Essay on Smoking
500 words essay on smoking.
One of the most common problems we are facing in today’s world which is killing people is smoking. A lot of people pick up this habit because of stress , personal issues and more. In fact, some even begin showing it off. When someone smokes a cigarette, they not only hurt themselves but everyone around them. It has many ill-effects on the human body which we will go through in the essay on smoking.


Ill-Effects of Smoking
Tobacco can have a disastrous impact on our health. Nonetheless, people consume it daily for a long period of time till it’s too late. Nearly one billion people in the whole world smoke. It is a shocking figure as that 1 billion puts millions of people at risk along with themselves.
Cigarettes have a major impact on the lungs. Around a third of all cancer cases happen due to smoking. For instance, it can affect breathing and causes shortness of breath and coughing. Further, it also increases the risk of respiratory tract infection which ultimately reduces the quality of life.
In addition to these serious health consequences, smoking impacts the well-being of a person as well. It alters the sense of smell and taste. Further, it also reduces the ability to perform physical exercises.
It also hampers your physical appearances like giving yellow teeth and aged skin. You also get a greater risk of depression or anxiety . Smoking also affects our relationship with our family, friends and colleagues.
Most importantly, it is also an expensive habit. In other words, it entails heavy financial costs. Even though some people don’t have money to get by, they waste it on cigarettes because of their addiction.
How to Quit Smoking?
There are many ways through which one can quit smoking. The first one is preparing for the day when you will quit. It is not easy to quit a habit abruptly, so set a date to give yourself time to prepare mentally.
Further, you can also use NRTs for your nicotine dependence. They can reduce your craving and withdrawal symptoms. NRTs like skin patches, chewing gums, lozenges, nasal spray and inhalers can help greatly.
Moreover, you can also consider non-nicotine medications. They require a prescription so it is essential to talk to your doctor to get access to it. Most importantly, seek behavioural support. To tackle your dependence on nicotine, it is essential to get counselling services, self-materials or more to get through this phase.
One can also try alternative therapies if they want to try them. There is no harm in trying as long as you are determined to quit smoking. For instance, filters, smoking deterrents, e-cigarettes, acupuncture, cold laser therapy, yoga and more can work for some people.
Always remember that you cannot quit smoking instantly as it will be bad for you as well. Try cutting down on it and then slowly and steadily give it up altogether.
Get the huge list of more than 500 Essay Topics and Ideas
Conclusion of the Essay on Smoking
Thus, if anyone is a slave to cigarettes, it is essential for them to understand that it is never too late to stop smoking. With the help and a good action plan, anyone can quit it for good. Moreover, the benefits will be evident within a few days of quitting.
FAQ of Essay on Smoking
Question 1: What are the effects of smoking?
Answer 1: Smoking has major effects like cancer, heart disease, stroke, lung diseases, diabetes, and more. It also increases the risk for tuberculosis, certain eye diseases, and problems with the immune system .
Question 2: Why should we avoid smoking?
Answer 2: We must avoid smoking as it can lengthen your life expectancy. Moreover, by not smoking, you decrease your risk of disease which includes lung cancer, throat cancer, heart disease, high blood pressure, and more.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App

Health Effects
Smoking leads to disease and disability and harms nearly every organ of the body.
More than 16 million Americans are living with a disease caused by smoking. For every person who dies because of smoking, at least 30 people live with a serious smoking-related illness. Smoking causes cancer, heart disease, stroke, lung diseases, diabetes, and chronic obstructive pulmonary disease (COPD), which includes emphysema and chronic bronchitis. Smoking also increases risk for tuberculosis, certain eye diseases, and problems of the immune system, including rheumatoid arthritis.
Secondhand smoke exposure contributes to approximately 41,000 deaths among nonsmoking adults and 400 deaths in infants each year. Secondhand smoke causes stroke, lung cancer, and coronary heart disease in adults. Children who are exposed to secondhand smoke are at increased risk for sudden infant death syndrome, acute respiratory infections, middle ear disease, more severe asthma, respiratory symptoms, and slowed lung growth.

Tobacco use increases the risk for many types of cancer, such as Lung cancer.

Heart Disease
Studies show a direct link between cigarette smoking and coronary heart disease.

Smoking, including during the teenage years, increases the risk of dying from COPD.

Smoking during pregnancy increases the risk for pregnancy complications.
Related Materials
- Health Effects of Cigarette Smoking
- Health Effects of Secondhand Smoke
- Tobacco-Related Mortality
- 50 Years of Progress: A Report of the Surgeon General [PDF–35.9 MB]
- U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General . Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2014 [accessed 2016 Dec 20].
To receive email updates about Smoking & Tobacco Use, enter your email address:
- Tips From Former Smokers ®
- Division of Cancer Prevention and Control
- Lung Cancer
- National Comprehensive Cancer Control Program
- Division of Reproductive Health

Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- MyAucklandUni
- Student Services Online
- Class search
- Student email
- Change my password
- MyCDES+ (job board)
- Course outlines
- Learning essentials
- Libraries and Learning Services
- Forms, policies and guidelines
- New students
- Enrol in courses
- Campus card
- Postgraduate students
- Summer school
- AskAuckland
- Student Hubs
- Student IT Hub
- Student Health and Counselling
- Harassment, bullying, sexual assault and other violence
- Complaints and incidents
- Career Development and Employability Services (CDES)
- Ratonga Hauātanga Tauira | Student Disability Services (SDS)
- Rainbow support
- Covid-19 information for our community
- Emergency information
- Report concerns, incidents and hazards
- Health and safety topics
- Staff email
- Staff intranet
- ResearchHub
- PeopleSoft HR
- Forms register
- Careers at the University
- Education Office
- Early childhood centres
- University Calendar
- Opportunities
- Update your details
- Make a donation
- Publications
- Photo galleries
- Video and audio
- Career services
- Virtual Book Club
- Library services
- Alumni benefits
- Office contact details
- Alumni and friends on social media
- No events scheduled for today You have no more events scheduled for today
- Next event:
- Show {0} earlier events Show {0} earlier event
- Event_Time Event_Name Event_Description
- My Library Account
- Change Password
- Edit Profile
- My GPA Grade Point Average About your GPA GPA not available Why can't I see my GPA?
- My Progress
- Points Required Completed points My Progress Progress not available All done!
- Student hubs
- Health and counselling
- All support
- Health, safety and well-being
Breadcrumbs List.
- News and opinion
A short essay on my relationship with tobacco
16 April 2020
Health and medicine , Faculty of Medical and Health Sciences
Opinion: Dr George Laking shares his journey with tobacco, from growing up in a smoking home and trying his first cigarette to his career as an expert in Nicotine Replacement Therapy.

Dad was a smoker when I grew up in the 1970s, his parents too. Mum’s side of the family didn’t. Mum told me of her experiences nursing people with respiratory illness, including a younger person who was killed by asthma. Dad’s father smoked the occasional cigar, I used to like the aroma around their house.
You can still buy “cigarette stink loads”. In 1978 I bought some from the local toyshop and fixed up one of Dad’s cigarettes. The prank made its presence known in the lounge but he just threw the cigarette away and started another one. Some scarily severe asthma attacks around 1982 convinced Dad to finally quit. Instead he took up distance running. He went on to a marathon personal best of 3:03 at Christchurch in 1988.
As kids we used to go into the woods and make forts and puff on bits of straw and cigarettes we’d buy from the old fella at the corner store. A store-owner who sold tobacco to primary students! He seemed ancient to us, but probably hit his teens in the Depression years. It was a different world. Anyhow, those first smokes made no great impression on me, because I had no idea about inhaling. We did learn to cover our tracks with peppermints.
I first inhaled tobacco smoke in a woolshed in Whiteman’s Valley, Upper Hutt, in 1985. Oh boy! Head spins!
It is one of life’s great misfortunes to enjoy a cigarette. Blessed are those who smoke and feel sick. They usually don’t repeat it.
Smoking never really worked for me because I was physically active, running or cycling. I could tell that smoking and sport were incompatible. I might enjoy a cigarette, usually with a drink, in the evening. The next day I would feel even worse. I still carry some nostalgia. Is that a curse? Indonesian clove cigarettes, with the sugar on the filter. The pop and crackle of burning clove oil at night. The stars spinning above me!
I studied medicine and was influenced by a surgeon from Australia who had amputated too many smokers’ limbs. He urged us to become active against tobacco. He said it would be the most effective thing we could do in our career. As a medical student I wrote a submission in support of Helen Clark’s 1990 Smokefree Environments Bill. More comical was to recently find a second submission, the one I didn’t send in, that argued the reverse on some points. I usually tried to understand a topic from different directions.
I spent the 1990s training for a career in medical oncology, with a focus on lung cancer. In 2010 I made a submission to the New Zealand Māori Affairs Select Committee inquiry into the tobacco industry in Aotearoa and consequences of tobacco use for Māori. It supported taxation, cessation services, protection of tamariki, and tikanga approaches to removing tobacco from Māori environments. In the 2010s I continued tobacco control work with Te Hotu Manawa Māori and the Smokefree Coalition. Since 2014 I have been with End Smoking New Zealand.
At the start of the decade I was optimistic about nicotine replacement (NRT) with patches and gum to help people quit, realising that some would need quite high doses. Alas NRT adds only 6–8% to the chance of a sustained quit at 6 months. Even with intensive behavioural support, the 6 month quit was not more than 23.2% in the 2018 Cochrane Review .
During the last decade I have seen tobacco control split over the issue of electronic cigarettes (e-cigarettes). It has often been said that tobacco is an addictive poison. Nicotine brings the addiction and tar brings the poison. Although not totally true, this statement is true in ways that matter.
My colleague Dr Penny Truman from End Smoking New Zealand is doing valuable work on the euphoriant properties of non-nicotine components of smoke. It does not surprise me that nicotine would not be the only euphoriant in smoke. Humans are likely to find smoke appealing, because it means food and warmth. This is in contrast to most animals, that will run away from smoke. Probable exceptions are rats and domestic animals that seek out humans. Penny suspects the combination of nicotine with other euphoriants gives tobacco smoke a double-whammy for addiction.
The marvel of e-cigarettes has been to separate the addiction from the poison in tobacco smoke. We found the same separation in tobacco control. It turns out tobacco control was an alliance between some who were more opposed to the poison of tobacco, and others who were more opposed to the addiction. This alliance was revealed, and strained or broken, by the arrival of e-cigarettes.
A subset of people, strongly opposed to the addictive potential of nicotine, have been trying very hard to find poison in e-cigarettes. In actual fact there is poison everywhere. It is 500 years since Paracelsus taught “everything is a poison – only the dose matters”. So there is an expanding literature reporting toxins in e-cigarette liquids, and effects of e-cigarette aerosols principally in animals, with a small number of studies in people.
There is still no literature to confirm actual physical harm, at a population level, to users of nicotine-containing e-cigarettes. A paper claiming that “some‐day and every‐day e‐cigarette use are associated with increased risk of having had a myocardial infarction” has been retracted .
Of course there must be controls on the ingredients of e-liquids. You probably wouldn’t want to try bitter almond flavour, for example. The main reason we can be confident that e-cigarettes are much safer than smoked tobacco is temperature. An e-cigarette atomises e-liquids at around 240 Celsius. A combustible cigarette burns tobacco leaf at around 900 Celsius. The higher temperature, and complex biological substrate, greatly increase the toxicity of tobacco smoke.
With more than 10 years but less than a lifetime’s experience, it remains possible that an adverse effect of e-cigarettes on population health will emerge. But if it did, that would be a surprise. Whereas we know for a fact that smoking combustible tobacco is highly harmful to health. Some people, motivated by their opposition to addiction, are trying hard to find physical harm in nicotine-containing e-cigarettes. For some people, e-cigarettes are scarily effective nicotine replacement.
Addiction is a harm. It takes away the person’s freedom to choose, and puts them at the mercy of others. In the case of tobacco, those others were an industry focused on profit, that twisted science to deny the harm of its products.
There is still a reckoning to be had with the tobacco industry over its historical actions. It remains to be seen whether the tobacco industry can reinvent itself, now there are finally safer nicotine products available.
I’ve tried a cartridge-based, nicotine salt e-cigarette. It popped and crackled like the clove cigarettes of my youth. That was pleasant enough, but fortunately for me I have not felt the need to go back to it. As a society, we tend to ascribe a power to addictive euphoriants that is near magical. “One puff and you will be hooked”. I have not forgotten my first puff in a woolshed in 1985. But there have been other things in my life that prevented me from returning.
As a society, we should ask what is driving our young people into the arms of tobacco . In 2002 my son chased me around the garden at a lunchtime barbecue, outraged that I was puffing on a cigar. He was right! Even at primary age, many young people are aware that smoking is harmful to health. In 2016 my son as a young adult took up smoking, while working at a restaurant. Fortunately he has since switched to vaping. I can’t deny I would prefer it if he stopped.
It is not always easy to be young, with doubt as to what the future holds for work, housing, and the world at large. Human beings have long turned to chemical relief for stress and anxiety. We should grow a kinder society. Until then, for those who turn to chemicals, they should at least have a safer option.
There is indeed a gateway between vaping and smoking, but the direction of travel is set by policy. Good policy pushes to vaping. Poor policy pushes to smoking. When I say “push”, I don’t mean “shove” or even the trendy “nudge”. I just mean that good policy helps people move in a better direction. There are many other gateways in the continuum from harm to health. Good policy helps people move towards health. To achieve good policy takes courage (to venture where others didn’t), faith (that policy will succeed), and commitment (to accept that good is not perfect, and keep improving).
Dr George Laking (Te Whakatōhea) is an Honorary Academic in oncology within the Faculty of Medical and Health Sciences. He is also the Chair of End Smoking New Zealand.
This article reflects the opinion of the author and not necessarily the views of the University of Auckland.
Used with permission from End Smoking New Zealand, A Short Essay on My Relationship with Tobacco , 15 April, 2020.
Media contact
Gilbert Wong | Research Communications Manager Mobile: 021 917 942 Email: gilbert.wong@auckland.ac.nz
Related links
- Q&A: Does NZ have a place for e-cigarettes?
- Vaping helps smokers quit
- Paper writing help
- Buy an Essay
- Pay for essay
- Buy Research Paper
- Write My Research Paper
- Research Paper Help
- Custom Research Paper
- Custom Dissertation
- Dissertation Help
- Buy Dissertation
- Dissertation Writer
- Write my Dissertation
- How it works
How To Write A Smoking Essay That Will Blow Your Classmates out of the Water

A smoking essay might not be your first choice, but it is a common enough topic, whether it is assigned by a professor or left to your choice. Today we’ll take you through the paces of creating a compelling piece, share fresh ideas for writing teen smoking essays, and tackle the specifics of the essential parts of any paper, including an introduction and a conclusion.
Why Choose a Smoking Essay?
If you are free to select any topic, why would you open this can of worms? There are several compelling arguments in favor, such as:
- A smoking essay can fit any type of writing assignment. You can craft an argumentative essay about smoking, a persuasive piece, or even a narration about someone’s struggle with quitting. It’s a rare case of a one-size-fits-all topic.
- There is an endless number of environmental essay topics ideas . From the reasons and history of smoking to health and economic impact, as well as psychological and physiological factors that make quitting so challenging.
- A staggering number of reliable sources are available online. You won’t have to dig deep to find medical or economic research, there are thousands of papers published in peer-reviewed journals, ready and waiting for you to use them.
Essential Considerations for Your Essay on Smoking
Whether you are writing a teenage smoking essay or a study of health-related issues, you need to stay objective and avoid including any judgment into your assignment. Even if you are firmly against smoking, do not let emotions direct your writing. You should also keep your language tolerant and free of offensive remarks or generalizations.
The rule of thumb is to keep your piece academic. It is an essay about smoking cigarettes you have to submit to your professor, not a blog post to share with friends.
How to Generate Endless Smoking Essay Topic Ideas
At first, it might seem that every theme has been covered by countless generations of your predecessors. However, there are ways to add a new spin to the dullest of topics. We’ll share a unique approach to generating new ideas and take the teenage smoking essay as an example. To make it fresh and exciting, you can:
- Add a historic twist to your topic. For instance, research the teenage smoking statistics through the years and theorize the factors that influence the numbers.
- Compare the data across the globe. You can select the best scale for your paper, comparing smoking rates in the neighboring cities, states, or countries.
- Look at the question from an unexpected perspective. For instance, research how the adoption of social media influenced smoking or whether music preferences can be related to this habit.
The latter approach on our list will generate endless ideas for writing teen smoking essays. Select the one that fits your interests or is the easiest to research, depending on the time and effort you are willing to put into essay writing .
How To Write An Essay About Smoking Cigarettes
A smoking essay follows the same rules as an academic paper on any other topic. You start with an introduction, fill the body paragraphs with individual points, and wrap up using a conclusion. The filling of your “essay sandwich” will depend on the topic, but we can tell for sure what your opening and closing paragraphs should be like.
Smoking Essay Introduction
Whether you are working on an argumentative essay about smoking or a persuasive paper, your introduction is nothing but a vessel for a thesis statement. It is the core of your essay, and its absence is the first strike against you. Properly constructed thesis sums up your point of view on the economic research topics and lists the critical points you are about to highlight. If you allude to the opposing views in your thesis statement, the professor is sure to add extra points to your grade.
The first sentence is crucial for your essay, as it sets the tone and makes the first impression. Make it surprising, exciting, powerful with facts, statistics, or vivid images, and it will become a hook to lure the reader in deeper.
Round up the introduction with a transition to your first body passage and the point it will make. Otherwise, your essay might seem disjointed and patchy. Alternatively, you can use the first couple of sentences of the body paragraph as a transition.
Smoking Essay Conclusion
Any argumentative and persuasive essay on smoking must include a short conclusion. In the final passage, return to your thesis statement and repeat it in other words, highlighting the points you have made throughout the body paragraphs. You can also add final thoughts or even a personal opinion at the end to round up your assignment.
Think of the conclusion as a mirror reflection of your introduction. Start with a transition from the last body paragraph, follow it with a retelling of your thesis statement, and complete the passage with a powerful parting thought that will stay with the reader. After all, everyone remembers the first and last points most vividly, and your opening and closing sentences are likely to have a significant influence on the final grade.
Bonus Tips on How to Write a Persuasive Essay About Smoking
With the most challenging parts of the smoking essay out of the way, here are a couple of parting tips to ensure your paper gets the highest grade possible:
- Do not rely on samples you find online to guide your writing. You can never tell what grade a random essay about smoking cigarettes received. Unless you use winning submissions from essay competitions, you might copy faulty techniques and data into your paper and get a reduced grade.
- Do not forget to include references after the conclusion and cite the sources throughout the paper. Otherwise, you might get accused of academic dishonesty and ruin your academic record. Ask your professor about the appropriate citation style if you are not sure whether you should use APA, MLA, or Chicago.
- Do not submit your smoking essay without editing and proofreading first. The best thing you can do is leave the piece alone for a day or two and come back to it with fresh eyes and mind to check for redundancies, illogical argumentation, and irrelevant examples. Professional editing software, such as Grammarly, will help with most typos and glaring errors. Still, it is up to you to go through the paper a couple of times before submission to ensure it is as close to perfection as it can get.
- Do not be shy about getting help with writing smoking essays if you are out of time. Professional writers can take over any step of the writing process, from generating ideas to the final round of proofreading. Contact our agents or skip straight to the order form if you need our help to complete this assignment.
We hope our advice and ideas for writing teen smoking essays help you get out of the slump and produce a flawless piece of writing worthy of an A. For extra assistance with choosing the topic, outlining, writing, and editing, reach out to our support managers .
Tobacco, Nicotine, and E-Cigarettes Research Report What are the physical health consequences of tobacco use?
Cigarette smoking harms nearly every organ in the body, 1,44 and smoking is the leading preventable cause of premature death in the United States. Although rates of smoking have declined, it is estimated that it leads to about 480,000 deaths yearly. 1 Smokers aged 60 and older have a twofold increase in mortality compared with those who have never smoked, dying an estimated 6 years earlier. 45 Quitting smoking results in immediate health benefits, and some or all of the reduced life expectancy can be recovered depending on the age a person quits. 46
Although nicotine itself does not cause cancer, at least 69 chemicals in tobacco smoke are carcinogenic, 1 and cigarette smoking accounts for at least 30 percent of all cancer deaths. 22 The overall rates of death from cancer are twice as high among smokers as nonsmokers, with heavy smokers having a four times greater risk of death from cancer than nonsmokers. 1
Foremost among the cancers caused by tobacco use is lung cancer. Cigarette smoking has been linked to about 80 to 90 percent of all cases of lung cancer, the leading cause of cancer death for both men and women, and it is responsible for roughly 80 percent of deaths from this disease. 22,47 Smoking increases lung cancer risk five to tenfold, with greater risk among heavy smokers. 48 Smoking is also associated with cancers of the mouth, pharynx, larynx, esophagus, stomach, pancreas, cervix, kidney, and bladder, as well as acute myeloid. 1 Cigarette smoking is not the only form of tobacco use associated with cancers. Smokeless tobacco (see " Other Tobacco Products ") has been linked to cancer of the pharynx, esophagus, stomach, and lung, as well as to colorectal cancer. 49
In addition to cancer, smoking causes lung diseases such as chronic bronchitis and emphysema, and it has been found to exacerbate asthma symptoms in adults and children. Cigarette smoking is the most significant risk factor for chronic obstructive pulmonary disease (COPD). 50 Survival statistics indicate that quitting smoking results in repair to much of the smoking-induced lung damage over time. However, once COPD develops, it is irreversible; COPD-related lung damage is not repaired with time.
Smoking also substantially increases the risk of heart disease, including stroke, heart attack, vascular disease, and aneurysm. 51,52 Cardiovascular disease is responsible for 40 percent of all smoking-related deaths. 53 Smoking causes coronary heart disease, the leading cause of death in the United States. Smoking is also linked to many other major health conditions—including rheumatoid arthritis, inflammation, and impaired immune function. 1 Even young smokers aged 26 to 41 report reduced health-related quality of life compared with nonsmoking peers, according to a cross-sectional population study. 54 Recent animal research also identified a pathway between the pancreas and a part of the brain active in nicotine intake, potentially linking cigarette smoking to the risk of developing Type 2 Diabetes.
Persuasive Essay Guide
Persuasive Essay About Smoking
Persuasive Essay About Smoking - Making a Powerful Argument with Examples

People also read
A Comprehensive Guide to Writing an Effective Persuasive Essay
200+ Persuasive Essay Topics to Help You Out
Learn How to Create a Persuasive Essay Outline
30+ Free Persuasive Essay Examples To Get You Started
Read Excellent Examples of Persuasive Essay About Gun Control
How to Write a Persuasive Essay About Covid19 | Examples & Tips
Crafting a Convincing Persuasive Essay About Abortion
Learn to Write Persuasive Essay About Business With Examples and Tips
Check Out 12 Persuasive Essay About Online Education Examples
Are you wondering how to write your next persuasive essay about smoking?
Smoking has been one of the most controversial topics in our society for years. It is associated with many health risks and can be seen as a danger to both individuals and communities.
Writing an effective persuasive essay about smoking can help sway public opinion. It can also encourage people to make healthier choices and stop smoking.
But where do you begin?
In this blog, we’ll provide some examples to get you started. So read on to get inspired!
- 1. What You Need To Know About Persuasive Essay
- 2. Persuasive Essay Examples About Smoking
- 3. Argumentative Essay About Smoking Examples
- 4. Tips for Writing a Persuasive Essay About Smoking
What You Need To Know About Persuasive Essay
A persuasive essay is a type of writing that aims to convince its readers to take a certain stance or action. It often uses logical arguments and evidence to back up its argument in order to persuade readers.
It also utilizes rhetorical techniques such as ethos, pathos, and logos to make the argument more convincing. In other words, persuasive essays use facts and evidence as well as emotion to make their points.
A persuasive essay about smoking would use these techniques to convince its readers about any point about smoking. Check out an example below:
Simple persuasive essay about smoking
Tough Essay Due? Hire Tough Writers!
Persuasive Essay Examples About Smoking
Smoking is one of the leading causes of preventable death in the world. It leads to adverse health effects, including lung cancer, heart disease, and damage to the respiratory tract. However, the number of people who smoke cigarettes has been on the rise globally.
A lot has been written on topics related to the effects of smoking. Reading essays about it can help you get an idea of what makes a good persuasive essay.
Here are some sample persuasive essays about smoking that you can use as inspiration for your own writing:
Persuasive speech on smoking outline
Persuasive essay about smoking should be banned
Persuasive essay about smoking pdf
Persuasive essay about smoking cannot relieve stress
Persuasive essay about smoking in public places
Speech about smoking is dangerous
Persuasive Essay About Smoking Introduction
Persuasive Essay About Stop Smoking
Short Persuasive Essay About Smoking
Stop Smoking Persuasive Speech
Check out some more persuasive essay examples on various other topics.
Argumentative Essay About Smoking Examples
An argumentative essay is a type of essay that uses facts and logical arguments to back up a point. It is similar to a persuasive essay but differs in that it utilizes more evidence than emotion.
If you’re looking to write an argumentative essay about smoking, here are some examples to get you started on the arguments of why you should not smoke.
Argumentative essay about smoking pdf
Argumentative essay about smoking in public places
Argumentative essay about smoking introduction
Check out the video below to find useful arguments against smoking:
Tips for Writing a Persuasive Essay About Smoking
You have read some examples of persuasive and argumentative essays about smoking. Now here are some tips that will help you craft a powerful essay on this topic.
Choose a Specific Angle
Select a particular perspective on the issue that you can use to form your argument. When talking about smoking, you can focus on any aspect such as the health risks, economic costs, or environmental impact.
Think about how you want to approach the topic. For instance, you could write about why smoking should be banned.
Check out the list of persuasive essay topics to help you while you are thinking of an angle to choose!
Research the Facts
Before writing your essay, make sure to research the facts about smoking. This will give you reliable information to use in your arguments and evidence for why people should avoid smoking.
You can find and use credible data and information from reputable sources such as government websites, health organizations, and scientific studies.
For instance, you should gather facts about health issues and negative effects of tobacco if arguing against smoking. Moreover, you should use and cite sources carefully.
Paper Due? Why Suffer? That's our Job!
Make an Outline
The next step is to create an outline for your essay. This will help you organize your thoughts and make sure that all the points in your essay flow together logically.
Your outline should include the introduction, body paragraphs, and conclusion. This will help ensure that your essay has a clear structure and argument.
Use Persuasive Language
When writing your essay, make sure to use persuasive language such as “it is necessary” or “people must be aware”. This will help you convey your message more effectively and emphasize the importance of your point.
Also, don’t forget to use rhetorical devices such as ethos, pathos, and logos to make your arguments more convincing. That is, you should incorporate emotion, personal experience, and logic into your arguments.
Introduce Opposing Arguments
Another important tip when writing a persuasive essay on smoking is to introduce opposing arguments. It will show that you are aware of the counterarguments and can provide evidence to refute them. This will help you strengthen your argument.
By doing this, your essay will come off as more balanced and objective, making it more convincing.
Finish Strong
Finally, make sure to finish your essay with a powerful conclusion. This will help you leave a lasting impression on your readers and reinforce the main points of your argument. You can end by summarizing the key points or giving some advice to the reader.
A powerful conclusion could either include food for thought or a call to action. So be sure to use persuasive language and make your conclusion strong.
To conclude,
By following these tips, you can write an effective and persuasive essay on smoking. Remember to research the facts, make an outline, and use persuasive language.
However, don't stress if you need expert help to write your essay! We're the best essay writing service for you!
Our persuasive essay writing service is fast, affordable, and trustworthy.
Try it out today!

