An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health


Nurse-Led Interventions in Chronic Obstructive Pulmonary Disease Patients: A Systematic Review and Meta-Analysis
Alejandra aranburu-imatz.
1 Department of Nursing, Maimonides Biomedical Research Institute of Cordoba (IMIBIC), University of Cordoba, 14004 Cordoba, Spain; se.ocu@amira2pe (A.A.-I.); moc.liamg@7raczepolnauj (J.d.l.C.L.-C.); se.ocu@aulom28n (A.M.-L.); moc.liamtoh@1991am_esoj (J.M.J.-P.); moc.liamg@abodrocoicorledairam (M.d.R.V.-L.); [email protected] (F.J.R.-C.); se.ocu@pubra27z (P.A.-B.); se.ocu@posol28n (P.J.L.-S.)
2 Department of Nursing, Pharmacology and Physiotherapy, University of Cordoba, 14004 Cordoba, Spain
3 Outpatient Clinic, Hospital Giovanni Paolo II, ULSS1 Dolomiti, 32044 Pieve di Cadore, Italy
Juan de la Cruz López-Carrasco
4 Department of Nursing, Reina Sofia University Hospital, 14004 Cordoba, Spain
Ana Moreno-Luque
José manuel jiménez-pastor, maría del rocío valverde-león, francisco josé rodríguez-cortés, pedro arévalo-buitrago, pablo jesús lópez-soto, ignacio morales-cané, associated data.
Not applicable.
Chronic obstructive pulmonary disease (COPD) is the third leading cause of death worldwide, causing 3.32 million deaths in 2019. COPD management has increasingly become a major component of general and hospital practice and has led to a different model of care. Nurse-led interventions have shown beneficial effects on COPD patient satisfaction and clinical outcomes. This systematic review was conducted to identify and assess nurse-led interventions in COPD patients in terms of mental, physical, and clinical status. The review was carried out following the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement. The relevance of each manuscript was assessed according to the inclusion criteria, and we retrieved full texts, as required, to reach our conclusions. Data extraction was performed independently by two reviewers, and the risk of bias was assessed using the Cochrane Risk of Bias tool. Forty-eight articles were included in the analysis, which focused on the management of COPD patients by hospital, respiratory and primary nursing care. Nursing management was shown to be highly effective in improving quality of life, emotional state, and pulmonary and physical capacity in COPD patients. In comparison, hospital and respiratory nurses carried out interventions with higher levels of effectiveness than community nurses.
1. Introduction
According to the World Health Organization [ 1 ], chronic diseases were the cause of 71% of deaths in the world in 2018 in ages ranging between 30 and 70 years old. Of these, chronic obstructive pulmonary disease (COPD) is the third leading cause of death worldwide, causing 3.23 million in 2019 [ 2 ].
Chronic obstructive pulmonary disease requires a complex, prolonged time period response, coordinating inputs from a wide range of professionals, specific kinds of drugs, and suitable monitoring equipment, and this care must ideally be embedded in a system that promotes patient empowerment. Many health systems are still largely built around an acute model of care, but the current challenge facing health policymakers is to figure out how to put in place a better response that meets COPD patient needs. As health systems differ widely, each must find its own solution. Even within similar systems, there may be marked differences in professional roles, coordination mechanisms, and care settings [ 3 ]. The national health systems have to face elderly multipathological population needs with a great economic and socio-health cost due to its great complexity. Multi-competence nurses accompany COPD patients in the management of all phases of the disease without generating an insurmountable economic burden for the coffers of the states, providing a good quality of care at home as well as in the hospital improving patient and family empowerment.
COPD management has increasingly become a key component of primary and hospital care leading to an evolving care model. International evidence has suggested that extending the role of primary and hospital nurses could improve the quality of life of COPD patients, adopting nurse-led care models to attain beneficial effects on patient satisfaction and clinical outcomes [ 4 , 5 ].
Fields of action in nursing range from health education to healthy lifestyles, correct management of inhalation pharmacology, early identification of signs of decompensation, respiratory rehabilitation, and palliative care. Nursing management of COPD patients achieves better outcomes in the day-to-day management of the disease, improving the patient’s knowledge of disease management [ 4 , 5 ]. Indeed, home visits and remote management with telemedicine at discharge time by hospital nurses and in primary care should be considered, not only for COPD patients but also for their families [ 6 ].
Given the benefits that nursing can bring to the care of COPD patients, it is essential to understand how nurse-led interventions affect COPD patients.
The purpose of this review was to analyze the effect of hospital or community nurse-led interventions in the follow-up and management of COPD patients in terms of mental, physical, and clinical status.
2. Materials and Methods
2.1. design.
The systematic review and meta-analyses were carried out following the Preferred Reporting Items of Systematic Reviews and Meta-Analyses (PRISMA) statement [ 7 ]. The CENTRAL and PROSPERO databases were consulted to see if there were any systematic reviews with the same characteristics. The systematic review was complemented by a review of the references of the selected manuscripts. The meta-analysis protocol was registered in PROSPERO (CRD42020161153).
2.2. Search Strategy
A systematic search was carried out for manuscripts published between January 2009–January 2021 in PubMed, Embase, and Web of Science databases. The complete search strategy is detailed in Table 1 .
Search strategy used for each database.
2.3. Inclusion Criteria
The inclusion criteria were: (a) observational studies (case–control, cohort and cross-sectional) or intervention study (randomized or non-randomized); (b) manuscripts that analyzed patients who had COPD or diseases characterized by airflow limitation of a progressive and not easily reversible nature; (c) studies in which nursing-led intervention was carried out in both primary care and hospital care; (d) studies in which some health outcome was evaluated (quality of life, exacerbations, hospital admissions, emergency department admissions, patient empowerment in disease management, home management of terminal phase of disease, etc.). Articles that did not meet any of the above inclusion criteria were excluded.
2.4. Study Selection
Once the search strategies were defined, the search on the databases was carried out from 1 June 2021 to 30 September 2021. The evaluation period was decided in order to take into account COVID pandemic period, the effect it had had on these patients, therefore from 2009 to 2019 there were 10 years plus two years of pandemic. Two investigators (AAI and IMC) independently assessed all references identified in the search. Firstly, duplicates were eliminated, and screening was performed by reading titles and abstracts. Secondly, manuscripts that met the inclusion criteria in the first phase were read in full text to determine their inclusion. In case of discrepancies between the two investigators, a third party (PJLS) was consulted.
