Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character

Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 181, NO. 4 CURRENT ISSUE pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
The Critical Relationship Between Anxiety and Depression
- Ned H. Kalin , M.D.
Search for more papers by this author
Anxiety and depressive disorders are among the most common psychiatric illnesses; they are highly comorbid with each other, and together they are considered to belong to the broader category of internalizing disorders. Based on statistics from the Substance Abuse and Mental Health Services Administration, the 12-month prevalence of major depressive disorder in 2017 was estimated to be 7.1% for adults and 13.3% for adolescents ( 1 ). Data for anxiety disorders are less current, but in 2001–2003, their 12-month prevalence was estimated to be 19.1% in adults, and 2001–2004 data estimated that the lifetime prevalence in adolescents was 31.9% ( 2 , 3 ). Both anxiety and depressive disorders are more prevalent in women, with an approximate 2:1 ratio in women compared with men during women’s reproductive years ( 1 , 2 ).
Across all psychiatric disorders, comorbidity is the rule ( 4 ), which is definitely the case for anxiety and depressive disorders, as well as their symptoms. With respect to major depression, a worldwide survey reported that 45.7% of individuals with lifetime major depressive disorder had a lifetime history of one or more anxiety disorder ( 5 ). These disorders also commonly coexist during the same time frame, as 41.6% of individuals with 12-month major depression also had one or more anxiety disorder over the same 12-month period. From the perspective of anxiety disorders, the lifetime comorbidity with depression is estimated to range from 20% to 70% for patients with social anxiety disorder ( 6 ), 50% for patients with panic disorder ( 6 ), 48% for patients with posttraumatic stress disorder (PTSD) ( 7 ), and 43% for patients with generalized anxiety disorder ( 8 ). Data from the well-known Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study demonstrate comorbidity at the symptom level, as 53% of the patients with major depression had significant anxiety and were considered to have an anxious depression ( 9 ).
Anxiety and depressive disorders are moderately heritable (approximately 40%), and evidence suggests shared genetic risk across the internalizing disorders ( 10 ). Among internalizing disorders, the highest level of shared genetic risk appears to be between major depressive disorder and generalized anxiety disorder. Neuroticism is a personality trait or temperamental characteristic that is associated with the development of both anxiety and depression, and the genetic risk for developing neuroticism also appears to be shared with that of the internalizing disorders ( 11 ). Common nongenetic risk factors associated with the development of anxiety and depression include earlier life adversity, such as trauma or neglect, as well as parenting style and current stress exposure. At the level of neural circuits, alterations in prefrontal-limbic pathways that mediate emotion regulatory processes are common to anxiety and depressive disorders ( 12 , 13 ). These findings are consistent with meta-analyses that reveal shared structural and functional brain alterations across various psychiatric illnesses, including anxiety and major depression, in circuits involving emotion regulation ( 13 ), executive function ( 14 ), and cognitive control ( 15 ).
Anxiety disorders and major depression occur during development, with anxiety disorders commonly beginning during preadolescence and early adolescence and major depression tending to emerge during adolescence and early to mid-adulthood ( 16 – 18 ). In relation to the evolution of their comorbidity, studies demonstrate that anxiety disorders generally precede the presentation of major depressive disorder ( 17 ). A European community-based study revealed, beginning at age 15, the developmental relation between comorbid anxiety and major depression by specifically focusing on social phobia (based on DSM-IV criteria) and then asking the question regarding concurrent major depressive disorder ( 18 ). The findings revealed a 19% concurrent comorbidity between these disorders, and in 65% of the cases, social phobia preceded major depressive disorder by at least 2 years. In addition, initial presentation with social phobia was associated with a 5.7-fold increased risk of developing major depressive disorder. These associations between anxiety and depression can be traced back even earlier in life. For example, childhood behavioral inhibition in response to novelty or strangers, or an extreme anxious temperament, is associated with a three- to fourfold increase in the likelihood of developing social anxiety disorder, which in turn is associated with an increased risk to develop major depressive disorder and substance abuse ( 19 ).
It is important to emphasize that the presence of comor‐bid anxiety symptoms and disorders matters in relation to treatment. Across psychiatric disorders, the presence of significant anxiety symptoms generally predicts worse outcomes, and this has been well demonstrated for depression. In the STAR*D study, patients with anxious major depressive disorder were more likely to be severely depressed and to have more suicidal ideation ( 9 ). This is consistent with the study by Kessler and colleagues ( 5 ), in which patients with anxious major depressive disorder, compared with patients with nonanxious major depressive disorder, were found to have more severe role impairment and more suicidal ideation. Data from level 1 of the STAR*D study (citalopram treatment) nicely illustrate the impact of comorbid anxiety symptoms on treatment. Compared with patients with nonanxious major depressive disorder, those 53% of patients with an anxious depression were less likely to remit and also had a greater side effect burden ( 20 ). Other data examining patients with major depressive disorder and comorbid anxiety disorders support the greater difficulty and challenge in treating patients with these comorbidities ( 21 ).
This issue of the Journal presents new findings relevant to the issues discussed above in relation to understanding and treating anxiety and depressive disorders. Drs. Conor Liston and Timothy Spellman, from Weill Cornell Medicine, provide an overview for this issue ( 22 ) that is focused on understanding mechanisms at the neural circuit level that underlie the pathophysiology of depression. Their piece nicely integrates human neuroimaging studies with complementary data from animal models that allow for the manipulation of selective circuits to test hypotheses generated from the human data. Also included in this issue is a review of the data addressing the reemergence of the use of psychedelic drugs in psychiatry, particularly for the treatment of depression, anxiety, and PTSD ( 23 ). This timely piece, authored by Dr. Collin Reiff along with a subgroup from the APA Council of Research, provides the current state of evidence supporting the further exploration of these interventions. Dr. Alan Schatzberg, from Stanford University, contributes an editorial in which he comments on where the field is in relation to clinical trials with psychedelics and to some of the difficulties, such as adequate blinding, in reliably studying the efficacy of these drugs ( 24 ).
In an article by McTeague et al. ( 25 ), the authors use meta-analytic strategies to understand the neural alterations that are related to aberrant emotion processing that are shared across psychiatric disorders. Findings support alterations in the salience, reward, and lateral orbital nonreward networks as common across disorders, including anxiety and depressive disorders. These findings add to the growing body of work that supports the concept that there are common underlying factors across all types of psychopathology that include internalizing, externalizing, and thought disorder dimensions ( 26 ). Dr. Deanna Barch, from Washington University in St. Louis, writes an editorial commenting on these findings and, importantly, discusses criteria that should be met when we consider whether the findings are actually transdiagnostic ( 27 ).
Another article, from Gray and colleagues ( 28 ), addresses whether there is a convergence of findings, specifically in major depression, when examining data from different structural and functional neuroimaging modalities. The authors report that, consistent with what we know about regions involved in emotion processing, the subgenual anterior cingulate cortex, hippocampus, and amygdala were among the regions that showed convergence across multimodal imaging modalities.
In relation to treatment and building on our understanding of neural circuit alterations, Siddiqi et al. ( 29 ) present data suggesting that transcranial magnetic stimulation (TMS) targeting can be linked to symptom-specific treatments. Their findings identify different TMS targets in the left dorsolateral prefrontal cortex that modulate different downstream networks. The modulation of these different networks appears to be associated with a reduction in different types of symptoms. In an editorial, Drs. Sean Nestor and Daniel Blumberger, from the University of Toronto ( 30 ), comment on the novel approach used in this study to link the TMS-related engagement of circuits with symptom improvement. They also provide a perspective on how we can view these and other circuit-based findings in relation to conceptualizing personalized treatment approaches.
Kendler et al. ( 31 ), in this issue, contribute an article that demonstrates the important role of the rearing environment in the risk to develop major depression. Using a unique design from a Swedish sample, the analytic strategy involves comparing outcomes from high-risk full sibships and high-risk half sibships where at least one of the siblings was home reared and one was adopted out of the home. The findings support the importance of the quality of the rearing environment as well as the presence of parental depression in mitigating or enhancing the likelihood of developing major depression. In an accompanying editorial ( 32 ), Dr. Myrna Weissman, from Columbia University, reviews the methods and findings of the Kendler et al. article and also emphasizes the critical significance of the early nurturing environment in relation to general health.
This issue concludes with an intriguing article on anxiety disorders, by Gold and colleagues ( 33 ), that demonstrates neural alterations during extinction recall that differ in children relative to adults. With increasing age, and in relation to fear and safety cues, nonanxious adults demonstrated greater connectivity between the amygdala and the ventromedial prefrontal cortex compared with anxious adults, as the cues were being perceived as safer. In contrast, neural differences between anxious and nonanxious youths were more robust when rating the memory of faces that were associated with threat. Specifically, these differences were observed in the activation of the inferior temporal cortex. In their editorial ( 34 ), Dr. Dylan Gee and Sahana Kribakaran, from Yale University, emphasize the importance of developmental work in relation to understanding anxiety disorders, place these findings into the context of other work, and suggest the possibility that these and other data point to neuroscientifically informed age-specific interventions.
Taken together, the papers in this issue of the Journal present new findings that shed light onto alterations in neural function that underlie major depressive disorder and anxiety disorders. It is important to remember that these disorders are highly comorbid and that their symptoms are frequently not separable. The papers in this issue also provide a developmental perspective emphasizing the importance of early rearing in the risk to develop depression and age-related findings important for understanding threat processing in patients with anxiety disorders. From a treatment perspective, the papers introduce data supporting more selective prefrontal cortical TMS targeting in relation to different symptoms, address the potential and drawbacks for considering the future use of psychedelics in our treatments, and present new ideas supporting age-specific interventions for youths and adults with anxiety disorders.
Disclosures of Editors’ financial relationships appear in the April 2020 issue of the Journal .
1 Substance Abuse and Mental Health Services Administration (SAMHSA): Key substance use and mental health indicators in the United States: results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18-5068, NSDUH Series H-53). Rockville, Md, Center for Behavioral Health Statistics and Quality, SAMHSA, 2018. https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHFFR2017/NSDUHFFR2017.htm Google Scholar
2 Kessler RC, Chiu WT, Demler O, et al. : Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication . Arch Gen Psychiatry 2005 ; 62:617–627, correction, 62:709 Crossref , Medline , Google Scholar
3 Merikangas KR, He JP, Burstein M, et al. : Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A) . J Am Acad Child Adolesc Psychiatry 2010 ; 49:980–989 Crossref , Medline , Google Scholar
4 Kessler RC, McGonagle KA, Zhao S, et al. : Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey . Arch Gen Psychiatry 1994 ; 51:8–19 Crossref , Medline , Google Scholar
5 Kessler RC, Sampson NA, Berglund P, et al. : Anxious and non-anxious major depressive disorder in the World Health Organization World Mental Health Surveys . Epidemiol Psychiatr Sci 2015 ; 24:210–226 Crossref , Medline , Google Scholar
6 Dunner DL : Management of anxiety disorders: the added challenge of comorbidity . Depress Anxiety 2001 ; 13:57–71 Crossref , Medline , Google Scholar
7 Kessler RC, Sonnega A, Bromet E, et al. : Posttraumatic stress disorder in the National Comorbidity Survey . Arch Gen Psychiatry 1995 ; 52:1048–1060 Crossref , Medline , Google Scholar
8 Brawman-Mintzer O, Lydiard RB, Emmanuel N, et al. : Psychiatric comorbidity in patients with generalized anxiety disorder . Am J Psychiatry 1993 ; 150:1216–1218 Link , Google Scholar
9 Fava M, Alpert JE, Carmin CN, et al. : Clinical correlates and symptom patterns of anxious depression among patients with major depressive disorder in STAR*D . Psychol Med 2004 ; 34:1299–1308 Crossref , Medline , Google Scholar
10 Hettema JM : What is the genetic relationship between anxiety and depression? Am J Med Genet C Semin Med Genet 2008 ; 148C:140–146 Crossref , Medline , Google Scholar
11 Hettema JM, Neale MC, Myers JM, et al. : A population-based twin study of the relationship between neuroticism and internalizing disorders . Am J Psychiatry 2006 ; 163:857–864 Link , Google Scholar
12 Kovner R, Oler JA, Kalin NH : Cortico-limbic interactions mediate adaptive and maladaptive responses relevant to psychopathology . Am J Psychiatry 2019 ; 176:987–999 Link , Google Scholar
13 Etkin A, Schatzberg AF : Common abnormalities and disorder-specific compensation during implicit regulation of emotional processing in generalized anxiety and major depressive disorders . Am J Psychiatry 2011 ; 168:968–978 Link , Google Scholar
14 Goodkind M, Eickhoff SB, Oathes DJ, et al. : Identification of a common neurobiological substrate for mental illness . JAMA Psychiatry 2015 ; 72:305–315 Crossref , Medline , Google Scholar
15 McTeague LM, Huemer J, Carreon DM, et al. : Identification of common neural circuit disruptions in cognitive control across psychiatric disorders . Am J Psychiatry 2017 ; 174:676–685 Link , Google Scholar
16 Beesdo K, Knappe S, Pine DS : Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V . Psychiatr Clin North Am 2009 ; 32:483–524 Crossref , Medline , Google Scholar
17 Kessler RC, Wang PS : The descriptive epidemiology of commonly occurring mental disorders in the United States . Annu Rev Public Health 2008 ; 29:115–129 Crossref , Medline , Google Scholar
18 Ohayon MM, Schatzberg AF : Social phobia and depression: prevalence and comorbidity . J Psychosom Res 2010 ; 68:235–243 Crossref , Medline , Google Scholar
19 Clauss JA, Blackford JU : Behavioral inhibition and risk for developing social anxiety disorder: a meta-analytic study . J Am Acad Child Adolesc Psychiatry 2012 ; 51:1066–1075 Crossref , Medline , Google Scholar
20 Fava M, Rush AJ, Alpert JE, et al. : Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report . Am J Psychiatry 2008 ; 165:342–351 Link , Google Scholar
21 Dold M, Bartova L, Souery D, et al. : Clinical characteristics and treatment outcomes of patients with major depressive disorder and comorbid anxiety disorders: results from a European multicenter study . J Psychiatr Res 2017 ; 91:1–13 Crossref , Medline , Google Scholar
22 Spellman T, Liston C : Toward circuit mechanisms of pathophysiology in depression . Am J Psychiatry 2020 ; 177:381–390 Link , Google Scholar
23 Reiff CM, Richman EE, Nemeroff CB, et al. : Psychedelics and psychedelic-assisted psychotherapy . Am J Psychiatry 2020 ; 177:391–410 Link , Google Scholar
24 Schatzberg AF : Some comments on psychedelic research (editorial). Am J Psychiatry 2020 ; 177:368–369 Link , Google Scholar
25 McTeague LM, Rosenberg BM, Lopez JW, et al. : Identification of common neural circuit disruptions in emotional processing across psychiatric disorders . Am J Psychiatry 2020 ; 177:411–421 Link , Google Scholar
26 Caspi A, Moffitt TE : All for one and one for all: mental disorders in one dimension . Am J Psychiatry 2018 ; 175:831–844 Link , Google Scholar
27 Barch DM : What does it mean to be transdiagnostic and how would we know? (editorial). Am J Psychiatry 2020 ; 177:370–372 Abstract , Google Scholar
28 Gray JP, Müller VI, Eickhoff SB, et al. : Multimodal abnormalities of brain structure and function in major depressive disorder: a meta-analysis of neuroimaging studies . Am J Psychiatry 2020 ; 177:422–434 Link , Google Scholar
29 Siddiqi SH, Taylor SF, Cooke D, et al. : Distinct symptom-specific treatment targets for circuit-based neuromodulation . Am J Psychiatry 2020 ; 177:435–446 Link , Google Scholar
30 Nestor SM, Blumberger DM : Mapping symptom clusters to circuits: toward personalizing TMS targets to improve treatment outcomes in depression (editorial). Am J Psychiatry 2020 ; 177:373–375 Abstract , Google Scholar
31 Kendler KS, Ohlsson H, Sundquist J, et al. : The rearing environment and risk for major depression: a Swedish national high-risk home-reared and adopted-away co-sibling control study . Am J Psychiatry 2020 ; 177:447–453 Abstract , Google Scholar
32 Weissman MM : Is depression nature or nurture? Yes (editorial). Am J Psychiatry 2020 ; 177:376–377 Abstract , Google Scholar
33 Gold AL, Abend R, Britton JC, et al. : Age differences in the neural correlates of anxiety disorders: an fMRI study of response to learned threat . Am J Psychiatry 2020 ; 177:454–463 Link , Google Scholar
34 Gee DG, Kribakaran S : Developmental differences in neural responding to threat and safety: implications for treating youths with anxiety (editorial). Am J Psychiatry 2020 ; 177:378–380 Abstract , Google Scholar
- Cited by None
- Neuroanatomy
- Neurochemistry
- Neuroendocrinology
- Other Research Areas
Eating disorders
Affiliations.
- 1 Institute of Psychiatry, Psychology and Neuroscience, King's College London, London, UK. Electronic address: [email protected].
- 2 Institute of Psychiatry, Psychology and Neuroscience, King's College London, London, UK; Serviço de Psiquiatria e Saúde Mental, Hospital de Santa Maria, Centro Hospitalar Universitário Lisboa Norte, Lisbon, Portugal.
- 3 Institute of Psychiatry, Psychology and Neuroscience, King's College London, London, UK; South London and Maudsley NHS Foundation Trust, London, UK.
- PMID: 32171414
- DOI: 10.1016/S0140-6736(20)30059-3
Eating disorders are disabling, deadly, and costly mental disorders that considerably impair physical health and disrupt psychosocial functioning. Disturbed attitudes towards weight, body shape, and eating play a key role in the origin and maintenance of eating disorders. Eating disorders have been increasing over the past 50 years and changes in the food environment have been implicated. All health-care providers should routinely enquire about eating habits as a component of overall health assessment. Six main feeding and eating disorders are now recognised in diagnostic systems: anorexia nervosa, bulimia nervosa, binge eating disorder, avoidant-restrictive food intake disorder, pica, and rumination disorder. The presentation form of eating disorders might vary for men versus women, for example. As eating disorders are under-researched, there is a great deal of uncertainty as to their pathophysiology, treatment, and management. Future challenges, emerging treatments, and outstanding research questions are addressed.
Copyright © 2020 Elsevier Ltd. All rights reserved.
Publication types
- Research Support, Non-U.S. Gov't
- Diagnosis, Differential
- Feeding and Eating Disorders* / diagnosis
- Feeding and Eating Disorders* / physiopathology
- Feeding and Eating Disorders* / psychology
- Feeding and Eating Disorders* / therapy
- Nutritional Status
- Search by keyword
- Search by citation
Page 1 of 8
Longitudinal studies of bipolar patients and their families: translating findings to advance individualized risk prediction, treatment and research
Bipolar disorder is a broad diagnostic construct associated with significant phenotypic and genetic heterogeneity challenging progress in clinical practice and discovery research. Prospective studies of well-c...
- View Full Text
Sociodemographic, clinical and treatment characteristics of current rapid-cycling bipolar disorder: a multicenter Chinese study
Rapid cycling bipolar disorder (RCBD), characterized by four or more episodes per year, is a complex subtype of bipolar disorder (BD) with poorly understood characteristics.
Type of cycle, temperament and childhood trauma are associated with lithium response in patients with bipolar disorders
Lithium stands as the gold standard in treating bipolar disorders (BD). Despite numerous clinical factors being associated with a favorable response to lithium, comprehensive studies examining the collective i...
How effective are mood stabilizers in treating bipolar patients comorbid with cPTSD? Results from an observational study
Multiple traumatic experiences, particularly in childhood, may predict and be a risk factor for the development of complex post-traumatic stress disorder (cPTSD). Unfortunately, individuals with bipolar disord...
Perceived loneliness and social support in bipolar disorder: relation to suicidal ideation and attempts
The suicide rate in bipolar disorder (BD) is among the highest across all psychiatric disorders. Identifying modifiable variables that relate to suicidal thoughts and behaviors (STBs) in BD may inform preventi...
Effectiveness of ultra-long-term lithium treatment: relevant factors and case series
The phenomenon of preventing the recurrences of mood disorders by the long-term lithium administration was discovered sixty years ago. Such a property of lithium has been unequivocally confirmed in subsequent ...
Prevention of suicidal behavior with lithium treatment in patients with recurrent mood disorders
Suicidal behavior is more prevalent in bipolar disorders than in other psychiatric illnesses. In the last thirty years evidence has emerged to indicate that long-term treatment of bipolar disorder patients wit...
Correlations between multimodal neuroimaging and peripheral inflammation in different subtypes and mood states of bipolar disorder: a systematic review
Systemic inflammation-immune dysregulation and brain abnormalities are believed to contribute to the pathogenesis of bipolar disorder (BD). However, the connections between peripheral inflammation and the brai...
Lithium: how low can you go?
Why is lithium [not] the drug of choice for bipolar disorder a controversy between science and clinical practice.
During over half a century, science has shown that lithium is the most efficacious treatment for bipolar disorder but despite this, its prescription has consistently declined internationally during recent deca...
Biomarkers for neurodegeneration impact cognitive function: a longitudinal 1-year case–control study of patients with bipolar disorder and healthy control individuals
Abnormalities in cerebrospinal fluid (CSF)-amyloid-beta (Aβ)42, CSF-Aβ40, CSF-Aβ38, CSF-soluble amyloid precursor proteins α and β, CSF-total-tau, CSF-phosphorylated-tau, CSF-neurofilament light protein (NF-L)...
Cognitive behavioural therapy for social anxiety disorder in people with bipolar disorder: a case series
Social anxiety disorder increases the likelihood of unfavourable outcomes in people with bipolar disorder. Cognitive behavioural therapy (CBT) is the first-line treatment for social anxiety disorder. However, ...
Lithium prescription trends in psychiatric inpatient care 2014 to 2021: data from a Bavarian drug surveillance project
Lithium (Li) remains one of the most valuable treatment options for mood disorders. However, current knowledge about prescription practices in Germany is limited. The objective of this study is to estimate the...
Lifetime risk of severe kidney disease in lithium-treated patients: a retrospective study
Lithium is an essential psychopharmaceutical, yet side effects and concerns about severe renal function impairment limit its usage.
Factors associated with suicide attempts in the antecedent illness trajectory of bipolar disorder and schizophrenia
Factors associated with suicide attempts during the antecedent illness trajectory of bipolar disorder (BD) and schizophrenia (SZ) are poorly understood.
Behavioral lateralization in bipolar disorders: a systematic review
Bipolar disorder (BD) is often seen as a bridge between schizophrenia and depression in terms of symptomatology and etiology. Interestingly, hemispheric asymmetries as well as behavioral lateralization are shi...
High lithium concentration at delivery is a potential risk factor for adverse outcomes in breastfed infants: a retrospective cohort study
Neonatal effects of late intrauterine and early postpartum exposure to lithium through mother’s own milk are scarcely studied. It is unclear whether described symptoms in breastfed neonates are caused by place...
Key questions on the long term renal effects of lithium: a review of pertinent data
For over half a century, it has been widely known that lithium is the most efficacious maintenance treatment for bipolar disorder. Despite thorough research on the long-term effects of lithium on renal functio...
Controversies regarding lithium-associated weight gain: case–control study of real-world drug safety data
The impact of long-term lithium treatment on weight gain has been a controversial topic with conflicting evidence. We aim to assess reporting of weight gain associated with lithium and other mood stabilizers c...
Differential diagnosis of unipolar versus bipolar depression by GSK3 levels in peripheral blood: a pilot experimental study
The differential diagnosis of patients presenting for the first time with a depressive episode into unipolar disorder versus bipolar disorder is crucial to establish the correct pharmacological therapy (antide...
Supra-second interval timing in bipolar disorder: examining the role of disorder sub-type, mood, and medication status
Widely reported by bipolar disorder (BD) patients, cognitive symptoms, including deficits in executive function, memory, attention, and timing are under-studied. Work suggests that individuals with BD show imp...
Association between childhood trauma, cognition, and psychosocial function in a large sample of partially or fully remitted patients with bipolar disorder and healthy participants
Childhood trauma (CT) are frequently reported by patients with bipolar disorder (BD), but it is unclear whether and how CT contribute to patients’ cognitive and psychosocial impairments. We aimed to examine th...
Countering the declining use of lithium therapy: a call to arms
For over half a century, it has been widely known that lithium is the most efficacious treatment for bipolar disorder. Yet, despite this, its prescription has consistently declined over this same period of tim...
Paediatric bipolar disorder: an age-old problem
Nrx-101 (d-cycloserine plus lurasidone) vs. lurasidone for the maintenance of initial stabilization after ketamine in patients with severe bipolar depression with acute suicidal ideation and behavior: a randomized prospective phase 2 trial.
We tested the hypothesis that, after initial improvement with intravenous ketamine in patients with bipolar disorder (BD) with severe depression and acute suicidal thinking or behavior, a fixed-dose combinatio...
The IBER study: a feasibility randomised controlled trial of imagery based emotion regulation for the treatment of anxiety in bipolar disorder
Intrusive mental imagery is associated with anxiety and mood instability within bipolar disorder and therefore represents a novel treatment target. Imagery Based Emotion Regulation (IBER) is a brief structured...
Mitochondrial genetic variants associated with bipolar disorder and Schizophrenia in a Japanese population
Bipolar disorder (BD) and schizophrenia (SZ) are complex psychotic disorders (PSY), with both environmental and genetic factors including possible maternal inheritance playing a role. Some studies have investi...
Differential characteristics of bipolar I and II disorders: a retrospective, cross-sectional evaluation of clinical features, illness course, and response to treatment
The distinction between bipolar I and bipolar II disorder and its treatment implications have been a matter of ongoing debate. The aim of this study was to examine differences between patients with bipolar I a...
Neonatal admission after lithium use in pregnant women with bipolar disorders: a retrospective cohort study
Lithium is the preferred treatment for pregnant women with bipolar disorders (BD), as it is most effective in preventing postpartum relapse. Although it has been prescribed during pregnancy for decades, the sa...
Rates and associations of relapse over 5 years of 2649 people with bipolar disorder: a retrospective UK cohort study
Evidence regarding the rate of relapse in people with bipolar disorder (BD), particularly from the UK, is lacking. This study aimed to evaluate the rate and associations of clinician-defined relapse over 5 yea...
Exploratory study of ultraviolet B (UVB) radiation and age of onset of bipolar disorder
Sunlight contains ultraviolet B (UVB) radiation that triggers the production of vitamin D by skin. Vitamin D has widespread effects on brain function in both developing and adult brains. However, many people l...
Characteristics of rapid cycling in 1261 bipolar disorder patients
Rapid-cycling (RC; ≥ 4 episodes/year) in bipolar disorder (BD) has been recognized since the 1970s and associated with inferior treatment response. However, associations of single years of RC with overall cycl...
Clinicians’ preferences and attitudes towards the use of lithium in the maintenance treatment of bipolar disorders around the world: a survey from the ISBD Lithium task force
Lithium has long been considered the gold-standard pharmacological treatment for the maintenance treatment of bipolar disorders (BD) which is supported by a wide body of evidence. Prior research has shown a st...
Phenotype fingerprinting of bipolar disorder prodrome
Detecting prodromal symptoms of bipolar disorder (BD) has garnered significant attention in recent research, as early intervention could potentially improve therapeutic efficacy and improve patient outcomes. T...
Predictors of adherence to electronic self-monitoring in patients with bipolar disorder: a contactless study using Growth Mixture Models
Several studies have reported on the feasibility of electronic (e-)monitoring using computers or smartphones in patients with mental disorders, including bipolar disorder (BD). While studies on e-monitoring ha...
Racial differences in the major clinical symptom domains of bipolar disorder
Across clinical settings, black individuals are disproportionately less likely to be diagnosed with bipolar disorder compared to schizophrenia, a traditionally more severe and chronic disorder with lower expec...
Methylomic biomarkers of lithium response in bipolar disorder: a clinical utility study
Response to lithium (Li) is highly variable in bipolar disorders (BD). Despite decades of research, no clinical predictor(s) of response to Li prophylaxis have been consistently identified. Recently, we develo...
A compelling need to empirically validate bipolar depression
Structured physical exercise for bipolar depression: an open-label, proof-of concept study.
Physical exercise (PE) is a recommended lifestyle intervention for different mental disorders and has shown specific positive therapeutic effects in unipolar depressive disorder. Considering the similar sympto...
Experiences that matter in bipolar disorder: a qualitative study using the capability, comfort and calm framework
When assessing the value of an intervention in bipolar disorder, researchers and clinicians often focus on metrics that quantify improvements to core diagnostic symptoms (e.g., mania). Providers often overlook...
Emotion regulation in bipolar disorder type-I: multivariate analysis of fMRI data
Bipolar disorder type-I (BD-I) patients are known to show emotion regulation abnormalities. In a previous fMRI study using an explicit emotion regulation paradigm, we compared responses from 19 BD-I patients a...
Lithium levels and lifestyle in patients with bipolar disorder: a new tool for self-management
Patients should get actively involved in the management of their illness. The aim of this study was to assess the influence of lifestyle factors, including sleep, diet, and physical activity, on lithium levels...
Reduced parenting stress following a prevention program decreases internalizing and externalizing symptoms in the offspring of parents with bipolar disorder
Offspring of parents with bipolar disorder (OBD) are at risk for developing mental disorders, and the literature suggests that parenting stress may represent an important risk factor linking parental psychopat...
Stigma in people living with bipolar disorder and their families: a systematic review
Stigma affects different life aspects in people living with bipolar disorder and their families. This study aimed to examining the experience of stigma and evaluating predictors, consequences and strategies to...
Lithium use in childhood and adolescence, peripartum, and old age: an umbrella review
Lithium is one of the most consistently effective treatment for mood disorders. However, patients may show a high level of heterogeneity in treatment response across the lifespan. In particular, the benefits o...
Risk of childhood trauma exposure and severity of bipolar disorder in Colombia
Bipolar disorder (BD) is higher in developing countries. Childhood trauma exposure is a common environmental risk factor in Colombia and might be associated with a more severe course of bipolar disorder in Low...
A systematic review on the effectiveness of dialectical behavior therapy for improving mood symptoms in bipolar disorders
Evidence-based psychotherapies available to treat patients with bipolar disorders (BD) are limited. Dialectical behavior therapy (DBT) may target several common symptoms of BD. We conducted a systematic review...
Bipolar disorder and sexuality: a preliminary qualitative pilot study
Individuals with mental health disorders have a higher risk of sexual problems impacting intimate relations and quality of life. For individuals with bipolar disorder (BD) the mood shifts might to a particular...
Long-term lithium therapy and risk of chronic kidney disease, hyperparathyroidism and hypercalcemia: a cohort study
Lithium is well recognized as the first-line maintenance treatment for bipolar disorder (BD). However, besides therapeutic benefits attributed to lithium therapy, the associated side effects including endocrin...
The association of genetic variation in CACNA1C with resting-state functional connectivity in youth bipolar disorder
CACNA1C rs1006737 A allele, identified as a genetic risk variant for bipolar disorder (BD), is associated with anomalous functional connectivity in adults with and without BD. Studies have yet to investigate the ...
- Editorial Board
- Sign up for article alerts and news from this journal
- ISSN: 2194-7511 (electronic)
- Research article
- Open access
- Published: 15 September 2015
Perceptions of the causes of eating disorders: a comparison of individuals with and without eating disorders
- Elizabeth H. Blodgett Salafia 1 ,
- Maegan E. Jones 1 ,
- Emily C. Haugen 1 &
- Mallary K. Schaefer 1
Journal of Eating Disorders volume 3 , Article number: 32 ( 2015 ) Cite this article
75k Accesses
19 Citations
28 Altmetric
Metrics details
In this study, we examined perceptions regarding the causes of eating disorders, both among those with eating disorders as well as those without. By understanding the differences in perceived causes between the two groups, better educational programs for lay people and those suffering from eating disorders can be developed.
This study used open-ended questions to assess the beliefs of 57 individuals with self-reported eating disorders and 220 without. Participants responded to the questions, “What do you think was (were) the cause(s) of your eating disorder?” and “What do you think is (are) the cause(s) of eating disorders?”.
A list of possible codes for the causes of eating disorders was created based on a thorough review of the literature. A manually-generated set of eight codes was then created from individuals' actual responses. Frequencies and chi square analyses demonstrated differences in rates of endorsement between those with eating disorders and those without. Participants with eating disorders most frequently endorsed psychological/emotional and social problems, with genetics/biology and media/culture ideals least endorsed. Participants without eating disorders most frequently endorsed psychological/emotional problems and media/culture ideals, with traumatic life events and sports/health least endorsed. There was a difference between groups in the endorsement of the media as a cause of eating disorders, suggesting that those without eating disorders may overly attribute the media as the main cause while those with eating disorders may not be fully aware of the media’s impact. Additionally, while both groups highly endorsed psychological/emotional problems, there was a noticeable stigma about eating disorders among those without eating disorders.
Conclusions
There were noteworthy differences between samples; such differences suggest that there is a need for more education on the topic of eating disorders. Furthermore, despite empirical support for the effects of genetics, sports, and family factors, these were infrequently endorsed as causes of eating disorders by both groups. Our results suggest that there is a need for more education regarding the factors associated with eating disorders, in order to reduce the stigma surrounding these disorders and to potentially aid the treatment process.
Eating disorders have increasingly become the focus of research studies due to their prevalence, especially in Western cultures. Of the adolescent and young adult populations in the United States, for example, between .3 and .9 % are diagnosed with anorexia nervosa (AN), between .5 and 5 % with bulimia nervosa (BN), between 1.6 and 3.5 % with binge eating disorder (BED), and about 4.8 % with eating disorder otherwise not specified (EDNOS) [ 1 – 4 ]. According to the fifth edition of the DSM, individuals that do not fit the criteria for AN, BN or BED are diagnosed with sub-threshold or atypical conditions that fit under other specified feeding or eating disorder (OSFED) [ 5 ]. Due in part to decreased thresholds for the diagnoses of AN, BN or BED in the DSM-V, rates of OSFED have been found to be lower than previous rates of EDNOS, while the rates of AN, BN or BED have stayed the same or slightly increased [ 6 ]. Furthermore, the age at onset is concerning, as most eating disorders originate during adolescence [ 4 ]. Despite the potentially serious health consequences that result from disordered eating [ 7 ], many in the general public believe that issues with eating are due to personal shortcomings [ 8 , 9 ]. This creates a foundation of stigma regarding why individuals develop an eating disorder (e.g., to be “skinny”) and the purpose the disorder serves (e.g., to gain control). Such stigma may dishonor the actual experience of those who have lived with an eating disorder, as people could assume eating disorders are self-inflicted. In turn, those developing unhealthy habits may be discouraged from seeking help [ 10 ].
Previous research has identified biological, psychological, and sociocultural factors related to the development of eating disorders. However, it is important to explore individual narratives to identify similarities and differences among individuals with and without eating disorders. Obtaining such knowledge can help scholars determine the public’s educational needs and better target missing gaps in their knowledge. More accurate information may reduce stigma regarding eating disorders, which may in turn encourage those experiencing symptoms to seek help sooner, as they may no longer fear the negative feedback from peers and family that such stigma causes.
Factors that contribute to eating disorders identified by research
Research has identified many risk factors, ranging from individual to sociocultural, that contribute to the development of eating disorders. Based on empirical literature, we present some of the most salient factors below.
Individual factors
Genetics and biology are individual factors that play a role in the development of eating disorders. Genetic contributions to the development of eating disorders have been suggested by twin studies, with heritability estimates ranging from 0.39 to 0.74, depending on the disorder [ 11 ]. Abnormalities in the regulation of certain neurochemicals, such as 5-Hydroxytryptamine (HT) and the serotonin-transporter-linked polymorphic region (5-HTTLPR), have been closely linked with eating disorders [ 11 – 13 ]. Further, recent research has identified mutations on two specific genes that have been associated with increased risk of developing eating disorders in families: estrogen-related receptor α (ESRRA) and histone deacetylase 4 (HDAC4) [ 14 ]. In addition, early puberty has also been associated with disordered eating behaviors, potentially due to increases or irregularities in circulating sex hormones, especially estrogen [ 15 , 16 ].
Body dissatisfaction has been commonly identified as an influential risk factor for eating disorders. Individuals dissatisfied with their bodies are at an increased risk of engaging in disordered eating behaviors such as bingeing and purging in order to gain satisfaction and move closer to the thin ideal [ 14 , 17 ]. Engaging in dieting behaviors also increases the risk for the occurrence of eating pathology such as binge eating and purging [ 15 , 18 ].
Researchers have recognized perfectionism as a specific risk factor in the development of eating disorders, as this personality trait may lead to a persistent pursuit of the thin ideal [ 15 , 19 , 20 ]. Perfectionism can also be a maintenance factor for disordered eating since it promotes dieting, bingeing, and purging, and enhances eating disorder symptoms, particularly when combined with low self-esteem [ 12 , 15 ]. Similarly, research has shown that negative affect in general, such as high levels of stress, guilt, hostility, anger, anxiety, and depressed mood, is associated with increases in eating disorder symptoms [ 12 , 13 , 17 – 21 ].
