Excellent Care from the Moment of Birth

Template for Notes and Presentations
Clinical rotations for students.
Although the official medical record is now entirely electronic, students may choose to write admission and follow-up notes on lined progress note paper. Whether notes are done electronically or on paper, it is important that the information is recorded and verbally presented in a logical, coherent manner and that a succinct assessment and plan is provided. Our suggested format for both admit and progress notes is presented on this page.
2/9/08 08:15
MS Admission Note
ID: 12 hour old term newborn
HPI: Baby Boy Brown was born at 39+3 weeks by NSVD to a 27yo G3P1011 mom with prenatal labs O+, Ab screen -, HBsAg-, VDRL non-reactive, GC/CT - , HIV -, PPD+/CXR-. Pregnancy was complicated by PIH, treated with Mag. ROM was 7 hours prior to delivery with clear fluid. Delivery was complicated by tight nuchal cord, cut before delivery. Apgars 3 and 9. Baby received PPV for 30 seconds to improve color and tone.
Baby has been doing well since birth, breastfed x3, stool x 1 and void x 1, VSS. Mom states that feeding are going well, but she complains of sore nipples.
FH: sibling under bili lights for 2 days in newborn nursery, negative for congenital diseases, childhood deaths, or atopic diseases.
SH: intact family, 3 yo sib; has all baby needs including car seat. Plans to receive care at LPCH clinic.
PE: wt - 3578g, length - 49.5cm, OFC - 34cm, temp 36.7 - 37.1, HR 145 - 160, RR 48 - 52
gen - well appearing, NL tone/color/activity, crying with exam
skin - no jaundice, + red macules with central papules scattered on chest and legs
HEENT- normocephalic, + fluctuent area over R parietal bone, does not cross sutures, + RR B eyes, ears NL set/shape, palate intact, tongue WNL
neck - WNL, clavicles intact B
lungs - clear B, - G/F/R
CV - RRR without m, pulses +2 B
abd - soft, non-distended, liver palpable 2 cm below RCM, umbilical stump intact/clamped
genitalia - NL male with testes descended B, anus patent
ext - hips stable B, all WNL
neuro- NL suck, grasp, Moro reflexes, DTRs +2 B
A/P: Term AGA newborn with low first apgar, with erythema toxicum rash and R parietal cephalohematoma. Mom with soreness during feeds.
Expect spontaneous resolution of rash within 1 -2 weeks
Expect spontaneous resolution of cephalohematoma, but follow clinically for jaundice, TBili to be drawn at 24 hours of life with newborn screen.
Discussed with mom expectations for feedings, RN to help with latch technique and position, recommended BF class.
Susan Student, MS 3, pager 19790
CoSignature of MD
MS Progress Note
ID: Term AGA male, DOL #2
S: baby did well O/N, mom reports much less pain with feedings
O: VSS, BF x 11, void x 2, stool x 5 (mec), TB at 26 hours of life - 6.5, algo was passed B
PE: wt - 3408g (down 5% from BW)
gen - well appearing, NL tone/color/activity, awake and alert
skin - mild facial jaundice, + red macules with central papules scattered on chest, abd, and legs
HEENT- normocephalic, + fluctuent area over R parietal bone unchanged from yest, + RR B eyes, ears NL set/shape, palate intact, tongue WNL
abd - soft, non-distended, liver palpable 2 cm below RCM, umbilical stump intact/dried
A/P: Term AGA male, DOL #2, now feeding better, with mild jaundice/cephalohematoma and TBili low int. risk on Bhutani graph.
Follow jaundice clinically, consider repeat TB in am if exam worsening.
Routine care.
- Daily Schedule
- Roles and Responsibilities
- Newborn Exam
- Notes and Presentations

- Gross motor development
- Fine motor development
- Speech and Language
- Social, emotional and behavioural
- Hearing and Vision
- Developmental Delay
- Autism Spectrum Disorder
- Child Protection
- HEADSSS Assessment
- Palliative Care
- Pierre Robin Sequence
- Down Syndrome
- Childhood Eczema
- Diabetic Ketoacidosis
- Hyperthyroidism
- Hypothyroidism
- Adrenal Cortical Insufficiency
- Anaphylaxis
- Approach to the seriously unwell child
- Basic Life Support
- Brief Resolved Unexplained Event (ALTE)
- Febrile Seizures
- Fluid Management
- Paediatric Shock
- Vital Signs and GCS
- Burns assessment
- Supracondylar fracture
- Clavicle fracture
- Cervical fracture
- Bite injuries
- Otitis Externa
- Mastoiditis
- Acute otitis media
- Otitis media with effusion
- Nasal trauma
- Peri-orbital cellulitis
- Foreign Bodies
- Epiglottitis
- Tonsillitis
- Peritonsillar Abscess
- Glandular Fever
- Laryngomalacia
- Gastro-Oesophageal Reflux Disease
- Coeliac Disease
- Cow’s Milk Protein Allergy
- Mesenteric Adenitis
- Gastroenteritis
- Crohns Disease
- Ulcerative Colitis
- Whooping Cough
- Bronchiolitis
- Bronchiectasis
- Cystic Fibrosis
- COVID-19 (coronavirus disease 2019)
- Cardiac Physiology in CHDs
- Foetal vs Adult circulation
- ECG interpretation
- Infective Endocarditis
- Acute Rheumatic Fever
- Patent Ductus Arteriosus
- Atrial Septal Defect
- Tetralogy of Fallot
- Transposition of the Great Arteries
- Ventricular Septal Defect
- Atrioventricular Septal Defects (AVSD)
- Tricuspid atresia
- Total Anomalous Pulmonary Venous Drainage
- Hypoplastic left heart syndrome
- Early onset neonatal sepsis
- Late-Onset Neonatal Sepsis
- Meconium Aspiration Syndrome
- Necrotising Enterocolitis
- Retinopathy of Prematurity
- The preterm infant
- Acute Lymphoblastic Leukaemia
- Acute Myeloid Leukaemia
- Sickle Cell Disease
- Haemophilia
- Ewing Sarcoma
- Nephroblastoma
- Neuroblastoma
- Osteosarcoma
- Primary Brain Tumours
- Oncological Emergencies
- Under construction
- Nephrotic Syndrome
- Kidney Stones
- Urinary Tract Infection
- Acute Appendicitis
- Gastroschisis
- Hirschsprung’s disease
- Inguinal Hernia
- Intussusception
- Omphalocele
- Pyloric stenosis
- Cryptorchidism
- Hypospadias
- Balanitis xerotica obliterans (BXO)
- Testicular torsion
- Epididymitis
- Paraphimosis
- Osteomyelitis
- Septic Arthritis
- Bone tumours
- Open fractures
- Principles of fracture management
- Hydrocephalus
- Intracranial infections
- Peri-operative care
- Cardiovascular Exam
- Respiratory exam
- Abdominal Exam
- Newborn Examination (NIPE)
Neonatology

Found an error? Is our article missing some key information? Make the changes yourself here!
Once you've finished editing, click 'Submit for Review', and your changes will be reviewed by our team before publishing on the site.
We use cookies to improve your experience on our site and to show you relevant advertising. To find out more, read our privacy policy .
Privacy Overview

Australian Journal of General Practice

Advertising
Common neonatal presentations to the primary care physician
Clinical history and examination are the most important tools in neonatal assessment. Babies often present with non-specific symptoms, but a thorough clinical assessment can identify the ‘unwell baby’ who requires immediate transfer to hospital. This includes babies with sepsis, moderate‑to‑severe dehydration or who are in acute cardiorespiratory compromise. A comprehensive neonatal assessment will also help to differentiate babies with significant conditions that may warrant further specialist input from those with normal neonatal development where parental support and reassurance may be sufficient.
This article is the first in a series on paediatric health. Articles in this series aim to provide information about diagnosis and management of presentations in infants, toddlers and pre-schoolers in general practice. Common neonatal (first 28 days of life post-term) 1 presentations to general practitioners (GPs) include fever, respiratory symptoms, feeding difficulties, unsettled babies, vomiting, constipation, jaundice and rashes. This article will discuss these clinical presentations and how to approach them in general practice. Table 1 outlines the general principles for a routine neonatal assessment. These principles can also be applied to babies who present for their first routine immunisations between six and eight weeks of age, to potentially identify rare but significant conditions that parents may not have been aware of.
Fever (rectal temperature >38°C) 2,3 in a newborn baby can be the first indicator of a serious invasive infective illness. Conversely, hypothermia (rectal temperature <36.5°C) 4 can also be a sign of sepsis, as neonates have difficulty regulating temperatures. 5 The health of neonates with sepsis can deteriorate rapidly; therefore, if a fever is detected (gold standard is to take the rectal temperature, but axillary or temporal artery temperature are acceptable), the baby requires immediate referral to the emergency department for a full septic workup, and hospital admission for empirical antibiotics. Ambulance retrieval may be necessary for babies who have associated signs of haemodynamic instability, acute respiratory distress and/or are non-responsive. A full septic workup should include a full blood count and film, blood culture, urine culture (through aseptic suprapubic aspiration), lumbar puncture and, if clinically indicated, a chest X-ray. 3 Where possible, it is recommended that neonates with suspected sepsis be admitted to hospital and treated with intravenous antibiotics; oral antibiotics may lead to only partial treatment and false‑negative culture results. 6
Respiratory symptoms
Respiratory symptoms are common and the majority will be benign. However, it is important not to miss the acutely unwell baby in respiratory distress, as these babies should be transferred to the emergency department via ambulance. 7 Table 2 outlines the signs and causes of acute respiratory distress outside the first 24 hours of life, and other common respiratory presenting concerns and conditions. In neonates, a cough can be due to a common viral upper respiratory tract infection, but it can also be a sign of a more significant pathology. Babies who have a cough and any associated ‘red flag’ signs or symptoms outlined in Table 2 should be referred for further investigation with a paediatrician. Clinical suspicion of pertussis infection warrants referral to the emergency department for laboratory confirmation, antimicrobials and monitoring, as these babies are at greatest risk of complications with apnoea, pneumonia, encephalopathy and death. 8
Neonates are obligatory nose breathers, and nasal congestion with mucus often results in noisy breathing. Normal saline drops or spray may relieve some of the nasal congestion. The most common pathological cause of noisy breathing is laryngomalacia. This developmental anomaly causes stridor through collapse of the supraglottic structures during inspiration. Babies with mild laryngomalacia who are feeding well and thriving can be regularly reviewed in the GP setting. Parents should be advised that stridor may become louder in the first six months of life, but will usually resolve by 12–18 months. Babies who have associated complications (eg poor feeding, gastro-oesophageal reflux [GOR]) should be referred to a respiratory paediatrician or otolaryngologist for further assessment. 9
Parental concerns regarding irregular breathing or pauses in their baby's breathing are also common GP presentations. In the majority of neonates, these irregularities will be due to ‘periodic breathing’, which is a normal developmental phenomenon. Periodic breathing is characterised by alternating cycles of five to 10 seconds of breathing and pauses in breathing. It is not associated with bradycardia or cyanosis. It increases in frequency between two and four weeks of age and resolves by six months of age. 10 Apnoea is defined as pauses in breathing of greater than 20 seconds, or shorter duration if accompanied by cyanosis or bradycardia. 10,11 This is of great concern, and a significant medical cause needs to be excluded. If a medical cause is not evident following clinical assessment, these babies are classified as having had a brief resolved unexplained event (BRUE). BRUE replaces the previous terminology: apparent life threatening event (ALTE). 10 BRUEs can be stratified into low risk and high risk, where low-risk BRUEs generally do not require hospital admission or invasive testing. 12 All neonatal BRUEs are categorised as high risk, given the age of the baby, 12 and should be reviewed by a paediatrician for further investigation. Table 2 summarises common causes of apnoea.
Gastrointestinal symptoms
Small amounts of effortless posseting or physiological GOR are common in babies. In otherwise well babies who are feeding adequately and thriving, parental reassurance that this is most likely to improve in the first year of life is sufficient. General measures, such as holding the baby in the prone position after feeds and thickening agents, may help reduce the vomiting. Acid-suppression agents (ie H2-agonists, proton-pump inhibitors) should be reserved for babies with associated complications, such as inadequate weight gain, oesophagitis or aspiration. 13 There is no clear causal link between GOR and infant irritability, and anti-reflux medication is generally not warranted in these instances. 14 Vomiting as a result of a more serious condition, such as pyloric stenosis, intestinal obstruction, sepsis or neurological cause (eg subdural or intracranial haemorrhage, hydrocephalus), needs to be promptly referred to the emergency department. Red flags for these conditions include projectile vomiting immediately post-feeds (associated with demands to be re-fed soon after), bilious vomiting, acute abdominal distension, fever, lethargy, dehydration or bulging fontanelle.
There is no universally agreed clinical definition of constipation for neonates. They may pass bowel motions several times a day or have more than a week between bowel motions. Formula-fed babies typically produce firmer and less frequent stools than breastfed babies, but unless these are hard and pellet-like, the baby is unlikely to be constipated. 15 Some babies will strain and cry for longer than 10 minutes before passing soft stools. This phenomenon, known as dyschezia, is caused by an inability to coordinate the increase in intra-abdominal pressure with pelvic floor relaxation. 16 It is a functional, self-limiting condition, and is not due to constipation. Caution should be applied and organic pathology excluded before prescribing laxatives in neonates. Clinical history and examination will detect some significant conditions, including:
- Hirschsprung's disease, alerted by a history of delayed meconium passage (after 48 hours of life)
- mechanical bowel obstruction suspected with firm abdominal distension on palpation
- spinal dysraphism leading to autonomic or sphincteric dysfunction.
Cutaneous lesions over the sacrococcygeal region may be indicative of closed spinal dysraphism.
It is also normal for newborn babies to have frequent, loose stools. Babies who have true diarrhoea will produce more watery and more frequent stools than usual. The most common causes of diarrhoea in neonates are viral or bacterial infections or cow’s milk protein allergy (CMPA). Babies with acute infective diarrhoea (gastroenteritis) need to be monitored closely for dehydration. Table 3 outlines the signs of dehydration and other signs of the unwell baby that should prompt early transfer to hospital. Admission to hospital should also be considered for those who are unlikely to maintain adequate oral intake at home. Antimicrobial therapy is rarely warranted in gastroenteritis, as most cases are viral and/or self-limiting.
Unsettled baby
All newborn babies cry. Normal infant crying patterns tend to increase in duration week by week, peaking at around six to eight weeks of age, and receding to lower, stable levels at around four to five months of age. 17,18 The typical presentation is clustered periods of inconsolable crying, some for more than two to three hours in duration, often in the late afternoon and evening. In otherwise well babies, reassurance, support and review in the first few months can be therapeutic tools in their own right. The exclusion of pain or ‘wind’ as the cause of crying will help to reassure parents. Box 1 lists some parental education resources on normal infant development, unsettled babies and breastfeeding. Alternative therapies, such as simethicone, herbal treatment, acupuncture and manipulation techniques, are not supported by the evidence. 19 Advice to change from breastmilk to formula, or to change between formula brands, should be avoided. 20 There is emerging evidence that probiotics may be helpful in settling breastfed babies, but currently there is no universal consensus for this to be a standard recommendation. 21,22
As part of the assessment of an unsettled baby, it is important not to miss a pathological cause. If there is a sudden onset of persistent crying, an acute pathology such as infection, hair tourniquet (ie strangulation of an appendage or digit by a thread-like material, such as hair), corneal abrasion and non-accidental injury should be considered.19 CMPA is a recognised cause for the unsettled baby. Supporting features for CMPA include blood and mucus in the stool, diarrhoea or constipation, inadequate weight gain, eczema, and family history of atopy. A cow’s milk exclusion diet (including mothers if breastfeeding) may be trialled in these babies to confirm the diagnosis. In babies who are formula-fed, a trial of extensively hydrolysed formula and/or amino acid formula will be required. Soy infant formulas are not recommended in infants younger than six months of age. Rice protein-based formulas can be used as a short-term, non-prescription alternative while awaiting specialist review. 23 Referral to a paediatrician or allergy specialist and dietitian is recommended for suspected cases of CMPA to ensure adequate parental education and future dietary management.
Feeding difficulties
Prematurity (gestation <37 weeks) is the most common cause of feeding difficulties in neonates. Their immature physiology can result in discoordination between sucking, swallowing and breathing. 24 Breastfeeding, however, can be a challenging process for any new mother. Support from a maternal child health nurse or lactation consultant can result in positive outcomes for both mothers and their babies. Tongue-tie, or ankyloglossia, has long been linked with difficult breastfeeding and maternal nipple pain. A Cochrane meta-analysis found that frenotomy (surgical release of tongue-tie) reduced maternal nipple pain in the short term, but did not find consistent positive effects on breastfeeding. 25 Maternal nipple pain is, however, a common reason for cessation of breastfeeding and early referral for frenotomy may prevent this. 26
Breastfeeding may not be a viable option for all mothers, and advice regarding infant formula, expressed breast milk, or a mixture of the two should be made available in a supportive and non-judgemental manner. Babies can lose up to 10% of their birthweight in the first week of life, and may take a further two weeks to regain their birthweight. 27,28
It is therefore more important to track the actual weight difference in grams between visits. Following the initial postpartum weight loss, newborns are expected to gain 30–40 grams per day on average. 28 ‘Failure to thrive’ or inadequate weight gain is most commonly a result of inadequate oral intake. If a baby continues to display inadequate weight gain despite increased feed frequency and/or supplementary feeds, referral to a paediatrician for further investigation and management should be made.
Jaundice, or hyperbilirubinaemia, is the result of bilirubin pigment deposition in the skin and mucous membranes. In the majority of cases, jaundice in neonates is due to unconjugated hyperbilirubinaemia. Conjugated hyperbilirubinaemia or ‘cholestatic jaundice’ is always pathological, and detection of this should prompt immediate review with a paediatric gastroenterologist. 29 The following discussion is in relation to unconjugated hyperbilirubinaemia.
Visual assessment of jaundice alone is an unreliable indicator of the degree of hyperbilirubinaemia. Assessment should include detection of any signs of bilirubin toxicity (Table 3), and identification of risk factors, including the following: 30
- prematurity
- jaundice within the first 24 hours
- blood group incompatibility
- cephalohaematoma or other birth-related trauma
- weight loss >10% of birthweight
- previous sibling with hyperbilirubinaemia requiring treatment.
Babies with jaundice and added signs of bilirubin toxicity require immediate referral to hospital. Babies with prolonged jaundice who are otherwise well looking, feeding adequately and with no risk factors are most likely to have physiological jaundice or breastmilk jaundice, and can be managed as outpatients. A bilirubin level (total and fractionated) should be checked with early follow-up for results and clinical review. Bilirubin threshold tables (www.nice.org.uk/guidance/cg98) should be used to determine whether the baby requires treatment with phototherapy or exchange transfusion. 31
In any baby who presents with a vesiculopustular rash, significant causes such as bacterial, viral and fungal infections need to be considered. If a rash is accompanied by systemic signs of being unwell, such as fever, lethargy or poor feeding, then the baby needs to be referred immediately to the emergency department for further assessment. Recent exposure to infectious diseases such as Varicella‑Zoster virus (VZV) or Herpes simplex virus (HSV), should also alert the physician to the possibility of an invasive infective disease.
Common benign rashes that may present in the newborn include erythema toxicum and milia. Erythema toxicum is a benign, self-limiting skin condition categorised by small erythematous papules, vesicles and pustules. It affects 30–70% of newborns, typically within the first two weeks of birth. 32 Erythema toxicum can be differentiated from an infective rash by its tendency to wax and wane over several days. It is also unusual for an individual erythema toxicum lesion to persist for more than one day. If the infant is otherwise well, no investigation or treatment is required, but recommendation for review should be made if the rash does not resolve after one to two weeks. Milia, which are a result of blocked pores, typically present as tiny, white cysts on the face in about 40–50% of newborns. 33 Most lesions resolve after one to two months. Parents should be reassured and advised to not squeeze or pick them as this may result in infection or scarring.
Neonatal assessment can be challenging because of the non-specific nature of presenting signs and symptoms. A thorough clinical assessment, including relevant maternal medical, antenatal, peripartum and postpartum histories, with a systematic physical examination, is the most important tool in the primary clinic setting.

