- Getting Published
- Open Research
- Communicating Research
- Life in Research
- For Editors
- For Peer Reviewers
- Research Integrity

How to communicate your research more effectively
Author: guest contributor.
by Angie Voyles Askham, Content Marketing Intern
"Scientists need to excite the public about their work in part because the public is paying for it, and in part because science has very important things to say about some of the biggest problems society faces."
Stephen S. Hall has been reporting and writing about science for decades. For the past ten years, he's also been helping researchers at New York University improve their writing skills through the school's unique Science Communication Workshops . In our interview below, he explains why the public deserves good science communication and offers some tips for how researchers can make their writing clear and engaging.
How would you descr ibe your role as a science journalist?
I’ve always made a distinction between "science writer" and a writer who happens to be interested in science. That may sound like wordplay, but I think it captures what we aspire to do. Even as specialists, science journalists wear several hats: we explain, we report, we investigate, we step back and provide historical context to scientific developments to help people understand what’s new, why something is controversial, who drove a major innovation. And like any writer, we look for interesting, provocative, and deeply reported ways to tell these stories.
I know you from the science communication workshop that’s offered to NYU graduate students. One of the most important things that I got out of the workshop, at least initially, was training myself out of the stuffy academic voice that I think a lot researchers fall into when writing academic papers. Why do you think scientists fall into this particular trap, and how do you help them get out of it?
Scientists are trained—and rightly so—to describe their work in neutral, objective terms, qualifying all observations and openly acknowledging experimental limitations. Those qualities play very well in scientific papers and talks, but are terrible for effective communication to the general public. In our Science Communication workshops at NYU, we typically see that scientists tend to communicate in dense, formal and cautious language; they tell their audiences too much; they mimic the scientific literature’s affinity for passive voice; and they slip into jargon and what I call “jargonish,” defensive language. Over ten years of conducting workshops, we’ve learned to attack these problems on two fronts: pattern recognition (training people to recognize bad writing/speaking habits and fixing them) and psychological "deprogramming" (it’s okay to leave some details and qualifications out!). And a key ingredient to successful communication is understanding your audience; there is no such thing as the "general public," but rather a bunch of different potential audiences, with different needs and different levels of expertise. We try to educate scientists to recognize the exact audience they're trying to reach—what they need to know and, just as important, what they don't need to know.
What are some other common mistakes that you see researchers making when they’re trying to communicate about their work, either with each other or with the public?
We see the same tendencies over and over again: vocabulary (not simply jargon, but common expressions—such as gene “expression”—that are second-hand within a field, but not clear to non-experts); abstract, complicated explanations rather than using everyday language; sentences that are too long; and “optics” (paragraphs that are too long and appear monolithic to readers). We’ve found that workshops are the perfect setting to play out the process of using everyday language to explain something without sacrificing scientific accuracy.
Why is it important for researchers to be better communicators?
Scientists need to learn to tell their own stories, first and foremost, because society needs their expertise, their perspective, their evidence-based problem solving skills for the future. But the lay public, especially in an era where every fact seems up for grabs, needs to be reminded of what the scientific method is: using critical thinking and rigorous analysis of facts to reach evidence-based conclusions. Scientists need to excite the public about their work in part because the public is paying for it, and in part because science has very important things to say about some of the biggest problems society faces—climate change, medical care, advanced technologies like artificial intelligence, among many other issues. As climate scientist Michael Mann said in a celebrated 2014 New York Times OpEd, scientists can no longer stay on the sidelines in these important public debates.
As a science journalist, part of your job is to hunt for interesting stories to tell. How can scientists make their work more accessible to people like you—or to other people outside of their specific area of research—so that their stories are told more widely?
The key word in your question is “stories.” Think like a writer. What’s the story behind your discovery? What were the ups and downs on the way to the finding? Where does this fit into a larger history of science narrative? Was there a funny incident or episode in the work (humor is a great way to draw and sustain public interest)? Was there a conflict or competition that makes the work even more interesting? Is there a compelling historical or contemporary figure involved that will help you humanize the science? It's been our-longstanding belief that scientists have a great intuitive feel for good storytelling (we incorporate narrative training in our workshops), but just don’t think about it when it comes to describing their own work. The other key thing is to explain why your research matters.
One of the ways that many researchers try to share their work is through Twitter, but I noticed that on the NYU website it says you’re a Twitter conscientious objector. Why is that? What effect do you think Twitter has had on science communication and journalism in general?
I actually think Twitter can be a great tool for science communication, and many of my colleagues use it deftly. I tend to gravitate toward stories that everyone is not talking about, so Twitter doesn’t help much in that regard. The larger reason I’m a Twitter “refusenik,” as my colleague Dan Fagin sometimes calls me, is that I think the technology has been widely abused to disseminate misinformation, intimidate enemies, and subvert democratic norms; I don’t use it primarily for those reasons.
Are there any other tips that you can offer researchers who want to be better communicators and just aren’t sure where to start?
One first step might be to see if your institution offers any communication training and to take advantage of those programs; if not, think about how you might establish a program. We’ve posted a few of the things we’ve learned at NYU on our website ; we’ve also established a publishing platform for science communicators at NYU called the Cooper Square Review , which is a good way for scientists to get experience publishing their own work and reaching a larger public.
Stephen S. Hall has been reporting and writing about science for nearly 30 years. In addition to numerous cover stories in the New York Times Magazine, where he also served as a Story Editor and Contributing Writer, his work has appeared in The New Yorker, The Atlantic Monthly, and a number of other outlets. He is also the author of six non-fiction books about contemporary science. In addition to teaching the Science Communication Workshops at NYU, he also teaches for NYU's Science, Health and Environmental Reporting Program (SHERP) and has taught graduate seminars in science writing and explanatory journalism at Columbia University.
Click here to learn how Springer Nature continues to support the needs of Early Career Researchers.
Guest Contributors include Springer Nature staff and authors, industry experts, society partners, and many others. If you are interested in being a Guest Contributor, please contact us via email: [email protected] .
- early career researchers
- research communication
- Tools & Services
- Account Development
- Sales and account contacts
- Professional
- Press office
- Locations & Contact
We are a world leading research, educational and professional publisher. Visit our main website for more information.
- © 2024 Springer Nature
- General terms and conditions
- Your US State Privacy Rights
- Your Privacy Choices / Manage Cookies
- Accessibility
- Legal notice
- Help us to improve this site, send feedback.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 26 April 2024
A guide to science communication training for doctoral students
- Christina Maher 1 na1 ,
- Trevonn Gyles ORCID: orcid.org/0000-0003-4635-5985 1 na1 ,
- Eric J. Nestler ORCID: orcid.org/0000-0002-7905-2000 1 , 2 &
- Daniela Schiller ORCID: orcid.org/0000-0002-0357-7724 1 , 2
Nature Neuroscience ( 2024 ) Cite this article
908 Accesses
70 Altmetric
Metrics details
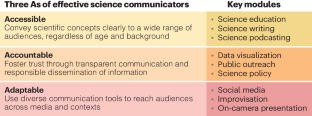
Effective science communication is necessary for engaging the public in scientific discourse and ensuring equitable access to knowledge. Training doctoral students in science communication will instill principles of accessibility, accountability, and adaptability in the next generation of scientific leaders, who are poised to expand science’s reach, generate public support for research funding, and counter misinformation. To this aim, we provide a guide for implementing formal science communication training for doctoral students.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Steinbeck, J. The Log From the Sea of Cortez (Penguin, 2001).
United Nations Educational, Scientific and Cultural Organization. UNESCO Science Report 2021: the Race Against Time for Smarter Development (United Nations, 2021).
Croxson, P. L., Neeley, L. & Schiller, D. Nat. Hum. Behav. 5 , 1466–1468 (2021).
Article PubMed Google Scholar
Rein, B. Cell 185 , 3059–3065 (2022).
Article CAS PubMed Google Scholar
Weingart, P. & Guenther, L. J. Sci. Commun. 15 , C01 (2016).
Article Google Scholar
Fischhoff, B. & Scheufele, D. A. Proc. Natl Acad. Sci. USA 110 , 14031–14032 (2013). (Suppl. 3).
Grorud-Colvert, K., Lester, S. E., Airamé, S., Neeley, E. & Gaines, S. D. Proc. Natl Acad. Sci. USA 107 , 18306–18311 (2010).
Article CAS PubMed PubMed Central Google Scholar
National Academies of Sciences, Engineering, and Medicine. Ending Discrimination Against People with Mental and Substance Use Disorders: the Evidence for Stigma Change (National Academies Press, 2016).
Neeley, L. et al. Front. Commun. 5 , 35 (2020).
Goldstein, C. M., Murray, E. J., Beard, J., Schnoes, A. M. & Wang, M. L. Ann. Behav. Med. 54 , 985–990 (2020).
Gascoigne, T. et al. (eds.) Communicating Science: A Global Perspective (ANU Press, 2020).
Rein, B. Neuroscience 530 , 192–200 (2023).
Download references
Acknowledgements
The authors thank P. Croxson for her involvement as co-founder of the effective science communication course. We also thank the various teaching assistants over the years, who were actively involved in shaping the course: T. Fehr, C. Lardner, C. Guevara and M. O’Brien.
Author information
These authors contributed equally: Christina Maher, Trevonn Gyles.
Authors and Affiliations
Nash Family Department of Neuroscience, Friedman Brain Institute, Icahn School of Medicine at Mount Sinai, New York, NY, USA
Christina Maher, Trevonn Gyles, Eric J. Nestler & Daniela Schiller
Department of Psychiatry, Icahn School of Medicine at Mount Sinai, New York, NY, USA
Eric J. Nestler & Daniela Schiller
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Daniela Schiller .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Maher, C., Gyles, T., Nestler, E.J. et al. A guide to science communication training for doctoral students. Nat Neurosci (2024). https://doi.org/10.1038/s41593-024-01646-y
Download citation
Published : 26 April 2024
DOI : https://doi.org/10.1038/s41593-024-01646-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Improving Communication in Clinical Research