Write Essay Within 60 Seconds!

Caleb S. has been providing writing services for over five years and has a Masters degree from Oxford University. He is an expert in his craft and takes great pride in helping students achieve their academic goals. Caleb is a dedicated professional who always puts his clients first.

Paper Due? Why Suffer? That’s our Job!
Keep reading

Home — Essay Samples — Nursing & Health — Addictions — Smoking
Essays About Smoking
Smoking essay, types of essay about smoking.
- Cause and Effect Essay: This type of essay focuses on the causes and effects of smoking. It discusses why people start smoking and the consequences of smoking on both the smoker and those around them.
- Argumentative Essay: This essay type aims to persuade the reader about the negative effects of smoking. It presents an argument and provides supporting evidence to convince the reader that smoking is harmful and should be avoided.
- Persuasive Essay: Similar to an argumentative essay, this type of essay aims to persuade the reader to quit smoking. It presents facts, statistics, and other relevant information to convince the reader to stop smoking.
Smoking Essay Example: Cause and Effect
- Identify the causes of smoking: Start by examining why people start smoking in the first place. Is it peer pressure, addiction, stress, or curiosity? Understanding the reasons why people smoke is crucial in creating an effective cause and effect essay.
- Discuss the effects of smoking: Highlight the impact smoking has on an individual's health and the environment. Discuss the risks associated with smoking, such as lung cancer, heart disease, and respiratory problems, and explain how smoking affects non-smokers through secondhand smoke.
- Use reliable sources: To make your essay more convincing, ensure that you use credible sources to back up your claims. Use scientific studies, government reports, and medical journals to support your arguments.
- Provide statistical evidence: Incorporate statistical data to make your essay more impactful. Use figures to show the number of people who smoke, the effects of smoking on the environment, and the costs associated with smoking.
- Offer solutions: Conclude your essay by suggesting solutions to the problem of smoking. Encourage smokers to quit by outlining the benefits of quitting smoking and offering resources for those who want to quit.
Smoking: Argumentative Essay
- Choose a clear position: The writer should choose a side on the issue of smoking, either for or against it, and be clear in presenting their stance.
- Gather evidence: Research and collect facts and statistics to support the writer's argument. They can find data from reliable sources like scientific journals, government reports, and reputable news organizations.
- Address counterarguments: A good argumentative essay will acknowledge opposing viewpoints and then provide a counterargument to refute them.
- Use persuasive language: The writer should use persuasive language to convince the reader of their position. This includes using rhetorical devices, such as ethos, pathos, and logos, to appeal to the reader's emotions and logic.
- Provide a clear conclusion: The writer should summarize the key points of their argument and reiterate their stance in the conclusion.
Persuasive Essay on Smoking
- Identify your audience and their beliefs about smoking.
- Present compelling evidence to support your argument, such as statistics, research studies, and personal anecdotes.
- Use emotional appeals, such as stories or images that show the negative impact of smoking.
- Address potential counterarguments and refute them effectively.
- Use strong and clear language to persuade the reader to take action.
- When choosing a topic for a smoking persuasive essay, consider a specific aspect of smoking that you would like to persuade the audience to act upon.
Hook Examples for Smoking Essays
Anecdotal hook.
Imagine a teenager taking their first puff of a cigarette, unaware of the lifelong addiction they're about to face. This scenario illustrates the pervasive issue of smoking among young people.
Question Hook
Is the pleasure derived from smoking worth the serious health risks it poses? Dive into the contentious debate over tobacco use and its consequences.
Quotation Hook
"Smoking is a habit that drains your money and kills you slowly, one puff after another." — Unknown. Explore the financial and health impacts of smoking in today's society.
Statistical or Factual Hook
Did you know that smoking is responsible for nearly 8 million deaths worldwide each year? Examine the alarming statistics and data associated with tobacco-related illnesses.
Definition Hook
What exactly is smoking, and what are the various forms it takes? Delve into the definitions of smoking, including cigarettes, cigars, pipes, and emerging alternatives like e-cigarettes.
Rhetorical Question Hook
Can we truly call ourselves a smoke-free generation when new nicotine delivery devices are enticing young people? Investigate the impact of vaping and e-cigarettes on the youth.
Historical Hook
Trace the history of smoking, from its ancient roots to its prevalence in different cultures and societies. Explore how perceptions of smoking have evolved over time.
Contrast Hook
Contrast the images of the suave, cigarette-smoking characters from classic films with the grim reality of tobacco-related diseases and addiction in the modern world.
Narrative Hook
Walk in the shoes of a lifelong smoker as they recount their journey from that first cigarette to a battle with addiction and the quest to quit. Their story reflects the struggles of many.
Shocking Statement Hook
Prepare to uncover the disturbing truth about smoking—how it not only harms the smoker but also affects non-smokers through secondhand smoke exposure. It's an issue that goes beyond personal choice.
The Harmful Effects of Smoking: Physical, Social, and Economic Consequences
Quitting smoking: strategies for success, made-to-order essay as fast as you need it.
Each essay is customized to cater to your unique preferences
+ experts online
Smoking Should Be Banned
The effects of smoking on your body, the effects of smoking on health, the importance of quitting smoking, let us write you an essay from scratch.
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
The History of Tobacco Use and Its Dangers
The dangers of smoke from cigarettes, a research paper on smoking cigarettes: should society ban it, effect of tobacco: why cigarette smoking should be banned, get a personalized essay in under 3 hours.
Expert-written essays crafted with your exact needs in mind
How Smoking Can Ruin Your Health
Fight addiction with the help willpower, should smoking be made illegal: argumentative, look of maturity: why smoking is "good" for you, nevada's smoking freedom at stake as joelle babula argues that local government should enforce strict laws, the effects of smoking ban, the challenges of quitting smoking, discussion on whether cigarette smoking should be banned in public places, the motif of smoking in all the pretty horses, the issue of smoking and alcohol drinking among adolescents, my personal experience of the effects of vaping, why vaping is bad for you: effects and dangers, feminist theory and communication, the toxic truth of smoking and vaping, the different harmful effects of smoking marijuana, pieces of advice that will help you to select the best vape shop in las vegas, facts of herbal cigarettes versus tobacco cigarettes, vaping: all you need to know about this trend, from cure to poison: the negative effects of tobacco, global efforts to diminish tobacco usage, relevant topics.
- Affordable Care Act
- Postpartum Depression
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
- Tobacco Products
- Public Health Education
Health Effects of Tobacco Use
Tobacco use has serious effects on the health of users. In fact, tobacco use remains the leading preventable cause of disease and death in the United States, 1 leading to more than 480,000 deaths each year.
Different tobacco products, however, pose varying levels of health risk to users. Combustible products that burn tobacco, like a cigarette, are the most harmful to a user’s health, while noncombustible products, such as e-cigarettes, may be less harmful. However, no tobacco product is considered safe.
Health Effects of Smoking
Cigarettes are responsible for the vast majority of all tobacco-related disease and death in the U.S. Smokers are exposed to a toxic mix of over 7,000 chemicals when they inhale cigarette smoke, 2 the consequences of which can threaten their health in many ways.
Order Free Print Version | Download Infographic

If you or a loved one are among the 34 million U.S. adults who smoke cigarettes in this country 9 and want to quit , there are resources to help you on your journey to living a smoke-free life .
COVID-19 and Smoking
Am I at risk for serious complications from COVID-19 if I smoke cigarettes?
Subscribe to CTP Email Newsletters
Stay up to date on tobacco product news and announcements from FDA’s Center for Tobacco Products (CTP) by subscribing to our email newsletters.
Yes. Data show that when compared to never smokers, cigarette smoking increases the risk of more severe illness from COVID-19, which could result in hospitalization, the need for intensive care, or even death. Smoking cigarettes can cause inflammation and cell damage throughout the body, and can weaken your immune system, making it less able to fight off disease.
There’s never been a better time to quit smoking. If you need resources to help you quit smoking, the FDA has supportive tips and tools to help you get closer to quitting for good .
If I vape tobacco or nicotine am I at risk for complications from COVID-19?
E-cigarette use can expose the lungs to toxic chemicals, but whether those exposures increase the risk of COVID-19 or the severity of COVID-19 outcomes is not known. However, many e-cigarette users are current or former smokers, and cigarette smoking increases the risk of respiratory infections, including pneumonia.
In the Health Effects of Tobacco Use Section
Nicotine Is Why Tobacco Products Are Addictive

Keep Your Air Clear: How Tobacco Can Harm Your Lungs

How Smoking Affects Heart Health

What It’s Like to Quit Smoking

Quitting Smoking and Other Tobacco Public Health Resources

- U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress. A Report of the Surgeon General. Atlanta, GA: US Dept of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014.
- U.S. Department of Health and Human Services (USDHHS). A Report of the Surgeon General: How Tobacco Smoke Causes Disease: What It Means to You (Consumer Booklet). Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2010.
- U.S. Department of Health and Human Services. Smoking and Cardiovascular Disease (Fact Sheet). Atlanta, GA: US Dept of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014.
- U.S. Department of Health and Human Services. Smoking and Cancer (Fact Sheet). Atlanta, GA: US Dept of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014.
- U.S. Department of Health and Human Services. National Diabetes Statistics Report. Atlanta, GA: US Dept of Health and Human Services, Centers for Disease Control and Prevention; 2020.
- U.S. Department of Health and Human Services. Smoking and Diabetes (Fact Sheet). Atlanta, GA: US Dept of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014.
- U.S. Department of Health and Human Services. Smoking and Respiratory Diseases (Fact Sheet). Atlanta, GA: US Dept of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014.
- Smoking during pregnancy. Centers for Disease Control and Prevention website. www.cdc.gov/tobacco/basic_information/health_effects/pregnancy/. Updated January 8, 2014. Accessed April 17, 2015.
- Cornelius ME, Wang TW, Jamal A, Loretan CG, Neff LJ. Tobacco Product Use Among Adults — United States, 2019. MMWR Morb Mortal Wkly Rep 2020;69:1736–1742.
Subscribe to CTPConnect
Get regular updates on the health effects of tobacco, public health educational resources, and highlights on current tobacco issues and regulations.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 24 March 2022
Tobacco and nicotine use
- Bernard Le Foll 1 , 2 ,
- Megan E. Piper 3 , 4 ,
- Christie D. Fowler 5 ,
- Serena Tonstad 6 ,
- Laura Bierut 7 ,
- Lin Lu ORCID: orcid.org/0000-0003-0742-9072 8 , 9 ,
- Prabhat Jha 10 &
- Wayne D. Hall 11 , 12
Nature Reviews Disease Primers volume 8 , Article number: 19 ( 2022 ) Cite this article
30k Accesses
63 Citations
68 Altmetric
Metrics details
- Disease genetics
- Experimental models of disease
- Preventive medicine
Tobacco smoking is a major determinant of preventable morbidity and mortality worldwide. More than a billion people smoke, and without major increases in cessation, at least half will die prematurely from tobacco-related complications. In addition, people who smoke have a significant reduction in their quality of life. Neurobiological findings have identified the mechanisms by which nicotine in tobacco affects the brain reward system and causes addiction. These brain changes contribute to the maintenance of nicotine or tobacco use despite knowledge of its negative consequences, a hallmark of addiction. Effective approaches to screen, prevent and treat tobacco use can be widely implemented to limit tobacco’s effect on individuals and society. The effectiveness of psychosocial and pharmacological interventions in helping people quit smoking has been demonstrated. As the majority of people who smoke ultimately relapse, it is important to enhance the reach of available interventions and to continue to develop novel interventions. These efforts associated with innovative policy regulations (aimed at reducing nicotine content or eliminating tobacco products) have the potential to reduce the prevalence of tobacco and nicotine use and their enormous adverse impact on population health.
Similar content being viewed by others

Adults who microdose psychedelics report health related motivations and lower levels of anxiety and depression compared to non-microdosers
Joseph M. Rootman, Pamela Kryskow, … Zach Walsh

The serotonin theory of depression: a systematic umbrella review of the evidence
Joanna Moncrieff, Ruth E. Cooper, … Mark A. Horowitz

Emotions and brain function are altered up to one month after a single high dose of psilocybin
Frederick S. Barrett, Manoj K. Doss, … Roland R. Griffiths
Introduction
Tobacco is the second most commonly used psychoactive substance worldwide, with more than one billion smokers globally 1 . Although smoking prevalence has reduced in many high-income countries (HICs), tobacco use is still very prevalent in low-income and middle-income countries (LMICs). The majority of smokers are addicted to nicotine delivered by cigarettes (defined as tobacco dependence in the International Classification of Diseases, Tenth Revision (ICD-10) or tobacco use disorder in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5)). As a result of the neuro-adaptations and psychological mechanisms caused by repeated exposure to nicotine delivered rapidly by cigarettes, cessation can also lead to a well-characterized withdrawal syndrome, typically manifesting as irritability, anxiety, low mood, difficulty concentrating, increased appetite, insomnia and restlessness, that contributes to the difficulty in quitting tobacco use 2 , 3 , 4 .
Historically, tobacco was used in some cultures as part of traditional ceremonies, but its use was infrequent and not widely disseminated in the population. However, since the early twentieth century, the use of commercial cigarettes has increased dramatically 5 because of automated manufacturing practices that enable large-scale production of inexpensive products that are heavily promoted by media and advertising. Tobacco use became highly prevalent in the past century and was followed by substantial increases in the prevalence of tobacco-induced diseases decades later 5 . It took decades to establish the relationship between tobacco use and associated health effects 6 , 7 and to discover the addictive role of nicotine in maintaining tobacco smoking 8 , 9 , and also to educate people about these effects. It should be noted that the tobacco industry disputed this evidence to allow continuing tobacco sales 10 . The expansion of public health campaigns to reduce smoking has gradually decreased the use of tobacco in HICs, with marked increases in adult cessation, but less progress has been achieved in LMICs 1 .
Nicotine is the addictive compound in tobacco and is responsible for continued use of tobacco despite harms and a desire to quit, but nicotine is not directly responsible for the harmful effects of using tobacco products (Box 1 ). Other components in tobacco may modulate the addictive potential of tobacco (for example, flavours and non-nicotine compounds) 11 . The major harms related to tobacco use, which are well covered elsewhere 5 , are linked to a multitude of compounds present in tobacco smoke (such as carcinogens, toxicants, particulate matter and carbon monoxide). In adults, adverse health outcomes of tobacco use include cancer in virtually all peripheral organs exposed to tobacco smoke and chronic diseases such as eye disease, periodontal disease, cardiovascular diseases, chronic obstructive pulmonary disease, stroke, diabetes mellitus, rheumatoid arthritis and disorders affecting immune function 5 . Moreover, smoking during pregnancy can increase the risk of adverse reproductive effects, such as ectopic pregnancy, low birthweight and preterm birth 5 . Exposure to secondhand cigarette smoke in children has been linked to sudden infant death syndrome, impaired lung function and respiratory illnesses, in addition to cognitive and behavioural impairments 5 . The long-term developmental effects of nicotine are probably due to structural and functional changes in the brain during this early developmental period 12 , 13 .
Nicotine administered alone in various nicotine replacement formulations (such as patches, gum and lozenges) is safe and effective as an evidence-based smoking cessation aid. Novel forms of nicotine delivery systems have also emerged (called electronic nicotine delivery systems (ENDS) or e-cigarettes), which can potentially reduce the harmful effects of tobacco smoking for those who switch completely from combustible to e-cigarettes 14 , 15 .
This Primer focuses on the determinants of nicotine and tobacco use, and reviews the neurobiology of nicotine effects on the brain reward circuitry and the functioning of brain networks in ways that contribute to the difficulty in stopping smoking. This Primer also discusses how to prevent tobacco use, screen for smoking, and offer people who smoke tobacco psychosocial and pharmacological interventions to assist in quitting. Moreover, this Primer presents emerging pharmacological and novel brain interventions that could improve rates of successful smoking cessation, in addition to public health approaches that could be beneficial.
Box 1 Tobacco products
Conventional tobacco products include combustible products that produce inhaled smoke (most commonly cigarettes, bidis (small domestically manufactured cigarettes used in South Asia) or cigars) and those that deliver nicotine without using combustion (chewing or dipping tobacco and snuff). Newer alternative products that do not involve combustion include nicotine-containing e-cigarettes and heat-not-burn tobacco devices. Although non-combustion and alternative products may constitute a lesser risk than burned ones 14 , 15 , 194 , no form of tobacco is entirely risk-free.
Epidemiology
Prevalence and burden of disease.
The Global Burden of Disease Project (GBDP) estimated that around 1.14 billion people smoked in 2019, worldwide, increasing from just under a billion in 1990 (ref. 1 ). Of note, the prevalence of smoking decreased significantly between 1990 and 2019, but increases in the adult population meant that the total number of global smokers increased. One smoking-associated death occurs for approximately every 0.8–1.1 million cigarettes smoked 16 , suggesting that the estimated worldwide consumption of about 7.4 trillion cigarettes in 2019 has led to around 7 million deaths 1 .
In most populations, smoking prevalence is much higher among groups with lower levels of education or income 17 and among those with mental health disorders and other co-addictions 18 , 19 . Smoking is also more frequent among men than women (Figs 1 – 3 ). Sexual and/or gender minority individuals have disproportionately high rates of smoking and other addictions 17 , 20 . In addition, the prevalence of smoking varies substantially between regions and ethnicities; smoking rates are high in some regions of Asia, such as China and India, but are lower in North America and Australia. Of note, the prevalence of mental health disorders and other co-addictions is higher in individuals who smoke compared with non-smokers 18 , 19 , 21 . For example, the odds of smoking in people with any substance use disorder is more than five times higher than the odds in people without a substance use disorder 19 . Similarly, the odds of smoking in people with any psychiatric disorder is more than three times higher than the odds of smoking in those without a psychiatric diagnosis 22 . In a study in the USA, compared with a population of smokers with no psychiatric diagnosis, subjects with anxiety, depression and phobia showed an approximately twofold higher prevalence of smoking, and subjects with agoraphobia, mania or hypomania, psychosis and antisocial personality or conduct disorders showed at least a threefold higher prevalence of smoking 22 . Comorbid disorders are also associated with higher rates of smoking 22 , 23 .
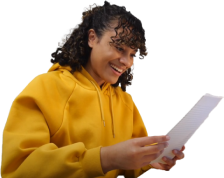
a | Number of current male smokers aged 15 years or older per country expressed in millions. b | Former male smokers aged 45–59 years per country expressed in millions. c | Former male smokers aged 45–59 years per country expressed as the percentage of smokers who stopped. The data shown are for male smokers for the period 2015–2019 from countries with direct smoking surveys. The prevalence of smoking among males is less variable than among females. Data from ref. 1 .
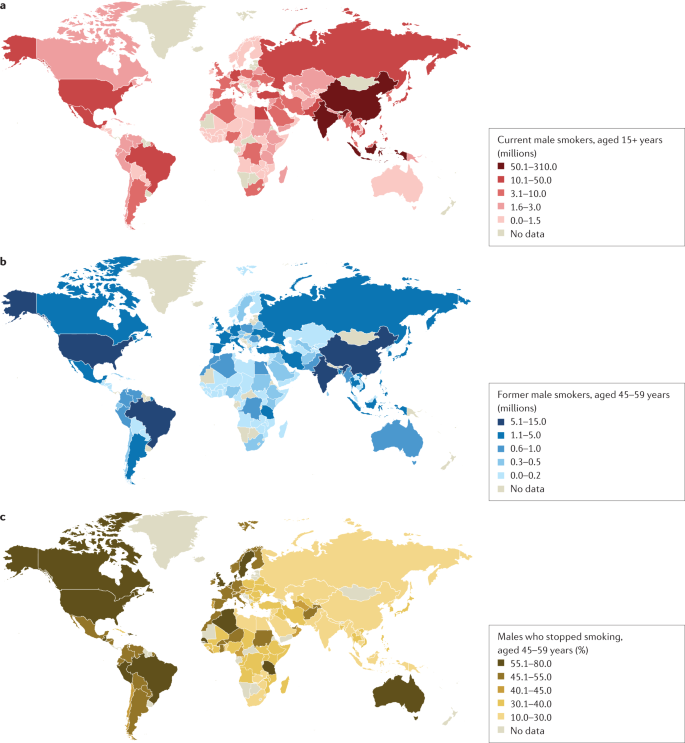
a | Number of current female smokers aged 15 years or older per country expressed in millions. b | Former female smokers aged 45–59 years per country expressed in millions. c | Former female smokers aged 45–59 years per country expressed as the percentage of smokers who stopped. The data shown are for female smokers for the period 2015–2019 from countries with direct smoking surveys. The prevalence of smoking among females is much lower in East and South Asia than in Latin America or Eastern Europe. Data from ref. 1 .
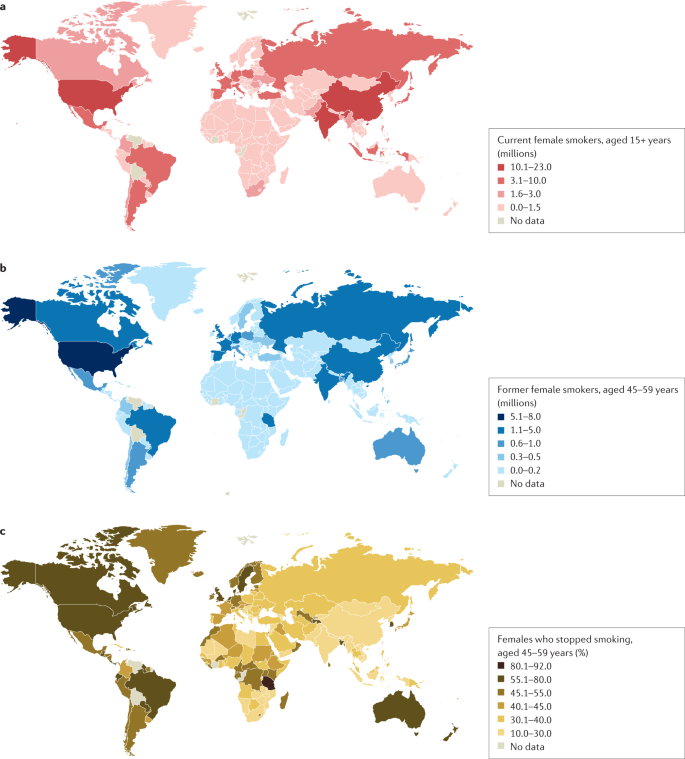
a | Number of current male and female smokers aged 15 years or older per country expressed in millions. b | Former male and female smokers aged 45–59 years per country expressed in millions. c | Former male and female smokers aged 45–59 years per country expressed as the percentage of smokers who stopped. The data shown are for the period 2015–2019 from countries with direct smoking surveys. Cessation rates are higher in high-income countries, but also notably high in Brazil. Cessation is far less common in South and East Asia and Russia and other Eastern European countries, and also low in South Africa. Data from ref. 1 .
Age at onset
Most smokers start smoking during adolescence, with almost 90% of smokers beginning between 15 and 25 years of age 24 . The prevalence of tobacco smoking among youths substantially declined in multiple HICs between 1990 and 2019 (ref. 25 ). More recently, the widespread uptake of ENDS in some regions such as Canada and the USA has raised concerns about the long-term effects of prolonged nicotine use among adolescents, including the possible notion that ENDS will increase the use of combustible smoking products 25 , 26 (although some studies have not found much aggregate effect at the population level) 27 .
Smoking that commences in early adolescence or young adulthood and persists throughout life has a more severe effect on health than smoking that starts later in life and/or that is not persistent 16 , 28 , 29 . Over 640 million adults under 30 years of age smoke in 22 jurisdictions alone (including 27 countries in the European Union where central efforts to reduce tobacco dependence might be possible) 30 . In those younger than 30 years of age, at least 320 million smoking-related deaths will occur unless they quit smoking 31 . The actual number of smoking-related deaths might be greater than one in two, and perhaps as high as two in three, long-term smokers 5 , 16 , 29 , 32 , 33 . At least half of these deaths are likely to occur in middle age (30–69 years) 16 , 29 , leading to a loss of two or more decades of life. People who smoke can expect to lose an average of at least a decade of life versus otherwise similar non-smokers 16 , 28 , 29 .
Direct epidemiological studies in several countries paired with model-based estimates have estimated that smoking tobacco accounted for 7.7 million deaths globally in 2020, of which 80% were in men and 87% were current smokers 1 . In HICs, the major causes of tobacco deaths are lung cancer, emphysema, heart attack, stroke, cancer of the upper aerodigestive areas and bladder cancer 28 , 29 . In some lower income countries, tuberculosis is an additional important cause of tobacco-related death 29 , 34 , which could be related to, for example, increased prevalence of infection, more severe tuberculosis/mortality and higher prevalence of treatment-resistant tuberculosis in smokers than in non-smokers in low-income countries 35 , 36 .
Despite substantial reductions in the prevalence of smoking, there were 34 million smokers in the USA, 7 million in the UK and 5 million in Canada in 2017 (ref. 16 ), and cigarette smoking remains the largest cause of premature death before 70 years of age in much of Europe and North America 1 , 16 , 28 , 29 . Smoking-associated diseases accounted for around 41 million deaths in the USA, UK and Canada from 1960 to 2020 (ref. 16 ). Moreover, as smoking-associated diseases are more prevalent among groups with lower levels of education and income, smoking accounts for at least half of the difference in overall mortality between these social groups 37 . Any reduction in smoking prevalence reduces the absolute mortality gap between these groups 38 .
Smoking cessation has become common in HICs with good tobacco control interventions. For example, in France, the number of ex-smokers is four times the number of current smokers among those aged 50 years or more 30 . By contrast, smoking cessation in LMICs remains uncommon before smokers develop tobacco-related diseases 39 . Smoking cessation greatly reduces the risks of smoking-related diseases. Indeed, smokers who quit smoking before 40 years of age avoid nearly all the increased mortality risks 31 , 33 . Moreover, individuals who quit smoking by 50 years of age reduce the risk of death from lung cancer by about two-thirds 40 . More modest hazards persist for deaths from lung cancer and emphysema 16 , 28 ; however, the risks among former smokers are an order of magnitude lower than among those who continue to smoke 33 .
Mechanisms/pathophysiology
Nicotine is the main psychoactive agent in tobacco and e-cigarettes. Nicotine acts as an agonist at nicotinic acetylcholine receptors (nAChRs), which are localized throughout the brain and peripheral nervous system 41 . nAChRs are pentameric ion channels that consist of varying combinations of α 2 –α 7 and β 2 –β 4 subunits, and for which acetylcholine (ACh) is the endogenous ligand 42 , 43 , 44 . When activated by nicotine binding, nAChR undergoes a conformational change that opens the internal pore, allowing an influx of sodium and calcium ions 45 . At postsynaptic membranes, nAChR activation can lead to action potential firing and downstream modulation of gene expression through calcium-mediated second messenger systems 46 . nAChRs are also localized to presynaptic membranes, where they modulate neurotransmitter release 47 . nAChRs become desensitized after activation, during which ligand binding will not open the channel 45 .
nAChRs with varying combinations of α-subunits and β-subunits have differences in nicotine binding affinity, efficacy and desensitization rate, and have differential expression depending on the brain region and cell type 48 , 49 , 50 . For instance, at nicotine concentrations found in human smokers, β 2 -containing nAChRs desensitize relatively quickly after activation, whereas α 7 -containing nAChRs have a slower desensitization profile 48 . Chronic nicotine exposure in experimental animal models or in humans induces an increase in cortical expression of α 4 β 2 -containing nAChRs 51 , 52 , 53 , 54 , 55 , but also increases the expression of β 3 and β 4 nAChR subunits in the medial habenula (MHb)–interpeduncular nucleus (IPN) pathway 56 , 57 . It is clear that both the brain localization and the type of nAChR are critical elements in mediating the various effects of nicotine, but other factors such as rate of nicotine delivery may also modulate addictive effects of nicotine 58 .

