An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Healthcare (Basel)


Current Issues on Research Conducted to Improve Women’s Health
Charalampos siristatidis.
1 Assisted Reproduction Unit, Second Department of Obstetrics and Gynecology, Medical School, National and Kapodistrian University of Athens, Aretaieion Hospital, 76 Vass Sofias, 11528 Athens, Greece
Vasilios Karageorgiou
2 2nd Department of Psychiatry, Medical School, National and Kapodistrian University of Athens, Attikon Hospital, 1 Rimini Street, 12642 Athens, Greece; moc.liamtoh@groegaraksav
Paraskevi Vogiatzi
3 Andromed Health & Reproduction Diagnostic Lab, 3 Mesogion Str, 15126 Maroussi, Greece; moc.liamg@iztaigovive
Associated Data
Not applicable.
There are varied lessons to be learned regarding the current methodological approaches to women’s health research. In the present scheme of growing medical literature and inflation of novel results claiming significance, the sheer amount of information can render evidence-based practice confusing. The factors that classically determined the impact of discoveries appear to be losing ground: citation count and publication rates, hierarchy in author lists according to contribution, and a journal’s impact factor. Through a comprehensive literature search on the currently available data from theses, opinion, and original articles and reviews on this topic, we seek to present to clinicians a narrative synthesis of three crucial axes underlying the totality of the research production chain: (a) critical advances in research methodology, (b) the interplay of academy and industry in a trial conduct, and (c) review- and publication-associated developments. We also provide specific recommendations on the study design and conduct, reviewing the processes and dissemination of data and the conclusions and implementation of findings. Overall, clinicians and the public should be aware of the discourse behind the marketing of alleged breakthrough research. Still, multiple initiatives, such as patient review and strict, supervised literature synthesis, have become more widely accepted. The “bottom-up” approach of a wide dissemination of information to clinicians, together with practical incentives for stakeholders with competing interests to collaborate, promise to improve women’s healthcare.
1. Introduction
Women’s health has been at the center of interest and growing concern in the last few decades. As a measurable outcome, it has been studied at the level of mortality [ 1 ], serious morbidity [ 2 ], and nutritional status [ 3 ] and through proven, evidence-based interventions. The implementation of such interventions is essential to guide national and international policies and programs, targeting the achievement of universal coverage of health services. In this respect, conducting the best quality of research (research that provides firm and ethical evidence adhering to the principles of professionalism, transparency, and auditability) with the use of robust methods is mandatory. Towards this goal, the current reality is far from encouraging.
In accordance with scientific literature guidelines and research quality guidelines (e.g., the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)), impact factors, and citation count are considered the norms in current research evaluation modalities. However, recent works in research methodology challenge this simplifying notion [ 4 , 5 , 6 ].
The pitfalls reported are associated with various—albeit specific—“cultural, ethical, operational, regulatory, and infrastructural factors” linked with a lack of adequately trained researchers and subject attrition bias [ 7 ]. As a result, the clinical research environment is more or less inseminated with various types of bias, leading to the discouragement of sponsors. The growing plethora of questionable quality trials and reviews is another issue to consider. “From 14 reports of trials published per day in 1980 [to] 75 trials and 11 systematic reviews of trials per day, a plateau in growth has not yet been reached”, stated a policy forum article reported in 2010 [ 8 ]; additionally, the authors noted that “the staple of medical literature synthesis remains the non-systematic narrative review”, further pointing out the need for freely available simple yet valid answers to most patients’ questions [ 8 ]. In the same context, current data concerning women’s health derived from protocols, full study reports, and participant-level datasets are rarely available to a wide audience. At the same time, selective reporting of methods and results plagues reports. With the reduced quality of information produced, a lot of money has been wasted; subsequently, the existence of all kinds of bias affect the research itself and jeopardize the validity of the findings and, consequently, the care of women [ 9 ].
Issues have been raised by exploring different approaches to evaluate the quality of scientific input to the community. The ultimate goal remains a robust and uniform literature evaluation system adapted to the evolving conduct of studies and to the application of modern tools to re-ensure robust methodology and reporting of data and results. Here, we perform a narrative overview on current issues in study quality assessment regarding clinical medicine. We electronically searched PubMed using the following keywords: “clinical trials”, “meta-analysis”, “IPD”, “sponsor”, “challenges”, “regulatory”, “women’s health”, “evidence-based medicine/trends”, “policy making”, “publishing”, “research methods and practices”, “consumers network”, “bias”, “industry-sponsored trials”, “biomedical bibliographic databases”, and “quality research”, trying to collect data irrespective of type of report and language. Based on this evidence, we propose a combination of interventions at various levels, underlining quality aspects that we consider significant, and other routes of judgments.
2. The “Standard” Factors
Citation count and publication rates in international databases, hierarchy in author lists according to contribution, and the impact factor of the journal are considered important factors in the quality of a study, especially for the “scientific reader” seeking quality information on a specific topic. This has been extensively studied by other workgroups [ 10 , 11 , 12 , 13 ] and represents a justified trend accounting for the prestige of a scientific journal and the publication itself, along with language and availability, and ultimately skewing scientific trends or potentially leaving some important contributions in obscurity. Even though previous works contemplate the importance of the aforementioned factors in the true quality of research studies and publications, all considerations are derived from a common denominator, that is, that the currently used quality standards either for the common user or for greater structures and institutions most probably do not reflect quality but rather popularity. In this context, the citation rate (including self-citation and “negative citing”) and an impact statement on the individual author (a concise summary of the impact of somebody’s career) have been proposed. In addition, other metrics, including altmetrics, bibliometrics, and H-index, combined with updated mathematical models, such as artificial neural networks, might be the tools of the future; these models constitute more accurate tools due to the special characteristics of these “learning through training” processes, resembling the capacity of the brain to learn and judge [ 14 ].
3. The Type of Research Question and Studies
Although multiple outcomes may be reported at once and variability in study designs fluctuates, a primary role belongs to the type of research question explored by a study or publication, which will inevitably determine the methodology to be followed. For example, in past years, there is a disproportionate output of Systematic Reviews (SRs) and meta-analyses from Asian countries produced on a massive scale [ 15 , 16 ] as a means of “publishing in order to publish” with questionable quality and methods. Their numbers are so high that, in some cases, it overtakes original trials. Of note, the use of such studies in the biomedical field was occasional until the 1990s [ 17 ]. Moreover, those from the Cochrane collaboration, the fundamental organization for good quality systematic reviews, are only a small fraction of this output [ 8 ].
With regard to Randomized Controlled Trials (RCTs), suggestions have been made in recent reports on better conduct [ 18 ]: trial protocols should be simple, reproducible, and well organized, with predefined and well-described study populations/participants and should have sound interventions, and representative comparisons and outcomes. Of note, these could be based on the conclusions of previously conducted SRs that often point out issues in quality and methodology of the original trials. Minimal deviations from protocols and a priori specification of useful core outcomes that translate directly to women’s wellbeing are the focus of the CROWN Initiative [ 19 ]. According to the authors, there has been a multi-targeted set of suggestions to “ensure that critical and important outcomes with good measurement properties are incorporated and reported, in advancing the usefulness of research, in informing readers, including guideline and policy developers, who are involved in decision-making, and in improving evidence-based practice”.
A priori description of the outcomes of interest can alleviate the known issues/biases associated with exploratory analyses. A change in outcome, especially in cases where the results do not support the rationale of the study, can mask the original intentions of the authors and can recontextualize the same results in a more positive manner [ 20 ]. Still, an exploratory analysis has a significant role in deducing potentially valuable conjectures for future studies. However, it is central for transparency that the authors explicitly state when this is the case, i.e., when an analysis is conducted post hoc. In order to ease the distinction of post hoc and a priori analyses by SR authors and readers, Dwan et al. (2014) proposed the publication of both protocols and pre-specified analyses [ 21 ].
We cannot anticipate that SRs can retrospectively solve the potential gaps and inconsistencies in the methodology and outcome reporting. For robust answers, research questions must be well defined from the start. However, more elaborate techniques of evidence synthesis can guide future research in more meaningful ways and are becoming more popular. Specifically, prospective and individual patient data meta-analyses (IPDMA) may need to become the norm in literature synthesis [ 22 , 23 ]. A major difficulty in IPDMA is the fact that securing sensitive patient data is a time-consuming task that demands the establishment of mutual trust. Even when representative evidence has been secured, data availability may still affect the pooled evidence. A recent study assessing IPDMA’s treating oncological topics suggested that studies for which they were available differed significantly from studies in which the authors did not share them [ 24 ]. Still, IPDMA is a trustworthy methodology that can assess the effect of patient-level covariates on treatment outcomes or diagnostic accuracy more thoroughly than the standard procedure of a meta-regression used in aggregate-data meta-analyses [ 25 ]. Given the current ethos of openness in clinical trials and common repositories becoming more widespread, IPDMA is likely to become the mainstay of critical synthesis of literature [ 26 ].
Finally, we have to include observational research in an effort to improve women’s health in the context of greater personalization of care and stratified medicine. Such studies have traditionally served as tools for understanding the nature of particular clinical conditions, for determining risk factors and mechanisms of actions, and for identifying potential intervention targets. Their disadvantages associated with methodological issues such as confounds and the fact that they are prone to limited internal validity could be restricted through guidelines such as the strengthening the reporting of observational studies in epidemiology (STROBE) statement [ 27 ].
4. The Inclusion of Young Authors
The encouragement of younger and/or less experienced scientists and ultimately their inclusion in the respective workgroups and in the list of contributors may provide an unexpected topic or question and a clearer view on established research schemes. The productivity of highly cited papers is related to the advanced age of their authors; adversely, better funding opportunities for younger researchers would give them unique chances to build strong productivity [ 28 ]. The advancement of knowledge taught during academic training as well as a higher probability of compliance with robust methods of reporting should encourage the inclusion of younger scientists. Tips and recommendations of young authors and early career scientists have been plenty, including collaborating with researchers within as well as outside their field and/or country, sending their research article to an appropriate journal, and adequately highlighting the novelty and impact of their research [ 29 , 30 ].
Towards this goal, the improvement of the scientific literacy of young scholars is the main step, and this burden falls on to the shoulders of the trainers. There are “uncomfortable truths” in training [ 31 ], but scientific research and the mode of thinking are processes continuously accumulated and must be taught by each director or responsible authority: they should improve the skills and capabilities of young scholars in scientific and technological literacy and in communication and productivity.
5. Quality in Reporting
Reporting quality must be ensured by avoiding bias, such as selective reporting, deliberate or not. Avoiding reporting insignificant data and outcomes could lead to severe distortion in the SR [ 32 ]. Thus, flaws in design, conduct, analysis, or reporting of RCTs can produce bias in the estimates of a treatment effect.
For example, in a large meta-epidemiological study of 1973 RCTs, a lack of blinding was associated with an average 22% exaggeration of treatment effects among trials that reported subjectively assessed outcomes [ 33 ]. This deviation is enough to adversely affect the interpretation of the results and further negatively influences regulatory settings and clinical practice.
Another example involves the evidence base on recent cancer drug approvals. Between 2014 and 2016, a quarter of the relevant studies were not RCTs; of the RCTs, the majority of them did not measure overall survival or quality of life outcomes as primary endpoints, and half of them were judged to be at high risk of bias; the authors’ judgments changed for a fifth of them when they relied on information reported in regulatory documents and scientific publications separately [ 34 ].
6. Strict Implementation of Rules in the Peer Review Processes
These processes first appeared in 1655 in a collection of scientific essays by Denis de Sallo in the Journal des Scavans , and almost 100 years later (1731), their implementation became a standard of practice by almost all biomedical journals [ 35 ]. Maintaining the quality and scientific integrity of publications; evaluating for competence, significance, and originality; and ensuring internal and external validity of submissions are crucial points. Similarly, the appropriate selection and training of reviewers to provide quality and specialized reviews without bias is an essential part of the process [ 36 ].
7. Sponsorship
Ethical and other issues surrounding sponsorships, to ensure credibility of a study, have been addressed in the past. One of the main sources of funding remains the industry [ 37 ]. Indeed, sponsored clinical research has always been questioned, influenced by reports of selective or biased disclosure of research results, ghostwriting and guest authorship, and inaccurate or incomplete reporting of potential conflicts of interest [ 38 ]. Although these may be a scarce incidence nowadays, active monitoring in funded studies should be implemented throughout in order to eliminate this possibility or any other conflicts of interest. An alarming analysis of 319 trials indicated that only a small minority (three out of 182 funded trials) were funded by multiple sponsors with competing interests. The presence of industry funding also almost tripled (OR = 2.8, 95% CI: 1.6, 4.7) the possibility of a study having reported favorable findings [ 39 ]. Furthermore, registered study protocols that announced funding were less likely to be published after their completion (non-publication rate: 32% vs. 18% [ 40 ].
8. Change in the Notion of Publishing
The change in notion and perception of the impact of outcomes is perhaps the most important part of the improvement in research conduct and implementation. This can be achieved through differentiation and modern adaptation of our scientific culture fighting inner and external incentives. Every scientific input should target a wider human benefit. A change in notion and incentives in publishing is crucial, from the level of the investigator aiming to publish/individual behaviors up to the social forces that provide affordances and incentives for those behaviors [ 41 , 42 , 43 ].
In a specific area of research, a clinical evaluation should precede publication in order to ensure relevance. A dramatic example is the scientific literature demonstrating an overload of various biomarkers for various diseases in which only a few of them have been confirmed by subsequent research and few have entered routine clinical practice [ 44 ]. In addition, biomarkers should also be judged on the grounds of cost-effectiveness and incremental net benefit [ 45 ]. Multiple indices may have comparable diagnostic accuracy, but their cost, an unavoidable concern in public health, may differ significantly.
Therefore, the selection of information to be published should be conducted on safer grounds and should be adequately supported by the authors, based on our knowledge on the scheme to date, and importantly, a summary of previous attempts should note the effective interventions and provide a concluding remark for the scientist through a good quality review.
9. Patient’s Contribution to Evaluation and Sex/Gender Analyses
In the era of evidence-based medicine, feedback from the recipients of healthcare development is gaining more importance and platforms for opinion exchange between patients and investigators have been established. This has already been implemented by the Cochrane Collaboration, where patient review is an integral part of the SR publication process and plain language summaries target a nontechnical audience. This process could be adopted as standard practice if accordingly modified. If the patient review, for example, is to be widely implemented in other journals, it would constitute a potentially radical paradigm shift that aims to solidify the review process. Of course, technical difficulties, such as acknowledgement and incentives for patients participating in review processes, are fields where further developments will enhance this policy [ 46 ].
It has been noted that the women population represents an “unequal majority” in health and health care. It is also well established that women’s health needs are dissimilar from those of men, resulting from the fact that both the woman’s body and brain functions differ critically from a man’s and that she reacts differently to even the same stimuli, such as medications or environmental events. It is indicative that, even though a large proportion of study protocols included women, only 3% of them planned an analytical approach for quantifying sex differences [ 47 ]; similarly, a recent report on therapies for atrial fibrillation concluded that the sex-specific reporting in trials comparing them was extremely low [ 48 ]. As a result, women have not received an ideal “personalized” health care, in many cases, so far. Thus, a specific design for studies on women’s health should be required.
There are several examples in the history of women’s health research where the contribution of the consumer women’s health movement in promoting research in women’s interests was critical. One of them concerned the collaborations between consumer groups and researchers in obtaining funding in the U.S. and France for a follow-up on a cohort of diethylstilboestrol-exposed people when the drug was discovered to be a transplacental carcinogen in pregnancy in 1971.
Another important issue is the nonavailability of sex/gender data from primary studies and consequently from SRs, which are the main tools to provide the necessary evidence for the formation of relevant policies [ 49 ]: the authors stated that even “Cochrane and the Campbell Collaboration have no specific policy on the reporting of sex/gender in systematic reviews, although Cochrane has endorsed the SAGER guidelines developed by the European Association of Science Editors” [ 50 ]. In their review, they found that the Methods sections of these collaborations included the most reports on sex/gender in both Campbell (50.8%) and Cochrane (83.1%) reviews, but the majority of these were descriptive considerations of sex/gender. They also reported that 62% of Campbell and 86% of Cochrane reviews did not report sex/gender in the abstract but included sex/gender considerations in a later section. A previous study on the subject reported that almost half of SRs described the sex/gender of the included populations but only 4% assessed sex/gender differences or included sex/gender when making judgments on the implications of the evidence [ 51 ].
10. An Improvement in the Dissemination of Studies
Despite advances in the dissemination of study information, half of health-related studies remain unpublished [ 52 ]. Problems in the publishing scheme in the selection of studies that appear to have a higher impact or that come from a respectable institution can lead to biased publishing. At the extreme, unsafe, ineffective, or even harmful interventions may enter clinical practice, as was the case with hormone replacement therapy [ 53 ]. In some instances, even a shift in healthcare resource allocation is reported [ 9 ]. It is standard practice in critical readings of literature to evaluate publication bias. This method attempts to address, with controversial success, precisely the unfortunate keenness of editors to promote positive results that imply novelty. A classic example of this inflation of positive and supposedly important results is the 2012 study by Fanelli [ 54 ], in which studies classified as related to clinical medicine showed a gradual increase in reporting positive findings. The author criticized the efficacy of measures taken to attenuate publication bias, e.g., protocol registration.
On the other hand, a respectable amount of research is published in other languages and not indexed in U.S. National Library of Medicine [ 55 ], while their quality remains controversial [ 56 ]; the authors of the above studies stated that peer review processes need to be improved through guidelines aiming to identify the authenticity of the studies.
The bulk of peer reviews remain a voluntary occupation, with the main motivation being recognition by peers. In addition, statistical review, a time-consuming process, is not performed in all published research. This process can be accelerated by practices that promote data and code sharing. It is also suggested that, even when papers are retracted, this could have been avoided with the simple measure of an active data sharing policy [ 57 ].
11. Role of the Stakeholders and Foundations
For the stakeholders and collaborative systems, a more energetic role is required in ensuring the conduct of multicenter massive-trials with increased clinical relevance. The main problem in the conduct of research is the lowered clinical value of the results from small sample sizes, even in RCTs. Mathematical models have been developed to predict sample sizes corresponding to the clinical value of the outcomes, while patient data from databases could easily increase the sample size of trials at much lower costs. Such paradigms could include the Health Care Systems Research Collaboratory and the Patient-Centered Outcomes Research Network (PCORnet) [ 58 ]. Also, new levels of patient engagement can raise the possibility of improving clinical outcomes on health. Involving multiple stakeholders (with potentially conflicting interests) in shared conversations on research has been proposed [ 59 ].
New foundations should be placed in research by focusing on the improvement of quality, such as NIH and PCORI [ 60 ]. The Cochrane Collaboration represents one of the very few large-scale initiatives in this context; importantly, both conduct high quality reviews, and participant education at all levels are based mostly from volunteers who care about science and high-quality evidence.
12. Cooperation of All Forces: The Role of Industry/Funding
The central point of problem is funding. USA-affiliated industry-funded trials and related activities represent more than 5% of US healthcare expenditure, with approximately $70 billion in commercial and $40 billion in governmental and non-profit funding annually. The NIH invests $41.7 billion annually in medical research: 80 percent is awarded for extramural research, through 50,000 competitive grants to more than 300,000 researchers at more than 2500 universities, medical schools, and other research institutions [ 61 ]. Concerns have been raised that this approach appears inefficient for how biomedical research is chosen, designed, regulated, financed, managed, disseminated, and reported [ 62 , 63 , 64 ].
The scheme, however, has been shifting in favor of Asian countries. Factors, such as ease of recruitment, population, and various epidemiological factors (e.g., increased incidence of infectious disease) have contributed positively to an inflation of local clinical trials [ 7 ]. Severe accusations regarding clinical data management have been raised, although the magnitude of the problem cannot be safely evaluated [ 65 ]. This unavoidably hinders the validity and future usefulness of these results despite initial enthusiasm from editors and the industry.
Economic forces are important, and ultimately, the industry seeks to maximize profit by providing new products and services to the medical market [ 66 ]. In industry-funded clinical research, intentional and unintentional commercial motives can control the study design and comparators. Governmental involvement [ 66 ] has an important role in distributing research funds in areas important for the protection and restoration of human health, even when the prospects for commercial profit are poor or nonexistent. The recruitment of specialized and qualified professionals should set higher standards of rigor when they are involved in commercial or unavoidably conflicted relationships and to disseminate the resources evenly, especially when nowadays these are scarce.
Funders and academic institutions are responsible for the moral status, as research usually initiates from there and determines any kind of shift in the process. Academics might be judged on the methodological rigor and full dissemination of their research, the quality of their reports, and the reproducibility of their findings. Previous reports suggest ways to increase the relevance and to optimize resource allocation in biomedical research, indicating how resource allocation should be conducted, along with revisions in the appropriateness of research design, methods, and analysis, with efficient research regulation and management fully accessible information, promoting unbiased and usable reports. Additionally, motivation must be given to authors to share their data [ 67 ], as has been performed in the field of genetics [ 68 ]. Of note, synthesis of evidence on the meta-epidemiological level cannot always confidently provide answers to practical clinical questions [ 69 ].
Compromised ethics should be traced and removed from independent research and academia, while journals should on no occasion put profit and publicity above quality. The solution to this lies on the progressive refinement of methods and improvement of the objective and controlled processes.
13. Training
Essential training and interprofessional learning of clinicians and other hands-on scientists in the medical field are an absolute must. There is a growing need to improve their scientific insight and judgment. Reviewers should learn how to apply an unbiased critical thinking and evaluation of the methods explored, of the study questions, and of the resulting impact towards good clinical practice and human welfare. This not only applies to organizational refinement by the Academic Institutes and Publishing Organizations but also to the scientists themselves to obtain the drive to train, along with methodologists and statisticians, so that specialization and knowledge is shared and every contributor works soundly towards a common cause.
14. Conclusions
Research is a solid foundation for the progression of sciences, and the key importance in maintaining the evolution of knowledge is “contributing and sharing”, but this has to be performed adequately. Although there are several criteria and controlled circumstances under which new data and overviews of data are published, research and publishing methods require continuous readjustments and modifications to ensure quality. An overview of the published literature on women’s health and its relevant subtopics is an excellent paradigm on a crucial field of the different types of research and publications that one may encounter but also an example of the vast variability in information available, not only in terms of results but also in terms of design, analysis, quality of information, and implementation of results. In clinical practice, it is imperative to assess information collectively a researcher, medical expert, funder, reviewer, and patient, and this should encourage the improvement of evidence-based patient management.
This review aimed to present the major nodal points of quality and to propose a combination of interventions at various levels, along with other routes of judgement. We also sought to address potential flaws and pitfalls in research conduct and to provide recommendations upon improvement of study designs/methods and scientific reporting to promote publication quality and stricter criteria for release with support from the appropriate structures. A summary of recommendations towards evidence implementation as presented in Table 1 could comprise valuable guidance to both the health experts and the health service recipients to which these standards are quality criteria. A meticulous study design that promotes the transparency of methods and potential conflicts allows a clear distinction of the pathologies and targeted groups and that provides substantial scientific background should be pursued by both researchers and readers. Robust implementation of the pre-stated methods and approaches of analysis, with active participation of collective fronts tied to the subject, should allow quality output to be published and should add value to the findings. Patient-first and common welfare should be considered throughout in conjunction with supporting and providing evidence on robust outcomes for the improvement of healthcare, that may be facilitated by healthy and network collaborations.
Summary of the recommendations for the steps towards evidence implementation.
How these recommendations should be accounted for, evaluated, and implemented relies on the individual discretion of the reader, the scientist, the author, or any entity affiliated with a publishing organization and should be customized to be applied individually for each specialized academic and scientific field but also tailored across continents and countries. The latter is derived from the realization that research conduct, funding, and even the monitoring authorities of clinical studies rely on nonuniform procedures among countries and unions and conforms to different legal frameworks across countries. Nevertheless, a core of actions, precautions, and a quality exemplar of golden standards should be constructed and widely applied to meet the standards that describe a representative scientific contribution, for example, uniform, widely accepted, and practiced standards through policies, guidelines, and rules on a national and/or international level created either by in-country legislation or by scientific entities; allocation of the resources for their implementation; and mechanisms of control for their application and adherence by all.
In conclusion, multiple steps throughout the long and costly process of trial conduct are prone to bias. Notably, increasing international competition favors faster and cheaper patient recruitment, conduct, and analysis and, in turn, produces questionable research. Literature synthesis through SRs and/or meta-analysis has a primarily retrospective role that guides future research and sheds light on arguable topics but cannot erase the wrongdoings of primary studies, which are often concealed. The “bottom-up” approach of a wide dissemination of information to clinicians, together with practical incentives for stakeholders with competing interests to collaborate, promise to improve women’s healthcare.
Author Contributions
C.S. conceived and designed the study and prepared the manuscript. P.V. and V.K. contributed to the design and reporting of the research. All authors approved the final version of the manuscript.
This research received no external funding. The APC was funded by the first author.
Informed Consent Statement
Not applicable due to the nature of this study.
Data Availability Statement
Conflicts of interest.
The authors have no conflicts of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Assessment of NIH Research on Women's Health
This study aims to fill gaps in our understanding of women's health research across all NIH Institutes and Centers. It will analyze how much funding is allocated to research on conditions that affect women specifically or are more common among women, and how these conditions are defined across different stages of life. The study will also assess sex differences and racial health disparities. Ultimately, the study will determine the funding needed to bridge gaps in women's health research at NIH.
Deadline: April 3, 2024
Call for Feedback
The National Academies' Committee on the Assessment of NIH Research on Women’s Health is inviting stakeholders and patients to share their perspectives on gaps in women’s health research, particularly across NIH Institutes and Centers. Please submit your comments by April 3, 2024.
Upcoming Events
Multiday Event | April 11-12, 2024
Publications
No publications are associated with this project at this time.
No projects are underway at this time.
Description
The National Academies of Sciences, Engineering, and Medicine (NASEM) will convene an ad hoc committee with specific scientific, ethical, regulatory, and policy expertise to develop a framework for addressing the persistent gaps that remain in the knowledge of women's health research across all NIH Institutes and Centers (ICs). Specifically, the study should be designed to analyze the proportion of research that the NIH funds on conditions that are female-specific and/or more common amongst women or that differently impact women (e.g., different pathophysiology or course of disease), establish how these conditions are defined and ensure that it captures conditions across the lifespan, evaluates sex differences and racial and ethnic health disparities. The committee should define women's health for the purpose of the report, taking into account today's social and cultural climate. Ultimately, the study should determine the appropriate level of funding that is needed to address gaps in women's health research at NIH.
The NASEM consensus committee, as a first step, will conduct an analysis and develop a matrix of identified NIH research on conditions that are female-specific, more common amongst women or that differently impact women, investigating sex differences, and centered on the unique health needs of women.
The committee will make recommendations for the following:
- Research priorities for NIH-supported research on women’s health
- NIH training and education efforts to build, support, and maintain a robust women’s health research workforce
- NIH structure (extra- and intra-mural), systems, review processes to optimize women’s health research
- NIH-wide workforce to effectively solicit, review and support women’s health research
- Allocation of funding needed to address gaps in women's health research at NIH.
The committee will identify metrics to ensure that research is tracked to meet the continuing health needs of women.
- Health and Medicine Division
- Board on Population Health and Public Health Practice
- Board on Health Care Services
- Board on Health Sciences Policy
In Progress
Consensus Study
- Health and Medicine
Contact the Public Access Records Office to make an inquiry, request a list of the public access file materials, or obtain a copy of the materials found in the file.
Committee Membership Roster Comments
Felina Cordova-Marks and Holly A. Ingraham were added on December 6, 2023. Bios were updated for Cheng, Golden, Kaplan, Lane, Salmon, and Secord on December 15, 2023, and for Burke on December 20, 2023. Bios for Cordova-Marks and Kaplan were updated on January 19, 2024. Crystal Schiller was added on January 25, 2024. The bio for Golden was updated on 3/5/2024.
Past Events
Multiday Event | March 7-8, 2024
3:30PM - 4:00PM (ET)
February 27, 2024
[Closed] Assessment of NIH Research on Women's Health: Evaluation criteria work group, Meeting #2
Multiday Event | January 30-31, 2024
[Closed] Assessment of NIH Research on Women's Health: Funding assessment work group, Meeting #1
Multiday Event | January 25-26, 2024
11:00AM - 12:00PM (ET)
January 18, 2024
[Closed] Assessment of NIH Research on Women's Health: Definitions work group, Meeting #1
Rachel Riley
(202) 334-3288
Responsible Staff Officers
- Amy Geller
Additional Project Staff
- Aimee Mead
- Magdaline Anderson
- Luz Brielle Dojer
- Rachel Riley
Women's Health Research Center

