tableau.com is not available in your region.

Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
- Starting the research process
- What Is Root Cause Analysis? | Definition & Examples
What Is Root Cause Analysis? | Definition & Examples
Published on January 6, 2023 by Tegan George . Revised on November 17, 2023.
Root cause analysis is a problem-solving approach that uses the analogy of roots and blooms to model cause-and-effect relationships. Rather than focusing on what’s above the surface, root cause analysis troubleshoots solutions to problems by analyzing what is causing them. Note Similarly to exploratory research , it’s important to remember that root cause analysis does not provide solutions to problems. Rather, it’s one method within a larger problem-solving landscape.
Root cause analysis is a form of quality management, often used in organizational management, quality control, and in healthcare fields like nursing. Root cause analysis can be a helpful study tool for students, too, when used for brainstorming or memorization exercises.
Table of contents
Root cause analysis template, the “5 whys” of root cause analysis, advantages and disadvantages of root cause analysis, other interesting articles, frequently asked questions.
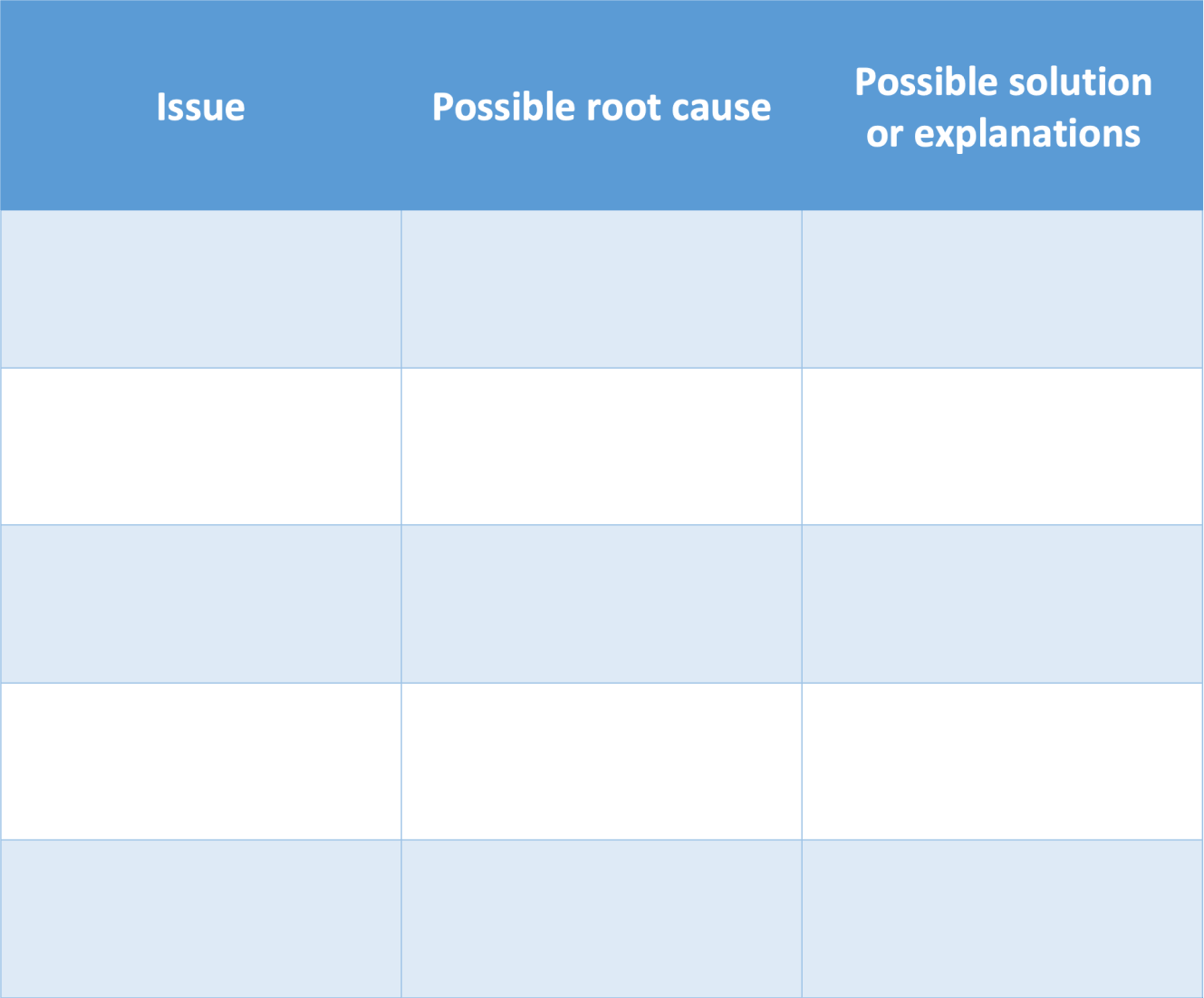
It’s easy to draw root cause analysis charts by hand, on a whiteboard or a big piece of paper. Many people use fishbone diagrams as well, or you can download our template below.
Here's why students love Scribbr's proofreading services
Discover proofreading & editing
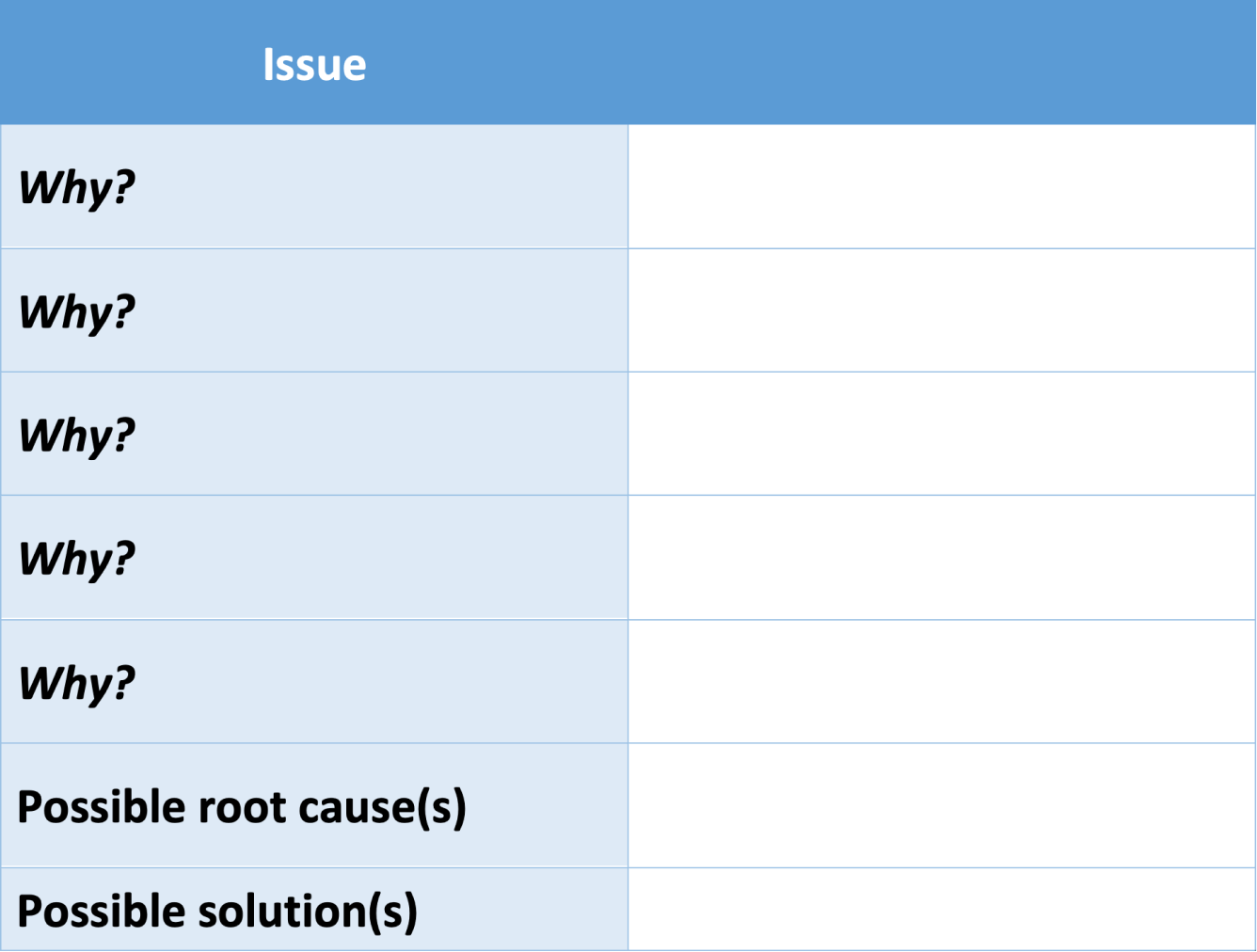
One of the most common ways to conduct root cause analysis is using the “5 Whys” method, popular in lean management. The 5 Whys are an interconnected method of analysis: after defining your problem, you ask “why?” and answer as concisely as possible. The first “why” often leads to the second, which leads to the third, etc.
In short, you continue to ask “why” until the answer provided is no longer a contributor to the broader issue, but a possible solution to that issue. In other words, as you strategize, you’ll sense it’s time to stop when a provided answer has the potential to stop the whole problem from occurring, rather than only one aspect of that problem. This often takes 3-5 “whys” but can definitely stretch out for longer.
You can use this template to map out your whys.
Root cause analysis is a great way to organize your thoughts, but its simplicity leads to a few downsides.
- Great brainstorming tool for individual or group projects.
- Can help identify causal relationships and clarify relationships between variables .
- “5 whys” system can help simplify complex issues and drive possible solutions.
Disadvantages
- Can be overly simplistic, not leaving much room for nuance or variations.
- Path dependence can occur if the wrong question is asked, leading to incorrect conclusions.
- Cannot provide answers, only suggestions, so best used in the exploratory research phase .
If you want to know more about the research process , methodology , research bias , or statistics , make sure to check out some of our other articles with explanations and examples.
Methodology
- Sampling methods
- Simple random sampling
- Stratified sampling
- Cluster sampling
- Likert scales
- Reproducibility
Statistics
- Null hypothesis
- Statistical power
- Probability distribution
- Effect size
- Poisson distribution
Research bias
- Optimism bias
- Cognitive bias
- Implicit bias
- Hawthorne effect
- Anchoring bias
- Explicit bias
Prevent plagiarism. Run a free check.
There are several common tools used for root cause analysis , the most popular of which include fishbone diagrams , scatterplots, and the “5 whys.”
A fishbone diagram is a method that can be used to conduct root cause analysis.
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
George, T. (2023, November 17). What Is Root Cause Analysis? | Definition & Examples. Scribbr. Retrieved April 9, 2024, from https://www.scribbr.com/research-process/root-cause-analysis/
Is this article helpful?
Tegan George
Other students also liked, what is a fishbone diagram | templates & examples, how to write a problem statement | guide & examples, how to define a research problem | ideas & examples, unlimited academic ai-proofreading.
✔ Document error-free in 5minutes ✔ Unlimited document corrections ✔ Specialized in correcting academic texts
- Teaching & Learning Home
- Becoming an Educator
- Become a Teacher
- California Literacy
- Career Technical Education
- Business & Marketing
- Health Careers Education
- Industrial & Technology Education
- Standards & Framework
- Work Experience Education (WEE)
- Curriculum and Instruction Resources
- Common Core State Standards
- Curriculum Frameworks & Instructional Materials
- Distance Learning
- Driver Education
- Multi-Tiered System of Supports
- Recommended Literature
- School Libraries
- Service-Learning
- Specialized Media
- Grade Spans
- Early Education
- P-3 Alignment
- Middle Grades
- High School
- Postsecondary
- Adult Education
- Professional Learning
- Administrators
- Curriculum Areas
- Professional Standards
- Quality Schooling Framework
- Social and Emotional Learning
- Subject Areas
- Computer Science
- English Language Arts
- History-Social Science
- Mathematics
- Physical Education
- Visual & Performing Arts
- World Languages
- Testing & Accountability Home
- Accountability
- California School Dashboard and System of Support
- Dashboard Alternative School Status (DASS)
- Local Educational Agency Accountability Report Card
- School Accountability Report Card (SARC)
- State Accountability Report Card
- Compliance Monitoring
- District & School Interventions
- Awards and Recognition
- Academic Achievement Awards
- California Distinguished Schools Program
- California Teachers of the Year
- Classified School Employees of the Year
- California Gold Ribbon Schools
- Assessment Information
- CA Assessment of Student Performance and Progress (CAASPP)
- CA Proficiency Program (CPP)
- English Language Proficiency Assessments for CA (ELPAC)
- Grade Two Diagnostic Assessment
- High School Equivalency Tests (HSET)
- National Assessment of Educational Progress (NAEP)
- Physical Fitness Testing (PFT)
- Smarter Balanced Assessment System
- Finance & Grants Home
- Definitions, Instructions, & Procedures
- Indirect Cost Rates (ICR)
- Standardized Account Code Structure (SACS)
- Allocations & Apportionments
- Categorical Programs
- Consolidated Application
- Federal Cash Management
- Local Control Funding Formula
- Principal Apportionment
- Available Funding
- Funding Results
- Projected Funding
- Search CDE Funding
- Outside Funding
- Funding Tools & Materials
- Finance & Grants Other Topics
- Fiscal Oversight
- Software & Forms
- Data & Statistics Home
- Accessing Educational Data
- About CDE's Education Data
- About DataQuest
- Data Reports by Topic
- Downloadable Data Files
- Data Collections
- California Basic Educational Data System (CBEDS)
- California Longitudinal Pupil Achievement Data System (CALPADS)
- Consolidated Application and Reporting System (CARS)
- Cradle-to-Career Data System
- Annual Financial Data
- Certificated Salaries & Benefits
- Current Expense of Education & Per-pupil Spending
- Data Governance
- Data Privacy
- Educational Data Governance (EDGO)
- Student Health & Support
- Free and Reduced Price Meal Eligibility Data
- Food Programs
- Data Requests
- School & District Information
- California School Directory
- Charter School Locator
- County-District-School Administration
- Private School Data
- Public Schools and District Data Files
- Regional Occupational Centers & Programs
- School Performance
- Postsecondary Preparation
- Specialized Programs Home
- Directory of Schools
- Federal Grants Administration
- Charter Schools
- Contractor Information
- Laws, Regulations, & Requirements
- Program Overview
- Educational Options
- Independent Study
- Open Enrollment
- English Learners
- Special Education
- Administration & Support
- Announcements & Current Issues
- Data Collection & Reporting
- Family Involvement & Partnerships
- Quality Assurance Process
- Services & Resources
- CA Equity Performance and Improvement Program
- Improving Academic Achievement
- Schoolwide Programs
- Statewide System of School Support (S4)
- Specialized Programs Other Topics
- American Indian
- Gifted & Talented Education
- Homeless Education
- Migrant/International
- Private Schools and Schooling at Home
- State Special Schools
- Learning Support Home
- Attendance Improvement
- School Attendance Review Boards
- Expanded Learning
- 21st Century Community Learning Centers
- After School Education & Safety Program
- Expanded Learning Opportunities Program
- Child Nutrition Information & Payment System (CNIPS)
- Rates, Eligibility Scales, & Funding
- School Nutrition
- Parents/Family & Community
- Clearinghouse for Multilingual Documents
- School Disaster and Emergency Management
- Learning Support Other Topics
- Class Size Reduction
- Education Technology
- Educational Counseling
- Mental Health
- Safe Schools
- School Facilities
- Transportation
- Youth Development
- Professional Learning Home
- Title II, Part A Resources and Guidance
- Specialized Programs
- Title I: Improving Academic Achievement
- Title I, Part A
Needs Assessment and Root Cause Analysis FAQs
These FAQs are intended to introduce local educational agencies (LEAs) to needs assessments and root cause analysis. This collection represents commonly asked questions, but is not intended to be a complete list of all possible questions.
Needs Assessment | Root Cause Analysis | Back to Continuous Improvement Resources
Expand All | Collapse All
Needs Assessment
What is a needs assessment.
A needs assessment is a tool used to identify a school’s and/or LEA’s strengths, weaknesses, and the areas in which improvement is needed. A needs assessment is sometimes called:
- Comprehensive Needs Assessment (CNA)
- Segmented Needs Assessment (SNA)
- Consolidated Needs Assessment
- Equity audit
- School Quality Review (SQR)
- Diagnostic assessment
- Diagnostic review
- Diagnostic inquiry
What is a needs assessment for improvement?
A needs assessment for improvement is a systemic process that is used to:
- Determine strengths and weaknesses of a school and/or LEA
- Understand the context and constraints of the school and/or LEA
- Perform a root-cause analysis
- Develop an improvement plan outlining changes considered most likely to bolster or build on strengths and to remediate weaknesses
- Be part of an ongoing continuous improvement cycle that includes both long-range performance goals and short-cycle implementation targets, and
- Include questions at the county office of education level, even if the focus is the LEA level
Why is a needs assessment important?
How do you know what kind of needs assessment to use.
A needs assessment is a point-in-time snapshot. Examples include:
- Comprehensive Needs Assessment–assessing all aspects of the district and its context (including its county office of education), and/or
- Segmented Needs Assessment–assessing only one or a few aspects of the district and its context.
Back to Top
Root Cause Analysis
Why is root cause analysis important.
Root cause analysis addresses the problem , rather than the symptom , eliminates wasted effort, conserves resources, and informs strategy selection.
- The California School Dashboard identifies symptoms of the problem. The problem causing those symptoms is revealed through root cause analysis.
What is root cause analysis?
Root cause analysis is part of the needs assessment process. It is a strategy to thoroughly examine practices, processes, and routines to determine their impact on outcomes. It answers the “Why?” behind each identified area of improvement.
- Root cause is defined as “the deepest underlying cause or causes of positive or negative symptoms within any process that, if dissolved, would result in elimination or substantial reduction of the symptom” (Preuss, 2003, p. 3).
Where does root cause analysis fit into the Continuous Improvement process?
Root cause analysis occurs:
- After gathering and analyzing data
- Before determining findings and creating action plans
Where does root cause analysis fit into the Local Control and Accountability Plan (LCAP) process?
- After gathering and analyzing data through the needs assessment process
- Before determining Actions and Services for the LCAP
Who participates in root cause analysis?
Representatives from all stakeholder groups can participate in root cause analysis and may include:
- California Department of Education personnel
- County offices of education personnel
- District personnel
- Local boards of education
- Families and community members
- School personnel
- District-hired external partners
What tools are available for root cause analysis?
Examples of some promising root cause analysis tools include:
- Fishbone Diagram (using the 5 Whys)
- Interrelationship Digraph
- Expert Convening
- Empathy Interviews
- Digging Into Data
- Process Mapping
- Driver Diagram
Preuss, P. 2003. Root Cause Analysis: School Leader’s Guide to Using Data to Dissolve Problems. New York: Routledge.
- Targeted/Additional Targeted Support & Improvement
- Title I Improving Academic Achievement
- Comprehensive Support and Improvement
- Title I, Part A Authorized Use of Funds
- ESSA Assistance Status Data Files
- Title I, Part A Parent and Family Engagement
- California's System of Support
- Title I, Part A Schoolwide Program
- Title I, Part A School Allocations
- ATSI Planning Summary
- FY 2023–24 GMART CSI LEA Reporting Instructions (added 02-Apr-2024) removed by RO --> Grant Management and Reporting Tool (GMART) instructions for local educational agencies (LEAs) with schools that meet the criteria for Comprehensive Support and Improvement (CSI) for Fiscal Year (FY) 2023–24. removed by RO -->
- Black Student Achievement (added 08-Mar-2024) removed by RO --> Information and resources for local educational agencies (LEAs) and educational partners to support academic achievement for Black/African American students. removed by RO -->
- ESSA CSI COE Subgrant Closeout (added 29-Feb-2024) removed by RO --> Information regarding the Every Student Succeeds Act (ESSA) Comprehensive Support and Improvement (CSI) county offices of education (COEs) Subgrant Closeout Timeline, Instructions, and Resources. removed by RO -->
- Business Essentials
- Leadership & Management
- Credential of Leadership, Impact, and Management in Business (CLIMB)
- Entrepreneurship & Innovation
- *New* Digital Transformation
- Finance & Accounting
- Business in Society
- For Organizations
- Support Portal
- Media Coverage
- Founding Donors
- Leadership Team