By: Anatoly Gorkun, MD, PhD, Chartered MCIPD Senior Manager, Global Clinical Development, PPD UK
Abstract: Effective communication skills in clinical research are vitally important. Due to many conflicting priorities however, clinical research professionals may not have time to manage soft skills. This increases the danger that something may go wrong. This article highlights real-life clinical research examples where communication problems affected deliverables or compliance. The principles of effective communication styles are discussed.
Introduction
Communication is a key tool for clinical researchers, yet problems due to inactive communication are common. It is important to monitor possible ineffective communication in order to develop effective solutions to proactively prevent the negative consequences of ineffective communication.
Some time ago, the author received feedback from two clinical trial managers (CTM) on the same clinical research associate (CRA) at the same time. One clinical trial manager said:
(CTM’s Name) “is perfectly performing as expected from an experienced CRA. Her time has been allocated to manage a few difficult sites. Due to her learning agility and deep experience, the situation is improving now. She is a very good team player.”
The other clinical trial manager told the author:
“I know this CRA is new to the company and is still learning; however, with the upcoming data cleaning, I need your help.
I would suggest she has a co-monitoring visit with someone who is experienced. She needs to understand that this reconciliation is not just making a match between source data vs. case report form but also questioning what is being reported and identifying gaps, and being able to address issues with the site staff.
I would appreciate your feedback and actions.”
Both studies were relatively similar, and in this specific example, the problem appeared to be the communication between the CRA and CTM.
The Importance of Communication in Clinical Research
There are various definitions of communication, including:.
“The imparting or exchanging of information by speaking, writing, or using some other medium.” ( oxforddictionaries.com )
“Two-way process of reaching mutual understanding, in which participants not only exchange (encode-decode) information, news, ideas, and feelings but also create and share meaning.” (businessdictionary.com).
The second definition is broader and reflects the nature of communication more accurately.
Poor communication in clinical research has many negative effects (Table 1) including stress, possible conflicts between clinical research professionals, and a breakdown in relationships. Other negative effects of poor communication are unmet expectations (ineffectiveness), wasted time because work is inefficient and must be re-done, non-compliance, possible harm to subjects, and possible invalidation of data.
As an example: an in-house CRA approached the line manager and said, “I’ve done what the project team wanted, but when I finished the task they said it was not what they expected.” The line manager asked if the CRA had checked with the project team before starting the task to clarify what they wanted. She said, “No, because the task seemed very clear.”
Communication that is free of assumptions is one of the characteristics of ideal communication (Table 2). It is important to listen, ask questions to ensure understanding of the task, agree to what needs to be done, and confirm the agreement. Communication is a two-way process that requires mutual understanding.
Successful Communication Methods
The most suitable method of communication depends upon the situation and to some extent, the receiver’s preferences. For urgent situations, a telephone call is best, followed by an email to summarize the call. The communicator should not bombard the person with emails, because he/she does not know whether the person is receiving and reading the emails. In some situations, more than one communication method is appropriate, such as emailing instructions and then following up with a telephone call.
Sometimes it happens that the site monitor and the in-house CRA as well as the project assistant may ask the research nurse at the site the same question. This may not be the most efficient approach. Communication should be streamlined in order to prevent it from being chaotic.
The following email communication is between a clinical trial manager (CTM) and a CRA on an urgent issue that required immediate attention. A delay in resolving the issue might affect deliverables and the company’s image.
- CTM → CRA, February 21: Check if all Adverse Events were entered into eCRF. Urgent, due in 2 days. Table attached.
- CTM → CRA, February 24: “A kind reminder, please.”
- CTM → CRA, February 24: “Please send me your answers today.”
- CTM → CRA, February 28: “I need your answers, please.”
- CTM → CRA, March 01: “Client requested us to provide the answer. Please complete this task.”
- CTM → CRA, March 06: “I need your answers URGENTLY please.”
- CTM → CRA, March 06: “Please do it tomorrow and let me know.”
- CRA → CTM, March 06: “I would do, but I don’t know what to check.”
- CTM → CRA, March 06: “The table is attached.”
- CTM → CRA, March 08: “Any news from the sites?”
- CRA → CTM, March 08: “Hopefully tomorrow.”
The clinical trial manager sent the first email to the CRA on February 21st and did not receive a reply from the CRA until March 6 th , nearly two weeks later. When the CRA responded that she did not know what to check, the CTM simply forwarded the same attachment. The CTM should have picked up the telephone and talked to the CRA.
Ideal communication is transparent. Transparency is:
“the perceived quality of intentionally shared information from a sender”
(Schnackenberg AK, Tomlinson EC. (March 2014). “Organizational transparency: a new perspective on managing trust in organization-stakeholder relationships,” Journal of Management . 10.1177/0149206314525202).
Transparency makes it easy for others to understand what actions have been completed and which actions need to be taken. It implies openness and accountability.
In another case, a project manager sent the following message to a line manager:
“As you know [name of CRA2] replaced [name of CRA1] at the end of March.
Unfortunately, by that date, the site performance decreased with late queries and SDV (Source Data Verification) backlog due to pending monitoring visits.
Until today both sites still have not been visited and the plan is not available. I appreciate if you guarantee to have both sites visited by the end of April.”
The line manager spoke to the CRA, who said that the visits had been scheduled a long time ago. The project manager had been on holiday. When the project manager came back, he did not speak with the CRA about the status of the visits but instead escalated the issue.
Considerations in using appropriate communication include:
- The purpose of the specific communication
- How communicating will benefit the situation
- Whether something different can be done
- Whether alternative communication is necessary, and if so, the best method to use.
In the example, considering these four questions would have enabled the project manager to realize that talking directly to the CRA was the appropriate communication method for this situation.
In this case, the CRA needed advice from the CTM:
CRA: “I need to complete a number of overdue study-specific learning items on my LMS (Learning Management System) but I don’t have time. I am so busy.”
CTM: “Then, do it wisely.”
The advice was not clear. Communication must also be concise. It is necessary to be clear about the purpose/goal of the message, to stick to the point, and to be brief.
Ideal communication is timely. In determining the best time for the message, the communicator must consider whether to communicate now or later. In some cases, it is better to wait and to communicate one message with another. It may also be helpful to pre-prepare the receiver of the communication with a brief heads-up.
A CRA was having communication issues with two clinical research sites. At the same time, this CRA had to deliver a presentation at a departmental meeting and wanted feedback from the line manager. The line manager knew that the sites were struggling to work with this CRA because of his insufficient communication skills. The line manager decided to wait a couple of days to speak with the CRA about his presentation/communication skills and the issue with the sites at the same time, as that was a good chance to demonstrate the importance of expressing thoughts clearly and explicitly.
It is also important to acknowledge receipt of an email or other communication when we are not going to provide our answer immediately. For example:
“I’ve received your message. It will take me a week to collect the requested information. I’ll get back to you by …”
Ideal communication is diplomatic and constructive. It is okay to disagree with someone; however, communication should focus on a person’s opinion or approach and not insult the person. For example, instead of saying,
“I don’t agree with you …,” say something like, “May I suggest that we discuss more options …”
An in-house CRA sent the following email message to a research nurse:
“I sent you my request 2 weeks ago, and it’s complete silence from your side. I find it so frustrating because we need to close all queries by the end of this week.”
The research nurse said that she would not respond to requests like this. After coaching the in-house CRA on communication methods, there was a visible improvement noticed, and the relationship with the site improved.
It is always better to be constructive. Avoid being very direct or pushy, and suggest options instead of criticizing or expressing frustration.
Ideal communication must be culturally respectful since clinical research is conducted internationally. Culturally respectful communication helps to avoid misunderstanding, to establish rapport, to build better relationships, and to facilitate more efficient work. Even among English-speaking countries, words or phrases can have slightly different meanings. For example, in the United States, “I hear what you say” means that the communicator accepts the other person’s point of view. In the United Kingdom, it may rather mean “I am not keen on discussing it further as I am not in agreement with this.” Also, accepting country or region-specific accents should be a part of cultural respect.
Ideal communication is also fair.
The following communication happened between a site monitor and a line manager.
Site monitor to line manager:
“I’m very busy and working very hard, however, I do not get enough support from the in-house CRA.”
The monitor’s line manager to in-house CRA’s line manager:
“I think that the in-house CRA might provide better support to the site monitor. Could you please check on the issue with the CRA’s performance and fix it?”
It turned out that the in-house CRA was doing a good job; however, the problem was that the site monitor needed to provide an explanation regarding the backlog of work that was created and decided to blame the in-house CRA for lack of support. Communication should be fair and should not blame other people unfairly.
Ideal communication is open, honest, and logical.
The following examples highlight communication between a line manager and a direct report during two performance reviews and a 1:1 meeting.
Mid-year performance review meeting, Line Manager to a direct report:
“You are leading a very important project really well. It’s going to be a great year for you!”
Monthly one-to-one meetings throughout the year:
The project delivery was on time and good quality. Every month, the line manager confirmed that she was happy with all of the work and there was nothing to improve.
End-of-year performance review meeting, Line Manager to a direct report:
“You’ve been struggling to deliver the project and managing it below expectations.”
The end-of-year performance review feedback was not logical because the previous messages were all positive. Ideal communication should avoid misunderstanding, conflicts, and disappointment.
Ideal communication is well-structured and compelling. Communicators should try not to tell a long story that makes it difficult for the receiver to determine what the communicator needs. This is important in everyday life with everyone, including communication with senior leaders and clinical investigators, both of whom are usually very busy.
The “rhetorical kipper” from Gareth Bunn can be used to plan communication. Using this model, communication is designed from the “tail of the kipper” and delivered from the “head.” After presenting the topic, three ideas or points are presented, and then finally, the request is made or the main message is delivered. The author’s direct reports found it useful to apply the rhetorical kipper method. Proper communication should be positive, assertive, and inspirational.
Case Study on Different Feedback
The case study presented at the beginning of this article illustrated different feedback from two clinical trial managers on the same CRA. One clinical trials managers stated that:
[CRA’s Name] “is perfectly performing as expected from an experienced CRA.
She has been allocated to manage a few difficult sites. Due to her learning agility and deep experience, the situation is improving now. She is a very good team player.”
I would suggest that she has a co-monitoring visit with someone experienced. She needs to understand that this reconciliation is not just making a match between source data vs. case report form but also questioning what is being reported and identifying gaps, being able to address issues with the site staff.
I would appreciate reviewing your feedback and actions.”
The reason for the different feedback was not different complexity of the studies but that the clinical trial manager was micro-managing the CRA. She had a different management style than the CRA was used to. The first clinical trial manager delegated the tasks and trusted the CRA to complete them. The second clinical trial manager required daily reports from the CRA, assuming that if there was no daily report, it meant that the job was not done. She also had negative experiences working with a previous CRA and assumed that the new CRA would act in the same way.
Thus, the second clinical trial manager’s style was based more on assumptions. After a root cause analysis of the situation, the CRA learned how to recognize different working styles and started working with the second CTM more efficiently.
Many skills are required for appropriate and effective communication (Table 3), including listening and observing, planning, and dealing with difficult situations dearly and empathetically. Methods of ensuring that communication is appropriate and effective include awareness of communication issues (Table 4). If we face a communication issue, we should not assume that it will disappear by itself. A root cause analysis should be done to determine the cause of the issue, and then a plan should be developed to manage the problem. The plan should include feedback to ensure that the other person understands and accepts the plan. Line managers can arrange for soft skills coaching and training for people who need to improve their communication skills. If nothing else works, such issues can be escalated.
In clinical research, it is important to monitor possible ineffective communication approaches and to proactively develop effective solutions to prevent negative consequences.
The Effects of Poor Communication in Clinical Research
- Possible conflicts and breakdowns in relationships
- Unmet expectations (ineffectiveness)
- Waste of time (inefficiency)
- Non-compliance
- Possible harm to subjects
- Possible invalidation of data
Ideal Communication
- Assumption-free
- Proper methods utilized
- Transparent
- Appropriate
- Clear and concise
- Diplomatic and constructive
- Culturally respectful
- Open, honest, and logical
- Well-structured and compelling
- Proper communication style
Communication Skills
- Listening and observing
- Nonverbal communication (body language, facial countenance)
- Negotiations
- Dealing with difficult situations
- Friendliness
- Flexibility (open-mind)
- Giving and receiving feedback
Communication Strategies to Prevent or Fix Issues
- Be aware of communication issues
- Observe and discover issues
- Do not assume that the issues disappear by themselves
- Perform root-cause analysis
- Feedback, and how to ensure that it is understood and accepted
- Soft skills coaching
- Soft skills training
- Escalating (if nothing else works)
6 thoughts on “Improving Communication in Clinical Research”
Nice article.thanks
Be sure to communicate in the mindset of a team member, or stakeholder with the same goals and not as an outsider looking in with judgement.
This is a great inspiring article.
Nice article! Thanks for sharing this informative post. Keep posting!
- Pingback: How To Succeed As A Clinical Trial Project Manager - Mosio
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Communicating and sharing your research

It is worthwhile considering what methods and communication channels you will use to share your research. Listed below are some common methods for communicating research with a range of audiences – academic, professional and general.
For academic purposes, share your research via these methods to increase the likelihood your research will be viewed, downloaded and cited. This will enable you to measure the impact and engagement of your work.
Researcher profiles
Creating and maintaining researcher profiles can foster connections with your research community, and maximises the visibility of your research outputs and impact. All RMIT researchers and HDR students are encouraged to have an ORCID profile. An ORCID profile can be used to display your research interests and activities, list your publications, qualifications and achievements, and link to other research and professional profiles. Some journals require researchers to provide their ORCID identifier when submitting articles for publication.
Blog, tweet, and post about your research
Consider writing a blog to share your research, or create a professional or academic Twitter or LinkedIn profile to connect with other researchers, share ideas and post links to your research writing and publications. Remember to include a DOI (Digital Object Identifier) when posting about your work – this will help you track citations, views and downloads. For more information regarding sharing using social media see the Library guide Social media for researchers .
For HDR Candidates
See the Thesis Whisperer and Research Whisperer blogs – both excellent resources for research students and early career researchers. If you have a Twitter profile, consider following their Twitter accounts. If you don’t use Twitter, consider signing up to the mailing list for either blog.
Watch this video for a brief introduction to using social media when communicating your research.
Communicate your research (2:14 mins)
“Communicate Your Research” by Andy Tattersall , ScHARR library is licensed under CC BY 4.0
Share your research data
Sharing your research data can be another method of promoting your research – the increased exposure may lead to new collaborations and new research projects with other researchers, or extra citations for your publications.
In some cases it may be mandated that you share your research data when submitting an article for publication. See the Library’s guide to Research Data Management for advice on managing and sharing your research data.
Test Your Knowledge
Research and Writing Skills for Academic and Graduate Researchers Copyright © 2022 by RMIT University is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book

← Back to blog
Published on August 5, 2019
Top tips and tools for effective research communication
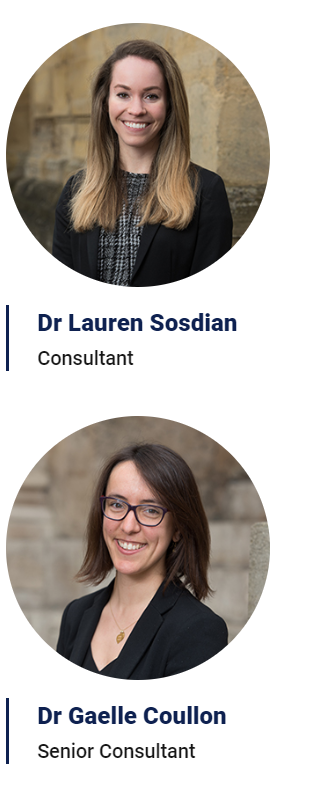
Academic researchers spend a significant proportion of their careers speaking to specialist audiences at conferences and applying for grants. However, sometimes even the best specialists struggle to clearly and concisely explain their work to a non-specialist audience. In the second article of our three-part series about the value of effective research communication, Oxentia consultants Dr Gaelle Coullon and Dr Lauren Sosdian explore some of the common mistakes researchers encounter when communicating to a non-specialist audience and provide a few tips and techniques to improve communication skills.
The ability to communicate with a non-specialist audience about the importance of your work doesn’t just make for a great TED talk. Research communication is a valuable skill for all academics to hone. It can help convince the listener about the importance of your work, it can facilitate interdisciplinary collaborations and improve how academics work with technology transfer offices, and it can help to make PhDs and Early Career Researchers more employable. We explored the benefits of good research communication in more detail in part one of this series .
Over the years, several different approaches have been taken to help researchers and entrepreneurs from all fields hone their communication skills. Below is a selection of four tools that we use when working with researchers and entrepreneurs which can help them tackle some of the challenges of research communication.
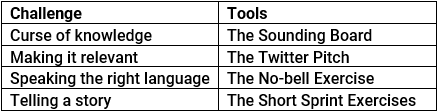
1. Curse of knowledge. Coined in Made to Stick 1 , the ‘curse of knowledge’ describes how knowing something very well means you become immune to the confusing and unique aspects of what you know. This can leave you unable to recognise when you are using technical terminology or jargon. However, at the other end of the spectrum, good research communication is not about ‘dumbing it down’. Good research communicators assume their audience is intelligent but just not equipped with the same technical expertise or language.
How can you overcome the curse of knowledge without ‘dumbing it down’? Complex ideas can be effectively communicated to any audience if the speaker can start by clearly explaining the core idea behind their research, using examples and metaphors to which we can all relate. Role-playing can help. For example, during our communication workshops, we would pair a researcher in microbiology who is preparing a marketing brief for her technology with a colleague in the department of sociology. Acting as a sounding board , this colleague would help her recognise the confusing elements of her work and identify better ways of explaining it.
2. Making it relevant. Even if researchers recognise that they aren’t communicating their work in a way that anyone can understand, many struggle in finding an alternative approach that would work better for a non-specialist audience. At a conference or in a journal publication, researchers are typically required to focus on technical descriptions of their methods and findings. With a non-specialist audience, the focus needs to be on the bottom-line of why we should care and what effect the research may have on the wider world. As pointed by Monica Metzler, founder and executive director of the Illinois Science Council (ISC), “the key difference between a technical talk and a lay audience talk is that we don’t want to know all about it” 2 .
One of the techniques we use to help researchers overcome the detail focus is a Twitter pitch . Used as part of a sprint toolkit workshop, this exercise takes participants out of their comfort zone by encouraging them to zero in on why we should care about their work and explain it in 280 characters.
3. Speaking the right language. When it comes to crafting the words used to describe their work, some researchers fail to recognise that some words, such as ‘theory’, ‘bias’ or ‘scheme’, have different meanings to different audiences. A Physics Today article 3 illustrates this point in relation to climate change – where the word ‘aerosol’ could easily be misunderstood by the public as a ’spray can’ when scientists actually mean ‘tiny atmospheric particle’.
Knowing your audience goes a long way in avoiding this pitfall. Understanding your audience will help convey why others should care about the research, but also help you tailor the story that you want to tell your audience. Don’t forget, the language you use when explaining your research at a public outreach conference will be very different to that which you use when pitching to an investor for a university spinout or how you explain your long days in the lab to your partner or friends.
One of the techniques that we use to help researchers better understand their audience is the no-bell exercise , a short exercise where participants pitch their work to colleagues from other departments who ring a bell if they hear a word or phrase that they do not understand. The objective is to finish the 3-minute pitch with no bells. This exercise forces participants to recognise when they are using jargon and then correct it, with the help of their colleagues.
4. Telling a story. Finally, really good research communicators tell a great story, one that uses clear, concise, and concrete language and examples. A brief history of the research project perhaps, the team who developed it, or how future work in this field could help improve someone’s life helps to engage your audience in the research question.
The series of short sprint exercises that we have developed as part of our training programmes are designed to help researchers craft compelling stories as well as new fun and interesting ways of talking about their research to a wide range of audiences. We explore how this works in practice in part three of our series.
How Oxentia can help
Oxentia, Oxford’s Global Innovation Consultancy, has worked with researchers in different disciplines at universities and institutions around the world for over fourteen years. Our experienced practitioner consultants work in over 70 countries for clients in governments, corporations, development agencies, and universities. This work has enabled us to develop training programmes featuring practical exercises and tool kits to help researchers better communicate their research to wider audiences, whether in STEM subjects or in the arts, humanities and social sciences.
Why do you think research communication is an important skill to develop in academia? Do researchers at your institution have access to communication training? Do you know other exercises and tips for effective research communication? Let us know in the comments on LinkedIn.
1 Chip Heath and Dan Heath (2007), “Made to Stick: Why Some Ideas Survive and Others Die”, Random House.
2 Science (2013), “Dispelling Myths About Science Communication”, https://www.sciencemag.org/careers/2013/02/dispelling-myths-about-science-communication
3 Somerville and Hassol (2011), “Communicating the science of climate change”, Physics Today 64(10), pp 48-53.
This website site uses cookies to improve your browsing experience. By continuing to use this site, you are agreeing to our use of cookies. Review our privacy policy .

