- Discussions
- Certificates
- Collab Space
- Course Details
- Announcements

This introductory level course provides a general overview of cholera including prevention and control principles. In addition, the course participants will learn about the Global Task Force for Cholera Control (GTFCC) and the Ending Cholera – A Global Roadmap to 2030 strategy. The target audience for this course is personnel responsible for prevention and control of cholera including those involved in cholera outbreak response.
Photo credits: WHO/ Olivia Acland

What you'll learn
- summarize the disease and main transmission routes;
- explain cholera prevention and control principles;
- describe the strategies of Ending Cholera – A Global Roadmap to 2030 and the role of the Global Task Force on Cholera Control (GTFCC); and
- recall additional Cholera resources.
Course contents
Module 1: cholera: the disease and its transmission:, module 2: prevention and control of cholera:, module 3: ending cholera: a global roadmap to 2030 and global task force on cholera control (gtfcc):, module 4: additional resources:, enroll me for this course, certificate requirements.
- Gain a Confirmation of Participation by completing at least 80% of the course material.
- World Health Organization
- Popular Categories
Powerpoint Templates
Icon Bundle
Kpi Dashboard
Professional
Business Plans
Swot Analysis
Gantt Chart
Business Proposal
Marketing Plan
Project Management
Business Case
Business Model
Cyber Security
Business PPT
Digital Marketing
Digital Transformation
Human Resources
Product Management
Artificial Intelligence
Company Profile
Acknowledgement PPT
PPT Presentation
Reports Brochures
One Page Pitch
Interview PPT
All Categories
Powerpoint Templates and Google slides for World Health Organization
Save your time and attract your audience with our fully editable ppt templates and slides..
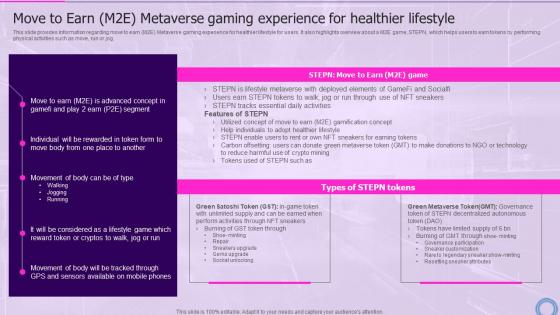
This slide provides information regarding move to earn M2E Metaverse gaming experience for healthier lifestyle for users. It also highlights overview about a M2E game, STEPN, which helps users to earn tokens by performing physical activities such as move, run or jog. Present the topic in a bit more detail with this Move To Earn M2e Healthier Decoding Digital Reality Of Physical World With Megaverse AI SS V. Use it as a tool for discussion and navigation on Experience, Information, Lifestyle. This template is free to edit as deemed fit for your organization. Therefore download it now.
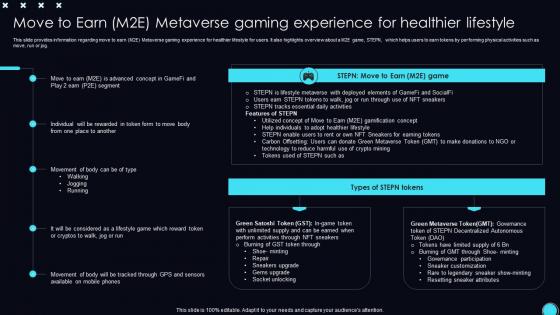
This slide provides information regarding move to earn M2E Metaverse gaming experience for healthier lifestyle for users. It also highlights overview about a M2E game, STEPN, which helps users to earn tokens by performing physical activities such as move, run or jog. Deliver an outstanding presentation on the topic using this Move To Experience For Healthier Lifestyle Unveiling Opportunities Associated With Metaverse World AI SS V. Dispense information and present a thorough explanation of Metaverse, Experience, Lifestyle using the slides given. This template can be altered and personalized to fit your needs. It is also available for immediate download. So grab it now.

Presenting World Health Organisation In Powerpoint And Google Slides Cpb slide which is completely adaptable. The graphics in this PowerPoint slide showcase three stages that will help you succinctly convey the information. In addition, you can alternate the color, font size, font type, and shapes of this PPT layout according to your content. This PPT presentation can be accessed with Google Slides and is available in both standard screen and widescreen aspect ratios. It is also a useful set to elucidate topics like World Health Organisation. This well structured design can be downloaded in different formats like PDF, JPG, and PNG. So, without any delay, click on the download button now.
Presenting our Worlds Healthiest Foods In Powerpoint And Google Slides Cpb PowerPoint template design. This PowerPoint slide showcases four stages. It is useful to share insightful information on Worlds Healthiest Foods This PPT slide can be easily accessed in standard screen and widescreen aspect ratios. It is also available in various formats like PDF, PNG, and JPG. Not only this, the PowerPoint slideshow is completely editable and you can effortlessly modify the font size, font type, and shapes according to your wish. Our PPT layout is compatible with Google Slides as well, so download and edit it as per your knowledge.

The below slide exhibits the role of microfinance in providing a solution for the sustainable development goal of good health and well-being. The major roles played are access to healthcare, health infrastructure, enhancing nutrition, etc. Increase audience engagement and knowledge by dispensing information using Good Health And Well Being Navigating The World Of Microfinance Basics To Innovation Fin SS. This template helps you present information on four stages. You can also present information on Access To Healthcare, Health Infrastructure, Enhancing Nutrition using this PPT design. This layout is completely editable so personaize it now to meet your audiences expectations.
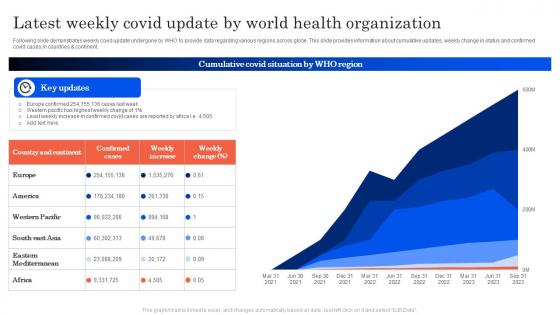
Following slide demonstrates weekly covid update undergone by WHO to provide data regarding various regions across globe. This slide provides information about cumulative updates, weekly change in status and confirmed covid cases in countries and continent. Introducing our latest weekly covid update by world health organization set of slides. The topics discussed in these slides are Country And Continent, Confirmed Cases, Weekly Increase. This is an immediately available PowerPoint presentation that can be conveniently customized. Download it and convince your audience.
Presenting World Health Organization Problems In Powerpoint And Google Slides Cpb slide which is completely adaptable. The graphics in this PowerPoint slide showcase Three stages that will help you succinctly convey the information. In addition, you can alternate the color, font size, font type, and shapes of this PPT layout according to your content. This PPT presentation can be accessed with Google Slides and is available in both standard screen and widescreen aspect ratios. It is also a useful set to elucidate topics like World Health Organization Problems This well-structured design can be downloaded in different formats like PDF, JPG, and PNG. So, without any delay, click on the download button now.
Presenting World Health Organization Burnout In Powerpoint And Google Slides Cpb slide which is completely adaptable. The graphics in this PowerPoint slide showcase three stages that will help you succinctly convey the information. In addition, you can alternate the color, font size, font type, and shapes of this PPT layout according to your content. This PPT presentation can be accessed with Google Slides and is available in both standard screen and widescreen aspect ratios. It is also a useful set to elucidate topics like Work Culture Adjectives. This well structured design can be downloaded in different formats like PDF, JPG, and PNG. So, without any delay, click on the download button now.
Presenting this set of slides with name - Buyer Health Care Growing World Population Food Security. This is an editable three stages graphic that deals with topics like Buyer Health Care, Growing World Population, Food Security to help convey your message better graphically. This product is a premium product available for immediate download, and is 100 percent editable in Powerpoint. Download this now and use it in your presentations to impress your audience.

Presenting this set of slides with name - World Health Assembly Global Initiative Financial Performance Audit. This is an editable four stages graphic that deals with topics like World Health Assembly, Global Initiative, Financial Performance Audit to help convey your message better graphically. This product is a premium product available for immediate download, and is 100 percent editable in Powerpoint. Download this now and use it in your presentations to impress your audience.
Microsoft PowerPoint Template and Background with doctor and nurses standing with world background
Presenting this set of slides with name World Health Organization Team Icon. This is a three stage process. The stages in this process are World Health Organization Team Icon. This is a completely editable PowerPoint presentation and is available for immediate download. Download now and impress your audience.

Presenting this set of slides with name Real World Data Analytics In Healthcare. This is a ten stage process. The stages in this process are Clinical Trials, Pharmacy Data, Device And Mobile. This is a completely editable PowerPoint presentation and is available for immediate download. Download now and impress your audience.

Bolster your presentation designs and make them impactful with our Powerpoint Template And Background With World Health Care Looking After The Planet. This cutting edge PPT will help you meet your audience expectations due to its interactive design. Useful content has been added to help you convey your ideas vision and principle aspects more proficiently. Throw light on what is important and take your presentation game a notch higher with this multipurpose design that comes with an assortment of features. No matter what is the purpose of your presentation conveying business ideas proposals analysis reports or any other you will find this creative design template perfect for all the scenarios. Also input any information and keep your audience hooked with this content ready template that is fully editable and customizable. Besides this you can represent large sets of complex data and information with this template design that can be adopted by any industry agency individual or group to deliver awe inspiring presentations.
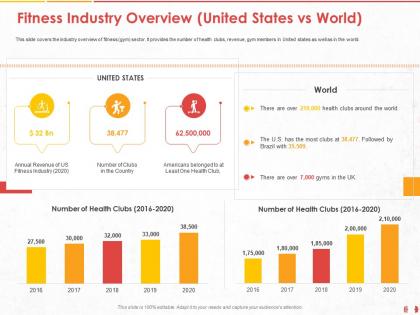
This slide covers the industry overview of fitness gym sector. It provides the number of health clubs, revenue, gym members in United states as well as in the world. Presenting this set of slides with name Fitness Industry Overview United States Vs World Health Ppt Powerpoint Presentation Outline Diagrams. The topics discussed in these slides are Revenue, Number Of Health, Country. This is a completely editable PowerPoint presentation and is available for immediate download. Download now and impress your audience.

Enhance your PowerPoint presentation and make them impressive with our Eye With World Map Painted Around It World Health Powerpoint Template. Using this attention-grabbing PPT, you can leave a significant impact on your audience and convince them. This handy template is entirely editable and portrays your ideas comprehensively. With this illustrative slide, emphasize the critical points and make your presentation praiseworthy. The color palette used in this PPT turns your dull presentation into a vibrant and attractive one. By utilizing our Eye With World Map Painted Around It World Health Powerpoint Template, you can engagingly describe the topic. Present your ideas, data insights, interpretation, analysis, and other crucial business information by using our professionally designed PPT. Showcase your skills and expertise in the domain of your choice with our visually appealing template which can be employed by any organization. Simply tweak this editable PPT and wow your audience. Take your presentation to the next level using this versatile PowerPoint theme which is equipped with attractive design elements.
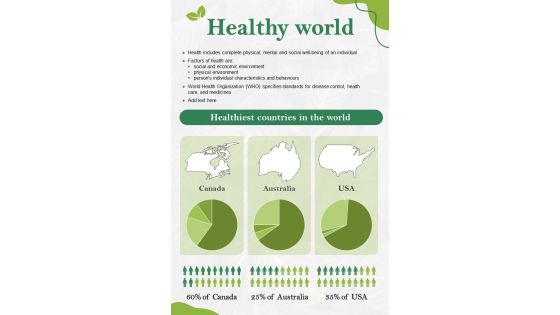
Introducing our captivating Infographic templates and one-pagers, designed to transform complex information into visually stunning stories. These user-friendly tools empower you to effortlessly communicate your ideas, data, and messages with clarity and impact. Our diverse collection offers a range of eye-catching designs, vibrant color schemes, and customizable elements, ensuring that every infographic or one-pager is tailored to your unique style and purpose. Whether you are presenting sales figures, explaining a process, or showcasing research findings, our templates provide the perfect canvas for your creativity. With intuitive editing features, even non-designers can effortlessly craft professional-grade visual content. You can simply tweak all the elements of the slide and enjoy the liberty of customizing all the components. Not only this, you can convert these slides in various formats including JPG, PNG, JPEG and PDF. Going well with Google Slides and major Microsoft versions, these templates can be presented on widescreen and standard screen seamlessly. the Grab attention, simplify complexity, and make a lasting impression with our Infographic templates and one-pagers, helping you turn information into unforgettable visual narrative. You can simply tweak all the elements of the slide and enjoy the liberty of customizing all the components. Not only this, you can convert these slides in various formats including JPG, PNG, JPEG and PDF. Going well with Google Slides and major Microsoft versions, these templates can be presented on widescreen and standard screen seamlessly.


Watch the replay
📌 World Bank Group Aims to Expand Health Services to 1.5 Billion People
- ABOUT THE EVENT
- Champions for Health
GO TO: SPEAKERS
Health care is a fundamental investment, one that can unlock human capital and economic dividends for countries, but the challenge to bring more care to more people requires political will, financing and partnership.
This was the main theme at the “Transforming Challenge into Action: Expanding Health Coverage for All” event where World Bank Group president Ajay Banga announced an ambitious plan to support countries in delivering quality, affordable health services to 1.5 billion people by 2030 .
During a fireside chat moderated by international broadcast journalist Shakuntala Santhiran, Ajay Banga and Tedros Adhanom Ghebreyesus, Director-General, World Health Organization spoke about the challenges to expanding health coverage and the urgency of doing so.
Banga said the new plan would “widen the aperture” of the Bank’s priorities from maternal and child health services to the health needs of people over their lifetimes, a move that also responds to rapidly aging populations, the surge in non-communicable diseases and the associated health care costs.
Following the fireside, Shun’ichi Suzuki, Minister of Finance, Japan announced the establishment of a Universal Health Care (UHC) Knowledge Hub to enhance health and finance ministries' capacity, an initiative also supported by the Bank and the World Health Organization.
Two separate panel discussions ensued with country and civil society leaders discussing what it will take to build resilient health systems, expand coverage and improve the health of populations so that countries can thrive. Panelists discussed the importance of political will, affordability, country ownership, partnerships with the private sector and the need for more financing in reaching universal health coverage for all.
Join the conversation on social media #WBGMeetings
01:53 Fireside Chat / Insights and Perspectives With World Bank Group President Ajay Banga and the Director-General of the World Health Organization Dr. Tedros Adhanom Ghebreyesus.
21:38 Remarks / National Strategies and Initiatives Reflecting on universal healthcare priorities and capacity-building efforts with Mr. Shun’ichi Suzuki, Japan's Minister of Finance.
27:15 Panel 1 / Achieving UHC: Opportunities and Challenges Hear from Dr. Muhammad Pate, Sri Mulyani Indrawati, and Dr. Senait Fisseha, as they share insights and experiences from Nigeria, Indonesia, and The Susan Thompson Buffett Foundation.
47:10 Panel 2 / How can we better finance health? Explore new approaches to health financing with Dr. Mohamed Maait, Egypt's Minister of Finance, as well as industry and civil society leaders Lamia Tazi and Joanne Carter.
The goal of Universal Health Coverage (UHC) is to ensure everyone receives the health services they need without facing financial hardship. Viewing health as an investment rather than an expense can unlock human capital and economic dividends for countries. Find out what our partners and UHC champions have to say about why Universal Health Coverage is so important, and what can be done to achieve this.
Rania A. Al-Mashat
Minister of International Cooperation, Egypt
"Investing in human capital by expanding health care services is key for sustainable development."
Global Director, Health and Nutrition, World Vision International
"Universal Health Coverage is a commitment to equity, gender equality, social inclusion, good nutrition, and mental health across the life cycle."
Janti Soeripto
President & CEO, Save the Children USA
"Achieving Universal Health Coverage is every child’s right."