Neurocircuitry of nicotine addiction
Nicotine has both rewarding effects (such as a ‘buzz’ or ‘high’) and aversive effects (such as nausea and dizziness), with the net outcome dependent on dose and others factors such as interindividual sensitivity and presence of tolerance 59 . Thus, the addictive properties of nicotine involve integration of contrasting signals from multiple brain regions that process reward and aversion (Fig. 4 ).
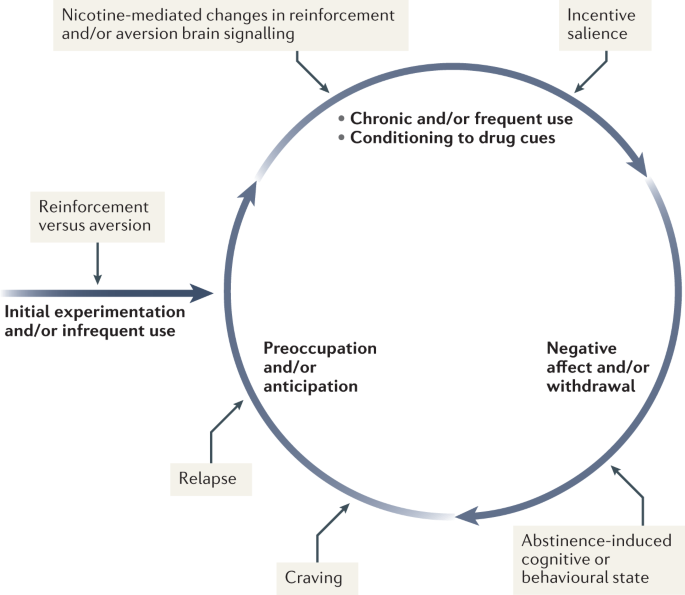
During initial use, nicotine exerts both reinforcing and aversive effects, which together determine the likelihood of continued use. As the individual transitions to more frequent patterns of chronic use, nicotine induces pharmacodynamic changes in brain circuits, which is thought to lead to a reduction in sensitivity to the aversive properties of the drug. Nicotine is also a powerful reinforcer that leads to the conditioning of secondary cues associated with the drug-taking experience (such as cigarette pack, sensory properties of cigarette smoke and feel of the cigarette in the hand or mouth), which serves to enhance the incentive salience of these environmental factors and drive further drug intake. When the individual enters into states of abstinence (such as daily during sleep at night or during quit attempts), withdrawal symptomology is experienced, which may include irritability, restlessness, learning or memory deficits, difficulty concentrating, anxiety and hunger. These negative affective and cognitive symptoms lead to an intensification of the individual’s preoccupation to obtain and use the tobacco/nicotine product, and subsequently such intense craving can lead to relapse.
The rewarding actions of nicotine have largely been attributed to the mesolimbic pathway, which consists of dopaminergic neurons in the ventral tegmental area (VTA) that project to the nucleus accumbens and prefrontal cortex 60 , 61 , 62 (Fig. 5 ). VTA integrating circuits and projection regions express several nAChR subtypes on dopaminergic, GABAergic, and glutamatergic neurons 63 , 64 . Ultimately, administration of nicotine increases dopamine levels through increased dopaminergic neuron firing in striatal and extrastriatal areas (such as the ventral pallidum) 65 (Fig. 6 ). This effect is involved in reward and is believed to be primarily mediated by the action of nicotine on α 4 -containing and β 2 -containing nAChRs in the VTA 66 , 67 .
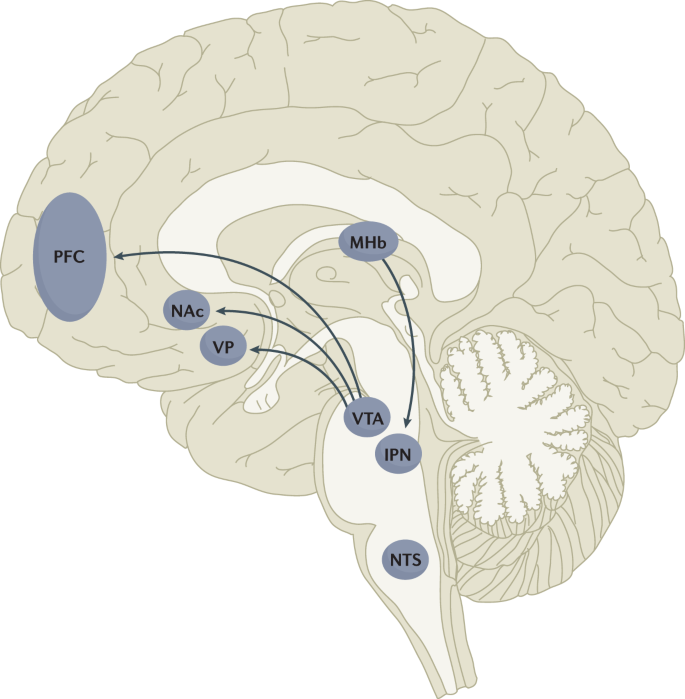
Multiple lines of research have demonstrated that nicotine reinforcement is mainly controlled by two brain pathways, which relay predominantly reward-related or aversion-related signals. The rewarding properties of nicotine that promote drug intake involve the mesolimbic dopamine projection from the ventral tegmental area (VTA) to the nucleus accumbens (NAc). By contrast, the aversive properties of nicotine that limit drug intake and mitigate withdrawal symptoms involve the fasciculus retroflexus projection from the medial habenula (MHb) to the interpeduncular nucleus (IPN). Additional brain regions have also been implicated in various aspects of nicotine dependence, such as the prefrontal cortex (PFC), ventral pallidum (VP), nucleus tractus solitarius (NTS) and insula (not shown here for clarity). All of these brain regions are directly or indirectly interconnected as integrative circuits to drive drug-seeking and drug-taking behaviours.
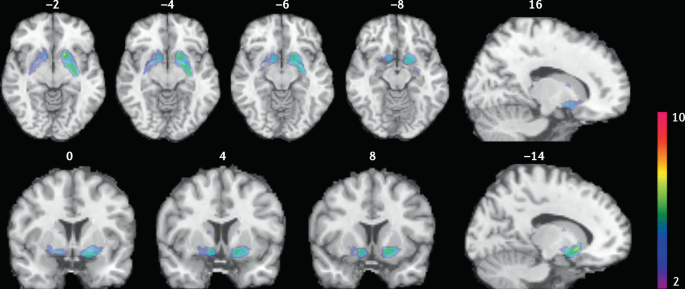
Smokers received brain PET scans with [ 11 C]PHNO, a dopamine D 2/3 PET tracer that has high sensitivity in detecting fluctuations of dopamine. PET scans were performed during abstinence or after smoking a cigarette. Reduced binding potential (BP ND ) was observed after smoking, indicating increased dopamine levels in the ventral striatum and in the area that corresponds to the ventral pallidum. The images show clusters with statistically significant decreases of [ 11 C]PHNO BP ND after smoking a cigarette versus abstinence condition. Those clusters have been superimposed on structural T1 MRI images of the brain. Reprinted from ref. 65 , Springer Nature Limited.
The aversive properties of nicotine are mediated by neurons in the MHb, which project to the IPN. Studies in rodents using genetic knockdown and knockout strategies demonstrated that the α 5 -containing, α 3 -containing and β 4 -containing nAChRs in the MHb–IPN pathway mediate the aversive properties of nicotine that limit drug intake, especially when animals are given the opportunity to consume higher nicotine doses 68 , 69 , 70 , 71 , 72 . In addition to nAChRs, other signalling factors acting on the MHb terminals in the IPN also regulate the actions of nicotine. For instance, under conditions of chronic nicotine exposure or with optogenetic activation of IPN neurons, a subtype of IPN neurons co-expressing Chrna5 (encoding the α 5 nAChR subunit) and Amigo1 (encoding adhesion molecule with immunoglobulin-like domain 1) release nitric oxide from the cell body that retrogradely inhibits MHb axon terminals 70 . In addition, nicotine activates α 5 -containing nAChR-expressing neurons that project from the nucleus tractus solitarius to the IPN, leading to release of glucagon-like peptide-1 that binds to GLP receptors on habenular axon terminals, which subsequently increases IPN neuron activation and decreases nicotine self-administration 73 . Taken together, these findings suggest a dynamic signalling process at MHb axonal terminals in the IPN, which regulates the addictive properties of nicotine and determines the amount of nicotine that is self-administered.
Nicotine withdrawal in animal models can be assessed by examining somatic signs (such as shaking, scratching, head nods and chewing) and affective signs (such as increased anxiety-related behaviours and conditioned place aversion). Interestingly, few nicotine withdrawal somatic signs are found in mice with genetic knockout of the α 2 , α 5 or β 4 nAChR subunits 74 , 75 . By contrast, β 2 nAChR-knockout mice have fewer anxiety-related behaviours during nicotine withdrawal, with no differences in somatic symptoms compared with wild-type mice 74 , 76 .
In addition to the VTA (mediating reward) and the MHb–IPN pathway (mediating aversion), other brain areas are involved in nicotine addiction (Fig. 5 ). In animals, the insular cortex controls nicotine taking and nicotine seeking 77 . Moreover, humans with lesions of the insular cortex can quit smoking easily without relapse 78 . This finding led to the development of a novel therapeutic intervention modulating insula function (see Management, below) 79 , 80 . Various brain areas (shell of nucleus accumbens, basolateral amygdala and prelimbic cortex) expressing cannabinoid CB 1 receptors are also critical in controlling rewarding effects and relapse 81 , 82 . The α 1 -adrenergic receptor expressed in the cortex also control these effects, probably through glutamatergic afferents to the nucleus accumbens 83 .
Individual differences in nicotine addiction risk
Vulnerability to nicotine dependence varies between individuals, and the reasons for these differences are multidimensional. Many social factors (such as education level and income) play a role 84 . Broad psychological and social factors also modulate this risk. For example, peer smoking status, knowledge on effect of tobacco, expectation on social acceptance, exposure to passive smoking modulate the risk of initiating tobacco use 85 , 86 .
Genetic factors have a role in smoking initiation, the development of nicotine addiction and the likelihood of smoking cessation. Indeed, heritability has been estimated to contribute to approximatively half of the variability in nicotine dependence 87 , 88 , 89 , 90 . Important advances in our understanding of such genetic contributions have evolved with large-scale genome-wide association studies of smokers and non-smokers. One of the most striking findings has been that allelic variation in the CHRNA5 – CHRNA3 – CHRNB4 gene cluster, which encodes α 5 , α 3 and β 4 nAChR subunits, correlates with an increased vulnerability for nicotine addiction, indicated by a higher likelihood of becoming dependent on nicotine and smoking a greater number of cigarettes per day 91 , 92 , 93 , 94 , 95 . The most significant effect has been found for a single-nucleotide polymorphism in CHRNA5 (rs16969968), which results in an amino acid change and reduced function of α 5 -containing nAChRs 92 .
Allelic variation in CYP2A6 (encoding the CYP2A6 enzyme, which metabolizes nicotine) has also been associated with differential vulnerability to nicotine dependence 96 , 97 , 98 . CYP2A6 is highly polymorphic, resulting in variable enzymatic activity 96 , 99 , 100 . Individuals with allelic variation that results in slow nicotine metabolism consume less nicotine per day, experience less-severe withdrawal symptoms and are more successful at quitting smoking than individuals with normal or fast metabolism 101 , 102 , 103 , 104 . Moreover, individuals with slow nicotine metabolism have lower dopaminergic receptor expression in the dopamine D2 regions of the associative striatum and sensorimotor striatum in PET studies 105 and take fewer puffs of nicotine-containing cigarettes (compared with de-nicotinized cigarettes) in a forced choice task 106 . Slower nicotine metabolism is thought to increase the duration of action of nicotine, allowing nicotine levels to accumulate over time, therefore enabling lower levels of intake to sustain activation of nAChRs 107 .
Large-scale genetic studies have identified hundreds of other genetic loci that influence smoking initiation, age of smoking initiation, cigarettes smoked per day and successful smoking cessation 108 . The strongest genetic contributions to smoking through the nicotinic receptors and nicotine metabolism are among the strongest genetic contributors to lung cancer 109 . Other genetic variations (such as those related to cannabinoid, dopamine receptors or other neurotransmitters) may affect certain phenotypes related to smoking (such as nicotine preference and cue-reactivity) 110 , 111 , 112 , 113 , 114 , 115 .
Diagnosis, screening and prevention
Screening for cigarette smoking.
Screening for cigarette smoking should happen at every doctor’s visit 116 . In this regard, a simple and direct question about a person’s tobacco use can provide an opportunity to offer information about its potential risks and treatments to assist in quitting. All smokers should be offered assistance in quitting because even low levels of smoking present a significant health risk 33 , 117 , 118 . Smoking status can be assessed by self-categorization or self-reported assessment of smoking behaviour (Table 1 ). In people who smoke, smoking frequency can be assessed 119 and a combined quantity frequency measure such as pack-year history (that is, average number of cigarettes smoked per day multiplied by the number of years, divided by 20), can be used to estimate cumulative risk of adverse health outcomes. The Association for the Treatment of Tobacco Use and Dependence recommends that all electronic health records should document smoking status using the self-report categories listed in Table 1 .
Owing to the advent of e-cigarettes and heat-not-burn products, and the popularity of little cigars in the US that mimic combustible cigarettes, people who use tobacco may use multiple products concurrently 120 , 121 . Thus, screening for other nicotine and tobacco product use is important in clinical practice. The self-categorization approach can also be used to describe the use of these other products.
Traditionally tobacco use has been classified according to whether the smoker meets criteria for nicotine dependence in one of the two main diagnostic classifications: the DSM 122 (tobacco use disorder) and the ICD (tobacco dependence) 123 . The diagnosis of tobacco use disorder according to DSM-5 criteria requires the presence of at least 2 of 11 symptoms that have produced marked clinical impairment or distress within a 12-month period (Box 2 ). Of note, these symptoms are similar for all substance use disorder diagnoses and may not all be relevant to tobacco use disorder (such as failure to complete life roles). In the ICD-10, codes allow the identification of specific tobacco products used (cigarettes, chewing tobacco and other tobacco products).
Dependence can also be assessed as a continuous construct associated with higher levels of use, greater withdrawal and reduced likelihood of quitting. The level of dependence can be assessed with the Fagerström Test for Nicotine Dependence, a short questionnaire comprising six questions 124 (Box 2 ). A score of ≥4 indicates moderate to high dependence. As very limited time may be available in clinical consultations, the Heaviness of Smoking Index (HSI) was developed, which comprises two questions on the number of cigarettes smoked per day and how soon after waking the first cigarette is smoked 125 . The HSI can guide dosing for nicotine replacement therapy (NRT).
Other measures of cigarette dependence have been developed but are not used in the clinical setting, such as the Cigarette Dependence Scale 126 , Hooked on Nicotine Checklist 127 , Nicotine Dependence Syndrome Scale 128 , the Wisconsin Inventory of Smoking Dependence Motives (Brief) 129 and the Penn State Cigarette Dependence Index 130 . However, in practice, these are not often used, as the most important aspect is to screen for smoking and encourage all smokers to quit smoking regardless of their dependence status.
Box 2 DSM-5 criteria for tobacco use disorder and items of the Fagerström Test for nicotine dependence
DSM-5 (ref. 122 )
Taxonomic and diagnostic tool for tobacco use disorder published by the American Psychiatric Association.
A problematic pattern of tobacco use leading to clinically significant impairment or distress as manifested by at least two of the following, occurring within a 12-month period.
Tobacco often used in larger amounts or over a longer period of time than intended
A persistent desire or unsuccessful efforts to reduce or control tobacco use
A great deal of time spent in activities necessary to obtain or use tobacco
Craving, or a strong desire or urge to use tobacco
Recurrent tobacco use resulting in a failure to fulfil major role obligations at work, school or home
Continued tobacco use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of tobacco (for example, arguments with others about tobacco use)
Important social, occupational or recreational activities given up or reduced because of tobacco use
Recurrent tobacco use in hazardous situations (such as smoking in bed)
Tobacco use continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by tobacco use
Tolerance, defined by either of the following.
A need for markedly increased amounts of tobacco to achieve the desired effect
A markedly diminished effect with continued use of the same amount of tobacco
Withdrawal, manifesting as either of the following.
Withdrawal syndrome for tobacco
Tobacco (or a closely related substance, such as nicotine) taken to relieve or avoid withdrawal symptoms
Fagerström Test for Nicotine Dependence 124
A standard instrument for assessing the intensity of physical addiction to nicotine.
How soon after you wake up do you smoke your first cigarette?
Within 5 min (scores 3 points)
5 to 30 min (scores 2 points)
31 to 60 min (scores 1 point)
After 60 min (scores 0 points)
Do you find it difficult not to smoke in places where you should not, such as in church or school, in a movie, at the library, on a bus, in court or in a hospital?
Yes (scores 1 point)
No (scores 0 points)
Which cigarette would you most hate to give up; which cigarette do you treasure the most?
The first one in the morning (scores 1 point)
Any other one (scores 0 points)
How many cigarettes do you smoke each day?
10 or fewer (scores 0 points)
11 to 20 (scores 1 point)
21 to 30 (scores 2 points)
31 or more (scores 3 points)
Do you smoke more during the first few hours after waking up than during the rest of the day?
Do you still smoke if you are so sick that you are in bed most of the day or if you have a cold or the flu and have trouble breathing?
A score of 7–10 points is classified as highly dependent; 4–6 points is classified as moderately dependent; <4 points is classified as minimally dependent.
DSM-5, Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
Young people who do not start smoking cigarettes between 15 and 25 years of age have a very low risk of ever smoking 24 , 131 , 132 . This age group provides a critical opportunity to prevent cigarette smoking using effective, evidence-based strategies to prevent smoking initiation and reduce escalation from experimentation to regular use 131 , 132 , 133 , 134 , 135 .
Effective prevention of cigarette uptake requires a comprehensive package of cost-effective policies 134 , 136 , 137 to synergistically reduce the population prevalence of cigarette smoking 131 , 135 . These policies include high rates of tobacco taxation 30 , 134 , 137 , 138 , widespread and rigorously enforced smoke-free policies 139 , bans on tobacco advertising and promotions 140 , use of plain packaging and graphic warnings about the health risks of smoking 135 , 141 , mass media and peer-based education programmes to discourage smoking, and enforcement of laws against the sale of cigarettes to young people below the minimum legal purchase age 131 , 135 . These policies make cigarettes less available and affordable to young people. Moreover, these policies make it more difficult for young people to purchase cigarettes and make smoking a much less socially acceptable practice. Of note, these policies are typically mostly enacted in HICs, which may be related to the declining prevalence of smoking in these countries, compared with the prevalence in LMICs.
Pharmacotherapy
Three evidence-based classes of pharmacotherapy are available for smoking cessation: NRT (using nicotine-based patches, gum, lozenges, mini-lozenges, nasal sprays and inhalers), varenicline (a nAChR partial agonist), and bupropion (a noradrenaline/dopamine reuptake inhibitor that also inhibits nAChR function and is also used as an antidepressant). These FDA-approved and EMA-approved pharmacotherapies are cost-effective smoking cessation treatments that double or triple successful abstinence rates compared with no treatment or placebo controls 116 , 142 .
Combinations of pharmacotherapies are also effective for smoking cessation 116 , 142 . For example, combining NRTs (such as the steady-state nicotine patch and as-needed NRT such as gum or mini-lozenge) is more effective than a single form of NRT 116 , 142 , 143 . Combining NRT and varenicline is the most effective smoking cessation pharmacotherapy 116 , 142 , 143 . Combining FDA-approved pharmacotherapy with behavioural counselling further increases the likelihood of successful cessation 142 . Second-line pharmacotherapies (for example, nortriptyline) have some potential for smoking cessation, but their use is limited due to their tolerability profile.
All smokers should receive pharmacotherapy to help them quit smoking, except those in whom pharmacotherapy has insufficient evidence of effectiveness (among adolescents, smokeless tobacco users, pregnant women or light smokers) or those in whom pharmacotherapy is medically contraindicated 144 . Table 2 provides specific information regarding dosing and duration for each FDA-approved pharmacotherapy. Extended use of pharmacotherapy beyond the standard 12-week regimen after cessation is effective and should be considered 116 . Moreover, preloading pharmacotherapy (that is, initiating cessation medication in advance of a quit attempt), especially with the nicotine patch, is a promising treatment, although further studies are required to confirm efficacy.
Cytisine has been used for smoking cessation in Eastern Europe for a long time and is available in some countries (such as Canada) without prescription 145 . Cytisine is a partial agonist of nAChRs and its structure was the precursor for the development of varenicline 145 . Cytisine is at least as effective as some approved pharmacotherapies for smoking cessation, such as NRT 146 , 147 , 148 , and the role of cytisine in smoking cessation is likely to expand in the future, notably owing to its much lower cost than traditional pharmacotherapies. E-cigarettes also have the potential to be useful as smoking cessation devices 149 , 150 . The 2020 US Surgeon General’s Report concluded that there was insufficient evidence to promote cytisine or e-cigarettes as effective smoking cessation treatments, but in the UK its use is recommended for smoking cessation (see ref. 15 for regularly updated review).
Counselling and behavioural treatments
Psychosocial counselling significantly increases the likelihood of successful cessation, especially when combined with pharmacotherapy. Even a counselling session lasting only 3 minutes can help smokers quit 116 , although the 2008 US Public Health Service guidelines and the Preventive Services Task Force 151 each concluded that more intensive counselling (≥20 min per session) is more effective than less intensive counselling (<20 min per session). Higher smoking cessation rates are obtained by using behavioural change techniques that target associative and self-regulatory processes 152 . In addition, behavioural change techniques that will favour commitment, social reward and identity associated with changed behaviour seems associated with higher success rates 152 . Evidence-based counselling focuses on providing social support during treatment, building skills to cope with withdrawal and cessation, and problem-solving in challenging situations 116 , 153 . Effective counselling can be delivered by diverse providers (such as physicians, nurses, pharmacists, social workers, psychologists and certified tobacco treatment specialists) 116 .
Counselling can be delivered in a variety of modalities. In-person individual and group counselling are effective, as is telephone counselling (quit lines) 142 . Internet and text-based intervention seem to be effective in smoking cessation, especially when they are interactive and tailored to a smoker’s specific circumstances 142 . Over the past several years, the number of smoking cessation smartphone apps has increased, but there the evidence that the use of these apps significantly increases smoking cessation rates is not sufficient.
Contingency management (providing financial incentives for abstinence or engagement in treatment) has shown promising results 154 , 155 but its effects are not sustained once the contingencies are removed 155 , 156 . Other treatments such as hypnosis, acupuncture and laser treatment have not been shown to improve smoking cessation rates compared with placebo treatments 116 . Moreover, no solid evidence supports the use of conventional transcranial magnetic stimulation (TMS) for long-term smoking cessation 157 , 158 .
Although a variety of empirically supported smoking cessation interventions are available, more than two-thirds of adult smokers who made quit attempts in the USA during the past year did not use an evidence-based treatment and the rate is likely to be lower in many other countries 142 . This speaks to the need to increase awareness of, and access to, effective cessation aids among all smokers.
Brain stimulation
The insula (part of the frontal cortex) is a critical brain structure involved in cigarette craving and relapse 78 , 79 . The activity of the insula can be modulated using an innovative approach called deep insula/prefrontal cortex TMS (deep TMS), which is effective in helping people quit smoking 80 , 159 . This approach has now been approved by the FDA as an effective smoking cessation intervention 80 . However, although this intervention was developed and is effective for smoking cessation, the number of people with access to it is limited owing to the limited number of sites equipped and with trained personnel, and the cost of this intervention.
Quality of life
Generic instruments (such as the Short-Form (SF-36) Health Survey) can be used to evaluate quality of life (QOL) in smokers. People who smoke rate their QOL lower than people who do not smoke both before and after they become smokers 160 , 161 . QOL improves when smokers quit 162 . Mental health may also improve on quitting smoking 163 . Moreover, QOL is much poorer in smokers with tobacco-related diseases, such as chronic respiratory diseases and cancers, than in individuals without tobacco-related diseases 161 , 164 . The dimensions of QOL that show the largest decrements in people who smoke are those related to physical health, day-to-day activities and mental health such as depression 160 . Smoking also increases the risk of diabetes mellitus 165 , 166 , which is a major determinant of poor QOL for a wide range of conditions.
The high toll of premature death from cigarette smoking can obscure the fact that many of the diseases that cause these deaths also produce substantial disability in the years before death 1 . Indeed, death in smokers is typically preceded by several years of living with the serious disability and impairment of everyday activities caused by chronic respiratory disease, heart disease and cancer 2 . Smokers’ QOL in these years may also be adversely affected by the adverse effects of the medical treatments that they receive for these smoking-related diseases (such as major surgery and radiotherapy).
Expanding cessation worldwide
