Understanding the Overlap Between Autism, Attention Deficit Hyperactivity Disorder (ADHD), and Anxiety

Autistic traits vary from person to person, impacting how individuals are identified as being autistic and when they receive their diagnosis, and they can also influence how individuals respond to different interventions. One factor contributing to this variability is the coexistence of autism with other conditions like anxiety and attention-deficit/hyperactivity disorder (ADHD).
Estimates suggest that 40-60% of autistic children also have anxiety and/or ADHD.
When autistic children have either anxiety or ADHD, it can make things more challenging for them in several ways. For instance, they may find it harder to manage their emotions, or they may face greater difficulties with things like sleeping and eating habits. It also impacts their academic performance. Because of this, understanding the impact of co-occurring anxiety and ADHD on the lives of autistic individuals is crucial. Currently, there’s limited knowledge about how these conditions affect autistic children, especially in early childhood. Furthermore, we lack insights into their influence on commonly used brain and behavioral measures employed in research and clinical trials.

To bridge these gaps, Kimberly Carpenter, PhD , assistant professor in the Duke Center for Autism and Brain Development, launched the Autism HERO study in 2021. This study takes a comprehensive approach, combining parent reports with play-based and brain assessments to examine how co-occurring anxiety and ADHD affect autistic children aged 4 to 7 years. Importantly, several challenges exist in understanding the unique impact of ADHD and anxiety on autistic individuals. These include difficulty differentiating between the conditions due to overlapping features, absence of guidelines for assessing anxiety and ADHD in autistic individuals, and reliance on measures created and standardized for non-autistic populations.
To address these challenges, Dr. Carpenter is collaborating with experts in ADHD diagnosis in autism (Drs. Naomi Davis, Julia Schechter, and Rachel Aiello from Duke University) and anxiety in autism (Dr. Connor Kerns from the University of British Columbia) to develop new diagnostic guidelines for co-occurring anxiety and ADHD in young autistic children. These guidelines will be coupled with assessments across various domains to better understand the distinct effects of anxiety and ADHD on clinical presentation, behavioral outcomes, and the neurobiology of autism. This research aims to support the development of early detection and intervention methods for co-occurring anxiety and ADHD in young autistic children, with the ultimate goal of improving the quality of life for all autistic individuals.
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support

AuDHD: When Autism and ADHD Co-Occur
The characteristics of these neurotypes overlap in surprising ways
Dr. Amy Marschall is an autistic clinical psychologist with ADHD, working with children and adolescents who also identify with these neurotypes among others. She is certified in TF-CBT and telemental health.
:max_bytes(150000):strip_icc():format(webp)/HeadShot2-0e5cbea92b2948a1a2013271d90c2d1f.jpg)
Claire Eggleston, LMFT-Associate is a neurodivergent therapist and specializes in and centers on the lived experiences of autistic and ADHD young adults, many of whom are also in the queer and disability communities. She prioritizes social justice and intertwines community care into her everyday work with clients.
:max_bytes(150000):strip_icc():format(webp)/DSC_03892-780ad18b393347f5806d4206ac4d16ec.jpg)
How Are Autism and ADHD Connected?
- Complications
Keep in Mind
Attention-deficit/hyperactivity disorder ( ADHD ) and autism spectrum disorder (ASD) are both noted as neurodevelopmental disorders in the DSM-5, however, contemporary perspectives emphasize that they're just different neurotypes from what is considered neurotypical. Even so, neurodivergence can lead to challenges, though neurodiversity reflects a variety of strengths among humanity.
While approximately 10% of the population has ADHD, some research has shown that 40% of autistic people have ADHD, with other studies suggesting that the rate may be closer to 70%. Conversely, while 2-3% of people are autistic, 20-50% of those with ADHD are also autistic.
In this article, we discuss the connection between ADHD and autism and how these diagnoses present when they co-exist.
Maskot / Getty Images
As the statistics above indicate, people with ADHD are significantly more likely to be autistic compared to those who do not have ADHD, and vice versa.
However, before 2013, the Diagnostic and Statistical Manual of Mental Disorders indicated that an individual could not meet the diagnostic criteria for both diagnoses. Despite this requirement, the comorbidity rate of diagnosing both autism and ADHD was 45% at this time.
ADHD and autism share common characteristics, including inattention, atypical movement (such as fidgeting or stimming behaviors ), social difficulties, and differences in learning style. Both autistic people and those with ADHD can experience sensory sensitivities as well.
Despite the overlap, though, current research indicates that ADHD and autism are distinct , separate diagnoses rather than one neurotype on the same spectrum.
Potential Complications
Due to symptom overlap, autistic individuals who also have ADHD might have more difficulty receiving an accurate diagnosis .
Many diagnostic scales emphasize symptoms—more commonly referred to as traits or characteristics—as they tend to manifest when the individual only meets the criteria for autism or ADHD rather than both diagnoses. So a unique combination of symptoms that may not neatly fit into just one diagnostic “box” can be overlooked or misunderstood.
Even though an autistic person is more likely to have ADHD than someone who is not autistic, and someone with ADHD is more likely to be autistic than someone who does not have ADHD, professionals often only assess for one diagnosis at a time.
If you have one diagnosis, it may be beneficial to request testing for the other if you feel that your existing diagnosis does not fully describe your experience.
Sometimes, autistic people with ADHD may have difficulty functioning in a world created for neurotypical brains. Sensory issues and executive dysfunction can make many daily tasks challenging. If you are struggling, look into what support services might be available to you.
Diagnosing AuDHD
ADHD and autism can both be diagnosed by specifically qualified medical and mental health professionals. Although many people have both diagnoses, providers may not evaluate for both unless you request it. A qualified evaluator will use a variety of diagnostic tools when determining if someone meets the diagnostic criteria for ADHD, autism, or both.
Most psychological evaluations for any diagnosis will include a diagnostic interview, during which they will ask several questions about history, symptoms, mental health, and traits that might be consistent with ADHD or autism. Since neurodevelopmental diagnoses like ADHD and autism occur from birth or early childhood, this interview will likely include questions about early developmental years.
If possible, the evaluator may ask to speak to someone who took care of you when you were a baby, but this information (called a collateral interview) is not essential in order to receive a diagnosis.
Diagnosing ADHD
Measures commonly used to diagnose ADHD include:
- Conners Rating Scales : There are Conners forms for ages 2 to 6 (Conners Early Childhood), 6 to 18 (Conners 4), and 18+ (Conners Adult ADHD Rating Scales). Depending on your age, there are self-report and observer rating scales that yield information about your symptoms and how closely those traits correlate with the diagnostic criteria for ADHD .
- Tests of Sustained Attention : Many different attention tasks exist, such as the Test of Variable Attention. These tasks require an individual to demonstrate their ability to focus on a task.
- Behavior Rating Inventory of Executive Functioning (BRIEF) : There are child and adult versions of this form, which assesses the individual’s ability to break down large projects, complete tasks, and sustain attention.
Diagnosing Autism
Measures used to diagnose autism include:
- Autism Diagnostic Observation Schedule. This test utilizes a series of tasks, which the evaluator uses to assess thought processes, behavior, and communication style for consistency with the diagnostic criteria for autism.
- Autism Spectrum Rating Scales. This observational form takes data from parents and teachers or childcare professionals to determine if a child’s behaviors are consistent with autism. It does not have a self-report form.
- Monteiro Interview Guidelines for Diagnosing the Autism Spectrum. This structured interview gathers history and current information about adults to determine if they meet the criteria for autism.
Depending on your presenting concerns, an evaluator might also complete a cognitive assessment (also known as an IQ test ). Some autistic people or those with ADHD have learning difficulties, and the IQ test may provide valuable information about how to support your learning.
They may also administer screeners for various other mental health issues, like anxiety or depression, that can co-occur with autism and ADHD.
Support for People with AuDHD
Since the world is not set up for autistic and ADHD brains, many people with either or both diagnoses need support for daily living, work, finances, or other areas. Traditionally, “ treatment ” for autism and ADHD has emphasized making the person act or appear neurotypical rather than supporting their needs. This has led to increased burnout and trauma symptoms and is increasingly discouraged.
These organizations offer more information on supporting autistic people with ADHD or for finding support regarding your own diagnoses:
- The Autistic Self-Advocacy Network : Created by and for the autistic community, ASAN provides educational information about autism and advocates for autistic-affirming policy changes.
- Neuroclastic : This online non-profit organization elevates autistic voices and stories as well as advocates for a neurodiversity-affirming world.
- CHADD : This organization provides information and community support for people with ADHD and their loved ones.
- ADDitude Mag : This magazine and blog provides medically accurate and community-based information about ADHD.
Rather than encouraging autistic people with ADHD to hide their traits, support looks like creating environments where their needs are met without having to hide or mask . Listen to community members, and make decisions about support based on what autistic and ADHD folks say is helpful to them.
Hours C, Recasens C, Baleyte JM. ASD and ADHD comorbidity: what are we talking about? Front Psychiatry . 2022;13:837424.
Rusting R. Decoding the overlap between autism and ADHD . Spectrum . Published online 2018.
American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders (4th ed., Text Revision). Washington, DC: Author.
Gordon-Lipkin E, Marvin AR, Law JK, Lipkin PH. Anxiety and mood disorder in children with autism spectrum disorder and ADHD . Pediatrics . 2018;141(4):e20171377.
Sokolova E, Oerlemans AM, Rommelse NN, et al. A causal and mediation analysis of the comorbidity between attention deficit hyperactivity disorder (Adhd) and autism spectrum disorder(Asd) . J Autism Dev Disord . 2017;47(6):1595-1604.
Mayes SD, Calhoun SL, Mayes RD, Molitoris S. Autism and ADHD: Overlapping and discriminating symptoms . Research in Autism Spectrum Disorders . 2012;6(1):277-285.
Higgins JM, Arnold SR, Weise J, Pellicano E, Trollor JN. Defining autistic burnout through experts by lived experience: Grounded Delphi method investigating #AutisticBurnout . Autism . 2021;25(8):2356-2369.
By Amy Marschall, PsyD Dr. Amy Marschall is an autistic clinical psychologist with ADHD, working with children and adolescents who also identify with these neurotypes among others. She is certified in TF-CBT and telemental health.
Understanding and Supporting Attention Deficit Hyperactivity Disorder (ADHD) in the Primary School Classroom: Perspectives of Children with ADHD and their Teachers
- Original Paper
- Open access
- Published: 01 July 2022
- Volume 53 , pages 3406–3421, ( 2023 )
Cite this article
You have full access to this open access article

- Emily McDougal ORCID: orcid.org/0000-0001-7684-7417 1 , 3 ,
- Claire Tai 1 ,
- Tracy M. Stewart ORCID: orcid.org/0000-0002-8807-1174 2 ,
- Josephine N. Booth ORCID: orcid.org/0000-0002-2867-9719 2 &
- Sinéad M. Rhodes ORCID: orcid.org/0000-0002-8662-1742 1
37k Accesses
6 Citations
16 Altmetric
Explore all metrics
Children with Attention Deficit Hyperactivity Disorder (ADHD) are more at risk for academic underachievement compared to their typically developing peers. Understanding their greatest strengths and challenges at school, and how these can be supported, is vital in order to develop focused classroom interventions. Ten primary school pupils with ADHD (aged 6–11 years) and their teachers (N = 6) took part in semi-structured interviews that focused on (1) ADHD knowledge, (2) the child’s strengths and challenges at school, and (3) strategies in place to support challenges. Thematic analysis was used to analyse the interview transcripts and three key themes were identified; classroom-general versus individual-specific strategies, heterogeneity of strategies, and the role of peers. Implications relating to educational practice and future research are discussed.
Similar content being viewed by others