Sania Nishtar
Chief Executive Officer, Gavi, The Vaccine Alliance
"Equitable access to vaccines and Universal Health Coverage are indivisible. Let us harness the transformative power of immunization and UHC to protect every community, with nobody left behind."
Chris Elias
President, Global Development, Bill & Melinda Gates Foundation
"Strong primary healthcare is at the core of well-functioning health systems."
Vanessa Kerry
CEO, Seed Global; Director-General Special Envoy for Climate Change and Health, WHO
"Access to healthcare, delivered by a skilled health worker, is essential to meet the challenges we face today."
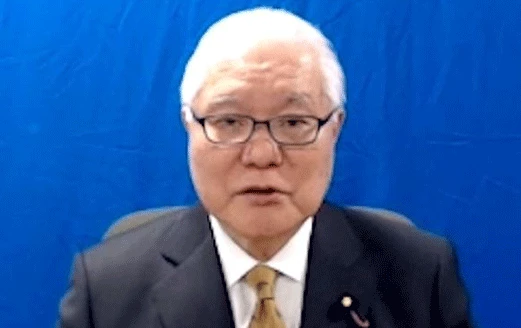
Keizo Takemi
Ministry of Health, Labour and Welfare, Government of Japan
"It is important to increase the scale of health financing in low- and middle-income countries."
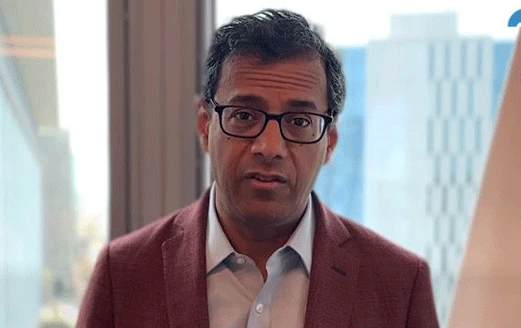
Atul Gawande
Assistant Administrator for Global Health, USAID
"Universal Health Coverage enables long and healthy lives for entire populations."
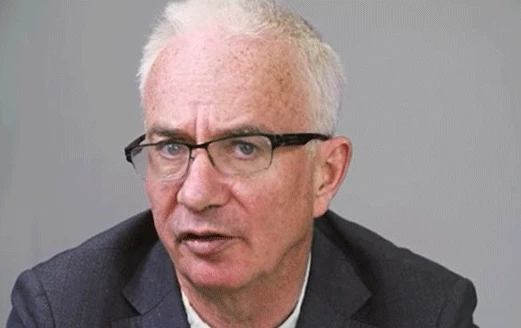
Peter Sands
Executive Director, The Global Fund to Fight AIDS, Tuberculosis & Malaria
"Accelerating progress towards Universal Health Coverage by tackling health inequalities is the only way to end the world's deadliest infectious diseases."

