Advertisement

Preventing foot ulceration in diabetes: systematic review and meta-analyses of RCT data
- Open access
- Published: 27 November 2019
- Volume 63 , pages 49–64, ( 2020 )
Cite this article
You have full access to this open access article
- Fay Crawford ORCID: orcid.org/0000-0002-0473-9959 1 , 2 ,
- Donald J. Nicolson 1 ,
- Aparna E. Amanna 1 ,
- Angela Martin 1 ,
- Saket Gupta 1 ,
- Graham P. Leese 3 ,
- Robert Heggie 4 ,
- Francesca M. Chappell 5 &
- Heather H. McIntosh 6
12k Accesses
34 Citations
43 Altmetric
Explore all metrics
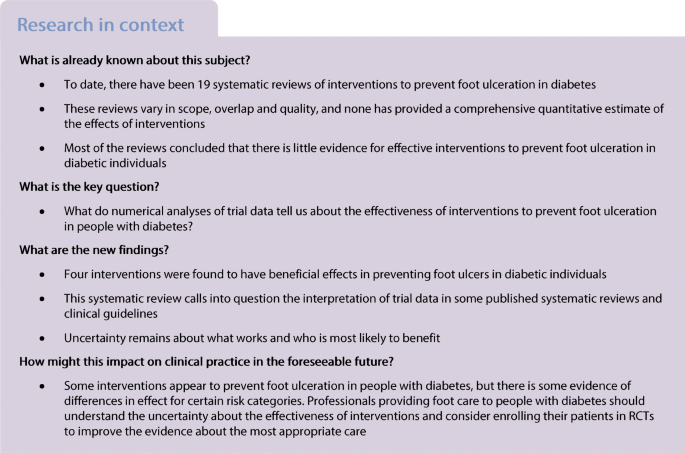
Aims/hypothesis
Foot ulceration is a serious complication for people with diabetes that results in high levels of morbidity for individuals and significant costs for health and social care systems. Nineteen systematic reviews of preventative interventions have been published, but none provides a reliable numerical summary of treatment effects. The aim of this study was to systematically review the evidence from RCTs and, where possible, conduct meta-analyses to make the best possible use of the currently available data.
We conducted a systematic review and meta-analysis of RCTs of preventative interventions for foot ulceration. OVID MEDLINE and EMBASE were searched to February 2019 and the Cochrane Central Register of Controlled Trials to October 2018. RCTs of interventions to prevent foot ulcers in people with diabetes who were free from foot ulceration at trial entry were included. Two independent reviewers read the full-text articles and extracted data. The quality of trial reporting was assessed using the Cochrane Risk of Bias tool. The primary outcome of foot ulceration was summarised using pooled relative risks in meta-analyses.
Twenty-two RCTs of eight interventions were eligible for analysis. One trial of digital silicone devices (RR 0.07 [95% CI 0.01, 0.55]) and meta-analyses of dermal infrared thermometry (RR 0.41 [95% CI 0.19, 0.86]), complex interventions (RR 0.59 [95% CI 0.38, 0.90], and custom-made footwear and offloading insoles (RR 0.53 [95% CI 0.33, 0.85]) showed beneficial effects for these interventions.
Conclusions/interpretation
Four interventions were identified as being effective in preventing foot ulcers in people with diabetes, but uncertainty remains about what works and who is most likely to benefit.
Similar content being viewed by others
Australian guideline on prevention of foot ulceration: part of the 2021 Australian evidence-based guidelines for diabetes-related foot disease
Michelle R. Kaminski, Jonathan Golledge, … on behalf of the Australian Diabetes-related Foot Disease Guidelines & Pathways Project

Epidemiology of diabetic foot disease and diabetes-related lower-extremity amputation in Australia: a systematic review protocol
Jaap J. van Netten, Mendel Baba & Peter A. Lazzarini

Australian guideline on wound healing interventions to enhance healing of foot ulcers: part of the 2021 Australian evidence-based guidelines for diabetes-related foot disease
Pamela Chen, Keryln Carville, … on behalf of the Australian Diabetes-related Foot Disease Guidelines & Pathways Project
Avoid common mistakes on your manuscript.
Introduction
Foot ulceration is a serious complication of diabetes that can result in high levels of morbidity for individuals and burdens health and social care systems with huge costs [ 1 , 2 ]. Predicting those people most likely to develop a foot ulcer has been the subject of much research and the independent risk factors have been established [ 3 , 4 ]. However, the value of prediction models to inform treatment decisions depends on the availability of effective interventions to modify risk [ 5 ].
As part of a wider research project to create a cost-effective, evidence-based pathway for assessing and managing the foot in diabetes, we conducted an overview of existing systematic reviews to synthesise the available evidence on treatment effects (PROSPERO registration: CRD42016052324). Although the overview identified 19 published reviews [ 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 ], it failed to provide reliable numerical summaries of effects because of limitations of the reviews in scope, overlap and quality [ 25 ]. A comprehensive review of RCTs was required to enable us to make the best possible use of the data currently available and re-explore the possibility of performing meta-analyses.
Our aim was to systematically review data from RCTs of interventions used to prevent foot ulcerations in diabetes, and to conduct meta-analyses to obtain pooled estimates of their effects. We included data from RCTs only, as this is the only method of clinical evaluation that controls for known, unknown and unmeasured confounding.
The protocol can be viewed at www.journalslibrary.nihr.ac.uk/programmes/hta/1517101 .
Eligibility criteria
Trials were permitted to include people of any age with a diagnosis of type 1 or type 2 diabetes, with or without a history of ulceration, but free from foot ulceration at trial entry.
Simple interventions (e.g. education aimed at individuals with diabetes or physicians, or the provision of footwear) and complex interventions (where several interventions were provided together) were eligible for inclusion. Standard care or active treatment were eligible as comparators.
Primary outcomes
We were primarily interested in foot ulcers (incident, primary and recurrent) reported as binary outcomes (present/absent). These could be defined, for example, as ‘a full-thickness skin defect that requires more than 14 days to heal’ [ 26 ] or according to a system of ulcer classification [ 27 ]. Primary outcomes were the absolute numbers of incident primary ulcers and of incident recurrent ulcers.
Secondary outcomes
In reports where foot ulceration was the primary outcome we also sought data on amputation (minor: involving the foot [intrinsic to the foot]; or major: involving the foot and leg); mortality; gangrene; infection; adverse events; harms; time to ulceration; quality of life (measured using the EuroQol five-dimensions questionnaire or the six- or 12-item Short Forms); timing of screening; self-care; hospital admissions; psychological (knowledge/behaviour); and adherence to therapy.
We searched OVID MEDLINE (see electronic supplementary material [ESM] Table 1 ) and OVID EMBASE (from inception to February 2019) and the Cochrane Central Register of Controlled Trials (to October 2018) for eligible RCTs, without language restrictions. ClinicalTrials.gov was searched for ongoing clinical trials (search date: 21 February 2019).
Trial selection and data extraction
One reviewer screened all titles and abstracts and a 10% random sample was checked by a second reviewer. Two reviewers working independently screened full-text articles and extracted data (D. J. Nicholson, and either F. Crawford or A. E. Amanna) about the included populations, including the risk classification, interventions, comparators and outcomes. For each trial we extracted absolute numbers on an intention-to-treat basis, where the numbers randomised to each group were available, and calculated RRs and 95% CIs. Where reports lacked information or clarity, we contacted the trial authors. Non-English language reports were translated.
Risk of bias (quality) assessment
We assessed the quality of trial reporting using the Cochrane Risk of Bias tool [ 28 ]. The five domains we assessed were: random sequence generation, allocation concealment, blinding of assessors to the outcome, incomplete outcome data and selective reporting [ 28 ]. We also noted whether an a priori sample size calculation was reported [ 29 ].
Data analysis
Absolute numbers were extracted and RRs and 95% CIs were calculated. Where it made clinical and statistical sense to pool the data, we undertook meta-analyses with trial data weighted according to the inverse variance method and assessed heterogeneity using the I 2 statistic [ 28 ]. Analyses were conducted using R version 3.4.2 ( https://cran.r-project.org ).
From 10,488 studies, 22 RCTs met our eligibility criteria [ 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 ]. A flow diagram showing the flow of information throughout the process of screening and selecting studies for inclusion in the review is presented in Fig. 1 and the characteristics of the included trials are described in Table 1 . Table 1 also incorporates the results from the risk of bias assessment; only five of the 22 trials [ 36 , 39 , 42 , 46 , 50 ] were judged to be at low risk of bias.
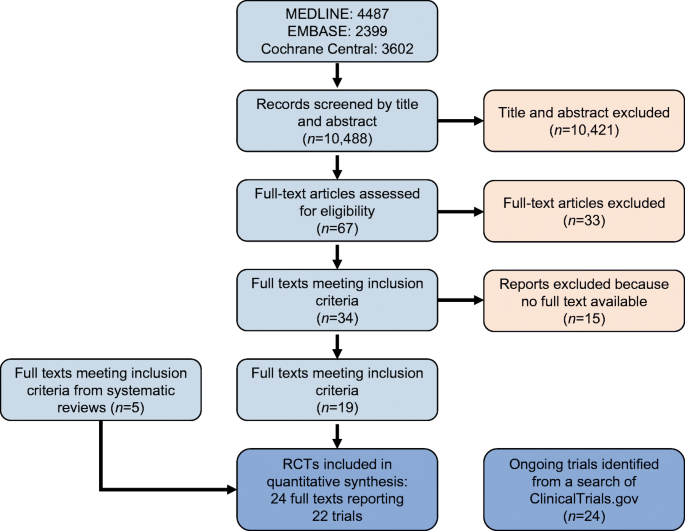
Flow diagram of study selection
Overall, the included trials assessed eight different types of interventions to prevent foot ulceration, which we grouped as follows: (1) education alone (three trials) [ 34 , 35 , 36 ]; (2) dermal infrared thermometry (four trials) [ 37 , 38 , 39 , 40 ]; (3) complex interventions (five trials) [ 41 , 42 , 43 , 44 , 45 ]; (4) custom-made footwear and offloading insoles (six trials) [ 46 , 47 , 48 , 49 , 50 , 51 ]; (5) digital silicone device (one trial) [ 32 ]; (6) antifungal treatment (one trial) [ 30 ]; (7) elastic compression stockings (one trial) [ 31 ]; and (8) podiatric care (one trial) [ 33 ].
Education alone
Three RCTs evaluated single-session education interventions of varying length and content for people at high risk of foot ulceration [ 34 , 35 , 36 ].
- Meta-analysis
( n = 423) (Fig. 2a ) showed no statistically significant difference in the incidence of foot ulceration at 6 months compared with standard care and advice (RR 1.04 [95% CI 0.54, 1.97]) [ 34 , 35 , 36 ]. The quality of the included trials was variable, with only one trial [ 36 ] judged to be at low risk of bias across all domains. Other sources of potential bias arose from one trial [ 34 ] being stopped early and another [ 35 ] reporting an interim analysis before target recruitment was reached [ 52 ].
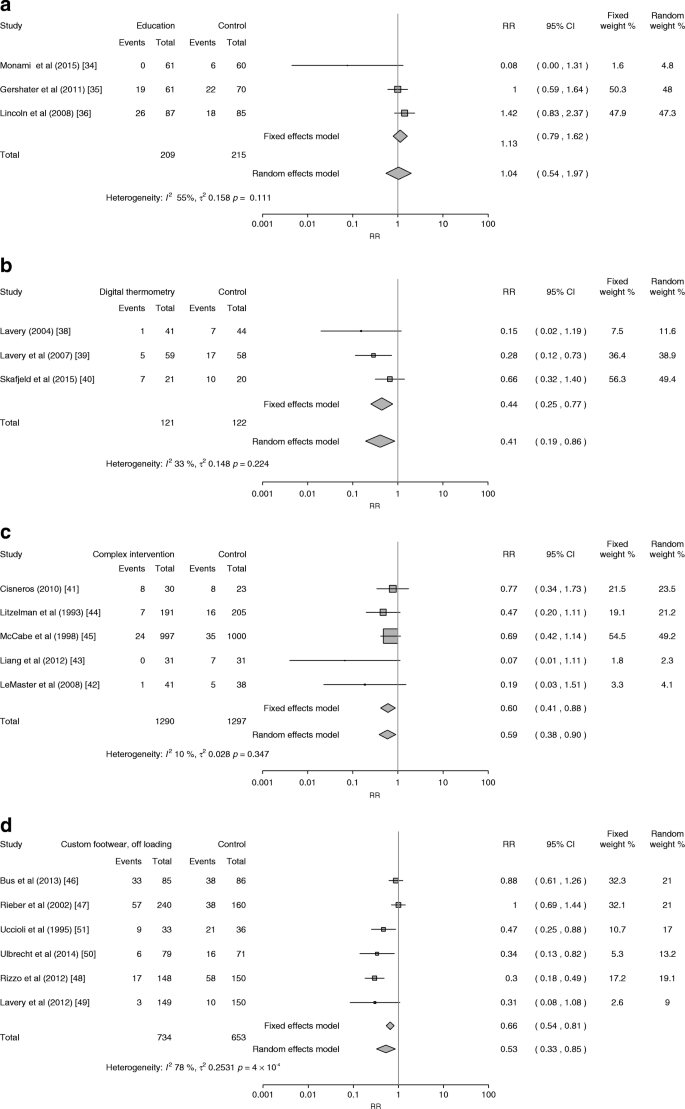
Forest plots of foot ulcers in people receiving standard care vs ( a ) education alone, ( b ) dermal infrared thermometry, ( c ) complex interventions and ( d ) custom-made footwear and offloading
Two trials of education interventions reported data on amputation [ 34 , 36 ], mortality [ 34 ], knowledge [ 34 ], behaviour [ 36 ] and/or quality of life [ 36 ]. No amputations were recorded for participants in either arm at 6 months’ follow-up in one trial [ 34 ]. The other trial reported 3/85 amputations in the intervention arm vs 0/85 in the control arm at 6 months, and no difference ( n = 9 in both arms) at 12 months [ 36 ].
One trial [ 34 ] reported that two participants, one in each arm, had died by 6 months. In the same trial, a statistically significant difference in knowledge (as measured by the Patient Interpretation of Neuropathy knowledge score) was observed in the intervention arm [ 34 ].
One trial [ 36 ] reported on quality of life and found no differences between the two arms on the Diabetic Foot Scale, but higher scores for those in the education arm on the Nottingham Assessment of Functional Footcare questionnaire, which assesses behaviour, compared with the control group.
Dermal infrared thermometry
Four RCTs involving 468 participants with diabetes were identified [ 37 , 38 , 39 , 40 ]. In one trial [ 37 ], the numbers of participants randomised to either dermal infrared thermometry or standard care were not known, and so an RR and 95% CI could not be calculated.
A pooled analysis of data from three RCTs ( n = 243) [ 38 , 39 , 40 ] found that dermal infrared thermometry reduced the number of foot ulcers in people with a history of foot ulceration (RR 0.41 [95% CI 0.19, 0.86]) (Fig. 2b ). Outcomes were collected between 6 and 15 months. The quality of these trials was variable, with only one trial [ 39 ] judged to be at low risk of bias across all domains.
Trials of dermal thermometry variously reported on amputation following infection [ 37 ], quality of life (36-item Short Form [SF-36]) [ 37 ], adherence to therapy [ 38 , 39 ] and time to ulceration [ 39 , 40 ].
In one trial, amputations following infections occurred in 0/41 participants in the intervention group vs 2/44 in the comparator group [ 38 ]. In the same trial there was no statistically significant difference in quality of life measured using SF-36 in any category or in the overall score [ 38 ].
Two trials [ 39 , 40 ] found no statistically significant difference between the dermal thermometry group and the comparator group in the time that prescribed footwear and insoles were worn, as measured using a self-report questionnaire containing an ordinal scale of <4 to >12 h/day. The time to ulceration was statistically significantly longer in the dermal thermometry treatment group compared with standard care in one trial [ 39 ] but not in another [ 40 ].
Complex interventions
Five RCTs evaluated the effects of complex interventions (i.e. integrated combinations of patient- or physician-level interventions and structural interventions) on the development of a foot ulcer [ 41 , 42 , 43 , 44 , 45 ].
A pooled analysis of data from five RCTs ( n = 2587) showed that complex interventions statistically significantly reduced the number of foot ulcers (RR 0.59 [95% CI 0.38, 0.90]) at 1 or 2 year follow-up (Fig. 2c ), with little evidence of statistical heterogeneity ( I 2 = 10%; Fig. 2c ) despite the variety of interventions tested. However, with the exception of one trial [ 42 ], all had a high risk of bias and the validity of these data may be compromised. One trial gave no information about the participants’ risk category [ 44 ], while three included people with no history of foot ulceration [ 41 , 43 ]. One trial included people who were at low/moderate or high risk of developing a foot ulcer, found that 75% of ulcers occurred in people with higher levels of risk; for the highest risk category (category 4), 2/6 individuals in the intervention group and 2/3 individuals in the comparator group developed foot ulcers [ 41 ].
