

Essay on Holistic Health
Students are often asked to write an essay on Holistic Health in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Holistic Health
What is holistic health.
Holistic health is about caring for the whole person. This means looking after your body, mind, and emotions. It’s not just about not being sick; it’s about feeling good in every way.
Taking care of your body is important. Eating healthy foods, being active, and getting enough sleep are all part of this. When your body feels good, you can do your best at school and play.
Mind and Emotions
Your thoughts and feelings are also key. Talking to friends, writing in a journal, or doing things you enjoy can keep your mind and heart happy.
Together as One
Holistic health means all parts of you work together. When your body, mind, and emotions are in harmony, you’re truly healthy. It’s like a team where every player is important.
250 Words Essay on Holistic Health
Understanding holistic health.
Holistic health is about caring for the whole person. This means not just focusing on one part of the body when someone is sick, but looking at everything—body, mind, and spirit. It’s like seeing a person as a big puzzle, and each piece is important to make the whole picture.
First, let’s talk about the body. When we think of health, we often think of eating right, exercising, and getting enough sleep. These are key parts of keeping our bodies working well. Eating fruits and vegetables, playing outside, and going to bed on time help us grow strong and stay healthy.
Next is the mind. This is about our feelings and thoughts. Being happy, worrying less, and doing well in school are signs of a healthy mind. It’s important to talk about our feelings and not keep them inside. Reading books, playing games that make us think, and spending time with friends can keep our minds sharp.
Lastly, there’s the spirit. This can mean different things to different people. It might be feeling calm, being kind, or believing in something bigger than ourselves. Some people find peace in nature, others in drawing or music, and some through faith. It’s about what makes us feel good inside.
Bringing It All Together
Holistic health means taking care of all parts of ourselves. It’s like a team, where the body, mind, and spirit work together. When all parts are cared for, we feel our best. Remember, every piece of the puzzle is important to be truly healthy.
500 Words Essay on Holistic Health
When we think about staying healthy, we often picture eating right and exercising. But there’s more to health than just that. Holistic health is about caring for the whole person. It means looking after our bodies, minds, and spirits all at the same time. Imagine you’re like a puzzle, with pieces that fit together to make you whole. Holistic health is about making sure all those pieces are in good shape.
First, let’s talk about the body. This part is about eating foods that are good for you, like fruits and vegetables, and staying active. When you run, play sports, or even walk, you help your body stay strong. It’s also about sleeping well so your body can rest and repair itself. Think of your body like a car; it needs the right fuel and regular maintenance to keep running smoothly.
Next is the mind. Just like you exercise your body, you need to keep your mind active too. This can be through reading, solving puzzles, or learning new things at school. It’s also important to talk about your feelings and not keep them bottled up inside. When you’re sad, worried, or angry, talking to friends, family, or a teacher can make a big difference. Your mind is like a garden; it needs to be looked after and given room to grow.
Then there’s the spirit. This doesn’t just mean religion, although for some people, that’s a part of it. It’s about feeling happy, loving yourself, and enjoying life. You can feed your spirit by doing things you love, like playing music, painting, or spending time in nature. Your spirit is like a bird; it needs space to soar and explore.
Connecting the Pieces
Holistic health is about connecting all these pieces. It’s like when you help a friend, you’re not just being kind; you’re also making your own spirit feel good. Or when you learn something new, you’re not just making your mind sharper; you’re also giving your spirit a boost because it feels great to learn.
Everyone Together
Holistic health isn’t something you do alone. Your family, friends, and community are all part of it. They can support you, cheer you on, and help you stay on track. It’s like being on a team where everyone wants you to win.
Small Steps
You don’t have to make big changes all at once to be more holistic. Small steps can make a big difference. Choose a fruit instead of a candy bar, take a walk instead of watching TV, or tell someone how you feel instead of keeping it to yourself. Each little choice adds up to a healthier you.
In Conclusion
Holistic health is a big idea, but it’s made up of small, simple parts. It’s about taking care of your body, mind, and spirit, and making sure they all work together. It’s like a team, where each player has a special job, but they all need to work together to win the game. By looking after all parts of yourself, you can feel your best and do your best in everything you do.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on Hollywood
- Essay on Homework Should Be Banned
- Essay on Pirates
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

The Holistic Health Promotion Model Overview Essay
Introduction, a holistic health promotion strategy, the importance of the preparation of a holistic health promotion strategy, assessment of data in the development of a holistic health promotion strategy, effective communication of the health promotion strategy to patients, reference list.
The holistic health promotion model offers better therapy, is very logical but at the same time narrow. It disqualifies other measures that are “like Cures”. The holistic approach takes the best possible perception of sickness, addressing the various possible causes, offering a therapy process that is multi-dimensional that is opposed to the cures that target specific illnesses. The model is concerned with an individual’s susceptibility towards disease as well as the transmission. The approach also assesses how people can try to get more hardy or disease-resistant before seeking intervention by medication or become more resilient before catching a disease. This paper will therefore address the concerns in a holistic approach that will include spiritual support and beliefs, physical concerns, and the possible distress in the context of a family; the significance of a holistic health strategy; the importance of the holistic approach, and development of the strategy.
Holistic support of health is an intervention strategy that takes into account factors that affect the wellbeing of human beings and these include the physical body, the emotional aspect, the mind, and the spiritual perception of human beings. The strategy also combines the best service in modern medicine about the diagnosis, monitoring, and prognosis as well as intervention (Berg, 2002, p. 385). In this case, ancient and innovative means of intervention can be used to support modern therapy in achieving better results.
The patients seem to be strict believers and therefore staunch followers of their religious beliefs as well as their cultural principles. This is evidenced by the fact that Manam who is a male aged 55 years of age suffers depression, anxiety as well as painful urination but does not want his wife to be notified of his condition. He also finds it very hard to discuss his problem with the female nurses. When asked questions that related to his other urinary symptoms, the patients feel very reluctant to inform the female nurses. In the first year, he had denied hematuria but he ultimately came to admit having experienced hematuria.
Shuba, the wife of Manan states that she had been using herbal drugs which have not worked for her, however. During the examination, the patient hesitated to take off her gown due to issues of modesty. Furthermore, she has continued taking foods that are high in carbohydrates and fats despite having been on high blood pressure drugs. The strategy of intervention, in this case, will be very critical since the patients will need to be monitored and treated in a way that they would feel that their spiritual or cultural beliefs are not infringed.
The holistic approach will work on the basis that good health is a very strong social and economic resource (Berg, 2002, p. 385). As a result, this would call for advocacy of better health. The patients will be counseled to understand that their cultural, environmental, social, and economic life dimensions can be tuned to favor good health. Otherwise if not properly managed, it could be very harmful.
‘Enabling’ will be the process of making the patients understand that the cultural and spiritual differences with the current medication state and ensure that the patients get the opportunity to utilize the resources that will make them achieve full health potential rather than focus on the herbal medicine that has not been working (Berg, 2002, p. 385). After understandings that medical problems are not just about the symptoms, the patients will be more likely to discuss with family members and as a result, actively get involved in the process of healing rather than sit back and be passive recipients of care.
A holistic approach is very important to the 21 st century as a way of achieving health intervention since it offers a solution to the entire problems that are underlying in this case. Good health is considered the most realistic and inalienable resource that can help an individual meet his/her social, economic, cultural, and even political satisfaction (Berg, 2002, p. 389). When the disease is healed then the patient will not only enjoy that absence of the symptoms but the dieses itself will be healed. And since the approach also covers the aspects of emotions and society, the patients experience a state of complete mental, physical and social comfort.
The process can integrate very well with moderns scientific discoveries in the medical practice. Therefore their preparation can go a long way in enhancing tee process of healing the patient. The process needs proper preparation since it involves some activities that could be tasking. This is because some of the intervention measures include exercise, observing a natural diet, relaxing, using an herbal medication, and use of additional nutrition supplements, spiritual and mental counseling as well as other self-regulated practices (Naidoo & Wills, 2000, p. 45).
The significance of a holistic approach in this process is that it will be able to address not only the symptoms but rather the whole person. As a craftsman, Manan will be able to get back to his work comfortably while his wife will b able to manage her weight and the cases of fatigue she suffered on exertion. The two granddaughters Achala and Gara will be helped to manage behavior problems and emotional issues due to the loss of parents respectively. The holistic process will address the current state of the patients who need counseling like in the case of Gara and Achala for them to get to terms with the life condition at home considering that their parents are dead and the grandparents are ailing. The process will be in this case addressing the prevention of further problems, emphasizing on maintenance of good health, achieving a very high degree of wellness and life longevity (Naidoo & Wills, 2000, p. 45). The process is a very successful paradigm in medication as it ensures the patient is an active participant in the process of healing.
Data assessment is very important in developing a holistic health plan as the strategy usually approaches the problems from a multi-dimensional perspective. It would be therefore very beneficial when the practitioners or the person administering therapy have a full understanding of the patients. To begin with, it’s imperative to understand how the lifestyle of the patient impacts the physical, emotional, economical intellectual, and spiritual elements (Naidoo & Wills, 2000, p. 49). From that, the practitioner can be able to find out how to develop a plan that would be effective and very appropriate in achieving the required results. This is of course after assessing the patient’s beliefs about such an 8intervention and counseling them on the process which would be very easy to attain since holistic intervention blends well with many forms of therapy (Naidoo & Wills, 2002, p. 78). The main focus here will be on personal resources which include mental aspects, physical wellbeing, and spiritual growth. Since the family in this context seems to be very religious and strict observers of their cultural beliefs, counseling, and understanding of the new therapies will be highly needed (Naidoo & Wills, 2000, p. 45). Knowing that Manan has a history of depression, anxiety and does not want to tell their wife about his problem that affects his urinary and reproductive system is evidence that he is somehow conservative due to culture or religion. The same goes for the wife, Shuba who feels uncomfortable undressing for the medical examination for modesty reasons. Achala has a character problem and hence finds a problem making new friends. Gara suffers emotionally and therefore develops a negative attitude towards medication due to the way they make her feel, “weird and different”.
Since the health promotion strategy in holistic healing involves covering several dimensions that affect the wellbeing of an individual, it’s usually a problem to communicate the aim of the process. Many people will be that their privacy is being infringed especially when discussing some spiritual matters they are not comfortable sharing out or are not allowed by religion (Naidoo & Wills, 2002, p. 78). For modesty reasons, Shuba feels uncomfortable taking off her gown, Manan on the other hand feels hesitant to tell female nurses about his urinary problem.
To effectively communicate that health promotion is important to patients, guiding and counseling will need to be used. Patients have to be made to understand that being healthy is the greatest resource a human being can ever have. From here, they need to be made to appreciate that all efforts have to be employed to ensure that health status is restored despite the conditions one has to go through (Naidoo & Wills, 2002, p. 78). There could be ethical concerns but when it comes to health issues the trained medical practitioners are required to assist as much as possible to save a life. The spiritual concerns of the patients can be compromised for life’s sake. The type of care to be administered is evidence-based and the patients have to be given the reassurance that the process serves in their best interests at heart (Naidoo & Wills, 2002, p. 78).
From ancient times, many communities have struggled to come up with several explanations or adopt new justifications and philosophies in their enthusiastic quest for better health. In some instances, sickness has been associated with evil spirits, microbes, and divine retribution. The contemporary approach on the other hand bases its arguments on the contagion illness theory and symptom control in diseases and hence promotes medicine and other measures that counter any damaging agents to the body. Health promotion and holistic approach hence aims at changing certain behaviors, managing risk factors, offering intervention and alleviating fears, and thus giving individuals alternative ways of life and medication that will enable them to achieve healthier lives.
Berg, G.V. (2002). A Holistic-Existential Approach To Health Promotion Scandinavian Journal Of Caring Sciences, 17 (4): 384 – 391
Naidoo J, & Wills J. (2000). Health Promotion : Foundations for Practice . 2 nd Ed. Edinburgh & New York: Baillière Tindall Pub.
Naidoo, J., & Wills, J. (2002). Complementary Therapies: A Resource for Integrated Practice . London: Elsevier Science Publishers.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, March 30). The Holistic Health Promotion Model Overview. https://ivypanda.com/essays/holistic-health-promotion/
"The Holistic Health Promotion Model Overview." IvyPanda , 30 Mar. 2024, ivypanda.com/essays/holistic-health-promotion/.
IvyPanda . (2024) 'The Holistic Health Promotion Model Overview'. 30 March.
IvyPanda . 2024. "The Holistic Health Promotion Model Overview." March 30, 2024. https://ivypanda.com/essays/holistic-health-promotion/.
1. IvyPanda . "The Holistic Health Promotion Model Overview." March 30, 2024. https://ivypanda.com/essays/holistic-health-promotion/.
Bibliography
IvyPanda . "The Holistic Health Promotion Model Overview." March 30, 2024. https://ivypanda.com/essays/holistic-health-promotion/.
- Holistic Care for Patient with Pressure Ulcer
- Holistic Rubric in Nursing Practice
- Moving Toward Holistic and Preventive Care
- Organ Donation: Donor Prevalence in Saudi Arabia
- Kawasaki Disease Analysis
- Reliability and Validity of Chart Audits
- Healthy People 2010 Targeted Objective
- How Pharmacy Practice Has Changed
What Is Holistic Health and Why Is It so Important?
Last Updated: June 8th, 2021

Holistic health has become a popular topic lately. Many medical practitioners and self help gurus are adopting the holistic approach, but it is more than just an ephemeral trend. Holistic healthcare is an integrative approach to health and wellbeing, which sees the person as a whole, not just a symptom to treat.
- What Is Holistic Health?
- Why Does Holistic Health Matter?
- What Is Holistic Medicine?
- The Holistic Approach to Work Life Balance During the COVID 19 Pandemic
- How to Build Our Own Pillars of Holistic Health and Wellness While COVID-19 We Are Stuck at Home
1 . What Is Holistic Health?
Holistic health is an approach to wellness that views the human being as a whole. To achieve holistic health, a certain harmonious interaction is needed between the body, the mind, the soul, the emotions, the environment, and all the other factors that influence living. Holistic health doesn’t believe in curing one symptom, instead it aims to elevate the whole living system, which is traditionally made of 8 key components. They are known as the 8 pillars of holistic health :
Physical health : It involves taking care of the physical body, by making sure to get enough sleep, to move and to exercise regularly.
Nutritional health : You are what you eat. Nutrition influences physical, emotional and intellectual health. It’s important to consume a diet rich in vegetables and fruits, and low in processed products. Pure and clean drinking water is also a must.
Intellectual health : Making sure to challenge the brain daily is essential, either by completing puzzles, or by constantly learning something new.
Emotional health : It means developing emotional awareness and intelligence. Allowing emotions to be expressed, recognized and honored. But also being aware of one’s emotional tank, what fills it up and what drains it.
Spiritual health : This pillar may mean different things to different people, but we all have that feeling of longing for more in common. Tending to our spiritual side gives us a sentiment of belonging and of purpose.
Environmental health : It means being ecologically conscious, honoring the blue planet and its resources while being aware that we are only visitors of this earth.
Social health : Humans are naturally social creatures. Tending to our social side makes us feel a part of a pack and a community. Having a trustworthy support system and a fulfilling social life are important aspects of social health.
Financial health : Money is an important resource for security and goal-attainment. Financial health means cultivating a positive relationship with money, and mindfully managing financial resources.

2 . Why Does Holistic Health Matter?
According to the World Health Organization, health is defined as a state of complete physical, mental and social well-being, and not merely the absence of disease or infirmity.
Conventional medicine only cares about disease and infirmity and doesn’t guarantee the full spectrum of health as defined above. In order to achieve this state of complete wellbeing, a holistic approach is mandatory, hence the importance of holistic health.
No one can contest with how much life has improved thanks to conventional medicine. But at the same time, we cannot deny the feelings of dissatisfaction, void, and loneliness that conventional medicine alone isn’t able to fix. Holistic health matters because conventional models of care are no longer enough.
3 . What Is Holistic Medicine?
Holistic medicine is an approach to healthcare that uses both conventional western medicine and alternative medicine as tools to ensure optimal health and wellbeing. Alternative treatments include nutrition and lifestyle interventions, therapies derived from traditional Chinese or Indian medicine, hypnosis, phototherapy, aromatherapy, meditation, and various self-development techniques.
Furthermore, in holistic medicine, the goal isn’t to cure a symptom, but rather to elevate the whole system. As a result, not only is the person healthy, but they are also the best version of themselves.
4 . The Holistic Approach to Work Life Balance During the COVID 19 Pandemic
Having a healthy work life balance is an essential part of healthy living . This has become even more important during our current situation. During the pandemic, many of us will continue to work from home, taking on multiple roles at the same time. Consider these tips to stay healthy and productive.
The COVID 19 pandemic has changed so many things in our lives. It has pushed us out of our comfort zones, and it made us face our doubts and deepest fears. Furthermore, since most people are either working or studying from home, it has made the line that separates life and work blurrier than before, hence the need now more than ever, to set healthy boundaries for work life balance.
Most people have already heard the mainstream advice about keeping a healthy work life balance, but the holistic approach would be to examine each health pillar individually. By adopting the holistic approach to work life balance, the goal isn’t simply to avoid burnout or disease, but it’s rather to become the most healthy, vibrant, and ideal version of yourself.
5 . How to Build Our Own Pillars of Holistic Health and Wellness While COVID-19 We Are Stuck at Home
We are living in unprecedented times. The current lockdown means that we are forced to live differently and work differently. Coronavirus can stir up all sorts of feelings, like fear, anxiety or stress. In this scenario, destress technique becomes crucial. This is the best time to find simple destress technique and build your own pillars of holistic health. Here are 11 tips to get holistic health . Keep reading to find out what they are.

Instead of viewing this time of quarantine and working from home as a period of boredom and loneliness, we can view it as a chance to learn and start practicing holistic wellness.
Whether you work or study from home, there are some common pillars for holistic wellness. First you need to take care of your physical body, by taking breaks during the day, going for walks, working out and keeping a healthy sleep schedule. Being stuck at home is also a great opportunity to cook healthy meals made from fresh in season ingredients. It’s helpful to be mindful of the environment you spend most of your day in, and to ensure it is clean and tidy. Keeping in contact with friends and family is important, since spending all day at home can make us long for human warmth. Emotionally, it’s essential to be aware of how you’re feeling, and to take the necessary steps to prevent burnout and mental health issues. Keeping a steady spiritual practice can immensely help with the doubt and uncertainty that plague us all. And last but not least, it’s important to be financially aware, and to avoid overspending (or overeating for that matter) to fill any emotional void you may carry.
If you work from home:
Prioritize self care! Tend to your needs before you take care of your job, because what good is a salary at the end of the month if you feel bad about yourself?
Due to the COVID-19 pandemic, more people are working from home than ever before. Whether you are new to working remotely or just want to upgrade, these tips from remote working professionals can help you stay productive and keep your balance.

