
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Variations in Fetal Position and Presentation |
During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front. At first, the fetus can move around easily or shift position as the mother moves. Toward the end of the pregnancy the fetus is larger, has less room to move, and stays in one position. How the fetus is positioned has an important effect on delivery and, for certain positions, a cesarean delivery is necessary. There are medical terms that describe precisely how the fetus is positioned, and identifying the fetal position helps doctors to anticipate potential difficulties during labor and delivery.
Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way.
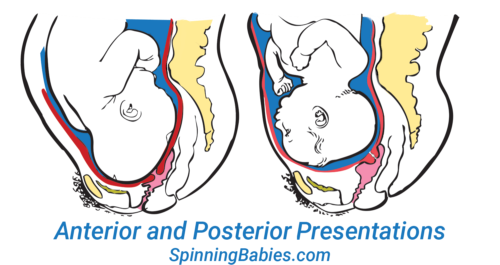
Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back).
Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique).
For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following:
Head first (called vertex or cephalic presentation)
Facing backward (occiput anterior position)
Spine parallel to mother's spine (longitudinal lie)
Neck bent forward with chin tucked
Arms folded across the chest
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible.
Variations in fetal presentation, position, or lie may occur when
The fetus is too large for the mother's pelvis (fetopelvic disproportion).
The uterus is abnormally shaped or contains growths such as fibroids .
The fetus has a birth defect .
There is more than one fetus (multiple gestation).

Position and Presentation of the Fetus
Variations in fetal position and presentation.
Some variations in position and presentation that make delivery difficult occur frequently.
Occiput posterior position
In occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back).
When a fetus faces up, the neck is often straightened rather than bent,which requires more room for the head to pass through the birth canal. Delivery assisted by a vacuum device or forceps or cesarean delivery may be necessary.
Breech presentation
In breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head).
When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first.
In a first delivery, these problems may occur more frequently because a woman’s tissues have not been stretched by previous deliveries. Because of risk of injury or even death to the baby, cesarean delivery is preferred when the fetus is in breech presentation, unless the doctor is very experienced with and skilled at delivering breech babies or there is not an adequate facility or equipment to safely perform a cesarean delivery.
Breech presentation is more likely to occur in the following circumstances:
Labor starts too soon (preterm labor).
The uterus is abnormally shaped or contains abnormal growths such as fibroids .
Other presentations
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.
In brow presentation, the neck is moderately arched so that the brow presents first.
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended.
In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
Breech, posterior, transverse lie: What position is my baby in?

Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. At the time of delivery, 97 percent of babies are head-down (cephalic presentation). But there are several other possibilities, including feet or bottom first (breech) as well as sideways (transverse lie) and diagonal (oblique lie).
Fetal presentation and position
During the last trimester of your pregnancy, your provider will check your baby's presentation by feeling your belly to locate the head, bottom, and back. If it's unclear, your provider may do an ultrasound or an internal exam to feel what part of the baby is in your pelvis.
Fetal position refers to whether the baby is facing your spine (anterior position) or facing your belly (posterior position). Fetal position can change often: Your baby may be face up at the beginning of labor and face down at delivery.
Here are the many possibilities for fetal presentation and position in the womb.
Medical illustrations by Jonathan Dimes
Head down, facing down (anterior position)
A baby who is head down and facing your spine is in the anterior position. This is the most common fetal presentation and the easiest position for a vaginal delivery.
This position is also known as "occiput anterior" because the back of your baby's skull (occipital bone) is in the front (anterior) of your pelvis.
Head down, facing up (posterior position)
In the posterior position , your baby is head down and facing your belly. You may also hear it called "sunny-side up" because babies who stay in this position are born facing up. But many babies who are facing up during labor rotate to the easier face down (anterior) position before birth.
Posterior position is formally known as "occiput posterior" because the back of your baby's skull (occipital bone) is in the back (posterior) of your pelvis.
Frank breech
In the frank breech presentation, both the baby's legs are extended so that the feet are up near the face. This is the most common type of breech presentation. Breech babies are difficult to deliver vaginally, so most arrive by c-section .
Some providers will attempt to turn your baby manually to the head down position by applying pressure to your belly. This is called an external cephalic version , and it has a 58 percent success rate for turning breech babies. For more information, see our article on breech birth .
Complete breech
A complete breech is when your baby is bottom down with hips and knees bent in a tuck or cross-legged position. If your baby is in a complete breech, you may feel kicking in your lower abdomen.
Incomplete breech
In an incomplete breech, one of the baby's knees is bent so that the foot is tucked next to the bottom with the other leg extended, positioning that foot closer to the face.
Single footling breech
In the single footling breech presentation, one of the baby's feet is pointed toward your cervix.
Double footling breech
In the double footling breech presentation, both of the baby's feet are pointed toward your cervix.
Transverse lie
In a transverse lie, the baby is lying horizontally in your uterus and may be facing up toward your head or down toward your feet. Babies settle this way less than 1 percent of the time, but it happens more commonly if you're carrying multiples or deliver before your due date.
If your baby stays in a transverse lie until the end of your pregnancy, it can be dangerous for delivery. Your provider will likely schedule a c-section or attempt an external cephalic version , which is highly successful for turning babies in this position.
Oblique lie
In rare cases, your baby may lie diagonally in your uterus, with his rump facing the side of your body at an angle.
Like the transverse lie, this position is more common earlier in pregnancy, and it's likely your provider will intervene if your baby is still in the oblique lie at the end of your third trimester.
Was this article helpful?
What to know if your baby is breech

What's a sunny-side up baby?

What happens to your baby right after birth

How your twins’ fetal positions affect labor and delivery

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
Ahmad A et al. 2014. Association of fetal position at onset of labor and mode of delivery: A prospective cohort study. Ultrasound in obstetrics & gynecology 43(2):176-182. https://www.ncbi.nlm.nih.gov/pubmed/23929533 Opens a new window [Accessed September 2021]
Gray CJ and Shanahan MM. 2019. Breech presentation. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK448063/ Opens a new window [Accessed September 2021]
Hankins GD. 1990. Transverse lie. American Journal of Perinatology 7(1):66-70. https://www.ncbi.nlm.nih.gov/pubmed/2131781 Opens a new window [Accessed September 2021]
Medline Plus. 2020. Your baby in the birth canal. U.S. National Library of Medicine. https://medlineplus.gov/ency/article/002060.htm Opens a new window [Accessed September 2021]

Where to go next

Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.
Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.

Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.

Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.

If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.

- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Make twice the impact
Your gift can go twice as far to advance cancer research and care!

- Mammary Glands
- Fallopian Tubes
- Supporting Ligaments
- Reproductive System
- Gametogenesis
- Placental Development
- Maternal Adaptations
- Menstrual Cycle
- Antenatal Care
- Small for Gestational Age
- Large for Gestational Age
- RBC Isoimmunisation
- Prematurity
- Prolonged Pregnancy
- Multiple Pregnancy
- Miscarriage
- Recurrent Miscarriage
- Ectopic Pregnancy
- Hyperemesis Gravidarum
- Gestational Trophoblastic Disease
- Breech Presentation
- Abnormal lie, Malpresentation and Malposition
- Oligohydramnios
- Polyhydramnios
- Placenta Praevia
- Placental Abruption
- Pre-Eclampsia
- Gestational Diabetes
- Headaches in Pregnancy
- Haematological
- Obstetric Cholestasis
- Thyroid Disease in Pregnancy
- Epilepsy in Pregnancy
- Induction of Labour
- Operative Vaginal Delivery
- Prelabour Rupture of Membranes
- Caesarean Section
- Shoulder Dystocia
- Cord Prolapse
- Uterine Rupture
- Amniotic Fluid Embolism
- Primary PPH
- Secondary PPH
- Psychiatric Disease
- Postpartum Contraception
- Breastfeeding Problems
- Primary Dysmenorrhoea
- Amenorrhoea and Oligomenorrhoea
- Heavy Menstrual Bleeding
- Endometriosis
- Endometrial Cancer
- Adenomyosis
- Cervical Polyps
- Cervical Ectropion
- Cervical Intraepithelial Neoplasia + Cervical Screening
- Cervical Cancer
- Polycystic Ovary Syndrome (PCOS)
- Ovarian Cysts & Tumours
- Urinary Incontinence
- Genitourinary Prolapses
- Bartholin's Cyst
- Lichen Sclerosus
- Vulval Carcinoma
- Introduction to Infertility
- Female Factor Infertility
- Male Factor Infertility
- Female Genital Mutilation
- Barrier Contraception
- Combined Hormonal
- Progesterone Only Hormonal
- Intrauterine System & Device
- Emergency Contraception
- Pelvic Inflammatory Disease
- Genital Warts
- Genital Herpes
- Trichomonas Vaginalis
- Bacterial Vaginosis
- Vulvovaginal Candidiasis
- Obstetric History
- Gynaecological History
- Sexual History
- Obstetric Examination
- Speculum Examination
- Bimanual Examination
- Amniocentesis
- Chorionic Villus Sampling
- Hysterectomy
- Endometrial Ablation
- Tension-Free Vaginal Tape
- Contraceptive Implant
- Fitting an IUS or IUD
Abnormal Fetal lie, Malpresentation and Malposition
Original Author(s): Anna Mcclune Last updated: 1st December 2018 Revisions: 12
- 1 Definitions
- 2 Risk Factors
- 3.2 Presentation
- 3.3 Position
- 4 Investigations
- 5.1 Abnormal Fetal Lie
- 5.2 Malpresentation
- 5.3 Malposition
The lie, presentation and position of a fetus are important during labour and delivery.
In this article, we will look at the risk factors, examination and management of abnormal fetal lie, malpresentation and malposition.
Definitions
- Longitudinal, transverse or oblique
- Cephalic vertex presentation is the most common and is considered the safest
- Other presentations include breech, shoulder, face and brow
- Usually the fetal head engages in the occipito-anterior position (the fetal occiput facing anteriorly) – this is ideal for birth
- Other positions include occipito-posterior and occipito-transverse.
Note: Breech presentation is the most common malpresentation, and is covered in detail here .
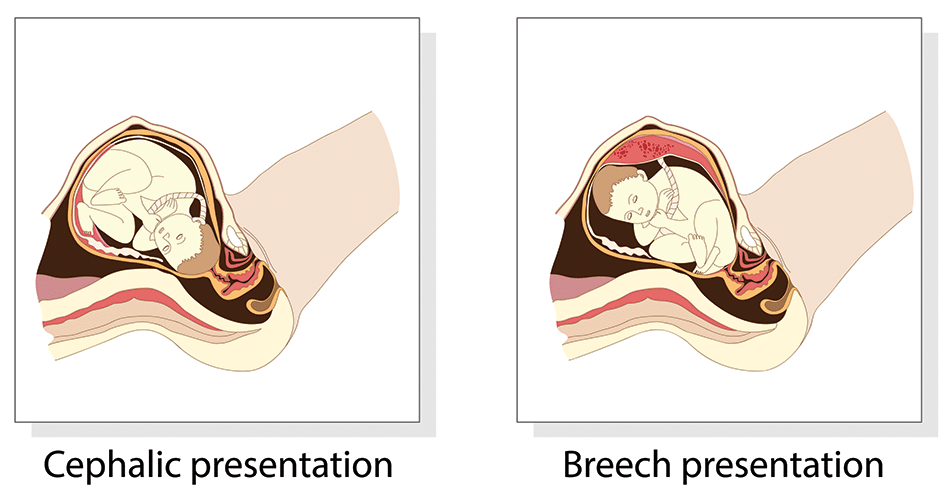
Fig 1 – The two most common fetal presentations: cephalic and breech.
Risk Factors
The risk factors for abnormal fetal lie, malpresentation and malposition include:
- Multiple pregnancy
- Uterine abnormalities (e.g fibroids, partial septate uterus)
- Fetal abnormalities
- Placenta praevia
- Primiparity
Identifying Fetal Lie, Presentation and Position
The fetal lie and presentation can usually be identified via abdominal examination. The fetal position is ascertained by vaginal examination.
For more information on the obstetric examination, see here .
- Face the patient’s head
- Place your hands on either side of the uterus and gently apply pressure; one side will feel fuller and firmer – this is the back, and fetal limbs may feel ‘knobbly’ on the opposite side
Presentation
- Palpate the lower uterus (above the symphysis pubis) with the fingers of both hands; the head feels hard and round (cephalic) and the bottom feels soft and triangular (breech)
- You may be able to gently push the fetal head from side to side
The fetal lie and presentation may not be possible to identify if the mother has a high BMI, if she has not emptied her bladder, if the fetus is small or if there is polyhydramnios .
During labour, vaginal examination is used to assess the position of the fetal head (in a cephalic vertex presentation). The landmarks of the fetal head, including the anterior and posterior fontanelles, indicate the position.
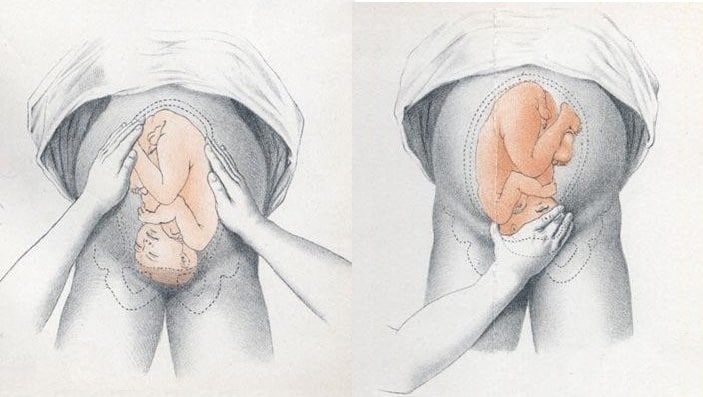
Fig 2 – Assessing fetal lie and presentation.
Investigations
Any suspected abnormal fetal lie or malpresentation should be confirmed by an ultrasound scan . This could also demonstrate predisposing uterine or fetal abnormalities.
Abnormal Fetal Lie
If the fetal lie is abnormal, an external cephalic version (ECV) can be attempted – ideally between 36 and 38 weeks gestation.
ECV is the manipulation of the fetus to a cephalic presentation through the maternal abdomen.
It has an approximate success rate of 50% in primiparous women and 60% in multiparous women. Only 8% of breech presentations will spontaneously revert to cephalic in primiparous women over 36 weeks gestation.
Complications of ECV are rare but include fetal distress , premature rupture of membranes, antepartum haemorrhage (APH) and placental abruption. The risk of an emergency caesarean section (C-section) within 24 hours is around 1 in 200.
ECV is contraindicated in women with a recent APH, ruptured membranes, uterine abnormalities or a previous C-section .
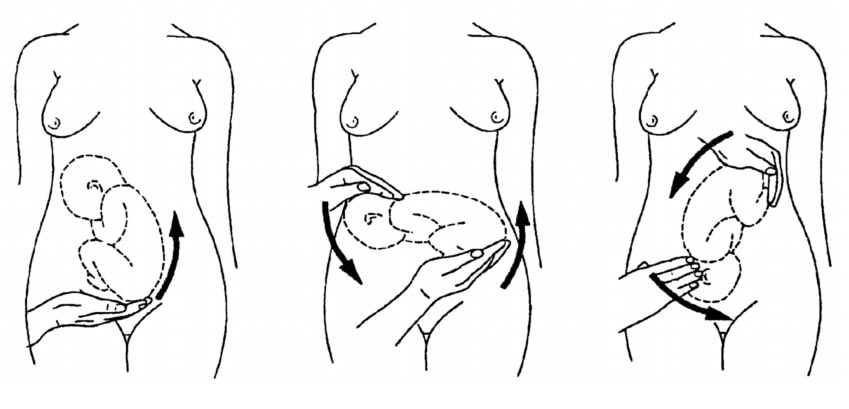
Fig 3 – External cephalic version.
Malpresentation
The management of malpresentation is dependent on the presentation.
- Breech – attempt ECV before labour, vaginal breech delivery or C-section
- Brow – a C-section is necessary
- If the chin is anterior (mento-anterior) a normal labour is possible; however, it is likely to be prolonged and there is an increased risk of a C-section being required
- If the chin is posterior (mento-posterior) then a C-section is necessary
- Shoulder – a C-section is necessary
Malposition
90% of malpositions spontaneously rotate to occipito-anterior as labour progresses. If the fetal head does not rotate, rotation and operative vaginal delivery can be attempted. Alternatively a C-section can be performed.
- Usually the fetal head engages in the occipito-anterior position (the fetal occiput facing anteriorly) - this is ideal for birth
If the fetal lie is abnormal, an external cephalic version (ECV) can be attempted - ideally between 36 and 38 weeks gestation.
- Breech - attempt ECV before labour, vaginal breech delivery or C-section
Found an error? Is our article missing some key information? Make the changes yourself here!
Once you've finished editing, click 'Submit for Review', and your changes will be reviewed by our team before publishing on the site.
We use cookies to improve your experience on our site and to show you relevant advertising. To find out more, read our privacy policy .
Privacy Overview