None of the individual trial results reached statistical significance and only one [ 42 ] reported an a priori sample size calculation; however, one trial [ 45 ] recruited everyone attending the foot care service.
Amputation [ 43 , 45 ], time to ulceration [ 41 ] and/or knowledge [ 43 ] were reported in three trials. In one trial [ 43 ] amputations occurred only in the control arm (2/31 vs 0/31 in the intervention arm), and in a second trial [ 45 ] there were fewer amputations in the intervention group (one major and six minor amputations) compared with the control group (12 major and 13 minor) [ 45 ]. The time to ulceration was shorter in the control group vs the intervention group in one trial, but this did not reach statistical significance [ 41 ].
In one trial participants’ knowledge about foot care, as measured using a diabetes knowledge questionnaire, was statistically significantly better in the intervention group compared with the control group [ 43 ].
Custom-made footwear and offloading insoles
Six RCTs evaluated custom-made footwear and offloading insoles [ 46 , 47 , 48 , 49 , 50 , 51 ].
A pooled estimate of data from six trials showed a beneficial association for custom-made footwear and offloading insoles on reducing the development of foot ulcers (pooled RR 0.53 [95% CI 0.33, 0.85]; Fig. 2d ) for outcomes collected at 12–24 months in 1387 people, of whom 464 had no history of foot ulceration. There was evidence of considerable statistical heterogeneity ( I 2 = 78%), which we explored using baseline risk of ulceration in a subgroup analysis (Fig. 3 ). This pooled analysis of four trials [ 46 , 47 , 50 , 51 ], all of which excluded people with no history of foot ulceration, failed to detect a statistically significant difference (RR 0.71 [95% CI 0.47, 1.06]). The six trials were of variable quality, with only two [ 46 , 50 ] having a low risk of bias across all five domains.
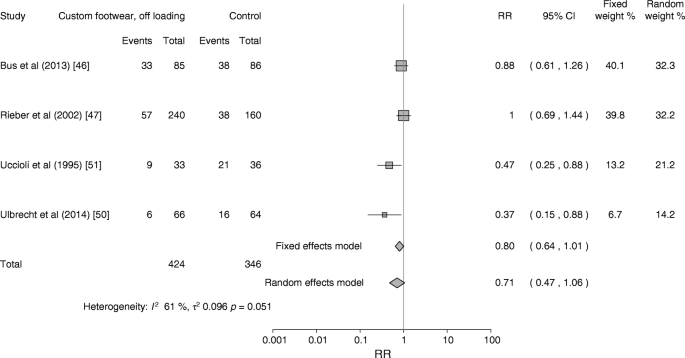
Subgroup analysis. Forest plot of foot ulcers in people with a history of foot ulceration receiving custom-made footwear and offloading vs standard care
Adherence [ 46 , 48 , 49 ] and/or cost [ 48 ] data were reported in four trials. One trial measured adherence using a temperature-based monitor placed inside the shoe, and found that 35/85 participants in the intervention group and 42/86 in the control group adhered to wearing their allocated footwear [ 46 ]. The trial authors conducted a subgroup analysis in participants who wore their allocated footwear, which showed a statistically greater reduction in ulcer recurrence in the intervention group; however, the analysis using data from the entire trial population failed to detect a beneficial association. A second trial of custom-made footwear and offloading insoles measured adherence using a self-reported physical activity questionnaire, and found that footwear and insole use was high in the groups who received cork inserts (83%) and prefabricated insoles (86%) [ 47 ]. A third trial measured participant compliance with footwear using self-reports of the number of hours per day that the shoes were worn. There were no statistically significant differences between each group in the number of people who wore the shoes for less than 4 h per day (23/149 vs 16/150), 4–8 h (77/149 vs 83/150), 8–12 h (38/149 vs 46/150) and 12–16 h (10/149 vs 6/150) [ 49 ].
Cost data collected in one trial published in 2012 found the cost of supplying footwear and insoles to be €675 per person per year [ 48 ].
Digital silicone devices
In one RCT of digital silicone devices [ 32 ], 167 participants with peripheral neuropathy, as defined by a vibration perception threshold of >25 V measured using a biothesiometer, and toe deformities (clawed toes, hallux valgus, interdigital lesions) were randomised to receive a bespoke silicone digital orthotic ( n = 89) or standard care ( n = 78). The number of ulcers was statistically significantly lower in the intervention group (RR 0.07 [95% CI 0.01, 0.55]) at 3 month follow-up. This trial had a low risk of bias in all domains except for allocation concealment, which was unclear.
Antifungal treatment
In a trial of antifungal nail lacquer, participants in the intervention group ( n = 34) received advice to inspect their feet daily and apply ciclopirox 8% to their toenails [ 30 ]. The control group ( n = 36) received advice about daily foot inspections. A history of foot ulcers was reported by 57% of participants. After 12 months there were two ulcerations in each group (RR 1.06 [95% CI 0.19, 5.76]). The risk of bias was unclear in two domains: allocation concealment and blinding of the outcome assessor.
Elastic compression stockings
An RCT of elastic stockings randomly allocated 160 people with no history of foot ulceration to either knee-length elastic stockings worn for 6 h/day or standard care [ 31 ]. There were three ulcers in the intervention group and ten in the control group, a difference that was not statistically significant (RR 0.37 [95% CI 0.11, 1.02]). The trial had a high or unclear risk of bias in the domains of sequence generation, allocation concealment and assessor blinding.
Thirteen limbs were reported as lost during the 48 month trial; 3/74 in the intervention arm and 10/75 in the control arm.
Podiatric care
One trial compared free chiropody care ( n = 47) with no chiropody care ( n = 44) for people all at high risk of foot ulceration [ 33 ]. Those receiving free chiropody were recommended to seek care at least once per month. The control group could seek chiropody if they were willing to pay for it, and their standard care included advice on the possible benefits of regular chiropody. There was no statistically significant difference in the number of ulcerations in the two groups (RR 0.67 [95% CI 0.43, 1.05]). This trial had a low risk of bias in all domains except assessor blinding to outcome data, which was unclear.
There were 2/47 amputations in the intervention arm vs 1/44 in the control arm. Deaths were recorded as 2/47 in the intervention arm vs 4/44 in the control arm [ 33 ].
Data for other secondary outcomes of interest, such as gangrene, self-care, hospital admissions, timing of screening and adverse events or harms, were absent from the trial reports.
Ongoing trials
The search for ongoing trials of foot ulcer prevention in diabetes from the ClinicalTrials.gov website found 24 studies being conducted worldwide. The stated interventions in these studies are: physiotherapy ( n = 1), skin temperature ( n = 6), hygiene ( n = 1), offloading insoles ( n = 10), risk stratification ( n = 2), PET-CT ( n = 1), amniotic tissue ( n = 1) and unclear ( n = 2). The list of these studies can be obtained from the corresponding author.
The purpose of this systematic review was to evaluate the evidence base and obtain summary statistics for preventative interventions for foot ulceration in diabetes to create a cost-effective, evidence-based care pathway. The meta-analyses of dermal infrared thermometry, complex interventions and therapeutic footwear with offloading insoles suggest that these interventions can help prevent foot ulceration in people with diabetes.
The meta-analysis of data from RCTs of dermal infrared thermometry in people with a history of foot ulceration and a moderate to high risk of ulceration indicates that this is a promising intervention deserving of further evaluation in randomised trials with larger participant samples, and we note from our search of the ClinicalTrials.gov trial registry that new trials are currently underway. If foot ulcer prevention can be confirmed in large, well-conducted trials, this form of self-monitoring could relieve pressure on healthcare systems. However, advising individuals to abstain from all weight-bearing activities when foot temperatures rise by more than 4°C may prove challenging, and poor adherence might diminish any benefit in a real-world context outside of a trial setting.
Specialist foot care, of the type evaluated in the included trials of complex interventions, is considered a marker of good-quality diabetes service delivery and it is intuitively correct to suppose it leads to improved outcomes. While a statistically significant reduction in foot ulcers was apparent in our meta-analysis, such an effect was not evident in any single trial. This does support the suggestion of others that very large sample sizes may be needed for trials of this nature [ 53 ]. Surprisingly, there was a low level of statistical heterogeneity in the pooled data, despite quite marked differences in the clinical care provided in the intervention arms of the trials and the participation of people with three different levels of ulcer risk.
Our review did not identify any trials of complex interventions that reflect the composition of multidisciplinary foot services as recommended in clinical guidelines [ 54 , 55 , 56 ]. These influential documents advise the involvement of diabetologists, podiatrists, vascular surgeons, diabetes specialist nurses and orthotists as the core team in a diabetes foot care service, but patient outcomes from such healthcare service arrangements have not been evaluated in RCTs. An evaluation of outcomes from people at different levels of ulceration risk who receive care in specialist foot care settings would be worthwhile.
The true value of therapeutic footwear and offloading insoles in preventing foot ulcers has been obscured by contradictory trial results and poor interpretation of data in systematic reviews; two larger trials involving only those with a history of foot ulcers both failed to detect evidence of effectiveness [ 46 , 47 ], and visual inspection of our analyses of pooled data from all six trials shows greatest beneficial effect in those where the majority of participants were considered to be at high or moderate risk but had not experienced a foot ulcer [ 48 , 49 ], albeit only one reached statistical significance [ 48 ]. Our subgroup analysis of data from four trials of participants with a history of foot ulceration found no statistically significant difference in the number of recurrent ulcers between the custom footwear and control groups.
This observation calls into question the conclusions of other systematic reviews evaluating footwear and insoles in the prevention of foot ulcers [ 6 , 17 , 24 ]. The most recent included randomised and non-randomised data and adopted a consensus approach to the analysis. The reviewers concluded that: ‘The evidence base to support the use of specific self-management and footwear interventions for the prevention of recurrent plantar foot ulcers is quite strong, but…is practically non-existent for the prevention of a first foot ulcer and non-plantar foot ulcer’ [ 24 ]. An individual participant data analysis using data from these six trials together with data from the ten ongoing studies of offloading insoles identified by our search of the ClinicalTrials.gov database could permit subgroup analyses to explore the value of footwear and offloading insoles in people with different baseline risks, and potentially resolve these ongoing uncertainties.
The marked reduction in ulcerations reported with the use of a dermal silicone device by individuals at high risk of ulceration is encouraging [ 32 ]. These devices are simple to make at the chair-side and easy for wearers to keep clean. Although they are a type of offloading intervention, we did not include these data in the meta-analysis of footwear and offloading insoles because they differ substantially in that they are only worn around the toes.
Three separate small trials [ 30 , 31 , 33 ] evaluating, respectively, the effects of a daily application of a fungal nail lacquer (ciclopirox 8%) with daily foot inspections, the use of elastic compression stockings and podiatry all failed to show a reduction in foot ulcers, possibly as a result of small sample sizes.
Strengths and limitations of this review
We have comprehensively reviewed a body of evidence from RCTs and made the fullest use of the data currently available to derive best estimates of treatment effects to inform a wider piece of work. In so doing we have highlighted uncertainties, gaps and limitations in the existing evidence base to inform practice, generated new research hypotheses and added value to this area of research.
The weaknesses of this review arise from the potential biases identified in many of the trial reports, especially for complex interventions, which may have produced unreliable results. Previous authors of systematic reviews have cited a lack of similarity between studies [ 13 ], lack of standardisation in terminology, prescription, manufacture and material properties of interventions [ 16 ], heterogeneity in study designs, methodology and participant populations [ 18 ], and differences in participant demographics [ 22 ] as reasons for not conducting meta-analyses, and we are aware of the potential limitations in the pooled analyses that we present here, both in the number and quality of trials. We have tried to produce conservative, less biased summary measures by adopting an intention-to-treat approach and a random-effects model. We acknowledge criticisms about the use of the latter [ 57 ], but believe the insights gleaned and the generation of new research hypotheses justifies our decision to pool data [ 58 ].
Conclusions
Our analyses found evidence of beneficial effects for four types of interventions used to prevent foot ulcers in people with diabetes, but considerable uncertainty remains about what works and who is most likely to benefit. Attention should be given to recommendations for the conduct of trials of interventions for the foot in diabetes, and researchers conducting future trials should endeavour to complete the trial to target recruitment as informed by an a priori sample size calculation [ 29 , 59 ].
Data availability
A copy of the extracted dataset can be obtained from the corresponding author.