2.5. Data Collection
The information extracted from the studies included using a standardized form specifically designed for the purpose: author, title, year, description of patient population, sample size, duration of follow-up period, nurses’ involvement in study, characteristics of intervention, comparators, and outcomes.
The data were collected on a form created by the authors based on the PICO [ 8 ] strategy (population, intervention, comparator, results). The information extracted was: type of nurses (specialties) who work in primary or hospital settings, characteristics of interventions (health education, respiratory rehabilitation, telecare, palliative care assistance, and application of specific techniques), and psychophysical or clinical outcomes: hospital admissions, emergency department admissions, exacerbations and patient empowerment in disease management.
For the quantitative analysis, a meta-analysis was performed using the Mantel–Hansen effects method with a 95% confidence interval for dichotomous variables, while the inverse variance random effects method was used for continuous variables. Statistical heterogeneity was assessed with the I2 statistic. The cut-off of I 2 ≤ 25%, I 2 with 26–50%, and I 2 > 50% was used to define low, moderate, and high heterogeneity, respectively [ 7 ]. Publication bias was assessed using funnel plots. Analyzes were performed with RevMan software, version 5.4.
2.6. Risk of Bias Assessment
The quality of the evidence was assessed using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) [ 9 ] tool, classifying the quality of the evidence as low, moderate, or high, by evaluating the risk of bias, imprecision, directionality, inconsistency, and suspected publication bias.
The risk of bias was assessed using the Cochrane risk of bias assessment tool, which assesses selection bias, performance bias, attrition bias, reporting bias, and other biases. A funnel plot was made with the Cochrane Review Manager (Rev Man) 5.4 software from Cochrane. The operation was performed and reviewed by two members of the research group.
3.1. Search Results
The study selection flowchart is shown in Figure 1 . A total of 19,486 references were identified, of which 5518 were duplicates. After reading the title and abstracts of 13,968 references, 13,766 did not meet the inclusion criteria. Reading the full text of 202 manuscripts, 154 were discarded for the following reasons: (i) no access to the full text was possible; (ii) different study design; (iii) several pathologies were analyzed; (iv) the manuscripts were assessment studies, and (v) nursing did not lead the intervention. Finally, 48 studies met the inclusion criteria for qualitative analysis, of which 25 were considered for meta-analysis.

PRISMA flowchart of the study selection process.
3.2. Characteristics of Studies Included
Studies were performed in 16 different countries from Europe, Asia, the Middle East, and Central and Northern America.
In the manuscripts included, the interventions were led by nurses in hospitals and in primary care settings by specialist respiratory nurses. The sample sizes of the studies ranged between 14 [ 10 ] to 516 participants [ 11 ] for a total of 5215 patients in 48 studies. The mean age of the intervention group was 60.85 years old, while in the control group it was 54.18 years old. In general terms, the populations included in the studies were homogeneous.
The participants were recruited on hospital discharge following an exacerbation, or from community hospitals. Inclusion criteria were based on a clinical diagnosis of COPD, and most studies also required there to be an airflow obstruction confirmed by spirometry. The minimum age for inclusion in studies varied from 18 to 80 years old. Sex distribution was variable across the studies (5 to 94% of males). Follow-up length also varied among studies, ranging from 8 weeks to 3 years.
3.2.1. Interventions
The review shows an upward trend in the number of publications since 2015. Heterogeneity was observed as regards the type of interventions and scope of care. The characteristics of the 48 studies selected are shown in Table S1 .
Specifically, twenty studies [ 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 ] reported data on hospital nurse management with a specific care plan of pharmacological management to empower COPD patients, i.e., correctly performed inhalation therapy training, use of oxygen therapy, and physical exercise, which are typically given on post-discharge home visits.
Twelve studies [ 11 , 19 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 ] analyzed the management of primary care nurses, the empowerment of COPD patients in activities of daily living, telemedicine, follow-up, and palliative care. Telemedicine for vital parameter monitoring and teleconsultation was led by hospital and community nurses in six manuscripts [ 40 , 41 , 42 , 43 , 44 , 45 ]. Additionally, the effect of nurse-led physical and respiratory rehabilitation interventions was analyzed in five studies [ 27 , 46 , 47 , 48 , 49 ].
Two studies [ 50 , 51 ] analyzed the collaboration between primary care nurses and hospital nurses at discharge time and the follow-up of COPD patients in the management of COPD disease, and four studies [ 15 , 16 , 52 , 53 ] analyzed inhalation drug training techniques given by specialized nurses with COPD patients.
3.2.2. Outcomes
The outcomes analyzed by the selected studies varied widely and focused on the psychophysical and clinical status of people with COPD: lung and vital capacity, dyspnea, mortality, hospital admission, use of health services, compliance and knowledge of drug therapy, use of oxygen therapy, patient satisfaction, health literacy, physical status, quality of life, anxiety, and depression. A quantitative analysis (meta-analysis) was performed on four specific outcomes: hospital admission, physical status, quality of life, and anxiety.
Hospital Admissions
The number of hospital admissions after the intervention was analyzed in seven studies [ 11 , 15 , 29 , 41 , 42 , 43 , 54 ] with 959 patients, after 3 months, 6 months, 12 months, and 18 months: the hospitalizations tended to be lower in the intervention group than in the control group [standard mean difference −0.44 (95% CI −0.92, 0.04), p = 0.07; I 2 = 87%], although heterogeneity was high ( Figure 2 ).

Number of hospital admissions and distance walked (6 MWT) [ 11 , 15 , 27 , 29 , 42 , 43 , 46 , 47 ].
Physical Status
The 6 m walking test (6 MWT) was used to verify the improvement of physical resistance in five studies [ 27 , 29 , 46 , 47 , 49 ] with 462 patients, after 3, 6 and 12 months: the patients improved in distance walked [SMD 0.66 (95% CI 0.10, 1.22), p = 0.02; I 2 = 82%] ( Figure 2 ).
Indeed, the Moderate to Vigorous Physical Activity (MVPA) and the International Physical Activity Questionnaire (IPAQ) were used in one study [ 11 ] with 411 patients, where after 12 months patients improved their physical activity, although the result was not statistically significant in the (MVPA) test ( p = 0.48) and (IPAQ) test ( p = 0.21). A walking diary was used in one study [ 47 ] with 24 patients, improving the number of minutes of walking per day at 8 weeks.