- about Merck
- Merck Careers
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Key Points |
Abnormal fetal lie or presentation may occur due to fetal size, fetal anomalies, uterine structural abnormalities, multiple gestation, or other factors. Diagnosis is by examination or ultrasonography. Management is with physical maneuvers to reposition the fetus, operative vaginal delivery , or cesarean delivery .
Terms that describe the fetus in relation to the uterus, cervix, and maternal pelvis are
Fetal presentation: Fetal part that overlies the maternal pelvic inlet; vertex (cephalic), face, brow, breech, shoulder, funic (umbilical cord), or compound (more than one part, eg, shoulder and hand)
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse
Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position.
Abnormal fetal lie, presentation, or position may occur with
Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal congenital anomalies
Uterine structural abnormalities (eg, fibroids, synechiae)
Multiple gestation
Several common types of abnormal lie or presentation are discussed here.

Transverse lie
Fetal position is transverse, with the fetal long axis oblique or perpendicular rather than parallel to the maternal long axis. Transverse lie is often accompanied by shoulder presentation, which requires cesarean delivery.
Breech presentation
There are several types of breech presentation.
Frank breech: The fetal hips are flexed, and the knees extended (pike position).
Complete breech: The fetus seems to be sitting with hips and knees flexed.
Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
Types of breech presentations
Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows. The head, which is the part with the largest diameter, can then be trapped during delivery.
Additionally, the trapped fetal head can compress the umbilical cord if the fetal umbilicus is visible at the introitus, particularly in primiparas whose pelvic tissues have not been dilated by previous deliveries. Umbilical cord compression may cause fetal hypoxemia.

Predisposing factors for breech presentation include
Preterm labor
Uterine abnormalities
Fetal anomalies
If delivery is vaginal, breech presentation may increase risk of
Umbilical cord prolapse
Birth trauma
Perinatal death

Face or brow presentation
In face presentation, the head is hyperextended, and position is designated by the position of the chin (mentum). When the chin is posterior, the head is less likely to rotate and less likely to deliver vaginally, necessitating cesarean delivery.
Brow presentation usually converts spontaneously to vertex or face presentation.
Occiput posterior position
The most common abnormal position is occiput posterior.
The fetal neck is usually somewhat deflexed; thus, a larger diameter of the head must pass through the pelvis.
Progress may arrest in the second phase of labor. Operative vaginal delivery or cesarean delivery is often required.
Position and Presentation of the Fetus
If a fetus is in the occiput posterior position, operative vaginal delivery or cesarean delivery is often required.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord.
For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Search Please fill out this field.
- Newsletters
- Sweepstakes
- Labor & Delivery
What Causes Breech Presentation?
Learn more about the types, causes, and risks of breech presentation, along with how breech babies are typically delivered.
What Is Breech Presentation?
Types of breech presentation, what causes a breech baby, can you turn a breech baby, how are breech babies delivered.
FatCamera/Getty Images
Toward the end of pregnancy, your baby will start to get into position for delivery, with their head pointed down toward the vagina. This is otherwise known as vertex presentation. However, some babies turn inside the womb so that their feet or buttocks are poised to be delivered first, which is commonly referred to as breech presentation, or a breech baby.
As you near the end of your pregnancy journey, an OB-GYN or health care provider will check your baby's positioning. You might find yourself wondering: What causes breech presentation? Are there risks involved? And how are breech babies delivered? We turned to experts and research to answer some of the most common questions surrounding breech presentation, along with what causes this positioning in the first place.
During your pregnancy, your baby constantly moves around the uterus. Indeed, most babies do somersaults up until the 36th week of pregnancy , when they pick their final position in the womb, says Laura Riley , MD, an OB-GYN in New York City. Approximately 3-4% of babies end up “upside-down” in breech presentation, with their feet or buttocks near the cervix.
Breech presentation is typically diagnosed during a visit to an OB-GYN, midwife, or health care provider. Your physician can feel the position of your baby's head through your abdominal wall—or they can conduct a vaginal exam if your cervix is open. A suspected breech presentation should ultimately be confirmed via an ultrasound, after which you and your provider would have a discussion about delivery options, potential issues, and risks.
There are three types of breech babies: frank, footling, and complete. Learn about the differences between these breech presentations.
Frank Breech
With frank breech presentation, your baby’s bottom faces the cervix and their legs are straight up. This is the most common type of breech presentation.
Footling Breech
Like its name suggests, a footling breech is when one (single footling) or both (double footling) of the baby's feet are in the birth canal, where they’re positioned to be delivered first .
Complete Breech
In a complete breech presentation, baby’s bottom faces the cervix. Their legs are bent at the knees, and their feet are near their bottom. A complete breech is the least common type of breech presentation.
Other Types of Mal Presentations
The baby can also be in a transverse position, meaning that they're sideways in the uterus. Another type is called oblique presentation, which means they're pointing toward one of the pregnant person’s hips.
Typically, your baby's positioning is determined by the fetus itself and the shape of your uterus. Because you can't can’t control either of these factors, breech presentation typically isn’t considered preventable. And while the cause often isn't known, there are certain risk factors that may increase your risk of a breech baby, including the following:
- The fetus may have abnormalities involving the muscular or central nervous system
- The uterus may have abnormal growths or fibroids
- There might be insufficient amniotic fluid in the uterus (too much or too little)
- This isn’t your first pregnancy
- You have a history of premature delivery
- You have placenta previa (the placenta partially or fully covers the cervix)
- You’re pregnant with multiples
- You’ve had a previous breech baby
In some cases, your health care provider may attempt to help turn a baby in breech presentation through a procedure known as external cephalic version (ECV). This is when a health care professional applies gentle pressure on your lower abdomen to try and coax your baby into a head-down position. During the entire procedure, the fetus's health will be monitored, and an ECV is often performed near a delivery room, in the event of any potential issues or complications.
However, it's important to note that ECVs aren't for everyone. If you're carrying multiples, there's health concerns about you or the baby, or you've experienced certain complications with your placenta or based on placental location, a health care provider will not attempt an ECV.
The majority of breech babies are born through C-sections . These are usually scheduled between 38 and 39 weeks of pregnancy, before labor can begin naturally. However, with a health care provider experienced in delivering breech babies vaginally, a natural delivery might be a safe option for some people. In fact, a 2017 study showed similar complication and success rates with vaginal and C-section deliveries of breech babies.
That said, there are certain known risks and complications that can arise with an attempt to deliver a breech baby vaginally, many of which relate to problems with the umbilical cord. If you and your medical team decide on a vaginal delivery, your baby will be monitored closely for any potential signs of distress.
Ultimately, it's important to know that most breech babies are born healthy. Your provider will consider your specific medical condition and the position of your baby to determine which type of delivery will be the safest option for a healthy and successful birth.
ACOG. If Your Baby Is Breech .
American Pregnancy Association. Breech Presentation .
Gray CJ, Shanahan MM. Breech Presentation . [Updated 2022 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
Mount Sinai. Breech Babies .
Takeda J, Ishikawa G, Takeda S. Clinical Tips of Cesarean Section in Case of Breech, Transverse Presentation, and Incarcerated Uterus . Surg J (N Y). 2020 Mar 18;6(Suppl 2):S81-S91. doi: 10.1055/s-0040-1702985. PMID: 32760790; PMCID: PMC7396468.
Shanahan MM, Gray CJ. External Cephalic Version . [Updated 2022 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
Fonseca A, Silva R, Rato I, Neves AR, Peixoto C, Ferraz Z, Ramalho I, Carocha A, Félix N, Valdoleiros S, Galvão A, Gonçalves D, Curado J, Palma MJ, Antunes IL, Clode N, Graça LM. Breech Presentation: Vaginal Versus Cesarean Delivery, Which Intervention Leads to the Best Outcomes? Acta Med Port. 2017 Jun 30;30(6):479-484. doi: 10.20344/amp.7920. Epub 2017 Jun 30. PMID: 28898615.
Related Articles

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Delivery presentations
Delivery presentation describes the way the baby is positioned to come down the birth canal for delivery.
Your baby must pass through your pelvic bones to reach the vaginal opening. The ease at which this passage will take place depends on how your baby is positioned during delivery. The best position for the baby to be in to pass through the pelvis is with the head down and the body facing towards the mother's back. This position is called occiput anterior (OA).
In breech position, the baby's bottom is facing down instead of the head. Your health care provider will most often detect this in an office visit before your labor begins. Most babies will be in the head-down position by about 34 weeks.
Part of your prenatal care after 34 weeks will involve making sure your baby is in the head-down position.
If your baby is breech, it is not safe to deliver vaginally. If your baby is not in a head-down position after your 36th week, your provider can explain your choices and their risks to help you decide what steps to take next.
Occiput Posterior (OP)
In occiput posterior position, your baby's head is down, but it is facing the mother's front instead of her back.
It is safe to deliver a baby facing this way. But it is harder for the baby to get through the pelvis. If a baby is in this position, sometimes it will rotate around during labor so that the head stays down and the body faces the mother's back (OA position).
The mother can walk, rock, and try different delivery positions during labor to help encourage the baby to turn. If the baby does not turn, labor can take longer. Sometimes, the provider may use forceps or a vacuum device to help get the baby out. If the baby stays in the OP position during labor, you have a higher risk of needing to deliver your baby by cesarean delivery (C-section).
Transverse Position
A baby in the transverse position is sideways. Often, the shoulders or back are over the mother's cervix. This is also called the shoulder, or oblique, position.
The risk for having a baby in the transverse position increases if you:
- Go into labor early
- Have given birth 3 or more times
- Have placenta previa
Unless your baby can be turned into head-down position, a vaginal birth will be too risky for you and your baby. A doctor will deliver your baby by cesarean birth ( C-section ).
Less Common Presentations
With the brow-first position, the baby's head extends backward (like looking up), and the forehead leads the way. This position may be more common if this is not your first pregnancy.
- Your provider rarely detects this position before labor. An ultrasound may be able to confirm a brow presentation.
- More likely, your provider will detect this position while you are in labor during an internal exam.
With face-first position, the baby's head is extended backwards even more than with brow first position.
- Most of the time, the force of contractions causes the baby to be in face-first position.
- It is also detected when labor does not progress.
In some of these presentations, a vaginal birth is possible, but labor will generally take longer. After delivery, the baby's face or brow will be swollen and may appear bruised. These changes will go away over the next few days.
Alternative Names
Pregnancy - delivery presentation; Labor - delivery presentation; Occiput posterior; Occiput anterior; Brow presentation
Barth WH. Malpresentations and malposition. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies . 8th ed. Philadelphia, PA: Elsevier; 2021:chap 17.
Thorp JM, Grantz KL. Clinical aspects of normal and abnormal labor. In: Lockwood CJ, Copel JA, Dugoff L, et al, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice . 9th ed. Philadelphia, PA: Elsevier; 2023:chap 40.
Vora S, Dobiesz VA. Emergency childbirth. In: Roberts JR, Custalow CB, Thomsen TW, eds. Roberts and Hedges' Clinical Procedures in Emergency Medicine and Acute Care . 7th ed. Philadelphia, PA: Elsevier; 2019:chap 56.
Review Date 11/21/2022
Updated by: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Related MedlinePlus Health Topics
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
INTRODUCTION
● The curvature of the fetal spine is oriented downward (also called "back down" or dorsoinferior), and the fetal shoulder presents at the cervix ( figure 1 ).
● The curvature of the fetal spine is oriented upward (also called "back up" or dorsosuperior), and the fetal small parts and umbilical cord present at the cervix.
(Note: Lie refers to the long axis of the fetus relative to the longitudinal axis of the uterus; the long axis of the fetus can be transverse to, oblique to, or parallel to [longitudinal lie] the longitudinal axis of the uterus. Presentation refers to the fetal part that directly overlies the pelvic inlet; it is usually cephalic [head] or breech [buttocks] but can be a shoulder, compound [eg, head and hand], or funic [umbilical cord]. Position is the relationship of a nominated site of the presenting part to a denominating location on the maternal pelvis [eg, right occiput anterior].)
Need to talk? Call 1800 882 436. It's a free call with a maternal child health nurse. *call charges may apply from your mobile
Is it an emergency? Dial 000 If you need urgent medical help, call triple zero immediately.
Share via email
There is a total of 5 error s on this form, details are below.
- Please enter your name
- Please enter your email
- Your email is invalid. Please check and try again
- Please enter recipient's email
- Recipient's email is invalid. Please check and try again
- Agree to Terms required
Error: This is required
Error: Not a valid value
Malpresentation
8-minute read
If you feel your waters break and you have been told that your baby is not in a head-first position, seek medical help immediately .
- Malpresentation is when your baby is not facing head-first down the birth canal as birth approaches.
- The most common type of malpresentation is breech — when your baby’s bottom or feet are facing downwards.
- A procedure called external cephalic version can sometimes turn a breech baby into a head-first position at 36 weeks.
- Most babies with malpresentation are born by caesarean, but you may be able to have a vaginal birth if your baby is breech.
- There is a serious risk of cord prolapse if your waters break and your baby is not head-first.
What are presentation and malpresentation?
‘Presentation’ describes how your baby is facing down the birth canal. The ‘presenting part’ is the part of your baby’s body that is against the cervix .
The ideal presentation is head-first, with the crown (top) of the baby’s head against the cervix, with the chin tucked into the baby’s chest. This is called ‘vertex presentation’.
If your baby is in any other position, it’s called ‘malpresentation’. Malpresentation can mean your baby’s face, brow, buttocks, foot, back, shoulder, arms or legs or the umbilical cord are against the cervix.
It’s safest for your baby’s head to come out first. If any other body part goes down the birth canal first, the risks to you and your baby may be higher. Malpresentation increases the chance that you will have a more complex vaginal birth or a caesarean.
If my baby is not head-first, what position could they be in?
Malpresentation is caused by your baby’s position (‘lie’). There are different types of malpresentation.
Breech presentation
This is when your baby is lying with their bottom or feet facing down. Sometimes one foot may enter the birth canal first (called a ‘footling presentation’).
Breech presentation is the most common type of malpresentation.
Face presentation
This is when your baby is head-first but stretching their neck, with their face against the cervix.
Transverse lie
This is when your baby is lying sideways. Their back, shoulders, arms or legs may be the first to enter the birth canal.
Oblique lie
This is when your baby is lying diagonally. No particular part of their body is against the cervix.
Unstable lie
This is when your baby continually changes their position after 36 weeks of pregnancy.
Cord presentation
This is when the umbilical cord is against the cervix, between your baby and the birth canal. It can happen in any situation where your baby’s presenting part is not sitting snugly in your pelvis. It can become an emergency if it leads to cord prolapse (when the cord is born before your baby, potentially reducing placental blood flow to your baby).
What is malposition?
If your baby is lying head-first, the best position for labour is when their face is towards your back.
If your baby is facing the front of your body (posterior position) or facing your side (transverse position) this is called malposition. Transverse position is not the same as transverse lie. A transverse position means your labour may take a bit longer and you might feel more pain in your back. Often your baby will move into a better position before or during labour.
Why might my baby be in the wrong position?
Malpresentation may be caused by:
- a low-lying placenta
- too much or too little amniotic fluid
- many previous pregnancies, making the muscles of the uterus less stable
- carrying twins or more
Often no cause is found.
Is it likely that my baby will be in the wrong position?
Many babies are in a breech position during pregnancy. They usually turn head-first as pregnancy progresses, and more than 9 in 10 babies in Australia have a vertex presentation (ideal presentation, head-first) at birth.
You are more likely to have a malpresentation if:
- this is your first baby
- you are over 40 years old
- you've had a previous breech baby
- you go into labour prematurely

