- Open access
- Published: 19 May 2020

The mediating effect of social support on uncertainty in illness and quality of life of female cancer survivors: a cross-sectional study
- Insook Lee ORCID: orcid.org/0000-0001-6090-7999 1 &
- Changseung Park 2
Health and Quality of Life Outcomes volume 18 , Article number: 143 ( 2020 ) Cite this article
2991 Accesses
20 Citations
Metrics details
Cancer survivors have been defined as those living more than 5 years after cancer treatment with no signs of recurrence or further growth; however, the National Coalition for Cancer Survivorship of the United States defined cancer survivors as those undergoing treatment after being diagnosed with cancer or those considered to be fully cured. The National Cancer Institute of the United States established the Office of Cancer Survivorship, with the American Society of Clinical Oncology including “patient and survivor management” as its 2006 annual objective [ 1 ], indicating the importance of cancer survivor management as a major agenda item.
Typically, breast and thyroid cancer diagnoses occur among women in their 40s and 50s, and patients who receive treatment have high survival rates. The majority of breast and thyroid cancer survivors return to their daily lives within a relatively short timeframe [ 2 ], making quality of life after treatment and important factor in cancer treatment [ 3 , 4 , 5 ].
Cancer survivors have reported experiencing a variety of physical difficulties during or after treatment, including fatigue, pain, loss of energy, sleeping disorders, and constipation [ 6 , 7 ]. They also have psychological concerns, such as fear of the cancer spreading, concerns about treatment results, and uncertainty about the future [ 8 ], as well as financial difficulties, issues with their sex lives, decreased body image, difficulties in interpersonal relationships, role disorders, and difficulty returning to work [ 7 ]. Thus, cancer patients require a diverse range of healthcare services, plus emotional and socioeconomic support, with an international study of the quality of life and symptoms of cancer survivors reporting that the quality of life among Asian patients to be the lowest of those than other country [ 6 ]. Survivors of breast cancer have reported low quality of life after treatment [ 9 , 10 ], which is influenced by emotional and psychological factors such as uncertainty, body image, lack of self-respect, and depression [ 9 , 10 , 11 ], as well as social factors including social, family, and spouse support [ 10 , 11 ].
Uncertainty among women diagnosed with malignant illnesses was found to be higher than that among women with a lump in the breast [ 12 ]. Uncertainty among breast cancer patients continues for a long period because of the fear of recurrence [ 13 ] and reduced quality of life [ 11 ]. Similarly, thyroid cancer survivors also show higher levels of fatigue, depression, and anxiety compared to those with no experience of cancer [ 14 , 15 , 16 ].
Social support is a complex and multidimensional concept that is characterized by mutual benefits that include social, psychological, and material support provided by the social support network [ 17 ]. In other words, social support means help provided by social relationships such as family, friends, and significant others, and plays an important role in directly and indirectly reducing uncertainty [ 18 , 19 ]. For cancer survivors, the need for social support is varied and depends largely on the adaptive tasks they face [ 20 ]. Social support is closely related to breast cancer survivor prognosis [ 21 ]; breast cancer survivors’ uncertainty was found to lower their quality of life, but their recognition of social support was found to improve it [ 11 ]. Recognition of social support and uncertainty played a key role in managing and maintaining quality of life. Research has shown that social support differs according to survival stage, as patients who are undergoing treatment receive active support from healthcare professionals and their family, but this support declines notably after the treatment ends [ 14 , 22 , 23 ].
With the number of cancer survivors steadily increasing, there has been an increase in the number of studies published on cancer survivors internationally [ 22 , 24 ]. In Korea in particular, there have been studies on recurrence-prevention behaviors and quality of life [ 25 ], the factors influencing quality of life [ 10 ], fatigue and quality of life [ 26 ], distress and quality of life [ 27 ], and symptoms and quality of life among breast cancer survivors [ 8 ]. Most of these studies focused on breast cancer survivors, but few studies focus on overall quality of life and the related influential factors. Few studies have analyzed the relationships between uncertainty in illness, quality of life, and social support among female breast and thyroid cancer survivors.
This study aimed to identify the relationships among uncertainty in illness, social support, and quality of life in female cancer survivors, and to verify the mediating role of social support, in the relationship between uncertainty in illness and quality of life. Social support may act as a generative mechanism influencing how uncertainty in illness, the predictor variable, affects quality of life, the outcome variable (Fig. 1 ) [ 28 ]. Therefore, this study will provide foundational data for devising practical and helpful intervention strategies to raise the quality of life of cancer survivors.
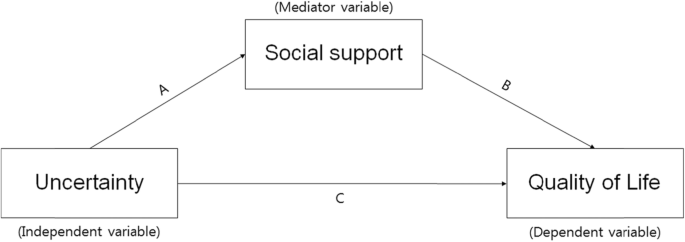
The theoretical research model showing the influence of uncertainty on quality of life and the mediating effect of social support
Participants
Participants were selected using convenience sampling of female cancer patients who were being treated by specialists in breast endocrinology at general hospitals located in J City of Korea. Among the 189 women (138 thyroid and 50 breast cancer patients) who agreed to participate, 156 surveys were collected (response rate: 82.5%). The final sample including 148 participants after excluding eight insincere responses. The data collection period was from April 21 to June 30, 2014. The completion of data collection through the mailed-in copies of surveys occurred on October 15, 2014. Participants were asked to complete the survey, put it in an opaque envelope, and seal it before returning it to the researchers. In cases in which on-site survey completion was difficult, participants were able to complete the survey at home and returned it by mail to the researcher.
The necessary sample size for the multiple regression analysis was confirmed utilizing G*power ver. 3.1.9 with a significance level (α) of .05; power of .80; effect size (f 2 ) of .15 (representing a medium effect size in the multiple regression analysis); and 13 independent variables (age, marital status, religion, level of education, occupation, satisfaction with economic status, smoking, drinking, diagnosis name, clinical stage of cancer, time passed since the end of treatment, uncertainty, and social support). The minimum sample size was determined to be 131. Since a maximum dropout rate of 40% was expected, information was collected from a total of 189 participants who fit the following inclusion criteria: 1) a diagnosis of cancer and no cognitive limitations; 2) the ability to understand and complete the survey in Korean; and 3) an understanding of the purpose of the study and consenting to participate. The exclusion criteria were those suffering from a mental illness, those with difficulties in communication, and those who did not wish to participate in the study.
Uncertainty in illness
Uncertainty occurs when an appropriate subjective interpretation of an illness or event is not formed. This study measured uncertainty using Mishel’s Uncertainty in Illness Scale (MUIS), which is composed of 33 items concerning uncertainty in illness. Mishel [ 19 ] originally developed the scale, and it has been translated into Korean by Lee [ 28 ]. The MUIS is a self-administered survey, with items scored on a 5-point scale from 5 ( strongly agree ) to 1 ( strongly disagree ). Positive items were measured backward, so that total scores ranged from 33 to 165. Higher scores indicated higher rates of uncertainty. The Cronbach’s α for the original 33-item tool was .91–.93; the Cronbach’s α for the tool used in the study of Korean breast cancer patients [ 29 ] was .83. In this study, the Cronbach’s α for the uncertainty scale was .88.
Social support
Social support was measured using Zimet et al.’s [ 30 ] Multidimensional Scale of Perceived Social Support (MSPSS). This 12-item measure is scored on a 7-point, Likert-type scale, and assessed the three dimensions of family, friends, and significant others. Its sub-domains are composed of four items. Overall social support scores are calculated by summing the scores for each item, with higher scores indicating higher levels of social support. At the time of development, the Cronbach’s α reliability was .91; Cronbach’s α for each subscale ranged from .90–.95. In this study, the Cronbach’s α of the social support scale was .95.
Quality of life
Quality of life was measured using a standardized tool that was translated into the Korean and verified validity of the Korean version of the EORTC QLQ-C30, which was developed through a process of international joint study from multiple countries, and it is the most widely used standardized tool to measure the quality of life of cancer patients. This tool is composed of three subdomains and 30 items. It includes two items on overall quality of life and five functional domains (i.e., physical, role, cognitive, emotional, and social functions) that include 15 items; three symptom domains (i.e., fatigue, pain, nausea/vomiting) that include seven items; and one item for each of the symptoms commonly reported by cancer patients (i.e., difficulties in breathing, loss of appetite, sleeping disorders, constipation, diarrhea, and financial hardship) [ 31 ]. The EORTC QLQ-C30 is converted into a score ranging between 0 and 100 points [ 31 ]; higher overall quality of life scores, higher functional domain scores, and lower symptom domain scores indicate higher quality of life. Moreover, overall quality of life can be understood as a measurement of comprehensive quality of life [ 31 ]. This study assess quality of life using the overall quality of life score. At the time of development, Cronbach’s α was .65–.73; the Cronbach’s α for the overall quality of life score in this study was .853.
Ethical considerations
This study was conducted after receiving approval of the research protocol from the Institutional Review Board (Approved number: 2014-L02–01). The purpose and method of the research was explained directly to participants by a trained research assistant. The participants then signed an informed consent form that stated the survey would be used for the purposes of the study only, and that their confidentiality would be safeguarded. The subjects who agreed to participate in the survey received a small amount of goods worth of KRW 3000, but there were no factors that could interfere with the answers in the survey.
Data analysis
The collected data were coded and analyzed using SPSS software (version 24.0; SPSS Inc., Chicago, IL) at .05 significance level. The analysis excluded missing data values. The general characteristics, illness-related characteristics, uncertainty, social support, and quality of life were measured using frequency, percentages, means, and standard deviations. The differences in uncertainty, social support, and quality of life in accordance with general and illness-related characteristics were analyzed using independent t -tests and one-way analysis of variance (ANOVA). Tukey’s post-hoc analysis was used for independent variables of more than three groups to identify which group contained the differences. Pearson’s correlation coefficient was calculated to identify correlations between uncertainty, social support, and quality of life. Multiple regression (stepwise method) was used to test the influence of uncertainty on social support and quality of life. To verify the mediating effects of social support in the relationship between uncertainty and quality of life, simple, and hierarchical multiple regression analyses were conducted as per the method proposed by Baron and Kenny [ 30 ]. The significance of the mediating effects of social support was verified using the Sobel test.
Demographic characteristics of subjects
The general characteristics of the female cancer survivors in this study indicated that their average age was 51.87 ( SD = 11.78) years, with the largest proportion (33.3%) of the population being in their 50s, followed by those in their 40s (30.1%), 60s and over (24.4%), and below 30 (12.2%). Most participants (76.2%) were married; 61.9% practiced a religion, and 66.7% had a high school education or below; 56.2% had jobs; 17.8% had lost their jobs as a result of their cancer diagnosis and treatment, and 73.1% indicated that their satisfaction with their financial status was average. They had an average of 2.26 ( SD = 1.19) children; 94.4% were non-smokers; 64.1% were non-drinkers; 29.1% of the subjects had breast cancer and 70.9% had thyroid cancer; 53.8% of the cancers were early stage, and 46.2% were advanced. The duration after cancer treatment averaged 17.64 ( SD = 31.30) months, with 70.3% reporting a duration of less than a year since they ended their treatment (Table 1 ).
Uncertainty in illness, social support, and quality of life
Average scores of uncertainty in illness, social support, and quality of life are given in Table 2 . The average uncertainty in illness score was 83.06 ( SD = 15.29; range: 44–127 points), and the average quality of life score was 66.90 ( SD = 20.32; range: 0–100 points). Average social support score was 62.62 ( SD = 17.09; range: 12–84 points), with family support being the highest (mean = 21.84, SD = 6.58), followed by support from significant others (mean = 21.28, SD = 5.93) and friends (mean = 19.45, SD = 6.70).
Differences in uncertainty in illness, social support, and quality of life according to general and illness-related characteristics
The results of the analysis of differences in uncertainty in illness, social support, and quality of life according to general and illness-related characteristics are given in Tables 3 and 4 . There were significant differences in uncertainty in illness by educational level ( t = 4.048, p < .001), satisfaction with financial status ( F = 3.760, p = .027), and smoking ( t = 2.195, p = .030). Uncertainty in illness was higher for subjects with less than a high school education, compared to those who had a university degree or higher, when they were dissatisfied with their financial status. Likewise, it was higher for smokers, compared to non-smokers.
Social support had statistically significant differences given satisfaction with financial status ( F = 5.151, p = .007) and duration since cancer treatment completion ( F = 4.292, p = .015). Social support was higher for subjects with average financial status satisfaction, and for subjects for whom it had been less than a year, or between 1 to 5 years, since they completed cancer treatment.
Quality of life significantly differed according to financial status satisfaction ( F = 6.648, p = .002). Participants had higher quality of life when they had high or average financial status satisfaction compared to dissatisfaction.
Correlation between uncertainty in illness, social support, and quality of life
The results of the correlation analyses indicated that uncertainty in illness had a significant negative correlation with social support ( r = −.335, p < .001) and quality of life ( r = −.312, p < .001); social support had a significant positive correlation with quality of life ( r = .321, p < .001). Correlations between the sub-factors of social support and quality of life indicate that there were significant positive correlations between quality of life and support from significant others ( r = .315, p < .001), friends ( r = .284, p = .001), and family ( r = .265, p = .001). Uncertainty and support from significant others ( r = −.326, p = .001), friends ( r = −.294, p = .002), and family ( r = −.244, p = .010) showed significant negative correlations; particularly, the highest correlation was between support from significant others and uncertainty (Table 5 ).
Mediating effect of social support
Four stages of regression analysis were conducted to verify whether social support had mediating effects in the process by which uncertainty in illness influenced quality of life. Prior to verifying the mediating effects of social support, this study examined the multicollinearity between variables. The residual limit was between 0.8–1.0, which is higher than 0.1; and the value of the variance inflation factor was between 1.0–1.2, which was lower than 10, indicating no issues with multicollinearity. Moreover, the Durbin-Watson test, which is the test of independence of residual error, indicated d = 1.903–1.944, which was close to two and met the independence condition, representing no issues with self-correlation.
Using the hierarchy regression, this confirmed the partial mediating effects of social support in the process of uncertainty influencing quality of life (Table 6 , Fig. 2 ). The first regression analysis indicated that the independent variable (uncertainty) had a statistically significant influence on the mediator variable (social support; β = − 0.335, p < .001), and the explanatory power for social support was 10.4%. The second stage regression analysis indicated that the mediator variable (social support) had a significant influence on the dependent variable (quality of life; β = 0.321, p < .001), and the explanatory power for quality of life was 9.7%. The third stage regression analysis indicated that the independent variable (uncertainty) had a significant influence on the dependent variable (quality of life; β = − 0.312, p = .001) with an explanatory power of 8.9%. At the fourth stage, this study aimed to test the influence of the independent variable (uncertainty) on the dependent variable (quality of life) with social support as the mediator variable. The results indicated that uncertainty (β = − 0.241, p = .014) and social support (β = 0.213, p = .030) were significant predictors of quality of life. When social support was set as the mediator variable, uncertainty was found to have a significant influence on quality of life; the unstandardized regression coefficient reduced from − 0.396 to − 0.398, indicating a partial mediation of social support. The explanatory power of these variables in terms of quality of life was 12.1%. This study executed the Sobel test to verify the significance of the mediating effects of social support, confirming that they were significant in the relationship between uncertainty and quality of life.
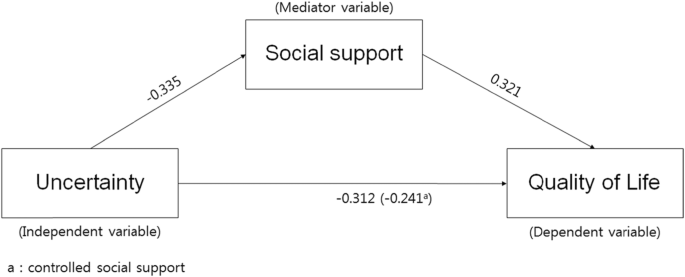
Model showing the influence of uncertainty on quality of life and the mediating effect of social support
Mullen divided the stages of cancer survival into three major classifications [ 32 , 33 ]. First is the acute stage, which marks the period after the cancer diagnosis. Second is the extended stage, in which the active treatment of cancer has ended and the patient is placed under tracking observation or engages in intermittent treatment. During this period, the majority of cancer survivors experience uncertainty toward their cancer treatment and fear recurrence, and they may experience physical and psychological issues. Lastly, the permanent stage marks a period in which the cancer is thought to be fully cured, or the patient is expected to survive long term, with a low risk of recurrence.
The participants in this study averaged a score of 66.90 for quality of life. As it is difficult to draw a direct comparison given the lack of research utilizing this measure, in converting quality of life into a scale of 100 points, this study’s results were similar to those found previously regarding post-hoc management following breast cancer treatment for 200 women [ 8 , 10 ]. However, a study covering regionally based, adult female breast cancer survivors between 6 months and 2 years after anti-cancer treatment completion reported lower scores (e.g., 60.13 points) compared to this study [ 27 ]. Likewise, a study of breast cancer survivors with completed surgeries and assistive treatments, breast cancer survivors whose treatment had ended had scores of 53.4 and 56.66 points, respectively for breast cancer survivors with completed surgeries and assistive treatments [ 25 , 26 ].
On the other hand, a report of 110 adult females with breast cancer or OB/GYN cancers [ 33 ] indicated that quality of life according to cancer survival stage was 58.7, 62.3, and 66.8 points during the acute, extended, and permanent stages, respectively. Quality of life in this study was similar to the level experienced by survivors during the permanent stage. Considering that the average time since treatment was 17.64 months, these results indicate a relatively high quality of life. While these differences cannot be accurately compared and discussed because of the lack of research covering the same variables, the majority of survivors had thyroid cancer (70.9%), and it is known that thyroid cancer has higher rates of survival. Going forward, it is important to develop interventions to improve quality of life by assessing survivors’ specific stages.
There were no significant relationships between quality of life and length of time since completing treatment. Existing research has suggested that quality of life was significantly higher for those surviving more than 5 years after cancer treatment completion [ 8 , 33 ], indicating that quality of life improves as duration of survival increases. The quality of life of these cancer survivors has been reported to improve with the passage of time [ 8 , 33 ]. Therefore, cross-sectional and longitudinal studies are required in the future to identify quality of life by survival stage and changes in quality of life over time.
On the other hand, qualitative studies of Korean female cancer survivors have indicated that the significant others and families of female cancer survivors wanted them to return to their pre-cancer lives to take care of their spouses and children, indicated the demands on female cancer survivors in Korea to fulfill their roles as wives and mothers before fully recovering from cancer [ 33 ]. Thus, customized interventions by survival stage for female cancer survivors are needed along with further research on the relationships between cultural specificity, role conflicts imposed on survivors because they are women, and their quality of life.
The uncertainty toward illness of the participants in this study was similar to existing research in breast cancer patients undergoing chemotherapy averaged 83.08 [ 34 ] and female thyroid cancer patients [ 35 ]. On the other hand, the level of uncertainty faced by cancer patients prior to surgery averaged 81.43 in a study of cancer patients hospitalized for breast, thyroid, and bladder cancer [ 36 ], which was slightly lower than the value found in this study. This appears to be because female cancer survivors in this study were mostly in the extended stage, which comes after the active treatment of their cancer [ 32 , 33 ]. Most cancer survivors face uncertainty toward cancer treatment and fear of recurrence [ 8 , 32 , 33 ]; thus, they experience a diverse range of physical and psychological problems [ 6 , 7 ]. On the other hand, a qualitative study of 25 breast cancer survivors aged over 30 who had undergone surgery and chemotherapy as their primary treatment for breast cancer [ 37 ] indicated that quality of life following treatment for breast cancer survivors saw a coexistence of anxiety and uncertainty about recurrence. A shorter duration of time since treatment led to higher confusion in their own health management efforts and health management in general.
These results indicate that there are limitations to comparing uncertainty results given the lack of domestic studies on cancer survivors; therefore, future studies are needed to fill this gap. Moreover, it is necessary to confirm uncertainty by cancer survival stage and develop interventions to reduce the uncertainty accompanying each stage.
Uncertainty in illness was higher for those with less than a high school education, compared to those with a university education or higher, when they were dissatisfied with their financial status, and for those who were smokers. These results were similar to previous research [ 36 ], which indicated high uncertainty for participants over 60 who had a low monthly income and low level of education. Therefore, it is necessary to consider these socioeconomic factors when developing uncertainty reducing strategies such as customized information delivery and communication.
The social support of female cancer survivors in this study was rather high, at 62.62 out of 84 points; family support was the highest, followed by support from significant others, and finally friends. Social support is known to play an important role in helping individuals reduce their levels of uncertainty [ 37 ]. Particularly, in Korea, family and healthcare professional support have been the most important support resources among all social support types [ 34 ]. The results of this study indicated that family support was the highest, which was in line with the results of existing studies. On the other hand, a qualitative study of 25 breast cancer survivors aged over 30 who had undergone surgery and chemotherapy as their primary breast cancer treatments [ 37 ] indicated that positive support and responses from family, patients with similar illnesses, and those surrounding them helped to strengthen positive self-suggestion, which also helped them to overcome their illnesses. Other studies have reported that patients undergoing treatment receive active support from healthcare professionals and their family, but they receive less support and interest from healthcare professionals, their family, and those surrounding them after the treatment ends [ 22 , 23 , 27 ]. Therefore, it is necessary to take a continuous interest in and facilitate social support for cancer survivors.
Social support was higher for participants with average satisfaction toward their financial status, and for those for whom less than a year, or between 1 and 5 years, had passed since the completion of their cancer treatment, compared to those for whom 5 years or more had passed since treatment. These results were similar to those of studies on cancer patients hospitalized for breast, thyroid, and bladder cancer surgery [ 36 ], which indicated social support differed according to the time that had passed since diagnosis. Moreover, these results are similar to those reporting that breast cancer survivors are required by their spouses or family to fulfill roles they had filled prior to their cancer diagnosis, and this was associated with decreasing support from family [ 38 ]. These results indicate that female cancer survivors require ongoing psychosocial support as well as education and access to information as they live out their lives.
According to Baik and Lim [ 20 ], who studied social support according to different stages of breast and gynecological cancer survival, the social support of patients in the acute stage was comparatively higher, but there were no significant differences in social support across the different stages, which was different from the findings of this study. While there were no significant differences, Baik and Lim [ 20 ] reported that the social support perceived by survivors decreased as they proceeded through the acute to the extended stage. The social support perceived by respondents decreased in the 2 years following the diagnosis but maintained the reduced rate through the permanent stage [ 20 ]. Long-term survivors had a greater need to meet other cancer patients and self-help groups [ 20 ]. Kwon and Yi [ 27 ] asserted that interest and support from family and the society in general are very important in raising breast cancer survivors’ quality of life and survival rates. Moreover, self-help groups were reported to be effective in providing emotional support for long- and short-term cancer survivors [ 39 ], which indicates the need for developing stage-specific social support interventions and various methods of facilitating social support groups. Moreover, further research is required concerning cancer survival stage-dependent social support and quality of life.
The results of this study showed that higher uncertainty in illness among female cancer survivors led to reduced social support and quality of life, while higher social support led to better quality of life. Support from others was found to be the most relevant aspect of the relationship between quality of life and uncertainty. These results were similar to those of studies on early-stage breast cancer patients [ 40 ] and on cancer patients hospitalized for breast, thyroid, and bladder cancer surgery [ 36 ], which indicated that perceived social support was lower as uncertainty increased.
Uncertainty was very influential on female cancer survivors’ quality of life. Higher uncertainty in illness among female cancer survivors led to lower social support and reduce quality of life; higher social support led to improved quality of life. The explanatory power of these variables on quality of life was 12.1%; uncertainty in illness and social support influenced the quality of life of female cancer survivors. Moreover, in the process of uncertainty in illness influencing subjects’ quality of life, social support was confirmed to play a significant, partially mediating, role in the relationship between uncertainty and quality of life. Higher uncertainty toward illness led to lower quality of life, higher social support led to higher quality of life, and social support influenced female cancer survivors’ quality of life by partially mediating its relationship with uncertainty. Social support plays an important role in directly and indirectly reducing uncertainty [ 18 , 19 ]. Social support is closely related to the prognosis of breast cancer survivors [ 21 ]. Uncertainty among breast cancer survivors has been found to lower their quality of life; however, social support has been found to improve quality of life [ 11 ]. Thus, the need for a diverse range of attempts, including developing and applying social support programs, to increase cancer survivors’ quality of life exists. On the other hand, the partially mediating effects of social support indicate that there are other mediating factors in uncertainty in illness’s influence on quality of life. Therefore, it is important for future studies to include other mediating factors in their examinations of what influences quality of life among female cancer survivors.
In Korea, studies on cancer survivors have been conducted since 2010, and the majority of these focused on breast cancer survivors. Particularly, as there has been no overall research into the healthy behaviors of cancer survivors, it is necessary to develop practical guidelines that befit Korea through studies concerning the development and application of health improvement programs based on the study of healthy behaviors, as per the assertion of Kim [ 32 ]. Moreover, attempts are needed to practically apply a diverse range of intervention studies to improve cancer survivors’ quality of life.
Moreover, future studies should include mediator variables other than social support that might influence quality of life. Additionally, both cross-sectional and longitudinal studies are needed to further investigate the quality of life and uncertainty according to the stages of survival.
Our results show that social support partial mediates the relationship between uncertainty and quality of life in female cancer survivors. The results of this study have great implications for improving cancer care, especially in how it relates to quality of life, and they also demonstrate how uncertainty can be decreased. Therefore, it is necessary to develop and apply intervention methods to improve social support thereby improving quality of life among female cancer survivors. A nurse-led social support program may especially contribute to enhancing the quality of life of cancer survivors by providing them with adequate health information and emotional support.
Availability of data and materials
The data used in this study were collected through questionnaires and analyzed by coding the original data. The datasets generated and/or analysed during the current study are not publicly available due [REASON WHY DATA ARE NOT PUBLIC] but are available from the corresponding author on reasonable request.
Abbreviations
Mishel’s Uncertainty in Illness Scale
Multidimensional Scale of Perceived Social Support
European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30
Obstetrics/Gynaecology
Lee JE, Shin DW, Cho BL. The current status of cancer survivorship care and a consideration of appropriate care model in Korea. Korean J Clin Oncol. 2014;10(2):58–62. https://doi.org/10.14216/kjco.14012 .
Article Google Scholar
Yoon HJ, Seok JH. Clinical factors associated with quality of life in patients with thyroid cancer. J Korean Thyroid Assoc. 2014;7(1):62–9. https://doi.org/10.11106/jkta.2014.7.1.62 .
Dow KH, Ferrell BR, Leigh S, Ly J, Gulasekaram P. An evaluation of the quality of life among long-term survivors of breast cancer. Breast Cancer Res Treat. 1996;39(3):261–73. https://doi.org/10.1007/BF01806154 .
Article CAS PubMed Google Scholar
Ferrell BR, Dow KH. Quality of life among long-term cancer survivors. Oncology. 1997;11:565–8.
CAS PubMed Google Scholar
Lee JE, Goo A, Lee KE, Park DJ, Cho B. Management of long-term thyroid cancer survivors in Korea. J Korean Med Assoc. 2016;59(4):287–93. https://doi.org/10.5124/jkma.2016.59.4.287 .
Article CAS Google Scholar
Molassiotis A, Yates P, Li Q, So WK, Pongthavornkamol K, Pittayapan P, et al. Mapping unmet supportive care needs, quality-of-life perceptions and current symptoms in cancer survivors across the Asia-Pacific region: results from the international STEP study. Ann Oncol. 2017;28(10):2552–8. https://doi.org/10.1093/annonc/mdx350 .
Yun YH, Kim YA, Sim JA, Shin AS, Chang YJ, Lee J, et al. Prognostic value of quality of life score in disease-free survivors of surgically-treated lung cancer. BMC Cancer. 2016;16(1):505–14. https://doi.org/10.1186/s12885-016-2504-x .
Article PubMed PubMed Central Google Scholar
Park JH, Jun EY, Kang MY, Joung YS, Kim GS. Symptom experience and quality of life in breast cancer survivors. J Korean Acad Nurs. 2009;39(5):613–21. https://doi.org/10.4040/jkan.2009.39.5.613 .
Article PubMed Google Scholar
Chae YR. Relationships of perceived health status, depression, and quality of life of breast cancer survivors. J Korean Adult Nurs. 2005;17:119–27.
Google Scholar
Kim YS, Tae YS. The influencing factors on quality of life among breast cancer survivors. J Korean Oncol Nurs. 2011;11(3):221–8. https://doi.org/10.5388/jkon.2011.11.3.221 .
Sammarco A, Konecny LM. Quality of life, social support, and uncertainty among Latina breast cancer survivors. Oncol Nurs Forum. 2008;35(5):844–9. https://doi.org/10.1188/08.ONF.844-849 .
Liao MN, Chen MF, Chen SC, Chen PL. Uncertainty and anxiety during the diagnostic period for women with suspected breast cancer. Cancer Nurs. 2008;31(4):274–83. https://doi.org/10.1097/01.NCC.0000305744.64452.fe .
Dirksen S, Erickson J. Well-being in Hispanic and non-Hispanic Caucasian survivors of breast cancer. Oncol Nurs Forum. 2002;29(5):820–6. https://doi.org/10.1188/02.ONF.820-826 .
Husson O, Haak HR, Buffart LM, Nieuwlaat WA, Oranje WA, Mols F, et al. Health-related quality of life and disease specific symptoms in long-term thyroid cancer survivors: a study from the population-based PROFILES registry. Acta Oncol. 2013;52(2):249–58. https://doi.org/10.3109/0284186X.2012.741326 .
Lee JI, Kim SH, Tan AH, Kim HK, Jang HW, Hur KY, et al. Decreased health-related quality of life in disease-free survivors of differentiated thyroid cancer in Korea. Health Qual Life Outcomes. 2010;8(1):101. https://doi.org/10.1186/1477-7525-8-101 .
Yang J, Yi M. Factors influencing quality of life in thyroid cancer patients with thyroidectomy. Asian Oncol Nurs. 2015;15(2):59–66. https://doi.org/10.5388/aon.2015.15.2.59 .
Oh KS. Social support as a prescription theory. J Nurs Query. 2006;15(1):134–54.
Lien CY, Lin HR, Kuo IT, Chen ML. Perceived uncertainty, social support and psychological adjustment in older patients with cancer being treated with surgery. J Clin Nurs. 2009;18(16):2311–9. https://doi.org/10.1111/j.1365-2702.2008.02549.x .
Mishel MH. Uncertainty in illness. Image J Nurs Sch. 1988;20(4):225–32. https://doi.org/10.1111/j.1547-5069.1988.tb00082.x .
Baik OM, Lim J. Social support in Korean breast and gynecological cancer survivors: comparison by the cancer stage at diagnosis and the stage of cancer survivorship. Korean J Family Soc Work. 2011;32(6):5–35.
Nausheen B, Kamal A. Familial social support and depression in breast cancer: an exploratory study on a Pakistani sample. Psychooncology. 2007;16(9):859–62. https://doi.org/10.1002/pon.1136 .
Alfano CM, Rowland JH. Recovery issues in cancer survivorship: a new challenge for supportive care. Cancer J. 2006;12(5):432–43. https://doi.org/10.1097/00130404-200609000-00012 .
Ashing KT, Padilla G, Tejero JS, Kagawa-Singer M. Understanding the breast cancer experience of Asian American women. Psychooncology. 2003;12(1):38–58. https://doi.org/10.1002/pon.632 .
Janz N, Mujahid M, Chung L, Lantz P, Hawley S, Morrow M, et al. Symptom experience and quality of life of women following breast cancer treatment. J Women's Health. 2007;16(9):1348–61. https://doi.org/10.1089/jwh.2006.0255 .
Min HS, Park SY, Lim JS, Park MO, Won HJ, Kim JI. A study on behaviors for preventing recurrence and quality of life in breast cancer survivors. J Korean Acad Nurs. 2008;38(2):187–94. https://doi.org/10.4040/jkan.2008.38.2.187 .
Kim GD. Impact of climacteric symptoms and fatigue on the quality of life in breast cancer survivors: the mediating effect of cognitive dysfunction. Asian Oncol Nurs. 2014;14(2):58–65. https://doi.org/10.5388/aon.2014.14.2.58 .
Kwon EJ, Yi M. Distress and quality of life in breast cancer survivors in Korea. Asian Oncol Nurs. 2012;12(4):289–96. https://doi.org/10.5388/aon.2012.12.4.289 .
Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–82. https://doi.org/10.1037/0022-3514.51.6.1173 .
Lee I. Uncertainty, appraisal and quality of life in patients with breast cancer across treatment phases. J Cheju Halla Collage. 2009;33:94–112.
Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the multidimensional scale of perceived social support. J Pers Assess. 1990;55(3–4):610–7. https://doi.org/10.1080/00223891.1990.9674095 .
Fayers PM, Aaronson NK, Bjordal K, Groenvold M, Curran D, Bottomley A, On behalf of the EORTC Quality of Life Group. EORTC QLQ-C30 scoring manual. 3rd ed. Brussels: European Organization for Research and Treatment of Cancer; 2001. p. 2001.
Kim SH. Understanding cancer survivorship and its new perspectives. J Korean Oncol Nurs. 2010;10(1):19–29.
Lim J, Han I. Comparison of quality of life on the stage of cancer survivorship for breast and gynecological cancer survivors. Korean J Soc Welf. 2008;60(1):5–27. https://doi.org/10.20970/kasw.2008.60.1.001 .
Ahn JY. The influence of symptoms, uncertainty, family support on resilience in patients with breast cancer receiving chemotherapy [master’s thesis]. Seoul: The Seoul National University; 2014.
Lee I, Park CS. Convergent effects of anxiety, depression, uncertainty, and social support on quality of life in women with thyroid cancer. J Korea Convergence Soc. 2017;8(8):163–76. https://doi.org/10.15207/JKCS.2017.8.8.163 .
Park YJ. Uncertainty, anxiety and social support among preoperative patients of cancer: A correlational study [master’s thesis]. Seoul: The Seoul National University; 2015.
Yun M, Song M. A qualitative study on breast cancer survivors’ experiences. Perspect Nurs Sci. 2013;10:41–51.
Ashing-Giwa KT. The contextual model of HRQoL: a paradigm for expanding the HRQoL framework. Qual Life Res. 2005;14(2):297–307. https://doi.org/10.1007/s11136-004-0729-7 .
Adamsen L, Rasmussen J. Sociological perspectives on self-help groups: reflections on conceptualisation and social processes. J Adv Nurs. 2001;35(6):909–17. https://doi.org/10.1046/j.1365-2648.2001.01928.x .
Kim HY, So HS. A structural model for psychosocial adjustment in patients with early breast cancer. J Korean Acad Nurs. 2012;42(1):105–15. https://doi.org/10.4040/jkan.2012.42.1.105 .
Download references
Acknowledgements
We would like to thank Dr. Min, a physician of the Endocrine surgery at Cheju Halla Hospital, for collecting the data. And, we would like to thank the IRB who approved the research and the Editage Company who edited the English.
Conflict of interest
“No conflict of interest has been declared by the author(s).”
The authors did not receive any financial support for this study. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
“This research did not received any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.”
Author information
Authors and affiliations.
Department of Nursing, Changwon National University, C.P.O. Box 51140, Changwon, Republic of South Korea
Division of Nursing, Cheju Halla University, Jeju, Republic of South Korea
Changseung Park
You can also search for this author in PubMed Google Scholar
Contributions
IL designed the study, searched the literature, analyzed the data, conducted the interpretation of data, drafted and edited the manuscript, and submitted the manuscript for publishing. CSP collected the data, searched the literature, and critically revised the initial manuscript. And all authors read and approved the final manuscript.
Corresponding author
Correspondence to Insook Lee .
Ethics declarations
Ethics approval and consent to participate.
This study approved by IRB in Cheju Halla Hospital (IRB No. 2014-L02) and informed consent to participate.
Consent for publication
This manuscript has never been published in any other journal, and all authors agree to be published in this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Lee, I., Park, C. The mediating effect of social support on uncertainty in illness and quality of life of female cancer survivors: a cross-sectional study. Health Qual Life Outcomes 18 , 143 (2020). https://doi.org/10.1186/s12955-020-01392-2
Download citation
Received : 08 December 2019
Accepted : 05 May 2020
Published : 19 May 2020
DOI : https://doi.org/10.1186/s12955-020-01392-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Health and Quality of Life Outcomes
ISSN: 1477-7525
- Submission enquiries: [email protected]
Select "Patients / Caregivers / Public" or "Researchers / Professionals" to filter your results. To further refine your search, toggle appropriate sections on or off.
Cancer Research Catalyst The Official Blog of the American Association for Cancer Research

Home > Cancer Research Catalyst > Cancer Survivors: In Their Words
Cancer Survivors: In Their Words
This year alone, an estimated 1.8 million people will hear their doctor say they have cancer. The individual impact of each person can be clouded in the vast statistics. In honor of National Cancer Survivor Month, Cancer Today would like to highlight several personal essays we’ve published from cancer survivors at different stages of their treatment.

