Home — Essay Samples — Nursing & Health — Drug Addiction — Drug Addiction: Choice or Disease?

Drug Addiction: Choice Or Disease?
- Categories: Drug Addiction Drugs
About this sample

Words: 677 |
Published: Sep 16, 2023
Words: 677 | Page: 1 | 4 min read
Table of contents
The choice argument, the disease model, psychological and sociological factors, a holistic perspective.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Prof. Kifaru
Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
4 pages / 1976 words
3 pages / 1587 words
5 pages / 2094 words
3 pages / 1486 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Drug Addiction
Drug abuse is a chronic disorder that has been a major problem affecting many people, especially the youth, for several decades. This problem has become a global concern that requires immediate attention, especially given the [...]
The issue of substance abuse presents a pervasive and multifaceted challenge, impacting individuals, families, and communities globally. Its consequences extend far beyond individual suffering, posing significant threats to [...]
Drug addiction has been a significant issue worldwide for many decades, impacting not only individuals addicted to illegal substances but also the society surrounding them. This essay aims to explore the influence of drug [...]
Millions of individuals are affected by the devastating consequences of substance abuse, making it a significant public health concern worldwide. As societies strive to address this issue, innovations in technology have emerged [...]
Drugabuse.gov. (2023). Commonly Abused Drugs Charts. National Institute on Drug Abuse. National Institute on Drug Abuse. (2022). Understanding Drug Use and Addiction DrugFacts. Retrieved from Press.
Teenage drug abuse is a deeply concerning issue that continues to cast a shadow over the lives of young Americans and their communities. As we grapple with this persistent challenge, it is essential to conduct an in-depth [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
- 5-Star Facility Tour

Is Addiction a Disease or Choice?

Addiction itself is often misunderstood. Some people argue that i t is a personal choice , and therefore anyone who is addicted to a substance has ended up there because of the lack of self-discipline or morality. Meanwhile others argue addiction is a disease, and as a result cannot be cured entirely or even resisted by discipline alone. The first view has been the most common understanding of addiction throughout history, and as a result there is a stigma surrounding people who struggle with drug abuse that often prevents them from willingly seeking help.
Recent studies over the past couple decades have brought evidence to question that understanding, and now the nature of addiction has become a common point of debate among specialists and the public itself . Does a person become locked into addiction because it is a choice that they are making and continue to make, or is it a disease that warps their brain and takes choice out of the equation? These are the two si des of the addiction debate , and which side wins plays a critical role in how medical professionals should approach addiction treatment .
The Misconception of Addiction
Much of the argument that addiction is a choice stems from misconceptions about the types of people who suffer from addiction. This is ti ed to th e stigma of addiction , which developed as a result of the individuals who were affected by addiction, such as people from specific social classes or ethnicities. Throughout history, substance abuse was most common among “ lesser” classes and people with l ower levels of education. Given that the scientists and researchers of the time were from a more prominent social class where addiction was less common, they drew a connection that poverty and a lack of education was the reason that these individuals were more likely to develop an addiction.
While this stigma is still common today, modern addiction can affect any person regardless of their socioeconomic class, ethnicity, and background. One use is all it takes for some drugs to set a person on the wrong course, and even legal drugs such as prescription opioids can easily catapult addiction if they are misused. This means that anyone wi th access to medical care is potentially at risk , and so long as old misconceptions continue to prevail, they are in greater danger than they would otherwise be .
Addiction as a Choice
Beyond the stigma, t here is a branch of modern researchers that strongly insists that addiction is a choice and uses evidence to support their argument . The primary figures on this side are behavioral scientists, and their belief is based on the idea that any activity capable of stimulating a person for pleasure or stress release holds a risk for addiction. This means that almost anything can potentially lead to an addiction, be it taking drugs, eating, or simply spending time on the internet. One of the ir most common arguments shines light on social media addiction. As social media has become a staple in modern society, many people have become hooked on this growing trend.
According to the neuroscientist Dr. Marc Lewis, this argument is largely based on the idea that when a person carries out an activity that they enjoy, it triggers pleasure in the brain and over time becomes a habitual act. Similar to how a person who wakes up at the same time most days for work , these processes easily become habit over time.
The main difference though is that that since it is connected to pleasure, which is the brain’s natural agent to tell the body what is good or bad for survival on a primal level, these habits form quicker and become more powerful than they otherwise would. A key point is that pleasure in this case does not necessarily need to be pleasure in the traditional sense, rather would be more accurately described as positive stimuli. This means that activities that do not cause pleasure but provide relief from negative feelings also present a strong habit-forming risk.
From a psychological standpoint, when this happens the brain has created special pathways for the activity to make it an easier trigger for that positive stimuli within the individual. Since drug us e frequently causes a wave of pleasure or at the very least relief from a negative feeling, these behavioral scientists argue that addiction is a case of repeated choice rather than a disorder. If an addict finds the self-control to stop using their chosen substance, t he expected result of this belief system is that the brain can fully recovery from addiction and eventually proceed in life as if it never occurred.
Addiction as a Disease
In recent decades, researchers began to label addiction as a disease rather than a behavioral choice. This decision stems primarily from how addiction a ffects the brain by changing it, progressively forcing an individual to crave the drug until use eventually becomes an unconscious act rather than a conscio us choice.
W hen a person begins abusing a substance or regularly us es prescription drugs for too long, their body will begin to adapt itself to account for its presence in order to maintain homeostasis , or balance . Over time, this leads to what is known as tolerance , which is when the body has adjusted itself enough that the individual will need to take more of their chosen drug in order to experience the same effects. This encourages them to further abuse the drug, and as this is happening, the individual’s brain will also be rewiring itself to desire more.
Eventually this leads to the development of dependence , which means that their body has been altered so much that it loses the ability to function normally without their chosen substance. If use stops , they will experience a series of painful side effects known as withdrawal , until either their body returns to its normal state without drugs or when they use again. The first option may take several days or weeks to accomplish, so many people opt for the latter as it is less painful . By choosing this option, the user becomes locked in a progressive cycle of addiction.
During this point, the part of the brain responsible for deciding to take the drug also shifts from the front of the brain to the back, which is the area in charge of regulating unconscious acts like breathing and blinking , as well as basic desires like hunger. As a result, drug abuse becomes fundamentally linked to their brain and is no longer a free choice.
To further complicate matters, some people are more prone to addiction than other s . One of the most common signs for determining if someone is as risk for addiction is to uncover whether there is a history of past addiction in their family. This supports the argument that addiction is a disease because if choice was the main factor in addiction, a person’s family history would have little bearing on their chance for becoming addicted as well.
Wrapping Up
A ddiction is a complicated subject filled with debate between researchers and scientists from a variety of backgrounds, and these debates have only grown as the years progress . Despite the complexity of the situation however, new evidence reveals the truth of the matter. While an addiction may begin from an individual’s personal choice, addiction itself is a mental disease rather than a continued choice.
The reason for this comes from t hree key points regarding how addiction affects an addict . The first of which is that a mental disease alters an individual’s brain and impacts their ability to function normally , and the second is that instead of returning to “ normal ” after treatment , a recovered individual will have to consciously work toward remaining sober each day, as relapse is always a possibility . The third point of note is that a person’s risk of addiction rises based on hereditary factors. If addiction were purely a choice, these three points would not exist al together.
Behavioral researchers like Dr. Lewis try to argue this by acknowledg ing that the brain does change during addiction, but they view it as a situation like playing with clay. The brain is altered by drugs , making poor choices more likely, but they believe that if the drugs are removed, the brain will eventually “remold” itself back to its normal shape.
However , many scientists now know that this does not happen, which is where th is argument quickly falls apart . Instead of returning to normal and no long being a problem, addiction is a process of ongoing recovery. Even years after being sober, a person who was once an addict will be at a higher risk for drug abuse than their peers who were never addicted. This is because the brain only reverts to normal functionality, but its makeup remains changed enough that recovering individuals can always struggle with temptation.
Choice argument s are also unable to account for the role of heredity in a person’s risk factors for developing an addiction. Once again, if it were solely choice based, addiction would affect each person as an individual and their family history would play no significant role.
As a disease, addiction is more difficult to treat than it would be if it were purely a choice. However, by recognizing it for what it really is, medical professionals can develop treatment plans that are more effective for helping their patients.
Providing the Highest-Quality of Addiction Treatment
Here at Brookdale Premier Addiction Recovery, we understand the complexity of substance use disorder and recognize the need for comprehensive treatment services . As such, every individual that comes to us for help, is treated with the highest level of compassion and understanding they deserve to materiali ze their potential into a Life…Recovered .
With customized detox protocols and clinical treatment strategies, our team of professionals wi ll work one-on-one with you to address your very specific needs and tailor of programs to best help you. If you are struggling with alcoholism or addiction, help is only one phone call away. Please contact us now at (855)575-1292 to learn more about our program or to begin the process of admission.
EXPERIENCE BROOKDALE - TOUR OUR 5-STAR FACILITY.
Drug Addiction: A Disease or a Choice?
Introduction, argument for, argument against, evaluation of arguments.
Despite numerous attempts to address the problem, drug addiction remains a serious health concern for contemporary society. Many thousands of individuals suffer from this issue and face the high risk of reduced quality of life or death. Although there is a long history of the problem, the is still a difference in opinions on whether drug addiction should be viewed as a disease requiring treatment or an individual’s choice. Today, numerous investigators offer their perspectives on the problem, supporting their assumptions with solid evidence and arguments. These views impact the attitudes to treatment, rehabilitation, and recovery.
The idea that drug addiction should be viewed as a disease is supported in the article “Addiction as a brain disease revised: why it still matters, and the need for consilience.” Heilig et al. (2021) assume that denying the fact that addiction is a severe brain disease might cause serious damage to populations suffering from this condition, as they will have limited access to healthcare services. The central idea introduced by the authors is that addiction promotes specific alterations in the brain’s work, meaning that it is critical to address the issue from the perspective of neuroscience (Heilig et al., 2021). It will help to acquire positive results and ideas for better treatment.
The premises of the authors’ argument are strongly supported by the existing research. Heilig et al. (2021) show that even if the initial decision to use drugs was conscious, a person acquires specific changes in brain function, leading to the development of the chronic and relapsing form of the disease. This statement is supported by the facts from neuroscience and recent investigations. As a result, the argument offered by the researchers is strong, and their assumption is justified by the existing body of knowledge, which makes it a potent source.
Moreover, the authors follow the logic while presenting the main arguments and discussing them from various perspectives. For instance, Heilig et al. (2021) say that following the traditional definition of the disease, drug use might not be viewed as an illness. Moreover, they appeal to the ideas introduced by Jellinek in his classic book, who views the state as a condition that should be analyzed and investigated (Heilig et al., 2021). However, the given assumption is followed by the existing evidence from the field of neuroscience, stating that addiction can be considered a chronic relapsing disease because of the observed changes in the brain and its function (Heilig et al., 2021). It helps to resist the opponents of the idea and refute their arguments.
Finally, another strength of the paper is that the authors avoid making narrowed conclusions. They accept the strengths of other parties’ arguments and offer the idea of considering drug addiction a critical problem that might benefit from combining various approaches to its management (Heilig et al., 2021). As a result, it is possible to compromise and agree on a multi-dimensional approach, which might help move forward and improve the current understanding of dependence and how to help individuals with this condition.
The opposing argument to the position described above is introduced by Lewis in the article “Addiction and the brain: Development, not disease”. In the academic, peer-reviewed article, the author speaks about the brain disease model, which is cultivated by medical authorities, and offers his counterarguments. The central idea offered by Lewis (2017) is that the disease model fails because the brain changes observed in addicted individuals are similar to those emerging during the development of deep habits, or Pavlovian learning. In other words, a person using drugs cultivates specific changes in brain function by his/her actions.
In such a way, the author emphasizes the idea that drug addiction should be viewed as a choice of an individual. The given assumption is linked to the ideas of self-organization and personality development. The author avoids introducing arguments without strong support from the current body of literature and appropriate research. Using the brain disease model as the basis for his cogitations, Lewis (2017) moves forward to introduce counterarguments and explain them by appealing to the existing studies in the field of addiction. It makes the ideas offered by the researcher stronger and helps to understand his central claims.
Moreover, the premises of the argument offered by the researcher are supported by the conclusion and the main ideas offered by him. Thus, Lewis (2017) moves from the idea of addiction as a brain disease to the opposite perspective by considering existing claims and factors supporting every statement. For instance, he says that the short duration of addictive rewards promotes the emergence of negative emotions and makes the learning cycle more effective (Lewis, 2017). It evidences the idea that similar to the acquired habit or skill, drug addiction evolves under the impact of an individual’s decisions and his/her willingness to continue.
In such a way, the author does not leave any assumptions unproven. Offering a particular argument, Lewis supports it with credible evidence from various sources, appealing to other authors or researchers working in the same field. It makes the work more meaningful and allows using it as the argument in the debate linked to the nature of addiction. Moreover, the researcher builds his arguments logically, moving from the discussion of the opposing view to the acceptance of a new one, which helps to understand his claims better. As a result, an enhanced understanding of the issue under research is acquired.
Evaluating the offered arguments, it is vital to admit several important aspects differentiating scholarly sources from popular ones. First of all, the authors use the previous research and support their assumptions with the facts proven by other researchers. For instance, the popular article about addiction lacks this aspect as it offers generalized ideas and leaves many premises unsupported by arguments (“Why is addiction a disease?” n.d.). As a result, popular sources’ quality, credibility, and relevance suffer. For this reason, scholarly papers such as those mentioned above can be used to discuss the problem of drug addiction and conclude about it.
Altogether, the problem of whether drug addiction can be viewed as a disease or a choice remains topical. The selected sources helped to acquire a better understanding of the issue. The arguments offered by the authors are robust and supported by credible evidence. Analyzing these studies, it is possible to conclude that viewing addiction as a disease seems more relevant; however, it is also critical to consider the fact that it depends on a person’s desire to stop using drugs and acquire the necessary treatment. The problem remains complex, and it is necessary to ensure the combined approach is used to address it to help patients.
Heilig, M., MacKillop, J., Martinez, D., Rehm, J., Leggio, L., & Vanderschuren, L. (2021). Addiction as a brain disease revised: why it still matters, and the need for consilience. Neuropsychopharmacology, 46 (10), 1715–1723.
Lewis M. (2017). Addiction and the brain: Development, not disease. Neuroethics , 10 (1), 7–18.
Why is addiction a disease? (2021). Web.
Cite this paper
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2023, August 3). Drug Addiction: A Disease or a Choice? https://studycorgi.com/drug-addiction-a-disease-or-a-choice/
"Drug Addiction: A Disease or a Choice?" StudyCorgi , 3 Aug. 2023, studycorgi.com/drug-addiction-a-disease-or-a-choice/.
StudyCorgi . (2023) 'Drug Addiction: A Disease or a Choice'. 3 August.
1. StudyCorgi . "Drug Addiction: A Disease or a Choice?" August 3, 2023. https://studycorgi.com/drug-addiction-a-disease-or-a-choice/.
Bibliography
StudyCorgi . "Drug Addiction: A Disease or a Choice?" August 3, 2023. https://studycorgi.com/drug-addiction-a-disease-or-a-choice/.
StudyCorgi . 2023. "Drug Addiction: A Disease or a Choice?" August 3, 2023. https://studycorgi.com/drug-addiction-a-disease-or-a-choice/.
This paper, “Drug Addiction: A Disease or a Choice?”, was written and voluntary submitted to our free essay database by a straight-A student. Please ensure you properly reference the paper if you're using it to write your assignment.
Before publication, the StudyCorgi editorial team proofread and checked the paper to make sure it meets the highest standards in terms of grammar, punctuation, style, fact accuracy, copyright issues, and inclusive language. Last updated: August 3, 2023 .
If you are the author of this paper and no longer wish to have it published on StudyCorgi, request the removal . Please use the “ Donate your paper ” form to submit an essay.