Quality of Life
Different tests were used to analyze the patient’s quality of life in 32 studies [ 10 , 11 , 12 , 13 , 16 , 19 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 37 , 38 , 40 , 46 , 47 , 48 , 50 , 51 , 52 , 54 , 55 ], such as the St. George’s Respiratory Questionnaire, Health Belief Scale, Self-Efficacy Scale, Stanford Self-Efficacy Score or World Health Organization Quality of Life Scale Abbreviated Version (QoL), among others.
Regarding St. George’s Respiratory Questionnaire, eleven studies [ 11 , 16 , 19 , 22 , 23 , 29 , 46 , 50 , 51 , 55 , 56 ] used it to assess quality of life (1.423 patients). Overall, no improvements were found in the intervention group when using this scale [SMD −0.11 (95% CI −0.95, 0.73); p = 0.79; I 2 = 90%]. However, studies which used the Barthel scale to assess the impact on activities of daily living [ 27 , 48 ] showed an improvement after nurse-led intervention [SMD 1.36 (95% CI 0.87, 1.74); p < 0.01; I 2 = 0%] ( Figure 3 ).

Activities of daily living (Barthel scale) and hospital anxiety and depression scale [ 11 , 17 , 27 , 37 , 48 , 54 ].
Anxiety was analyzed using different scales in eight studies [ 10 , 11 , 17 , 19 , 28 , 30 , 37 , 54 ], such as the hospital anxiety and depression scale (HADS), anxiety and depression symptoms inventory scale (SCL), self-rating anxiety scale (SAS), and hospital anxiety scale (HAC).
Hospital anxiety and depression scale (HADS) was used in five studies [ 10 , 11 , 14 , 17 , 37 ] with 746 patients. Anxiety levels decreased in all the studies after the nurse-led intervention, except in Scheerens et al. [ 37 ]. Overall, the decrease in anxiety levels was significant [SMD −0.21 (95% CI −0.35, −0.07); p = 0.003; I 2 = 0%] ( Figure 3 ).

Risk of Bias in Selected Studies
Almost all the studies ( n = 48) have a moderate risk of bias due to the study design. Eighteen manuscripts [ 10 , 13 , 14 , 15 , 16 , 25 , 28 , 30 , 31 , 32 , 39 , 41 , 46 , 50 , 52 , 53 , 54 , 55 ] were not randomized and five did not have a control group [ 14 , 25 , 31 , 52 , 53 ].
Due to the characteristics of the studies where the nurse had to follow and train patients, the double-blind was impossible; however, performance bias was accepted as correct or not present in twelve studies and there was a selection bias in 10% of studies [ 13 , 36 , 45 , 50 , 54 ]. Overall, five studies were considered as high methodological quality [ 21 , 22 , 29 , 33 , 34 , 40 ]. A detection bias was present in 75% studies [ 10 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 23 , 24 , 26 , 27 , 28 , 30 , 32 , 36 , 37 , 38 , 39 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 56 , 57 ].
4. Discussion
This systematic review and meta-analysis analyzed different types of nurse-led interventions in COPD patients which obtained improvements in physical status, quality of life, and anxiety and/or reductions in hospital admissions. Although there are several systematic reviews on the effects of interventions in the management of COPD patients, to our knowledge this is the first systematic review to analyze the effect of nurse-led interventions in this population.
As mentioned, interventions are led by different types of nurses: general hospital, community, palliative, and respiratory nurses [ 58 ]. In general, these professionals work in different areas using different techniques: home telemonitoring, telecare, palliative care both in hospital and at home, health education through continuous training or training in inhalation techniques and oxygen management at the home, hospital and home respiratory rehabilitation or telerehabilitation, self-efficacy and training in smoking cessation techniques.
Hospital nurse-led interventions use various types of nursing care models, including the health belief model; humanistic nursing care model; self-management education model; bidirectional quality feedback nursing model; psychological, cognitive-behavioral model; physical-functional model, and a nursing care model based on the information, knowledge, attitude, and practice (IKAP) theory. In general, the studies analyzed reports that these models had improved patients’ health status by empowering them to manage the disease.
Early identification of signs of COPD decompensation is a fundamental part of patient education, as is training on the correct use of pharmacological therapy, especially in inhalation techniques such as the use of oxygen therapy. In the present review, all the nurse-led interventions have been shown to have a positive impact on the patients’ stress levels and the number of hospitalizations [ 12 , 13 , 15 , 20 , 21 , 22 , 24 , 27 , 28 , 29 , 50 , 51 , 55 , 57 ].
Incorrect inhaler technique is very common among COPD patients, resulting in decreased efficacy of drug therapy and worsening patient health [ 59 ]. Inhaler training by the specialized nurse has been shown to significantly improve patient performance [ 16 , 53 ].
Anxiety and depression are common symptoms among COPD patients. The uncertainty of not knowing when an acute breathlessness attack may occur worsens the patient’s emotional situation, leaving them to cope with the anxiety and depression it produces. These findings suggest that psychological therapy, including cognitive behavioral therapy and counseling, can improve depressive and anxiety symptoms in COPD patients [ 60 , 61 ]. The present review also reports that nurses using special techniques such as cognitive behavioral therapy or minimal psychological intervention help the patients learn to manage anxiety successfully [ 11 , 14 , 17 , 19 , 28 , 30 , 55 ].
Home visits by the hospital nurse after hospital discharge have not shown a significant decrease in the number of readmissions, but patients reported feeling better and more confident, with greater knowledge of disease management and decreasing anxiety levels [ 12 , 50 , 52 , 55 ].
Such monitoring and telemonitoring of vital parameters and teleconsultation by the hospital nurse has reduced the number of admissions, days of hospitalization, access to emergency services, reduced levels of anxiety and depression, and improved quality of life [ 11 , 25 , 33 , 42 , 43 , 44 , 45 , 56 ]. This intervention, for a limited period of fewer than 6 months, has demonstrated efficacy. The only study that required more time was that by Taylor et al. [ 62 ], which increased morale but not the patient quality of life after one year of follow-up.
Community nurse-led education and telecare only resulted in reducing the number of days of hospitalization [ 41 ] and level of dyspnea—in the Medical Research Council Questionnaire and SF-36 physical score fields [ 30 ]—while the FEV1%, FEV1 FVC% ratio, FEV1 (L), number of ED visits were worse compared to the control group in several studies [ 38 , 40 ]. Similarly, the study by Baker et al. [ 63 ] in a primary care setting shows benefits in the management of COPD patients, decreased number of physician visits and anxiety, but the results were not significant and therefore no firm conclusions on efficacy can be drawn.