Evidence-Based Assessment and Intervention for ADHD in School Psychology
The ecology of adhd in the schools.
Effective Assessment and Intervention for Children with ADHD in Rural Elementary School Settings
Avoid common mistakes on your manuscript.
Characterised by persistent inattention, hyperactivity and impulsivity (APA, 2013), ADHD is a neurodevelopmental disorder thought to affect around 5% of children (Russell et al., 2014 ) although prevalence estimates vary (Sayal et al., 2018 ). Although these core symptoms are central to the ADHD diagnosis, those with ADHD also tend to differ from typically developing children with regards to cognition and social functioning (Coghill et al., 2014 ; Rhodes et al., 2012 ), which can negatively impact a range of life outcomes such as educational attainment and employment (Classi et al., 2012 ; Kuriyan et al., 2013 ). Indeed, academic outcomes for children with ADHD are often poor, particularly when compared with their typically developing peers (Arnold et al., 2020 ) but also compared to children with other neurodevelopmental disorders, such as autism (Mayes et al., 2020 ). Furthermore, children with ADHD can be viewed negatively by their peers. For example, Law et al. ( 2007 ) asked 11–12-year-olds to read vignettes describing the behaviour of a child with ADHD symptoms, and then use an adjective checklist to endorse those adjectives that they felt best described the target child. The four most frequently ascribed adjectives were all negative (i.e. ‘careless’, ‘lonely’, ‘crazy’, and ‘stupid’). These negative perceptions can have a significant impact on the wellbeing of individuals with ADHD, including self-stigmatisation (Mueller et al., 2012 ). There is evidence that teachers with increased knowledge of ADHD report more positive attitudes towards children with ADHD compared to those with poor knowledge (Ohan et al., 2008 ) and thus research that identifies the characteristics of gaps in knowledge is likely to be important in addressing stigma.
Previous research of teachers' ADHD knowledge is mixed, with the findings of some studies indicating that teachers have good knowledge of ADHD (Mohr-Jensen et al., 2019 ; Ohan et al., 2008 ) and others suggesting that their knowledge is limited (Latouche & Gascoigne, 2019 ; Perold et al., 2010 ). Ohan et al. ( 2008 ) surveyed 140 primary school teachers in Australia who reported having experience of teaching at least one child with ADHD. Teachers completed the ADHD Knowledge Scale which consisted of 20 statements requiring a response of either true or false (e.g. “A girl/boy can be appropriately labelled as ADHD and not necessarily be over-active ”). They found that, on average, teachers answered 76.34% of items correctly, although depth of knowledge varied across the sample. Almost a third of the sample (29%) had low knowledge of ADHD (scoring less than 69%), with just under half of teachers (47%) scoring in the average range (scores of 70–80%). Only a quarter (23%) had “high knowledge” (scores above 80%) suggesting that knowledge varied considerably. Furthermore, Perold et al. ( 2010 ) asked 552 teachers in South Africa to complete the Knowledge of Attention Deficit Disorders Scale (KADDS) and found that on average, teachers answered only 42.6% questions about ADHD correctly. Responses of “don’t know” (35.4%) and incorrect responses (22%) were also recorded, indicating gaps in knowledge as well as a high proportion of misconceptions. Similar ADHD knowledge scores were reported in Latouche and Gascoigne’s ( 2019 ) study, who found that teachers enrolled into their ADHD training workshop in Australia had baseline KADDS scores of below 50% accuracy (increased to above 80% accuracy after training).
The differences in ADHD knowledge reported between Ohan et al. ( 2008 ) and the more recent studies could be due to the measures used. Importantly, when completing the KADDS, respondents can select a “don’t know” option (which receives a score of 0), whereas the ADHD Knowledge Scale requires participants to choose either true or false for each statement. The KADDS is longer, with a total of 39 items, compared to the 20-item ADHD Knowledge Scale, offering a more in-depth knowledge assessment. The heterogeneity of measures used within the described body of research is also highlighted within Mohr-Jensen et al. ( 2019 ) systematic review; the most frequently used measure (the KADDS) was only used by 4 out of the 33 reviewed studies, showing little consensus on the best way to measure ADHD knowledge. Despite these differences in measurement, the findings from most studies indicate that teacher ADHD knowledge is lacking.
Qualitative methods can provide rich data, facilitating a deeper understanding of phenomena that quantitative methods alone cannot reveal. Despite this, there are very few examples in the literature of qualitative methods being used to understand teacher knowledge of ADHD. In one example, Lawrence et al. ( 2017 ) interviewed fourteen teachers in the United States about their experiences of working with pupils with ADHD, beginning with their knowledge of ADHD. They found that teachers tended to focus on the external symptoms of ADHD, expressing knowledge of both inattentive and hyperactive symptoms. Although this provided key initial insights into the nature of teachers’ ADHD knowledge, only a small section of the interview schedule (one out of eight questions/topics) directly focused on ADHD knowledge. Furthermore, none of the questions asked directly about strengths, with answers focusing on difficulties. It is therefore difficult to determine from this study whether teachers are aware of strengths and difficulties outside of the triad of symptoms. A deeper investigation is necessary to fully understand what teachers know, and to identify areas for targeted psychoeducation.
Importantly, improved ADHD knowledge may impact positively on the implementation of appropriate support for children with ADHD in school. For example, Ohan et al. ( 2008 ) found that teachers with high or average ADHD knowledge were more likely to perceive a benefit of educational support services than those with low knowledge, and teachers with high ADHD knowledge were also more likely to endorse a need for, and seek out, those services compared to those with low knowledge. Furthermore, improving knowledge through psychoeducation may be important for improving fidelity to interventions in ADHD (Dahl et al., 2020 ; Nussey et al., 2013 ). Indeed, clinical guidelines recommend inclusion of psychoeducation in the treatment plan for children with ADHD and their families (NICE, 2018 ). Furthermore, Jones and Chronis-Tuscano ( 2008 ) found that educational ADHD training increased special education teachers’ use of behaviour management strategies in the classroom. Together, these findings suggest that understanding of ADHD may improve teachers’ selection and utilisation of appropriate strategies.
Child and teacher insight into strategy use in the classroom on a practical, day-to-day level may provide an opportunity to better understand how different strategies might benefit children, as well as the potential barriers or facilitators to implementing these in the classroom. Previous research with teachers has shown that aspects of the physical classroom can facilitate the implementation of effective strategies for autistic children, for example to support planning with the use of visual timetables (McDougal et al., 2020 ). Despite this, little research has considered the strategies that children with ADHD and their teachers are using in the classroom to support their difficulties and improve learning outcomes. Moore et al. ( 2017 ) conducted focus groups with UK-based educators (N = 39) at both primary and secondary education levels, to explore their experiences of responding to ADHD in the classroom, as well as the barriers and facilitators to supporting children. They found that educators mostly reflected on general inclusive strategies in the classroom that rarely targeted ADHD symptoms or difficulties specifically, despite the large number of strategies designed to support ADHD that are reported elsewhere in the literature (DuPaul et al., 2012 ; Richardson et al., 2015 ). Further to this, when interviewing teachers about their experiences of teaching pupils with ADHD, Lawrence et al. ( 2017 ) specifically asked about interventions or strategies used in the classroom with children with ADHD. The reported strategies were almost exclusively behaviourally based, for example, allowing children to fidget or move around the classroom, utilising rewards, using redirection techniques, or reducing distraction. This lack of focus on cognitive strategies is surprising, given the breadth of literature focusing on the cognitive difficulties in ADHD (e.g. Coghill, et al., 2014 ; Gathercole et al., 2018 ; Rhodes et al., 2012 ). Furthermore, to our knowledge research examining strategy use from the perspective of children with ADHD themselves, or strengths associated with ADHD, is yet to be conducted.
Knowledge and understanding of ADHD in children with ADHD has attracted less investigation than that of teachers. In a Canadian sample of 8- to 12-year-olds with ADHD (N = 29), Climie and Henley ( 2018 ) found that ADHD knowledge was highly varied between children; scores on the Children ADHD Knowledge and Opinions Scale ranged from 5 to 92% correct (M = 66.53%, SD = 18.96). The authors highlighted some possible knowledge gaps, such as hyperactivity not being a symptom for all people with ADHD, or the potential impact upon social relationships, however the authors did not measure participant’s ADHD symptoms, which could influence how children perceive ADHD. Indeed, Wiener et al ( 2012 ) has shown that children with ADHD may underestimate their symptoms. If this is the case, it would also be beneficial to investigate their understanding of their own strengths and difficulties, as well as of ADHD more broadly. Furthermore, if children do have a poor understanding of ADHD, they may benefit from psychoeducational interventions. Indeed, in their systematic review Dahl et al. ( 2020 ) found two studies in which the impact of psychoeducation upon children’s ADHD knowledge was examined, both of which reported an increase in knowledge as a consequence of the intervention. Understanding the strengths and difficulties of the child, from the perspective of the child and their teacher, will also allow the design of interventions that are individualised, an important feature for school-based programmes (Richardson et al., 2015 ). Given the above, understanding whether children have knowledge of their ADHD and are aware of strategies to support them would be invaluable.
Teacher and child knowledge of ADHD and strategies to support these children is important for positive developmental outcomes, however there is limited research evidence beyond quantitative data. Insights from children and teachers themselves is particularly lacking and the insights which are available do not always extend to understanding strengths which is an important consideration, particularly with regards to implications for pupil self-esteem and motivation. The current study therefore provides a vital examination of the perspectives of both strengths and weaknesses from a heterogeneous group of children with ADHD and their teachers. Our sample reflects the diversity encountered in typical mainstream classrooms in the UK and the matched pupil-teacher perspectives enriches current understandings in the literature. Specifically, we aimed to explore (1) child and teacher knowledge of ADHD, and (2) strategy use within the primary school classroom to support children with ADHD. This novel approach, from the dual perspective of children and teachers, will enable us to identify potential knowledge gaps, areas of strength, and insights on the use of strategies to support their difficulties.
Participants
Ten primary school children (3 female) aged 7 to 11 years (M = 8.7, SD = 1.34) referred to Child and Adolescent Mental Health Services (CAMHS) within the NHS for an ADHD diagnosis were recruited to the study. All participant characteristics are presented in Table 1 . All children were part of the Edinburgh Attainment and Cognition Cohort and had consented to be contacted for future research. Children who were under assessment for ADHD or who had received an ADHD diagnosis were eligible to take part. Contact was established with the parent of 13 potential participants. Two had undergone the ADHD assessment process with an outcome of no ADHD diagnosis and were therefore not eligible to take part, and one could not take part within the timeframe of the study. The study was approved by an NHS Research Ethics Committee and parents provided informed consent prior to their child taking part. Co-occurrences data for all participants was collected as part of a previous study and are reported here for added context. All of the children scored above the cut-off (T-score > 70) for ADHD on the Conners 3 rd Edition Parent diagnostic questionnaire (Conners, 2008 ). The maximum possible score for this measure is 90. At the point of interview, seven children had received a diagnosis of ADHD, two children were still under assessment, and one child had been referred for an ASD diagnosis (Table 1 ). The ADHD subtype of each participant was not recorded, however all children scored above the cut-off for both inattention (M = 87.3, SD = 5.03) and hyperactivity (M = 78.6, SD = 5.8) which is indicative of ADHD combined type. Use of stimulant medication was not recorded at the time of interview.
Following the child interview and receipt of parental consent, each child’s school was contacted to request their teacher’s participation in the study. Three teachers could not take part within the timeframe of the study, and one refused to take part. Six teachers (all female) were successfully contacted and gave informed consent to participate.
Due to the increased likelihood of co-occurring diagnoses in the target population, we also report Autism Spectrum Disorder (ASD) symptoms and Developmental Co-ordination Disorder (DCD) symptoms using the Autism Quotient 10-item questionnaire (AQ-10; Allison et al., 2012 ) and Movement ABC-2 Checklist (M-ABC2; Henderson et al., 2007 ) respectively, both completed by the child’s parent.
Scores of 6 and above on the AQ-10 indicates referral for diagnostic assessment for autism is advisable. All but one of the participants scored below the cut-off on this measure (M = 3.6, SD = 1.84).
The M-ABC2 checklist categorises children as scoring green, amber or red based on their scores. A green rating (up to the 85th percentile) indicates no movement difficulty, amber ratings (between 85 and 95th percentile) indicate risk of movement difficulty, and red ratings (95th percentile and above) indicate high likelihood of movement difficulty. Seven of the participants received a red rating, one an amber rating, and two green ratings.
Socioeconomic status (SES) is also known to impact educational outcomes, therefore the SES of each child was calculated using the Scottish Index of Multiple Deprivation (SIMD), which is an area-based measure of relative deprivation. The child’s home postcode was entered into the tool which provided a score of deprivation on a scale of 1 to 5. A score of 1 is given to the 20% most deprived data zones in Scotland, and a score of 5 indicates the area was within the 20% least deprived areas.
Semi-Structured Interview
The first author, who is a psychologist, conducted interviews with each participant individually, and then a separate interview with their teacher. This was guided by a semi-structured interview schedule (see Appendix A, Appendix B) developed in line with our research questions, existing literature, and using authors (T.S. and J.B.) expertise in educational practice. The questions were adapted to be relevant for the participant group. For example, children were asked “If a friend asked you to tell them what ADHD is, what would you tell them?” and teachers were asked, “What is your understanding of ADHD or can you describe a typical child with ADHD?”. The schedule comprised two key sections for both teachers and children. The first section focused on probing the participant’s understanding and knowledge of ADHD broadly. The second section focused on the participating child’s academic and cognitive strengths and weaknesses, and the strategies used to support them. Interviews with children took place in the child’s home and lasted between 19 and 51 min (M = 26.3, SD = 10.9). Interviews with teachers took place at their school and were between 28 and 50 min long (M = 36.5, SD = 7.61). Variation in interview length was mostly due to availability of the participant and/or age of the child (i.e. interviews with younger children tended to be shorter). All interviews were recorded on an encrypted voice recorder and transcribed by the first author prior to data analysis. Pseudonyms were randomly generated for each child to protect anonymity.
Reflexive thematic analysis was used to analyse the data (Braun & Clarke, 2019 ). This flexible approach allows the data to drive the analysis, putting the participant at the centre of the research and placing high value on the experiences and perspectives of individual participants (Braun & Clarke, 2006 ). The six phases of reflexive thematic analysis as outlined by Braun and Clarke were followed: (1) familiarisation, (2) generating codes, (3) constructing themes, (4) revising themes, (5) defining themes, (6) producing the report. Due to the exploratory nature of this study, bottom-up inductive coding was used. Two of the authors (E.M. and C.T.) worked collaboratively to construct and subsequently define the themes using the process described above. More specifically, one author (E.M.) generated codes, with support from another author (C.T.). Collated codes and data were then abstracted into potential themes, which were reviewed and refined using relevant literature, as well as within the wider context of the data. This process continued until all themes were agreed upon.
In the first part of the analysis, focus was placed on summarising the participants’ understanding of ADHD, as well as what they thought their biggest strengths and challenges were at school. Following this, an in-depth analysis of the strategies used in the classroom was conducted, taking into account the perspective of both teachers and children, aiming to generate themes from the data.
Knowledge of ADHD
Children and teachers were asked about their knowledge of ADHD. When asked if they had ever heard of ADHD, the majority of children said yes. Some of the children could not explain to the interviewer what ADHD was or responded in a way that suggested a lack of understanding ( “it helps you with skills” – Niall, 7 years; “ Well it’s when you can’t handle yourself and you’re always crazy and you can just like do things very fast”— Nathan, 8 years). Very few of the children were able to elaborate accurately on their understanding of ADHD, which exclusively focused on inattention. For example, Paige (8 years) said “ its’ kinda like this thing that makes it hard to concentrate ” and Finn (10 years) said “ they get distracted more just in different ways that other people would ”. This suggests that children with ADHD may lack or have a limited awareness or understanding of their diagnosis.
When asked about their knowledge of ADHD, teachers tended to focus on the core symptoms of ADHD. All teachers directly mentioned difficulties with attention, focus or concentration, and most directly or indirectly referred to hyperactivity (e.g. moving around, being in “ overdrive ”). Most teachers also referred to social difficulties as a feature of ADHD, including not following social rules, reacting inappropriately to other children and appearing to lack empathy, which they suggested could be linked to impulsivity. For example, “ reacting in social situations where perhaps other children might not react in a similar way” (Paige’s teacher) and “ They can react really really quickly to things and sometimes aggressively” (Eric’s teacher). Although no teachers directly mentioned cognitive difficulties, some referred to behaviours indicative of cognitive difficulties, for example, “ they can’t store a lot of information at one time” (Eric’s teacher) and, “ it’s not just the concentration it’s the amount they can take in at a time as well” (Nathan’s teacher), which may reflect processing or memory differences. Heterogeneity was mentioned, in that ADHD can mean different things for different children (e.g., “ I think ADHD differs from child to child and I think that’s really important” —Nathan’s teacher). Finally, academic difficulties as a feature of ADHD were also mentioned (e.g., “ a child… who finds some aspects of school life, some aspects of the curriculum challenging ”—Jay’s teacher).
After being asked to give a general description of ADHD, each child was asked about their own strengths at school and teachers were also asked to reflect on this topic for the child taking part.
When asked what they like most about school, children often mentioned art or P.E. as their preferred subjects. A small number of children said they enjoyed maths or reading, but this was not common and the majority described these subjects as a challenge or something they disliked. There was also clear link between the aspects of school children enjoyed, and what they perceived to be a strength for them. For example, when asked what he liked about school, Eric (10 years) said, “ Math, I’m pretty good at that”, or when later asked what they were good at, most children responded with the same answers they gave when asked what they liked about school. It is interesting to note that subjects such as art or P.E. generally have a different format to more traditionally academic subjects such as maths or literacy. Indeed, Felicity (11 years) said, “ I quite like art and drama because there’s not much reading…and not really too much writing in any of those” . Children also tended to mention the non-academic aspects of school, such as seeing their friends, or lunch and break times.
Teachers’ descriptions of the children’s strengths were much more variable compared to strengths mentioned by children. Like the children, teachers tended to consider P.E and artistic activities to be a strength for the child with ADHD. Multiple teachers referred to the child having a good imagination and creative skills. For example, “ she’s a very imaginative little girl, she has a great ability to tell stories and certainly with support write imaginative stories” (Paige’s teacher) . Teachers referred to other qualities or characteristics of the child as strengths, although these varied across teachers. These included openness, both socially but also in the context of willingness to learn or being open to new challenges, being a hard worker, or an enjoyable person to be around (e.g., “ he is the loveliest little boy, I’ve got a lot of time for [Nathan]. He makes me smile every day, you know, he just comes out with stuff he’s hilarious”— Nathan’s teacher). The most noticeable theme that emerged from this data was that when some teachers began describing one of the child’s strengths, it was suffixed with a negative. For example, Henry’s teacher said, “ He’s got a very good imagination, his writing- well not so much the writing of the stories, he finds writing quite a challenge, but his verbalising of ideas he’s very imaginative”. This may reflect that while these children have their own strengths, these can be limited by difficulties. Indeed, Paige’s teacher said, “ I think she’s a very able little girl without a doubt, but there is a definite barrier to her learning in terms of her organisation, in terms of her focus” , which reinforces this notion.
Children were asked directly about what they disliked about school, and what they found difficult. Children tended to focus more on specific subjects, with maths and aspects of literacy being the most frequently mentioned of these. Children referred to difficulties with or a dislike for reading, writing and/or spelling activities, for example, Rory (9 years) said “ Well I suppose spelling because … sometimes we have to do some boring tasks like we have to write it out three times then come up with the sentence for each one which takes forever and it’s hard for me to think of the sentences if I’m not ready” . Linking this with known cognitive difficulties in ADHD, it is interesting to note that both memory and planning are implicated in this quote from Rory about finding spelling challenging. In terms of writing, children referred to both the physical act of writing (e.g., “ probably writing cause sometimes I forget my finger spaces ”—Paige, 8 years; “ [writing the alphabet is] too hard… like the letters joined together … [and] I make mistakes” —Jay, 7 years) as well as the planning associated with writing a longer piece of work (e.g. “ when I run out of ideas for it, it’s really hard to think of some more so I don’t usually get that much writing done ”—Rory (9 years) .
Aside from academic subjects, several children referred to difficulties with focus or attention (e.g. “ when I find it hard to do something I normally kind of just zone out ”—Felicity, 11 years, “ probably concentrating sometimes ”—Rory, 9 years), but boredom was also a common and potentially related theme (e.g. “ Reading is a bit hard though … it just sometimes gets a bit boring” —Finn, 10 years, “ I absolutely hate maths … ‘cause it’s boring ”—Paige, 8 years). It could be that children with ADHD find it more difficult to concentrate during activities they find boring. Indeed, when Jay (7 years) was asked how it made him feel when he found something boring, he said “ it made me not do my work ”. Some children also alluded to the social difficulties faced at school, which included bullying and difficulties making friends (e.g. “ just making all kind of friends [is difficult] ‘cause the only friend that I’ve got is [name redacted] ”—Nathan, 8 years; “ sometimes finding a friend to play with at break time [is difficult] ” – Paige, 8 years; “ there’s a lot of people in my school that they bully me” —Eric, 10 years).
When asked what they thought were the child’s biggest challenges at school, teachers' responses were relatively variable, although some common themes were identified. As was the case for children, teachers reflected on difficulties with attention, which also included being able to sit at the table for long periods of time (e.g. “ I would say he struggles the most with sitting at his table and focusing on one piece of work ”—Henry’s teacher). Teachers did also mention difficulties with subjects such as maths and literacy, although this varied from child to child, and often they discussed these in the context of their ADHD symptom-related difficulties. For example, Eric’s teacher said, “ we’ve struggled to get a long piece of writing out of him because he just can’t really sit for very long ”. This quote also alludes to difficulties with evaluating the child’s academic abilities, due to their ADHD-related difficulties, which was supported by other teachers (e.g. “ He doesn’t particularly enjoy writing and he’s slow, very slow. And I don’t know if that’s down to attention or if that’s something he actually does find difficult to do ” —Henry’s teacher). Furthermore, some teachers reflected on the child’s confidence as opposed to a direct academic difficulty. For example, Luna’s teacher said, “ I think it’s she lacks the confidence in maths and reading like the most ” and later, elaborated with “ she’ll be like “I can’t do it” but she actually can. Sometimes she’s … even just anxious at doing a task where she thinks … she might not get it. But she does, she’s just not got that confidence”.
Teachers also commonly mentioned social difficulties, and referred to these difficulties as a barrier to collaborative learning activities (e.g. “ he doesn’t always work well with other people and other people can get frustrated” —Henry’s teacher; “ [during] collaborative group work [Paige] perhaps goes off task and does things she shouldn’t necessarily be doing and that can cause friction within the group” —Paige’s teacher). Teachers also mentioned emotion regulation, mostly in relation to the child’s social difficulties. For example, Eric’s teacher said “ I think as well he does still struggle with his emotions like getting angry very very quickly, and being very defensive when actually he’s taken the situation the wrong way” , which suggests that the child’s difficulty with regulating emotions may impact on their social relationships.
Strategy Use in the Classroom
Strategies to support learning fell into one of four categories: concrete or visual resources, information processing, seating and movement, and support from or influence of others. Examples of codes included in each of these strategy categories are presented in Table 2 .
Concrete or visual resources were the most commonly mentioned type of strategy by teachers and children, referring to the importance of having physical representations to support learning. Teachers spoke about the benefit of using visual aids (e.g. “ I think [Henry] is quite visual so making sure that there is visual prompts and clues and things like that to help him ”—Henry’s teacher), and teachers and children alluded to these resources supporting difficulties with holding information in mind. For example, when talking about the times table squares he uses, Rory said “ sometimes I forget which one I’m on…and it’s easier for me to have my finger next to it than just doing it in my head because sometimes I would need to start doing it all over again ”.
Seating and movement were also commonly mentioned, which seemed to be specific to children with ADHD in that it was linked to inattention and hyperactivity symptoms. For example, teachers referred to supporting attention or avoiding distraction by the positioning of a child’s location in the classroom (e.g. “ he’s so easily distracted, so he has an individual desk in the room and he’s away from everyone else because he wasn’t coping at a table [and] he’s been so much more settled since we got him an individual desk” —Eric’s teacher). Some teachers also mentioned the importance of allowing children to move around the room where feasible, as well as giving them errands to perform as a movement break (e.g. “ if I need something from the printer, [Nathan] is gonna go for it for me…because that’s down the stairs and then back up the stairs so if I think he’s getting a bit chatty or he’s not focused I’ll ask him to go and just give him that break as well” —Nathan’s teacher). Children also spoke about these strategies but didn’t necessarily describe why or how these strategies help them.
Information processing and cognitive strategies included methods that supported children to process learning content or instructions. For example, teachers frequently mentioned breaking down tasks or instructions into more manageable chunks (e.g. “ with my instructions to [Eric] I break them down … I’ll be like “we’re doing this and then we’re doing this” whereas the whole class wouldn’t need that ”—Eric’s teacher). Teachers and children also mentioned using memory strategies such as songs, rhymes or prompts. For example, Jay’s teacher said, “ if I was one of the other children I could see why it would be very distracting but he’s like he’s singing to himself little times table songs that we’ve been learning in class” , and Paige (8 years) referred to using mnemonics to help with words she struggles to spell, “ I keep forgetting [the word] because. But luckily we got the story big elephants can always understand little elephants [which helps because] the first letter of every word spells because” .
Both groups of participants mentioned support from and influence of others, and referred to working with peers, the teacher–child relationship, and one-to-one teaching. Peer support was a common theme across the data and is discussed in more detail in the thematic analysis findings, where teachers and children referred to the importance of the role of peers during learning activities. Understanding the child well and adapting to them was also seen as important, for example, Luna’s teacher said, “ with everything curricular [I] try and have an art element for her, just so I know it’ll engage her [because] if it’s like a boring old written worksheet she’s not gonna do it unless you’re sitting beside her and you’re basically telling her the answers” . As indicated in this quote, teachers also referred to the effectiveness of one-to-one or small group work with the child (e.g. “ when somebody sits beside her and explains it, and goes “come on [Paige] you know how to do this, let’s just work through a couple of examples”… her focus is generally better ” – Paige’s teacher), however this resource is not always available (e.g. “ I’d love for someone to be one-to-one with [Luna] but it’s just not available, she doesn’t meet that criteria apparently ” – Luna’s teacher). Children also referred to seeking direct support from their teacher (e.g. “if I can’t get an idea of what I’m doing then I ask the teacher for help” – Paige, 8 years), but were more likely to mention seeking support from their peers than the teacher.
Thematic Analysis
In addition to summarising the types of strategies that teachers and children reported using in the classroom, the data were also analysed using thematic analysis to generate themes. These are now presented. The theme names, definitions, and example quotes for each theme are presented in Table 3 .
Theme 1: Classroom-General Versus Individual-Specific Strategies
During the interviews, teachers spoke about strategies that they use as part of their teaching practice for the whole class but that are particularly helpful for the child/children with ADHD. These tended to be concrete or visual resources that are available in the classroom for anyone, for example, a visual timetable or routine checklist (e.g. “ there’s also a morning routine and listing down what’s to be done and where it’s to go … it’s very general for the class but again it’s located near her” —Paige’s teacher).
Teachers also mentioned using strategies that have been implemented specifically for that child, and these strategies tended to focus on supporting attention. For example, Nathan’s teacher spoke about the importance of using his name to attract his attention, “ maybe explaining to the class but then making sure that I’m saying “[Nathan], you’re doing this”, you know using his name quite a lot so that he knows it’s his task not just the everybody task ”, and this was a strategy that multiple teachers referred to using with the individual child and not necessarily for other children. Other strategies to support attention with a specific child also tended to be seating and movement related, such as having an individual desk or allowing them to fidget. For example, Luna’s teacher said, “ she’s a fidgeter so she’ll have stuff to fidget with … [and] even if she’s wandering around the classroom or she’s sitting on a table, I don’t let other kids do that, but as long as she’s listening, it’s fine [with me]” .
Similar to teachers, children spoke about strategies or resources that were in place for them specifically as well as about general things in the classroom that they find helpful. That said, it was less common for children to talk about why particular strategies were in place for them and how they helped them directly.
In addition to recognising strategies that teachers had put in place for them, children also referred to using their own strategies in the classroom. The most frequently mentioned strategy was fidgeting, and although some of the younger children spoke about having resources available in the classroom for fidgeting, some of the older children referred to using their own toy or an object that was readily available to them but not intended for fidgeting. For example, Finn (10 years) and Rory (9 years) both spoke about using items from their pencil case to fiddle with, and explained that this would help them to focus. (“ Sometimes I fidget with something I normally just have like a pencil holder under the table moving about … [and] it just keeps my mind clear and not from something else ”—Rory; “ Sometimes I fiddle with my fingers and that sometimes helps, but if not I get one of my coloured pencils and have a little gnaw on it because that actually takes my mind off some things and it’s easier for me to concentrate when I have something to do ”—Finn). Henry (9 years) spoke about being secretive with his fidgeting as it was not permitted in class, “ if you just bring [a fidget toy] in without permission [the teacher will] just take it off of you, so it has to be something that’s not too big. I bring in a little Lego ray which is just small enough that she won’t notice ”. Although some teachers did mention having fidget toys available, not all teachers seemed to recognise the importance of this for the child, and some children viewed fidgeting as a behaviour they should hide from the teacher.
Another strategy mentioned uniquely by children was seeing their peers as a resource for ideas or information. This is discussed in more detail in Theme 3—The role of peers , but reinforces the notion that children also develop their own strategies, independently from their teacher, rather than relying only on what is made available to them.
Theme 2: Heterogeneity of Strategies
Teachers spoke about the need for a variety of strategies in the classroom, for two reasons: (1) that different strategies work for different children (e.g. “ some [strategies] will work for the majority of the children and some just don’t seem to work for any of them ”—Jay’s teacher), and (2) what works for a child on one occasion may not work consistently for the same child (e.g. “ I think it’s a bit of a journey with him, and some things have worked and then stopped working, so I think we’re constantly adapting and changing what we’re doing ”—Eric’s teacher). One example of both of these challenges of strategy use came from Luna’s teacher, who spoke about using a reward chart with Luna and another child with ADHD, “ [Luna] and another boy in my class [with ADHD] both had [a reward chart]… but I think whereas the boy loved his and still loves his, she was getting a bit “oh I’m too cool for this” or that sort of age… so I stopped doing that for her and she’s not missing that at all” . These quotes demonstrate that strategies can work differently for different children, highlighting the need for a variety of strategies for teachers to access and trial with children.
Some children also referred to the variability of whether a strategy was helpful or not; for example, Henry (9 years) said that he finds it helpful to fidget with a toy but that sometimes it can distract him and prevent him from listening to the teacher. He said, “ Well, [the fidget toy] helps but it also gets me into trouble when the teacher spots me building it when I’m listening…but then sometimes I might not listen in maths and [use the fidget toy] which might make it worse”. This highlights that both children and teachers might benefit from support in understanding the contexts in which to use particular strategies, as well as why they are helpful from a psychological perspective.
For teachers, building a relationship with and understanding the child was also highly important in identifying strategies that would work. Luna’s teacher reflected upon the difference in Luna’s behaviour at the start of the academic year, compared to the second academic term, “ at the start of the year, we would just clash the whole time. I didn’t know her, she didn’t know me … and then when we got that bond she was absolutely fine so her behaviour has got way better ”. Eric’s teacher also reflected on how her relationship with Eric had changed, particularly after he received his diagnosis of ADHD, “ I think my approach to him has completely changed. I don’t raise my voice, I speak very calmly, I give him time to calm down before I even broach things with him. I think our relationship’s just got so much better ‘cause I kind of understand … where he’s coming from ”. She also said, “ it just takes a long time to get to know the child and get to know what works for them and trialling different things out ”, which demonstrates that building a relationship with and understanding the child can help to identify the successful strategies that work with different children.
Theme 3: The Role of Peers
Teachers and children spoke about the role of the child’s peers in their learning. Teachers talked about the benefit of partnering the child with good role models (e.g. “ I will put him with a couple of good role models and a couple of children who are patient and who will actually maybe get on with the task, and if [Jay] is not on task or not on board with what they’re doing at least he’s hearing and seeing good behaviour ”—Jay’s teacher), whereas children spoke more about their peers as a source of information, idea generation, or guidance on what to do next. For example, when asked what he does to help him with his writing, Henry (9 years) said, “ [I] listen to what my partner’s saying… my half of the table discuss what they’re going to do so I can literally hear everything they’re doing and steal some of their ideas ”. Henry wasn’t the only child to use their peers as a source of information, for example, Niall (7 years) said, “ I prefer working with the children because some things I might not know and the children might help me give ideas ”, and with a more specific example, Rory (9 years) said, “ somebody chose a very good character for their bit of writing, and I was like “I think I might choose that character”, and somebody else said “my setting was going to be the sea”, and I chose that and put that in a tiny bit of my story ”.
Some children also spoke about getting help from their peers in other ways, particularly when completing a difficult task. Paige (8 years) said, “ if the question isn’t clear I try and figure it out, and if I can’t figure it out then… don’t tell my teacher this but I sometimes get help from my classmates ”, which suggests some guilt associated with asking for help from her peers. This could be related to confidence and self-esteem, which teachers mentioned as a difficulty for some children with ADHD. In some instances, children felt it necessary to directly copy their peers’ work; for example, Nathan (8 years) spoke about needing a physical resource (i.e. “ fuzzies ”) to complete maths problems, but that when none were available he would “ just end up copying other people ”. This could also be related to a lack of confidence, as he may feel as though he may not be able to complete the task on his own. Indeed, Nathan’s teacher mentioned that when he is given the option to choose a task from different difficulty levels, Nathan would typically choose something easier, and that it was important to encourage him to choose something more difficult to build his confidence, “ I quite often say to him “come on I think you can challenge yourself” and [will] use that language”.
Peers clearly play an important role for the children with ADHD, and this is recognised both by the children themselves, and by their teachers. Teachers also mentioned that children with ADHD respond well to one-to-one learning with staff, indicating that it is important for these children to have opportunities to learn in different contexts: whole classroom learning, small group work and one-to-one.
In this study, a number of important topics surrounding ADHD in the primary school setting were explored, including ADHD knowledge, strengths and challenges, and strategy use in the classroom, each of which will now be discussed in turn before drawing together the findings and outlining the implications.
ADHD Knowledge
Knowledge of ADHD varied between children and their teachers. Whilst most of the children claimed to have heard of ADHD, very few could accurately describe the core symptoms. Previous research into this area is limited, however this finding supports Climie and Henley’s ( 2018 ) finding that children’s knowledge of ADHD can be limited. By comparison, all of the interviewed teachers had good knowledge about the core ADHD phenotype (i.e. in relation to diagnostic criteria) and some elaborated further by mentioning social difficulties or description of behaviours that could reflect cognitive difficulties. This supports and builds further upon existing research into teachers’ ADHD knowledge, demonstrating that although teachers understanding may be grounded in a focus upon inattention and hyperactivity, this is not necessarily representative of the range of their knowledge. By interviewing participants about their ADHD knowledge, as opposed to asking them to complete a questionnaire as previous studies have done (Climie & Henley, 2018 ; Latouche & Gascoigne, 2019 ; Ohan et al., 2008 ; Perold et al., 2010 ), the present study has demonstrated the specific areas of knowledge that should be targeted when designing psychoeducation interventions for children and teachers, such as broader aspects of cognitive difficulties in executive functions and memory. Improving knowledge of ADHD in this way could lead to increased positive attitudes and reduction of stigma towards individuals with ADHD (Mueller et al., 2012 ; Ohan et al., 2008 ), and in turn improving adherence to more specified interventions (Bai et al., 2015 ).
Strengths and Challenges
A range of strengths and challenges were discussed, some of which were mentioned by both children and teachers, whilst others were unique to a particular group. The main consensus in the current study was that art and P.E. tended to be the lessons in which children with ADHD thrive the most. Teachers elaborated on this notion, speaking about creative skills, such as a good imagination, and that these skills were sometimes applied in other subjects such as creative writing in literacy. Little to no research has so far focused on the strengths of children with ADHD, therefore these findings identify important areas for future investigation. For example, it is possible that these strengths could be harnessed in educational practice or intervention.
Although a strength for some, literacy was commonly mentioned as a challenge by both groups, specifically in relation to planning, spelling or the physical act of writing. Previous research has repeatedly demonstrated that literacy outcomes are poorer for children with ADHD compared to their typically developing peers (DuPaul et al., 2016; Mayes et al., 2020 ), however in these studies literacy tended to be measured using a composite achievement score, where the nuance of these difficulties can be lost. Furthermore, in line with a recent systematic review and meta-analysis (McDougal et al., 2022 ) the present study’s findings suggest that cognitive difficulties may contribute to poor literacy performance in ADHD. This issue was not unique to literacy, however, as teachers also spoke about academic challenges in the context of ADHD symptoms being a barrier to learning, such as finding it difficult to remain seated long enough to complete a piece of work. Children also raised this issue of engagement, who referred to the most challenging subjects being ‘boring’ for them. This link between attention difficulties and boredom in ADHD has been well documented (Golubchik et al., 2020 ). The findings here demonstrate the need for further research into the underlying cognitive difficulties leading to academic underachievement.
Both children and teachers also mentioned social and emotional difficulties. Research has shown that many different factors may contribute to social difficulties in ADHD (for a review see Gardner & Gerdes, 2015 ), making it a complex issue to disentangle. That said, in the current study teachers tended to attribute the children’s relationship difficulties to behaviour, such as reacting impulsively in social situations, or going off task during group work, both of which could be linked to ADHD symptoms. Despite these difficulties, peers were also considered a positive support. This finding adds to the complexity of understanding social difficulties for children with ADHD, demonstrating the necessity and value of further research into this key area.
The three key themes of classroom-general versus individual-specific strategies , heterogeneity of strategies and the role of peers were identified from the interview transcripts with children and their teachers. Within the first theme, classroom-general versus individual-specific strategies, it was clear that teachers utilise strategies that are specific to the child with ADHD, as well as strategies that are general to the classroom but that are also beneficial to the child with ADHD. Previously, Moore et al. ( 2017 ) found that teachers mostly reflected on using general inclusive strategies, rather than those targeted for ADHD specifically, however the methods differ from the current study in two key ways. Firstly, Moore et al.’s sample included secondary and primary school teachers, for whom the learning environment is very different. Secondly, focus groups were used as opposed to interviews where the voices of some participants can be lost. The merit of the current study is that children were also interviewed using the same questions as teachers; we found that children also referred to these differing types of strategies, and reported finding them useful, suggesting that the reports of teachers were accurate. Interestingly, children also mentioned their own strategies that teachers did not discuss and may not have been aware of. This finding highlights the importance of communication between the child and the teacher, particularly when the child is using a strategy considered to be forbidden or discouraged, for example copying a peer’s work or fidgeting with a toy. This communication would provide an understanding of what the child might find helpful, but more importantly identify areas of difficulty that may need more attention. Further to this, most strategies specific to the child mentioned by teachers aimed to support attention, and few strategies targeted other difficulties, particularly other aspects of cognition such as memory or executive function, which supports previous findings (Lawrence et al., 2017 ). The use of a wide range of individualised strategies would be beneficial to support children with ADHD.
Similarly, the second theme, heterogeneity of strategies , highlighted that some strategies work with some children and not others, and some strategies may not work for the same child consistently. Given the benefit of a wide range of strategy use, for both children with ADHD and their teachers, the development of an accessible tool-kit of strategies would be useful. Importantly, and as recognised in this second theme, knowing the individual child is key to identifying appropriate strategies, highlighting the essential role of the child’s teacher in supporting ADHD. Teachers mostly spoke about this in relation to the child’s interests and building rapport, however this could also be applied to the child’s cognitive profile. A tool-kit of available strategies and knowledge of which difficulties they support, as well as how to identify these difficulties, would facilitate teachers to continue their invaluable support for children and young people with ADHD. This links to the importance of psychoeducation; as previously discussed, the teachers in our study had a good knowledge of the core ADHD phenotype, but few spoke about the cognitive strengths and difficulties of ADHD. Children and their teachers could benefit from psychoeducation, that is, understanding ADHD in more depth (i.e., broader cognitive and behavioural profiles beyond diagnostic criteria), what ADHD and any co-occurrences might mean for the individual child, and why certain strategies are helpful. Improving knowledge using psychoeducation is known to improve fidelity to interventions (Dahl et al., 2020 ; Nussey et al., 2013 ), suggesting that this would facilitate children and their teachers to identify effective strategies and maintain these in the long-term.
The third theme, the role of peers , called attention to the importance of classmates for children with ADHD, and this was recognised by both children and their teachers. As peers play a role in the learning experience for children with ADHD, it is important to ensure that children have opportunities to learn in small group contexts with their peers. This finding is supported by Vygotsky’s ( 1978 ) Zone of Proximal Development; it is well established in the literature that children can benefit from completing learning activities with a partner, especially a more able peer (Vygotsky, 1978 ).
Relevance of Co-Occurrences
Co-occurring conditions are common in ADHD (Jensen & Steinhausen, 2015 ), and there are many instances within the data presented here that may reflect these co-occurrences, in particular, the overlap with DCD and ASD. For ADHD and DCD, the overlap is considered to be approximately 50% (Goulardins et al., 2015 ), whilst ADHD and autism also frequently co-occur with rates ranging from 40 to 70% (Antshel & Russo, 2019 ). It was not an aim of the current study to directly examine co-occurrences, however it is important to recognise their relevance when interpreting the findings. Indeed, in the current sample, scores for seven children (70%) indicated a high likelihood of movement difficulty. One child scored above the cut-off for autism diagnosis referral on the AQ-10, indicating heightened autism symptoms. Further to this, some of the discussions with children and teachers seemed to be related to DCD or autism, for example, the way that they can react in social situations, or difficulties with the physical act of handwriting. This finding feeds into the ongoing narrative surrounding heterogeneity within ADHD and individualisation of strategies to support learning. Recognising the potential role of co-occurrences should therefore be a vital part of any psychoeducation programme for children with ADHD and their teachers.
Limitations
Whilst a strong sample size was achieved for the current study allowing for rich data to be generated, it is important to acknowledge the issue of representativeness. The heterogeneity of ADHD is recognised throughout the current study, however the current study represents only a small cohort of children and young people with ADHD and their teachers which should be considered when interpreting the findings, particularly in relation to generalisation. Future research should investigate the issues raised using quantitative methods. Also on this point of heterogeneity, although we report some co-occurring symptoms for participants, the number of co-occurrences considered here were limited to autism and DCD. Learning disabilities and other disorders may play a role, however due to the qualitative nature of this study it was not feasible to collect data on every potential co-occurrence. Future quantitative work should aim to understand the complex interplay of diagnosed and undiagnosed co-occurrences.
Furthermore, only some of the teachers of participating children took part in the study; we were not able to recruit all 10. It may be, for example, that the six teachers who did take part were motivated to do so based on their existing knowledge or commitment to understanding ADHD, and the fact that not all child-teacher dyads are represented in the current study should be recognised. Another possibility is the impact of time pressures upon participation for teachers, particularly given the increasing number of children with complex needs within classes. Outcomes leading from the current study could support teachers in this respect.
It is also important to recognise the potential role of stimulant medication. Although it was not an aim of the current study to investigate knowledge or the role of stimulant medication in the classroom setting, it would have been beneficial to record whether the interviewed children were taking medication for their ADHD at school, particularly given the evidence to suggest that stimulant medication can improve cognitive and behavioural symptoms of ADHD (Rhodes et al., 2004 ). Examining strategy use in isolation (i.e. with children who are drug naïve or pausing medication) will be a vital aim of future intervention work.
Implications/Future Research
Taking the findings of the whole study together, one clear implication is that children and their teachers could benefit from psychoeducation, that is, understanding ADHD in more depth (i.e., broader cognitive and behavioural profiles beyond diagnostic criteria), what ADHD might mean for the individual child, and why certain strategies are helpful. Improving knowledge using psychoeducation is known to improve fidelity to interventions (Dahl et al., 2020 ; Nussey et al., 2013 ), suggesting that this would facilitate children and their teachers to identify effective strategies and maintain these in the long-term.
To improve knowledge and understanding of both strengths and difficulties in ADHD, future research should aim to develop interventions grounded in psychoeducation, in order to support children and their teachers to better understand why and in what contexts certain strategies are helpful in relation to ADHD. Furthermore, future research should focus on the development of a tool-kit of strategies to account for the heterogeneity in ADHD populations; we know from the current study’s findings that it is not appropriate to offer a one-size-fits-all approach to supporting children with ADHD given that not all strategies work all of the time, nor do they always work consistently. In terms of implications for educational practice, it is clear that understanding the individual child in the context of their ADHD and any co-occurrences is important for any teacher working with them. This will facilitate teachers to identify and apply appropriate strategies to support learning which may well result in different strategies depending on the scenario, and different strategies for different children. Furthermore, by understanding that ADHD is just one aspect of the child, strategies can be used flexibly rather than assigning strategies based on a child’s diagnosis.
This study has provided invaluable novel insight into understanding and supporting children with ADHD in the classroom. Importantly, these insights have come directly from children with ADHD and their teachers, demonstrating the importance of conducting qualitative research with these groups. The findings provide clear scope for future research, as well as guidelines for successful intervention design and educational practice, at the heart of which we must acknowledge and embrace the heterogeneity and associated strengths and challenges within ADHD.
Allison, C., Auyeung, B., & Baron-Cohen, S. (2012). Autism spectrum quotient: 10 items (AQ-10). Journal of the American Academy of Child and Adolescent Psychiatry., 51 (2), 202–212.
Article PubMed Google Scholar
Antshel, K. M., & Russo, N. (2019). Autism spectrum disorders and ADHD: Overlapping phenomenology, diagnostic issues, and treatment considerations. Current Psychiatry Reports, 21 (5), 34. https://doi.org/10.1007/s11920-019-1020-5
Arnold, L. E., Hodgkins, P., Kahle, J., Madhoo, M., & Kewley, G. (2020). Long-term outcomes of ADHD: Academic achievement and performance. Journal of Attention Disorders, 24 (1), 73–85. https://doi.org/10.1177/1087054714566076
Bai, G., Yang, L., Wang, Y., & Niu, W.-Y. (2015). Effectiveness of a focused, brief psychoeducation program for parents of ADHD children: Improvement of medication adherence and symptoms. Neuropsychiatric Disease and Treatment, . https://doi.org/10.2147/NDT.S88625
Article PubMed PubMed Central Google Scholar
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3 (2), 77–101. https://doi.org/10.1191/1478088706qp063oa
Article Google Scholar
Braun, V., & Clarke, V. (2019). Reflecting on reflexive thematic analysis. Qualitative Research in Sport, Exercise and Health, 11 (4), 589–597. https://doi.org/10.1080/2159676X.2019.1628806
Classi, P., Milton, D., Ward, S., Sarsour, K., & Johnston, J. (2012). Social and emotional difficulties in children with ADHD and the impact on school attendance and healthcare utilization. Child and Adolescent Psychiatry and Mental Health, 6 (1), 33. https://doi.org/10.1186/1753-2000-6-33
Climie, E. A., & Henley, L. (2018). Canadian parents and children’s knowledge of ADHD. Vulnerable Children and Youth Studies, 13 (3), 266–275. https://doi.org/10.1080/17450128.2018.1484975
Coghill, D. R., Seth, S., & Matthews, K. (2014). A comprehensive assessment of memory, delay aversion, timing, inhibition, decision making and variability in Attention Deficit Hyperactivity Disorder: Advancing beyond the three-pathway models. Psychological Medicine, 44 (9), 1989–2001. https://doi.org/10.1017/S0033291713002547
Conners, C. K., & Multi-Health Systems Inc. (2008). Conners Comprehensive Behavior Rating Scales (Conners CBRS): Manual . North Tonawanda, N.Y: Multi-Health Systems.
Dahl, V., Ramakrishnan, A., Spears, A. P., Jorge, A., Lu, J., Bigio, N. A., & Chacko, A. (2020). Psychoeducation interventions for parents and teachers of children and adolescents with ADHD: A systematic review of the literature. Journal of Developmental and Physical Disabilities, 32 (2), 257–292. https://doi.org/10.1007/s10882-019-09691-3
DuPaul, G. J., Eckert, T. L., & Vilardo, B. (2012). The effects of school-based interventions for Attention Deficit Hyperactivity Disorder: A meta-analysis. School Psychology Review, 41 (4), 387412. https://doi.org/10.1080/02796015.2012.12087496
Gardner, D. M., & Gerdes, A. C. (2015). A review of peer relationships and friendships in youth with ADHD. Journal of Attention Disorders, 19 (10), 844–855. https://doi.org/10.1177/1087054713501552
Gathercole, S. E., Astle, D. A., Manly, T., the CALM Team, & Holmes, J. (2018). Cognition and behaviour in learning difficulties and ADHD: A dimensional approach [Preprint]. Animal Behavior and Cognition . https://doi.org/10.1101/260265
Golubchik, P., Manor, I., Shoval, G., & Weizman, A. (2020). Levels of proneness to boredom in children with Attention-Deficit/Hyperactivity Disorder on and off methylphenidate treatment. Journal of Child and Adolescent Psychopharmacology, 30 (3), 173–176. https://doi.org/10.1089/cap.2019.0151
Goulardins, J. B., Rigoli, D., Licari, M., Piek, J. P., Hasue, R. H., Oosterlaan, J., & Oliveira, J. A. (2015). Attention Deficit Hyperactivity Disorder and developmental coordination disorder: Two separate disorders or do they share a common etiology. Behavioural Brain Research, 292 , 484–492. https://doi.org/10.1016/j.bbr.2015.07.009
Henderson, S. E., Sugden, D. A., & Barnett, A. L. (2007). Movement assessment battery for children – (2nd ed.). Harcourt Assessment.
Google Scholar
Jensen, C. M., & Steinhausen, H.-C. (2015). Comorbid mental disorders in children and adolescents with Attention-Deficit/Hyperactivity Disorder in a large nationwide study. ADHD Attention Deficit and Hyperactivity Disorders, 7 (1), 27–38. https://doi.org/10.1007/s12402-014-0142-1
Jones, H. A., & Chronis-Tuscano, A. (2008). Efficacy of teacher in-service training for attention-deficit/hyperactivity disorder: Teacher in-service training for ADHD. Psychology in the Schools, 45 (10), 918–929. https://doi.org/10.1002/pits.20342
Kuriyan, A. B., Jr., Molina, B. S. G., Waschbusch, D. A., Gnagy, E. M., Sibley, M. H., Babinski, D. E., Walther, C., Cheong, J., Yu, J., & Kent, K. M. (2013). Young adult educational and vocational outcomes of children diagnosed with ADHD. Journal of Abnormal Child Psychology, 41 , 27–41. https://doi.org/10.1007/s10802-012-9658-z
Latouche, A. P., & Gascoigne, M. (2019). In-service training for increasing teachers’ ADHD knowledge and self-efficacy. Journal of Attention Disorders, 23 (3), 270–281. https://doi.org/10.1177/1087054717707045
Law, G. U., Sinclair, S., & Fraser, N. (2007). Children’s attitudes and behavioural intentions towards a peer with symptoms of ADHD: Does the addition of a diagnostic label make a difference? Journal of Child Health Care, 11 (2), 98–111. https://doi.org/10.1177/1367493507076061
Lawrence, K., Estrada, R. D., & McCormick, J. (2017). Teachers’ experiences with and perceptions of students with Attention Deficit/hyperactivity Disorder. Journal of Pediatric Nursing, 36 , 141–148. https://doi.org/10.1016/j.pedn.2017.06.010
Mayes, S. D., Waschbusch, D. A., Calhoun, S. L., & Mattison, R. E. (2020). Correlates of academic overachievement, nondiscrepant achievement, and learning disability in ADHD, autism, and general population samples. Exceptionality, 28 (1), 60–75. https://doi.org/10.1080/09362835.2020.1727324
McDougal, E., Gracie, H., Oldridge, J., Stewart, T. M., Booth, J. N., & Rhodes, S. M. (2022). Relationships between cognition and literacy in children with attention‐deficit/hyperactivity disorder: A systematic review and meta‐analysis. British Journal of Developmental Psychology , 40 (1), 130–150. https://doi.org/10.1111/bjdp.12395
McDougal, E., Riby, D. M., & Hanley, M. (2020). Teacher insights into the barriers and facilitators of learning in autism. Research in Autism Spectrum Disorders, 79 , 101674. https://doi.org/10.1016/j.rasd.2020.101674
Mohr-Jensen, C., Steen-Jensen, T., Bang-Schnack, M., & Thingvad, H. (2019). What do primary and secondary school teachers know about ADHD in children? Findings from a systematic review and a representative, nationwide sample of Danish teachers. Journal of Attention Disorders, 23 (3), 206–219. https://doi.org/10.1177/1087054715599206
Moore, D. A., Russell, A. E., Arnell, S., & Ford, T. J. (2017). Educators’ experiences of managing students with ADHD: A qualitative study: Educators’ management of ADHD. Child: Care, Health and Development, 43 (4), 489–498. https://doi.org/10.1111/cch.12448
Mueller, A. K., Fuermaier, A. B., Koerts, J., & Tucha, L. (2012). Stigma in attention deficit hyperactivity disorder. Attention Deficit and Hyperactivity Disorders, 4 (3), 101–114. https://doi.org/10.1007/s12402-012-0085-3
National Institute for Health and Care Excellence (NICE). (2018). Attention deficit hyperactivity disorder: Diagnosis and management . Retrieved August 2021, from https://www.nice.org.uk/guidance/ng87/chapter/Recommendations#managing-adhd .
Nussey, C., Pistrang, N., & Murphy, T. (2013). How does psychoeducation help? A review of the effects of providing information about Tourette syndrome and attention-deficit/hyperactivity disorder: A review of psychoeducational approaches in TS and ADHD. Child Care, Health and Development, 39 (5), 617–627. https://doi.org/10.1111/cch.12039
Ohan, J. L., Cormier, N., Hepp, S. L., Visser, T. A. W., & Strain, M. C. (2008). Does knowledge about attention-deficit/hyperactivity disorder impact teachers’ reported behaviors and perceptions? School Psychology Quarterly, 23 (3), 436–449. https://doi.org/10.1037/1045-3830.23.3.436
Perold, M., Louw, C., & Kleynhans, S. (2010). Primary school teachers’ knowledge and misperceptions of attention deficit hyperactivity disorder (ADHD). South African Journal of Education, 30 (3), 457–473.
Rhodes, S. M., Coghill, D. R., & Matthews, K. (2004). Methylphenidate restores visual memory, but not working memory function in attention deficit-hyperkinetic disorder. Psychopharmacology (berl), 175 (3), 319–330. https://doi.org/10.1007/s00213-004-1833-7
Rhodes, S. M., Park, J., Seth, S., & Coghill, D. R. (2012). A comprehensive investigation of memory impairment in attention deficit hyperactivity disorder and oppositional defiant disorder: Memory in ADHD and ODD. Journal of Child Psychology and Psychiatry, 53 (2), 128–137. https://doi.org/10.1111/j.1469-7610.2011.02436.x
Richardson, M., Moore, D. A., Gwernan-Jones, R., Thompson-Coon, J., Ukoumunne, O., Rogers, M., Whear, R., Newlove-Delgado, T. V., Logan, S., Morris, C., Taylor, E., Cooper, P., Stein, K., Garside, R., & Ford, T. J. (2015). Non-pharmacological interventions for attention-deficit/hyperactivity disorder (ADHD) delivered in school settings: Systematic reviews of quantitative and qualitative research. Health Technology Assessment, 19 (45), 1–470. https://doi.org/10.3310/hta19450
Russell, G., Rodgers, L. R., Ukoumunne, O. C., & Ford, T. (2014). Prevalence of parent-reported ASD and ADHD in the UK: Findings from the millennium cohort Study. Journal of Autism and Developmental Disorders, 44 (1), 31–40. https://doi.org/10.1007/s10803-013-1849-0
Sayal, K., Prasad, V., Daley, D., Ford, T., & Coghill, D. (2018). ADHD in children and young people: Prevalence, care pathways, and service provision. The Lancet. Psychiatry, 5 (2), 175–186. https://doi.org/10.1016/S2215-0366(17)30167-0
Vygotsky, L. S. (1978). Mind in society: The development of higher psychological processes . Harvard University Press.
Wiener, J., Malone, M., Varma, A., Markel, C., Biondic, D., Tannock, R., & Humphries, T. (2012). Children’s perceptions of their ADHD symptoms: Positive illusions, attributions, and stigma. Canadian Journal of School Psychology, 27 (3), 217–242. https://doi.org/10.1177/0829573512451972
Download references
The funding was provided by Waterloo Foundation Grant Nos. (707-3732, 707-4340, 707-4614).
Author information
Authors and affiliations.
Centre for Clinical Brain Sciences, Child Life and Health, University of Edinburgh, Edinburgh, United Kingdom
Emily McDougal, Claire Tai & Sinéad M. Rhodes
Moray House School of Education and Sport, University of Edinburgh, Edinburgh, United Kingdom
Tracy M. Stewart & Josephine N. Booth
School of Psychology, University of Surrey, Guildford, United Kingdom
Emily McDougal
You can also search for this author in PubMed Google Scholar
Contributions
E.M. Conceptualization, Methodology, Investigation, Data Curation, Formal Analysis, Writing - original draft, C.T. Formal Analysis, Writing - review & editing, T.M.S., J.N.B. and S.M.R. Conceptualization, Methodology, Writing - review & editing.
Corresponding author
Correspondence to Sinéad M. Rhodes .
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Interview Schedule—Teacher
Demographic/experience.
How many years have you been teaching?
Are you currently teaching pupils with ADHD and around how many?
If yes, do you feel competent/comfortable/equipped teaching pupils with ADHD?
If no, how competent/comfortable/equipped would you feel to teach pupils with ADHD?
Would you say your experience of teaching pupils with ADHD is small/moderate/significant?
Psychoeducation
What is your understanding of ADHD/Can you describe a typical child with ADHD?
Probe behaviour knowledge
Probe cognition knowledge
Probe impacts of behaviour/cognition difficulties
Probe knowledge that children with ADHD differ from each other
Probe knowledge that children with ADHD have co-occurring difficulties as the norm
(If they do have some knowledge) Where did you learn about ADHD?
e.g. specific training, professional experience, personal experience, personal interest/research
Cognitive skills and strategies
Can you tell me about the pupil’s strengths?
Can you tell me about the pupil’s biggest challenges/what they need most support with?
When you are supporting the pupil with their learning, are there any specific things you do to help them? (i.e. strategies)
Probe internal
Probe external
Probe whether they think those not mentioned might be useful/feasible/challenges
Probe if different for different subjects/times of the day
In your experience, which of these you have mentioned are the most useful for the pupil?
Probe for examples of how they apply it to their learning
Probe whether these strategies are pupil specific or broadly relevant
Probe if specific to particular subjects/times of the day
In your experience, which of these you have mentioned are the least useful for the pupil?
What would you like to be able to support the pupil with that you don’t already do?
Probe why they can’t access this currently e.g. lack of training, resources, knowledge, time
Is there anything you would like to understand better about ADHD?
Probe behaviour
Probe cognition
Interview Schedule—Child
Script: We’re going to have a chat about a few different things today, mostly about your time at school. This will include things like how you get on, how you think, things you’re good at and things you find more difficult. I’ve got some questions here to ask you but try to imagine that I’m just a friend that you’re talking to about these things. There are no right or wrong answers, I’m just interested in what you’ve got to say. Do you have any questions?
Script: First we’re going to talk about ADHD (Attention Deficit Hyperactivity Disorder).
Have you ever heard of/has anyone ever told you what ADHD is?
(If yes) If a friend asked you to tell them what ADHD is, what would you tell them?
Is there anything you would like to know more about ADHD?
Cognition/strategy use
Script: Now we’re going to talk about something a bit different. Everyone has things they are good at, and things they find more difficult. For example, I’m quite good at listening to what people have to say, but I’m not so good at remembering people’s names. I’d like you to think about when you’re in school, and things you’re good at and things you are not so good at. It doesn’t just have to be lessons, it can be anything.
Do you like school?
Probe why/why not?
Probe favourite lessons
What sort of things do you find you do well at in school?
Is there anything you think that you find more difficult in school?
Probe: If I asked your teacher/parent what you find difficult, what would they say?
Probe: Is there anything at school you need extra help with?
Probe: Is there anything you do to help yourself with that?
Script: Some people do things to try to help themselves do things well. For example, when someone tells me a number to remember, I repeat it in my head over and over again.
Can you try to describe to me what you do to help you do these things?
Solving a maths problem
Planning your writing
Doing spellings
Trying to remember something
Concentrating/ignoring distractions
Listening to the teacher
Remaining seated in class when doing work
Working with other children in the class
Probe: Do you use anything in lessons to help you with your work?
Probe: What kind of things do you think could help you with your work?
Probe: Is there anything you do at home, such as when you’re doing your homework, to help you finish what you are doing to do it well?
Probe: Does someone help you with your homework at home? If yes, what do they do that helps? If no, what do you think someone could do to help?
Script: In this last part we’re going to talk about your time at school.
How many teachers are in your class?
Is there anyone who helps you with your work?
Do you work mostly on your own or in groups?
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
McDougal, E., Tai, C., Stewart, T.M. et al. Understanding and Supporting Attention Deficit Hyperactivity Disorder (ADHD) in the Primary School Classroom: Perspectives of Children with ADHD and their Teachers. J Autism Dev Disord 53 , 3406–3421 (2023). https://doi.org/10.1007/s10803-022-05639-3
Download citation
Accepted : 06 June 2022
Published : 01 July 2022
Issue Date : September 2023
DOI : https://doi.org/10.1007/s10803-022-05639-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Child and teacher interviews
- Strengths and difficulties
- Learning strategies
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 25 May 2020
Guidance for identification and treatment of individuals with attention deficit/hyperactivity disorder and autism spectrum disorder based upon expert consensus
- Susan Young 1 ,
- Jack Hollingdale 2 ,
- Michael Absoud 3 , 4 ,
- Patrick Bolton 2 ,
- Polly Branney 5 ,
- William Colley 6 ,
- Emily Craze 7 ,
- Mayuri Dave 8 ,
- Quinton Deeley 7 ,
- Emad Farrag 9 ,
- Gisli Gudjonsson 10 ,
- Peter Hill 11 ,
- Ho-lan Liang 12 ,
- Clodagh Murphy 13 , 14 ,
- Peri Mackintosh 7 ,
- Marianna Murin 15 ,
- Fintan O’Regan 16 ,
- Dennis Ougrin 17 ,
- Patricia Rios 18 ,
- Nancy Stover 19 ,
- Eric Taylor 17 &
- Emma Woodhouse 14
BMC Medicine volume 18 , Article number: 146 ( 2020 ) Cite this article
55k Accesses
56 Citations
92 Altmetric
Metrics details
Individuals with co-occurring hyperactivity disorder/hyperactivity disorder (ADHD) and autism spectrum disorder (ASD) can have complex presentations that may complicate diagnosis and treatment. There are established guidelines with regard to the identification and treatment of ADHD and ASD as independent conditions. However, ADHD and ASD were not formally recognised diagnostically as co-occurring conditions until the Diagnostic and Statistical Manual of Mental Disorders 5 (DSM-5) was published in 2013. Hence, awareness and understanding of both conditions when they co-occur is less established and there is little guidance in the clinical literature. This has led to uncertainty among healthcare practitioners when working with children, young people and adults who present with co-existing ADHD and ASD. The United Kingdom ADHD Partnership (UKAP) therefore convened a meeting of professional experts that aimed to address this gap and reach expert consensus on the topic that will aid healthcare practitioners and allied professionals when working with this complex and vulnerable population.
UK experts from multiple disciplines in the fields of ADHD and ASD convened in London in December 2017. The meeting provided the opportunity to address the complexities of ADHD and ASD as a co-occurring presentation from different perspectives and included presentations, discussion and group work. The authors considered the clinical challenges of working with this complex group of individuals, producing a consensus for a unified approach when working with male and female, children, adolescents and adults with co-occurring ADHD and ASD. This was written up, circulated and endorsed by all authors.
The authors reached a consensus of practical recommendations for working across the lifespan with males and females with ADHD and ASD. Consensus was reached on topics of (1) identification and assessment using rating scales, clinical diagnostic interviews and objective supporting assessments; outcomes of assessment, including standards of clinical reporting; (2) non-pharmacological interventions and care management, including psychoeducation, carer interventions/carer training, behavioural/environmental and Cognitive Behavioural Therapy (CBT) approaches; and multi-agency liaison, including educational interventions, career advice, occupational skills and training, and (3) pharmacological treatments.
Conclusions
The guidance and practice recommendations (Tables 1, 4, 5, 7, 8 and 10) will support healthcare practitioners and allied professionals to meet the needs of this complex group from a multidisciplinary perspective. Further research is needed to enhance our understanding of the diagnosis, treatment and management of individuals presenting with comorbid ADHD and ASD.
Peer Review reports
Approximately 5% of the population worldwide is reported to have a diagnosis of hyperactivity disorder/hyperactivity disorder (ADHD) [ 1 ], a disorder often associated with co-occurring conditions that can complicate identification and treatment [ 2 ]; autism spectrum disorder (ASD) is among those conditions that are commonly found to co-exist with those diagnosed with ADHD at a reported rate (obtained by meta-analysis) of 21% [ 3 ].
There are established guidelines regarding the identification and treatment of ADHD and ASD as independent conditions. Indeed, this comorbidity was not formally recognised diagnostically until the fifth revision of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) [ 4 ]; hence, awareness and understanding of them as co-occurring conditions is less established. This has led to uncertainty among healthcare practitioners when working with children, young people and adults who present with both ADHD and ASD. It is further complicated by the expansion of the concept of ASD in recent years, which means that (although ASD is a neurodevelopmental disorder) many people in the spectrum are intellectually and emotionally able and their ‘impairment’ primarily relates to stigmatisation within society (for instance, in being excluded unnecessarily from employment). Nevertheless, mental health needs may arise from co-existing conditions (such as anxiety and ADHD). This consensus therefore included the needs of those who are functionally impaired as well as those who are more broadly considered ‘neurodiverse’.
hyperactivity disorder/hyperactivity disorder
ADHD is a childhood onset, neurodevelopmental disorder with genetic and environmental origins [ 5 ] characterised by pervasive behavioural symptoms of hyperactivity, inattentiveness and impulsivity that have been present for at least 6 months and adversely impact on daily functioning and development [ 4 ]. ADHD is highly prevalent. Research combining data from multiple sources and analysed using meta-regression reported a worldwide-pooled estimate of 5.29–7.2% in children [ 1 , 6 ], 2.5% in adults [ 7 ] and between 2.8% in older adulthood [ 8 ]. Symptoms must persist across the lifespan, although the relative balance and the specific manifestations of inattentive and hyperactive-impulsive characteristics vary across individuals, and may change over the course of development, e.g. in particular hyperactive-impulsive symptoms commonly reduce with age [ 9 , 10 ].
The diagnostic criteria for ADHD are presented in DSM-5 [ 4 ] and the World Health Organization’s International Statistical Classification of Diseases, 11th edition beta, (ICD-11) [ 11 ]. Whilst the basic symptom criteria did not change from the revision of DSM-IV [ 12 ], DSM-5 increased the typical age of onset to age 12 (previously age 7). The definition of ADHD was expanded to more accurately characterise the experience of adults, and the number of symptoms was relaxed for adults (> 17 years) who are now required to have five or more symptoms that have persisted for at least 6 months in the inattention and/or hyperactive-impulsive domains. For a diagnosis made in childhood, the number of symptoms remained as 6, respectively. Symptoms must be pervasive and interfere with or reduce the quality of social, academic and occupational functioning. They must not be better explained by other conditions, such as intellectual disability. The change in nomenclature from ‘subtypes’ in DSM-IV to ‘presentations’ in DSM-5 reflects increasing evidence that symptoms are often fluid within individuals across their lifespan rather than stable traits. The ‘presentation’ represents the person’s current symptomatology which may change over time: For example, in ADHD, inattentiveness may be relatively stable across development, but hyperactivity and impulsiveness often wane with age. Also, importantly, ASD is no longer an exclusion criterion, which is a fundamental change from DSM-IV and this, together with other comorbid conditions, should be noted. The advance preview of ICD-11 was published in June 2018, and this no longer refers to ADHD as hyperkinetic disorder. Other than that, it appears to be essentially similar to DSM-5 [ 13 , 14 ].
Multi-morbidity is common in both children and adults of both sexes. In children, around one-half will have at least one psychiatric disorder comorbid to ADHD and around one-quarter will have two or more comorbid disorders [ 15 ]. These are typically ‘current’ episodes of comorbidity, the most frequent in childhood being disruptive behavioural disorders (e.g. oppositional defiant disorder, conduct disorder), anxiety (e.g. generalised anxiety disorder, social anxiety, obsessive-compulsive disorder) and mood (e.g. depression, bipolar disorder). Others include specific developmental disorders of language, learning and motor development, autism spectrum disorders and intellectual disability, many of which present across the lifespan [ 3 , 15 , 16 , 17 , 18 ]. Adults with ADHD also experience high rates of co-occurring conditions, especially anxiety, mood and substance use disorders (including cigarette smoking) [ 19 , 20 ]. Therefore, the clinical presentation is complex, and this is often further complicated by academic and social impairments, leading to academic and occupational failure, delinquent and antisocial behaviour [ 20 , 21 , 22 ].
Autism spectrum disorders
The worldwide prevalence of ASD is around 1%, but some data suggest it may be higher [ 23 , 24 ]. Following the publication of DSM-5 in 2013, ASD is now characterised by two categories: (1) persistent deficits in the ability to initiate and to sustain reciprocal social interaction and social communication and (2) restricted, repetitive and inflexible patterns of behaviour, interests or activities, including differences in sensory sensitivities and interests. Individuals with ASD exhibit a range of intellectual and language functioning. Symptoms typically present in early childhood (by 2–3 years of age) with or without language delay and may be associated with early developmental delays and/or loss of social or language skills. However, many people may not receive a diagnosis of ASD until adulthood. This may be due to a variety of factors including lack of awareness of ASD across the lifespan, poor recognition of ASD in females and/or lack of services [ 25 ]. DSM-5 notes that symptoms must be associated with clinically significant impairment in personal, family, social, educational, occupational or other important areas of functioning. Symptoms are usually a pervasive feature of the individual’s functioning which are observable across settings. However, they may vary according to social, educational or other contexts and may be masked by ‘camouflaging’. Symptoms are relatively stable across the lifespan [ 26 , 27 ], although there may be some developmental gains in adolescence and adulthood due to increased interest in social interaction, behavioural improvement associated with interventions and/or compensations applied and/or the environmental supports provided.
The DSM-5 made substantial amendments to the diagnostic criteria of ASD from previous publications, the most striking being the removal of Asperger’s disorder and pervasive developmental disorder ‘not otherwise specified’ as distinct subtypes and these are now subsumed under the general diagnosis of a scalable severity of ASD. The latter is introduced by a hierarchical classification of the level of support required by the individual, i.e. level 1 ‘requiring support’, level 2 ‘requiring substantial support’ and level 3 ‘requiring very substantial support’. Severity of social communication difficulties and restricted, repetitive behaviours are rated separately, with the recognition that severity may vary by context and fluctuate over time. Additional specifiers should be included recording (a) with or without accompanying intellectual impairment (intellectual disability and ASD frequently co-occur, but symptoms should not be better explained by intellectual disability or global developmental delay); (b) with or without language impairment (assessed and described by the current level of verbal functioning, e.g. no intelligible speech, single words only, phrase speech, full sentences, fluent speech). Both receptive and expressive language is considered separately since the former may be relatively delayed in ASD; (c) whether ASD is associated with a known medical or genetic condition or environmental factor; (d) whether ASD is associated with another neurodevelopmental, mental or behavioural disorder; and (e) whether ASD is associated with catatonia.
Hence, DSM-5 has moved away from a polarised distinction of ‘high’ and ‘low’ ASD functioning and instead focuses on whether the condition is associated with or without accompanying intellectual impairments. Severity is classified by the level of support required by an individual, ranging across three levels. DSM-5 further separated out ASD from social communication disorder (SCD); impairments in social communication without the presence of repetitive, restricted or stereotyped behaviours may meet criteria for SCD.
At the time of writing, the ICD-10 is under revision and a detailed version of ICD-11 has yet to be published [ 28 ]. It is anticipated that ICD-11 will align with DSM-5, in that ASD can occur with other neurodevelopmental and mental health conditions (including ADHD) if full diagnostic criteria are met. Moreover, Asperger’s syndrome and other generalised developmental disorders will be included within the broader classification of autism and the diagnostic criteria will be organised under the same two categories presented in DSM-5, i.e. (1) difficulties in interaction/social communication and (2) repetitive behaviours (although it seems that ICD-11 will not include sensory sensitivities). Hence, the characteristic specifically relating to language problems has been removed, although ICD-11 seems to consider the loss of previously acquired competencies (such as language, self-care, toileting, motor skills) as a characteristic that should be considered when making a diagnosis. Further, ICD-11 will place less emphasis on the type of play children partake in due to variations across countries and culture but instead focus more of whether children follow or impose strict rules when they play.
ASD co-occurs with several neurodevelopmental, psychiatric and neurological conditions [ 29 , 30 ]. Indeed, 70% of children with ASD will have at least one co-occurring psychiatric condition and 41% will have two or more, the most common being social anxiety, ADHD and oppositional defiant disorder. Adults also experience high rates of comorbidity, the most common being mood disorders, anxiety disorder and ADHD [ 31 ]. Patterns of comorbidity are similar across the lifecycle, however, with individuals presenting with a range of anxiety and mood disorders, including panic attacks, generalised anxiety disorder, obsessive-compulsive disorder and unipolar and bipolar disorders. Hence, as for people with ADHD, the presentation of people with ASD may be complex from both a clinical and behavioural perspective but outcomes for those with ASD are often more marked in terms of functional impairments. Many adults with ASD live independently in adulthood but describe difficulties across a variety of educational and occupational settings and require support (formal or otherwise) from family or professionals [ 32 ].
Co-occurring ADHD and ASD
Previous publications of the DSM prohibited clinicians from making a concurrent ADHD and ASD diagnosis. The change in diagnostic approach taken by DSM-5 most likely reflects a growing body of research over the past decade that has identified both shared and distinct risk factors and phenotypic manifestations, including:
Many copy number variants (CNVs) and chromosome abnormalities confer risks for ADHD and ASD [ 33 ]. A genome-wide association study across five major psychiatric disorders including ADHD and ASD found evidence of shared genetic risk factors between ADHD and ASD, and common molecular pathways and functional domains that are affected by the disorders [ 34 , 35 ].
Both conditions frequently co-occur and cluster in families. Multiple interacting genetic factors and their interplay with environmental factors constitute the main causative determinants of both ADHD and ASD [ 36 ]. This interaction can affect epigenetic expression such as DNA methylation, histone modification and microRNA expression leading to altered development.
Brain structure and functional imaging studies show both shared and distinct neuronal features and activities [ 37 ]. For example, functional brain magnetic resonance imaging (fMRI) studies report both disorder-specific differences and shared deficits in functional brain activation and behavioural performance in tasks of sustained attention [ 38 ] and temporal discounting [ 39 ] in youth with ADHD and ASD. The largest structural brain MRI investigation to date of young people and adults with ADHD and ASD notes maturational differences, with ADHD-specific smaller intracranial volume in children and adolescents and ASD-specific thicker frontal cortices in adults [ 40 ].
Both disorders have a male predominance [ 2 , 38 ]. Although some specific distinctions are present between the two conditions, generally both are commonly associated with social difficulties, executive dysfunction and language and cognitive delays [ 36 , 41 , 42 , 43 ].
Rates of co-occurrence vary. In children, clinical studies investigating ADHD symptoms in ASD report a co-occurrence ranging between 53 and 78% [ 44 , 45 ]; whereas in community samples, it is lower at 28–31% [ 30 , 46 ]. A meta-analysis of the co-occurrence of ASD symptoms in young people from both clinical and community ADHD samples found a comorbid rate of 21% [ 3 ]. This suggests that ADHD symptoms may be more likely to be found in people with ASD than vice versa and a meta-analysis of rates of ASD in people with ADHD employing a similar methodology as Hollingdale and colleagues [ 3 ] would be helpful to consolidate the available data.
The co-occurrence of ADHD and ASD presents in those both with and without intellectual disability. In a personal communication from Dr. Bhathika Perera, Chair of the Royal College of Psychiatrists’ ADHD in Intellectual Disability Group (a sub-group of their Neurodevelopmental Disorder Special Interest Group), we were informed of a recent UK national audit (in preparation) that showed 70% of people with intellectual disability and ADHD also have autism. When working with this group, however, one needs to be mindful that there may be a difference in conceptualising ADHD in mildly intellectually disabled, verbal ASD individuals in contrast to those who are non-verbal and severely intellectually disabled. This has implications for treatment; for example, agitated states in severely intellectually disabled non-verbal autistic individuals may be confused with hyperactivity, leading to the underlying core problem not being understood and addressed. In turn, this may lead to greater risk of deterioration in the individual’s clinical presentation and associated functioning.
As discussed, comorbidity is very common in both conditions but for those in whom it co-occurs, this may be considerably more marked. Research from a community sample by Simonoff and colleagues [ 30 ] found that when ASD was comorbid with ADHD, the risk of receiving a further comorbid diagnosis increased by 14% (from 70% for the ASD group to 84% for the co-occurrence of ASD and ADHD). A prison study of 390 male inmates with ADHD reported that 21.9% screened positive for ASD, and this group with co-occurring ADHD and ASD was at higher risk of developing comorbid psychiatric symptoms than inmates in either group alone [ 47 ]. Thus, the co-occurrence of both conditions may increase the risk of developing further psychiatric conditions; indeed, persisting states of anxiety and dysphoria are common in ASD (alone or with comorbid ADHD) and risk of suicide in this group is a concern [ 48 , 49 ]. However, many individuals do not progress to a level of emotional ‘disorder’ that persists for a substantial period but instead experience mood instability, characterised by extreme fluctuations in mood that change rapidly over the course of a day [ 50 ]. This may be perceived by healthcare practitioners as less debilitating and of lower concern, but for the individual (and their families/carers), these extreme fluctuating emotional states are exhausting and deeply distressing.
There are diagnostic challenges for both conditions especially for those with subtle or ‘mild’ presentations, when difficulties are ‘masked’ by other comorbid conditions, ‘camouflaged’ by compensatory strategies, and/or when there is limited information about childhood functioning when making the diagnosis of ADHD or ASD for the first time in adults. Other challenges relate to teasing out symptoms and difficulties that may be adaptive in certain situations or settings. For example, an individual may be friendly and socially proactive, but the quality of these interactions may be gauche or ‘odd’ in nature. Concentration problems and/or overactivity may be less evident when individuals are engrossed in a topic or activity of special interest. Distraction, in terms of switching tasks by moving from one incomplete activity to another, may also be influenced by the level of interest in the task and/or modified by a tendency to become preoccupied with the task or due to a resistance to change. There are also diagnostic challenges when working with individuals at the other end of the spectrum, i.e. when assessing ASD in severely/profoundly disabled children with physical disabilities and/or young people.
It seems that the co-occurrence of ADHD and ASD confers additive vulnerability and complexity; hence, the United Kingdom ADHD Partnership (UKAP) convened a consensus meeting, attended by multidisciplinary experts working in the field, to address the complexities of ADHD and ASD from different perspectives, consider the clinical challenges of working with this complex group of patients and how to resolve them. A list of abbreviations can be found at the beginning of the manuscript.
Experts in the fields of ADHD and ASD convened in December 2017 in London, UK, for a meeting hosted by the United Kingdom ADHD Partnership (UKAP; www.UKADHD.com ). The attendees represented a multidisciplinary group of prescribing and non-prescribing clinical and academic experts with extensive experience working with individuals with ADHD and ASD (covering the fields of psychiatry, paediatrics, general practice, clinical psychology, social work, speech and language therapy, psychotherapy and clinical academic research). We were also fortunate to have representation from the field of education. The meeting included presentations summarising research on the topic. Following the presentations, attendees separated into three sub-groups. Each group was tasked to produce a framework of guidance with specific regards to:
Identification and assessment of children and adults with both ADHD and ASD
Interventions and treatments for children with both ADHD and ASD
Intervention and treatments for adults with both ADHD and ASD
The discussions during the breakout sessions were facilitated by group leaders and summarised by note-takers. The methodological orientation that underpinned the focus of the discussion groups was phenomenological, drawing on the empirical research base and their clinical experience. The sub-group leaders then presented their conclusions to all the meeting attendees for another round of discussion and debate until consensus was agreed.
The entire meeting was audio recorded and later transcribed (sub-group discussions were recorded by note-takers). The medical writer consolidated the meeting transcription, electronic slide presentations and breakout session notes into a draft manuscript. It was then revised by the lead author following further consultation with some authors and other expert colleagues who had been unavailable to attend the consensus meeting. The final draft was then circulated again to all authors to review and to agree the final consensus. The consensus reflects the views of the authors based on their practical experience and published research and provides a unified approach for working with children and adults with co-occurring ADHD and ASD.
Identification and assessment
A summary of the consensus reached regarding the identification and assessment of ADHD and ASD when this presents as a comorbid diagnosis is presented in Table 1 .
When conducting an assessment for either disorder or when considering the possibility of both co-occurring, it is essential to apply a multifaceted assessment approach that may include the use of standardised and semi-standardised measures. As ADHD and ASD are both complex neurodevelopmental conditions, a comprehensive assessment should include background information (including developmental, clinical and family history, and a current mental state examination), rating scales, a clinical diagnostic interview (including a detailed assessment of symptoms and examples of impairment and, if required, a risk assessment), observational data and an assessment of intellectual ability. Collectively, the information gained from this approach will guide the diagnostic decision. No single point of evaluation or instrument should be conclusive in making a diagnostic decision.
The high rate of co-occurrence between ADHD and ASD means that both conditions should be considered when one of the conditions is present; ASD may confer greater risk for co-existing ADHD where the prevalence of the dual diagnoses appears to be somewhat higher [ 3 , 44 , 45 ]. Indeed, young children presenting with an initial diagnosis of ASD should be continually monitored through development for ADHD, particularly given that the average age of diagnosis for the two conditions is discrepant.
Some individuals with ADHD find their symptoms substantially improve in young adulthood; others continue to sustain symptoms that cause impairment well into middle to late adulthood. In adolescence, people with ASD and/or intellectual disability may experience small improvements in their social functioning, but gains can be limited, and their difficulties and/or impairments persist across the lifespan [ 26 , 51 ]. Symptoms associated with ‘mild’ ASD may not be recognised (or not prioritised) in children with challenging behaviours associated with severe ADHD; however, this may change with priorities reversing in young adulthood when ADHD symptoms may start to remit for many young people. For this reason, a comprehensive assessment needs to be conducted that obtains detailed information about the person’s functioning spanning many years. It is important to get this right, as a neurodevelopmental diagnosis has the potential to help and guide understanding and necessary support.
It is therefore of concern that assessments (and diagnoses) are made by practitioners with limited training and skills and without a comprehensive appreciation of the variation and idiosyncrasies in the presentation of both conditions. The recent revisions to diagnostic criteria (DSM-5 and ICD-11) have been substantial, and this further emphasises the need for healthcare practitioners to obtain appropriate training for their continuing professional development. Aside from ensuring they access appropriate training, it is essential that practitioners refer to the diagnostic criteria to guide their clinical decision and apply the various clinical tools that are available to support it, rather than rely on a ‘general sense’ of the conditions. In such cases, there is a risk for missed or misdiagnosis. For example, a diagnosis of ASD might not be made because the individual is able to sustain eye contact and will initiate conversations on topics of interest. A diagnosis of ADHD might not be made because the individual does not present with hyperactivity and is able to settle or can ‘hyper-focus’ on a topic of interest or one that provides immediate gratification.
Research on gender differences suggests that girls may be consistently under-identified for both ADHD and ASD [ 52 , 53 ]. This may be due to multiple reasons. Females with ADHD are reported to have fewer hyperactive/impulsive symptoms and more inattentive symptoms compared with males with ADHD [ 52 , 54 ]. This may lead to a referral bias as they may not present with behavioural problems that are challenging to manage. Indeed, the lower rates of disruptive behaviour in females with ADHD (compared with males) may contribute to the ‘gender gap’ of 3:1 between males and females respectively [ 14 ]. Similarly, there is a ‘gender gap’ in ASD but it is more marked at 4:1, respectively [ 4 ]. Females with ASD are more likely than males to have comorbid intellectual disability; hence, those without accompanying intellectual impairments or language delays may not be recognised [ 4 ]. It has also been reported that females may acquire superficial learned social skills and exhibit milder restrictive stereotyped behaviour [ 55 ], which may mask their underlying social difficulties. The problem is further compounded when rating scales are used as few have separate gender norms, most being predominantly comprised of males. Hence, rating scales may lack the sensitivity and specificity to identify symptoms in females.
Some diagnostic measures have been validated in different cultural contexts [ 56 , 57 ], but the majority have been developed and standardised in western societies. Cultural issues are likely to impact the assessment, for example, expectations regarding the use of eye contact vary in different parts of the world, and hyperactivity in low- to middle-income countries may be beneficial in some settings but challenging within a post-industrial western educational system [ 58 ]. In the criteria for ASD, it seems that ICD-11 will disregard the type of play that children partake in since this may be sensitive to cultural influence but place greater emphasis on the approach they take to play (e.g. whether they follow or impose strict rules), i.e. behaviour which is less culturally specific. Cultural issues may also influence the diagnosis of children with ADHD. A UK study found that children from immigrant Asian families were rated by teachers as much less overactive and inattentive compared with actometer, observation and psychological test variables compared with their white English contemporaries, the rater bias perhaps reflecting higher expectations and/or symptoms not being noticed in Asian children [ 59 ].
When conducting neurodevelopmental assessments, it is common for family members to be involved, especially when assessing children, but also for adults where possible. Heritability estimates of both conditions are high (ranging between 70 and 80% for ADHD and 37 and > 90% for ASD) [ 4 , 14 ], and it is not uncommon for individuals to present for first diagnosis in adulthood prompted by a diagnosis of autism or ADHD in the family. Hence, it is important to be mindful that informants who are family members may also have (undiagnosed) ADHD or ASD and in turn this may impact their judgement of ‘typical’ behaviour. It is therefore important for the assessor to obtain specific examples of behaviour from the informant and use these examples to make clinically informed judgements, rather than relying upon the informants’ perception of what is ‘typical’ or ‘atypical’.
Whenever possible, the assessor should also obtain collateral information from independent sources. A wealth of useful information may be obtained from observing a child in school and speaking directly with teachers. When assessing adults, perusal of school, college and/or employment reports (if available) can be helpful.
Due to the high rates of comorbidity reported to be present in individuals with either ASD or ADHD (see the ‘ Background ’ section), practitioners should always consider possible comorbid conditions. In general, females are at greater risk of developing internalising conditions (e.g. anxiety, depression) than males, whereas males are at greater risk of developing externalising conditions (e.g. disruptive behaviour disorders). Positive outcomes may be hampered by unrecognised and untreated co-occurring mental health conditions. Intellectual disability is one of the most common comorbidities of both ADHD and ASD, 46% [ 60 ] and up to 70% [ 61 ] respectively. Adults with ASD and severe impairments requiring substantial support may lack the capacity to make decisions (this is less likely for those with ADHD without co-occurring ASD); hence, an assessment of capacity may be warranted. This needs to be managed carefully and sensitively, especially when there is a discrepancy between the wishes of the individual and those of their family or caregivers.
Symptoms of both ADHD and ASD may be masked for many reasons, which may cloud clinical judgement. Environmental accommodations may be applied at home, e.g. family outings, social events and school trips may be avoided in order to avoid embarrassing emotional ‘meltdowns’ in public. As it is often easier for accommodations to be made at home than at school, this may result in impairments in functioning not appearing to be pervasive across settings. Adults may also make accommodations; adults with ADHD may select occupations that are not ‘office bound’, which maximise the opportunity to be creative and/or stimulated and minimise the need for administration and organisational skills. Adults with ASD may select and be highly valued in occupations that match their special interests and skills.
Symptoms may also be masked by compensatory strategies and coping mechanisms, which may lead to an underestimation of their underlying difficulties. By the time individuals reach adulthood, it is not uncommon for such techniques to have been developed (especially by those with stronger language and intellectual abilities). These usually facilitate the individual to behave in an appropriately acceptable manner in public for a short time and/or in specific settings. These ‘camouflaging behaviours’ usually have an adaptive or functional purpose, for example, adults with ASD may develop a good understanding of social expectations in formal situations (such as a time-limited consultation with medical professionals). Adults with ADHD may employ strategies to remain focused and/or control the urge to fidget during an important appointment or meeting. Nevertheless, it takes great effort to maintain a social façade of this nature for any length of time and doing so may cause the individual to feel fatigued, stressed and distressed.
The strategies and mechanisms applied may not always be adaptive and functional; however, the assessor should be mindful of strategies applied that are dysfunctional. These may be obvious such as drinking alcohol or taking illicit drugs to manage social anxiety or low mood. Others may be less obvious, such as avoiding specific events, settings and/or people, not facing up to difficulties and problems, withdrawal and spending too much time locked away in a room online and/or not engaging in help-seeking behaviours. Some individuals may seek to obtain a social network by forming damaging relationships such as joining a gang, making themselves sexually available, engaging in promiscuous and unsafe sexual practices and/or being used by others for criminal activities.
There may appear to be some symptom overlap across the two conditions, which can complicate clinical assessment. Rating scales may not pick up on qualitative differences in presentation, especially when these are subtle, requiring the assessor to probe for detailed examples of behaviour. For example, when considering abnormal social reciprocity—a person with ADHD may be over-talkative and dominate a conversation, speaking with energy and passion, speak too loud, stand too close, be tangential and frequently change the topic, lose their train of thought mid-sentence, interrupt people’s conversations and illustrate what they are saying with gesture. A person with ASD may be over-talkative and dominate a conversation regarding a special interest, dogmatically stick to that topic and bring the conversation back to it when the other person tries to talk about something else. They may avoid making eye contact, tone and conversation style may seem ‘flat’, and they appear to have limited interest in the other person and lack awareness of social rules and cues (e.g. not asking questions, making inappropriate comments). Both examples indicate limited social reciprocity, but the clinical quality of the deficits is markedly different.
An individual with a co-occurring ADHD and ASD may show a combination of both characteristics in different situations. However, to meet diagnostic criteria for an additional comorbid diagnosis, there must be enough evidence for the second diagnosis over and above what would be expected for the first diagnosis. The assessor therefore should take a parsimonious approach, i.e. they should not ‘double count’ symptoms. For example, if ‘talkativeness’ has been rated as an ADHD symptom, then it should only be re-counted as an ASD symptom if it is distinctly different (i.e. odd and monotonous). Similarly, if invading personal space has already been counted as a symptom of ADHD it should not be counted again as an ASD symptom.
Rating scales
Rating scales may be used for two purposes: (1) to screen for a suspected condition and (2) to monitor responses to treatment and interventions. Rating scales are often used to aid clinical assessment, and they are useful tools for monitoring clinical progress; however, when used for screening purposes, it should be borne in mind that they are non-specific markers of potential problems, the results of which should be interpreted cautiously [ 62 ]. Rigid adherence to cut-offs is likely to lead to a high proportion of false positives and negatives and unnecessary concerns and anxiety among carer interventionss and caregivers.
There are many rating scales available with varying merits and limitations, and we present in Table 2 some that are in common use in the UK. Some are available in multiple languages and those that are free of charge are indicated with an asterisk (*).
The Strengths and Difficulties Questionnaire (SDQ) is a widely used brief behavioural screening questionnaire tool that evaluates emotional symptoms, conduct problems, hyperactivity/inattention, peer relationship problems and antisocial behaviour in children age 3–16 years. Translated into over 80 languages, it is therefore a helpful rating scale for use in children with both ADHD and ASD. Depending on the circumstances, there is a charge for using the SDQ.
Specific populations (such as females, younger children higher functioning young people and individuals with intellectual disability) may require adaptations to be made to a rating scale, if one cannot be identified that better addresses their functional abilities. For example, it is common for people with ASD (with or without intellectual disability) to have difficulty identifying or describing their thoughts, feelings and sensations. In such cases, observational tools such as visual representations of mood states, visual analogue scales, sketches and drawings may be useful aids. It is important to be mindful that norms for many screening tools are often based predominantly on male samples, which may disadvantage their use in females (in which case greater emphasis should be placed on carer interventionsal and school reports if female norms are not available).
Rating scales for adult use often rely on self-report. Adults with specific learning or motor difficulties may need support to complete them. Another problem is that some (but not all) individuals may have limited insight into their current and past difficulties (this is the case for individuals of any age, both with and without intellectual impairment). For those with ASD, an additional problem may arise for those with language problems, e.g. they may struggle with seemingly arbitrary phrasing and/or undefined concepts (for example, having to select the frequency of a behaviour from a choice of terms such as ‘occasionally’ and ‘sometimes’). People with ADHD tend to make careless errors due to poor concentration, and it is not uncommon for items to be completely missed out in questionnaires and/or for more than one response to be endorsed on a scale by accident. Hence, questionnaire responses need to be carefully checked and, in some cases, interpreted with caution.
Accepting the limitations of rating scales used for purposes of screening described above when used in clinical settings, there may be merit for using rating scales to screen children in educational settings who are regularly excluded from school and/or who are under-achieving academically. Similarly, it may be helpful to screen children at risk in social care.
Clinical interview
The interview should always commence with current concerns as well as background information (including family, past psychiatric and medical history) and move on to obtain a detailed developmental and clinical history that assesses the onset, trajectory, persistence and pervasiveness of symptoms as this will assist with differentiating between ADHD, ASD and other comorbid conditions. A current mental state examination should always be included as this is helpful for indicating the presence of comorbid psychiatric conditions and the assessment of risk. If indicated, some individuals may require referral for development coordination disorder.
It is critical to consider the extent to which the individual’s functioning is both age and developmentally appropriate. A child’s chronological age relates to their date of birth, and it may differ substantially from their developmental age. Their developmental age is the age at which they function emotionally, physically, cognitively and socially. For example, a child may be 12 years of age, but developmentally, they display emotions or behaviours that make them seem much younger. Hence, it is important not to focus solely on a child’s intellectual limitations or chronological age but to be mindful of a child’s developmental limitations more broadly. For example, a child of 12 years may have an IQ that falls within normal limits, but their emotional and social functioning may be highly discrepant with other functioning and developmentally inappropriate. Hence, one has to consider the broader developmental functioning of the child.
Environmental factors may also be salient. It is important to obtain examples of how difficulties interfere in the person’s functioning and development at home and education/work environments. For example, are unhelpful factors and dynamics present, which exacerbate symptoms and affect the person’s ability to cope? Does fluorescent or harsh lighting, hot or cold temperatures, smells of air fresheners or pets, general clutter, or noises from the TV, trains or road traffic have a negative effect? Can these factors be changed or can the individual’s reaction to them be changed?
Semi-structured clinical diagnostic interviews are particularly helpful as they guide the healthcare practitioner to complete a comprehensive developmental and clinical interview. There are fewer clinical interviews to choose from compared with rating scales and, as with rating scales, these have varying merits and limitations. We present in Table 2 some that are in common use in the UK. Some are available in multiple languages and those that are free of charge are indicated with an asterisk (*).
Administering semi-structured and structured interviews can be resource intensive and costly. It can be seen from the above that most clinical interviews specific to autism must be purchased, whereas most interviews specific to assessing ADHD are free of charge. Most require administration by trained interviewers. ADHD clinical interviews such as ACE, ACE+ and DIVA-2 have been developed to directly map onto diagnostic criteria, but most autism interviews have not; hence, if using the ADI-R for example, it is advised that this is done manually (i.e. by cross referencing the information obtained in the interview with the diagnostic criteria). The recently launched Diagnostic Autism Spectrum Interview (DASI) [ 78 ] also maps directly onto diagnostic criteria and to our knowledge is the only autism diagnostic tool that is free of charge. Whilst ‘mapping’ the clinical information onto the diagnostic criteria, the persistence and pervasiveness of symptoms should be considered, as well as differential diagnoses. In complex cases, this requires a skilled and experienced multidisciplinary team. ACE and ACE+ are the only clinical interviews that include an integral option for the assessor to apply either DSM or ICD criteria and include a prompt to consider comorbid conditions. For autism, the DASI also includes a prompt to consider comorbid conditions. The DAWBA can be used to assess ASD, ADHD and associated comorbidities at the same time. It is modular in format via a ‘package’ of questionnaires designed to make a range of psychiatric diagnoses that can be completed online (using self- or informant-report, as appropriate) or via interview.
Risk assessment of harm to self and others and from others should be included in the assessment for both ADHD and ASD. The vulnerabilities associated with those who have both conditions may elevate risk further. There is evidence that adolescents with ASD are at higher risk of suicidal thinking, making suicidal plans and engaging in self-harm with suicidal intent than young people without ASD [ 46 ]; similar evidence has also been found for individuals with ADHD [ 84 ]. Young people with ASD and an IQ that falls within the average range appear to be at particular risk [ 85 ]. Although the association is documented to emerge in adolescence, clinicians gave anecdotal accounts at the meeting that this is also a serious problem in younger children. It was a concern of the group that young people with ASD may act on suicidal ideation due to their tendency to rigidly adhere to ideas. Young people with ADHD, by contrast, may become distracted and/or make inadequate plans. They may nevertheless act impulsively on an idea (as may young people with ASD).
A risk assessment should therefore be included for children and young people, as well as adults, that enquires about suicidal ideation; use of illicit drugs/substances and alcohol; antisocial attitudes and behaviours; any harm to self and others, or from others; excessive internet use; unsafe sexual practices; victimisation of bullying and assault; and sexual/financial/social exploitation. For individuals with ASD, a risk assessment should take account of sensory deficits, such as seeming oblivious to pain or to significant temperature changes.
When conducting clinical assessments in adults, a developmental history should be obtained, where possible, which can be difficult when this is self-reported. Whenever possible, this should be provided by an informant, such as a carer interventions/carer, although this may also be challenging due to the passage of time. A helpful prompt may be to ask the carer interventions/carer to look at childhood developmental health records, photographs and school reports and/or to think about key transitions in the child’s life (such as moves from home, change of school). However, the assessor needs to be mindful of the need for symptoms to be consistent and pervasive over time and across settings; difficulties should not be better explained by a situation-specific event that required the child to adapt to substantial change in their life (such as moving home or school). The assessor should also consider whether difficulties are being masked by compensatory strategies and/or ‘accommodations’ (i.e. adjustments) made by others.
In some cases, a carer interventions/carer may not be available, in which case collateral information should be obtained from another close family member. If a suitable informant cannot be identified who knew (and can recall) the individual well during their early childhood, it is valuable to obtain information from an informant who currently knows the individual well (e.g. a partner) as they can supplement self-reported information with an objective perspective. If available, reports from childhood (for example, school, social service and/or previous clinical reports) are likely to be informative.
Objective assessments
Objective assessments range from direct observation of an individual in a specific setting (e.g. in clinic, at home or at school) that provides qualitative information about the individual’s behaviour to standardised assessments that compare an individual’s behaviour or performance against norms obtained from a general and/or other specific populations. The assessor should be mindful of caveats that may influence outcomes. For example, if the individual is in a novel environment and/or aware of being observed, he may appear more socially able than usual due to ‘surface skills’ that he is able to apply and manage for a short period of time. In particular, the use of compensatory strategies may minimise deficits in social communication and interaction. With respect to more formal testing, problems with mobility may limit performance and/or the individual may perform relatively well on novel tasks, especially when these are delivered via a mode of interest (e.g. computerised tests). Moreover, a test environment is often arranged to be one that optimises performance (i.e. it is conducted in a quiet room that minimises distraction by an assessor who provides individual attention to ensure the person understands the test instructions and who provides prompts, encouragement and feedback). Hence, outcomes may lack ecological validity as they may not reflect performance in the ‘real world’.
The Autism Diagnostic Observation Schedule Second Edition (ADOS-2) [ 86 , 87 ] is a widely used semi-structured standardised measure of communication, social interaction, play/imagination and restricted/repetitive behaviours. It is used with individuals who have suspected ASD. The ADOS-2 requires a trained assessor to administer structured and semi-structured tasks and questions to elicit a range of responses in children (including toddlers) and adults. Although the title includes ‘diagnostic’, it is not a diagnostic instrument but a useful measure to be used in support of a clinical assessment. Females may develop superficial learned social skills, which may ‘camouflage’ underlying difficulties or exhibit milder restrictive stereotyped behaviours [ 55 ] leading them to score lower on the ADOS-2 compared with males.
An intellectual assessment should always be considered (especially in cases when intellectual impairment or an uneven cognitive profile is suspected). Practitioners should maintain a low threshold for administering the most recent versions of available cognitive tests such as the Wechsler intelligence scales for children or adults (i.e. currently the WAIS-IV and the WISC-5 [ 88 , 89 ] together with an assessment of adaptive functioning, such as the ABAS-3 [ 90 ] or the Vineland-3 [ 91 ]). The Kaufman Assessment Battery for Children (KABC-II NU) is a measure of cognitive ability that is culturally fair and includes a non-verbal option and standardisation samples that include people with ASD and ADHD [ 92 ]. Cognitive assessments of this nature will inform the psychological treatment approach as those with low intellectual abilities and/or poor verbal skills may respond better to interventions that focus more on a behavioural approach delivered directly to the individual and/or via carer interventionss/carers.
For both conditions, uneven cognitive profiles are commonly seen which may complicate the determination of an individual’s general intellectual abilities (i.e. the Full Scale IQ). In such cases, it is more informative to focus on the four individual intellectual sub-scales or indices that summarise the person’s verbal abilities, performance abilities, working memory and processing speed. The inclusion of an intellectual assessment is particularly useful for both young people in school/further education and adults as it provides information about the individual’s cognitive strengths and weaknesses, which in turn informs goals for treatment by indicating specific areas of cognitive weakness that can then be targeted with appropriate interventions in educational settings.
Neuropsychological testing is neither necessary nor sufficient for a diagnosis of ADHD; however, tests that assess executive dysfunction are helpful in determining deficits in higher order processing skills such as task switching, perseveration, planning, sequencing and organising information. Some have been specifically developed for use with an ADHD population and focus on assessing attention, impulsivity and vigilance in children and adults, e.g. Go-No-Go tasks, Stop tasks and continuous performance tests. Those most commonly used in clinical practice include the Conners’ Continuous Performance Test, third edition (CPT 3 [age 8+]) [ 93 ] and the QbTest [ 94 ]. These tests are not specific markers of ADHD, but they augment clinical decision-making by providing useful information regarding a person’s cognitive functioning. The assessor should be mindful of the limitations of formal tests and test environments raised above.
Outcome of the assessment