Addiction Is a Choice
Many activities that are not themselves diseases can cause diseases, and a foolish, self-destructive activity is not necessarily a disease. When we find a parallel between physiological processes and mental or personality processes, we can mistakenly assume the physiological process is what is really going on, and the mental process is just a passive result of the physical process.
(Please see Counterpoint article by by John H. Halpern, M.D.)
Is addiction a disease, or is it a choice? To think clearly about this question, we need to make a sharp distinction between an activity and its results. Many activities that are not themselves diseases can cause diseases. And a foolish, self-destructive activity is not necessarily a disease.
With those two vital points in mind, we observe a person ingesting some substance: alcohol, nicotine, cocaine or heroin. We have to decide, not whether this pattern of consumption causes disease nor whether it is foolish and self-destructive, but rather whether it is something altogether distinct and separate: Is this pattern of drug consumption itself a disease?
Scientifically, the contention that addiction is a disease is empirically unsupported. Addiction is a behavior and thus clearly intended by the individual person. What is obvious to common sense has been corroborated by pertinent research for years (Table 1).
The person we call an addict always monitors their rate of consumption in relation to relevant circumstances. For example, even in the most desperate, chronic cases, alcoholics never drink all the alcohol they can. They plan ahead, carefully nursing themselves back from the last drinking binge while deliberately preparing for the next one. This is not to say that their conduct is wise, simply that they are in control of what they are doing. Not only is there no evidence that they cannot moderate their drinking, there is clear evidence that they do so, rationally responding to incentives devised by hospital researchers. Again, the evidence supporting this assertion has been known in the scientific community for years (Table 2).
My book Addiction Is a Choice was criticized in a recent review in a British scholarly journal of addiction studies because it states the obvious (Davidson, 2001). According to the reviewer, everyone in the addiction field now knows that addiction is a choice and not a disease, and I am, therefore, "violently pushing against a door which was opened decades ago." I'm delighted to hear that addiction specialists in Britain are so enlightened and that there is no need for me to argue my case over there.
In the United States, we have not made so much progress. Why do some persist, in the face of all reason and all evidence, in pushing the disease model as the best explanation for addiction?
I conjecture that the answer lies in a fashionable conception of the relation between mind and body. There are several competing philosophical theories about that relation. Let us accept, for the sake of argument, the most extreme "materialist" theory: the psychophysical identity theory. Accordingly, every mental event corresponds to a physical event, because it is a physical event. The relation between mind and the relevant parts of the body is, therefore, like the relation between heat and molecular motion: They are precisely the same thing, observed in two different ways. As it happens, I find this view of the relation between mind and body very congenial.
However, I think it is often accompanied by a serious misunderstanding: the notion that when we find a parallel between physiological processes and mental or personality processes, the physiological process is what is really going on and the mental process is just a passive result of the physical process. What this overlooks is the reality of downward causation , the phenomenon in which an emergent property of a system can govern the position of elements within the system (Campbell, 1974; Sperry, 1969). Thus, the complex, symmetrical, six-pointed design of a snow crystal largely governs the position of each molecule of ice in that crystal.
Hence, there is no theoretical obstacle to acknowledging the fact that thoughts, desires, values and other mental phenomena can dominate bodily functions. Suppose that a man's mother dies, and he undergoes the agonizing trauma we call unbearable grief . There is no doubt that if we examine this man's bodily processes we will find many physical changes, among them changes in his blood and stomach chemistry. It would be clearly wrong to say that these bodily changes cause him to be grief-stricken. It would be less misleading to say that his being grief-stricken causes the bodily changes, but this is also not entirely accurate. His knowledge of his mother's death (interacting with his prior beliefs and values) causes his grief, and his grief has blood-sugar and gastric concomitants, among many others.
There is no dispute that various substances cause physiological changes in the bodies of people who ingest them. There is also no dispute, in principle, that these physiological changes may themselves change with repeated doses, nor that these changes may be correlated with subjective mental states like reward or enjoyment.
I say "in principle" because I suspect that people sometimes tend to run away with these supposed correlations. For example, changes in dopamine levels have often been hypothesized as an integral part of the reward/reinforcement process. Yet research shows that dopamine in the nucleus accumbens does not mediate primary or unconditioned food reward in animals (Aberman and Salamone, 1999; Nowend et al., 2001; Salamone et al., 2001; Salamone et al., 1997). According to Salamone, the theory that drugs of abuse turn on a natural reward system is simplistic and inaccurate: "Dopamine in the nucleus accumbens plays a role in the self-administration of some drugs (i.e., stimulants), but certainly not all" (personal communication, Nov. 26, 2001).
Garris et al. (1999) reached similar conclusions: "Dopamine may therefore be a neural substrate for novelty or reward expectation rather than reward itself." They concluded:
[T]here is no correlation between continual bar pressing during [intracranial self-stimulation] and increased dopaminergic neurotransmission in the nucleus accumbensour results are consistent with evidence that the dopaminergic component is not associated with the hedonistic or 'pleasure' aspects of rewardLikewise, the rewarding effects of cocaine do not require dopamine; mice lacking the gene for the dopamine transporter, a major target of cocaine, will self-administer cocaine. However, increased dopamine neurotransmission in the nucleus accumbens shell is seen when rats are transiently exposed to a new environment. The increase in extracellular dopamine quickly returns to normal levels and remains there during continued exploration of the new environmentdopamine release in the nucleus accumbens is related to novelty, predictability or some other aspects of the reward process, rather than to hedonism itself.
Perhaps, then, some people have been too ready to jump to conclusions about specific mechanisms. Be that as it may, chemical rewards have no power to compel--although this notion of compulsion may be a cherished part of clinicians' folklore. I am rewarded every time I eat chocolate cake, but I often eschew this reward because I feel I ought to watch my weight.
Experience with addiction treatment must surely make us even more dubious about the theory that addiction is a disease. The most popular way of helping people manage their addictive behavior is Alcoholics Anonymous (AA) and its various 12-step offshoots. Many observers have recognized the essentially religious nature of AA. The U.S. courts are increasingly regarding AA as a religious activity. In United States v Seeger (1965), the U.S. Supreme Court stated that the test to be applied as to whether a belief is religious is to enquire whether that belief "occupies a place in the life of its possessor parallel to that filled by the orthodox belief in God" in religions more widely accepted in the United States. This requirement is met by members of AA and other secular programs that help people with addictive behaviors and encourage their members to turn their will and lives over to the care of a supreme being. What kind of disease is this for which the best available treatment is religion (Antze, 1987)? Clinical applications are based on explanations for why the behavior occurs. An activity based on a religious belief masquerading as a clinical form of treatment tells us something about what the activity really is--an ethical, not medical, problem in living.
What passes as clinical treatment for addiction is psychotherapy, which essentially consists of various forms of conversation or rhetoric (Szasz, 1988). One person, the therapist, tries to influence another person, the patient, to change their values and behavior. While the conversation called therapy can be helpful, most of the conversation that occurs in therapy based on the disease model is potentially harmful. This is because the therapist misleads the patient into believing something that is simply untrue--that addiction is a disease, and, therefore, addicts cannot control their behavior. Preaching this falsehood to patients may encourage them to abandon any attempt to take responsibility for their actions.
The treatment of drug effects, at the patient's request, is well within the domain of medicine, what passes as evidence for the theory that addiction is a disease is merely clinical folklore.
References:
Aberman JE, Salamone JD (1999), Nucleus accumbens dopamine depletions make rats more sensitive to high ratio requirements but do not impair primary food reinforcement. Neuroscience 92(2):545-552.
Antze P (1987), Symbolic action in Alcoholics Anonymous. In: Constructive Drinking: Perspectives on Drink From Anthropology, Douglas M, ed. New York: Cambridge University Press, pp149-181.
Campbell DT (1974), 'Downward causation' in hierarchically organized biological systems. In: Studies in the Philosophy of Biology: Reduction and Related Problems, Ayala FJ, Dobzhansky T, eds. London: Macmillan.
Davidson R (2001), Conspiracy, cults and choices. Addiction Research & Theory 9(1):92-92 [book review].
Garris PA, Kilpatrick M, Bunin MA et al. (1999), Dissociation of dopamine release in the nucleus accumbens from intracranial self-stimulation. Nature 398(6722):67-69.
Nowend KL, Arizzi M, Carlson BB, Salamone JD (2001), D1 or D2 antagonism in nucleus accumbens core or dorsomedial shell suppresses lever pressing for food but leads to compensatory increases in chow consumption. Pharmacol Biochem Behav 69(3-4):373-382.
Salamone JD, Cousins MS, Snyder BJ (1997), Behavioral functions of nucleus accumbens dopamine: empirical and conceptual problems with the anhedonia hypothesis. Neurosci Biobehav Rev 21(3):341-359.
Salamone JD, Wisniecki A, Carlson BB, Correa M (2001), Nucleus accumbens dopamine depletions make animals highly sensitive to high fixed ratio requirements but do not impair primary food reinforcement. Neuroscience 105(4):863-870.
Sperry W (1969), A modified concept of consciousness. Psychol Rev 76(6):532-536.
Szasz TS (1988), The Myth of Psychotherapy: Mental Healing as Religion, Rhetoric, and Repression. Syracuse, N.Y.: Syracuse University Press.
United States v Seeger, 980 US 163 (1965).

Addiction & Substance Use in Psychiatric Times

How to Talk to Teenagers About Substance Use
National Alcohol Screening Day 2024

Lloyd Sederer, MD: A Conversation About Addiction and the Opioid Epidemic

COVID-19 Research Roundup: March 22, 2024

Child and Adolescent Psychiatry Research Roundup: March 15, 2024
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Open access
- Published: 22 February 2021
Addiction as a brain disease revised: why it still matters, and the need for consilience
- Markus Heilig 1 ,
- James MacKillop ORCID: orcid.org/0000-0003-4118-9500 2 , 3 ,
- Diana Martinez 4 ,
- Jürgen Rehm ORCID: orcid.org/0000-0001-5665-0385 5 , 6 , 7 , 8 ,
- Lorenzo Leggio ORCID: orcid.org/0000-0001-7284-8754 9 &
- Louk J. M. J. Vanderschuren ORCID: orcid.org/0000-0002-5379-0363 10
Neuropsychopharmacology volume 46 , pages 1715–1723 ( 2021 ) Cite this article
85k Accesses
97 Citations
322 Altmetric
Metrics details
The view that substance addiction is a brain disease, although widely accepted in the neuroscience community, has become subject to acerbic criticism in recent years. These criticisms state that the brain disease view is deterministic, fails to account for heterogeneity in remission and recovery, places too much emphasis on a compulsive dimension of addiction, and that a specific neural signature of addiction has not been identified. We acknowledge that some of these criticisms have merit, but assert that the foundational premise that addiction has a neurobiological basis is fundamentally sound. We also emphasize that denying that addiction is a brain disease is a harmful standpoint since it contributes to reducing access to healthcare and treatment, the consequences of which are catastrophic. Here, we therefore address these criticisms, and in doing so provide a contemporary update of the brain disease view of addiction. We provide arguments to support this view, discuss why apparently spontaneous remission does not negate it, and how seemingly compulsive behaviors can co-exist with the sensitivity to alternative reinforcement in addiction. Most importantly, we argue that the brain is the biological substrate from which both addiction and the capacity for behavior change arise, arguing for an intensified neuroscientific study of recovery. More broadly, we propose that these disagreements reveal the need for multidisciplinary research that integrates neuroscientific, behavioral, clinical, and sociocultural perspectives.
Similar content being viewed by others
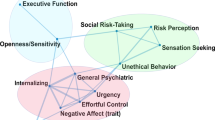
Subtypes in addiction and their neurobehavioral profiles across three functional domains
Gunner Drossel, Leyla R. Brucar, … Anna Zilverstand

Drug addiction: from bench to bedside
Julian Cheron & Alban de Kerchove d’Exaerde