Respiratory rehabilitation in home telecare with different types of tools, such as mobile phones and the Bandura technique, improved patient quality of life in the study [ 46 ], in which the FEV1 FC1% ratio, baseline dyspnea index (BDI), and 6MWT scale scores improved; in the studies by Nguyen et al. [ 23 ], Khoshkesht et al. [ 36 ] and Mohammadi et al. [ 48 ], the self-efficacy scale, Barthel scale, fatigue severity scale (FSS) and SF36 scale also improved; only the study by Cameron-Tuker et al. [ 47 ] showed no improvement in smoking, nutrition, alcohol consumption, physical activity, psychosocial well-being or the symptom management scales.
Last but not least, evidence of the benefits of smoking cessation in COPD has been demonstrated, including decreased disease progression, and reduced symptoms and mortality [ 6 ]. Nurse interventions focused on reducing smoking have been covered in two studies [ 11 , 49 ] but only in Jolly et al. [ 11 ], the number of smokers decreased after 12 months.
This systematic review has several limitations. Although the search strategy has been exhaustive, using several keywords and three databases, it may be possible that not all the articles related to the study topic have been included. On the other hand, although the number of articles included is large, the heterogeneity in the study designs, the different outcome variables, and the different measurement tools have made it difficult to carry out a quantitative analysis. Finally, the evaluation of the quality of the evidence reported a medium level. Therefore, the findings obtained in this review must be taken with caution.
5. Conclusions
Nurse-led interventions in different fields, using different techniques and approaches, have demonstrated their effectiveness in improving quality of life, emotional state, hospital admissions, and physical capacity in COPD patients. In comparison, hospital nursing and respiratory nurse management have presented levels of effectiveness compared to community ones. However, these conclusions may be affected by the heterogeneity of the studies and their level of evidence, so a greater number of quality studies addressing this issue would be necessary.
Regarding the implications for clinical practice, this manuscript provides a broad view of the interventions that nurses could carry out in both community and hospital care.
The findings invite us to motivate, assess, and guide future nursing professionals to design steps to control and monitor chronic pathologies. Apparently simple actions such as health education can provide great benefits for both the patient and their family.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph19159101/s1 , Table S1: Characteristics of studies focusing on nurse-led COPD patients; Figure S1. Assessment of publication bias. Funnel Plots; Figure S2. Risk of bias of all selected studies.
Funding Statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author Contributions
Conceptualization, A.A.-I., P.J.L.-S. and I.M.-C.; methodology, A.A.-I., J.d.l.C.L.-C., A.M.-L., P.J.L.-S. and I.M.-C.; software, A.A.-I., J.d.l.C.L.-C., A.M.-L., J.M.J.-P. and F.J.R.-C.; validation, A.A.-I., P.J.L.-S. and I.M.-C.; formal analysis, A.A.-I., J.d.l.C.L.-C., A.M.-L., P.J.L.-S. and I.M.-C.; investigation, A.A.-I., J.d.l.C.L.-C. and A.M.-L.; resources, M.d.R.V.-L. and P.A.-B.; data curation, A.A.-I., J.d.l.C.L.-C. and A.M.-L.; writing—original draft preparation, A.A.-I., J.d.l.C.L.-C., A.M.-L., P.J.L.-S. and I.M.-C.; writing—review and editing, all authors; visualization, M.d.R.V.-L. and P.A.-B.; supervision, P.A.-B., P.J.L.-S. and I.M.-C.; project administration, A.A.-I., P.J.L.-S. and I.M.-C.; funding acquisition, P.J.L.-S. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Informed consent statement, data availability statement, conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Nursing Research on Patients with Chronic Obstructive Pulmonary Disease and Respiratory Failure Based on Big Data
Affiliations.
- 1 Department of Respiratory and Critical Care Medicine, Shanghai Chest Hospital, Shanghai Jiao Tong University, Shanghai 200030, China.
- 2 Emergency Department, Shanghai Chest Hospital, Shanghai Jiao Tong University, Shanghai 200030, China.
- PMID: 34630978
- PMCID: PMC8494542
- DOI: 10.1155/2021/2541751
This work organically integrates a systematic and individualized nursing plan with big data technology and applies it to the care of patients with chronic obstructive pulmonary disease (COPD) and respiratory failure (RF) and explores the continuous care model based on modern big data technologies to improve COPD and RF. It aims to relieve the symptoms of COPD and RF, reduce the number of acute episodes of COPD and RF and the number of hospitalizations, and improve the quality of life of patients. One hundred COPD and RF patients hospitalized in the respiratory medicine department of a tertiary hospital were selected and were categorized into control and experimental group. The nursing mode of the patients in the control group was the original telephone follow-up in the department, and the contents of the follow-up were determined according to the questions of the patients on the telephone at that time. Based on the original nursing in the department, the experimental group adopted individualized continual nursing plans based on the Internet and big data techniques for patients to conduct a pulmonary rehabilitation-related functional assessment, functional exercise guidance, and health guidance. Experimental results show that, compared with traditional continuous care, individualized continuous care combined with big data techniques can improve the lung function of patients with stable COPD and RF, reduce the number of acute COPD and RF attacks and the number of readmissions, and improve self-management ability and quality of life. The method can be applied and implemented in continuous nursing care.
Copyright © 2021 Yongqing Chen and Luyi Pan.
Publication types
- Retracted Publication
- Nursing Research*
- Pulmonary Disease, Chronic Obstructive*
- Quality of Life
- Respiratory Insufficiency*
Chronic Obstructive Pulmonary Disease (COPD)
Learn about the nursing care management of patients with chronic obstructive pulmonary disease in this study guide .
Table of Contents
- What is Chronic Obstructive Pulmonary Disease?
Chronic Bronchitis
Pathophysiology, epidemiology, clinical manifestations, complications, assessment and diagnostic findings, pharmacologic therapy, management of exacerbations, surgical management, nursing assessment, planning & goals, nursing priorities, nursing interventions, discharge and home care guidelines, documentation guidelines, what is chronic obstructive pulmonary disease.
Nurses care for patients with COPD across the spectrum of care, from outpatient to home care to emergency department, critical care, and hospice settings.
- Chronic Obstructive Pulmonary Disease (COPD) is a condition of chronic dyspnea with expiratory airflow limitation that does not significantly fluctuate.