The major global challenge is to consider individual and population-based strategies that could increase the substantially low rates of adult cessation in most LMICs and indeed strategies to ensure that even in HICs, cessation continues to increase. In general, the most effective tools recommended by WHO to expand cessation are the same tools that can prevent smoking initiation, notably higher tobacco taxes, bans on advertising and promotion, prominent warning labels or plain packaging, bans on public smoking, and mass media and educational efforts 29 , 167 . The effective use of these policies, particularly taxation, lags behind in most LMICs compared with most HICs, with important exceptions such as Brazil 167 . Access to effective pharmacotherapies and counselling as well as support for co-existing mental health conditions would also be required to accelerate cessation in LMICs. This is particularly important as smokers living in LMICs often have no access to the full range of effective treatment options.
Regulating access to e-cigarettes
How e-cigarettes should be used is debated within the tobacco control field. In some countries (for example, the UK), the use of e-cigarettes as a cigarette smoking cessation aid and as a harm reduction strategy is supported, based on the idea that e-cigarette use will lead to much less exposure to toxic compounds than tobacco use, therefore reducing global harm. In other countries (for example, the USA), there is more concern with preventing the increased use of e-cigarettes by youths that may subsequently lead to smoking 25 , 26 . Regulating e-cigarettes in nuanced ways that enable smokers to access those products whilst preventing their uptake among youths is critical.
Regulating nicotine content in tobacco products
Reducing the nicotine content of cigarettes could potentially produce less addictive products that would allow a gradual reduction in the population prevalence of smoking. Some clinical studies have found no compensatory increase in smoking whilst providing access to low nicotine tobacco 168 . Future regulation may be implemented to gradually decrease the nicotine content of combustible tobacco and other nicotine products 169 , 170 , 171 .
Tobacco end games
Some individuals have proposed getting rid of commercial tobacco products this century or using the major economic disruption arising from the COVID-19 pandemic to accelerate the demise of the tobacco industry 172 , 173 . Some tobacco producers have even proposed this strategy as an internal goal, with the idea of switching to nicotine delivery systems that are less harmful ( Philip Morris International ). Some countries are moving towards such an objective; for example, in New Zealand, the goal that fewer than 5% of New Zealanders will be smokers in 2025 has been set (ref. 174 ). The tobacco end-game approach would overall be the best approach to reduce the burden of tobacco use on society, but it would require coordination of multiple countries and strong public and private consensus on the strategy to avoid a major expansion of the existing illicit market in tobacco products in some countries.
Innovative interventions
The COVID-19 pandemic has shown that large-scale investment in research can lead to rapid development of successful therapeutic interventions. By contrast, smoking cessation has been underfunded compared with the contribution that it makes to the global burden of disease. In addition, there is limited coordination between research teams and most studies are small-scale and often underpowered 79 . It is time to fund an ambitious, coordinated programme of research to test the most promising therapies based on an increased understanding of the neurobiological basis of smoking and nicotine addiction (Table 3 ). Many of those ideas have not yet been tested properly and this could be carried out by a coordinated programme of research at the international level.
GBD 2019 Tobacco Collaborators. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990-2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet 397 , 2337–2360 (2021). This study summarizes the burden of disease induced by tobacco worldwide .
Google Scholar
West, R. Tobacco smoking: health impact, prevalence, correlates and interventions. Psychol. Health 32 , 1018–1036 (2017).
PubMed PubMed Central Google Scholar
West, R. The multiple facets of cigarette addiction and what they mean for encouraging and helping smokers to stop. COPD 6 , 277–283 (2009).
PubMed Google Scholar
Fagerström, K. Determinants of tobacco use and renaming the FTND to the Fagerström test for cigarette dependence. Nicotine Tob. Res. 14 , 75–78 (2012).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General (Centers for Disease Control and Prevention, 2014).
Doll, R. & Hill, A. B. Smoking and carcinoma of the lung; preliminary report. Br. Med. J. 2 , 739–748 (1950).
CAS PubMed PubMed Central Google Scholar
Royal College of Physicians. Smoking and health. Summary of a report of the Royal College of Physicians of London on smoking in relation to cancer of the lung and other diseases (Pitman Medical Publishing, 1962).
Henningfield, J. E., Smith, T. T., Kleykamp, B. A., Fant, R. V. & Donny, E. C. Nicotine self-administration research: the legacy of Steven R. Goldberg and implications for regulation, health policy, and research. Psychopharmacology 233 , 3829–3848 (2016).
Le Foll, B. & Goldberg, S. R. Effects of nicotine in experimental animals and humans: an update on addictive properties. Hand. Exp. Pharmacol. https://doi.org/10.1007/978-3-540-69248-5_12 (2009).
Article Google Scholar
Proctor, R. N. The history of the discovery of the cigarette–lung cancer link: evidentiary traditions, corporate denial, global toll. Tob. Control. 21 , 87–91 (2012).
Hall, B. J. et al. Differential effects of non-nicotine tobacco constituent compounds on nicotine self-administration in rats. Pharmacol. Biochem. Behav. 120 , 103–108 (2014).
Musso, F. et al. Smoking impacts on prefrontal attentional network function in young adult brains. Psychopharmacology 191 , 159–169 (2007).
CAS PubMed Google Scholar
Goriounova, N. A. & Mansvelder, H. D. Short- and long-term consequences of nicotine exposure during adolescence for prefrontal cortex neuronal network function. Cold Spring Harb. Perspect. Med. 2 , a012120 (2012).
Fagerström, K. O. & Bridgman, K. Tobacco harm reduction: the need for new products that can compete with cigarettes. Addictive Behav. 39 , 507–511 (2014).
Hartmann-Boyce, J. et al. Electronic cigarettes for smoking cessation. Cochrane Database Syst. Rev. 9 , CD010216 (2021).
Jha, P. The hazards of smoking and the benefits of cessation: a critical summation of the epidemiological evidence in high-income countries. eLife https://doi.org/10.7554/eLife.49979 (2020).
Article PubMed PubMed Central Google Scholar
Palipudi, K. M. et al. Social determinants of health and tobacco use in thirteen low and middle income countries: evidence from Global Adult Tobacco Survey. PLoS ONE 7 , e33466 (2012).
Goodwin, R. D., Pagura, J., Spiwak, R., Lemeshow, A. R. & Sareen, J. Predictors of persistent nicotine dependence among adults in the United States. Drug Alcohol. Depend. 118 , 127–133 (2011).
Weinberger, A. H. et al. Cigarette use is increasing among people with illicit substance use disorders in the United States, 2002-14: emerging disparities in vulnerable populations. Addiction 113 , 719–728 (2018).
Evans-Polce, R. J., Kcomt, L., Veliz, P. T., Boyd, C. J. & McCabe, S. E. Alcohol, tobacco, and comorbid psychiatric disorders and associations with sexual identity and stress-related correlates. Am. J. Psychiatry 177 , 1073–1081 (2020).
Hassan, A. N. & Le Foll, B. Survival probabilities and predictors of major depressive episode incidence among individuals with various types of substance use disorders. J. Clin. Psychiatry https://doi.org/10.4088/JCP.20m13637 (2021).
Article PubMed Google Scholar
Smith, P. H., Mazure, C. M. & McKee, S. A. Smoking and mental illness in the U.S. population. Tob. Control. 23 , e147–e153 (2014).
Bourgault, Z., Rubin-Kahana, D. S., Hassan, A. N., Sanches, M. & Le Foll, B. Multiple substance use disorders and self-reported cognitive function in U.S. adults: associations and sex-differences in a nationally representative sample. Front. Psychiatry https://doi.org/10.3389/fpsyt.2021.797578 (2022).
Reitsma, M. B. et al. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and initiation among young people in 204 countries and territories, 1990-2019. Lancet Public Health 6 , e472–e481 (2021).
Warner, K. E. How to think–not feel–about tobacco harm reduction. Nicotine Tob. Res. 21 , 1299–1309 (2019).
Soneji, S. et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 171 , 788–797 (2017).
Levy, D. T. et al. Examining the relationship of vaping to smoking initiation among US youth and young adults: a reality check. Tob. Control. 28 , 629–635 (2019).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The health consequences of smoking — 50 years of progress: a report of the Surgeon General (Centers for Disease Control and Prevention, 2014).
Jha, P. & Peto, R. Global effects of smoking, of quitting, and of taxing tobacco. N. Engl. J. Med. 370 , 60–68 (2014). This review covers the impact of tobacco, of quitting smoking and the importance of taxation to impact prevalence of smoking .
Jha, P. & Peto., R. in Tobacco Tax Reform: At the Crossroads of Health and Development . (eds Marquez, P. V. & Moreno-Dodson, B.) 55–72 (World Bank Group, 2017).
Jha, P. et al. 21st-century hazards of smoking and benefits of cessation in the United States. N. Engl. J. Med. 368 , 341–350 (2013).
Banks, E. et al. Tobacco smoking and all-cause mortality in a large Australian cohort study: findings from a mature epidemic with current low smoking prevalence. BMC Med. 13 , 38 (2015).
Pirie, K. et al. The 21st century hazards of smoking and benefits of stopping: a prospective study of one million women in the UK. Lancet 381 , 133–141 (2013).
Jha, P. et al. A nationally representative case-control study of smoking and death in India. N. Engl. J. Med. 358 , 1137–1147 (2008).
Chan, E. D. et al. Tobacco exposure and susceptibility to tuberculosis: is there a smoking gun? Tuberculosis 94 , 544–550 (2014).
Wang, M. G. et al. Association between tobacco smoking and drug-resistant tuberculosis. Infect. Drug Resist. 11 , 873–887 (2018).
Jha, P. et al. Social inequalities in male mortality, and in male mortality from smoking: indirect estimation from national death rates in England and Wales, Poland, and North America. Lancet 368 , 367–370 (2006).
Jha, P., Gelband, H, Irving, H. & Mishra, S. in Reducing Social Inequalities in Cancer: Evidence and Priorities for Research (eds Vaccarella, S et al.) 161–166 (IARC, 2018).
Jha, P. Expanding smoking cessation world-wide. Addiction 113 , 1392–1393 (2018).
Jha, P. Avoidable global cancer deaths and total deaths from smoking. Nat. Rev. Cancer 9 , 655–664 (2009).
Wittenberg, R. E., Wolfman, S. L., De Biasi, M. & Dani, J. A. Nicotinic acetylcholine receptors and nicotine addiction: a brief introduction. Neuropharmacology 177 , 108256 (2020).
Boulter, J. et al. Functional expression of two neuronal nicotinic acetylcholine receptors from cDNA clones identifies a gene family. Proc. Natl Acad. Sci. USA 84 , 7763–7767 (1987).
Couturier, S. et al. A neuronal nicotinic acetylcholine receptor subunit (α7) is developmentally regulated and forms a homo-oligomeric channel blocked by α-BTX. Neuron 5 , 847–856 (1990).
Picciotto, M. R., Addy, N. A., Mineur, Y. S. & Brunzell, D. H. It is not “either/or”: activation and desensitization of nicotinic acetylcholine receptors both contribute to behaviors related to nicotine addiction and mood. Prog. Neurobiol. 84 , 329–342 (2008).
Changeux, J. P. Structural identification of the nicotinic receptor ion channel. Trends Neurosci. 41 , 67–70 (2018).
McKay, B. E., Placzek, A. N. & Dani, J. A. Regulation of synaptic transmission and plasticity by neuronal nicotinic acetylcholine receptors. Biochem. Pharmacol. 74 , 1120–1133 (2007).
Wonnacott, S. Presynaptic nicotinic ACh receptors. Trends Neurosci. 20 , 92–98 (1997).
Wooltorton, J. R., Pidoplichko, V. I., Broide, R. S. & Dani, J. A. Differential desensitization and distribution of nicotinic acetylcholine receptor subtypes in midbrain dopamine areas. J. Neurosci. 23 , 3176–3185 (2003).
Gipson, C. D. & Fowler, C. D. Nicotinic receptors underlying nicotine dependence: evidence from transgenic mouse models. Curr. Top. Behav. Neurosci. 45 , 101–121 (2020).
Hamouda, A. K. et al. Potentiation of (α4)2(β2)3, but not (α4)3(β2)2, nicotinic acetylcholine receptors reduces nicotine self-administration and withdrawal symptoms. Neuropharmacology 190 , 108568 (2021).
Lallai, V. et al. Nicotine acts on cholinergic signaling mechanisms to directly modulate choroid plexus function. eNeuro https://doi.org/10.1523/ENEURO.0051-19.2019 (2019).
Benwell, M. E., Balfour, D. J. & Anderson, J. M. Evidence that tobacco smoking increases the density of (-)-[3H]nicotine binding sites in human brain. J. Neurochem. 50 , 1243–1247 (1988).
Perry, D. C., Davila-Garcia, M. I., Stockmeier, C. A. & Kellar, K. J. Increased nicotinic receptors in brains from smokers: membrane binding and autoradiography studies. J. Pharmacol. Exp. Ther. 289 , 1545–1552 (1999).
Marks, M. J. et al. Nicotine binding and nicotinic receptor subunit RNA after chronic nicotine treatment. J. Neurosci. 12 , 2765–2784 (1992).
Le Foll, B. et al. Impact of short access nicotine self-administration on expression of α4β2* nicotinic acetylcholine receptors in non-human primates. Psychopharmacology 233 , 1829–1835 (2016).
Meyers, E. E., Loetz, E. C. & Marks, M. J. Differential expression of the beta4 neuronal nicotinic receptor subunit affects tolerance development and nicotinic binding sites following chronic nicotine treatment. Pharmacol. Biochem. Behav. 130 , 1–8 (2015).
Zhao-Shea, R., Liu, L., Pang, X., Gardner, P. D. & Tapper, A. R. Activation of GABAergic neurons in the interpeduncular nucleus triggers physical nicotine withdrawal symptoms. Curr. Biol. 23 , 2327–2335 (2013).
Jensen, K. P., Valentine, G., Gueorguieva, R. & Sofuoglu, M. Differential effects of nicotine delivery rate on subjective drug effects, urges to smoke, heart rate and blood pressure in tobacco smokers. Psychopharmacology 237 , 1359–1369 (2020).
Villanueva, H. F., James, J. R. & Rosecrans, J. A. Evidence of pharmacological tolerance to nicotine. NIDA Res. Monogr. 95 , 349–350 (1989).
Corrigall, W. A., Coen, K. M. & Adamson, K. L. Self-administered nicotine activates the mesolimbic dopamine system through the ventral tegmental area. Brain Res. 653 , 278–284 (1994).
Nisell, M., Nomikos, G. G., Hertel, P., Panagis, G. & Svensson, T. H. Condition-independent sensitization of locomotor stimulation and mesocortical dopamine release following chronic nicotine treatment in the rat. Synapse 22 , 369–381 (1996).
Rice, M. E. & Cragg, S. J. Nicotine amplifies reward-related dopamine signals in striatum. Nat. Neurosci. 7 , 583–584 (2004).
Mameli-Engvall, M. et al. Hierarchical control of dopamine neuron-firing patterns by nicotinic receptors. Neuron 50 , 911–921 (2006).
Picciotto, M. R., Higley, M. J. & Mineur, Y. S. Acetylcholine as a neuromodulator: cholinergic signaling shapes nervous system function and behavior. Neuron 76 , 116–129 (2012).
Le Foll, B. et al. Elevation of dopamine induced by cigarette smoking: novel insights from a [11C]-+-PHNO PET study in humans. Neuropsychopharmacology 39 , 415–424 (2014). This brain imaging study identified the brain areas in which smoking elevates dopamine levels .
Maskos, U. et al. Nicotine reinforcement and cognition restored by targeted expression of nicotinic receptors. Nature 436 , 103–107 (2005). This article discusses the implication of the β 2 - containing nAChRs in the VTA in mammalian cognitive function .
Picciotto, M. R. et al. Acetylcholine receptors containing the beta2 subunit are involved in the reinforcing properties of nicotine. Nature 391 , 173–177 (1998). This article discusses the implication of the β 2 - containing nAChRs in addictive effects of nicotine .
Fowler, C. D., Lu, Q., Johnson, P. M., Marks, M. J. & Kenny, P. J. Habenular alpha5 nicotinic receptor subunit signalling controls nicotine intake. Nature 471 , 597–601 (2011). This article discusses the implication of the α5 nicotinic receptor located in the MHb in a mechanism mediating the aversive effects of nicotine .
Elayouby, K. S. et al. α3* Nicotinic acetylcholine receptors in the habenula-interpeduncular nucleus circuit regulate nicotine intake. J. Neurosci. https://doi.org/10.1523/JNEUROSCI.0127-19.2020 (2020).
Ables, J. L. et al. Retrograde inhibition by a specific subset of interpeduncular α5 nicotinic neurons regulates nicotine preference. Proc. Natl Acad. Sci. USA 114 , 13012–13017 (2017).
Frahm, S. et al. Aversion to nicotine is regulated by the balanced activity of β4 and α5 nicotinic receptor subunits in the medial habenula. Neuron 70 , 522–535 (2011).
Jackson, K. J. et al. Role of α5 nicotinic acetylcholine receptors in pharmacological and behavioral effects of nicotine in mice. J. Pharmacol. Exp. Ther. 334 , 137–146 (2010).
Tuesta, L. M. et al. GLP-1 acts on habenular avoidance circuits to control nicotine intake. Nat. Neurosci. 20 , 708–716 (2017).
Salas, R., Pieri, F. & De Biasi, M. Decreased signs of nicotine withdrawal in mice null for the β4 nicotinic acetylcholine receptor subunit. J. Neurosci. 24 , 10035–10039 (2004).
Salas, R., Sturm, R., Boulter, J. & De Biasi, M. Nicotinic receptors in the habenulo-interpeduncular system are necessary for nicotine withdrawal in mice. J. Neurosci. 29 , 3014–3018 (2009).
Jackson, K. J., Martin, B. R., Changeux, J. P. & Damaj, M. I. Differential role of nicotinic acetylcholine receptor subunits in physical and affective nicotine withdrawal signs. J. Pharmacol. Exp. Ther. 325 , 302–312 (2008).
Le Foll, B. et al. Translational strategies for therapeutic development in nicotine addiction: rethinking the conventional bench to bedside approach. Prog. Neuropsychopharmacol. Biol. Psychiatry 52 , 86–93 (2014).
Naqvi, N. H., Rudrauf, D., Damasio, H. & Bechara, A. Damage to the insula disrupts addiction to cigarette smoking. Science 315 , 531–534 (2007). This article discusses the implication of the insular cortex in tobacco addiction .
Ibrahim, C. et al. The insula: a brain stimulation target for the treatment of addiction. Front. Pharmacol. 10 , 720 (2019).
Zangen, A. et al. Repetitive transcranial magnetic stimulation for smoking cessation: a pivotal multicenter double-blind randomized controlled trial. World Psychiatry 20 , 397–404 (2021). This study validated the utility of deep insula/prefrontal cortex rTMS for smoking cessation .
Le Foll, B., Forget, B., Aubin, H. J. & Goldberg, S. R. Blocking cannabinoid CB1 receptors for the treatment of nicotine dependence: insights from pre-clinical and clinical studies. Addict. Biol. 13 , 239–252 (2008).
Kodas, E., Cohen, C., Louis, C. & Griebel, G. Cortico-limbic circuitry for conditioned nicotine-seeking behavior in rats involves endocannabinoid signaling. Psychopharmacology 194 , 161–171 (2007).
Forget, B. et al. Noradrenergic α1 receptors as a novel target for the treatment of nicotine addiction. Neuropsychopharmacology 35 , 1751–1760 (2010).
Garrett, B. E., Dube, S. R., Babb, S. & McAfee, T. Addressing the social determinants of health to reduce tobacco-related disparities. Nicotine Tob. Res. 17 , 892–897 (2015).
Polanska, K., Znyk, M. & Kaleta, D. Susceptibility to tobacco use and associated factors among youth in five central and eastern European countries. BMC Public Health 22 , 72 (2022).
Volkow, N. D. Personalizing the treatment of substance use disorders. Am. J. Psychiatry 177 , 113–116 (2020).
Li, M. D., Cheng, R., Ma, J. Z. & Swan, G. E. A meta-analysis of estimated genetic and environmental effects on smoking behavior in male and female adult twins. Addiction 98 , 23–31 (2003).
Carmelli, D., Swan, G. E., Robinette, D. & Fabsitz, R. Genetic influence on smoking–a study of male twins. N. Engl. J. Med. 327 , 829–833 (1992).
Broms, U., Silventoinen, K., Madden, P. A. F., Heath, A. C. & Kaprio, J. Genetic architecture of smoking behavior: a study of Finnish adult twins. Twin Res. Hum. Genet. 9 , 64–72 (2006).
Kendler, K. S., Thornton, L. M. & Pedersen, N. L. Tobacco consumption in Swedish twins reared apart and reared together. Arch. Gen. Psychiat 57 , 886–892 (2000).
Saccone, N. L. et al. The CHRNA5-CHRNA3-CHRNB4 nicotinic receptor subunit gene cluster affects risk for nicotine dependence in African-Americans and in European-Americans. Cancer Res. 69 , 6848–6856 (2009).
Bierut, L. J. et al. Variants in nicotinic receptors and risk for nicotine dependence. Am. J. Psychiatry 165 , 1163–1171 (2008). This study demonstrates that nAChR gene variants are important in nicotine addiction .
Bierut, L. J. et al. Novel genes identified in a high-density genome wide association study for nicotine dependence. Hum. Mol. Genet. 16 , 24–35 (2007).
Berrettini, W. et al. α-5/α-3 nicotinic receptor subunit alleles increase risk for heavy smoking. Mol. Psychiatry 13 , 368–373 (2008).
Sherva, R. et al. Association of a single nucleotide polymorphism in neuronal acetylcholine receptor subunit alpha 5 (CHRNA5) with smoking status and with ‘pleasurable buzz’ during early experimentation with smoking. Addiction 103 , 1544–1552 (2008).
Thorgeirsson, T. E. et al. Sequence variants at CHRNB3-CHRNA6 and CYP2A6 affect smoking behavior. Nat. Genet. 42 , 448–453 (2010).
Ray, R., Tyndale, R. F. & Lerman, C. Nicotine dependence pharmacogenetics: role of genetic variation in nicotine-metabolizing enzymes. J. Neurogenet. 23 , 252–261 (2009).
Bergen, A. W. et al. Drug metabolizing enzyme and transporter gene variation, nicotine metabolism, prospective abstinence, and cigarette consumption. PLoS ONE 10 , e0126113 (2015).
Mwenifumbo, J. C. et al. Identification of novel CYP2A6*1B variants: the CYP2A6*1B allele is associated with faster in vivo nicotine metabolism. Clin. Pharmacol. Ther. 83 , 115–121 (2008).
Raunio, H. & Rahnasto-Rilla, M. CYP2A6: genetics, structure, regulation, and function. Drug Metab. Drug Interact. 27 , 73–88 (2012).
CAS Google Scholar
Patterson, F. et al. Toward personalized therapy for smoking cessation: a randomized placebo-controlled trial of bupropion. Clin. Pharmacol. Ther. 84 , 320–325 (2008).
Rodriguez, S. et al. Combined analysis of CHRNA5, CHRNA3 and CYP2A6 in relation to adolescent smoking behaviour. J. Psychopharmacol. 25 , 915–923 (2011).
Strasser, A. A., Malaiyandi, V., Hoffmann, E., Tyndale, R. F. & Lerman, C. An association of CYP2A6 genotype and smoking topography. Nicotine Tob. Res. 9 , 511–518 (2007).
Liakoni, E. et al. Effects of nicotine metabolic rate on withdrawal symptoms and response to cigarette smoking after abstinence. Clin. Pharmacol. Ther. 105 , 641–651 (2019).
Di Ciano, P. et al. Influence of nicotine metabolism ratio on [11C]-(+)-PHNO PET binding in tobacco smokers. Int. J. Neuropsychopharmacol. 21 , 503–512 (2018).
Butler, K. et al. Impact of Cyp2a6 activity on nicotine reinforcement and cue-reactivity in daily smokers. Nicotine Tob. Res. https://doi.org/10.1093/ntr/ntab064 (2021).
Benowitz, N. L., Swan, G. E., Jacob, P. 3rd, Lessov-Schlaggar, C. N. & Tyndale, R. F. CYP2A6 genotype and the metabolism and disposition kinetics of nicotine. Clin. Pharmacol. Ther. 80 , 457–467 (2006).
Liu, M. et al. Association studies of up to 1.2 million individuals yield new insights into the genetic etiology of tobacco and alcohol use. Nat. Genet. 51 , 237–244 (2019).
McKay, J. D. et al. Large-scale association analysis identifies new lung cancer susceptibility loci and heterogeneity in genetic susceptibility across histological subtypes. Nat. Genet. 49 , 1126–1132 (2017).
Chukwueke, C. C. et al. The CB1R rs2023239 receptor gene variant significantly affects the reinforcing effects of nicotine, but not cue reactivity, in human smokers. Brain Behav. 11 , e01982 (2021).
Ahrens, S. et al. Modulation of nicotine effects on selective attention by DRD2 and CHRNA4 gene polymorphisms. Psychopharmacology 232 , 2323–2331 (2015).
Harrell, P. T. et al. Dopaminergic genetic variation moderates the effect of nicotine on cigarette reward. Psychopharmacology 233 , 351–360 (2016).
Lerman, C. et al. Role of functional genetic variation in the dopamine D2 receptor (DRD2) in response to bupropion and nicotine replacement therapy for tobacco dependence: results of two randomized clinical trials. Neuropsychopharmacology 31 , 231–242 (2006).
Le Foll, B., Gallo, A., Le Strat, Y., Lu, L. & Gorwood, P. Genetics of dopamine receptors and drug addiction: a comprehensive review. Behav. Pharmacol. 20 , 1–17 (2009).
Chukwueke, C. C. et al. Exploring the role of the Ser9Gly (rs6280) dopamine D3 receptor polymorphism in nicotine reinforcement and cue-elicited craving. Sci. Rep. 10 , 4085 (2020).
The Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel, Liaisons, and Staff A clinical practice guideline for treating tobacco use and dependence: 2008 update: a U.S. Public Health Service report. Am. J. Prev. Med. 35 , 158–176 (2008).
Hackshaw, A., Morris, J. K., Boniface, S., Tang, J. L. & Milenković, D. Low cigarette consumption and risk of coronary heart disease and stroke: meta-analysis of 141 cohort studies in 55 study reports. BMJ 360 , j5855 (2018).
Qin, W. et al. Light cigarette smoking increases risk of all-cause and cause-specific mortality: findings from the NHIS cohort study. Int. J. Env. Res. Public Health https://doi.org/10.3390/ijerph17145122 (2020).