- Strategy development
- Commercialisation Services
- Accelerators
- Privacy Policy
Stay up to date
- © 2024 Oxentia Limited
- [email protected]
- Privacy Statement
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.1; 2022 Dec
- PMC10194302
Novel approaches to communication skills development: The untapped potential of qualitative research immersion
Amy s. porter.
a St. Jude Children’s Research Hospital, Memphis, TN, USA
Cameka Woods
Erica c. kaye, associated data.
Participation in qualitative research, particularly analysis of recorded medical dialogue, offers real-time, longitudinal immersion that can strengthen clinical trainee communication skills. The study objective was to explore how qualitative research participation impacts clinical trainees’ self-perceived communication skills development and practice.
In this study, a 17-member multidisciplinary working group of child life specialists, advanced practice providers, undergraduate/medical students, residents, fellows, attending physicians, social scientists, and career researchers with recent qualitative and communication research experience assembled to discuss this topic using a structured discussion guide. Content analysis was used to identify concepts and themes.
Three key themes characterizing the impact of qualitative research participation on aspiring clinicians’ communication skills development and practice arose – the 3Cs: (1) C onnection, therapeutic alliance, and accompaniment; (2) C larity and prognostic communication; (3) C ompassion, empathy, and understanding. Participants emphasized that qualitative research learning improved their understanding of patient/family lived experiences, preparing them for future clinical encounters, strengthening their emotional intelligence, and promoting self-care, resilience, and professional affirmation.
Conclusions
Immersion in clinical communication through participation in qualitative research is an under-utilized resource for supporting clinical trainees in communication skills development.
The process of collaborative knowledge production through the collective exploration of an a priori question related to group members’ collective experiences is methodologically innovative. Further, re-thinking qualitative research participation as an underutilized educational opportunity is pedagogically novel, and leaders in medical education and qualitative research should collaborate to realize the potential of this teaching tool.
- • Qualitative research participation offers immersion in clinical communication.
- • Participation impact characterized by the 3 C’s: 1) Connection, 2) Clarity, 3) Compassion.
- • This is an under-utilized medical education resource for communication skills development.
- • Medical education and qualitative research leaders should collaborate.
1. Introduction
Communication training for clinical trainees often involves single timepoint simulation as a “gold standard” for practicing navigation of challenging conversations [ [1] , [2] , [3] , [4] , [5] , [6] , [7] , [8] , [9] , [10] , [11] , [12] ]. Due to time, staffing, and resource constraints, medical educators face challenges realizing high volume of real-time communication learning opportunities [ 1 ]. Clinicians-in-training are exposed infrequently and inconsistently to in-depth, communication-heavy encounters between clinicians and patients and their families during difficult moments in the illness course [ 5 , 13 , 14 ]. As a result, trainees lack robust opportunities to witness communication and consider which modeled approaches they want to integrate into their own communication toolboxes. Further, depending on supervisory ratios, trainees may not have sufficient opportunities to observe clinicians with a range of emotional dexterity skills to learn and reflect on how (or how not) to communicate during challenging medical encounters.
Healthcare communication science researchers have amassed large repositories of recorded medical dialogue to answer questions about best practices for communication between patients, families, and healthcare professionals; however, little precedent exists for collaboration between communication researchers and medical education leaders to optimize use of this under-utilized resource to offer learners opportunities for developing communication skills through participation in communication research. Existing literature explores how guided reflection activities such as “The Healer’s Art” and other self-contemplative didactics positively impact trainees’ communication skills, empathy, self-awareness, and overall clinical practice [ [15] , [16] , [17] ], yet the potential educational value and impact of qualitative research experiences on trainees’ learning and communication skills remains understudied and poorly understood.
To address this knowledge gap, we convened a multidisciplinary working group of students, clinicians, and researchers to consider the question: “How does engaging in qualitative communication research (i.e., listening to audio recordings and/or reading transcripts of recorded clinical encounters) impact trainees as professionals (both clinicians and researchers) and as individuals holistically?” The Qu alitative research as E ducation for S tudents and clinicians-in- Tr aining (QUEST) working group comprised individuals affiliated with a communication research lab within an academic institution who each had recent experiences participating in qualitative research on topics related to communication. The working group examined whether engaging in qualitative research involving patients and families could influence the way students and clinicians-in-training learn and practice communication. In this article, we summarize findings from the QUEST working group and propose immersion in qualitative research datasets as an innovative alternative or complement to standardized simulated communication skills training.
In this study, we used an adaptation of autoethnography to bring together a team of authors with common experiences related to qualitative research participation, collectively share our perceptions and generate reflective data about our experiences with qualitative research, and collaborate with one another to analyze the data and present our insights. In traditional autoethnographic methods, an individual uses a reliable process to generate data from their own experience, observations, and reflections and then reflects on and synthesizes these data to inform a larger context [ 18 ]. Koopman et al describes autoethnography as the ultimate form of reflexivity, a mechanism by which to explore personal perceptions, values, and beliefs through the lens of lived experience, culture, and self-other interactions [ 19 ]. In this project, our authorship team wished to gain deeper insights into the potential influence of qualitative research participation on communication education for students and clinicians. In deciding to study ourselves, we developed a modified form of autoethnography, which we describe below. This paper reports the findings from the QUEST working group with all group members represented as authors; there were not separate groups representing “researchers” and “study participants,” but rather one collaborative group working together to explore an a priori question related to our collective experiences. As such, the project did not require IRB approval.
The authorship team convened as the QUEST working group, comprising a 17-member group of students, staff, and faculty with recent qualitative communication research experience, including undergraduate/medical students, residents, fellows, child life specialists, advanced practice providers, and clinical research staff. Within the Quality of Life and Palliative Care Research Division, all learners who had participated in communication research by listening to recorded medical dialogue or reading transcripts of interviews with patients, families, and clinicians at a particular academic institution over the past 3 years were invited via email to participate (n = 21). No exclusionary requirements were applied. Though all invited individuals expressed interest in joining the QUEST working group, a total of 17 people ultimately participated. Individuals agreed to participate in working group conversations by responding in writing to the email invitation. All working group members had participated in analysis of at least one qualitative data set related to communication, with most participating in qualitative research for at least one year (although outliers included 1 member with a 2-month qualitative research elective and 1 member with 5+ years of qualitative research participation). Most of the group was comprised of nursing/medical trainees (e.g., undergraduate, graduate, nursing, and medical students; fellows; n=13); the group also included 2 clinical research staff who engage in communication with patients and families, 1 child life specialist who participated in qualitative research, and 1 clinician-researcher who oversees qualitative research studies. Members’ training, roles, and experiences interfacing with different types of qualitative data are presented in Table 1 .
QUEST working group member characteristics.
The three lead authors crafted a semi-structured working group discussion guide, with iterative revisions to refine questions for content and language. Supplemental Figure presents the guide, encompassing a semi-structured outline of questions prompts and probes to organize and support cooperative conversation. Working group members were encouraged via email to join a virtual 120-minute discussion; those who could not attend were given an opportunity to respond to the questions in writing. A physician-medical anthropologist with training and expertise in group engagement facilitated the virtual discussion. Twelve QUEST working group members, including the three lead authors, attended the recorded virtual session using WebEx (an online platform for virtual group meetings). The conversation introduction included reminders about the importance of reflexivity and how participants’ positionality influences (and may bias) perspectives. Throughout the virtual discussion session, each participant remained engaged and interacted with most question probes, yielding multiple responses for each question. A working group format was used intentionally to explore the targeted question, given the positive potential for group dynamics to help with idea generativity and allow reflections to build upon others’ thoughts and observations [ 20 , 21 ]. Most working group members were students and trainees or clinical research staff, interacting within similar hierarchical tiers. Recognizing the potential for hierarchy to constrain conversation, the one faculty member in a supervisory position observed quietly, engaging only when asked a direct question by another working group member.
Five working group members were unable to attend the virtual discussion due to their training schedules, and they wished to participate in the exploratory question. To ensure inclusion of their voices and perspectives, they were given an opportunity to provide written reflection responses to each item in the structured discussion guide; these lengthy responses were shared via email to contribute their perspectives to the conversation.
Following data generation, the three lead authors initially conducted memo-writing of the recorded discussion and written responses to begin reflecting on and discussing emerging patterns in working group conversation content [ 22 ]. Memo-writers purposefully represented different perspectives from a current clinical trainee, a research staff member, and a faculty member, with iterative discussions held in person and via email to explore how different viewpoints influenced reflections in memos and examine internal biases shaping thoughts and assessments. Content analysis was used to synthesize working group transcripts as this method provides a rigorous process for identification of concepts and themes within text. As concepts were inductively generated via memo-writing, findings were shared with all QUEST members for iterative reflection and input. The QUEST working group collaborated to synthesize and review key themes, with cycles of review and refinement among authors [ 23 , 24 ]. The final report was presented to the working group for member-checking [ 25 ], with confirmation from all authors that thematic findings reflected the comprehensive content of working group discussions.
Working group members consistently emphasized the value of immersion in qualitative research, highlighting the utility of engagement with audio recorded and/or transcribed clinical encounters that included challenging communication scenarios ( Fig. 1 ). Nearly all members described the impact of qualitative research experiences on their personal communication skills and practice, and two driving themes emerged to characterize the “value added” by qualitative research: 1) the tangible benefits of exposure to difficult medical communication prior to real-life encounters; and 2) the potential for long-lasting impact and sustained influence of qualitative research experiences on future clinical practice, including three specific impacts on communication skills (“the 3Cs”).

Influences of qualitative research immersion on learner communication skills.
3.1. Immersive learning prior to real-life training and practice
For many working group members, communication challenges in healthcare were largely hypothetical prior to their participation in qualitative research. Coding real clinical encounters as part of qualitative research revealed the complexity of interpersonal communication and offered lessons for how to navigate difficult conversations with actual patients and families: “I really saw models of what this actually looks like and how do patients and their families respond to different styles.” Authors with limited previous exposure to clinical encounters also shared how immersion in raw qualitative data helped them recognize the emotional intensity experienced by patients, families, and clinicians:
“Listening [to audio-recorded medical dialogue] really helped me to understand how much tension there can be in a room… Just listening to long pauses of silence helped me understand that [prognostic communication] can be really challenging emotionally, both on the clinician side and the family and patient side, how challenging it can be to navigate that both as a parent and as a clinician.”
Another member described how her participation in qualitative research as a medical student informed her future practice as a resident:
“I began intern year in the intensive care unit and had several patients die within my first two to three weeks of residency. Communicating with these families about the goals or priorities of their loved one and then having to tell them when that person had died required attention to detail, meticulous word choice, and rapport building. All of these skills were taught or honed by the coding experience.”
Universally, working group members highlighted how exposure to “real” clinical encounters offered them unique experiences to observe communication skills and reflect on interpersonal dynamics that they could carry forward into their future clinical practice.
3.2. Sustained influence on future clinical practice
Overall, working group members agreed that participating in qualitative research had a greater impact than they anticipated on the way that they provide clinical care. One child life specialist explained specifically how real clinical encounters still shape her everyday clinical practice:
“I was not anticipating the coding experience [would] play such an influential role in my day-to-day clinical practice. The process has made me more reflective in my everyday interactions with patients and families, as I have various narratives to refer back to, and [they] are typically at the forefront of my thoughts when interacting with families now.”
A palliative care physician explained how specific clinician-patient or clinician-family interactions persist in a clinician’s mind through years of clinical practice: “Some of the quotes stick with you and influence your practice.” Many working group members echoed this idea of staying power – conversations witnessed through reading transcripts or listening to audio recordings remained impressed on their minds as reference points for choosing language, reflecting on clinical encounters, and remembering the complexities of patients’ and families’ experiences.
The working group also identified three key themes characterizing how immersion in qualitative communication research influenced aspiring clinicians’ self-perceived communication skills development – the 3Cs ( Table 2 ): 1) C onnection, therapeutic alliance, and accompaniment; 2) C larity and prognostic communication; and 3) C ompassion, empathy, and understanding.
3Cs: Key themes characterizing the impact of qualitative research participation on learners’ communication skills development.
3.3. Skills for aspiring clinicians: connection
Working group members described how witnessing clinicians’ approaches for establishing connection and building therapeutic alliance with patients and families helped them learn how to develop their own skills. Many mentioned the importance of listening carefully to patients and families, as well as the value of silence:
“This experience helped me further develop active listening skills. I think silence is something that often makes people uncomfortable; however, this experience made me realize how many families…want and need a space to process and have others actively listen to their thoughts and emotions. It was very humbling to be a part of that process.”
As detailed in Table 2 , others discussed how they came to realize that affirming patients’ and families’ emotions is essential to establishing therapeutic alliance and how witnessing clinicians establish rapport with families led them to aspire to do the same in their own clinical practice.
Several working group members contemplated the sensation of privilege upon entering what felt like experiencing prognostic communication with the patient and family – accompanying them through the illness trajectory. One nurse practitioner explained that, despite having been a bedside oncology nurse prior to participating in qualitative research, listening to recorded conversations was the first time she had been “in the room” during prognostic disclosure:
“What really struck me was how you do feel like you’re living through the process with the family… Living all those intense moments with the family feels extremely different than even what the providers themselves might feel.”
Some participants felt the emotion of experiencing disease reevaluation discussions with the families so intensely that they became uncomfortable and concerned they might be intruding: “In a way, it almost feels like you are listening to a private conversation, like you’re impinging on their privacy.” All participants agreed that reviewing transcripts and recordings represented more than a research task – for many, it felt like an honor to witness families most challenging moments.
3.4. Skills for aspiring clinicians: clarity
One working group member, who began qualitative research as an undergraduate student and is currently a medical resident, explained how her prior experiences with qualitative research actively motivate her to be clearer in her communication with patients and families:
“My experience with [reading transcripts] has…informed core beliefs I have regarding communication with patients, especially related to giving bad news… Remembering how [a particular] family felt from not discussing the full extent of the truth encourages me to…talk about all possible outcomes early… It also motivates me to be honest, even when it is hard. So many parents [in interviews]…said they didn’t want someone to ‘beat around the bush.’ I want to tell the truth in a kind way and set the scene for success.”
Another member, who was exposed to qualitative research while practicing as a child life specialist, also underscored how qualitative research training has helped her better understand the value of intentionality when communicating bad news, including exploring and accepting patients’ and families’ reactions to the news conveyed:
“The experience of coding has definitely influenced my clinical practice. One parent…shared that her first thought when our team offered legacy building interventions was: ‘Are you f***ing kidding me?’ I find myself actively thinking about this parent and her reaction every time that I am about to offer these types of interventions – and furthermore thinking about the themes that emerged when coding this data that reiterated the various ways our introduction of these interventions may be improved.”
Several working group members also explained that clinical communication research projects led them to develop heightened awareness of the impact of language on patients/families: “[I developed] awareness that the words that we use can have these long-lasting ramifications and impact. It gives you a heightened cognizance of how important the language and interactions are.”
3.5. Skills for aspiring clinicians: compassion
Compassion through understanding and empathy was a pervasive theme across working group members’ reflections on participating in qualitative research: “I think [participation in qualitative research] helps foster empathy and compassion. Medicine can be very draining; there are many systemic barriers to providing care in a patient-centered, thoughtful, and kind way.” Many articulated how qualitative research participation helped them to dig deeper into patients’ and families’ stories, not just limited to clinical encounters in clinical spaces: “Seeing the stories, not just the patients. This work inherently teaches you about the value of the story.” One author explained that this sense of walking with patients and families helped foster patience: “I think [patience] comes from having more perspective into their narrative and giving them the benefit of the doubt because you have not just the hospital, clinical side – you have more insight into the other side of things.” Working group members emphasized how more complex understandings of patients’ and families’ lives generated deeper understanding and compassion, which they recognized as skills integral to provision of high-quality medical care in their future careers.
3.6. Unanticipated impact: Self-care and professional affirmation
Working group members identified various unexpected positive outcomes from participation in qualitative research, including how it influenced perceptions of self-care and professional affirmation. Witnessing the strength and wisdom of parents of children with serious illness and/or bereaved parents inspired many learners. One member explained that studying communication through qualitative research methods allowed her to be less harsh on herself in evaluating her own communication: “This experience has provided me with the space to allow myself grace when I know I could have completed an intervention in a different way.” Several also shared that the research experience has affirmed their decisions into go into healthcare professions:
“I remember sitting down and really listening to one of the conversations, and immediately, I was so filled with emotion that tears really filled my eyes, partly because of the emotion of the conversation but also because I had been longing for this viewpoint, as it addressed why I had become really passionate about nursing. It reignited my passion for nursing and healthcare.”
Another echoed this same idea, explaining that the work reinvigorated her medical studies: “Seeing how this life experience affects these parents each and every day really allowed me to see the gravity of the situation and gave me the motivation to continue on this journey towards becoming a doctor.”
An additional unexpected benefit of qualitative research participation was deconstruction of hierarchy in clinical medicine. The process through which team members from various roles and statuses came together to reach consensus in coding belied self-perceived hierarchical identities:
“I was surprised by the richness of diligence and detail involved in the work, including check mechanisms that produced consensus. I found the reconciliation process to be a perfect example of this. The meetings were equal parts presentation of fact and defense of personal standpoint that involved everyone as an equal partnered contributor.”
An author who participated in this research as an undergraduate emphasized the power of connection among team members that overrode the difference of education level or training experience: “We connected on raw emotion that we felt from the conversation – even though we may be at very different stages of life, we still felt the same responses to some scenarios.”
Working group members emphasized that qualitative research participation also helped them develop skills in teaching and mentoring, as well as influenced how they approached the development of communications training programs and curricula in the future. Finally, they explained that it inspired them to continue self-reflection on communication, driving them to develop their practices of life-long learning. Table 3 articulates both benefits in more detail. Alongside these positive benefits, working group members also identified unexpected challenges, acknowledging the emotional weight of accompanying families, bearing witness, and feeling responsible for empathetic and compassionate communication, detailed in Table 4 .
Benefits of qualitative research participation as educators and life-long learners.
Unexpected challenges of participation in qualitative research: the emotional weight of accompanying families, bearing witness, and feeling responsible for empathetic and compassionate communication.
4. Discussion and conclusion
4.1. discussion.
Clinician-researchers with immersive experience in qualitative research identified the value of research participation on gaining and sustaining important communication skills. Key lessons from the working group are summarized in Fig. 2 .