- Chronic Obstructive Pulmonary Disease has been defined by The Global Initiative for Chronic Obstructive Lung Disease as “a preventable and treatable disease with some significant extrapulmonary effects that may contribute to the severity in individual patients.”
- This updated definition is a broad description of COPD and its signs and symptoms.
Classification
There are two classifications of COPD: chronic bronchitis and emphysema. These two types of COPD can be sometimes confusing because there are patients who have overlapping signs and symptoms of these two distinct disease processes.
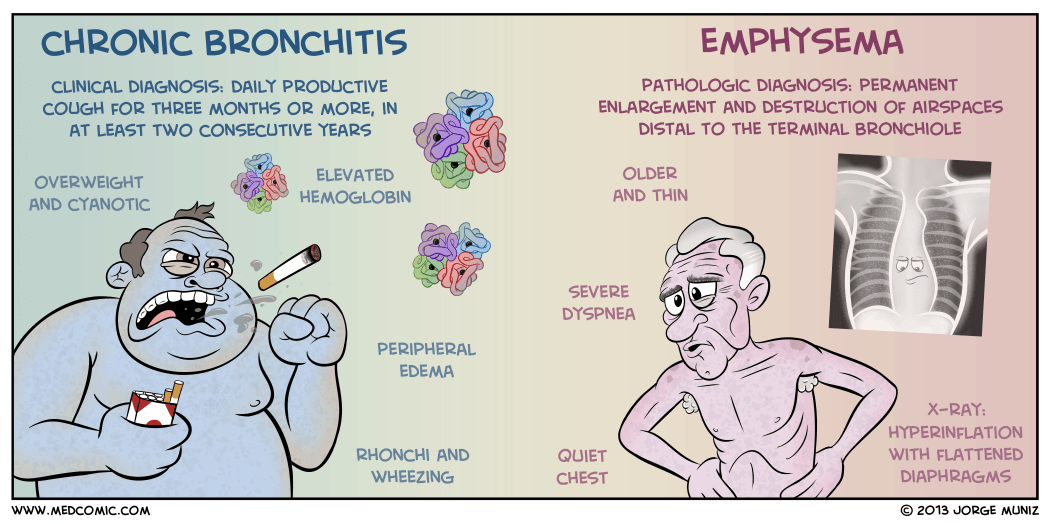
- Chronic bronchitis is a disease of the airways and is defined as the presence of cough and sputum production for at least 3 months in each of 2 consecutive years .
- Chronic bronchitis is also termed as “blue bloaters” .
- Pollutants or allergens irritate the airways and leads to the production of sputum by the mucus-secreting glands and goblet cells.
- A wide range of viral, bacterial, and mycoplasmal infections can produce acute episodes of bronchitis.
- Pulmonary Emphysema is a pathologic term that describes an abnormal distention of airspaces beyond the terminal bronchioles and destruction of the walls of the alveoli.
- People with emphysema are also called “pink puffers”.
- There is impaired carbon dioxide and oxygen exchange, and the exchange results from the destruction of the walls of overdistended alveoli.
- In panlobular , there is destruction of the respiratory bronchiole, alveolar duct, and alveolus.
- All spaces in the lobule are enlarged.
- In centrilobular , pathologic changes occur mainly in the center of the secondary lobule.
In COPD, the airflow limitation is both progressive and associated with an abnormal inflammatory response of the lungs to noxious gases or particles.
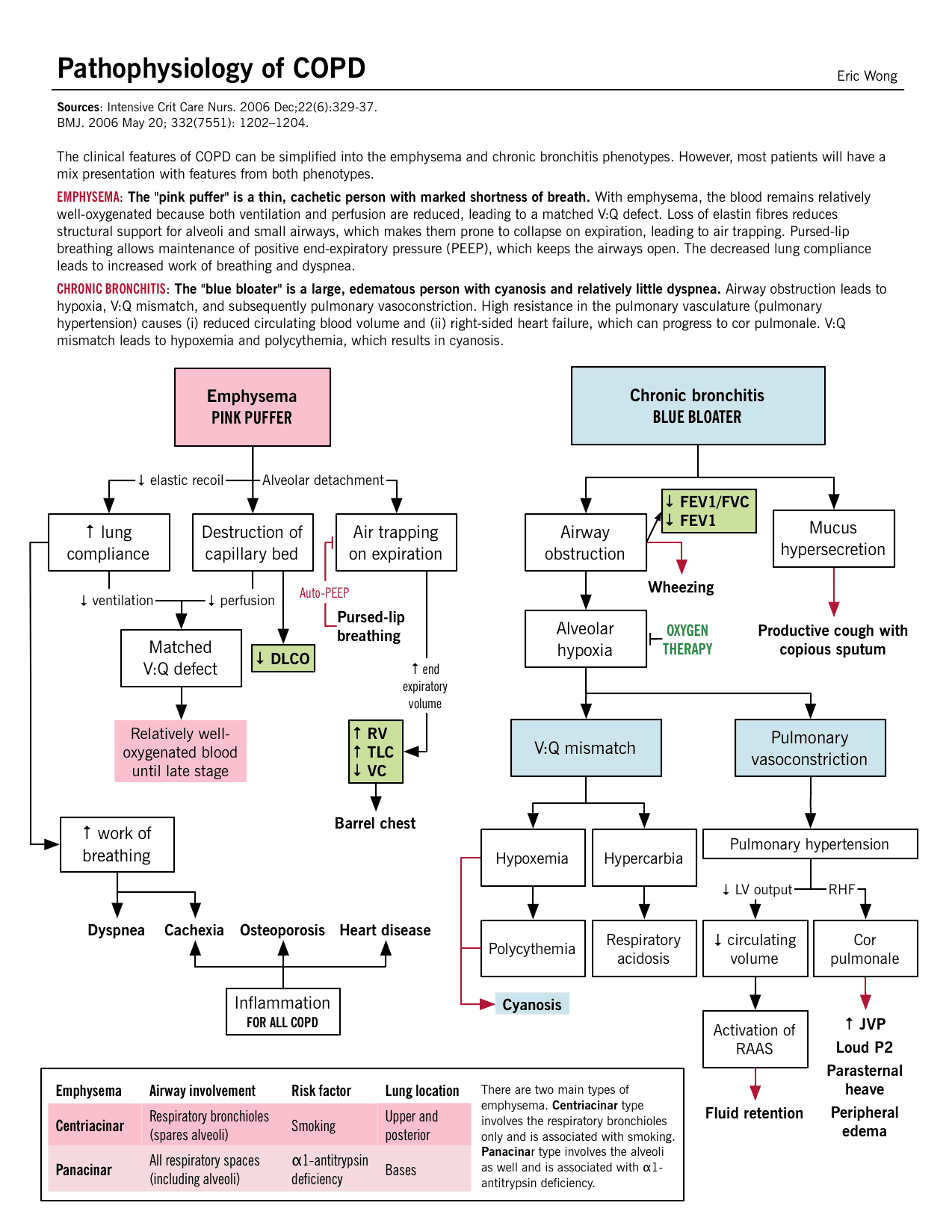
- An inflammatory response occurs throughout the proximal and peripheral airways, lung parenchyma, and pulmonary vasculature.