The outcome of the assessment should include a diagnostic formulation as well as an aetiological formulation that includes protective, predisposing, precipitating and perpetuating factors that inform a comprehensive care plan which considers of the needs of the individual and how these may be met across settings. This might include suggested pharmacological and/or psychological interventions to manage co-occurring difficulties such as anxiety or low mood, to minimise presenting risks, difficulties in social communication and behaviour and improve cognitive skills, study skills and social skills. For children and young people at school or in further education, a comprehensive formulation of current strengths and difficulties could be shared with educational establishments and other professionals involved in their care, should the young person consent. A comprehensive clinical assessment report should be copied to the patient and referrer. See Table 3 for a summary of suggested content.
Non-pharmacological interventions for ADHD and ASD
Those with comorbid ADHD and ASD present with additional layers of complexity, often requiring psychological and/or environmental interventions. In order to maximise the likelihood of positive outcomes from any therapeutic intervention, the influence of the individual’s relational and situational context must be considered. This includes both the home and education/work environments. There may be unhelpful factors and dynamics exacerbating symptoms and affecting the person’s ability to cope, such as fluorescent or harsh lighting, temperatures, smells (air fresheners or pets), noises both internal (e.g. TV) or external sources (e.g. trains or road traffic), unclear labels (e.g. for toilets) and/or a cluttered environment with obstacles that they need to navigate. A systemic approach is therefore advised.
Due to the unique presentation and difficulties experienced by children and adults with ADHD and ASD, non-pharmacological interventions must be tailored to meet their individual needs. This may relate to ‘internal’ change that the individual can make themselves (e.g. by developing functional coping mechanisms and adaptive techniques that they can apply) as well as ‘external’ changes that can be made within the environment (e.g. systemic adaptations working with the family/carers and/or school in order to optimise achievement). The approach taken depends on the developmental level of the individual, their clinical and behavioural presentation and their social communication skills.
It is important to ensure that individuals and/or carer interventionss/carers have realistic expectations of the patient’s abilities and what may be achieved by interventions (both medical and non-medical). The rationale for taking medication, if prescribed, needs to be explained (e.g. what it is, how it works, what it does, why they are taking it, what the expectations are). This approach will foster understanding and personal collaboration that will aid compliance.
Due to the high estimates of heritability for neurodevelopmental conditions, some carer interventionss may also have symptoms of ADHD and/or ASD symptoms, so interventions targeted at carer interventionss should be delivered in a way that will facilitate their acquisition of knowledge and skills.
We consider below specific interventions for (1) working with children, young people and their carer interventionss/carers and (2) working with adults. It is important that proposed intervention plans are included in the individual’s care plan and shared with all relevant personnel. Positive Behavioural Support plans focus on providing consistency of interventions between different caregivers or staff and the individual. This will increase awareness and understanding of caregivers and staff of early warning signs (both external as in the example, but also precursory behaviours of the individual that may indicate an emotional outburst is imminent) and develop proactive strategies.
Working with children, young people and their carer interventionss/carers
A summary of the consensus reached regarding non-pharmacological clinical interventions for children and adolescents with comorbid ADHD and ASD is presented in Table 4 .
Psychoeducation
Psychoeducation is helpful for improving the experience and long-term outcomes for individuals with ADHD and ASD and their carer interventionss/carers. It may be delivered in various formats: as a ‘stand-alone’ one-on-one intervention delivered to individuals, parents/carers and/or others (such as teachers) or in a group format (most commonly to individuals and/or parents/carers).
In addition to ‘stand-alone’ delivery (either in individual sessions or in group format), psychoeducation should also be included as a precursor to all other interventions provided (both medical and therapeutic). Indeed, psychoeducation is an integral part of all therapeutic interventions and every face-to-face meeting with the individual and/or parents/carers is an opportunity to provide information and education about ADHD and ASD.
The aim of psychoeducation is to provide information about the condition(s) (ADHD and ASD): This might include topics on aetiology, symptom presentation and associated difficulties, common comorbidities, treatments provided or available, and ‘trigger points’ for increased stress (both small scale, such as going on holiday or attending social events, and large scale, such as change of school, moving home, transitioning between junior and senior school, transitioning between child and adult health services, transitioning to further education or work), local resources and support services. When delivered on a one-to-one basis, input from parent/carers should be included in the development of the individual’s care plan in order to ensure that the rationale for the approach taken in the care of the individual is clear and understood by all.
Due to the ongoing need for psychoeducational interventions, a lifespan approach should be adopted; follow-up sessions are essential to provide information, support and key points of transition. Hence, psychoeducational intervention should not be considered to be a ‘one off course’ but ‘drip fed’ over time with reinforcement at regular intervals. However, uptake rates may be low, perhaps because parents/carers perceive psychoeducation as a lower priority than therapeutic interventions. Practitioners at the consensus meeting commented that feedback from parents/carers is that they find the content too generic and/or that they are too busy or too tired to commit to sessions. Therefore, it is important to consider the resources of the family—in terms of time, emotion and support—and structure the content so it is relevant to the needs of the child (and taking account of the child’s chronological age or developmental age). For example, psychoeducational programmes should differ for children and adolescent populations with the latter including issues relating to transition, sexuality and risk.
Parent/carer interventions
Most commonly referred to as parenting interventions, there are two types of intervention that may be offered to parents/carers: (1) parent/carer support interventions and (2) parent/carer-mediated interventions. Ideally, an integration of both approaches is likely to lead to better outcomes, especially with the inclusion of a psychoeducational component.
Families may experience enormous strain in having to persistently support a child with co-occurring ADHD and ASD. Parent/carer support interventions are designed to provide a supportive and contained ‘space’ where they can meet and share experiences with others who are in similar circumstances. These programmes may be time limited or ongoing ‘drop in’ meetings. Sessions may introduce some basic behavioural management strategies, but the focus is predominantly on the parent/carer with the child being the indirect beneficiary via the parent /carer feeling better supported and learning to better cope with their own feelings of stress, distress and feelings of isolation. Discussion topics may include improving coping skills (that of the parent/carer and the child), managing stigma, coping with the impact of the child’s behaviour on family relationships, balancing the demands of employment and family life, building routines and structure, introducing visual schedules, building in ‘me time’ and respite care, accessing supportive networks, enhancing competency in advocating for their child, improving safety in the home and community, applying a sensory diet and using rewards sanctions and reinforcers, as well as reminders and prompts.
Parent/carer-mediated interventions are designed to teach parents/carers to deliver interventions to their child. It is therefore technique focused, and the parent/carer is the agent of change with the child being the direct beneficiary. They are usually delivered in a time-limited group format (up to 12 sessions). There is some evidence base for the use of behavioural interventions of this nature in children with ASD, ADHD, oppositional defiant disorder and conduct disorders with findings for improved parenting skills and decreased levels of family distress [ 95 , 96 , 97 , 98 ].
The aim of these interventions is to support the child to develop skills and reduce maladaptive behaviours. For children with both ADHD and ASD, the content should include greater focus on social communication skills and methods to address disruptive behaviour, aggression, feeding, sleep and toileting problems. The inclusion of environmental adaptations, whenever possible, is likely to maximise success. It is important to acknowledge the difficulties experienced by parents/carers in coping with a child with complex needs by including aspects in the programme content that will help the parents/carers to manage their own feelings of isolation, stress, anxiety and depression. Sessions should be supplemented with written and/or pictorial handouts summarising the information covered and interventions need to be pitched at a realistic level to achieve success. Small gains are better than no gains, and no gains may be the outcome if goals are perceived to be unrealistic or overwhelming.
Behavioural and environmental interventions
Following psychoeducational and parenting programmes, and depending on the individual’s needs and presenting difficulties, specific therapeutic interventions may be offered. Depending on the level of ability, these are often behavioural and environmental interventions that are specifically tailored to the child’s needs and modified to account for their unique presentation, comorbid and associated problems. Most commonly those around the child (parents, carers, teachers) are the agents of change in addition to physical environmental modifications being made in order to optimise outcomes.
For both children and adults with ASD and challenging behaviour, environmental interventions are often preceded by a Functional Behavioural Analysis. This is an observational technique that systematically records the Antecedents, Behaviours and Consequences of behaviour (known as an ABC chart). Typically, an individual is observed in a specific setting (or if appropriate across settings) for a period of time and interacting with different people. The antecedents to behaviour are noted in a chart (i.e. what was happening immediately before the behaviour occurred, what makes it worse, what makes it better), and the behaviour itself is described in detail and its consequences (i.e. what happened afterwards, how the individual and those around him/her responded). The recording and analysing of behaviour using this method provide insight into the triggers and motivations of challenging behaviour and factors that may maintain the behaviour. In turn, this informs the method and goals of treatment. For example, in the case of a functional analysis being conducted to identify triggers of severe emotional outbursts, it is determined that these are precipitated by ‘spinning noises’ such as a washing machine or dishwasher. The interventions may include making parents/carers aware of the trigger, removing the child from the environment before the items are turned on, changing the times they are in use (if possible) and/or moving the child to a calming environment to help them reduce feelings of distress in reaction to the noise. Some behavioural interventions have been specifically developed for toddlers with ASD drawing on this approach, probably the most common being the Applied Behaviour Analysis (ABA) [ 99 ].
Other therapeutic interventions
Individual sessions working directly with the child are sometimes provided, especially for those with severe symptoms and intellectual limitations and/or those who are unable to tolerate group sessions for other reasons (e.g. excessive hyperactivity, poor social communication). These typically draw on ‘traditional’ therapeutic interventions with modifications as appropriate such as the inclusion of visual analogues and materials. They may also be delivered via their teachers and/or parents/carers. Two semi-structured programmes are available to support this type of intervention which have been specifically developed for young children with cognitive, emotional, social and/or behavioural problems: one for individual delivery [ 100 ] and the other for group delivery [ 101 , 102 , 103 ].
When delivered directly with the child, more sessions may be required but of slower pace and shorter duration and/or including mid-session breaks. Greater structure and adherence to a clear agenda will help to reduce uncertainty and anxiety. The therapist should also consider whether environmental adaptations are needed to minimise sensory discomfort and distractions (e.g. sensitivity to light and sounds). It is advisable to involve parents/carers (and in some cases teachers, if appropriate) since many people with ASD struggle to generalise from one context to another. Parents/carers can support them to apply strategies they have learned in therapy when they are in different contexts.
For those individuals without intellectual limitations, narrative therapy aims to enhance children and young people’s awareness of their strengths and how to utilise them through the sharing and recounting of ‘stories’ the person tells himself/herself about the world. It aims to promote social adaptation, so the person is better able to manage change in their life by strengthening their self-esteem and self-efficacy. This approach has been found to be useful by some services, but its effectiveness has yet to be robustly researched.
An adapted cognitive behavioural therapy (CBT) approach is likely to be more suitable for young people in adolescence than younger children, although the balance between cognitive and behavioural interventions may need to favour the latter when treating children with ADHD and co-existing ASD. Useful topics include social skills training; emotion recognition, ‘reading’ body language and facial expressions; impulse control; emotional control; methods to improve attention and memory; addressing low self-esteem; assertiveness training; coping with peer pressure; identifying and recognising risky behaviours; managing family and social relationships; constructive planning skills; and problem solving techniques.
Adolescence is an important time to support an individual with ADHD and ASD as it is a time they face many transitions, e.g. between health services, between education settings, leaving education, entering the workplace and hormonal and personal body changes. Peer relationships (or difficulties with them) become more salient. Therefore, when working with adolescents, issues relating to sexual development, desires and sexual behaviour should be included, in addition to risk behaviours and attitudes (e.g. antisocial, psychosexual, alcohol and substance use).
Individuals may require support in resolving difficulties that arise within the criminal justice system if their conduct is deemed to reach critical thresholds. The carrying of ‘alert cards’ may help in triggering additional communication supports at moments of crisis. The alert card may specify the disability and provide contact details of family members/carers and/or professionals involved in their care. This simple intervention may be influential in ensuring the individual receives fair and just treatment.
Those people with ASD that do get involved with the criminal justice system, however, may be disadvantaged by some test processes. For example, the probation service in the UK has started using mandatory polygraph (‘lie detector’) testing for high-risk sex offenders under their supervision [ 104 ]. The police can also use polygraphs on a ‘voluntary’ basis. The use of the polygraph is controversial due to problems with its validity [ 105 ], and this may be amplified for suspects and offenders with autism, who are likely to be particularly vulnerable to erroneous outcomes (both false-positive and false-negative error rates) due to their social communication difficulties.
Education and classroom interventions
A summary of the consensus reached regarding educational interventions for children and adolescents with comorbid ADHD and ASD is presented in Table 5 .
Unfortunately, many children with complex and comorbid presentations may fail multiple times in school before any action is taken to help them. Difficulties may be compounded by late diagnosis or delay in recognition of primary diagnosis, and/or comorbid disorders following an initial diagnosis and lack of awareness of ADHD and ASD. Education professionals in collaboration with health and social care professionals should be mindful of the range of presentations associated with both conditions and sensitive to the less overt behaviours (inattention/daydreaming) which may indicate a level of risk in pupils (especially, but not exclusively, females) who might not be perceived as particularly challenging or oppositional. Screening tools such as the Strengths and Difficulties Questionnaire [ 75 ] could be applied in educational establishments to screen ‘at risk’ pupils and guide the type and direction of intervention that may be required (which may be referral for further assessment).
The current evidence base for the effectiveness of school-based interventions for either ASD or ADHD remains poor and is almost non-existent for comorbid presentations. However, the Collaborative Life Skills Program (CLS), a 12-week psychosocial intervention programme for primary school students with ADHD symptoms, has been tested in a randomised controlled trial and shows promise. CLS integrates school, parent and student treatments delivered by school-based mental health providers. Following the program, students from the CLS-assigned schools had significantly greater improvement on parent and teacher ratings of ADHD symptom severity and organisational functioning, teacher-rated academic performance and parent ratings of oppositional defiant disorder symptoms and social/interpersonal skills. During the following school year, CLS-assigned schools had significantly greater improvement on parent, but not teacher, ratings of ADHD symptom severity, organisational functioning and global impairment. Within-group analysis indicated that parent- and teacher-reported post-treatment gains for CLS in ADHD and oppositional defiant disorder symptoms, organisational skills and academic competence were maintained into the next school year [ 106 , 107 ].
Nevertheless, due to the paucity of research in this area, the guidance below has been largely derived from practitioner observations with the recommendation that benefits are likely to be maximised where support plans are individualised to pupil needs, where comprehensive assessments extend beyond the diagnostic profile and where education staff have the skills and experience to make regular adjustments as each pupil develops (i.e. dynamic assessment of need).
Significant differences exist between primary, secondary school and college settings in terms of both the executive demands made of children and young people, and the capacity of staff to monitor and track pupil progress. In general, the logistical challenges in secondary schools make it difficult to gain an overview of how a student is performing with multiple teachers and across multiple subject areas, and it is thus vital to ensure that all concerned are fully aware of an individual’s needs and understand of the importance of providing regular feedback to the special educational needs coordinator [SENCO], or equivalent. This is particularly important where treatment is being titrated or novel preparations are being trialled, or when there are changes in a pupil’s presentation in terms of their general health and well-being.
It is important that teachers acknowledge that students with ASD and/or ADHD are not labelled as ‘naughty’ or ‘disruptive’ per se as this may set a precedent within the school environment and stigmatise the child. The attitude and approach in managing a student within his/her peer group and the school at large will define the child’s experience in education.
Special attention should be given to periods of transition, particularly from primary to secondary education, and proactive individual planning for this should be thought through with the student, the school and others involved in the students care (if appropriate) in order to minimise the potential negative impact of this event and feelings of stress.
Given that both ADHD and ASD are associated with specific learning difficulties such as dyslexia and dyscalculia, it is sensible to consider how these might impact on learning and to systematically screen this high-risk population as a matter of course. Likewise, any language or communication deficits should be identified early in primary school settings so that appropriate interventions can be introduced before they have a significant impact on learning, social function and development. Allied health professionals (speech and language therapists, occupational therapists) can assess receptive and expressive language capabilities and movement function (e.g. posture, pencil grip) as well as adaptive behaviour functioning and contribute to educational support plans. Children with autism may find generalising functional skills across different contexts particularly difficult. It is therefore important that school staff work in multi-agency teams, especially in cases where the risk of disengagement is high, or pupil needs are complex. Disengagement from school, possibly to the extent of exclusion, rarely benefits the child, and a proactive approach that supports the child both academically and behaviourally may divert the child from a negative course.
Given the known association between language deficits, challenging behaviour and academic under-attainment, staff may benefit from specific training to understand the significance of subtle difficulties in understanding in the way that children both learn in the classroom and interact with their peers. Such difficulties can lead to heightened anxiety and frustration and both academic under-attainment and social isolation (and thus reduced opportunities for social learning).
Similarly, teachers should be aware of any sensory challenges that a child or young person may face. Given that anxiety may be the principal barrier to social inclusion and learning in school settings, understanding both the social and sensory needs of a pupil can enable staff to make the necessary adjustments (e.g. avoidance of congested spaces, loud noises) to reduce stress and promote learning and engagement. Occupational therapists can support schools to provide the sensory diets needed by many children and young people with comorbid disorders.
Pupils with extreme demand avoidant profiles may require a higher level of individualised support in order to sustain their participation in mainstream settings, and school staff should be aware of the high level of neurodevelopmental risk in the pupil population considered to be ‘school refusers’.
It is helpful for teachers to be aware of both the developmental age of any pupil diagnosed with comorbid ADHD and ASD and their cognitive ability to ensure that curricular demands are appropriate. By the early teenage years, pupils with ADHD may function at a level 2 to 3 years behind their peers as a result of delayed cortical maturation and this may help to explain apparent under-attainment, difficulties with task adherence, or problematic behaviours and social isolation [ 108 ].
School can be a challenging environment for children with ADHD and ASD (either alone or when co-occurring). At school, children are academically compared with their peers in class (e.g. rated in position of the class, put into streams according to achievement); however, teachers and teaching assistants may not fully appreciate the ‘achievement gap’ between chronological age and developmental age especially for children who are being educated in mainstream school. This needs to be clearly addressed in the child’s Education, Health and Care Plan (EHCP), or equivalent (e.g. a Coordinated Support Plan in Scotland), which in England and Wales is a legal document which describes a child or young person’s special educational needs, the support they need and the outcomes they would like to achieve. The EHCP should be developed and regularly updated with input from all those involved in the child’s care, including parents/carers.
Difficulties may not relate solely to academic performance but also to social demands (managing peer relationships, team sports, free play during breaks in playground, after school clubs and activities). This may be due to a variety of reasons including peer relationship problems, being intimidated and bullied, social anxiety, perceived sense of failure, stigma, difficulties adapting to school routines and/or sensory sensitivities. Children with ADHD and ASD are often perceived as being so ‘different’ from their peers that they become the subject of ridicule and bullying. They may feel isolated and deeply distressed in the school setting, leading to some children refusing to attend school. When this happens, it is important that educational services develop comprehensive coordinated support plans to help the child and prevent school refusals in advance. This may include allowing flexible school attendance or home tutoring, with the aim of gradual reintegration back into school. Prior to that, adjustments may be made in the school setting to support pupils by providing quiet spaces during breaks and lunch times, supported social groups and higher levels of staff supervision during these times. It is important that support staff (e.g. teaching assistants) are both trained in recognising different levels and types of need and encouraged to raise concerns and contribute to planning meetings.
The poor long-term outcomes for this high-risk population suggest that preventative measures may be helpful and necessary in order to avert later risk (such as unplanned pregnancy, sexually transmitted infections, substance misuse and mental health difficulties). The inclusion of health and well-being topics within the curriculum may be beneficial.
For those with co-occurring ADHD and ASD, a personalised education plan (PEP), or equivalent (e.g. Individualised Educational Programme (IEP), Pupil Support Plan, Co-ordinated Support Plan or Child’s Plan in Scotland), is recommended. See Table 6 for a summary of specific educational interventions that may be helpful for children and adolescents.
Working with adults
A summary of the consensus reached regarding non-pharmacological clinical interventions for adults with comorbid ADHD and ASD is presented in Table 7 .
Parents/carers are recognised as a valuable source of expertise in the care needs and specific educational and occupational challenges faced by their child with co-occurring ASD and ADHD. However, parents/carers may experience a sense of exclusion when their child is transitioning into adulthood. This is particularly true if the individual wishes to advocate more for themselves and restrict access to information and decisions regarding their care. Services need to manage the interface between an individual’s right to confidentiality and the need to draw on the expertise that parents/carers have developed over time. Any information shared with parents/carers must be done so with the individual’s knowledge and consent. The issue of guardianship may need to be considered and long-term financial planning arrangements put in place (e.g. setting up a trust fund), particularly when intellectual disability has also been diagnosed. In such cases, signposting to reputable services that can provide advice on these topics may be helpful.
Poor timekeeping and organisation skills may lead to disengagement from important services (e.g. GP, mental/physical health, dentist) and additional structure may be necessary to sustain appointments, treatment regimens and medication (e.g. use of text, phone app reminders). There may often be difficulties in self-regulating behaviour and decision-making, leading to poor lifestyle choices, which may result in poor physical and mental health (e.g. anxiety, depression, forgetting to take medication, dental care), poor financial management, homelessness and social isolation.
Many individuals with ADHD and ASD become parents themselves. However, for a minority, their capacity to support children may be questioned if appropriate support and guidance is not provided. Their commitment to family welfare may be misconstrued if, for example, problems with planning and organisation are interpreted as evidence of neglect. If unnecessary disruption to family life is to be avoided, all professionals involved need to understand how ADHD and ASD may impact on the person’s daily functioning in order to identify the most appropriate types of support that may be required.
There is a dearth of research on the needs of adults with ADHD and ASD who are negotiating transitions in later life, e.g. in middle-age, at retirement and in geriatric patients. Professionals in primary care settings should be conscious of the current under-diagnosis of both conditions in the adult population and mindful of the risks that may become evident in clinical settings, as well as the treatment options available. Likewise, social care professionals may benefit from understanding the range of presentations that these cohorts may demonstrate when demands are made for their services.
The approach for working with adults is similar to that applied to working with children and adolescents, especially for those with severe intellectual impairments (i.e. by providing systemic support and psychoeducation, functional behavioural analysis and the implementation of behavioural environmental interventions, and the provision of individual cognitive behavioural interventions, when appropriate). There are however some key adaptations that will be addressed here. As for children, interventions should be integrated into a bespoke collaborative care plan for the individual.
The management of consent and capacity may need to be carefully considered in adults as it impacts on the individual’s decision-making capacity and legal rights. It also needs to be managed sensitively, especially in the presence of conflicting perspectives and opinions. Even in the absence of issues of consent and capacity, there may be discrepancies between how the individuals themselves want to live and the wishes of their family or carers. In such cases, there needs to be close communication with families and carers, often involving psychoeducation with both the individual and carers. Indeed, there may be a need to work systemically on family relationships and/or with carers on placement rather than applying a solution-focused approach, e.g. with a focus on values and trust, and establish who to go to for what information and guidance.
Positive Behavioural Support planning is strongly recommended to provide consistency in how carers and staff work with the individual. This will enable them to better understand subtle differences in presentation, identify early warning signals of specific behaviours and develop proactive strategies of prevention and/or intervention.
For adolescents and adults, it is important that individuals develop common sense practices regarding unsupervised use of medications (if appropriate). This may be achieved by providing information about how the medication may impact on their performance in adult activities (including work) and the risks of not taking the medication. They should also learn about the consequences of sharing or selling medications to others, both from a legal perspective as well as from a health perspective (i.e. the potential harm that may arise from supplying medications to others).
Psychoeducation for young people and adults should also address the use of alcohol and illicit drugs, impulsivity, antisocial attitudes and behaviours and their potential outcomes. Sex education is a topic that is sometimes excluded, yet these young people are experiencing sexual feelings and desires. They may engage in promiscuous behaviour to gain friends and, due to their vulnerability, they may be at risk of sexual exploitation. Often, these are issues that they have never spoken about and it may be necessary to ‘give them the language’ to articulate their thoughts and feelings, supplemented with visual analogues and materials and in some cases with anatomically correct dolls.
Pregnancy rates for young women with ADHD are elevated [ 111 , 112 ] suggesting that this may also be a risk for females with both ADHD and ASD. As young parents themselves, they may need a great deal of support else they may become increasingly vulnerable, particularly if they are the sole caregivers for their children. Hence, specific tailored assessments, support plans and social interventions are needed for this vulnerable group. There is currently limited literature on this topic and more research is required.
Psychological interventions
Group work may be challenging for some people with ADHD and ASD, especially those with intellectual limitations, as they may lack concentration and struggle with the social communication demands of group work. They often find it difficult to settle and inhibit their urge to interrupt. Nevertheless, adults may be better able to cope with group delivered treatments than children and adolescents, especially when specific adaptations are arranged, for example by increasing the number of group facilitators to ensure individual support can be provided during group meetings. If possible, it is preferable for individuals to be grouped in some relational way, e.g. by age and/or gender. For those who are unable to tolerate a group format, some content may be appropriately adapted and provided on an individual basis.
The R&R2 for ADHD youths and adults programme, which has a good evidence base when delivered in group sessions in the community [ 113 , 114 , 115 ], has been successfully adapted in adults with moderate intellectual impairment. The programme covers topics of relevance to both ADHD and ASD, including the development of prosocial competence skills, cognitive and executive functioning skills, critical analysis and consequential thinking, emotional control, negotiation skills, social problems solving skills, assertiveness training and moral reasoning skills.
The R&R2 is tailored to the needs of its recipients, and compared to the original R&R, it includes more visual material, simpler language and some modified examples and exercises [ 116 ].
In addition to the structured or semi-structured group interventions described above, individuals may benefit from attending peer group support interventions (i.e. a peer version of the parent/carer support interventions described in the previous section).
There is evidence that interventions adopting a cognitive paradigm are effective interventions for adults with ADHD (e.g. those drawing on cognitive remediation strategies to address core symptoms and those drawing on CBT strategies to address associated mental health and social problems), and there is increasing evidence for its use with adults with ASD [ 117 , 118 , 119 , 120 , 121 , 122 ]. Although there is no published evidence base yet for modified cognitive interventions for adults with both ASD and ADHD, the consensus was to endorse this treatment paradigm in individual sessions for adults with both conditions, provided the therapist has expertise in working with adults with ASD and ADHD. The content of therapy needs to reflect topical issues of importance (to be determined by the patient and the therapist together), such as symptoms of ASD/ADHD, anxiety, low mood, friendships, primary-to-secondary school transitions, sexuality, puberty, management of intimate relationships, substance and alcohol misuse, pregnancy and parenting.
As when working with children, there may need to be specific adaptions to meet individual needs associated with varying social communication and intellectual abilities, including greater support and supervision by the therapist. The content of modified CBT sessions may need to be more practically and behaviourally oriented and include topics such as goal setting, sequencing information and priority setting, planning skills, time management and organisation, budgeting and managing finances, social relationships and social communication skills, problem solving skills, understanding and recognising body language, emotional dysregulation and impulsive behaviour, methods to improve concentration and memory skills. Specific strategies may also need to be taught for low mood, anxiety management, frustration and anger. As when working with young people, in some cases, it may be helpful to involve a family member or carer in the treatment to support them to apply strategies they learn in therapy to different contexts (as people with ASD may struggle to generalise from one context to another). If an adult patient does not specifically request this level of support, their consent needs to be obtained.
Further education, career advice and occupational skills training
A summary of the consensus reached regarding educational and occupational interventions for adults with comorbid ADHD and ASD is presented in Table 8 .
The educational approach for young people in further education is not dissimilar to that outlined in the previous section focused on the education of children. Across the contexts of both further education and occupation, each area of disability may magnify the other and multiply the number of potential educational and occupational challenges for a person with both ADHD and ASD. Other additional comorbidities and specific learning difficulties (e.g. dyslexia, dyspraxia, dyscalculia) are also likely to contribute to poorer outcomes.
Transition planning should occur at least 1 year before a young person moves from adolescent to adult services so that appropriate supports may be identified, and a range of potential positive destinations recognised [ 123 , 124 ]. It is important to consider the strategies and person-centered planning services that can be applied to support transitions (between services, between education settings, leaving education, entering the workplace, between employments, independent/semi-independent living etc.). A successful transition should involve everyone in the person’s circle of support. Significant life-path transitions (e.g. parental bereavement) should also trigger enhanced planning, as should geographical re-location or major relationship changes.
All young people and adults require career advice, and for this vulnerable group, who may have limitations but also strengths in what they can achieve, it is essential that career officers, special educational needs coordinators and occupational therapists collaborate to ensure the young people in their care are directed appropriately towards aspirational and realistic career goals and independent living.
Standardised disability provisions in tertiary education settings (e.g. the practice of allotting extra time to complete an examination) may not be appropriate for individuals in this group. Student support services should be aware of the difficulties that might arise with elevated levels of anxiety, difficulties in living independently, sleep disruption, social isolation and substance use. The groups’ recommendation is to consider a holistic assessment of needs, informed by, and incorporated into a personalised education plan or equivalent (see also section on this topic in the child and adolescent section). See Table 9 for a summary of specific educational and occupational interventions that may be helpful for adults.
Positive and creative approaches should be used to help individuals to spend their time effectively and identify job opportunities. This may include voluntary and supported work placements in order for the individual to gain an understanding about the expectations of being in a work setting. For those able to tolerate them, shared skill groups may help in the training process as well as provide a setting to develop social communication skills and reduce isolation. Formal professional support in this respect is not routinely provided, however, and it often falls to parents/carers or friends to provide guidance and support in navigating occupational expectations.
Those with co-occurring ADHD and ASD may often require support with applications and interviews, and in negotiating the recruitment process. This will also involve consideration of the best way and time to disclose the person has a disability. Occupational testing may include objective tests that require a person to consider interpersonal scenarios and these may not be appropriate for use with people with ASD. One such assessment is the Civil Service Judgement Test, which is commonly used in the UK for the recruitment of staff by the civil service [ 125 ]. People with ASD may be disadvantaged by both the content and process of this type of assessment, which includes a requirement they consider online interpersonal scenarios and rate how they would respond (from a 4-point multiple-choice format). This requires the applicant to infer information such as the beliefs, intents, desires, emotions and/or knowledge of those interacting in these brief scenarios (presented in text only or by both text and video). This process, known as ‘theory of mind’, may be challenging for some people with ASD due to their difficulty attributing mental states to both themselves and to others. A person with ASD may be hampered in their ability to decide on the best course of action because they have insufficient information to consider and select a response from fixed options (which may be perceived as arbitrary undefined concepts, such as ‘counterproductive, ineffective, fairly effective, effective'). In ‘real life’, they would be able to draw on environmental cues and contextual information.
Many young people and adults struggle with daily demands which challenge their executive functioning leading to difficulties with punctuality, time management, organising and prioritising work, managing their workload and meeting deadlines. Helpful supports at work include mentoring, pairing with a more experienced ‘buddy’ peer, supportive monitoring and adopting technological aids such as apps and generic software applications. To avoid confusion and/or misguided task prioritisation, it is recommended that expectations and information is explicitly communicated to the employee (both verbally and in writing).
Many occupations involve an interpersonal aspect (e.g. dealing with the public, team working with colleagues, attending meetings, giving presentations, appreciation of and adherence to line-management systems). Individuals with ADHD and ASD may struggle to manage workplace relationships, especially those who actively avoid social communication; lack an appreciation of ‘office politics’, occupational expectations and boundaries (which are often not explicit); and/or do not fully understand the need to adhere to established hierarchies. They may become very anxious, irritable and in some cases aroused and confrontational. They may need help to resolve differences with colleagues before they escalate to more formal disputes. Workplace disputes (both performance-related and interpersonal-related) may be avoided by coaching to understand (1) the organisational structure of the work setting and (2) the expectations of how to dress and behave at work and how this differs from when at home or when socialising with friends. These problems are exacerbated when ADHD and ASD co-occur, resulting in more complex needs and service provision.
Workforce tolerance may be enhanced by providing training in neurodiversity to improve general understanding among colleagues. Employers need to be mindful of equalities legislation, such as the UK Equality Act, 2010, Autism Act 2009 (the first ever disability-specific legislation in England) and Think Autism 2014, and the importance of making reasonable adjustments in order to avoid the potential for disability discrimination.
Some individuals with ADHD and ASD will enjoy a level of independence in terms of their occupation and living arrangements, but it is not uncommon for them to struggle with managing their personal finances. Coaching support may be necessary to help them to learn how to plan and budget for financial commitments to ensure that essential bills (e.g. rent, utilities, phone) are paid on time and/or, if necessary, reduce and amalgamate debts.
Pharmacological treatment for ADHD and ASD in children and adults
A summary of the consensus reached regarding pharmacological interventions for ADHD and ASD when these conditions present as a comorbid diagnosis (in both children and adults) is presented in Table 10 .
The pharmacological treatment for co-occurring ASD and ADHD in children and adults is no different from the treatment of each disorder separately. In the UK, the National Institute for Health and Care Excellence (NICE) guidelines should be followed for the pharmacological treatment of ADHD as a separate condition; medication is commonly offered to treat ADHD symptoms (usually stimulant and non-stimulant medications) in both people with ADHD and those with co-occurring ADHD and ASD. ADHD medications should not be offered to treat people with ASD (without co-occurring ADHD) as there is no evidence for a positive effect in this population [ 126 , 127 , 128 ].
Indeed, there is no orthodox pharmacological treatment for ASD in either children or adults that has an evidence base for treatment effect [ 128 ]. Antipsychotic medication for core ASD symptoms has been used widely in certain countries; however, the evidence base supporting its use in this population is negligible and the risk of adverse effects is high. The second-generation antipsychotics, particularly risperidone and aripiprazole, have been used for the short-term treatment of angry outbursts in children and adolescents with ASD, some of whom will have ADHD [ 129 ]. Low doses, regular reviews and short-term use are advised. However, there are variable degrees of official approval for their use between countries and behavioural and environmental interventions are first-line treatments. Selective serotonin reuptake inhibitor [SSRI] medications are not clearly helpful for treating repetitive behaviours in children and adults with comorbid ASD and ADHD [ 130 ].
When an individual has a diagnosis of both ADHD and ASD, the trigger point for prescribing medication is when the ADHD symptom presentation is severe and/or associated with impairments that hamper personal, social and educational development and achievement. However, given the substantial symptom overlap between the two conditions, when an individual (child or adult) presents with both, there is merit in commencing with psychological/environmental interventions to treat the associated difficulties of ASD, monitor outcomes and review the need for medication as appropriate. In childhood and adolescence, should psychological/environmental interventions fail, then ADHD medications (stimulant and non-stimulant) are helpful for the characteristic symptoms of inattention, hyperactivity and impulsivity when these are clearly evident (e.g. distinguishing agitation for hyperactivity) and arise from ADHD [ 131 , 132 , 133 ]. However, in adults with co-occurring ASD and ADHD, medication to treat their ADHD should be offered as appropriate, with regular monitoring, and should not wait until psychological treatment has been completed. This is especially the case where there is a shortage of specialised ASD/ADHD adult psychology services and where medication for ADHD may be a more immediately available treatment option. Medication for ADHD may also enable adults to better concentrate and maximise benefits from psychological treatment.
Prescribers need to be mindful of the presence of conditions or problems co-existing with combined ADHD and ASD and, if appropriate, prescribe medication, e.g. melatonin may help with the insomnia associated with stimulants. An SSRI may be prescribed to treat depression and/or curb anxiety, though should be used with caution, e.g. SSRI's can interact adversely with amfetamine and in the USA their dispensed packaging carries a 'black box' warning about suicidality in the young, (although this practice is not paralleled in te UK or Europe). The use of second-generation antipsychotics to reduce aggressive behaviour, especially in association with comorbid oppositional defiant or conduct disorder, is mentioned above. There is only limited evidence to suggest that stimulants worsen tics [ 134 ], although the possibility of an increase in tics in some individuals should not be ignored and medication adjusted accordingly.
Treatment with (any) medication should not be given to compensate for deficits in the individual’s environment, such as inadequate staffing levels or lack of training and skills. Medications should only be used for the shortest time possible with clearly specified goals and measures of effectiveness in place. The outcomes of treatment should be closely monitored, including vigilant monitoring for side effects. Any medication that is not effective should be stopped.
A significant proportion of people with ASD may have difficulty identifying or describing their thoughts, feelings and sensations, which may cause difficulty with obtaining subjective reports of treatment outcome and side effects (even by those without intellectual disability). This may be facilitated by visual representations of mood states, visual analogue scales, sketches and drawings. These methods may also assist practitioners to obtain informed consent in cases when this is problematic.
When treating people with co-occurring ADHD and ASD, practitioners need to be particularly mindful of the following:
There is limited data on treating patients who have both ADHD and ASD with ADHD medications, and a careful and circumspect approach should be taken when treating children and adults with co-occurring ADHD and ASD (in comparison to prescribing for ADHD alone). Prescribers should ‘start low and go slow’ as people with the both conditions may be more treatment resistant and more sensitive to the effects of medication, especially with respect to side effects. Some individuals may have lower thresholds for experiencing side effects from medication, which include sleep difficulties, decreased appetite, tics, mood volatility and irritability [ 131 ].
In collaboration with the child and parents/carers, clear goals and outcome measures should be specified and monitored to determine the effectiveness of medications prescribed, including medication for aggression, anxiety and sleep problems.
Due to sensory issues and physical difficulties, individuals with ASD may experience difficulties with consumption of the medications in tablet form (e.g. difficulty swallowing, aversion to tablets). Many medications are available in liquid or sprinkle preparations.
Young people with ADHD are at higher risk of teenage pregnancy [ 111 , 112 ], and it is not advisable to treat pregnant females with stimulant medications. It is important that alternative support is set in place for those who are taken off medication for this reason (see non-pharmacological interventions section).
A medication management plan should be provided to the individual and/or parents/carers, as appropriate, detailing information about the individual’s pharmacological treatments. This involves specifying the indication for the use of medication, the medication used, measures of effects and side effects, and the plan for stepwise adjustments of dosage and drug switching or augmentation, should that be necessary.
The co-occurrence of ADHD and ASD is common, and the presence of both conditions exacerbates difficulties above those experienced by either condition alone. The identification and assessment of ADHD and ASD is complex due to shared aetiologies, overlapping symptoms and shared characteristics. The intervention and management of both conditions is complicated by the core features of both disorders and by co-occurring neurodevelopmental and mental health conditions. These may have a significant impact on engagement, effectiveness and outcomes of both pharmacological and psychological interventions. Neurodevelopmental conditions are often missed in children and adults, especially when they present with high rates of comorbidity that healthcare practitioners are more readily able to recognise, e.g. anxiety and depression. This is further complicated by the change in symptom presentation as young people grow up, with reported decline in hyperactive/impulsive symptoms in ADHD and improved social communication in ASD. These ‘improvements’ however may be offset by the development of additional mental health problems and associated impairments that persist into adulthood.
Hence, UKAP hosted a meeting of experts in ADHD and ASD from a range of disciplines with the aim of reaching a consensus regarding the most appropriate methods of identifying and assessing co-occurring ADHD and ASD. We further sought to agree the most effective interventions and treatments for ADHD and ASD in children and adults. The consensus recommendations for practice are summarised in Tables 1 , 4 , 5 , 7 , 8 and 10 .
Barriers to achieving positive outcomes exist within the clinical, social, and educational spheres. These include poor access to care; lack of training for healthcare staff, teachers and allied professionals; inadequate knowledge about female presentation; lack of care coordination and poor inter-agency working; high rates of comorbidity and functional problems that limit the individual’s ability to engage effectively with a service; inability of the individual to advocate for themselves; stigma (even within the family); need for age-appropriate psychoeducational initiatives; poor coping strategies and substance misuse issues which may significantly impact on an individual’s ability to engage with a service and/or in specific interventions. Unfortunately, some barriers are a result of rigid adherence to the same clinical plan that has been in effect over many years without modifications being made in line with the developments in presentation and needs of the child or adult. A willingness to make changes to accommodate the varied needs of individuals with co-occurring ADHD and ASD over the years will help to eradicate the barriers.
In view of their complex needs, children and adults with co-occurring ADHD and ASD are ‘resource intense patients’ and the experience for the service-user is often that they are passed from service to service. This delays the individual and parents/carers being able to access appropriate treatment and support, sometimes for many years. Individuals with ADHD and ASD should not be denied proper assessment, especially when a screen indicates this is warranted, in order to ensure that their fundamental needs are identified and met as appropriate. Services are better geared to support individuals with intellectual disabilities (i.e. with specialist inpatient services or residential community care settings), but community outpatient services for those without intellectual disabilities are fewer, especially for adults, leaving service-user led charity and support services to ‘fill the gap’. Given the amount of ‘common ground’ shared by those with ADHD and ASD, the implementation of integrated neurodevelopmental services with comprehensive input from a multidisciplinary team working across community and residential settings will be an efficient, cost-effective and user-friendly provision of service and lead to better outcomes for all concerned. This model has been successfully implemented by the Integrated Children’s Service (ICS) in parts of the UK. More and better service provisions are urgently required to meet the complex needs of those with co-occurring ADHD and ASD.
There is a clear need for training about ADHD and ASD, both individually and as comorbid conditions, in health care and allied services. Unfortunately, despite international clinical guidelines to the contrary, ‘lay’ scepticism and resistance to the validity of ADHD may affect perceptions of care needs. Due to the complexity of the presentation when both conditions are present, inter-agency collaborations are required to ensure a successful provision of care drawing on the expertise of professionals working in social care, health and education services. When appropriate, multi-agency input should be included in the individual’s care plan and shared accordingly. Aside from training in the recognition of ADHD, ASD or both conditions in children and adults, training needs to be provided about the additional comorbidities that may be present, gender differences in presentation, appropriate assessment protocols and the referral process, the treatment and interventions available (both medical and psychological), the needs of family and caregivers, inter-agency collaborations and key transitional points of need across the lifespan.
It is hoped that this consensus will support healthcare and allied professionals across a range of disciplines to effectively identify and treat individuals with ADHD and ASD. Accurate and timely diagnoses and appropriate interventions will undoubtedly increase positive outcomes across the lifespan. There is a dearth of research on ADHD and ASD as co-occurring conditions, including gender differences and long-term outcomes (both with and without treatment). In particular, further research is needed to establish an evidence base for the most effective treatments for children and adults, both males and females, who have both conditions.
Abbreviations
Developmental, Dimensional and Diagnostic Interview
Antecedents, Behaviours and Consequences (chart)
ADHD Child Evaluation
Attention deficit/hyperactivity disorder
Autism Diagnostic Interview-Revised
Autism Diagnostic Observation Schedule, second edition
Autism spectrum disorder
Adult ADHD Self-report Rating Scale
Conners’ Adult Rating Scales
Cognitive Behavioural Therapy
Collaborative Life Skills Program
Copy number variants
Conners’ Comprehensive Behavior Rating Scales
Conners’ Continuous Performance Test, third edition
Diagnostic Autism Spectrum Interview
Development and Well-Being Assessment
Diagnostic Interview for Social Communication Disorders
Diagnostic Interview of Adult ADHD
Diagnostic and Statistical Manual of Mental Disorders
Educational, Health and Care Plan
Functional Behavioural Analysis
International Classification of Diseases
Information and communication technology
Individualised Education Programme
Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version
Learning disability
United Kingdom’s National Institute for Health Care Excellence
Personalised education plan
Quantified Behavior Test
Reasoning and Rehabilitation Programme
Schedule for Affective Disorders and Schizophrenia
Social communication disorder
Social and Communication Disorders Checklist
Social Communication Questionnaire
Strengths and Difficulties Questionnaire
Special Education Needs Coordinator
Swanson, Nolan, and Pelham-IV Questionnaire
Social Responsiveness Scale
Selective serotonin reuptake inhibitor
Sexually transmitted disease
United Kingdom ADHD Partnership
Wechsler Adult Intelligence Scale
Wechsler Intelligence Scale for Children
Polanczyk G, De Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007;164(6):942–8.
Article PubMed Google Scholar
Thapar A, Cooper M. Attention deficit hyperactivity disorder. Lancet. 2016;387(10024):1240–50. https://doi.org/10.1016/S0140-6736(15)00238-X .
Hollingdale J, Woodhouse E, Young S, Fridman A, Mandy W. Autistic spectrum disorder symptoms in children and adolescents with attention deficit/hyperactivity disorder: a meta-analytical review. Psychol Med, BMC Psychiatry. 19:404. https://doi.org/10.1186/s12888-019-2284-3 .
Diagnostic and statistical manual of mental disorders. 5th ed (DSM-5). Arlington, VA: American Psychiatric Association. 2013.
Spencer TJ, Biederman J, Mick E. Attention-deficit/hyperactivity disorder: diagnosis, lifespan, comorbidities, and neurobiology. J Pediatr Psychol. 2007;32(6):631–42.
Thomas R, Sanders S, Doust J, Beller E, Glasziou P. Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Pediatrics. 2015;135(4). doi: https://doi.org/10.1542/peds.2014-3482 .
Simon V, Czobor P, Bálint S, Mészáros A, Bitter I. Prevalence and correlates of adult attention-deficit hyperactivity disorder: meta-analysis. Br J Psychiatry. 2009;194(3):204–11. https://doi.org/10.1192/bjp.bp.107.048827 .
Michielsen M, Semeijn E, Comijs HC, Van de Ven P, Beekman TF, Deeq DJH, et al. Prevalence of attention-deficit hyperactivity disorder in older adults in the Netherlands. Br J Psychiatry. 2012;201(4):298–305.
Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006;36(2):159–65.
Weiss G, Hechtman LT. Hyperactive children grown up: ADHD in children, adolescents, and adults. 2nd ed. New York: Guilford Press; 1993.
World Health Organization. (2016). International classification of diseases 11th ed (ICD-11) . http://www.who.int/classifications/icd/en/ . Accessed 21 Apr 2019.
Diagnostic and statistical manual of mental disorders, text revision. 4th ed (DSM-IV). Washington, DC: American Psychiatric Association. 2000.
World Health Organization. (2018). International classification of diseases 11th ed (ICD-11) . Update. https://icd.who.int/dev11/f/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f821852937 . Accessed 21 Apr 2019.
Kooij JJS, Bijlenga D, Salerno L, Jaeschke R, Bitter I, Balázs J, et al. Updated European consensus statement on diagnosis and treatment of adult ADHD. Eur Psychiatry. 2019;56:14–34 https://www.sciencedirect.com/science/article/pii/S0924933818301962 .
Article CAS PubMed Google Scholar
Jensen CM, Steinhausen HC. Comorbid mental disorders in children and adolescents with attention-deficit/hyperactivity disorder in a large nationwide study. Atten Defic Hyperact Disord. 2015;7(1):27–38.
Spencer T, Biederman J, Wilens T. Attention-deficit/hyperactivity disorder and comorbidity. Pediatr Clin N Am. 1999;46(5):915–27.
Article CAS Google Scholar
Pliszka SR, Carlson CL, Swanson JM. ADHD with comorbid disorders: clinical assessment and management. New York: Guilford Press; 1999.
Google Scholar
Mancini C, Van Ameringen M, Oakman JM, Figueiredo D. Childhood attention deficit/hyperactivity disorder in adults with anxiety disorders. Psychol Med. 1999;29(3):515–25.
Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163(4):716–23.
Article PubMed PubMed Central Google Scholar
Fayyad J, Sampson NA, Hwang I, Adamowski T, Aquilar-Gaxiola S, Al-Hamzawi A, et al. The descriptive epidemiology of DSM-IV adult ADHD in the World Health Organization World Mental Health Surveys. Atten Defic Hyperact Disord. 2017;9(1):47–65. https://doi.org/10.1007/s12402-016-0208-3 Epub 2016 Nov 19.
Young S, Moss D, Sedgwick O, Fridman M, Hodgkins P. A meta-analysis of the prevalence of attention deficit hyperactivity disorder in incarcerated populations. Psychol Med. 2015;45(2):247–58.
Young S, Sedgwick O, Fridman M, Gudjonsson G, Hodgkins P, Lantigua M, et al. Co-morbid psychiatric disorders among incarcerated ADHD populations: a meta-analysis. Psychol Med. 2015;45(12):2499–510.
Article CAS PubMed PubMed Central Google Scholar
Elsabbagh M, Divan G, Koh Y-J, Kim YS, Kauchali S, Marcín C, et al. Global prevalence of ASD and other pervasive developmental disorders. Autism Res. 2012;5(3):160–79.
Christensen DL, Maenner MJ, Bilder D, Constantino JN, Daniels J, Durkin MS, et al. Prevalence and characteristics of autism spectrum disorder among children aged 4 years – early autism and developmental disabilities monitoring network, seven sites, United States, 2010, 2012, and 2014. MMWR Surveill Summ. 2019;68(2):1–19. https://doi.org/10.15585/mmwr.ss6802a1 .
Murphy CM, Wilson CE, Robertson DM, Ecker C, Daly EM, Hammond N, et al. Autism spectrum disorder in adults: diagnosis, management, and health services development. Neuropsychiatr Dis Treat. 2016;12:1669–86.
Pourcain BS, Mandy WP, Heron J, Golding J, Smith GD, Skuse DH. Links between co-occurring social-communication and hyperactive-inattentive trait trajectories. J Am Acad Child Adolesc Psychiatry. 2011;50(9–6):892–902 e5.
Article Google Scholar
Robinson EB, Munir K, Munafò MR, Hughes M, McCormick MC, Koenen KC. Stability of autistic traits in the general population: further evidence for a continuum of impairment. J Am Acad Child Adolesc Psychiatr. 2011;50(4):376–84.
World Health Organization. (2018). WHO releases new International Classification of Diseases (ICD 11). June 18, 2018. https://icd.who.int/browse11/lm/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f437815624 . Accessed 23 June 2019.
Levy SE, Giarelli E, Lee LC, Schieve LA, Kirby RS, Cunniff C, et al. Autism spectrum disorder and co-occurring developmental, psychiatric, and medical conditions among children in multiple populations of the United States. J Dev Behav Pediatr. 2010;31(4):267–75.
Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47(8):921–9.
Hofvander B, Delorme R, Chaste P, Nydén A, Wentz E, Ståhlberg O, et al. Psychiatric and psychosocial problems in adults with normal-intelligence autism spectrum disorders. BMC Psychiatry. 2009;9(1):35.
Howlin P, Magiati I. Autism spectrum disorder: outcomes in adulthood. Curr Opin Psychiatry. 2017;30(2):69–76.
Rommelse NN, Franke B, Geurts HM, Hartman CA, Buitelaar JK. Shared heritability of attention-deficit/hyperactivity disorder and autism spectrum disorder. Eur Child Adolescent Psychiatry. 2010;19(3):281–95.
Lee SH, Ripke S, Neale BM, Faraone SV, Purcell SM, Perlis RH, et al. Genetic relationship between five psychiatric disorders estimated from genome-wide SNPs. Nat Genet. 2013;45(9):984–94.
Ronald A, Simonoff E, Kuntsi J, Asherson P, Plomin R. Evidence for overlapping genetic influences on autistic and ADHD behaviours in a community twin sample. J Child Psychol Psychiatry. 2008;49(5):535–42.
Antshel KM, Zhang-James Y, Faraone SV. The comorbidity of ADHD and autism spectrum disorder. Expert Review Neurother. 2013;13(10):1117–28.
Jung M, Tu Y, Park J, Jorgenson K, Lang C, Song W, et al. Surface-based shared and distinct resting functional connectivity in attention deficit hyperactivity disorder and autism spectrum disorder. Br J Psychiatry. 2019;214(6):339–44.
Christakou A, Murphy CM, Chantiluke K, Cubillo AI, Smith AB, Giampietro V, et al. Disorder-specific functional abnormalities during sustained attention in youth with attention deficit hyperactivity disorder (ADHD) and with autism. Mol Psychiatry. 2013;18(2):236–44. https://doi.org/10.1038/mp.2011.185 .
Chantiluke K, Christakou A, Murphy CM, Giampietro V, Daly EM, Ecker C, et al. Disorder-specific functional abnormalities during temporal discounting in youth with attention deficit hyperactivity disorder (ADHD), autism and comorbid ADHD and autism. Psychiatry Res. 2014;223(2):113–20.
Boedhoe PSW, van Rooij D, Hoogman M, Twisk JWR, Schmaal L, Abe Y, et al. Subcortical brain volume, regional cortical thickness and surface area variations across attention-deficit/hyperactivity disorder (ADHD), autism spectrum disorder (ASD), and obsessive-compulsive disorder (OCD). In submission. Am J Psychiatry Preprint available doi. https://doi.org/10.1101/673012 .
Kern JK, Geier DA, Sykes LK, Geier MR, Deth RC. Are ASD and ADHD a continuum? A comparison of pathophysiological similarities between the disorders. J Atten Disord. 2015;19(9):805–27.
Corbett BA, Constantine LJ, Hendren R, Rocke D, Ozonoff S. Examining executive functioning in children with autism spectrum disorder, attention deficit hyperactivity disorder and typical development. Psychiatry Res. 2009;166(2–3):210–22.
Leitner Y. The co-occurrence of autism and attention deficit hyperactivity disorder in children – what do we know? Front Hum Neurosci. 2014;8(268):1–8. https://doi.org/10.3389/fnhum.2014.00268 .
Sinzig J, Walter D, Doepfner M. Attention deficit/hyperactivity disorder in children and adolescents with autism spectrum disorder: symptom or syndrome? J Atten Disord. 2009;13(2):117–26.
Lee DO, Ousley OY. Attention-deficit hyperactivity disorder symptoms in a clinic sample of children and adolescents with pervasive developmental disorders. J Child Adolescent Psychopharmacol. 2007;16(6):737–46.
Leyfer OT, Folstein SE, Bacalman S, Davis NO, Dinh E, Morgan J, et al. Comorbid psychiatric disorders in children with autism: interview development and rates of disorders. J Autism Dev Disord. 2006;36(7):849–61.
Young S, González R, Mullens H, Mutch L, Mallet-Lambert I, Gudjonsson GH. Neurodevelopmental disorders in prison inmates: comorbidity and combined associations with psychiatric symptoms and behavioural disturbance. Psychiatry Res. 2018;261:109–15.
Culpin I, Mars B, Pearson RM, Golding J, Heron J, Bubak I, et al. Autistic traits and suicidal thoughts, plans, and self-harm in late adolescence: population-based cohort study. J Am Acad Child Adolesc Psychiatry. 2018;57(5):313–20.
Hirvikoski T, Mittendorfer-Rutz E, Boman M, Larsson H, Lichtenstein P, Bölte S. Premature mortality in autism spectrum disorder. Br J Psychiatry. 2016;208(3):232–8.
Skirrow C, McLoughlin G, Kuntsi J, Asherson P. Behavioral, neurocognitive and treatment overlap between attention-deficit/hyperactivity disorder and mood instability. Expert Rev Neurother. 2009;9(4):489–503. https://doi.org/10.1586/ern.09.2 .
Karam RG, Breda V, Picon FA, Rovaris DL, Victor MM, Salgado CAI, et al. Persistence and remission of ADHD during adulthood: a 7-year clinical follow-up study. Psychol Med. 2015;45(10):2045–56.
Gershon J. A meta-analytic review of gender differences in ADHD. J Atten Disord. 2002;5(3):143–54.
Lai MC, Lombardo MV, Auyeung B, Chakrabarti B, Baron-Cohen S. Sex/gender differences and autism: setting the scene for future research. J Am Acad Child Adolesc Psychiatry. 2015;54(1):11–24.
Gaub M, Carlson CL. Gender differences in ADHD: a meta-analysis and critical review. J Am Acad Child Adolesc Psychiatry. 1997;36(8):1036–45.
Mandy W, Chilvers R, Chowdhury U, Salter G, Seigal A, Skuse D. Sex differences in autism spectrum disorder: evidence from a large sample of children and adolescents. J Autism Dev Disord. 2012;42(7):1304–13.
Sun X, Allison C, Auyeung B, Zhang Z, Matthews FE, Baron-Cohen S, et al. Validation of existing diagnosis of autism in mainland China using standardised diagnostic instruments. Autism. 2015;19(8):1010–7.
Becker MM, Wagner MB, Bosa CA, Schmidt C, Longo D, Papaleo C, et al. Translation and validation of Autism Diagnostic Interview-Revised (ADI-R) for autism diagnosis in Brazil. Arq Neuropsiquiatr. 2012;70(3):185–90.
Matson JL, Worley JA, Fodstad JC, Chung KM, Suh D, Jhin HK, et al. A multinational study examining the cross-cultural differences in reported symptoms of autism spectrum disorders: Israel, South Korea, the United Kingdom, and the United States of America. Res Autism Spectr Disord. 2011;5(4):1598–604.
Sonuga-Barke EJS, Minocha K, Taylor EA, Sandberg S. Inter-ethnic bias in teachers’ ratings of childhood hyperactivity. Br J Dev Psychol. 1993;11(2):187–200.
Larson K, Russ SA, Kahn RS, Halfon N. Patterns of comorbidity, functioning, and service use for US children with ADHD, 2007. Pediatrics. 2011;127(3):462–70.
La Malfa G, Lassi S, Bertelli M, Salvini R, Placidi GF. Autism and intellectual disability: a study of prevalence on a sample of the Italian population. J Intellect Disabil Res. 2004;48(3):262–7.
Wigham S, Rodgers J, Berney T, Le Couteur A, Ingham B, Parr JR. Psychometric properties of questionnaires and diagnostic measures for autism spectrum disorders in adults: a systematic review. Autism. 2019;23(2):287–305.
Rutter M, Bailey A, Lord C. The Social Communication Questionnaire (SCQ). Manual. 2003. Los Angeles: Western Psychological Services.
Constantino JN. Social Responsiveness Scale (SRS™-2), second edition. Manual. 2012.
Skuse DH, Mandy WP, Scourfield J. Measuring autistic traits: heritability, reliability, and validity of the social communication disorders checklist. Br J Psychiatry. 2005;187:568–72.
Conners KC. Comprehensive behavior rating scales. Manual. 2008.
Conners KC, Erhardt D, Sparrow E. Conners’ Adult ADHD Rating Scales (CAARS). Manual. 1999.
Swanson JM. The SNAP-IV Teacher and Parent Rating Scale. University of California, Irvine, CA 92715. http://www.shared-care.ca/files/scoring_for_snap_iv_guide_26-item.pdf . Accessed 24 Apr 2020.
Ustun B, Adler LA, Rudin C, Faraone SV, Spencer TJ, Berglund P, et al. The World Health Organization adult attention-deficit/hyperactivity disorder self-report screening scale for DSM-5. JAMA Psychiatry. 2017;74(5):520–6.
Young S. RATE and RATE-C Scales. 2007. https://www.psychology-services.uk.com/adhd.htm . Accessed 24 Apr 2020.
Wolraich M. The Vanderbilt ADHD diagnostic rating scale. https://psychology-tools.com/test/vadrs-vanderbilt-adhd-diagnostic-rating-scale . Assessed 23 June 2019.
Scoring instructions for the NICHQ Vanderbilt Assessment Scales (pdf). American Academy of Pediatrics. https://www.nichq.org/sites/default/files/resource-file/NICHQ_Vanderbilt_Assessment_Scales.pdf . Assessed 23 June 2019.
K-SADS-PL Screener (2016). https://www.kennedykrieger.org/sites/default/files/library/documents/faculty/ksads-dsm-5-screener.pdf . Accessed 21 Apr 2019.
K-SADS-PL DSM-5 Supplement 4: Neurodevelopmental, disruptive and conduct disorders supplement (2016). https://www.pediatricbipolar.pitt.edu/sites/default/files/KSADS_DSM_5_Supp4_DevelopmentalDisruptiveDO_Final.pdf . Accessed 21 Apr 2019.
The Strengths and Difficulties Questionnaire. http://sdqinfo.org/py/sdqinfo/b0.py . Accessed 21 Apr 2019.
Goodman R, Ford T, Richards H, Gatward R, Meltzer H. The development and well-being assessment: description and initial validation of an integrated assessment of child and adolescent psychopathology. J Child Psychol Psychiatry Allied Disciplines. 2000;41:645–55.
McEwen FS, Steward CS, Colvert E, Woodhouse E, Curran s, Gillan N, et al.et al. Diagnosing autism spectrum disorder in community settings using the Development and Well-Being Assessment: validation in a UK population-based twin sample. J Child Psychol Psychiatry 2016; 57(2):161–170.
Young S. Diagnostic Autism Specftrum Interview. 2020. https://www.psychology-services.uk.com/autism . Accessed 24 Apr 2020.
Rutter M, Le Couteur A, Lord C. ADRI-R: Autism Diagnostic Interview-Revised (ADI-R). 2003. Western Psychological Services, Los Angeles. https://www.scirp.org/(S(351jmbntvnsjt1aadkposzje))/reference/ReferencesPapers.aspx?ReferenceID=1423674 Accessed 21 Apr 2019.
Wing L, Leekam S, Libby S, Gould J, Larcombe M. The diagnostic interview for social and communication disorders: background, inter-rater reliability and clinical use. J Child Psychol Psychiatry. 2002;43(3):307–25.
Skuse D, Warrington R, Bishop D, Chowdhury U, Lau J, Mandy W, et al. The developmental, dimensional and diagnostic interview (3Di): a novel computerized assessment for autism spectrum disorders. J Am Acad Child Adolesc Psychiatry. 2004;43(5):548–58.
Young S. ACE: ADHD Child Interview. 2015. https://www.psychology-services.uk.com/adhd . Accessed 24 Apr 2020.
Young S. ACE+: ADHD Interview Adult. 2016. https://www.psychology-services.uk.com/adhd . Accessed 24 Apr 2020.
Kooij JJ. Adult ADHD: diagnostic assessment and treatment. 3rd ed. London: Springer; 2013.
Book Google Scholar
Furczyk K, Thorne J. Adult ADHD and suicide. Atten Defic Hyperact Disord. 2014;6(3):153–8.
Veenstra-VanderWeele J. Recognizing the problem of suicidality in autism spectrum disorder. J Am Acad Child Adolesc Psychiatry. 2018;57(5):302–3.
Lord C, Luyster RJ, Gotham K, Guthrie W. Autism diagnostic observation schedule, second edition (ADOS-2) manual (part II): toddler module. Torrance: Western Psychological Services; 2012.
Lord C, Rutter M, DiLavore PC, Risi S, Gotham K, Bishop S. Autism diagnostic observation schedule, second edition (ADOS-2) manual (part I): modules 1–4. Torrance: Western Psychological Services; 2012.
Wechsler D. Wechsler intelligence scale for children-fifth edition. Bloomington: Pearson; 2014.
Wechsler D. Wechsler adult intelligence scale - fourth edition. Bloomington: Pearson; 2008.
Harrison P, Oakland T. Adaptive behavior assessment (ABAS-3) – third edition. Bloomington: Pearson; 2015.
Sparrow SS, Cicchetti DV, Saulnier CA. Vineland adaptive behavior scales (Vineland-3) - third edition. Bloomington: Pearson; 2016.
Kaufman AS, Kaufman NL. Kaufman assessment battery for children. Second edition. Normative update. Bloomington: Pearson; 2018.
Conners CK. Conners’ continuous performance test - third edition. Bloomington: Pearson; 2014.
Ulberstad F. QbTest technical manual. rev. ed. Stockholm: QbTech AB; 2012.
Young S, Amarasinghe JA. Practitioner review: non-pharmacological treatments for ADHD: a lifespan approach. J Child Psychol Psychiatry. 2010;51(2):116–33.
Pickles A, Le Couteur A, Leadbitter K, Salomone E, Cole-Fletcher R, Tobin H, et al. Parent-mediated social communication therapy for young children with autism (PACT): long-term follow-up of a randomized controlled trial. Lancet. 2016;388(10059):2501–9.
Green J, Charman T, McConachie H, Aldred C, Slonims V, Howlin P, et al. Parent-mediated communication-focused treatment in children with autism (PACT): a randomized controlled trial. Lancet. 2010;375(9732):2152–60.
Kasan C, Gulsrud A, Paparella T, Hellemann G, Berry K. Randomized comparative efficacy study of parent-mediated interventions for toddlers with autism. J Consult Clin Psychol. 2015;83(3):554–63.
Smith T, Iadarola S. Evidence base update for autism spectrum disorder. J Clin Child Adolesc Psychol. 2015;44(5):897–922.
Young S, Smith J. Helping Children with ADHD: A CBT Guide for Practitioners, Parents and Teachers. Chichester: Wiley; 2017.
Young S. The STAR detective facilitator manual: a cognitive behavioral group intervention to develop skilled thinking and reasoning for children with cognitive, behavioral, emotional and social problems. London: Jessica Kingsley; 2017.
Young S. Becoming a STAR detective!: your detective’s notebook for finding clues to how you feel. London: Jessica Kingsley; 2017.
Marshall D, Thomas T. Polygraphs and sex offenders: the truth is out there. Probation J. 2015;62(2):128–39.
Gudjonsson GH, Vrij A. A review of the current scientific status and fields of application of polygraphic deception of detection. Leicester: British Psychological Society; 2004. p. 1–31.
Pfiffner LJ, Rooney M, Haack L, Villodas M, Delucchi K, McBurnett K. A randomized controlled trial of a school-implemented school-home intervention for attention-deficit/hyperactivity disorder symptoms and impairment. J Am Acad Child Adolesc Psychiatry. 2016;55(9):762–70.
Pfiffner LJ, Rooney ME, Jiang Y, Haack LM, Beaulieu A, McBurnett K. Sustained effects of collaborative school-home intervention for attention-deficit/hyperactivity disorder symptoms and impairment. J Am Acad Child Adolesc Psychiatry. 2018;57(4):245–51.
Shaw P, Eckstrand K, Sharp W, Blumenthal J, Lerch JP, Greenstein D, et al. Attention-deficit/hyperactivity disorder is characterized by a delay in cortical maturation. Proc Natl Acad Sci U S A. 2007;104(49):19649–54 Epub 2007 Nov 16.
The Joint Council for Qualifications. https://www.jcq.org.uk/ . Accessed 28 Apr 2019.
The Scottish Qualifications Authority. https://www.sqa.org.uk/sqa/70972.html . Accessed 28 Apr 2019.
Harpin VA. The effect of ADHD on the life of an individual, their family, and community from preschool to adult life. Arch Dis Child. 2005;90(suppl 1):i2–7.
Østergaard SD, Dalsgaard S, Faraone SV, Munk-Olsen T, Laursen TM. Teenage parenthood and birth rates for individuals with and without attention-deficit/hyperactivity disorder: a nationwide cohort study. J Am Acad Child Adolesc Psychiatry. 2017;56(7):578–84 e3.
Emilsson, Gudjonsson G, Sigurdsson JF, Einarsson E, Baldursson G, Olafsdottir H, et al. Cognitive behaviour therapy in medication-treated adults with ADHD and persistent symptoms: a randomized controlled trial. BMC Psychiatry. 2011;11:116 https://doi.org/10.1186/1471-244X-11-116 .
Young S, Khondoker M, Emilsson B, Sigurdsson JF, Philipp-Wiegmann F, Baldursson G, et al. A randomized controlled trial reporting functional outcomes of cognitive behavioural therapy in medication-treated adults with ADHD and comorbid psychopathology. Eur Arch Psychiatry Clin Neurosci. 2017;267(3):267–76. https://doi.org/10.1007/s00406-016-0735-0 .
Young S, Khondoker M, Emilsson B, Sigurdsson JF, Philipp-Wiegmann F, Baldursson G, Olafsdottir H, Gudjonsson G. Cognitive behavioral therapy in medication-treated adults with ADHD and comorbid psychopathology: a randomized controlled trial using multi-level analysis. Psychol Med. 2015;45(13):2793–804 https://doi.org/10.1017/S0033291715000756 .
Waugh A, Gudjonsson GH, Rees-Jones A, Young S (2014). A feasibility study of the Reasoning and Rehabilitation Mental Health Programme (R&R2MHP) in male offenders with intellectual disability. Criminal Behaviour Mental Health. 2014; (24)222–4.
Bramham J, Young S, Bickerdike Spain D, McCartan D, Xenitidis K. Evaluation of group cognitive behavioral therapy for adults with ADHD. J Atten Disord. 2009;12(5):434–41.
Knouse LE, Teller J, Brooks MA. Meta-analysis of cognitive–behavioral treatments for adult ADHD. J Consult Clin Psychol. 2017;85(7):737–50.
Spain D, Sin J, Chalder T, Murphy D, Happe F. Cognitive behaviour therapy for adults with autism spectrum disorders and psychiatric co-morbidity: a review. Res Autism Spectr Disord. 2015;9:151–62.
Solanto MV, Marks DJ, Wasserstein J, Mitchell K, Abikoff H, Alvir JM, et al. Efficacy of meta-cognitive therapy for adult ADHD. Am J Psychiatry. 2010;167(8):958–68.
Russell AJ, Jassi A, Fullana MA, Mack H, Johnston K, Heyman I, et al. Cognitive behavior therapy for comorbid obsessive-compulsive disorder in high-functioning autism spectrum disorders: a randomized controlled trial. Depress Anxiety. 2013;30(8):697–708.
Russell AJ, Mataix-Cols D, Anson MA, Murphy DG. Psychological treatment for obsessive-compulsive disorder in people with autism spectrum disorders – a pilot study. Psychother Psychosom. 2009;78(1):59–61.
Young S, Adamou M, Asherson P, Coghill D, Colley B, Gudjonsson G, et al. Recommendations for the transition of patients with ADHD from child to adult healthcare services: a consensus statement from the UK Adult ADHD Network. BMC Psychiatry. 2016;16:301. https://doi.org/10.1186/s12888-016-1013-4 .
Young S, Murphy C, Coghill D. Avoiding the ‘twilight zone’: guidance and recommendations on ADHD and the transition between child and adult services. BMC Psychiatry. 2011;11:174 https://doi.org/10.1186/1471-244X-11-174 .
Civil Service Judgement Test: A guide for candidates. Accessed 07 May 2019. https://www.google.com/search?client=safari&rls=en&q=Civil+Service+Situational+Judgment+Test&ie=UTF-8&oe=UTF-8 .
Sturman N, Deckx L, van Driel ML. Methylphenidate for children and adolescents with autism spectrum disorder. Cochrane Database Syst Rev. 2017; https://doi.org/10.1002/14651858.CD011144.pub2 .
Reichow B, Volkmar FR, Bloch MH. Systematic review and meta-analysis of pharmacological treatment of the symptoms of attention-deficit/hyperactivity disorder in children with pervasive developmental disorders. J Autism Dev Disord. 2013;43(10):2435–41.
Howes OD, Rogdaki M, Findon JL, Wichers RH, Charman T, King BH, et al. Autism spectrum disorder: consensus guidelines on assessment, treatment and research from the British Association for Psychopharmacology. J Psychopharmacol. 2018;32(1):3–29.
Taylor DM, Barnes TR, Young AH. The Maudsley prescribing guidelines in psychiatry, 13th edition. Chichester: Wiley; 2018.
Reiersen AM, Handen B. Commentary on ‘selective serotonin reuptake inhibitors (SSRIs) for autism spectrum disorders (ASD)’. Evid Based Child Health. 2011;6(4):1082–5.
Santosh PJ, Baird G, Pityaratstian N, Tavare E, Gringras P. Impact of comorbid autism spectrum disorders on stimulant response in children with attention deficit hyperactivity disorder: a retrospective and prospective effectiveness study. Child Care Health Dev. 2006;32(5):575–83.
Politte LC, Scahill L, Figuera J, McCracken JT, King B, McDougle CJ. A randomized, placebo-controlled trial of extended-release guanfacine in childrenwith autism spectrum disorder and ADHD symptoms: an analysis of secondary outcome measures. Neuropsychopharmacol. 2018;43:1772–8.
Handen BL, Aman MG, Arnold LE, Hyman SL, Tumuluru RV, Lecavalier L, et al. Atomoxetine, parent training, and their combination in children with autism spectrum disorder and attention-deficit/hyperactivity disorder. J Am Acad ChildAdolesc Psychiatry. 2015;54:905–15.
Friedland S And Walkup, J T. Meta-assurance: no tic exacerbation caused by stimulants. J Am Acad Child Adolesc Psychiatry 2015;54(9):706–708.
Download references
Acknowledgements
We are grateful to the assistance of Hannah Stynes, Luke Aldridge-Waddon and Alex Nolan who attended the consensus meeting and made notes during the breakout sessions. When addressing reviewers’ comments, we consulted with Dr. Bhathika Perera, the Chair of the Royal College of Psychiatrist’s ADHD in Intellectual Disability group (which is a sub-group of their Neurodevelopmental Disorder Special Interest Group), and we thank him for his input.
The meeting was funded by the UK ADHD Partnership (UKAP), who has been in receipt of unrestricted educational donations from Takeda. Takeda has had no influence or involvement in determining the topic and arrangements of the day, the consensus process and outcomes, or writing the final manuscript. SY, PB, WC, EF, PH, JH, EW and GG were on the UKAP committee at the time of the meeting. Other than reimbursement of travel expenses to attend the meeting, none of the authors received any financial compensation for attending the meeting or writing the manuscript, aside from NS who received funds for medical writing assistance.
Author information
Authors and affiliations.
Psychology Services Limited, London, UK
Susan Young
South London & Maudsley NHS Foundation Trust, Service for Complex Autism and Associated Neurodevelopmental Disorders, London, UK
Jack Hollingdale & Patrick Bolton
Department of Children’s Neurosciences, Evelina London Children’s Hospital, Guy’s and St Thomas’ NHS Foundation Trust, London, UK
Michael Absoud
Department of Women & Children’s Health, King’s College, London, UK
Oxford ADHD & Autism Centre, Oxford, UK
Polly Branney
CLC Consultancy, Perth, UK
William Colley
South London & Maudsley NHS Foundation Trust, National Autism Unit, Kent, UK
Emily Craze, Quinton Deeley & Peri Mackintosh
Positive Behaviour, Learning Disability, Autism and Mental Health Service (PALMS) Hertfordshire Communication Disorders Clinics, Hertfordshire Community NHS Trust, St Albans, UK
Mayuri Dave
South London & Maudsley NHS Foundation Trust, Maudsley Health, Abu Dhabi, UAE
Emad Farrag
Department of Psychology, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, UK
Gisli Gudjonsson
Private Practice, London, UK
Great Ormond Street Hospital, London, UK
Ho-lan Liang
Behavioural and Developmental Psychiatry Clinical Academic Group, Behavioural Genetics Clinic, National Adult Autism and ADHD Service, South London and Maudsley Foundation NHS Trust, London, UK
Clodagh Murphy
Department of Forensic and Neurodevelopmental Sciences, Institute of Psychiatry, Psychology & Neuroscience, King’s College London, London, UK
Clodagh Murphy & Emma Woodhouse
Anna Freud Centre, London, UK
Marianna Murin
Helen Arkell Centre, Guildford, UK
Fintan O’Regan
Department of Child and Adolescent Psychiatry, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, UK
Dennis Ougrin & Eric Taylor
Diagnostic Assessments and Treatment Services (DATS), Hertfordshire, UK
Patricia Rios
Stover Consultancy, Santa Barbara, CA, USA
Nancy Stover
You can also search for this author in PubMed Google Scholar
Contributions
SY and EW contributed to the planning and scientific input of this consensus statement. All authors (except NS, QD, ET and GG) attended the consensus meeting. NS completed the first draft of the manuscript with input from EW and JH. It was substantially revised by SY; further input was obtained from GG, ET, JH, BC, FO and QD. The second draft was circulated to all authors for comment and endorsement of the consensus. The final draft was circulated once more, and all authors have read and approved the final manuscript.
Corresponding author
Correspondence to Susan Young .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
In the last 5 years, SY has received honoraria for consultancy and educational talks years from Janssen, HB Pharma and/or Shire. She is an author of the RATE Scales [ 70 ]; the Diagnostic Autism Spectrum Interview (DASI) [ 78 ]; the ADHD Child Evaluation (ACE) [ 82 ] and ACE+ for adults [ 83 ]; Helping Children with ADHD CBT programme [ 101 ]; The Star Programme for children with cognitive, behavioural, emotional and social problems [ 102 , 103 ]; and R&R2 for ADHD Youths and Adults [ 113 ]. PH has received honoraria for consultancy and educational talks in the last 5 years from Shire, Janssen and Flynn. He has acted as an expert witness for Lilly. PB has received honoraria for educational talks from Shire and research grants from Action Medical Research and the UK Tuberous Sclerosis Association for research on ASD and ADHD. In addition, SY, PB, WC, PH, FOR, PR, NS and EW are affiliated on a full-time basis with consultancy firms/private practices. The remaining authors have no disclosures.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Young, S., Hollingdale, J., Absoud, M. et al. Guidance for identification and treatment of individuals with attention deficit/hyperactivity disorder and autism spectrum disorder based upon expert consensus. BMC Med 18 , 146 (2020). https://doi.org/10.1186/s12916-020-01585-y
Download citation
Received : 02 August 2019
Accepted : 03 April 2020
Published : 25 May 2020
DOI : https://doi.org/10.1186/s12916-020-01585-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- hyperactivity disorder/hyperactivity disorder (ADHD)
- Autism spectrum disorder (ASD)
- Comorbidity
- Interventions
BMC Medicine
ISSN: 1741-7015
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 16 November 2023
Clinical implications of ADHD, ASD, and their co-occurrence in early adulthood—the prospective ABIS-study
- Andrea Lebeña 1 ,
- Åshild Faresjö 2 ,
- Tomas Faresjö 2 &
- Johnny Ludvigsson 1 , 3
BMC Psychiatry volume 23 , Article number: 851 ( 2023 ) Cite this article
1527 Accesses
5 Altmetric
Metrics details
Attention-deficit/hyperactivity disorder (ADHD) and autism spectrum disorder (ASD) are childhood-onset disorders associated with functional and psychosocial impairments that may persist into adulthood, leading to serious personal and societal costs.
This study aimed to examine the socio-economic difficulties, physical and mental comorbidities, and psycho-social vulnerabilities associated with ADHD, ASD, and their co-occurrence among young adults.
16 365 families with children born 1997–1999, were involved in the prospective population-based ABIS study (All Babies in Southeast Sweden). A total of 6 233 ABIS young adults answered the questionnaire at the 17–19-year follow-up and were included in this case–control study. Diagnoses of ADHD and ASD from birth up to 17 years of age were obtained from the Swedish National Diagnosis Register. N =182 individuals received a single diagnosis of ADHD, n =78 of ASD, and n =51 received both diagnoses and were considered the co-occurrence group. Multiple multinomial logistic regression analyses were performed.
In the univariate analyses all three conditions were significantly associated with concentration difficulties, worse health quality, lower socio-economic status, lower faith in the future, less control over life, and lower social support. In the adjusted analyses, individuals with ADHD were almost three-times more likely to have less money compared with their friends (aOR 2.86; p < .001), experienced worse sleep quality (aOR 1.50; p = .043) and concentration difficulties (aOR 1.96; p < .001). ASD group were two-fold more likely to experience concentration difficulties (aOR 2.35; p = .002) and tended not to have faith in the future (aOR .63; p = .055), however, showed lesser risk-taking bahaviours (aOR .40; p < .001). Finally, the co-occurrence was significantly associated with unemployment (aOR 2.64; p = .007) and tended to have a higher risk of autoimmune disorders (aOR 2.41; p = .051), however, showed a 51% lower risk of stomach pain (aOR .49; p = .030).
Conclusions
All these conditions significantly deteriorated several areas of life. ADHD/ASD co-occurrence is a heavy burden for health associated with several psychosocial vulnerabilities, that shared a similar morbidity pattern with ADHD although showed less risk cognitive and behavioral profile, similar to the ASD group. Long-term follow-up and support for individuals with these conditions over the life course are crucial.
Peer Review reports
Introduction
Attention-deficit/hyperactivity disorder (ADHD) and autism spectrum disorder (ASD) are common childhood-onset neurodevelopmental disorders [ 1 , 2 ] generally persisting into adulthood [ 3 , 4 , 5 ]. The challenges for these persons are twofold: they face age-related effects experienced by the general population, such as new social challenges and biological and emotional transition to adulthood, alongside disorder-specific effects [ 6 ].
The phenotypes of neurodevelopmental disorders (NDDs) are heterogeneous, and their complexity is compounded by high comorbidity rates with several conditions (i.e., gastrointestinal disturbances, congenital anomalies, and immunological disorders) [ 7 ]. In previous studies, ADHD and ASD have been associated with coexisting psychiatric and neurological conditions, such as oppositional and conduct disorders, tic disorders, epilepsy, depression, anxiety, and substance use disorders [ 8 , 9 ]. Moreover, both disorders have been found to be associated with psychosocial functional impairments and a range of adverse outcomes in patients and their families [ 4 , 5 , 10 , 11 ]. Children and adults with ADHD or ASD often experience emotional and social difficulties, which also negatively impact their quality of life [ 3 , 4 , 5 ].
It has also been shown that psychological, physical, and sexual forms of abuse and household dysfunction such as substance abuse, mental illness, and violence were associated with risk behaviours like binge drinking and smoking, poor health in general, and a higher risk of obesity, myocardial infarction, and stroke [ 12 ]. Risk-taking behaviours and unhealthy habits are mostly established during adolescence and are often carried into adulthood, having long-term effects on lifestyle and health [ 13 ]. Finally, several studies have suggested that ASD and ADHD may be even associated with an increased risk of mortality due to both natural and non-natural causes [ 14 , 15 , 16 ].
Despite the growing body of research pointing at the impact of ADHD and ASD on health and quality of life, little is known regarding their co-occurrence, which could be associated with greater impairment than a single condition and could be less responsive to standard treatments for either disorder. The current study aimed to examine the socio-economic difficulties, physical and mental comorbidities, and psycho-social vulnerabilities associated with ADHD, ASD, and especially their co-occurrence in early adulthood.
Study population
This study includes data from the ABIS-Study (All Babies in Southeast Sweden), a longitudinal, population-based cohort study based on data collected from 16 365 families with children born between October 1997 and October 1999 in Southeast Sweden. ABIS-Study aims to investigate how environmental and genetic factors influence the development of immune-mediated diseases, which include ADHD and ASD, where immune mechanisms may play a role [ 17 ]. The children included in the ABIS-Study have been followed from birth onwards, and questionnaires data, biological samples, and register data of diseases (based on medical records) have been collected at birth and age of 1, 3, 5, 8, 10–12, 17–19, and 23–25 years. A total of 6 233 young adults who were included in the ABIS-Study at birth and answered the questionnaire at 17–19 years follow-up, were included in this prospective case–control sub study (Fig. 1 ).
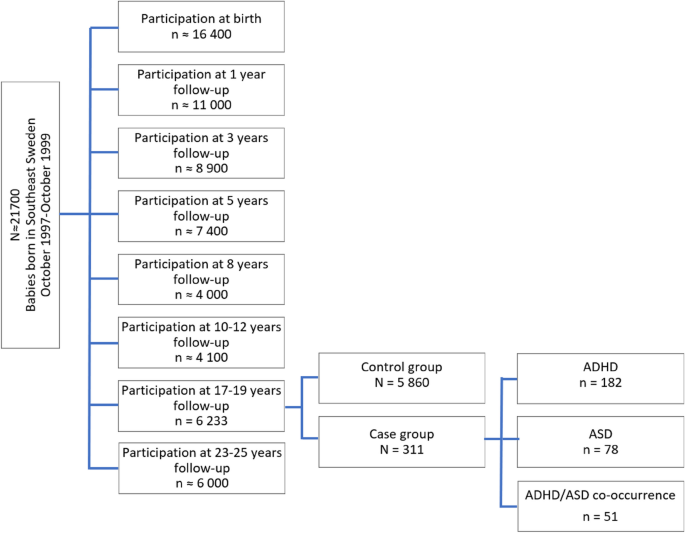
Study population flow-chart
Definition of case and control groups based on the cumulative incidence rates for ADHD, ASD, and their co-occurrence from birth until 17 years of age. ADHD indicates attention-deficit/hyperactivity disorder, while ASD indicates autism spectrum disorder
Diagnosis of ADHD, ASD, and their co-occurrence
The diagnoses of ADHD, ASD, and their co-occurrence were obtained from birth until 17 years of age for the 17–19 years follow-up participants ( n = 6 233), by cross-linking with the Swedish National Patient Register (NPR), containing all hospital inpatients (since 1973) and outpatients (since 2001) International Classification of Diseases (ICD-8 to ICD-10) based on doctor-set diagnoses [ 18 ]. According to ICD-10, F90 (F90.0, F90.1, F90.8, and F90.9) and F84 (F84.0, F84.1, F84.2, F84.3, F84.4, F84.5, F84.8, and F84.9) were the diagnostic codes used for ADHD and ASD, respectively. Those participants who got a unique diagnosis of ADHD ( n = 182), those who received a unique ASD diagnosis ( n = 78), and those who got both diagnoses (ADHD and ASD co-occurrence) ( n = 51), according to the NPR, are the three-case groups. The rest of the study population constitutes the control group ( N = 5 860) (Fig. 1 ).
The parents were given oral and written information before giving informed consent to participate in the study. The ABIS study was approved by the research ethics committees at Linköping University (Dnr 96–287, Dnr 99–321, and Dnr 03–092) and Lund University (LU 83–97) in Sweden, and connection of the ABIS registers to National registers was approved by the Research Ethics Committee in Linköping (Dnr 2013/253–32). All methods were carried out following relevant guidelines and regulations.
The items from the web survey answered at 17–19 years of age (see Additional file 1 ), were categorized into four major areas:
Socio-economic indicators
Included if they have enough money to do the same thing as their friends, and questions regarding occupation (studying, working or unemployed).
Health-related factors
Comprised questions regarding health quality (ranged from 1 very poor to 5 excellent), exercise until get sweaty (dichotomic), weekdays and weekends screen time exposure (categorized in less or more than 4hs per day, according to The American Academy of Pediatrics—AAP) [ 19 ], sleep quality (ranged from 1 very poor to 5 excellent), headache, stomach, and joint pain (ranged from 1 never to 5 almost every day), if they have been or being severely ill (dichotomic), if they have allergies, and BMI (underweight < 18.36, normal 18.37–26.35, overweight 26.36–30.11, or obese > 30.12). Doctor-set diagnoses of autoimmune diseases: celiac disease, psoriasis, immune thrombocytopenic purpura, hypothyroidism, thyrotoxicosis (hyperthyroidism), autoimmune thyroiditis, type 1 diabetes mellitus, arteritis, Crohn’s disease, ulcerative colitis, vitiligo, juvenile arthritis, Kawasaki syndrome, and Sjögren syndrome, were obtained by cross-linking with the Swedish National Patient Register (NPR).
Psychosocial vulnerability
Involved questions about faith in the future, control over life, perceived stress during the last month (ranged from 1 not at all to 10 very much), and being bullied (ranged from 1 never to 5 always). If they feel down or depressed, worried or anxious, and concentration difficulties (ranged from 1 never to 5 almost every day) were also added. Questions regarding job or academic feelings/performance , and social support (from friends, family, or school) were included as well. It also involved if the participants had been exposed to serious life events in the last two years, including death or severe illness in the family (death of parent, sibling, or grandparents, and severe illness within the family), unstable family situation (many conflicts between adults, divorced or separated parents, sole custody with regular or no/sporadic contact with the non-custodial parent, new adults in the family, new children in the family, contact with a supportive family), contact with social authorities for support, if they were sexually or physically abused (by an adult or peer), and robbery victim. An index of stressful life events was developed based on the cumulative frequency of the described stressful events (none, one or two, more than three).
Risk-taking behaviours and perceptions of risks
The questionnaire included 5 dichotomic items regarding tobacco smoking, e-cigarette use, hashish/marijuana smoking, snuff use, and alcohol consumption. An index with a max. score of 5 points was made and a higher score corresponded to many unhealthier/risk-taking behaviours. The questionnaire also included other 5 items that assessed particpants´perceptions of the above-mentioned risk-taking behaviours (eg. “imagine someone that smokes 2–3 times/day: how harmful do you think this is for health?”). All items ranged from 1 (not harmful at all) to 5 (extremely harmful), the index had a max. score of 25. Scores from 5 to 15 were considered slightly/moderately harmful, while scores between 16 and 25 were considered extremely/quite harmful.
Statistical analyses
All statistical analyses were performed in SPSS software version 28.0 (IBM SPSS Inc., Chicago, IL, USA). Dichotomous variables were presented as frequencies and percentages, and differences between groups were assessed using the Chi-squared test. A p -value ≤ 0.05 was considered statistically significant, and multiple comparisons between the three case-groups were adjusted using Bonferroni correction (Tables 1 , 2 , 3 and 4 ). A comparison was made between those who participated in the 17–19 year follow-up and those who did not to evaluate the risk of skewness in participation over time. Identification of statistically independent discriminators used a backward elimination algorithm in which all univariately statistically significant discriminators (Unadjusted model – Table 5 ) were entered into a single full model in the multiple multinomial logistic regression analyses (Adjusted model – Table 5 ). Effect sizes were reported as odds ratios (OR) within 95% confidence intervals (95% CI) and 2-tailed p -values.
All case-groups showed lower participation in the 17–19 years follow-up compared to the controls. Females constitute 36.5% of NDDs cases, 48.4% of ADHD, 37.2% of ASD, and 37.3% of the co-occurrence group, were women. All three conditions reported having less money than friends, while ASD and the co-occurrence groups were more likely to be unemployed (Table 1 ).
Health-related outcomes
All three case-groups reported worse health quality compared with the control group. The ADHD group reported having somatic complaints (stomach and joint pain) more regularly, lower physical activity, and worse sleep quality than the control group did. ASD group reported having severe illness in the last two years, lower physical activity, and were more likely to be overweight/obese. The ASD group also reported longer screen exposure (> 4 h/day) than the control group. The co-occurrence group was more likely to have a severe illness and autoimmune diseases, tended to be underweight or overweight/obese, and reported worse sleep quality than the control group did. The co-occurrence group also reported longer screen exposure (> 4 h/day) during weekends but was not significant (Table 2 ).
All three case-groups reported having contacted social authorities for support, regular concentration difficulties, lower faith in the future, and a lack of social support, compared with the control group. The ADHD and the co-occurrence groups were more likely to experienced 3 or more serious life events in the last two years, however, those events were more violence-related (physical abuse by an adult or peer and robberies) in the ADHD group, while death/illness in the family and unstable family situation where predominantly associated with the co-occurrence group. Both groups also indicated worse job or academic feelings/performance, frequent anxious and depressed feelings, and being bullied (did not rich the significance in the ADHD group). The ADHD group also reported greater perceived stress, and less control over life than the control group did. The ASD group, like the ADHD group, reported less control over life (Table 3 ).
Tobacco, e-cigarettes, hashish/marijuana smoking, and snuff use, were more frequently reported among the ADHD group. ASD group reported instead e-cigarettes and hashish/marijuana smoking, but also alcohol consumption to a lesser extent than the control group did. The co-occurrence group was also less likely to alcohol consumption compared with the control group. Regarding perceptions of risks, tobacco and e-cigarettes smoking every day, and hashish/marijuana smoking and snuff use every week, were considered less harmful among the ADHD group compared to the control group (Table 4 ).
Case-group comparisons
The ADHD group showed lower participation in the 17–19 year follow-up than ASD and reported lower unemployment rates than the co-occurrence group. The co-occurrence group, compared to the ADHD were more likely to be either underweight or overweight/obese and to report severe illness, while ADHD reported having stomach pain more frequently than ASD and the co-occurrence group. The ASD group reported longer screen exposure (during weekends) than the ADHD group, and better sleep quality than the ADHD and the co-occurrence group. In terms of vulnerability, the co-occurrence group reported having contact with social authorities to a greater extent than the ADHD group and being bullied more often compared to the ASD group. The ADHD group perceived higher stress levels than the ASD group did. What concerns about risk-taking behaviours, the ADHD group was more likely to smoke e-cigarettes and consume alcohol than ASD and the co-occurrence group, but also used snuff to a greater extent than the ASD group. Oppositely, the ASD group reported tobacco and hashish/marijuana smoking to a lesser extent than the ADHD and the co-occurrence group. Regarding perceptions of risk-taking behaviours, the co-occurrence group considered smoking hashish/marijuana every week as more harmful than the ADHD group, and alcohol consumption every week than the ASD group (case-groups comparisons column, Tables 1 , 2 , 3 and 4 ).
Statistically independent effects
Less money than friends, concentration difficulties, and bad sleep quality remain significant for ADHD in the multiple multinomial logistic regression analyses, while perceptions of risks showed a tendential effect (Table 5 ). Regarding the ASD group, concentration difficulties, and fewer risk-taking behaviours were the ones that remained significant in the multiple multinomial logistic regression analyses, together with a lower faith in the future, lower perceived stress levels, and less money than friends, all of them showed a tendential effect. Finally, being unemployed, and having less stomach pain were the ones statistically associated with the co-occurrence group, while having an autoimmune disease was tendential.
This is the first-ever prospective study evaluating the impact of ADHD, ASD, and their co-occurrence on socio-economic, health, psychosocial vulnerabilities, risk-taking behaviours, and perceptions of risks in early adulthood. The observed associations suggested that socio-economic status, health quality, faith in the future, control over life, and social support are significantly compromised in individuals with any of these conditions. Our aim was especially to study the impact of the co-occurrence of both disorders, since it was shown that between 30 and 50% of individuals with ASD manifest ADHD symptoms, and two-thirds of individuals with ADHD show features of ASD [ 20 ].
The co-occurrence condition shared several morbidities with the ADHD group, thus both often experienced depressed and anxious feelings and worse sleep quality. Previous studies have found that as many as 80% of adults with ADHD have at least one coexisting psychiatric disorder [ 21 , 22 ], including depression and anxiety, bipolar disorder, and substance use disorder (SUD) [ 23 , 24 ]. Despite some studies also reporting higher lifetime rates of psychiatric comorbidities (major depressive disorder, anxiety, social phobia, and obsessive–compulsive disorder) in persons with autism [ 25 , 26 , 27 ], in this study the ASD group did not report depression or anxious feelings, neither higher perceived stress. Considering the association observed in this study between the co-occurrence and ADHD and serious life events, we could hypothesize that these individuals experienced, alongside the disorder-specific challenges, a more hostile environment (violence-related in the ADHD and more psychosocial in the co-occurrence), which can make them more prone to develop comorbid psychiatric symptomatology. In this line, it was also observed in this study that the co-occurrence group reported being bullied more often. Previous studies found that ADHD adults were more likely to have been divorced and less satisfied with their personal, social, and professional lives [ 28 ], while adults with autism often have satisfying social relationships [ 29 ]. Despite that, a lack of social support was reported as a common experience among all three conditions and could be attributed to social communication difficulties [ 30 ]. Interestingly the co-occurrence, but not each condition separately, was associated with a high risk of having an autoimmune disorder, which may suggest that both disorders could share the same autoimmune etiological mechanism. In previous studies celiac disease, ulcerative colitis, psoriasis, and T1D were linked to ADHD [ 31 , 32 ], similarly, a study on adults on the spectrum reported a high prevalence of immune conditions (70.2%) in their sample [ 33 ].
In this study, individuals with ASD or those with the co-occurrence condition, were more likely to be unemployed, on this line, studies consistently reported unemployment rates around 30–40% in adults with autism [ 34 , 35 ]. In accordance also with ASD, unlike the ADHD group, the co-occurrence was associated with lesser risk-taking behaviours and perceptions of risks. ADHD is accompanied by less activation of the frontoparietal networks associated with deficient inhibition, and impairments in executive functioning and decision-making [ 36 ], which may explain why this group perceived tobacco, e-cigarette, hashish/marijuana smoking, snuff use, and alcohol consumption as less harmful and therefore was more prone to these risk-taking behaviours. This same mechanism could also explain the association of ADHD with externalizing disorders such as conduct disorder and oppositional defiant disorder [ 37 ]. However, it could also be that drug use, through its pharmacological effects, make these persons less concerned with the consequences of their actions or more willing to become involved in risky behaviours or bad lifestyle to support a drug dependency or addiction [ 38 ]. Intriguingly, although there is a reported association between ADHD and overweight, we did not find a significant association, which may depend on the pharmacological treatment for ADHD, which is known to reduce appetite [ 39 ]. The co-occurrence however, showed a high risk of being underweight or overweight (similar to the ASD group). In the same direction as our results, some studies have reported higher rates of common chronic health conditions related to obesity, such as hypertension, dyslipidemia, diabetes, and in general poorer health outcomes in adults with autism [ 40 ]. Another study found self-rating general health as worse in a higher proportion of adults with autism [ 41 ]. In this study, despite all case-groups showing low health quality, the co-occurrence and ASD groups reported severe illness in the last two years in greater proportion than the control group did.
According to the results observed in this study, the individuals with ADHD seem to be exposed to different challenges than those with ASD. The ADHD group was characterized by more frequent somatic complaints (especially stomach and joint pain). In this line, a study found that adults with ADHD visited physicians 10 times more often and had rates of emergency room visits and hospitalization three times greater than controls [ 42 ]. This group also had worse job or academic feelings/performance, and lower physical activity. The ASD group also showed lower physical activity and longer screen exposure during weekends (> 4h/day). Establishing social relationships often comes with unique challenges for young-adults with ASD. One study found that subjects with autism who use social networking sites were found more likely to have close friends [ 43 ], which could explain the longer screen exposure of this group during weekends. A better understanding of the relative impact of these conditions in several areas of life could provide clues for enhanced specific-treatment options.
Strengths and limitations
Our study has important strengths as our results are based on a large prospective birth cohort from the general population with a follow-up for more than 20 years and the strength of merging doctor-set diagnoses of ADHD, ASD, and autoimmune disorders via the National Diagnosis Register. However, our study also has some limitations. Besides diagnosis and household income, all other data are based on self-reported questionnaires, and therefore they could potentially be subject to recall bias, even though it is unlikely that this can explain our results. The attrition analyses showed that the families of young adults that responded to the 17–19 year questionnaire, have higher household income, higher parental education level, both parents were born in Sweden, and live together. If anything, this makes our observed associations even more obvious, suggesting that socio-economic status, health quality, faith in the future, control over life and social support are significantly compromised in individuals with any of these conditions. In addition, more young females than males participated, but we saw the same trends in both sexes. Future studies should gather information from sources beyond self-reports of individuals with ADHD and ASD, especially if they have psychiatric comorbidities. It might also be warranted to consider pharmacological treatment in subjects with ADHD in relation to different comorbidities.
ADHD, ASD, and their co-occurrence significantly deteriorated socio-economic status, health quality, faith in the future, control over life, and social support. The co-occurrence of both disorders is a heavy burden for health, it is associated with several psychosocial vulnerabilities, and shares a similar morbidity pattern with ADHD while a less risk-taking behaviours and perceptions, according to the ASD group. Subjects with ADHD are exposed to different challenges than those with ASD. Understanding the impact of ADHD, ASD, and their co-occurrence allows improving the chance of prevention and development of early treatments with the potential to change the specific trajectory of morbidity later in life.
Availability of data and materials
Deidentified participant data can be shared on reasonable request and ethical approval for a specified purpose, after approval by Johnny Ludvigsson ([email protected]) through a signed data access agreement.
Global Burden of Disease Child and Adolescent Health Collaboration, Kassebaum N, Kyu HH, et al. Child and Adolescent Health From 1990 to 2015: Findings From the Global Burden of Diseases, Injuries, and Risk Factors 2015 Study [published correction appears in JAMA Pediatr. 2017 Jun 1;171(6):602] [published correction appears in JAMA Pediatr. 2017 Oct 1;171(10):1019]. JAMA Pediatr . 2017;171(6):573–592. https://doi.org/10.1001/jamapediatrics.2017.0250
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019 [published correction appears in Lancet. 2020 Nov 14;396(10262):1562]. Lancet . 2020;396(10258):1204–1222. https://doi.org/10.1016/S0140-6736(20)30925-9
Thapar A, Cooper M, Rutter M. Neurodevelopmental disorders. Lancet Psychiatry. 2017;4(4):339–46. https://doi.org/10.1016/S2215-0366(16)30376-5 .
Article PubMed Google Scholar
Lord C, Elsabbagh M, Baird G, Veenstra-Vanderweele J. Autism spectrum disorder. Lancet. 2018;392(10146):508–20. https://doi.org/10.1016/S0140-6736(18)31129-2 .
Article PubMed PubMed Central Google Scholar
Posner J, Polanczyk GV, Sonuga-Barke E. Attention-deficit hyperactivity disorder. Lancet. 2020;395(10222):450–62. https://doi.org/10.1016/S0140-6736(19)33004-1 .
Sonido M, Arnold S, Higgins J, et al. Autism in Later Life: What Is Known and What Is Needed? Curr Dev Disord Rep. 2020;7:69–77. https://doi.org/10.1007/s40474-020-00192-z .
Article Google Scholar
Muskens JB, Velders FP, Staal WG. Medical comorbidities in children and adolescents with autism spectrum disorders and attention deficit hyperactivity disorders: a systematic review. Eur Child Adolesc Psychiatry. 2017;26(9):1093–103. https://doi.org/10.1007/s00787-017-1020-0 .
Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47(8):921–9. https://doi.org/10.1097/CHI.0b013e318179964f .
Hossain MM, Khan N, Sultana A, et al. Prevalence of comorbid psychiatric disorders among people with autism spectrum disorder: An umbrella review of systematic reviews and meta-analyses. Psychiatry Res. 2020;287:112922. https://doi.org/10.1016/j.psychres.2020.112922 .
Nourredine M, Gering A, Fourneret P, et al. Association of Attention-Deficit/Hyperactivity Disorder in Childhood and Adolescence With the Risk of Subsequent Psychotic Disorder: A Systematic Review and Meta-analysis. JAMA Psychiat. 2021;78(5):519–29. https://doi.org/10.1001/jamapsychiatry.2020.4799 .
Drmic IE, Szatmari P, Volkmar F. Life Course Health Development in Autism Spectrum Disorders. In: Halfon N, Forrest CB, Lerner RM, Faustman EM, eds. Handbook of Life Course Health Development . Cham (CH): Springer; November 21, 2017.237–274.
Campbell JA, Walker RJ, Egede LE. Associations Between Adverse Childhood Experiences, High-Risk Behaviors, and Morbidity in Adulthood. Am J Prev Med. 2016;50(3):344–52. https://doi.org/10.1016/j.amepre.2015.07.022 .
Jackson CA, Henderson M, Frank JW, Haw SJ. An overview of prevention of multiple risk behaviour in adolescence and young adulthood. J Public Health (Oxf). 2012;34(Suppl 1):i31–40. https://doi.org/10.1093/pubmed/fdr113 .
Catalá-López F, Hutton B, Page MJ, et al. Mortality in Persons With Autism Spectrum Disorder or Attention-Deficit/Hyperactivity Disorder: A Systematic Review and Meta-analysis. JAMA Pediatr. 2022;176(4):e216401. https://doi.org/10.1001/jamapediatrics.2021.6401 .
Sun S, Kuja-Halkola R, Faraone SV, et al. Association of Psychiatric Comorbidity With the Risk of Premature Death Among Children and Adults With Attention-Deficit/Hyperactivity Disorder. JAMA Psychiat. 2019;76(11):1141–9. https://doi.org/10.1001/jamapsychiatry.2019.1944 .
Smith GS, Fleming M, Kinnear D, et al. Mortality in 787,666 school pupils with and without autism: A cohort study. Autism. 2021;25(1):300–4. https://doi.org/10.1177/1362361320944037 .
Bölte S, Girdler S, Marschik PB. The contribution of environmental exposure to the etiology of autism spectrum disorder. Cell Mol Life Sci. 2019;76(7):1275–97. https://doi.org/10.1007/s00018-018-2988-4 .
Article CAS PubMed Google Scholar
Ludvigsson JF, Almqvist C, Bonamy AK, et al. Registers of the Swedish total population and their use in medical research. Eur J Epidemiol. 2016;31(2):125–36. https://doi.org/10.1007/s10654-016-0117-y .
COUNCIL ON COMMUNICATIONS AND MEDIA. Media Use in School-Aged Children and Adolescents. Pediatrics. 2016;138(5):e20162592. https://doi.org/10.1542/peds.2016-2592 .
Article CAS Google Scholar
Russell G, Rodgers LR, Ukoumunne OC, Ford T. Prevalence of parent-reported ASD and ADHD in the UK: findings from the Millennium Cohort Study. J Autism Dev Disord. 2014;44(1):31–40. https://doi.org/10.1007/s10803-013-1849-0 .
Torgersen T, Gjervan B, Rasmussen K. ADHD in adults: a study of clinical characteristics, impairment and comorbidity. Nord J Psychiatry. 2006;60(1):38–43. https://doi.org/10.1080/08039480500520665 .
Sobanski E, Brüggemann D, Alm B, et al. Psychiatric comorbidity and functional impairment in a clinically referred sample of adults with attention-deficit/hyperactivity disorder (ADHD). Eur Arch Psychiatry Clin Neurosci. 2007;257(7):371–7. https://doi.org/10.1007/s00406-007-0712-8 .
Das D, Cherbuin N, Butterworth P, Anstey KJ, Easteal S. A population-based study of attention deficit/hyperactivity disorder symptoms and associated impairment in middle-aged adults. PLoS ONE. 2012;7(2):e31500. https://doi.org/10.1371/journal.pone.0031500 .
Article CAS PubMed PubMed Central Google Scholar
Philipsen A, Graf E, Jans T, et al. A randomized controlled multicenter trial on the multimodal treatment of adult attention-deficit hyperactivity disorder: enrollment and characteristics of the study sample. Atten Defic Hyperact Disord. 2014;6(1):35–47. https://doi.org/10.1007/s12402-013-0120-z .
Lever AG, Geurts HM. Psychiatric Co-occurring Symptoms and Disorders in Young, Middle-Aged, and Older Adults with Autism Spectrum Disorder. J Autism Dev Disord. 2016;46(6):1916–30. https://doi.org/10.1007/s10803-016-2722-8 .
Arnold S, Foley KR, Hwang YIJ, et al. Cohort profile: the Australian Longitudinal Study of Adults with Autism (ALSAA). BMJ Open. 2019;9(12):e030798. Published 2019 Dec 4. doi: https://doi.org/10.1136/bmjopen-2019-030798
Cvejic RC, Arnold SRC, Foley KR, Trollor JN. Neuropsychiatric profile and psychotropic medication use in adults with autism spectrum disorder: results from the Australian Longitudinal Study of Adults with Autism. BJPsych Open . 2018;4(6):461–466. Published 2018 Nov 13. https://doi.org/10.1192/bjo.2018.64
Biederman J, Faraone SV. The effects of attention-deficit/hyperactivity disorder on employment and household income. MedGenMed . 2006;8(3):12. Published 2006 Jul 18.
Alvarez-Fernandez S, Brown HR, Zhao Y, et al. Perceived social support in adults with autism spectrum disorder and attention-deficit/hyperactivity disorder. Autism Res. 2017;10(5):866–77. https://doi.org/10.1002/aur.1735 .
Ee D, Hwang YIJ, Reppermund S, et al. Loneliness in Adults on the Autism Spectrum. Autism Adulthood. 2019;1(3):182–93. https://doi.org/10.1089/aut.2018.0038 .
Chen MH, Su TP, Chen YS, et al. Comorbidity of Allergic and Autoimmune Diseases Among Patients With ADHD. J Atten Disord. 2017;21(3):219–27. https://doi.org/10.1177/1087054712474686 .
Nielsen PR, Benros ME, Dalsgaard S. Associations Between Autoimmune Diseases and Attention-Deficit/Hyperactivity Disorder: A Nationwide Study. J Am Acad Child Adolesc Psychiatry. 2017;56(3):234-240.e1. https://doi.org/10.1016/j.jaac.2016.12.010 .
Bishop-Fitzpatrick L, Rubenstein E. The Physical and Mental Health of Middle Aged and Older Adults on the Autism Spectrum and the Impact of Intellectual Disability. Res Autism Spectr Disord. 2019;63:34–41. https://doi.org/10.1016/j.rasd.2019.01.001 .
Coleman DM, Adams JB. Survey of vocational experiences of adults with autism spectrum disorders, and recommendations on improving their employment. J Vocat Rehabil. 2018;49(1):67–78. https://doi.org/10.3233/JVR-180955 .
Frank F, Jablotschkin M, Arthen T, et al. Education and employment status of adults with autism spectrum disorders in Germany - a cross-sectional-survey. BMC Psychiatry . 2018;18(1):75. Published 2018 Mar 27. https://doi.org/10.1186/s12888-018-1645-7 36
Mowinckel AM, Pedersen ML, Eilertsen E, Biele G. A meta-analysis of decision-making and attention in adults with ADHD. J Atten Disord. 2015;19(5):355–67. https://doi.org/10.1177/1087054714558872 .
Tistarelli N, Fagnani C, Troianiello M, Stazi MA, Adriani W. The nature and nurture of ADHD and its comorbidities: A narrative review on twin studies. Neurosci Biobehav Rev. 2020;109:63–77. https://doi.org/10.1016/j.neubiorev.2019.12.017 .
Barkley RA, Fischer M, Smallish L, Fletcher K. Young adult follow-up of hyperactive children: antisocial activities and drug use. J Child Psychol Psychiatry. 2004;45(2):195–211. https://doi.org/10.1111/j.1469-7610.2004.00214.x .
Faraone SV, Banaschewski T, Coghill D, et al. The World Federation of ADHD International Consensus Statement: 208 Evidence-based conclusions about the disorder. Neurosci Biobehav Rev. 2021;128:789–818. https://doi.org/10.1016/j.neubiorev.2021.01.022 .
Croen LA, Zerbo O, Qian Y, et al. The health status of adults on the autism spectrum. Autism. 2015;19(7):814–23. https://doi.org/10.1177/1362361315577517 .
Rydzewska E, Hughes-McCormack LA, Gillberg C, Henderson A, MacIntyre C, Rintoul J, et al. General health of adults with autism spectrum disorders - a whole country population cross-sectional study. Res Autism Spectr Disord. 2019;60:59–66. https://doi.org/10.1016/j.rasd.2019.01.004 .
Kirino E, Imagawa H, Goto T, Montgomery W. Sociodemographics, Comorbidities, Healthcare Utilization and Work Productivity in Japanese Patients with Adult ADHD. PLoS One . 2015;10(7):e0132233. Published 2015 Jul 6. https://doi.org/10.1371/journal.pone.0132233
Mazurek MO. Social media use among adults with autism spectrum disorders. Comput Hum Behav. 2013;29(4):1709–14. https://doi.org/10.1016/j.chb.2013.02.004 .
Download references
Acknowledgements
We are grateful to all the participating families who take part in ABIS ongoing cohort study and all the staff at Obstetric Department and Well-Baby Clinics. Sincere thanks to Prof. Fredrikson (Department of Biomedical and Clinical Sciences, Linköping University) for the supervision of the statistical analysis.
Open access funding provided by Linköping University. ABIS-study has received funding from the County Council of Östergötland, Swedish Research Council (K2005-72X-11242-11A and K2008-69X-20826–01-4), Swedish Child Diabetes Foundation (Barndiabetesfonden), Juvenile Diabetes Research Foundation, Wallenberg Foundation (K 98-99D-12813-01A), Medical Research Council of Southeast Sweden (FORSS), Swedish Council for Working Life and Social Research (FAS2004–1775), Östgöta Brandstodsbolag, and Joanna Cocozza Foundation.
Author information
Authors and affiliations.
Division of Pediatrics, Department of Biomedical and Clinical Sciences, Linköping University, Linköping, Sweden
Andrea Lebeña & Johnny Ludvigsson
Department of Medicine and Health, Community Medicine, Linköping University, Linköping, Sweden
Åshild Faresjö & Tomas Faresjö
Crown Princess Victoria Children’s Hospital, Region Östergötland, Linköping, Sweden
Johnny Ludvigsson
You can also search for this author in PubMed Google Scholar
Contributions
JL. created and still leads the ABIS study. JL. collected all data, supported this study, including funding acquisition. ÅF. and TF. led the design of the study. AL. and JL. wrote the initial and final drafts of the manuscript. AL. and ÅF. performed the statistical analyses. All authors contributed to the interpretation of findings, critical revisions, and redrafting of the manuscript. The first and last authors (the manuscript’s guarantors) affirm that the manuscript is an honest, accurate, and transparent account of the study being reported and that no important aspects of the study have been omitted. All authors have confirmed the final version of the manuscript.
Corresponding author
Correspondence to Andrea Lebeña .
Ethics declarations
Ethics approval and consent to participate.
ABIS-study was conducted according to the Helsinki Declaration and was approved by the Research Ethics Committees of the Faculty of Health Science at Linköping University (Dnr: LiU 287–96, LiU 2011/53–32, LiU 2003–092). Informed consent after both written and oral information was obtained from all parents of the participating ABIS-children. All data used in this study were also anonymized.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