Improving the health of women
Mayo Clinic Women's Health Research Center is a leader in providing evidence to improve healthcare for women and educating the next generation of women's health investigators and healthcare professionals.
The Mayo Clinic Women's Health Research Center advances scientific discoveries to improve the health of women through all stages of life.
The center is at the forefront of a new era in women's health, based on the understanding that the female body isn't simply a smaller version of the male form. Women and men have different chromosomes and hormones. Thus, disease risk, diagnosis and response to treatments — including some medicines — are often different for women and men.
Yet current medical treatments are often based on research that was conducted mainly on men. Or, when women were included, the research didn't account for differences between women and men.
Mayo Clinic is transforming women's health by advancing research and studies specifically focused on the unique needs and abilities of the female body through all stages of life.
Investigators in the Women's Health Research Center are studying why certain illnesses occur more often — or sometimes only — in women or manifest differently in women than in men. Armed with this information, healthcare professionals can better prevent, diagnose and treat some of today's most debilitating diseases.
For more than 150 years, Mayo Clinic research has changed the face of medicine, enabling healthcare professionals around the world to provide lifesaving care to millions of people. Now, Mayo is advancing research focused on women's health so that medical care can be personalized for women and men.
Right now, there are more than 1,400 research studies related to women's health across Mayo Clinic campuses in Arizona, Florida and Minnesota. Mayo researchers are dedicated to addressing the health issues women face, with the goal of improving women's health and quality of life.
- View Complete Calendar
Mayo Clinic Women's Health Research Center
Mayo Clinic Women's Health Research Center director Kejal Kantarci, M.D., former director, Virginia M. Miller, Ph.D., and colleagues talk about research in the Women's Health Research Center.
Center leadership
Associate Director
Mayo Clinic Footer
- Request Appointment
- About Mayo Clinic
- About This Site
Legal Conditions and Terms
- Terms and Conditions
- Privacy Policy
- Notice of Privacy Practices
- Notice of Nondiscrimination
- Manage Cookies
Advertising
Mayo Clinic is a nonprofit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised.
- Advertising and sponsorship policy
- Advertising and sponsorship opportunities
Reprint Permissions
A single copy of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic," "MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research.
Women’s Health

Women’s Health Activities
Women’s health science.
Read selected scientific findings and publications regarding the health of women and girls.
Healthy Living
Learn about specific health challenges women and girls face throughout their lifespan.
Women’s Health Features

Women’s Unseen Battle: Shining a Light on Lupus
CDC and partners are working to make lupus visible by raising awareness about this disease. Read on to learn more about lupus among women. Share this information in your community!

Celebrating Women’s Health Week!
National Women’s Health Week starts each year on Mother’s Day to encourage women and girls to make their health a priority. Learn more about how to live a safer and healthier life.

Working Together to Reduce Black Maternal Mortality
Black Maternal Health Week is recognized each year from April 11-17 to bring attention and action in improving Black maternal health. Everyone can play a role in working to prevent pregnancy-related deaths and improving maternal health outcomes.

Supporting Women with Disabilities to Achieve Optimal Health
An estimated 37.5 million women in the U.S. report having a disability. Learn about the challenges women with disabilities experience and how you can help support disability awareness.
Sign up for our free newsletter
Read our latest newsletter.
- Breastfeeding Report Card, United States, 2022
- Gynecologic Cancer Awareness
- Pregnancy-Related Deaths: Data from Maternal Mortality Review Committees in 36 US States, 2017–2019
- Fetal Alcohol Spectrum Disorders: Resources for Prevention and Care
- Geographic Examination of COVID-19 Test Percent Positivity and Proportional Change in Cancer Screening Volume, National Breast and Cervical Cancer Early Detection Program
Journal of Women's Health: Report from the CDC
- Addressing Racial Disparities in Pregnancy-Related Deaths: An Analysis of Maternal Mortality-Related Federal Legislation, 2017–2021
- Surveillance of Hypertension Among Women of Reproductive Age: A Review of Existing Data Sources and Opportunities for Surveillance Before, During, and After Pregnancy
- Summary of Current Guidelines for Cervical Cancer Screening and Management of Abnormal Test Results: 2016–2020
To receive email updates about this page, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 13 June 2023
It’s about time to focus on women’s health
Nature Reviews Bioengineering volume 1 , page 379 ( 2023 ) Cite this article
1703 Accesses
19 Altmetric
Metrics details
- Biomedical engineering
- Health care
Women’s health has long been overlooked in both fundamental and clinical research, which, sadly, also holds true for the bioengineering field — albeit things are slowly changing.
Only 3.7% of all clinical trials from 2007 to 2020 focused on gynaecology 1 , and there is an undeniable gender disparity in the allocation of research funds 2 ; a disproportionate share of resources is dedicated to diseases that affect primarily males 3 , at the expense of funding for research on conditions that disproportionately affect females , such as pregnancy disorders, autoimmune diseases and reproductive tract disorders. A report by the Global Health Alliances in 2014 suggested that neglect in medical research and funding is directly responsible for delayed diagnosis, severe disease progression and premature death of women 4 . So, it is fair to say that women’s health is overlooked in fundamental and clinical research. Therefore, it is about time for our field to adapt, tailor and optimize our engineered models and platforms for the investigation of the health of individuals who identify as women, regardless of their sex at birth.
“…it is about time for our field to adapt, tailor and optimize our engineered models and platforms for the investigation of the health of individuals who identify as women, regardless of their sex at birth.”
“Before I was diagnosed with lupus, I did not understand that medicine had a gender problem,” writes Elinor Cleghorn at the beginning of her book ‘Unwell Women’ 5 . What follows is her personal story of suffering from undiagnosed pain for years, an experience that is all too familiar for many women affected by lupus and other autoimmune diseases, such as Graves’ disease. Of note, women make up approximately 80% of people with autoimmune diseases 6 . The mechanisms underlying many autoimmune diseases remain to be identified, and, accordingly, their diagnosis and treatment are often delayed and ineffective. The bioengineering field has put great effort into investigating, manipulating and engineering the immune system, resulting in notable progress in immunotherapy, vaccine technologies and in vitro immune tissue models. The same immunoengineering efforts could be dedicated to the investigation of autoimmune diseases; for example, to improve the early detection of lupus, biomaterial models can be designed to study how immune cells interact with blood vessels to shed light on the pathogenesis of this disease 7 .
Endometriosis, which is a chronic disease that affects roughly 10% (190 million) of reproductive age women and girls globally , is associated with severe, life-impacting pain. Yet, diagnosis of endometriosis remains difficult and there is currently no known cure. A key strength of bioengineering is the design of in vitro models, such as organoids and organs-on-chips, to investigate disease and test drugs. Such model systems can also be designed for modelling the endometrium to investigate diagnostic tools and treatments for endometriosis; for example, endometrial organoids can be derived from menstrual flow to non-invasively diagnose endometriosis 8 , or they can be engineered from human tissue-derived cells using synthetic matrices 9 . The progress made in the design of clinically relevant in vitro models is reflected in the US Food and Drug Administration (FDA) Modernization Act 2.0, authorizing the use of certain alternatives, including cell-based assays, to animal testing. Therefore, research efforts in optimizing endometrial organoids may well result in the development of new diagnosis and treatment strategies for endometriosis.
Similarly, the advanced design of drug delivery systems has contributed to breakthroughs in the treatment and prevention of many diseases. However, these systems rarely consider the barriers, challenges and microenvironments unique to the female body 10 . In this issue, Michael J. Mitchell and colleagues discuss the design and optimization of therapeutic nanoparticle and biomaterial systems to deliver drugs for the treatment of conditions in non-pregnant and pregnant women. Importantly, the authors emphasize that drug delivery systems intended for the treatment of women’s health conditions must be specifically engineered to penetrate female-specific biological barriers, such as the vaginal mucosa, and potentially consider placental transport, and maternal and fetal safety. Nanoscale systems can now be designed to overcome complex biological barriers (even the blood–brain barrier) and target specific tissues and cells in the human body — the next challenge should be to study and tailor their behaviour in the female body.
The list could go on — from menopause and long COVID to accounting for the role of sex in tissue engineering. There is lots to tackle for the bioengineering community.
Steinberg, J. R. et al. Early discontinuation, results reporting, and publication of gynecology clinical trials from 2007 to 2020. Obstet. Gynecol. 139 , 821–831 (2022).
Article Google Scholar
[No authors listed]. Women’s health: end the disparity in funding. Nature 617 , 8 (2023).
Mirin, A. A. Gender disparity in the funding of diseases by the U.S. National Institutes of Health. J. Womens Health 30 , 956–963 (2021).
Bonita, R. & Beaglehole, R. Women and NCDs: overcoming the neglect. Glob. Health Action 7 , 1 (2014).
Cleghorn, E. Unwell Women: A Journey Through Medicine and Myth in a Man-Made World (W&N, 2021).
Invernizzi, P., Pasini, S., Selmi, C., Gershwin, M. E. & Podda, M. Female predominance and X chromosome defects in autoimmune diseases. J. Autoimmun. 33 , 12–16 (2009).
Silberman, J. et al. Modeled vascular microenvironments: immune-endothelial cell interactions in vitro. Drug Deliv. Transl. Res. 11 , 2482–2495 (2021).
Cindrova-Davies, T. et al. Menstrual flow as a non-invasive source of endometrial organoids. Commun. Biol. 4 , 651 (2021).
Hernandez-Gordillo, V. et al. Fully synthetic matrices for in vitro culture of primary human intestinal enteroids and endometrial organoids. Biomaterials 254 , 120125 (2020).
Poley, M. et al. Sex-based differences in the biodistribution of nanoparticles and their effect on hormonal, immune, and metabolic function. Adv. NanoBiomed Res. 2 , 2200089 (2022).
Download references
Rights and permissions
Reprints and permissions
About this article
Cite this article.
It’s about time to focus on women’s health. Nat Rev Bioeng 1 , 379 (2023). https://doi.org/10.1038/s44222-023-00081-1
Download citation
Published : 13 June 2023
Issue Date : June 2023
DOI : https://doi.org/10.1038/s44222-023-00081-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
- For Consumers
- Women's Health
- Women's Health Research
- About OWH Research
Women's Health Research Roadmap
From the FDA Office of Women's Health (OWH)
On this page: About the roadmap | Research priority areas | Related links
Download the Research Roadmap (PDF, 9.20 MB)
About the Women’s Health Research Roadmap
A strategy for science and innovation to improve the health of women
Since its inception, the FDA Office of Women’s Health (OWH) has worked closely with FDA’s centers to expand existing research projects and foster new collaborations related to advancing the science of women’s health. OWH has also worked with other government agencies, academia, women’s research organizations, and other stakeholders to foster and facilitate research projects and scientific forums. These combined efforts have helped to advance our understanding of women’s health issues. They have furthered the development of new tools and approaches for informing FDA decisions about the harm or the safety and effectiveness of FDA-regulated products that are used not only by women, but by all Americans.
The Women’s Health Research Roadmap builds on knowledge gained from previously funded research and is intended to assist OWH in coordinating future research activities with other FDA research programs and with external partners. The Roadmap outlines priority areas where new or enhanced research is needed. Although many critical women’s health issues may warrant further examination, future OWH-funded research should focus on areas where advancements will be directly relevant to FDA as it makes regulatory decisions. The Roadmap creates strategic direction for OWH to help maximize the impact of OWH initiatives and ultimately promote optimal health for women.
Research priority areas
- Advance safety and efficacy : Advance the safety and efficacy and reduce the toxicity of FDA-regulated products used by women
- Improve clinical study design and analyses : Improve clinical study design and conduct to better identify and evaluate possible sex differences related to FDA-regulated products
- Novel modeling and simulation approaches : Evaluate and promote the adoption of novel modeling and simulation approaches that can aid in regulatory evaluation of FDA-regulated products
- Advances in biomarker science : Develop tools and methods that can help identify, evaluate, and qualify predictive or prognostic clinical and non-clinical biomarkers and surrogate endpoints
- Expand data sources and analysis : Identify, develop, and evaluate data sources and efficient techniques for data mining, data linkage, and large data set analysis that can be used to assess the postmarket toxicity or the safety and effectiveness of FDA-regulated products
- Improve health communications : Develop, evaluate, and use tools and methods to foster the creation and easy availability of clear and useful information about FDA-regulated products used by women to help women and their health care professionals make informed health-related decisions
- Emerging technologies : Support the identification of sex differences related to the use of emerging technologies
Related links
- OWH information on BAA funding
- Extramural Research - Women's Health (including funding information)
- Annual Awards
- Mission and Vision
- Share Your Story
- Women’s Health Research
- Board of Directors
- Collaborations
- Partner with SWHR
- Philanthropy
- Job Opportunities
- Alzheimer’s Disease
- Endometriosis and Fibroids
- Roundtables
- Science Events
- Advisory Council
- Women’s Health Policy Agenda
- Position Statements
- Policy Letters
- Legislation
- Policy Events
- Read My Lips
- Women’s Health Equity Initiative
- Coronavirus
- Publications
- Peer-Reviewed Articles
- Guides & Toolkits
- SWHR in the News
- Read Women’s Health Stories
- Annual Awards 2024
- Annual Awards 2023
- Annual Awards 2018-2022
Home » About » Women’s Health Research
Women’s health Research
What is women’s health research.
Women’s health research is the study of health across a woman’s lifespan in order to preserve wellness and to prevent, diagnose, and treat disease. It includes all health conditions for which women and men experience differences in risk, presentation, and treatment response, as well as health issues specific to women, such as pregnancy and menopause.
Women’s health research considers both sex and gender differences and how these differences affect disease risk, pathophysiology, symptoms, diagnosis, and treatment.

Sex vs. gender
What’s the difference.
While the terms sex and gender are often used interchangeably in society, they have distinct definitions that apply in scientific research. Both sex and gender are variables that should be considered in scientific research, from the development and design of studies to the analysis and reporting of study results.
is a multidimensional biological construct based on anatomy, physiology, genetics, and hormones. These components are sometimes referred to together as “sex traits.”
is broadly defined as a multidimensional construct that encompasses gender identity and expression, as well as social and cultural expectations about status, characteristics, and behavior as they are associated with certain sex traits. Understandings of gender vary throughout historical and cultural contexts.
the health gap for women
Until about 25 years ago, essentially all health research was conducted on men..
Women were actively excluded from participating in most clinical trials. Why? Because of the persistent idea that female hormonal cycles were too difficult to manage in experiments — including the fear of harming potential pregnancies — and that using only one sex would reduce variation in results. This exclusion of females in health research wasn’t just limited to humans. It extended to research on female animals, cells, and tissue. Researchers assumed that they could simply extrapolate their male-only study results to females, a dangerous precedent that overlooked fundamental differences between women and men.
Fortunately, thanks to advocacy by the Society for Women’s Health Research and other groups, Congress passed the National Institutes of Health Revitalization Act of 1993, mandating the inclusion of women and minorities in NIH-funded clinical trials. In the same year, the Food and Drug Administration changed its policies to require the inclusion of women in efficacy studies and in the analysis of data on sex differences.
Then, in 2016, the NIH implemented a new policy stating that sex as a biological variable should be factored into preclinical research and reporting in vertebrate animal and human studies. Today, all NIH-funded researchers must either include both female and male research subjects or explain why they do not.
Although researchers have been playing catch-up for the past couple of decades, this longtime bias put the health of women at risk and created a huge gap in knowledge about women’s health and the role that differences between women and men play in health and disease.
Differences exist
The biological differences between women and men go beyond basic anatomy. Researchers must consider sex differences down to the cellular level in order to discover crucial information about the varied development, function, and biology between women and men.

of women with sleep apnea go undiagnosed
because they may not report the same “textbook” symptoms as men.
of those with Alzheimer’s disease are women
and some research suggests women are at greater risk for AD than men.
of people with osteoporosis are women
and they experience rapid bone loss at menopause due to hormonal changes.
The Inclusion of Women in Research
1977 · The Food and Drug Administration (FDA) bars women of child bearing potential from participating in most early phase clinical research.
1985 · A United States Public Health Service task force concludes that exclusion of women from clinical research was detrimental to women’s health.
1986 · The National Institutes of Health (NIH) adopts guidelines urging the inclusion of women in NIH-sponsored clinical research.
1990 · The Society for Women’s Health Research is founded and asks the General Accounting Office (GAO) to examine whether NIH is following its 1986 guideline.
1990 · A GAO report reveals that the NIH guidelines are not being followed. The Physician’s Health or “aspirin” study, designed to examine the impact of taking aspirin on cardiovascular disease, is one of many large studies not included women highlighted by the report.
1993 · The NIH Revitalization Act of 1993 mandates that the NIH must ensure that women and members of minorities and their subpopulations are included in all human subject research. 1993 · The FDA rescinds earlier guidelines barring the participation of women with child-bearing potential from most early phase research.
2000 · The GAO concludes that although women are now included in clinical research proportionate to their representation in the population, analysis by sex of subjects is rare.
2001 · The GAO concludes FDA not effectively monitoring research data to determine how sex differences affect drug safety and effectiveness.
2006 · The Organization for the Study of Sex Differences is established. It is the brain child of basic and clinical scientists with established research commitments to the study of sex differences, and staff members of SWHR.
2012 · Food and Drug Administration Safety and Innovation Act (FDASIA) signed into law, requiring FDA to provide a special report and accounting of trials by sex, race, and ethnicity.
2014 · The National Institutes of Health (NIH) enact new policies to address sex differences by will be requiring applicants to report their cell and animal inclusion plans as part of preclinical experimental design.
2015 · The FDA launched the website Drug Trials Snapshots that provide consumers with information about who participated in clinical trials that supported the FDA approval of new drugs. The site is is part of an overall FDA effort to make demographic data more available and transparent.
2016 · NIH implemented a policy that expects scientists to account for the possible role of sex as a biological variable (SABV) in vertebrate animal and human studies.
Both sex and gender influence health across the lifespan, and SWHR strives to comprehensively address both sex and gender as they relate to women’s health. When citing research, SWHR uses terminology consistent with what is used in the cited study. As inclusive language practices continue to evolve in the scientific and medical communities, we will reassess our language as usage to promote accuracy and inclusivity. Please note that not all language will be updated retroactively.
SWHR acknowledges that there are valued groups of people that may benefit from our materials who do not identify as women. We encourage those who identify differently to engage with us and our content.
- Departments & Services
- Directions & Parking
- Medical Records
- Physical Therapy (PT)
- Primary Care
Header Skipped.
- Department of Medicine
Division of Women's Health
Division of women's health research.
The Division of Women’s Health’s research goals are: to lead scientific and clinical discoveries that identify and explain sex- and gender-based differences in health and disease, prioritize disorders specific to women, and ultimately improve the overall health and access to care for women and men. Faculty in the Division of Women’s Health pursue a wide range of research topics dedicated to advancing knowledge of women’s health and sex differences in health and disease. To learn more about specific research programs and areas, visit our research website: Women's Health Research .
Research Areas
- Cancer Screening & Prevention
- Cardiovascular Disease
- Clinical Neuroscience & Neuroendocrinology
- Gender, Violence & Trauma
- Global Women’s Health
- Life Course & Reproductive Epidemiology
- Women’s Health Policy Research & Advocacy
Research Faculty
- Kathryn Rexrode, MD, MPH Professor of Medicine Division Chief
- Laura Holsen, PhD Assistant Professor of Psychiatry
- Ingrid Katz, MD, MHSc Associate Professor of Medicine
- Annie Lewis-O'Connor, MSN, MPH, PhD Instructor in Medicine
- Roseanna Means, MD Associate Professor of Medicine, Part-time
- Lydia Pace, MD, MPH Assistant Professor of Medicine
- Alexandra Purdue-Smithe, PhD Instructor in Medicine
- Janet Rich-Edwards, ScD, MPH Associate Professor of Medicine
- Eve Rittenberg, MD Assistant Professor of Medicine
- Meghan Rudder, MD Instructor in Medicine
- Hanni Stoklosa, MD, MPH Instructor in Medicine
- Jennifer J. Stuart, ScD Instructor in Medicine
Affiliate Faculty
- Deborah Bartz, MD, MPH
- Kari Braaten, MD, MPH
- Ann Celi, MD
- Ming Hui Chen, MD, MMSc, FACC, FASE
- Alisa Goldberg, MD, MPH
- Jill Goldstein, PhD
- Tamarra James-Todd, PhD, MPH
- Elizabeth Janiak, ScD
- Tamara Bockow Kaplan, MD
- Bharti Khurana, MD
- Nomi Levy-Carrick, MD
- Rose L. Molina, MD, MPH
- Maria Nardell, MD
- Jennifer Scott, MD, MBA, MPH
- Caren Solomon, MD, MPH
- Paula Emma Voinescu, MD, PhD
Learn more about Brigham and Women's Hospital
For over a century, a leader in patient care, medical education and research, with expertise in virtually every specialty of medicine and surgery.
Stay Informed. Connect with us.
- X (formerly Twitter)

- Current Projects
- Yale OCD Research Clinic
- Publications
INFORMATION FOR
- Residents & Fellows
- Researchers
25 Years of Women’s Health Research at Yale
Making every year count, 25 years of women's health research at yale.
Women's Health Research at Yale marks 25 years of investigating conditions of high morbidity and mortality in women and understanding sex and gender differences that affect health outcomes.
Google came online the same year Women’s Health Research at Yale (WHRY) was created. Each, as it turned out, would fill a void in the search for information.
It was 1998, soon after the National Institutes of Health issued a grant requirement that women be included as participants in clinical research. Without this requirement, the existing gap in what was known about the health of women would continue. This directive also meant that the largest single funder of biomedical research in the world was changing the ground rules about who was studied and calling for data on the health of women beyond the existing focus of reproductive health.
And so, the search for information began.
Through our Pilot Project Program, WHRY began generating studies on the causes, mechanisms, and interventions for the health conditions that affect women and broadening the scope of what was considered women’s health. These studies also allowed Yale faculty to collect the necessary feasibility data required to secure new NIH grants for further study on the wide span of critical women’s health topics.