Did you know you can now log your CPD with a click of a button?
- World Health Organization. Health topics: Infant, newborn. Geneva: WHO, 2017. Available at www.who.int/topics/infant_newborn/en [Accessed 24 Nov 2017]. Search PubMed
- Hui C, Neto G, Tsertsvadze A, et al. Diagnosis and management of febrile infants (0–3 months). Evid Report Technol Assess (Full Rep) 2012;(205):1–297. Search PubMed
- The Royal Children's Hospital. Clinical practice guidelines: Febrile child. Melbourne: RCH, 2011. Available at www.rch.org.au/clinicalguide/guideline_index/Febrile_child [Accessed 24 Nov 2017]. Search PubMed
- World Health Organization. Thermal protection of the newborn: A practical guide. Geneva: WHO, 1997. Search PubMed
- Hofer N, Müller W, Resch B. Neonates presenting with temperature symptoms: Role in the diagnosis of early onset sepsis. Pediatr Int 2012;54(4):486–90. Search PubMed
- Zea-Vera A, Ochoa TJ. Challenges in the diagnosis and management of neonatal sepsis. J Trop Pediatr 2015;61(1):1–13. Search PubMed
- Edwards MO, Kotecha SJ, Kotecha S. Respiratory distress of the term newborn infant. Paediatr Respir Rev 2013;14(1):29–36. Search PubMed
- Winter K, Zipprich J, Harriman K, et al. Risk factors associated with infant deaths from pertussis: A case-control study. Clin Infect Dis 2015;61(7):1099–106. Search PubMed
- Carter J, Rahbar R, Brigger M, et al. International Pediatric ORL Group (IPOG) laryngomalacia consensus recommendations. Int J Pediatr Otorhinolaryngol 2016;86:256–61. Search PubMed
- Patrinos ME, Martin RJ. Apnea in the term infant. Semin Fetal Neonatal Med 2017;22(4):240–44. Search PubMed
- Kondamudi NP, Wilt AS. Apnea, Infant. StatPearls. Treasure Island, FL: StatPearls Publishing, 2017. Search PubMed
- Tieder JS, Bonkowsky JL, Etzel RA, et al. Brief resolved unexplained events (formerly apparent life-threatening events) and evaluation of lower-risk infants. Pediatrics 2016;137(5). Search PubMed
- The Royal Children's Hospital. Clinical practice guidelines: Gastroesophageal reflux in infants. Melbourne: RCH, 2017. Available at www.rch.org.au/clinicalguide/guideline_index/gastrooesophageal_reflux_in_infants [Accessed 24 Nov 2017]. Search PubMed
- Heine RG, Jaquiery A, Lubitz L, Cameron DJ, Catto-Smith AG. Role of gastro-oesophageal reflux in infant irritability. Arch Dis Child 1995;73(2):121–25. Search PubMed
- den Hertog J, van Leengoed E, Kolk F, et al. The defecation pattern of healthy term infants up to the age of 3 months. Arch Dis Child Fetal Neonatal Ed 2012;97(6):F465–70. Search PubMed
- Kramer EA, den Hertog-Kuijl JH, van den Broek LM, et al. Defecation patterns in infants: A prospective cohort study. Arch Dis Child 2015;100(6):533–36. Search PubMed
- Barr RG. Crying behaviour and its importance for psychosocial development in children. Montreal, Quebec: Encyclopedia on Early Childhood Development, 2006. Available at www.child-encyclopediacom/crying-behaviour/according-experts/crying-behaviour-and-its-importance-psychosocial-development [Accessed 14 July 2017]. Search PubMed
- Hiscock H, Jordan B. Problem crying in infancy. Med J Aust 2004;181(9):507–12. Search PubMed
- Halpern R, Coelho R. Excessive crying in infants. J Pediatr (Rio J) 2016;92(3 Suppl 1):S40–45. Search PubMed
- Akhnikh S, Engelberts AC, van Sleuwen BE, L'Hoir MP, Benninga MA. The excessively crying infant: Etiology and treatment. Pediatr Ann 2014;43(4):e69–75. Search PubMed
- Harb T, Matsuyama M, David M, Hill RJ. Infant colic – What works: A systematic review of interventions for breast-fed infants. J Pediatr Gastroenterol Nutr 2016;62(5):668–86. Search PubMed
- Xu M, Wang J, Wang N, Sun F, Wang L, Liu XH. The efficacy and safety of the probiotic bacterium lactobacillus reuteri DSM 17938 for infantile colic: A meta-analysis of randomized controlled trials. PLoS One 2015;10(10):e0141445. Search PubMed
- Australasian Society of Clinical Immunology and Allergy. Food allergy clinical update for health professionals. Perth: ASCIA, 2017. Available at www.allergy.org.au/images/stories/pospapers/ASCIA_HP_Clinical_Update_Food_Allergy_2017_HP_version.pdf [Accessed 1 November 2017]. Search PubMed
- Rommel N, De Meyer AM, Feenstra L, Veereman-Wauters G. The complexity of feeding problems in 700 infants and young children presenting to a tertiary care institution. J Pediatr Gastroenterol Nutr 2003;37(1):75–84. Search PubMed
- O'Shea JE, Foster JP, O'Donnell CP, et al. Frenotomy for tongue-tie in newborn infants. Cochrane Database Syst Rev 2017;3:CD011065. Search PubMed
neonates ongoing medical education paediatrics
Open Access is an initiative that aims to make scientific research freely available to all. To date our community has made over 100 million downloads. It’s based on principles of collaboration, unobstructed discovery, and, most importantly, scientific progression. As PhD students, we found it difficult to access the research we needed, so we decided to create a new Open Access publisher that levels the playing field for scientists across the world. How? By making research easy to access, and puts the academic needs of the researchers before the business interests of publishers.
We are a community of more than 103,000 authors and editors from 3,291 institutions spanning 160 countries, including Nobel Prize winners and some of the world’s most-cited researchers. Publishing on IntechOpen allows authors to earn citations and find new collaborators, meaning more people see your work not only from your own field of study, but from other related fields too.
Brief introduction to this section that descibes Open Access especially from an IntechOpen perspective
Want to get in touch? Contact our London head office or media team here
Our team is growing all the time, so we’re always on the lookout for smart people who want to help us reshape the world of scientific publishing.
Home > Books > Neonatology
Selected Topics in Neonatal Care

Book metrics overview
19,781 Chapter Downloads
Impact of this book and its chapters
Total Chapter Downloads on intechopen.com
Total Chapter Views on intechopen.com
Overall attention for this book and its chapters
Book Citations
Total Chapter Citations
Academic Editor
Austral University of Chile , Chile
Published 27 June 2018
Doi 10.5772/65564
ISBN 978-1-78923-363-6
Print ISBN 978-1-78923-362-9
eBook (PDF) ISBN 978-1-83881-248-5
Copyright year 2018
Number of pages 248
Neonatology is one of the areas of greatest development and evolution within pediatrics. The technoscientific advances in this area have led to an increase in the survival of premature infants who sometimes require sophisticated care. However, there is essential care that must be included in all centers that care for high-risk babies. This book includes important topics related to neonatal care gr...
Neonatology is one of the areas of greatest development and evolution within pediatrics. The technoscientific advances in this area have led to an increase in the survival of premature infants who sometimes require sophisticated care. However, there is essential care that must be included in all centers that care for high-risk babies. This book includes important topics related to neonatal care grouped into four sections. In 14 chapters that address relevant issues about neonatal care, the book seeks to contribute to the clinical work of the health teams of neonatal units. Specialists in the field of neonatology from different countries have developed these chapters and through them they hope to share part of their experience.
By submitting the form you agree to IntechOpen using your personal information in order to fulfil your library recommendation. In line with our privacy policy we won’t share your details with any third parties and will discard any personal information provided immediately after the recommended institution details are received. For further information on how we protect and process your personal information, please refer to our privacy policy .
Cite this book
There are two ways to cite this book:
Edited Volume and chapters are indexed in
Table of contents.
By R. Mauricio Barría
By Teja Škodič Zakšek, Anita Jug Došler, Ana Polona Mivšek and Petra Petročnik
By Petja Fister and Štefan Grosek
By Štefan Grosek and Petja Fister
By Adauto Dutra Moraes Barbosa, Israel Figueiredo Júnior and Gláucia Macedo de Lima
By Selim Öncel
By Lidia Decembrino, Nunzia Decembrino and Mauro Stronati
By Rejane P. Neves, Ana Maria R. de Carvalho Parahym, Carolina M. da Silva, Danielle P.C. Macêdo, André F.G. Leal, Henrique J. Neves and Reginaldo G. Lima-Neto
By Esra Caliskan
By Carlos Baeza Herrera, Alin Villalobos Castillejos and Ricardo Cortés García
By Kriengkrai Srithanaviboonchai
By Koichi Miyake, Noriko Miyake and Takashi Shimada
By Maria Slomczynska, Malgorzata Grzesiak and Katarzyna Knapczyk- Stwora
By Hippolite O. Amadi and Mohammed B. Kawuwa
IMPACT OF THIS BOOK AND ITS CHAPTERS
19,781 Total Chapter Downloads
3,775 Total Chapter Views
10 Crossref Citations
4 Web of Science Citations
19 Dimensions Citations
3 Altmetric Score
Order a print copy of this book
Available on

Delivered by
£119 (ex. VAT)*
Hardcover | Printed Full Colour
FREE SHIPPING WORLDWIDE
* Residents of European Union countries need to add a Book Value-Added Tax Rate based on their country of residence. Institutions and companies, registered as VAT taxable entities in their own EU member state, will not pay VAT by providing IntechOpen with their VAT registration number. This is made possible by the EU reverse charge method.
As an IntechOpen contributor, you can buy this book for an Exclusive Author price with discounts from 30% to 50% on retail price.
Log in to your Author Panel to purchase a book at the discounted price.
For any assistance during ordering process, contact us at [email protected]
Related books
Update on critical issues on infant and neonatal care.
Edited by René Mauricio Barría
Topics on Critical Issues in Neonatal Care
Cohort studies in health sciences, selected topics in breastfeeding, neonatal bacterial infection.
Edited by Bernhard Resch
Neonatal Medicine
Edited by Antonina Chubarova
Pediatric and Neonatal Surgery
Edited by Joanne Baerg
Neonatal Care
Edited by Zoe Iliodromiti
Infant Feeding
Edited by Isam Jaber Al-Zwaini
Selected Topics on Infant Feeding
Call for authors, submit your work to intechopen.

- Second Opinion
The Neonatal Intensive Care Unit (NICU)
The birth of a baby is a wonderful and very complex process. Many physical and emotional changes occur for both mother and baby.
A baby must make many physical adjustments to life outside the mother's body. Leaving the uterus means that a baby can no longer depend on the mother's blood supply and placenta for important body functions.

Before birth, the baby depends on functions from the mother. These include breathing, eating, elimination of waste, and immune protection. When a baby leaves the womb, its body systems must change. For example:
The lungs must breathe air.
The cardiac and pulmonary circulation changes.
The digestive system must begin to process food and excrete waste.
The kidneys must begin working to balance fluids and chemicals in the body and excrete waste.
The liver and immune systems must begin working on their own.
Your baby's body systems must work together in a new way. In some cases, a baby has trouble making the transition outside the womb. Preterm birth, a difficult birth, or birth defects can make these changes more challenging. But a lot of special care is available to help newborn babies.
What is the neonatal intensive care unit (NICU)?
Newborn babies who need intensive medical care are often put in a special area of the hospital called the neonatal intensive care unit (NICU). The NICU has advanced technology and trained healthcare professionals to give special care for the tiniest patients. NICUs may also care areas for babies who are not as sick but do need specialized nursing care. Some hospitals don’t have the staff for a NICU and babies must be moved to another hospital. Babies who need intensive care do better if they are born in a hospital with a NICU than if they are moved after birth.
Some newborn babies will require care in a NICU. Giving birth to a sick or premature baby can be unexpected for any parent. The NICU can be overwhelming. This information is to help you understand why a baby may need to be in the NICU. You will also find out about some of the procedures that may be needed for the care of your baby.
Which babies need special care?
Most babies admitted to the NICU are preterm (born before 37 weeks of pregnancy), have low birth weight (less than 5.5 pounds), or have a health condition that needs special care. In the U.S., nearly half a million babies are born preterm. Many of these babies also have low birth weights. Twins, triplets, and other multiples often are admitted to the NICU. This is because they tend to be born earlier and smaller than single birth babies. Babies with health conditions such as breathing trouble, heart problems, infections, or birth defects are also cared for in the NICU.
Below are some factors that can place a baby at high risk and increase the chances of being admitted to the NICU. But each baby must be assessed to see if he or she needs the NICU. High-risk factors include the below.
Maternal factors include:
Being younger than age 16 or older than age 40
Drug or alcohol use
High blood pressure (hypertension)
Sexually transmitted diseases
Multiple pregnancy (twins, triplets, or more)
Too little or too much amniotic fluid
Premature rupture of membranes (also called the amniotic sac or bag of waters)
Delivery factors include:
Changes in a baby’s organ systems due to lack of oxygen (fetal distress or birth asphyxia)
Buttocks delivered first (breech birth) or other abnormal position
The baby's first stool (meconium) passed during pregnancy into the amniotic fluid
Umbilical cord wrapped around the baby's neck (nuchal cord)
Forceps or cesarean delivery
Baby factors include:
Baby born at gestational age of less than 37 weeks or more than 42 weeks
Birth weight less than 5 pounds, 8 ounces (2,500 grams) or over 8 pounds, 13 ounces (4,000 grams)
Small for gestational age
Medicine or resuscitation in the delivery room
Birth defects
Respiratory distress including rapid breathing, grunting, or stopping breathing (apnea)
Infection such as herpes, group B streptococcus, chlamydia
Low blood sugar (hypoglycemia)
Need for extra oxygen or monitoring, IV (intravenous) therapy, or medicines
Need for special treatment or procedures such as a blood transfusion
Who will care for your baby in the NICU?
Some of the specially-trained healthcare providers who may care for your baby include:
Neonatologist. This is a pediatrician with extra training in the care of sick and premature babies. The neonatologist (often called the attending physician) supervises pediatric fellows and residents, nurse practitioners, and nurses who care for babies in the NICU.
Neonatal fellow. This is a pediatrician getting extra training in the care of sick and premature babies. He or she may do procedures and direct your child's care.
Pediatric resident. This is a doctor who is getting extra training in the care of children. He or she may do or assist in procedures and help direct your child's care.
Neonatal nurse practitioner. This is a registered nurse with extra training in the care of newborn babies. He or she can do procedures and help direct your child's care.
Respiratory therapist. This is a person with special training in giving respiratory support. This includes managing breathing machines and oxygen.
Physical, occupational, and speech therapists. These types of therapists make sure a baby is developing well. They also help with care including positioning and soothing methods. Speech therapists help babies learn to eat by mouth.
Dietitians. Dietitians ensure the babies are growing well and getting good nutrition. They watch your baby's intake of calories, protein, vitamins, and minerals.
Lactation consultants. These are healthcare providers with extra training and certification in helping women and babies breastfeed. They can help with pumping, maintaining milk supply, and starting and continuing breastfeeding.
Pharmacists. Pharmacists help in the NICU by assisting the care providers choose the best medicines. They check medicine doses and levels. They keep the team aware of possible side effects and monitoring that may be needed.
Social workers. Social workers help families cope with many things when a child is ill. They give emotional support. They help families get information from healthcare providers. They support the family with other more basic care needs, too. These can include money problems, transportation, or arranging home healthcare.
Hospital chaplain. The hospital chaplain may be a priest, minister, lay pastor, or other religious advisor. The chaplain can give spiritual support and counseling to help families cope with the stress of the NICU.
NICU team members work together with parents to create a plan of care for high-risk newborns. Ask about the NICU's parent support groups and other programs designed to help parents.

Supporing each delivery with nurturing care and outstanding comfort
Related links.
- Neonatology Care
- Neonatal Intensive Care Unit
- Parent Support
- Road to Home
- Pediatric Cardiology
- Our Services
- Chiari Malformation Center at Stanford Medicine Children's Health
Related Topics
Developmental Care for Babies in the NICU
Equipment That Is Used in the NICU
Intravenous (IV) Line and Tubes
Connect with us:
Download our App:
- Leadership Team
- Vision, Mission & Values
- The Stanford Advantage
- Government and Community Relations
- Get Involved
- Volunteer Services
- Auxiliaries & Affiliates
© 123 Stanford Medicine Children’s Health
- Search Menu
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Urban Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Archaeology
- Greek and Roman Papyrology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Agriculture
- History of Education
- History of Emotions
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Acquisition
- Language Variation
- Language Families
- Language Evolution
- Language Reference
- Lexicography
- Linguistic Theories
- Linguistic Typology
- Linguistic Anthropology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Modernism)
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Religion
- Music and Culture
- Music and Media
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Science
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Lifestyle, Home, and Garden
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Oncology
- Medical Toxicology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Clinical Neuroscience
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Medical Ethics
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Neuroscience
- Cognitive Psychology
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Strategy
- Business History
- Business Ethics
- Business and Government
- Business and Technology
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic Systems
- Economic Methodology
- Economic History
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Theory
- Political Behaviour
- Political Economy
- Political Institutions
- Politics and Law
- Public Administration
- Public Policy
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Developmental and Physical Disabilities Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