- Harvard Business School →
- HBS Online →
- Business Insights →
Business Insights
Harvard Business School Online's Business Insights Blog provides the career insights you need to achieve your goals and gain confidence in your business skills.
- Career Development
- Communication
- Decision-Making
- Earning Your MBA
- Negotiation
- News & Events
- Productivity
- Staff Spotlight
- Student Profiles
- Work-Life Balance
- Alternative Investments
- Business Analytics
- Business Strategy
- Business and Climate Change
- Design Thinking and Innovation
- Digital Marketing Strategy
- Disruptive Strategy
- Economics for Managers
- Entrepreneurship Essentials
- Financial Accounting
- Global Business
- Launching Tech Ventures
- Leadership Principles
- Leadership, Ethics, and Corporate Accountability
- Leading with Finance
- Management Essentials
- Negotiation Mastery
- Organizational Leadership
- Power and Influence for Positive Impact
- Strategy Execution
- Sustainable Business Strategy
- Sustainable Investing
- Winning with Digital Platforms
Root Cause Analysis: What It Is & How to Perform One
- 07 Mar 2023
The problems that affect a company’s success don’t always result from not understanding how to solve them. In many cases, their root causes aren’t easily identified. That’s why root cause analysis is vital to organizational leadership .
According to research described in the Harvard Business Review , 85 percent of executives believe their organizations are bad at diagnosing problems, and 87 percent think that flaw carries significant costs. As a result, more businesses seek organizational leaders who avoid costly mistakes.
If you’re a leader who wants to problem-solve effectively, here’s an overview of root cause analysis and why it’s important in organizational leadership.
Access your free e-book today.
What Is Root Cause Analysis?
According to the online course Organizational Leadership —taught by Harvard Business School professors Joshua Margolis and Anthony Mayo— root cause analysis is the process of articulating problems’ causes to suggest specific solutions.
“Leaders must perform as beacons,” Margolis says in the course. “Namely, scanning and analyzing the landscape around the organization and identifying current and emerging trends, pressures, threats, and opportunities.”
By working with others to understand a problem’s root cause, you can generate a solution. If you’re interested in performing a root cause analysis for your organization, here are eight steps you must take.
8 Essential Steps of an Organizational Root Cause Analysis
1. identify performance or opportunity gaps.
The first step in a root cause analysis is identifying the most important performance or opportunity gaps facing your team, department, or organization. Performance gaps are the ways in which your organization falls short or fails to deliver on its capabilities; opportunity gaps reflect something new or innovative it can do to create value.
Finding those gaps requires leveraging the “leader as beacon” form of leadership.
“Leaders are called upon to illuminate what's going on outside and around the organization,” Margolis says in Organizational Leadership , “identifying both challenges and opportunities and how they inform the organization's future direction.”
Without those insights, you can’t reap the benefits an effective root cause analysis can produce because external forces—including industry trends, competitors, and the economy—can affect your company’s long-term success.
2. Create an Organizational Challenge Statement
The next step is writing an organizational challenge statement explaining what the gap is and why it’s important. The statement should be three to four sentences and encapsulate the challenge’s essence.
It’s crucial to explain where your organization falls short, what problems that poses, and why it matters. Describe the gap and why you must urgently address it.
A critical responsibility is deciding which gap requires the most attention, then focusing your analysis on it. Concentrating on too many problems at once can dilute positive results.
To prioritize issues, consider which are the most time-sensitive and mission-critical, followed by which can make stakeholders happy.
3. Analyze Findings with Colleagues
It's essential to work with colleagues to gain different perspectives on a problem and its root causes. This involves understanding the problem, gathering information, and developing a comprehensive analysis.
While this can be challenging when you’re a new organizational leader, using the double helix of leadership —the coevolutionary process of executing organizational leadership's responsibilities while developing the capabilities to perform them—can help foster collaboration.
Research shows diverse ideas improve high-level decision-making, which is why you should connect with colleagues with different opinions and expertise to enhance your root cause analysis’s outcome.
4. Formulate Value-Creating Activities
Next, determine what your company must do to address your organizational challenge statement. Establish three to five value-creating activities for your team, department, or organization to close the performance or opportunity gap you’ve identified.
This requires communicating organizational direction —a clear and compelling path forward that ensures stakeholders know and work toward the same goal.
“Setting direction is typically a reciprocal process,” Margolis says in Organizational Leadership . “You don't sit down and decide your direction, nor do you input your analysis of the external context into a formula and solve for a direction. Rather, setting direction is a back-and-forth process; you move between the value you'd like to create for customers, employees, investors, and your grasp of the context.”

5. Identify Necessary Behavior Changes
Once you’ve outlined activities that can provide value to your company, identify the behavior changes needed to address your organizational challenge statement.
“Your detective work throughout your root cause analysis exposes uncomfortable realities about employee competencies, organizational inefficiencies, departmental infighting, and unclear direction from leadership at multiple levels of the company,” Mayo says in Organizational Leadership .
Factors that can affect your company’s long-term success include:
- Ineffective communication skills
- Resistance to change
- Problematic workplace stereotypes
Not all root cause analyses reveal behaviors that must be eliminated. Sometimes you can identify behaviors to enhance or foster internally, such as:
- Collaboration
- Innovative thinking
- Creative problem-solving
6. Implement Behavior Changes
Although behaviors might be easy to pinpoint, putting them into practice can be challenging.
To ensure you implement the right changes, gauge whether they’ll have a positive or negative impact. According to Organizational Leadership , you should consider the following factors:
- Motivation: Do the people at your organization have a personal desire for and commitment to change?
- Competence: Do they have the skills and know-how to implement change effectively?
- Coordination: Are they willing to work collaboratively to enact change?
Based on your answers, decide what behavior changes are plausible for your root cause analysis.
7. Map Root Causes
The next step in your analysis is mapping the root causes you’ve identified to the components of organizational alignment. Doing so helps you determine which components to adjust or change to implement employee behavior changes successfully.
Three root cause categories unrelated to behavior changes are:
- Systems and structures: The formal organization component, including talent management, product development, and budget and accountability systems
- People: Individuals’ profiles and the workforce’s overall composition, including employees’ skills, experience, values, and attitudes
- Culture: The informal, intangible part of your organization, including the norms, values, attitudes, beliefs, preferences, common practices, and habits of its employees
8. Create an Action Plan
Using your findings from the previous steps, create an action plan for addressing your organizational problem’s root cause and consider your role in it.
To make the action plan achievable, ensure you:
- Identify the problem’s root cause
- Create measurable results
- Ensure clear communication among your team
“One useful way to assess your potential impact on the challenge is to understand your locus of control,” Mayo says in Organizational Leadership , “or the extent to which you can personally drive the needed change or improvement.”
The best way to illustrate your control is by using three concentric circles: the innermost circle being full control of resources, the middle circle representing your ability to influence but not control, and the outermost circle alluding to shifts outside both your influence and control.
Consider these circles when implementing your action plan to ensure your goals don’t overreach.

The Importance of Root Cause Analysis in Organizational Leadership
Root cause analysis is a critical organizational leadership skill for effectively addressing problems and driving change. It helps you understand shifting conditions around your company and confirm that your efforts are relevant and sustainable.
As a leader, you must not only effect change but understand why it’s needed. Taking an online course, such as Organizational Leadership , can enable you to gain that knowledge.
Using root cause analysis, you can identify the issues behind your organization’s problems, develop a plan to address them, and make impactful changes.
Are you preparing to transition to a new leadership role? Enroll in our online certificate course Organizational Leadership —one of our leadership and management courses —and learn how to perform an effective root cause analysis to ensure your company’s long-term success. To learn more about what it takes to be an effective leader, download our free leadership e-book .