- Due to the chronic inflammation, changes and narrowing occur in the airways.
- There is an increase in the number of goblet cells and enlarged submucosal glands leading to hypersecretion of mucus.
- Scar formation. This can cause scar formation in the long term and narrowing of the airway lumen.
- Wall destruction . Alveolar wall destruction leads to loss of alveolar attachments and a decrease in elastic recoil.
- The chronic inflammatory process affects the pulmonary vasculature and causes thickening of the vessel lining and hypertrophy of smooth muscle .
Mortality for COPD has been increasing ever since while other diseases have decreasing mortalities.
- COPD is the fourth leading cause of death in the United States.
- COPD also account for the death of 125, 000 Americans every year.
- Mortality from COPD among women has increased, and in 2005, more women than men died of COPD.
- Approximately 12 million Americans live with a diagnosis of COPD.
- An additional 2 million may have COPD but remain undiagnosed.
- The annual cost of COPD is approximately $42.6 billion with overall healthcare expenditures of $26.7 billion.
Causes of COPD includes environmental factors and host factors. These includes:
- Smoking depresses the activity of scavenger cells and affects the respiratory tract’s ciliary cleansing mechanism.
- Occupational exposure. Prolonged and intense exposure to occupational dust and chemicals, indoor air pollution, and outdoor air pollution all contribute to the development of COPD.
- Genetic abnormalities . The well-documented genetic risk factor is a deficiency of alpha1- antitrypsin, an enzyme inhibitor that protects the lung parenchyma from injury .
The natural history of COPD is variable but is a generally progressive disease.
- Chronic cough . Chronic cough is one of the primary symptoms of COPD.
- Sputum production . There is a hyperstimulation of the goblet cells and the mucus-secreting gland leading to overproduction of sputum.
- Dyspnea on exertion . Dyspnea is usually progressive, persistent, and worsens with exercise.
- Dyspnea at rest . As COPD progress, dyspnea at rest may occur.
- Weight loss . Dyspnea interferes with eating and the work of breathing is energy depleting.
- Barrel chest . In patients with emphysema, barrel chest thorax configuration results from a more fixed position of the ribs in the inspiratory position and from loss of elasticity.
Prevention of COPD is never impossible. Discipline and consistency are the keys to achieving freedom from chronic pulmonary diseases.
- Smoking cessation . This is the single most cost-effective intervention to reduce the risk of developing COPD and to stop its progression.
- Healthcare providers should promote cessation by explaining the risks of smoking and personalizing the “at-risk” message to the patient.
There are two major life-threatening complications of COPD: respiratory insufficiency and failure.
- Respiratory failure . The acuity and the onset of respiratory failure depend on baseline pulmonary function, pulse oximetry or arterial blood gas values, comorbid conditions, and the severity of other complications of COPD.
- Respiratory insufficiency . This can be acute or chronic, and may necessitate ventilator support until other acute complications can be treated.
Diagnosis and assessment of COPD must be done carefully since the three main symptoms are common among chronic pulmonary disorders.
- Health history . The nurse should obtain a thorough health history from patients with known or potential COPD.
- Pulmonary function studies . Pulmonary function studies are used to help confirm the diagnosis of COPD, determine disease severity, and monitor disease progression.
- Spirometry . Spirometry is used to evaluate airway obstruction, which is determined by the ratio of FEV1 to forced vital capacity.
- ABG . Arterial blood gas measurement is used to assess baseline oxygenation and gas exchange and is especially important in advanced COPD.
- Chest x-ray . A chest x-ray may be obtained to exclude alternative diagnoses.
- CT scan . Computed tomography chest scan may help in the differential diagnosis.
- Screening for alpha1-antitrypsin deficiency . Screening can be performed for patients younger than 45 years old and for those with a strong family history of COPD.
- Chest x-ray: May reveal hyperinflation of lungs, flattened diaphragm, increased retrosternal air space, decreased vascular markings/bullae (emphysema), increased bronchovascular markings (bronchitis), normal findings during periods of remission ( asthma ).
- Pulmonary function tests: Done to determine cause of dyspnea, whether functional abnormality is obstructive or restrictive, to estimate degree of dysfunction and to evaluate effects of therapy, e.g., bronchodilators. Exercise pulmonary function studies may also be done to evaluate activity tolerance in those with known pulmonary impairment/progression of disease.
- The forced expiratory volume over 1 second (FEV 1 ): Reduced FEV 1 not only is the standard way of assessing the clinical course and degree of reversibility in response to therapy, but also is an important predictor of prognosis.
- Total lung capacity (TLC), functional residual capacity (FRC), and residual volume (RV): May be increased, indicating air-trapping. In obstructive lung disease, the RV will make up the greater portion of the TLC.
- Arterial blood gases ( ABGs ): Determines degree and severity of disease process, e.g., most often Pao 2 is decreased, and Paco 2 is normal or increased in chronic bronchitis and emphysema , but is often decreased in asthma ; pH normal or acidotic, mild respiratory alkalosis secondary to hyperventilation (moderate emphysema or asthma ).
- D L CO test: Assesses diffusion in lungs. Carbon monoxide is used to measure gas diffusion across the alveocapillary membrane. Because carbon monoxide combines with hemoglobin 200 times more easily than oxygen, it easily affects the alveoli and small airways where gas exchange occurs. Emphysema is the only obstructive disease that causes diffusion dysfunction.
- Bronchogram: Can show cylindrical dilation of bronchi on inspiration; bronchial collapse on forced expiration ( emphysema ); enlarged mucous ducts (bronchitis).
- Lung scan: Perfusion/ventilation studies may be done to differentiate between the various pulmonary diseases. COPD is characterized by a mismatch of perfusion and ventilation (i.e., areas of abnormal ventilation in area of perfusion defect).