The neurobiology of drug addiction: cross-species insights into the dysfunction and recovery of the prefrontal cortex
Ahmet O. Ceceli, Charles W. Bradberry & Rita Z. Goldstein
Introduction
Close to a quarter of a century ago, then director of the US National Institute on Drug Abuse Alan Leshner famously asserted that “addiction is a brain disease”, articulated a set of implications of this position, and outlined an agenda for realizing its promise [ 1 ]. The paper, now cited almost 2000 times, put forward a position that has been highly influential in guiding the efforts of researchers, and resource allocation by funding agencies. A subsequent 2000 paper by McLellan et al. [ 2 ] examined whether data justify distinguishing addiction from other conditions for which a disease label is rarely questioned, such as diabetes, hypertension or asthma. It concluded that neither genetic risk, the role of personal choices, nor the influence of environmental factors differentiated addiction in a manner that would warrant viewing it differently; neither did relapse rates, nor compliance with treatment. The authors outlined an agenda closely related to that put forward by Leshner, but with a more clinical focus. Their conclusion was that addiction should be insured, treated, and evaluated like other diseases. This paper, too, has been exceptionally influential by academic standards, as witnessed by its ~3000 citations to date. What may be less appreciated among scientists is that its impact in the real world of addiction treatment has remained more limited, with large numbers of patients still not receiving evidence-based treatments.
In recent years, the conceptualization of addiction as a brain disease has come under increasing criticism. When first put forward, the brain disease view was mainly an attempt to articulate an effective response to prevailing nonscientific, moralizing, and stigmatizing attitudes to addiction. According to these attitudes, addiction was simply the result of a person’s moral failing or weakness of character, rather than a “real” disease [ 3 ]. These attitudes created barriers for people with substance use problems to access evidence-based treatments, both those available at the time, such as opioid agonist maintenance, cognitive behavioral therapy-based relapse prevention, community reinforcement or contingency management, and those that could result from research. To promote patient access to treatments, scientists needed to argue that there is a biological basis beneath the challenging behaviors of individuals suffering from addiction. This argument was particularly targeted to the public, policymakers and health care professionals, many of whom held that since addiction was a misery people brought upon themselves, it fell beyond the scope of medicine, and was neither amenable to treatment, nor warranted the use of taxpayer money.
Present-day criticism directed at the conceptualization of addiction as a brain disease is of a very different nature. It originates from within the scientific community itself, and asserts that this conceptualization is neither supported by data, nor helpful for people with substance use problems [ 4 , 5 , 6 , 7 , 8 ]. Addressing these critiques requires a very different perspective, and is the objective of our paper. We readily acknowledge that in some cases, recent critiques of the notion of addiction as a brain disease as postulated originally have merit, and that those critiques require the postulates to be re-assessed and refined. In other cases, we believe the arguments have less validity, but still provide an opportunity to update the position of addiction as a brain disease. Our overarching concern is that questionable arguments against the notion of addiction as a brain disease may harm patients, by impeding access to care, and slowing development of novel treatments.
A premise of our argument is that any useful conceptualization of addiction requires an understanding both of the brains involved, and of environmental factors that interact with those brains [ 9 ]. These environmental factors critically include availability of drugs, but also of healthy alternative rewards and opportunities. As we will show, stating that brain mechanisms are critical for understanding and treating addiction in no way negates the role of psychological, social and socioeconomic processes as both causes and consequences of substance use. To reflect this complex nature of addiction, we have assembled a team with expertise that spans from molecular neuroscience, through animal models of addiction, human brain imaging, clinical addiction medicine, to epidemiology. What brings us together is a passionate commitment to improving the lives of people with substance use problems through science and science-based treatments, with empirical evidence as the guiding principle.
To achieve this goal, we first discuss the nature of the disease concept itself, and why we believe it is important for the science and treatment of addiction. This is followed by a discussion of the main points raised when the notion of addiction as a brain disease has come under criticism. Key among those are claims that spontaneous remission rates are high; that a specific brain pathology is lacking; and that people suffering from addiction, rather than behaving “compulsively”, in fact show a preserved ability to make informed and advantageous choices. In the process of discussing these issues, we also address the common criticism that viewing addiction as a brain disease is a fully deterministic theory of addiction. For our argument, we use the term “addiction” as originally used by Leshner [ 1 ]; in Box 1 , we map out and discuss how this construct may relate to the current diagnostic categories, such as Substance Use Disorder (SUD) and its different levels of severity (Fig. 1) .
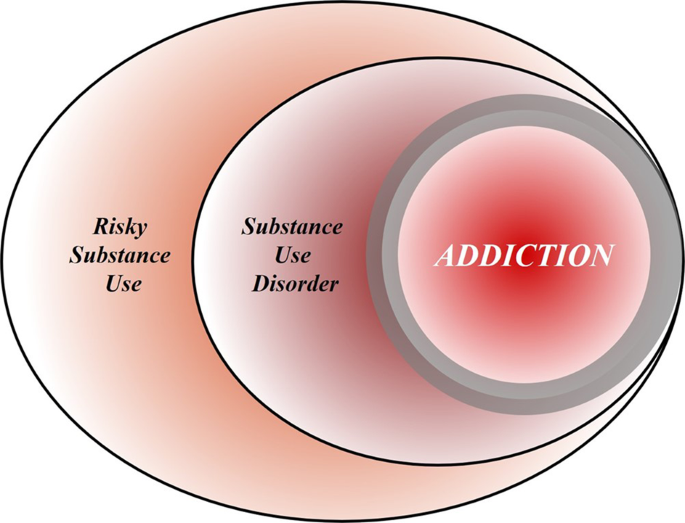
Risky (hazardous) substance use refers to quantity/frequency indicators of consumption; SUD refers to individuals who meet criteria for a DSM-5 diagnosis (mild, moderate, or severe); and addiction refers to individuals who exhibit persistent difficulties with self-regulation of drug consumption. Among high-risk individuals, a subgroup will meet criteria for SUD and, among those who have an SUD, a further subgroup would be considered to be addicted to the drug. However, the boundary for addiction is intentionally blurred to reflect that the dividing line for defining addiction within the category of SUD remains an open empirical question.
Box 1 What’s in a name? Differentiating hazardous use, substance use disorder, and addiction
Although our principal focus is on the brain disease model of addiction, the definition of addiction itself is a source of ambiguity. Here, we provide a perspective on the major forms of terminology in the field.
Hazardous Substance Use
Hazardous (risky) substance use refers to quantitative levels of consumption that increase an individual’s risk for adverse health consequences. In practice, this pertains to alcohol use [ 110 , 111 ]. Clinically, alcohol consumption that exceeds guidelines for moderate drinking has been used to prompt brief interventions or referral for specialist care [ 112 ]. More recently, a reduction in these quantitative levels has been validated as treatment endpoints [ 113 ].
Substance Use Disorder
SUD refers to the DSM-5 diagnosis category that encompasses significant impairment or distress resulting from specific categories of psychoactive drug use. The diagnosis of SUD is operationalized as 2 or more of 11 symptoms over the past year. As a result, the diagnosis is heterogenous, with more than 1100 symptom permutations possible. The diagnosis in DSM-5 is the result of combining two diagnoses from the DSM-IV, abuse and dependence, which proved to be less valid than a single dimensional approach [ 114 ]. Critically, SUD includes three levels of severity: mild (2–3 symptoms), moderate (4–5 symptoms), and severe (6+ symptoms). The International Classification of Diseases (ICD) system retains two diagnoses, harmful use (lower severity) and substance dependence (higher severity).
Addiction is a natural language concept, etymologically meaning enslavement, with the contemporary meaning traceable to the Middle and Late Roman Republic periods [ 115 ]. As a scientific construct, drug addiction can be defined as a state in which an individual exhibits an inability to self-regulate consumption of a substance, although it does not have an operational definition. Regarding clinical diagnosis, as it is typically used in scientific and clinical parlance, addiction is not synonymous with the simple presence of SUD. Nowhere in DSM-5 is it articulated that the diagnostic threshold (or any specific number/type of symptoms) should be interpreted as reflecting addiction, which inherently connotes a high degree of severity. Indeed, concerns were raised about setting the diagnostic standard too low because of the issue of potentially conflating a low-severity SUD with addiction [ 116 ]. In scientific and clinical usage, addiction typically refers to individuals at a moderate or high severity of SUD. This is consistent with the fact that moderate-to-severe SUD has the closest correspondence with the more severe diagnosis in ICD [ 117 , 118 , 119 ]. Nonetheless, akin to the undefined overlap between hazardous use and SUD, the field has not identified the exact thresholds of SUD symptoms above which addiction would be definitively present.
Integration
The ambiguous relationships among these terms contribute to misunderstandings and disagreements. Figure 1 provides a simple working model of how these terms overlap. Fundamentally, we consider that these terms represent successive dimensions of severity, clinical “nesting dolls”. Not all individuals consuming substances at hazardous levels have an SUD, but a subgroup do. Not all individuals with a SUD are addicted to the drug in question, but a subgroup are. At the severe end of the spectrum, these domains converge (heavy consumption, numerous symptoms, the unambiguous presence of addiction), but at low severity, the overlap is more modest. The exact mapping of addiction onto SUD is an open empirical question, warranting systematic study among scientists, clinicians, and patients with lived experience. No less important will be future research situating our definition of SUD using more objective indicators (e.g., [ 55 , 120 ]), brain-based and otherwise, and more precisely in relation to clinical needs [ 121 ]. Finally, such work should ultimately be codified in both the DSM and ICD systems to demarcate clearly where the attribution of addiction belongs within the clinical nosology, and to foster greater clarity and specificity in scientific discourse.
What is a disease?
In his classic 1960 book “The Disease Concept of Alcoholism”, Jellinek noted that in the alcohol field, the debate over the disease concept was plagued by too many definitions of “alcoholism” and too few definitions of “disease” [ 10 ]. He suggested that the addiction field needed to follow the rest of medicine in moving away from viewing disease as an “entity”, i.e., something that has “its own independent existence, apart from other things” [ 11 ]. To modern medicine, he pointed out, a disease is simply a label that is agreed upon to describe a cluster of substantial, deteriorating changes in the structure or function of the human body, and the accompanying deterioration in biopsychosocial functioning. Thus, he concluded that alcoholism can simply be defined as changes in structure or function of the body due to drinking that cause disability or death. A disease label is useful to identify groups of people with commonly co-occurring constellations of problems—syndromes—that significantly impair function, and that lead to clinically significant distress, harm, or both. This convention allows a systematic study of the condition, and of whether group members benefit from a specific intervention.
It is not trivial to delineate the exact category of harmful substance use for which a label such as addiction is warranted (See Box 1 ). Challenges to diagnostic categorization are not unique to addiction, however. Throughout clinical medicine, diagnostic cut-offs are set by consensus, commonly based on an evolving understanding of thresholds above which people tend to benefit from available interventions. Because assessing benefits in large patient groups over time is difficult, diagnostic thresholds are always subject to debate and adjustments. It can be debated whether diagnostic thresholds “merely” capture the extreme of a single underlying population, or actually identify a subpopulation that is at some level distinct. Resolving this issue remains challenging in addiction, but once again, this is not different from other areas of medicine [see e.g., [ 12 ] for type 2 diabetes]. Longitudinal studies that track patient trajectories over time may have a better ability to identify subpopulations than cross-sectional assessments [ 13 ].
By this pragmatic, clinical understanding of the disease concept, it is difficult to argue that “addiction” is unjustified as a disease label. Among people who use drugs or alcohol, some progress to using with a quantity and frequency that results in impaired function and often death, making substance use a major cause of global disease burden [ 14 ]. In these people, use occurs with a pattern that in milder forms may be challenging to capture by current diagnostic criteria (See Box 1 ), but is readily recognized by patients, their families and treatment providers when it reaches a severity that is clinically significant [see [ 15 ] for a classical discussion]. In some cases, such as opioid addiction, those who receive the diagnosis stand to obtain some of the greatest benefits from medical treatments in all of clinical medicine [ 16 , 17 ]. Although effect sizes of available treatments are more modest in nicotine [ 18 ] and alcohol addiction [ 19 ], the evidence supporting their efficacy is also indisputable. A view of addiction as a disease is justified, because it is beneficial: a failure to diagnose addiction drastically increases the risk of a failure to treat it [ 20 ].
Of course, establishing a diagnosis is not a requirement for interventions to be meaningful. People with hazardous or harmful substance use who have not (yet) developed addiction should also be identified, and interventions should be initiated to address their substance-related risks. This is particularly relevant for alcohol, where even in the absence of addiction, use is frequently associated with risks or harm to self, e.g., through cardiovascular disease, liver disease or cancer, and to others, e.g., through accidents or violence [ 21 ]. Interventions to reduce hazardous or harmful substance use in people who have not developed addiction are in fact particularly appealing. In these individuals, limited interventions are able to achieve robust and meaningful benefits [ 22 ], presumably because patterns of misuse have not yet become entrenched.
Thus, as originally pointed out by McLellan and colleagues, most of the criticisms of addiction as a disease could equally be applied to other medical conditions [ 2 ]. This type of criticism could also be applied to other psychiatric disorders, and that has indeed been the case historically [ 23 , 24 ]. Today, there is broad consensus that those criticisms were misguided. Few, if any healthcare professionals continue to maintain that schizophrenia, rather than being a disease, is a normal response to societal conditions. Why, then, do people continue to question if addiction is a disease, but not whether schizophrenia, major depressive disorder or post-traumatic stress disorder are diseases? This is particularly troubling given the decades of data showing high co-morbidity of addiction with these conditions [ 25 , 26 ]. We argue that it comes down to stigma. Dysregulated substance use continues to be perceived as a self-inflicted condition characterized by a lack of willpower, thus falling outside the scope of medicine and into that of morality [ 3 ].
Chronic and relapsing, developmentally-limited, or spontaneously remitting?
Much of the critique targeted at the conceptualization of addiction as a brain disease focuses on its original assertion that addiction is a chronic and relapsing condition. Epidemiological data are cited in support of the notion that large proportions of individuals achieve remission [ 27 ], frequently without any formal treatment [ 28 , 29 ] and in some cases resuming low risk substance use [ 30 ]. For instance, based on data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) study [ 27 ], it has been pointed out that a significant proportion of people with an addictive disorder quit each year, and that most afflicted individuals ultimately remit. These spontaneous remission rates are argued to invalidate the concept of a chronic, relapsing disease [ 4 ].
Interpreting these and similar data is complicated by several methodological and conceptual issues. First, people may appear to remit spontaneously because they actually do, but also because of limited test–retest reliability of the diagnosis [ 31 ]. For instance, using a validated diagnostic interview and trained interviewers, the Collaborative Studies on Genetics of Alcoholism examined the likelihood that an individual diagnosed with a lifetime history of substance dependence would retain this classification after 5 years. This is obviously a diagnosis that, once met, by definition cannot truly remit. Lifetime alcohol dependence was indeed stable in individuals recruited from addiction treatment units, ~90% for women, and 95% for men. In contrast, in a community-based sample similar to that used in the NESARC [ 27 ], stability was only ~30% and 65% for women and men, respectively. The most important characteristic that determined diagnostic stability was severity. Diagnosis was stable in severe, treatment-seeking cases, but not in general population cases of alcohol dependence.
These data suggest that commonly used diagnostic criteria alone are simply over-inclusive for a reliable, clinically meaningful diagnosis of addiction. They do identify a core group of treatment seeking individuals with a reliable diagnosis, but, if applied to nonclinical populations, also flag as “cases” a considerable halo of individuals for whom the diagnostic categorization is unreliable. Any meaningful discussion of remission rates needs to take this into account, and specify which of these two populations that is being discussed. Unfortunately, the DSM-5 has not made this task easier. With only 2 out of 11 symptoms being sufficient for a diagnosis of SUD, it captures under a single diagnostic label individuals in a “mild” category, whose diagnosis is likely to have very low test–retest reliability, and who are unlikely to exhibit a chronic relapsing course, together with people at the severe end of the spectrum, whose diagnosis is reliable, many of whom do show a chronic relapsing course.
The NESARC data nevertheless show that close to 10% of people in the general population who are diagnosed with alcohol addiction (here equated with DSM-IV “dependence” used in the NESARC study) never remitted throughout their participation in the survey. The base life-time prevalence of alcohol dependence in NESARC was 12.5% [ 32 ]. Thus, the data cited against the concept of addiction as a chronic relapsing disease in fact indicate that over 1% of the US population develops an alcohol-related condition that is associated with high morbidity and mortality, and whose chronic and/or relapsing nature cannot be disputed, since it does not remit.
Secondly, the analysis of NESARC data [ 4 , 27 ] omits opioid addiction, which, together with alcohol and tobacco, is the largest addiction-related public health problem in the US [ 33 ]. This is probably the addictive condition where an analysis of cumulative evidence most strikingly supports the notion of a chronic disorder with frequent relapses in a large proportion of people affected [ 34 ]. Of course, a large number of people with opioid addiction are unable to express the chronic, relapsing course of their disease, because over the long term, their mortality rate is about 15 times greater than that of the general population [ 35 ]. However, even among those who remain alive, the prevalence of stable abstinence from opioid use after 10–30 years of observation is <30%. Remission may not always require abstinence, for instance in the case of alcohol addiction, but is a reasonable proxy for remission with opioids, where return to controlled use is rare. Embedded in these data is a message of literally vital importance: when opioid addiction is diagnosed and treated as a chronic relapsing disease, outcomes are markedly improved, and retention in treatment is associated with a greater likelihood of abstinence.
The fact that significant numbers of individuals exhibit a chronic relapsing course does not negate that even larger numbers of individuals with SUD according to current diagnostic criteria do not. For instance, in many countries, the highest prevalence of substance use problems is found among young adults, aged 18–25 [ 36 ], and a majority of these ‘age out’ of excessive substance use [ 37 ]. It is also well documented that many individuals with SUD achieve longstanding remission, in many cases without any formal treatment (see e.g., [ 27 , 30 , 38 ]).
Collectively, the data show that the course of SUD, as defined by current diagnostic criteria, is highly heterogeneous. Accordingly, we do not maintain that a chronic relapsing course is a defining feature of SUD. When present in a patient, however, such as course is of clinical significance, because it identifies a need for long-term disease management [ 2 ], rather than expectations of a recovery that may not be within the individual’s reach [ 39 ]. From a conceptual standpoint, however, a chronic relapsing course is neither necessary nor implied in a view that addiction is a brain disease. This view also does not mean that it is irreversible and hopeless. Human neuroscience documents restoration of functioning after abstinence [ 40 , 41 ] and reveals predictors of clinical success [ 42 ]. If anything, this evidence suggests a need to increase efforts devoted to neuroscientific research on addiction recovery [ 40 , 43 ].
Lessons from genetics
For alcohol addiction, meta-analysis of twin and adoption studies has estimated heritability at ~50%, while estimates for opioid addiction are even higher [ 44 , 45 ]. Genetic risk factors are to a large extent shared across substances [ 46 ]. It has been argued that a genetic contribution cannot support a disease view of a behavior, because most behavioral traits, including religious and political inclinations, have a genetic contribution [ 4 ]. This statement, while correct in pointing out broad heritability of behavioral traits, misses a fundamental point. Genetic architecture is much like organ structure. The fact that normal anatomy shapes healthy organ function does not negate that an altered structure can contribute to pathophysiology of disease. The structure of the genetic landscape is no different. Critics further state that a “genetic predisposition is not a recipe for compulsion”, but no neuroscientist or geneticist would claim that genetic risk is “a recipe for compulsion”. Genetic risk is probabilistic, not deterministic. However, as we will see below, in the case of addiction, it contributes to large, consistent probability shifts towards maladaptive behavior.
In dismissing the relevance of genetic risk for addiction, Hall writes that “a large number of alleles are involved in the genetic susceptibility to addiction and individually these alleles might very weakly predict a risk of addiction”. He goes on to conclude that “generally, genetic prediction of the risk of disease (even with whole-genome sequencing data) is unlikely to be informative for most people who have a so-called average risk of developing an addiction disorder” [ 7 ]. This reflects a fundamental misunderstanding of polygenic risk. It is true that a large number of risk alleles are involved, and that the explanatory power of currently available polygenic risk scores for addictive disorders lags behind those for e.g., schizophrenia or major depression [ 47 , 48 ]. The only implication of this, however, is that low average effect sizes of risk alleles in addiction necessitate larger study samples to construct polygenic scores that account for a large proportion of the known heritability.
However, a heritability of addiction of ~50% indicates that DNA sequence variation accounts for 50% of the risk for this condition. Once whole genome sequencing is readily available, it is likely that it will be possible to identify most of that DNA variation. For clinical purposes, those polygenic scores will of course not replace an understanding of the intricate web of biological and social factors that promote or prevent expression of addiction in an individual case; rather, they will add to it [ 49 ]. Meanwhile, however, genome-wide association studies in addiction have already provided important information. For instance, they have established that the genetic underpinnings of alcohol addiction only partially overlap with those for alcohol consumption, underscoring the genetic distinction between pathological and nonpathological drinking behaviors [ 50 ].
It thus seems that, rather than negating a rationale for a disease view of addiction, the important implication of the polygenic nature of addiction risk is a very different one. Genome-wide association studies of complex traits have largely confirmed the century old “infinitisemal model” in which Fisher reconciled Mendelian and polygenic traits [ 51 ]. A key implication of this model is that genetic susceptibility for a complex, polygenic trait is continuously distributed in the population. This may seem antithetical to a view of addiction as a distinct disease category, but the contradiction is only apparent, and one that has long been familiar to quantitative genetics. Viewing addiction susceptibility as a polygenic quantitative trait, and addiction as a disease category is entirely in line with Falconer’s theorem, according to which, in a given set of environmental conditions, a certain level of genetic susceptibility will determine a threshold above which disease will arise.
A brain disease? Then show me the brain lesion!
The notion of addiction as a brain disease is commonly criticized with the argument that a specific pathognomonic brain lesion has not been identified. Indeed, brain imaging findings in addiction (perhaps with the exception of extensive neurotoxic gray matter loss in advanced alcohol addiction) are nowhere near the level of specificity and sensitivity required of clinical diagnostic tests. However, this criticism neglects the fact that neuroimaging is not used to diagnose many neurologic and psychiatric disorders, including epilepsy, ALS, migraine, Huntington’s disease, bipolar disorder, or schizophrenia. Even among conditions where signs of disease can be detected using brain imaging, such as Alzheimer’s and Parkinson’s disease, a scan is best used in conjunction with clinical acumen when making the diagnosis. Thus, the requirement that addiction be detectable with a brain scan in order to be classified as a disease does not recognize the role of neuroimaging in the clinic.
For the foreseeable future, the main objective of imaging in addiction research is not to diagnose addiction, but rather to improve our understanding of mechanisms that underlie it. The hope is that mechanistic insights will help bring forward new treatments, by identifying candidate targets for them, by pointing to treatment-responsive biomarkers, or both [ 52 ]. Developing innovative treatments is essential to address unmet treatment needs, in particular in stimulant and cannabis addiction, where no approved medications are currently available. Although the task to develop novel treatments is challenging, promising candidates await evaluation [ 53 ]. A particular opportunity for imaging-based research is related to the complex and heterogeneous nature of addictive disorders. Imaging-based biomarkers hold the promise of allowing this complexity to be deconstructed into specific functional domains, as proposed by the RDoC initiative [ 54 ] and its application to addiction [ 55 , 56 ]. This can ultimately guide the development of personalized medicine strategies to addiction treatment.
Countless imaging studies have reported differences in brain structure and function between people with addictive disorders and those without them. Meta-analyses of structural data show that alcohol addiction is associated with gray matter losses in the prefrontal cortex, dorsal striatum, insula, and posterior cingulate cortex [ 57 ], and similar results have been obtained in stimulant-addicted individuals [ 58 ]. Meta-analysis of functional imaging studies has demonstrated common alterations in dorsal striatal, and frontal circuits engaged in reward and salience processing, habit formation, and executive control, across different substances and task-paradigms [ 59 ]. Molecular imaging studies have shown that large and fast increases in dopamine are associated with the reinforcing effects of drugs of abuse, but that after chronic drug use and during withdrawal, brain dopamine function is markedly decreased and that these decreases are associated with dysfunction of prefrontal regions [ 60 ]. Collectively, these findings have given rise to a widely held view of addiction as a disorder of fronto-striatal circuitry that mediates top-down regulation of behavior [ 61 ].
Critics reply that none of the brain imaging findings are sufficiently specific to distinguish between addiction and its absence, and that they are typically obtained in cross-sectional studies that can at best establish correlative rather than causal links. In this, they are largely right, and an updated version of a conceptualization of addiction as a brain disease needs to acknowledge this. Many of the structural brain findings reported are not specific for addiction, but rather shared across psychiatric disorders [ 62 ]. Also, for now, the most sophisticated tools of human brain imaging remain crude in face of complex neural circuit function. Importantly however, a vast literature from animal studies also documents functional changes in fronto-striatal circuits, as well their limbic and midbrain inputs, associated with addictive behaviors [ 63 , 64 , 65 , 66 , 67 , 68 ]. These are circuits akin to those identified by neuroimaging studies in humans, implicated in positive and negative emotions, learning processes and executive functions, altered function of which is thought to underlie addiction. These animal studies, by virtue of their cellular and molecular level resolution, and their ability to establish causality under experimental control, are therefore an important complement to human neuroimaging work.
Nevertheless, factors that seem remote from the activity of brain circuits, such as policies, substance availability and cost, as well as socioeconomic factors, also are critically important determinants of substance use. In this complex landscape, is the brain really a defensible focal point for research and treatment? The answer is “yes”. As powerfully articulated by Francis Crick [ 69 ], “You, your joys and your sorrows, your memories and your ambitions, your sense of personal identity and free will, are in fact no more than the behavior of a vast assembly of nerve cells and their associated molecules”. Social and interpersonal factors are critically important in addiction, but they can only exert their influences by impacting neural processes. They must be encoded as sensory data, represented together with memories of the past and predictions about the future, and combined with representations of interoceptive and other influences to provide inputs to the valuation machinery of the brain. Collectively, these inputs drive action selection and execution of behavior—say, to drink or not to drink, and then, within an episode, to stop drinking or keep drinking. Stating that the pathophysiology of addiction is largely about the brain does not ignore the role of other influences. It is just the opposite: it is attempting to understand how those important influences contribute to drug seeking and taking in the context of the brain, and vice versa.
But if the criticism is one of emphasis rather than of principle—i.e., too much brain, too little social and environmental factors – then neuroscientists need to acknowledge that they are in part guilty as charged. Brain-centric accounts of addiction have for a long time failed to pay enough attention to the inputs that social factors provide to neural processing behind drug seeking and taking [ 9 ]. This landscape is, however, rapidly changing. For instance, using animal models, scientists are finding that lack of social play early in life increases the motivation to take addictive substances in adulthood [ 70 ]. Others find that the opportunity to interact with a fellow rat is protective against addiction-like behaviors [ 71 ]. In humans, a relationship has been found between perceived social support, socioeconomic status, and the availability of dopamine D2 receptors [ 72 , 73 ], a biological marker of addiction vulnerability. Those findings in turn provided translation of data from nonhuman primates, which showed that D2 receptor availability can be altered by changes in social hierarchy, and that these changes are associated with the motivation to obtain cocaine [ 74 ].
Epidemiologically, it is well established that social determinants of health, including major racial and ethnic disparities, play a significant role in the risk for addiction [ 75 , 76 ]. Contemporary neuroscience is illuminating how those factors penetrate the brain [ 77 ] and, in some cases, reveals pathways of resilience [ 78 ] and how evidence-based prevention can interrupt those adverse consequences [ 79 , 80 ]. In other words, from our perspective, viewing addiction as a brain disease in no way negates the importance of social determinants of health or societal inequalities as critical influences. In fact, as shown by the studies correlating dopamine receptors with social experience, imaging is capable of capturing the impact of the social environment on brain function. This provides a platform for understanding how those influences become embedded in the biology of the brain, which provides a biological roadmap for prevention and intervention.
We therefore argue that a contemporary view of addiction as a brain disease does not deny the influence of social, environmental, developmental, or socioeconomic processes, but rather proposes that the brain is the underlying material substrate upon which those factors impinge and from which the responses originate. Because of this, neurobiology is a critical level of analysis for understanding addiction, although certainly not the only one. It is recognized throughout modern medicine that a host of biological and non-biological factors give rise to disease; understanding the biological pathophysiology is critical for understanding etiology and informing treatment.
Is a view of addiction as a brain disease deterministic?
A common criticism of the notion that addiction is a brain disease is that it is reductionist and in the end therefore deterministic [ 81 , 82 ]. This is a fundamental misrepresentation. As indicated above, viewing addiction as a brain disease simply states that neurobiology is an undeniable component of addiction. A reason for deterministic interpretations may be that modern neuroscience emphasizes an understanding of proximal causality within research designs (e.g., whether an observed link between biological processes is mediated by a specific mechanism). That does not in any way reflect a superordinate assumption that neuroscience will achieve global causality. On the contrary, since we realize that addiction involves interactions between biology, environment and society, ultimate (complete) prediction of behavior based on an understanding of neural processes alone is neither expected, nor a goal.
A fairer representation of a contemporary neuroscience view is that it believes insights from neurobiology allow useful probabilistic models to be developed of the inherently stochastic processes involved in behavior [see [ 83 ] for an elegant recent example]. Changes in brain function and structure in addiction exert a powerful probabilistic influence over a person’s behavior, but one that is highly multifactorial, variable, and thus stochastic. Philosophically, this is best understood as being aligned with indeterminism, a perspective that has a deep history in philosophy and psychology [ 84 ]. In modern neuroscience, it refers to the position that the dynamic complexity of the brain, given the probabilistic threshold-gated nature of its biology (e.g., action potential depolarization, ion channel gating), means that behavior cannot be definitively predicted in any individual instance [ 85 , 86 ].
Driven by compulsion, or free to choose?
A major criticism of the brain disease view of addiction, and one that is related to the issue of determinism vs indeterminism, centers around the term “compulsivity” [ 6 , 87 , 88 , 89 , 90 ] and the different meanings it is given. Prominent addiction theories state that addiction is characterized by a transition from controlled to “compulsive” drug seeking and taking [ 91 , 92 , 93 , 94 , 95 ], but allocate somewhat different meanings to “compulsivity”. By some accounts, compulsive substance use is habitual and insensitive to its outcomes [ 92 , 94 , 96 ]. Others refer to compulsive use as a result of increasing incentive value of drug associated cues [ 97 ], while others view it as driven by a recruitment of systems that encode negative affective states [ 95 , 98 ].
The prototype for compulsive behavior is provided by obsessive-compulsive disorder (OCD), where compulsion refers to repeatedly and stereotypically carrying out actions that in themselves may be meaningful, but lose their purpose and become harmful when performed in excess, such as persistent handwashing until skin injuries result. Crucially, this happens despite a conscious desire to do otherwise. Attempts to resist these compulsions result in increasing and ultimately intractable anxiety [ 99 ]. This is in important ways different from the meaning of compulsivity as commonly used in addiction theories. In the addiction field, compulsive drug use typically refers to inflexible, drug-centered behavior in which substance use is insensitive to adverse consequences [ 100 ]. Although this phenomenon is not necessarily present in every patient, it reflects important symptoms of clinical addiction, and is captured by several DSM-5 criteria for SUD [ 101 ]. Examples are needle-sharing despite knowledge of a risk to contract HIV or Hepatitis C, drinking despite a knowledge of having liver cirrhosis, but also the neglect of social and professional activities that previously were more important than substance use. While these behaviors do show similarities with the compulsions of OCD, there are also important differences. For example, “compulsive” substance use is not necessarily accompanied by a conscious desire to withhold the behavior, nor is addictive behavior consistently impervious to change.
Critics question the existence of compulsivity in addiction altogether [ 5 , 6 , 7 , 89 ], typically using a literal interpretation, i.e., that a person who uses alcohol or drugs simply can not do otherwise. Were that the intended meaning in theories of addiction—which it is not—it would clearly be invalidated by observations of preserved sensitivity of behavior to contingencies in addiction. Indeed, substance use is influenced both by the availability of alternative reinforcers, and the state of the organism. The roots of this insight date back to 1940, when Spragg found that chimpanzees would normally choose a banana over morphine. However, when physically dependent and in a state of withdrawal, their choice preference would reverse [ 102 ]. The critical role of alternative reinforcers was elegantly brought into modern neuroscience by Ahmed et al., who showed that rats extensively trained to self-administer cocaine would readily forego the drug if offered a sweet solution as an alternative [ 103 ]. This was later also found to be the case for heroin [ 103 ], methamphetamine [ 104 ] and alcohol [ 105 ]. Early residential laboratory studies on alcohol use disorder indeed revealed orderly operant control over alcohol consumption [ 106 ]. Furthermore, efficacy of treatment approaches such as contingency management, which provides systematic incentives for abstinence [ 107 ], supports the notion that behavioral choices in patients with addictions remain sensitive to reward contingencies.
Evidence that a capacity for choosing advantageously is preserved in addiction provides a valid argument against a narrow concept of “compulsivity” as rigid, immutable behavior that applies to all patients. It does not, however, provide an argument against addiction as a brain disease. If not from the brain, from where do the healthy and unhealthy choices people make originate? The critical question is whether addictive behaviors—for the most part—result from healthy brains responding normally to externally determined contingencies; or rather from a pathology of brain circuits that, through probabilistic shifts, promotes the likelihood of maladaptive choices even when reward contingencies are within a normal range. To resolve this question, it is critical to understand that the ability to choose advantageously is not an all-or-nothing phenomenon, but rather is about probabilities and their shifts, multiple faculties within human cognition, and their interaction. Yes, it is clear that most people whom we would consider to suffer from addiction remain able to choose advantageously much, if not most, of the time. However, it is also clear that the probability of them choosing to their own disadvantage, even when more salutary options are available and sometimes at the expense of losing their life, is systematically and quantifiably increased. There is a freedom of choice, yet there is a shift of prevailing choices that nevertheless can kill.
Synthesized, the notion of addiction as a disease of choice and addiction as a brain disease can be understood as two sides of the same coin. Both of these perspectives are informative, and they are complementary. Viewed this way, addiction is a brain disease in which a person’s choice faculties become profoundly compromised. To articulate it more specifically, embedded in and principally executed by the central nervous system, addiction can be understood as a disorder of choice preferences, preferences that overvalue immediate reinforcement (both positive and negative), preferences for drug-reinforcement in spite of costs, and preferences that are unstable ( “I’ll never drink like that again;” “this will be my last cigarette” ), prone to reversals in the form of lapses and relapse. From a contemporary neuroscience perspective, pre-existing vulnerabilities and persistent drug use lead to a vicious circle of substantive disruptions in the brain that impair and undermine choice capacities for adaptive behavior, but do not annihilate them. Evidence of generally intact decision making does not fundamentally contradict addiction as a brain disease.
Conclusions
The present paper is a response to the increasing number of criticisms of the view that addiction is a chronic relapsing brain disease. In many cases, we show that those criticisms target tenets that are neither needed nor held by a contemporary version of this view. Common themes are that viewing addiction as a brain disease is criticized for being both too narrow (addiction is only a brain disease; no other perspectives or factors are important) or too far reaching (it purports to discover the final causes of addiction). With regard to disease course, we propose that viewing addiction as a chronic relapsing disease is appropriate for some populations, and much less so for others, simply necessitating better ways of delineating the populations being discussed. We argue that when considering addiction as a disease, the lens of neurobiology is valuable to use. It is not the only lens, and it does not have supremacy over other scientific approaches. We agree that critiques of neuroscience are warranted [ 108 ] and that critical thinking is essential to avoid deterministic language and scientific overreach.
Beyond making the case for a view of addiction as a brain disease, perhaps the more important question is when a specific level of analysis is most useful. For understanding the biology of addiction and designing biological interventions, a neurobiological view is almost certainly the most appropriate level of analysis, in particular when informed by an understanding of the behavioral manifestations. In contrast, for understanding the psychology of addiction and designing psychological interventions, behavioral science is the natural realm, but one that can often benefit from an understanding of the underlying neurobiology. For designing policies, such as taxation and regulation of access, economics and public administration provide the most pertinent perspectives, but these also benefit from biological and behavioral science insights.
Finally, we argue that progress would come from integration of these scientific perspectives and traditions. E.O. Wilson has argued more broadly for greater consilience [ 109 ], unity of knowledge, in science. We believe that addiction is among the areas where consilience is most needed. A plurality of disciplines brings important and trenchant insights to bear on this condition; it is the exclusive remit of no single perspective or field. Addiction inherently and necessarily requires multidisciplinary examination. Moreover, those who suffer from addiction will benefit most from the application of the full armamentarium of scientific perspectives.
Funding and disclosures
Supported by the Swedish Research Council grants 2013-07434, 2019-01138 (MH); Netherlands Organisation for Health Research and Development (ZonMw) under project number 912.14.093 (LJMJV); NIDA and NIAAA intramural research programs (LL; the content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health); the Peter Boris Chair in Addictions Research, Homewood Research Institute, and the National Institute on Alcohol Abuse and Alcoholism grants AA025911, AA024930, AA025849, AA027679 (JM; the content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health).
MH has received consulting fees, research support or other compensation from Indivior, Camurus, BrainsWay, Aelis Farma, and Janssen Pharmaceuticals. JM is a Principal and Senior Scientist at BEAM Diagnostics, Inc. DM, JR, LL, and LJMJV declare no conflict of interest.
Leshner AI. Addiction is a brain disease, and it matters. Science. 1997;278:45–7.
Article CAS PubMed Google Scholar
McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–95.
Schomerus G, Lucht M, Holzinger A, Matschinger H, Carta MG, Angermeyer MC. The stigma of alcohol dependence compared with other mental disorders: a review of population studies. Alcohol Alcohol. 2011;46:105–12.
Heyman GM. Addiction and choice: theory and new data. Front Psychiatry. 2013;4:31.
Article PubMed PubMed Central Google Scholar
Heather N, Best D, Kawalek A, Field M, Lewis M, Rotgers F, et al. Challenging the brain disease model of addiction: European launch of the addiction theory network. Addict Res Theory. 2018;26:249–55.
Article Google Scholar
Pickard H, Ahmed SH, Foddy B. Alternative models of addiction. Front Psychiatr.y 2015;6:20.
Google Scholar
Hall W, Carter A, Forlini C. The brain disease model of addiction: is it supported by the evidence and has it delivered on its promises? Lancet Psychiatr. 2015;2:105–10.
Hart CL. Viewing addiction as a brain disease promotes social injustice. Nat Hum Behav. 2017;1:0055.
Heilig M, Epstein DH, Nader MA, Shaham Y. Time to connect: bringing social context into addiction neuroscience. Nat Rev Neurosc.i 2016;17:592–9.
Article CAS Google Scholar
Jellinek EM. The disease concept of alcoholism. Hillhouse Press on behalf of the Christopher J. Smithers Foundation: New Haven, CT; 1960.
Stevenson A. Oxford dictionary of English. 3 ed. New York, NY: Oxford University Press; 2010.
Fan J, May SJ, Zhou Y, Barrett-Connor E. Bimodality of 2-h plasma glucose distributions in whites: the Rancho Bernardo study. Diabetes Care 2005;28:1451–6.
King AC, Vena A, Hasin D, De Wit D, O’Connor CJ, Cao D. Subjective responses to alcohol in the development and maintenance of alcohol use disorder (AUD). Am J Psychiatry. 2021. https://doi.org/10.1176/appi.ajp.2020.20030247 .
GBD. 2016 Alcohol and Drug Use Collaborators. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry. 2018;5:987–1012.
Edwards G, Gross MM. Alcohol dependence: provisional description of a clinical syndrome. Br Med J. 1976;1:1058–61.
Article CAS PubMed PubMed Central Google Scholar
Epstein DH, Heilig M, Shaham Y. Science-based actions can help address the opioid crisis. Trends Pharm Sci. 2018;39:911–16.
Amato L, Davoli M, Perucci CA, Ferri M, Faggiano F, Mattick RP. An overview of systematic reviews of the effectiveness of opiate maintenance therapies: available evidence to inform clinical practice and research. J Subst Abus Treat. 2005;28:321–9.
Cahill K, Stevens S, Perera R, Lancaster T. Pharmacological interventions for smoking cessation: an overview and network meta-analysis. Cochrane Datab System Rev. 2013;5:CD009329.
Jonas DE, Amick HR, Feltner C, Bobashev G, Thomas K, Wines R, et al. Pharmacotherapy for adults with alcohol use disorders in outpatient settings a systematic review and meta-analysis. JAMA. 2014;311:1889–900.
Article PubMed CAS Google Scholar
Mark TL, Kranzler HR, Song X. Understanding US addiction physicians’ low rate of naltrexone prescription. Drug Alcohol Depend. 2003;71:219–28.
Article PubMed Google Scholar
Nutt DJ, King LA, Phillips LD. Drug harms in the UK: a multicriteria decision analysis. Lancet. 2010;376:1558–65.
Wilk AI, Jensen NM, Havighurst TC. Meta-analysis of randomized control trials addressing brief interventions in heavy alcohol drinkers. J Gen Intern Med. 1997;12:274–83.
Laing RD. The divided self; a study of sanity and madness. London: Tavistock Publications; 1960.
Foucault M, Khalfa J. History of madness. New York: Routledge; 2006.
Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL. et al.Comorbidity of mental disorders with alcohol and other drug abuse. Results Epidemiologic Catchment Area (ECA) study.JAMA. 1990;264:2511–8.
Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–16.
Lopez-Quintero C, Hasin DS, de Los Cobos JP, Pines A, Wang S, Grant BF, et al. Probability and predictors of remission from life-time nicotine, alcohol, cannabis or cocaine dependence: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Addiction. 2011;106:657–69.
Humphreys K. Addiction treatment professionals are not the gatekeepers of recovery. Subst Use Misuse. 2015;50:1024–7.
Cohen E, Feinn R, Arias A, Kranzler HR. Alcohol treatment utilization: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2007;86:214–21.
Sobell LC, Cunningham JA, Sobell MB. Recovery from alcohol problems with and without treatment: prevalence in two population surveys. Am J Public Health. 1996;86:966–72.
Culverhouse R, Bucholz KK, Crowe RR, Hesselbrock V, Nurnberger JI Jr, Porjesz B, et al. Long-term stability of alcohol and other substance dependence diagnoses and habitual smoking: an evaluation after 5 years. Arch Gen Psychiatry. 2005;62:753–60.
Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830–42.
Skolnick P. The opioid epidemic: crisis and solutions. Annu Rev Pharm Toxicol. 2018;58:143–59.
Hser YI, Evans E, Grella C, Ling W, Anglin D. Long-term course of opioid addiction. Harv Rev Psychiatry. 2015;23:76–89.
Mathers BM, Degenhardt L, Bucello C, Lemon J, Wiessing L, Hickman M. Mortality among people who inject drugs: a systematic review and meta-analysis. Bull World Health Organ. 2013;91:102–23.
Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, et al. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72:757–66.
Article PubMed PubMed Central CAS Google Scholar
Lee MR, Sher KJ. “Maturing Out” of binge and problem drinking. Alcohol Res: Curr Rev. 2018;39:31–42.
Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ. Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction. 2005;100:281–92.
Berridge V. The rise, fall, and revival of recovery in drug policy. Lancet. 2012;379:22–23.
Parvaz MA, Moeller SJ, d’Oleire Uquillas F, Pflumm A, Maloney T, Alia-Klein N, et al. Prefrontal gray matter volume recovery in treatment-seeking cocaine-addicted individuals: a longitudinal study. Addict Biol. 2017;22:1391–401.
Korponay C, Kosson DS, Decety J, Kiehl KA, Koenigs M. Brain volume correlates with duration of abstinence from substance abuse in a region-specific and substance-specific manner. Biol Psychiatry Cogn Neurosci Neuroimaging. 2017;2:626–35.
PubMed PubMed Central Google Scholar
Janes AC, Datko M, Roy A, Barton B, Druker S, Neal C, et al. Quitting starts in the brain: a randomized controlled trial of app-based mindfulness shows decreases in neural responses to smoking cues that predict reductions in smoking. Neuropsychopharmacology. 2019;44:1631–38.
Humphreys K, Bickel WK. Toward a neuroscience of long-term recovery from addiction. JAMA Psychiatry. 2018;75:875–76.
Verhulst B, Neale MC, Kendler KS. The heritability of alcohol use disorders: a meta-analysis of twin and adoption studies. Psychol Med. 2015;45:1061–72.
Goldman D, Oroszi G, Ducci F. The genetics of addictions: uncovering the genes. Nat Rev Genet. 2005;6:521–32.
Kendler KS, Jacobson KC, Prescott CA, Neale MC. Specificity of genetic and environmental risk factors for use and abuse/dependence of cannabis, cocaine, hallucinogens, sedatives, stimulants, and opiates in male twins. AJ Psychiatry. 2003;160:687–95.
Schizophrenia Working Group of the Psychiatric Genomics C. Biological insights from 108 schizophrenia-associated genetic loci. Nature. 2014;511:421–7.
Wray NR, Ripke S, Mattheisen M, Trzaskowski M, Byrne EM, Abdellaoui A, et al. Genome-wide association analyses identify 44 risk variants and refine the genetic architecture of major depression. Nat Genet. 2018;50:668–81.
Wray NR, Lin T, Austin J, McGrath JJ, Hickie IB, Murray GK, et al. From basic science to clinical application of polygenic risk scores: a primer. JAMA Psychiatry. 2021;78:101–9.
Walters RK, Polimanti R, Johnson EC, McClintick JN, Adams MJ, Adkins AE, et al. Transancestral GWAS of alcohol dependence reveals common genetic underpinnings with psychiatric disorders. Nat Neurosci. 2018;21:1656–69.
Visscher PM, Wray NR. Concepts and misconceptions about the polygenic additive model applied to disease. Hum Hered. 2015;80:165–70.
Heilig M, Leggio L. What the alcohol doctor ordered from the neuroscientist: theragnostic biomarkers for personalized treatments. Prog Brain Res. 2016;224:401–18.
Rasmussen K, White DA, Acri JB. NIDA’s medication development priorities in response to the Opioid Crisis: ten most wanted. Neuropsychopharmacology. 2019;44:657–59.
Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. AJ Psychiatry. 2010;167:748–51.
Kwako LE, Schwandt ML, Ramchandani VA, Diazgranados N, Koob GF, Volkow ND, et al. Neurofunctional domains derived from deep behavioral phenotyping in alcohol use disorder. AJ Psychiatry. 2019;176:744–53.
Kwako LE, Bickel WK, Goldman D. Addiction biomarkers: dimensional approaches to understanding addiction. Trends Mol Med. 2018;24:121–28.
Xiao P, Dai Z, Zhong J, Zhu Y, Shi H, Pan P. Regional gray matter deficits in alcohol dependence: a meta-analysis of voxel-based morphometry studies. Drug Alcohol Depend. 2015;153:22–8.
Ersche KD, Williams GB, Robbins TW, Bullmore ET. Meta-analysis of structural brain abnormalities associated with stimulant drug dependence and neuroimaging of addiction vulnerability and resilience. Curr Opin Neurobiol. 2013;23:615–24.
Klugah-Brown B, Di X, Zweerings J, Mathiak K, Becker B, Biswal B. Common and separable neural alterations in substance use disorders: a coordinate-based meta-analyses of functional neuroimaging studies in humans. Hum Brain Mapp. 2020;41:4459–77.
Volkow ND, Fowler JS, Wang GJ. The addicted human brain: insights from imaging studies. J Clin Investig. 2003;111:1444–51.
Goldstein RZ, Volkow ND. Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications. Nat Rev Neurosci. 2011;12:652–69.
Goodkind M, Eickhoff SB, Oathes DJ, Jiang Y, Chang A, Jones-Hagata LB, et al. Identification of a common neurobiological substrate for mental illness. JAMA Psychiatry. 2015;72:305–15.
Scofield MD, Heinsbroek JA, Gipson CD, Kupchik YM, Spencer S, Smith AC, et al. The nucleus accumbens: mechanisms of addiction across drug classes reflect the importance of glutamate homeostasis. Pharm Rev. 2016;68:816–71.
Korpi ER, den Hollander B, Farooq U, Vashchinkina E, Rajkumar R, Nutt DJ, et al. Mechanisms of action and persistent neuroplasticity by drugs of abuse. Pharm Rev. 2015;67:872–1004.
Luscher C, Malenka RC. Drug-evoked synaptic plasticity in addiction: from molecular changes to circuit remodeling. Neuron. 2011;69:650–63.
Everitt BJ. Neural and psychological mechanisms underlying compulsive drug seeking habits and drug memories–indications for novel treatments of addiction. Eur J Neurosci. 2014;40:2163–82.
Lesscher HM, Vanderschuren LJ. Compulsive drug use and its neural substrates. Rev Neurosci. 2012;23:731–45.
Cruz FC, Koya E, Guez-Barber DH, Bossert JM, Lupica CR, Shaham Y, et al. New technologies for examining the role of neuronal ensembles in drug addiction and fear. Nat Rev Neurosci. 2013;14:743–54.
Crick F. The astonishing hypothesis: the scientific search for the soul. Scribner; Maxwell Macmillan International: New York, NY; 1994.
Vanderschuren LJ, Achterberg EJ, Trezza V. The neurobiology of social play and its rewarding value in rats. Neurosci Biobehav Rev. 2016;70:86–105.
Venniro M, Zhang M, Caprioli D, Hoots JK, Golden SA, Heins C, et al. Volitional social interaction prevents drug addiction in rat models. Nat Neurosci. 2018;21:1520–29.
Martinez D, Orlowska D, Narendran R, Slifstein M, Liu F, Kumar D, et al. Dopamine type 2/3 receptor availability in the striatum and social status in human volunteers. Biol Psychiatry. 2010;67:275–8.
Wiers CE, Shokri-Kojori E, Cabrera E, Cunningham S, Wong C, Tomasi D, et al. Socioeconomic status is associated with striatal dopamine D2/D3 receptors in healthy volunteers but not in cocaine abusers. Neurosci Lett. 2016;617:27–31.
Morgan D, Grant KA, Gage HD, Mach RH, Kaplan JR, Prioleau O, et al. Social dominance in monkeys: dopamine D2 receptors and cocaine self-administration. Nat Neurosci. 2002;5:169–74.
Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017;2:e356–e66.
Gilbert PA, Zemore SE. Discrimination and drinking: a systematic review of the evidence. Soc Sci Med 2016;161:178–94.
Oshri A, Gray JC, Owens MM, Liu S, Duprey EB, Sweet LH, et al. Adverse childhood experiences and amygdalar reduction: high-resolution segmentation reveals associations with subnuclei and psychiatric outcomes. Child Maltreat. 2019;24:400–10.
Holmes CJ, Barton AW, MacKillop J, Galván A, Owens MM, McCormick MJ, et al. Parenting and salience network connectivity among African Americans: a protective pathway for health-risk behaviors. Biol Psychiatry. 2018;84:365–71.
Brody GH, Gray JC, Yu T, Barton AW, Beach SR, Galván A, et al. Protective prevention effects on the association of poverty with brain development. JAMA Pediatr. 2017;171:46–52.
Hanson JL, Gillmore AD, Yu T, Holmes CJ, Hallowell ES, Barton AW, et al. A family focused intervention influences hippocampal-prefrontal connectivity through gains in self-regulation. Child Dev. 2019;90:1389–401.
Borsboom D, Cramer A, Kalis A. Brain disorders? Not really… why network structures block reductionism in psychopathology research. Behav Brain Sci. 2018;42:1–54.
Field M, Heather N, Wiers RW. Indeed, not really a brain disorder: Implications for reductionist accounts of addiction. Behav Brain Sci. 2019;42:e9.
Pascoli V, Hiver A, Van Zessen R, Loureiro M, Achargui R, Harada M, et al. Stochastic synaptic plasticity underlying compulsion in a model of addiction. Nature. 2018;564:366–71.
James W. The dilemma of determinism. Whitefish, MT: Kessinger Publishing; 2005.
Gessell B. Indeterminism in the brain. Biol Philos. 2017;32:1205–23.
Jedlicka P. Revisiting the quantum brain hypothesis: toward quantum (neuro)biology? Front Mol Neurosci. 2017;10:366.
Heyman GM. Addiction: a disorder of choice. Cambridge, MA: Harvard University Press; 2010.
Heather NQ. Is addiction a brain disease or a moral failing? A: Neither. Neuroethics. 2017;10:115–24.
Ahmed SH, Lenoir M, Guillem K. Neurobiology of addiction versus drug use driven by lack of choice. Curr Opin Neurobiol. 2013;23:581–7.
Hogarth L, Lam-Cassettari C, Pacitti H, Currah T, Mahlberg J, Hartley L, et al. Intact goal-directed control in treatment-seeking drug users indexed by outcome-devaluation and Pavlovian to instrumental transfer: critique of habit theory. Eur J Neurosci. 2019;50:2513–25.
Mathis V, Kenny PJ. From controlled to compulsive drug-taking: the role of the habenula in addiction. Neurosci Biobehav Rev. 2019;106:102–11.
Luscher C, Robbins TW, Everitt BJ. The transition to compulsion in addiction. Nat Rev Neurosci. 2020;21:247–63.
Robinson TE, Berridge KC. Addiction. Annu Rev Psychol. 2003;54:25–53.
Everitt BJ, Robbins TW. Neural systems of reinforcement for drug addiction: from actions to habits to compulsion. Nat Neurosci. 2005;8:1481–89.
Koob GF, Volkow ND. Neurocircuitry of addiction. Neuropsychopharmacology. 2010;35:217–38.
Tiffany ST. A cognitive model of drug urges and drug-use behavior: role of automatic and nonautomatic processes. Psychol Rev. 1990;97:147–68.
Robinson TE, Berridge KC. The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Res Rev. 1993;18:247–91.
Koob GF, Le Moal M. Plasticity of reward neurocircuitry and the ‘dark side’ of drug addiction. Nat Neurosci. 2005;8:1442–4.
Stein DJ, Costa DLC, Lochner C, Miguel EC, Reddy YCJ, Shavitt RG, et al. Obsessive-compulsive disorder. Nat Rev Dis Prim. 2019;5:52.
Vanderschuren LJ, Everitt BJ. Drug seeking becomes compulsive after prolonged cocaine self-administration. Science 2004;305:1017–9.
American_Psychiatric_Association. Diagnostic and statistical manual of mental disorders: DSM-5™. 5th ed. Arlington, VA, US: American Psychiatric Publishing, Inc; 2013.
Book Google Scholar
Spragg SDS. Morphine addiction in chimpanzees. Comp Psychol Monogr. 1940;15:132–32.
Lenoir M, Cantin L, Vanhille N, Serre F, Ahmed SH. Extended heroin access increases heroin choices over a potent nondrug alternative. Neuropsychopharmacology. 2013;38:1209–20.
Caprioli D, Venniro M, Zeric T, Li X, Adhikary S, Madangopal R, et al. Effect of the novel positive allosteric modulator of metabotropic glutamate receptor 2 AZD8529 on incubation of methamphetamine craving after prolonged voluntary abstinence in a rat model. Biol Psychiatry. 2015;78:463–73.
Augier E, Barbier E, Dulman RS, Licheri V, Augier G, Domi E, et al. A molecular mechanism for choosing alcohol over an alternative reward. Science. 2018;360:1321–26.
Bigelow GE. An operant behavioral perspective on alcohol abuse and dependence. In: Heather N, Peters TJ, Stockwell T, editors. International handbook of alcohol dependence and problems. John Wiley & Sons Ltd; 2001. p. 299–315.
Higgins ST, Heil SH, Lussier JP. Clinical implications of reinforcement as a determinant of substance use disorders. Annu Rev Psychol. 2004;55:431–61.
Satel S, Lilienfeld SO. Brainwashed: the seductive appeal of mindless neuroscience. New York, NY: Basic Books; 2015.
Wilson EO. Consilience: the unity of knowledge. New York, NY: Vintage Books; 1999.
Saunders JB, Degenhardt L, Reed GM, Poznyak V. Alcohol use disorders in ICD-11: past, present, and future. Alcohol Clin Exp Res 2019;43:1617–31.
Organization. WH. ICD-11 for mortality and morbidity statistics. 2018. https://icd.who.int/browse11/l-m/en . Accessed 21 Oct 2020.
Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, brief intervention, and referral to treatment (SBIRT): toward a public health approach to the management of substance abuse. Subst Abus. 2007;28:7–30.
Witkiewitz K, Hallgren KA, Kranzler HR, Mann KF, Hasin DS, Falk DE, et al. Clinical validation of reduced alcohol consumption after treatment for alcohol dependence using the World Health Organization risk drinking levels. Alcohol Clin Exp Res 2017;41:179–86.
Hasin DS, O’Brien CP, Auriacombe M, Borges G, Bucholz K, Budney A, et al. DSM-5 criteria for substance use disorders: recommendations and rationale. AJ Psychiatry. 2013;170:834–51.
Rosenthal RJ, Faris SB. The etymology and early history of ‘addiction’. Addict Res Theory. 2019;27:437–49.
Martin CS, Steinley DL, Verges A, Sher KJ. The proposed 2/11 symptom algorithm for DSM-5 substance-use disorders is too lenient. Psychol Med. 2011;41:2008–10.
Degenhardt L, Bharat C, Bruno R, Glantz MD, Sampson NA, Lago L, et al. Concordance between the diagnostic guidelines for alcohol and cannabis use disorders in the draft ICD-11 and other classification systems: analysis of data from the WHO’s World Mental Health Surveys. Addiction. 2019;114:534–52.
PubMed Google Scholar
Lago L, Bruno R, Degenhardt L. Concordance of ICD-11 and DSM-5 definitions of alcohol and cannabis use disorders: a population survey. Lancet Psychiatry. 2016;3:673–84.
Lundin A, Hallgren M, Forsman M, Forsell Y. Comparison of DSM-5 classifications of alcohol use disorders with those of DSM-IV, DSM-III-R, and ICD-10 in a general population sample in Sweden. J Stud Alcohol Drugs. 2015;76:773–80.
Kwako LE, Momenan R, Litten RZ, Koob GF, Goldman D. Addictions neuroclinical assessment: a neuroscience-based framework for addictive disorders. Biol Psychiatry. 2016;80:179–89.
Rehm J, Heilig M, Gual A. ICD-11 for alcohol use disorders: not a convincing answer to the challenges. Alcohol Clin Exp Res. 2019;43:2296–300.
Download references
Acknowledgements
The authors want to acknowledge comments by Drs. David Epstein, Kenneth Kendler and Naomi Wray.
Author information
Authors and affiliations.
Center for Social and Affective Neuroscience, Department of Biomedical and Clinical Sciences, Linköping University, Linköping, Sweden
Markus Heilig
Peter Boris Centre for Addictions Research, McMaster University and St. Joseph’s Healthcare Hamilton, Hamilton, ON, Canada
- James MacKillop
Homewood Research Institute, Guelph, ON, Canada
New York State Psychiatric Institute and Columbia University Irving Medical Center, New York, NY, USA
Diana Martinez
Institute for Mental Health Policy Research & Campbell Family Mental Health Research Institute, Centre for Addiction and Mental Health (CAMH), Toronto, ON, Canada
Jürgen Rehm
Dalla Lana School of Public Health and Department of Psychiatry, University of Toronto (UofT), Toronto, ON, Canada
Klinische Psychologie & Psychotherapie, Technische Universität Dresden, Dresden, Germany
Department of International Health Projects, Institute for Leadership and Health Management, I.M. Sechenov First Moscow State Medical University, Moscow, Russia
Clinical Psychoneuroendocrinology and Neuropsychopharmacology Section, Translational Addiction Medicine Branch, National Institute on Drug Abuse Intramural Research Program and National Institute on Alcohol Abuse and Alcoholism Division of Intramural Clinical and Biological Research, National Institutes of Health, Baltimore and Bethesda, MD, USA
Lorenzo Leggio
Department of Population Health Sciences, Unit Animals in Science and Society, Faculty of Veterinary Medicine, Utrecht University, Utrecht, the Netherlands
Louk J. M. J. Vanderschuren
You can also search for this author in PubMed Google Scholar
Contributions
All authors jointly drafted the paper.
Corresponding author
Correspondence to Markus Heilig .
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions

About this article
Cite this article.
Heilig, M., MacKillop, J., Martinez, D. et al. Addiction as a brain disease revised: why it still matters, and the need for consilience. Neuropsychopharmacol. 46 , 1715–1723 (2021). https://doi.org/10.1038/s41386-020-00950-y
Download citation
Received : 10 November 2020
Revised : 11 December 2020
Accepted : 14 December 2020
Published : 22 February 2021
Issue Date : September 2021
DOI : https://doi.org/10.1038/s41386-020-00950-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Persistent impacts of smoking on resting-state eeg in male chronic smokers and past-smokers with 20 years of abstinence.
- Yoonji Jeon
- Dongil Chung
Scientific Reports (2023)
A contextualized reinforcer pathology approach to addiction
- Samuel F. Acuff
- James G. Murphy
Nature Reviews Psychology (2023)
Functional genomic mechanisms of opioid action and opioid use disorder: a systematic review of animal models and human studies
- Camille Falconnier
- Alba Caparros-Roissard
- Pierre-Eric Lutz
Molecular Psychiatry (2023)
A neuromarker for drug and food craving distinguishes drug users from non-users
- Leonie Koban
- Tor D. Wager
Nature Neuroscience (2023)
Does a Survivorship Model of Opioid Use Disorder Improve Public Stigma or Policy Support? A General Population Randomized Experiment
- Jarratt D. Pytell
- Geetanjali Chander
- Emma E. McGinty
Journal of General Internal Medicine (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Psychiatry
Addiction and Choice: Theory and New Data
Gene m. heyman.
1 Department of Psychology, Boston College, Boston, MA, USA
Addiction’s biological basis has been the focus of much research. The findings have persuaded experts and the public that drug use in addicts is compulsive. But the word “compulsive” identifies patterns of behavior, and all behavior has a biological basis, including voluntary actions. Thus, the question is not whether addiction has a biology, which it must, but whether it is sensible to say that addicts use drugs compulsively. The relevant research shows most of those who meet the American Psychiatric Association’s criteria for addiction quit using illegal drugs by about age 30, that they usually quit without professional help, and that the correlates of quitting include legal concerns, economic pressures, and the desire for respect, particularly from family members. That is, the correlates of quitting are the correlates of choice not compulsion. However, addiction is, by definition, a disorder, and thereby not beneficial in the long run. This is precisely the pattern of choices predicted by quantitative choice principles, such as the matching law, melioration, and hyperbolic discounting. Although the brain disease model of addiction is perceived by many as received knowledge it is not supported by research or logic. In contrast, well established, quantitative choice principles predict both the possibility and the details of addiction.
Introduction
Addictive drugs change the brain, genetic studies show that alcoholism has a substantial heritability, and addiction is a persistent, destructive pattern of drug use (e.g., Cloninger, 1987 ; American Psychiatric Association, 1994 ; Robinson et al., 2001 ). In scientific journals and popular media outlets, these observations are cited as proof that “addiction is a chronic, relapsing brain disease, involving compulsive drug use” (e.g., Miller and Chappel, 1991 ; Leshner, 1999 ; Lubman et al., 2004 ; Quenqua, 2011 ). Yet, research shows that addiction has the highest remission rate of any psychiatric disorder, that most addicts quit drugs without professional help, and that the correlates of quitting are those that attend most decisions, such as financial and familial concerns (e.g., Biernacki, 1986 ; Robins, 1993 ; Stinson et al., 2005 ; Klingemann et al., 2010 ). However, addiction is “disease-like” in the sense that it persists even though on balance its costs outweigh the benefits (e.g., most addicts eventually quit). Thus, in order to explain addiction, we need an account of voluntary behavior that predicts the persistence of activities that from a global bookkeeping perspective (e.g., long-term) are irrational. That is, addiction is not compulsive drug use, but it also is not rational drug use. Several empirical choice principles predict the possibility of relatively stable yet suboptimal behavior. They include the matching law, melioration, and hyperbolic discounting (e.g., Herrnstein, 1990 ; Ainslie, 1992 ). These principles were discovered in the course of experiments conducted in laboratories and natural settings, and in experiments these same principles also distinguish addicted from non-addicted drug users (e.g., Kirby et al., 1999 ). For example, ex and current heavy drug users were more likely to suboptimally “meliorate” than were non-addicts in a choice procedure that invited both long-term maximizing and melioration (Heyman and Dunn, 2002 ). Thus, we have on hand a research based, non-disease account of the defining features of addiction, which is to say its destructive and irrational aspects. As this essay is based on how those we call addicts behave, it would be most efficient to begin with a brief summary of key aspects of the natural history of addiction.
Likelihood of Remission and Time Course of Addiction
Figure Figure1 1 shows the cumulative frequency of remission as a function of the onset of dependence in a nation-wide representative sample of addicts (United States, Lopez-Quintero et al., 2011 ). The researchers first recruited a sample of more than 42,000 individuals whose demographic characteristics approximated those of the US population for individuals between the ages of 18 and 64 (Grant and Dawson, 2006 ). The participants were interviewed according to a questionnaire designed to produce an APA diagnosis when warranted. For those who currently or in the past met the criteria for “substance dependence” (the APA’s term for addiction), there were additional questions aimed at documenting the time course of clinically significant levels of drug use. Figure Figure1 1 summarizes the findings regarding remission and the duration of dependence.