Sabin Nsanzimana
Minister of Health, Rwanda
"Rwanda has committed to promoting UHC by calling for evidence-based policy reforms that will guide a long-term model for health service delivery and financing in the country."
[Shakuntala Santhiran]
Hello and welcome to the 2024 Spring Meetings of the World Bank Group and IMF. We have a full room here. I'm Shakuntala Santhiran, Shaks for short. Over the next hour, we'll discuss how countries can accelerate progress toward universal health coverage, where everyone, everywhere has access to quality, affordable health care when they need it. You can share your thoughts on this topic at any time using the hashtag #WBGMeetings. We have experts in multiple languages standing by to answer your questions online at live.worldbank.org. Please, post your questions in the live chat if you're joining us online, or by using the QR codes displayed on the chairs in front of you and around the room if you're here with us. Now, later in the program, we'll hear from ministers of Health and Finance, leaders in the private sector, civil society, and philanthropy to explore the issues and opportunities. First up, let's get the perspective of two people very familiar with the topic who understand what we need to make urgent progress. Please, join me in welcoming Ajay Banga, President of the World Bank Group, and Dr. Tedros Adhanom Ghebreyesus, who's Director General of the World Health Organization. [Audience applauds]
Greetings, gentlemen. Thank you so very much for being here with us today. Ajay, first, quickly, you've been doing a lot of work fixing the plumbing of the World Bank Group. Why and what's the aim of that?
[Ajay Banga]
This plumbing question is getting asked a few times, and I think that's because I made the statement that I believe that if you make the Bank better and more effective, quicker, faster, simpler to navigate, then that allows you to raise your ambition on the kind of things that you can do because your ability to execute gets enhanced many times over by the quality of your foundation. So, I use plumbing to describe it because I say that you can't build a new house with poor plumbing. That is the logic. What we're trying to do is to improve the speed, turnaround time. It used to take us 19 months to get a project approved from the time we started talking about it to approval, we're down by three months. We want to bring down another three months by the middle of next year. If we get it down to a year, that's really good, given the complexity of what we deal with. We're trying to do things with combining our structure in different countries, 20 countries. We're going to put one country ahead on top of IFC, MIGA, IBRD all together. So, our client has to deal with one person, one World Bank Group, and cut out some of the silos that otherwise are visible. We're working on capital adequacy, change the Vision and Mission of the Bank to include Livable Planet. There's a whole series of these partnerships with the multilateral banks. We're about to launch a co-financing platform, a digital one, which will enable all the MDBs to work together on co-financing deals. We're looking at standardizing standards across procurement. I mean, I could keep going. It's all the plumbing. It's what makes the bank and its people work quicker, faster, better.
So, streamlining everything.
Here we are today talking about health with the world facing so many pressing issues. Why are we talking about health care today?
Because I think health care is foundational. I think that at the end of the day, if you look at people struggling with either the cost of health care or the inability to access health care, it leads to the worst possible outcomes. I went to Indonesia and saw the work they're doing on stunting. The reality is that a child in the first 1,000 days of their existence doesn't get the right kind of nutrition, that has an impact economically forever for that child. They earn between 15% and 20% less every year, forever. If you look at climate change and what it's doing to heat impact on diseases, another issue. Tedros can talk about this ad nauseam, but 2 billion people in this world do not have access to health care in a way that they get insurance or they get it free. They end up paying for it out of pocket. That puts them in a cycle of poverty for a long time to come. We've got to fix what is a fundamental requirement for human existence in the form of health care, and we have to make it available at a price that's affordable. That's not that complex to get around your head. It's hard to get done, but you will hear from the Japanese Finance Minister in a short while, they knew how to do it well. And that's what we are trying to do as well.
So, “no health, no wealth,” as the saying goes. Thank you for spelling that out for us, Ajay. So, Dr. Tedros, where does the world stand on universal health coverage that you've long championed?
[Dr. Tedros Adhanom Ghebreyesus]
Now, thank you. First of all, I would like to thank my friend Ajay for inviting me to this very important session. And second, I fully agree with him, health is the foundation. As you rightly said, “health is wealth.” That's why Ajay and the World Bank takes it seriously. And we're very, very glad to say this. By the way, our partnership is increasing from time to time now. We partner on UHC, we partner on Global Preparedness and Monitoring Board, we partner on Pandemic Fund, we partner on also leading the Health and Finance Task Force, you name it. It's a long list, by the way. So, thank you so much for your leadership, Ajay. And on the status of UHC, 140 countries have recognized health as a fundamental right in their constitutions. This is very important because it's recognizing health as a fundamental human right, which is a political choice that can help us to do the rest, financing or everything. So, that's good. Then the second part is, since the birth of WHO, that's 76 years ago, life expectancy has increased from 46 to now 74, average. This is good progress. Of course, this is living condition improved, improvements in medicine, improvements in public health. It's overall development. It shows overall development. We're progressing, but if you see the SDG goals directly, if you compare it with the SDG goals, we're off track.
Yeah, very.
[Dr. Tedros Adhanom Ghebreyesus]
I don't think without a very serious catch-up, we may even reach the SDGs. So, we have to work harder, and that's why we're partnering with the World Bank and other partners, the whole UN, with countries, especially countries at the center, to push forward to achieve the SDG goals.
So, partnerships, clearly, key, Dr. Tedros, just talk us through quickly. What are some of the key challenges to achieving universal health coverage?
So, the challenges are twofold. One, in terms of service coverage, and second, financial. I think Ajay had already said that. In terms of service coverage, 4.5 million do not have access to basic services, and 2 billion, Ajay said it, face financial hardship, trying to seek service. And even as a result, some of them descend into poverty. So, that's one of the challenges. Coverage, the first one, the 4.5, but also, the financial hardship, which is the 2 billion who can’t afford. These are the two main ones. But of course, there are problems like shortage of the workforce that we need to address. There is, of course, a long list of challenges.
And overall aging population as well.
Aging population, urbanization, and now with the pandemics, climate and health because the climate crisis is a health crisis. So, the major trends and problems actually that complicate the health problem.
So, those are some very stark figures and daunting challenges. So, Ajay, in the face of this, what is the World Bank Group doing to support countries to get health care to more people?
By the way, one thing I understand. One thing I would like to say, the issue of, for example, workforce shortages is also an opportunity because if you think about Africa, and Tedros is an Ethiopian, and if you think about the whole continent, the number of young people who are going to be looking for jobs in the coming 10 to 15 years, one of the ways to give them a really good job is give them the chance to get skilled to provide the kind of service that's going to be required from the investment we're going to make in the coming 10 years in this space. He's absolutely correct. It is a problem today, but we also see it, both of us, as a way forward for young people. Back to your point, what are we going to do? The Bank has been working in 100 countries for a while on what I would call “maternal and neonatal” kind of effort to improve the delivery of care to women and young babies, and they've done a decent job of doing so. The question really is if you want to widen your aperture to include the diseases across adolescents and older age. So, if you just think about heart attacks, diabetes, blood pressure, those are diseases that are challenging, in older life as well. So, if you want to broaden the access for those, then you have to widen your aperture to include that. And that's what we are trying to do in this effort, reach 1.5 billion people over the coming period with the WHO, with other partners, and make that happen by 2030. Reach them means really reach them. I don't mean reach as in you put up a center and everybody in the area is counted. This is actually touching the person with a medical appointment, either physical or telehealth, working on this expanded range of noncommunicable diseases, and maybe in those 100 countries, but maybe expanded geographies in those countries or new countries as well. That's the effort we're going to try and put in by now in 2030.
That's one and a half billion people in essentially five years. How are you going to do that? [Ajay Banga] Six years, but who's counting? [Panelists laugh]
Six years. How are we going to do that? [Shakuntala Santhiran] How are you going to do that?
How are we going to do that? I think it takes a lot of hard work, a lot of knowledge, a lot of financing, and a lot of partnerships. Let me quickly walk through a little bit of it. Financing is the obvious one. We've got money, yes. We're a money bank and a knowledge bank, but even the money we can put to work will never be enough. We're talking about putting to work 50% more money per year than what we used to spend in healthcare pre the pandemic. You're still going to need money from governments. You're going to need money from the private sector. Let me walk you through this a little bit. If you talk about the countries that are at the lowest end of affordability, mostly IDA countries, they spend relatively little amounts of money per person, 21 dollars per person per year on health care. That's not going to get you health care workers in remote areas that we're talking about. We have to give them share financing, concessional and grant financing. But if you're a middle-income country, you may have more money available, but you may not have the right regulatory policies to create the multiplier that you want to create by also bringing in the private sector, but also clarifying how to get more energy going into this space. I think there we can help with incentivizing them through our money to create the right regulatory platforms, the right policies. Tedros can talk to you about regulatory policies all day long, but that could help a lot. If you get the private sector involved, once they have some clarity, you could do things like focusing them on the manufacturing of PPE, manufacturing of essential medicines, something that Tedros had a nightmare of during COVID. Ask him, he will tell you. If you could also get them involved with, for example, putting the right vitamin supplements into processed foods so that you enhance health right from the basic consumption. So, there's a number of things. Some of these are more likely to happen in some countries, some in others. The point is this financing has to be catered for the country and its stage of development. In the same way, knowledge has to be catered for the country and its stage of development. If it's basic knowledge, are you talking about putting our primary health center or a hospital, which is better at what stage of development? Tough choice, but a conversation to be had. If it's later discussions and conversations about, does this country need geographic expansion? Does this country need new skills? Does this country need affordability? What's the logic of what that country needs to break through its barriers on delivering its share of the 1.5 billion? That's kind of the knowledge part. The partnership part, there are a lot of people in the audience. I'm sure Gavi is here and others are here. They're all part of this game. You kind of need to bring all shoulders to the wheel. But since we've got Tedros here, he has what I would call “domain expertise” beyond limit, technical expertise beyond limit. What do we bring? We bring a diversification of knowledge. We understand water, we understand climate, we understand agriculture, we understand different things. We understand how those connect to health challenges. We can bring that knowledge as a partner, not just our financing, not just our ability to advise governments on regulatory policy, but our ability to help even him understand the intersections between these different causes of health care problems in the intertwined challenges that we are going through. So, it's a long answer. It needs a lot of work. It's going to be really hard work between now and 2030. I'm sure we will make mistakes along the way, but we are determined to get this done.
You certainly got your work cut out for you, right? So, partnerships, financing, and the sharing of knowledge, all vital. Dr. Tedros, what do you hope to see in global health in five years? Or six years?
[Dr. Tedros Adhanom Ghebreyesus] [Laughs]
In six years.
[Shakuntala Santhiran laughs]
By the way, the two things which are very important with regards to making progress are, one, a political commitment. I can add to that. Of course, financial commitment also, you had said that. Political commitment, we have 140 countries who recognize health as a human right, and we have 140 countries who recognize health as a fundamental human right, and we hope the other countries will do, because health is a political choice. When they do that, then the rest comes, including finance. Then, the second is the financial commitment. In the financial commitment, there is a way. There are finance ministers here, and we expect you to increase public spending. Commitment to Universal Health Coverage or Health For All, of course, it's ambitious, but it's possible. One example that comes to mind is the United Kingdom. After the Second World War, when its economy was in its knees, it actually declared Universal Health Coverage. The Lord Beveridge model started immediately after the Second World War. So, economic status cannot be an issue. You can start with what you have. The key is the commitment, and then you can build up. So, I think the political commitment and finance are important. Then what do I expect in the next? Of course, I said earlier, to get better or to add years into your life, life expectancy, then we need, especially to focus on mothers and children, to reduce mortality. It can be done. By the way, Ajay raised that when I was Minister of Health in Ethiopia, just in a few years, with the introduction of primary health care, that maternal and under-five mortality started to decline significantly. That's what I wish in the next five, six years. Still, there could be a significant cut in many of the countries, especially who have high burden of maternal and child health. This could be done through a combination of promoting health, especially addressing the root causes of ill health, focusing on the determinants, because many of the health problems are in the food we eat, in the air we breathe, in the environment we live in, our lifestyle, and so on. We should start from there. The second is the access issue we said, Universal Health Coverage, but with primary health care at the foundation, because primary health care is key to cover the basic services. More than 80%, by the way, can be covered using primary health care. Primary health care is also the ears and eye of the health system, and it can help us to prevent outbreaks, but at the same time, if not to detect early and manage. So, investment in primary health care is key. From my own experience in Ethiopia, World Bank was a major player in building the primary health care, which made a good impact. Of course, the pandemic preparedness is very important, and we're investing in that. Then, investment in science, data, and technology is very important. And, like the World Bank, reforming WHO itself to be fit for purpose will be very important. But all this, the center is the country. What do we do at the country level and what capacity do we build at the country level and how do we help countries to achieve is crucial. At the end of the day, the ownership is the countries. We are only here to help. The World Bank and WHO, that's exactly what we're saying. The results come at the country level, I cannot say we'll get this result, but sure, if we can partner effectively and if countries can commit on and take it as a political choice, and if we can support them to the fullest we can, we can turn the tide and hopefully we can achieve SDGs, because that's what we aim for, and we don't need to have another goal. Let's stick to that and make it happen. I'm hopeful that we can do that.
A resounding call to action. Dr. Tedros, Ajay, thank you very much indeed for highlighting not only the challenges that we're facing, [Audience applauds]
but also, the enormous opportunity that we can realize if people have access to quality affordable health care. It's not just the individual, but also, communities and entire countries who will benefit from such investments. Thank you both again. Now, Japan is a leader in the pursuit of Universal Health Coverage and understands the level of partnership and collaboration it will take to make progress. We are honored to be joined now by His Excellency, Shun’ichi Suzuki. [Speaking in foreign language] This is Japan's Minister of Finance. [Audience applauds] [Speaking in foreign language]
Thank you, sir. Thank you.
[Shun’ichi Suzuki]
First of all, I would like to thank President Banga and Director General Tedros for a very insightful discussion. It is my great honor to make a short statement on Japan's efforts to promote UHC. Japan has long been emphasizing the critical importance of UHC as a foundation for human capital development and sustainable growth. Japan has also been advocating that finance-health collaboration is essential to achieve UHC. For this reason, Japan hosted the first G20 joint Finance-Health Ministers’ Meeting in 2019 at the emergence of the G20, Osaka summit. In this context, I am pleased today to see various stakeholders, including finance and health experts meeting to discuss UHC. Japan has been closely working with the World Bank and WHO in supporting developing countries towards the achievement of UHC, including through financial contributions to technical assistance in this area. In order to further accelerate our efforts, I am delighted to announce today that Japan, together with the Bank and the WHO, will establish a UHC knowledge hub in Japan in 2025. [Audience applauds]
The hub will support knowledge sharing on UHC as well as capacity building for finance and health authorities. It leverages the expertise of the Bank and the WHO while drawing on Japan's experience, such as our efforts to maintain quality UHC amid an aging and declining population. At the Bank, the discussion on IDA21 is ongoing. IDA plays a crucial role in mainstreaming UHC in low-income countries. It is imperative to help them secure adequate financing resources for a well-functioning health care system. Japan expects that IDA21 maintains UHC as one of the policy priorities. Today, I look forward to a lively debate about the challenges and the policy efforts to achieve UHC in each country. Building on today's discussion, Japan will continue to help step up efforts to promote UHC across the world. Thank you. [Audience applauds]
[Shakuntala Santhiran speaking in foreign language] [Shakuntala Santhiran]
Many thanks, Minister Suzuki, for your important message and for Japan's continued commitment to global health.
Yes, yes, thank you.
Thank you very much, sir. Thank you. Now, we have three questions for you, our audience, here in person and watching online, not just to test your knowledge, but also to help illustrate the scope of the challenge. Please, use the QR codes to participate, and we'll share the correct answers with you later in the event. Question number one. It's a sad reality that women in low-income countries are more likely to die due to childbirth compared to women in high-income countries. But by how much? Is it 4 times more likely, 14 times, 34 times, or is it 140 times more likely? Our second question for you. There's a shortage of health care workers in countries everywhere. What percentage of countries have fewer than one doctor for every 1,000 people? Is it 3% of countries, 18%, 33%, or is it 43% of countries? Our third question, what do you think is the single most important thing that can help accelerate progress toward universal health coverage? Please, let us know in just one word. We'll share all your ideas later in this event. So, achieving Universal Health Coverage brings opportunities and challenges, as we've heard, and will require country reforms. Let's now welcome His Excellency Dr. Muhammad Pate, Nigeria's Minister of Health. Her Excellency, Sri Mulyani Indrawati Minister Finance of Indonesia, and Dr. Senait Fisseha, Vice President of Global Programs at The Susan Thompson Buffett Foundation. [Dr. Muhammad Ali Pate] Very good.
Welcome to you all.
[Sri Mulyani Indrawati]
Thank you very much for taking the time to be here. Muhammad, if we could start with you, please. You are leading your country through critical health reforms. What's your vision and how is it going to change health coverage for Nigeria's poorest and most vulnerable people?
[Dr. Muhammad Ali Pate]
We are a young and fast-growing country, and our health outcomes have been improving over time, but there are other elements like noncommunicable diseases that are rising as the fastest-growing segment for morbidity and mortality. Under the President's Health Sector Renewal Investment Initiative, we're expanding access to quality basic health care through the primary health care system, expanding the primary health care centers that are functional from 8,800 to 17,000, retraining 120,000 frontline health workers and enabling them with digital technology to function, expanding the affordability through the Vulnerable Groups Fund to ensure the poorest and most vulnerable are able to afford the services that they need, to improve maternal and child health, immunization, as well as deal with other elements of the evolving epidemiology that we are seeing of hypertension, diabetes, and other diseases. That is the approach that we are taking so that we can guarantee basic health care to all Nigerians over time, to raise the domestic resources, and to work with our partners in a sector-wide manner as a federal system between the federal government and the state government, as well as development partners and civil society, so that we pull in the same direction to improve health outcomes. Over time, we expect that Nigeria's health outcomes trajectory will improve, that life expectancy can improve, and that maternal mobility and mortality will reduce because many of the diseases are actually preventable with simple things that can be delivered at the primary health care centers. On our path to UHC, these reforms are getting us closer to saving more lives, reducing physical and financial pain, producing health, and to do it for all Nigerians so that we don't leave anyone behind. That's what we are undertaking right now in Nigeria.
That's the vision. That's the goal. How's it going? What challenges are you facing in implementing and also sustaining these reforms?
It's been an exciting journey. I think we've got the highest level of political leadership from the President. And as Tedros says, it's a political choice. Nigeria made a political choice to prioritize health investment and the well-being of Nigerians. So, we're seeing that ease in the path. State governors are joining along, and development partners like the Bank, like the WHO and others also are rallying around this effort. Challenges of human resources are certainly ones that are not limited to us. We've doubled the intakes for our physicians, nurses, midwives, pharmacists to increase the production of health workforce in our country, to redistribute them, and also, to create the enabling environment so that they can stay and function. That's one challenge. But financing is a key one. The financing gap that we have, certainly, we're very encouraged when we hear Ajay mentioned 1.5 billion, and that's a significant commitment by the Bank to actually do that. But then backing it with the resources that are needed, you can scale. For Nigeria, for instance, we can deliver 100 million out of that 1.5 billion if the resources are there. We're really seeing appetite from our development partners to contribute. Some of these are doing this quietly, and some of them are actually working programmatically, in addition to a technical support, to get us closer to our aspiration as laid out by the President in his agenda.
It's an immense task, but one that needs doing. Mulyani, we know that getting health care in many countries' countries comes at a very high cost. It puts a heavy financial burden on individuals, on families, especially the poor. Why is this of concern? Why should this be of concern to a finance minister?
Well, I think for the finance minister, the focus of the quality of human capital is very important. At the end of the day, if the economy and the country have a human capital with a better quality, whether on education and health, that definitely is going to create much better quality of growth, inclusive, equal growth in this case. And for countries like Indonesia, with the young demographic dividend, just like Nigeria, this is very important, investing at the very early stage. And that's why Indonesia is putting quite significant resources, both on education and health. And on health, we have the legislation which is mandatory for us to create a universal health access. That's very costly, certainly, if you look at the cost, but the rate of return is definitely very high. Indonesia currently has 95%, which they are all the people registered on a health insurance system, the biggest single player of the health insurance in Indonesia. And that will provide, especially the budget, our fiscal policy tools, providing support for the poorest families and the members of the family to be registered free of pay. That means we are going to be the ones who pay, and that provides an access to education without out-of-pocket for those poor families. The problem now is more on a demand side. It's created with those. Then, supply constraints. And that's why reform on supply side is going to be very important. And this is one of the most important reforms of health in Indonesia. Indonesia is a very big country, 273 million, comprising of local governments, and health is actually delegated to the local government. You can have an uneven quality of health services across Indonesia. That's why providing a good support, technical capacity, competency, human resources, medical workers, I think that's going to be very important. Currently, Indonesia is launching this comprehensive reform on health, which is supported by many of the MDBs, and that's why the World Bank is now hosting this talk show with us.
To conduct, to make these reforms happen, you need financing, and Indonesia has been quite successful in mobilizing financing for these reforms. How have you done so?
First, I think the MDBs really look at the country, and they love to have a country who has a strong ownership, they call it, and leadership. The Minister of Health is important. They have a good Minister of Health with leadership, they know what they are doing, do the reform. We passed the reform legislation, which is very important for the Indonesia health system. This totally overhauled in terms of how we are going to educate the medical doctors, how we are going to manage the local government hospitals as well as health services, especially on a primary level. Then also how this is going to be connected with the insurance system. These have all become one important reform, which is not only curative but also preventive. This is one integrated from the lifestyle into early detection of the disease up to the whole services from the primary, secondary, rural level hospital Of course, we have to make sure that people have a better health and lifestyle so that it can create a much better… That kind of ownership as well as leadership and a comprehensive health vision is very important to gain confidence from the source of funding, specifically the MDBs. The MDBs, which is a combination of not only World Bank, but also Islamic Development Bank, Asian Development Bank. What is good about this combination of co-financing is they are all now looking at the procurement system, one combined simple process, with President Ajay Banga already launching this plumbing improvement by having it [being] simpler, faster; and hopefully that’s true for us, so that is going to deliver a much better and also supporting the reform in a credible way. Because legislation has been passed, the discussion with many stakeholders is already being conducted, and so, we are going to then support it with the financing.
Thank you, Mulyani. Now, Senait, you have been in the field of global health for many years. You're a physician yourself and a globally recognized leader in reproductive health and rights. How do you think we can collectively do more with the funding that's currently available for health?
[Senait Fisseha]
Thank you, Shaks. I don't think any of the things I would say would come as a surprise, at least to this audience. What we see globally is vertical programming. I think the single most impactful way to maximize our limited resources is to fund a primary healthcare system instead of individualized vertical diseases. We, as you rightly said, I work in reproductive health. Imagine a woman seeking care, going to one clinic for HIV, another clinic for contraception, and somewhere else for her children's immunization. So, rather than doing that, if we pool our resources and essentially do what Minister Pate was talking about and invest it in strengthening the health system and provide integrated service delivery, we can push our resources further. We at the foundation, at The Buffett Foundation, have seen that. We are a single-issue foundation committed to advancing the health and well-being and rights of women and girls. But by funding governments and strengthening health systems and responding to the government's mandate, we have seen that we can reach many more women at scale, and the services are scalable and sustainable. Unfortunately, global funding doesn't work like that, but I think there are examples we can glean. If you look at the Bank's investments, for example, at the global financing facility, and take workforce as an example. If you focus on workforce, you're primarily focusing on ensuring essential health services are available, but these are also the tools for strong preparedness, for pandemic preparedness. If you look at climate response, first-line responders are healthcare providers. And a shout out to my colleagues in Women in Global Health for so long who've been advocating, women are the frontline providers. So, 90% of healthcare providers are women. So, by investing in them and paying them and creating a career ladder, you're also then working on gender equity. So, I think there's just a lot we could do to pull these strands together and maximize our resources by putting it in a systems lens as opposed to an individual disease lens approach. Thanks. [Shakuntala Santhiran] Thank you, Senait. [Audience applause]