Supplementary Information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Lebeña, A., Faresjö, Å., Faresjö, T. et al. Clinical implications of ADHD, ASD, and their co-occurrence in early adulthood—the prospective ABIS-study. BMC Psychiatry 23 , 851 (2023). https://doi.org/10.1186/s12888-023-05298-3
Download citation
Received : 27 June 2023
Accepted : 23 October 2023
Published : 16 November 2023
DOI : https://doi.org/10.1186/s12888-023-05298-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Co-occurrence
- Impact on health
- Psychosocial vulnerabilities
- Young adults
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]

What Is AuDHD?
A common comorbidity or a separate diagnosis.
Posted May 4, 2024 | Reviewed by Abigail Fagan
- What Is Autism?
- Find a therapist to help with autism
- AuDHD is a term coined by the neurodiversity community to describe the co-existence of ADHD and autism.
- Whether AuDHD represents a comorbidity or a separate phenomena is a topic of exploration.
- Research suggests that there may be brain dynamics unique to AuDHD.
When I first came across the term "AuDHD," I thought it was a typo. It wasn't. While AuDHD is not listed in the DSM-5 , the acronym has been utilized to describe the co-occurrence of ADHD and autism. Rather than the American Psychiatric Association, AuDHD was identified by the neurodiversity community. In recent years, research has engaged the construct with the inclusion of neurodivergent researchers and emphasis on its lived experience (Bertilsdotter et al., 2023).
Comorbidity or a New Diagnosis?
Although AuDHD may be new as a descriptor, the construct is not novel. The co-existence of ADHD and autism traits in the same person has been a noted phenomenon for some time. So much so that in earlier years controversy existed as to whether both conditions should ever be diagnosed in the same person (Gargo et al., 2011) given the level of overlap in impact on areas like executive functioning and attention .
As an undergraduate, I was taught that autistic folks often struggled with transitions in attention, with more sustained attention, while ADHDers would need novelty focus and do better on tasks of divided attention. As research has progressed, the picture appears more muddied. ADHD can also be associated with hyper-focus (Hupfeld et al., 2019) and autism with distractibility (Irvine et al., 2024). In addition, sensory hypersensitivities and bottom-up processing blur the image even further when exploring the relationship between autism and attention.
Today the two are often diagnosed together. Research indicates that as many as 50-70% of autistics may also meet the criteria for ADHD (Hours et al., 2022). A question could be asked if this particular comorbidity represents a separate condition on its own.
FMRI research has suggested some unique brain dynamics in individuals with co-occurrence of autism and ADHD that may be separate from the influence of either condition by itself (Watanabe and Watanabe, 2023). Although further research is needed before declaring AuDHD an official diagnosis, it is one of investigation. The findings will be interesting to see and may affirm a group of individuals whose neurodivergence doesn't currently fall well within a listed diagnostic category.
If AuDHD is a distinct condition, investigation would also be necessary into how interventions affect this phenotype.
Embracing Neurodiversity
Regardless of whether AuDHD is simply shorthand for the ADHD and autism combination, or a condition on its own, AuDHD individuals benefit from understanding and affirmation of neurodiversity. This may look like work toward self-acceptance and educating others on neurodivergence.
In a school or work setting, care can be taken to outline and meet diverse needs for any diagnosis. Still, as AuDHD is an emerging diagnosis, finding the most helpful accommodations becomes more individualized. We can also celebrate the strengths that AuDHD individuals bring to the world. With different ways of thinking comes innovation and fresh perspectives.
These are all things that we can start today.
Bertilsdotter Rosqvist, H., Hultman, L., Österborg Wiklund, S., Nygren, A., Storm, P., & Sandberg, G. (2023). Naming ourselves, becoming neurodivergent scholars. Disability & Society , 1-20.
Gargaro, B. A., Rinehart, N. J., Bradshaw, J. L., Tonge, B. J., & Sheppard, D. M. (2011). Autism and ADHD: how far have we come in the comorbidity debate?. Neuroscience & Biobehavioral Reviews , 35 (5), 1081-1088.
Hours, C., Recasens, C., & Baleyte, J. M. (2022). ASD and ADHD comorbidity: What are we talking about?. Frontiers in psychiatry , 13 , 837424.
Hupfeld, K. E., Abagis, T. R., & Shah, P. (2019). Living “in the zone”: hyperfocus in adult ADHD. ADHD Attention Deficit and Hyperactivity Disorders , 11 , 191-208.
Irvine, B., Elise, F., Brinkert, J., Poole, D., Farran, E. K., Milne, E., ... & Remington, A. (2024). ‘A storm of post-it notes’: Experiences of perceptual capacity in autism and ADHD. Neurodiversity , 2 , 27546330241229004.
Watanabe, D., & Watanabe, T. (2023). Distinct frontoparietal brain dynamics underlying the co-occurrence of autism and ADHD. eneuro , 10 (7).