Kerr M (2017) Diabetic foot care in England: an economic study. Diabetes UK, London
Google Scholar
Kerr M, Barron E, Chadwick P et al (2019) The cost of diabetic foot ulcers and amputations to the National Health Service in England. Diabet Med 36(8):995–1002
CAS PubMed Google Scholar
Crawford F, Cezard G, Chappell FM, on behalf of the PODUS group (2018) The development and validation of a multivariable prognostic model to predict foot ulceration in diabetes using a systematic review and individual patient data meta-analyses. Diabet Med 35(11):1480–1493
Monteiro-Soares M, Ribas R, Pereira da Silva C et al (2017) Diabetic foot ulceration development risk classifications’ validation: a multicentre prospective cohort study. Diabetes Res Clin Pract 127:105–114
Steyerberg EW (2009) Clinical prediction models: a practical approach to development, validation, and updating. Springer, New York
Arad Y, Fonseca V, Peters A, Vinik A (2011) Beyond the monofilament for the insensate diabetic foot: a systematic review of randomized trials to prevent the occurrence of plantar foot ulcers in patients with diabetes. Diabetes Care 34(4):1041–1046
PubMed PubMed Central Google Scholar
Binning J, Woodburn J, Bus SA, Barn R (2019) Motivational interviewing to improve adherence behaviours for the prevention of diabetic foot ulceration. Diabetes Metab Res Rev 35(2):e3105
PubMed Google Scholar
Dorresteijn JA, Kriegsman DM, Assendelft WJ, Valk GD (2012) Patient education for preventing diabetic foot ulceration. Cochrane Database Syst Rev, Issue 10, Art. no.: CD001488. https://doi.org/10.1002/14651858.CD001488.pub4
He JD, Zhang L, Liu L, Zhu YJ (2013) Intensive versus routine education on diabetes mellitus for prevention diabetic foot ulcer: a systematic review. Chinese J Evid Based Med 13(12):1470–1474
Hoogeveen RC, Dorresteijn JA, Kriegsman DM, Valk GD (2015) Complex interventions for preventing diabetic foot ulceration. Cochrane Database Syst Rev, Issue 8, Art. no.: CD007610
Kaltenthaler E, Morrell CJ, Booth A, Akehurst RL (1998) The prevention and treatment of diabetic foot ulcers: a review of clinical effectiveness studies. J Clin Effect 3(3):99–104
Mason J, O’Keeffe C, McIntosh A, Hutchinson A, Booth A, Young RJ (1999) A systematic review of foot ulcer in patients with type 2 diabetes mellitus. I: Prevention. Diabet Med 16(10):801–812
O’Meara S, Cullum N, Majid M, Sheldon T (2000) Systematic reviews of wound care management: (3) antimicrobial agents for chronic wounds; (4) diabetic foot ulceration. Health Technol Assess 4(21):1–237
Spencer SA (2000) Pressure relieving interventions for preventing and treating diabetic foot ulcers. Cochrane Database Syst Rev, Issue 3, Art. no. CD002302. https://doi.org/10.1002/14651858.CD002302
Buckley CM, Perry IJ, Bradley CP, Kearney PM (2013) Does contact with a podiatrist prevent the occurrence of a lower extremity amputation in people with diabetes? A systematic review and meta-analysis. BMJ Open 3(5):pii: e002331
Bus SA, Valk GD, van Deursen RW et al (2008) The effectiveness of footwear and offloading interventions to prevent and heal foot ulcers and reduce plantar pressure in diabetes: a systematic review. Diabetes Metab Res Rev 24(Suppl 1):S162–S180
Bus SA, van Deursen RW, Armstrong DG, Lewis JE, Caravaggi CF, Cavanagh PR on behalf of the International Working Group on the Diabetic Foot (IWGDF) (2015) Footwear and offloading interventions to prevent and heal foot ulcers and reduce plantar pressure in patients with diabetes: a systematic review. Diabetes Metab Res Rev 32(Suppl 1):99–118
Healy A, Naemi R, Chockalingam N (2013) The effectiveness of footwear as an intervention to prevent or to reduce biomechanical risk factors associated with diabetic foot ulceration: a systematic review. J Diabetes Complicat 27(4):391–400
Heuch L, Streak Gomersall J (2016) Effectiveness of offloading methods in preventing primary diabetic foot ulcers in adults with diabetes: a systematic review. JBI Database System Rev Implement Rep 14(7):236–265
Maciejewski ML, Reiber GE, Smith DG, Wallace C, Hayes S, Boyko EJ (2004) Effectiveness of diabetic therapeutic footwear in preventing reulceration. Diabetes Care 27(7):1774–1782
Mayfield JA, Sugarman JR (2000) The use of the Semmes-Weinstein monofilament and other threshold tests for preventing foot ulceration and amputation in persons with diabetes. J Fam Pract 49(11 Suppl):S17–S29
Paton J, Bruce G, Jones R, Stenhouse E (2011) Effectiveness of insoles used for the prevention of ulceration in the neuropathic diabetic foot: a systematic review. J Diabetes Complicat 25(1):52–62
Ahmad Sharoni SK, Minhat HS, Mohd Zulkefli NA, Baharom A (2016) Health education programmes to improve foot self-care practices and foot problems among older people with diabetes: a systematic review. Int J Older People Nursing 11(3):214–239
van Netten JJ, Price PE, Lavery LA et al (2016) Prevention of foot ulcers in the at-risk patient with diabetes: a systematic review. Diabetes Metab Res Rev 32(Suppl 1):84–98
Ballard M, Montgomery P (2017) Risk of bias in overviews of review: a scoping review of methodological guidance and four-item checklist. Res Synth Methods 8(1):92–108
Boyko EJ, Ahroni JH, Stensel V, Forsberg RC, Davignon DR, Smith DG (1999) A prospective study of risk factors for diabetic foot ulcer: the Seattle Diabetic Foot Study. Diabetes Care 22(7):1036–1042
Frykberg RG (2002) Diabetic foot ulcers: pathogenesis and management. Am Fam Physician 66(9):1655–1662
Higgins JPT, Green S (eds) (2011) Cochrane handbook for systematic reviews of interventions 5.1.0 [updated March 2011]. The Cochrane Collaboration. Available from www.Cochrane-handbook.org
Jeffcoate WJ, Bus SA, Game FL, Hinchliffe RJ, Price PE, Schaper NC (2016) Reporting standards of studies and papers on the prevention and management of foot ulcers in diabetes: required details and markers of good quality. Lancet Diabetes Endocrinol 4(9):781–788
Armstrong DG, Holtz K, Wu S (2005) Can the use of a topical antifungal nail lacquer reduce risk for diabetic foot ulceration? Results from a randomised controlled pilot study. Int Wound J 2(2):166–170
Belcaro G, Laurora G, Cesarone MR, Pomante P (1992) Elastic stockings in diabetic microangiopathy. Long term clinical and microcirculatory evaluation. Vasa 21(2):193–197
Scirè V, Leporati E, Teobaldi I, Nobili LA, Rizzo L, Piaggesi A (2009) Effectiveness and safety of using Podikon digital silicone padding in the primary prevention of neuropathic lesions in the forefoot of diabetic patients. J Am Podiatr Med Assoc 99(1):28–34
Plank J, Haas W, Rakovac I et al (2003) Evaluation of the impact of chiropodist care in the secondary prevention of foot ulcerations in diabetic subjects. Diabetes Care 26(6):1691–1695
Monami M, Zannoni S, Gaias M, Nreu B, Marchionni N, Mannucci E (2015) Effects of a short educational program for the prevention of foot ulcers in high-risk patients: a randomized controlled trial. Int J Endocrinol 2015:615680
Annersten Gershater M, Pilhammar E, Apelqvist J, Alm-Roijer C (2011) Patient education for the prevention of diabetic foot ulcers: interim analysis of a randomised controlled trial due to morbidity and mortality of participants. Eur Diabetes Nurs 8(3):102b–107b
Lincoln NB, Radford KA, Game FL, Jeffcoate WJ (2008) Education for secondary prevention of foot ulcers in people with diabetes: a randomised controlled trial. Diabetologia 51(11):1954–1961
Armstrong DG, Holtz-Neiderer K, Wendel C, Mohler MJ, Kimbriel HR, Lavery LA (2007) Skin temperature monitoring reduces the risk for diabetic foot ulceration in high-risk patients. Am J Med 120(12):1042–1046
Lavery LA (2004) Home monitoring of skin temperatures to prevent ulcerations. Diabetes Care 27(11):2642–2647
Lavery LA, Higgins KR, Lanctot DR et al (2007) Preventing diabetic foot ulcer recurrence in high-risk patients: use of temperature monitoring as a self-assessment tool. Diabetes Care 30(1):14–20
Skafjeld A, Iversen MM, Holme I, Ribu L, Hvaal K, Kilhovd BK (2015) A pilot study testing the feasibility of skin temperature monitoring to reduce recurrent foot ulcers in patients with diabetes—a randomized controlled trial. BMC Endocr Disord 15:55
Cisneros LL (2010) Evaluation of a neuropathic ulcers prevention program for patients with diabetes. Rev Bras Fisioter 14(1):31–37
LeMaster JW, Mueller MJ, Reiber GE, Mehr DR, Madsen RW, Conn VS (2008) Effect of weight-bearing activity on foot ulcer incidence in people with diabetic peripheral neuropathy: feet first randomized controlled trial. Phys Ther 88(11):1385–1398
Liang R, Dai X, Zuojie L, Zhou A, Meijuan C (2012) Two-year foot care program for minority patients with type 2 diabetes mellitus of Zhuang tribe in Guangxi, China. Can J Diabetes 36(1):15–18
Litzelman DK, Slemenda CW, Langefeld CD et al (1993) Reduction of lower extremity clinical abnormalities in patients with non-insulin-dependent diabetes mellitus: a randomized, controlled trial. Ann Intern Med 119(1):36–41
McCabe CJ, Stevenson RC, Dolan AM (1998) Evaluation of a diabetic foot screening and protection programme. Diabet Med 15(1):80–84
Bus SA, Waaijman R, Arts M et al (2013) Effect of custom-made footwear on foot ulcer recurrence in diabetes: a multicenter randomized controlled trial. Diabetes Care 36(12):4109–4116
Reiber GE, Smith DG, Wallace C et al (2002) Effect of therapeutic footwear on foot reulceration in patients with diabetes: a randomized controlled trial. JAMA 287(19):2552–2558
Rizzo L, Tedeschi A, Fallani E et al (2012) Custom-made orthesis and shoes in a structured follow-up program reduces the incidence of neuropathic ulcers in high-risk diabetic foot patients. Int J Low Extrem Wounds 11(1):59–64
Lavery LA, Lafontaine J, Higgins KR, Lanctot DR, Constantinides G (2012) Shear-reducing insoles to prevent foot ulceration in high-risk diabetic patients. Adv Skin Wound Care 25(11):519–524
Ulbrecht JS, Hurley T, Mauger DT, Cavanagh PR (2014) Prevention of recurrent foot ulcers with plantar pressure-based in-shoe orthoses: the CareFUL prevention multicenter randomized controlled trial. Diabetes Care 37(7):1982–1989
Uccioli L, Faglia E, Monticone G et al (1995) Manufactured shoes in the prevention of diabetic foot ulcers. Diabetes Care 18(10):1376–1378
Pocock S (1992) When to stop a clinical trial. BMJ 305(6847):235–240
CAS PubMed PubMed Central Google Scholar
Jeffcoate WJ (2011) Stratification of foot risk predicts the incidence of new foot disease, but do we yet know that the adoption of routine screening reduces it? Diabetologia 54(5):991–993
SIGN (2010; updated 2017) SIGN 116: management of diabetes: a national clinical guideline. Available from www.sign.ac.uk/assets/sign116.pdf . Accessed 5 June 2019
National Institute for Health and Care Excellence (2015) Diabetic foot problems: prevention and management. Available from www.nice.org.uk/guidance/ng19/resources/diabetic-foot-problems-prevention-and-management-pdf-1837279828933 . Accessed 6 June 2019
IWGDF (2019) IWGDF guidelines on the prevention and management of diabetic foot disease. Available from https://iwgdfguidelines.org/wp-content/uploads/2019/05/IWGDF-Guidelines-2019.pdf . Accessed 5 June 2019
Kirkwood BR, Sterne JAC (2003) Essential medical statistics, 2nd edn. Blackwell Science, Oxford
Freemantle N, Wood J, Crawford F (1998) Evidence into practice, experimentation and quasi experimentation: are the methods up to the task? J Epidemiol Community Health 52(2):75–81
Jeffcoate WJ, Vileikyte L, Boyko EJ, Armstrong DG, Boutlon AJM (2018) Current challenges and opportunities in the prevention and management of diabetic foot ulcers. Diabetes Care 41(4):645–652
Download references
Acknowledgements
We thank M. Smith (NHS Fife librarian) and our public partner W. Morrison (Dunfermline, UK) for their help and enthusiasm during the project. We also thank the following for their kind replies to our requests for clarification and additional information about their trials: D. G. Armstrong (University of Southern California, Los Angeles, CA, USA), L. Cisernos (Universidad Federal de Minas Gerais, Brazil), C. Chan (University of Alberta, Edmonton, AB, Canada), J. Everett (University of Calgary, AB, Canada), M. Gershater (Malmö University, Sweden), T. Kelechi (Medical University of South Carolina, Charleston, SC, USA), L. Lavery (University of Texas, Austin, TX, USA), D. Litzelman (Indiana University, Bloomington, IN, USA), S. Morgan (University of Washington, Seattle, WA, USA) and A. Piaggesi (University of Pisa, Italy). We appreciate the help received from two anonymous journal referees for their insightful comments and suggestions for improving our manuscript.
Members of the wider project team who were not directly involved in this research were: K. Gray (R&D Department, NHS Fife), D. Weller (Department of General Practice, University of Edinburgh), J. Brittenden (Institute of Cardiovascular and Medical Sciences, University of Glasgow), J. Lewsey and N. Hawkins (both Health Economics and Health Technology Assessment [HEHTA], Institute of Health and Wellbeing, University of Glasgow).
This systematic review was funded by the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) Programme (HTA project: 15/171/01) as part of a wider project. The views expressed are those of the authors and not necessarily those of the NIHR or the UK Department of Health and Social Care.
Author information
Authors and affiliations.
NHS Fife, Queen Margaret Hospital, Dunfermline, KY12 0SU, UK
Fay Crawford, Donald J. Nicolson, Aparna E. Amanna, Angela Martin & Saket Gupta
School of Medicine, University of St Andrews, Fife, UK
Fay Crawford
NHS Tayside, Dundee, UK
Graham P. Leese
Health Economics and Health Technology Assessment (HEHTA) Institute of Health and Wellbeing College of Medical, Veterinary and Life Sciences, University of Glasgow, Glasgow, UK
Robert Heggie
The Centre for Clinical Brain Sciences (CCBS) Neuroimaging Sciences, University of Edinburgh, Edinburgh, UK
Francesca M. Chappell
Healthcare Improvement Scotland, Glasgow, UK
Heather H. McIntosh
You can also search for this author in PubMed Google Scholar
Contributions
All authors made substantial contributions to the concept or design of the work or the acquisition, analysis or interpretation of data for the work and have drafted the manuscript critically and approved the final version. FC, FMC and HHM are the guarantors of this research and accept full responsibility for the work and/or the conduct of the study, had access to the data and controlled the decision to publish.
Corresponding author
Correspondence to Fay Crawford .
Ethics declarations
The authors declare that there is no duality of interest associated with this manuscript.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
(PDF 407 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Reprints and permissions
About this article
Crawford, F., Nicolson, D.J., Amanna, A.E. et al. Preventing foot ulceration in diabetes: systematic review and meta-analyses of RCT data. Diabetologia 63 , 49–64 (2020). https://doi.org/10.1007/s00125-019-05020-7
Download citation
Received : 03 July 2019
Accepted : 20 August 2019
Published : 27 November 2019
Issue Date : January 2020
DOI : https://doi.org/10.1007/s00125-019-05020-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Evidence-based healthcare
- Systematic review
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 20 October 2022
Reliability of the evidence to guide decision-making in foot ulcer prevention in diabetes: an overview of systematic reviews
- Fay Crawford ORCID: orcid.org/0000-0002-0473-9959 1 ,
- Donald J. Nicolson 2 ,
- Aparna E. Amanna 2 &
- Marie Smith 2
BMC Medical Research Methodology volume 22 , Article number: 274 ( 2022 ) Cite this article
2587 Accesses
2 Citations
1 Altmetric
Metrics details
Reliable evidence on the effectiveness of interventions to prevent diabetes-related foot ulceration is essential to inform clinical practice. Well-conducted systematic reviews that synthesise evidence from all relevant trials offer the most robust evidence for decision-making. We conducted an overview to assess the comprehensiveness and utility of the available secondary evidence as a reliable source of robust estimates of effect with the aim of informing a cost-effective care pathway using an economic model. Here we report the details of the overview. [PROSPERO Database (CRD42016052324)].
Medline (Ovid), Embase (Ovid), Epistomonikos, Cochrane Database of Systematic Reviews (CDSR), Database of Abstracts of Reviews of Effectiveness (DARE), and the Health Technology Assessment Journals Library were searched to 17th May 2021, without restrictions, for systematic reviews of randomised controlled trials (RCTs) of preventive interventions in people with diabetes. The primary outcomes of interest were new primary or recurrent foot ulcers. Two reviewers independently extracted data and assessed the risk of bias in the included reviews.
The overview identified 30 systematic reviews of patient education, footwear and off-loading, complex and other interventions. Many are poorly reported and have fundamental methodological shortcomings associated with increased risk of bias. Most concerns relate to vague inclusion criteria (60%), weak search or selection strategies (70%) and quality appraisal methods (53%) and inexpert conduct and interpretation of quantitative and narrative evidence syntheses (57%). The 30 reviews have collectively assessed 26 largely poor-quality RCTs with substantial overlap.
Interpretation
The majority of these systematic reviews of the effectiveness of interventions to prevent diabetic foot ulceration are at high risk of bias and fail to provide reliable evidence for decision-making. Adherence to the core principles of conducting and reporting systematic reviews is needed to improve the reliability of the evidence generated to inform clinical practice.
Peer Review reports
Diabetes mellitus is a major global public health problem. In 2019, 463 million adults around the world were living with diabetes and projections predict an increase in prevalence to 578 million by 2030 and 700 million by 2045 [ 1 ]. In the UK alone it is estimated that 5 million people will have diabetes by 2030 [ 2 ]. People with diabetes are more at risk of developing foot problems with those affected experiencing higher rates of foot ulceration, lower-limb amputation and premature death [ 3 , 4 ]. The healthcare costs of diabetic foot ulcers and amputations to the NHS in England has been estimated at between £837 and £962 million, almost 1% of the NHS budget, with more than 90% of that expenditure related to ulceration [ 3 ].
Reliable evidence on the clinical effectiveness of preventive interventions is imperative to design effective care pathways that can reduce the risk of foot ulceration and its adverse consequences for people with diabetes and the associated healthcare costs. As part of a wider research project to develop an evidence-based care pathway we sought to obtain numerical estimates of effect from randomised controlled trials (RCTs) of interventions to prevent diabetic foot ulceration as RCTs have the advantage over other study designs when evaluating interventions because only a randomly allocated control group comparison can prevent systematic differences at baseline influencing the results and support reliable claims about cause and effect [ 5 , 6 ].
Systematic review methods are widely used to summarise the evidence generated by multiple individual primary studies of alternative interventions to support decision-making and inform clinical practice, guidelines and health policy [ 6 , 7 ]. Well-conducted systematic reviews based on explicit methods that identify, appraise and summarise the findings from all relevant primary studies of the same and alternative interventions can determine which results are sufficiently reliable to inform practice and provide more accurate estimates of effect than individual studies alone. It is however becoming increasingly common to find multiple systematic reviews in the published literature that address the same clinical questions [ 8 , 9 ]. In this situation an overview can provide a comprehensive summary of the evidence base and reduce the research duplication and waste that is generated by conducting unnecessary additional reviews [ 10 , 11 ]. Overviews have a similar structure and methodology to systematic reviews but include reviews rather than primary studies [ 12 ].
Several published systematic reviews of preventative interventions for foot ulceration in diabetes are known to exist, some of which reach conflicting conclusions [ 13 , 14 ]. We conducted an overview to assess the comprehensiveness and utility of the available secondary evidence as a reliable source of robust estimates of effect with the aim of informing a cost-effective care pathway using an economic model, based on numerical data [ 5 ]. Although we identified 19 systematic reviews (one of which had been updated) limitations in scope, overlap and quality meant we had to undertake an additional systematic review in order to make the best possible use of the available data [ 14 ]. The purpose of this overview is to update the original searches for eligible reports and to consider the quality and reliability of systematic reviews of preventative interventions for foot ulceration in diabetes.
The overview protocol was registered on the PROSPERO Database (registration number: CRD42016052324).
The literature search, selection and appraisal methods are summarised here and reported in detail elsewhere [ 5 ].