In this essay , psychiatrist Adam P. Stern’s cerebral processing of his metastatic kidney cancer diagnosis gives rise to piercing questions. When he drops off his 3-year-old son to daycare, he ponders a simple exchange: his son’s request for a routine morning hug before he turns to leave. “Will he remember me, only a little, just enough to mythologize me as a giant who used to carry him up the stairs? As my health declines, will he have to learn to adjust to a dad who used to be like all the other dads but then wasn’t?” he questions.

In another essay from a parent with a young child, Amanda Rose Ferraro describes the abrupt change from healthy to not healthy after being diagnosed with acute myeloid leukemia in May 2017. After a 33-day hospital stay, followed by weeklong chemotherapy treatments, Ferraro’s cancer went into remission, but a recurrence required more chemotherapy and a stem cell transplant. Ferraro describes harrowing guilt over being separated from her 3-year-old son, who at one point wanted nothing to do with her. “Giving up control is hard, but not living up to what I thought a mother should be was harder. I had to put myself first, and it was the hardest thing I had ever done,” she writes.
In January 1995, 37-year-old Melvin Mann was diagnosed with chronic myelogenous leukemia, which would eventually mean he would need to take a chance on a phase I clinical trial that tested an experimental drug called imatinib—a treatment that would go on to receive U.S. Food and Drug Administration approval under the brand name Gleevec. It would also mean trusting a system with a documented history of negligence and abuse of Black people like him: “Many patients, especially some African Americans, are afraid they will be taken advantage of because of past unethical experiments like the infamous Tuskegee syphilis study,” Mann writes, before describing changes that make current trials safer. Mann’s been on imatinib ever since and has enjoyed watching his daughter become a physician and celebrating 35 years of marriage.

In another essay , Carly Flumer addresses the absurdity of hearing doctors reassure her that she had a good cancer after she was diagnosed with stage I papillary thyroid cancer in 2017. “What I did hear repeatedly from various physicians was that I had the ‘good cancer,’ and that ‘if you were to have a cancer, thyroid would be the one to get,’” she writes.
In another piece for Cancer Today , Flumer shares how being diagnosed with cancer just four months after starting a graduate program shaped her education and future career path.
For Liza Bernstein, her breast cancer diagnosis created a paradox as she both acknowledged and denied the disease the opportunity to define who she was. “In the privacy of my own mind, I refused to accept that cancer was part of my identity, even though it was affecting it as surely as erosion transforms the landscape,” she writes . “Out in the world, I’d blurt out, ‘I have cancer,’ because I took questions from acquaintances like ‘How are you, what’s new?’ literally. Answering casual questions with the unvarnished truth wasn’t claiming cancer as my identity. It was an attempt to dismiss the magnitude of it, like saying ‘I have a cold.’” By her third primary breast cancer diagnosis, Bernstein reassesses and moves closer to acceptance as she discovers her role as advocate.

As part of the staff of Cancer Today , a magazine and online resource for cancer patients, survivors and caregivers, we often refer to a succinct tagline to sum up our mission: “Practical knowledge. Real hope.” Part of providing information is also listening closely to cancer survivors’ experiences. As we celebrate National Cancer Survivor Month, we elevate these voices, and all patients and survivors in their journeys.
Cancer Today is a magazine and online resource for cancer patients, survivors, and caregivers published by the American Association for Cancer Research. Subscriptions to the magazine are free to cancer patients, survivors and caregivers who live in the U.S.
- About This Blog
- Blog Policies
- Tips for Contributors

FDA Workshop to Address Need for Non-clinical Models to Advance Immuno-oncology

Annual Meeting 2022: Transitions at the National Cancer Institute

Why We Need Tailored Tobacco-control Strategies
Cancel reply
Your email address will not be published. Required fields are marked *
Join the Discussion (max: 750 characters)...
This site uses Akismet to reduce spam. Learn how your comment data is processed .
- Share Your Story
- National Cancer Research Month
- National Cancer Survivor Month
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Substance Use Disorders Among US Adult Cancer Survivors
- 1 New England Geriatric Research Education and Clinical Center, VA Boston Healthcare System, Boston, Massachusetts
- 2 Department of Population Health Sciences, Duke University School of Medicine, Durham, North Carolina
- 3 Division of General Internal Medicine, Department of Medicine, University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania
- Comment & Response Substance Use Disorders Among Cancer Survivors Alain Braillon, MD, PhD JAMA Oncology
Question What is the cancer type–specific prevalence of substance use disorder (SUD) among adult US cancer survivors?
Findings In this cross-sectional study of 6101 adult cancer survivors who responded to the National Survey on Drug Use and Health for 2015 through 2020, the overall prevalence of active SUD (within the past 12 months) was approximately 4%, with higher prevalence in some subpopulations, including survivors of head and neck cancer (approximately 9%) and esophageal and gastric cancer (approximately 9%). Alcohol use disorder was the most common SUD.
Meaning Findings of this study highlight subpopulations of adult cancer survivors who may benefit from efforts to integrate cancer and addiction care.
Importance Some individuals are predisposed to cancer based on their substance use history, and others may use substances to manage cancer-related symptoms. Yet the intersection of substance use disorder (SUD) and cancer is understudied. Because SUD may affect and be affected by cancer care, it is important to identify cancer populations with a high prevalence of SUD, with the goal of guiding attention and resources toward groups and settings where interventions may be needed.
Objective To describe the cancer type–specific prevalence of SUD among adult cancer survivors.
Design, Setting, and Participants This cross-sectional study used data from the annually administered National Survey on Drug Use and Health (NSDUH) for 2015 through 2020 to identify adults with a history of solid tumor cancer. Substance use disorder was defined as meeting at least 1 of 4 Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition) criteria for abuse or at least 3 of 6 criteria for dependence.
Main Outcomes and Measures Per NSDUH guidelines, we made adjustments to analysis weights by dividing weights provided in the pooled NSDUH data sets by the number of years of combined data (eg, 6 for 2015-2020). The weighted prevalence and corresponding SEs (both expressed as percentages) of active SUD (ie, within the past 12 months) were calculated for respondents with any lifetime history of cancer and, in secondary analyses, respondents diagnosed with cancer within 12 months prior to taking the survey. Data were analyzed from July 2022 to June 2023.
Results This study included data from 6101 adult cancer survivors (56.91% were aged 65 years or older and 61.63% were female). Among lifetime cancer survivors, the prevalence of active SUD was 3.83% (SE, 0.32%). Substance use disorder was most prevalent in survivors of head and neck cancer (including mouth, tongue, lip, throat, and pharyngeal cancers; 9.36% [SE, 2.47%]), esophageal and gastric cancer (9.42% [SE, 5.51%]), cervical cancer (6.24% [SE, 1.41%]), and melanoma (6.20% [SE, 1.34%]). Alcohol use disorder was the most common SUD (2.78% [SE, 0.26%]) overall and in survivors of head and neck cancer, cervical cancer, and melanoma. In survivors of esophageal and gastric cancers, cannabis use disorder was the most prevalent SUD (9.42% [SE, 5.51%]). Among respondents diagnosed with cancer in the past 12 months, the overall prevalence of active SUD was similar to that in the lifetime cancer survivor cohort (3.81% [SE, 0.74%]). However, active SUD prevalence was higher in head and neck (18.73% [SE, 10.56%]) and cervical cancer survivors (15.70% [SE, 5.35%]). The distribution of specific SUDs was different compared with that in the lifetime cancer survivor cohort. For example, in recently diagnosed head and neck cancer survivors, sedative use disorder was the most common SUD (9.81% [SE, 9.17%]).
Conclusions and Relevance Findings of this study suggest that SUD prevalence is higher among survivors of certain types of cancer; this information could be used to identify cancer survivors who may benefit from integrated cancer and SUD care. Future efforts to understand and address the needs of adult cancer survivors with comorbid SUD should prioritize cancer populations in which SUD prevalence is high.
Read More About
Jones KF , Osazuwa-Peters OL , Des Marais A , Merlin JS , Check DK. Substance Use Disorders Among US Adult Cancer Survivors. JAMA Oncol. 2024;10(3):384–389. doi:10.1001/jamaoncol.2023.5785
Manage citations:
© 2024
Artificial Intelligence Resource Center
Oncology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Welcome to the Survivor's Review
Encouraging the creative expression of cancer survivors.
Our goal at the Survivor's Review is to publish stories, essays, and poems that are powerful, poignant, and unflinchingly honest. Whether you are a cancer survivor, caregiver, or friend, we invite you to peruse the features in this issue.
We also hope to encourage all survivors to use writing as a tool for emotional and physical healing. In each issue, guest contributors will offer ideas and prompts to get you started. Click here to begin writing now!
Our evolving resources page lists books, websites, and other links with information on the benefits of writing and creative expression.
Also, if you're a cancer survivor or caregiver who has written a piece that has the potential to touch another's soul, please consider submitting your work to the Survivor's Review . We make every effort to respond as soon as possible.
We are interested in your feedback . Please contact us with your comments and suggestions.
We hope you enjoy this issue of Survivor's Review and that you will share this site with other survivors, caregivers and friends.
Question: Who is a cancer survivor? Answer: Anyone living with a history of cancer from the moment of diagnosis through the remainder of life.
Please join our email list so we can alert you to future issues and events. Your information is private and will never be shared.
The Survivor's Review was founded and is maintained by a small all-volunteer staff. As our readership continues to grow, we are finding ourselves in need of another committed volunteer to join our team. If you are inspired by our mission and have writing/reading/editing experience and basic computer skills, we would like to hear from you.
Our goal is to publish two issues per year, in fall and spring, and we are seeking an Associate Editor who will read and catalogue submissions and readers' interest messages, respond via email to writers and readers, and meet via Zoom for a few editorial meetings twice per year. The workload will average no more than three or four hours a month, with those hours concentrated more in the spring and fall, six weeks prior to publication. If interested, please share a bit about your interest and background with our editor, Sheree Kirby, at [email protected] .
DigitalCommons@UNMC
Home > Eppley Institute > Theses & Dissertations
Theses & Dissertations: Cancer Research
Theses/dissertations from 2024 2024.
Novel Spirocyclic Dimer (SpiD3) Displays Potent Preclinical Effects in Hematological Malignancies , Alexandria Eiken
Therapeutic Effects of BET Protein Inhibition in B-cell Malignancies and Beyond , Audrey L. Smith
Identifying the Molecular Determinants of Lung Metastatic Adaptation in Prostate Cancer , Grace M. Waldron
Identification of Mitotic Phosphatases and Cyclin K as Novel Molecular Targets in Pancreatic Cancer , Yi Xiao
Theses/Dissertations from 2023 2023
Development of Combination Therapy Strategies to Treat Cancer Using Dihydroorotate Dehydrogenase Inhibitors , Nicholas Mullen
Overcoming Resistance Mechanisms to CDK4/6 Inhibitor Treatment Using CDK6-Selective PROTAC , Sarah Truong
Theses/Dissertations from 2022 2022
Omics Analysis in Cancer and Development , Emalie J. Clement
Investigating the Role of Splenic Macrophages in Pancreatic Cancer , Daisy V. Gonzalez
Polymeric Chloroquine in Metastatic Pancreatic Cancer Therapy , Rubayat Islam Khan
Evaluating Targets and Therapeutics for the Treatment of Pancreatic Cancer , Shelby M. Knoche
Characterization of 1,1-Diarylethylene FOXM1 Inhibitors Against High-Grade Serous Ovarian Carcinoma Cells , Cassie Liu
Novel Mechanisms of Protein Kinase C α Regulation and Function , Xinyue Li
SOX2 Dosage Governs Tumor Cell Identity and Proliferation , Ethan P. Metz
Post-Transcriptional Control of the Epithelial-to-Mesenchymal Transition (EMT) in Ras-Driven Colorectal Cancers , Chaitra Rao
Use of Machine Learning Algorithms and Highly Multiplexed Immunohistochemistry to Perform In-Depth Characterization of Primary Pancreatic Tumors and Metastatic Sites , Krysten Vance
Characterization of Metastatic Cutaneous Squamous Cell Carcinoma in the Immunosuppressed Patient , Megan E. Wackel
Visceral adipose tissue remodeling in pancreatic ductal adenocarcinoma cachexia: the role of activin A signaling , Pauline Xu
Phos-Tag-Based Screens Identify Novel Therapeutic Targets in Ovarian Cancer and Pancreatic Cancer , Renya Zeng
Theses/Dissertations from 2021 2021
Functional Characterization of Cancer-Associated DNA Polymerase ε Variants , Stephanie R. Barbari
Pancreatic Cancer: Novel Therapy, Research Tools, and Educational Outreach , Ayrianne J. Crawford
Apixaban to Prevent Thrombosis in Adult Patients Treated With Asparaginase , Krishna Gundabolu
Molecular Investigation into the Biologic and Prognostic Elements of Peripheral T-cell Lymphoma with Regulators of Tumor Microenvironment Signaling Explored in Model Systems , Tyler Herek
Utilizing Proteolysis-Targeting Chimeras to Target the Transcriptional Cyclin-Dependent Kinases 9 and 12 , Hannah King
Insights into Cutaneous Squamous Cell Carcinoma Pathogenesis and Metastasis Using a Bedside-to-Bench Approach , Marissa Lobl
Development of a MUC16-Targeted Near-Infrared Antibody Probe for Fluorescence-Guided Surgery of Pancreatic Cancer , Madeline T. Olson
FGFR4 glycosylation and processing in cholangiocarcinoma promote cancer signaling , Andrew J. Phillips
Theses/Dissertations from 2020 2020
Cooperativity of CCNE1 and FOXM1 in High-Grade Serous Ovarian Cancer , Lucy Elge
Characterizing the critical role of metabolic and redox homeostasis in colorectal cancer , Danielle Frodyma
Genomic and Transcriptomic Alterations in Metabolic Regulators and Implications for Anti-tumoral Immune Response , Ryan J. King
Dimers of Isatin Derived Spirocyclic NF-κB Inhibitor Exhibit Potent Anticancer Activity by Inducing UPR Mediated Apoptosis , Smit Kour
From Development to Therapy: A Panoramic Approach to Further Our Understanding of Cancer , Brittany Poelaert
The Cellular Origin and Molecular Drivers of Claudin-Low Mammary Cancer , Patrick D. Raedler
Mitochondrial Metabolism as a Therapeutic Target for Pancreatic Cancer , Simon Shin
Development of Fluorescent Hyaluronic Acid Nanoparticles for Intraoperative Tumor Detection , Nicholas E. Wojtynek
Theses/Dissertations from 2019 2019
The role of E3 ubiquitin ligase FBXO9 in normal and malignant hematopoiesis , R. Willow Hynes-Smith
BRCA1 & CTDP1 BRCT Domainomics in the DNA Damage Response , Kimiko L. Krieger
Targeted Inhibition of Histone Deacetyltransferases for Pancreatic Cancer Therapy , Richard Laschanzky
Human Leukocyte Antigen (HLA) Class I Molecule Components and Amyloid Precursor-Like Protein 2 (APLP2): Roles in Pancreatic Cancer Cell Migration , Bailee Sliker
Theses/Dissertations from 2018 2018
FOXM1 Expression and Contribution to Genomic Instability and Chemoresistance in High-Grade Serous Ovarian Cancer , Carter J. Barger
Overcoming TCF4-Driven BCR Signaling in Diffuse Large B-Cell Lymphoma , Keenan Hartert
Functional Role of Protein Kinase C Alpha in Endometrial Carcinogenesis , Alice Hsu
Functional Signature Ontology-Based Identification and Validation of Novel Therapeutic Targets and Natural Products for the Treatment of Cancer , Beth Neilsen
Elucidating the Roles of Lunatic Fringe in Pancreatic Ductal Adenocarcinoma , Prathamesh Patil
Theses/Dissertations from 2017 2017
Metabolic Reprogramming of Pancreatic Ductal Adenocarcinoma Cells in Response to Chronic Low pH Stress , Jaime Abrego
Understanding the Relationship between TGF-Beta and IGF-1R Signaling in Colorectal Cancer , Katie L. Bailey
The Role of EHD2 in Triple-Negative Breast Cancer Tumorigenesis and Progression , Timothy A. Bielecki
Perturbing anti-apoptotic proteins to develop novel cancer therapies , Jacob Contreras
Role of Ezrin in Colorectal Cancer Cell Survival Regulation , Premila Leiphrakpam
Evaluation of Aminopyrazole Analogs as Cyclin-Dependent Kinase Inhibitors for Colorectal Cancer Therapy , Caroline Robb
Identifying the Role of Janus Kinase 1 in Mammary Gland Development and Breast Cancer , Barbara Swenson
DNMT3A Haploinsufficiency Provokes Hematologic Malignancy of B-Lymphoid, T-Lymphoid, and Myeloid Lineage in Mice , Garland Michael Upchurch
Theses/Dissertations from 2016 2016
EHD1 As a Positive Regulator of Macrophage Colony-Stimulating Factor-1 Receptor , Luke R. Cypher
Inflammation- and Cancer-Associated Neurolymphatic Remodeling and Cachexia in Pancreatic Ductal Adenocarcinoma , Darci M. Fink
Role of CBL-family Ubiquitin Ligases as Critical Negative Regulators of T Cell Activation and Functions , Benjamin Goetz
Exploration into the Functional Impact of MUC1 on the Formation and Regulation of Transcriptional Complexes Containing AP-1 and p53 , Ryan L. Hanson
DNA Polymerase Zeta-Dependent Mutagenesis: Molecular Specificity, Extent of Error-Prone Synthesis, and the Role of dNTP Pools , Olga V. Kochenova
Defining the Role of Phosphorylation and Dephosphorylation in the Regulation of Gap Junction Proteins , Hanjun Li
Molecular Mechanisms Regulating MYC and PGC1β Expression in Colon Cancer , Jamie L. McCall
Pancreatic Cancer Invasion of the Lymphatic Vasculature and Contributions of the Tumor Microenvironment: Roles for E-selectin and CXCR4 , Maria M. Steele
Altered Levels of SOX2, and Its Associated Protein Musashi2, Disrupt Critical Cell Functions in Cancer and Embryonic Stem Cells , Erin L. Wuebben
Theses/Dissertations from 2015 2015
Characterization and target identification of non-toxic IKKβ inhibitors for anticancer therapy , Elizabeth Blowers
Effectors of Ras and KSR1 dependent colon tumorigenesis , Binita Das
Characterization of cancer-associated DNA polymerase delta variants , Tony M. Mertz
A Role for EHD Family Endocytic Regulators in Endothelial Biology , Alexandra E. J. Moffitt
Biochemical pathways regulating mammary epithelial cell homeostasis and differentiation , Chandrani Mukhopadhyay
EPACs: epigenetic regulators that affect cell survival in cancer. , Catherine Murari
Role of the C-terminus of the Catalytic Subunit of Translesion Synthesis Polymerase ζ (Zeta) in UV-induced Mutagensis , Hollie M. Siebler
LGR5 Activates TGFbeta Signaling and Suppresses Metastasis in Colon Cancer , Xiaolin Zhou
LGR5 Activates TGFβ Signaling and Suppresses Metastasis in Colon Cancer , Xiaolin Zhou
Theses/Dissertations from 2014 2014
Genetic dissection of the role of CBL-family ubiquitin ligases and their associated adapters in epidermal growth factor receptor endocytosis , Gulzar Ahmad
Strategies for the identification of chemical probes to study signaling pathways , Jamie Leigh Arnst
Defining the mechanism of signaling through the C-terminus of MUC1 , Roger B. Brown
Targeting telomerase in human pancreatic cancer cells , Katrina Burchett
The identification of KSR1-like molecules in ras-addicted colorectal cancer cells , Drew Gehring
Mechanisms of regulation of AID APOBEC deaminases activity and protection of the genome from promiscuous deamination , Artem Georgievich Lada
Characterization of the DNA-biding properties of human telomeric proteins , Amanda Lakamp-Hawley
Studies on MUC1, p120-catenin, Kaiso: coordinate role of mucins, cell adhesion molecules and cell cycle players in pancreatic cancer , Xiang Liu
Epac interaction with the TGFbeta PKA pathway to regulate cell survival in colon cancer , Meghan Lynn Mendick
Theses/Dissertations from 2013 2013
Deconvolution of the phosphorylation patterns of replication protein A by the DNA damage response to breaks , Kerry D. Brader
Modeling malignant breast cancer occurrence and survival in black and white women , Michael Gleason
The role of dna methyltransferases in myc-induced lymphomagenesis , Ryan A. Hlady
Design and development of inhibitors of CBL (TKB)-protein interactions , Eric A. Kumar
Pancreatic cancer-associated miRNAs : expression, regulation and function , Ashley M. Mohr
Mechanistic studies of mitochondrial outer membrane permeabilization (MOMP) , Xiaming Pang
Novel roles for JAK2/STAT5 signaling in mammary gland development, cancer, and immune dysregulation , Jeffrey Wayne Schmidt
Optimization of therapeutics against lethal pancreatic cancer , Joshua J. Souchek
Theses/Dissertations from 2012 2012
Immune-based novel diagnostic mechanisms for pancreatic cancer , Michael J. Baine
Sox2 associated proteins are essential for cell fate , Jesse Lee Cox
KSR2 regulates cellular proliferation, transformation, and metabolism , Mario R. Fernandez
Discovery of a novel signaling cross-talk between TPX2 and the aurora kinases during mitosis , Jyoti Iyer
Regulation of metabolism by KSR proteins , Paula Jean Klutho
The role of ERK 1/2 signaling in the dna damage-induced G2 , Ryan Kolb
Regulation of the Bcl-2 family network during apoptosis induced by different stimuli , Hernando Lopez
Studies on the role of cullin3 in mitosis , Saili Moghe
Characteristics of amyloid precursor-like protein 2 (APLP2) in pancreatic cancer and Ewing's sarcoma , Haley Louise Capek Peters
Structural and biophysical analysis of a human inosine triphosphate pyrophosphatase polymorphism , Peter David Simone
Functions and regulation of Ron receptor tyrosine kinase in human pancreatic cancer and its therapeutic applications , Yi Zou