Jennifer Gerlach, LCSW, is a psychotherapist based in Southern Illinois who specializes in psychosis, mood disorders, and young adult mental health.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 01 October 2022
Exploring the causal effects of genetic liability to ADHD and Autism on Alzheimer’s disease
- Panagiota Pagoni ORCID: orcid.org/0000-0002-8090-512X 1 , 2 na1 ,
- Christina Dardani 2 , 3 na1 ,
- Beate Leppert 1 , 2 ,
- Roxanna Korologou-Linden 1 , 2 ,
- George Davey Smith ORCID: orcid.org/0000-0002-1407-8314 1 , 2 ,
- Laura D. Howe 1 , 2 ,
- Emma L. Anderson 1 , 2 &
- Evie Stergiakouli ORCID: orcid.org/0000-0003-3586-0927 1 , 2
Translational Psychiatry volume 12 , Article number: 422 ( 2022 ) Cite this article
3005 Accesses
3 Citations
12 Altmetric
Metrics details
- Autism spectrum disorders
Few studies suggest possible links between attention deficit hyperactivity disorder (ADHD), autism spectrum disorder (ASD) and Alzheimer’s disease but they have been limited by small sample sizes, diagnostic and recall bias. We used two-sample Mendelian randomization (MR) to estimate the bidirectional causal association between genetic liability to ADHD and ASD on Alzheimer’s disease. In addition, we estimated the causal effects independently of educational attainment and IQ, through multivariable Mendelian randomization (MVMR). We employed genetic variants associated with ADHD (20,183 cases/35,191 controls), ASD (18,381 cases/27,969 controls), Alzheimer’s disease (71,880 cases/383,378 controls), educational attainment ( n = 766,345) and IQ ( n = 269,867) using the largest GWAS of European ancestry. There was limited evidence to suggest a causal effect of genetic liability to ADHD (odds ratio [OR] = 1.00, 95% CI: 0.98–1.02, P = 0.39) or ASD (OR = 0.99, 95% CI: 0.97–1.01, P = 0.70) on Alzheimer’s disease. Similar causal effect estimates were identified as direct effects, independent of educational attainment (ADHD: OR = 1.00, 95% CI: 0.99–1.01, P = 0.76; ASD: OR = 0.99, 95% CI: 0.98–1.00, P = 0.28) and IQ (ADHD: OR = 1.00, 95% CI: 0.99–1.02. P = 0.29; ASD: OR = 0.99, 95% CI: 0.98–1.01, P = 0.99). Genetic liability to Alzheimer’s disease was not found to have a causal effect on risk of ADHD or ASD (ADHD: OR = 1.12, 95% CI: 0.86–1.44, P = 0.37; ASD: OR = 1.19, 95% CI: 0.94–1.51, P = 0.14). We found limited evidence to suggest a causal effect of genetic liability to ADHD or ASD on Alzheimer’s disease; and vice versa.
Similar content being viewed by others