If you study from home:
We have all seen the news and are currently understanding the world situation, so we need to find effective ways to study or work at home. Take this time to reflect on your future and the things you want to become. Remember that studying is just one way to make your dreams come true. Also take this time to learn other skills that will help you in your career.
Studying at home does not have to be boring or unnecessarily complicated. Here are 5 study tips and you can combine with your own tips and tricks and set a schedule to make the most productive entrepreneurs jealous.
Remember to take regular breaks and use your free time to do things that will make you smile and feel good. There are many things you can do during the quarantine period, including cooking, playing video games, completing online courses, etc. So this is an excellent time to develop on all levels.
6 . Conclusion
Holistic wellness is an approach to healthcare that sees the person as a whole and not just a symptom. The goal of holistic wellness is to ensure optimal wellbeing and not just being free of disease. Being stuck at home because of the COVID 19 pandemic is a great opportunity to become more aware of our health, and to learn and incorporate more holistic wellness into our daily life.
Use the Wellness Wheel Worksheet to help you to identify what areas of your life are fulfilled and healthy and what areas need improvement and attention
Let Start to Practice Holistic Health


Personalize Your Experience
Log in or create an account for a personalized experience based on your selected interests.
Already have an account? Log In
Free standard shipping is valid on orders of $45 or more (after promotions and discounts are applied, regular shipping rates do not qualify as part of the $45 or more) shipped to US addresses only. Not valid on previous purchases or when combined with any other promotional offers.
Register for an enhanced, personalized experience.
Receive free access to exclusive content, a personalized homepage based on your interests, and a weekly newsletter with topics of your choice.
Home / Living Well / A holistic approach to integrative medicine
A holistic approach to integrative medicine
As studies continue to reveal the important role the mind plays in healing and in fighting disease, a transformation is taking place in hospitals and clinics across the country. Meta description: Discover principles and benefits of integrative medicine, a comprehensive approach combining conventional and complementary therapies.
Please login to bookmark

Interested in integrative medicine? Read the following excerpt from the Mayo Clinic Guide to Integrative Medicine .
People who take an active role in their health care experience better health and improved healing. It’s a commonsense concept that’s been gaining scientific support for several years now.
As studies continue to reveal the important role the mind plays in healing and in fighting disease, a transformation is taking place in hospitals and clinics across the country. Doctors, in partnership with their patients, are turning to practices once considered alternative as they attempt to treat the whole person — mind and spirit, as well as body. This type of approach is known today as integrative medicine.
Incorporate integrative medicine alongside your treatments
Integrative medicine describes an evolution taking place in many health care institutions. This evolution is due in part to a shift in the medical industry as health care professionals focus on wellness as well as on treating disease. This shift offers a new opportunity for integrative therapies.
Integrative medicine is the practice of using conventional medicine alongside evidence-based complementary treatments. The idea behind integrative medicine is not to replace conventional medicine, but to find ways to complement existing treatments.
For example, taking a prescribed medication may not be enough to bring your blood pressure level into a healthy range, but adding meditation to your daily wellness routine may give you the boost you need — and prevent you from needing to take a second medication.
Integrative medicine isn’t just about fixing things when they’re broken; it’s about keeping things from breaking in the first place. And in many cases, it means bringing new therapies and approaches to the table, such as meditation, mindfulness and tai chi. Sometimes, integrative approaches help lead people into a complete lifestyle of wellness.
What types of integrative medicines are available?
What are some of the most promising practices in integrative medicine? Here’s a list of 10 treatments that you might consider for your own health and wellness:
- Acupuncture is a Chinese practice that involves inserting very thin needles at strategic points on the body.
- Guided imagery involves bringing to mind a specific image or a series of memories to produce certain responses in the body.
- Hypnotherapy involves a trancelike state where the mind is more open to suggestion.
- Massage uses pressure to manipulate the soft tissues of the body. There are many different kinds of massage, and some have specific health goals in mind.
- Meditation involves clearing and calming the mind by focusing on your breathing or a word, phrase or sound.
- Music therapy can influence both your mental and physical health.
- Spinal manipulation, which is also called spinal adjustment, is practiced by chiropractors and physical therapists.
- Spirituality has many definitions, but its focus is on an individual’s connection to others and to the search for meaning in life.
- Tai chi is a graceful exercise in which you move from pose to pose.
- Yoga involves a series of postures that often include a focus on breathing. Yoga is commonly practiced to relieve stress, as well as treat heart disease and depression.
Who can integrative medicine help?
A number of surveys focused on the use of integrative medicine by adults in the United States suggest that more than a third of Americans are already using these practices as part of their health care.
These surveys demonstrate that although the United States has the most advanced medical technology in the world, Americans are turning to integrative treatments — and there are several reasons for this trend. Here are three of the top reasons why more and more people are exploring integrative medicine.
Integrative medicine for people engaged in their health
One reason integrative medicine is popular is that people in general are taking a greater, more active role in their own health care. People are more aware of health issues and are more open to trying different treatment approaches.
Internet access is also helping to fuel this trend by playing a significant role in improving patient education. Two decades ago, consumers had little access to research or reliable medical information. Today, clinical trials and pharmaceutical developments are more widely available for public knowledge.
For example, people who have arthritis can find a good deal of information about it online. They may find research showing that glucosamine, for example, helps with joint pain and doesn’t appear to have a lot of risks associated with it. With this information in hand, they feel empowered to ask their doctors if glucosamine might work with their current treatment plans.
Integrative medicine for an aging population
A second reason for the wider acceptance of integrative treatments is the influence of the baby boomer generation. This generation is open to a variety of treatments as it explores ways to age well. In addition, baby boomers are often dealing with several medical issues, from weight control to joint pain, high blood pressure and elevated cholesterol. Not everyone wants to start with medication; many prefer to try complementary methods first.
Integrative medicine for the chronically stressed
A third reason for the growth, interest and use of integrative therapies is the degree of chronic stress in the American lifestyle. Workplace stress, long commutes, relationship issues and financial worries are just some of the concerns that make up a long list of stressors.
Although medications can effectively treat short-term stress, they can become just as damaging — and even as life-threatening — as stress itself is when taken long term. Integrative medicine, on the other hand, offers several effective, evidence-based approaches to dealing with stress that don’t involve medication. Many otherwise healthy people are learning to manage the stress in their lives successfully by using complementary methods such as yoga, meditation, massage and guided imagery.
Considering that many healthy people are engaging in integrative practices, it isn’t surprising to find out that they’re turning to these treatments in times of illness, as well. Here are just a few ways integrative medicine is used to help people cope with medical conditions:
- Meditation can help manage the anxiety and discomfort of medical procedures.
- Massage has been shown to improve recovery rates after heart surgery.
- Gentle tai chi or yoga can assist the transition back to an active life after illness or surgery.
Conventional Western medicine doesn’t have cures for everything. Many people who have arthritis, back pain, neck pain, fibromyalgia and anxiety look to integrative treatments to help them manage these often-chronic conditions without the need for medications that may have serious side effects or that may be addictive.
The risks and benefits of integrative medicine
As interest in integrative medicine continues to grow, so does the research in this field. Researchers are studying these approaches in an effort to separate evidence-based, effective therapies from those that don’t show effectiveness or may be risky. In the process, this research is helping to identify many genuinely beneficial treatments. In essence, both consumer interest and scientific research have led to further review of these therapies within modern medicine.
As evidence showing the safety and efficacy of many of these therapies grows, physicians are starting to integrate aspects of complementary medicine into conventional medical care. Ultimately, this is what has led to the current term integrative medicine.
Ask your healthcare team about integrative medicine and wellness
If you’re interested in improving your health, many integrative medicine practices can help. Not only can they speed your recovery from illness or surgery, but they can also help you cope with a chronic condition. In addition, complementary practices such as meditation and yoga can work to keep you healthy and may actually prevent many diseases.

Relevant reading
Mayo Clinic First-Aid Guide for Outdoor Adventures
The first-ever first-aid book from medical experts at Mayo Clinic, the most trusted name in medicine. Welcome to the jungle! Or the mountains! Or the high seas! Wherever your travels take you, Mayo Clinic First Aid Guide for the Outdoor Adventures is here to help you survive your next trek…

Discover more Living Well content from articles, podcasts, to videos.
You May Also Enjoy

Privacy Policy
We've made some updates to our Privacy Policy. Please take a moment to review.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Public Health Ethics
- PMC10849326