With one of the first pilot project grants, Bruce Haffty, MD, Professor of Therapeutic Radiology, found, in a rare 15-year follow-up study of women with breast cancer, that women with BRCA1 or BRCA2 mutations were more likely to develop breast cancer recurrence in either breast than women without this genetic risk factor. These findings became crucially important to women weighing treatment options at the time of diagnosis and developing plans for follow-up.

Dr. Haffty’s study was one of many that demonstrated rapid benefit derived from our pilot studies. Another offered girls with autism spectrum disorder (ASD) a new treatment option. Traditionally, girls with ASD have been under-represented in research. Pamela Ventola, PhD, Associate Professor in the Child Study Center, demonstrated that Pivotal Response Therapy (PRT), a social-behavioral treatment could help girls, along with boys, with ASD. Dr. Ventola showed that girls benefited from PRT and made larger net gains than did boys, resulting in its therapeutic use today in both girls and boys.
Similar to an internet search, some research studies can provide swift answers, while others require longer investigation. Here’s an example of research that requires a longer-term commitment.
Previous studies have shown women have a higher risk for parathyroid disorders, such as hypoparathyroidism in which insufficient parathyroid hormone is secreted. Women are also more likely to develop thyroid cancer requiring surgical treatment, which often comes with the unintended consequence of damage to the parathyroid glands. In either case, lifelong hypoparathyroidism can result. This means that parathyroid hormone is not available to maintain needed calcium levels in the blood. Without proper calcium levels, patients are at risk for painful muscle spasms, seizures, and brain fog when the condition is mild and can develop a life-threatening calcium deficiency when it is severe. Treating hypoparathyroidism with calcium supplements, which is the standard of care, is often ineffective for maintaining the proper calcium balance, in addition to causing unwanted side effects.

As the Associate Director of Yale’s Stem Cell Center, Diane Krause, MD, PhD, Anthony N. Brady Professor of Laboratory Medicine, has taken on the intensive work of turning patients’ stem cells into parathyroid cells to give patients the capacity to produce parathyroid hormone on their own. The round-the-clock effort is a multi-year process involving five stages of development. Dr. Krause and her team established a protocol to orchestrate the molecular cues that mimic the natural development process of turning stem cells into parathyroid cells. This protocol, which will provide a revolutionary new treatment option, has been validated in collaborating laboratories, and is now being fine-tuned to improve the efficiency of parathyroid cell differentiation.
Dr. Krause’s work is the result of believing that the current standard of treatment can be improved. She is among the many researchers who have used WHRY’s Pilot Project Program seed grants to explore novel ideas and shape the future of health care.

Samit Shah, MD, PhD, Assistant Professor of Medicine (Cardiology) focused his grant on creating a new approach to improve the diagnosis of heart disease in women. Most heart attacks in women and men are due to blockage of major cardiac arteries, thus preventing blood flow to the heart. However, chest pain and heart attacks can also be caused by constriction or spasm of the small vessels that feed the heart. Known as microvascular disease, this cause is more common in women and it is not detected by routine diagnostic protocols that are designed to detect major blockages. Consequently, women are more likely to be left without a diagnosis or appropriate treatment. Dr. Shah’s research focuses on this physiological difference between women and men and, if a cholesterol blockage is not found during cardiac catheterization, he uses specialized techniques to determine whether there is another cause of reduced blood flow, such as microvascular disease. In women without blockages, nearly 90 percent of women who underwent testing were found to have a cause of reduced blood flow to the heart, despite having no significant plaque blockage in the large blood vessels. This advanced testing helps patients find an accurate diagnosis and allows providers to develop precision treatment plans.

Other novel advances in treating a particular disease have now turned out to be useful for other disorders. For example, the innovative approach used in two different pilot studies by Akiko Iwasaki, PhD, Sterling Professor of Immunobiology, to treat herpes infections is now being applied to the fight against Covid-19. In her first WHRY study, Dr. Iwasaki focused her research on the role of mucous membranes in understanding why women are more susceptible than men to viral genital herpes infections. Her second study expanded upon that knowledge and created a treatment strategy dubbed “prime and pull” that would prime the immune system to create a memory response to the herpes simplex virus and then pull those immune memory cells to the site of infection to stop the virus. In a third WHRY study at the start of the COVID-19 pandemic, Dr. Iwasaki showed sex differences in immune response to the novel SARS-CoV-2 virus and is now using her combined expertise on this virus and viral transmission to develop an intranasal vaccine to create mucosal immunity that would stop the virus at the site of infection – the nasal muscosa.

The importance of ingenuity in scientific discovery is also evident in the ovarian and breast cancer research by Peter Glazer, MD, PhD, Robert E. Hunter Professor of Therapeutic Radiology. Dr. Glazer, along with James Hansen, MD, began investigating a nontoxic lupus antibody that can penetrate cancer cells for its potential as a mechanism for cancer treatment. In his WHRY study, he found that this specific lupus antibody could be used to inhibit the DNA repair component of the cancer cell in a manner that stops the cancer cell from sustaining itself. Further research showed efficacy in the antibody destroying specifically those cancer cells associated with mutations in the tumor suppressing BRCA1/2 genes. As mutations in these BRCA genes lead to higher rates of breast and ovarian cancer, this research is of great value for BRCA-related cancers that affect many women around the world. The antibody has now been developed into a therapy to fight these cancers and clinical trials are planned for later this year.
Women’s Health Research at Yale’s search for information began 25 years ago to address the scarcity of information on women’s health. It has led to knowledge on a myriad of conditions and uncovered vital sex and gender differences that influence the health of all people.
As this sampling of WHRY funded studies show, there is much to learn that can advance the health of women and men. And so, the search continues.
- Basic Science Research
- Clinical research
- Cardiology and Vascular
- Ovarian Cancer
- Breast Cancer
- Immunology & Immunobiology
- Translational Research
- Heart Disease

Featured in this article
- Carolyn M. Mazure, PhD Norma Weinberg Spungen and Joan Lebson Bildner Professor in Women's Health Research and Professor of Psychiatry and of Psychology
- Bruce Haffty, MD
- Diane Krause, MD, PhD Anthony N. Brady Professor of Laboratory Medicine and Professor of Pathology; Vice Chair for Research Affairs, Laboratory Medicine; Assoc. Director, Yale Stem Cell Center; Assoc. Director, Transfusion Medicine Service; Medical Director, Clinical Cell Processing Laboratory; Medical Director, Advanced Cell Therapy Laboratory
- Samit Shah, MD, PhD, FACC, FSCAI Assistant Professor of Medicine; Director, VA Connecticut Cardiac Catheterization Laboratory
- Akiko Iwasaki, PhD Sterling Professor of Immunobiology and Professor of Dermatology and of Molecular, Cellular, and Developmental Biology and of Epidemiology (Microbial Diseases); Investigator, Howard Hughes Medical Institute
- Peter M. Glazer, MD, PhD Robert E. Hunter Professor of Therapeutic Radiology and Professor of Genetics; Chair, Therapeutic Radiology
- Pamela Ventola, PhD Associate Professor Child Study Center
- Frontiers in Communication
- Health Communication
- Research Topics
Centering Women, Health, and Health Equity in Health Communication
Total Downloads
Total Views and Downloads
About this Research Topic
Gendered patterns of labor and ongoing patriarchal attitudes mean that women’s voices, worldviews, and cultural frames of reference are systematically neglected in the production of health knowledge and communication around health. For example, male-identified researchers tend to produce far more research on ...
Keywords : Health Equity, Gender, Women, Race, Critical Cultural Communication, Health communication
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, recent articles, submission deadlines, participating journals.
Manuscripts can be submitted to this Research Topic via the following journals:
total views
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.
- Share full article
Advertisement
Supported by
Biden Signs Executive Order to Expand Research on Women’s Health
The president said that improving women’s health was crucial to ensuring a healthy, stable economy.
Biden Signs Executive Order to Boost Women’s Health Research
The executive order is aimed at addressing the underrepresentation of women in health research..
We’ve launched the first ever White House initiative on women’s health research to pioneer the next generation of scientific research and discovery in women’s health. Think of all the breakthroughs we’ve made in medicine across the board, but women have not been the focus. And today — [applause] today, we’re jumpstarting that investment by dedicating $200 million in the National Institutes of Health to tackle some of the most pressing health problems facing women today. With the executive order I’m about to sign, I’m directing the most comprehensive set of executive actions ever taken to improve women’s health — ever taken. And I’m going to ensure that women’s health is integrated and prioritized across the entire federal government. It’s not just in women’s health, not just at N.I.H., the National Science Foundation or the Defense Department, the Environmental Protection Agency. I mean, across the board. This is really serious.

By Zolan Kanno-Youngs
Reporting from Washington
President Biden on Monday signed an executive order to expand the federal government’s research into women’s health, including midlife conditions like menopause, arthritis and heart disease, as well as issues specifically affecting women in the military.
In what the White House described as the “most comprehensive” action by a president on women’s health research, Mr. Biden directed federal agencies to ensure that they are using federal funds to research health conditions and diseases that disproportionately affect women.
Standing alongside the first lady, Jill Biden, and Vice President Kamala Harris, Mr. Biden said improving women’s health was crucial to guaranteeing a healthy, stable economy.
“There’s not a damn thing a man can do a woman can’t do,” Mr. Biden said. “To state the obvious, if you want to have the strongest economy in the world, you can’t leave half of the country behind.”
Carolyn M. Mazure, a psychologist and a professor at the Yale School of Medicine, who is the chairwoman of the White House initiative on Women’s Health Research, told reporters on Sunday night that health conditions like heart disease, Alzheimer’s, menopause and fibroids would be a focus of the expanded research effort.
“I’m not even a betting woman,” said Maria Shriver, the former first lady of California, who also attended the event, “but I’ll bet today that this is the first time a president of the United States has ever signed an executive order that mentions the words ‘menopause’ and ‘women’s midlife health’ in it.”
After the U.S. Supreme Court overturned Roe v. Wade in 2022 and the Alabama Supreme Court ruled last month that frozen embryos should be considered children , threatening in vitro fertilization, the Biden campaign has increasingly accused Republicans of undermining women’s health. During his State of the Union address this month, Mr. Biden said such decisions would motivate women to vote in the November election, while also saying his White House would commit to investing in women’s health in the year ahead.
“You can’t lead America with old ideas and take us backwards,” Mr. Biden said, adding, “To lead the land of possibilities, you need a vision for the future laying out what we can and should do and what we’re going to do.”
Mr. Biden’s executive order will require agencies to report annually their investments in women’s health research and to study ways that artificial intelligence can be used to advance such research. The National Institutes of Health will increase by 50 percent investments in small businesses focused on women’s health. The Defense Department also plans to invest $10 million to learn more about cancers and mental health issues affecting women in active military service.
The White House has called on Congress to pass a plan to invest $12 billion to create a new fund for women’s health research at the National Institutes of Health. In the meantime, the executive order signed on Monday directed the N.I.H. to spend $200 million on women’s health research. Dr. Biden traveled to Cambridge, Mass., last month to announce the first step of the women’s health initiative: $100 million to support women’s health researchers and start-up companies.
Zolan Kanno-Youngs is a White House correspondent, covering President Biden and his administration. More about Zolan Kanno-Youngs
What we do and do not know about women and kidney diseases; Questions unanswered and answers unquestioned: Reflection on World Kidney Day and International Woman's Day
Affiliations.
- 1 1 Department of Clinical and Biological Sciences, University of Torino , Torino, Italy.
- 2 2 Department of Nephrology, Centre Hospitalier Le Mans , Le Mans, France.
- 3 3 Department of Medicine, Dubai Medical College , Dubai, United Arab Emirates.
- 4 4 National Clinical Research Center of Kidney Diseases, Jinling Hospital, Nanjing University School of Medicine , Nanjing, China.
- 5 5 Department of Nephrology, Moscow City Hospital n.a. S.P. Botkin , Moscow, Russian Federation.
- 6 6 Department of Nephrology, Moscow State University of Medicine and Dentistry , Moscow, Russian Federation.
- 7 7 Department of Nephrology, Russian Medical Academy of Continuous Professional Education , Moscow, Russian Federation.
- 8 8 Division of Nephrology, Department of Medicine, The University of British Columbia , Vancouver, BC, Canada.
- PMID: 29602290
- DOI: 10.1556/2060.105.2018.1.6
Chronic kidney disease (CKD) affects approximately 10% of the world's adult population; it is within the top 20 causes of death worldwide, and its impact on patients and their families can be devastating. World Kidney Day and International Women's Day in 2018 coincide, thus offering an opportunity to reflect on the importance of women's health and specifically their kidney health, on the community, and the next generations, as well as to strive to be more curious about the unique aspects of kidney disease in women so that we may apply those learnings more broadly. Girls and women, who make up approximately 50% of the world's population, are important contributors to society and their families. Gender differences continue to exist around the world in access to education, medical care, and participation in clinical studies. Pregnancy is a unique state for women, which not only offers an opportunity for diagnosis of kidney disease, but also states where acute and chronic kidney diseases may manifest, and which may impact future generations with respect to kidney health. There are various autoimmune and other conditions that are more likely to impact women with profound consequences for childbearing, and on the fetus. Women have different complications on dialysis than men and are more likely to be donors than recipients of kidney transplants. In this editorial, we focus on what we do and do not know about women, kidney health, and kidney disease and what we might learn in the future to improve outcomes worldwide.
Keywords: access to care; acute and chronic kidney diseases; inequities; kidney health; women.
Publication types
- Global Health*
- Health Promotion*
- Health Status
- Kidney Diseases* / diagnosis
- Kidney Diseases* / epidemiology
- Kidney Diseases* / therapy
- Renal Dialysis
- Risk Factors
- Treatment Outcome
- Women's Health*
Read our research on: Abortion | Podcasts | Election 2024
Regions & Countries
What the data says about abortion in the u.s..
Pew Research Center has conducted many surveys about abortion over the years, providing a lens into Americans’ views on whether the procedure should be legal, among a host of other questions.
In a Center survey conducted nearly a year after the Supreme Court’s June 2022 decision that ended the constitutional right to abortion , 62% of U.S. adults said the practice should be legal in all or most cases, while 36% said it should be illegal in all or most cases. Another survey conducted a few months before the decision showed that relatively few Americans take an absolutist view on the issue .
Find answers to common questions about abortion in America, based on data from the Centers for Disease Control and Prevention (CDC) and the Guttmacher Institute, which have tracked these patterns for several decades:
How many abortions are there in the U.S. each year?
How has the number of abortions in the u.s. changed over time, what is the abortion rate among women in the u.s. how has it changed over time, what are the most common types of abortion, how many abortion providers are there in the u.s., and how has that number changed, what percentage of abortions are for women who live in a different state from the abortion provider, what are the demographics of women who have had abortions, when during pregnancy do most abortions occur, how often are there medical complications from abortion.
This compilation of data on abortion in the United States draws mainly from two sources: the Centers for Disease Control and Prevention (CDC) and the Guttmacher Institute, both of which have regularly compiled national abortion data for approximately half a century, and which collect their data in different ways.
The CDC data that is highlighted in this post comes from the agency’s “abortion surveillance” reports, which have been published annually since 1974 (and which have included data from 1969). Its figures from 1973 through 1996 include data from all 50 states, the District of Columbia and New York City – 52 “reporting areas” in all. Since 1997, the CDC’s totals have lacked data from some states (most notably California) for the years that those states did not report data to the agency. The four reporting areas that did not submit data to the CDC in 2021 – California, Maryland, New Hampshire and New Jersey – accounted for approximately 25% of all legal induced abortions in the U.S. in 2020, according to Guttmacher’s data. Most states, though, do have data in the reports, and the figures for the vast majority of them came from each state’s central health agency, while for some states, the figures came from hospitals and other medical facilities.
Discussion of CDC abortion data involving women’s state of residence, marital status, race, ethnicity, age, abortion history and the number of previous live births excludes the low share of abortions where that information was not supplied. Read the methodology for the CDC’s latest abortion surveillance report , which includes data from 2021, for more details. Previous reports can be found at stacks.cdc.gov by entering “abortion surveillance” into the search box.
For the numbers of deaths caused by induced abortions in 1963 and 1965, this analysis looks at reports by the then-U.S. Department of Health, Education and Welfare, a precursor to the Department of Health and Human Services. In computing those figures, we excluded abortions listed in the report under the categories “spontaneous or unspecified” or as “other.” (“Spontaneous abortion” is another way of referring to miscarriages.)
Guttmacher data in this post comes from national surveys of abortion providers that Guttmacher has conducted 19 times since 1973. Guttmacher compiles its figures after contacting every known provider of abortions – clinics, hospitals and physicians’ offices – in the country. It uses questionnaires and health department data, and it provides estimates for abortion providers that don’t respond to its inquiries. (In 2020, the last year for which it has released data on the number of abortions in the U.S., it used estimates for 12% of abortions.) For most of the 2000s, Guttmacher has conducted these national surveys every three years, each time getting abortion data for the prior two years. For each interim year, Guttmacher has calculated estimates based on trends from its own figures and from other data.
The latest full summary of Guttmacher data came in the institute’s report titled “Abortion Incidence and Service Availability in the United States, 2020.” It includes figures for 2020 and 2019 and estimates for 2018. The report includes a methods section.
In addition, this post uses data from StatPearls, an online health care resource, on complications from abortion.
An exact answer is hard to come by. The CDC and the Guttmacher Institute have each tried to measure this for around half a century, but they use different methods and publish different figures.
The last year for which the CDC reported a yearly national total for abortions is 2021. It found there were 625,978 abortions in the District of Columbia and the 46 states with available data that year, up from 597,355 in those states and D.C. in 2020. The corresponding figure for 2019 was 607,720.
The last year for which Guttmacher reported a yearly national total was 2020. It said there were 930,160 abortions that year in all 50 states and the District of Columbia, compared with 916,460 in 2019.
- How the CDC gets its data: It compiles figures that are voluntarily reported by states’ central health agencies, including separate figures for New York City and the District of Columbia. Its latest totals do not include figures from California, Maryland, New Hampshire or New Jersey, which did not report data to the CDC. ( Read the methodology from the latest CDC report .)
- How Guttmacher gets its data: It compiles its figures after contacting every known abortion provider – clinics, hospitals and physicians’ offices – in the country. It uses questionnaires and health department data, then provides estimates for abortion providers that don’t respond. Guttmacher’s figures are higher than the CDC’s in part because they include data (and in some instances, estimates) from all 50 states. ( Read the institute’s latest full report and methodology .)
While the Guttmacher Institute supports abortion rights, its empirical data on abortions in the U.S. has been widely cited by groups and publications across the political spectrum, including by a number of those that disagree with its positions .
These estimates from Guttmacher and the CDC are results of multiyear efforts to collect data on abortion across the U.S. Last year, Guttmacher also began publishing less precise estimates every few months , based on a much smaller sample of providers.
The figures reported by these organizations include only legal induced abortions conducted by clinics, hospitals or physicians’ offices, or those that make use of abortion pills dispensed from certified facilities such as clinics or physicians’ offices. They do not account for the use of abortion pills that were obtained outside of clinical settings .
(Back to top)
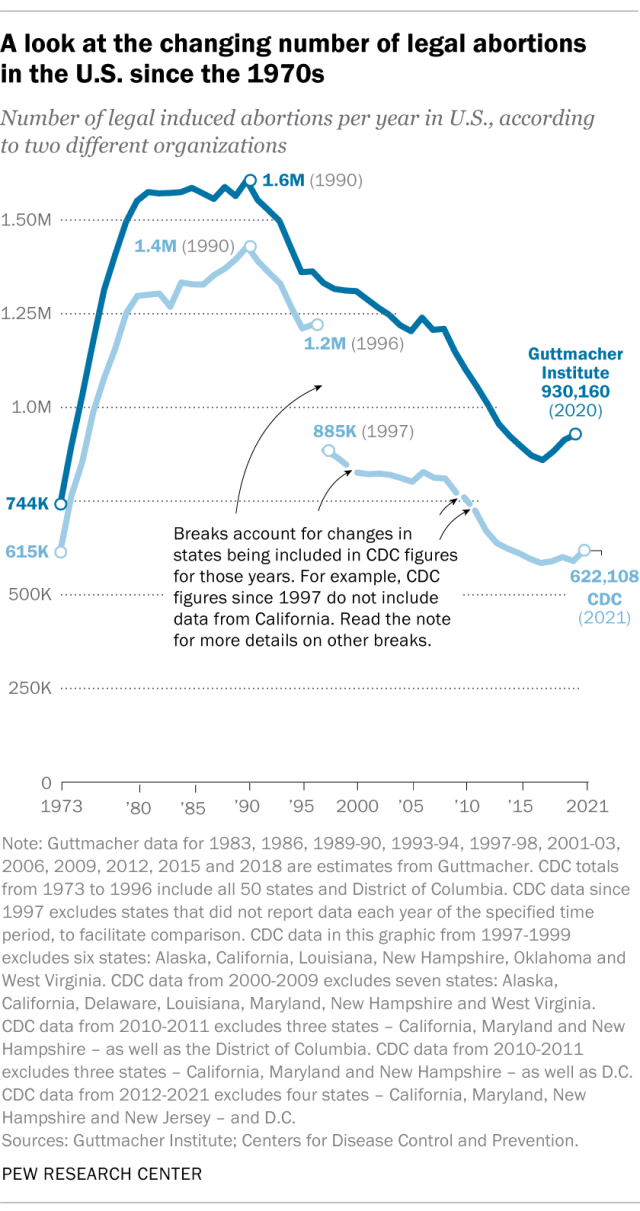
The annual number of U.S. abortions rose for years after Roe v. Wade legalized the procedure in 1973, reaching its highest levels around the late 1980s and early 1990s, according to both the CDC and Guttmacher. Since then, abortions have generally decreased at what a CDC analysis called “a slow yet steady pace.”
Guttmacher says the number of abortions occurring in the U.S. in 2020 was 40% lower than it was in 1991. According to the CDC, the number was 36% lower in 2021 than in 1991, looking just at the District of Columbia and the 46 states that reported both of those years.
(The corresponding line graph shows the long-term trend in the number of legal abortions reported by both organizations. To allow for consistent comparisons over time, the CDC figures in the chart have been adjusted to ensure that the same states are counted from one year to the next. Using that approach, the CDC figure for 2021 is 622,108 legal abortions.)
There have been occasional breaks in this long-term pattern of decline – during the middle of the first decade of the 2000s, and then again in the late 2010s. The CDC reported modest 1% and 2% increases in abortions in 2018 and 2019, and then, after a 2% decrease in 2020, a 5% increase in 2021. Guttmacher reported an 8% increase over the three-year period from 2017 to 2020.
As noted above, these figures do not include abortions that use pills obtained outside of clinical settings.
Guttmacher says that in 2020 there were 14.4 abortions in the U.S. per 1,000 women ages 15 to 44. Its data shows that the rate of abortions among women has generally been declining in the U.S. since 1981, when it reported there were 29.3 abortions per 1,000 women in that age range.
The CDC says that in 2021, there were 11.6 abortions in the U.S. per 1,000 women ages 15 to 44. (That figure excludes data from California, the District of Columbia, Maryland, New Hampshire and New Jersey.) Like Guttmacher’s data, the CDC’s figures also suggest a general decline in the abortion rate over time. In 1980, when the CDC reported on all 50 states and D.C., it said there were 25 abortions per 1,000 women ages 15 to 44.
That said, both Guttmacher and the CDC say there were slight increases in the rate of abortions during the late 2010s and early 2020s. Guttmacher says the abortion rate per 1,000 women ages 15 to 44 rose from 13.5 in 2017 to 14.4 in 2020. The CDC says it rose from 11.2 per 1,000 in 2017 to 11.4 in 2019, before falling back to 11.1 in 2020 and then rising again to 11.6 in 2021. (The CDC’s figures for those years exclude data from California, D.C., Maryland, New Hampshire and New Jersey.)
The CDC broadly divides abortions into two categories: surgical abortions and medication abortions, which involve pills. Since the Food and Drug Administration first approved abortion pills in 2000, their use has increased over time as a share of abortions nationally, according to both the CDC and Guttmacher.
The majority of abortions in the U.S. now involve pills, according to both the CDC and Guttmacher. The CDC says 56% of U.S. abortions in 2021 involved pills, up from 53% in 2020 and 44% in 2019. Its figures for 2021 include the District of Columbia and 44 states that provided this data; its figures for 2020 include D.C. and 44 states (though not all of the same states as in 2021), and its figures for 2019 include D.C. and 45 states.
Guttmacher, which measures this every three years, says 53% of U.S. abortions involved pills in 2020, up from 39% in 2017.
Two pills commonly used together for medication abortions are mifepristone, which, taken first, blocks hormones that support a pregnancy, and misoprostol, which then causes the uterus to empty. According to the FDA, medication abortions are safe until 10 weeks into pregnancy.
Surgical abortions conducted during the first trimester of pregnancy typically use a suction process, while the relatively few surgical abortions that occur during the second trimester of a pregnancy typically use a process called dilation and evacuation, according to the UCLA School of Medicine.
In 2020, there were 1,603 facilities in the U.S. that provided abortions, according to Guttmacher . This included 807 clinics, 530 hospitals and 266 physicians’ offices.
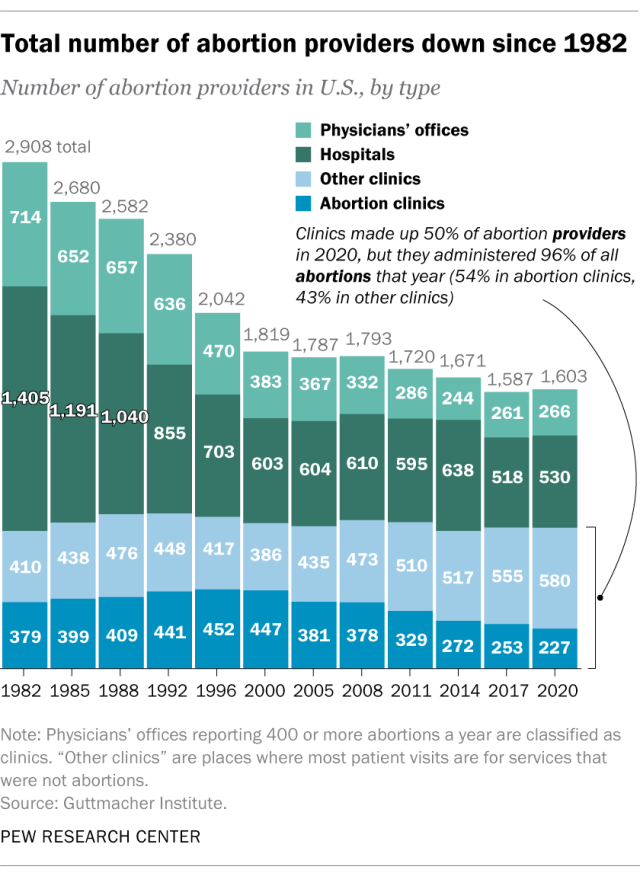
While clinics make up half of the facilities that provide abortions, they are the sites where the vast majority (96%) of abortions are administered, either through procedures or the distribution of pills, according to Guttmacher’s 2020 data. (This includes 54% of abortions that are administered at specialized abortion clinics and 43% at nonspecialized clinics.) Hospitals made up 33% of the facilities that provided abortions in 2020 but accounted for only 3% of abortions that year, while just 1% of abortions were conducted by physicians’ offices.
Looking just at clinics – that is, the total number of specialized abortion clinics and nonspecialized clinics in the U.S. – Guttmacher found the total virtually unchanged between 2017 (808 clinics) and 2020 (807 clinics). However, there were regional differences. In the Midwest, the number of clinics that provide abortions increased by 11% during those years, and in the West by 6%. The number of clinics decreased during those years by 9% in the Northeast and 3% in the South.
The total number of abortion providers has declined dramatically since the 1980s. In 1982, according to Guttmacher, there were 2,908 facilities providing abortions in the U.S., including 789 clinics, 1,405 hospitals and 714 physicians’ offices.
The CDC does not track the number of abortion providers.
In the District of Columbia and the 46 states that provided abortion and residency information to the CDC in 2021, 10.9% of all abortions were performed on women known to live outside the state where the abortion occurred – slightly higher than the percentage in 2020 (9.7%). That year, D.C. and 46 states (though not the same ones as in 2021) reported abortion and residency data. (The total number of abortions used in these calculations included figures for women with both known and unknown residential status.)
The share of reported abortions performed on women outside their state of residence was much higher before the 1973 Roe decision that stopped states from banning abortion. In 1972, 41% of all abortions in D.C. and the 20 states that provided this information to the CDC that year were performed on women outside their state of residence. In 1973, the corresponding figure was 21% in the District of Columbia and the 41 states that provided this information, and in 1974 it was 11% in D.C. and the 43 states that provided data.
In the District of Columbia and the 46 states that reported age data to the CDC in 2021, the majority of women who had abortions (57%) were in their 20s, while about three-in-ten (31%) were in their 30s. Teens ages 13 to 19 accounted for 8% of those who had abortions, while women ages 40 to 44 accounted for about 4%.
The vast majority of women who had abortions in 2021 were unmarried (87%), while married women accounted for 13%, according to the CDC , which had data on this from 37 states.
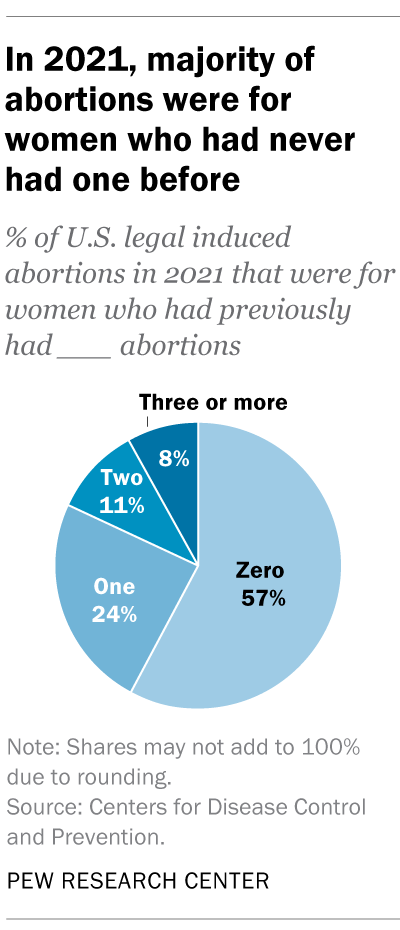
In the District of Columbia, New York City (but not the rest of New York) and the 31 states that reported racial and ethnic data on abortion to the CDC , 42% of all women who had abortions in 2021 were non-Hispanic Black, while 30% were non-Hispanic White, 22% were Hispanic and 6% were of other races.
Looking at abortion rates among those ages 15 to 44, there were 28.6 abortions per 1,000 non-Hispanic Black women in 2021; 12.3 abortions per 1,000 Hispanic women; 6.4 abortions per 1,000 non-Hispanic White women; and 9.2 abortions per 1,000 women of other races, the CDC reported from those same 31 states, D.C. and New York City.
For 57% of U.S. women who had induced abortions in 2021, it was the first time they had ever had one, according to the CDC. For nearly a quarter (24%), it was their second abortion. For 11% of women who had an abortion that year, it was their third, and for 8% it was their fourth or more. These CDC figures include data from 41 states and New York City, but not the rest of New York.
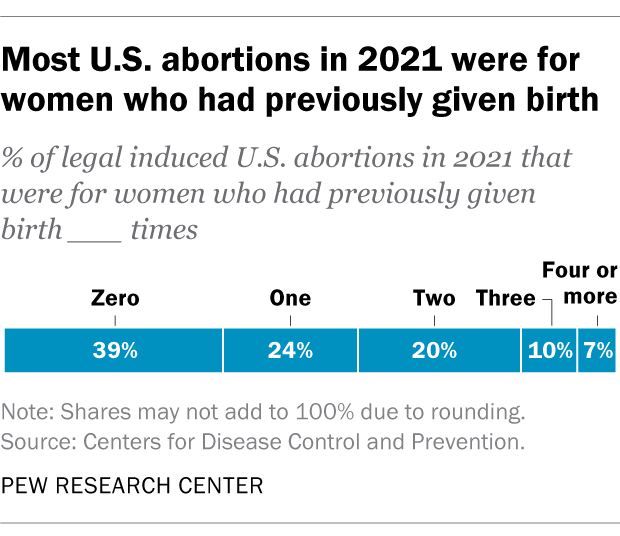
Nearly four-in-ten women who had abortions in 2021 (39%) had no previous live births at the time they had an abortion, according to the CDC . Almost a quarter (24%) of women who had abortions in 2021 had one previous live birth, 20% had two previous live births, 10% had three, and 7% had four or more previous live births. These CDC figures include data from 41 states and New York City, but not the rest of New York.
The vast majority of abortions occur during the first trimester of a pregnancy. In 2021, 93% of abortions occurred during the first trimester – that is, at or before 13 weeks of gestation, according to the CDC . An additional 6% occurred between 14 and 20 weeks of pregnancy, and about 1% were performed at 21 weeks or more of gestation. These CDC figures include data from 40 states and New York City, but not the rest of New York.
About 2% of all abortions in the U.S. involve some type of complication for the woman , according to an article in StatPearls, an online health care resource. “Most complications are considered minor such as pain, bleeding, infection and post-anesthesia complications,” according to the article.
The CDC calculates case-fatality rates for women from induced abortions – that is, how many women die from abortion-related complications, for every 100,000 legal abortions that occur in the U.S . The rate was lowest during the most recent period examined by the agency (2013 to 2020), when there were 0.45 deaths to women per 100,000 legal induced abortions. The case-fatality rate reported by the CDC was highest during the first period examined by the agency (1973 to 1977), when it was 2.09 deaths to women per 100,000 legal induced abortions. During the five-year periods in between, the figure ranged from 0.52 (from 1993 to 1997) to 0.78 (from 1978 to 1982).
The CDC calculates death rates by five-year and seven-year periods because of year-to-year fluctuation in the numbers and due to the relatively low number of women who die from legal induced abortions.
In 2020, the last year for which the CDC has information , six women in the U.S. died due to complications from induced abortions. Four women died in this way in 2019, two in 2018, and three in 2017. (These deaths all followed legal abortions.) Since 1990, the annual number of deaths among women due to legal induced abortion has ranged from two to 12.
The annual number of reported deaths from induced abortions (legal and illegal) tended to be higher in the 1980s, when it ranged from nine to 16, and from 1972 to 1979, when it ranged from 13 to 63. One driver of the decline was the drop in deaths from illegal abortions. There were 39 deaths from illegal abortions in 1972, the last full year before Roe v. Wade. The total fell to 19 in 1973 and to single digits or zero every year after that. (The number of deaths from legal abortions has also declined since then, though with some slight variation over time.)
The number of deaths from induced abortions was considerably higher in the 1960s than afterward. For instance, there were 119 deaths from induced abortions in 1963 and 99 in 1965 , according to reports by the then-U.S. Department of Health, Education and Welfare, a precursor to the Department of Health and Human Services. The CDC is a division of Health and Human Services.
Note: This is an update of a post originally published May 27, 2022, and first updated June 24, 2022.