- < Previous
- Next chapter >
1 Common Neonatal Presentations
- Published: October 2020
- Cite Icon Cite
- Permissions Icon Permissions
Parents of newborns, particularly first-time parents, are often concerned that their infant has a physical examination finding or behavior that is out of range of normal. Neonates have a variety of common findings and diagnoses specific to this age group. However, their range of behaviors is limited, and they are unable to communicate, complicating evaluation. Caring for neonates in the emergency department requires knowledge of newborn-specific conditions as well as the range of normal behaviors. Common chief complaints include jaundice, feeding difficulties, vomiting, irritability and crying, breathing difficulty, and rash. Emergency department providers must be familiar with the range of normal behaviors and common diagnoses seen in neonates. This chapter presents an overview of common concerns parents have about their neonates.
Introduction
Caring for neonates in the emergency department (ED) requires knowledge of newborn-specific conditions as well as the range of normal behaviors. Common chief complaints include jaundice, feeding difficulties, vomiting, irritability and crying, breathing difficulty, and rash. Fewer than one-third are admitted, with the most common diagnoses being jaundice, fever, vomiting, and respiratory infections.
Birth and perinatal history are key data when evaluating neonates. Practitioners should ask about gestational age; vaginal versus cesarean birth; birth weight; prenatal, birth, and postnatal complications; and age at discharge (often 48 hours if no complications). The newborn’s clothes must be removed to adequately examine for findings such as increased work of breathing, bruises and sentinel injuries of non-accidental trauma, and umbilical cord abnormalities. In addition, while addressing the parents’ specific concern, the ED provider should also assess common areas of concern, such as feeding, stooling, sleeping, breathing patterns, and umbilical cord issues. If possible, neonates should be isolated from other ED patients with potential infections, particularly respiratory infections.
Parents are commonly concerned about a behavior or physical finding in the newborn. New parents may be wondering if the finding is “normal,” and even experienced parents may be worried if their newborn differs from older siblings.
Feeding, Growth, and Stooling Patterns
Assess growth by comparing current weight to birth weight. Neonates initially lose 5–10% of their birth weight, and they typically regain birth weight by age 10–14 days. Once birth weight is regained, neonates are expected to gain a minimum of 30 g/day.
A feeding history should include breast versus bottle versus mixed, any difficulties encountered, how the parent is mixing powdered or concentrated formula if used, frequency and amount (minutes per side for breastfeeding and ounces for bottle feeding) of feeds, and total feeds in a 24-hour period. Most newborns feed every 2 or 3 hours, or 8–12 times in a 24-hour period—10 minutes per side for breastfed infants and 1 or 2 oz for bottle-fed infants, increasing to 2 or 3 oz by age 2 weeks. Adequacy of feeding can also be assessed by quantifying the number of wet diapers (for urine) in a 24-hour period. A history of delayed time to passage of first meconium stool after birth, particularly >48 hours, raises concerns for Hirschsprung disease.
Breastfeeding infants initially feed colostrum; the milk “comes in” at approximately 3 or 4 days of life. Early on, infants may not completely empty the mother’s breast, causing engorgement. The rapid letdown of engorged breasts can cause infants to sputter and choke at the initiation of feeds. If this is occurring, mothers can be instructed to allow the rapid letdown to flow into a container or cloth and then put the infant back on to breastfeed.
Formula-fed infants can be given ready-to-feed formula without any mixing required, but it is expensive. Liquid concentrated formula is mixed with 1 oz of formula concentrate to 1 oz of water. The most commonly used form is powdered formula, which is mixed one scoop formula to 2 oz of water (must use the scoop that comes with the can of formula). Sometimes parents are mixing the formula incorrectly, often overdiluting because of perceived constipation or to save money, which may result in electrolyte abnormalities.
Assess outputs such as spit up, urine, and stools. Overfed neonates (>3 or 4 oz at a time) may spit up. A small amount of spit up, often with burping, is common and normal. Adequately fed neonates should have five or six wet (urine) diapers per day (although they may have only two or three in the first few days of life). Initially, neonates have thick, dark green–black meconium stools. By day of life 2–4, the stools start to transition. Breastfed infants’ stools are yellow, seedy, and runny, and breastfed infants often stool six or more times a day, sometimes after every feed. Parents may mistake this normal stool pattern for diarrhea. Formula-fed infants’ stools are pastier, yellow to tan, less frequent, and become more malodorous. Stool frequency usually lessens as neonates age, to a mean of four per day by 1 month of age and sometimes as infrequent as one per week in the second month of life.
Treatment and Disposition
Any neonate not back to birth weight by 14 days of age, or not gaining 30 g/day after that, should be followed up closely (1 or 2 days) with the pediatrician. If weight gain is extremely abnormal, such as well below birth weight at 14 days of age, gaining <30 g/day, or losing weight, admit the patient for further evaluation and monitoring. Further workup and possible admission are warranted if there have been no wet diapers for 8 hours. If the neonate is feeding well, not vomiting excessively, has a benign abdominal examination without distension, and has normal vital signs, reassurance and close follow-up with the pediatrician are all that is generally needed for concerns about stool frequency.
Neonates sleep the majority of the day but wake frequently to feed, resulting in parental exhaustion despite the total amount of time newborns spend sleeping. Recommended sleep duration for infants aged 0–3 months is 14–17 hours per day (range, 11–19 hours). Initially, neonates often have day–night reversal, where they sleep more in the daytime and are awake at night, which can also be challenging for parents.
Reassurance and education regarding sleeping norms are generally all that are needed. Assess support for the primary caregiver, such as spouse, grandparent, other relative, or even hired aides, to reduce parental frustration and exhaustion from lack of sleep. Sometimes parents’ concerns are the opposite—their infant is sleeping too much. Newborns not waking for feeds can be stimulated through diaper changes, undressing and re-dressing, gentle rubbing, and baby “exercises” such as bicycling the legs or lifting the arms. Parents can slowly change day–night reversal by working to keep the infant awake during the day. Parents should be told to place the infant to sleep on their back and to avoid co-sleeping or placement of fluffy items such as blankets, thick bumpers, or stuffed animals in the sleeping area because these are important measures to reduce sudden infant death syndrome (see Chapter 4 ).
Crying and Colic
Crying is normal in newborns; it is a primary method of communication. The median number of hours per day spent crying at age 2 weeks is 1.75 hours, and this usually increases to a peak of 2.75 hours at age 6–8 weeks and then slowly declines by age 3 or 4 months. Crying tends to be most frequent in the late afternoon and evening hours. There is considerable variation in frequency, duration, and character of crying bouts from infant to infant, and parents may be concerned because a newborn’s crying bouts are different from those of an older sibling when the sibling was a newborn.
Colic is excessive crying beyond the standard and is classically described by Wessel’s rule of threes: crying for more than 3 hours per day, more than 3 days per week, with these episodes occurring for more than 3 weeks. Approximately 10–20% of infants are “colicky” by this definition. Similar to normal crying, colic tends to begin at 3 or 4 weeks of age, peak at 6–8 weeks of age, and improve by 3 or 4 months of age. Parents often think their child has gas pains or another cause of pain. Some breastfeeding mothers alter their own diet and parents who formula feed their infants change formula types and brands in an effort to reduce colic. These treatments, however, have not been shown to be uniformly helpful.
Pathologic crying must be excluded before diagnosing colic. A thorough history and physical examination should be performed to rule out treatable causes of crying, such as otitis media; ocular foreign body; glaucoma; frenulum tear (which is a sentinel injury for child abuse in a nonmobile child); oral thrush; acute abdomen; hair tourniquet on a digit or penis or, very rarely, clitoris; testicular torsion; incarcerated inguinal hernia; anal fissure; trauma and fracture; neonatal drug withdrawal; hydrocephalus; meningitis; and rash. Corneal abrasions have classically been taught as a potential cause of excessive crying, although Shope et al. found that 49% of asymptomatic infants seen at well-child visits had corneal abrasions. Fluorescein examination should be reserved for infants with corroborating signs, such as conjunctival injection or apparent eye pain, or as part of the workup of the inconsolable infant.
If the infant is still feeding and growing well, has a normal physical examination and no concerning historical factors, and is either consoled by the motion of the ride to the ED, as commonly happens, or is consolable in the ED, reassurance and education are all that is needed. Assess for support and availability of other caretakers to help the parent(s). Parents can be taught Dr. Harvey Karp’s “5 S’s” for soothing colicky infants: swaddling, side or stomach positioning (with the caveat that infants should sleep or be left alone in the crib only on their backs), shushing noises (or white noise), swinging and other motion (car ride, baby swing, walk in stroller, rocking, or carried by parent), and suck (on a pacifier or parent’s clean pinky finger). Parents should be warned to never shake the infant and instructed that if they become very frustrated, they should either place the crying infant in a safe place such as a crib or hand the infant off to another caretaker. They can be reassured that a period of crying will not be harmful to the newborn. Medications such as simethicone or anticholinergics and herbal remedies such as chamomile tea have not shown efficacy and should not be recommended by ED providers. Similarly, changes in maternal diet or formula type or brand should be left to the primary care provider.
If the infant is not consolable in the ED, perform an initial abbreviated workup such as fluorescein examination and urine to rule out infection and for toxicologic screen, and observe the infant while continuing attempts to console through the 5 S’s, feeding, burping, and changing the diaper. If the infant remains inconsolable despite a period of observation and attempts to console, consider expanding the workup to include laboratory tests, blood culture, lumbar puncture, electrocardiogram (ECG), abdominal ultrasound, and skeletal survey. In addition, consider head computed tomography and admitting the patient for empiric antibiotics for possible sepsis. It is extremely rare to get to this step, however.
Head Bumps and Bald Spots
The newborn’s soft, flexible skull and lack of fused sutures allow for molding with gravitational pressure. In addition to open sutures, the anterior fontanelle is widely patent and does not close until 18–24 months of age, and the posterior fontanelle is also patent, closing in the first few months of life or as late as 12–24 months.
Deformational plagiocephaly, an abnormally shaped head due to pressure forces on the skull, may be birth related (i.e., from the birth canal or from forceps) or related to sleep positioning, particularly due to the campaign to encourage sleeping supine only. Excessive supine positioning, particularly in combination with torticollis leading to a fixed neck position, can lead to flattening of the occiput and/or a bald spot in that area.
Several birth-related head swellings may not be noticed by parents until after nursery discharge. Caput succedaneum is a soft subdermal or subcutaneous edema that can cross midline and suture lines, occurring due to pressure applied to the head during vaginal birth and/or from vacuum extraction. There may be overlying skin discoloration with erythema or even petechiae. Caput succedaneum usually self-resolves during the first week of life.
Cephalohematoma is a collection of blood from ruptured subperiosteal veins that occurs in 1% or 2% of newborns, particularly those delivered using vacuum or forceps. It is usually unilateral, more discrete than caput succedaneum, and does not cross midline nor suture lines. Due to slow accumulation of blood, size peaks in the middle of the first week of life. The hematoma then organizes and becomes firmer, and it is slowly resorbed during the first 1 or 2 months of life. Rarely, cephalohematomas can become infected, most commonly with Escherichia coli . Suspect infected cephalohematoma if a previously stable hematoma is enlarging and/or the infant is ill-appearing or febrile.
Subgaleal hemorrhage, also more common in vacuum-assisted deliveries, collects between the galea aponeurotica and the periosteum of the skull. This is a large potential space, and bleeding significant enough to cause anemia and even shock can occur. Suspect subgaleal hemorrhage when there is a large fluctuance ballooning out the scalp that is easily moved to other parts of the head as in a fluid wave, signs of anemia, or a rapid increase in head circumference in the first 24–48 hours. Hematocrit should be checked and followed.
If the timeline fits one of the previously discussed diagnoses and the patient is hemodynamically stable, neurologically normal, and does not have a rapidly growing head circumference, reassurance and close follow-up with the primary care provider are all that is needed. Imaging is not indicated unless there is a suspicion for infected cephalohematoma, hydrocephalus, or non-accidental trauma or a new swelling developing several days beyond birth. Differential diagnosis of a new enlarging swelling includes growing skull fracture, or leptomeningeal cyst, a rare complication of a previously unrecognized skull fracture. Infants with infected cephalohematomas require a complete sepsis workup and admission for empiric broad-spectrum antibiotics. Consult a neurosurgeon for neonates with subgaleal hemorrhage who are not hemodynamically stable. Counsel parents of infants with deformational plagiocephaly to place their infant in supervised “tummy time” prone positioning while awake and to alternate which end of the crib the infant’s head is in to encourage variation in head positioning.
Eye Discharge
Neonatal conjunctivitis can have several causes, which are differentiated by time of onset and physical examination findings.
Chemical conjunctivitis is less common now that silver nitrate is not used in the United States for ocular prophylaxis after birth. However, silver nitrate is more effective for gonorrhea prophylaxis than the erythromycin ointment recommended in the United States, and silver nitrate may be used in areas with high rates of gonorrhea. The trade-off is that silver nitrate is ineffective against chlamydia. Silver nitrate-induced chemical conjunctivitis starts a few hours after application of the drops and lasts for 24–36 hours, presenting as conjunctival injection and watery eye discharge/tearing.
Gonococcal conjunctivitis carries the most morbidity of the various causes of neonatal conjunctivitis. It typically presents in the first week of life, often within 48 hours of birth. In addition to conjunctival injection, there can be erythema and edema of the eyelids and chemosis. There is typically profuse purulent discharge.
Chlamydial conjunctivitis presents in the second week of life (5–14 days) up to 1 month of age as either unilateral or bilateral conjunctival injection, sometimes with eyelid edema, pseudomembrane formation, or papillary conjunctival involvement. Discharge is initially watery, unlike gonococcal conjunctivitis, but becomes more mucopurulent over time. Chlamydia pneumonitis concomitantly occurs in up to half of infected neonates.
Herpes simplex virus (HSV) conjunctivitis presents at age 6–14 days with conjunctival injection and sometimes eyelid redness and swelling. Discharge is watery. Vesicles may be present around the eye. There may be no known history of maternal HSV. Perform a fluorescein examination to look for dendritic lesions.
Bacterial conjunctivitis caused by a multitude of other bacteria, such as Staphylococcus species, Streptococcus pneumonia , or Moraxella catarrhalis , is more frequent than the previously mentioned causes.
Nasolacrimal duct stenosis is a common disorder affecting up to 20% of newborns. Initial presentation is in the first weeks to months of life with excessive tearing, particularly in the medial canthal area. If the child has a viral upper respiratory infection, the discharge can become mucoid and more evident. If the eye becomes superinfected, there may be purulent discharge.
Dacrocystitis (Figure 1.1 ), an infection of the nasolacrimal system, is a rare serious complication of nasolacrimal duct stenosis. Infants present with acute-onset redness, swelling, tenderness, and fluctuance around the medial canthal area, sometimes with purulent discharge. Infants may be febrile, and the infection can progress to periorbital or orbital cellulitis. Mean age of onset is in the first 1–3 weeks of life. Diagnosis is clinical, and the infecting organism is confirmed through bacterial culture of purulent discharge (expressed if necessary).

Dacrocystitis.
Confirmatory testing (culture and polymerase chain reaction) should be performed for all suspected infectious causes of conjunctivitis.
If gonococcal conjunctivitis is suspected, the infant should be admitted for intravenous (IV) antibiotics and frequent ocular lavage with normal saline. Intramuscular 50 mg/kg of ceftriaxone may be considered if IV access is difficult. Similarly, if HSV is suspected, infants should undergo testing of other sites (oral, nasopharyngeal, rectal swabs, and lumbar puncture) and be admitted for IV acyclovir. For the rare case of dacryocystitis, patients should be admitted for broad-spectrum IV antibiotics. All three of these suspected diagnoses warrant emergent consultation with an ophthalmologist.
Chemical conjunctivitis will resolve spontaneously, but it is often treated with a topical antibiotic ointment for prophylaxis and emollient purposes. Chlamydial conjunctivitis should be treated with oral erythromycin for at least 14 days due to the common involvement of other sites such as the lungs; additional topical antibiotics are not needed. Routine bacterial conjunctivitis can be treated with topical erythromycin ointment. Ointment is preferred to drops for young infants because it is easier to apply and is not as easily washed out.
Oral Findings
Oral thrush is a very common problem in neonates due to the ubiquity of Candida species and the neonate’s weaker immune system. It presents as patchy white exudate commonly on the buccal mucosa and tongue. Infants may be noted to have poorer feeding. It is differentiated from residual milk in that it cannot be scraped off with a tongue depressor. There may or may not be an associated candida diaper rash. Breastfeeding mothers may have infection evidenced by red, cracked, sore, or itchy nipples.
Ankyloglossia, commonly called “tongue-tie,” is a shortened lingual frenulum that inserts near the tip of the tongue. In neonates, it may impair feeding, particularly breastfeeding.
Several benign oral findings may concern parents. Natal teeth are present at birth, and neonatal teeth emerge during the neonatal period. Both can be an early eruption of normal primary teeth or an extra supernumary tooth. Epstein pearls are tiny firm white bumps on the midline palate or sometimes the gums that stem from entrapment of keratin during development. Bohn nodules are small, <3-mm gray–white cystic nodules on the alveolar gums and occasionally the palate.
Oral thrush is treated with oral nystatin, 100,000 units/mL, 0.5 mL in each buccal pouch (right and left side), four times a day for 5–10 days (or until a few days after no further white exudate is seen). Any concomitant candidal diaper rash should also be treated. Instruct parents to sterilize bottle nipples and pacifiers by cleaning them in a hot dishwasher or placing them briefly in boiling water. Breastfeeding mothers with evidence of nipple candidiasis can be given topical nystatin or clotrimazole to apply to the nipples after each feed (it should be absorbed into the skin by the next feed).
Ankyloglossia that is not inhibiting feeding can be followed by the primary care provider and will often resolve spontaneously. Consider consultation with a lactation specialist for breastfeeding infants or an occupational therapist for other feeding issues. Sometimes frenectomy is performed, but not by emergency physicians.
Reassurance and follow-up with the primary care provider are sufficient for natal and neonatal teeth, Epstein pearls, and Bohn nodules. Only very loose teeth that pose an aspiration risk need to be managed emergently; these can be removed with a simple pull if they are very loose, or a dental or oral and maxillofacial surgery specialist can be consulted. Ensure that the patient has received vitamin K prophylaxis before removing any teeth.
Torticollis
Congenital muscular torticollis is a common newborn abnormality, particularly in cases in which the birth was difficult. It is due to shortening and fibrosis of one of the sternocleidomastoid muscles (SCMs), which is sometimes palpable as a firm mass at 3 or 4 weeks of age. The shortened muscle causes the head to be tilted toward the affected SCM and rotated such that the chin points away from the affected SCM. There is decreased passive range of motion when tilting the chin toward the affected SCM or rotating the head away from the affected SCM (any movement that requires stretching of that SCM). Because the infant prefers to hold the head in a position that does not stretch the affected SCM, positional plagiocephaly and facial asymmetry can occur. The diagnosis is clinically made, and the infant should be otherwise well-appearing, afebrile, feeding normally, and neurologically normal.
Initial management is conservative, including gentle passive stretching exercises—three sets held for 30–60 seconds at a time, performed six to eight times per day—and placement of the infant in the crib so as to encourage turning the head in the direction opposite preferred in order to see out toward the middle of the room/door. Prone positioning tummy time while awake is also recommended. Patients can be discharged to follow up with the primary care provider.
Breast Issues
Neonatal breast hypertrophy occurs in both female and male infants as a result of exposure to maternal estrogen in utero. There may even be a few drops of milky discharge (“witch’s milk”). Hypertrophy is typically noticed in the first 1 or 2 weeks of life, and it resolves within a few weeks in male infants and within a few months in female infants.
Mastitis must be differentiated from benign breast hypertrophy. It presents as erythematous, tender, indurated breast tissue that is usually unilateral. Mastitis also occurs in both females and males, and incidence peaks at age 2 weeks. It may progress to abscess formation, and there may be associated purulent nipple discharge or systemic symptoms such as fever.
Reassurance and education are all that is needed for benign neonatal breast hypertrophy. Parents should be instructed to avoid stimulating the area, such as palpating it to check for resolution or squeezing the nipple to express discharge, because this may prolong hypertrophy through a hormonal feedback loop, irritate the area, and increase the risk of mastitis.
Neonates with mastitis should be admitted for parenteral broad-spectrum antibiotics, and a pediatric surgeon should be consulted to follow the patient in case of abscess formation.
Periodic Breathing
Parents sometimes present with concerns that their neonate has stopped breathing. True apnea is defined as cessation of breathing for 20 seconds or longer, often associated with bradycardia, cyanosis and oxygen desaturation, pallor, and/or hypotonia. True apnea is more common in preterm infants and can be associated with respiratory syncytial virus infection.
Periodic breathing is a much more common finding in neonates through age 6 months, consisting of alternating short 5- to 10-second periods of normal respirations or even tachypnea followed by a short period of lack of breathing. There should be no hypoxia, cyanosis, bradycardia, or tone changes. Parents often overestimate the duration of lack of breathing, so timing with a stopwatch can be useful.
A short period of observation on a cardiorespiratory monitor to rule out true apnea and to reassure the parents is warranted. Once periodic breathing is identified and confirmed, parental education and reassurance are all that is needed.
Heart Murmur
During examination for another chief complaint, an incidental heart murmur may be heard. Or, less commonly, the infant may be referred by an outside provider for heart murmur assessment. Innocent heart murmurs are very common in pediatrics, and less than 1% of all pediatric murmurs are due to a congenital heart defect. Characteristics concerning for pathologic murmur include grade 4–6, harsh, diastolic (except venous hum) or holosystolic. Associated findings concerning for congenital heart disease include gallop rhythm, poor feeding or poor weight gain, sweating with feeding, increased work of breathing, liver edge palpable more than 2 or 3 cm below the right subcostal margin, cyanosis or hypoxemia, and pulse or blood pressure or oxygen saturation differential between preductal (right upper extremity) and postductal (either lower extremity).
If a pathologic heart murmur is suspected, ECG and chest radiograph may be helpful. Infants with normal feeding, growth, oxygen saturation, ECG for age, and chest radiograph can be followed by primary care and cardiologist referral as needed. Consultation with a pediatric cardiologist should occur if a congenital lesion is suspected.
The differential diagnosis for vomiting in a neonate is broad, ranging from normal spit up or overfeeding to highly morbid conditions such as midgut volvulus. Other serious conditions that can present with vomiting in the neonate include pyloric stenosis, necrotizing enterocolitis, inborn error of metabolism, neonatal withdrawal syndrome, tracheoesophageal fistula, salt-wasting congenital adrenal hyperplasia, hydrocephalus and increased intracranial pressure, non-accidental trauma, Hirschsprung disease, urinary tract infection, sepsis, meningitis, and omphalitis. Any of the following findings warrant further workup and potentially admission to rule out a serious etiology of vomiting: bilious vomiting (concerning for volvulus), projectile vomiting (concerning for pyloric stenosis), hematemesis, inability to tolerate any oral intake, dehydration or reduced number of wet diapers, abnormal abdominal examination including even mild distension, poor growth, abnormal vital signs (especially fever or hypotension), and lethargy or irritability. Demonstrating tolerance of a small oral intake trial (e.g., 0.5–1 oz) is useful. When in doubt, screening urinalysis, electrolytes, and abdominal radiography to assess for signs of obstruction, free air, pneumatosis intestinalis, and evidence of malrotation or toxic megacolon, and also a period of observation while awaiting results of this abbreviated workup, may aid the assessment.
Gastroesophageal reflux is a very common finding in neonates and infants due to developmental laxity in the gastroesophageal sphincter. This natural reflux peaks at approximately age 4 months and often resolves by age 1 year. It is not termed gastroesophageal disease unless there are pathologic consequences such as poor weight gain, recurrent aspiration pneumonia, or esophagitis.
Neonates with concerning history, physical examination, laboratory, or radiography findings should be admitted for further evaluation and management. If borderline, a period of observation either in the ED or as an inpatient is warranted; vomiting in the neonate is a symptom to take seriously, and high morbidity entities often progress rapidly. Ondansetron is not recommended for this age group.
If the neonate is growing well, has no red flag history or physical examination findings, is not unusually irritable (i.e., is a “happy spitter”), and tolerates an oral intake trial in the ED, the parents can be reassured and sent home to follow up with the primary care provider. Conservative interventions such as smaller, more frequent, and sometimes thickened feeds and also keeping the infant upright for 20–30 minutes after feeds may be trialed. Or, management trials can be left to the primary care provider. If the parents are giving >2 oz per feed, overfeeding is a possibility, and these infants may also benefit from smaller, more frequent feeds.
Jaundice (icterus), manifested by a yellow tinge to the skin and the sclerae of the eyes, is one of the most common complaints for which neonates are brought to medical attention. There are several benign etiologies, but very high levels can cause kernicterus, neurologic sequelae from bilirubin crossing the blood–brain barrier, and direct central nervous system toxicity. Also, conjugated (direct) hyperbilirubinemia carries a wide differential of pathologic causes, most notably biliary atresia.
Physiologic jaundice is due to immature development of liver enzymes that conjugate excess bilirubin, among other developmentally related causes. Bilirubin level peaks in the first 3–5 days of life, usually at <6 mg/dL, but higher at 10 mg/dL in Asian neonates, and the bilirubin is unconjugated (indirect). A bilirubin level >17 mg/dL in an infant 96 hours old or older should not be attributed to benign physiologic jaundice.
Breastfeeding jaundice differs from breast milk jaundice and is due to inadequate oral intake from either breast milk not fully coming in or difficulties with breastfeeding. It typically potentiates the effect of physiologic jaundice in the first week of life, contributing to an elevated unconjugated (indirect) bilirubin level. Dehydration may be present. Assess adequacy of breastfeeding (should be 8–12 times per day), wet diapers, and weight gain. Offer mothers support and/or consultation with a lactation specialist. Formula supplementation may be needed.
Breast milk jaundice is a separate entity of unknown mechanism, but it is thought to be due to some component of human breast milk inhibiting liver enzyme conjugation of bilirubin. This type of jaundice presents as an unconjugated (indirect) hyperbilirubinemia that starts in the second week of life (days 6–14) and may continue for up to 3 months. A brief pause in breastfeeding (with the mother pumping and saving breast milk so her production is not impaired) can be diagnostic and therapeutic—the bilirubin level should decline by 3 mg/dL per day.
Cholestasis is indicated by conjugated (direct) hyperbilirubinemia, and although the differential diagnosis for the underlying etiology is broad, biliary atresia is one of the most important causes to identify. These infants develop jaundice in the first few weeks of life. They remain well-appearing, with normal feeding and growth, but become jaundiced and have acholic or clay-colored stools. Jaundice thought to be physiologic but persisting beyond 2 weeks of life or acholic stools should prompt a laboratory workup including direct bilirubin level, liver enzymes, and γ-glutamyltransferase to identify cholestasis.
Well-appearing low-risk infants can be screened with a transcutaneous bilirubin measurement (“bilimeter”). Although transcutaneous measurements correlate well with serum bilirubin, they are less accurate at higher serum bilirubin levels. If the value is >13 mg/dL or ≥70% of the serum bilirubin level requiring intervention, then a serum bilirubin level should be obtained to confirm.
Standard laboratory studies when drawing blood include total and indirect bilirubin and hemoglobin. If not previously found to be normal, direct bilirubin should also be measured; an abnormal level should prompt admission and further workup for cholestatic disease. If hemoglobin reveals anemia or if there is potential for isoantibodies (particularly with mother blood type O or Rh negative), perform a complete blood count, type and screen, and direct antibody (Coomb’s) test. For significantly jaundiced infants, urinalysis to rule out urinary tract infection, reticulocyte count, and glucose-6-phosphate dehydrogenase level are recommended.
Most physiologic jaundice requires no specific treatment. If breastfeeding jaundice is present, offer mothers support and/or consultation with a lactation specialist. Formula supplementation may be needed. Close follow-up to ensure adequate intake is important. Breast milk jaundice can be treated by a brief pause in breastfeeding (while the mother pumps her milk), but providers should not suggest that the mother stop breastfeeding. Sunlight exposure, thought to work similarly to phototherapy, has previously been recommended but carries the risk of overexposure and sunburn.
If the unconjugated bilirubin level approaches 25 mg/dL in a term infant or 20 mg/dL in an infant with other risk factors, kernicterus may develop. Infants at intermediate or high risk for such complications should be admitted for phototherapy, and if the level is very high, exchange transfusion should be considered. A 2004 American Academy of Pediatrics nomogram for infants born at ≥35 weeks of gestation uses gestational age, hours since birth, total bilirubin level (not just indirect), and the presence of other risk factors such as hemolysis to define the threshold level for intervention. Bilitool, a useful online calculator, returns the results from this nomogram ( http://www.bilitool.org ). If the level is in the moderate- to high-risk zone, phototherapy should be begun in the ED if inpatient admission cannot occur immediately.
Umbilicus Concerns
Umbilical granuloma results from inflamed granulation tissue, and it presents as a 3- to 10-mm round, pink, sometimes pedunculated lesion that may be moist. Umbilical granuloma is a clinical diagnosis.
Urachal abnormalities arise in the urachus, an embryologic connection between the umbilicus and the bladder that normally closes and forms a fibrous cord. Urachal abnormalities can often be assessed by ultrasound.
Patent urachus allows free flow of urine to the umbilicus and results in an umbilical cord area that is constantly wet or draining. It occasionally results in urinary tract infection.
Urachal sinus is closed at one end (either bladder or umbilical) and may present with periumbilical redness, pain, and drainage at the umbilicus. In sinuses opening to the bladder, urinary tract infection can occur.
Urachal cyst is a mid-remnant cyst, as the urachus closes on both ends but not completely in the middle. It presents as a palpable periumbilical mass and, if infected, as a red, tender, usually infraumbilical swelling associated with abdominal pain.
Omphalomesenteric (vitelline) duct patent remnant connecting the intestinal tract and the umbilicus may result in fecal drainage at the umbilicus.
Delayed cord separation becomes a concern when a neonate reaches 3 weeks of age without cord separation. Mean cord separation is usually 7–15 days. The significance is that delayed cord separation may be a harbinger of leukocyte adhesion disorder, a rare immunologic disease.
Umbilical granulomas are treated with silver nitrate applications. Take care to apply only to the granuloma because the silver nitrate can burn and discolor the surrounding skin. Additional applications by the primary care provider will be required.
Suspicion of urachal or omphalomesenteric remnants or delayed cord separation requires subspecialty referral (by the primary care provider). A bacterial superinfection requires admission and parenteral antibiotics.
The cord should be kept clean and dry, and the diaper should be folded down below the level of the cord. The base of the stump can be gently cleaned with rubbing alcohol several times a day to help dry it out. Avoid application of large amounts of liquid alcohol, which can be systemically absorbed.
Genital and Inguinal Complaints
Inguinal hernia occurs when the processus vaginalis does not fully close, allowing bowel to pass through. It typically presents as an inguinal or scrotal swelling that comes out with Valsalva, such as when crying, and returns into the abdomen when the infant is relaxed. Inguinal hernias are more common in male and preterm infants. Vomiting and intolerance of oral intake, redness and tenderness overlying the mass, inability to push the mass back into the abdomen, and ill appearance may indicate incarceration.
Hydrocele occurs when the processus vaginalis closes enough to exclude bowel, but fluid passes through into the scrotum. It presents as a nonreducible fluid-filled scrotal swelling that is palpable separate from the almond-sized testis and that transilluminates with a bright light source. The swelling of hydroceles is typically more discrete than that of hernia.
Vaginal withdrawal bleeding sometimes occurs in the first few weeks of life. The female fetus may develop an endometrial lining due to stimulation from maternal estrogen in utero. Once the infant is born and that hormonal influence wanes, shedding of the lining results in a light bloody discharge that can be distressing to parents.
Easily reduced inguinal hernias can be nonurgently referred to a surgeon for elective herniorrhaphy. Return instructions include signs and symptoms of incarceration. Trendelenburg positioning, continuous gentle pressure, and sometimes sedation are required to reduce incarcerated hernias. If unsuccessful, consult a surgeon emergently.
Hydroceles usually resolve spontaneously during the first few years of life. Vaginal withdrawal bleeding is a single self-limited event. For both of these diagnoses, reassurance and parental education are sufficient.
Diaper Rash
Irritant diaper dermatitis (Figure 1.2 ) is the most common diaper rash. It is caused either by the soiled diaper chafing the infant’s skin or by a contact dermatitis reaction to diaper or wipe material. Erythematous papules, plaques, and erosions are on the parts of the skin that touch the diaper; the skin creases are spared. Parents should be asked about a recent increase in stool volume and about a change in brand of diapers or wipes used.