Discordant associations of educational attainment with ASD and ADHD implicate a polygenic form of pleiotropy
Genetic risk for attention-deficit/hyperactivity disorder predicts cognitive decline and development of Alzheimer’s disease pathophysiology in cognitively unimpaired older adults
Bidirectional genetic overlap between autism spectrum disorder and cognitive traits
Introduction.
Attention deficit hyperactivity disorder (ADHD) and autism spectrum disorder (ASD) are lifelong neurodevelopmental conditions associated with large societal costs [ 1 , 2 , 3 ]. It has been estimated that the largest proportion of these costs is attributed to the increased physical care and psychosocial support needs of the affected individuals during adulthood [ 4 , 5 ]. Despite increasing interest on the adult outcomes of ADHD and ASD, there is currently limited evidence on the associations of both neurodevelopmental conditions with one of the most debilitating conditions of old age, Alzheimer’s disease. Research in this area is of great importance in order to inform family support and financial planning as well as societal policies and services.
ADHD is characterised by difficulties in several areas of neurocognitive functioning, including memory, attention and inhibitory control [ 6 ]. In later life, these difficulties could be risk factors for an Alzheimer’s disease diagnosis [ 7 , 8 ]. This relationship might be mediated by educational attainment and IQ [ 9 ]. ADHD has been associated with lower educational attainment and IQ in observational and genetic studies [ 9 , 10 ], and they in turn confer increased risk for Alzheimer’s [ 11 , 12 ].
In the case of ASD, it has been suggested that abnormal synaptogenesis, connectivity, and hyper plasticity of the brain identified recently in ASD, could be protective against Alzheimer’s disease [ 13 ]. Adding to this, a protective effect of ASD on the risk of Alzheimer’s could be further hypothesized based on evidence suggesting strong positive genetic correlations of ASD with IQ and educational attainment [ 14 ], which could therefore mediate any associations between the two conditions.
Beyond these hypotheses, little is currently known on the possible associations between ADHD, ASD and Alzheimer’s. There is only a small number of case-control studies on ADHD, suggesting a higher frequency of ADHD symptoms in patients with dementia with Lewy body and a higher risk of dementia in adults with ADHD [ 15 , 16 , 17 ]. However, these studies are limited by small sample sizes and the possibility of diagnostic and recall bias, since sample definition has mostly relied on self or informant reports [ 18 ]. In addition, longitudinal studies require a long follow-up period (from childhood to late adulthood) and could be biased by attrition and confounding. Finally, despite the availability of genome-wide association study (GWAS) data on ADHD, ASD and Alzheimer’s disease [ 14 , 19 , 20 ] studies have focused solely on the genetic correlation between the three phenotypes, showing limited evidence of a genetic overlap [ 14 , 19 , 20 ].
The release of the latest ADHD and ASD GWASs provides a unique opportunity to investigate the possible causal associations between genetic liability to ADHD, ASD and Alzheimer’s, through a method that overcomes limitations of observational studies: Mendelian randomization. Mendelian randomization is an instrumental variables (IVs) approach using genetic variants as proxies for exposures to investigate the causal effects of these exposures on health outcomes [ 21 ]. As genetic variants are randomly allocated at meiosis and fixed at conception, the method is robust to confounding and reverse causation [ 22 ].
For these reasons, we aimed to investigate the bidirectional causal associations between genetic liability to ADHD, ASD and Alzheimer’s using two-sample Mendelian randomization. Next, we performed multivariable Mendelian randomization to estimate the direct causal effects of genetic liability to ADHD and ASD on risk of Alzheimer’s, independent of educational attainment and IQ to explore the possibility that the causal effect of ADHD and ASD on Alzheimer’s are being masked by IQ or educational attainment.
Materials and methods
Two-sample mendelian randomization (mr).
MR relies on strict assumptions that the genetic variants should satisfy in order to be considered valid instruments and therefore yield unbiased causal effect estimates. Specifically, the genetic variants:
must be strongly associated with the exposure,
independently of any confounders of the exposure-outcome association, and
are associated with the outcome only via their effect on the exposure (i.e., absence of horizontal pleiotropy).
In the context of the present study, we applied two-sample MR [ 23 ], a method that enhances statistical power and the precision of the causal effect estimates. This is because the method does not require data on exposure, outcome, and genotype in a single sample. Instead, instrument-exposure and instrument-outcome effect sizes and standard errors are extracted from GWAS conducted in independent samples of the same underlying population.
GWAS summary data
We used GWAS summary data from the latest publicly available GWASs on the exposures of interest. Table 1 provides a summary of the studies utilized. Detailed information can be found in the original publications [ 14 , 19 , 20 , 24 , 25 ].
Instrument extraction
For each exposure of interest independent genetic variants were identified ( r 2 < 0.01 within a 10,000 kb window, p < 5 × 10 −08 ) and corresponding log odds ratios and standard errors were extracted from the publicly available datasets. An exception was ASD, where only two independent variants were identified. Therefore, in order to increase the power of our study, we relaxed the significance threshold ( p < 5 × 10 −07 ) for instrument selection. A similar approach for ASD instrument selection has been used in a previous study [ 26 ]. Exposure instruments were extracted from the outcome GWAS. When a genetic variant was not present in the outcome GWAS, we identified proxy variants using the LDLink online tool [ 27 ] ( r 2 < 0.01 within a 10,000 kb window).
Harmonisation
As instrument-exposure effect estimates were coded to express the effect estimate per increasing allele, the alleles of the variants identified in the outcome were harmonised so that their effect estimates corresponded to the alleles of the exposure. The GWAS summary data of ADHD and ASD do not offer information on effect allele frequencies. Therefore, for variants where the alignment of the alleles between the exposure and outcome variants was not possible, were excluded as palindromic. Information on the genetic variants included in the analysis can be found in Supplementary material (Supplementary Tables 1 – 3 ). The analytic process that was followed across the analyses of the present study is illustrated in Supplementary material (Supplementary Fig. 1 ).
Statistical analyses
Causal effect estimates were generated using the Inverse-Variance-Weighted (IVW) method. IVW can be used to summarize the causal effects of multiple genetic variants, as it is equivalent to fitting a weighted linear regression of the gene-outcome associations on the gene-exposure associations, with the intercept term constrained to zero [ 28 , 29 ]. Thus, IVW estimates assume that all genetic variants are valid instruments with no pleiotropic effects.
Sensitivity analyses
In order to explore the validity of MR assumptions, we compared the estimated total causal effects obtained from univariable MR to the effects obtained using the MR-Egger regression and the Weight median estimator [ 30 , 31 ]. Briefly, MR-Egger regression unlike the IVW method, allows for an unconstrained intercept term and therefore the intercept term is a formal statistical test for the presence of horizontal pleiotropy, while the slope provides a causal effect estimate accounting for pleiotropic bias. The Weighted median estimator provides a causal effect estimate even when up to half of the genetic variants are invalid instruments, by estimating the causal effect as the median of the weighted ratio estimates. Consistent results across the above methods are indicative of a true causal effect.
In addition, as the validity of MR results depends largely on the strength of the genetic instruments, we used F-statistic to ensure that weak instrument bias will not affect our results [ 32 ]. F-statistic estimates the instrument strength of a genetic variant, which is a function of the variance explained by a set of genetic variants (R 2 ), the number of genetic variants used and the sample size. An F-statistic smaller than 10 indicates the presence of weak instrument bias and that causal effect estimates are likely to be influenced.
The influence of each genetic variant on the outcome, was assessed via a leave-one out analysis, in which genetic variants are systematically removed and causal effects of the remaining SNPs on the outcome are re-estimated [ 33 ]. Finally, the Cochran’s Q statistic was used, to assess whether the causal estimates of the genetic variants were comparable [ 31 ]. Observed substantial heterogeneity was used as an indication that genetic variants may not be valid instruments.
Multivariable MR
MVMR is an extension of MR that can be utilized in cases that multiple exposures seem to be strongly genetically related and are considered to have possible causal effects on an outcome. MVMR allows the estimation of the direct effects of each exposure on the outcome by entering the exposures within the same model. Detailed information on the method can be found in the original publication [ 34 ].
Analyses restricted to clinically diagnosed Alzheimer’s disease cases
The main analyses conducted in the present study used summary data from Phase 3 of the Alzheimer’s GWAS, which included proxy-cases of Alzheimer’s disease in UK Biobank (Table 1 ). This might be problematic as: i. participants were defined as cases, based on family history, ii. which was self-reported, iii. and they were asked about broad dementia and not Alzheimer’s specifically. In addition, UK Biobank is an overlapping sample across the Alzheimer’s, educational attainment and intelligence GWASs and this might bias current analyses [ 35 ]. More specifically, the overlap of participants between the Alzheimer’s and educational attainment GWAS was 58% and 72% with IQ GWAS.
Considering the above limitations, we conducted a second round of analyses using summary data of the meta-analysis of Korologou- Linden et al. [ 36 ] which corresponds to Phase 1 of the Alzheimer’s GWAS. Thus, it included only clinically diagnosed cases and the sample overlap between the Alzheimer’s GWAS and the educational attainment GWAS reduced to 1%.
All statistical analysis was performed in R 3.6.1, TwoSampleMR and MendelianRandomization packages were used for the harmonization of datasets and estimation of causal effects. All statistical tests were two-sided.
Instrument strength
Instrument strength as estimated by the F-statistic did not indicate weak instrument bias as it ranged from 30 to 51 for ADHD, 25 to 35 for ASD and 30 to 945 for Alzheimer’s instruments.
Causal effects of genetic liability to ADHD on Alzheimer’s
Bidirectional total causal effects.
A total of 10 genetic variants were used to estimate the total causal effect of genetic liability to ADHD on Alzheimer’s disease. We found limited evidence of a causal effect of genetic liability to ADHD (OR = 1.00, 95% CI: 0.98–1.02, P = 0.39) on Alzheimer’s disease. Horizontal pleiotropy was unlikely to bias the result, as suggested by the MR-Egger intercept term (OR = 0.99, 95% CI: 0.99–1.00, P = 0.91). Moreover, MR-Egger and weighted median estimators yielded similar results to the IVW estimator for ADHD (Table 2 ). No substantial heterogeneity was observed between the genetic variants, as indicated by Cochrane’s Q statistic ( Q = 6.52, P = 0.68), and leave-one out analyses did not identify any SNP as influential (Supplementary Fig. 2A ).
In the reverse direction, 31 genetic variants were available to be used for the estimation of the total causal effect. The IVW estimator suggested limited evidence of a causal effect of genetic liability to Alzheimer’s on ADHD (OR = 1.12, 95% CI: 0.86 to 1.44, P = 0.37). MR-Egger and Weight median estimators were directionally consistent with the IVW (Table 2 ). Heterogeneity among the variants was unlikely to bias the results ( Q = 39.84, P = 0.10), and leave-one out analysis did not point out any genetic variant as influential (Supplementary Fig. 2B ).
Direct effects
Following the exclusion of all palindromic SNPs during harmonization and after clumping the final set of genetic variants (to ensure that only independent variants are included in our analysis), a total of 643 and of 180 variants were available for inclusion in the ADHD-EA-AD and ADHD-IQ-AD multivariable analyses, respectively.
The estimate of the direct causal effect of genetic liability to ADHD on Alzheimer’s, independent of educational attainment, remained virtually the same (OR = 1.00, 95% CI: 0.99–1.01, P = 0.76) (Table 3A ). A similar causal effect was identified after estimating the direct causal effect of genetic liability to ADHD on Alzheimer’s, independent of IQ (OR = 1.00, 95%CI: 0.99–1.02. P = 0.29) (Table 3B ).
The results were comparable—in univariable and multivariable MR analyses—to the ones obtained from the MR analyses using Phase 1 of the Alzheimer’s disease GWAS which did not include proxy cases (Supplementary Tables 4 , 5 ).
Causal effects of genetic liability to ASD on Alzheimer’s
A total of nine genetic variants were used to estimate the total causal effect of genetic liability to ASD on Alzheimer’s disease. We found very little evidence for a causal effect of genetic liability to ASD (OR = 0.99, 95% CI: 0.97–1.01, P = 0.70) on Alzheimer’s disease. MR-Egger and weighted median estimators produced directionally comparable results to the IVW estimator (Table 4 ). In addition, no indication of horizontal pleiotropy was identified by the MR-Egger intercept term (OR = 1.00, 95% CI: 0.99–1.00, P = 0.58). No considerable heterogeneity was observed between the genetic variants ( Q = 6.07, P = 0.63) and leave-one out analyses did not identify any SNP as influential (Supplementary Fig. 3A ).
In the opposite direction, a total of 32 genetic variants were used to estimate the total causal effect. We observed weak evidence that genetic liability to Alzheimer’s was associated with a higher risk of ASD (OR = 1.19, 95% CI: 0.94–1.51, P = 0.14). MR-Egger and weighted median estimators were directionally consistent with the IVW for the genetic liability of Alzheimer’s on ASD (Table 4 ). We had no indication that horizontal pleiotropy influenced our results as indicated by the MR-Egger intercept term (OR = 1.00, 95% CI: 0.99–1.01, P = 0.53) and by Cochrane’s Q statistic ( Q = 36.65, P = 0.22). Moreover, leave-one out analysis did not point out any genetic variant as influential (Supplementary Fig. 3B ).
A total of 662 SNPs and 185 variants were available for inclusion in the ASD-EA-AD and ASD-IQ-AD multivariable analyses respectively. Genetic liability to ASD was not found to have direct effects on Alzheimer’s disease when educational attainment was entered in the models (OR = 0.99, 95% CI: 0.98–1.00, P = 0.28) (Table 5A ). In addition, there was limited evidence to suggest a direct, independent of IQ, causal effect of genetic liability to ASD on Alzheimer’s (OR = 0.99, 95% CI: 0.98–1.01, P = 0.99) (Table 5B ).
The results were comparable to the ones obtained from the MR analyses using Phase 1 of the Alzheimer’s disease GWAS which did not include proxy cases (Supplementary Tables 6 , 7 ).
Within a two-sample Mendelian randomization framework, we found limited evidence of causal effects between genetic liability to ADH and ASD on Alzheimer’s. To exclude the possibility that any causal effects might be masked by educational attainment or IQ, we conducted MVMR to estimate the direct effects of each phenotype on risk of Alzheimer’s. There was limited evidence to suggest direct causal effects of genetic liability to ADHD and ASD on Alzheimer’s risk. Finally, genetic liability to Alzheimer’s was not found to be associated with risk of ADHD and ASD.
Despite current hypotheses stemming out from observational studies that neurocognitive deficits characterizing ADHD could be associated with increased risk for Alzheimer’s disease, in the present study there was limited evidence to support this. Previous genetic studies investigating the associations between polygenic risk for Alzheimer’s and neurocognitive deficits, IQ, as well as brain structural abnormalities in childhood, have found limited evidence of associations between these cognitive measures and genome-wide significant polygenic risk score for Alzheimer’s [ 37 , 38 ]. Most of the associations were identified with a polygenic risk score of Alzheimer’s using a liberal p-value threshold, suggesting possible pleiotropic pathways instead of childhood neurocognitive functioning as an early manifestation of Alzheimer’s risk [ 37 ].
A recently published large cross-generational study suggested that there was a familial association between ADHD and Alzheimer’s disease, and this association was attenuated with decreasing genetic relatedness [ 39 ]. These results contradict with our findings suggesting limited evidence of causal effects between genetic liability to ADH and Alzheimer’s. This could be explained by uncontrolled confounding introduced due to environmental factors (e.g., educational attainment, socioeconomic status, obesity) shared by family members.
However, ADHD is not a phenotypically uniform condition. Specifically, the affected children present with variable neurocognitive profiles [ 40 ], in some cases manifestations of ADHD will remit in adulthood [ 41 , 42 ] and in some cases ADHD will first manifest later in life and not necessarily in childhood (late-onset ADHD) [ 43 , 44 ]. Therefore, different manifestations of ADHD might present different links to Alzheimer’s disease. The ADHD GWAS study we used, included a broad range of children and adults with ADHD and did not allow for testing any possible differential causal associations of genetic liability to ADHD sub-phenotypes with Alzheimer’s.
In the case of ASD, despite the hypothesis that the hyper plasticity of the ASD brain and the strong positive genetic correlations with IQ and educational attainment would reveal a protective effect against Alzheimer’s, we found limited evidence to support this. This could be attributed to the heterogeneity characterising the spectrum [ 45 , 46 ], as in the case of ADHD, and possible differential causal associations across the different dimensions of the spectrum with Alzheimer’s could be speculated. Another consideration in the present study is that we included instruments at a relaxed p -value threshold of p < 5 × 10 −07 , as only five genome-wide significant hits were identified in the ASD GWAS. This might have led to the inclusion of weak instruments, biasing the causal effect estimates towards the null [ 32 ]. However, the sensitivity analyses to test for the different MR assumptions we conducted and the estimation of the strength of the included instruments, suggest that this possibility is unlikely.
Regarding both the ADHD and ASD findings of the present study, an important consideration is the possible influence of survival bias. ADHD seems to be associated with increased risk of mortality compared to the general population, which seems to arise from engagement in high-risk behaviours, suicide and psychiatric comorbidity [ 47 , 48 , 49 ]. Similarly, medication-related side effects, chronic health conditions and intellectual disabilities seem to be associated with increased mortality risk in the case of ASD [ 50 , 51 , 52 , 53 , 54 ]. Therefore, it is possible that excess mortality associated with ADHD and ASD might bias any associations between the two conditions and Alzheimer’s and future research is necessary in order to assess this possibility.
Strengths and limitations
The present study is the first investigating the possible causal associations between genetic liability to ADHD, ASD and Alzheimer’s disease within a Mendelian randomization framework. This method allowed us to investigate causal relationships in the largest samples to date for the three phenotypes of interest, without the presence of confounding. In addition, we scrutinised the validity of our findings through sensitivity analyses as well as Multivariable MR that allowed us to assess whether any causal effects were masked by IQ and educational attainment.
However, there are limitations that should be considered. The common variants that have been currently identified in the ADHD and ASD GWAS and we used as instruments, explain only a small proportion of the genetic variance of the phenotypes [ 14 , 19 ]. More importantly, rare variation seems to play an important part in the aetiopathogenesis of both ADHD and ASD [ 53 , 54 ]. We could not investigate the possible impact of rare variants associated with ADHD and ASD on risk of Alzheimer’s within the context of MR.
Also, we could not assess the possibility our MVMR results being biased due to possible sample overlap in the education attainment and Alzheimer’s GWASs, as both include samples from UK Biobank and TwinGene. However, results remained virtually the same, when we used Phase 1 of the Alzheimer’s disease GWAS which did not include proxy cases and thus had an inconsiderable overlap (1%).
Future directions
Investigating the possible associations of ADHD and ASD with Alzheimer’s disease is an important area of research that can have important implications for the affected individuals, their families and policy makers. It is important therefore, for future GWAS studies to offer subtype specific data in order to explore any possible differential associations of ADHD and ASD subtypes with Alzheimer’s. In addition, although longitudinal designs for this question could be difficult, the availability of registry data (e.g., Swedish registry data) can offer a unique opportunity to investigate the associations between ADHD, ASD and Alzheimer’s disease as well as the possible role of educational attainment through their extensive clinical and academic records.
Conclusions
This is the first study to investigate the possible causal associations between genetic liability to ADHD, ASD and Alzheimer’s disease using the largest sample sizes publicly available for each phenotype, within a Mendelian randomization framework. We found limited evidence to suggest total and direct effects of genetic liability to ADHD and ASD on risk of Alzheimer’s disease. We hope that this will be an important step towards encouraging future research into possible differential associations of ADHD and ASD subtypes and risk of Alzheimer’s disease as well as utilizing longitudinal data.
Data availability
ADHD and ASD GWAS summary data were accessed from [ https://www.med.unc.edu/pgc/download-results/ ]. Educational attainment GWAS summary data were accessed from [ https://www.thessgac.org/data ]. Summary GWAS data for Intelligence (IQ) and Alzheimer’s disease (Phase 3) were accessed from [ https://ctg.cncr.nl/software/summary_statistics ].
Le HH, Hodgkins P, Postma MJ, Kahle J, Sikirica V, Setyawan J, et al. Economic impact of childhood/adolescent ADHD in a European setting: the Netherlands as a reference case. Eur Child Adolesc Psychiatry. 2014;23:587–98. https://doi.org/10.1007/s00787-013-0477-8 .
Article PubMed Google Scholar
Birnbaum HG, Kessler RC, Lowe SW, Secnik K, Greenberg PE, Leong SA, et al. Costs of attention deficit-hyperactivity disorder (ADHD) in the US: excess costs of persons with ADHD and their family members in 2000. Curr Med Res Opin. 2005;21:195–206. https://doi.org/10.1185/030079904X20303 .
Buescher AV, Cidav Z, Knapp M, Mandell DS. Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatr. 2014;168:721–8. https://doi.org/10.1001/jamapediatrics.2014.210 .
Doshi JA, Hodgkins P, Kahle J, Sikirica V, Cangelosi MJ, Setyawan J, et al. Economic impact of childhood and adult attention-deficit/hyperactivity disorder in the United States. J Am Acad Child Adolesc Psychiatry. 2012;51:990–1002.e2. https://doi.org/10.1016/j.jaac.2012.07.008 .
Ganz ML. The lifetime distribution of the incremental societal costs of autism. Arch Pediatr Adolesc Med. 2007;161:343–9. https://doi.org/10.1001/archpedi.161.4.343 .
Barkley RA. Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull. 1997;121:65–94. https://doi.org/10.1037/0033-2909.121.1.65 .
Ivanchak N, Abner EL, Carr SA, Freeman SJ, Seybert A, Ranseen J, et al. Attention-deficit/hyperactivity disorder in childhood is associated with cognitive test profiles in the geriatric population but not with mild cognitive impairment or Alzheimer’s disease. J Aging Res. 2011;2011:729801 https://doi.org/10.4061/2011/729801 .
Article CAS PubMed PubMed Central Google Scholar
Ivanchak N, Fletcher K, Jicha GA. Attention-deficit/hyperactivity disorder in older adults: prevalence and possible connections to mild cognitive impairment. Curr Psychiatry Rep. 2012;14:552–60. https://doi.org/10.1007/s11920-012-0305-8 .
Article PubMed PubMed Central Google Scholar
Fried R, Petty C, Faraone SV, Hyder LL, Day H, Biederman J. Is ADHD a risk factor for high school dropout? a controlled study. J Atten Disord. 2016;20:383–9. https://doi.org/10.1177/1087054712473180 .
Daley D, Birchwood J. ADHD and academic performance: why does ADHD impact on academic performance and what can be done to support ADHD children in the classroom? Child Care Health Dev. 2010;36:455–64. https://doi.org/10.1111/j.1365-2214.2009.01046.x .
Article CAS PubMed Google Scholar
Anderson EL, Howe LD, Wade KH, Ben-Shlomo Y, Hill WD, Deary IJ, et al. Education, intelligence and Alzheimer’s disease: evidence from a multivariable two-sample Mendelian randomization study. Int J Epidemiol. 2020;49:1163–72. https://doi.org/10.1093/ije/dyz280 .
Larsson SC, Traylor M, Malik R, Dichgans M, Burgess S, Markus HS, et al. Modifiable pathways in Alzheimer’s disease: Mendelian randomisation analysis. BMJ. 2017;359:j5375 https://doi.org/10.1136/bmj.j5375 .
Oberman LM, Pascual-Leone A. Hyperplasticity in Autism Spectrum Disorder confers protection from Alzheimer’s disease. Med Hypotheses. 2014;83:337–42. https://doi.org/10.1016/j.mehy.2014.06.008 .
Demontis D, Walters RK, Martin J, Mattheisen M, Als TD, Agerbo E, et al. Discovery of the first genome-wide significant risk loci for attention deficit/hyperactivity disorder. Nat Genet. 2019;51:63–75. https://doi.org/10.1038/s41588-018-0269-7 .
Fluegge K, Fluegge K. Antecedent ADHD, dementia, and metabolic dysregulation: a U.S. based cohort analysis. Neurochem Int. 2018;112:255–58. https://doi.org/10.1016/j.neuint.2017.08.005 .
Golimstok A, Rojas JI, Romano M, Zurru MC, Doctorovich D, Cristiano E. Previous adult attention-deficit and hyperactivity disorder symptoms and risk of dementia with Lewy bodies: a case-control study. Eur J Neurol. 2011;18:78–84. https://doi.org/10.1111/j.1468-1331.2010.03064.x .
Tzeng NS, Chung CH, Lin FH, Yeh CB, Huang SY, Lu RB, et al. Risk of dementia in adults with ADHD: a nationwide, population-based cohort study in Taiwan. J Atten Disord. 2019;23:995–1006. https://doi.org/10.1177/1087054717714057 .
Callahan BL, Bierstone D, Stuss DT, Black SE. Adult ADHD: risk factor for dementia or phenotypic mimic. Front Aging Neurosci. 2017;9:260. https://doi.org/10.3389/fnagi.2017.00260 .
Grove J, Ripke S, Als TD, Mattheisen M, Walters RK, Won H, et al. Identification of common genetic risk variants for autism spectrum disorder. Nat Genet. 2019;51:431–44. https://doi.org/10.1038/s41588-019-0344-8 .
Jansen IE, Savage JE, Watanabe K, Bryois J, Williams DM, Steinberg S, et al. Genome-wide meta-analysis identifies new loci and functional pathways influencing Alzheimer’s disease risk. Nat Genet. 2019;51:404–13. https://doi.org/10.1038/s41588-018-0311-9 .
Davey Smith G, Ebrahim S. ‘Mendelian randomization’: can genetic epidemiology contribute to understanding environmental determinants of disease? Int J Epidemiol. 2003;32:1–22.
Article Google Scholar
Davies NM, Holmes MV, Davey Smith G. Reading Mendelian randomisation studies: a guide, glossary, and checklist for clinicians. BMJ. 2018;362:k601. https://doi.org/10.1136/bmj.k601 .
Lawlor DA. Commentary: Two-sample Mendelian randomization: opportunities and challenges. Int J Epidemiol. 2016;45:908–15. https://doi.org/10.1093/ije/dyw127 .
Lee JJ, Wedow R, Okbay A, Kong E, Maghzian O, Zacher M, et al. Gene discovery and polygenic prediction from a genome-wide association study of educational attainment in 1.1 million individuals. Nat Genet. 2018;50:1112–21. https://doi.org/10.1038/s41588-018-0147-3 .
Savage JE, Jansen PR, Stringer S, Watanabe K, Bryois J, de Leeuw CA, et al. Genome-wide association meta-analysis in 269,867 individuals identifies new genetic and functional links to intelligence. Nat Genet. 2018;50:912–19. https://doi.org/10.1038/s41588-018-0152-6 .
Gao X, Meng LX, Ma KL, Liang J, Wang H, Gao Q, et al. The bidirectional causal relationships of insomnia with five major psychiatric disorders: a Mendelian randomization study. Eur Psychiatry. 2019;60:79–85. https://doi.org/10.1016/j.eurpsy.2019.05.004 .
Machiela MJ, Chanock SJ. LDlink: a web-based application for exploring population-specific haplotype structure and linking correlated alleles of possible functional variants. Bioinformatics. 2015;31:3555–7. https://doi.org/10.1093/bioinformatics/btv402 .
Burgess S, Butterworth A, Thompson SG. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol. 2013;37:658–65. https://doi.org/10.1002/gepi.21758 .
Burgess S, Scott RA, Timpson NJ, Davey Smith G, Thompson SG, Consortium E-I. Using published data in Mendelian randomization: a blueprint for efficient identification of causal risk factors. Eur J Epidemiol. 2015;30:543–52. https://doi.org/10.1007/s10654-015-0011-z .
Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44:512–25. https://doi.org/10.1093/ije/dyv080 .
Bowden J, Davey Smith G, Haycock PC, Burgess S. Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol. 2016;40:304–14. https://doi.org/10.1002/gepi.21965 .
Burgess S, Thompson SG, Collaboration CCG. Avoiding bias from weak instruments in Mendelian randomization studies. Int J Epidemiol. 2011;40:755–64. https://doi.org/10.1093/ije/dyr036 .
Burgess S, Thompson SG. Interpreting findings from Mendelian randomization using the MR-Egger method. Eur J Epidemiol. 2017;32:377–89. https://doi.org/10.1007/s10654-017-0255-x .
Sanderson E, Davey Smith G, Windmeijer F, Bowden J. An examination of multivariable Mendelian randomization in the single-sample and two-sample summary data settings. Int J Epidemiol. 2018;48:713–27. https://doi.org/10.1093/ije/dyy262 .
Article PubMed Central Google Scholar
Burgess S, Davies NM, Thompson SG. Bias due to participant overlap in two-sample Mendelian randomization. Genet Epidemiol. 2016;40:597–608. https://doi.org/10.1002/gepi.21998 .
Korologou-Linden R, Anderson EL, Howe LD, Millard LAC, Ben-Shlomo Y, Williams DM, et al. The causes and consequences of Alzheimer’s disease: phenome-wide evidence from Mendelian randomization. medRxiv. 2020:2019.12.18.19013847. https://doi.org/10.1101/2019.12.18.19013847 .
Korologou-Linden R, Anderson EL, Jones HJ, Davey Smith G, Howe LD, Stergiakouli E Polygenic risk scores for Alzheimer’s disease, and academic achievement, cognitive and behavioural measures in children from the general population. Int J Epidemiol. 2019. https://doi.org/10.1093/ije/dyz080 .
Axelrud LK, Santoro ML, Pine DS, Talarico F, Gadelha A, Manfro GG, et al. Polygenic risk score for Alzheimer’s Disease: implications for memory performance and hippocampal volumes in early life. Am J Psychiatry. 2018;175:555–63. https://doi.org/10.1176/appi.ajp.2017.17050529 .
Zhang L, Du Rietz E, Kuja-Halkola R, Dobrosavljevic M, Johnell K, Pedersen NL, et al. Attention-deficit/hyperactivity disorder and Alzheimer’s disease and any dementia: a multi-generation cohort study in Sweden. Alzheimers Dement. 2021. https://doi.org/10.1002/alz.12462 .
Wahlstedt C, Thorell LB, Bohlin G. Heterogeneity in ADHD: neuropsychological pathways, comorbidity and symptom domains. J Abnorm Child Psychol. 2009;37:551–64. https://doi.org/10.1007/s10802-008-9286-9 .
Biederman J, Mick E, Faraone SV. Age-dependent decline of symptoms of attention deficit hyperactivity disorder: impact of remission definition and symptom type. Am J Psychiatry. 2000;157:816–8. https://doi.org/10.1176/appi.ajp.157.5.816 .
Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006;36:159–65. https://doi.org/10.1017/S003329170500471X .
Faraone SV, Biederman J, Spencer T, Mick E, Murray K, Petty C, et al. Diagnosing adult attention deficit hyperactivity disorder: are late onset and subthreshold diagnoses valid. Am J Psychiatry. 2006;163:1720–9. https://doi.org/10.1176/ajp.2006.163.10.1720 .
Caye A, Rocha TB, Anselmi L, Murray J, Menezes AM, Barros FC, et al. Attention-deficit/hyperactivity disorder trajectories from childhood to young adulthood: evidence from a birth cohort supporting a late-onset syndrome. JAMA Psychiatry. 2016;73:705–12. https://doi.org/10.1001/jamapsychiatry.2016.0383 .
Ronald A, Happe F, Bolton P, Butcher LM, Price TS, Wheelwright S, et al. Genetic heterogeneity between the three components of the autism spectrum: a twin study. J Am Acad Child Adolesc Psychiatry. 2006;45:691–99. https://doi.org/10.1097/01.chi.0000215325.13058.9d
Betancur C. Etiological heterogeneity in autism spectrum disorders: more than 100 genetic and genomic disorders and still counting. Brain Res. 2011;1380:42–77. https://doi.org/10.1016/j.brainres.2010.11.078 .
Barbaresi WJ, Colligan RC, Weaver AL, Voigt RG, Killian JM, Katusic SK. Mortality, ADHD, and psychosocial adversity in adults with childhood ADHD: a prospective study. Pediatrics. 2013;131:637–44. https://doi.org/10.1542/peds.2012-2354 .
Dalsgaard S, Ostergaard SD, Leckman JF, Mortensen PB, Pedersen MG. Mortality in children, adolescents, and adults with attention deficit hyperactivity disorder: a nationwide cohort study. Lancet. 2015;385:2190–6. https://doi.org/10.1016/S0140-6736(14)61684-6 .
London AS, Landes SD. Attention deficit hyperactivity disorder and adult mortality. Prev Med. 2016;90:8–10. https://doi.org/10.1016/j.ypmed.2016.06.021 .
Bilder D, Botts EL, Smith KR, Pimentel R, Farley M, Viskochil J, et al. Excess mortality and causes of death in autism spectrum disorders: a follow up of the 1980s Utah/UCLA autism epidemiologic study. J Autism Dev Disord. 2013;43:1196–204. https://doi.org/10.1007/s10803-012-1664-z .
Gillberg C, Billstedt E, Sundh V, Gillberg IC. Mortality in autism: a prospective longitudinal community-based study. J Autism Dev Disord. 2010;40:352–7. https://doi.org/10.1007/s10803-009-0883-4 .
Smith DaWalt L, Hong J, Greenberg JS, Mailick MR. Mortality in individuals with autism spectrum disorder: predictors over a 20-year period. Autism. 2019;23:1732–39. https://doi.org/10.1177/1362361319827412 .
Ganna A, Satterstrom FK, Zekavat SM, Das I, Kurki MI, Churchhouse C, et al. Quantifying the impact of rare and ultra-rare coding variation across the phenotypic spectrum. Am J Hum Genet. 2018;102:1204–11. https://doi.org/10.1016/j.ajhg.2018.05.002 .
Demontis D, Satterstrom K, Duan J, Lescai F, Dinesen Østergaard S, Lesch K-P, et al. The Role of Ultra-Rare Coding Variants In ADHD. Eur Neuropsychopharmacol. 2019;29:S724–S25. https://doi.org/10.1016/j.euroneuro.2017.06.042 .
Download references
Acknowledgements
This work was supported by a grant from the BRACE Alzheimer’s charity (BR16/028). PP, BL, RKL, ELA, GDS, LDH and ES work in a unit that receives funding from the University of Bristol and the UK Medical Research Council (MC_UU_00011/1, MC_UU_00011/3 and MC_UU_00011/6). CD is funded by the Wellcome Trust (grant ref: 108902/B/15/Z). BL was supported by a research grant from the Wellcome Trust (grant ref: 204895/Z/16/Z). RKL is supported by a Wellcome Trust PhD studentship (Grant ref: 215193/Z18/Z). LDH and ELA are funded by a Career Development Award from the UK Medical Research Council (MR/M020894/1 and MR/P014437/1, respectively). This publication is the work of the authors, and ES will serve as a guarantor for the contents of this paper.
Author information
These authors contributed equally: Panagiota Pagoni, Christina Dardani.
Authors and Affiliations
MRC Integrative Epidemiology Unit, University of Bristol, Bristol, UK
Panagiota Pagoni, Beate Leppert, Roxanna Korologou-Linden, George Davey Smith, Laura D. Howe, Emma L. Anderson & Evie Stergiakouli
Population Health Sciences, Bristol Medical School, University of Bristol, Bristol, UK
Panagiota Pagoni, Christina Dardani, Beate Leppert, Roxanna Korologou-Linden, George Davey Smith, Laura D. Howe, Emma L. Anderson & Evie Stergiakouli
Centre of Academic Mental Health, Population health Sciences, Bristol Medical School, University of Bristol, Bristol, UK
Christina Dardani
You can also search for this author in PubMed Google Scholar
Contributions
Conception: PP, ELA and ES; Methodology: PP, CD, ELA and ES; Data acquisition and curation: PP; Data analysis: PP; Paper preparation—writing: PP and CD; Paper preparation—reviewing and editing: PP, CD, BL, RKL, GDS, LDH, ELA and ES; Final approval of the version to be published: PP, CD, BL, RKL, GDS, LDH, ELA and ES; Funding acquisition: GDS, LDH, ELA and ES.
Corresponding author
Correspondence to Panagiota Pagoni .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary material, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Pagoni, P., Dardani, C., Leppert, B. et al. Exploring the causal effects of genetic liability to ADHD and Autism on Alzheimer’s disease. Transl Psychiatry 12 , 422 (2022). https://doi.org/10.1038/s41398-022-02150-2
Download citation
Received : 30 December 2021
Revised : 25 August 2022
Accepted : 02 September 2022
Published : 01 October 2022
DOI : https://doi.org/10.1038/s41398-022-02150-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Psychiatry
ASD and ADHD Comorbidity: What Are We Talking About?
Associated data.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
According to the scientific literature, 50 to 70% of individuals with autism spectrum disorder (ASD) also present with comorbid attention deficit hyperactivity disorder (ADHD). From a clinical perspective, this high rate of comorbidity is intriguing. What is the real significance of this dual diagnosis? Is ADHD in fact always present in such cases? Might the attentional impairment reported among our ASD patients actually be a distinct trait of their ASD—namely, impaired joint attention—rather than an ADHD attention deficit? Could their agitation be the consequence of this joint attention impairment or related to a physical restlessness etiologically very different from the agitation typical of ADHD? The neurobiological reality of ASD-ADHD comorbidity is a subject of debate, and amphetamine-based treatment can have paradoxical or undesirable effects in the ASD population. Consequently, does a dual diagnosis, notwithstanding its currency in the literature, prevent us from shedding sufficient light on major physiopathologic questions raised by the clinical picture of ASD?
Introduction
The semiology of autism spectrum disorder (ASD) and attention deficit hyperactivity disorder (ADHD) presented in current nosography, which helps clinicians to identify these disorders, makes it clear that they are different entities, affecting children and their developmental histories in ways that are clearly distinct. In the first case, we are primarily describing distracted children who pay little attention in academic settings, lose their belongings, and have difficulty sustaining mental effort. In the second case, we are talking about children who seldom associate with others, have a hard time interacting and communicating, and may display unique motor or verbal behaviors, including stereotypies, echolalia, and idiosyncratic language. Whereas, children with ADHD tend to be relatively boisterous and talkative, and eager rather than apprehensive of interactions with peers or adults, autistic children may be distinguished by their repetitive and less coordinated motor function, difficulty communicating, emotions in sync with their sensory reality more than with their social setting, and uniform behaviors that keep the unpredictable at bay.
Epidemiologically, these two disorders also differ in their incidence. Their diagnoses are made at different ages. Children with ASD can be identified before they are 3 years old, while ADHD is diagnosed later on. Both fall into the wider category of neurodevelopmental disorders, within which “comorbidities” are considered relatively frequent.
The prevalence of ADHD in people with ASD ranges from 50 to 70%, according to the literature ( 1 ). Where does this figure come from? How was it obtained, which studies and semiological criteria were applied, and how were the relevant clinical data collected?
This figure is the product of meta-analyses. It is important to note the variability of findings between studies—more than a mean prevalence, a precise yet illusory value reflecting the view that this comorbidity is a clearly measurable entity—because it admits an alternative interpretation of the phenomenon in question. Indeed, reported rates of comorbidity range from 10 to 90%. In the logic of meta-analysis, variation is often explained through methodological arguments: studies diverging from the mean are said to describe different populations, apply less valid methods of measurement, or gather their data in atypical ways. Yet, in part, what may be described as “bias” could betray an unsound theoretical foundation, accommodating a multitude of experimental paradigms measuring what is thought to be the same phenomenon.
This article thus aims to recall the attentional features inherent to ASD; to describe and analyze the variability of data reported in the literature; and finally, to draw on studies of factors related to attention, such as memory, sensorimotor function, executive functioning, and intellectual disability, for a better understanding of the role these variables play in the expression of cognitive capacity within the ASD population.
Autism and Attention
Attention is defined as a process of selection applied to the product of perception, and may even be directed toward memories. To direct attention on a perceptual or internally represented entity, our working memory must be trained on a goal for the duration of the task at hand. Attention encompasses essential elements of the executive functions and can be further broken down into sustained attention; focused attention; visual search, whereby the target of attention is defined using a template stored in working memory; voluntary or reflexive orienting and disengagement; attentional filtering; and expectation ( 2 ).
In people with ASD, these components of attention have a characteristic profile: sustained and focused attention is stronger than in normal subjects; visual search is also, though this seems to reflect the quality of perceptual processing more than attention; and the ability to orient attention toward non-social stimuli is deficient, as are reflexive and voluntary disengagement, in certain settings. Attentional filtering is not compromised in ASD patients having no intellectual disability. Higher-functioning ASD patients have a specific attentional impairment not observed among other ASD patients ( 3 ). Joint attention also appears to be lacking.
Can the comorbidity of ASD and ADHD truly be established by considering executive functions alone, as several studies suggested ( 4 )? The developmental cognitive specificities of ASD have been well described as they are linked with perception aspects but their executive or attentional aspects have been relatively neglected. “Attentional impairments in autism tend to be more of the ‘not listening' and ‘difficulty shifting focus' type than of the ‘short attention span' and ‘excessive distractibility' type 1 .” These distinct clinical particulars suggest attentional symptoms inherent to ASD rather than comorbid ADHD.
What Do Comorbidity Studies Address?
While the DSM-4 and ICD-10 give mutually exclusive diagnoses of ADHD and ASD, the DSM-5 mentions each condition in its description of the other, admitting the possibility of comorbidity.
Sprenger et al. ( 5 ) concluded that autistic symptoms were significantly more severe, especially in the area of social interaction (as evaluated by the social responsiveness scale and autism diagnostic interview), in patients with dual ASD-ADHD diagnoses than in those with ASD alone. Yet this conclusion might also illustrate the frequent clinical confusion of these disorders: could the severe autism they describe not just as well itself be the cause of a more symptomatic attention deficit, without suggesting the presence of ADHD? Similarly, Green et al. ( 6 ) stated that autistic symptoms were more prevalent in children with ADHD. Their study considered a group of children aged 6 to 10 divided into an ADHD subgroup and a control subgroup without ADHD. It seems questionable to conclude that autistic symptoms are more prevalent in ADHD patients without recognizing that the severity of ASD is independently at the origin of pronounced attentional deficiencies. The study also concluded that the intensity of hyperactive and impulsive symptoms directly impacts the severity of ASD symptoms, without inversely considering that, again, the severity of ASD might independently explain signs of psychomotor agitation and attentional deficiencies. Furthermore, findings did not differ by ADHD subtype, which further supports the hypothesis that the observed attentional deficit and motor hyperactivity are more directly explained by severe autism than comorbid ADHD.
Some studies have reported structural differences in attentional functions between ASD and ADHD patients, while others suggest these disorders present identical deficiencies ( 7 , 8 ).
Barnard-Brak ( 9 ) reported varying ability to distinguish individuals with ASD from those with ADHD on the basis of their performance on different cognitive tasks that assess sustained attention. However, the rapid letter naming task, which is thought to predict surface reading ability and other reading skills, did reveal significant differences between ASD and ADHD children: the former spent more time on the task and performed better. Thus, the interpretation of performance on cognitive-attentional tasks evaluating sustained attention requires special caution to avoid confusing the two disorders. This study also highlighted the effect of environment on the performance of attentional tasks by those with ASD: the setting under which individuals complete diagnostic tests can greatly influence results.
Hochhauser et al. ( 10 ) described specific attentional traits related to social interaction in young adults with ASD that may, however, be the consequences of another form of cognitive impairment. Several studies have reported cognitive characteristics affecting attentional skills in the ASD population, including difficulty disengaging, significantly greater processing of local details, or heightened perception yet “context blindness”. These elements in turn influence processing speed. Processing speed is therefore not impaired directly, but rather, differences in how perceptual data are processed have an impact on attention. Hence, it would seem more appropriate to speak of attentional traits of ASD, rather than attentional anomalies or deficits, thereby distinguishing them from ADHD.
Mayes et al. ( 11 ) demonstrated that disruptive mood dysregulation disorder was extremely prevalent among children with ASD, significantly more so than among ADHD and neurotypical children. Moreover, 91% of the children with disruptive mood dysregulation disorder symptoms also satisfied criteria for oppositional defiant disorder, revealing the very high prevalence of externalizing behaviors in ASD. The presence of psychomotor agitation cannot be automatically attributed to ADHD motor hyperactivity but does suggest an emotional dysregulation disorder more directly linked to the behavioral effects of irritability.
Physiopathologic Aspects: Imaging and Eeg Data
Is observed agitation then a sign of the prefrontal inhibitory deficit underlying ADHD or rather a state of restlessness, a minimal expression of cerebellar dysfunction, characterizing an etiologically distinct entity? The association of ASD with alterations in specific brain regions is becoming increasingly clearer. The affected regions include the orbitofrontal cortex, superior temporal sulcus, fusiform gyrus, amygdala, and cerebellum ( 12 ), and the latter plays a role in learning processes, memorization, several executive functions, and cognition. In light of these facts, might it not be risky to diagnose ADHD, a disorder linked with an altered prefrontal cortex, in the ASD population?
ADHD and ASD are described as frequently co-occurring, sharing certain cognitive phenotypes. However, it is important to be able to trace these shared features back to a common physiopathology and identify the physiopathologic characteristics of comorbidity, which may present additional neurofunctional deficits. Chantiluke et al. ( 13 ) compared prefrontal function in four groups of youth with ASD, ADHD, comorbid ASD and ADHD, or neither disorder (controls) through a temporal discounting task, using fMRI. They revealed anomalies shared by the non-control groups, in addition to distinct features unique to each of these three groups. In comparison with the non-comorbid and control groups, the comorbid group presented unique and more severe impairments affecting the lateral and ventromedial prefrontal cortex, ventral striatum, and anterior cingulate cortex. These physiopathologic findings suggest that ASD-ADHD comorbidity does not correspond to a mere combination or addition of both disorders: it is neurofunctionally distinct and merits further study for more accurate characterization.
As shown by Lau-Zhu et al. ( 14 ), ASD and ADHD are each associated with unique attention processing traits. Studies of event-related potentials (ERPs)—concerned with inhibitory control and performance monitoring in ADHD ( 15 – 17 ), and social or emotional processing as well as executive functioning in ASD ( 18 )—mostly involving adolescents have reported distinct abnormal cognitive profiles for ADHD and ASD. Both disorders are associated with atypical allocation of attentional resources and atypical performance monitoring. However, the structural impairments underlying them are very different. With regards to attention, ADHD impairment tends to reflect difficulty detecting clues that would otherwise enable anticipation, while ASD impairment is more directly related to a heightened perceptual capacity and weaker orientation toward new inputs, with longer retention of stimuli in working memory and unique social, emotional, and executive functioning features. ADHD, unlike ASD, is more immediately linked to impaired inhibition. It is important to recall that impaired inhibition, the root physiopathologic feature of ADHD, has not been studied in cohorts of ASD patients. Sensory processing impairments, such as those observed in ASD, ultimately have repercussions on attentional processes. The causes of the attentional deficiencies seen in these two disorders would thus appear to be very distinct.
Research applying quantitative EEG has demonstrated atypical profiles for ADHD, principally concerning theta and beta frequency bands ( 17 , 19 ), and for ASD, mainly related to alpha, beta, and gamma frequency bands ( 20 ). ASD and ADHD have distinct and overlapping features in “four neurocognitive domains: attention processing, performance monitoring, face processing and sensory processing” ( 14 ). Yet studies comparing the two disorders or considering dual diagnoses have yet to be undertaken. Further investigation into the neural bases of co-occurring ADHD and ASD would be of particular interest.
To better understand the distinct neuropsychological profiles of ADHD and ASD patients, it seems appropriate to consider visuospatial exploration strategies. In terms of visuospatial abilities, ADHD patients in a study by Cardillo et al. ( 21 ) exhibited a heterogeneous profile with more severely impaired visuospatial processing speed, while ASD patients and typically developing subjects had similar profiles. The authors also state that the local-global processing index effectively distinguishes these groups on the basis of performance on visuo-constructive tasks. Accordingly, a more detailed understanding of the neurocognitive specificities of each disorder might be acquired by accounting for the various domains of visuospatial processing.
It has often been stated in the literature that ASD and ADHD are difficult to distinguish when making a diagnosis. Mayes et al. ( 22 ), considering 847 children with ASD and 158 with ADHD, report that ADHD symptoms were commonly observed in ASD youth. Ratings of attention deficit, impulsivity, and hyperactivity were no different between children with ASD of any severity and children with ADHD-Combined type. Autism is very distinct from ADHD, but the core symptoms of ADHD-Combined type, i.e., attention deficit, impulsivity, and hyperactivity, would appear to also be features of autism. ASD and ADHD are neurobiological disorders characterized by similar underlying neuropsychological “deficits”. A similar observation is made by Van der Meer et al. ( 23 ). According to the authors, ASD and ADHD are different manifestations of one overarching disorder. They made the hypothesis there is a single continuum in which emotion regulation is a crucial common factor. In the same way, Ghirardi et al. ( 24 ) demonstrated there do exist a genetic overlap between clinical ASD and ADHD, suggesting an underestimation of this overlap by genomic studies. Van der Meer et al. also added that children with a ADHD phenotype without ASD symptoms can clearly be identified while the opposite is not true. These observations corroborated the assumption attention disorder is an inherent feature of ASD. Though Mayes et al. quickly conclude that “attention deficits” in ASD and ADHD are similar, they do report an interesting difference between ASD and ADHD children in this domain: selective attention is significantly more common among children with ASD (98%), no matter the severity of their disorder, than among those with ADHD-Inattentive type or ADHD-Combined type (21%). Whereas, children with ADHD have difficulty fixing their attention on a given task, those with ASD do have the capacity to focus on activities that interest them, e.g., puzzle assembly, reading, or repetitive drawing. Consequently, the authors reach the conclusion that ASD and ADHD can be distinguished by certain symptoms that differ considerably. While autistic symptoms are rarely seen in ADHD, there are specific ADHD symptoms that are particularly common in autism. Accordingly, we maintain that the definition of autism must take into account those symptoms that mirror or overlap with symptoms of ADHD, thereby better representing both the clinical reality of ASD, whose symptoms vary in intensity along a spectrum, and its neurobiological reality, i.e., the cortical dysfunction of which the clinical symptoms are an expression.
Mayes et al. also found no significant difference between children of normal intelligence with ASD, ADHD-Combined type, or ASD-Inattentive type in terms of performance on neuropsychological tests that evaluated attention, working memory, processing speed, and graphomotor skills.
Can comorbidity of ASD and ADHD truly be established by considering executive functions alone, as suggested by some studies ( 3 )? Carter Leno et al. ( 25 ) reported that multiple executive functioning impairments typically associated with ADHD are also found in people with ASD. Neuropsychological evaluations of executive functions do not fully account for the complexity of symptoms, and broader studies that consider additional brain functions could provide more clinical data essential for diagnoses. The study by Carter Leno et al. emphasized the limits of executive function exploration for discriminating ASD, ADHD, and oppositional defiant disorder subgroups. The authors evaluated the performance of four groups of youth ages 10 to 16—a typically developing group ( N = 43) and three groups of individuals clinically diagnosed with ADHD ( N = 21), oppositional defiant disorder ( N = 26), and ASD ( N = 41), respectively—on go-no-go and switch tasks, and detected deficits shared by the ADHD, oppositional defiant disorder, and ASD groups, such as increased reaction time variability. After controlling for symptoms of ADHD and oppositional defiant disorder, differences in reaction time variability between groups were no longer significant. For cognitive flexibility, as evaluated by the switch task, there was also no observed difference between groups. The ASD group alone exhibited impaired response inhibition and premature responsiveness, relative to the typically developing group. Carter Leno et al. thus concluded that executive functioning impairments specifically described as present in ADHD are also found in ASD. This stresses the need to explore and precisely define the characteristics of attentional impairment in autism. These characteristics, their causes, and their consequences should be included in the definition of ASD, to more accurately represent its specificities.
These findings are supported by those of Rosello et al. ( 26 ), who reported significantly more ADHD symptoms and poorer learning behaviors in ASD children than in those exhibiting typical development. Furthermore, behavioral regulation problems and impaired executive functioning associated with ADHD symptoms significantly impacted performance for ASD children, objectively demonstrating the effect of ADHD symptoms on these children's learning behaviors.
The attentional impairment best described for ASD is diminished joint attention. It is also said to give rise to later social communication impairments, especially in connection with oromotor skills ( 27 – 29 ). Recent functional neuroimaging studies reveal the influence of neural mechanisms through which sensory processing and attention may be modulated by the affective impact of a stimulus. The amygdala plays a central role in the production of direct and indirect top-down signals along sensory pathways, shaping how emotional events are represented. “These modulatory effects implement specialized mechanisms of ‘emotional attention' that might supplement but also compete with other sources of top-down control on perception ( 30 ).” When interpreting attentional abilities, it therefore seems necessary to account for the role of neural processes and temporo-spatial dynamics of the brain determining how cognitive and affective elements are integrated into attention and behavior. These factors are fundamental to the study of attentional abilities in ASD patients in whom amygdalar dysfunction has been described. We may refer to the findings of Liss et al. ( 31 ), who demonstrated that sensory overreactivity is associated with overselective, hyperreactive and overfocused attention; perseverative and stereotyped behaviors; and excellent memory skills—but also with major social deficits. Sensory-seeking behaviors are strongly linked to overfocused attention. This kind of excessive attention can be mistaken for ADHD inattention.
With respect to psychomotor agitation, it has been posited that ASD patients have atypical arousal systems, their state of overexcitement reflecting both excessive and fluctuating cortical activation by the brain stem. Dopaminergic hyperactivity along the nigrostriatal (explaining stereotypies) and mesolimbic (explaining interpersonal and perceptual deficits) pathways is a hypothesis gaining wider support. It would explain the perceived effectiveness of dopamine antagonists, vs. agonists, on all symptoms of autism. The above confirms the need to include the characteristics of hyperfocus among the diagnostic criteria for autism. Hyperfocus is a dimension also suggested by MEG studies ( 32 ) pointing to long-range underconnectivity in ASD patients.
Mundy et al. ( 33 ) explain that joint attention plays a key role in the functional development of a distributed cortical system involving both anterior (prefrontal and insular cortices) and posterior (temporal and parietal cortices) neural networks. Hence, early impairment of joint attention has direct repercussions on all aspects of intero- and exteroceptive data integration, altering cortical processing. Interestingly, ASD patients are described as being slow to orient their attention. Harris et al. ( 34 ) show, in children with ASD, that delay in orienting attention to visual stimuli correlates with severity of cerebellar hypoplasia, as evaluated by MRI. No correlations were found with the sizes of other brain regions. When interpreting the unique cognitive traits of people with ASD, particular attention must be paid to the role of the cerebellum. This may afford a broader understanding of the neurocognitive processes involved in ASD and a clinical perspective that better reflects the neurobiological facts.
To date, the mixed findings of etiologic ASD-ADHD comorbidity studies do not permit a clinical description of the physiopathologic comorbidity of these disorders. When speaking of comorbidity, are we not rather describing the severity of an attentional trait, with disabling functional effects, present in all ASD children?
These studies themselves demonstrate that children diagnosed with a comorbid disorder have more severe ASD. This suggests that—rather than an ASD-ADHD comorbidity, as authors conclude—the causes and consequences of a major attentional deficit typical of ASD are responsible for these patients' profiles. If so, this attentional trait should be included in the clinical definition and description of ASD. Instead of an ADHD explanation, we might then adopt an alternative etiologic perspective on these neurocognitive peculiarities and more fully account for the various brain impairments observed. As we have shown, children with ASD are affected much more by heightened attentional abilities than by a primary attention deficit, although the latter may be mistakenly (and dangerously) suggested by their clinical presentation. Therefore, we highlight the urgent need to develop new clinical and electrophysiological instruments to best fractionate and analyze these important neuropsychological features. This would be of crucial interest in particular for those modeling aspects of the co-morbidity in IPSC lines or animal models but also for the optimization of treatments use.
The attentional specificities observed in ASD, and their consequences, which are a direct reflection of unique brain functioning again challenge the validity of polythetic diagnoses in psychiatry. Attention deficits are key behavioral phenotypes of a considerable number of neurological and genetic diseases characterized by complex psychiatric disorders. Might the error lie in conflating such deficits with the unique, and very different, attentional traits of autism? In other words, are the attentional characteristics of disorders ignored by making an erroneous generalization?
Though further description of these characteristics is necessary, are they not key clinical symptoms of ASD in their own right—justifying their inclusion in the definition of this disorder—and potentially sufficient for its diagnosis?
Data Availability Statement
Author contributions.
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
1 https://caddra.ca/pdfs/caddraGuidelines2011Chapter02.pdf .