The cumulative frequency of remission as a function of time since the onset of dependence, based on Lopez-Quintero et al.’s ( 2011 ) report . The proportion of addicts who quit each year was approximately constant. The smooth curves are based on the negative exponential equations listed in the figure.
On the x- axis is the amount of time since the onset of dependence. On the y -axis is the cumulative frequency of remission, which is the proportion of individuals who met the criteria for lifetime dependence but for the past year or more had been in remission. The fitted curves are negative exponentials, based on the assumption that each year the likelihood of remitting remained constant, independent of the onset of dependence (Heyman, 2013 ).
The cumulative frequency of remission increased each year for each drug. Indeed, the theoretical lines so closely approximated the observations that the simplest account is that each year a constant proportion of those who had not yet remitted did so regardless of how long they had been addicted. By year 4 (since the onset of dependence) half of those who were ever addicted to cocaine had stopped using cocaine at clinically significant levels; for marijuana the half-life of dependence was 6 years; and for alcohol, the half-life of dependence was considerably longer, 16 years. As the typical onset age for dependence on an illicit drug is about 20 (Kessler et al., 2005a ), the results say that most people who become addicted to an illicit drug are “ex-addicts” by age 30. Of course, addicts may switch drugs rather than quit drugs, but other considerations indicate that this does not explain the trends displayed in Figure Figure1. 1 . For example, dependence on any illicit drug decreases markedly as a function of age, which would not be possible if addicts were switching from one drug to another (Heyman, 2013 ).
The graph also shows that there is much individual variation. Among cocaine users, about 5% continued to meet the criteria for addiction well into their 40s; among marijuana users, about 8% remained heavy users well into their 50s, and for alcoholics, more than 15% remained heavy drinkers well into their 60s. Thus, for both legal and illegal drugs some addicts conform to the expectations of the “chronic disease” label. However, as noted below, the correlates of quitting drugs are the correlates of decision making, not the correlates of the diseases addiction is said to be similar to.
Can We Trust the Data?
The results in Figure Figure1 1 replicate the findings of previous nation-wide surveys and targeted studies that selected participants so as to obtain representative samples (e.g., Robins and Murphy, 1967 ; Anthony and Helzer, 1991 ; Robins, 1993 ; Warner et al., 1995 ; Kessler et al., 2005a , b ). For instance, in every national scientific survey of mental health in the United States, most of those who met the criteria for dependence on an illicit drug no longer did so by age 30, and addiction had the highest remission rate of any other psychiatric disorder. However, research on remission faces well-known methodological pitfalls. Those in remission may relapse at some post-interview date, and the subject rosters of the large epidemiological studies may be biased in favor of those addicts who do quit. For instance, addicts who remain heavy drug users may not cooperate with researchers or may be hard to contact because of their life style, illnesses, or have higher mortality rates. These issues have been discussed in some detail elsewhere (Heyman, 2013 ). The key results were that remission after age 30 was reasonably stable, and that it was unlikely that there were enough missing or dead addicts to alter significantly the trends displayed in Figure Figure1 1 .
The Correlates of Quitting and the Role of Treatment
The correlates of quitting include the absence of additional psychiatric and medical problems, marital status (singles stay addicted longer), economic pressures, fear of judicial sanctions, concern about respect from children and other family members, worries about the many problems that attend regular involvement in illegal activities, more years spent in school, and higher income (e.g., Waldorf, 1983 ; Biernacki, 1986 ; Waldorf et al., 1991 ; Warner et al., 1995 ). Put in more personal terms, addicts often say that they quit drugs because they wanted to be a better parent, make their own parents proud of them, and not further embarrass their families (e.g., Premack, 1970 ; Jorquez, 1983 ). In short, the correlates of quitting are the practical and moral concerns that affect all major decisions. They are not the correlates of recovery from the diseases addiction is said to be like, such as Alzheimer’s, schizophrenia, diabetes, heart disease, cancer, and so on (e.g., Leshner, 1999 ; McLellan et al., 2000 ; Volkow and Li, 2004 ).
Much of what we know about quitting drugs has been provided by researchers who study addicts who are not in treatment (e.g., Klingemann et al., 2010 ). This is because most addicts do not seek treatment. For instance, in the survey that provided the data for Figure Figure1, 1 , only 16% of those who currently met the criteria for dependence were in treatment, and treatment was broadly defined so as to include self-help organizations as well as services by trained clinicians (Stinson et al., 2005 ). Since most addicts quit, the implication is that most addicts quit without professional help. Research supports this logic (e.g., Fiore et al., 1993 ).
A Non-Disease Etiology for Persistent Self-Destructive Drug Use
Although self-destructive, irrational behavior can be a sign of pathology, it need not be. The self-help industry is booming, which reflects the tendency of so many of us to procrastinate, overeat, skip exercising, and opt for whatever is most convenient. Why buy a book or go to a lecture on how to improve your life if you did not realize that (1) you were behaving imprudently, (2) knew you probably could change, but (3) so far have not taken the requisite steps. Similarly, human irrationality drives the story-line of most novels, memoirs, movies, and plays. Agamemnon sacrifices his own daughter to advance his political and personal goals but then publicly embarrasses Achilles his most powerful and skillful warrior. Both actions are selfish, and the second undermines the goals of the first, which anyone could have foretold. However, Homer is portraying human nature not writing a psychiatric text. Thus, it seems fair to say that who cite selfishness and myopic choices as evidence of pathology (e.g., “she has to be sick because she bought drugs rather than groceries”) naively misread human nature.
In support of the poet’s as opposed to the brain disease account of human nature, behavioral psychologists and economists have discovered principles that predict self-defeating, selfish patterns of behavior. They include “hyperbolic discounting,” “melioration,” and the “matching law” (Herrnstein, 1970 , 1990 ; Rachlin and Green, 1972 ; Ainslie, 1992 ; Rachlin, 2007 ). These are quantitative, empirical laws of choice that predict how different species, including humans, choose between different commodities and activities, such as food, water, and exercise. Their relevance to addiction and other self-defeating behaviors is that under some conditions they predict relatively stable yet suboptimal patterns of behavior. For example, Heyman and Herrnstein ( 1986 ) arranged an experiment in which the matching predicted the lowest possible rate of reinforcement. As predicted the subjects shifted to matching, lowering their overall reinforcement rate as they did so. This finding has been replicated numerous times (e.g., Herrnstein et al., 1997 ), and it is analogous as to what happens as drug use turns into addiction.
Or, put another way, general principles that apply to everyday choices, also predict compulsive-like consumption patterns that are consistent with the behavior of addicts.
These choice laws reflect a basic, but often overlooked property, of most choice situations. There is more than one “optimal” strategy (Heyman, 2009 ). One is optimal from the perspective of the most immediate circumstances, such as the current values of the options, taking into account just the most pressing needs and goals. The others are optimal in terms of wider time horizons and the perspectives of others. For example, in settings in which current choices affect the values of future options, it is possible for the current best choice to be the worst long-term choice (e.g., Herrnstein et al., 1993 ; Heyman and Dunn, 2002 ). This is relevant because a common feature of addictive drugs is that they provide immediate benefits but delayed costs. Thus, it is possible that the drug is the best choice when the frame of reference is restricted to the current values of the immediately available options but the worst choice when the frame of reference expands to include future costs and other people’s needs. According to this account, persistent drug use reflects the workings of a local optimum, whereas controlled drug use or abstinence reflects the workings of a global optimum. Put somewhat differently, whether or not drug use persists depends on the factors that influence decision making, particularly values that emphasize global as opposed to a local frame of reference (e.g., values related to family, the future, one’s reputation, and so on). Scores of studies support this analysis (e.g., Waldorf, 1983 ; Biernacki, 1986 ; Mariezcurrena, 1994 ; Klingemann et al., 2010 ).
Old Clinical Follow-Up Studies: Empirical Support for the Disease Account
Imagine that what we knew about addiction was restricted to those individuals who make up the right-hand tails of the cumulative distribution curves in Figure Figure1. 1 . We would have good reason to believe that addiction is a chronic relapsing disease. This is precisely the situation for much of the history of addiction research. Until the mid 1970s virtually all empirical studies of addicts were based on individuals who had been in treatment, which was most often detoxification in American prison/hospitals or similar institutions (e.g., Brecher, 1972 ; Vaillant, 1973 ; Maddux and Desmond, 1980 ; Hser et al., 1993 ). In some studies virtually all of the participants were males with extensive arrest records, poor work histories, lower than average marriage rates, and lower than average educational achievement (e.g., Vaillant, 1973 ). That is, the understanding of addiction as a chronic disorder was based on a population of drug users whose demographic characteristics – we now know – match those that predict not quitting (e.g., Klingemann et al., 2010 ). In the 1960s illicit drug use spread to college campuses and upscale neighborhoods. This new generation of addicts included individuals who were employed, married, and well-educated (e.g., Waldorf et al., 1991 ). With these demographic changes, the natural history of addiction changed. More often than not, the pressures of family, employment, and the hassles of an illegal life style eventually trumped getting high. Figure Figure1, 1 , which is representative of every major epidemiological study conducted over the past 30 years, reflects this reality; received opinion does not.
But Drugs Change the Brain
With the exception of alcohol, addictive drugs produce their biological and psychological changes by binding to specific receptor sites throughout the body. As self-administered drug doses greatly exceed the circulating levels of their natural analogs, persistent heavy drug use leads to structural and functional changes in the nervous system. It is widely – if not universally – assumed that these neural adaptations play a causal role in addiction. In support of this interpretation brain imaging studies often reveal differences between the brains of addicts and comparison groups (e.g., Volkow et al., 1997 ; Martin-Soelch et al., 2001 ) However, these studies are cross-sectional and the results are correlations. There are no published studies that establish a causal link between drug-induced neural adaptations and compulsive drug use or even a correlation between drug-induced neural changes and an increase in preference for an addictive drug. For example, in a frequently referred to animal study, Robinson et al. ( 2001 ) found dendritic changes in the striatum and the prefrontal cortex of rats who had self-administered cocaine. They concluded that this was a “recipe for addiction.” However, they did not evaluate whether their findings with rodents applied to humans, nor did they even test if the dendritic modifications had anything to do with changes in preference for cocaine in their rats. In principle then it is possible that the drug-induced neural changes play little or no role in the persistence of drug use. This is a testable hypothesis.
First, most addicts quit. Thus, drug-induced neural plasticity does not prevent quitting. Second, in follow-up studies, which tested Robinson et al.’s claims, there were no increases in preference for cocaine. For instance in a preference test that provided both cocaine and saccharin, rats preferred saccharin (Lenoir et al., 2007 ) even after they had consumed about three to four times more cocaine than the rats in the Robinson et al study, and even though the cocaine had induced motoric changes which have been interpreted as signs of the neural underpinnings of addiction (e.g., Robinson and Berridge, 2003 ). Third, Figure Figure1 1 shows that the likelihood of remission was constant over time since the onset of dependence. Although this is a surprising result, it is not without precedent. In a longitudinal study of heroin addicts, Vaillant ( 1973 ) reports that the likelihood of going off drugs neither increased nor decreased over time (1973), and in a study with rats, Serge Ahmed and his colleagues (Cantin et al., 2010 ) report that the probability of switching from cocaine to saccharin (which was about 0.85) was independent of past cocaine consumption. Since drugs change the brain, these results suggest that the changes do not prevent quitting, and the slope of Figure Figure1 1 implies that drug-induced neural changes do not even decrease the likelihood of quitting drugs once dependence is in place.
But There is a Genetic Predisposition for Addiction
Twin and adoption studies have repeatedly demonstrated a genetic predisposition for alcoholism (e.g., Cloninger, 1987 ), and the limited amount of research on the genetics of illicit drug use suggests the same for drugs such as heroin, cocaine, and marijuana (Tsuang et al., 2001 ). However, all behavior has a genetic basis, including voluntary acts. The brain is the organ of voluntary action, and brain structure and development follow the blueprint set by DNA. Thus, there is no necessary connection between heritability and compulsion. In support of this point, monozygotic twins are much more likely to share similar religious and political beliefs than are dizygotic twins, even when they are separated before the age of 1 year old (e.g., Waller et al., 1990 ; McCourt et al., 1999 ). That is, learned, voluntary religious and political beliefs have substantial heritabilities just as do many involuntary human characteristics. The relevance to addiction is that a genetic predisposition is not a recipe for compulsion, just as brain adaptations are not a recipe for compulsion.
Addiction involves an initial “honey moon” period, followed by alternating periods of remission and relapse, and then an eventual return to a more sober life. Most addicts quit using drugs at clinically significant levels, they typically quit without professional help, and in the case of illicit drugs, they typically quit before the age of 30. The correlates of quitting include many of the factors that influence voluntary acts, but not, according to Figure Figure1, 1 , drug exposure once drug use meets the criteria for dependence. Thus, we can say that addiction is ambivalent drug use, which eventually involves more costs than benefits (otherwise why quit?). Behavioral choice principles predict ambivalent preferences, semi-stable suboptimal behavior patterns, and the capacity to shift from one option to another. In contrast, the brain disease account of addiction fails to predict the high quit rates; it fails to predict the correlates of quitting; it fails to predict the temporal pattern of quitting; and it is tied to unsupportable assumptions, such as the claims that neural adaptations, heritability, and irrationality are prima facie evidence of disease. To be sure “compulsion” and “choice” can be seen as points on a continuum, but Figure Figure1 1 and research on quitting make it clear that addiction is not a borderline case.
It is time to think about addiction in terms of what the research shows, particularly the more recent epidemiological studies, and it is time to abandon the medical model of addiction. It does not fit the facts. The matching law, melioration, and hyperbolic discounting predict that drugs and similar commodities will become the focus of destructive, suboptimal patterns of behavior. These same choice models also predict that individuals caught in a destructive pattern of behavior retain the capacity to improve their lot and that they will do so as a function of changes in their options and/or how they frame their choices. This viewpoint fits the facts of addiction and provides a practical guide to measures that will actually help addicts change for the better.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
- Ainslie G. (1992). Picoeconomics: The Strategic Interaction of Successive Motivational States Within the Person . Cambridge: Cambridge University Press [ Google Scholar ]
- American Psychiatric Association (1994). Diagnostic and Statistical Manual of Mental Disorders: DSM-IV , 4th Edn Washington, DC: American Psychiatric Association [ Google Scholar ]
- Anthony J. C., Helzer J. E. (1991). “Syndromes of drug abuse and dependence,” in Psychiatric Disorders in America , eds Robins L. N., Regier D. A. (New York: The Free Press; ), 116–154 [ Google Scholar ]
- Biernacki P. (1986). Pathways from Heroin Addiction: Recovery Without Treatment . Philadelphia, PA: Temple University Press [ Google Scholar ]
- Brecher E. M. (1972). Licit and Illicit Drugs; The Consumers Union Report on Narcotics, Stimulants, Depressants, Inhalants, Hallucinogens, and Marijuana–Including Caffeine, Nicotine, and Alcohol , 1st Edn Boston, MA: Little, Brown [ Google Scholar ]
- Cantin L., Lenoir M., Augier E., Vanhille N., Dubreucq S., Serre F., et al. (2010). Cocaine is low on the value ladder of rats: possible evidence for resilience to addiction . PLoS ONE 5 :e11592. 10.1371/journal.pone.0011592 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cloninger C. R. (1987). Neurogenetic adaptive mechanisms in alcoholism . Science 236 , 410–416 10.1126/science.2882604 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fiore M. C., Newcomb P., McBride P. (1993). “Natural history of tobacco use and addiction,” in Nicotine Addiction: Principles and Management , eds. Orleans C. T., Slade J. (New York: Oxford University Press; ), 89–104 [ Google Scholar ]
- Grant B. F., Dawson D. A. (2006). Introduction to the National epidemiologic survey on alcohol and related conditions . Alcohol Res. Health 29 , 74–78 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Herrnstein R. J. (1970). On the law of effect . J. Exp. Anal. Behav. 13 , 243–266 10.1901/jeab.1970.13-243 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Herrnstein R. J. (1990). Behavior, reinforcement, and utility . Psychol. Sci. 1 , 217–224 10.1111/j.1467-9280.1990.tb00203.x [ CrossRef ] [ Google Scholar ]
- Herrnstein R. J., Rachlin H., Laibson D. I. (1997). The Matching Law: Papers in Psychology and Economics . New York: Russell Sage Foundation [ Google Scholar ]
- Herrnstein R. J., Loewenstein G. F., Prelec D., Vaughan W. (1993). Utility maximization and melioration: internalities in individual choice . J. Behav. Decis. Mak. 6 , 149–185 10.1002/bdm.3960060302 [ CrossRef ] [ Google Scholar ]
- Heyman G. M. (2009). Addiction: A Disorder of Choice . Cambridge, MA: Harvard University Press [ Google Scholar ]
- Heyman G. M. (2013). Quitting drugs: quantitative and qualitative features . Annu. Rev. Clin. Psychol. 9 , 29–59 10.1146/annurev-clinpsy-032511-143041 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Heyman G. M., Dunn B. (2002). Decision biases and persistent illicit drug use: an experimental study of distributed choice in drug clinic patients . Drug Alcohol Depend. 67 , 192–203 10.1016/S0376-8716(02)00071-6 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Heyman G. M., Herrnstein R. J. (1986). More on concurrent interval ratio schedules . J. Exp. Anal. Behav. 46 , 331–351 10.1901/jeab.1986.46-331 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hser Y. I., Anglin D., Powers K. (1993). A 24-year follow-up of California narcotics addicts . Arch. Gen. Psychiatry 50 , 577–584 10.1001/archpsyc.1993.01820190079008 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jorquez J. S. (1983). The retirement phase of heroin using careers . J. Drug Issues 13 , 343–365 [ Google Scholar ]
- Kessler R. C., Berglund P., Demler O., Jin R., Merikangas K. R., Walters E. E. (2005a). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National comorbidity survey replication . Arch. Gen. Psychiatry 62 , 593–602 10.1001/archpsyc.62.6.617 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kessler R. C., Chiu W. T., Demler O., Merikangas K. R., Walters E. E. (2005b). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National comorbidity survey replication . Arch. Gen. Psychiatry 62 , 617–627 10.1001/archpsyc.62.6.617 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kirby K., Petry N., Bickel W. (1999). Heroin addicts discount delayed rewards at higher rates than non-drug-using controls . J. Exp. Psychol. Gen. 128 , 78–87 10.1037/0096-3445.128.1.78 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Klingemann H. K., Sobell M. B., Sobell L. C. (2010). Continuities and changes in self-change research . Addiction 105 , 1510–1518 10.1111/j.1360-0443.2009.02770.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lenoir M., Serre F., Cantin L., Ahmed S. H. (2007). Intense sweetness surpasses cocaine reward . PLoS ONE 2 :e698. 10.1371/journal.pone.0000698 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Leshner A. I. (1999). Science-based views of drug addiction and its treatment . J. Am. Med. Assoc. 282 , 1314–1316 10.1001/jama.282.14.1314 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lopez-Quintero C., Hasin D. S., de los Cobos J. P., Pines A., Wang S., Grant B. F., et al. (2011). Probability and predictors of remission from life-time nicotine, alcohol, cannabis or cocaine dependence: results from the National epidemiologic survey on alcohol and related conditions . Addiction 106 , 657–669 10.1111/j.1360-0443.2010.03194.x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lubman D. I., Yucel M., Pantelis C. (2004). Addiction, a condition of compulsive behaviour? Neuroimaging and neuropsychological evidence of inhibitory dysregulation . Addiction 99 , 1491–1502 10.1111/j.1360-0443.2004.00808.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Maddux J. F., Desmond D. P. (1980). New light on the maturing out hypothesis in opioid dependence . Bull. Narc. 32 , 15–25 [ PubMed ] [ Google Scholar ]
- Mariezcurrena R. (1994). Recovery from addictions without treatment: literature review . Scand. J. Behav. Ther. 23 , 131–154 10.1080/16506079409455971 [ CrossRef ] [ Google Scholar ]
- Martin-Soelch C., Chevalley A.-F., Kunig G., Missimer J., Magyar S., Mino A., et al. (2001). Changes in reward-induced brain activation in opiate addicts . Eur. J. Neurosci. 14 , 1360–1368 10.1046/j.0953-816x.2001.01753.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McCourt K. B., Thomas J., Jr., Lykken D. T., Tellegen A., Keyes M. (1999). Authoritarianism revisited: genetic and environmental influences examined in twins reared apart and together . Pers. Individ. Differ. 27 , 985–1014 10.1016/S0191-8869(99)00048-3 [ CrossRef ] [ Google Scholar ]
- McLellan A. T., Lewis D. C., O’Brien C. P., Kleber H. D. (2000). Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation . J. Am. Med. Assoc. 284 , 1689–1695 10.1001/jama.284.13.1689 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Miller N. S., Chappel J. N. (1991). History of the disease concept . Psychiatr. Ann. 21 , 196–205 [ Google Scholar ]
- Premack D. (1970). “Mechanisms of self-control,” in Learning Mechanisms in Smoking , ed. Hunt W. A. (Chicago: Aldine; ), 107–123 [ Google Scholar ]
- Quenqua D. (2011). July 10. Rethinking Addiction’s Roots, and Its Treatment . New York Times; Available at: http://www.nytimes.com/2011/07/11/health/11addictions.html [ Google Scholar ]
- Rachlin H. (2007). In what sense are addicts irrational? Drug Alcohol Depend. 90 ( Suppl. ), S92–S99 10.1016/j.drugalcdep.2006.07.011 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rachlin H., Green L. (1972). Commitment, choice, and self-control . J. Exp. Anal. Behav. 17 , 15–22 10.1901/jeab.1972.17-15 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Robins L. N. (1993). Vietnam veterans’ rapid recovery from heroin addiction: a fluke or normal expectation? Addiction 188 , 1041–1054 10.1111/j.1360-0443.1993.tb02123.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Robins L. N., Murphy G. (1967). Drug use in a normal population of young Negro men . Am. J. Public Health Nations Health 57 , 1580–1596 10.2105/AJPH.57.9.1580 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Robinson T. E., Berridge K. E. (2003). Addiction . Ann. Rev. Psychol. 54 , 25–53 10.1146/annurev.psych.54.101601.145237 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Robinson T. E., Gorny G., Mitton E., Kolb B. (2001). Cocaine self-administration alters the morphology of dendrites and dendritic spines in the nucleus accumbens and neocortex . Synapse 39 , 257–266 10.1002/1098-2396(20010301)39:3<257::AID-SYN1007>3.0.CO;2-1 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stinson F. S., Grant B. F., Dawson D., Ruan W. J., Huang B., Saha T. (2005). Comorbidity between DSM-IV alcohol and specific drug use disorders in the United States: results from the National epidemiological survey on alcohol and related conditions . Drug Alcohol Depend. 80 , 105–116 10.1016/j.drugalcdep.2005.03.009 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tsuang M. T., Bar J. L., Harley R. M., Lyons M. J. (2001). The Harvard twin study of substance abuse: what we have learned . Harv. Rev. Psychiatry 9 , 267–279 10.1080/10673220127912 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vaillant G. E. (1973). A 20-year follow-up of New York narcotic addicts . Arch. Gen. Psychiatry 29 , 237–241 10.1001/archpsyc.1973.04200020065009 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Volkow N. D., Li T. K. (2004). Drug addiction: the neurobiology of behaviour gone awry . Nat. Rev. Neurosci. 5 , 963–970 10.1038/nrn1539 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Volkow N. D., Wang G. J., Fowler J. S. (1997). Decreased striatal dopaminergic responsiveness in detoxified cocaine-dependent subjects . Nature 386 , 830–833 10.1038/386827a0 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Waldorf D. (1983). Natural recovery from opiate addiction: some social-psychological processes of untreated recovery . J. Drug Issues 13 , 237–279 [ Google Scholar ]
- Waldorf D., Reinarman C., Murphy S. (1991). Cocaine Changes: The Experience of Using and Quitting . Philadelphia, PA: Temple University Press [ Google Scholar ]
- Waller N. G., Kojetin B. A., Bouchard T. (1990). Genetic and environmental influences on religious interests, attitudes, and values: a study of twins reared apart and together . Psychol. Sci. 1 , 138–142 10.1111/j.1467-9280.1990.tb00083.x [ CrossRef ] [ Google Scholar ]
- Warner L. A., Kessler R. C., Hughes M., Anthony J. C., Nelson C. B. (1995). Prevalence and correlates of drug use and dependence in the United States. results from the National comorbidity survey . Arch. Gen. Psychiatry 52 , 219–229 10.1001/archpsyc.1995.03950150051010 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Find Providers
- Medical Services
- Get Care Now
- Schedule an Appointment
- Find a Career
- Log in to My IU Health
- Thrive by IU Health
- We are IU Health
- Patient Stories
- Health & Wellness
Is Addiction Really a Disease?
September 02, 2020.
Is addiction really a disease or a matter of choice? Ask the mother who lost her 19-year-old son — the laughing family prankster who earned a full-ride college scholarship as a solid student and star second baseman — to drugs.
The moody, angry dropout who survived overdoses to get caught breaking into cars wasn't the boy she raised. What she knew, like the families and friends of the more than 15,000 Hoosiers who've died due to overdose since 1999, is that addiction's not a life anyone would choose.
Most medical professionals agree. The American Medical Association (AMA) classified alcoholism as a disease in 1956 and included addiction as a disease in 1987.
In 2011 the American Society of Addiction Medicine (ASAM) joined the AMA, defining addiction as a chronic brain disorder, not a behavior problem, or just the result of making bad choices.
Research and input from top addiction authorities, addiction medicine doctors, neuroscientists and experts from the National Institute on Drug Abuse agree in classifying addiction as a disease. Like other chronic diseases such as diabetes and heart disease, experts are still learning about how and why the disease develops. This blog post will help you understand addiction and how IU Health addiction treatment can help those struggling.
What is addiction?
Alcohol or drug addiction, also known as substance use disorder, is a chronic disease of the brain that can happen to anyone. Severe substance use disorder happens when substance use becomes an uncontrollable habit that hurts your day-to-day life, showing up as struggles at work or in school, conflicts with relationships, legal or money problems.
Addiction changes the brain
Addiction changes the way the brain works, rewiring its structure. Drugs and alcohol hack into your brain's communication system and interfere with how nerve cells send, receive and process information.
The brain’s reward system activates when we do something we like—eating a piece of our favorite pie, hanging out with friends, or going for a run, for instance. That reward comes in the chemical dopamine. Drugs or alcohol trigger the release of dopamine.
Addiction causes the brain to ask for more
Dopamine makes us feel good and want to keep doing what we're doing. It also teaches the brain to repeat the behavior. Cues trigger the reward system, fuel cravings and create a habit loop. The smell of pie baking can make you salivate in anticipation of the taste. Addiction fuels habits too—craving a cigarette every morning with coffee or wanting a hit when you drive past the house where you used to do drugs.
When you take a drug, your brain releases a flood of dopamine, much more than it would when you're eating your favorite pie. Your brain overreacts and cuts back on dopamine production to bring it down to a normal level.
As you continue to use drugs, your body produces less dopamine. Things that brought you pleasure—that pie, friends, and even drugs—don't anymore. Once you're addicted, it takes more and more drugs just to feel normal.
An addicted brain impacts behavior
Research has shown how addiction changes the areas of the brain in charge of judgment, decision making, learning and memory, and controlling behavior. Those changes can lead to a good student flunking out, a wife lying about draining the family savings account or an overdose in a grocery parking lot, with kids watching from their car seats.
Once substance use changes the brain, willpower changes too. If you try to quit using substances, your brain tries to protect you from the pain and intensity of withdrawal symptoms. Addiction fuels your brain's response to do whatever it takes to stop the cravings and discomfort. That can mean overruling the will to "just say no" by taking a drink or using a drug.