Sign up for our weekly newsletter
Fresh data delivered Saturday mornings
Key facts about the abortion debate in America
Public opinion on abortion, three-in-ten or more democrats and republicans don’t agree with their party on abortion, partisanship a bigger factor than geography in views of abortion access locally, do state laws on abortion reflect public opinion, most popular.
About Pew Research Center Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
- Research article
- Open access
- Published: 22 July 2016
Social capital – a mixed blessing for women? A cross-sectional study of different forms of social relations and self-rated depression in Moscow
- Sara Ferlander 1 ,
- Andrew Stickley 1 , 2 , 3 ,
- Olga Kislitsyna 4 ,
- Tanya Jukkala 1 ,
- Per Carlson 5 &
- Ilkka Henrik Mäkinen 6
BMC Psychology volume 4 , Article number: 37 ( 2016 ) Cite this article
5621 Accesses
29 Citations
1 Altmetric
Metrics details
An Erratum to this article was published on 19 June 2017
Depression is a major health problem worldwide, especially among women. The condition has been related to a number of factors, such as alcohol consumption, economic situation and, more recently, to social capital. However, there have been relatively few studies about the social capital-depression relationship in Eastern Europe. This paper aims to fill this gap by examining the association between different forms of social capital and self-rated depression in Moscow. Differences between men and women will also be examined, with a special focus on women.
Data was obtained from the Moscow Health Survey, which was conducted in 2004 with 1190 Muscovites aged 18 years or above. For depression, a single-item self-reported measure was used. Social capital was operationalised through five questions about different forms of social relations. Logistic regression analysis was undertaken to estimate the association between social capital and self-rated depression, separately for men and women.
More women (48 %) than men (36 %) reported that they had felt depressed during the last year. An association was found between social capital and reported depression only among women. Women who were divorced or widowed or who had little contact with relatives had higher odds of reporting depression than those with more family contact. Women who regularly engaged with people from different age groups outside of their families were also more likely to report depression than those with less regular contact.
Conclusions
Social capital can be a mixed blessing for women. Different forms of social relations can lead to different health outcomes, both positive and negative. Although the family is important for women’s mental health in Moscow, extra-familial relations across age groups can be mentally distressing. This suggests that even though social capital can be a valuable resource for mental health, some of its forms can be mentally deleterious to maintain, especially for women. More research is needed on both sides to social capital. A special focus should be placed on bridging social relations among women in order to better understand the complex association between social capital and depression in Russia and elsewhere.
Peer Review reports
Depression is a common mental disorder that is characterised by “sadness, loss of interest or pleasure, feelings of guilt or low self-worth, disturbed sleep or appetite, feelings of tiredness, and poor concentration” [ 1 ]. According to the World Health Organisation (WHO) [ 2 ], depression is the third leading contributor to the global burden of disease and is anticipated to become the highest contributing factor by 2030. Nevertheless, for women, depression is already the leading cause of disease worldwide [ 2 ]. Significant gender differences have been found in many countries, with depression being about twice as common among women than among men [ 3 , 4 ].
In low- and middle-income countries, among which most Eastern European countries are included, depression is also the leading cause of the global disease burden [ 2 ]. In their study of 23 countries, Van de Velde et al. [ 4 ] found that the prevalence of depression was highest in the Eastern and Central European countries. In Russia, however, relatively little is known about depression [ 5 ]. Nonetheless, some studies have shown that levels of depression are high in Russia [ 6 ], and especially among women [ 7 ]. For example, in a study in Novosibirsk in 1999–2000, depression was reported by 23 % of men and 44 % of women [ 8 ]. During the same years, in Arkhangelsk, depression, anxiety and/or sleeping disorders affected 33 % of men and 69 % of women [ 9 ]. Consequently, there is a significant gender difference in depression in Russia.
Depression has been related to a number of factors, such as alcohol consumption [ 10 ], economic situation [ 8 ] and social capital [ 11 ]. However, as recently stated by Levecque and Van Rossem: “Although depression is widespread, the complex mechanisms causing depression are still not clearly understood” ([ 12 ], p. 50). Among the causes of depression, social capital may be of particular importance [ 13 ]. The association between social capital and depression is often traced back to the work of Emile Durkheim, who found a link between social integration and suicide rates in different societies [ 14 ]. In the WHO report Promoting Mental Health , social capital is suggested as one of the factors that might promote better mental health [ 15 ]. Unfortunately, despite the potential importance of the social capital-mental health relationship, relatively few studies have been conducted on this topic in Eastern Europe [ 16 ]. Although there have been reports on the prevalence of depression in Russia, few studies have examined how this disorder affects each gender [ 5 , 17 ]. Women have generally been overlooked in health studies in Russia, as men have suffered the heaviest burden of mortality [ 18 ]. The aim of this article therefore is to fill these research gaps by studying the association between different forms of social capital and self-rated depression in Moscow. Women and men will be analysed separately, with a special focus on women.
Social capital
Social capital is often described as a valuable resource accessed through social relations. Bourdieu defines it as “the actual or potential resources which are linked to possession of a durable network of more or less institutionalised relationships of mutual acquaintances and recognition – or in other words, to membership of a group” ([ 19 ], p. 248). Putnam writes that “the core idea of social capital is that social networks have a value” ([ 20 ], p. 18). Coleman also views social capital as a valuable resource, but acknowledges that “a given form of social capital that is valuable in facilitating certain actions may be useless or even harmful for others” ([ 21 ], p. 98). This argument supports the view that there can be a negative side to social capital [ 22 ].
Different forms of social capital
Although social capital has been defined in various ways, most definitions include two aspects: one structural and the other cognitive, i.e. the social relations themselves and their more qualitative aspects, such as trust and reciprocity. Structural social capital is often divided into informal and formal forms [ 21 , 23 ]. The former comprises casual relations with family and friends, whereas the latter involves more rule-bound networks, such as voluntary associations. Among informal contacts, a further distinction can be made between relations within and outside of one’s family. Family is often viewed as the main form of social capital [ 24 , 25 ], i.e. family-based social capital. Family has been defined as both immediate family and extended family (the latter e.g. relatives) [ 26 ]. As put by Astone et al.: “Family behaviours, including marriage and childrearing, remain the classic examples of investment in social capital” ([ 27 ], p. 18). More recent sociological research has also stressed the importance of family as social capital [ 28 ]. In contemporary society, however, social relations often extend beyond family. People have access to a variety of relationships: a few family relations and perhaps hundreds of peripheral ones [ 29 ].
Whereas Bourdieu and Coleman focused on strong familial ties, Putnam, especially in his early work, focused on the weaker, more formal ties outside the family that, for instance, can be accessed via voluntary associations [ 23 ]. Weak ties refer to relations among people who are distant from each other, such as acquaintances [ 30 ]. A more recent distinction is the one between bonding and bridging social capital [ 31 ]. Bonding relations are homogenous in terms of certain social characteristics, such as age or educational level, whereas bridging relations are heterogeneous and link people across different groups, such as intergenerational relations. Although these distinctions are related, they are not synonymous. Strong ties exist between people who are emotionally close, bonding ties between people who are similar. Weak ties unite emotionally distant people, whereas bridging ties connect people who are different from each other. For a more detailed discussion of the different forms of social capital, see Ferlander [ 32 ].
Social capital and mental health
There is consistent evidence linking social capital to physical health, but fewer studies have linked social capital with mental health [ 33 ]. Though they may not have used the term social capital, many earlier studies found a positive link between strong family ties and mental health [ 34 , 35 ]. It has been shown, for example, that married individuals exhibit fewer depressive symptoms than non-married individuals [ 36 ]. Marriage generally has a positive effect on well-being through the exchange of emotional support and increased economic well-being [ 37 ]. More extended family, i.e. relatives, play an important role in terms of social support [ 38 ]. Marriage and other family relations are vital buffers against stress [ 39 ]. Strong and bonding relations, however, can also be a source of strain, leading to feelings of obligation and poor health [ 22 , 40 ].
In a study in a low-income area of the US, Mitchell and LaGory found that bonding social capital increased mental distress, whereas bridging contacts decreased it [ 41 ]. The authors concluded that the obligations of bonding social capital might be a burden and a source of stress for people living in economically deprived areas. Similarly Caughy and colleagues [ 42 ] found that higher levels of social capital among parents were related to higher levels of depression among children in poor areas. In wealthy areas, however, higher parental social capital was associated with better mental health in children. Thus, the social capital-mental health link varies not only between different forms of social capital, but also between different groups. In relation to this, many scholars have stressed the importance of comparing different groups when studying the association between social capital and health [ 43 ]. Vyncke et al. ([ 44 ], p. 960), for instance, recently wrote that: “Future studies should seek to identify subgroups for whom social capital might be particularly influential, by transcending ‘simple’ dyads such as ‘men versus women’”.
Social capital, gender and mental health
Gender differences have received relatively little attention in social capital research [ 44 ]. It has been found, though, that women tend to be more family-oriented, often occupying the role of “kin-keeper” in the family [ 45 ]. Spending more time performing this role, women might socialise less outside the family, as shown by the observation that women belong to fewer voluntary associations than men [ 46 ]. However, women tend to bear the cost of creating social capital, while deriving fewer benefits from it than men [ 45 ]. Although generally ignoring gender issues in relation to social capital, Bourdieu argues that women enable men to accumulate social capital through social activities, such as the exchange of gifts and telephone calls [ 47 ]. A recent study in Russia gives an example of this by showing that women spend more time providing unpaid assistance than men, even though they face a greater risk of nonreciprocation [ 48 ].
It has also been claimed that women do not receive the same health benefits from their contacts as their male counterparts. A number of studies have found a positive link between social capital and self-rated health among men, but not among women [e.g. 49 , 50 ]. Pertaining to depression, nevertheless, social relations seem to have a stronger effect on women [ 33 , 51 ]. In their classic work, Brown and Harris found that women with a close confidant were less likely to become depressed during traumatic life events [ 52 ]. There is also some evidence that the effect of divorce in terms of depression is greater for women than for men [ 53 ]. Similar findings have also been reported for Eastern Europe, for instance in Ukraine where it was recently shown that divorce and widowhood are associated with female depression [ 54 ].
In contrast, social relations may also increase levels of mental illness among women with fewer economic resources. Kawachi and Berkman argue that differences in gender support may partly account for the higher prevalence of psychological distress among women compared to men, particularly if social relations involve strain associated with obligations to provide support for others [ 55 ]. In two different studies of mothers in low-income settings, social capital was associated with a higher risk of mental health problems [ 56 , 57 ]. The authors hypothesised that participating in many social activities may have placed an additional burden on already overextended mothers. Similar effects have been found among mothers in Russia [ 58 , 59 ].
Social capital in Russia
Russia is often described as being characterised by a weak civil society and low levels of institutional trust [ 60 , 61 ]. As a large number of the social safety nets that were available in the Soviet period, such as childcare and maternity benefits, either weakened or disappeared after the collapse of communism [ 62 , 63 ], many Russians, particularly women, have turned to their informal contacts for social and emotional support [ 64 ]. Family and friends are argued to be vital forms of social capital in Eastern Europe [ 65 ], and in Russia, it has been suggested that the “family may be the only island of stability in the boundless ocean of uncertainty” ([ 66 ], p. 367).
In most Russian families, the link between generations is strong. For instance, studies have shown that relations between daughters and mothers in Russia are very amicable [ 67 ]. Women’s family relations often involve exchanges of emotional support across generations, but they can also be fraught with hierarchical and internal power relations, particularly between women of different ages [ 58 , 59 ]. This ambivalence towards intergenerational relations is also shown by Minnigaleeva and her colleagues, who found that the general view of the elderly outside one’s family in Russia is negative—they are often described as poor, passive and unable to adapt to modern life [ 68 ]. However, when people speak about the elderly within their family, the image is more positive, with the elderly being described as “active, kind, wise and caring” ([ 68 ], p. 64–65).
In Russia, family may be even more important for women than for men, as women tend to be more economically dependent than men [ 69 ]. Although the high levels of female employment present during the Soviet period have persisted, women’s position in the labour market has deteriorated as a result of gender discrimination [ 70 ]. For example, a recent national report showed that the ratio of female to male earnings was 65 % [ 71 ]. Single women are thus at risk of living in poverty [ 17 ]. Moreover, conservative attitudes suggesting that women should return to their ‘traditional’ role in the home have re-emerged [ 58 ]. Gender roles are highly traditional in Russia, with women undertaking most of the domestic and child-caring duties [ 63 , 72 ]. In trying to balance home with work, the ‘double burden’ is heavy for many Russian women [ 17 ].
There has been a trend towards smaller families in Russia with decreasing rates of marriage and increasing divorce rates [ 59 , 66 ]. Attitudes are also beginning to change in Russia, especially among the young and highly educated, who have more liberal attitudes towards gender roles [ 73 ]. It has also been argued that there has been an increase in detached relations, i.e. relations with low levels of emotional closeness, among Russian women [ 67 ]. Among divorced Muscovites, there is a high prevalence of loneliness, and more women than men report that they often feel lonely [ 74 ]. This might have negative health effects, as in a society with weak social safety nets, the most exposed groups are probably those without strong ties. Indeed, it has been hypothesised that social capital might be particularly strongly related to mental health in these types of societies [ 33 ]. The need for more studies on the social capital-depression link in low- and middle-income countries, such as Russia, has also recently been emphasised [ 13 ].
The data used in this study came from the Moscow Health Survey, which was conducted in 2004. The survey aimed to study self-rated health in Moscow in relation to social and economic factors. As earlier research had indicated that social capital might be an important factor in the health of Russians [ 75 ], the survey explicitly incorporated a range of social capital measures. The use of this dataset in the current study thus makes it possible to explore the association between different forms of social capital and self-reported depression in a representative sample of the population in the largest city in Eastern Europe - where social capital might be especially important given the social and economic turmoil that has characterised post-Soviet Russia for a long period [ 60 – 64 ]. Indeed, according to Rose [ 75 ], Russia is especially suitable for studying social capital and health, as the collapse of the Soviet Union was far more pervasive in its effects than the social crisis Durkheim, in his time, referred to as causing anomie and suicide [ 14 ].
A gender- and age-stratified random sampling method was used across the 125 municipal districts of Greater Moscow, where the city telephone network formed the sampling frame (nearly all of Moscow’s flats had a telephone in 2004). Face-to-face interviews were done by trained interviewers with Muscovites aged 18 and above based upon a structured questionnaire. The final sample consisted of 1190 individuals with a response rate of 47 %. Fifty-seven percent of the respondents were women. The average age of the sample was 47 years. More than half of the respondents (53 %) had a high level of education, whereas one-fifth (19 %) had a low educational level. Thirty-six percent of the sample had many (2 or more) economic problems. Except for an over-representation of the highly educated, the sample was generally representative of Moscow’s population. The gender and age distributions closely mirrored those of Greater Moscow as a whole. For a more detailed discussion of the survey methodology, see Vågerö and colleagues [ 76 ].
Information on self-rated depression, the dependent variable, was obtained by asking: ‘During the last 12 months, have you had any of the following health problems? If yes, were they severe or mild?’ One of the response categories was ‘nervous disorders, depression.’ The answers were then dichotomised into ‘depression‘ (severe or mild) and ‘no depression’ . Single-item measures of self-rated mental health are increasingly being used in health research and population health surveys, as they reduce the burden for the respondents compared to longer scales [ 77 ]. Similar measures of depression have been used previously in Russia [ 9 ] and elsewhere. For example, in a study of 29 countries using World Value Survey data, the question, ‘During the past weeks, did you ever feel… Depressed or very unhappy?’ was used to assess depression [ 3 ].
Five indicators of structural social capital were used as independent variables. Following previous studies, for instance by Coleman [ 25 ], Helliwell and Putnam [ 78 ], and Furstenberg [ 79 ], marital status and the frequency of visiting relatives were used as indicators of family-based social capital. Marital status was divided into three categories: ‘married or cohabiting’, ‘divorced or widowed’ and ‘never married’. Contact with relatives was measured by the question, ‘Do you tend to visit relatives?’ There were three response categories—‘often, rarely or never’—which were recoded into two categories: ‘regular’ (often) and ‘little (rarely/never) contact’.
The other social capital indicators focused on extra-familial relations: contacts with friends and acquaintances, age-bridging contacts with people from different age groups and membership in voluntary associations. The first two were measured with the following questions: ‘Do you tend to visit friends and acquaintances?’, which is a common indicator of social capital [ 80 ], and ‘How often do you mix with people from different age groups (outside the family)?’ There were three response categories—‘often, rarely or never’—which were recoded into two categories: ‘regular’ (often) and ‘little (rarely/never) contact’. In addition to measuring social capital outside the family, the first question also measures both strong (friends) and weak (acquaintances) ties [ 30 ], whereas the second, following Mitchell and LaGory’s [ 41 ] study, measures bridging relations in terms of contact with people from different age groups outside the family. In this study, the latter is labelled age-bridging contacts, as age is the cross-cutting factor in focus.
Membership in a voluntary association measures a more formal type of social capital. It is probably the most common indicator of social capital in general including in mental health studies [ 81 ]. Associational membership was measured with the question: ‘Are you a member of any of the following organisations or associations: a) sports club, b) environmental organisation, c) cultural, musical, dance or theatre society, d) women’s organisation, e) temperance organisation, f) local action group, g) political party, h) trade union, i) business or employer’s organisation, j) religious organisation, k) other club or association?’ There were three response categories —‘yes, active member’, ‘yes, ordinary member’ and ‘no’—which were recoded into ‘member’ (active or ordinary member of at least one voluntary association) and ‘non-member’.
As in other studies about social capital and health [ 16 , 49 ], demographic (age) and socioeconomic (educational level and economic situation) variables were included in the analysis. Educational level was divided into three groups: ‘high’ (higher or incomplete higher), ‘medium’ (specialised secondary or vocational technical school) and ‘low’ (common secondary or less). To assess the economic situation, the respondents were asked whether, during the previous twelve months, their family ‘had to rely on outside help to pay regular expenses on time (e.g., rent)’, ‘could not have meat or fish more than once or twice a week’, ‘had to refrain from purchasing necessary clothes or footwear’, and ‘involuntarily had to refrain from taking part in social or cultural activities, such as going to a restaurant, cinema, theatre, etc.?’ The answers were added to create a scale from 0–4, which was further divided into two groups: those experiencing ‘few’ (0–1) and ‘many’ (2 or more) types of economic problem.
Statistical analysis
First, descriptive statistics were calculated to determine the levels of depression and social capital in Moscow (Table 1 ). Women and men were compared using a chi-square analysis. Logistic regression analysis was then undertaken to estimate the association between different forms of social capital and self-rated depression separately for men and women, while controlling for the effects of age, educational level and economic problems (Table 2 ). There were two regression models: in Model 1, the association between each variable and reported depression was separately examined while adjusting only for age; in Model 2, the association was examined while adjusting for all the other variables in the model.
The results of these analyses led to a further analysis of the association between age-bridging contacts outside the family and women’s reported depression (Table 3 ). Logistic regression analyses between these variables were performed for subgroups divided according to age, educational level, economic situation, marital status, presence of small children and the nature of their work, controlling for all other variables. The results are presented as odds ratios (OR) with 95 % confidence intervals (CI) and p -values. The level of statistical significance was set at p < 0.05, with statistically significant p -values presented with at least one asterisk (*).
To overcome the potential problem of over-representation of the highly educated in the analysis, the data were weighted in order to match the educational distribution given in the All-Russia Population Census 2002 for Moscow city [ 82 ]. Proportional weights were calculated for the three educational groups and separately for men and women. See also the study by Jukkala et al. [ 83 ]. Finally, to examine the validity of the dependent variable, an additional analysis was undertaken where the association between self-rated depression and other aspects of major depressive disorder (i.e. insomnia and problematic weight loss) was examined through a chi-square test.
Descriptive results
Table 1 shows that more than two-fifths (43 %) of the sample reported that they had felt depressed during the last twelve months. Twenty-nine percent reported that they had experienced severe depression. A chi-square analysis showed that the prevalence of self-rated depression (severe and mild) was significantly higher among women (48 %) than among men (36 %). Nearly one-third (32 %) of all women in Moscow reported that they had felt severely depressed.
Regarding family-based social capital (i.e. family relations; Table 1 ), 57 % of the sample was married or cohabiting and more than two-fifths (42 %) visited relatives regularly. In terms of extra-familial relations, almost half (48 %) of the respondents visited friends or acquaintances regularly and more than half (55 %) regularly mixed with people from other age groups outside the family (i.e. age-bridging contacts). A quarter of the sample (25 %) were members of at least one voluntary association. There were also some statistically significant gender differences in social capital. Two-thirds of the men in the sample were married or cohabiting (66 %), compared to only half of the women (50 %). Approximately half of the men (52 %), as compared to less than half of women (46 %), maintained regular contact with friends and acquaintances. Thirty percent of men were members of some form of voluntary association, compared to 22 % of women. No statistically significant gender differences were found in contact with relatives and contact with different age groups outside the family (i.e. age-bridging contacts).
Multivariable results
Table 2 shows that neither age nor educational level was significantly associated with self-rated depression, although economic problems were. In the fully adjusted model, Model 2, the odds of reporting depression among men experiencing many economic problems were more than twice as high compared to those among men with few economic problems (odds ratio (OR) for men = 2.49), whereas the corresponding OR for women was 1.52.
For social capital, a statistically significant association was found between family relations and women’s reported depression in both models. Women who were divorced or widowed had higher odds of reporting depression (OR = 1.49) than those who were married or cohabiting. Women who had little contact with relatives were also more likely to feel depressed than those with more regular contact (OR = 1.57). Concerning extra-familial social relations, there was no association between contact with friends or membership in voluntary associations and self-rated depression for either sex. A statistically significant association was found, however, between age-bridging contacts outside the family and women’s depression in both models. Women who had little contact with people from other age groups outside the family were less likely to feel depressed (OR = 0.72) than those who had more regular contact. Hence, age-bridging social capital outside the family seems to increase the risk of reporting depression among women in Moscow.
To examine the above finding further, the regression analysis between age-bridging contacts and women’s reported depression was repeated for a number of groupings within the sample in Table 3 . The protective effect of having fewer age-bridging contacts was statistically significant in four subgroups: women 18–40 years old, those with a high educational level, those with few economic problems and those with small (0–5 years) children. The latter was the subgroup that had the strongest effect of age-bridging contacts to reported depression, but that had a lower significance level than the others due to the reduced number of cases in that group. Among the variables with a higher significance level (**), age had the strongest effect. Accordingly, young women and women with small children seem to be especially affected by these forms of social relations.
This study examined the association between social capital and self-rated depression in Moscow, with a special focus on women. In accordance with previous studies in Russia, there was a high level of depression in Moscow [ 6 ], especially among women [ 7 ]. There were also gender differences in social capital. Women were less likely to be married, have contact with friends or be members of voluntary associations than men [ 46 ]. Gender differences in the relationship between social capital and depression were also found. A significant association between the two was found only among women, supporting the idea that, in terms of depression, social capital has a stronger effect on women than on men [ 51 ]. For women in Moscow, family relations seem to decrease the risk of depression, whereas contacts across age groups outside the family seem to increase mental distress. In line with previous family studies in Russia [ 58 ], these findings indicate that social capital can constitute a mixed blessing for women in Moscow.
Family relations and women’s depression
Divorced or widowed women and women who had little contact with their relatives had higher odds of reporting depression than those with more family-based social capital. This finding supports theories stressing that the family is a valuable form of social capital [ 24 , 25 ], particularly for women [ 45 ]. It also supports studies that show that in Russia, where civil society is weak and institutional trust is low [ 61 ], the family is a significant form of social capital [ 66 ].
The importance of the family for mental health has been stressed in a number of previous studies, both in Russia and elsewhere [ 52 ]. Marriage and kin relations provide resources in the form of emotional, instrumental and social support [ 37 , 38 ], such as having someone to talk to about problems, which can reduce stress [ 39 ]. In Russia, studies have found that relations between daughters and mothers are very amicable and that most young married women have regular contact with their mothers for emotional support [ 67 ]. The findings are supported by evidence showing that marital status is a stronger predictor of depressive symptoms for women than for men in general [ 53 ], as well as in Eastern Europe [ 54 ]. This might be especially true in Russia, as the collapse of communism created stressful conditions for women, such as losing access to societal support and being at greater risk of living in poverty as single parents [ 17 , 62 ]. Also, women in Moscow may rely more on relatives as they have less social capital than men – being less likely to be married and having fewer contacts outside of immediate family members.
Age-bridging relations and women’s depression
The results of this study also indicate that there can be negative aspects of social capital, as women with regular contacts across age groups outside the family were more likely to report depression than those with less bridging relations. This finding supports arguments that certain forms of social capital might be harmful [ 21 , 22 ], and especially for certain groups [ 42 ]. However, it contradicts more general findings suggesting that bonding social capital is most strongly related to poor mental health [ 41 ]. In this study, bridging relations were related to self-rated depression among women.
These findings might be explained by workplace research in general [ 84 ] and Bourdieu’s argument [ 24 ] that there are generational conflicts over economic and cultural resources. Different work values across generations can lead to conflict. In a study of Russian culture [ 85 ], generational differences were found, with people below the age of forty converging more towards Western social values than older generations. In terms of Russian family relations, although women’s networks across generations often involve an exchange of emotional support, there are also elements of unequal power relations, conflict and tensions [ 58 ]. According to Utrata [ 59 ], who studies Russian single-mother families, there is an intersection between age and gender that produces constraints, with age being the primary organising principle of power. As women in Moscow seem to have less access to social capital than men, it may also be hypothesised that women may have more conflict within the social relations that they have.
If this observation is also mirrored in extra-familial relations, it may help explain our findings, as, through performing their dual role, many women come into contact with numerous extra-familial figures of various ages, through child-care institutions or employers, for example, where inequalities in power can be keenly felt. This inequality might be especially burdening for mothers who are already strained [ 57 – 59 ]. Several studies have found that parents, especially mothers, are more psychologically distressed than non-parents [ 37 ]. In Russia, there is marked gender discrimination in the labour market [ 70 ], with women, and especially mothers [ 86 ], often being discriminated against by employers [ 87 ]. Polls among professional women have shown that what could be labelled sexist at a Western workplace is viewed as normal in Russian work relations [ 88 ]. There is extensive evidence that bullying and job strain, which is more common among women, is related to depression [ 89 ]. Given this, it is possible that many women in Moscow, and elsewhere, experience more mental distress than men due to gender discrimination, conflict and strain from extra-familial ties across generations, leading to feelings of depression.
Other factors and depression
Neither age nor educational level was significantly related to self-rated depression in Moscow, in accordance with various studies indicating that depression affects individuals across the population [ 2 ]. The respondents’ economic situation, though, had a strong link with their reported depression, particularly among men, which confirms findings from previous studies in Russia [ 6 ]. Being unable to meet one’s basic needs increased the odds of reporting depression for both genders. Economic problems may be a source of anxiety and mental distress [ 90 ], especially in Russia, where many of the social safety nets that were available during the Soviet period have weakened or disappeared [ 62 , 63 ]. Despite the importance of economy for depression, however, social capital was statistically significantly associated with women’s reported depression in Moscow.
Methodological limitations
This study has some methodological limitations that should be mentioned. In social research, measurement error is always a possibility. For self-rated depression, as in several other studies [ 3 , 9 , 77 ], a single-item measure was used. Previous research about the reliability and validity of single-item depression measures has found that results can vary between different contexts and populations [ 91 ]. However, there has been relatively little research on these measures in the general adult population. A meta-analysis of studies of primary care patients showed that the single-item test had poor sensitivity, correctly identifying less than one-third with depression [ 92 ]. A more recent study of chronic pain patients, however, has indicated that these measures can correctly identify most depressed patients [ 93 ], while other studies have found high sensitivity but lower specificity [ 94 , 95 ]. The only large-scale (US) general population study we could locate concluded that a single-item question worked well in detecting depressed adults [ 96 ]. However, using previous research to judge the quality of our measure is difficult. Given this, we analysed it in relation to other aspects of major depressive disorder [ 97 ]. This showed that respondents who were depressed were also significantly more likely to report suffering from insomnia and problematic weight loss in the past year compared to those who were not depressed (chi-square test, p < 0.01). Although caution should be exercised given that our question on depression was not formally validated, the clustering of depressive symptoms among the same individuals suggests that our single-item measure can be used as an adequate measure of depression.
Measuring social capital is also a complex task. One of the most serious criticisms in relation to social capital is that measurements do not match the theory. Although social capital is a multi-dimensional concept, many studies rely on one-dimensional measures [ 98 ]. Few existing instruments measure the various forms of social capital. There is also a lack of consistency among studies. For instance, Mitchell and LaGory [ 41 ] measured bonding social capital via associational membership, whereas others [ 99 ] have used the same measure as an indicator of bridging social capital. The value of separating the level of family that exists within social capital has recently been stressed [ 79 ]. In this article, an attempt has been made to measure different forms of social relations, distinguishing mainly between social capital within and outside the family. This may be especially important in Russia where forms other than associational membership are important [ 65 , 66 ]. Although these forms are conceptually different, in reality there is, of course, much overlap between the different forms of social capital [ 32 ]. Further, due to the cross-sectional nature of the study, it was not possible to determine the direction of causality. Feeling depressed might be a cause rather than an effect of differences in social capital. A recent study has shown, for example, that the social capital-health relationship is bidirectional: while high levels of social capital promote better health, social capital also depends on health [ 100 ]. Based on previous studies and theoretical explanations, however, it is widely recognised and theoretically plausible that social capital has an impact on mental health [ 16 ]. A final limitation of this study concerns the regression analyses between age-bridging extra-familial contacts and women’s self-rated depression. Due to the reduced number of cases in the subgroups, the results should be interpreted with some caution. However, the results do give an indication of the groups within which the effects of this kind of social capital are larger (i.e. young women and women with small children). Although intersectional studies are being conducted more frequently to reveal power relations, much work remains to be done, especially in relation to age [ 59 ]. Consequently, this topic is important and requires further investigation.
Social capital can be a mixed blessing for women. Different forms of social relations can lead to different health outcomes, both positive and negative. Family is an important resource promoting women’s mental health in Moscow, whereas extra-familial relations across age groups can be mentally distressing. Socialising among women within families often involves an exchange of support, but maintaining ties across age groups outside the family can be stressful due to value disparity, conflict and discrimination. These findings constitute an important contribution from a theoretical perspective because even though the downside of social capital is increasingly being discussed in the literature, it has, until now, rarely been shown empirically. Consequently, this study adds to the few studies on the social capital-depression association that provide empirical evidence for negative mental health aspects of social capital. In conclusion, although social capital can be seen as a valuable resource for mental health, some of its forms can be mentally deleterious to maintain, especially among women.
More research, both quantitative and qualitative, is needed about both sides to social capital – the positive and the negative health aspects of social capital. In relation to this, future research should examine how the social capital-depression association varies by different forms of social relations and by different groups. It is important to continue distinguishing between different forms of social capital, as they imply different resources and constraints. Researchers should try to identify the forms of social relations that are most valuable as well as most burdening for various groups. When studying social capital and depression, as noted by Vyncke et al. [ 44 ], a combination of dimensions, such as gender and age, should be analysed. A special focus should be placed on bridging social relations among women, particularly mothers with small children, to better understand the complex association between social capital, gender and depression in Russia and elsewhere.
Abbreviations
CI, Confidence interval; ISESP, Institute for Social and Economic Studies of Population; OR, Odds ratio; RAS, Russian Academy of Sciences; SCOHOST, Stockholm Centre for Health and Social Change; WHO, World Health Organisation.
WHO. Website of WHO. http://www.who.int/topics/depression/en/ . Accessed 17 Jul 2016.
WHO. The global burden of disease: 2004 update. Geneva: W.H.O; 2008.
Google Scholar
Hopcroft RL, Bradley DB. The sex difference in depression across 29 countries. Soc Forces. 2007;85:1483–507.
Article Google Scholar
Van de Velde S, Bracke P, Levecque K. Gender differences in depression in 23 European countries. Cross-national variation in the gender gap in depression. Soc Sci Med. 2010;71:305–13.
Article PubMed Google Scholar
Zhan W, Shaboltas AV, Skochilov RV, Kozlov AP, Krasnoselskikh TV, Abdala N. Depressive symptoms and unprotected sex in St. Petersburg, Russia. J Psychosom Res. 2012;72:371–5.
Article PubMed PubMed Central Google Scholar
Nicholson A, Pikhart H, Pajak A, Malyutina S, Kubinova R. Peasey et al. Socio-economic status over the life-course and depressive symptoms in men and women in Eastern Europe. J Affect Disord. 2008;105:125–36.
Hinote BP, Cockerham WC, Abbott P. Psychological distress and dietary patterns in eight post-Soviet republics. Appetite. 2009;53:24–33.
Bobak M, Pikhart H, Pajak A, Kubinova R, Malyutina S, Sebakova H, et al. Depressive symptoms in urban population samples in Russia, Poland and the Czech Republic. Brit J Psychiat. 2006;188:359–65.
Averina M, Nilssen O, Brenn T, Brox J, Arkhipovsky VL, Kalinin AG. Social and lifestyle determinants of depression, anxiety, sleeping disorders and self-evaluated quality of life in Russia. A population-based study in Arkhangelsk. Soc Psych Psych Epid. 2005;40:511–8.
Åhlin J, Hallgren M, Öjehagen A, Källmén H, Forsell Y. Adults with mild to moderate depression exhibit more alcohol related problems compared to the general adult population: a cross sectional study. BMC Public Health. 2015;15:542.
Almedom A, Glandon D. Social capital and mental health: an updated interdisciplinary review of primary evidence. In: Kawachi I, Subramanian SV, Kim D, editors. Social capital and health. New York: Springer; 2008. p. 191–214.
Chapter Google Scholar
Levecque K, Van Rossem R. Depression in Europe: does migrant integration have mental health payoffs? A cross-national comparison of 20 countries. Ethn Health. 2015;20:49–65.
Ehsan AM, De Silva M. J. Social capital and common mental disorder: a systematic review. J Epidemiol Commun H. 2015;69:1021–8.
Durkheim E. Suicide: a study in sociology. Glencoe: Free Press; 1897.
WHO. Promoting mental health. Concepts, emerging evidence, practice. Geneva: W.H.O; 2005.
Goryakin Y, Suhrcke M, Rocco L, Roberts B, McKee M. Social capital and self-reported general and mental health in nine former Soviet Union countries. Health Econ Policy Law. 2014;9:1–24.
Barrett JB, Buckley C. Gender and perceived control in the Russian Federation. Europe-Asia Stud. 2009;61:29–49.
Hinote BP, Cockerham WC, Abbott P. Women and alcohol in eight post-Soviet states. Soc Sci Med. 2009;68:1254–62.
Bourdieu P. The forms of capital. In: Richardson J, editor. Handbook of theory and research for the sociology of education. New York: Greenwood; 1986. p. 241–58.
Putnam R. Bowling alone: the collapse and revival of American community. New York: Simon & Schuster; 2000.
Book Google Scholar
Coleman JS. Social capital in the creation of human capital. Am J Sociol. 1988;94:95–121.
Portes A. Social capital: its origins and applications in modern sociology. Annu Rev Sociol. 1998;24:1–24.
Putnam R. Making democracy work: civic traditions in modern Italy. Princeton: Princeton University Press; 1993.
Bourdieu P. Sociology in question. London: Sage Ltd; 1994.
Coleman J. Prologue: constructed social organisations. In: Bourdieu P, Coleman J, editors. Social theory for a changing society. Boulder: Westview; 1991. p. 1–14.
Widmer ED. Who are my family members? Bridging and binding social capital in family configurations. J Soc Pers Relat. 2006;23:979–98.
Astone NM, Nathanson CA, Schoen R, Kim YJ. Family demography, social theory, and investment in social capital. Popul Dev Rev. 1999;25:1–31.
Furstenberg FF, Kaplan SB. Social capital and the family. In: Richards M, Scott J, Treas J, editors. Blackwell companion to the sociology of families. London: Blackwell; 2003. p. 218–32.
Fingerman KL. Consequential strangers and peripheral ties: the importance of unimportant relationships. J Fam Theor Rev. 2009;1:69–86.
Granovetter MS. The strength of weak ties. Am J Sociol. 1973;78:1360–80.
Woolcock M. Social capital and economic development: towards a theoretical synthesis and policy framework. Theor Soc. 1998;27:151–208.
Ferlander S. The importance of different forms of social capital for health. Acta Sociol. 2007;50:115–28.
Riumallo-Herl CJ, Kawachi I, Avendano M. Social capital, mental health and biomarkers in Chile: assessing the effects of social capital in a middle-income country. Soc Sci Med. 2014;105:47–58.
Cobb S. Social support as a moderator of life stress. Psychosom Med. 1976;38:300–14.
House J, Landis K, Umberson D. Social relationships and health. Science. 1988;241:540–5.
Dean A, Kolody B, Wood P. Effects of social support from various sources on depression in elderly persons. J Health Soc Behav. 1990;31:148–61.
Ross CE, Mirowsky J, Goldsteen K. The impact of the family on health: a decade in the review. J Marriage Fam. 1990;52:1059–78.
Agneessens F, Waege H, Lievens J. Diversity in social support by role relations: a typology. Soc Networks. 2006;28:427–41.
Siegrist J. Place, social exchange and health: proposed sociological framework. Soc Sci Med. 2000;51:1283–93.
Moore S, Daniel M, Gauvin L, Dubé L. Not all social capital is good capital. Health Place. 2009;15:1071–7.
Mitchell CU, LaGory M. Social capital and mental distress in an impoverished community. City Community. 2002;1:199–217.
Caughy MO, O’Campo PJ, Muntaner C. When being alone might be better: neighborhood poverty, social capital, and child mental health. Soc Sci Med. 2006;57:227–37.
Eriksson M, Ng N. Changes in access to structural social capital and its influence on self-rated health over time for middle-aged men and women: a longitudinal study from northern Sweden. Soc Sci Med. 2015;130:250–8.
Vyncke V, Hardyns W, Peersman W, Pauwels L, Groenewegen P, Willems S. How equal is the relationship between social capital and psychological distress? A gendered analysis using cross-sectional data from Ghent (Belgium). BMC Public Health. 2014;14:960.
O’Neill B, Gidengil E. Gender and social capital. New York: Routledge; 2006.
Norris P, Inglehart R. Gendering social capital. Bowling in women’s leagues? In: O’Neil B, Gidengil E, editors. Gender and social capital. New York: Routledge; 2006. p. 73–98.
Bourdieu P. Masculine domination. Stanford: Stanford University Press; 2001.
Ashwin S, Tartakovskaya I, Ilyina M, Lytkina T. Gendering reciprocity: solving a puzzle of nonreciprocation. Gend Soc. 2013;27:396–421.
Carlson P. The European health divide: a matter of financial or social capital? Soc Sci Med. 2004;59:1985–92.
Ferlander S, Mäkinen IH. Social capital, gender and self-rated health. Evidence from the Moscow Health Survey 2004. Soc Sci Med. 2009;69:1323–32.
Umberson D, Chen M, House J, Hopkins K, Slaten E. The effect of social relationships on psychological well-being: are men and women so different? Am Sociol Rev. 1996;61:837–57.
Brown G, Harris T. Social origins of depression. A study of psychiatric disorder in women. New York: Free Press; 1978.
Simon RW. Revisiting the relationships among gender, marital status, and mental health. Am J Sociol. 2002;107:1065–96.
Ivanenko O. Socioeconomic determinants of poor health in Ukraine: a cross-sectional study in Stakhanov City. Stockholm: CHESS, Stockholm University/Karolinska Institute; 2011.
Kawachi I, Berkman L. Social ties and mental health. J Urban Health. 2001;78:458–67.
De Silva MJ, Huttly SR, Harpham T, Kenward MG. Social capital and mental health: a comparative analysis of four low income countries. Soc Sci Med. 2007;64:5–20.
Thuy NTM, Berry HL. Social capital and mental health among mothers in Vietnam who have children with disabilities. Glob Health Act. 2013;6:18886.
Kosterina I. Young married women in the Russian countryside: women’s networks, communication and power. Europe-Asia Stud. 2012;64:1870–92.
Utrata J. Youth privilege: doing age and gender in Russia’s single-mother families. Gend Soc. 2011;25:616–41.
Evans A, Henry L, McIntosh SL. Russian civil society: a critical assessment. New York: ME Sharpe; 2006.
Stickley A, Ferlander S, Jukkala T, Carlson P, Kislitsyna O, Mäkinen IH. Institutional trust in contemporary Moscow. Europe-Asia Stud. 2009;61:779–96.
Cockerham WC. The intersection of life expectancy and gender in a transitional state: the case of Russia. Sociol Health Ill. 2012;34:943–57.
Rimachevskaya N. Family and children during the economic transition. In: Twigg J, Schecter K, editors. Social capital and social cohesion in post-Soviet Russia. New York: M.E. Sharpe; 2003. p. 74–97.
Ashwin S, Yakubovich V. Cherchez la femme: women as supporting actors in the Russian labour market. Eur Sociol Rev. 2005;21:149–63.
Pichler F, Wallace C. Patterns of formal and informal social capital in Europe. Eur Sociol Rev. 2007;23:423–35.
Zubkov V. Russian families. Marriage Fam Rev. 2007;41:361–92.
Nauck B. Affection and conflict in intergenerational relationships of women in sixteen areas in Asia, Africa, Europe, and America. Comp Pop Stud. 2014;39:647–78.
Minnigaleeva G, Demina K, Zulkarnaev T, Jusupova L, Hizhnajakova I. The image of older people today. Psihologija Zrelosti i Starenija. 2013;4:51–66.
Balabanova E. Women’s economic dependency: nature, causes and consequences. Sotsiologicheskie Issledovaniya. 2007;46:5–21.
Gerber TP, Mayorova O. Dynamic gender differences in a post-socialist labor market: Russia, 1991–1997. Soc Forces. 2006;84:2047–75.
Bobylev S. National human develop report in the Russian Federation 2010, Millennium development goals in Russia: looking into the future. Moscow: UNDP; 2010.
Cubbins LA, Vannoy D. Socioeconomic resources, gender traditionalism, and wife abuse in urban Russian couples. J Marriage Fam. 2005;67:37–52.
Motiejunaite A, Kravchenko Z. Family policy, employment and gender-role attitudes: a comparative analysis of Russia and Sweden. J Eur Soc Policy. 2008;18:38–49.
Stickley A, Koyanagi A, Leinsalu M, Ferlander S, Sabawoon W, McKee M. Loneliness and health in Eastern Europe: findings from Moscow, Russia. Public Health. 2015;129:403–10.
Rose R. How much does social capital add to individual health? A survey study of Russians. Soc Sci Med. 2000;51:1421–35.
Vågerö D, Kislitsyna O, Ferlander S, Migranova L, Carlson P, Rimashevskaya N. Moscow Health Survey 2004 – Social surveying under difficult circumstances. Int J Public Health. 2008;53:171–9.
Ahmad F, Jhajj AK, Stewart DE, Burghardt M, Bierman AS. Single item measures of self-rated mental health: a scoping review. BMC Health Serv Res. 2014;14:398.
Helliwell JF, Putnam RD. The social context of wellbeing. Phil Trans R Soc. 2004;359:1435–46.
Furstenberg FF. Banking on families: how families generate and distribute social capital. J Marriage Fam. 2005;67:809–21.
Stone W. Measuring social capital. Towards a theoretically informed measurement framework for researching social capital in family and community life. Research paper no 24. Melbourne: Australian Institute of Family Studies; 2001.
De Silva M. Systematic review of the methods used in studies of social capital and mental health. In: Kenzie K, Harpham T, editors. Social capital and mental health. London: Jessica Kingsley Publishers; 2006. p. 39–70.
All-Russia Population Census 2002. Retrieved from https://rg.ru/2004/03/31/perepis-dok.html .
Jukkala T, Mäkinen IH, Kislitsyna O, Ferlander S, Vågerö D. Economic strain, social relations, gender, and binge drinking in Moscow. Soc Sci Med. 2008;66:663–74.
Karp H, Sirias D. Generational conflict. Gestalt Rev. 2001;5:71–87.
Naumov A, Puffer S. Measuring Russian culture using Hofstede’s dimensions. Appl Psychol - Int Rev. 2000;49:709–78.
Teplova T. Welfare state transformation, childcare, and women’s work in Russia. Soc Policy. 2007;14:284–322.
White A. Gender roles in contemporary Russia: attitudes and expectations among women students. Europe-Asia Stud. 2005;57:429–55.
Kolchik S. Women talk: sexual harassment or attention-seeking? RIA novosti. 2011.
Theorell T, Hammarström A, Aronsson G, Träsksman Bendz L, Grape T, Hogstedt C, et al. A systematic review including meta-analysis of work environment and depressive symptoms. BMC Pubic Health. 2015;15:738.
Wilkinson R. Unhealthy societies: the afflictions of inequality. London: Routledge; 1996.
McCormack B, Boldy D, Lewin G, McCormack GR. Screening for depression among older adults referred to home care services: a single-item depression screener versus the geriatric depression scale. Home Health Care Manag Pract. 2011;23:13–9.
Mitchell AJ, Coyne JC. Do ultra-short screening instruments accurately detected depression in primary care? A pooled analysis and meta-analysis of 22 studies. Br J Gen Pract. 2007;57:144–51.
PubMed PubMed Central Google Scholar
Reme SE, Eriksen HR. Is one question enough to screen for depression? Scand J Public Health. 2010;38:618–24.
Carey M, Jones KA, Yoong SL, D’Este C, Boyes AW, Paul C, Inder KJ, Sanson-Fisher R. Comparison of a single self-assessment item with the PHQ-9 for detecting depression in general practice. Fam Pract. 2014;31:483–9.
Donker T, van Straten A, Marks I, Cuijpers P. Brief self-rated screening for depression on the internet. J Affect Disord. 2010;122:253–9.
Le Strat Y, Dubertret C. A single question to screen for major depression in the general population. Compr Psychiatry. 2013;54:831–4.
American Psyciatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: APA Press; 2013.
Vyncke V, Peersman W, De Maeseneer JD, Willems S. Measuring the immeasurable? Operationalising social capital in health research. Health. 2012;4:555–66.
Van Oorschot W, Arts W, Gelissen J. Social capital in Europe: measurement and social and regional distribution of a multifaceted phenomenon. Acta Sociol. 2006;49:149–68.
Sirven N, Debrand T. Social capital and health of older Europeans: from reverse causality to health inequalities. Paris: IRDES Working Paper; 2011.
Download references
Acknowledgements
We would like to thank our colleagues at the Institute for Social and Economic Studies of Population (ISESP), at the Russian Academy of Sciences (RAS) in Moscow, especially Natalia Rimachevskaya and Ludmila Migranova, who helped to set up the study. Many thanks also to the 30 interviewers and all the respondents in Moscow who answered our questions. Special thanks to Kristina Abiala, Alireza Behtoui, Abbas Emami, Mall Leinsalu, Apostolis Papakostas and Katharina Wesolowski at Södertörn University for their valuable comments on earlier drafts of this paper. Finally, we want to thank the reviewers for their helpful comments.
This research was funded by the Foundation for Baltic and East European Studies.
Availability of data and materials
Data will not be made publically available in order to protect the participants’ identities. Nevertheless, the authors will consider individual requests for the use of the data.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Authors’ contribution
SF had the idea for the study. She drafted and wrote most of the manuscript. PC, SF and OK was involved in the survey design and the data collection. SF analysed and interpreted the data together with PC, TJ and IHM. AS contributed to the critical revision. All authors commented on the manuscript and provided input for its content. They also read and approved the final version.
Ethical approval and consent to participate
Ethical approval for the study was provided by the Institute for Social and Economic Studies of Population at the Russian Academy of Sciences. The study was conducted in accordance with the Helsinki Declaration and local ethical guidelines with all participants providing their informed consent for participation.
Author information
Authors and affiliations.
Stockholm Centre for Health and Social Change (SCOHOST), Department of Sociology, School of Social Sciences, Södertörn University, 141 89, Huddinge, Sweden
Sara Ferlander, Andrew Stickley & Tanya Jukkala
European Centre on Health of Societies in Transition (ECOHOST), London School of Hygiene and Tropical Medicine, London, UK
Andrew Stickley
Department of Human Ecology, Graduate School of Medicine, University of Tokyo, Tokyo, Japan
Department of Quality of Life Measurement Problems at the Institute of Economics, Russian Academy of Sciences, Moscow, Russia
Olga Kislitsyna
Stockholm Centre for Health and Social Change (SCOHOST), Department of Social Work, School of Social Sciences, Södertörn University, Huddinge, Sweden
Per Carlson
Department of Sociology, Uppsala University, Uppsala, Sweden
Ilkka Henrik Mäkinen
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Sara Ferlander .
Additional information
An erratum to this article is available at http://dx.doi.org/10.1186/s40359-017-0190-3 .
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Ferlander, S., Stickley, A., Kislitsyna, O. et al. Social capital – a mixed blessing for women? A cross-sectional study of different forms of social relations and self-rated depression in Moscow. BMC Psychol 4 , 37 (2016). https://doi.org/10.1186/s40359-016-0144-1
Download citation
Received : 02 March 2016
Accepted : 11 July 2016
Published : 22 July 2016
DOI : https://doi.org/10.1186/s40359-016-0144-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental Health
- Social Capital
- Social Relation
- Significant Gender Difference
- Mental Distress
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
- Open access
- Published: 04 August 2022
What next for the polyclinic? New models of primary health care are required in many former Soviet Union countries
- Nigel Edwards 1 &
- Igor Sheiman ORCID: orcid.org/0000-0002-5238-4187 2
BMC Primary Care volume 23 , Article number: 194 ( 2022 ) Cite this article
2430 Accesses
Metrics details
There is unfinished reform in primary care in Russia and other former Soviet Union (FSU) countries. The traditional ‘Semashko’ multi-specialty polyclinic model has been retained, while its major characteristics are increasingly questioned. The search for a new model is on a health policy agenda. It is relevant for many other countries.
In this paper, we explore the strengths and weaknesses of the multi-specialty polyclinic model currently found in Russia and other FSU countries, as well as the features of the emerging multi-disciplinary and large-scale primary care models internationally. The comparison of the two is a major research question. Health policy implications are discussed.
We use data from two physicians’ surveys and recent literature to identify the characteristics of multi-specialty polyclinics, indicators of their performance and the evaluation in the specific country context. The review of the literature is used to describe new primary care models internationally.
The Semashko polyclinic model has lost some of its original strengths due to the excessive specialization of service delivery. We demonstrate the strengths of extended practices in Western countries and conclude that FSU countries should “leapfrog” the phase of developing solo practices and build a multi-disciplinary model similar to the extended practices model in Europe. The latter may act as a ‘golden mean’ between the administrative dominance of the polyclinic model and the limited capacity of solo practices. The new model requires a separation of primary care and outpatient specialty care, with the transformation of polyclinics into centers of outpatient diagnostic and specialty services that become part of hospital services while working closely with primary care.
The comprehensiveness of care in a big setting and potential economies of scale, which are major strengths of the polyclinic model, should be retained in the provision of specialty care rather than primary care. Internationally, there are lessons about the risks associated with models based on narrow specialization in caring for patients who increasingly have multiple conditions.
• The Semashko polyclinic model has lost strengths due to excessive specialization.
• Solo and group PHC practices are no longer suitable to manage multimorbidity.
• A new ‘extended general practice’ reorients the health system towards PHC.
• Restructuring polyclinics is possible by transforming them into outpatient specialty units of hospital structures.
Peer Review reports
In the former Soviet Union (FSU) and some Central and Eastern European (CEE) countries, the traditional ‘Semashko’ Soviet multi-specialty polyclinic model, originally developed in the 1930s, has been retained [ 1 ]. However, in many rural and some urban areas of FSU countries, the traditional polyclinic model shifted towards solo and group primary care practices in the 1990s in response to policymakers’ demands for stronger primary health care (PHC). This shift towards solo and group practices continues today in many countries of this region [ 2 ].
The existing PHC models are currently facing a number of challenges. The professionals running standalone practices are struggling to respond to a growing proportion of people with multi-morbidity and complex healthcare needs, in a context of underdeveloped and underfunded supportive services, such as social care, rehabilitation, long-term care and palliative care [ 3 ]. While in theory, the mostly urban polyclinic-based generalists could be delivering more comprehensive care, in practice, patients seek out ‘narrow’ specialists based in polyclinics (cardiologists, neurologists, etc., further referred as specialists) instead for the management of relatively common conditions that would be in the scope of PHC providers in other countries [ 1 ]. Neither the polyclinic approach taken in urban areas nor the rural solo/group practice are functioning well and new approaches are needed.
In this paper, we focus on the Russian Federation and consider a number of questions that policy makers, payers and medical leaders could discuss when planning changes to their services. Firstly, what are the current strengths and weaknesses of the polyclinic model currently found in Russia and other FSU countries and does this mean that there are some aspects that should be preserved. Secondly, what are the features of the emerging multi-disciplinary and large-scale primary care models internationally. Thirdly, which elements of the new models of primary care could be adapted to the Russian and other similar settings. We argue the case that polyclinics should be transformed – not into the model of standalone or small group practices that is common – but instead into the ‘extended general practice’ model seen across Europe that re-orients the health system towards comprehensive PHC delivered by multi-disciplinary teams.
The evidence on the strengths and weaknesses of the polyclinic model set out in this paper is based on a review of the literature and two physician surveys. The review is focused on: a) determining characteristics of multi-specialty polyclinics in Russia, indicators of their performance and the evaluation in the specific country context; b) description of the emerging extended PHC practices internationally; c) comparison of the two models. We searched MEDLINE using the query: (Ambulatory Care Facilities[mh] OR polyclinic) AND (model OR type OR semashko) AND (USSR OR russia OR europe OR european union) AND 1990:2022[dp]. 1614 findings were checked manually and 36 were relevant. We also used sources snowballed from these reports and the grey literature related to Russian health care, including those in limited circulation, unpublished documents, memorandums, and presentations from our personal collections covering more than twenty years.
The surveys of Russian physicians are designed to explore the managerial environment for their performance of the staff in polyclinics. Firstly, the managerial control is evaluated via questions like: Is the number of patient visits planned by the polyclinics’ administrators? Does the failure to implement plans can cause a reduction in physicians’ remuneration? Who determines the average length of a patient visit and what happens if it is regularly violated? Are physicians involved in managerial actions to improve the performance of polyclinics?
Secondly, we assess the level of physicians’ clinical autonomy. The examples of questions: Do you select patients for check-ups and screening or rely on administrative decisions? Do your referrals to hospital admissions and CT/MRI tests require the authorization of polyclinics administrators? Which indicators of performance are used for your reporting to the administration?
Thirdly, teamwork and coordination of providers in polyclinics is evaluated. We ask questions about their joint planning of curative activities, inter-discipline consultations and training sessions, as well as the leading role of district physicians in the team—in joint planning and managing chronic cases.
International comparisons of primary care performance are based on the national and OECD databases.
A small-scale survey of polyclinics’ physicians was conducted in January 2020 in three urban polyclinics in Moscow city and Moscow oblast (the region near Moscow). They represent a big multi-specialty urban polyclinic with an average number of staff of around 80–90 health workers. In Moscow city, these polyclinics have been consolidated into bigger outpatient centers with three to five polyclinics each. But this new level of administration was not taken into account, to reflect the usual pattern of administration of polyclinics in Russian big cities. The questions relate only to the staff of individual polyclinics (not their amalgamation). The special area of interest is the attitude of generalists and specialists. A list of 13 questions (appendix 1 ) was sent to all three polyclinics’ physicians through the Russian social network “Vkontakte”. This survey was anonymous, respondents were not compensated and were reassured that any negative feedback would not affect them. The postgraduate students of the National Research University Higher School of Economics (Moscow) dispersed the survey. It was sent to 129 physicians, 103 physicians (80%) responded, including 67 district physicians and 37 specialists. The questionnaire had the same questions to all respondents, and the latter were required to answer all questions by the design of the survey. Therefore, the response rate was the same for all questions. Similarly, the fraction of participants and respondents was the same for each question. Ten physicians on the list were randomly selected and approached directly for face-to-face interviews.
This small-scale survey doesn’t represent all physicians in the country, but it can provide additional evidence to our observations on the limitations of professional autonomy in polyclinics. Some questions from this survey were also used in our recent study of the national preventive program [ 4 ].
This survey was designed to receive more detailed evidence of the level of interaction between professionals in polyclinics, including the exchange of information about patients’ emergency calls, the level of awareness of patients’ hospital admissions, the involvement of polyclinics' physicians in the rehabilitation activities after hospital admissions of stroke and heart attack cases. A special area of interest is the referral pattern of district physicians: what is the share of first visits that is referred to specialists?
The second survey was conducted online in October 2020 in the middle of the COVID-19 pandemic through the mobile ap “Handbook of Physician” (available in Google Play and AppStore) with 540 thousand registered users. 2316 physicians responded to the survey. They represented 81 of 85 regions of the country. 1118 respondents worked in polyclinics (48%), 1068 – in hospitals (46%), the rest – in other settings. Since the survey was designed to look at broader issues of service integration (between polyclinics, hospitals, emergency care centers, etc.), we selected respondents that worked in polyclinics and studied their responses to the questions about the level of integration within polyclinics. All questions were asked with the note “in regular conditions of work before March 2020”. This part of the questionnaire is provided in appendix 2 .
Survey 2 covers generalists and specialists in the staff of polyclinics in practically all types of primary care settings in Russia which vary in size. A high popularity of the ap in all Russian regions and a substantial number of respondents that represent various medical organizations and physician specialties make the survey a reliable instrument of the study.
The polyclinic model
The polyclinic model was established in the USSR in the early 1930s and inherited by FSU and some CEE countries. The polyclinic is a multi-specialty entity providing both primary care and most outpatient specialty care. Typically, there are separate clinics for adults and children and each has a catchment area and a patient list managed mostly by district therapists, district pediatricians and general practitioners (GPs) – all of which are collectively referred to as ‘district physicians’ (DPs). Mental health care is not provided by this service – this is the area of specialty organizations. GPs with a broad task profile are only emerging and account for only 15% of DPs. The catchment population of polyclinics in big urban areas ranges from 30,000 to 120,000 people [ 5 ].
People can choose a polyclinic, and most choose the provider closest to their place of residence. Patients enrolled in a polyclinic form the patient list. According to federal regulations, DPs and GPs act as gatekeepers and refer patients to specialists and hospitals. But many regions loosen the requirements of gatekeeping: patients increasingly see specialists directly without a referral from primary-care physicians.
There has been a trend towards specialization within PHC since the 1990s. The Semashko model of a district unit with mainly a district physician has given way to multi-specialist polyclinics, which currently employ 15–20 categories of specialists in big urban areas (including for example, cardiology, gynecology, surgery, etc.), and three to five categories in small cities. Rural and small city areas are served mostly by small solo practices. Outpatient specialists account for around two-thirds of polyclinic staff and service activity [ 5 ]. It is important to note that the increased professional diversity of the polyclinic staff has been based on a growing number of medical specialists rather than nurses and other allied health professionals. The role of nurses is limited to non-clinical functions. The nurses to physicians ratio is only 2.1, as against 3.0 in Germany, 3.8 in Canada and 4.3 in the US ([ 6 ], p.179).
Legislation defines the polyclinic as a PHC model, which consists of ‘primary physician service’ (care provided by DPs) and ‘specialty primary care’. The latter includes some care equivalent to that provided by outpatient specialists in Western countries, but also care that is effectively managed by family doctors elsewhere, for example, angina and type 2 diabetes.
The governance of polyclinics is highly centralized. The regional health authority appoints directors of polyclinics and manages their performance, most of the rules and patterns of care provision are set by the federal Ministry of Health. The administration of polyclinics is a multilayered structure: a director, a medical director, a few deputies, the head of the district unit, and heads of specialty and diagnostic units. Most polyclinics are state owned and staffed with salaried medical personnel. The growing private sector is also based on this model.
The majority of a polyclinic’s financial revenue is derived from a regional mandatory health insurance (MHI) fund on a capitation basis. But the revenue of a polyclinic can be reduced if it has not reached a minimum number of visits. This target is set and controlled by the regional health authority and MHI fund (which jointly act as a purchaser of care). When there is a risk of not reaching a planned number of visits, the administration of polyclinics has to encourage multiple referrals of patients. Polyclinics’ preventive services are paid for on a fee-for-service basis. The rates of payment are set for a fixed package of services under a so called “program of dispensarization” (a nation-wide vertical program of check-ups and screenings). The control of the actual number of preventive services is conducted by MHI funds and administration of polyclinics. While this method of payment motivates physicians to implement the program, it limits their professional autonomy on the choice of preventive services for an individual. They have to provide the entire bundle of services to be reimbursed, irrespective of the actual need of a patient [ 4 ].
The salary of medical personnel has fixed and variable parts. The latter is based on some pay-for-performance indicators, including the number of visits managed by the individual physician, number of patient complaints and some preventive services. The variable part is determined individually by administration.
Evaluation of the model
There is an unfavourable context for the operation of the urban polyclinic model in modern Russia. There are low levels of health funding (currently, public funding is around 3.5% of GDP), there is a 30% shortage of district therapists, structural distortions in the workforce which are explored below, a hospital-centred model and little focus on chronic disease management [ 7 ].
A major strength of the model is its capacity to provide an easy access to primary and specialist care, at least in theory. Patients can see a DP, receive diagnostic services and have consultations with specialists ‘under one roof’. Specialists may or may not be located in the same premises. But even if they are, this does not mean that patients can have tests and see specialists the same day. This process usually takes weeks because of the shortage of specialists [ 7 ].
Polyclinics have a number of potential advantages due to the consolidation of service delivery. These include additional leverage to implement care pathways and shared use of capital investment resources. Polyclinics can also centralize administrative and support services, with potential economies of scale. Furthermore, large settings can redistribute resources across geographic areas through setting up small branches in remote areas and polyclinic workers can stand in for each other in case of illness or holidays. There is evidence that these strengths are not fully realized in Russia and managerial action is needed to deal with this [ 8 ].
Another potential strength of the polyclinic model is better financial sustainability relative to solo and group practices. The model has enabled the introduction of a fundholding scheme in some regions of Russia, with polyclinics as major financial risk-bearers. Within a short period of its implementation (four to five years in most regions), this has allowed strong economic incentives to be used to increase the role of PHC in the health system [ 5 ].
The larger scale of polyclinics also allows them to respond to national health programs more effectively. For example, larger scale has allowed the implementation of the recent federal program called “Resource-saving polyclinics” that covers most big polyclinics in the country. The objective is to improve the efficiency of internal processes through new appointment systems, separation of patient flows across individual providers, improve electronic communication and develop better organization of the working space, etc. These innovations are more cost effective in big settings. The response to COVID-19 is also facilitated by large-scale facilities.
There are, however, a number of major weaknesses of the polyclinic model.
First, strong administrative pressure on physicians in polyclinics and their limited professional autonomy . Physicians are poorly involved in the management of polyclinics. They work according to the rules determined by polyclinics’ administrators, who in turn follow the commands of the federal and regional health authorities. Administrators set DPs’ catchment areas, plan the number of patient visits, develop the norms for the average length of a patient visit, determine the scope of preventive services and their coverage, ration expensive diagnostic resources for each physician and approve referrals to hospital.
The first survey provided evidence of managerial control and limited professional autonomy:
66% of physicians reported that plans for the number of patient visits are developed by the polyclinics’ administrators. Only 34% plan this activity themselves.
59% indicated that the failure to implement plans on the number of visits can cause a reduction in their remuneration.
66% reported ‘administrative action’ if the norms for the average length of a patient visit are regularly violated.
Only 25% of physicians select patients for check-ups and screening programmes themselves after assessing their risk factors. The rest rely on administrative decisions on the targeted populations. The share of those who select patients for chronic disease management themselves is higher though – 69%.
Just under 50% reported that their referral of patients to hospital requires the authorization of heads of specialty units, 15% – the deputy director, 12% – medical commissioners and 6% – other actors. There is a similar distribution of responses for the authorization of CT and MRI referrals.
28% of respondents reported administrators’ ‘excessive administrative regulation’ of clinical decisions.
Second, the loss of the primary care providers’ leading curative and coordination roles . In Russia, DPs are traditionally seen as gatekeepers for access to specialty services. Theoretically, they are supposed to act as a patient’s guide through the health system and ensure continuity of treatment. However, a high level of polyclinic care specialization distorts the coordination role of primary care providers. In a big multi-specialist entity with a growing division of labour and many specialists working together, many traditional curative functions of DPs are delegated to specialists. It is hard for DP to resist the temptation to refer a patient to a specialist next door. Clinical recommendations, pathways and quality control actors tend to incentivise specialist consultation. Polyclinics’ administrators often encourage referrals to specialists to meet the specified minimum number of visits. The task profile of DPs’ curative work therefore gradually narrows. They deal with a few simple diseases, and the majority of patient care (even gastritis, ulcer, bronchitis) is managed by specialists [ 5 ]. Contrary to GPs, district physicians are allowed to practice without postgraduate training. As a result, a DP’s coordination role also narrows.
The first survey provides the following evidence of a lack of cooperation and coordination in the urban polyclinic:
35.5% of DPs said that the development of plans for the joint management of cases by DPs and specialists did not occur, 45.2% said it ‘rarely’ occurred, 9.7% said it ‘sometimes’ occurred and only 1.6% said it ‘always’ happened. This is contrary to the expectation that a big entity facilitates joint working.
Training sessions for DPs with the involvement of specialists were reported as a regular event by only 4% of polyclinics’ physicians, as a rare event by 35%, while the rest of the respondents indicated their absence.
Only 3.2% of respondents reported medical case conferences as a regular event.
This survey allows us to determine a task profile of DPs and their role in a multi-specialty team:
Only 29,7% of DPs reported that they referred to specialists less than 10% of patients, that is had referral patterns similar to European GPs who referred from 5 to 15% of patients to specialists [ 2 ]. The bulk of Russian physicians referred every second patient to specialists, indicating an excessive specialization of primary care and a limited task profile of generalists. Unsurprisingly, only 26% of DPs reported themselves as “captains of the team” in joint planning of curative activities.
The second survey provides a more detailed evidence of a level of integration in Russian polyclinics. Its results were compared with similar estimates made in 2012 [ 9 ].
An important indicator of the interaction of polyclinics and hospitals is the level of information exchange between them. Only 19.6% of respondents said that their polyclinics received the information about all hospital admissions of patients in their catchment area in 2020; 18.5%—didn’t receive it at all; 23.9% could not answer this question, which was close to the negative answer. The level of physicians’ awareness of hospital admissions in 2020 was even less than in 2012 (Fig. 1 ). This in turn complicates the continuity of care after hospitals admissions. The survey indicates that even for “catastrophic” cases of a stroke or a myocardial infarction the practice of visiting patients within the first days of their hospital admission is not common: it is reported only by 45.5% of respondents (Fig. 2 ).
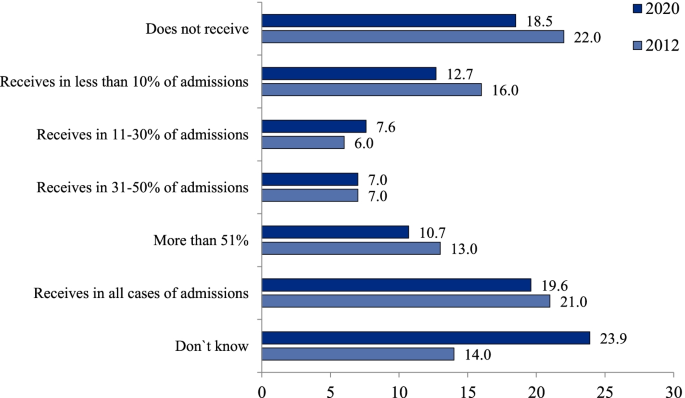
Distribution of polyclinic physicians’ responses to the question `How often does your polyclinic receive information about hospital admissions of patients in the catchment area`, % (survey 2)
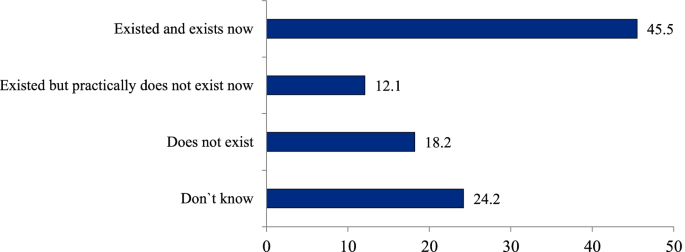
Distribution of polyclinic physicians’ responses to the question `Does your polyclinic have a regular practice of visiting patients within first days after their hospital admission with a stroke or a myocardial infarction`, % (survey 2)
Substantial efforts have been undertaken recently in introducing modern IT in medical facilities, but a national electronic medical record system has not been built yet. Only a few big cities have a system that covers both outpatient and inpatient facilities. The majority of outpatient physicians don’t know much about care utilization on other stages of service delivery.
Third, the limitation of outpatient specialists’ task profile and curative competences. For the reasons mentioned above, a multi-specialist polyclinic generates demand for specialty care . This demand is served by two specific types of specialist who provide only outpatient care: those who work in polyclinics dealing only with simple cases as first-contact providers; and those who provide only inpatient care for complex cases. The former face the problem of professional isolation from their counterparts in hospitals and have limited clinical competences, for example, they do not carry out operations or manage difficult cases. The latter have very limited responsibilities for outpatient consultations. Thus, a multi-specialist polyclinic not only generates demand but also requires a growing supply of specialists. Only 13% of physicians in Russia are generalists [ 5 ], compared with 27% in the UK, 29% in France and 48% in Canada, with 23% being the average for the OECD countries [ 6 ].
Fourth, the lack of economic incentives in a multi-specialty polyclinic . A salaried status and the principle of a ‘common pot’ inherent in a big entity decrease the economic motivation of polyclinics’ health workers relative to their self-employed counterparts in solo and group practices. The first survey of physicians indicates that their income is poorly linked to the financial revenue of the polyclinic: 49% of respondents reported that they did not see this link, 37% saw the link, while the rest did not answer.
Fifth, a low potential for patient choice of PHC providers and their competition . Russian citizens have a strong interest in provider choice but the majority cannot choose due to the prevalence of big entities. Also, there is a growing interest in physician practices that are smaller and therefore closer to patients’ homes.
Some indicators of polyclinics’ performance
Large-scale provision of primary care in polyclinics might be expected to reduce the burden on hospitals, but this has not been the case. In spite of a relatively high number of outpatient physician consultations (9.9 per person), the hospital admission rate in Russia is 52% higher than the OECD average and even higher than in European countries, including Estonia, which had similar high levels of admission in the first post-Soviet period and then had rejected a multi-specialty polyclinic model. A poor-performing primary care system in Russia increases the probability of acute deterioration in people living with asthma, chronic obstructive pulmonary disease, congestive heart failure and some other illnesses, therefore requires hospital admissions that are avoided internationally. Together with a high average length of hospital stay, a significant frequency of admissions produce a very high total utilization of inpatient care: bed-days per capita in Russia is more than two times higher than the OECD average (Table 1 ). Similarly, the utilization of emergency care per capita in Russia is nearly three times higher than the average for OECD countries [ 5 ].
This can be attributed to a number of factors. Firstly, inpatient care remains a major priority of health policy, with a major proportion of funding going to this sector. Secondly, the curative capacity of outpatient specialists in polyclinics is lower than that of their counterparts in hospitals because they deal only with relatively simple cases. Thirdly, patients prefer to be admitted to a hospital due to a traditional mistrust of polyclinic physicians. Administrative pressure – a major characteristic of the model – does not allow patients’ trust to increase.
A theoretically important feature of the polyclinic model is its focus on preventive activities but this does not happen in practice. Physicians and other professionals have no discretion over their patients’ involvement in large-scale health programs and cannot adapt them to the specific environment of their work. An example is the current federal program of ‘dispensarization’, which covers all adults with check-ups and screenings and is implemented according to standard rules. Polyclinics’ physicians are not involved in the design of the program and cannot choose the scope of preventive activities, the targeted populations or the forms of follow-up activities for identified cases of chronic disease. This has caused a number of serious problems: an overburden on DPs, distortions in reporting, poor communication between providers of preventive and curative services, excessive prescribing of diagnostic tests and a lack of follow-up activities for identified cases. The survey of physicians conducted online in April 2019 (randomly selected 1103 physicians) demonstrated that only 7.7% of respondents indicated that a set of actual curative activities met the requirements of a pattern of dispensary surveillance issued by the Federal Ministry of Health. The analysis of medical records of 7043 patients after their hospital admissions with a stroke or a myocardial infarction indicates that nearly half of these patients have not seen a doctor during the year prior to admission [ 11 ].
Heart attacks and other cardiac ischemia mortality rate in Russia is 310 per 100 000 population (in 2019) – nearly three time higher than the average OECD (110). There is a similar gap is for stroke mortality (180 vs 60) ([ 10 ] p. 91).
Polyclinics’ responses to challenges resulting from the COVID-19 pandemic demonstrate both the strengths and weaknesses of the model. There is some evidence of its potential for the mobilization of resources, which has allowed polyclinics to allocate resources to the most vulnerable areas of service delivery and organize flexible testing and tracing of patients and their contacts. This has been facilitated by polyclinics being instructed to implement government policy through decrees and commands. On the other hand, physicians in polyclinics do not have the competences required to take on a major role in triaging or managing new cases. Hospitals have become overburdened as they have taken on this role. The excessive specialization of primary care has also prevented continuity of outpatient care for people with coronavirus.
Discussion: where next for primary care in FSU countries?
Developing a new approach – learning from elsewhere.
FSU and some CEE countries are seeking a new model of PHC that combines the strengths of solo, close-to-home practices and large multi-specialist polyclinics while addressing their weaknesses. A shift to the model of small independent primary care practices, that have been common in Western Europe, may not be a reasonable alternative to the polyclinic model. Firstly, because patients in Russia do not favour this model and its historic legacy means they will try to bypass it. Secondly, the scale of change in the workforce required would be very large and potentially impractical. Thirdly, and most significantly, it would potentially mean losing the opportunity to adopt a more modern and appropriate approach to primary care rather than copying an old model that is starting to exhibit difficulties.
In a number of countries there has been growing interest in the development of larger multidisciplinary primary care practices or networks in response to the growing complexity of patients, the desire to provide more care locally, demand for extended hours and pressures on the workforce. In Spain [ 12 ], France [ 13 ] and the UK [ 14 ] it is increasingly common for primary care services to cover in excess of 20,000 population and these are very different from the existing polyclinics as they rely on a much wider spectrum of primary care expertise including pharmacists, a number of different therapy disciplines, mental health professionals, dentists, opticians, hearing aid technicians and dieticians. They also have an extensive role for nurses. They may also provide a base for social work and staff who can assist patients with non-medical problems and who can direct people to services that can help them. Larger units may have administrative staff to reduce the time taken on non-clinical tasks by health professionals.
The main points of difference to the current multi-specialty polyclinic model in Russia are the following:
The level of narrow specialization of care is much higher in the polyclinic model than in an ‘extended general practice’ model. Groenengen et al. (2015) [ 15 ] found that the median number of additional professionals in extended general practice is five to six in Australia, England, Iceland, New Zealand, Poland, Slovenia, Spain and Sweden, while in Russia it may reach 20 categories [ 5 ]. This excessive specialization has destroyed the polyclinic’s original design as a centre of PHC based on teamwork, coordination and continuity of care and resulted in a fragmented provision of services with the duplication of specialists in outpatient and inpatient settings.
The curative and coordination role of generalists remains central in the extended practices in Western Europe, while it tends to be small in the polyclinic model: specialists replace rather than supplement generalists.
Polyclinics have extended their scope through the introduction of new categories of outpatient specialists. In contrast, while some new primary care models may include some specialists, they rely on GPs with a wide range of skills, including the ability to manage many conditions.
Paediatric and adult care are generally provided under the same roof in the new extended primary care models, rather than in separate clinics as is often the case in urban areas in FSU countries.
Clinicians in the new extended primary care practices are expected to follow guidelines and are subject to quality audit, but generally have more autonomy in decision-making than doctors in polyclinics.
Developing multi-disciplinary group practices
With some considerable work, the existing polyclinics could be transformed into the type of multidisciplinary group practices described above. These would be linked to smaller satellite primary care centres to enable easy access for patients. These networks should take responsibility for the primary care of the whole population – including children – and where they are in separate facilities they should be brought together. A minimum population of 20–30,000 people will provide a critical mass to allow a wide range of primary care services, as around 10–15 GPs working together would justify hiring other professionals, including nurses and pharmacists. Larger networks, which are easier to create in urban areas, could allow even more services to be developed, including diagnostic imaging and a base for visiting specialists.
At the core of the ‘extended general practice’ model are GPs. District therapists and some of the narrow specialists would need extensive retraining to undertake the role of GP. In those systems that have retained paediatricians, it may be better to improve their capability as clinicians for children through enhanced training and to integrate them into the primary care centres, working alongside family doctors. Such a change may be easier than trying to retrain doctors who have had a purely paediatric training to work in family medicine (and vice versa) – not least because in many FSU countries, sub-specialisation in paediatrics takes place very early in training. This is also likely to be more acceptable to the population, who are used to taking children to see paediatricians, and there is some evidence that specialist primary care for children produces better outcomes [ 16 , 17 ]. Locating GPs and paediatricians in the same practice would also allow issues relating to the whole family context to be understood.
Nurses in the multidisciplinary group practices would need to deliver many more services than the quasi-administrative roles that many currently undertake. There would need to be a significant programme of training for them and the wider range of primary care professionals that the model requires (mental health workers, social workers, physiotherapists etc.). Changes in regulatory rules will be required in a number of countries to allow for this, in particular to permit nurse prescribing.
The existing model, in which a lot of activity has been generated by annual screening, pre-employment checks, the issuing of sick certificates and referral to other providers, would need to be replaced. A more proactive approach based on risk assessment and the selection of preventive services for each individual patient would also be required. The new model would also necessitate a significant change in the mindset of staff and patients.
The long-term goal for the extended general practice model is that it will encompass the broad range of primary care services including rapid access for immediate problems and the management of many long-term conditions. Elements of women’s health and less serious mental health conditions would be part of this. For long-term conditions the role of specialists would be to provide assistance with diagnosis, develop management plans, provide advice where changes in these plans are needed, support or take over the management of very complex or refractory cases and, where required, periodically review the care plans and the patient’s progress. To do this means that specialists will see fewer patients and these will be more complex. They will also need to be available by phone or email to provide advice and there will be more emphasis on support, education and training provided to primary care clinicians. The reimbursement system will need to recognise this and, in those countries where it is an issue, also consider the income lost to doctors from informal payments.
The goal of integrated care would take a long time to realize, which requires a set of integrative activities in both multidisciplinary group practices and hospitals. These include:
expanding capacity for direct information exchange
joint planning of care through the chain of providers
establishing process and outcome indicators for chronic disease management
increasing people’s economic motivation for integration
restoring GPs’ gatekeeping function and coordination role
Most importantly, regulation is needed to promote a greater interaction of GPs with specialists and hospitals beyond a simple referral system. This could include the provision of email and telephone advice, education and training, clinical supervision and other joint activities.
Specialists who currently work in polyclinics would need to be retrained either to work in primary care or to bring their skills up to a level that is appropriate for hospital outpatient/ inpatient services.
The preferable option for outpatient centres is to employ specialists who work in both inpatient and outpatient settings. To facilitate this process, the centres should become structural units of hospitals. This would avoid specialists’ professional isolation and may decrease demand for the number of specialists in the entire health system.
In most cases, access to specialist opinion would be provided by hospital outpatients departments and would be by referral from a primary care doctor (and over time by other clinicians). This would need to be supported by the development of guidelines and pathways. To be most effective, primary care would need to have access to a range of laboratory and imaging tests to help improve the appropriateness of referrals.
One area where more rapid progress could be made is in the development of primary care and outpatient consultations by digital means. Health systems have been rapidly adopting such approaches in response to the COVID-19 pandemic, although there were already a number of examples before the crisis where substantial amounts of care were delivered through these means. In common with many other countries, rural areas have great difficulty recruiting medical and nursing staff but access to smartphones with internet capability is growing rapidly and, subject to there being reasonable mobile phone coverage, a combination of digital and mobile services could help to fill this gap.
FSU countries should ‘leapfrog over’ the phase of developing solo practices and build a multidisciplinary model similar to the extended general practice model seen across much of Europe. The latter may act as a ‘golden middle point’ between the excessive specialization and administrative dominance of the polyclinic model and the limited capacity of solo practices. The new model requires a separation of primary care and outpatient specialty care, with the transformation of polyclinics into centres of outpatient diagnostic and specialty services that become structural units of hospitals. A transition to this model requires retraining specialists, extending the task profile of traditional district physicians, therapists and paediatricians, consolidation of adult and child primary care, and increasing the role of nurses and other professionals. The comprehensiveness of care in a big setting and potential economies of scale, which are major strengths of the polyclinic model, would be retained in the provision of specialty care in hospitals rather than primary care.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Kuhlbrandt C. Primary care reforms in countries of the former Soviet Union: success and challenges. In: Rechel B, Richardson E, McKee M, editors. Trends in health systems in the former Soviet countries. Copenhagen: World Health Organization; 2014.
Google Scholar
Kringos D, Boerma W, Hutchinson A, Saltman R. Building primary care in a changing Europe. Vol. 1, No. 38. Copenhagen: The European Observatory on Health Systems and Health Policies; 2015.
Jakab M, Farrington J, Borgermans L, Mantingh F. Health systems respond to noncommunicable diseases: time for ambition. Copenhagen: WHO Regional Office for Europe; 2018. p. 137 ( http://www.euro.who.int/__data/assets/pdf_file/0009/380997/Book-NCD-HS.pdf?ua=1 [Accessed 10 03 21]).
Sheiman I, Shishkin S, Sazhina SV. Vertical program of screenings and check-ups in the Russian Federation: design, implementation and lessons learnt. Arch Public Health. 2022;80:123 (Article 123).
Article Google Scholar
Sheiman I, Shevsky V, Shishkin S. The evolving Semashko model of primary health care: the case of the Russian Federation. Risk Manage Healthc Policy. 2018;11:209–20.
OECD (2019) Health at a Glance 2019: OECD indicators. OECD Publishing, Paris,p. 179. https://doi.org/10.1787/98e2d5de-en [Accessed 10 03 21].
Sheiman I, Gerry C. Too many and too few: the paradoxical case of physicians in the Russian Federation. Int J Health Plann Manage. 2018;33(1):391–402.
Sheiman I, Shevsky V. Concentration of health care providers: does it contribute to integration of service delivery? Risk Manage Healthc Policy. 2019;12:153–66.
Article CAS Google Scholar
Sheiman I, Shevski V. Evaluation of health care delivery integration: the case of the Russian Federation. Health Policy. 2014;115(2–3):128–37.
OECD. Health at a Glance 2021: OECD indicators. Paris: OECD Publishing; p. 135–9. https://doi.org/10.1787/4dd50c09-en .
Sheiman I, Shishkin S, Shevsky V, Sazhina S, Ponkratova O. Dispanserization of the population: expectation and reality. Mir Rossii// Mir Rossii. 2021;4:6–29. https://doi.org/10.17323/1811-038X-2021-30-4-6-29 ([in Russian]).
Dedeu T, Marti T. Multiprofile primary health care teams in Catalonia, Spain: a population-based effective model of service delivery. Copenhagen: World Health Organization; 2018. ( https://www.euro.who.int/en/health-topics/Health-systems/health-systems-response-to-ncds/publications/2018/multiprofile-primary-health-care-teams-in-catalonia,-spain-a-population-based-effective-model-of-services-delivery-2018 [Accessed 10 03 21]).
Ministère des Solidarités et de la Santé. Les maisons de santé. Paris: Ministère des Solidarités et de la Santé; 2020. ( https://solidarites-sante.gouv.fr/systeme-de-sante-et-medico-social/structures-de-soins/article/les-maisons-de-sante-300889 [Accessed 10 03 21]).
Kumpunen S, Natasha Curry, Maddy Farnworth, Rebecca Rosen. Collaboration in general practice: Surveys of GP practice and clinical commissioning groups. Nuffield Trust, Royal College of General Practitioners; 2017. https://www.nuffieldtrust.org.uk/research/collaboration-in-general-practice-surveys-of-gp-practice-and-clinical-commissioning-groups
Groenewegen P, Heinemann S, Greb S, Scharfer W. Primary care practice composition in 34 countries. Health Policy. 2015;119:1576–83.
Wolfe I, Thompson M, Gill P, Tamburlini G, Blair M, van den Bruel A, et al. Health services for children in western Europe. Lancet. 2013;381(9873):1224–34 ( https://pubmed.ncbi.nlm.nih.gov/23541056/ [Accessed 10 03 21]).
Wolfe I, Cass H, Thompon MJ, Craft A, Peile E, Wiegersma PA, et al. Improving child health services in the UK: insights from Europe and their implications for the NHS reforms. BMJ. 2011;342:d1277 ( https://www.bmj.com/content/342/bmj.d1277.full [Accessed 10 03 21]).
Download references
Acknowledgements
This paper is an output of the research project implemented as a part of the Basic Research Program at the National Research University Higher School of Economics in Moscow, Russian Federation. The authors are grateful to Rowan Dennison and Svetlana Sazhina for their kind assistance.
No funding for the paper.
Author information
Authors and affiliations.
Nuffield Trust, 59 New Cavendish St, London, W1G 7LP, UK
Nigel Edwards
National Research University Higher School of Economics, 0 Myasnitskaya str., 101000, Moscow, Russian Federation
Igor Sheiman
You can also search for this author in PubMed Google Scholar
Contributions
Nigel Edwards (NE) participated in the design of the study, collection of literature, writing and reviewing the text. Igor Sheiman (IS) participated in conducting physicians’ surveys and face-to-face interviews, writing and reviewing the text. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Igor Sheiman .
Ethics declarations
Ethics approval and consent to participate.
Two surveys of physicians were taken in the study. Methods of surveys were carried out in accordance with relevant guidelines and regulations. These methods were approved by the “Commission on the intra university surveys and ethical reviews of empirical research projects” of the National Research University High School of Economics https://www.hse.ru/org/hse/irb/ . Informed consent was obtained from all subjects.
Consent for publication
Nigel Edwards and Igor Sheiman agree to publish the paper”What next of the polyclinic? New models of primary health care are required in many Former Soviet countries”.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., additional file 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Edwards, N., Sheiman, I. What next for the polyclinic? New models of primary health care are required in many former Soviet Union countries. BMC Prim. Care 23 , 194 (2022). https://doi.org/10.1186/s12875-022-01812-w
Download citation
Received : 16 November 2021
Accepted : 12 July 2022
Published : 04 August 2022
DOI : https://doi.org/10.1186/s12875-022-01812-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Primary health care
- Multi-specialty model
BMC Primary Care
ISSN: 2731-4553
- General enquiries: [email protected]
PCOS symptoms are still difficult for doctors to diagnose and treat. Here's why.
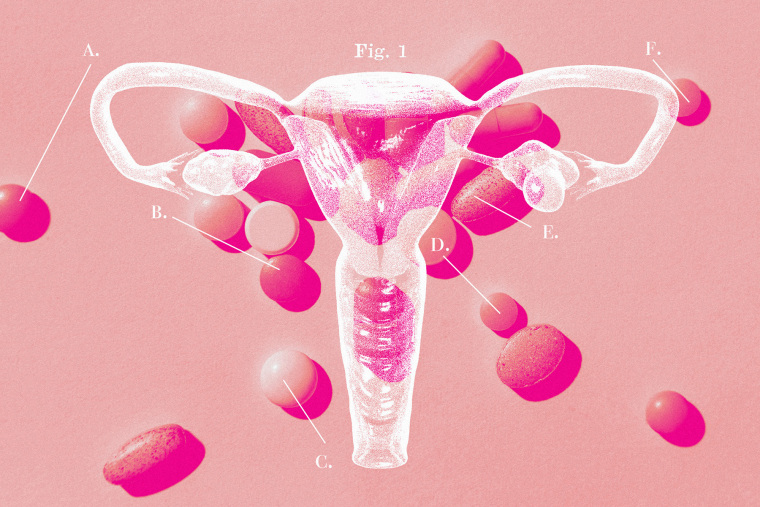
Every morning, Jeni Gutke swallows 12 pills. In the evening, she takes 15 more, then another before bed. She also takes an injectable medication once weekly, and two other medications as needed.
Gutke, of Joliet, Illinois, has polycystic ovary syndrome, or PCOS, and the medications and supplements help the 45-year-old cope with migraines, high blood pressure, diabetes, high cholesterol, anxiety and depression that come with the complex hormonal condition.
Not one of Gutke’s medications are technically “PCOS drugs.”