Sexual, physical, and emotional abuse have all received empirical support as risk factors for psychiatric difficulties, which can include eating disorders [ 22 ]. Specifically, research has shown that sexual abuse can occur in 29 % of individuals with eating disorders, and physical abuse may occur in 57 % of individuals [ 23 , 24 ]. Additionally, emotional abuse is a significant predictor of eating disorder symptoms among women when other types of abuse are controlled for, suggesting that emotional abuse may be particularly salient [ 12 , 25 ].
Sociocultural factors
Many sociocultural factors affect the development of eating disorders. In families, for example, mothers’ and fathers’ own body dissatisfaction and dieting behaviors have been associated with their children’s eating-related attitudes and behaviors [ 26 , 27 ]. Parental weight-related teasing, negative comments about body shape, pressure to lose weight, and encouragement to diet have also been associated with body dissatisfaction, dieting, disordered eating behaviors, and eating disorders among both females and males [ 12 , 15 , 26 , 28 – 31 ]. Furthermore, parents who engage in high levels of parental control, expressed emotionality, critical comments, hostility, or emotional overinvolvement and negate their child’s emotional needs are more likely to have children who develop eating disorders [ 12 , 32 ].
Peer influences on the development of eating disorders can also be broken down into a variety of factors. Peer pressure to conform to cultural ideals has been consistently identified as an important factor associated with the development of disordered eating behaviors, especially among adolescents [ 29 , 33 ]. In particular, girls may learn attitudes and behaviors from their peers, such as the importance of being thin and dieting behaviors, through modeling, teasing, and conversations about body image and eating [ 12 , 33 ]. Similarly, romantic partners play a significant role in the development of eating disorders through negative comments about appearance and encouragement to lose weight, which can lead to weight concerns, body dissatisfaction, and disordered eating behaviors among both men and women [ 34 , 35 ].
It is also worth mentioning that eating disorders among athletes are common, as there is a large focus not only on being in shape, but on being the fittest and therefore the “best” [ 36 , 37 ]. There is an even greater risk of developing an eating disorder with participation in certain competitive sports that focus on leanness, such as gymnastics [ 38 ]. Athletes who believe that being leaner will increase their performance are more likely to engage in disordered eating [ 39 ]. This belief may be encouraged or reinforced by coaches and instructors, further increasing athletes’ risk for developing disordered habits [ 40 ].
Lastly, the media has an influential, if often controversial, role in the development of eating behaviors due its representation of the thin ideal. There is support that, regardless of the level of internalized thin ideal, women who were warned that a thin media image was altered experienced lower body dissatisfaction in comparison to those who were not warned the image was altered [ 41 ]. A preference for a thin and virtually unattainable body has been associated with the development of eating disorders, particularly AN [ 42 ].
A relatively small number of studies have examined individuals’ perceptions regarding the causes of eating disorders [ 10 , 36 , 43 – 55 ]. Some studies have solely focused on the perceptions of either the general public [ 10 , 43 – 47 ] or those with eating disorders [ 36 , 37 , 50 – 55 ]. Both types of studies have identified a common set of risk factors, with public perceptions and the perceptions of individuals with eating disorders varying slightly [e.g. 48,49]. Overall, both populations have a basic understanding of what eating disorders are and characteristics of each eating disorder [ 10 , 36 , 43 – 55 ]. However, despite this knowledge, many adults without eating disorders may be unsympathetic to those suffering from eating disorders, believe that having an eating disorder would not be distressing, and report that eating disorders are not difficult to treat [ 9 ].
Public perceptions of factors that contribute to eating disorders
The studies to date that have focused on identifying public perceptions of the factors associated with the development of eating disorders have surveyed individuals drawn from communities or schools. Typically, these samples have been quite large, numbering over 100 [ 43 , 44 ] or even several hundred [ 10 , 45 , 46 ], and have included both females and males [ 10 , 43 , 44 , 46 – 48 ]. Despite the importance of large samples, all of these studies have been limited in that the researchers did not ask open-ended questions; rather, participants responded to forced-answer questions where they either had to identify which item was a cause of eating disorders or identify to what degree a particular item was a cause.
The public commonly places blame on individuals with eating disorders, suggesting that they have control over their “self-inflicted” illnesses [ 48 ]. Of the individual factors associated with the development of eating disorders, the majority of people who do not have eating disorders identify psychological explanations such as emotional state, personality, and low self-esteem [ 10 , 43 , 46 – 48 ]. The general public also believes that individuals’ own behaviors and attitudes related to body image such as dieting, a desire to be thin, and body image distortion are important factors in the development of eating disorders [ 43 , 47 , 48 ]. Traumatic events, genetics, and sexual abuse were rarely discussed or, if they were mentioned, rated low on the level of significance in causing eating disorders [ 10 , 47 ].
Although sociocultural factors are less commonly identified as causal factors of eating disorders among the general public, a few factors have received support. Of all the sociocultural factors, family issues were the factors most often identified [ 43 , 46 , 48 , 49 ]. Pressure from friends as well as social isolation and loneliness were also perceived to be factors contributing to eating disorders [ 46 , 47 ]. In one study, the portrayal of thin women in the media was a highly significant cause endorsed by adult women [ 45 ].
Perceptions of individuals with eating disorders regarding causes
In contrast to studies investigating the perceptions of the general public regarding factors associated with the development of eating disorders, most studies we found that focused on individuals with eating disorders used open-ended measures, either via interview or questionnaires. Despite this, one pitfall of the research to date is that it has often involved relatively small sample sizes, ranging from 15 to 36 [ 36 , 37 , 49 – 51 ]. Only two studies have included samples over 50 individuals [ 52 , 53 ]. Additionally, almost all of these studies have focused exclusively on women, with only two including a limited number of men [ 37 , 50 ]. Furthermore, although research has included assessments of individuals with AN [ 36 , 50 , 54 ] and BN [ 53 , 55 ] or both [ 49 , 51 , 52 ], studies have failed to examine if differences existed in the perceptions of those with AN versus BN, or include individuals with other eating disorders such as BED, EDNOS, or OSFED.
Similar to public perceptions of causal factors, people with eating disorders also identify individual and sociocultural factors. Individual factors commonly identified among samples of those who were diagnosed with eating disorders include perfectionism, emotional problems or distress, stress, unhappiness with appearance, high expectations of self, and lack of control [ 36 , 48 , 50 – 54 ]. Behaviors and attitudes related to body image, such as weight loss activities, body image distortion, and a belief that thinness equals happiness, were also frequently identified as factors that related to the development of their disorders [ 48 , 53 , 55 ]. Hereditary factors and sexual abuse were not indicated.
Sociocultural influences identified by individuals with eating disorders included the media, family, peers, and sports. Although rarely mentioned, the media was occasionally identified as playing a role through the importance it places on thinness and self-comparison to the thin ideal [ 36 , 37 ]. Family factors, in contrast, were often cited and included poor parental care, controlling parents, poor relationship with parents, family tension or high amounts of conflict, critical family environment, emotional abuse, and an emphasis on weight [ 36 , 37 , 48 – 51 , 53 , 55 ]. Factors associated with peers and sports were also common and included receiving comments or pressure from friends and coaches about appearance, a need to lose weight for sports performance, and poor relationships with peers [ 36 , 37 , 53 , 55 ].
Comparisons of individuals with and without eating disorders
We could only find two studies that examined the perceptions of both individuals with and without eating disorders. First, Haworth-Hoeppner [ 49 ] interviewed 21 women with an eating disorder (either AN or BN) and 11 without, asking open-ended questions about the development of eating disorders. In this study, no comparisons were made across the two groups, likely due to the qualitative nature of the project as well as the small sample size. Second, Holliday and colleagues [ 48 ] used larger samples of individuals with and without AN and made comparisons across groups regarding the causes of eating disorders and the most important causes. However, this study was limited in that it did not allow participants to describe their own beliefs. Instead, participants responded to a list of eighteen pre-identified causes of eating disorders, which did not allow for individual perspectives and greater depth into the complexity of eating disorders.
The present study
With the prevalence of eating disorders and young age of onset, examining people’s perceptions of the factors contributing to eating disorders is important. Such efforts can enhance public education and potentially decrease the stigma surrounding eating disorders. The present study specifically examined the differences between what people with and without eating disorders perceived to be the causes of eating disorders in order to better understand people’s experiences with eating disorders as well as to better educate the larger population. We also examined differences regarding the causes of eating disorders according to type of eating disorder, including AN, BN, both, and other (e.g., BED, EDNOS, or OSFED). This study strengthens existing research by utilizing qualitative, open-ended responses as opposed to forced-answer questionnaires so that participants could identify causes using their own opinions.
Participants and procedure
This study was reviewed and approved by the university’s Institutional Review Board. Our sample was recruited from flyers and emails distributed at local universities as well as from flyers distributed to local hospitals and clinics in a medium-sized, Midwestern U.S. city. A secure Internet link was provided, which participants used to indicate consent, provide demographic information, and answer several open-ended questions. All participants were first asked, “Do/did you have an eating disorder?” with the answer choices of “yes, currently,” “yes, in the past,” and “no.” Individuals who answered as having an eating disorder, whether past or current, were asked to specify which eating disorder they had/have and for how long.
The total sample consisted of 277 participants: 57 individuals who had a past or current eating disorder and 220 who did not. Consistent with the ethnic composition of the city, most of the sample identified themselves as White (93 %). There were 234 females (84.5 %) and 43 males (15.5 %). The age range of participants was from 18 to 51 (M = 22.39, SD = 5.77).
Sample with eating disorders
Of the 57 individuals who had an eating disorder, 26 had AN (46 %), 12 had BN (21 %), 11 had both AN and BN (19 %), and 8 had another type of eating disorder such as BED or EDNOS/OSFED (14 %). Participants reporting having an eating disorder from between 4 months and 22 years (M = 3.70 years, SD = 4.55 years). Similar to the demographics of the entire sample, 93 % identified as White, and the majority of individuals in this sample were female (96.5 %; n = 55). Participants ranged in age from 18 to 47 (M = 23.70, SD = 5.84).
Sample without eating disorders
Of the 220 individuals who did not have an eating disorder, 93 % identified as White. In addition, 81 % identified as female ( n = 179). Participants ranged in age from 18 to 51 (M = 22.05, SD = 5.71). In terms of ethnicity and age, both samples were similar; there were no statistically significant differences between samples ( p = .80 and p = .11, respectively). There was, however, a statistically significant difference in gender ( p = .01).
Survey questions and compensation
After completing a series of demographic questions using the secure Internet link, individuals who had an eating disorder were asked the open-ended question, “What do you think was (were) the cause(s) of your eating disorder?” Individuals who did not have an eating disorder were asked a similar open-ended question, “What do you think is (are) the cause(s) of eating disorders?” These participants were then asked to report why they believed that these were the causes or how they learned about them. All participants were invited to participate in a random drawing for one of four $50 giftcards. Interested individuals were given another secure Internet link to provide their contact information if they wished to enter the drawing; this was done to keep the survey responses anonymous.
Coding of participants’ reponses
We initially created a list of possible codes for the causes of eating disorders commonly specified in previous research articles (as identified by overview articles on the risk factors or causes of eating disorders [e.g., 12, 15]). This provided us with a basic framework for content analysis [ 56 ]. Next, we manually generated a set of codes from actually reading individuals’ responses to the questions, “What do you think was (were) the cause(s) of your eating disorder?” and “What do you think is (are) the cause(s) of eating disorders?” Thus, we were able to identify a unique but relevant set of eight key themes. The eight themes that emerged from the data were: 1) traumatic life events, 2) family problems, 3) social problems, 4) psychological and emotional problems, 5) genetics and biology, 6) media and culture ideals, 7) sports and health, and 8) body image and eating.
Participants’ responses were then grouped under each of these categories. Many participants identified multiple causes of eating disorders, which were therefore grouped under multiple categories. The responses were coded independently by three research assistants, then checked by an additional research assistant and the first author for consistency. This was done to ensure interrater reliability [ 56 ]. When a difference in coding existed, the research team discussed the differences and mutually agreed upon a solution. See Table 1 for sample responses in each category.
Frequencies of individuals reporting each cause
A Chi square test for goodness of fit indicated that the participants in this sample showed significantly different rates of endorsement among the causes of eating disorders, χ 2 (7, n = 108) = 41.63, p < .05. Specifically, psychological and emotional ( n = 30) and social problems ( n = 22) were most frequently endorsed, with the lowest number of endorsements for genetics and biology ( n = 2) and media and culture ideals ( n = 5).
Individuals with AN most commonly indicated psychological and emotional problems as the cause ( n = 13), followed by body image and eating problems ( n = 9). Individuals with BN reported psychological and emotional ( n = 8) and social ( n = 7) as the primary causes. Those with both AN and BN listed all types of problems as causes, so there was not a clear primary cause, although social ( n = 5) and psychological and emotional problems ( n = 4) were slightly more frequently endorsed. Finally, those with other eating disorders most frequently cited psychological and emotional problems ( n = 5) and traumatic life events ( n = 3). See Table 2 for a complete listing of the frequencies of individuals citing each causal category.
A Chi square test for goodness of fit indicated that the participants in this sample showed significantly different rates of endorsement among the causes of eating disorders, χ 2 (7, n = 414) = 326.95, p < .05. Specifically, psychological and emotional problems ( n = 141) and media and culture ideals ( n = 104) were most frequently endorsed, with the lowest number of endorsements for family problems ( n = 28), genetics and biology ( n = 18), traumatic life events ( n = 5), and sports and health ( n = 4). Clearly, this sample differed from the sample of individuals with eating disorders in what they viewed as the primary causes. See Table 2 for the frequencies.
Differences between samples
Chi square tests for independence indicated that there was not a significant relationship between type of eating disorder (AN, BN, both, or other) and the causes specified. Furthermore, there were no significant relationships among each pairing of eating disorder sub-groups. The lack of statistically significant findings here could be the result of our small sample sizes for each group. See Table 3 for a summary of results from these chi square tests for independence.
Of particular noteworthiness, results from a chi square test of independence indicated that there was a significant relationship between eating disorder versus non-eating disorder groups and the causes specified, χ 2 (7, n = 522) = 77.96, p < .05, Phi = .39. This suggests that individuals with and without eating disorders had significantly different views regarding the causes of eating disorders, with each group likely to endorse causes at different rates. In conducting follow-up analyses of each cause separately, we found significant differences in the endorsement of family problems (χ 2 (1, n = 39) = 7.41, p < .05), social problems (χ 2 (1, n = 79) = 15.51, p < .05), psychological and emotional problems (χ 2 (1, n = 171) = 72.05, p < .05), genetics and biology (χ 2 (1, n = 20) = 12.80, p < .05), media and culture (χ 2 (1, n = 109) = 89.92, p < .05), and body image and eating (χ 2 (1, n = 71) = 26.04, p < .05) among those with and without eating disorders. More specifically, individuals with eating disorders more often endorsed family problems, and social problems while individuals without eating disorders more often endorsed psychological and emotional problems, genetics and biology, media and culture, and body image and eating.
Additionally, there were significant relations between each individual type of eating disorder versus non-eating disorder and the causes specified. See Table 3 for these results. This suggests, for example, that individuals without eating disorders had different levels of endorsement for each cause than the group of individuals with AN. The same was true for the sub-groups of BN, both, and other, when compared to individuals without eating disorders.
This is the only known study that assessed subjective perceptions of the causes of eating disorders among a relatively large sample of individuals with and without eating disorders. The results support differences between the general public and individuals suffering from eating disorders, which hopefully can be used to provide proper education. Specifically, the general public largely believed that the media causes eating disorders, a perception that is not shared among individuals with an eating disorder. Similarly, sports, body image, and traumatic events were listed less frequently by participants without eating disorders than participants with eating disorders. However, psychological and emotional problems were highly endorsed by all. Together, these findings indicate differences in opinion regarding the causes of eating disorders between those who have an eating disorder and those who do not.
The open-ended questions used in the present study enabled us to gain insight into individuals’ personal opinions regarding factors associated with the development of their disorders, ultimately providing a greater understanding for both clinicians and lay people. Psychological and emotional problems were the most frequently reported causes for those with an eating disorder, supporting the need for greater availability of support systems. In considering the perspectives of individuals who had an eating disorder, it is difficult to know if their perceptions align accurately with the actual causes. However, professionals working with these individuals could help assess the discrepancy between perceived and actual causes. For many postmodern therapists, understanding the perception of the eating disorder from the client perspective and helping him or her make meaning of the experience is more important than determining the actual cause of the disorder [ 57 , 58 ]. This, therefore, provides reinforcement for the role of psychologists and family therapists within the field of eating disorders, yet many currently lack sufficient training to address eating disorders and instead must refer clients to specialists, who are often expensive and not widely located.
The role of the media
Our findings revealed a definite contrast between how people with and without eating disorders perceive media as a risk factor for developing an eating disorder. A large percentage of people without eating disorders identified media as a cause (47 %), but only five total participants with eating disorders did. There is a clear separation in the experience of those with eating disorders and with society’s conceptualization of them [ 36 , 37 ]. Thus, it seems that lay individuals may overemphasize the role of the media as one of the main causes of eating disorders, while those with eating disorders may not be fully aware of the potential impact of the media [ 50 ]. Whereas specific media variables such as depiction of the thin ideal and unrealistic body standards may be correlated with eating disorders [ 42 ], they do not fully explain disordered behaviors. Our findings should be used to educate consumers of media on the complexity of eating disorders, and as evidence for the need to change the types of messages regarding body image ideals that are currently available in the media.
- Psychological and emotional problems
Psychological and emotional problems were one of the highest named causes of eating disorders by both groups, which is consistent with prior research [ 43 , 46 , 48 ]. However, upon close examination of the data, we noticed a contrast between the written answers of those who had eating disorders and those who did not. More specifically, individuals with eating disorders listed personal reasons, such as “a bad relationship that caused a lot of low self-esteem,” or simple statements such as “stress, depression.” In contrast, there was a negative stigma surrounding some of the answers from participants without eating disorders. These answers included phrases such as “no self-confidence” and “mental disabilities.” This difference is worth noting, because it demonstrates a stigma towards those with eating disorders, which may result in a fear of judgment from others that often prevents those suffering from eating disorders to seek help [ 59 ]. Reduction of this stigma through educational programs could encourage individuals who are developing disordered eating habits to speak up, as well as encourage friends and family to begin a non-judgmental, supportive dialogue with individuals about their habits.
Other factors
Traumatic life events were only listed by 2 % of the non-eating disorder group, versus 23 % of those with eating disorders. This once again emphasizes the need for education geared towards the general public. However, there is also a need for better education for those with eating disorders, as the number of people listing traumatic events was quite low. Many individuals may not make the connection between a traumatic event, such as sexual assault, and the beginning of their disorder, despite empirical support for the effects of abuse [ 22 ].
Similar to previous studies, genetics as a cause of disordered eating was only listed by two participants with eating disorders and eight participants without eating disorders [ 10 , 47 ], making it the least endorsed cause. This indicates a need for the dissemination of information regarding the genetic component of eating disorders, as this could potentially help with the negative stigma surrounding eating disorders [ 60 ].
Similarly, and in line with previous studies, only twelve participants with eating disorders and 28 participants without listed family problems as a cause of disordered eating [ 43 , 46 , 48 , 49 ]. There are numerous studies, however, that show the impact that mothers, fathers, and siblings can have on the development of disordered eating in an individual (e.g., [ 26 , 27 ]). If education efforts could help improve understanding of how eating disorders develop within families, parents and siblings can take steps towards preventing the occurrence of these issues and can work towards developing healthier habits for themselves as well.
Sports and health were also listed more frequently as causes by those with eating disorders (19 %), whereas only 2 % of those without eating disorders mentioned them. However, these numbers are both still low. The general public, and specifically coaches, need to be aware of how an intense focus on the body can lead to negative outcomes and strive to support healthy methods of getting and staying in shape.
Body image was listed as a cause of eating disorders by 26 % of participants without an eating disorder, and 25 % of those with experience with disorder eating; these numbers represent a substantial portion of participants. Poor body image often provides a foundation for the development of an eating disorder [ 15 , 17 ], and understanding what issues underlie an eating disorder can help not only those struggling to recover, but those trying to assist them.
Another highly-endorsed cause of eating disorders was social problems, as 26 % of those without eating disorders and 39 % of those with eating disorders listed them. While these numbers are considerably higher than other groups, only one fourth of those without eating disorders acknowledged social problems as a cause, while a much larger number of those with eating disorders indicated social problems as a cause. However, many individuals may not realize the effect that external events can have on their internal belief systems, once again indicating the need to incorporate this finding into general education, as well as into the treatment process as a way of lessening the blame that those suffering may place on themselves.
Summary of findings
This study provides insight into the educational resources needed to inform the lay audience regarding eating disorders as well as some factors to consider in the education or prevention of eating disorders among those affected. There is a clear difference between perceived causes of eating disorders from those who have experienced them and those who have not. Those who had not struggled with an eating disorder were more likely to believe that media and cultural ideals influenced eating disorders. For those who had lived with an eating disorder, this was one of the least likely perceived causes. Social problems, in contrast, were frequently listed by participants with eating disorders and less frequently listed by participants without. Genetics and traumatic events were listed most infrequently by both groups, and there were also relatively low levels of endorsement for traumatic life events, sports and health, and family problems among both groups. Both groups listed body image as a fairly frequent cause, and although both groups highly endorsed psychological and emotional problems as causes, there was a clear negative stigma surrounding psychological and emotional problems when listed by non-disordered participants. Improved educational programs should seek to give those who are uninformed a greater understanding of how psychological, social, and relational factors influence those with eating disorders. Increased opportunities for those who have lived with eating disorders to share their stories and perspectives are also needed. With the opportunity to provide first-hand knowledge, these individuals can be an excellent asset for researchers, professionals, and lay people.
Limitations
Our sample was a relatively homogenous group in terms of gender and ethnicity, so separate analyses could not be conducted examining differences among men and women or among various ethnic groups. Thus, care should be taken when generalizing the results to males and non-white individuals. Furthermore, in order to utilize open-ended questions, no measurement scales were used to determine eating disorder pathology. Therefore, eating disorder status was determined solely by self-report and may not be clinically accurate. In retrospect, it may have been useful to at least provide participants with a self-report survey to assess their eating disorder symptomatology. However, we do note that our sample was recruited not only from local universities but directly from hospitals and clinics that included eating disorder treatment facilities. As a result, we hope that participants were able to appropriately reflect on the nature of their symptomatology. Further, our type of questioning allowed for only two groups of samples, those with eating disorders and those without; individuals who have subclinical symptoms or undiagnosed eating disorders may have been inaccurately placed in the category of non-eating disorder due to their own assessment. Similarly, those who identified themselves as having an eating disorder may have been self-diagnosed, and therefore may not technically meet clinical standards for a disorder.
Additionally, two different questions were asked of participants. Specifically, we asked participants with an eating disorder: “What do you think was (were) the cause(s) of your eating disorder?”, and we asked participants without an eating disorder: “What do you think is (are) the cause(s) of eating disorders?” This allows individuals to add a personal dimension to their analysis of the causes of eating disorders. As such, they may believe that the cause of their disorder is very different than the cause of someone else’s disorder. Similarly, individuals with an eating disorder may have focused more on life events or recent triggers without a reflection on more general risk factors.
Lastly, because this study was completed online, it could be considered relatively impersonal, whereas in-person interviews would have most likely been more in depth. However, because the main interest of the study was to examine participants’ instinctive reactions to eating disorders, the completely anonymous online survey was the most beneficial means of execution.
Despite limitations, this study contributes to the field in a variety of ways. The sample size of those with eating disorders ( n = 57) is somewhat larger than samples currently in the literature. Furthermore, while many studies focus only on AN or BN, this study included those with self-reported AN, BN, BED and EDNOS/OSFED, allowing for more inclusive results. It also allowed us to separately assess perceived causes of eating disorders according to the type of eating disorder. For example, individuals with AN most frequently indicated psychological and emotional problems as well as body image and eating problems; individuals with BN often reported psychological and emotional problems as well as social problems; individuals with both AN and BN listed all types of problems; and individuals with BED, EDNOS, or OSFED primarily cited psychological and emotional problems as well as traumatic life events. Although these differences in perceptions were not statistically significant, it may suggest that each type of disorder is unique, with potentially unique causes attributed to the disorder. Future research should continue to examine these differences, and education should focus on the unique nature of each type of eating disorder.
The use of an open-ended qualitative assessment allowed for a complete picture of individuals’ perceptions of the causes of eating disorders. It also allowed individuals to write about more than one perceived cause of the disorders, which is not always possible with close-ended questions with limited answer options. An additional strength of this study is that it contributes to the relatively small pool of current literature discussing perceptions of eating disorders. Within this limited research, most examine perceptions of the general public or perceptions of those with eating disorders separately. Our study is also one of very few studies to examine differences between these two groups.
Overall, it appears that all individuals would benefit from learning more about eating disorders and their causes. Knowing this could be particularly helpful for individuals going through eating disorder treatment, especially for therapists to use when educating those close to someone struggling with an eating disorder. This could help facilitate greater support and connection between family members and friends, and help to end the stigma surrounding these problems and allow those in trouble to seek help.
Le Grange D, Swanson SA, Crow SJ, Merikangas KR. Eating disorder not otherwise specified presentation in the US population. Int J Eat Disord. 2012;45:711–8.
Article PubMed Central PubMed Google Scholar
Hudson J, Hiripi E, Pope H, Kessler R. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61:348–58.
Rosen DS. Identification and management of eating disorders in children and adolescents. Pediatr. 2010;126:1240–53.
Article Google Scholar
Swanson SA, Crow SJ, LeGrange D, Swendsen J, Merikangas KR. Prevalence and correlates of eating disorders in adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. Arch Gen Psych. 2011;68:714–23.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
Google Scholar
Quick V, Berg KC, Bucchianeri MM, Byrd-Bredbenner C. Identification of eating disorder pathology in college students: a comparison of DSM-IV-TR and DSM-5 diagnostic criteria. Adv Eat Disord. 2014;2:112–24.
Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders: a meta-analysis of 36 studies. Arch Gen Psych. 2011;68:724–31.
Lee NM, Lucke J, Hall WD, Meurk C, Boyle FM, Carter A. Public views on food addiction and obesity: implications for policy and treatment. PLoS One. 2013;8, e74836.
Article PubMed Central CAS PubMed Google Scholar
Mond JM, Arrighi A. Gender differences in perceptions of the severity and prevalence of eating disorders. Early Int Psych. 2011;5:41–9.
Mond JM, Hay PJ. Public perceptions of binge eating and its treatment. Int J Eat Disord. 2008;41:419–26.
Article PubMed Google Scholar
Yilmaz Z, Hardaway AJ, Bulik CM. Genetics and epigenetics of eating disorders. Adv Genomics Genet. 2015;5:131–50.
Polivy J, Herman CP. Causes of eating disorders. Annu Rev Psychol. 2002;53:187–214.
Lee Y, Lin PY. Association between serotonin transporter gene polymorphism and eating disorders: a meta-analytic study. Int J Eat Disord. 2010;43:498–504.
Cui H, Moore J, Ashimi SS, Mason BL, Drawbridge JN, Han S, et al. J Clin Invest. 2013;123:4706–13.
Stice E. Risk and maintenance factors for eating pathology: a meta-analytic review. Psychol Bull. 2002;128:825–48.
Zehr JL, Culbert KM, Sisk CL, Klump KL. An association of early puberty with disordered eating and anxiety in a population of undergraduate women and men. Horm Behav. 2007;52:427–35.
Wertheim EH, Koerner J, Paxton SJ. Longitudinal predictors of restrictive eating and bulimic tendencies in three different age groups of adolescent girls. J Youth Adolesc. 2001;30:69–82.
Leon GR, Fulkerson JA, Perry CL, Keel PK, Klump KL. Three to four year prospective evaluation of personality and behavioral risk factors for later disordered eating in adolescent girls and boys. J Youth Adolesc. 1999;28:181–96.
Fairburn CG, Cooper Z, Doll HA, Welch SL. Risk factors for anorexia nervosa: three integrated case–control comparisons. Arch Gen Psychiatry. 1999;56:468–76.
Article CAS PubMed Google Scholar
Tyrka AR, Waldron I, Graber JA, Brooks-Gunn J. Prospective predictors of the onset of anorexic and bulimic syndromes. Int J Eat Disord. 2002;32:282–90.
Tylka TL. The relation between body dissatisfaction and eating disorder symptomatology: an analysis of moderating variables. J Couns Psychol. 2004;51:178–91.
Neumark‐Sztainer D, Story M, Hannan PJ, Beuhring T, Resnick MD. Disordered eating among adolescents: associations with sexual/physical abuse and other familial/psychosocial factors. Int J Eat Disord. 2000;28:249–58.
Treuer T, Koperdák M, Rózsa S, Füredi J. The impact of physical and sexual abuse on body image in eating disorders. Eur Eat Disord Rev. 2005;13:106–11.
Wonderlich SA, Rosenfeldt S, Crosby RD, Mitchell JE, Engel SG, Smyth J, et al. The effects of childhood trauma on daily mood lability and comorbid psychopathology in bulimia nervosa. J Traum Stress. 2007;20:77–87.
Fischer S, Stojek M, Hartzell E. Effects of multiple forms of childhood abuse and adult sexual assault on current eating disorder symptoms. Eat Behav. 2010;11:190–2.
Fulkerson JA, McGuire MT, Neumark-Sztainer D, Story M, French SA, Perry CL. Weight-related attitudes and behaviors of adolescent boys and girls who are encouraged to diet by their mothers. Int J Obes. 2002;26:1579–87.
Article CAS Google Scholar
Keery H, Eisenberg M, Boutelle K, Neumark-Sztainer D, Story M. Relationships between maternal and adolescent weight-related behaviors and concerns: the role of perception. J Psychosom Res. 2006;61:105–11.
Tremblay L, Lariviere M. The influence of puberty onset, body mass index, and pressure to be thin on disordered eating behaviors in children and adolescents. Eat Behav. 2009;10:75–83.
Wertheim EH, Paxton SJ, Schutz HK, Muir SL. Why do adolescent girls watch their weight? An interview study examining sociocultural pressures to be thin. J Psychosom Res. 1997;42:345–55.
Ata RN, Ludden AB, Lally MM. The effects of gender and family, friend, and media influences on eating behaviors and body image during adolescence. J Youth Adolesc. 2007;36:1024–37.
Vincent MA, McCabe MP. Gender differences among adolescents in family, and peer influences on body dissatisfaction, weight loss, and binge eating behaviors. J Youth Adolesc. 2000;29:205–21.
Kluck AS. Family factors in the development of disordered eating: integrating dynamic and behavioral explanations. Eat Behav. 2008;9:471–83.
van den Berg P, Thompson JK, Obremski-Brandon K, Coovert M. The tripartite influence model of body image and eating disturbance: a covariance structure modeling investigation testing the meditational role of appearance comparison. J Psychosom Res. 2002;53:1007–20.
Sheets V, Ajmere K. Are romantic partners a source of college students' weight concern? Eat Behav. 2005;6:1–9.
Weller JE, Dziegielewski SF. The relationship between romantic partner support styles and body image disturbance. J Hum Behav Soc Environ. 2004;10:71–92.
Dignon A, Beardsmore A, Spain S, Kuan A. ‘Why I won’t eat’: patient testimony from 15 anorexics concerning the causes of their disorder. J Health Psychol. 2006;11:942–56.
Woods S. Untreated recovery from eating disorders. Adolescence. 2004;39:361–71.
PubMed Google Scholar
Kong P, Harris LM. The sporting body: body image and eating disorder symptomatology among female athletes from leanness focused and nonleanness focused sports. J Psychol. 2015;149:141–60.
Krentz EM, Warschburger P. A longitudinal investigation of sports-related risk factors for disordered eating in aesthetic sports. Scand J Med Sci Sports. 2013;23:303–10.
Thompson RA, Sherman R. Reflections on athletes and eating disorders. Psychol Sport Exerc. 2014;15:729–34.
Slater A, Tiggemann M, Firth B, Hawkins K. Reality check: an experimental investigation of the addition of warning labels to fashion magazine images on women's mood and body dissatisfaction. J Soc Clin Psychol. 2012;31:105–22.
Ahern AL, Bennett KM, Hetherington MM. Internalization of the ultra-thin ideal: positive implicit associations with underweight fashion models are associated with drive for thinness in young women. Eat Disord. 2008;16:294–307.
Furnham A, Hume-Wright A. Lay theories of anorexia nervosa. J Clin Psychol. 1992;48:20–36.
Furnham A, Manning R. Young people's theories of anorexia nervosa and obesity. Couns Psychol Q. 1997;10:389–414.
Mond JM, Hay PJ, Rodgers B, Owen C, Beumont PJ. Beliefs of women concerning causes and risk factors for bulimia nervosa. Aust N Z J Psychiatry. 2004;38:463–9.
Smith MC, Pruitt JA, Mann LM, Thelen MH. Attitudes and knowledge regarding bulimia and anorexia nervosa. Int J Eat Disord. 1986;5:545–53.
Lee S. How lay is lay? Chinese students' perceptions of anorexia nervosa in Hong Kong. Soc Sci Med. 1997;44:491–502.
Holliday J, Wall E, Treasure J, Weinman J. Perceptions of illness in individuals with anorexia nervosa: a comparison with lay men and women. Int J Eat Disord. 2005;37:50–6.
Haworth-Hoeppner S. The critical shapes of body image: the role of culture and family in the production of eating disorders. J Marriage Fam. 2000;62:212–27.
Button EJ, Warren RL. Living with anorexia nervosa: the experience of a cohort of sufferers from anorexia nervosa 7.5 years after initial presentation to a specialized eating disorders service. Eur Eat Disord Rev. 2001;9:74–96.
Patching J, Lawler J. Understanding women’s experiences of developing an eating disorder and recovering: a life-history approach. Nurs Inq. 2009;16:10–21.
Tozzi F, Sullivan PF, Fear JL, McKenzie J, Bulik CM. Causes and recovery in anorexia nervosa: the patient's perspective. Int J Eat Disord. 2003;33:143–54.
Rossotto E, Rorty-Greenfield M, Yager J. What causes and maintains bulimia nervosa? Recovered and nonrecovered women's reflections on the disorder. Eat Disord: J Treat Prev. 1996;4:115–27.
Nilsson K, Abrahamsson E, Torbiornsson A, Hägglöf B. Causes of adolescent onset anorexia nervosa: patient perspectives. Eat Disord. 2007;15:125–33.
Lacey J, Coker S, Birtchnell SA. Bulimia: factors associated with its etiology and maintenance. Int J Eat Disord. 1986;5:475–87.
Patton MQ. Qualitative research and evaluation methods. Thousand Oaks, CA: Sage Publications; 2002.
Gergen K. An invitation to social construction. London: Sage Publications Ltd; 2009.
White M, Epston D. Narrative means to therapeutic ends. New York: W.W. Norton; 1990.
Becker AE, Arrindell AH, Perloe A, Fay K, Striegel-Moore RH. A qualitative study of perceived social barriers to care for eating disorders: perspectives from ethnically diverse health care consumers. Int J Eat Disord. 2010;43:633–47.
Easter MM. “Not all my fault”: genetics, stigma, and personal responsibility for women with eating disorders. Soc Sci Med. 2012;75:1408–16.
Download references
Acknowledgements
We thank our undergraduate and graduate research assistants at the North Dakota State University Eating Disorders and Body Image Lab for their assistance with coding the data.