- Complete blood count (CBC) and differential: Increased hemoglobin (advanced emphysema ), increased eosinophils (asthma).
- Blood chemistry: alpha 1 -antitrypsin is measured to verify deficiency and diagnosis of primary emphysema .
- Sputum culture: Determines presence of infection , identifies pathogen.
- Cytologic examination: Rules out underlying malignancy or allergic disorder.
- Electrocardiogram ( ECG ): Right axis deviation, peaked P waves (severe asthma); atrial dysrhythmias (bronchitis), tall, peaked P waves in leads II, III, AVF (bronchitis, emphysema ); vertical QRS axis (emphysema).
- Exercise ECG, stress test: Helps in assessing degree of pulmonary dysfunction, evaluating effectiveness of bronchodilator therapy, planning/evaluating exercise program.
Medical Management
Healthcare providers perform medical management by considering the assessment data first and matching the appropriate intervention to the existing manifestation.
- Bronchodilators . Bronchodilators relieve bronchospasm by altering the smooth muscle tone and reduce airway obstruction by allowing increased oxygen distribution throughout the lungs and improving alveolar ventilation.
- Corticosteroids . A short trial course of oral corticosteroids may be prescribed for patients to determine whether pulmonary function improves and symptoms decrease.
- Other medications . Other pharmacologic treatments that may be used in COPD include alpha1-antitrypsin augmentation therapy, antibiotic agents, mucolytic agents, antitussive agents, vasodilators , and narcotics .
- Optimization of bronchodilator medications is first-line therapy and involves identifying the best medications or combinations of medications taken on a regular schedule for a specific patient.
- Hospitalization . Indications for hospitalization for acute exacerbation of COPD include severe dyspnea that does not respond to initial therapy, confusion or lethargy, respiratory muscle fatigue , paradoxical chest wall movement, and peripheral edema .
- Oxygen therapy . Upon arrival of the patient in the emergency room, supplemental oxygen therapy is administered and rapid assessment is performed to determine if the exacerbation is life-threatening.
- Antibiotics . Antibiotics have been shown to be of some benefit to patients with increased dyspnea, increased sputum production, and increased sputum purulence.
Patients with COPD also have options for surgery to improve their condition.
- Bullectomy . Bullectomy is a surgical option for select patients with bullous emphysema and can help reduce dyspnea and improve lung function.
- Lung Volume Reduction Surgery . Lung volume reduction surgery is a palliative surgery in patients with homogenous disease or disease that is focused in one area and not widespread throughout the lungs.
- Lung Transplantation . Lung transplantation is a viable option for definitive surgical treatment of end-stage emphysema.
Nursing Management
Management of patients with COPD should be incorporated with teaching and improving the respiratory status of the patient. Learn about the nursing care management of patients with Chronic Obstructive Pulmonary Disease using the nursing process in this guide.
SEE ALSO: 8 Chronic Obstructive Pulmonary Disease (COPD) Nursing Care Plans for a comprehensive nursing care plan and management guide
Assessment of the respiratory system should be done rapidly yet accurately.
- Assess patient’s exposure to risk factors.
- Assess the patient’s past and present medical history.
- Assess the signs and symptoms of COPD and their severity.
- Assess the patient’s knowledge of the disease.
- Assess the patient’s vital signs.
- Assess breath sounds and pattern.
Diagnosis of COPD would mainly depend on the assessment data gathered by the healthcare team members.
- Impaired gas exchange due to chronic inhalation of toxins.
- Ineffective airway clearance related to bronchoconstriction, increased mucus production, ineffective cough, and other complications.
- Ineffective breathing pattern related to shortness of breath, mucus, bronchoconstriction, and airway irritants.
- Self-care deficit related to fatigue.
- Activity intolerance related to hypoxemia and ineffective breathing patterns.
Goals to achieve in patients with COPD include:
- Improvement in gas exchange.
- Achievement of airway clearance.
- Improvement in breathing pattern.
- Independence in self-care activities.
- Improvement in activity intolerance .
- Ventilation/oxygenation adequate to meet self-care needs.
- Nutritional intake meeting caloric needs.
- Infection treated/prevented.
- Disease process/prognosis and therapeutic regimen understood.
- Plan in place to meet needs after discharge.
- Maintain airway patency.
- Assist with measures to facilitate gas exchange.
- Enhance nutritional intake.
- Prevent complications, slow progression of condition.
- Provide information about disease process/prognosis and treatment regimen.
Patient and family teaching is an important nursing intervention to enhance self-management in patients with any chronic pulmonary disorder.
To achieve airway clearance:
- The nurse must appropriately administer bronchodilators and corticosteroids and become alert for potential side effects.
- Direct or controlled coughing . The nurse instructs the patient in direct or controlled coughing, which is more effective and reduces fatigue associated with undirected forceful coughing.
To improve breathing pattern:
- Inspiratory muscle training . This may help improve the breathing pattern.
- Diaphragmatic breathing . Diaphragmatic breathing reduces respiratory rate, increases alveolar ventilation, and sometimes helps expel as much air as possible during expiration.
- Pursed lip breathing . Pursed lip breathing helps slow expiration, prevents collapse of small airways, and control the rate and depth of respiration.
To improve activity intolerance:
- Manage daily activities . Daily activities must be paced throughout the day and support devices can be also used to decrease energy expenditure.
- Exercise training . Exercise training can help strengthen muscles of the upper and lower extremities and improve exercise tolerance and endurance.
- Walking aids . Use of walking aids may be recommended to improve activity levels and ambulation .
To monitor and manage potential complications:
- Monitor cognitive changes . The nurse should monitor for cognitive changes such as personality and behavior changes and memory impairment.
- Monitor pulse oximetry values . Pulse oximetry values are used to assess the patient’s need for oxygen and administer supplemental oxygen as prescribed.
- Prevent infection . The nurse should encourage the patient to be immunized against influenza and S. pneumonia because the patient is prone to respiratory infection.
During evaluation , the effectiveness of the care plan would be measured if goals were achieved in the end and the patient:
- Identifies the hazards of cigarette smoking.
- Identifies resources for smoking cessation.
- Enrolls in smoking cessation program.
- Minimizes or eliminates exposures.
- Verbalizes the need for fluids.
- Is free of infection.
- Practices breathing techniques.
- Performs activities with less shortness of breath.
It is important for the nurse to assess the knowledge of patient and family members about self-care and the therapeutic regimen.
