or illegal drugs, and is often the first drug tried. Signs and symptoms of recent use can include: A sense of euphoria or feeling "high". A heightened sense of visual, auditory and taste perception. Increased blood pressure and heart rate.
Drug abuse refers to the excessive and frequent consumption of drugs. Drug abuse can have several harmful effects on our mental and physical health. Ronald Reagan, the 40th President of the USA, passed the Anti-Drug Abuse Act of 1986 and initiated the War on Drugs. He said, 'Let us not forget who we are. Drug abuse is a repudiation of ...
500 Words Essay on Addiction Understanding Addiction. Addiction is a serious issue that affects many people around the world. It is a state where a person cannot stop using a substance or engaging in a behavior, even if it is harmful. The person becomes dependent on the substance or the activity to feel good or normal. Types of Addiction
500 Words Essay on Addiction. As we all know that excess of anything can be very dangerous, the same way, addiction of any kind can hamper the life quality of an individual. The phrase states that addiction is a family disease as one person uses and the whole family suffers. The above statement stands true in all its essence as the addict does ...
Presence of needles, syringes, etc. Steps for de-addiction: (i) Pyarmacotherapy — Treatment by medicine. (ii) Psychosocial therapy — Supportive care by family members and friends. (iii) Health restoration — Care taken to restore health, lost due to drugs, (iv) Psychological treatment — By experienced doctors.
How to prevent Drug addiction (essay) Illegal drugs tend to be highly addictive compared to those that are legal and cause far more damage to the body and organs than prescribed drugs. Unfortunately, consumers continue to buy and consume illegal drugs through the illegal drug trade that includes several developing countries that make a fortune ...
Page: 1. This essay sample was donated by a student to help the academic community. Papers provided by EduBirdie writers usually outdo students' samples. Cite This Essay. Download. As a student, I have read lots of stories and articles about the use of illegal drugs and drug addiction. I, too, have seen and heard various news about this topic ...
In a recent New York Times essay, a professor of anesthesia and pain management recently protested the Drug Enforcement Administration's opioid manufacturing quotas and micromanagement of doctors treating their patients' pain. At a time when DEA S.W.A.T. teams frequently raid doctors' offices for "inappropriate" prescribing, the professor's essay demonstrated boldness. Unfortunately, the ...
The Disease Model of Addiction. As mentioned above, the disease model of addiction has been firmly established in medical knowledge. The nurses are educated on it (Kaye et al., 2014, p. 231), including the matter of the lack of Vitamin B as a result of alcohol usage (Kaye et al., 2014, p. 237).
The drugs may vary from prescribed medications to narcotic drugs such cocaine, hashish, heroine etc. The use of these substances produces a craving or a physical addiction, which leads to regular intake of these drugs and is called 'Drug Addiction'. In severe cases the drug addict can neither lead a normal life nor survive without drugs.
"Serial" returns with a history of Guantánamo told by people who lived through key moments in Guantánamo's evolution, who know things the rest of us don't about what it's like to be ...