So, Muhammad, you've seen this issue from many different perspectives, from the global level to the country level from the private sector now to the public sector. You're a medical doctor as well. You've worked in an emergency room. You know this issue inside out. If we were to meet in one year from now, what do you hope will have shifted in the global and country discussions on universal health coverage?
Well, first on the UHC agenda, I think even before COVID, we knew that we were not on track at the pace that we are making progress. Pandemic came and drilled us even further. So going forward, continuing on the same path will not meet our objectives. So, there are some shifts that are needed. And with countries at the center, and what we're trying to do in Nigeria is articulate a division, a direction, defragmented the landscape with the subnational levels also aligned with us, and having our supportive global partners come to back us up with financing, with technical support, but following leadership of government and using national systems that are more sustainable, and let's hold each other accountable. If that shift occurs where we're really real from the global perspective to really deploy the resources, then we will see the shift in progress with UHC. So as long as we continue with the model that we had, where, as Senait mentioned, we have vertical funding, hyper fragmentation and various interests here and there, the reality is for the pregnant woman, for the child who is sick, they go to the primary health care center. They want to be assessed, they want the health worker to see them, they want the commodities to be there, they want to be able to afford the care. An integrated perspective is what is needed. In the case of Nigeria, the Health Sector Renewal Investment Initiative, which was launched by our President, is precisely trying to do that, to pull everyone in one direction, subnational units, development partners, but with a laser focus on results and results at scale, not results in one district or one state, and also results focusing on the most vulnerable, the poorest who are left out. That's really the shift that I hope we can begin to see in the next year or so. I will also reiterate for us, for the Bank colleagues that are here, for GFF who are doing an amazing job with us and many other partners that are also trying to support Nigeria in this journey, that we can put on the table at least 100 million population that can be reached with access to basic health care services. If the Bank is really going to go all out for this, Nigeria, now this is where we are and this is where we are going. Thank you. [Audience applauds]
Thank you, Muhammed. Senait, last words to you. What gives you hope? Is there anything that gives you hope in the pursuit for global health?
Sure. We're living in very fragile times, and it's very easy to give up hope. But the truth is there's a lot to be hopeful for, especially post-pandemic. I think the global narrative and conversation on global health has shifted in such a way that we cannot go back. And for me, what I see at this table, the leadership from the Global South, gives me incredible hope. The leadership that I see in international institutions, seeing someone like Tedros, who delivered health care for millions of people as a health minister leading the WHO, or Juan Pablo [Uribe], who is a Health Minister in Colombia sitting at the GFF and the Health Nutrition and Population at the World Bank, tells us that the world, as we know, it is changing. I think external funders need to rally support and throw themselves around some of this change that we're seeing. Eighty years of development, I think we've made very, very little progress. I think you all agree with me. We've made progress, but when you look at our expenditure, it should have been much more. And part of it is this very colonial, outdated model of development is not fit for purpose for the time we're in. There's a lot of exciting stuff around the world. When I see what Minister Pate is doing in Nigeria, I recently met with President Ruto and his commitment to deploy 140,000 community health workers. Look at Rwanda boldly doubling down to quadruple workforce in four years because if they continue at the current pace, it will take 100 plus years to meet the WHO's minimum requirement for workforce. There's really strong momentum and leadership. How are we going to position ourselves to support this change, to support this dynamic, and invest in such a way that allows governments to have ownership? Again, the Bank, I know, needs to improve a lot of things, including speed, the way we manage projects, but it's a country-led ownership. It's a country-led process. I think I'm really hopeful, when I look at my own continent, and Africa CDC, and a new voice for Africa in a unified way to negotiate, we've seen what happened in the pandemics and who was left behind, so, I think it's really hopeful that the world as a whole is awakened to this new reality. I think if we all rally around that and reform ourselves to be fit for purpose, we can be inching closer to achieving UHC Health For All in the real meaningful way.
Thank you very much indeed. Thank you all for joining us together to discuss this important issue with smart country reforms and strong government leadership. Change is possible. It's also clear that health and finance ministries need to be working together because without adequate financing, health care reforms cannot happen. Once again, thank you all very much indeed. [Audience applauds]
Now, before we invite our next panel to the stage, let's hear from some frontline health workers. We asked them to tell us one thing that has helped them improve health services for their patients. Here's what they said.
[Dr. Chidinma S. Ononogbu]
And one of the greatest innovations that has been able to help with care is being able to get ambulance services on time. And that's one of the things that has helped us to be able to care for our patient urgently.
[Dr. Longtila M. Sangtam]
And another intervention that really helps us is the installation of solar light and rainwater harvesting facility for our center.
[Dr. Eustaquio Solis] [Speaks in Spanish] This telemedicine program also contributes to comprehensive patient care.
[Dr. Nii Ayikwei A. Addo-Quaye]
And one of the greatest innovations that has been able to help with this has been the electronic health management systems, which helps me to be able to have continuity of care with my patients, so that none are left behind them and we carry them along. [Shakuntala Santhiran] So very important to hear from these local heroes. They need our support to continue their good work, improving and expanding health care services to people in need. Now, here are the answers to our quiz. The numbers are staggering and really underscore the need for urgent action. Women in low-income countries are 34 times more likely to die from childbirth than women in higher-income countries, and 43% countries have fewer than one doctor for every thousand people. Clearly, we need better progress, and that will require more investments in health. To talk about this, please join me on stage now, His Excellency Dr. Mohamed Maait, Minister of Finance of Egypt. Hello, sir. Lamia Tazi. Hello. Lamia is CEO of Sothema, a pharmaceutical manufacturing company in Morocco. And Dr. Joanne Carter, Executive Director of RESULTS… [Audience applauds]
An organization committed to ending poverty. We appreciate you being here, taking the time to be here with us today. We just heard Ajay announced that new commitment by the World Bank Group to help countries get health services to more people, one and a half billion people in five or six years. Joanne, you lead a global advocacy network in Africa, Asia, the US, Europe, and the Pacific. From where you sit, what will it take to really deliver on this, especially in terms of how we prioritize financing?
[Joanne Carter]
Yeah. Well, one thing I would say is I'm not quite sure we celebrated enough that target because the target that was just announced is a doubling of reach and a doubling of ambition. [Audience applauds]
I think we ought to just notice that and celebrate it. That's huge. What I would say, though, first thing is, ambitious targets need ambitious funding to match. Maybe you expected me to say that as an advocate. Of course, it starts with domestic budgets. Our advocacy partners across the world work with their governments, including parliamentary champions, to increase investment in health and nutrition, especially for the most marginalized. But I would say we urgently need also more external grant and concessional financing, especially for the lowest income countries and those facing debt distress. And that's why donor support for an ambitious, robust IDA replenishment, along with support for other key global health institutions, Gavi, the Global Fund, the World Health Organization, the Global Financing Facility is so critical. And also, prioritization of health and nutrition within IDA. And the other thing I would just say about targets is that targets can and should drive us, but we also know from experience that top-line targets, even bold ones, can actually obscure inequities. We need to ensure that financing reaches the most marginalized, and that only happens if it is specifically targeted to do so. To deliver on a goal like this, we need equity between countries and within countries. Just a few really quick thoughts about what we can do. You heard this earlier in the last panel, but a focus on investment in primary health care. Primary health care at the community level, especially for the most marginalized, has to be the leading edge of Universal Health Coverage investment. To measure IDA's impact on UHC, this has to be where we start, focusing on the numbers of people reached with primary health care and measuring it with an equity lens, increasing the share of resources going to the lowest quintiles. I would also just add that global health security matters, and it matters a lot, but it also matters how we define it. A narrow investment in health security does not reach UHC, and theoretical global readiness actually falls apart if we actually don't have the support and capacity at community level. Just really final point. We also need to build PHC starting there and then going further with human capital investments. I think it's also a real strength of IDA to start with primary health care, but also ensure access to emergency and higher-level care and nutrition supports across this spectrum and across sectors, social sector and program support and gender investments, because bold targets for UHC matter and why they don't guarantee equity? We can do things in targeting an investment that ensures equity. Country ambition needs investment, and that needs to include donors. [Shakuntala Santhiran] Thank you, Joanne. [Audience applauds]
Now, we've heard over and over today the need for political commitment. Minister Maait, what is your government doing to ensure that all Egyptians have access to effective health care?
[Mohamed Maait]
I think Egypt, although it was one of the first countries to introduce health insurance in 1962, the objective was to cover all the population. However, by that time, we found that the system did not cover all the population, it’d become financially unsustainable, inefficient, and also it didn't achieve its objective. So, four years ago, we decided to change and introduce universal health insurance with a different model and different design. And it is based on that we have to split the financing of the system from the affordability, or the ability of the Minister of Finance to provide finance or not that depends on how the budget is, to create an independent power and create all the sources needed to ensure that the system will be financially sustainable for a long time. This is number one. Number two, to ensure that we cover the whole families. Number three, to ensure that private and public sector will compete and to ensure that the government is no longer responsible to provide health care, but to buy health care for the citizen. If citizens want to receive the service, we have to create one public arm to provide the health care and to compete with the private sector. And a third organization, which will be the regulator. This regulator will be given the accreditation. So, three different organizations. One is a buyer, one is a public provider, one is the regulator accreditation and control of quality. Over the four years, we were able to start rolling out the new system with the government, and we created financing from different sources. One is social insurance contribution, be it by the employee and the employers. The second one, earmarking tax and tax coming from the budget. The third one is that the State will pay the contribution for those who are vulnerable or unable. Every one or two years, we review the system, from the actuarial point of view, to ensure this system is sustainable. We created a mechanism to ensure that the pricing of the health services will be attractive for the private sector and public sector at the same level. So, all will compete. So, the buyer is just buying the services for the citizen. Over the four years, we were able to cover around five governments out of 27, and we are continuing to do that. Satisfaction level. The Wallet Bank, JICA, and the others with us review the level of satisfaction and fix it if the system is having something in the design.
You were saying the private sector and the public sector need to compete, but you mean in terms of pricing, right?
They need to compete in satisfaction for the citizen because at the end, the citizen has the option to choose a provider, whether it is public or private. So, this is number one. Number two, they need not to compete on the main cost of the services, but on the quality of the services, because we have an independent committee which includes private, public, and the independent who price the services to the people. But again, we're choosing the slogan of “Money will follow the patient,” so, whenever the patient chooses to go for a specific provider, money will go to this provider. And we said the government is not responsible to provide the services, but to buy the services. And this helped us to ensure that citizens will go where they can find quality of their services and they are satisfied with that. The other thing is to ensure some independence for the financing sources. I worked as a First Deputy Minister of Health before I became Minister of Finance. I felt that leaving the Health Services at the mercy of the Minister of Finance is not a good idea.
After one year of working as a First Deputy Minister of Health, and I was awarded Bachelor of Medicine, after one year, so I said, “When I become a Minister of Finance, I will ensure not to put the system and the financing of the system depending on whether the budget is in good health so they can allocate more money or not, no.” We were able to build a huge reserve in the first four years of implementing such a system.
Thank you, Minister Maait. Let's look more closely now at the private sector and the public sector. There are also opportunities to cooperate, right? Because they can complement each other. Lamia, you're there in the private sector. In your experience, how can the private and public sectors best complement each other? For example, in developing a vaccine, you need a partnership, don't you, between the private and public sectors?
[Lamia Tazi]
Yeah. Thanks, Shaks. Thanks for inviting me to have the chance to discuss about contribution of pharma industry in the health coverage. As you said, I'm leading a company which is located in Morocco. In 2021, His Majesty, Our King, decided to give the health coverage for all, which was a very courageous decision, knowing that we had to add 22 new inhabitants in Morocco in this health coverage. So, I was very pleased to be part of this big challenge. And it's exactly the title of the panel, “How to move the challenge to action.” And I think Morocco took the good decision to go there. And after two years, I can say that it is a success. This success cannot be here if there is no collaboration between public and private sector. Of course, the chance we had in Morocco is that we had a strong pharma industry before. Thanks to some incentives given by the public sector, by our Ministry of Health, we had some incentives to push local manufacturing. In 2021, 70% of the needs in medications were manufactured locally. Knowing that in health coverage, 30% of expenses are coming from medication. It was very important to have this availability of the products, and it was manufactured locally, which gives us, and give to the public, the availability and the accessibility to give the equity for all Moroccans. At the end, I can say that collaboration is very important. This local production affords the products in term of quantity because it was planned, it was discussed before. In terms of quantities and in terms also of kind of medication, knowing that our region may need some molecules that do not exist, perhaps in other countries. So local production was able to afford these kinds of molecules. In terms of vaccines, we discussed about vaccines. My company had the chance to be part of the big adventure in COVID. So, it was a real partnership between public and private. I had the chance to conduct the first clinical trials in vaccines in Morocco and then manufacture the vaccines before. Really, it was done by very close collaboration between pharma industry, between my company and the Ministry of Health.
We're going to look more closely at the benefits of local production very shortly. First, Mr. Maait, is the government of Egypt working together with the private sector in any way?
What I insist on when we designed this system, I said there was no possibility to success in ensuring this system will achieve its objectives without private sector. Why? When we move to some government rates, the infrastructure, the public infrastructure is not there. I have to rely more on the private sector to ensure that they will be able to provide the service. But how can I attract the private sector? How I can convince the private sector to be with me? Number one, to be part of pricing the services. Dynamic. Dynamic, I mean by dynamic if the inflation is changed, they can call for a committee tomorrow. We need to change the pricing. And they can at any time, because they are part of the committee who are pricing for the whole Republic of Egypt. They can change it on a weekly basis, on a monthly basis, in order to ensure that they are always seeing the system, responding to their success, because eventually, they look for profit. Eventually, they look to get more business. At least, unless this business is attractive for them, they will not be joining me. This is number one. Number two, I'm trying to ensure that the capacity they have will be built-in in the system itself. They are on the price, on the provider side, and I give them the opportunity to do more and more business. Egypt has roughly 115 million people living in it, and in some areas, the private sector has more infrastructure, more capabilities, so I believe with good prices, with good volume of business, and with good infrastructure, they’ll come with us. Also, we always make contracts with them on a regular basis to join us. Even the insurance companies. I said to the insurance companies, “You can work with us.” Why? Because at some level of different categories of population, insurance companies are more efficient to deal with those who have the financial capabilities and want some special health system. So, I say, “Okay, I have a price list, and this price list will be applied to all, because the private sector and the independent experts were there in pricing. So, let the insurance companies make the contract with the employers and provide whatever services they want, and at the end, for every quarter or so, we can make a financial settlement. You are happy, we are happy.” At the end, the government wants what? They want the citizen to enjoy a good health service. For me, I want it to be efficient. I want to ensure that this system will continue to be sustainable. This system will earn the satisfaction of the citizen, regardless of who will provide the service, the public or private sector. This is not my job. My job is to make citizens happy. I created the money which can support that. I said, “The money cannot get from one source.” If it is only the budget, I will be under the mercy of the budget and the Minister of Finance. So, I said, “No.” We need to get social insurance contribution directly deducted from people's salaries and from the employers to the system. This is number one. Number two, earmarking tax on tobacco and cigarettes and everything should come directly to us. So, the tax authority collects this money and doesn’t give it to the Minister of Finance, it gives it directly to the system. At the end, the Minister of Finance is responsible for financing a part of the system, particularly the population who are not able to finance themselves.
Thank you, Minister Maait. Now, let's go back to that point about local production. There were important lessons during the COVID-19 pandemic for many countries about not having medical equipment, tools, and drugs, pharmaceutical drugs, not being produced locally. You manufacture locally in Morocco, in Senegal. You're looking to expand into East Africa and also the Middle East. So outside of health emergencies, how does local production actually help increase health coverage?
We know all that COVID pandemic was a really crash test for all, and especially for the health systems. Even I know in rich countries, there are many issues of shortage of medications, of all medical devices. So, Morocco had the chance to have a good experience on it because of this local production. We were able to provide all medication needed when all important products were stopped. By the way, Sothema is working also in Africa, and we were providing also, with the Moroccan approval, our African countries and partners, because there were shortages in many, many products. So, it was very important to have this local production to permit the pandemic to pass away. I think without this local production, Morocco and Africa will have issues. Now, I can talk about opportunities in the health coverage. I discussed about all that pharma industry gives for the health coverage. Of course, in this pharma industry, as Mr. Minister said, we have also opportunities as producers. Of course, it makes the quantities more important because of the economy of scale, so, we reduce the price. We reduced the price so we can afford more quantities with accessibility, and we know how the cost of the product is very important in the health coverage. So, this opportunity is in affordability and also in creating an ecosystem. Helping this local production is pushing investors to invest more, invest more in new technologies, which is a very important point for me. Primary care is very important, but in our region, we also face the same issues in chronic diseases. We have oncology, we have cardiovascular, and these molecules are very expensive for countries like us. So, giving the opportunity to local producers, it's to push them also to invest on new technology, to create an ecosystem in R&D. R&D is not existing in our countries. So, I think that, as you said, partnership between public and private is really a win-win situation for all. And from my side, I'm very happy to participate in this adventure. It permits us to think about going outside Morocco and outside our region, which is very important for the economy and for bringing in the outside. So, at the end, it's a win-win situation.
[Shakuntala Santhiran] Thank you, Lamia.[Joanne Carter] Yes. [Shakuntala Santhiran] Joanne… [Joanne Carter] Yes.
In closing, you've been a strong advocate for universal health coverage, throughout your career you've worked very hard to bring many different players to tackle the major diseases of poverty. How do you think we can keep funding an action for global health as a top priority?
Well, thanks. I would say the thing that I come back to start with is that we cannot achieve these targets for primary health care, for Universal Health Coverage without more funding for these priorities. That is so clear. It's also clear that countries and the most impacted communities need to lead on what's needed, and they need to do domestic financing in ways to protect the most impoverished. But we so need donors to also do their part in the financing. Increasing, again, grant and concessional finance through increasing support for the IDA replenishment, which is in play right now, as well as for other key global health institutions, is absolutely essential for supporting domestic investment and ambition. Also, the Global Financing Facility, which is housed here at the Bank, is one of the instruments that can help support countries to crowd in more IDA resources and also more domestic resources for health. I would say, really importantly, where countries are stepping up domestic investment in health and areas like nutrition, this has to be an incentive for donors to do more and not an excuse to do less. I would also say it was really exciting to hear about the local production, and the UHC will require everyone at the table. I would also say that in health delivery, we need also a core, strong public health system. I think that is another strength of IDA because it actually works across the public health sectors to support that. I guess, finally, I would say to your question of what do we need to do. We need ministers of finance who are leaders like this. We need ministers of health. We need the private sector and things like dispersed manufacturing. We also need members of Parliament; I know that there's members of Parliament here from around the world whose role on budgets and oversight, and as champions, is really key. And absolutely central is the role of local leaders, civil society, and especially directly affected communities for setting direction for holding governments and institutions accountable and also for resource mobilization. I would just say to wrap up, I've worked with the US and other donor governments for decades as an advocate, and I know that we have strong allies in those places for global health, and I also know the constraints that they face, right? But those constraints are political and not fundamentally economic. These are political decisions, and so we need to provide public backing for our allies and our champions, but we cannot let donor countries step back at this time. We need them to step up, to fund what matters, and to be partners with countries so that countries can fund what matters to the communities and the most vulnerable. And ultimately, and Dr. Tedros said this at the start, this is a political choice, and we cannot accept that there isn't enough money for this agenda, and we cannot expect countries to try to do more with less. We actually need to increase support for IDA and other key global health institutions so that we can support countries to do lots more on primary health care, on UHC with more. We all need to work together to make that happen. Thank you [Shakuntala Santhiran] Bravo. [Audience applauds]
Thank you all for being part of this very necessary conversation. Partnerships are clearly key to making a dent in improving and increasing health services. Partnerships with civil society organizations who know the situation on the ground. Partnerships with governments who prioritize health and the financing for it, and partnerships with the private sector that can help fill gaps, especially when it comes to medical supplies and delivery. Many thanks to all our guests once again, and thank you to everyone who took part in our quiz who answered the question, what is the one thing most crucial to accelerate progress toward universal health coverage? Here is what you said, the cloud is up there. We see money, affordability. Yes, we need more affordable services. All those answers are correct. You've all clearly been paying attention to our expert speakers. Underpinning all of this, political will, and of course, the funding, the money, funding for healthcare ultimately is a fundamental investment for the benefit of all that will unlock future human capital and economic progress. Thank you very much for taking part, for sharing your thoughts. That brings us to the end of this event. We hope it's been informative and engaging for you. You can watch the replay of this session and our other events at live.worldbank.org. Please, do continue sharing your comments online with the hashtag #WBGMeetings. We'd love to hear from you. We thank you for joining us. Thank you. [Audience applauds] [Music]
EVENT HIGHLIGHTS
"If you make the Bank better and more effective—quicker, faster, simpler to navigate—that allows you to raise your ambition and the kind of things you can do because your ability to execute gets enhanced many times over by the quality of your foundation.”
Ajay Banga, World Bank President
“On our path to Universal Health Coverage, these reforms are getting us closer to saving more lives, reducing physical and financial pain, producing health, and to do it for all Nigerians, so that we don’t leave anyone behind.”
Muhammed Ali Pate, Minister of Health, Nigeria
"If the economy and the country have human capital with better quality on education and health, that definitely will create much better quality, inclusive and equal growth."
Sri Mulyani Indrawati, Minister of Finance, Indonesia
Learning Resources
- Tracking Universal Health Coverage: 2023 Global Monitoring Report
- Digital-in-Health: Unlocking the Value for Everyone
- The Economic Burden of COVID-19 Infections amongst Health Care Workers
- Health Financing in a Time of Global Shocks
- Increasing Access to Health Services Through Inclusive Digital Health
- Brief: Expanding Health Coverage for All
Stories and Blogs
Transforming challenge to action: new health target announced at spring meetings, human capital ministerial conclave: realizing the potential of digital technology and ai.
- Investing in Health Blogs
- Filling the Prescription for Better Medical Equipment
- How Health-Tech is Delivering Life-Saving Innovation in Kenya
Additional resources
- Universal Health Coverage
- World Bank and Health
- IFC and Health
Read the Latest