The Food and Drug Administration has not approved a medication specifically for PCOS, which is often linked to infertility, irregular or missed periods, weight problems, and other debilitating symptoms. Gutke’s array of medications is typical of how many of the estimated 5 million women in the U.S. diagnosed with PCOS deal with it.
“It’s such a vast syndrome that affects everything from your head to your toes,” she said. She was diagnosed with endometrial cancer — another risk linked to PCOS — at age 37.
After nearly a century of disagreements over what, exactly, defines the condition, as well as a lack of research, PCOS is still poorly understood. The symptoms vary so widely that any single drug would be unlikely to help all patients, said Dr. Heather Huddleston, a reproductive endocrinologist at the University of California, San Francisco and director of UCSF’s PCOS Clinic.
Women with PCOS and the doctors who care for them say they want better options — treatments for the condition’s root causes rather than bandages for individual symptoms. Even as calls for better treatments grow, the lack of investment in PCOS research has limited doctors’ ability to help their patients.
“It gets very messy to try to identify one treatment that’s going to work for everybody,” Huddleston said.
Many women with the condition end up taking off-label prescriptions — meaning drugs technically approved for other conditions, like diabetes or obesity — to help PCOS-related symptoms. Navigating insurance coverage for off-label prescriptions can be challenging.
“There’s no magic pill,” said Tallene Hacatoryan, 31, a registered dietician from Orange County, California. “There are too many components for there to be a one-size-fits-all treatment.”