Author information
Authors and affiliations.
Department of Human Development and Family Science, North Dakota State University, 283-H EML Hall, #2615, P.O. Box 6050, Fargo, North Dakota, 58108, USA
Elizabeth H. Blodgett Salafia, Maegan E. Jones, Emily C. Haugen & Mallary K. Schaefer
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Elizabeth H. Blodgett Salafia .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contributions
EHBS conceived of and designed the study, developed codes for and analysed the data, and wrote the manuscript. MEJ co-wrote and formatted the manuscript. ECH coded data and co-wrote the manuscript. MKS coded data and co-wrote the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Blodgett Salafia, E.H., Jones, M.E., Haugen, E.C. et al. Perceptions of the causes of eating disorders: a comparison of individuals with and without eating disorders. J Eat Disord 3 , 32 (2015). https://doi.org/10.1186/s40337-015-0069-8
Download citation
Received : 13 April 2015
Accepted : 04 September 2015
Published : 15 September 2015
DOI : https://doi.org/10.1186/s40337-015-0069-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Eating disorders
- Perceptions
Journal of Eating Disorders
ISSN: 2050-2974
- General enquiries: [email protected]
Treatment, Symptoms, and Prevention of Bipolar Disorder Essay
Introduction.
Bipolar disorder is a mental disorder that is manifested by drastic mood changes — bipolar manifests in two main extremes, namely depression, and mania (Peacock, 2000). Depression manifests when an individual feels tired and sad. On the other hand, mania manifests when an individual experiences periods of extreme excitement and restlessness. Symptoms of bipolar depend on the extreme that individual experiences at a certain period.
In many cases, an individual is diagnosed with clinical depression and later with bipolar. During an episode of depression, individuals experience feelings that include hopelessness, extreme sadness, worthlessness, lethargy, and irritability (Peacock, 2000). In severe cases, an individual might contemplate suicide. On the other hand, episodes of mania are characterized by feelings of happiness, joy, irritability, and extreme creativity.
Prevalence and incidence
According to the World Health Organization, more than 10 million individuals have bipolar in the United States (Peacock, 2000). The disorder is a leading cause of disability in the world. It has a lifetime prevalence of approximately 3% around the globe. Statistics have revealed that more than 0.8% of the American population experiences at least a manic episode at one time in their life.
On the other hand, 0.5% of the population experiences a hypomanic episode. 6.4% of the American population has been shown to have bipolar spectrum disorder (Peacock, 2000). Studies have revealed that the incidence of bipolar disorder among men and women is the same. The incidence rate is similar across people of different origins and ethnic backgrounds.
However, its severity varies across the world. In the U.S., the rate of incidence is higher among African Americans than among Americans of European descent (Peacock, 2000). The disorder affects people mainly in their adolescence and early adulthood years. In many cases, individuals with experienced bipolar episodes of mania after the age of fifty.
Symptoms of bipolar disorder depend on the mood that an individual experiences at a certain period. Individuals experience extreme mood changes that affect their behaviors and thinking patterns. Mania is characterized by over-excitement, while depression is characterized by extreme sadness.
During episodes of depression, individuals experience feelings of sadness, hopelessness, worthlessness, and loss of interest in activities they previously enjoyed, such as sex and social interaction (Fink & Kraynak, 2012). Their thinking is predominantly negative, and they rarely see the positive aspects of their lives. Their behavior also changes. They are restless, irritable, indecisive, and insomniac. Moreover, they experience problems with concentration and memory (Peacock, 2000).
Symptoms of mania
Symptoms of mania include hyperactivity, high quantities of energy, extreme irritability, impulsive behavior, restlessness, risk-taking, extreme happiness, and excitement, as well as unrealistic belief in personal capabilities (Fink & Kraynak, 2012).
Hypomania is a less severe form of mania that is characterized by moderate productivity and happiness. In other cases, both episodes of depression and mania might manifest at the same time. During such episodes, individuals become insomniac, agitated, and may harbor sundial thoughts (Fink & Kraynak, 2012).
Treatment of bipolar disorder includes us of both medication and therapy (Miklowitz, 2011). Bipolar is a disorder that affects individuals for the rest of their lives. Therefore, combining medication with therapy lowers the prevalence of the various mood changes associated with the disorder (Fink & Kraynak, 2012).
The recurrence of a maniac and depressive episodes makes life difficult for victims. Successful treatment of bipolar disorder involves the use of different treatment remedies. According to studies, medication alone is not enough to treat bipolar disorder effectively. One of the most important aspects of bipolar treatment is education and awareness about causes and ways of management.
Victims should read extensively about the disorder, join support groups, and make lifestyle changes that enable them to manage their symptoms (Ketter, 2007). The most common treatment methods for bipolar include medication, psychotherapy, education, lifestyle changes, and support. Drugs such as mood stabilizers aid in the minimization of symptoms. The most common and most effective mood stabilizer used to treat bipolar is lithium (Ketter, 2007).
Antidepressants such as Prozac and Amitriptyline are also used. Antipsychotic medications include Ariplazole, Quetiapine, Risperidone, and Clozapine (Ketter, 2007). Other drugs used together with mood stabilizers include Lamictal, Symbax, Zyprexa, and Seroquel. Psychotherapy teaches individuals different ways of coping with difficult times and different mood changes (Fink & Kraynak, 2012). Types of therapy available to individuals include cognitive-behavioral therapy and family-focused therapy (Ketter, 2007).
Education involves understanding the various symptoms of bipolar and their management. Finally, support involves interacting with individuals with the disorder for moral, emotional, and psychological support. Support groups facilitate the sharing of experiences that could be helpful to other individuals with similar challenges (Ketter, 2007). Complementary treatments include acupuncture, deep meditation, as well as light and dark therapy.
Prevention of a bipolar disorder
To prevent bipolar disorder, it is important to learn about it to control mood changes and other symptoms. It is also important to practice lifestyle management. Lifestyle management involves changes such as alcohol avoidance, practicing meditation, physical exercise, and thinking positively (Miklowitz, 2011).
Prevention of bipolar disorder mainly focuses on stress reduction. High levels of stress increase the risk of developing bipolar for genetically susceptible individuals. Stress reduction can be achieved through regular physical exercise and participating in relaxation methods such as meditation and yoga (Ketter, 2007).
Risk factors
Bipolar disorder’s risk factors include genetics, lifestyle, alcohol and drug abuse, high-stress levels, environment, and major life changes. Research has revealed that bipolar disorder has a basis in the genes of individuals. Therefore, the risk is very high for individuals who come from families with a history of the disorder. Research has shown that children from families in which one or both the parents have the disorder have a high risk of developing the disorder (Fink & Kraynak, 2012).
Major life changes such loss of a loved one, sexual abuse, or traumatic events such as accidents increase the risk of developing the disorder. Individuals who undergo prolonged periods of stress are also at high risk of developing the disorder (Fink & Kraynak, 2012). Medical practitioners recommend physical exercise and meditation as two of the most effective methods of reducing stress. Alcohol and drug abuse also increase the risk of developing the disorder.
Environment plays a critical role in the development o bipolar disorder. For instance, children who grow in abusive and violent families have a very high risk of developing bipolar (Miklowitz, 2011). Stressful environments play a key role in triggering depressive episodes that herald the development of bipolar.
Diagnosis is carried out through evaluation by a medical professional following diagnosis guidelines as provided in the Diagnostic and Statistical Manual of Mental disorder (DSM) (Fink & Kraynak, 2012). Successful diagnosis is mainly based on the observation of major changes in mood patterns and behavior. After a successful diagnosis, a patient is given medication based on past medical history and the severity of the condition.
Bipolar disorder is a mental disorder that is characterized by extreme mood changes that range from mania to depression. Risk factors include lifestyle, genetics, environment, drug and alcohol abuse, and major life changes such as death or abuse. Symptoms depend on the type of mod. Symptoms observed during the mania phase include hyperactivity, risk-taking, restlessness, and unrealistic belief in one’s capabilities.
During the depression phase, symptoms include insomnia, poor concentration, lack of appetite, loss of interest in activities that were once enjoyable, and feelings of hopelessness as well as helplessness. In severe cases, individuals contemplate suicide. Effective treatment involves the use of both drugs and psychotherapy. Drugs used include mood stabilizers, antidepressants, and psychotic medication.
Forms of therapy applied to include cognitive-behavioral therapy, family-centered therapy, as well as interpersonal and social rhythm therapy. Prevention involves participation in physical exercise and stress reduction activities such as meditation and yoga. According to the World Health Organization, more than 10 million individuals have bipolar in the United States.
On the other hand, 3% of the world’s population suffers from the disorder. Research has revealed that bipolar disorder has a basis in the genes of individuals. Therefore, the risk is very high for individuals who come from families with a history of the disorder. Research has shown that children from families in which one or both the parents have the disorder have a high risk of developing the disorder.
Fink, C., & Kraynak, J. (2012). Bipolar Disorder for Dummies . New York: John Wiley & sons.
Ketter, T. (2007). Advances in Treatment of Bipolar Disorder . New York: American Psychiatric Publishers.
Miklowitz, D. J. (2011). The Bipolar Disorder Survival Guide, Second Edition: What You and your Family Need to Know . New York: Gilford Press.
Peacock, J. (2000). Bipolar Disorder . New York: Capstone.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2020, April 5). Treatment, Symptoms, and Prevention of Bipolar Disorder. https://ivypanda.com/essays/bipolar-disorder-essay/
"Treatment, Symptoms, and Prevention of Bipolar Disorder." IvyPanda , 5 Apr. 2020, ivypanda.com/essays/bipolar-disorder-essay/.
IvyPanda . (2020) 'Treatment, Symptoms, and Prevention of Bipolar Disorder'. 5 April.
IvyPanda . 2020. "Treatment, Symptoms, and Prevention of Bipolar Disorder." April 5, 2020. https://ivypanda.com/essays/bipolar-disorder-essay/.
1. IvyPanda . "Treatment, Symptoms, and Prevention of Bipolar Disorder." April 5, 2020. https://ivypanda.com/essays/bipolar-disorder-essay/.
Bibliography
IvyPanda . "Treatment, Symptoms, and Prevention of Bipolar Disorder." April 5, 2020. https://ivypanda.com/essays/bipolar-disorder-essay/.
- Bipolar Mania and Nursing Interventions
- Bipolar Disorder and Its Main Phases
- Bipolar and Mania Disorders
- Bipolar Disorder: Causes, Symptoms and Facts
- The Bipolar Disorder and Its Management
- Managing Bipolar Disorder
- Bipolar Expeditions: Mania and Depression
- Bipolar Disorder in Asian American Woman
- Bipolar Disorder and Current Treatment Options
- Cognitive-Behavioral Therapy for Bipolar Disorder
- Various Anxiety Disorders' Comparison
- Psychiatric Issues: Schizophrenia's Demystify
- Hypoactive Sexual Desire Disorder
- Medical Issues: Mental Illness
- Social Non-Comformity in Books of K. Kesey and S. Kaysen