Irritant diaper dermatitis.
Candidal diaper dermatitis is another common presentation, with erythematous patches, plaques, and erosions. Differentiating from irritant etiology, candidal rashes tend to be brighter red, more moist appearing, involve the skin creases, and have satellite lesions—small discrete papules around the borders of the main rash. Recent antibiotic therapy disrupts the normal skin flora and is a risk factor for candidiasis.
Seborrheic dermatitis can cause a diaper rash in addition to rash on the scalp, face, ears, and neck. Etiology may be due to Malassezia yeast species. The rash consists of scaly red papules and plaques and can be mistaken for psoriasis. Unlike irritant diaper dermatitis, the rash does involve the skin creases. There may be greasy yellow scales similar to scalp seborrheic dermatitis.
Parents of infants with irritant diaper dermatitis should be instructed to check the diaper every few hours for soiling and to change the diaper frequently. Scented wipes, soaps, and other potential irritants should be avoided; severe rash should be cleansed with a clean towel and warm water only. A thick layer of zinc oxide-based diaper rash cream should be applied with each diaper change to act as a barrier between the infant’s skin and the diaper. When the infant is sleeping, the diaper can be removed entirely and the infant laid on a cloth diaper. Severe inflammation may benefit from low-potency topical steroid cream (e.g., 1% hydrocortisone) applied in a thin layer twice daily. Combination steroid and antifungal creams should be avoided because the steroid component is too potent for neonatal skin.
Candidal diaper dermatitis is treated with topical antifungal creams, such as nystatin or clotrimazole, applied four times per day. Treat any concomitant oral thrush.
Seborrheic dermatitis is treated with topical steroid cream as for irritant and/or topical ketoconazole cream, applied once a day.
Jerks and Jitteriness
Moro (startle) reflex is a normal newborn reflex in which, when the infant is held in supine position and then the head is suddenly dropped back a few inches, the infant abducts both arms and then brings them back in toward midline. Parents who have elicited a Moro reflex from their infant may be concerned as to whether it is normal. The Moro reflex usually extinguishes by 3 or 4 months of age.
Benign sleep myoclonus presents as symmetric, bilateral extremity jerks occurring during non-rapid eye movement sleep, typically starting in the first 2 weeks of life. They occur in rhythmic clusters and may be multiple or single; they occur only when the infant is falling asleep or sleeping. They may be difficult to differentiate from true epileptic seizures, and a normal electroencephalogram (EEG) is useful in establishing the diagnosis. Benign sleep myoclonus typically self-resolves by age 4 months.
Neonatal jitteriness may be a normal finding in response to overstimulation. The jitteriness presents as typically symmetric bilateral tremors with oscillations of equal amplitude and frequency. Unlike with seizures, tremors can be reduced with consoling the neonate or holding the affected extremity. Although common in normal newborns, the differential diagnosis includes pathologic conditions such as hypoglycemia, hypocalcemia, neonatal drug withdrawal, and hypoxic–ischemic encephalopathy.
Neonatal seizures can be subtle in presentation and can involve eye twitching, nystagmus, lip smacking or rhythmic chewing movements, tongue protrusion, bicycling/swimming movements or thrashing of extremities, and salaam bowing-style infantile spasms.
Unless history and physical examination clearly support the diagnosis of benign Moro reflex or benign sleep myoclonus, it is wise to check glucose, sodium, and calcium levels to rule out immediately treatable hypoglycemia, hyponatremia, or hypocalcemia. Also consider obtaining an ECG to screen for rare long QT syndrome producing seizures. If the infant is feeding and growing normally, has normal vital signs and an otherwise normal physical examination (especially neurologic examination), has no periods of apnea or cyanosis, and there are no historical factors that place the infant at high risk for a pathologic process (e.g., birth asphyxia), the patient can be discharged home with close primary care follow-up. Outpatient imaging and EEG may be indicated. If these discharge criteria are not met, or if the movements are frequent and distressing, admission for monitoring and inpatient neurology consultation may be warranted.
Neonatal Skin Findings
Cutis marmorata is flat symmetric reticular mottling of the trunk and extremities exacerbated by cold. It is usually relieved by warming the skin.
Harlequin color change, reddening of one half of the body with a clear demarcation at midline, occurs when the infant lies on one side. Onset is sudden, and the discoloration lasts seconds to minutes, resolving with increased activity or crying. It is most commonly seen from day of life 2 to 5, and it may continue to occur for the first 3 weeks of life.
Acrocyanosis peripherally of the feet, hands, and lips is common in cold temperatures, and it resolves with warming. Central cyanosis requires investigation, but isolated acrocyanosis is benign.
Erythema toxicum is a common neonatal rash characterized by pink macules, papules, and pustules on a blotchy erythematous base. Lesions typically develop on day of life 2 or 3 and resolve spontaneously over 5–7 days. Lesions are found on the face, trunk, and extremities, but not the palms and soles. Recurrences can occur during the next several weeks.
Transient neonatal pustular melanosis (TNPM) is an uncommon benign vesiculopustular rash seen more often in Black neonates. Lesions include pustules and hyperpigmented macules, often surrounded by a fine collarette of scale, and can be diffuse, including on the palms and soles. Differentiation from more severe causes of vesicles and pustules (e.g., HSV infection) can be difficult, and thus TNPM is generally an ED diagnosis of exclusion.
Neonatal acne (Figure 1.3 ) is a common finding due to the effects of maternal hormones. Acneiform comedones are found most often on the forehead, nose, and cheeks, although they may also occur on the chest and back. Neonatal acne usually resolves spontaneously during the first year of life, but severe lesions may require treatment.

Neonatal acne.
Seborrheic dermatitis has unknown etiology, although Malassezia furfur yeast may play a role. It causes the very common “cradle cap” rash consisting of thick, greasy, yellow adherent scales on the scalp. Rash may also occur on the face, ears, neck, and diaper area, consisting of erythematous papules and plaques, sometimes with scale. The plaques may have a shiny, moist appearance. Seborrheic dermatitis typically resolves spontaneously during the first year of life.
Milia are tiny, pearly white to yellow papules commonly found on the nose, forehead, cheeks, and chin due to retained keratin. They resolve spontaneously during the first month of life.
Miliaria crystallina occur due to retained sweat in eccrine ducts. They present as tiny vesicles with no surrounding erythema on the head, neck, and trunk.
Miliaria rubra (heat rash) occurs due to a similar mechanism but with inflammation. It presents as small erythematous prickly appearing papules and vesicles, typically on areas of the body covered by clothing. A history of bundling or overheating may be obtained.
Dermal melanosis, previously termed “Mongolian spots,” presents as flat irregular patches of blue-gray discoloration, commonly on the lower back and buttocks. It is more common in Asian, Native American, Hispanic, and Black infants. It should not be mistaken for bruising.
Nevus simplex, or “stork bite” or “salmon patch,” presents as a blanchable, flat, salmon-colored pink macule commonly seen on the nape of the neck, eyelid, nose, and scalp. Lesions can be bilateral and symmetric, and they typically fade during the first year of life.
Nevus flammeus, or “port-wine stain,” presents as a unilateral, blanchable, flat, dark red to purple, often large, macule. If it involves the part of the face innervated by the trigeminal nerve ophthalmic portion (V1), there may be associated Sturge–Weber syndrome, glaucoma, and seizures. Nevus flammeus, unlike nevus simplex, does not fade over time.
Hemangiomas are usually not present at birth but appear in the first days to months of life. They first appear as a subtle telangiectasia and then proliferate during the next 6–12 months into a larger bright red (strawberry hemangioma) or bluish (deep subcutaneous hemangioma) swelling. They spontaneously involute during the next several years of life. Unless complicated by infection, bleeding, or obstructing vision or airway, no acute treatment is needed.
Most of the benign skin findings require no more than reassurance, parental education, and follow-up with the primary care provider. Significant seborrheic dermatitis may respond to low-potency topical steroid (e.g., 1% hydrocortisone cream) or topical ketoconazole applied once daily. Parents of infants with miliaria rubra should be instructed to avoid overheating. Parents can be reassured that the amount of clothing a newborn requires is similar to what is comfortable for a parent in the current environmental temperatures. When pustules or vesicles are present, practitioners must consider more serious skin conditions such as HSV.
Neonates have a narrow range of behaviors: sleeping, feeding, urinating and defecating, and some quiet alert time. ED practitioners must be familiar with the typical normal patterns for these behaviors.
When evaluating the neonate, obtaining a prenatal, perinatal, and birth history is key.
Weight gain compared to birth weight should be assessed for adequacy.
ED providers must be familiar with common physical examination findings and benign diagnoses seen in neonates. With this familiarity, providers can avoid unnecessary diagnostic testing and admission.
Not fully removing the infant’s clothing during examination may result in missing signs of increased work of breathing, problems with umbilical cord healing, sentinel injuries concerning for non-accidental trauma, and other important findings.
Not checking the umbilical cord may result in missing evidence of infection, congenital abnormality, or delayed cord separation.
Even if not the chief complaint, jaundiced infants should be assessed to ensure that they do not meet criteria for phototherapy.
Further Reading
Aby, J. Photo Gallery. Stanford Medicine Newborn Nursery at Lucile Packard Children’s Hospital. https://med.stanford.edu/newborns/professional-education/photo-gallery.html . Accessed April 24, 2019.
Burgos T , Turner S. BiliTool. http://www.bilitool.org . Accessed April 27, 2019.
Karp, H. The 5 S’s for Soothing Babies. Happiest Baby. https://www.happiestbaby.com/blogs/baby/the-5-s-s-for-soothing-babies . Accessed April 24, 2019.
Lowe MC , Woolridge DP. The normal newborn exam, or is it? Emerg Med Clin North Am . 2007 ;25:921–946. 10.1016/j.emc.2007.07.013
Maisels MJ , Bhutani VK , Bogen D, et al. Hyperbilirubinemia in the newborn infant ≥35 weeks’ gestation: An update with clarifications. Pediatrics 2009 ;124(4):1193–1198. 10.1542/peds.2009-0329
Google Scholar
Shope TR , Rieg TS , Kathiria NN. Corneal abrasions in young infants. Pediatrics 2010 Mar;125(3):e565–e569. PMID 20142290. 10.1542/peds.2008-2023
Web of Science
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Your Browser is Out of Date
To provide you with the best experience, our websites uses features that are not supported by your current browser. For the best experience on Childrenshospitals.org, please open this site in a different browser such as Google Chrome
- Product/Program
NICU Course Library

This comprehensive online NICU education program ensures learners receive evidence-based, standardized education focused on the specifics of neonatal care. Help your NICU clinicians develop the clinical judgement to manage and deliver quality care to their patients.
NICU Library courses
Advanced Concepts in Respiratory Physiology Anemia and Polycythemia in the Neonate Apnea of Prematurity Basic Principles of Oxygen Therapy, Specialty Gases and Noninvasive Ventilation Blood Exchange Transfusion Bronchopulmonary Dysplasia Cardiovascular Laboratory Procedures: Diagnostic and Interventional Care of the Small Baby Caring for a Child with a Tracheostomy Caring for the Pediatric Patient in Shock Central Lines in the Neonate Comprehensive Assessment of the Neonate Congenital Diaphragmatic Hernia Congenital Heart Disease: Acyanotic Defects Congenital Heart Disease: An Overview Congenital Heart Disease: Cyanotic Defects Congestive Heart Failure Continuous Renal Replacement Therapy Developmental Care of the Newborn Disseminated Intravascular Coagulation Esophageal Atresia and Tracheoesophageal Fistula Extrauterine Life: Assessment of the Neonate's Transition Extrauterine Life: Fetal to Neonatal Circulation Family-Centered Care In the NICU Gastroschisis and Omphalocele Glucose Homeostasis In the Neonate Hemodialysis Hemodynamic Monitoring Hydrocephalus Hyperbilirubinemia Hypoxic Ischemic Encephalopathy Intracranial Pressure Monitoring and Management Introduction to Arterial Blood Gas Interpretation Management of Peripheral IV Complications in the Pediatric Patient Maternal Factors Affecting the Newborn Mechanical Ventilation: Introduction to Pediatric Practices Meconium Aspiration Syndrome Metabolic Disorders of the Newborn NAVA Necrotizing Enterocolitis Neonatal Abstinence Syndrome Neonatal Cranial Hemorrhage Neonatal Nutrition Neonatal Pain Assessment and Management Neonatal Pharmacokinetics Neonatal Respiratory Distress Syndrome Neonatal Seizures Neonatal Sepsis Neonatal Skin Care Nursing Management of Chest Tubes Pediatric Peripheral IV Care & Management Peritoneal Dialysis Persistent Pulmonary Hypertension of the Newborn (PPHN) Pneumothorax in the Neonate Preventing Surgical Site Infections Preventing Ventilator-Associated Pneumonia Renal Failure in the Pediatric Patient Retinopathy of Prematurity Thermoregulation of the Newborn Infant Transient Tachypnea of the Newborn Understanding Abnormal Blood Gases Vasoactive Medications
View a Demo
Learn more by participating in a live session or viewing course demos.
For more information, contact:
Pediatric Learning Solutions’ online education provides the foundational knowledge clinicians need to master the competencies and skills for safe and effective patient care.
Related Content
Courses to prepare for certification exams.

Standardized Curriculum Decreases Length of Nurse Onboarding in the NICU

Care of the Small Baby Course Overview

Pediatric Learning Solutions offers preparatory resources to help clinicians prepare for career-advancing certification exams.

Neonatal educators reduce NICU orientation cost and time across facilities.