Search strategy
A librarian (MS) developed strategies to identify systematic reviews in Medline OVID and Embase OVID (initially from inception to December 2019 then re-run to update the searches until 17th May 2021) without restrictions. The first searches were de duplicated using RefWorks. The electronic search strategies were informed by the strategies reported elsewhere [ 11 ] and include methodological search terms (see Additional file 1 : supplementary files). The Cochrane Database of Systematic Reviews (CDSR), the Database of Abstracts of Reviews of Effectiveness (DARE), and the Health Technology Assessment (HTA) Journals Library and (for the update search only, Epistomonikos) were also searched. Systematic reviews in progress were identified via PROSPERO ( https://www.crd.york.ac.uk/prospero/ ) and checked for subsequent completion or publication. Reference lists in all eligible reviews were browsed for additional relevant reviews. Additional data and clarifications about their reviews were sought from review authors.
Eligibility criteria
Systematic reviews of RCTs of interventions to prevent foot ulceration in people with type 1 or type 2 diabetes whether at high, medium, or low risk, with or without a history of foot ulceration but no existing foot ulcers at baseline were eligible for inclusion. The outcomes of interest were incident primary or recurrent foot ulcers and Lower Extremity Amputations (LEA) derived from RCTs comparing single-component or complex interventions (comprising several interacting components provided together) with standard care or alternative interventions. We excluded reviews of surgical procedures. Systematic reviews that included RCTs and other study designs were eligible for inclusion but only data from the relevant RCTs was used for the purpose of the overview.
Selection and data extraction
One reviewer (DJN or FC) screened all titles and abstracts to identify potentially relevant reviews with a second reviewer (FC or HMc) screening a 10% random sample to minimise the risk of errors of judgement. Reviewers working in pairs (DJN, AEA, FC or HMc) independently assessed the selected full text articles for eligibility and resolved disagreements in discussion with a third reviewer. Reviewers (DJN, AEA, FC or HMc) independently extracted data from the included reviews using a bespoke data extraction tool and resolved disagreements through discussion.
Quality assessment
Reviewers working in pairs (DJN, AEA, FC or HMc) independently assessed the risk of bias in the included reviews using the Risk of Bias in Systematic Reviews (ROBIS) tool and reached agreement by discussion [ 12 ]. Concerns with the process of reviews are assessed using 4 domains; (i) study eligibility criteria, (ii) the identification and selection of studies, (iii) data collection and study appraisal and (iv) synthesis and findings.
A diagram showing the flow of information through the process of identifying and selecting reviews for inclusion in the overview is presented in Fig. 1 .
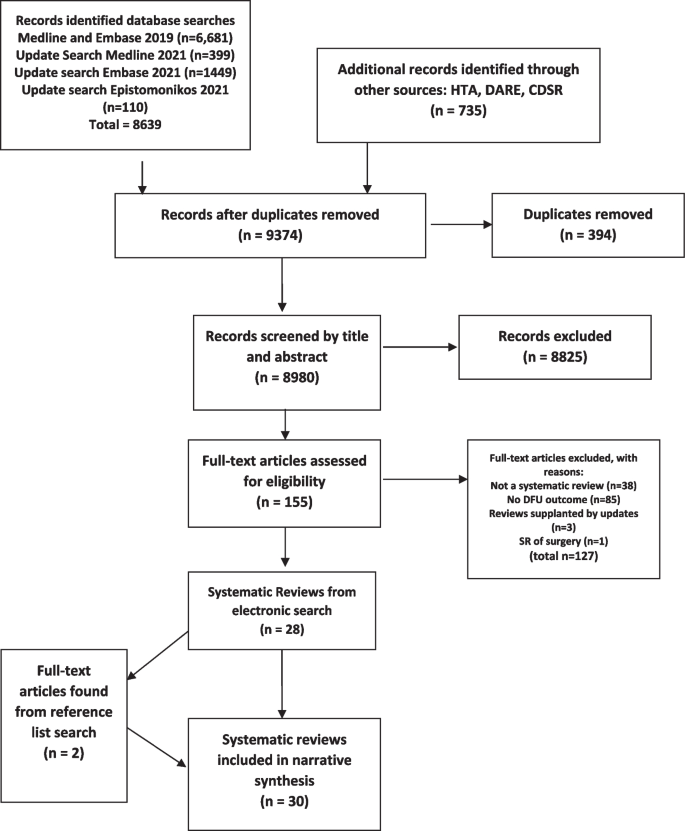
Flow diagram. Additional searches: CDSR – Cochrane Database of Systematic Reviews; DARE – Database of Abstracts of Reviews of Effectiveness; HTA – Health Technology Assessment Journals Library

Included reviews
Thirty-two reviews met the criteria for inclusion in the overview [ 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 ]. Two were updates of previously published reviews and the earlier versions were excluded to avoid the double-counting of data [ 31 , 33 ]. Of the 30 reviews, 14 included only RCTs [ 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 ] and 16 included RCTs together with various other study designs [ 27 , 28 , 29 , 30 , 32 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 ]. The reviews were published between 1998 and 2021 in professional or scientific journals, four in the Cochrane Library, one was published in the UK National Institute of Health Research (NIHR) Health Technology Assessment (HTA) journals library and one for the Agency for Healthcare Research and Quality (AHRQ), USA [ 15 , 16 , 19 , 20 , 24 , 41 ]. Other key characteristics of the included reviews are summarised in Table 1 .
Overall, the 30 reviews included a total of 26 RCTs relevant to the overview (See Additional file 2 : Supplementary references S1–S26). The majority of the RCTs were included in more than one review, only three being included only once (see Additional file 2 : Supplementary references S16, S18, S20).
Risk of bias
The ROBIS assessment results are summarised in Table 2 . Six were judged to have a low risk of bias in all four domains assessed using the ROBIS tool [ 15 , 16 , 19 , 20 , 23 , 24 ]. Nineteen reviews (65%) were judged to be at high risk of bias [ 13 , 17 , 18 , 21 , 22 , 27 , 28 , 29 , 32 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 42 , 43 , 44 ]. The most common reasons for concern about bias in the reviews related to the lack of clarity in eligibility criteria specification (60%) [ 13 , 17 , 18 , 21 , 22 , 27 , 28 , 29 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 ] methods used to identify and select eligible studies (70%) [ 13 , 14 , 17 , 18 , 21 , 22 , 25 , 26 , 28 , 29 , 32 , 34 , 35 , 36 , 37 , 38 , 40 , 41 , 42 , 43 , 44 ] data collection and study appraisal (53%) [ 13 , 17 , 18 , 21 , 22 , 27 , 28 , 29 , 30 , 32 , 34 , 36 , 37 , 38 , 42 , 43 ] and the synthesis and findings (57%) [ 13 , 17 , 18 , 21 , 22 , 25 , 28 , 29 , 32 , 35 , 37 , 38 , 39 , 40 , 42 , 43 , 44 ]. Only nine of the 26 non-Cochrane reviews reported the registration or existence of a review protocol [ 14 , 19 , 23 , 24 , 28 , 30 , 32 , 39 , 41 ]. The reviews used a variety of tools to assess the validity and risk of bias in trials with the Cochrane risk of bias tool being the most frequently used [ 6 , 13 , 14 , 15 , 16 , 17 , 18 , 20 , 23 , 24 , 25 , 26 , 29 , 32 , 41 , 42 ]. Other assessment tools were, the JBL, [ 28 , 39 , 40 , 45 ] reporting recommendations for trials of interventions for the foot in diabetes [ 27 , 30 , 46 ] PEDro [ 44 , 47 ], the source of the risk of bias tool not reported [ 19 , 22 ] QUADAS and other assessments for diagnostic tests [ 34 , 37 , 48 , 49 ] Downs and Black [ 35 , 50 ], McMaster Critical Review Form [ 38 , 51 ]. Quality assessment not reported in two reviews [ 21 , 43 ] preventative services veterans task force [ 36 , 52 ].
Fifteen of the 26 non-Cochrane reviews either did not provide any information about sources of funding or declared none [ 17 , 18 , 22 , 26 , 27 , 28 , 29 , 30 , 32 , 35 , 37 , 38 , 39 , 42 , 43 ].
Evidence of effectiveness of preventive interventions
Patient education.
Evidence was available from four systematic reviews of patient education interventions that included four RCTs relevant to the overview [ 13 , 15 , 17 , 29 ]. The risk of bias in the Cochrane review was judged to be low [ 15 ] while three non-Cochrane reviews were considered to be at high risk of bias [ 13 , 17 , 29 ].
The Cochrane review [ 15 ] published in 2014 identified two RCTs which excluded people with foot ulcers at baseline (Additional file 2 : Supplementary references S1, S2). These RCTs compared intensive foot care education programmes with brief educational interventions in people at high risk of ulceration and reported contradictory results. Clinical heterogeneity precluded meta-analysis in the review as a whole which concluded there was insufficient robust evidence that patient education was effective in preventing foot ulcers.
A review comparing intensive with routine patient education published in 2013 [ 17 ] pooled the results from the same two RCTs (Additional file 2 : Supplementary references S1, S2) included in the Cochrane review with results from five other trials. The meta-analysis showed a lower incidence of foot ulceration in favour of intensive education but the pooled effect estimate is unlikely to be reliable because it combined results from trials involving people with and without existing foot ulcers [ 53 ] (Additional file 2 : Supplementary references S1, S2), and the authors concede some trials did not provide details of the randomisation procedure and selection bias is possible.
A subsequent review and meta-analysis [ 13 ] included six RCTs of which three met the criteria for the overview: one (Additional file 2 : Supplementary reference S24) included in the Cochrane review, one (Additional file 2 : Supplementary reference S3) published after completion of the Cochrane review, and interim findings from a trial (Additional file 2 : Supplementary reference S4) that the Cochrane review classified as awaiting final results. One of the RCTs (Additional file 2 : Supplementary reference S1) included in the previous reviews was omitted. This review was rated high for risk of bias with particular concerns about the synthesis of findings casting doubt on the reliability of the results. Meta-analysis of ulcer incidence data pooled results from trials in people with and without existing foot ulcers and failed to take account of the risk of bias in the primary studies and inconsistency in their results (I 2 = 92%). The review’s positive conclusion, that intensive educational intervention reduced the incidence of foot ulcers compared with brief educational intervention, was based on a single meta-analysis which was interpreted as being statistically significant ( p = 0.05). This review also pooled LEA data from dissimilar trials as reported in the earlier review by He et al. [ 17 ].
A review that intended to include only RCTs to assess the effectiveness of health education programmes to improve foot self-care and reduce foot problems in older people with diabetes expanded its scope to include non-randomised studies due to ‘the dearth of information’ identified [ 29 ]. The review method raised concerns about its ability to identify relevant studies. Ultimately it included 14 studies of various types and the only RCT (Additional file 2 : Supplementary reference S2) was included in the earlier reviews we identified.
Systematic reviews that addressed the question of the effectiveness of a broad range of preventive interventions provided no additional evidence on the effectiveness of patient education from RCTs relevant to the overview. The most recent of these, an update of a previous review, undertaken to inform International Working Group on the Diabetic Foot (IWGDF) guidance on the prevention of foot ulcers in at-risk patients [ 30 , 31 ] considered evidence from four RCTs (Additional file 2 : Supplementary references S2, S3, S4, S14) alongside results from non-controlled studies. Conclusions were informed by a system for grading evidence-based guidelines [ 46 ] and reached by consensus. The reviews of assorted preventative interventions which included RCTs of patient education either included or pre-dated the patient education RCTs already described and identified no others [ 14 , 18 , 19 , 21 , 22 , 25 , 30 , 41 ].
Overall these systematic reviews all found that there is inadequate evidence upon which to base recommendations about patient education to prevent foot ulceration in diabetes, [ 13 , 15 , 17 , 29 ] except one which concluded that patient education is effective in preventing foot ulcers [ 13 ].
Reviews of psychosocial interventions
Three reviews assessed the evidence for psychosocial interventions to prevent foot ulcers [ 23 , 24 , 27 ], two of which were judged to be at low risk of bias [ 23 , 24 ].
One published in the Cochrane library [ 24 ] and included a single RCT of home monitoring of foot skin temperature which included theory-based counselling for people whose foot skin temperature was raised (Additional file 2 : Supplementary reference S25). A second review of psychosocial interventions included six RCTs relevant to our overview, all of which had previously been reviewed by others mostly within reviews of educational interventions [ 23 ].
A review of the effect of motivational interviewing to improve adherence behaviours for the prevention of diabetic foot ulceration was judged to be at high risk of bias [ 27 ]. The only RCT data included were the interim findings from the trial (Additional file 2 : Supplementary reference S4) previously included in the review of educational interventions by Adiewere et al. [ 13 ].
These reviews all concluded there was a lack of evidence of effectiveness for psychosocial interventions or motivational interviewing and the authors of one suggested randomised controlled trials of theoretically informed interventions to assess clinical outcomes are required [ 23 ].
Footwear and off-loading
Eight reviews [ 20 , 28 , 32 , 34 , 35 , 36 , 38 , 40 ] aimed to evaluate footwear and/or offloading interventions and a further eight reviews of assorted interventions included footwear and offloading [ 14 , 18 , 19 , 21 , 22 , 25 , 30 , 41 ], collectively identified nine RCTs relevant to the overview (Additional file 2 : Supplementary references S5–S10, S16, S18, S19). Only two reviews were judged to be at low risk of bias [ 19 , 20 ] and ten others were considered to be at high risk [ 18 , 21 , 22 , 28 , 32 , 34 , 35 , 36 , 38 , 40 ].
A Cochrane review published in 2000 [ 20 ] identified one quasi-randomised trial, in which patients were allocated alternately, not randomly, showed a significant reduction in recurrent ulceration with therapeutic shoes compared with standard footwear (Additional file 2 : Supplementary reference S5).
Two subsequent reviews of the effectiveness of therapeutic footwear for preventing re-ulceration [ 34 , 36 ] restricted inclusion of studies to those published in English, included one additional RCT (Additional file 2 : Supplementary reference S6) and other study designs. The authors concluded that the evidence to support footwear interventions to prevent re-ulceration is conflicting because non-randomised and observational studies reported positive results while the RCT showed no benefit.
The quasi-randomised trial (Additional file 2 : Supplementary reference S5) was the only study with an outcome relevant to the overview that was included in a review of the effectiveness of insoles for the prevention of ulcer recurrence [ 35 ]. This review considered evidence from mixed study designs which did not support its overly positive conclusions.
A review that focussed on the effectiveness of off-loading interventions to prevent primary (first) diabetic foot ulcers was restricted to studies published in English and failed to identify any relevant RCTs with ulceration as an outcome [ 28 ].
A review [ 32 ] (updating a previous version [ 33 ]) to inform IWGDF guidance on footwear and off-loading interventions to prevent and heal diabetic foot ulcers included five additional RCTs (Additional file 2 : Supplementary references S7–S11). This review considered the findings from the RCTs (including the quasi-randomised trial) alongside results from cohort studies. The authors conclude that the evidence supporting the use of specific footwear interventions to prevent recurrent plantar ulcers is quite strong and that sufficient good quality evidence supports the use of therapeutic footwear with demonstrated pressure relief to prevent plantar ulcer recurrence [ 32 ]. This finding appeared to be based on the results from a subgroup analysis within a single RCT (Additional file 2 : Supplementary reference S7).
A review of the effects of footwear and insoles published in 2020 [ 38 ] identified five RCTs, only one of which had not been included in a review previously (Additional file 2 : Supplementary reference S19). The RCT ( n = 51) compared ridged with semi ridged rocker soles in people at high risk of foot ulceration and found a statistically significantly reduction in ulcers in those allocated to the ridged rocker sole. The review concluded there was limited evidence to inform the use of footwear and insoles to prevent foot ulceration. A more recent review [ 40 ] included one RCT evaluating the use of a mobile phone to alert patients of increased foot pressures which was out with the search dates of all other systematic reviews (Additional file 2 : Supplementary reference S18). The proof of concept trial allocated 90 patients who were at high risk of foot ulceration to an insole system where either audio-visual alerts via a smartwatch and offloading instructions were sent to the patients’ phones when increased pressures were detected or, in the control group, no alerts were sent. The trial had a large loss to follow up (36%) and no statistically significant difference in the number of ulcerations was observed but time to event analyses found the intervention group were ulcer-free for longer. The review concludes there was difficulty in singling out the most effective weight-redistributing preventative features in shoes and insoles but concluded that this type of intervention appears to be effective.
Eight other reviews of assorted preventative interventions were identified and again either included or pre-dated RCTs of footwear and/or offloading already described and identified no others [ 14 , 18 , 19 , 21 , 22 , 25 , 30 , 41 ]. Meta-analyses of RCT data were presented in two of the more recent reviews [ 14 , 25 ]. These suggest that footwear and insoles can reduce foot ulceration but further research to examine the most effective features of footwear and insoles and their effect in people with different risk profiles is merited.