In the brain, bursts of beta rhythms implement cognitive control
Bursts of brain rhythms with “beta” frequencies control where and when neurons in the cortex process sensory information and plan responses. Studying these bursts would improve understanding of cognition and clinical disorders, researchers argue in a new review.
The brain processes information on many scales. Individual cells electrochemically transmit signals in circuits but at the large scale required to produce cognition, millions of cells act in concert, driven by rhythmic signals at varying frequencies. Studying one frequency range in particular, beta rhythms between about 14-30 Hz, holds the key to understanding how the brain controls cognitive processes—or loses control in some disorders—a team of neuroscientists argues in a new review article.
Drawing on experimental data, mathematical modeling and theory, the scientists make the case that bursts of beta rhythms control cognition in the brain by regulating where and when higher gamma frequency waves can coordinate neurons to incorporate new information from the senses or formulate plans of action. Beta bursts, they argue, quickly establish flexible but controlled patterns of neural activity for implementing intentional thought.
“Cognition depends on organizing goal-directed thought, so if you want to understand cognition, you have to understand that organization,” said co-author Earl K. Miller , Picower Professor in The Picower Institute for Learning and Memory and the Department of Brain and Cognitive Sciences at MIT. “Beta is the range of frequencies that can control neurons at the right spatial scale to produce organized thought.”
Miller and colleagues Mikael Lundqvist, Jonatan Nordmark and Johan Liljefors at the Karolinska Institutet and Pawel Herman at the KTH Royal Institute of Technology in Sweden, write that studying bursts of beta rhythms to understand how they emerge and what they represent would not only help explain cognition, but also aid in diagnosing and treating cognitive disorders.
“Given the relevance of beta oscillations in cognition, we foresee a major change in the practice for biomarker identification, especially given the prominence of beta bursting in inhibitory control processes … and their importance in ADHD, schizophrenia and Alzheimer’s disease,” they write in the journal Trends in Cognitive Sciences .
Experimental studies covering several species including humans, a variety of brain regions, and numerous cognitive tasks have revealed key characteristics of beta waves in the cortex, the authors write: Beta rhythms occur in quick but powerful bursts; they inhibit the power of higher frequency gamma rhythms; and though they originate in deeper brain regions, they travel within specific locations of cortex. Considering these properties together, the authors write that they are all consistent with precise and flexible regulation, in space and time, of the gamma rhythm activity that experiments show carry signals of sensory information and motor plans.
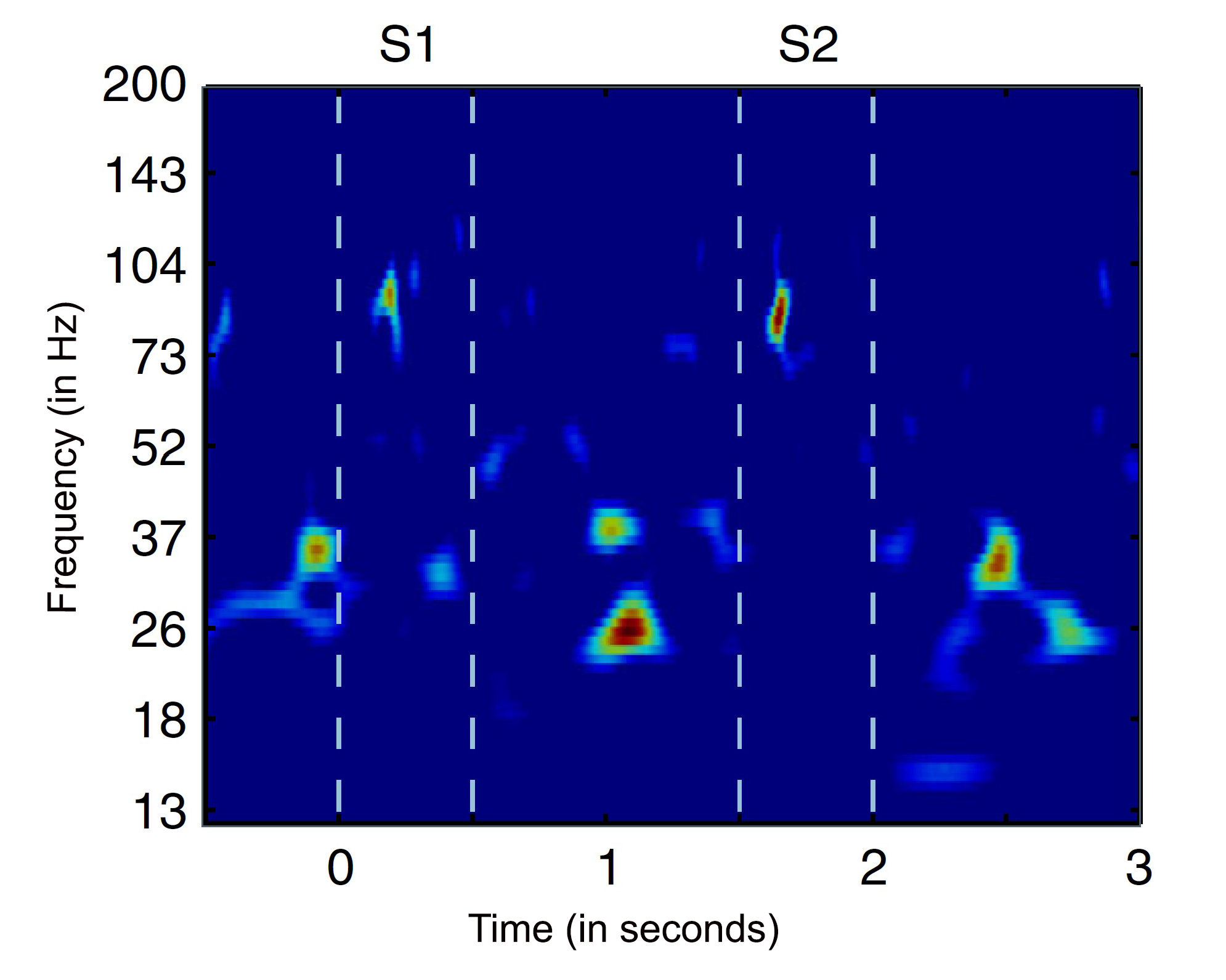
“Beta bursts thus offer new opportunities for studying how sensory inputs are selectively processed, reshaped by inhibitory cognitive operations and ultimately result in motor actions,” the authors write.
For one example, Miller and colleagues have shown in animals that in the prefrontal cortex in working memory tasks, beta bursts direct when gamma activity can store new sensory information, read out the information when it needs to be used, and then discard it when it’s no longer relevant. For another example, other researchers have shown that beta rises when human volunteers are asked to suppress a previously learned association between word pairs, or to forget a cue because it will no longer be used in a task.
In a paper last year, Lundqvist, Herman, Miller and others cited several lines of experimental evidence to hypothesize that beta bursts implement cognitive control spatially in the brain , essentially constraining patches of the cortex to represent the general rules of a task even as individual neurons within those patches represent the specific contents of information. For example, if the working memory task is to remember a pad lock combination, beta rhythms will implement patches of cortex for the general steps “turn left,” “turn right,” “turn left again,” allowing gamma to enable neurons within each patch to store and later recall the specific numbers of the combination. The two-fold value of such an organizing principle, they noted, is that the brain can rapidly apply task rules to many neurons at a time and do so without having to re-establish the overall structure of the task if the individual numbers change (i.e. you set a new combination).
Another important phenomenon of beta bursts, the authors write, is that they propagate across long distances in the brain, spanning multiple regions. Studying the direction of their spatial travels, as well as their timing, could shed further light on how cognitive control is implemented.
New ideas beget new questions
Beta rhythm bursts can differ not only in their frequency, but also their duration, amplitude, origin and other characteristics. This variety speaks to their versatility, the authors write, but also obliges neuroscientists to study and understand these many different forms of the phenomenon and what they represent to harness more information from these neural signals.
“It quickly becomes very complicated, but I think the most important aspect of beta bursts is the very simple and basic premise that they shed light on the transient nature of oscillations and neural processes associated with cognition,” Lundqvist said.“This changes our models of cognition and will impact everything we do. For a long time we implicitly or explicitly assumed oscillations are ongoing which has colored experiments and analyses. Now we see a first wave of studies based on this new thinking, with new hypothesis and ways to analyze data, and it should only pick up in years to come.”
The authors acknowledge another major issue that must be resolved by further research—How do beta bursts emerge in the first place to perform their apparent role in cognitive control?
“It is unknown how beta bursts arise as a mediator of an executive command that cascades to other regions of the brain,” the authors write.
The authors don’t claim to have all the answers. Instead, they write, because beta rhythms appear to have an integral role in controlling cognition, the as yet unanswered questions are worth asking.
“We propose that beta bursts provide both experimental and computational studies with a window through which to explore the real-time organization and execution of cognitive functions,” they conclude. “To fully leverage this potential there is a need to address the outstanding questions with new experimental paradigms, analytical methods and modeling approaches.”
Related Articles
Paper: to understand cognition—and its dysfunction—neuroscientists must learn its rhythms.