Key takeaway lessons from exploratory investigation of influences of participation in qualitative research on clinicians-in-training.
These findings raise the possibility that opportunities for participation in qualitative research alongside communication scientists may be an under-utilized resource for medical educators seeking to support trainees in developing important communication skills. Theories of experiential learning [ 26 , 27 ] and reflexive learning [ 28 , 29 ] underscore the potential educational benefit of qualitative research participation [ 30 ], in that they suggest that learning through doing and informally and formally reflecting on experiences may be more effective at conveying key lessons in clinical communication than didactics, small group discussions, or other instruction on the topic. We encourage medical educators and communication researchers to explore strategies for collaboration through engagement of undergraduate, graduate, medical, and post-graduate clinicians- and researchers-in-training. Rethinking the potential of qualitative research to improve clinical education may be bidirectionally beneficial, strengthening communication skills training while also reinforcing the value of qualitative research.
Further, these data preliminarily suggest that regular immersion in qualitative data may support resilience building for learners, and future research is needed to explore this potential. Listening to recordings or reading transcripts from clinical encounters offers trainees a unique opportunity to bear witness and experience diagnostic or prognostic communication, metaphorically standing alongside the patient and family, while still maintaining space to reflect, question, cry, otherwise respond, pause, discuss, and debrief the encounter. DIPEx International and other similar resources amalgamating qualitative research data can be incorporated into learning opportunities that enable more clinical trainees to conduct qualitative research.
The research team functions as a support group within which researchers can process the emotional weight and lessons learned from the encounter. This “practice run” prior to driving difficult conversations offers trainees the chance to develop communications skills and bolster both their approach and confidence prior to patient encounters [ 31 ]. Prior qualitative research experiences enable trainees to avoid feeling overwhelmed, hitting the ground running, prepared for the emotional burden and capable of listening, leaving room for silence, building empathy, and prioritizing compassion. Working group members felt prepared not only to practice skillful communication, but also to teach strategies.
Findings from the work should be interpreted in the context of limitations. Working group members all had participated in qualitative research previously and thus likely had a predisposition for engagement with and enthusiasm for communication research and qualitative methodology. It is possible that a different group of learners – perhaps those who tend toward a more positivist sensibility – may not find participation in qualitative research as useful for communication skills development. Additionally, not all QUEST working group members had an opportunity to participate in collective, generative dialogue to build upon ideas in real time. Several members participated by sharing their perspectives in writing, and although this allowed for enrichment of perspectives and experiences, it is not possible to know how additional interaction may have shaped the collective message.
Innovation: We offer two innovative approaches to healthcare professions education. First, we offer an innovative research methodology – an adaptation of autoethnography that involves collaboration among a group of people who share an experience (i.e., qualitative research participation), generate reflective data about that experience, and then work together to analyze those data. The methodology carried out by the collaborative working group to explore an a priori question related to our collective experiences is innovative, in that there was no division between “researchers” and “study participants” and thus the process was not traditional “research” but rather collaborative generation of knowledge. Inspired by autoethnographic methods, in which one person generates data from their own experiences, observations, and reflections and then analyzes those data, we have embarked upon a modified autoethnographic endeavor in which we collected data from ourselves as a working group made up of people with shared qualitative communication research participation experience and then analyzed and interpreted those data collectively. Different members of the working group participated in different ways to generate and analyze the data; we generated our own data and then studied our own experiences by analyzing the data. This methodology enables and may even empower health professions educators to study their own educational innovations.
Second, we offer a pedagogical innovation for health professions education, in which participation in qualitative research provides a learning experience for students in the health professions. We found that experience in qualitative research about communication facilitated learning about how to connect with patients and families, communicate clearly, and practice with empathy and compassion. Beyond the communication domain, additional applications of qualitative research experience as a learning opportunity might involve topics such as resilience, mindfulness, meaning-making, and self-reflection as tools to combat burnout or compassion fatigue.
With regards to application of findings, rethinking qualitative research participation as an underutilized educational opportunity is pedagogically innovative and should inspire medical education leaders to collaborate with communication researchers in engagement of undergraduate, graduate, medical, and post-graduate trainees. Collaborations between health professions educators and qualitative researchers could lead beyond communication, expanding to teaching about self-awareness, humility, active listening, quiet observation, and the critical importance of triangulating data to deepen information synthesis and interpretation. Rich opportunities exist to further probe how students immersed in qualitative research gain knowledge and skills. Further research also is needed to explore the benefits of partnerships between medical education and qualitative research teams in development of immersion-based communication learning.
4.2. Conclusion
Exposing clinical trainees to communication through participation in qualitative research has the potential to enhance self-perceived communication competency in three key domains: (1) Connection, (2) Clarity, and (3) Compassion, preparing them for future clinical encounters. Further, such exposure may have the potential to strengthen emotional intelligence and promote self-care, professional affirmation, and resilience.
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Credit author statement
Amy Porter: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Writing – original draftWriting
Cameka Woods: Data curation, Formal analysis, Investigation, Methodology, Project administration, Writing – review & editing.
Erica Kaye: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Writing – original draft
All other authors: Data curation, Formal analysis, Investigation, Methodology, Writing – review & editing
Declaration of Competing Interest
Acknowledgements.
We thank working group members’ qualitative research mentors and collaborators for providing teaching and support throughout their qualitative research experiences.
Appendix A Supplementary data to this article can be found online at https://doi.org/10.1016/j.pecinn.2022.100079 .
Contributor Information
Taylor aglio, jacob applegarth.
b Oakland University William Beaumont School of Medicine, Royal Oak, MI, USA (Jacob)
Tharwa Bilbeisi
c University of Memphis, Memphis, TN, USA
d Rhodes College, Memphis, TN, USA
Katie Greer
e University of California Davis Children’s Hospital, Sacramento, CA, USA
Rachel Huber
Ashley kiefer autrey.
f Children’s Hospital of New Orleans, New Orleans, LA, USA
Sarah Rockwell
g Emory University, Atlanta, GA, USA
Marta Salek
Melanie stall.
h University of Texas Southwestern Medical Center, Dallas, TX, USA
Mariela Trejo
i University of Maryland School of Medicine, Baltimore, MD, USA
j University of Tennessee Health Sciences Center, Memphis, TN, USA
Kristina Zalud
k St. Louis Children’s Hospital, St. Louis, MO, USA
Appendix A. Supplementary data
QUEST Working Group Discussion Guide

- Advisers & Contacts
- Bachelor of Arts & Bachelor of Science in Engineering
- Prerequisites
- Declaring Computer Science for AB Students
- Declaring Computer Science for BSE Students
- Class of '25, '26 & '27 - Departmental Requirements
- Class of 2024 - Departmental Requirements
- COS126 Information
- Important Steps and Deadlines
- Independent Work Seminars
- Guidelines and Useful Information
- Undergraduate Research Topics
- AB Junior Research Workshops
- Undergraduate Program FAQ
- How to Enroll
- Requirements
- Certificate Program FAQ
- Interdepartmental Committee
- Minor Program
- Funding for Student Group Activities
- Mailing Lists and Policies
- Study Abroad
- Jobs & Careers
- Admissions Requirements
- Breadth Requirements
- Pre-FPO Checklist
- FPO Checklist
- M.S.E. Track
- M.Eng. Track
- Departmental Internship Policy (for Master's students)
- General Examination
- Fellowship Opportunities
- Travel Reimbursement Policy
- Communication Skills
- Course Schedule
- Course Catalog
- Research Areas
- Interdisciplinary Programs
- Technical Reports
- Computing Facilities
- Researchers
- Technical Staff
- Administrative Staff
- Graduate Students
- Undergraduate Students
- Graduate Alumni
- Climate and Inclusion Committee
- Resources for Undergraduate & Graduate Students
- Outreach Initiatives
- Resources for Faculty & Staff
- Spotlight Stories
- Job Openings
- Graduate Program
Advice on Research Communications Skills
Great researchers are great communicators. This page provides some resources to help you develop your communication skills.
- How to read a paper . S. Keshav. Note: The general principles here are very useful (read a paper in several iterations of increasing depth depending upon your objectives and interest). However, the amount of time it may take you to read a paper will vary greatly depending on the paper and the area. Assuming you can understand a paper deeply in just a few hours may be unrealistic for some papers in some areas. It may take you days or weeks. Do not get discouraged if it takes you more time than suggested here.
- Go to Princeton colloquia, job talks, area meetings, general exams, pre-FPOs and FPOs. Think about what speakers in each context are doing well (or not so well) to communicate their content effectively and memorably.
- How to give a great research talk . Simon Peyton Jones.
- Presenting a technical talk . Nick Feamster and Alex Gray.
General Advice & Courses
- Read more . Of anything that is well written. Doing so improves your vocabulary and exposes you to varied sentence structures. For instance, subscribe to National Geographic or the Atlantic. Start immediately. Improving communication skills is a long-term project and it pays to start immediately.
- Take one of Princeton's writing seminars for graduate students when you have time.
- Join one of Princeton's dissertation boot camps (which doesn't just have to be for writing your thesis, but could be for writing a paper)
- Take Stanford's free online writing class for the sciences when you have time.
- Read article on Mathematical Writing
Internet Articles
- The science of scientific writing . George Gopen and Judith Swan.
- Writer's block is not a struggle with your writing but with your thinking . Write your way out of it.
- Story-telling 101: Writing tips for academics . Nick Feamster and Alex Gray.
- Dave Patterson's writing advice . Dave Patterson.
- How to write a great research paper . Simon Peyton Jones.
- The curse of knowledge . Benjamin Pierce.
- How to give a bad talk (circa 1983) . Dave Patterson.
- Style: Toward clarity and grace . Joseph Williams.
- How to write a lot: A practical guide to academic writing . Paul Silvia.
- The elements of style . William Strunk and E. B. White.
- Writing for computer science. Justin Zobel.
Book a discovery call • [email protected] • +43 660 378 2939

Practical, engaging communication training for researchers and scientists
We’re here to help researchers and scientists hone their communication skills and use them to promote their work., clearly, confidently, and without “dumbing things down”..