Health as Complete Well-Being: The WHO Definition and Beyond
Thomas schramme.
Department of Philosophy, University of Liverpool, Gillian Howie House, Mulberry Street, Liverpool, L69 7SH, UK
The paper defends the World Health Organisation (WHO) definition of health against widespread criticism. The common objections are due to a possible misinterpretation of the word complete in the descriptor of health as ‘complete physical, mental and social well-being’. Complete here does not necessarily refer to perfect well-being but can alternatively mean exhaustive well-being, that is, containing all its constitutive features. In line with the alternative reading, I argue that the WHO definition puts forward a holistic account, not a notion of perfect health. I use historical and analytical evidence to defend this interpretation. In the second part of the paper, I further investigate the two different notions of health (holistic health and perfect health). I argue that both ideas are relevant but that the holistic interpretation is more adept for political aims.
Introduction
‘Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity’ ( World Health Organisation [WHO], 1948 : 100). In this paper, I argue that this famous WHO definition of health is fully adequate. Criticism that has been levied against it is based on a specific interpretation that is not the only alternative. In addition to defending the WHO definition, I will discuss two different meanings of the concept of health, which can lead to confusion if not properly kept apart. This is important, for historical and analytical reasons, because the WHO definition can indeed be interpreted in different ways and because we need to get to grips with the differences between types of definitions of health. My second aim in this paper is hence to explain and to properly keep apart two different conceptualisations of health. 1
As regards the WHO definition, I will claim that critics have read the word complete in the phrase ‘complete physical, mental and social well-being’ in a way that goes against the likely intentions of the draftees of the definition. The common objections, for instance, accusing the WHO definition of utopianism and overreach, are based on an implicit assumption, according to which complete is a quantitative term. In other words, critics assume that the phrase means that health is a state of well-being to the largest degree. I will call this interpretation perfect health . So, the critics claim that the WHO identifies health with the largest degree of well-being, that is, with perfect well-being or—in less technical terms—with happiness.
However, the term complete can also have a qualitative meaning. 2 When we say that something is a complete specimen of its kind, then we mean that it has all the features that are constitutive of it. For instance, a complete dinner is one that contains a starter, a main dish and a dessert. Accordingly, complete well-being might be understood as a state that is exhaustive of all constitutive features of well-being. These are, according to the WHO, physical, mental and social aspects. I will call this holistic health . 3 In brief, I will claim that the WHO endorses a holistic account of health, not a perfectionist account. 4
In the second section, I briefly introduce the most important objections to the WHO definition. They have mainly to do with an alleged confusion of health with happiness, which then purportedly leads to a form of medicalisation of human life. In the third section, I discuss the likely intentions behind the WHO definition. I do this by referring to the two readings mentioned before, perfect health and holistic health. There are systematic and historical reasons as to why the WHO plausibly intended a holistic interpretation of health. In the fourth section, I discuss the two interpretations of health in their own right. I introduce their purposes and some objections to either notion. As is the case with many concepts we use, there is no single right or wrong conceptualisation of health. However, I argue that a holistic concept of health is better suited for the purposes of the WHO and more generally for political and economic agendas.
Criticism of the WHO Definition
The health definition of the WHO has often been dismissed by philosophers of medicine and medical scientists (for an overview, see Leonardi, 2018 ). One of the main reasons has been the alleged confusion of health and happiness, that is, a state of complete well-being. 5 If health is understood as happiness, it has been argued, there are many highly problematic consequences, most importantly the medicalisation of people’s lives. After all, health is also interpreted as a basic human right in the same document: ‘The enjoyment of the highest attainable standard of health is one of the fundamental rights of every human being without distinction of race, religion, political belief, economic or social condition’ ( WHO, 1948 : 100). If people fall short of the ideal of perfection, that is, if they are not in a state of complete well-being, their health ought to be enhanced. With health care being an important instrument to reach health, the lives of people seem to fall under the remit of health-related institutions, especially medicine, in all their aspects. For instance, if someone is sad, they lack health in the sense of complete well-being. Accordingly, following the WHO constitution, they apparently have a justified claim to be made healthy, that is, happy, potentially by using mood-enhancing drugs or other medical means.
A prominent and influential critique of the WHO definition stems from Daniel Callahan: ‘[T]he most specific complaint about the WHO definition is that its very generality, and particularly its association of health and general well-being as a positive ideal, has given rise to a variety of evils. Among them are the cultural tendency to define all social problems, from war to crime in the streets, as “health” problems’ ( Callahan, 1973 : 78; see also Kass, 1975 : 14, for a very similar critique). This is an example of the critique of overreach (cf. Bickenbach, 2017 : 962), that is, of applying a medical concept to areas that pose other types of problems than healthcare problems.
Another problem that has repeatedly been pointed out is the utopianism of the definition. It seems that ‘[t]he requirement for complete health “would leave most of us unhealthy most of the time”’ ( Huber et al ., 2011 : 235; quoting Smith, 2008 ; see also Saracci, 1997 : 1409, 1409; Card, 2017 ). This can specifically be deemed problematic in relation to people with disabilities, chronic diseases and people of advanced age. They would by definition permanently be missing out on health and accordingly on well-being. However, such a view seems to conflict with the perspectives of relevant groups of people themselves ( Fallon and Karlawish, 2019 : 1104).
Despite the widespread criticism from many different disciplinary backgrounds, the WHO never amended their definition of health. It seems that they did not see a need to change their point of view. In the following section, I will argue that the critique is indeed based on a misunderstanding of the WHO’s perspective.
Interpreting the WHO Definition of Health
As explained, I will argue that the WHO defines health as holistic health, not as perfect health. To bolster this claim about the intentions of the institution, I need to consider the history of its constitution. In this section, I will therefore rely on historical documents, which are in the public domain. In addition, I have benefitted from an enormously helpful recent publication by Lars Thorup Larsen (2022) , who gives a detailed account specifically of the genealogy of the WHO definition, based on archival research.
An important fact that supports my reading of the WHO’s intentions is that the word complete was only inserted into the definition at the very final stages of its conception. It is fairly obvious that it was as a form of editorial amendment, not a substantial change, because otherwise it would have required extensive debate. If the word complete would have fixed the intended definition of health to a perfectionist account, this would have either stirred up a debate or would have had to be uncontroversial. However, there is no evidence in the relevant documents that the draftees of the WHO constitution definitely understood health as perfection. The term complete , according to my reading, was rather intended to clarify the phrase ‘physical, mental and social well-being’, the latter of which had been part of the definition since the drafting period. 6 The word complete summarises and jointly describes the three aspects of well-being. It also adds a rhetorical contrast to the second part of the sentence that denies the sufficiency of the absence of disease or infirmity for health. A perhaps better way to express the notion would have been to state that: health is a state of complete well-being, that is, a state that comprises physical, mental and social elements. But this locution would not have worked straightforwardly in a one-sentence definition, which was apparently aimed at by the WHO.
The late arrival of the term complete of course does not present conclusive evidence that the WHO did not intend to push an account of perfect health. The historical records are not sufficient in this respect. The final draft of the constitution, which had been penned by the Technical Preparatory Committee, was discussed at a meeting in New York City in 1946. 7 The relevant draft definition reads: ‘Health is not only the absence of disease, but also a state of physical and mental well-being and fitness resulting from positive factors, such as adequate feeding, housing and training’ ( WHO, 1947 : 58). The final version, which was eventually adopted, had been prepared by the so-called Committee I, which ‘had given careful consideration to amendments submitted by the delegations of South Africa, Mexico, Australia, Belgium, Netherlands, Chile, United Kingdom, Iran, China, Philippines, Poland, Venezuela, United States of America and Canada’ ( WHO, 1948 : 44). Unfortunately, there are no published minutes or other forms of evidence in relation to this decisive period—decisive, as far as the introduction of the term complete is concerned. We simply do not know who added the word. This would have been important, though, to get a better grasp of the intentions behind the addition. 8
Importantly, many members of the Technical Preparatory Committee, who had been involved to different degrees in the drafting of the WHO constitution, came from a public health background ( Farley, 2008 : 12ff.; Cueto et al ., 2019 : 39ff.). Renowned proponents of so-called social medicine, such as Andrija Štampar, René Sand, Karl Evang and Thomas Parran, were leading members of the drafting group. This is significant because public health usually has a different understanding of the concept of health than clinical medicine. Whereas for the latter, health can be defined as absence of disease ( Smith, 2008 ), that is, in absolute terms, health in public health is a multifarious and scalar notion ( Schramme, 2017 ; Valles, 2018 : 31ff.).
In clinical medicine, health is often understood as absence of disease. This makes sense because the focus is on individual patients. These either have a disease or not. Patients might suffer from a more or less severe disease, but that does not mean that they are more or less diseased than others. Similarly, health over and above the absence of disease is not usually the focus of clinical medicine. If there is no disease, then that is sufficient to establish health. There is no need to refer to health in a positive way, that is, to define it in its own terms.
In contrast, public health scientists usually refer to populations. In their parlance, chosen populations can be more or less healthy than comparison groups. For instance, it might be declared that mine workers are less healthy than millionaires. This does not mean that all mine workers acutely suffer from a disease; rather, it means that they are more likely to fall ill, due to their circumstances of life. Public health has traditionally studied the causes of disease and has made big strides in the prevention of disease. Accordingly, its focus is upstream, as it is sometimes put ( Marmot, 2010 : 41; Venkatapuram, 2011 : 189), towards the conditions that make disease more likely. Health becomes a dispositional term that allows for different grades.
From a public health perspective, it is fairly obvious that health is ‘more than the absence of disease’. It is more in the sense of additionally requiring dispositional elements, not because it is a quantitatively better condition than medical normality (i.e. the absence of disease). People who live in destitute circumstances might not suffer from a disease, but they are often lacking in terms of a sufficient disposition to maintain minimal health.
The public health perspective, therefore, is a gradual perspective on health, allowing parlance of more and less health, or being healthier than others. Although such a perspective does not necessarily lead to an account of perfect health, it is nevertheless compatible with the latter. People with a perfect health disposition—marked by a very low probability to fall ill—might accordingly be deemed in a state of perfect health. Importantly, falling below the ideal point of perfection on a scale does not imply having a disease. In other words, not being perfectly healthy would not constitute a condition of being un healthy; it would merely mean being less healthy than others ( Schramme 2019 : 29ff.). This shows that some of the criticism levied against the WHO definition, even if understood as a perfectionist account, is implausible. More specifically, it does not necessarily follow that, for instance, people with disabilities would be constantly deemed unhealthy because they lack perfect health. As explained, health is not a binary term according to the relevant perspective.
So far, I have argued that the WHO definition is supposed to allow for grades of health. For that purpose, it takes its cue from public health perspectives, though I do not want to claim that it is identical to it. After all, the WHO definition still incorporates the traditional medical perspective on health as absence of disease. There are, nevertheless, important qualms to do with the notion of perfect health. The WHO refers to health as a state of well-being and this might itself be deemed problematic. To be sure, the conceptual connection between health and the good life for human beings has long been established ( Temkin, 1973 ). 9 The connection also makes sense from an experiential point of view. Health has indeed to do with how we fare. Still, if we read the definition as a perfectionist account of health, it would define health as perfect well-being. If that were the case, this would apparently lead to the alleged dangerous confusion of health and happiness mentioned earlier. After all, sufficient health but not happiness seems to be the business of welfare state institutions. It is true, of course, that health care from a public health perspective includes vastly more than just medical care, especially aspects to do with work, education and the environment. Yet, we normally see good reasons to restrict the remit of state institutions to a form of needs provision, basic security and enablement of self-determination (cf. Goodin, 1988 : 363ff.). So, if perfect health were the focus of the state, it would probably end up becoming unjustifiably expansive.
I do not believe that the WHO is guilty of this charge. To be sure, there are reasons for thinking that a public health perspective occasionally tends towards an expansive view of health politics (cf. Preda and Voigt, 2015 ). Yet, it is hardly imaginable that a nascent institution—still precarious in its status at the time of drafting its constitution including the health definition—would intend to basically take over the whole established welfare state agenda and indeed even to expand it by making perfect health a political aim. This is even less credible, as one of the global health institutions predating the WHO, the League of Nations Health Organization , had come under fire for its alleged political overreach during these times of increasing national isolationism ( Cueto et al ., 2019 : 20ff.). There were, accordingly, strong political reasons not to endorse a perfectionist health definition, or at least to keep such ambitions hidden from plain view, especially in 1946, with very fresh memories of the dangers of totalitarianism being abundant. 10
A more science-oriented reason as to why the WHO is unlikely to have opted for an account of perfect health is that such an ideal is not measurable. After all, it refers to an abstract point of reference. To quantify the health statuses of populations, scientists need metrics and they need to determine thresholds. In other words, they need to plot health along a scale. If health were only a hypothetical point on a limitless scale, it would hardly be a useful metric for scientific purposes. Again, this is not a decisive reason to reject the perfectionist interpretation of the WHO definition. But there are numerous publications by health scientists who use the WHO definition without running into the mentioned problems ( Breslow, 1972 ; Greenfield and Nelson, 1992 ). So, it seems that many scientists do not assume the perfectionist health interpretation (see also Ware et al ., 1981 : 621). 11
In contrast, the holistic health interpretation leads to the following point of view: Health is seen as a state of well-being with numerous aspects—physical, mental and social. 12 Given these dimensions of well-being, health statuses can be assessed in a combined approach, taking the full range of health-related factors into account. Importantly, health is not a fictional point at the end of the scale, but any point along a scale. Some people might have a comparatively bad health status, some might be in good health; all will be positioned along a spectrum. From the health definition itself, nothing follows as to when health is good enough or so bad that state institutions need to interfere. In other words, important political decisions regarding thresholds of sufficient health are not prejudged if we follow a holistic health definition. Such a perspective is much more amenable to the political remit of the WHO, which ended up with fairly limited interventionist power (cf. Packard, 2016 : 99ff.; Larsen, 2022 : 123ff.).
The overarching focus of the holistic health interpretation is maintenance of health. It is thereby acknowledged that to counter the various threats to health not only medical means are required, but a dynamic level of physical, mental and social assets. This has been an insight of early public health practitioners. For instance, Henry Sigerist, who evidently had a significant indirect influence on the WHO definition via Raymond Gautier’s draft ( Larsen, 2022 : 119), had already been concerned with the aim of health maintenance. 13 This provides a dynamic element in the conceptualisation of health, which is also implicit in the WHO definition, despite its reference to a state , which seemingly suggests a static view. When Sigerist writes that ‘health is more than the absence of disease’ ( Sigerist, 1932 : 293), this is meant as a conclusion to an argument acknowledging the environmental and social determinants of health. His point becomes quite clear in a later quote:
A healthy individual is a man [ sic! ] who is well balanced bodily and mentally, and well adjusted to his physical and social environment. He is in full control of his physical and mental faculties, can adapt to environmental changes, so long as they do not exceed normal limits; and contributes to the welfare of society according to his ability. Health is, therefore, not simply the absence of disease: it is something positive, a joyful attitude toward life, and a cheerful acceptance of the responsibilities that life puts upon the individual ( Sigerist, 1941 : 100). 14
Sigerist’s terminology, referring to being well balanced, adjusted and in full control, is not aiming towards an ideal of perfection. Rather, he is stating several elements of a good human life within the limits of reality. He believes that health enables an affirmative view of individuals towards their life, not unlimited happiness.
In this section, I have discussed the WHO definition partly from an analytical point of view, in that I distinguished two possible interpretations, a perfectionist and a holistic account of health. I have added historical information regarding the drafting period. Both analytical and historical reasons speak in favour of my thesis that the WHO definition should be read as defining health in a holistic way. Health as complete well-being refers to the full range of factors determining a specific disposition of people to prevent ill health (cf. Ware et al ., 1981 ). This ties in nicely with a more recent official statement by the WHO, the Ottawa Charter, which I will cite as final support of my thesis: ‘[H]ealth is a resource for everyday life, not the objective of living. Health is a positive concept emphasizing social and personal resources, as well as physical capacities’ ( WHO, 1986 ). Health is not the best possible state of well-being but a multifarious instrument, including external as well as internal resources, to pursue a good life.
Why We Need to Distinguish Between Holistic Health and Perfect Health
I have not argued that a conceptualisation of perfect health is wrong-headed or even harmful. Rather, I claimed that perfect health is not the notion that the WHO has been after. It is of import to distinguish between the two notions of health introduced earlier, because confusing them will lead to cross-purposes, not merely in respect to the WHO definition. In this section I will take a closer look at the two health conceptions and discuss the purposes which they can serve. I will also hint at problems with both interpretations that might eventually call for terminological reform.
Holistic health allows to pursue multiple political and economic purposes. For instance, it enables comparisons between groups of people and is especially adept to highlight social inequalities that have an impact on population health. This makes it more pertinent for political purposes than a negative conceptualisation of health as the absence of disease. The latter is absolute or non-comparative and hence does not allow for any interesting information about health-related inequalities between persons.
Importantly, in contrast to perfect health, the scope of holistic health can be contoured by thresholds. As explained, complete well-being can be understood as having all elements that are constitutive of it. What exactly that means in relation to health is of course contested, and I have already insinuated that the WHO did not set a threshold, perhaps intentionally. Still, the required level of holistic health could be determined via political decision-making processes. This makes holistic health open for different substantial interpretations and hence political ambitions.
Despite these advantages, the conceptualisation of health as holistic health has serious drawbacks. 15 Most significantly, the distinction between health conditions and determinants of health becomes blurry ( Bickenbach, 2017 : 968, 968; van Druten et al ., 2022 : 2). 16 Environmental and social determinants of health come with certain probabilities, sometimes unknown, to fall ill or to stay healthy, but they are not constituents of medical conditions themselves; rather, they are their presumed causes ( Whitbeck, 1981 : 617). As we have seen in the previous example of miners’ health, a poor health disposition is not the same as being unhealthy, that is, suffering from disease or illness. 17
The potential confusion between poor health dispositions and disease or illness leads to normative confusion as well, especially when we are assessing claims of justice. Disease has a different normative status than a relatively bad health disposition. Arguably, disease has an immediate urgency in relation to human needs, in terms of threatening or involving harm. A comparatively high propensity to fall ill or membership in a vulnerable population as such does not obviously have such normative urgency. Important normative discussions about health justice are short-circuited if we transfer direct urgency to alleviating relatively poor holistic health statuses without thinking about the impact on the lives of real people and merely consider relative positions.
One way forward would be to acknowledge the basic insights of a holistic conceptualisation of health but to nevertheless distinguish between health as a condition of an individual and health-related traits and circumstances that have an impact on the maintenance of individual and population health. We would accordingly need a more adequate term than health for combining both of these aspects—an organismic condition, that is, health in the more narrowly medical sense, and a set of health-related resources. Such a revisionary conceptual perspective can only be alluded to here (see Davies and Schramme, 2022 ).
Accounts of perfect health have a different purpose than accounts of holistic health. The former set an ideal; an ambitious target for individual or social aspiration. According to this perspective, a person can always be potentially healthier, because there is no fixed point on a scale which suffices for health. It seems to me that such an interpretation of health is fully adequate for specific purposes, for instance, introducing a utopian goal and to stop people from becoming complacent about an important element of a good human life. Perfect health shares features with traditional accounts of the virtues, although it is not itself supposed to be a virtue. Virtues are similar to perfect health in that they describe human excellences. Virtues are excellences of character, or perfect dispositions to act fully adequately; health is excellence in relation to well-being, or a perfect organismic disposition to keep harmful and disadvantageous conditions at bay. Becoming virtuous can be an aspiration for human beings and so can becoming perfectly healthy.
However, there is a danger of imposing such an ideal on everyone. If we always have to strive for more health, then we might lose sight of other values, such as pursuing friendships, taking risks or enjoying unhealthy choices. This is a real risk in many modern societies, where health has been turned into a kind of religion and individual mission ( Katz, 1997 ). Socially, similar developments can be studied in relation to so-called ‘healthism’ and generally the moralisation of health ( Conrad, 1992 ). 18 The problems intensify if health dispositions and risk factors are not clearly distinguished from health conditions. Every single action a person pursues might have an impact on their health, according to the perfectionist health account. Hence, if combined with a prescriptive reading of the ideal—as something to be sought—then health can turn into a totalitarian imperative. This would clearly undermine the initial purpose of setting an ideal.
Whether perfect health will fail to meet its purposes will be established by experience and through history. It is not a necessary feature of the account. As mentioned, there are warning signs. However, more importantly, there is a need to clearly distinguish between holistic health and perfect health because perfect health, in contrast to holistic health, should never be the remit of state institutions.
Conclusions
‘Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity’ ( WHO, 1948 : 100). This definition allows for two different interpretations. A perfectionist account, where health describes a hypothetical, perfect state of well-being, or a holistic account, where health is a state of exhaustive well-being, including all relevant dimensions of its constitutive elements. I have argued that the WHO intended to support a holistic account. I provided analytical and historical reasons for this point of view.
To distinguish between the two interpretations of health is important for systematic reasons as well, not merely in relation to the proper interpretation of the WHO’s definition of health. The two different accounts serve different purposes and run into different types of problems, as I have highlighted in this paper. Still, both are perfectly valid notions of health.
Acknowledgements
I would like to thank Lars Thorup Larsen and one of the two anonymous reviewers for helpful comments.
1 There can, of course, be even more than just these two conceptualisations of health. For instance, many would probably define health simply in terms of the absence of disease or illness. Indeed, one of the reasons why the WHO definition has raised concerns is probably due to its explicit diversion from the widespread conceptualisation in negative terms, that is, as absence of something.
2 The Oxford Dictionary of English (2015) entry on the adjective forms of complete states: ‘1. having all the necessary or appropriate parts: a complete list of courses offered by the university | no woman’s wardrobe is complete without this pretty top ( … ) 2. [attributive] (often used for emphasis) to the greatest extent or degree; total: a complete ban on smoking | their marriage came as a complete surprise to me ’.
3 The term holistic has been used in relation to health by Lennart Nordenfelt (see Nordenfelt, 1995 : 12ff., 35ff.). By using this term, I do not want to claim that Nordenfelt endorses the WHO definition.
4 A slightly different distinction between two meanings of the concept of complete— complete in an ‘all-or-nothing sense’ and in a sense that ‘admits of degrees’—has been drawn by Sissela Bok in relation to the WHO definition ( Bok, 2008 : 592). In passing, I also want to note that the label perfectionist is of course not supposed to refer to perfectionism in value theory, where it denotes an objective theory of the good.
5 Possibly the first philosopher of medicine to take note of this feature and the likely consequences was Owsei Temkin: ‘I do not think that I read too much into this formula [the WHO definition] if I believe that it tends to include moral values and to identify health with happiness. ( … ) But is the pursuit of happiness itself wholly a medical matter? Our life has many values and ( … ) happiness can sometimes be achieved at the sacrifice of health. ( … ) [I]f health is defined so broadly as to include morality, then the danger exists that the physician will also be burdened with all the duties of the medieval priest’ ( Temkin, 1949 : 20).
6 This needs to be qualified, because the term social was introduced fairly late in the drafting process. However, the point I am making here is to do with the fact that elements of well-being had been listed for some time during the drafting period and that the word complete was added to characterise these elements jointly.
7 The Technical Preparatory Committee itself relied on earlier drafts of senior members of related institutional bodies, especially the League of Nations Health Organization ( Larsen, 2022 ). Larsen gives a detailed account of the origins of the WHO definition, tracing it back to Henry Sigerist’s influential publications in the history, sociology and philosophy of medicine, dating mainly from the 1930ies. Sigerist’s ideas were not revisionary or highly original, though, at least not in its focus on positive health. The idea that health includes elements that cannot be captured by the phrase ‘absence of disease’ goes back to antiquity. Especially the notion of health as a form of equilibrium and—in modern terms—resilience has been known for centuries ( Edelstein, 1967 : 303ff.). So, even if Sigerist’s work probably had a role in finding the relevant formulations, the underlying ideas had been prevalent.
8 One of the members of the Technical Preparatory Committee, Szeming Sze, recalled 40 years later that James H.S. Gear ‘improved the wording’ ( WHO, 1988 : 33). However, there is no identifiable evidence to corroborate Sze’s recollection.
9 The notion of well-being here is a state of a person including their circumstances. It should not be interpreted as a mental state only, that is, as a kind of feeling.
10 It should also not be forgotten that the early focus of public health institutions, including the precursors of the WHO, was on the prevention of diseases, specifically communicable diseases. This speaks against assuming a focus on health enhancement.
11 Indeed, numerous researchers claim that although the WHO definition sets a political ambition, its main purpose is to set a framework that makes health measurable ( Salomon et al ., 2003 ; Rubinelli et al ., 2018 ; cf. Chatterji et al ., 2002 ).
12 In line with this reading, in more recent years, there was also a discussion in the WHO whether to add spiritual well-being to the definition ( WHO, 1997 : 2; cf. Larson, 1996 ; Nordenfelt, 2016 : 214). The discussion around a fourth aspect of well-being did not lead to official changes, though.
13 Bok also mentions that Sigerist was a close friend of Štampar’s, who was—as mentioned earlier—a member of the drafting group ( Bok, 2008 : 594).
14 Georges Canguilhem similarly declared that ‘[h]ealth is a set of securities and assurances ( … ), securities in the present, assurances for the future’ ( Canguilhem, 1966 : 198).
15 Surely not everyone would see the political negotiability of adequate health thresholds as an advantage. However, I am here concerned with a relative advantage over the perfectionist account of health.
16 Once the determinants of health are confused with health itself, there is an additional danger of conceptualising immorality and incivility as forms of health disruptions (cf. Farley 2008 : 56). WHO officials were not immune to this problem. For instance, in a memorandum called International Health of the Future (1943), Gautier wrote: ‘For health is more than the absence of illness; the word health implies something positive, namely physical, mental, and moral fitness. This is the goal to be reached’ ( Larsen, 2022 : 117; see also Chisholm, 1946 : 16; cf. Cueto et al ., 2019 : 33).
17 The otherwise philosophically important distinction between disease and illness does not matter for the purposes of my essay. I use the terms interchangeably for ease of reading.
18 An important and still highly recommendable early critique of the utopian standard of health is Rene Dubos’s Mirage of Health ( Dubos, 1959) .
- Bickenbach, J. (2017). WHO’s Definition of Health: Philosophical Analysis . In Schramme, T. and Edwards, S. (eds), Handbook of the Philosophy of Medicine . Dordrecht: Springer, pp. 961–974. [ Google Scholar ]
- Bok, S. (2008). WHO Definition of Health, Rethinking the . In Heggenhougen, H. K. (ed.), International Encyclopedia of Public Health . Amsterdam: Elsevier, pp. 590–597. [ Google Scholar ]
- Breslow, L. (1972). A Quantitative Approach to the World Health Organization Definition of Health: Physical, Mental and Social Well-being . International Journal of Epidemiology , 1 , 347–355. [ PubMed ] [ Google Scholar ]
- Callahan, D. (1973). The WHO Definition of “Health” . The Hastings Center Studies , 1 , 77–87. [ PubMed ] [ Google Scholar ]
- Canguilhem, G. (1966). The Normal and the Pathological . New York: Zone Books. [ Google Scholar ]
- Card, A. (2017). Moving Beyond the WHO Definition of Health: A New Perspective for an Aging World and the Emerging Era of Value-Based Care . World Medical & Health Policy , 9 , 127–137. [ Google Scholar ]
- Chatterji, S., Ustün, B. L., Sadana, R., Salomon, J. A., Mathers, C. D. and Murray, C. J. L. (2002). The Conceptual Basis for Measuring and Reporting on Health . Global Programme on Evidence for Health Policy Discussion Paper No. 45, World Health Organization. [ Google Scholar ]
- Chisholm, G. B. (1946). The Reëstablishment of Peacetime Society . Journal of the Biology and the Pathology of Interpersonal Relations , 9 , 3–20. [ Google Scholar ]
- Conrad, P. (1992). Medicalization and Social Control . Annual Review of Socioliology 18 , 209–232. [ Google Scholar ]
- Cueto, M., Brown, T. M., and Fee, E. (2019). The World Health Organization: A History . Cambridge: Cambridge University Press. [ Google Scholar ]
- Davies, B., Schramme, T. (2022). Health Capital and its Significance for Health Justice . Manuscript. [ Google Scholar ]
- Dubos, R. (1959). Mirage of Health: Utopias, Progress, and Biological Change . New York: Harper & Brothers. [ Google Scholar ]
- Edelstein, L. (1967). Ancient Medicine: Selected Papers of Ludwig Edelstein . Edited by Owsei T. and Lilian Temkin, C. Baltimore: John Hopkins University Press. [ Google Scholar ]
- Fallon, C. K. and Karlawish, J. (2019). Is the WHO Definition of Health Aging Well? Frameworks for “Health” After Three Score and Ten . AJPH , 109 , 1104–1106. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Farley, J. (2008). Brock Chisholm, The World Health Organization, and the Cold War . Vancouver: UBC Press. [ Google Scholar ]
- Goodin, R. E. (1988). Reasons for Welfare. The Political Theory of the Welfare State . Princeton: Princeton University Press. [ Google Scholar ]
- Greenfield, S. and Nelson, E. C. (1992). Recent Developments and Future Issues in the Use of Health Status Assessment Measures in Clinical Settings . Medical Care , 30 , MS23–MS41. [ PubMed ] [ Google Scholar ]
- Huber, M., et al.. (2011). Health: How Should We Define It ? British Medical Journal , 343 , 235–237. [ Google Scholar ]
- Kass, L. (1975) Regarding the End of Medicine and the Pursuit of Health . Public Interest 40 : 11–42. [ PubMed ] [ Google Scholar ]
- Katz, S. (1997). Secular Morality . In Brandt, A. M. and Rozin, P. (eds.), Morality and Health . London: Routledge, pp. 297–330. [ Google Scholar ]
- Larsen, L. T. (2022). Not Merely the Absence of Disease: A Genealogy of the WHO’s Positive Health Definition . History of the Human Sciences , 35 , 111–131. [ Google Scholar ]
- Larson, J. S. (1996). The World Health Organization’s Definition of Health: Social Versus Spiritual Health . Social Indicators Research , 38 , 181–192. [ Google Scholar ]
- Leonardi, F. (2018). The Definition of Health: Towards New Perspectives . International Journal of Health Services , 48 , 735–748. [ PubMed ] [ Google Scholar ]
- Marmot, M. (2010). Fair Society, Healthy Lives—The Marmot Review . Institute of Health Equity. [ Google Scholar ]
- Nordenfelt, L. (1995). On the Nature of Health: An Action-Theoretic Approach . 2nd Revised and Enlarged Edition. Dordrecht: Kluwer. [ Google Scholar ]
- Nordenfelt, L. (2016). A Defence of a Holistic Concept of Health . In Giroux, É. (ed.) Naturalism in the Philosophy of Health: Issues and Implications . Heidelberg: Springer, pp. 209–225. [ Google Scholar ]
- Oxford Dictionary of English. 3rd edn. Edited by Stevenson, A. Oxford University Press. Current Online Version: 2015 [ Google Scholar ]
- Packard, R. M. (2016). A History of Global Health: Interventions into the Lives of Other Peoples . Baltimore: John Hopkins University Press. [ Google Scholar ]
- Preda, A. and Voigt, K. (2015). The Social Determinants of Health: Why Should We Care ? The American Journal of Bioethics , 15 , 25–36. [ PubMed ] [ Google Scholar ]
- Rubinelli, S., Cieza, A., and Stucki, G. (2018). Health and Functioning in Context . In Riddle, C. A. (ed.), From Disability Theory to Practice: Essays in Honor of Jerome E. Bickenbach . Lanham: Lexington Books, pp. 121–131. [ Google Scholar ]
- Salomon, J. A., Mathers, C. D., Chatterji, S., Sadana, R., Üstün, T. B., and Murray, C. J. L. (2003). Quantifying Individual Levels of Health: Definitions, Concepts, and Measurement Issues . In Evans, D. B. and Murray, C. J. L. (eds), Health Systems Performance Assessment . Geneva: World Health Organization, pp. 301–318. [ Google Scholar ]
- Saracci, R. (1997). The World Health Organisation Needs to Reconsider Its Definition of Health . BMJ , 314 , 1409–1410. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schramme, T. (2017). Health as Notion in Public Health . In Schramme, T. and Edwards, S. (eds), Handbook of the Philosophy of Medicine . Dordrecht: Springer, pp. 975–984. [ Google Scholar ]
- Schramme, T. (2019). Theories of Health Justice: Just Enough Health . London: Rowman & Littlefield Int. [ Google Scholar ]
- Sigerist, H. E. (1932). Man and Medicine . New York: W.W. Norton. [ Google Scholar ]
- Sigerist, H. E. (1941). Medicine and Human Welfare . New Haven: Yale University Press. [ Google Scholar ]
- Smith, R. (2008). The End of Disease and the Beginning of Health . The BMJ Blog , available from: https://blogs.bmj.com/bmj/2008/07/08/richard-smith-the-end-of-disease-and-the-beginning-of-health/ [accessed 12 October 2022].
- Temkin, O. (1949). Medicine and the Problem of Moral Responsibility . Bulletin of the History of Medicine , 23 , 1–20. [ PubMed ] [ Google Scholar ]
- Temkin, O. (1973). Health and Disease . In Wiener, P. P. (ed.), Dictionary of the History of Ideas . New York: Scribner, pp. 395–407. [ Google Scholar ]
- Valles, S. A. (2018). Philosophy of Population Health: Philosophy for a New Public Health Era . Abingdon: Routledge. [ Google Scholar ]
- van Druten, V. P., Bartels, E. A., van de Mheen, D., de Vries, E., Kerckhoffs, A. P. M. and Nahar-van Venrooij, L. M. W. (2022). Concepts of Health in Different Contexts: A Scoping Review . BMC Health Services Research , 22 , 1–21. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Venkatapuram, S. (2011). Health Justice: An Argument from the Capabilities Approach . Cambridge: Polity Press. [ Google Scholar ]
- Ware, J. E., Brook, R. H., Davies, A. R. and Lohr, K. N. (1981). Choosing Measures of Health Status for Individuals in General Populations . American Journal of Public Health , 71 , 620–625. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Whitbeck, C. (1981). A Theory of Health . In Caplan, A. L., Engelhardt, H. T.Jr. and McCartney, J. J. (eds), Concepts of Health and Disease: Interdisciplinary Perspectives . Reading: Addison-Wesley, pp. 611–626. [ Google Scholar ]
- World Health Organization (1947). Minutes of the Technical Preparatory Committee for the International Health Conference Held in Paris from 18 March to 5 April 1946 . World Health Organization, available from: https://apps.who.int/iris/handle/10665/85572 [ Google Scholar ]
- World Health Organization (1948). Summary Reports on Proceedings Minutes and Final Acts of the International Health Conference held in New York from 19 June to 22 July 1946 . World Health Organization, available from: https://apps.who.int/iris/handle/10665/85573 [ Google Scholar ]
- World Health Organization (1986). The Ottawa Charter for Health Promotion . Geneva: World Health Organization, available from: https://www.euro.who.int/__data/assets/pdf_file/0004/129532/Ottawa_Charter.pdf [ Google Scholar ]
- World Health Organization. (1988). Forum Interview with Szeming Sze. WHO: From Small Beginnings . World Health Forum , 9 , 34, available from: https://apps.who.int/iris/handle/10665/46414 [ PubMed ] [ Google Scholar ]
- World Health Organization (1997). Review of the Constitution and regional arrangements of the World Health Organization . Geneva: World Health Organization, available from: https://apps.who.int/iris/handle/10665/78112 [ Google Scholar ]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 18 March 2020
A philosophy of health: life as reality, health as a universal value
- Julian M. Saad ORCID: orcid.org/0000-0002-9323-1021 1 &
- James O. Prochaska 1
Palgrave Communications volume 6 , Article number: 45 ( 2020 ) Cite this article
43k Accesses
3 Citations
5 Altmetric
Metrics details
- Health humanities
- Medical humanities
Emphases on biomarkers (e.g. when making diagnoses) and pharmaceutical/drug methods (e.g. when researching/disseminating population level interventions) in primary care evidence philosophies of health (and healthcare) that reduce health to the biological level. However, with chronic diseases being responsible for the majority of all cause deaths and being strongly linked to health behavior and lifestyle; predominantly biological views are becoming increasingly insufficient when discussing this health crisis. A philosophy that integrates biological, behavioral, and social determinants of health could benefit multidisciplinary discussions of healthy publics. This manuscript introduces a Philosophy of Health by presenting its first five principles of health. The philosophy creates parallels among biological immunity, health behavior change, social change by proposing that two general functions— precision and variation —impact population health at biological, behavioral, and social levels. This higher-level of abstraction is used to conclude that integrating functions, rather than separated (biological) structures drive healthy publics. A Philosophy of Health provides a framework that can integrate existing theories, models, concepts, and constructs.
Similar content being viewed by others