An overview of physiological differences and specific care management considerations unique to the small baby.
Neonatology/Newborn Issues
Circumcision
Resuscitation of a Newborn
Heart Disease (Congenital) in Infants
Breastfeeding
Examination of a Newborn
Patient Education, Self-Care
Hip Dysplasia (Congenital)
Fetal Alcohol Spectrum Disorders
Screenings for Newborns
Respiratory Distress
Premature Infant/Outpatient Care of Former Premature Infant
Editorials and Letters
Postpartum Counseling/First Well Child Visit
Intestinal Obstruction
Recently Added
Popular afp topics.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
- Adolescent Medicine
- Alternative Medicine
- Developmental Pediatrics
- General Pediatrics
- Immunodeficiencies
- Infectious Diseases
- Laboratory Medicine
- Medical Procedures
- Medico-Legal Issues
Neonatology
- Pediatric Anesthesia
- Pediatric Cardiology
- Pediatric Critical Care
- Pediatric Dentistry
- Pediatric Dermatology
- Pediatric Endocrinology
- Pediatric GI and Hepatology
- Pediatric Hematology
- Pediatric Nephrology
- Pediatric Neurology
- Pediatric Oncology
- Pediatric Ophthalmology
- Pediatric Orthopedics
- Pediatric Pulmonology
- Pediatric Radiology
- Pediatric Rheumatology
- Pediatric Surgery
- Vaccinology
Partner Sites
Infection in Children - Part 3
- Kids Corner
- Diagnostic Aid
- Ask a Doctor
- Diagnostic Dilemma
- Question of the Week
- Pediatric Blogs
- Spot Diagnosis
- Grand Rounds
- Current Issue
- Advance Access
- About the Journal
- Submit Article
- Pediatric Oncall
- Medical Calculators
- Vaccine Reminder
- Pediatric Oncall Journal
- Drug Center
- Upcoming Conferences
- Conference Abstracts
Common neonatal presentations to the primary care physician
Affiliation.
- 1 MBBS, FRACP, MPH, General and Developmental Paediatrician, Senior Research Officer, Murdoch Children@s Research Institute, Melbourne, Vic. [email protected].
- PMID: 29621858
- DOI: 10.31128/AFP-09-17-4326
Background: Newborn babies are very vulnerable in their first weeks of life. Timely and appropriate management of neonatal conditions is paramount for health and developmental outcomes.
Objective: The aim of this article is to provide an overview of common neonatal presentations to general practice, and highlight significant conditions that may require referral to the emergency department and/or other specialist.
Discussion: Clinical history and examination are the most important tools in neonatal assessment. Babies often present with non-specific symptoms, but a thorough clinical assessment can identify the ‘unwell baby’ who requires immediate transfer to hospital. This includes babies with sepsis, moderate‑to‑severe dehydration or who are in acute cardiorespiratory compromise. A comprehensive neonatal assessment will also help to differentiate babies with significant conditions that may warrant further specialist input from those with normal neonatal development where parental support and reassurance may be sufficient.
- Feeding Behavior
- Fever / diagnosis
- Fever / etiology
- Gastrointestinal Diseases / diagnosis
- Gastrointestinal Diseases / therapy
- Infant Health / trends*
- Infant, Newborn
- Medical History Taking / methods
- Primary Health Care / methods*
- Primary Health Care / trends
- Respiratory Physiological Phenomena
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
Contributor Disclosures
Please read the Disclaimer at the end of this page.
The following represent additions to UpToDate from the past six months that were considered by the editors and authors to be of particular interest. The most recent What's New entries are at the top of each subsection.
ORTHOPEDICS AND SPORTS MEDICINE
Running injuries in high school and collegiate athletes (March 2024)
Although running is the most common form of exercise, few high-quality reviews of running-related injuries have been published. A recent systematic review that included 24 prospective cohort studies (nearly 2000 adolescent and young adult competitive runners) found that female runners sustained more injuries than their male counterparts [ 1 ]. All runners, but particularly females, with risk factors for relative energy deficiency in sport (REDS) experienced higher injury rates; athletes with weak hip and thigh muscles were at increased risk of developing anterior knee pain (eg, patellofemoral pain). This study also confirmed known risk factors, such as a history of prior running-related injury. Overall, study quality and certainty of evidence were low to moderate. These findings reinforce the importance of sound nutrition and adjunct strength training to prevent running injuries. (See "Running injuries of the lower extremities: Risk factors and prevention", section on 'Sex and age' .)
Concussion and mental health disorders in children and adolescents (March 2024)
Ongoing research continues to examine the complex relationship between concussion and mental health disorders. In a recent case-control study of over 18,000 children (≤17 years old) with concussion and over 37,000 matched controls, concussion was associated with an increased risk for a new diagnosis of a behavior disorder at two and four years after injury [ 2 ]. For most diagnoses, the absolute numbers were low. Confidence in a causal relationship is limited by risk of confounding and reliance on an electronic medical record for establishing lack of baseline behavioral problems prior to injury. Whether pediatric concussion is an independent risk factor for new behavioral problems after recovery remains unclear. (See "Concussion in children and adolescents: Management", section on 'Mental health disorders' .)
Overuse injuries, overtraining, and burnout in children and adolescents (February 2024)
Greater numbers of children and adolescents now specialize in a single sport, thereby increasing the risk for overuse injuries, overtraining, and burnout. The American Academy of Pediatrics has issued a new clinical report that reviews the medical literature about these conditions and summarizes key findings pertaining to risk factors, clinical presentation, and prevention [ 3 ]. The report emphasizes the importance of achieving a healthy balance between stress and recovery. Specific recommendations include taking one to two days off from competition and sport-specific training each week and two to three months away from any specific sport each year. Discussions of endurance sports and weekend tournaments are included. (See "Overtraining syndrome in athletes", section on 'Special considerations in the young athlete' .)
Risk of reinjury following ACL repair (February 2024)
Despite advances in surgical techniques, the risk of reinjury following repair of a ruptured anterior cruciate ligament remains substantial, ranging from 5 to 15 percent depending on the patient's age and activities. According to a systematic review of 71 studies involving over 600,000 patients, factors associated with an increased risk for retear following surgery include male sex, younger age, preoperative high-grade knee laxity, return to a high activity level or sport, and concomitant medial collateral ligament injury [ 4 ]. The modifiable factors identified highlight the importance of following a rigorous rehabilitation program and allowing time for complete healing before returning to sport. (See "Anterior cruciate ligament injury", section on 'Risk of reinjury' .)
Return to sport following stress fracture (November 2023)
Evidence is limited regarding return to sport (RTS) following stress fracture. A new systematic review of 76 studies involving nearly 3000 cases,provides some guidance; most of the studies were retrospective and involved predominately male athletes [ 5 ]. The lowest overall rates for RTS were reported for injuries of the femoral neck (55 percent), talus (69 percent), anterior tibial shaft (76 percent), and tarsal navicular (83 percent). The longest average times for RTS were reported for stress fractures of the tarsal navicular (127 days), femoral neck (107 days), and medial malleolus (106 days). These figures are averages, and healing for individuals may vary substantially given the many factors involved, including location within the bone, radiologic grade, duration of symptoms, compliance with treatment, and underlying bone health. Nevertheless, these findings inform treatment decisions and anticipatory guidance for athletes. (See "Overview of stress fractures", section on 'Return to activity' .)
Heavy load resistance exercise for tendinopathy (November 2023)
Evidence supporting the effectiveness of resistance exercise for the treatment of chronic (overuse) tendinopathy is growing. A recent systematic review and meta-analysis of 110 studies with just under 4000 subjects assessed research primarily involving the rotator cuff, Achilles, lateral elbow, and patellar tendons [ 6 ]. While noting that resistance dose was not well documented in many studies, researchers found consistent evidence that rehabilitation programs using resistance loads in excess of body weight and performed less frequently (ie, less than daily) demonstrated greater efficacy. These findings are consistent with our approach to treatment. (See "Overuse (persistent) tendinopathy: Overview of management", section on 'Heavy-load resistance training' .)
Avulsion fractures of hip and pelvis in children (October 2023)
There are few large-scale studies of pelvic avulsion fractures in children. A retrospective review of over 700 children with pelvic or hip avulsion fractures from a single tertiary care hospital reported the average patient age was just over 14 years and nearly 80 percent were sustained by males [ 7 ]. The anterior-superior and inferior iliac spines and ischial tuberosity were the most common sites, accounting for over 80 percent of fractures. Most injuries were sustained while the patient was running or kicking during sport, most often football (soccer). The incidence of avulsion fracture rose substantially during the study period, 2005 to 2020. (See "Pelvic trauma: Initial evaluation and management", section on 'Epidemiology and mechanism' .)
GENERAL PEDIATRICS AND ADOLESCENT MEDICINE
Management of children with mild sleep-disordered breathing (February 2024)
For children with mild sleep-disordered breathing (SDB) and relevant symptoms, little evidence has been available to guide a choice between adenotonsillectomy and watchful waiting. In a randomized trial in 459 children 3 to <13 years with tonsillar hypertrophy and mild SDB (defined by habitual snoring with occasional episodes of obstruction with apnea per hour of sleep), executive function and attention were similar for individuals assigned to adenotonsillectomy compared with watchful waiting at 12 months follow-up [ 8 ]. However, children treated with adenotonsillectomy had greater decrease in snoring, obstruction with apnea or hypopnea, blood pressure, and caregiver-reported symptoms (sleep symptoms, behavioral problems, sleepiness) as well as increased quality of life. These findings support our suggestion to offer adenotonsillectomy to children with mild obstructive sleep apnea and relevant symptoms although watchful waiting is a reasonable alternative. (See "Management of obstructive sleep apnea in children", section on 'Adenotonsillectomy' .)
Cannabinoids and mental health in adolescents (December 2023)
Cannabis use is associated with an increased risk of mental health disorders. However, little is known about the effects of cannabidiol (CBD), a nonpsychoactive component of cannabis used for anorexia and childhood epilepsy, or of recreational synthetic cannabinoids. In a school-based survey from the United Kingdom that included over 6500 adolescents ages 13 to 14 years, reported use of cannabis, CBD, or synthetic cannabinoids were each associated with probable depression, anxiety disorder, or conduct disorder, as well as with auditory hallucinations [ 9 ]. For each disorder, the risk appeared greatest with synthetic cannabinoids. This study highlights the need for further investigation into the association between mental health effects in youth and the different types of cannabinoids. We advise adolescents (and younger children) to avoid cannabis consumption, including CBD. (See "Substance use disorder in adolescents: Epidemiology, clinical features, assessment, and diagnosis", section on 'Cannabis, cannabidiol, and synthetic cannabinoids' .)
High blood lead levels in US children after eating cinnamon applesauce pouches (November 2023)
The Centers for Disease Control and Prevention have issued a health alert following reports of high blood lead levels from several states for a total of 22 children who were fed cinnamon-containing applesauce pouches that were subsequently found to contain extremely high concentrations of lead [ 10 ]. Children who have eaten a recalled product should undergo blood lead testing. Clinicians should advise parents, primary caregivers, and guardians to not buy specific cinnamon-containing apple puree or applesauce products named in the US Food and Drug Administration announcement and to discard any recalled products that they have purchased. (See "Childhood lead poisoning: Exposure and prevention", section on 'Food' and "Childhood lead poisoning: Clinical manifestations and diagnosis", section on 'Laboratory evaluation' and "Childhood lead poisoning: Management" .)
Long distance effect of wildfire smoke on asthma symptoms (October 2023)
Wildfire fine particulate matter (PM 2.5) has been shown to affect respiratory health; however, previous work has focused on populations residing near and directly affected by wildfires. In June 2023, smoke from wildfires in Canada drifted hundreds of miles to New York City, resulting in increased ambient PM 2.5 . During smoke waves, emergency department visits for asthma in both pediatric and adult patients increased to 261 per day (reference during nonsmoke periods, 181.5 per day; incidence rate ratio 1.4) [ 11 ]. Wildfires have health effects far from their source and are particularly hazardous to those with underlying lung disease. (See "Climate emergencies", section on 'Changing wildfire exposure' .)
ALLERGY, IMMUNOLOGY, AND RHEUMATOLOGY
Baricitinib for refractory juvenile idiopathic arthritis (November 2023)
Janus kinase (JAK) inhibitors are one of several options for children with polyarticular juvenile idiopathic arthritis (pJIA) that is refractory to conventional therapy (eg, methotrexate with or without a biologic tumor necrosis factor inhibitor). In a phase 3, randomized trial of 220 children aged 2 to 17 years with JIA (66 percent with pJIA) who had inadequate response or intolerance to standard therapy, patients assigned to the investigational JAK inhibitor baricitinib had a longer time to disease flare compared with placebo [ 12 ]. During the study period, fewer patients receiving baricitinib had a flare compared with placebo (17 versus 51 percent, respectively), but more infections occurred in the baricitinib group than the placebo group. However, rates of serious adverse events were similar in both groups. Baricitinib compares favorably with tofacitinib , another JAK inhibitor used in refractory pJIA, but is not yet approved for this indication. (See "Polyarticular juvenile idiopathic arthritis: Treatment", section on 'Baricitinib' .)
DEVELOPMENTAL AND BEHAVIORAL PROBLEMS
Pharmacotherapy for ADHD and mortality risk (April 2024)
Attention deficit hyperactivity disorder (ADHD) is associated with higher mortality than in the general population; whether treatment modifies that risk is unclear. In an observational study of nearly 149,000 individuals with ADHD in Sweden (mean age 17 years), initiation of medication within three months of diagnosis was associated with lower all-cause mortality over two years (hazard ratio [HR] 0.79) as well as lower mortality from unnatural causes (eg, suicide, unintentional injury, and accidental poisoning; HR 0.75) [ 13 ]. While the study could not control for unmeasured confounders that may have impacted mortality risk (eg, lifestyle factors, social support), these data generally lend further support for pharmacotherapy of ADHD. (See "Attention deficit hyperactivity disorder in adults: Treatment overview", section on 'Benefits of stimulant treatment' .)
Infertility and autism spectrum disorder (December 2023)
Patients with infertility often ask about the impact of the disorder and its treatment on risk of autism spectrum disorder (ASD) in offspring. In a large population-based cohort study comparing ASD risk among children whose parents had subfertility (an infertility consultation without treatment), infertility treatment, or neither (unassisted conception), children in the subfertility and infertility treatment groups had a small increased risk of ASD compared with unassisted conception but the absolute risk was low (2.5 to 2.7 per 1000 person-years versus 1.9 per 1000 person-years with unassisted conception) [ 14 ]. The increased risk was similar in the subfertile and infertility treatment groups, suggesting that infertility treatment was not a major risk factor. Obstetrical and neonatal factors (eg, preterm birth) appeared to mediate a sizeable proportion of the increased risk for ASD. (See "Assisted reproductive technology: Infant and child outcomes", section on 'Confounders' .)
ENDOCRINOLOGY
Proposed formal diagnostic criteria for hypophosphatasia in children and adults (March 2024)
Hypophosphatasia is a rare form of osteomalacia caused by pathogenic variants in the tissue nonspecific alkaline phosphatase gene ( ALPL ). Missed or delayed diagnosis is common, in part due to lack of formal diagnostic criteria. An international working group has proposed diagnostic criteria for hypophosphatasia in both children and adults [ 15 ]. Two major criteria or one major and two minor criteria are considered sufficient for diagnosis. For both children and adults, major criteria include a pathogenic (or likely pathogenic) variant in ALPL and elevated natural substrate concentrations (eg, pyridoxal 5'-phosphate). Additional major criteria for adults are atypical femoral fracture and recurrent metatarsal fractures and, for children, early loss of primary teeth and radiographic evidence of rickets. These criteria highlight the variable phenotypic expression of hypophosphatasia and the importance of considering this diagnosis in individuals with metabolic bone disease. (See "Clinical manifestations, diagnosis, and treatment of osteomalacia in adults", section on 'Low alkaline phosphatase (hypophosphatasia)' and "Skeletal dysplasias: Specific disorders", section on 'Hypophosphatasia' .)
Janus kinase inhibition to preserve insulin secretion in early onset type 1 diabetes (January 2024)
In type 1 diabetes, the janus kinase (JAK)/signal transducer and activator of transcription (STAT) pathway has been implicated in immune-mediated beta cell destruction. In a trial in 91 individuals (aged 10 to 30 years) with new-onset type 1 diabetes (diagnosed within 100 days), participants were randomly assigned to daily treatment with the oral JAK1/2 inhibitor baricitinib (n = 60) or placebo (n = 31) [ 16 ]. After 48 weeks of therapy, insulin secretion was greater with baricitinib compared with placebo (median stimulated mean C-peptide level 0.65 versus 0.43 nmol/L per minute, respectively). A1C, frequency of hypoglycemia, and the percentage of time spent in the target glucose range (70 to 180 mg/dL [3.9 to 10 mmol/L]) were not significantly different between groups. JAK/STAT pathway inhibition is a promising strategy for preserving insulin secretion in new-onset type 1 diabetes. (See "Type 1 diabetes mellitus: Prevention and disease-modifying therapy", section on 'Cytokine-directed therapies' .)
Investigational once-weekly basal insulin therapy (insulin icodec) for the treatment of adults with type 1 diabetes (November 2023)
Ultra-long-acting insulin icodec is an investigational basal insulin therapy that requires only once-weekly dosing. In a trial in 655 adults with type 1 diabetes (mean A1C approximately 7.6 percent), participants were randomly assigned to basal insulin therapy with once-weekly insulin icodec or once-daily insulin degludec [ 17 ]. After 26 weeks, the mean reduction in A1C was similar in the icodec and degludec groups (-0.47 and -0.51 percentage points, respectively). However, insulin icodec led to a nearly twofold higher combined rate of clinically significant (<54 mg/dL [<3 mmol/L]) or severe hypoglycemia (2836 versus 1495 events with insulin degludec). Additional studies are needed to determine whether risk of hypoglycemia will limit the use of ultra-long-acting insulin in individuals with type 1 diabetes. (See "General principles of insulin therapy in diabetes mellitus", section on 'Basal insulin analogs' .)
GASTROENTEROLOGY, HEPATOLOGY, AND NUTRITION
Budesonide oral suspension for eosinophilic esophagitis (March 2024)
In patients with eosinophilic esophagitis (EoE), use of topical glucocorticoids has been limited by lack of regulatory approval and potentially inconsistent drug delivery. Budesonide oral suspension is a formulation that was recently approved by the US Food and Drug Administration for treating EoE in adults and pediatric patients ages 11 years and older [ 18,19 ]. Approval was informed by clinical trials showing that topical budesonide resulted in higher rates of histologic remission and symptomatic improvement compared with placebo. We anticipate using budesonide oral suspension as the preferred topical glucocorticoid for treating EoE. (See "Treatment of eosinophilic esophagitis (EoE)", section on 'Topical glucocorticoids' .)
Dupilumab for refractory eosinophilic esophagitis (February 2024)
Few data are available on the use of dupilumab (a monoclonal antibody) for treating refractory eosinophilic esophagitis. In a cohort study of 46 patients with refractory eosinophilic esophagitis, dupilumab therapy was associated with histologic remission (defined as <15 eosinophils/high-power field) in 37 patients (80 percent) and with symptomatic improvement in 42 patients (91 percent) after a median of six months [ 20 ]. These data support our approach of using dupilumab for patients with eosinophilic esophagitis who have not responded to other therapies (eg, topical glucocorticoids). (See "Treatment of eosinophilic esophagitis (EoE)", section on 'Dupilumab' .)
Testing for hepatitis C virus infection in infants with perinatal exposure (November 2023)
Perinatally acquired hepatitis C virus (HCV) infection in the United States has increased sharply since 2010. New guidance from the Centers for Disease Control and Prevention recommends early testing for infants with perinatal exposure to HCV ( algorithm 1 ) [ 21 ]:
● Test for HCV RNA during early infancy after two months of age, and ideally before six months of age.
● After 18 months of age, test any infant who has not previously been tested by measuring anti-HCV antibodies, with reflexive testing for HCV RNA.
A negative HCV RNA result at any time point after two months of age virtually excludes HCV infection and further testing is not required. Children with a positive HCV RNA test before three years of age should have repeat testing for HCV RNA before initiating antiviral therapy to determine whether they have spontaneously cleared the infection. This new guidance is consistent with our previous recommendations for early testing for infants with perinatal exposure to HCV. (See "Hepatitis C virus infection in children", section on 'How to test' .)
GENETIC AND METABOLIC DISORDERS
Investigational gene therapy for autosomal recessive deafness (March 2024)
Gene therapies for single gene disorders are an area of active study. In two recent studies, children with autosomal recessive deafness 9, a type of congenital deafness, were treated with gene therapy to supply functional otoferlin, encoded by the OTOF gene, using an adeno-associated virus vector injected into cochlear cells [ 22,23 ]. Of eight treated children, seven had significant improvements in hearing. This therapy has not been approved by the US Food and Drug Administration. (See "Overview of gene therapy, gene editing, and gene silencing", section on 'Inherited single gene disorders' .)
N-acetyl-l-leucine (NALL) for Niemann-Pick disease type C (February 2024)
Niemann-Pick disease type C (NPD-C) is a rare lysosomal disease with a wide phenotypic spectrum; most patients have onset in childhood with cerebellar ataxia and slowly progressive neurologic deterioration. Investigational therapies include N-acetyl-l-leucine (NALL), a putative neuroprotective agent that improves cellular energy production and reduces neuroinflammation. In a recent placebo-controlled, 12-week crossover trial of 60 patients (age ≥4 years) with NPD-C, treatment with NALL was well tolerated and led to improved neurologic status on a scale that measures ataxia and other neurologic signs and symptoms [ 24 ]. While these results are promising, longer-term trials are needed to determine if NALL is beneficial for patients with NPD-C. (See "Overview of Niemann-Pick disease", section on 'Experimental therapies' .)
HEMATOLOGY AND ONCOLOGY
New international guideline for PK deficiency (March 2024)
A new international expert guideline for diagnosis and treatment of pyruvate kinase (PK) deficiency has been published [ 25 ]. Key recommendations include testing in any individual with nonimmune hemolytic anemia after exclusion of hemoglobin and red blood cell (RBC) membrane disorders, acceptance of genetic testing alone for diagnosis, regular RBC transfusions for children <5 years with symptomatic anemia, monitoring for iron overload and its complications, use of mitapivat for symptomatic anemia in adults who are not receiving transfusions and do not have two nonmissense mutations, and discontinuing mitapivat for lack of efficacy. These guidelines are consistent with the advice in UpToDate. (See "Pyruvate kinase deficiency", section on 'Treatment' .)
Hemoglobin nadir in transfusion-dependent thalassemia (March 2024)
Thalassemia experts generally target a nadir hemoglobin of 9.5 to 10.5 in patients with transfusion-dependent thalassemia (TDT), but supporting evidence for this has been very limited. A new retrospective study evaluated outcomes in 779 patients with TDT and reported that higher pretransfusion hemoglobin (the nadir between regular transfusions) correlated with improved 10-year survival [ 26 ]. The survival benefit was not seen with ferritin >1000 ng/mL, emphasizing the importance of addressing iron overload. While several caveats apply to interpretation, this study supports our practice of targeting a nadir of 9.5 to 10.5 g/dL in TDT. (See "Management of thalassemia", section on 'Supporting evidence' .)
No benefit of routine thromboprophylaxis for children with ALL (January 2024)
Whether routine thromboprophylaxis reduces the risk of thrombotic complications in patients with acute lymphoblastic leukemia (ALL) has been debated. In a multicenter randomized trial of over 500 children and adolescents with newly diagnosed pre-B or T cell ALL, patients assigned to prophylactic anticoagulation with apixaban compared with standard care alone had similar rates of symptomatic venous thrombosis (1.6 versus 2.3 percent, respectively) and asymptomatic venous thrombosis (11 versus 15 percent) [ 27 ]. Nonmajor bleeding episodes (mostly epistaxis) occurred more frequently in the apixaban group (4 versus 1 percent). These data do not support the routine use of thromboprophylaxis in children with ALL, although it may be warranted in selected patients with additional risk factors for thrombosis. (See "Thromboembolism in children with cancer", section on 'Primary prevention' .)
Maintenance eflornithine in high-risk neuroblastoma (January 2024)
For patients with high-risk neuroblastoma (HRNBL), there is interest in investigating novel maintenance therapies such as eflornithine, an ornithine decarboxylase inhibitor. In an externally controlled analysis of almost 100 patients with HRNBL who completed multimodality treatment and maintenance immunotherapy, extended maintenance therapy with eflornithine was associated with improved overall survival (hazard ratio 0.38) [ 28 ]. Based on these data, the US Food and Drug Administration approved eflornithine as maintenance therapy in patients with HRNBL who achieve at least a partial response to prior systemic agents and complete maintenance immunotherapy. Since maintenance eflornithine is not standard across all institutions, this agent may be offered on a case-by-case basis. (See "Treatment and prognosis of neuroblastoma", section on 'Eflornithine' .)
Methemoglobinemia in infants due to contaminated hospital water supply (January 2024)
Methemoglobinemia is a potentially life-threatening condition in which heme iron becomes oxidized, preventing oxygen delivery. A report from a hospital in Japan described methemoglobinemia in 10 neonates who were fed infant formula prepared with tap water from the general hospital water supply [ 29 ]. The cause was identified as high levels of nitrites, and the source was traced to contamination by an anticorrosion agent from the heating system that entered the water supply due to a malfunctioning valve. All 10 survived, although 3 required methylene blue therapy. Infants are especially susceptible to methemoglobinemia because they have lower baseline levels of the enzyme that converts heme iron back to its normal state. (See "Methemoglobinemia", section on 'Nitrates and nitrites (from foods, drugs, preservatives, and chemicals)' .)
INFECTIOUS DISEASES AND IMMUNIZATIONS
Nirsevimab effectiveness in infants (March 2024)
During the 2023-24 respiratory syncytial virus (RSV) season, infants could receive the monoclonal antibody nirsevimab for the first time to protect against RSV-related hospitalization. In a case-control study of almost 700 infants <8 months old who were hospitalized in the United States for an acute respiratory illness during this RSV season, almost 60 percent tested positive for RSV; almost all of these patients had not received nirsevimab [ 30 ]. Among infants who tested negative for RSV, 18 percent had received nirsevimab. Estimated effectiveness against RSV-associated hospitalization among nirsevimab recipients was 90 percent. These data provide additional support for recommendations to administer nirsevimab to all infants <8 months old upon entering their first RSV season and to all newborns during the RSV season unless the birthing parent received RSV vaccination during pregnancy. (See "Respiratory syncytial virus infection: Prevention in infants and children", section on 'Immunoprophylaxis' .)
Short-course antibiotic therapy in children with febrile UTI (February 2024)
In children with urinary tract infection (UTI) without suspected kidney involvement, there is controversy about the duration of empiric antibiotic therapy. In an unblinded trial from Italy of amoxicillin-clavulanate to treat UTI, 142 children three months to five years of age were randomly assigned to a 10-day course (standard) or a 5-day course (short) of antibiotics [ 31 ]. Fewer children assigned to the short course had recurrent UTI within 30 days of antibiotic completion (2.8 versus 14.3 percent [difference -11.5 percent, 95% CI -20.5 to -2.5]). Rates of resistance to amoxicillin-clavulanate within 5 days following completion of antibiotics (1.4 versus 4.3 percent) and within 30 days (1.4 versus 0 percent) were similar. This trial lends further support for a 5-day course of antibiotics to treat UTI when kidney involvement is not suspected. (See "Urinary tract infections in infants older than one month and children less than two years: Acute management, imaging, and prognosis", section on 'Preferred empiric oral regimens' .)
R21/Matrix-M vaccine to prevent malaria in children (November 2023, Modified February 2024)
