

Office of Quality Compliance
Main navigation.
The Standard Operating Procedures (SOPs) in this library have been established to ensure consistency and compliance with Federal & State regulations, institutional policies, and Good Clinical Practice guidelines that are common to clinical research of all types. By standardizing these SOPs, we are aligning our clinical research activities across campus with the 1U4U vision.
The SOPs in this library define clinical research and clinical trial as:

Standard Operating Procedure Library
- UUSOP-01 STANDARD OPERATING PROCEDURE PROCESS
- UUSOP-02 FDA INSPECTIONS
- UUSOP-02-A FDA INSPECTIONS SUPPLEMENT A
- UUSOP-03 PROTOCOL TRAINING FOR INVESTIGATORS AND STUDY STAFF
- UUSOP-04 INVESTIGATOR RESPONSIBILITIES
- UUSOP-05 DELEGATION OF AUTHORITY
- UUSOP-06 STUDY RECORDS MANAGEMENT
- UUSOP-06-A STUDY RECORDS MANAGEMENT SUPPLEMENT A
- UUSOP-07 DEVIATIONS: DOCUMENTATION AND REPORTING
- UUSOP-08 OBTAINING WRITTEN INFORMED CONSENT
- UUSOP-09 CASE REPORT FORM COMPLETION STANDARD
- UUSOP-10 MONITORING VISITS FOR EXTERNALLY SPONSORED CLINICAL TRIALS
- UUSOP-11 Investigational New Drug Applications in FDA-Regulated Research
- UUSOP-12 Investigational Device Exemption Applications in FDA-Regulated Research
- UUSOP-13 CLINICAL RESEARCH INSTITUTIONAL FEE SCHEDULE
- UUSOP-13-A CLINICAL RESEARCH INSTITUTIONAL FEE SCHEDULE SUPPLEMENT A – COST STRUCTURE RATIONALE
- UUSOP-14 Clinical Trial Safety Assessment and Reporting
- UUSOP-15 internal monitoring of university of utah clinical studies
UPDATES TO CLINICAL RESEARCH SOPS
SUGGESTIONS FOR CLINICAL RESEARCH SOPS
CRCG BYLAWS
ADDITIONAL U OF U SOPS AND POLICIES
CONTACT CRCG
CRCG OFFICERS & MEMBERSHIP
Who should use these?
This library of Standard Operating Procedures is a resource for anyone conducting clinical research at the University of Utah as applicable to the research being done.
As a research institution, the University of Utah must comply with laws, policies and regulations established by the Food and Drug Administration (FDA), the Office for Human Research Protections (OHRP), the International Conference on Harmonization guidelines (ICH), and the State of Utah.
Our University clinical research SOPs define processes in-line with the laws, policies and regulations governing human subject research and should be utilized by all personnel conducting such research at the University of Utah.
My department already has SOPs on these topics but they have more details specific to my group. Which SOPs should I use?
In an effort to standardize all clinical research efforts at the University, and to align with the 1U initiative, the Office of Quality Compliance highly promotes the utilization of these SOPs. However, if additional details or processes specific to individual departments/divisions need to be followed, Working Guidelines should be developed as a supplement to the SOPs in this library.
Departmental leadership or their delegates should develop these Working Guidelines for use by the individual departments/divisions. Any department/divisional Working Guidelines should not conflict with the SOPs in this library and should follow the same basic principles and standards.
What do I do with my current SOPs?
Any SOPs that are of the same topic and similar process should be retired and the University SOP should be implemented. Each group is encouraged to create supplemental working guidelines as needed to further direct their department/study processes.
What should I do if there are procedures in the SOP that cannot be followed by our individual team?
Every effort should be made to adhere to the processes outlined in these SOPs. If an exception to an SOP is needed, the department should clearly document, in writing, what part of the SOP cannot be adhered to and an alternative process that will be followed.
What is the difference between an SOP and a guideline or work practice document (WPD)?
An SOP is the chief document to describe what is to be done for a given procedure, who is responsible for doing it, and when it is to be performed. If instructions on how to perform the procedure are relatively simple, they may be included in the SOP.
However, if the steps are especially detailed or change depending on department practices then a separate, department-specific Guidance Document/WPD should be created to describe the full details.
A Guidance or Work Practice Document is a supportive document that describes in detail how a specific procedure is to be performed or suggest direction on operational processes and workflows. Refer to UU SOP-01 , Sections “Definitions and Acronyms”, 1.1. and 2.2.
I have other SOPs on topics that are not found in this library, what do I do with those?
You can continue to utilize your other SOPs as long as they do not contain contradicting processes to the SOPs in this library.
How should teams be trained on these SOPs?
Training and documentation of training should be carried out by the individual departments as part of their current training plan.
Optional Resources
- If you need an example of a general training log, please see this link .
- A certificate to document review of each SOP can be obtained here .
Will I be held accountable?
The Office of Quality Compliance may conduct periodic audits to identify areas where researchers may need additional training, or to alert the office of any SOPs that should be created or amended.
Whom should I contact with questions or concerns?
Please submit any questions or comments and someone from the SOP Collaboration Team will contact you within 2-3 business days.
U of U SOPs Contact Us
What is the CRCG Clinical Research SOP Development Process?
Clinical research sop development process.

1 SOP needs are identified by the following methods: • Request from University employee (either by email to [email protected] or through the CRCG web form ) • Multiple Google searches for specific content (identified through Google analytics report) • Need identified and suggested by CRCG member(s) 2 CRCG is the Clinical Research SOP Collaboration Group. 3 CRCG approval is performed by voting members, according to bylaws . 4 CRC is the Clinical Research Committee, chaired by the School of Medicine Associate Dean of Clinical Research. 5 VPR is the Vice President for Research
How are Source Documents, study worksheets, and Case Report Forms (CRFs) similar and different? A comparison of purpose, creation, and use.
FAQ - Source Documents vs CRFs vs Worksheets
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- PLoS Comput Biol
- v.16(9); 2020 Sep

Ten simple rules on how to write a standard operating procedure
Susanne hollmann.
1 Potsdam University, Potsdam, Germany
2 SB Science Management UG (haftungsbeschränkt), Berlin, Germany
Marcus Frohme
3 Technical University of Applied Sciences, Wildau, Germany
Christoph Endrullat
Andreas kremer.
4 ITTM Information Technology for Translational Medicine, Esch-sur-Alzette, Luxemburg
Domenica D’Elia
5 Institute for Biomedical Technologies, National Research Council, Bari, Italy
Babette Regierer
Alina nechyporenko.
6 Kharkiv National University of Radio Electronics, Kharkiv, Ukraine
Research publications and data nowadays should be publicly available on the internet and, theoretically, usable for everyone to develop further research, products, or services. The long-term accessibility of research data is, therefore, fundamental in the economy of the research production process. However, the availability of data is not sufficient by itself, but also their quality must be verifiable. Measures to ensure reuse and reproducibility need to include the entire research life cycle, from the experimental design to the generation of data, quality control, statistical analysis, interpretation, and validation of the results. Hence, high-quality records, particularly for providing a string of documents for the verifiable origin of data, are essential elements that can act as a certificate for potential users (customers). These records also improve the traceability and transparency of data and processes, therefore, improving the reliability of results. Standards for data acquisition, analysis, and documentation have been fostered in the last decade driven by grassroot initiatives of researchers and organizations such as the Research Data Alliance (RDA). Nevertheless, what is still largely missing in the life science academic research are agreed procedures for complex routine research workflows. Here, well-crafted documentation like standard operating procedures (SOPs) offer clear direction and instructions specifically designed to avoid deviations as an absolute necessity for reproducibility.
Therefore, this paper provides a standardized workflow that explains step by step how to write an SOP to be used as a starting point for appropriate research documentation.