About the Author
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Root cause analysis and medical error prevention.
Gunjan Singh ; Raj H. Patel ; Joshua Boster .
Affiliations
Last Update: May 30, 2023 .
- Continuing Education Activity
The term "medical error" encompasses diverse events that vary in magnitude and can potentially harm the patient. According to the 2019 World Health Organization (WHO) Patient Safety Factsheet, adverse events due to unsafe patient care are among the top 10 causes of death and disability worldwide. However, it is essential to understand that healthcare delivery involves multiple variables in a dynamic environment, with many critical decisions made quickly. As such, the healthcare system cannot implement rigid protocols used by other high-risk industries, such as aviation. Reducing medical errors requires a multifaceted approach at various levels of healthcare. In the event of a sentinel occurrence or adverse patient outcomes, a thorough evaluation is warranted to prevent such events. Root cause analyses provide a method of evaluation for these situations so that a system-based intervention can be implemented rather than blaming individual providers. This activity reviews the root cause analysis process in medical error prevention. The course highlights the interprofessional team's role in performing this analysis to prevent medical errors and improve clinical outcomes.
- Demonstrate effective root cause analysis of a sentinel event and implement strategies for its prevention.
- Apply root cause analysis reporting standards in accordance with the Joint Commission requirements.
- Identify the indications for reporting sentinel events to the Joint Commission and the steps that should be taken following the occurrence of such incidents.
- Collaborate within an interprofessional team to prevent the most common types of clinical errors and improve clinical outcomes.
- Introduction
Medical error is an unfortunate reality of the healthcare industry and a topic that is continuously discussed due to its grave impact on patient care and outcomes. In a 1999 publication by the Institute of Medicine (IOM), it was highlighted that deaths resulting from medical error exceeded those attributed to motor vehicle accidents, breast cancer, or AIDS. [1]
Subsequent reports that discuss potential etiologies of medical errors have blamed systemic issues. Others have focused attention on certain groups of patients that may be more vulnerable to medical error than others. [2] [3] Recently, the impact of medical errors on patient family members and healthcare professionals has been emphasized due to its effects on exacerbating burnout, poor work performance, mental health decline, and even suicidality. [4] [5]
Though it may be challenging to pinpoint the definitive cause of medical error in certain situations, it is important to evaluate strategies that can be used to mitigate and prevent these adverse events from occurring in the first place. One such method is root cause analysis, which has been previously shown to reduce clinical and surgical errors in various specialties by establishing a quality improvement framework. [6] This article will discuss the application of root cause analysis in medical error prevention and strategies for maintaining continuous quality improvement in the healthcare setting.
The Institute of Medicine defines a medical error as "the failure of a planned action to be completed as intended or the use of a wrong plan to achieve an aim." [1] It is essential to recognize the differences between medical malpractice and medical error. An adverse event in a healthcare setting may be attributed to medical error while not meeting the threshold of malpractice or negligence. Medical errors generally result from the improper execution of a plan or improper planning of a method of execution. Medical errors can also occur during preventative care measures, for example, if a provider overlooks a patient's allergy when administering medication. Thus, the complexity of the occurrence of a medical error can range widely and manifest in any aspect of patient care, from admission to discharge and in the outpatient setting. It is essential to recognize that medical errors may occur without causing direct harm to the patient. Regardless, it is critical to evaluate the cause of all medical errors, whether or not the patient is harmed, and develop guidelines and strategies to prevent future occurrences.
If medical errors harm the patient, they are classified as preventable adverse events or sentinel events. Sentinel events are preventable adverse outcomes that warrant urgent investigation to determine the cause of the error. [7] These events are not only debilitating to patients but can also impact the livelihood of healthcare providers. It is important to note that sentinel events are unrelated to the patient's underlying medical condition and are attributable to improper medical intervention or improper technique. If a patient receives medication and experiences an anaphylactic reaction, it must be determined whether the reaction was due to the medication itself or the provider's failure to review the patient's allergies before administration. Thus, these cases must be critically reviewed to delineate whether or not the etiology of the error was preventable, which is often a challenging task.
Root cause analysis (RCA) is a process for identifying the causal factors underlying variations in performance. In the case of medical error, this variation in performance may result in a sentinel event. A standardized RCA process is mandated by the Joint Commission to identify the cause of medical errors and thus allow healthcare institutions to develop strategies to mitigate future errors. [7] Despite its wide adoption in the business, engineering, and industrial sectors, its use in the medical field has been limited. It is important to note that the RCA process aims not to assign individual blame but to identify lapses in system-level processes that can be restructured to prevent patient harm and reduce the likelihood of future sentinel events. Thus, identifying the root cause of a medical error can better direct the need for additional training and resources.
Applying Root Cause Analysis
For accreditation purposes, the Joint Commission requires that healthcare institutions have a comprehensive process for systematically analyzing sentinel events. The RCA process is one of the most commonly utilized tools for this purpose. Through the RCA process, healthcare institutions can optimize patient care and enact measures to mitigate adverse events that compromise patient safety. In addition to improving patient safety and quality metrics, an RCA's purpose includes optimizing process flow and outcomes.
RCA emphasizes lapses in system-level processes. It does not emphasize individual actions. A designated RCA team must be assembled to review and identify necessary changes at the systematic level that can improve performance and reduce the likelihood of a repeat sentinel event. [8] Failure to perform an RCA within 45 days of a sentinel event may result in the healthcare institution being placed on an 'accreditation watch,' which is public information. Repeat violations may result in an onsite review by the Joint Commission that may jeopardize accreditation. [9]
The first step of an RCA is to form an interprofessional team to analyze and define the problem. There should be a designated process to communicate with senior leadership throughout the journey while meeting deadlines internally and with the Joint Commission. After identifying the problem, the team should evaluate systematic factors that may have contributed to the error. Throughout the process, collecting data regarding the potential underlying causes is important. The team should propose and implement immediate changes so that a repeat sentinel event does not occur during the RCA process. Next, the team should evaluate the list of root causes and consider their interrelationships. During the RCA process, the team will explore risk-reduction and process improvement strategies to prevent future errors at the systematic level. After identifying process improvement strategies, the team must communicate with senior leadership and key stakeholders to evaluate whether the proposed process modifications are acceptable.
The Joint Commission has created a framework and series of 24 questions to aid in organizing an RCA. This framework should be utilized as a general template when preparing the RCA report that will eventually be submitted to the Joint Commission after thorough evaluation. The 24-question framework recommended by the Joint Commission considers various situational factors that may have contributed to a sentinel event. This includes examining the systematic process, human factors, equipment malfunctions, environmental factors, uncontrollable external factors, organizational factors, staffing and qualifications, contingency plans, performance expectations, informational disruptions, communication, environmental risks, training, and technology. [7]
With detailed consideration of each of these topics, an in-depth analysis of the cause of the sentinel event can occur. One factor that makes an appearance in several questions is communication. Communication within the team and with leadership is critical to maintaining organizational structure. It can be difficult to convey messages effectively and efficiently without proper communication systems. Environmental factors should also be examined to determine if any situational issues were ongoing at the time of the sentinel event that may have impacted the outcome. Staffing is another important topic that should be examined during an RCA review to determine if the staff were appropriately qualified, competent, and portioned for their assigned duties.
After discussion, evaluation, and analysis, corrective actions should be developed, identifying areas for targeted improvement. While utilizing the 24-question framework, it is important to always consider causative etiologies because it will help determine the specific area that can be restructured to reduce risk. The root cause analysis should be clear and precise while providing appropriate depth and scope.
The Joint Commission has identified a series of adverse events subject to their purview. Primarily, this would be a sentinel event that has resulted in death or permanent loss of function unrelated to any underlying medical conditions. Alternatively, a sentinel event can also be considered as one of the following, even if the event did not cause death or severe harm:
- Patient suicide of any patient receiving care (including emergency department care), treatment, or services within the healthcare setting or 72 hours following their discharge
- Full-term infant having an unanticipated death
- An infant discharged to the wrong family
- Abduction of any patient receiving care, treatment, or services
- Elopement of a patient within a healthcare setting, leading to their harm
- Hemolytic transfusion reaction requiring administration of blood products
- Rape, assault, or homicide of anyone on scene at the healthcare premises
- Wrong patient, site, or procedure for all invasive procedures, including surgery
- Unintended retention of a foreign body in a patient following surgery
- Severe neonatal hyperbilirubinemia
- Prolonged fluoroscopy with cumulative dose to the wrong body region
- Fire, flame, or unanticipated smoke, heat, or flashes during patient care
- Intrapartum maternal death
- Severe maternal morbidity
The finalized RCA report must follow a set standard to meet the Joint Commission's requirement. It must include the following:
- Participation of the organization's leadership and key stakeholders involved in the process/system under review
- Thorough explanation of all findings
- Consideration of any relevant or applicable literature
- Internal accuracy and consistency, without contradictions or unanswered questions
Case Illustrations with RCA Interventions
Case Example 1
A 42-year-old primigravida woman at 34 weeks gestation was brought to the obstetric emergency department at midnight with complaints of severe headache, blurry vision, and right upper quadrant pain for the last 5 to 6 hours. She noted gradually increasing lower extremity edema and facial swelling as well. She has a history of gestational hypertension and was prescribed labetalol 200 mg twice a day a week before this presentation. On initial evaluation, her blood pressure was 190/110 mm Hg on 2 separate occasions, 5 minutes apart. She had gained 2 kilograms since her last antenatal checkup in the clinic a week ago.
The patient was diagnosed with severe preeclampsia. The senior obstetric resident ordered a loading dose of magnesium sulfate to prevent imminent seizure. The hospital protocol used an intravenous (IV) and intramuscular (IM) regimen where the patient receives a 4-gram (20% concentration) intravenous solution bolus and a 10-gram intramuscular dose (50% concentration) administered as 5 grams in each buttock. The senior resident verbally provided the order for magnesium sulfate administration to the junior resident, who subsequently verbally communicated the order to the nurse.
This magnesium sulfate dosing regimen is complex, with multiple doses in different locations, and was incorrectly prepared by the nurse who felt rushed in an urgent situation. A chart displaying magnesium sulfate's preparation in the drug preparation room was present but had become faded. Therefore the nurse prepared the medication relying on her memory. Before administering the medicine to the patient, as a part of the protocol, she repeated the dose strength aloud to another nurse, who cross-checked it from a printed chart and picked up the error in time. The senior resident also identified the error as the dose was communicated aloud and stopped administering the drug.
RCA with Corrective Measures
A root cause analysis was performed, and measures were taken to avoid this problem in the future. Magnesium sulfate was marked as a high-alert medication, as the Institute of Safe Medication Practices recommended. Furthermore, premixed solutions prepared by the pharmacy for the bolus dosing were instituted instead of requiring nurses to mix this high-risk medication on the unit. The second nurse verification measure was retained, with the second nurse instructed to double-check all doses, pump settings, drug names, and concentrations before administration of any drugs.
Moreover, the RCA recommended that all medication orders be provided in writing and/or entered in the electronic medical record using computerized provider order entry (CPOE) systems, regardless of the urgency of the situation, to avoid any dosing errors. The RCA team emphasized that verbal communication for medication administration should always be avoided. If verbal communications are necessary or unavoidable, the RCA recommended that the nurse taking the order should read back the order given to the prescribing physician to minimize any prescribing errors.
Case Example 2 (The name and date of birth used in this example are imaginative, used for illustrative purposes, and do not represent an actual patient. Any similarities, if noted, are purely coincidental.)
Anna Joy (date of birth October 30, 1991) was admitted to a busy obstetric ward. She was a primigravida woman at 30 weeks of gestation with complaints of intermittent cramping abdominal pain. She had come to visit her sister living in Boston from Spain. The patient's ability to communicate in English was limited, and she preferred speaking Spanish. However, her husband and sister were fluent in English and assisted with translation throughout the history, exam, and admission. The patient was seen by an obstetrician who advised routine investigations for threatened preterm labor and observation.
Another patient Ann Jay (date of birth September 30, 1991), was also admitted to the same obstetric ward. She was 34 weeks gestation and was admitted because of gestational diabetes mellitus with hyperglycemia. Her obstetrician advised an endocrinology referral, and the endocrinologist advised glucose monitoring and insulin administration. The nurse taking care of the patient was provided with the instructions, performed a finger-stick blood glucose check, and informed the endocrinologist about the results over the phone. The endocrinologist advised six units of regular insulin before lunch. The nurse also informed the obstetrician that the patient felt a decrease in fetal movements. The obstetrician advised ongoing observation and fetal kick counts.
The family members of the first patient, Anna Joy, informed the nurse that they were going to lunch. The morning shift nurse later required a half-day leave because of personal issues and quickly handed over her patients to another nurse. The ward was busy and running at full capacity. The new nurse decided to give the insulin injection first as the patient was about to receive her lunch. She did not know that Anna Joy preferred communication in Spanish. The nurse asked a few questions and rushed through patient identification with the help of two unique patient identifiers. She administered the insulin injection to the first patient and later realized it was supposed to be given to the second patient, Ann Jay. The attending obstetrician and the endocrinologist were informed. They took the necessary measures and closely monitored the patient for the next few hours. No inadvertent effects were noted.
A root cause analysis was performed, and measures were taken to avoid this problem in the future. The RCA team noted that the nurse caring for both patients had worked in the hospital for 5 years and was recently transitioned to the obstetric ward. This had never happened to her before. The team recognized that the modern patient care delivery process relies on the efficient and effective integration of an interprofessional care team. A clear, consistent, and standardized communication method between the team members contributes to safe patient care and minimizes the risk of adverse outcomes. The RCA team did not lay blame on the nurse involved. They instead instituted a standardized handoff platform and required all patient handoffs to occur using this format in the future. During shift change, the handoff between clinicians and nurses is pivotal in providing high-quality care. The aim should be to provide the oncoming team with up-to-date, accurate, and complete information. The RCA team outlined clinical education programs for nurses and clinicians to ensure high-quality and effective handoff occurs at every shift change and patient handoff.
They also instituted mandatory use of hospital-based interpreters when communicating with patients who are not fluent in English. The hospital procedure for verifying patient identification using two unique patient identifiers, the name and the date of birth, was retained. However, an additional mandatory step of verifying the patient's identity using an arm-band barcode was instituted before every medication administration. They also instituted the highlighting of patient charts and rooms when patients had similar names and dates of birth.
Case Example 3
A 26-year-old primigravida woman with labor pains was admitted to a busy hospital's labor and delivery suite at 39 weeks of gestation. There were no associated high-risk factors. The patient was admitted to the labor ward and managed according to routine protocol. She progressed in spontaneous labor, but the cardiotocograph showed prolonged fetal bradycardia lasting for 3 and a half minutes at 4 centimeters (cm) cervical dilatation. The fetal bradycardia did not resolve with initial conservative measures.
The patient was transferred to the operating room for a category one emergent cesarean section. A category one cesarean section means the baby should be delivered within 30 minutes of the procedure's decision. It is done when there is an immediate threat to the life of the mother or the baby. The baby was delivered in good condition, with no intraoperative complications. Before closure, the operating obstetrician asked the scrub nurse to perform a surgical count. The scrub nurse reported that there might be a missing gauze piece from the surgical trolley. The count was performed several times by the scrub and the floor nurse at this time. A second on-call obstetrician was called to assist the primary surgeon in checking for the surgical field's missing gauze piece.
The surgical gauze had a heat-bonded barium sulfate marker embedded in the fabric to assist with x-ray identification. An intraoperative x-ray was obtained to evaluate for intraperitoneal gauze, and the results were negative. The case was discussed with the department chief, and abdominal closure was performed. Due to the associated delays, the operative time was increased significantly (2 hours and 30 minutes).
An RCA of the event revealed that there were inconsistent practices regarding surgical count before the initiation of a procedure. Moreover, only one person (the scrub nurse) was charged with making this count. The RCA team highlighted that the surgical count is critical and must be performed in a standardized fashion to eliminate variation and minimize the possibility of human error. They highlighted international standards that recommend standardizing the counting process and systematically tracking the instruments, gauze, and sponges in the sterile field. They instituted World Health Organization's Surgical Safety Checklist as a mandatory step for all procedures regardless of the urgency of the procedure. They also recommended that the counting process be concurrently audible and visual to eliminate errors. The RCA recommended that the counting process should be performed by the scrub nurse and the circulating nurse independently, both before and after every procedure. They emphasized that the best practices for surgical count should always be followed regardless of the clinical situation.
Case Example 4
A 25-year-old man presented for bilateral LASIK surgery at a same-day surgery center. The operating surgeon examined the patient, a community-based surgeon who does not routinely operate at this facility. Informed consent was obtained by the operating surgeon preoperatively. The refractive error was -4 D for the right eye and – 5D for the left eye. The plan was to remove the refractive error altogether. There was a timeout to ensure the correct patient and procedure. The LASIK was started by making corneal flaps on both eyes, which was completed uneventfully. The second step was the excimer laser-guided corneal power correction.
The patient was adjusted on the operating microscope so that the first eye was directly under the excimer laser, and iris recognition was attempted. The machine did not recognize the iris pattern after 3 attempts. The surgeon decided to proceed without iris recognition. The technician thought that this was rare and that they had good iris recognition rates for this month (>98%). However, he did not want to contradict the surgeon.
Before the procedure, the circulating nurse noted that the patient's table was adjusted to the wrong side, and the left eye was under the laser instead of the right. She pressed the emergency stop button, and the treatment was terminated. After identifying the mistake, the surgeon and technician restarted the machine to treat the correct sequence's correct eyes.
Compared to unilateral procedures, bilateral procedures are especially challenging, particularly if the treatment varies between the 2 sides. An example is LASIK, where both eyes are typically corrected simultaneously, and there is no obvious pathology on the eye except for the refractive error. The correction is determined preoperatively, and the result is not immediately titrated. There is a significant chance for wrong-site procedures, given these ambiguities. To avoid this disaster, the RCA team implemented a verification procedure where the optometrist, technician, and surgeon were ALL required to verify each eye's refractive error before the procedure and after programming the laser.
Some advanced laser machines have an inbuilt layer of defense where the iris pattern of the eye is uniquely identified via iris recognition, which helps determine the correct eye and enhances the treatment fidelity. Some treatments, however, do not include iris recognition, and therefore the onus lies on the technicians, nurses, and surgeons to identify the appropriate eye correctly.
Case Example 5
A community clinic treats approximately 110 patients per day. The clinic is run by 2 primary care physicians, with the assistance of 2 nurses and scribes. A 10-year-old boy was brought to the clinic by his parents. The child had a runny nose for the last ten days. On examination, the primary care physician noted simple allergic rhinitis and advised them to use over-the-counter cetirizine. One of the scribes had called in sick that day, so a secretary was assisting the physician. The physician advised the parents that cetirizine is an over-the-counter medication, and they can go to their pharmacy of choice to obtain the medication. After 2 days, the patient's mother returned to the clinic and reported that the child was lethargic. The clinic's front desk stated that they would convey the information to the physician, who was very busy that day. The physician said it is typical for children taking cetirizine to be slightly sleepy. He said that they should inform the parents to ask the child to avoid going to school for the next few days. The message was conveyed to the mother.
The patient's mother, however, decided to take the child to another specialist as she was concerned regarding the sedation. At this visit, it was noted that the child was taking a 10-mg cetirizine tablet 2 times a day, which is higher than typically recommended.
An RCA review was performed at the primary clinic. It was noted that there was a typographical error in the instructions given to the patient, saying 10 mg twice a day instead of 5 mg twice a day, which the physician had intended. The RCA recommended a verification procedure for all prescription recommendations made during the clinic visit. They instituted verbal and written verification with the prescribing physicians of all drugs and doses transcribed by the scribes and/or office personnel to avoid this error in the future. The RCA team also recommended that the physician and the team should read prescription and over-the-counter drug recommendations with their intended doses to the patient/attendant in the clinic from the summary instructions and verify that it matches their notes.
The RCA also mandated a document review for all patient callbacks or return visits before any patient communication is made to avoid such errors in the future.
Case Example 6
All-Eyes Laser Center is a busy same-day ophthalmic laser center with multiple laser procedures being performed throughout the day. The center specializes in retinal and anterior segment lasers.
A 60-year-old man, JM, suffers from chronic angle-closure glaucoma and has been advised to undergo a YAG (Yttrium-Aluminum-Garnett) laser iridotomy. This procedure involves creating a small hole in the peripheral part of the iris to increase the aqueous flow between the anterior chamber and the posterior chamber to prevent a possible angle-closure attack and/or further glaucoma progression.
This was an unusually busy day at the laser center. The laser surgeon was running behind. There were 5 patients ahead of JM, and there was an anticipated delay of around 2 hours. As is the practice at the center, the nurse practitioner prepares the patients before the laser, and then the laser surgeon performs the procedure. The preparation involves checking the history, confirming the examination findings, and then instilling eye drops to prepare the procedure's eyes. This laser surgeon does 2 types of laser procedures. YAG iridotomy needs the eyes constricted with 2% pilocarpine eye drops, which ensures a good exposure of the peripheral iris crypts where the laser is directed to create a small iridotomy. The second procedure is a YAG capsulotomy. The posterior capsule in a pseudophakic eye is lasered to create an opening to counter an after-cataract posterior capsular opacity and improve vision. The YAG laser platform is a combined platform where both procedures can be performed with one machine.
The surgeon arrived at the laser suite and started the lasers. When JM's turn came, a proper timeout was confirmed, including the correct eye and procedure. However, when the patient was positioned at the laser machine, the surgeon noticed that the pupil was dilated rather than constricted. The surgeon again verified the patient's tag and name and the correct procedure. It was confirmed that the patient was indeed the correct one, and the procedure intended was YAG iridotomy. It would have been dangerous to attempt an iridotomy in a dilated pupil. The surgeon did not proceed with the procedure, and the patient was transferred out of the laser suite. The patient was counseled regarding the error and instructed that he would be rescheduled for the correct procedure in a few days. The error was misattributed to the nurse administering the wrong eye drop, secondary to high patient volume and practice inconsistencies.
A root cause analysis was performed, and measures were taken to avoid this problem in the future. This error did not result in harm to the patient. However, there is a significant chance of the wrong type of procedure being performed. Considering this, the RCA team recommended segregating patients for YAG capsulotomy and YAG iridotomy to different seating areas that were clearly labeled. The 2 eye drops, tropicamide and pilocarpine, were kept only in these areas, and the staff was not allowed to carry these drops out from the designated area. A barcode-based verification was also instituted to be used each time the drop was instilled.
There are precautions in place for similar-sounding medications and similar-sounding patient names. However, in a mixed clinic where multiple procedures are being performed with a relatively quick turnover, the pre-procedure medications can be mixed, especially if there is no designated 'bedside area' for the patient. Therefore using the precautions noted above can avoid incorrect medication administration.
- Issues of Concern
The IOM identifies medical errors as a leading cause of death and injury. [1] According to the 2019 World Health Organization (WHO) Patient Safety Factsheet, adverse events due to unsafe patient care are among the top ten causes of death and disability worldwide. Preventable adverse events in the United States of America (US) cause an estimated 44,000 to 98,000 hospital deaths annually. [1] This exceeds the number of deaths attributable to motor vehicle accidents and is estimated to cost the community between 37.6 to 50 billion dollars in terms of added health care cost, disability, and loss of productivity. [1]
Patients and their families face the most critical and severe consequences of medical errors. Therefore, identifying system processes that lead to medical errors and implementing corrective measures is the primary goal in treating this problem. An RCA and response can help identify system-based measures that can minimize the risk of adverse events and improve clinical outcomes.
Types of Medical Errors
It is essential to recognize that medical errors constitute diverse events. The "error" is not always a human miscalculation or miscommunication, as outlined by the cases above. Some errors are inherent to clinical situations, such as patient falls in hospital settings and healthcare-associated infections. The commonly recognized "types" of medical errors are outlined below.
- Medication error is widely accepted as the most common and preventable cause of patient injury. [10] Medication errors include giving the wrong drug or dose, via the wrong route, at an incorrect time, or to the wrong patient. The reported incidence of medication error-associated adverse events in acute hospitals is around 6.5 per 100 admissions. [10] Medication errors in the peri-discharge from an acute care facility are the most easily overlooked or missed errors. [10]
- Another common medical error is a diagnostic error with failure to correctly identify the cause of the clinical condition promptly. [10] Diagnostic errors are "missed opportunities to make a correct or timely diagnosis based on the available evidence, regardless of patient harm." [11]
- In hospitalized patients, wound infections, pressure ulcers, falls, healthcare-associated infections, and technical complications constitute another group of preventable medical errors. [10]
- The most common systems-error is failure to disseminate drug knowledge and patient information. This, in essence, is a communication failure, whether with the patient or other providers. [10]
- Failure to employ indicated tests is another medical error that can lead to diagnostic delays or errors. [1]
- Similarly, using outdated tests or treatments or failing to respond to the results of tests or monitoring also constitutes a type of medical error. [1]
- Treatment errors include errors during the performance of a test or procedure and inappropriate treatment. [1]
When applying root cause analysis for medical error prevention, it is essential to consider several patient-related factors and underlying issues that may hinder or impede the ability to generate an efficacious root cause analysis. Awareness of particular safety hazards for specific patient demographics and groups can often help mitigate common medical errors and encourage patients to take responsibility for their safety.
Elderly patients represent such a group as various common medical illnesses may result from age-related changes within this group. Elderly patients tend to be prone to falls due to their age-related changes in vision or cardiovascular problems. This patient group also tends to be prone to balance issues and muscle weakness over time, leading to ambulatory dysfunction. Having fall-prevention protocols in place, identifying potential high-risk areas within the home, and mitigating them through safety measures can improve patient safety and outcomes. [7] Age-associated hearing and cognitive decline increase the likelihood of communication errors regarding medications. Ensuring appropriate communication skills tailored to distinct patient groups is key to preventing such errors. Young children and infants are similarly prone to common medical errors due to the lack of direct participation in decision-making and patient care. Thus, specialized communication is needed to convey medical instructions to this population. It is essential to involve both the family and the child to ensure no lapses in communication.
Reducing diagnostic errors requires a more comprehensive approach. Common conditions misdiagnosed yearly include cancer, coronary artery disease, and surgical complications. [12] [13] Clinicians within these specialties must be aware of the high rate of misdiagnoses and attempt to combat this through additional measures. Many of these misdiagnoses are easily preventable by implementing standardized protocols, which can be integrated into electronic medical record software. [14] According to a 2015 New England Journal of Medicine article, "trigger tools" are essential in reducing this type of medical error. [15] "Trigger tools" are electronic algorithms that identify potential adverse events. This is accomplished by searching electronic health records and flagging specific occurrences. The use of trigger tools has been shown to decrease the rate of misdiagnoses in recent studies. [15]
Another important realization clinicians should be aware of is using an interpreter to aid in effective communication. A skilled medical interpreter may be crucial in effectively communicating instructions and information to the patient. Physicians need to utilize an unbiased and neutral medical interpreter, as family members may often be biased in communication.
Communication deficits among medical staff members are another essential root cause of medical errors that can be mitigated through standardized protocols. [16] The healthcare institution must recognize all staff members' inclusion in communication protocol development and identify processes for clinicians and pharmacists to exchange information regarding medication orders. Training staff to participate in error recognition and medication safety training is another valuable tool that can be implemented within a healthcare institution. Controlling the storage, access, and labeling of medications is another strategy that can be implemented and monitored to prevent errors that can be easily mitigated by storing medications in the accepted manner or by identifying protocols to ensure that similar medications are properly labeled to avoid mismatching. Managing the availability of information within the healthcare organization is also important. Ensuring staff members can readily access important updates and protocol changes can help prevent unnecessary medical errors.
- Clinical Significance
RCA has important implications in helping healthcare organizations study events that resulted in patient harm or undesired clinical outcomes and identify strategies to reduce future errors and improve patient care and safety. Most notably, RCA can help identify medication errors such as illegible handwritten prescriptions, similar name packaging or misleading drug strength or dosage presentations, ineffective control of prescription labels, and lapsed concentration due to interruptions. [17] Clinician participation in root cause analysis is vital as these initiatives recognize and address important patient care aspects.
Through a review of data gathered by the Joint Commission, six common categories of clinical error resulting in patient death, which can be prevented through root cause analysis, have been identified. These sentinel events account for a significant proportion of morbidity and mortality within the hospital setting. The six most common categories of clinical errors resulting in patient deaths include: [7]
- Wrong-site surgeries
- Patient suicide
- Surgical complications
- Medical treatment delays
- Medication errors
- Patient falls.
Wrong-site surgery is a major cause of medical errors that can be mitigated through various safety checkpoints preoperatively and has been the subject of a sentinel event alert by the Joint Commission. [7] [18] This type of error has most commonly been noted in orthopedic surgeries. [19] Risk factors include several surgeons involved in surgical care or transfers to another surgeon for patient care, multiple procedures on a single patient, time constraint pressures, and unique circumstances requiring unusual or special positioning during a surgical procedure. [18] This error can easily be mitigated by ensuring proper pre-operative measures, such as labeling the correct surgical site with an indelible pen or distinctively marking the nonsurgical site before the surgery. Intraoperative radiography can also assist in aiding the correct surgical site during the procedure.
Patient suicide is an unfortunate cause of death commonly seen in psychiatric care settings. [7] Several risk-reduction methods can be implemented for this adverse event, including ensuring a controlled environment free of hazardous materials, frequent patient observation, effective communication, adequate staffing in the facility, suicide assessment upon admission, regular psychiatric evaluation, and assessment for the presence of contraband.
Delays in medical treatment are preventable adverse events that may result in patient death and permanent injuries. This may result from misdiagnoses, delayed diagnostic test results, lack of staffing or physician availability, delays in order fulfillment, inadequate treatment, and delays within the emergency department. It is important to recognize this root cause and implement steps to improve timeliness, completeness and check the accuracy of medical communication to prevent such errors.
Medication administration errors are a common and avoidable adverse event that can occur at various patient care levels, involving many individuals in a multidisciplinary patient care team. [17] The primary tool of prevention for this type of error is communication. A standardized protocol for communication between the physician, nurse, pharmacist, and other clinicians involved in patient care is essential to ensure that patients receive the correct medication at the appropriate dosage, route, and frequency.
Similarly, patient falls are a constant source of error within healthcare facilities. It is important to recognize patients at high risk for falls and take appropriate safety precautions. Standardized protocols can reduce fall rates by ensuring a safe environment for risk-prone patients. Patient factors contributing to falls include advanced age, mobility impairment, and surgery. [20] Organizational factors contributing to falls include nurse staffing and the proportion of new nurses. [20] Instuting fall prevention protocols in hospitals and long-term care facilities have significantly impacted reducing these errors. Studies have shown that fall risk assessments using standardized scales such as the Morse Fall Scale can decrease patient falls. [21] Institutional interventions such as staff education, patient mobility training with rehabilitation professionals, and nutritionist support have also been shown to reduce patient falls. [21]
- Enhancing Healthcare Team Outcomes
Medical errors are undeniably an important cause of patient morbidity and mortality within the United States healthcare system. These errors are prevalent at rampant levels, and the consequences of such errors can have severe impacts on the patient, family members, and clinicians. The interprofessional healthcare team plays an invaluable role in preventing medical errors; team effort is crucial in identifying strategies and solutions to reduce the burden of medical error on the healthcare system. Nurses, pharmacists, rehabilitation professionals, nutritionists, and physicians are integral to the patient care team and crucial in preventing medical errors. Practitioners who work in error-prone environments must recognize their roles as healthcare team members who are responsible for reducing unnecessary errors. [22] The interprofessional team members comprising the RCA team should include professionals from all disciplines to ensure an effective and accurate RCA occurs.[Level 5]
Clinicians should not hesitate to provide their peers with assistance in recognizing particular sources of common medical errors to deliver better patient care. Equal accountability and responsibility of all healthcare team members are critical in preventing errors and providing superior patient safety. [1]
Quality assurance teams should employ RCAs with every sentinal event, especially in situations when the identification of medical errors becomes difficult or complex due to many underlying factors. RCAs can help identify factors within the healthcare delivery process that may impede the ability to provide quality patient care. Given the preventable nature of most medical errors, a thorough RCA can improve patient safety and allow healthcare organizations to serve as a model for others.
Healthcare professionals should be aware of common medical error sources and work as a team to identify possible risks when they become apparent. Doing so will increase the quality and efficiency of the healthcare industry and patient trust in the healthcare system. When an RCA is performed, the cooperation of all healthcare team members and clinicians involved in patient care is critical to understanding the "Why" behind the source of medical error and identifying future strategies to mitigate such errors and improve patient outcomes.[Level 5]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Gunjan Singh declares no relevant financial relationships with ineligible companies.
Disclosure: Raj Patel declares no relevant financial relationships with ineligible companies.
Disclosure: Joshua Boster declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Singh G, Patel RH, Boster J. Root Cause Analysis and Medical Error Prevention. [Updated 2023 May 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Medical Error Reduction and Prevention. [StatPearls. 2024] Medical Error Reduction and Prevention. Rodziewicz TL, Houseman B, Hipskind JE. StatPearls. 2024 Jan
- Prevention of Surgical Errors. [StatPearls. 2024] Prevention of Surgical Errors. Santos G, Jones MW. StatPearls. 2024 Jan
- Pilot Medical Certification. [StatPearls. 2024] Pilot Medical Certification. Matthews MJ, Stretanski MF. StatPearls. 2024 Jan
- Review Tuberculosis. [Major Infectious Diseases. 2017] Review Tuberculosis. Bloom BR, Atun R, Cohen T, Dye C, Fraser H, Gomez GB, Knight G, Murray M, Nardell E, Rubin E, et al. Major Infectious Diseases. 2017 Nov 3
- Review Suffering in Silence: Medical Error and its Impact on Health Care Providers. [J Emerg Med. 2018] Review Suffering in Silence: Medical Error and its Impact on Health Care Providers. Robertson JJ, Long B. J Emerg Med. 2018 Apr; 54(4):402-409. Epub 2018 Feb 1.
Recent Activity
- Root Cause Analysis and Medical Error Prevention - StatPearls Root Cause Analysis and Medical Error Prevention - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Aerospace Overview
- Light Aircraft
- Construction
- Entertainment
- Financial Institutions
- Food and Agriculture
- Higher Education
- Life Sciences
- Manufacturing
- Nonprofit Overview
- Affordable Housing Insurance and Consulting for Nonprofits
- Human Services Consulting
- Showguard™ Event Insurance
- PEO and Temporary Staffing
- Private Equity and M&A
- Public Sector & K-12 Education
- Real Estate and Hospitality
- Restaurants
- Senior Living
- Transportation
- Alternative Risk & Captives
- Business Continuity Planning and Resiliency Services
- Claims Overview
- Commercial Lines Claims Contacts
- Small Business Lines Claims Contacts
- Home and Property Lines Claims Contacts
- Claims Management & Advocacy
- Claims Management and Third Party Administration
- Commercial Surety Bonds
- Construction Bonds
- Credit and Political Risk
- Crisis Resilience Insurance & Consulting
- Data and Analytics
- Enterprise Risk Management
- Environmental
- Executive and Financial Risk
- Global Risk Management
- Loss Control
- Multinational Services Overview
- Asia Pacific
- Personal Lines
- Product Recall
- Reinsurance
- Small Business
- Supplier Diversity
- Workers Compensation
- Insurance and Risk Management Webinars
- Compensation Consulting and Total Rewards Programs
- Compensation Survey Reports
- Compliance Consulting Overview
- Healthcare Reform Toolkit
- Diversity, Equity and Inclusion (DEI) Consulting
- Employee Communications Consulting
- Engagement Solutions
- ESG Consulting
- Executive Benefits
- Executive Compensation Consulting
- Executive Search Overview
- Executive Career Opportunities
- Health and Welfare Consulting
- Healthcare Analytics Consulting
- Human Resources and Compensation Consulting Overview
- Meet the Human Resource Compensation Consulting Team
- Human Resources Consulting
- Human Resources Technology Consulting
- Individual Life and Wealth Consulting
- Investment and Fiduciary Consulting
- Leadership Advisors
- Multinational Benefits and HR Consulting
- Pharmacy Benefit Management Consulting
- Physical and Emotional Wellbeing Consulting
- Physician Compensation and Valuation
- Research and Insights
- Retirement Plan Consulting
- Voluntary Benefits Consulting
- News & Insights
- Investor Relations
- Our Purpose
- Executive Team
- The Gallagher Way
- Gallagher Companies
- Recognition & Awards
- How We Work Overview
- Mission Statement
- Gallagher Better Works
- Tools and Applications
- Merge with Gallagher
- Gallagher Global Network
- Office Locations
- Partnerships
- Inclusion and Diversity
- Global Standards
- Compensation Disclosure
Root Cause Analysis in Higher Education
Author: John Watson
Historically there have been two recognized causes of accidents; unsafe acts (human error) or unsafe conditions. More recently, accident investigation is being adapted to recognize that typically, the cause is more complex than a simple unsafe act or condition. Most serious losses are caused by multiple factors, which when carefully analyzed, normally point to a flaw in the management system of an organization. In line with this new perspective in accident investigation, the traditional concept of root cause analysis (RCA) 1 is being enhanced. Almost all accidents have a contributory and a root cause. For example, if a higher education employee is electrocuted because of a failure to lockout an electrical system, the contributory cause is the failure to properly de-energize the system. Too often, the investigation stops there, with a recommendation to retrain the higher education employee in the lockout procedure. However, a good RCA will dig into the factors of why the higher education employee did not follow the procedure. A well-done RCA can often find the hidden flaw in the management system and fix not just that single incident, but also many others like it, enacting real change toward preventing future losses for your educational institution.
Benefits of Root Cause Analysis
- Add value to the organization
- Create the potential for cost reduction or improved allocation of resources
- Provide a learning process for better understanding of relationships, causes and effects, solutions, and ownership of risk
- Provide a logical approach to problem solving using data that already exists
- Reduce recurring risk
- Mitigate likelihood of similar losses
- Improve performance
- Support development of more robust and resilient systems
How Higher Education Institutions Can Use Root Cause Analysis
There are times when a “team” root cause analysis is called for. Examples of this type of root cause analysis might be when:
- There has been a significant event or loss such as a serious injury, death, or large property loss.
- There are repeated losses, e.g., multiple similar injuries in a work unit or job function, similar types of property losses across campus, and repeated accidents in a specific location.
- There is an awareness of repeated “near misses” which are leading indicators of a future large loss.
- An audit determines that required practices are no longer followed or are ineffective (e.g., training, reporting, and submission of credentials before being given access to facilities, programs or property).
- There has been a change in organizational risk appetite and past accepted loss levels must be decreased.
Risk managers may be in a unique position to organize the institutional effort to create a RCA task force. Loss patterns may be recognized through claims and loss data, campus police or Title IX reports, incident reports and other types of data analysis.
Who Should Be Involved
Participants in an RCA task force will depend on what is being investigated, but a typical higher education team would be composed of the following:
- Management responsible for and familiar with the area where the losses or non-compliance appear
- Higher education employee(s) who conduct the operation in question
- Risk Management
- Safety officer
- Internal Audit
- Legal Counsel
- Other campus personnel that might be beneficial: investigator from campus police, laboratory or research safety specialists, workers comp specialist, etc.
Root Cause Analysis Techniques
There are many different techniques used in performing RCA. Each higher education institution should use a method that best suits their needs, resources, and operational model:
- Ishikawa Diagrams (fishbone diagrams 2 )
- The 5 Whys 3 Method
- Fault Tree Analysis 4
- Failure Mode Effects Analysis (FME) 5
Institutions that may need repeated RCAs, because of their size or other factors, can also easily find affordable training programs on how to perform RCAs by contacting your Broker, referring to the IIA website6, or reviewing scholarly articles available online.
Engaging in RCA following a serious loss will clearly benefit the higher education institution if the information is used to help prevent future losses. It can also benefit the school’s insurance program if the analysis process and the follow-up loss prevention practices are reported back to the institution’s insurers, creating a positive circle of reinforcement that the institution is engaged in improvement for the benefit of all.
Want more tips and tricks from our higher education team? Subscribe here.
Author Information:

John Watson
Executive director, higher education practice.
- Camarillo, CA
1 American Society for Quality. “What is Root Cause Analysis (RCA)?” 2 Project Management Skills. “Fishbone Diagram Cause and Effect Analysis” 3 iSixSigma. “Determine the Root Cause: 5 Whys” 4 eDrawsoft. “What is Fault Tree Analysis (FTA)? – The Beginner’s Guide” 5 ScienceDirect. “Failure Mode and Effect Analysis” 6 The Institute of Internal Auditors North America website
Root Cause Analysis Methods
Why is it that some of our best-laid plans don’t work out the way they’re supposed to? No matter how…

Why is it that some of our best-laid plans don’t work out the way they’re supposed to? No matter how hard we try, some problems seem insurmountable.
Root Cause Analysis (RCA) is a helpful tool in our problem-solving challenges. Root cause analysis methods involve identifying the root of a problem to arrive at a solution. It helps us dig deeper into the origin of a problem. Additionally, it can help us identify patterns that are inefficient. Organizations deploy several types of root cause analysis methods to prevent unnecessary business interruptions, regulations, or fines.
The two most popular root cause analysis methods that can help eliminate underlying obstacles are:
- The 5 Whys Method
For effective root cause analysis, 5 Whys is one of the most preferred root cause analysis methods. The technique helps you get to the bottom of the problem. Every ‘why’ is followed up by more ‘whys’, allowing one to unravel the layers and access more information. Let’s look at these root cause examples to better understand the 5 Whys technique:
A company launches a new marketing initiative to promote its new product. But the new marketing strategy fails to attract customers. By asking the 5 Whys, you can get to the bottom of the problem.
- The first why:
Why did the new marketing initiative fail? Because the team could not meet their deadlines.
The second why:
Why did the team member fail to meet their deadlines? Because nobody was tracking individual and overall progress.
The third why:
Why did nobody track the progress of the initiative? Because nobody collaborated or discussed their respective milestones.
The fourth why:
Why did nobody collaborate and communicate individual progress? Because there was no opportunity for them to sit and brainstorm together. ( biergardenencinitas.com )
The fifth why:
Why were there no group brainstorming sessions? Because the team leader believed that group sessions were a futile activity.
From the above root cause analysis 5 whys example, it’s clear that the team leader should have conducted brainstorming sessions for the marketing team. These root cause analysis examples go a long way in identifying underlying causes.
Harappa Education’s Creating Solutions course will teach you how to effectively analyze and get to the bottom of workplace problems through root cause analysis. The 5 Whys model, in particular, will help you get to the root cause of problems by following a chain of “why” questions.
- The Fishbone Diagram Method
The root cause analysis fishbone diagram is another popular and effective technique for problem-solving . It’ll encourage you to visualize your problems by helping you draw a mental map of cause-and-effect. It lets you map out multiple branching paths that’ll lead to potential causes.
The fishbone diagram is also called the Ishikawa diagram, after the Japanese organizational theorist Kaoru Ishikawa. The diagram is named so because it resembles a fish’s skeleton. The process is kicked-off by placing the major challenge at the center. So, the issue to be addressed becomes the spine of the fish’s skeleton. Other causes and sub-causes branch out from the main spine or problem. By raising questions at each level of the branch, you get closer to the root cause.
Let’s take the following root cause analysis examples to understand the fishbone technique clearly:
- An organization is lagging in productivity and finding it difficult to meet its monthly targets. A root cause analysis fishbone structure will help you categorize your problem under different heads like ‘people’ or ‘environment’. You can further branch out the underlying factors affecting the ‘people’ category into ‘leadership’, ‘ teamwork ’, and ‘training’. You can work towards the areas that need improvement.
- The rules of a fishbone diagram can also be applied in personal life. Imagine trying to meet your friends at a pub just after the lockdown has been lifted in your city but you’re unable to. You can classify the problems into ‘internal’ and ‘external’ categories. Underlying factors that can be included in the external category are ‘time’, ‘location’, and ‘safety’.
Root Cause Analysis Steps
The root cause analysis methods involve five steps. These are:
- Define The Problem:
It involves finding out what exactly is happening and what the specific indicators of the problem are.
- Collect Data:
If you can understand how long the problem has lasted or what the impact of the problem has been, it can maximize the effectiveness of root cause analysis.
- Identify Potential Causal Factors:
Understanding the sequence of events that has led to the final event helps to study potential factors that allowed the problems to occur.
- Identify Root Cause Technique:
In this step, you try to find out why the causal factors exist. You may want to use root cause analysis 5 Whys or the fishbone diagram to discover the root cause.
- Recommend Solutions:
If you can use your knowledge to prevent mistakes from repeating in the future, you can mitigate risks and arrive at efficient solutions.
Remember, running away from any problem only increases the distance from the solution. The easiest way to escape from the problem is to solve it. So face your problems head-on and get to their root. Be a problem-solver and stand out at your workplace!
Explore topics such as Root Cause Analysis , 5 Whys Analysis & Pareto Analysis from our Harappa Diaries blog section and develop your skills.
Witness the power of one: new worktech innovations coming April 16. Register in Americas/EMEA timezone and Register in APAC timezone
- Our platform With Eptura’s all-in-one platform, you can bring together your entire world of work, so your people — and your business — can reach their full potential
- Product portfolio
Eptura for Business
Eptura for Education
Eptura for Energy and Transportation
Eptura for Government
Eptura for Healthcare
Eptura for Manufacturing
Eptura for Software & Tech
Partnering with the best local experts to meet your needs
Building future-proofed workplaces ready for tomorrow
Transforming space utilization for the future of work
Integrating seamlessly with the tools you use every day
Collaborating to create a better world of work for everyone
Access a wealth of expert resources for yourself, your team, and your organization.
Read insightful articles filled with can’t-miss tips and research
Listen to thought-provoking conversations with industry experts
Catch up on all the latest from Eptura HQ
Browse our upcoming live and virtual events
See how we’re building a future where everyone can thrive
Discover what motivates our work
Learn how we support workplace equality and the planet
Get to know the people behind our mission
Find us in locations around the world
Join our growing team of innovators
How to implement root cause analysis (RCA): Explanation and examples
Everything you need to avoid failures and recreate successes using root cause analysis (RCA), including clear definitions and easy-to-understand examples.
April 10, 2024

Root cause analysis (RCA) is a process for finding the fundamental cause of a problem, issue, or incident. It’s also how you determine corrective actions and outline and implement steps to reduce the risk of future occurrences. If an organization only ever treats the symptoms without addressing their source, you waste time and money reacting to the same failures.

What is the definition of root cause analysis (RCA)?
Just like the name implies, it’s the process of finding the original cause for an incident. To fully understand that definition, you need to know the answers to two questions:
- What’s the difference between accidents and incidents?
- What’s the difference between a cause and a symptom?
Incidents vs accidents
Strictly speaking, an incident is something that happened, usually as the result of an earlier event. So, someone gets arrested after committing a crime. Or someone gets promoted after boosting uptime and cutting costs in a facility.
In one case, it’s something positive. In the other, it’s negative. But both are incidents, and this fact is important to remember when looking at RCA. Your root cause can be the reason why something didn’t work but it can also be the reason why something did.
Accidents, though, are always bad. Separate from questions about who’s to blame or if it was avoidable or not, you don’t want accidents.
Causes and symptoms
Causes are the reasons why. Symptoms are the results. The classic example is when you get sick and suffer from:
- Headache
- Sore throat
Everything on that list is a symptom, a result of your being sick. But they are not the reason you’re sick. The reason is likely a bacteria or viral infection. Why is the distinction important?
If you only ever treat symptoms, you always run the risk of getting sick again. Sure, you can use all kinds of medicine to lessen the effects of the symptoms, but because you aren’t attacking the root of the problem, it can come back.
What are the benefits of root cause analysis?
RCA helps you reveal the real reasons something happened, which helps you both now and in the future. First, you can more easily fix a problem when you know what’s causing it. For example, if a piece of equipment has a leak, you can patch it, dealing only with the symptoms. But if you dig deeper and discover the leak is the result of a broken internal seal, you can replace the seal, both stopping the leak now and avoiding leaks in the future.
The second benefit comes from how you can take what you learned with the broken seal and apply it to other equipment. You might decide, after a bit more digging for the root cause, that the team is not inspecting the seals often enough, leading you to add more preventive maintenance inspections and tasks to the schedule. Or it might be the case that your seals are generally low quality, and moving forward, you want to change suppliers. In either case, RCA helps you develop insights into your operations, which leads to better decision-making.
What are the common strategies and examples of RCA?
There are various methods, but they’re all connected.
5-whys method
The first method for root cause analysis is to ask yourself why something happened. Sounds easy at first, but it can become challenging as you drill down.
There’s a story about a Ph.D. candite defending his doctoral thesis in astrophysics. Everything was going fine until close to the end when one of the professors ask him what seemed like a simple question: “Why is the sky blue?”
Every time he answered, he was met with, “Could you be more specific?” And so, he kept digging deeper, until he was at the level of explaining molecular energies, optics, and the inner workings of the human eye.
RCA works the same way. You keep asking yourself why something happened until you’re about five or so levels down. Five is the general rule of thumb for root cause analysis. In some cases, you only need to dig down twice, while in others, it’s deeper.
Examples of the 5-whys method for RCA
So, back to our earlier example of the leaking equipment. How could you use the 5 whys?
Why is it leaking? The connection between the two pieces is not tight enough to keep the liquid from coming out.
Why is it not tight enough? The rubber seal is damaged, preventing a tight fit.
Why is the seal damaged? It was not installed properly. When the techs tightened the pieces together, the threads bit into the seal, damaging it.
Why did the techs install it improperly? The seals are different than the ones they’re used to working with, and they did not receive new training.
So, why is there a leak? The root cause of the leak is a lack of proper training on how to install the new seals.
Change analysis and event analysis
In the leaking example, we’re drilling down from one connected cause to the next, looking for the root cause.
For change and event analysis, we’re sorting through different changes, looking for the one that was the root cause. We must decide if each change leading up to the incident was unrelated, correlated, contributing, or the root cause.
Unrelated means there is no relationship, and the change did not cause the incident. Correlated means there is a relationship, but the change did not cause the incident. How is this possible?
The classic example of “correlation is not causation” is murder and ice cream. Whenever ice cream sales increase, there is a corresponding increase in the murder rate. For example, a small increase in sales is followed by a small increase in murder. But ice cream is not affecting the crime rate. Instead, there is a lurking variable in the background pushing up both numbers: heat. When the temperature rises, people eat more ice cream. And they have much shorter fuses.
Contributing means the change helped but wasn’t the only cause.
Example of change analysis and event analysis for RCA
The maintenance manager notices an increase in the monthly close-out rate for preventive maintenance inspections and tasks. Hoping to recreate the success, they come up with the following list of recent changes that could explain it:
- A new tech started two months ago
- The maintenance department switched supplies for some parts and materials
- A different tech has been taking care of the PMs while the regular tech is on vacation
Which change is the root cause? The first one turns out to be unrelated. The new tech was hired specifically for a maintenance project that’s separate from the PM program. Looking at the parts and materials, it’s hard to say they’re affecting close-out rates. They might last longer and cost less, but that wouldn’t make them easier to use.
But are they easier to find? The manager notices that the packaging is better. The writing is nice and clear, and many of the boxes are color coded. It’s a small change, and likely only saving the techs a few minutes per PM, so the manager decides it’s only a contributing cause.
That leaves the fact that a different tech had been doing the PMs, which looks great for the tech. But is it the root cause for the better close-out numbers? When the maintenance manager compares the new tech to the old one, they’re very similar, with roughly the same amounts of experience and time with the company.
Digging deeper and asking between two and 5 whys, the manager finds the root cause. The first tech tends to work on a later shift, which means they’re constantly being called away to deal with on-demand work orders. The second tech usually works the earlier shift, before any equipment has had a chance to break down. They’re able to get more PMs closed out because no one is reprioritizing the work order schedule.
Now that the manager has found the root cause, they can recreate that success by actively scheduling more of PMs for the earlier shift.
In this example, the maintenance manager was able to find a root cause they could control. That’s not always the case. There are times when you can easily identify the root cause, but you can’t easily do anything about it. What if the difference between the two techs was that one had a young baby at home and the other one didn’t? Because the baby’s up all night, the tech’s not getting enough sleep, and it’s affecting their performance? RCA can tell us why something happened, but that doesn’t mean it also always tells us the best way to fix it.
Ishikawa or fishbone diagrams (aka Fishikawa)
When you’re first brainstorming possible causes, there’s no such thing as a bad idea. But once you have all the ideas out in front of you, it’s time to start organizing them, deciding which are the best.
Ishikawa diagrams, named after Kaoru Ishikawa, a key figure in Japanese quality management innovations, show the causes leading up to an event. The name fishbone diagram comes from their resemblance to a fish skeleton with the effect at the head.
By building out the diagram, you can get a better understanding of the causes, their relationships to one another, and their relative contribution to the final effect. From there, you can work on finding ways to either re-enforce or remove them.
What connects these RCA methods is the need for good data and careful thinking.
“What you really want people to do is think through in a very logical, evidence-based fashion as to why things happen,” explains Bob Latino, principal at Prelical Solutions, LLC, in an episode of the Asset Champion podcast.
How can maintenance departments implement root cause analysis?
Now that you know what it is, it’s time to get it working for you. One of your most important goals needs to be getting accurate information. If you want to prevent a problem from popping up again, you need to know why it happened in the first place. But we know that there are times when getting to the bottom of things can be challenging.
Make reporting incidents easier
When something goes wrong, is there a process in place for reporting it? How comfortable are the techs using this process? Does it encourage them to be open and honest?
There are different ways to approach the situation. For example, you can have a frank discussion with the team, assuring them that you’re more interested in avoiding problems than punishing people. And when you have the chance, go out of your way to show that you mean it.
You can also look at ways to allow for anonymous reporting. Techs might feel more comfortable if their name is not attached to the report.
Get standardized maintenance processes with an asset management solution
Before you can reliably use RCA, the maintenance team needs to be performing inspections and tasks the same way every time. If your processes are not standardized, there’s no way for you to look back for changes. Remember, with change and event analysis, you’re looking for what was different. If the team does the work differently every time, it’s harder to find root causes.
Modern asset and facility management platforms help you standardize processes with work orders packed with step-by-step instructions and customizable checklists. Now, instead of techs winging it when they must complete an unfamiliar task, they can easily access the department’s best practices.
And if they have any questions, they can quickly reach out from anywhere by using the software to add comments directly to work orders.
Capture accurate data
With paper- and spreadsheet-based methods, there’re too many chances for bad data to creep in. Old-fashioned paperwork makes it hard to create copies, which are then easy to lose. And with spreadsheets, you can make many copies quickly, but you don’t have any way to keep them all connected and up to date.
Modern maintenance management solutions keep everything in a central database your team can access from any connected device, from desktops to smartphones. And because everyone is working from the same data, it’s always accurate and up to date.
And that means when you go back and start looking for causes, you know you can trust your data.

By Jonathan Davis
Jonathan writes about asset management, maintenance software, and SaaS solutions in his role as a digital content creator at Eptura. He covers trends across industries, including fleet, manufacturing, healthcare, and hospitality, with a focus on delivering thought leadership with actionable insights. Earlier in his career, he wrote textbooks, edited NPC dialogue for video games, and taught English as a foreign language. He hold a master's degree in journalism.
Find this article useful? Why not share it
You might also like.

Workplace portals: how to support flex work and the hybrid office

NFMT Baltimore 2024: facility management conference and expo recap

How to reduce idle time and cut costs
Ready to learn more.
Sign up to stay in the loop on new product updates, the latest innovations in worktech, and tips & tricks to help you work your world.
Keep me updated
- Search Menu
- About BJA Education
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Active and latent errors, executive errors, slips and lapses, planning errors, knowledge based, rule based and mental model mistakes, team-working errors, error within complex systems, incident reporting systems, root cause analysis, 1. getting started, 2. gathering and mapping the information, 3. identifying care and service delivery problems, 4. analysing the information—identifying contributory factors and root causes, 5. generating recommendations and solutions, 6. implementing solutions, 7. writing the report, declaration of interest.
- < Previous
Error and Root Cause Analysis
- Article contents
- Figures & tables
- Supplementary Data
Mhairi Jhugursing, Valerie Dimmock, Haresh Mulchandani, Error and Root Cause Analysis, BJA Education , Volume 17, Issue 10, October 2017, Pages 323–333, https://doi.org/10.1093/bjaed/mkx019
Errors can be defined as an act of commission or omission leading to an undesirable outcome or potentially undesirable outcome.
Error can be classified as active or latent, individual or system based.
Addressing the individual error may prevent the person repeating the same error, whereas addressing latent errors and contributing human factors may prevent an entire organization from making the error again.
In the NHS, incident reporting systems are a form of voluntary staff-led error data collection and collation.
Root cause analysis is a systematic process whereby the factors that contribute to an incident are identified and learned from.
‘Knowledge and error flow from the same mental sources, only success can tell one from the other.’ 1
An error is an act that can lead to an undesirable outcome. Everyone makes mistakes; it is part of the human condition. Cognitive psychologists believe that slips, lapses, and mistakes are inevitable, as they are the price we pay for advanced higher cerebral function. Specifically, a medical error is a preventable adverse effect of care, whether or not it is evident or harmful to the patient. This might include an inaccurate or incomplete diagnosis or treatment of a disease, injury, behaviour, infection, or other ailment. But how do we reconcile this with modern health care, where safe effective patient care is the pinnacle of our practice? James Reason, a British psychologist, founded the framework of error classification and management in health care in the 1990s. As health care has evolved over time, so has our understanding of error and its management. Reason’s work forms the basis of the rapidly expanding field of patient safety. Anaesthesia was one of the first specialities to introduce patient safety guidelines into practice. Patient safety was further highlighted by the Elaine Bromiley case in 2005. This article explores the theory of error occurrence and systems we use to learn from it.
Errors can be defined as an act of commission or omission leading to an undesirable outcome or potential undesirable outcome. 2 Fortunately, not all errors lead to actual patient harm.
The time point the error occurred relative to the error identification, i.e. active and latent errors.
The thought process related to the error, poor planning, or poor execution of a task.
The conscious movement away from established rules within an organization, i.e. violations and malevolent acts.
Team-working errors.
Errors can be thought of as active or latent ( Fig. 1 ).
Active and latent errors diagram.
Active errors occur at the ‘sharp end’ of health care, where an action directly causes an error in real time. 8 , – 10 These errors tend to be person/individual related or immediate equipment failures. Examples include an anaesthetist administering an incorrect drug dose to a patient or not turning on the oxygen flow for pre-oxygenation in a rapid sequence induction of anaesthesia. Active errors are usually picked up quickly at the time of the incident and therefore more easily identified.
Latent errors occur at the ‘blunt end’ of health care. They do not directly cause the error and occur upstream of the event. These errors are wide ranging—the building/room layout, organizational processes, human resources, equipment failure, or medication error. These errors tend to be ‘systems’ related. They are the factors that have contributed to the event. 8–10 For example, many drugs have similar packaging (see Fig. 2 ), and the wrong drug or concentration could easily be administered. Some pumps have multiple steps to their programming, making it difficult to check the correct data have been entered. An example of a human resource error is not enough anaesthetists available to attend a crisis in another theatre during a normal working day.

Drugs with similar packaging.
Latent errors can lie dormant for a long period of time before a situation arises that leads to the error being identified. There has been extensive investment in latent error reduction in many high-risk industries, with human factors engineering playing an important role.
To use an analogy, ‘active failures are like mosquitoes. They can be swatted one by one, but they still keep coming. The best remedies are to create more effective defences and to drain the swamps in which they breed. The swamps, in this case, are the ever present latent conditions.’ 11
An executive error is an active error occurring at an individual level. A task broadly has two stages—the planning phase and the action phase. An executive error occurs when an intended outcome is not achieved because of a deficit in the actions carried out. 8 Executive errors can be further divided into slips and lapses.
Slips are due to attentional failures, usually when undertaking familiar tasks. Familiar tasks have usually been undertaken many times previously and are almost an automatic behaviour, requiring little conscious effort 3 , 8 , 12 . A slip can take the form of intrusions where you are thinking about the management of another difficult case ahead and, for example, inadvertently draw up ephedrine into the intended metaraminol syringe. Slips tend to happen with familiar skill-based tasks.
Lapses are due to memory failures. The tasks involved tend to be complex or have multiple steps, 8 , 12 e.g. forgetting to flush the central venous catheter with 0.9% saline before inserting it or forgetting to give surgical antibiotic prophylaxis prior to making an incision (see Fig. 3 ).

Summary of error types. Adapted from St Pierre et al. 8
A planning error is a form of active error, where the intended outcome is not achieved because of a deficit in the planning before execution of the task and is termed as a mistake. Planning relies on thought processes, and it applies largely to unfamiliar tasks. It is a conscious effort and requires more focus and energy than automatic familiar tasks. Problem solving is required to formulate a plan, and there are three common cognitive tools used to facilitate the process: knowledge based, rule application, and a mental model. 8 , 12
Knowledge-based mistakes are generated by lack of facts related to the problem. 8 , 9 , 12 For example, suxamethomium can trigger malignant hyperthermia; and patients with diabetes can have gastric autonomic neuropathy, increasing the risk of acid reflux and aspiration.
Rule application concerns the use of a set of learned guidelines. Mistakes can occur in the misapplication of a ‘good’ rule, e.g. giving a beta-blocker to a patient with fast atrial fibrillation to control the heart rate, but the patient has asthma. Using the ‘wrong’ rule also causes mistakes, 8 e.g. using the pneumonia guidelines to treat a patient with pulmonary embolus.
Mental models are psychological representations of a situation. We often rely on previous experience when encountering a new situation and tend to use a mental model that best fits when we previously felt in control. However, this may not be the reality of the situation. 8 For example, a general anaesthetic is administered to an obstetric patient because of inadequate epidural anaesthesia for urgent Caesarean section. The patient becomes hypotensive and is resuscitated with i.v. fluids. Previous experience has been of obstetric hypotension caused by maternal haemorrhage, and aggressive blood transfusion is commenced. The obstetricians have achieved haemostasis, but the mental model persists and further fluids and blood products are given for presumed occult blood loss. The blood pressure remains low and the oxygen saturations drop as fluid overload manifests. The mental model has falsely reassured the anaesthetist who has overlooked or dismissed other causes of hypotension, such as a ‘high’ regional block. Mental models should not be relied upon and should be frequently re-evaluated.
As an anaesthetist progresses through his/her career, the likelihood of particular error types changes. In the early stages of a doctor’s career, knowledge-based errors are more likely. As the novice advances and acquires his/her basic competencies his/her practice is guided by a basic set of rules, hence rule-based error usually occurs at this point. As an anaesthetic consultant, the majority of activities have become automatic skills, and slips and lapses can creep in. 8
Slips, lapses, and mistakes are unintentional behaviours that may lead to patient harm. Violations differ as they are deliberate acts that deviate from the accepted guidelines of safe practice. In some rare instances, they are malevolent acts, where staff deliberately cause harm to patients, equipment, or other staff members. However, the majority of violations are committed with the intention of making a task easier or quicker, despite falling outside the safety guidelines. Such ‘shortcuts’ may on the surface seem to be a better trade-off between efficiency and risk but may cause patient harm. Continued violation of a safety protocol at an individual or department level will lead to a bare minimum safety margin, where serious harm could occur. 8 An example would be preoperative assessment of elective cases in the anaesthetic room. This would be time saving but would need to be balanced against the risk of pressure to proceed with surgery, even with insufficient investigations. In most occasions, all required information will be available and anaesthesia will proceed safely.
Active errors from the individual can be minimized by the use of checklists, briefings, guidelines, structured handovers, read backs, and double checks, ‘Do not enter—anaesthesia in progress’ signs, and simulation training (see Table 1 ).
Latent errors within a system can be minimized by automated systems, standardization of equipment and drugs, and optimal equipment design with forced functions (i.e. equipment or systems that only allow specific standardized options to minimize error) (see Table 2 ).
Measures to reduce active errors 6 , 9 , 10 , 15
Measures to reduce latent errors 9 , 10 , 15
No department is error proof. Reason proposed the ‘Swiss Cheese’ model to describe the trajectory of an error (see Fig. 4 ). 9 Multiple safeguards are put in place to avoid errors in a system. Each layer of protection will have an area of weakness, representing a hole in the defence. With multiple layers, even if an error breaches one layer, the next layer will catch the error before it causes patient harm. This model can be 100% effective in a static environment, but the NHS is a complex dynamic system with multiple ‘moving’ layers of protection, thus at some point the ‘holes’ in each layer can align, allowing a straight path to patient harm. There are, however, limitations to the ‘Swiss Cheese’ model in that it implies linear determinism. While that may be true in some industries such as nuclear and aviation, in health care it seldom is, as events rarely unfold in a single straightforward pattern, and are usually much more complicated and interrelated. 3 , 8 , 12 A comparably complex situation to health care is in the prediction of extreme weather events. It is not always possible to predict the occurrence of a severe hurricane or flood, as there are numerous factors that interplay to lead to one, but once one has occurred, the factors leading up to it can be analysed in retrospect in great detail.

Swiss Cheese model. 9
Error theory is constantly evolving. Suggested theories and solutions are more applicable to a static environment; however, health care is a dynamic environment. An expanding population, with increasing levels of co-morbidity, coupled with demand outstripping resources, means the health care environment will only get more complex over time. Kinnear proposed a different approach accepting the fluidity of the health care environment and focusing on our innate ability to problem solve through resilience engineering. 16 This is examining what works well in this challenging environment, in addition to went wrong. Resilience engineering involves building a flexible organization that anticipates the dynamic nature of errors and continually revises risk models to reduce errors before they occur. 11
Errors will occur within every health care system. It is important that these errors are identified and lessons drawn from these cases to improve patient safety. Incident reporting systems (IRS) collect error data with the aim of facilitating learning and improving patient safety. They are passive processes where data are voluntarily reported by staff on the front line. Voluntary incident reporting is highly variable and does not truly reflect the incidence of errors, which are generally under-reported within health care. However, these passive systems are relatively inexpensive and empower staff to identify and learn from error. If lessons are appropriately disseminated to the right people, the required changes can be made to prevent recurrence. Increased reporting can be encouraged with an open ‘fair blame’ culture ensuring timely feedback and improvements. 7 , 14 A ‘fair blame’ culture achieves a balance of openly investigating the factors leading up to an incident and our individual responsibility and behaviour as health care professionals to maintain good practice and safety. In the UK, 75% of Trusts use the Datix web-based software programme for incident reporting. Once reported, the process of learning and improving patient safety begins with root cause analysis (RCA). There are two general approaches to error investigation: person based and system based.
The person-based approach focuses directly on the unsafe act committed by the person causing the incident and implies that the error is specific to that individual, separating the incident from the latent errors and human factors contributing to it. Unfortunately, the person-based approach is prevalent throughout many organizations. 8 With this approach, it is easier to blame an individual for his/her carelessness, inattention, recklessness, or lack of education. This tends to lead to a ‘naming, blaming and shaming’ culture, where if a similar circumstance were to occur again, the likelihood is that the same error would happen. In addition, the morale and confidence of the individuals involved may be permanently damaged. This is not an effective approach to error reduction in health care. The Berwick Report (2013) on patient safety in the NHS stated we should ‘abandon blame as a tool’. 17
The basic premise in the system-based approach is that humans are fallible and errors are expected, even in the best organizations.
The systems-based approach is far more applicable to the NHS and considers the organizational processes and chain of events that lead to the error. Errors are seen as consequences rather than causes, having their origins not so much in the perversity of human nature as in the ‘upstream’ systemic factors. 11 Countermeasures are based on the assumption that though we cannot change the human condition, we can change the conditions under which humans work. RCA examines both aspects, but with particular emphasis on the systems-based approach. 8
RCA is the structured, thorough investigation of a patient safety incident to determine the underlying causes and contributing factors, and then analyse these to draw out any learning points. 7 The learning points can be actioned to reduce the chance of the same or similar incident reoccurring. The Berwick Report stated as its main objective regarding patient safety, ‘A promise to learn—a commitment to act: improving the safety of patients in England’. 17 The most widely adopted RCA template is from the National Patient Safety Agency (NPSA), which is detailed below. The process of RCA can be broken down into seven steps 18 (see Fig. 5 ).

The RCA investigation process.
The RCA investigation process
Worked Example
Incident Report System (Datix) summary from theatres:
Vascular surgery emergency open abdominal aortic aneurysm (AAA) repair (failed endovascular aortic repair (EVAR)): Incorrect dose of heparin administered during surgery, patient suffered coagulopathy causing major surgical haemorrhage and cardiovascular instability requiring multiple blood product administrations. Patient admitted to intensive care unit postoperatively. Patient remains intubated with high oxygen requirements secondary to transfusion related acute lung injury (TRALI) and is receiving renal replacement therapy due to acute renal impairment. Anaesthetist who administered heparin had drawn up the incorrect dose. There are two different heparin vial concentrations in the anaesthetic room drug cupboard, heparin 100 units/ml and 1000 units/ml.
Level 1 – No harm (‘near miss’)/low harm/moderate harm. A concise investigation usually handled by one local person, comprising a one-page summary.
Level 2 – Severe harm or death. A comprehensive investigation, an in-depth assessment requiring a multidisciplinary team, which was not involved in the incident, or in the locality or directorate. There may be expert opinion sought.
Level 3 – Severe harm, death, or public interest. As above, plus incidents of public interest or notifiable serious incidents (e.g. never events). These investigations are carried out by investigators external to the organization.
The RCA team will routinely comprise a person trained in RCA, expert(s) in the incident field, an administrator, and a non-executive person (layperson or patient representative). 18
Patient safety incident Level 2 (severe harm), requiring comprehensive investigation by RCA team. RCA team assembled. Consultant anaesthetist (not involved in the incident), consultant vascular surgeon (not involved in the incident), medical secretary, pharmacist, and patient advisory liaison officer.
This step is about gathering all relevant facts surrounding the incident, avoiding opinions and other bias, e.g. the cultural bias ‘this is the way it has always been done here’. The sources of information may include medical notes, staff statements, staff rotas (to ascertain staff numbers and skill mix), interviews, local and national policies, guidelines and inspection of equipment and drugs. Interviews can be challenging, highly emotive situations and individuals frequently have poor or altered event recollection. Group interviews suffer from hierarchical impedance whereby in a group of nurses and doctors, nurses may tend to speak up less frequently. Similarly, in a mixed group of junior doctors and consultants, the junior doctors may be less likely to express their concerns. It is important to have an experienced facilitator during group interviews with sensitive and concise questioning to obtain the facts.
All facts should be collected, including conflicting information. Expert opinion should be obtained. Data gaps should be identified and areas of good practice should be identified. This is a fact-finding mission at this stage of the RCA, and the temptation to analyse the data should be resisted. 17 The mapping of information can be recorded via a tabular timeline or a time/person grid (see Worked example on the previous page). 18
Care delivery problems (CDPs) and service delivery problems (SDPs) include all acts of commission and omission. CDPs generally involve failure to monitor, observe, or act. 18
Not noticing the intravenous cannula has ‘tissued’ during total intravenous anaesthesia (TIVA).
A trainee not escalating an ASA 4 cardiovascularly unstable vascular patient to the consultant before commencing anaesthesia.
Not giving antibiotic prophylaxis to a patient undergoing hemiarthroplasty, with subsequent joint infection.
Failure to ask for assistance when spinal anaesthesia has failed in a category 1 Caesarean section with a delay in delivery, resulting in a neonate with poor Apgar scores.
The decision to skip the team briefing in the morning before the list starts, which subsequently leads to a specific piece of surgical equipment not being available for a difficult case.
Unintentionally using 2% instead of 1% propofol in the TIVA pump, causing cardiovascular instability in a patient.
The administration of neat potassium chloride solution in a paediatric burette to an adult patient causing an unpredictable infusion rate, resulting in cardiac arrhythmias.
Continued shortage of central venous catheters in the operating theatre area.
Inadvertently giving local anaesthetics drugs intravenously, causing cardiovascular instability.
Inadequate handover of septic patient, causing delay in treatment.
CDP: Failure to identify correct vial of heparin for vascular procedure by anaesthetic registrar, anaesthetic registrar failure to register, or read the heparin vial label correctly. Consultant failed to check the heparin concentration before administration.
SDP: Two different concentrations of heparin available beside each other in the anaesthetic drug cupboard. Anaesthetic registrar had drawn up multiple drugs over short space of time, while on phone to haematology department.
Contributory factors:
Equipment and resources: Two different concentrations of heparin vials available in the anaesthetic drug cupboard with similar packaging and labels.
Patient factors: Emergency ASA 4e patient cardiovascularly unstable requiring multiple anaesthetic interventions.
Individual factors. Anaesthetic registrar fatigue.
Task factors: Anaesthetist carrying out multiple tasks at once.
Communication factors
Consultant did not ask to see the vial of heparin to check the dose he was administering. Poor communication between surgeon and anaesthetist leading to delay in identification of the problem—assumption excessive haemorrhage was due to surgical trauma, assumption anaesthetist aware of unusually excessive bleeding. Delay in direct communication with haematologist on-call to receive advice about coagulopathy management. No allocated person to liaise with haematology team.
Team and social factors
Multiple activities occurring—additional anaesthetic staff available, but not requested. Theatre staff unaware of error until late in chain of events. If had information earlier could allocate more staff to assist.
Education and training factors
Anaesthetic registrar not aware of two different concentrations of heparin available as he/she is new to the hospital.
Working c onditions
Error occurred during busy night shift, but appropriate level of staffing available.
Organizational and strategic factors
Drugs available in anaesthetic cupboard vary between each theatre and different packaging for same drug.
Root cause:
Equipment latent error
Heparin drug vials of different concentrations found together with similar packaging and similar labels.
Active i ndividual slip
Not reading fully the label on the heparin vial before drawing the drug up by the anaesthetic registrar.
Routine violation
Consultant anaesthetist not rechecking the drug vial before administering to patient (as he did not personally draw up the drug).
Reliance in part on mental models by surgeons and anaesthetists leading to delayed recognition of the error.
Team work error
Poor communication between all groups involved, deficient situational awareness, suboptimal task prioritization, and task allocation

Using the Fishbone (Ishikawa) Diagram to analyse the information- identifying the contributory factors and root causes.
Human actions, e.g. teamwork, handovers, and skills.
Administrative actions, e.g. procedures, policies, guidelines, training, and supervision
Physical actions, e.g. similar product packaging changed and equipment with forced functions. 18
Solutions with a large impact within an entire organization are often more difficult to achieve than more localized ones. Therefore, solutions that work on both levels should be considered to achieve optimal safe working environments and practices (see Fig. 7 ). 18 Constructing a Pareto chart may be useful to focus interventions to gain maximum benefits. A Pareto chart is a combined bar and line graph, which indicates the reduction in an event occurrence relative to specific interventions.

Generating recommendations and solutions.
Physical action: Have single-set concentration of heparin for intraoperative boluses available in the anaesthetic drug cupboard in theatres, with the second concentration for infusions in recovery drug cupboard within the next 2 weeks. This should be standardized across the trust within next 4 months.
Review and reduce drug packaging similarities across trust in all clinical areas over next 12 months.
Human actions: leadership and team working training for theatre staff, focusing on human factors in crisis situations. Training to be initiated within the next 3 months.
Administrative actions: Major haemorrhage protocol review, focusing on improving line of communication between theatres, maternity, emergency department, and haematology team. Aim to complete review within next 4 months.
Implementing a solution is an ongoing dynamic process involving communication, dissemination, diffusion, adoption, spread, and sustainability. An action plan must be specific, measurable, achievable, relevant and timely (SMART). A common template used is an Action Plan Document (see Worked example on the next page). This document encourages the consideration of common factors required for a successful solution implementation. 18 A successful solution implementation is evidenced by measurement of the intended effect. This is akin to a quality improvement project where the Plan, Do, Study, Act (PDSA) cycle continuously assesses and refines the value of the activity.
There are report templates (concise, comprehensive, and external) on the NPSA website; however, each trust will have its own modified template. It is important when analysing investigation findings to be aware of, and try to avoid, hindsight bias and outcome bias. Hindsight bias is the tendency for people with the ‘benefit of hindsight’ to falsely believe, once all the facts become clear, that the actions that should have been taken to prevent an incident seem obvious, or that they could have predicted the outcome of the event. 18 Outcome bias is the tendency to judge a past decision or action by its success or failure, instead of based on the quality of the decision made at the time. No decision maker knows for sure whether or not the future will turn out for the best following any decision they make. Individuals whose judgements are influenced by outcome bias can hold decision makers responsible for events beyond their control. 18 Similarly, if an incident leads to death it is often considered very differently and critically, compared with an incident that results in no harm, even where the incident or error is exactly the same. When people are judged one way when the outcome is good, and another when the outcome is poor, accountability levels become inconsistent and unfair. To avoid the influence of outcome bias, one should evaluate the decision or action taken at the time it was taken, and given what was known or going on at that time, irrespective of the successful or failed outcome. When producing the report, it is important to bear in mind which differing groups will have access to and be reading the report. This may include clinical staff, patient(s) involved and their relatives, hospital patient safety committee, hospital board, Department of Health, coroners, solicitors, general public, and media. It is therefore important to set the right tone, format, and style for all the interested parties. The report must be clear, concise, logical, and show an open and fair approach, and be in the third person. The report should be anonymized and avoid negative or inflammatory descriptors. It is best to record facts and reasoned conclusions, not opinions and assumptions. Link care and service delivery problems with their root cause and then demonstrate the shared learning derived from that. 18 The RCA report must be completed within 60 days of identification of the incident by the patient safety team.
The amalgamation of the entire RCA, ensuring tone, language, and data, are suitable for each group of people who may be reading it. The report should include the analysis, all recommendations and actions with time frames, and identified personnel who will be responsible for ensuring compliance.
To err is human, to cover up is unforgivable, to fail to learn is inexcusable. 19
None declared.
The associated MCQs (to support CME/CPD activity) can be accessed at http://www.oxforde-learning.com/journals/ by subscribers to BJA Education .
Mach E. Knowledge and Error . Dordrecht, Holland: Reidel, 1976 (originally published in German , 1905 )
Google Scholar
Google Preview
Wachter RM. Understanding Patient Safety , 2nd Edn. New York: McGraw-Hill Lange , 2012 ; 33 – 51
Wachter RM. Understanding Patient Safety , 2nd Edn. New York: McGraw-Hill Lange , 2012 ; 21 – 31
Wachter RM. Understanding Patient Safety , 2nd Edn. New York: McGraw-Hill Lange , 2012 ; 149 – 59
Wachter RM. Understanding Patient Safety , 2nd Edn. New York: McGraw-Hill Lange , 2012 ; 111 – 23
Wachter RM. Understanding Patient Safety , 2nd Edn. New York: McGraw-Hill Lange , 2012 ; 303 – 19
Wachter RM. Understanding Patient Safety , 2nd Edn. New York: McGraw-Hill Lange , 2012 ; 233 – 53
St Pierre M , Hofinger G , Buerschaper C , Simon R. Crisis Management in Acute Care Setting , 2nd Edn. New York: Springer , 2015 ; 41 – 59
Gregory B , Kaprielian VS. Anatomy of Error Module Duke University of Medicine. Available from http://patientsafetyed.duhs.duke.edu/module_e/module_overview.html (accessed 3 June 2016)
Wheeler SJ , Wheeler DW. Medication errors in anaesthesia and critical care . Anaesthesia 2000 ; 60 : 257 – 73
Reason J. Human error: models and management . BMJ 2000 ; 320 : 768 – 70
Zhang J , Patel VL , Johnson TR , Shortliffe EH. A cognitive taxonomy of medical errors . J Biomed Inform 2004 ; 37 : 193 – 204
Fortune PM , Davis M , Hanson J , Philips B ; Advanced Life Support Group . Human Factors in the Health Care Setting . New Jersey, USA, London, Oxford: Wiley-Blackwell , 2013 ; 20 – 35
Carthey J , Clarke J. Implementing human factors in healthcare PDF. Patient Safety First Group. Available from www.weahsn.net/wp-content/uploads/Human-Factors-How-to-Guide-v1.2.pdf (accessed 3 June 2016)
Human Factors and Managing Error . NHS Education for Scotland. Available from https://learn.nes.nhs.scot/Resource/View/800 (accessed 3 May 2017)
Kinnear J. Presentation—Damage Limitation—Minimising Unintentional Harm: Complexity, Team Working & Human Factors . The Royal College of Anaesthetists, Patient Safety in Peri-Operative Practice , 2014
Berwick D. A Promise to Learn—A Commitment to Act. Improving the Safety of Patients in England. Commissioned by NHS England, 2013
Root Cause Analysis . National Patient safety Agency. Available from www.nrls.npsa.nhs.uk (accessed 3 June 2016)
Donaldson L. Twitter account quote. 2011
Affiliations

- Online ISSN 2058-5357
- Print ISSN 2058-5349
- Copyright © 2024 The British Journal of Anaesthesia Ltd
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

RCA2: Improving Root Cause Analyses and Actions to Prevent Harm
This tool describes best practices for conducting a comprehensive Root Cause Analyses and Actions (RCA2) to improve patient safety by reducing medical errors, adverse events, and near misses; the Action Hierarchy tool helps identify which specific actions will have the strongest effect for successful and sustained system improvement.
- Root Cause Analyses and Actions (RCA2) event review process
- Action Hierarchy tool instructions, example, and template
Root cause analysis (RCA) is a process widely used by health professionals to learn how and why errors occurred, but there have been inconsistencies in the success of these initiatives.
To identify best practices around RCAs and develop guidelines to help health professionals standardize the process and improve the way they investigate medical errors, adverse events, and near misses, we have concentrated on the ultimate objective: preventing future harm. Prevention requires actions to be taken, and so we have renamed the process Root Cause Analyses and Actions, or RCA 2 (RCA “squared”) to emphasize this point.
The purpose of RCA 2 is to identify and implement sustainable systems-based improvements that make patient care safer in settings across the continuum of care. The approach is two-pronged:
- Identify methodologies and techniques that will lead to more effective and efficient RCA 2
- Provide tools to evaluate individual RCA 2 reviews so that significant flaws can be identified and remediated to achieve the ultimate objective of improving patient safety
The intent of an RCA 2 review is to identify system vulnerabilities so that they can be eliminated or mitigated; the review is not to be used to focus on or address individual performance, since individual performance is a symptom of larger systems-based issues.
After completing the RCA 2 investigation and analysis process, RCA 2 teams work to identify corrective actions to mitigate root causes of the adverse event. A tool such as the Action Hierarchy will assist clinical teams in identifying which actions will have the strongest effect for successful and sustained system improvement.
- Before filling out the templates, first save the PDF files to your computer. Then open and use that version of the tool. Otherwise, your changes will not be saved.
- IHI does not endorse any software or training for the RCA 2 process that is not directly provided by IHI.
How to Cite These Documents: RCA 2 : Improving Root Cause Analyses and Actions to Prevent Harm . Boston: National Patient Safety Foundation; 2015.
Patient Safety Essentials Toolkit: Action Hierarchy Tool . Boston: Institute for Healthcare Improvement; 2019. (Available at ihi.org)
Additional Information
- RCA 2 Frequently Asked Questions
- RCA 2 Endorsements
Related Content
- Patient Safety Essentials Toolkit
What Is RCA 2 ?
Download RCA2 and Action Hierarchy Tools
* Required fields
Related Resources
Root Cause Analysis (RCA), Explained

Root Cause Analysis (RCA) is the best way to find out what causes an issue in your IT operations (ITOps) . In other words, it is a great versatile analysis method for corrective action that is inherent to the ITIL framework . It’s a comprehensive approach that all managers can appreciate.
In the IT industry, this method is invaluable since its ability to swiftly and effectively address problems is what distinguishes proactive IT Service Management (ITSM) . But it’s not just for solving-problem that is valuable; RCA fosters a culture of continuous improvement , learning, and innovation without playing the blaming game.
So, if you want to transform problems to predictable and manageable events in the hopes of navigating the complexities of your IT operations with confidence, keep on reading.
We’ll explore everything that is to know about RCA and how to tailor a method that aligns with your organization’s goals.
Let 's get started.
Table of contents
Itil and root cause analysis, why do you need rca, 5 root cause analysis methods.
- How do you do RCA?
- 5 Root Cause Analysis examples
Root Cause Analysis is a method used to understand the causes of a problem or incident. It’s pretty much the rubric used within the ITIL framework to standardize Problem Management .
As you may know, Problem Management is one of the processes under the Service Operation phase of ITIL , which aims to manage the lifecycle of all problems that could or do affect IT services.
Both ITIL and RCA embody the principle of continuous improvement. In theory, such integration is not just a procedural requirement, it's a strategic approach. And in practice, the synergy between both happens when this method is used to investigate the cause of problems so we can implement solutions long-term instead of temporary fixes.
All of these lead to fewer disruptions and more reliable services. With that comes a robust knowledge base that will help your team make informed decisions when preventing future problems.
The Definitive Guide to Problem Management
It goes without saying that organizations need a problem-solving method that is effective. And more importantly, one that doesn’t merely address the immediate symptoms of a failure.
Keep in mind that problems are often complex, with not just a single cause but multiple contributing factors. Hence, there is a lot of value in digging deeper into problems to improve your operations.
So, why do you need to implement RCA ? Because not only your business resilience depends on preemptively mitigating potential disruptions and downtime , but also because understanding root causes is as much about preventing negative outcomes as it is about replicating success.
Benefits of performing RCA
- RCA helps in streamlining processes and removing bottlenecks that lower your IT team’s productivity.
- On that note, an environment with fewer disruptions also contributes to better work quality and employee morale.
- With this method the likelihood of customers facing the same issues repeatedly diminishes. Reliable products and services improve consumer satisfaction and loyalty.
- Over time, root cause analysis saves an organization time, money, and resources because repeated repairs or adjustments are not necessary.
- Most importantly, you’ll get peace of mind, since you are building a stable and predictable operational environment.

9 Ways to Do Proactive IT Support – And Switch From The Break/Fix Model
In fact, there are several ways in which your organization can conduct Root Cause Analysis . The choice of method depends on the complexity of the issue, the level of detail required in the analysis, the available data and resources, and the desired outcome of the RCA process.
Let’s check them out.
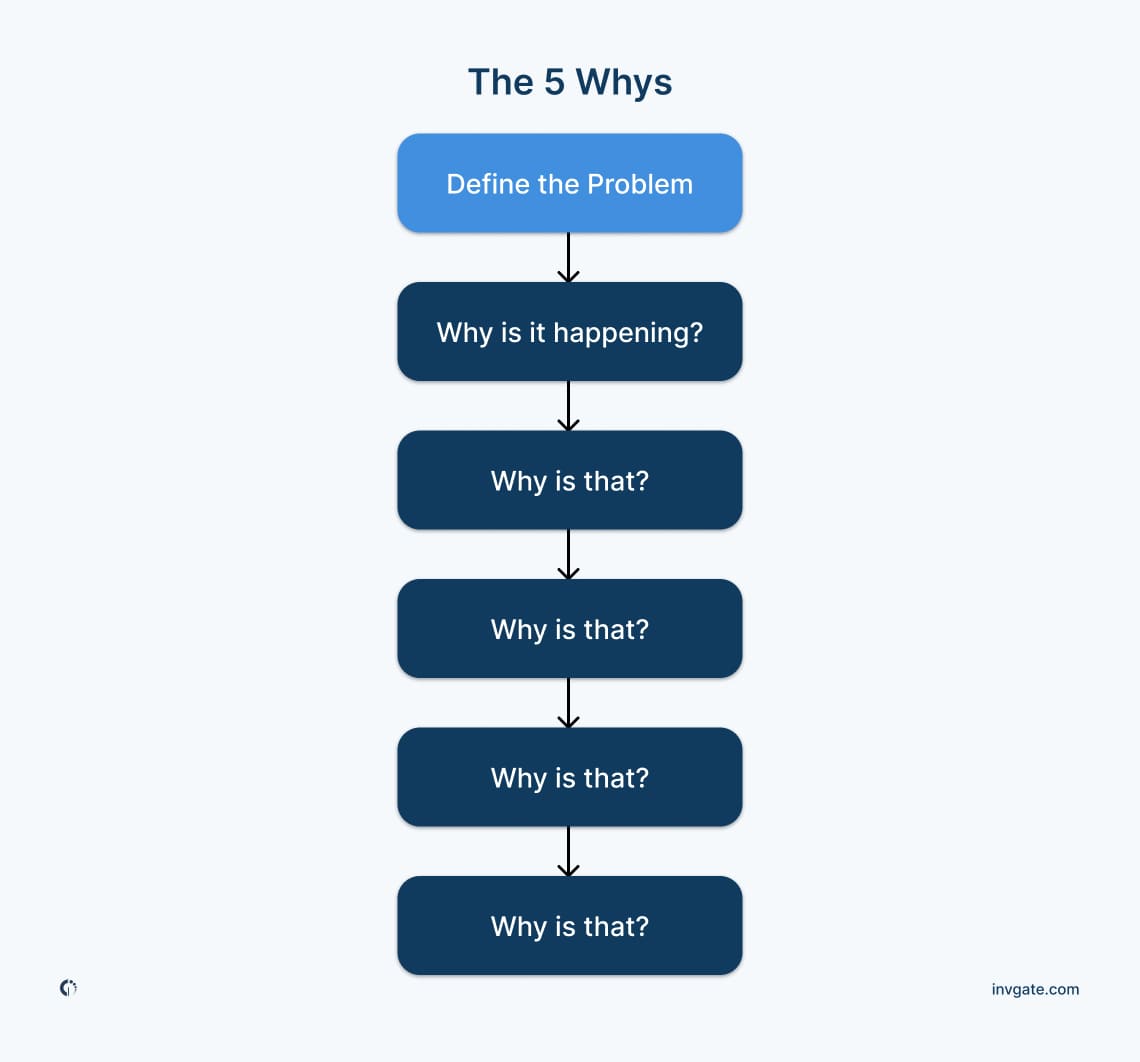
The 5 Whys method involves asking the question "Why?" repeatedly to peel away the layers of symptoms and reach the core issue. It's a straightforward technique that doesn't require statistical analysis, making it accessible for anyone to use. However, its simplicity can also be a limitation, as it might not be suitable for complex problems with multiple root causes.
For instance, let’s say users are experiencing slow response times when accessing the company's internal Customer Relationship Management (CRM) system .
- Why? The CRM system's server is experiencing high latency.
- Why? The server's CPU usage is consistently at 100% during peak business hours.
- Why? A recent update to the CRM software introduced a memory leak that increases CPU usage over time.
- Why? The update was not fully tested in a simulated production environment before deployment.
- Why? The IT department has been under-resourced and couldn't allocate time for comprehensive testing due to back-to-back project deadlines.
2. Failure Mode and Effects Analysis (FMEA)
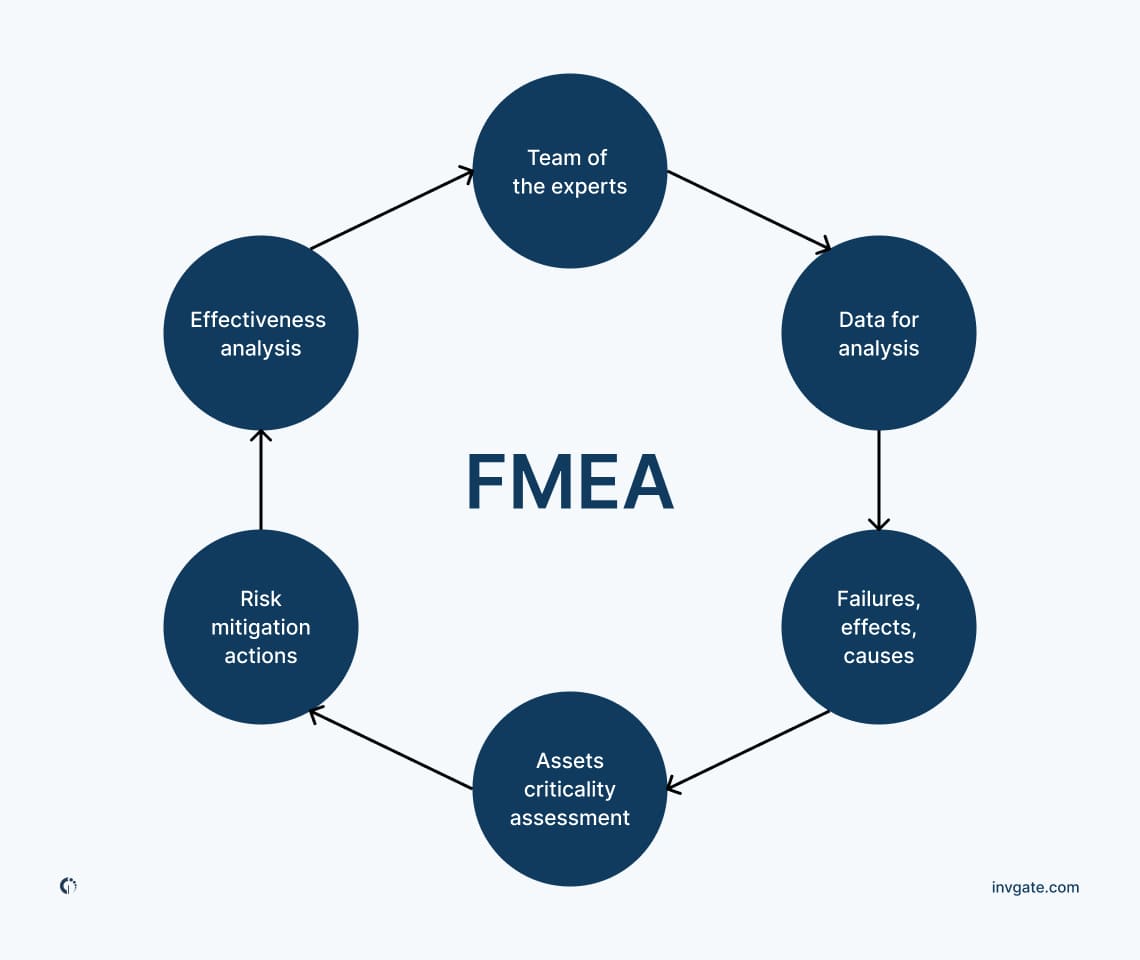
FMEA is a step-by-step approach for identifying all possible failures in a design, a manufacturing or assembly process, or a product or service. It's particularly useful in early stages of development, as it helps to prevent problems before they occur. FMEA evaluates the severity, likelihood, and detectability of failures to prioritize which ones need to be addressed first.
3. Fishbone Diagram (Ishikawa Diagram)
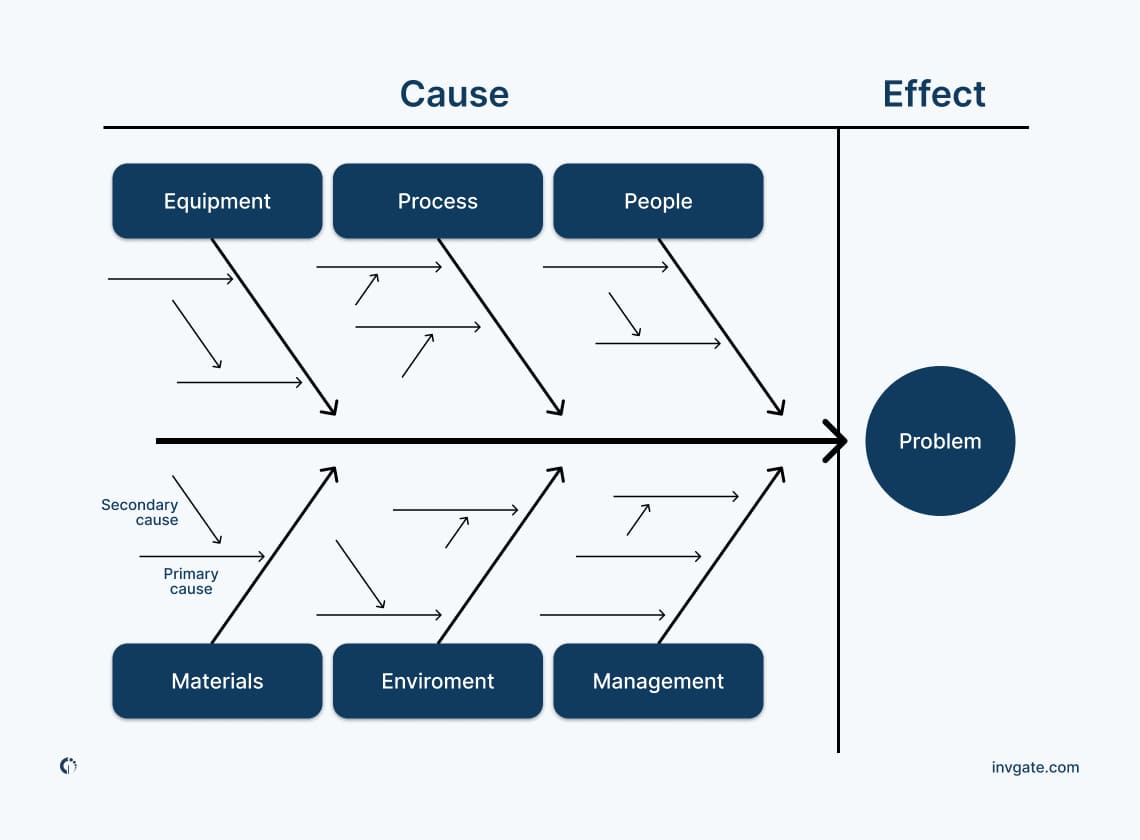
When your issue is complex and you need a structured analysis, the Fishbone Diagram , also known as the Ishikawa Diagram, is a visual tool used to systematically identify and present all possible causes of a deeper problem. It helps teams brainstorm and categorize causes into groups such as methods, machines, materials, people, environment, and measurement.
4. Pareto Analysis
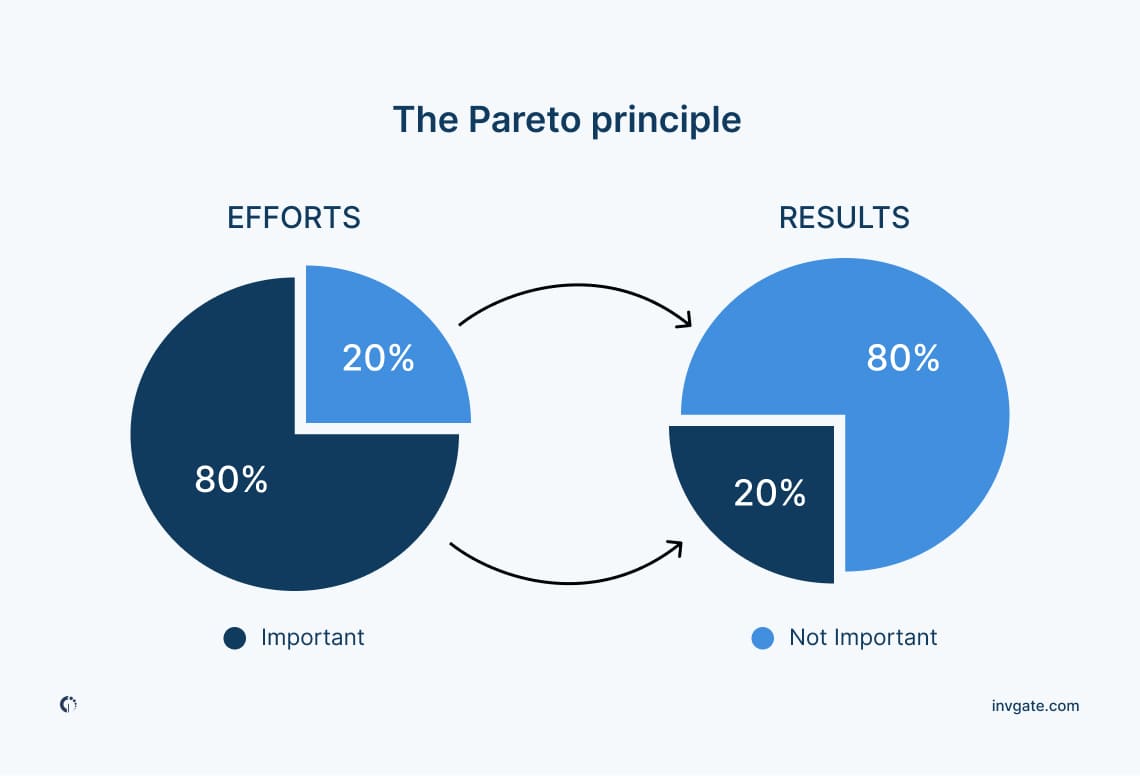
To focus on where to allocate the efforts of your team as well as identifying the most significant issues go with Pareto Analysis , based on the Pareto Principle (80/20 rule). It’s used to prioritize problems or causes to focus on those that will have the greatest impact if solved. Your team will create a Pareto chart, where causes are listed on the X-axis, and the frequency or impact of the causes is shown on the y-axis.
5. Fault Tree Analysis (FTA)
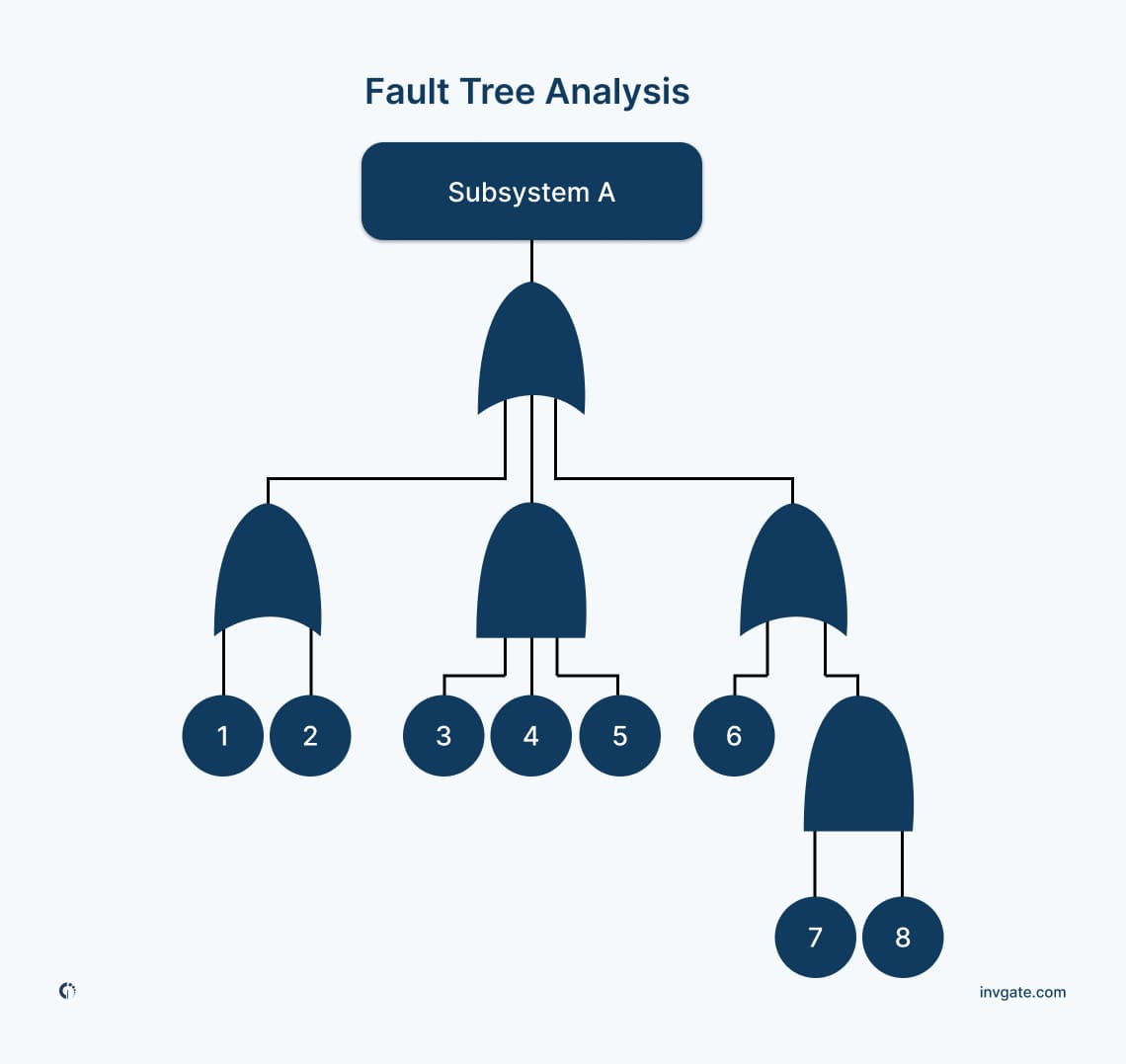
Fault Tree Analysis is a top-down, deductive analytical method used to explore the causes of specific events (usually adverse events). It uses a graphical representation of various parallel and sequential causes that can lead to the event. FTA is particularly useful in industries like aerospace and nuclear power, where preventing failures is critical.
How to choose the right RCA method?
The context of the issue at hand will help you choose the right RCA method , as each one has its own strengths. These are some of the considerations you could take when choosing a method that that aligns with the issue's nature, your objectives, and your organization's capabilities:
- Simple issues only need basic methods like the 5 Whys, while complex problems require detailed analysis techniques like FMEA or FTA.
- Data-intensive methods like FMEA are suitable when detailed information is available. With limited data, the Fishbone Diagram is key as it’s based on expert judgment.
- Consider the expertise within your team and the resources to dedicate. Some methods require specialized knowledge or tools.
- Remember that compliance with industry-specific RCA standards may dictate the method choice as it is the case for aviation.
How to do Root Cause Analysis?
RCA is based on the premise that it is more effective to systematically prevent and solve underlying issues rather than just treating symptoms. The process is relatively straightforward and typically involves these key steps to perform RCA :
- Knowing the problem : Clearly defining the problem or issue that has occurred.
- Collecting data : Gathering all relevant information about the problem, including when and where it occurred, and under what conditions.
- Analyzing data : Using various RCA methods (such as the 5 Whys, Fishbone Diagram, FMEA, etc.) to explore potential causes.
- Identifying the root cause(s) : Determining the underlying factors that led to the problem.
- Developing solutions : Proposing and implementing solutions that address these root causes.
- Monitoring : Assessing the effectiveness of the solutions over time to ensure the problem does not recur.
Now, to integrate RCA within the broader organizational processes, you might also consider these actions or principles:
- Don’t isolated problem-solving, instead make RCA a standard practice across all levels and departments.
- Encourage the formation of cross-functional teams, since perspectives can shed light on overlooked aspects of a problem.
- Focus on improvements and solutions, not on the blaming game.
- Prioritize root causes based on their impact and the feasibility of implementing solutions, which means dealing with the most critical aspects first.
- Go deeper. The first conclusions may not always uncover the deepest root cause.
- Find proper evidence. Assumptions, guesses, and opinions are not sufficient.
- Invest in specialized software tools can streamline the RCA process. AI-driven RCA tools hold great promise.
- Establish mechanisms to monitor and review the outcomes of RCA efforts regularly.
- Shift the focus from reactive problem-solving to prevention. How can your team anticipate potential issues and be prepared?
8 Steps to Build a Solid Problem Management Process
5 root cause analysis examples.
The root analysis approach is versatile and systematic, which means it’s applicable to various fields such as ITSM , manufacturing, aviation, healthcare, and more.
These are some examples of RCA adaptability and impact on our everyday lives.
1. Car manufacture defects
If a car manufacturer notices an unusual rate of returns due to a specific engine component failure a simple RCA could reveal that the component is failing due to a flaw in the manufacturing process where incorrect temperature settings during heat treatment weaken the metal.
The root cause is identified as a misconfigured machine. All your team has to do is to reconfigure the machine settings and retrain staff on the correct procedures.
2. Ineffective sterilization process at a hospital
In case a hospital experiences a higher than average rate of post-surgical infections in one of its wards, a root analysis may uncover that the sterilization process for surgical instruments was compromised.
The cause is traced back to a recently changed cleaning solution that was not effective against all types of bacteria. The most reasonable thing to do is for the hospital to return to the previously effective cleaning solution and probably do additional checks for sterilization effectiveness.
3. IT system outages
This is generic, but think of an IT company that faces frequent, unexplained outages of its customer service platform. Through RCA, it's discovered that the outages coincide with high traffic volumes that exceed the system's capacity.
At this point it is obvious that what happened is due to inadequate scaling policies for cloud resources. So what has to be done is to invest in more robust infrastructure to handle peak loads.
4. Equipment failure in aviation
Let’s say an airline finds that a particular model of aircraft frequently requires unscheduled maintenance for landing gear issues. RCA identifies that the landing gear problem is due to premature wear of a hydraulic seal.
Further investigation reveals that the issue stems from a recent switch to a cheaper hydraulic fluid that lacks certain lubricative properties. The best they can do is to switch back to the original hydraulic fluid and replace the affected seals.
5. A retail chain experiences a high employee turnover
Lastly, imagine that a retail chain is experiencing higher than industry average turnover rates among its store employees. An RCA conducted through exit interviews and employee surveys reveals that the primary cause of dissatisfaction is inflexible scheduling that doesn't consider employee availability or preferences.
The company implements a new scheduling system that allows for greater employee input into their schedules.
Final thoughts
Our advice would be that you build a constructive RCA process focused on understanding how and why a problem occurred, rather than attributing blame to individuals or teams. If you take this principle into consideration, you’ll encourage a culture of openness and learning, where the goal is improvement rather than punishment.
Also, when it comes to problem-solving through RCA, causes and symptoms are equally necessary to track down for knowledge base purposes, but the aim is to go to the root of the problem. Identify them and allocate your team’s efforts accordingly. And so, be methodical and evidence-driven as we know from experience that identifying patterns makes all potential issues predictable events.
Lastly, for IT operations, where the complexity and volume of data are substantial, AI-driven RCA would be particularly beneficial to better forecast potential future disruptions. As this technology develops, we’ll see quick diagnosed issues in software and hardware, predicting failures, and suggesting corrective actions.
With this in mind, we might be exploring self-optimization, freeing up IT teams to focus on strategic initiatives rather than being bogged down by routine problem-solving.
The key is to focus on investing, involving, and integrating!
Read other articles like this : ITIL , Problem Management , root cause analysis
Read other articles like this:
Evaluate invgate as your itsm solution, 30-day free trial - no credit card needed.