Complex interventions
We classified three systematic reviews of the effectiveness of interventions as complex [ 16 , 37 , 39 ]. One review was judged to be at low risk of bias [ 16 ], two others being judged to be at high risk. There were eight reviews of assorted interventions [ 14 , 18 , 19 , 21 , 22 , 25 , 30 , 41 ] which included integrated foot care or complex interventions, and collectively all reviews included six RCTs relevant to the overview (Additional file 2 : Supplementary references S1, S13–S16, S24).
A Cochrane review published in 2015 which assessed complex interventions defined as combinations of preventive strategies identified three RCTs relevant to the overview [ 16 ]. One RCT of an education-focused intervention in low to medium-risk patients (Additional file 2 : Supplementary reference S12) reported a reduction in the incidence of foot ulceration compared with usual care but may not be reliable because the cluster-randomisation design was reportedly not accounted for in the analysis. One of two RCTs that compared more intensive and comprehensive complex interventions with usual care in high-risk patients showed no difference in the incidence of foot ulceration but a significant reduction in LEA (Additional file 2 : Supplementary reference S13) whereas the other trial reported the opposite (Additional file 2 : Supplementary reference S14). This review judged all three RCTs at high risk of bias and the pooling of data in a meta-analysis inappropriate due to marked heterogeneity. Overall, it concluded there was insufficient evidence to support the effectiveness of complex interventions.
A review of monofilament and other threshold tests for preventing foot ulceration was judged at high risk of bias across all 4 ROBIS domains and included only one RCT evaluating the prevention of foot ulceration and amputation in people with diabetes which was also included in the Cochrane review (Additional file 2 : Supplementary reference S13) [ 37 ]. The review produced overly positive conclusions about the value of screening in preventing of foot ulcers and amputations given the trial found no statistically significant difference in the incidence of foot ulcers in the two groups [ 37 ].
The same trial was excluded from a review to inform IWGDF guidance on the prevention of foot ulcers in at-risk patients because of concerns about the comparability of the intervention and control groups [ 30 ].
The review undertaken to inform IWGDF guidance included studies of integrated foot care, defined as care given by one or multiple collaborating professionals treating patients on multiple occasions with multiple interventions [ 30 ]. It excluded the trial by McCabe et al. (Additional file 2 : Supplementary reference S13) but included an RCT of chiropodist care (Additional file 2 : Supplementary reference S15), (which was classified in other reviews as patient education) as well as unpublished data from an additional RCT of podiatric care (Additional file 2 : Supplementary reference S16) which contributed to the assessment alongside data from non-controlled studies. No conclusion could be drawn about first ulcer prevention, and the suggestion that integrated foot care may be beneficial in preventing recurrent ulceration was largely based on the results from uncontrolled studies.
A systematic review of the effect of contact with a podiatrist, working within a team, on the incidence of foot ulceration did not identify any RCTs which met its own eligibility criteria [ 39 ].
The eight reviews of assorted interventions, details of which are presented below, identified no additional trials of complex interventions [ 14 , 18 , 19 , 21 , 22 , 25 , 31 , 41 ].
Reviews of telehealth interventions and foot temperature monitoring
The overview identified two systematic reviews evaluating telehealth interventions to prevent foot ulceration [ 42 , 43 ]. Both reviews were judged to be at high risk of bias across all 4 ROBIS domains but only one included any RCTs. The review by Hazenberg et al. [ 42 ] analysed data from 4 RCTs of home-monitoring of foot skin temperature and presented a meta-analysis showing a reduction in the number of foot ulcers when abnormal temperatures were recorded and patients’ avoided weight-bearing until their foot temperature lowered (Additional file 2 : Supplementary references S21–S23, S25). These same 4 RCTs were pooled by Ena et al. [ 26 ] in a review of temperature monitoring and were also included in three systematic reviews of assorted interventions [ 14 , 25 , 30 ].
The two reviews conclude that further research is required, [ 42 , 43 ] one also acknowledge the limitations in the studies and that a larger evidence base is required before this technology could be widely implemented in practice [ 42 ]. However, the review by Ena et al. concludes that daily measurement of skin temperature when measured using a handheld infrared thermometer reduces the appearance of new foot ulcers and notes the risk of bias in the same 4 RCTs is low (Additional file 2 : Supplementary references S21–S23, S25) [ 26 ]. The three reviews of assorted interventions all concluded that the available data suggest this intervention may prevent foot ulcers developing [ 14 , 25 , 30 ] but two noted the need for further evaluation and the possibility that the intervention might not be feasible in real world settings [ 14 , 25 ].
Reviews of physical activity
We found one systematic review of physical activity which we judged to be at high risk of bias in its evaluation of the effect of exercise of the prevention of foot ulceration [ 44 ]. It included one RCT in which foot ulceration was an outcome (Additional file 2 : Supplementary reference S24). The reviewers’ conclusion that exercise can delay the development of foot ulcers is not supported by the trial results (Additional file 2 : Supplementary reference S24). The RCT was also included in three separate systematic reviews of assorted interventions [ 14 , 30 , 41 ].
Reviews of assorted preventative interventions
Eight systematic reviews included a variety of interventions to prevent foot ulcers [ 14 , 18 , 19 , 21 , 22 , 25 , 30 , 41 ] only one was judged to be at low risk of bias [ 19 ]. Four were judged to have an unclear risk of bias because of approaches they took to the selection of studies or the analysis [ 14 , 25 , 30 , 41 ] and three were judged at high risk of bias [ 18 , 21 , 22 ].
Collectively they assessed the evidence from 26 RCTs, 2 of which were not included in intervention-specific reviews presented above. Two reviews included a trial of elastic compression stockings as a preventive intervention [ 14 , 19 ]. The incidence of foot ulcers in people randomised to elastic compression stockings compared with those who did not receive hosiery was not found to be statistically significantly different. The trial population was at high risk of foot ulceration (Additional file 2 : Supplementary reference S26).
Three reviews [ 14 , 31 , 41 ] included one RCT of patient instruction to apply antifungal nail lacquer as a way to increase the frequency of foot self-inspection but found no difference in the incidence of first or recurrent ulcers when compared with standard care (Additional file 2 : Supplementary reference S17).
Systematic reviews are widely regarded as the cornerstone of evidence-based healthcare. Harnessing that evidence has become increasingly challenging as the prevalence of systematic reviews in the biomedical literature continues to increase with one recent estimate suggesting a publication rate of more than 8000 per year [ 9 ]. It is therefore unsurprising that we identified 30 systematic reviews of interventions to prevent diabetic foot ulceration that met the criteria for inclusion in our overview, with one-third having been published in the last 5 years. Yet, this surfeit of systematic reviews does not provide a wholly reliable source of evidence for decision-making.
The ability of an overview to provide useful decision-support is reliant on the quality of the conduct and reporting of the systematic reviews available. As stated, our original purpose was to conduct an overview of reviews to obtain numerical summaries of the effects of preventative interventions for foot ulcers in diabetes to populate an economic model, but two-thirds of the reviews we included had methodological shortcomings associated with a high risk of bias and reliable meta-analyses of trial data were first published in 2020 [ 14 , 25 ].
Those reviews without protocols made it difficult to ascertain whether the reviews’ methods were pre-defined, adhered to or decided or modified during the review process. The absence of pre specified primary study inclusion criteria in a third of the reviews also made it hard to judge whether reviewers’ decisions about including studies during the conduct of the reviews could have introduced bias. The evident inadequate development of search strategies may suggest a lack of familiarity with the principles of searching electronic databases and working with an information specialist who possesses the skills to construct and implement robust search strategies. Searches were frequently compromised by involving few sources, limited search terms and unjustified restrictions. Only around half of the reviews searched without language restrictions and few searched sources of unpublished data. More than half of the reviews included various study designs as well as RCTs but few considered the influence that study design could have on the results.
The conduct of evidence synthesis was another common cause for concern about bias in most of the reviews we identified. Quantitative synthesis of RCT data was performed in only five of the reviews but we found problems with meta-analyses that included data from patients who did not meet predefined eligibility criteria, errors in the interpretation of meta-analytical statistics and failure to explore reasons for heterogeneity. Narrative approaches largely entailed study-by-study narrative summaries which may indicate a lack of awareness or expertise in methods for the conduct of narrative synthesis in systematic reviews. Whatever the approach used, interpretation of the findings often ignored or glossed over the potential for bias in the included studies and other important between-study differences. The upshot of this is seen in overly positive conclusions that are not supported by the evidence reviewed.
Guidance for conducting overviews is accumulating but challenges remain [ 54 ] and some limitations to our overview warrant consideration. We could have missed some relevant systematic reviews by not searching a wider range of sources but, finding more reviews is unlikely to have altered our concern about the reliability of the evidence base as a whole. We may also have failed to find reviews including RCTs of other relevant interventions. We used ROBIS [ 12 ] to appraise the quality of the included systematic reviews but found that using this validated tool often relied on subjective judgment, especially in the absence of review protocols, resulting in lengthy deliberations to resolve disagreements. Research published by others has shown inadequate inter-rater reliability among professional reviewers using ROBIS [ 55 ] and we concur that the tool and guidance need revision to improve its reliability and utility. We suggest that reviewers who intend to use ROBIS to assess the risk of bias in systematic reviews clarify and agree the reasons for allocating specific ratings during the development of the protocol and again periodically during the conduct of the overview.
In any overview of multiple systematic reviews evaluating alternative intervention options some overlap in the included primary studies is to be expected and has to be assessed to avoid introducing bias [ 56 , 57 ]. This overview revealed how substantial the overlapping nature of the evidence from systematic reviews of RCTs addressing diabetic foot ulcer prevention is and crucially, the same (largely poor-quality) trials being reviewed over and over again without our understanding about what works to improve patient outcomes becoming any clearer [ 14 ].
The predominance of low-quality trials that are subsequently included in systematic reviews without due consideration is a concern for journal editors as it undermines confidence in systematic reviews to reliably inform clinical practice [ 58 ]. From the overview it appears some editors do not share those concerns and may not even be aware of the methodological flaws in the systematic reviews their journals have published. This is at odds with the endorsement of the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guidelines [ 59 ] by most of those journals in their instructions to authors and is also hard to reconcile with a robust peer review process. These systematic reviews were published over two decades, but we saw little improvement in the quality of conduct and reporting over time. This mirrors the pattern observed more widely in the biomedical literature by researchers who have recommended certified training for journal editors in how to implement PRISMA and facilitate its use by peer reviewers as one way to improve the value of systematic reviews [ 9 ]. The same challenges might also exist for the recent reporting guidelines for literature searches in systematic reviews, PRISMA-S, despite the clear intention to improve the reproducibility of searches in reviews [ 60 ].
Practitioners involved in developing international guidelines on the prevention of diabetic foot ulcers recognise the need to improve the quality of the intervention studies that are conducted and submitted for publication [ 46 ]. They have drawn attention to the omission of core details from many trial reports that hinders appraisal of study quality and clinical relevance in systematic reviews. This has implications for relying on overviews to understand the evidence base if it is not possible to tell from systematic review reports whether missing details were absent from the included trial reports or overlooked by the reviewers. The proposed reporting standards checklist for studies on the management and prevention of foot ulcers in diabetes should inform the conduct of systematic reviews as well primary studies alongside PRISMA and CONSORT (Consolidated Standards of Reporting Trials) [ 59 , 61 ] to improve the quality of published research in this area. Other researchers engaged in synthesizing evidence of health technologies for clinical conditions other than the foot in diabetes may also find condition-specific reporting standards helpful when undertaking an assessment of relevant literature.
Using evidence from unreliable systematic reviews to inform clinical practice has obvious negative consequences including invalid clinical guidelines recommendations which could result in the provision of suboptimal care that will not lead to improved outcomes for patients. There is already evidence that the number of overviews of systematic reviews of healthcare interventions is rising and their quality is variable [ 62 ]. Given the abundance of systematic reviews summarising poor-quality trials of interventions to prevent diabetic foot ulcers, it may only be a matter of time before uncritical overviews also start to proliferate. Those who conduct, fund, peer review and publish research in this area have a joint responsibility to ensure that the evidence base does not serve the interests of researchers and publishers rather than improving outcomes for people living with diabetes.
Availability of data and materials
All data generated or analysed during the current study are included in this published article and its supplementary information files.
International Diabetes Federation. IDF diabetes atlas. 9th ed. Brussels; 2019. Available from: https://www.diabetesatlas.org . Cited 2020 Nov 1
Diabetes UK. Facts and figures. Available from: https://www.diabetes.org.uk/professionals/position-statements-reports/statistics . Cited 2020 Nov 1.
Kerr M, Barron E, Chadwick P, Evans T, Kong WM, Rayman G, et al. The cost of diabetic foot ulcers and amputations to the National Health Service in England. Diabet Med. 2019;36(8):995–1002.
Article CAS PubMed Google Scholar
Saluja S, Anderson SG, Hambleton I, Shoo H, Livingston M, Jude EB, et al. Foot ulceration and its association with mortality in diabetes mellitus: a meta-analysis. Diabet Med. 2020;37(2):211–8.
Crawford F, Chappell FM, Lewsey J, Riley R, Hawkins N, Nicolson DJ, et al. Risk assessments and structured care interventions for prevention of foot ulceration in diabetes: development and validation of a prognostic model. Health Technol Assess. 2020;24(62):1.
Article PubMed PubMed Central Google Scholar
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al. Cochrane handbook for systematic reviews of interventions. 2nd ed. Chichester: Wiley; 2019.
Book Google Scholar
Systematic Reviews. CRD’s guidance for undertaking reviews in health care: Centre for Reviews and Dissemmination, University of York; 2009. Available from: https://www.york.ac.uk/crd/guidance/
Google Scholar
Moher D. The problem of duplicate systematic reviews. BMJ. 2013;347:f5040.
Article PubMed Google Scholar
Page MJ, Shamseer L, Altman DG, Tetzlaff J, Sampson M, Tricco AC, et al. Epidemiology and reporting characteristics of systematic reviews of biomedical research: a cross-sectional study. PLoS Med. 2016;13(5):e1002028.
Smith V, Devane D, Begley CM, Clarke M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol. 2011;11(1):15.
Wu L, Norman G, Dumville JC, O’Meara S, Bell-Syer SE. Dressings for treating foot ulcers in people with diabetes: an overview of systematic reviews. Cochrane Database Syst Rev. 2015;(7) Available from: http://doi.wiley.com/10.1002/14651858.CD010471.pub2 .
Whiting P, Savović J, Higgins JP, Caldwell DM, Reeves BC, Shea B, et al. ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016;69:225–34.
Adiewere P, Gillis R, Imran Jiwani S, Meal A, Shaw L, Adams GG. A systematic review and meta-analysis of patient education in preventing and reducing the incidence or recurrence of adult diabetes foot ulcers (DFU). Heliyon. 2018;4(5):e00614.
Article CAS PubMed PubMed Central Google Scholar
Crawford F, Nicolson DJ, Amanna AE, Martin A, Gupta S, Leese GP, et al. Preventing foot ulceration in diabetes: systematic review and meta-analyses of RCT data. Diabetologia. 2020;63(1):49–64.
Dorresteijn JA, Kriegsman DM, Assendelft WJ, Valk GD. Patient education for preventing diabetic foot ulceration. Cochrane Database Syst Rev. 2014;(12) Available from: http://doi.wiley.com/10.1002/14651858.CD001488.pub5 .
Hoogeveen RC, Dorresteijn JA, Kriegsman DM, Valk GD. Complex interventions for preventing diabetic foot ulceration. Cochrane Database Syst Rev. 2015;(8) Available from: http://doi.wiley.com/10.1002/14651858.CD007610.pub3 .
He J, Zhang L, Liu L, Zhu Y. Intensive versus routine education on diabetes mellitus for prevention of diabetic foot ulcer: a systematic review [Chinese]. Chinese J Evidence-Based Med. 2013;13(12):1470–4.
Arad Y, Fonseca V, Peters A, Vinik A. Beyond the monofilament for the insensate diabetic foot. A systematic review of randomized trials to prevent the occurrence of plantar foot ulcers in patients with diabetes. Diabetes Care. 2011;34(4):1041–6.
O’Meara S, Cullum N, Majid M, Sheldon T. Systematic reviews of wound care management: (3) antimicrobial agents for chronic wounds; (4) diabetic foot ulceration. Health Technol Assess. 2000;4(21):1–237.
PubMed Google Scholar
Spencer SA. Pressure relieving interventions for preventing and treating diabetic foot ulcers. Cochrane Database Syst Rev. 2000;(3) Available from: http://doi.wiley.com/10.1002/14651858.CD002302 .
Mason J, O’Keeffe C, McIntosh A, Hutchinson A, Booth A, Young RJ. A systematic review of foot ulcer in patients with type 2 diabetes mellitus. I: prevention. Diabet Med. 1999;16(10):801–12.
Kaltenthaler E, Morrell CJ, Booth A, Akehurst RL. The prevention and treatment of diabetic foot ulcers: a review of clinical effectiveness studies. J Clin Eff. 1998;3(3):99–104.