Theses/Dissertations from 2011 2011
Coordinate detection of new targets and small molecules for cancer therapy , Kurt Fisher
The role of c-Myc in pancreatic cancer initiation and progression , Wan-Chi Lin
The role of inosine triphosphate pyrophosphatase (ITPA) in maintanence [sic] of genomic stability in human cells , Miriam-Rose Menezes
- Eppley Institute Website
- McGoogan Library
Advanced Search
- Notify me via email or RSS
- Collections
- Disciplines
Author Corner
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
Survivors learn to live fully with a cancer diagnosis
Steffanie, age 57, describes herself as an artist, a gardener, an associate creative director and a cancer survivor. When she was diagnosed with cancer in 2021, she asked about 20 people she knew who were cancers survivors the same question: When it comes to treatment, what would you always choose to do again? One person told her something that changed her life: Talk to a cancer therapist.
“I’d never heard of a cancer therapist,” says Steffanie, who met with Bonnie McGregor, Ph.D., at Seattle’s Orion Center for Integrative Medicine, a program of Harmony Hill. “She helped me manage the emotional aspects of dealing with a life-threatening illness. For me, it was mainly anxiety and fear. That hasn’t gone away completely, but I now have skills like visualization and breathing exercises that continue to help immensely.”
“Science clearly supports the connection between emotional well-being and overall physical health,” says McGregor, who has contributed to dozens of research studies exploring the mind-body connection in cancer patients and survivors. “But we don’t see emotional health included as part of the prescription for people with a cancer diagnosis, offered alongside nutrition, sleep, exercise, and medication. That’s changing but it’s a slow journey, taking as long as 17 years for peer-reviewed research to make its way into clinical practice.”
Health-related quality of life
Research at the National Cancer Institute shows that, like Steffanie, nearly 70% of people diagnosed with cancer will live five-plus years. But just because the disease is in remission, that doesn’t mean life returns to normal for survivors. One study published in the journal Cancer examined nearly 500 cancer patients for post-traumatic stress disorder markers. Nearly 22% of patients experienced markers of PTSD six months post-diagnosis, and about one-third of those patients were still experiencing persistent symptoms — in many cases worsening — at the four-year follow-up.
Research is also finding a direct relationship between a person’s Health-Related Quality of Life, an individual’s perceived physical and mental health over time, and health outcomes. Conditions such as social isolation, stress and/or depression can be associated with key biological processes promoting tumor progression as well as poorer survival.
Harmony Hill’s retreats and other programs, designed and led by medical professionals, therapists and a chaplain, offer a host of techniques and experiences that promote a sense of connection with others and life, reduce fear and stress, encourage self-care and promote wellness. Harmony Hill’s outcomes demonstrate that over 90% of cancer retreat participants report:
- Increased sense of well-being.
- Increased awareness of the value of self-care.
- Increased sense of connection with others and with life.
- Decreased stress.
- Decreased fear and anxiety.
Community support is key for cancer survivors
McGregor referred Steffanie to an 11-week virtual support group she leads for those undergoing cancer treatment and survivors, Living SMART with Cancer. Participants learn mindfulness and relaxation practices to reduce stress and enhance overall well-being, as well build community.
“These were people with different types of cancer, in different stages, who all knew what I was going through,” Steffanie says. “They could give me perspective and support in a way no one else could. It was such an inspiring and healing place to be every week, with other like souls who were not afraid to be themselves. Not afraid to be afraid.”
Steffanie and about a dozen of her Smart Group members later met for a Harmony Hill three-day Cancer Retreat. One of the last things they did was to write letters to their future selves. Steffanie wrote, in part: “I’m writing to remind you what’s important to you: peace, love, joy, and real connection — deep connection. Remember what it felt like to be in your body and take good care of it. Remember what it felt like to be in truth and fully in heart. Remember what’s important. Remember to show compassion for self and others. Remember that the fog will lift, and the beauty that was there the entire time will show itself. Be kind and compassionate to yourself today. Make the time to love yourself and enjoy the gifts of the moment.”
“As a cancer survivor there will always be a little voice inside your head that reminds you of your illness and how precious life is,” says Steffanie, who has been cancer-free since 2022. “And now I also have the skills to soothe myself, quiet the negative thoughts and fears when they arise.”
Harmony Hill inspires healthy living, transforming the lives of those affected by cancer, health care professionals and others experiencing challenges. Harmony Hill and their Seattle location at Orion Center for Integrative Medicine teach the art and science of emotional healing.
Advertisement
Challenges of Survivorship for Older Adults Diagnosed with Cancer
- Geriatric Oncology (L Balducci, Section Editor)
- Published: 14 March 2022
- Volume 24 , pages 763–773, ( 2022 )
Cite this article

- Margaret I. Fitch 1 ,
- Irene Nicoll 2 ,
- Lorelei Newton 3 &
- Fay J. Strohschein 4
2792 Accesses
5 Citations
7 Altmetric
Explore all metrics
Purpose of Review
The purpose of this brief review is to highlight significant recent developments in survivorship research and care of older adults following cancer treatment. The aim is to provide insight into care and support needs of older adults during cancer survivorship as well as directions for future research.
Recent Findings
The numbers of older adult cancer survivors are increasing globally. Increased attention to the interaction between age-related and cancer-related concerns before, during, and after cancer treatment is needed to optimize outcomes and quality of life among older adult survivors. Issues of concern to older survivors, and ones associated with quality of life, include physical and cognitive functioning and emotional well-being. Maintaining activities of daily living, given limitations imposed by cancer treatment and other comorbidities, is of primary importance to older survivors. Evidence concerning the influence of income and rurality, experiences in care coordination and accessing services, and effectiveness of interventions remains scant for older adults during survivorship.
There is a clear need for further research relating to tailored intervention and health care provider knowledge and education. Emerging issues, such as the use of medical assistance in dying, must be considered in this population.
Similar content being viewed by others
Older adults with cancer and their caregivers — current landscape and future directions for clinical care