In October 2023, the World Health Organization (WHO) approved the R21/Matrix-M vaccine for prevention of malaria in children [ 32 ]. In a placebo-controlled randomized trial of 4800 children (age 5 to 36 months) in four African countries, 12-month efficacy of a three-dose vaccine series against clinical malaria was 75 percent at sites with seasonal transmission and 68 percent at sites with year-round transmission [ 33,34 ]. The vaccine was well tolerated. Injection site pain and fever were the most frequent adverse events. Together with the RTS,S/AS01 vaccine (recommended by the WHO in 2021), this approval is expected to facilitate sufficient vaccine supply to benefit all children living in areas where malaria is a public health risk. (See "Malaria: Epidemiology, prevention, and control", section on 'R21/Matrix-M vaccine' .)
Nirsevimab to prevent severe respiratory syncytial virus in infants (January 2024)
Nirsevimab is a new antibody that prevents severe respiratory syncytial virus (RSV) infection in infants. In a trial conducted in France, Germany, and the United Kingdom, more than 8000 otherwise healthy infants ≤12 months, born at ≥29 weeks' gestation, and entering their first RSV season were assigned to receive one dose of nirsevimab or no intervention [ 35 ]. The group who received nirsevimab had fewer hospitalizations for RSV-associated lower respiratory tract infection (0.3 versus 1.5 percent, efficacy 83.2 percent, 95% CI 67.8-92.0) and fewer infants with an oxygen saturation <90 percent (0.1 versus 0.5 percent, efficacy 75.7 percent, 95% CI 32.8-92.9). These findings further support the use of nirsevimab for RSV immunoprophylaxis in infants. (See "Respiratory syncytial virus infection: Prevention in infants and children", section on 'Immunoprophylaxis' .)
Updated guidance for pneumococcal vaccination in children in the Unites States (October 2023)
The Centers for Disease Control and Prevention (CDC) has provided updated guidance for pneumococcal vaccination, endorsing use of either the 15-valent or 20-valent pneumococcal conjugate vaccine ( PCV15 or PCV20) for routine vaccination in infancy and childhood [ 36 ]. The primary vaccine schedule otherwise remains unchanged. For infants who previously received the 13-valent vaccine ( PCV13 ), the series may be completed with PCV15 or PCV20; restarting the series is not necessary. Children with high-risk conditions( table 1 1) may require additional pneumococcal vaccination with either PCV20 or the polysaccharide vaccine ( PPSV23 ) after age two years if their primary series did not include at least one dose of PCV20. We agree with the updated CDC guidance. Guidelines for pneumococcal vaccination in other countries may differ. (See "Pneumococcal vaccination in children", section on 'In the United States' .)
Immunoprophylaxis for severe respiratory syncytial virus in infants (October 2023)
Nirsevimab is a new monoclonal antibody that targets the prefusion conformation of the respiratory syncytial virus (RSV) F glycoprotein [ 37 ]. It has a longer half-life than palivizumab , an existing antibody that requires five monthly injections to provide immunoprophylaxis against severe RSV infection. The efficacy and safety of nirsevimab were demonstrated in two randomized placebo-controlled trials, one involving 1490 infants ≥35 weeks' gestation and the other involving >1400 preterm infants (29 to <35 weeks' gestation) [ 38,39 ]. In both trials, a single intramuscular dose of nirsevimab lowered rates of RSV-related medical evaluation and hospital admissions for RSV. In line with American Academy of Pediatrics and United States Centers for Disease Control and Prevention guidance, we now recommend that infants <8 months old receive one dose of nirsevimab during their first RSV season if the birthing parent did not receive RSV vaccination between 32 and 36 weeks of gestation and at least 14 days prior to delivery. Palivizumab may be used in high-risk infants if nirsevimab is not available. (See "Respiratory syncytial virus infection: Prevention in infants and children", section on 'Immunoprophylaxis' .)
NEONATOLOGY
Neurodevelopmental effects of donor versus birth parent milk (March 2024)
For very low birth weight infants, feeding fortified human milk from the birth parent rather than preterm formula appears to have beneficial effects on cognitive development and significantly reduces the risk of necrotizing enterocolitis (NEC); whether cognitive benefits are seen with donor milk is unclear. In a randomized trial of 483 extremely preterm infants without access to birth parent milk that compared fortified donor milk with preterm formula during the birth hospitalization, individuals assigned to donor milk had similar cognitive development outcomes at approximately two years of age but had a lower risk of NEC during hospitalization (adjusted risk difference -5 percent) [ 40 ]. Despite the lack of benefit on cognitive outcomes, these findings support our suggestion to use fortified donor milk rather than preterm formula for very low birth weight infants without access to birth parent milk. (See "Human milk feeding and fortification of human milk for premature infants", section on 'Use of donor milk' .)
No benefit of early treatment of PDA in extremely preterm neonates (January 2024)
The optimal timing for intervention in extremely preterm (EPT) neonates with patent ductus arteriosus (PDA) is debated; some centers favor early pharmacologic treatment while others favor expectant supportive care initially. In a multicenter, placebo-controlled trial involving >650 EPT neonates with large PDA, early treatment with ibuprofen resulted in higher rates of PDA closure by three weeks of age, but it did not reduce mortality, moderate or severe bronchopulmonary dysplasia, or other neonatal morbidities [ 41 ]. Based on these findings and results from prior clinical trials, we suggest expectant supportive care for PDA rather than early pharmacologic therapy.(See "Patent ductus arteriosus (PDA) in preterm infants: Management and outcome", section on 'Comparison of approaches' .)
Delayed cord clamping in preterm births (December 2023)
Increasing evidence supports delaying cord clamping in preterm births. In an individual participant data meta-analysis of randomized trials of delayed versus immediate cord clamping at births <37 weeks (over 3200 infants), delaying cord clamping for >30 seconds reduced infant death before discharge (6 versus 8 percent) [ 42 ]. In a companion network meta-analysis evaluating the optimal duration of delay, a long delay (≥120 seconds) significantly reduced death before discharge compared with immediate clamping; reductions also occurred with delays of 15 to <120 seconds but were not statistically significant [ 43 ]. For preterm births that do not require resuscitation, we recommend delayed rather than immediate cord clamping. We delay cord clamping for at least 30 to 60 seconds as approximately 75 percent of blood available for placenta-to-fetus transfusion is transfused in the first minute after birth. (See "Labor and delivery: Management of the normal third stage after vaginal birth", section on 'Preterm infants' .)
Long-term neurodevelopmental outcomes for preterm infants receiving minimally invasive surfactant (November 2023)
The technique of administering surfactant via thin intratracheal catheter (called minimally invasive surfactant therapy [MIST]) to preterm neonates with respiratory distress syndrome reduces the risk of bronchopulmonary dysplasia (BPD), but the long-term impact is uncertain. In a recent follow-up report of a multicenter international trial, infants who received MIST had lower rates of hospitalization for respiratory illness at two years but similar neurodevelopmental outcomes compared with those in the control group [ 44 ]. These findings and results from prior trials suggest that MIST improves short- and long-term pulmonary outcomes (ie, reduced need for intubation, reduced incidence of BPD, and reduced respiratory illnesses during the first two years). However, these benefits may not translate into meaningful improvements in long-term neurodevelopmental outcomes. Nevertheless, we continue to use MIST in appropriate candidates given the demonstrated pulmonary benefits. (See "Respiratory distress syndrome (RDS) in preterm infants: Management", section on 'Minimally invasive surfactant therapy (MIST)' .)
NEPHROLOGY AND UROLOGY
Single versus divided doses of oral corticosteroids for nephrotic syndrome (March 2024)
Prednisone or prednisolone is the initial treatment of choice for children with idiopathic nephrotic syndrome (NS). In a randomized trial in 60 children with a first episode of NS, a single daily dose and divided-dose therapy both induced remission within six weeks in all participants [ 45 ]. Suppression of the hypothalamic-pituitary-adrenal axis after six weeks of therapy was more common in children treated with divided-dose therapy (100 percent) compared with those treated with single-dose therapy (83 percent). These findings support our practice of using single daily doses of prednisone for this condition. (See "Treatment of idiopathic nephrotic syndrome in children", section on 'Initial steroid course' .)
Serial amnioinfusions for bilateral renal agenesis (January 2024)
Bilateral renal agenesis (BRA) is incompatible with extrauterine life because prolonged oligohydramnios results in pulmonary hypoplasia, leading to postnatal respiratory failure. A prospective study (RAFT) assessed use of serial amnioinfusions to treat 18 cases of BRA diagnosed at <26 weeks of gestation [ 46 ]. Of the 17 live births, 14 survived ≥14 days and had placement of dialysis access, but only 6 survived to hospital discharge. Of the 4 children alive at 9 to 24 months of age, 3 had experienced a stroke and none had undergone transplant. These findings show that serial amnioinfusions for BRA mitigates pulmonary hypoplasia and increases short-term survival and access to dialysis; however, long-term outcome remains poor with no survival to transplantation. Serial amnioinfusions remain investigational and should be offered only as institutional review board-approved research. (See "Renal agenesis: Prenatal diagnosis", section on 'Investigative role of therapeutic amnioinfusion' .)
Nedosiran for primary hyperoxaluria type 1 (October 2023)
For children with primary hyperoxaluria type 1 (PH1), a rare inborn error of glyoxylate metabolism, treatment with lumasiran , an RNA interference agent (RNAi), in combination with standard care (hyperhydration, crystallization inhibitors, and/or pyridoxine supplements), reduces urinary oxalate excretion and progression to kidney failure. In a randomized trial that included 18 children and adults with PH1, subcutaneous injection of nedosiran , a new RNAi, significantly decreased urinary oxalate excretion and achieved sustained normal or near-normal excretion levels compared with placebo with no significant safety concerns [ 47,48 ]. Based upon these findings, nedosiran has been approved for treatment of PH1 by the US Food and Drug Administration. For patients with PH1, we recommend RNAi therapy (either nedosiran or lumasiran) in addition to other measures to reduce kidney calcium oxalate deposition. (See "Primary hyperoxaluria", section on 'Additional therapies for primary hyperoxaluria type 1' .)
Antibiotic prophylaxis for children with high-grade vesicoureteral reflux (October 2023)
The management of vesicoureteral reflux (VUR) varies. Children with high-grade VUR (grade III to V ( figure 1 )) typically receive antibiotic prophylaxis to prevent urinary tract infection (UTI). In a recent randomized, open-label trial in over 290 young infants (mean age 3 months, about 75 percent uncircumcised males) with high-grade VUR and no prior UTI, antibiotic prophylaxis (primarily amoxicillin-clavulanate ) over two years reduced the proportion of patients with a first symptomatic UTI compared with placebo (21 versus 36 percent, hazard ratio 0.55) [ 49 ]. Antibiotic resistance was more common in urine cultures obtained from children receiving prophylaxis. These findings confirm the benefit of antibiotic prophylaxis in young infants with high-grade VUR and no prior UTI. (See "Management of vesicoureteral reflux", section on 'Evidence' .)
Benign acute childhood myositis (January 2024)
Benign acute childhood myositis (BACM) is a self-limited syndrome associated with calf pain and creatinine kinase elevation, often following infection with influenza. In a retrospective study of 65 patients with BACM, the median age was 6.6 years and 66 percent of patients were male [ 50 ]. The most common symptoms were bilateral calf pain, refusal to walk, and diffuse weakness. The median creatinine kinase was 1827 U/L, which normalized after an average of seven days. Early recognition of this syndrome allows the clinician to avoid an unnecessary evaluation for other muscle diseases. (See "Overview of viral myositis", section on 'Benign acute childhood myositis' .)
Vamorolone for Duchenne muscular dystrophy (December 2023)
Glucocorticoid treatment with prednisone or deflazacort for Duchenne muscular dystrophy (DMD) is associated with improved motor function, but adverse effects include weight gain, slowing of growth, and bone loss. Vamorolone , a novel steroid, was designed to reduce adverse effects of glucocorticoid therapy for DMD. In the VISION-DMD trial, vamorolone treatment led to improvement on several motor outcomes compared with placebo, while efficacy was similar compared with prednisone [ 51 ]. Prednisone treatment (but not vamorolone) led to growth deceleration and bone biomarker abnormalities. Based on these findings, the US Food and Drug Administration approved vamorolone for children age ≥2 years with DMD [ 52 ]. We suggest glucocorticoid treatment for children with DMD and anticipate using vamorolone as an alternative to prednisone and deflazacort. (See "Duchenne and Becker muscular dystrophy: Glucocorticoid and disease-modifying treatment", section on 'Benefits of glucocorticoid therapy' .)
Acute encephalopathy with biphasic seizures and late reduced diffusion (November 2023)
Acute encephalopathy with biphasic seizures and late reduced diffusion (AESD) is a parainfectious syndrome characterized by presentation with febrile status epilepticus (FSE) followed by a brief seizure-free period before recurrence of seizures in clusters. In a retrospective study from Japan of 55 patients presenting with FSE, the development of AESD in 11 patients was associated with longer time from seizure onset to hospital arrival, presence of hypoxia, and later treatment with antiseizure medications [ 53 ]. These findings suggest that shortening the seizure duration by early effective treatment and preventing hypoxia during ambulance transportation might reduce the risk of AESD. (See "Clinical features and evaluation of febrile seizures", section on 'Acute encephalopathy with biphasic seizures and late reduced diffusion' .)
Expert panel on epilepsy with eyelid myoclonia (November 2023)
Epilepsy with eyelid myoclonia (EEM; Jeavons syndrome) is a female-predominant generalized epilepsy syndrome with onset from 3 to 12 years of age characterized by eyelid myoclonia, photosensitivity, and eye closure-induced seizures or paroxysms on electroencephalography (EEG). Recently, an international expert panel found a strong consensus that EEM is often underdiagnosed, that a correct diagnosis can only be made with EEG including photic stimulation, and that an earlier age at onset is associated with an increased risk of intellectual disability and drug-resistant epilepsy [ 54 ]. Management generally involves reducing exposure to provoking factors (eg, visual stimuli, various sources of natural and artificial light) and use of antiseizure medication such as levetiracetam or valproate [ 55 ]. (See "Photosensitive epilepsies", section on 'Epilepsy with eyelid myoclonia (Jeavons syndrome)' .)
New guidelines for the treatment of neonatal seizures (October 2023)
New guidelines from the International League Against Epilepsy (ILAE) recommend phenobarbital as first-line antiseizure medication (ASM) therapy for treating most etiologies of neonatal seizures [ 56 ]. The one exception is that sodium channel blockers ( phenytoin / fosphenytoin or carbamazepine ) are considered a first-line therapy for neonates with a channelopathy. Phenytoin, levetiracetam , midazolam , and lidocaine are considered second-line ASMs for infants who continue to have seizures despite first-line therapy. Our approach is in accordance with the ILAE guidelines. (See "Treatment of neonatal seizures", section on 'Phenobarbital for most etiologies' .)
Fatal immune reaction after gene therapy for Duchenne muscular dystrophy (September 2023)
Recombinant adeno-associated virus (rAAV) vectors used to deliver gene therapy can be associated with a risk of severe immune reactions. This was illustrated by a report of a 27-year-old patient with advanced Duchenne muscular dystrophy (DMD) and impaired cardiopulmonary function who was treated with a high dose of rAAV containing a CRISPR-based transgene designed to upregulate dystrophin [ 57 ]. After treatment, he developed worsening cardiac dysfunction, acute respiratory distress syndrome, and fatal cardiac arrest. Laboratory and postmortem studies suggested his death was due to an innate immune reaction. Further research to develop safer approaches and identify high-risk patients may help to mitigate the acute toxic effects of rAAV gene therapy. (See "Overview of gene therapy, gene editing, and gene silencing", section on 'Potential concerns with gene therapy' and "Duchenne and Becker muscular dystrophy: Glucocorticoid and disease-modifying treatment", section on 'Risk of immune reactions with AAV vectors' .)
Management of spinal deformities in children with NF1 (September 2023)
New consensus-based guidelines on the management of spinal deformities, including scoliosis in children with neurofibromatosis type 1 (NF1), have been published [ 58 ]. The guidelines recommend screening for spine deformity by physical examination at diagnosis and yearly thereafter. To limit radiation exposure in the pediatric population, diagnostic spine imaging is suggested only if clinical suspicion for a spinal abnormality arises from patient history or physical examination. Spinal tumor burden must be assessed preoperatively in any patient with NF1 undergoing surgery for scoliosis because instrumentation that impedes visualization of spinal tumors by magnetic resonance imaging is not recommended when spinal tumor burden is high. (See "Neurofibromatosis type 1 (NF1): Management and prognosis", section on 'Scoliosis' .)
- Joachim MR, Kuik ML, Krabak BJ, et al. Risk Factors for Running-Related Injury in High School and Collegiate Cross-country Runners: A Systematic Review. J Orthop Sports Phys Ther 2024; 54:1.
- Delmonico RL, Tucker LY, Theodore BR, et al. Mild Traumatic Brain Injuries and Risk for Affective and Behavioral Disorders. Pediatrics 2024; 153.
- Brenner JS, Watson A, COUNCIL ON SPORTS MEDICINE AND FITNESS. Overuse Injuries, Overtraining, and Burnout in Young Athletes. Pediatrics 2024; 153.
- Zhao D, Pan JK, Lin FZ, et al. Risk Factors for Revision or Rerupture After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis. Am J Sports Med 2023; 51:3053.
- Hoenig T, Eissele J, Strahl A, et al. Return to sport following low-risk and high-risk bone stress injuries: a systematic review and meta-analysis. Br J Sports Med 2023; 57:427.
- Pavlova AV, Shim JSC, Moss R, et al. Effect of resistance exercise dose components for tendinopathy management: a systematic review with meta-analysis. Br J Sports Med 2023; 57:1327.
- Ferraro SL, Batty M, Heyworth BE, et al. Acute Pelvic and Hip Apophyseal Avulsion Fractures in Adolescents: A Summary of 719 Cases. J Pediatr Orthop 2023; 43:204.
- Redline S, Cook K, Chervin RD, et al. Adenotonsillectomy for Snoring and Mild Sleep Apnea in Children: A Randomized Clinical Trial. JAMA 2023; 330:2084.
- Hotham J, Cannings-John R, Moore L, et al. Association of cannabis, cannabidiol and synthetic cannabinoid use with mental health in UK adolescents. Br J Psychiatry 2023; 223:478.
- Health Alert Network: High Blood Lead Levels in Children Consuming Recalled Cinnamon Applesauce Pouches. HAN00500. Centers for Disease Control and Prevention. . Atlanta, GA, November 13, 2023. https://emergency.cdc.gov/han/2023/han00500.asp?ACSTrackingID=USCDC_511-DM117142&ACSTrackingLabel=HAN%20500%20-%20General%20Public&deliveryName=USCDC_511-DM117142 (Accessed on November 14, 2023).
- Chen K, Ma Y, Bell ML, Yang W. Canadian Wildfire Smoke and Asthma Syndrome Emergency Department Visits in New York City. JAMA 2023; 330:1385.
- Ramanan AV, Quartier P, Okamoto N, et al. Baricitinib in juvenile idiopathic arthritis: an international, phase 3, randomised, double-blind, placebo-controlled, withdrawal, efficacy, and safety trial. Lancet 2023; 402:555.
- Li L, Zhu N, Zhang L, et al. ADHD Pharmacotherapy and Mortality in Individuals With ADHD. JAMA 2024; 331:850.
- Velez MP, Dayan N, Shellenberger J, et al. Infertility and Risk of Autism Spectrum Disorder in Children. JAMA Netw Open 2023; 6:e2343954.
- Khan AA, Brandi ML, Rush ET, et al. Hypophosphatasia diagnosis: current state of the art and proposed diagnostic criteria for children and adults. Osteoporos Int 2024; 35:431.
- Waibel M, Wentworth JM, So M, et al. Baricitinib and β-Cell Function in Patients with New-Onset Type 1 Diabetes. N Engl J Med 2023; 389:2140.
- Russell-Jones D, Babazono T, Cailleteau R, et al. Once-weekly insulin icodec versus once-daily insulin degludec as part of a basal-bolus regimen in individuals with type 1 diabetes (ONWARDS 6): a phase 3a, randomised, open-label, treat-to-target trial. Lancet 2023; 402:1636.
- Budesonide oral suspension. US Food & Drug Administration, approval letter. February 2024. https://www.accessdata.fda.gov/drugsatfda_docs/appletter/2024/213976Orig1s000ltr.pdf (Accessed on February 12, 2024).
- Budesonide oral suspension. United States Prescribing Information, February 2024. US Food & Drug Administration. https://www.accessdata.fda.gov/drugsatfda_docs/label/2024/213976s000lbl.pdf (Accessed on February 13, 2024).
- Lee CJ, Dellon ES. Real-World Efficacy of Dupilumab in Severe, Treatment-Refractory, and Fibrostenotic Patients With Eosinophilic Esophagitis. Clin Gastroenterol Hepatol 2024; 22:252.
- Panagiotakopoulos L, Sandul AL, DHSc, et al. CDC Recommendations for Hepatitis C Testing Among Perinatally Exposed Infants and Children - United States, 2023. MMWR Recomm Rep 2023; 72:1.
- Qi J, Tan F, Zhang L, et al. AAV-Mediated Gene Therapy Restores Hearing in Patients with DFNB9 Deafness. Adv Sci (Weinh) 2024; 11:e2306788.
- Lv J, Wang H, Cheng X, et al. AAV1-hOTOF gene therapy for autosomal recessive deafness 9: a single-arm trial. Lancet 2024.
- Bremova-Ertl T, Ramaswami U, Brands M, et al. Trial of N-Acetyl-l-Leucine in Niemann-Pick Disease Type C. N Engl J Med 2024; 390:421.
- Al-Samkari H, Shehata N, Lang-Robertson K, et al. Diagnosis and management of pyruvate kinase deficiency: international expert guidelines. Lancet Haematol 2024; 11:e228.
- Musallam KM, Barella S, Origa R, et al. Pretransfusion hemoglobin level and mortality in adults with transfusion-dependent β-thalassemia. Blood 2024; 143:930.
- O'Brien SH, Rodriguez V, Lew G, et al. Apixaban versus no anticoagulation for the prevention of venous thromboembolism in children with newly diagnosed acute lymphoblastic leukaemia or lymphoma (PREVAPIX-ALL): a phase 3, open-label, randomised, controlled trial. Lancet Haematol 2024; 11:e27.
- Oesterheld J, Ferguson W, Kraveka JM, et al. Eflornithine as Postimmunotherapy Maintenance in High-Risk Neuroblastoma: Externally Controlled, Propensity Score-Matched Survival Outcome Comparisons. J Clin Oncol 2024; 42:90.
- Takahashi S, Ishige T, Takizawa T. Methemoglobinemia Outbreak in a Neonatal ICU and Maternity Ward. N Engl J Med 2023; 389:2395.
- Moline HL, Tannis A, Toepfer AP, et al. Early Estimate of Nirsevimab Effectiveness for Prevention of Respiratory Syncytial Virus-Associated Hospitalization Among Infants Entering Their First Respiratory Syncytial Virus Season - New Vaccine Surveillance Network, October 2023-February 2024. MMWR Morb Mortal Wkly Rep 2024; 73:209.
- Montini G, Tessitore A, Console K, et al. Short Oral Antibiotic Therapy for Pediatric Febrile Urinary Tract Infections: A Randomized Trial. Pediatrics 2024; 153.
- WHO recommends R21/Matrix-M vaccine for malaria prevention in updated advice on immunization. World Health Organization, 2023. Available at: https://www.who.int/news/item/02-10-2023-who-recommends-r21-matrix-m-vaccine-for-malaria-prevention-in-updated-advice-on-immunization (Accessed on October 06, 2023).
- Datoo MS, Dicko A, Tinto H, et al. Safety and efficacy of malaria vaccine candidate R21/Matrix-M in African children: a multicentre, double-blind, randomised, phase 3 trial. Lancet 2024; 403:533.
- https://papers.ssrn.com/sol3/papers.cfm?abstract_id=4584076 (Accessed on October 06, 2023).
- Drysdale SB, Cathie K, Flamein F, et al. Nirsevimab for Prevention of Hospitalizations Due to RSV in Infants. N Engl J Med 2023; 389:2425.
- ACIP Updates: Recommendations for Use of 20-Valent Pneumococcal Conjugate Vaccine in Children - United States, 2023. MMWR Morb Mortal Wkly Rep 2023; 72:1072.
- FDA Approves New Drug to Prevent RSV in Babies and Toddlers. Press Release, US Food and Drug Administration, 2023. https://www.fda.gov/news-events/press-announcements/fda-approves-new-drug-prevent-rsv-babies-and-toddlers (accessed 10/4/23)
- Griffin MP, Yuan Y, Takas T, et al. Single-Dose Nirsevimab for Prevention of RSV in Preterm Infants. N Engl J Med 2020; 383:415.
- Hammitt LL, Dagan R, Yuan Y, et al. Nirsevimab for Prevention of RSV in Healthy Late-Preterm and Term Infants. N Engl J Med 2022; 386:837.
- Colaizy TT, Poindexter BB, McDonald SA, et al. Neurodevelopmental Outcomes of Extremely Preterm Infants Fed Donor Milk or Preterm Infant Formula: A Randomized Clinical Trial. JAMA 2024; 331:582.
- Gupta S, Subhedar NV, Bell JL, et al. Trial of Selective Early Treatment of Patent Ductus Arteriosus with Ibuprofen. N Engl J Med 2024; 390:314.
- Seidler AL, Aberoumand M, Hunter KE, et al. Deferred cord clamping, cord milking, and immediate cord clamping at preterm birth: a systematic review and individual participant data meta-analysis. Lancet 2023; 402:2209.
- Seidler AL, Libesman S, Hunter KE, et al. Short, medium, and long deferral of umbilical cord clamping compared with umbilical cord milking and immediate clamping at preterm birth: a systematic review and network meta-analysis with individual participant data. Lancet 2023; 402:2223.
- Dargaville PA, Kamlin COF, Orsini F, et al. Two-Year Outcomes After Minimally Invasive Surfactant Therapy in Preterm Infants: Follow-Up of the OPTIMIST-A Randomized Clinical Trial. JAMA 2023; 330:1054.
- Khan T, Akhtar S, Mukherjee D, et al. Single- versus Divided-Dose Prednisolone for the First Episode of Nephrotic Syndrome in Children: An Open-Label RCT. Clin J Am Soc Nephrol 2023; 18:1294.
- Miller JL, Baschat AA, Rosner M, et al. Neonatal Survival After Serial Amnioinfusions for Bilateral Renal Agenesis: The Renal Anhydramnios Fetal Therapy Trial. JAMA 2023; 330:2096.
- Baum MA, Langman C, Cochat P, et al. PHYOX2: a pivotal randomized study of nedosiran in primary hyperoxaluria type 1 or 2. Kidney Int 2023; 103:207.
- Manufacturer's prescibing information for RIFLOZA, October 2023. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/215842s000lbl.pdf (Accessed on October 08, 2023).
- Morello W, Baskin E, Jankauskiene A, et al. Antibiotic Prophylaxis in Infants with Grade III, IV, or V Vesicoureteral Reflux. N Engl J Med 2023; 389:987.
- Attaianese F, Costantino A, Benucci C, et al. Benign acute children myositis: 5 years experience in a tertiary care pediatric hospital. Eur J Pediatr 2023; 182:4341.
- Guglieri M, Clemens PR, Perlman SJ, et al. Efficacy and Safety of Vamorolone vs Placebo and Prednisone Among Boys With Duchenne Muscular Dystrophy: A Randomized Clinical Trial. JAMA Neurol 2022; 79:1005.
- Muscular Dystrophy Association-supported drug Agamree (vamorolone) approved for the treatment of Duchenne muscular dystrophy by the FDA. Available at: https://www.mda.org/press-releases/mda-supported-drug-agamree-vamorolone-approved-for-the-treatment-of-duchenne-muscular-dystrophy-by-the-fda (Accessed on December 07, 2023).
- Arai Y, Okanishi T, Kanai S, et al. Risk Factors of Prehospital Emergency Care for Acute Encephalopathy in Children With Febrile Status Epilepticus. Pediatr Neurol 2023; 147:95.
- Smith KM, Wirrell EC, Andrade DM, et al. Clinical presentation and evaluation of epilepsy with eyelid myoclonia: Results of an international expert consensus panel. Epilepsia 2023; 64:2330.
- Smith KM, Wirrell EC, Andrade DM, et al. Management of epilepsy with eyelid myoclonia: Results of an international expert consensus panel. Epilepsia 2023; 64:2342.
- Pressler RM, Abend NS, Auvin S, et al. Treatment of seizures in the neonate: Guidelines and consensus-based recommendations-Special report from the ILAE Task Force on Neonatal Seizures. Epilepsia 2023; 64:2550.
- Lek A, Wong B, Keeler A, et al. Death after High-Dose rAAV9 Gene Therapy in a Patient with Duchenne's Muscular Dystrophy. N Engl J Med 2023; 389:1203.
- Xu AL, Suresh KV, Gomez JA, et al. Consensus-Based Best Practice Guidelines for the Management of Spinal Deformity and Associated Tumors in Pediatric Neurofibromatosis Type 1: Screening and Surveillance, Surgical Intervention, and Medical Therapy. J Pediatr Orthop 2023; 43:e531.
Skip to content
Neonatology Research
Division of neonatology.
The Division of Neonatology has a robust research program that focuses on several key areas: understanding the fundamental biology of preterm birth and its complications, meticulously testing new therapeutics in newborns through expertly designed clinical trials, developing new knowledge about risk factors for poor outcomes in sick neonates through rigorous observational studies, and developing new understanding of the social and medical impact of the organization and economy of healthcare delivery structures on maternal and child health. In addition, the Division also serves as a national leader in the development and conduct of multicenter and single-center clinical trials. As a member of the National Institute of Child Health and Human Development’s Neonatal Research Network, the Division is at the forefront of academic centers in clinical and epidemiological research in the United States.
The Division has recognized strength in neonatal follow-up and outcomes research; laboratory research into the fetal origins of adult disease, the causes of preterm birth and fetal growth restriction, inflammatory lung diseases, and drug discovery for rare genetic diseases; and research in neonatal infectious disease, antibiotic stewardship, and the microbiome and its impact of long-term health.
In collaboration with CHOP’s Research Institute , we oversee the work of more than 150 investigators pursuing hundreds of active research projects.
Division of Neonatology Areas of Research
Children's environmental health.
- Rebeccca A. Simmons, MD
- Colin Conine, PhD
- Scott Gordon, MD, PhD
- Heather H. Burris, MD
- Scott A. Lorch, MD, MSCE
Clinical Trials/Neonatal Research Network
- Eric C. Eichenwald, MD
- Sara B. DeMauro, MD, MSCE
- Erik Jensen, MD, MSCE
Developmental Origins of Health and Disease
Fetal/Neonatal Lung Disease
- Krithika Lingappan, MD, PhD, MS
- G. Scott Worthen, MD
- Shaon Sengupta, MBBS, MPH
- Danielle A. Callaway, MD, PhD
- Nicolas Bamat, MD, MSCE
March of Dimes Preterm Birth Research Center
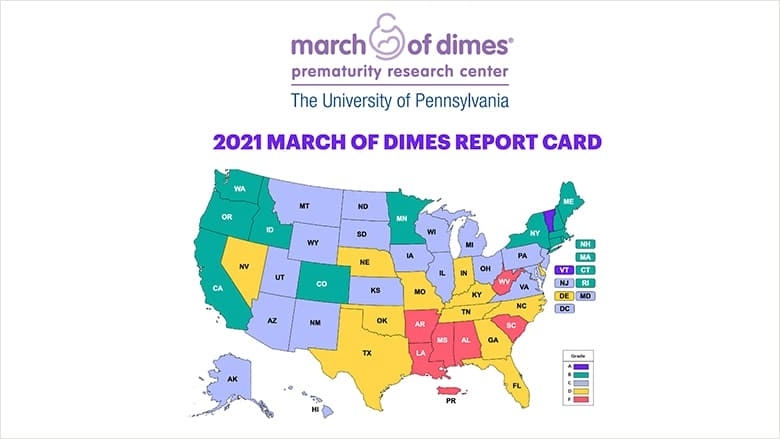
Neonatal Follow-Up/Long-Term Outcomes of Premature Birth
- Andrea F. Duncan, MD, MS
- Sara DeMauro, MD, MSCE
Neonatal Immunology and Infectious Disease
- Kathryn Rubey, MD
- Dustin D. Flannery, DO, MSCE
- Lakshmi Srinivasan, MD, FAAP
- Mary C. Harris, MD
- Karen M. Puopolo, MD, PhD
- Sagori Mukhopadhyay, MD, MMSc
- Carolyn McGann, MD
Neonatal Outcomes and Health Services Research
Health Policy
- Diana Montoya-Williams, MD
- Sara Handley, MD, MSCE
Racial/Ethnic Disparities
Quality of Care Assessment
Community Drivers of Outcomes
Hospital Characteristics and Systems
Resuscitation
- Heidi Herrick, MD
- Elizabeth E. Foglia, MD, MA, MSCE
You Might Also Like