Rodu, B. & Plurphanswat, N. Mortality among male smokers and smokeless tobacco users in the USA. Harm Reduct. J. 16 , 50 (2019).
Kasza, K. A. et al. Tobacco-product use by adults and youths in the United States in 2013 and 2014. N. Engl. J. Med. 376 , 342–353 (2017).
Richardson, A., Xiao, H. & Vallone, D. M. Primary and dual users of cigars and cigarettes: profiles, tobacco use patterns and relevance to policy. Nicotine Tob. Res. 14 , 927–932 (2012).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental disorders 5th edn (American Psychiatric Association, 2013).
World Health Organization. Tobacco fact sheet. WHO https://www.who.int/news-room/fact-sheets/detail/tobacco (2021).
Heatherton, T. F., Kozlowski, L. T., Frecker, R. C. & Fagerström, K. O. The Fagerström test for nicotine dependence: a revision of the Fagerström tolerance questionnaire. Br. J. Addict. 86 , 1119–1127 (1991).
Heatherton, T. F., Kozlowski, L. T., Frecker, R. C., Rickert, W. & Robinson, J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br. J. Addict. 84 , 791–799 (1989).
Etter, J. F., Le Houezec, J. & Perneger, T. V. A self-administered questionnaire to measure dependence on cigarettes: the cigarette dependence scale. Neuropsychopharmacology 28 , 359–370 (2003).
DiFranza, J. R. et al. Measuring the loss of autonomy over nicotine use in adolescents: the DANDY (Development and Assessment of Nicotine Dependence in Youths) study. Arch. Pediatr. Adolesc. Med. 156 , 397–403 (2002).
Shiffman, S., Waters, A. & Hickcox, M. The Nicotine Dependence Syndrome Scale: a multidimensional measure of nicotine dependence. Nicotine Tob. Res. 6 , 327–348 (2004).
Smith, S. S. et al. Development of the Brief Wisconsin Inventory of Smoking Dependence Motives. Nicotine Tob. Res. 12 , 489–499 (2010).
Foulds, J. et al. Development of a questionnaire for assessing dependence on electronic cigarettes among a large sample of ex-smoking E-cigarette users. Nicotine Tob. Res. 17 , 186–192 (2015).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Preventing tobacco use among youth and young adults: a report of the Surgeon General (Centers for Disease Control and Prevention, 2012).
World Health Organization. Tobacco control to improve child health and development. Thematic brief (WHO, 2021).
Lantz, P. M. et al. Investing in youth tobacco control: a review of smoking prevention and control strategies. Tob. Control. 9 , 47–63 (2000).
Leão, T., Kunst, A. E. & Perelman, J. Cost-effectiveness of tobacco control policies and programmes targeting adolescents: a systematic review. Eur. J. Public Health 28 , 39–43 (2018).
Royal College of Physicians. Smoking and health 2021: a coming of age for tobacco control? (RCP, 2021).
Higashi, H. et al. Cost effectiveness of tobacco control policies in Vietnam: the case of population-level interventions. Appl. Health Econ. Health Policy 9 , 183–196 (2011).
Ranson, M. K., Jha, P., Chaloupka, F. J. & Nguyen, S. N. Global and regional estimates of the effectiveness and cost-effectiveness of price increases and other tobacco control policies. Nicotine Tob. Res. 4 , 311–319 (2002).
International Agency for Research on Cancer. I ARC Handbooks of Cancer Prevention: Tobacco control Vol. 14 (IARC, 2011).
Frazer, K. et al. Legislative smoking bans for reducing harms from secondhand smoke exposure, smoking prevalence and tobacco consumption. Cochrane Database Syst. Rev. 2 , CD005992 (2016).
Hoffman, S. J. & Tan, C. Overview of systematic reviews on the health-related effects of government tobacco control policies. BMC Public Health 15 , 744 (2015).
McNeill, A. et al. Tobacco packaging design for reducing tobacco use. Cochrane Database Syst. Rev. 4 , CD011244 (2017).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Smoking cessation: a report of the Surgeon General (Department of Health and Human Services, 2020).
Lindson, N. et al. Different doses, durations and modes of delivery of nicotine replacement therapy for smoking cessation. Cochrane Database Syst. Rev. 4 , CD013308 (2019).
Krist, A. H. et al. Interventions for tobacco smoking cessation in adults, including pregnant persons: US Preventive Services Task Force recommendation statement. JAMA 325 , 265–279 (2021).
Tutka, P. & Zatonski, W. Cytisine for the treatment of nicotine addiction: from a molecule to therapeutic efficacy. Pharmacol. Rep. 58 , 777–798 (2006).
Courtney, R. J. et al. Effect of cytisine vs varenicline on smoking cessation: a randomized clinical trial. JAMA 326 , 56–64 (2021).
Walker, N. et al. Cytisine versus nicotine for smoking cessation. N. Engl. J. Med. 371 , 2353–2362 (2014). This study validated the utility of cytisine for smoking cessation .
West, R. et al. Placebo-controlled trial of cytisine for smoking cessation. N. Engl. J. Med. 365 , 1193–1200 (2011).
Hajek, P. et al. E-cigarettes compared with nicotine replacement therapy within the UK Stop Smoking Services: the TEC RCT. Health Technol. Assess. 23 , 1–82 (2019).
Walker, N. et al. Nicotine patches used in combination with e-cigarettes (with and without nicotine) for smoking cessation: a pragmatic, randomised trial. Lancet Respir. Med. 8 , 54–64 (2020).
Siu, A. L., U.S. Preventive Services Task Force. Behavioral and pharmacotherapy interventions for tobacco smoking cessation in adults, including pregnant women: U.S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 163 , 622–634 (2015).
Black, N. et al. Behaviour change techniques associated with smoking cessation in intervention and comparator groups of randomized controlled trials: a systematic review and meta-regression. Addiction 115 , 2008–2020 (2020).
Center for Substance Abuse and Treatment. Detoxification and Substance Abuse Treatment (Center for Substance Abuse and Treatment, 2006).
Cahill, K., Hartmann-Boyce, J. & Perera, R. Incentives for smoking cessation. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD004307.pub5 (2015).
Secades-Villa, R., Aonso-Diego, G., García-Pérez, Á. & González-Roz, A. Effectiveness of contingency management for smoking cessation in substance users: a systematic review and meta-analysis. J. Consult. Clin. Psychol. 88 , 951–964 (2020).
Cahill, K. & Perera, R. Competitions and incentives for smoking cessation. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD004307.pub4 (2011).
Trojak, B. et al. Transcranial magnetic stimulation combined with nicotine replacement therapy for smoking cessation: a randomized controlled trial. Brain Stimul. 8 , 1168–1174 (2015).
Wing, V. C. et al. Brain stimulation methods to treat tobacco addiction. Brain Stimul. 6 , 221–230 (2013).
Dinur-Klein, L. et al. Smoking cessation induced by deep repetitive transcranial magnetic stimulation of the prefrontal and insular cortices: a prospective, randomized controlled trial. Biol. Psychiatry 76 , 742–749 (2014).
Goldenberg, M., Danovitch, I. & IsHak, W. W. Quality of life and smoking. Am. J. Addict. 23 , 540–562 (2014).
Heikkinen, H., Jallinoja, P., Saarni, S. I. & Patja, K. The impact of smoking on health-related and overall quality of life: a general population survey in Finland. Nicotine Tob. Res. 10 , 1199–1207 (2008).
Moayeri, F., Hsueh, Y. A., Dunt, D. & Clarke, P. Smoking cessation and quality of life: insights from analysis of longitudinal Australian data, an application for economic evaluations. Value Health 24 , 724–732 (2021).
Taylor, G. M. et al. Smoking cessation for improving mental health. Cochrane Database Syst. Rev. 3 , CD013522 (2021).
López-Nicolás, Á., Trapero-Bertran, M. & Muñoz, C. Smoking, health-related quality of life and economic evaluation. Eur. J. Health Econ. 19 , 747–756 (2018).
Morris, A. Linking nicotine addiction and T2DM. Nat. Rev. Endocrinol. 16 , 6 (2020).
Willi, C., Bodenmann, P., Ghali, W. A., Faris, P. D. & Cornuz, J. Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. Jama 298 , 2654–2664 (2007).
World Health Organization. WHO report on the global tobacco epidemic (WHO, 2019).
Donny, E. C. et al. Randomized trial of reduced-nicotine standards for cigarettes. N. Engl. J. Med. 373 , 1340–1349 (2015). This study tested the impact of reducing the quantity of nicotine present in cigarettes on smoking .
Benowitz, N. L. & Henningfield, J. E. Establishing a nicotine threshold for addiction. The implications for tobacco regulation. N. Engl. J. Med. 331 , 123–125 (1994).
Benowitz, N. L. & Henningfield, J. E. Reducing the nicotine content to make cigarettes less addictive. Tob. Control. 22 , i14–i17 (2013).
Gottlieb, S. & Zeller, M. A nicotine-focused framework for public health. N. Engl. J. Med. 377 , 1111–1114 (2017).
Hall, W. & West, R. Thinking about the unthinkable: a de facto prohibition on smoked tobacco products. Addiction 103 , 873–874 (2008).
Ioannidis, J. P. A. & Jha, P. Does the COVID-19 pandemic provide an opportunity to eliminate the tobacco industry? Lancet Glob. Health 9 , e12–e13 (2021).
Smokefree. Smokefree 2025. Smokefree https://www.smokefree.org.nz/smokefree-in-action/smokefree-aotearoa-2025 (2021).
Morgan, C. J., Das, R. K., Joye, A., Curran, H. V. & Kamboj, S. K. Cannabidiol reduces cigarette consumption in tobacco smokers: preliminary findings. Addict. Behav. 38 , 2433–2436 (2013).
Elsaid, S., Kloiber, S. & Le Foll, B. Effects of cannabidiol (CBD) in neuropsychiatric disorders: a review of pre-clinical and clinical findings. Prog. Mol. Biol. Transl. Sci. 167 , 25–75 (2019).
Butler, K. & Le Foll, B. Novel therapeutic and drug development strategies for tobacco use disorder: endocannabinoid modulation. Expert Opin. Drug Discov. 15 , 1065–1080 (2020).
D’Souza, D. C. et al. Efficacy and safety of a fatty acid amide hydrolase inhibitor (PF-04457845) in the treatment of cannabis withdrawal and dependence in men: a double-blind, placebo-controlled, parallel group, phase 2a single-site randomised controlled trial. Lancet Psychiatry 6 , 35–45 (2019).
Robinson, J. D. et al. Pooled analysis of three randomized, double-blind, placebo controlled trials with rimonabant for smoking cessation. Addict. Biol. 23 , 291–303 (2018).
Gueye, A. B. et al. The CB1 neutral antagonist AM4113 retains the therapeutic efficacy of the inverse agonist rimonabant for nicotine dependence and weight loss with better psychiatric tolerability. Int. J. Neuropsychopharmacol. https://doi.org/10.1093/ijnp/pyw068 (2016).
Yammine, L. et al. Exenatide adjunct to nicotine patch facilitates smoking cessation and may reduce post-cessation weight gain: a pilot randomized controlled trial. Nicotine Tob. Res. 23 , 1682–1690 (2021).
Eren-Yazicioglu, C. Y., Yigit, A., Dogruoz, R. E. & Yapici-Eser, H. Can GLP-1 be a target for reward system related disorders? A qualitative synthesis and systematic review analysis of studies on palatable food, drugs of abuse, and alcohol. Front. Behav. Neurosci. 14 , 614884 (2020).
Vanderkam, P. et al. Effectiveness of drugs acting on adrenergic receptors in the treatment for tobacco or alcohol use disorders: systematic review and meta-analysis. Addiction 116 , 1011–1020 (2021).
Sokoloff, P. & Le Foll, B. The dopamine D3 receptor, a quarter century later. Eur. J. Neurosci. 45 , 2–19 (2017).
David, S. P., Lancaster, T., Stead, L. F., Evins, A. E. & Prochaska, J. J. Opioid antagonists for smoking cessation. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD003086.pub3 (2013).
Ray, L. A. et al. Efficacy of combining varenicline and naltrexone for smoking cessation and drinking reduction: a randomized clinical trial. Am. J. Psychiatry 178 , 818–828 (2021).
Mooney, M. E. et al. Bupropion and naltrexone for smoking cessation: a double-blind randomized placebo-controlled clinical trial. Clin. Pharmacol. Ther. 100 , 344–352 (2016).
Justinova, Z., Le Foll, B., Redhi, G. H., Markou, A. & Goldberg, S. R. Differential effects of the metabotropic glutamate 2/3 receptor agonist LY379268 on nicotine versus cocaine self-administration and relapse in squirrel monkeys. Psychopharmacology 233 , 1791–1800 (2016).
Le Foll, B., Wertheim, C. E. & Goldberg, S. R. Effects of baclofen on conditioned rewarding and discriminative stimulus effects of nicotine in rats. Neurosci. Lett. 443 , 236–240 (2008).
Franklin, T. R. et al. The GABA B agonist baclofen reduces cigarette consumption in a preliminary double-blind placebo-controlled smoking reduction study. Drug Alcohol. Depend. 103 , 30–36 (2009).
Lotfy, N., Elsawah, H. & Hassan, M. Topiramate for smoking cessation: systematic review and meta-analysis. Tob. Prev. Cessat. 6 , 14 (2020).
Shanahan, W. R., Rose, J. E., Glicklich, A., Stubbe, S. & Sanchez-Kam, M. Lorcaserin for smoking cessation and associated weight gain: a randomized 12-week clinical trial. Nicotine Tob. Res. 19 , 944–951 (2017).
Higgins, G. A., Fletcher, P. J. & Shanahan, W. R. Lorcaserin: a review of its preclinical and clinical pharmacology and therapeutic potential. Pharmacol. Ther. 205 , 107417 (2020).
Stead, L. F. & Lancaster, T. Interventions to reduce harm from continued tobacco use. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD005231.pub2 (2007).
Download references
Acknowledgements
B.Le F. is supported by a clinician-scientist award from the Department of Family and Community Medicine at the University of Toronto and the Addiction Psychiatry Chair from the University of Toronto. The funding bodies had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication. The authors thank H. Fu (University of Toronto) for assistance with Figs 1–3.
Author information
Authors and affiliations.
Translational Addiction Research Laboratory, Campbell Family Mental Health Research Institute, Centre for Addiction and Mental Health, University of Toronto, Toronto, Ontario, Canada
Bernard Le Foll
Departments of Family and Community Medicine, Psychiatry, Pharmacology and Toxicology, University of Toronto, Toronto, Ontario, Canada
Department of Medicine, University of Wisconsin, Madison, WI, USA
Megan E. Piper
University of Wisconsin Center for Tobacco Research and Intervention, Madison, WI, USA
Department of Neurobiology and Behaviour, University of California Irvine, Irvine, CA, USA
Christie D. Fowler
Section for Preventive Cardiology, Department of Endocrinology, Morbid Obesity and Preventive Medicine, Oslo University Hospital, Oslo, Norway
Serena Tonstad
Department of Psychiatry, Washington University School of Medicine, St. Louis, MO, USA
Laura Bierut
Institute of Mental Health, Peking University Sixth Hospital, Peking University, Beijing, China
National Institute on Drug Dependence, Peking University Health Science Center, Beijing, China
Centre for Global Health Research, Unity Health Toronto, University of Toronto, Toronto, Ontario, Canada
- Prabhat Jha
National Centre for Youth Substance Use Research, The University of Queensland, St Lucia, Queensland, Australia
Wayne D. Hall
Queensland Alliance for Environmental Health Sciences, The University of Queensland, Woolloongabba, Queensland, Australia
You can also search for this author in PubMed Google Scholar
Contributions
Introduction (B.Le F.); Epidemiology (P.J. and W.D.H.); Mechanisms/pathophysiology (C.D.F., L.B., L.L. and B.Le F.); Diagnosis, screening and prevention (P.J., M.E.P., S.T. and B.Le F.); Management (M.E.P., S.T., W.D.H., L.L. and B.Le F.); Quality of life (P.J. and W.D.H.); Outlook (all); Conclusions (all). All authors contributed substantially to the review and editing of the manuscript.
Corresponding author
Correspondence to Bernard Le Foll .
Ethics declarations
Competing interests.
B.Le F. has obtained funding from Pfizer (GRAND Awards, including salary support) for investigator-initiated projects. B.Le F. has received some in-kind donations of cannabis product from Aurora and medication donation from Pfizer and Bioprojet and was provided a coil for TMS study from Brainsway. B.Le F. has obtained industry funding from Canopy (through research grants handled by CAMH or the University of Toronto), Bioprojet, ACS, Indivior and Alkermes. B.Le F. has received in-kind donations of nabiximols from GW Pharma for past studies funded by CIHR and NIH. B.Le F. has been an advisor to Shinoghi. S.T. has received honoraria from Pfizer the manufacturer of varenicline for lectures and advice. All other authors declare no competing interests.
Peer review
Peer reviewer information.
Nature Reviews Disease Primers thanks Jamie Brown, Elisardo Iglesias and Ming Li for their contribution to the peer review of this work.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
CTRI website: https://d3futrf33lk36a.cloudfront.net/wp-content/uploads/sites/240/2019/04/Meds-Chart.pdf
Philip Morris International: https://www.pmi.com/
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Le Foll, B., Piper, M.E., Fowler, C.D. et al. Tobacco and nicotine use. Nat Rev Dis Primers 8 , 19 (2022). https://doi.org/10.1038/s41572-022-00346-w
Download citation
Accepted : 07 February 2022
Published : 24 March 2022
DOI : https://doi.org/10.1038/s41572-022-00346-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Integrated mrna- and mirna-sequencing analyses unveil the underlying mechanism of tobacco pollutant-induced developmental toxicity in zebrafish embryos.
- Jiasheng Chen
- Xiaoping Zhong
Journal of Translational Medicine (2024)
Reductions in smoking due to ratification of the Framework Convention for Tobacco Control in 171 countries
- Guillermo Paraje
- Mauricio Flores Muñoz
Nature Medicine (2024)
Impact of benzoic acid and 2,2’-methylenebis (6-tert-butyl-4-methylphenol) on the metabolome of flue-cured tobacco and rhizosphere microbial communities: implications for continuous cropping obstacles
- Qiulian Peng
- Jiayan Zhang
Plant and Soil (2024)
When smoke meets gut: deciphering the interactions between tobacco smoking and gut microbiota in disease development
- Guangyi Zeng
- Changtao Jiang
Science China Life Sciences (2024)
Effectiveness of health promotion intervention on the knowledge and selected practices related with oral cancer among a group of vulnerable youth in Sri Lanka
- Manori Dhanapriyanka
- Kanthi RDFC
- Prasanna Jayasekara
BMC Public Health (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Banning the use of Tobacco Essay
Introduction, why the use of tobacco should be banned, works cited.
Tobacco is a product of a species of plant that has nicotine content. Harvested as leaves of that particular plant, tobacco can be used to control pests or even as medicine.
It is however widely used as a drug through smoking, snuffing, chewing among others. This paper seeks to support the banning of the use of tobacco. The paper will give reasons in support of the opinion.
Tobacco and cardiovascular diseases
Tobacco like many other drugs has varied side effects that call for the control of its use. These negative impacts are manifested in individuals and ends up costing lives in the long run. One of the reasons why tobacco should be banned is its danger in relation to cardiovascular diseases.
Cardiovascular diseases are complications that are associated with the heart and blood vessels in the body such as arteries which carry blood to body parts. Once a cardiovascular disease is induced in a person, it manifests in different ways causing threats to a person’s health and thus life.
A significant percentage of heart complications related deaths have, for example, been associated with tobacco smoking with reports ranging this value at about thirty percent. One of the contents of tobacco, carbon monoxide, has for example been identified to have an impact on the oxygen carrying capacity of blood.
Consequently, a person who is under the influence of tobacco will suffer from insufficient supply of oxygen to vital body parts that include the “heart, lungs, brain and other vital body organs” (Wvdhhr 1).
The nicotine content of tobacco also induces increased “heart beat rate and blood pressure” (Wvdhhr 1) as a result, the blood circulatory system is over worked and exposed to risks of being damaged.
This in the long run results in cases such as “heart attacks, high blood pressure, blood clots, strokes, hemorrhages” (Wvdhhr 1) among other disorders. A person who smokes is thus endangered by a number of complications that will negatively hinder the person’s operations and subsequently his or her life due to malfunctioning body parts.
These effects can be easily transferred to aspects such as economic instability of the tobacco victim and immediate family members if the victim was the sole bread winner and is put down by such cardiovascular complications.
A government’s responsibility over the welfare of its citizens therefore calls for a step to control such cardiovascular complications and subsequent impacts and one of the primary ways to do this is by banning the consumption of tobacco.
Tobacco and cancers
Another reason why tobacco should be banned is because of its effect in causing a number of cancers in the body. Cancer is characterized by an induced growth of malignant cells in a person’s body.
These cancerous growths also have an effect of malfunctioning of specified body organs despite the level of pain that might be associated with it. Tobacco smoking has been identified to; for example, cause about “ninety percent of laryngeal cancer and lung cancer and a significant percentage of oral, esophageal and stomach cancers” (Tobacco 1).
Once the cancerous cells start to grow in the body parts, they impair the parts and might even spread causing wounds in the body with subsequent dangers such as death. Lung cancer will, for example, be characterized with growth of foreign cells in the lungs and a corresponding damage of the normal cells.
As a result, the normal functionality of the lungs such as the absorption of oxygen into the body and the elimination of carbon dioxide from the body will be impaired. Respiratory processes that require oxygen and are necessary for cellular activities of the body will therefore be compromised.
Stomach cancer may also impair digestive processes and subsequent poor supply of nutrients to the body. The other cancers such as oral or esophageal may also be associated with a level of pain that can even discourage an individual from eating.
As a result, there will be poor nutritional habit in a victim of these cancers due to insufficient supply of nutrients to the body cells and subsequent insufficient energy generated by the body.
Tobacco therefore with respect to its induced cancers affects the functionality of body organs and the overall health of an individual. These complications have been associated with significant percentage of premature deaths among tobacco users (Tobacco 1).
Tobacco and Addiction
Another reason for alarm over the use of tobacco is the threat of addiction that it poses to its users. Like in cases of other drugs, and induced by its nicotine content, tobacco compels its users into addiction which makes them to even overlook the side effects that the drug has in their lives.
Following the addiction, individual addicts together with help that they receive from social society is not sufficient to help them out of the drug. The only viable control is thus an authoritative step to ban the drug (Dugdale 1).
The use of tobacco is identifiably unhealthy following its risks to the user’s health that is then spread to other members of the society through social and economic costs. Since the drug is addictive, individual users can not easily and willingly stop the consumption the drug. The significant control measure therefore lies in banning usage of the drug.
Dugdale, David. Drug dependence . NCBI, 20101. Web.
Tobacco. Dangers of tobacco . Tobacco Facts, n.d. Web. < http://www.tobacco-facts.info/dangers_of_tobacco.htm >
Wvdhhr. Tobacco and CVD . WVDHHR, n.d. Web. < http://www.wvdhhr.org/bph/cvd/page1.htm >
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2023, December 5). Banning the use of Tobacco. https://ivypanda.com/essays/banning-the-use-of-tobacco/
"Banning the use of Tobacco." IvyPanda , 5 Dec. 2023, ivypanda.com/essays/banning-the-use-of-tobacco/.
IvyPanda . (2023) 'Banning the use of Tobacco'. 5 December.
IvyPanda . 2023. "Banning the use of Tobacco." December 5, 2023. https://ivypanda.com/essays/banning-the-use-of-tobacco/.
1. IvyPanda . "Banning the use of Tobacco." December 5, 2023. https://ivypanda.com/essays/banning-the-use-of-tobacco/.
Bibliography
IvyPanda . "Banning the use of Tobacco." December 5, 2023. https://ivypanda.com/essays/banning-the-use-of-tobacco/.
- Should Cigarettes Be Banned? Essay
- Pharmacology of Nicotine: Absorption and Distribution
- Bisphenol-A Should be Banned
- Nicotine Addiction Research and Assessment
- Nicotine: E-Cigarettes and Tobacco Use
- Banning Violent Video Games Argumentative Essay
- Arguments for and Against Banning All Forms of Child Labour
- Tobacco and COVID-19 Relations
- Banning Gender Affirming Care: Denying Transgenders Access to Healthcare
- Banning Texting while Driving Saves Lives
- Impact of Culture on Communication in a Health Setting
- Workplace Stress Problem
- Health Outcome of Tobacco Use: Lung Cancer
- The Different Lifestyle Issues that Affect People’s Health
- The Influence on Health of Economic Inequality
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Committee on the Public Health Implications of Raising the Minimum Age for Purchasing Tobacco Products; Board on Population Health and Public Health Practice; Institute of Medicine; Bonnie RJ, Stratton K, Kwan LY, editors. Public Health Implications of Raising the Minimum Age of Legal Access to Tobacco Products. Washington (DC): National Academies Press (US); 2015 Jul 23.

Public Health Implications of Raising the Minimum Age of Legal Access to Tobacco Products.
- Hardcopy Version at National Academies Press
4 The Effects of Tobacco Use on Health
The scope of the burden of disease and death that cigarette smoking imposes on the public's health is extensive. Cigarette smoking is the major focus of this chapter because it is the central public health problem, but the topics of secondhand smoke exposure, smoking of other combustible tobacco products, smokeless tobacco, and electronic nicotine delivery systems (ENDS) are also considered. The magnitude of the public health threat posed by cigarette smoking stems from two factors: (1) the prevalence of cigarette smoking is so high, and (2) smoking causes so many deleterious health effects. A policy change that reduces the prevalence of cigarette smoking will result in a commensurate reduction in the population burden of disease and death caused by cigarette smoking. The associations between cigarette smoking and the adverse health effects caused by smoking are dose-dependent ( HHS, 2014 ). Thus, a public health benefit would be realized if a policy change led to reduced exposure to cigarette smoke via means other than reducing the prevalence of smoking. For example, additional reduction in the population burden of smoking-caused disease and death will be generated if the policy also results in delayed initiation of cigarette smoking. The population health benefit from delayed initiation, although potentially large, will be less than the benefit from a commensurate reduction in smoking prevalence because delayed initiation is associated with reduced exposure to cigarette smoking rather than with the complete prevention of the exposure. A decrease in the prevalence of cigarette smoking will have additional downstream benefits by reducing the potential for nonsmokers to be exposed to secondhand tobacco smoke.
- TIME HORIZON FOR THE HEALTH EFFECTS OF CIGARETTE SMOKING
Cigarette smoking causes chronic diseases that appear at older ages, such as lung cancer, as well as adverse health effects that occur in the short run. The immediate and short-term adverse health effects of cigarette smoking are less likely to be directly fatal than the long-term health effects. Nevertheless, they are important public health indicators because they lead to suboptimal health status throughout the life course in smokers and because many of the short-term physiologic effects mechanistically contribute to the etiology of smoking-caused diseases that usually do not become clinically apparent until later adulthood.
The short-term adverse health effects caused by cigarette smoking can be observed in smokers immediately or soon after they begin smoking. The health effects of cigarette smoking thus begin at or near the age of initiation of cigarette smoking, which is usually in adolescence. To highlight the immediacy of the adverse impact of smoking on health, this report uses a life-course perspective by considering health effects of smoking according to the various stages of life, which include childhood, adolescence, and young adulthood as well as middle and late adulthood, when most of the chronic disease burden imposed by smoking occurs. A particularly vulnerable time during the life course is pregnancy (for both mother and fetus) and the months following birth (for the infant); for this reason, this stage of life is considered separately. In this report, the term “immediate health effects” refers to effects that occur within days of cigarette smoking, while “long-term health effects” refers to the clinical morbidity and mortality that occur primarily in middle and late adulthood, and the term “intermediate health effects” is used to refer broadly to the health outcomes that occur between the immediate and long-term health effects.
- SPECTRUM OF HEALTH EFFECTS
Cigarette smoke contains more than 7,000 chemicals ( HHS, 2010 ). Inhaling cigarette smoke exposes the cigarette smoker to these numerous toxins, which include the various tobacco constituents and the products of pyrolysis. As summarized below, exposure to this complex chemical mixture causes immediate adverse physiologic effects shortly after the exposure occurs ( HHS, 2010 ).
The ultimate harm caused by exposure to the toxic agents in cigarette smoke is determined in large part by the extent of the exposure, and most adult cigarette smokers tend to smoke many cigarettes per day for decades ( HHS, 2014 ). This repeated inhalation of the complex mixture of cigarette smoke toxicants at high daily doses, often sustained over the course of many years, causes a broad spectrum of short-term and long-term health effects that affect most major organ systems (see Tables 4-1 through 4-3 ). In the short run, cigarette smoking causes the smoker to have overall diminished health status as measured by a diverse array of indices, including biomarkers of physiologic disadvantage, lower self-reported health, susceptibility to acute illnesses and respiratory symptoms, and absence from school and work. Among the long-term health effects are smoking-caused diseases that are the major causes of death in middle- and upper-income nations: coronary heart disease, cancer, and chronic obstructive pulmonary disease, or COPD ( HHS, 2014 ).
Immediate Adverse Health Outcomes Causally Associated with Cigarette Smoking Based on Surgeon General's Reports.
Long-Term Adverse Health Outcomes Causally Associated with Cigarette Smoking Based on Surgeon General's Reports.
The net result of the broad spectrum of short-term and long-term deleterious health effects caused by cigarette smoking and the substantial prevalence of smoking is that cigarette smoking is the single most important cause of preventable disease and premature mortality in the United States and in many other high-income nations ( Thun et al., 2012 ). For example, in the United States cigarette smoking is estimated to account for at least 480,000 deaths per year ( HHS, 2014 ). The magnitude of this burden is a direct function of two key facts: (1) cigarette smoking causes an incredibly broad spectrum of short-term and long-term deleterious health effects, and (2) a large proportion of the population is exposed (i.e., the prevalence of smoking is very high).
In assessing the potential public health impact of enacting a new tobacco policy such as raising the minimum age of legal access to tobacco products (MLA), it is worth keeping in mind that this lengthy catalogue of well-established consequences of cigarette smoking will continue to expand as scientific knowledge advances and more definitive evidence is generated concerning additional health outcomes. Thus, the characterization of the potential impact of a policy change that reduces exposure to cigarette smoke is a conservative estimate of the true public health impact. For example, in addition to the many adverse health outcomes established as causally related to tobacco smoke and summarized in Tables 4-1 , 4-2 , and 4-3 , Tables 4-4 and 4-5 summarize health outcomes for which the evidence summarized in the 2014 Surgeon General's report is currently considered strong enough to be considered suggestive of a causal association but not yet strong enough to be rated as causal. These are outcomes for which the currently existing body of evidence falls short of being definitive, but the association between cigarette smoking and these outcomes remains under active investigation.
Intermediate Adverse Health Outcomes Causally Associated with Cigarette Smoking Based on Surgeon General's Reports.
Intermediate Adverse Health Outcomes with Evidence Suggestive of a Causal Association with Cigarette Smoking Based on Surgeon General's Reports.
Long-Term Adverse Health Outcomes with Evidence Suggestive of a Causal Association with Cigarette Smoking Based on Surgeon General's Reports.
Tables 4-1 through 4-3 summarize the preclinical health effects and morbidity caused by cigarette smoking, organized according to whether the effects occur in the immediate, intermediate, or long-term time horizon and by the stages of life usually affected by the health outcome.
Immediate Health Effects
Cigarette smoking causes a constellation of subclinical health effects that occur shortly after initiation of smoking. As described below, these immediate adverse health effects include increased oxidative stress; depletion of selected bioavailable antioxidant micronutrients; increased inflammation; impaired immune status; altered lipid profiles; poorer self-rated health status; respiratory symptoms, including coughing, phlegm, wheezing, and dyspnea; and nicotine addiction. Taken in combination, these detrimental effects detract from a smoker's overall health status and lead to what has been referred to as “diminished health status” ( HHS, 2004 ). Physiologic markers of diminished health status include subclinical outcomes such as increased oxidative stress, reduced antioxidant defenses, increased inflammation, impaired immune status, and altered lipid profiles (see Tables 4-1 through 4-3 ). Smoking's impacts on such short-term physiologic outcomes impair the smoker's overall health status, which in turn renders the smoker more susceptible to various adverse health outcomes, such as developing acute illnesses, respiratory symptoms, and a lessened capacity to heal wounds. One downstream marker of the diminished health status induced by cigarette smoking is that smokers are more likely to miss school and work. In short, soon after the initiation of smoking, an array of smoking-induced short-term deleterious health effects sets in motion a lifelong trajectory that leaves persistent smokers highly disadvantaged compared to their counterparts who never smoked. By looking at the immediate and intermediate adverse health effects of cigarette smoking, it is clear that cigarette smoking contributes in important ways to suboptimal health beginning shortly after smoking initiation—long before the chronic diseases that smoking causes at older ages become clinically apparent ( HHS, 2004 ).
Physiologic Markers of Diminished Health Status
Increased oxidative stress.
Cigarette smoke contains free radicals and other oxidants in abundance. A single puff of a cigarette exposes the smoker to more than 10 15 free radicals in the gas phase and additional radicals and oxidants in the tar phase ( Pryor and Stone, 1993 ).
The biological impacts of the oxidative stress induced by cigarette smoking have been extensively documented in humans ( HHS, 2004 ). These include oxidative injury to proteins, DNA, and lipids. Assaying protein carbonyls is one method of measuring oxidative damage to proteins, and protein carbonyl concentrations have been observed to be significantly higher in smokers than in nonsmokers ( Kapaki et al., 2007 ; Marangon et al., 1999 ; Padmavathi et al., 2010 ). One way of quantifying the oxidative damage to DNA is to measure the DNA damage in peripheral white blood cells induced by the hydroxyl radical at the C8 position of guanine, 8-hydroxy-deoxyguanosine (8-OH-dG). Most of the available evidence indicates that current smokers have concentrations of 8-OH-dG in peripheral leukocytes that are at least 20 percent higher than nonsmokers ( HHS, 2004 ). Studies of 8-OH-dG in DNA extracted from urine provide corroborative evidence, with 8-OH-dG concentrations that are 6 to 50 percent higher in smokers than in nonsmokers ( Campos et al., 2011 ; HHS, 2004 ; Lowe et al., 2009 ; Seet et al., 2011 ). Measures of lipid peroxidation include F2-isoprostanes and malondialdehyde (MDA). Many studies have demonstrated that current smokers have substantially higher concentrations of isoprostanes in both plasma and urine than nonsmokers ( Bloomer et al., 2008 ; HHS, 2004 ; Kocyigit et al., 2011 ; Ozguner et al., 2005 ; Seet et al., 2011 ; Taylor et al., 2008 ). The results of several studies indicate that MDA concentrations are 30 percent more abundant in current-versus-nonsmokers, suggesting cigarette smoking directly increases MDA concentrations ( Bloomer et al., 2008 ; Jain et al., 2009 ; Kocyigit et al., 2005 ; Ozguner et al., 2005 ). This is further corroborated by evidence from several studies that have found concentrations of thiobarbituric acid–reactive substances (TBARS) found in MDA range from 6 percent to 118 percent more in smokers than in people who have never smoked ( HHS, 2004 ).
Cigarette smoking clearly generates substantial quantities of oxidative stress, as indicated by a consistent body of evidence indicating that cigarette smoking significantly increases biomarkers of oxidative damage to proteins, DNA, and lipids. Cigarette smokers experience measurable and immediate oxidative damage. This oxidative damage, experienced over long periods of time, is one pathway contributing to smoking-caused disease and death ( HHS, 2010 ).
Depletion of circulating antioxidant micronutrient concentrations
Cigarette smoking exposes the smoker to potential oxidative damage not experienced by the nonsmoker. One direct result of the exposure to oxidative stress is the depletion of the body's defenses against oxidative stress. For example, the antioxidant defense system is partly comprised of antioxidant micronutrients ( Evans and Halliwell, 2001 ). Antioxidant status provides a biomarker of health status because oxidative damage is thought to be centrally involved in the aging process as well as in enhanced susceptibility to a wide range of specific diseases. Evidence from a number of studies firmly establishes that smokers have circulating concentrations of ascorbic acid and provitamin A carotenoids such as a-carotene, b-carotene, and cryptoxanthin that are more than 25 percent lower than nonsmokers ( Alberg, 2002 ). Considered in total, a strong and diverse body of evidence consistently implicates oxidative stress from cigarette smoking in the depletion of antioxidant micronutrients in circulation. Furthermore, the results across studies are consistent with a dose–response relationship, with the amount of smoking being inversely related to the circulating concentrations of vitamin C and provitamin A carotenoids ( HHS, 2004 ).
The immediate effects of cigarette smoking on these concentrations have been examined with measurements of circulating micronutrient concentrations taken before and after a smoker stops smoking. One such study, for example, found substantially increased concentrations of vitamin C and provitamin A carotenoids after 84 hours without a cigarette ( Brown, 1996 ). In another study, the exposure of plasma to the equivalent of six puffs of cigarette smoke completely depleted the ascorbic acid present in the serum ( Eiserich et al., 1995 ). In yet another, measurements taken at baseline and 20 minutes after smoking a cigarette found decreased circulating micronutrient concentrations ( Yeung, 1976 ). Results such as these highlight the immediate impact that smoking a cigarette can have on health status. Cigarette smoking causes depletion of antioxidant micronutrients, leading smokers to have lower circulating concentrations of these antioxidant micronutrients than nonsmokers. The direct immediate result on the smoker's lower concentrations of antioxidant micronutrients such as vitamin C is to reduce the smoker's antioxidant defenses, and thus the smoker's cells throughout the body are more prone to the damaging effects of oxidative stress. Oxidative stress is hypothesized to be associated with premature aging and greater risk of disease ( Laher, 2014 ).
Increased inflammation
The direct pro-oxidant effects of cigarette smoke are further exacerbated by additional endogenous oxidant formation via the smoking-induced inflammatory-immune response ( van der Vaart et al., 2004 ; Yao and Rahman, 2011 ). Another measure of smokers' poorer health is the chronically higher level of inflammatory response experienced by smokers compared to nonsmokers. Chronic inflammation is hypothesized to play a role in the pathogenesis of numerous chronic diseases ( Pawelec et al., 2014 ; Prasad et al., 2012 ).
For example, cigarette smoking is strongly and consistently associated with higher leukocyte concentrations ( HHS, 2004 ); this suggests that smoking induces a sustained, long-term inflammatory response. Compared to nonsmokers, current smokers have been uniformly found, across many studies, to have approximately 20 percent higher leucocyte counts. Furthermore, leucocyte counts increase with a greater degree of smoking, measured either by the number of cigarettes smoked per day or the depth of inhalation ( HHS, 2004 ). Prospective cohort studies that evaluate how changes in smoking status relate to changes in leucocyte counts provide evidence that eliminating cigarette smoking leads to reductions in leucocyte counts ( HHS, 2004 ). Leucocytes are a marker of chronic inflammation, but cigarette smoking is also associated with markers of the acute inflammatory response, such as C-reactive protein ( HHS, 2014 ).
Impaired immune status
The 2014 Surgeon General's report was the first report of the Surgeon General to review thoroughly the contribution of cigarette smoking to impaired immune status. Cigarette smoking was found to adversely impact the two major immune pathways, innate immunity and adaptive immunity. Recognizing the extreme complexity of the immune system, with its built-in compensatory mechanisms, the conclusion of the Surgeon General's report was that the evidence is sufficient to infer that cigarette smoking compromises the immune system and compromises immune homeostasis by diminishing both innate and adaptive immunity ( HHS, 2014 ). The impact of the adverse effects on immune status would be to make smokers more susceptible to disease, which in turn contributes to the etiology of acute infectious and chronic diseases above and beyond the way in which cigarette smoking contributes to acute and chronic inflammation.
Altered lipid profiles
Cigarette smoking causes altered lipid metabolism ( HHS, 2010 ). The alterations in the lipid profile induced by cigarette smoking create a higher risk profile: Compared with nonsmokers, cigarette smokers have significantly higher serum cholesterol, triglyceride, and low-density lipoprotein (LDL) levels and lower high-density lipoprotein (HDL) levels ( Ambrose and Barua, 2004 ). In a meta-analysis of 54 epidemiologic studies, smokers were found to have serum concentrations of cholesterol, triglycerides, and very low density lipoprotein (VLDL) cholesterol that were 3 percent, 9 percent, and 10 percent higher, respectively, and HDL cholesterol concentrations that were 6 percent lower than nonsmokers ( Craig et al., 1989 ). Furthermore, clear dose–response associations were observed, with these associations growing stronger as the number of cigarettes smoked per day increased. The alteration of the lipid profile in the direction of increased cardiovascular disease risk has been extensively documented not only in adults but also in children and adolescents. In a meta-analysis of studies in which study participants ranged from 8 to 19 years of age, adolescents who smoked cigarettes had serum LDL cholesterol and triglyceride concentrations that were significantly higher than in nonsmokers, whereas smokers had lower serum concentrations of HDL cholesterol than nonsmokers ( Craig et al., 1990 ). These differences are likely due to a direct effect of cigarette smoking. In a cohort of middle school students in Germany, those who initiated smoking had significantly lower HDL cholesterol levels than nonsmokers after 2 years of follow-up despite there having been similar baseline levels of HDL cholesterol in the two groups—those who would remain nonsmokers and those who would go on to begin smoking ( Dwyer et al., 1988 ).
Poorer Self-Rated Health Status
The adverse impact of smoking on health status has been directly measured by comparing self-rated health in smokers versus nonsmokers. Studies of varying design have uniformly shown that smokers tend to rate their overall health status lower than nonsmokers do ( HHS, 2004 , 2014 ). The consistent reporting of poorer self-rated health among smokers compared to nonsmokers across numerous dimensions of health status provides direct evidence that smoking impairs the health of cigarette smokers in ways that are perceptible to the smoker even in the absence of clinical disease.
Respiratory Symptoms: Coughing, Phlegm, Wheezing, Dyspnea
The immediate adverse health effects of cigarette smoking are not limited to subclinical measures; they can also result in physical symptoms. In reviewing the evidence separately for children/adolescents and adults, the 2004 Surgeon General's report concluded that cigarette smoking was causally associated with all major respiratory symptoms in both age groups ( HHS, 2004 ). The specific symptoms caused by cigarette smoking are coughing, phlegm, wheezing, and dyspnea. The consistent presence of the causal association across the life course supports the classification of these symptoms as an immediate health effect based on the definition used in this report.
Nicotine Addiction
Another clinical, immediate adverse health effect of cigarette smoking is nicotine addiction. The 2012 Surgeon General's report concluded that cigarette smoking was causally associated with nicotine addiction, beginning in adolescence ( HHS, 2012 ). The onset of nicotine addiction begins soon after smoking initiation.
The importance of nicotine addiction as an immediate adverse health effect cannot be underestimated. Nicotine addiction, via its role in propagating sustained smoking, assumes a role as a central determinant of the entire catalogue of downstream health effects of cigarette smoking. The often long-term, sustained addiction to nicotine is the underlying factor driving the long-term, sustained exposure to the toxins in tobacco smoke that drive the adverse health effects of cigarette smoking.
Finding 4-1: Cigarette smoking is causally associated with a broad spectrum of adverse health effects that begin soon after the onset of regular smoking and that, in total, significantly diminish the health status of the smoker compared to nonsmokers .
Intermediate-Term Effects on Morbidity
The health effects included in the category of “intermediate adverse health effects” consist largely of health outcomes that are not dependent on having smoked a cigarette in the immediate past but rather require a more extensive smoking history for the adverse outcome to become manifest. For example, intermediate adverse health effects are often direct sequellae of some of the immediate health effects of smoking, such as absenteeism and medical care utilization, or else they are diagnoses that are precursors of subsequent, more severe disease endpoints, such as type 2 diabetes and subclinical atherosclerosis. Cigarette smoking cessation diminishes the risk of experiencing these intermediate adverse health effects, but individuals with a past history of cigarette smoking still have greater risks than those who never smoked.
Absenteeism
Another indicator of diminished health status is absence from work. Among the many factors that contribute to attendance, health status is clearly a major determinant. Thus, attendance patterns are potential markers of health status ( Alberg et al., 2003 ).
Cigarette smoking is a determinant of absence. A substantial body of evidence on the association in adults between cigarette smoking and absence from work consistently demonstrates that smokers are significantly more likely to have greater workplace absenteeism ( HHS, 2004 ). The likelihood of workplace absence increases with the number of cigarettes smoked per day ( HHS, 2004 ). Furthermore, smoking cessation is associated with reduced absence rates ( HHS, 2004 ). In addition to smokers having more episodes of absence than nonsmokers, smokers tend to stay out longer when they are sick than nonsmokers. Thus, smokers miss more cumulative work time than nonsmokers ( HHS, 2004 ).
A strong and consistent body of evidence demonstrates that cigarette smoking is associated with a greater likelihood of absence from work. This association could be at least partially due to smoking being a marker for other causes of absenteeism, such as mental illness and abuse of other substances. In considering the societal toll of cigarette smoking, attendance is not only a useful marker of diminished health status, but also a marker of other downstream costs. On the individual level, workplace absenteeism can lead to problems on the job and even result in unemployment. At the societal level, absenteeism decreases productivity and is a drain on the economy.
Increased Utilization of Medical Services
Utilization of medical services provides an additional indicator of health status. Despite the complexities inherent in studying the association between cigarette smoking and use of medical services, the evidence reviewed in the 2004 and 2014 Surgeon General's reports yields a clear signal indicating that cigarette smokers generate higher medical care costs and have more inpatients and outpatient visits than those who do not smoke ( HHS, 2004 , 2014 ). Among patients admitted to the hospital, smokers have longer lengths of stay and incur greater expenses per admission than nonsmokers.
Subclinical Atherosclerosis
Atherosclerosis is a cardiovascular disease precursor that begins early in life; it is the underlying pathogenic mechanism that ultimately leads to many cardiovascular disease endpoints. The epidemiologic evidence has been consistent in demonstrating a strong, dose-dependent association between cigarette smoking and subclinical atherosclerosis as measured by carotid intimal–medial thickness. Consequently, cigarette smoking has been established as a cause of atherosclerosis ( HHS, 2004 ). Establishing the link between cigarette smoking and atherosclerosis provides a strong, biologically plausible rationale for the role of cigarette smoking in the pathogenesis of clinical cardiovascular endpoints that occur as a consequence of atherosclerosis.
Impaired Lung Development and Accelerated Decline in Function
In addition to smoking's long-term health effects on the respiratory system from diseases such as lung cancer and COPD, some adverse respiratory effects experienced by adolescent cigarette smokers manifest themselves shortly after smoking initiation. Compared to nonsmokers, adolescents who smoke cigarettes are more likely to experience impaired lung growth, early onset in the decline of lung function, and asthma-related symptoms ( HHS, 2004 ). Among adults who smoke cigarettes, lung function begins to decline at younger ages, and the age-related decline in lung function occurs faster ( HHS, 2004 ).
Increased Susceptibility to Infectious Lung Diseases
Due at least in part to its adverse impact on immune status, cigarette smoking predisposes the smoker to developing acute infectious respiratory illnesses such as pneumonia. Established effects of cigarette smoking on the immune system provide a clear biological basis for the increased likelihood that has been observed among smokers of developing an infection after exposure to microbes that cause respiratory infections and also of developing a clinically apparent disease once infected ( HHS, 2004 ). Further, impaired cilia function in the trachea and bronchi also contributes to the increased risk of respiratory infections in smokers ( Simet et al., 2010 ). Thus, it is no surprise that cigarette smokers have an increased susceptibility to respiratory infections.
Cigarette smoking is causally associated with an increased risk of pneumonia ( HHS, 2004 ). The 2014 Surgeon General's report was the first to review the evidence on the association between cigarette smoking and tuberculosis. A strong statistical association has been observed between cigarette smoking and risk of M. tuberculosis infection and also the risk, once infected, of progressing to tuberculosis disease, but showing a clear causal connection between smoking and risk of tuberculosis has been challenging because cigarette smokers often have a much higher risk profile than nonsmokers for these outcomes because of other social determinants of health. These challenges notwithstanding, the evidence has now coalesced to the point that cigarette smoking is causally associated with tuberculosis disease and tuberculosis mortality ( HHS, 2014 ).
Type 2 diabetes mellitus is a leading underlying cause of mortality from cardiovascular disease, and it also leads to other adverse consequences such as kidney failure and blindness ( HHS, 2014 ). Obesity has long been established as a major risk factor for diabetes, but the association between cigarette smoking and diabetes has only more recently been elucidated. The results of a meta-analysis of 51 prospective cohort studies in the 2014 Surgeon General's report demonstrated that cigarette smokers have a 30–40 percent greater risk of diabetes than nonsmokers and that there is a strong dose–response relationship, with the risk increasing with the number of cigarettes smoked per day ( HHS, 2014 ). In addition to having an increased risk of developing diabetes, evidence also indicates that, among patients with diabetes, cigarette smokers are more likely to suffer cardiovascular complications and to have higher mortality rates. Based on this body of evidence, the 2014 Surgeon General's report concluded that cigarette smoking is a cause of diabetes ( HHS, 2014 ).
Periodontitis
A synthesis of the evidence in the 2004 Surgeon General's report revealed a strong, consistent, and dose-dependent relationship between cigarette smoking and the risk of periodontitis. Based on this evidence, cigarette smoking was judged to be causally associated with periodontitis. Approximately one-half of all diagnoses of adult periodontitis are attributable to cigarette smoking ( HHS, 2004 ).
Asthma Exacerbation
The fact that cigarette smoking is causally associated with so many outcomes that are relevant to asthma has long raised suspicions that cigarette smoking is a risk factor for asthma. Examples of these asthma-relevant factors are persistent inflammation, diminished immune status, and the respiratory symptoms of coughing, phlegm, wheezing, and dyspnea. At the present time, the evidence is considered suggestive but not sufficient to infer a causal association between cigarette smoking and the risk of developing asthma in adolescents or adults or between smoking and the risk of asthma exacerbations in adolescents ( HHS, 2014 ). However, the 2014 Surgeon General's report did conclude that cigarette smoking is causally associated with asthma exacerbation in adults ( HHS, 2014 ).