Research Methods: Outcomes and Survivorship Research in Geriatric Oncology

Avoid common mistakes on your manuscript.
Introduction
Older adults constitute one of the fastest-growing subgroups in the cancer population [ 1 ]. Over the next decade, the number of individuals 65 years and older who are diagnosed with cancer is expected to double, accounting for 67% of new cancer cases and reaching levels of 14 million worldwide [ 2 ]. Given advances in screening, treatment, and supportive care which have resulted in improved cancer outcomes, the population of older adult cancer survivors is also expected to escalate [ 3 ].
The aftermath of cancer treatment can have a significant impact on survivors [ 4 , 5 ]. Physical, emotional, and practical changes during and after treatment may carry consequences that have a significant impact on the quality of life of survivors [ 6 ], carrying implications for recovery and maintenance of autonomy and independence. Early evidence illustrates that immediate recovery following cancer treatment and improvements in survival for older adults following cancer is slower than for younger survivors [ 7 ••]. For older adults, who may be already dealing with other comorbid conditions and effects of aging, the added burden of late and long-term effects may be particularly troublesome [ 8 ].
Challenges emerging during survivorship add to the complexity of meeting the needs of older adults after cancer [ 9 , 10 ••]. Evidence is beginning to accumulate regarding the unique, multi-dimensional needs of older adults following cancer [ 11 •], and, with it, an understanding of challenges they may face as cancer survivors [ 12 ]. However, further work is needed to fully understand survivorship experiences for this population, gaps in care delivery, and how those gaps could be mitigated.
This paper highlights significant recent developments in survivorship research and care for older adults following cancer. We define survivorship as the interval from completion of primary cancer treatment until the identification of recurrent or progressive disease [ 13 ]. Our aim is to provide insight into care and support needs of older adults during cancer survivorship as well as directions for future research.
A brief review of literature from the last 3 years reporting on older adult cancer survivors aged 65 years and older was undertaken. Relevant topics were identified through consultation with experts in the field and used for search purposes. Keywords used together with “older adults” and “cancer survivors” were accelerated aging, polypharmacy, late/long-term effects, cognitive changes, neuropathy, comprehensive geriatric assessment, survivorship care plans, depression, ethics, and MAiD. A search of Medline via PubMed using the keywords identified relevant English publications from the past 3 years. All article types were considered (e.g., reviews, perspectives papers, descriptive/intervention studies). Each article was reviewed, significant findings identified, and results grouped into broad topic areas. These broad topics are summarized below, presenting significant developments regarding research and care of older cancer survivors reported over the past 3 years.
Aging and Cancer Survival
Four articles addressed patterns of survival among older adults and the impact of little research that considers age-related concerns on patterns and quality of survival in this group. There have been consistent improvements in cancer survival over the past two decades; however, these improvements are smaller for those aged 75 years and older at diagnosis and there is greater variation in 5-year survival across countries for this age group [ 7 ••]. Cellular and molecular changes that occur in non-cancerous cells with aging contribute to a microenvironment that promotes tumor progression and to treatment responses that may impact outcomes, including survival, but are seldom considered in pre-clinical trials [ 14 •]. In addition, a lack of inclusion of older adults in clinical trials, and consideration of outcomes of importance to older adults, means that treatment decisions for older adults with cancer are often based on evidence acquired from younger adults with fewer comorbidities, less polypharmacy, and different physiology [ 15 ].
Accelerated Aging
Not only does aging impact the experience of cancer, but the disease and treatment can also impact the experience of aging among cancer survivors. There is increasing work documenting patterns of accelerated or accentuated aging among people who have experienced cancer treatment [ 16 , 17 ••, 18 ]. Aging is often understood as the “time-dependent accumulation of cellular damage” [ 14 •]. Accelerated or accentuated aging occurs when cancer and cancer treatments contribute to genotoxic and cytotoxic damage that contributes to anatomic and functional changes that mirror those expected with aging, but at a younger age or to a greater degree than would occur in the absence of cancer [ 17 ••]. We identified seven articles exploring relationships among physiological markers of aging, behavioral or functional changes associated with aging, and the receipt of cancer treatment. The aging phenotype caused by cancer and its treatment has been characterized by adverse physical and cognitive consequences, including fatiguability and poor endurance [ 19 ], persistent cognitive impairment [ 20 ], onset of chronic health conditions [ 16 , 21 ••, 22 ], and decreased survival [ 17 ••, 22 ]. Researchers are exploring physiological mechanisms that may contribute to this accelerated aging phenotype among cancer survivors, including DNA damage [ 17 ••, 22 ], stem cell depletion [ 17 ••], alterations in cerebral blood flow [ 20 ], shortening of telomere length [ 16 ], cellular senescence [ 17 ••, 21 ••], and disruption of pathways that mitigate the damaging effects of inflammation and oxidative stress [ 20 , 21 ••]. These physiological changes may be reflected in clinical measures of functional status, frailty, and cognitive function, including subjective measures, such as self-report measures of activities of daily living, and objective measures, such as gait speed and grip strength [ 17 ••]. These changes may also be reflected in biological measures. The authors of recent reviews present a thorough discussion of the biomarkers associated with aging that may be used to assess and/or predict accelerated aging [ 17 ••] or resilience [ 21 ••].
To increase understanding of cancer treatment on aging, appropriate clinical and biological measures of aging of must be incorporated into clinical trials [ 17 ••]. Resilience, defined as capacity to resist or regain physical, cognitive, or psychological function and well-being after a stressor, diminishes with aging and may be defined by age-related biologic processes [ 21 ••]. If so, then clinical and biological measures of aging may also predict resilience in older survivors, and identifying associated physiological and molecular mechanisms may promote the identification of protective factors and strategies to promote resilience and well-being in survivorship [ 21 ••]. Some strategies to prevent accelerated aging include treatment with pharmaceuticals or nutraceuticals that reduce inflammation, treat cardiovascular risk, or improve cardiac function, as well as behavioral strategies including exercise-based interventions considering the unique needs of survivors [ 16 ].
Issues of Particular Concern Among Older Adult Survivors
Eighteen articles describing physical issues, comorbidities, and polypharmacy for older cancer survivors were identified. Ten were studies of older cancer survivors, five focused on older breast cancer survivors, and others addressed issues with older survivors of hematological, oral-digestive and prostate cancers, and non-Hodgkin’s lymphoma.
Physical Issues
Studies about older adults following cancer treatment have chiefly focused on physical health and function [ 10 ••, 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 ••, 31 , 32 , 33 , 34 , 35 , 36 , 37 ]. The impaired physical function has been studied as a result of treatment [ 25 , 26 , 27 , 28 ] and several studies compared symptom burden with non-cancer controls or younger cancer survivors [ 23 , 26 , 28 , 29 , 30 ••, 31 , 32 , 33 , 35 ]. In a Canadian survey of over 3000 cancer survivors 75 years or older, 80% reported physical concerns [ 11 •]. Specifically impaired physical function, decline in cardiovascular and other health conditions, fatigue, and depression were studied. The effect of cancer treatment on cardiovascular systems, physical balance, mobility, and neuropathy were reported as significant in older cancer survivors [ 10 ••, 25 , 28 ].
While the importance of physical function in older cancer survivors was explored in some studies, cognitive impairment was highlighted in more than half. Cognitive decline was observed as common in older cancer survivors, but findings varied, ranging from 12 to 75% [ 33 ]. One study observed no association between chemotherapy and cognitive function [ 27 ]. In others, older cancer survivors were shown to demonstrate the decline in executive functioning and verbal memory more frequently than younger adults following treatment [ 26 , 33 ]. Regier et al. [ 33 ] found up to 40% of older cancer survivors exhibited cancer-related cognitive impairment (sustained attention, memory, and verbal fluency) 18 months post-diagnosis while survivors who exhibited high psychoneurological symptoms at diagnosis were more likely to experience greater cognitive decline post-treatment [ 25 , 30 ••, 35 ].
Comorbidities and Polypharmacy
It is estimated 25% of older adults with cancer have five or more comorbid conditions [ 10 ••]. In a recent Canadian study, over 70% of adult survivors 75 years and older reported comorbidities, the four most common being cardiovascular/heart disease (45%); arthritis, osteoarthritis, or other rheumatic diseases (40%); diabetes (16%); and mental health (7%) [ 11 •]. Given the prevalence of other diseases and medical conditions, it is interesting that less than half of the articles addressed comorbidities and fewer discussed the importance of polypharmacy and its implications. While older adults comprise less than 15% of the population of the USA, for example, they account for over 30% of both non-prescription and prescription medications [ 30 ••]. Magnusson et al. [ 30 ••] state that polypharmacy is defined as the use of five or more medications but recognize that researchers less often address appropriate versus inappropriate polypharmacy (lacking evidence base, adverse reactions, etc.). On average, older adults with cancer take nearly 10 different medications and many are uncertain about the reasons they need these medications [ 10 ••]. The impacts of adverse drug effects (e.g., falls, cognitive issues) and drug and disease interactions can be severe. In addition, Guerard et al. [ 10 ••] note that a fragmented group of providers is often responsible for the provision of healthcare to older adults which can result in a lack of communication and coordination among the various specialists involved [ 30 ••] and uncertainty on the part of survivors about where they should seek assistance for an issue [ 12 ].
Overall cancer and its treatments are associated with higher levels of symptom burden and greater loss of well-being over time in older adult survivors, as compared to older adults without cancer, suggesting the need for greater surveillance and opportunities for intervention [ 31 ]. In addition, many older adults are at risk for experiencing physical, emotional, and practical concerns following cancer treatment yet are not obtaining desired help [ 12 ]. Coughlin et al. noted that given prevalent age-related issues such as comorbidities, osteoporosis, symptoms, physical functioning, cognitive functioning, nutrition, and physical activity [ 37 ], appropriate surveillance, screening (including pre-screening for at-risk individuals), and interventions both during and post-treatment are critical to improve associated functional/neurological changes and improve the overall quality of life [ 24 , 30 ••, 31 , 32 , 33 ]. Future research is needed about the nature and extent of disability and symptom burden to develop survivorship programs for this distinct patient population [ 29 ] and inform the development of guidelines and policies in conjunction with patients’ preferences and goals [ 10 ••].
Factors Influencing Quality of Life in Older Adult Survivors
A primary direction of research regarding older adult cancer survivors has been identifying factors that influence quality of life. Health-related quality of life (HRQOL) is seen as a primary outcome given that priorities and values for older adults shift as they age [ 38 ] and acknowledge they have few remaining years. However, age alone is insufficient to explain variations in this populations’ HRQOL. Both cancer (e.g., cancer type, treatment modality, recurrence) and non-cancer-related (e.g., education, income, residence) factors contribute [ 38 , 39 , 40 ].
Most studies reviewed included survivors of breast, prostate, lung, and colorectal cancers, making use of existing databases and frequently resulting in sizeable sample sizes (121 [ 41 ] to 271,640 [ 42 •]. Studies involved various time intervals following completion of treatment (1 to > 10 years), definitions of older adults (e.g., 60+, 75+, 70+, 75+, and 80+ years) and combinations of physical, psychological, emotional, social, and demographic variables. Overall, there is agreement that HRQOL is lower in older adult survivors than in general older adult populations [ 42 •, 43 ].
Consistently physical variables have the strongest associations with HRQOL. Although these variables were measured in various ways, (e.g., physical well-being [ 44 •], functional health limitations [ 38 ] disability [ 45 ], mobility [ 46 , 47 ], and physical health status [ 48 ], the capacity to manage activities of daily living and maintain independence were critical for older adult survivors and contributed to HRQOL. Cancer type [ 49 •], the number of comorbidities [ 42 •, 45 ], length of time dealing with side effects, side effect severity [ 43 , 50 , 51 ], duration of chronic illness [ 39 ], and deteriorating health status [ 41 , 45 ] are key variables with negative influence on HRQOL. Experiencing fatigue [ 44 •], frailty [ 53 ••], difficulty performing Activities of Daily Living (ADLs) [ 53 ••], difficulty walking [ 46 ],) and increased risk for falls [ 47 , 48 ] are challenges associated with poor HRQOL outcomes [ 53 ••] in older survivors. In a sample of 3274 older cancer survivors, when asked to identify the main challenge, they experienced in transitioning to survivorship, over 68% identified physical limitations [ 11 •].
Psychosocial variables have not been explored as frequently as physical variables in older cancer survivors. Depression [ 40 , 50 ], body image (appearance) [ 51 , 54 ], reduced optimism [ 55 ], altered sexual intimacy [ 56 ], treatment decision regret [ 57 ], chronic stress (55), lack of emotional support [ 39 ], and post-traumatic growth [ 41 ] are associated with reduced HRQOL. Depression is concerning in this population, reaching levels of 30% in community-dwelling older survivors [ 40 ]. Increased levels of depression are associated with female gender, number of symptoms [ 50 ], living alone [ 40 ], reduced income [ 40 ], and recurrence [ 40 ]. Additionally, social well-being, which is associated with social support and satisfaction with psychosocial need fulfillment [ 58 ], is associated with QOL [ 41 ]. Attending to environmental barriers which hinder engagement in social activities and reintegration in the community is important for older survivors given isolation contributes to reduced QOL [ 58 ].
Two variables beginning to receive attention in survivor populations are income and rurality. A larger proportion of older cancer survivors with low household income have concerns and seek help for physical, emotional, and practical issues than those with higher incomes [ 59 ]. However, similar proportions of low- and high-income older survivors experienced difficulty obtaining help for their concerns. In general, lower levels of subjective socioeconomic status are associated with lower QOL across all domains [ 39 , 41 , 49 •], non-adherence in purchasing medicines and supplies [ 60 ], and foregoing tests, procedures, and care [ 61 ].
Although rurality has been investigated regarding access to screening, diagnostic, and treatment services, few studies have looked at access to services for survivorship care, especially for older adults. Access to services presents different challenges for survivors than for cancer patients; survivors want services close to home rather than traveling for specialist treatment [ 62 ]. Moss et al. [ 42 •] reported QOL is higher for older survivors living in urban settings where access to ancillary services such as social work, physiotherapy, and support groups is easier. The need to leverage the higher social integration in rural communities to enhance emotional support for older adult survivors is recommended.
Interventions for Older Adult Cancer Survivors
Few studies regarding the effectiveness of interventions designed for older adult cancer survivors were identified in our search. Interventions receiving the most attention included incorporating comprehensive geriatric assessment (CGA) and physical exercise.
Comprehensive Geriatric Assessment
Older adults present a wide variation in health and functional status that may be exacerbated by cancer treatment and present various life challenges [ 63 ]. The use of screening and other assessment tools is helpful for identifying patient needs and planning appropriate interventions, particularly for distinct populations such as older adults.
Comprehensive Geriatric Assessment (CGA) is a process of evaluating and improving functional ability, physical health, cognition and mental health, and socio-environmental circumstances of older adults. Assessment results are reviewed by healthcare teams, discussed with patients, and incorporated into care plans. Nishuima et al. [ 64 •], for example, propose an approach to CGA comprised of assessments in 10 impairment domains (cognition, mood, communication, mobility, balance, bowels, bladder, nutrition, daily activities, and social) and a single comorbidity domain. Geriatric assessed impairments were associated with increased hospitalizations and long-term care use in older adults with cancer [ 65 ]. Benefits of CGA include treatment effectiveness and efficacy, prediction of mortality and cancer treatment tolerance, and decision-making to establish the appropriate treatment of cancer [ 66 ••]. CGA also helps identify significant comorbidities and polypharmacy [ 67 ] and patients who might benefit from less invasive and more tolerable evidence-based treatments [ 68 ]. Studies have shown that participants receiving CGA-based intervention report significantly better HRQOL [ 63 ].
While GA is helpful in identifying deficits in older adults with cancer and is considered a critical component in oncology treatment planning, with demonstrated feasibility and effectiveness, it is not widely implemented [ 63 , 65 , 67 , 68 ]. The incorporation of geriatric screening can be taxing to this population particularly if multiple surveys/screening tools related to geriatric domains are used in addition to those related to distress and patient-reported outcomes. In addition, healthcare providers find the incorporation of CGA into daily practice time-consuming [ 63 ]. Successful implementation requires the involvement of the multi-disciplinary team, strong administrative and patient scheduling support, and planning [ 66 ••]. Given the complexities of care for older adults with cancer, the introduction of CGA in post-treatment care, as an aspect of survivorship care planning, for example, could assist in isolating survivors’ critical health issues, identifying appropriate therapies, and enhancing survivorship care coordination.
Physical Activity/Exercise
More than 50% of older cancer survivors are not achieving standards for physical activity (PA) [ 44 •, 54 ]. Given the potential impact of PA on recovery and capacity to perform activities of daily living (ADLs), finding relevant and effective physical programming for older adults with cancer has become a priority. Unfortunately, current guidelines are based on research with younger populations. A recent systematic review of the effectiveness of PA interventions in older survivors identified 14 studies [ 69 ••]. However, interventions varied in duration (1 to 12 months), intensity, settings, and outcome measurements, making it difficult to draw conclusions about specific approaches for older survivors.
Given the choice about what interventions to pursue in one study, older adults selected PA [ 70 ]. Older survivors reported they used PA programs to increase engagement and performance of ADLs and reduce sleep disturbances and fatigue [ 70 , 71 , 72 ]. In addition, interventions help with issues of body image and psychosocial distress [ 44 •, 54 , 72 ]. Barriers included time, transportation, lack of facilities, weather, and pain [ 44 •, 70 , 72 ] while their preferences included structured programs incorporated with cancer care, having supervision, and being able to use equipment aids [ 70 , 72 ].
Older Adult Survivor Perspectives Regarding Experiences with Care
A small but growing body of evidence is emerging which captures survivors’ perspectives about experiences with cancer care delivery and suggestions for improvement. Given the complexity of needs and challenges in addressing concerns, it is important to understand the views of older survivors who have accessed services.
In quantitative investigations, higher access to services and higher self-reported health status were associated with better care experiences [ 73 ]. Variations in care experiences exist by education, gender, and cancer types. Scores indicating patient perceptions of higher care coordination are associated with living rurally at diagnosis, having fewer specialists involved in care, and more frequent visits with a family doctor [ 74 ]. Low scores are reported by women with metastatic disease, those with higher education, and individuals over 80 years of age [ 74 ].
A thematic analysis from Canada described perspectives of older adults regarding challenges experienced during survivorship care and suggestions for improvements. Themes regarding challenges included: “Getting back on my feet,” “Adjusting to life changes,” and “Finding the support I need” [ 11 •], while those regarding suggestions for improvements were, “Offer me support,” “Make access easy for me,” and “Show me you care” [ 36 ]. In this same study, communication, information, and access to a range of services were considered important yet remained gaps in service delivery by 82% of respondents.
During the COVID-19 pandemic, older adult survivors were reported to be among one of the most disadvantaged groups and needed special consideration in terms of support [ 75 ]. One qualitative study reported older survivors [ 76 ] indicated they understood the situation but that they missed interactions with others. Survivors found virtual clinic appointments were helpful, especially in reducing needs for transportation, but they were not as beneficial for social interaction as in-person visits.
Suggestions Regarding Future Research and Care Across Articles
Many articles contained recommendations about screening to identify at-risk individuals and utilizing deeper assessment of needs to build tailored interventions. Incorporating self-report by older survivors for aspects such as physical health, mobility, and emotional distress was emphasized [ 43 , 48 , 50 ] together with a relevant discussion of preferences [ 38 ]. Older survivors are a heterogeneous population with unique and complex needs. The priorities in unmet needs vary [ 12 ] and what will be most effective in meeting those needs differs from other age groups [ 77 ]. Yet health care professionals report a lack of confidence in caring for this population [ 78 ]. Enhancing knowledge and skill for survivorship care of older adults, guided by standards for optimizing care for this population [ 78 , 79 ], needs consideration.
Several areas of interventions used with other populations may have potential relevance for the older adult survivor cohort and could be considered for future program design and implementation. Lay Navigation [ 80 ], nurse coordination models [ 74 ], home telehealth [ 74 , 76 ], use of survivorship care plans [ 81 , 82 ], and active involvement of caregivers/partners in care planning [ 83 , 84 ] could be explored given the interventions were designed with the unique needs of older survivors in mind.
An Emerging Consideration from Clinical Care
An emerging issue regarding the clinical care of older adults with cancer is the marked increase in requests for medical assistance in dying (MAiD) [ 85 ]. The concept of MAiD encompasses the terms assisted suicide and euthanasia [ 86 •] with MAiD legislation originally aimed to ease the burden of suffering of imminent death. Conversation of the right to access MAiD most often centers on individual autonomy and dying with dignity (e.g., Selby et al. [ 87 •]), conceptualized as having control over one’s destiny. It has been strongly associated with an unacceptable situation of being dependent and a burden to the family. Definitions and restrictions of MAiD, guided by healthcare providers’ standards of practice, organizational policies, and professional codes of ethics, vary depending on jurisdiction-specific legislation. MAiD is often framed as a procedure; however, this patient choice also represents an extensive social movement in which a multitude of legal, ethical, regulatory, and clinical factors converge with highly personal values and beliefs involved. No discussion about this issue emerged in the literature regarding older adult cancer survivors, leaving little guidance for negotiating the difficulty of providing ethical options while also countering ageist discourses influencing patient choices.
The majority of people who consider MAiD have a pre-existing cancer diagnosis [ 88 •, 89 , 90 , 91 •]. A recent Canadian survey of oncologists reported 70% encountered a patient request for MAiD [ 92•• ]. Nurses also grapple with requests for medical assistance in dying (MAiD) among older adults with cancer, perceiving it to be a response to suffering, being a burden in survivorship, and not wanting to engage in treatment or transition to palliative care [ 80 ]. Concerns that uncontrolled physical and psychological symptoms may prompt premature requests for MAiD are warranted [ 91 •]. Furthermore, understanding the interplay of depression and demoralization, factors which are often undertreated and unaddressed in older adults, with MAiD requests is essential. The research provides a better understanding of these influences and provides guidance for practice underway [ 93 •].
In support of appropriate access and choice regarding MAiD, current evidence supports that clear and direct discussions with an interdisciplinary approach enhance therapeutic relationships [ 91• , 94 , 95 ]. At the same time, MAiD must remain person-centered to humanize a medicalized activity [ 96 ••]. Such conversations have implications for all patients, and more specifically older adults with cancer. The conversations are apt to occur within a largely unquestioned backdrop of system-level ageism, an often unaccounted for force impacting cancer care [ 36 ]. Healthcare professionals must consider messages they transmit when they commit to having explicit conversations about assistance for dying but not to the assistance required for living with the challenging side effects of cancer and subsequent treatment as patients move in and through survivorship. Evidence-informed guidelines are essential to support the transition through active treatment to survivorship. Clearly, there is need for further research in this area in the context of survivorship.
Existing Guidelines to Inform Intervention
Guidelines established by the National Comprehensive Cancer Network [NCCN] [ 97 ] and the American Society of Clinical Oncology [ 98 ] provide a framework for assessing and managing age-related concerns prior to and during cancer treatment. In addition, priorities to optimize care of older adults with cancer have been identified [ 79 , 99 , 100 ] and recommendations to support quality of life during all phases of the cancer trajectory, including survivorship, have been developed [ 101 ].
The body of evidence for guiding care of older adult cancer survivors is growing and confirms the unique and complex needs of this population. Screening at-risk individuals and connecting them to appropriate resources is important. Tailored assessments and interventions before, during, and after treatment are necessary to optimize survivorship care. However, additional research is required to design truly age appropriate and effective care approaches. By strengthening the evidence base to better inform treatment decision-making, outcomes for older adults with cancer may be improved, both in terms of survival and quality of life in survivorship.
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Miller KD, Nogueira L, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019;69:363–85.
Article Google Scholar
Pilleron S, Sarfati D, Janssen-Heijnen M, et al. Global cancer incidence in older adults, 2012 and 2035: a population-based study. Int J Cancer. 2019;144:49–58.
Article CAS Google Scholar
Parry C, Kent EE, Mariotto AB, et al. Cancer survivors: a booming population. Cancer Epidemiol Biomarkers Prev. 2011;20:1996–2005.
Lerro CC, Stein KD, Smith T, Virgo KS. A systematic review of large-scale surveys of cancer survivors conducted in North America, 2000–2011. J Cancer Survivorship. 2012;6:115–45. https://doi.org/10.1007/s11764-012-0214-1 .
Hewitt M, Greenfield S, Stovall E. From cancer patient to cancer survivor: Lost in transition. Institute of Medicine, Washington, DC: The National Academies Press. 2006
Hamrood R, Hamrood H, Merhasin I, Kenan-Boker L. Chronic pain and other symptoms among breast cancer survivors: prevalence predictors and effects on quality of life. Breast Cancer Res Treat. 2018;167(1):157–69. https://doi.org/10.1007/s10549-017-4485-0 ( Epub 2017 Aug 31 ).
Arnold M, Rutherford MJ, Bardot A, Ferlay J, Andersson TML, Myklebust TÅ… Bray F. Progress in cancer survival, mortality, and incidence in seven high-income countries 1995-2014 (ICBP SURVMARK-2): A population-based study. Lancet Oncol. 2019;20(11);1493–1505. https://doi.org/10.1016/S1470-2045(19)30456-5 . Longitudinal, population-based study in which researchers analyzed patient-level data of 3.9 million patients drawn from population-based cancer registries in seven countries. They calculated age-standardized net survival at 1 and 5 years by tumor site, age group, and period of diagnosis.
Corbett T, Bridges J. Multimorbidity in older adults living with and beyond cancer. Current Opinion in Supportive and Palliative Care. 2019;13:220–4. https://doi.org/10.1097/SPC.0000000000000439 .
Article PubMed Google Scholar
Rowland JH, Bellizzi KM. Cancer Survivorship Issues Life after treatment and implications for an aging population. Journal of Clinical Oncology. 2014;32:2662–8. https://doi.org/10.1200/JCO.2014.55.836 .
Article PubMed PubMed Central Google Scholar
Guerard EJ, Nightingale G, Bellizzi K, Burhenn P, Rosko A, Artz AS, et al. Survivorship care for older adults with cancer: U13 Conference Report. J Geriatr Oncol. 2016;(4):305-12. https://doi.org/10.1016/j.jgo.2016.06.005 . This article presents a summary of the Cancer and Aging Research Group (National Institute on Aging and National Cancer Institute) 2015 conference that discussed survivorship care for older adults. Emerging themes included that survivorship must evolve to meet the needs of older adults; older adult survivors require tailored survivorship care and plans; the suitability of the interdisciplinary team to provide older adult survivorship care; and patient advocacy is needed throughout the care continuum.
Fitch MI, Nicoll I, Lockwood G, Strohschein FJ, Newton L. Main challenges in survivorship transitions: perspectives of older adults with cancer. J Geriatr Oncol. 2021;12(4):632–640. https://doi.org/10.1016/j.jgo.2020.09.024 . A secondary analysis of early cancer survivorship for older adults revealing gaps in care and raises concerns about unexamined ageism within the Canadian cancer care system, with the concurrent need for comprehensive geriatric assessments along with multi-modal proactive treatment plans.
Fitch MI, Nicoll I, Lockwood G, Strohschein FJ, Newton L. Cancer survivors 75 years and older: physical, emotional and practical needs. BMJ Support Palliat Care. 2021; Apr 21. https://doi.org/10.1136/bmjspcare-2020-002855 .
Earle CC. Failing to plan is planning to fail: improving the quality of care with survivorship care plans. J Clin Oncol. 2006;24(32):5112–6. https://doi.org/10.1200/JCO.2006.06.5284 .
Fane M, Weeraratna AT. How the ageing microenvironment influences tumour progression. Nat Rev Cancer. 2020;20(2):89–106. https://doi.org/10.1038/s41568-019-0222-9 . A review in which the authors discuss how the ageing microenvironment contributes to tumor progression and responses to cancer therapy, including survival.
Outlaw D, Williams GR. Is the lack of evidence in older adults with cancer compromising safety? Expert Opin Drug Saf. 2020;19(9):1059–61.
Armenian SH, Gibson CJ, Rockne RC, Ness KK. Premature aging in young cancer survivors. J Natl Cancer Inst. 2019; 111(3):226–232.
Guida JL, Ahles TA, Belsky D, Campisi J, Cohen HJ, Degregori J… Hurria, A. Measuring aging and identifying aging phenotypes in cancer survivors. J Natl Cancer Inst 2019;111(12):1245–1254. https://doi.org/10.1093/jnci/djz136 . Provides a summary of the National Cancer Institute’s 2018 interdisciplinary think tank concerning aging-related consequence of cancer and cancer treatment, which addressed conceptual, measurement, and methodological challenges in this field.
Sedrak MS, Hurria A. Cancer in the older adult: implications for therapy and future research. Cancer. 2018;124(6):1108–10. https://doi.org/10.1002/cncr.31236 .
Gresham G, Dy SM, Zipunnikov V, Browner IS, Studenski SA, Simonsick EM, Ferrucci L, Schrack JA. Fatigability and endurance performance in cancer survivors: analyses from the Baltimore Longitudinal Study of Aging. Cancer. 2018;124(6):1279–87.
Carlson BW, Craft MA, Carlson JR, Razaq W, Deardeuff KK, Benbrook DM. Accelerated vascular aging and persistent cognitive impairment in older female breast cancer survivors. Geroscience. 2018;40(3):325–36. https://doi.org/10.1007/s11357-018-0025-z .
Article CAS PubMed PubMed Central Google Scholar
Sedrak MS, Gilmore NJ, Carroll JE, Muss HB, Cohen HJ, Dale W. Measuring biologic resilience in older cancer survivors. J ClinOncol. 2021;39(19):2079–2089. In this review, authors highlight the emerging concept of resilience in older cancer survivors, considering potential biomarkers and interventions that may promote resilience in this population.
Slavin TP, Sun CL, Chavarri-Guerra Y, Sedrak MS, Katheria V, Castillo D, et al. Older breast cancer survivors may harbor hereditary cancer predisposition pathogenic variants and are at risk for clonal hematopoiesis. J Geriatr Oncol. 2020;11(2):316–9. https://doi.org/10.1016/j.jgo.2019.09.004 .
Bevilacqua L, Dulak D, Schofield E, Starr TD, Nelson CJ, Roth AJ. Prevalence and predictors of depression, pain, and fatigue in older- versus younger-adult cancer survivors. Psycho-oncology. 2018;27(3):900–7. https://doi.org/10.1002/pon.4605 .
Blackwood J, Rybicki K, Huang M. Cognitive measures in older cancer survivors: An examination of validity, reliability, and minimal detectable change. J Geriatr Oncol. 2021;1:146–51. https://doi.org/10.1016/j.jgo.2020.06.015 .
La Carpia D, Liperoti R, Guglielmo M, Di Capua B, Devizzi LF, Matteucci P, et al. Cognitive decline in older long-term survivors from Non-Hodgkin Lymphoma: a multicenter cross-sectional study. J Geriatr Oncol. 2020;11(5):790–5. https://doi.org/10.1016/j.jgo.2020.01.007 .
Morin RT, Midlarsky E. Treatment with chemotherapy and cognitive functioning in older adult cancer survivors. Arch Phys Med Rehabil. 2018;99(2):257–63. https://doi.org/10.1016/j.apmr.2017.06.016 .
Fino PC, Horak FB, El-Gohary M, Guidarelli C, Medysky ME, Nagle SJ, Winters-Stone KM. Postural sway, falls, and self-reported neuropathy in aging female cancer survivors. Gait Posture. 2019;69:136–42. https://doi.org/10.1016/j.gaitpost.2019.01.025 .
Götze H, Köhler N, Taubenheim S, Lordick F, Mehnert A. Polypharmacy, limited activity, fatigue and insomnia are the most frequent symptoms and impairments in older hematological cancer survivors (70+): Findings from a register-based study on physical and mental health. J Geriatr Oncol. 2019;10(1):55–9. https://doi.org/10.1016/j.jgo.2018.05.011 .
Magnuson A, Sattar S, Nightingale G, Saracino R, Skonecki E, Trevino KM. A practical guide to geriatric syndromes in older adults with cancer: a focus on falls, cognition, polypharmacy, and depression. Am Soc Clin Oncol Educ Book. 2019n;39:e96–e109. https://doi.org/10.1200/EDBK_237641 . Identifies potential screening tools to identify geriatric syndromes and highlights the significance of falls, cognitive impairment, polypharmacy, and depression in older adults with cancer.
Mandelblatt JS, Zhai W, Ahn J, Small BJ, Ahles TA, Carroll JE, et al. Symptom burden among older breast cancer survivors: the Thinking and Living with Cancer (TLC) study. Cancer. 2020;126(6):1183–92. https://doi.org/10.1002/cncr.32663 .
Meneses K, Benz R, Bail JR, Vo JB, Triebel K, Fazeli P, et al. Speed of processing training in middle-aged and older breast cancer survivors (SOAR): results of a randomized controlled pilot. Breast Cancer Res Treat. 2018;168(1):259–67. https://doi.org/10.1007/s10549-017-4564-2 .
Regier NG, Naik AD, Mulligan EA, Nasreddine ZS, Driver JA, Sada YH, Moye J. Cancer-related cognitive impairment and associated factors in a sample of older male oral-digestive cancer survivors. Psycho-oncology. 2019;28(7):1551–8. https://doi.org/10.1002/pon.5131 .
Shah R, Chou LN, Kuo YF, Raji MA. Long-term opioid therapy in older cancer survivors: a retrospective cohort study. J Am Geriatr Soc. 2019;67(5):945–52. https://doi.org/10.1111/jgs.15945 .
Tometich DB, Small BJ, Carroll JE, Zhai W, Luta G, Zhou X, et al. Thinking and Living with Cancer (TLC) Study. Pretreatment psychoneurological symptoms and their association with longitudinal cognitive function and quality of life in older breast cancer survivors. J Pain Symptom Manage. 2019;57(3):596–606. https://doi.org/10.1016/j.jpainsymman.2018.11.015 .
Fitch MI, Nicoll I, Lockwood G, Newton L, Strohschein FJ. Improving survivorship care: perspectives of cancer survivors 75 years and older. J Geriatr Oncol. 2021;12(3):453–60. https://doi.org/10.1016/j.jgo.2020.09.012 .
Coughlin SS, Paxton RJ, Moore N, Stewart JL, Anglin J. Survivorship issues in older breast cancer survivors. Breast Cancer Res Treat. 2019;174(1):47–53. https://doi.org/10.1007/s10549-018-05078-8 .
Lapinsky E, Man LC, MacKenzie AR. Health-related quality of life in older adults with colorectal cancer. Curr Oncol Rep. 2019;21(9):81. https://doi.org/10.1007/s11912-019-0830-2 ( PMID: 31359163 ).
Doran P, Burden S, Shryane N. Older people living well beyond cancer: the relationship between emotional support and quality of life. J Aging Health. 2019;31(10):1850–71. https://doi.org/10.1177/0898264318799252 .
Doege D, Thong MSY, Koch-Gallenkamp L, Jansen L, Bertram H, Eberle A, et al. Age-specific prevalence and determinants of depression in long-term breast cancer survivors compared to female population controls. Cancer Med. 2020;9(22):8713–21. https://doi.org/10.1002/cam4.3476 .
Yang S-K, Ha Y. Exploring the relationships between posttraumatic growth, wisdom, and quality of life in older cancer survivors. Asian Pac J Cancer Prev. 2019;20(9):2667–72. https://doi.org/10.31557/APJCP.2019.20.9.2667 .
Moss JL, Pinto CN, Mama SK, Rincon M, Kent EE, Yu M, Cronin KA. Rural–urban differences in health-related quality of life: patterns for cancer survivors compared to other older adults. Qual Life Res. 2021;30:1131–1143. https://doi.org/10.1007/s11136-020-02683-3 . This study has a very large sample size and one of the first to explore rural-urban differences among older cancer survivors.
Winters-Stone KM, Medysky ME, Savin MA. Patient-reported and objectively measured physical function in older breast cancer survivors and cancer-free controls. J Geriatr Oncol. 2019;10(2):311–6. https://doi.org/10.1016/j.jgo.2018.10.006 .
Shuk D, Cheung T, Takemura N, Chau PH, Yee A, Ng M, Xu X, Lin CC. Exercise levels and preferences on exercise counselling and programming among older cancer survivors: a mixed-methods study. JGO. 2021;12(8):1173–1180. https://doi.org/10.1016/j.jgo.2021.05.00 . Study provides interesting insight into the preferences of older adult survivors regarding how exercise programs could be designed with their needs in mind.
Diemling GT, Pappada H, Ye M, Nalepa E, Ciaralli S, Phelps E, Burant CJ. Factors affecting perceptions of disability and self-rated health among older adult, long-term cancer survivors. J Aging Health. 2019;31(4):667–84. https://doi.org/10.1177/0898264317745745 .
Brown JC, Narhay MO, Harhay MN. Self-reported major mobility, disability and mortality among cancer survivors. J Geriatr Oncol. 2018; 9(5):459–463. 1016/j.jgo.2018.03.004
Huang MH, Blackwood J, Godoshian M, Pfalzer L. Predictors of falls in older survivors of breast and prostate cancer: a retrospective cohort study of surveillance, epidemiology and end results-Medicare health outcomes survey linkage. J Geriatr Oncol. 2019;10(1):89–97. https://doi.org/10.1016/j.jgo.2018.04.009 .
Sulicka J, Pac A, Puzianowska-Kuźnicka3 M, Zdrojewski T, Chudek J, Tobiasz-Adamczyk B, et al., Health status of older cancer survivors—results of the PolSenior study. J Cancer Survivorship. 2018;12:326–333 https://doi.org/10.1007/s11764-017-0672-6
Ramsey SD, Hall IJ, Smith JL, Ekwueme DU, Fedorenko CR, Kreizenbeck K, et al. A comparison of general, genitourinary, bowel, and sexual quality of life among long term survivors of prostate, bladder, colorectal, and lung cancer. J Geriatr Oncol. 2021;12(2):305–311. https://doi.org/10.1016/j.jgo.2020.07.014 . This study offers insight into an often-overlooked aspect of quality of life in older adults (sexual activity). It includes a sample of various cancer types.
Levkovich I, Cohen, Alon S, Evron E, Pollack S, Fried, et al. Symptom cluster of emotional distress, fatigue and cognitive difficulties among young and older breast cancer survivors: the mediating role f subjective stress. J Geriatr Oncol. 2018;9(5):469–475. 1016/j.jgo.2018.05.002
Davis C, Tami P, Ramsay D, Melanson L, MacLean L, Nersesian S, Ramjeesingh R. Body image in older breast cancer survivors: a systematic review. Psycho-Oncology. 2020;29:823–32. https://doi.org/10.1002/pon.5359 .
Koll TT, Semin JN, Brodsky R, Fisher AL, High R, Beadle JN. Health-related and sociodemographic factors associated with physical frailty among older cancer survivors. J Geriatr Oncol. 2021;12(1):96–101. https://doi.org/10.1016/j.jco.2020.04.015 .
Blackwood J, Karczewski H, Huang MH, Pfalzer L. Katz activities of daily living disability in older cancer survivors by age, stage, and cancer type. J Cancer Surviv. 2020;14(6):769–778. https://doi.org/10.1007/s11764-020-00891-x . This article describes the range of potential impairments in activities of daily living cancer survivors could experience. It is a strong case for screening for ADL impairments as a regular aspect of care for older survivors.
Zhang X, Pennell ML, Bernardo BM, Crane T, Shadyab AH, Paskett ED, et al. Body image, physical activity and psychological health in older female cancer survivors. J Geriatr Oncol. 2021;12(7):1059–67. https://doi.org/10.1016/j.jgo2021.04.007 .
Chow PI, Shaffer LM, Lohman MC, LeBaron VT, Fortuna KL, Ritterband LM. Examining the relationship between changes in personality and depression in older adult cancer survivors. Aging Ment Health. 2019;24(8):1237–45. https://doi.org/10.1080/13607863.2019.1594158 .
Arthur EK, Wordy B, Carpenter KM, Krok-Schoen JL, Quick AM, Jenkins LC, et al. Let’s get it on: addressing sex and intimacy in older cancer survivors. JGO. 2021;12(2):312–5. https://doi.org/10.1016/j.jgo.2020.08.033 .
Karauturi MS, Lei X, Shen Y, Giordano SH, Swanick CW, Smith BD. Long-term decision regret surrounding systemic therapy in older breast cancer survivors: a population-based survey study. J Geriatr Oncol. 2019;10(6):973–9. https://doi.org/10.1016/j.jgo.2019.03.013 .
Loew K, Lynch MF, Lee J. Social support, basic psychological needs, and social well-being among older cancer survivors. Int J Aging Hum Dev. 2021;92:100–14. https://doi.org/10.1177/0091415019887688 .
Fitch MI, Nicoll I, Lockwood G, Loiselle CG, Longo CJ, Newton L, Strohschein FJ. Exploring the relationships between income and emotional/practical concerns and help-seeking by older adult cancer survivors: a secondary analysis. J Geriatr Oncol. 2021. https://doi.org/10.1016/j.jgo.2021.11.007 .
Gu D, Shen C. Cost-related medication nonadherence and cost-reduction strategies among elderly cancer survivors with self-reported symptoms of depression. Popul Health Manag. 2020;23(2):132–9. https://doi.org/10.1089/pop.2019.0035 .
Longo CJ, Fitch MI. Unequal distribution of financial toxicity among people with cancer and its impact on access to care: a rapid review. Current Opinion (ePub 2021) https://doi.org/10.1097/spc.0000000000000561
Fitch MI, Lockwood G, Nicoll I. Physical, emotional, and practical concerns, help-seeking and unmet needs of rural and urban dwelling adult cancer survivors. J Eur Oncol Nurs. 2021;53:101976. https://doi.org/10.1016/j.ejon.2021.101976 .
Fitch MI, Strohschein FJ, Nyrop K. Measuring quality of life in older people with cancer. Curr Opin Support Palliat Care. 2021;15(1):39–47. https://doi.org/10.1097/SPC.0000000000000535 .
Nishijima TF, Shimokawa M, Esaki T, Morita M, Toh Y, Muss HB. A 10-item frailty index based on a Comprehensive Geriatric Assessment (FI-CGA-10) in Older Adults with Cancer: Development and construct validation. Oncologist. 2021;26(10):e1751–e1760. https://doi.org/10.1002/onco.13894 . Study of the creation and testing of a user-friendly frailty index based on comprehensive geriatric assessment with over 500 older adults with various cancer types. Results were determined more quickly and interpreted in a more clinically sensible manner than existing tools.
Williams GR, Dunham L, Chang Y, Deal AM, Pergolotti M, Lund JL, et al. Geriatric assessment predicts hospitalization frequency and long-term care use in older adult cancer survivors. J Oncol Pract. 2019;15(5):e399–409. https://doi.org/10.1200/JOP.18.00368 .
Overcash J, Ford N, Kress E, Ubbing C, Williams N. Comprehensive Geriatric Assessment as a versatile tool to enhance the care of the older person diagnosed with cancer. Geriatrics (Basel). 2019;24;4(2):39. https://doi.org/10.3390/geriatrics4020039 . Examination of how a comprehensive geriatric assessment can be tailored to ambulatory geriatric oncology programs in academic cancer centers and to community oncology practices with varying levels of resources.
Williams GR, Kenzik KM, Parman M, Al-Obaidi M, Francisco L, Rocque GB, et al. Integrating geriatric assessment into routine gastrointestinal (GI) consultation: the Cancer and Aging Resilience Evaluation (CARE). J Geriatr Oncol. 2020;11(2):270–3. https://doi.org/10.1016/j.jgo.2019.04.008 .
Cope DG, Reb A, Schwartz R, Simon J. Older adults with lung cancer: assessment, treatment options, survivorship issues, and palliative care strategies. Clin J Oncol Nurs. 2018;22(6):26–35. https://doi.org/10.1188/18.CJON.S2.26-35 .
Forbes C, Swan F, Greenley SL, Lind M, Johnson MJ. Physical activity and nutrition interventions for older adults with cancer: A systematic review. Journal of Cancer Survivorship. 2020;14:689–711. https://doi.org/10.1007/s11764-020-00883-x / Published online: 24 April 2020. A recent literature review of effectiveness of physical activity interventions for older adult cancer survivors describes various interventions and can inform future designs.
Lyons KD, Newman R, Adachi-Mejia AM, Whipple J, Hegel MT. Content analysis of a participant-directed intervention to optimize activity engagement of older adult cancer survivors. OTJR: Occup Participation Health. 2018;38(1):38–45. https://doi.org/10.1177/1539449217730356
Paulo TRS, Rossi FE, Viezel J, Tosello GT, Seidinger SG, Simões RR, et al. The impact of an exercise program on quality of life in older breast cancer survivors undergoing aromatase inhibitor therapy: a randomized controlled trial. Health Qual Life. 2019;17:17. https://doi.org/10.1186/s12955-019-1090-4 .
Perry CK, Ali WB, Solanki E, Winters-Stone K. Attitudes and beliefs of older female breast cancer survivors and providers about exercise in cancer care. ONF. 2020;47(1):56–69. https://doi.org/10.1188/20.ONF.56-69
Halpern MT, Urato MP, Lines LM, Cohen JB, Arora NK, Kent EE, et al. Healthcare experience among older cancer survivors: analysis of the SEER-CAHPS dataset. J Geriatr Oncol. 2018;9:194–203. https://doi.org/10.1016/j.jgo.2017.11.005 .
Mollica MA, Buckenmaier SS, Halpern MT, McNeel TS, Weaver SJ, Doose M, Kent EE. Perceptions of care coordination among older adult cancer survivors: a SEER-CAHPS study 2020. J Geriatr Oncol. 2021;12:446–52. https://doi.org/10.1016/j.jgo.2020.09.003 .
Galica J, Liu Z, Kain D, Merchant S, Booth C, Koven R, Brundage M, Haase KR. Coping during COVID-19: a mixed methods study of older cancer survivors. Support Care Cancer. 2021;29(6):3389–3398. https://doi.org/10.1007/s00520-020-05929-5 . Erratum in: Support Care Cancer. 2021.
Haase KR, Kain D, Merchant S, Booth C, Koven R, Brundage M, Galica J. Older survivors of cancer in the COVID-19 pandemic: reflections and recommendations for future care. J Geriatr Oncol. 2021;12(3):461–466. https://doi.org/10.1016/j.jgo.2020.11.009 .
Strohschein FJ. Newton L. Fitch MI, Haase K, Puts MTE, Jin R, Loucks A, Kenis C. Optimizing care of older adults with cancer: Canadian perspectives on challenges, solutions, and the need for interprofessional collaboration. Canadian Association of Psychosocial Oncology National Virtual Conference, July 14-16, 2020.
Puts M, Hsu T, Szumacher E, Dawe D, Fitch M, Jones J, Fulop T, Alibhai S, Strohschein F. Never too old to learn new tricks: surveying Canadian health care professionals about learning needs in caring for older adults with cancer. Curr Oncol. 2019;26(2):71–2. https://doi.org/10.3747/co.26.4833 .
Strohschein FJ, Newton L, Puts M, Jin R, Haase, K, Plante A, Loucks A, Kenis C, Fitch MI. Optimizing the care of older Canadians with cancer and their families: a statement articulating the position and contribution of Canadian oncology nurses. Can Oncol Nurs J = Revue canadienne de nursing oncologique. 2021;31(3):352–356.
Pisu M, Rocque GB, Jackson BE, Kenzik KM, Sharma P, Williams CP… Meneses K. Lay navigation across the cancer continuum for older cancer survivors: equally beneficial for Black and White survivors? J Geriatr Oncol. 2019;10(5):779–786. https://doi.org/10.1016/j.jgo.2018.10.013
Krok-Schoen JL, DeSalvo J, Klemanski D, Stephens C, Noonan AM, Brill S, Lustberg MB. Primary care physicians’ perspectives of the survivorship care for older breast cancer survivors: a pilot study. Support Care Cancer. 2020;28(2):645–52. https://doi.org/10.1007/s00520-019-04855-5 .
Krok-Schoen JL, Naughton MJ, Noonan AM, Pisegna J, DeSalvo J, Lustberg MB. Perspectives of survivorship care plans among older breast cancer survivors: a pilot study. Cancer Control. 2020;27(1):1073274820917208. https://doi.org/10.1177/1073274820917208 .
Cohee AA, Bigatti SM, Shields CG, Johns SA, Stump T, Monahan PO, Champion VL. Quality of life in partners of young and old breast cancer survivors. Cancer Nurs. 2018;41(6):491–7. https://doi.org/10.1097/NCC.0000000000000556 .
Kadambi S, Loh KP, Dunne R, Magnuson A, Maggiore R, Zittel J, Mohile S. Older adults with cancer and their caregivers - current landscape and future directions for clinical care. Nat Rev Clin Oncol. 2020;17(12):742–55. https://doi.org/10.1038/s41571-020-0421-z .
Van Den Noortgate N, Van Humbeeck L. Medical assistance in dying and older persons in Belgium: trends, emerging issues and challenges. Age Ageing. 2021;50(1):68–71. https://doi.org/10.1093/ageing/afaa116 .
Beuthin R, Bruce A, Scaia M. Medical assistance in dying (MAiD): Canadian nurses’ experiences. Nurs Forum . 2018;53:511–520. https://doi.org/10.1111/nuf.12280 . A Canadian descriptive narrative inquiry examining nurses’ experiences in the first six months of MAiD legalization, highlighting professional impacts of, and the importance of, open and non-judgemental communication with and between patients, families and the multidisciplinary healthcare team.
Selby, D, Bean, S, Isenberg-Grzeda, E, Bioethics, B, & Nolen, A. Medical Assistance in Dying (MAiD): A Descriptive study from a Canadian tertiary care hospital. Am J Hospice Palliat Care. 2020;37(1):58–64. https://doi.org/10.1177/1049909119859844 . A retrospective chart review was conducted to better understand the nature of MAiD requests in a Canadian healthcare institution, finding similarities with requests to other jurisdictions, and indicating that earlier assessments and more careful monitoring would be beneficial for this group at high risk for loss of capacity.
Blanke C, LeBlanc M, Hershman D, Ellis L, Meyskens F. (2017). Characterizing 18 years of the death with dignity act in Oregon. JAMA Oncol 2017;3(10):1403–1406. https://doi.org/10.1001/jamaoncol.2017.0243 . This analysis of publicly available data illuminates how MAiD in the USA is enacted and corroborates how cancer is the prevalent diagnosis of those choosing this option.
Emanuel IJ, Onwuteaka-Philipsen BD, Unwin JW, Cohen J. Attitudes and practices of euthanasia and physician-assisted suicide in the United States, Canada and Europe. JAMA. 2016;316:79–90. Comprehensive review of practices across Europe and North America with extensive data on differing approaches and experiences.
Health Canada. Second Annual Report on Medical Assistance in Dying in Canada: 2020. Ottawa, ON; June 2021. Accessed December 2, 2021 from: https://www.canada.ca/content/dam/hc-sc/documents/services/medical-assistance-dying/annual-report-2020/annual-report-2020-eng.pdf
Selby D, Bean S. Oncologists communicating with patients about assisted dying. Curr Opin Support Palliat Care. 2019;13(1):59–63. https://doi.org/10.1097/SPC.0000000000000411 . A review of recent literature regarding MAiD and communication revealed key themes of perceived barriers and benefits, including the importance of pragmatic and proactive approaches o develop and support best practices
Chandhoke G, Pond G, Levine O, Oczkowski S. Oncologists and medical assistance in dying: where do we stand? Results of a national survey of Canadian oncologists. Curr Oncol (Toronto, Ont.), 2020;27(5):263–269. https://doi.org/10.3747/co.27.6295 . An overview of survey finding to better understand Canadian oncologists’ experiences with MAiD, in which 70% of respondents received MAiD requests, supporting calls for standardized guidelines to safeguard equitable access for oncology patients.
Li M, Shapiro GK, Klein R, et al. Medical Assistance in Dying in patients with advanced cancer and their caregivers: a mixed methods longitudinal study protocol. BMC Palliat Care, 2021;117. https://doi.org/10.1186/s12904-021-00793-4 . This Canadian study is aimed to excavate the prevalence and determinants of depression and demoralization and how these states influence desire for death and MAiD requests, pointing to the importance of appropriate access and further consideration as the legislation for MAiD is broadening.
Jackson ML. Transitional Care: methods and processes for transitioning older adults with cancer in a post-acute setting. Clin J Oncol Nurs. 2018;22(6):37–41. https://doi.org/10.1188/18.CJON.S2.37-41 .
Suva G, Penney T, McPherson CJ. Medical assistance in dying: a scoping review to inform nurses’ practice. J Hospice Palliat Nurs. 2019;21(1):46–53. https://doi.org/10.1097/NJH.0000000000000486 .
Pesut B, Thorne S, Schiller C, Greig M, Roussel J, Tishelman C. (2020). Constructing good nursing practice for medical assistance in dying in Canada: an interpretive descriptive study. Glob QualNurs Res. 2020;7:2333393620938686 https://doi.org/10.1177/2333393620938686 . The purpose of this qualitative study was to explore ‘good nursing practice’ in the context of MAiD to humanize a somewhat medicalized experience, which includes establishing relationships, planning and supporting the family and underscores the need for best practice guidelines development.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): Older adult oncology (Version 1.2021). 2021. Available from: www.nccn.org . Accessed 2 Jan 2022.
Mohile SG, Dale W, Somerfield MR, Schonberg MA, Boyd CM, Burhenn PS, et al. Practical assessment and management of vulnerabilities in older patients receiving chemotherapy: ASCO guideline for geriatric oncology. J Clin Oncol. 2018;36:2326–47.
Extermann M, Brain E, Canin B, Cherian MN, Cheung K-L, de Glas N, et al. Priorities for the global advancement of care for older adults with cancer: an update of the International Society of Geriatric Oncology Priorities Initiative. Lancet Oncol. 2021;22(1):e29–36.
Puts M, Strohschein F, Oldenmenger W, Haase K, Newton L, Fitch M, et al. Position statement on oncology and cancer nursing care for older adults with cancer and their caregivers of the International Society of Geriatric Oncology Nursing and Allied Health Interest Group, the Canadian Association of Nurses in Oncology Oncology & Aging Special Interest Group, and the European Oncology Nursing Society. J Geriatr Oncol. 2021;12(7):1000–4.
Scotté F, Bossi P, Carola E, Cudennec T, Dielenseger P, Gomes F, et al. Addressing the quality of life needs of older patients with cancer: a SIOG consensus paper and practical guide. Ann Oncol. 2018;29(8):1718–26.
Download references
Author information
Authors and affiliations.
Bloomberg Faculty of Nursing, University of Toronto, 207 Chisholm Ave, Toronto, ON, M4C 4V9, Canada
Margaret I. Fitch
Health Care Consultant, Toronto, Canada
Irene Nicoll
School of Nursing, STN CSC, University of Victoria, PO Box 1700, Victoria, BC, V8W 2Y2, Canada
Lorelei Newton
Faculty of Nursing, University of Calgary, Calgary, AB, Canada
Fay J. Strohschein
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Margaret I. Fitch .
Ethics declarations
Conflict of interest.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Geriatric Oncology
Rights and permissions
Reprints and permissions
About this article
Fitch, M.I., Nicoll, I., Newton, L. et al. Challenges of Survivorship for Older Adults Diagnosed with Cancer. Curr Oncol Rep 24 , 763–773 (2022). https://doi.org/10.1007/s11912-022-01255-7
Download citation
Accepted : 05 January 2022
Published : 14 March 2022
Issue Date : June 2022
DOI : https://doi.org/10.1007/s11912-022-01255-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Older adults
- Survivorship
- Quality of life
- Literature review
- Find a journal
- Publish with us
- Track your research
- International website
- Find courses
- Find research
- Find organisation
Suleiman Abuhasanein: New and rapid ways to detect bladder cancer
Investigation of patients suspected of having urinary bladder cancer (UBC) is resource-intensive. Often, it requires a camera examination through the urethra, which can cause discomfort and complications. Suleiman Abuhasanein’s thesis reveals new and rapid methods for early detection of UBC, potentially reducing costs for society and suffering for patients.