Hacatoryan was diagnosed with PCOS at age 18 and now works as a diet and lifestyle coach for women with PCOS.
Although research is murky when it comes to the best diet for women with PCOS, the most up-to-date international guidelines recommend exercise and a healthy diet. There’s no evidence that any particular diet improves symptoms, although some women have found lifestyle coaching helpful.
Insufficient funding for research
Among the reported 315 medical conditions that receive federal support from the National Institutes of Health , PCOS ranks near the bottom, with an estimated $10 million earmarked for research in 2024. Until 2022, PCOS was so underfunded that it wasn’t included as a line item in the NIH list. And the condition is not explicitly included in the $100 million the Department of Health and Human Services announced recently to research neglected areas of women’s health. Neither is PCOS mentioned in President Joe Biden’s recent executive order to advance women’s health , which includes $200 million for NIH research grants, or the White House’s calls for Congress to allocate $12 billion to fund women’s health research.
A spokesperson at the NIH said that it’s too early to know which women’s health conditions will receive funding under the new initiative.
“Given how common PCOS is, the amount of funding it’s gotten is proportionately extremely small,” Huddleston said.
Government funding is just one part of the total research budget for a given disease. While it’s tough to pin down a dollar figure for private industry spending, experts say the lack of FDA-approved PCOS treatments reflects a lack of investment from drugmakers, too.
Developing PCOS treatments requires a better understanding of the condition. This, in turn, requires far more research tracking thousands of women over many years, which can be extremely expensive, experts say.
However, there are some promising signs.
Although research is early and only in a few dozen women, there are a handful of small drug companies studying possible PCOS treatments. A Menlo Park, California-based company called May Health , for instance, is developing a one-time surgical procedure it thinks could help with PCOS. Spruce Bio, a San Francisco biotech firm, is running a small clinical trial with a drug called tildacerfont for PCOS. It is not clear yet if the oral drug works. President and CFO Samir Gharib said larger clinical trials will depend on the company’s ability to “secure additional financing” or partner with another drug company.
More women's health news
- First over-the-counter birth control pills hit store shelves.
- Common medical errors harm or kills hundreds of thousands each year, especially women.
- Increasing protein from plants may help protect women against many chronic diseases.
The FDA recently attended a meeting with advocacy group PCOS Challenge where women shared their experiences with the agency’s scientists and drug companies. No PCOS drug trials were announced after the meeting, but the FDA’s interest shows a growing push for improved treatment, said William Patterson, a spokesperson for PCOS Challenge.
No known cure for PCOS
Doctors recommend hormonal contraceptives — most commonly the birth control pill — to regulate heavy, irregular periods;, acne;, and unwanted hair growth. Others say taking the pill just masks, rather than treats, their PCOS symptoms and the symptoms return as soon as they stop taking it.
“PCOS is unfortunately not curable, so treatment is about managing its symptoms,” said Dr. Jessica Chan, a reproductive endocrinologist at Cedars-Sinai. Chan said birth control can be a good option for some, but not all, of her PCOS patients.
For women with PCOS whose main concerns are insulin resistance or stubborn weight gain, Chan often prescribes off-label diabetes medications like metformin.
Some doctors who treat PCOS, including OB-GYNs or endocrinologists, have also begun prescribing GLP-1 agonists like Ozempic and Wegovy, which have shown promise for some women with PCOS, although studies have been small and early -stage.
Novo Nordisk, the company that makes Ozempic and Wegovy, said it has no plans as of now to seek FDA approval for PCOS. Still, the company mentions PCOS on its Truth About Weight website, part of its marketing campaign for Wegovy
Causes and symptoms of PCOS
“We don’t know the initial spark leading to PCOS or where it arises from,” Chan said.
PCOS affects an estimated 6% to 12% of reproductive-age women in the U.S. The real prevalence is likely higher since an estimated 70% of cases go undetected.
Experts generally agree that PCOS, at its core, is a hormone-related condition. Women with PCOS have higher levels of androgen hormones, which can cause a range of symptoms, including:
- Missing, irregular, or heavy periods
- Excess hair growth on the face or body
- Thinning or balding scalp hair
According to endocrinologist Dr. Andrea Dunaif, some doctors have been pushing to separate PCOS into two different diagnoses: one having more to do with the reproductive cycle and fertility issues and another having more to do with metabolism, high body weight, and diabetes.
“PCOS looks to be at least two or three different conditions we’re lumping together, but they’re genetically distinct,” said Dunaif, the chief of the endocrinology, diabetes and bone disease division of Mount Sinai Health System and the Icahn School of Medicine.
The confusion surrounding PCOS diagnosis is partly why it’s been hard to get large pharmaceutical companies to invest in PCOS treatment, she said.
In Dunaif’s view, it’s not accurate to call the condition “PCOS” at all, because it has more to do with excess hormones than it does with actual cysts on the ovaries. PCOS got its name from the bumps on the ovaries appearing like cysts on an ultrasound image. These are not cysts, but instead egg follicles that are, as Dunaif described them, “arrested in development.”
As it is, many doctors diagnose the condition based on two of three factors:
- Irregular periods
- High androgen levels
- Multiple follicles on the patient’s ovaries
But these three factors don’t account for some of the most challenging symptoms of PCOS: insulin resistance and stubborn weight gain. Excess androgen hormones can spike insulin levels, which interferes with how the body processes sugar. Doctors aren’t sure whether the hormonal dysregulation causes insulin resistance, or whether insulin resistance causes excess androgen hormones.
Either way, women with PCOS have a higher risk of diabetes, excess weight gain, high cholesterol, and high blood pressure. Yet these metabolic conditions aren’t included in the criteria many doctors use to diagnose PCOS. The result? A missed diagnosis.
This was initially the case for Candice Bolden, 35, who started noticing acne and excess facial and body hair several years before she was diagnosed with PCOS in 2021. Bolden, a lifelong dancer, also had unusually low energy.