FEATURE STORY

Feature Story
You Asked Our Expert

David Wilson
Program Director, Health Nutrition & Population, World Bank Group
2024 Spring Meetings
Watch the event replays, read the recaps, and find out about the latest announcements on increasing energy access across Africa and expanding health coverage worldwide . We received over 600 questions online, and our experts responded to over 200 of them in the chat during the live sessions.

World Bank Group Flagship Events

President, World Bank Group

Tedros Adhanom Ghebreyesus
Director-General, World Health Organization

Shun’ichi Suzuki
Minister of Finance, Japan
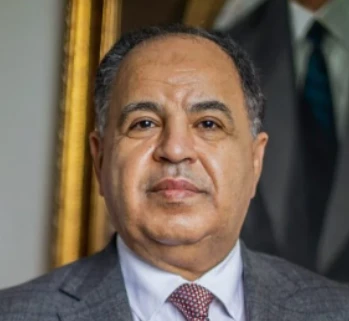
Mohamed Maait
Minister of Finance, Arab Republic of Egypt

Muhammad Ali Pate
Minister of Health, Nigeria

Sri Mulyani Indrawati
Minister of Finance, Indonesia

Joanne Carter
Executive Director, RESULTS

CEO, Sothema

Senait Fisseha
Vice President of Global Programs, The Susan Thompson Buffett Foundation

Shakuntala Santhiran
International broadcast journalist
2024 Spring Meetings on World Bank Live

April 17, 2024
Energizing Africa: What Will It Take to Accelerate Access and Improve Lives?

April 11, 2024
2024 Spring Meetings Opening Press Conference
Receive updates about upcoming events.
I agree with the terms of the Privacy Notice and consent to my personal data being processed, to the extent necessary, to receive these updates.
Status message
Thank you for requesting an event reminder for email We have just sent you a confirmation.
Error message
It looks as though the e-mail address: email is already registered for reminders for this event.
Something went wrong
WORLD HEALTH ORGANIZATION Read less
Recommended
More related content, what's hot, what's hot ( 20 ), similar to who ppt., similar to who ppt. ( 20 ), recently uploaded, recently uploaded ( 20 ).
- 1. AISHWARYA HIREMATH M –PHARM Industrial Pharmacy. 1 Bapuji College Of Pharmacy Davanagere (WHO)
- 3. The World Health Organization is a specialized agency of United Nations. WHO was established on 7th April 1948. The headquarters of WHO is located in Geneva. WHO serves as the directing and coordinating authority for International health matters and public health. 3
- 4. First global health organization. In latter half of 19 th century, severe cholera epidemics was occurred. At that time, series of international sanitary conferences were held in Europe to co-ordinate policy & practice around quarantine & disease management. The League of Nations established a health organization in 1920. 4
- 5. Establishment of the United Nations is in 1945, marked as a period of aggressive internationalism & international organization building & though health was not initially thought to be under the U.N. After its motion started by Brazilian & Chinese delegates to establish an international health organization and that was generally accepted. 5
- 6. Finally, WHO’s constitution came into force on 7 th April 1948. This date celebrates every year as “ WORLD HEALTH DAY” by all over world. 6 A group of health experts, working on emergency relief in World War II were charged with the task of drafting a constitution to define the structure & mandate of the body that would become known as the World Health Organization (WHO).
- 7. To develop & implement multisectorial public policies for health, integrated gender- & age- sensitive approaches that facilitate community empowerment, together with action for health promotion, self-care & health protection throughout the life course in cooperation with the relevant national and International partners. 7
- 8. The world health assembly is the supreme decision making body for WHO. It generally meets in Geneva in may each year, and is attended by delegations from all 194 member states. 8 i. WORLD HEALTH ASSEMBLY (Parliament)
- 9. The health assembly appoints the Director-General. . The current director general of WHO is Dr. Tedros Adhanom an Ethiopian nationalist, who started his 5 year term on 1st July 2017. 9
- 10. For the first time (5th oct 2017), an Indian Doctor has been appointed as deputy DG of WHO. Dr.Soumya Swaminathan, she was untill now the DG of Indian Council of Medical Research. New Delhi. 10 Dr.Soumya swaminathan (Deputy Director General of WHO)
- 11. 11World Health Assembly
- 12. Main functions of assembly are: 1.To determine international health policy and programme. 2. To review the work of past years 3.To approve the Budget. 4.To elect member state to designate a person to serve for 3 years on executive board. 5. Supervises the financial policies of the organization and reviews and approves the proposed program budget. 12
- 13. The executive board is composed of 34 members technically qualified in the field of health. Members are elected for 3 year terms. The main functions of the board are to give effect to the decisions and policies of the health assembly, to advise it and generally to facilitate its work. 13 EXECUTIVE BOARD
- 14. The current Chairman of executive board is Dr. ASSAD hafeez. 14 Dr. Assad Hafeez
- 15. 15Executive Board
- 16. The secretariat of WHO is staffed by some 8000 health and other experts and support staff on fixed-term appointment, working at headquarters in the 6 regional offices. 16 . There are 5 assistant Director General and there responsibility is assigned by DG in different Divisions.
- 17. African Region Brazzaville, Congo Region of the Americas, Washington , USA South East Asia Region , New Delhi, India European Region, Copenhagen, Denmark Eastern Mediterranean Region , Egypt Cairo, Western Pacific Region, Manila, Philippines 17
- 19. “The attainment by all people the highest level of health”. MISSION “To lead strategic collaborative efforts among Member States and other partners to promote equity in health, to combat disease, and to improve the quality of, and lengthen, the lives of the all peoples of the world” 19
- 20. Prevention and control of specific diseases Development of comprehensive health services To improve the Family health Environmental health Health statistics Bio-medical research Assembling of Health literature and information Cooperation with other organizations to get the equilibrium in improved health status. 20
- 21. “Health is a state of complete physical, mental and social well-being, and not merely the absence of disease or infirmity” WHO’S LOGO WHO's logo was chosen by the first World Health Assembly in 1948. The logo consists of the United Nations symbol surmounted by a staff with a snake coiling around it. The staff with the snake has long been a symbol of medicine and the medical profession. 21
- 22. Neutral Organization to all member state. Nearly universal membership. Global presence and Networking. No parallel Organization in tackling diseases. Large no. of Expertise in all health issues. Strong coordination and convincing ability. Strong fund collecting ability Global cooperation, collaboration and investment 22
- 23. Membership into WHO is open to all countries. All countries that are part of the UN are also members of WHO. WHO GLOBAL SERVICE CENTRE WHO Global Service Centre is an integral part of WHO’s global strategy, in helping WHO to deliver its global mandate and implement its programmes in a timely and cost effective manner. 23
- 24. 1. Promoting development 2. Encourage health security 3. Strengthening health systems 4. Encouraging research, information & evidence 5. Enhancing partnerships 6. Improving performance of health developping organiztions. 24
- 25. Providing leadership on matters critical to health and engaging in partnerships where joint action is needed, Shaping the research agenda and stimulating the generation, translation and spreading of valuable knowledge. Setting norms and standards and promoting and monitoring their implementation. Articulating ethical and evidence based policy options. 25
- 26. Providing technical support, catalizing change, and building sustainable institutional capacity. Monitoring the health situation and assessing health trends. 26
- 27. “Although WHO has both opportunities and challenges; Its contribution is great to increase the quality of life and living standard globally.” 27
- 28. www.who.com www.wikipedia.net 28
- 29. 29 THANK YOU…..
- Open access
- Published: 18 April 2024
Research ethics and artificial intelligence for global health: perspectives from the global forum on bioethics in research
- James Shaw 1 , 13 ,
- Joseph Ali 2 , 3 ,
- Caesar A. Atuire 4 , 5 ,
- Phaik Yeong Cheah 6 ,
- Armando Guio Español 7 ,
- Judy Wawira Gichoya 8 ,
- Adrienne Hunt 9 ,
- Daudi Jjingo 10 ,
- Katherine Littler 9 ,
- Daniela Paolotti 11 &
- Effy Vayena 12
BMC Medical Ethics volume 25 , Article number: 46 ( 2024 ) Cite this article
701 Accesses
6 Altmetric
Metrics details
The ethical governance of Artificial Intelligence (AI) in health care and public health continues to be an urgent issue for attention in policy, research, and practice. In this paper we report on central themes related to challenges and strategies for promoting ethics in research involving AI in global health, arising from the Global Forum on Bioethics in Research (GFBR), held in Cape Town, South Africa in November 2022.
The GFBR is an annual meeting organized by the World Health Organization and supported by the Wellcome Trust, the US National Institutes of Health, the UK Medical Research Council (MRC) and the South African MRC. The forum aims to bring together ethicists, researchers, policymakers, research ethics committee members and other actors to engage with challenges and opportunities specifically related to research ethics. In 2022 the focus of the GFBR was “Ethics of AI in Global Health Research”. The forum consisted of 6 case study presentations, 16 governance presentations, and a series of small group and large group discussions. A total of 87 participants attended the forum from 31 countries around the world, representing disciplines of bioethics, AI, health policy, health professional practice, research funding, and bioinformatics. In this paper, we highlight central insights arising from GFBR 2022.
We describe the significance of four thematic insights arising from the forum: (1) Appropriateness of building AI, (2) Transferability of AI systems, (3) Accountability for AI decision-making and outcomes, and (4) Individual consent. We then describe eight recommendations for governance leaders to enhance the ethical governance of AI in global health research, addressing issues such as AI impact assessments, environmental values, and fair partnerships.
Conclusions
The 2022 Global Forum on Bioethics in Research illustrated several innovations in ethical governance of AI for global health research, as well as several areas in need of urgent attention internationally. This summary is intended to inform international and domestic efforts to strengthen research ethics and support the evolution of governance leadership to meet the demands of AI in global health research.
Peer Review reports
Introduction
The ethical governance of Artificial Intelligence (AI) in health care and public health continues to be an urgent issue for attention in policy, research, and practice [ 1 , 2 , 3 ]. Beyond the growing number of AI applications being implemented in health care, capabilities of AI models such as Large Language Models (LLMs) expand the potential reach and significance of AI technologies across health-related fields [ 4 , 5 ]. Discussion about effective, ethical governance of AI technologies has spanned a range of governance approaches, including government regulation, organizational decision-making, professional self-regulation, and research ethics review [ 6 , 7 , 8 ]. In this paper, we report on central themes related to challenges and strategies for promoting ethics in research involving AI in global health research, arising from the Global Forum on Bioethics in Research (GFBR), held in Cape Town, South Africa in November 2022. Although applications of AI for research, health care, and public health are diverse and advancing rapidly, the insights generated at the forum remain highly relevant from a global health perspective. After summarizing important context for work in this domain, we highlight categories of ethical issues emphasized at the forum for attention from a research ethics perspective internationally. We then outline strategies proposed for research, innovation, and governance to support more ethical AI for global health.
In this paper, we adopt the definition of AI systems provided by the Organization for Economic Cooperation and Development (OECD) as our starting point. Their definition states that an AI system is “a machine-based system that can, for a given set of human-defined objectives, make predictions, recommendations, or decisions influencing real or virtual environments. AI systems are designed to operate with varying levels of autonomy” [ 9 ]. The conceptualization of an algorithm as helping to constitute an AI system, along with hardware, other elements of software, and a particular context of use, illustrates the wide variety of ways in which AI can be applied. We have found it useful to differentiate applications of AI in research as those classified as “AI systems for discovery” and “AI systems for intervention”. An AI system for discovery is one that is intended to generate new knowledge, for example in drug discovery or public health research in which researchers are seeking potential targets for intervention, innovation, or further research. An AI system for intervention is one that directly contributes to enacting an intervention in a particular context, for example informing decision-making at the point of care or assisting with accuracy in a surgical procedure.
The mandate of the GFBR is to take a broad view of what constitutes research and its regulation in global health, with special attention to bioethics in Low- and Middle- Income Countries. AI as a group of technologies demands such a broad view. AI development for health occurs in a variety of environments, including universities and academic health sciences centers where research ethics review remains an important element of the governance of science and innovation internationally [ 10 , 11 ]. In these settings, research ethics committees (RECs; also known by different names such as Institutional Review Boards or IRBs) make decisions about the ethical appropriateness of projects proposed by researchers and other institutional members, ultimately determining whether a given project is allowed to proceed on ethical grounds [ 12 ].
However, research involving AI for health also takes place in large corporations and smaller scale start-ups, which in some jurisdictions fall outside the scope of research ethics regulation. In the domain of AI, the question of what constitutes research also becomes blurred. For example, is the development of an algorithm itself considered a part of the research process? Or only when that algorithm is tested under the formal constraints of a systematic research methodology? In this paper we take an inclusive view, in which AI development is included in the definition of research activity and within scope for our inquiry, regardless of the setting in which it takes place. This broad perspective characterizes the approach to “research ethics” we take in this paper, extending beyond the work of RECs to include the ethical analysis of the wide range of activities that constitute research as the generation of new knowledge and intervention in the world.
Ethical governance of AI in global health
The ethical governance of AI for global health has been widely discussed in recent years. The World Health Organization (WHO) released its guidelines on ethics and governance of AI for health in 2021, endorsing a set of six ethical principles and exploring the relevance of those principles through a variety of use cases. The WHO guidelines also provided an overview of AI governance, defining governance as covering “a range of steering and rule-making functions of governments and other decision-makers, including international health agencies, for the achievement of national health policy objectives conducive to universal health coverage.” (p. 81) The report usefully provided a series of recommendations related to governance of seven domains pertaining to AI for health: data, benefit sharing, the private sector, the public sector, regulation, policy observatories/model legislation, and global governance. The report acknowledges that much work is yet to be done to advance international cooperation on AI governance, especially related to prioritizing voices from Low- and Middle-Income Countries (LMICs) in global dialogue.
One important point emphasized in the WHO report that reinforces the broader literature on global governance of AI is the distribution of responsibility across a wide range of actors in the AI ecosystem. This is especially important to highlight when focused on research for global health, which is specifically about work that transcends national borders. Alami et al. (2020) discussed the unique risks raised by AI research in global health, ranging from the unavailability of data in many LMICs required to train locally relevant AI models to the capacity of health systems to absorb new AI technologies that demand the use of resources from elsewhere in the system. These observations illustrate the need to identify the unique issues posed by AI research for global health specifically, and the strategies that can be employed by all those implicated in AI governance to promote ethically responsible use of AI in global health research.