Limited Evidence of a Link Between Acetaminophen and Autism or ADHD
By Kate Yandell
Posted on February 22, 2023 | Updated on April 26, 2024 | Corrected on May 30, 2023 | Clarification on June 6, 2023
Q: Is the use of acetaminophen during pregnancy linked to autism or ADHD?
A: There is currently no strong evidence that acetaminophen use during pregnancy causes autism or ADHD in children. Expert groups continue to recommend use of the drug during pregnancy when necessary and in consultation with a doctor.
FULL QUESTION
Does Tylenol have links to Autism?
Is Tylenol a threat for pregnant people and tied to asd [autism] and adhd?
FULL ANSWER
Readers have asked whether Tylenol (acetaminophen) is connected to autism or ADHD, also known as attention-deficit/hyperactivity disorder. One person forwarded a sponsored Facebook post from the page “Child Autism & ADHD from Tylenol during pregnancy” stating that “parents of children with autism or ADHD whose mother took Tylenol while pregnant may be eligible for legal compensation.” The page continues to run similar advertisements , as do various other pages . Parents have filed lawsuits against retailers of acetaminophen, stating that their children developed autism or ADHD due to exposure to acetaminophen taken during pregnancy.

Some studies have indeed shown a relationship between acetaminophen taken during pregnancy and autism or ADHD in children, but they do not demonstrate that the acetaminophen use caused the elevated rates of autism and ADHD, researchers say. For example, a pregnant person who takes acetaminophen may have a child with ADHD or autism because of other factors, such as genetics.
Experts agree that acetaminophen has a role in pregnancy but that it should be used only when necessary and in consultation with a doctor. Avoiding use of acetaminophen for fever or pain during pregnancy may have negative consequences . For instance, an uncontrolled fever in early pregnancy can harm brain development.
A Food and Drug Administration spokesperson told us via email that the available evidence is “too limited to make any recommendations based on these studies at this time.”
The American College of Obstetricians and Gynecologists said in a 2021 statement that studies “show no clear evidence that proves a direct relationship between the prudent use of acetaminophen during any trimester and fetal developmental issues.” An ACOG representative told us that the statement is the most up-to-date communication on the topic. And a 2017 Society for Maternal-Fetal Medicine statement , which a representative also confirmed to be the most up-to-date document, found the evidence on a causal link between acetaminophen and neurobehavioral disorders to be “inconclusive.”
Update, Dec. 19: A federal judge ruled Dec. 18 that testimony from experts purporting to show acetaminophen causes autism and ADHD was inadmissible. The ruling applied to a consolidated case involving hundreds of lawsuits against retailers of store-branded acetaminophen and the manufacturer of Tylenol. The judge wrote that “there is no generally accepted scientific conclusion that in utero exposure to acetaminophen causes either ASD or ADHD. As explained below, the plaintiffs’ experts have not reliably opined so either.”
Update, April 26: A large study published April 9 in JAMA found no association between using acetaminophen during pregnancy and autism or ADHD in children, when comparing siblings. Analysis without using sibling controls did find an association between acetaminophen use and slight increased rates of autism and ADHD. Rather than the acetaminophen causing the increased risks, the researchers wrote, it appears that factors related to the parents influenced both acetaminophen use and the likelihood of having a child with autism or ADHD. For instance, there is evidence that pregnant people with genetic risk factors for ADHD or autism are both more likely to use acetaminophen and to have a child with one of these conditions.
Studies of Acetaminophen During Pregnancy Have Weaknesses
Acetaminophen, called paracetamol outside the U.S., is used widely during pregnancy to treat pain and fever. It is an ingredient in many over-the-counter and prescription medications, including Tylenol, Excedrin and Vicodin, as well as some versions of DayQuil, NyQuil, Sudafed, Mucinex and Midol.
As we said, some studies have found that women who reported using acetaminophen during pregnancy were more likely than those who didn’t to have children who later developed autism or ADHD. A 2018 paper published in the American Journal of Epidemiology that aimed to comprehensively analyze data from multiple studies, for example, found a 34% and 19% higher risk of ADHD and autism, respectively, in children whose mothers took acetaminophen in pregnancy compared with those whose mothers did not.

But this doesn’t necessarily mean acetaminophen is to blame for the conditions. These studies were observational , meaning that researchers simply noted levels of acetaminophen exposure, generally based on reports from the parents in the studies. Randomized controlled trials — in which one group receives a medication or treatment and another group receives a placebo or standard care — are the gold standard for determining whether a causal relationship exists.
It is possible that people who take more acetaminophen are more likely to have characteristics that predispose them to have a child with autism or ADHD — including the illnesses or other health conditions that might have prompted a pregnant person to take acetaminophen in the first place.
The authors of the 2018 study recognized this issue, writing that the results “should be interpreted with caution given that the available evidence consists of observational studies and is susceptible to several potential sources of bias.”
Sura Alwan , a birth defects epidemiologist and co-director of the Teratogen Information System at the University of Washington, told us in an email that genetic factors might also help explain the results, adding that not all studies have found an association between prenatal acetaminophen and neurodevelopmental outcomes like autism and ADHD.
In any case, she said, the studies “do not necessarily imply a causal link, which means that there isn’t enough evidence to say that taking acetaminophen causes those behavioral or cognitive concerns.”
Some researchers do think the associations are worrisome enough to caution women taking acetaminophen during pregnancy. In 2021, an international group of scientists, clinicians, and public health professionals published what they called a “ consensus statement ” in Nature Reviews Endocrinology, which made news for calling for “precautionary action” based on data indicating acetaminophen might alter fetal development, with an increasing impact with increasing duration of exposure.
“We recognize that limited medical alternatives exist to treat pain and fever; however, we believe the combined weight of animal and human scientific evidence is strong enough for pregnant women to be cautioned by health professionals against its indiscriminate use, both as a single ingredient and in combination with other medications,” the researchers wrote.
The statement proved controversial, however, with other groups of scientists pushing back to add context and explain why acetaminophen might not have caused the links seen in the studies.
“In my opinion, the level of evidence out there is poor, and I do not believe that there is any causal or any other association between at least short-term use of acetaminophen during pregnancy and ensuing increased risk of childhood ADHD or ASD [autism],” Dr. Per Damkier , a professor and clinical pharmacologist at Odense University Hospital and University of Southern Denmark, told us in an interview. Damkier was one of the scientists who pushed back at the consensus statement.
Multiple factors contribute to autism and ADHD . These conditions “are variable in clinical presentation, very difficult to assess and associate with a single causal factor,” Alwan said.
Damkier emphasized that many studies do not adequately take into account whether the parents had ADHD or autism , which run in families. He pointed to one study that suggested accounting for ADHD in parents likely weakens the relationship between this disorder and acetaminophen.
Many studies also rely on questionnaires filled out by parents, Damkier said. These may identify children at increased risk of ADHD or autism but do not replace an official diagnosis.
Finally, Damkier said that even if you accepted the analyses in the studies showing increased risk as valid, “which you should not,” the risk levels — typically 20% to 30% increased risk during childhood — represent a “weak association,” especially since there is typically a fair to moderate degree of uncertainty surrounding the numbers.
A Closer Look at Cord Blood
A 2019 JAMA Psychiatry study , which is cited in legal advertisements , did not rely on self-reported data, instead looking at concentrations of broken down acetaminophen components in blood collected at Boston Medical Center from umbilical cords at birth and stored for future study.
The children with acetaminophen exposure in the top third — meaning the highest concentrations of the drug components in cord blood — had 2.86 times higher odds of an ADHD diagnosis and 3.62 times higher odds of an autism diagnosis compared with children with exposure in the bottom third. “Our findings support previous studies regarding the association between prenatal and perinatal acetaminophen exposure and childhood neurodevelopmental risk and warrant additional investigations,” the authors wrote.
The authors themselves noted some limitations of the paper at the time of publication. The cord blood measurements did not give a sense of acetaminophen exposure throughout pregnancy, instead showing recent use by people who had just given birth. Further, “caution is needed to apply our findings to other populations with different characteristics,” they wrote. Finally, one author pointed out in a press release that the study does not show that Tylenol causes ADHD or autism.
Damkier and others said that some observations and the characteristics of the children in the study appeared unusual, making it hard to draw general conclusions. Every cord blood sample showed acetaminophen exposure, he noted, and there were extremely high rates of ADHD and autism among the children. The study also lacked information on the mothers’ use of drugs or history of psychiatric disease.
Acetaminophen Treats Pain and Fever During Pregnancy
Expert groups said that acetaminophen can have benefits for pregnant people experiencing pain or fever, and there may not be good alternatives. The ACOG statement reads: “ACOG and obstetrician-gynecologists across the country have always identified acetaminophen as one of the only safe pain relievers for pregnant individuals during pregnancy.”
Nonsteroidal anti-inflammatory drugs, such as ibuprofen and aspirin, can have risks during pregnancy. Taking these drugs during later portions of pregnancy can lead to problems including insufficient amniotic fluid volume and premature closing of a major blood vessel in the fetus. Opioids can also harm the fetus and lead to withdrawal at birth, as well as pose risks for the mother.
Avoiding acetaminophen could have consequences for both mother and child. Fever early in pregnancy can lead to defects in the neural tube affecting the formation of the brain or spinal cord, Alwan said, noting that it is “critically important to treat fever in pregnancy.”
The Society for Maternal-Fetal Medicine statement calls acetaminophen “a reasonable and appropriate medication choice for the treatment of pain and/or fever during pregnancy.”
The authors of the 2021 Nature Reviews Endocrinology statement suggested doing more research into acetaminophen during pregnancy and cautioned women to “forego APAP [acetaminophen] unless its use is medically indicated; consult with a physician or pharmacist if they are uncertain whether use is indicated and before using on a long-term basis; and minimize exposure by using the lowest effective dose for the shortest possible time.”
This advice is in line with longstanding recommendations for pregnant people. “ACOG’s clinical guidance remains the same and physicians should not change clinical practice until definitive prospective research is done. Most importantly, patients should not be frightened away from the many benefits of acetaminophen. However, as always, any medication taken during pregnancy should be used only as needed, in moderation, and after the pregnant patient has consulted with their doctor,” the ACOG statement said.
“It is important for pregnant women and all women of reproductive age who may become pregnant to always consult their health care provider to find the best treatment option for pain or fever in pregnancy, which may be taking the recommended dose of acetaminophen and making sure to stay well hydrated and getting lots of rest,” Alwan said. People with questions about medications during pregnancy or breastfeeding can contact organizations like MotherToBaby , she added.
An FDA spokesperson told us in an email: “The FDA is aware of and understands the concerns arising from reports questioning the safety of prescription and over-the-counter (OTC) pain medicines when used during pregnancy. As a result, we evaluated research studies on acetaminophen published in the medical literature and determined that they are too limited to make any recommendations based on these studies at this time. Because of this uncertainty, the use of pain medicines during pregnancy should be carefully considered. We urge pregnant persons to always discuss all medicines with their health care professionals before using them. Acetaminophen labels contain the following information regarding pregnancy: ‘If pregnant or breast feeding, ask a health professional before use.’ The FDA continues to review the published literature and to monitor the potential impacts of acetaminophen.”
The spokesperson concluded by sharing a link to a 2015 Drug Safety Communication describing an FDA review of the risks of pain medicine during pregnancy. The document noted that severe and persistent pain, when not treated effectively, can lead to depression, anxiety and high blood pressure for the pregnant individual.
Correction, May 30: An earlier version of this article incorrectly stated that acetaminophen is an ingredient in oxycodone. Oxycodone is an opioid that is sometimes combined with acetaminophen. We thank the reader who brought this to our attention.
Clarification, June 6: An earlier version of this article listed drugs that contain acetaminophen, but did not make clear that acetaminophen is only in some versions of several of the drugs. We have updated the article to clarify this point. We thank the reader who brought this to our attention.
Editor’s note: SciCheck’s articles providing accurate health information and correcting health misinformation are made possible by a grant from the Robert Wood Johnson Foundation. The foundation has no control over FactCheck.org’s editorial decisions, and the views expressed in our articles do not necessarily reflect the views of the foundation.
Acetaminophen – ASD/ADHD Products Liability Litigation. MDL No. 3043. Transfer Order . United States Judicial Panel on Multidistrict Litigation. 5 Oct 2022.
Ji, Yuelong et al. “ Association of Cord Plasma Biomarkers of In Utero Acetaminophen Exposure With Risk of Attention-Deficit/Hyperactivity Disorder and Autism Spectrum Disorder in Childhood .” JAMA Psychiatry. 30 Oct 2019.
Bauer, Ann Z. et al. “ Paracetamol Use during Pregnancy — a Call for Precautionary Action .” Nature Reviews Endocrinology. 23 Sep 2021.
Masarwa, Reem et al. “ Prenatal Exposure to Acetaminophen and Risk for Attention Deficit Hyperactivity Disorder and Autistic Spectrum Disorder: A Systematic Review, Meta-Analysis, and Meta-Regression Analysis of Cohort Studies .” American Journal of Epidemiology. 24 Apr 2018.
Damkier, Per et al. “ Handle with Care — Interpretation, Synthesis and Dissemination of Data on Paracetamol in Pregnancy .” Nature Reviews Endocrinology. 14 Dec 2021.
Alwan, Sura et al. “ Paracetamol Use in Pregnancy — Caution over Causal Inference from Available Data .” Nature Reviews Endocrinology. 14 Dec 2021.
O’Sullivan, Joseph et al. “ Paracetamol Use in Pregnancy — Neglecting Context Promotes Misinterpretation .” Nature Reviews Endocrinology. 11 March 2022.
“ ACOG Response to Consensus Statement on Paracetamol Use During Pregnancy .” American College of Obstetricians and Gynecologists. 29 Sep 2021.
Society for Maternal-Fetal Medicine (SMFM) Publications Committee. “ Prenatal Acetaminophen Use and Outcomes in Children .” American Journal of Obstetrics and Gynecology. 23 Jan 2017.
“ ACETAMINOPHEN |TERIS agent – 1017 .” Teratogen Information System. Accessed 17 Feb 2023.
“ Common Medicines with Acetaminophen .”KnowYourDose.org. Accessed 20 Feb 2023.
Cueto, Isabella. “ New research cautions about possible risks of acetaminophen use during pregnancy .” STAT. 23 Sep 2021.
Tingley, Kim. “ Why Is Good Medical Advice for Pregnant Women So Hard to Find? ” New York Times Magazine. 21 Oct 2021.
Ystrom, Eivind et al. “ Prenatal Exposure to Acetaminophen and Risk of ADHD .” Pediatrics. 1 Nov 2017.
Liew, Zeyan et al. “ Maternal use of acetaminophen during pregnancy and risk of autism spectrum disorders in childhood: A Danish national birth cohort study .” Autism Research. 21 Dec 2015.
“ What Is Autism Spectrum Disorder? ” CDC. Updated 9 Dec 2022.
“ What Is ADHD? ” CDC. Updated 9 Aug 2022.
Masarwa, Reem et al. “ Acetaminophen use during pregnancy and the risk of attention deficit hyperactivity disorder: A causal association or bias ?” Paediatric and Perinatal Epidemiology. 9 Jan 2020.
“ Expert Reaction to Study Looking at Paracetamol in Pregnancy and Autism, ADHD and Other Developmental Disabilities in Children .” Science Media Centre. 30 Oct 2019.
Bauer, Ann Z. et al. “ Reply to ‘Paracetamol use in pregnancy — caution over causal inference from available data’; ‘Handle with care — interpretation, synthesis and dissemination of data on paracetamol in pregnancy ’” Nature Reviews Endocrinology. 14 Dec 2021.
ACOG Committee on Clinical Practice Guidelines–Obstetrics. “ Headaches in Pregnancy and Postpartum: ACOG Clinical Practice Guideline No. 3 .” Obstetrics and Gynecology. 1 May 2022.
“ FDA Recommends Avoiding Use of NSAIDs in Pregnancy at 20 Weeks or Later Because They Can Result in Low Amniotic Fluid .” FDA. 15 Oct 2020.
“ About Opioid Use during Pregnancy .” CDC. Updated 28 Nov 2022.
“ FDA Drug Safety Communication: FDA has reviewed possible risks of pain medicine use during pregnancy .” FDA. 9 Jan 2015.
Family History Of Autism And ADHD Vary With Recruitment Approach And SES
Olivia Guy-Evans, MSc
Associate Editor for Simply Psychology
BSc (Hons) Psychology, MSc Psychology of Education
Olivia Guy-Evans is a writer and associate editor for Simply Psychology. She has previously worked in healthcare and educational sectors.
Learn about our Editorial Process
Saul Mcleod, PhD
Editor-in-Chief for Simply Psychology
BSc (Hons) Psychology, MRes, PhD, University of Manchester
Saul Mcleod, PhD., is a qualified psychology teacher with over 18 years of experience in further and higher education. He has been published in peer-reviewed journals, including the Journal of Clinical Psychology.
Autism and ADHD are neurodevelopmental conditions that impact an individual’s behavior, communication, and cognitive processes. Autism is characterized by challenges in social interaction, restricted interests, and repetitive behaviors, while ADHD is associated with inattention, hyperactivity, and impulsivity. Research suggests a strong genetic component to both conditions, with increased likelihood of diagnosis among individuals who have a sibling or parent with autism or ADHD. Moreover, there is significant co-occurrence between autism and ADHD, further indicating potential shared genetic underpinnings. Understanding the heritability and familial patterns of these conditions is crucial for early identification, intervention, and support for individuals and families affected by autism and ADHD.

- The prevalence of family history (FH) of autism and ADHD varies depending on the recruitment approach used in developmental studies. Rates were 3-9% for diagnosed cases.
- The highest rate of FH-autism/ADHD was in the sample recruited through an online participant pool, which also had the most socio-economically diverse families.
- Lower parental education and income were associated with higher rates of FH-ADHD. Lower parental education was associated with increased FH-autism.
- Recruitment strategies meaningfully impact sample neurodiversity and the generalizability of findings. Online crowdsourced samples may be more representative than university databases/social media.
Autism and ADHD are highly heritable neurodevelopmental conditions. Children with a parent or sibling diagnosed with autism or ADHD have a significantly higher likelihood of receiving a diagnosis themselves (Chen et al., 2017; Constantino et al., 2010; Messinger et al., 2013; Miller et al., 2019; Risch et al., 2014).
Around 30-40% of individuals with autism or ADHD have a co-occurring diagnosis of the other condition (Lai et al., 2019; Rong et al., 2021).
However, family history of autism/ADHD is not often considered during recruitment for developmental studies, despite the high recurrence rates and impact on neurodivergent development.
This study aimed to examine how rates of FH-autism/ADHD vary across different recruitment methods and family socioeconomic factors in young children.
The researchers looked at rates of autism or ADHD among family members of children who are autistic or have ADHD.
Participants were 1055 children aged 9-46 months from three UK-based samples recruited using different methods. The samples varied in socioeconomic diversity.
- The rate of FH-autism or FH-ADHD was 3–9% for diagnosed cases.
- The rate was highest in the sample recruited through an online participant pool, which also consisted of the most socio-economically diverse families.
- Lower parental education and family income were associated with higher rates of FH-ADHD. Lower parental education was associated with increased FH-autism.
This study provides important insights into how recruitment methods and family socioeconomic factors relate to rates of FH-autism/ADHD in developmental research samples.
The finding that online crowdsourced samples had the highest rates of FH-autism/ADHD and greatest socioeconomic diversity suggests this recruitment approach may yield more representative samples than university databases or social media.
The associations between lower parental education/income and higher rates of FH-ADHD/autism align with previous research linking autism and ADHD to socioeconomic status (Durkin et al., 2017; Russel et al., 2016).
Future research should examine potential mechanisms underlying these associations and take family history and socioeconomic diversity into account when developing recruitment strategies.
Below are some notable strengths with this study:
- Examined rates of FH-autism/ADHD across multiple samples recruited using different methods
- Large total sample size of over 1,000 participants
- Included socioeconomically diverse families
Limitations
Below are some of the limitations of this study:
- Samples were all from the UK, limiting geographic generalizability
- Family history was based on parent-report, not verified diagnoses
- Cross-sectional design prevents causal conclusions about links between socioeconomic factors and FH-autism/ADHD
Implications
The results suggest that developmental researchers should carefully consider how their recruitment strategies may impact the neurodiversity and representativeness of their samples.
In particular, online crowdsourcing may be an effective way to recruit more socioeconomically diverse samples with higher rates of FH-autism/ADHD compared to traditional university or social media-based approaches.
Clinically, the findings highlight the importance of screening for family history, especially among socioeconomically disadvantaged families, to identify children at higher likelihood of autism/ADHD.
Finally, the socioeconomic associations underscore the need for policies and services that support neurodivergent individuals and families across the socioeconomic spectrum.
Primary reference
Bazelmans, T., Scerif, G., Holmboe, K., Gonzalez‐Gomez, N., & Hendry, A. (2024). Rates of family history of autism and ADHD varies with recruitment approach and socio‐economic status. British Journal of Developmental Psychology, 42 (2), 117–132. https://doi.org/10.1111/bjdp.12469
Other references
Chen, Q., Brikell, I., Lichtenstein, P., Serlachius, E., Kuja‐Halkola, R., Sandin, S., & Larsson, H. (2017). Familial aggregation of attention‐deficit/hyperactivity disorder. Journal of Child Psychology and Psychiatry , 58 (3), 231-239. https://doi.org/10.1111/jcpp.12616
Constantino, J. N., Zhang, Y. I., Frazier, T., Abbacchi, A. M., & Law, P. (2010). Sibling recurrence and the genetic epidemiology of autism. American Journal of Psychiatry , 167 (11), 1349-1356. https://doi.org/10.1176/appi.ajp.2010.09101470
Durkin, M. S., Maenner, M. J., Baio, J., Christensen, D., Daniels, J., Fitzgerald, R., … & Yeargin-Allsopp, M. (2017). Autism spectrum disorder among US children (2002–2010): Socioeconomic, racial, and ethnic disparities. American journal of public health , 107 (11), 1818-1826. https://doi.org/10.2105/AJPH.2017.304032
Lai, M. C., Kassee, C., Besney, R., Bonato, S., Hull, L., Mandy, W., Szartmari, P., & Ameis, S. H. (2019). Prevalence of co-occurring mental health diagnoses in the autism population: a systematic review and meta-analysis. The Lancet Psychiatry , 6 (10), 819-829. https://doi.org/10.1016/S2215-0366(19)30289-
Messinger, D. S., Young, G. S., Webb, S. J., Ozonoff, S., Bryson, S. E., Carter, A., … & Zwaigenbaum, L. (2015). Early sex differences are not autism-specific: A Baby Siblings Research Consortium (BSRC) study. Molecular autism , 6 , 1-12. https://doi.org/10.1186/s13229-015-0027-y
Miller, M., Musser, E. D., Young, G. S., Olson, B., Steiner, R. D., & Nigg, J. T. (2019). Sibling recurrence risk and cross-aggregation of attention-deficit/hyperactivity disorder and autism spectrum disorder. JAMA pediatrics , 173 (2), 147-152.
Risch, N., Hoffmann, T. J., Anderson, M., Croen, L. A., Grether, J. K., & Windham, G. C. (2014). Familial recurrence of autism spectrum disorder: evaluating genetic and environmental contributions. American Journal of Psychiatry , 171 (11), 1206-1213. https://doi.org/10.1176/appi.ajp.2014.13101359
Rong, Y., Yang, C. J., Jin, Y., & Wang, Y. (2021). Prevalence of attention-deficit/hyperactivity disorder in individuals with autism spectrum disorder: A meta-analysis. Research in Autism Spectrum Disorders , 83 , 101759. https://doi.org/10.1016/j.rasd.2021.101759
Russell, A. E., Ford, T., Williams, R., & Russell, G. (2016). The association between socioeconomic disadvantage and attention deficit/hyperactivity disorder (ADHD): a systematic review. Child Psychiatry & Human Development , 47 , 440-458. https://doi.org/10.1007/s10578-015-0578-3
Keep Learning
Here are some potential discussion questions for a college class on this paper:
- How might researchers weigh the pros and cons of different recruitment strategies in light of these findings? What additional factors should they consider?
- What potential mechanisms might explain the associations between lower socioeconomic status and higher rates of FH-autism/ADHD? How could future research test these mechanisms?
- How can developmental research become more inclusive and representative of the full spectrum of neurodiversity? What other steps, beyond broadening recruitment, may be needed?
- What are the implications of these findings for clinical screening and support services for families of children with or at risk for autism/ADHD? How can we ensure equitable access?
- How might intersectionality between neurodivergence and socioeconomic disadvantage shape individuals’ and families’ experiences and outcomes? What related research questions does this study raise?
Related Articles

Clinical Psychology
Sleep Loss and Emotion: A Systematic Review and Meta-Analysis

Measuring And Validating Autistic Burnout

A Systematic Review of Grief and Depression in Adults

Anxiety in Early Adolescents During the Covid-19 Pandemic

Accommodation of PTSD Symptoms

Gut Microbiome Diversity and Emotional Well-Being

Why autism and ADHD self-diagnosis may be inaccurate
E very few months, 52-year-old Peter* would find himself in trouble with his wife. Sitting silently during an argument and unable to speak, he couldn’t process anything levelled at him. He didn’t know what was wrong, except noticing that he had a weird pattern of “getting stuck in a rut”, hyper-fixating on interests such as programming and PC gaming at the expense of spending time with his wife.
Then, by chance, Peter discovered the autism spectrum quotient (AQ) test on Facebook and scored two times higher than an average adult – a strong indication that he might be autistic. Following that, he went down the rabbit hole of autism self-diagnosis and spent all his evenings watching YouTube channels like Mom on the Spectrum and That Autistic Guy.
“From then, I went on to find other diagnostic tests. So many of the experiences people talked about mirrored my own life experiences, and then the tests all came back saying my responses were indicative of likely having autism,” he recalls.
Peter got hooked on r/AutismTranslated, a Reddit forum for those who are on the quest to explore their autistic identity. Of over 45,000 members, many people are self-diagnosers like him. Adjacent to this growing community, there is now also a booming cast of autistic influencers. Paul Micallef, the creator of Autism from the Inside – one of Peter’s favourite YouTube channels – has over 300,000 subscribers on the platform. Celebrities such as the pop singer Sia and the TV personality Christine McGuinness are also opening up about their late-diagnosed autism , prompting many people to wonder if they could be autistic as well after years of feeling isolated.
In fact, recently published research would suggest that there are tens of thousands of people who believe that something is amiss.
A new report from health think tank Nuffield Trust has shown that the number of people in England awaiting an autism or ADHD diagnosis has ballooned fivefold in four years ; in April 2019, just 17,409 people had an open referral for suspected autism. In December that year the figure was 32,233 and by December 2023 this had risen to 172,022.
And while there is no national data on referrals for ADHD, it’s been reported that between 2019/20 and 2022/23 there was a 51 per cent increase in the number of people prescribed with medication for the condition.
Diagnosis, or the hope of an official diagnosis, is one thing but first there are the enormous waiting lists to navigate. The median wait on the NHS for the first appointment (of many) to decide whether or not a patient is autistic is currently nine months – for some areas of the country, this can rise to over two years.
With such a long and stringent official diagnosis process, it’s little wonder then that people who feel they may better fit into the neurodiverse rather than neurotypical category are seeking out their own diagnoses.
Self-diagnosis rocketed during the pandemic thanks in part to social media and other internet platforms. In 2021, the #autism hashtag became the ninth most-viewed health-related hashtag on TikTok. Autism-related hashtags generated an astounding 11.5 billion views on the platform in 2023.
While it all feels very current, the groundswell of self-diagnosis began decades ago. Following the emergence of the autism self-advocacy movement in North America in the 1990s, the internet then provided a text-based way for autistic people, who can struggle in social situations, to connect with each other. Then DSM-IV: Diagnostic and Statistical Manual of Mental Health Disorders , essentially the classification handbook of mental disorders used by psychologists and psychiatrists worldwide, became available in the public domain so even by the early 2000s, self-diagnosis began to gain traction.
The AQ test, one of the most popular self-reporting tools, was developed by Cambridge researchers in 2001 and was soon popularised by Wired magazine. But it was never intended to be a diagnostic measure; the test was designed for screening purposes only. Many clinicians have criticised it for being misleading on the grounds that it only indicates autistic traits.
“Lots of people might show autistic traits like being sensitive to sounds in the environment or struggling in some social situations,” explains Laura Crane, a professor of autism studies at the University of Birmingham. “And some people show several such traits. But it’s not the case that these isolated traits mean that someone is autistic. It’s when a person’s traits interfere significantly with their daily life and map on to some specific diagnostic criteria (as determined by a multidisciplinary clinical team) that they would be considered for a diagnosis.”
While the new diagnosis figures appear extraordinary and would point to the fact that vast swathes of the population are suddenly being struck down with ADHD and autism, according to Sir Simon Wessely, a regius professor of psychiatry at King’s College London, who was interviewed by the Today programme on the subject, this is just not the case. “We know… [for ADHD] it’s about 2 per cent of the school population for example,” he said, adding that those figures have remained constant for decades and there is no evidence of the disorder becoming more common despite the wild rise in diagnosis requests. “The changes that we’re seeing now are dramatic,” he continued. “We don’t normally see that sort of change anywhere in medicine.” Explanations for the sudden lurch include wider societal awareness of neurodiverse conditions and a broader definition of autism.
According to Prof Wessely, GPs are reporting that while they’re being inundated with patients wanting a formal diagnosis for ADHD or autism, patients are not looking for medical treatment, be it prescriptions or talking therapies; what they’re looking for is “validation and recognition”.
“They don’t want treatment and they don’t necessarily think they are ill. They think they are different.”
While Prof Wessely is calling for society to have a complete “redefinition of thinking about these problems”, stating that the NHS is not coping now and will never cope with an exponential increase in open referrals, at present the situation is such that tens of thousands of people are left feeling “different” and undiagnosed.
As for Peter, he contacted the local NHS team after his initial suspicion, but the staff members “did their best to discourage” him from taking it further.
“They cited that the waiting list is 18 months and told me that I’d got through life this far without a diagnosis so I should be able to cope without getting one. I was made to feel that my diagnosis request wouldn’t be welcome, so I decided not to apply,” he said.
Can you self-diagnose autism and ADHD?
Nevertheless, Dr Sam Fellowes, a history of autism specialist at Lancaster University, warns of the inaccuracies of autism self-diagnosis: “My concern is that people will primarily self-diagnose with psychiatric diagnoses which are more well known, which means they do not consider diagnoses that are less well known but more accurate descriptions of them.” Schizoid personality disorder, for example, can look very similar to autism at first sight. But the former is characterised by a lack of social motivation rather than the inability to read social cues.
And Peter is worried about the legitimacy of some people’s claims on social media; a recent study warns that more than half of neurodiverse content on TikTok could be misleading.
“Knowing other people share some of the same life experiences and troubles does make me feel less alone. But I have seen lots of fakers. I trust the long-form videos on YouTube the most, and the soundbites on Instagram and TikTok the least,” says Peter.
After a year of investigating his potential autism, Peter is still reading and watching all the materials he can find on the internet to ascertain his self-diagnosis. He is now suspecting he might also have ADHD, which presents in 50 to 70 per cent of autistic individuals, along with other conditions including pathological demand-avoidance syndrome and rejection-sensitive dysphoria.
Tim Nicholls, head of influencing and research at the National Autistic Society, says he recognises the importance of autism self-diagnosis but still recommends those who have doubts to obtain an official diagnosis to receive “the right help and support at school, home and work”. He is also concerned about the current long waits for autism assessment as “for many, this will mean struggling without support or eventually reaching crisis point”.
For Peter and many other self-diagnosers, their new apparent autistic identity provides a long-waited explanation of who they are but he has been reconsidering an official autism diagnosis. He has heard about the “right to choose” system on TikTok, which offers faster assessments through private healthcare providers by NHS referral. Since last year, researching autism has become Peter’s special interest. He has done all the tests available online and is late for bed every day – his wife thought he was gaming all the time.
“A formal diagnosis won’t really give me solutions to my problems. After all, I can’t rewire how my brain works, so it will keep doing things the way it always does,” he says. “But then I can stop doing all the research and get to bed sooner each night. I’d also stop feeling like an impostor and having to continually find ways to support my belief, and possibly I might have better protection at work if I’m officially disabled.”
Naturally, there are criticisms that we are in danger, as a society, of medicalising normal human variety and that instead of trying to label every personality trait, we should spend less time navel-gazing and more time getting on with things. However, that viewpoint probably won’t be held by the growing number desperate for answers on NHS waiting lists.
“It’s important to remember that people seek a diagnosis because, very often, they’re struggling in some way,” explains Prof Crane. “Even if a person went for an assessment and didn’t receive the diagnosis they were expecting, we can’t negate their lived experience and it doesn’t mean that they don’t need support.
“Neurodivergences like autism and ADHD mean that a person experiences the world differently to other people, and because of the way society is set up, they may experience more challenges. Perhaps the question shouldn’t be about whether we are in danger of pathologising normal human differences but [should] be whether society is really set up in a way that values difference and diversity?”
*Name has been changed
Recommended
The truth about ADHD: separating fact from fiction
Play The Telegraph’s brilliant range of Puzzles - and feel brighter every day. Train your brain and boost your mood with PlusWord, the Mini Crossword, the fearsome Killer Sudoku and even the classic Cryptic Crossword.

PERSPECTIVE article
Asd and adhd comorbidity: what are we talking about.