SULEIMAN ABUHASANEIN Dissertation defense: 31 May 2024 (click for details) Doctoral thesis: Optimizing the early diagnosis process of urinary bladder cancer Research area: Urology Sahlgrenska Academy, The Institute of Clinical Sciences
A new urine test and an innovative AI technique can simplify the investigation of bladder cancer (UBC). That’s what Suleiman Abuhasanein’s research shows.
UBC is a common form of cancer. Visible blood in the urine (macroscopic hematuria) is often the first symptom. A delay in diagnosis is linked to a worse prognosis. Therefore, it’s crucial to detect the disease as early as possible.
However, current investigation methods such as cystoscopy (a camera examination inserted through the urethra) and computed tomography urography (CTU) are expensive and resource-intensive.
“They also have known complications, and only about 10–15 percent of the patients examined actually have underlying urinary tract cancer. Simple diagnostic methods for patients presenting with macroscopic hematuria like urine tests to rule out UBC are lacking,” says Suleiman Abuhasanein, a urology specialist at Uddevalla Hospital and currently pursuing a doctorate at the Institute of Clinical Sciences.
New ways to investigate UBC
What is the focus of your research? “The main aim of my thesis is to examine how the investigation of macroscopic hematuria has evolved over time. And to study the effects of this development and find possible improvements in the investigation process. We have therefore studied how early detection of UBC can affect tumor characteristics,” says Suleiman Abuhasanein, and continues:
“We have also evaluated the potential of CTU as a standalone investigation method and AI interpretation of CTU to improve the investigation of patients with suspected UBC. Finally, we have evaluated a new simple urine test with an mRNA panel to detect or exclude UBC with high diagnostic certainty.”

“A rapid process”
What are the key research findings? “Prompt investigation after observing blood in the urine can reduce the risk of developing more dangerous tumors. CTU imaging can reliably examine patients with blood in the urine. We have developed an innovative AI technique that enables automatic identification of bladder cancer on CTU imaging. With a new urine test, we can now detect or exclude bladder cancer in patients experiencing macroscopic hematuria. Finally, we have developed a new diagnostic framework for examining macroscopic hematuria.”
What could the research findings mean for this patient group? “These findings eliminate the need for camera examinations in the bladder, an examination that can cause both discomfort and complications. Faster diagnoses become possible, reducing the burden on urological clinics. A rapid process also reduces society’s costs for patients undergoing investigations.”
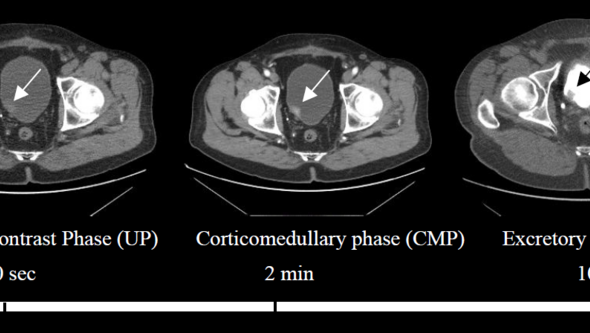
“Scientific euphoria”
What has been enjoyable and rewarding about the doctoral project? “It is enriching to contribute to new knowledge in the field. Knowing that one’s work can have a real impact and contribute to progress in the field gives a feeling of pride and achievement. In addition, the opportunity to participate in conferences and meetings within the research community has been inspiring and provided new perspectives,” says Suleiman Abuhasanein, adding:
“What I find most fascinating about research, what I call scientific euphoria, is when you have a hypothesis, collect data over a long period, sit down and start analyzing… and suddenly completely new results with new insights and sometimes surprising findings emerge.”
And what have been the biggest challenges? “Handling the large amount of information and needing to stay updated with the latest research in the field has been demanding. In addition, balancing research, clinical work, and other things in life has been challenging. Despite these challenges, the project has given me the opportunity to grow both as a researcher and as a person, and I look forward to continuing my research journey.”
Text: Jakob Lundberg
- Share full article
Advertisement
Supported by
In Reversal, Expert Panel Recommends Breast Cancer Screening at 40
Some researchers said the advice did not go far enough. The panel also declined to recommend extra scans for women with dense breast tissue.

By Roni Caryn Rabin
Citing rising breast cancer rates in young women, an expert panel on Tuesday recommended starting regular mammography screening at age 40, reversing longstanding and controversial guidance that most women wait until 50.
The panel, the U.S. Preventive Services Task Force, finalized a draft recommendation made public last year . The group issues influential advice on preventive health, and its recommendations usually are widely adopted in the United States.
In 2009, the task force raised the age for starting routine mammograms to 50 from 40, sparking wide controversy. At the time, researchers were concerned that earlier screening would do more harm than good, leading to unnecessary treatment in younger women, including alarming findings that lead to anxiety-producing procedures that are invasive but ultimately unnecessary.
But now breast cancer rates among women in their 40s are on the rise, increasing by 2 percent a year between 2015 and 2019, said Dr. John Wong, vice chair of the task force. The panel continues to recommend screening every two years for women at average risk of breast cancer, though many patients and providers prefer annual screening.
“There is clear evidence that starting screening every other year at age 40 provides sufficient benefit that we should recommend it for all women in this country to help them live longer and have a better quality of life,” said Dr. Wong, a primary care clinician at Tufts Medical Center who is the director of comparative effectiveness research for the Tufts Clinical Translational Science Institute.
The recommendations have come under harsh criticism from some women’s health advocates, including Representative Rosa DeLauro, Democrat of Connecticut, and Representative Debbie Wasserman Schultz, Democrat of Florida, who say the advice does not go far enough.
In a letter to the task force in June , they said that the guidance continued to “fall short of the science, create coverage gaps, generate uncertainty for women and their providers, and exacerbate health disparities.”
Weighing in again on a hotly debated topic, the task force also said there was not enough evidence to endorse extra scans, such as ultrasounds or magnetic resonance imaging, for women with dense breast tissue.
That means that insurers do not have to provide full coverage of additional screening for these women, whose cancers can be missed by mammograms alone and who are at higher risk for breast cancer to begin with. About half of all women aged 40 and older fall into this category.
In recent years, more mammography providers have been required by law to inform women when they have dense breast tissue and to tell them that mammography may be an insufficient screening tool for them.
Beginning in September, all mammography centers in the United States will be required to give patients that information.
Doctors often prescribe additional or “supplementary” scans for these patients. But these patients frequently find they have to pay all or some of the charges themselves, even when the additional tests are performed as part of preventive care, which under law should be offered without cost.
Medicare, the government health plan for older Americans, does not cover the additional scans. In the private insurance market, coverage is scattershot, depending on state laws, the type of plan and the plan’s design, among other factors.
The task force sets the standards for what preventive care services must be covered by law by health insurers at no cost to patients.
The panel’s decision not to endorse the extra scans has significant implications for patients, said Robert Traynham, a spokesman for AHIP, the association that represents health insurance companies.
“What that means for coverage is that there is no mandate to cover these specific screenings for women with dense breasts at zero-dollar cost-sharing,” he said.
While some employers may choose to have their health insurance plans do so, it is not required by law, Mr. Traynham said.
Kathleen Costello, a retiree in Southern California who was diagnosed with breast cancer in 2017 when she was 59, said she was convinced that mammograms missed her cancer for many years.
She underwent screening annually, and every year she received a letter saying that she was cancer-free. The letters also told her that she had dense breast tissue and that additional screening was available but not covered by insurance.
Six months after an all-clear mammogram in 2016, she told her doctor that her right breast felt stiff. The doctor ordered a mammogram and an ultrasound.
“In 30 seconds, the ultrasound found the cancer,” Ms. Costello said in an interview, adding that she knew because “the technician blanched and left the room.”
The mass was four centimeters in size, Ms. Costello added: “It’s hard for me to accept that it grew in six months from undetectable to four centimeters.”
But Dr. Wong, of the task force, said there was no scientific evidence to prove that supplemental imaging, by either M.R.I. or ultrasound, reduces breast cancer progression and extends life for women with dense breast tissue.
There is ample evidence, on the other hand, that supplemental screenings may lead to frequent false-positive findings and to biopsies, contributing to stress and unnecessary invasive procedures.
“It’s tragic,” Dr. Wong said. “We are as frustrated as women are. They deserve to know whether supplemental screenings would be helpful.”
But medical organizations like the American College of Radiology endorse supplemental screening for women with dense breast tissue. There is research showing that ultrasound in conjunction with mammography does detect additional cancers in patients with dense tissue, said Dr. Stamatia Destounis, chair of the college’s breast imaging commission.
For women with dense breasts who are at average risk of breast cancer, recent research indicates that M.R.I. is the best supplemental scan, Dr. Destounis said, “with far better cancer detection and more favorable positive predictive values.”
The college also recommends annual screening for women at average cancer risk, rather than screening every two years as recommended by the panel. The radiologists group is pressing for a recommendation that all women should be assessed for breast cancer risk before age 25, so that women at high risk can start screening even before they turn 40.
Growing evidence shows that Black, Jewish and other minority women develop breast cancer and die from it before age 50 more frequently than do other women, Dr. Destounis noted.
Trans men who have not had mastectomies must continue to be screened for breast cancer, she added, and trans women, whose hormone use puts them at greater risk for breast cancer than the average man, should discuss screening with their doctor.
While the panel’s advice to start screening at age 40 is “an improvement,” Dr. Destounis said, the final recommendations “do not go far enough to save women’s lives.”
Roni Caryn Rabin is a Times health reporter focused on maternal and child health, racial and economic disparities in health care, and the influence of money on medicine. More about Roni Caryn Rabin
The Fight Against Breast Cancer
Citing rising breast cancer rates in young women, the U.S. Preventive Services Task Force recommended starting regular mammography screening at age 40 , reversing longstanding guidance that most women wait until 50.
Clinics around the United States are starting to offer patients a new service: having their mammograms read not just by a radiologist, but also by an A.I. model .
Risk calculators can offer a more personalized picture of an individual patient’s breast cancer risk. But experts warn that the results need to be interpreted with the help of a doctor.
We asked doctors to weigh in on the new mammograms guidelines and how younger women can understand and mitigate their breast cancer risk .
Scientists have long known that dense breast tissue is linked to an increased risk of breast cancer. A recent study adds a new twist .
Skip to Content
Geologists, biologists unearth the atomic fingerprints of cancer
Cancerous growths in the liver of a mouse. (Credit: Imaging/tissue extraction by Anthony B. Eason; lab of Dirk Dittmer, University of North Carolina Lineberger Comprehensive Cancer Center. Mice maintained by UNC Animal Studies Core; staining by UNC Animal Histopathology Core)
- Share via Twitter
- Share via Facebook
- Share via LinkedIn
- Share via E-mail
Scientists at CU Boulder and Princeton University have, for the first time, employed a tool often used in geology to detect the atomic fingerprints of cancer.
In a case of medicine meets earth science, the researchers discovered that cancer cells may be made from a different assortment of hydrogen atoms than healthy tissue. The findings could give doctors new strategies for studying how cancer grows and spreads—and may even, one day, lead to new ways to spot cancer early on in the body.
The team, led by CU Boulder geochemist Ashley Maloney, published their findings May 6 in the Proceedings of the National Academy of Sciences.
“This study adds a whole new layer to medicine, giving us the chance to look at cancer at the atomic level,” said Maloney, a research associate in the Department of Geological Sciences .
She explained that in nature, hydrogen comes in two main flavors, or isotopes. Some hydrogen atoms, called deuterium, are a little heavier, while others, usually just known as hydrogen, are a little lighter. On Earth, hydrogen atoms outnumber deuterium atoms by a ratio of about 6,420 to one. For decades, scientists from a number of fields have turned to the natural distribution of these atoms to reveal clues about the history of our planet. Climate scientists, for example, examine the hydrogen atoms trapped in the ice on Antarctica to infer how hot or cool Earth was hundreds of thousands of years ago.
In the new study, Maloney and her colleagues wondered: Could those same tiny atoms provide hints about the lives of complex biological organisms?
Yeast grow under controled conditions in a lab at Princeton University. (Credit: Ashley Maloney)
Yeast cells under a microscope. (Credit: CC image via Wikimedia Commons )
To find out, the team grew cultures of yeast and mouse liver cells in the lab, then analyzed their hydrogen atoms. The team found that cells that are growing really fast, such as cancer cells, contain a much different ratio of hydrogen versus deuterium atoms. Think of it like cancer leaving a fingerprint on the doorknob of a crime scene.
The research is still in its early stages, and the team isn’t sure how this signal might appear, or not, in the bodies of real cancer patients. But the potential could be big, said Sebastian Kopf, a co-author of the study and an assistant professor in geological sciences.
“Your chances of survival are so much higher if you catch cancer early on,” Kopf said. “If this isotopic signal is strong enough that you could detect it through something like a blood test, that could give you an important hint that something is off.”
The metabolism of cancer
The study centers around a concept that has intrigued cancer researchers for years: metabolism.
Under normal conditions, the cells of organisms like yeast and animals generate energy through a process called respiration, in which they take in oxygen and release carbon dioxide. But that’s not the only way to get a sugar high. Colonies of baker’s yeast (Saccharomyces cerevisiae), for example, can produce energy via fermentation, in which organisms break down sugars without help from oxygen and produce alcohol. It’s the same process that gives you beer.
“In humans, if an athlete performs beyond their aerobic limit, their muscles will also start fermenting, which doesn’t use oxygen,” Kopf said. “That gives you a quick energy boost.”
As it turns out, many cancer cells also fuel their growth through a similar get-rich-quick strategy.
Scientists have long searched for more ways to track these metabolic changes in cancer cells. Maloney, who led the new study as a Harry Hess Postdoctoral Fellow at Princeton, and her advisor Xinning Zhang decided to follow hydrogen.
Inside the cell
Today, Maloney manages CU Boulder’s Earth Systems Stable Isotope Lab, one of more than 20 Core Facilities on campus. As a graduate student, she explored hydrogen atoms in algae from tropical islands. Her current work was inspired by an unlikely source: her father, a dermatologist.
“He takes skin cancer cells off people all the time,” Maloney said. “I wondered how the metabolism of those cells might be different from the cells growing next to them.”
To understand that question, it helps to know how hydrogen winds up in cells in the first place. In some cases, those atoms come from a hard-to-pronounce, but critically important, enzyme known as nicotinamide adenine dinucleotide phosphate (NADPH). Among its many roles in cells, NADPH collects hydrogen atoms then passes them to other molecules in the process of making fatty acids, an important building block for life.
NADPH, however, doesn’t always draw from the same pool of hydrogen. Previous research led by Zhang and focusing on bacteria suggested that, depending on what other enzymes in a cell are doing, NADPH may sometimes use different hydrogen isotopes more or less often.
Which raised the question: If cancer rewires a cell’s metabolism, could it also alter how NADPH gets its hydrogen, ultimately altering the atomic makeup of a cell?
Window into cancer
To begin to find out, the researchers set up jars filled with flourishing colonies of yeast in labs at Princeton and CU Boulder. Separately, biologists at Princeton conducted an experiment with colonies of healthy and cancerous mouse liver cells. The researchers then pulled the fatty acids from the cells and used a machine called a mass spectrometer to identify the ratio of hydrogen atoms within.
“When we started the study, I thought, ‘Ooh, we have a chance to see something cool,” Maloney said. “It ended up creating a huge signal, which I didn’t expect.”
Fermenting yeast cells, the kind that resemble cancer, contained roughly 50 percent fewer deuterium atoms on average than the normal yeast cells, a startling change. Cancerous cells exhibited a similar but not quite as strong shortage in deuterium.
Zhang, the study’s senior author and an assistant professor of geosciences at Princeton, is hopeful the research could one day help families around the world.
“Cancer, and other illnesses, are unfortunately a huge theme in many people’s lives. Seeing Ashley’s data was special, profound moment,” Zhang said. “It meant that a tool used to track planetary health might also be applied to track health and disease in lifeforms, hopefully one day in humans. Growing up in a family challenged by cancer, I hope to see this area expand.”
News Headlines
Related articles.
National Cancer Research Month: 7 CU Boulder discoveries that could improve, save lives

Teen ‘Game Changers’ confronting youth violence crisis head-on

Why do we move slower the older we get? New study delivers answers
- Arts & Humanities
- Business & Entrepreneurship
- Climate & Environment
- Education & Outreach
- Health & Society
- Law & Politics
- Science & Technology
Campus Community
- Administration
- Announcements & Deadlines
- Career Development
- Getting Involved
- Mind & Body
Events & Exhibits
- Arts & Culture
- Conferences
- Lectures & Presentations
- Performances & Concerts
- Sports & Recreation
- Workshops & Seminars
Subscribe to CUBT
Sign up for Alerts
Administrative eMemos
Buff Bulletin Board
Events Calendar

IMAGES
VIDEO
COMMENTS
The HNC survivors surveyed (n=918; 62.4% male; median age 65.6 years) were more likely than matched (sex, age, survey year) non-cancer controls (4:1 ratio: n=3,672) and matched survivors of 25 other types of cancers (n=3,672) to be experiencing: a) one or more common symptoms of depression (e.g., feeling "hopeless") and/or anxiety (e.g ...
A previous study in the United States also showed that cancer survivors with a higher healthy lifestyle score (3-5) had a substantially lower risk of all-cause and non-cancer mortality. 37 Besides, a prospective study that enrolled 1425 newly diagnosed stages I-III colorectal cancer survivors found having a lifestyle highly in line with the ...
The financial effects of a breast cancer diagnosis can be long-lasting. When assessing QOL in breast cancer survivors at an average of 12.5 years postdiagnosis, Hsu et al. found that breast cancer patients had EORTC financial impact subscores 6.3% higher than cancer-free age-matched controls (21).
Cancer patients' rates of insomnia and other sleep disturbances exceed those found in non-cancer populations, with problems reported in about 30% to 87% of cancer patients (J. Savard et al., 2001) compared to 16% to 20% in the general population (Ohayon, 2002). For example, in a prospective study of 823 patients of mixed cancer types
Demographic characteristics of subjects. The general characteristics of the female cancer survivors in this study indicated that their average age was 51.87 (SD = 11.78) years, with the largest proportion (33.3%) of the population being in their 50s, followed by those in their 40s (30.1%), 60s and over (24.4%), and below 30 (12.2%).Most participants (76.2%) were married; 61.9% practiced a ...
A common side effect of breast cancer treatment, is change in cognitive function, which research indicates is experienced by 30-60% of breast cancer survivors (Player, Mackenzie, Willis, & Loh, 2014). Symptoms may be subtle or dramatic, and include changes in memory, concentration, language, and executive function.
The cancer survival rate in the USA has steadily improved over the past decade. The 5-year relative survival rate for all cancers combined currently stands at 67% overall, 68% in whites, and 62% in blacks [].Cancer prevalence reports as of January 2019 indicate that the majority of cancer survivors (68%) were diagnosed 5 or more years ago, and 18% were diagnosed 20 or more years ago [].
health behaviours of cancer survivors in the United Kingdom (UK), and the lifestyle information available to them. This thesis used a range of methodologies to try and address some of these gaps in the literature. Study 1 showed that on a population level, there is little evidence that cancer survivors make positive changes to their lifestyle
Breast cancer survivors may need to prepare for ongoing psychosocial challenges in survivorship and proactively seek sup-port to overcome these. Keywords Breast cancer · Survivorship · Qualitative · Meta-review · Systematic review Introduction Breast cancer (BC), while highly prevalent globally (highest incidence cancer among women in 159/ ...
older people with cancer, and secondly the quality of life of cancer survivors, was the primary focus of the research. The complexity of the topic, that is the interplay between cancer, older people, and social support, led to integrating qualitative and quantitative cancer.
Cancer survivors were more likely to contact their GP for psychosocial problems compared with noncancer controls. Survivors were more likely to use antidepressants compared with controls, although 71% of survivors preferred depression treatment to be "talking therapy only." Overall, GPs and patients mostly agreed that GPs are the preferred ...
Introduction Individuals with metastatic cancer experience many medical, physical, and emotional challenges due to changing medical regimens, oscillating disease states, and side effects. The purpose of this study was to describe the type and prevalence of survivorship concerns reported by individuals with metastatic cancer, and their associations with cancer diagnosis, treatment, and socio ...
3.3 Breast Cancer worldwide. Breast cancer is the most common type of cancer in women around the globe. It affects women from low, middle and high-income countries (Rohani, Abedi, Omranipour, & Langius-Eklöf, 2015, 2). Breast cancer prevalence has increased within the last few years in middle- and low-income countries.
Cancer Survivors: In Their Words. June 20, 2020by Marci Landsmann. This year alone, an estimated 1.8 million people will hear their doctor say they have cancer. The individual impact of each person can be clouded in the vast statistics. In honor of National Cancer Survivor Month, Cancer Today would like to highlight several personal essays we ...
My thesis is about the power of telling narratives about one's life-changing memories. I am very ... 1.5.1!Parents of young adult cancer survivors. .....14! 1.5.2!Parent-child communication and children's narrative identity.....15! 1.5.3!Maternal dispositional optimism. ...
Results The result shows that the overall number of cancer survivors is 673 per 100.000 older adults and is higher in Urban areas (874 per 100.000) than in rural areas (535 per 100.000). 43.7% of ...
Key Points. Question What is the cancer type-specific prevalence of substance use disorder (SUD) among adult US cancer survivors?. Findings In this cross-sectional study of 6101 adult cancer survivors who responded to the National Survey on Drug Use and Health for 2015 through 2020, the overall prevalence of active SUD (within the past 12 months) was approximately 4%, with higher prevalence ...
Howard Cabiao. During the summer of 2003, I plunged into a two week nightmare. I felt robbed of my dreams and my hopes for sharing another year with my grandfather, or at least to utter the words of goodbye. On July 28th, 2003 my grandfather, Pantaleon Cabiao, passed away just a day after his birthday, from Prostate Cancer.
Survivor's Review Encouraging the creative expression of cancer survivors. Our goal at the Survivor's Review is to publish stories, essays, and poems that are powerful, poignant, and unflinchingly honest. Whether you are a cancer survivor, caregiver, or friend, we invite you to peruse the features in this issue.. We also hope to encourage all survivors to use writing as a tool for emotional ...
Theses/Dissertations from 2022. PDF. Omics Analysis in Cancer and Development, Emalie J. Clement. PDF. Investigating the Role of Splenic Macrophages in Pancreatic Cancer, Daisy V. Gonzalez. PDF. Polymeric Chloroquine in Metastatic Pancreatic Cancer Therapy, Rubayat Islam Khan. PDF. Evaluating Targets and Therapeutics for the Treatment of ...
More than one-fourth of cancer survivors reported having a physical disability that diminished their mobility, according to study results published in Journal of Clinical Oncology.Nearly 10% ...
Community support is key for cancer survivors. McGregor referred Steffanie to an 11-week virtual support group she leads for those undergoing cancer treatment and survivors, Living SMART with ...
A primary direction of research regarding older adult cancer survivors has been identifying factors that influence quality of life. Health-related quality of life (HRQOL) is seen as a primary outcome given that priorities and values for older adults shift as they age [] and acknowledge they have few remaining years.However, age alone is insufficient to explain variations in this populations ...
Investigation of patients suspected of having urinary bladder cancer (UBC) is resource-intensive. Often, it requires a camera examination through the urethra, which can cause discomfort and complications. Suleiman Abuhasanein's thesis reveals new and rapid methods for early detection of UBC, potentially reducing costs for society and suffering for patients.
Breast cancer rates among women in their 40s are on the rise, increasing by 2 percent a year between 2015 and 2019. Credit... Michael Hanschke/picture alliance, via Getty Images
A new study suggests that these same tiny atoms could one day lead to new ways to track the growth of cancer. ... With new medications extending the lives of advanced cancer patients, many live for years in the face of radical uncertainty. A new CU Boulder-born therapy has been shown to reduce trauma, depression, anxiety and fear.
Cancer; Cardiovascular Disease; ... about the importance of centering patients in research and treatment. ... newsletter to read each week's best First Opinion essays. About the Author ...