Addiction is a disease with complex risk factors
Addiction doesn't discriminate. High-rent districts, "seedy" neighborhoods, age, race, sex or income—addiction weaves its way through all walks of life. No one thing can predict your risk of developing a substance use disorder. But researchers agree there are a combination of factors involved that can increase your risk.
Risk factors for drug or alcohol addiction:
- Genetics —Yes, if addiction runs in the family, the National Institute on Drug Addiction says you have up to a 60% greater risk of becoming addicted too.
- Environment —Just like growing up in a home where fried foods, soda and sugary sweets increase your risk for heart disease and diabetes, growing up in a home with adults who use drugs increases the risk of addiction.
- Development —Using drugs as a teenager up to age 25 when the brain is still developing increases your chances of addiction and can cause serious, lasting damage.
Addiction is a chronic disease
A disease is a condition that changes the way an organ functions. Chronic disease can be treated and managed, but it can't be cured. Addiction is a chronic disease of the brain the way diabetes is a chronic disease of the pancreas, and heart disease is one of the heart.
Getting treatment for addiction is a choice
Everyone makes a choice about using drugs or taking a drink for the first time. You don't have a choice about how your brain reacts, however. Willpower and shaming won't undo the changes in the brain and cure addiction. There is no cure, but treatment helps you manage and successfully live with the disease.
Just as someone with diabetes or heart disease has to choose to exercise and change to a healthy diet to control their disease, someone with addiction has to choose treatment. A court order or family's ultimatum may be behind that choice. But often, someone chooses on their own, wanting a life without addiction and the problems that come with it more than the drugs.
Scientists don't know why some people can successfully quit using drugs on their own, and others can't. For most people, recovery takes intervention with things like Indiana inpatient substance abuse treatment, behavioral therapy , and medications to help control cravings and encourage the brain to adapt to functioning without drugs.
Addiction relapses are a reality, but not failure
Getting sober is hard. Staying on track is too. That's the nature of living with a chronic disease. Success takes managing the changes in the brain and learning how to change deeply rooted behaviors. And then the toughest part for many: committing to managing new behaviors for the rest of your life. Sometimes it's too much. Relapses happen, often many times. They're not a treatment failure, but a cue to get back on track. That can mean making adjustments with or changing treatment.
Find hope and help for drug addiction in Indiana
Addiction is treatable and it is never too early or too late to ask for help. There are Indiana opioid treatment programs, inpatient or outpatient alcohol rehab, and many other options throughout Indiana, like several IU Health locations , including Indianapolis, Bloomington and Muncie.
How to find addiction help in Indiana
- Call 211 for help 24 hours a day, 7 days a week, or connect with help online .
- Visit the Indiana Addiction Treatment website for resources in Indiana.
- Learn more about Addiction Treatment services available at IU Health.
Outpatient drug and alcohol treatment at IU Health
IU Health provides full-service drug and alcohol treatment designed for the individual. We offer virtual and in-person visits for substance abuse treatment. Options include withdrawal and detox, ongoing treatments such as medications and therapy, and intensive outpatient programs. In some locations, crisis appointments are available. Find an IU Health addiction treatment and recovery center near you .
Start Outpatient Addiction Treatment
Get immediate access to full-service substance use intervention services at IU Health Addiction Treatment & Recovery Centers.
Featured Services
Addiction treatment & recovery.
Addiction treatment depends on your individual needs. Services span from outpatient therapy and medication appointments to more intensive inpatient treatments.
- View: Providers | Details
- Share full article
Advertisement
Supported by
Should Addiction Be Viewed as a Disease?
More from our inbox:, conservatives and climate change, those undeserving of political donations, olympians, join the rest of us, my refuge: shooting hoops.