Norman G, Westby MJ, Vedhara K, Game F, Cullum NA. Effectiveness of psychosocial interventions for the prevention and treatment of foot ulcers in people with diabetes: a systematic review. Diabet Med. 2020;37:1256–65.
McGloin H, Devane D, McIntosh CD, Winkley K, Gethin G. Psychological interventions for treating foot ulcers, and preventing their recurrence, in people with diabetes. Cochrane Database Syst Rev. 2021;(2):CD012835. https://doi.org/10.1002/14651858.CD012835.pub2 .
Alkahoon C, Fernando M, Galappaththy C, Matthews EO, Lazzarini P, Moxon JV, et al. Meta-analysis of randomised controlled trials reporting the effect of home foot temperature monitoring, patient education or off-loading footwear on the incidence of diabetes related foot ulcers. Diabet Med. 2020;37(8):1266–79.
Article Google Scholar
Ena J, Carretero-Gomez J, Arevalo-Lorido C, SanchezaArdila C, Zapatero-Gaviria A, Gomez-Huelgas G. The association between elevated foot skin temperature and the incidence of diabetic foot ulcers: a meta-analysis. Int J Low Extrem Wounds. 2020:1–8. https://doi.org/10.1177/1534734619897501 .
Binning J, Woodburn J, Bus SA, Barn R. Motivational interviewing to improve adherence behaviours for the prevention of diabetic foot ulceration. Diabetes Metab Res Rev. 2019;35(2):e3105.
Heuch L, Gomersall JS. Effectiveness of offloading methods in preventing primary diabetic foot ulcers in adults with diabetes: a systematic review. JBI Database Syst Rev Implement Rep. 2016;14(7):236–65.
Ahmad Sharoni S, Minhat H, Mohd Zulkefli N, Baharom A. Health education programmes to improve foot self-care practices and foot problems among older people with diabetes: a systematic review. Int J Older People Nursing. 2016;11(3):214–39.
van Netten JJ, Raspovic A, Lavery LA, Moneiro-Soares, Rasmussen A, Sacco ICN, et al. Patient prevention of foot ulcers in the at-risk patient with diabetes: a systematic review. Diabetes Metab Res Rev. 2020;36(S1):e3270. https://doi.org/10.1002/dmrr.3270 .
van Netten JJ, Price PE, Lavery LA, Monteiro-Soares M, Rasmussen A, Jubiz Y, et al. Prevention of foot ulcers in the at-risk patient with diabetes: a systematic review. Diabetes Metab Res Rev. 2016;32(Suppl 1):84–98.
Bus SA, van Deursen RW, Armstrong DG, Lewis JEA, Caravaggi CF, Cavanagh PR. Footwear and offloading interventions to prevent and heal foot ulcers and reduce plantar pressure in patients with diabetes: a systematic review. Diabetes Metab Res Rev. 2015;32(Suppl 1):99–118.
Bus SA, Valk GD, van Deursen RW, Armstrong DG, Caravaggi C, Hlavácek P, et al. The effectiveness of footwear and offloading interventions to prevent and heal foot ulcers and reduce plantar pressure in diabetes: a systematic review. Diabetes Metab Res Rev. 2008;24(Suppl 1):S162–80.
Healy A, Naemi R, Chockalingam N. The effectiveness of footwear as an intervention to prevent or to reduce biomechanical risk factors associated with diabetic foot ulceration: a systematic review. J Diabetes Complicat. 2013;27(4):391–400.
Paton J, Bruce G, Jones R, Stenhouse E. Effectiveness of insoles used for the prevention of ulceration in the neuropathic diabetic foot: a systematic review. J Diabetes Complicat. 2011;25(1):52–62.
Maciejewski M, Reiber G, Smith D, Wallace C, Hayes S, Boyko EJ. Effectiveness of diabetic therapeutic footwear in preventing reulceration. Diabetes Care. 2004;27(7):1774–82.
Mayfield J, Sugarman J. The use of the Semmes-Weinstein monofilament and other threshold tests for preventing foot ulceration and amputation in persons with diabetes. J Fam Pract. 2000;49(11):S17–29.
CAS PubMed Google Scholar
Ahmed S, Barwick A, Butterworth P, Nancarrow S. Footwear and insole design features that reduce neuropathic plantar foot ulcer risk in people with diabetes: a systematic literature review. J Foot Ankle Res. 2020;13:30. https://doi.org/10.1186/s13047-020-00400-4 .
Blanchette V, Brousseau-Foley M, Cloutier L. Effect of contact with podiatry in a team approach context on diabetic foot ulcer and lower extremity amputation: systematic review and meta analysis. J Foot Ankle Res. 2020;13(15). https://doi.org/10.1186/s13047-020-0380-8 .
Collings R, Freeman J, Latour JM, Paton J. Footwear and insole design features for offloading the diabetic at risk foot-a systematic review and meta analysis. Endocrinol Diabetes Metab. 2020. https://doi.org/10.1002/edm2.132 .
Dy SM, Bennett WL, Sharma R, Zhang A, Waldfogel JM, Nebit SA, Yeh H-C, Chelladurai Y, Feldman D, Wilson LM, Robinson KA. Preventing complications and treating symptoms of diabetic peripheral neuropathy. AHRQ publication no. 17-EHC005-EF. 2017.
Hazenberg CEVB, aan de Stegge WB, Van Baal SG, Moll FL, Bus SA. Telehealth and telemedicine applications for the diabetic foot: a systematic review. Diabetes Metab Res Rev. 2019;36(3). https://doi.org/10.1002/dmrr.3247 .
Da Silva AFR, de Carvalho FJ, Guimaraes MR, Bernardes RA, Brito VRR, da Silva ARV. Tecnologia movel no cuidado com os pes em pessoas com diabetes mellitus: revisao integrativa. Cienc Cuid Saude. 2020;19:e5036.
Matos M, Mendes R, Silva AB, Sousa N. Physical activity and exercise on diabetic foot related outcomes: a systematic review. Diabetes Res Clin Pract. 2018;139:81–90.
JBI checklist for randomised controlled trials. Checklist_for_RCTs.docx (live.com) . Accessed 11 May 2022.
Jeffcoate WJ, Bus SA, Game FL, Hinchliffe RJ, Price PE, Schaper NC. Reporting standards of studies and papers on the prevention and management of foot ulcers in diabetes: required details and markers of good quality. Lancet Diabetes Endocrinol. 2016;4(9):781–8.
Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713–21. https://doi.org/10.1093/ptj/83.8.713 .
Whiting P, Rutjes AWS, Reitsma JB, Bossuyt PMM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic test accuracy included in systematic reviews. BMC Med Res Methodol. 2003;3:25.
Jaeschke R, Guyatt G, Sackett DL, the Evidence-Based Medicine Working Group. Users’ guides to the medical literature: III. How to use an article about a diagnostic test: are the results of the study validity. JAMA. 1994;271:389–91.
Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–84.
Letts L, Wilkins S, Law MC, Stewart DA, Bosch J, Westmorland MG. Guidelines for critical review form - qualitative studies (version 2.0): McMaster University Occupational Therapy Evidence-Based Practice Research Group; 2007.
Harris RP, Helfland M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, et al. Current methods of the U. S. Preventive Services Task Force: a review of the process. Am J Prev Med. 2001;20(Suppl 3):21–35.
Malone J, Snyder M, Anderson G, Bernard VM, Holloway GA, Bunt TJ. Prevention of amputation by diabetic education. Am J Surg. 1989;158:520–4.
Gates M, Gates A, Guitard S, Pollock M, Hartling L. Guidance for overviews of reviews continues to accumulate, but important challenges remain: a scoping review. Syst Rev. 2020;9(1):254.
Gates M, Gates A, Duarte G, Cary M, Becker M, Prediger B, et al. Quality and risk of bias appraisals of systematic reviews are inconsistent across reviewers and centers. J Clin Epidemiol. 2020;125:9–15.
Pollock M, Fernandes R, Newton A, Scott S, Hartling L. The impact of different inclusion decisions on the comprehensiveness and complexity of overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):18.
Ballard M, Montgomery P. Risk of bias in overviews of reviews: a scoping review of methodological guidance and four-item checklist. Res Synth Methods. 2017;8(1):92–108.
Horton R. Offline: the gravy train of systematic reviews. Lancet. 2019;394(10211):1790.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10:89.
Rethlefsen, M.L., Kirtley, S., Waffenschmidt, S. et al. PRISMA-S: an extension to the PRISMA statement for reporting literature searches in systematic reviews. Syst Rev 2021;10: 39. https://doi.org/ https://doi.org/10.1186/s13643-020-01542- .
Schulz K, Altman D, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332.
Pieper D, Buechter R, Jerinic P, Eikermann M. Overviews of reviews often have limited rigor: a systematic review. J Clin Epidemiol. 2012;65(12):1267–73.
Download references
Acknowledgments
We thank our public partner Mr. William Morrison for his help and enthusiasm during the project and Xin Wang, PhD candidate at the University of Edinburgh for her English translation of the review published in Chinese [ 17 ]. We also thank the following for their kind replies to our requests for clarification and additional information about their reviews; Dr. Susan O’Meara, the University of Leeds; Professor Dirk Stengel Unfallkrankenhaus, Berlin. Thanks are also due to Dr. Heather M McIntosh (independent researcher) for her assistance with risk of bias assessments and study selection and data extraction of the reviews identified in the update searches and Angela Martin (Podiatry Principal, NHS Fife) for her clinical advice.
This overview was funded as part of a wider project by the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) Programme (HTA project: 15/171/01). The views expressed are those of the authors and not necessarily those of the NIHR or UK Department of Health and Social Care.
Author information
Authors and affiliations.
The School of Medicine, The University of St Andrews, North Haugh, St Andrews, KY16 9TF, UK
Fay Crawford
NHS Fife, Kirkcaldy, UK
Donald J. Nicolson, Aparna E. Amanna & Marie Smith
You can also search for this author in PubMed Google Scholar
Contributions
M.S. developed and implemented the search strategies. D.J.N. screened titles and abstracts to identify relevant reviews, assessed full text articles for eligibility, assessed risk of bias and extracted data from the included reviews. A.E.A. assessed full text articles for eligibility. F.C. designed the study, screened titles and abstracts, assessed risk of bias, and extracted data from the included reviews. H.Mc. participated in the data extraction and risk of bias assessments. F.C. interpreted the data and wrote the manuscript. M.S., D.J.N., A.E.A., read and approved the final manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Fay Crawford .
Ethics declarations
Ethics approval and consent to participate.
Not Applicable.
Consent for publication
Competing interests, additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., additional file 2., medline strategy.
exp foot orthoses/
exp health education/
exp primary health care/
exp emollients/
insole*.mp.
footwear.mp.
educat*.mp.
specialist car*.mp.
multi disciplinary team*.mp.
multidisciplinary team*.mp.
routine podiatry car*.mp.
exp general practice/
exp community health services/
off load*.mp.
offload*.mp.
emollient*.mp.
exp foot diseases/
exp diabetic foot/
exp diabetic neuropathies/
exp diabetes mellitus/
exp diabetic angiopathies/
exp diabetes complications/
exp podiatry/
exp foot ulcer/
exp skin ulcer/
exp ischemia/
exp bacterial infections/
(diabet* adj3 ulcer*).mp.
(diabet* adj3 (foot or feet)).mp.
(diabet* adj3 wound*).mp.
(diabet* adj3 amputat*).mp.
systematic* review*.mp.
meta-analysis as topic/
(meta-analytic* or meta-analysis or metanalysis or metaanalysis or meta analysis or meta synthesis or meta-synthesis or metasynthesis or meta-regression or metaregression or meta regression).mp.
(synthes* adj3 literature).mp.
(synthes* adj3 evidence).mp.
(integrative review or data synthesis).mp.
(research synthesis or narrative synthesis).mp.
(systematic study or systematic studies).mp.
(systematic comparison* or systematic overview*).mp.
((evidence based or comprehensive or critical or quantitative or structured) adj review).mp.
(realist adj (review or synthesis)).mp.
(medline or pubmed or embase or cinahl or psyc?lit or psyc?info).mp.
((literature or database* or bibliographic or electronic or computeri?ed. or internet) adj3 search*).mp.
(electronic adj3 database*).mp.
included studies.mp.
(inclusion adj3 studies).mp.
((inclusion or selection or predefined or predetermined) adj criteria).mp.
(assess* adj3 (quality or validity)).mp.
(select* adj3 (study or studies)).mp.
(data adj3 extract*).mp.
extracted data.mp.
(data adj3 abstraction).mp.
published intervention*.mp.
((study or studies) adj2 evaluat*).mp.
(intervention* adj2 evaluat*).mp.
(confidence interval* or heterogeneity or pooled or pooling or odds ratio*).mp.
(Jadad or coding).mp.
(review* adj4 (papers or trials or studies or evidence or intervention* or evaluation*)).mp.
48 or 67 or 69 or 70
editorial.pt.
comment.pt.
72 or 73 or 74
19 and 36 and 76
Embase search strategy
exp foot orthosis/
emollient agent/
footwear*.mp.
general practice/
exp community care/
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18
exp foot disease/
diabetic foot/
diabetic neuropathy/
exp diabetic angiopathy/
(diabet* adj3 complicat*).mp.
foot ulcer/
exp bacterial infection/
(diabet* adj 3 wound*).mp.
20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35
meta analysis/
((literature or database* or bibliographic or electronic or computer?ed. or internet) adj3 search*).mp.
(jadad or coding).mp.
exp. animals/not humans/
78.76 not 77
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Crawford, F., Nicolson, D.J., Amanna, A.E. et al. Reliability of the evidence to guide decision-making in foot ulcer prevention in diabetes: an overview of systematic reviews. BMC Med Res Methodol 22 , 274 (2022). https://doi.org/10.1186/s12874-022-01738-y
Download citation
Received : 24 February 2021
Accepted : 19 September 2022
Published : 20 October 2022
DOI : https://doi.org/10.1186/s12874-022-01738-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Systematic reviews
- Evidence-based health care
BMC Medical Research Methodology
ISSN: 1471-2288
- General enquiries: [email protected]
- Research article
- Open access
- Published: 20 March 2020
Diabetic foot care: knowledge and practice
- Aydin Pourkazemi 1 ,
- Atefeh Ghanbari ORCID: orcid.org/0000-0002-7949-5717 2 ,
- Monireh Khojamli 1 ,
- Heydarali Balo 1 ,
- Hossein Hemmati 1 ,
- Zakiyeh Jafaryparvar 1 &
- Behrang Motamed 3
BMC Endocrine Disorders volume 20 , Article number: 40 ( 2020 ) Cite this article
34k Accesses
49 Citations
1 Altmetric
Metrics details
Diabetic foot ulcers (DFUs) are common problems in diabetes. One of the most important factors affecting the quality of diabetes care is knowledge and practice. The current study aimed at determining the knowledge and practice of patients with diabetes regarding the prevention and care of DFUs.
The current analytical, cross sectional study was conducted in Guilan Province (north of Iran) on 375 patients registered in the medical records as type 2 diabetes mellitus. Demographic characteristics, knowledge, and practice of participants were recorded in a questionnaire during face-to-face interviews conducted by the researcher. Descriptive and inferential statistics were performed using SPSS version18.
The mean score of knowledge was 8.63 ± 2.5 out of 15, indicating that the majority of participants had a poor knowledge (84.8%). The mean practice score was 7.6 ± 2.5 out of 15, indicating that a half of them had poor performance (49.6%). There was a significant and direct correlation between knowledge and practice. Knowledge level, place of residence, marital status, and history of admission due to diabetic foot were predictors of practice score.
Conclusions
According to the low level of knowledge and practice in patients with diabetes regarding the prevention and care of DFUs, and considering the significant relationship of some demographics of patients with knowledge and practice scores, a targeted educational program is needed to promote knowledge of patients with diabetes.
Peer Review reports
What is already known about this subject?
Diabetes accounted for 1.3 million deaths (2.4% of all death). The prevalence of diabetes varies among countries in Eastern Mediterranean Region (EMR).
Prevalence of diabetes mellitus in Iran ranged 20 to 30% in different provinces with higher frequency among females from 1990 to 2013.
Among people living with diabetes mellitus, 20% are at risk for foot ulceration as a result of neuropathy.
Diabetic foot ulcers (DFUs) are one of most common diabetes complications with 0–4% prevalence.
Good knowledge and practice regarding DFU reduces the risk of diabetic foot complications and ultimately amputation.
What are the new findings?
- In the current study, 84.8% of the participants had poor knowledge and only 8.8% had good practice. There was a direct and significant correlation between knowledge and practice.
The lowest knowledge scores belonged to the use of talcum powder or other powders and not using lotions between the toes.
The strongest variables related to practice were knowledge, place of residence, marital status, and history of admission due to diabetic foot, indicating that these four variables were the predictors of practice score.
How might this impact on clinical practice in the foreseeable future?