Study reveals a universal pattern of brain wave frequencies
Anesthesia blocks sensation by cutting off communication within the cortex

Anesthesia technology precisely controls unconsciousness in animal tests

- See us on facebook
- See us on twitter
- See us on youtube
- See us on linkedin
- See us on instagram
Brain organoids and assembloids are new models for elucidating, treating neurodevelopmental disorders
Stanford Medicine research on Timothy syndrome — which predisposes newborns to autism and epilepsy — may extend well beyond the rare genetic disorder to schizophrenia and other conditions.
April 24, 2024 - By Bruce Goldman, Erin Digitale

In this 2019 photo, Timothy syndrome patient Holden Hulet, left, rides in a side-by-side ATV driven by his dad, Kelby Hulet, at sand dunes near their home in southern Utah. Courtesy of the Hulet family
For a long time, no one understood that Holden Hulet was having seizures.
“He would just say ‘I feel tingly, and my vision kind of goes blurry,’” said Holden’s mom, JJ Hulet. “But he couldn’t communicate exactly what was going on.”
JJ and Kelby Hulet could see their son was having short spells of incoherent speech, rapid back-and-forth eye movements and odd physical changes. “He’d kind of go — I don’t want to say ‘limp’ because he would stand just fine — but his body would just be in zombie mode,” JJ said. The episodes lasted less than a minute.
The parents were puzzled and worried, as they had been many times since Holden was born in 2008 and they learned that their newborn had an extremely rare genetic disease. “I was thinking it was his heart,” Kelby Hulet, Holden’s dad, said.
Holden’s condition, Timothy syndrome, causes long, irregular gaps in heart rhythm. He spent his first six months hospitalized in a neonatal intensive care unit in his family’s home state of Utah while he grew big enough to receive an implantable cardioverter defibrillator. The device sends an electrical signal to restart his heart when it pauses for too long.
As a small child, Holden would sometimes pass out before the defibrillator shocked his heart back into action. When Holden started telling his parents about the blurry-vision episodes at age 6, Kelby initially believed it was a new version of the same problem, and he kept a time stamp on his phone for each episode. But the records from Holden’s defibrillator showed that these times did not line up with any heart-rhythm problems.
The family’s pediatrician was confused, too. Perhaps Holden was having periods of low blood sugar, another possible Timothy syndrome complication, he suggested. Initial testing at the local medical center did not turn up clear answers.
But Kelby, who was training to become an operating room nurse, realized Holden’s episodes reminded him of what he was learning about warning signs for stroke. JJ called Holden’s cardiologist in Utah and asked for a detailed neurologic evaluation, which enabled the mysterious episodes to be diagnosed as seizures. Holden began taking anti-seizure medication, which helped, to his parents’ great relief.
Researching a rare disease
A few months after Holden was born, Sergiu Pasca , MD, arrived at Stanford Medicine to pursue a postdoctoral fellowship in the lab of Ricardo Dolmetsch, PhD, then an assistant professor of neurobiology, who was redirecting his research to autism spectrum disorder. At the time, Pasca did not know the Hulet family. But his work soon became focused on the disorder that has shaped Holden’s life.
Caused by a defective gene on the 12th chromosome, Timothy syndrome is vanishingly rare, with no more than 70 diagnosed cases. Children with this disorder rarely survive to late adolescence. It is caused by a mutation in the gene coding for a type of calcium channel — a protein containing a pore that selectively opens or closes, respectively permitting or blocking the flow of calcium across cells’ membranes. While a prominent feature — severe heart malfunction — can be tackled with a pacemaker, most children with Timothy syndrome will end up with lifelong brain disorders including autism, epilepsy and schizophrenia.
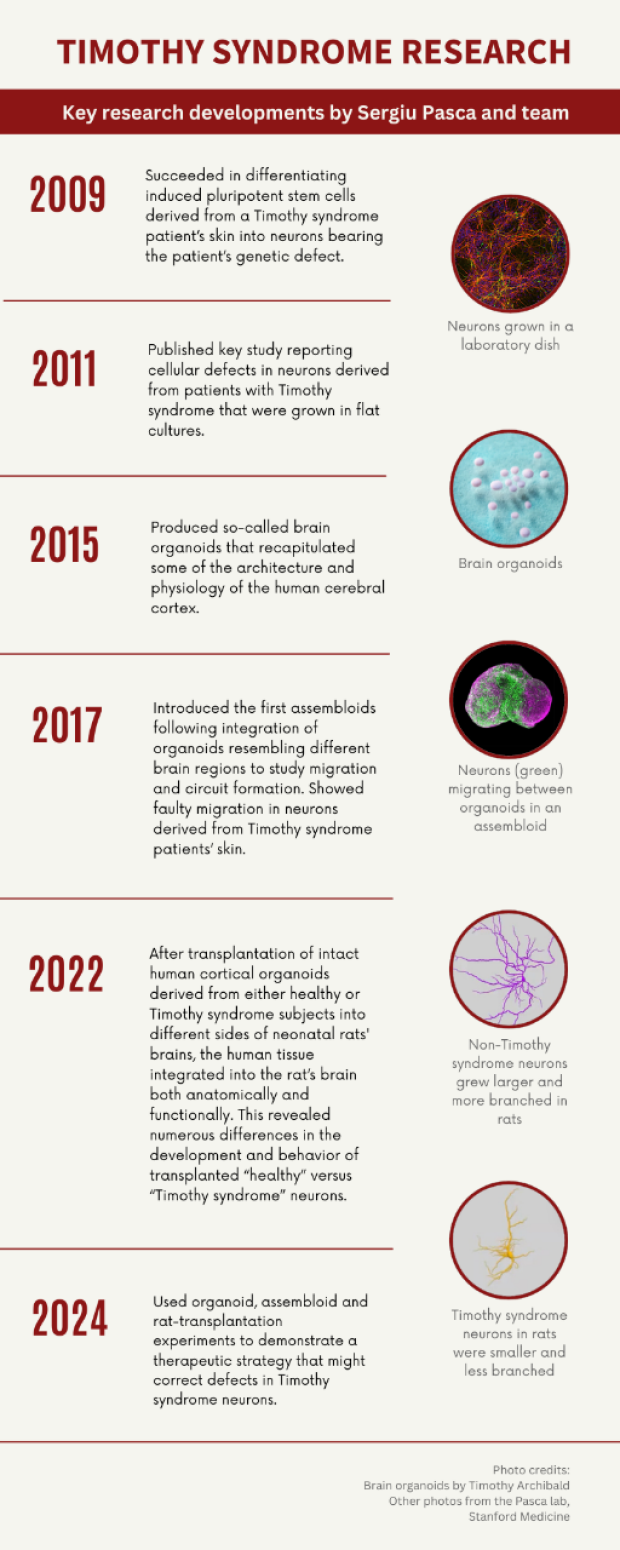
By mid-2009, Pasca had succeeded in generating nerve cells from induced pluripotent stem cells (which can be induced to form virtually any of the body’s numerous cell types). These included cells derived from the skin of two patients with Timothy syndrome. Later that year he observed defects in how the patient-derived neurons were handling calcium. This advance — the creation of one of the initial in-a-dish models of brain disease, built from neurons with defects that precisely mirrored those of a patient’s brain — was published in Nature Medicine in 2011.
Pasca and colleagues continued to monitor these Timothy-syndrome neurons in standard two-dimensional culture — growing as single layers in petri dishes — over the next few years. While this two-dimensional culture method was limited in its ability to sustain viable neurons, it was soon superseded by a genuine scientific breakthrough.
Pioneering the first assembloids
The constraints of two-dimensional culture, including the inability to keep these neurons for long periods of time so that they could reach key stages of neural development, prompted Pasca in 2011 to start developing an unprecedented three-dimensional method. The novel technology produced what came to be known as brain organoids. These constructs recapitulated some of the architecture and physiology of the human cerebral cortex. The organoids can survive for several years in culture, enabling neuroscientists to view, non-invasively, the developing human brain up close and in real time. The scientists wrote a seminal Nature Methods paper , published in 2015, that described their discovery.
Pasca’s group subsequently showed that culturing brain organoids in different ways could generate organoids representing different brain regions (in this case, the cerebral cortex and a fetal structure called the subpallium). In a breakthrough set of experiments, Pasca’s team found ways to bring these organoids into contact so that they fuse and forge complex neuronal connections mimicking those that arise during natural fetal and neonatal development. Pasca named such constructs assembloids.
In their paper on the research, which was published in Nature in 2017, Pasca’s team showed that after fusion, a class of inhibitory neurons originating in the subpallium migrates to the cortex, proceeding in discrete, stuttering jumps. (See animation .) These migrating neurons, called interneurons, upon reaching their destinations — excitatory neurons of the cortex — form complex circuits with those cortical neurons.
But in assembloids derived from Timothy syndrome patients, the motion of interneurons as they migrate from the subpallium is impaired — they jump forward more often, but each jump is considerably shorter, so they fail to integrate into the appropriate circuitry in the cortex. This wreaks havoc with signaling in cortical circuits. Pasca’s team tied this aberrant neuronal behavior on the part of Timothy syndrome neurons to the key molecular consequence of the genetic defect responsible for the condition: namely, malfunction of the critical channels through which calcium must pass to cross neurons’ outer membranes.
A family’s struggles
While Pasca was developing assembloids, the Hulet family was progressing through their own journey of discovery with Holden. They faced painful uncertainty at every stage, starting when Holden was discharged from the NICU in the summer of 2009, after several months of hospitalization and multiple heart surgeries.
“Even when we brought him home, [his doctors] said ‘Don’t get your hopes up. We don’t usually see them make it past age 2,” JJ recalled. Many children with Timothy syndrome die from cardiac failure in early life.
“It’s really hard to be positive in that kind of situation, and for a long time I did let it get to me,” JJ said. “I finally got to a point where I said, ‘I have to live my life and we just keep fighting.’”
JJ runs a child care center and has years of experience working with special-needs kids, which motivated her to push for an autism evaluation when she saw signs of autism in Holden. He’s much more verbal than many children with autism, which paradoxically made it more difficult to get an official diagnosis.
“That was frustrating,” JJ said. Although the family’s pediatric cardiologist in Salt Lake City was familiar with the vagaries of Timothy syndrome, their local caregivers in the small town where they live in southern Utah were not. “They kept saying ‘Oh, no, it’s just developmental delays because he was so premature,’” she said. She wonders whether it would have been easier to have Holden’s autism diagnosed had more been known about Timothy syndrome at the time.
“I think research is important so that parents and children have the support they need,” she said, noting how lonely and painful it can be to advocate for a child when his condition is poorly understood — and when, as a parent, you may be doubted by medical professionals. “It’s a really hard thing to deal with.”
Her voice breaks briefly. She continues, “I think research brings validity to that.”

Sergiu Pasca
Implanting organoids
In 2022, Pasca published a study in Nature describing the transplantation of human cortical organoids into neonatal rats’ brains, which resulted in the integration of human neurons along with supporting brain cells into the brain tissue of rats to form hybridized working circuits. The implanted human organoids survived, thrived and grew. Individual neurons from the human organoids integrated into young rats’ brains were at least six times as big as those — generated the same way, at the same time — that remained in a dish. The transplanted neurons also exhibited much more sophisticated branching patterns. Pasca and his colleagues observed marked differences in the electrical activity of, on one hand, human neurons generated from a Timothy syndrome patient, cultured as organoids and transplanted into one side of a rat’s brain, and, on the other hand, those generated from a healthy individual and transplanted, as an organoid, into the corresponding spot on the other side of the same rat’s brain. The Timothy syndrome neurons were also much smaller and were deficient in sprouting branching, brush-like extensions called dendrites, which act as antennae for input from nearby neurons.
“We’ve learned a lot about Timothy syndrome by studying organoids and assembloids kept in a dish,” Pasca said. “But only with transplantation were we able to convincingly see these neuronal-activity-related differences.”
That same year, the FDA Modernization Act 2.0 was signed into law, exempting certain categories of new drug-development protocols from previously mandated animal testing. The act was predicated on the understanding that recent advancements in science offer increasingly viable alternatives to animal testing, so the findings based on the organoid- and assembloid-culture technologies may be adequate to justify clinical trials in some neurodevelopmental conditions.
Most recently, in a Nature paper published April 24, Pasca and his colleagues demonstrated, in principle, the ability of antisense oligonucleotides (ASOs) to correct the fundamental defects that lead to Timothy syndrome by nudging calcium-channel production toward another form of the gene that does not carry the disease-causing mutation. Using ASOs to guide production of the functional rather than defective form of this channel reversed the defect’s detrimental downstream effects: Interneuronal migration proceeded similarly to that procedure in healthy brains, and the altered electrical properties of the calcium channel reverted to normalcy. This therapeutic correction was demonstrated in a lab dish — and, critically, in rat-transplantation experiments, suggesting that this therapeutic approach can work in a living organism.
Pasca is now actively searching the globe for carriers of the genetic defect, in preparation for the pursuit of a clinical trial at Stanford Medicine to test the safety and therapeutic potential of ASOs in mitigating the pathological features of Timothy syndrome.
“We are also actively engaged in conversations with other scientists, clinicians in the field and ethicists about the best way to move forward and safely bring this therapeutic approach into the clinic,” he said.
Pasca added that the calcium channel that is mutated in Timothy syndrome is, in fact, “the hub” of several neuropsychiatric diseases including schizophrenia and bipolar disorder. So it may be that the lessons learned — and the therapies derived — from his 15-year focus on a rare disease may have broad application in a number of widespread and troubling psychiatric conditions.
‘Amazing’ teenager
Today, in defiance of his doctors’ warning that he might not live past age 2, Holden Hulet is 15 years old and doing well.
“I think a lot of times, autism is perceived as ‘They’re not neurotypical and they’re not capable of certain things.’ But he is brilliant,” JJ said. “He’s amazing with techie stuff or Legos. He’s funny and super honest and very self-aware.”
Kelby often takes Holden to visit the farm where he grew up. Holden loves to ride the farm equipment and enjoys hanging out with the animals, especially the farm dogs and calves. Like a lot of kids, he keeps an eye out for good rocks, Kelby said with a chuckle.
“He’s always either throwing them or collecting them,” JJ said. “That’s something I really like about him: He’s always got a pocket full of something.”
Although navigating a rare disease is one of the most challenging things they have faced, the Hulets see light in their situation, and would offer encouragement to any family facing a new Timothy syndrome diagnosis.
“There is hope,” JJ said. “There are people out there who care, people out there who fight for you who don’t even know you. I think that’s what is so important about research — that you’re fighting a battle for people you don’t even know.”
The study published April 24 was supported by the National Institute of Mental Health (grants R01 MH115012 and K99 MH119319P), the Wu Tsai Neuroscience Institute, the Autism Speaks Postdoctoral Fellowship, the Kwan Funds, the Senkut Funds, the Coates Foundation, the Ludwig Family Foundation, the Alfred E. Mann Foundation, and the Stanford Maternal and Child Health Research Institute Postdoctoral Fellowship.

About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu .
Artificial intelligence
Exploring ways AI is applied to health care

Research method finds new use in diagnosis of genetic disorders
- How the hand muscles have evolved
- Patient’s leg saved by Baylor Medicine surgeon
- Understanding the neural dynamics of emotional processing in treatment-resistant depression
- Prevent trouble with your tattoo

Researchers at Baylor College of Medicine have tested the feasibility of using human cell transdifferentiation with RNA sequencing to facilitate diagnoses of Mendelian disorders. The approach generated an overall diagnostic yield of 25.4% in a cohort of Undiagnosed Diseases Network cases. The findings are published in the American Journal of Human Genetics .
RNA sequencing, which reads the transcriptome or gene expression in a cell, is often needed to support a genetic diagnosis obtained through exome sequencing or whole genome sequencing. However, the effectiveness of RNA sequencing is limited by expression of disease-associated genes in clinically accessible tissues like blood or skin fibroblasts, cells that contribute to the formation of connective tissue.

“This is especially problematic in neurological diseases because the gene causing the disorder may not be expressed in blood and skin cells,” said corresponding author Dr. Pengfei Liu , associate professor of molecular and human genetics and director of the ACGME-accredited Laboratory Genetics and Genomics Fellowship Program at Baylor.
Research method helps overcome obstacles to genetic diagnoses
To overcome this challenge, researchers led by first author Dr. Shenglan Li , staff scientist in Liu’s lab at Baylor, converted fibroblasts obtained in skin biopsies to neurons in a process called transdifferentiation. “This method activates neuron-specific gene expression and increases the probability that we can accurately characterize disease-causing mutations in these cells,” Li said.
For clinical validation, researchers generated these induced neurons for a cohort of 71 individuals with neurological characteristics in the Undiagnosed Diseases Network. RNA sequencing of the induced neurons led to a diagnosis in 18 individuals (25.4%); five of those cases could not have been diagnosed with RNA sequencing of fibroblasts alone.
This study shows that fibroblast-to-neuron transdifferentiation followed by RNA sequencing is a simple, low-cost and reproducible approach with a reasonable turnaround time, making it feasible for clinical implementation,” Liu said. “This new testing method represents a paradigm shift in laboratory genetics, moving from the traditional DNA-centric approach to one that focuses on the patient’s cells.”
“It’s exciting to apply this well-established technique, which previously has been used to study mechanisms of neurodegenerative diseases, for a new use in genetic diagnostics,” Li said.
Other authors of this work include Sen Zhao, Jefferson C. Sinson, Aleksandar Bajic, Jill A. Rosenfeld, Matthew B. Neeley, Mezthly Pena, Kim C. Worley, Lindsay C. Burrage, Monika Weisz-Hubshman, Shamika Ketkar, William J. Craigen, Gary D. Clark, Seema Lalani, Carlos A. Bacino, Keren Machol, Hsiao-Tuan Chao, Lorraine Potocki, Lisa Emrick, Jennifer Sheppard, My T.T. Nguyen, Anahita Khoramnia, Paula Patricia Hernandez, Sandesh C. S. Nagamani, Zhandong Liu, Christine M. Eng and Brendan Lee. They are affiliated with one or more of the following institutions: Baylor College of Medicine, Jan and Dan Duncan Neurological Research Institute at Texas Children’s Hospital, Texas Children’s Hospital, McNair Medical Institute at the Robert and Janice McNair Foundation and Baylor Genetics.
The research was supported by the National Institutes of Health Common Fund (U01HG007709 and U01HG007942), the National Human Genome Research Institute (R35HG011311) and the BCM Intellectual and Developmental Disabilities Research Center funded by the Eunice Kennedy Shriver National Institute of Child Health & Human Development (P50HD103555). For a full list of funding sources, see the publication .
By Molly Chiu
Follow From the Labs on X @BCMFromtheLabs and Instagram !
Receive From the Labs via email
Enter your email address to subscribe to this blog and receive notifications of new posts by email.
Email Address
Share this:
- Click to share on Facebook (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to email a link to a friend (Opens in new window)
You May Also Like