Transforming Care for Extremely Premature Babies
CHOP researchers design a unique womb-like, fluid-filled environment to bridge critical time from mother’s womb to outside world.

Research on ECMO
Children’s Hospital of Philadelphia is advancing extracorporeal life support technologies for the most critically ill children.

Support for Short Bowel Syndrome Beyond the N/IICU
This case study highlights the care of an infant with necrotizing enterocolitis (NEC) that led to short bowel syndrome (SBS), one of the most devastating complications of prematurity.

Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches

12 templates

68 templates

el salvador
32 templates

41 templates
48 templates

33 templates
Neonatal ICU Medical Center
Neonatal icu medical center presentation, free google slides theme and powerpoint template.
Welcoming a newborn into the world should be a joyous occasion, but for some families, it can quickly turn into a worrisome experience. That's why Neonatal Intensive Care Units (NICUs) exist. If you're in charge of promoting your medical center, we have the perfect template for you. Our professional and elegant template is designed to showcase your center's services and help parents feel at ease. Filled with images and pictures that are related to the topic, this template is sure to catch the eye of those who need it most.
Features of this template
- 100% editable and easy to modify
- 35 different slides to impress your audience
- Contains easy-to-edit graphics such as graphs, maps, tables, timelines and mockups
- Includes 500+ icons and Flaticon’s extension for customizing your slides
- Designed to be used in Google Slides and Microsoft PowerPoint
- 16:9 widescreen format suitable for all types of screens
- Includes information about fonts, colors, and credits of the resources used
How can I use the template?
Am I free to use the templates?
How to attribute?
Attribution required If you are a free user, you must attribute Slidesgo by keeping the slide where the credits appear. How to attribute?
Related posts on our blog.

How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.

Premium template
Unlock this template and gain unlimited access

- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
The Research-Backed Benefits of Daily Rituals
- Michael I. Norton