Patients’ knowledge about foot ulcer prevention should be promoted based on guidelines both in community and hospitals.
Adherence to guidelines prevents DFU; targeted interventions directed toward patients/health care providers can lead to reduced DFU complications.
Diabetes mellitus is a group of common metabolic disease characterized by hyperglycemia. Due to multiple and prolonged complications, diabetes affects almost all systems of the body [ 1 ]. Diabetes caused 1.3 million deaths (2.4% of all death) and 56 million disability adjusted life years (DALYs) in 2013. The diabetes DALY rate increased from 589.9 per 100,000 in 1990 to 883.5 per 100,000 populations in 2013. Total DALYs from diabetes increased by 148.6% during 1990–2013; population growth accounted for a 62.9% increase, and aging and increase in age-specific DALY rates accounted for 31.8 and 53.9%, respectively [ 2 ]. The prevalence of diabetes varies among countries in EMR. In Saudi Arabia, the prevalence of diabetes was reported 13.4% Saudis aged 15 years or older [ 3 ] and in Pakistan 12.1% for males and 9.8% for females aged ≥25 years [ 2 ]. A systematic review on the prevalence of type 2 diabetes in Iran showed a range of 3 to 20% in different provinces [ 4 ].
Of people living with diabetes, 20% are at high risk of foot ulceration as a result of neuropathy [ 5 ]. Diabetic foot ulcers (DFU S ) comprise 12–15% of total estimated cost of diabetes in the developed countries, increasing to 40% in the developing countries [ 6 ]. DFUs are one of the most common diabetes complications with 4 to 10% prevalence in the affected population [ 7 ]. The overall incidence of DFU is 5.8–6.0% in some particular diabetic in the U. S, while it is 2.1–2.2% in smaller populations in Europe [ 8 ]. Treating foot ulcers can be expensive and it is evident that about 49–85% of all DFU S can be prevented by raising awareness and taking proper measures [ 7 ]..
Among the complications of diabetes, DFU S affects the patient’s quality of life in case of amputation. However, it is possible to prevent amputation using educational and care strategies [ 9 ]. Data show that 25% of patients with diabetes develop a foot ulcer in their lifetime and that the cost of treating a DFU S is more than twice that of any other chronic ulcer [ 10 ]. Diabetic foot amputation remains an unpleasant impact on patients’ life more than other complications [ 11 , 12 ]. Delays in referral of serious foot problems are of particular concern [ 5 ]. Ndosi et al., reported that 15.1% of patients died within the year of presentation, the ulcer had healed in 45.5%, but recurred in (9.6%). Participants with a single ulcer on their index foot had a higher incidence of healing than those with multiple ulcers (hazard ratio 1.90, 95% CI 1.18 to 3.06) [ 13 ].
Understanding the level of knowledge and practice in patients with diabetes is important in planning for the better control of diabetes and its complications. A study by Ahmad and Ahmad on 124 patients with diabetes in North India reported that 60.5 and 79.0% got lower scores in knowledge and practice toward diabetes, respectively [ 14 ]. Jackson IL et al., reported that 79.5% of patients with diabetes in Nigeria had more than 70% of overall knowledge about self-care [ 15 ]. The results of a study in Malaysia showed that the most patients (58%) had poor knowledge and 61.8% of them had poor practice of foot care [ 16 ].
Among diabetes complications, the foot ulcers are considered as the most preventable ones. Risk factors of DFU S are correlated with poor practices and knowledge. Good knowledge and practice toward diabetic foot care reduces the risk of diabetic foot complications and ultimately amputation [ 7 ]. According to American Diabetes Association, annual assessments of knowledge, skills and behaviors are necessary for patients with diabetes [ 15 ].. The current study was conducted to assess patients’ knowledge and practice toward diabetic foot care. No similar study is conducted in Rasht City (the capital of Guilan Province, Northern Iran) thus far; therefore, the present study aimed at evaluating the level of practice and knowledge toward foot care in patients with type 2 diabetes mellitus. Health system can prevent DFU and amputation by applying a strategy to raise knowledge in patients.
Study design and subjects
The current analytical, cross sectional study was conducted at a clinic in Razi Hospital, affiliated to Guilan University of Medical Sciences, which is the only endocrine disease referral center across the province. Data were gathered from May to July 2017 and the subjects were selected by consecutive sampling. To Diagnostic and classify the patients, the American Diabetic Association, the diagnostic criteria were utilized [ 17 ]. Patients with diabetes receive care, education, treatment, and other services at this center. The center also delivers healthcare services to outpatients and inpatients, as well as routine training. The research project was approved by the Deputy of Research, Guilan University of Medical Sciences. Participation in the study was voluntarily and the subjects were informed about their right to withdraw from the study at any stage. The participant’s privacy was respected, and data were kept confidential and utilized for study purposes only. Participants were asked to read and sign an informed consent form. Inclusion criteria were: receiving the diagnosis of type 2 diabetes mellitus, age 18 years or above, taking anti-diabetic medications for at least 1 month prior to the study, having clinical records at the center, and willing to participate in the study. The exclusion criteria were: critically ill patients with diabetes, pregnant or newly diagnosed (less than 1 month) patients, receiving any other treatment or therapy, and having major psychiatric problems. A structured datasheet was used to collect demographic and clinical information of the patients using paper-based and digital records archives. Some information was also collected by a medical student through face-to-face interviews. A paper-based questionnaire was distributed among both outpatients and inpatients. Wagner DFU classification system was used to classify the patients based on ulcers. In this hospital, we assessed peripheral neuropathy, retinopathy and peripheral vascular disease (PVD), respectively by using monofilament testing, optometrist or ophthalmologist reports and the clinical diagnosis documented by the surgeon or, if available, images taken through arterial Doppler or angiography. Macro vascular disease was defined as any macro vascular complications other than PVD including prior myocardial infarction, angioplasty, coronary artery bypass grafting, ischemic heart disease, or stroke [ 18 ].
In the current study, having one or two more complications was considered a positive condition. The sample size was determined 375 considering 95% confidence interval with d = 0.05 and P = 0.58. A total of 375 out of 395 distributed questionnaires were completed and returned; the response rate was 94.4%.
A three-section questionnaire was used in the current study. First section included demographic characteristics such as age, gender, and duration of diabetes mellitus, place of residence, occupation, and level of education, marital status, and body mass index. Second part consisted of 15 questions about knowledge scored based on nominal (yes/no/I don’t know) scale, and third part with 15 questions focusing on practice was scored based on “yes/no” scale. The questionnaire was used to measure the level of knowledge and practice of subjects toward diabetic foot care. Patients’ demographic data were collected to analyze factors associated with knowledge and practice toward diabetic foot care. Each correct answer was given 1 point; however, wrong answers or choosing “I don’t know” option was given 0 point. The total score for each part ranged 0 to 15. Good or poor level of knowledge was determined based on the 75% of the maximum score of the questionnaire; therefore, the scores higher than 11.25 were considered good and those lower than 11.25 were considered poor. Examples of the questions included “Do you care about your diabetes?”; “Do you wash your feet every day?”; “Do you check the water temperature before using it?” and “Do you dry your feet after washing?”
The questionnaire was translated into the Persian language. Following the translations conducted by an Iranian professor of English literature, a native bilingual English speaker translated it back into English. Content validity was determined by gathering the views of 15 medical and nursing professionals after reviewing the questionnaire. Content validity ratio (CVR) and content validity index (CVI) of the questionnaire were assessed. Mean scores of CVI and CVR were higher than 0.80. Cronbach’s α coefficients were computed to evaluate reliability of knowledge and practice, which were 0.80 and 0.85, respectively.
Statistical analysis
After collecting data, descriptive statistics (frequency, mean, and standard deviation) were employed to summarize patients’ socio-demographic data and Chi-square test to investigate association between predictors (factors) and knowledge and practice level. In order to assess the differences between groups, the Wilcoxon, Mann-Whitney, and Kruskal-Willis tests were used for continuous variables. Factors related to knowledge and practice was estimated by multiple regressions. In this research, wrong answers and “I don’t know” merged as poor awareness. In order to assess the relationship between individual variables with knowledge and practice, we had to integrate these two items in order to have a better analysis. Variables with a P -value of < 0.1 were included in the multi-variate models. P -value < 0.05 was considered as the level of significance. All analyses were performed using SPSS version 18.
The mean (± SD) age of the 375 participants was 55.4 (±12.9) years, and 56.4% were female. Majority of patients had diabetes for less than 10 years (54.1%), were female (56.5%), urban residents (62.1%), illiterate or had elementary education (73.1%), did not have normal BMI (69.8%), and (10.6%) patients had 2 and more complications (Table 1 ). In terms of knowledge, only 57 participants (15.2%) had good knowledge, most of them (84.8%) had poor knowledge, and the mean score of patients’ knowledge was 8.63 ± 2.65. The highest percentage of correct answers was found with the knowledge about “The need for meeting or consulting a physician, if there were signs of wounding” (88.8%), followed by “Not walking without shoes” (83.5%) and “Washing and changing socks” (9.81%). The lowest knowledge was about “The use of talcum powder or other powders between the toes” (3.5%), followed by “Not using lotion between the toes” (22.24%), and “The proper method of trimming the toenails” (23.2%).
In terms of practice, only 33 patients (8.8%) had a good practice; most of them (91.2%) had a poor practice (Table 2 ), and the mean score of patients’ practice was 7.6 (± 2.5). The participants reported their best practice toward “Importance of diabetes control” (80.5%), followed by “Meeting or consulting a physician, in case of signs of DFU” (79.2%). The poorest practice was toward “The use of talcum powder between the toes” (2.7%), followed by “Proper method of trimming the toenails” (25.9%), and “Keeping the foot skin soft” (30.9%).
There was a direct and significant correlation between knowledge and practice ( P < 0.0001, r < 0.8) (Fig. 1 ). There was a significant relationship between knowledge score and gender, duration of diabetes, occupation, level of education, place of residence, having DFU, hospital stay history, and amputation history.

Correlation Between Khowledge and Practice
The study results showed that patients with more than 10 years history of diabetes, history of DFU, history of hospital stay or experience of lower limb amputation due to DFU, female gender, and the ones with complications had higher knowledge ( P < 0.05).
There was a significant correlation between practice score and gender, duration of diabetes, occupation, level of education, and place of residence (P < 0.05) (Table 3 ).
Also, based on multiple regression, the strongest variables related to practice were knowledge score ( P < 0.0001), place of residence ( P < 0.03), marital status ( P = 0.008), and DFU ( P = 0.02), indicating that these four variables were the predictors of foot care practices in the current study (Table 4 ).
In the current study, majority of patients with diabetes had lower levels of education. Studies report that level of knowledge depends on the level of education [ 14 , 19 ]. Understanding this variable is highly important in designing strategies to prevent diabetes.
In the current study, most patients had lower scores of knowledge and practice toward foot care, and the mean practice score was lower than the mean knowledge score, which was similar to the findings of Muhammad-Lutfi’s and Kim’s studies [ 16 , 20 ]. A study conducted on patients with diabetes in Western Nepal reported poor KAP (knowledge, attitude and practices) score; they indicated that the plausible factors could be lack of knowledge, lack of information, and literacy level of the studied population [ 21 ]. Another study on young Saudi females with diabetes also reported poor KAP scores [ 19 ]. Some studies reported that patients with diabetes had good level of knowledge about diabetes [ 7 , 16 , 22 , 23 ]. The differences in knowledge about foot care among patients with diabetes across the studies could be due to different trainings on diabetes care provided by the health care professionals in different settings [ 23 ] and also the literacy level of the studied subjects.
Several studies reported poor foot care practices among patients with diabetes. Kheir et al., reported poor practices toward regular inspection of feet among patients in Qatar [ 24 ]. Hamidah et al., from Malaysia observed that 28.4% of patients newly diagnosed with diabetes practiced good habits towards foot care [ 25 ]. Desalu et al., from Nigeria observed that only 10.2% of patients with diabetes had good foot care practices [ 26 ]. It was difficult to compare the results of the current study with those of other studies since the nature of the study populations and the applied measurements were different.
In the current study, there was a direct and significant correlation between knowledge and practice scores; therefore, with an increase in the knowledge score, the practice score also increased. Other studies also showed that patients who receive trainings on foot care checked their feet regularly [ 20 ]. Patients who are advised to take care of their feet and the ones whose feet are regularly checked by physicians have better practices toward foot care [ 27 ].
In the current study, the lowest knowledge scores were regarding the application of talcum powder or other powders and not using lotions between the toes, and the proper way of trimming the toenails; while the lowest practice scores were related to the application of talcum powder between the toes, the proper way of trimming the toenails; keeping the foot skin soft, and avoid dryness.
It should also be noted that due to wet climate in the North of Iran, use of lotion between the toes is not common. Nevertheless, it also needs training. Patients with diabetes need to keep between their toes dry using talcum powder and avoid the application of lotion since it is important as a hygienic measure for feet in preventing fungal infection [ 28 ]. Patients should also use skin moisturizers daily to keep the skin of their feet soft and should trim their toenails straight across (not rounded) to prevent damage to their toes [ 29 ].
In the current study, gender, duration of disease, occupation, place of residence, level of education, having DFU, and a history of hospitalization, amputation, and complication had significant relationships with knowledge. Also, gender, duration of disease, place of residence, occupation, and level of education had significant relationships with practice. It was found that knowledge level was higher in females, patients with a diabetes history of more than 10 years, and the ones underwent amputation due to DFU compared to the others; in addition, females, patients with a diabetes history of more than 10 years, and urban residents had better performance. The current study results showed that males were usually reluctant to disclose their health problems and seek professional care. Also, males presented greater deficit in self-care compared to females [ 30 ].
In the study by Muhammad-Lotfi, age, gender, level of education, and duration of diabetes had no significant relationship with knowledge and practice. This finding was in agreement with that of the current study [ 16 ], but another study indicated a significant relationship between the level of education and knowledge [ 31 ].
People with higher education are expected to be more likely to read and receive information about their illness and foot care and understand the information provided by medical staff in health care settings.
But in the current study, there was no significant relationship between the level of education and knowledge or practice, which could be due to the poor and inadequate resources of information about diabetes at the community level, since both educated and uneducated groups had inadequate information. It may also be due to the fact that in spite of possessing knowledge, due to the lack of time, heavy work load, and lack of adequate insurance coverage, patients could not take good care of their feet in practice, which requires more studies to root out the causes.
Nevertheless, the attitude of patients toward self-care in addition to sufficient knowledge was not studied in the current study. As observed in the present study, patients with a history of DFU or hospital stay, and even amputation and complication had higher knowledge level. It could be due to the fact that while completing the questionnaire, the current knowledge level of the subjects was questioned, which indicated that training medical centers can raise the level of knowledge in patients with DFU. In many Iranian state hospitals, diabetic training programs are not well organized, and the existing programs are weak. It is believed that knowledge about diabetes in the general population as well as patients with diabetes in Iran is not enough and there is a dire need for a good program for diabetes [ 32 ].
The collected data indicated that patients with diabetes had poor practice and knowledge about foot care. This is basically due to lack of proper communication between patients and medical team and inadequate education. Based on nurses’ opinion, recommendations and guidelines play an effective role in prevention, treatment, and reduction of complication among patients with DFU. Therefore, adaptation, implementation, and evaluation of the educational programs were recommended [ 33 ].
Thus, patients should be trained for foot ulcer prevention based on clinical practice guidelines for diabetes mellitus both in the community and hospitals. The results of the current study encouraged a positive outlook: A diabetes educator should give necessary advices to patients during every visit, in order to improve their perception about disease, diet, and lifestyle changes and help them control their glycemic level and overcome the complications of diabetes.
According to the principle of “prevention is better than cure” and considering the predictive factors in the current study including poor knowledge, urban residency, being single, and lack of DFU, more attention should be paid to patients possessing risk factors .
Knowledge and practice toward foot care were poor in most patients with diabetes. There was a significant relationship between some demographic characteristics of patients and knowledge and practice toward foot care. The level of knowledge, place of residence, marital status, and history of hospital stay due to DFU were the predictors of practice in patients with diabetes.
The strength of the current study was that it was the first, study to discuss this important issue in Guilan Province. The study also had some limitations; first, since the work had a cross sectional design, the direction of relationships and causal relationships cannot be determined. Second, the result of the study should be interpreted with caution, since they were obtained from a single center; a clinic-based study. Hospital-based studies cannot provide a true picture of knowledge and practice in the community. The current study sample did not represent the whole Iranian population consisting of several ethnicities. In this research, responses of the wrong answers and “I don’t know” have been grouped together, in order to achieve better analysis. Perhaps with increasing sample size, we could solve this problem in future studies.
Adequate knowledge and good practices are important to effectively control diabetes mellitus. Patients require continuous support of family members and community in order to modify their lifestyle and behaviors and make sustainable changes in order to better control their diabetes disease. Also, education about diabetes mellitus and its risk factors should be provided through mass media in order to effectively control it in the community.