“The final straw was excess weight gain that I could not take off no matter what I did,” said Bolden, who lives in Los Angeles. “All the other things I had kind of just stuffed under the rug. I’d just chalked it up to being a hairy, Haitian woman.”
After gaining 35 pounds, the 5-foot-2-inch Bolden, who exercised twice a day and followed strict diets, saw multiple doctors who she said ignored her symptoms.
“Doctors kept telling me I was fine, and to go home, work out, and eat clean,” she said. “It was the most frustrating thing ever.”
‘We don’t have to live underneath this dark cloud’
Women living with PCOS say the rise of online communities, including on social media apps like TikTok and Instagram, has given them a place to speak out, share the treatment approaches working for them, and meet other women with PCOS.
When Bolden finally got a diagnosis, she wasn’t sure what to do next. Gutke and Hacatoryan had similar experiences.
“I was like, ‘Wait, I have so many questions,’ and the doctor just told me, ‘It is what it is,’” Hacatoryan said.
Hacatoryan calls women in her online community her “cysters.”
Bolden said she’s noticed more women turning to social media to learn how others manage their PCOS and share their own stories.
On her own social media accounts, she’s been trying to change the narrative about PCOS being primarily a fertility problem, which she sees as an outdated perception.
“When I was diagnosed, my doctor mentioned PCOS being the No. 1 reason for infertility, and that shattered me,” said Bolden, who was newly engaged at the time and eager to start a family. “I was happy I was diagnosed, because it showed me something was actually happening and I wasn’t just crazy. But I was heartbroken.”
Things changed after Bolden moved; found a new doctor; and worked closely with her husband and the online PCOS community to find a system that worked to manage her PCOS symptoms.
Bolden is now pregnant and expecting a baby girl.
“I want people diagnosed with PCOS to know there’s hope, and we don’t have to live underneath this dark cloud all the time,” she said.
NBC News contributor Caroline Hopkins is a health and science journalist who covers cancer treatment for Precision Oncology News. She is a graduate of the Columbia University Graduate School of Journalism.
Dr. Loh: Women have been underrepresented in clinical research
In prior columns I’ve alluded to the inapplicability of clinical trial results to certain populations, often as a result of non-inclusion of those patient groups into the study cohort. Recognition of those disparities has resulted in active efforts by the US Food and Drug Administration to include those underrepresented populations into these projects so that the results actually reflect what can be expected in those patient groups.
There are many barriers to the inclusion of these patients on both sides of the equation, that is, from the research side based on cost and effort, and from the patient side based on ability and trust to allow participation. I am part of an academic proposal to bridge those obstacles, but that is a subject for a future column. For this column, I’d like to focus on a major effort to include about half of our population that has been underrepresented in clinical research and for which more information is absolutely required. Although those barriers have usually been based on racial or ethnic criteria, it turns out that being female has been a bias that has finally been recognized and is being addressed.
This month, the Biden administration announced an executive order proposing a $12 billion fund to improve our long-overdue understanding of women’s health and to strengthen women’s health research standards across federal agencies. In his remarks, President Biden called this first Initiative on Women’s Health Research the “most comprehensive executive actions ever taken to improve women’s health” and said it highlighted the administration’s efforts to enhance economic gains for women. “Our administration has turned around the economy because we focused on women. … If you want to have the strongest economy in the world, you can’t leave half the workforce behind.”
Within this order, the National Science Foundation and Department of Health and Human Services are instructed to research ways to use artificial intelligence (another one of my favorite topics) to advance women’s health research, including a national network of women’s research centers. There certainly are gaps in medical knowledge concerning how to diagnose, manage, and treat diseases that affect women more than men, and evaluate illnesses that affect women differently than men.
So this order will create a Fund for Women’s Heath Research at the National Institutes of Health (NIH). It also directs the HHS to expand data collection on women’s midlife health and launch an agenda that can guide investments toward menopause-related research in heart, brain, and bone health. Menopause, I suspect that’s a word that has never before seen the light of day in an executive order. Employers estimate that the U.S. economy loses $26.6 billion annually due to menopause-related symptoms and many have been promoting menopause benefits to mitigate those losses.
In addition, impactful conditions like endometriosis and fibroids, plus breast cancer, Alzheimer’s disease and autoimmune disorders disproportionately affect women. As a practicing cardiologist for over four decades, I can tell you that we became aware that women present with heart attacks differently that men only because it became apparent the we were taught “classical symptoms” generated by data acquired in studying men and not women.
New topics targeted for investigation will include wider range subjects including computational research, data standardization, engineering biomechanics, and environmental factors. Simplification of the arduous process of getting funding is also part of this initiative. Lest one think that this is yet another governmental bureaucracy, this initiative also calls on public (ARPA-H)-private (SBIR) engagement to meet these goals. I have known and worked with both of those entities and can tell you they are the best of the best when it comes to guiding meaningful projects to successful conclusions.
And since the overturning of Roe v. Wade in June 2022, the ability of women to make decisions about their own healthcare and bodily integrity has also been top of mind for many. This order reminds us all that women’s issues go far beyond abortion, but are also included under the umbrella of women’s health. It’s also about whether one thinks it’s OK for the government to tell you how to manage your family decisions, like whether you should have children, when you should have them, and how to educate them by constraining what they can learn.
Parents should be able to decide whether or not to even become parents, and once they are, be able to make educational decisions with their children. Beyond health and safety of children and the community at large, the government should support and not dictate to women.
To be fair, there is bipartisan support for this endeavor. To paraphrase Jack Harlow in Bloomberg, we must realize there are supporters of he-who-must-not-be-named who believe that women exist to bear children (Handmaid’s, as it were), make dinner (in Katie Britt’s kitchen, I suspect) while pouring a cocktail for the man of the house, do laundry while cleaning the house, and do women’s work (like raising the children) while the men do real work.
Let’s see if the men in the Congress try to cut this funding out of the 2025 federal budget. Some of these men endorsed by HWMNBN who are running for office are even suggesting that women should not be allowed to vote. None of these men have ever met my wife. And God help them if they ever do.
Irving Kent Loh, M.D., is a preventive cardiologist and the director of the Ventura Heart Institute in Thousand Oaks. Email him at [email protected].