Research and science communication training
We offer online, blended-learning, hybrid and in-person workshops and training programmes to equip researchers, academics and scientists with the communication skills they need to talk about their work – with non-experts and experts, in a way that is clear, authentic and confident.
Where do you want to go today?
Here’s an overview of the themes we cover
Are you looking for something else? Would you like us to tailor a programme for your group? Tell us more and we’ll send you a custom proposal based on your needs →
Personal branding & visibility
Building a brand and online presence for your research career, networking for success for scientists and researchers, how to "wow" when it's all online in the research world, speaking & presenting, storytelling and narrative skills for researchers, crafting clear, focused key messages for communcating research, presentation & speaking skills for researchers, media awareness and interview training for researchers, easy elevator pitches for researchers, visual, social media & design, website design & management skills for researchers and research groups, podcasting skills for researchers, poster design skills for researchers.
- Social media for researchers
Infographics & data visualisation for researchers
Interpersonal skills, navigating different communication styles for researchers and research groups, non-verbal communication skills for researchers, building cross-cultural intelligence for researchers, bite-sized learning & workshops, short, fast-paced mini-workshops, short online sessions for large groups, information-packed presentations, short talks and webinars.
Fancy a chat? Who we help


APPLY NOW --> REQUEST INFO
Apply Today
Ready to apply to Penn LPS Online? Apply Now
Learn more about Penn LPS Online
Request More Information
Why excellent communication skills are vital to a successful science career

What is communication in science?
Science communication involves taking technically complex scientific topics and crafting them into accessible, informative, and compelling content for specific audiences. This audience could be scientific peers, the media, potential investors, government or other leadership decision-makers, or the general public. Successful communication requires strong scientific and industry expertise and practical messaging skills to bridge the knowledge gap between researchers and other diverse groups.
Academics, journalists, technical writers, marketing and public relations professionals, and environmental advocates may also benefit from building strong rhetorical abilities to help further society’s understanding of scientific research. Whether you aspire to become a scientist or a writer, to be a successful science communicator you must develop the skills necessary to explain relevant findings and why people should care.
Different types of science communication
In the past, the preferred channels for science communication included scientific journals, books, conferences, and traditional forms of mass media. But with advances in technology—and changes in the way people consume information—science communication has branched out into documentaries, podcasts, webinars, digital newsletters and magazines, social media, and virtual or in-person presentations such as TED Talks.
With an increase in online misinformation and a decrease in trust in the scientific community from certain members of the public and government, it’s more critical than ever to identify engaging ways to reinforce the validity of scientific research. The types of communication you may develop as a scientist include presentations to foster partnerships, academic papers to inform peers, grant proposals to obtain funding for research, or features and interviews with media outlets to educate the world.
Strategies for science communication
Strong communication skills are essential for networking, collaborating, educating, and succeeding in a career as a scientist. Below are important strategies you can employ to strengthen your science communication and help ensure your message is received.
1. Pinpoint your communication goals
The first step in creating effective science messaging is to identify your goals. According to the American Association for the Advancement of Science (AAAS), examples of short-term objectives for science communication include raising awareness of a particular topic and making scientists, and science in general, more relatable. Common long-term goals include engaging the public to build trust, influence policy, improve scientific research, advocate for change, and create a positive dialogue.
The goals for your science communication will vary depending on the topic and target audience. If you’re communicating research on the efficacy of the flu vaccine to the general public, your goal is likely to educate people on the importance of vaccination and convince them to make an appointment. But if you’re speaking to mass media, your messaging may focus on rising hospitalization rates and the vaccine’s effectiveness to establish relevance.
2. Tailor messaging to your audiences
Multiple audiences consume scientific communications, so it’s essential to customize your messaging to align with each group’s interests and needs. For instance, messaging for potential research funders should include hard numbers highlighting the possible return on the investment. In contrast, conversations with a potential partner may focus on the expertise of the research team, prior successes, and the benefits of collaborating.
The AAAS recommends asking the following questions to frame your narrative more effectively:
- Which audience interests may align with my research topic?
- What do I have in common with the target audience?
- What types of questions might the audience have?
If you’re eager to enhance your rhetorical prowess to help you advance your career, CLCH 3000: Communicating Science at Penn LPS Online is the course for you. Focusing on climate change issues, you’ll learn how to refine your communication skills to relate scientific concepts and quantitative data through messaging customized for different audiences. You must take at least two undergraduate-level physical science or life science courses before enrolling to set you up for success in this course.
3. Lead with the most critical information
Although scientists generally present key findings at the end of research papers, when communicating to the public, journalists, or fundraising stakeholders, the best practice is to lead with the most important takeaways. The AAAS recommends starting with the big picture and using a three-point structure to build your messaging around how it impacts your audience, including supporting details. Depending on the audience, these could be three conclusions of your research, applications of your findings, or critical data points that indicate a potential solution to a problem.
For instance, in an article in Smithsonian Magazine on top scientific discoveries in 2021, three notable conclusions on a study of the cancer-prone lemon frost gecko include:
- Discovering that a gene called SPINT1, linked to skin cancer in humans, is responsible for the geckos’ golden color and skin tumors
- Studying SPINT1 could help scientists better understand how certain cancers develop in humans
- Researching how the gene is expressed in geckos that don’t develop cancer could help inspire new melanoma treatments
4. Avoid using jargon
Jargon refers to scientific terminology, including abbreviations, acronyms, or other technical terms, that could alienate a broader audience unfamiliar with their meaning. Even within the scientific community, similar language can have completely different connotations, so including jargon can dilute the impact of your messaging. The American Geophysical Union, a leading non-profit scientific association and publisher, recommends asking the following questions to determine whether your phrasing includes jargon:
- Does it have a different meaning in regular conversation?
- Do you only use it when discussing your research?
- Would friends, family, or neighbors be able to explain or define it?
- Does it serve as a barrier to communication rather than a bridge?
- Are there alternatives that would be more widely understood?
An excellent way to avoid jargon and increase relatability in your science communication is to incorporate analogies and anecdotes that make complex topics more accessible. And if you want to engage your audience, it’s vital to appeal to them in a way that allows for dialogue and addresses misconceptions, such as those promulgated on social media, rather than denouncing the people who espouse them.
5. Include data-based visuals
Another strategy to improve the efficacy of your science storytelling is incorporating different media forms to explain research data. This includes photography, illustrations, animation, video, infographics, charts, and graphs. The more interactive you can make the experience, the better. An added benefit of creating visually compelling digital stories, images, and reels is that they are easily shared on social media networks like Facebook, Instagram, Twitter, or Tik Tok. This is a significant advantage because it is easy to customize this media for your target audience, build awareness, and—if you’re successful in your execution—convince your followers to share your communications.
Why is science communication important?
Science communication is important because, when done correctly, it can build trust, educate, and inspire people to do good. In a 2019 review article featured in Frontiers , various accepted definitions of the goals of science communication were cited, including one from The National Academies of Science, Engineering, and Medicine that included:
- Sharing recent findings and generating excitement for science
- Developing and growing the public appreciation of science
- Increasing general knowledge and understanding of science
- Influencing opinions, policy preferences, or behavior
- Ensuring a diversity of perspectives is included when pursuing scientific solutions
When research findings are communicated concisely and coherently, there are many benefits to society and the scientific community. According to academic and professional publisher Sciendo, effectual and open-access dissemination of research can build support for science, influence behavior, and support informed decision-making at the individual, community, and governmental levels to help solve societal issues.
This is particularly important when it comes to an urgent subject such as climate change or the proliferation of a virus like COVID-19, as these require actions such as passing evidence-based climate policy initiatives and educating the public on symptoms, risks, and treatments.
Another benefit of compelling science communication is the ability to inspire the next generation of scientists to investigate methods to prevent and cure disease, develop new technologies, and make a positive difference in the world. Read on to learn about five rewarding careers in science that you may want to investigate.
1. Biochemist or biophysicist
Biochemists and biophysicists study the chemical and physical properties of living things and biological processes like cell development, growth, disease, and heredity. The minimum education requirement to work in some entry-level positions in this field is a bachelor’s or master’s degree in biochemistry, biology, chemistry, or physics. However, a PhD is needed to work in independent research-and-development roles.
2. Computer and information research scientist
Computer and information research scientists study and design computing technology to solve complex issues in business, medicine, science, and other fields. Employers typically require a minimum of a master’s degree in computer science or computer engineering for consideration, but certain employers may prefer those with doctorate degrees.
3. Environmental scientist
Environmental scientists specialize in using their expertise to protect the environment and human health by cleaning up pollution, advising policymakers, and working with industries to reduce waste and other hazards. Although some entry-level positions may require a minimum of a bachelor’s degree in natural science or a related field, you may need to obtain a master’s degree to qualify for higher-level roles.
4. Forensic scientist
If you're a true crime buff, you may be familiar with forensic scientists. Responsible for collecting and analyzing evidence, forensic science technicians typically specialize in laboratory analysis or crime scene investigations. Employers may prefer applicants with bachelor’s degrees in biology, physical science, or forensic science, and this role typically requires a significant amount of on-the-job training.
5. Medical scientist
Medical scientists conduct research to help prevent and cure disease and improve overall human health, often through clinical trials and other investigative methods. Medical scientists typically obtain a PhD in biology, chemistry, or a related field. However, some may opt to earn a medical degree instead of, or in addition to, a doctorate.
Start your scientific journey at Penn LPS Online
Whether your career goal in science involves combatting biodiversity losses, mitigating the impacts of global warming and increasing gas emissions, or tracking the epidemiology of new diseases and viruses, you must be capable of convincing others why your research matters.
With the Certificate in Science Foundations at Penn LPS Online, you can enhance your understanding of physical and life sciences and develop the groundwork needed for further study. The Ivy League courses in this program are designed to provide the scientific and mathematical tools to allow you to evaluate data, apply logic, and effectively communicate complex scientific concepts to diverse audiences. The scientific skills and knowledge you acquire may be relevant to careers in health and science adjacent fields of education, public health, and law.
If you want to complete your Bachelor of Applied Arts and Sciences (BAAS) while developing a solid interdisciplinary scientific foundation, the concentration in Physical and Life Sciences may be an ideal fit. With course requirements covering biology, chemistry, and physics, you’ll learn the scientific method, analyze and research alternate points of view, interpret quantitative and qualitative evidence, and communicate scientific findings through oral, visual, and written media. The expertise you obtain may be applicable in health, research, and clinical settings and provides a foundation for pursuing further graduate study.
Ready to get started? Apply today to the Physical and Life Sciences concentration for the BAAS program or enroll in the Science Foundations Certificate . If you haven’t already, fill out our online application form or view our course guide to explore your options.