In memoriam of genetics pioneer Dr. C. Thomas Caskey

Sorting out what drives Huntington’s disease

Thinking outside the box to fight back neurodegeneration
Leave a reply cancel reply.
Your email address will not be published. Required fields are marked *
Notify me of follow-up comments by email.
Notify me of new posts by email.
Ozempic Hurts the Fight Against Eating Disorders
I t’s impossible to escape the soaring popularity of Ozempic and similar drugs these days—daily headlines, celebrity “success” stories, and apparent ease in procuring prescriptions (even Costco sells them now) abound. But the cumulative effect of all of this has many experts in the eating disorder field worried about how this might affect their patients. This makes sense—even for those without eating disorders, these drugs can feel both triggering and enticing. After all, research tells us about 90% of women are dissatisfied with their bodies. This sounds like a quick fix.
Then, I started hearing reports—first anecdotal, then published —that some doctors were prescribing weight loss drugs like Ozempic to their patients with eating disorders. As in, to help treat them.
As a journalist who has extensively researched the harms of eating disorders and the barriers to recovery—and as a woman who had suffered from eating disorders on and off for much of my own life—I thought I must have misunderstood. Yes, we as a society are in the midst of Ozempic Fever—and by “fever,” I’m referring to excitement, rather than a possible side effect of the drug (which it is). Researchers are continuing to find new potential applications for these drugs, initially developed to treat type 2 diabetes. In March, the FDA approved a new indication for the weight-loss drug Wegovy (which has the same active ingredient as Ozempic), allowing it to be used as a treatment to reduce the risk for heart attack and stroke. Ozempic, a diabetes drug, used off-label for weight loss, is also being studied to treat anxiety and depression , polycystic ovary syndrome, substance abuse, Alzheimer’s , and now—eating disorders.
Read More: Ozempic Exposed the Cracks in the Body Positivity Movement
It’s early days and research hasn’t yet caught up with the enthusiasm. But our cultural misunderstanding of eating disorders, even by well-meaning practitioners, could exacerbate the illnesses for those who suffer from them—and have dire consequences.
The new class of weight loss drugs mimics the body’s GLP-1 hormone , stimulating insulin production, and lowering blood sugar levels, helpful to those with type 2 diabetes. The drugs also curb appetite and slow the speed that food moves into the small intestine—you feel full more quickly and eat less. Many patients without eating disorders who take these drugs, have reported a reduction of “food noise” in their minds—referring to obsessive thoughts and preoccupation with food. (Though, as philosopher Kate Manne wisely posited in a recent New York Times piece , isn’t “food noise,” simply, hunger?)
For folks suffering from binge eating disorder (BED) or bulimia nervosa (BN), a drug that decreases appetite may seem to make sense. Both illnesses are characterized by eating large amounts of food, eating until uncomfortably full, and feeling distress around that (bulimia is distinguished by purging after a binge).
Binge eating often emerges as part of a cycle of restriction—dieting, fasting, or eliminating entire food groups—like carbs, for example. “Many people struggling with BED view the binge episodes as the problem and the restriction as something to strive for,” said Alexis Conason, a psychologist specializing in the treatment of binge eating disorder. “When people with BED take a GLP-1 medication that dampens their appetite, many are excited that they can be ‘better’ at restriction and consume very little throughout the day.” Subsequently, Conason adds, there is a dangerous potential for BED to then morph into anorexia, starving oneself with possibly life-threatening complications.
Eating disorders are complex illnesses that aren’t yet fully understood, even by experts in the field. Underneath the behaviors around food is often an intricate web of trauma, anxiety, and even genetic predisposition, all set against the backdrop of a culture that prizes thinness . Low weight is frequently (incorrectly) conflated with good health, and people in larger bodies are often subjected to bullying, negative stereotypes, and discrimination in the workplace .
Read More: Ozempic Gets the Oprah Treatment in a New TV Special
Emerging research strongly supports that for many, eating disorders are brain-based illnesses and in most cases, there exists a co-morbidity like anxiety, mood disorders, or substance abuse.
“GLP-1’s can’t help someone deal with their stress, anxiety, [and] trauma-history,” said psychologist Cynthia Bulik, one of the world’s leading eating disorder researchers, and Founding Director of the University of North Carolina Center of Excellence of Eating Disorders. “All of that background distress—fundamental distress that might be driving the BED in the first place—is temporarily bypassed by removing the desire to eat.”
Nearly 30 million Americans will have an eating disorder in their lifetime, but only about 6% of those are medically diagnosed as “underweight,” according to the National Association of Anorexia Nervosa and Associated Disorders. This means that a person may exhibit all of the diagnostic hallmarks of anorexia, for example, extreme restriction and even malnourishment, but still present as average weight or even overweight. They may even be told by a physician to lose weight, despite the fact that they are already going to dangerous extremes to chase that “goal.”
“We tend to think that everyone in a larger body with an eating disorder must have BED and everyone in a smaller body must have anorexia, but this couldn’t be further from the truth,” said Conason. “So many people with BED seek help in weight loss settings instead of seeking eating disorder treatment; many view the problem as their weight and think they need more help sticking to their diet” when in reality, an end to the restriction would more likely regulate their eating.
It’s much easier to get weight loss treatment than help for an eating disorder. There is no standard of care for eating disorders in this country and treatment is unregulated. While there are some promising, evidenced-based treatments (cognitive behavioral therapy for adults, and family-based treatment for children and teens), they don’t work for everyone. If a person is fortunate to be diagnosed and receive adequate treatment, relapses are common and full recovery can be elusive.
Further, these drugs are often intended to be taken for a person’s entire life. “When they go off the drug, or can’t access it due to supply problems, the urge to binge comes right back and they have not developed any psychological (or) behavioral skills to manage the urge,” Bulik told me. Just like with a diet, any lost weight will likely be regained when a person stops taking the drugs. Weight fluctuations, themselves ,may increase a person’s risk of chronic illnesses like type 2 diabetes, according to multiple studies.
“The focus on weight and erasing the desire to eat could indeed do harm,” cautioned Bulik. “The potential for abuse is high and will become higher with new preparations that don’t require an injection … Remember, these drugs are ‘for life.’ Stop them, and everything comes rushing back.”
The long-term side effects of GLP-1’s are not yet known. But the harms of eating disorders are: eating disorders have one of the highest mortality rates of any mental illness (second only to opioid overdose). People with eating disorders are more likely to attempt suicide, and during COVID-19, emergency room visits and inpatient admissions for eating disorders at pediatric hospitals skyrocketed, particularly for young women. According to the CDC, emergency room visits for 12-17 year old girls who suffer from eating disorders doubled during the pandemic. Those numbers, as shown by recent studies , have not returned to pre-pandemic levels.
An even greater concern is that the gaps in comprehensive care for eating disorders invite experimental, potentially harmful treatments and leave patients vulnerable. GLP-1’s may seem like a short-term “fix,” but they won’t graze the deeper issues nor will they diminish the eating disorder crisis in this country. And it is a crisis—every year, eating disorders cost the U.S. more than $65 billion .
I know too well that if a doctor advises their patient with an eating disorder “here’s something to make you eat less” most patients would happily oblige. That’s part of the pathology of the illness. It’s the eating disorder talking. Ideally, it wouldn’t be your doctor’s voice, too.
More Must-Reads From TIME
- The 100 Most Influential People of 2024
- Coco Gauff Is Playing for Herself Now
- Scenes From Pro-Palestinian Encampments Across U.S. Universities
- 6 Compliments That Land Every Time
- If You're Dating Right Now , You're Brave: Column
- The AI That Could Heal a Divided Internet
- Fallout Is a Brilliant Model for the Future of Video Game Adaptations
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at [email protected]

April 22, 2024
Substance use disorders are underdiagnosed and undertreated among formerly incarcerated Virginians, new VCU-led study finds
Research collaboration with the virginia department of medical assistance services highlights health disparities affecting medicaid members with addiction – and some of the barriers they face., share this story.
- Share on Twitter
- Share on Facebook
- Share on LinkedIn
By Olivia Trani
People recently released from prison experience some of the highest rates of substance use disorder, but they are also the least likely to have access to providers who can diagnose and treat their addiction. New research led by Virginia Commonwealth University’s School of Population Health is shedding light on the magnitude of these health disparities in Virginia and what policies might help people receive lifesaving care.
National estimates suggest as many as 85% of people who are incarcerated have substance use disorders. While most of these adults are eligible for Medicaid services after their release, the VCU-led study found that only 17% of formerly incarcerated Medicaid members were diagnosed with substance use disorders in Virginia. Even fewer received medications as treatment for their addiction.
“We know that substance use disorders are prevalent health issues among incarcerated populations, but this research shows that many people aren’t getting the medical attention they need as they transition back to their communities,” said Peter Cunningham , Ph.D., who led the new research and is interim chair of the Department of Health Policy at VCU’s School of Population Health. Other contributors to the report include Sarah Marks and Hannah Shadowen – both M.D.-Ph.D. students at VCU’s School of Population Health – as well as Peyton Bernstein, a master’s student at the College of William & Mary.
The study is part of a collaboration between VCU and the Virginia Department of Medical Assistance Services to better understand health disparities impacting Medicaid members with opioid and other substance use disorders. Using data from both DMAS and the Virginia Department of Corrections, the researchers measured the number of people being diagnosed and treated for a substance use disorder following their release from prison.
According to the VCU research team’s analysis, 4,652 adults were released from county jails and state prisons in 2022, with 85% enrolling in Medicaid within one month of release. Among those enrolled in Medicaid, only 17% had seen health care providers and were diagnosed with a substance use disorder within three months, including 13% with an opioid use disorder.
Of those who were formerly incarcerated and diagnosed with an opioid use disorder, only about 25% went on to receive medications to treat their addiction. By comparison, 78% of all Medicaid members diagnosed with an opioid use disorder in Virginia received medications.
“The good news is that we see a high number of individuals enrolling in Medicaid soon after they are released from prison, and that is in large part due to the state expanding Medicaid coverage in 2019,” Cunningham said. “However, based on national statistics, we expected more people to receive a diagnosis and treatment for opioid addiction. This is concerning because having an undiagnosed, untreated opioid use disorder greatly increases the risk of overdose.”
The researchers noted that a number of barriers might be contributing to these gaps in addiction treatment, such as the instability many formerly incarcerated adults experience after their release, as well as limitations in access to Medicaid services set by federal policies.
While the vast majority of individuals in the criminal justice system qualify for Medicaid, only emergency hospital services are covered as they serve their sentence. Most other benefits – including treatments for substance use disorders – are prohibited by federal law until after a person is released from prison.
“The first few months after a person is released from incarceration is a particularly vulnerable time. They often have to figure out all aspects of their life at the same time,” said Shadowen. “Many people don’t have a stable residence, mailing address or phone number, which makes it difficult for the Medicaid agency to contact them for health services.”
“It can also take some time for a person to be registered as eligible for Medicaid and schedule an appointment with a provider,” added Marks. “Even having the required photo identification and Medicaid card to visit a doctor’s office is going to be much harder to do during this period of tremendous instability.”
Increasing access to treatment prior to release can help to facilitate transitions to the community and ensure continuity of treatment following release from incarceration, Cunningham explained. “If providers are able to diagnose substance use disorders and initiate treatment plans before a person is released from prison, this might reduce the risk of overdoses and improve health outcomes when they return to their community.”
Looking ahead, the researchers are surveying formerly incarcerated Medicaid members to pinpoint some of the barriers they experience when seeking addiction treatment after prison.
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.
Related stories

Medicaid beneficiaries report less financial stress following enrollment, VCU study finds

Report: Virginia has significantly expanded access to addiction treatment services through Medicaid

Study: Opioid treatment for pregnant women has increased but racial inequities exist
Most popular

April 16, 2024
A new home for creativity and collaboration at VCU

April 15, 2024
Richmonders, cast a ballot in a special election this month – and you can wear the winner this fall

April 17, 2024
Class of 2024: Deja Cooke returned to college to pursue a dream of a career in criminal justice

Class of 2024: Hope Ollivant found artistic expression in many forms
Latest headlines

April 25, 2024
Class of 2024: Lasting friendships put Angela-Marie Rone on a path to social work

VCU students and alums deliver the entrepreneurial pitch at Demo Day

Capital News Service and VCU InSight, two powerful proving grounds for journalism students, reach notable milestones
April 24, 2024
Class of 2024: Mohammed AlAwadh delves into the intricacies of drug development
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.12(7); 2022

Original research
University students’ understanding and opinions of eating disorders: a qualitative study, millie manning.
1 College of Medical and Dental Sciences, University of Birmingham, Birmingham, UK
Sheila Greenfield
2 Institute of Applied Health Research, College of Medical and Dental Sciences, University of Birmingham, Birmingham, UK
Associated Data
bmjopen-2021-056391supp001.pdf
Data are available upon reasonable request. All requests for data should be made to the corresponding author.
Eating disorders (EDs) affect 1.25 million people in the UK. Evidence suggests the public display stigma and poor mental health literacy (MHL) towards EDs. There is a high prevalence of EDs in university populations, so it is important to determine the MHL of this at-risk group. Qualitative research exploring the MHL of this population is incomplete.
Explore university students’ beliefs and opinions of EDs, their knowledge of symptoms, treatment and help sources and how these are influenced by biological sex.
A qualitative study, using semistructured interviews analysed using inductive thematic analysis.
The University of Birmingham.
Participants
Seven female and seven male University of Birmingham students.
Analysis revealed six themes, each with subthemes: ED characteristics, causes, body image, seeking help, stigma and awareness. Students displayed poor awareness towards ED signs and symptoms, causes and help sources. Students were not stigmatising towards EDs, but many perceived them as a female problem and believed society to be stigmatising. Many referenced informal sources of information such as social media and expressed a desire for ED teaching. Sex did not have a significant influence on knowledge or opinions of EDs in this study; however, there were some differences, for example, some males were more likely to see EDs as a weakness and to perceive themselves as having low levels of knowledge.
Conclusions
University students show broad awareness of EDs; however, knowledge of certain aspects of ED-MHL including help sources and symptom recognition was lacking. Although students were not stigmatising of EDs themselves, many perceived high levels of public stigma. This, alongside poor knowledge, may delay help-seeking. Campaigns educating students and the public about EDs would aid earlier diagnosis, improving long-term outcomes. Further research into awareness and knowledge in other populations would be beneficial.
Strengths and limitations of this study
- First qualitative exploration of knowledge and understanding of eating disorders (EDs) in UK university students.
- Qualitative methodology allowed broad exploration and insight about perceptions of EDs in this at-risk population.
- Member validation and analyst triangulation with an experienced qualitative researcher strengthen the methodology.
- Some participants may have been hesitant to disclose their true views due to social desirability bias.
- Study was advertised as research about EDs, so participants could have volunteered because they have an interest and therefore more knowledge about EDs.
Introduction
Eating disorders (EDs) are a class of severe mental illnesses 1 that affect 1.25 million people in the UK. 2 They are characterised by abnormal eating behaviours and attitudes that have a significant impact on the physical health of those suffering, 3 resulting in complications including osteoporosis and cardiac arrhythmias. 4 These go hand in hand with psychiatric comorbidities, such as depression. 5 For these reasons, one ED subtype, anorexia nervosa (AN), has the highest mortality rate of any psychiatric condition. 6
Notwithstanding the significant mortality and morbidity associated with EDs, statistics show it takes individuals an average of 91 weeks to realise they have an ED, on top of the 58 weeks they typically wait before presenting to their doctor. 7 Recent data suggest a shorter duration of untreated ED is associated with increased likelihood of remission. 8 However, fewer than 20% of individuals who screen positive for an ED go on to receive treatment, 9 10 highlighting a significant treatment gap and leaving individuals vulnerable to suffering debilitating long-term outcomes.
This delay in health-seeking is postulated to be due, in part, to poor mental health literacy (MHL) and the fear of stigma attached to EDs. 11 MHL refers to an individual’s ‘knowledge and beliefs about mental disorders that aid the recognition, management or prevention of these disorders’. 12 Studies show members of the public attribute EDs to personal shortcomings and perceive ED sufferers as vain and self-obsessed. 13 14 This can result in high levels of self-stigma, whereby an ED sufferer turns public stigma towards themselves, 15 lowering self-worth and self-efficacy and further delaying help-seeking. 16
The ability to recognise ED behaviours has been shown to be a significant factor in improving early intervention and help-seeking. 17 Furthermore, an ED sufferer’s social network has been shown to be fundamental in improving ED identification and encouraging treatment-seeking. 18
However, research indicates the public display poor MHL towards various mental illnesses, 19 including EDs, 20 21 suggesting the ability of the public to recognise an ED in themselves or in others is suboptimal. In addition, ED-MHL appears less systematically investigated than MHL relating to other mental illnesses, and therefore research in this area lacks the ability to inform relevant health promotion and early intervention programmes that seek to reduce the burden of these conditions. 22 23
In the UK, the highest incidence of EDs occurs in girls between 15 and 19 years of age, 24 with symptom duration often lasting 5–8 years. 2 Unsurprisingly, there is a high prevalence of EDs in university populations, 25 where normalisation of ED behaviours such as restrictive dietary intake and overexercising alongside a loss of external accountability can exacerbate symptoms and lead to the development of new, unhealthy food behaviours. 26 Furthermore, in a survey of UK university students by the ED charity Beat, 32% of students with an ED were diagnosed at university; however, 69% reported difficulties accessing treatment. 27
The literature suggests that men constitute at least 25% of UK ED cases. 28 However, research indicates the public expectation that EDs are primarily a female issue limits young men’s ability to recognise their symptoms and delays them from seeking appropriate help. 29 30 Sex bias is also indicated, with studies indicating that men hold more negative attitudes towards EDs 31 32 and have generally poorer MHL than females. 20
The majority of previous studies into ED-MHL have been quantitative, and have taken place outside of the UK, where different cultural norms, health systems and mental health education may mean results are not necessarily transferrable to the UK. 33 Although useful for determining the general scope of ED knowledge and associated stigma, the pre-prepared questions in such studies do not allow for volunteering of further opinions not expressed in the questionnaires. Additionally, it does not allow in-depth exploration of individual beliefs and attitudes.
Therefore, there is a need for extensive qualitative research to be carried out in this area. Yet, the existing UK qualitative literature into ED-MHL is lacking, only seeking responses from females, 34 meaning difference in responses between males and females cannot be inferred. Some qualitative literature exists from other countries, but this literature is also incomplete, focussing only on ED causes, 21 or solely on AN. 35 Furthermore, none of these studies concentrated on at-risk populations such as university students.
Research focused on university students, to determine if differences in understanding and opinions of EDs exist between these at-risk young males and females can give an insight into the ED-MHL of this population, identifying areas where greater education is needed to improve help-seeking and reduce stigma. This paper reports on a qualitative interview study, which aimed to determine university students’ ED-MHL, exploring beliefs and opinions of EDs and their knowledge of ED symptoms, treatment and sources of help. It also sought to determine the impact of sex on ED perceptions and knowledge.
Materials and methods
Participants were recruited from a convenience sample of English-speaking University of Birmingham students, 36 chosen purposively to ensure equal numbers of male and female participants were recruited. 37 To investigate lay perceptions of EDs, students with a previous formal diagnosis of an ED were excluded, alongside students studying a healthcare degree or psychology, as they were assumed to have greater ED knowledge than other university students. 38 To focus on UK perceptions, international students and international exchange students were also excluded.
Recruitment
Participants were recruited via advertisements placed around the university campus and posted on a University of Birmingham Facebook group. 39
Participants who responded were emailed a participant information sheet and eligibility questionnaire to enable purposive sampling based on sex, and ensure any non-eligible individuals were excluded, for example, those who had previously been diagnosed with an ED. 37
Participant recruitment continued until data saturation was reached ( figure 1 ).

Participant recruitment process. Individuals who responded contacted the researcher to enquire about the study. Non-responders either did not return the eligibility questionnaire or did not confirm interest in the study. Five participants were not required as data saturation was reached.
Data collection
Data were collected using face to face, semi-structured, audio-recorded interviews. 40 These took place in a private room in the University of Birmingham library during January and February 2020. No repeat interviews were undertaken. Written, informed consent was obtained from each participant prior to their interview.
All interviews were carried out by MM, a female, white British medical student intercalating in psychological medicine. Interview duration ranged between 20 and 37 min, with a mean of 28 min. The researcher did not know any participant prior to study initiation, and all were aware of the interviewer’s demographics as outlined in the participant information sheet, prior to their interview. On interview completion, each participant received a £15 Amazon voucher to thank them for their time.
An interview guide ( online supplemental file 1 ) of open-ended questions informed by the relevant literature 34 41 42 was used to explore key areas of MHL, 43 including knowledge of ED symptoms, causes, characteristics, treatments and recovery, and personal help-seeking behaviours (see online supplemental file 1 for specific questions relating to these areas). These topics were chosen to reflect a broad overview of ED-MHL, to ensure participants were able to share their full knowledge and perceptions they have of EDs, ensuring the research question was answered. The interview guide ensured consistency across interviews and was piloted on participants known to the researcher who met the eligibility criteria to ensure questions were accessible to participants. Pilot data were not included in the study.
Supplementary data
Data analysis.
Following each interview, field notes were taken to contextualise interviews and reflect on the researcher’s impact on the interviews. 44 Interviews were transcribed verbatim by MM and listened to twice to ensure transcript accuracy. To establish participant anonymity and confidentiality, each was allocated a numerical ID used for data collection and analysis.
Data were thematically analysed using Braun and Clarke’s six-step process, 45 as it allows rich interpretation of data. An inductive approach was taken, therefore analysis was data driven, rather than theory driven. 46 Transcripts were read twice to ensure familiarisation. Open coding was then performed manually, and codes inputted into the software NVivo for clarity and organisation. 47 As analysis progressed, codes were refined and sorted into themes and subthemes using an Excel spreadsheet, NVivo and thematic maps. 48 This allowed codes to be compared between participants and between sexes.
To enhance the quality of the analytic process, investigator triangulation occurred. 49 Two transcripts were coded independently by SG, an experienced qualitative researcher. MM and SG then met to discuss analysis and agree on themes, before meeting again to further refine and define themes. Furthermore, to ensure credibility of results, member validation occurred. Participants were sent their interview’s main themes and asked to confirm these reflected the intent of their responses. Overall, 11 participants responded confirming this was an accurate representation of their views. 50 Data are reported in accordance with the Consolidated criteria for reporting qualitative research checklist. 51
Patient and public involvement
Patients and members of the public were not involved in study design or development. Participants were involved in study analysis through member validation.
Seven male and seven female participants took part in the study, their characteristics are described in table 1 . A total of 86% were White British ethnicity, and the ages of participants ranged from 18 to 26 years old. Participants studied a wide range of university courses, with the majority reading either the arts and law or social sciences.
Participant characteristics
Participant age ranged from 18 to 26. Equal numbers of male and female participants took part in the study and 86% of participants were of White British ethnicity. Participants studied a range of university courses, including arts and law and social sciences.
Six themes, each with subthemes, were interpreted from the data: ED characteristics, causes, body image, seeking help, stigma and awareness. Themes represent central attitudes and ideas discussed throughout interviews. Some reflect areas of the interview guide; however, others, such as stigma, were mentioned by participants without directly being led by the interview guide. Figure 2 summarises the links between themes and the impact of sex on results.