Introduction
Nowadays, digital technologies are integral to how knowledge is produced and shared, and science is organized. Data availability is a critical feature for an efficient, progressive, and, ultimately, self-correcting scientific ecosystem that generates credible findings and has become a relevant element of scientific integrity [ 1 ]. However, the anticipated benefits of sharing are achieved only if data are of reliable quality and reusable [ 2 , 3 ]. Despite this need, it has been shown that fewer than one-third of (biomedical) papers can be reproduced in general [ 4 , 5 ]. Further studies showed that suboptimal data curation, unclear analysis specification, and reporting errors could impede reuse and analytic reproducibility, undermining the utility of data sharing and the credibility of scientific findings [ 6 – 9 ]. Standard operating procedures (SOPs) for industrial processes to achieve efficiency, quality, and uniformity of performance have existed since a long time ago. SOPs ensure that the user operates following consistent processes that meet best practice standards. Moreover, the use of SOPs ensures that processes are reviewed and updated regularly and that researchers inside and outside the same group or institute are enabled to reproduce or reuse results to enlarge the study or for other studies. Despite their importance, the need for the use of standards in life science research has emerged as crucial for the quality and reproducibility of research findings only in recent years [ 9 ]. The question of data quality and reproducibility poses new scientific and societal challenges for individual researchers, universities, scientific organizations, infrastructure facilities and funders, and the broader society [ 10 ]. The scientific community started to talk about a crisis of reproducibility and its dramatic impact on the economy and credibility of the research system [ 9 , 11 ] around 2016. Many community-driven initiatives such as the Research Data Alliance (RDA) [ 12 ] and the European Commission prompted a series of initiatives in support of the scientific community to cope with problems related to the need of new tools and strategies to improve the harmonization of standard initiatives [ 13 – 14 ] and the implementation of standards in the daily research work to improve research quality and data reuse. Since then, many steps forwards have been made in different fields of biological research [ 15 – 20 ].
There are recommendations providing guidelines for maintaining reproducible results by just applying simple rules. Those rules include the use of error annotations for produced data that are viable for evaluating the impact and credibility of single data associated with the generated results. Furthermore, it is essential to use annexes when research project results are published. Annexes aid the traceability of findings and the reproducibility of performed experiments and can be linked to the aforementioned error classifications. Input files, along with information of the applied software versions, perfectly fit into annexes and play a pivotal role for reproducing results. Finally, adopting these simple rules in the routine research practice within an SOP format aid the transparency of results and exert a decisive impact on scientific reproducibility [ 21 ]. Against this background, the implementation of a minimal quality assurance (QA) system as a systematic approach to review practices and procedures is inherent logical [ 22 ]. QA systems enable the users to identify possible improvements and errors and provide a mechanism for their use, for example, by developing and deploying a failure mode and effects analysis (FMEA) [ 23 ]. The basis of each quality system is a high-quality record providing a string of documents for the verifiable origin and quality of data. Also, the general documentation improves the traceability and transparency of research findings to prove the reliability of results. Such quality control systems should be based on and be in line with good laboratory practices (GLP), well-defined and validated protocols, and comprehensive SOPs [ 24 – 25 ]. The advantages of implementing SOPs in the daily workflow of academic researchers might not be immediately obvious and enlighten everyone. At first, it seems to be unnecessary and avoidable extra work. Indeed, without appropriate training, the setup of an SOP is time-consuming and does not appear to be a relevant asset. However, because each SOP describes one procedure only and not a series of complex procedures the efforts to be done remain feasible. For this reason, we provide you here with “10 Simple Rules on How To Write an SOP” that will enable you to produce a reliable and verifiable set of your research data.
The Ten Rules
Fig 1 demonstrates the workflow of SOP writing along the line from its preparation, validation, and approval to its implementation and follow-up processes, which will be detailed in the following 10 rules.

Workflow of SOP development, its implementation, and monitoring.
Rule 1: Knowing when to write an SOP
SOPs are always needed when critical processes or workflows need to be repeated in a reproducible way or when defined procedures are obliged by compliance guidelines. In other words, SOPs are vital instruments for maintaining consistent quality. Hence, every research institution which faces such processes, compliance requirements or has demand for quality should be encouraged to develop new or follow existing SOPs. Crosscheck within your institution for templates. There is no need to reinvent the wheel. Often templates are existing in your institution, but their existence might not be well communicated. Contact your data or quality manager for information. There also often exists a shared team server or cloud, containing all internal SOPs being accessible for each appropriate member or user, respectively. If your institute or department does not have official templates, ask other groups if they already have SOPs in use. If so, your colleagues should be happy to share their knowledge with you. If there is no template available, you have a pioneering role. In this case you can run a quick online search for SOP templates to be used as a starting point. It is wise to involve the technicians of your lab as well as the leader of your group or department and the quality manager and/or data manager of your institution. The initial step is now to draft a cover sheet and discuss the content of the SOP with the relevant stakeholders (reviewers and approvers) of your institution (Rules 3 and 6). Depending on the peculiarity of research you can choose an appropriate SOP format or develop your own. The resulting unique template can then be further used by all members of your group, department, or institution and by your wider community of practice.
Rule 2: Write the introduction: describe the purpose (the why)
An essential aspect of any SOP is introduction and purpose forming. The introduction section specifies the need and capability of the procedures for the research environment in which the process is being established. Identify the specific reason you decided to write your SOP. Which specific process do you address? Which specific procedures will be covered, and which are not covered? Clarifying what the specific focus of your document is will facilitate the use of your SOP by your colleagues. Richie Norton writes, “Simplicity is complex. It's never simple to keep things simple. Simple solutions require the most advanced thinking” [ 26 ]. The way you frame the information describing the process matters. Consider "less is more." Trying to tackle too much at once will mostly only lead to confusion. Represent the complex aspects of a process in a way to make it as simple as possible to make it also understandable even for users who are not from your field.
Rule 3: Set up the document structure
Every single SOP should consist of three sections:
The cover page
- The sequence of steps or tasks (metadata) for the given procedure (Rule 4)
- A list of references and definitions (Rule 5)
The cover page represents a control block used to house the document control information required to configure management and compliance standards.
It should contain the following information ( Fig 1 ):
- administrative information about the institution and/or department
- a title that clearly identifies the activity or procedure
The SOP’s cover page should provide information about traceability of the SOP, including information about the purpose and scope, its author, issuing, any changes made, and its status (draft, approved, revised, or removed).
- page number and total number of pages of the SOP
- the date of issue (or of versioning)
- possible safety instructions
- the names of individuals who prepared and approved the SOP
- the name of the reviewers, including the date of the review
- a description of the purpose and field of application
- the name and function of the author
- the name and function of the approver
There are standardized abbreviations to describe elements of the respective SOP on the cover page. Table 2 provides a list of typical abbreviations for an SOP category.
It is recommended to use a digital object identifier (DOI) for the identification of the SOP in accordance with ISO 26324:2012 [ 27 ].
Each following page should have a heading and/or footing note mentioning ( Table 3 )
All SOP pages should have an identifier referring to the cover page and consist of administrative information about the institution and/or department, the short title of the SOP, the page number out of the total number, the date, and approval and/or version number.
- short title of the SOP
- date of approval and/or version number
A version number can be assigned in accordance with semantic versioning [ 28 ] recommendations as guidelines used in source control systems like GitHub [ 29 ].
The presentation of dates, including date of issue, versioning, date of review, and approval should be in accordance with the format specified in ISO 8601 [ 30 ].
The final step in creating your SOP template should involve a note on the styles, fonts, and margins that you intend to use. You can download a full template SOP at Zenodo as a writable PDF [ 31 ].
Rule 4: Fill in the content
The procedure.
Start at page 2 to compile the metadata. In this step you describe the activities and the sequence of steps or tasks for the given procedure. Always consider the aim of the SOP; this will help you to focus on the specific procedure you describe. However, an SOP may contain multiple SOPs provided that each one is cited by number and full information is provided. Every user should be able to understand your work instructions. As George Orwell said, "Good [writing] is like a windowpane" [ 32 ]. Consider the knowledge and skills of potential users and the level of detail to present the process description. Long preambles should be avoided. Work instructions should follow a single style and follow a stepwise process strictly. Balance the level of detail, avoid unnecessary specification (e.g., “blue-cap tubes”) and alternatives; if alternatives are necessary, explain what dictates which action. Ensure consistency in terms of terminology, layout, media, and method and, as much as possible, avoid polysyllabic words, complex sentences, jargon, acronyms, or too many terms (without explaining them). To facilitate handling of the different data types and formats within the same workflow, the impact of such diversity to the usability of data and metadata should be minimized. Consider the different work cultures and different circumstances within people’s work and explain and describe the how and what to do. To optimize the structure of you SOP.
- break the process into sections
- break the sections into specific steps
- number the steps or add bullet points for clarity.
Describe each task in detail, including timeframes and tools required to complete assignments and achieve expected outcomes.
