An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMC Res Notes


A teenager with uncontrolled hypertension: a case report
Abdul wadud chowdhury.
1 Department of Cardiology, Dhaka Medical College Hospital, Dhaka, Bangladesh
ATM Hasibul Hasan
2 Department of Medicine (Outdoor Patient Department), Dhaka Medical College Hospital, Dhaka, Bangladesh
SME Jahan Kabir
Km nurus sabah.
Takayasu Arteritis is a vasculitis occurring mostly in young females which may present in diverse ways. Here we report a teenager with Takayasu Arteritis who presented with uncontrolled hypertension. This case depicts an atypical presentation of this disease where the girl visited many physicians for controlling the level of hypertension and put a diagnostic dilemma about the underlying etiology of young hypertension.
Case presentation
A 13 year old girl presented with epistaxis, persistent headache and uncontrolled hypertension. Her clinical examination revealed normal radial, very feeble femoral and absent other lower limb pulses. There was a blood pressure discrepancy of 50/40 mm of Hg between two arms. There were bruits over multiple areas including the abdominal aorta. She had features of left ventricular hypertrophy. Her Arch aortogram showed hugely dilated arch of aorta which became abruptly normal just after origin of left subclavian artery. There was ostio-proximal stenosis of right bracheocephalic artery, left common carotid and left subclavian artery with post stenotic dilatation of all the vessels. Abdominal aortogram revealed critical stenosis of abdominal aorta above the origin of renal arteries with a pressure gradient of 80/11 mm of Hg.
Takayasu’s Arteritis should also be kept in mind while searching for the cause of uncontrolled hypertension in the young age group.
The estimated prevalence of hypertension in pediatric age group is between 2%–5% [ 1 ]. The usual form of hypertension in young is attributable to secondary causes. The most common cause is the renovascular one (60–70%) [ 2 , 3 ]. Cushing syndrome, hyperthyroidism, pheochromocytoma, essential hypertension, coarctation of aorta, SLE are also found less commonly with hypertension in children and adeloscent [ 4 ]. With the growing knowledge and awareness of hypertension, the rate of diagnosis is increasing in children [ 1 ]. Evidences are increasing regarding early development of atherosclerosis in child and their possible relation to hypertension and coronary artery disease [ 5 ]. Several studies have reported the correlation between pediatric hypertension and family H/O hypertension, low birth weight, excess body weight [ 6 , 7 ]. Here we describe a 13 year old girl presenting with epistaxis, headache and uncontrolled hypertension despite poly drug therapy, abnormal peripheral pulses and unequal blood pressure in upper limbs. Further investigations were done to determine the cause of hypertension. The arch and abdominal aortography further correlated the uncontrolled hypertension with Takayasu’s disease according to American College Rheumatology (ACR) criteria. KS Chugh et al. described Takayasu Arteritis as the most common cause of renovascular hypertension in India [ 8 ]. Takayasu Arteritis is a large vessel vasculitis of unknown origin characterized by granulomatous inflammation of aorta and its major branches, leading to stenosis, thrombosis and aneurysm formation.
A 13 year old girl presented with three episodes of spontaneous profuse nasal bleeding within last three years which had remission without specific therapy. She had diffuse persistent headache without nausea or vomiting and uncontrolled hypertension, despite taking amlodipine and atenolol. She gave no H/O chest pain, shortness of breath, fever, prolonged cough, pulsatile tinnitus, light headedness, arthralgia, skin rash, weight loss, claudication or colour changes on cold exposure. There was no history of contact with TB patient. She did not give any H/O dizziness or syncope. On examination, both radial pulses were 80 beats/min, regular, high volume and surprisingly apparently symmetrical on both sides. There was no radio-femoral delay. Both the femoral pulses were feeble. All other lower limb pulses were absent. BP on right arm was 120/80 mmHg and on left arm was 170/120mmHg. There were bruits over both carotids, suprasternal, supraclavicular areas and over abdominal aorta. On precordial examination-apex beat was palpable at left 5th intercostal space just lateral to the midclavicular line. It was heaving in nature. A 2 was loud, there was no added sound. All other systemic examinations including optic fundi were normal. On investigation, Hemoglobin was 11.2 gm/dl, Total Count-5100/mm [ 3 ], Neutrophil- 51%, Lymphocyte- 35%, Monocyte- 03%, Eosinophil-07%, Erythrocyte sedimentation rate (ESR)- 30 mm in 1st hour. Mantoux test (MT) and C-reactive protein (CRP) were negative. Blood glucose, Serum creatinine, urine analysis were normal. Chest X-ray showed cardiomegaly with LV type apex (Figure (Figure1 1 A).

A: CXR P-A view. Cardiomegaly with LV type apex. B ECG. Left ventricular hypertrophy.
ECG fulfilled the voltage criteria of left ventricular hypertrophy (Figure (Figure1B). 1 B). 2D, M-mode and Doppler echocardiography revealed concentric left ventricular hypertrophy, aneurysmal dilatation of aortic arch, proximal stenosis and post stenotic dilatation of brachiocephalic, left common carotid and left subclavian artery and narrowing of descending thoracic aorta beyond the origin of left subclavian artery. Arch Aortogram showed hugely dilated (70 mm) arch of aorta which became abruptly normal (35 mm) just after origin of left subclavian artery. Right bracheocephalic artery had ostio-proximal stenosis with marked post stenotic dilatation (Figure (Figure2A: 2 A: white arrow). There was also ostio-proximal stenosis of left common carotid and left subclavian artery with post stenotic dilatation (Figure (Figure2B: 2 B: white arrow). Abdominal aortogram revealed critical stenosis of abdominal aorta (8.9 mm) above the origin of renal arteries (Figure (Figure2C: 2 C: white arrow). Renal arteries were however normal. Pressure study in abdominal aorta showed a pressure tracing of 200/106 mm of Hg above and 120/95 mm of Hg below the stenosis (Figure (Figure3 3 ).

A: Arch Aortogram. Hugely dilated (70 mm) arch of aorta which became abruptly normal (35 mm) just after origin of left subclavian artery. Right bracheocephalic artery had ostio-proximal stenosis with marked post stenotic dilatation (white arrow). B : Arch Aortogram. Ostio-proximal stenosis of left common carotid and left subclavian artery with post stenotic dilatation (white arrow). C : Abdominal Aortogram critical stenosis of abdominal aorta (8.9 mm) above the origin of renal arteries (white arrow).

Pressure tracing in abdominal aorta.
She fulfilled four of the six major ACR (American College of Rheumatology) criteria for Takayasu’s disease eg, onset of age is 13 years (<40years), 50 mm of Hg pressure difference between systolic BP between arms (>10mm of Hg pressure difference), subclavian and aortic bruit and narrowing of major branches of aorta. She was prescribed Amlodipine 10 mg, Atenolol 100mg, Prazosin 6mg, Hydrochlorthiazide 50mg and Amiloride 5mg. Methotrexate 5mg weekly with Folinic acid supplementation were given too. Plan for Angioplasty and Stenting of abdominal aortic stenosis was provided to the patient.
Takayasu’s Arteritis (TA) is a chronic inflammatory large vessel vasculitis of unknown origin, predominantly affecting aorta and its major branches. It is also called Aortic arch syndrome, Pulse less disease, Occlusive thromboaortopathy, Martorell syndrome [ 9 ]. The first scientific description of Takayasu’s Arteritis was given by Mikito Takaysu, Professor of Opthalmology at Kanazawa University, Japan, in 1905 at 12th Annual conference of Japanese Ophthalmology Society [ 10 ]. He presented a 21year old woman with a peculiar form of arteriovenus anastomoses at optic fundi. K Onishi and T Kagosha also contributed with their patients of absent radial pulse in the same conference [ 10 ]. But the first ever documented description of this arteritis dates back to 1830. Rokushu Yamamoto who practiced Japanese oriental medicine, described a case of 45 years old man presenting with absent pulse in one upper limb and feeble pulse in another one following a year long history of high grade fever. During the period of follow up the patient subsequently became emaciated, dyspnoeic and died suddenly after 11 years [ 10 ]. The world wide prevalence of Takayasu’s disease is 3.3/million. The disease is more common in East Asia and in Asian descendants in other countries [ 11 ]. TA commonly presents in 2nd or 3rd decade of life, with a high female preponderance. But the female to male ratio declines from Eastern Asia to the West [ 12 ]. TA may manifest as asymptomatic pulseless disease to catastrophic neurological impairements. The disease may present in two phase, a prepulseless phase of nonspecific inflammatory signs, followed by a chronic phase of vascular insufficiency [ 13 - 15 ]. Presentation of TA varies among the races. Japanese patients are predominantly female, presents with pulslessness, dizziness, vertigo, aortic regurgitation, inflammatory process commonly affecting the arch and its major branches, whereas Indian patients are male dominant. Indian cases present with more hypertension, headache, LV hypertrophy and vasculitic involvement of abdominal aorta and renal arteries [ 15 ]. Diminished or absent pulse along with upper limb claudication and blood pressure difference is found in 84–96% of cases [ 16 ]. Vascular bruits involving carotid, subclavian and abdominal vessels are also common (80–94%) [ 17 ]. Hypertension is associated with 33–83% patients of TA [ 15 , 17 ]. Our index case was also a young girl with feeble femoral pulse and absent other peripheral pulses in lower limb, blood pressure discrepancy between arms, bruits over multiple areas of chest and neck and hypertension. The blood pressure discrepancy of 50/40 mm of Hg is probably due to the difference in percentage of stenosis among the brachiocephalic (70–80% stenosis) and left subclavian vessels (50–60% stenosis). Retinopathy, aortic regurgitation, congestive heart failure, cardiomyopathy, myocardial ischemia, headache, dizziness, seizure are less common association of TA. From common findings of TA, American College of Rheumatology has devised some diagnostic criteria for TA in 1990. Angiography remains the gold standard investigation for diagnosis. The main differential diagnosis include other causes of large vessel vasculitis eg inflammatory vasculitis (Syphilis, Tuberculosis, Behchets, SLE); development abnormalities (Coarctation of aorta, Marfans syndrome) and neurofibromatosis. TA has been classified on the basis of angiographic findings. The new classification was described at Takayasu Arteritis Conference in 1994 based on vessel involvement. Type-I involving branches from aortic arch, Type-IIa denoting ascending aorta, aortic arch and its branches, Type-IIb including Type-Ia plus descending thoracic aorta. Type-III means descending thoracic aorta, abdominal aorta and/ or renal arteries. Type-IV involves abdominal aorta and/ or renal arteries. Type-V is combined features of Type-IIb and Type-IV [ 15 ]. Ishikawa classified different clinical groups based on natural history and complications. He described Group-I as uncomplicated disease with or without pulmonary artery involvement, Group-IIA as mild/moderate single complication together with uncomplicated disease, Group-IIB as severe single complication together with uncomplicated disease, Group-III as two or more complications together with uncomplicated disease [ 17 ]. Ishikawa defined Takayasu retinopathy, Secondary hypertension, Aortic regurgitation, Aneurysm formation as four most important complications. Our index case met the angiographic criteria of Type-IV Takayasu Arteritis class and Group-III of Ishikawa class [ 17 ]. Ishikawa class caries a prognostic significance not only for the Japanese patients but also for the Indians. The overall five year survival rate is 83%. The survival rate is 100% in Group-I and 70% in Group-IIb and Group-III. The most common cause of mortality is cerebrovascular disease and cardiac failure. Regarding treatment strategy steroid had been the mainstay of treatment. Shelhamer et al. showed half of the TA patients on steroid won’t respond [ 18 ]. Kerr et al. showed overall remission rate of 33% with immunosuppressive drugs in steroid unresponsive patients [ 16 ]. Methotrexate though not more efficacious than others, became popular due to its well tolerability [ 19 , 20 ]. The combination of steroid and methotrexate demonstrated a remission rate of 81% in steroid unresponsive patients [ 21 ]. Treatment of hypertension and prevention of thrombosis are also important aspects of therapy. Treatment of hypertension with ACE inhibitors requires careful monitoring for renal artery stenosis. Surgery may be needed in patients with critical renal artery stenoses, limb claudication limiting the daily activities, stenosis of three or more cerebral vessels, moderate aortic regurgitation. Stenoses of renal artery are best treated by Percutaneous Transluminal Angioplasty [ 21 ]. Stent placement following angioplasty is a safe and effective procedure [ 22 ]. Takayasu’s Arteritis is a chronic progressive vasculopathy. So long term follow up is recommended. Markers of acute phase response are unreliable during follow up. Doppler studies and MRA are can help to determine the vessel wall thickness and lumen configuration.
Takaysu’s Arteritis can have varied presentation. So a young female patient presenting with absent pulse, unequal blood pressure between arms and hypertension should be suspected clinically for Takayasu’s disease.
Written informed consent was obtained from the patient’s guardian for publication of this case report and for all the accompanying images.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
AWC is the first author and was involved in diagnosis by performing the angiography and writing a part of the manuscript. ATMHH is the communicating author and was involved in writing the manuscript. SMEJK and KMNS were responsible for the management of the patient. All the authors read and approved the final manuscript.
Acknowledgement
We acknowledge Professor H I Lutfur Rahman Khan for providing the overall support to us.
- Sorof JM, Lai D, Turner J, Poffenbarger T, Portman RJ. Overweight, ethnicity, and the prevalence of hypertension in school-aged children. Pediatrics. 2004; 113 (3 pt 1):475–482. [ PubMed ] [ Google Scholar ]
- Ooi BS, Chen BTM, Toh CCS, Khoo OT. “Cause of Hypertension in Young” Br Med J. 1970; 3 :744–746. doi: 10.1136/bmj.3.5725.744. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Flynn JT. Evaluation and management of hypertension in childhood. Prog Pediatr Cardiol. 2001; 12 :177–188. doi: 10.1016/S1058-9813(00)00071-0. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004; 114 (2 suppl 4th report):555–576. [ PubMed ] [ Google Scholar ]
- Luma GB, Spoitta RT. “Hypertension in Children and Adeloscent” Am Fam Physician. 2006; 73 (9):1558–1566. [ PubMed ] [ Google Scholar ]
- Franco MC, Christofalo DM, Sawaya AL, Ajzen SA, Sesso R. Effects of low birth weight in 8- to 13-yearold children: implications in endothelial function and uric acid levels. Hypertension. 2006; 48 (1):45–50. doi: 10.1161/01.HYP.0000223446.49596.3a. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moore WE, Stephens A, Wilson T, Wilson W, Eichner JE. Body mass index and blood pressure screening in a rural public school system: the Healthy Kids Project. Prev Chronic Dis. 2006; 3 (4):A114. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chugh KS, Jain S, Sakhuja V. Renovascular hypertension due to Takayasu’s Arteritis among Indian patients. QJM. 1992; 85 :833–843. [ PubMed ] [ Google Scholar ]
- Lupi-Herrera E, Sánchez-Torres G, Marcushamer J. Takayasu Arteritis. Clinical study of 107 cases. Am Heart J. 1977; 93 :94–103. doi: 10.1016/S0002-8703(77)80178-6. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Numano F, Okawara M, Inomata H. Takayasu’s Arteritis. Lancet. 2000; 356 :1023–1025. doi: 10.1016/S0140-6736(00)02701-X. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Watts R, Al Taiar A, Mooney J, Scott D, MacGregor A. The Epidemiology of Takayasu Arteritis in the UK. Rheumatology. 2009; 48 :1008–1011. doi: 10.1093/rheumatology/kep153. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Johnston SL, Lock RJ, Gompels MM. Takayasu Arteritis: a review. J Clin Pathol. 2002; 55 :481–486. doi: 10.1136/jcp.55.7.481. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moriwaki R, Noda M, Yajima M. Clinical manifestations of Takayasu Arteritis in India and Japan—new classification of angiographic findings. Angiology. 1997; 48 :369–379. [ PubMed ] [ Google Scholar ]
- Jain S, Sharma N, Singh S. Takayasu Arteritis in children and young Indians. Int J Cardiol. 2000; 75 :S153–S157. [ PubMed ] [ Google Scholar ]
- Subramanyan R, Joy J, Balakrishnan KG. Natural history of aortoarteritis (Takayasu’s disease) Circulation. 1989; 80 :429–437. doi: 10.1161/01.CIR.80.3.429. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kerr GS, Hallahan CW, Giordano J. Takayasu Arteritis. Ann Intern Med. 1994; 120 :919–929. [ PubMed ] [ Google Scholar ]
- Ishikawa K. Natural history and classification of occlusive thromboaortopathy (Takayasu’s disease) Circulation. 1978; 57 :27–35. doi: 10.1161/01.CIR.57.1.27. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shelhamer JH, Volkman DJ, Parrillo JE. Takayasu’s Arteritis and its therapy. Ann Intern Med. 1985; 103 :121–126. [ PubMed ] [ Google Scholar ]
- Hoffman GS, Leavitt RY, Kerr GS. Treatment of Takayasu’s Arteritis (TA) with methotrexate (MTX) Arthritis Rheum. 1991; 34 :S74. [ PubMed ] [ Google Scholar ]
- Hoffmann GS, Leavitt RY, Kerr GS. Treatment of glucocorticoid-resistant or relapsing Takayasu Arteritis with methotrexate. Arthritis Rheum. 1994; 37 :578–582. doi: 10.1002/art.1780370420. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Giordano JM. Surgical treatment of Takayasu’s Arteritis. Int J Cardiol. 2000; 75 :S123–S128. [ PubMed ] [ Google Scholar ]
- Sharma BK, Jain S, Bali HK. A follow-up study of balloon angioplasty and de-novo stenting in Takayasu Arteritis. Int J Cardiol. 2000; 75 :S147–S152. [ PubMed ] [ Google Scholar ]
- Research article
- Open access
- Published: 22 May 2019
Uncontrolled hypertension and associated factors among adult hypertensive patients in Ayder comprehensive specialized hospital, Tigray, Ethiopia, 2018
- Gebrewahd Bezabh Gebremichael ORCID: orcid.org/0000-0001-7374-595X 1 ,
- Kalayou Kidanu Berhe 1 &
- Teklewoini Mariye Zemichael 2
BMC Cardiovascular Disorders volume 19 , Article number: 121 ( 2019 ) Cite this article
17k Accesses
41 Citations
10 Altmetric
Metrics details
Despite the availability and improvement in diagnostic and therapeutic interventions with proven benefits in reducing cardiovascular morbidity and mortality, control rates of hypertension remain poor and grossly inadequate. Around one billion individuals are living with uncontrolled hypertension globally. Uncontrolled hypertension among hypertensive patients on treatment in Ethiopia ranges from 11.4 to 69.9%. Therefore, the aim of this study was to determine the magnitude and associated factors of uncontrolled hypertension among hypertensive patients in Ayder comprehensive specialized hospital, Tigray, Ethiopia 2018.
Methods and materials
Hospital-based cross-sectional study design was conducted from February 16–April 30/2018. Simple random sampling method was used to select 320 participants. Data was collected using interviewer administered standard structured questionnaire. Self-care practice measuring tool was adopted from hypertension self-care activity level effects (H-scale). Data was entered to and cleaned by Epi Info version 7 and it was exported to SPSS version 22 for analysis. Binary logistic regression model (AOR, 95% CI and p -value < 0.05) was used to determine the predictors of uncontrolled hypertension.
From the total respondents, 164 (51.2%) were females. The mean age of the respondents was 53.83 + 14.52 years. Prevalence of uncontrolled hypertension was found 52.5%. Overweight (AOR = 4.527, 95% CI: 2.247–9.123), co-morbidity (AOR = 2.112, 95% CI: 1.218–3.662), non-adherence to anti-hypertensive medication (AOR = 2.062, 95% CI: 1.030–4.129), non-adherence to physical activity (AOR = 1.931, 95% CI: 1.074–3.470) and non-adherence to alcohol abstinence (AOR = 2.093, 95% CI: 1.109–3.948) are independent predictors of uncontrolled hypertension.
the prevalence of uncontrolled hypertension is high. Patients’ adherence to antihypertensive medication, physical exercise and alcohol abstinence should be maximized. Weight reduction and early identification and management of co-morbidities are also crucial.
Peer Review reports
Uncontrolled hypertension is a major public health problem among hypertensive patients both in developed and developing countries [ 1 , 2 , 3 , 4 ]. Despite the availability and improvement in diagnostic options and therapeutic interventions of hypertension with proven benefits in reducing cardiovascular morbidity and mortality; BP control rates are grossly inadequate (< 30% controlled to < 140/90 mmHg) even among those diagnosed as hypertensive and taking anti-hypertension treatment [ 5 , 6 ]. Around one billion individuals are living with uncontrolled hypertension globally [ 7 ].
Systolic Blood Pressure Intervention Trial (SPRINT) reported, intensive versus standard BP control (systolic BP of < 120 vs. < 140 mmHg) in adults with hypertension results in 25% risk reduction in major cardiovascular events and 27% reduction in all-cause mortality [ 8 ]. However, when hypertension remains uncontrolled, risks for long-term sequelae such as myocardial infarction, heart failure, stroke, and kidney disease significantly increase. For every 20 mmHg increase in systolic BP) to > 115 mmHg (or 10 mmHg increase in diastolic BP to > 75 mmHg), the risk of major cardiovascular and stroke events doubles [ 9 ]. Uncontrolled hypertension increases the risk of all-cause and cardiovascular disease mortality [ 10 , 11 ] .
Majority of studies in Africa had shown that less than a third of patients achieve treatment goals [ 12 ]. A meta-analysis also showed that in most Sub-Saharan Africa (SSA), the control of BP to the target level (140/90) is less than 30% [ 13 ]. Few studies conducted in Ethiopia revealed that the prevalence of uncontrolled hypertension among patients on treatment varied from 11.4% in Gondar University Hospital to 59.9% in Tikur Anbessa Hospital and 69.9% in Zewditu Memorial Hospital [ 14 , 15 , 16 ].
Even though there is inconsistency among studies, multiple factors were found to contribute for uncontrolled hypertension. Non-adherence to anti-hypertensive therapy and dietary approach to stop hypertension (DASH diet), high salt intake, alcohol intake, smoking, physical inactivity and overweight/obesity are among the major contributing factors to uncontrolled hypertension [ 14 , 17 , 18 , 19 ]. Other factors such as sex, age, disease duration and co-morbidities also have association with uncontrolled hypertension [ 17 , 20 ].
One of the key Sustainable Development Goals adopted by the World Health Assembly in 2013 was to lower the prevalence of raised blood pressure by 25% by 2025 [ 21 ]. Improvement in the management and control of hypertension will require an understanding of the factors that affect blood pressure control. Although there are a few attempts the reasons for uncontrolled hypertension remain unclear in low income countries and have been insufficiently studied in Ethiopia. Thus, this study aimed to assess the prevalence and predictors of uncontrolled blood pressure in hypertensive patients attending in Ayder comprehensive specialized hospital, Tigray, Ethiopia.
Study area and period
ACSH is a university hospital in Mekelle, Tigray region commenced rendering all the specialized and non-specialized services including special clinic services [ 22 ]. The hospital provided follow-up care for 540 hypertensive patients according to data registered in 2017 prior to data collection period. The study was conducted from February 16 to April 30/2018.
Study design and population
Hospital-based cross-sectional study design was conducted among adult hypertensive patients attending in Ayder comprehensive specialized hospital.
Inclusion and exclusion criteria
All adult (≥ 18 years old) hypertensive patients who were on anti-hypertensive treatment and follow up for at least 6 months at time of data collection were included in this study. However unconscious and critical ill hypertensive patients and pregnant mothers were excluded.
Sample size determination
Sample size was determined using single population proportion formula and considering the following assumptions: Prevalence (p) uncontrolled hypertension 0.7 [ 16 ], 푍 = standard normal distribution at 95% confidence level of 푍훼/2 = 1.96 and margin of error (푑) = 5%:
Sampling procedure and techniques
A sampling frame was created using the patients’ medical registration number and participants were selected using simple random sampling technique from the sampling frame.
Study variables
Independent variables.
The independent variables were socio-demographic variables ( age, sex, household monthly income in Ethiopian birr, marital status, religion, educational status, occupation, ethnicity and residence), clinical characteristics of patients ( family history of hypertension, Body mass index, availability of BP cuff at home, BP monitoring at home or any else, presence of co-morbidity, duration of the disease and number and type of medication) and behavioral practices (adherence to anti-hypertensive medication physical activity, dietary management, moderation of alcohol and smoking status) of the participants.
Dependent variable
Uncontrolled hypertension was the dependent variable.
Data collection tool
Data was collected using interviewer-administered structured questionnaire and document review. The questionnaire contains two parts. Part I contains socio-demographic characteristics, clinical profile and knowledge about hypertension and its management. Part II contains questions related to hypertension self-care practices such as medication adherence, dietary management (low salt diet and DASH diet), smoking status, physical activity, weight management and alcohol intake. The self-care practice measuring tool was adopted from hypertension self-care activity level effects (H-scale) [ 23 ].
Operational definitions
Educational status.
Is categorized in to four mutually exclusive categories. Can’t read and write includes participants who are not able to read and write. Can read and write includes participants who never took or followed formal education; however they might take informal education (e.g. religious education) thus they are able to read and write. Primary includes participants who followed primary level formal education. Secondary educational status includes participants who followed secondary level formal education. College and above includes participants who are honored of college diploma and above.
- Uncontrolled hypertension
Is defined as systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg in patients taking anti-hypertensive treatment [ 24 ].
Scoring method
Hypertension Self-Care Activity Level Effects (H-SCALE) includes:
Medication adherence
Three items were used to assess the number of days in the last week that an individual: [ 1 ] takes blood pressure medication, [ 2 ] takes it at the same time every day and [ 3 ] takes the recommended dosage. Responses were summed (range, 0–21), and participants reported that they followed these 3 recommendations on 7 out of 7 days were considered adherent (score = 21).
Dietary management (Low-salt diet and DASH diet)
Twelve items were used to assess practices related to eating a healthy diet, avoiding salt while cooking and eating, and avoiding foods high in salt content. A mean score was calculated. A score of 6 or better (indicating that participants followed low-salt diet practices on 6 out of 7 days) was considered adherent.
Physical activity
Physical activity was assessed by 2 items. “How many of the past 7 days did you do at least 30 minutes total physical activity?” and “how many of the past 7 days did you do a specific exercise activity (such as swimming, walking or biking) other than what you do around the house or as part of your work?” Responses were summed (range, 0–14). Participants who scored ≥8 were coded as adhering to physical activity recommendations.
Smoking status was assessed with 1 item, “How many of the past 7 days did you smoke a cigarette or cigar, even just one puff?” Respondents who reported 0 days were considered a nonsmoker. All others were categorized as smokers.
Weight management
Ten items were used to assess activities undertaken in the past 30 days to manage weight through dietary practices and physical exercise. Response categories ranged from strongly disagree [ 1 ] to strongly agree [ 5 ]. Participants who agree or strongly agree with all 10 items (score ≥ 40) were considered to be following good weight management practices.
Adherence to JNC7 recommendations was deemed to be alcohol abstinent. Participants who reported not drinking any alcohol in the last 7 days or who indicated that they usually didn’t drink at all was considered abstainers. All others were non adherent [ 23 ].
Knowledge about lifestyle management of hypertension
Good knowledge: knowledge score above the mean value on hypertension evaluation of lifestyle and management (HELM) scale.
Poor knowledge : knowledge score below the mean value on hypertension evaluation of lifestyle and management (HELM) scale.
Hypertension evaluation of lifestyle and management scale which included 14 items was used to assess respondents’ knowledge [ 25 ]. The numbers of questions are modified to 10 as questions “7 and 8” are country specific and questions “12 and 13” does not meet the study objectives. The tool contains selected response items with the right answer coded as “1” and wrong answer as “0”.
Data quality assurance
Data collectors and supervisors were trained for 1 day on the data collection approach of the study. The questionnaire was translated to Tigrigna language and back translated into English by another person to check for consistency and meaning and data was collected using the Tigrigna version questionnaire. A Pretest was conducted in 5% of the sample size in Axum comprehensive specialized hospital to see the applicability of the instruments and was ratified accordingly. Continuous follow-up and supervision was made by the supervisor and principal investigator throughout the data collection period. Collected data was reviewed and checked daily for completeness and consistency at the spot during data collection time.
Data processing and analysis
Data was checked, cleaned and entered into Epi Info version 7 and then it was exported to SPSS version 22.0 for analysis. Descriptive statistics including frequencies, percentages, ranges, mean and standard deviations were done and presented using tables, figures and texts. Binary logistic regression was done to identify factors which were associated with the self-care practice. Variables which were found to have an association with the outcome variable at P -value < 0.25 in the bivariate regression analysis were entered to the multivariable logistic regression model. The magnitude of association between independent and dependent variables was measured using odds ratios and 95% confidence interval (CI) with significant level ( P -value < 0.05).
Ethical consideration
Ethical clearance was received from Mekelle University Collage of Health Science research committee. Informed consent was obtained and participation was fully based on the willingness of participants. The respondents were allowed to refuse or discontinue participation at any time. Information was recorded anonymously. Confidentiality and privacy were ensured throughout the study.
Socio-demographic characteristics
A total of 320 adult hypertensive respondents were interviewed using a structured questionnaire and all questionnaires were included in the analysis which makes 100% of response rate. More than half of the total respondents (51.2%) were females. The mean age of the respondents was 53.83 + 14.52 years with a minimum age of 19 years old and maximum age of 85 years old. Majority of the respondents 227 (70.9%) were less than 65 years old and 230 (71.9%) of respondents were married. Most of the respondents 253 (79.1%) were orthodox Christian followers and 288 (90%) respondents were Tigrawot in ethnicity. One hundred thirty-eight (43.1%) of the respondents were not able to read and write and 86 (26.9%) of the respondents were self-employed. Majority of the study participants 177 (55.3%) had low monthly income and 232 (72.5%) of the respondents were urban residents (See Table 1 ).
Mean score of knowledge of respondents was 4.3 + 1.19 with a minimum score of 1 and a maximum score of 8 (See Table 2 ).
Health profile related factors
Ninety-seven (30.3%) of the total respondents had a family history of hypertension and only 13 (4.1%) of the respondents had BP cuff at home. The mean duration of hypertension was 3.50 + 3.07 with a minimum of 0.5 year and a maximum of 20 years. A significant number of respondents,215 (67.2%) had normal BMI. One hundred sixty-two of the respondents(50.3%) had medically confirmed co-morbidity. One hundred thirty-seven (42.8%) of the respondents checked their BP regularly at least twice a month at home, health institution or any else. Ninety-six respondents (30%) had ever missed follow-ups. Majority of the respondents, 228 (71.2%) took less than or equal to two types of antihypertensive medication (See Table 3 ).
Uncontrolled hypertension and associated factors
The magnitude of uncontrolled hypertension was found to 52.5% (95% CI, 47.2–58.1%). Fifteen variables were found significantly associated variables in the bivariate logistic regression. However, only five variables (BMI, co-morbidity, adherence to medication and physical activity and alcohol abstinence) were found statistically significant predictors of uncontrolled hypertension at p -value < 0.05 in the Multivariable logistic regression model.
Overweight patients were found 4.527 more likely to have uncontrolled hypertension compared to those with normal weight (AOR = 4.527, 95% CI: 2.247–9.123). Hypertensive patients with co-morbidity had 2.112 more risk of uncontrolled hypertension than their counterparts (AOR = 2.112, 95% CI: 1.218–3.662). Hypertensive patients who were non-adherent to anti-hypertensive medication had 2.062 more risk of uncontrolled hypertension (AOR = 2.062, 95% CI: 1.030–4.129). Non-adherence to physical activity had1.931more risk of uncontrolled hypertension (AOR = 1.931, 95% CI: 1.074–3.470). Similarly, non-adherence to alcohol abstinence had 2.093 more risk of uncontrolled hypertension (AOR = 2.093, 95% CI: 1.109–3.948) (See Table 4 ).
The magnitude of uncontrolled hypertension was found high, 52.5% (95% CI: 47.2–58.1%). The rate of uncontrolled hypertension is in line with the study findings done in Thailand (53.4%) [ 26 ], Kwazulu-Natal (51%) [ 27 ], South Asia (58.0%) [ 28 ], Ghana (57.7%) [ 29 ], Nigeria 53.6% [ 30 ] and Jimma university hospital, Ethiopia (52.7%) [ 19 ]. However, this is higher than the findings reported from Israel (35.9%) and Gondar university hospital, Ethiopia (37%) [ 31 , 32 ]. This could be explained by the lower rates of medication adherence and a slightly higher magnitude of co-morbidity in our study compared to the study done in Gondar, Ethiopia. The difference in the operational definition of uncontrolled hypertension among the studies could also be responsible for the discrepancy of the study results [ 32 ]. In addition, this might be due to sociocultural and behavioral differences of the population and healthcare services differences of the study settings.
In contrary, the magnitude of uncontrolled hypertension in this is lower than the study done in Panama (66.7%) [ 33 ], Western India 63.6% [ 34 ], Southern China (55.4%) [ 35 ], Morocco 82.8% [ 36 ], Kinshasa, Democratic Republic of the Congo (77.5%) [ 37 ], South Africa (75.5%) [ 38 ], Zimbabwe (67.2%) [ 39 ], Cameron (63.2%) [ 40 ], Ethiopia (63%) [ 41 ] and Zewditu Memorial Hospital, Ethiopia (69.9%) [ 16 ]. This inconsistency could be due to the difference in the; anti-hypertensive medication adherence rate, proportion of overweight and obesity, magnitude of co-morbidity, operational definition of hypertension, adherence to alcohol abstinence and age of study participants.
Compared to the other studies, our study reported a higher rate of medication adherence [ 33 , 34 , 37 , 38 , 41 ]. The other studies reported a higher prevalence of overweight and obesity [ 33 , 35 , 36 , 39 , 40 ]. Our study also had a low prevalence of co-morbidity among hypertensive patients. Most of the studies had high proportion co-morbidities or exclusively done among hypertensive patients with chronic co-morbidities [ 33 , 36 , 38 , 39 , 40 ]. The study done in democratic republic Congo has operationally defined uncontrolled hypertension as BP of ≥130/80 for hypertensive patients with chronic co-morbidities [ 37 ]. So that, this lower cut point could contribute to the increased prevalence of uncontrolled hypertension. Our study revealed higher adherence to alcohol abstinence compared to other study done in Ethiopia [ 41 ]. Compared to our study the studies done in China, Morocco, Democratic Republic of Congo, South Africa and Zimbabwe had higher proportion of older adults and even some of them were done exclusively among older adults [ 35 , 36 , 37 , 38 , 39 ]. Even though our study didn’t show significant association of age with uncontrolled hypertension, many previous studies revealed advanced age is an independent predictor of uncontrolled hypertension [ 19 , 36 , 41 , 42 ]. Aging causes hypertension referred to as isolated systolic hypertension which is found primarily in elderly people by stiffening of the aorta [ 43 ].
Overweight was found significant predictor of uncontrolled hypertension. This is supported by the studies done in China and Zimbabwe [ 35 , 39 ]. Other study done in Jimma university hospital, Ethiopia also revealed overweight and obesity were independent predictors of uncontrolled hypertension [ 19 ]. Higher BMI (overweight and obesity) is one major contributing factor for hypertension and many health studies have consistently identified that BMI and blood pressure have a direct and apparent dose-response relationship [ 44 ]. The mechanism by which obesity directly causes hypertension is under investigation. Activation of the sympathetic nervous system, the amount of intra-abdominal and intra-vascular fat, sodium retention leading to increase in renal reabsorption, and the renin-angiotensin system are considered to have important functions in the pathogenesis of obesity related hypertension [ 45 ].
Co-morbidity had a significant association with uncontrolled hypertension. This is consistent with the studies done in South Asia and China, which showed diabetic and kidney disease co-morbidities were associated with uncontrolled hypertension [ 28 , 35 ]. This is also in line with the study done in Gondar university hospital, Ethiopia which showed co-morbid hypertensive patients were more likely to have uncontrolled hypertension [ 32 ]. Many chronic diseases are secondary causes of hypertension so that controlling hypertension among hypertensive patients with other chronic co-morbidities might be challengeable.
Non-adherence to anti-hypertensive medication was an independent predictor of uncontrolled hypertension. This is in line with studies done in and Southern California [ 46 ], South Asia [ 28 ] and Zimbabwe [ 39 ] and Cameron [ 40 ] in which good adherence to antihypertensive medication was found protective to uncontrolled hypertension. It is also supported by the study done in Ghana and University of Gondar hospital, Ethiopia which showed poor adherence or non-adherence to anti-hypertensive medication was found statistically associated with uncontrolled hypertension [ 29 , 32 ]. This congruency could be due to the good adherence to antihypertensive medication is essential to control hypertension and reduces blood pressure. Anti-hypertensive medications lower and control high blood pressure by increasing vasodilatation and decreasing vasoconstriction, increasing urine output and blocking the sympathetic activation of heart [ 47 ].
Non-adherence to physical activity was associated with uncontrolled hypertension. This is similar with the study done in China which showed that lack of physical activity was statistically associated with uncontrolled hypertension [ 35 ]. Epidemiological studies have evidenced that physical activity results in significant BP and weight reduction. Sedentary life, which is a known predictor of obesity, is one of the major risk factors of high blood pressure and thus non-adherence to physical exercise makes difficult to control hypertension [ 44 ]. Although precise mechanisms have yet to be fully elucidated, available data have provided enough information to establish biologically plausible mechanisms for the relationship between physical activity and hypertension. Physical exercise may prevent increases in BP through beneficial alterations in insulin sensitivity, and autonomic nervous system function and vasoconstriction regulation. It also decreases high blood pressure by decreasing body weight and increasing renal function [ 48 ].
Non-adherence to alcohol abstinence was found significantly associated with uncontrolled hypertension. This is consistent with studies done in South Africa [ 38 ], Zimbabwe [ 39 ] and Jimma university teaching hospital, Ethiopia [ 19 ]. Health studies evidenced that Alcohol is one of the risk factors and is accountable for significant population burden of hypertension. Non-adherence of hypertensive patients to recommendations of alcohol intake makes more difficult to control hypertension [ 44 ]. Stimulation of the endothelium to release vasoconstrictors and loss of relaxation due to inflammation and oxidative injury of the endothelium by angiotensin II leading to inhibition of endothelium-dependent nitric oxide production is the major contributors of the alcohol-induced hypertension [ 49 ].
Limitations
There might be recall bias and social desirability bias since the behavioral practice of the study participants were based on self-reports and performance of these behaviors was not observed and could not be confirmed. Since our study design is a cross-sectional study it doesn’t show temporal relationship. Hence, it is also difficult to confirm the cause and effect between the dependent and predictor variables. Besides the study was conducted in a relatively small sample size which may have an effect on generalizability.
The magnitude of uncontrolled hypertension was found high. Non-adherence to anti-hypertensive medications, overweight, co-morbidity, non-adherence to physical exercise and non-adherence to alcohol abstinence were the independent predictors of uncontrolled hypertension. So that health care professionals and other stakeholders should promote overweight hypertensive patients to reduce their weight and maximize patients’ adherence to antihypertensive therapy, physical exercise and alcohol abstinence. Early identification and management of co-morbidities among hypertensive patients is crucial to control hypertension.
Abbreviations
- Ayder comprehensive specialized hospital
Adjusted odds ratio
Body max index
Blood pressure
Confidence interval
Crude odds ratio
Cardiovascular disease
Dietary approaches to stop hypertension
Degree of freedom
Hypertension evaluation of lifestyle and management
Hypertension self-care activity level effect
Hypertension
Joint National Commission
Non-communicable disease
Statistical package for social sciences
United state
World Health Organization
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Journal of the American Society of Hypertension. 2018;12(8):579–e1
Kingue S, Ngoe CN, Menanga AP, Jingi AM, Noubiap JJN, Fesuh B, et al. Prevalence and risk factors of hypertension in urban areas of Cameroon: a nationwide population-based cross-sectional study. J Clin Hypertens. 2015;17(10):819–24.
Article Google Scholar
Dzudie A, Kengne AP, Muna WF, Ba H, Menanga A, Kouam CK, et al. Prevalence, awareness, treatment and control of hypertension in a self-selected sub-Saharan African urban population: a cross-sectional study. BMJ Open. 2012;2(4):e001217.
Iloh GU, Ofoedu JN, Njoku PU, Amadi AN, Godswill-Uko EU. Medication adherence and blood pressure control amongst adults with primary hypertension attending a tertiary hospital primary care clinic in eastern Nigeria. Afr J Prim Health Care Fam Med. 2013;5(1):446.
Elder K, Ramamonjiarivelo Z, Wiltshire J, Piper C, Horn WS, Gilbert KL, et al. Trust, medication adherence, and hypertension control in southern African American men. Am J Public Health. 2012;102(12):2242–5.
Hill MN, Miller NH, DeGeest S, Group ASoHW. Adherence and persistence with taking medication to control high blood pressure. J Am Soc Hypertens. 2011;5(1):56–63.
Mendis S, Puska P, Norrving B. World Health Organization. Global atlas on cardiovascular disease prevention and control. Geneva: World Health Organization; 2011.
Google Scholar
Group SR. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103–16.
Weber MA, Schiffrin EL, White WB, Mann S, Lindholm LH, Kenerson JG, et al. Clinical practice guidelines for the management of hypertension in the community. J Clin Hypertens. 2014;16(1):14–26.
Zhou D, Xi B, Zhao M, Wang L, Veeranki SP. Uncontrolled hypertension increases risk of all-cause and cardiovascular disease mortality in US adults: the NHANES III linked mortality study. Sci Rep. 2018;8(1):9418.
Lanti M, Puddu PE, Vagnarelli OT, Laurenzi M, Cirillo M, Mancini M, et al. Antihypertensive treatment is not a risk factor for major cardiovascular events in the Gubbio residential cohort study. J Hypertens. 2015;33(4):736–44.
Article CAS Google Scholar
Kayima J, Wanyenze RK, Katamba A, Leontsini E, Nuwaha F. Hypertension awareness, treatment and control in Africa: a systematic review. BMC Cardiovasc Disord. 2013;13(1):54.
Ataklte F, Erqou S, Kaptoge S, Taye B, Echouffo-Tcheugui JB, Kengne AP. Burden of undiagnosed hypertension in sub-saharan Africa: a systematic review and meta-analysis. Hypertension. 2015;65(2):291–8.
Abegaz TM, Abdela OA, Bhagavathula AS, Teni FS. Magnitude and determinants of uncontrolled blood pressure among hypertensive patients in Ethiopia: hospital based observational study. Pharm Pract. 2018;16(2):1173.
Tesfaye A, Kumela K, Wolde M. Blood pressure control associates and antihypertensive pharmacotherapy patterns in Tikur Anbessa general specialized hospital chronic care department, Addis Ababa, Ethiopia. Am J Biol Life Sci. 2015;3(3):41–8.
Yazie D, Shibeshi W, Alebachew M, Berha A. Assessment of Blood Pressure Control among Hypertensive Patients in Zewditu Memorial Hospital, Addis Ababa, Ethiopia: A Cross-Sectional Study. J Bioanal Biomed. 2018;10:80–7.
Teshome DF, Demssie AF, Zeleke BM. Determinants of blood pressure control amongst hypertensive patients in Northwest Ethiopia. PLoS One. 2018;13(5):e0196535.
Animut Y, Assefa AT, Lemma DG. Blood pressure control status and associated factors among adult hypertensive patients on outpatient follow-up at University of Gondar Referral Hospital, Northwest Ethiopia: a retrospective follow-up study. Integr Blood Press Control. 2018;11:37.
Tesfaye B, Haile D, Lake B, Belachew T, Tesfaye T, Abera H. Uncontrolled hypertension and associated factors among adult hypertensive patients on follow-up at Jimma University teaching and specialized hospital: cross-sectional study. Research Reports in Clinical Cardiology. 2017;8:21–9.
Olomu AB, Gourineni V, Huang JL, Pandya N, Efeovbokhan N, Samaraweera J, et al. Rate and predictors of blood pressure control in a federal qualified health center in Michigan: a huge concern? J Clin Hypertens. 2013;15(4):254–63.
World Health Organization. Global action plan for the prevention and control of noncommunicable diseases 2013–2020. [Internet]. 2013. Available from: http://africahealthforum.afro.who.int/first-edition/IMG/pdf/global_action_plan_for_the_prevention_and_control_of_ncds_2013-2020.pdf . [cited 15 Jan 2018]
Mekelle University. Ayder Comprehensive Specialized Hospital [Internet]. 2018 Available from: http://www.mu.edu.et/chs/index.php/ayder-referral-hospital . [cited 15 Jan 2018]
Warren-Findlow J, Seymour RB. Prevalence rates of hypertension self-care activities among African Americans. J Natl Med Assoc. 2011;103(6):503–12.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. Jama. 2003;289(19):2560–71.
Schapira MM, Fletcher KE, Hayes A, Eastwood D, Patterson L, Ertl K, et al. The development and validation of the hypertension evaluation of lifestyle and management knowledge scale. J Clin Hypertens. 2012;14(7):461–6.
Sangsuwan T, Jamulitrat S. Prevalence of uncontrolled blood pressure in hypertensive patients attending the primary care unit of Songklanagarind hospital. Songklanagarind Medical Journal. 2018;36(1):11–27.
Olowe OA, Ross AJ. Knowledge, adherence and control among patients with hypertension attending a peri-urban primary health care clinic, KwaZulu-Natal. Afri J Prim Health Care Fam Med. 2017;9(1):1–5.
Jafar TH, Gandhi M, Jehan I, Naheed A, de Silva HA, Shahab H, Alam D, Luke N, Wee Lim C, COBRA-BPS Study Group. Determinants of uncontrolled hypertension in rural communities in South Asia—Bangladesh, Pakistan, and Sri Lanka. American journal of hypertension. 2018;31(11):1205–14.
Sarfo FS, Mobula LM, Burnham G, Ansong D, Plange-Rhule J, Sarfo-Kantanka O, et al. Factors associated with uncontrolled blood pressure among Ghanaians: evidence from a multicenter hospital-based study. PLoS One. 2018;13(3):e0193494.
Ojo OS, Malomo SO, Sogunle PT, Ige AM. An appraisal of blood pressure control and its determinants among patients with primary hypertension seen in a primary care setting in Western Nigeria. S Afr Fam Pract. 2016;58(6):192–201.
Weitzman D, Chodick G, Shalev V, Grossman C, Grossman E. Prevalence and factors associated with resistant hypertension in a large health maintenance organization in Israel. Hypertension. 2014;64(3):501–7.
Abdu O, Diro E, Abera Balcha MA, Ayanaw D, Getahun S, Mitiku T, et al. Blood pressure control among hypertensive patients in University of Gondar Hospital, Northwest Ethiopia: a cross sectional study. Hypertension. 2017;140(1):6.
Chen Camano RR. Uncontrolled hypertension and associated factors in hypertensive patients at the primary healthcare center Luis H. Moreno, Panama: a feasibility study; 2013.
Choudhary R, Sharma SM, Kumari V, Gautam D. Awareness, treatment adherence and risk predictors of uncontrolled hypertension at a tertiary care teaching hospital in Western India. Indian Heart J. 2016;68(Suppl 2):S251.
Yang L, Xu X, Yan J, Yu W, Tang X, Wu H, et al. Analysis on associated factors of uncontrolled hypertension among elderly hypertensive patients in southern China: a community-based, cross-sectional survey. BMC Public Health. 2014;14(1):903.
Berraho M, El Achhab Y, Benslimane A, Rhazi KE, Chikri M, Nejjari C. Hypertension and type 2 diabetes: a cross-sectional study in Morocco (EPIDIAM study). Pan Afr Med J. 2012;11(1):52.
Kika T, Kintoki E, M’Buyamba-Kabangu J, Lepira F, Makulo J, Sumaili E, et al. Uncontrolled hypertension among patients managed in primary healthcare facilities in Kinshasa, democratic republic of the Congo. Cardiovasc J Afr. 2016;27(6):361.
Adeniyi OV, Yogeswaran P, Longo-Mbenza B, Ter Goon D. Uncontrolled hypertension and its determinants in patients with concomitant type 2 diabetes mellitus (T2DM) in rural South Africa. PLoS One. 2016;11(3):e0150033.
Goverwa TP, Masuka N, Tshimanga M, Gombe NT, Takundwa L, Bangure D, et al. Uncontrolled hypertension among hypertensive patients on treatment in Lupane District, Zimbabwe, 2012. BMC Res Notes. 2014;7(1):703.
Menanga A, Edie S, Nkoke C, Boombhi J, Musa AJ, Mfeukeu LK, et al. Factors associated with blood pressure control amongst adults with hypertension in Yaounde, Cameroon: a cross-sectional study. Cardiovasc Diagn Ther. 2016;6(5):439.
Berhe DF, Taxis K, Haaijer-Ruskamp FM, Mulugeta A, Mengistu YT, Mol PG. Hypertension treatment practices and its determinants among ambulatory patients: retrospective cohort study in Ethiopia. BMJ Open. 2017;7(8):e015743.
Kanungo S, Mahapatra T, Bhowmik K, Saha J, Mahapatra S, Pal D, et al. Patterns and predictors of undiagnosed and uncontrolled hypertension: observations from a poor-resource setting. J Hum Hypertens. 2017;31(1):56.
Weber MA, Schiffrin EL, White WB, Mann S, Lindholm LH, Kenerson JG, et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertens. 2014;16(1):14–26.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):e127–248.
Jiang SZ, Lu W, Zong XF, Ruan HY, Liu Y. Obesity and hypertension. Exp Ther Med. 2016;12(4):2395–9.
Elperin DT, Pelter MA, Deamer RL, Burchette RJ. A large cohort study evaluating risk factors associated with uncontrolled hypertension. J Clin Hypertens. 2014;16(2):149–54.
Bell K, Twiggs J, Olin BR, Date IR. Hypertension: the silent killer: updated JNC-8 guideline recommendations. Alabama Pharmacy Association. 2015;334:4222.
Diaz KM, Shimbo D. Physical activity and the prevention of hypertension. Curr Hypertens Rep. 2013;15(6):659–68.
Husain K, Ansari RA, Ferder L. Alcohol-induced hypertension: mechanism and prevention. World J Cardiol. 2014;6(5):245–52.
Download references
Acknowledgments
We would like to acknowledge Mekelle University for providing of financial support to the accomplishment of this project. We are grateful to the data collectors for their cooperation in the data collection process. We would like also to give our heartfelt thanks to our study participants for their cooperation in the provision of their information.
Financial support was obtained from Mekelle University.
Availability of data and materials
Raw data can be made available on request to the corresponding author.
Author information
Authors and affiliations.
School of Nursing College of Health Science, Mekelle Univesity, Tigray, Ethiopia
Gebrewahd Bezabh Gebremichael & Kalayou Kidanu Berhe
Department of Nursing College of Health Science, Axum University, Tigray, Ethiopia
Teklewoini Mariye Zemichael
You can also search for this author in PubMed Google Scholar
Contributions
GBG: conception, design, acquisition, data collection, analysis and interpretation of data and drafting the manuscript. KKB critically reviewed the design, analysis, interpretation and the drafted manuscript. TMG participate in reviewing of the design, analysis, interpretation and the drafted manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Gebrewahd Bezabh Gebremichael .
Ethics declarations
Ethics approval and consent to participate.
Permission to proceed with the study Ethical approval was receipt from the Health Research Ethics Review Committee (HRERC) of Mekelle university college of health science (ERC 1293/2018). Written informed consent was also obtained from all participants.
Consent for publication
Written informed consent was obtained from all participants for publication of the result.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Gebremichael, G.B., Berhe, K.K. & Zemichael, T.M. Uncontrolled hypertension and associated factors among adult hypertensive patients in Ayder comprehensive specialized hospital, Tigray, Ethiopia, 2018. BMC Cardiovasc Disord 19 , 121 (2019). https://doi.org/10.1186/s12872-019-1091-6
Download citation
Received : 26 October 2018
Accepted : 30 April 2019
Published : 22 May 2019
DOI : https://doi.org/10.1186/s12872-019-1091-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
BMC Cardiovascular Disorders
ISSN: 1471-2261
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Case Report
- Open access
- Published: 29 November 2012
A teenager with uncontrolled hypertension: a case report
- Abdul Wadud Chowdhury 1 ,
- ATM Hasibul Hasan 2 ,
- SME Jahan Kabir 1 &
- KM Nurus Sabah 1
BMC Research Notes volume 5 , Article number: 659 ( 2012 ) Cite this article
10k Accesses
2 Citations
Metrics details
Takayasu Arteritis is a vasculitis occurring mostly in young females which may present in diverse ways. Here we report a teenager with Takayasu Arteritis who presented with uncontrolled hypertension. This case depicts an atypical presentation of this disease where the girl visited many physicians for controlling the level of hypertension and put a diagnostic dilemma about the underlying etiology of young hypertension.
Case presentation
A 13 year old girl presented with epistaxis, persistent headache and uncontrolled hypertension. Her clinical examination revealed normal radial, very feeble femoral and absent other lower limb pulses. There was a blood pressure discrepancy of 50/40 mm of Hg between two arms. There were bruits over multiple areas including the abdominal aorta. She had features of left ventricular hypertrophy. Her Arch aortogram showed hugely dilated arch of aorta which became abruptly normal just after origin of left subclavian artery. There was ostio-proximal stenosis of right bracheocephalic artery, left common carotid and left subclavian artery with post stenotic dilatation of all the vessels. Abdominal aortogram revealed critical stenosis of abdominal aorta above the origin of renal arteries with a pressure gradient of 80/11 mm of Hg.
Takayasu’s Arteritis should also be kept in mind while searching for the cause of uncontrolled hypertension in the young age group.
The estimated prevalence of hypertension in pediatric age group is between 2%–5% [ 1 ]. The usual form of hypertension in young is attributable to secondary causes. The most common cause is the renovascular one (60–70%) [ 2 , 3 ]. Cushing syndrome, hyperthyroidism, pheochromocytoma, essential hypertension, coarctation of aorta, SLE are also found less commonly with hypertension in children and adeloscent [ 4 ]. With the growing knowledge and awareness of hypertension, the rate of diagnosis is increasing in children [ 1 ]. Evidences are increasing regarding early development of atherosclerosis in child and their possible relation to hypertension and coronary artery disease [ 5 ]. Several studies have reported the correlation between pediatric hypertension and family H/O hypertension, low birth weight, excess body weight [ 6 , 7 ]. Here we describe a 13 year old girl presenting with epistaxis, headache and uncontrolled hypertension despite poly drug therapy, abnormal peripheral pulses and unequal blood pressure in upper limbs. Further investigations were done to determine the cause of hypertension. The arch and abdominal aortography further correlated the uncontrolled hypertension with Takayasu’s disease according to American College Rheumatology (ACR) criteria. KS Chugh et al. described Takayasu Arteritis as the most common cause of renovascular hypertension in India [ 8 ]. Takayasu Arteritis is a large vessel vasculitis of unknown origin characterized by granulomatous inflammation of aorta and its major branches, leading to stenosis, thrombosis and aneurysm formation.
A 13 year old girl presented with three episodes of spontaneous profuse nasal bleeding within last three years which had remission without specific therapy. She had diffuse persistent headache without nausea or vomiting and uncontrolled hypertension, despite taking amlodipine and atenolol. She gave no H/O chest pain, shortness of breath, fever, prolonged cough, pulsatile tinnitus, light headedness, arthralgia, skin rash, weight loss, claudication or colour changes on cold exposure. There was no history of contact with TB patient. She did not give any H/O dizziness or syncope. On examination, both radial pulses were 80 beats/min, regular, high volume and surprisingly apparently symmetrical on both sides. There was no radio-femoral delay. Both the femoral pulses were feeble. All other lower limb pulses were absent. BP on right arm was 120/80 mmHg and on left arm was 170/120mmHg. There were bruits over both carotids, suprasternal, supraclavicular areas and over abdominal aorta. On precordial examination-apex beat was palpable at left 5th intercostal space just lateral to the midclavicular line. It was heaving in nature. A 2 was loud, there was no added sound. All other systemic examinations including optic fundi were normal. On investigation, Hemoglobin was 11.2 gm/dl, Total Count-5100/mm [ 3 ], Neutrophil- 51%, Lymphocyte- 35%, Monocyte- 03%, Eosinophil-07%, Erythrocyte sedimentation rate (ESR)- 30 mm in 1st hour. Mantoux test (MT) and C-reactive protein (CRP) were negative. Blood glucose, Serum creatinine, urine analysis were normal. Chest X-ray showed cardiomegaly with LV type apex (Figure 1 A).
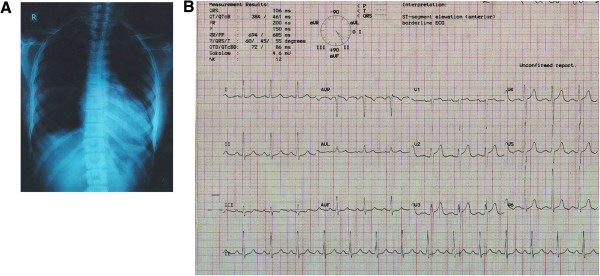
A: CXR P-A view. Cardiomegaly with LV type apex. B ECG. Left ventricular hypertrophy.
ECG fulfilled the voltage criteria of left ventricular hypertrophy (Figure 1 B). 2D, M-mode and Doppler echocardiography revealed concentric left ventricular hypertrophy, aneurysmal dilatation of aortic arch, proximal stenosis and post stenotic dilatation of brachiocephalic, left common carotid and left subclavian artery and narrowing of descending thoracic aorta beyond the origin of left subclavian artery. Arch Aortogram showed hugely dilated (70 mm) arch of aorta which became abruptly normal (35 mm) just after origin of left subclavian artery. Right bracheocephalic artery had ostio-proximal stenosis with marked post stenotic dilatation (Figure 2 A: white arrow). There was also ostio-proximal stenosis of left common carotid and left subclavian artery with post stenotic dilatation (Figure 2 B: white arrow). Abdominal aortogram revealed critical stenosis of abdominal aorta (8.9 mm) above the origin of renal arteries (Figure 2 C: white arrow). Renal arteries were however normal. Pressure study in abdominal aorta showed a pressure tracing of 200/106 mm of Hg above and 120/95 mm of Hg below the stenosis (Figure 3 ).
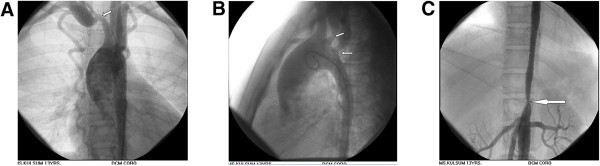
A: Arch Aortogram. Hugely dilated (70 mm) arch of aorta which became abruptly normal (35 mm) just after origin of left subclavian artery. Right bracheocephalic artery had ostio-proximal stenosis with marked post stenotic dilatation (white arrow). B : Arch Aortogram. Ostio-proximal stenosis of left common carotid and left subclavian artery with post stenotic dilatation (white arrow). C : Abdominal Aortogram critical stenosis of abdominal aorta (8.9 mm) above the origin of renal arteries (white arrow).
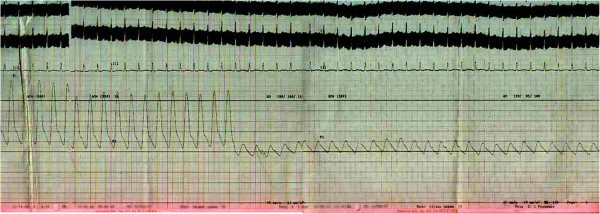
Pressure tracing in abdominal aorta.
She fulfilled four of the six major ACR (American College of Rheumatology) criteria for Takayasu’s disease eg, onset of age is 13 years (<40years), 50 mm of Hg pressure difference between systolic BP between arms (>10mm of Hg pressure difference), subclavian and aortic bruit and narrowing of major branches of aorta. She was prescribed Amlodipine 10 mg, Atenolol 100mg, Prazosin 6mg, Hydrochlorthiazide 50mg and Amiloride 5mg. Methotrexate 5mg weekly with Folinic acid supplementation were given too. Plan for Angioplasty and Stenting of abdominal aortic stenosis was provided to the patient.
Takayasu’s Arteritis (TA) is a chronic inflammatory large vessel vasculitis of unknown origin, predominantly affecting aorta and its major branches. It is also called Aortic arch syndrome, Pulse less disease, Occlusive thromboaortopathy, Martorell syndrome [ 9 ]. The first scientific description of Takayasu’s Arteritis was given by Mikito Takaysu, Professor of Opthalmology at Kanazawa University, Japan, in 1905 at 12th Annual conference of Japanese Ophthalmology Society [ 10 ]. He presented a 21year old woman with a peculiar form of arteriovenus anastomoses at optic fundi. K Onishi and T Kagosha also contributed with their patients of absent radial pulse in the same conference [ 10 ]. But the first ever documented description of this arteritis dates back to 1830. Rokushu Yamamoto who practiced Japanese oriental medicine, described a case of 45 years old man presenting with absent pulse in one upper limb and feeble pulse in another one following a year long history of high grade fever. During the period of follow up the patient subsequently became emaciated, dyspnoeic and died suddenly after 11 years [ 10 ]. The world wide prevalence of Takayasu’s disease is 3.3/million. The disease is more common in East Asia and in Asian descendants in other countries [ 11 ]. TA commonly presents in 2nd or 3rd decade of life, with a high female preponderance. But the female to male ratio declines from Eastern Asia to the West [ 12 ]. TA may manifest as asymptomatic pulseless disease to catastrophic neurological impairements. The disease may present in two phase, a prepulseless phase of nonspecific inflammatory signs, followed by a chronic phase of vascular insufficiency [ 13 – 15 ]. Presentation of TA varies among the races. Japanese patients are predominantly female, presents with pulslessness, dizziness, vertigo, aortic regurgitation, inflammatory process commonly affecting the arch and its major branches, whereas Indian patients are male dominant. Indian cases present with more hypertension, headache, LV hypertrophy and vasculitic involvement of abdominal aorta and renal arteries [ 15 ]. Diminished or absent pulse along with upper limb claudication and blood pressure difference is found in 84–96% of cases [ 16 ]. Vascular bruits involving carotid, subclavian and abdominal vessels are also common (80–94%) [ 17 ]. Hypertension is associated with 33–83% patients of TA [ 15 , 17 ]. Our index case was also a young girl with feeble femoral pulse and absent other peripheral pulses in lower limb, blood pressure discrepancy between arms, bruits over multiple areas of chest and neck and hypertension. The blood pressure discrepancy of 50/40 mm of Hg is probably due to the difference in percentage of stenosis among the brachiocephalic (70–80% stenosis) and left subclavian vessels (50–60% stenosis). Retinopathy, aortic regurgitation, congestive heart failure, cardiomyopathy, myocardial ischemia, headache, dizziness, seizure are less common association of TA. From common findings of TA, American College of Rheumatology has devised some diagnostic criteria for TA in 1990. Angiography remains the gold standard investigation for diagnosis. The main differential diagnosis include other causes of large vessel vasculitis eg inflammatory vasculitis (Syphilis, Tuberculosis, Behchets, SLE); development abnormalities (Coarctation of aorta, Marfans syndrome) and neurofibromatosis. TA has been classified on the basis of angiographic findings. The new classification was described at Takayasu Arteritis Conference in 1994 based on vessel involvement. Type-I involving branches from aortic arch, Type-IIa denoting ascending aorta, aortic arch and its branches, Type-IIb including Type-Ia plus descending thoracic aorta. Type-III means descending thoracic aorta, abdominal aorta and/ or renal arteries. Type-IV involves abdominal aorta and/ or renal arteries. Type-V is combined features of Type-IIb and Type-IV [ 15 ]. Ishikawa classified different clinical groups based on natural history and complications. He described Group-I as uncomplicated disease with or without pulmonary artery involvement, Group-IIA as mild/moderate single complication together with uncomplicated disease, Group-IIB as severe single complication together with uncomplicated disease, Group-III as two or more complications together with uncomplicated disease [ 17 ]. Ishikawa defined Takayasu retinopathy, Secondary hypertension, Aortic regurgitation, Aneurysm formation as four most important complications. Our index case met the angiographic criteria of Type-IV Takayasu Arteritis class and Group-III of Ishikawa class [ 17 ]. Ishikawa class caries a prognostic significance not only for the Japanese patients but also for the Indians. The overall five year survival rate is 83%. The survival rate is 100% in Group-I and 70% in Group-IIb and Group-III. The most common cause of mortality is cerebrovascular disease and cardiac failure. Regarding treatment strategy steroid had been the mainstay of treatment. Shelhamer et al. showed half of the TA patients on steroid won’t respond [ 18 ]. Kerr et al. showed overall remission rate of 33% with immunosuppressive drugs in steroid unresponsive patients [ 16 ]. Methotrexate though not more efficacious than others, became popular due to its well tolerability [ 19 , 20 ]. The combination of steroid and methotrexate demonstrated a remission rate of 81% in steroid unresponsive patients [ 21 ]. Treatment of hypertension and prevention of thrombosis are also important aspects of therapy. Treatment of hypertension with ACE inhibitors requires careful monitoring for renal artery stenosis. Surgery may be needed in patients with critical renal artery stenoses, limb claudication limiting the daily activities, stenosis of three or more cerebral vessels, moderate aortic regurgitation. Stenoses of renal artery are best treated by Percutaneous Transluminal Angioplasty [ 21 ]. Stent placement following angioplasty is a safe and effective procedure [ 22 ]. Takayasu’s Arteritis is a chronic progressive vasculopathy. So long term follow up is recommended. Markers of acute phase response are unreliable during follow up. Doppler studies and MRA are can help to determine the vessel wall thickness and lumen configuration.
Takaysu’s Arteritis can have varied presentation. So a young female patient presenting with absent pulse, unequal blood pressure between arms and hypertension should be suspected clinically for Takayasu’s disease.
Written informed consent was obtained from the patient’s guardian for publication of this case report and for all the accompanying images.
Sorof JM, Lai D, Turner J, Poffenbarger T, Portman RJ: Overweight, ethnicity, and the prevalence of hypertension in school-aged children. Pediatrics. 2004, 113 (3 pt 1): 475-482.
Article PubMed Google Scholar
Ooi BS, Chen BTM, Toh CCS, Khoo OT: “Cause of Hypertension in Young”. Br Med J. 1970, 3: 744-746. 10.1136/bmj.3.5725.744.
Article PubMed CAS PubMed Central Google Scholar
Flynn JT: Evaluation and management of hypertension in childhood. Prog Pediatr Cardiol. 2001, 12: 177-188. 10.1016/S1058-9813(00)00071-0.
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents: The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004, 114 (2 suppl 4th report): 555-576.
Article Google Scholar
Luma GB, Spoitta RT: “Hypertension in Children and Adeloscent”. Am Fam Physician. 2006, 73 (9): 1558-1566.
PubMed Google Scholar
Franco MC, Christofalo DM, Sawaya AL, Ajzen SA, Sesso R: Effects of low birth weight in 8- to 13-yearold children: implications in endothelial function and uric acid levels. Hypertension. 2006, 48 (1): 45-50. 10.1161/01.HYP.0000223446.49596.3a.
Article PubMed CAS Google Scholar
Moore WE, Stephens A, Wilson T, Wilson W, Eichner JE: Body mass index and blood pressure screening in a rural public school system: the Healthy Kids Project. Prev Chronic Dis. 2006, 3 (4): A114-
PubMed PubMed Central Google Scholar
Chugh KS, Jain S, Sakhuja V: Renovascular hypertension due to Takayasu’s Arteritis among Indian patients. QJM. 1992, 85: 833-843.
PubMed CAS Google Scholar
Lupi-Herrera E, Sánchez-Torres G, Marcushamer J: Takayasu Arteritis. Clinical study of 107 cases. Am Heart J. 1977, 93: 94-103. 10.1016/S0002-8703(77)80178-6.
Numano F, Okawara M, Inomata H: Takayasu’s Arteritis. Lancet. 2000, 356: 1023-1025. 10.1016/S0140-6736(00)02701-X.
Watts R, Al Taiar A, Mooney J, Scott D, MacGregor A: The Epidemiology of Takayasu Arteritis in the UK. Rheumatology. 2009, 48: 1008-1011. 10.1093/rheumatology/kep153.
Johnston SL, Lock RJ, Gompels MM: Takayasu Arteritis: a review. J Clin Pathol. 2002, 55: 481-486. 10.1136/jcp.55.7.481.
Moriwaki R, Noda M, Yajima M: Clinical manifestations of Takayasu Arteritis in India and Japan—new classification of angiographic findings. Angiology. 1997, 48: 369-379.
Jain S, Sharma N, Singh S: Takayasu Arteritis in children and young Indians. Int J Cardiol. 2000, 75: S153-S157.
Subramanyan R, Joy J, Balakrishnan KG: Natural history of aortoarteritis (Takayasu’s disease). Circulation. 1989, 80: 429-437. 10.1161/01.CIR.80.3.429.
Kerr GS, Hallahan CW, Giordano J: Takayasu Arteritis. Ann Intern Med. 1994, 120: 919-929.
Ishikawa K: Natural history and classification of occlusive thromboaortopathy (Takayasu’s disease). Circulation. 1978, 57: 27-35. 10.1161/01.CIR.57.1.27.
Shelhamer JH, Volkman DJ, Parrillo JE: Takayasu’s Arteritis and its therapy. Ann Intern Med. 1985, 103: 121-126.
Hoffman GS, Leavitt RY, Kerr GS: Treatment of Takayasu’s Arteritis (TA) with methotrexate (MTX). Arthritis Rheum. 1991, 34: S74-
Hoffmann GS, Leavitt RY, Kerr GS: Treatment of glucocorticoid-resistant or relapsing Takayasu Arteritis with methotrexate. Arthritis Rheum. 1994, 37: 578-582. 10.1002/art.1780370420.
Giordano JM: Surgical treatment of Takayasu’s Arteritis. Int J Cardiol. 2000, 75: S123-S128.
Sharma BK, Jain S, Bali HK: A follow-up study of balloon angioplasty and de-novo stenting in Takayasu Arteritis. Int J Cardiol. 2000, 75: S147-S152.
Download references
Acknowledgement
We acknowledge Professor H I Lutfur Rahman Khan for providing the overall support to us.
Author information
Authors and affiliations.
Department of Cardiology, Dhaka Medical College Hospital, Dhaka, Bangladesh
Abdul Wadud Chowdhury, SME Jahan Kabir & KM Nurus Sabah
Department of Medicine (Outdoor Patient Department), Dhaka Medical College Hospital, Dhaka, Bangladesh
ATM Hasibul Hasan
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to ATM Hasibul Hasan .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contributions
AWC is the first author and was involved in diagnosis by performing the angiography and writing a part of the manuscript. ATMHH is the communicating author and was involved in writing the manuscript. SMEJK and KMNS were responsible for the management of the patient. All the authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Authors’ original file for figure 2, authors’ original file for figure 3, authors’ original file for figure 4, authors’ original file for figure 5, authors’ original file for figure 6, rights and permissions.
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Chowdhury, A.W., Hasan, A.H., Kabir, S.J. et al. A teenager with uncontrolled hypertension: a case report. BMC Res Notes 5 , 659 (2012). https://doi.org/10.1186/1756-0500-5-659
Download citation
Received : 25 September 2012
Accepted : 23 November 2012
Published : 29 November 2012
DOI : https://doi.org/10.1186/1756-0500-5-659
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Takayasu’s Arteritis (TA)
BMC Research Notes
ISSN: 1756-0500
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State
Differential Diagnoses
Hypertension differential diagnosis.
One of the most dangerous aspects of hypertension is that it may be asymptomatic. The early stages of hypertension may present with no clinical manifestations other than elevated blood pressure.

Diagnosis of hypertension requires blood pressure measurement on at least two separate occasions. These two measurements are then averaged. Requirements for these measurements include no smoking or caffeine intake within the previous thirty minutes and that the two blood pressure readings must be at least 2 minutes apart (Mayo Clinic, 2014a).
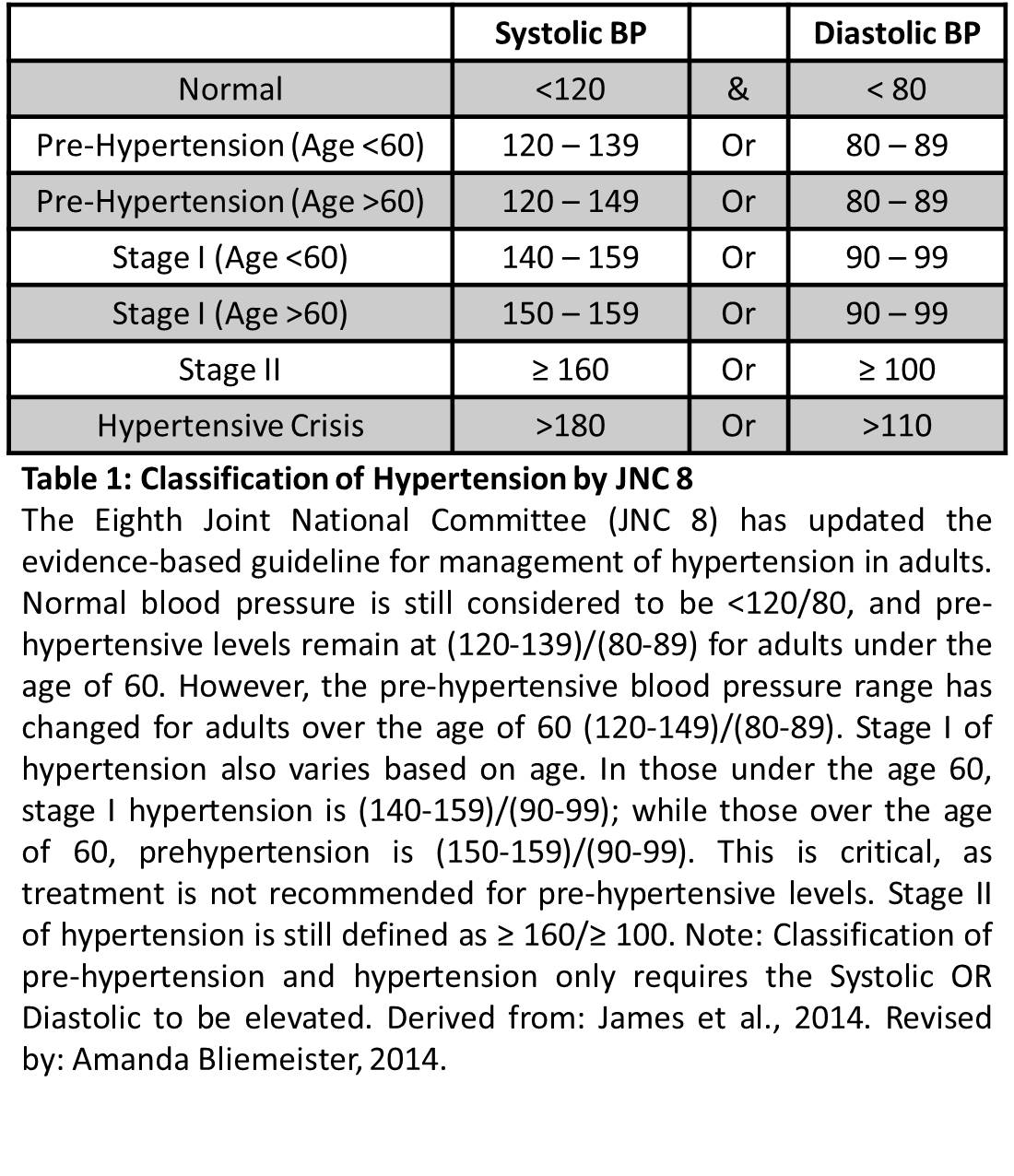
Differential Diagnosis I: Primary Hypertension
Due to patient’s age, BMI, lifestyle, consecutive hypertensive blood pressures, and description of headaches (bilateral temporal throbbing – occurring throughout day with decreased intensity as the day progresses), lower extremity edema, and knowledge that primary hypertension is the most common form of hypertension and mild to moderate primary (essential) hypertension is largely asymptomatic for many years, combined provide rationale for this differential diagnosis.
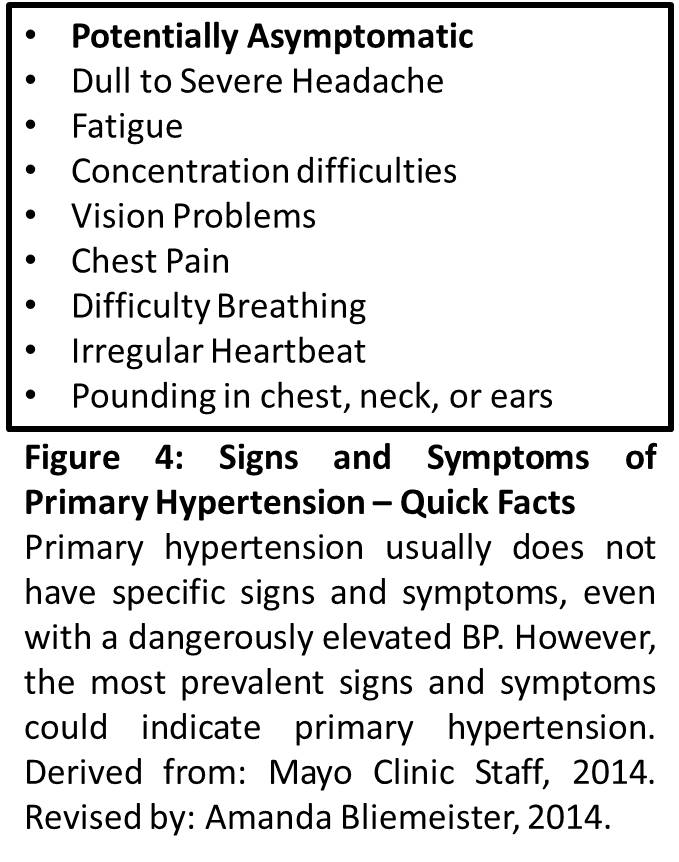
Differential Diagnosis II: Secondary Hypertension
Patient’s description of headaches, consecutive hypertensive blood pressures, combined with the knowledge that secondary hypertension is the second most common type of hypertension provides rationale for this differential diagnosis. Presentation of secondary hypertension is similar to primary hypertension in that it may be asymptomatic despite a dangerously elevated blood pressure (Mayo Clinic, 2014b).

Differential Diagnosis III: Complicated Hypertension
Patient’s description of headaches, swelling of the lower extremities, consecutive uncontrolled hypertensive blood pressures, combined with the potential for chronic hypertensive damage leading to organ dysfunction, provides rationale for this differential diagnosis. Potential organ damage and/or dysfunction include: heart, kidney, eyes, arteries, brain, bone loss, difficulty sleeping, and sexual dysfunction (Mayo Clinic 2014c).
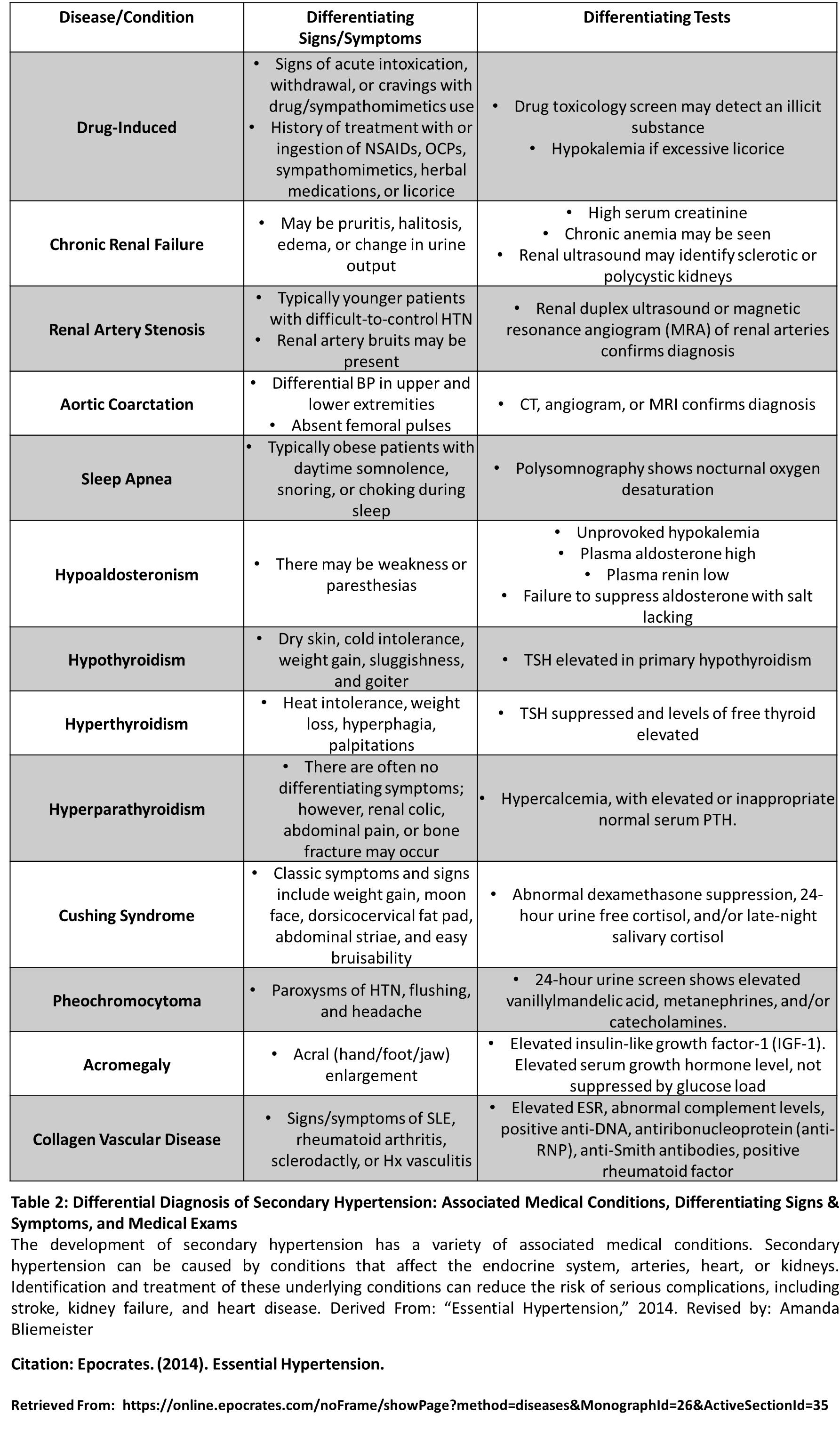
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Special Issue: Current evidence and perspectives for hypertension management in Asia
- Published: 05 April 2022
Latest hypertension research to inform clinical practice in Asia
- Kazuomi Kario 1 ,
- Masaki Mogi 2 &
- Satoshi Hoshide 1
Hypertension Research volume 45 , pages 555–572 ( 2022 ) Cite this article
6021 Accesses
16 Citations
3 Altmetric
Metrics details
Despite the challenges associated with the coronavirus pandemic, the last 2 years have been active periods for hypertension research and initiatives in Asia. There are new hypertension guidelines from the World Health Organization that can be interpreted and applied locally. This is also the case for data from the latest Blood Pressure Lowering Treatment Trialists’ Collaboration meta-analysis, which showed that greater reductions in systolic blood pressure (BP) are associated with lower risks of cardiovascular events. The randomized controlled Strategy of Blood Pressure Intervention in the Elderly Hypertensive study and the Salt Substitute and Stroke Study provide local data to inform practice. Other initiatives to help reduce high salt intake in Asia are also underway. Both drug-resistant and nocturnal hypertension are appropriate areas of focus in Asia, and there are an increasing number of pharmacological and non-pharmacological treatment options for these conditions. Digital therapeutics to promote uptake and implementation of lifestyle interventions are showing promise, and other digital-based strategies such as telemedicine, wearable BP monitors to detect beat-by-beat BP and artificial intelligence will no doubt become integral parts of future strategies to reduce the burden of hypertension and hypertension-related disease. A number of initiatives from the Hypertension Cardiovascular Outcome Prevention and Evidence in Asia Network and Japanese Society of hypertension are underway, and there is good reason for optimism regarding the ongoing and future management of hypertension in Asia based on these and the active research activities in the region.

Introduction
As the second year of the coronavirus pandemic comes to an end, global issues around low rates of achievement of blood pressure (BP) control have not improved, and hypertension remains a prevalent and significant health issue worldwide [ 1 , 2 ]. This is due, at least in part, to the reluctance of patients with chronic diseases to seek medical care due to fear of infection with SARS-CoV-2, and the worsening economic situation. However, the greater burden of coronavirus illness (COVID-19) in patients with comorbid diseases such as hypertension [ 3 ] highlights the importance of continuing to pursue important hypertension goals, including the global non-communicable disease target of reducing the prevalence of elevated BP by 25% compared with 2010 levels by 2025 [ 4 ].
Despite these challenges, the last 2 years have been active periods of hypertension research [ 5 ] and implementation of hypertension-related action plans in Asia. These data continue to highlight the need for both population-based primary prevention strategies and more effective treatments for high-risk patients with hypertension [ 6 ], something that should be achievable in all countries [ 2 ]. As has been documented previously, effective prevention and management of hypertension in Asia requires country- and region-specific approaches that take into account the Asia-specific characteristics of hypertension [ 7 , 8 , 9 ].
This article provides an up-to-date overview on the latest hot topics, clinical trial data, new pharmacological and non-pharmacological treatment options, and technological advances (including digital therapeutics, wearable monitoring devices, the Internet of Things [IoT] and artificial intelligence [AI]) (Fig. 1 ). Asian action approaches to improve the management of hypertension are also highlighted.
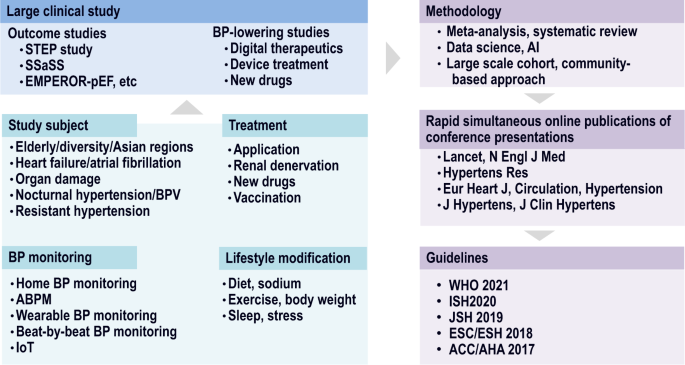
Summary of hypertension research activities to inform clinical practice. ABPM ambulatory blood pressure monitoring, ACC American College of Cardiology, AHA American Heart Association, AI artificial intelligence, BP blood pressure, BPV blood pressure variability, EMPEROR-pEF EMPagliflozin outcomE tRial in Patients With chrOnic heaRt Failure With Preserved Ejection Fraction, ESC European Society of Cardiology, ESH European Society of Hypertension, IoT Internet of Things, ISH International Society of Hypertension, JSH Japanese Society of Hypertension, WHO World Health Organization
Latest WHO guidelines
In 2021, the World Health Organization (WHO) published new guidelines for the pharmacological treatment of hypertension [ 10 ]. Summarizing the evidence to date, the guidelines recommend that high-risk patients should be treated promptly and reliably, starting earlier, at lower BP levels, and that the BP target should be gradually decreased. Initiation of antihypertensive therapy is recommended when BP is ≥140/90 mmHg, even in the absence of cardiovascular disease or risk factors. For patients who do have existing cardiovascular disease or cardiovascular disease risk factors and/or comorbid conditions (e.g., diabetes mellitus or chronic kidney disease [CKD]), antihypertensive drug treatment should be initiated when systolic BP (SBP) is 130–139 mmHg. In order to achieve a reliable antihypertensive effect, thiazide and thiazide-like diuretics, angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs), and long-acting dihydropyridine calcium channel blockers (CCBs) are recommended as first-line agents. In addition, fixed-dose single pill combinations (SPCs) are recommended to reduce the number of tablets taken and improve adherence. Target BP during treatment is <140/90 mmHg in all patients without comorbidities, while reducing SBP to <130 mmHg is recommended in patients with known cardiovascular disease or those with high cardiovascular risk [ 10 ].
BPLTTC meta-analysis data
The results of the largest ever meta-analysis of antihypertensive therapy, including data from the Systolic Blood Pressure Intervention Trial (SPRINT) [ 11 ], were published in 2021 by the Blood Pressure Lowering Treatment Trialists’ Collaboration (BPLTTC) [ 12 ]. This included data from 344,716 patients who participated in 48 randomized controlled trials that compared antihypertensive drug therapy versus placebo, different classes of antihypertensive agents, or intensive versus standard antihypertensive therapy [ 12 ].
Although changes in office SBP varied between studies, the meta-analysis showed that greater reductions in SBP were associated with lower risks of cardiovascular disease events. A 5-mmHg reduction in SBP was associated with an approximately 10% reduction in the rate of major vascular events, although the magnitude of risk reduction varied by the type of event (Fig. 2 ). The beneficial cardiovascular effects of BP lowering were consistent across baseline SBP categories and occurred regardless of baseline cardiovascular disease status [ 12 , 13 ]. Pharmacological reduction of BP was also found to be effective across all age groups (including participants aged ≥85 years) [ 13 ].
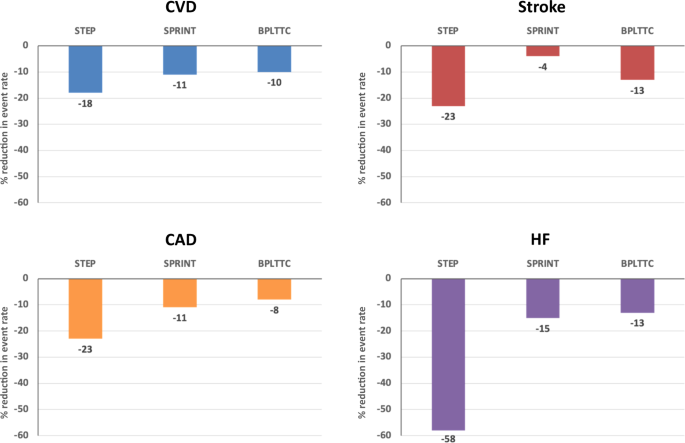
Estimated cardiovascular risk reduction associated with a 5-mmHg reduction in office systolic blood pressure (SBP) in the STEP [ 17 ] and SPRINT [ 11 ] studies, and the BPLTTC meta-analysis [ 12 ]. BPLTTC Blood Pressure Lowering Treatment Trialists’ Collaboration, CAD coronary artery disease (myocardial infarction [MI]/acute coronary syndrome), CVD cardiovascular disease, HF heart failure, SPRINT Systolic Blood Pressure Intervention Trial, STEP Strategy of Blood Pressure Intervention in the Elderly Hypertensive Patients. *CVD definitions as follows: STEP—composite of stroke (ischemic or hemorrhagic), acute coronary syndrome (acute MI and hospitalization for unstable angina), acute decompensated HF, coronary revascularization, atrial fibrillation, or death from cardiovascular causes; SPRINT—composite of MI, acute coronary syndrome not resulting in MI, stroke, acute decompensated HF, or death from cardiovascular causes; BPLTTC—composite of fatal or non-fatal stroke, fatal or non-fatal MI or ischemic heart disease, or heart failure causing death or requiring hospital admission
Overall, the BPLTTC meta-analysis findings suggest that a fixed degree of BP lowering is effective for both the primary and secondary prevention of major cardiovascular events, and that these benefits are seen even at BP levels that are below currently recommended thresholds for antihypertensive treatment initiation [ 12 ]. In addition, drug treatment of hypertension should be considered for patients of all ages, and the removal of age-related BP thresholds from international treatment guidelines was recommended [ 13 ]. The utility of antihypertensive drug therapy in older individuals is also highlighted by data showing that regimens designed to achieve intensive BP lowering tended to be more effective than standard BP-lowering treatment in trials of older patients with hypertension (age ≥70 years) (Fig. 3 ) [ 14 ]. Furthermore, BPLTTC data show that reducing BP is an effective strategy for preventing new-onset type 2 diabetes mellitus in patients with hypertension, especially when treatment includes an ACE inhibitor or ARB [ 15 ].
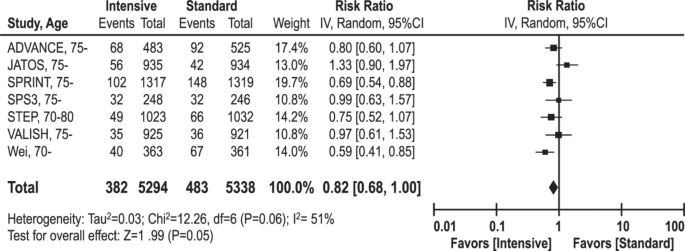
Effect of intensive blood pressure-lowering during pharmacological antihypertensive therapy on the risk of composite cardiovascular events in older patients. Boxes and horizontal lines represent the risk ratio (RR) and 95% confidence interval (CI) values for individual trials, and the size of boxes is proportional to the weight of that trial result. The diamond represents the pooled RR and 95% CI for pooled estimates of effect. Reproduced, with permission, from Rakugi et al. (2022) [ 14 ]
Another BPLTTC meta-analysis investigated the usefulness of antihypertensive treatment with SPCs for the primary prevention of cardiovascular disease [ 16 ]. Data from three large, randomized trials were included, and the results showed that treatment strategies including an SPC substantially reduced rates of cardiovascular disease, including myocardial infarction, revascularization, stroke and cardiovascular death. These findings were consistent for SPCs that did or did not include aspirin, and occurred irrespective of the presence of cardiometabolic risk factors [ 16 ].
High-impact clinical trials in Asia
The Strategy of Blood Pressure Intervention in the Elderly Hypertensive (STEP) [ 17 ] and Salt Substitute and Stroke Study (SSaSS) [ 18 ] were both conducted in China and the results were published in 2021.
The randomized, controlled STEP study is a Chinese version of the SPRINT trial [ 11 ], providing specific data on the value of intensive BP lowering in an Asian population [ 17 ]. It enrolled 8511 older patients with hypertension (age 60–80 [mean 66] years) who were treated with intensified (target SBP 110–130 mmHg) or standard (target SBP 130–150 mmHg) antihypertensive therapy [ 17 ]. All subjects used smartphones and home BP monitors to continuously monitor BP, and worked with physicians to adjust medications. Over a mean follow-up of 3.34 years, the mean reduction in SBP was 19.4 mmHg in the intensified treatment group and 10.1 mmHg in the standard treatment group (between-group difference: 9.3 mmHg). The difference between treatment groups in SBP was seen early after treatment initiation and was maintained throughout the study [ 17 ].
In China, as in Japan, early morning hypertension is attracting attention, and BP in the morning before taking antihypertensive medication is widely recognized as a blind spot for drug treatment. In the STEP study, there was initially almost no difference in early morning home SBP between the two treatment groups, but this difference gradually increased over time, such that the mean SBP reduction during the study period was about 7.5 mmHg greater in the intensified versus standard treatment group [ 17 ]. The risk of the composite primary outcome (a composite of stroke, acute coronary syndrome, acute uncompensated heart failure, coronary revascularization, atrial fibrillation (AF), and cardiovascular death) was reduced by 26% in patients managed using intensified treatment compared with standard treatment (hazard ratio [HR] 0.74, 95% confidence interval [CI] 0.60–0.92]; p = 0.007). Both stroke and acute coronary syndrome risk was reduced by 33% with intensive versus standard treatment (HR 0.67, 95% CI 0.47–0.97 and HR 0.67, 95% CI 0.47–0.94, respectively), and intensified treatment reduced the risk of acute uncompensated heart failure was reduced by almost three-quarters compared with standard therapy (HR 0.27, 95% CI 0.08–0.98). These results clearly demonstrate the benefits of intensive BP lowering.
In the STEP study, a 5-mmHg reduction in SBP was associated with an 18% reduction in the risk of major cardiovascular disease events. This is nearly twice the reduction seen in the BPLTTC meta-analysis (Fig. 2 ). Reductions in the risk of individual endpoint events were also numerically greater in the STEP study compared with the BPLTTC meta-analysis [ 12 ] and SPRINT [ 11 ] (Fig. 2 ), indicating that the benefits of BP reduction may be greater in elderly Asian populations compared with western patients. However, this issue needs to be evaluated in future studies.
The STEP study was discussed during a Super-Express Session at the Japanese Society of Hypertension (JSH) 2021 conference, and has been the subject of several editorial comments published in Hypertension Research [ 14 , 19 , 20 ]. Dr Hiromi Rakugi noted that mean BP achieved in the intensified treatment group of the STEP study (127.5 mmHg) should prompt reconsideration of the target BP level for elderly patients with hypertension in a variety of international guidelines [ 14 ]. He also noted that the results of this study should be used to educate physicians and help overcome clinical inertia [ 14 ], which is a contributing factor to low treatment rates and poor BP control [ 21 ]. Although antihypertensive medication titration and BP targets were based on office measurements, Dr Takayoshi Okubo highlighted the importance of collecting home BP data using smartphone applications, as performed in the STEP study [ 20 ]. However, the study population was limited to those able to competently use a smartphone and relevant applications, which may not be the case in unselected patients treated during routine clinical practice [ 20 ]. As noted by the author (K. Kario) in another editorial, data from the online supplement accompanying the STEP study publication showed that the prevalence of masked morning hypertension appeared to increase in the standard treatment group over time, whereas this was not the case in the intensive BP control group [ 19 ]. This shows that standard treatment based on office BP is insufficient to provide good control of morning BP during long-term follow-up. Thus, the STEP study findings, along with data showing a close association between poorly controlled morning BP and cardiovascular events [ 22 , 23 , 24 , 25 ], highlight the importance of controlling morning BP and the use of digital hypertension management strategies focusing on early morning BP [ 19 , 26 , 27 ].
Higher salt intake and salt sensitivity are likely to be key factors driving high rates of hypertension and the BP profile in Asia. In addition to being genetically predisposed to salt sensitivity [ 28 ], Asians also have a high salt intake [ 29 ], which exceeds the WHO-recommended level of <5 g/day [ 30 ]. Use of a salt substitute in which a proportion of the sodium chloride is replaced by potassium chloride is a valid way to reduce dietary salt intake. This also has the benefit of decreasing the urinary sodium/potassium ratio. Increases in the urinary sodium/potassium ratio have been shown to be associated with increases in both SBP and diastolic BP (DBP) [ 31 , 32 ], and is a useful indicator of adherence to WHO-recommended sodium intake levels [ 33 ].
In addition to increasing BP, high salt intake has been linked to a variety of negative cardiovascular outcomes. For example, household salt intake was significantly associated with the long-term risk of all-cause, cardiovascular, cerebrovascular and stroke mortality over 24 years of follow-up in a representative Japanese population [ 34 ]. Although both dietary sodium reduction and dietary potassium supplementation have been shown to have BP-lowering effects [ 35 , 36 ], the effects of these approaches on the cardiovascular disease burden had not previously been investigated.
SSaSS was a cluster randomized trial that evaluated the effects of using a salt substitute (25% potassium chloride/75% sodium chloride) compared with standard salt (100% sodium chloride) on rates of stroke, major cardiovascular events and death in patients with hypertension plus age ≥60 years or a history of stroke from a group of 60 villages in China [ 18 ]. Villages were randomly assigned to the intervention (salt substitute) or control (standard salt) groups. The intervention groups used salt substitute instead of regular salt for all cooking, seasoning and food preservation purposes at similar amounts to their usual salt usage. The mean follow-up was 4.74 years. Patients who used the salt substitute showed a 14% reduction in stroke risk, a 30% reduction in rates of a non-fatal acute coronary syndrome, and a 12% reduction in total mortality compared with the standard salt group [ 18 ]. The observed benefits from the salt substitute were broadly consistent across participant subgroups and prespecified exploratory outcome analyses of stroke, other vascular events, and death [ 18 ]. The absence of any increased risk of clinical hyperkalemia in the intervention group supports the safety of salt substitution in this patient population [ 18 ].
Other salt intake-related studies and initiatives
A study conducted in rural India randomized patients to the use of a salt substitute (30% potassium chloride/70% sodium chloride) or regular salt [ 37 ]. Over the 3-month follow-up period, mean SBP/DBP was 4.66/1.14 mmHg lower in participants using the salt substitute compared to those using standard salt ( p < 0.001/ p = 0.02). In addition, compared with the control group, there was a significant increase in 24-h urinary potassium excretion and a significant decrease in the urinary sodium/potassium ratio in the salt substitute group.
Asian countries have implemented many programs to reduce population salt intake. The Chinese government has included the reduction of salt intake as a key component of “Healthy Lifestyle for All”, which is part of the country’s health development agenda [ 38 ]. A series of programs were created and implemented nationwide by Action on Salt China, a unit funded by the National Institute of Health Research. These included a salt awareness campaign, education on salt reduction at home, and reducing salt usage in restaurants and processed food [ 38 ]. In addition, a significant reduction in salt intake for both children and adults was achieved through the School-based Education Program to Reduce Salt Intake in Children and Their Families (School-EduSalt) [ 39 ].
Multi-component strategies have been a feature of most successful dietary sodium intake reduction programs. For example, the JSH set up at Salt Reduction Committee in 2005 to promote the reduction of population salt consumption. In 2019, the JSH announced the “Tokyo Declaration in Promotion of Salt Reduction” [ 40 ]. This included a six-strategy action plan designed to reduce salt intake to <6 g/day. Key components were: (1) educate citizens on the harms of excessive salt intake and the importance of reducing salt intake; (2) recommend assessment of salt intake of individuals or populations, and propose adequate methods to reduce salt intake; (3) promote salt reduction in children as a part of dietary education at school; (4) promote salt reduction in restaurant meals, prepared dishes, canteens, and school lunches; (5) encourage companies to develop and spread low-salt foods; and (6) encourage the government to take measures to promote salt reduction. In addition, the JSH hypertension management guidelines include clear recommendations around reducing salt intake [ 41 ]. More broadly, The Okinawa Declaration on the unity of hypertension societies in Asian countries and regions to overcome hypertension and hypertension-related diseases was announced in 2021 [ 42 ].
Hypertension and atrial fibrillation
After heart failure, aging and valvular heart disease, hypertension is the fourth-most common risk factor for AF [ 43 ]. However, as by far the most prevalent of these risk factors, hypertension is an important contributor to AF burden in the population [ 44 , 45 ]. Data from epidemiological studies show that hypertension is associated with a 1.8-fold increase in the risk of developing new-onset AF and a 1.5-fold increased risk of progression to permanent AF [ 43 , 46 ]. In an elderly Chinese population, there was a U-shaped relationship between both SBP and DBP and prevalent AF, with the lowest risk of AF seen with high-normal BP levels [ 47 ]. AF alone increases the risk of stroke and systemic emboli, but the risk is even greater in presence of both AF and hypertension [ 48 , 49 ]. Nevertheless, a recent study conducted in China showed that even after AF is detected, the proportion of patients treated with appropriate oral anticoagulant therapy was extremely low [ 50 ]. Therefore, the early detection and appropriate treatment of AF and associated comorbidities such as hypertension are essential.
Detection of AF in patients with hypertension
A home BP monitoring (HBPM) device equipped with a new algorithm for pulse wave analysis for the detection of AF was evaluated in 75 subjects with confirmed AF based on an echocardiogram and 205 who were in sinus rhythm [ 51 ]. Based on the pulse wave extracted by changing each pulse pressure after cuff deflation in three consecutive home BP measurements, the interval of pulse peak (IPP15) was defined as: [interval of pulse peak – the average of the interval of the pulse peak] ≥ the average of the interval of the pulse peak × 15%, and irregular heart beat (IHB) was defined as beats of IPP ≥ total pulse × 20%. The sensitivities of IPP15 for diagnosing AF defined as two or three IHBs of three readings were 1.0 and 0.99, and the corresponding specificities were 0.97 and 0.99, respectively. This shows that this AF detection algorithm mounted on a HBPM device had high diagnostic accuracy for detecting AF [ 51 ]. Its association with a standard and widely available technique for monitoring home BP suggests that it could be widely implemented to monitor heart rhythm as well as BP in patients with hypertension over the long term, although additional research is needed to facilitate implementation of this potential tool into clinical practice.
A wrist-type pulse wave monitor also showed high sensitivity and specificity for the diagnosis of AF in patients with hypertension in a case–control study that used similar definitions for IPP and IHB [ 52 ]. This is another promising approach to facilitate AF detection in patients with hypertension.
BP management in patients with AF
Current guidelines recommend a target BP of 130/80 mmHg in patients with AF receiving anticoagulant therapy [ 41 , 53 , 54 ]. However, patients with AF have often been excluded from hypertension treatment trials because of their fluctuating and unstable BP. The prospective, multicenter, observational, longitudinal All Nippon AF In Elderly Registry was designed to collect data on the clinical status of elderly patients with nonvalvular AF [ 55 ]. A total of 5204 patients aged ≥75 years were included and evaluated using HBPM. This allows the white coat effect to be eliminated and a high frequency of measurements allowed the impact of BP on embolic and hemorrhagic events in patients with AF to be assessed over approximately 2 years of follow-up. Overall, 77.5% of patients with nonvalvular AF had hypertension. Office BP was ≥130 mmHg (i.e., uncontrolled based on guideline recommendations) in 48.9% of patients, and even in the 51.1% of patients who had office BP < 130 mmHg, more than half (52.5%) still had uncontrolled morning home BP [ 55 ]. This shows that a high proportion of high-risk elderly patients with nonvalvular AF have inadequate control of morning home BP, which could contribute to a higher risk of morning cerebrovascular and cardiovascular events in these patients.
Another study from Japan highlights the importance of good BP control in patients with hypertension before the development of AF [ 56 ]. Using data from the Japan Medical Data Center Co., Ltd database, this retrospective analysis investigated the impact of pre-existing hypertension and BP control status prior to AF onset on subsequent prognosis [ 56 ]. Based on data from 7885 patients with new-onset nonvalvular AF and BP data from prior to AF onset, those with pre-existing hypertension has a significantly higher rate of AF-related cardiovascular endpoint events compared to those without hypertension (10.3 vs. 4.4 per 1000 patient-years; p < 0.001). In addition, there was a significant association between lower SBP before AF onset (<120 mmHg) and a lower incidence of cardiovascular events after the development of AF [ 56 ]. This highlights the importance of tight BP control for reducing not only the development of AF but also the risk of subsequent cardiovascular events after an AF diagnosis.
There are a number of mechanisms by which antihypertensive therapy has the potential to prevent AF. These include the improvement of structural and electrical cardiac remodeling, and prevention of heart failure, all of which contribute to the development of AF [ 57 ]. Analysis of data from the SPRINT study suggested that intensive antihypertensive treatment (target SBP < 120 mmHg) in patients with hypertension at high risk of cardiovascular disease has the potential to reduce the risk of AF [ 58 ]. However, patients with AF still appear to be at increased cardiovascular risk even when BP is reduced to <120/80 mmHg during antihypertensive therapy [ 59 ]. Therefore, additional data from prospective clinical trials are needed to clearly define the role of antihypertensive therapy in the prevention and management of AF.
Drug-resistant hypertension defined using out-of-office BP measurement
Resistant hypertension is defined as a BP level that exceeds goal despite concurrent treatment with agents from three different antihypertensive drug classes, usually including a renin-angiotensin system blocker, a CCB and a diuretic, or when treatment with ≥4 agents is needed to achieve BP control [ 41 , 53 , 54 , 60 ]. However, making a true diagnosis of resistant hypertension requires the measurement of out-of-office BP (i.e., home and/or ambulatory BP) [ 60 ]. This allows white coat hypertension, where patients have an elevated office BP reading but normal out-of-office readings, to be excluded. In clinical practice, this is relevant to management decisions because patients with uncomplicated white coat hypertension do not have increased cardiovascular risk compared with normotensive individuals [ 61 ]. Thus, patients with true resistant hypertension have uncontrolled BP based on both office and out-of-office measurements, as defined in recent studies [ 62 , 63 ].
Treatment-resistant hypertension confirmed using HBPM or 24-h ambulatory BP monitoring (ABPM) has been shown to be a risk factor for cardiovascular disease, including heart failure [ 62 , 63 ].
The Japan Morning Surge Home BP study was the first to report an association between treatment-resistant hypertension based on HBPM and cardiovascular risk [ 63 ]. The study included 4261 Japanese subjects who performed HBPM in the morning and evening for 14 days. Treatment-resistant hypertension was defined as uncontrolled home BP using three classes of medications including diuretics or controlled/uncontrolled home BP during treatment with ≥4 classes of medication. Over a mean 6.2 ± 3.8 years of follow-up, the adjusted total cardiovascular disease risk was significantly increased in patients with treatment-resistant hypertension compared with those whose BP was controlled using <3 antihypertensive drug classes (HR 2.20, 95% CI 1.38–2.94 using a home BP of 135/85 mmHg, and HR 1.81, 95% CI 1.23–2.65 using a home BP of 130/80 mmHg) [ 63 ].
Most recently, the Japan Ambulatory Blood Pressure Monitoring Prospective (JAMP) study investigated the effects of uncontrolled resistant hypertension diagnosed using ABPM on the risk of heart failure and overall cardiovascular events in 5839 patients [ 62 ]. True treatment-resistant hypertension was defined as a 24-h ambulatory BP of ≥130/80 mmHg. The adjusted risk of total cardiovascular events (HR 1.66, 95% CI 1.12–2.48; p = 0.012), and especially HF events (HR 2.24, 95% CI 1.17–4.30; p = 0.015), was significantly increased in patients with true resistant versus controlled nonresistant hypertension [ 62 ]. The findings from both of these studies confirm the importance of diagnosing treatment-resistant hypertension using out-of-office BP measurement, and then determining a treatment regimen that reduces BP to target.
Nocturnal hypertension
Heart failure risk.
When BP rises, a large amount of salt is eliminated from the body, but if the body is prone to storing salt (e.g., Asians, and patients with CKD, metabolic syndrome and/or obesity), salt intake increases BP not only during the day but also at night. This compensatory increase in nighttime BP increases cardiac workload and has adverse effects on the cardiovascular system and kidneys.
Control of elevated nighttime BP (nocturnal hypertension) is a key component of managing patients with hypertension and heart failure [ 64 , 65 , 66 , 67 ]. There are several mechanisms by which nocturnal hypertension has negative effects in patients with heart failure, as summarized previously [ 64 , 68 ]. Briefly, when the patient is in the supine position during sleep, circulating blood volume shifts from the periphery to the upper body by about 800 mL, causing the heart to expand and increasing preload. In this situation, high nighttime BP (i.e., afterload) further increases preload, and increases strain on the left ventricular wall.
There are four different circadian patterns of nighttime BP variability: dipper (nighttime BP decreases by 10–20 mmHg compared with the daytime); non-dipper (nighttime BP does not decrease); riser (nighttime BP increases); and extreme dipper (nighttime BP decreases significantly). In the JAMP study, 6359 Japanese subjects underwent 24-h ABPM at baseline to determine the nighttime BP dipping pattern and were then followed for a mean of 4.5 years [ 69 ]. The results showed that each 20-mmHg increase in nighttime SBP was associated with a 21% increase in the risk of stroke and coronary artery disease, and a 36% increase in the risk of heart failure [ 69 ]. In addition, the risk of developing heart failure was 2.45 times higher in patients with a riser versus dipper pattern of nighttime BP ( p = 0.004), even after adjustment for 24 h, daytime, and nighttime BP. Even in patients with well-controlled BP, those with a riser or non-dipper pattern of nighttime BP still showed substantially and significantly elevated heart failure risk [ 69 ]. This highlights the importance of monitoring and controlling nighttime BP even if BP otherwise appears to be well controlled. Effective control of nighttime BP can also help to attenuate left ventricular hypertrophy and renal dysfunction, further reducing heart failure risk [ 64 ].
New sodium-releasing drugs
Reducing circulating volume is an important part of strategies to reduce nighttime BP and ameliorate nocturnal hypertension. The heart failure drugs sodium-glucose cotransporter 2 (SGLT2) inhibitors, angiotensin receptor-neprilysin inhibitors (ARNI) and selective mineralocorticoid receptor antagonists (MRA) are now covered by insurance in Japan for the treatment of hypertension. Recent data are summarized below.
SGLT2 inhibitors
This group of agents is currently only indicated in patients with heart failure or diabetes mellitus. However, there is a growing body of evidence to suggest that they also have benefits beyond their hypoglycemic activity, including beneficial effects on BP [ 70 ]. The Japanese SGLT2 inhibitor and Angiotensin Receptor Blocker Combination Therapy in Patients With Diabetes and Uncontrolled Nocturnal Hypertension (SACRA) study [ 71 ], the EMPA-REG BP trial [ 72 ], the LUSCAR study [ 73 ], the Y-AIDA trial [ 74 ], other studies with dapagliflozin and empagliflozin [ 75 , 76 ], and a post-hoc analysis of data from the Canagliflozin and Renal Events in Diabetes With Established Nephropathy Clinical Evaluation (CREDENCE) trial [ 77 ] have all reported reductions in out-of-office BP measurements (including nighttime BP) during treatment with a variety of SGLT2 inhibitors. Taken together, these recent data make this class of agents a potential new option for reducing BP, along with cardiovascular risk, in patients with heart failure—although more studies are needed in this area [ 78 , 79 ].
Dual inhibition of the angiotensin-1 receptor and neprilysin has multiple beneficial effects on the cardiovascular system [ 80 ]. The first-in-class ARNI sacubitril/valsartan is being seen as a potential treatment option for resistant hypertension and may be ideally suited to a salt-sensitive hypertension phenotype, which is common in Asia [ 80 ]. Sacubitril/valsartan was approved in Japan for the treatment of hypertension in September 2021 [ 81 ]. This approval was supported by data from several rigorous clinical studies showing the BP-lowering effects of sacubitril/valsartan, especially over the important nighttime period [ 82 , 83 , 84 , 85 ]. In the most recent publication, data from a multicenter, randomized, double-blind, parallel-group study conducted in Japanese patients with mild to moderate systolic hypertension experienced a greater reduction in mean seated SBP and achieved a higher BP control rate during treatment with sacubitril/valsartan compared with olmesartan [ 83 ]. However, as recently noted, additional follow-up data are required to confirm the role of sacubitril/valsartan for the long-term treatment of hypertension [ 86 ].
MRAs are effective for the treatment of resistant hypertension, but use of earlier generation agents was associated with problematic adverse events, including hyperkalemia (with both spironolactone and eplerenone) and gynecomastia (spironolactone) [ 87 , 88 , 89 ]. Esaxerenone is a newer non-steroidal selective MRA that received approval in the hypertension indication in Japan in January 2019 [ 90 ]. In addition to studies documenting BP reductions in patients with hypertension treated with esaxerenone [ 91 , 92 , 93 , 94 , 95 , 96 ], a recent Japanese analysis highlighted the BP-lowering activity of esaxerenone through the important nighttime period [ 97 ]. Nighttime SBP decreased in all patients after 28 weeks’ treatment with esaxerenone 2.5–5 mg/day, regardless of nocturnal BP dipping status, although BP reductions were greatest in those with a riser pattern. In addition, the prevalence of the undesirable riser and non-dipper patterns of nighttime BP decreased during esaxerenone therapy [ 97 ]. Therefore, esaxerenone may be a useful treatment option for patients who have nocturnal hypertension, and especially those with a riser pattern of nighttime BP.