Explore Jobs
- Jobs Near Me
- Remote Jobs
- Full Time Jobs
- Part Time Jobs
- Entry Level Jobs
- Work From Home Jobs
Find Specific Jobs
- $15 Per Hour Jobs
- $20 Per Hour Jobs
- Hiring Immediately Jobs
- High School Jobs
- H1b Visa Jobs
Explore Careers
- Business And Financial
- Architecture And Engineering
- Computer And Mathematical
Explore Professions
- What They Do
- Certifications
- Demographics
Best Companies
- Health Care
- Fortune 500
Explore Companies
- CEO And Executies
- Resume Builder
- Career Advice
- Explore Majors
- Questions And Answers
- Interview Questions
The Most Important Research Skills (With Examples)
- What Are Hard Skills?
- What Are Technical Skills?
- What Are What Are Life Skills?
- What Are Social Media Skills Resume?
- What Are Administrative Skills?
- What Are Analytical Skills?
- What Are Research Skills?
- What Are Transferable Skills?
- What Are Microsoft Office Skills?
- What Are Clerical Skills?
- What Are Computer Skills?
- What Are Core Competencies?
- What Are Collaboration Skills?
- What Are Conflict Resolution Skills?
- What Are Mathematical Skills?
- How To Delegate
Find a Job You Really Want In
Research skills are the ability to find out accurate information on a topic. They include being able to determine the data you need, find and interpret those findings, and then explain that to others. Being able to do effective research is a beneficial skill in any profession, as data and research inform how businesses operate.
Whether you’re unsure of your research skills or are looking for ways to further improve them, then this article will cover important research skills and how to become even better at research.
Key Takeaways
Having strong research skills can help you understand your competitors, develop new processes, and build your professional skills in addition to aiding you in finding new customers and saving your company money.
Some of the most valuable research skills you can have include goal setting, data collection, and analyzing information from multiple sources.
You can and should put your research skills on your resume and highlight them in your job interviews.
What are research skills?
Why are research skills important, 12 of the most important research skills, how to improve your research skills, highlighting your research skills in a job interview, how to include research skills on your resume, resume examples showcasing research skills, research skills faqs.
- Sign Up For More Advice and Jobs
Research skills are the necessary tools to be able to find, compile, and interpret information in order to answer a question. Of course, there are several aspects to this. Researchers typically have to decide how to go about researching a problem — which for most people is internet research.
In addition, you need to be able to interpret the reliability of a source, put the information you find together in an organized and logical way, and be able to present your findings to others. That means that they’re comprised of both hard skills — knowing your subject and what’s true and what isn’t — and soft skills. You need to be able to interpret sources and communicate clearly.
Research skills are useful in any industry, and have applications in innovation, product development, competitor research, and many other areas. In addition, the skills used in researching aren’t only useful for research. Being able to interpret information is a necessary skill, as is being able to clearly explain your reasoning.
Research skills are used to:
Do competitor research. Knowing what your biggest competitors are up to is an essential part of any business. Researching what works for your competitors, what they’re doing better than you, and where you can improve your standing with the lowest resource expenditure are all essential if a company wants to remain functional.
Develop new processes and products. You don’t have to be involved in research and development to make improvements in how your team gets things done. Researching new processes that make your job (and those of your team) more efficient will be valued by any sensible employer.
Foster self-improvement. Folks who have a knack and passion for research are never content with doing things the same way they’ve always been done. Organizations need independent thinkers who will seek out their own answers and improve their skills as a matter of course. These employees will also pick up new technologies more easily.
Manage customer relationships. Being able to conduct research on your customer base is positively vital in virtually every industry. It’s hard to move products or sell services if you don’t know what people are interested in. Researching your customer base’s interests, needs, and pain points is a valuable responsibility.
Save money. Whether your company is launching a new product or just looking for ways to scale back its current spending, research is crucial for finding wasted resources and redirecting them to more deserving ends. Anyone who proactively researches ways that the company can save money will be highly appreciated by their employer.
Solve problems. Problem solving is a major part of a lot of careers, and research skills are instrumental in making sure your solution is effective. Finding out the cause of the problem and determining an effective solution both require accurate information, and research is the best way to obtain that — be it via the internet or by observation.
Determine reliable information. Being able to tell whether or not the information you receive seems accurate is a very valuable skill. While research skills won’t always guarantee that you’ll be able to tell the reliability of the information at first glance, it’ll prevent you from being too trusting. And it’ll give the tools to double-check .
Experienced researchers know that worthwhile investigation involves a variety of skills. Consider which research skills come naturally to you, and which you could work on more.
Data collection . When thinking about the research process, data collection is often the first thing that comes to mind. It is the nuts and bolts of research. How data is collected can be flexible.
For some purposes, simply gathering facts and information on the internet can fulfill your need. Others may require more direct and crowd-sourced research. Having experience in various methods of data collection can make your resume more impressive to recruiters.
Data collection methods include: Observation Interviews Questionnaires Experimentation Conducting focus groups
Analysis of information from different sources. Putting all your eggs in one source basket usually results in error and disappointment. One of the skills that good researchers always incorporate into their process is an abundance of sources. It’s also best practice to consider the reliability of these sources.
Are you reading about U.S. history on a conspiracy theorist’s blog post? Taking facts for a presentation from an anonymous Twitter account?
If you can’t determine the validity of the sources you’re using, it can compromise all of your research. That doesn’t mean just disregard anything on the internet but double-check your findings. In fact, quadruple-check. You can make your research even stronger by turning to references outside of the internet.
Examples of reliable information sources include: Published books Encyclopedias Magazines Databases Scholarly journals Newspapers Library catalogs
Finding information on the internet. While it can be beneficial to consulate alternative sources, strong internet research skills drive modern-day research.
One of the great things about the internet is how much information it contains, however, this comes with digging through a lot of garbage to get to the facts you need. The ability to efficiently use the vast database of knowledge that is on the internet without getting lost in the junk is very valuable to employers.
Internet research skills include: Source checking Searching relevant questions Exploring deeper than the first options Avoiding distraction Giving credit Organizing findings
Interviewing. Some research endeavors may require a more hands-on approach than just consulting internet sources. Being prepared with strong interviewing skills can be very helpful in the research process.
Interviews can be a useful research tactic to gain first-hand information and being able to manage a successful interview can greatly improve your research skills.
Interviewing skills involves: A plan of action Specific, pointed questions Respectfulness Considering the interview setting Actively Listening Taking notes Gratitude for participation
Report writing. Possessing skills in report writing can assist you in job and scholarly research. The overall purpose of a report in any context is to convey particular information to its audience.
Effective report writing is largely dependent on communication. Your boss, professor , or general reader should walk away completely understanding your findings and conclusions.
Report writing skills involve: Proper format Including a summary Focusing on your initial goal Creating an outline Proofreading Directness
Critical thinking. Critical thinking skills can aid you greatly throughout the research process, and as an employee in general. Critical thinking refers to your data analysis skills. When you’re in the throes of research, you need to be able to analyze your results and make logical decisions about your findings.
Critical thinking skills involve: Observation Analysis Assessing issues Problem-solving Creativity Communication
Planning and scheduling. Research is a work project like any other, and that means it requires a little forethought before starting. Creating a detailed outline map for the points you want to touch on in your research produces more organized results.
It also makes it much easier to manage your time. Planning and scheduling skills are important to employers because they indicate a prepared employee.
Planning and scheduling skills include: Setting objectives Identifying tasks Prioritizing Delegating if needed Vision Communication Clarity Time-management
Note-taking. Research involves sifting through and taking in lots of information. Taking exhaustive notes ensures that you will not neglect any findings later and allows you to communicate these results to your co-workers. Being able to take good notes helps summarize research.
Examples of note-taking skills include: Focus Organization Using short-hand Keeping your objective in mind Neatness Highlighting important points Reviewing notes afterward
Communication skills. Effective research requires being able to understand and process the information you receive, either written or spoken. That means that you need strong reading comprehension and writing skills — two major aspects of communication — as well as excellent listening skills.
Most research also involves showcasing your findings. This can be via a presentation. , report, chart, or Q&A. Whatever the case, you need to be able to communicate your findings in a way that educates your audience.
Communication skills include: Reading comprehension Writing Listening skills Presenting to an audience Creating graphs or charts Explaining in layman’s terms
Time management. We’re, unfortunately, only given 24 measly hours in a day. The ability to effectively manage this time is extremely powerful in a professional context. Hiring managers seek candidates who can accomplish goals in a given timeframe.
Strong time management skills mean that you can organize a plan for how to break down larger tasks in a project and complete them by a deadline. Developing your time management skills can greatly improve the productivity of your research.
Time management skills include: Scheduling Creating task outlines Strategic thinking Stress-management Delegation Communication Utilizing resources Setting realistic expectations Meeting deadlines
Using your network. While this doesn’t seem immediately relevant to research skills, remember that there are a lot of experts out there. Knowing what people’s areas of expertise and asking for help can be tremendously beneficial — especially if it’s a subject you’re unfamiliar with.
Your coworkers are going to have different areas of expertise than you do, and your network of people will as well. You may even know someone who knows someone who’s knowledgeable in the area you’re researching. Most people are happy to share their expertise, as it’s usually also an area of interest to them.
Networking involves: Remembering people’s areas of expertise Being willing to ask for help Communication Returning favors Making use of advice Asking for specific assistance
Attention to detail. Research is inherently precise. That means that you need to be attentive to the details, both in terms of the information you’re gathering, but also in where you got it from. Making errors in statistics can have a major impact on the interpretation of the data, not to mention that it’ll reflect poorly on you.
There are proper procedures for citing sources that you should follow. That means that your sources will be properly credited, preventing accusations of plagiarism. In addition, it means that others can make use of your research by returning to the original sources.
Attention to detail includes: Double checking statistics Taking notes Keeping track of your sources Staying organized Making sure graphs are accurate and representative Properly citing sources
As with many professional skills, research skills serve us in our day to day life. Any time you search for information on the internet, you’re doing research. That means that you’re practicing it outside of work as well. If you want to continue improving your research skills, both for professional and personal use, here are some tips to try.
Differentiate between source quality. A researcher is only as good as their worst source. Start paying attention to the quality of the sources you use, and be suspicious of everything your read until you check out the attributions and works cited.
Be critical and ask yourself about the author’s bias, where the author’s research aligns with the larger body of verified research in the field, and what publication sponsored or published the research.
Use multiple resources. When you can verify information from a multitude of sources, it becomes more and more credible. To bolster your faith in one source, see if you can find another source that agrees with it.
Don’t fall victim to confirmation bias. Confirmation bias is when a researcher expects a certain outcome and then goes to find data that supports this hypothesis. It can even go so far as disregarding anything that challenges the researcher’s initial hunch. Be prepared for surprising answers and keep an open mind.
Be open to the idea that you might not find a definitive answer. It’s best to be honest and say that you found no definitive answer instead of just confirming what you think your boss or coworkers expect or want to hear. Experts and good researchers are willing to say that they don’t know.
Stay organized. Being able to cite sources accurately and present all your findings is just as important as conducting the research itself. Start practicing good organizational skills , both on your devices and for any physical products you’re using.
Get specific as you go. There’s nothing wrong with starting your research in a general way. After all, it’s important to become familiar with the terminology and basic gist of the researcher’s findings before you dig down into all the minutia.
A job interview is itself a test of your research skills. You can expect questions on what you know about the company, the role, and your field or industry more generally. In order to give expert answers on all these topics, research is crucial.
Start by researching the company . Look into how they communicate with the public through social media, what their mission statement is, and how they describe their culture.
Pay close attention to the tone of their website. Is it hyper professional or more casual and fun-loving? All of these elements will help decide how best to sell yourself at the interview.
Next, research the role. Go beyond the job description and reach out to current employees working at your desired company and in your potential department. If you can find out what specific problems your future team is or will be facing, you’re sure to impress hiring managers and recruiters with your ability to research all the facts.
Finally, take time to research the job responsibilities you’re not as comfortable with. If you’re applying for a job that represents increased difficulty or entirely new tasks, it helps to come into the interview with at least a basic knowledge of what you’ll need to learn.
Research projects require dedication. Being committed is a valuable skill for hiring managers. Whether you’ve had research experience throughout education or a former job, including it properly can boost the success of your resume .
Consider how extensive your research background is. If you’ve worked on multiple, in-depth research projects, it might be best to include it as its own section. If you have less research experience, include it in the skills section .
Focus on your specific role in the research, as opposed to just the research itself. Try to quantify accomplishments to the best of your abilities. If you were put in charge of competitor research, for example, list that as one of the tasks you had in your career.
If it was a particular project, such as tracking the sale of women’s clothing at a tee-shirt company, you can say that you “directed analysis into women’s clothing sales statistics for a market research project.”
Ascertain how directly research skills relate to the job you’re applying for. How strongly you highlight your research skills should depend on the nature of the job the resume is for. If research looks to be a strong component of it, then showcase all of your experience.
If research looks to be tangential, then be sure to mention it — it’s a valuable skill — but don’t put it front and center.
Example #1: Academic Research
Simon Marks 767 Brighton Blvd. | Brooklyn, NY, 27368 | (683)-262-8883 | [email protected] Diligent and hardworking recent graduate seeking a position to develop professional experience and utilize research skills. B.A. in Biological Sciences from New York University. PROFESSIONAL EXPERIENCE Lixus Publishing , Brooklyn, NY Office Assistant- September 2018-present Scheduling and updating meetings Managing emails and phone calls Reading entries Worked on a science fiction campaign by researching target demographic Organizing calendars Promoted to office assistant after one year internship Mitch’s Burgers and Fries , Brooklyn, NY Restaurant Manager , June 2014-June 2018 Managed a team of five employees Responsible for coordinating the weekly schedule Hired and trained two employees Kept track of inventory Dealt with vendors Provided customer service Promoted to restaurant manager after two years as a waiter Awarded a $2.00/hr wage increase SKILLS Writing Scientific Research Data analysis Critical thinking Planning Communication RESEARCH Worked on an ecosystem biology project with responsibilities for algae collection and research (2019) Lead a group of freshmen in a research project looking into cell biology (2018) EDUCATION New York University Bachelors in Biological Sciences, September 2016-May 2020
Example #2: Professional Research
Angela Nichols 1111 Keller Dr. | San Francisco, CA | (663)-124-8827 |[email protected] Experienced and enthusiastic marketer with 7 years of professional experience. Seeking a position to apply my marketing and research knowledge. Skills in working on a team and flexibility. EXPERIENCE Apples amp; Oranges Marketing, San Francisco, CA Associate Marketer – April 2017-May 2020 Discuss marketing goals with clients Provide customer service Lead campaigns associated with women’s health Coordinating with a marketing team Quickly solving issues in service and managing conflict Awarded with two raises totaling $10,000 over three years Prestigious Marketing Company, San Francisco, CA Marketer – May 2014-April 2017 Working directly with clients Conducting market research into television streaming preferences Developing marketing campaigns related to television streaming services Report writing Analyzing campaign success statistics Promoted to Marketer from Junior Marketer after the first year Timberlake Public Relations, San Francisco, CA Public Relations Intern – September 2013–May 2014 Working cohesively with a large group of co-workers and supervisors Note-taking during meetings Running errands Managing email accounts Assisting in brainstorming Meeting work deadlines EDUCATION Golden Gate University, San Francisco, CA Bachelor of Arts in Marketing with a minor in Communications – September 2009 – May 2013 SKILLS Marketing Market research Record-keeping Teamwork Presentation. Flexibility
What research skills are important?
Goal-setting and data collection are important research skills. Additional important research skills include:
Using different sources to analyze information.
Finding information on the internet.
Interviewing sources.
Writing reports.
Critical thinking.
Planning and scheduling.
Note-taking.
Managing time.
How do you develop good research skills?
You develop good research skills by learning how to find information from multiple high-quality sources, by being wary of confirmation bias, and by starting broad and getting more specific as you go.
When you learn how to tell a reliable source from an unreliable one and get in the habit of finding multiple sources that back up a claim, you’ll have better quality research.
In addition, when you learn how to keep an open mind about what you’ll find, you’ll avoid falling into the trap of confirmation bias, and by staying organized and narrowing your focus as you go (rather than before you start), you’ll be able to gather quality information more efficiently.
What is the importance of research?
The importance of research is that it informs most decisions and strategies in a business. Whether it’s deciding which products to offer or creating a marketing strategy, research should be used in every part of a company.
Because of this, employers want employees who have strong research skills. They know that you’ll be able to put them to work bettering yourself and the organization as a whole.
Should you put research skills on your resume?
Yes, you should include research skills on your resume as they are an important professional skill. Where you include your research skills on your resume will depend on whether you have a lot of experience in research from a previous job or as part of getting your degree, or if you’ve just cultivated them on your own.
If your research skills are based on experience, you could put them down under the tasks you were expected to perform at the job in question. If not, then you should likely list it in your skills section.
University of the People – The Best Research Skills for Success
Association of Internet Research Specialists — What are Research Skills and Why Are They Important?
MasterClass — How to Improve Your Research Skills: 6 Research Tips
How useful was this post?
Click on a star to rate it!
Average rating / 5. Vote count:
No votes so far! Be the first to rate this post.

Sky Ariella is a professional freelance writer, originally from New York. She has been featured on websites and online magazines covering topics in career, travel, and lifestyle. She received her BA in psychology from Hunter College.
Recent Job Searches
- Registered Nurse Jobs Resume Location
- Truck Driver Jobs Resume Location
- Call Center Representative Jobs Resume Location
- Customer Service Representative Jobs Resume
- Delivery Driver Jobs Resume Location
- Warehouse Worker Jobs Resume Location
- Account Executive Jobs Resume Location
- Sales Associate Jobs Resume Location
- Licensed Practical Nurse Jobs Resume Location
- Company Driver Jobs Resume
Related posts

Most Important Administrative Skills (With Examples)
What Is A Visual Learner?

Domain Knowledge: What Is It And Examples

The Most Important Clerical Skills (With Examples)
- Career Advice >
- Hard Skills >
- Research Skills
Our websites may use cookies to personalize and enhance your experience. By continuing without changing your cookie settings, you agree to this collection. For more information, please see our University Websites Privacy Notice .
UConn Today
- School and College News
- Arts & Culture
- Community Impact
- Entrepreneurship
- Health & Well-Being
- Research & Discovery
- UConn Health
- University Life
- UConn Voices
- University News
April 25, 2024 | Matt Engelhardt
DOE Grants Fund Collaborative Clean Energy Projects
UConn is one of dozens of beneficiaries in funding program to bolster research into hydrogen energy and related projects
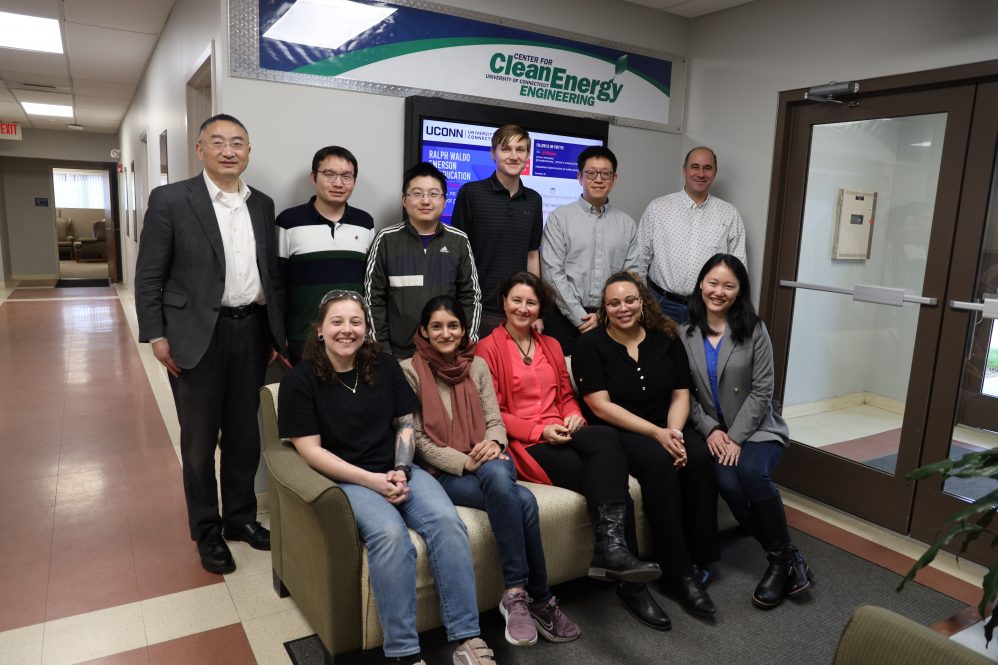
Researchers from the Center for Clean Energy Engineering are conducting collaborative projects funded by the federal Department of Energy.
UConn is a partner in three important projects with industry that have been selected to receive significant federal funding as the Department of Energy (DOE) seeks to advance hydrogen energy technology.
In March, the DOE announced $750 million in funding for 52 projects nationwide, many of them pairing university research with industrial production. The funding is the first phase of the Bipartisan Infrastructure Law, which authorizes $1.5 billion for clean energy projects and aims to create thousands of new jobs. Additionally, the selected projects will provide support to 32 disadvantaged communities across the country.
“Clean energy technology presents so many opportunities for our state and country,” says Pamir Alpay, UConn’s vice president for research, innovation, and entrepreneurship. “Beyond the critical importance of producing clean, renewable energy that mitigates the impact of climate change, the industry’s growth brings with it excellent employment opportunities and the chance to establish Connecticut as a leader in the field.”
UConn faculty are directly involved with three of the funded projects, each relating to electolyzers – devices utilized to split water atoms into hydrogen and oxygen, allowing generation of green hydrogen as a clean energy carrier and a carbon-free feedstock for a number of industrial processes. The work continues a legacy of University researchers collaborating with private and public entities to advance fuel cell technology.
“This is the largest hydrogen program ever to come out of the Department of Energy,” says Jasna Jankovic, an associate professor of Materials Science and Engineering and Center for Clean Energy Engineering (C2E2), and one the primary investigators being funded. “This is really a huge moment in the story of clean energy and we are very happy to be selected with our collaborators to continue our work.”
Jankovic is involved in two of the projects as the UConn PI. She and co-PI Qian Yang, Assistant Professor in the School of Computing, are collaborating with the National Renewable Energy Laboratory (NREL) and Plug Power Inc., the lead of the project, on gigawatt-scale electolyzer component manufacturing and assembly, a project receiving $45.7 million in total funding. UConn will receive approximately $1.9 million of that funding.
Associate research professor for the UConn C2E2 Stoyan Bliznakov is a co-P.I. with Jankovic on a second manufacturing project. They are working with the Farmington-based Mott Corporation on advanced porous transport layer design and manufacturing for electrolyzers. UConn’s portion of the $10 million grant is approximately $2.1 million.
C2E2 and UConn researchers, PI Xiao-Dong Zhou and Co-PIs S. Bliznakov, S. Santos, Y. Wang, and N. Xu, are beneficiaries of the third grant, led by NexTech (d.b.a. Nexceris), funding work on scaleup and demonstration of high temperature electrolysis technology. Collaborators include Georgia Tech, the Idaho National Laboratory, Clark Atlanta University, and Florida A&M. Of the $30 million for the project, UConn will receive close to $1.7 million.
According to C2E2 Director Xiao-Dong Zhou, UConn’s role will continue to build understanding of best techniques to manufacture fuel cells. The industry collaborations allow researchers to understand scaling through the interpretation of system-level data.
“In many ways, producing hydrogen focuses in green energy by using water as the source,” Zhou says. “Dr. Jankovic and her team are focused on the low-temperature side of things. Other members are working on hydrogen sourcing. UConn has expertise and experience in both areas.”
UConn’s research and interest in clean energy technology runs deep. President Radenka Maric – herself a world-renowned researcher and expert in clean energy – has declared climate change as one of the most critical issues facing the world.
“These projects support the initiatives that President Maric lay the foundation for and will contribute to our recognition as leaders,” Jankovic says.
The DOE estimates that the awarded projects will create 1,500 new jobs and reduce the cost of clean energy production. Thousands of additional jobs will support regional economic activity as communities grow the industry.
Stephany Santos, UConn’s executive director of the Vergnano Institute for Inclusion, is pleased with the DOE’s mission to support underserved communities. She says that the process of generation clean energy can sometimes have “dirty” side effects, notably the sources of materials used.
“We are supporting communities that have historically been marginalized,” Santos says. “We are ensuring that those involved are not being exploited and that resources are cleanly sourced.”
At UConn, the projects are creating invaluable opportunities for students to learn from top faculty, as well as contribute to research. Fullbright Scholar Mariah Batool, a Ph.D. candidate in Materials Science, who will work as a postdoctoral fellow on the project with Plug Power, says she has been presented with a huge opportunity.
“It is allowing me to employ all my knowledge and expertise in a more practical approach to bringing forth clean energy advancement, not just only in the academic sense but also in practical and industrial spaces.”
Recent Articles