- Service universitaire de Psychiatrie de l'Enfant et de l'Adolescent, Centre hospitalier Intercomunal de Créteil, Créteil, France
According to the scientific literature, 50 to 70% of individuals with autism spectrum disorder (ASD) also present with comorbid attention deficit hyperactivity disorder (ADHD). From a clinical perspective, this high rate of comorbidity is intriguing. What is the real significance of this dual diagnosis? Is ADHD in fact always present in such cases? Might the attentional impairment reported among our ASD patients actually be a distinct trait of their ASD—namely, impaired joint attention—rather than an ADHD attention deficit? Could their agitation be the consequence of this joint attention impairment or related to a physical restlessness etiologically very different from the agitation typical of ADHD? The neurobiological reality of ASD-ADHD comorbidity is a subject of debate, and amphetamine-based treatment can have paradoxical or undesirable effects in the ASD population. Consequently, does a dual diagnosis, notwithstanding its currency in the literature, prevent us from shedding sufficient light on major physiopathologic questions raised by the clinical picture of ASD?
Introduction
The semiology of autism spectrum disorder (ASD) and attention deficit hyperactivity disorder (ADHD) presented in current nosography, which helps clinicians to identify these disorders, makes it clear that they are different entities, affecting children and their developmental histories in ways that are clearly distinct. In the first case, we are primarily describing distracted children who pay little attention in academic settings, lose their belongings, and have difficulty sustaining mental effort. In the second case, we are talking about children who seldom associate with others, have a hard time interacting and communicating, and may display unique motor or verbal behaviors, including stereotypies, echolalia, and idiosyncratic language. Whereas, children with ADHD tend to be relatively boisterous and talkative, and eager rather than apprehensive of interactions with peers or adults, autistic children may be distinguished by their repetitive and less coordinated motor function, difficulty communicating, emotions in sync with their sensory reality more than with their social setting, and uniform behaviors that keep the unpredictable at bay.
Epidemiologically, these two disorders also differ in their incidence. Their diagnoses are made at different ages. Children with ASD can be identified before they are 3 years old, while ADHD is diagnosed later on. Both fall into the wider category of neurodevelopmental disorders, within which “comorbidities” are considered relatively frequent.
The prevalence of ADHD in people with ASD ranges from 50 to 70%, according to the literature ( 1 ). Where does this figure come from? How was it obtained, which studies and semiological criteria were applied, and how were the relevant clinical data collected?
This figure is the product of meta-analyses. It is important to note the variability of findings between studies—more than a mean prevalence, a precise yet illusory value reflecting the view that this comorbidity is a clearly measurable entity—because it admits an alternative interpretation of the phenomenon in question. Indeed, reported rates of comorbidity range from 10 to 90%. In the logic of meta-analysis, variation is often explained through methodological arguments: studies diverging from the mean are said to describe different populations, apply less valid methods of measurement, or gather their data in atypical ways. Yet, in part, what may be described as “bias” could betray an unsound theoretical foundation, accommodating a multitude of experimental paradigms measuring what is thought to be the same phenomenon.
This article thus aims to recall the attentional features inherent to ASD; to describe and analyze the variability of data reported in the literature; and finally, to draw on studies of factors related to attention, such as memory, sensorimotor function, executive functioning, and intellectual disability, for a better understanding of the role these variables play in the expression of cognitive capacity within the ASD population.
Autism and Attention
Attention is defined as a process of selection applied to the product of perception, and may even be directed toward memories. To direct attention on a perceptual or internally represented entity, our working memory must be trained on a goal for the duration of the task at hand. Attention encompasses essential elements of the executive functions and can be further broken down into sustained attention; focused attention; visual search, whereby the target of attention is defined using a template stored in working memory; voluntary or reflexive orienting and disengagement; attentional filtering; and expectation ( 2 ).
In people with ASD, these components of attention have a characteristic profile: sustained and focused attention is stronger than in normal subjects; visual search is also, though this seems to reflect the quality of perceptual processing more than attention; and the ability to orient attention toward non-social stimuli is deficient, as are reflexive and voluntary disengagement, in certain settings. Attentional filtering is not compromised in ASD patients having no intellectual disability. Higher-functioning ASD patients have a specific attentional impairment not observed among other ASD patients ( 3 ). Joint attention also appears to be lacking.
Can the comorbidity of ASD and ADHD truly be established by considering executive functions alone, as several studies suggested ( 4 )? The developmental cognitive specificities of ASD have been well described as they are linked with perception aspects but their executive or attentional aspects have been relatively neglected. “Attentional impairments in autism tend to be more of the ‘not listening' and ‘difficulty shifting focus' type than of the ‘short attention span' and ‘excessive distractibility' type 1 .” These distinct clinical particulars suggest attentional symptoms inherent to ASD rather than comorbid ADHD.
What Do Comorbidity Studies Address?
While the DSM-4 and ICD-10 give mutually exclusive diagnoses of ADHD and ASD, the DSM-5 mentions each condition in its description of the other, admitting the possibility of comorbidity.
Sprenger et al. ( 5 ) concluded that autistic symptoms were significantly more severe, especially in the area of social interaction (as evaluated by the social responsiveness scale and autism diagnostic interview), in patients with dual ASD-ADHD diagnoses than in those with ASD alone. Yet this conclusion might also illustrate the frequent clinical confusion of these disorders: could the severe autism they describe not just as well itself be the cause of a more symptomatic attention deficit, without suggesting the presence of ADHD? Similarly, Green et al. ( 6 ) stated that autistic symptoms were more prevalent in children with ADHD. Their study considered a group of children aged 6 to 10 divided into an ADHD subgroup and a control subgroup without ADHD. It seems questionable to conclude that autistic symptoms are more prevalent in ADHD patients without recognizing that the severity of ASD is independently at the origin of pronounced attentional deficiencies. The study also concluded that the intensity of hyperactive and impulsive symptoms directly impacts the severity of ASD symptoms, without inversely considering that, again, the severity of ASD might independently explain signs of psychomotor agitation and attentional deficiencies. Furthermore, findings did not differ by ADHD subtype, which further supports the hypothesis that the observed attentional deficit and motor hyperactivity are more directly explained by severe autism than comorbid ADHD.
Some studies have reported structural differences in attentional functions between ASD and ADHD patients, while others suggest these disorders present identical deficiencies ( 7 , 8 ).
Barnard-Brak ( 9 ) reported varying ability to distinguish individuals with ASD from those with ADHD on the basis of their performance on different cognitive tasks that assess sustained attention. However, the rapid letter naming task, which is thought to predict surface reading ability and other reading skills, did reveal significant differences between ASD and ADHD children: the former spent more time on the task and performed better. Thus, the interpretation of performance on cognitive-attentional tasks evaluating sustained attention requires special caution to avoid confusing the two disorders. This study also highlighted the effect of environment on the performance of attentional tasks by those with ASD: the setting under which individuals complete diagnostic tests can greatly influence results.
Hochhauser et al. ( 10 ) described specific attentional traits related to social interaction in young adults with ASD that may, however, be the consequences of another form of cognitive impairment. Several studies have reported cognitive characteristics affecting attentional skills in the ASD population, including difficulty disengaging, significantly greater processing of local details, or heightened perception yet “context blindness”. These elements in turn influence processing speed. Processing speed is therefore not impaired directly, but rather, differences in how perceptual data are processed have an impact on attention. Hence, it would seem more appropriate to speak of attentional traits of ASD, rather than attentional anomalies or deficits, thereby distinguishing them from ADHD.
Mayes et al. ( 11 ) demonstrated that disruptive mood dysregulation disorder was extremely prevalent among children with ASD, significantly more so than among ADHD and neurotypical children. Moreover, 91% of the children with disruptive mood dysregulation disorder symptoms also satisfied criteria for oppositional defiant disorder, revealing the very high prevalence of externalizing behaviors in ASD. The presence of psychomotor agitation cannot be automatically attributed to ADHD motor hyperactivity but does suggest an emotional dysregulation disorder more directly linked to the behavioral effects of irritability.
Physiopathologic Aspects: Imaging and Eeg Data
Is observed agitation then a sign of the prefrontal inhibitory deficit underlying ADHD or rather a state of restlessness, a minimal expression of cerebellar dysfunction, characterizing an etiologically distinct entity? The association of ASD with alterations in specific brain regions is becoming increasingly clearer. The affected regions include the orbitofrontal cortex, superior temporal sulcus, fusiform gyrus, amygdala, and cerebellum ( 12 ), and the latter plays a role in learning processes, memorization, several executive functions, and cognition. In light of these facts, might it not be risky to diagnose ADHD, a disorder linked with an altered prefrontal cortex, in the ASD population?
ADHD and ASD are described as frequently co-occurring, sharing certain cognitive phenotypes. However, it is important to be able to trace these shared features back to a common physiopathology and identify the physiopathologic characteristics of comorbidity, which may present additional neurofunctional deficits. Chantiluke et al. ( 13 ) compared prefrontal function in four groups of youth with ASD, ADHD, comorbid ASD and ADHD, or neither disorder (controls) through a temporal discounting task, using fMRI. They revealed anomalies shared by the non-control groups, in addition to distinct features unique to each of these three groups. In comparison with the non-comorbid and control groups, the comorbid group presented unique and more severe impairments affecting the lateral and ventromedial prefrontal cortex, ventral striatum, and anterior cingulate cortex. These physiopathologic findings suggest that ASD-ADHD comorbidity does not correspond to a mere combination or addition of both disorders: it is neurofunctionally distinct and merits further study for more accurate characterization.
As shown by Lau-Zhu et al. ( 14 ), ASD and ADHD are each associated with unique attention processing traits. Studies of event-related potentials (ERPs)—concerned with inhibitory control and performance monitoring in ADHD ( 15 – 17 ), and social or emotional processing as well as executive functioning in ASD ( 18 )—mostly involving adolescents have reported distinct abnormal cognitive profiles for ADHD and ASD. Both disorders are associated with atypical allocation of attentional resources and atypical performance monitoring. However, the structural impairments underlying them are very different. With regards to attention, ADHD impairment tends to reflect difficulty detecting clues that would otherwise enable anticipation, while ASD impairment is more directly related to a heightened perceptual capacity and weaker orientation toward new inputs, with longer retention of stimuli in working memory and unique social, emotional, and executive functioning features. ADHD, unlike ASD, is more immediately linked to impaired inhibition. It is important to recall that impaired inhibition, the root physiopathologic feature of ADHD, has not been studied in cohorts of ASD patients. Sensory processing impairments, such as those observed in ASD, ultimately have repercussions on attentional processes. The causes of the attentional deficiencies seen in these two disorders would thus appear to be very distinct.
Research applying quantitative EEG has demonstrated atypical profiles for ADHD, principally concerning theta and beta frequency bands ( 17 , 19 ), and for ASD, mainly related to alpha, beta, and gamma frequency bands ( 20 ). ASD and ADHD have distinct and overlapping features in “four neurocognitive domains: attention processing, performance monitoring, face processing and sensory processing” ( 14 ). Yet studies comparing the two disorders or considering dual diagnoses have yet to be undertaken. Further investigation into the neural bases of co-occurring ADHD and ASD would be of particular interest.
To better understand the distinct neuropsychological profiles of ADHD and ASD patients, it seems appropriate to consider visuospatial exploration strategies. In terms of visuospatial abilities, ADHD patients in a study by Cardillo et al. ( 21 ) exhibited a heterogeneous profile with more severely impaired visuospatial processing speed, while ASD patients and typically developing subjects had similar profiles. The authors also state that the local-global processing index effectively distinguishes these groups on the basis of performance on visuo-constructive tasks. Accordingly, a more detailed understanding of the neurocognitive specificities of each disorder might be acquired by accounting for the various domains of visuospatial processing.
It has often been stated in the literature that ASD and ADHD are difficult to distinguish when making a diagnosis. Mayes et al. ( 22 ), considering 847 children with ASD and 158 with ADHD, report that ADHD symptoms were commonly observed in ASD youth. Ratings of attention deficit, impulsivity, and hyperactivity were no different between children with ASD of any severity and children with ADHD-Combined type. Autism is very distinct from ADHD, but the core symptoms of ADHD-Combined type, i.e., attention deficit, impulsivity, and hyperactivity, would appear to also be features of autism. ASD and ADHD are neurobiological disorders characterized by similar underlying neuropsychological “deficits”. A similar observation is made by Van der Meer et al. ( 23 ). According to the authors, ASD and ADHD are different manifestations of one overarching disorder. They made the hypothesis there is a single continuum in which emotion regulation is a crucial common factor. In the same way, Ghirardi et al. ( 24 ) demonstrated there do exist a genetic overlap between clinical ASD and ADHD, suggesting an underestimation of this overlap by genomic studies. Van der Meer et al. also added that children with a ADHD phenotype without ASD symptoms can clearly be identified while the opposite is not true. These observations corroborated the assumption attention disorder is an inherent feature of ASD. Though Mayes et al. quickly conclude that “attention deficits” in ASD and ADHD are similar, they do report an interesting difference between ASD and ADHD children in this domain: selective attention is significantly more common among children with ASD (98%), no matter the severity of their disorder, than among those with ADHD-Inattentive type or ADHD-Combined type (21%). Whereas, children with ADHD have difficulty fixing their attention on a given task, those with ASD do have the capacity to focus on activities that interest them, e.g., puzzle assembly, reading, or repetitive drawing. Consequently, the authors reach the conclusion that ASD and ADHD can be distinguished by certain symptoms that differ considerably. While autistic symptoms are rarely seen in ADHD, there are specific ADHD symptoms that are particularly common in autism. Accordingly, we maintain that the definition of autism must take into account those symptoms that mirror or overlap with symptoms of ADHD, thereby better representing both the clinical reality of ASD, whose symptoms vary in intensity along a spectrum, and its neurobiological reality, i.e., the cortical dysfunction of which the clinical symptoms are an expression.
Mayes et al. also found no significant difference between children of normal intelligence with ASD, ADHD-Combined type, or ASD-Inattentive type in terms of performance on neuropsychological tests that evaluated attention, working memory, processing speed, and graphomotor skills.
Can comorbidity of ASD and ADHD truly be established by considering executive functions alone, as suggested by some studies ( 3 )? Carter Leno et al. ( 25 ) reported that multiple executive functioning impairments typically associated with ADHD are also found in people with ASD. Neuropsychological evaluations of executive functions do not fully account for the complexity of symptoms, and broader studies that consider additional brain functions could provide more clinical data essential for diagnoses. The study by Carter Leno et al. emphasized the limits of executive function exploration for discriminating ASD, ADHD, and oppositional defiant disorder subgroups. The authors evaluated the performance of four groups of youth ages 10 to 16—a typically developing group ( N = 43) and three groups of individuals clinically diagnosed with ADHD ( N = 21), oppositional defiant disorder ( N = 26), and ASD ( N = 41), respectively—on go-no-go and switch tasks, and detected deficits shared by the ADHD, oppositional defiant disorder, and ASD groups, such as increased reaction time variability. After controlling for symptoms of ADHD and oppositional defiant disorder, differences in reaction time variability between groups were no longer significant. For cognitive flexibility, as evaluated by the switch task, there was also no observed difference between groups. The ASD group alone exhibited impaired response inhibition and premature responsiveness, relative to the typically developing group. Carter Leno et al. thus concluded that executive functioning impairments specifically described as present in ADHD are also found in ASD. This stresses the need to explore and precisely define the characteristics of attentional impairment in autism. These characteristics, their causes, and their consequences should be included in the definition of ASD, to more accurately represent its specificities.
These findings are supported by those of Rosello et al. ( 26 ), who reported significantly more ADHD symptoms and poorer learning behaviors in ASD children than in those exhibiting typical development. Furthermore, behavioral regulation problems and impaired executive functioning associated with ADHD symptoms significantly impacted performance for ASD children, objectively demonstrating the effect of ADHD symptoms on these children's learning behaviors.
The attentional impairment best described for ASD is diminished joint attention. It is also said to give rise to later social communication impairments, especially in connection with oromotor skills ( 27 – 29 ). Recent functional neuroimaging studies reveal the influence of neural mechanisms through which sensory processing and attention may be modulated by the affective impact of a stimulus. The amygdala plays a central role in the production of direct and indirect top-down signals along sensory pathways, shaping how emotional events are represented. “These modulatory effects implement specialized mechanisms of ‘emotional attention' that might supplement but also compete with other sources of top-down control on perception ( 30 ).” When interpreting attentional abilities, it therefore seems necessary to account for the role of neural processes and temporo-spatial dynamics of the brain determining how cognitive and affective elements are integrated into attention and behavior. These factors are fundamental to the study of attentional abilities in ASD patients in whom amygdalar dysfunction has been described. We may refer to the findings of Liss et al. ( 31 ), who demonstrated that sensory overreactivity is associated with overselective, hyperreactive and overfocused attention; perseverative and stereotyped behaviors; and excellent memory skills—but also with major social deficits. Sensory-seeking behaviors are strongly linked to overfocused attention. This kind of excessive attention can be mistaken for ADHD inattention.
With respect to psychomotor agitation, it has been posited that ASD patients have atypical arousal systems, their state of overexcitement reflecting both excessive and fluctuating cortical activation by the brain stem. Dopaminergic hyperactivity along the nigrostriatal (explaining stereotypies) and mesolimbic (explaining interpersonal and perceptual deficits) pathways is a hypothesis gaining wider support. It would explain the perceived effectiveness of dopamine antagonists, vs. agonists, on all symptoms of autism. The above confirms the need to include the characteristics of hyperfocus among the diagnostic criteria for autism. Hyperfocus is a dimension also suggested by MEG studies ( 32 ) pointing to long-range underconnectivity in ASD patients.
Mundy et al. ( 33 ) explain that joint attention plays a key role in the functional development of a distributed cortical system involving both anterior (prefrontal and insular cortices) and posterior (temporal and parietal cortices) neural networks. Hence, early impairment of joint attention has direct repercussions on all aspects of intero- and exteroceptive data integration, altering cortical processing. Interestingly, ASD patients are described as being slow to orient their attention. Harris et al. ( 34 ) show, in children with ASD, that delay in orienting attention to visual stimuli correlates with severity of cerebellar hypoplasia, as evaluated by MRI. No correlations were found with the sizes of other brain regions. When interpreting the unique cognitive traits of people with ASD, particular attention must be paid to the role of the cerebellum. This may afford a broader understanding of the neurocognitive processes involved in ASD and a clinical perspective that better reflects the neurobiological facts.
To date, the mixed findings of etiologic ASD-ADHD comorbidity studies do not permit a clinical description of the physiopathologic comorbidity of these disorders. When speaking of comorbidity, are we not rather describing the severity of an attentional trait, with disabling functional effects, present in all ASD children?
These studies themselves demonstrate that children diagnosed with a comorbid disorder have more severe ASD. This suggests that—rather than an ASD-ADHD comorbidity, as authors conclude—the causes and consequences of a major attentional deficit typical of ASD are responsible for these patients' profiles. If so, this attentional trait should be included in the clinical definition and description of ASD. Instead of an ADHD explanation, we might then adopt an alternative etiologic perspective on these neurocognitive peculiarities and more fully account for the various brain impairments observed. As we have shown, children with ASD are affected much more by heightened attentional abilities than by a primary attention deficit, although the latter may be mistakenly (and dangerously) suggested by their clinical presentation. Therefore, we highlight the urgent need to develop new clinical and electrophysiological instruments to best fractionate and analyze these important neuropsychological features. This would be of crucial interest in particular for those modeling aspects of the co-morbidity in IPSC lines or animal models but also for the optimization of treatments use.
The attentional specificities observed in ASD, and their consequences, which are a direct reflection of unique brain functioning again challenge the validity of polythetic diagnoses in psychiatry. Attention deficits are key behavioral phenotypes of a considerable number of neurological and genetic diseases characterized by complex psychiatric disorders. Might the error lie in conflating such deficits with the unique, and very different, attentional traits of autism? In other words, are the attentional characteristics of disorders ignored by making an erroneous generalization?
Though further description of these characteristics is necessary, are they not key clinical symptoms of ASD in their own right—justifying their inclusion in the definition of this disorder—and potentially sufficient for its diagnosis?
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author Contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ADHD, attention deficit hyperactivity disorder; ASD, autism spectrum disorder.
1. ^ https://caddra.ca/pdfs/caddraGuidelines2011Chapter02.pdf .
1. Rong Y, Yang C-J, Jin Y, Wang Y. Prevalence of attention-deficit/hyperactivity disorder in individuals with autism spectrum disorder: a meta-analysis. Res Autism Spectr Disord. (2021) 83:101759. doi: 10.1016/j.rasd.2021.101759
CrossRef Full Text | Google Scholar
2. Rosenberg MD, Finn ES, Scheinost D, Constable RT, Chun MM. Characterizing attention with predictive networks models. Trends Cogn Sci. (2017) 21:290–302. doi: 10.1016/j.tics.2017.01.011
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Mansour R, Ward AR, Lane DM, Loveland KA, Aman MG, Jerger S, et al. Severity as a predictor of cognitive task performance in children with autism spectrum disorder (ASD). Res Dev Disabil. (2021) 111:103882. doi: 10.1016/j.ridd.2021.103882
4. Gargaro BA, Rinehart NJ, Bradshaw JL, Tonge BJ, Sheppard DM. Autism and ADHD: how far have we come in the comorbidity debate? Neurosci Biobehav Rev. (2011) 35:1081–8. doi: 10.1016/j.neubiorev.2010.11.002
5. Sprenger L, Bühler E, Poustka L, Bach C, Heinzel-Gutenbrunner M, Kamp-Becker I, et al. Impact of ADHD symptoms on autism spectrum disorder symptom severity. Res Dev Disabil. (2013) 34:3545–52. doi: 10.1016/j.ridd.2013.07.028
6. Green JL, Rinehart N, Anderson V, Nicholson JM, Jongeling B, Sciberras E. Autism spectrum disorder symptoms in children with ADHD: a community-based study. Res Dev Disabil. (2015) 47:175–84. doi: 10.1016/j.ridd.2015.09.016
7. Landry R, Bryson SE. Impaired disengagement of attention in young children with autism. J Child Psychol Psychiatry. (2004) 45:1115–22. doi: 10.1111/j.1469-7610.2004.00304.x
8. Kennedy DM, Banks RS. The ADHD Autism Connection: a Step Toward More Accurate Diagnosis and Effective Treatment . Colorado Spings, Colo: Waterbrook Press (2002).
Google Scholar
9. Barnard-Brak L. The difference between autism and ADHD is in the eye of the cognitive task? Personal Individ Differ. (2011) 50:1305–8. doi: 10.1016/j.paid.2011.02.007
10. Hochhauser M, Aran A, Grynszpan O. Investigating attention in young adults with autism spectrum disorder (ASD) using change blindness and eye tracking. Res Autism Spectr Disord. (2021) 84:101771. doi: 10.1016/j.rasd.2021.101771
11. Mayes SD, Waxmonsky J, Calhoun SL, Kokotovich C, Mathiowetz C, Baweja R. Disruptive mood dysregulation disorder (DMDD) symptoms in children with autism, ADHD, and neurotypical development and impact of co-occurring ODD, depression, and anxiety. Res Autism Spectr Disord. (2015) 18:64–72. doi: 10.1016/j.rasd.2015.07.003
12. Li D, Karnath H-O, Xu X. Candidate biomarkers in children with autism spectrum disorder: a review of MRI studies. Neurosci Bull. (2017) 33:219–37. doi: 10.1007/s12264-017-0118-1
13. Chantiluke K, Christakou A, Murphy CM, Giampietro V, Daly EM, Ecker C, et al. Disorder-specific functional abnormalities during temporal discounting in youth with attention deficit hyperactivity disorder (ADHD), autism and comorbid ADHD and Autism. Psychiatry Res. (2014) 223:113–20. doi: 10.1016/j.pscychresns.2014.04.006
14. Lau-Zhu A, Fritz A, McLoughlin G. Overlaps and distinctions between attention deficit/hyperactivity disorder and autism spectrum disorder in young adulthood: Systematic review and guiding framework for EEG-imaging research. Neurosci Biobehav Rev. (2019) 96:93–115. doi: 10.1016/j.neubiorev.2018.10.009
15. Barry RJ, Clarke AR, McCarthy R, Selikowitz M, Brown CR, Heaven PCL. Event-related potentials in adults with attention-deficit/hyperactivity disorder: an investigation using an inter-modal auditory/visual oddball task. Int J Psychophysiol Off J Int Organ Psychophysiol. (2009) 71:124–31. doi: 10.1016/j.ijpsycho.2008.09.009
16. Johnstone SJ, Barry RJ, Clarke AR. Ten years on: a follow-up review of ERP research in attention-deficit/hyperactivity disorder. Clin Neurophysiol Off J Int Fed Clin Neurophysiol. (2013) 124:644–57. doi: 10.1016/j.clinph.2012.09.006
17. Tye C, McLoughlin G, Kuntsi J, Asherson P. Electrophysiological markers of genetic risk for attention deficit hyperactivity disorder. Expert Rev Mol Med. (2011) 13:e9. doi: 10.1017/S1462399411001797
18. Jeste SS, Nelson CA. Event related potentials in the understanding of autism spectrum disorders: an analytical review. J Autism Dev Disord. (2009) 39:495–510. doi: 10.1007/s10803-008-0652-9
19. Barry RJ, Clarke AR, Johnstone SJ. A review of electrophysiology in attention-deficit/hyperactivity disorder: I. Qualitative and quantitative electroencephalography. Clin Neurophysiol Off J Int Fed Clin Neurophysiol. (2003) 114:171–83. doi: 10.1016/S1388-2457(02)00362-0
20. Billeci L, Sicca F, Maharatna K, Apicella F, Narzisi A, Campatelli G, et al. On the application of quantitative EEG for characterizing autistic brain: a systematic review. Front Hum Neurosci. (2013) 7:442. doi: 10.3389/fnhum.2013.00442
21. Cardillo R, Vio C, Mammarella IC. A comparison of local-global visuospatial processing in autism spectrum disorder, nonverbal learning disability, ADHD and typical development. Res Dev Disabil. (2020) 103:103682. doi: 10.1016/j.ridd.2020.103682
22. Mayes SD, Calhoun SL, Mayes RD, Molitoris S. Autism and ADHD: Overlapping and discriminating symptoms. Res Autism Spectr Disord. (2012) 6:277–85. doi: 10.1016/j.rasd.2011.05.009
23. Van der Meer JMJ, Oerlemans AM, Van Steijn DJ, Lappenschaar MGA, de Sonneville LMJ, Buitelaar JK, et al. Are autism spectrum disorder and attention-deficit/hyperactivity disorder different manifestations of one overarching disorder? Cognitive and symptom evidence from a clinical and population-based sample. J Am Acad Child Adolesc Psychiatry . (2012) 51:1160–72.e3. doi: 10.1016/j.jaac.2012.08.024
24. Ghirardi L, Brikell I, Kuja-Halkola R, Freitag CM, Franke B, Asherson P et al. The familial co-aggregation of ASD and ADHD: a register-based cohort study. Mol Psychiatry. (2017) 23:257–62. doi: 10.1038/mp.2017.17
25. Carter Leno V, Chandler S, White P, Pickles A, Baird G, Hobson C, et al. Testing the specificity of executive functioning impairments in adolescents with ADHD, ODD/CD and ASD. Eur Child Adolesc Psychiatry. (2018) 27:899–908. doi: 10.1007/s00787-017-1089-5
26. Rosello B, Berenguer C, Baixauli I, Colomer C, Miranda A. ADHD symptoms and learning behaviors in children with ASD without intellectual disability. A mediation analysis of executive functions. PloS ONE. (2018) 13:e0207286. doi: 10.1371/journal.pone.0207286
27. Dalton JC, Crais ER, Velleman SL. Joint attention and oromotor abilities in young children with and without autism spectrum disorder. J Commun Disord. (2017) 69:27–43. doi: 10.1016/j.jcomdis.2017.06.002
28. Charman T. Why is joint attention a pivotal skill in autism? Philos Trans R Soc Lond B Biol Sci. (2003) 358:315–24. doi: 10.1098/rstb.2002.1199
29. Oberwelland E, Schilbach L, Barisic I, Krall SC, Vogeley K, Fink GR, et al. Young adolescents with autism show abnormal joint attention network: a gaze contingent fMRI study. NeuroImage Clin. (2017) 14:112–21. doi: 10.1016/j.nicl.2017.01.006
30. Vuilleumier P. How brains beware: neural mechanisms of emotional attention. Trends Cogn Sci. (2005) 9:585–94. doi: 10.1016/j.tics.2005.10.011
31. Liss M, Saulnier C, Fein D, Kinsbourne M. Sensory and attention abnormalities in autistic spectrum disorders. Autism Int J Res Pract. (2006) 10:155–72. doi: 10.1177/1362361306062021
32. O'Reilly C, Lewis JD, Elsabbagh M. Is functional brain connectivity atypical in autism? A systematic review of EEG and MEG studies. PloS One. (2017) 12:e0175870. doi: 10.1371/journal.pone.0175870
33. Mundy P, Gwaltney M, Henderson H. Self-referenced processing, neurodevelopment and joint attention in autism. Autism Int J Res Pract. (2010) 14:408–29. doi: 10.1177/1362361310366315
34. Harris NS, Courchesne E, Townsend J, Carper RA, Lord C. Neuroanatomic contributions to slowed orienting of attention in children with autism. Brain Res Cogn Brain Res. (1999) 8:61–71. doi: 10.1016/S0926-6410(99)00006-3
Keywords: autism, attention deficit and hyperactivity disorder, attention, agitation, restlessness, comorbidity, autism spectrum disorder
Citation: Hours C, Recasens C and Baleyte J-M (2022) ASD and ADHD Comorbidity: What Are We Talking About? Front. Psychiatry 13:837424. doi: 10.3389/fpsyt.2022.837424
Received: 16 December 2021; Accepted: 24 January 2022; Published: 28 February 2022.
Reviewed by:
Copyright © 2022 Hours, Recasens and Baleyte. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Camille Hours, camille.hours@chicreteil.fr
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Signs and Symptoms
- Living with Autism Spectrum Disorder
- Frequently Asked Questions (FAQs)
- Data and Statistics on Autism Spectrum Disorder
- Autism Materials and Resources
- Diagnosis ASD
- Information on ASD for Healthcare Providers
- Acceptance Month Partner Toolkit
- 2023 Community Report on Autism
- Autism Data Visualization Tool
Autism Prevalence Studies Data Table
What to know.
- This data table summarizes information from peer-reviewed autism prevalence studies. Information reported from each study includes the autism prevalence estimate and additional study characteristics (such as case ascertainment and criteria).
- The information on this page is intended for healthcare providers, public health professionals, and those interested in reviewing additional scientific articles about ASD.

A PubMed search was conducted to identify studies using the search terms: autism (title/abstract) OR autistic (title/abstract) AND prevalence (title/abstract). Data were abstracted and included if the study fulfilled the following criteria:
- The study was published in English;
- The study produced at least one autism prevalence estimate; and
- The study was population-based (any age range) within a defined geographic area.
Autism prevalence studies data table
Originating source: https://data.cdc.gov/Public-Health-Surveillance/autism-prevalence-studies/9mw4-6adp
To suggest additional autism prevalence studies for inclusion in the data table, please email [email protected] .
Description of data table
Data column descriptions.
Note: blank cells indicate data not available.
Title —publication title
Year published —publication year
Country —country where the study was conducted
Area(s) —the city or specific geographical area(s) where the study was conducted
Age range (years) —age range (in years) of the population studied
Study years —the study period (in years)
Case identification method —study source record(s)* used to identify individuals with autism (registry; health records; education records; survey [specify type: in-person, phone, mail, online]; service provider records; other [define]) *more than one method may be used
Case criterion —criteria* used to identify individuals with autism (DSM [specify edition]; ICD [specify version]; Rutter(1); Kanner(2); clinical impression; autism test [specify test]; special education classification; self-report; parental report; receipt of autism-specific services; other [define]) * more than one case criterion may be used
- Rutter M. Diagnosis and definition of childhood autism. Journal of Autism and Childhood Schizophrenia. 1978;8(2):139-161.
- Kanner L. Autistic disturbances of affective contact. Nervous Child. 1943;2:217-250.
Sample size —study population size (prevalence denominator)
Number of cases —individuals with autism (prevalence numerator)
Autism prevalence estimate —autism prevalence estimate per 1,000 population; autism prevalence estimates were reported or calculated by CDC under the following conditions. Autism prevalence was reported separately for multiple study years with no overall estimate (data from the most recent study year was reported to highlight the most up-to-date data); autism prevalence for multiple age ranges was reported separately with no overall estimate (the age range with the largest sample size or best quality data, as reported by study authors, was used); autism prevalence for multiple birth cohorts of data was reported separately with no overall estimate (the most recent birth cohort to date was used to highlight the most-up-to-date data); autism prevalence was reported separately by subtype of autism or separately by geographic area with no overall estimate (number of individuals with autism in each subgroup combined or combined geographic areas were used to estimate autism prevalence if possible. If not possible [for example, denominator for subgroup was not available], the estimate with the best quality data, as indicated by the author, was reported)
Confidence interval (CI) —95% confidence interval (CI) for the autism prevalence estimate; if a CI was not reported in the study, a CI was calculated using the Wilson method with this online tool: http://www.hutchon.net/Wilsons.htm
Male:female ratio —male to female ratio of individuals with autism
Non-Hispanic White:Hispanic prevalence ratio —non-Hispanic White to Hispanic ethnicity autism prevalence ratio
White:Black prevalence ratio —White to Black race autism prevalence ratio
Diagnosis age range (months) —age range (in months) of cases at time of autism diagnosis
Diagnosis mean age (months) —mean age (in months) of cases at time of autism diagnosis
Diagnosis median age (months) —median age (in months) of cases at time of autism diagnosis
IQ <70 (%) —percentage of individuals with autism with an IQ (intelligence quotient) less than 70
Adaptive score <70 (%) —percentage of individuals with autism with an adaptive score less than 70
Non-verbal or minimally verbal (%) —percentage of individuals with autism that are non-verbal or minimally verbal
Percentage of individual co-occurring conditions (%) —percentage of co-occurring conditions reported in individuals with autism (attention deficit disorder [ADD] or attention deficit hyperactivity disorder [ADHD]; anxiety; cerebral palsy [CP]; congenital rubella; depression; Down syndrome; encephalopathy; epilepsy/seizure disorder; fetal alcohol syndrome; fragile X; language delay; learning disability; mood disorder; neonatal abstinence syndrome; obsessive compulsive disorder [OCD]; oppositional defiant disorder [ODD]; prematurity; Rett syndrome*; sudden infant death syndrome [SIDS]; sickle cell disease [SCD]; Tourette syndrome; tuberous sclerosis) * For cases of Rett syndrome: if Rett syndrome cases were included in the autism prevalence estimate, Rett syndrome was not included as a co-occurring condition. If authors separated Rett syndrome from the autism prevalence estimate, it was included as a co-occurring condition and excluded from the prevalence estimate.
Autism types included —subtypes of autism included in the study as reported by the authors (early or classic infantile autism, autistic syndrome, autistic mental retardation, childhood autism, autistic-like conditions, pervasive developmental disorder [PDD], pervasive developmental disorder–not otherwise specified [PDD-NOS], autistic disorder, atypical autism, Asperger's syndrome, childhood disintegrative disorder [CDD], autism spectrum disorder [ASD])
Publication link —link to publication
CDC calculated values —indicates values calculated by CDC's abstractor (e.g., converting age range from months to years, calculating confidence interval [CI], calculating overall autism prevalence estimate when prevalence was reported separately for autism subtype or for geographic study area; calculating percentages of individuals with autism by IQ categories or with co-occurring conditions when only individual case numbers are reported)
Autism Spectrum Disorder (ASD)
Autism spectrum disorder (ASD) is a developmental disability that can cause significant social, communication and behavioral challenges. CDC is committed to continuing to provide essential data on ASD and develop resources that help identify children with ASD as early as possible.
For Everyone
Health care providers, public health.
- School of Medicine Columbia
- Location Location
- Contact Contact
- Colleges and Schools
- Centers and Institutes
- Center for Disability Resources
- SC Assistive Technology Program
- Trainings and Workshops
09-05-24 - Learn how AI rapidly improves reading skills for students with dyslexia, ADHD and autism with BuddyBooks
Registration.
Participants must register in order to recieve the Webinar link. REGISTER NOW.
About the Program
Target Audience: Special Educators, Dyslexia Interventionists, Reading Specialists, Administrators
Participants will Learn:
- Learners will identify how state-of-the-art technology and research are combined to provide engaging and effective oral reading practice.
- Learners will identify 2 state-of-the-art technologies and 3 peer-reviewed research strands that make using AI based co-reading viable and feasible.
- Learners will identify 2 methods of computer-based remediation that have been demonstrated to improve oral reading prosody.
About the Presenter

Jason Stewart - ObjectiveEd
Jason is Director of Customer Success for ObjectiveEd. He is a former teacher, educational diagnostician, and district level administrator with over 20 years of educational experience. His passion for education is now focused on helping students achieve their best educational outcomes through educational technology. Jason has a master’s in special education from the University of Texas at Tyler.
Accommodations
CART captioning is provided for all SCATP webinars. If you need an additional accommodation to participate, please contact us at least one week prior to the webinar via e-mail or by phone at 803-935-5263.
Webinars are recorded and archived on our training page .
Challenge the conventional. Create the exceptional. No Limits.
Services for Guests Who Are Neurodivergent
Disney is committed to delivering a wide range of innovative support services aimed at helping our guests with disabilities visiting our theme parks. explore ways and resources for guests with neurodivergent disabilities to use throughout the theme parks and in the resort hotel areas. some tools found on this page may benefit a variety of individuals and are not limited to guests with neurodivergent disabilities., know what to expect at the parks.
For more information, download the Accessibility Planning Guide & Recommendations.
How to Prepare
Plan a visual schedule.
Next, fill in the remaining times with possible attractions and use a question mark or a change card to build flexibility into the schedule. Review the visual schedule with your family member before your visit so they have an idea of what to expect.
By providing a possible timeline, you can help the Guest with a neurodivergent disability understand what to expect—such as crowds, sights, sounds, and smells—and so that they can learn the routine.
For an example of a timeline, please download our Accessibility Planning Guide & Recommendations .
Study Location Maps
Review the maps with the Guest with a neurodivergent disability and try to lay out a plan for the day. We recommend that you consider downloading the My Disney Experience app to have information on your mobile device, including entertainment showtimes. You can even order food and beverages via the My Disney Experience app .
What to Bring
Being prepared for a day at Walt Disney World Resort goes beyond the parks. Plan ahead by bringing along an assortment of items.
Some suggestions include:
- A Safety Bracelet or Nametag
- Ear Plugs or Headphones
- A Favorite Device or Activity
- A Sensory Toy
Practice Waiting in Line
To prepare, practice waiting with the Guest with a neurodivergent disability at home or in lines at places they might already frequent.
Attraction Planning Resources
Sensory experience details.
Review a list of details about Walt Disney World experiences—including details about scents, lighting effects, attraction vehicle speeds and more.
Accessing Attraction Queues
Walt Disney World Resort offers tips and a variety of programs to help Guests with disabilities access attraction queues including Rider Switch, Single Rider, Disability Access Service and more.
At the Parks
Companion restrooms.
Learn more about restrooms
Choose a Meeting Location
Should they get lost, stress the importance to the Guest with a neurodivergent disability of finding a Cast Member who will assist in attempting to reunite you. In addition, there are also designated locations in each park where lost persons can be escorted.
It is recommended that you take a photo of the Guest with a neurodivergent disability on your mobile device or digital camera, especially if they tend to wander off. You may also consider making a nametag that includes their name, as well as your name and mobile phone number.
Take a Break
Some examples include:
Magic Kingdom Park:
- Main Street, U.S.A. – Center Street
- Adventureland – Area near Swiss Family Treehouse; Area next to the Pirates of the Caribbean restrooms
- Frontierland – Miner’s Cove; Area near Tiana’s Bayou Adventure restrooms
- Liberty Square – Area behind Ye Old Christmas Shoppe; Area next to the Hall of Presidents
- Fantasyland – Area near the Wishing Well; Area outside Pete’s Silly Sideshow
- Tomorrowland – Pathway near TRON Lightcycle/Run leading towards Fantasyland; Area between Space Mountain and the Rockettower Plaza Stage; Area near Walt Disney’s Carousel of Progress
- World Celebration – Areas throughout
- World Nature – Area between the Seas with Nemo and Friends and the Coral Reef Restaurant; Imagination Pavilion near the restrooms
- World Discovery – Area near Mission: SPACE and Guardians of the Galaxy: Cosmic Rewind
- Mexico Pavilion – Accessible ramp to right of pavilion
- Norway Pavilion – Corridor between Norway and China
- China Pavilion – Area next to the Temple of Heaven
- Italy Pavilion – Seating nook next to Pizza Al Taglio
- America Pavilion – Corridor between Joffrey’s Coffee and Regal Eagle Smokehouse: Craft Drafts & Barbecue
- Japan Pavilion – Garden seating area
- Morocco Pavilion – Near Restaurant Marrakesh and Lamps of the Wonder
- France Pavilion – Between France and the United Kingdom near the water
- United Kingdom Pavilion – Garden area
- Canada Pavilion – Garden walkway towards Le Cellier Steakhouse
Disney’s Hollywood Studios:
- Sunset Boulevard – Courtyard near Lightning McQueen’s Racing Academy
- Sunset Boulevard & Hollywood Boulevard – Area next to The Hollywood Brown Derby restaurant
- Animation Courtyard – Near the restrooms
- Pixar Place – End of block near archway
- Toy Story Land – Corridor between Toy Story Land and Star Wars: Galaxy’s Edge
- Star Wars: Galaxy’s Edge – Area next to First Order Cargo; Area between Oga’s Cantina at the Walt Disney World Resort and Millennium Falcon: Smugglers Run; Area next to Toydarian Toymaker
- Grand Avenue – Corridor on right just before Star Wars: Galaxy’s Edge; Pathway between Muppet Vision 3D and Mama Melrose’s Ristorante Italiano
- Echo Lake – Area by Indiana Jones Adventure Outpost to the right of 50’s Prime Time Café
Disney’s Animal Kingdom Theme Park:
- Discovery Island: Areas throughout
- DinoLand USA – Area next to theater
- Asia – Maharajah Jungle Trek (locations throughout) and the pathway next to Caravan Road leading to Africa
- Rafiki’s Planet Watch – Locations throughout
- Africa – Gorilla Falls Exploration Trail (locations throughout)
All Parks – First Aid and quick-service restaurant seating areas (during non-peak periods).
Learn more about break areas in the Accessibility Planning Guide & Recommendations.
Dietary Accommodations
View more information about special dietary requests throughout the Resort.
Guest Health Care Services Presented by AdventHealth

IMAGES
VIDEO
COMMENTS
1.1. Evaluation of ADHD. The current diagnostic criteria for ADHD can be found in the DSM-5 [] and in the International Statistical Classification of Diseases and Related Health Problems, eleventh revision, from the World Health Organization [].Various evaluation instruments are used to identify ADHD, from general assessments via broad scales such as the Wechsler scale, to more specific tests ...
Case study - assessing a boy with Autistic Spectrum Condition (ASC) initially diagnosed with ADHD. Less common mental health conditions include autism spectrum disorders (ASD), eating disorders, tic disorders, and a number of very low prevalence conditions. About one in fifty (2.1%) 5 to 19year olds were identified with one or more of these ...
ADHD (Symptoms) in Children with ASD. A significant percentage of children with ASD seeking services at clinical centers present with comorbid symptoms of ADHD, with rates ranging between 37% (Gadow et al., 2006) and 85% (Lee and Ousley, 2006) across studies conducted in the United States and Europe (Rao and Landa, 2013).ADHD was the third most common disorder identified in a community sample ...
CASE STUDY 10-year-old boy diagnosed with ADHD These case studies, each submitted by a Certified HANDLE® Practitioner, demonstrate outcomes ... The HANDLE paradigm for understanding behaviors and their root causes is thoroughly explained in The Fabric of Autism: Weaving the Threads into a Cogent Theory, by Judith Bluestone, ...
To bridge these gaps, Kimberly Carpenter, PhD, assistant professor in the Duke Center for Autism and Brain Development, launched the Autism HERO study in 2021.This study takes a comprehensive approach, combining parent reports with play-based and brain assessments to examine how co-occurring anxiety and ADHD affect autistic children aged 4 to 7 years.
ADHD and autism share common characteristics, including inattention, atypical movement (such as fidgeting or stimming behaviors ), social difficulties, and differences in learning style. Both autistic people and those with ADHD can experience sensory sensitivities as well. Despite the overlap, though, current research indicates that ADHD and ...
Discussion. Approximately 1 in 8 children currently diagnosed with ADHD were also diagnosed with current ASD (13.0%). The prevalence of ASD among children currently diagnosed with ADHD was higher among younger children (ages 4-11) (18.7%) when compared to older children (ages 12-17) (10.0%).
Autism spectrum disorder (ASD) is a congenital or early-acquired complex neurodevelopmental disorder characterised by difficulties in social interaction, impaired social communication and restricted behavioural patterns (Association, Citation 2013; Wing & Gould, Citation 1979).The symptoms must be present in the early developmental period, typically before age of three, and usually persist ...
For ADHD and DCD, the overlap is considered to be approximately 50% (Goulardins et al., 2015), whilst ADHD and autism also frequently co-occur with rates ranging from 40 to 70% (Antshel & Russo, 2019). It was not an aim of the current study to directly examine co-occurrences, however it is important to recognise their relevance when ...
Approximately 5% of the population worldwide is reported to have a diagnosis of hyperactivity disorder/hyperactivity disorder (ADHD) [], a disorder often associated with co-occurring conditions that can complicate identification and treatment []; autism spectrum disorder (ASD) is among those conditions that are commonly found to co-exist with those diagnosed with ADHD at a reported rate ...
Studies were also excluded if they did not specify the status of diagnosis examined or focusing on diagnosed individuals and studies that do not mention the terms "Attention Deficit Hyperactivity Disorder," "Autistic," "ADHD," "Autism" or "ASD." Case studies and studies on genetics, medication and scale development were ...
In this study, despite all case-groups showing low health quality, the co-occurrence and ASD groups reported severe illness in the last two years in greater proportion than the control group did. According to the results observed in this study, the individuals with ADHD seem to be exposed to different challenges than those with ASD.
Children with Autism Spectrum Disorders: Three Case Studies. Speech-language pathologists play a critical role in screening, assessing, diagnosing, and treating the language and social communication disorders of individuals with autism spectrum disorders (ASD). People with ASD use a variety of communication modes including speech, facial ...
Preventing school exclusion: a case study of a primary aged autistic child with ADHD and a PDA profile GAP,19,2, 2018 35 Christie, Gould, Viding and Happé, 2013) as there was a feeling that interventions typically indicated for a child with autism and ADHD were unsuccessful. Although never designed as a diagnostic tool, the EDAQ is
Details about study-specific case and control selection criteria and how individuals ... Anckarsater, H. & Lichtenstein, P. Symptoms of autism and ADHD: a Swedish twin study examining their ...
Anholt, G. E. et al. Autism and adhd symptoms in patients with ocd: Are they associated with specific oc symptom dimensions or oc symptom severity. J. Autism Dev. Disord. 40 , 580-589 (2010).
AuDHD is a term coined by the neurodiversity community to describe the co-existence of ADHD and autism. Whether AuDHD represents a comorbidity or a separate phenomena is a topic of exploration ...
There is only a small number of case-control studies on ADHD, suggesting a higher frequency of ADHD symptoms in patients with dementia with Lewy body and a higher risk of dementia in adults with ...
Furthermore, findings did not differ by ADHD subtype, which further supports the hypothesis that the observed attentional deficit and motor hyperactivity are more directly explained by severe autism than comorbid ADHD. Some studies have reported structural differences in attentional functions between ASD and ADHD patients, while others suggest ...
Case Study 1 - Jack Jack is a 7 year old male Grade 1 student who lives in Toronto with his parents. He is the only child to two parents, both of whom have completed post-graduate education. There is an extended family history of Attention Deficit/Hyperactivity Disorder (ADHD), mental health concerns as well as academic excellence.
Associate's Name: Lynn Schoeneck, OTR/L Associate's Organization: Porter Academy Client: 7-year-old boy, Autism Spectrum Disorder, ADHD Presenting Problem: Difficulties with anxiety, social interactions, attention, expressive and receptive language, poor organization, fine motor coordination and gross motor coordination Therapeutic Goals: Improve social interaction with both peers and ...
A 2018 paper published in the American Journal of Epidemiology that aimed to comprehensively analyze data from multiple studies, for example, found a 34% and 19% higher risk of ADHD and autism ...
The prevalence of family history (FH) of autism and ADHD varies depending on the recruitment approach used in developmental studies. Rates were 3-9% for diagnosed cases. The highest rate of FH-autism/ADHD was in the sample recruited through an online participant pool, which also had the most socio-economically diverse families.
Cross sectional studies have shown that children with ADHD often exhibit overlapping autism symptoms as measured on the ADOS and a large epidemiological study showed that up to 13% of youth with ADHD were diagnosed with cooccurring ASD (Antshel & Russo, 2019; Hatch et al., 2023).
There are several case studies of individual CBT in autistic adults, which had promising results ... ADHD: 43 (19) 1 (1) 0.66** Dyslexia: 15 (6) 3 (4) n.s. Dyspraxia/DCD ... In this study, individual autism factors included sensory and cognitive differences that make social interaction more challenging than rewarding and having low levels of ...
A new report from health think tank Nuffield Trust has shown that the number of people in England awaiting an autism or ADHD diagnosis has ballooned fivefold in four years; in April 2019, just ...
Furthermore, findings did not differ by ADHD subtype, which further supports the hypothesis that the observed attentional deficit and motor hyperactivity are more directly explained by severe autism than comorbid ADHD. Some studies have reported structural differences in attentional functions between ASD and ADHD patients, while others suggest ...
This data table provides a collection of information from peer-reviewed autism prevalence studies. Information reported from each study includes the autism prevalence estimate and additional study characteristics (e.g., case ascertainment and criteria). A PubMed search was conducted to identify studies published at any time through September ...
Study; Colleges and Schools; School of Medicine Columbia; Centers and Institutes; Center for Disability Resources; SC Assistive Technology Program; Services; Trainings and Workshops; 09-05-24 - Learn how AI rapidly improves reading skills for students with dyslexia, ADHD and autism with BuddyBooks
Blind & Low Vision. For assistance with your Walt Disney World vacation, including resort/package bookings and tickets, please call (407) 939-5277. For Walt Disney World dining, please book your reservation online. 7:00 AM to 11:00 PM Eastern Time. Guests under 18 years of age must have parent or guardian permission to call. Find information ...