Renal denervation
Renal denervation (RDN) is a non-drug option for reducing nocturnal BP via suppression of the sympathetic nervous system and improving salt sensitivity. This technique showed great theoretical promise, but progress was stalled by the equivocal results of early sham-controlled trials. These sometimes conflicting results have recently been summarized in a meta-analysis and systematic review to provide a more accurate estimate of the effects of this non-pharmacological intervention on BP in patients with hypertension [ 98 ]. Taken together, data from 1555 patients (885 treated with RDN and 670 with a sham control) suggest a modest but statistically significant reduction in both office (−3.31 mmHg) and 24-h ambulatory (−5.25 mmHg) BP at 26 months after RDN (Fig. 4 ), and this was consistent across devices and in the presence or absence of antihypertensive medication [ 98 ]. This analysis also showed that RDN significantly reduced nighttime SBP by 3.2 mmHg from baseline [ 98 ]. The authors suggested that this may be clinically relevant for reducing cardiovascular event risk in patients with hypertension given the limitations of pharmacological treatment for effectively lowering nighttime BP [ 98 ].
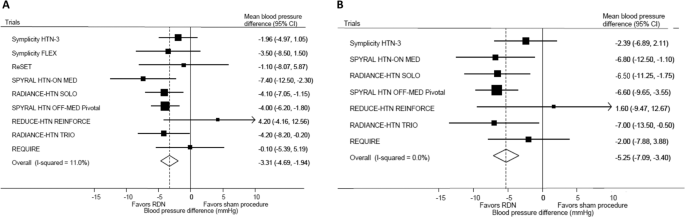
Effects of renal denervation (RDN) on 24-h ambulatory ( A ) and office ( B ) blood pressure in patients with hypertension (reproduced, with permission, from Ogoyama et al. (2021)) [ 98 ]. Horizontal lines show 95% confidence intervals (CI) with the point estimate at the center of the box. Boxes are proportional to the sample size from each study. Diamonds represent summary data centered on the pooled estimate and their width spans the corresponding 95% CI
There are several Asia-specific characteristics of hypertension that mean that RDN may be particularly suited to the Asian hypertension phenotype [ 99 , 100 ]. Subanalyses from the Global SYMPLICITY Registry showed significant and sustained BP reductions after RDN in treated individuals from Korea and Taiwan [ 101 , 102 , 103 ]. In addition, the magnitude of BP reductions in patients from Korea was greater than that in a matched group of European patients [ 101 , 102 ]. Based on these data, the Asia Renal Denervation Consortium has suggested that RDN could be considered as an initial therapy option for the treatment of hypertension in Asia, either alone or in combination with antihypertensive medication [ 99 ].
A survey conducted recently in Japan determined patient preference for treatment with RDN, and included 2393 patients with hypertension [ 104 ]. A total of 755 survey participants (31.6%) stated a preference for RDN to treat their hypertension; males, younger individuals, and those with higher SBP, poor adherence to antihypertensive medication, heart failure and adverse effects during antihypertensive treatment were more likely to express a preference for RDN.
Going forward, challenges to be overcome with respect to the implementation of RDN in clinical practice include procedural guidance, identification of responders, and durability of effects [ 105 ]. Based on currently available data, Asian patients with hypertension might be good candidates for RDN, but additional research is needed.
Advances in non-pharmacological treatment
As highlighted by the RDN-related survey findings above and other research, individual patients will have different preferences for antihypertensive therapy [ 106 , 107 ]. This means that patient preference should be central to decisions regarding the management of hypertension, and is a key component in shared decision making (Fig. 5 ) [ 108 ]. As part of this strategy, there are a growing number of other non-pharmacological options that can be utilized to facilitate the management of hypertension. Some of these are highlighted below.
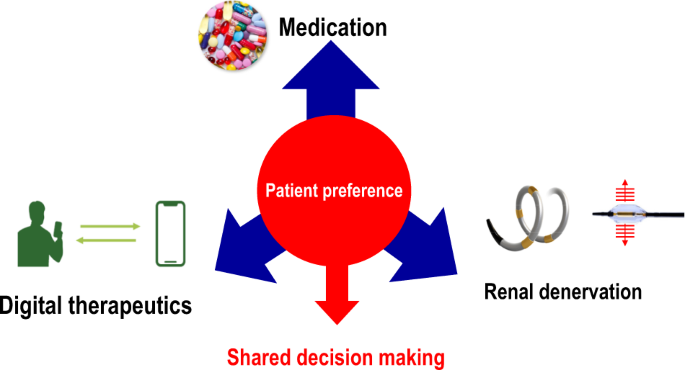
Patient preference and shared decision making for the future management of hypertension (adapted from Kario (2020) [ 108 ], with permission)
Digital therapy with hypertension treatment application
Digital therapeutics refer to the use of evidence-based therapeutic interventions driven by high-quality software programs to treat, manage, or prevent a medical condition [ 109 ]. In the field of hypertension, new non-pharmacological digital methods of lowering BP are now approaching clinical implementation.
The world’s first application for hypertension treatment, HERB, is an approach to hypertension management that aims to lower BP by encouraging patients to change their behavior [ 110 ]. The app contains information on non-pharmacological therapies that have evidence to support their effectiveness in the treatment of hypertension (salt reduction, weight loss, reducing alcohol intake, exercise, stress management and sleep). The aim of the program is to help patients to acquire the correct knowledge about these lifestyle modifications and implement changes in their daily life. Patients record home BP and other information in the app, and their physicians check treatment status on the internet and provide individual guidance [ 110 ].
In a pivotal study of treatment-motivated patients who were not receiving pharmacological antihypertensive therapy (HERB-DH1), patients managed using the HERB digital system had a significantly greater reduction in 24-h BP at 12 weeks than the control group (who were managed conventionally with home BP recording) (−4.9 vs. −2.5 mmHg; between-group difference: 2.4 mmHg, p = 0.024) [ 110 ]. The greatest difference between groups was seen in early morning BP (−10.6 vs. −6.2 mmHg; between-group difference: 4.3 mmHg, p < 0.001) [ 110 ]. Normally, BP can be lowered by about 2 mmHg by monitoring home BP alone, and by about 6 mmHg with general guidance and individualized instruction from a physician. This matches the reduction in early morning BP seen in the HERB-DH1 study control group who were managed in this way, but BP reductions in the intervention group exceeded this by 4.3 mmHg. These findings support a bright future for app-based individualized therapy to promote lifestyle modifications that support hypertension management.
Hypertension vaccine
Vaccines addressing several different targets are being investigated for the prevention and treatment of hypertension [ 111 ]. One such agent is a modified angiotensin II DNA vaccine (AGMG0201) that was recently evaluated in a double-blind randomized, placebo-controlled phase I/IIa trial [ 112 ]. Patients aged 18–79 years with mild to moderate hypertension received two vaccine injections 30 days apart and were monitored for 360 days after the second dose. Treatment-related adverse events were generally mild or moderate in severity, and included injection site pain and erythema. Vaccination triggered the production of anti-angiotensin II antibodies, especially at the highest dose [ 112 ]. This is an innovative area of research that is of future interest.
Digital hypertension research and anticipation medicine
The JSH has defined digital hypertension as the application of rapidly evolving digital health technologies and AI to hypertension healthcare and research [ 113 ]. This approach shows great promise for providing further insights into the pathophysiology of this significant public health issue and identifying potential new therapeutic targets [ 114 ]. In addition, it is central to the implementation of predictive, personalized, and preemptive approaches in clinical practice [ 114 ].
Digital hypertension encompasses many aspects, including BP monitoring, wearable devices, digital therapeutics (as described above), telemedicine, big data, and mobile health (Fig. 6 ). Ultimately, information obtained from these sources using a digital hypertension approach is to predict cardiovascular events using AI. This is particularly relevant in hypertension due to the regular variations in BP (beat-by-beat, orthostatic, diurnal, daily, short term, between-visit and seasonal) and the important contribution that this makes to cardiovascular risk [ 115 ]. The goal is to use digital information to create personalized solutions for anticipation medicine, thereby substantially reducing (or even eliminating) cardiovascular risk [ 116 ].
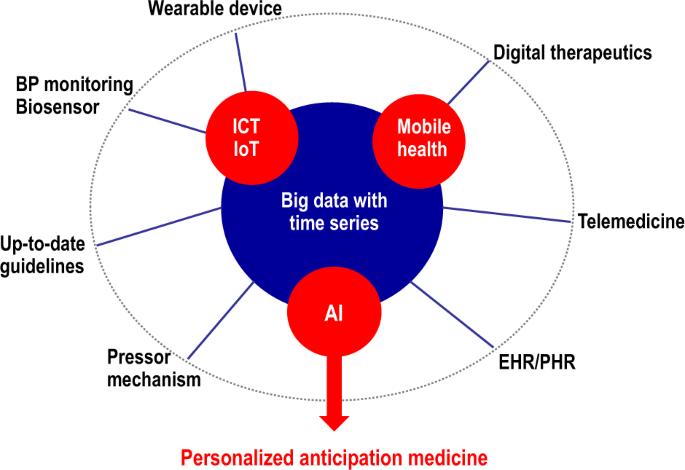
Digital hypertension management to facilitate personalized anticipation medicine. AI artificial intelligence, BP blood pressure, EHR electronic health record, ICT information and communication technology, IoT Internet of Things, PHR personal health record
Telemedicine and digital patient management
HBPM is a central component in telemedicine strategies for hypertension management. It has been shown to significantly reduce BP and improve BP control [ 117 ]. However, remote monitoring of BP is just one component of digital hypertension strategies. HBPM can be combined with other support/interventions, as documented with the HERB digital therapeutics program [ 110 ].
As recently summarized [ 118 ], there is a growing body of evidence for the beneficial effects of telemedicine strategies on a variety of indices, including BP, mediation adherence and lifestyle modification. Telemedicine has a number of advantages, including patient engagement/empowerment and enhanced patient–physician relationships [ 118 , 119 ]. In addition, telemedicine strategies have shown their value for the management of chronic medical conditions to ensure continuity of care during the COVID-19 pandemic and associated restrictions on face-to-face interactions [ 120 , 121 , 122 , 123 , 124 ]. However, there are also a number of barriers and challenges that need to be overcome. These include access to equipment and internet connectivity, technological competence of users, data privacy, and the need for relevant training, certification and licensing [ 118 , 125 ].
Thus, although additional work is needed to fully define the role of telemonitoring and telemedicine in routine clinical care across a range of settings, it is clear that these approaches have an important part to play in the future management of hypertension.
Wearable wrist-type BP monitoring
There are a wide variety of factors that can impact BP at any one time, including physical activity, mental stress, environmental factors, and sleep disturbance. These are important because, for example, seasonal factors such as changes in temperature have been shown to have an important effect on BP and cardiovascular risk [ 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 ]. The combination of one or more of these factors with other periods where BP might increase naturally, such as the early morning period, could elevate BP enough to trigger a series of events, starting with plaque disruption or hemorrhage, that culminate in a cardiovascular event (referred to as the synergistic resonance hypothesis) [ 135 ], even when office BP is apparently controlled. Previously, the only way to get regular data on changes in BP throughout the 24-h period was to use ABPM. Automated HBPM devices capable of determining nighttime BP are also available, and are being developed to also monitor other risk factors such as environmental conditions and physical activity, and may have the potential to detect arrhythmias [ 126 , 131 , 136 , 137 , 138 ]. However, conventional upper arm measurement of BP can be inconvenient for patients and is associated with sleep disturbance [ 139 ].
This highlights the value of small wearable BP monitoring devices that can provide regular or continuous data on BP status, and potentially other triggers, in an individual patient [ 140 ]. One of these devices has been shown to be able to detect changes in BP under different conditions, including emotional stress, location, body position and physical activity [ 141 ]. BP was found to increase by a mean of 7.9 mmHg during negative emotions (anxiety, tension) compared with positive emotions (happiness, calm), by 4.6 mmHg at work versus at home, and by 4.5 mmHg during moderate exercise compared with rest [ 141 ]. Furthermore, BP determined using a wearable device correlated well with the left ventricular mass index on cardiac magnetic resonance imaging in patients with hypertension [ 142 ].
To prepare for more widespread usage of wearable BP devices, it is important that these are validated and accurate compared with conventional methods of measuring out-of-office BP. The first comparison of a wrist-worn watch-type oscillometric BP monitoring device (HeartGuide; Omron Healthcare) with traditional ABPM found that the wearable device produced BP readings that showed an acceptable level of similarity to brachial cuff inflation ABPM [ 143 ]. In addition, patients found the wearable device more comfortable, less burdensome, and less intrusive than ABPM [ 143 ].
The use of wearable devices to continuously monitor nighttime BP is an important potential application, given the close association between nighttime BP and cardiovascular risk [ 144 , 145 , 146 ]. In a recent Japanese study, use of a new algorithm-equipped wrist nocturnal HBPM device (HEM-9601T, NightView; Omron Healthcare) was found to record BP values that were similar to those obtained with an upper arm HBPM device and be clinically reliable. Further studies such as this will help to better define the role and application of wearable BP monitoring devices in real-world clinical settings.
Beat-by-beat continuous BP monitoring
There are a number of methods by which small wearable monitoring devices determine beat-by-beat continuous BP. One of these is applanation tonometry [ 147 ]. The radial artery at the wrist is ideally suited to this method because it is fixed on a radial bone and is shallow beneath the skin [ 116 ]. A small beat-by-beat monitoring device based on tonometry has been shown to provide continuous BP readings that correlate well with other validated conventional devices [ 147 ]. Although wearable devices using tonometry appear to do well under static conditions [ 148 ], accuracy is lower under ambulatory conditions due to the movement of the sensor during measurements [ 149 ]. This is something that will clearly need to be resolved before this can be widely utilized in clinical settings.
Another method that can be used to continuously monitor BP is pulse transit time (PTT). This is the interval of the pulse wave propagation between two arterial sites, is inversely proportional to BP, and has been shown to provide a good estimate of BP [ 150 , 151 , 152 , 153 , 154 ]. PTT can be estimated without the need for an ECG using an array of bioimpedance sensors placed on the wrist [ 155 ]. This has been shown to allow continuous and accurate BP measurement in a way that patients found comfortable [ 155 ]. In addition, beat-to-beat monitoring using a PTT approach showed good agreement with intermittent measurements, especially with respect to average BP values and BP variability [ 156 ].
Artificial intelligence for prediction
Combining the data that can be obtained from digital platforms and wearable BP monitoring devices with AI is an area with great potential. Such approaches have already been shown to facilitate the development of a model predicting the development of hypertension in a general population based on information on vascular stiffness [ 157 ], and to predict both mean BP and BP variability [ 158 ]. With respect to BP variability, morning home SBP data over 56 days, plus data on prescription medications, age, height, weight, past BP changes and temperature changes, were used to develop an algorithm for predicting future BP changes using AI (deep neural network) [ 158 ]. This model was able to predict changes in BP over the next month within a range of about 10 mmHg on a weekly basis; the accuracy of the model was greater when patient information and time-series environmental information were included [ 158 ].
Other potential applications of AI in the field of hypertension include predicting disease incidence and related clinical outcomes, and the prediction of BP levels with new technologies (such as the wearable devices highlighted above) [ 159 ]. Although there is much research still needed into applying developing AI technology to facilitate the diagnosis and management of hypertension, it is likely that it will make an important contribution to the future digital management of this common condition.
Actions for better hypertension management in Asia
The Asian continent is large and diverse but hypertension is a prevalent and burdensome condition throughout the region [ 1 ]. Absolute BP levels in Asia are now amongst the highest in the world and BP control rates are relatively low [ 1 , 6 , 8 ], although there is variation within the region [ 160 , 161 , 162 ]. Thus, while Asian peoples not only share some cultures, customs and genetic factors, this diversity between regions also influences the development and treatment of hypertension and hypertension-related diseases in Asian countries and regions.
A variety of factors contribute to the development and severity of hypertension in Asia (Fig. 7 ) [ 7 ]. This highlights the need for a coordinated approach to hypertension management in the region, with the tailoring of approaches for each individual country/region.
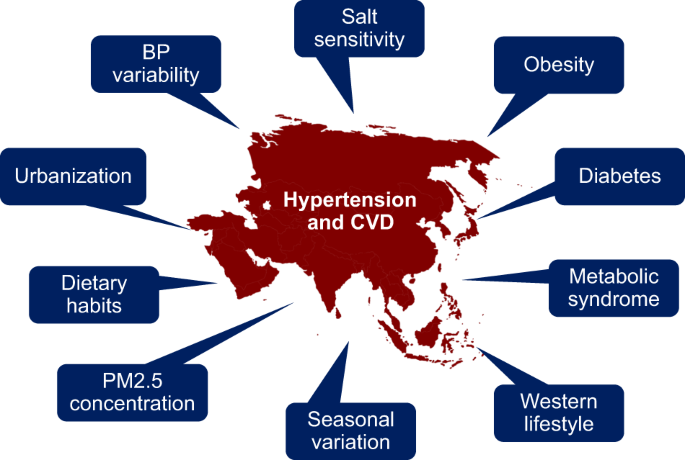
Factors contributing to hypertension and cardiovascular disease in Asia (reproduced, with permission, from Kario et al. (2020)) [ 7 ]. BP blood pressure, CVD cardiovascular disease, PM2.5 fine particulate matter <2.5 μg
The Hypertension Cardiovascular Outcome Prevention and Evidence in Asia (HOPE Asia) Network was established in 2016 and is now both a member of the organization of the World Hypertension League (WHL) and affiliated with the International Society of Hypertension. To help contribute to the WHL’s mission of confronting the global hypertension epidemic and associated burden of disability and premature mortality, the HOPE Asia Network’s goal is to improve the management of hypertension to protect against target organ damage, with the ultimate aim of reducing the number of cardiovascular events in Asia to zero [ 163 , 164 ]. To facilitate this, the HOPE Asia Network has published several consensus documents and Asia-specific guidelines covering a variety of topics relating to hypertension and its management [ 165 , 166 , 167 , 168 , 169 ].
HOPE Asia Network action approach
Most recently, the HOPE Asia Network has outlined seven action approaches for improving the management of hypertension in Asia [ 170 ]. These are as follows:
Strict reduction of sodium intake.
Strict BP control.
Use of home BP to guide hypertension management.
Reduce morning home BP first, followed by nighttime BP, in high-risk patients.
Choose appropriate antihypertensive agents for local populations.
Implement widespread screening to improve awareness.
Use telemedicine strategies.
It is hoped that these strategies will make a significant contribution to reducing the burden of hypertension in Asia.
Okinawa declaration
To date, collaborative research in Asian countries and regions, including Japan, has contributed much to hypertension research. As part of the next stage, the “Okinawa Declaration of the Asian Hypertension Network” was presented at the 43rd Annual Meeting of the JSH in 2021 [ 42 ]. Its aim is to build a network to overcome hypertension and hypertension-related diseases in Asia by sharing evidence and experience. The hypertension societies of Asian countries and regions will continue their efforts to achieve this goal by creating and cooperating on a concrete action plan, as follows:
Actively promote clinical and experimental investigations for hypertension research to encourage participation from researchers and practitioners from Asia.
Share Asian evidence to promote the establishment of standardized management of hypertension in Asia.
Continue to work toward developing Asian consensus guidance for the management of hypertension, using a collaborative approach and taking into account diversities within Asia.
Create an Asian multidisciplinary network for the management of hypertension and hypertension-related diseases.
JSH future plan in the “new normal” with COVID-19
In 2018, the JSH formulated a plan for the future in terms of overcoming hypertension with the slogan “Healthy 100-year life with good blood pressure” [ 113 ]. However, the plan was recently revised due to the COVID-19 pandemic and now includes the phrase “new normal”, and promotion of the three pillars—medical system, academic research and social awareness—was accelerated [ 171 , 172 ].
With respect to the healthcare system, this focuses on the establishment of a telemedicine system to accurately assess BP and the complications of hypertension complications. In addition, the need for the establishment of a multidisciplinary telemedicine team is recognized. This will help to ensure that lifestyle changes required to prevent infection with SARS-CoV-2 do not lead to suboptimal eating and exercise habits, and increased mental stress. Having a robust telemedicine system will also contribute to preventing the spread of COVID-19 because patients can be managed remotely rather than face-to-face.
It is suggested that academic research focuses on strategies to enable the prevention, prediction and control of hypertension using AI, big data, and IoT-based telemedicine. Bioinformatics obtained from continuous digital information regarding BP and heart rate can be applied to BP management, and also could be used to predict the onset of cerebral infarction and myocardial infarction, and worsening of heart failure. In addition, research on hypertension in aging-related diseases such as frailty and dementia, and prevention of cardiovascular diseases in the elderly, will be promoted.
A key component of social awareness is the development of a society where citizens take responsibility for managing their own BP. In Asia, reducing salt intake is a key component of this. Thus, the JSH is focusing on self-monitoring of salt intake, issuing health guidance in this area, and improving access to low-salt foods.
All of these activities, both in Japan and elsewhere in Asia, will be facilitated by the dedication of Asian countries to the Kyoto declaration on hypertension research in Asia, which aspires to generate novel solutions for common hypertension-related problems in Asia based on a deeper understanding of Asian hypertension through cooperative efforts [ 173 ].
There is good reason for optimism regarding the ongoing and future management of hypertension in Asia based on the active research activities and initiatives taking place in the region. Both regional and international collaborations will continue to drive advances in technology and patient care that contribute to reducing the burden of hypertension and hypertension-related disease. Challenges still remain, but the increased usage of digital approaches and therapeutics, the drive towards personalized medicine and shared decision making, and treatment advances are key contributors to improved patient outcomes.
Zhou B, Perel P, Mensah GA, Ezzati M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat Rev Cardiol. 2021;18:785–802.
Article PubMed PubMed Central Google Scholar
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398:957–80.
Article Google Scholar
Lippi G, Wong J, Henry BM. Hypertension in patients with coronavirus disease 2019 (COVID-19): a pooled analysis. Pol Arch Intern Med. 2020;130:304–9.
PubMed Google Scholar
World Health Organization. Global NCD Target. Reduce high blood pressure. https://www.who.int/beat-ncds/take-action/policy-brief-reduce-high-blood-pressure.pdf . Accessed 10 Jan 2021.
Mogi M, Higashi Y, Bokuda K, Ichihara A, Nagata D, Tanaka A, et al. Annual reports on hypertension research 2020. Hypertension Res. 2022;45:15–31.
Hisamatsu T, Segawa H, Kadota A, Ohkubo T, Arima H, Miura K. Epidemiology of hypertension in Japan: beyond the new 2019 Japanese guidelines. Hypertens Res. 2020;43:1344–51.
Article CAS PubMed Google Scholar
Kario K, Chia YC, Sukonthasarn A, Turana Y, Shin J, Chen CH, et al. Diversity of and initiatives for hypertension management in Asia—why we need the HOPE Asia Network. J Clin Hypertens (Greenwich). 2020;22:331–43.
Kario K, Wang JG. Could 130/80 mm Hg be adopted as the diagnostic threshold and management goal of hypertension in consideration of the characteristics of Asian populations? Hypertension. 2018;71:979–84.
Arima H, Murakami Y, Lam TH, Kim HC, Ueshima H, Woo J, et al. Effects of prehypertension and hypertension subtype on cardiovascular disease in the Asia-Pacific Region. Hypertension. 2012;59:1118–23.
World Health Organization. Guideline for the pharmacological treatment of hypertension in adults. 2021. https://apps.who.int/iris/bitstream/handle/10665/344424/9789240033986-eng.pdf . Accessed 11 Jan 2022.
Wright JT Jr., Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–16.
Blood Pressure Lowering Treatment Trialists’ Collaboration. Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant-level data meta-analysis. Lancet. 2021;397:1625–36.
Blood Pressure Lowering Treatment Trialists’ Collaboration. Age-stratified and blood-pressure-stratified effects of blood-pressure-lowering pharmacotherapy for the prevention of cardiovascular disease and death: an individual participant-level data meta-analysis. Lancet. 2021;398:1053–64.
Rakugi H. Step for breaking free from clinical inertia. Hypertension Res. 2022;45:5–7.
Nazarzadeh M, Bidel Z, Canoy D, Copland E, Wamil M, Majert J, et al. Blood pressure lowering and risk of new-onset type 2 diabetes: an individual participant data meta-analysis. Lancet. 2021;398:1803–10.
Article CAS PubMed PubMed Central Google Scholar
Joseph P, Roshandel G, Gao P, Pais P, Lonn E, Xavier D, et al. Fixed-dose combination therapies with and without aspirin for primary prevention of cardiovascular disease: an individual participant data meta-analysis. Lancet. 2021;398:1133–46.
Zhang W, Zhang S, Deng Y, Wu S, Ren J, Sun G, et al. Trial of intensive blood-pressure control in older patients with hypertension. N Engl J Med. 2021;385:1268–79.
Neal B, Wu Y, Feng X, Zhang R, Zhang Y, Shi J, et al. Effect of salt substitution on cardiovascular events and death. N Engl J Med. 2021;385:1067–77.
Kario K, Sakima A, Ohya Y. STEP to estimate cardiovascular events by home blood pressure in the era of digital hypertension. Hypertension Res. 2022;45:11–14.
Ohkubo T. Utility of the “Strategy of Blood Pressure Intervention in Elderly Hypertensive Patients” for home blood pressure management in a real-world setting. Hypertens Res. 2022;45:8–10.
Article PubMed Google Scholar
Augustin A, Coutts L, Zanisi L, Wierzbicki AS, Shankar F, Chowienczyk PJ, et al. Impact of therapeutic inertia on long-term blood pressure control. Hypertension. 2021;77:1350–9.
Hoshide S, Yano Y, Haimoto H, Yamagiwa K, Uchiba K, Nagasaka S, et al. Morning and evening home blood pressure and risks of incident stroke and coronary artery disease in the Japanese general practice population: The Japan Morning Surge-Home Blood Pressure Study. Hypertension. 2016;68:54–61.
Kario K, Saito I, Kushiro T, Teramukai S, Tomono Y, Okuda Y, et al. Morning home blood pressure is a strong predictor of coronary artery disease: The HONEST Study. J Am Coll Cardiol. 2016;67:1519–27.
Fujiwara T, Yano Y, Hoshide S, Kanegae H, Kario K. Association of cardiovascular outcomes with masked hypertension defined by home blood pressure monitoring in a Japanese general practice population. JAMA Cardiol. 2018;3:583–90.
Narita K, Hoshide S, Kario K. Difference between morning and evening home blood pressure and cardiovascular events: the J-HOP Study (Japan Morning Surge-Home Blood Pressure). Hypertens Res. 2021;44:1597–605.
Kario K. Home blood pressure monitoring: current status and new developments. Am J Hypertension. 2021;34:783–94.
Kario K, Shimbo D, Hoshide S, Wang JG, Asayama K, Ohkubo T, et al. Emergence of home blood pressure-guided management of hypertension based on global evidence. Hypertension. 2019;74:Hypertensionaha11912630.
Katsuya T, Ishikawa K, Sugimoto K, Rakugi H, Ogihara T. Salt sensitivity of Japanese from the viewpoint of gene polymorphism. Hypertens Res. 2003;26:521–5.
Powles J, Fahimi S, Micha R, Khatibzadeh S, Shi P, Ezzati M, et al. Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open. 2013;3:e003733.
World Health Organization. Global action plan for the prevention and control of NCDs 2013-20. https://www.who.int/publications/i/item/9789241506236 . Accessed 14 Jan 2022.
Hedayati SS, Minhajuddin AT, Ijaz A, Moe OW, Elsayed EF, Reilly RF, et al. Association of urinary sodium/potassium ratio with blood pressure: sex and racial differences. Clin J Am Soc Nephrol. 2012;7:315–22.
Thi Minh Nguyen T, Miura K, Tanaka-Mizuno S, Tanaka T, Nakamura Y, Fujiyoshi A, et al. Association of blood pressure with estimates of 24-h urinary sodium and potassium excretion from repeated single-spot urine samples. Hypertens Res. 2019;42:411–8.
Iwahori T, Miura K, Ueshima H, Tanaka-Mizuno S, Chan Q, Arima H, et al. Urinary sodium-to-potassium ratio and intake of sodium and potassium among men and women from multiethnic general populations: the INTERSALT Study. Hypertension Res. 2019;42:1590–8.
Article CAS Google Scholar
Shima A, Miyamatsu N, Miura K, Miyagawa N, Okuda N, Yoshita K, et al. Relationship of household salt intake level with long-term all-cause and cardiovascular disease mortality in Japan: NIPPON DATA80. Hypertension Res. 2020;43:132–9.
Huang L, Trieu K, Yoshimura S, Neal B, Woodward M, Campbell NRC, et al. Effect of dose and duration of reduction in dietary sodium on blood pressure levels: systematic review and meta-analysis of randomised trials. BMJ. 2020;368:m315.
Filippini T, Naska A, Kasdagli MI, Torres D, Lopes C, Carvalho C, et al. Potassium intake and blood pressure: a dose-response meta-analysis of randomized controlled trials. J Am Heart Assoc. 2020;9:e015719.
Yu J, Thout SR, Li Q, Tian M, Marklund M, Arnott C, et al. Effects of a reduced-sodium added-potassium salt substitute on blood pressure in rural Indian hypertensive patients: a randomized, double-blind, controlled trial. Am J Clin Nutr. 2021;114:185–93.
Zhang P, He FJ, Li Y, Li C, Wu J, Ma J, et al. Reducing salt intake in China with “Action on Salt China” (ASC): protocol for campaigns and randomized controlled trials. JMIR Res Protoc. 2020;9:e15933.
Li X, Jan S, Yan LL, Hayes A, Chu Y, Wang H, et al. Cost and cost-effectiveness of a school-based education program to reduce salt intake in children and their families in China. PLoS One. 2017;12:e0183033.
Tsuchihashi T, Ishimitsu T, Ando K, Kusaka M, Ichihara A, Miura K, et al. JSH Statement: Tokyo declaration promoting salt reduction by the Japanese Society of Hypertension-the JSH Tokyo declaration. Hypertens Res. 2020;43:1133–4.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Ohya Y, Kario K, Itoh H, Nishiyama A, Ishimitsu T, Ichihara A, et al. Statement of the Asian Hypertension Society Network: the Okinawa Declaration on the unity of hypertension societies in Asian countries and regions to overcome hypertension and hypertension-related diseases. Hypertens Res. 2022;45:1–2.
Benjamin EJ, Levy D, Vaziri SM, D’Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA. 1994;271:840–4.
Huxley RR, Lopez FL, Folsom AR, Agarwal SK, Loehr LR, Soliman EZ, et al. Absolute and attributable risks of atrial fibrillation in relation to optimal and borderline risk factors: the Atherosclerosis Risk in Communities (ARIC) study. Circulation. 2011;123:1501–8.
Lau YF, Yiu KH, Siu CW, Tse HF. Hypertension and atrial fibrillation: epidemiology, pathophysiology and therapeutic implications. J Hum Hypertens. 2012;26:563–9.
de Vos CB, Pisters R, Nieuwlaat R, Prins MH, Tieleman RG, Coelen RJ, et al. Progression from paroxysmal to persistent atrial fibrillation clinical correlates and prognosis. J Am Coll Cardiol. 2010;55:725–31.
Chen Y, Huang QF, Sheng CS, Lei L, Xu SK, Zhang W, et al. Cross-sectional association between blood pressure status and atrial fibrillation in an elderly Chinese population. Am J Hypertens. 2019;32:777–85.
Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001;285:2864–70.
Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137:263–72.
Chen Y, Huang QF, Sheng CS, Zhang W, Shao S, Wang D, et al. Detection rate and treatment gap for atrial fibrillation identified through screening in community health centers in China (AF-CATCH): a prospective multicenter study. PLoS Med. 2020;17:e1003146.
Watanabe T, Tomitani N, Yasui N, Kabutoya T, Hoshide S, Kario K. Assessment of a new algorithm to detect atrial fibrillation in home blood pressure monitoring device among healthy adults and patients with atrial fibrillation. J Clin Hypertens (Greenwich). 2021;23:1085–8.
Kabutoya T, Takahashi S, Watanabe T, Imai Y, Uemoto K, Yasui N, et al. Diagnostic accuracy of an algorithm for detecting atrial fibrillation in a wrist-type pulse wave monitor. J Clin Hypertens (Greenwich). 2019;21:1393–8.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:1269–324.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
Kario K, Hasebe N, Okumura K, Yamashita T, Akao M, Atarashi H, et al. High prevalence of masked uncontrolled morning hypertension in elderly non-valvular atrial fibrillation patients: Home blood pressure substudy of the ANAFIE Registry. J Clin Hypertens (Greenwich). 2021;23:73–82.
Kario K, Abe T, Kanegae H. Impact of pre-existing hypertension and control status before atrial fibrillation onset on cardiovascular prognosis in patients with non-valvular atrial fibrillation: a real-world database analysis in Japan. J Clin Hypertens (Greenwich). 2020;22:431–7.
Zhang W, Wang JG. Prevention of atrial fibrillation by intensive antihypertensive treatment. Hypertension. 2020;75:1414–6.
Soliman EZ, Rahman AF, Zhang ZM, Rodriguez CJ, Chang TI, Bates JT, et al. Effect of intensive blood pressure lowering on the risk of atrial fibrillation. Hypertension. 2020;75:1491–6.
Parcha V, Patel N, Kalra R, Kim J, Gutiérrez OM, Arora G, et al. Incidence and implications of atrial fibrillation/flutter in hypertension: insights from the SPRINT Trial. Hypertension. 2020;75:1483–90.
Carey RM, Calhoun DA, Bakris GL, Brook RD, Daugherty SL, Dennison-Himmelfarb CR, et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72:e53–e90.
Kario K, Thijs L, Staessen JA. Blood pressure measurement and treatment decisions. Circ Res. 2019;124:990–1008.
Kario K, Hoshide S, Narita K, Okawara Y, Kanegae H, Aoki K, et al. Cardiovascular prognosis in drug-resistant hypertension stratified by 24-hour ambulatory blood pressure: The JAMP Study. Hypertension. 2021;78:1781–90.
Narita K, Hoshide S, Kario K. Association of treatment-resistant hypertension defined by home blood pressure monitoring with cardiovascular outcome. Hypertension Res. 2022;45:75–86.
Kario K, Williams B. Nocturnal hypertension and heart failure: mechanisms, evidence, and new treatments. Hypertension. 2021;78:564–77.
Asayama K, Fujiwara T, Hoshide S, Ohkubo T, Kario K, Stergiou GS, et al. Nocturnal blood pressure measured by home devices: evidence and perspective for clinical application. J Hypertens. 2019;37:905–16.
Li Y, Wang JG. Isolated nocturnal hypertension: a disease masked in the dark. Hypertension. 2013;61:278–83.
Ruilope LM, Ruiz-Hurtado G, Lucia A. Preventing and managing hypertension: do not forget the night. Hypertens Res. 2021;44:1674–5.
Kario K. Nocturnal hypertension: new technology and evidence. Hypertension. 2018;71:997–1009.
Kario K, Hoshide S, Mizuno H, Kabutoya T, Nishizawa M, Yoshida T, et al. Nighttime blood pressure phenotype and cardiovascular prognosis: practitioner-based nationwide JAMP study. Circulation. 2020;142:1810–20.
Tanaka A, Node K. Hypertension in diabetes care: emerging roles of recent hypoglycemic agents. Hypertens Res. 2021;44:897–905.
Kario K, Okada K, Kato M, Nishizawa M, Yoshida T, Asano T, et al. Twenty-four-hour blood pressure-lowering effect of an SGLT-2 inhibitor in patients with diabetes and uncontrolled nocturnal hypertension: results from the randomized, placebo-controlled SACRA study. Circulation. 2018;139:2089–97.
Article PubMed Central Google Scholar
Tikkanen I, Narko K, Zeller C, Green A, Salsali A, Broedl UC, et al. Empagliflozin reduces blood pressure in patients with type 2 diabetes and hypertension. Diabetes Care. 2015;38:420–8.
Kario K, Okada K, Murata M, Suzuki D, Yamagiwa K, Abe Y, et al. Effects of luseogliflozin on arterial properties in patients with type 2 diabetes mellitus: the multicenter, exploratory LUSCAR study. J Clin Hypertens (Greenwich). 2020;22:1585–93.
Kinguchi S, Wakui H, Ito Y, Kondo Y, Azushima K, Osada U, et al. Improved home BP profile with dapagliflozin is associated with amelioration of albuminuria in Japanese patients with diabetic nephropathy: the Yokohama add-on inhibitory efficacy of dapagliflozin on albuminuria in Japanese patients with type 2 diabetes study (Y-AIDA study). Cardiovasc Diabetol. 2019;18:110.
Ferdinand KC, Izzo JL, Lee J, Meng L, George J, Salsali A, et al. Antihyperglycemic and blood pressure effects of empagliflozin in black patients with type 2 diabetes mellitus and hypertension. Circulation. 2019;139:2098–109.
Papadopoulou E, Loutradis C, Tzatzagou G, Kotsa K, Zografou I, Minopoulou I, et al. Dapagliflozin decreases ambulatory central blood pressure and pulse wave velocity in patients with type 2 diabetes: a randomized, double-blind, placebo-controlled clinical trial. J Hypertens. 2021;39:749–58.
Ye N, Jardine MJ, Oshima M, Hockham C, Heerspink HJL, Agarwal R, et al. Blood pressure effects of canagliflozin and clinical outcomes in type 2 diabetes and chronic kidney disease: insights from the CREDENCE Trial. Circulation. 2021;143:1735–49.
Kario K, Ferdinand KC, Vongpatanasin W. Are SGLT2 inhibitors new hypertension drugs? Circulation. 2021;143:1750–3.
Kario K, Ferdinand KC, O’Keefe JH. Control of 24-hour blood pressure with SGLT2 inhibitors to prevent cardiovascular disease. Prog Cardiovasc Dis. 2020;63:249–62.
Yamamoto K, Rakugi H. Angiotensin receptor-neprilysin inhibitors: comprehensive review and implications in hypertension treatment. Hypertens Res. 2021;44:1239–50.
Otsuka Pharmaceutical Co. Ltd. Otsuka announces that Novartis Pharma’s ENTRESTO® received a new indication for treatment of hypertension in Japan (media release; 27 Sep 2021). https://www.otsuka.co.jp/en/company/newsreleases/2021/20210927_2.html . Accessed 25 Jan 2022.
Kario K, Sun N, Chiang FT, Supasyndh O, Baek SH, Inubushi-Molessa A, et al. Efficacy and safety of LCZ696, a first-in-class angiotensin receptor neprilysin inhibitor, in Asian patients with hypertension: a randomized, double-blind, placebo-controlled study. Hypertension. 2014;63:698–705.
Rakugi H, Kario K, Yamaguchi T, Sasajima T, Gotou H, Zhang J. Efficacy of sacubitril/valsartan versus olmesartan in Japanese patients with essential hypertnesion: a randomized, double-blind, multicenter study. Hypertens Res. 2022. (In press).
Ruilope LM, Dukat A, Böhm M, Lacourcière Y, Gong J, Lefkowitz MP. Blood-pressure reduction with LCZ696, a novel dual-acting inhibitor of the angiotensin II receptor and neprilysin: a randomised, double-blind, placebo-controlled, active comparator study. Lancet. 2010;375:1255–66.
Williams B, Cockcroft JR, Kario K, Zappe DH, Brunel PC, Wang Q, et al. Effects of sacubitril/valsartan versus olmesartan on central hemodynamics in the elderly with systolic hypertension: the PARAMETER study. Hypertension. 2017;69:411–20.
Lin DS, Wang TD, Buranakitjaroen P, Chen CH, Cheng HM, Chia YC, et al. Angiotensin receptor neprilysin inhibitor as a novel antihypertensive drug: evidence from Asia and around the globe. J Clin Hypertens (Greenwich). 2021;23:556–67.
Epstein M, Duprez DA. Resistant hypertension and the pivotal role for mineralocorticoid receptor antagonists: a clinical update 2016. Am J Med. 2016;129:661–6.
Takahashi S, Katada J, Daida H, Kitamura F, Yokoyama K. Effects of mineralocorticoid receptor antagonists in patients with hypertension and diabetes mellitus: a systematic review and meta-analysis. J Hum Hypertens. 2016;30:534–42.
Narayan H, Webb DJ. New evidence supporting the use of mineralocorticoid receptor blockers in drug-resistant hypertension. Curr Hypertens Rep. 2016;18:34.
Duggan S. Esaxerenone: first global approval. Drugs. 2019;79:477–81.
Ito S, Itoh H, Rakugi H, Okuda Y, Yamakawa S. Efficacy and safety of esaxerenone (CS-3150) for the treatment of essential hypertension: a phase 2 randomized, placebo-controlled, double-blind study. J Hum Hypertens. 2019;33:542–51.
Ito S, Itoh H, Rakugi H, Okuda Y, Iijima S. Antihypertensive effects and safety of esaxerenone in patients with moderate kidney dysfunction. Hypertension Res. 2021;44:489–97.
Ito S, Itoh H, Rakugi H, Okuda Y, Yoshimura M, Yamakawa S. Double-blind randomized phase 3 study comparing esaxerenone (CS-3150) and eplerenone in patients with essential hypertension (ESAX-HTN Study). Hypertension. 2020;75:51–58.
Itoh H, Ito S, Rakugi H, Okuda Y, Nishioka S. Efficacy and safety of dosage-escalation of low-dosage esaxerenone added to a RAS inhibitor in hypertensive patients with type 2 diabetes and albuminuria: a single-arm, open-label study. Hypertens Res. 2019;42:1572–81.
Rakugi H, Ito S, Itoh H, Okuda Y, Yamakawa S. Long-term phase 3 study of esaxerenone as mono or combination therapy with other antihypertensive drugs in patients with essential hypertension. Hypertens Res. 2019;42:1932–41.
Satoh F, Ito S, Itoh H, Rakugi H, Shibata H, Ichihara A, et al. Efficacy and safety of esaxerenone (CS-3150), a newly available nonsteroidal mineralocorticoid receptor blocker, in hypertensive patients with primary aldosteronism. Hypertens Res. 2021;44:464–72.
Kario K, Ito S, Itoh H, Rakugi H, Okuda Y, Yamakawa S. Effect of esaxerenone on nocturnal blood pressure and natriuretic peptide in different dipping phenotypes. Hypertension Res. 2022;45:97–105.
Ogoyama Y, Tada K, Abe M, Nanto S, Shibata H, Mukoyama M, et al. Effects of renal denervation on blood pressures in patients with hypertension: a systematic review and meta-analysis of randomized sham-controlled trials. Hypertens Res. 2022;45:210–20. https://doi.org/10.1038/s41440-021-00761-8 .
Kario K, Kim BK, Aoki J, Wong AY, Lee YH, Wongpraparut N, et al. Renal denervation in Asia: Consensus Statement of the Asia Renal Denervation Consortium. Hypertension. 2020;75:590–602.
Kario K, Wang TD. Perspectives of renal denervation from hypertension to heart failure in Asia. Hypertens Res. 2022;45:193–7. https://doi.org/10.1038/s41440-021-00751-w .
Kim BK, Böhm M, Mahfoud F, Mancia G, Park S, Hong MK, et al. Renal denervation for treatment of uncontrolled hypertension in an Asian population: results from the Global SYMPLICITY Registry in South Korea (GSR Korea). J Hum Hypertens. 2016;30:315–21.
Kim BK, Kim HS, Park SJ, Park CG, Seung KB, Gwon HC, et al. Long-term outcomes after renal denervation in an Asian population: results from the Global SYMPLICITY Registry in South Korea (GSR Korea). Hypertens Res. 2021;44:1099–104.
Lee CK, Wang TD, Lee YH, Fahy M, Lee CH, Sung SH, et al. Efficacy and safety of renal denervation for patients with uncontrolled hypertension in Taiwan: 3-year results from the Global SYMPLICITY Registry-Taiwan (GSR-Taiwan). Acta Cardiol Sin. 2019;35:618–26.
PubMed PubMed Central Google Scholar
Kario K, Kagitani H, Hayashi S, Hanamura S, Ozawa K, Kanegae H. A Japan nationwide web-based survey of patient preference for renal denervation for hypertension treatment. Hypertens Res. 2022;45:232–40. https://doi.org/10.1038/s41440-021-00760-9 .
Katsurada K, Shinohara K, Aoki J, Nanto S, Kario K. Renal denervation: basic and clinical evidence. Hypertens Res. 2022;45:198–209.
Nishigaki N, Shimasaki Y, Yoshida T, Hasebe N. Physician and patient perspectives on hypertension management and factors associated with lifestyle modifications in Japan: results from an online survey. Hypertens Res. 2020;43:450–62.
Yoshida T, Nishigaki N, Saita S, Shimasaki Y, Hasebe N. Perspectives of patients and physicians regarding hypertensive management from an online survey for excellence: a subanalysis of the PARADOX study by physician categories. Hypertens Res. 2020;43:431–41.
Kario K. Perfect 24-hr blood pressure control: up-to-date 2020. Curr Hypertens Rev. 2020;16:2–10.
Digital Therapeutics Alliance. Digital Therapeutics Definitin and Core Principles. 2019. https://dtxalliance.org/wp-content/uploads/2021/01/DTA_DTx-Definition-and-Core-Principles.pdf . Accessed 22 Nov 2021.
Kario K, Nomura A, Harada N, Okura A, Nakagawa K, Tanigawa T, et al. Efficacy of a digital therapeutics system in the management of essential hypertension: the HERB-DH1 pivotal trial. Eur Heart J. 2021;42:4111–22.
Nakagami H, Hayashi H, Shimamura M, Rakugi H, Morishita R. Therapeutic vaccine for chronic diseases after the COVID-19 era. Hypertension Res. 2021;44:1047–53.
Nakagami H, Ishihama T, Daikyoji Y, Sasakura C, Yamada E, Morishita R. Brief report on a phase I/IIa study to assess the safety, tolerability, and immune response of AGMG0201 in patients with essential hypertension. Hypertens Res. 2022;45:61–65.
Node K, Kishi T, Tanaka A, Itoh H, Rakugi H, Ohya Y, et al. The Japanese Society of Hypertension—digest of plan for the future. Hypertens Res. 2018;41:989–90.
Matsuoka R, Akazawa H, Kodera S, Komuro I. The dawning of the digital era in the management of hypertension. Hypertens Res. 2020;43:1135–40.
Kario K. Prognosis in relation to blood pressure variability: pro side of the argument. Hypertension. 2015;65:1163–9. discussion 1169
Kario K. Evidence and perspectives on the 24-hour management of hypertension: hemodynamic biomarker-initiated ‘Anticipation Medicine’ for zero cardiovascular event. Prog Cardiovasc Dis. 2016;59:262–81.
Duan Y, Xie Z, Dong F, Wu Z, Lin Z, Sun N, et al. Effectiveness of home blood pressure telemonitoring: a systematic review and meta-analysis of randomised controlled studies. J Hum Hypertension. 2017;31:427–37.
Omboni S, McManus RJ, Bosworth HB, Chappell LC, Green BB, Kario K, et al. Evidence and recommendations on the use of telemedicine for the management of arterial hypertension: an international expert position paper. Hypertension. 2020;76:1368–83.
Wang JG, Li Y, Chia YC, Cheng HM, Minh HV, Siddique S, et al. Telemedicine in the management of hypertension: evolving technological platforms for blood pressure telemonitoring. J Clin Hypertens (Greenwich). 2021;23:435–9.
Bhaskar S, Bradley S, Chattu VK, Adisesh A, Nurtazina A, Kyrykbayeva S, et al. Telemedicine as the new outpatient clinic gone digital: position paper from the Pandemic Health System REsilience PROGRAM (REPROGRAM) International Consortium (Part 2). Front Public Health. 2020;8:410.
Bhaskar S, Bradley S, Chattu VK, Adisesh A, Nurtazina A, Kyrykbayeva S, et al. Telemedicine across the globe—position paper from the COVID-19 Pandemic Health System Resilience PROGRAM (REPROGRAM) International Consortium (Part 1). Front Public Health. 2020;8:556720.
Keesara S, Jonas A, Schulman K. Covid-19 and health care’s digital revolution. N Engl J Med. 2020;382:e82.
Latifi R, Doarn CR. Perspective on COVID-19: finally, telemedicine at center stage. Telemed J E Health. 2020;26:1106–9.
Monaghesh E, Hajizadeh A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health. 2020;20:1193.
Yatabe J, Yatabe MS, Ichihara A. The current state and future of internet technology-based hypertension management in Japan. Hypertens Res. 2021;44:276–85.
Kubozono T, Akasaki Y, Kawasoe S, Ojima S, Kawabata T, Makizako H, et al. The relationship between home blood pressure measurement and room temperature in a Japanese general population. Hypertens Res. 2021;44:454–63.
Modesti PA. The shifted focus of interest in the temperature-blood pressure relationship: from load to variability. Hypertens Res. 2021;44:1548–50.
Park S, Kario K, Chia YC, Turana Y, Chen CH, Buranakitjaroen P, et al. The influence of the ambient temperature on blood pressure and how it will affect the epidemiology of hypertension in Asia. J Clin Hypertens (Greenwich). 2020;22:438–44.
Stergiou GS, Palatini P, Modesti PA, Asayama K, Asmar R, Bilo G, et al. Seasonal variation in blood pressure: evidence, consensus and recommendations for clinical practice. Consensus statement by the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. J Hypertens. 2020;38:1235–43.
Tsao TM, Tsai MJ, Hwang JS, Su TC. Health effects of seasonal variation in cardiovascular hemodynamics among workers in forest environments. Hypertens Res. 2019;42:223–32.
Umishio W, Ikaga T, Kario K, Fujino Y, Suzuki M, Ando S, et al. Impact of indoor temperature instability on diurnal and day-by-day variability of home blood pressure in winter: a nationwide Smart Wellness Housing survey in Japan. Hypertens Res. 2021;44:1406–16.
Narita K, Hoshide S, Fujiwara T, Kanegae H, Kario K. Seasonal variation of home blood pressure and its association with target organ damage: the J-HOP Study (Japan Morning Surge-Home Blood Pressure). Am J Hypertens. 2020;33:620–8.
Narita K, Hoshide S, Kario K. Seasonal variation in blood pressure: current evidence and recommendations for hypertension management. Hypertens Res. 2021;44:1363–72.
Narita K, Hoshide S, Kario K. Relationship between home blood pressure and the onset season of cardiovascular events: the J-HOP Study (Japan Morning Surge-Home Blood Pressure). Am J Hypertens. 2021;34:729–36.
Kario K. New insight of morning blood pressure surge into the triggers of cardiovascular disease—synergistic resonance of blood pressure variability. Am J Hypertension. 2015;29:14–16.
Kario K, Tomitani N, Kanegae H, Yasui N, Nishizawa M, Fujiwara T, et al. Development of a new ICT-based multisensor blood pressure monitoring system for use in hemodynamic biomarker-initiated anticipation medicine for cardiovascular disease: The National IMPACT Program Project. Prog Cardiovasc Dis. 2017;60:435–49.
Watanabe T, Hoshide S, Kario K. Noninvasive method to validate the variability of blood pressure during arrhythmias. Hypertens Res. 2021. https://doi.org/10.1038/s41440-021-00835-7 .
Watanabe T, Tomitani N, Kario K. Perspectives on an ambulatory blood pressure monitoring device with novel technology for pulse waveform analysis to detect arrhythmias. J Clin Hypertens (Greenwich). 2020;22:1525–9.
Tomitani N, Hoshide S, Kario K. Accurate nighttime blood pressure monitoring with less sleep disturbance. Hypertens Res. 2021;44:1671–3.
Kario K. Management of hypertension in the digital era: small wearable monitoring devices for remote blood pressure monitoring. Hypertension. 2020;76:640–50.
Tomitani N, Kanegae H, Suzuki Y, Kuwabara M, Kario K. Stress-induced blood pressure elevation self-measured by a wearable watch-type device. Am J Hypertens. 2021;34:377–82.
Kario K, Tomitani N, Morimoto T, Kanegae H, Lacy P, Williams B. Relationship between blood pressure repeatedly measured by a wrist-cuff oscillometric wearable blood pressure monitoring device and left ventricular mass index in working hypertensive patients. Hypertens Res. 2022;45:87–96.
Kario K, Shimbo D, Tomitani N, Kanegae H, Schwartz JE, Williams B. The first study comparing a wearable watch-type blood pressure monitor with a conventional ambulatory blood pressure monitor on in-office and out-of-office settings. J Clin Hypertens (Greenwich). 2020;22:135–41.
Fujiwara T, Hoshide S, Kanegae H, Kario K. Cardiovascular event risks associated with masked nocturnal hypertension defined by home blood pressure monitoring in the J-HOP Nocturnal Blood Pressure Study. Hypertension. 2020;76:259–66.
Kario K, Kanegae H, Tomitani N, Okawara Y, Fujiwara T, Yano Y, et al. Nighttime blood pressure measured by home blood pressure monitoring as an independent predictor of cardiovascular events in general practice. Hypertension. 2019;73:1240–8.
Mokwatsi GG, Hoshide S, Kanegae H, Fujiwara T, Negishi K, Schutte AE, et al. Direct comparison of home versus ambulatory defined nocturnal hypertension for predicting cardiovascular events: The Japan Morning Surge-Home Blood Pressure (J-HOP) Study. Hypertension. 2020;76:554–61.
Ota Y, Kokubo A, Yamashita S, Kario K. Development of small and lightweight beat-by-beat blood pressure monitoring device based on tonometry. Annu Int Conf IEEE Eng Med Biol Soc. 2021;2021:5455–8.
Nair D, Tan SY, Gan HW, Lim SF, Tan J, Zhu M, et al. The use of ambulatory tonometric radial arterial wave capture to measure ambulatory blood pressure: the validation of a novel wrist-bound device in adults. J Hum Hypertens. 2008;22:220–2.
Komori T, Eguchi K, Hoshide S, Williams B, Kario K. Comparison of wrist-type and arm-type 24-h blood pressure monitoring devices for ambulatory use. Blood Press Monit. 2013;18:57–62.
Geddes LA, Voelz MH, Babbs CF, Bourland JD, Tacker WA. Pulse transit time as an indicator of arterial blood pressure. Psychophysiology. 1981;18:71–74.
Mukkamala R, Hahn JO, Inan OT, Mestha LK, Kim CS, Toreyin H, et al. Toward ubiquitous blood pressure monitoring via pulse transit time: theory and practice. IEEE Trans Biomed Eng. 2015;62:1879–901.
Smith RP, Argod J, Pepin JL, Levy PA. Pulse transit time: an appraisal of potential clinical applications. Thorax. 1999;54:452–7.
Thomas SS, Nathan V, Chengzhi Z, Akinbola E, Aroul AL, Philipose L, et al. BioWatch – a wrist watch based signal acquisition system for physiological signals including blood pressure. Conf Proc IEEE Eng Med Biol Soc. 2014;2014:2286–9.
Google Scholar
Thomas SS, Nathan V, Zong C, Soundarapandian K, Shi X, Jafari R. BioWatch: a noninvasive wrist-based blood pressure monitor that incorporates training techniques for posture and subject variability. IEEE J Biomed Health Inf. 2016;20:1291–1300.
Ibrahim B, Jafari R. Continuous blood pressure monitoring using wrist-worn bio-impedance sensors with wet electrodes. IEEE Biomed Circuits Syst Conf. 2018;2018:10.1109.
Hoshide S, Yoshihisa A, Tsuchida F, Mizuno H, Hiroki T, Kasai T, et al. Comparison of pulse transit time estimated blood pressure between beat-to-beat and intermittent measurement. Hypertens Res. 2022. (In press).
Kanegae H, Suzuki K, Fukatani K, Ito T, Harada N, Kario K. Highly precise risk prediction model for new-onset hypertension using artificial intelligence techniques. J Clin Hypertens (Greenwich). 2020;22:445–50.
Koshimizu H, Kojima R, Kario K, Okuno Y. Prediction of blood pressure variability using deep neural networks. Int J Med Inf. 2020;136:104067.
Tsoi K, Yiu K, Lee H, Cheng HM, Wang TD, Tay JC, et al. Applications of artificial intelligence for hypertension management. J Clin Hypertens (Greenwich). 2021;23:568–74.
Tomitani N, Hoshide S, Buranakitjaroen P, Chia YC, Park S, Chen CH, et al. Regional differences in office and self-measured home heart rates in Asian hypertensive patients: AsiaBP@Home study. J Clin Hypertens (Greenwich). 2021;23:606–13.
Tomitani N, Wanthong S, Roubsanthisuk W, Buranakitjaroen P, Hoshide S, Kario K. Differences in ambulatory blood pressure profiles between Japanese and Thai patients with hypertension /suspected hypertension. J Clin Hypertens (Greenwich). 2021;23:614–20.
Kario K, Tomitani N, Buranakitjaroen P, Chia YC, Park S, Chen CH, et al. Home blood pressure control status in 2017-8 for hypertension specialist centers in Asia: Results of the Asia BP@Home study. J Clin Hypertens (Greenwich). 2018;20:1686–95.
Kario K. The HOPE Asia Network for “zero” cardiovascular events in Asia. J Clin Hypertens (Greenwich). 2018;20:212–4.
Kario K. The HOPE Asia Network activity for “zero” cardiovascular events in Asia: overview 2020. J Clin Hypertens (Greenwich). 2020;22:321–30.
Chia YC, Buranakitjaroen P, Chen CH, Divinagracia R, Hoshide S, Park S, et al. Current status of home blood pressure monitoring in Asia: statement from the HOPE Asia Network. J Clin Hypertens (Greenwich). 2017;19:1192–201.
Kario K, Morisawa Y, Sukonthasarn A, Turana Y, Chia YC, Park S, et al. COVID-19 and hypertension-evidence and practical management: guidance from the HOPE Asia Network. J Clin Hypertens (Greenwich). 2020;22:1109–19.
Kario K, Park S, Chia YC, Sukonthasarn A, Turana Y, Shin J, et al. 2020 Consensus summary on the management of hypertension in Asia from the HOPE Asia Network. J Clin Hypertens (Greenwich). 2020;22:351–62.
Kario K, Shin J, Chen CH, Buranakitjaroen P, Chia YC, Divinagracia R, et al. Expert panel consensus recommendations for ambulatory blood pressure monitoring in Asia: The HOPE Asia Network. J Clin Hypertens (Greenwich). 2019;21:1250–83.
Park S, Buranakitjaroen P, Chen CH, Chia YC, Divinagracia R, Hoshide S, et al. Expert panel consensus recommendations for home blood pressure monitoring in Asia: the Hope Asia Network. J Hum Hypertens. 2018;32:249–58.
Kario K, Chia YC, Siddique S, Turana Y, Li Y, Chen CH, et al. Seven action approaches for the management of hypertension in Asia – The HOPE Asia Network. J Clin Hypertens (Greenwich). 2022. (In press).
Rakugi H. Further promotion of “the JSH plan for the future” conscious of new normal after/with COVID-19: message from the new president of the Japanese Society of Hypertension. Hypertens Res. 2021;44:4–6.
Shibata S, Arima H, Asayama K, Hoshide S, Ichihara A, Ishimitsu T, et al. Hypertension and related diseases in the era of COVID-19: a report from the Japanese Society of Hypertension Task Force on COVID-19. Hypertens Res. 2020;43:1028–46.
Ito M, Ishimitsu T, Ichihara A, Itoh H, Ohishi M, Ohkubo T, et al. JSH Statement: Kyoto declaration on hypertension research in Asia. Hypertens Res. 2019;42:759–60.
Download references
Acknowledgements
Medical writing assistance was provided by Nicola Ryan, independent medical writer, and Ayako Okura, medical writer, funded by Jichi Medical University.
Author information
Authors and affiliations.
Division of Cardiovascular Medicine, Department of Medicine, Jichi Medical University School of Medicine, Tochigi, Japan
Kazuomi Kario & Satoshi Hoshide
Department of Pharmacology, Ehime University, Graduate School of Medicine, Ehime, Japan
- Masaki Mogi
You can also search for this author in PubMed Google Scholar
Contributions
KK wrote the first draft of the manuscript. All authors drafted and reviewed the manuscript critically and gave final approval of the paper.
Corresponding author
Correspondence to Kazuomi Kario .
Ethics declarations
Conflict of interest.
KK reports research grant from A&D, Omron Healthcare, Fukuda Denshi, Otsuka Pharmaceutical, Otsuka Holdings, CureApp, Sanwa Kagaku Kenkyusho, Daiichi Sankyo, Taisho Pharmaceutical, Sumitomo Dainippon Pharma, Takeda Pharmaceutical, Mitsubishi Tanabe Pharma, Teijin Pharma, Boehringer Ingelheim Japan, Pfizer Japan, Fukuda Lifetec, Bristol-Myers Squibb, Mochida Pharmaceutical, Roche Diagnostics; and Consulting fees from A&D, JIMRO, Omron Healthcare, CureApp, Kyowa Kirin, Sanwa Kagaku Kenkyusho, Terumo, Fukuda Denshi, Mochida Pharmaceutical; and Honoraria from Idorsia, Omron Healthcare, Daiichi Sankyo, Novartis Pharma, Mylan EPD; and Participation in Advisory Board of Daiichi Sankyo, Novartis Pharma, Fukuda Denshi outside the submitted work. All other authors declare no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Kario, K., Mogi, M. & Hoshide, S. Latest hypertension research to inform clinical practice in Asia. Hypertens Res 45 , 555–572 (2022). https://doi.org/10.1038/s41440-022-00874-8
Download citation
Received : 01 February 2022
Accepted : 02 February 2022
Published : 05 April 2022
Issue Date : April 2022
DOI : https://doi.org/10.1038/s41440-022-00874-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Hypertension
- Antihypertensives
- Cardiovascular risk
- Digital therapeutics
- Artificial intelligence
- Blood pressure monitoring
This article is cited by
A tryst of ‘blood pressure control- sex- comorbidities’: the odyssey of basic public health services in yunnan in quest for truth.
- Linhong Pang
- Lakshme Kottu
BMC Public Health (2024)
The Editorial Structure 2024 of Hypertension Research for global initiatives
- Kazuomi Kario
- Satoshi Hoshide
Hypertension Research (2024)
The WHO Global report 2023 on hypertension warning the emerging hypertension burden in globe and its treatment strategy
- Ayako Okura
Five special focuses of Hypertension Research: digital hypertension, home blood pressure-centered approach, renal denervation, Asians, for guidelines
Hypertension Research (2023)
Topics 2023 in Hypertension Research leading to guidelines in Asia
Quick links.
- Explore articles by subject
- Guide to authors
- Editorial policies
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Use of progestogens...
Use of progestogens and the risk of intracranial meningioma: national case-control study
- Related content
- Peer review
This article has a correction. Please see:
- Use of progestogens and the risk of intracranial meningioma: national case-control study - March 28, 2024
- Noémie Roland , general practitioner and epidemiologist 1 ,
- Anke Neumann , senior statistician 1 ,
- Léa Hoisnard , epidemiologist 2 ,
- Lise Duranteau , endocrinologist and gynaecologist 3 ,
- Sébastien Froelich , professor of neurosurgery 4 ,
- Mahmoud Zureik , professor of epidemiology and head of department 1 5 ,
- Alain Weill , senior epidemiologist and deputy director 1
- 1 EPI-PHARE Scientific Interest Group, French National Agency for Medicines and Health Products Safety, French National Health Insurance, Saint-Denis, France
- 2 EpiDermE Epidemiology in Dermatology and Evaluation of Therapeutics, EA7379, Paris Est Créteil University UPEC, Créteil, France
- 3 Department of Medical Gynaecology, Bicêtre Hospital, Assistance Publique-Hôpitaux de Paris, Paris Saclay University, 94270, Le Kremlin-Bicêtre, France
- 4 Department of Neurosurgery, Lariboisière University Hospital, Paris-Cité University, Assistance Publique-Hôpitaux de Paris, Paris, France
- 5 University Versailles St-Quentin-en-Yvelines, Montigny le Bretonneux, France
- Correspondence to: N Roland noemie.roland{at}assurance-maladie.fr (@NoemieRoland11 @EPIPHARE on X)
- Accepted 22 February 2024
Objective To assess the risk of intracranial meningioma associated with the use of selected progestogens.
Design National case-control study.
Setting French National Health Data System (ie, Système National des Données de Santé ).
Participants Of 108 366 women overall, 18 061 women living in France who had intracranial surgery for meningioma between 1 January 2009 and 31 December 2018 (restricted inclusion periods for intrauterine systems) were deemed to be in the case group. Each case was matched to five controls for year of birth and area of residence (90 305 controls).
Main outcome measures Selected progestogens were used: progesterone, hydroxyprogesterone, dydrogesterone, medrogestone, medroxyprogesterone acetate, promegestone, dienogest, and intrauterine levonorgestrel. For each progestogen, use was defined by at least one dispensation within the year before the index date (within three years for 13.5 mg levonorgestrel intrauterine systems and five years for 52 mg). Conditional logistic regression was used to calculate odds ratio for each progestogen meningioma association.
Results Mean age was 57.6 years (standard deviation 12.8). Analyses showed excess risk of meningioma with use of medrogestone (42 exposed cases/18 061 cases (0.2%) v 79 exposed controls/90 305 controls (0.1%), odds ratio 3.49 (95% confidence interval 2.38 to 5.10)), medroxyprogesterone acetate (injectable, 9/18 061 (0.05%) v 11/90 305 (0.01%), 5.55 (2.27 to 13.56)), and promegestone (83/18 061 (0.5%) v 225/90 305 (0.2 %), 2.39 (1.85 to 3.09)). This excess risk was driven by prolonged use (≥one year). Results showed no excess risk of intracranial meningioma for progesterone, dydrogesterone, or levonorgestrel intrauterine systems. No conclusions could be drawn concerning dienogest or hydroxyprogesterone because of the small number of individuals who received these drugs. A highly increased risk of meningioma was observed for cyproterone acetate (891/18 061 (4.9%) v 256/90 305 (0.3%), odds ratio 19.21 (95% confidence interval 16.61 to 22.22)), nomegestrol acetate (925/18 061 (5.1%) v 1121/90 305 (1.2%), 4.93 (4.50 to 5.41)), and chlormadinone acetate (628/18 061 (3.5%) v 946/90 305 (1.0%), 3.87 (3.48 to 4.30)), which were used as positive controls for use.
Conclusions Prolonged use of medrogestone, medroxyprogesterone acetate, and promegestone was found to increase the risk of intracranial meningioma. The increased risk associated with the use of injectable medroxyprogesterone acetate, a widely used contraceptive, and the safety of levonorgestrel intrauterine systems are important new findings.
Introduction
Meningiomas account for 40% of primary tumours of the central nervous system. 1 2 The incidence of meningioma in the United States is 9.5 per 100 000 person years. 2 Meningiomas are mostly slow growing, histologically benign tumours but can nevertheless compress adjacent brain tissue and thus patients may require surgical decompression. 3 The incidence of meningiomas increases with age, rising sharply after the age of 65 years. Conversely, meningiomas are rare before the age of 35. Other recognised risk factors for meningioma are being female, intracranial exposure to ionising radiation, neurofibromatosis type 2 2 , and, as shown only recently, prolonged use (≥one year) to high doses of three potent progestogens: cyproterone acetate, 4 5 chlormadinone acetate, 4 and nomegestrol acetate. 4
The link between female sexual hormones, in particular progesterone, and intracranial meningioma is biologically plausible. 6 Progesterone receptors are present in more than 60% of meningiomas 7 and the volume of these tumours has been observed to increase during pregnancy and to decrease post partum. 8 However, previous pregnancy does not appear to be an unequivocal risk factor for meningioma. 9 Studies have also shown a link, albeit a weak one, between breast cancer and meningiomas. 10
No significant association between exogenous female hormones and risk of meningioma has been shown to date for hormonal contraceptives (either combined or progestogen only pills). 11 12 Additionally, data for hormone replacement treatment for menopause are contradictory. Several studies have shown a slight excess risk of meningioma associated with the use of hormone replacement treatment for menopause, 11 13 whereas others have reported no deleterious effects of these molecules. 14 By contrast, the excess risk of meningioma observed with the use of high doses of cyproterone acetate among cis women, men, and trans women has been shown to be very high 5 15 16 and somewhat lower, but still substantial, for chlormadinone acetate and nomegestrol acetate. 4 Discontinuation of each of these three progestogens generally leads to a reduction in meningioma volume, 17 18 which avoids the need for surgery and its associated risk of complications for most patients.
Whether progestogens other than these three oral progestogens at high doses have a similar effect depending on their route of administration is still unknown. Our study aimed to assess the real-life risk of intracranial meningioma associated with the use of progestogens from an extensive list (progesterone, hydroxyprogesterone, dydrogesterone, medrogestone, medroxyprogesterone acetate, promegestone, dienogest, and levonorgestrel intrauterine systems) with different routes of administration (oral, percutaneous, intravaginal, intramuscular, and intrauterine). Although some of the progestogens studied are used in France (promegestone) or in only a few countries (medrogestone), others are widely used worldwide in various doses and for various indications (progesterone, levonorgestrel, hydroxyprogesterone, medroxyprogesterone) (supplementary table A). Certain progestogens may also be risky at some doses when used over a long period of time, but not at lower doses or when used for a short period of time. Our secondary objectives were to describe the characteristics of the women who were in the cases group (age, grade, and anatomical location of the meningiomas) and to approximate the number of surgically treated meningiomas attributable to the use of the concerned progestogens.
Study design and data source
This observational population based study used data derived from the French national health data system ( Système National des Données de Santé (SNDS)). Given the analysis of multiple exposure situations (different exposure definitions and lookback periods) in our study, we opted for a case-control design rather than a cohort study, thus including long term users of the considered medications. 19
The SNDS database contains information on all health spending reimbursements for over 99% of the population residing in France and is linked to the French hospital discharge database. 20 SNDS is currently one of the largest healthcare databases in the world and is widely used in pharmacoepidemiological studies. 4 5 21 22 23 24
Definition of cases and selection of controls
The eligible cases in this study were women residing in France of all ages who underwent surgery for intracranial meningioma between 1 January 2009, and 31 December 2018. For each case, the start date of the corresponding admission to hospital marked the index date. Women with a pregnancy beginning in the two years before the index date were excluded from the study (pregnancies were defined as those that had resulted in childbirth or medical termination of the pregnancy after 22 weeks of amenorrhoea).
Surgery for intracranial meningioma was defined by the simultaneous combination of the following diagnoses and procedures recorded for the same hospital stay: a meningeal tumour (codes D32, D42, or C70 according to the 10 th revision of the International Classification of Diseases (ICD-10)) coded as the main diagnosis of the admission to hospital and an intracranial surgery act (supplementary table B). These codes have already been used in our previous studies. 4 5
Five women in the control group were randomly matched to each woman in the case group for the year of birth and area of residence (“ département ”, a French geographical subdivision, n=101). Matching was based on the risk set sampling approach. 25 The traceability of the controls in the SNDS was ensured by selecting only women who had had at least one service reimbursed in the calendar year before the index date and the two to three calendar years preceding the index date. This criterion was also applied to the selection of cases.
For analyses relating to intrauterine systems, subsets of these cases and the matched controls were considered to ensure sufficiently long lookback periods. For the hormonal intrauterine systems containing 52 mg levonorgestrel and copper intrauterine devices, the cases and controls from the years 2011 to 2018 were retained. For the hormonal intrauterine systems containing 13.5 mg levonorgestrel, the inclusion period was restricted to 2017 to 2018 (start of commercialisation in France in 2013).
Definition of exposure
Exposure to the progestogen of interest was defined according to WHO’s anatomical, therapeutic, and chemical (ATC) classification. The list included progesterone (oral and intravaginal: 100, 200 mg (ATC code G03DA04); percutaneous: 25 mg per bar (G03DA04)), dydrogesterone (10 mg, or in association with oestrogen: 5 or 10 mg (G03DB01, G03FA14, G03FB08)), hydroxyprogesterone (500 mg (G03DA03)), medrogestone (5 mg (G03DB03)), promegestone (0.125, 0.25, or 0.5 mg (G03DB07)), medroxyprogesterone acetate (injectable contraceptive, 150 mg/3 mL (G03AC06, L02AB02 partially)), dienogest (in association with oestrogen, 2 mg (G03FA15)), levonorgestrel (52 mg intrauterine systems (G02BA03); 13.5 mg intrauterine systems (G02BA03)) (supplementary tables C and D). As drospirenone, which is a spironolactone derivative, is not reimbursed in France, we were unable to access data concerning its use. We therefore chose to study the use of spironolactone (25, 50, and 75 mg), even though its indications may be very different. The code used to identify spironolactone was C03DA01. The indications for these various progestogens in France are available in table 1 .
Main indications (marked as x), in France, for the progestogens under study
- View inline
For oral, intravaginal, percutaneous, or intramuscular progestogens, exposure was defined as at least one dispensation of the progestogen of interest in the 365 days before the index date. For intrauterine progestogens, a dispensation was sought within three years before the index date for levonorgestrel 13.5 mg (as the duration of efficacy of this intrauterine system is three years before any change or withdrawal of the device) and within five years before the index date for levonorgestrel 52 mg intrauterine systems (duration of contraceptive efficacy of five to six years according to current recommendations during the study period).
Exposure was described by three modes for each progestogen as follows: 1) exposure to the progestogen concerned, 2) exposure during the three years preceding the index date to at least one of the three high dose progestogens known to increase the risk of meningioma (ie, chlormadinone acetate, nomegestrol acetate, and cyproterone acetate), and 3) absence of exposure to the progestogen considered or to the three high dose progestogens (the reference for the analyses).
Definition of covariates
The description of sociodemographic and medical characteristics included age, area of residence, existence of neurofibromatosis type 2 (ICD-10 code Q85.1), and, for cases only, the year of surgery, anatomical site (anterior, middle, or posterior base of the skull, convexity, falx and tentorium, others; supplementary table C), and grade of severity of the meningioma (according to WHO’s classification 1 : benign, malignant, or atypical, supplementary table E).
Adjuvant radiotherapy was also sought from three months before the index date to six months after (supplementary table F). Additionally, all causes mortality at two and five years after the index date was assessed in cases, as well as the use of antiepileptic drugs in the third year after the index date (supplementary table G).
Statistical analysis
Logistic regression models conditioned on matched pairs were used to estimate odds ratios and their 95% confidence intervals (CIs) for the association between exposure to the progestogens of interest and meningioma (odds ratio of exposure relative to non-exposure). Additionally, the effect of history of neurofibromatosis type 2 on the risk of meningioma was estimated, as well as the effect of chlormadinone acetate, nomegestrol acetate, and cyproterone acetate exposure, all serving as positive controls for exposure to validate our results. In parallel, exposure to a copper intrauterine device was used as a negative control for exposure (codes in supplementary table H).
The risk of meningioma associated with progestogen use was also estimated for each oral, percutaneous, intravaginal, and intramuscular progestogen according to the duration of use: short term (at least one dispensation in the year before the index date but no dispensation in the second year before the index date) and prolonged use (at least one dispensation in the year before the index date and at least one dispensation in the second year before the index date).
The population attributable fraction was approximated from the odds ratio obtained for each progestogen. The formula used was as follows: population attributable fraction=p c (1-1/odds ratio), where p c is the prevalence of the use of the progestogen concerned (isolated exposure) among the cases. 26 Lastly, sensitivity analyses were performed. Analyses were stratified for age (<35 years, 35-44 years, 45-54 years, 55-64 years, and ≥65 years) and for the location and grade of severity of the tumours whenever a positive association was found between exposure to the considered progestogen and meningioma surgery.
Data were analysed using SAS software version 9.4 (SAS Institute Inc). A P value of less than 0.05 was considered statistically significant (two tailed tests).
The present study was authorised by decree 2016–1871 on 26 December 2016. 27 As an authorised permanent user of the SNDS, the author’s team was exempt from approval from the institutional review board. This work was declared, before implementation, on the register of studies of the EPI-PHARE Scientific Interest Group with register reference T-2023-01-437.
Patient and public involvement
The list of progestogens of interest (supplementary table B) was drawn up in consultation with a temporary scientific advisory board comprised of representatives of the French National Agency for Medicines and Health Products Safety, patient organisations, and healthcare professionals (neurosurgery, endocrinology, gynaecology, and general medicine).
Description of cases and controls
In total, 108 366 women were included in the study during the inclusion period of 2009 to 2018, consisting of 18 061 women in the case group were matched with 90 305 in the control group ( fig 1 ).

Flowchart for the analyses of oral, percutaneous, intravaginal, and intramuscular progestogens. Index date is defined as the date of hospital admission
- Download figure
- Open in new tab
- Download powerpoint
Among them, 15 162 cases and 75 810 controls were retained for the analyses of intrauterine systems and copper intrauterine devices using 52 mg of levonorgestrel (restricted inclusion period: 2011 to 2018) (supplementary figure A) and 4048 cases and their 20 240 controls for the analysis of intrauterine systems of 13.5 mg of levonorgestrel (2017-18) (supplementary figure B). Descriptions of cases and controls for the analyses of intrauterine devices are detailed in supplementary I and J.
The mean age of all women was 57.6 years (standard deviation 12.8 years). The most highly represented age groups were 45-54 (26.7%), 55-64 (26.4%), and 65-74 (21.5%) years ( table 2 ).
Description of the cases and controls (overall inclusion period 2009-18). Data are number of individuals (percentage), unless otherwise specified
The number of cases steadily increased from 1329 in 2009 to 2069 in 2018. Meningiomas requiring surgery were most frequently located at the base of the skull (a total of 10 046/18 061 cases (55.6%); anterior skull base: 3979/18 061 (22.0%), middle: 3911/18 061 (21.7%), posterior: 2156/18 061 (11.9%)), followed by the convexity (6468/18 061 (35.8%)). Concerning tumour grade, most meningioma cases were benign (16 662/18 061, 92.3%) and 1047/18 061 (5.8%) were classified as atypical and 352/18 061 (1.9%) as malignant. Among cases, 28.8% (5202/18 061) of women used antiepileptic drugs three years after the index date of surgery. Mortality was also higher among cases than controls: 502 cases/18 061 (2.8%) died within two years ( v 1.2% of controls) and 951/18 061 (5.3%) within five years ( v 3.4% of controls). Mortality was higher for the cases with malignant tumours, 12.5% of whom died within two years and 20.7% within five.
The comparison of the cases and controls in the subsets used to analyse hormonal intrauterine systems is included the supplementary data (supplementary tables I and J).
Progestogens (others than intrauterine)
Exposure among cases.
Among the 18 061 women admitted to hospital for meningioma surgery between 2009 and 2018, 329 (1.8%) had used oral or intravaginal progesterone, 90 (0.5%) percutaneous progesterone, zero hydroxyprogesterone, 156 (0.9%) dydrogesterone, 42 (0.2%) medrogestone, nine (<0.1%) medroxyprogesterone acetate, 83 (0.5%) promegestone, three (<0.1%) dienogest, and 264 (1.5%) spironolactone ( table 3 , supplementary figure C). These numbers excluded 2999 women who had been exposed to cyproterone acetate, nomegestrol acetate, or chlormadinone acetate, or a combination, within the previous three years (among these 2999 women, 68 had also been exposed to oral progesterone, 47 to percutaneous progesterone, 0 to hydroxyprogesterone, 43 to dydrogesterone, 10 to medrogestone, 0 to medroxyprogesterone acetate, 17 to promegestone, 1 to dienogest, and 56 to spironolactone). The median cumulative doses of progestogens for cases and exposed controls are shown in supplementary table K.
Associations between use of oral, percutaneous, intravaginal, and intramuscular progestogen and risk of surgically treated intracranial meningioma. Data are number of individuals (percentage), unless otherwise specified
Effect on meningioma risk
No significant association with an increased risk of intracranial meningioma surgery was noted with exposure to oral or intravaginal progesterone (odds ratio of 0.88 (95% CI 0.78 to 0.99)) or percutaneous progesterone (1.11 (0.89 to 1.40)), dydrogesterone (0.96 (0.81 to 1.14)), or spironolactone (0.95 (0.84 to 1.09)) ( table 3 , supplementary figure C). Exposure to dienogest was rare, with only 14 women who were exposed (3/18 061 among cases and 11/90 305 among controls) and, consequently, the estimated odds ratio had a very large confidence interval (1.48 (0.41 to 5.35)). Additionally, we could not assess the odds ratio concerning hydroxyprogesterone because no exposed cases were found ( fig 2 ).

Associations between various progestogens and risk of intracranial meningioma requiring surgery (case control design, 2009-18). Odds ratio in logarithmic scale. CI=confidential interval; LNG=levonorgestrel; SNDS=French National Health Data System ( Système National des Données de Santé ). *LNG had different denominators due to restricted inclusion periods (10/4048 cases, 48/20 240 controls; 566/15 162 cases, 3888/75 810 controls)
By contrast, an excess risk of meningioma was associated with the use of medrogestone (3.49 (2.38 to 5.10)), medroxyprogesterone acetate (5.55 (2.27 to 13.56)), and promegestone (2.39 (1.85 to 3.09)). As expected, an excess risk of meningioma for women with positive control exposure neurofibromatosis type 2 (18.93 (10.50 to 34.11)), as well as those exposed to chlormadinone acetate (3.87 (3.48 to 4.30)), nomegestrol acetate (4.93 (4.50 to 5.41)), and cyproterone acetate (19.21 (16.61 to 22.22)) was also noted ( fig 2 ).
The duration of exposure to medrogestone, medroxyprogesterone acetate, promegestone, chlormadinone, nomegestrol, and cyproterone acetate for exposed cases and controls is presented in supplementary table L. The results show that three quarters of the women in the cases group who had been exposed for more than a year had been exposed for more than three years. As for medrogestone, medroxyprogesterone acetate, and promegestone, the excess risk associated with prolonged use was higher than that measured for short term and prolonged exposure combined. Specifically, prolonged use of promegestone had an odds ratio of 2.74 (2.04 to 3.67) (versus 2.39 for all durations of exposure) and short term use an odds ratio of 1.62 (0.95 to 2.76). For prolonged use of medrogestone, the odds ratio was 4.08 (2.72 to 6.10) (versus 3.49 for all durations of exposure combined), and for medroxyprogesterone acetate, the odds ratio was 5.62 (2.19 to 14.42). No significant association was reported for either short or prolonged periods of use for any of the other progestogens studied.
Meningiomas before age 45 years were rare in cases of exposure to medrogestone (n=3/42), medroxyprogesterone acetate (n=3/9), or promegestone (n=10/83), and only one (medroxyprogesterone) was observed before the age of 35.
Concerning medrogestone, the most frequent locations of meningiomas in exposed cases were the base of the skull (n=21/42; 13 in the middle) and the convexity (n=19/42) (supplementary tables M, N and O). The excess risk of meningioma for the middle of the base of the skull was particularly high (odds ratio 8.30 (95% CI 3.70 to 18.63)). Additionally, the estimated excess risk among women aged 45-54 years was slightly higher than that in the main analysis (4.53 (2.73 to 7.53) v 3.49 (2.38 to 5.10)).
In women in the cases group who were exposed to promegestone, meningiomas were preferentially located at the front of the base of the skull (n=25/83), the convexity (n=25/83), and the middle of the base of the skull (n=22/83). The excess risk of meningioma linked to promegestone use was slightly higher in the group who were older than 65 years (odds ratio 3.21 (95% CI 1.39 to 7.43)) and for meningiomas located at the front or middle of the base of the skull (3.15 (1.95 to 5.10) and 3.03 (1.82 to 5.02), respectively).
We found no malignant grade tumours among cases exposed to medrogestone, medroxyprogesterone acetate, or promegestone (for information, the same analyses were carried out for chlormadinone acetate, nomegestrol acetate, and cyproterone acetate in supplementary table N).
Levonorgestrel intrauterine systems
In total, 566/15 162 users of hormonal levonorgestrel 52 mg were among the cases with meningioma surgery between 2011 and 2018 (3.7%) ( table 3 ). For the intrauterine systems with 13.5 mg of levonorgestrel, 10 of 4048 users were reported among the cases from 2017 and 2018 (0.2% of all cases). Again, women who had been exposed to cyproterone acetate, nomegestrol acetate, or cyproterone acetate, or a combination, within the previous three years were not counted (among them, 95 were exposed to the intrauterine systems of 52 mg levonorgestrel and three to intrauterine systems of 13.5 mg levonorgestrel).
No excess risk of meningioma was reported with the use of hormonal intrauterine systems containing 52 mg (odds ratio 0.94 (95% CI 0.86 to 1.04)) or 13.5 mg (1.39 (0.70 to 2.77)) of levonorgestrel ( fig 2).
Exposure to copper intrauterine devices, used as a negative control for exposure in this study, had an odds ratio of 1.13 (1.01 to 1.25).
Attributable cases
The population attributable fractions, which are relative to the observed overall number of surgically treated intracranial meningiomas, were 0.17% for exposure to medrogestone, 0.04% for medroxyprogesterone acetate, and 0.27% for promegestone. For comparison, they were calculated as 2.58% for chlormadinone acetate, 4.08% for nomegestrol acetate, and 4.68% for cyproterone acetate. The numbers for the attributable cases are presented in supplementary figure D.
Principal findings
Although the risk of meningioma was already known for three progestogens, this study is the first to assess the risk associated with progestogens that are much more widely used for multiple indications, such as contraception.
This population based study shows an association between the prolonged use of medrogestone (5 mg), medroxyprogesterone acetate injection (150 mg), and promegestone (0.125, 0.25, 0.5 mg) and a risk of intracranial meningioma requiring surgery. No such risk was reported for less than one year of use of these progestogens. However, we found no excess risk of meningioma with the use of progesterone (25, 100, 200 mg; oral, intravaginal, percutaneous), dydrogesterone (10 mg, combined with oestrogen: 5, 10 mg), or spironolactone (25, 50, 75 mg), neither with short term nor prolonged use, and with the use of levonorgestrel intrauterine systems (13.5, 52 mg). A small number of women were exposed to dienogest (2 mg, in association with oestrogen) and hydroxyprogesterone (500 mg), therefore we cannot draw any conclusions concerning the association between use of these progestogens and the risk of meningioma.
No malignant meningiomas were noted for women exposed to medrogestone, medroxyprogesterone acetate, or promegestone. Moreover, the number of cases of surgically treated intracranial meningioma attributable to use of these progestogens was much lower than the number of cases attributable to the intake of chlormadinone acetate, nomegestrol acetate, and, in particular, cyproterone acetate. This finding is explained by both a lower excess risk of meningioma (for medrogestone and promegestone) and lower rates of use in France (particularly low for medroxyprogesterone acetate, with less than 5000 women exposed each quarter during the inclusion period of the study of 2009-18).
Specific considerations on meningiomas
Meningioma is a predominantly benign tumour. Between 2011 and 2015, 80.5% of the meningiomas diagnosed in the United States were grade 1, 17.7% grade 2, and 1.7% grade 3. 1 Even in the absence of malignancy, meningiomas can cause potentially disabling symptoms. In such cases, first line treatment is surgery, even for the oldest patients, entailing a risk of complications and morbidity. 28 29
Age is an important factor both for the indication of progestogens and for considering intracranial surgery. In our study, the mean age of women in the cases group was 57.6 years. Medrogestone, medroxyprogesterone acetate, and promegestone can be used both by women of childbearing age and by premenopausal and postmenopausal women. In our study, only one user of these progestogens who had undergone meningioma surgery was younger than 35 years (medroxyprogesterone).
Postoperative complications are not uncommon for meningioma surgery. Depending on the exact location of meningiomas, the surgical risk varies but surgery may have severe neurological consequences due to the immediate proximity of highly functional cortical area and critical neurovascular structures. Cognitive function tends to improve after surgery for meningioma, 30 31 but several studies have suggested a potential for postoperative anxiety and depression and a high intake of antidepressants and sedatives in the medium term, 32 33 although other studies have reported conflicting findings for depression. 34 Seizures are also a possible short term complication of surgery, 35 leading to a need to take antiepileptic drugs in the years following the operation. In our study, almost three in 10 women (28.8% of cases) were using antiepileptic drugs three years after the operation, which was consistent with previously published findings. 36 Additionally, results showed that progestin related meningiomas tend to occur more frequently at the skull base and that surgery for lesions in this location is much more challenging. The recent evidence supporting stabilisation or regression of meningiomas after stopping chlormadinone acetate, nomegestrol acetate, and cyproterone acetate has reduced the surgical indications for these patients, thus avoiding potential complications. 17 18 A recent report showed that although the tissue portion of the meningioma most often regresses in size, the hyperostosis associated with meningiomas further increases, which may require surgical intervention, not for oncological purposes but only for decompression of the structures nerves and relief of symptoms. 37
Use of the studied progestogens in France and worldwide
Medrogestone is indicated in France for the treatment of menstrual cycle disorders and luteal insufficiency (eg, dysmenorrhea, functional menorrhagia or fibroid-related menorrhagia, premenstrual syndrome, and irregular cycles), endometriosis, mastodynia, and hormone replacement therapy for menopause. In the United States, medrogestone has never been approved by the US Food and Drug Administration. Outside of France, this molecule is also used in Germany, in combination with oestrogen (0.3 mg/5 mg, 0.6 mg/2 mg, 0.6 mg/5 mg). 38 The use of medrogestone increased significantly in France in 2019, notably as a result of postponements in the prescription of chlormadinone acetate, nomegestrol acetate, and cyproterone acetate, following the French and European recommendations to reduce the risk of meningioma attributable to these progestogens in 2018 and 2019. 39 40 As therapeutic alternatives have not shown an increased risk of meningioma, switching from products that notoriously increase this risk to medrogestone should be reconsidered.
Worldwide, in 2019, 3.9% of women of childbearing age were using injectable contraception (medroxyprogesterone), that is, 74 million users, but figures vary widely between world regions (from 1.8% in high income countries to 8.7% in low income countries). 41 This method of contraception is the most widely used in Indonesia (13 million women), 42 Ethiopia (4.6 million women), and South Africa (3.6 million women). 41 In the USA, medroxyprogesterone acetate is used in more than 2 million prescriptions in 2020 and more than one of five sexually active American women report having used injected medroxyprogesterone acetate (150 mg/3 mL) in their lifetime. 43 44 Injectable contraceptives are much less widely used in Europe (3.1% of women of childbearing age in the UK and 0.2% in France 41 ). Our results support preliminary findings from studies of meningioma cases exposed to chronic use of medroxyprogesterone acetate or cases of high dose administration. 45 46 47 48 49 In particular, our results show similarities with those of a retrospective review of 25 patients diagnosed with meningioma who had a history of chronic medroxyprogesterone acetate use and were treated at the University of Pittsburgh Medical Center between 2014 and 2021 concerning the characteristics of cases exposed to medroxyprogesterone acetate (women (mean age of 46 years) with meningiomas commonly located at the base of the skull). 48 In addition, medroxyprogesterone acetate used as an injected contraceptive is known to be prescribed to specific populations, especially people with mental illnesses. 50 The protection of these vulnerable populations from additional drug risks is particularly important. Depot medroxyprogesterone acetate (150 mg) is registered for use as a form of birth control in more than 100 countries worldwide. 41 In countries that have high numbers of people using medroxyprogesterone acetate, the number of meningiomas attributable to this progestogen may be potentially high. Furthermore, medroxyprogesterone (non-acetate) is also used orally, at lower doses, in some countries other than France (notably in the US), for which no data exists on a risk of meningioma so far.
Promegestone was only available in France (not marketed in any other country) and was withdrawn from the market in 2020. This drug was indicated for the relief of premenopausal symptoms and hormone replacement therapy for menopause. With the discontinuation of its marketing, some users could have switched to medrogestone in 2020, a molecule also implicated in the risk of meningioma in our results. Clinicians therefore must remain vigilant because meningioma risk could last beyond market withdrawal and a potential switch to another progestogen.
The FDA defines a therapeutic class as “all products (…) assumed to be closely related in chemical structure, pharmacology, therapeutic activity, and adverse reactions”. 51 52 Various subtypes of progestogens exist depending on the molecule from which the progestogen is derived (ie, progesterone, testosterone, and spironolactone) (supplementary table B). 53 Their chemical structures and pharmacological properties differ according to this classification, which explains why no class effect is reported for certain benefits and risks associated with their use (eg, breast cancer and cardiovascular risk). 54 55 56 57 Progestogens have distinct affinities for different target organ steroid receptors, which may vary even within a subclass, determining their activity.
Our study suggests that 17-OH-hydroprogesterone and 19-norprogesterone derivatives, both progesterone derivatives, have a class effect on meningioma risk. Four of five progestogens belonging to the 17-OH-hydroprogesterone group have shown an increase in the risk of meningioma (supplementary table R). However, the fact that we found different sizes of risk appears to be more a question of duration and cumulative dose than that of belonging to a progestogen class. We could not draw any conclusions about hydroxyprogesterone (due to a lack of power), the fifth progestogen in the subclass, but its main indication (assisted reproductive technology) corresponded to fewer women exposed and very short exposure (approximately 15 days), which could explain why this drug differs from the others. Finally, to date, at the doses considered in the study, no excess risk of meningioma associated with testosterone derivatives has been shown. However, the risk of meningioma associated with the use of these derivatives at other doses and in other regimens needs to be investigated.
Strengths and limitations
To our knowledge, this study of meningioma risk is the first to expand the list of progestogens of interest beyond chlormadinone acetate, nomegestrol acetate, and cyproterone acetate, detailing the risk associated with each progestogen, with different modes of administration. This study was conducted on a national scale for women of all ages for both the cases and their controls. The SNDS database allowed the use of exhaustive real-world data from over a period of 12 years (2006-18; postoperative information was searched even up to 2022), thus preventing recall bias.
The exclusion of women with a pregnancy beginning in the two years preceding the index date ensured that estimates of the risks associated with progestogen use were reliable. Pregnancy is a unique state, affecting exposure to progestogens (of endogenous or exogenous origin), the likelihood of a meningioma appearing or increasing in volume, 9 58 59 and the likelihood of admission to hospital for surgery (possibly with a lower surgery rate, depending on the symptoms, maternal and foetal health, and tumour characteristics). 59
Another potentially important confounding factor, use of chlormadinone acetate, nomegestrol acetate, or cyproterone acetate, was considered in the analyses by modelling exposure to each progestogen of interest with a separate mode of prior or simultaneous exposure to these drugs. Furthermore, the results obtained for the negative and positive control exposure, including exposure to chlormadinone acetate, nomegestrol acetate, and cyproterone acetate, support the appropriateness of the method chosen for this study.
However, this study also had several limitations. As a result of the scarcity of historical data in the SNDS (which began in 2006, and did not have information for some reimbursement schemes during the first few years), we have only three years of lookback period for the oldest meningioma cases (2009-06), and 12 years for the most recent. The SNDS does not provide information on non-reimbursed drugs, which obliged us to study dienogest in association with oestrogen rather than dienogest alone. Further studies will therefore be necessary. Similarly, we were unable to study other progestogens, such as norgestimate, gestodene, and norethisterone, contained in non-reimbursed products (supplementary table B). Conversely, desogestrel is available and reimbursed in France. Its dosage is much lower and, thus, we chose not to study the drug. Further study to assess a dose-response association in the event of prolonged use would be needed. The progestogen implants (etonogestrel) are also rarely used in France, and concern young women, for whom the risk of meningioma is probably very low. 60 61 We have also not studied the risk associated with the use of hormonal intrauterine systems containing 19.5 mg levonorgestrel because its marketing in France was too recent (2018). However, any excess risk associated with the use of the levonorgestrel 19.5 mg intrauterine systems is unlikely because this dose of levonorgestrel is lower than that of the levonorgestrel 52 mg intrauterine systems, for which we observed no risk.
Moreover, the SNDS does not provide information on all the clinical details and medical indications for which progestogens are prescribed. These missing data mean assessing the risk-benefit ratio of prescriptions is not possible, which could be favourable in the absence of an effective alternative, for example, in the case of relief of endometriosis symptoms. We only have some indirect idea of the indication, depending on the age of the user, and the molecule used (progesterone is not indicated for endometriosis, for example, and dydrogesterone is indicated for endometriosis but is rarely used in this indication). Nevertheless, a risk-benefit assessment was not the aim of our study and will require further studies using other sources of data for product efficacy. Furthermore, no evidence suggests that an increase in meningioma risk depends on the medical indication for the progestogen prescription. In the study of Weill and colleagues in 2021, the excess risk of meningioma associated with the use of cyproterone acetate was equivalent for men and women, who, nevertheless, use cyproterone acetate for radically different indications. 5
In this study, only admission to hospital for meningioma surgery was used as the outcome of interest. However, meningiomas can also be treated with radiotherapy (in rare cases) or simply monitored. Therefore, this study is highly likely to have underestimated the prevalence of meningiomas attributable to the use of progestogens by limiting itself solely to symptomatic tumours that require surgery. However, using admission to hospital for surgery as the outcome ensured diagnostic specificity and thus limited classification bias. The SNDS does not specify the histological characteristics of the meningiomas or the isolated or multiple nature of the tumour, both of which are important criteria in determining severity and the choice of appropriate treatment. Nevertheless, for the cases selected for this study, WHO’s severity grade of the meningioma is coded via the main diagnosis, which is entered according to the ICD-10 code at the end of the hospital stay after a reading of the pathology report. As such, we had indirect information about the histology of the tumours.
Our study has several confounding factors. The two main risk factors identified for meningioma, in addition to age (which was considered in this study) and being female (only women were included in this study), are genetic predisposition, attributed, in particular, to hereditary mutations of the neurofibromatosis type 2 gene, and medical or environmental exposure to high doses of ionising radiation. Radiotherapy for brain cancer (especially during childhood) is probably the most important of the possible medical reasons for intracranial radiation exposure, but only a small proportion of individuals in the general population had cerebral radiotherapy or a malignant brain tumour during childhood.
The progestogens investigated in our study that did not result in an increase to risk of meningioma should be considered under the specific conditions of use in France. These results may not be generalised to the use of these progestogens for other indications, increased doses, or increased duration of use. Similarly, the use of one or more of these progestogens might increase the meningioma risk, when the patient had previously received another type of progestogen.
Prescribers need to be aware of previous progestogen use of any kind and any changes in type of progestogen prescribed that may have occurred and should consider the cumulative dose of progestogens for each patient. The list of progestogens we studied is wide ranging, covering a variety of indications (summarised in table 1 ) for women of all ages (childbearing, premenopausal, and menopausal). As in hormone replacement therapy for menopause, progestogens can be easily substituted for each other, and thus progesterone appears to be the safest alternative. For endometriosis, however, therapeutic alternatives are much more limited, and each indication must be discussed on the basis of the personal benefit to risk ratio. If a high risk progestogen is to be continued, clinical and radiological monitoring and compliance with recommendations are essential.
Finally, we did not estimate the effect of concomitant oestrogen use on the risk of meningioma. In a previous report, having a concomitant oestrogen prescription was weakly but significantly associated with meningioma risk, with an age adjusted hazard ratio of 1.6 (95% CI 1.1 to 2.4) for use of cyproterone acetate. In our previous studies, the simultaneous prescription of oestrogen with chlormadinone acetate (hazard ratio 0.8 (0.5 to 1.3)) and nomegestrol acetate (1.0 (0.7 to 1.7)) was not significantly associated with a risk of meningioma. 28 62 In addition, in these two studies, which were cohort studies of women initiating treatment with the progestogen considered, the proportion of women with a simultaneous prescription of oestrogen at the initiation of progestogen treatment was relatively low (6.8%, and 5.0%, respectively per study).
Conclusions
Prolonged use of medrogestone, medroxyprogesterone acetate, and promegestone was found to be associated with an increased risk of meningioma. Future studies should further clarify the association between the duration of use and risk for the progestogens studied, and extend the discussion of meningioma risk to dienogest and hydroxyprogesterone. Finally, no excess risk of meningioma was associated with the use of progesterone, dydrogesterone, or spironolactone, or the hormonal intrauterine systems used worldwide, regardless of the dose of levonorgestrel they contained.
Further studies are also needed to assess the meningioma risk with the use of medroxyprogesterone acetate, which, in this study, was considered at a dose of 150 mg and corresponded to a second line injectable contraceptive that is rarely used in France. Studies from countries with a broader use of this product, which, furthermore, is often administered to vulnerable populations, are urgently needed to gain a better understanding of its dose-response association.
What is already known on this topic
Known risk factors for intracranial meningioma include age, female sex, neurofibromatosis type 2, exposure to ionising radiation, and use of high dose progestogens: nomegestrol, chlormadinone, and cyproterone acetate
Many other progestogens are widely used for multiple indications for which the risk of meningioma associated with their use has not been estimated individually
What this study adds
Prolonged use of medrogestone (5 mg, oral), medroxyprogesterone acetate (150 mg, injectable), and promegestone (0.125/0.5 mg, oral) was found to be associated with an excess risk of intracranial meningioma
In countries for which the use of medroxyprogesterone acetate for birth control is frequent (74 million users worldwide), the number of attributable meningiomas may be potentially high
The results for oral, intravaginal, and percutaneous progesterone, as well as dydrogesterone and levonorgestrel intrauterine systems, are reassuring, supporting the absence of excess meningioma risk
Ethics statements
Ethical approval.
The present study was authorised by decree 2016–1871 on December 26, 2016. 27 As a permanent user of the SNDS, the author’s team was exempt from approval from the institutional review board. This work was declared, before implementation, on the register of studies of the EPI-PHARE Scientific Interest Group requiring use of the SNDS (register reference: EP-0437).
Data availability statement
Under the terms of the SNDS data use agreement, the complete study data cannot be shared with other investigators ( https://www.snds.gouv.fr ). However, the authors try to share publication related data as much as possible: algorithms and other additional information are provided in the supplemental data; aggregated data can be supplied upon request by contacting the corresponding author at noemie.roland{at}assurance-maladie.fr .
Acknowledgments
We thank Bérangère Baricault and Pauline Dayani for their help in responding to the reviewers, and Sylvie Fontanel and Emmanuelle Mignaton for reviewing the manuscript. We also thank Alex Edelman and Associates for proofreading the English version.
Contributors: AW had the idea for the study. NR, AN, LH, and AW conceived and planned the study. NR and AN drafted the manuscript. AN and LH performed the data management. AN, LH, and NR performed the statistical analyses. AW and MZ ensured project and study management. All authors approved the final manuscript. The corresponding author (NR) attests that all listed authors meet the authorship criteria and that no others meeting the criteria have been omitted. AW is the guarantor.
Funding: This research was funded by the French National Health Insurance Fund (Cnam) and the French National Agency for Medicines and Health Products Safety (ANSM) via the Health Product Epidemiology Scientific Interest Group (ANSM-Cnam EPI-PHARE Scientific Interest Group). NR, AN, and AW are employees of the French National Health Insurance Fund, MZ is an employee of the French National Agency for Medicines and Health Products Safety. The funders had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at https://www.icmje.org/disclosure-of-interest/ and declare: support from French National Health Insurance Fund (Cnam) and the Health Product Epidemiology Scientific Interest Group (ANSM-Cnam EPI-PHARE Scientific Interest Group) for the submitted work, no financial relationships with any organizations that might have an interest in the submitted work in the previous three years, and no other relationships or activities that could appear to have influenced the submitted work.
Transparency: The lead author affirms that the manuscript is an honest, accurate, and transparent account of the study being reported, that no important aspects of the study have been omitted, and that any discrepancies from the study as originally planned (and, if relevant, registered) have been explained.
Dissemination to participants and related patient and public communities: The results were presented for the first time on 12 June 2023, at a meeting organised by the French National Agency for Medicines and Health Products Safety to invited patient association representatives, gynaecologists, endocrinologists, neurosurgeons, and general practitioners. The report on this study (in French) was than published on 26 June 2023, on the EPI-PHARE, ANSM (Agence nationale de sécurité du médicament et des produits de santé), and Cnam (Caisse nationale de l’assurance maladie) websites and was sent to the European Medicine Agency.
Provenance and peer review: Not commissioned; externally peer reviewed.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- Ostrom QT ,
- Kruchko C ,
- Barnholtz-Sloan JS
- Kshettry VR ,
- Al-Mefty O ,
- Barnett GH ,
- Hoisnard L ,
- Laanani M ,
- Passeri T ,
- Mariniello G ,
- Guadagno E ,
- Barbato M ,
- Corvino S ,
- Del Basso De Caro M
- Baxter DS ,
- Rosenfeld JV ,
- Mathiesen T
- Casabella AM ,
- Urakov TM ,
- Pettersson-Segerlind J ,
- Mathiesen T ,
- Elmi-Terander A ,
- Degeneffe A ,
- De Maertelaer V ,
- De Witte O ,
- Michaud DS ,
- Schlehofer B ,
- Lemaire I ,
- Raffin Sanson ML
- Benson VS ,
- Kirichek O ,
- Korhonen K ,
- Raitanen J ,
- Haapasalo H ,
- Salminen T ,
- Wiepjes CM ,
- de Blok CJM ,
- Mikkelsen AP ,
- Greiber IK ,
- Scheller NM ,
- Lidegaard Ø
- Bernat AL ,
- Voormolen EHJ ,
- Champagne PO ,
- Pottegård A
- Lassalle R ,
- Billioti de Gage S ,
- Desplas D ,
- Baricault B ,
- Jabagi MJ ,
- Bertrand M ,
- Lassalle M ,
- Dray-Spira R
- Mansournia MA ,
- Hernán MA ,
- Greenland S
- ↵ JORF. Décret no 2016-1871 du 26 décembre 2016 relatif au traitement de données à caractère personnel dénommé “ système national des données de santé”» 2016-1871, JORF n°0301. 26 December 2016. https://www.legifrance.gouv.fr/affichTexte.do?cidTexte=JORFTEXT000033702840
- Goldbrunner R ,
- Stavrinou P ,
- Jenkinson MD ,
- Lorenzetti M ,
- Franca RA ,
- Esposito F ,
- Gehring K ,
- Rutten GJM ,
- Sitskoorn MM
- Ruhland JM ,
- Wiestler B ,
- van der Vossen S ,
- Schepers VPM ,
- Berkelbach van der Sprenkel JW ,
- Visser-Meily JMA ,
- Skoglund T ,
- Neumann A ,
- Florea SM ,
- Abbritti R ,
- Gelbe Liste Online
- Duranteau L ,
- United Nations
- Maharani A ,
- Sujarwoto S ,
- ClinCalc DrugStats Database
- Daniels K ,
- Hensiek AE ,
- Kellerman AJ ,
- Wahyuhadi J ,
- Heryani D ,
- Malueka RG ,
- Hartanto RA ,
- Setyawan NH ,
- Abou-Al-Shaar H ,
- Wrigley R ,
- Mallela AN ,
- Zenonos GA ,
- Pozzati E ,
- Zucchelli M ,
- Schiavina M ,
- Contini P ,
- Foschini MP
- McCloskey LR ,
- Wisner KL ,
- Cattan MK ,
- Betcher HK ,
- ↵ The Food and Drug Administration (FDA). Federal register. 2008. Guidance for industry on diabetes mellitus-evaluating cardiovascular risk in new antidiabetic therapies to treat type 2 diabetes. https://www.federalregister.gov/documents/2008/12/19/E8-30086/guidance-for-industry-on-diabetes-mellitus-evaluating-cardiovascular-risk-in-new-antidiabetic
- Furberg CD ,
- Herrington DM ,
- Schindler AE ,
- Campagnoli C ,
- Druckmann R ,
- Sitruk-Ware R ,
- Stanczyk FZ ,
- Hapgood JP ,
- Mishell DR Jr .
- Palacios S ,
- Hipolito Rodrigues MA ,
- Carbone L ,
- Le Guen M ,
- Rouzaud-Cornabas M ,
- Health Barometer group 2016

Study links birth control, menopause treatment to higher risk for brain tumors
T he contraceptive injection Depo-Provera and two drugs used for menopause relief could be linked to a heightened risk for brain tumors in some women, a new study warns.
Depo-Provera (medroxyprogesterone acetate) increased the risk of intracranial meningioma 5.6-fold if used for longer than a year, researchers report in the BMJ .
"In countries for which the use of medroxyprogesterone acetate for birth control is frequent [74 million users worldwide], the number of attributable meningiomas may be potentially high," concluded the research team led by Noémie Roland , a general practitioner and epidemiologist with French National Health Insurance in Saint-Denis, France.
Further, the menopausal hormone therapy drugs medrogestone and promegestone increased the risk of intracranial meningiomas by 4.1-fold and 2.7-fold, respectively, results show.
Intracranial meningiomas are mostly non-cancerous tumors that grow in the layers of tissue that cover the brain and spinal cord, researchers said. Meningiomas account for 40% of cancers in the central nervous system.
The three drugs all contained progestogens, which are similar to the natural hormone progesterone. This class of drugs also are used to treat conditions like endometriosis and ovarian cysts .
For the study, researchers analyzed French health system data for more than 18,000 women who underwent surgery for intracranial meningioma between 2009 and 2018.
Each case was matched to five other women who didn't have an intracranial meningioma.
The research team tracked women's use of the progestogen drugs progesterone, hydroxyprogesterone, dydrogesterone, medrogestone, medroxyprogesterone acetate, promegestone, dienogest and levonorgestrel.
Prolonged use was defined as a year or more, as there appeared to be no risk posed by using the drugs for less than one year, researchers said.
None of the other drugs showed an increased risk for meningioma, including levonorgestrel, a hormone used in IUD contraceptive devices and in emergency contraceptives like Plan B.
Researchers warned that because this was an observational study, it couldn't draw a direct cause-and-effect link between the drugs and brain tumors.
More research is needed to understand why these specific drugs might increase tumor risk in some women.
"Future studies should further clarify the association between the duration of use and risk for the progestogens studied," the team said.
Progesterone receptors are present in more than 60% of meningiomas, which could provide one potential explanation, researchers said.
More information
The National Cancer Institute has more about meningioma .
Copyright © 2024 HealthDay. All rights reserved.


COMMENTS
Several studies have reported the correlation between pediatric hypertension and family H/O hypertension, low birth weight, excess body weight [6,7]. Here we describe a 13 year old girl presenting with epistaxis, headache and uncontrolled hypertension despite poly drug therapy, abnormal peripheral pulses and unequal blood pressure in upper limbs.
Introduction. According to data from the National Health and Nutrition Examination Survey (NHANES) 2017 to 2018, 56.3% of US adults with hypertension have uncontrolled blood pressure (BP), defined by systolic BP (SBP) ≥140 mm Hg or diastolic BP (DBP) ≥90 mm Hg. 1 In October 2020, the US Surgeon General published a Call to Action to Control Hypertension that emphasized improving the ...
Resistant hypertension is a common clinical problem faced by both primary care clinicians and specialists. While the exact prevalence of resistant hypertension is unknown, clinical trials suggest that it is not rare, involving perhaps 20% to 30% of study participants. As older age and obesity are 2 of the strongest risk factors for uncontrolled ...
Multiple social vulnerabilities to health disparities and hypertension and death in the REGARDS study. Hypertension. 2022; 79:196-206. doi: 10.1161/HYPERTENSIONAHA.120.15196 Link Google Scholar; 22. U.S. Department of Health and Human Services Office of Disease Prevention and Health Promotion. Healthy people 2030, social determinants of health.
1 Introduction. Resistant hypertension represents a condition where blood pressure levels remain uncontrolled despite the use of at least three drugs or if the control happens with four or more drugs. Many evidences suggest that approximately the 20% of resistant hypertension recognize secondary causes. Among these, primary aldosteronism (PA) is the most common form.
In conclusion, this case study reports a secondary care medical intervention for a cardiovascular adverse event, resulting from case finding of uncontrolled hypertension at the dentist in primary ...
In men, there was an increased odds of uncontrolled hypertension with heavy alcohol drinking compared to light-or-never (adjusted odds ratio 1.34, 95% CI 1.10-1.63), with low as well as with ...
Dr. Sally A. Ingham (Medicine): A 45-year-old woman was admitted to this hospital because of dyspnea on exertion, fatigue, and confusion. The patient had been in her usual state of health until 18 ...
Uncontrolled hypertension: the greatest challenge and perspectives in Asia. A cross-sectional analysis of a community-based cohort study in Tarumizu demonstrated that patients with uncontrolled ...
Uncontrolled hypertension is a major public health problem among hypertensive patients both in developed and developing countries [1,2,3,4].Despite the availability and improvement in diagnostic options and therapeutic interventions of hypertension with proven benefits in reducing cardiovascular morbidity and mortality; BP control rates are grossly inadequate (< 30% controlled to < 140/90 mmHg ...
The estimated prevalence of hypertension in pediatric age group is between 2%-5% [ 1 ]. The usual form of hypertension in young is attributable to secondary causes. The most common cause is the renovascular one (60-70%) [ 2, 3 ]. Cushing syndrome, hyperthyroidism, pheochromocytoma, essential hypertension, coarctation of aorta, SLE are also ...
109 deliver health coaching for hypertension. We used a case-control design that consisted of two 30-110 day phases comprising a health awareness phase and a health coaching phase. The first phase of 111 the study involved a self-measured blood pressure (SMBP) program. The goal of this phase was
Diagnosis of hypertension requires blood pressure measurement on at least two separate occasions. These two measurements are then averaged. Requirements for these measurements include no smoking or caffeine intake within the previous thirty minutes and that the two blood pressure readings must be at least 2 minutes apart (Mayo Clinic, 2014a).
A wrist-type pulse wave monitor also showed high sensitivity and specificity for the diagnosis of AF in patients with hypertension in a case-control study that ... DH1 study control group who ...
Hence, we conduct the randomized controlled study protocol to explore the effect of management of nursing case on blood pressure control in hypertension patients. 2 Materials and methods. This is a randomized controlled study which will be carried out from May 2021 to May 2022 at the People's Hospital of Chengyang District.
We conducted a test-negative case-control study to assess the effectiveness of EV-A71 vaccines in preventing EV-A71-associated HFMD. Children aged 6-71 months with HFMD were enrolled as participants. The case group comprised those who tested positive for EV-A71, while the control group comprised those who tested negative for EV-A71.
METHODS: This retrospective case-control study used Colorado's All Payer Claims Database (2012-2019). We identified index stroke events in young adults (aged 18-55 years), matched 1:3 to stroke-free controls, by (1) sex, (2) age±2 years, (3) insurance type, and (4) prestroke period.
Objective To assess the risk of intracranial meningioma associated with the use of selected progestogens. Design National case-control study. Setting French National Health Data System (ie, Système National des Données de Santé ). Participants Of 108 366 women overall, 18 061 women living in France who had intracranial surgery for meningioma between 1 January 2009 and 31 December 2018 ...
For the study, researchers analyzed French health system data for more than 18,000 women who underwent surgery for intracranial meningioma between 2009 and 2018.