Adverse Surgical Outcomes: Wound Healing and Respiratory Complications
The fact that smoking causes diminished health status by impairing factors such as immune response and lung function provides a strong reason to believe that cigarette smoking could be associated with a worse prognosis after surgical procedures. Based on a large and diverse body of evidence with outcomes that ranged from short- and long-term complications of surgery to survival, the 2004 Surgeon General's report concluded that cigarette smoking is a cause of adverse surgical outcomes ( HHS, 2004 ).
Finding 4-2: Cigarette smoking causes many adverse health effects classified as “intermediate,” which include increased absence from work, the increased use of medical services, subclinical atherosclerosis, impaired lung development and function, an increased risk of lung infections, diabetes, periodontitis, the exacerbation of asthma in adults, subclinical organ injury, and adverse surgical outcomes .
Long-Term Morbidity
Cigarette smoking contributes to a major portion of the population burden of many of the chronic diseases that typically occur in middle and late adulthood, such as cancer, cardiovascular disease, and COPD ( HHS, 2004 ). As noted below, the full scope of long-term morbidity attributable to cigarette smoking also extends to numerous other disease endpoints. Cessation of cigarette smoking diminishes the risk of experiencing these long-term adverse health effects, but a past history of cigarette smoking is still associated with increased risk compared to never having smoked ( HHS, 2014 ).
Cigarette smoking is causally associated with 12 different types of malignancy and is responsible for approximately 30 percent of all cancer deaths in the United States ( ACS, 2007 ; HHS, 2014 ). Cigarette smoking has been known for many years to be a cause of cancers of the lung, oral cavity, larynx, esophagus, bladder, pancreas, kidney, uterine cervix, and stomach, and of acute myeloid leukemia. The conclusions of the 2014 report of the Surgeon General indicate that cigarette smoking is also causally associated with colorectal cancer and liver cancer. Furthermore, cigarette smoking is causally associated with clinical precursors of cancer lesions, such as colorectal adenomatous polyps ( HHS, 2014 ).
Vascular Disease
Cigarette smoking is associated with numerous clinical cardiovascular disease endpoints, including coronary heart disease, stroke, and abdominal aortic aneurism. Coronary heart disease is a leading cause of death in the United States and most high-income countries. Cigarette smoking has been established as a major cause of coronary heart disease for decades. The impact of cigarette smoking is particularly strong among younger age groups, as it causes 40 percent of ischemic heart disease deaths in 35- to 64-year-olds ( HHS, 2004 ).
Cigarette smoking has long been identified as a major cause of cerebrovascular disease. As with coronary heart disease, the impact of cigarette smoking is proportionally larger in relatively younger adults. Among 35- to 64-year-olds, more than 40 percent of all cerebrovascular disease deaths are attributable to cigarette smoking ( HHS, 2004 ).
Cigarette smoking is an established cause of abdominal aortic aneurysm ( HHS, 2004 ). This condition is often fatal and accounts for more than 10,000 deaths per year in the United States.
The process of inhaling cigarette smoke brings the smoker's respiratory system into direct contact with heavy doses of tobacco toxins. Given these profound levels of exposure, it is not surprising that cigarette smoking's deleterious effects on the respiratory system extend well beyond lung cancer. Cigarette smoking is estimated to have caused 7.5 million prevalent cases of COPD in the United States in 2009 ( Rostron et al., 2014 ). More than 138,000 Americans died from COPD in 2010, making it the third leading cause of death in the United States ( Heron, 2013 ). As the predominant cause of COPD, cigarette smoking is responsible for approximately 80 percent of the mortality burden from COPD ( HHS, 2004 ).
Eye Disease: Age-Related Macular Degeneration and Nuclear Cataracts
Cigarette smoking also adversely affects eye health, causing nuclear cataracts ( HHS, 2004 ). The body of evidence linking cigarette smoking with age-related macular degeneration that was accumulated over the past two decades has now been judged to be strong and consistent enough to prove a causal association between the two ( HHS, 2014 ).
Rheumatoid Arthritis
Cigarette smoking also causes joint disease. More than 1 million Americans have been diagnosed with rheumatoid arthritis, a disease linked to immune dysregulation. Enough supportive evidence has been accumulated to indicate a clear link between cigarette smoking and rheumatoid arthritis. The conclusions of the 2014 Surgeon General's report contained the conclusion that a causal association has been established between cigarette smoking and rheumatoid arthritis ( HHS, 2014 ).
Bone Health: Hip Fractures and Bone Density
Cigarette smoking has adverse consequences for bone health. Cigarette smoking is causally associated with hip fractures. In postmenopausal women, a causal association has been established between cigarette smoking and low bone density ( HHS, 2004 ).
Finding 4-3: Cigarette smoking is causally associated with a broad spectrum of adverse long-term health effects which cause suffering, impaired quality of life, and death .
Maternal/Fetal and Infancy Health Effects
Pregnancy represents a particularly vulnerable time of life for both the mother and the developing fetus, and this critical time window extends into the neonatal period and infancy. Because of the unique features of this period of enhanced vulnerability and its critical public health importance, the topic is considered separately. Cigarette smoking is an established cause of a broad spectrum of health effects to the mother, fetus, and infant, including decreased likelihood of becoming pregnant, increased risk of experiencing adverse pregnancy outcomes, and adverse effects on the newborn that can range from organ impairment to congenital malformations to death, as summarized in Table 4-6 . Table 4-6 also includes the immediate physiologic effects of smoking from Table 4-1 to emphasize the point that pregnant women who smoke incur the same short-term adverse health effects incurred by all cigarette smokers. It is estimated that more than 400,000 infants are exposed each year to maternal smoking in utero. Furthermore, recent data indicate that more than 1.2 million births each year in the United States occur among mothers under 25 years of age. In the United States in 2012, 31 percent of all births were to mothers less than 25 years old (1,225,871/3,952,841); of these, 90,095 were to mothers less than 18 years old, 85,310 were to mothers who were 18 years old, and 1,050,466 were to mothers who were 19–24 years old ( Martin et al., 2013 ).
Maternal, Fetal, and Infant Adverse Health Outcomes Causally Associated with Cigarette Smoking Based on Surgeon General's Reports.
Decreased Likelihood of Conception
Cigarette smoking is associated with a decreased likelihood of pregnancy because of smoking's adverse effects on the female and the male reproductive systems. Cigarette smoking is causally associated with reduced fertility in women ( HHS, 2004 ). Further, the 2014 Surgeon General's report pointed to a diverse body of research evidence supported by a strong biologic rationale to conclude that cigarette smoking is a cause of erectile dysfunction in men.
Pregnancy Complications
Maternal smoking during pregnancy reduces the likelihood of a full-term gestational period with optimal fetal growth. Cigarette smoking by pregnant women adversely affects pregnancy by making it more likely they will experience ectopic pregnancies, complications of pregnancy such as premature rupture of the membranes, placenta previa, and placental abruption. Furthermore, cigarette smoking in expectant mothers causes preterm delivery and shortened gestation ( HHS, 2004 ).
Outcomes: Childbirth, Infancy, and Survival
Maternal cigarette smoking during pregnancy directly harms the fetus and, later, the infant in several ways ( HHS, 2004 ). Cigarette smoking is causally associated with stunted fetal growth and is an important cause of shortened gestation. In combination, stunted fetal growth and premature delivery are major determinants of low birth weight. Cigarette smoking causes congenital malformations, specifically orofacial clefts. Cigarette smoking is also associated with impaired organ function, specifically reduced lung function ( HHS, 2014 ).
Based on these many severe effects, it is logical to infer that cigarette smoking negatively affects the viability of the fetus and child. Specifically, smoking is causally associated with fetal deaths, or stillbirths; furthermore, among live births smoking is an established cause of overall infant mortality. That is, compared with infants of mothers who do not smoke, infants with mothers who smoke during or after pregnancy experience higher rates of death before reaching 1 year of age. One specific cause of increased mortality of infants whose mothers smoke is sudden infant death syndrome, which is more likely to strike those infants than infants whose mothers do not smoke ( HHS, 2004 ).
After birth, children who are exposed to secondhand smoke (SHS) via parental smoking suffer numerous adverse health effects as a consequence. In infants, symptoms associated with SHS exposure include increased lower respiratory illnesses, otitis media, middle ear effusion, reduced lung function, and the respiratory symptoms of coughing, phlegm, wheezing, and dyspnea ( HHS, 2006 ). In addition to the increased risk of symptoms, infants of smoking mothers are more likely to experience subclinical immediate adverse health effects of cigarette smoke exposure as well. For example, evidence indicates that infant exposure to parental smoking is associated with physiologic markers of diminished health status, such as increased oxidative damage to DNA and lipids. As noted above, 8-OH-dG can be used as a measure of oxidative damage to DNA, and neonatal levels of urinary 8-OH-dG have been found to be significantly associated with exposure to the toxicants from tobacco smoke due to the mother's smoking ( Hong et al., 2001 ). Newborns with mothers who smoked had concentrations of 8-OH-dG that were 333 percent higher than newborns whose mothers did not smoke ( Hong et al., 2001 ).
Finding 4-4: Maternal smoking during pregnancy and secondhand smoke exposure during infancy are causally associated with many adverse health outcomes. This not only leaves exposed infants prone to short- and long-term health risks but also can result in death .
Age of Initiation and Health Outcomes
The following four factors were used to assess the effects that the age of initiation had on an individual's cigarette smoking trajectory and subsequent health effects: (1) nicotine dependence, (2) the number of cigarettes smoked per day (smoking intensity), (3) the likelihood of smoking cessation (or, conversely, the likelihood of remaining a smoker), and (4) health outcomes. These four factors are closely interrelated. Nicotine dependence is associated with smoking intensity ( Hu et al., 2006 ), and both of these measures are in turn associated with the likelihood of remaining a smoker in the long term. The interrelationships among the factors involve both smoking intensity (number of cigarettes per day) and smoking duration (number of years smoked) and hence also the effects of the lifetime cumulative exposure to cigarette smoking. Many of the established deleterious health effects of cigarette smoking are dose-dependent, thus providing a mechanistic explanation for how earlier age of initiation could exert a powerful contribution on smoking-caused health effects that is mediated by leading to increased doses of exposure to cigarette smoke.
In particular, the mechanistic basis for a powerful influence of the age of initiation on smoking-caused adverse health outcomes is grounded in the evidence, reviewed in Chapter 3 , that those who start smoking earlier are more likely to (1) have a greater degree of nicotine dependence ( Breslau and Peterson, 1996 ; Buchmann et al., 2013 ; HHS, 2012 ; Hu et al., 2006 ; Lando et al., 1999 ; Park et al., 2004 ), (2) smoke cigarettes more frequently ( Breslau, 1993 ; Buchmann et al., 2013 ; Chen and Millar, 1998 ; D'Avanzo et al., 1994 ; Escobedo et al., 1993 ; Everett et al., 1999 ; Fernandez et al., 1999 ; Hu et al., 2006 ; Lando et al., 1999 ; Reidpath et al., 2014 ; Taioli and Wynder, 1991 ), and (3) remain smokers for longer periods of time ( Breslau and Peterson, 1996 ; Chen and Millar, 1998 ; D'Avanzo et al., 1994 ; Eisner et al., 2000 ; Everett et al., 1999 ; Khuder et al., 1999 ). These associations all point toward an association between a younger age of initiation and greater exposure to the toxicants in cigarette smoke, which because of well-established dose–response relationships would therefore be expected to lead to higher risk of smoking-caused disease and death. A further negative consequence of starting to smoke at younger ages is that tissues and organ systems that are still in the growth and maturation phase may be particularly vulnerable to the toxicants in smoke, so that even a given exposure dose to cigarette smoke may be more harmful when exposure occurs during childhood and adolescence than during adulthood.
Younger age of initiation has been found to be associated with one short-term health effect in particular: an increased risk of hospital inpatient stay during the previous year ( Lando et al., 1999 ). Concerning long-term health effects, the lung is exquisitely sensitive to the adverse consequences of cigarette smoke because it is directly exposed to inhaled cigarette smoke and is further exposed to harmful smoke toxicants via the circulation of those toxicants in the blood. In a prospective cohort study, a strong association was observed between an earlier age of smoking initiation and an increased risk of respiratory disease ( Kenfield et al., 2008 ). Compared to people who have never smoked, the relative odds (and 95 percent confidence intervals) of contracting respiratory disease were 7.0 (3.9–12.4) for those who started smoking at 26 years old or older; 8.1 (5.5–11.9) for those who started between 22 and 25; 10.2 (9.9–13.2) for smoking initiation between 18 and 21; and 13.4 (9.8–18.2) for those who started smoking at 17 or younger; the age trend is highly statistically significant (a p-value of 0.001). The same study also observed a statistically significant trend for the risk of lung cancer, which was not grouped under respiratory disease ( Kenfield et al., 2008 ); this finding was also observed in another population-based cohort study ( Prizment et al., 2014 ). The strong association between an earlier age of starting to smoke and increased lung cancer risk was summarized in a meta-analysis of 69 studies, which estimated that the summary odds ratio for lung cancer was 10.3 (95 percent confidence interval of 8.0–13.3) for starting to smoke around the age of 14 years; 7.5 (5.9–9.4) for starting to smoke at approximately 18 years; and 3.9 (3.3–4.6) for starting to smoke at age 26 years ( Lee et al., 2012 ). Thus, an earlier age of initiation is strongly associated with an increased risk of respiratory diseases (primarily COPD) and lung cancer.
The evidence for cardiovascular disease has been mixed. The risk of cardiovascular disease increased significantly with younger age of initiation in the ARIC prospective cohort study ( Huxley et al., 2012 ), but the results of the Nurses' Health Study did not find a significant effect ( Kenfield et al., 2008 ). In another study, younger age of initiation was significantly associated with peripheral artery disease ( Planas et al., 2002 ).
Overall, the evidence is consistent in finding that the younger the age of initiation, the greater the risk of nicotine dependence, smoking intensity, and persistent smoking/reduced likelihood of cessation. The associations between a younger age of initiation and these outcomes holds true even after accounting for time from first cigarette to first daily smoking. The findings consistently show a dose–response trend, with younger ages of initiation associated with a higher likelihood of nicotine dependence, greater smoking intensity, and reduced likelihood of cessation. The absence of any apparent age threshold on these associations or any diminution of the associations across the age continuum indicates that any delay in initiation, regardless of the ages affected (e.g., late childhood to early adolescence, early to mid-adolescence, or adolescence to young adulthood) would be expected to have measurable benefits in reducing the lifetime consumption of cigarettes and hence in reducing the risk for smoking-caused disease and death. The adverse consequences of a younger age of initiation appear to manifest at young ages and be sustained over the life course.
Finding 4-5: A younger age of initiation is associated with an increased risk of many adverse health outcomes, such as a hospital inpatient stay in the past year and lifetime risk of respiratory disease, especially chronic obstructive pulmonary disease and lung cancer .
Other Tobacco Products and Sources of Exposure
So far, the discussion has focused specifically on cigarette smoking. SHS exposure and other tobacco products and nicotine delivery devices are discussed below.
Secondhand Smoke Exposure
The health effects of cigarette smoking are not limited to the adverse health effects on the smoker; they also include the health consequences that exposure to SHS has on nonsmokers ( HHS, 2014 ). SHS exposure has now been linked with a host of adverse health effects in addition to the long-established causal associations with lung cancer and heart disease.
As cigarette smokers, parents who smoke cigarettes increase their personal risk for all of the adverse health outcomes described above. If parents smoke in the presence of their children, they also negatively affect the health of their children by exposing them to SHS. The health effects of SHS exposure are not limited to long-term enhanced susceptibility to chronic diseases, but, as in the case of cigarette smoking, they also include immediate and substantial effects that leave SHS-exposed individuals prone to short-term health risks (see Table 4-7 ).
Adverse Health Outcomes Causally Associated with Secondhand Smoke Exposure Based on Surgeon General's Reports.
Thus, as is the case with cigarette smoking, SHS exposure is associated with diminished health status. Exposure to SHS is associated with increased oxidative damage to DNA and lipids. As noted above, MDA can be used as a measure of lipid peroxidation, and children exposed to SHS have been found to have significantly higher circulating levels of MDA and also significantly lower levels of glutathione peroxidase ( Zalata et al., 2007 ). Concerning antioxidant micronutrients, the evidence for SHS exposure mirrors the evidence for smoking. Compared to nonsmokers not exposed to SHS, nonsmokers exposed to SHS have significantly reduced circulating concentrations of vitamin C and provitamin A carotenoids, indicating that even low-dose cigarette smoke exposures lower circulating antioxidant micronutrient concentrations. Evidence of lowered circulating antioxidant micronutrient concentrations has also been observed in children of smokers ( Wilson et al., 2011 ; Yilmaz et al., 2009 ; Zalata et al., 2007 ). Children whose mothers were smokers had 29 percent and 26 percent lower circulating concentrations of vitamin E and vitamin A, respectively, than children whose mothers did not smoke ( Yilmaz et al., 2009 ).
Nonsmokers exposed to SHS have also been found to have lessened immune status ( HHS, 2010 ). The body of evidence firmly indicates that among nonsmokers, SHS exposure is associated with greater oxidative damage, lower circulating antioxidant micronutrient concentrations, and lessened immune status. Given the consistent body of evidence and the clear biological rationale based on the causal associations seen with cigarette smoking these associations are likely to be rated as causal in the future, but the evidence base has not yet reached the standard for these associations to be judged as causal in the Surgeon General's report.
Consistent with the health effects observed for cigarette smoking, the health effects of SHS exposure also include reduced lung function and the respiratory symptoms of coughing, phlegm, wheezing, and dyspnea. SHS exposure in children causes numerous adverse health effects, including lower respiratory illnesses, otitis media, and middle ear effusion ( HHS, 2006 ).
In adults, SHS exposure is also causally associated with increased risk of long-term chronic diseases, just as in the case of cigarette smoking. These diseases include lung cancer, coronary heart disease, stroke, and inflammatory bowel disease.
As expected, based on the lower-exposure doses of exposure to tobacco toxins that result from secondhand smoke, the health risks of SHS exposure for most health outcomes tend to be less than the risks of cigarette smoking. Nevertheless, the fact that these risks are incurred even at very low doses indicates that there is no safe threshold for exposure to cigarette smoke. The importance of this public health challenge is accentuated by the fact that these health risks are incurred as the result of smoking by others rather by the affected individuals themselves.
Finding 4-6: Secondhand smoke exposure is causally associated with adverse health effects .
It is worth keeping in mind that this lengthy catalogue of well-established consequences of SHS exposure will continue to grow as more definitive evidence coalesces for additional health outcomes. For example, Table 4-8 summarizes health outcomes for which the evidence summarized in the 2014 Surgeon General's report is currently considered strong enough to be considered suggestive of a causal association but not yet strong enough to be rated as causal.
Adverse Health Outcomes with Evidence Suggestive of a Causal Association with Secondhand Smoke Exposure Based on Surgeon General's Reports.
Smoking of Pipes, Cigars, and Other Combustible Tobacco Products
Combustible tobacco products other than cigarettes are also associated with the same sort of chronic disease outcomes associated with cigarette smoking, such as cancer and cardiovascular disease. Pipe and cigar smoke contain similar profiles of harmful toxins to those found in cigarette smoke ( HHS, 2014 ). A key distinction in the health risks is that the doses of toxins delivered to the smoker are often less for pipes and cigars than for cigarettes because pipes and cigars are usually smoked less frequently and the smoke tends to be inhaled less deeply ( HHS, 1998 ). For example, pipe and cigar smoking pose risks for malignancies of the larynx, oral cavity, and esophagus that are similar to the risks associated with smoking cigarettes ( HHS, 1998 ). Pipes and cigars are causally associated with lung cancer, even though the risks are less than observed for cigarette smoking because compared to cigarette smoking pipes and cigars are smoked on average less frequently and the smoke is inhaled less deeply ( Alberg et al., 2013 ). The available evidence indicating that pipe and cigar smoking have similar adverse health effects to cigarette smoking thus supports the conclusion that the impact of a policy change that resulted in lower uptake or delayed initiation of pipes or cigars would have a significant impact on public health but would be expected to be less than a similar reduction in cigarette smoking because of the lower exposure to tobacco toxins due to the manner in which pipes and cigars are smoked.
Another way to smoke tobacco is with a hookah, or waterpipe. From an exposure assessment perspective, the distinctive features of this tobacco smoke delivery system are that the tobacco is sometimes indirectly heated and that the smoke passes through a water column prior to inhalation ( Akl et al., 2010 ). Hookah use is becoming more common throughout the world, including in the United States ( Cobb et al., 2010 ; Jawad et al., 2013 ). In a study comparing the urinary concentrations of the tobacco-specific nitrosamine 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol (NNAL) in cigarette smokers, hookah smokers, and nonsmokers, it was found that hookah smokers had significantly higher NNAL concentrations than nonsmokers but significantly lower concentrations than cigarette smokers ( Radwan et al., 2013 ). In a study in which urine samples were collected from hookah smokers before and after they smoked from the hookah, significant post-smoking increases were noted in the urinary concentrations of nicotine, cotinine, NNAL, and volatile organic compounds ( St. Helen et al., 2014 ). Expired carbon monoxide concentrations ( Jacob et al., 2011 ) and benzene exposure ( Jacob et al., 2013 ) tend to be much higher for hookah smoking than for cigarette smoking. Studies have assessed the association between hookah smoking and selected health outcomes, but there is a paucity of evidence available on this topic, and the body of evidence is generally of low quality ( Akl et al., 2010 ). In a meta-analysis of data from four studies, hookah smoking was significantly associated with an increased lung cancer risk (odds ratio, 2.1; 95 percent confidence interval, 1.3–3.4) ( Akl et al., 2010 ). In this same systematic review, only one study each was identified to assess the association between hookah smoking and cancers of the bladder, esophagus, and nasopharynx, and none of the observed associations were statistically significant ( Akl et al., 2010 ). With respect to pregnancy outcomes, three studies found hookah smoking to be associated with a significantly increased risk of low birth weight (2.1; 1.1–4.2) ( Akl et al., 2010 ). In one study, hookah smoking was found to be associated with a significantly increased risk of respiratory illness (2.3; 1.1–5.1) ( Akl et al., 2010 ). Definitive conclusions on the risks associated with hookah smoking versus cigarette smoking are not possible with the limited quality and quantity of the evidence currently available.
Little evidence on the health effects of newer combustible tobacco products has been generated. In attempting to estimate risks, it is important to account for the specific product features. For example, the 2014 Surgeon General's report points out that when considering the emergence of small cigarette-like cigars, the health risks may more closely parallel those of cigarettes than of the traditional cigar because of the way that small cigarette-like cigars are used ( HHS, 2014 ). This line of reasoning emphasizes that the health risks of tobacco use are directly linked to doses of exposure to disease-causing toxins, which is a function not only of the tobacco product but also of the frequency and duration of and the manner in which the product is smoked, when factors such as depth of inhalation are accounted for. This concept is also critical to thinking about the health risks of dual use or poly-use of combustible tobacco products and ENDS, an exposure pattern that will likely increase in the future but for which data on health risks are needed.
Finding 4-7: Smoking of combustible tobacco products other than cigarettes, such as pipes and cigars, is causally associated with a broad spectrum of adverse health effects .
Smokeless Tobacco Products
The marketplace for smokeless tobacco products has diversified considerably in recent years. In addition to the traditional smokeless tobacco products of chewing tobacco and snuff, a number of new products have been introduced, such as snus and dissolvable tobacco products.
The 1986 Surgeon General's report examined the evidence concerning smokeless tobacco and concluded that it was a cause of cancer of the oral cavity. Smokeless tobacco use can also lead to oral leukoplakia, gingival recession, and nicotine addiction. A 2007 monograph of the International Agency for Research on Cancer (IARC) that focused on smokeless tobacco concluded that smokeless tobacco is a Group 1 carcinogen, meaning that it is a human carcinogen ( IARC, 2007 ). The IARC review of the evidence led to the conclusion, “Smokeless tobacco causes cancers of the oral cavity and pancreas” ( IARC, 2007 , p. 370). Smokeless tobacco may also be linked to an increased risk of esophageal cancer ( IARC, 2012 ).
These earlier reviews of the evidence concerning the health effects of smokeless tobacco use were primarily based on evidence related to traditional smokeless tobacco products and did not take into account the newer products. A more recent review of the epidemiologic evidence for Swedish-type snus, a moist snuff, suggests that the use of snus may be less harmful than cigarette smoking ( Lee, 2011 ). How the health risks of Swedish-type snus differ from the more traditional smokeless tobacco products has yet to be precisely characterized; furthermore, direct epidemiologic evidence is not yet available on the health effects of the Swedish-type snus products presently marketed in the United States.
Finding 4-8: The use of smokeless tobacco products is causally associated with oral cancer .
The marketplace for tobacco products and devices that deliver nicotine has recently expanded in response to the smoking bans that have increasingly limited the locations where traditional cigarette smoking is allowed ( Jawad et al., 2013 ; Kamerow, 2013 ; Popova and Ling, 2013 ; Schuster et al., 2013 ). Electronic nicotine delivery systems, or ENDS, have experienced a rapid upsurge in use and are now marketed by the major U.S. tobacco companies ( Dockrell et al., 2013 ; Kamerow, 2013 ; Li et al., 2013 ; Popova and Ling, 2013 ).
Monitoring this expansion in products and how the products are used is important to tobacco control. An ENDS product that decreases the delivery of tobacco toxins would ostensibly also reduce the risk of developing smoking-caused disease if current cigarette smokers were to switch from cigarettes to exclusive use of the ENDS. On the other hand, the risk of smoking-caused disease could be increased if the ENDS maintained nicotine addiction and its users continued to smoke cigarettes and to use multiple products that deliver nicotine. Furthermore, these alternative products, particularly those that involve flavorings attractive to adolescents, may serve as a gateway for adolescents to initiate smoking and thus start on a path that eventually leads to tobacco addiction. Currently there is a paucity of data on issues such as these; along with the direct adverse health effects associated with use of these alternative products, these remain important lines of inquiry for future research. Definitive evidence on the long-term health effects of ENDS products will not be available for many years because any long-term health effects associated with these products will take decades to emerge. Furthermore, generating the needed evidence base will be complicated by the facts that there are so many different ENDS products and the products and their contents are evolving.