April 30, 2024
Celebrating UConn’s Class of 2024
Read the article

Neag School Class of 2024 Student Profile: Jennette Lopez

Neag School Class of 2024 Student Profile: Dale Erickson

An official website of the Department of Health & Human Services
- Search All AHRQ Sites
- Email Updates

1. Use quotes to search for an exact match of a phrase.
2. Put a minus sign just before words you don't want.
3. Enter any important keywords in any order to find entries where all these terms appear.
- The PSNet Collection
- All Content
- Perspectives
- Current Weekly Issue
- Past Weekly Issues
- Curated Libraries
- Clinical Areas
- Patient Safety 101
- The Fundamentals
- Training and Education
- Continuing Education
- WebM&M: Case Studies
- Training Catalog
- Submit a Case
- Improvement Resources
- Innovations
- Submit an Innovation
- About PSNet
- Editorial Team
- Technical Expert Panel
Technology as a Tool for Improving Patient Safety
Introduction .
In the past several decades, technological advances have opened new possibilities for improving patient safety. Using technology to digitize healthcare processes has the potential to increase standardization and efficiency of clinical workflows and to reduce errors and cost across all healthcare settings. 1 However, if technological approaches are designed or implemented poorly, the burden on clinicians can increase. For example, overburdened clinicians can experience alert fatigue and fail to respond to notifications. This can lead to more medical errors. As a testament to the significance of this topic in recent years, several government agencies [(e.g. the Agency for Healthcare Research and Quality (AHRQ) and the Centers for Medicare and Medicaid services (CMS)] have developed resources to help healthcare organizations integrate technology, such as the Safety Assurance Factors for EHR Resilience (SAFER) guides developed by the Office of the National Coordinator for Health Information Technology (ONC). 2,3,4 However, there is some evidence that these resources have not been widely used.5 Recently, the Centers for Medicare & Medicaid Services (CMS) started requiring hospitals to use the SAFER guides as part of the FY 2022 Hospital Inpatient Prospective Payment Systems (IPPS), which should raise awareness and uptake of the guides. 6
During 2022, research into technological approaches was a major theme of articles on PSNet. Researchers reviewed all relevant articles on PSNet and consulted with Dr. A Jay Holmgren, PhD, and Dr. Susan McBride, PhD, subject matter experts in health IT and its role in patient safety. Key topics and themes are highlighted below.
Clinical Decision Support
The most prominent focus in the 2022 research on technology, based on the number of articles published on PSNet, was related to clinical decision support (CDS) tools. CDS provides clinicians, patients, and other individuals with relevant data (e.g. patient-specific information), purposefully filtered and delivered through a variety of formats and channels, to improve and enhance care. 7
Computerized Patient Order Entry
One of the main applications of CDS is in computerized patient order entry (CPOE), which is the process used by clinicians to enter and send treatment instructions via a computer application. 8 While the change from paper to electronic order entry itself can reduce errors (e.g., due to unclear handwriting or manual copy errors), research in 2022 showed that there is room for improvement in order entry systems, as well as some promising novel approaches.
Two studies looked at the frequency of and reasons for medication errors in the absence of CDS and CPOE and demonstrated that there was a clear patient safety need. One study found that most medication errors occurred during the ordering or prescribing stage, and both this study and the other study found that the most common medication error was incorrect dose. Ongoing research, such as the AHRQ Medication Safety Measure Development project, aims to develop and validate measure specifications for wrong-patient, wrong-dose, wrong-medication, wrong-route, and wrong-frequency medication orders within EHR systems, in order to better understand and capture health IT safety events.9 Errors of this type could be avoided or at least reduced through the use of effective CPOE and CDS systems. However, even when CPOE and CDS are in place, errors can still occur and even be caused by the systems themselves. One study reviewed duplicate medication orders and found that 20% of duplicate orders resulted from technological issues, including alerts being overridden, alerts not firing, and automation issues (e.g., prefilled fields). A case study last year Illustrated one of the technological issues, in this case a manual keystroke error, that can lead to a safety event. A pharmacist mistakenly set the start date for a medication to the following year rather than the following day , which the CPOE system failed to flag. The authors recommended various alerts and coding changes in the system to prevent this particular error in the future.
There were also studies in 2022 that showed successful outcomes of well-implemented CPOE systems. One in-depth pre-post, mixed-methods study showed that a fully implemented CPOE system significantly reduced specific serious and commonly occurring prescribing and procedural errors. The authors also presented evidence that it was cost-effective and detailed implementation lessons learned drawn from the qualitative data collected for the study. A specific CPOE function that demonstrated statistically significant improvement in 2022 was automatic deprescribing of medication orders and communication of the relevant information to pharmacies. Deprescribing is the planned and supervised process of dose reduction or stopping of a medication that is no longer beneficial or could be causing harm. That study showed an immediate and sustained 78% increase in successful discontinuations after implementation of the software. A second study on the same functionality determined that currently only one third to one half of medications are e-prescribed, and the study proposed that e-prescribing should be expanded to increase the impact of the deprescribing software. It should be noted, however, that the systems were not perfect and that a small percentage of medications were unintentionally cancelled. Finally, an algorithm to detect patients in need of follow-up after test results was developed and implemented in another study . The algorithm showed some process improvements, but outcome measures were not reported.
Usability
Usability of CDS systems was a large focus of research in 2022. Poorly designed systems that do not fit into existing workflows lead to frustrated users and increase the potential for errors. For example, if users are required to enter data in multiple places or prompted to enter data that are not available to them, they could find ways to work around the system or even cease to use it, increasing the potential for patient safety errors. The documentation burden is already very high on U.S. clinicians, 10 so it is important that novel technological approaches do not add to this burden but, if possible, alleviate it by offering a high level of usability and interoperability.
One study used human-factored design in creating a CDS to diagnose pulmonary embolism in the Emergency Department and then surveyed clinician users about their experiences using the tool. Despite respondents giving the tool high usability ratings and reporting that the CDS was valuable, actual use of the tool was low. Based on the feedback from users, the authors proposed some changes to increase uptake, but both users and authors mentioned the challenges that arise when trying to change the existing workflow of clinicians without increasing their burden. Another study gathered qualitative feedback from clinicians on a theoretical CDS system for diagnosing neurological issues in the Emergency Department. In this study too, many clinicians saw the potential value in the CDS tool but had concerns about workflow integration and whether it would impact their ability to make clinical decisions. Finally, one study developed a dashboard to display various risk factors for multiple hospital-acquired infections and gathered feedback from users. The users generally found the dashboard useful and easy to learn, and they also provided valuable feedback on color scales, location, and types of data displayed. All of these studies show that attention to end user needs and preferences is necessary for successful implementation of CDS. However, the recent market consolidation in Electronic Health Record vendors may have an impact on the amount of user feedback gathered and integrated into CDS systems. Larger vendors may have more resources to devote to improving the usability and design of CDS, or their near monopolies in the market may not provide an incentive to innovate further. 11 More research is needed as this trend continues.
Alerts and Alarms
Alerts and alarms are an important part of most CDS systems, as they can prompt clinicians with important and timely information during the treatment process. However, these alerts and alarms must be accurate and useful to elicit an appropriate response. The tradeoff between increased safety due to alerts and clinician alert fatigue is an important balance to strike. 12
Many studies in 2022 looked at clinician responses to medication-related alerts, including override and modification rates. Several of the studies found a high alert override rate but questioned the validity of using override rates alone as a marker of CDS effectiveness and usability. For example, one study looked at drug allergy alerts and found that although 44.8% of alerts were overridden, only 9.3% of those were inappropriately overridden, and very few overrides led to an adverse allergic reaction. A study on “do not give” alerts found that clinicians modified their orders to comply with alert recommendations after 78% of alerts but only cancelled orders after 26% of alerts. A scoping review looked at drug-drug interaction alerts and found similar results, including high override rates and the need for more data on why alerts are overridden. These findings are supported by another study that found that the underlying drug value sets triggering drug-drug interaction alerts are often inconsistent, leading to many inappropriate alerts that are then appropriately overridden by clinicians. These studies suggest that while a certain number of overrides should be expected, the underlying criteria for alert systems should be designed and regularly reviewed with specificity and sensitivity in mind. This will increase the frequency of appropriate alerts that foster indicated clinical action and reduce alert fatigue.
There also seems to be variability in the effectiveness of alert systems across sites. One study looked at an alert to add an item to the problem list if a clinician placed an order for a medication that was not indicated based on the patient’s chart. The study found about 90% accuracy in alerts across two sites but a wide difference in the frequency of appropriate action between the sites (83% and 47%). This suggests that contextual factors at each site, such as culture and organizational processes, may impact success as much as the technology itself.
A different study looked at the psychology of dismissing alerts using log data and found that dismissing alerts becomes habitual and that the habit is self-reinforcing over time. Furthermore, nearly three quarters of alerts were dismissed within 3 seconds. This indicates how challenging it can be to change or disrupt alert habits once they are formed.
Artificial Intelligence and Machine Learning
In recent years, one of the largest areas of burgeoning technology in healthcare has been artificial intelligence (AI) and machine learning. AI and machine learning use algorithms to absorb large amounts of historical and real-time data and then predict outcomes and recommend treatment options as new data are entered by clinicians. Research in 2022 showed that these techniques are starting to be integrated into EHR and CDS systems, but challenges remain. A full discussion of this topic is beyond the scope of this review. Here we limit the discussion to several patient-safety-focused resources posted on PSNet in 2022.
One of the promising aspects of AI is its ability to improve CDS processes and clinician workflow overall. For example, one study last year looked at using machine learning to improve and filter CDS alerts. They found that the software could reduce alert volume by 54% while maintaining high precision. Reducing alert volume has the potential to alleviate alert fatigue and habitual overriding. Another topic explored in a scoping review was the use of AI to reduce adverse drug events. While only a few studies reviewed implementation in a clinical setting (most evaluated algorithm technical performance), several promising uses were found for AI systems that predict risk of an adverse drug event, which would facilitate early detection and mitigate negative effects.
Despite enthusiasm for and promising applications of AI, implementation is slow. One of the challenges facing implementation is the variable quality of the systems. For example, a commonly used sepsis detection model was recently found to have very low sensitivity. 13 Algorithms also drift over time as new data are integrated, and this can affect performance, particularly during and after large disturbances like the COVID-19 pandemic. 14 There is also emerging research about the impact of AI algorithms on racial and ethnic biases in healthcare; at the time of publication of this essay, an AHRQ EPC was conducting a review of evidence on the topic. 15 These examples highlight the fact that AI is not a “set it and forget it” application; it requires monitoring and customization from a dedicated resource to ensure that the algorithms perform well over time. A related challenge is the lack of a strong business case for using high-quality AI. Because of this, many health systems choose to use out-of-the-box AI algorithms, which may be of poor quality overall (or are unsuited to particular settings) and may also be “black box” algorithms (i.e., not customizable by the health system because the vendor will not allow access to the underlying code). 16 The variable quality and the lack of transparency may cause mistrust by clinicians and overall aversion to AI interventions.
In an attempt to address these concerns, one article in 2022 detailed best practices for AI implementation in health systems, focusing on the business case. Best practices include using AI to address a priority problem for the health system rather than treating it as an end itself. Additionally, testing the AI using the health system’s patients and data to demonstrate applicability and accuracy for that setting, confirming that the AI can provide a return on investment, and ensuring that the AI can be implemented easily and efficiently are also important. Another white paper described a human-factors and ergonomics framework for developing AI in order to improve the implementation within healthcare systems, teams, and workflows. The federal government and international organizations have also published AI guidelines, focusing on increasing trustworthiness (National Artificial Intelligence Initiative) 17 and ensuring ethical governance (World Health Organization). 18
Conclusion and Next Steps
As highlighted in this review, the scope and complexity of technology and its application in healthcare can be intimidating for healthcare systems to approach and implement. Researchers last year thus created a framework that health systems can use to assess their digital maturity and guide their plans for further integration.
The field would benefit from more research in several areas in upcoming years. First and foremost, high-quality prospective outcome studies are needed to validate the effectiveness of the new technologies. Second, more work is needed on system usability, how the systems are integrated into workflows, and how they affect the documentation burden placed on clinicians. For CDS specifically, more focus is needed on patient-centered CDS (PC CDS), which supports patient-centered care by helping clinicians and patients make the best decisions given each individual’s circumstances and preferences. 19 AHRQ is already leading efforts in this field with their CDS Innovation Collaborative project. 20 Finally, as it becomes more common to incorporate EHR scribes to ease the documentation burden, research on their impact on patient safety will be needed, especially in relation to new technological approaches. For example, when a scribe encounters a CDS alert, do they alert the clinician in all cases?
In addition to the approaches mentioned in this article, other emerging technologies in early stages of development hold theoretical promise for improving patient safety. One prominent example is “computer vision,” which uses cameras and AI to gather and process data on what physically happens in healthcare settings beyond what is captured in EHR data, 21 including being able to detect immediately that a patient fell in their room. 22
As technology continues to expand and improve, researchers, clinicians, and health systems must be mindful of potential stumbling blocks that could impede progress and threaten patient safety. However, technology presents a wide array of opportunities to make healthcare more integrated, efficient, and safe.
- Cohen CC, Powell K, Dick AW, et al. The Association Between Nursing Home Information Technology Maturity and Urinary Tract Infection Among Long-Term Residents . J Appl Gerontol . 2022;41(7):1695-1701. doi: 10.1177/07334648221082024. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9232878/
- https://www.healthit.gov/topic/safety/safer-guides
- https://cds.ahrq.gov/cdsconnect/repository
- https://www.cms.gov/about-cms/obrhi
- McBride S, Makar E, Ross A, et al. Determining awareness of the SAFER guides among nurse informaticists. J Inform Nurs. 2021;6(4). https://library.ania.org/ania/articles/713/view
- Sittig DF, Sengstack P, Singh H. Guidelines for US hospitals and clinicians on assessment of electronic health record safety using SAFER guides. J ama . 2022;327:719-720.
- https://library.ahima.org/doc?oid=300027#.Y-6RhXbMKHt
- https://www.healthit.gov/faq/what-computerized-provider-order-entry#:~:text=Computerized%20provider%20order%20entry%20(CPOE,paper%2C%20fax%2C%20or%20telephone
- https://digital.ahrq.gov/2018-year-review/research-spotlights/leveragin…
- Holmgren AJ, Downing NL, Bates DW, et al. Assessment of electronic health record use between US and non-US health systems. JAMA Intern Med. 2021;181:251-259. https://doi.org/10.1001/jamainternmed.2020.7071
- Holmgren AJ, Apathy NC. Trends in US hospital electronic health record vendor market concentration, 2012–2021. J Gen Intern Med. 2022. https://link.springer.com/article/10.1007/s11606-022-07917-3#citeas
- Co Z, Holmgren AJ, Classen DC, et al. The tradeoffs between safety and alert fatigue: data from a national evaluation of hospital medication-related clinical decision support. J Am Med Inform Assoc. 2020;27:1252-1258. https://pubmed.ncbi.nlm.nih.gov/32620948/
- Wong A, Otles E, Donnelly JP, et al. External validation of a widely implemented proprietary sepsis prediction model in hospitalized patients. JAMA Intern Med. 2021;181:1065-1070. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2781307
- Parikh RB, Zhang Y, Kolla L, et al. Performance drift in a mortality prediction algorithm among patients with cancer during the SARS-CoV-2 pandemic. J Am Med Inform Assoc. 2022;30:348-354. https://academic.oup.com/jamia/advance-article/doi/10.1093/jamia/ocac221/6835770?login=false
- https://effectivehealthcare.ahrq.gov/products/racial-disparities-health…
- https://www.statnews.com/2022/05/24/market-failure-preventing-efficient-diffusion-health-care-ai-software/
- https://www.ai.gov/strategic-pillars/advancing-trustworthy-ai/
- Ethics and governance of artificial intelligence for health (WHO guidance). Geneva: World Health Organization; 2021. https://www.who.int/publications/i/item/9789240029200
- Dullabh P, Sandberg SF, Heaney-Huls K, et al. Challenges and opportunities for advancing patient-centered clinical decision support: findings from a horizon scan. J Am Med Inform Assoc. 2022: 29(7):1233-1243. doi: 10.1093/jamia/ocac059. PMID: 35534996; PMCID: PMC9196686.
- https://cds.ahrq.gov/cdsic
- Yeung S, Downing NL, Fei-Fei L, et al. Bedside computer vision: moving artificial intelligence from driver assistance to patient safety. N Engl J Med. 2018;387:1271-1273. https://www.nejm.org/doi/10.1056/NEJMp1716891
- Espinosa R, Ponce H, Gutiérrez S, et al. A vision-based approach for fall detection using multiple cameras and convolutional neural networks: a case study using the UP-Fall detection dataset. Comput Biol Med. 2019;115:103520. https://doi.org/10.1016/j.compbiomed.2019.103520
This project was funded under contract number 75Q80119C00004 from the Agency for Healthcare Research and Quality (AHRQ), U.S. Department of Health and Human Services. The authors are solely responsible for this report’s contents, findings, and conclusions, which do not necessarily represent the views of AHRQ. Readers should not interpret any statement in this report as an official position of AHRQ or of the U.S. Department of Health and Human Services. None of the authors has any affiliation or financial involvement that conflicts with the material presented in this report. View AHRQ Disclaimers
Perspective
Perspectives on Safety
Annual Perspective
Patient Safety Innovations
Suicide Prevention in an Emergency Department Population: ED-SAFE
WebM&M Cases
The Retrievals. August 9, 2023
Agent of change. August 1, 2018
Amid lack of accountability for bias in maternity care, a California family seeks justice. August 16, 2023
Mirror, Mirror on the Wall: An Update on the Quality of American Health Care Through the Patient's Lens. April 12, 2006
Improving patient safety by shifting power from health professionals to patients. October 25, 2023
Patient Safety Primers
Discharge Planning and Transitions of Care
Medicines-related harm in the elderly post-hospital discharge. March 27, 2019
Emergency department crowding: the canary in the health care system. November 3, 2021
Advancing Patient Safety: Reviews From the Agency for Healthcare Research and Quality's Making Healthcare Safer III Report. September 2, 2020
Exploring Alternatives To Malpractice Litigation. January 15, 2014
Making Healthcare Safer III. March 18, 2020
Special Section: Patient Safety. May 24, 2006
The Science of Simulation in Healthcare: Defining and Developing Clinical Expertise. November 19, 2008
Compendium of Strategies to Prevent HAIs in Acute Care Hospitals 2014. September 1, 2014
Quality, Safety, and Noninterpretive Skills. November 11, 2015
Patient Safety. November 21, 2018
Ambulatory Safety Nets to Reduce Missed and Delayed Diagnoses of Cancer
Remote response team and customized alert settings help improve management of sepsis.
Using sociotechnical theory to understand medication safety work in primary care and prescribers' use of clinical decision support: a qualitative study. May 24, 2023
Human factors and safety analysis methods used in the design and redesign of electronic medication management systems: a systematic review. May 17, 2023
Journal Article
Reducing hospital harm: establishing a command centre to foster situational awareness.
The potential for leveraging machine learning to filter medication alerts. May 4, 2022
Improving the specificity of drug-drug interaction alerts: can it be done? April 6, 2022
A qualitative study of prescribing errors among multi-professional prescribers within an e-prescribing system. December 23, 2020
The tradeoffs between safety and alert fatigue: data from a national evaluation of hospital medication-related clinical decision support. July 29, 2020
Assessment of health information technology-related outpatient diagnostic delays in the US Veterans Affairs health care system: a qualitative study of aggregated root cause analysis data. July 22, 2020
Reducing drug prescription errors and adverse drug events by application of a probabilistic, machine-learning based clinical decision support system in an inpatient setting. August 21, 2019
Improving medication-related clinical decision support. March 7, 2018
The frequency of inappropriate nonformulary medication alert overrides in the inpatient setting. April 6, 2016
The effect of provider characteristics on the responses to medication-related decision support alerts. July 15, 2015
Best practices: an electronic drug alert program to improve safety in an accountable care environment. July 1, 2015
Impact of computerized physician order entry alerts on prescribing in older patients. March 25, 2015
Differences of reasons for alert overrides on contraindicated co-prescriptions by admitting department. December 17, 2014