- Setting goals. If the COPD is mild, the objectives of the treatment are to increase exercise tolerance and prevent further loss of pulmonary function, while if COPD is severe, these objectives are to preserve current pulmonary function and relieve symptoms as much as possible.
- Temperature control. The nurse should instruct the patient to avoid extremes of heat and cold because heat increases the temperature and thereby raising oxygen requirements and high altitudes increase hypoxemia.
- Activity moderation. The patient should adapt a lifestyle of moderate activity and should avoid emotional disturbances and stressful situations that might trigger a coughing episode.
- Breathing retraining. The home care nurse must provide the education and breathing retraining necessary to optimize the patient’s functional status.
Documentation is an essential part of the patient’s chart because the interventions and medications given and done are reflected on this part.
- Document assessment findings including respiratory rate, character of breath sounds; frequency, amount and appearance of secretions laboratory findings and mentation level.
- Document conditions that interfere with oxygen supply.
- Document plan of care and specific interventions.
- Document liters of supplemental oxygen.
- Document client’s responses to treatment, teaching, and actions performed.
- Document teaching plan.
- Document modifications to plan of care.
- Document attainment or progress towards goals.
See also: Respiratory System NCLEX Practice Questions and Reviewer (220 Questions)
5 thoughts on “Chronic Obstructive Pulmonary Disease (COPD)”
This article is very helpful with nursing plans with first semester nursing students. Thank you.
VERY HELPFUL WITH NURSING CARE PLAN. THANK YOU
VERY INFORMATIVE…
Hey Suzanne, Thanks a lot! 😊 Glad you found it helpful.
Very helpful for work use and outside of work use
Leave a Comment Cancel reply

IMAGES
VIDEO
COMMENTS
1. Introduction. According to the World Health Organization [], chronic diseases were the cause of 71% of deaths in the world in 2018 in ages ranging between 30 and 70 years old.Of these, chronic obstructive pulmonary disease (COPD) is the third leading cause of death worldwide, causing 3.23 million in 2019 [].Chronic obstructive pulmonary disease requires a complex, prolonged time period ...
Chronic obstructive pulmonary disease (COPD) is the third leading cause of death worldwide, causing 3.32 million deaths in 2019. COPD management has increasingly become a major component of general and hospital practice and has led to a different model of care. Nurse-led interventions have shown beneficial effects on COPD patient satisfaction and clinical outcomes. This systematic review was ...
Chronic obstructive pulmonary disease (COPD) is a chronic, progressive disease process characterized by dyspnea, chronic cough, and mucus production. Despite frequent referral of these patients, COPD does not require specialty management under most conditions. This article provides primary care providers with a concise review on the diagnosis and management of COPD in the primary care setting ...
Chronic obstructive pulmonary disease (COPD) is an important cause of morbidity and mortality but widely underdiagnosed. This thesis explores methods to improve case finding for COPD in primary care. It includes two systematic reviews- the first evaluated the diagnostic accuracy of screening tests and showed that handheld flow meters are more
INTRODUCTION. Chronic obstructive pulmonary disease (COPD) is a major global health problem due to its high prevalence (about 10% of the adult population), rising incidence (related in part to the aging of the population) and very significant associated personal, social, and economic costs ().The World COPD Day (November 18, 2020) is organized by the Global Initiative for Chronic Obstructive ...
With COPD: A Concurrent Mixed Methods Study of the Role of the General Practice Nurse Neil Wilson A thesis submitted in partial fulfilment of the requirements of the Manchester Metropolitan University for the degree of Doctor of Philosophy Department of Nursing Manchester Metropolitan University 2019. i Abstract Background Chronic Obstructive ...
This work organically integrates a systematic and individualized nursing plan with big data technology and applies it to the care of patients with chronic obstructive pulmonary disease (COPD) and respiratory failure (RF) and explores the continuous care model based on modern big data technologies to improve COPD and RF.
A Chronic Obstructive Pulmonary Disease Self-Management Packet to Reduce 30-Day Readmissions By Josette Askratni. MSN, University of South Alabama, 2012. Project Submitted in Partial Fulfillment Of the Requirements for the Degree of Doctor of Nursing Practice. Walden University February 2018.
Patient and family teaching is an important nursing intervention to enhance self-management in patients with any chronic pulmonary disorder. To achieve airway clearance: The nurse must appropriately administer bronchodilators and corticosteroids and become alert for potential side effects. Direct or controlled coughing.
Introduction. Chronic obstructive pulmonary disease (COPD) is the field closer to implementing a precision medicine. a approach to diagnosis and treatment. leading cause of death and disability worldwide. Although COPD is heterogeneous, defining features include persistent airflow obstruction and respiratory symptoms.
Nursing management of COPD patients achieves better outcomes in the day-to-day management of the disease, improving the patient's knowledge of disease management [4,5]. Indeed, home visits and remote manage-ment with telemedicine at discharge time by hospital nurses and in primary care should be
Muscle exercise training, a major component of pulmonary rehabilitation, is a key element in the treatment of patients with COPD [Citation 99, Citation 100] as it exerts beneficial effects on skeletal muscle performance, while favoring exercise capacity and physical activity in patients with COPD [Citation 99-101] in a safely manner [Citation ...
Abstract Most nurses, not just specialist nurses, will routinely encounter people with chronic obstructive pulmonary disease in their care. Although there
referred to as COPD (Chronic obstructive pulmonary. disease), is a group of progressive lun g diseases. The. most common are emphyse ma and chronic. bronchitis [1]. Many people with COPD have both ...
This work organically integrates a systematic and individualized nursing plan with big data technology and applies it to the care of patients with chronic obstructive pulmonary disease (COPD) and respiratory failure (RF) and explores the continuous care model based on modern big data technologies to improve COPD and RF. It aims to relieve the symptoms of COPD and RF, reduce the number of acute ...
The four key findings of this thesis are a) COPD patients with and without CVD have similar CV risk; b) the elevated aortic stiffness in COPD is modifiable through pulmonary rehabilitation (PR) and that this reduction is related to physical activity (PA); c) aortic stiffness reduction is maintained for at least six weeks following PR and ...
COPD Case Study Essay. Chronic obstructive pulmonary disease is a chronic progressive lung disease caused predominantly by smoking National Institute for Health and Clinical Excellence NICE, 2010. It is characterised by airflow obstruction which is not fully reversible. The airflow obstruction does not change markedly over several months and is ...