How is malpresentation diagnosed?
Malpresentation is normally diagnosed when your doctor or midwife examines you, from 36 weeks of pregnancy. If it’s not clear, it can be confirmed with an ultrasound.
Can my baby’s position be changed?
If you are 36 weeks pregnant , it may be possible to gently turn your baby into a head-first position. This is done by an obstetrician using a technique called external cephalic version (ECV).
Some people try different postures or acupuncture to correct malpresentation, but there isn’t reliable evidence that either of these work.
Will I need a caesarean if my baby has a malpresentation?
Most babies with a malpresentation close to birth are born by caesarean . You may be able to have a vaginal birth with a breech baby, but you will need to go to a hospital that can offer you and your baby specialised care.
If your baby is breech, an elective (planned) caesarean is safer for your baby than a vaginal birth in the short term. However, in the longer term their health will be similar, on average, regardless of how they were born.
A vaginal birth is safer for you than an elective caesarean. However, about 4 in 10 people planning a vaginal breech birth end up needing an emergency caesarean . If this happens to you, the risk of complications will be higher.
Your doctor can talk to you about your options. Whether it’s safe for you to try a vaginal birth will depend on many factors. These include how big your baby is, the position of your baby, the structure of your pelvis and whether you’ve had a caesarean in the past.
What are the risks if I have my baby when it’s not head-first?
If your waters break when your baby is not head-first, there is a risk of cord prolapse. This is an emergency.
Vaginal breech birth
Risks to your baby can include:
- Erb’s palsy
- fractures, dislocations or other injuries
- bleeding in your baby’s brain
- low Apgar scores
- their head getting stuck – this is an emergency
Risks to you include:
- blood loss or blood clots
- infection in the wound
- problems with the anaesthetic
- damage to other organs nearby, such as your bladder
- a higher chance of problems in future pregnancies
- a longer recovery time than after a vaginal birth
Risks to your baby include:
- trouble with breathing — this is temporary
- getting a small cut during the surgery
Will I have a malpresentation in my future pregnancies?
If you had a malpresentation in one pregnancy, you have a higher chance of it happening again, but it won’t necessarily happen in future pregnancies. If you’re worried, it may help to talk to your doctor or midwife so they can explain what happened.

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call . Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content .
Last reviewed: July 2022
Related pages
Labour complications.
- Interventions during labour
- Giving birth - stages of labour
Breech pregnancy
Search our site for.
- Caesarean Section
- Foetal Version
Need more information?
Top results
When a baby is positioned bottom-down late in pregnancy, this is called the breech position. Find out about 3 main types and safe birthing options.
Read more on Pregnancy, Birth & Baby website

Breech Presentation at the End of your Pregnancy
Breech presentation occurs when your baby is lying bottom first or feet first in the uterus (womb) rather than the usual head first position. In early pregnancy, a breech position is very common.
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website

Breech presentation and turning the baby
In preparation for a safe birth, your health team will need to turn your baby if it is in a bottom first ‘breech’ position.
Read more on WA Health website

External Cephalic Version for Breech Presentation - Pregnancy and the first five years
This information brochure provides information about an External Cephalic Version (ECV) for breech presentation
Read more on NSW Health website

Presentation and position of baby through pregnancy and at birth
Presentation and position refer to where your baby’s head and body is in relation to your birth canal. Learn why it’s important for labour and birth.
Even if you’re healthy and well prepared for childbirth, there’s always a chance of unexpected problems. Learn more about labour complications.
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Call us and speak to a Maternal Child Health Nurse for personal advice and guidance.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Government Accredited with over 140 information partners
We are a government-funded service, providing quality, approved health information and advice
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
© 2024 Healthdirect Australia Limited
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is a Transverse Baby Position?
Why It Happens, How to Turn Your Baby, and Tips for a Safe Delivery
Causes and Risk Factors
Turning the fetus, complications, frequently asked questions.
A transverse baby position, also called transverse fetal lie, is when the fetus is sideways—at a 90-degree angle to your spine—instead of head up or head down. This development means that a vaginal delivery poses major risks to both you and the fetus.
Sometimes, a transverse fetus will turn itself into the head-down position before you go into labor. Other times, a healthcare provider may be able to turn the position.
If a transverse fetus can't be turned to the right position before birth, you're likely to have a cesarean section (C-section).
This article looks at causes and risk factors for a transverse baby position. It also covers how it's diagnosed and treated, the possible complications, and how you can plan ahead for delivery.
Marko Geber / Getty Images
How Common Is Transverse Baby Position?
An estimated 2% to 13% of babies are in an unfavorable position at delivery —meaning they're not in the head-down position .
Certain physiological issues can lead to a transverse fetal lie. These include:
- A bicornuate uterus : The uterus has a deep V in the top that separates the uterus into two sides; it may only be able to hold a near-term fetus sideways.
- Oligohydramnios or polyhydramnios : Abnormally low or high amniotic fluid volume (respectively).
Several risk factors can make it more likely for the fetus to be in a transverse lie, such as:
- The placenta being in an unusual position, such as blocking the opening to the cervix ( placenta previa ), which doesn't allow the fetus to reach the head-down position
- Going into labor early, before the fetus has had a chance to get into the right position
- Being pregnant with twins or other multiples, as the uterus is crowded and may not allow for much movement
- An abnormal pelvic structure that limits fetal movement
- Having a cyst or fibroid tumor blocking the cervix
Transverse fetal positioning is also more common after your first pregnancy.
It’s not uncommon for a fetus to be in a transverse position during the earlier stages of pregnancy. In most cases, though, they shift on their own well before labor begins. The transverse fetal position doesn't cause any signs or symptoms.
Healthcare professionals diagnose a transverse lie through an examination called Leopold’s Maneuvers. That involves feeling your abdomen to determine the fetal position. It's usually confirmed by an ultrasound.
You may also discover a transverse fetal lie during a routine ultrasound.
Timing of Transverse Position Diagnosis
The ultrasound done at your 36-week checkup lets your healthcare provider see the fetal position as you get closer to labor and delivery. If it's still a transverse lie at that time, your medical team will look at options for the safest labor and delivery.
Approximately 97% of deliveries involve a fetus positioned with the head down, in the best position to slide out. That makes a vaginal delivery easier and safer.
A transverse position only happens in about 1% of deliveries. In that position, the shoulder, arm, or trunk of the fetus may present first. This isn't a good scenario for either of you because a vaginal delivery is nearly impossible.
In these cases, you have two options:
- Turning the fetal position
- Having a C-section
If the fetus is in a transverse lie late in pregnancy, you or your healthcare provider may be able to change the position. Turning into the proper head-down position may help you avoid a C-section.
Medical Options
A healthcare provider can use one of the following techniques to attempt re-positioning a fetus:
- External cephalic version (ECV) : This procedure typically is performed at or after 36 weeks of pregnancy; involves using pressure on your abdomen where the fetal head and buttocks are.
- Webster technique : This is a chiropractic method in which a healthcare professional moves your hips to allow your uterus to relax and make more room for the fetus to move itself. (Note: No evidence supports this method.)
A 2020 study reported a 100% success rate for trained practitioners who used turning to change a transverse fetal lie. Real-world success rates are closer to 60%.
At-Home Options
You may be able to encourage a move out of the transverse position at home. You can try:
- Getting on your hands and knees and gently rocking back and forth
- Lying on your back with your knees bent and feet flat on the floor, then pushing your hips up in the air (bridge pose)
- Talking or playing music to stimulate the fetus to become more active
- Applying some cold to your abdomen where the fetal head is, which may make them want to move away from it
These methods may or may not work for you. While there's anecdotal evidence that they sometimes work, they haven't been researched.
Talk to your healthcare provider before attempting any of these techniques to ensure you're not doing anything unsafe.
Can Babies Go Back to Transverse After Being Turned?
Even if the fetus does change position or is successfully moved, it is possible that it could return to a transverse position prior to delivery.
Whether your child is born via C-section or is successfully moved so you can have a vaginal delivery, potential complications remain.
Cesarean Sections
C-sections are extremely common and are generally safe for both you and the fetus. Still, some inherent risks are associated with the procedure, as there are with any surgery.
The transverse position can force the surgeon to make a different type of incision, as the fetal lie may be right where they'd usually cut. Possible C-section complications for you can include:
- Increased bleeding
- Bladder or bowel injury
- Reactions to medicines
- Blood clots
- Death (very rare)
In rare cases, a C-section can result in potential complications for the baby , including:
- Breathing problems, if fluid needs to be cleared from their lungs
Most C-sections are safe and result in a healthy baby and parent. In some situations, a surgical delivery is the safest option available.
Vaginal Delivery
If the fetus is successfully moved out of the transverse lie position, you'll likely be able to deliver it vaginally. However, a few complications are possible even after the fetus has been moved:
- Labor typically takes longer.
- Your baby’s face may be swollen and appear bruised for a few days.
- The umbilical cord may be compressed, potentially causing distress and leading to a C-section.
Studies suggest that ECV is safe, effective, and may help lower the C-section rate.
Planning Ahead
As with any birth, if you experience a transverse fetal position, you should work with your healthcare provider to develop a delivery plan. If the transverse position has been maintained throughout the pregnancy, the medical team will evaluate the position at about 36 weeks and make plans accordingly.
Remember that even if the fetal head is down late in pregnancy, things can change quickly during labor and delivery. That means it's worthwhile to discuss options for different types of delivery in case they become necessary.
A transverse baby position, or transverse fetal lie, is the term for a fetus that's lying sideways in the uterus. Vaginal delivery usually isn't possible in these cases.
If the fetus is in this position near the time of delivery, the options are to turn it to make vaginal delivery possible or to have a C-section. A trained healthcare provider can use turning techniques. You may also be able to get the fetus to turn at home with some simple techniques.
Both C-section and vaginal delivery pose a risk of certain complications. However, these problems are rare and the vast majority of deliveries end with a healthy baby and parent.
A Word From Verywell
Pregnancy comes with many unknowns, and the surprises can continue up through labor and delivery.
Talking to your healthcare provider early on about possible scenarios can give you time to think about possible outcomes. This helps to avoid a situation where you’re considering risks and benefits during labor when quick decisions need to be made.
Ideally, a baby should be in the cephalic position (head down) at 32 weeks. If not, a doctor will examine the fetal position at around the 36-week mark and determine what should happen next to ensure a smooth delivery. Whether this involves a cesarian section will depend on the specific case.
Less than 1% of babies are born in the transverse position. In many cases, a doctor might recommend a cesarian delivery to ensure a more safe delivery. The risk of giving birth in the transverse lie position is greater before a due date or if twins or triplets are also born.
A planned cesarian section , or C-section, is typically performed in the 39th week of gestation. This is done so the fetus is given enough time to grow and develop so that it is healthy.
In some cases, a doctor may perform an external cephalic version (ECV) to change a transverse fetal lie. This involves the doctor using their hands to apply firm pressure to the abdomen so the fetus is moved into the cephalic (head-down) position.
Most attempts of ECV are successful, but there is a chance the fetus can move back to its previous position; in these cases, a doctor can attempt ECV again.
The American College of Obstetricians and Gynecologists. If your baby is breech .
Tempest N, Lane S, Hapangama D. Babies in occiput posterior position are significantly more likely to require an emergency cesarean birth compared with babies in occiput transverse position in the second stage of labor: a prospective observational study . Acta Obstet Gynecol Scand . 2020;99(4):537-545. doi:10.1111/aogs.13765
National Institutes of Health, U.S. National Library of Medicine: MedlinePlus. Congenital uterine anomalies .
Figueroa L, McClure EM, Swanson J, et al. Oligohydramnios: a prospective study of fetal, neonatal and maternal outcomes in low-middle income countries . Reprod Health. 2020;17 (article 19). doi:10.1186/s12978-020-0854-y
National Institutes of Health, U.S. National Library of Medicine: MedlinePlus. Placenta previa .
National Institutes of Health, U.S. National Library of Medicine: MedlinePlus. Your baby in the birth canal .
Van der Kaay DC, Horsch S, Duvekot JJ. Severe neonatal complication of transverse lie after preterm premature rupture of membranes . BMJ Case Rep . 2013;bcr2012008399. doi:10.1136/bcr-2012-008399
Oyinloye OI, Okoyomo AA. Longitudinal evaluation of foetal transverse lie using ultrasonography . Afr J Reprod Health ; 14(1):129-133.
Nishikawa M, Sakakibara H. Effect of nursing intervention program using abdominal palpation of Leopold’s maneuvers on maternal-fetal attachment . Reprod Health 2013;10 (article 12). doi.org/10.1186/1742-4755-10-12
National Institutes of Health, U.S. National Library of Medicine: MedlinePlus. Delivery presentations .
Dalvi SA. Difficult deliveries in Cesarean section . J Obstet Gynaecol India . 2018;68(5):344-348. doi:10.1007/s13224-017-1052-x
Zhi Z, Xi L. Clinical analysis of 40 cases of external cephalic version without anesthesia . J Int Med Res . 2021;49(1):300060520986699. doi:10.1177/0300060520986699
National Institutes of Health, U.S. National Library of Medicine: MedlinePlus. Questions to ask your doctor about labor and delivery .
Nemours KidsHealth. Cesarean sections .
By Elizabeth Yuko, PhD Yuko has a doctorate in bioethics and medical ethics and is a freelance journalist based in New York.
Why would posterior position matter in labor? The head is angled so that it measures larger. The top of the head molds less than the crown.
Baby’s spine is extended, not curled, so the crown of the head is not leading the way. Baby can’t help as much during the birth process to the same degree as the curled up baby.
Some posteriors are easy, while others are long and painful, and there are several ways to tell how your labor will be beforehand. After this, you may want to visit What to do when….in Labor .
Belly Mapping ® Method tips: The Right side of the abdomen is almost always firmer, but the direct OP baby may not favor one side or the other. Baby’s limbs are felt in front, on both sides of the center line. A knee may slide past under the navel.