Root Cause Analysis: Drilling Down to True Causes to Solve and Prevent Problems
- Resource Person
Course Name
May 06, 2024 - May 08, 2024
Schedule via Zoom:
May 6, 7, & 8, 2024
Monday - Wednesday
8:30 am - 12:30 pm
Regular Rate:
Early Eagle Rate:
Valid Until:
April 22, 2024
Because we operate in a fast-paced work environment, we do our work as quickly as possible, including solving problems. Sometimes the solution works, but often the problems come back because the solutions did not address the true root causes of the problems. The risk of repeated problems in today’s world is significant: lack of credibility to customers, lost business, frustrated employees, high operational cost, and many more.
This workshop will focus on root cause analysis, providing you with a simple and effective method to identify and verify the true root causes of problems. This will enable you to come up with the right solutions to resolve and prevent the recurrence of problems.
Relevant to all employees especially those leading teams
At the end of the workshop, you will be able to:
1. Validate the problem with data to ensure the right problem is being worked on;
2. Perform an effective root cause analysis by following a step-by-step process of identifying and verifying causes; and
3. Identify the right solutions that will eliminate or control the true root causes.
I. Introduction to Root Cause Analysis (RCA): A. Symptom vs Problem vs Cause B. What Is Root Cause Analysis? C. Conducting RCA
II. Describe and validate the problem A. Writing a focused problem statement B. Validating the problem with data
III. Identify potential causes A. Brainstorming, 5 Whys, Fishbone diagram, Causal tree, Might-cause check
IV. Prioritize, investigate and pin-point the true root causes A. Effort-Impact diagram B. Verification techniques
V. Develop effective solutions (linked to the true causes) to solve and prevent recurrence of the problem
Ms. Anamaria M. Mercado is a certified Six Sigma Master Black Belt and Lean Practitioner. She received her certification after six weeks of training in the US and a two-year full-time assignment as a Six Sigma Deployment Manager. She is also the Program Director of Six Sigma Certification Programs at the Ateneo Graduate School - Center for Continuing Education.
As a Deployment Manager, she helped launch the continuous improvement initiative in her former company. She managed multiple projects across the organization, improving process performance and customer satisfaction while delivering financial benefits.
Further, she has professional experience in sales and marketing management, as well as in training and development. Over the years, Ms. Mercado has concentrated on providing training and coaching services to various clients across industries, particularly in the areas of business process improvement and service excellence.
Ms. Mercado has a degree in Business Economics and post-graduate units in Professional Education from the University of the Philippines. She also holds a Masters degree in Business Administration from the Ateneo Graduate School of Business.
- Inside Ateneo CCE
- Register Now
- Program Calendar
- RCA 101 – 5-Why Analysis (Free Training)
- RCA 201 – Basic Failure Analysis
- RCA 301 – PROACT® RCA Certification
- RCA 401 – RCA Train The Trainer
- Other Trainings
- 5 Whys Root Cause Analysis Template
- RCA Template
- Chronic Failure Calculator
5 Root Cause Analysis Examples That Shed Light on Complex Issues

By Sebastian Traeger
Updated: April 12, 2024
Reading Time: 7 minutes
What is Root Cause Analysis?
Example 1: engineering – bridge collapse, example 2: mining – equipment failure, example 3: manufacturing – product defects, example 4: healthcare – medication errors, example 5: businesses – customer complaints, applications beyond individual operations.
With over two decades in business – spanning strategy consulting, tech startups, and executive leadership – I am committed to helping your organization thrive.
At Reliability, we’re on a mission to help enhance strategic decision-making and operational excellence through the power of Root Cause Analysis, and I hope this article will be helpful!
Our goal is to help you better understand root cause analysis by offering insights and practical tips based on years of experience. Whether you’re new to doing RCAs or a seasoned pro, we trust this will be useful in your journey towards working hard and working smart.
When it comes to addressing complex issues, Root Cause Analysis can help with identifying the underlying factors that contribute to problems. But what exactly is Root Cause Analysis and why should we care about it?
At its core, Root Cause Analysis involves delving deep into an issue to identify the fundamental reason behind it. This method goes beyond simply addressing surface-level symptoms and aims to uncover the underlying causes that lead to recurring problems. By understanding these root causes, organizations can implement targeted solutions that prevent issues from resurfacing.
Why Should You Care?
The significance of Root Cause Analysis becomes evident when we consider its real-life impact. Through this approach, businesses and industries have witnessed a significant reduction in the recurrence of issues, leading to improved process efficiency and decreased downtime. Moreover, by accurately identifying root causes, organizations have been able to enhance product quality and track the time taken to address underlying issues effectively.
Furthermore, monitoring customer satisfaction and feedback after implementing corrective actions has demonstrated the tangible benefits of Root Cause Analysis. Notably, this proactive approach has decreased the number of incidents and associated costs across various sectors.
In essence, embracing Root Cause Analysis isn’t just about troubleshooting; it’s about fostering a culture of continuous improvement by addressing issues at their core. Here are 5 examples of root cause analysis that shed light on complex issues:
A bridge unexpectedly collapsed, causing significant damage and disrupting transportation. The RCA revealed that the cause was a design flaw in the bridge’s suspension system, which failed to account for the weight distribution under specific conditions. The solution involved redesigning the suspension system and implementing more rigorous testing procedures for future projects.
Root Cause Found: A detailed analysis revealed that the root cause of the bridge collapse was a critical design flaw in the suspension system. Specifically, the design did not adequately account for the dynamic load distribution caused by varying traffic patterns and environmental conditions.
Technique Used: The engineering team employed the Fault Tree Analysis (FTA) technique , which helped them systematically trace the failure path back to the original design flaw.
- Define the Problem : the unexpected bridge collapse resulting from a design flaw in the suspension system.
- Identify the Top Event : The primary undesired outcome, the bridge collapse, is the focal point of investigation.
- Identify Contributing Factors : List all potential factors contributing to the collapse, such as design flaws, material defects, environmental factors, and human error. Given the prior identification of a design flaw, focus efforts on analyzing specific elements of the suspension system design.
- Construct the Fault Tree : Develop a fault tree diagram to visually represent the logical relationships between the top event and contributing factors. Include events such as “suspension system failure,” “dynamic load imbalance,” and “inadequate material strength.”
- Identify Primary and Secondary Causes : Distinguish between primary causes (directly leading to the top event) and secondary causes (contributing to primary causes). Highlight the design flaw in the suspension system as the primary cause, with secondary causes potentially including inadequate testing procedures or oversight of environmental conditions.
- Analyze the Fault Tree : Evaluate the fault tree to prioritize the most likely paths to the top event. This analysis guides the focus toward addressing critical factors to prevent similar failures in the future.
Solution: To address this issue, the suspension system was redesigned to incorporate more robust materials and a more flexible structure that could accommodate varying loads. Additionally, the team introduced more rigorous testing protocols, including simulations and stress tests, to ensure the new design could withstand real-world conditions.
A mining company faced recurring failures of critical equipment, leading to downtime and lost productivity. The RCA identified that the root cause was the use of substandard materials in the equipment’s components. As a result, the company implemented stricter quality control measures for material selection and increased the frequency of maintenance checks to detect and address potential issues early.
Root Cause Found: The recurring equipment failures were traced back to the use of substandard materials in critical components, which were prone to wear and tear under harsh mining conditions.
Technique Used: The team used the 5 Whys technique , asking “why” repeatedly until they reached the root cause of the problem, which was the procurement of low-quality materials.
- Why did the equipment fail?
- Why were the critical components failing?
- Why were substandard materials used in the critical components?
- Why were there issues in the procurement process?
- Why were there insufficient quality control measures in place?
- Answer : There were insufficient quality control measures because the company did not prioritize or implement rigorous checks for material quality during procurement.
Solution: The mining company implemented stricter quality control measures for material procurement and increased the frequency of maintenance checks. They also established partnerships with reputable suppliers to ensure that all materials met the required standards.
A manufacturing plant experienced a high rate of product defects, affecting customer satisfaction and sales. The RCA found that the root cause was a misalignment in the assembly line, causing inconsistencies in the final product. The solution involved realigning the assembly line and introducing regular calibration checks to ensure consistent product quality.
Root Cause Found: The investigation revealed that a misalignment in the assembly line was causing inconsistencies in the final product, leading to defects.
Technique Used: The Cause and Effect Diagram (the Ishikawa or Fishbone Diagram ) was used to identify potential factors contributing to the product defects, ultimately pinpointing the assembly line misalignment.
- Identify the Problem : Recognize the high rate of product defects affecting customer satisfaction and sales.
- Define the Effect : Clearly define the problem statement. In this case, it would be the high rate of product defects.
- Brainstorm Potential Causes : Generate potential causes such as human error, equipment malfunction, etc.
- Create the Diagram and Categorize Causes : Construct a ‘Cause and Effect’ Diagram representing potential causes. Group potential causes into categories like equipment, process, people, etc.
- Identify Root Causes : Drill down to specific root causes within each category.
- Verify Root Causes and Develop Solutions : Confirm root causes through data analysis, observation, and brainstorming solutions
Solution: The assembly line was realigned, and regular calibration checks were introduced to maintain alignment. The manufacturing plant also implemented a quality control system that included random sampling and inspection of products at various stages of production.
A hospital reported an increase in medication errors, posing a risk to patient safety. The RCA determined that the root cause was a lack of standardized procedures for medication administration. The hospital implemented a standardized protocol, including double-checks and electronic medication management systems, to reduce the risk of errors.
Root Cause Found: The RCA identified a lack of standardized procedures for medication administration as the root cause, leading to inconsistencies and errors in dosing and delivery.
Technique Used: The healthcare team used the Failure Mode and Effects Analysis (FMEA) technique to systematically evaluate the medication administration process and identify areas where errors could occur.
- Establishing the FMEA Team: A multidisciplinary team was assembled, led by a designated leader.
- Define the Scope: The scope was narrowed to focus on the hospital’s medication administration process.
- Identifying Failure Modes: Potential failure modes within medication administration were systematically identified.
- Assessing Effects: Each failure mode’s impact on patient safety and outcomes was evaluated.
- Determining Causes and Assigning Ratings: Root causes contributing to each failure mode were analyzed. Severity, occurrence, and detection ratings were assigned to each failure mode.
- Calculating RPNs: Risk Priority Numbers were computed to prioritize attention to high-risk failure modes.
- Developing Mitigation Strategies: Strategies were devised to reduce occurrence, enhance detection, and minimize impact.
Solution: The hospital implemented a standardized medication administration protocol, which included steps like double-checking medication orders, using electronic medication management systems, and providing additional training to staff. This helped to reduce the risk of errors and improve patient safety.
A company noticed a spike in customer complaints regarding its service. The RCA revealed that the root cause was inadequate training of customer service representatives. The company addressed the issue by revamping its training program, focusing on communication skills and product knowledge, significantly reducing complaints.
Root Cause Found: The increase in customer complaints was traced back to inadequate training of customer service representatives, leading to poor communication and misunderstanding of product features.
Technique Used: The team used the Pareto Analysis technique to categorize the complaints and identify the most common issues, which pointed to gaps in the training program.
- Data Collection : Gathered customer complaints data.
- Categorization : Classified complaints into different types.
- Frequency Count : Tally occurrences for each category.
- Cumulative Percentage : Calculated cumulative frequency and percentage.
- Pareto Chart : Constructed a chart to visualize key issues.
- Identified Priorities : Focused on vital few categories causing most complaints.
- Action Plan : A revamped training program to address the root cause.
Solution: The company revamped its training program, focusing on enhancing the communication skills, product knowledge, and problem-solving abilities of the customer service team. They also introduced regular assessments and feedback sessions to ensure continuous improvement.
In each of these examples, RCA provided a systematic approach to identifying and addressing the underlying causes of problems. By implementing effective solutions, these industries were able to improve their operations, enhance safety, and increase customer satisfaction.
The application of Root Cause Analysis extends beyond individual operations; it underscores the importance of proactive risk management and continuous improvement in industrial settings.
By understanding and addressing the root causes of safety incidents, companies can mitigate risks, prevent accidents, and ensure the well-being of their workforce. Moreover, the lessons learned from applying Root Cause Analysis in safety can be extrapolated to other industries, emphasizing the value of systematic problem-solving and proactive safety measures.
In essence, Root Cause Analysis serves as a vital tool for enhancing industrial safety, empowering organizations to identify and address the underlying factors that contribute to safety incidents. This approach not only protects employees from harm but also promotes operational efficiency and sustainability in the long run.
By integrating this problem-solving technique into your decision-making processes, you’ll navigate challenges effectively. Embrace opportunities for growth by dissecting root causes and devising targeted solutions as you navigate through both professional and personal journeys.
I hope you found these examples of root cause analysis insightful and actionable! Stay tuned for more thought-provoking articles as we continue to share our knowledge. Success is rooted in a thorough understanding and consistent application, and we hope this article was a step in unlocking the full potential of Root Cause Analysis for your organization.
Reliability runs initiatives such as an online learning center focused on the proprietary PROACT® RCA methodology and EasyRCA.com software. For additional resources, visit Reliability Resources .
- Root Cause Analysis /
Recent Posts
Root Cause Analysis with 5 Whys Technique (With Examples)
What Is Fault Tree Analysis (FTA)? Definition & Examples
Guide to Failure Mode and Effects Analysis (FMEA)
Root Cause Analysis Software
Our RCA software mobilizes your team to complete standardized RCA’s while giving you the enterprise-wide data you need to increase asset performance and keep your team safe.
Root Cause Analysis Training
[email protected]
Tel: 1 (800) 457-0645
Share article with friends:

IMAGES
VIDEO
COMMENTS
Root cause analysis is one part of a broader continuous improvement process, which is outlined in the U.S. Department of Education's (ED's) Non-Regulatory Guidance: Using Evidence to Strengthen Education Investments. The first step in evidence use described in the non-regulatory guidance (Step 1: Identify Local Needs) includes gathering and examining needs assessment data "to understand ...
Root Cause Analysis: Background . Excerpted from: Preuss, P.G. (2003). School Leader's Guide to Root Cause Analysis: Using Data to dissolve Problems. Larchmont, NY: Eye on Education. What is "Root Cause"? Rather than assume knowledge of what a ―root cause‖ is, let's first look at several definitions:
Using Root Cause Analysis as Part of the Continuous Improvement Process in Education. A root cause analysis process is a systematic investigation of the contributing and foundational (or "root") causes of the problems that organizations or institutions face. 1 In practice, root cause analysis is an approach to problem solving that uses data analysis and discussion to dig deeper than the ...
What is Root Cause Analysis? Root Cause Analysis (RCA) is a problem-solving process designed to unearth the root and fundamental reasons for identified concerns. It requires a systematic investigation of the central causes of the student performance problems that schools and educators may face. 1. RCA helps educators identify
•What is a root cause •Root cause analysis: The big picture •An essential starting place: Key indicators of student success •Root cause analysis: Key elements and techniques •Root cause technique: IDC's Success Gaps Toolkit •Root cause analysis in South Carolina 5
Root cause analysis (RCA) is the process of discovering the root causes of problems in order to identify appropriate solutions. RCA assumes that it is much more effective to systematically prevent and solve for underlying issues rather than just treating ad hoc symptoms and putting out fires. Root cause analysis can be performed with a ...
Root cause analysis is a problem-solving approach that uses the analogy of roots and blooms to model cause-and-effect relationships. Rather than focusing on what's above the surface, root cause analysis troubleshoots solutions to problems by analyzing what is causing them. Note. Similarly to exploratory research, it's important to remember ...
It describes how to carry out a descriptive analysis of disparities in school discipline and how to conduct a root cause analysis to systematically address school-based factors that contribute to disparities. ... Center on Safe Supportive Learning Environments Web site were assembled under contracts from the U.S. Department of Education, Office ...
Keywords: root cause analysis, medical education, quality improvement, patient safety, curriculum, simulation. Introduction. ... Reported preparedness to conduct and teach root cause analysis among 93 alumni of the Chief Resident in Quality and Safety program. Chief Resident in Quality and Safety alumni are US-based clinicians from various ...
A root cause is defined as a factor that caused a nonconformance and should be permanently eliminated through process improvement. The root cause is the core issue—the highest-level cause—that sets in motion the entire cause-and-effect reaction that ultimately leads to the problem (s). Root cause analysis (RCA) is defined as a collective ...
Frequently asked questions (FAQs) about needs assessments and root cause analysis. These FAQs are intended to introduce local educational agencies (LEAs) to needs assessments and root cause analysis. This collection represents commonly asked questions, but is not intended to be a complete list of all possible questions.
Root Cause Analysis. This step involves identifying the underlying causes behind the priority performance challenges identified during data analysis. Root causes are statements that describe the deepest underlying cause, or causes, of performance challenges and they become the focus of major improvement strategies.
What Is Root Cause Analysis? According to the online course Organizational Leadership—taught by Harvard Business School professors Joshua Margolis and Anthony Mayo—root cause analysis is the process of articulating problems' causes to suggest specific solutions. "Leaders must perform as beacons," Margolis says in the course. "Namely, scanning and analyzing the landscape around the ...
A root cause analysis was performed, and measures were taken to avoid this problem in the future. The RCA team noted that the nurse caring for both patients had worked in the hospital for 5 years and was recently transitioned to the obstetric ward.
Benefits of Root Cause Analysis. Add value to the organization. Create the potential for cost reduction or improved allocation of resources. Provide a learning process for better understanding of relationships, causes and effects, solutions, and ownership of risk. Provide a logical approach to problem solving using data that already exists.
Root Cause Analysis (RCA) is a helpful tool in our problem-solving challenges. Root cause analysis methods involve identifying the root of a problem to arrive at a solution. It helps us dig deeper into the origin of a problem. Additionally, it can help us identify patterns that are inefficient. Organizations deploy several types of root cause ...
The Root Cause Analysis Process in 5 Simple Steps. Root Cause Analysis Process. As shown in the diagram above, the root cause analysis steps are: Realize the problem. Gather data. Determine possible causal factors. Identify the root cause. Recommend and implement solutions. Going through each step in detail, here's how you can perform root ...
Root cause analysis (RCA) is a process for finding the fundamental cause of a problem, issue, or incident. It's also how you determine corrective actions and outline and implement steps to reduce the risk of future occurrences. If an organization only ever treats the symptoms without addressing their source, you waste time and money reacting ...
Root cause analysis RCA is the structured, thorough investigation of a patient safety incident to determine the underlying causes and contributing factors, and then analyse these to draw out any learning points. 7 The learning points can be actioned to reduce the chance of the same or similar incident reoccurring.
Education Overview Learn, connect, and grow with numerous IHI educational opportunities, designed with your needs in mind. Conferences Training ... Root cause analysis (RCA) is a process widely used by health professionals to learn how and why errors occurred, but there have been inconsistencies in the success of these initiatives. ...
Root Cause Analysis is a method used to understand the causes of a problem or incident. It's pretty much the rubric used within the ITIL framework to standardize Problem Management . As you may know, Problem Management is one of the processes under the Service Operation phase of ITIL , which aims to manage the lifecycle of all problems that ...
This workshop will focus on root cause analysis, providing you with a simple and effective method to identify and verify the true root causes of problems. ... Ms. Mercado has a degree in Business Economics and post-graduate units in Professional Education from the University of the Philippines. She also holds a Masters degree in Business ...
Example 1: Engineering - Bridge Collapse. A bridge unexpectedly collapsed, causing significant damage and disrupting transportation. The RCA revealed that the cause was a design flaw in the bridge's suspension system, which failed to account for the weight distribution under specific conditions.