Rule 5: References and definitions: Specify tools required for the task
The workflow elements may involve different types of resources and tools. Depending on a particular task, the selection of tools can also comprise modeling and simulation tools, data repositories, and compiler construction tools. Do not forget to add relevant references. Reference materials can include normative documents, instructions, and standards as well as research papers, graphical material, photographs, and even different SOPs. Provide all definitions of terms and abbreviations that are to be used in the procedure. Harmonize and align with standard terminologies used within your field. These should be provided as an annex.
Rule 6: Set up responsibilities and nominate reviewers and approvers
Reviewers should be nominated and appointed responsible for each particular task. These persons should have appropriate scientific knowledge and expertise as well as experience in the field. Usually, the initial SOP-author(s) is/are responsible for monitoring and reviewing the SOP. They will ensure that the SOP reflects the tasks described in the document. Open discussion on controversial aspects related to the SOP should be allowed among reviewers to guarantee a proper revision. Changes to SOPs should preferably be made by the creator. Each change needs again to be reviewed and approved by the responsible persons and by an increase of the revision number (Rule 8). The team of reviewers should agree on a timeframe to monitor and align the current state-of-the-art SOP.
Rule 7: Test with a colleague: Perform training
Congratulations! By reaching this step you wrote your first SOP. Now it is time to check if the SOP is clear and understandable for all potential users. Hence ask a colleague (it can be a researcher or a technician) to read the SOP and, if feasible, execute a test run. Ask the test person to be constructive and critical and wait for his or her feedback or questions. Consider that the test person should be able to run the experiment without any support. Do not interfere while testing to receive authentic feedback and to avoid falsifying the result.
Once written, it is essential that all staff is appropriately trained with and familiarized in the use of the new SOP. This can easily be integrated within the annual safety instructions or as part of a running seminar series. Retraining should be conducted regularly but also when there is a change in SOPs. Ensure that showing attendance at training is documented.
Rule 8: Review and approve
Once your SOP is tested, make it available for the reviewers’ team for a final check. Once substantial comments are received, discuss them with your colleagues to ensure a successful outcome and that the SOP is clear for everybody. Include all relevant edits to improve the document. Repeat the procedure until the SOP is agreed by all stakeholders and, subsequently, send the document to the quality manager for approval afterwards. The final document should be sent to the assigned SOP approvers, who will sign it. In case an SOP is out of date due to the introduction of new technologies or changes in the organizational structure, the SOP should be terminated, labelled (out of date), and archived for traceability. The new and valid version should be distributed. All valid versions should be stored and accessible in a folder at a central location. By this, you ensure that valid and approved SOPs exist and every employee receives the information necessary for their work. To keep track of any deviations from existing SOPs, the establishment and deployment of an exception log might be a powerful instrument. This log should ideally entail a documentation of any deviation, the reason for the deviation, the outcome, any troubleshooting which has been applied, and resolutions and appropriate communication. Regarding the latter, issues or reasons for deviations as well as necessary changes or modifications in the SOP should be discussed with and signed by all involved stakeholders and supervisors, respectively [ 33 ].
Rule 9: Update document: Specify validation and periodic review date
Do not forget to review and update an SOP regularly to keep it up to date and useful for current and future use. Your SOP should be validated and reviewed periodically to improve the document and reflect any changes that have been made or are necessary. All changes should be entered into a revision form, which comprises version number, change data, reason and description for change, reviewers’ data, and signatures. The revised or updated document should be shared immediately with all respective users, while clarifying that the former SOP is outdated. The SOP compliance maintenance could be easily implemented by using an electronic lab notebook (ELN), which might keep track of all deviations automatically, dependent on software and functions.
In this case, ensure the interoperability of used formats to enable export of the data into other systems. Furthermore, regular mandatory user training should be set up for the most important SOPs to ensure compliance.
Rule 10: Publish
It's all very good to have work instructions, but what is their value if they are only available in your office when the users who need them are somewhere else? The people performing the work should have easy access to the work instructions anytime and anywhere, most easily accomplished by setting up a secured team server or cloud on which all latest versions are uploaded. To add value to your SOP, make it available to a broad user community you should upload your SOP also in open access public repositories such as Zenodo [ 34 ], SEEK [ 18 ], OpenAIRE [ 35 ], FAIRsharing [ 36 – 37 ], or another.
Nowadays digital technologies and advanced computational methods are an integral part of daily laboratory practice. To best manage the generated data and avoid reproducibility issues, scientists need to implement FAIR data principles, suitable DMPs, and appropriate documentation. The lack of reproducibility within laboratory research discourages successful implementation of the wide-spread adoption of research results in the scientific community. One way to improve it is to provide consistency and traceability of existing standards and laboratory practices that are achievable with precise and clearly written SOPs.
Acknowledgments
This publication is based upon work from COST Action CHARME CA15110 [ 14 ] supported by COST (European Cooperation in Science and Technology). www.cost.eu .
Funding Statement
This work has been funded by COST (European Cooperation in Science and Technology) CA15110. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Standard Operating Procedures for Clinical Trials (SOPs)
The Clinical Trials Unit at Kilimanjaro Christian Medical Center has prepared numerous Standard Operating Procedures (SOPs) for clinical trials that meet NIH requirements. DGHI is pleased to share these documents with others who are working in resource-limited locations. Although most of these SOPs were developed for AIDS clinical trials, many of these documents can be modified and extrapolated to meet your specific project needs.
SOPs are available in the areas of:
Administrative ( Download PDF Bundle - 93KB Zip File )
- Procurement
- Vehicle use
Clinical ( Download PDF Bundle - 1.6MB Zip File )
- Clinic Flow policies & procedures
- Clinical research management plan
- Protocol implementation
- Source documentation
- Essential documents
- Office charts
- Study visits and missed visits
- Study medications
- Toxicity management
- Subject recruitment
- Subject logs and codes
- Transportation reimbursement
- Ethics committee submission checklist
- New protocol evaluation survey
- Orientation manual
- Quality management plan
- Research coordinator checklist
- Study nurse checklist
- Monitoring visits
- Regulatory affairs
- Site assessment
- Site responsibility
- Patient and study identification numbers
- Safety reports
- Training record
- Venipuncture
Data Management ( Download PDF Bundle - 92KB Zip File )
- Case report forms (CRF) completion
- CRF scanning
- Data security
- Definitions
- International communications
- Query resolution
- Power failure during data entry
- CRF quality assurance
- Table of contents
Laboratory ( Download PDF Bundle - 2.9MB Zip File )
- Over 60 SOPs regarding laboratory equipment, supplies, and tests
Pharmacy ( Download PDF Bundle - 316KB Zip File )
- Infant prescriptions
- Pharmacy plan
- Study accountability records
- Post trial ARV access
- Refrigerator temperature logs
- Room temperature logs
- Site pharmacist checklist
- Policies and Procedures
- Disposal of unfit pharmaceuticals
- Disposal of unfit products
- Importing study products
- Prescription numbering
- Drug transfer form
- Quick Links
- Make An Appointment
- Our Services
- Price Estimate
- Price Transparency
- Pay Your Bill
- Patient Experience
- Careers at UH
Schedule an appointment today

Research Standard Operating Procedures

Download the Clinical Research SOP Manual (DWP)
- Glossary of Terms for Standard Operating Procedures
- Tip Sheet: How to Download Individual SOPs
What are Standard Operating Procedures (SOP)?
“Detailed, written instructions to achieve uniformity of the performance of a specific function.” ( ICH GCP 1.55 )
In simple terms an SOP is a written process and a way for the clinical site to perform a task the same way each time it is completed.
SOPs are used to:
- Identify the responsible person for each task;
- Describe what is to be completed;
- Train staff; and
- Monitor site performance.
What are the benefits of using SOPs?
- SOPs ensure that sites follow Federal Regulations, International Conference on Harmonization Good Clinical Practice Guidelines, and UH Institutional Policies to protect the rights and welfare of human study participants.
- They improve quality of data collected and improves research,
- Provide a reference and guideline for conducting research, and
- Act as a training tool for new employees and/or trainees.
Tips for writing SOPs
- Determine a single task to focus on.
- List all the steps currently used to complete that task.
- Take each step in the task and make it more efficient and easier to follow.
- Following the template, fill in each step.
- Use clear, concise language.
- Use the active voice when writing.