Availability of data and materials
The datasets used and /or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Content validity index
Content validity ratio
Diabetic foot ulcers
Eastern Mediterranean Region
World health organization
Janmohammadi N, Moazzezi Z, Ghobadi P, et al. Evaluation of the risk factors of diabetic foot ulcer and its treatment in diabetic patients, Babol, North of Iran. Iranian J Endocrinol Metab. 2010;11(2):121–5. https://doi.org/10.1155/2018/7631659 .
Article Google Scholar
Moradi-Lakeh M, Forouzanfar MH, El Bcheraoui C, et al. High fasting plasma glucose, diabetes, and its risk factors in the eastern mediterranean region, 1990–2013: findings From the Global Burden of Disease Study 2013. Diabetes Care. 2017;40(1):22–9. https://doi.org/10.2337/dc16-1075 Epub 2016 Oct 26.
Article PubMed Google Scholar
Bcheraoui C, Basulaiman M, Tuffaha M, et al. Status of the diabetes epidemic in the kingdom of Saudi Arabia, 2013. Int J Public Health. 2014;59:1011–21.
Haghdoost AA, Rezazadeh-Kermani M, Sadghirad B, Baradaran HR. Prevalence of type 2 diabetes in the Islamic Republic of Iran: systematic review and meta-analysis. East Mediterr Health J. 2009;15:591–9.
Article CAS Google Scholar
Paisey R, Abbott A, Levenson R, et al. Diabetes-related major lower limb amputation incidence is strongly related to diabetic foot service provision and improves with enhancement of services: peer review of the south-west of England. Diabet Med. 2018;35(1):53–62. https://doi.org/10.1111/dme.13512 Epub 2017 Oct 11.
Article CAS PubMed Google Scholar
Solan YM, Kheir HM, Mahfouz MS, et al. Diabetic Foot Care: Knowledge and Practice. J Endocrinol Metab. 2017;6(6):172–7. https://doi.org/10.14740/jem388e .
Haq NU, Durrani P, Nasim A, et al. Assessment of Knowledge and Practice of Diabetes Mellitus Patients Regarding Foot Care in Tertiary Care Hospitals in Quetta, Pakistan. Specialty J Med Res Health Sci. 2017;2(4):35–43.
Google Scholar
Jeffcoate WJ, Boyko EJ, Vileikyte L, et al. Current Challenges and Opportunities in the Prevention and Management of Diabetic Foot Ulcers. Diabetes Care. 2018;41:645–52. https://doi.org/10.2337/dc17-1836 .
Morey-Vargas OL, Smith SA. Be Smart: Strategies for foot care and prevention of foot complications in patients with diabetes. Prosthet Orthot Int. 2015;39(1):48–60.
Hurlow JL, Hamphreys GI, Bowling FL, et al. Diabetic foot infection: a critical complication. Int Wound J. 2018:1–8. https://doi.org/10.1177/0309364614535622 .
Clarke P, Gray A, Holman R. Estimating utility values for health states of type 2 diabetic patients using the EQ-5D (UKPDS 62). Med Decis Mak. 2002;22(4):340–9. https://doi.org/10.1177/0272989X0202200412 .
Laiteerapong N, Karter AJ, Liu JY, et al. Correlates of quality of life in older adults with diabetes. Diabetes Care. 2011;34(8):1749–53. https://doi.org/10.2337/dc10-2424 Epub 2011 Jun 2.
Article PubMed PubMed Central Google Scholar
Ndosi M, Wright-Hughes A, Brown S, et al. Prognosis of the infected diabetic foot ulcer: a 12-month prospective observational study. Diabet Med. 2018;35(1):78–88. https://doi.org/10.1111/dme.13537 Epub 2017 Nov 20.
Ahmad S, Ahmad MT. Assessment of knowledge, attitude and practice among diabetic patients attending a health care facility in North India. Indian J Basic Appl Med Res. 2015;4(3):501–9.
Jackson IL, Adibe MO, Okonta MJ, et al. Knowledge of self-care among type 2 diabetes patients in two states of Nigeria. Pharmacy Pract. 2014;12(3) PMID:25243026,PMCID:PMC4161403.
Muhammad-Lutfi A, Zaraihah M, Anuar-Ramdhan I. Knowledge and practice of diabetic foot care in an in-patient setting at a tertiary medical center. Malays Orthop J. 2014;8(3):22. https://doi.org/10.5704/MOJ.1411.005 .
Article CAS PubMed PubMed Central Google Scholar
American Diabetes Association. Classification and diagnosis of diabetes: standards of medical Care in Diabetes 2019. Diabetes Care. 2019;42(Suppl. 1):S13–28. https://doi.org/10.2337/dc19-S002 .
Jeyaraman K, Berhane T, Hamilton M, et al. Mortality in patients with diabetic foot ulcer: A retrospective study of 513 cases from a single Centre in the Northern Territory of Australia. BMC Endocr Disord. 2019;19:1. https://doi.org/10.1186/s12902-018-0327-2 .
Saadia Z, Rushdi S, Alsheha M, et al. A study of knowledge attitude and practices of Saudi women towards diabetes mellitus. A (KAP) study in Al-Qassim region. Internet J Health. 2010;11(2). https://doi.org/10.4236/jdm.2015.52014 .
Kim A, Hongsranagon P. Preventive behaviors regarding foot ulcers in diabetes type II patients at BMA health center no. 48, Bangkok, Thailand. J Health Res. 2008;22(suppl):21–8.
Gautam A, Bhatta DN, Aryal UR. Diabetes related health knowledge, attitude and practice among diabetic patients in Nepal. BMC Endocr Disord. 2015;15(1):25. https://doi.org/10.1186/s12902-015-0021-6 .
Saleh F, Mumu SJ, Ara F, et al. Knowledge and self-care practices regarding diabetes among newly diagnosed type 2 diabetics in Bangladesh: a cross-sectional study. BMC Public Health. 2012;12(1):1112. https://doi.org/10.1186/1471-2458-12-1112 .
Gul N. Knowledge, attitudes and practices of type 2 diabetic patients. J Ayub Med Coll Abbottabad. 2010;22(3):128–31 PMID: 22338437.
PubMed Google Scholar
Kheir N, Greer W, Yousif A, et al. Knowledge, attitude and practices of Qatari patients with type 2 diabetes mellitus. Int J Pharm Prac. 2011;19(3):185–91. https://doi.org/10.1111/j.2042-7174.2011.00118.x .
Hamidah H, Santhna L, Ruth RP, et al. Foot care strategy for the newly diagnosed DM Type 2 patients with low educational and socio-economic background: a step towards future. Clin Ter. 2012;163(6):473–8.
CAS PubMed Google Scholar
Desalu O, Salawu F, Jimoh A, et al. Diabetic foot care: self-reported knowledge and practice among patients attending three tertiary hospital in Nigeria. Ghana Med J. 2011;45(2):60–5 PMID: 21857723.
Bell RA, Arcury TA, Snively BM, et al. Diabetes foot self-care practices in a rural, triethnic population. Diabetes Educ. 2005;31(1):75–83. https://doi.org/10.1177/0145721704272859 .
Aalami HB, Aalami HA, Siavashi B. Diabetic foot ulcer management review of literature. Iran J Surgery. 2009;16(4):1–7. https://doi.org/10.17795/jssc23312 .
Hasnain S, Sheikh NH. Knowledge and practices regarding foot care in diabetic patients visiting diabetic clinic in Jinnah hospital, Lahore. J Pak Med Assoc. 2009;59(10):687 PMID: 19813683.
Rossaneis MA, Haddad MD, Mathias T, et al. Differences in foot self-care and lifestyle between men and women with diabetes mellitus. Rev Lat Am Enfermagem. 2016;24:e2761. https://doi.org/10.1590/1518-8345.1203.2761 .
Chiwanga FS, Njelekela MA. Diabetic foot: prevalence, knowledge, and foot self-care practices among diabetic patients in Dar es Salaam, Tanzania–a cross-sectional study. J Foot Ankle Res. 2015;8(1):20. https://doi.org/10.1186/s13047-015-0080-y .
Delavari A, Alikhani S, Nili S, et al. Quality of care of diabetes mellitus type II patients in Iran. AIM . 2009;12(5):492–5 PMID: 19722773.
Ghanbari A, Rahmatpour P,Jafaraghaee et al .Quality assessment of Diabetic Foot ulcer clinical practice guildeline. J Evid Based Med .2018; 11(3):200–207. doi: https://doi.org/10.1111/jebm.12304 .
Download references
Acknowledgements
The authors wish to thank all the individuals who helped throughout the study, especially Razi Clinical Research Development Center.
The study was funded by the Deputy for Research; Guilan University of Medical Sciences. The funder had no role in the study design, data analysis and interpretation, and writing of the manuscript.
Author information
Authors and affiliations.
Razi Clinical Research Development unit, Guilan university of medical sciences, Rasht, Iran
Aydin Pourkazemi, Monireh Khojamli, Heydarali Balo, Hossein Hemmati & Zakiyeh Jafaryparvar
Social Determinants of Health Research center, nursing and midwifery school, Guilan University of medical sciences, Rasht, Iran
Atefeh Ghanbari
Department of internal medicine , Razi Hospital ,School of Medicine, Guilan university of Medical Sciences, Rasht, Iran
Behrang Motamed
You can also search for this author in PubMed Google Scholar
Contributions
PA, KM, and GA: the study design; PA,KM and MB: data collection; PA, KM, GA, HH, and BH: data analysis; PA, GA, KM, BH, HH, MB and JZ: data interpretation and drafting of the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Correspondence to Atefeh Ghanbari .
Ethics declarations
Ethics approval and consent to participate.
Written informed consent was obtained from participations and verbal consent from illiterate participants following a detailed explanation of the study objectives. The study was conducted in accordance with the ethical principles and its protocol was approved by the Ethics Committee of Guilan University of Medical Sciences (ethical code: IR.GUMS.REC.1396.8).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Pourkazemi, A., Ghanbari, A., Khojamli, M. et al. Diabetic foot care: knowledge and practice. BMC Endocr Disord 20 , 40 (2020). https://doi.org/10.1186/s12902-020-0512-y
Download citation
Received : 07 January 2019
Accepted : 25 February 2020
Published : 20 March 2020
DOI : https://doi.org/10.1186/s12902-020-0512-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Diabetic foot
- Diabetes mellitus
BMC Endocrine Disorders
ISSN: 1472-6823
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Abstract. Diabetic foot ulceration is a devastating complication of diabetes that is associated with infection, amputation, and death, and is affecting increasing numbers of patients with diabetes mellitus. The pathogenesis of foot ulcers is complex, and different factors play major roles in different stages. The refractory nature of foot ulcer ...
Results. Following the search of databases, 9275 articles were screened and 10 met the inclusion criteria. Studies were RCTs (n = 5), non-RCTs (n = 1), and prepoststudies (n = 4).Informal caregivers through the intervention programmes were engaged in diverse roles that resulted in improved foot ulcer prevention and/or management outcomes such as improved foot care behaviors, increased diabetes ...
recommend treatment of diabetic foot osteomyelitis with antibiotic therapy for no longer than 6 weeks. • Assessment of perfusion in the diabetic foot can be challenging. The level of perfusion required to heal a foot ulcer depends on multiple factors such as ulcer size and location, presence/extent of gangrene and infection. The Global
Diabetes is a condition that can lead to foot ulcers that often progress to amputation of a limb. Providing patients with education about foot care is crucial because it can help to prevent or minimize the incidence of foot ulcer development and amputation of a limb. Foot care education as a strategy not only empowers patients with proper foot care
for individuals with a diabetic foot ulcer is approximately 30%, exceeding 70% for those with. a major amputation. The mortality rate for people with diabetic foot ulcers is 231 deaths per. 1000 ...
1. INTRODUCTION. Diabetic foot ulceration (DFU) is among the most common and debilitating complications of diabetes, with a lifetime incidence of up to 25% in people with this condition. 1 DFU represents a major health problem in this population because of its deleterious impact on physical and psychosocial functioning 2 and increased risks of DFU recurrence, 3 amputation, 1 and mortality. 4 ...
Foot ulceration is a serious complication of diabetes that can result in high levels of morbidity for individuals and burdens health and social care systems with huge costs [1, 2].Predicting those people most likely to develop a foot ulcer has been the subject of much research and the independent risk factors have been established [3, 4].However, the value of prediction models to inform ...
Diabetes mellitus is a major global public health problem. In 2019, 463 million adults around the world were living with diabetes and projections predict an increase in prevalence to 578 million by 2030 and 700 million by 2045 [].In the UK alone it is estimated that 5 million people will have diabetes by 2030 [].People with diabetes are more at risk of developing foot problems with those ...
that is, venous stasis ulcers, arterial insufficiency ulcers in patients without diabetes, pressure ulcers, and atyp-ical ulcers, in the same sample were excluded. Atyp-ical ulcer is defined as any and all ulcers/wounds not falling under the heading of DFU, pressure ulcer, venous stasis ulcer, or ischemic ulcer (due to
2.2 Types of diabetes. There are three most common Types of diabetes, which are type 1 diabetes (T1D), type 2 di-abetes (T2D) and gestational diabetes mellitus(GDM). Type 1 diabetes is the most common and severe metabolic disorder in childhood, and the incidence increases with age until puber-ty (Craig et al. 2009).
Abstract. Foot problems are commonly involved in diabetes, and the most common presentation of diabetes is an ulcer. Diabetic foot ulcer is a complex problem caused by reduced blood supply, nerve ...
1 INTRODUCTION. Diabetes mellitus is a common chronic clinical disease, now classified as type I and type II diabetes, and its incidence is increasing year by year. 1 Diabetic foot ulcer (DFU) is one of the common serious complications in diabetic patients. 2 The pathogenesis of diabetic foot is still unclear, and the existing theory is that the patient is in a long-term hyperglycemic state ...
Core tip: Diabetic foot ulcer (DFU) is the most common complication of diabetes mellitus that usually fail to heal, and leading to lower limb amputation. Early effective management of DFU as follows: education, blood sugar control, wound debridement, advanced dressing, offloading, advance therapies and in some cases surgery, can reduce the severity of complications, and also can improve ...
Diabetic foot ulcers (DFUs) are common problems in diabetes. One of the most important factors affecting the quality of diabetes care is knowledge and practice. The current study aimed at determining the knowledge and practice of patients with diabetes regarding the prevention and care of DFUs. The current analytical, cross sectional study was conducted in Guilan Province (north of Iran) on ...
society.( Working Group on the Diabetic Foot, 2019.) The aim of the thesis is to find out how nurse's role is described in prevention of diabetic foot ulcers through reviewing of existing literature. The purpose of the thesis is to offer in-formation and knowledge related to prevention of diabetic foot ulcers to nursing students
Introduction Diabetic foot ulcer (DFU) is a common complication of diabetes mellitus, and it develops around 25% of diabetic patients. 60 80 % of DFUs will heal, and approximately 10 15% of the ...
2.2 Diabetic foot ulcer and risk factors Diabetic foot ulcers is defined as the manifestation of infection, ulceration and any damage of deep tissues in connection to neurological problems or any level of peripheral arterial disease (PAD) around the foot of a diabetic person (Yazdanpanah et al., 2018). Foot ulcerations starts
Science, Practice and Education. Living with diabetic foot ulceration can have a significant impact on a person's physical and psychological health. All members of the multi- disciplinary team have a responsibility to consider the importance of wellbeing assessment and to be mindful of a number of suggested approaches.
Diabetic foot ulcers are some of the most common complications of diabetes, and they are associated with a high risk of lower-limb amputation and, as a result, reduced life expectancy. Timely detection and periodic ulcer monitoring can considerably decrease amputation rates. Recent research has demonstrated that computer vision can be used to ...
localized to the foot and its pathology. ―Peripheral sensory neuropathy in the face of unperceived. trauma is the primary factor leading to diabetic foot ulcerations (24, 27, 46, 49). Approximately 45% to 60% of all diabetic ulcerations. are purely neuropathic, while up to 45% have neuropathic and. ischemic.
Abstract. Diabetic foot ulcers (DFU) are one of the most challenging complications of diabetes. Up to one-third of patients with diabetes mellitus (DM) may suffer from DFUs during their life. DFU is one of the leading causes of morbidity in patients with DM. The treatment period is challenging, and the recurrence rate of DFUs is high.
DIABETIC FOOT ULCER: A CASE REPORT. February 2017. European Journal Pharmaceutical and Medical Research 4 (3):481-483. Authors: Shraddha Devarshi. Indira College of Pharmacy. Vinod Kumar ...
Diabetic foot ulcers account for more than 50% of non traumatic amputations and are associated with high rates of mortality, re-amputation and contra lateral limb amputation. India has 30 million diabetics at present and in the year 2025 India is predicted to have 57 million diabetics. Incidence in India Foot Ulcer : 1-4% Toe amputation : 2.6%