RECs and the regulation of research involving AI
RECs represent an important element of the governance of AI for global health research, and thus warrant further commentary as background to our paper. Despite the importance of RECs, foundational questions have been raised about their capabilities to accurately understand and address ethical issues raised by studies involving AI. Rahimzadeh et al. (2023) outlined how RECs in the United States are under-prepared to align with recent federal policy requiring that RECs review data sharing and management plans with attention to the unique ethical issues raised in AI research for health [ 13 ]. Similar research in South Africa identified variability in understanding of existing regulations and ethical issues associated with health-related big data sharing and management among research ethics committee members [ 14 , 15 ]. The effort to address harms accruing to groups or communities as opposed to individuals whose data are included in AI research has also been identified as a unique challenge for RECs [ 16 , 17 ]. Doerr and Meeder (2022) suggested that current regulatory frameworks for research ethics might actually prevent RECs from adequately addressing such issues, as they are deemed out of scope of REC review [ 16 ]. Furthermore, research in the United Kingdom and Canada has suggested that researchers using AI methods for health tend to distinguish between ethical issues and social impact of their research, adopting an overly narrow view of what constitutes ethical issues in their work [ 18 ].
The challenges for RECs in adequately addressing ethical issues in AI research for health care and public health exceed a straightforward survey of ethical considerations. As Ferretti et al. (2021) contend, some capabilities of RECs adequately cover certain issues in AI-based health research, such as the common occurrence of conflicts of interest where researchers who accept funds from commercial technology providers are implicitly incentivized to produce results that align with commercial interests [ 12 ]. However, some features of REC review require reform to adequately meet ethical needs. Ferretti et al. outlined weaknesses of RECs that are longstanding and those that are novel to AI-related projects, proposing a series of directions for development that are regulatory, procedural, and complementary to REC functionality. The work required on a global scale to update the REC function in response to the demands of research involving AI is substantial.
These issues take greater urgency in the context of global health [ 19 ]. Teixeira da Silva (2022) described the global practice of “ethics dumping”, where researchers from high income countries bring ethically contentious practices to RECs in low-income countries as a strategy to gain approval and move projects forward [ 20 ]. Although not yet systematically documented in AI research for health, risk of ethics dumping in AI research is high. Evidence is already emerging of practices of “health data colonialism”, in which AI researchers and developers from large organizations in high-income countries acquire data to build algorithms in LMICs to avoid stricter regulations [ 21 ]. This specific practice is part of a larger collection of practices that characterize health data colonialism, involving the broader exploitation of data and the populations they represent primarily for commercial gain [ 21 , 22 ]. As an additional complication, AI algorithms trained on data from high-income contexts are unlikely to apply in straightforward ways to LMIC settings [ 21 , 23 ]. In the context of global health, there is widespread acknowledgement about the need to not only enhance the knowledge base of REC members about AI-based methods internationally, but to acknowledge the broader shifts required to encourage their capabilities to more fully address these and other ethical issues associated with AI research for health [ 8 ].
Although RECs are an important part of the story of the ethical governance of AI for global health research, they are not the only part. The responsibilities of supra-national entities such as the World Health Organization, national governments, organizational leaders, commercial AI technology providers, health care professionals, and other groups continue to be worked out internationally. In this context of ongoing work, examining issues that demand attention and strategies to address them remains an urgent and valuable task.
The GFBR is an annual meeting organized by the World Health Organization and supported by the Wellcome Trust, the US National Institutes of Health, the UK Medical Research Council (MRC) and the South African MRC. The forum aims to bring together ethicists, researchers, policymakers, REC members and other actors to engage with challenges and opportunities specifically related to research ethics. Each year the GFBR meeting includes a series of case studies and keynotes presented in plenary format to an audience of approximately 100 people who have applied and been competitively selected to attend, along with small-group breakout discussions to advance thinking on related issues. The specific topic of the forum changes each year, with past topics including ethical issues in research with people living with mental health conditions (2021), genome editing (2019), and biobanking/data sharing (2018). The forum is intended to remain grounded in the practical challenges of engaging in research ethics, with special interest in low resource settings from a global health perspective. A post-meeting fellowship scheme is open to all LMIC participants, providing a unique opportunity to apply for funding to further explore and address the ethical challenges that are identified during the meeting.
In 2022, the focus of the GFBR was “Ethics of AI in Global Health Research”. The forum consisted of 6 case study presentations (both short and long form) reporting on specific initiatives related to research ethics and AI for health, and 16 governance presentations (both short and long form) reporting on actual approaches to governing AI in different country settings. A keynote presentation from Professor Effy Vayena addressed the topic of the broader context for AI ethics in a rapidly evolving field. A total of 87 participants attended the forum from 31 countries around the world, representing disciplines of bioethics, AI, health policy, health professional practice, research funding, and bioinformatics. The 2-day forum addressed a wide range of themes. The conference report provides a detailed overview of each of the specific topics addressed while a policy paper outlines the cross-cutting themes (both documents are available at the GFBR website: https://www.gfbr.global/past-meetings/16th-forum-cape-town-south-africa-29-30-november-2022/ ). As opposed to providing a detailed summary in this paper, we aim to briefly highlight central issues raised, solutions proposed, and the challenges facing the research ethics community in the years to come.
In this way, our primary aim in this paper is to present a synthesis of the challenges and opportunities raised at the GFBR meeting and in the planning process, followed by our reflections as a group of authors on their significance for governance leaders in the coming years. We acknowledge that the views represented at the meeting and in our results are a partial representation of the universe of views on this topic; however, the GFBR leadership invested a great deal of resources in convening a deeply diverse and thoughtful group of researchers and practitioners working on themes of bioethics related to AI for global health including those based in LMICs. We contend that it remains rare to convene such a strong group for an extended time and believe that many of the challenges and opportunities raised demand attention for more ethical futures of AI for health. Nonetheless, our results are primarily descriptive and are thus not explicitly grounded in a normative argument. We make effort in the Discussion section to contextualize our results by describing their significance and connecting them to broader efforts to reform global health research and practice.
Uniquely important ethical issues for AI in global health research
Presentations and group dialogue over the course of the forum raised several issues for consideration, and here we describe four overarching themes for the ethical governance of AI in global health research. Brief descriptions of each issue can be found in Table 1 . Reports referred to throughout the paper are available at the GFBR website provided above.
The first overarching thematic issue relates to the appropriateness of building AI technologies in response to health-related challenges in the first place. Case study presentations referred to initiatives where AI technologies were highly appropriate, such as in ear shape biometric identification to more accurately link electronic health care records to individual patients in Zambia (Alinani Simukanga). Although important ethical issues were raised with respect to privacy, trust, and community engagement in this initiative, the AI-based solution was appropriately matched to the challenge of accurately linking electronic records to specific patient identities. In contrast, forum participants raised questions about the appropriateness of an initiative using AI to improve the quality of handwashing practices in an acute care hospital in India (Niyoshi Shah), which led to gaming the algorithm. Overall, participants acknowledged the dangers of techno-solutionism, in which AI researchers and developers treat AI technologies as the most obvious solutions to problems that in actuality demand much more complex strategies to address [ 24 ]. However, forum participants agreed that RECs in different contexts have differing degrees of power to raise issues of the appropriateness of an AI-based intervention.
The second overarching thematic issue related to whether and how AI-based systems transfer from one national health context to another. One central issue raised by a number of case study presentations related to the challenges of validating an algorithm with data collected in a local environment. For example, one case study presentation described a project that would involve the collection of personally identifiable data for sensitive group identities, such as tribe, clan, or religion, in the jurisdictions involved (South Africa, Nigeria, Tanzania, Uganda and the US; Gakii Masunga). Doing so would enable the team to ensure that those groups were adequately represented in the dataset to ensure the resulting algorithm was not biased against specific community groups when deployed in that context. However, some members of these communities might desire to be represented in the dataset, whereas others might not, illustrating the need to balance autonomy and inclusivity. It was also widely recognized that collecting these data is an immense challenge, particularly when historically oppressive practices have led to a low-trust environment for international organizations and the technologies they produce. It is important to note that in some countries such as South Africa and Rwanda, it is illegal to collect information such as race and tribal identities, re-emphasizing the importance for cultural awareness and avoiding “one size fits all” solutions.
The third overarching thematic issue is related to understanding accountabilities for both the impacts of AI technologies and governance decision-making regarding their use. Where global health research involving AI leads to longer-term harms that might fall outside the usual scope of issues considered by a REC, who is to be held accountable, and how? This question was raised as one that requires much further attention, with law being mixed internationally regarding the mechanisms available to hold researchers, innovators, and their institutions accountable over the longer term. However, it was recognized in breakout group discussion that many jurisdictions are developing strong data protection regimes related specifically to international collaboration for research involving health data. For example, Kenya’s Data Protection Act requires that any internationally funded projects have a local principal investigator who will hold accountability for how data are shared and used [ 25 ]. The issue of research partnerships with commercial entities was raised by many participants in the context of accountability, pointing toward the urgent need for clear principles related to strategies for engagement with commercial technology companies in global health research.
The fourth and final overarching thematic issue raised here is that of consent. The issue of consent was framed by the widely shared recognition that models of individual, explicit consent might not produce a supportive environment for AI innovation that relies on the secondary uses of health-related datasets to build AI algorithms. Given this recognition, approaches such as community oversight of health data uses were suggested as a potential solution. However, the details of implementing such community oversight mechanisms require much further attention, particularly given the unique perspectives on health data in different country settings in global health research. Furthermore, some uses of health data do continue to require consent. One case study of South Africa, Nigeria, Kenya, Ethiopia and Uganda suggested that when health data are shared across borders, individual consent remains necessary when data is transferred from certain countries (Nezerith Cengiz). Broader clarity is necessary to support the ethical governance of health data uses for AI in global health research.
Recommendations for ethical governance of AI in global health research
Dialogue at the forum led to a range of suggestions for promoting ethical conduct of AI research for global health, related to the various roles of actors involved in the governance of AI research broadly defined. The strategies are written for actors we refer to as “governance leaders”, those people distributed throughout the AI for global health research ecosystem who are responsible for ensuring the ethical and socially responsible conduct of global health research involving AI (including researchers themselves). These include RECs, government regulators, health care leaders, health professionals, corporate social accountability officers, and others. Enacting these strategies would bolster the ethical governance of AI for global health more generally, enabling multiple actors to fulfill their roles related to governing research and development activities carried out across multiple organizations, including universities, academic health sciences centers, start-ups, and technology corporations. Specific suggestions are summarized in Table 2 .
First, forum participants suggested that governance leaders including RECs, should remain up to date on recent advances in the regulation of AI for health. Regulation of AI for health advances rapidly and takes on different forms in jurisdictions around the world. RECs play an important role in governance, but only a partial role; it was deemed important for RECs to acknowledge how they fit within a broader governance ecosystem in order to more effectively address the issues within their scope. Not only RECs but organizational leaders responsible for procurement, researchers, and commercial actors should all commit to efforts to remain up to date about the relevant approaches to regulating AI for health care and public health in jurisdictions internationally. In this way, governance can more adequately remain up to date with advances in regulation.
Second, forum participants suggested that governance leaders should focus on ethical governance of health data as a basis for ethical global health AI research. Health data are considered the foundation of AI development, being used to train AI algorithms for various uses [ 26 ]. By focusing on ethical governance of health data generation, sharing, and use, multiple actors will help to build an ethical foundation for AI development among global health researchers.
Third, forum participants believed that governance processes should incorporate AI impact assessments where appropriate. An AI impact assessment is the process of evaluating the potential effects, both positive and negative, of implementing an AI algorithm on individuals, society, and various stakeholders, generally over time frames specified in advance of implementation [ 27 ]. Although not all types of AI research in global health would warrant an AI impact assessment, this is especially relevant for those studies aiming to implement an AI system for intervention into health care or public health. Organizations such as RECs can use AI impact assessments to boost understanding of potential harms at the outset of a research project, encouraging researchers to more deeply consider potential harms in the development of their study.
Fourth, forum participants suggested that governance decisions should incorporate the use of environmental impact assessments, or at least the incorporation of environment values when assessing the potential impact of an AI system. An environmental impact assessment involves evaluating and anticipating the potential environmental effects of a proposed project to inform ethical decision-making that supports sustainability [ 28 ]. Although a relatively new consideration in research ethics conversations [ 29 ], the environmental impact of building technologies is a crucial consideration for the public health commitment to environmental sustainability. Governance leaders can use environmental impact assessments to boost understanding of potential environmental harms linked to AI research projects in global health over both the shorter and longer terms.
Fifth, forum participants suggested that governance leaders should require stronger transparency in the development of AI algorithms in global health research. Transparency was considered essential in the design and development of AI algorithms for global health to ensure ethical and accountable decision-making throughout the process. Furthermore, whether and how researchers have considered the unique contexts into which such algorithms may be deployed can be surfaced through stronger transparency, for example in describing what primary considerations were made at the outset of the project and which stakeholders were consulted along the way. Sharing information about data provenance and methods used in AI development will also enhance the trustworthiness of the AI-based research process.
Sixth, forum participants suggested that governance leaders can encourage or require community engagement at various points throughout an AI project. It was considered that engaging patients and communities is crucial in AI algorithm development to ensure that the technology aligns with community needs and values. However, participants acknowledged that this is not a straightforward process. Effective community engagement requires lengthy commitments to meeting with and hearing from diverse communities in a given setting, and demands a particular set of skills in communication and dialogue that are not possessed by all researchers. Encouraging AI researchers to begin this process early and build long-term partnerships with community members is a promising strategy to deepen community engagement in AI research for global health. One notable recommendation was that research funders have an opportunity to incentivize and enable community engagement with funds dedicated to these activities in AI research in global health.
Seventh, forum participants suggested that governance leaders can encourage researchers to build strong, fair partnerships between institutions and individuals across country settings. In a context of longstanding imbalances in geopolitical and economic power, fair partnerships in global health demand a priori commitments to share benefits related to advances in medical technologies, knowledge, and financial gains. Although enforcement of this point might be beyond the remit of RECs, commentary will encourage researchers to consider stronger, fairer partnerships in global health in the longer term.
Eighth, it became evident that it is necessary to explore new forms of regulatory experimentation given the complexity of regulating a technology of this nature. In addition, the health sector has a series of particularities that make it especially complicated to generate rules that have not been previously tested. Several participants highlighted the desire to promote spaces for experimentation such as regulatory sandboxes or innovation hubs in health. These spaces can have several benefits for addressing issues surrounding the regulation of AI in the health sector, such as: (i) increasing the capacities and knowledge of health authorities about this technology; (ii) identifying the major problems surrounding AI regulation in the health sector; (iii) establishing possibilities for exchange and learning with other authorities; (iv) promoting innovation and entrepreneurship in AI in health; and (vi) identifying the need to regulate AI in this sector and update other existing regulations.
Ninth and finally, forum participants believed that the capabilities of governance leaders need to evolve to better incorporate expertise related to AI in ways that make sense within a given jurisdiction. With respect to RECs, for example, it might not make sense for every REC to recruit a member with expertise in AI methods. Rather, it will make more sense in some jurisdictions to consult with members of the scientific community with expertise in AI when research protocols are submitted that demand such expertise. Furthermore, RECs and other approaches to research governance in jurisdictions around the world will need to evolve in order to adopt the suggestions outlined above, developing processes that apply specifically to the ethical governance of research using AI methods in global health.
Research involving the development and implementation of AI technologies continues to grow in global health, posing important challenges for ethical governance of AI in global health research around the world. In this paper we have summarized insights from the 2022 GFBR, focused specifically on issues in research ethics related to AI for global health research. We summarized four thematic challenges for governance related to AI in global health research and nine suggestions arising from presentations and dialogue at the forum. In this brief discussion section, we present an overarching observation about power imbalances that frames efforts to evolve the role of governance in global health research, and then outline two important opportunity areas as the field develops to meet the challenges of AI in global health research.
Dialogue about power is not unfamiliar in global health, especially given recent contributions exploring what it would mean to de-colonize global health research, funding, and practice [ 30 , 31 ]. Discussions of research ethics applied to AI research in global health contexts are deeply infused with power imbalances. The existing context of global health is one in which high-income countries primarily located in the “Global North” charitably invest in projects taking place primarily in the “Global South” while recouping knowledge, financial, and reputational benefits [ 32 ]. With respect to AI development in particular, recent examples of digital colonialism frame dialogue about global partnerships, raising attention to the role of large commercial entities and global financial capitalism in global health research [ 21 , 22 ]. Furthermore, the power of governance organizations such as RECs to intervene in the process of AI research in global health varies widely around the world, depending on the authorities assigned to them by domestic research governance policies. These observations frame the challenges outlined in our paper, highlighting the difficulties associated with making meaningful change in this field.
Despite these overarching challenges of the global health research context, there are clear strategies for progress in this domain. Firstly, AI innovation is rapidly evolving, which means approaches to the governance of AI for health are rapidly evolving too. Such rapid evolution presents an important opportunity for governance leaders to clarify their vision and influence over AI innovation in global health research, boosting the expertise, structure, and functionality required to meet the demands of research involving AI. Secondly, the research ethics community has strong international ties, linked to a global scholarly community that is committed to sharing insights and best practices around the world. This global community can be leveraged to coordinate efforts to produce advances in the capabilities and authorities of governance leaders to meaningfully govern AI research for global health given the challenges summarized in our paper.
Limitations
Our paper includes two specific limitations that we address explicitly here. First, it is still early in the lifetime of the development of applications of AI for use in global health, and as such, the global community has had limited opportunity to learn from experience. For example, there were many fewer case studies, which detail experiences with the actual implementation of an AI technology, submitted to GFBR 2022 for consideration than was expected. In contrast, there were many more governance reports submitted, which detail the processes and outputs of governance processes that anticipate the development and dissemination of AI technologies. This observation represents both a success and a challenge. It is a success that so many groups are engaging in anticipatory governance of AI technologies, exploring evidence of their likely impacts and governing technologies in novel and well-designed ways. It is a challenge that there is little experience to build upon of the successful implementation of AI technologies in ways that have limited harms while promoting innovation. Further experience with AI technologies in global health will contribute to revising and enhancing the challenges and recommendations we have outlined in our paper.
Second, global trends in the politics and economics of AI technologies are evolving rapidly. Although some nations are advancing detailed policy approaches to regulating AI more generally, including for uses in health care and public health, the impacts of corporate investments in AI and political responses related to governance remain to be seen. The excitement around large language models (LLMs) and large multimodal models (LMMs) has drawn deeper attention to the challenges of regulating AI in any general sense, opening dialogue about health sector-specific regulations. The direction of this global dialogue, strongly linked to high-profile corporate actors and multi-national governance institutions, will strongly influence the development of boundaries around what is possible for the ethical governance of AI for global health. We have written this paper at a point when these developments are proceeding rapidly, and as such, we acknowledge that our recommendations will need updating as the broader field evolves.
Ultimately, coordination and collaboration between many stakeholders in the research ethics ecosystem will be necessary to strengthen the ethical governance of AI in global health research. The 2022 GFBR illustrated several innovations in ethical governance of AI for global health research, as well as several areas in need of urgent attention internationally. This summary is intended to inform international and domestic efforts to strengthen research ethics and support the evolution of governance leadership to meet the demands of AI in global health research.
Data availability
All data and materials analyzed to produce this paper are available on the GFBR website: https://www.gfbr.global/past-meetings/16th-forum-cape-town-south-africa-29-30-november-2022/ .
Clark P, Kim J, Aphinyanaphongs Y, Marketing, Food US. Drug Administration Clearance of Artificial Intelligence and Machine Learning Enabled Software in and as Medical devices: a systematic review. JAMA Netw Open. 2023;6(7):e2321792–2321792.
Article Google Scholar
Potnis KC, Ross JS, Aneja S, Gross CP, Richman IB. Artificial intelligence in breast cancer screening: evaluation of FDA device regulation and future recommendations. JAMA Intern Med. 2022;182(12):1306–12.
Siala H, Wang Y. SHIFTing artificial intelligence to be responsible in healthcare: a systematic review. Soc Sci Med. 2022;296:114782.
Yang X, Chen A, PourNejatian N, Shin HC, Smith KE, Parisien C, et al. A large language model for electronic health records. NPJ Digit Med. 2022;5(1):194.
Meskó B, Topol EJ. The imperative for regulatory oversight of large language models (or generative AI) in healthcare. NPJ Digit Med. 2023;6(1):120.
Jobin A, Ienca M, Vayena E. The global landscape of AI ethics guidelines. Nat Mach Intell. 2019;1(9):389–99.
Minssen T, Vayena E, Cohen IG. The challenges for Regulating Medical Use of ChatGPT and other large Language models. JAMA. 2023.
Ho CWL, Malpani R. Scaling up the research ethics framework for healthcare machine learning as global health ethics and governance. Am J Bioeth. 2022;22(5):36–8.
Yeung K. Recommendation of the council on artificial intelligence (OECD). Int Leg Mater. 2020;59(1):27–34.
Maddox TM, Rumsfeld JS, Payne PR. Questions for artificial intelligence in health care. JAMA. 2019;321(1):31–2.
Dzau VJ, Balatbat CA, Ellaissi WF. Revisiting academic health sciences systems a decade later: discovery to health to population to society. Lancet. 2021;398(10318):2300–4.
Ferretti A, Ienca M, Sheehan M, Blasimme A, Dove ES, Farsides B, et al. Ethics review of big data research: what should stay and what should be reformed? BMC Med Ethics. 2021;22(1):1–13.
Rahimzadeh V, Serpico K, Gelinas L. Institutional review boards need new skills to review data sharing and management plans. Nat Med. 2023;1–3.
Kling S, Singh S, Burgess TL, Nair G. The role of an ethics advisory committee in data science research in sub-saharan Africa. South Afr J Sci. 2023;119(5–6):1–3.
Google Scholar
Cengiz N, Kabanda SM, Esterhuizen TM, Moodley K. Exploring perspectives of research ethics committee members on the governance of big data in sub-saharan Africa. South Afr J Sci. 2023;119(5–6):1–9.
Doerr M, Meeder S. Big health data research and group harm: the scope of IRB review. Ethics Hum Res. 2022;44(4):34–8.
Ballantyne A, Stewart C. Big data and public-private partnerships in healthcare and research: the application of an ethics framework for big data in health and research. Asian Bioeth Rev. 2019;11(3):315–26.
Samuel G, Chubb J, Derrick G. Boundaries between research ethics and ethical research use in artificial intelligence health research. J Empir Res Hum Res Ethics. 2021;16(3):325–37.
Murphy K, Di Ruggiero E, Upshur R, Willison DJ, Malhotra N, Cai JC, et al. Artificial intelligence for good health: a scoping review of the ethics literature. BMC Med Ethics. 2021;22(1):1–17.
Teixeira da Silva JA. Handling ethics dumping and neo-colonial research: from the laboratory to the academic literature. J Bioethical Inq. 2022;19(3):433–43.
Ferryman K. The dangers of data colonialism in precision public health. Glob Policy. 2021;12:90–2.
Couldry N, Mejias UA. Data colonialism: rethinking big data’s relation to the contemporary subject. Telev New Media. 2019;20(4):336–49.
Organization WH. Ethics and governance of artificial intelligence for health: WHO guidance. 2021.
Metcalf J, Moss E. Owning ethics: corporate logics, silicon valley, and the institutionalization of ethics. Soc Res Int Q. 2019;86(2):449–76.
Data Protection Act - OFFICE OF THE DATA PROTECTION COMMISSIONER KENYA [Internet]. 2021 [cited 2023 Sep 30]. https://www.odpc.go.ke/dpa-act/ .
Sharon T, Lucivero F. Introduction to the special theme: the expansion of the health data ecosystem–rethinking data ethics and governance. Big Data & Society. Volume 6. London, England: SAGE Publications Sage UK; 2019. p. 2053951719852969.
Reisman D, Schultz J, Crawford K, Whittaker M. Algorithmic impact assessments: a practical Framework for Public Agency. AI Now. 2018.
Morgan RK. Environmental impact assessment: the state of the art. Impact Assess Proj Apprais. 2012;30(1):5–14.
Samuel G, Richie C. Reimagining research ethics to include environmental sustainability: a principled approach, including a case study of data-driven health research. J Med Ethics. 2023;49(6):428–33.
Kwete X, Tang K, Chen L, Ren R, Chen Q, Wu Z, et al. Decolonizing global health: what should be the target of this movement and where does it lead us? Glob Health Res Policy. 2022;7(1):3.
Abimbola S, Asthana S, Montenegro C, Guinto RR, Jumbam DT, Louskieter L, et al. Addressing power asymmetries in global health: imperatives in the wake of the COVID-19 pandemic. PLoS Med. 2021;18(4):e1003604.
Benatar S. Politics, power, poverty and global health: systems and frames. Int J Health Policy Manag. 2016;5(10):599.
Download references
Acknowledgements
We would like to acknowledge the outstanding contributions of the attendees of GFBR 2022 in Cape Town, South Africa. This paper is authored by members of the GFBR 2022 Planning Committee. We would like to acknowledge additional members Tamra Lysaght, National University of Singapore, and Niresh Bhagwandin, South African Medical Research Council, for their input during the planning stages and as reviewers of the applications to attend the Forum.
This work was supported by Wellcome [222525/Z/21/Z], the US National Institutes of Health, the UK Medical Research Council (part of UK Research and Innovation), and the South African Medical Research Council through funding to the Global Forum on Bioethics in Research.
Author information
Authors and affiliations.
Department of Physical Therapy, Temerty Faculty of Medicine, University of Toronto, Toronto, Canada
Berman Institute of Bioethics, Johns Hopkins University, Baltimore, MD, USA
Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, USA
Department of Philosophy and Classics, University of Ghana, Legon-Accra, Ghana
Caesar A. Atuire
Centre for Tropical Medicine and Global Health, Nuffield Department of Medicine, University of Oxford, Oxford, UK
Mahidol Oxford Tropical Medicine Research Unit, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand
Phaik Yeong Cheah
Berkman Klein Center, Harvard University, Bogotá, Colombia
Armando Guio Español
Department of Radiology and Informatics, Emory University School of Medicine, Atlanta, GA, USA
Judy Wawira Gichoya
Health Ethics & Governance Unit, Research for Health Department, Science Division, World Health Organization, Geneva, Switzerland
Adrienne Hunt & Katherine Littler
African Center of Excellence in Bioinformatics and Data Intensive Science, Infectious Diseases Institute, Makerere University, Kampala, Uganda
Daudi Jjingo
ISI Foundation, Turin, Italy
Daniela Paolotti
Department of Health Sciences and Technology, ETH Zurich, Zürich, Switzerland
Effy Vayena
Joint Centre for Bioethics, Dalla Lana School of Public Health, University of Toronto, Toronto, Canada
You can also search for this author in PubMed Google Scholar
Contributions
JS led the writing, contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. JA contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. CA contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. PYC contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. AE contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. JWG contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. AH contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. DJ contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. KL contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. DP contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. EV contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper.
Corresponding author
Correspondence to James Shaw .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Shaw, J., Ali, J., Atuire, C.A. et al. Research ethics and artificial intelligence for global health: perspectives from the global forum on bioethics in research. BMC Med Ethics 25 , 46 (2024). https://doi.org/10.1186/s12910-024-01044-w
Download citation
Received : 31 October 2023
Accepted : 01 April 2024
Published : 18 April 2024
DOI : https://doi.org/10.1186/s12910-024-01044-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Artificial intelligence
- Machine learning
- Research ethics
- Global health
BMC Medical Ethics
ISSN: 1472-6939
- General enquiries: [email protected]
Sealy Center on Aging
utmb.edu/scoa
Global web ALERT button