The OP position (occiput posterior fetal position) is when the back of the baby’s head is against the mother’s back. Here are drawings of an anterior and posterior presentation.
- When is Breech an Issue?
- Belly Mapping® Breech
- Flip a Breech
- When Baby Flips Head Down
- Breech & Bicornuate Uterus
- Breech for Providers
- What if My Breech Baby Doesn't Turn?
- Belly Mapping ®️ Method
- After Baby Turns
- Head Down is Not Enough
- Sideways/Transverse
- Asynclitism
- Oblique Lie
- Left Occiput Transverse
- Right Occiput Anterior
- Right Occiput Posterior
- Right Occiput Transverse
- Face Presentation
- Left Occiput Anterior
- OP Truths & Myths
- Anterior Placenta
- Body Balancing

Look at the above drawing. The posterior baby’s back is often extended straight or arched along the mother’s spine. Having the baby’s back extended often pushes the baby’s chin up.
Attention: Having the chin up is what makes the posterior baby’s head seem larger than the same baby when it’s in the anterior position.
Because the top of the head enters (or tries to enter) the pelvis first, baby seems much bigger by the mother’s measurements. A posterior head circumference measures larger than the anterior head circumference.
A large baby is not the same issue, however. The challenge with a posterior labor is that the top of the head, not the crown of the head leads the way.
A baby with their spine straight has less ability to wiggle and so the person giving birth has to do the work of two. This can be long and challenging or fast and furious. Also, there are a few posterior labors that are not perceived different than a labor with a baby curled on the left.
Why? Anatomy makes the difference. Learn to work with birth anatomy to reduce the challenge of posterior labor by preparing with our Three Balances SM and more.
What to do?
- Three Balances SM
- Dip the Hip
- Psoas Release
- Almost everything on this website except Breech Tilt
In Labor, do the above and add,
- Abdominal Lift and Tuck
- Other positions to Open the Brim
- Open the Outlet during pushing
There are four posterior positions
The direct OP is the classic posterior position with the baby facing straight forward. Right Occiput Transverse (ROT) is a common starting position in which the baby has a bit more likelihood of rotating to the posterior during labor than to the anterior. Right Occiput Posterior usually involves a straight back with a lifted chin (in the first-time mother). Left Occiput Posterior places the baby’s back opposite the maternal liver and may let the baby flex (curl) his or her back and therefore tuck the chin for a better birth. These are generalities, of course. See a bit more about posterior positions in Belly Mapping ® on this website. Want to map your baby’s position? Learn how with the Belly Mapping ® Workbook .
Pregnancy may or may not show symptoms. Just because a woman’s back doesn’t hurt in pregnancy doesn’t mean the baby is not posterior. Just because a woman is quite comfortable in pregnancy doesn’t mean the baby is not posterior. A woman can’t always feel the baby’s limbs moving in front to tell if the baby is facing the front.
The four posterior fetal positions
Four starting positions often lead to (or remain as) direct OP in active labor. Right Occiput Transverse (ROT), Right Occiput Posterior (ROP), and Left Occiput Posterior (LOP) join direct OP in adding labor time. The LOP baby has less distance to travel to get into an LOT position.
As labor begins, the high-riding, unengaged Right Occiput Transverse baby slowly rotates to ROA , working past the sacral promontory at the base of the spine before swinging around to LOT to engage in the pelvis. Most babies go on to OA at the pelvic floor or further down on the perineal floor.
If a baby engages as a ROT, they may go to OP or ROA by the time they descend to the midpelvis. The OP baby may stay OP. For some, once the head is lower than the bones and the head is visible at the perineum, the baby rotates and helpers may see the baby’s head turn then! These babies finish in the ROA or OA positions.
Feeling both hands in front, in two separate but low places on the abdomen, indicates a posterior fetal position. This baby is Left Occiput Posterior.
Studies estimate 15-30% of babies are OP in labor. Jean Sutton in Optimal Fetal Positioning states that 50% of babies trend toward posterior in early labor upon admission to the hospital. Strong latent labor swings about a third of these to LOT before dilation begins (in “pre-labor” or “false labor”).
Recent research shows about 50% of babies are in a posterior position when active labor begins, but of these, 3/4 of them rotate to anterior (or facing a hip in an occiput transverse, head down position.
Jean Sutton’s observations, reported in her 1996 book, indicates that some babies starting in a posterior position will rotate before arriving to the hospital. Ellice Lieberman observed most posteriors will rotate out of posterior into either anterior or to facing a hip throughout labor. Only 5-8% of all babies emerge directly OP (13% with an epidural in Lieberman’s study). At least 12% of all cesareans are for OP babies that are stuck due to the larger diameter of the OP head in comparison to the OA head. It’s more common for ROT, ROP, and OP babies to rotate during labor and to emerge facing back (OA). Some babies become stuck halfway through a long-arc rotation and some will need a cesarean anyway.
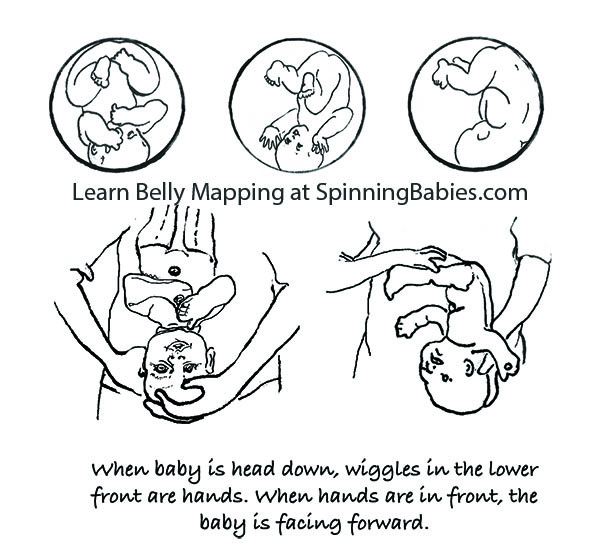
The three anterior starting positions for labor

Why not ROA? ROA babies may have their chins up and this deflexed position may lengthen the course of labor. Less than 4% of starting positions are ROA, according to a Birmingham study. This might not be ideal for first babies, but is not a posterior position either.
The spectrum of ease across posterior labors

Purchase Parent Class
Baby’s posterior position may matter in labor
With a posterior presentation, labor may or may not be significantly affected. There is a spectrum of possibilities with a posterior baby. Some women will not know they had a posterior baby because no one mentions it. Either the providers didn’t know, or didn’t notice. If labor moved along, they may not have looked at fetal position clues since there was no reason to figure out why labor wasn’t progressing. If a woman didn’t have back labor (more pain in her back than in her abdomen), the provider may not have been “clued into” baby’s position.
Some posterior babies are born in less than 8 hours and position did not slow down labor. Some posterior babies are born in less than 24 hours and position did not slow down labor enough to be out of the norm. Some posterior babies are born in less than 36-48 hours without the need for interventions.
Some posterior labors are manageable when women are mobile, supported, and eat and drink freely, as needed. Some posterior labor needs extra support that a well-trained and experienced doula may provide, but that typically a mate or loved one would not have the skills or stamina to keep up with. Some posterior labors progress only with the help of a highly-trained pregnancy bodyworker or deep spiritual, or otherwise a non-conventional model of care. Or, they seem only able to finish with medical intervention.
Some posterior labors are served by an epidural, meaning the pelvic floor relaxes enough for the baby to rotate and come out. Some epidurals, on the other hand, make it so that a woman can not finish the birth vaginally.
NOTE: Parents should know — some birth researchers, like Pediatrician John Kennell, are seriously asking whether a mother’s epidural turns off her body’s release of pain-relieving hormones which a baby relies on during childbirth. Some babies can’t turn and can’t be born vaginally and must be born by cesarean. This is a spectrum of possibilities. I’ve seen every one of the above possibilities several times and can add the wonderful experience of seeing a woman laughing pleasurably and squatting while her posterior baby slid out on to her bedroom floor.
Possible posterior effects, some women will have one or two and some will have many of these:

The forehead that overlaps the pubic bone after labor starts must turn and drop into the pelvis to allow the birth to happen naturally. A cesarean finish of the labor is possible. Look at Abdominal Lift and Tuck in Techniques to guide you to solutions for easier engagement and progress.
- Longer pregnancy (some research shows this and some doesn’t)
- The amniotic sac breaking (water breaks, membranes open, rupture of membranes) before labor (1 in 5 OP labors)
- Not starting in time before induction is scheduled
- Labor is longer and stronger and less rhythmic than expected
- Start and stop labor pattern
- The baby may not engage, even during the pushing stage
- Longer early labor
- Longer active labor
- Back labor (in some cases)
- Pitocin may be used when labor stalls (but a snoring good rest followed by oatmeal may restore a contraction pattern, too)
- Longer pushing stage
- Maybe a woman has all three phases of labor lengthened by the OP labor or one or two of the three phases listed
- Sometimes the baby’s head gets stuck turned halfway to anterior – in the transverse diameter. This may be called a transverse arrest (not a transverse lie ).
- More likely to tear
- More likely to need a vacuum (ventouse) or forceps
- More likely to need a cesarean
These effects are in comparison to a baby in the left occiput anterior or left occiput transverse fetal position at the start of labor.
Who might have a hard time with a posterior baby?
This family just had a fast posterior birth of their second child! Ease in labor includes other factors beyond baby position.
- A first-time mom
- A first-time mom whose baby hasn’t dropped into the pelvis by 38 weeks gestation (two weeks before the due date)
- A woman with an android pelvis (“runs like a boy,” often long and lanky, low pubis with narrow pubic arch and/or sitz bones close together, closer than or equal to the width of a fist)
- A woman whose baby, in the third trimester, doesn’t seem to change position at all, over the weeks. He or she kicks in the womb and stretches, but whose trunk is stationary for weeks. This mother’s broad ligament may be so tight that she may be uncomfortable when baby moves.
- A woman who has an epidural early in labor (data supports this), before the baby has a chance to rotate and come down.
- A woman who labors lying in bed
- Low-thyroid, low-energy woman who has gone overdue (this is my observation)
- A woman who lacks support by a calm and assured woman who is calming and reassuring to the birthing mother (a doula)
- A woman put on the clock
- A woman who refuses all help when the labor exceeds her ability to physically sustain her self (spilling ketones, dehydration, unable to eat or rest in a labor over X amount of hours which might be 24 for some or 48 for others)
- A woman whose birth team can’t match an appropriate technique to the needs of the baby for flexion, rotation, and/or descent from the level of the pelvis where the baby is currently at when stuck
Who is likely to have an easy time with a posterior baby?
- A second-time mom who’s given birth readily before (and pushing went well)
- A posterior baby with a tucked chin on his or her mama’s left side with a round pelvic brim
- An average-sized or smaller baby
- Someone whose posterior baby changes from right to left after doing inversions and other balancing work , though the baby is still posterior
- A woman with a baby in the Left Occiput Posterior, especially if the baby’s chin is tucked or flexed
- A woman who gets bodywork, myofascial release, etc.
- A woman whose posterior baby engages, and does not have an android (triangular) pelvis or a small outlet
- And of all of these, what is necessary is a pelvis big enough to accommodate the baby’s extra head size
- A woman who uses active birthing techniques — vertical positions, moves spontaneously and instinctively or with specific techniques from Spinning Babies ® , and other good advice
- A woman in a balanced nervous state, not so alert and “pumped up,” on guard, etc.
Any woman may also have an easier time than public opinion might indicate, too, just because she isn’t on this list. Equally, just because she is on the “hard” list doesn’t mean she will have a hard time for sure. These are general observations. They are neither condemnations nor promises. Overall, some posterior babies will need help getting born, while some posterior babies are born easily (easy being a relative term).
Let’s not be ideological about posterior labors.
While most posterior babies do eventually rotate, that can still mean there is quite a long wait – and a lot of physical labor during that wait. Sometimes it means the doula, midwife, nurse, or doctor is asking the mother to do a variety of position changes, techniques, and even medical interventions to help finish the labor. Patience works for many, but for some a cesarean is really the only way to be born. Read What To Do When…in Labor .
What causes a baby to be posterior?
There is a rising incidence of posterior babies at the time of birth. We know now that epidural anesthesia increases the rate of posterior position at the time of birth from about 4% (for women who don’t choose an epidural in a university birth setting) up to about 13% (Lieberman, 2005). Low thyroid function is associated with fetal malposition such as posterior or breech. (See Research & References .)
Most babies who are posterior early in labor will rotate to anterior once labor gets going. Some babies rotate late in labor, even just before emerging. Studies such as Lieberman’s show that at any given phase of labor, another 20% of posterior babies will rotate so that only a small number are still posterior as the head emerges.
My observations are that the majority of babies are posterior before labor. The high numbers of posterior babies at the end of pregnancy and in the early phase of labor is a change from what was seen in studies over ten years old. Perhaps this is from our cultural habits of sitting at desks, sitting in bucket seats (cars), and leaning back on the couch (slouching). Soft tissues such as the psoas muscle pair or the broad ligament also seem to be tight more often from these postures, from athletics (quick stops, jolts, and falls), from accidents, and from emotional or sexual assault.
Being a nurse or bodyworker who turns to care for people in a bed or on a table will also twist the lower uterine segment (along with some of the previously mentioned causes). This makes the baby have to compensate in a womb that is no longer symmetrical. Less often, the growing baby settles face-forward over a smaller pelvis, or a triangular-shaped pelvis (android). At the end of pregnancy, the baby’s forehead has settled onto a narrower than usual pubic bone, and if tight round ligaments hold the forehead there, the baby may have a tough time rotating. These are the moms and babies that I’m most concerned with in my work at Spinning Babies®. A baby that was breech beyond week 30 – 34 of pregnancy will flip head down in the posterior position. A woman with a history of breech or posterior babies is more likely to have a breech or posterior baby in the next pregnancy. However, she may not have an as long labor.
The best way to tell if your baby is OP or not, usually, is if you feel little wiggles in the abdomen right above your pubic bone. These are the fingers. They’d feel like little fingers wiggling, not like a big thunk or grinding from the head, though you might feel that, too. The little fingers will be playing by the mouth. This is the easiest indication of OP. The wiggles will be centered in the middle of your lower abdomen, close to the pubic bone. If you feel wiggles far to the right, near your hip, and kicks above on the right, but not near the center and none on the left, then those signal an OA or LOT baby (who will rotate to the OA easily in an active birth). After this, you might go to What to do when…in Labor.
Check out our current references in the Research & References section.

Pin It on Pinterest

- Pregnancy Week By Week
- Ovulation Calculator
Malpresentation and Malposition of the Fetus
A malpresentation or malposition of the fetus is when the fetus is in any abnormal position, other than vertex (head down) with the occiput anterior or posterior.
The following are considered malpresentations or malpositions:
Unstable lie
- Transverse presentation
- Oblique presentation
Face presentation
Brow presentation
Shoulder presentation
High head at term
- Prolapsed arm
The cause of a malpresentation can often not be clearly identified but it can be associated with the following:
- Preterm pregnancy
- Uterine anomalies
- Pelvic tumors eg f ibroids
- Placenta previa
- Grandmultiparty
- Contracted maternal pelvis
- Multiple gestation
- Too much amniotic fluyid (polyhydramnios)
- Short umbilical cord
- Fetal anomalies (e.g. anencephaly, hydro-cephalus)
- Abnormal fetal motor ability
There is an increased risk of neonatal and maternal complications associated with a malpresentation including neonatal and maternal trauma. If delivery is indicated, doing a cesarean delivery can significantly decrease the risk of complications.
Transverse lie
Oblique lie
In most cases of a normal vertex (head down) presentation, the baby's head is flexed with the chin close to the baby's chest. In these cases, the presenting part is the occiput, the posterior part of the baby's head. If the baby's head is more but not completekly extended then the baby's brow presents towards the vagina. A brow presentation is rare, maybe happening in about 1 in 2,000 births, more likely in pwomen with their second or subsequent births. A baby with a brow presentation can only deliver vaginally if the head flexes or extends.
Prolapsed arm
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Surg J (N Y)
- v.6(Suppl 2); 2020 Jul

Clinical Tips of Cesarean Section in Case of Breech, Transverse Presentation, and Incarcerated Uterus
1 Department of Obstetrics and Gynecology, Faculty of Medicine, Juntendo University, Tokyo, Japan
Gen Ishikawa
2 Department of Obstetrics and Gynecology, Chiba Hokusoh Hospital, Nippon Medical School, Chiba, Japan
Satoru Takeda
Cesarean section in breech or transverse presentation involves more complicated procedures than cesarean section in cephalic presentation because the former requires additional manipulations for guiding the presenting part of the fetus, liberation of the arms, and the after-coming head delivery; therefore, those cesarean sections are likely to be more invasive. Making a rather wide uterine incision to prevent uterine injury during delivery of the fetus facilitates smooth delivery of the fetus. Furthermore, in cases of breech or transverse presentation, it is important to initially identify the presenting part of the fetus and guide it to the incision opening in the lower uterine segment, because delivering the presenting part of the fetus first is a basic rule of delivery of the fetus. Smooth delivery of the fetus by means of breech extraction can prevent excessive stress or injury to the fetus. Therefore, it is important to acquire the knowledge and skills necessary to perform these techniques, including the internal version. Smooth delivery of the fetus is also less invasive for the mother because an extension of the uterine excision or injury to arteries and veins in the uterus and parametrium can be avoided. Incarcerated uterus occurring in cases of pregnancy with intrapelvic adhesion, endometriosis, cervical myoma, or extended cervix may result in excessive uterine and cervical injury when a transverse incision of the lower uterine segment is performed without caution. These conditions may result in difficulty in fetal delivery. Therefore, it is important to identify risks in advance and to choose the incision line with great care. Countermeasures for difficult delivery of the fetus need to be mastered by all practitioners of obstetrics. If the transverse incision fails to reach the uterine cavity, an inverted T-shaped or J-shaped incision should be made. Risks of complications such as injury to the cervical canal, the vagina, the bladder or ureter, and massive hemorrhage must be kept in mind.
Cesarean Section in Case of Breech or Transverse Presentation
Preoperative evaluation.
The presentation, position, and attitude of the fetus should be confirmed by transabdominal ultrasonography on admission and at departure from the ward for cesarean section. It is important to have images of the course of the surgery and delivery of the fetus by confirming the fetal position, location of the placenta and umbilical cord, and volume of amniotic fluid. The operation should be performed by imaging the descent, presentation, position, and attitude of the fetus through external examination according to Leopold's maneuver before laparotomy. Such imaging facilitates learning of the cesarean section techniques and obstetric management in the long run.
We basically use a transverse incision or a subumbilical longitudinal midline incision technique for skin incision. However, in cases of transverse or oblique presentation, a longitudinal incision is recommended by considering the possible extension of the incision wound. When performing a transverse incision, the Pfannenstiel incision is used as a rule, and the site of incision should be 3 to 5 cm above the pubic bone. It is important to secure the field of view; an incision at a higher site may cause difficulty in delivery of the fetus or may exacerbate uterine injury. If a higher incision site is required, caution should be exercised to secure the field of view for an incision of the rectus abdominis muscle, according to the original Maylard incision. In cases with a history of cesarean section or laparotomy or those with obesity, a sufficient field of view may be difficult to obtain; the selection and length of the skin incision line can affect the subsequent course of the operation.
Explanation of Procedures
Before the surgical procedure is initiated, the surgeon studies the images of the course of the operation and delivery of the fetus based on the findings obtained by ultrasonography in the ward or by external examination prior to the incision. The gravid uterus is not bilaterally symmetrical. In particular, the midline is difficult to find when left uterine displacement has been provided for preventing supine hypotensive syndrome or when the operating table is tilted ( Fig. 1 ). 3 When performing fasciotomy and peritoneotomy, caution should be exercised to avoid tearing of the abundant subfascial vessels. Before incision of the uterus wall, the position of presentation, leg position, and location and descent of the presenting part of the fetus should be confirmed by palpation from the serous surface of the uterus. Then, the uterine rotation status should be confirmed, and the incision line decided. This is useful for avoiding injury to the fetus and allows us to quickly reach the uterine cavity.

Selection of the skin incision line. In cases of cesarean section, it is common to perform left uterine displacement by placing a pillow under the right side of the waist or by tilting the operating table immediately after inducing spinal subarachnoid anesthesia, aiming at preventing the occurrence of supine hypotensive syndrome. Because the surgical field is subsequently disinfected and the patient is draped, the midline becomes more difficult to identify. In addition, the abdominal skin is not bilaterally equal or symmetrical, depending on the position of presentation, fetal attitude, and rotation of the uterus. Therefore, the location of the skin incision line should be decided promptly but with care. (Reproduced with permission from Ishikawa G. Cesarean section for breech, transverse presentation and incarcerated uterus. In: Hiramatsu Y, Konishi I, Sakuragi N, Takeda S, eds. Mastering the Essential Surgical Procedures OGS NOW, No.3. Cesarean section. (Japanese). Tokyo: Medical View; 2010: 72–81. Copyright © Medical View).
Incision of the Lower Uterine Segment
To facilitate delivery of the fetus, the presenting part of the fetus should be touched from the serosal side of the uterus and manually elevated toward the maternal head. Then, the loose vesicouterine serosa is grasped with tweezers and incised transversely with scissors. The bladder is gently dissected from the underlying lower uterine segment. After this bladder separation, a transverse incision should be made in the lower uterine segment, in the same manner as in a cesarean section for a cephalic presentation ( Fig. 2 ). 3 The incision made with a surgical knife to reach the uterine cavity can be extended manually or sharply with Cooper scissors ( Fig. 3 ). 3 In either case, it is necessary to take care to avoid injury to the uterine artery and vein that lie on the extension line of the incision. Surgical techniques performed without due caution may cause additional injuries while guiding the fetus, liberating the arms, or after-coming head delivery in breech presentation, leading to major bleeding.

Transverse incision in the lower uterine segment. While holding the lower uterine segment with two fingers of the left hand, the operator incises the lower segment with a round-edged knife to prevent bleeding and identify the location. The assistant aids in securing the field of view with the left hand and supports the wound surface with Pean forceps to facilitate a prompt incision. (Reproduced with permission from Ishikawa G. Cesarean section for breech, transverse presentation and incarcerated uterus. In: Hiramatsu Y, Konishi I, Sakuragi N, Takeda S, eds. Mastering the Essential Surgical Procedures OGS NOW, No.3. Cesarean section. (Japanese). Tokyo: Medical View; 2010: 72–81. Copyright © Medical View).

Extension of the transverse incision in the lower uterine segment. In our institution, it is common to extend the uterine incision manually by “smiling up” the lateral apices. In cases of malpresentation, such as breech presentation at the cesarean section, Cooper scissors may be used, considering the possibility that subsequent delivery of the fetus might extend or injure the incision. The incision in the uterus is extended with Cooper scissors. Guiding with two fingers of the left hand, the lateral apices of the incision are cut in an arc shape toward the uterine fundus to make the “smiling up” incision. (Reproduced with permission from Ishikawa G. Cesarean section for breech, transverse presentation and incarcerated uterus. In: Hiramatsu Y, Konishi I, Sakuragi N, Takeda S, eds. Mastering the Essential Surgical Procedures OGS NOW, No.3. Cesarean section. (Japanese). Tokyo: Medical View; 2010: 72–81. Copyright © Medical View).
In a transverse or oblique presentation, smooth delivery of the fetus may be achieved by transverse incision of the uterine body based on the fetal presentation, as carefully determined in advance. The operator preoccupied with the lower uterine segment may make an incision in a narrow lower uterine segment, thereby possibly inducing injury at the incision site while guiding the fetus manually. Incising the lower segment is advantageous, considering the concerns of repeated cesarean section in the future and protection of the wound by suture and repair after incision of the peritoneal reflection of the vesicouterine pouch. However, a transverse incision of the uterine body might be more advantageous with regard to the patency of the guiding path for the fetus. A J-shaped or U-shaped incision may be superior on the assumption that the fetus in oblique or transverse presentation will be delivered without rotation ( Fig. 4 ). 1 4 However, if an incision is made at a high position without considering the positional relationship between the fetus and uterus, it may be difficult to guide the fetal buttocks located at a lower position to the incised opening.

Extension of the uterine incision. A slightly wider incision is made into the myometrium. For a difficult delivery, the incision is preferably extended upward to a J-shape ( A ) or U-shape ( B ) or an inverted T-shape ( C ). If a transverse incision does not reach the uterine cavity such as uterine incarceration, the incision should be extended upward to make a J shape or be extended into an inverted T shape. (Reproduced with permission from Takeda S. Important point of emergency cesarean section. In: Takeda S, Makino S, Takeda J, eds. Management of Breech Delivery and Shoulder Dystocia. (Japanese). Tokyo: Medical View;2019:106–110. Copyright © Takeda S).
Delivery of the Fetus
The presenting part of the fetus should be identified by finding the fetus from the incision in the uterus. In cases of footling presentation, the operator should hold the legs and proceed to the subsequent guiding process. Because holding the legs and subsequent guiding and extraction place a burden on the joints of the lower limbs (ankle, knee, and hip joints) of the fetus, it is recommended that both hips be held if possible. In cases of complete or frank breech presentation, both hips (iliac crest to inguinal region) should be held. In cases of fetal presentation in which the fetal back is facing the maternal back (sacrum posterior positions: sacrum posterior, left sacrum posterior, and right sacrum posterior), the fetal back should be guided to rotate around the long axis of the fetal body toward the maternal ventral side, to allow the spinal column in the fetal back to move toward the anterior portion of the maternal body (sacrum anterior position). This corresponds to the position of presentation at the end of the second rotation during vaginal delivery in breech presentation. This maneuver is advantageous in that it facilitates liberation of the arms and delivery of the fetal head following delivery of the fetal legs and trunk. Furthermore, this maneuver allows the passage of the fetus to more appropriately correspond to the incisional opening of the uterus.
In case of transverse or oblique presentation, since the presenting part is not often palpable, the operator probes the foot to grasp and deliver the infant. To touch the foot, the operator rotates the fetus, using fingers inserted through the vagina and placed on the external uterine wall. If the foot is palpable, the operator should grasp the ankle ( Fig. 5 ). 1 Grasping of the lower legs or thighs may cause fractures. If the foot is difficult to find, extending the incision of the myometrium in the direction where the foot may be located would facilitate grasping of the foot for performing the internal version. If the delivery is difficult, one should not hesitate to extend the incision to a J- or U-shape, or an inverted T-shape to facilitate the delivery ( Fig. 4 ). 1 4 There is a question as to whether the fetal head or the buttocks should be guided as the presenting part. Because the hips and legs of the fetus are easier to hold and guide than the fetal head, the buttocks are guided as the presenting part in principle. However, there is no concern as to setting the fetal head as the presenting part if smooth manipulation is secured. In this case, delivery of the fetus is in accordance with a cesarean section in cephalic presentation.

Internal version technique by grasping of the fetal feet. The operator grasps the fetal ankle over the medial and lateral malleoli with three fingers (thumb, index, and middle fingers), pulling toward the incision. Simultaneously, the operator leads the fetal buttocks to the incision, placing the hand on the external uterine wall. 1 (Reproduced with permission from Takeda S. Important point of emergency cesarean section. In: Takeda S, Makino S, Takeda J, eds. Management of Breech Delivery and Shoulder Dystocia. (Japanese). Tokyo: Medical View;2019:106–110. Copyright © Takeda S).
The presenting part should be guided to the incision opening of the uterus and extracted toward the maternal feet while holding both fetal hips securely. The goal is to keep the fetus horizontal while extracting the fetus until the upper back (inferior scapular angle) of the fetus is delivered ( Fig. 6 ). 3

Delivery of the fetus. The presenting part of the fetus is extracted while holding both fetal hips securely. If the fetus is deflected or elevated upward with excessive consideration of the subsequent delivery of the fetal head, it increases the risk of injuries at the incision, such as extension of the uterine incision. (Reproduced with permission from Ishikawa G. Cesarean section for breech, transverse presentation and incarcerated uterus. In: Hiramatsu Y, Konishi I, Sakuragi N, Takeda S, eds. Mastering the Essential Surgical Procedures OGS NOW, No.3. Cesarean section. (Japanese). Tokyo: Medical View; 2010: 72–81. Copyright © Medical View).
In cases of footling presentation, the fetus is initially guided and extracted while holding both legs, and then the hip (iliac crest to inguinal region), of the fetus. However, in cases of breech presentation, the hip of the fetus is held basically from the beginning. In cases of complete breech presentation, the operator may be tempted to guide the fetal legs first, but caution is necessary because there is concern that the uterine incision might be damaged because of the process by which the fetal legs bent at the hip and knee joints extend during passage through the incisional opening. If the fetus is guided while holding the hips after elevating the lowest part of the fetus toward the maternal head, a frank breech presentation in the uterus may be obtained, leading to smooth delivery of the trunk.
After delivering the fetus horizontally toward the maternal feet until the inferior scapular angle emerges, the operator should proceed to deliver the fetus in the manner of the Bracht maneuver for vaginal delivery in breech presentation ( Figs. 6 , ,7 7 ). 3 Namely, the fetal trunk should be elevated and dorsiflexed ( Fig. 7A ), 3 and then rotated toward the maternal ventral side in an arc with the uterine incision serving as the fulcrum ( Fig. 7B ). 3

Delivery of the arms and the after-coming head using the Bracht maneuver. After extracting the trunk horizontally ( Fig. 6 ), the operator should proceed to liberation of the arms and delivery of the fetal head in the manner of the Bracht maneuver ( A, B ). The operator should try to achieve smooth delivery without interruption following delivery of the trunk. Whenever liberation of the arms is performed using the classic technique, with delivery of the fetal head according to the Mauriceau maneuver, these manipulations should be conducted smoothly at a constant pace and in a consistent manner with flexibility, as needed, to adapt to circumstances. (Reproduced with permission from Ishikawa G. Cesarean section for breech, transverse presentation and incarcerated uterus. In: Hiramatsu Y, Konishi I, Sakuragi N, Takeda S, eds. Mastering the Essential Surgical Procedures OGS NOW, No.3. Cesarean section. (Japanese). Tokyo: Medical View; 2010: 72–81. Copyright © Medical View).
When the arms are not brought down by the Bracht maneuver during delivery of the fetus, the procedures of liberation of the arms and delivery of the after-coming head should be performed. In cases of difficult delivery, the arms should be liberated in the manner of the classic method of liberating the arms. More specifically, while the fetal trunk is elevated anteriorly to the maternal body, the arm emerging on the maternal feet side of the uterine incision opening should be liberated with the index finger hooked in the fetal elbow joint. After both arms are liberated in this manner, the fetus should be kept dorsiflexed and elevated anteriorly to the maternal body; the after-coming head is subsequently delivered ( Fig. 7B ). 3 In cases of vaginal delivery in breech presentation, the fetal back is rotated laterally to the maternal body, and the arms located posteriorly are liberated in the first and second breech presentations. In cases of cesarean section, uniaxial rotation of the fetus should not be performed by exerting force. This is because the uterine incision wound extends in the horizontal direction of the maternal body, and the mode of spread of the birth canal is different from that in vaginal delivery in breech presentation. The key to successful liberation of the arms is to guide the arm to be liberated in the manner of wiping the forehead of the fetus with the palmar side of the arm. If the arm is initially guided without due caution in the downward direction, the uterine incision may be damaged by the fetal elbow, the fetal upper arm may be injured as fracture, or an excessive burden may be imposed on joints of the fetus. Although successful liberation of the arms usually leads to delivery of the after-coming head without difficulty, delivery of the fetal head is assisted by the Mauriceau or Veit-Smellie maneuver. The fetal trunk is already dorsiflexed and elevated anteriorly to the maternal body by the Bracht maneuver, showing the occipital protuberance of the fetal head. Therefore, it is not necessary to perform extraction posteroinferiorly to the maternal body according to the Mauriceau maneuver during vaginal delivery in breech presentation.
When the head is entrapped, the incision should be extended to a J-shape to deliver the infant. If time permits, administration of nitroglycerin can release the myometrial tone to enable a smooth delivery. In cases of cesarean delivery of preterm infants and those with a sufficient descent of the head or breech presentation, the anesthesiologists should be alerted beforehand to prepare nitroglycerin.
After removal of the placenta, the cervical os should be observed. If the cervical os is closed, it should be dilated during or after the operation to allow the lochia to flow outward. The uterine cavity should be bluntly removed using gauze to eliminate retained membranes.
Closure of the Abdomen
The uterine incision wound should be closed by suture using 0-synthetic absorbable suture, such as Vicryl or Monocryl. The interrupted suture or Z-suture on the bilateral cut end should be performed for ligation of thick branches of the uterine artery and prevention of dead space or hematoma. The uterine incision is closed basically with two layers. The first layer is sutured by employing interrupted sutures such that both endometrial layers meet precisely. Continuous sutures on the inner side of the uterine wall are not employed because a history of continuous sutures on the inner side of the uterine wall might influence the development of placenta accreta in patients with prior cesarean section. 5 The second layers may be sutured by employing a continuous interlocking suture or interrupted sutures.
There is no need for suturing the serosa on the vesicouterine pouch to prevent elevation and adhesion of the bladder, covering over the uterine wound. Douglas pouch, both sides of the peritoneal cavity, and the vesicouterine pouch should be examined to determine the hemostasis state and presence/absence of any abnormalities. The uterine adnexa should also be checked for any lesions or abnormalities.
The peritoneal cavity is sufficiently irrigated with 2000 to 3000 mL of physiological saline. A continuous closed suction drain is inserted into the Douglas pouch, if needed.
Absorbable adhesion barrier, such as Seprafilm, is applied to the wounds on the uterus and abdominal wall to prevent development of subsequent adhesion. The serosa, fascia, subcutaneous tissue, and epidermis are sutured to close the wound. The patency of the uterine os and outflow of lochia are confirmed by speculum and pelvic examinations. Then, the position of the uterine fundus and propriety of uterine contractions are confirmed to complete the operation.
Cesarean Section in Case of Incarcerated Uterus or the Cervical Elongation
Preoperative preparation.
In cases of cesarean section for an incarcerated uterus, the success of the operation depends on whether cervical elongation and retroverted uterus can be detected preoperatively and whether the cesarean section procedure is smooth and minimally invasive to the maternal body. Incarceration of the uterus may not be recognized in early pregnancy. However, when extreme anterior-upward displacement of the cervix of the uterus or globular tumorous sensation in the posterior vaginal fornix is found by vaginal examination on admission for cesarean section or preoperative examination before departure from the hospital ward, the uterine cervix located anterosuperior to the bladder should be further examined by transabdominal ultrasonography to determine whether there is either elongation of the cervix or incarceration of the uterus. The height of the lower uterine segment and site of the uterine cavity should be examined by ultrasonography to decide the cutting level of the uterus before the operation.
If a diagnosis of the incarcerated uterus was made at term, elective cesarean section should be performed with special attention. When a cesarean section is performed without the recognition of an incarcerated uterus, it might be difficult to deliver the fetus because it will not reach the uterine cavity and consequently result in fetal asphyxia. Several complications such as complete cutting of the cervix or the vagina, extended uterine incision, incision on the posterior wall of the uterus through the vagina, or laceration due to massive hemorrhage may occur, because the lower uterine segment is dislocated extremely to the upper site compared with that in an ordinary cesarean section. 3 4 6 Therefore, a strategy for a safe cesarean section to avoid special complications of incarceration should be developed.
The incarcerated gravid uterus is recognized as being in a state of uterine retroflexion by pelvic examination or transvaginal ultrasonography in early pregnancy. As gestational weeks increase, the degree of retroflexion increases, resulting in embedding of the uterine fundus in the Douglas' pouch at the end of pregnancy ( Fig. 8 ). 4 When there is elongation and elevation of the cervix due to cervical myoma in the posterior wall of the uterus or myoma in the lower uterine segment, cervical findings are similar to those in cases with an incarcerated gravid uterus ( Fig. 9 ). 4

Incarcerated uterus. Pelvic examination readily leads to a diagnosis of incarcerated gravid uterus because this examination yields characteristic findings. However, it is likely to be overlooked on ultrasonography alone. Because the cervix and uterine wall are thin at the end of pregnancy, it is difficult to diagnose retroflexion and incarceration of the uterus. The placenta attached to the posterior wall can be misdiagnosed as low-lying placenta or placenta previa. (Reproduced with permission from Takeda S. Cesarean section for incarcerated uterus and elongation of the uterine cervix. In: Hiramatsu Y, Konishi I, Sakuragi N, Takeda S, eds. Mastering the Essential Surgical Procedures OGS NOW, No.10. Massive Obstetric Hemorrhage: Critical Care for Intractable Bleeding and Definite Strategies of Hemostasis. (Japanese). Tokyo: Medical View; 2012: 154–159. Copyright © Medical View).