- Avoid names; use job functions instead.
Things to Remember
- The Principal Investigator should approve all SOPs and designate an effective date.
- SOPs should be reviewed on a regular basis (usually annually) to ensure policy based regulations are up-to-date.
- Previous versions of SOPs should be retained.
- All staff should have SOP training (document this training)
- SOPs should be accessible to staff
- SOPs are an integral part of good research practice!

- FlashLine Login
- Phone Directory
- Maps & Directions
- Research Involving Animals (IACUC) Overview
- Overview of the IACUC Process
- IACUC Forms
- Required Training
- IACUC Meeting Dates
- IACUC Regulations, Guidance, FAQs
- IACUC Approval Timeline
- Research with Human Subjects (IRB) Overview
- Approval Timelines & IRB Process
- Meeting Dates, Deadlines & Reviewers
Clinical Research Standard Operating Procedures
List of Standard Operating Procedures
- SOP #101- Writing SOPs
- SOP #102 - Training Personnel
- SOP #103 - Responsibilities of Research Team
- SOP #104 - Conduct of Clinical Study
- SOP #105 - Document Control
- SOP #201 - Regulatory Documentation (regulatory binder)
- SOP #202 - Privacy and Confidentiality
- SOP #203 - IRB Submission
- SOP #204 - Adverse Event Reporting
- SOP #205 - Conflicts of Interest
- SOP #301 - Study Feasibility
- SOP #302 - Site Qualification visit
- SOP #303 - Site Initiation visit
- SOP #304 - Communication Practices
- SOP #305 - Investigational Product Accountability
- SOP #306 - Randomization and Blinding
- SOP #307 - Venipuncture
- SOP #308 - Specimens Collection and Management
- SOP #309 - Preparing Injectable Medications
- SOP #310 - Site Monitoring Visit
- SOP #311 - Site Closeout Visit
- SOP #312 - Protocol Compliance
- SOP # 401 - Subject Recruitment
- SOP #402 - Informed Consent
- SOP #403 - Eligibility and Enrollment
- SOP #404 - Protecting Confidentiality of Study Subjects
- SOP #405 - Study Visits
- SOP #406 - Payments to Subjects
- SOP #501 - Case Report Forms
- SOP #502 - Source Documentation
- SOP #503 - Electronic Records
- SOP #504 - Archiving Study Records
- SOP #505 - Printing and Certifying Medical Records
- SOP #601 - Quality Control
- SOP #602 - FDA Audits
- SOP #603 - Corrective and Preventative Action Plan
- SOP #604 - Equipment Maintenance and Calibration
- SOP #605 - Temperature Monitoring
- Source Documentation Checklist
- Research Involving Animals (IACUC)
- Research with Human Subjects (IRB)

Street Address
Mailing address.
- 330-672-3000
- [email protected]
- Kent State Kent Campus - facebook
- Kent State Kent Campus - twitter
- Kent State Kent Campus - youtube
- Kent State Kent Campus - instagram
- Kent State Kent Campus - linkedin
- Kent State Kent Campus - snapchat
- Kent State Kent Campus - pinterest
- Accessibility
- Annual Security Reports
- Emergency Information
- For Our Alumni
- For the Media
- Health Services
- Jobs & Employment
- Privacy Statement
- HEERF CARES/CRRSAA/ARP Act Reporting and Disclosure
- Website Feedback
Writing Standard Operating Procedures (SOPS)
Standard operating procedures (sops) are standardized written procedures, with detailed instructions to record routine operations, processes and procedures followed within a business organization..
In clinical research, SOPs help define the group’s (e.g., unit, division, department, institution, etc...) standard practices and daily processes conducted to assure execution of research tasks in accordance with institutional, state and federal guidance. SOPs should contain enough detail to guide research staff through a particular procedure and thereby establish uniformity in the everyday functions of the department. The SOP should have a specific aim but be written in a general format to allow for easy implementation across a broad set of venues and circumstances. The SOP however, should contain specifically defined procedures that can be followed without deviation.
All SOPs for the department should be written in the same format with consistent font size, unit title, and section headers. It should include page numbers, date of initial approval, date it was effective within the department and date of revision if applicable. The body of the SOP at a minimum should include the objective of the SOP, definition of key terms and acronyms, defined list of responsible individuals and details outlining the procedures with attachments of examples if applicable. It is important to reference applicable guidance and regulations within the SOP, such as ICH E6 Good Clinical Practice and 21 CFR 50. The SOP should also include the signature of the Administrator or Director of the group with the date of approval. Existing SOPs should be reviewed at regular intervals to reassess applicability of the policy. Annual review is recommended and review prior to sponsor interactions is encouraged.
Distribution, education, and training on new departmental SOPs should be consistent. In-service training and Computer Based Learning modules (CBLs) are typical methods that can be used to educate and train staff on SOPs. It is important to document the date responsible research staff has been appropriately trained and agree to comply with new SOPs that are implemented by the department. Research staff should be monitored consistently to ensure compliance and receive refresher training at regular intervals.
Common SOPs
- GCP Training
- Authority and Delegations of Responsibilities of Research Staff
- Subject Screening and Recruitment
- Informed Consent Process and Documentation
- Eligibility Confirmation
- Source Documentation
- Data Management
- Protocol Deviations
- Adverse Events and Serious Adverse Events Reporting
- Confidentiality of Information
- Drug/Device Storage, Accountability, and Management
- Regulatory Document Submission Process (Initial Submissions, Amendments and Continuing Reviews)
- Sample Processing and Shipping Training
- Monitoring Visits
- Sponsor, CRO and Internal Audits
- Writing SOPs
- Record Organization and Retention
- Sub-Site Management
See also Standard Operating Procedure for Good Clinical Practice .
If you have a disability and experience difficulty accessing this content, please submit an email to [email protected] for assistance.
Policies, Procedures & Guidance
Standard operating procedures (sops) for clinical research.
Standard Operating Procedures (SOPs) for Clinical Research are established to ensure we articulated our expectation for clinical research execution standards that adhere to federal and state regulations and institutional policies.
Sponsor SOPs
Sponsor sops detail the roles and responsibilities for those who serve as regulatory sponsors for investigator initiated clinical trials..
SOP 001 — Sponsor Responsibilities
SOP 002 — Vendor Selection and Qualification
SOP 003 — Investigational Product Management
SOP 004 — Sponsor Monitoring
SOP 005 — Pharmacovigilance and Safety Reporting
SOP 006 — Sponsor Qualification Registration
Outline purchasing and billing compliance review processes.
Finance sops.
SOP 300 — Research Billing Compliance Review
SOP 301 — NETC Parallel Review
Detail expectations for clinical investigators adherence to federal state and institutional requirements
Compliance sops.
SOP 200 — Compliance Reviews
SOP 201 — Regulatory Inspections
SOP 202 — Report of Compliance concerns in Clinical Research
SOP 203 — FDA Form 1572 Policy
SOP 205 — Dissemination Plan for Clinical Trial Results for NIH Funded Clinical Trials
SOP 206 — ClinicalTrials.gov
SOP 206 Attachment — ClinicalTrials.gov Attachment
SOP 207 — External IND Safety Reports
Operational / Research Technology SOPs detail the requirements for the use of clinical research systems
Operational / research technology sops.
SOP 400 — CRMS Requirements
SOP 402 — PennChart Research Associations
SOP 403 — PennChart Research Study Maintenance
SOP 404 — PennChart Research Billing
SOP 405 — REDCap Training and Access
SOP 406 — External Monitoring
SOP 407 — PennVault Training Access
SOP 408 — PennVault eTMF Study Access
SOP 409 — Veeva SVE Access Change Control
SOP 410 — Research Honest Broker Access Process
Manufacturing SOPs detail the requirements to register manufacturing activity and detail the training requirements for all manufacturers
Manufacturing sops.
SOP 100 — Manufacturing Qualification, Registration and Training
SOP 101 — Good Documentation Practices
SOP 102 — Deviations and Corrective Action and Preventative Plan
SOP 102 — Form Deviation CAPA
SOP 104 — Training
Training SOPs detail the training requirements for all research team members
Training sops.
SOP 401 — Clinical Research Training for PSOM Faculty and Staff
Other Clinical Research SOPs
IRB SOPs
ePHI/ Security
EVD Policies
Clinical Research Guidance
The following are guidelines developed for Penn Medicine clinical research teams and links to helpful external resources. They have been developed in partnership with relevant offices across Penn Medicine.
Research Space Allocation
Requests for space to support the conduct of clinical research may require allocation of UPHS space. Such requests may be triaged for consideration by the Office of Clinical Research in conjunction with the hospital Space Committee who will assist investigators in identifying space and in properly specifying suballocations of space with shared research and clinical research uses for clinical research professionals.
Binder Guidance
Clinical Research Space Allocation Guidance
Requirements for Protecting PHI and Clinical Research Document Storage
PSOM Incremental Space Request
Patient Safety / Adverse Event Documentation
The intent of the PSOM Guidance for Adverse Event (AE) Assessment is to provide early, mid and senior career investigators a roadmap on how to investigate, perform, and confirm AE assessments.
Clinicaltrials.gov
Registering studies and submitting results to clinicaltrials.gov.
The following guidance is designed to help the clinical research team navigate the ClinicalTrials.gov (i.e., the Protocol Registration and Results System or PRS system) registration process. If you have any further questions about the process of setting up an account and submitting information to ClinicalTrials.gov, PRS has published a detailed PRS Users Guide found at https://prsinfo.clinicaltrials.gov/prs-users-guide.html or contact OCR at [email protected] .
Click to review how to Registering Studies and Submitting Results to ClinicalTrials.gov
NIH Data Management & Sharing Plan Requirements
NIH Data Management & Sharing Policy (2023)
This page is intended to inform the Penn community about the new National Institutes of Health (NIH) policy . The current NIH policy on sharing research data expires January 25, 2023.
More Information on how Penn is preparing and providing resource: https://guides.library.upenn.edu/NIH
- What is new about the 2023 NIH Data Management and Sharing Policy?
- Beginning on January 25, 2023, ALL grant applications or renewals that generate Scientific Data must include a detailed plan for managing and sharing data through the entire funded period with plans for data dissemination. You must provide this information in a Data Management and Sharing Plan (DMSP). In addition, once the award is made and plan approved, compliance with the DMSP will be a determining condition of the work, meaning it can impact future funding decisions.
- Why is the NIH making these changes?
- The NIH is emphasizing good data stewardship with the goals of advancing rigorous and reproducible research and promoting public trust in scientific endeavors.
- How does the NIH define scientific data?
- Scientific Data are "the recorded factual material commonly accepted in the scientific community as of sufficient quality to validate and replicate research findings, regardless of whether the data are used to support scholarly publications. Scientific data do not include laboratory notebooks, preliminary analyses, completed case report forms, drafts of scientific papers, plans for future research, peer reviews, communications with colleagues, or physical objects, such as laboratory specimens."
- Am I required to share my data?
- The policy encourages efforts to maximize appropriate sharing, but recognizes exceptions (i.e., legal, ethical, or technical reasons). These reasons must be communicated in the NIH DMSP. In addition, sharing plans must be communicated in informed consent documents. In the end, ALL data must be managed, even if not all data can be shared.
Permissions & Guidance:
- IRB Regarding Approvals
- Clinical Trials.gov
- Privacy Policies and Guidance
- Penn Clinical and Biospecimen Data Sharing
- Federal and State-Specific Laws - HIPAA Waiver Form (Search HIPAA on left hand side menu, and click update)
Data Management:
- DART website regarding secure storage and computing options
- Penn Research Analytic Storefront regarding where to find clinical data for research
- Data Analytics Center (DAC) for submitting data request
Sharing Plan:
- ORS regarding research inventory system for submitting DUA, MTA, BAA, etc.
- Scholarly Commons
Privacy and Clinical Research
Data classification/ sensitivity.
Penn Medicine/ University of Penn classifies data into three categories based on the level of data sensitivity, government regulations and existing PSOM or Penn Medicine policies.
More information on this and the Penn Data Classification policy can be found here. This includes information on Penn Box and what information can and cannot be stored there.
- PSOM Data Handling Policy
- Cures Act FAQ - see guidance section on Cures Act and Research
Use of PHI in Email for Research
These guidance documents are important to the use of email and PHI in communication with patients and other Penn Medicine staff and employees. Penn Medicine’s Privacy Office and Information Security Office’s has issued guidance on avoiding and minimizing PHI in email communications. The Office of Clinical Research has collaborated with the Office of Audit Compliance and Privacy (OACP) to create a specific guidance on the use of email during the conduct of research studies and clinical trials.
These guidance documents are titled: Avoid and Minimize PHI in Email and Use of Email During the Conduct of Research
As the guidance specifies, spreadsheets of PHI should never be emailed. You may use secure share as an alternative.
Another option to utilize is Penn Medicine MS Teams. This tip sheet and PowerPoint provide additional guidance and information on how to use MS Teams to share PHI securely via Teams. As a reminder, the minimum of PHI should always be used and shared.
Use of PHI in Text for Research
The purpose of this document is to provide guidance to researchers considering using texting as a form of communication with study participants. Please note texting may raise privacy concerns on behalf of recipients, especially before subjects have signed consent.
Updated guidance coming soon . Contact the Office of Clinical Research for interim questions.
Certificate of Confidentiality (CoC)
Certificate of Confidentiality (CoC) protects the privacy of research subjects by prohibiting the disclosure of identifiable, sensitive research related data to anyone not connected directly to the research except when a patient/research subject consents to the sharing.
Attached guidance and tipsheet provides a high-level overview of a certificate of confidentiality. In addition, it highlights workflows in PennChart that should be used to support the CoC provisions are maintained.
Cures Act and Research
The 21st Century Cures Act and the new ruling from the Health and Human Services department of the Federal Government, Penn Medicine is required to allow patients increased access to their electronic medical record. The purpose of this Act is to promote the patient’s right to electronically access their information, expand the electronic exchange of health information, standardize & expand the content of the health information dataset, reduce barriers for electronic health information exchange, and prevent health information exchange blocking.
The 21 st Century Cures Act also regulates how to share information with patients including research results. The law has provisions for holding results if the release would reveal the results of the study, hence we need the insight of the research team confirming the need to hold or release research results. For more information refer to the guidance document, HERE
Telemedicine
General guidance.
- Penn Medicine (UPHS And PSOM) Guidance Video Conference Platforms and HIPAA Protected Health Information (“PHI”). For more information about specifically using telemedicine in research that overlaps with standard of care, continuity of care or any research that involves billing to insurance or mixed billing please refer to the following document/ Clinical Research Connected Health Telemedicine Guidance .
- Telemedicine Document Guidance Tips
- Appendix 1 How to tell if you are using Penn Medicine or University Meeting Services
- Appendix 2 How to configure services for privacy and compliance
- Out of State Telemedicine Guidance and FAQs
- Out of State Physician Licensing Guide
Subject Payment
Subjects are often offered monetary or non-monetary payments for their participation in research studies. While many options exist, the decision to provide payment to research subjects is generally made to facilitate timely recruitment of subjects for the study and thereby decrease time to study completion, with the consideration of ethics and effectiveness. Accepted justification of research subject payment include reimbursement for expenses that the subject may incur to participate in the research and/or payment for the subject's time and inconvenience. It is never acceptable to use payment as a benefit to offset the risks of a study. The payment procedures must be detailed in the HS-ERA Protocol Application Form and reviewed by the IRB prior to implementation.
TYPES OF SUBJECT COMPENSATION
Subject compensation are typically classified as either reimbursement or remuneration.
- Reimbursement refers to payment, monetary or other form, paid to a subject for out-of-pocket expenses, such as study-related travel, lodging, meals or lost wages.
- Remuneration refers to payment, monetary or other form, paid to subjects as repayment for their personal time and effort committed to study participation.
All subject payment procedures should be described in the study protocol, HS-ERA Protocol, and the Informed Consent Form, which must be approved by the IRB prior to study initiation.
Note: Although the IRB may approve a subject payments for a protocol, this does not imply that the payment method is allowable under University Financial Policy . The IRB reviews payments to ensure that they will not unduly influence a subject's decision to participate, but they do not review the payment procedures to ensure they follow University Financial Policy. It is the responsibility of the investigator or research coordinator to ensure that the proposed payment procedures are in compliance with University Financial Policy.
The Business Office’s Guide for Approving Human Subject Payments provides information and guidance on remuneration and reimbursement of out-of-pocket expenditures provided to research subjects participating in research trials.
21 CFR 11 Compliant Electronic Signatures
This guidance has been generated to help distinguish electronic signatures, from part 11 compliant signatures, and digital signatures. DocuSign signatures are considered part 11 compliant if access via the Office of Clinical Research and PMACS/ DART. Other types of DocuSign or access points are not compliant.
Note: This document does not cover the use of digital or electronic signatures related to contracting, business administration, grant/proposal submission systems, or the effort reporting system (ERS).
See Guidance: USE OF ELECTRONIC DOCUMENTS AND SIGNATURES IN RESEARCH AND 21 CFR PART 11 COMPLIANCE
This document outlines the step by step instructions for creating a compliant adobe eSignature. The purpose of this document is to promote the adoption of digital signatures, by individuals using a PMACS/DART or UPHS managed computer in clinical research, by providing the processes of how to create a signature in Adobe Acrobat and how to verify it to meet 21 CFR Part 11 compliance
Create and Verify a Self-Signed Digital Signature in Adobe Acrobat
The purpose of this document is to instruct users on how to use the “Repository” method to document an Adobe Acrobat self-signed digital-signature certificate information so that it may be verified. The purpose of verification is to provide assurance of the signer, thus meeting 21 CFR Part 11 compliance.
Verification Process for Self-signed Digital Signatures
Social Media and Research
The following documents outline best practices and requirements when using social media to support research recruitment or other research related activities.
- Guidance on Recruitment & Research Using Social Media (link out to Penn IRB's website)
- Social Media Best Practices (requires Penn Login)
Vendormate is a 3 rd party vendor Penn Medicine uses to back ground check pharmaceutical company representatives, and their immunization status. This to mostly protect patients especially immunocompromised patients in clinic spaces. Registration in Vendormate costs about $250 per year to register. This requires yearly renewal by the company, and updates of the representatives immunization records. The cost for this is included in the budget template by OCR Finance so teams can incorporate it before they negotiate with the pharmaceutical sponsor. The pharmaceutical representative category is also extended to CRO/ sponsor monitors that will be in clinic spaces.
- The link below is a brief step by step of how a Pharmaceutical vendor rep registers on the platform, and the screen shot below is that of the main website, and video tutorial that the vendor can accesses at: https://registersupplier.ghx.com/reg/network/vendor/
- Step-by-Step guide document
- The policy that refers to Vendormate and pharmaceutical representatives resides on the UPHS Intranet at (Document is password protected. Copy-paste link in browser if clicking does not open it): https://pennmedaccess.uphs.upenn.edu/f5-w-687474703a2f2f75706873786e65742e757068732e7570656e6e2e656475$$/pahhome/pahpolicies/M15.pdf
- Contact for Vendormate at Penn: Robert Fisher Director, Materials Management Hospital of the University of Pa Tel: 215-662-4741 Email: [email protected]/ [email protected]
Artificial Intelligence (AI) and Human Subjects Research
Artificial Intelligence, AI, is the process of imparting data, information, and human intelligence to machines. The main goal of Artificial Intelligence is to develop self-reliant machines that can think and act like humans. These machines can mimic human behavior and perform tasks by learning and problem-solving. Most of the AI systems simulate natural intelligence to solve complex problems.
Machine learning is a subfield of artificial intelligence, or an application of AI, which is broadly defined as the capability of a machine to imitate intelligent human behavior. It allows a system to automatically learn and improve experience. Artificial intelligence systems are used to perform complex tasks in a way that is similar to how humans solve problems.
Deep Learning is a subset of machine learning that uses vast volumes of data and complex algorithms to train a model.
There are several different ways that AI might be used in research but of particular note are uses of Electronic Medical Record (EMR) data in order to conduct modeling, predict care pathways or interact with patients.
Penn Medicine’s Position on AI and Research:
New artificial intelligence (AI) and machine learning (ML) capabilities, methods, and platforms offer great promise for patient care and research. Notably, large language models such as ChatGPT have been gaining traction and driving imagination on potential applications in healthcare and clinical research – particularly to increase efficiency and productivity. While we support and encourage exploration of AI/ML capabilities, this guidance provides compliance reminders and guardrails to ensure that we continue to protect patients’ privacy and deliver patient care following validated standards.
Patient Privacy Protection: It is not permissible under HIPAA or Penn Medicine policy to share patient or research participant information in connection with public AI/ML services, such as ChatGPT. This is because, as currently configured, such public services can use and share any data without regard to HIPAA restrictions and other protections. Therefore, individual patient data and patient data sets (even if deidentified) may not be exposed to AI/ML services.
Penn Medicine will contribute to the evaluation and development of innovative technologies, in a manner that is compliant with HIPAA and other privacy laws, Penn policies and guidance.
FDA Regulations and AI as a Device
The use of AI in research
FDA Main Page: Artificial Intelligence and Machine Learning in Software as a Medical Device
https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-and-machine-learning-software-medical-device
FDA regulation of AI/ML is evolving, as the field continues to rapidly evolve. Additional information can be found at the following link: https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-and-machine-learning-software-medical-device#regulation
Need additional information or have questions?
Contact OCR Regulatory – [email protected] or 215-662-4484
Penn IRB Research with Devices information: https://irb.upenn.edu/homepage/biomedical-homepage/guidance/types-of-biomedical-research/research-with-device-products/
Sharing Data and Biological Samples with Third Parties
Penn Medicine has developed guidance on the sharing of clinical data and biological samples, whether deidentified or not, with third parties. The guidance is maintained between OACP and OCR and maybe found HERE
Digital Health
Broadly, ‘digital health’ refers to wearable devices, telehealth, and health information technology. Digital health technologies (DHTs) use computing platforms, software, connectivity, and sensors for medical and healthcare uses.
- Penn’s Center for Digital Health: https://healthcareinnovation.upenn.edu/center-for-digital-health
- “The Digital Health Center of Excellence (DHCoE) is part of the planned evolution of the Digital Health Program in the Center for Devices and Radiological Health (CDRH) and will align and coordinate digital health work across the FDA. It marks the beginning of a comprehensive approach to digital health technology, setting the stage for advancing and realizing the potential of digital health.”
- Outlines recommendations to facilitate the use of digital health technologies (DHTs) in clinical investigations evaluating medical products.
Software/ Mobile Medical Apps
Mobile medical apps are software programs that can run on smartphones and other mobile devices. Some apps are aimed at patients/consumers, and other are aimed at healthcare providers. The FDA regulated mobile medical apps via a risk-based approach. The following links can provide additional information:
- Describes mobile medical apps, discusses how FDA regulates device software functions, and lists device software functions that are the focus of FDA oversight.
- FDA Guidance: Policy for Device Software Functions and Mobile Medical Applications: https://www.fda.gov/media/80958/download
- CDSS is a type of software intended to provide decision support in the diagnosis, treatment, prevention, cure, or mitigation of diseases. This guidance applies to CDSS intended to be used by healthcare professionals.
- Provides guidance about recommended documentation for premarket submissions of device software functions (i.e. Investigational Device Exemptions (IDE), among others).
- Recommended for review if you are considering incorporating off-the-shelf software in developing a medical device.
Data Management Tools and Research
For studies where data management is being performed by individual research teams, there are a series of documents to assist with overall data management. Find these in the Forms, Tools, & Templates library .
Some of these are high level like:
- Electronic Database Build and Activation Log
- Database Activation Authorization
- CRF Testing Script
- CRF Testing Tracker
- CRF Build and Schedule of Events Tracker
- Data Base Lock Down and CRMS Examples
- Data Management Plan Creation Guidance
Others are more system specific to using the Penn CRMS as an EDC/ Database:
- Testing CRFs Overview in Penn CRMS
- Penn CRMS EDC Guidelines and Tips
- Understanding Using an EDC-CRMS Workflows
Research, Quality Improvement, Privacy and Data Use Restrictions
Coming soon
Site Guidance for Source Documents
Guidance Document for Source Documentation
This document contains information about Source Documentation for clinical trials. Contents • What Are Source Documents? • Why Are Source Documents Required? • Source Document vs. Case Report Form (CRF) • Location of Source Documents

UNMC Center for Clinical & Translational Research
Standard Operating Procedures
- Clinical Research Spotlight Award
- Clinical Research Development Fund
- Clinical Recruiting Resources
- Biostatistics
- Clinical Research Center (CRC)
- Utilizing CRC Clinical Services
- Clinical Research Units
- Study Intake
- Study Monitoring
- Site Information Sheet
- Clinical Research Services
- Standard Operating Procedures
- Clinical Research Education
- Fees
- Contact Us
- Electronic Health Record Data Access Core
- Research Pharmacy
- Sponsored Programs Administration
- Biomedical Informatics
- Disease Specific Biobanks & Registries
- Nebraska Biobank
- Research Policies
- Uploading Radiologic Images for Research Studies
- Pathology Samples for Clinical Research
- UNeHealth Guidebook
Clinical Research Center Standard Operating Procedures
Below are the Standard Operating Procedures of the Clinical Research Center. They are categorized into 4 sections, Study Management, Clinical Operations, Administrative, and Emergency Preparedness. You may edit and adapt for your department.
Study Management
- SM01- Assessing Protocol Feasibility
- SM02- Site Qualification Visit
- SM03- Study Intake Process
- SM11- Regulatory Binder
- SM12- Management of Regulatory Documents- eReg
- SM13- Management of Regulatory Documents
- SM14- IRB Approval
- SM15- Staff Protocol Training
- SM16- DOA Log Combinded
- SM17- Site Initiation Visit
- SM31- Recruitment of Subjects
- SM34- Informed Consent
- SM35- General Correspondence
- SM36- Protocol Amendments
- SM37- Release of Information - Monitoring
- SM38- Audits and Inspections
- SM39- Case Report Forms
- SM40- Redacting Source Documents
- SM41- Certified Copies of EMR
- SM42- Adverse Events
- SM44- Review of Laboratory Results
- SM45- Home Health
- SM51- Closeout (Termination) Visit
- SM52- Insufficient Accrual
Clinical Operations
- CO01- Staff Competencies
- CO02- CRC Laboratory Orientation
- CO03- Laboratory Orientation
- CO04- Performing an ECG
- CO05- Monoclonal Antibody Admisitration
- CO21- Equipment Calibration and Maintenance
- CO22- Eyewash Maintenance
- CO31- Using CRC Space
- CO32- High Containment Space Utilization
- CO33- Scheduling Visits
- CO34- Offsite Work Activities
- CO41- Kit Destruction
- CO42- Allergy Hypersensitivity Management
- CO43- Medication Storage
- CO50- Infection Control
- CO51- Removing Paper Consent from COVID+ Room
- CO52- COVID Equipment Removal
Administrative
- AD01- Staff Orientation and Training
- AD02- Dress Code
- AD03- Attendance and Leave Requests
- AD05- Key Control
- AD06- Guidelines for Effective Remote Working
- AD07- Travel
- AD08- Professional Development
- AD21- Development and Review of Policies and SOP's
- AD22- Educational Grants from Sponsors
Emergency Preparedness
- EP01- Medical Emergency (Code Blue)
- EP02- Hazardous Materials
- EP03- Power Outage
- EP04- Essential Staffing
- EP05- External Disaster
- EP07- Severe Weather
- Opted-In Subject Recruitment Policy (CRC-SOP-51)
- Recruitment Request Form (Attachment B: Fillable PDF)
Access the UNMC Policies & Procedures Wiki
Standard operating procedures for clinical research departments
Affiliation.
- 1 BMKConsultants, 1611 Carroll Avenue, #1, Saint Paul, MN 55104, USA. [email protected]
- PMID: 22283077
A set of standard operating procedures (SOPs) provides a clinical research department with clear roles, responsibilities, and processes to ensure compliance, accuracy, and timeliness of data. SOPs also serve as a standardized training program for new employees. A practice may have an employee that can assist in the development of SOPs. There are also consultants that specialize in working with a practice to develop and write practice-specific SOPs. Making SOPs a priority will save a practice time and money in the long run and make the research practice more attractive to corporate study sponsors.
- Biomedical Research / organization & administration*
- Biomedical Research / standards*
- Quality Control*
- United States
- UNC Chapel Hill
SOM Clinical Research SOPs
The SOM CRSO is creating Standard Operating Procedures (SOPs) to address risks and inefficiencies in clinical research operations and provide clear and consistent instructions to support investigators and study teams in carrying out the research in compliance with the Code of Federal Regulations, Good Clinical Practice, institutional policies and procedures, and identified best practices, as applicable. SOM SOPs support uniformity and quality in the performance of specific activities that are required by these comprehensive and often complex regulations.
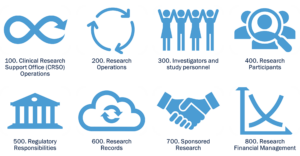
The SOPs are widely applicable to all human subjects research conducted across the SOM as represented in the following 8 SOP categories:
Once draft SOPs are developed and undergo multi-level review, they are disseminated for public review and feedback to seek input from all SOM personnel. The CRSO SOP on SOPs details the full process for developing, implementing, and maintaining SOPs.
Click here to access SOM Clinical Research SOP Repository
- Cancer Center /
- Researchers and Clinicians /
- Clinical Research /
Clinical Trial Resources
Investigator resources.
Access these resources and contacts for assistance in conducting clinical trials.
New Trial Development Brian Chung, PhD: (414) 805-7694 | [email protected]
Trial Management and Resources Ben George, MD, CTO Medical Director: (414) 805-4600| [email protected]
Clinical Research Committees Jennifer Bollmer, PhD: (414) 805-1947 | [email protected]
IIT Steering Committee The Investigator-Initiated Trial (IIT) Steering Committee provides support and mentorship to principal investigators in developing a concept into a full clinical trial protocol for submission to the Scientific Review Committee.
- Steering Committee Roster (PDF)
- Steering Committee Charter (PDF)
- Concept Submission Form
- Clinical Trials Protocol Template (March 2021) (DOCX)
- Concept Development Process (PDF)
- Protocol Activation Process (PDF)
- Scientific Review Committee New Trial Submission Form (PDF)
Disease-Oriented Teams Sixteen integrated Disease-Oriented Teams are comprised of basic, translational, clinical, and population health scientists focused on specific organ/disease groups. Each group meets monthly to exchange ideas and evaluate their research portfolio (active and pending trials). Teams discuss the feasibility and merit of new concepts and protocols proposed by members, as well as protocol prioritization.
- Disease-Oriented Team Chairs
- Disease-Oriented Team Charter (PDF)
Feasibility Committees Adult trials are reviewed by the Feasibility Review Committee (FRC), to ensure new studies are rigorously vetted for patient population availability, competition with trials already in the portfolio, and operational resource utilization (personnel, financial, material). The FRC is charged with identifying any issue that may impact the success of a trial, making the Disease-Oriented Team aware of the issue, and helping to resolve the issue if possible. Pediatric trials are reviewed by the Pediatric Disease-Oriented Team which has a similar feasibility review function.
- Adult Feasibility Review Committee Roste r (PDF)
- Pediatric Feasibility Review Committee Roster (PDF)
- Feasibility Review Charter (PDF)
Scientific Review Committee Comprised of members from a range of disease groups and modalities, as well as representatives from basic science, nursing, biostatistics, pharmacy, and the community, the Scientific Review Committee (SRC) plays a vital role in protocol review and monitoring to ensure trials are scientifically sound and that approved trials maintain patient accrual goals and scientific progress.
- Scientific Review Committee Roster (PDF)
- Scientific Review Committee Charter (PDF)
Data and Safety Monitoring Committee The Data and Safety Monitoring Committee (DSMC) reviews trials for data quality and patient safety and focuses solely on MCW Cancer Center investigator-initiated interventional trials.
- Data and Safety Monitoring Committee Roster (PDF)
- Data and Safety Monitoring Plan (PDF)
Clinical Research Executive Committee The Clinical Research Executive Committee provides a forum for senior clinical research faculty and administrative leaders to discuss and resolve issues related to the conduct and support of clinical trials at the Medical College of Wisconsin Cancer Center.
- Clinical Research Executive Committee Roster (PDF)
- Clinical Research Executive Committee Charter (PDF)
Standard Operating Procedures
Adult Site Profile
Glossary of Terms and Definitions (Apr. 10, 2015) (PDF)
IRB Policies and Procedures
Clinical Research, Investigational Drug Policy (PDF)
Formulary Management of Biosimilars (PDF)
Investigational Drug Accountability and Inventory Management (PDF)
Investigational Drug Disposition and Destruction Policy (PDF)
Investigational Drug Record Retention (PDF)
Investigational Drug Temperature Monitoring Temperature Exclusion Policy (PDF)
Monitoring Visit Policy (PDF)
Priming and Administering Intravenous Investigational Agents Guideline (PDF)
SOP Process Change Management (Feb. 11, 2022) (PDF)
SOP on SOPs (Nov. 5, 2021) (PDF)
Management of EAP and Treatment Use Protocols (June 10, 2020) (PDF)
Study Subject Randomization (Feb. 11, 2022) (PDF)
Protocol Implementation Meetings (March 16, 2020) (PDF)
Required Protocol Training (June 19, 2019) (PDF)
Patient Screening and Enrollment (Nov. 5, 2021) (PDF)
Study Subject Unblinding (March 16, 2020) (PDF)
Completing the FDA 1572, Financial Disclosures and CVs (Feb. 11, 2022) (PDF)
Consenting Study Subjects (Nov. 5, 2021) (PDF)
Documenting Delegation of Authority (Sept. 2, 2021) (PDF)
Employee Resignation (March 16, 2020) (PDF)
External Audits (Nov. 5, 2021) (PDF)
External Safety Reports: Cooperative Groups (Nov. 5, 2021) (PDF)
External Safety Reports: Industry Sponsored (Nov. 5, 2021) (PDF)
Internal Quality Assurance Reviews (June 10, 2020) (PDF)
Investigator Brochure Version Control (Nov. 5, 2021) (PDF)
Investigator Review of Subject Laboratory Reports (Nov. 5, 2021) (PDF)
Laboratory Processes (March 16, 2020) (PDF)
Planned Study Transition Between CTO Employees (Feb. 20, 2018) (PDF)
Study Monitors and Monitoring Visits (Aug. 15, 2023) (PDF)

IMAGES
VIDEO
COMMENTS
The Standard Operating Procedures (SOPs) in this library have been established to ensure consistency and compliance with Federal & State regulations, institutional policies, and Good Clinical Practice guidelines that are common to clinical research of all types. By standardizing these SOPs, we are aligning our clinical research activities ...
Standard Operating Procedures (SOPs) are uniformly written procedures, with detailed instructions to record routine operations, processes and practices followed within a business organization. In clinical research, SOPs help define the group's (e.g., unit, division, department, institution, etc.) standard practices and daily processes ...
The Ten Rules. Fig 1 demonstrates the workflow of SOP writing along the line from its preparation, validation, and approval to its implementation and follow-up processes, which will be detailed in the following 10 rules. Fig 1. SOP workflow. Workflow of SOP development, its implementation, and monitoring.
The Clinical Trials Unit at Kilimanjaro Christian Medical Center has prepared numerous Standard Operating Procedures (SOPs) for clinical trials that meet NIH requirements. DGHI is pleased to share these documents with others who are working in resource-limited locations. Although most of these SOPs were developed for AIDS clinical trials, many ...
Standard Operating Procedure (SOP) - Detailed written instructions to maintain standardization of a specific function. Please reference the Standard Operating Procedures Glossary of Terms for complete definitions of terms in this SOP. 5. POLICY STATEMENT: This SOP must be used as a guide to write, format, implement, and maintain Research
What are Standard Operating Procedures (SOP)? "Detailed, written instructions to achieve uniformity of the performance of a specific function." (ICH GCP 1.55) In simple terms an SOP is a written process and a way for the clinical site to perform a task the same way each time it is completed. SOPs are used to:
Contact. Meredith Fitz-Gerald, MSN, RN Director, Clinical Research Support Program [email protected] 205-975-2758. Home. Clinical Research. Clinical Services. Clinical Research Support Program. Implementation. Standard Operating Procedures Library. Implementation.
Developing site standard operating procedures is an important aspect of launching an effective clinical trial site. Institutional Commitment. Infrastructure and Resources. Standard Operating Procedures. ... Setting up a clinical research program in the community hospital setting.
generating the clinical trial data are performing per the required specifications. CAPA is a structured approach to investigating, correcting, and preventing a deficiency/issue in a process/system . The main elements of a DAIDS required QMS are: • Standard Operating Procedures (SOPs) • Clinical Quality Management Plan (CQMP)
A consistent concern when implementing a quality system for clinical research is the level of standardization and organization to impose within each department. Standard operating procedures (SOPs) and operational guidelines (OGs), describing how each member of the clinical research team should conduct the various activities associated within ...
Clinical Research Standard Operating Procedures. List of Standard Operating Procedures. SOP #101- Writing SOPs. SOP #102 - Training Personnel. SOP #103 - Responsibilities of Research Team. SOP #104 - Conduct of Clinical Study. SOP #105 - Document Control. SOP #201 - Regulatory Documentation (regulatory binder)
In clinical research, SOPs help define the group's (e.g., unit, division, department, institution, etc...) standard practices and daily processes conducted to assure execution of research tasks in accordance with institutional, state and federal guidance. SOPs should contain enough detail to guide research staff through a particular procedure and thereby establish uniformity in the everyday ...
Abstract. A consistent concern when implementing a quality system for clinical research is the level of standardization and organization to impose within each department. Standard operating ...
Standard Operating Procedures (SOPs) for Clinical Research. Standard Operating Procedures (SOPs) for Clinical Research are established to ensure we articulated our expectation for clinical research execution standards that adhere to federal and state regulations and institutional policies.
Clinical Research Center Standard Operating Procedures. Below are the Standard Operating Procedures of the Clinical Research Center. They are categorized into 4 sections, Study Management, Clinical Operations, Administrative, and Emergency Preparedness. You may edit and adapt for your department. Study Management. SM01- Assessing Protocol ...
Abstract. A set of standard operating procedures (SOPs) provides a clinical research department with clear roles, responsibilities, and processes to ensure compliance, accuracy, and timeliness of data. SOPs also serve as a standardized training program for new employees. A practice may have an employee that can assist in the development of SOPs.
Standard Operating Procedure (SOP) for Clinical Research at FMRC; Version 2. Revision 1 . Prepared : : Dr. Shivashankara A.R., Faculty of Father Muller Research Center and Member Secretary of FMIEC Reviewed: Dr .Varadraj Shenoy, Professor of Pediatrics and Chairman Scientific Committee, Father Muller Medical College. Mangalore 575002
The SOM CRSO is creating Standard Operating Procedures (SOPs) to address risks and inefficiencies in clinical research operations and provide clear and consistent instructions to support investigators and study teams in carrying out the research in compliance with the Code of Federal Regulations, Good Clinical Practice, institutional policies and procedures, and identified best practices, as ...
This special contribution provides insight into the role that standard operating procedures (SOPs) play in an imaging department and their value in building a high-quality research site. If you have ever participated in a clinical trial, many of the principles described in this article should be familiar. However, this article goes a step further by presenting information from a pharmaceutical ...
Expandable List Version 9.0 - effective June 6, 2023. Standard Operating Procedures (SOPs) for Clinical Research conducted by investigators affiliated with McMaster University's Faculty of Health Sciences teaching hospitals are available by contacting Health Research Services.The SOPs are also available for users located at St. Joseph's Healthcare Hamilton and Hamilton Health Sciences ...
The NIAID Clinical Research Toolkit has been developed with contributions from all NIAID divisions. ... guidance documents, standard operating procedures, and templates are applicable across all NIAID-funded clinical research. Additional division-specific policies, procedures, and resources are located on division websites listed below. All ...
703.2. The [Title] in the clinical research depart-ment will be responsible for the prepara-tion of the clinical study report at the conclusion of the study and after receipt of the final clean database (SOP 406). 703.3. The clinical study report (or the summary) must be translated into the national lang-uage if it is to be used in a country in ...
Clinical Research Committees Jennifer Bollmer, PhD: (414) 805-1947 ... Standard Operating Procedures (SOPs) help ensure consistency and compliance with Federal and State regulations, institutional policies, and Good Clinical Practice guidelines common to clinical research of all types. ... Adult site, profile glossary, IRB procedures. Adult ...
SOP-10: Procedure for Archival of Study Documents. 10.1. Purpose: The purpose of this Standard Operating Procedure (SOP) is to describe the procedures used by the Principal Investigator and his / her team to archive the study documents at the end of the study. 10.2. Scope: Applicable and to be used by the PI and clinical research staff who are ...