Welcome The Sealy Center on Aging at UTMB: Leading Aging Research Since 1995
Quick links.
- Texas Resource Center on Minority Aging Research (RCMAR)
- Claude D. Pepper Older Americans Independence Center (OAIC)
- World Health Organization / Pan Merican Health Organization (WHO/PAHO)
- Center for Comparative Effectiveness Research on Cancer in Texas (CERCIT)
- Health of Older Minorities Training (T32)
- Medical Student Aging Research Training (MSTAR)
Share this website:
The Sealy Center on Aging focuses on improving the health and well-being of older adults through interdisciplinary research, education, and community service by integrating the resources and activities relevant to aging at UTMB. The Center also implements our research findings in hospitals and clinics, bringing excellence and visibility to our health care system, and improving the health of older adults.
Current Events

University of Texas Medical Branch Sealy Center on Aging (SCoA) 301 University Blvd. Galveston, TX 77555-0177 Directions and Maps Phone: (409) 747-0008 Email: [email protected]

Postdoctoral Fellowship Position
Texas rcmar presentation april 23.
Join us for the next Texas RCMAR Scholar presentation on April 23, 2024. "Data available from the Data Management and Analysis Core for Comparative Effectiveness Research on Cancer in Texas," is presented by Yong-Fang Kuo, PhD, Professor and Chair, Department of Biostatistics & Data Science at 3 PM via zoom.
Research Programs Supported in part by the Sealy Center on Aging

The Texas Resource Center on Minority Aging Research
Claude d. pepper older americans independence center.

World Health Organization/Pan American Health Organization
Comparative effectiveness research on cancer in texas.

Health of Older Minorities Pre and Postdoctoral Training
Medical student in aging research program.

Rebeca Wong, PhD
Sheridan Lorenz Distinguished Professor in Aging and Health, Professor, Department of Population Health and Health Disparities, School of Public and Population Health; Director, WHO/ PAHO Collaborating Center on Aging and Health; Co-Director, Claude Pepper Older American Independence Center; Director ad interim, Sealy Center on Aging

James S. Goodwin, MD
George and Cynthia Mitchell Distinguished Chair of Geriatric Medicine; Co-director, Claude D Pepper Older Americans Independence Center; Senior Associate Director, Sealy Center on Aging
Social Media
UTMB Sealy Center on Aging
World Bank Group Aims to Expand Health Services to 1.5 Billion People
The World Bank Group announced an ambitious plan to support countries in delivering quality, affordable health services to 1.5 billion people by 2030. This is part of a larger global effort to provide a basic standard of care through every stage of a person’s life – infancy, childhood, adolescence, and adulthood.
For decades, the World Bank Group has helped provide health services for women and children in more than 100 countries. A focused effort to become faster, work better with partners, and bring in the private sector has enabled the 80-year-old institution to pursue greater scale and impact.
The strategy to reach 1.5 billion people is focused on three core elements:
- Expanding focus from maternal and child health to include coverage throughout a person’s lifetime, including non-communicable diseases.
- Expanding operations to hard-to-reach areas, including remote villages, cities, and countries.
- Working with governments to cut unnecessary fees and other financial barriers to health care.
To be counted toward this goal, a person must be seen and treated by a health-care worker via an in-person visit or telehealth.
Today, around 2 billion people face severe financial hardship when paying for health services. Intertwined challenges, such as climate change, pandemics, conflicts, societal aging, and a projected shortfall of 10 million healthcare workers by 2030, exacerbate the cycle of poverty and inequality.
The World Bank Group will combine financing, knowledge, and partnerships to address this challenge.
- All elements of the Bank’s financing capabilities are positioned to be called upon depending on a country’s unique need and stage of development to reach 1.5 billion people.
- For countries most in need, IDA financing will make it possible to bring health-care workers into communities where people may otherwise have no access to services.
- In middle-income countries, IBRD will deploy financing to incentivize government investments in health and regulations that move a country forward.
- With regulatory certainty and reliable governance in place, it opens the door for more private sector investments, especially in local production of medications and protective gear.
- Strong partnerships will be critical for the World Bank Group to achieve results in health. The World Bank Group will fall short if it doesn’t work hand-in-hand – faster and better – with non-government organizations, the private sector, and civil society.
- The World Bank Group welcomes Japan’s announcement to launch a Universal Health Coverage (UHC) Knowledge Hub to enhance health and finance ministries' capacity, an initiative supported by the Bank and the World Health Organization.
The goal to deliver quality, affordable health services to 1.5 billion people by 2030 is one of the more recent examples of the World Bank Group’s commitment to become more impact-oriented and is the byproduct of a concerted effort to build a better bank.
Contact: In Washington: Alexandra Humme, [email protected]
For more information: visit www.worldbank.org/en/topic/health and follow @WBG_Health
This site uses cookies to optimize functionality and give you the best possible experience. If you continue to navigate this website beyond this page, cookies will be placed on your browser. To learn more about cookies, click here .
- Warning Signs and Symptoms
- Mental Health Conditions
- Common with Mental Illness
- Mental Health By the Numbers
- Individuals with Mental Illness
- Family Members and Caregivers
- Kids, Teens and Young Adults
- Veterans & Active Duty
- Identity and Cultural Dimensions
- Frontline Professionals
- Mental Health Education
- Support Groups
- NAMI HelpLine
- Publications & Reports
- Podcasts and Webinars
- Video Resource Library
- Justice Library
- Find Your Local NAMI
- Find a NAMIWalks
- Attend the NAMI National Convention
- Fundraise Your Way
- Create a Memorial Fundraiser
- Pledge to Be StigmaFree
- Awareness Events
- Share Your Story
- Partner with Us
- Advocate for Change
- Policy Priorities
- NAMI Advocacy Actions
- Policy Platform
- Crisis Intervention
- State Fact Sheets
- Public Policy Reports
- Get Involved
Mental Health Awareness Month
May is Mental Health Awareness Month. Since its inception in 1949, Mental Health Awareness Month has been a cornerstone of addressing the challenges faced by millions of Americans living with mental health conditions. Throughout the month, NAMI actively participates in this national movement, dedicated to eradicating stigma, extending support, fostering public education and advocating for policies that prioritize the well-being of individuals and families affected by mental illness.
Take the Moment
Download the toolkit, share on social media, sharing is caring, nami helplines, more ways to get involved this mental health awareness month.
This year, NAMI is celebrating Mental Health Awareness Month with the Take the Moment campaign. We encourage you to join us in fostering open dialogues, cultivating empathy and understanding. We also urge you to share our resources to support individuals and families on their journey towards mental wellness. Through "Take the Moment," we shine a spotlight on NAMI's array of signature programs including: NAMI Basics , NAMI Family-to-Family , NAMI Family & Friends , NAMI Homefront , NAMI In Our Own Voice , NAMI Peer-to-Peer , NAMI Support Groups and our invaluable NAMI HelpLine , which is a free, nationwide peer-support service providing information, resource referrals and support to people living with a mental health condition, their family members and caregivers, mental health providers and the public.
This campaign also champions the importance of destigmatizing mental health by normalizing the practice of taking moments to prioritize mental health care without guilt or shame.
We at NAMI National have created this in order to support NAMI State Organizations, NAMI Affiliates, partners and ambassadors in efforts to promote Mental Health Awareness Month.
Join us, take the moment and let's make a difference together. Download our toolkit for more insights on this campaign, downloadable graphics, and more!
Throughout May, we invite you to share with us on social media why or how you are taking moments to prioritize your mental health. Please use the hashtag #TakeAMentalHealthMoment in your posts.
Also, this page will be updated with more resources and ways to get involved during the months of April and May. You can bookmark this webpage, so you can easily access this information.
To help get you get started, we have provided sample posts and graphics below you can use on social media. Don’t forget to tag us at @NAMICommunicate on Instagram, Threads and X and @NAMI on LinkedIn, TikTok and Facebook.
Sample Captions
Take the Moment: Join NAMI's Mental Health Awareness Month campaign as we spotlight our signature programs! Let's break the stigma together! nami.org/mham #TakeAMentalHealthMoment #MentalHealthMonth
Our mental health journey starts with a single moment. Take it! NAMI's 2024 campaign is here to empower you with resources like NAMI Family-to-Family. Let's prioritize mental well-being together. nami.org/mham #TakeAMentalHealthMoment #MentalHealthMonth
Seeking mental health support? Look no further than NAMI's comprehensive suite of programs! Join us in making a difference today! nami.org/mham #TakeAMentalHealthMoment #MentalHealthMonth
Join us and NAMI this month in normalizing the practice of taking moments to prioritize mental health care without guilt or shame. Programs. nami.org/mham #TakeAMentalHealthMoment #MentalHealthMonth
Share some of our graphics below ( access our full set of graphics here ). Don’t forget to tag us at @NAMICommunicate on Instagram and Twitter and @NAMI on TikTok and Facebook and use our hashtag #TakeAMentalHealthMoment #MentalHealthMonth!