Links between themes and impact of biological sex. Each box contains one theme and associated subthemes. Links between themes are represented by a black line. ED, eating disorder.
Themes are displayed with supporting quotations, presented with biological sex-specific pseudonyms to maintain confidentiality. Superfluous text within quotations has been removed and is represented by an ellipsis […].
ED characteristics
Types of ed.
All participants mentioned AN, and most were able to attempt a definition. Many participants also cited over-eating as an ED; however, only three specifically defined binge ED. Though 12 participants were able to name bulimia nervosa (BN), many were hesitant to define and describe it:
I think most people have some kind of idea of what anorexia is, bulimia, I think it’s more complicated (David, 21)
Defining EDs
Many participants believed EDs to be a psychological issue and defined them as a mental illness. Furthermore, EDs were frequently recognised as a spectrum, a scale between disordered eating and a severe ED:
I think they’re almost like a spectrum, I think some people have a really bad eating disorder and it affects them in a really bad way but I think a lot of people can have unhealthy relationships with food that but they stay at a sort of stable weight but it’s more of the mental thoughts they have about it (Chelsea, 22)
Overall, 12 participants perceived EDs as a predominantly female problem, with few mentioning EDs in men. They were also frequently associated with younger people, believed to affect those of school and university age:
Younger women are the main category, so teenagers to like early mid-twenties I’d say, so that captures students (Rebecca, 21) If I see a guy and he’s skinny […] I don’t think there’s any chance of it being an eating disorder, he’s just skinny (David, 21)
The perception that individuals with EDs are ‘skinny’ or ‘skeletal’ was held by 13 participants, and many described the impact of EDs as severe, believing sufferers to appear ‘ill-looking’ and ‘gaunt’:
So skinny that you can see their hip bones protruding, knee bones look massive in comparison to the rest of their leg because they’re so big and like clothes hanging off them (Katie, 19)
While the majority of participants recognised EDs as challenging and impactful, some male participants were more likely to associate EDs with vulnerability, perceiving sufferers as ‘fragile’:
I’d see them as more fragile I think, I’d see them more […] like a vase (William, 19)
There was the view that individuals with EDs are obsessive and seeking perfection, with two students commenting on a ‘type A’ personality putting someone at increased risk of an ED 52 :
If you’re quite neurotic so you’re a bit strung, highly strung up maybe they’re a perfectionist or someone really has to be yeah really controlling about things in life (Callum, 26)
Control was mentioned by five participants, four of whom were female. EDs were seen as a coping mechanism, by which individuals can take control of aspects of their lives:
They get some sort of, I wouldn’t say enjoyment but satisfaction with having the control of food especially if they don’t have the control of anything else (Katie, 19)
Image conscious
Seven students believed ED sufferers hold a low self-worth, perceiving them to care a lot about their own image and what others thought of them:
Lack of confidence as a trait would also make you a lot more sort of conscious of how you’re seen (Shaun, 19)
Signs and symptoms
Perceived signs and symptoms freely volunteered by participants are presented in table 2 . Students were generally unaware of specific ED symptoms and which symptoms were associated with specific EDs. Some symptoms were recognised more than others, specifically under-eating and over-eating. Vomiting and binge eating and purging were also frequently mentioned, and all participants that recognised these symptoms associated them with BN. Despite seven participants describing EDs as visible illnesses with numerous physical signs, many perceived difficulties in recognising signs and symptoms, describing EDs as conditions that are not easy to spot:
Perceived signs and symptoms of eating disorders (EDs)
Perceived signs and symptoms of EDs alongside frequency stated by participants and a supporting quotation.
It’s not really as apparent, we don’t see people naked or in their underwear every day, you just assume someone’s fine (Danielle, 21)
Causes of EDs
Many male students were unaware of potential causes on initial questioning. Perceived causes, after prompting in many cases, are presented in table 3 . Several students referenced internal factors such as a psychological comorbidity or low self-worth as major ED causes. Of the seven individuals who believed low self-worth could contribute, five were male. Nevertheless, many students attributed social causes to be the most influential:
Perceived causes of eating disorders (EDs)
Perceived causes of EDs alongside frequency stated and a supporting quotation.
Social factors would probably play a larger role (Katie, 19)
Participants perceived poor body image as both an ED cause and a consequence of repeated pressure from the media. Many commented that poor body image was common, and referenced their own personal experience of a poor relationship with their body:
I think it affects lots of people, like sort of body dysmorphia in general, I think like in some kind of mild forms (Adam, 21)
‘The perfect body’
‘The perfect body’ was something that had been repeatedly presented to many participants from a young age, with individuals with this body type deemed more attractive to society and the opposite sex:
If you don’t look like that, or you’re not like aiming to look like that […] then you’re unhealthy or you’re not good enough or you’re not attractive […] because you have to fit into like one of the groups, one of the standards presented (Grace, 22)
All students cited media pressure as a cause of poor body image, with many reflecting on increased pressure due to the rise in social media, resulting in a constant comparison of oneself against others:
Because of social media, you’re always comparing yourself to other people, I think people feel more in competition with other people all the time […] I don’t think it’s healthy on body image (Rebecca, 21)
Many students believed females to be under greater pressure, citing increased female body representation in the media and sexist viewpoints towards female bodies as mechanisms for this. Ten participants referred to the ‘female ideal’ of being slim:
What you’d see in something like London fashion week, tall skinny models that would have potentially a thigh gap, a flat stomach, no stretch marks, not much cellulite (Katie, 19)
Contrastingly, the ‘male ideal’ was described as heavily muscular:
A six pack, like well-toned, just a good size of muscles like all over (Andrew, 19)
Male body image
Despite acknowledging that males also experience pressure to look a certain way, students generally inferred that males care less about image and are not bothered about how other people perceived them. This was supported by male participants being more likely to comment that body image worries did not personally affect them:
Myself I'm not too bothered, but men in general if I had to be very stereotypical, I would say men don’t care as much about their image (Joshua, 20)
Various students commented on the societal stigma they believe exists around men’s bodies, with male body image viewed as less inclusive and spoken about than female body image. Due to this, some participants commented that many males do not talk about their bodies:
The stereotype of not showing weakness may mean that they’re less willing to open up (Shaun, 19)
Seeking help
With prompting, 12 participants were able to suggest some sources of professional help available to support those with EDs. Seven participants recognised the importance of seeking social support. Many students commented on potential treatment barriers, including perceived negatives of medical treatment and worries about self-image.
Professional
Twelve participants recognised therapy as a potential treatment. Further sources of formal treatment included treatment in specialist hospitals and nasogastric feeding. Many participants, especially females, commented on issues with seeking medical treatment, including perceived lack of treatment availability and the belief that doctors would not take EDs seriously:
With the NHS they have so much on their plate and there’s underfunding and stuff so I just personally wouldn’t want to go there for them. And as well GPs can be a bit snappy and try and like rush you and stuff (Chelsea, 22)
Ten participants said they would be willing to seek professional help, the majority mentioned consulting their General Practitioner or seeking a therapist. Male participants were more likely to seek only professional support or seek social support after first pursuing professional support. Furthermore, some mentioned first researching online about what help was available for EDs:
Probably look on NHS website first I’m sure they’d probably say go to a doctor and then I’d probably get a referral from the doctor (Callum, 26)
The majority perceived social support as vital in both recovery and maintaining recovery. Five participants mentioned greater willingness to seek social rather than professional support, highlighting the ability of the social network to encourage help-seeking:
I’d probably ask for someone’s advice on whether I should go to the doctor (Grace, 22)
Despite perceived benefits of seeking social support, many commented on potential barriers that would prevent them from seeking social support, including not wanting to bother others with their problems and a fear of being judged. All male participants worried about being perceived differently by peers:
If I suspected one of my friends of having an eating disorder I’d see them as fragile and delicate, I wouldn’t want the people close to me to see me as fragile and delicate cos I wouldn’t want people’s opinions to change about me (William, 19)
The desire to help those with an ED was emphasised by 13 participants; however, 6 participants recognised that helping someone with an ED was often difficult. Participants were generally sympathetic, suggesting a need to be supportive and encourage those suffering to seek professional support:
I’d encourage them, and if they were like I want to get medical help I’d like come with them (Thomas, 18)
Notwithstanding the support offered, many participants predicated a subconscious change in behaviour that would come with knowing someone had an ED. Nine participants mentioned a need to act carefully around those with EDs, particularly in situations involving food. Five participants also recognised the need to maintain a sense of normality:
I’d want to be a lot more careful with how I acted around them but then again whilst I’d be a lot more careful I’d also very much try to act that nothing has changed, so around them I’d try and act exactly the same (William, 19)
Internal barriers
The extent that personal beliefs and coping mechanisms limited help-seeking was also discussed. Seven participants highlighted the struggles that come with seeking help, perceiving EDs as difficult to discuss, and help-seeking as embarrassing and scary:
I can imagine that would be a really hard conversation, to say like mate I think you might have an eating disorder, I wouldn’t want to hear that, I don’t think anyone would want to hear that (Thomas, 18)
The internalisation of one’s problems was mentioned by three participants. This came hand in hand with a perception that EDs are not a serious issue, and therefore something that could be easily dealt with by oneself. Furthermore, many participants held the belief that individuals with EDs may not want to recover, or may lack the intuition to realise they have a problem:
I imagine some people just don’t even know that they, it’s a problem for themselves and they could be putting themselves at risk (Grace, 22)
Eleven participants believed it was possible to recover from an ED. Despite this, participants made frequent reference to the idea that the ED would remain with you, and that it would be easy to relapse. Ten participants commented on the ease of falling back into previous behaviours or thoughts:
I think it would be difficult for them to never have them same thoughts in their head again. So, I think the thoughts will always be there it just depends, they can probably learn to live with it rather than them let it take over their life (Chelsea, 22)
The majority of participants recognised EDs, and mental health conditions in general, as highly publicly stigmatised.
Some participants commented on the impact of EDs on image. Five students perceived EDs as conditions that are shamed within society, commenting that society has a tendency to label people with mental health issues:
I wouldn’t want it to be perceived as a part of my identity, I wouldn’t want to be known as the boy with an eating disorder rather than anything else about me, I wouldn’t want that to be what people sort of defined me as (Shaun, 19)
EDs being seen as a ‘weakness’ was mainly specified by male participants, with three participants stating this as a reason they would not tell anyone they had an ED:
I think I’d find it hard to tell my friends about it as well, like show weakness rather than just coming across as someone who’s laid back and calm (Shaun, 19)
A number of students saw EDs as conditions that are rarely discussed by society. Many held the perception that mental illnesses were ‘taboo’. Additionally, six students commented on EDs being poorly understood within the community, seeing society as ignorant towards the seriousness of the conditions:
I feel like for a long time it wasn’t really recognised and therefore people didn’t, if you had an eating disorder it was sort of why are you be being difficult rather than being like oh let’s work, let’s find a way to work around this (Andrew, 19)
In addition, a number of students saw EDs as conditions that were ‘difficult to relate to’, citing this as a reason why many find it hard to understand EDs:
If someone’s feeling anxious they can talk to their friends about it, there’d be some level of empathy and them understanding that, I think it would be much harder to talk to a friend and expect them to, well have them understand an eating disorder, because it’s not a shared thing (David, 21)
Throughout the interviews there was a general hesitancy and lack of awareness when discussing certain aspects of EDs.
Lack of knowledge
Ten participants, the majority of whom were male, perceived themselves to have poor knowledge about certain aspects of EDs. Many were hesitant to answer, and lacked confidence in their answers:
I don’t know a huge amount, so I definitely don’t have great knowledge on it (Callum, 26)
Furthermore, many participants stated their knowledge as ‘assumptions’ or ‘clichés’, with male participants particularly worried that their answers were incorrect or would be interpreted improperly:
I don’t want my opinions to come across like I know what I’m talking about almost, if you know what I mean (Joshua, 20)
Nine participants mentioned knowing an ED sufferer, evidencing the frequently held perception that EDs are common. Many cited experiences of these individuals as sources of their knowledge, particularly around treatment and symptoms:
I think now they’re quite common, I feel like everyone knows someone who’s struggled with an eating disorder (Rebecca, 21)
Six participants mentioned being formally taught about EDs in school; however, many reflected that these lessons were ‘basic’ and were unable to recollect what specifics they had been taught:
We had like the basic kind of PSHE lessons about it but nothing that could have like helped anyone, or not enough I don’t think (Chelsea, 22)
The majority of participants cited informal sources such as social media and films as their sources of ED knowledge:
A lot of what I think about eating disorders is from movies and TV shows, rather than fact (Grace, 22)
However, some participants acknowledged that they were sceptical about the accuracy of this information. Furthermore, a number of students made comment about how the representation of EDs in the media, and their perceived commonness within the younger generation had made them sensitised to the signs and consequences of EDs:
With the lens of social media […] when I first found out about eating disorders, at 14 or 15, made it seem almost, I don’t want to say too ok but it almost normalised it to a point where I actually didn’t realise for a little bit how serious an eating disorder was’ (Thomas, 18)
Improving awareness
Seven participants commented on the need to improve ED teaching. For many, the need to educate individuals about the signs and symptoms and promote help-seeking was of particular importance:
It flagged them up as being as issue but never really went into depth with what to do about them or how to act with someone who has those and so I found that I had to learn it for myself rather than learning from like lessons and things (Shaun, 19)
Despite the perceived need for better teaching, a number of students commented on positive steps in society that are improving ED awareness. Many commented on improving body representation in the media and five students commented on sources of positive ED representation, believing this to be beneficial to those suffering.
I got a lot of knowledge from social media and stuff like that, a lot of it really positive stuff, you know hashtags on twitter or stuff on Tumblr, people sharing their experiences and stories and it’s all been from a very supportive, positive light (Thomas, 18)
Main findings
This study, to the best of the author’s knowledge, is the first UK qualitative study exploring ED-MHL in university students. Generally, the study highlighted the university students interviewed had a broad awareness of EDs, for example, a good general awareness of symptoms and signs and treatment options; however, there were areas where knowledge was lacking, even in this highly educated group.
While many students were able to state AN and BN as EDs, many were hesitant to define and describe BN, and only a few were able to suggest further ED types. Furthermore, though many students were able to name some signs and symptoms when prompted, there was a great deal of uncertainty, and many struggled to link particular symptoms to specific EDs. The findings of this study are in keeping with a previous quantitative study of members of the public, in which participants showed difficulty discriminating between ED diagnoses. 53 There was no apparent difference in ED identification between sexes, in contrast to a previous vignette study of Canadian postsecondary students, in which males had greater difficulty identifying ED diagnoses. 54 Awareness of ED symptoms is important, as poor symptom recognition is associated with reduced likelihood of help-seeking, and increased risk of long-term outcomes. 55 56 Many students in this study perceived EDs as a female problem. This perception was also reported in a previous qualitative study of young people, who also believed AN to be a female issue. 35 EDs are already considered underdiagnosed in men, 57 therefore this belief, in this at risk population, can result in young men being less likely to recognise their symptoms as indicative of an ED, and in them being less likely to seek help. 30
The greatest perceived cause of EDs was media pressure. These results are similar to a previous qualitative study in members of the public, in which media ideals were a major perceived cause of EDs. 21 Furthermore, many participants made reference to the ‘thin ideal’ presented to young women in the media. This perception is common, with previous research in UK students highlighting how a desire for a thin, often unattainable body type is associated with ED development. 58
Although participants in this study did not generally hold stigmatising attitudes towards EDs, several perceived EDs as highly stigmatised in the community. This perception is in line with previous studies, which have shown public attitudes towards EDs are highly conductive to stigma. 14 59 Higher educational status is correlated with liberal views towards mental illness, which may explain the low levels of stigmatisation apparent in the participants of this study. 60 Many students cited fear of public stigma as a reason for not seeking help, further enhancing the idea that fear of public stigma is a major cause of delayed help-seeking. 11 Previous studies focused on ED stigma in university students have highlighted significant sex bias, with males exhibiting higher ED stigma than females. 31 61 The results of this study are not in keeping with this literature, as differences in stigmatising viewpoints were not as apparent between male and female participants, though some differences were observed.
Encouragingly, the majority of participants said they would seek professional help for an ED; however, many were unsure of what help is available, and many made comments about perceived negatives of professional support, such as not being taken seriously. These worries are in keeping with previous research 62 and could act as an explanation as to why those with EDs take so long to seek treatment. 8 Most participants expressed sympathy and a desire to help those with an ED, and many recognised the importance of social support, which has been shown to be highly influential in ED recovery. 63
Many participants perceived themselves as having poor or inaccurate knowledge. With this in mind, the majority of participants referenced informal sources such as social media as their main informants, similarly to recent quantitative research in Italian students. 64 However, these sources of ED information are likely to be damaging and inaccurate. 65 66 Students in a previous Australian study highlighted a desire for greater ED teaching in schools, 54 a sentiment similarly expressed by participants of this study, many of whom perceived their ED teaching as inadequate.
Previous research in members of the public showed significantly poorer MHL in male participants. 60 Contrary to this, differences in the ED-MHL between the male and female participants of this study were not significantly apparent. However, there were some disparities. Male participants were more likely to perceive themselves to have low levels of knowledge and appeared more reluctant to seek social support, making more reference to perceived social stigma, such as being perceived differently by their peers.
Strengths and limitations
To the best of the authors’ knowledge, this study is the first in-depth, qualitative exploration of knowledge and understanding of EDs in UK university students. This is a major strength of the research as the interviews enabled broad exploration of knowledge and enable further insight into individual perceptions of EDs and beliefs about stigma and treatment barriers in a highly specific, at-risk population. The use of member validation and analyst triangulation with an experienced qualitative researcher further strengthens the study. Data saturation was reached with 14 participants, which reflects recommended sample sizes in a study of this type. 67
However, there are a number of limitations. The study was advertised as looking at EDs, therefore participants could have volunteered because they had a greater interest or perceived themselves to have greater ED knowledge. Furthermore, some participants may have been reluctant to disclose their true views about EDs due to social desirability bias, 68 and may have held more stigmatising viewpoints than was apparent from interviews. Participants’ lack of awareness in certain areas may reflect this bias and therefore they may have been reluctant to discuss answers they knew may have been rooted in stereotypical assumptions. Methods to minimise the impact of social desirability bias, such as self-administered questionnaires may be beneficial for future research. 69
Research and policy recommendations
This study, alongside others, highlights there are poor levels of ED knowledge in this population in certain areas, including symptom recognition and awareness of treatment options. Further research in this at-risk population using vignette studies may be beneficial to draw further inferences about individual perceptions about EDs.
Furthermore, this study also emphasised a desire from participants for greater ED teaching. Therefore, ED educational campaigns within schools or universities would be crucial to improving awareness of symptoms and treatments and may encourage earlier help-seeking and improve treatment uptake in this at-risk group. Additionally, university, school and college welfare services need to be suitably prepared to support individuals with EDs. Improving ED education in university and school staff, through courses such as Beat’s ‘bridging the gap’, can increase early detection of EDs and ensure individuals with EDs are given the support they need. 70
Despite antistigma campaigns such as Beat’s ‘ED awareness week’, 71 participants still perceived EDs as stigmatised within the community. There is a need for research into the efficacy of ED antistigma campaigns to determine which methods work, allowing for more successful future campaigns. Findings from a small-scale trial suggest the delivery of information emphasising the biological basis of EDs can help reduce stigmatising attitudes towards EDs, 72 hence further research into provision of this information would be beneficial. There is also a need for research involving participants of different educational levels and ages. This would be more indicative of public knowledge and understanding and would help inform educational and antistigma campaigns targeted at a broader audience. The perception of EDs as a ‘female issue’ is still a major problem, and therefore antistigma campaigns targeted at males may be useful to address the sex-specific stigma associated with EDs and improve symptom recognition and help-seeking in men.
This study demonstrates that although this group of UK university students demonstrated a broad general awareness of EDs, there remain areas where knowledge is lacking. There is a need for health campaigns targeted at at-risk, younger individuals to better educate them about EDs, including information about symptoms and treatment options to better aid recognition and improve help-seeking, with the hope of lowering the significant treatment gap apparent in these conditions. Further research is necessary to better determine the ED-MHL of the general public and to develop effective methods of tackling the stigma surrounding EDs and other mental health conditions.
Supplementary Material
Acknowledgments.
We would like to thank Rachel Marchant for her support during analysis. We would also like to thank all the study participants, without whom this project would not have been possible. A conference abstract of this work has been published as M Manning, S Greenfield, University students' understanding and options of eating disorders: A qualitative study. Eur J Public Health 2021; 31. doi: 10.1093/eurpub/ckab165.575.
Contributors: MM designed the study, wrote the study protocol, obtained ethical approval, undertook recruitment, carried out interviews, analysed the data and produced the final manuscript. SG provided expert supervision, contributed to the study design, protocol and analysis and provided revisions to manuscript drafts. SG, as guarantor, accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Funding: This research was funded by the BMedSc Population Sciences and Humanities programme at the University of Birmingham (no award/grant number). SG is part funded by the National Institute for Health Research and Collaboration for Leadership in Applied Health Research and Care.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Ethics statements, patient consent for publication.
Not applicable.
Ethics approval
This study involves human participants. Ethical approval was granted by the BMedSc Population Sciences and Humanities Internal Ethics Review Committee at the University of Birmingham, Reference: IREC2019/Student 1638594. Participants gave informed consent to participate in the study before taking part.
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
Teens and social media: Key findings from Pew Research Center surveys