IMAGES
COMMENTS
The "bottom-up" approach of a wide dissemination of information to clinicians, together with practical incentives for stakeholders with competing interests to collaborate, promise to improve women's healthcare. Keywords: research quality, methodology, evidence-based medicine, systematic review. Go to: 1. Introduction.
The FDA Office of Women's Health (OWH) awards research grants for 1-2 year studies to address regulatory research questions related to women's health issues and the impact of sex differences on ...
Assessment of NIH Research on Women's Health. This study aims to fill gaps in our understanding of women's health research across all NIH Institutes and Centers. It will analyze how much funding is allocated to research on conditions that affect women specifically or are more common among women, and how these conditions are defined across ...
Mayo Clinic is transforming women's health by advancing research and studies specifically focused on the unique needs and abilities of the female body through all stages of life. Investigators in the Women's Health Research Center are studying why certain illnesses occur more often — or sometimes only — in women or manifest differently in ...
Women's health information, tips, and research from the Centers for Disease Control and Prevention. Skip directly to site content Skip ... Inclusion of Women and Racial and Ethnic Minorities in Research; Health Matters for Women Newsletter; Social_govd. Get Email Updates. To receive email updates about this page, enter your email address: Email ...
Women's health has long been overlooked in both fundamental and clinical research, which, sadly, also holds true for the bioengineering field — albeit things are slowly changing.
However, a number of very large studies, including the Women's Health Initiative Dietary Modification Trial, an eight-year study of 49,000 women, the Nurses' Health Study and the Health ...
Helen Verdeli. Eleni Vousoura. 8,250 views. 4 articles. Advances our understanding of the health issues for women globally, especially in low-middle income countries. It aligns with the UN Sustainable Development Goals and promotes physical and mental w...
The Women's Health Research Roadmap (Roadmap), outlined here, builds on knowledge gained from previously funded research and is intended to assist OWH in coordinating future research activities ...
Depression is the most common mental health problem for women and suicide a leading cause of death for women under 60. Helping sensitise women to mental health issues, and giving them the confidence to seek assistance, is vital. Noncommunicable diseases: In 2012, some 4.7 million women died from noncommunicable diseases before they reached the ...
Women's health research is the study of health across a woman's lifespan in order to preserve wellness and to prevent, diagnose, and treat disease. It includes all health conditions for which women and men experience differences in risk, presentation, and treatment response, as well as health issues specific to women, such as pregnancy and ...
To identify evidence gaps to inform women's health, the EPC Program examined all reviews conducted by an EPC from December 2017 through February 2022 that addressed a research topic in women's health. Women's health is defined as a health topic that exclusively affects women (e.g., reproductive health) or other health conditions of ...
The Division of Women's Health's research goals are: to lead scientific and clinical discoveries that identify and explain sex- and gender-based differences in health and disease, prioritize disorders specific to women, and ultimately improve the overall health and access to care for women and men. Faculty in the Division of Women's ...
Women's Health Research at Yale marks 25 years of investigating conditions of high morbidity and mortality in women and understanding sex and gender differences that affect health outcomes. Google came online the same year Women's Health Research at Yale (WHRY) was created. Each, as it turned out, would fill a void in the search for information.
The aim of this Research Topic is to explore women-centered understandings of health and health communication from a variety of perspectives in order to address gender, racial, and cultural gaps in the production of knowledge. As part of the inaugural "Women in Communication'' collection, this Research Topic centers women and advances ...
Sec. 2. Definitions. For purposes of this order: (a) The term "women's health research" means research aimed at expanding knowledge of women's health across their lifespans, which includes ...
In the meantime, the executive order signed on Monday directed the N.I.H. to spend $200 million on women's health research. Dr. Biden traveled to Cambridge, Mass., last month to announce the ...
The latest report from the National Center for Health Statistics says that 1,205 women in the US died of maternal causes in 2021. The maternal mortality rate had jumped more than 60% over the ...
World Kidney Day and International Women's Day in 2018 coincide, thus offering an opportunity to reflect on the importance of women's health and specifically their kidney health, on the community, and the next generations, as well as to strive to be more curious about the unique aspects of kidney disease in women so that we may apply those ...
The CDC says that in 2021, there were 11.6 abortions in the U.S. per 1,000 women ages 15 to 44. (That figure excludes data from California, the District of Columbia, Maryland, New Hampshire and New Jersey.) Like Guttmacher's data, the CDC's figures also suggest a general decline in the abortion rate over time.
Depression is a major health problem worldwide, especially among women. The condition has been related to a number of factors, such as alcohol consumption, economic situation and, more recently, to social capital. However, there have been relatively few studies about the social capital-depression relationship in Eastern Europe. This paper aims to fill this gap by examining the association ...
The comparison of the two is a major research question. Health policy implications are discussed. ... Elements of women's health and less serious mental health conditions would be part of this. For long-term conditions the role of specialists would be to provide assistance with diagnosis, develop management plans, provide advice where changes ...
Neither is PCOS mentioned in President Joe Biden's recent executive order to advance women's health, which includes $200 million for NIH research grants, or the White House's calls for ...
So this order will create a Fund for Women's Heath Research at the National Institutes of Health (NIH). It also directs the HHS to expand data collection on women's midlife health and launch ...