Cervical elongation due to a myoma in the cervix. ( A ) In cases with cervical myoma in the posterior wall of the uterus or myoma in the lower uterine segment, the cervix is elongated. Therefore, myometrial incision at the usual level fails to reach the uterine cavity. In particular, in the case of performing a Pfannenstiel transverse incision, upward deviation of the lower uterine segment may be overlooked because the field of view in the peritoneal cavity is limited. Therefore, a transverse incision in the myometrium at the usual site fails to reach the amniotic cavity and the cervix is cut instead. ( B ) Incision at the usual site will result in cutting the cervix cross-sectionally or cutting into myoma in the posterior wall. (Reproduced with permission from Takeda S. Cesarean section for incarcerated uterus and elongation of the uterine cervix. In: Hiramatsu Y, Konishi I, Sakuragi N, Takeda S, eds. Mastering the Essential Surgical Procedures OGS NOW, No.10. Massive Obstetric Hemorrhage: Critical Care for Intractable Bleeding and Definite Strategies of Hemostasis. (Japanese). Tokyo: Medical View; 2012: 154–159. Copyright © Medical View).
There are characteristic pelvic examination findings; the uterovaginal region is deviated anteriorly and superiorly to the pubis to an extreme degree. The protruded uterus and myoma are palpable in the Douglas' pouch. Colposcopy may fail to identify the uterovaginal region because it is deviated superiorly. It is common for the uterine fundus to be lower according to the gestational week, causing elongation of the bladder.
If the incarcerated gravid uterus is not recognized until the end of pregnancy, pelvic examination may raise suspicion because the uterovaginal region is deviated anteriorly and superiorly to an extreme degree, although the cervix is difficult to identify on transabdominal ultrasonography. 7
On ultrasonography, the cervix is deviated anteriorly and superiorly, and the bladder appears to be suspended upward. 7 If incarcerated gravid uterus is suspected, magnetic resonance imaging can provide a definitive diagnosis based on the locations of the vagina, cervix, and bladder in the sagittal view. 8 It is important to determine the level of the skin incision and the site of the uterine incision wound in advance, by confirming the level of entry into the uterine cavity by ultrasonography prior to implementation of cesarean section. 3 4 Intraoperative ultrasonography is also useful.
Cesarean section for an incarcerated uterus is basically the same as a routine cesarean section. However, to facilitate subsequent surgical manipulations, a longer than usual incision should be made to provide a large field of view. A subumbilical longitudinal midline skin incision is preferred because of a wider field of view. The possibility that the incision is cut upward to the navel during the operation should be assumed.
When the cervix is elongated because of myoma, the positional relationships between the myoma, the cervix, the uterine body, and the round ligament of the uterus, and the bladder need to be confirmed. The bladder may be located extremely low but can also be elevated. The bladder should be palpated directly, and the urethral catheter be confirmed. If the bladder is extremely elevated, the upper end must be confirmed and separated.
Uterine Incision
As for incision in the myometrium, the peritoneal reflection of the vesicouterine pouch cannot be the target, as would routinely be the case, and the boundary between the uterine body and isthmus is ambiguous. Therefore, we can rely only on preoperative ultrasonographic findings in such cases.
The location of the uterine cavity should be confirmed by intraoperative ultrasonography, whenever possible. Because the vaginal wall and cervical canal in the final stages of pregnancy are thin, it may not be possible to confirm the location of the internal cervical os. It is also important to make sure of the distance to the uterine cavity. There is no need to strictly adhere to the use of deep transverse incision. If the cervix and the lower uterine segment are not distinguishable, longitudinal uterine incision is also a reasonable choice. Depending on the length of the elongated cervix, a longitudinal or transverse incision is made in the muscular layer near the umbilical region. When a transverse incision does not reach the amniotic cavity, the incision should be extended upward in the direction toward the uterine body in the manner of an inverted T-shaped or J-shaped incision.
In cases of cephalic presentation, cephalic delivery should be performed by employing a mild Kristeller maneuver via the incision opening of the uterus. In cases of breech presentation, the trunk should be delivered according to the cesarean section in breech presentation procedure, followed by liberation of the arms and delivery of the fetal head. These procedures are the same as those in cesarean section in breech or transverse presentation, but the patency of the uterine os is more difficult to confirm.
The myometrium should be sutured by placing simple interrupted sutures with absorbable thread. The second layer of suturing is performed for reinforcement. When an inverted T-shaped incision is made, the intersecting point should be joined firmly by Z or equivalent sutures. Suture and ligation should be carefully performed to obtain accurate matching of the layered planes to avoid piercing penetration of the myometrium. These procedures are the same as in those for cesarean section in breech or transverse presentation.
Postoperative Management
When there is a cervical myoma ( Fig. 9 ), 4 outflow of lochia from the cervical canal may be inhibited by the myoma. Therefore, frequent and meticulous follow-up observations for retention of lochia are necessary. Although incarcerated uterus may undergo reduction spontaneously after cesarean section, a careful follow-up is also necessary because there is concern about retention of lochia when there are no distinct changes in cervical elongation or incarceration status.
Complications
Repair of the cut cervical canal, control of bleeding.
If there is bleeding or difficulty in delivering the fetus, it is important to secure the field of view. If the skin incision is narrow, and the field of view is insufficient, the incision should be extended. When the Pfannenstiel transverse incision is performed, the rectus abdominis muscle may be cut unilaterally or bilaterally (Maylard method), or the rectus abdominis fascia can be cut in a T shape toward the pubis or separated and cut in an inverted T shape. Alternatively, both of these procedures may be performed to secure the field of view.
After delivery of the fetus, it is difficult to move the uterus outside the body because of adhesions to the Douglas pouch, which makes suturing difficult. The bleeding point should be clamped with serrated forceps, and the positional relationships between the cesarean section wound, vagina, cervix, body of the uterus, and surrounding organs including the bladder, ureter, uterine artery and vein, and the cardinal ligament need to be ascertained and well understood. Bleeding from the paravaginal tissue and cardinal ligament is an important issue. If the bladder is located low or separated sufficiently, injury to the bladder and ureter is avoidable.
Suture and Hemostasis of the Cervical Canal
If the lumen of the cervical canal is obscure, orientation can be obtained by insertion of the fingers or forceps from the vagina or by insertion of a urethral balloon catheter into the cervical canal. Even when the cervical canal is cut cross-sectionally, a catheter should be passed through it, and the upper and lower cut ends can then be sutured by simple interrupted suture with 2–0 or 1–0 absorbable thread. Attention should be paid to possible rupturing of the suture after repair, and it should thus be ensured that a drain is inserted in the vicinity of the sutured portion.
Injuries of the Bladder and the Ureter
If abdominal closure is performed without recognizing the presence of injury to the bladder or ureter, an echo free space will appear in the peritoneal cavity alongside an increase in blood urea nitrogen and creatinine within a few days. Patients may complain of mild symptoms such as a vague feeling of discomfort and lassitude, or may sometimes be minimally symptomatic. There may also be leukocytosis and a slight increase in C-reactive protein. Caution should be exercised regarding massive transfusion-related hyperpotassemia, hepatic dysfunction, hemolytic reaction, etc.
Conflict of Interest None.
Tips and Warnings
Characteristics of Emergency Cesarean Sections in Breech Delivery
Emergency cesarean sections that have been switched from vaginal breech delivery involve the following specific characteristics: in most cases, the indication is non-reassuring fetal status caused by a sudden and rapid onset of cord compression due to a forelying or prolapsed cord; the baby must be delivered as quickly as possible; and it may be associated with rupture of the membranes and/or thin myometrium caused by effacement and elongation of the uterine isthmus because of progression in the descent of the presenting part ( Table 1 ). 1 Thus, caution should be exercised during an incision of the myometrium because the fetus can be injured. To deliver the fetus, the operator grasps the fetal buttocks, hooking his/her index finger on the fetal bilateral groins, and pulls the fetal body gently, similar to the usual breech extraction maneuver. The femoral region must never be pulled with a finger over it. This can result in fetal femur fractures, which have been reported after cesarean breech delivery.
Obstetricians should understand and learn such characteristics of and strategies for cesarean delivery for breech presentation and establish a system to conduct an emergency cesarean section at any given time. For this purpose, obstetricians should consult with each other and form a multidisciplinary team that includes anesthesiologists, pediatricians, midwives, nurses, and paramedical staff to share information, cooperate immediately and closely, and receive simulation training. 1 2
Management of a Case with Cord Prolapse or Non-Reassuring Fetal Heart Rate Patterns
In cases of sudden onset of persistent fetal bradycardia and/or cord prolapse, vaginal examination should be performed to identify the causes and position of the cord. To relieve cord compression, the fetal presenting part should be elevated and tocolysis with nitroglycerin or ritodrine hydrochloride should be considered before transfer to the operating room. In most cases, the fetal heart rate is restored. Elevation of the presenting part using fingers through the vagina should be continued until delivery of the fetus. 1
Finally, the incision sizes of the skin and fascia should be confirmed at this point before a transverse incision is made on the lower uterine segment. An incision that is too small and excessive tension of the fascia and rectus abdominis muscle may cause difficulty during the delivery of the fetus. Therefore, the incision should be extended at this point, if necessary. After making a transverse incision of the lower uterine segment, the operation usually proceeds expeditiously enough that no modifications can be made.
A cesarean section in breech presentation involves more complicated procedures than a cesarean section in cephalic presentation because the former requires additional manipulations for guiding the presenting part of the fetus, liberation of the arms, and the after-coming head delivery. Therefore, a cesarean section in breech presentation is likely to be more invasive. Making a rather wide uterine incision to prevent uterine injury during the delivery of a fetus facilitates smooth delivery of the fetus. At this point, it is important to “smile up” the lateral apices of the incision in an arc shape toward the uterine fundus.
A “smile up” rather than a straight-line, incision is commonly used.
For identifying the lowest presenting part of the fetus, four fingers (index to little fingers) of one hand (on the maternal caudal side) of the operator, in principle, are initially used. Later, the fetus should be held mainly with two or three fingers, that is, the index finger, (middle finger) and thumb, of both hands. There is concern that careless holding with five fingers may result in extension of the uterine incision and injury to the uterine artery and vein. When the operator is not skilled enough in performing cesarean section in breech presentation or when a sufficient abdominal incision or uterine incision is lacking (such as in patients with a history of surgery or obesity), the operator is apt to apply excessive force when attempting to hold the fetus. It is useful to place gauze between the holding fingers and fetus to prevent slippage. This allows the fetus to be held more firmly and facilitates smooth delivery of the fetus. If the presenting part descends deeply, the assistant manually elevates the presenting part through the vagina and then the operator attempts to deliver the infant.
In cases of transverse or oblique presentation, the operator's hand tends to be inserted deeply into the uterus. Therefore, more attention is needed to avoid extension of the uterine incision or injury to the uterine artery and vein in transverse or oblique presentation than in breech presentation. Namely, careless manipulation during manual exploration and rotation of the fetus may result in extension of the uterine incision, injury to lateral blood vessels of the uterus, or laceration on the cervical side of the uterine incision. Due caution is necessary to avoid these problems.
If liberation of the arms and delivery of the after-coming head are found to be difficult, the operator should not hesitate to attempt extension of the uterine incision. It is important to extend the incision in an upward direction toward the uterine fundus as a J-shaped incision to prevent injury to the uterine artery and vein. It may also be helpful to add an incision at the center of the uterine incision toward the uterine fundus to make an inverted T-shaped incision. It is recommended that the decision to perform extension of the uterine incision or add an inverted T-shaped incision should be made in advance as the second-best procedure, which should be performed without hesitation by the operator or the first assistant in the event of a difficult delivery. Continuation of surgical manipulations, without sufficient caution, which reduces the success in liberation of the arms and delivery of the fetal head, may unnecessarily exacerbate injury to the uterine incision and result in complications. The J-shaped and inverted T-shaped incisions are methods that allow for extension of the incision, but do not cause injury to the incision. They not only facilitate delivery in difficult cases but also prevent maternal injury, thereby leading to decreased surgical stress to the maternal body and decreased blood loss.
Pathophysiology of the Incarcerated Uterus
Pregnancies complicated by myoma, endometriosis, and/or pelvic adhesion have been increasing with recent tendencies toward later marriages, increased pregnancy rates in women of advanced maternal age, and advancements in fertility treatments. Along with these trends, elongation of the uterine cervix has been attracting close attention as a reason for near-misses during cesarean section. Related near-miss cases, such as delivery of the fetus from the posterior wall of the uterus after incising the cervix and vaginal wall, failure to reach the uterine cavity during uterine myometrium incision, and massive hemorrhage, have been reported. Although uterine retroflexion before 12 gestational weeks is found at a frequency of 11 to 19% (15%), incarcerated gravid uterus is recognized in 1 out of 3,000 pregnant cases. 7 Risk factors include pelvic inflammatory disease, adhesion after gynecological surgery, endometriosis, myoma in the posterior wall of the uterus, and congenital anomalies of the uterus. 7
There are complications such as injury to the bladder or ureter, difficulty delivering the fetus, cervical incision, vaginal wall incision, and delivery of the fetus from the posterior wall of the uterus. Massive hemorrhage resulting in hysterectomy has also been reported.
Because uterine ruptures resulting from an attempt at vaginal delivery have occurred in the past, the current rule is that cesarean section should basically be selected for delivery in all cases with an incarcerated gravid uterus.
Symptoms become prominent after 13 to 17 gestational weeks, varying from none to pollakiuria, urinary retention, dysuria, incontinence, abdominal pain, suprapubic pain, low back pain, feeling of anal pressure, feeling of abdominal distension, and constipation. Symptoms may be intermittent or improve in some cases.
If the same doctor is in charge of ongoing medical check-ups of the patient from early in the pregnancy, it is relatively easy for the doctor to diagnose incarcerated gravid uterus, and cesarean section can be performed with this risk in mind. However, if multiple doctors see this patient, as in university hospitals, a problem may arise. Namely, uterine retroflexion might be missed as the uterus grows larger because of poor processes when one doctor takes over from another.
If transvaginal ultrasonography alone is used for medical check-ups of pregnant women, without performing the proper pelvic examinations, incarcerated gravid uterus may be overlooked. Placenta attached to the posterior wall of the uterus may be misdiagnosed as placenta previa or low-lying placenta.
In pregnancy with uterine myoma, cervical myoma and myoma in the lower uterine segment can cause the problem of cervical elongation. In particular, in cases with myoma in the posterior wall of the uterus, it is possible for cesarean section to be performed without due caution because there is no myoma at the site of incision in the myometrium. However, problems may arise during surgery because the cervix might be unexpectedly elongated.
It is common for the posterior wall of the uterus to be firmly adherent to the Douglas pouch in cases with an incarcerated gravid uterus, and the uterus may not be elevated outside the body cavity at the time of myometrial suture. If the wound area is elongated or the cervical canal is cut inadvertently, it is difficult to secure the field of view, and this results in difficulty with suturing. Suture during heavy bleeding and suture of the uterine wound without orientation may result in misalignment of the wound edges or failure in achieving clean closure of the wound.
In Cases of Failure to Reach the Uterine Cavity
If pregnancy progresses with the uterus in an incarcerated state, the uterine cervix becomes extended and elongated. In this case, if a uterine incision is made in the peritoneal reflection of the vesicouterine pouch, it enters the cervical canal. As a result, delivery of the fetus cannot be achieved, and the paracervical tissue or posterior wall of the uterus may be incised erroneously, leading to massive hemorrhage. The cervical canal may also be cross-sectioned. In any event, the operator may lose orientation and become disconcerted.
If the uterine cavity is not reached by incising the expected thickness of the myometrium, an inverted T-shaped or J-shaped incision should be made from the midline without hesitation, keeping this condition in mind ( Fig. 4 ). When cutting upward, the intestinal tract should be protected using a bladder spatula or intestinal spatula. If the uterine cavity is reached, the fetal membranes will bulge and may even rupture. Because the fetus is to be delivered from the lower part, rupture may occur unless a wide incision is made.
If the incision is deepened without recognizing this condition, the uterine cavity is reached from the posterior wall of the uterus. There is a report of the fetus being delivered twice via the vagina. 6 There are also cases in which the cervical canal was cut cross-sectionally without realizing that this had taken place or in which the fetus was delivered from the posterior wall of the uterus after partial incision.
Precautions to Avoid Complications of the Bladder Injury
When performing laparotomy for cesarean section, it is important to routinely confirm the location of the bladder. The trainer should make sure that the trainee understands the location of the bladder, initially by direct palpation of the organ. Even when the bladder is elevated and thereby mimics the appearance of the uterine wall, manually holding it up from the both sides allows palpation and confirmation of the bladder, preventing injury to this organ.
In cesarean section cases, it is important to routinely estimate the amount of amniotic fluid, thickness of the myometrium in the lower uterine segment, space between the lowest part of the fetus and the myometrium, etc., by palpating the lowest part of the fetus via the uterine wall prior to making an incision in the myometrium. This will provide a clue as to whether, in this condition, an incision made to the depth of the estimated thickness of the myometrium would fail to reach the uterine cavity.
Fetal Lie or Baby Position in womb – Does it really matter?
Medically Reviewed by: Dr. Veena Shinde (M.D, D.G.O, PG – Assisted Reproductive Technology (ART) from Warick, UK) Mumbai, India
- >> Post Created: March 22, 2022
- >> Last Updated: April 26, 2024

Fetal Lie or baby position in the womb - All you need to know - Content flow
It is an absolute wonder how a tiny life grows inside a womb – from the size of an apple seed to a small, but complete human baby.
Within the womb, this growing fetus moves around till it grows big enough to run out of space and is ready to enter this world.
The baby’s position , also referred to as the ‘ fetal lie ,’ in the last month of pregnancy decides the mother’s journey through labor and delivery.
If words like anterior position , posterior position , breech , or transverse baby position shows up in your test reports while describing your baby’s position, then this article will help you decode what it means.
This article will help you understand about all the various types of fetal lie or various different positions your baby could be in while growing in your womb.
Understanding fetal lie/fetal position
Fetal lie/fetal position or the baby’s position in the womb is of utmost importance generally towards the end of your pregnancy, i.e. generally in the last month of your pregnancy.
When the fetus is still growing, it moves around in the womb, but as it grows, it settles in one particular position – the most common position is the head-down position or also referred to as cephalic position and the vertex presentation. In this position the baby is facing the mother’s back with its head entering the pelvis.
The head-down position/cephalic position is the optimal position for delivery, where the baby’s head is right above the birth canal.
The birth canal comprises of the mother’s cervix (uterus’ outlet), vagina, and vulva. The birth canal can be seen as an elastic tunnel through which the baby passes to come into this world.
However, the fetus can settle in other not-so-desirable positions as well, which have their own set of challenges.
Fetal Lie/fetal position vs. fetal presentation
To describe the baby’s accurate position in the womb, medical professionals use both the terms – fetal position and fetal presentation.
Fetal lie/fetal position , also referred to as baby position in womb before labor, establishes where the baby’s face is – toward the mother’s back or her belly.
Fetal presentation actually tells you what part of the baby’s body will lead the way out of the birth canal. With this, one can determine the direction the baby’s head and feet are.
Together these terms tell a doctor the baby’s exact position in the womb and whether it is an optimal one or in one of those positions that may cause some hiccups in the delivery.
Types of fetal lie/fetal positions
An unborn baby instinctively just knows when it is time for it to come into this world and accordingly settles in the best position for delivery just before labor. This generally happens between 32 and 36 weeks of pregnancy.
However, some babies get comfortable in other not-very-favorable positions, which can cause some delay or difficulty in labor, calling for a caesarean delivery.
Occiput anterior position (OA position)
Your child is said to be in the occiput anterior position /occiput anterior fetal lie, when your baby is positioned head-down (near the cervix), feet up (near the ribs), facing the mother’s back with the head resting against the mother’s belly.
The occiput anterior position/occiput anterior fetal lie is not only the most common position but also the best position for a smooth delivery, as it helps the baby fit in and move through the birth canal in the easiest way.
The fetal presentation here is the baby’s head (crown to be precise).
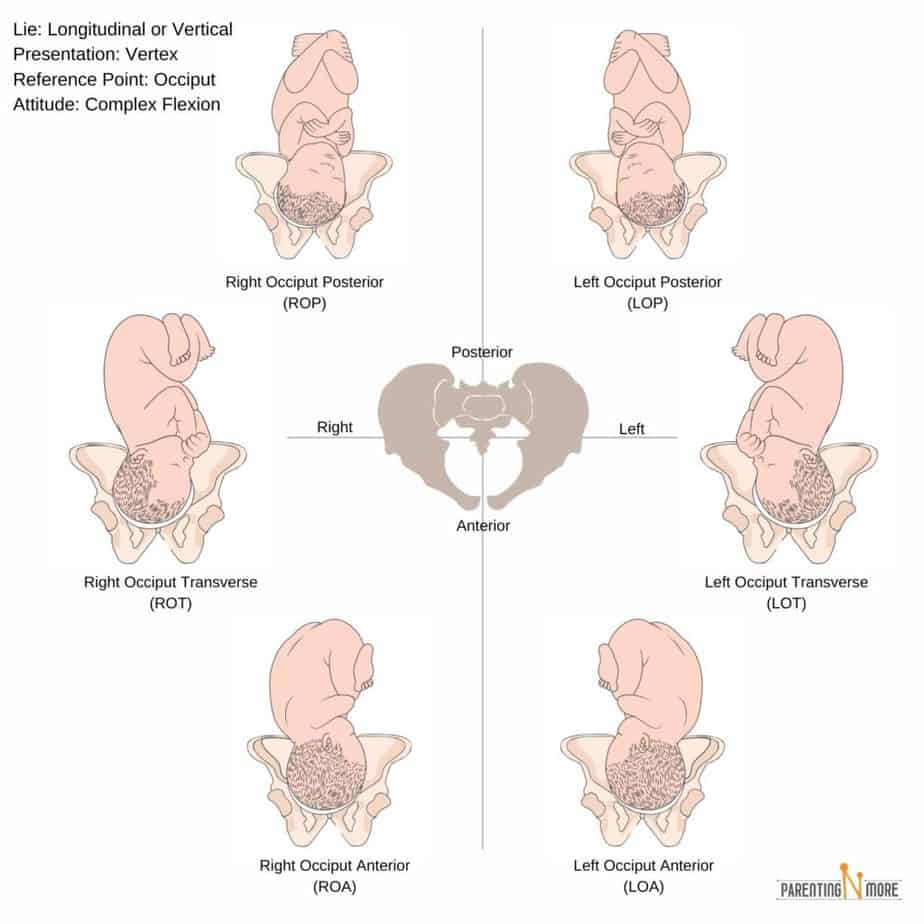
Occiput posterior position (OP baby position)
Occiput posterior position /occiput posterior fetal lie is similar to the occiput anterior fetal lie, with the only difference being that instead of facing the mother’s back, the baby faces the mother’s belly, with its back against the mother’s back.
Hence, the occiput posterior position/occiput posterior fetal lie is also referred to as the back-to-back position.
The fetal presentation in the occiput posterior position is the head, but the baby comes out face-up; hence, this is also titled the sunny-side up position .
Labor is a little more painful if the baby is in the occiput posterior position, as the mother experiences pressure on her spine. In this fetal lie/fetal position, the baby is unable to tuck its chin down to fit into the birth canal as easily as OA baby position , and hence, labor can be longer here. Your doctor may analyze your situation and may recommend a C-section.
Breech position
In this position, the baby takes up the position that is exact opposite to that of OA baby position – it settles in the head-up, feet-down position. This is one of the uncommon baby positions – merely 3-4% of
Almost all breech fetal positions require a caesarean delivery.
There are different types of breech positions –
- Complete breech : Here, the baby’s bottom is above the birth canal (making it the fetal presentation if vaginal delivery was possible), knees bent, and feet close to the bottom.
- Frank breech baby position : Again, baby’s bottom is near the birth canal, but here baby lies in V-shape, with its legs straight up near the head.
- Footling breech : Baby has one or both legs near the birth canal, making its feet the fetal presentation here.
- Flexed breech : Here one or both of the baby’s knees are bent and the buttocks and feet are at the birth canal opening.
Oblique fetal position/oblique fetal lie/oblique lie
The oblique lie , as the name says, indicates that your baby is in a diagonal or slanted position in the womb just before labor. It is one of the rarest baby positions which is also risky at the same time.
In the oblique fetal lie, the baby’s head or any other body part is not aligned with the opening of the birth canal, which can result in umbilical cord compression, and hence, lead to an emergency.
Oblique lie is risky in case of a vaginal delivery, and it can cause injuries to the baby or even be life threatening.
Therefore, if the baby cannot be turned in a proper head-down position, your doctor may recommend a C-section.
Transverse baby position/transverse lie
In the transverse baby position , the baby lies horizontally or sideways in the mother’s womb. It can have either its shoulder, back, hands, or even feet near the birth canal when in a transverse baby position. This is an extremely rare fetal lie for a full-term baby.
The transverse baby position carries the risk of damaging the placenta during delivery or in an attempt to turn the baby into a more favorable position. Here as well, the risk of umbilical cord prolapse looms, which can turn into a medical emergency. Your
doctor will examine your condition before deciding on a C-section.
Continue reading below ↓
Read this next
Vertex Presentation: How does it affect your labor & delivery?

Everything you need to know about Placenta Position & Placenta Health – with FAQs

The Ultimate List of Baby Must Haves
What is the reason behind uncommon fetal positions.
Most mothers might feel they are responsible in some way for the baby not settling in the best position. That is never the case. However, some physical traits/issues, like an unusual shape of the uterus, fibroids, or the alignment of the hip, etc. might be some of the reasons that the baby takes up unusual positions.
But do not be disheartened, there are a few ways to try to fix the baby’s position.
How to tell what position the baby is in the womb?
So, how can a mother understand the baby’s position?
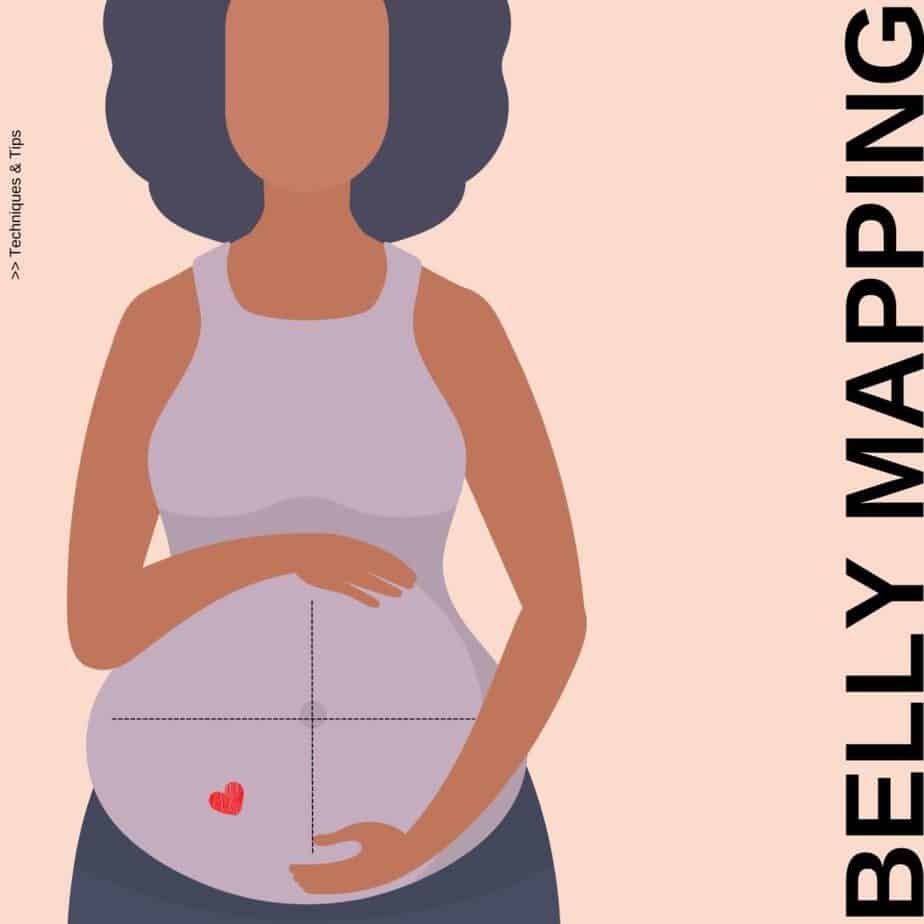
After you enter the 8 th month of pregnancy, i.e. around 32 weeks of your pregnancy, you can try belly mapping to know what baby position/fetal lie your little one is settling into.
It is recommended that you try this method right after you visit your doctor so that you have an idea where the baby’s head is placed.
All you need is non-toxic, washable paint or marker for doing this – i.e. mapping the position of your baby on your belly.
- Divide your belly area with the marker with 2 lines – one horizontal and one vertical intersecting in the middle, such that your belly is divided into 4 quadrants.
- Start by lying down and putting slight pressure with your hand on the pelvic region to feel your baby’s head. It will feel like a small bowling ball. Mark it.
- Use a fetoscope to detect your baby’s heartbeat and mark it on your belly as its heart, as shown in the image.
- Your baby’s bottom will be hard and round. You will get an idea of where exactly it can be once you know where the head is.
- Remember where you feel the baby’s movements. Its kicks and wiggles can give you an idea of where its legs and knees are. Mark it on your belly.
Mothers or their caretakers can then draw a baby on the belly to understand the exact position on their own. Of course, an ultrasound scan is the best way to know this.
Can I turn my baby in the womb?
Yes! If you are aware that your baby is not in the optimal occiput anterior position, then you can try certain simple methods to try to turn your baby before you get into labor.
- Whenever you sit, do so in such a way that your pelvis is tilted forward instead of backward.
- Sitting on exercise ball or birth ball.
- When seated, ensure that your hips are always higher than your knees.
- Do not sit continuously in one place, do move around at regular intervals.
- In a car, sit on a cushion to lift and tilt your bottom forward.
- A few times in a day go on your hands and knees (like what you do while scrubbing the floor) to encourage your baby to move to the OA fetal lie.
- Some also recommend using temperature changes as a guiding tool. A baby in the womb dislikes extreme cold temperatures and moves towards a warm one.
It is recommended to put a bag of frozen peas near the baby’s head and a warm bottle where you intend the head to be for the best position. The baby will move away from the cold towards the warmth.
- Music too is recommended; place the speakers on your belly where you want the baby’s head for the optimal position.
- Visiting a chiropractor who has an expertise in the Webster technique can also help in changing the fetal lie.
- Acupuncture is also said to help some times
These techniques do not necessarily work, as there is no scientific evidence to back them. But then, what’s the harm in trying? Do talk to you doctor in case you have doubts.
Your doctor too can use a few techniques to cajole your baby to turn to a more desirable fetal position/fetal lie for delivery. If a baby is turned to occiput anterior fetal lie, then a vaginal birth is possible.
Medically the procedure to try to turn the baby in the uterus is called External Cephalic Version (ECV) .
External (because the procedure is done externally)
Cephalic (head-down position)
Version (turning the baby)
Your doctor can attempt to turn the baby in the uterus, provided –
- The pregnancy is about 36 to 42 weeks
- Labor has not begun
- Labor has begun, but the water has not broken
- The baby has aplenty amniotic fluid to move in
- The baby is not touching the entrance of the birth canal
- The mother is carrying a single baby, not carrying twins or multiples
- The mother has had previous delivery/deliveries, which makes the stomach muscles less firm
- You are in a hospital; in case an emergency C-section is required while trying to turn the baby
Performing ECV:
To perform this, the doctor gently massages and puts firm pressure at specific places on the belly to encourage the baby to move into the OA cephalic position. This works about 65% of the time and it can help you avoid a breech baby C-section surgery .
During the procedure , the mother might be given an injection to relax her muscles or a numbing (epidural) medication to keep her comfortable. However, an epidural is not recommended in certain specific cases.
The mother and baby’s heart rate will be monitored to avoid any issues. The baby’s movements during the procedure will be monitored through an ultrasound to check if the technique is working.
The mother and baby’s health are taken into account before this procedure and the baby is closely monitored during the process to ensure it isn’t taking this negatively.
During the procedure if the mother’s contractions get stronger, water breaks or baby moves near or enters partly into the birth canal, the ECV is abandoned and an urgent C-section is done for a safe delivery.
How do I know I am ready for labor?
As the pregnancy comes to its full-term, a mother on her own will feel as though her baby has dropped lower in the abdomen. This is called Lightening .
While readying itself for delivery, the baby settles deeper in the mother’s pelvis, taking the pressure off from her diaphragm, making it easier to breathe. The baby dropping lower in the belly is among the first signs that the big day is close.
In a nutshell
Baby position/fetal lie should not be a concern until after 36 weeks of pregnancy. It is quite common that a baby might adjust its position by itself by the time the mother gets into labor or even if she is already in labor. Contractions can also help the baby turn. It is necessary that the mother stays relaxed and positive to aid this.
If the fetal lie is not in an ideal position for birth, then it is necessary that you go to the hospital for delivery in case an emergency C-section is required. It is important that skilled and experienced doctors handle a delivery with unusual baby positions.
Hope our article provides you with detailed understanding about a fetal lie and how it affects your pregnancy and labor.
Your baby’s position/fetal lie before labor may change the course of your labor and delivery experience, but at the end of it all, what matters is having a happy, healthy baby in your arms.
Happy Pregnancy!
Khushboo Kirale
You may also be interested in.

Sequential Screening – Why is it so important for you to get it done?

Placenta Previa or Low Lying Placenta: How much should you be concerned?

Looking for Diapers on Sale? Here’s where you can get great diaper deals on buying bulk diapers
Lateral Placenta: How does this placenta position impact pregnancy and delivery?

hCG levels twins vs. singleton – What’s the difference?
Anterior Placenta Position – How It Affects Pregnancy, Labor and Delivery
3 thoughts on “fetal lie or baby position in womb – does it really matter”.
so much excellent info on here, : D.
Enjoyed looking through this, very good stuff, regards.
Best Content I Have Found Every Time On This Site, Best Of Luck.
Comments are closed.
Subscribe to get our latest posts on parenting and we will make sure you don’t miss a thing!
Privacy Policy - Terms and Conditions

IMAGES
VIDEO
COMMENTS
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.. In brow presentation, the neck is moderately arched so that the brow presents first.. Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor.
Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. ... (transverse lie) and diagonal (oblique lie). Advertisement | page continues below. Photo credit: Jonathan Dimes for BabyCenter. Fetal presentation and position.
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse. Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position. Abnormal fetal lie, presentation, or position may occur with. Fetopelvic disproportion (fetus too large for the pelvic inlet)
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
Definitions. Lie - the relationship between the long axis of the fetus and the mother.. Longitudinal, transverse or oblique; Presentation - the fetal part that first enters the maternal pelvis.. Cephalic vertex presentation is the most common and is considered the safest; Other presentations include breech, shoulder, face and brow
The baby will slip head down during the contraction. Repeating the Side-lying Release in labor may also help any oblique lie whether 1 or 2 or more babies. Begin SLR before 3 cm as a preventative measure. A similar article, here on Spinning Babies ®, to serve your baby's position is the one about the Transverse Lie, and while the fetal ...
During routine prenatal care, clinicians assess fetal lie and presentation with physical examination in the late third trimester. Ultrasonography can also be done. If breech presentation is detected, external cephalic version can sometimes move the fetus to vertex presentation before labor, usually at 37 or 38 weeks.
With frank breech presentation, your baby's bottom faces the cervix and their legs are straight up. This is the most common type of breech presentation. ... Another type is called oblique ...
Delivery presentations. Delivery presentation describes the way the baby is positioned to come down the birth canal for delivery. Your baby must pass through your pelvic bones to reach the vaginal opening. The ease at which this passage will take place depends on how your baby is positioned during delivery. The best position for the baby to be ...
In an oblique position, doctors explain that the head is just at the side of the pelvic inlet. This is close to the optimal head-down position because if the baby moves slightly to put its head at the center of the pelvic inlet, it can have the vertex presentation at the time of delivery. On the other hand, the oblique position can also become ...
In the cephalic presentation, the baby is head down, chin tucked to chest, facing their mother's back. This position typically allows for the smoothest delivery, as baby's head can easily move down the birth canal and under the pubic bone during childbirth. While that's not to say there can't be complications, this is the ideal position ...
When a fetus is in a noncephalic or nonvertex presentation, it is considered malpresentation. Fetal malposition is a term used to describe a fetus that is rotated so that it is in the occiput posterior or occiput transverse positions. Both of these conditions are associated with increased rates of adverse maternal and perinatal events ...
INTRODUCTION. Transverse lie refers to a fetal presentation in which the fetal longitudinal axis lies perpendicular to the long axis of the uterus. It can occur in either of two configurations: The curvature of the fetal spine is oriented downward (also called "back down" or dorsoinferior), and the fetal shoulder presents at the cervix ( figure ...
Face presentation. This is when your baby is head-first but stretching their neck, with their face against the cervix. Transverse lie. This is when your baby is lying sideways. Their back, shoulders, arms or legs may be the first to enter the birth canal. Oblique lie. This is when your baby is lying diagonally.
A transverse baby position, also called transverse fetal lie, is when the fetus is sideways—at a 90-degree angle to your spine—instead of head up or head down. This development means that a vaginal delivery poses major risks to both you and the fetus. Sometimes, a transverse fetus will turn itself into the head-down position before you go ...
There are four posterior positions. The direct OP is the classic posterior position with the baby facing straight forward. Right Occiput Transverse (ROT) is a common starting position in which the baby has a bit more likelihood of rotating to the posterior during labor than to the anterior. Right Occiput Posterior usually involves a straight back with a lifted chin (in the first-time mother).
The oblique position in pregnancy refers to a fetal presentation where the baby lies diagonally in the uterus, neither in a head-down… 1 min read · Jul 21, 2023 See all from Arjun Narayan
Oblique lie Face presentation Brow presentation . In most cases of a normal vertex (head down) presentation, the baby's head is flexed with the chin close to the baby's chest. In these cases, the presenting part is the occiput, the posterior part of the baby's head.
In a transverse or oblique presentation, smooth delivery of the fetus may be achieved by transverse incision of the uterine body based on the fetal presentation, as carefully determined in advance. The operator preoccupied with the lower uterine segment may make an incision in a narrow lower uterine segment, thereby possibly inducing injury at ...
A malpresentation is diagnosed when any part of the baby is presenting to the maternal pelvis other than the vertex of the fetal head. A malposition is diagnosed when the fetal head is in any position other than occipito-anterior (OA) flexed vertex. Both malpresentation and malposition are associated with prolonged or obstructed labour, fetal and maternal morbidity, and potential mortality, if ...
To describe the baby's accurate position in the womb, medical professionals use both the terms - fetal position and fetal presentation. Fetal lie/fetal position, also referred to as baby position in womb before labor, establishes where the baby's face is - toward the mother's back or her belly.. Fetal presentation actually tells you what part of the baby's body will lead the way ...