Connect With Us
Sign up for Email Updates
To sign up for updates or to access your subscriber preferences, please enter your email address below.
Agency for Healthcare Research and Quality
5600 Fishers Lane Rockville, MD 20857 Telephone: (301) 427-1364
- Accessibility
- Disclaimers
- Electronic Policies
- HHS Digital Strategy
- HHS Nondiscrimination Notice
- Inspector General
- Plain Writing Act
- Privacy Policy
- Viewers & Players
- U.S. Department of Health & Human Services
- The White House
- Don't have an account? Sign up to PSNet
Submit Your Innovations
Please select your preferred way to submit an innovation.
Continue as a Guest
Track and save your innovation
in My Innovations
Edit your innovation as a draft
Continue Logged In
Please select your preferred way to submit an innovation. Note that even if you have an account, you can still choose to submit an innovation as a guest.
Continue logged in
New users to the psnet site.
Access to quizzes and start earning
CME, CEU, or Trainee Certification.
Get email alerts when new content
matching your topics of interest
in My Innovations.

IMAGES
VIDEO
COMMENTS
Whether you're giving a conference talk, writing a grant, or explaining your work to a family member, the ability to effectively communicate about your research is an essential skill for an Early Career Researcher (ECR) to develop.Read on for our interview with science writer Stephen S. Hall to learn how he helps researchers improve their communication skills, and why that matters.
Interspecialist science communication skills are emphasized in multidisciplinary research projects, internal communication at research institutions, educational purposes, and communication with decision-makers and business partners. Such skilled communicators often have thought and speech patterns typical of their discipline that have been ...
Let's read why communicating research is important. It helps boost awareness of your work: Communicating research findings to wider audiences can help bridge the gap between academic research and public understanding and goes a long way in boosting researcher credibility. When the public is informed about your research, it increases the ...
The impact of scientific research relies on the communication of discoveries among members of the research community. Sharing research—allowing other researchers to critique and build upon it—is a fundamental part of the scientific research process. ... Communication Skills for Success in Science. The National Academies of Sciences ...
Effective science communication is necessary for engaging the public in scientific discourse and ensuring equitable access to knowledge. Training doctoral students in science communication will ...
By: Anatoly Gorkun, MD, PhD, Chartered MCIPD Senior Manager, Global Clinical Development, PPD UK Abstract: Effective communication skills in clinical research are vitally important. Due to many conflicting priorities however, clinical research professionals may not have time to manage soft skills. This increases the danger that something may go wrong. This article highlights real-life
Soft skills that senior researchers should build. Soft skills encompass a wide range of abilities, including communication, teamwork, problem-solving, adaptability, and leadership. These skills enable individuals to navigate complex professional environments, work effectively in teams, and build meaningful relationships.
The role of verbal communication skills. You may feel that as a researcher you don't need to worry about verbal communication because you primarily need to focus on written communication - in the form of emails or journal articles. This is not true. As a researcher, you need to heavily rely on verbal communication for several things:
Research and Writing Skills for Academic and Graduate Researchers. Communicating and sharing your research Photo by Tony Stoddard on Unsplash. It is worthwhile considering what methods and communication channels you will use to share your research. Listed below are some common methods for communicating research with a range of audiences ...
Researcher Connect is a series of short interactive modules for researchers at any stage of their career and from any academic discipline. It focuses on the development of excellent communication skills using English language in international, multi-cultural contexts. It is appropriate for B2 (Upper Intermediate) level learners and above, and ...
In the second article of our three-part series about the value of effective research communication, Oxentia consultants Dr Gaelle Coullon and Dr Lauren Sosdian explore some of the common mistakes researchers encounter when communicating to a non-specialist audience and provide a few tips and techniques to improve communication skills.
Results. Three key themes characterizing the impact of qualitative research participation on aspiring clinicians' communication skills development and practice arose - the 3Cs: (1) Connection, therapeutic alliance, and accompaniment; (2) Clarity and prognostic communication; (3) Compassion, empathy, and understanding.Participants emphasized that qualitative research learning improved their ...
Doing so improves your vocabulary and exposes you to varied sentence structures. For instance, subscribe to National Geographic or the Atlantic. Start immediately. Improving communication skills is a long-term project and it pays to start immediately. Take one of Princeton's writing seminars for graduate students when you have time.
Our science communication training and workshops are designed for researchers in science, technology, engineering, medicine and social sciences. If you are interested in building your skills, the skills of a group, or simply raise awareness about science communication at a scientific event, there are several ways that we can help you.
Strategies for science communication. Strong communication skills are essential for networking, collaborating, educating, and succeeding in a career as a scientist. Below are important strategies you can employ to strengthen your science communication and help ensure your message is received. 1. Pinpoint your communication goals.
RDF, to deliver skills training that will help researchers progress in their career and function at an international level. Why choose the Researcher Connect The Researcher Connect approach was formed by our expert development team after many years' analysis and practice of effective communication in multiple cultures around the world.
Purpose: This article presents a systematic review of research into the teaching and learning of communication skills in social work education.Methods: We conducted a systematic review, adhering to the Cochrane Handbook of Systematic Reviews for Interventions and PRISMA reporting guidelines for systematic reviews and meta-analyses.Results: Sixteen records reporting on fifteen studies met the ...
Referred to as "performance-based" or "competence-oriented tests" within the field of competence research, such tests seek to represent holistically the individual's capabilities to act (Blömeke et al., 2015; Shavelson et al., 2018 ). Thus, even the designation of a "competence-oriented examination" of communication skills, for ...
Say it with your body. In face-to-face conversation, body language plays an important role. Communication is 55 percent non-verbal, 38 percent vocal (tone and inflection), and 7 percent words, according to Albert Mehrabian, a researcher who pioneered studies on body language [].Up to 93 percent of communication, then, does not involve what you are actually saying.
Try incorporating their feedback into your next chat, brainstorming session, or video conference. 4. Prioritize interpersonal skills. Improving interpersonal skills —or your ability to work with others—will feed into the way you communicate with your colleagues, managers, and more.
Seven of eight communication skills identified in previous research (Burleson & Samter, 1990; Frymier & Houser, 2000) were perceived by students to be important in the teacher‐student relationship.
Research skills are the ability to find out accurate information on a topic. They include being able to determine the data you need, find and interpret those findings, and then explain that to others. Being able to do effective research is a beneficial skill in any profession, as data and research inform how businesses operate.
modifying or even changing in behaviour. Specifically, communication is held to. share feelings and thoughts for several purposes that aim to connect with others. such as: inspiring, motivati ng ...
Communication skills, such as listening, open-mindedness, empathy, and confidence, are essential for personal and professional development and play a significant role in many disciplines ...
Researchers have found these skills to be associated with numerous desirable performance (e.g., productivity) and health outcomes (e.g., reduced burnout). Therefore, the demand for occupational initiatives which can develop transferable skills is growing and workplaces are increasingly looking outside of work settings for training and ...
C2E2 and UConn researchers, PI Xiao-Dong Zhou and Co-PIs S. Bliznakov, S. Santos, Y. Wang, and N. Xu, are beneficiaries of the third grant, led by NexTech (d.b.a. Nexceris), funding work on scaleup and demonstration of high temperature electrolysis technology. ... Building Communication Skills in Natural Environments. Read the article. April 25 ...
This research aims to compare the developmental profiles of children with autism spectrum disorder (ASD) and children with Down Syndrome (DS) between the ages of 3 and 6 years. The study examines whether these developmental disorders share common developmental milestones or exhibit distinctive characteristics. A total of 43 children, 23 with DS and 20 with ASD, participated in the study.
In the past several decades, technological advances have opened new possibilities for improving patient safety. Using technology to digitize healthcare processes has the potential to increase standardization and efficiency of clinical workflows and to reduce errors and cost across all healthcare settings.1 However, if technological approaches are designed or implemented poorly, the burden on ...