NAMI’s signature programs are where people and communities can find help, hope and healing. We encourage you to share or sign up for these programs if you or someone you know needs mental health support.
- NAMI Basics : A six-session education program for parents, caregivers and other family members who provide care for youth (ages 22 and younger) who are experiencing mental health symptoms.
- NAMI Family-to-Family : A free, eight-session educational program for family, significant others and friends of people with mental health conditions.
- NAMI Family & Friends: A free 90-minute or four-hour seminar that informs people who have loved ones with a mental health condition how to best support them.
- NAMI Homefront : A free, six-session program for families, caregivers and friends of military members and veterans with mental health conditions. Plus, find free online resources available 24/7.
- NAMI In Our Own Voice : Free presentations that provide a personal perspective of mental health conditions, as leaders with lived experience talk openly about what it's like to have a mental health condition.
- NAMI Peer-to-Peer : A free, eight-session educational program for adults with mental health conditions who are looking to better understand themselves and their recovery.
- NAMI Support Groups : NAMI support groups are peer-led and offer participants an opportunity to share their experiences and gain support from other attendees.
In Need of Help or Support?
You are not alone! If you are struggling with your mental health, the NAMI HelpLine is here for you. Connect with a NAMI HelpLine specialist or Teen & Young Adult HelpLine specialist today.
The NAMI HelpLine is a free, nationwide peer-support service providing information, resource referrals and support to people living with a mental health condition, their family members and caregivers, mental health providers and the public.
The NAMI Teen & Young Adult (T&YA) HelpLine offers a direct connection with another young person who shares similar experiences and is prepared to offer information, resources, and support to help you move through difficult times to a better place.
Available Monday Through Friday, 10 A.M. – 10 P.M. ET

Call 1-800-950-NAMI (6264) , text "HelpLine" to 62640 or chat with us at nami.org/help .
Call 1-800-950-NAMI (6264) , text "HelpLine" to 62640 or chat with us at nami.org/talktous .
Need Immediate Help in A Crisis?
988 Suicide & Crisis Lifeline – Dial or text 988 if you or someone you know is having thoughts of suicide or experiencing a mental health crisis and get connected to a trained crisis counselor 24 hours a day, 7 days a week. Crisis counselors listen empathetically and without judgment. Your crisis counselor will work to ensure that you feel safe and help identify options and information about mental health services in your area.
Attend An Event
NAMIWalks : Is more than just a walk—it's a powerful movement for change in mental health. Bringing together individuals, families, and communities, NAMIWalks raises funds, spreads awareness, and fights stigma surrounding mental illness. By participating, you join a nationwide effort to value mental health and promote compassion and understanding for those affected by mental illness.
Partner With Us
Become an advocate : NAMI advocates with elected officials to ensure people get help early, people get the best possible care, and people get diverted from justice system involvement. But, we can’t do this without you. Your voice makes a difference.
Volunteer: Get involved with your local NAMI and make a difference in your community or apply to be a volunteer with our national HelpLine.

Know the warning signs of mental illness

Learn more about common mental health conditions
NAMI HelpLine is available M-F, 10 a.m. – 10 p.m. ET. Call 800-950-6264 , text “helpline” to 62640 , or chat online. In a crisis, call or text 988 (24/7).
Advancing social justice, promoting decent work ILO is a specialized agency of the United Nations

World Day for Safety and Health at Work 2024
As climate change intensifies, workers around the globe find themselves at an increased risk of exposure to hazards such as excessive heat , ultraviolet radiation , extreme weather events , air pollution , vector-borne diseases and agrochemicals .
The time to act is now!
- Press Release: Climate change creates a ‘cocktail’ of serious health hazards for 70 per cent of the world’s workers, ILO report finds

Global debate on climate change and occupational safety and health
Experts, employers, workers and other guests discussed how to address impacts of climate change on occupational safety and health.
- View the recording of the event

Ensuring safety and health at work in a changing climate
- Report at a glance
- Promotional Materials

News and Updates
- Press Conference at the United Nations, Geneva (22 April 2024)

Email: [email protected]

Email: [email protected]
- UN Audiovisual for Professionals
- UN Photo - Digital Asset Management System
- Media Accreditation and Liaison
- Meetings Coverage
- Media Stakeouts
- Press Conferences
Agencies, Funds & Programmes
- Conferences
- Economic and Social Council
- General Assembly
- High Level Events
- Human Rights Council
- Human Rights Treaty Bodies
- International Court of Justice
- Security Council
- Side Events
- Trusteeship Council
- Audiovisual Library of International Law
- Hungry Planet Series (IFAD)
- News Stories
- UN Dag Hammarskjöld Library
- Secretary-General
- Deputy Secretary-General
- Live Schedule
Global Event: Climate change and safety and health…
25 April 2024
Global Event: Climate change and safety and health at work
The ILO will launch its NEW report Ensuring safety and health at work in a changing climate which reveals alarming new data on the impact of climate change on workers' safety and health.
This report will be launched in the context of the commemoration of the World Day for Safety and Health at Work 2024.
As climate change intensifies, workers around the globe find themselves at an increased risk of exposure to hazards such as excessive heat, ultraviolet radiation, extreme weather events, air pollution, vector-borne diseases and agrochemicals. The time to act is now!

IMAGES
VIDEO
COMMENTS
The World Health Assembly is the decision-making body of WHO and is attended by delegations from all Member States. Governance. Accountability and funding. We are committed to the principle of accountability - a core value for an organization that is entrusted by countries and other donors to use limited resources effectively to protect and ...
2014-2016, the World Health Organization (WHO) adopted a plan for research and development (R&D) -this is known as the R&D Blueprint •The R&D Blueprint is a global strategy to enable rapid activation of research during epidemics and fast-track development of diagnostics, vaccines and medicines. •WHO convened the first global COVID-19
65 likes • 50,053 views. S. Suvarta Maru. [email protected]. Education. 1 of 15. Download now. Download to read offline. WORLD HEALTH ORGANIZATION ( WHO ) - Download as a PDF or view online for free.
WHO principles for effective communications. WHO's work is designed to support the adoption of healthy behaviours and the implementation of policies to protect health. Understanding the relevant knowledge level, attitudes, and current behaviors of the target audience increases the success of your communication materials and messages.
Tool 4. Presentation template - 28 April 2021. 28 April 2021. COVID-19: Critical preparedness, readiness and response. Download (3.8 MB) WHO Team. WHO Headquarters (HQ) Reference numbers. WHO Reference Number: WHO-2019-nCoV-Country-IAR-templates-presentation-2021.1.
Presentation of the response by the Ministry of Health. Suggested points to present: Overview of existing capacities prior to the COVID-19 response. Capacities developed for and during the COVID-19 response. Response strategy. Response timeline during the period under review. Be sure to pre load the MOH presentation . World Health Organization ...
In 2005 the World Health Assembly through its resolution WHA58.28 on eHealth urged Member States "to consider drawing up a long-term strategic plan for developing and implementing eHealth services…to develop the infrastructure for information and communication technologies for health…to promote equitable,
The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever ... 2 Thirteenth General Programme of Work 2019-2023: promote health, keep the world safe, serve the vulnerable. Geneva: World Health Organization; 2019 (https://apps.who.int/iris/
The World Health Organization (WHO) is divided into six regions with regional offices, each responsible for addressing health challenges and promoting public health within its designated geographical area. ... By using the Datasets or any presentations of data derived from them, or by using our APIs in connection with the Datasets, you agree to ...
The official public health information Youtube channel of the World Health Organization (WHO) WHO Mission: Providing leadership on global health matters - Shaping the health research agenda ...
21. Future Targets Public Health Area Target Date Global interruption of transmission of poliomyelitis, except Nigeria Interruption of transmission poliomyelitis in Nigeria 2009 Measles Measles Reduce the number of measles deaths worldwide by 90% compared to 2000 level 2010 Immunization Ensure full immunization of children under one year of age, at 90% coverage nationally, with at least 80% ...
WHO (WORLD HEALTH ORGANIZATION) Mar 25, 2019 • Download as PPTX, PDF •. 106 likes • 32,920 views. Saurabh Singh. Follow. World health organization will help you to gain complete knowledge regarding WHO. it is one of the largest and essential international health agency in the world. Read more. Healthcare. 1 of 30.
PK !ñsŠ‚ú _ ppt/presentation.xmlì˜[ ã& Çß+õ;X~6 ߢɬœ™MUiªF›Ù À8$±- Èܪ~÷ ¾ádjÔæ)Äç ‡ Ç`¸ýòv Î á¢dÕÜ 7 ë ª`›²ÚÍÝïOK/u !qµÁ"Udî¾ á~¹ûõ—ÛzVs"H%±T®Ž S‰ ž»{)ë™ï‹bO XÜ°šTʶeü€¥úËwþ†ãW þ@} ± Àeå¶þügüÙv[ ä Çƒê¾ Â 5yˆ}Y‹.Zý3ÑìQŒS {öº®IQbº¢â¯ê©""¬éfî*H ¿ õñY ¹d ...
Overview: Cholera is an acute diarrhoeal infection caused by ingestion of contaminated water or food. It can lead to dehydration, and death in patients with severe forms of the disease. Cholera is an indicator of inequity and lack of social development. Its prevention and control should be multisectoral and well-coordinated integrating ...
Sexual and reproductive health and rights: central to health, well-being and sustainable futures. The United Nations agency working to promote health, keep the world safe and serve the vulnerable.
Introducing our latest weekly covid update by world health organization set of slides. The topics discussed in these slides are Country And Continent, Confirmed Cases, Weekly Increase. This is an immediately available PowerPoint presentation that can be conveniently customized. Download it and convince your audience.
This WHO-Themed Presentation Slides can be used as an excellent alternative for your hospital presentation, encompassing your company profile effectively. It contains 11 slides with the following PowerPoint shapes and themes: Introduction template showing global presence. World health assembly with an image of gathering.
Download Free and Premium World Health Organization PowerPoint Templates. Choose and download World Health Organization PowerPoint templates, and World Health Organization PowerPoint Backgrounds in just a few minutes.And with amazing ease of use, you can transform your "sleep-inducing" PowerPoint presentation into an aggressive, energetic, jaw-dropping presentation in nearly no time at all.
With World Bank Group President Ajay Banga and the Director-General of the World Health Organization Dr. Tedros Adhanom Ghebreyesus. 21:38 Remarks / National Strategies and Initiatives Reflecting on universal healthcare priorities and capacity-building efforts with Mr. Shun'ichi Suzuki, Japan's Minister of Finance.
WHO ppt. 1. AISHWARYA HIREMATH M -PHARM Industrial Pharmacy. 1 Bapuji College Of Pharmacy Davanagere (WHO) 2. 2. 3. The World Health Organization is a specialized agency of United Nations. WHO was established on 7th April 1948. The headquarters of WHO is located in Geneva. WHO serves as the directing and coordinating authority for ...
The forum consisted of 6 case study presentations, 16 governance presentations, and a series of small group and large group discussions. A total of 87 participants attended the forum from 31 countries around the world, representing disciplines of bioethics, AI, health policy, health professional practice, research funding, and bioinformatics.
The World Health Organization is the global coordinating agency for the response to the COVID-19 pandemic. The Organization works with Member States and partners on all aspects of the pandemic response, including facilitating research, developing guidance, coordinating vaccine development and distribution, and monitoring daily case numbers and ...
Join us for the next Texas RCMAR Scholar presentation on April 23, 2024. ... World Health Organization/Pan American Health Organization. Comparative Effectiveness Research on Cancer in Texas. Health of Older Minorities Pre and Postdoctoral Training. Medical Student in Aging Research Program.
Dissemination, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 2476; fax: +41 22 791 4857; email: [email protected]). Requests for permission to reproduce or ... The designations employed and the presentation of the material in this publication do not imply the
The World Bank Group announced an ambitious plan to support countries in delivering quality, affordable health services to 1.5 billion people by 2030. This is part of a larger global effort to provide a basic standard of care through every stage of a person's life - infancy, childhood, adolescence, and adulthood.
May is Mental Health Awareness Month. Since its inception in 1949, Mental Health Awareness Month has been a cornerstone of addressing the challenges faced by millions of Americans living with mental health conditions. Throughout the month, NAMI actively participates in this national movement, dedicated to eradicating stigma, extending support ...
Coronavirus disease (COVID-19) is an infectious disease caused by the SARS-CoV-2 virus. Most people infected with the virus will experience mild to moderate respiratory illness and recover without requiring special treatment. However, some will become seriously ill and require medical attention. Older people and those with underlying medical ...
World Day for Safety and Health at Work 2024. Climate change and safety and health at work. Facebook Twitter Linkedin As climate change ... International Labour Organization. 4 route des Morillons. CH-1211 Geneva 22. Switzerland. Follow us on. Instagram Facebook
Prompted by the life-saving impact of messenger ribonucleic acid (mRNA) vaccines during the COVID-19 pandemic, the World Health Organization's (WHO) Science Council has released a report reviewing the potential benefits and limitations of mRNA vaccine technology. The report conveys the importance of research and development (R&D) efforts to COVID-19 mRNA vaccines and outlines challenges of ...
The ILO will launch its NEW report Ensuring safety and health at work in a changing climate which reveals alarming new data on the impact of climate change on workers' safety and health. This report will be launched in the context of the commemoration of the World Day for Safety and Health at Work 2024.