A survey of more than 130 HBR readers asked how they use rituals to start their days, psych themselves up for stressful challenges, and transition when the workday is done.
While some may cringe at forced corporate rituals, research shows that personal and team rituals can actually benefit the way we work. The authors’ expertise on the topic over the past decade, plus a survey of nearly 140 HBR readers, explores the ways rituals can set us up for success before work, get us psyched up for important presentations, foster a strong team culture, and help us wind down at the end of the day.
“Give me a W ! Give me an A ! Give me an L ! Give me a squiggly! Give me an M ! Give me an A ! Give me an R ! Give me a T !”
- Michael I. Norton is the Harold M. Brierley Professor of Business Administration at the Harvard Business School. He is the author of The Ritual Effect and co-author of Happy Money: The Science of Happier Spending . His research focuses on happiness, well-being, rituals, and inequality. See his faculty page here .
Partner Center
Disclaimer » Advertising
- HealthyChildren.org
- Facebook Icon
- Twitter Icon
- LinkedIn Icon
Pediatric Care Online Webinars
Presentations from distinguished experts on important and timely topics in pediatrics.
Let’s Increase Vaccination Rates in Children: Updates to the 2023 Child and Adolescent Immunization Schedule
Henry (Hank) Bernstein, DO, MHCM, FAAP
In this webinar, Dr. Bernstein reviews the latest updates to the 2023 Recommended Childhood and Adolescent Immunization Schedule, discusses the update to COVD-19 vaccines for children, and highlights concern for vaccine hesitancy. View slide presentation
View Webinar
Time Stamps
2:08 - Review latest updates to the 2023 Recommended Childhood and Adolescent Immunization Schedule 28:16 - Update to COVID-19 vaccines for children 39:13 - Highlight concern for vaccine hesitancy
- AAP Policy Statement: Recommended Childhood and Adolescent Immunization Schedule: United States, 2023
- Immunization Schedules for 2023
- Red Book Online Immunization Strategies and Resources
What Makes Kids Tic: Tourette Syndrome, Tic Disorders & Tik Tok Tics
Jessica Goldstein, MD, FAAP | Jaclyn Martindale, DO
This webinar defines the term "tics" and discusses clinical criteria, pathophysiology, and comorbidities of tic disorders, as well as diagnostic work-up and management of a child presenting with tics. View slide presentation
February 2023
Hope on the horizon: emerging therapies for sma and dmd.
Ashutosh Kumar, MBBS, FAAP
In this webinar, Dr. Kumar discusses when to suspect and how to make the diagnosis of Spinal Muscular Atrophy (SMA) and Duchenne Muscular Dystrophy (DMD), as well as the natural history and treatment status of both. View slide presentation
October 2022
Management of hyperbilirubinemia in the newborn infant ≥35 weeks’ gestation: overview of the 2022 revised guideline.
Alex R. Kemper, MD, MPH, MS, FAAP | Thomas B. Newman, MD, MPH, FAAP
Dr. Kemper and Dr. Newman discuss the new 2022 AAP “Clinical Practice Guideline Revision: Management of Hyperbilirubinemia in the Newborn Infant 35 or More Weeks of Gestation” of which they are both authors. View slide presentation
Bridging the Gap: Practical Mental Health Interventions for Pediatric Clinicians
Rebecca Baum, MD, FAAP | Cody Hostutler, PhD | Jeff Shahidullah, PhD
In this webinar, the presenters discuss practical strategies to help pediatricians implement mental health care for their child and adolescent patients. View slide presentation
Seizure Rescue Medications
Rachel Gottlieb-Smith, MD, MHPE, FAAP
In this short webinar, Dr. Gottlieb-Smith describes when to prescribe and administer outpatient seizure rescue medications and compares three routes of administration: rectal, intranasal, and enteral. View slide presentation
December 2021
Long-term follow-up care for childhood, adolescent, and young adult cancer survivors.
Melissa M. Hudson, MD, FAAP
Melissa M. Hudson, MD, FAAP discusses how primary care pediatricians can efficiently access resources to guide them in providing evidence-based care for survivors of pediatric cancer. View slide presentation
Introducing the New Mental Health Clinical Support Chart
Jane Meschan Foy, MD, FAAP | Cori M. Green, MD, MS, FAAP
Dr. Foy and Dr. Green discuss care of common pediatric mental health problems within pediatric practice and use of a clinical support tool in decision-making about mental health care. View slide presentation
September 2021
Positional molding vs. craniosynostosis.
David Chesler, MD, PhD, FAANS, FAAP | Elias Rizk, MD, MSc, FAANS
In this webinar, Dr. Chesler and Dr. Rizk discuss positional molding and craniosynostosis, including: basic pathology underlying positional molding; treatment options for positional molding and when they should be employed; basic pathologies underlying nonsyndromic and syndromic craniosynostosis; circumstances and timing under which it is necessary and appropriate to refer for neurosurgical consultation; and treatment options for syndromic and nonsyndromic craniosynostosis and when they should be employed. View slide presentation
A Multidisciplinary Approach to Infants with GERD-like Symptoms: A New Paradigm
Mark Fishbein, MD, FAAP
Listen as Dr. Fishbein discusses a multidisciplinary approach to infants with gastroesophageal reflux disease (GERD)-like symptoms. Objectives of this webinar include: understanding GERD-like symptoms in infants; distinguishing GERD-like symptoms from GER and GERD; and recognizing the symptoms of dysphagia and colic and the role of therapy to address these conditions. View slide presentation
Acute Kidney Injury in Children
Brian Stotter, MD, FAAP
In this webinar, Dr. Stotter discusses how to formulate a differential diagnosis for causes of acute kidney injury (AKI) based on clinical and laboratory findings, as well as how to describe the initial management of AKI and recall the indications for renal replacement therapy. View slide presentation
Thank you for participating in the Pediatric Nephrology on the Go curriculum. We value your feedback—your responses to the following three surveys will assist the AAP Section on Nephrology (SONp) in assessing the impact of the presentation, improving the quality of the content, and identifying future topics to better serve you and the greater pediatrics community. The surveys should take 2–3 minutes each and your responses are confidential. Acute Kidney Injury in Children survey
Hematuria in Children
In this webinar, Dr. Stotter identifies the different causes of hematuria in children; evaluates the source of hematuria based on history, physical exam, and diagnostic studies; and distinguishes between isolated hematuria and hematuria associated with other renal and systemic manifestations that would require nephrology follow-up. View slide presentation
Hematuria in Children survey
Pediatric Hypertension
In this webinar, Dr. Stotter defines and confirms elevated blood pressure and hypertension in children; lists common causes of hypertension in children across different age ranges; and describes the diagnostic evaluation of a child presenting with suspected hypertension based on history and physical exam findings. View slide presentation
Pediatric Hypertension survey
Identifying Infants and Young Children With Developmental Disorders Through Developmental Surveillance and Screening
Paul H. Lipkin, MD, FAAP | Michelle M. Macias, MD, FAAP
Listen as Dr Lipkin and Dr Macias summarize the recommended steps for effective developmental surveillance and screening, identify components of developmental surveillance, and identify AAP partner initiatives and resources available to assist with implementation of developmental screening, referral, and follow-up. View slide presentation
Identification, Evaluation, and Management of Children with Autism Spectrum Disorder
Susan L. Hyman, MD, FAAP | Susan E. Levy, MD, MPH, FAAP
In this webinar, Dr. Hyman and Dr. Levy describe effective methods for screening and early identification of children with autism spectrum disorder (ASD) in primary care; report the components of diagnostic and etiologic evaluation of children with ASD; identify evidence-based interventions for the core deficits of ASD and associated co-occurring conditions; and report strategies to engage in shared decision-making and partnership with families/caregivers of children and youth with ASD. View slide presentation
November 2019
Introducing the new aap clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents.
Mark L. Wolraich, MD, FAAP | Joseph F. Hagan, Jr., MD, FAAP
In this webinar Dr Mark Wolraich and Dr Joseph Hagan, Jr. review the 2019 ADHD clinical practice guideline revision and its Key Action Statements; describe the clinical care algorithm for primary care management; and assess existing barriers to care. View slide presentation
August 2019
Confessions of a car seat junkie: what every pediatrician needs to know about child passenger safety.
Benjamin Hoffman, MD, FAAP, CPST-I
Listen as Dr. Hoffman discusses basic principles of child passenger safety (CPS) science (epidemiology, physics, anatomy and physiology of children, crash dynamics) and best practice recommendations for appropriate child passenger restraint); 5 ways car safety seats help prevent injury to children; and how to identify and access CPS resources, including for children with special health care needs. View slide presentation
Making Bright Futures Work! How Evidence, the Periodicity Schedule, and the Bright Futures Guidelines Impact Practice
Joseph F. Hagan, Jr., MD, FAAP
Learn how to use Bright Futures in practice as Dr. Hagan reviews new clinical content in the Bright Futures Guidelines and the associated Periodicity Schedule, and discusses how to use evidence to decide on content for your practice's health supervision visits and how to identify strategies, tools, and resources to maximize efficiency for health promotion and preventive services. View slide presentation
PPE: Preparticipation Physical Evaluation
David T. Bernhardt, MD, FAAP | William O. Roberts, MD, MS, FACSM, FAAFP
In this webinar, Dr. Bernhardt and Dr. Roberts discuss how to use the 5th edition of the Preparticipation Physical Examination (PPE) in practice, including justifying student athletes needing to undergo a PPE prior to participation in sports, understanding this is more than preventing sudden death or injury or filling out a waiver form, and that the medical home and the primary care provider are the ideal environment and provider for the PPE. View slide presentation
AAP Infantile Hemangioma Webinar
Ilona J. Frieden, MD, FAAP FAAD | Anthony J. Mancini, MD, FAAP, FAAD
View this webinar to increase your knowledge on how to risk-stratify infantile hemangiomas, understand the natural history of hemangiomas and how this affects referral and management, and increase your awareness of treatment options for infantile hemangiomas requiring treatment. View slide presentation
January 2019
Clinical practice guideline: maintenance intravenous fluids in children.
Leonard G. Feld, MD, PhD, MMM, FAAP | Michael L. Moritz, MD, FAAP | Matthew D. Garber, MD, FHM, FAAP | Sahar N. Rooholamini, MD, MPH, FAAP
Drs Leonard G. Feld, Michael L. Moritz, and Matthew D. Garber, on behalf of the AAP Subcommittee on Fluid and Electrolyte Therapy, discuss the new AAP guideline "Clinical Practice Guideline: Maintenance Intravenous Fluids in Children." During this webinar, the presenters review the following topics: definitions; objective; background; methods; results; and conclusions and limitations. View slide presentation
Guidelines for Adolescent Depression in Primary Care: Navigating the GLAD-PC Recommendations and Toolkit
Rachel A. Zuckerbrot, MD, FAAP | Nerissa S. Bauer, MD, MPH, FAAP
In this webinar, Rachel Zuckerbrot, MD, FAAP and Nerissa Bauer, MD, MPH, FAAP review the recently published Guidelines for Adolescent Depression in Primary Care (GLAD-PC): Part I. Practice Preparation, Identification, Assessment, and Initial Management and Part II. Treatment and Ongoing Management, and the GLAD-PC Toolkit. View slide presentation
September 2018
Pediatric headache.
Robert C. Stowe, MD | Irene R. Patniyot, MD
Listen to a short review of an effective history and physical in a patient presenting with headache as described through a trainee and expert discussion. View slide presentation
August 2018
Symptomatic gastroesophageal reflux in the preterm infant: fantasy or real.
Eric C. Eichenwald, MD, FAAP
Dr. Eric Eichenwald discusses symptomatic gastroesophageal reflux (GER) in the preterm infant. In this webinar. Dr. Eichenwald identifies the pathophysiology and effects of treatment of GER in the preterm infant; discusses diagnostic modalities for GER; and explains the possible causal relationship of GER and apnea of prematurity. View slide presentation
January 2018
Working together to reduce infant sleep-related deaths: what you need to know now.
Michael Goodstein, MD, FAAP
In this webinar, Dr. Goodstein discusses sleep safety for infants and helps viewers to understand the definition of SUID and SIDS; be familiar with statistics on SIDS and accidental sleep deaths; be aware of the basic pathophysiology of SIDS; be able to engage families for education on the 2016 AAP recommendations on SIDS risk reduction and suffocation prevention; and realize the importance of safe sleep modeling and education in the hospital setting. View slide presentation
December 2017
Neonatal abstinence syndrome.
Jatinder Bhatia, MD, FAAP
Listen as Jatinder Bhatia, MD, FAAP discusses neonatal abstinence syndrome, covering definition, incidence, commonly used/abused drugs, signs and symptoms, complications, testing, and prevention and treatment. View slide presentation
November 2017
2017 aap guidelines for childhood hypertension.
Joseph T. Flynn, MD, MS, FAAP
Dr. Flynn discusses changes to the new American Academy of Pediatrics childhood hypertension guideline and how these changes will affect the management of children and adolescents with high blood pressure. View slide presentation
September 2017
Addressing early childhood emotional and behavioral problems in primary care.
Mary Margaret Gleason, MD, FAAP
In this webinar, Dr. Gleason discusses the following objectives: familiarity with the prevalence of early childhood mental health concerns; recognition of screening tools and the rationale for their use; and familiarity with Common Factors approaches to early childhood mental health in primary care. View slide presentation
Mind-Body Therapies in Children and Youth
Hilary McClafferty, MD, FAAP | Timothy Culbert, MD, FAAP | Lawrence Rosen, MD, FAAP
Drs. McClafferty, Culbert, and Rosen, members of the AAP Section on Integrative Medicine, discuss the concept of mind-body therapies, mind-body therapies as part of an appropriate treatment plan for children with behavioral and medical issues, yoga, biofeedback, guided imagery, meditation, and hypnosis for pediatric patients, and where to get further training in mind-body therapies. View slide presentation
December 2016
Providing evidence-based medical care to immigrant children.
Janine Young, MD, FAAP | Julie M. Linton, MD, FAAP
Drs Janine Young and Julie Linton discuss providing evidence-based medical care to immigrant children. Specifically, they review pertinent background regarding the care of immigrant children and recommendations regarding comprehensive medical evaluation of newly arriving immigrant children, in addition to identifying strategies to integrate care of immigrant children into a family-centered medical home. View slide presentation
November 2016
Infantile spasms.
Mary L. Zupanc, MD, FAAP
In this webinar, Dr. Mary Zupanc discusses the causes of infantile spasms and the importance of early recognition. She also explains the differences between infantile spasms and febrile seizures. View slide presentation
August 2016
Poverty and child health in the united states: strategies to lessen the stress.
James Duffee, MD, MPH, FAAP
Describe the epidemiology of child poverty in the U.S.; trends in health disparities; connection between early childhood adversity and lifelong health; apply family-centered, trauma-informed care elements; screen for social determinants of health; and identify strategies for prevention and early intervention. View slide presentation
Rescue Medication and Seizure Emergency Planning in Education Settings
Sarah Doerrer, CPNP
Learn about seizure emergency and school action plans, medications and considerations, IEP and 504 plans, and community resources to help parents with medical care in their child's school. View slide presentation
Brief Resolved Unexplained Events
Joel S. Tieder, MD, MPH, FAAP
Learn historical framework and epidemiology, ALTE vs. BRUE terminology, event characterization, risk stratification, new recommendations, and tools to implement practice change. View slide presentation
December 2015
High-risk newborns and nutrition.
Understand global incidence and long-term consequences of prematurity and the associate morbidity and mortality; as well as the rationale for aggressive early and sustained nutritional goals and choice of feeding in the hospital and post-discharge. View slide presentation
Care of Infants with Bronchopulmonary Dysplasia
This webinar defines bronchopulmonary dysplasia (BPD), lists the risk factors, identifies current strategies to prevent and manage BPD, and discusses the implications for practicing pediatricians. View slide presentation
January 2015
Evaluating failure to thrive: a growing body of evidence.
Joyee G. Vachani, MD, M.Ed | Maria R. Mascarenhas, MBBS
Apply evidence in the literature on Failure to Thrive (FTT) patients on admission criteria, growth assessment, utilization of laboratory data, and discharge criteria; discuss quality metrics, including cost data, to provide improvement opportunities for the hospitalist; and integrate a systematic approach to the differential diagnosis and management algorithm for FTT into practice. View slide presentation
December 2014
Quality improvement charts.
Sanjay Mahant, MD, FRCPC, MSc
Understand the basic anatomy of charts used in quality improvement (QI), specifically run charts and process control charts, as well as some of the basics to interpreting QI charts. View slide presentation
August 2014
Medical management of the pediatric spinal fusion patient.
Erin Shaughnessy, MD, FAAP
This webinar explains the role of the pediatric hospitalist in co-managing spinal fusion patients; describes three common medical complications following spinal fusion surgery; and discusses two approaches to prevent respiratory and gastrointestinal complications in the postoperative period. View slide presentation
ACL Injuries: Diagnosis, Treatment and Prevention
Cynthia R. LaBella, MD, FAAP | William Hennrikus, MD, FAAP | Timothy E. Hewett, PhD, FACSM
Discusses epidemiology, injury mechanisms, risk factors, diagnosis, treatment, and prevention of ACL injuries. View slide presentation
December 2013
Returning to learning following a concussion.
Mark Halstead, MD, FAAP | Cynthia Di Laura Devore, MD, FAAP | Karen McAvoy, PsyD
Understand background, signs/symptoms of concussion, Return to Learning Team Concept, strategies, readiness assessment, and assistance with prolonged symptoms
Diagnosis and Management of Acute Bacterial Sinusitis in Children: 2013 Guideline from the AAP
Ellen R. Wald, MD, FAAP
Understand updates from 2001 guideline; including worsening course, effectiveness of antibiotics, observation, and diagnosis without imaging
AAP Clinical Practice Guideline: Management of Newly Diagnosed Type 2 Diabetes Mellitus in Children and Adolescents
Janet Silverstein, MD | Kenneth C. Copeland, MD
Case–based exploration of diagnosis, treatment, and management clinical practice guidelines.
November 2012
Sport–related concussions in children and adolescents: what you need to know.
Mark Halstead, MD, FAAP
Understand epidemiology, in–office evaluation, the role of computerized neurocognitive assessment, and appropriate return to play protocols
Type 1 and Type 2 Diabetes in Children and Youth: What’s New and What’s True
Francine Ratner Kaufman, MD, FAAP
Learn genetic and environmental contributions to diabetes, prevention strategies, new treatment options, and challenges
New National Heart Lung and Blood Institute (NHLBI) Expert Panel Guidelines for Cardiovascular Health and Risk Reduction in Childhood
Rae-Ellen W. Kavey, MD, MPH, FAAP
Discuss the evidence base and review process behind the 2011 guidelines, new evidence-based dietary recommendations for cardiovascular health, lipid screening and management, and risk factor-specific information
Fever and Antipyretic Use in Children
Janice E. Sullivan, MD
Reviews the primary concerns regarding fever and the treatment goals for a febrile child, as well as discusses the parental educational opportunities regarding fever, illness, and medication practices.
Advertising Disclaimer »
Affiliations
- Editorial Board
- Residents and Medical Students Subscriptions
- Online ISSN 2767-6617
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations, advertising.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account
- Environment
How does Tampa Bay fare with ‘kitten season’?
- Hannah Farrow Times staff
It’s the time of year when animal shelters are inundated with cats: pregnant cats, baby cats, hormonal cats.
Aka, kitten season.
“Spring and summer are the classical times for shelters getting overwhelmed with kittens that need homes,” said Julie Levy, a professor of shelter medicine at the University of Florida College of Veterinary Medicine, in an email to the Tampa Bay Times.
Felines start going into heat in January as daylight begins to linger longer, and pregnancy rates peak in March. Cats give birth nine weeks after fertilization, and they can have multiple pregnancies in one year, meaning spring and summer months welcome a plethora of kittens.
The spike in births causes animal shelters to be flooded with cats, and many can’t keep up; there are too many cats and not enough adopters, said Sherry Silk, CEO of the Humane Society of Tampa Bay.
“It’s a terrible time of year for animal shelters,” Silk said. “It really is.”
One solution many shelters implement is a trap, neuter, vaccinate and return program for feral cats. People in the community can safely trap a cat, bring it to a shelter where a veterinarian will sterilize and vaccinate it, and the cat can be adopted out or returned to where it was found. This process helps cut down on feral cats, but it only scratches the surface, according to Silk.
As summer months near and kitten season approaches its peak, here are a few things to know about how to handle feral felines.
How do feral cats affect Tampa Bay’s ecosystems?
A single free-ranging cat may kill 100 or more birds and mammals per year, making them a major threat to native wildlife, according to the Florida Fish and Wildlife Conservation Commission .
These cats are also known to spread disease, including toxoplasmosis, which can kill other mammals.
While the wildlife commission doesn’t play a major role in handling the populations, its policy is “to protect native wildlife from predation, disease and other impacts presented by feral and free-ranging cats.”
The agency’s website says not to feed outdoor cats, yet Silk encourages people to put out food.
“If their tummies are full because someone puts out a bowl of food for them every night … and they don’t have the hormones racing through, they’re much less likely to kill birds,” Silk said.
But “it’s more complicated” than that, said Grant Sizemore, the director of invasive species programs at the American Bird Conservancy, a nonprofit that conserves wild birds and their habitats.
Keep up with Tampa Bay’s top headlines
Subscribe to our free DayStarter newsletter
You’re all signed up!
Want more of our free, weekly newsletters in your inbox? Let’s get started.
Anyone who’s played with a cat — like with a feather toy or fake mice — knows that cats engage in predatory behaviors. “We call it play,” Sizemore said.
Wild cats engage in the same behavior, except instead of toy mice and birds, they attack living wildlife, Sizemore said.
Does climate play any role in kitten season?
Kitten births are controlled by daylight, not temperature, said UF’s Levy. Still, she said, climate plays a role.
Warm weather brings more people outside — which creates opportunities for more interactions between humans and cats — and encourages more cats to wander out in public spaces, Levy said.
It also enhances the chances that kittens survive.
A newborn litter that loses its mother doesn’t have a high chance of surviving on its own, according to Jasmine Simmons, a veterinarian for Hillsborough County Pet Resource Center.
“Kittens are extremely fragile,” Simmons said. “They don’t do a great job, like most mammals do, of being able to produce their own body heat. So even in Florida, even in the hottest temperatures, they can still sometimes get too cold.”
The shelter has multiple incubators and other warming devices to keep the kittens alive.
What role do Tampa Bay shelters play?
Since the implementation of the Humane Society of Tampa Bay’s trap, neuter, vaccinate and return program in 2007, Silk estimates the shelter has spayed and neutered over 87,000 feral cats. People in the area today can bring feral cats to the shelter’s two surgeons, who sterilize about 100 cats every week.
“You would think with that many cats being spayed or neutered, we would have this under control,” Silk said. “But it’s not. It’s getting worse each and every year.”
Silk said her shelter sees many cats who’ve been abandoned by people who move away.
“For whatever reason, when they think of moving, whether it’s across town or out of state, they’ll take the family dogs, but they will leave the cat behind,” Silk said.
A similar pattern happens at Hillsborough County’s shelter, where doctors spay and neuter five times a week. Simmons said it takes about 30 seconds to neuter a male cat, as it’s a minimally invasive surgery, and three to four minutes to spay a female cat. (Simmons’ record is 52 sterilizations in one day.)
Last week, just a few adult cats were in the “cat condos” when you first entered the shelter, available for adoption, and a 2-day-old litter was in one of the incubators in the back, keeping warm. While it felt empty, Simmons said this is just the beginning.
“Right now, we’re still ahead of it,” Simmons said. “Once it gets to be in the heat of kitten season, it’s going to be absolutely full.”
Last summer, the shelter reached 500% capacity.
What to do if you encounter cats in the wild?
When encountering a feral feline, check to see if one of its ears is clipped, an international sign that a cat has been vaccinated and sterilized, Silk said. And if you’d like to trap a cat to have it spayed or neutered, the Humane Society rents live traps for $5, and they’ll show you how to use it.
But no matter how much you want to help the little creatures out, the best care for them is to keep litters with their moms, Simmons said.
“They require very, very tailored care. And the best to provide that care is their mom,” Simmons said. ”Although that may seem a little bit alarming to people, it’s better not to just go and grab that litter of kittens, because you’re probably stealing them from mom, who’s doing an amazing job taking care of them, and giving them things that we never can.”
Hannah Farrow is a newsletter and social media producer. You can reach her at [email protected].
MORE FOR YOU
- Advertisement
ONLY AVAILABLE FOR SUBSCRIBERS
The Tampa Bay Times e-Newspaper is a digital replica of the printed paper seven days a week that is available to read on desktop, mobile, and our app for subscribers only. To enjoy the e-Newspaper every day, please subscribe.

IMAGES
VIDEO
COMMENTS
Our suggested format for both admit and progress notes is presented on this page. 2/9/08 08:15. MS Admission Note. ID: 12 hour old term newborn. HPI: Baby Boy Brown was born at 39+3 weeks by NSVD to a 27yo G3P1011 mom with prenatal labs O+, Ab screen -, HBsAg-, VDRL non-reactive, GC/CT - , HIV -, PPD+/CXR-.
The neonatal period. 5 Topics. TeachMe Paediatrics. Part of the TeachMe Series. The medical information on this site is provided as an information resource only, and is not to be used or relied on for any diagnostic or treatment purposes. This information is intended for medical education, and does not create any doctor-patient relationship ...
Nonimmune hydrops fetalis in the neonate: Causes, presentation, and overview of neonatal management. View in. Overview of the routine management of the healthy newborn infant. View in Prenatal substance exposure and neonatal abstinence syndrome (NAS): Management and outcomes ... Neonatal screening. Newborn screening for critical congenital ...
Erythema toxicum is a benign, self-limiting skin condition categorised by small erythematous papules, vesicles and pustules. It affects 30-70% of newborns, typically within the first two weeks of birth. 32 Erythema toxicum can be differentiated from an infective rash by its tendency to wax and wane over several days.
Selected Topics in Neonatal Care. Edited by: R. Mauricio Barría. ISBN 978-1-78923-362-9, eISBN 978-1-78923-363-6, PDF ISBN 978-1-83881-248-5, Published 2018-06-27. Neonatology is one of the areas of greatest development and evolution within pediatrics. The technoscientific advances in this area have led to an increase in the survival of ...
Neonatal Quality at Hot Topics is a one-day conference focused on quality improvement and patient safety in neonatology. Didactic presentations, panel discussions, and interactive workshops will showcase best practices in newborn care, and will offer a pragmatic approach to using quality methods and tools to improve newborn outcomes.
Chapter 16: The Nursing Role in Providing Comfort During Labor and Birth, PowerPoint Presentation; Chapter 17: Nursing Care of a Postpartal Family, PowerPoint Presentation; Chapter 18: Nursing Care of a Family With a Newborn, PowerPoint Presentation; Chapter 19: Nutritional Needs of a Newborn, PowerPoint Presentation
The Neonatal Intensive Care Unit (NICU) The birth of a baby is a wonderful and very complex process. Many physical and emotional changes occur for both mother and baby. A baby must make many physical adjustments to life outside the mother's body. Leaving the uterus means that a baby can no longer depend on the mother's blood supply and placenta ...
Initially, neonates have thick, dark green-black meconium stools. By day of life 2-4, the stools start to transition. Breastfed infants' stools are yellow, seedy, and runny, and breastfed infants often stool six or more times a day, sometimes after every feed. Parents may mistake this normal stool pattern for diarrhea.
Every Newborn: an action plan to end preventable deaths is a global initiative that aims to save millions of lives by improving the quality and coverage of newborn care. This powerpoint presentation summarizes the key findings and recommendations of the Every Newborn Lancet series, which provides the latest evidence and analysis on the global burden, causes, and interventions for newborn ...
This comprehensive online NICU education program ensures learners receive evidence-based, standardized education focused on the specifics of neonatal care. Help your NICU clinicians develop the clinical judgement to manage and deliver quality care to their patients. NICU Library courses. Advanced Concepts in Respiratory Physiology
Neonatology/Newborn Issues. This collection features the best content from AFP, as identified by the AFP editors, on neonatology and newborn issues and related topics, including breastfeeding ...
Chapter 10: Nursing Care during Labor and Birth, PowerPoint Presentation; Chapter 11: Assisted Delivery and Cesarean Birth, PowerPoint Presentation; Chapter 12: The Postpartum Woman, PowerPoint Presentation; Chapter 13: Nursing Assessment of Newborn Transition, PowerPoint Presentation; Chapter 14: Nursing Care of the Normal Newborn, PowerPoint ...
Care of the Newborn. Common Physiologic problems in the Newborn. Hearing Screening in NICU Graduates. Hypocalcemia in Neonates. Kernicterus. Necrotizing Enterocolitis (NEC) Neonatal Apnea. Neonatal Respiratory Distress and treatment modalities. Neonatal Resuscitation.
10.1016/j.nwh.2019.04.002; nwhjournal.org. e23. Acknowledgements. Neonatal Nursing: Clinical Competencies and Education Guide (7th ed.) has been reviewed by members the Association of Women's Health, Obstetric and Neonatal Nurses (AWHONN). These reviewers were selected because of their expertise in neonatal care, nursing education, or ...
Background: Newborn babies are very vulnerable in their first weeks of life. Timely and appropriate management of neonatal conditions is paramount for health and developmental outcomes. Objective: The aim of this article is to provide an overview of common neonatal presentations to general practice, and highlight significant conditions that may require referral to the emergency department and ...
The American Academy of Pediatrics has issued a new clinical report that reviews the medical literature about these conditions and summarizes key findings pertaining to risk factors, clinical presentation, and prevention . The report emphasizes the importance of achieving a healthy balance between stress and recovery.
Division of Neonatology. 20 Locations. Contact Us. 215-590-1653. Referrals. 215-590-3083. Physicians and scientists from the Division of Neonatology at The Children's Hospital of Philadelphia continue to lead basic and clinical research into many conditions affecting newborns and infants.
Explores the field of fetal and neonatal medicine, aiming for reports that provide a valid and clear message for scientists and clinicians. ... Research Topics; Type at least 3 characters 118 Research Topics Guest edit your own article collection Suggest a topic. Submission.
This resource is a learning module featuring three multistep cases covering common neonatal presentations that medical students may encounter. The cases are focused on the topics of neonatal jaundice, vomiting in an infant, and copious secretions in a newborn. Each case works through the appropriate management, diagnosis, and treatment of the ...
Neonatal ICU Medical Center Presentation . Medical . Free Google Slides theme and PowerPoint template . Welcoming a newborn into the world should be a joyous occasion, but for some families, it can quickly turn into a worrisome experience. ... Filled with images and pictures that are related to the topic, this template is sure to catch the eye ...
Pictures: Pictures can communicate complex ideas quickly and memorably but choosing the right images is key. Images or pictures should be big (perhaps 20-25% of the page), bold, and have a clear ...
The authors' expertise on the topic over the past decade, plus a survey of nearly 140 HBR readers, explores the ways rituals can set us up for success before work, get us psyched up for ...
Presentations from distinguished experts on important and timely topics in pediatrics. March 2023 Let's Increase Vaccination Rates in Children: Updates to the 2023 Child and Adolescent Immunization Schedule Henry (Hank) Bernstein, DO, MHCM, FAAP In this webinar, Dr. Bernstein reviews the latest updates to the 2023 Recommended Childhood and Adolescent Immunization Schedule, discusses the ...
Housing is one of the most common non‐wage benefits provided to workers on dairy farms (Dairy Farmer Survey, n=71, 2018) Latino Workers. 100% received housing and utilities. US Workers. Housing provided by 62% of farms, Utilities provided by 53% of farms. Housing options differ for US worker compared to migrant dairy farmworkers.
Aka, kitten season. "Spring and summer are the classical times for shelters getting overwhelmed with kittens that need homes," said Dr. Julie Levy, a professor of shelter medicine at the ...