- IMPACT OF CIGARETTE SMOKING ON MORTALITY
Cigarette smoking contributes significantly to the population burden of many of the leading causes of chronic disease deaths that typically occur in middle and late adulthood, such as cancer, cardiovascular disease, and COPD ( HHS, 2004 ).
The combined death toll linked to cigarette smoking is staggering. Cigarette smoking is estimated to account for approximately 480,000 deaths per year in the United States ( HHS, 2014 ). In 2010 the four leading causes of death in the United States were heart disease (597,700 deaths), cancer (574,700 deaths), chronic lower respiratory diseases (138,100 deaths), and stroke and cerebrovascular disease (129,500) ( Heron, 2013 ). Cigarette smoking is a major cause of all four of these diseases. Furthermore, smoking is also a cause of the seventh (diabetes, 69,000 deaths) and eighth (influenza/pneumonia, 50,100 deaths) leading causes of death ( Heron, 2013 ).
As a cause of 12 different types of malignancy, cigarette smoking is responsible for 163,700 cancer deaths per year in the United States ( HHS, 2014 ; NCHS, 2013 ). Most of this mortality burden (130,700 deaths) is due to lung cancer, but cigarette smoking also caused 36,000 deaths from other malignancies ( HHS, 2014 ).
Cardiovascular Disease
Cigarette smoking is estimated to cause 160,600 cardiovascular disease deaths per year in the United States ( HHS, 2014 ). The majority of the smoking-caused cardiovascular deaths (99,300 deaths) are due to coronary heart disease, but smoking also causes 25,500 deaths from other forms of heart disease. Furthermore, cigarette smoking causes 15,300 deaths from cerebrovascular disease and 11,500 deaths from other forms of vascular disease.
Type 2 diabetes mellitus is a leading underlying cause of mortality from cardiovascular disease, and it also leads to other adverse consequences such as kidney failure and blindness ( HHS, 2014 ). It is the seventh leading cause of death in the United States ( Heron, 2013 ). Cigarette smoking is estimated to cause 9,000 deaths from type 2 diabetes per year in the United States ( HHS, 2014 ).
More than 138,000 Americans died from COPD in 2010 ( Heron, 2013 ), making it the third leading cause of death in the United States. Cigarette smoking is the predominant cause of COPD. Estimates indicate that 100,600 COPD deaths per year in the United States are attributable to cigarette smoking ( HHS, 2014 ).
Cigarette smoking is causally associated with an increased risk of pneumonia ( HHS, 2004 ) and tuberculosis mortality ( HHS, 2014 ). Cigarette smoking is estimated to cause 12,500 deaths from these infectious diseases per year.
- IMPACT OF EXPOSURE TO SECONDHAND SMOKE ON MORTALITY
Due to its causal associations with coronary heart disease and lung cancer, secondhand smoke exposure is estimated to cause more than 41,300 deaths per year in the United States ( HHS, 2014 ). The majority of these (almost 34,000 deaths) are due to coronary heart disease, while more than 7,000 deaths per year are from lung cancer ( HHS, 2014 ). Furthermore, parental smoking is estimated to cause approximately 600 deaths per year from prenatal conditions and 400 deaths per year from sudden infant death syndrome ( HHS, 2014 ).
Finding 4-9: Tobacco use is causally associated with premature mortality from a variety of causes, such as lung infections, chronic obstructive pulmonary disease, coronary heart disease, and a variety of cancers .
- ACS (American Cancer Society). Cancer facts & figures 2007. Atlanta, GA: American Cancer Society; 2007.
- Akl EA, Gaddam S, Gunukula SK, Honeine R, Jaoude PA, Irani J. The effects of waterpipe tobacco smoking on health outcomes: A systematic review. International Journal of Epidemiology. 2010; 39 (3):834–857. [ PubMed : 20207606 ]
- Alberg AJ. The influence of cigarette smoking on circulating concentrations of antioxidant micronutrients. Toxicology. 2002; 180 (2):121–137. [ PubMed : 12324189 ]
- Alberg AJ, Diette GB, Ford JG. Attendance and absence as markers of health status—The example of active and passive cigarette smoking. American Journal of Epidemiology. 2003; 157 (10):870–873. [ PubMed : 12746238 ]
- Alberg AJ, Brock MV, Ford JG, Samet JM, Spivack SD. Epidemiology of lung cancer: Diagnosis and management of lung cancer, 3rd ed.: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013; 143 (5 Suppl):e1S–e29S. [ PMC free article : PMC4694610 ] [ PubMed : 23649439 ]
- Ambrose JA, Barua RS. The pathophysiology of cigarette smoking and cardiovascular disease: An update. Journal of the American College of Cardiology. 2004; 43 (10):1731–1737. [ PubMed : 15145091 ]
- Bloomer RJ, Solis AD, Fisher-Wellman KH, Smith WA. Postprandial oxidative stress is exacerbated in cigarette smokers. British Journal of Nutrition. 2008; 99 (5):1055–1060. [ PubMed : 17925054 ]
- Breslau N. Daily cigarette consumption in early adulthood: Age of smoking initiation and duration of smoking. Drug and Alcohol Dependence. 1993; 33 (3):287–291. [ PubMed : 8261892 ]
- Breslau N, Peterson EL. Smoking cessation in young adults: Age at initiation of cigarette smoking and other suspected influences. American Journal of Public Health. 1996; 86 (2):214–220. [ PMC free article : PMC1380330 ] [ PubMed : 8633738 ]
- Brown AJ. Acute effect of smoking cessation on antioxidant status. Journal of Nutritional Biochemistry. 1996; 7 (1):29–39.
- Buchmann AF, Blomeyer D, Jennen-Steinmetz C, Schmidt MH, Esser G, Banaschewski T, Laucht M. Early smoking onset may promise initial pleasurable sensations and later addiction. Addiction Biology. 2013; 18 (6):947–954. [ PubMed : 21966958 ]
- Campos C, Guzman R, Lopez-Fernandez E, Casado A. Urinary biomarkers of oxidative/nitrosative stress in healthy smokers. Inhalation Toxicology. 2011; 23 (3):148–156. [ PubMed : 21391783 ]
- Chen J, Millar WJ. Age of smoking initiation: Implications for quitting. Health Reports. 1998; 9 (4):39–46. [ PubMed : 9836879 ]
- Cobb C, Ward KD, Maziak W, Shihadeh AL, Eissenberg T. Waterpipe tobacco smoking: An emerging health crisis in the United States. American Journal of Health Behavior. 2010; 34 (3):275–285. [ PMC free article : PMC3215592 ] [ PubMed : 20001185 ]
- Craig WY, Palomaki GE, Haddow JE. Cigarette smoking and serum lipid and lipoprotein concentrations: An analysis of published data. BMJ. 1989; 298 (6676):784–788. [ PMC free article : PMC1836079 ] [ PubMed : 2496857 ]
- Craig WY, Palomaki GE, Johnson AM, Haddow JE. Cigarette smoking-associated changes in blood lipid and lipoprotein levels in the 8- to 19-year-old age group: A meta-analysis. Pediatrics. 1990; 85 (2):155–158. [ PubMed : 2136949 ]
- D'Avanzo B, La Vecchia C, Negri E. Age at starting smoking and number of cigarettes smoked. Annals of Epidemiology. 1994; 4 (6):455–459. [ PubMed : 7804500 ]
- Dockrell M, Morison R, Bauld L, McNeill A. E-cigarettes: Prevalence and attitudes in Great Britain. Nicotine & Tobacco Research. 2013; 15 (10):1737–1744. [ PMC free article : PMC3768337 ] [ PubMed : 23703732 ]
- Dwyer JH, Rieger-Ndakorerwa GE, Semmer NK, Fuchs R, Lippert P. Low-level cigarette smoking and longitudinal change in serum cholesterol among adolescents. The Berlin-Bremen study. JAMA. 1988; 259 (19):2857–2862. [ PubMed : 3367451 ]
- Eiserich JP, van der Vliet A, Handelman GJ, Halliwell B, Cross CE. Dietary antioxidants and cigarette smoke-induced biomolecular damage: A complex interaction. American Journal of Clinical Nutrition. 1995; 62 (6 Suppl):1490S–1500S. [ PubMed : 7495250 ]
- Eisner MD, Yelin EH, Katz PP, Shiboski SC, Henke J, Blanc PD. Predictors of cigarette smoking and smoking cessation among adults with asthma. American Journal of Public Health. 2000; 90 (8):1307–1311. [ PMC free article : PMC1446347 ] [ PubMed : 10937016 ]
- Escobedo LG, Marcus SE, Holtzman D, Giovino GA. Sports participation, age at smoking initiation, and the risk of smoking among U.S. high school students. JAMA. 1993; 269 (11):1391–1395. [ PubMed : 8441214 ]
- Evans P, Halliwell B. Micronutrients: Oxidant/antioxidant status. British Journal of Nutrition. 2001; 85 (Suppl 2):S67–S74. [ PubMed : 11509092 ]
- Everett SA, Warren CW, Sharp D, Kann L, Husten CG, Crossett LS. Initiation of cigarette smoking and subsequent smoking behavior among U.S. high school students. Preventive Medicine. 1999; 29 (5):327–333. [ PubMed : 10564623 ]
- Fernandez E, Schiaffino A, La Vecchia C, Borras JM, Nebot M, Salto E, Tresserras R, Rajmil L, Villalbi JR, Segura A. Age at starting smoking and number of cigarettes smoked in Catalonia, Spain. Preventive Medicine. 1999; 28 (4):361–366. [ PubMed : 10090865 ]
- Heron M. Deaths: Leading causes for 2010. National Vital Statistics Reports. 2013; 62 (6):1–96. [ PubMed : 24364902 ]
- HHS (Department of Health and Human Services). Smoking and tobacco control monograph 9: Cigars: Health effects and trends. Bethesda, MD: U.S. Department of Health and Human Services; Office on Smoking and Health; National Cancer Institute. Original edition, Bethesda, MD; 1998.
- HHS (Department of Health and Human Services). The health consequences of smoking: A report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2004.
- HHS (Department of Health and Human Services). The health consequences of involuntary exposure to tobacco smoke: A report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2006. [ PubMed : 20669524 ]
- HHS (Department of Health and Human Services). How tobacco smoke causes disease: The biology and behavioral basis for smoking-attributable disease: A report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2010. [ PubMed : 21452462 ]
- HHS (Department of Health and Human Services). Preventing tobacco use among youth and young adults: A report of the Surgeon General. Atlanta GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2012. [ PubMed : 22876391 ]
- HHS (Department of Health and Human Services). The health consequences of smoking—50 years of progress: A report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [ PubMed : 24455788 ]
- Hong YC, Kim H, Im MW, Lee KH, Woo BH, Christiani DC. Maternal genetic effects on neonatal susceptibility to oxidative damage from environmental tobacco smoke. Journal of the National Cancer Institute. 2001; 93 (8):645–647. [ PubMed : 11309442 ]
- Hu MC, Davies M, Kandel DB. Epidemiology and correlates of daily smoking and nicotine dependence among young adults in the United States. American Journal of Public Health. 2006; 96 (2):299–308. [ PMC free article : PMC1470478 ] [ PubMed : 16380569 ]
- Huxley RR, Yatsuya H, Lutsey PL, Woodward M, Alonso A, Folsom AR. Impact of age at smoking initiation, dosage, and time since quitting on cardiovascular disease in African Americans and whites: The Atherosclerosis Risk in Communities Study. American Journal of Epidemiology. 2012; 175 (8):816–826. [ PMC free article : PMC3390013 ] [ PubMed : 22396389 ]
- IARC (International Agency for Research on Cancer). IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Vol. 89. 2007. Smokeless tobacco and some tobacco-specific n-nitrosamines. [ PMC free article : PMC4781254 ] [ PubMed : 18335640 ]
- IARC (International Agency for Research on Cancer). IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Pt E. Vol. 100. 2012. Personal habits and indoor combustions. Volume 100e. A review of human carcinogens. [ PMC free article : PMC4781577 ] [ PubMed : 23193840 ]
- Jacob P III, Abu Raddaha AH, Dempsey D, Havel C, Peng M, Yu L, Benowitz NL. Nicotine, carbon monoxide, and carcinogen exposure after a single use of a water pipe. Cancer Epidemiology, Biomarkers and Prevention. 2011; 20 (11):2345–2353. [ PMC free article : PMC3210932 ] [ PubMed : 21908725 ]
- Jacob P III, Abu Raddaha AH, Dempsey D, Havel C, Peng M, Yu L, Benowitz NL. Comparison of nicotine and carcinogen exposure with water pipe and cigarette smoking. Cancer Epidemiology, Biomarkers and Prevention. 2013; 22 (5):765–772. [ PMC free article : PMC3650103 ] [ PubMed : 23462922 ]
- Jain A, Agrawal BK, Varma M, Jadhav AA. Antioxidant status and smoking habits: Relationship with diet. Singapore Medical Journal. 2009; 50 (6):624–627. [ PubMed : 19551318 ]
- Jawad M, McEwen A, McNeill A, Shahab L. To what extent should waterpipe tobacco smoking become a public health priority? Addiction. 2013; 108 (11):1873–1884. [ PubMed : 23863044 ]
- Kamerow D. Big tobacco lights up e-cigarettes. BMJ. 2013; 346 :f3418. [ PubMed : 23709584 ]
- Kapaki E, Liappas I, Lyras L, Paraskevas GP, Mamali I, Theotoka I, Bourboulis N, Liosis I, Petropoulou O, Soldatos K. Oxidative damage to plasma proteins in patients with chronic alcohol dependence: The effect of smoking. In Vivo. 2007; 21 (3):523–528. [ PubMed : 17591364 ]
- Kenfield SA, Stampfer MJ, Rosner BA, Colditz GA. Smoking and smoking cessation in relation to mortality in women. JAMA. 2008; 299 (17):2037–2047. [ PMC free article : PMC2879642 ] [ PubMed : 18460664 ]
- Khuder SA, Dayal HH, Mutgi AB. Age at smoking onset and its effect on smoking cessation. Addictive Behaviors. 1999; 24 (5):673–677. [ PubMed : 10574304 ]
- Kocyigit A, Keles H, Selek S, Guzel S, Celik H, Erel O. Increased DNA damage and oxidative stress in patients with cutaneous leishmaniasis. Mutation Research. 2005; 585 (1-2):71–78. [ PubMed : 16005255 ]
- Kocyigit A, Selek S, Celik H, Dikilitas M. Mononuclear leukocyte DNA damage and oxidative stress: The association with smoking of hand-rolled and filter cigarettes. Mutation Research. 2011; 721 (2):136–141. [ PubMed : 21295155 ]
- Laher I. Systems biology of free radicals and antioxidants. Berlin: Springer Reference; 2014.
- Lando HA, Thai DT, Murray DM, Robinson LA, Jeffery RW, Sherwood NE, Hennrikus DJ. Age of initiation, smoking patterns, and risk in a population of working adults. Preventive Medicine. 1999; 29 (6 Part 1):590–598. [ PubMed : 10600442 ]
- Lee PN. Summary of the epidemiological evidence relating snus to health. Regulatory Toxicology and Pharmacology. 2011; 59 (2):197–214. [ PubMed : 21163315 ]
- Lee PN, Forey BA, Coombs KJ. Systematic review with meta-analysis of the epidemiological evidence in the 1900s relating smoking to lung cancer. BMC Cancer. 2012; 12 :385. [ PMC free article : PMC3505152 ] [ PubMed : 22943444 ]
- Li J, Bullen C, Newcombe R, Walker N, Walton D. The use and acceptability of electronic cigarettes among New Zealand smokers. New Zealand Medical Journal. 2013; 126 (1375):48–57. [ PubMed : 23824024 ]
- Lowe FJ, Gregg EO, McEwan M. Evaluation of biomarkers of exposure and potential harm in smokers, former smokers and never-smokers. Clinical Chemistry and Laboratory Medicine. 2009; 47 (3):311–320. [ PubMed : 19676143 ]
- Marangon K, Devaraj S, Jialal I. Measurement of protein carbonyls in plasma of smokers and in oxidized LDL by an ELISA. Clinical Chemistry. 1999; 45 (4):577–578. [ PubMed : 10102923 ]
- Martin JA, Hamilton BE, Osterman MJK, Curtin SC, Mathews TJ. Births: Final data for 2012. National Vital Statistics Reports. 2013; 64 (1):1–65. [ PubMed : 25603115 ]
- NCHS (National Center for Health Statistics). Faststats: Leading causes of death. 2013. [January 7, 2015]. http://www .cdc.gov/nchs /fastats/leading-causes-of-death.htm .
- Ozguner F, Koyu A, Cesur G. Active smoking causes oxidative stress and decreases blood melatonin levels. Toxicology and Industrial Health. 2005; 21 (1-2):21–26. [ PubMed : 15986573 ]
- Padmavathi P, Reddy VD, Kavitha G, Paramahamsa M, Varadacharyulu N. Chronic cigarette smoking alters erythrocyte membrane lipid composition and properties in male human volunteers. Nitric Oxide. 2010; 23 (3):181–186. [ PubMed : 20561918 ]
- Park SM, Son KY, Lee YJ, Lee HC, Kang JH, Lee YJ, Chang YJ, Yun YH. A preliminary investigation of early smoking initiation and nicotine dependence in Korean adults. Drug and Alcohol Dependence. 2004; 74 (2):197–203. [ PubMed : 15099663 ]
- Pawelec G, Goldeck D, Derhovanessian E. Inflammation, ageing and chronic disease. Current Opinion in Immunology. 2014; 29 :23–28. [ PubMed : 24762450 ]
- Planas A, Clara A, Marrugat J, Pou JM, Gasol A, de Moner A, Contreras C, Vidal-Barraquer F. Age at onset of smoking is an independent risk factor in peripheral artery disease development. Journal of Vascular Surgery. 2002; 35 (3):506–509. [ PubMed : 11877699 ]
- Popova L, Ling PM. Alternative tobacco product use and smoking cessation: A national study. American Journal of Public Health. 2013; 103 (5):923–930. [ PMC free article : PMC3661190 ] [ PubMed : 23488521 ]
- Prasad S, Sung B, Aggarwal BB. Age-associated chronic diseases require age-old medicine: Role of chronic inflammation. Preventive Medicine. 2012; 54 (Suppl):S29–S37. [ PMC free article : PMC3340492 ] [ PubMed : 22178471 ]
- Prizment AE, Yatsuya H, Lutsey PL, Lubin JH, Woodward M, Folsom AR, Huxley RR. Smoking behavior and lung cancer in a biracial cohort: The Atherosclerosis Risk in Communities Study. American Journal of Preventive Medicine. 2014; 46 (6):624–632. [ PMC free article : PMC4030495 ] [ PubMed : 24842739 ]
- Pryor WA, Stone K. Oxidants in cigarette smoke: Radicals, hydrogen peroxide, peroxynitrate, and peroxynitrite. Annals of the New York Academy of Sciences. 1993; 686 :12–27. [ PubMed : 8512242 ]
- Radwan G, Hecht SS, Carmella SG, Loffredo CA. Tobacco-specific nitrosamine exposures in smokers and nonsmokers exposed to cigarette or waterpipe tobacco smoke. Nicotine & Tobacco Research. 2013; 15 (1):130–138. [ PMC free article : PMC3524061 ] [ PubMed : 22573723 ]
- Reidpath DD, Davey TM, Kadirvelu A, Soyiri IN, Allotey P. Does one cigarette make an adolescent smoker, and is it influenced by age and age of smoking initiation? Evidence of association from the U.S. Youth Risk Behavior Surveillance System (2011). Preventive Medicine. 2014; 59 :37–41. [ PubMed : 24270054 ]
- Rostron BL, Chang CM, Pechacek TF. Estimation of cigarette smoking–attributable morbidity in the United States. JAMA Internal Medicine. 2014; 174 (12):1922–1928. [ PubMed : 25317719 ]
- Schuster RM, Hertel AW, Mermelstein R. Cigar, cigarillo, and little cigar use among current cigarette-smoking adolescents. Nicotine & Tobacco Research. 2013; 15 (5):925–931. [ PMC free article : PMC3621583 ] [ PubMed : 23072873 ]
- Seet RCS, Lee CY, Loke WM, Huang SH, Huang H, Looi WF, Chew ES, Quek AM, Lim EC, Halliwell B. Biomarkers of oxidative damage in cigarette smokers: Which biomarkers might reflect acute versus chronic oxidative stress? Free Radical Biology and Medicine. 2011; 50 (12):1787–1793. [ PubMed : 21420490 ]
- Simet SM, Sisson JH, Pavlik JA, DeVasure JM, Boyer C, Liu X, Kawasaki S, Sharp JG, Rennard SI, Wyatt TA. Long-term cigarette smoke exposure in a mouse model of ciliated epithelial cell function. American Journal of Respiratory Cell and Molecular Biology. 2010; 43 (6):635–640. [ PMC free article : PMC2993085 ] [ PubMed : 20042711 ]
- St. Helen G, Benowitz NL, Dains KM, Havel C, Peng M, Jacob P III. Nicotine and carcinogen exposure after water pipe smoking in hookah bars. Cancer Epidemiology, Biomarkers & Prevention. 2014; 23 (6):1055–1066. [ PMC free article : PMC4047652 ] [ PubMed : 24836469 ]
- Taioli E, Wynder EL. Effect of the age at which smoking begins on frequency of smoking in adulthood. New England Journal of Medicine. 1991; 325 (13):968–969. [ PubMed : 1881424 ]
- Taylor AW, Bruno RS, Traber MG. Women and smokers have elevated urinary F(2)-isoprostane metabolites: A novel extraction and LC-MS methodology. Lipids. 2008; 43 (10):925–936. [ PMC free article : PMC2770443 ] [ PubMed : 18751751 ]
- Thun M, Peto R, Boreham J, Lopez AD. Stages of the cigarette epidemic on entering its second century. Tobacco Control. 2012; 21 (2):96–101. [ PubMed : 22345230 ]
- van der Vaart H, Postma DS, Timens W, Ten Hacken NHT. Acute effects of cigarette smoke on inflammation and oxidative stress: A review. Thorax. 2004; 59 (8):713–721. [ PMC free article : PMC1747102 ] [ PubMed : 15282395 ]
- Wilson KM, Finkelstein JN, Blumkin AK, Best D, Klein JD. Micronutrient levels in children exposed to secondhand tobacco smoke. Nicotine & Tobacco Research. 2011; 13 (9):800–808. [ PubMed : 21558135 ]
- Yao H, Rahman I. Current concepts on oxidative/carbonyl stress, inflammation and epigenetics in pathogenesis of chronic obstructive pulmonary disease. Toxicology and Applied Pharmacology. 2011; 254 (2):72–85. [ PMC free article : PMC3107364 ] [ PubMed : 21296096 ]
- Yeung DL. Relationships between cigarette smoking, oral contraceptives, and plasma vitamins A, E, C, and plasma triglycerides and cholesterol. American Journal of Clinical Nutrition. 1976; 29 (11):1216–1221. [ PubMed : 998536 ]
- Yilmaz G, Isik Agras P, Hizli S, Karacan C, Besler HT, Yurdakok K, Coskun T. The effect of passive smoking and breast feeding on serum antioxidant vitamin (A, C, E) levels in infants. Acta Paediatrica. 2009; 98 (3):531–536. [ PubMed : 19006535 ]
- Zalata A, Yahia S, El-Bakary A, Elsheikha HM. Increased DNA damage in children caused by passive smoking as assessed by comet assay and oxidative stress. Mutation Research. 2007; 629 (2):140–147. [ PubMed : 17368083 ]
- Cite this Page Committee on the Public Health Implications of Raising the Minimum Age for Purchasing Tobacco Products; Board on Population Health and Public Health Practice; Institute of Medicine; Bonnie RJ, Stratton K, Kwan LY, editors. Public Health Implications of Raising the Minimum Age of Legal Access to Tobacco Products. Washington (DC): National Academies Press (US); 2015 Jul 23. 4, The Effects of Tobacco Use on Health.
- PDF version of this title (6.0M)
In this Page
Related information.
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- The Effects of Tobacco Use on Health - Public Health Implications of Raising the... The Effects of Tobacco Use on Health - Public Health Implications of Raising the Minimum Age of Legal Access to Tobacco Products
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
500 Words Essay On Smoking. One of the most common problems we are facing in today's world which is killing people is smoking. A lot of people pick up this habit because of stress, personal issues and more. In fact, some even begin showing it off. When someone smokes a cigarette, they not only hurt themselves but everyone around them.
Introduction. Tobacco use, including smoking, has become a universally recognized issue that endangers the health of the population of our entire planet through both active and second-hand smoking. Pro-tobacco arguments are next to non-existent, while its harm is well-documented and proven through past and contemporary studies (Jha et al., 2013).
Tobacco use is a global epidemic among young people. As with adults, it poses a serious health threat to youth and young adults in the United States and has significant implications for this nation's public and economic health in the future (Perry et al. 1994; Kessler 1995). The impact of cigarette smoking and other tobacco use on chronic disease, which accounts for 75% of American spending ...
Nicotine works on your brain to create a relaxing, pleasurable feeling that makes it tough to quit. But smoking tobacco puts you at risk for cancer, stroke, heart attack, lung disease and other health issues. Nicotine replacements and lifestyle changes may help you quit. How smoking affects the heart animation.
Health impact of smoking. Table Table1 1 lists the main causes of death from smoking. Tobacco smoking is estimated to lead to the premature death of approximately 6 million people worldwide and 96,000 in the UK each year (Action on Smoking and Health, 2016b; World Health Organization, 2013).A 'premature death from smoking' is defined as a death from a smoking-related disease in an ...
Health Effects. Smoking leads to disease and disability and harms nearly every organ of the body. More than 16 million Americans are living with a disease caused by smoking. For every person who dies because of smoking, at least 30 people live with a serious smoking-related illness. Smoking causes cancer, heart disease, stroke, lung diseases ...
Tobacco kills more than 8 million people each year, including an estimated 1.3 million non-smokers who are exposed to second-hand smoke (4). Around 80% of the world's 1.3 billion tobacco users live in low- and middle-income countries. In 2020, 22.3% of the world's population used tobacco: 36.7% of men and 7.8% of women.
The Hazards of Smoking: Effects, Bans, and Prevention Essay. Smoking has numerous health effects, both short-term and long-term. Some of the short-term effects include bad breath, yellow teeth, and decreased sense of taste and smell. The long-term effects, however, are much more severe.
Smoking can result in stroke and heart attacks since it hinders blood flow, interrupting oxygen to various parts of the body, such as feet and hands. Introduction of cigarettes with low tar does not reduce these effects since smokers often prefer deeper puffs and hold the smoke in lungs for a long period. This smoking practice draws the tar ...
1 hour! Gilman Sander L. and Xhou Zun. Smoke: A GlobalHistory of Smoking. Reaktion Books; illustrated edition edition, 2004. This essay, "Smoking: Causes and Effects" is published exclusively on IvyPanda's free essay examples database. You can use it for research and reference purposes to write your own paper.
Opinion: Dr George Laking shares his journey with tobacco, from growing up in a smoking home and trying his first cigarette to his career as an expert in Nicotine Replacement Therapy. Dad was a smoker when I grew up in the 1970s, his parents too. Mum's side of the family didn't.
A smoking essay can fit any type of writing assignment. You can craft an argumentative essay about smoking, a persuasive piece, or even a narration about someone's struggle with quitting. It's a rare case of a one-size-fits-all topic. ... Any argumentative and persuasive essay on smoking must include a short conclusion. In the final passage ...
Essay on Tobacco. Sort By: Page 1 of 50 - About 500 essays. Decent Essays. Tobacco And Tobacco. 1278 Words; 6 Pages; Tobacco And Tobacco. of Americans younger than 18 years will likely die from a tobacco-related illness if tobacco use persists at the current rate among youth in the United States (1). Tobacco use is the largest preventable cause ...
Foremost among the cancers caused by tobacco use is lung cancer. Cigarette smoking has been linked to about 80 to 90 percent of all cases of lung cancer, the leading cause of cancer death for both men and women, and it is responsible for roughly 80 percent of deaths from this disease. 22,47 Smoking increases lung cancer risk five to tenfold ...
These carcinogens cause cancer and negatively affect human health. Lung, throat, brain, bladder, cervical cancer as well as other forms are caused by smoking. The symptoms are often detected at the time when the smoker's health condition is already chronic. Cancer is one of the leading causes of death world wide.
Here are some sample persuasive essays about smoking that you can use as inspiration for your own writing: Persuasive speech on smoking outline. Persuasive essay about smoking should be banned. Persuasive essay about smoking pdf. Persuasive essay about smoking cannot relieve stress. Persuasive essay about smoking in public places.
Smoking Essay Smoking is a widespread habit that involves inhaling smoke from the burning of tobacco. It is a highly addictive habit that has numerous negative effects on the body, including lung cancer, heart disease, and respiratory issues. Writing an essay on smoking can be a challenging task, but it is an important topic to discuss.
The topic of passive or involuntary smoking was first addressed in the 1972 U.S. Surgeon General's report (The Health Consequences of Smoking, U.S. Department of Health, Education, and Welfare [USDHEW] 1972), only eight years after the first Surgeon General's report on the health consequences of active smoking (USDHEW 1964). Surgeon General Dr. Jesse Steinfeld had raised concerns about ...
Continue reading this short essay about smoking. Eradication Of Smoking. Although everyone is aware of the dangers of smoking, no one is motivated to give up the habit. The vilest habit among the 1.2 billion smokers worldwide is smoking. It offers neither smokers nor society any advantages. The effects of smoking on society go beyond health and ...
The secret of their Nicotiana tabacum blend was closely guarded by the Spanish - it was against the law to share seeds or plants with non-Spaniards - but travelers or merchants would do so anyway. When England began to colonize North America in the late 16th century CE, Sir Walter Raleigh (l. c. 1552-1618 CE) introduced the older, rougher, strain of tobacco - N. rustica - to Britain.
Tobacco Product Use Among Adults — United States, 2019. MMWR Morb Mortal Wkly Rep 2020;69:1736-1742. Content current as of: 03/23/2022. Regulated Product(s) Tobacco; Health Effects of Tobacco Use.
Tobacco smoking is a major determinant of preventable morbidity and mortality worldwide. ... B. et al. Impact of short access nicotine self-administration on expression of α4β2* nicotinic ...
Conclusion. The use of tobacco is identifiably unhealthy following its risks to the user's health that is then spread to other members of the society through social and economic costs. Since the drug is addictive, individual users can not easily and willingly stop the consumption the drug. The significant control measure therefore lies in ...
Banning Tobacco Essay. Tobacco Tobacco has been around for many years, and it should be stopped, but can the economy handle it. The tobacco is reaching young children, and not to mention the nonsmokers as well. The medical effects alone should convince people to stop smoking.
The scope of the burden of disease and death that cigarette smoking imposes on the public's health is extensive. Cigarette smoking is the major focus of this chapter because it is the central public health problem, but the topics of secondhand smoke exposure, smoking of other combustible tobacco products, smokeless tobacco, and electronic nicotine delivery systems (ENDS) are also considered.