To the Editor:
Re “ Calling Addiction a Disease Is Misleading ,” by Carl Erik Fisher (Opinion guest essay, Sunday Review, Jan. 16):
Dr. Fisher’s opinion piece about addiction was misleading and polarizing. His arguments ignore decades of biomedical and behavioral research that have taught so much about the nature of substance use disorder, as it is now called, and what to do about it.
First, the originators of the concept did not say that addiction is only a brain disease; we acknowledged how important behavioral and social elements are to its development and to recovery.
Moreover, the concept that substance use disorder is a brain disease does not at all imply that “drugs hold all the power.” No one would ever assert, for example, that people are powerless to affect their hypertension or diabetes by changing their behavior, as well as taking their medicine.
Let’s not revert to an outdated conception of the drug problem as only either biological or behavioral and ignore the decades of scientific research that have led to combined treatments and policy approaches that work far better than either alone.
Alan I. Leshner Potomac, Md. The writer is former director (1994-2001) of the National Institute on Drug Abuse, National Institutes of Health.
Dr. Carl Erik Fisher is correct in arguing that thinking of addiction as a disease has the risk of simplifying a very complex interaction of factors, overemphasizing the biological factors at the expense of the myriad social and psychological factors that are also major contributors to addiction.
However, emphasizing the fact that addiction, like other mental disorders such as depression, has a significant biological component has served to reduce the stigma and shame surrounding addiction and increased individuals’ willingness to seek treatment.
While the pendulum has perhaps swung so far in the direction of biology that other important factors are being overlooked, it is important not to jeopardize the headway made over the past 50 years.
Michael B. First Richard B. Kruger New York The writers are doctors with the Columbia University Department of Psychiatry. Dr. First is the editor of the forthcoming Diagnostic and Statistical Manual of Mental Disorders-5 text revision.
Dr. Carl Erik Fisher did not mention the most important reason that alcoholism was classified as a disease. Before Alcoholics Anonymous, alcoholism was widely considered a human failing, a weakness of character, a sin. These people could stop drinking if they wanted to!
But this was not true. Many wanted to stop but could not. By defining alcoholism as a disease the shame of being an alcoholic was removed. No longer were alcoholics seen as morally deficient. Alcoholism/addiction has nothing to do with morals.
This understanding of addiction as a disease has opened the door of recovery wide to many of us who may not have sought help for an affliction if we thought we should be able to “fix” it by ourselves — by just being “better” people. We are not bad people. We are sick people, deserving of help. Classifying addiction as a disease does not narrow the opportunities for healing; it expands them.
Vanessa S. Oakland, Calif. The writer, 35 years sober, requested anonymity in keeping with A.A.’s tradition.
I believe that Dr. Carl Erik Fisher is correct in his view that addiction is not just one thing, which is to say “a disease.” There are certainly medical elements, for example our imperfect but growing understanding of the genetics of addictive behavior. But, in essence, addiction must still be seen and treated as a behavior . And, as with most behaviors, addiction has huge sociologic and economic inputs.
By making medicine the principal portal for accessing treatment of any harmful behavior is to seriously tie our hands as a society seeking a cure. As a practicing physician of 40 years, I might feel differently if we had had more success treating behavioral problems as medical problems. We’ve had our chance.
John R. Bennett Snohomish, Wash.
Having lost a father (to alcoholism), a sister (to smoking cigarettes and alcoholism) and a son (to opioid addiction), I believe it would be a tremendous boon if research could determine the difference between those who can be treated successfully for their addiction and those who are not helped by the current methods of treatment.
Dr. Carl Erik Fisher concludes by saying that dropping the idea of disease and opening a fuller picture of addiction will allow for more nuance, care and compassion. I think there is an abundance of those currently. What is needed is an understanding of the biology and differences that lead to addiction as a death sentence for some and a chronic disease for others.
Amie Schantz Arlington, Mass.
One of the important reasons to call addiction a disease is that it reframes the discussion away from the court system/incarceration and toward treatment. This is extremely important as the United States leads the world in incarceration , much of which is related to illicit drug use or trade.
Steven Persky Marina del Rey, Calif.
Re “ U.S. Greenhouse Gas Emissions Bounced Back Sharply in 2021 ” (news article, Jan. 10):
Many Republicans oppose Build Back Better simply because the Democrats support it, others because it limits coal and oil industries, which they perceive as critical to their states. But many oppose it because it is a key culture war issue.
It and other initiatives like the Green New Deal represent the things conservatives fear most: change, a substitution of a new order for the old, and the possibility that they will lose their hard-earned place in the world.
Despite the climate disasters of the past year, programs that limit greenhouse gas emissions are going nowhere. The fact that the recovery of the economy is so closely tied to a rise in greenhouse gases is sobering and deeply worrying.
Climate change will soon be a problem so large that even conservatives won’t be able to deny it. Whether we will then be able to do anything about it remains to be seen.
Tim Shaw Cambridge, Mass.
Re “ After Jan. 6, Donor Pause Was Short ” (Business, Jan. 7):
As the former chair of a major biopharmaceutical company’s political action committee and general counsel of the industry’s principal trade association, I appreciate the importance of making contributions to supportive lawmakers, regardless of their positions on unrelated issues.
However, the continuing strength of our democracy and the rule of law are not unrelated matters. They are as vital to the industry as prices and patents. No contributions should be made to lawmakers who refuse to recognize and act on the threats to our Constitution.
Bruce Kuhlik Washington The writer is former general counsel of Merck & Co. and of the Pharmaceutical Research and Manufacturers of America.
Re “ To Avoid Virus, Olympians Bend Over Backward ” (front page, Jan. 24):
I chuckled with recognition at the extensive restrictions that Olympic athletes are putting on themselves to avoid being infected with Covid-19 before the Games begin next month. That’s how we seniors have been living for nearly two years! I believe we deserve a medal.
Debbie Duncan Stanford, Calif.
Dan Barry’s contemplative, healing story of outdoor solo basketball in wintertime resonates with my lifetime passion for the sport (“ A Story of Covid Exile, Told in Never-Ending Arcs, ” Sports, Jan. 18). The rhythm of shoot-miss/shoot-swish soothes my soul in times both good and troubled.
This phenomenon reached an unprecedented high a decade ago. After receiving a lifesaving stem transplant, I was confined to weeks of isolation to prevent post-procedure infection. Solo basketball on a neighborhood court was my refuge.
During my first outing, even as I missed most shots, I was overcome with the emotion of a medical procedure enabled by an anonymous donor, a young college student whom I would meet in person a year later. Weeping profusely, with the hoop as my witness, I shot my heart out, overcome with gratitude for life and for every shot, made and missed.
Now a septuagenarian, I continue to play solo in frigid weather, warmed by the hoop and ball that have been my companions during the ebb and flow over decades of a life well lived.
Allen White Brookline, Mass.
Addiction: A Disease Or A Choice?
Several people argue whether drug addiction is a disease or a choice. Today, I will be discussing this argument in hopes to have a better understanding as to why this topic is so controversial. Throughout my research, I easily found information on this topic and I am still not sure I have found any answers. The biggest argument is that addiction is a choice not a disease. For those on the other side of the argument they claim just the opposite.
According to a source on the Internet entitled Alcohol and Drug Treatment: The Disease Concept Of Substance Abuse and Addiction, the idea of drugs and alcohol being a disease is a very controversial and debated topic . For the purposes of this essay, I am forced to agree that drug addiction is a choice. People get high and drink because they want to and if they are not careful they can become an addict. The research I found on this particular topic seemed to have the most support and facts to dismiss the idea that addiction is a disease.
I also beeivle if there was enough evidence to support the idea of addiction being a disease it would not be such a controversial topic. According to a Website entitled Saint Jude Retreat House, alcoholism and drug addiction are not diseases because those types of behaviors can be avoided and there is help available to change these behaviors. Although it has been found true that drug and alcohol dependency can be passed down through hereditary there is no concrete evidence I have found that proves that this is a disease.
In a book entitled Treating Substance Abuse , Theory and Technique 2nd edition, says This first and probably least controversial of the disease models can be termed the medical consequences model. (Page 11). This statement seems to be saying that because this topic is so controversial and not enough medical proof is available it has been given a generic name. It is true that drugs and alcohol can cause diseases , but does that make the addiction problem a disease? Perhaps this topic is so controversial because of the lack of knowledge or understanding of drug addiction.
On a Website entitled Addiction is a Chronic Disease , the source was comparing diabetes and cancer to support their idea that drug addiction to is a chronic disease. The Website did not give any additional support and provided no examples. In the Encyclopedia Of Psychoactive Drugs: The Addictive Personality, page fifteen of the book states that there are three components of the disease. The three components included: the substance in which the person does, who the person is, and the society in which they came from.
In addition to the research I also interviewed an ex-addict who wishes to stay unknown. She has been clean and sober now for seven years and was an addict for about twenty years. In her recovery, she was told that her addiction was a disease, however, she was not sure that she really believed that. To this day she questions that theory, because it really is a choice. To every argument there is at least two sides and not every argument has an answer, a real reason, or a specific situation. It is amazing that such a question can be so controversial and not even say what the real controversy is.
I am going to continue on my search to find the information I am looking for in regards to this topic. There has to be more information to support the idea and the controversy that addiction is a disease. Although I stated earlier in this paper that I agreed to the idea of addiction not being a disease I would like to make a descant based on more information. For the purposes of this paper , and for the need to seek more in depth of this controversy I will find different avenues to find the information I need so that I can then inform you later with an update.
To export a reference to this essay please select a referencing style below:
Related essays:
- Fantasys Integral Role In Creation Of A Monster
- Fantasy’s Integral Role In The Creation Of A Monster
- Cause Of Addiction Essay
- Fetal Alcohol Syndrome
- Investigative Report Of Internet Addiction
- None Provided, Alcoholism
- An Objection to Mandatory Drug Testing in High Schools
- Models Of Conceptualizing Addiction
- Alcohol Abuse Essay
- Should The United States End Drug Prohibition
- Sex Addiction Research
Drug Addiction a Disease or a Choice
Introduction.
There are different types of addictions in the world that include drug, sexual, eating, and television addictions. Over 40% of the American population is affected by one or more addictions (Ross, 2010). Addictions are habits that one acquires, and after practicing the habits for sometimes, it becomes impossible to function without practicing the given habit. Drug addiction is a condition that emanates from taking drugs such as alcohol and cocaine for fun. Soon the body becomes dependent on drugs, and one cannot function without the drugs.
There is a constant debate on whether drug addiction is a disease or a habit. If classified as a choice, it encourages addicts to take the initiative and say no to drugs. They acquire the necessary will power to stop the addiction. If addiction is termed as a disease, addicts stop feeling ashamed of their condition and seek treatment. Addiction can therefor fall under the disease or choice category depending on how one approaches the issue. It is a choice because one requires the mind to decide, while it is a diseasebecause one needs medication to heal.This paper is therefore focused on discussing whether addiction is a choice or a disease depending on how one gets addicted and how they get out of addiction.
People get addicted to drugs for different reasons. When one is born, they are born with a free will and are also free from any preference. A child does not know what is bad or good, but they learn as they grow up. Consequently, a child or an adult is exposed to drugs as they grow up. For instance, a child can know about drugs through parents who use them. A child can also learn about drugs on the television or through friends. As the child learns about drugs, they either get attracted or repel the drugs. Those who become drug addicts choose to drink or take hard drugs. Further, if one’s parents are addicts, they are also likely to become addicts themselves. Therefore, addiction can be termed as either a choice that a person makes or a disease that is awakened by a slight use of drugs.
Addiction settles in when one takes drugs and is unable to control how they use them(Schaler, 2011). Further, the drugs become their priority and everything else including studies and family are dictated by drug usage. Drug usage starts as a normal routine where in most instance one uses alcohol or cigarettes to relax with friends. As the habit continues, one becomes a regular at a bar and they take more than what they used to take before the addiction took over. Addiction becomes full blown when one is unable to live without the usage of drugs and they make the drugs a priority. The drug addict should go for rehabilitation or therapy to help them stop the habit. Further, one should make up their mind that they will not use drugs anymore for the treatment to work.
Unborn children can become exposed to drugs if their parents, especially the mother, takes drugs while pregnat or while breast feeding. The unborn baby can take drugs through the placenta as it is transferred from the mother to them. Similarly, a breastfeeding mother can pass drugs to the child through the breast milk. As the child grows up they can easily become addicts of they involve themselves with drugs because the drugs are already in their systems. However, it is not a guarantee that the child must be an addict because it depends on whether they will start taking the drugs or not. Addiction can therefore be far fetched from the time the child is unborn to when they are toddlers. A mother preparing to get pregnantis also advised against using any drugs so that hersystem can be free of any drugs when they get the baby. If there are strong drugs in the system, they might affect theunbornbaby andif the baby grows up and uses drugs, they can easily become addicts.
A choice is a conscious decision that one makes, as they have to select between two or more options(Gruenert, 2010). One makes a choice depending on their preference and goals in life. One might have a preference of going to the bar or choosing friends who use drugs. As a result, they end up becoming addicts as they choose to have addicted friends. Moreover, drug addiction can be termed as a choice because a drug user decides whether to take a drug or not. For instance, if a boy goes to a friend’s party and get free alcohol and heroine being used, he can decide whether to take the alcohol and use the heroine. The decision to take Alcohol or heroine is however dictated by their personal preference, their principles, background, and what they want in life.one might chose to use the drugs because everyone else is doing so, therefore, showing that they are easily influenced by the latest trends. If one choses to abstain from the drugs, it shows that they have strong principles. Addiction can therefore be termed as a choice as one has the free will to decide whether they want to take a drug or not.
While undergoing treatment, drug addiction is termed as a choice. One should decide to stop taking drugs for him or her to stop being addicts(Gruenert, 2010). Over a half of addicts who check in rehabilitation centers relapse. On the contrary, over 10% of or drug addicts who decide to do away with the addiction and do not go for any treatment but are able to stop the addiction successfully. This is a clear indication that drug addiction is a choice that one makes in their mind. One can choose to stop the addiction or to refrain from becoming an addict altogether. Decisions that one makes concerning drugs should be made wisely because addiction is expensive to maintain.
If one comes from a family of drug addicts, they are in many cases likely to become addicts. However, this depends on their choice to start drugs or to refrain from them. If one does not use drugs then they will not awaken the addiction. However, if one takes the drugs they are most likely to become addicts because they already have the drugs in their system through their bloodline. Similarly, people who were addicts before can easily relapse if they choose to take drugs again. The choice to take drugs depends on one’swillpower to say no to drugs. One can choose to stay away from situations and people who make them use drugs. Further, they can choose to stay clean for the sake of their own dignity and to be able to achieve their goals. Addictiontherefore depends on ones ability to choosebetweenrefraining from drugs or taking them.
A disease is commonly expounded as the malfunction of a specific body part, has signs and symptoms, and does not necessarily emerge from physical injury(Hensher, Rose & Greene, 2015). If an arm is aching, it means that the arm could be infected. Addiction fits the definition of a disease because it affects the mind fist. The mind becomes sick not because of any physical injury but because of the thinking that an addict does. Drugs stimulate the brain first and excite the user. As a result, the user takes more drugs to continue exciting their minds. The more drugs one takes, the more they become dependent on drugs. Addiction therefore settles in because of the mind malfunctioning. Drugs change the normal functioning of the brain and as a result, a drug addict is sick in the brain. The condition affects the way one thinks as they only choose to take drugs in a bid to excite their brains.
Addiction can be termed as a disease because it can be inherited(“Drug Addiction and Families”, 2007). For instance, if a father is an addict, a child can easily become an addict if he or she uses drugs at one point in their lives. Addiction is therefore in an addict’s blood and only waits to be awakened by the use of drugs. Thus, addiction can be classified together with other diseases such as hypertension where the user is a patient is more likely to suffer if their parents suffered from the condition. As an inherited disease, addiction affects those people who got access to drugs as fetus or as toddlers. Children whose mothers took drugs while pregnant or while breastfeeding are candidates of the addiction disease. Addiction can therefore be passed on from parents to childrenjust like obesity as it is in the genes.
For drug addiction to be termed as a disease, there should be symptoms and signs. For instance, the condition of excessive drug usage can be termed as an addiction if the user is dependent on drugs to function. Sometimes addicts shake or develop other complications such as liver failure due to excessive usage of drugs(Gruenert, 2010). During treatment, drug addiction is treated like a disease because one has to undergo medical treatment. Patients are detoxified in a bid to remove the toxic drugs in their system. Rehabilitation centers are a common place where addicts get the necessary treatment. Besides using medicine, addicts are taught to avoid relapse by changing things that prompt them to use drugs.Therapy is also an important part of drug treatment as a patient is able to talk about their problem to a therapist of a group of other addicts. The therapy sessions are similar tothose that depression patients undergo and therefore drug addiction can be termed as a disease just like depression.
Drug addiction prompts debate on whether it is a disease or a choice. Choices are made consciously, but a disease settles in unexpectedly. If termed as a decease, it shows that addiction comes in without the addict or those around him or her noticing. Most of the time, people get into addiction due to their change in habits. Those around an addict are more aware that an addict is getting into addiction. While getting into addition, an addict can be a frequent at a bar or a drug den. They become more familiar with the people at the bar or get to know who is a dealer in a given estate.
As the addiction becomes more noticeable when the patient starts showingphysical signs to other people such as sleepinga lot or shaking while not high on drugs. It is a clear indication that their body is already programed to function with the help of drugs.an addict is most likely to stop their daily routine to pursue taking drugs. They can stop going to school or work to be able to buy and take drugs. They can stop going to school or work to be able to buy and take drugs. If they run out of money, they easily steal or borrow to get drugs. The brain is no longer excited by the use of drugs as it was initially, but it becomes dependent on the drugs, as it cannotfunctionwithout drugs. The brain shuts down when an addict is not ion drugs and that is why addicts sleep for long hours.
Addiction can, therefore, be termed as a choice because an addict has a choice to take drugs or not. If one comes from an addicted bloodline, they also have a choice to take drugs or not. The moment they start taking drugs they awaken the addiction in them. While treating addiction in rehabilitation centers, an addict is taught how to say no to drugs by restructuring their minds. The addict’s choice to say no to drugs extends to avoiding the people who lure them to addiction. If an addicted is not fully decided to stop the addiction, they will most likely get back to the addiction. Teaching addicts how to say no to drugs shows that addiction is more of a mind system where one can say no.An addict finds reasons and not excuses saying no. for instance, they find the reason of getting back to school rather than an excuse of been seen sober.Saying no or yes makes all the difference because those are choices. Addiction can, therefore, be classified as a choice rather than a disease.
Addiction starts as a habit where one makes frequent visits to a bar. At this point one has a choice to say no to drugs and can avoid taking drugs. Moreover, when one gets very addicted to drugs, they can decide that they do not want to take drugs and seek help. Help is foundin family, friends, church, and rehabilitation centers. The addicts who do not take the rehabilitation path become clean by changing their habits and their friends. It is therefore possible to put an end to an addiction if one decides. One’s brain is their strongest assetand therefore one can make a decision to stop drugs. Deciding to stop drugs can sometimes be accompanied by medication if the patient had contracted other conditions such as liver disease. However, firm decision-making cannot be substituted by any kind of treatment. Deciding to stop drugs can sometimes be accompanied by medication if the patient had contracted other conditions such as liver disease. However, firm decision-making cannot be substituted by any kind of treatment.
Rehabilitation canters only act as places to help people make the right decision, but they cannot prevent an individual from going back to drugs. The over 50% addicts who relapse are not fully decided to fightaddiction. One has to decidethat they will not take drugs no matter how stressed or available the drugs are. Personal choices are what influence addiction and therefore addiction is a choice andnot as disease.
Drug addiction can be termed as a disease or a choice depending on how one looks at it. It is a choice because a person who takes drugs has the willpower to say no to drugs. Further, one takes drug because they want to take them. On the other hand, it is a disease because when an addict gets deep in the addiction, they cannot function without the drugs. They depend on medical treatment to get well. Detoxing is a major way that drug addiction utilizes medication for treatment. Drug addiction can be termed as a choice with the goal of helping addicts say no to drugs. Further, the addicts can be encouraged to seek treatment by telling them that they are sick.An addict can put a stop to their addiction by making the right choices without necessarily going for treatment. For a person to undergo treatment and remain clean, they should make up their mind to stop drugs.Rehabilitation, medication, and therapyare ways of helping an addict get sober faster butare not a means of getting addictsentirelyclean.Addiction can be termed as a choice rather than a disease.
Cite this page
Drug Addiction a Disease or a Choice. (2018, Sep 22). Retrieved from https://supremestudy.com/drug-addiction-a-disease-or-a-choice/
"Drug Addiction a Disease or a Choice." supremestudy.com , 22 Sep 2018, https://supremestudy.com/drug-addiction-a-disease-or-a-choice/
supremestudy.com. (2018). Drug Addiction a Disease or a Choice . [Online]. Available at: https://supremestudy.com/drug-addiction-a-disease-or-a-choice/ [Accessed: 14 Apr. 2024]
"Drug Addiction a Disease or a Choice." supremestudy.com, Sep 22, 2018. Accessed April 14, 2024. https://supremestudy.com/drug-addiction-a-disease-or-a-choice/
"Drug Addiction a Disease or a Choice," supremestudy.com , 22-Sep-2018. [Online]. Available: https://supremestudy.com/drug-addiction-a-disease-or-a-choice/ . [Accessed: 14-Apr-2024]
supremestudy.com. (2018). Drug Addiction a Disease or a Choice . [Online]. Available at: https://supremestudy.com/drug-addiction-a-disease-or-a-choice/ [Accessed: 14-Apr-2024]
Drug Addiction a Disease or a Choice. (2018, Sep 22). Retrieved April 14, 2024 , from https://supremestudy.com/drug-addiction-a-disease-or-a-choice/
This paper was written and submitted by a fellow student
Our verified experts write your 100% original paper on any topic
Having doubts about how to write your paper correctly?
Our editors will help you fix any mistakes and get an A+!
Leave your email and we will send a sample to you.
Please check your inbox
Sorry, copying content is not allowed on this website
Please indicate where to send you the sample.