For the latest survey data on social media and tech use among teens, see “ Teens, Social Media, and Technology 2023 .”
Today’s teens are navigating a digital landscape unlike the one experienced by their predecessors, particularly when it comes to the pervasive presence of social media. In 2022, Pew Research Center fielded an in-depth survey asking American teens – and their parents – about their experiences with and views toward social media . Here are key findings from the survey:
Pew Research Center conducted this study to better understand American teens’ experiences with social media and their parents’ perception of these experiences. For this analysis, we surveyed 1,316 U.S. teens ages 13 to 17, along with one parent from each teen’s household. The survey was conducted online by Ipsos from April 14 to May 4, 2022.
This research was reviewed and approved by an external institutional review board (IRB), Advarra, which is an independent committee of experts that specializes in helping to protect the rights of research participants.
Ipsos invited panelists who were a parent of at least one teen ages 13 to 17 from its KnowledgePanel , a probability-based web panel recruited primarily through national, random sampling of residential addresses, to take this survey. For some of these questions, parents were asked to think about one teen in their household. (If they had multiple teenage children ages 13 to 17 in the household, one was randomly chosen.) This teen was then asked to answer questions as well. The parent portion of the survey is weighted to be representative of U.S. parents of teens ages 13 to 17 by age, gender, race, ethnicity, household income and other categories. The teen portion of the survey is weighted to be representative of U.S. teens ages 13 to 17 who live with parents by age, gender, race, ethnicity, household income and other categories.
Here are the questions used for this report, along with responses, and its methodology .
Majorities of teens report ever using YouTube, TikTok, Instagram and Snapchat. YouTube is the platform most commonly used by teens, with 95% of those ages 13 to 17 saying they have ever used it, according to a Center survey conducted April 14-May 4, 2022, that asked about 10 online platforms. Two-thirds of teens report using TikTok, followed by roughly six-in-ten who say they use Instagram (62%) and Snapchat (59%). Much smaller shares of teens say they have ever used Twitter (23%), Twitch (20%), WhatsApp (17%), Reddit (14%) and Tumblr (5%).
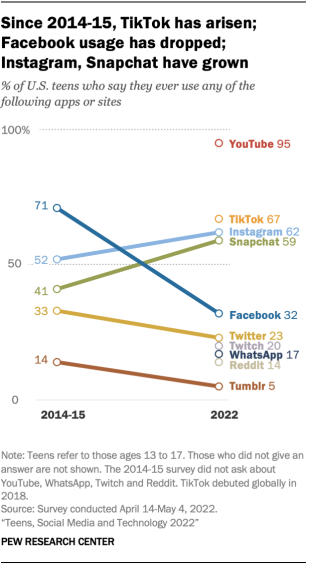
Facebook use among teens dropped from 71% in 2014-15 to 32% in 2022. Twitter and Tumblr also experienced declines in teen users during that span, but Instagram and Snapchat saw notable increases.
TikTok use is more common among Black teens and among teen girls. For example, roughly eight-in-ten Black teens (81%) say they use TikTok, compared with 71% of Hispanic teens and 62% of White teens. And Hispanic teens (29%) are more likely than Black (19%) or White teens (10%) to report using WhatsApp. (There were not enough Asian teens in the sample to analyze separately.)
Teens’ use of certain social media platforms also varies by gender. Teen girls are more likely than teen boys to report using TikTok (73% vs. 60%), Instagram (69% vs. 55%) and Snapchat (64% vs. 54%). Boys are more likely than girls to report using YouTube (97% vs. 92%), Twitch (26% vs. 13%) and Reddit (20% vs. 8%).
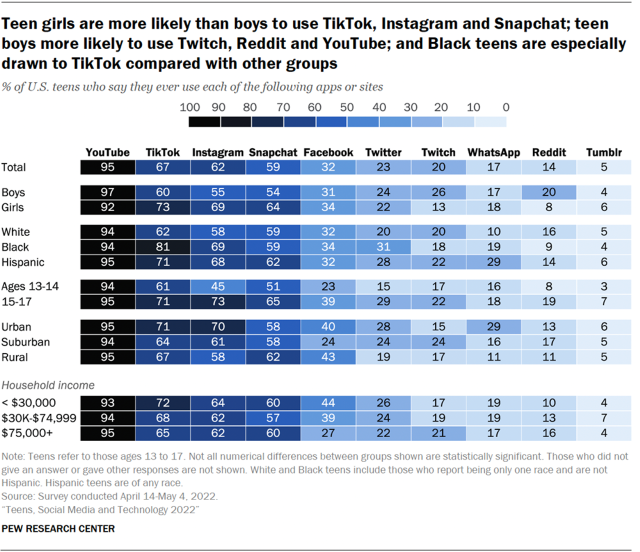
Majorities of teens use YouTube and TikTok every day, and some report using these sites almost constantly. About three-quarters of teens (77%) say they use YouTube daily, while a smaller majority of teens (58%) say the same about TikTok. About half of teens use Instagram (50%) or Snapchat (51%) at least once a day, while 19% report daily use of Facebook.
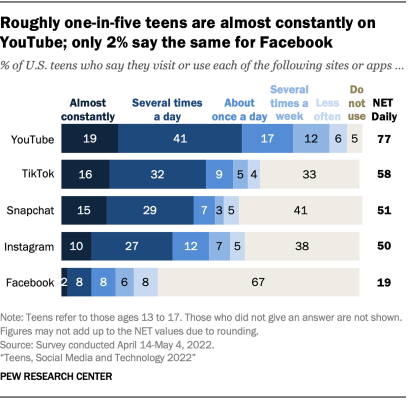
Some teens report using these platforms almost constantly. For example, 19% say they use YouTube almost constantly, while 16% and 15% say the same about TikTok and Snapchat, respectively.
More than half of teens say it would be difficult for them to give up social media. About a third of teens (36%) say they spend too much time on social media, while 55% say they spend about the right amount of time there and just 8% say they spend too little time. Girls are more likely than boys to say they spend too much time on social media (41% vs. 31%).
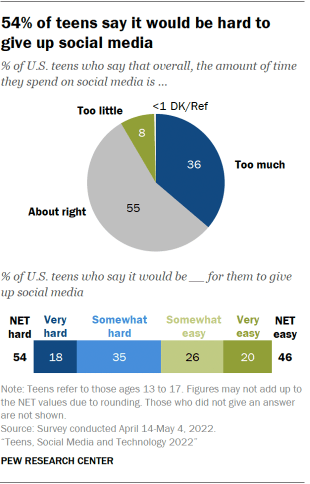
Teens are relatively divided over whether it would be hard or easy for them to give up social media. Some 54% say it would be very or somewhat hard, while 46% say it would be very or somewhat easy.
Girls are more likely than boys to say it would be difficult for them to give up social media (58% vs. 49%). Older teens are also more likely than younger teens to say this: 58% of those ages 15 to 17 say it would be very or somewhat hard to give up social media, compared with 48% of those ages 13 to 14.
Teens are more likely to say social media has had a negative effect on others than on themselves. Some 32% say social media has had a mostly negative effect on people their age, while 9% say this about social media’s effect on themselves.
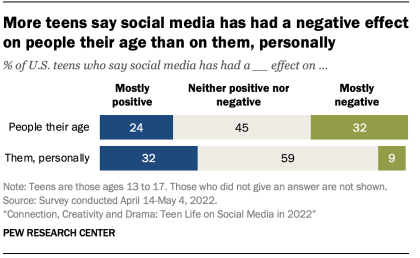
Conversely, teens are more likely to say these platforms have had a mostly positive impact on their own life than on those of their peers. About a third of teens (32%) say social media has had a mostly positive effect on them personally, while roughly a quarter (24%) say it has been positive for other people their age.
Still, the largest shares of teens say social media has had neither a positive nor negative effect on themselves (59%) or on other teens (45%). These patterns are consistent across demographic groups.
Teens are more likely to report positive than negative experiences in their social media use. Majorities of teens report experiencing each of the four positive experiences asked about: feeling more connected to what is going on in their friends’ lives (80%), like they have a place where they can show their creative side (71%), like they have people who can support them through tough times (67%), and that they are more accepted (58%).
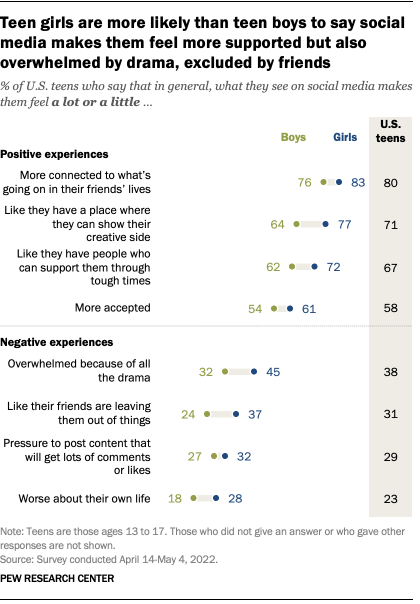
When it comes to negative experiences, 38% of teens say that what they see on social media makes them feel overwhelmed because of all the drama. Roughly three-in-ten say it makes them feel like their friends are leaving them out of things (31%) or feel pressure to post content that will get lots of comments or likes (29%). And 23% say that what they see on social media makes them feel worse about their own life.
There are several gender differences in the experiences teens report having while on social media. Teen girls are more likely than teen boys to say that what they see on social media makes them feel a lot like they have a place to express their creativity or like they have people who can support them. However, girls also report encountering some of the pressures at higher rates than boys. Some 45% of girls say they feel overwhelmed because of all the drama on social media, compared with 32% of boys. Girls are also more likely than boys to say social media has made them feel like their friends are leaving them out of things (37% vs. 24%) or feel worse about their own life (28% vs. 18%).
When it comes to abuse on social media platforms, many teens think criminal charges or permanent bans would help a lot. Half of teens think criminal charges or permanent bans for users who bully or harass others on social media would help a lot to reduce harassment and bullying on these platforms.
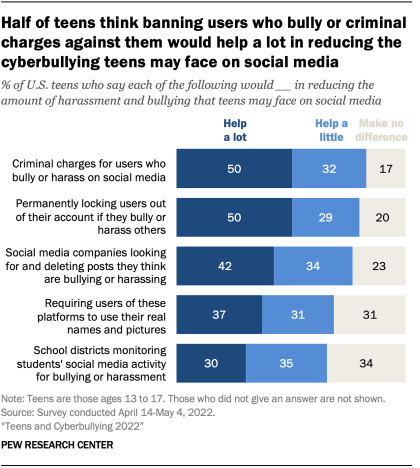
About four-in-ten teens say it would help a lot if social media companies proactively deleted abusive posts or required social media users to use their real names and pictures. Three-in-ten teens say it would help a lot if school districts monitored students’ social media activity for bullying or harassment.
Some teens – especially older girls – avoid posting certain things on social media because of fear of embarrassment or other reasons. Roughly four-in-ten teens say they often or sometimes decide not to post something on social media because they worry people might use it to embarrass them (40%) or because it does not align with how they like to represent themselves on these platforms (38%). A third of teens say they avoid posting certain things out of concern for offending others by what they say, while 27% say they avoid posting things because it could hurt their chances when applying for schools or jobs.
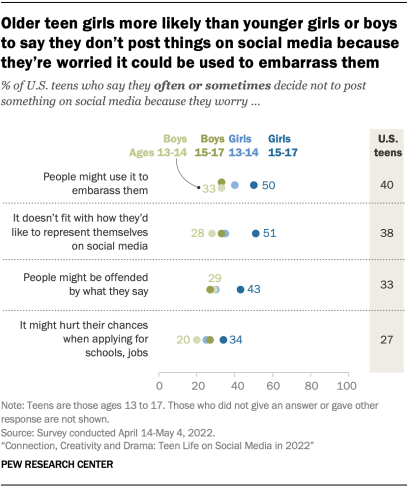
These concerns are more prevalent among older teen girls. For example, roughly half of girls ages 15 to 17 say they often or sometimes decide not to post something on social media because they worry people might use it to embarrass them (50%) or because it doesn’t fit with how they’d like to represent themselves on these sites (51%), compared with smaller shares among younger girls and among boys overall.
Many teens do not feel like they are in the driver’s seat when it comes to controlling what information social media companies collect about them. Six-in-ten teens say they think they have little (40%) or no control (20%) over the personal information that social media companies collect about them. Another 26% aren’t sure how much control they have. Just 14% of teens think they have a lot of control.
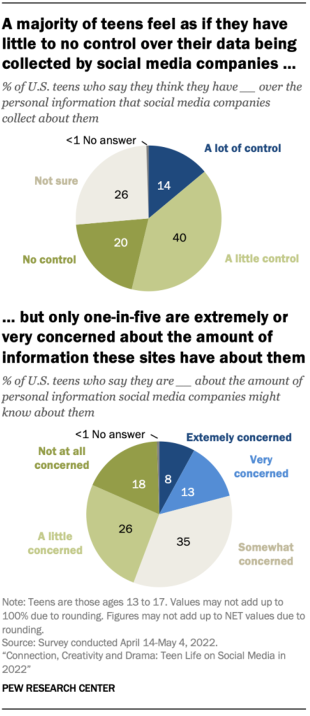
Despite many feeling a lack of control, teens are largely unconcerned about companies collecting their information. Only 8% are extremely concerned about the amount of personal information that social media companies might have and 13% are very concerned. Still, 44% of teens say they have little or no concern about how much these companies might know about them.
Only around one-in-five teens think their parents are highly worried about their use of social media. Some 22% of teens think their parents are extremely or very worried about them using social media. But a larger share of teens (41%) think their parents are either not at all (16%) or a little worried (25%) about them using social media. About a quarter of teens (27%) fall more in the middle, saying they think their parents are somewhat worried.
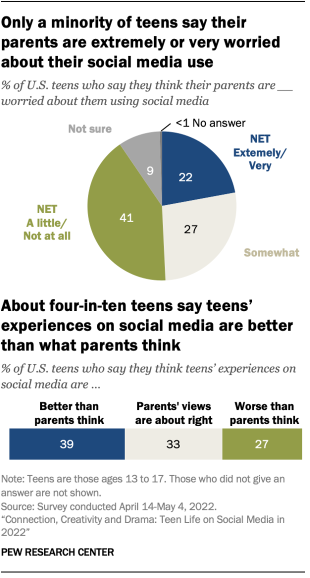
Many teens also believe there is a disconnect between parental perceptions of social media and teens’ lived realities. Some 39% of teens say their experiences on social media are better than parents think, and 27% say their experiences are worse. A third of teens say parents’ views are about right.
Nearly half of parents with teens (46%) are highly worried that their child could be exposed to explicit content on social media. Parents of teens are more likely to be extremely or very concerned about this than about social media causing mental health issues like anxiety, depression or lower self-esteem. Some parents also fret about time management problems for their teen stemming from social media use, such as wasting time on these sites (42%) and being distracted from completing homework (38%).
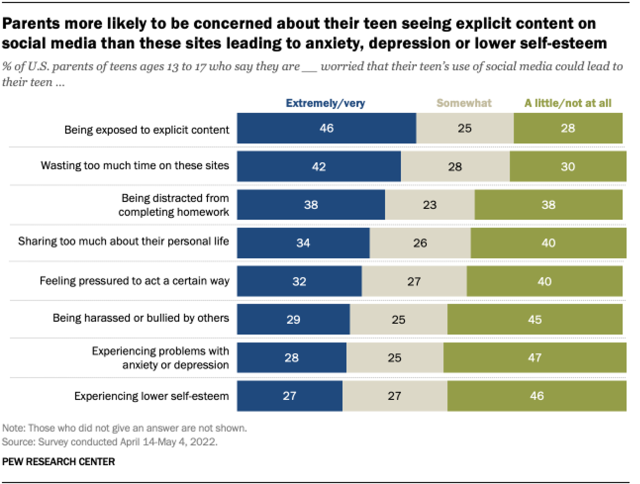
Note: Here are the questions used for this report, along with responses, and its methodology .
CORRECTION (May 17, 2023): In a previous version of this post, the percentages of teens using Instagram and Snapchat daily were transposed in the text. The original chart was correct. This change does not substantively affect the analysis.
- Age & Generations
- Age, Generations & Tech
- Internet & Technology
- Platforms & Services
- Social Media
- Teens & Tech
- Teens & Youth
Emily A. Vogels is a former research associate focusing on internet and technology at Pew Research Center

Risa Gelles-Watnick is a research analyst focusing on internet and technology research at Pew Research Center
How Teens and Parents Approach Screen Time
Who are you the art and science of measuring identity, u.s. centenarian population is projected to quadruple over the next 30 years, older workers are growing in number and earning higher wages, teens, social media and technology 2023, most popular.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Coronavirus (COVID-19)
- Economy & Work
- Family & Relationships
- Gender & LGBTQ
- Immigration & Migration
- International Affairs
- Methodological Research
- News Habits & Media
- Non-U.S. Governments
- Other Topics
- Politics & Policy
- Race & Ethnicity
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Terms & Conditions
Privacy Policy
Cookie Settings
Reprints, Permissions & Use Policy

IMAGES
VIDEO
COMMENTS
The findings revealed a 19% concurrent comorbidity between these disorders, and in 65% of the cases, social phobia preceded major depressive disorder by at least 2 years. In addition, initial presentation with social phobia was associated with a 5.7-fold increased risk of developing major depressive disorder. These associations between anxiety ...
Personality disorders (PDs) can be described as the manifestation of extreme personality traits that interfere with everyday life and contribute to significant suffering, functional limitations, or both. They are common and are frequently encountered in virtually all forms of health care. PDs are associated with an inferior quality of life (QoL ...
Anxiety disorders are the most prevalent psychiatric disorders. There is a high comorbidity between anxiety (especially generalized anxiety disorders or panic disorders) and depressive disorders or between anxiety disorders, which renders treatment more complex. ... Thibaut F. Gender does matter in clinical research. Eur Arch Psychiatry Clin ...
Advances and the current status of evidence‐based treatment and outcomes for the main eating disorders, anorexia nervosa, bulimia nervosa and BED are discussed with focus on first‐line psychological therapies. Deficits in knowledge and directions for further research are highlighted, particularly with regard to treatments for BED and ARFID ...
Anxiety disorders form the most common group of mental disorders and generally start before or in early adulthood. Core features include excessive fear and anxiety or avoidance of perceived threats that are persistent and impairing. Anxiety disorders involve dysfunction in brain circuits that respond to danger. Risk for anxiety disorders is influenced by genetic factors, environmental factors ...
Personality Disorders: Theory, Research, and Treatment® ( PD:TRT) publishes a wide range of cutting-edge research on personality disorders and related psychopathology from a categorical and/or dimensional perspective including laboratory and treatment outcome studies, as well as integrative conceptual manuscripts and practice reviews that ...
Depression and anxiety disorders are together responsible for 8% of years lived with disability globally. ... Recent research has established a bidirectional causal relationship between poverty and mental illness. ... D. A. Cobb-Clark, S. Dahmann, N. Kettlewell, "Depression, risk preferences and risk-taking behavior," research paper 12285 ...
Aims and scope. Journal of Eating Disorders is the first open access, peer-reviewed journal publishing leading research in the science and clinical practice of eating disorders. It disseminates research that provides answers to the important issues and key challenges in the field of eating disorders and to facilitate translation of evidence ...
Eating disorders are disabling, deadly, and costly mental disorders that considerably impair physical health and disrupt psychosocial functioning. Disturbed attitudes towards weight, body shape, and eating play a key role in the origin and maintenance of eating disorders. Eating disorders have been increasing over the past 50 years and changes in the food environment have been implicated.
Eating disorders are disabling, deadly, and costly mental disorders that considerably impair physical health and disrupt psychosocial functioning. Disturbed attitudes towards weight, body shape, and eating play a key role in the origin and maintenance of eating disorders. Eating disorders have been increasing over the past 50 years and changes ...
The nine item avoidant/restrictive food intake disorder screen (NIAS) is a short and practical assessment tool specific to ARFID with three ARFID phenotypes such as "Picky eating," "Fear," and "Appetite". This... Hakan Öğütlü, Meryem Kaşak, Uğur Doğan, Hana F. Zickgraf and Mehmet Hakan Türkçapar. Journal of Eating Disorders ...
Bipolar disorder is a broad diagnostic construct associated with significant phenotypic and genetic heterogeneity challenging progress in clinical practice and discovery research. Prospective studies of well-c... Anne Duffy and Paul Grof. International Journal of Bipolar Disorders 2024 12 :12.
This research paper embarks on a comprehensive exploration of the multifaceted landscape of neurological disorder treatments, offering insights into the genetic and molecular underpinnings of ...
Eating disorders have increasingly become the focus of research studies due to their prevalence, especially in Western cultures. Of the adolescent and young adult populations in the United States, for example, between .3 and .9 % are diagnosed with anorexia nervosa (AN), between .5 and 5 % with bulimia nervosa (BN), between 1.6 and 3.5 % with binge eating disorder (BED), and about 4.8 % with ...
A psychological disorder is a condition characterized by abnormal thoughts, feelings, and behaviors. Psychopathology is the study of psychological disorders, including their symptoms, etiology (i ...
1. Introduction. Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder (NDD) presenting with inattention, hyperactivity, and impulsivity. It can be classified in three subtypes, depending on the intensity of the symptoms: predominantly inattentive, predominantly hyperactive-impulsive, and combined [ 1, 2 ].
W ellington, 6012, New Zealand. EXPLANA TION OF EA TING DISORDERS 1. Abstract. Eating disorders (EDs) are one of the most severe and complex mental health problems. facing researchers and ...
Conclusion. Bipolar disorder is a mental disorder that is characterized by extreme mood changes that range from mania to depression. Risk factors include lifestyle, genetics, environment, drug and alcohol abuse, and major life changes such as death or abuse. Symptoms depend on the type of mod.
Bursts of brain rhythms with "beta" frequencies control where and when neurons in the cortex process sensory information and plan responses. Studying these bursts would improve understanding of cognition and clinical disorders, researchers write.
Stanford Medicine research on Timothy syndrome — which predisposes newborns to autism and epilepsy — may extend well beyond the rare genetic disorder to schizophrenia and other conditions. Brain organoids and assembloids are new models for elucidating, treating neurodevelopmental disorders | News Center | Stanford Medicine
At least four-in-ten U.S. adults (41%) have experienced high levels of psychological distress at some point during the pandemic, according to four Pew Research Center surveys conducted between March 2020 and September 2022. Young adults are especially likely to have faced high levels of psychological distress since the COVID-19 outbreak began: 58% of Americans ages 18 to 29 fall into this ...
Research method helps overcome obstacles to genetic diagnoses To overcome this challenge, researchers led by first author Dr. Shenglan Li, staff scientist in Liu's lab at Baylor, converted fibroblasts obtained in skin biopsies to neurons in a process called transdifferentiation. "This method activates neuron-specific gene expression and ...
Emerging research strongly supports that for many, eating disorders are brain-based illnesses and in most cases, there exists a co-morbidity like anxiety, mood disorders, or substance abuse.
Abstract and Figures. There is a commonly held view that eating disorders are lifestyle choice. Eating disorders are actually serious and often fatal illnesses, obsessions with food, body weight ...
April 22, 2024. Substance use disorders are underdiagnosed and undertreated among formerly incarcerated Virginians, new VCU-led study finds Research collaboration with the Virginia Department of Medical Assistance Services highlights health disparities affecting Medicaid members with addiction - and some of the barriers they face.
Introduction. Eating disorders (EDs) are a class of severe mental illnesses 1 that affect 1.25 million people in the UK. 2 They are characterised by abnormal eating behaviours and attitudes that have a significant impact on the physical health of those suffering, 3 resulting in complications including osteoporosis and cardiac arrhythmias. 4 These go hand in hand with psychiatric comorbidities ...
Gene editing has the potential to solve fundamental challenges in agriculture, biotechnology, and human health. CRISPR-based gene editors derived from microbes, while powerful, often show significant functional tradeoffs when ported into non-native environments, such as human cells. Artificial intelligence (AI) enabled design provides a powerful alternative with potential to bypass ...
The FY24 Defense Appropriations Act provides funding for the Alcohol and Substance Use Disorders Research Program (ASUDRP) to support research of exceptional scientific merit in the area of alcohol, opioid and other substance use disorders research. The managing agent for the anticipated program announcements/funding opportunities is the CDMRP ...
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions.