Heart Attack Symptoms, Risk, and Recovery
What is a heart attack.
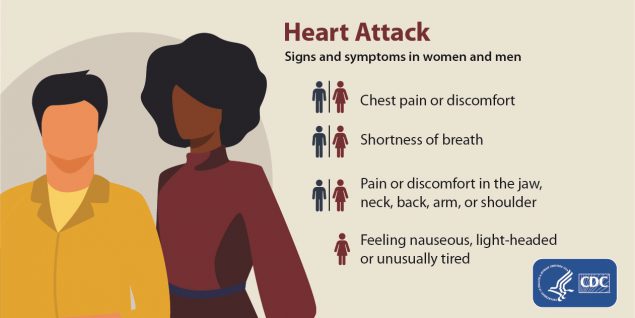
Heart attack signs and symptoms in men and women: Chest pain or discomfort; Shortness of breath; Pain or discomfort in the jaw, neck, back, arm, or shoulder; Feeling nauseous, light-headed, or unusually tired.
A heart attack, also called a myocardial infarction, happens when a part of the heart muscle doesn’t get enough blood.
The more time that passes without treatment to restore blood flow, the greater the damage to the heart muscle.
Coronary artery disease (CAD) is the main cause of heart attack. A less common cause is a severe spasm, or sudden contraction, of a coronary artery that can stop blood flow to the heart muscle.

What are the symptoms of heart attack?
The major symptoms of a heart attack are
- Chest pain or discomfort. Most heart attacks involve discomfort in the center or left side of the chest that lasts for more than a few minutes or that goes away and comes back. The discomfort can feel like uncomfortable pressure, squeezing, fullness, or pain.
- Feeling weak, light-headed, or faint. You may also break out into a cold sweat.
- Pain or discomfort in the jaw, neck, or back.
- Pain or discomfort in one or both arms or shoulders.
- Shortness of breath. This often comes along with chest discomfort, but shortness of breath also can happen before chest discomfort.
Other symptoms of a heart attack could include unusual or unexplained tiredness and nausea or vomiting. Women are more likely to have these other symptoms. Learn more about women and heart disease .
Every 40 seconds, someone in the United States has a heart attack. 1 Learn more facts about heart attack and heart disease.
Call 9-1-1 if you notice symptoms of a heart attack.
If you notice the symptoms of a heart attack in yourself or someone else, call 9-1-1 immediately . The sooner you get to an emergency room, the sooner you can get treatment to reduce the amount of damage to the heart muscle. At the hospital, health care professionals can run tests to find out if a heart attack is happening and decide the best treatment.
In some cases, a heart attack requires cardiopulmonary resuscitation (CPR) or an electrical shock (defibrillation) to the heart to get the heart pumping again. Bystanders trained to use CPR or a defibrillator may be able to help until emergency medical personnel arrive.
Remember, the chances of surviving a heart attack are better the sooner emergency treatment begins.
What are the risk factors for heart attack?
Several health conditions, your lifestyle, and your age and family history can increase your risk for heart disease and heart attack. These are called risk factors. About half of all Americans have at least one of the three key risk factors for heart disease: high blood pressure, high blood cholesterol, and smoking. 2
Some risk factors cannot be controlled, such as your age or family history. But you can take steps to lower your risk by changing the factors you can control.
Learn more about risk factors for heart disease and heart attack.
What can I do to recover after a heart attack?
If you’ve had a heart attack, your heart may be damaged. This could affect your heart’s rhythm and its ability to pump blood to the rest of the body. You may also be at risk for another heart attack or conditions such as stroke , kidney disorders, and peripheral arterial disease (PAD).
You can lower your chances of having future health problems following a heart attack with these steps:
- Physical activity —Talk with your health care team about the things you do each day in your life and work. Your doctor may want you to limit work, travel, or sexual activity for some time after a heart attack.
- Lifestyle changes —Eating a healthier diet, increasing physical activity, quitting smoking, and managing stress—in addition to taking prescribed medicines—can help improve your heart health and quality of life. Ask your health care team about attending a program called cardiac rehabilitation to help you make these lifestyle changes.
- Physical activity
- Education about healthy living, including healthy eating, taking medicine as prescribed, and ways to help you quit smoking
- Counseling to find ways to relieve stress and improve mental health
A team of people may help you through cardiac rehab, including your health care team, exercise and nutrition specialists, physical therapists, and counselors or mental health professionals.

More Information
- American Heart Association: Heart Attack
- National Heart, Lung, and Blood Institute: Heart Attack
- Tsao CW, Aday AW, Almarzooq ZI, Beaton AZ, Bittencourt MS, Boehme AK, et al. Heart Disease and Stroke Statistics—2023 Update: A Report From the American Heart Association . 2023;147:e93–e621.
- Fryar CD, Chen T-C, Li X. Prevalence of uncontrolled risk factors for cardiovascular disease: United States, 1999–2010 [PDF-494K] . NCHS data brief, no. 103. Hyattsville, MD: National Center for Health Statistics; 2012. Accessed May 9, 2019.
Division for Heart Disease and Stroke Prevention
- High Blood Pressure
- Cholesterol
- Million Hearts ®
- WISEWOMAN Program
- Physical Activity
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Myocardial infarction.
Niranjan Ojha ; Amit S. Dhamoon .
Affiliations
Last Update: August 8, 2023 .
- Continuing Education Activity
Myocardial infarction (MI), colloquially known as "heart attack," is caused by decreased or complete cessation of blood flow to a portion of the myocardium. Myocardial infarction may be"silent," and go undetected, or it could be a catastrophic event leading to hemodynamic deterioration and sudden death. Most myocardial infarctions are due to underlying coronary artery disease, the leading cause of death in the United States. With coronary artery occlusion, the myocardium is deprived of oxygen. Prolonged deprivation of oxygen supply to the myocardium can lead to myocardial cell death and necrosis. Patients can present with chest discomfort or pressure that can radiate to the neck, jaw, shoulder, or arm. In addition to the history and physical exam, myocardial ischemia may be associated with ECG changes and elevated biochemical markers such as cardiac troponins. This activity describes the pathophysiology, evaluation, and management of myocardial infarction and highlights the role of the interprofessional team in improving care for affected patients.
- Review the basic pathophysiology of myocardial infarction.
- Explain the management protocol when presented with acute myocardial infarction, including all necessary laboratory and other diagnostic testing.
- Summarize the long-term management and rehabilitation for a patient post-MI.
- Explain interprofessional team strategies for improving care coordination and communication to advance the prevention and management of myocardial infarction leading to improved outcomes.
- Introduction
Myocardial infarction (MI), colloquially known as “heart attack,” is caused by decreased or complete cessation of blood flow to a portion of the myocardium. Myocardial infarction may be “silent” and go undetected, or it could be a catastrophic event leading to hemodynamic deterioration and sudden death. [1] Most myocardial infarctions are due to underlying coronary artery disease, the leading cause of death in the United States. With coronary artery occlusion, the myocardium is deprived of oxygen. Prolonged deprivation of oxygen supply to the myocardium can lead to myocardial cell death and necrosis. [2] Patients can present with chest discomfort or pressure that can radiate to the neck, jaw, shoulder, or arm. In addition to the history and physical exam, myocardial ischemia may be associated with ECG changes and elevated biochemical markers such as cardiac troponins. [3] [4]
As stated above, myocardial infarction is closely associated with coronary artery disease. INTERHEART is an international multi-center case-control study which delineated the following modifiable risk factors for coronary artery disease: [5] [6]
- Abnormal lipid profile/blood apolipoprotein (raised ApoB/ApoA1)
- Hypertension
- Diabetes mellitus
- Abdominal obesity (waist/hip ratio) (greater than 0.90 for males and greater than 0.85 for females)
- Psychosocial factors such as depression, loss of the locus of control, global stress, financial stress, and life events including marital separation, job loss, and family conflicts
- Lack of daily consumption of fruits or vegetables
- Lack of physical activity
- Alcohol consumption (weaker association, protective)
The INTERHEART study showed that all the above risk factors were significantly associated with acute myocardial infarction except for alcohol consumption, which showed a weaker association. Smoking and abnormal apolipoprotein ratio showed the strongest association with acute myocardial infarction. The increased risk associated with diabetes and hypertension were found to be higher in women, and the protective effect of exercise and alcohol was also found to be higher in women. [5]
Other risk factors include a moderately high level of plasma homocysteine, which is an independent risk factor of MI. Elevated plasma homocysteine is potentially modifiable and can be treated with folic acid, vitamin B6, and vitamin B12. [7]
Some non-modifiable risk factors for myocardial infarction include advanced age, male gender (males tend to have myocardial infarction earlier in life), genetics (there is an increased risk of MI if a first-degree relative has a history of cardiovascular events before the age of 50). [6] [8] The role of genetic loci that increase the risk for MI is under active investigation. [9] [10]
- Epidemiology
The most common cause of death and disability in the western world and worldwide is coronary artery disease. [11] Based on 2015 mortality data from the National Health Interview Survey (NHIS-CDC), MI mortality was 114,023, and MI any-mention mortality (i.e., MI is mentioned as a contributing factor in the death certificate) was 151,863.
As per the National Health and Nutrition Examination Survey (NHANES)-CDC data from 2011 to 2014, an estimated 16.5 million Americans older than 20 years of age have coronary artery disease, and the prevalence was higher in males than females for all ages. As per the NHANES 2011 through 2014, the overall prevalence of MI is 3.0% in US adults older than 20 years of age.
Prevalence of MI in the US Sub-populations
Non-Hispanic Whites
- 4.0% (Male)
- 2.4% (Female)
Non-Hispanic Blacks
- 3.3% (Male)
- 2.2% (Female)
- 2.9% (Male)
- 2.1% (Female)
Non-Hispanic Asians
- 2.6% (Male)
- 0.7% (Female)
Based on the Atherosclerosis Risk in Communities Study (ARIC) performed by National Heart, Lung, and Blood Institute (NHLBI) collected between 2005 and 2014, the estimated annual incidence is 605,000 new MIs and 200,000 recurrent MIs. [12]
The ARIC study also found that the average age at first MI is 65.6 years for males and 72.0 years for females. In the past decades, several studies have shown a declining incidence of MI in the United States. [12]
- Pathophysiology
The acute occlusion of one or multiple large epicardial coronary arteries for more than 20 to 40 minutes can lead to acute myocardial infarction. The occlusion is usually thrombotic and due to the rupture of a plaque formed in the coronary arteries. The occlusion leads to a lack of oxygen in the myocardium, which results in sarcolemmal disruption and myofibril relaxation. [2] These changes are one of the first ultrastructural changes in the process of MI, which are followed by mitochondrial alterations. The prolonged ischemia ultimately results in liquefactive necrosis of myocardial tissue. The necrosis spreads from sub-endocardium to sub-epicardium. The subepicardium is believed to have increased collateral circulation, which delays its death. [2] Depending on the territory affected by the infarction, the cardiac function is compromised. Due to the negligible regeneration capacity of the myocardium, the infarcted area heals by scar formation, and often, the heart is remodeled characterized by dilation, segmental hypertrophy of remaining viable tissue, and cardiac dysfunction. [13]
- History and Physical
The imbalance between oxygen supply and the demand leads to myocardial ischemia and can sometimes lead to myocardial infarction. The patient’s history, electrocardiographic findings, and elevated serum biomarkers help identify ischemic symptoms. Myocardial ischemia can present as chest pain, upper extremity pain, mandibular, or epigastric discomfort that occurs during exertion or at rest. Myocardial ischemia can also present as dyspnea or fatigue, which are known to be ischemic equivalents. [14] The chest pain is usually retrosternal and is sometimes described as the sensation of pressure or heaviness. The pain often radiates to the left shoulder, neck, or arms with no obvious precipitating factors, and it may be intermittent or persistent. The pain usually lasts for more than 20 minutes. [15] It is usually not affected by positional changes or active movement of the region. Additional symptoms, such as sweating, nausea, abdominal pain, dyspnea, and syncope, may also be present. [14] [16] [17] The MI can also present atypically with subtle findings such as palpitations, or more dramatic manifestations, such as cardiac arrest. The MI can sometimes present with no symptoms. [18]
The three components in the evaluation of the MI are clinical features, ECG findings, and cardiac biomarkers.
The resting 12 lead ECG is the first-line diagnostic tool for the diagnosis of acute coronary syndrome (ACS). It should be obtained within 10 minutes of the patient’s arrival in the emergency department. [17] Acute MI is often associated with dynamic changes in the ECG waveform. Serial ECG monitoring can provide important clues to the diagnosis if the initial EKG is non-diagnostic at initial presentation. [14] Serial or continuous ECG recordings may help determine reperfusion or re-occlusion status. A large and prompt reduction in ST-segment elevation is usually seen in reperfusion. [14]
ECG findings suggestive of ongoing coronary artery occlusion (in the absence of left ventricular hypertrophy and bundle branch block): [19]
ST-segment elevation in two contiguous lead (measured at J-point) of
- Greater than 5 mm in men younger than 40 years, greater than 2 mm in men older than 40 years, or greater than 1.5 mm in women in leads V2-V3 and/or
- Greater than 1 mm in all other leads
ST-segment depression and T-wave changes
- New horizontal or down-sloping ST-segment depression greater than 5 mm in 2 contiguous leads and/or T inversion greater than 1 mm in two contiguous leads with prominent R waves or R/S ratio of greater than 1
The hyperacute T-wave amplitude, with prominent symmetrical T waves in two contiguous leads, maybe an early sign of acute MI that may precede the ST-segment elevation. Other ECG findings associated with myocardial ischemia include cardiac arrhythmias, intraventricular blocks, atrioventricular conduction delays, and loss of precordial R-wave amplitude (less specific finding). [14]
ECG findings alone are not sufficient to diagnose acute myocardial ischemia or acute MI as other conditions such as acute pericarditis, left ventricular hypertrophy (LVH), left bundle branch block (LBBB), Brugada syndrome, Takatsubo syndrome (TTS), and early repolarization patterns also present with ST deviation.
ECG changes associated with prior MI (in the absence of left ventricular hypertrophy and left bundle branch block):
- Any Q wave in lead V2-V3 greater than 0.02 s or QS complex in leads V2-V3
- Q wave > 03 s and greater than 1 mm deep or QS complex in leads I, II, aVL, aVF or V4-V6 in any two leads of contiguous lead grouping (I, aVL; V1-V6; II, III, aVF)
- R wave > 0.04 s in V1-V2 and R/S greater than 1 with a concordant positive T wave in the absence of conduction defect.
Biomarker Detection of MI
Cardiac troponins (I and T) are components of the contractile apparatus of myocardial cells and expressed almost exclusively in the heart. Elevated serum levels of cardiac troponin are not specific to the underlying mode of injury (ischemic vs. tension) [14] [20] . The rising and/or falling pattern of cardiac troponins (cTn) values with at least one value above the 99 percentile of upper reference limit (URL) associated with symptoms of myocardial ischemia would indicate an acute MI. Serial testing of cTn values at 0 hours, 3 hours, and 6 hours would give a better perspective on the severity and time course of the myocardial injury. Depending on the baseline cTn value, the rising/falling pattern is interpreted. If the cTn baseline value is markedly elevated, a minimum change of greater than 20% in follow up testing is significant for myocardial ischemia. Creatine kinase MB isoform can also be used in the diagnosis of MI, but it is less sensitive and specific than cTn level. [4] [21]
Different imaging techniques are used to assess myocardial perfusion, myocardial viability, myocardial thickness, thickening and motion, and the effect of myocyte loss on the kinetics of para-magnetic or radio-opaque contrast agents indicating myocardial fibrosis or scars. [14] Some imaging modalities that can be used are echocardiography, radionuclide imaging, and cardiac magnetic resonance imaging (cardiac MRI). Regional wall motion abnormalities induced by ischemia can be detected by echocardiography almost immediately after the onset of ischemia when greater than 20% transmural myocardial thickness is affected. Cardiac MRI provides an accurate assessment of myocardial structure and function. [14]
- Treatment / Management
Acute Management
Reperfusion therapy is indicated in all patients with symptoms of ischemia of less than 12-hours duration and persistent ST-segment elevation. Primary percutaneous coronary intervention (PCI) is preferred to fibrinolysis if the procedure can be performed <120 minutes of ECG diagnosis. If there is no immediate option of PCI (>120 minutes), fibrinolysis should be started within 10 minutes of STEMI after ruling out contraindications. If transfer to a PCI center is possible in 60 to 90 minutes after a bolus of the fibrinolytic agent and patient meets reperfusion criteria, a routine PCI can be done, or a rescue PCI can be planned. [19] [17] If fibrinolysis is planned, it should be carried out with fibrin-specific agents such as tenecteplase, alteplase, or reteplase (class I). [19]
Relief of pain, breathlessness, and anxiety: The chest pain due to myocardial infarction is associated with sympathetic arousal, which causes vasoconstriction and increased workload for the ischemic heart. Intravenous opioids (e.g., morphine) are the analgesics most commonly used for pain relief (Class IIa). [19] The results from CRUSADE quality improvement initiative have shown that the use of morphine may be associated with a higher risk of death and adverse clinical outcomes. [22] The study was done from the CIRCUS (Does Cyclosporine Improve outcome in STEMI patients) database, which showed no significant adverse events associated with morphine use in a case of anterior ST-segment elevation MI. [23] A mild anxiolytic (usually a benzodiazepine) may be considered in very anxious patients (class IIa). Supplemental oxygen is indicated in patients with hypoxemia (SaO2 <90% or PaO2 <60mm Hg) (Class I). [19]
Nitrates: Intravenous nitrates are more effective than sublingual nitrates with regard to symptom relief and regression of ST depression (NSTEMI). The dose is titrated upward until symptoms are relieved, blood pressure is normalized in hypertensive patients, or side effects such as a headache and hypotension are noted. [17]
Beta-blockers: This group of drugs reduces myocardial oxygen consumption by lowering heart rate, blood pressure, and myocardial contractility. They block beta receptors in the body, including the heart, and reduce the effects of circulating catecholamines. Beta-blockers should not be used in suspected coronary vasospasm.
Platelet inhibition: Aspirin is recommended in both STEMI and NSTEMI in an oral loading dose of 150 to 300 mg (non-enteric coated formulation) and a maintenance dose of 75 to 100 mg per day long-term regardless of treatment strategy (class I). [17] Aspirin inhibits thromboxane A2 production throughout the lifespan of the platelet. [24]
Most P2Y12 inhibitors are inactive prodrugs (except for ticagrelor, which is an orally active drug that does not require activation) that require oxidation by hepatic cytochrome P450 system to generate an active metabolite which selectively inhibits P2Y12 receptors irreversibly. Inhibition of P2Y12 receptors leads to inhibition of ATP induced platelet aggregation. The commonly used P2Y12 inhibitors are clopidogrel, prasugrel, and ticagrelor.
The loading dose for clopidogrel is 300 to 600 mg loading dose followed by 75 mg per day.
Prasugrel, 60 mg loading dose, and 10 mg per day of a maintenance dose have a faster onset when compared to clopidogrel. [19]
Patients undergoing PCI should be treated with dual antiplatelet therapy (DAPT) with aspirin + P2Y12 inhibitor and a parenteral anticoagulant. In PCI, the use of prasugrel or ticagrelor is found to be superior to clopidogrel. Aspirin and clopidogrel are also found to decrease the number of ischemic events in NSTEMI and UA. [17]
The anticoagulants used during PCI are unfractionated heparin, enoxaparin, and bivalirudin. The bivalirudin is recommended during primary PCI if the patient has heparin-induced thrombocytopenia. [19]
Long-Term Management
Lipid-lowering treatment: It is recommended to start high-intensity statins that reduce low-density lipoproteins (LDLs) and stabilize atherosclerotic plaques. High-density lipoproteins are found to be protective. [19]
Antithrombotic therapy: Aspirin is recommended lifelong, and the addition of another agent depends on the therapeutic procedure done, such as PCI with stent placement.
ACE inhibitors are recommended in patients with systolic left ventricular dysfunction, or heart failure, hypertension, or diabetes.
Beta-blockers are recommended in patients with LVEF less than 40% if no other contraindications are present.
Antihypertensive therapy can maintain a blood pressure goal of less than 140/90 mm Hg.
Mineralocorticoid receptor antagonist therapy is recommended in a patient with left ventricular dysfunction (LVEF less than 40%).
Glucose lowering therapy in people with diabetes to achieve current blood sugar goals. [19]
Lifestyle Modifications
Smoking cessation is the most cost-effective secondary measure to prevent MI. Smoking has a pro-thrombotic effect, which has a strong association with atherosclerosis and myocardial infarction. [6]
Diet, alcohol, and weight control: A diet low in saturated fat with a focus on whole grain products, vegetables, fruits, and the fish is considered cardioprotective. The target level for bodyweight is body mass index of 20 to 25 kg/m2 and waist circumference of <94 cm for the men and <80 cm for the female. [25]
- Differential Diagnosis
- Angina pectoris
- Non-ST segment elevation myocardial infarction (NSTEMI)
- ST-segment elevation myocardial infarction (STEMI)
- Pulmonary embolism
- Pneumothorax
Despite many advances in treatment, acute MI still carries a mortality rate of 5-30%; the majority of deaths occur prior to arrival to the hospital. In addition, within the first year after an MI, there is an additional mortality rate of 5% to 12%. The overall prognosis depends on the extent of heart muscle damage and ejection fraction. Patients with preserved left ventricular function tend to have good outcomes. Factors that worsen prognosis include:
- Advanced age
- Delayed reperfusion
- Low ejection fraction
- Presence of congestive heart failure
- Elevations in C-reactive protein and B-type natriuretic peptide ( BNP ) levels
- Complications
Type and Manifestation
I: Ischemic
- Reinfarction
- Extension of infarction
II: Arrhythmias
- Supraventricular or ventricular arrhythmia
- Sinus bradycardia and atrioventricular block
III: Mechanical
- Myocardial dysfunction
- Cardiac failure
- Cardiogenic shock
- Cardiac rupture (Free wall rupture, ventricular septal rupture, papillary muscle rupture)
IV: Embolic
- Left ventricular mural thrombus,
- Peripheral embolus
V: Inflammatory
- Pericarditis (infarct associated pericarditis, late pericarditis, or post-cardiac injury pericarditis)
- Pericardial effusion
- Enhancing Healthcare Team Outcomes
The diagnosis and management of patients with ischemic heart disease are best done with an interprofessional team. In most hospitals, there are cardiology teams that are dedicated to the management of these patients.
For patients who present with chest pain, the key to the management of MI is time to treatment. Thus, healthcare professionals, including nurses who work in the emergency department, must be familiar with the symptoms of MI and the importance of rapid triage. A cardiology consult should be made immediately to ensure that the patient gets treated within the time frame recommendations. Because MI can be associated with several serious complications, these patients are best managed in an ICU setting.
There is no cure for ischemic heart disease, and all treatments are symptom-oriented. The key to improving outcomes is to prevent coronary artery disease. The primary care provider and nurse practitioner should educate the patient on the benefits of a healthy diet, the importance of controlling blood pressure and diabetes, exercising regularly, discontinuing smoking, maintaining healthy body weight, and remaining compliant with medications. The pharmacist should educate the patient on types of medication used to treat ischemic heart disease, their benefits, and potential adverse effects.
Only through such a team approach can the morbidity and mortality of myocardial infarction be lowered. [Level 5]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Myocardial Infarction (Heart Attack) Warning Signs in Women. U.S. Department of Health and Human Services Office on Women's Health
ECG With Pardee Waves Indicating AMI. Pardee waves indicate acute myocardial infarction in the inferior leads II, III, and aVF with reciprocal changes in the anterolateral leads. Wikimedia Commons, Glenlarson
Transesophageal echocardiography, Thrombo embolism, Pulmonary artery, Pulmonary Embolism, Thromboembolic , Right Pulmonary artery, TE, RPA, Acute ECG segment elevation mimicking myocardial infarction in a patient with pulmonary embolism Contribute by (more...)
Ischemic ventricular tachycardia in a patient with an old inferior myocardial infarction Contributed by Alina Negru, MD
Disclosure: Niranjan Ojha declares no relevant financial relationships with ineligible companies.
Disclosure: Amit Dhamoon declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Ojha N, Dhamoon AS. Myocardial Infarction. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Myocardial Infarction (Nursing). [StatPearls. 2024] Myocardial Infarction (Nursing). Ojha N, Dhamoon AS, Chapagain R. StatPearls. 2024 Jan
- Review Context-independent identification of myocardial ischemia in the prehospital ECG of chest pain patients. [J Electrocardiol. 2024] Review Context-independent identification of myocardial ischemia in the prehospital ECG of chest pain patients. Swenne CA, Ter Haar CC. J Electrocardiol. 2024 Jan-Feb; 82:34-41. Epub 2023 Nov 7.
- Enhanced External Counterpulsation (EECP): An Evidence-Based Analysis. [Ont Health Technol Assess Ser....] Enhanced External Counterpulsation (EECP): An Evidence-Based Analysis. Medical Advisory Secretariat. Ont Health Technol Assess Ser. 2006; 6(5):1-70. Epub 2006 Mar 1.
- Association of Silent Myocardial Infarction and Sudden Cardiac Death. [JAMA Cardiol. 2019] Association of Silent Myocardial Infarction and Sudden Cardiac Death. Vähätalo JH, Huikuri HV, Holmström LTA, Kenttä TV, Haukilahti MAE, Pakanen L, Kaikkonen KS, Tikkanen J, Perkiömäki JS, Myerburg RJ, et al. JAMA Cardiol. 2019 Aug 1; 4(8):796-802.
- Review Prevention of ventricular fibrillation, acute myocardial infarction (myocardial necrosis), heart failure, and mortality by bretylium: is ischemic heart disease primarily adrenergic cardiovascular disease? [Am J Ther. 2004] Review Prevention of ventricular fibrillation, acute myocardial infarction (myocardial necrosis), heart failure, and mortality by bretylium: is ischemic heart disease primarily adrenergic cardiovascular disease? Bacaner M, Brietenbucher J, LaBree J. Am J Ther. 2004 Sep-Oct; 11(5):366-411.
Recent Activity
- Myocardial Infarction - StatPearls Myocardial Infarction - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Healthdirect Free Australian health advice you can count on.
Medical problem? Call 1800 022 222. If you need urgent medical help, call triple zero immediately
healthdirect Australia is a free service where you can talk to a nurse or doctor who can help you know what to do.
Heart attack
12-minute read
Share via email
There is a total of 5 error s on this form, details are below.
- Please enter your name
- Please enter your email
- Your email is invalid. Please check and try again
- Please enter recipient's email
- Recipient's email is invalid. Please check and try again
- Agree to Terms required
Error: This is required
Error: Not a valid value
Call triple zero (000) for an ambulance immediately if you or someone else may be having a heart attack.
- A heart attack occurs when the blood supply to your heart is blocked and your heart muscle can’t get enough oxygen.
- Common symptoms of a heart attack are chest pain, feeling breathless and sweating.
- Heart attacks are mostly caused by coronary heart disease.
- You can reduce your risk of having a heart attack by adopting a healthy lifestyle.
What is a heart attack?
To work properly, your heart needs a continuous supply of blood. It normally receives this from blood vessels called coronary arteries.
When a coronary artery suddenly becomes blocked, oxygen can’t get to your heart muscle. This causes a heart attack (or ‘myocardial infarction’).
A heart attack is a medical emergency: without oxygen, your heart muscle begins to die and your heart can become permanently damaged.
Heart attacks can be fatal — every day, 17 Australians die from a heart attack. One patient is admitted to hospital due to heart attack every 13 minutes.
What are the symptoms of a heart attack?
If you have any of the symptoms below, you could be having a heart attack. If symptoms are severe, get worse, or last longer than 10 minutes, call triple zero (000) immediately and ask for an ambulance. If calling triple zero (000) does not work on your mobile, try calling 112.
The most common symptoms of a heart attack are:
- chest pain — pressure or tightness in your chest that may spread to your jaw, neck or left arm
- suddenly feeling dizzy , faint , light-headed or anxious
- nausea or vomiting
- a feeling of indigestion
- sweating, or a cold sweat
- looking pale
- shortness of breath or difficulty breathing
- palpitations (being aware of your heart beating)
Chest pain may come and go.
Heart attack symptoms in females
Females may experience different symptoms, such as:
- breathlessness and generally feeling unwell
- tightness or discomfort in your arms
- chest pain that feels more like burning, throbbing, tightness or like trapped wind
- a feeling of indigestion or upper tummy pain
- upper back pain or pressure
Heart attack symptoms differ from person to person. Some people experience no warning signs before a heart attack. It’s possible to not feel any chest pain at all.
CHECK YOUR SYMPTOMS — Use the Symptom Checker and find out if you need to seek medical help.
What causes heart attacks?
The most common cause of a heart attack is coronary artery disease . This is where fatty deposits, cholesterol and other substances build up in the walls of your coronary arteries that supply oxygen to your heart.
Over time, this build-up hardens into cholesterol plaques. The plaque can rupture (burst) and cause a blood clot which blocks your artery.
In some cases, heart attacks have another cause.
- Coronary artery spasm (variant angina) is an unusual narrowing of blood vessels that can stop blood flow to your heart.
- Spontaneous coronary artery dissection is a sudden tear in the wall of your coronary artery.
Certain lifestyle factors are shown to increase your chances of having a heart attack. These include:
- an unhealthy diet high in saturated fat , salt and added sugar
- not getting enough physical activity
- having high blood pressure
- having high cholesterol
- having diabetes
- being overweight or obese
When should I see my doctor?
Call triple zero (000) immediately and ask for an ambulance, if you or someone near you experiences symptoms of a heart attack that are:
- getting worse, or
- lasting longer than 10 minutes
If calling triple zero (000) does not work on your mobile, try calling 112. Early treatment could save a life.
See your doctor regularly to manage your health. Your doctor can test for heart disease risk factors and help you take steps to prevent a heart attack.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
How are heart attacks diagnosed?
If you think you might be having a heart attack, you need immediate assessment in hospital. There, a doctor will assess your symptoms and check your vital signs, including your blood pressure , pulse and temperature.
There are several tests that help show if you’ve had a heart attack, and whether any damage was caused. These include:
- electrocardiogram (ECG) — electrical leads are placed on your chest, arms and legs to record the electrical signals travelling through your heart muscle
- troponin blood tests
- chest x-ray
- angiography (or, cardiac catheterisation ) — a small tube (catheter) is inserted into an artery in your groin or your wrist, which can then be guided to your heart where a special dye is injected into the coronary arteries to show if there is a narrowing or blockage
- echocardiogram — an ultrasound scan of your heart
- CT scan or MRI scan of the heart
How are heart attacks treated?
When treating a heart attack it is important to restore blood flow to your heart quickly. Heart muscle cells depend on oxygen and the longer your heart is without oxygen, the more permanent and widespread the damage.
Treating the blocked artery
Treatments that can restore blood flow to your heart include the following.
- Coronary angioplasty is a procedure where the blocked coronary artery is opened up from the inside using a special balloon inserted during cardiac catheterisation. Your artery may then be kept open with a special metal tube (stent).
- Thrombolytic therapy uses a medicine to dissolve the blood clot in your blocked coronary artery.
- Bypass surgery ( coronary artery bypass graft surgery , or CABG) is open heart surgery that involves redirecting blood to bypass (go around) the blockage in your coronary artery.
Medications
Medicines are given to treat a heart attack and prevent the risk of another heart attack. These include:
- pain relievers
- medicines that reduce the blood’s clotting action, such as aspirin , or other blood-thinning medicines
- nitrate medicines to improve blood flow through the coronary arteries
- heart and blood pressure medicines ( ACE inhibitors, angiotensin II receptor blockers , beta blockers )
- cholesterol-lowering medicines
Cardiac rehabilitation
If you are recovering from a heart attack you may be referred for cardiac rehabilitation. This service provides support during your recovery and helps reduce your risk of heart disease.
ASK YOUR DOCTOR — Preparing for an appointment? Use the Question Builder for general tips on what to ask your GP or specialist.
How can I prevent a heart attack?
Making positive lifestyle changes is the best way to lower your risk of a heart attack.
There are a number of ways you can improve your heart health:
- quitting smoking
- eating a healthy diet
- seeing your doctor to help manage your cholesterol and blood pressure
- staying physically active and exercising regularly
- maintaining a healthy weight
- drinking alcohol in moderation
- reducing stress and looking after your mental wellbeing
There are also other risk factors that you can’t control, like your: age, sex, ethnicity and family history .
Speak with your doctor if you’re concerned about your risk factors. They can give you tips on how you can reduce your risk of a heart attack.
ARE YOU AT RISK? — Are you at risk of type 2 diabetes, heart disease or kidney disease? Use the Risk Checker to find out.
NEED TO LOSE WEIGHT? — Use the BMI Calculator to find out if your weight and waist size are in a healthy range.
Complications of a heart attack
Complications following a heart attack can be serious. Some complications include the following:
- Arrhythmias — your heart may develop an abnormal heartbeat following a heart attack due to your damaged heart muscle disrupting electrical signals.
- Heart failure — your heart may have difficulty pumping enough blood, due to the muscles being too weak or too stiff.
- Cardiogenic shock — a life-threatening condition where your heart suddenly can’t pump enough blood to your body.
- Heart rupture — this is a rare but serious complication in which your heart’s muscles, walls or valves split apart.
Is a cardiac arrest the same thing as a heart attack?
A cardiac arrest and a heart attack are both medical emergencies. However, they are not the same thing.
During a cardiac arrest, the electrical system that controls your heart rate and rhythm stops working properly, and your heart stops beating.
Someone having a cardiac arrest will collapse and have no pulse. They may not breathe properly, or not at all, and they will lose consciousness.
If someone has a cardiac arrest, they need help immediately. Call 000 (triple zero) for an ambulance.
While waiting for the ambulance to arrive, begin chest compressions (cardiopulmonary resuscitation or CPR). Use a device called a defibrillator , if available.
Sometimes a heart attack can progress into a cardiac arrest.
Does COVID-19 cause heart attacks?
A heart attack is a possible complication of COVID-19 . COVID-19 can also worsen existing heart conditions.
When people with cardiovascular disease catch COVID-19, they have a higher risk of severe complications.
Get vaccinated against COVID-19 and the flu to help protect yourself and others.
The Heart Foundation has more information about COVID-19 and heart disease .
Life after a heart attack
Recovering from a heart attack can be both emotionally and physically challenging. Hearing stories from others who have experienced a heart attack can help.
The Heart Foundation have shared several people’s "heart stories" on their website.
Resources and support
Support and information on heart attack and heart health are also available from the Heart Foundation .
The Heart Foundation has a warning signs of heart attack action plan . There are instructions on what to do if you have chest pain or other possible signs of a heart attack.
You can also call the healthdirect helpline on 1800 022 222 (known as NURSE-ON-CALL in Victoria). A registered nurse is available to speak with 24 hours a day, 7 days a week.
Other languages
Do you prefer to read languages other than English? The Heart Foundation has fact sheets on heart health translated into more than 25 languages .
Learn more here about the development and quality assurance of healthdirect content .
Last reviewed: November 2022
Related pages
- Heart attack symptoms: men vs women
Search our site for
- Heart health
- Angiography
- Troponin Test
Need more information?
These trusted information partners have more on this topic.
Top results
Will you recognise your heart attack?
What are the warning signs of a heart attack?
Read more on Heart Foundation website

Heart attack - Better Health Channel
Heart attack is an emergency. If you have warning signs of heart attack, get help fast. Call triple zero (000) and ask for an ambulance.
Read more on Better Health Channel website

Having one or more signs or symptoms of a heart attack means this is a life-threatening emergency—call triple zero (000) for an ambulance immediately.
Read more on St John Ambulance Australia website

Heart Attack | Heart Foundation
Understand what a heart attack is, its causes, the warning signs to look out for and what to do if you or someone you know is having one. Read more now
Heart attack - MyDr.com.au
A heart attack (myocardial infarction) means the blood supply to part of the heart muscle has become blocked. Early treatment can reduce muscle damage.
Read more on myDr website

Heart attack recovery – first month | The Heart Foundation
A heart attack can be a life-changing event. Find out what to expect from your recovery in the first month after your heart attack. Read our guide.
Acute Coronary Syndromes (Heart Attack and Suspected Heart Attack) Clinical Care Standard: Consumer fact sheet | Australian Commission on Safety and Quality in Health Care
Acute Coronary Syndromes (Heart Attack and Suspected Heart Attack) Clinical Care Standard: Consumer fact sheet Downloads Acute Coronary Syndromes (Heart Attack and Suspected Heart Attack) Clinical Care Standard: Consumer fact sheet Publication year 2014 Resource type Fact sheet or brochure Topics Clinical Care Standards Health conditions, diseases and treatments
Read more on Australian Commission on Safety and Quality in Health Care website

Physical activity after a heart attack | The Heart Foundation
With the ok from your doctor, it’s important to start doing physical activity after a heart attack. A cardiac rehab program is a great place to start.
Support after a heart attack | The Heart Foundation
Many different thoughts may go through your head after a heart attack and you may be presented with complicated medical info. Know where to get support.
Pericarditis - Better Health Channel
Pericarditis symptoms may be similar to those of heart attack and include chest pain and abnormal heart rhythms.
Cardiovascular disease risk factors and heart attack warning signs in women I Heart Foundation
Information for healthcare professionals and the public on cardiovascular disease risk factors and warning signs affecting women.
Quicker access to medical advice and life saving cardiac therapy
In the past, a doctor had to be with a person to diagnose a heart attack, but a new service that is being introduced in NSW allows an ECG to be sent quickly to a specialist doctor who may be many kilometres away. This means that people are treated much faster and, in many cases, even before they see a doctor.
Read more on ACI - Agency for Clinical Innovation website

Decision Aid: Statin/Aspirin Choice - Australasian Menopause Society
The electronic version of the Statin/Aspirin Choice Decision Aid, a randomised trial tested tool to help patients and clinicians discuss the pros and cons of statin and aspirin use to reduce the risk of heart attacks. The risk calculator allows you to use one of three methods of assessing risk of cardiovascular disease and whether the patient should be on extra medication. The best known is the Framingham calculator which has been used for many years. The Reynolds calculator has been designed
Read more on Australasian Menopause Society website


Troponin | Pathology Tests Explained
This test measures the level of troponin in your blood. Troponin is a protein found in muscle that helps it contract. There are three different troponins: tr
Read more on Pathology Tests Explained website

Creatine kinase MB (CKMB) | Pathology Tests Explained
CK–MB is one of three forms (or isoenzymes) of the enzyme creatine kinase (CK). CK–MB is found mostly in heart muscle. It rises when there is any damage to h
Creatine kinase (CK) | Pathology Tests Explained
Creatine kinase (CK) is a chemical known as an enzyme which is found in many tissues of the body and in several forms. When CK is routinely measured in the b
Lipoprotein (a) | Pathology Tests Explained
Lipoprotein (a) (Lp (a)) is a type of so-called `bad’ lipoprotein. Lipoproteins are tiny particles that carry cholesterol in the bloodstream. High levels of
Lactate dehydrogenase (LDH) | Pathology Tests Explained
Lactate dehydrogenase (LD) is an enzyme that is found in cells throughout the body. Only a small amount of LD is usually detectable in the
Clinical Management of Acute Coronary Syndromes | Ausmed
Acute coronary syndrome (ACS) is an umbrella term used to describe any situation where the blood supply to the heart is suddenly obstructed, including unstable angina and acute myocardial infarction. The main cause is atherosclerosis, a condition where plaque builds up and thickens the artery walls.
Read more on Ausmed Education website

Troponins in myocardial infarction and injury - Australian Prescriber
The detection of cardiac troponins in the blood is no longer synonymous with acute coronary syndrome.
Read more on Australian Prescriber website

Healthdirect Australia is not responsible for the content and advertising on the external website you are now entering.
Healthdirect 24hr 7 days a week hotline
24 hour health advice you can count on
1800 022 222
Government Accredited with over 140 information partners
We are a government-funded service, providing quality, approved health information and advice
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
© 2024 Healthdirect Australia Limited
Support for this browser is being discontinued
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.

Free first aid powerpoint presentations
Heart Attack
This medical emergency presentation covers heart attacks. Topics include
- What is a heart attack?
- Signs and symptoms of a heart attack
- First aid treatment for a heart attack
- Use of Aspirin
Download PowerPoint Presentation
Like us on Facebook!
Our powerpoint presentations.
- Basic First Aid Presentations
- Medical Emergencies Presentations
- Trauma Presentations
- Pediatric First Aid Presentations
- Advanced First Aid Presentations
Pin It on Pinterest
Appointments at Mayo Clinic
- Strategies to prevent heart disease
You can help prevent heart disease by following a heart-healthy lifestyle. Here are strategies to help you protect your heart.
Heart disease is a leading cause of death. You can't change some risk factors for it, such as family history, sex at birth or age. But you can take plenty of other steps to lower your risk of heart disease.
Get started with these eight tips to boost your heart health:
1. Don't smoke or use tobacco
One of the best things you can do for your heart is to stop smoking or using smokeless tobacco. Even if you're not a smoker, be sure to stay away from secondhand smoke.
Chemicals in tobacco can damage the heart and blood vessels. Cigarette smoke lowers the oxygen in the blood, which raises blood pressure and heart rate. That's because the heart has to work harder to supply enough oxygen to the body and brain.
There's good news though. The risk of heart disease starts to drop in as little as a day after quitting. After a year without cigarettes, the risk of heart disease drops to about half that of a smoker. No matter how long or how much you smoked, you'll start reaping rewards as soon as you quit.
2. Get moving: Aim for at least 30 to 60 minutes of activity daily
Regular, daily physical activity can lower the risk of heart disease. Physical activity helps control your weight. It also lowers the chances of getting other conditions that may put a strain on the heart. These include high blood pressure, high cholesterol and type 2 diabetes.
If you haven't been active for a while, you may need to slowly work your way up to these goals. But in general, you should aim for at least:
- 150 minutes a week of moderate aerobic exercise, such as walking at a brisk pace.
- 75 minutes a week of vigorous aerobic activity, such as running.
- Two or more strength training sessions a week.
Even shorter bouts of activity offer heart benefits. So if you can't meet those guidelines, don't give up. Just five minutes of moving can help. Activities such as gardening, housekeeping, taking the stairs and walking the dog all count toward your total. You don't have to exercise hard to benefit. But you can see bigger benefits if you boost the intensity, length and frequency of your workouts.
3. Eat a heart-healthy diet
A healthy diet can help protect the heart, improve blood pressure and cholesterol, and lower the risk of type 2 diabetes. A heart-healthy eating plan includes:
- Vegetables and fruits.
- Beans or other legumes.
- Lean meats and fish.
- Low-fat or fat-free dairy foods.
- Whole grains.
- Healthy fats such as olive oil and avocado.
Two examples of heart-healthy food plans include the Dietary Approaches to Stop Hypertension (DASH) eating plan and the Mediterranean diet.
Take in less of the following:
- Salt or high-sodium meals.
- Sugar or sweetened beverages.
- Highly refined carbohydrates.
- Highly processed food, such as processed meats.
- Saturated fat, which is found in red meat, full-fat dairy products, palm oil and coconut oil.
- Trans fat, which is found in some fried fast food, chips and baked goods.
4. Maintain a healthy weight
Being overweight — especially around the middle of the body — raises the risk of heart disease. Extra weight can lead to conditions that raise the chances of getting heart disease. These conditions include high blood pressure, high cholesterol and type 2 diabetes.
The body mass index (BMI) uses height and weight to find out whether a person is overweight or obese. A BMI of 25 or higher is considered overweight. In general, it's linked with higher cholesterol, higher blood pressure, and an increased risk of heart disease and stroke.
Waist circumference also can be a useful tool to measure how much belly fat you have. The risk of heart disease is higher if the waist measurement is greater than:
- 40 inches (101.6 centimeters, or cm) for men.
- 35 inches (88.9 cm) for women.
Even a small weight loss can be good for you. Reducing weight by just 3% to 5% can help lower certain fats in the blood called triglycerides. It can lower blood sugar, also called glucose. And it can cut the risk of type 2 diabetes. Losing even more helps lower blood pressure and blood cholesterol levels.
5. Get quality sleep
People who don't get enough sleep have a higher risk of obesity, high blood pressure, heart attack, diabetes and depression.
Most adults need at least seven hours of sleep each night. Children usually need more. So make sure you get enough rest. Set a sleep schedule and stick to it. To do that, go to bed and wake up at the same times each day. Keep your bedroom dark and quiet too, so it's easier to sleep.
Talk to a member of your health care team if you feel like you get enough sleep but you're still tired throughout the day. Ask if you need to be evaluated for obstructive sleep apnea. It's a condition that can raise your risk of heart disease. Symptoms of obstructive sleep apnea include loud snoring, stopping breathing for short times during sleep and waking up gasping for air. Treatment for obstructive sleep apnea may involve losing weight if you're overweight. It also might involve using a device that keeps your airway open while you sleep. This is called a continuous positive airway pressure (CPAP) device.
6. Manage stress
Ongoing stress can play a role in higher blood pressure and other risk factors for heart disease. Some people also cope with stress in unhealthy ways. For example, they may overeat, drink or smoke. You can boost your health by finding other ways to manage stress. Healthy tactics include physical activity, relaxation exercises, mindfulness, yoga and meditation.
If stress becomes overwhelming, get a health care checkup. Ongoing stress may be linked with mental health conditions such as anxiety and depression. These conditions also are tied to heart disease risk factors, including higher blood pressure and less blow flow to the heart. If you think you might have depression or anxiety, it's important to get treatment.
7. Get regular health screening tests
High blood pressure and high cholesterol can damage the heart and blood vessels. But if you don't get checked for these conditions, you likely won't know whether you have them. Regular screening tests can tell you what your numbers are and whether you need to take action.
Blood pressure. Regular blood pressure screenings usually start in childhood. Starting at age 18, blood pressure should be measured at least once every two years. This checks for high blood pressure as a risk factor for heart disease and stroke.
If you're between 18 and 39 and have risk factors for high blood pressure, you'll likely be screened once a year. People age 40 and older also are given a blood pressure test yearly.
- Cholesterol levels. The National Heart, Lung, and Blood Institute (NHLBI) recommends that cholesterol screenings start between the ages of 9 and 11. Earlier testing may be recommended if you have other risk factors, such as a family history of early-onset heart disease. After the first cholesterol test, screenings should be repeated every five years. Then the timing changes with age. The NHLBI recommends that women ages 55 to 65 and men ages 45 to 65 get screened every 1 to 2 years. People over 65 should get their cholesterol tested once a year.
- Type 2 diabetes screening. Diabetes involves ongoing high blood sugar levels. It raises the chances of getting heart disease. Risk factors for diabetes include being overweight and having a family history of diabetes. If you have any of the risk factors, your health care team may recommend early screening. If not, screening is recommended starting at age 45. Then you get your blood sugar levels tested again every three years.
If you have a condition such as high cholesterol, high blood pressure or diabetes, talk with your health care team. Your doctor may prescribe medicines and recommend lifestyle changes. Make sure to take your medicines exactly as prescribed, and follow a healthy-lifestyle plan.
8. Take steps to prevent infections
Certain infections may lead to heart problems. For instance, gum disease may be a risk factor for heart and blood vessel diseases. So brush and floss daily. Get regular dental checkups too.
Other illnesses caused by infections can make existing heart problems worse. Vaccines help protect against infectious diseases. So stay up to date on the following shots:
- Yearly flu vaccine.
- COVID-19 vaccine, which lowers the chances of getting very sick.
- Pneumococcal vaccine, which reduces the risk of certain illnesses caused by bacteria.
- Tdap vaccine, which protects against tetanus, diphtheria and pertussis.
Ask your health care professional if you need any other vaccines too.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Know your risk for heart disease. Centers for Disease Control and Prevention. https://www.cdc.gov/heartdisease/risk_factors.htm. Accessed May 15, 2023.
- Heart disease facts. Centers for Disease Control and Prevention. https://www.cdc.gov/heartdisease/facts.htm. Accessed May 15, 2023.
- Hennekens CH. Overview of primary prevention of coronary heart disease and stroke. https://www.uptodate.com/contents/search. Accessed May 15, 2023.
- How to prevent heart disease at any age. American Heart Association. https://www.heart.org/en/healthy-living/healthy-lifestyle/how-to-help-prevent-heart-disease-at-any-age. Accessed May 15, 2023.
- Heart-healthy lifestyle changes. National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health-topics/heart-healthy-lifestyle-changes. Accessed May 15, 2023.
- Smokeless tobacco: Health effects. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/smokeless/health_effects/index.htm. Accessed May 15, 2023.
- How smoking affects heart health. U.S. Food and Drug Administration. https://www.fda.gov/tobacco-products/health-information/how-smoking-affects-heart-health. Accessed May 15, 2023.
- Benefits of quitting. American Lung Association. https://www.lung.org/stop-smoking/i-want-to-quit/benefits-of-quitting.html. Accessed May 15, 2023.
- Physical Activity Guidelines for Americans. 2nd ed. U.S. Department of Health and Human Services. https://health.gov/our-work/physical-activity/current-guidelines. Accessed May 15, 2023.
- How does sleep affect your heart health? Centers for Disease Control and Prevention. https://www.cdc.gov/bloodpressure/sleep.htm. Accessed May 15, 2023.
- Sleep apnea. National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health-topics/sleep-apnea. Accessed May 15, 2023.
- AskMayoExpert. Screening, immunization, and prevention (child). Mayo Clinic; 2022.
- AskMayoExpert. Screening, immunization, and prevention (adult). Mayo Clinic; 2022.
- Sleep and chronic disease. https://www.cdc.gov/sleep/about_sleep/chronic_disease.html. Accessed May 15, 2023.
- AskMayoExpert. Hypertension (adult). Mayo Clinic; 2023.
- Lopez-Jimenez F (expert opinion). June 19, 2023.
- Stress and heart health. American Heart Association. https://www.heart.org/en/healthy-living/healthy-lifestyle/stress-management/stress-and-heart-health. Accessed June 20, 2023.
- Blood cholesterol: Diagnosis. National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health/blood-cholesterol/diagnosis. June 20, 2023.
- Wilder RS, et al. Overview of gingivitis and periodontitis in adults. https://www.uptodate.com/contents/search. Accessed June 20, 2023.
- What vaccines are recommended for you? Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/adults/rec-vac/index.html. Accessed June 20, 2023.
Products and Services
- Blood Pressure Monitors at Mayo Clinic Store
- A Book: Live Younger Longer
- A Book: Future Care
- Health foods
- Atkins Diet
- Automated external defibrillators: Do you need an AED?
- Blood Basics
- Blood tests for heart disease
- Bradycardia
- Transplant advances
- Butter vs. margarine
- Calcium supplements: A risk factor for heart attack?
- Can vitamins help prevent a heart attack?
- Cardiac ablation
- Cardiac amyloidosis — Treatment options
- Cardiac amyloidosis — What is amyloid and how does it affect the heart
- Cardiac catheterization
- Cardioversion
- Chelation therapy for heart disease: Does it work?
- Chest X-rays
- Complete blood count (CBC)
- Coronary angiogram
- Coronary angioplasty and stents
- Coronary artery bypass surgery
- Coronary artery spasm: Cause for concern?
- Daily aspirin therapy
- Don't get tricked by these 3 heart-health myths
- Echocardiogram
- Ejection fraction: What does it measure?
- Electrocardiogram (ECG or EKG)
- Heart transplant to treat dilated cardiomyopathy: Elmo's story
- Erectile dysfunction: A sign of heart disease?
- Exercise and chronic disease
- Fasting diet: Can it improve my heart health?
- Flu Shot Prevents Heart Attack
- Flu shots and heart disease
- Grass-fed beef
- Healthy Heart for Life!
- Heart arrhythmia
- Heart attack
- Heart attack prevention: Should I avoid secondhand smoke?
- Heart attack symptoms
- Heart Attack Timing
- Heart disease
- Heart disease in women: Understand symptoms and risk factors
- Heart-healthy diet: 8 steps to prevent heart disease
- Heart murmurs
- Heart transplant
- Herbal supplements and heart drugs
- Holter monitor
- Honey: An effective cough remedy?
- Implantable cardioverter-defibrillators (ICDs)
- Leg swelling
- Mediterranean diet
- Menus for heart-healthy eating
- NSAIDs: Do they increase my risk of heart attack and stroke?
- Nuclear stress test
- Nuts and your heart: Eating nuts for heart health
- Omega-3 in fish
- Omega-6 fatty acids
- Organ transplant in highly sensitized patients
- Pericardial effusion
- Polypill: Does it treat heart disease?
- Pseudoaneurysm: What causes it?
- Pulmonary edema
- Red wine, antioxidants and resveratrol
- Shortness of breath
- Silent heart attack
- Sitting risks: How harmful is too much sitting?
- Stress symptoms
- Stress test
- Tachycardia
- The Last Brother's Heart
- Integrative approaches to treating pain
- Nutrition and pain
- Pain rehabilitation
- Self-care approaches to treating pain
- Triathlete transplant
- Coronary angioplasty
- Video: Heart and circulatory system
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
News releases.
News Release
Monday, December 10, 2007
Heart Attack Symptoms in Women — Are they Different?
Chest pain is still the most common sign of a heart attack for most women, although studies have shown that women are more likely than men to have symptoms other than chest pain or discomfort when experiencing a heart attack or other form of acute coronary syndrome (ACS), according to an article "Symptom Presentation of Women With Acute Coronary Syndromes — Myth vs. Reality" published online Dec. 10 in the Archives of Internal Medicine . The study was funded by the National Heart, Lung, and Blood Institute (NHLBI) of the National Institutes of Health.
Researchers examined 35 years of research that yielded 69 studies 69 studies and found that, depending on the size of the study (which ranged from large trials to single centers and interviews), between 30 percent and 37 percent of women did not have chest discomfort during a heart attack. In contrast, 17 percent to 27 percent of men did not experience chest discomfort. Overall, the majority of women — and men — in the reviewed studies had chest discomfort with heart attack (two-thirds to three-quarters, depending on study size).
Study authors also found that older people are more likely to have heart attack without chest discomfort. However, because women are on average nearly a decade older than men at the time of their initial heart attack, the researchers call for more studies to determine the degree to which gender independently influences heart attack symptoms.
They conclude that current research does not indicate a need to differentiate heart attack symptoms in women from those in men, and public health messages should continue to emphasize chest pain or discomfort, shortness of breath, and other common signs of heart attack. Coronary heart disease is the leading cause of death among U.S. women, and affects one in 10 women over the age of 18.
The authors also report that women are more likely than men to experience other forms of cardiac chest pain syndromes, such as unstable angina, and they appear to report a wider range of symptoms associated with ACS. For example, women are more likely to report pain in the middle or upper back, neck, or jaw; shortness of breath; nausea or vomiting; indigestion; loss of appetite; weakness or fatigue; cough; dizziness; and palpitations.
Absence of chest discomfort is a strong predictor for missed diagnosis and treatment delays. Noting that many studies exclude patients who do not report chest pain, the researchers call for additional research from well-designed studies to further investigate gender differences in heart attack symptoms. This includes expanding symptom definitions and greater standardization in data collection and reporting of women's symptoms.
Study co-author George Sopko, M.D., Medical Officer with NHLBI's Division of Cardiovascular Diseases, is available for comment. To schedule interviews, contact the NHLBI Communications Office at 301-496-4236 or at [email protected].
NHLBI is part of the National Institutes of Health (NIH), the Federal Government’s primary agency for biomedical and behavioral research. NHLBI press releases and fact sheets, including information on the Women’s Health Initiative and on overweight and obesity can be found online at www.nhlbi.nih.gov .
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov .
NIH…Turning Discovery Into Health ®
- Act In Time To Heart Attack Signs is an NHLBI education campaign that that urges physicians to educate their patients about heart attack risk, warning signs, and survival. For information on heart attack warning signs for both the public and health care professionals, http://www.nhlbi.nih.gov/actintime/haws/haws.htm .
- The Heart Truth, NHLBI's national awareness campaign for women about heart disease, aims to spread the word that heart disease is largely preventable. For midlife women, the most common risk factors for heart disease in order of greatest prevalence include overweight/obesity, high blood cholesterol, diabetes, and high blood pressure. For more on The Heart Truth, http://www.hearttruth.gov .
- For current recommendations for heart health, see Your Guide to a Healthy Heart, http://www.nhlbi.nih.gov/health/public/heart/other/your_guide/healthyheart.htm .
Connect with Us
- More Social Media from NIH

Heart Attack
Sep 28, 2014
391 likes | 992 Views
Heart Attack. The Disease. What is a heart Attack?. when blood flow is blocked from reaching part of the heart prevents sufficient oxygen from reaching heart causes heart muscle to become damaged or die. also known as myocardial infarction. What are the Causes?.
Share Presentation
- coronary artery
- heart attack
- heart muscle
- heart attack overview
- heart attack warning signs

Presentation Transcript
Heart Attack The Disease
What is a heart Attack? • when blood flow is blocked from reaching part of the heart • prevents sufficient oxygen from reaching heart • causes heart muscle to become damaged or die • also known as myocardial infarction
What are the Causes? Heart attacks are caused by: • blood clots blocking the coronary arteries • this stops blood flow and heart cells die • clot forms because coronary arteries becomes narrowed by plaque (atherosclerosis) • plaque cracks and triggers clot • less commonly from blood vessel problems and severe coronary artery spasm • spasm could be related to drugs, stress, smoking
Diabetes Family history of Coronary Artery Disease (CAD) High fat diet Race: higher risk in African Americans, Mexican Americans, Native Americans, and Native Hawaiians High blood pressure Increasing age Smoking Unhealthy cholesterol levels Lack of exercise Stress Sex: men over 45, women over 55 Am I at Risk? Risk Factors
Shortness of breath Loss of consciousness Perspiration Severe crushing pain Tightness or squeezing in chest (Angina) Pain possibly spreading to left arm, shoulder, neck or jaw Light-headedness Many attacks begin slowly with mild pain May feel like heartburn/indigestion Nausea and vomiting How do I know if I am having a Heart Attack? Symptoms DO NOT IGNORE SYMPTOMS!
Diagnosing a Heart Attack • Physician uses stethoscope to find abnormal heart rhythms/sounds • Check pulse and blood pressure • Electrocardiograms (ECG) detect irregular heart beat (arrhythmia) or blocked coronary artery • Blood tests • High level of cardiac enzymes indicate damaged heart muscle • CK (creatine kinase), MB (myoglobin) and troponin released from damaged heart muscle (proteins)
Treating a Heart Attack Victim • While heart attack is occurring: • Take aspirin at home to help dissolve clot • Ambulance/Doctors will administer clot busters such as streptokinase and nitrates • Surgery may be needed to clear/open arteries • Put on oxygen • CPR may be needed or defibulation to restore heart beat • Morphine administered • Relieves pain, sedates, and reduces oxygen demand
After person is stabilized: • Thrombolytic Therapy • Medicine given to dissolve blood clots • Beta- Blockers • Decrease workload for heart, relieve pains, and correct arrhythmia • ACE (angiotensin-converting enzymes) inhibitors • Lower blood pressure, reduce strain for heart • Anticoagulents • Thin blood and prevent clots from forming • Antiplatelet Medicine • Stop platelets from clumping together
More Advanced Treatments • Angioplasty • Open coronary arteries • Catheter with balloon is threaded through blood vessel to blocked artery • Balloon then inflates pushing plaque aside • Doctors sometimes place a stent in the artery • Coronary Artery Bypass Grafting • Arteries or veins are taken from other parts of the body to bypass arteries • These arteries/veins are then sewn in place • Open-heart surgery could be required if heart ruptures
Rehabilitation • Discharged from hospital after a week at earliest • Activites slowly increase over 8 weeks • Resume full schedule after 2 months out of the hospital • Long term treatment with beta-blockers and aspirin • Drugs to lower cholesterol are given • Badly damaged heart requires warfarin (anticoagulent) for 3 months
Facts • 40% of heart attacks are fatal • Half of these deaths occur in first hour • Over 1.1 million heart attacks in United States each year • One of the leading killers in America • Males have higher risks for heart attacks
Don’t smoke Healthy diet Control blood sugar Exercise Lose weight if obese Control BP Low fat diet Lower salt intake Lower cholesterol Control diabetes Reducing Your Risk Prevention
References Internet sources • Berger, A. (2009). Heart Attack- Overview. Retrieved April 23, 2009, from http://www.umm.edu/ency/article/000195.htm • Heart Attack: Warning Signs and Tips on Prevention. (2009). FamilyDoctor.org. Retrieved May 14, 2009, from http://familydoctor.org/online/famdocen/home/common/heartdisease/basics/291.html • Heart Attack. (2008, March). National Heart Lung and Blood Institute (all articles on side used). Retrieved May 14, 2009, from http://www.nhlbi.nih.gov/health/dci/Diseases/HeartAttack/HeartAttack_whatis.html
Book Sources • Bunch, Bryan. (2003). Heart Attack. “Diseases” (Vol. 4 pp. 70-72) Danbury: Scientific Publishing, Inc. • Margolis, S. (2005). Heart Attack. In medical guide to Health After 50 (pp. 376-380). New York, NY: Black Dog & Leventhal, Inc. Pictures • http://www.daviddarling.info/encyclopedia/C/coronary_artery.html • http://myhealth.ucsd.edu/library/healthguide/en-us/support/topic.asp?hwid=zm2431 • http://farm4.static.flickr.com/3205/2723962050_284c85ccf9.jpg • http://www.crestock.com/image/763286-heart-monitor-screen.aspx • http://www.firstaidmonster.com/images/products/FAM_ASPIRIN_1000-1520.jpg • http://www.nhlbi.nih.gov/health/dci/Diseases/Angioplasty/Angioplasty_All.html • http://www.usageorge.com/Jokes/Jokes/No-smoking-sign.gif
Video • http://www.healthcentral.com/cholesterol/understanding-cholesterol-13-115.html
- More by User
HEART ATTACK
?. AMI. HEART ATTACK. Coronary SUPPLY. Pumping Cardiac Work DEMAND (O 2 ). O 2. ATP. G. FFA. O 2. G. O 2. O 2. ATP. O 2. O 2. G. O 2. FFA. G. FFA. O 2. ATP. INCREASED DEMAND. IMPAIRED SUPPLY. ISCHEMIC HEART DISEASE [IHD]. Coronary SUPPLY.
536 views • 38 slides
HEART ATTACK. Signs & Symptoms. Statistics
544 views • 15 slides

The Heart attack
The Heart attack . Problem/Question. Will different caffeinated drinks raise heart rates at varying rates?. Hypothesis.
329 views • 16 slides
Heart attack
Heart attack . Div 407 7/14/08 Juan Quintanilla . objective. The objective of this project is so you can learn how to give first aid to people who have heart attacks. .
202 views • 6 slides
. BY Griselda Hernandez. Heart Attack . Introduction .
222 views • 10 slides

HEART ATTACK!!
HEART ATTACK!! . Did you know..?!. Heart disease is the leading cause of death African Americans are at greater risk for heart disease Prevalence of heart disease in black females is 44.7% compared to 32.4% in white females
353 views • 11 slides

Heart Attack & Stroke
Heart Attack & Stroke. Heart Attack. Myocardial Infarction : Death ( necrosis ) of a portion of the heart muscle caused by coronary artery obstruction causing interruption of normal blood flow to an area of the heart ( Ischemia ) Angina pectoris : chest pain caused by myocardial ischemia.
356 views • 12 slides