IMAGES
VIDEO
COMMENTS
Drug addiction is a complex and contentious issue that has sparked debates for decades. At the heart of this debate is the question of whether drug addiction should be viewed as a choice made by individuals or as a disease that requires medical treatment. This essay will explore the multifaceted nature of drug addiction, examining both the ...
Drug addiction, in the simplest terms is the strong compulsion to get and use substances, even though a number of undesirable and dangerous consequences are likely to occur. Addiction has been described as a "medical disorder that affects the brain and changes behavior." 1 Various substances including alcohol, illicit drugs, prescription ...
In Addiction: A disorder of choice, Gene Heyman surveys a broad array of evidence—historical, anthropological, survey, clinical, and laboratory-based to build an argument about the role of basic choice processes in the phenomena that comprise drug addiction. He makes a compelling, multifaceted argument that conceptualizing drug addiction as a chronic disease (like schizophrenia or diabetes ...
Addiction itself is often misunderstood. Some people argue that i t is a personal choice, and therefore anyone who is addicted to a substance has ended up there because of the lack of self-discipline or morality. Meanwhile others argue addiction is a disease, and as a result cannot be cured entirely or even resisted by discipline alone. The first view has been the most common understanding of ...
Argument For. The idea that drug addiction should be viewed as a disease is supported in the article "Addiction as a brain disease revised: why it still matters, and the need for consilience.". Heilig et al. (2021) assume that denying the fact that addiction is a severe brain disease might cause serious damage to populations suffering from ...
These distinctive features of addiction as a disease are shared with other neuropsychiatric disorders, 43 - 49 raising the possibility that addiction is not only a mental illness, but also a prototypical one. Although substance use disorders are unique in that disease expression (as an addiction) requires exposure to a drug, other psychiatric disorders also need external triggers.
Addiction Is a Choice. Many activities that are not themselves diseases can cause diseases, and a foolish, self-destructive activity is not necessarily a disease. When we find a parallel between physiological processes and mental or personality processes, we can mistakenly assume the physiological process is what is really going on, and the ...
Drug Addiction has become a serious issue in society today, with an increase in controversy leading towards the topic of whether drug addiction is a disease or a choice. Addiction and disease are two different things and understanding them is very important when it comes to drugs and how it affects the mind and body.
The view that substance addiction is a brain disease, although widely accepted in the neuroscience community, has become subject to acerbic criticism in recent years. These criticisms state that ...
Although the brain disease model of addiction is perceived by many as received knowledge it is not supported by research or logic. In contrast, well established, quantitative choice principles predict both the possibility and the details of addiction. Keywords: addiction, choice theory, remission, correlates of recovery, brain disease model.
The reality is that addiction is a disease, and the research is there to support it. Drugs physically change the brain and create a compulsive drive to continue using while inhibiting normal decision-making abilities. This development has huge implications for those who are living with and fighting against addiction.
Chronic disease can be treated and managed, but it can't be cured. Addiction is a chronic disease of the brain the way diabetes is a chronic disease of the pancreas, and heart disease is one of the heart. Getting treatment for addiction is a choice. Everyone makes a choice about using drugs or taking a drink for the first time.
My experiences and those of my patients seem more in line with how 16th- and 17th-century writers described addiction: a disordered choice, decisions gone awry. ... addiction, and drug problems ...
No - It's Not a Choice. "It's a disease.". Many scientists label addiction as a disease. They argue that those struggling with substance abuse have literally lost control. The disease has taken over their bodies and they no longer have a choice. The National Institute on Drug Abuse defines drug addiction as a "disease that will ...
To the Editor: Re "Calling Addiction a Disease Is Misleading," by Carl Erik Fisher (Opinion guest essay, Sunday Review, Jan. 16): Dr. Fisher's opinion piece about addiction was misleading ...
The biggest argument is that addiction is a choice not a disease. For those on the other side of the argument they claim just the opposite. According to a source on the Internet entitled Alcohol and Drug Treatment: The Disease Concept Of Substance Abuse and Addiction, the idea of drugs and alcohol being a disease is a very controversial and ...
Drug addiction is a constant craving, seeking, and using of a substance, despite the negative consequences it may have on the addict or those around them. When drug use becomes more frequent, it is considered drug abuse. Once an individual's drug abuse is can no longer be controlled, and they are using the drug to get through everyday life ...
Drugs change the normal functioning of the brain and as a result, a drug addict is sick in the brain. The condition affects the way one thinks as they only choose to take drugs in a bid to excite their brains. Addiction can be termed as a disease because it can be inherited ("Drug Addiction and Families", 2007).
physical, psychological, or social effects and typically causing well-defined symptoms (such. as anxiety, irritability, tremors, or nausea) upon withdrawal or abstinence ", to simply put it ...
Addiction can be characterised as a physical need, cognitive choice, emotional instability, psychological failure, neuroadaptation or a disease. Drug addiction, for instance, involves opiate substances (Boshears, Boeri, & Harbry, 2011). Since the 21st century, in Western industrialised societies, addiction is said to be a disease by most of the ...
Many people who oppose the fact that addiction is a disease say that it is a choice. People argue saying "addiction is self-acquired and is not transmissible, contagious, autoimmune, hereditary, degenerative, or traumatic. Treatment consists of little more than stopping a given behavior.
Get your custom essay on. Having considered and carried a lot of research on this controversial issue, my stand remains that drug abuse or drug addict is wholly a matter of choice and not a disease. The time one is born, he/she does not know anything. You are introduced into the new world with your own will.