The transition from genomics to phenomics in personalized population health
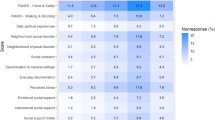
Measuring social determinants of health in the All of Us Research Program

The Project Baseline Health Study: a step towards a broader mission to map human health
A philosophy of health.
What is health? Is it a state of the body or the mind? Is health primarily a natural, biological state or a holistic, value-laden state? Naturalistic and holistic philosophies of health have provided very important, but very different, perspectives of population health. Naturalistic views (e.g. as seen in Boorse, 1997 ) provide insight into physical, natural, biological, or physiological processes that are tangible (in the material sense), observable, and measurable with modern technology. Complementarily, holistic views contend that value-laden phenomena (e.g. vital goals, meaning, and purpose) play a central role in population health (Nordenfeldt, 2007 ).
A dialog, or as we see it, an important dialectic among naturalistic and holistic perspectives plays out between the Biostatistical Theory of Health (BST) and the Holistic Theory of Health (HTH). The BST posits that a person is healthy if and only if, all natural organs function normally given a statistically normal environment (Boorse, 1997 ). The HTH posits that a person is healthy if and only if (given standard circumstances) he/she has the ability to attain their vital goals (Nordenfeldt, 2007 ).
In addition to defining health, each philosophy defines disease. The BST poses that disease is the internal state of impairment to the normal functioning of organs (Boorse, 1997 ). In the HTH, an organ dysfunction is a disease if and only if the organ’s process reduces the person’s ability to pursue vital goals or life-purpose (Nordenfelt, 2007 ). In BST health is the absence of disease; and in HTH, health is not the absence of biological disease, but is the whole person’s ability to function in relation to vital goals.
Both naturalistic and holistic perspectives guide important observations of health and disease. When one considers health through the BST one pays close attention to the functions of the internal, biological functioning of the human being. When one considers health through the HTH, one pays close attention to the functioning of an individual, in relation to their external, societal/cultural functions. Is there a hybrid model that accounts for both internal and external functioning?
Wakefield’s ( 2014 ) harmful dysfunction analysis (HDA) creates a hybrid model that integrates natural- and value-laden phenomena when conceptualizing disease. HDA asserts that a person suffers from a disorder/disease if (1) the condition causes harm (as judged by the standards of the person’s culture); or if (2) the person’s internal, natural processes cannot perform normal functioning (as judged by the standards set by evolution). HDA creates a hybrid model that can integrate perspectives of the BST (i.e. by considering internal organ functioning); and the HTH (i.e. by considering external societal/goal functioning). However, while HDA may define health processes in relation to disease, it serves primarily as an integrative model of disease . Is there an integrative model of health that can account for natural and value-laden functions?
Schroeder ( 2012 ) identifies a significant, common thread among these competing (or perhaps complementing) philosophies: functionalism . The researcher suggests that each philosophy is concerned with the functioning of organisms. Although the BST, HTH, and the HDA might not agree on which functions inform the first principles of health, Schroder ( 2012 ) uses higher-level abstraction to identify one common first principle: the state of functioning in an organism impacts its state of health . When paralleling the three philosophies based upon functioning one might observe that (1) BST declares an individual healthy if its organs function normally; (2) HTH declares an individual healthy if he/she can function in relation to vital goals; and (3) HDA declares an individual unhealthy if internal mechanisms cannot perform natural, evolutionary functions, and/or when a condition prevents a person from functioning in relation to goals/norms/values. Through this higher-level abstraction, an integration of seemingly separate philosophies of health is made possible.
Learning from leaders in the field
As we attend to these philosophies of health, we too observe how discussions about functions and functioning produce integrative perspectives. Although a definition of “function” is not explicitly stated in the above research, it appears that Nordenfeldt ( 2007 ), Boorse ( 1997 ), Wakefield ( 2014 ), and Schroeder ( 2012 ) are each discussing functions as pre-existent (i.e. either from evolution, personal goal-setting, cultural tradition) processes - with - purposes . Whether one is describing a value-laden function (e.g. decision-making in pursuit of a valuable career) or an evolutionary-biological function (e.g. the heart beating for circulation), each process (i.e. decision-making processes or cardiac processes) serves identifiable purposes (e.g. maintained financial stability or maintained blood flow). Whether an organ is functioning normally in relation to the body or a human being is functioning in relation to vital goals, it appears that both perspectives consider if an active “process” (i.e. an organ’s activity, an individual’s activity) can express its “purpose” (i.e. evolutionary-purpose, life-purpose).
In the present manuscript we will propose that naturalistic and holistic perspectives can be integrated within a single philosophy of health. We will propose two universal functions—termed precision and variation —that can account for both natural functions and value-laden functions of the existing philosophies. This functional language will support a higher level of abstraction that integrates, rather than separates, biological functions, behavioral functions, and social functions under A Philosophy of Health.
The need for new perspectives in population health
The chronic disease crisis beckons the need for an updated philosophy of health that can account for biological, behavioral, and social functioning. Why? Chronic diseases, which account for 60% of all-cause deaths worldwide (Chartier and Cawthorpe, 2016 ), do not emerge from naturalistic, biological, or physical contact with an illness. Rather, chronic diseases do emerge in biological functions (e.g. tumor proliferation in an organ) after prolonged contact with health risk behaviors and lifestyle factors that active the conditions (Mokdad et al., 2018 ; Edington, 2009 ; Li et al., 2018 ). Chronic diseases are not curable by purely naturalistic or biological means (e.g. pharmaceuticals). Rather, some diseases may be effectively prevented or intervened on through healthy behavior (Dansinger et al., 2005 ; Daubenmier et al., 2007 ).
Population health risk behaviors are unique determinants of population health because researchers can actively observe how they simultaneously alter biological functioning (e.g. chronic smoking alters cells in lung tissue), behavioral functioning (e.g. chronic smoking alters decision-making and daily habits) and social functioning (e.g. chronic smoking creates an economic, social, and healthcare burden) of the population. These behaviors not only have biological, behavioral, and social implications for the individual doing the behavior, but also have intergenerational and interpersonal effects. The individual who binges on refined sugar not only puts themselves at risk of diabetes, but can put their future offspring at risk. The individual who smokes two packs of cigarettes per day not only puts themselves at risk of lung cancer, but can put their housemates at risk of lung cancer from second-hand smoke. Therefore, the chronic disease crisis is neither purely naturalistic, nor purely value-laden; rather it reflects an integration of natural and value-laden phenomena. There remains a real need for principles of health that can integrate existing naturalistic and holistic perspectives of population health.
The principles
Since April 7, 1948, the Constitution of the World Health Organization ( 2010 ) has utilized an intuitive definition of health by suggesting that health is “a state of complete physical, mental, and social well-being.” While this definition might be intuitive and even accessible to a wide audience; the defininition is not necessarily researchable across health disciplines. Integrating principles of health might begin with a common-sense definition of health that can also be upheld across existing naturalistic and holistic perspectives. Without operationally defining functions that drive physical, mental, and social well-being, it is a challenge for multidisciplinary collaborators to unite under the WHO mission. Further, without a common definition of health, important communications from patients to doctors, from subjects to researchers, from researchers to collaborators, and from peer-reviewers to peer-reviewees, can become fragmented or lost in translation. In the proceeding sections, a common-sense definition of health is used to present the first principles of A Philosophy of Health.

Principle 1: “Health” is the state of maintainable-ease of functioning . A “disease” is a state of prolonged-dysfunction that prevents ease
Chronic diseases emerge from prolonged exposure to dysfunctional behaviors like smoking, alcohol abuse, unhealthy diet, and inactivity (Mokdad et al., 2018 ) that also create dysfunctional expressions of life functions. Smoking creates dysfunctional breathing; alcohol abuse creates dysfunctional drinking; sugar binging creates dysfunctional eating; and sedentary behavior creates dysfunctional moving. When these health risk behaviors lead to chronic disease, they have already prolonged dysfunctional breathing, drinking, eating, and/or moving.
The chronic smoker breathes in smoke so frequently that he no longer experiences an ease-of-breathing. Rather, his breathing becomes short and shallow. Prior to the emergence of lung tumors, the chronic smoker prolongs dysfunctional patterns of breathing. The “couch potato” sits so frequently that he no longer experiences an ease-of-movement. Rather his movement becomes rigid and limited. Prior to the emergence of cardiovascular dysfunction or obesity, the sedentary person prolongs dysfunctional patterns of movement.
If chronic smoking facilitates prolonged-dysfunction in breathing, and sedentary behavior facilitates prolonged-dysfunction in movement, what do functional breathing and moving look like? Healthy breathing and moving (as well as eating and drinking) are characteristic of an ease of one’s functioning that can be maintained in normal conditions. For example, the chronic smoker and the “couch potato” might report momentary-ease in breathing and posture when engaging in their health risk behaviors; but they do not maintain that ease outside of smoking or sitting. Conversely, the yogi might report that their yoga practices expose them to momentary dis-ease in breathing and moving that lead to maintainable-ease in breathing and movement in everyday life. In contrast to disease as a prolonged-dysfunction, healthy functioning can be commonly sensed as a maintainable - ease of functioning .
When observing a disease, perhaps we are observing a prolonged-dysfunction that prevents ease. Rather than define health as the absence of disease (as seen in BST), notice here how we instead define disease in relation to health; and we define health in relation to maintainability , ease , and functioning . Consideration of “maintainable-ease of functioning” will allow us to consider how not all “dis-ease” is bad (i.e. exposure to acute dis-ease/stress maintains healthy functioning in the long-term); and not all “ease” is good (i.e. avoidance of stress and prolonged “comfort” creates fragility seen in sedentary behavior). We propose that:
Dysfunction parallels a state of “dis-ease”; and prolonged -dysfunction parallels the state of Disease.
Function parallels a state of “ease”; and maintainable-ease of functioning parallels the state of Health.
This definition of health will be applied in the proceeding principles to integrate naturalistic and holistic perspectives of population health.
Principle 2: Health emerges from maintainable-ease of functioning at multiple levels . Maintainable-ease of functioning in the general population can be observed at the level of the cell , the self , and the society simultaneously
Cooperation across multiple levels of functioning is required for the organization and adaptation of living systems (Nowak and Sigmund, 2005 ; Antonucci and Webster, 2014 ). When developing an integrative model of health, it is important to consider how biological cells, individuals, and the larger society simultaneously play a role in population health (Xavier da Silveira dos Santos and Liberali, 2019 ; Antonucci and Webster, 2014 ). In this philosophy, we define health from three levels: cells , selves, and societies . What happens when these levels do not function in cooperation?
When the functioning of cells disrupts the functioning of the self, a state dis-ease in the self can follow. For example, prolonged dysfunction in autoimmune conditions can lead to prolonged dysfunction for the (individual’s sense of) self by triggering depression, decreased motivation, or anxiety (Lougee et al., 2000 ; Garud et al., 2009 ). The reverse can also be true. When the functioning of the self (i.e. one individual) disrupts the functioning of their cells, a state dis-ease in the cells can also follow. For example, prolonged sugar binging and addictive eating can lead to prolonged high blood sugar and pancreatic dysfunction seen in diabetes (De Koning et al., 2011 ; Imamura et al., 2015 ). Cells and selves are not separate.
When the functioning of the self disrupts the functioning of the society we observe a state dis-ease in the society. For example, one person’s unprotected sex with multiple partners can also lead to epidemics and social conflicts. The reverse can also be true. When the functioning of the society disrupts the functioning of the individual, a state dis-ease in the self can follow. For example, dysfunctional social conditions (as seen in Rutter, 1998 ), can lead to prolonged psychological and behavioral dysfunctions of individuals. Selves and societies are not separate.
When the functioning of society disrupts the functioning of cells, a state of dis-ease in the cells can also follow. For example, prolonged dysfunction in society in the form of misguided values about cleanliness, can lead to over-sanitization practices that create superbugs and antibiotic-resistant bacteria (Zaccheo et al., 2017 ; Finkelstein et al., 2014 ; Bower and Daeschel, 1999 ). The reverse can also be true. When the functioning of cells disrupts the functioning of the society, a state of dis-ease in the society can follow. Prolonged dysfunction in cells from naturally occurring parasites (e.g. Yersinia pestis [Cui et al., 2013 ]) can lead to prolonged dysfunctions like the economic collapse following 14th century Black Death (Haensch et al., 2010 ). Cells and societies are not separate.
What does health look like when these levels work together? Recent reports on the Blue Zones (i.e. the areas of the world where populations live significantly longer and healthier than the average) demonstrate that healthy functioning at these levels enhances physical longevity and mental wellbeing in populations (Buettner, 2012 ; Poulain et al., 2013 ). Buettner ( 2012 ) reports on how Blue-Zone populations intentionally and habitually enrich their physical bodies with healthy eating and physical activity. In addition to integrating physical and behavioral practices, these communities also integrate behavioral and social practices, such as, goal-setting, meditations/prayer, social engagement, pursuit of purpose, and community gathering. Humor is used by individuals and groups as a means to practice ease when challenges present themselves (Buettner, 2012 ). Blue Zone communities place value upon physical/natural, behavioral and social processes, generating them intentionally and habitually.
Both states of ease and dis-ease can teach us about the contributions of cells, selves, and societies to population health. Although it is important to be able to observe the levels separately to describe their contributions, it is also important to consider how the levels integrate to impact healthy publics. We acknowledge that meaningful changes can be observed above and below these levels (e.g. at the level of the biosphere and genome). However, this initial paper will introduce levels that are most proximal and accessible to the experience of a general readership (Fig. 1 ).
Principle 3: Health emerges from systems whose primary purpose is to generate maintainable-ease of functioning at a respective level
We propose that systems exist at each level with the purpose of generating maintainable-ease of functioning at that level. The biological immune system, an individual’s system of health behaviors, and the social system will be observed as systems that generate maintainable-ease of functioning in cells, selves, and societies respectively (Fig. 2 ).
Principle 3a: The biological immune system is directly responsible for maintainable-ease of functioning at the level of the cell
Throughout the course of human evolution, the complexity and biodiversity of the human body continued to increase (Rodríguez et al., 2012 ). What keeps the trillions of cells and microorganisms in cooperation in a human body? The biological immune system maintains functional cells (Rodríguez et al., 2012 ). Although it is documented that the functioning of the biological immune system has implications for behavioral functioning (Ader, 1974 , 2000 ; Johnston et al., 1992 ; CDC, 2016 ) and social functioning (CDC, 2016 ; Reidel, 2005 ; Cutler and Miller, 2005 ) the system’s primary purpose is supporting functioning in the cellular/biological system.
Principle 3b: Health behavior is directly responsible for maintainable-ease of functioning at the level of the self
Throughout the course of time, the complexity of human behavior, has continued to increase (Boulding and Khalil, 2002 ). What keeps an individual in a state of balance during times of rapid change? One’s system of health behaviors (e.g. one’s practices of breathing, drinking, eating, and moving) maintain a functional self. Although it is well documented that the behavior of the individual impacts biological functioning (Fadel, 2013 , 2015 ) and social functioning (Omer et al., 2009 ), one’s system of health behaviors directly impacts one’s experience of (or one’s ‘sense of’) their “self”.
Principle 3c: The social system is directly responsible for maintainable-ease of functioning at the level of the society
Throughout history, the social diversity of human societies continued to increase. During periods of rapid increases in social diversity and cultural integration, what supported cooperation in the society? Social systems (e.g. public governments, private social organizations, religious/spiritual organizations) emerge to maintain a functional society. Although it is well documented that a social system can impact biological functioning (CDC, 2016 ; Riedel, 2005 ; Cutler and Miller, 2005 ) and behavioral functioning (Buettner, 2012 ), the social system’s primary role is to maintain functions at the level of the society.
Principle 3d: By considering health as maintainable-ease of functioning generated by systems , we have the ability generalize health across levels
To observe health at the level of the cell, the self, and the society simultaneously, we consider systems that support maintainable-ease of biological, behavioral, and social functioning. The biological immune system, an individual’s system of health behaviors, and the social system make meaningful contributions to the functioning of cells, selves, and societies, respectively. While these systems are not the only systems that impact each level (e.g. one’s cardiovascular system impacts cells, one’s “personality” impacts the self, the environment impacts society), the biological immune system, health behavior, and the social system have great implications for population health from their respective levels; and they can be operationalized at these levels based upon their functions .
By considering health as maintainable-ease of functioning (rather than maintained biological structures) at multiple levels, we set a point of reference from which to integrate important determinants of population health. When taking the structuralist’s perspective, the biological immune system, health behavior, and social systems appear as distinctly separated. When taking a functionalist’s perspective, the biological immune system (i.e. the integration of host defense functions and microbiota functions), one’s (system of) health behaviors (i.e. the integration of decision-making/executive functions and habits/habitual life functions), and the social system (i.e. the integration of population values and population behaviors) appear together in A Philosophy of Health.
Principle 4: Each system employs two general functions— variation and precision —to generate maintainable-ease of functioning at a level
The functionalist perspective allows us to observe systems based upon their functions . The biological immune system will be observed as an integration of host defense functions and microbiota functions (Hooper and Littman Macpherson, 2012 ); (2) an individual’s system of health behaviors will be observed as an integration of decisions/executive functions and habits/habitual life functions (de Bruin et al., 2016 ; Verplankern, 2005 ; Norman et al., 1998 ; Prochaska et al., 1994 ; Prochaska et al., 1991 ); and the social system will be observed as an integration of actively functioning values and population-wide behaviors that function in relation to those values (Dowling and Pfeffer, 1975 ; Cotgrove and Duff, 1981 ).
By researching the role of these functions at each level, we distilled two general functions of each system: variation and precision. Variation appears in the functions of each system that generate a range of abilities, the “varied-abilities”, that sustain health in presently changing conditions. The microbiota, habits/habitual life functions and population behaviors will be observed (in Principle 4a) as the variation-functions of the biological immune system, health behavior, and the social system, respectively. Precision appears in those functions that prioritize and organize the patterns of variation that can sustain health at a level in future, changing conditions. The host-defense functions, decision-making/executive functions, and values systems will be observed (in Principle 4b) as the precision-functions in the biological immune system, health behavior, and the social system, respectively.
Consideration of a complementary relationship among precision and variation is not novel. Precision and variation have been discussed as central to the development of neural and biological systems (Hiesinger and Bassem, 2018 ). Discussions of precision and variation have also provided important insight into research on the biological immune system (Albert-Vega et al., 2018 ; Brodin et al., 2015 ). Through this philosophy, one can go beyond biological systems to observe how precision (in the form of host-defense functions, decision-making/executive functions, and values) and variation (in the form of microbiota functions, habits/habitual life functions, and population-wide behaviors) integrate to generate to maintainable-ease of functioning in cells, selves, and societies simultaneously (Fig. 3 ).
Principle 4a: Variation is responsible for generating the range of abilities, the “varied-abilities”, that can express ease-of-functioning in presently changing conditions
Without functional variation, life is fragile because the present environment is always changing (Taleb and Blyth, 2011 ). Fragile systems’ inability to experience changing conditions (in part) relates to limited variability. Conversely, adaptive system’s ability to experience changing conditions (in part) relates to functional variability (Taleb, 2012 ). When one microorganism in the microbiome takes over, biological fragility reflects a state of infection. When one habit takes over, behavioral fragility reflects a state of an addiction/dependence. When one population behavior takes over (e.g. when economic participation or access to food is restricted to a small percentage of the population) social fragility reflects a state of social/civil unrest.
The human microbiota is comprised of trillions of microorganisms, such as bacteria, fungi, and viruses. When variability in the human microbiota exists, an ease of functioning, or “homeostasis” in cells can be expressed in the present biological/ecological environment (Parfrey and Knight, 2012 ; Bogaert et al., 2011 ; Claesson et al., 2011 ). Research demonstrates that variation in the microbiota impacts the health of human cells by metabolizing complex carbohydrates, converting proteins to neural signals, and modulating diurnal rhythms that maintain biological homeostasis (Clemente et al., 2012 ; Rothe and Blaut, 2012 ; Blaut and Clavel, 2007 ; De Vadder et al., 2014 ). When variation in the microbiota is dramatically limited or changed (e.g. following antibiotic overuse), cellular tissue in the human body is fragile and vulnerable to infections, allergies, and inflammatory outbreaks (Francino, 2016 ).
When one’s habitual life functions (e.g. breathing, drinking, eating, and moving) and one’s healthy habits (e.g. one’s weekly exercise schedule, or weekly meal preparation) can be expressed freely, an ease of functioning is felt by one-self in the present environment. When life functions are no longer expressed with ease (e.g. breathing and movement are compromised due to prolonged sedentary lifestyle), or when a single habit takes over one’s lifestyle (e.g. smokes breaks “must” occur every 30 min), an individual is vulnerable to stressful outbreaks and chronic states (Al’Absi, 2011 ; Conrad et al., 2007 ; Suess et al., 1980 ; León and Sheen, 2003 ; Parrott, 1999 ; Koob, 2008 ).
When the basic human rights in a society are preserved in the present (e.g. right to life, freedom of speech; right to property), human populations have the ability to freely engage in the population - wide behaviors (e.g. health behaviors, social behaviors, economic behaviors) that support a functioning society. Health behaviors drive health and longevity. Social behaviors drive communication and cooperation. Economic behaviors drive goods and resources. When these population-wide behaviors are chronically restricted in a population (e.g. poor access to health care, oppression of free-speech, economic crash), societies become vulnerable to social/civil unrest [as commented historically by Victor Frankl ( 1985 ), Alexander Solzhenitsyn ( 2003 ), Franklin D. Roosevelt ( 1941 ), and Dr. Martin Luther King ( 1985 )].
Variation is essential so that a system has varied-abilities that can express ease-of-functioning in present environmental conditions . Dramatic and prolonged restrictions to variation in the microbiota, habits/habitual life functions, and population-wide behaviors characterize fragile and vulnerable states in cells, selves, and societies. Conversely, functional-variation supports resilience, robustness, and antifragility (Taleb, 2012 ). This does not mean that infinite variation is desirable; however, in this philosophy, precision is responsible for organizing expressions of variation so that the system does not degrade into unpredictably random variation or chaos (see Principle 4b).
Principle 4b: Precision is responsible for prioritizing and organizing the patterns of variation that maintain ease-of-functioning in future, changing conditions
Some environmental changes are too challenging for ease to be expressed in the present. However, following an exposure to challenging conditions, some systems adapt and become more functional (Taleb, 2012 ). Without the ability to functionally organize after stressors, a system degrades into disorder or chaos over time. Host-defense functions, decision-making/executive functions and values systems prioritize and organize variation in the microbiota, habits/habitual life functions, and population behaviors respectively.
When a pathogen invades the biological system, precise responses must occur to organize this potentially chaotic situation. At the level of the cell, a functional host-defense system (comprised of the innate, adaptive and complement immune system branches) organizes the biological system so that functional invaders (i.e. symbionts) and healthy cells are maintained and dysfunctional invaders (i.e. pathogens) and damaged cells are removed (Hoeb et al., 2004 ; Janeway, 1992 ; Janeway and Medzhitov, 2002 ; Janeway et al., 2014 ). When precision is dysfunctional, the host-defense system may (1) fail to prioritize responses to a costly invasion, leading to a state of infection; or (2) the host-defense system might prioritize dysfunctional responses to the cells of body that prolong a state of autoimmunity (Naor and Tarcic, 1982 ).
When a bad habit emerges, precise responses must occur to organize this potentially chaotic situation. At the level of the self, functional decision-making (or at smaller scales executive functioning) prioritizes and organizes behavior so that functional expressions of habit (or at smaller scales, habitual life functions) are prioritized regularly, and dysfunctional ones are replaced or minimized (de Bruin et al., 2016 ; Prochaska et al., 1994 ; Prochaska and Prochaska, 2016 ; Prochaska et al., 1988 ; Redding et al., 2011 ; Weissenborn and Duka, 2003 ; Bickel et al., 2012 ). When dysfunctional, decisions may (1) fail to prioritize responses that remove a costly expression of habit (e.g. a teen started smoking cigarettes to “be cool” and now has to smoke in the bathroom before each class to get through the day; by not deciding to move at work, one’s breathing becomes shallow and movement becomes rigid); or decisions may (2) prioritize habits that prolong dysfunction despite knowing the dangerous consequences (e.g. an adult continues smoking cigarettes despite knowing the family’s history of lung cancer; an adolescent continues binge on sugar despite a diabetes diagnosis).
When dangerous population-wide behaviors threaten life in a society, precise responses must occur to organize this potentially chaotic situation. At the level of society, the agreed upon values organize the social system so that functional population behaviors are prioritized and dysfunctional population behaviors are minimized. Functional values prioritize behaviors that support the society (e.g. as seen when societies mandate that students get certain vaccines before attending University), while also setting standards that remove/replace behaviors that threaten the society (e.g. new laws create legal repercussions for risk behaviors in society). Without values that functionally prioritize population-wide behavior, society may (1) fail to prioritize responses to a dysfunctional population behavior (e.g. as seen during AIDS epidemic of the 1980s due to insufficient public health values around safe sex); or society may (2) prioritize dangerous behaviors that can prolong societal dysfunction (e.g. the antibiotic resistance crisis (Ventola, 2015 ; Michael et al., 2014 ) has been attributed in part to the over-valuing or over-use of antibiotic medications in healthcare practices).
Precision is essential so that a system can maintain ease-of-functioning in future, changing conditions . When precision does not adequately detect the presence of costly conditions, a response may not be prioritized (e.g. as seen during acute infection, addiction/dependence following a surgery, the AIDs outbreak in the 1980s). When precision prioritizes responses that prevent ease longitudinally, dysfunction is prolonged (e.g. autoimmunity, continued smoking despite family history of cancer, misguided values that create an antibiotic-resistant bacteria). Through dysfunctional -precision, the conditions for life in cells, selves, and societies becomes disordered over time. Through functional -precision, a system prioritizes responses that maintain ease-of-functioning in future conditions. Prioritizing functional microorganisms (i.e. symbionts) supports the developing life of cells; prioritizing functional habits (e.g. weekly exercise) and habitual life functions (e.g. diaphragmatic breathing and relaxed movement) supports the developing life of the self; and prioritizing functional population behaviors (e.g. access to functional health care, economic resources; access to social support) supports the developing life of the society.
Principle 5: Health is valued by a system when precision-and-variation generate maintainable-ease of functioning. Health is de-valued by a system when precision or variation prevent maintainable-ease of functioning
By defining precision-and-variation, we can better understand maintainable-ease of functioning in population health:
Functional-Variation generates ease-of-functioning in the present (e.g. fluid and variable motion reflects an ease and variability of one’s movement); while Functional-Precision prioritizes expressions that can maintain ease-of-functioning in the future (e.g. prioritizing challenging exercise for 20 min each day may lead to an ease in bodily movement long term).
Dysfunctional-Variation prevents ease-of-functioning in the present (e.g. prolonged sitting might lead to rigid movement and shallow breathing); while Dysfunctional-Precision might prioritize expressions that prevent ease in the future (e.g. rather than focus on relaxing breathing and movement on work breaks, one decides to drink alcohol to relax).
Without functional-variation, life is fragile and vulnerable to changing conditions of the present. Without functional-precision, life becomes disorganized from the system’s exposure to changing conditions across time. When functional-and-integrated, precision-and-variation value maintainable-ease of functioning in cells, selves, and societies. When dysfunctional or fragmented, precision or variation can de-value maintainable-ease of functioning in cells, selves, or societies. If maintainable-ease of functioning can be valued in cells, selves, and societies, we will likely observe healthy publics.
Five principles of health are presented: (1) Health is the maintainable-ease of functioning; (2) Maintainable-ease of functioning emerges from multiple levels ; (3) At each level, maintainable-ease of functioning is generated by systems ; (4) Each system employs two functions, precision - and - variation , that generate maintainable-ease of functioning ; and (5) Health is valued by a system if precision-and-variation generate maintainable-ease of functioning. Through these five principles, both naturalistic and holistic perspectives can be considered simultaneously because maintainable-ease of functioning is relevant to biological functioning (e.g. as described in BST) and personal/social, goal-oriented functioning (e.g. as described in HTH). This philosophy can also be used to investigate how naturalistic and holistic phenomena have informed past healthcare interventions. What do vaccine interventions, behavior change interventions, and social change interventions have in common? When successful, these interventions enhance both precision and variation.
Vaccine interventions can enhance both the precision of the host-defense functions and variation in the microbiome. During a vaccine intervention, the microbiome is exposed to a new variation in the form of a new virus (Reidel, 2005 ). Through this exposure, the precision of host defense functions can adapt to prioritize maintainable-ease of functioning in the microbiome in the future. How? The host-defense system produces antibodies that allow the immune system to respond effectively and efficiently to this virus when exposed to it again in the future (Janeyway, 2014 ). Although the precision of the immune system has been enhanced to handle historical threats through vaccines (e.g. for small pox, chickenpox, measles), new viruses like the coronavirus can still emerge. With this philosophy, vaccine developers and public health officials might not only ask the question, “How do we combat the coronavirus?” Researchers, vaccine developers and public health officials may also ask the functional question: “How do we enhance the precision of the host-defense system and the variation of the human microbiome to adapt following an exposure to the coronavirus?”
Behavior change interventions can enhance both the precision in one’s decisions and the variation in one’s habits. During a behavior change intervention, a person’s existing habits are exposed to a new variation in habit. For example, the beginning of a new exercise intervention exposes the individual’s current habits/habitual functioning to changes in movement and breathing (i.e. exercise) that may also change their patterns of eating and hydration. Through this exposure, a person’s decision-making might adapt to prioritize maintainable-ease of functioning in the individual’s lifestyle. How? Some behavior change interventions train one’s decision-making to remove or “counter-condition” unhealthy habits, by replacing them with healthy habits (Prochaska et al., 1988 ). Although modern behavior change interventions have shaped the precision of decision-making during health behavior change (e.g. of smoking, diet, alcohol use, inactivity), new problems for health behavior still emerge when the individual is exposed to a new, potentially addictive technology. With this philosophy, behavior change interventionists and health officials might not only ask the question, “How do we support good decision-making of individuals?” Researchers, behavior change technology developers, and public health officials may also ask the functional question: “How do we enhance the precision of one’s decisions and the variation of one’s habits following the exposure to a new, potentially addictive technology?”
Public health campaigns disseminated by social organizations can enhance the precision of the population’s health values and variation in population-wide health behaviors. Leading up to first Surgeon General’s Advisory Committee on Smoking and Health (1964), the U.S. Department of Health had become increasingly aware of (i.e. exposed to) variations in a population health behavior. If populations smoked, then populations were more likely to develop lung cancer, laryngeal cancer, or chronic bronchitis (CDC, 2018 ). Following this exposure to (the consequences of) population smoking behavior, society’s values shifted to prioritize health. How? The Federal Cigarette Labeling and Advertising Act of 1965 was adopted, and the Public Health Cigarette Smoking Act of 1969 was adopted to create new health values. This shift in values prioritized new variations in population health behavior by: (1) requiring a health warning on cigarette packages; (2) banning cigarette advertising in the broadcasting media; and (3) calling for an annual report on the health consequences of smoking (CDC, 2018 ). Since these first initiatives adult smoking rates have fallen from about 43% (in 1965) to about 18% today; and mortality rates from lung cancer, the leading cause of cancer death, are declining (Department of Health and Human Services, 2014 ). Although the precision of the population’s values has been enhanced to impact population behaviors (e.g. the tobacco laws described above supported healthy change), new chronic states can still emerge following exposure to social changes (e.g. the invention of the Juul impacted high school and college aged populations). With this philosophy, public policy officials and public health researchers might not only ask the question, “How do we create new laws to protect population health from nicotine addiction?” They may also ask the functional question: “How do we enhance the precision of the population’s values and the variation of the population’s behavior following the invention of a new nicotine delivery system technology (e.g. flavored Juuls)?”
Previously we described that without functional variation, life is fragile when exposed to present changing conditions; and without functional precision, life becomes disorganized from exposure to changing conditions across time. When successful, the above interventions upon biological, behavioral, and social functioning have a common theme: each facilitates exposures to biological, behavioral or social conditions that support (1) increasingly complex/diverse variation; and (2) increasingly organizable precision. Exposure, not avoidance , has facilitated population health in these interventions. While healthcare systematically prioritizes biological exposures in the form of vaccine interventions, they do not systematically prioritize behavioral or social exposures. However, it is documented that exposure to healthy behaviors in youth prevents risk behaviors in adolescence (Velicer et al., 2000 ); and exposure to community-based health initiatives can support population health (Dulin et al., 2018 ; CDC, 2018 ). Given that systematic biological exposures in the form of vaccination have led to a global control of some acute infectious diseases (Tangermann et al., 2007 ); might systematic behavioral and social exposures (especially in youth) be needed to enhance global campaigns toward the control of chronic disease?
A functional language of health is central to the success of a Philosophy of Health. Why? The levels are not separate, but rather are continuously connecting with one another. A good philosophy of health should have the ability to discuss assessment, diagnosis, intervention, and prevention across levels, across systems, across cultural populations, and across time. Using the common language of precision and variation creates discussions that connect the levels and integrate research disciplines.
A case (to) study: mental health as between-level functioning in this philosophy
Historically, and still too often, health professionals have an expertise at one level, that limits their prescription of interventions to that level. This can actually create barriers to a complete solution when a health problem is multileveled. While a person’s mental health is typically assessed based upon their first-person experience of thoughts, feelings, and behaviors; symptoms can be triggered by biological, physiological, behavioral, psychological, and/or social dysfunction. Most clinicians typically do not have the ability to assess and address all forms functioning. So if one person, John, is meeting with a clinician who specializes in primary care medicine, he may only be prescribed a biological intervention like medication. If John is meeting with a clinician who specializes in behavioral medicine, he may only be prescribed a health behavior change intervention. If John is meeting with a clinician who specializes in a certain theory of psychotherapy, he may only be prescribed a psychotherapy intervention based on the clinician’s training. If John is meeting with a clinician who specializes in social work, he may only be prescribed a group, community or social intervention. While the above specializations have been helpful in establishing an empirical bases for mental health interventions, over-specialization can be problematic when a multi-leveled solution is needed. In addition, it can also be problematic when a level-specific solution is needed that the clinician cannot provide (e.g. when psychotherapy is needed but a clinician only has the ability to prescribe psychiatric medication).
Technology poses a multileveled issue for population mental health in 2020. Selves have more social connection then ever in history, yet societies are characterized by increasing rates of depression and loneliness (Sum et al., 2008 ; Hammond, 2020 ; Srivastava and Tiwari, 2013 ; Twenge, 2017 ). Researchers might use this Philosophy of Health to facilitate between-level conversations that address seemingly paradoxical outcomes that emerge during this new age of rapid technological growth. To do this, a researcher might first begin by asking questions about functioning at each level ; second , ask questions about processes between the levels ; and third , concurrently ask questions at and between levels .
First: Begin by asking questions at each level
Novel challenges face the iGeneration (and their parents) due to technology’s novel impacts on the development of individual and social functioning (Twenge, 2017 ). For example, if John’s decisions (self-precision) and habits (self-variation) remain consistent during school hours because his parents do not let him have a phone; but his class’ social behaviors around him (society-variation) change dramatically because everyone else at school uses the newest smartphone application to talk during class; will John’s mental health suffer? Although his parents’ intentions are to protect John, the contrast between his behavior (self’s precision-and-variation) and the population social behavior (society-variation) can impact John’s health. Notice here how we have not yet considered functions that connect the self to the society (e.g. John’s thoughts and feelings). Rather we first consider (or contrast) functioning at the level of the self (i.e. John’s decisions-and-habits) and the society (i.e. population social behavior) in accordance with Principles 1–5 (see Figs 1 – 3 ).
Second: Look for functional processes that connect the levels
One person’s thoughts and emotions/feelings are processes that help to integrate the functioning of one-self within the functioning of a society. How might John’s thoughts and feelings connect his (sense of) self to his society? Perhaps John’s parents teach him that it is important to feel separate from his classmates during class so he can think clearly in class; and that he can feel connected to his friends by inviting them over to communicate together after school. This parenting may impact John’s thoughts and feelings during school. If John’s parents do not talk with him about this topic, John may experience different thoughts and feelings during school hours. When kept to one-self, thoughts and emotions are foundational to an internal sense of self as one functions in the larger society; and, when acted upon, thoughts and feelings can become verbal communication (e.g. speech) and non-verbal communication (e.g. body language, facial expressions) that form an external sense of self that is visible to the society. The (internal) experience of and (external) communication of thoughts, feelings and actions form the foundation of all systems of psychotherapy (Prochaska and Norcross, 2018 ). This view can be particularly helpful as researchers begin to investigate how smart technology impacts developmental changes to the self within the society beginning in youth.
Third: Concurrently ask questions at and between levels
Perhaps, a clinical researcher is interested in investigating protective mental health factors in the iGeneration; and they hypothesize that lower rates of loneliness, anxiety, and depression will be seen in subjects that do not respond to text messages immediately. The researcher might investigate further by using the philosophy to develop questions for the research subjects: “(1) Do you use conscious decision-making (self-precision) to prevent yourself from habitually responding to your phone when a text appears (self-variation)? (2) How fast do other’s in your social group typically respond to texts (society-variation)? (3) What changes in thoughts and feelings are experienced (internal self-society connection) after you communicate via text (external self-society connection)?” Perhaps this researcher also wants to investigate how those who are addicted to the technology perceive non-responders. The clinical researcher might again apply the philosophy: “(1) How fast do other’s in your social group typically respond to your texts (society-variation)? (2) Do you experience changes in thought and feeling (internal self-society connection) when others do not respond to you within an hour (society-variation)? (3) How do you communicate those thoughts and feelings (external self-society connection) with others when they do not respond for a prolonged period of time (society-variation)?” Future research might use this method to gather and organize levels of information on mental health factors across different self- and societal-conditions.
The processes that form our mental health form a functional connection between self and society. If mental health is a reflection of the self–society connection, what might be a reflection of the self–cell connection? Physiological health evidences a functional connection between our sense of self and our cells. For example, aerobic exercise is a health behavior that stimulates changes to variations in breathing and movement. By engaging in this behavior, the biological cells of the body are also stimulated via various physiological processes. Breathing will stimulate cellular functioning via the cardiovascular and respiratory systems; and movement will stimulate cellular functioning via the cardiovascular, musculoskeletal, and central nervous systems. While all physiological systems are working in collaboration in the body, certain changes to behavioral and biological functioning will stimulate certain physiological systems. By viewing health through this lens, between-level observations join the philosophy: biological functions emerge at the level of the cell; physiological functioning emerges as the cell–self connection; behavioral functions emerge at the level of the self; psychological/mental functioning emerges as the self–society connection; and social functions emerge at the level of the society. Future papers will explore maintainable-ease of functioning at and between levels.
Future directions: new images of healthcare integration and new perspectives of healthcare innovation
By considering this integrative philosophy, one can define health based upon a tangible connectedness, rather than separateness, of cells, selves, and societies. We provide Image 4 as a way to visualize the common paths to the health of healthy publics. When researchers observe that a host defense system is changing cellular functions following an infection, they may also expect these changes to have an impact [along Path 1] on expressions of habitual or physiological functions (e.g. immune function can stimulate the sensation of “achiness” or “pain” altering one’s physical movement, breath rate, hydration, and hunger) (Kelley, 2003 ; Johnson et al., 1992 ; Danzer, 2009 ). When researchers observe an individual deciding to engage in health behavior change following an addiction, they may also expect these changes to have an impact [along Path 2] on the group-behavior of their family system or social systems. When researchers observe changes to society’s values following a newly detected problem (e.g. laws ban Cigarette Advertising in broadcasting media; public health standards mandate certain vaccines before attending school), they may also expect that these changes can have an impact on behavioral functions of individuals [along Path 2] and biological functions of cells/organs [along Path 3]. These levels are continually integrating along these common paths to the health of healthy publics (Fig. 4 ).
When attending to this connectedness new, important questions can have new answers. What function does modern technology serve in population health and healthcare? If technology algorithms prioritize variations in population behaviors, then they fulfill a role as society-level precision. When modern technologies like machine learning (ML) technology and Computer Tailored Interventions (CTI) prioritize patterns of population behavior, we can see profound impacts on social change in a society. Although one might argue that technologies can be used by individual-level functions, the algorithms that are currently deployed and updated on devices interface with big-data gathered on population behaviors (Manogaran and Lopez, 2017 ; Dinov, 2016 ; Mullainathan and Spiess, 2017 ; Cheng et al., 2017 ).
In this paper, we identified that precision can be functional or dysfunctional. Similarly, technologies can support or prevent healthy population behavior. Some technologies prioritize health behavior in populations by tracking physical activity and providing feedback on activity progress; while others prevent healthy behavior by prioritizing sedentary behavior through video-gaming. Some social media technologies facilitate social communication with distant friends and relatives that supports wellbeing; while others facilitate conflictual communication that diminishes wellbeing. Given that modern technology can support or hinder health, we believe it is important that healthcare can prioritize technological innovations that value health in cells, selves, and societies. To do this, technology innovators might seek to value a higher order construct (e.g. maintainable-ease of functioning) in their algorithms.
Medical technology is currently used to titrate the doses of vaccines so that maintainable-ease of biological functioning (i.e. inoculation) is made available to the general population. When biological exposures are not properly titrated, infections can become active in the population and health is no longer valued at the level of the cell. Similarly, when behavioral and social exposures are not tailored to the needs of individuals and groups, populations can become resistant to healthy change, and health is no longer valued at the level of the self and the society. Behavior change researchers Prochaska and Prochaska ( 2016 ) report that when individuals and populations are not ready for a change, interventions that force individuals or populations to take action can increase resistance and prolong dysfunction. By tailoring (or what they term “staging”) behavioral and social level interventions, Computer Tailored Interventions upon behavioral and social functioning are made possible (Prochaska et al., 2001 ; Velicer et al., 2000 , Prochaska and Prochaska, 2016 ). Despite these advances, there remains a need for technological advances that can make maintainable-ease of behavioral and social functioning available to the general population.
Future healthcare interventions could benefit from ML algorithms that tailor behavioral and social exposures to enhance precision-and-variation. Research already demonstrates that tailoring interventions for biological precision (Albert-Vega et al., 2018 ) and biological variation (Brodin et al., 2015 ) can impact long-term biological functioning. Future innovations might seek to use technology to tailor behavioral and social interventions to generate maintainable-ease of functioning. Through the functional language used in this paper we hope readers are inspired to present new questions, new comments, and new perspectives about needed healthcare innovations.
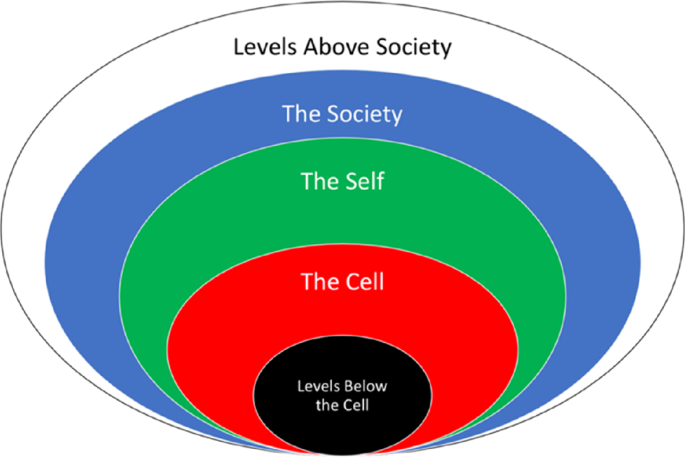
This philosophy of health investigates three levels of health: cell, self, and society. The level of the cell accounts for biological functioning within human beings. The level of the self accounts for first-person functioning of each human being. The level of the society accounts for group functioning of human beings.
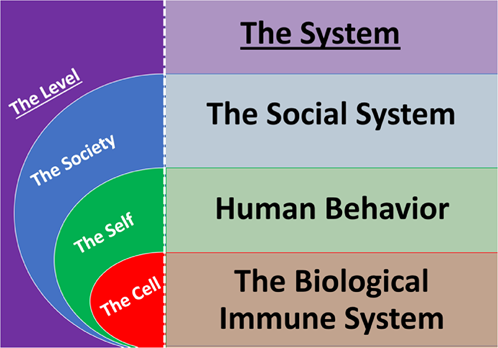
Each system is responsible for generating maintainable-ease of functioning at a level. The biological immune system is responsible at the level of the cell. A human's system of health behaviors is responsible at the level of the self. The social system is responsible at the level of the society.
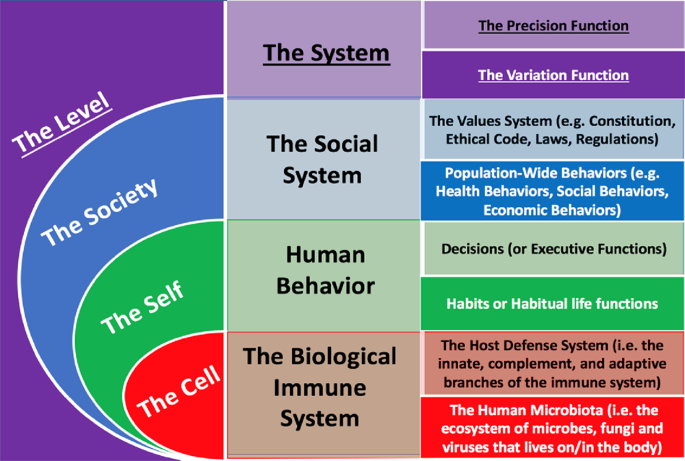
Maintainable-ease of functioning is generated by two functions in each system: precision and variation. The human microbiota, habits, and population-wide behaviors evidence variation in cells, selves and societies respectively. The host defense system, decisions, and values evidence precision in cells, selves and societies respectively.
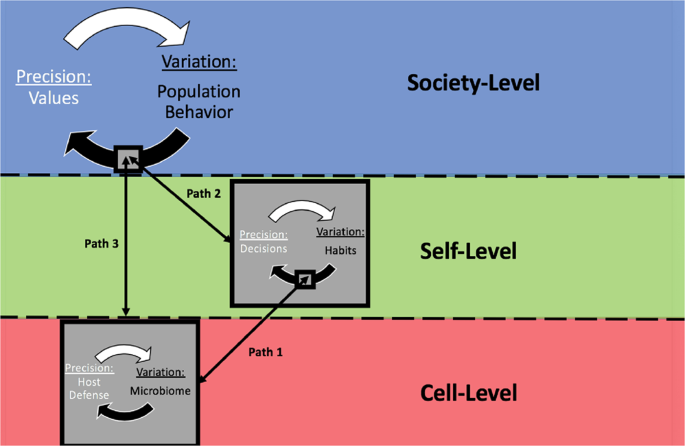
Population health is generated along common paths that integrate the levels. The biological functioing of cells impacts fluctuations of habits/habitual functioning; and vice versa. The behavioral functioning of each self impacts fluctuations in population behavior; and vice versa. The biological functioning of cells also can impact fluctations in population behavior; and vice versa.
Ader R (1974) Behaviorially conditioned immunosuppression. Psychosom Med 36(2):183–184
Article CAS PubMed Google Scholar
Ader R (2000) On the development of psychoneuroimmunology. Eur J Pharmacol 405(1–3):167–176
Al’Absi M (2011) Stress and addiction: biological and psychological mechanisms. Elsevier
Albert-Vega C, Tawfik DM, Trouillet-Assant S, Vachot L, Mallet F, Textoris J (2018) Immune functional assays, from custom to standardized tests for precision medicine. Front Immunol 9:2367
Article CAS PubMed PubMed Central Google Scholar
Antonucci TC, Webster NJ (2014) Rethinking cells to society. Res Hum Dev 11(4):309–322
Article PubMed PubMed Central Google Scholar
Bickel WK, Jarmolowicz DP, Mueller ET, Gatchalian KM, McClure SM (2012) Are executive function and impulsivity antipodes? A conceptual reconstruction with special reference to addiction. Psychopharmacology 221(3):361–387
Blaut M, Clavel T (2007) Metabolic diversity of the intestinal microbiota: implications for health and disease. J Nutr 137(3):751–755
Article Google Scholar
Bogaert D, Keijser B, Huse S, Rossen J, Veenhoven R, Van Gils E, Bruin J, Montijn R, Bonten M, Sanders E (2011) Variability and diversity of nasopharyngeal microbiota in children: a metagenomic analysis. PLoS ONE 6(2):e17035
Article ADS CAS PubMed PubMed Central Google Scholar
Boorse C (1997) A rebuttal on health. In: What is disease? Humana Press, Totowa. Springer. pp. 1–134
Boulding K, Khalil E (2002) Evolution, order and complexity. Routledge
Bower CK, Daeschel MA (1999) Resistance responses of microorganisms in food environments. Int J food Microbiol 50(1-2):33–44
Brodin P, Jojic V, Gao T, Bhattacharya S, Lopez Angel CJ, Furman D, Shen-Orr S, Dekker CL, Swan GE, Butte AJ, Maecker HT, Davis MM (2015) Variation in the human immune system is largely driven by non-heritable influences. Cell 160(1–2):37–47
Buettner D (2012) The blue zones: 9 lessons for living longer from the people who’ve lived the longest. National Geographic Books
Centers for Disease Control and Prevention (2016) CDC history of smallpox. https://www.cdc.gov/smallpox/history/history.html
Centers for Disease Control and Prevention (2018) History of the Surgeon General’s reports on smoking and health 2(28), 07. https://www.cdc.gov/tobacco/data_statistics/sgr/history/index.htm
Chartier G, Cawthorpe D (2016) From ‘Big 4’to ‘Big 5’: a review and epidemiological study on the relationship between psychiatric disorders and World Health Organization preventable diseases. Curr Opin Psychiatry 29(5):316–321
Article PubMed Google Scholar
Cheng Q, Li TM, Kwok CL, Zhu T, Yip PS (2017) Assessing suicide risk and emotional distress in Chinese social media: a text mining and machine learning study. J Med Internet Res 19(7):e243
Claesson MJ, Cusack S, O'Sullivan O, Greene-Diniz R, de Weerd H, Flannery E (2011) Composition, variability, and temporal stability of the intestinal microbiota of the elderly. Proc Natl Acad Sci USA 108:4586–4591
Article ADS PubMed Google Scholar
Clemente JC, Ursell LK, Parfrey LW, Knight R (2012) The impact of the gut microbiota on human health: an integrative view. Cell 148(6):1258–1270
Conrad A, Müller A, Doberenz S, Kim S, Meuret AE, Wollburg E, Roth WT (2007) Psychophysiological effects of breathing instructions for stress management. Appl Psychophysiol Biofeedback 32(2):89–98
Cotgrove S, Duff A (1981) Environmentalism, values, and social change. Br J Sociol 1:92–110
Cui Y, Yu C, Yan Y, Li D, Li Y, Jombart T, Weinert LA, Wang Z, Guo Z, Xu L, Zhang Y (2013) Historical variations in mutation rate in an epidemic pathogen, Yersinia pestis. Proc Natl Acad Sci 110(2):577–582
Cutler D, Miller G (2005) The role of public health improvements in health advances: the twentieth-century United States. Demography 42(1):1–22
Dansinger ML, Gleason JA, Griffith JL, Selker HP, Schaefer EJ (2005) Comparison of the atkins, ornish, weight watchers, and zone diets for weight loss and heart disease risk reduction. JAMA 293(1):43
Dantzer R (2009) Cytokine, sickness behavior, and depression. Immunol Allergy Clin North Am 29(2):247–264
Daubenmier JJ, Weidner G, Sumner MD, Mendell N, Merritt-Worden T, Studley J, Ornish D (2007) The contribution of changes in diet, exercise, and stress management to changes in coronary risk in women and men in the Multisite Cardiac Lifestyle Intervention Program. Ann Behav Med 33(1):57–68
de Bruin EI, van der Zwan JE, Bögels SM (2016) A RCT comparing daily mindfulness meditations, biofeedback exercises, and daily physical exercise on attention control, executive functioning, mindful awareness, self-compassion, and worrying in stressed young adults. Mindfulness 7(5):1182–1192
De Koning L, Malik VS, Rimm EB, Willett WC, Hu FB (2011) Sugar-sweetened and artificially sweetened beverage consumption and risk of type 2 diabetes in men. Am J Clin Nutr 93(6):1321–1327
De Vadder F, Kovatcheva-Datchary P, Goncalves D, Vinera J, Zitoun C, Duchampt A, Bäckhed F, Mithieux G (2014) Microbiota-generated metabolites promote metabolic benefits via gut–brain neural circuits. Cell 156(1–2):84–96
Dinov ID (2016) Volume and value of big healthcare data. J Med Stat Inform 4(1):3
Dowling J, Pfeffer J (1975) Organizational legitimacy: social values and organizational behavior. Pac Sociol Rev 18(1):122–136
Dulin A, Risica PM, Mello J, Ahmed R, Carey KB, Cardel M, Howe CJ, Nadimpalli S, Gans KM (2018) Examining neighborhood and interpersonal norms and social support on fruit and vegetable intake in low-income communities. BMC Public Health 18(1):455
Edington DW (2009). Zero trends: health as a serious economic strategy. UM-HMRC
Fadel PJ (2013) Neural control of the circulation during exercise in health and disease Front Physiol 4:224
Fadel PJ (2015) Reflex control of the circulation during exercise. Scand J Med Sci sports 25:74–82
Finkelstein JA, Dutta-Linn M, Meyer R, Goldman R (2014) Childhood infections, antibiotics, and resistance: what are parents saying now? Clin Pediatr 53(2):145–150
Francino MP (2016) Antibiotics and the human gut microbiome: dysbioses and accumulation of resistances. Front Microbiol 6:1543
Frankl VE (1985) Man’s search for meaning. Simon and Schuster
Garud S, Leffler D, Dennis M, Edwards‐George J, Saryan D, Sheth S, Schuppan D, Jamma S, Kelly CP (2009) Interaction between psychiatric and autoimmune disorders in coeliac disease patients in the Northeastern United States. Aliment Pharmacol Ther 29(8):898–905
Haensch S, Bianucci R, Signoli M, Rajerison M, Schultz M, Kacki S, Vermunt M, Weston DA, Hurst D, Achtman M, Carniel E (2010) Distinct clones of Yersinia pestis caused the black death. PLoS Pathog 6(10):e1001134
Hammond C (2020) https://www.bbc.co.uk/programmes/articles/2yzhfv4DvqVp5nZyxBD8G23/who-feels-lonely-the-results-of-the-world-s-largest-loneliness-study
Hiesinger PR, Hassan BA (2018) The evolution of variability and robustness in neural development. Trends Neurosci 41(9):577–586
Hooper LV, Littman DR, Macpherson AJ (2012) Interactions between the microbiota and the immune system. Science 336(6086):1268–1273
Imamura F, O’Connor L, Ye Z, Mursu J, Hayashino Y, Bhupathiraju SN, Forouhi NG (2015) Consumption of sugar sweetened beverages, artificially sweetened beverages, and fruit juice and incidence of type 2 diabetes: systematic review, meta-analysis, and estimation of population attributable fraction. BMJ 351:h3576
Janeway CA (1992) The immune system evolved to discriminate infectious nonself from noninfectious self. Immunol Today 13(1):11–16
Janeway CA, Medzhitov R (2002) Innate immune recognition. Annu Rev Immunol 20(1):197–216
Janeway Jr CA, Travers P, Walport M, Shlomchik MJ (2014) Immunobiology: the immune system in health and disease, vol. 2001. Garland Science, New York, pp. 620–626
Google Scholar
Johnson EO, Kamilaris TC, Chrousos GP, Gold PW (1992) Mechanisms of stress: a dynamic overview of hormonal and behavioral homeostasis. Neurosci Biobehav Rev 16(2):115–130
Kelley KW, Bluthé RM, Dantzer R, Zhou JH, Shen WH, Johnson RW, Broussard SR (2003) Cytokine-induced behavior. Brain Behav Immun 17(1):112–118
King ML (1985) I have a dream: a speech. Thee Hellbox Press
Koob GF (2008) A role for brain stress systems in addiction. Neuron 59(1):11–34
León P, Sheen J (2003) Sugar and hormone connections. Trends Plant Sci 8(3):110–116
Li Y, Pan A, Wang DD, Liu X, Dhana K, Franco OH, Kaptoge S, Di Angelantonio E, Stampfer M, Willett WC, Hu FB (2018) Impact of healthy lifestyle factors on life expectancies in the US population. Circulation 138(4):345–355
Lougee L, Perlmutter SJ, Nicolson R, Garvey MA, Swedo SE (2000) Psychiatric disorders in first-degree relatives of children with pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS). J Am Acad Child Adolesc Psychiatry 39(9):1120–1126
Manogaran G, Lopez D (2017) A survey of big data architectures and machine learning algorithms in healthcare. Int J Biomed Eng Technol 25(2–4):182–211
Michael CA, Dominey-Howes D, Labbate M (2014) The antimicrobial resistance crisis: causes, consequences, and management. Front Public Health 2:145
Mokdad AH, Ballestros K, Echko M, Glenn S, Olsen HE, Mullany E, Lee A, Khan AR, Ahmadi A, Ferrari AJ, Kasaeian A (2018) The state of US health, 1990–2016: burden of diseases, injuries, and risk factors among US states. JAMA 319(14):1444–1472
Mullainathan S, Spiess J (2017) Machine learning: an applied econometric approach. J Econ Perspect 31(2):87–106
Naor D, Tarcic N (1982) Control of autoimmune responses induced with modified self antigens. Ann NY Acad Sci 392(1):178–190
Article ADS CAS PubMed Google Scholar
Nordenfelt L (2007) The concepts of health and illness revisited. Med Health Care Philos 10(1):5
Norman GJ, Velicer WF, Fava JL, Prochaska JO (1998) Dynamic typology clustering within the stages of change for smoking cessation. Addict Behav 23(2):139–153
Nowak MA, Sigmund K (2005) Evolution of indirect reciprocity. Nature 437(7063):1291–1298
Omer SB, Salmon DA, Orenstein WA, Dehart MP, Halsey N (2009) Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. N Engl J Med 360(19):1981–1988
Parfrey LW, Knight R (2012) Spatial and temporal variability of the human microbiota. Clin Microbiol Infect 18:5–7
Parrott AC (1999) Does cigarette smoking cause stress? Am Psychol 54(10):817
Poulain M, Herm A, Pes G (2013) The Blue Zones: areas of exceptional longevity around the world. Vienna Yearb Popul Res 11(1):87–108
Prochaska JO, Norcross JC, DiClemente CC (1994) Changing for good. Avon Books, New York
Prochaska JO, Velicer WF, DiClemente CC, Fava J (1988) Measuring processes of change: applications to the cessation of smoking. J Consult Clin Psychol 56(4):520
Prochaska JO, Velicer WF, Guadagnoli E, Rossi JS, DiClemente CC (1991) Patterns of change: dynamic typology applied to smoking cessation. Multivar Behav Res 26(1):83–107
Article CAS Google Scholar
Prochaska JO, Velicer WF, Fava JL, Rossi JS, Tsoh JY (2001) Evaluating a population-based recruitment approach and a stage-based expert system intervention for smoking cessation. Addict Behav 26(4):583–602
Prochaska JO, Norcross JC (2018) Systems of psychotherapy: a transtheoretical analysis. Oxford University Press
Prochaska JO, Prochaska JM (2016) Changing to thrive: using the stages of change to overcome the top threats to your health and happiness. Simon and Schuster
Redding CA, Prochaska JO, Paiva A, Rossi JS, Velicer W, Blissmer BJ, Greene GW, Robbins ML, Sun X (2011) Baseline stage, severity, and effort effects differentiate stable smokers from maintainers and relapsers. Subst Use Misuse 46(13):1664–1674
Riedel S (2005) Edward Jenner and the history of smallpox and vaccination. In: Baylor University Medical Center Proceedings, January 1, vol. 18(1). Taylor & Francis, pp. 21–25
Rodríguez RM, López-Vázquez A, López-Larrea C (2012) Immune systems evolution. Sensing in nature. Springer, New York, pp. 237–251
Book Google Scholar
Roosevelt FD (1941) Message to congress. Retrieved 20 Mar 2012
Rothe M, Blaut M (2012) Evolution of the gut microbiota and the influence of diet. Benef Microbes 4(1):31–37
Rutter M (1998) Developmental catch-up, and deficit, following adoption after severe global early privation. J Child Psychol Psychiatry 39(4):465–476
Schroeder SA (2012) Rethinking health: healthy or healthier than? Br J Philos Sci 64(1):131–159
Solzhenitsyn A (2003) The Gulag Archipelago, 1918–56: an experiment in literary investigation. Random House
Srivastava A, Tiwari RP (2013) Effect of excess use of cell phone on adolescent’s mental health and quality of life. Int Multidiscip e-J 2(1):1–0
Suess WM, Alexander AB, Smith DD, Sweeney HW, Marion RJ (1980) The effects of psychological stress on respiration: a preliminary study of anxiety and hyperventilation. Psychophysiology 17(6):535–540
Sum S, Mathews RM, Hughes I, Campbell A (2008) Internet use and loneliness in older adults. CyberPsychol Behav 11(2):208–211
Taleb NN, Blyth M (2011) The black swan of Cairo: how suppressing volatility makes the world less predictable and more dangerous. Foreign Aff 2011:33–39
Taleb NN (2012) Antifragile: things that gain from disorder. Random House Incorporated
Tangermann RH, Nohynek H, Eggers R (2007) Global control of infectious diseases by vaccination programs. In: Pediatric infectious diseases revisited: Birkhäuser advances in infectious diseases BAID, Springer. vol. 1. pp. 1–41
Twenge JM (2017) iGen: Why today’s super-connected kids are growing up less rebellious, more tolerant, less happy–and completely unprepared for adulthood–and what that means for the rest of us. Simon and Schuster.
US Department of Health and Human Services (2014) The health consequences of smoking—50 years of progress. A report of the Surgeon General
Velicer WF, Prochaska JO, Fava JL, Rossi JS, Redding CA, Laforge RG, Robbins ML (2000) Using the transtheoretical model for population-based approaches to health promotion and disease prevention. Homeost Health Dis 40:174–195
Ventola CL (2015) The antibiotic resistance crisis: part 1: causes and threats. Pharm Ther 40(4):277
Verplanken B (2005) Habits and implementation intentions. The ABC of behavioural change. Elsevier, pp. 99–109
Wakefield JC (2014) The biostatistical theory versus the harmful dysfunction analysis, part 1: is part-dysfunction a sufficient condition for medical disorder? J Med Philos 39(6):648–682
Weissenborn R, Duka T (2003) Acute alcohol effects on cognitive function in social drinkers: their relationship to drinking habits. Psychopharmacology 165(3):306–312
World Health Organization (2010) Basic documents. World Health Organization
Xavier da Silveira dos Santos A, Liberali P (2018) From single cells to tissue self‐organization. FEBS J 286(8):1495–1513
Zaccheo A, Palmaccio E, Venable M, Locarnini-Sciaroni I, Parisi S (2017) Biocides and “superbugs”. Anthropological cross cultural perspectives, vol. 1. Springer, Cham, pp. 63–72
Download references
Acknowledgements
This research was supported by funding from the National Institutes of Health’s (NIH) National Cancer Institute (NCI).
Author information
Authors and affiliations.
Cancer Prevention Research Center, The University of Rhode Island, 130 Flagg Rd, Kingston, RI, 02881, USA
Julian M. Saad & James O. Prochaska
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Julian M. Saad .
Ethics declarations
Competing interests.
The authors declared the following potential competing interests: JOP, Ph.D. is a founder of the Transtheoretical Model (TTM) of Behavior Change, and is the Director of the Cancer Prevention Research Center at the University of Rhode Island. JMS, M.Ed. is currently a Ph.D. student conducting dissertation research on population health and behavior change under JOP’s supervision at the University of Rhode Island.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Saad, J.M., Prochaska, J.O. A philosophy of health: life as reality, health as a universal value. Palgrave Commun 6 , 45 (2020). https://doi.org/10.1057/s41599-020-0420-9
Download citation
Received : 28 September 2019
Accepted : 27 February 2020
Published : 18 March 2020
DOI : https://doi.org/10.1057/s41599-020-0420-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Holism in Health Care: Patient as Person
- Living reference work entry
- First Online: 01 January 2015
- Cite this living reference work entry

- Simon Woods 3
752 Accesses
2 Citations
This chapter explores the place of holism within the philosophy of medicine. It is organized into three sections which explore three related aspects of holism in the context of medicine and health care. The chapter begins with an introduction which places the holism debate within the wider history of ideas and the evolution of medicine as a scientifically grounded practice. An early consideration in section one is whether holism can be positively defined or whether it can be discussed only in terms of its relationship with reductionism – the holism/reductionism dyad. A key question is whether medicine’s reliance upon the natural sciences requires the adoption of a form of reductionism that is incompatible with holism. Developing the analysis of reductionism the question of the compatibility of reductionism with holism is explored further. Section two deals with the question of whether holism is actually antireductionist. Here several strands are explored in order to show that the holism/reductionism dyad is not merely a scientific, philosophical debate but in addition has important normative implications for understanding the very raison d’être of medicine. Section three continues the analysis of the normative issues by exploring the holism/reductionism dyad in the context of medical ethics.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Institutional subscriptions
Beauchamp TL, Childress JF (1979) The principles of biomedical ethics. Oxford University Press, Oxford
Google Scholar
Beecher HK (1966) Ethics and clinical research. N Engl J Med 274(24):1354–1360
Article Google Scholar
Borrel-Carrió F, Suchman AL, Epstein RM (2004) The biopsychosocial model 25 years later: principles, practice, and scientific enquiry. Ann Fam Med 2(6):576–582
Brandon RN (1996) Concepts and methods in evolutionary biology. Cambridge University Press, Cambridge
Cantopher T (2012) Depressive illness: the curse of the strong, 3rd edn. Sheldon Press, London
Carlson RJ (1979) Holism and reductionism as perspectives in medicine and patient care, In Orthodox medicine, humanistic medicine and holistic health care – a forum. West J Med 131:466–470
Chilvers CED, Bagenal FS, Easton DF, Harris E, McElwain TJ (1990) Survival of patients with breast cancer attending Bristol Cancer Help Centre. The Lancet 336(8715):606–610
Clouser KD, Gert B (1999) A critique of principlism. J Med Philos 15(2):219–236
Descartes R (1637/1991) The philosophical writings of descartes, vol III (trans: Cottingham J, Stoothoff R, Kenny A, Murdoch D). Cambridge University Press, Cambridge
Engel GL (1981) The clinical application of the biopsychosocial model. J Med Philos 6:101–123
Faulder C (1985) Whose body is it?: the troubling issue of informed consent. Virago, London
Foss L (1989) The challenges to biomedicine: a foundations perspective. J Med Philos 14:165–191
Foucault M (1965) The birth of the clinic: an archaeology of medical perception. Vintage Books, New York
Goodare H (2007) The media and cancer survival. J R Soc Med 100(10):483–484
Hunt L (1993) News of death greatly exaggerated: the report on the Bristol Cancer Help Centre was damning. It was also highly inaccurate. These ex-patients want the world to be told, and they are tired of waiting. The Independent Newspaper. Monday, 15 Nov 1993. http://www.independent.co.uk/life-style/news-of-death-greatly-exaggerated-the-report-on-the-bristol-cancer-help-centre-was-damning-it-was-also-highly-inaccurate-these-expatients-want-the-world-to-be-told-and-they-are-tired-of-waiting-liz-hunt-reports-1504475.html#. Accessed 8 Aug 2015
Illich I (1974) Medical nemesis. Marion Boyars, New York
Kearney M (1992) Palliative medicine – just another speciality? Palliat Med 6:39–46
Koppelman L, Moskop J (1981) The holistic health movement: a survey and critique. J Med Philos 6:209–235
Loeb J (1912) Mechanistic conception of life. The University of Chicago Press, Chicago
Book Google Scholar
Loewy EEH, Loewy Springer R. (2006) Textbook of healthcare ethics. 2d ed. Dordrecht: Kluwer Academic Publishers
Montalenti G (1974) Chapter 2, From Aristotle to Democritus via Darwin: a short survey of a long historical and logical journey. In: Ayala FJ, Dobzhansky TG (eds) Studies in the philosophy of biology: reduction and related problems. University of California Press, Berkley, pp 3–20
Chapter Google Scholar
Nagel E (1961) The structure of science. Problems in the logic of explanation. Harcourt, Brace & World, New York
Nightingale F (1860/2006) Notes on nursing what it is, and what it is not . Hard Press, London
Pappworth MH (1967) Human guinea pigs: experimentation on man. Routledge and Kegan Paul, London
Pellegrino ED (1976) Philosophy of medicine: problematic and potential. J Med Philos 1(1):5–31
Peplau H (1952) Interpersonal relations in nursing: a conceptual frame of reference for psychodynamic nursing. Putnam, New York
Phillips DC (1976) Holistic thought in the social sciences. California University Press, Stanford
Quigley C (2012) Dissection on display: cadavers, anatomists and public spectacle. McFarland & Co, Jefferson
Ramsey P (1970) The patient as person: explorations in medical ethics. Yale University Press, New Haven
Rogers ME (1970) An introduction to the theoretical basis of nursing. Davis Company, Philadelphia
Rosenberg C (1998) Holism in twentieth-century medicine. In: Lawrence C, Weisz G (eds) Greater than the parts: holism in biomedicine 1920–1950. Oxford University Press, Oxford, pp 335–355
Saunders C (2005) Watch with me: inspiration for a life in hospice care. Observatory Publications, Lancaster
Smuts JC (1926) Holism and evolution. Macmillan, New York
Szasz TS (1961/1974) The myth of mental illness: foundations of a theory of personal conduct. Harper & Row, New York
Tauber QI (2002) The ethical imperative of holism in medicine. In: Van Regenmortel MHV, Hull DI (eds) Promises and limits of reductionism in biomedical sciences. Wiley, West Sussex, pp 261–277
Tauber AI (2003) Sick autonomy. Perspect Biol Med 46(4):484–495
Thomasma DC (1990) Establishing the moral basis of medicine: Edmund d. Pellegrino’s philosophy of medicine. J Med Philos 15:245–267
Van Riel R, Van Gulick R (2014) Scientific reduction. In: Zalta EN (ed) The Stanford encyclopedia of philosophy, Summer 2014 edn. http://plato.stanford.edu/archives/sum2014/entries/scientific-reduction/
Watson A (2011) Nursing: human science and human care, 2nd edn. Jones & Bartlett, New York
Woods S (1998a) Holism in nursing. In: Edwards SD (ed) Philosophical issues in nursing. Macmillan Press, London
Woods S (1998b) A theory of holism for nursing. Med Health Care Philos 1(3):255–261
Woods S (2007) Death’s dominion: ethics at the end of life. Facing death. Open University Press
World Health Organization (1946/1958) Preamble to the constitution , adopted by the International Health Conference. New York 19 June to 22 July 1946. In: The first ten years of the World Health Organization . WHO, Geneva
Zucker A (1981) Holism and reductionism: a view from genetics. J Med Philos 6:145–163
Download references
Author information
Authors and affiliations.
PEALS (Policy, Ethics & Life Sciences) Research Centre, Newcastle University, 4th Floor Claremont Bridge, NE1 7RU, Newcastle upon Tyne, UK
Simon Woods
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Simon Woods .
Editor information
Editors and affiliations.
Philosophisches Seminar, Universität Hamburg, Hamburg, Germany
Thomas Schramme
Philosophy, History and Law, Swansea University, Swansea, United Kingdom
Steven Edwards
Rights and permissions
Reprints and permissions
Copyright information
© 2015 Springer Science+Business Media Dordrecht
About this entry
Cite this entry.
Woods, S. (2015). Holism in Health Care: Patient as Person. In: Schramme, T., Edwards, S. (eds) Handbook of the Philosophy of Medicine. Springer, Dordrecht. https://doi.org/10.1007/978-94-017-8706-2_21-1
Download citation
DOI : https://doi.org/10.1007/978-94-017-8706-2_21-1
Received : 09 August 2015
Accepted : 01 September 2015
Published : 07 October 2015
Publisher Name : Springer, Dordrecht
Online ISBN : 978-94-017-8706-2
eBook Packages : Springer Reference Religion and Philosophy Reference Module Humanities and Social Sciences Reference Module Humanities
- Publish with us
Policies and ethics
- Find a journal
- Track your research
We use cookies to enhance our website for you. Proceed if you agree to this policy or learn more about it.
- Essay Database >
- Essay Examples >
- Essays Topics >
- Essay on Health
Free Essay About 'holistic Health' And Its Application In Health Promotion
Type of paper: Essay
Topic: Health , Alternative Medicine , Medicine , Marketing , Holism , Disease , Promotion , Wellness
Words: 1400
Published: 02/20/2020
ORDER PAPER LIKE THIS
Health promotion has received numerous definitions over time, with differences dependent on the emphasis and perspective one has, rather than any core substance disagreement (Irvin et.al 9). However, the most characteristic one is probably that of Perry and Jessor (1985), who define health promotion as “The implementation of efforts to foster improved health and well-being in all four domains of health [physical, social, psychological and personal]” (22). So, taking into account the aforementioned definition of health promotion, one can say that holistic health and medicine are indeed dedicated to health promotion, in more ways than one, that will be further analyzed throughout this paper.
Basic Principles of Holistic Health/Medicine
Holistic health or holistic medicine is a field of alternative medicine that focuses on the whole of a human existence, meaning the physical, emotional, mental and spiritual health of each individual (American Cancer Society). To holistic medicine, if the body, or mind suffers the whole person’s health is affected, which is why it is believed that all four pre mentioned elements of a human existence interconnect to bring health to an individual. For that reason, when a person is ill or unhealthy for some reason, holistic health will focus on the whole person, rather than trying to manage the disease and cure the specific illness or part of the body that suffers (American Cancer Society). In other words, holistic health targets maximum well-being, where all four elements that comprise humans, function the best possible way. So, it becomes obvious that holistic health is a direct example of health promotion, as already defined by Perry and Jessor. With respect to the law of nature, holistic health forwards the concept that everything around us is closely connected with one another. For example, the earth is made up of various, independent systems, like land, water, animals and air. Although independent, if one system faces a problem, the other systems are also affected, which is exactly what happens to individuals: if something goes wrong in physical, emotional, mental or spiritual level, overall health is negatively impacted (Walter). For instance, if one is stressed because they have missed the bus and will be late for work, all the nervousness might as well cause a physical reaction, like a stomach ache. Studies have shown that suppressed anger, or anger turned inward is a reason for migraines (Boyle, Church & Byrnes 47), which demonstrates the interconnection of emotional and physical health. The good thing about holistic health is that it is an ongoing process, where the current health status of an individual does not block cure; everyone can achieve overall wellbeing, despite potential mishaps that may occur on the way (Walter). It is widely accepted that lifestyle choices affect health and elevate the risk for developing a disease, if one choses to not take care of their overall health (Genetic Science Learning Center). The most prevailing dangers that jeopardize one’s health is smoking, drugs, alcohol, lack of exercise and unhealthy eating habits, while some of the equally dangerous, yet not as recognized, dangers to health, include sugar and of course, negative attitudes towards life and low self-esteem (Walter). But, if what is inside the human being is of low quality, due to the bad lifestyle choices one makes, illness might take hold. What holistic health does is to promote people towards eating healthy, exercising, taking care of their inner self and balance and allow a healthy mind and spirit live in a healthy body, exactly like the Latin quotation “Mens sana in corpore sano” (Juvenal, line 356), meaning “a sound mind in a healthy body”.
Applications of Holistic Medicine in Health Promotion
Some mainstream doctors and other health care professionals chose to add non-mainstream, or complementary treatments to the care they provide patients with, which is called holistic care, or most widely known as integrative care (American Cancer Association). Integrative medicine or integrative health is a completely patient-centered care that not only educate, but also empowers individuals to take a very active role in their own health care and wellness (Bravewell Collaborative). So, with integrative care, optimal health and healing is achieved with an integration of the best medicine used in the West and a greater understanding of the very nature of any disease, illness and suffering, as a means to promote healing and wellbeing. However, there are practically myriads of healing arts that are based in holistic health/medicine, who can get involved in integrative medicine, there is a wide array of different approaches and applications of holistic medicine to patients. For example, health care professionals can work with acupuncturists, massage therapists, practitioners using Ayuvedic medicine or nutritionists, among others. Holistic Health is considered part of alternative and complementary medicine (Passarelli) and according to the National Center for Complementary and Alternative Medicine, approximately 38 percent of adults in the US and about 12 percent of children prefer some form of a complementary and alternative medicine (nih.gov). The population of the UK also show a preference for contemporary and alternative medicine, given that about one third of them use the aforementioned medicine (Hill). Contemporary and Alternative Medicine, in general, appears to be experiencing an increase in recent years, especially within biomedical health care, although many are still skeptical on the use of holistic health (Hill). It is for sure that health promotion must partner with other professions, in light of the 21st century, in order to promote public health (Hill).
Holistic Health is considered by many part of Contemporary and Alternative medicine and is believed to promote health in various ways. If health promotion is indeed implementing ways to foster improved health on all major elements that comprise the human nature, that of the body, mind and soul, the holistic health has lots to demonstrate. It relies on basic principles that treat an individual as a whole and not every illness or body part that aches separately. By caring for the entire “human ecosystem”, holistic health promotes overall health and well-being, and educates people on how to achieve high levels of wellness. Truth is that for the last 20 years holistic health and complementary and alternative medicine have become the pole of serious criticism; however, it is vital that health promotion joints forces with holistic health, since they both have the same goad: public health. According to the latest statistics and figures, about a third of the population in the US and the UK have started using complementary and alternative medicine, which shows that people are in fact trying to enhance their wellbeing and life a healthier, happier life. And, when people want health, governments are obliged to take the necessary action to provide them with exactly that.
Works Cited:
American Cancer Society (2013). “Holistic Medicine”. Web. Nov. 9, 2013 <http://www.cancer.org/treatment/treatmentsandsideeffects/complementaryandalternativemedicine/mindbodyandspirit/holistic-medicine> Boyle, Scott, Church II, Wesley and Byrnes, Edward (2005). “Migraine Headaches and Anger”. Print. Best Practices in Mental Health, Vol. 1, No. 1, Winter 2005. Lyceum Books, Inc. The Bravewell Collaborative (n.d). “Elements of Integrative Care”. Web. Nov. 8, 2013 <http://www.bravewell.org/integrative_medicine/integrative_care/> Genetic Science Learning Center (n.d). “Lifestyle Choices and Risks”. The University of Utah. Web. Nov. 8, 2013. < http://learn.genetics.utah.edu/content/health/history/lifestyle/> Hill, Faith (2003). “Complementary and alternative medicine: the next generation of health promotion?”. Oxford Journals. Health Promotion International 18 (3): 265-272 Irvin, Rootman, et.al (2001). “Evaluation in Health Promotion: Principles and Perspectives”. WHO Regional Publications European Series, No 92 Juvenal, edited by Courtney & Rudd (1991). “Juvenal: Satires I, III, X”. Print. Bristol Classical Press; 2 edition. National Center for Complementary and Alternative Medicine (2008). “The Use of Complementary and Alternative Medicine in the United States”. US Department of Health and Human Services: National Institutes of Health. Web. Nov. 8, 2013 <http://nccam.nih.gov/news/camstats/2007/camsurvey_fs1.htm> Passarelli, Tonya (2008). “Complementary and Alternative Medicine in the United States». Print. <http://www.cwru.edu/med/epidbio/mphp439/complimentary_meds.pdf> Perry, C.L. and Jessor, R (1985). “The concept of health promotion and the prevention of adolescent drug abuse. Health Education Quarterly, 12 (2): 169-184 Walter, Susan (n.d). “Holistic Health”. American Holistic Health Association. Web. Nov. 9, 2013 < http://ahha.org/rosen.htm>

Cite this page
Share with friends using:
Removal Request

Finished papers: 1140
This paper is created by writer with
If you want your paper to be:
Well-researched, fact-checked, and accurate
Original, fresh, based on current data
Eloquently written and immaculately formatted
275 words = 1 page double-spaced

Get your papers done by pros!
Other Pages
Quarantine research papers, child psychology research papers, gases research papers, dream job college essays, because i could not stop for death by emily dickinson literature review, essay on quality daily physical exercise, essay on significance of study, ethics in business essay, comparison of the efficiency of ajax and hand sanitizer report, essay on the temptations of dishonesty, calculate analyze current ratios and acid test case study, research paper on research support for parent involvement, essay on water pollution, research paper on general impact of international law, report on field of the invention, news media course work, article review on gender and identity, sample essay on managing people team, good endangered species research project blue whale research paper example, free market structures essay sample, sample essay on bollywood film review krrish, good essay about the perils of writing utopia, good poland essay example, essay on a rhetorical analysis of john f kennedys inaugural speech, good essay about health care services, example of thesis proposal on using near infrafed spectroscopy to probe brain oxygenation by waveforms, free research paper about toys r us, mosier essays, pauper essays, jager essays, industrial techno essays, kingdom of jordan essays, livers essays, trautman essays, bassano essays, jacopo bassano essays, coq au vin essays, french cuisine essays, defense policy essays, libyan essays, metaplastic essays, animal planet essays, vasoconstriction essays.
Password recovery email has been sent to [email protected]
Use your new password to log in
You are not register!
By clicking Register, you agree to our Terms of Service and that you have read our Privacy Policy .
Now you can download documents directly to your device!
Check your email! An email with your password has already been sent to you! Now you can download documents directly to your device.
or Use the QR code to Save this Paper to Your Phone
The sample is NOT original!
Short on a deadline?
Don't waste time. Get help with 11% off using code - GETWOWED
No, thanks! I'm fine with missing my deadline

“The Doctor as a Humanist”: The Viewpoint of the Students
Conference Report and Reflection by Poposki Ognen (University Pompeu Fabra); Castillo Gualda Paula (University of Balearic Islands); Barbero Pablos Enrique (University Autonoma de Madrid); Pogosyan Mariam (Sechenov University); Yusupova Diana (Sechenov University); and Ahire Akash (Sechenov University)

The practice of Medicine as a profession has become very technical; doctors rely on fancy investigations, treatment algorithms and standardized guidelines in treating patients. In a lot of universities, medical students and residents are trained without appreciating the importance of art and the humanities in delivering good care to patients and their families. Factual knowledge is imposed on us, as students, from scientific evidence delivered by highly specialized professionals: those who know more and more about niche subjects.
As a result, when someone decides to become a doctor , it seems that scientific training is the sole priority, with most attention being given to the disease-treatment model. As medical students, we are taught very specific subjects, leaving little or no space or time for any cultural enrichment programs. And yet, Personal growth as a doctor and a human being cannot be achieved unless one is exposed to the whole range of human experience. Learning from art and artists can be one such means of gaining these enriching experiences. We can learn from historians, and from eminent painters, sculptors, and writers, as well as from great scientists. How do we achieve these ends? The following essay summarizes and reviews one attempt at providing answers. The 2nd “Doctor as a Humanist” Symposium took place at Sechenov University in Moscow from the 1 st to the 3 rd of April, 2019, to explore the holistic perspective of interpersonal treatment.
To begin our essay, we would like to clarify some key concepts, such as culture, humanism and humanities, as they were employed at the conference. Culture is a complex phenomenon that includes knowledge, beliefs, artistic production, morals, customs and skills acquired by being part of a society, which can be transmitted consciously or unconsciously, by individuals to others and through different generations.
The humanities are academic disciplines that study the cultural aspects and frailties of being human, and use methods that are primarily analytical, critical, or speculative, which distinguish them from the approaches of the natural sciences. Humanism is the practice of making the human story central. Consequently, the studies of humanities, so invested in human stories, is one aspect of practicing humanism.
Technological and practical progress in medicine has been impressive in the past fifty years. Nevertheless, patients still suffer from chronic conditions such as heart failure, chronic lung disease, depression, and many others. These are conditions where technology cannot significantly change the outcomes or reverse the underlying condition. One of the ways to alleviate suffering is through compassion and empathy where the doctor is a professional who listens to, understands and comforts the patient, as well as engaging the patient as a fellow human being. We need arts and humanities as doctors’ tools to comfort and, perhaps, even to heal. We also need them to remind us that we are ‘merely human’ ourselves, and that we share our humanity with our patients, as equals.
Unquestionably, there are fundamental requirements that every physician must internalize; the conference goal was to explain that one such requirement is the humanistic view. Opera, poetry, philosophy, history, the study of dialectics, biographical readings, and even volunteering abroad can be means of engaging the world for positive change. Sometimes called “soft” skills, these are in fact necessary and valuable qualities to empower ourselves as persons, as well as doctors. The 2nd The Doctor as a Humanist Symposium placed the corner stone in a global project that aims to understand medicine as a multidisciplinary subject, and to establish the concept of humanistic medicine both as a science and an art where the patient and the doctor are human beings working together.

STUDENT PARTICIPATION
The event united experts in Medicine and the Humanities from all over the world. The speakers (doctors, nurses and students) were from Russia, the USA, the UK, Spain, Italy, Germany, Mexico and more. Each day’s program was both intense and diverse, and included plenary lectures and panel sessions. Medical students were highly involved in all parts of the conference, offering us a great chance to introduce our projects, share our opinions on various topics, and discuss our questions connected with the role of the humanities in medicine.We participated in roundtable discussions, which were chaired by experts from different countries. Even though this made us nervous, at the same time it was very important for us, as students, to be a part of it. We discussed the future of medical humanities from various perspectives, and above all our thoughts and ideas were listened to and commented on, on an equal basis with the world’s experts. For once, we could see that our views were being taken into consideration, and we hope that in the future this will be the norm and NOT the exception. We are the future of medicine, and our voices should be heard, too.
At the end of the first day there was a students’ session, where we gave our opinions on the relative importance of the medical humanities from a multicultural viewpoint, and on this particular roundtable there were students from Russia, Spain, Iran, Mexico, Italy, as well as a Nursing resident. One of the students during the session shared her view that “I would like to see medicine through the lens of humanism and empathy, and also implement all its principles in my professional life on a daily basis”. All participants agreed, and although we were representing different countries and cultures there was no disagreement about this. Even though we have not yet faced many of the obstacles of the world of medicine, we can see the role of compassion in clinical practice better perhaps than our seniors. We shared our points of view about this question and its relevance in the different countries. It was an incredible moment, as experts and professors demonstrated a great interest in our ideas.
The program was extremely diverse; however, the main idea that most speakers expressed was how to find, sustain and not lose humanist goals. Brandy Schillace gave an impressive presentation entitled “Medical Humanities today: a publisher’s perspective”, which studied the importance of writing and publishing not only clinical trials, but also papers from historians, literary scholars, sociologists, and patients with personal experiences. The nurses Pilar d’Agosto and Maria Arias made a presentation on the topic of the Nursing Perspective that is one of the main pillars of medical practice. Professor Jacek Mostwin (Johns Hopkins University) shared his thoughts on patients’ memoirs. An Italian student, Benedetta Ronchi presented the results of an interview on medical humanities posed to the participants and speakers during the symposium. The plurality of perspectives made this conference an enriching event and showed us how diverse ideas can help us become better doctors. More importantly, it reminded us of our common humanity.
A significant part of the symposium was dedicated to Medicine and Art. Prof Josep Baños and Irene Canbra Badii spoke about the portrayal of physicians in TV medical dramas during the last fifty years. The book “The role of the humanities in the teaching of medical students” was presented by these authors and then given to participants as gifts. Dr Ourania Varsou showed how Poetry can influence human senses through her own experience in communicating with patients. She believed that many of the opinions and knowledge that we have internalized should be unlearned in order to have a better understanding of the human mind. The stimulus of poetry makes this possible. Poetry allows us to find new ways to express ourselves, and thus increase our emotional intelligence and understanding of other people’s feelings.
One of the most impressive lectures was by Dr Joan.B Soriano, who spoke about “Doctors and Patients in Opera” and showed how the leading roles of physicians in opera have changed over the centuries. People used to consider the doctor as the antihero, but with time this view has transformed into a positive one that plays a huge role in history.
It is important to be professional in your medical career, but also to be passionate about the life surrounding you; for instance, Dr Soriano is also a professional baritone singer. For students, this Symposium was full of obvious and hidden messages, which gave us much lot of food for thought. As Edmund Pellegrino, the founding editor of the Journal of Medicine and Philosophy , said: “Medicine is the most humane of sciences, the most empiric of arts, and the most scientific of humanities.”

CHOOSING ONE WORD
To conclude our summary of the students’ viewpoint each of us chose One word to encapsulate our thoughts about the symposium.
The Doctor as a Humanist is a multicultural event where everyone can learn and contribute to this global necessity to put the heart and soul back into medicine. Of course, we are aware and delighted that other organizations are championing the cause of the Humanities in Medicine, and in some cases, such as https://www.dur.ac.uk/imh/ , they have been doing so for many years.
As medical students, we appreciate how we have been placed at the centre of the symposium, which we believe has made this new initiative rather special. We hope that students of Medicine and from other disciplines come and participate in future symposia.
If you want to learn more, and see how you can participate, please contact the International student representatives, Mariam ( [email protected] ) and David ( [email protected] ).
Acknowledgements
Assistance provided by Jonathan McFarland (c) and Joan B. Soriano (University Autonoma de Madrid) was greatly appreciated during the planning and the development of the article.
Analysis and discussion of research | Updates on the latest issues | Open debate
All BMJ blog posts are published under a CC-BY-NC licence
BMJ Journals
Holistic Health Essays
Harmony amid climate turmoil, popular essay topics.
- American Dream
- Artificial Intelligence
- Black Lives Matter
- Bullying Essay
- Career Goals Essay
- Causes of the Civil War
- Child Abusing
- Civil Rights Movement
- Community Service
- Cultural Identity
- Cyber Bullying
- Death Penalty
- Depression Essay
- Domestic Violence
- Freedom of Speech
- Global Warming
- Gun Control
- Human Trafficking
- I Believe Essay
- Immigration
- Importance of Education
- Israel and Palestine Conflict
- Leadership Essay
- Legalizing Marijuanas
- Mental Health
- National Honor Society
- Police Brutality
- Pollution Essay
- Racism Essay
- Romeo and Juliet
- Same Sex Marriages
- Social Media
- The Great Gatsby
- The Yellow Wallpaper
- Time Management
- To Kill a Mockingbird
- Violent Video Games
- What Makes You Unique
- Why I Want to Be a Nurse
- Send us an e-mail

AIMEE LONG, CNHP
Certified natural health professional diplomate of holistic iridology zyto technology specialist.
Aimee Long earned a Bachelor of Science degree from the University of Scranton in 1988. While originally scheduled to graduate the year prior, an unexpected leukemia diagnosis not only delayed graduation, but ultimately shifted her focus away from allopathic medicine and toward holistic/alternative studies.
Aimee became a Certified Natural Health Professional (CNHP) through the Trinity School of Natural Health and then eventually earned the title of Diplomate of Holistic Iridology through the International College of Iridology; she has attended iridology conferences all throughout the US, as well as in Canada and in France. She is also a specialist in ZYTO technology, a software that uses galvanic skin response to analyze energy frequencies and provide valuable health insight. Aimee's primary interests/specialties include iridology, herbology, women’s hormone health, children’s developmental health, nutritional biochemistry, homeopathy, parasitology, Bach flower remedies, and Lifewave light therapy.
Outside the office, Aimee spends most of her time with her husband - together they enjoy hiking, foraging for herbs, gardening, cross-country skiing, repurposing antiques, creating art projects, and traveling. Aimee has three grown sons, all of whom were raised with the knowledge of natural/holistic health practices.
Advertisement
Supported by
Ukraine Needs Money to Fight. Can Seized Russian Assets Help?
Kyiv’s supporters are discussing how to use the interest earned by frozen Russian assets to help pay for weapons and postwar reconstruction.
- Share full article

By Steven Erlanger
Steven Erlanger has written extensively about the diplomacy around Russia’s war against Ukraine.
As much as $300 billion in Russian assets, frozen in the West since the invasion of Ukraine , is piling up profits and interest income by the day. Now, Europe and the United States are considering how to use those gains to aid the Ukrainian military as it wages a grueling battle against Russian forces.
There has been a debate for months about whether it would be legal or even wise to confiscate the frozen assets altogether. While the United States and Britain have favored confiscations, significant objections have come from countries like France, Germany, Indonesia, Italy, Japan and Saudi Arabia, as well as from officials like Christine Lagarde, the head of the European Central Bank.
They argue that confiscation would be a bad precedent, a violation of sovereignty and could lead to legal challenges, financial instability and retaliatory seizures of Western assets abroad.
So the idea of confiscation appears dead for now. But proposals to seize and use the profits earned on those Russian assets — the interest on accumulated cash stemming from the sanctions, said Euroclear , a financial services company — are gaining considerable ground. Both the Europeans and Americans believe that those profits could be used without raising the same legal challenges or risks to the global financial system.
But they have competing ideas on how to use the funds. The Europeans would like to transfer them to Ukraine yearly or every two years. The Americans want to find a way to get more money to Ukraine more quickly.
The debate over which approach to use is intensifying in the run-up to the Group of 7 summit meeting in Italy next month, when it is hoped an agreement will be reached. Here’s a closer look at the plans.
The European Plan
The European Union is expected next week to formally adopt a contentious and long-hatched plan to use most of the interest gained on the Russian assets frozen in Europe to help arm Ukraine and make Russia pay for the country’s reconstruction.
After months of talks, E.U. nations approved the policy in March . Last week, they agreed in principle that they would be willing to use 90 percent of the profits to buy arms for Ukraine through the European Peace Facility, an E.U. structure to finance military aid and its own military missions.
The remaining 10 percent would go to reconstruction and nonlethal purchases, to satisfy countries like Ireland, Austria, Cyprus and Malta, which are militarily neutral.
The European proposal only targets profits made by Belgium’s central securities depository Euroclear, where about €190 billion of Russian central bank assets are held.
The European Commission expects Euroclear to hand over about €3 billion a year that would be transferred to the bloc’s funds every two years, with a first payout expected in July. That is something roughly equivalent to what Britain promises to provide Ukraine next year, but it is small compared with the $61 billion the United States recently authorized.
Euroclear has made about €5 billion in net profits from the Russian assets since the invasion. Profits made until February of this year will be retained by Euroclear in case of legal claims, but the European Commission has judged that Moscow has no legal right to the profits.
The American Plan
With Ukraine losing ground to Russia and in need of funds to buy more ammunition and pay salaries, the Americans argue that it is preferable to get more money to Ukraine as soon as possible.
The United States holds only a small amount of Russian assets, estimated at around $5 billion. But the Americans propose giving Ukraine some $60 billion up front, and then using the profits from the Russian assets being held in Europe to pay back the debt over time.
Such a step, they argue, would send an important signal of Western commitment to both Ukraine and Russia. Their plan does not preclude the European one, but would follow it and then potentially replace it. And it could be arranged before the November election.
Daleep Singh, a U.S. security adviser and a key architect of the Western sanctions on Russia, described the idea last month in Kyiv .
The Biden administration wanted to make use of interest income on frozen Russian assets in order to “maximize the impact of these revenues , both current and future, for the benefit of Ukraine today,” he said.
“Instead of just transferring the yearly profits from the reserves,” he said, “it’s conceptually possible to transfer the 10 years of profits or 30 years of profits,” he said. “The present value of those profits adds up to a very large number.”
Mujtaba Rahman, managing director for Europe for the Eurasia Group, who has explored the issue extensively, said that the advantage of the American plan was that it is a form of “future proofing.”
That should avoid the kind of recent, deeply politicized delay to approve aid to Ukraine from the Congress. It would, Mr. Rahman said, get “ahead of a possible Trump presidency and around Congress as well.”
The Argument
The American plan has raised objections from Brussels that it undermines European control over the assets and entails greater risks.
If interest rates drop, Europeans argue, the money earned from the Russian assets may not be enough to pay back the debt. So who would be responsible for covering the shortfall, the United States or the European Union?
Second, if the war ends in a negotiation before the bond matures, what happens if the sanctions on Russia are lifted and Russian assets are returned? Or what if they are finally confiscated to pay for Ukrainian reconstruction? In either scenario, who would be responsible?
European officials suggest that the United States should be the guarantor, while the Americans want the Europeans to take responsibility, Mr. Rahman said. Some officials suggest that the Group of 7 take responsibility and even issue the bond, but some countries may have legal objections to that plan.
Some Europeans suggest that the European Commission should issue the bond, since the assets are in Europe, and thereby have more say over how the money is spent — predominantly on European arms manufacturers or companies, for instance, rather than American ones. And Europe would not have to worry about a reluctant Donald J. Trump or Congress.
Confiscation?
The argument about outright confiscation continues, even if it remains unlikely. Seizing the money would be a way to force Russia to pay for the expensive reconstruction of Ukraine , estimated to cost at least $500 billion if not twice that, since it is unlikely to volunteer to do so.
Nigel Gould-Davies, a former British diplomat now at the International Institute for Strategic Studies, a research institution, says that Western fears of financial instability are unrealistic.
“Freezing the assets was a far more decisive step than confiscating them and caused no market turbulence,” he said. “If the countries that issue the major currencies — dollar, euro, sterling and yen — move together, there is nowhere else for large funds of money to be safely held.”
In a recent essay , Mr. Gould-Davies said that as with weapons supplies to Ukraine, “an exaggerated fear of adverse consequences is the latest form of chronic self-deterrence in economic affairs.”
Such hesitation is especially foolish, he argues, because economics are “the West’s greatest area of natural strength, one against which Russia cannot effectively retaliate.”
Matina Stevis-Gridneff contributed reporting from Brussels.
Steven Erlanger is the chief diplomatic correspondent in Europe and is based in Berlin. He has reported from over 120 countries, including Thailand, France, Israel, Germany and the former Soviet Union. More about Steven Erlanger
Our Coverage of the War in Ukraine
News and Analysis
Secretary of State Antony Blinken met with President Volodymyr Zelensky of Ukraine in Kyiv, assuring him that American military aid is on its way at a “challenging time” for the country.
As Moscow seeks more support for its war in Ukraine, President Vladimir Putin of Russia will visit China’s top leader, Xi Jinping, testing their “no limits” partnership .
Putin replaced his minister of defense , Sergei Shoigu, with the economist Andrei Belousov , shaking up his national security team for the first time since his invasion of Ukraine.
Rebuilding Ukrainian Villages: The people of the Kherson region have slowly rebuilt their livelihoods since Ukraine’s military forced out Russian troops. Now they are bracing for another Russian attack .
Replenishing the Army’s Ranks: Ukraine’s Parliament passed a bill that will allow some convicts to serve in the military in exchange for the possibility of parole at the end of their service.
Ukraine’s Unidentified Dead: Families of some Ukrainian soldiers say they have spent months trying to get official confirmation of their loved ones’ deaths , adding to their anguish.
How We Verify Our Reporting
Our team of visual journalists analyzes satellite images, photographs , videos and radio transmissions to independently confirm troop movements and other details.
We monitor and authenticate reports on social media, corroborating these with eyewitness accounts and interviews. Read more about our reporting efforts .

IMAGES
VIDEO
COMMENTS
250 Words Essay on Holistic Health Understanding Holistic Health. Holistic health is about caring for the whole person. This means not just focusing on one part of the body when someone is sick, but looking at everything—body, mind, and spirit. It's like seeing a person as a big puzzle, and each piece is important to make the whole picture.
A Holistic Health Promotion Strategy. Holistic support of health is an intervention strategy that takes into account factors that affect the wellbeing of human beings and these include the physical body, the emotional aspect, the mind, and the spiritual perception of human beings. The strategy also combines the best service in modern medicine ...
Essay On Holistic Health. 1514 Words7 Pages. When exploring what is health, it looks at the idea of an individual being free from illness or injuries (World Health Organization 1948). WHO further explains that it is the state of complete: physical, mental, and social well-being and not the absence of disease or infirmity (health context, 2018 ...
Holistic health is an approach to wellness that views the human being as a whole. To achieve holistic health, a certain harmonious interaction is needed between the body, the mind, the soul, the emotions, the environment, and all the other factors that influence living. Holistic health doesn't believe in curing one symptom, instead it aims to ...
A holistic approach to integrative medicine. As studies continue to reveal the important role the mind plays in healing and in fighting disease, a transformation is taking place in hospitals and clinics across the country. Meta description: Discover principles and benefits of integrative medicine, a comprehensive approach combining conventional ...
In contrast, the holistic health interpretation leads to the following point of view: Health is seen as a state of well-being with numerous aspects—physical, mental and social. 12 Given these dimensions of well-being, health statuses can be assessed in a combined approach, taking the full range of health-related factors into account ...
This definition of health will be applied in the proceeding principles to integrate naturalistic and holistic perspectives of population health. Principle 2: Health emerges from maintainable-ease ...
It uses holistic interventions to financial status, social networks, and education. 81% of those who used the service felt that it had helped them to achieve their goals and 99% rated it as good or excellent. Taking a holistic approach and working to address the causes of the causes undoubtedly helps to reduce health inequalities.
Holistic Health Essay Originating over five thousand years ago in China and India, holistic health focuses on considering all potential contributing factors which may affect a person's well-being when assessing a person's overall health (Wikipedia, 2011). Since each factor influences at least one other factor and the whole, all factors ...
health outcomes. Studies on the Sars-CoV virus suggest Holistic lessons from a pandemicÉprevention is better than cure STUDENT ESSAY Virtual Reality , a painting by medical student Freya Elliott, Barts and The London School of Medicine and Dentistry, exploring the theme of solitude and the encounter in healthcare during the Covid-19 pandemic.
Engel, in a series of papers from the early 1960s, had been working to reconcile medicine's dual commitment to being scientifically grounded and to resolving the problems of the patient or person. ... The holistic health movement: a survey and critique. J Med Philos 6:209-235. Article Google Scholar Loeb J (1912) Mechanistic conception of ...
Holistic View Of Health Essay. Decent Essays. 756 Words. 4 Pages. Open Document. In the Holistic view of health and illness, there is a definite distinction made between the outcomes of healing and cure. One of the ideas stated in the reading is that healing can occur even in the absence of cure. Do you agree or disagree with this statement?
1. The Health Promoting Schools approach and its development. The Ottawa Charter, adopted in 1986, was a milestone in the development of a holistic and positive understanding of health that requires actions at different levels, from healthy public policy to the development of personal skills, using different strategies, such as enabling and advocacy approaches ().
Holistic health or holistic medicine is a field of alternative medicine that focuses on the whole of a human existence, meaning the physical, emotional, mental and spiritual health of each individual (American Cancer Society). To holistic medicine, if the body, or mind suffers the whole person's health is affected, which is why it is believed ...
The 2nd "Doctor as a Humanist" Symposium took place at Sechenov University in Moscow from the 1 st to the 3 rd of April, 2019, to explore the holistic perspective of interpersonal treatment. To begin our essay, we would like to clarify some key concepts, such as culture, humanism and humanities, as they were employed at the conference.
Holistic Health Essay. 690 Words2 Pages. Health is considered a complete wellness of a body including physical, mental and social well-being and Holistic Health is considered a wellness of a whole body including mind, body and spirit. According to American Holistic Medicine Association "Holistic medicine is the art and science of healing that ...
Essay On Holistic Health Care. In holism there is a belief that wellbeing is more than what is going on in the body physically in terms of illness or disease, but also on a deeper level with psychological, spiritual, emotional, social and environmental aspects. These aspects are all equally important and essential for optimal and sustainable ...
Holistic Health Essays. Harmony Amid Climate Turmoil. Introduction Global climate changes, which are generated by people's actions such as the burning of fossil fuel, deforestation, or others, may lead to various dangerous consequences for Earth. To this end, however, there are myriads of complex and socio-political-economic problems that ...
Reflective practice is as a medium for an individual's reflective capacity to be communicated and examined both internally and externally. Self directed learning is emphasised through reflective writing as students engage in a more holistic approach which uncovers the reasons behind their actions. Related Articles.
New York Essays - database with more than 65.000 college essays for A+ grades Check out this FREE essay on Holistic health ️ and use it to write your own unique paper. Free Essays
Holistic health is an approach to full-person wellness. Every aspect of the person is enriched and nourished — to feed the mind-body connection and provide our souls with the path to freedom, to ...
Holistic Health Essay - Free download as PDF File (.pdf) or read online for free. This is an essay on the new evidences that support the new approach on human health, taking into consideration all the dimensions of a person (spiritually, emotionally , mentally and physically) as a whole, in order to make a diagnosis of his/her real causes of disease.
Aimee became a Certified Natural Health Professional (CNHP) through the Trinity School of Natural Health and then eventually earned the title of Diplomate of Holistic Iridology through the International College of Iridology; she has attended iridology conferences all throughout the US, as well as in Canada and in France.
A fighter fly-past returned to Russia's World War II commemorations, where President Vladimir V. Putin permitted himself a single reference to his "special military operation."
Ukraine's forces are stretched thin and have minimal reserves to draw on, the chief of military intelligence said, in addition to shortages of weapons.
A new law accelerates the weaning of U.S. electric utilities from using Russian enriched uranium to power America's nuclear plants.
places for health-related teaching, learning and development, need to adapt. Where does the Health Promoting School approach stand today, more than 30 years after the Ottawa Charter on health promotion? Can the Health Promoting School, with its holistic orientation, deliver on its promise of addressing health inequalities and improving children's
Moscow seeks more support for its war in Ukraine. But Beijing risks alienating Europe, a key trading partner needed to help revive China's economy.
The secretary of state, a longtime guitarist, strummed along to a song chosen to underscore a central message of President Biden's foreign policy.
In a recent essay, Mr. Gould-Davies said that as with weapons supplies to Ukraine, "an exaggerated fear of adverse consequences is the latest form of chronic self-deterrence in economic affairs."