Early Heart Attack Care
Early Heart Attack Care. Heart attacks have beginnings. For Questions, call Amy Fraulini, MSN, RN Director of Critical Care and Heart Services (740)356-8305 [email protected]. Heart Attack:. A community problem… with a community solution. Cardiovascular Disease Mortality Rates.
653 views • 43 slides
Early Heart Attack Care. Heart Attacks Have Beginnings. Heart Attack: A Community Problem With A Community Solution. Course Outline. Anatomy and Physiology 101: Your Heart A Heart Attack in Progress Concepts of Early Heart Attack Care Recognition and Intervention Delay and Denial
615 views • 39 slides
Preventing Heart Attack
Preventing Heart Attack. Dr. Prashant Jagtap M.D. D.M. FACC Wockhardt Heart Hospital. WHO Prediction. 100 million heart patients in 2010 (60% of world population) Treating 50 million heart patient will cost Rs.6,90,000 crores ($ 150 billion). ehi.
426 views • 31 slides
Heart Attack. By: Young Liu. What is a Heart Attack?. A heart attack occurs when blood flow to a section of heart muscle becomes blocked. If the flow of blood isn’t restored quickly, the section of heart muscle becomes damaged from lack of oxygen and begins to die. What is the cause?.
539 views • 6 slides
Heart Attack. Sudden Cardiac Arrest. Missouri House Bill 1337 requiring students to learn CPR in high school should not be passed. N o funding No certified instructors No emotional consideration. Lacks Funding. $405 from the AED Superstore. $380 from the AED Superstore.
246 views • 12 slides

?. ?. AMI. HEART ATTACK. DRUGS IN HYPERLIPIDEMIA. DRUGS IN HYPERLIPIDEMIA. ILOs. By the end of those 2 lectures [23 slides for studing ] you will be able to:. Define hyperlipidemia vs normal lipid levels
558 views • 41 slides
Heart attack. By: Jasmine Parker, Ariyel Cheatham, and Qyaira Colbert. A Description of A heart attack. A heart attack is when a blood clot cuts off most or all of blood supply to the heart. Pictures of a heart attack. Symptoms of a heart attack.
542 views • 7 slides
Dental Health and Heart Attack
Most of us are not aware that our dental health can also be one of the reasons of heart attack.
146 views • 4 slides
Heart attack, Heart Attack Symptoms, Open Heart Surgery - Consult Lybrate
Found any symptoms of heart attack? Then, get in touch with lybrate.com for open heart surgery and any heart related diseases. They will provide you with world class treatment of diseases. Visit us : https://www.lybrate.com/heart-attack
169 views • 2 slides
heart attack treatment-randhawahospital-heart failure treatment
Randhawa Hospital offers heart attack treatment, ecp therapy with treatment in India
118 views • 6 slides
Heart Attack Symptoms Women, How To Stay Healthy, Heart Attack Warning Signs In Men, Heart Attack
http://grow-younger-blood.good-info.co ---<br><br>Heart Attack Symptoms Women, How To Stay Healthy, Heart Attack Warning Signs In Men, Heart Attack.<br><br>Is blood the secret to life?<br><br>It's funny how when new scientific breakthroughs happen, we find out we sort of knew all along.<br><br>In this video John explains how every power and vulnerability we have in our lives is encoded in our blood.<br><br>including whether we are about to be crippled by a stroke and how to prevent it.<br><br>And should we be surprised?<br><br>Since the dawn of time, we always sort of knew there was something special almost magical about the nature of our blood.<br><br>In the Jewish bible, old temple sacrifices were only valid if the blood of the animal was poured on the altar.<br><br>In the Christian bible, Jesus talks of his blood being salvation for mankind.<br><br>In family conversations (and disputes), people say "You're my blood," to declare unity or to demand obligation.<br><br>So why should we be surprised at John discovery, that the secret to changing your life, lies in simply adjusting your blood's chemistry with a few fairly easy steps?<br><br>It really is that simple Click Here.<br><br>http://grow-younger-blood.good-info.co
78 views • 5 slides
Cardiac Emergency Services at Aga Khan University Hospital. https://hospitals.aku.edu/pakistan/
54 views • 3 slides
Heart Attack And Heart Disease Triggered
Consider portion control. The truth is that foods that have fat in them taste good. It is hard to cut them out entirely and unless there is a medical problem that specifically prevents you from doing so, you can continue eating them. The trick is to make sure that you do not eat them to excess, however! Take some time and really consider what you can do eat in moderation; learn about acceptable portion sizes in order to avoid heart disease.
19 views • 1 slides
Silent heart attack market
Silent Heart Attack Market Research Report: By Diagnosis (CT, MRI, ECG, Blood Tests), Treatment (Medications, Coronary Angioplasty And Stenting, Coronary Artery Bypass Surgery), End User (Hospital, Clinic, Diagnostic Center) - Global Forecast till 2023
32 views • 3 slides

Germany Silent heart attack Market
38 views • 3 slides

IMAGES
VIDEO
COMMENTS
Others have severe symptoms. Some people have no symptoms. Common heart attack symptoms include: Chest pain that may feel like pressure, tightness, pain, squeezing or aching. Pain or discomfort that spreads to the shoulder, arm, back, neck, jaw, teeth or sometimes the upper belly. Cold sweat.
Heart attack signs and symptoms in men and women: Chest pain or discomfort; Shortness of breath; Pain or discomfort in the jaw, neck, back, arm, or shoulder; Feeling nauseous, light-headed, or unusually tired. View Larger. A heart attack, also called a myocardial infarction, happens when a part of the heart muscle doesn't get enough blood.
Myocardial infarction, commonly known as a heart attack, is the irreversible necrosis of heart muscle secondary to prolonged ischemia. This usually results from an imbalance in oxygen supply and demand, which is most often caused by plaque rupture with thrombus formation in a coronary vessel, resulting in an acute reduction of blood supply to...
The First 90 Days After a Heart Attack: Life After a Heart Attack. Join the Nation of Lifesavers today! Learn CPR. Save a Life. You could be the difference between life and death for someone experiencing a cardiac event. Be ready to act by learning CPR. Learn more and find a CPR course.
A heart attack occurs when blood flow that brings oxygen-rich blood to the heart muscle is severely reduced or cut off. This is due to a buildup of fat, cholesterol and other substances (plaque) that narrows coronary arteries. This process is called atherosclerosis. When plaque in a heart artery breaks open, a blood clot forms.
Myocardial infarction (MI), colloquially known as "heart attack," is caused by decreased or complete cessation of blood flow to a portion of the myocardium. Myocardial infarction may be "silent" and go undetected, or it could be a catastrophic event leading to hemodynamic deterioration and sudden death.[1] Most myocardial infarctions are due to underlying coronary artery disease, the ...
Symptoms of a heart attack include: Discomfort, pressure, heaviness, tightness, squeezing, or pain in your chest, arm, or below your breastbone. Discomfort that goes into your back, jaw, throat ...
Heart attacks occur when there is a lack of blood supply to the heart. Symptoms include: chest pain, pressure, or tightness. pain that may spread to arms, neck, jaw, or back. nausea and vomiting ...
A heart attack is when blood flow to the heart is blocked. It's a circulation problem. With sudden cardiac arrest (SCA), the heart malfunctions and suddenly stops beating. Sudden cardiac arrest is an electrical problem caused by irregular heart rhythms called arrhythmias.
Prevention. 9 /10. If you smoke, stop. It will immediately cut your chances of a heart attack by a third. Get exercise and eat right. The American Heart Association recommends 30 minutes of ...
J Am Heart Assoc. 2014; 3:e000586. DOI: 10.1161/JAHA.113.000586. Link Google Scholar; 2 Canto JG, Canto EA, Goldberg RJ. Time to standardize and broaden the criteria of acute coronary syndrome symptom presentations in women. Can J Cardiol. 2014; 30:721-728. Crossref Medline Google Scholar
breathlessness and generally feeling unwell. tightness or discomfort in your arms. chest pain that feels more like burning, throbbing, tightness or like trapped wind. a feeling of indigestion or upper tummy pain. upper back pain or pressure. Heart attack symptoms differ from person to person.
3. Pinterest. This medical emergency presentation covers heart attacks. Topics include. What is a heart attack? Signs and symptoms of a heart attack. First aid treatment for a heart attack. Use of Aspirin. Loading….
Get started with these eight tips to boost your heart health: 1. Don't smoke or use tobacco. One of the best things you can do for your heart is to stop smoking or using smokeless tobacco. Even if you're not a smoker, be sure to stay away from secondhand smoke. Chemicals in tobacco can damage the heart and blood vessels.
It lasts more than a few minutes, or goes away and comes back. Pain or discomfort in one or both arms, the back, neck, jaw or stomach. Shortness of breath with or without chest discomfort. Other signs such as breaking out in a cold sweat, nausea or lightheadedness. As with men, women's most common heart attack symptom is chest pain or discomfort.
For people who have never experienced angina or a heart attack, it may present as chest tightness, or pain or discomfort that can spread to the shoulders, back, chest, and jaw. Angina happens when the arteries in the heart get narrow. A heart attack can cause permanent heart damage. If this is your first time experiencing chest pain, seek ...
Chest pain is still the most common sign of a heart attack for most women, although studies have shown that women are more likely than men to have symptoms other than chest pain or discomfort when experiencing a heart attack or other form of acute coronary syndrome (ACS), according to an article "Symptom Presentation of Women With Acute ...
Heart attacks are caused by: • blood clots blocking the coronary arteries • this stops blood flow and heart cells die • clot forms because coronary arteries becomes narrowed by plaque (atherosclerosis) • plaque cracks and triggers clot • less commonly from blood vessel problems and severe coronary artery spasm • spasm could be ...
Get enough sleep. Getting a good night's sleep every night is vital to your heart health. The amount and quality of sleep you get can influence your eating habits, mood, memory, internal organs and more. Too much or too little can be harmful. Adults should aim for an average of 7 to 9 hours a night.
However, some researchers also doubted that study, because the placebo scientists used might have caused heart attacks. Yes, this is confusing, and that is the point: With nutrition, we need to be ...