
- Case Examples
Based on a composite of a number of real sentinel event reports to The Joint Commission, Case Examples can be used for educational purposes to identify lapses in patient safety and missed opportunities for developing a safety culture. This learning resource highlights safety actions and strategies to have a better result. Stay current with what is happening at The Joint Commission by subscribing to our free publications.
- Joint Commission Online
- Quick Safety
- What is HSO?

In recognition of Canadian Patient Safety Week 2022, we are pleased to share these case studies featuring diverse examples of how our healthcare partners are applying the Canadian Quality and Patient Safety Framework in their settings. We hope you find them useful.
Access the Canadian Quality and Patient Safety Framework Evaluation here .


Early adoption of the Canadian Quality and Patient Safety Framework at Eating Disorders Nova Scotia : A useful tool for self‑assessment, education, and program development
Shaleen Jones is the Executive Director of Eating Disorders Nova Scotia . The community‑based organization has been around for nearly 25 years. Eating Disorders Nova Scotia operates on a core belief that no one should have to go through an eating disorder alone, and everyone should have access to the resources and supports needed for recovery. Along with peer‑support programs, the organization provides psychologists, dieticians, and other professional supports, based on clients’ preferences and needs. Operating out of Nova Scotia, the organization has extended its services from in‑person to virtual and now serves people across Canada through their Peer Support Programs. The pandemic helped spur the transition. “We wanted to reach more people with the resources available, and once we went virtual, it opened up a whole new world … we’ve had a 400% increase in service,” said Jones. Read More

Aligning quality and patient safety with policy and practice at Nova Scotia Health : Applying the Canadian Quality and Patient Safety Framework
“We have seen progress and benefits of our initiatives and the Canadian Quality and Patient Safety Framework . It really helps to focus and guide our work,” says Gail Blackmore, Senior Director of Quality Improvement and Safety at Nova Scotia Health . Blackmore is using the Framework to align policy and practice. The organization can embed Framework goals into daily practice by ensuring that reporting templates and other everyday practices align with the broader goals of patient safety and quality. “When there’s alignment, it’s more likely to be successful,” she says. Read More

Canadian Quality and Patient Safety Framework : A tool supporting organizational priorities, quality and safety process improvements
St. Joseph’s Health Care London is a leading teaching hospital in Ontario and part of London’s academic sciences community. As a Catholic health care organization, St. Joseph’s is a values‑driven organization with the aim of caring for the community, particularly, poor, marginalized, and underserved populations. Members of the St. Joseph’s Quality Council and representatives from the Quality Committee of the Board participated in a case study to learn about their experiences and views on the Canadian Quality and Patient Safety Framework. The Framework and its implementation resources aim to accelerate quality and patient safety across the Canadian health systems by focusing stakeholders on five goals for safe and quality care. These goals include people‑centred care, safe care, accessible care, appropriate care, and integrated care. Participants said the Framework validated their organizational quality and safety processes and has the potential to support improvements aligned with St. Joseph’s strategic goals. They recommended professional colleges and training organizations consider the Framework to strengthen quality and integration practices. Read More
Canadian Patient Safety Week Webinar: Safety Conversations Start with a Safe Workplace and Workforce
In partnership with Health Excellence Canada , we are hosting a joint webinar on Thursday, October 27, from 12 -1 pm ET. This interactive webinar will convene a panel of senior leaders to share their experience designing and implementing the new Health Standards Organization (HSO) Workforce Survey on Well-Being, Quality and Safety (WSWQS). Participants will hear about the survey methodology, validation process, and learnings from early adopter health care organizations.
Learn More and Register
Cookies on the NHS England website
We’ve put some small files called cookies on your device to make our site work.
We’d also like to use analytics cookies. These send information about how our site is used to a service called Google Analytics. We use this information to improve our site.
Let us know if this is OK. We’ll use a cookie to save your choice. You can read more about our cookies before you choose.
Change my preferences I'm OK with analytics cookies
Patient safety review and response case studies by clinical specialty
This page shows case studies, listed by clinical specialty, of where the National Patient Safety Team worked with partners to address issues identified through its review of recorded patient safety events.
Urgent/emergency care
General medicine, intensive care, obstetrics and gynaecology/midwifery, paediatrics and child health, primary care.
You can find out more about our processes for identifying new and under recognised patient safety issues on our using patient safety events data to keep patients safe and reviewing patient safety events and developing advice and guidance web pages.
- COVID-19 swab snapped in tracheostomy
- Risk of dose error when using intraosseous lidocaine in children
- ePrescribing systems and insulin combinations
- Risks of ingestion of alcohol-based hand sanitiser
- Risk of airway obstruction from green anaesthetic swabs
- Dual purpose naso-gastric tubes with ENFit® connectors and the risk of aspiration
- Diagnosis and management of supraglottitis
- Sucrose vial cap identified as potential choking hazard in babies
- The risk of aspiration from orally administered contrast media with spigotted nasogastric tubes
- Metacarpal wrong site surgery – inconsistent terminology used to describe anatomy
- Osmotic Demyelination Syndrome from rapid correction of severe hypo/hypernatraemia
- Ensuring timely updates to clinical risk assessment and management triage tools in emergency departments
- Ingested gel toilet discs
- Delayed oxygenation of neonate during resuscitation when oxygen not ‘flicked’ on
- Equipment falling onto critically ill patients during intrahospital transfers
- Misapplication of spinal collars resulting in harm from unsecured spinal injury
- Ensuring compatibility between defibrillators and associated defibrillator pads
- Ensuring pregnant women with COVID-19 symptoms access appropriate care
- Overdose of oral vitamin D related to frequency and duration of treatment
- Administration of chemotherapy and reactivation of Hepatitis B
- Delay in treatment with prothrombin complex concentrate (PCC)
- Harm from catheterisation in patients with implanted artificial urinary sphincters
- Confusion between different strength preparations of alfentanil
- Distinguishing between haemofilters and plasma filters to reduce mis-selection
- Variation in use of cardiac telemetry
- Ceftazidime as a 24-hour infusion
- Tacrolimus – risk of overdose when converting from oral to intravenous route
- Haloperidol prescribing for confused/agitated/delirious patients
- Ensuring oxygen delivery when using two step humification systems
- Pregnancy tests not performed before anaesthesia
- Ventilator left in standby mode
- Sudden patient deterioration due to secretions blocking heat and moisture exchanger filters
- Anaesthetic machines used as ventilators: issues with circuit set up
- Importance of ‘tug test’ for checking oxygen hose when transferring a patient to a portable ventilator
- Use of trimethoprim in women of child-bearing age
- Assessment of risk of venous thromboembolism (VTE) when prescribing combined hormonal contraceptives
- Harm from prescribing and administering Syntometrine when contraindicated to woman with significantly raised BP
- Unnecessary caesarean section for breech presentation if not scanned on the day
- HIV prophylaxis in women and new-borns
- Ensuring the safe use of plastic cord clamps at caesarean section
- Warning on the use of ethyl chloride during fetal blood sampling
- Risk of babies becoming unwell following move to virtual home midwifery visits
- Testing ammonia levels in children
- Unintentional perforation of oesophagus in neonates from invasive procedures
- Chemical burn to a neonate from use of chlorhexidine
- Risk of harm from spinal administration of anaesthetic agent containing preservative
- Hip cement – different expiry dates for separate components in the same pack
- Bone cement implantation syndrome
- Surgical skin preparation solution entering the eye during surgery
- Retained surgical instrumentation and complex procedures involving multiple teams and equipment
- Unintentional retention of bone cement following hip surgery
- Monitoring patients taking nitrofurantoin for potential lung disease
- Unintended bolus of medication if infused at speed from residual space in giving set
- Infrared temperature screening to detect COVID-19
Patient Safety and Communication Case Studies

Hawai‘i Pacific Health was named a 2019 HIMSS Davies Enterprise Award recipient for leveraging the value of health information and technology to improve outcomes. The three case studies below cover patient safety workflow enhancements, virtual communication solutions and reducing length of stay.
Case Studies
1. i-pass nurse handoffs.
Hawai‘i Pacific Health recognized that communication amongst nurses at shift change in the neonatal intensive care unit was a patient safety improvement opportunity for the high volume, high acuity unit. In order to address this, they aimed to apply high reliability techniques and leverage EHR-based tools to bring the evidence-based I-PASS handoff structure to nursing handoffs. To learn more, listen to the use case video below or download the use case presentation.
2. Putting the IT in CapITation
Hawai‘i Pacific Health recognized there were a variety of opportunities to ensure its growing patient population received quality care in a timely fashion and was challenged by a limited supply of physicians and a changing health care environment to do so. To combat these challenges, cross-functional teams worked together to implement virtual e-visits and other patient communication tools.
3. Decreasing Case-Mix Adjusted Average Length of Stay
Hawai‘i Pacific Health recognized that safely decreasing length of stay was a means to increase service capacity while reducing internal costs. In order to address this, Hawai‘i Pacific Health set a system level goal to reduce case-mix adjusted average length of stay (CMI-adjusted ALOS) by a half-day over a period of five years.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Qual Health Care
- PMC10656601
Improving patient safety governance and systems through learning from successes and failures: qualitative surveys and interviews with international experts
Peter d hibbert.
Australian Institute of Health Innovation, Faculty of Medicine, Health and Human Sciences, Macquarie University, 75 Talavera Rd, Macquarie Park, NSW 2109, Australia
IIMPACT in Health, Allied Health and Human Performance, University of South Australia, GPO Box 2471, Adelaide SA 5001, Australia
Sasha Stewart
Louise k wiles, jeffrey braithwaite, william b runciman, matthew j w thomas.
Appleton Institute, School of Health, Medical and Applied Sciences, Central Queensland University, 114-190 Canning Street, Rockhampton, Queensland 4700, Australia
Associated Data
The dataset generated and analysed during the current study is not publicly available.
Patient harm is a leading cause of global disease burden with considerable morbidity, mortality, and economic impacts for individuals, families, and wider society. Large bodies of evidence exist for strategies to improve safety and reduce harm. However, it is not clear which patient safety issues are being addressed globally, and which factors are the most (or least) important contributors to patient safety improvements. We aimed to explore the perspectives of international patient safety experts to identify: (1) the nature and range of patient safety issues being addressed, and (2) aspects of patient safety governance and systems that are perceived to provide value (or not) in improving patient outcomes. English-speaking Fellows and Experts of the International Society for Quality in Healthcare participated in a web-based survey and in-depth semistructured interview, discussing their experience in implementing interventions to improve patient safety. Data collection focused on understanding the elements of patient safety governance that influence outcomes. Demographic survey data were analysed descriptively. Qualitative data were coded, analysed thematically (inductive approach), and mapped deductively to the System-Theoretic Accident Model and Processes framework. Findings are presented as themes and a patient safety governance model. The study was approved by the University of South Australia Human Research Ethics Committee. Twenty-seven experts (59% female) participated. Most hailed from Africa (n = 6, 22%), Australasia, and the Middle East (n = 5, 19% each). The majority were employed in hospital settings (n = 23, 85%), and reported blended experience across healthcare improvement (89%), accreditation (76%), organizational operations (64%), and policy (60%). The number and range of patient safety issues within our sample varied widely with 14 topics being addressed. Thematically, 532 textual segments were grouped into 90 codes (n = 44 barriers, n = 46 facilitators) and used to identify and arrange key patient safety governance actors and factors as a ‘system’ within the System-Theoretic Accident Model and Processes framework. Four themes for improved patient safety governance were identified: (1) ‘safety culture’ in healthcare organizations, (2) ‘policies and procedures’ to investigate, implement, and demonstrate impact from patient safety initiatives, (3) ‘supporting staff’ to upskill and share learnings, and (4) ‘patient engagement, experiences, and expectations’. For sustainable patient safety governance, experts highlighted the importance of safety culture in healthcare organizations, national patient safety policies and regulatory standards, continuing education for staff, and meaningful patient engagement approaches. Our proposed ‘patient safety governance model’ provides policymakers and researchers with a framework to develop data-driven patient safety policy.
Introduction
Avoidable patient harm remains one of the leading causes of global disease burden, despite considerable progress being made, especially in developing nations [ 1 ]. In high-income countries, approximately one in ten patients experiences an adverse event [ 2 ]. In low- and middle-income countries, it is estimated that 134 million adverse events occur in hospitals per year contributing to 2.6 million deaths annually [ 2 ].
An increasing recognition of the importance of patient safety has catalyzed the formation of international and national quality and safety alliances to set priorities and shape policy, and there is now a large body of evidence relating to improvement strategies for reducing harm in health care [ 3–6 ]. Recent international efforts include the World Health Organization’s Global Patient Safety Action Plan [ 2 ] and the Organization for Economic Co-operation and Development’s safety measurement system [ 7 ].
Despite extensive resources and efforts to reduce harm, more evidence is needed in relation to which aspects of patient safety governance provide value in terms of improving outcomes for patients and health systems, versus those that are not effective and therefore waste resources. This study aimed to examine the perspectives of international patient safety experts to identify the [ 1 ]: nature and range of patient safety issues being addressed, and [ 2 ] aspects of patient safety governance and systems that are perceived to provide value (‘successes’) or are not effective (‘failures’) in improving outcomes for patients.
Study design, sample, and setting
A case study methodology [ 8 ] using surveys and interviews was employed and is described according to the Standards for Reporting Qualitative Research Checklist ( Supplementary Appendix 1 ). Case study approaches are appropriate to generate an in-depth, multifaceted understanding of a complex issue such as patient safety interventions and governance in its real-life context [ 9 ]. We studied multiple cases simultaneously (a collective case study approach) to enable a broad understanding of the effectiveness of patient safety governance [ 9 , 10 ]. Experts, Fellows, and Academy members (International Academy of Quality and Safety, IAQS) from the International Society for Quality in Healthcare (ISQua) were made aware of this study via ISQua communication channels (including website notices, newsletters, and email circulations) which directed them to the study website. ISQua is a global professional organization that focuses on facilitating improvements in the quality and safety of health care [ 11 ]. At the time of the study, ISQua had 1555 Experts, Fellows, and Academy members, with representation across 83 countries and 6 continents [ 12 ]. All participants provided written informed consent prior to study enrolment. Participation was voluntary and no compensation was provided. Participants were assured that no identifiable information would be collected or reported. The study received ethics approval from the University of South Australia Human Research Ethics Committee (no. 203 467).
Data collection
Data collection occurred between May and September 2021, and comprised internet-based surveys (Microsoft Forms) ( Supplementary Appendix 2 and 3 ) and one-on-one in-depth semistructured interviews (telephone or web-based platform; Zoom) ( Supplementary Appendix 4 ). Two researchers (P.D.H. and S.S.) conducted all interviews; both have patient safety experience, with one (P.D.H.) being an ISQua Fellow. Surveys and interviews sought to explore and understand experts’ experiences about patient safety initiatives in which they were involved. Participants were invited to discuss (via case report or interview) an example of either a patient safety ‘success’, or a persistent problem (‘failure’), and to reflect on the lessons learnt and factors perceived as contributing to improvements or failure to achieve the desired outcomes. Interviews were audio-recorded and transcribed verbatim. All data were anonymized for reporting.
Data analysis
Survey and interview data were analysed thematically using inductive and deductive approaches [ 13 ]. Participants’ perspectives on the key barriers and facilitators to effective patient safety efforts (taken from case study ‘successes’ and ‘failures’) were coded and deductively mapped to the System-Theoretic Accident Model and Processes (STAMP) framework [ 14 ]. STAMP is generally applied to accidents or hazard analysis; however, it has been used to analyse systems for governance, for example in road safety [ 15 ], electronic medical record safety [ 16 ], and risk management in hospitals [ 17 ]. It is underpinned by systems and control theory, and considers constraints and controls across system development and operations. STAMP recognizes that in today’s complex world, the causes of accidents are generally nonlinear, inter-related, and represented across multiple layers in the system. Patient safety governance can also be considered as a complex sociotechnical system with a series of hierarchical control structures that impose constraints from high levels to low levels [ 18 ]. The resistance and inertia in improving patient safety at scale may be related to its characteristic as a complex sociotechnical system.
The aspects of patient safety governance and systems perceived to provide value or not in improving outcomes for patients were analysed inductively (thematic analysis) [ 19 ].
Using the constant comparison method, participants’ perspectives were deductively mapped to the content of the STAMP framework [ 20–22 ], and then iteratively refined into a novel overarching systems model with key themes for patient safety governance and improvement. Example quotes from interviewed participants were selected for publication.
Rigor and trustworthiness
The interview schedule was pilot tested on three non-ISQua members with patient safety experience—their data were not included in the study. All interviews were coded by one researcher (S.S.), with a random subsample (n = 6, 22%) coded independently by a second researcher (L.K.W.). The two researchers met to ensure code consistency, before agreeing on the final coding frame and resultant themes and subthemes. Interview data analysis was undertaken by one researcher (L.K.W.) and verified by another (S.S.). Further discussions were held to confirm saturation across sampling, data collection, and analysis domains for each approach [ 23 ]. In the inductive analysis, the researchers ensured that no new codes or themes were being generated and no new theoretical insights gained from the data [ 23 ]. For the deductive component, the two researchers ensured that the STAMP framework hierarchical levels were adequately represented in the data (i.e. that all levels within the formulated overarching systems model were sufficiently replete with examples from the data). Interview transcripts and summaries of the analysis were sent to participants to ensure they were satisfied with interpretations of their data, with no suggested amendments received.
Study sample
Twenty-seven ISQua participants (n = 16, 59% female) completed the survey and then an interview, representing a response rate of 1.7%. Most hailed from Africa (n = 6, 22%), and Australasia or the Middle East (n = 5, 19% each) and were employed in hospital settings (n = 23, 85%). Participants reported a blend of experience across healthcare improvement (89%), accreditation (76%), organizational operations (64%), and policy (60%). According to participants and illustrated via case study descriptions, the nature and range of patient safety issues being addressed in our sample varied in topic (n = 14), with specific examples of adverse events and patient harm most commonly discussed (n = 5, 38%) ( Table 1 ).
Table 1.
Participant profile.
Synthesis and interpretation
Thematically, a total of 532 textual segments (n = 247 barriers, n = 285 facilitators) were grouped into 90 factors (n = 44 barriers, n = 46 facilitators) and were used to identify key factors relating to patient safety governance which were aligned with prioritized STAMP framework hierarchical levels [ 14 ] ( Figure 1 ). Factors were also used to synthesize four distinct yet interrelated and overlapping themes (n = 12 subthemes) relating to aspects of patient safety governance and systems perceived as valuable or ineffective; these are discussed below and summarized, with illustrative quotes, in Tables 2–4 . A matrix of codes, STAMP framework hierarchical levels, and themes appears in Supplementary Appendix 5 .

Adapted STAMP systems model for patient safety governance [ 14 ]. Note: Control and Feedback mechanisms in italics. Key factors related to patient safety governance and systems are noted in boxes with borders; deeper coloured boxes with bolded text show factors with ten or more responses from participants. These are organised into different STAMP hierarchical levels in plain bold text and sub-levels in boxes with borders. Factors were aggregated including across barriers and facilitators and renamed into neutral factors (for example, lack of access to healthcare (a barrier) and access to healthcare (a facilitator) were aggregated and renamed access to healthcare. Factors mentioned by less than 3 participants were excluded. See Supplementary Appendix 5 for full dataset results.
Table 2.
Theme 1 (organizational culture, safety and quality mindset) summary, illustrated with participant quotations.
Theme 1: Organizational culture, safety, and quality mindset
The organizational culture, safety, and quality mindset was the most frequently mentioned barrier or facilitator by participants comprising 412 (or 77% of) textual segments ( Supplementary Appendix 5 ).
Organizational culture and leadership priorities
Participants were emphatic that a health service organization’s culture is ‘critical’ to setting its safety, quality mindset and efforts. The approaches and activities prioritized by leadership and management teams are indicative of culture and reflect their commitment to safety and quality. These filter through the organization in discussions and meetings with staff ( Table 2 ).
Participants reported that leaders’ priorities are largely shaped by their accountabilities and how success is measured within the organization (e.g. financial key performance indicators versus quality outcomes), and these priorities can either promote or downgrade the importance placed on safety and quality. Safety should be ensconced within the organizational development of health services through adequate clinical representation on Boards, and by employing models of safety improvement with proven track records. The efforts of individual safety managers who can leverage political networks and priorities make a real difference in producing positive outcomes for the community ( Table 2 ).
Staff engagement
Many participants suggested that safety culture and awareness could be deepened with meaningful staff engagement through partnership in nonhierarchical consultations rather than imposing preconceived solutions, thereby engendering ownership of issues and initiatives. Leaders also need to provide consistent clear messaging and follow-up with actions that align with stated patient safety priorities ( Table 2 ).
Endorsement of quality
Healthcare employees’ behaviour is guided by decisions from their management teams; therefore, quality improvement initiatives must be endorsed by organizational leaders. If the organization promotes reflective practice and staff-led safety and quality improvement initiatives, a sustainable culture of improvement can grow. On the other hand, factors identified as negatively influencing safety culture included ‘cover up’ activities borne out of concerns for reputational protection and a heavy focus on accreditation compliance as an endpoint rather than business-as-usual. There was a clear consensus that nonpunitive approaches that seek to unearth learnings for future improvement best support patients and staff ( Table 2 ).
Theme 2: Policies and processes to investigate, implement, and demonstrate impact
Factors related to policies and processes to investigate, implement, and demonstrate impact comprised 68% (361/532) of the textual segments mentioned by participants ( Supplementary Appendix 5 ).
National-level reporting and legislative mandates were considered an important drive for organizations to prioritize safety programs and promote transparency in incident reports and learnings ( Table 3 ).
Table 3.
Theme 2 (policies and processes to investigate, implement, and demonstrate impact) summary, illustrated with participant quotations.
Regulatory bodies
Regulation agencies and accreditation processes were considered key to ensuring accountability, particularly when underpinned by government support and industry-based partnerships. National-level standards were viewed favourably; however, potential negative consequences of ‘setting the accreditation bar too high’ included the closure rather than development and improvement of ‘problematic’ health services. Other potential limitations of accreditation included setting patient safety standards too low, inadequate assessment, and failure to partner with health services to undertake the necessary improvements ( Table 3 ).
Processes—data informing and informed by practice
Many participants described the value of high-quality data systems such as incident reporting and trigger tools that align with key safety priorities. It was noted, however, that incident reporting systems do not provide the complete picture. Nontraditional data sources should be used to validate and enhance information from reporting systems and identify issues that are not routinely reported (e.g. use of low value procedures, rates of and time to patient follow-up care). Data ‘drill-downs’ should be undertaken by dedicated quality and safety managers, in conjunction with staff discussions, to flesh out the underlying reasons for ‘why’ and ‘how’ things go wrong. Engagement by healthcare professionals is often low due to a failure of organizations to ‘close the loop’ in response to identified issues, coupled with the burden of completing often lengthy incident forms ( Table 3 ).
Implementation, interpretation, and demonstrating impact
Participants espoused the value of implementation approaches that ‘start somewhere’ and are ‘clinically relevant’, such as risk stratification and pain score assessments on hospital presentation. Contrarily, strategies undertaken at the level of paperwork (e.g. hospital procedural documents) are sometimes viewed as not resulting in meaningful improvements and done ‘for show’ ( Table 3 ).
Some examples of limitations to demonstrating impact from initiatives included inadequate assessment of safety issues, rolling out off-the-shelf solutions rather than tailored context-sensitive approaches, inappropriate selection of outcome measures (i.e. flawed unidimensional short-range metrics), and too much focus on either celebrating improvements or calling out residual deficiencies (e.g. acceptability thresholds for hand hygiene rates). Political imperatives can lead to patient safety issues ‘of the moment’ gaining attention at the expense of others, such as increased health service activity or ambulance queuing, or hospital readmission rates ( Table 3 ).
Theme 3: Staff support, upskilling, and shared learning
Factors related to staff support, upskilling, and shared learning comprised 68% (374/532) of the textual segments mentioned by participants ( Supplementary Appendix 5 ).
Staff support and capacity
A supportive organizational ethos that focuses on learning rather than blame will develop staff as agents of patient safety change. Staff can then feel comfortable to report issues, fostering positive reporting practices within the organization. Staff in safety and quality roles needs to be supported with sufficient resourcing to ensure a critical mass of field teams and managers, and allowed license to balance their safety responsibilities with other clinical pressures ( Table 4 ).
Table 4.
Theme 3 (staff support, upskilling, and shared learning) and Theme 4 (Patient engagement, experiences, and expectations) summary, illustrated with participant quotations.
Staff upskilling
Healthcare workers often lack safety-specific technical knowledge and skills to adequately understand and drive improvement agendas within their organizations. Thus, career-long safety education should be made available. Responsibility for continuous learning falls within the remit of both university and teaching hospital sectors and is reflective of an organization’s commitment to building capacity for safety. Practical and experiential learning opportunities are especially valuable in helping staff to appreciate the nature and range of patient safety problems ( Table 4 ).
Education on foundational topics is also essential and should encompass the influence of social determinants of health to enhance understanding of responsible management of health funding and use of cost-effectiveness measures. Human factors were also highlighted as a key educational target. Shaping helpful staff attitudes, behaviours, and communication skills is critical to these being perpetuated within healthcare organizations ( Table 4 ).
Shared learning
To achieve ongoing improvement in the patient safety space, there must be opportunities for all stakeholders to share information and learnings which tend to increase buy-in from all sides. Webinars and other virtual modalities were suggested as a means of communication across a country ( Table 4 ).
Theme 4: Patient engagement, experience, and expectations
Factors related to patient engagement, experience, and expectations comprised 22% (118/532) of the textual segments mentioned by participants ( Supplementary Appendix 5 ).
Patient engagement and experience
There was widespread recognition that patient engagement is pivotal to patient safety. However, in some regions, patient-centeredness is still a relatively new concept that is not embedded in organizational policies, education, and practice. Nevertheless, there was general agreement that hearing patients’ personal stories positively influences healthcare professionals’ attitudes towards patient safety, with some subsequently attracted to patient safety roles. Leadership training, in particular, could benefit from incorporating ‘patient experience’ first-hand from patient advocates ( Table 4 ).
Patient expectations
Patients’ health literacy influences their own expectations and attitudes towards safety. Where levels of health literacy are low, it was reported that some patients almost ‘expect and accept’ adverse events. Conversely, participants reflected that well-informed patients are active partners in their own care, and can advocate for their own safety especially when things go wrong. Public education, implemented early and with due sensitivity of cultural nuances, may enhance patients’ self-efficacy through a heightened understanding of basic healthcare principles. Collaborative person-centred approaches and general improvements in health literacy can help drive public pressure and expectations of the healthcare system, and organizations must keep pace with these developments.
Statement of principal findings
The nature and range of patient safety issues being addressed in our sample varied in topic (n = 14), with specific examples of adverse events and patient harm, relating to medical procedures (e.g. postpartum haemorrhage, transvalvular percutaneous aortic valve replacement, and central line infection) most commonly discussed (n = 5, 38%). Four themes for improving patient safety emerged from this study [ 1 ]: an organizational culture that prioritizes patient safety [ 2 ]; policies and processes to investigate patient safety issues, and implement and demonstrate impact from initiatives [ 3 ]; supporting staff to foster appetite, capacity, and participation in safety efforts, and offering upskilling and shared learning opportunities; and [ 4 ] engaging patients to explore and enhance their experiences and expectations of safe health care. Barriers and facilitators, and the strategies identified for addressing them, were related to the crafted themes and interconnected within a broader patient safety system.
While these four themes may appear particularly familiar in the context of the patient safety agenda over the past few decades, the results of this study underpin that these areas remain a priority. Further, given the relative lack of new emergent themes, the broader results of the study could be interpreted from the perspective that our recent efforts in these areas have not been sufficient, especially in the face of the many barriers identified by the experts in this study.
Strengths and limitations
Case design methodology is suitable to answer questions of ‘how’ and ‘why’ in a real-life context [ 8 ]. Our sample size of 27 experts was appropriate to explore study aims and achieve data saturation, within pragmatic considerations [ 24 ]. The response rate (1.7%) was low but consistent with expectations for a large-scale email circulation approach [ 25 ]. Our findings are a function of the convenience sampling approach used. A key study strength was the international perspectives captured through ISQua members, and the triangulation of contexts across countries, health services, and policy settings [ 26 ]. Data collection sought case study examples of aspects underpinning high-value and/or ineffective patient safety governance; however, participants’ responses varied in detail. To enhance credibility, we double-coded data from a 20% participant subsample and used a combined deductive-inductive analytical approach. Our findings are a reflection of the STAMP framework chosen for analysis; additional or alternative groupings of critical patient safety governance and system factors may have surfaced from deductive mapping to other frameworks, especially those that centre around or more broadly represent ‘culture’, which comprised 77% of mentioned factors by our participants. Data collection occurred in English; for some experts, this was not their first language which could introduce bias. To mitigate this, we cross-checked interview transcriptions against the audio files to correct for language mistakes. Study participants worked mostly in hospital settings and developing countries; therefore, it is unclear how experts from other settings experience patient safety and how this might affect future studies and recommendations.
Interpretation within the context of the wider literature
When examined as a whole, common to each of the themes is a focus on the primary actors in patient safety: the patient; the healthcare workforce; and the organization. The Institute for Healthcare Improvement’s framework for respectful management of serious clinical adverse events first emphasised these layers over a decade-ago [ 27 ], and the findings of our research emphasize that globally our work needs to continue to develop across each of these ‘layers’ a culture that underpins safety and quality.
Reflecting the outermost layer of the ‘organization’, the study’s most frequently mentioned barrier or facilitator, ‘organizational culture and safety and quality mindset’, features prominently in the well-documented ‘third age in safety’ [ 28 ]. Here, the focus is on trying to understand and strengthen everyday features of work within complex sociotechnological systems that promote safety [ 29 ]. The achievement of a ‘restorative just culture’ has become an important component of this. Its function is to fashion appropriate responses to evidence of errors and failures and to preserve the possibility of learning while holding people accountable for unacceptable behaviours [ 29 ]. Therefore, our study’s key contribution to the literature lies in the findings embodying restorative just culture principles [ 30 ], and operationalizing these within a patient safety governance system [ 31 ]. Restorative responses to patient safety incidents are ‘a voluntary, relational process where all those affected by an adverse event come together in a safe and supportive environment, with the help of skilled facilitators, to speak openly about what happened, to understand the human impacts, and to clarify responsibility for the actions required for healing and learning’ [ 32 ]. This definition speaks directly to the themes identified by study participants, with our findings further supported by a recent systematic review [ 33 ] which framed trust as a key tenet to just culture in hospital settings, and achievable through strategies that address organizational and team factors (e.g. management support and commitment, transparent incident reporting, close supervisory relationships, discussion of the nature of errors) and staff experience (e.g. clinical skill confidence, knowledge of reporting systems) [ 33 ]. Mirroring related literature, restorative approaches are scaffolded by adequate resourcing [ 31 ] and accreditation processes within a ‘quality-of-care (accreditation, inspection and public reporting)’ [ 34 ] paradigm. In this way, data-driven solutions can be formulated to ‘close the loop’ and facilitate sustained learning, implementation, and evaluation of patient safety initiatives [ 35 , 36 ].
With respect to the ‘layer’ reflecting the healthcare workforce, healthcare professionals are often the ‘second victims’ of patient safety incidents, with many personally traumatized and professionally (e.g. blamed) as a result [ 37 ]. Continuing the focus on the need for continued efforts to support a culture of safety, the theme of supporting staff in nonpunitive pro-learning environments has been reported in the literature and can assist their wellbeing and motivate reflective practice and behavioural change [ 37–39 ]. Support resources for those affected by patient safety incidents aim to provide psychological first aid, foster coping strategies, and promote individual resilience [ 40 ]. The Institute for Healthcare Improvement’s framework for respectful management of serious clinical adverse events [ 27 ] addresses the second victim phenomenon and has been adopted within national-level patient safety responses [ 41 ].
At the core of health care is the ‘layer’ that represents those that receive care and are consumers of our health services, and again, this was a clear theme within the findings of this study. There is increasing global momentum in promoting the patient voice in patient safety initiatives [ 42 ]. Recent systematic review evidence supports the benefits of patient engagement when developing health services and policy, resulting in positive health outcomes (e.g. reduced neonatal mortality) and the identification of broader healthcare priorities (e.g. environmental, educational, employment conditions) [ 43 ]. In support of our findings, barriers to patient safety engagement are currently based on an unwillingness to participate from patients (e.g. fear of reprisals, health literacy) and healthcare professionals (e.g. potential legal ramifications, attitude/knowledge limitations), coupled with organizational constraints (e.g. power-dynamic cultures, limited resourcing) [ 43 ]. Based on available evidence [ 44 ], future engagement approaches should be proactive and employ collaborative patient-professional partnerships, user-friendly patient safety feedback systems (e.g. succinct, plain language, integrated with documentation systems), and strategies to empower patients and improve confidence and seek organizational sponsorship (e.g. transparent value-based culture, staff consistency/training, whole of agency support).
Implications for policy, practice, and research
Policymakers can use our findings to identify and target current gaps in patient safety directives with national and international improvement initiatives that are tailored to a country’s own stage of evolution. These include accreditation processes, consistent and continuous undergraduate and postgraduate education, data reporting systems and infrastructure for benchmarking, and the establishment of clinical collaboratives for shared learnings and work towards national and international priorities. Study themes could inform further explorations of key factors for effective patient safety governance via implementation mechanistic and logic modelling [ 45 ], with findings used to design and pilot test interventional approaches across healthcare organizations and settings to explore outcomes and the relative cost-effectiveness in varying contexts.
Exploring the perspectives of international experts towards patient safety governance revealed aspects that provide value in improving patient outcomes. The quality and sustainability of patient safety governance relies on a strong safety culture in healthcare organizations, national policies and regulatory standards, continuing education for staff, and meaningful patient engagement approaches. The proposed ‘patient safety governance model’ provides policymakers and researchers with a framework to develop data-driven policy and initiatives.
Supplementary Material
Mzad088_supp, acknowledgements.
Funding for this research was provided by a grant from the Australian Patient Safety Foundation. The authors would like to acknowledge the assistance of the International Society for Quality in Health Care (ISQua) and the participants who contributed their valuable time and expertise.
Contributor Information
Peter D Hibbert, Australian Institute of Health Innovation, Faculty of Medicine, Health and Human Sciences, Macquarie University, 75 Talavera Rd, Macquarie Park, NSW 2109, Australia. IIMPACT in Health, Allied Health and Human Performance, University of South Australia, GPO Box 2471, Adelaide SA 5001, Australia.
Sasha Stewart, Australian Institute of Health Innovation, Faculty of Medicine, Health and Human Sciences, Macquarie University, 75 Talavera Rd, Macquarie Park, NSW 2109, Australia.
Louise K Wiles, Australian Institute of Health Innovation, Faculty of Medicine, Health and Human Sciences, Macquarie University, 75 Talavera Rd, Macquarie Park, NSW 2109, Australia. IIMPACT in Health, Allied Health and Human Performance, University of South Australia, GPO Box 2471, Adelaide SA 5001, Australia.
Jeffrey Braithwaite, Australian Institute of Health Innovation, Faculty of Medicine, Health and Human Sciences, Macquarie University, 75 Talavera Rd, Macquarie Park, NSW 2109, Australia.
William B Runciman, IIMPACT in Health, Allied Health and Human Performance, University of South Australia, GPO Box 2471, Adelaide SA 5001, Australia.
Matthew J W Thomas, Appleton Institute, School of Health, Medical and Applied Sciences, Central Queensland University, 114-190 Canning Street, Rockhampton, Queensland 4700, Australia.
Supplementary data
Supplementary data is available at INTQHC online.
SS and LKW received University of South Australia funding with a grant from the Australian Patient Safety Foundation.
Data availability statement
Contributorship.
P.H., M.T., S.S., and W.B.R. designed the study. P.H. and S.S. conducted the interviews, S.S. and L.K.W. analysed the interview data, and P.H., M.T., and W.B.R. contributed to interpretation of interview data. All authors contributed to writing of the manuscript and approved the final manuscript.
Ethics and other permissions
All participants provided written informed consent prior to participating in the study. The study received Human Research Ethics Committee approval by the University of South Australia Human Research Ethics Committee (203 467).

ASHRM President O’Sullivan’s March Message
We thrive together at ashrm.

Emerging Roles of Risk Managers in Senior Living and Skilled Nursing

Handling Disagreements Between Telehealth Critical Care and Bedside Providers

Strategies for Communication and Apology are Critical for Front-line Staff

Risk Professionals Ideal to Lead Health Care ESG Journey

- Uncategorized
Case Studies in Patient Safety
- Google Plus
Storytelling has been key to learning since the beginning of humankind. Case studies are a form of storytelling that often includes learning objectives, reflection and analysis. This book by Julie K. Johnson, Helen W. Haskell and Paul R. Barach uses storytelling to explore medical cases from the viewpoints of surviving family members. The amount of effort to collect such stories must have been astounding, but the reader benefits in incalculable ways.
The book’s stories illuminate how the industry might move from a clinician-centered system of care to a patient and family-centered system of care. The authors refer to Paul Batalden’s quote, “Every system is perfectly designed to get the results it gets.” For example, the results of the current medical educations system are knowledgeable diagnosticians who are focused on the individual physician-patient dyad. The authors examined 153 competencies across disciplines internationally that seem to correlate with good outcomes. The book’s stories are organized by these competencies:
- Medical knowledge, patient care
- Professionalism
- Interpersonal/communication skills
- Practice-based learning and improvement
- System-based practice
- Interprofessional collaboration
- Personal and professional development
One sees where professionalism and interpersonal/communication skills are greater important deficits for the families than knowledge or patient care aspects. This sets up the challenge for the reader, as the authors promote, to think differently about how to emotionally and intellectually engage patients and providers in healthcare transformation.
Discussed are 24 cases resulting from in- and out-patient settings in locations throughout the English-speaking world. One poignant case concerned a routine endoscopic procedure, an endoscopic retrograde cholangiopancreatography (ERCP). Post discharge, the patient began regurgitating, perspiring and was in pain. A telephone call to the office nurse resulted in a Tylenol suggestion. Then the physician called and suggested soup. A family member demanded a direct admission. The patient arrived at the emergency room with no forwarding message from the physician so she waited 12 hours for pain meds, but a full workup was achieved. The physician was not returning any emergency room calls as it was after 5 p.m. and the covering colleague said “not my patient.” As the patient deteriorated, a catheter was inserted. Then she was moved to the ICU and then to CCU. Diagnosis: sepsis. No record was ever found for the catheter order nor the ICU or CCU admissions. By now hospital specialists were attending to the patient with no sign of the original surgeon. The first code blue was noted.
With pneumonia and sepsis prevailing, staff placed a ventilator. Physicians mentioned pancreatitis after ERCP. They said it was not uncommon and the patient should recover. Eleven days later the patient had a cardiac arrest and coded. There were conflicting stories whether this occurred during a bath or during some suctioning. The code was unsuccessful. The family was not called by nursing per the protocol.
The CEO called the family back about a month after the death. New management had taken over the hospital. The CEO was trying to set a meeting with the family and physician, but the physician refused. After a year from the death, the physician accepted a meeting. Evidently, he felt comfortable because the family had not requested an autopsy so there was no way to prove whether the surgeon should have done the procedure in the first place or if he had done it wrong. The family regrets the omission of the autopsy because they saw there was no redress possible without it. After a complaint, the state medical board saw no wrong doing on the part of the surgeon. The state’s health services department did cite the emergency room for the lack of care of the patient.
The family felt abandoned by the surgeon, wrote a book about the event and discovered that adverse events were not nearly as common as they were led to believe. The book reviews further insight and notes ERCP is now widely overused.
In conclusion, this book presents poignant case studies that prompt one to think about various sides of stories and how systems, cultures and technical skills intertwine to affect life and death. One sees how the lack of communication can trump all of the aforementioned items to create a disaster. However, the reader is not left depressed, but instead inspired by the people sharing their stories and by the subsequent critical thinking that can occur after reading them.
Johnson, J., Haskell, H., & Barach, P. (2016) Case Studies in Patient Safety. Subury, MA: Jones and Bartlett Learning
You may also like
Building a High-Reliability Organization: A Toolkit for Success

ASHRM Whitepaper – Telemedicine: Risk Management Considerations


Stronger: Develop the Resilience You Need to Succeed
Sign up for ashrm forum updates.
Provide your information below to subscribe to ASHRM email communications
ASHRM Forum
- Submit an Article
Recent Articles
- ASHRM President O’Sullivan’s March Message March 20, 2024
- We thrive together at ASHRM January 10, 2024
- Emerging Roles of Risk Managers in Senior Living and Skilled Nursing October 16, 2023
- Handling Disagreements Between Telehealth Critical Care and Bedside Providers September 12, 2023
- Strategies for Communication and Apology are Critical for Front-line Staff September 7, 2023
- January 2024
- October 2023
- September 2023
- November 2022
- February 2022
- January 2022
- December 2021
- December 2020
- October 2020
- September 2020
- August 2020
- February 2020
- November 2019
- September 2019
- August 2019
- February 2019
- January 2019
- December 2018
- October 2018
- September 2018
- August 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- February 2017
- November 2016
- October 2016
- September 2016
- ASHRM Academy
- ASHRM President Message
- ASHRM Updates
- Behavioral Health
- Book Review
- Emergency Preparedness
- Enterprise Risk Management (ERM
- Human Capital
- Legal & Regulatory
- Letter from the Chair
- Member Profile
- Operational
- Patient Safety/Clinical Care
- Sustainibility
- Angela Lucas, MSN, BSN, RN, CCRN-K
- Anne Huben-Kearney, RN, BSN, MPA, CPHRM, CPHQ, CPPS, DFASHRM
- Arlene Luu, RN, BSN, JD, CPHRM
- Barbara McCarthy RN, MPH, CIC, CPHQ, CPHRM, FASHRM
- Benedict Hane
- Chad Follmer, ARM, MBA
- Dan Corcoran
- Dan Groszkruger, JD, MPH, CPHRM, DFASHRM
- Deborah Lessard CPHRM, FASHRM, MS and Leigh Ann Yates, AIC, MBA, CPHRM, DFASHRM
- Deborah Lessard, Esq., RN, JD, MA, BSN, CPHRM, FASHRM
- Denise Shope, RN, MHSA, ARM, CPHRM, DFASHRM and Nancy Connelly, RN, BA, CPHRM, DFASHRM
- Denise Winiarski JD, CPHRM Emily Klatt, JD Amir Kazerouninia, MD, PhD
- Ferdinando L. Mirarchi, DO, FAAEM, FACEP
- Forum Task Force Chair Leigh Ann Yates, AIC, MBA, CPHRM, DFASHRM
- Franchesca J. Charney, RN, MS, CPHRM, CPPS, CPSO, DFASHRM and Guy Whittall-Scherfee, MS
- Heidi Harrison, CPHRM
- Jessica J. Ayd, Esq.; Sherri Hobbs, MSM, MSN, RN, CPHQ; Heather Joyce-Byers, MSJ, BS, RN, CCRN-K, CPHRM; Shannon M. Madden, Esq.
- Joan Porcaro, RN, BSN, MM, CPHRM
- John C. West, JD, MHA, DFASHRM, CPHRM,
- John D. Banja, PhD
- Julie Radford, JD, CPHRM
- Karen Garvey, DFASHRM, CPHRM, and CPPS
- Karen Wright RN, BSN, ARM, CPHRM
- Kathleen Shostek, RN ARM FASHRM CPHRM CPPS
- Kenita Hill, MSA, CPHRM, LNHA, LPN
- Larry Veltman, MD, FACOG, CPHRM, DFASHRM
- Leigh Ann Yates and Stephanie Nadasi
- Leigh Ann Yates, MBA, CPHRM, AIC, DFASHRM
- Mackenzie C. Monaco
- Maggie Neustadt, JD CPHRM, FASHRM
- Margaret Curtin, MPA, HCA, CPHRM, DFASHRM
- Mark Dame, MHA, CPHRM, FACHE
- Melanie Osley and Holly Taylor
- Melanie Osley, RN, MBA, CPHRM, CPHQ, CPPS, ARM, DFASHRM
- Melanie Taylor, Esq.
- Melinda Van Niel, BA, MBA and Doug Wojcieszak, MA, MS, BS
- Michael G. Lloyd, MBA, CPCU, ARM, CPHRM
- Monica Cooke BSN, MA, RNC, CPHQ, CPHRM, FASHRM
- Nancy Connelly, RN, BA, CPHRM, DFASHRM
- Nancy Connelly, RN, BA, CPHRM, DFASHRM and Kenita Hill, MSA, CPHRM, LNHA, LPN
- Paula Caballero
- Rhonda DeMeno, RN, MS,MPM, BSHRM, CBIC, CPHRM and Joan Porcaro, RN, BSN, MM, CPHRM
- Rita Barrett-Cosby, CPHRM
- Robin Diamond
- Ryan Solomon, JD
- Sarah B. Roberts, MPH, CHES, CPHQ, CPHRM, ARM, AIS, AINS
- Scripps La Jolla Memorial Quality Team Memorial Quality Team
- Steven D. Weiner and Mario Giannettino
- Sue Boisvert, BSN, MHSA, CPHRM, FASHRM
- Susan Lucot, MSN RN
- Suzanne Natbony
- Tatum O’Sullivan, RN, BSN, MHSA, CPHRM, DFASHRM, CPPS
- Tricia Brooks-Phillips, MSN, RN, CPHRM
- Vallerie H. Propper, JD, MPH
- Vicki J. Missar
- Log In / Register
- Education Platform
- Newsletter Sign Up
Case Studies

- How to Improve
- Improvement Stories
- Publications
- IHI White Papers
- Audio and Video
Case studies related to improving health care.
first < > last
- An Extended Stay A 64-year-old man with a number of health issues comes to the hospital because he is having trouble breathing. The care team helps resolve the issue, but forgets a standard treatment that causes unnecessary harm to the patient. A subsequent medication error makes the situation worse, leading a stay that is much longer than anticipated.
- Mutiny The behavior of a superior starts to put your patients at risk. What would you do? The University of Rochester’s Dr. Paul Griner presents the final installment in a series of case studies for the IHI Open School.
- On Being Transparent You are the CEO and a patient in your hospital dies from a medication error. What do you do next? The University of Rochester’s Dr. Paul Griner presents the fourth in a series of case studies.
- Locked In A cancer diagnosis leads to tears and heartache. But is it correct? Dr. Paul Griner, Professor Emeritus of Medicine at the University of Rochester, presents the third in a series of case studies for the IHI Open School.
- Confidentiality and Air Force One A difficult patient. A difficult decision. The University of Rochester’s Dr. Paul Griner presents the second in a series of case studies.
- The Protective Parent During a 50-year career in medicine, Dr. Paul Griner accumulated hundreds of patient stories. Most of his stories – including this case study "The Protective Parent" - are from the 1950s and 1960s, prior to what we now refer to as “modern medicine.”
- Advanced Case Study Between Sept. 30th and Oct. 14th, 2010, students and residents all over the world gathered in interprofessional teams and analyzed a complex incident that resulted in patient harm. Selected teams presented their work to IHI faculty during a series of live webinars in October.
- A Downward Spiral: A Case Study in Homelessness Thirty-six-year-old John may not fit the stereotype of a homeless person. Not long ago, he was living what many would consider a healthy life with his family. But when he lost his job, he found himself in a downward spiral, and his situation dramatically changed. John’s story is a fictional composite of real patients treated by Health Care for the Homeless. It illustrates the challenges homeless people face in accessing health care and the characteristics of high-quality care that can improve their lives.
- What Happened to Alex? Alex James was a runner, like his dad. One day, he collapsed during a run and was hospitalized for five days. He went through lots of tests, but was given a clean bill of health. Then, a month later, he collapsed again, fell into a deep coma, and died. His father wanted to know — what had gone wrong? Dr. John James, a retired toxicologist at NASA, tells the story of how he uncovered the cause of his son’s death and became a patient safety advocate.
- Improving Care in Rural Rwanda When Dr. Patrick Lee and his teammates began their quality improvement work in Kirehe, Rwanda, last year, the staff at the local hospital was taking vital signs properly less than half the time. Today, the staff does that task properly 95% of the time. Substantial resource and infrastructure inputs, combined with dedicated Rwandan partners and simple quality improvement tools, have dramatically improved staff morale and the quality of care in Kirehe.


An official website of the Department of Health and Human Services

Browse Topics
Priority populations.
- Children/Adolescents
- Racial/Ethnic Minorities
- Rural/Inner-City Residents
- Special Healthcare Needs
- Clinicians & Providers
- Data & Measures
- Digital Healthcare Research
- Education & Training
- Hospitals & Health Systems
- Prevention & Chronic Care
- Quality & Patient Safety
- Publications & Products
- AHRQ Publishing and Communications Guidelines
- Search Publications
Research Findings & Reports
- Evidence-based Practice Center (EPC) Reports
- Fact Sheets
- Grantee Final Reports: Patient Safety
- Making Healthcare Safer Report
- National Healthcare Quality and Disparities Reports
- Technology Assessment Program
- AHRQ Research Studies
National Healthcare Quality and Disparities Report
Latest available findings on quality of and access to health care
- Data Infographics
- Data Visualizations
- Data Innovations
- All-Payer Claims Database
- Healthcare Cost and Utilization Project (HCUP)
- Medical Expenditure Panel Survey (MEPS)
- AHRQ Quality Indicator Tools for Data Analytics
- State Snapshots
- United States Health Information Knowledgebase (USHIK)
- Data Sources Available from AHRQ
Funding & Grants
Notice of funding opportunities, research policies.
- Notice of Funding Opportunity Guidance
- AHRQ Grants Policy Notices
- AHRQ Informed Consent & Authorization Toolkit for Minimal Risk Research
- HHS Grants Policy Statement
- Federal Regulations & Authorities
- Federal Register Notices
- AHRQ Public Access Policy
- Protection of Human Subjects
Funding Priorities
- Special Emphasis Notices
- Staff Contacts
Training & Education Funding
Grant application, review & award process.
- Grant Application Basics
- Application Forms
- Application Deadlines & Important Dates
- AHRQ Tips for Grant Applicants
- Grant Mechanisms & Descriptions
- Application Receipt & Review
- Study Sections for Scientific Peer Review
- Award Process
Post-Award Grant Management
- AHRQ Grantee Profiles
- Getting Recognition for Your AHRQ-Funded Study
- Grants by State
- No-Cost Extensions (NCEs)
AHRQ Grants by State
Searchable database of AHRQ Grants
AHRQ Projects funded by the Patient-Centered Outcomes Research Trust Fund.
- Press Releases
- AHRQ Social Media
- Impact Case Studies
- AHRQ News Now
- AHRQ Research Summit on Diagnostic Safety
- AHRQ Research Summit on Learning Health Systems
- National Advisory Council Meetings
- AHRQ Research Conferences
- AHRQ's 35th Anniversary
- Mission and Budget
- AHRQ's Core Competencies
- National Advisory Council
- Careers at AHRQ
- Maps and Directions
- Other AHRQ Web Sites
- Other HHS Agencies
- Testimonials
Organization & Contacts
- Centers and Offices
- Organization Chart
- Key Contacts
- Evidence-based Practice Center Reports
- National Healthcare Quality & Disparities Reports
- Making Health Care Safer II
- Making Healthcare Safer III
Making Healthcare Safer IV
- Making Health Care Safer
- Making Healthcare Safer Comparison
A Continuous Updating of Patient Safety Harms and Practices
Making Healthcare Safer reports I, II, and III have shown a positive impact of patient safety practices on the reduction of medical errors. However, threats to patient safety are still emerging and evolving in a dynamic world.
Patient safety research is growing, spanning across more healthcare settings, and considers a wide array of contextual factors. The combination of emerging patient safety threats and the growing amount of published patient safety research, patient safety resources, and accrediting body standards makes it increasingly difficult to prioritize adoption and implementation of evidence-based practices. AHRQ’s fourth iteration of Making Healthcare Safer intends to address this issue by publishing evidence-based reviews of patient safety practices and topics as they are completed. This intentional release of updated reviews will aid healthcare organization leaders in prioritizing implementation of evidence-based practices in a timelier way. The report also will help researchers identify where more research is needed in a timelier way and assist policymakers in understanding which patient safety practices have the supporting evidence for promotion. Reviews will be posted below as they are completed.
Making Healthcare Safer IV was commissioned in 2022. To kick off the report, AHRQ explored the potential harms that may be associated with telehealth, which has grown exponentially during the wake of the COVID-19 pandemic to facilitate healthcare during a time when in-person clinical encounters between a patient and clinician was significantly reduced to help slow the spread of the virus. Because the benefits of telehealth became evident during the pandemic, the harms and patient safety practices to reduce the risk for medical errors, misdiagnosis, and privacy concerns are still being assessed. This review will serve as a baseline for the evidence of harms and patient safety practices to prevent or mitigate harms associated with the use of telehealth.
Making Healthcare Safer IV began with a horizon scan to identify emerging trends and needs in the patient safety field. A technical expert panel (TEP) was convened to prioritize which topics and patient safety practices, including updates to the ones covered in the previous Making Healthcare Safer reports, would be most beneficial to the field if addressed throughout the years of the fourth report. These discussions are summarized in the Prioritization Report .
AHRQ determined that the first rapid review would be on the potential harms that may be associated with telehealth, which has grown exponentially during the wake of the COVID-19 pandemic to facilitate healthcare during a time when in-person clinical encounters between a patient and clinician was significantly reduced to help slow the spread of the virus. Because the benefits of telehealth became evident during the pandemic, the harms and patient safety practices to reduce the risk for medical errors, misdiagnosis, and privacy concerns are still being assessed. This review will serve as a baseline for the evidence of harms and patient safety practices to prevent or mitigate harms associated with the use of telehealth. Since AHRQ asked for this topic to be explored first, it was not discussed during the TEP convening.
The first three Making Healthcare Safer reports, published in 2001 , 2013 , and 2020 , have each served as a consolidated source of information for healthcare providers, health system administrators, researchers, and government agencies. A set of tables compares the patient safety practices among the reports.
Prioritization of Patient Safety Practices for Making Healthcare Safer IV
Potential Harms Resulting From Video-Based Telehealth
Patient and Family Engagement
Surgical Report Cards and Outcome Measurements
Opioid Stewardship
Reducing Adverse Events Related to Anticoagulants
Implicit Bias Training
Deprescribing
Computerized Clinical Decision Support To Prevent Medication Errors and Adverse Drug Events
Failure To Rescue—Rapid Response Systems
Transmission-Based Precautions for Multidrug-Resistant Organisms
Sepsis Prediction, Recognition, and Intervention
Engaging Family Caregivers
Fatigue and Sleepiness of Clinicians Due to Hours of Service
Infection Surveillance for Clostridiodes difficile , Methicillin-Resistant Staphylococcus aureus (MRSA), Carbapenem-Resistant Enterobacterales (CRE), and Candida auris
Internet Citation: Making Healthcare Safer IV. Content last reviewed April 2024. Agency for Healthcare Research and Quality, Rockville, MD. https://www.ahrq.gov/research/findings/making-healthcare-safer/mhs4/index.html
Nursing Case Study Jessica’s Suicide
This essay about a nursing case study investigates the tragic suicide of Jessica, a young patient with a history of severe depression and anxiety. It critically examines the factors contributing to her death, emphasizing the need for vigilant mental health care and responsive adjustments in treatment based on a patient’s changing emotional state. The analysis points out failures in communication within the healthcare team and inadequate family involvement, suggesting that better informed support networks could prevent similar crises. The essay advocates for integrated care approaches, including psychological, psychiatric, and social support, to enhance patient-centered care and potentially save lives. This reflective analysis underscores the importance of training and awareness in healthcare settings to better manage and support patients experiencing mental health challenges.
How it works
Suicide is a critical public health issue that necessitates comprehensive understanding and sensitive intervention, particularly within the healthcare setting. This analysis delves into a poignant nursing case study centered around Jessica, a young patient who tragically ended her life. By examining Jessica’s case, we aim to shed light on the complex interplay of mental health challenges and the healthcare strategies that could potentially mitigate such devastating outcomes.
Jessica, a 24-year-old female, had been battling severe depression and anxiety for several years.
Her medical history reveals multiple previous attempts at suicide, each coinciding with periods of extreme emotional distress. Jessica’s situation underscores a critical aspect of mental health care: the necessity for vigilant, ongoing assessments and interventions tailored to individual patient histories and circumstances.
Upon her last admission to the hospital, Jessica appeared particularly withdrawn and despondent. Nursing notes indicated that she expressed feelings of hopelessness and a decreased interest in engaging with both staff and her own family members. Despite these clear warning signs, the response from the healthcare team was not sufficiently tailored to her acute need for intensive psychological support. This case points to the first significant lesson: the importance of responsive care adjustments based on a patient’s evolving emotional and psychological state.
One pivotal factor in Jessica’s care was the communication between her nurses and the broader psychiatric team. Effective communication in healthcare settings is crucial and can often be the deciding factor in preventing a crisis. For Jessica, the lapse in conveying critical information about her worsening depressive state and potential suicidal ideation might have contributed to the lack of timely interventions. Therefore, enhancing communication protocols within hospital settings could serve as a preventive measure, ensuring that all team members are aware of a patient’s current mental health status and are acting accordingly.
Additionally, Jessica’s case highlights the role of family involvement in managing mental health crises. It appears that her family was not fully aware of the gravity of her condition nor the potential for imminent risk. Increasing family engagement and education about mental health conditions could bridge this gap, providing a support system that is more attuned and responsive to the patient’s needs.
In addressing these issues, healthcare providers can learn from Jessica’s case to better manage similar situations. Implementing routine and more detailed psychological evaluations can help identify at-risk individuals before a crisis occurs. Training for nursing staff in recognizing the subtleties of mental health deterioration and the importance of assertive communication can also be crucial.
Furthermore, integrating multidisciplinary approaches that include psychological, psychiatric, and social support can create a more holistic care model. Such integration ensures that patients like Jessica receive not only medical treatment but also comprehensive psychosocial support, potentially alleviating the sense of isolation and despair that can lead to suicide.
Finally, healthcare institutions must foster an environment where mental health care is prioritized and where all staff members are equipped with the necessary tools and training to effectively intervene. This requires ongoing education and awareness programs that emphasize the complexities of mental health issues and the critical role of tailored, patient-centered care.
Jessica’s tragic outcome serves as a somber reminder of what might happen when systemic and individual care components fail to adequately align with the needs of those at risk. Through this case study, we learn the invaluable lessons of vigilance, communication, and an integrated approach to mental health within the nursing profession. It is only through such committed efforts that we can hope to prevent such losses in the future and better support our patients through their most challenging times.
Cite this page
Nursing Case Study Jessica's Suicide. (2024, Apr 14). Retrieved from https://papersowl.com/examples/nursing-case-study-jessicas-suicide/
"Nursing Case Study Jessica's Suicide." PapersOwl.com , 14 Apr 2024, https://papersowl.com/examples/nursing-case-study-jessicas-suicide/
PapersOwl.com. (2024). Nursing Case Study Jessica's Suicide . [Online]. Available at: https://papersowl.com/examples/nursing-case-study-jessicas-suicide/ [Accessed: 14 Apr. 2024]
"Nursing Case Study Jessica's Suicide." PapersOwl.com, Apr 14, 2024. Accessed April 14, 2024. https://papersowl.com/examples/nursing-case-study-jessicas-suicide/
"Nursing Case Study Jessica's Suicide," PapersOwl.com , 14-Apr-2024. [Online]. Available: https://papersowl.com/examples/nursing-case-study-jessicas-suicide/. [Accessed: 14-Apr-2024]
PapersOwl.com. (2024). Nursing Case Study Jessica's Suicide . [Online]. Available at: https://papersowl.com/examples/nursing-case-study-jessicas-suicide/ [Accessed: 14-Apr-2024]
Don't let plagiarism ruin your grade
Hire a writer to get a unique paper crafted to your needs.

Our writers will help you fix any mistakes and get an A+!
Please check your inbox.
You can order an original essay written according to your instructions.
Trusted by over 1 million students worldwide
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers

An official website of the Department of Health & Human Services
- Search All AHRQ Sites
- Email Updates

1. Use quotes to search for an exact match of a phrase.
2. Put a minus sign just before words you don't want.
3. Enter any important keywords in any order to find entries where all these terms appear.
- The PSNet Collection
- All Content
- Perspectives
- Current Weekly Issue
- Past Weekly Issues
- Curated Libraries
- Clinical Areas
- Patient Safety 101
- The Fundamentals
- Training and Education
- Continuing Education
- WebM&M: Case Studies
- Training Catalog
- Submit a Case
- Improvement Resources
- Innovations
- Submit an Innovation
- About PSNet
- Editorial Team
- Technical Expert Panel
Book/Report
Patient Safety: A Case-based Innovative Playbook for Safer Care. Second Edition.
Agrawal A, Bhatt J, eds. Cham, Switzerland, Springer Nature; 2023. ISBN: 9783031359330.
This publication describes and analyzes clinical cases to illustrate patient safety concepts and types of medical errors to engage clinicians in improvement work. The second edition includes chapters devoted to safety challenges that emerged in prominence due to the COVID-19 pandemic (health disparities, inequities and nursing home care failures), as well as core topics such as high reliability, human factors engineering and the opioid epidemic.
Advances in Human Factors and Ergonomics in Healthcare and Medical Devices. September 11, 2019
Error Reduction and Prevention in Surgical Pathology, Second Edition. August 28, 2019
Cognitive Errors and Diagnostic Mistakes: A Case-Based Guide to Critical Thinking in Medicine. July 10, 2019
Mistakes, Errors and Failures across Cultures. April 15, 2020
Diagnoses Without Names: Challenges for Medical Care, Research, and Policy. October 12, 2022
Textbook of Patient Safety and Clinical Risk Management. January 20, 2021
Clinical Uncertainty in Primary Care: The Challenge of Collaborative Engagement. March 5, 2014
Cognitive Informatics: Reengineering Clinical Workflow for Safer and More Efficient Care. August 21, 2019
Occupational Health and Organizational Culture within a Healthcare Setting: Challenges, Complexities, and Dynamics. January 17, 2024
Decision Making in Emergency Medicine: Biases, Errors and Solutions. June 30, 2021
Global Burden of Preventable Medication-related Harm in Health Care: A Systematic Review. March 20, 2024
New evidence on stemming low-value prescribing. May 1, 2019
Making Healthcare Safe: The Story of the Patient Safety Movement. June 9, 2021
Building a Culture of Patient Safety Through Simulation: An Interprofessional Learning Model. June 10, 2015
Patient Safety in Dialysis Access. February 25, 2015
Quality and Safety in Nursing: a Competency Approach to Improving Outcomes, Second Edition. May 17, 2017
High Reliability Organizations: A Healthcare Handbook for Patient Safety & Quality. May 25, 2016
A Socio-cultural Perspective on Patient Safety. February 22, 2012
Zero Harm: How to Achieve Patient and Workforce Safety in Healthcare. July 31, 2019
Medication Safety for Look-alike, Sound-alike Medicines. November 15, 2023
SHOT Annual Report. July 19, 2023
Procuring Interoperability: Achieving High-Quality, Connected, and Person-Centered Care. October 24, 2018
The Essential Guide for Patient Safety Officers, Second Edition. September 22, 2010
Enhancing Patient Safety and Reducing Errors in Health Care. March 6, 2005
Handbook of Perioperative and Procedural Patient Safety. February 7, 2024
Oxford Professional Practice: Handbook of Patient Safety. July 27, 2022
Health Care Errors and Patient Safety. May 13, 2009
Improving Usability, Safety and Patient Outcomes With Health Information Technology. February 27, 2019
Right Kind of Wrong: Why Learning to Fail can Teach us to Thrive. October 18, 2023
ICN Position Statement: Patient Safety. September 6, 2023
Broken Trust: Making Patient Safety More than Just a Promise. July 19, 2023
Systems Approach in Healthcare. October 31, 2018
Perioperative Handoffs. August 2, 2023
Patient Safety in Anesthetic Practice. March 27, 2005
Quality and Safety. July 29, 2015
Engaging Patients for Patient Safety: Advocacy Brief. February 14, 2024
Fragmented: A Doctor's Quest to Piece Together American Health Care. September 27, 2023
SAFER Electronic Health Records: Safety Assurance Factors for EHR Resilience. May 13, 2015
Organizing for Reliability: A Guide for Research and Practice. January 30, 2019
Around the Patient Bed: Human Factors and Safety in Health Care. October 23, 2013
The Nurse's Role in Medication Safety, Second Edition. January 11, 2012
Errors in Organizations. August 1, 2012
Optimal Resources for Surgical Quality and Safety. August 16, 2017
New Horizons in Patient Safety: Understanding Communication: Case Studies for Physicians. April 5, 2017
Improving Patient Safety Through Teamwork and Team Training. January 29, 2014
Putting Patients First: Best Practices in Patient-Centered Care. Second Edition. February 4, 2009
Advancing Diagnostic Excellence for Maternal Health Care: Proceedings of a Workshop–in Brief. November 15, 2023
Influencing the Quality, Risk and Safety Movement in Healthcare: In Conversation with International Leaders. November 4, 2015
Communicating Radiation Risks in Paediatric Imaging: Information to Support Healthcare Discussions About Benefit and Risk. July 13, 2016
Ethical Issues in Patient Safety Research: Interpreting Existing Guidance. August 7, 2013
Global Patient Safety Action Plan 2021-2030: Towards Eliminating Avoidable Harm in Health Care. August 18, 2021
Medication Safety Officer's Handbook. July 23, 2014
Cognitive Systems Engineering in Health Care. February 11, 2015
Delivering Quality Health Services: A Global Imperative for Universal Health Coverage. July 18, 2018
Safety in Medication Use. June 8, 2016
Teaching Clinical Reasoning. August 26, 2015
Optimizing Crisis Resource Management to Improve Patient Safety and Team Performance--A Handbook for Acute Care Health Professionals. September 13, 2017
Quality and Safety in Anesthesia and Perioperative Care. July 17, 2019
Global State of Patient Safety 2023. December 20, 2023
Patient Safety and Quality. March 3, 2010
Burnout in Healthcare. September 24, 2014
Patient Safety in Emergency Medicine. February 17, 2010
Artificial Intelligence in Health Care: The Hope, the Hype, the Promise, the Peril. December 1, 2019
Situational Awareness and Patient Safety: A Learning Package. December 7, 2011
The Sociology of Healthcare Safety and Quality. February 17, 2016
Implication of the COVID-19 Pandemic for Patient Safety: A Rapid Review. August 24, 2022
Systematically Identified Failure Is the Route to a Successful Health System. March 9, 2016
Resilience Engineering in Practice: a Guidebook. January 12, 2011
WHO Patient Safety Curriculum Guide: Multi-Professional Edition. November 23, 2011
Enhancing Patient Care: A Practical Guide to Improving Quality and Safety in Hospitals. November 4, 2009
Patient Safety. December 13, 2006
Language Barriers in Health Care. February 6, 2008
Merry and McCall Smith's Errors, Medicine, and the Law. 2nd ed. March 6, 2005
Ethics & Governance of Artificial Intelligence for Health. July 14, 2021
Safety and Ethics in Healthcare: A Guide to Getting it Right. October 10, 2007
Medical Device Use Error: Root Cause Analysis. March 2, 2016
Hospital bosses ignored months of doctors' warnings about Lucy Letby. August 30, 2023
Racial, Ethnic, and Payer Disparities in Adverse Safety Events: Are there Differences across Leapfrog Hospital Safety Grades? June 21, 2023
Vital Signs: Core Metrics for Health and Health Care Progress. May 20, 2015
Judgment under Uncertainty: Heuristics and Biases. March 6, 2005
Lessons from the Covid War: An Investigative Report. May 10, 2023
Patient Safety. January 12, 2022
Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. September 19, 2012
Optimizing Graduate Medical Trainee (Resident) Hours and Work Schedules to Improve Patient Safety. February 27, 2008
Reporting and Learning Systems for Medication Errors: The Role of Pharmacovigilance Centres. November 19, 2014
Patient Safety Culture: Theory, Methods and Application. January 21, 2015
Impact of the Care Quality Commission on Provider Performance: Room for Improvement? November 21, 2018
Global Patient Safety: Law, Policy and Practice. August 14, 2019
Human Factors Engineering for Healthcare Applications. April 14, 2010
Patient Safety: An Old and New Issue. August 22, 2007
Anesthesia Patient Safety Foundation Newsletter. January 4, 2006
Identification and Prevention of Common Adverse Drug Events in the Intensive Care Unit. June 16, 2010
Principles of Risk Management and Patient Safety. March 9, 2011
Impact of Medical Errors and Malpractice on Health Economics, Quality, and Patient Safety. April 26, 2017
Patient Safety: Perspectives on Evidence, Information and Knowledge Transfer. June 4, 2014
Improving Healthcare Team Communication: Building on Lessons from Aviation and Aerospace. June 25, 2008
Clinical Risk Management. Enhancing Patient Safety. 2nd ed. March 27, 2005
Quality and Safety. November 2, 2022
RFID tags reduce restocking errors of anesthesia medications. September 27, 2023
Diagnosis: Reducing Errors and Improving Quality. November 2, 2022
WebM&M Cases
Advancing Diagnostic Excellence for Older Adults: Proceedings of a Workshop in Brief. July 21, 2022 - July 21, 2022
Improved Diagnostic Accuracy Through Probability-Based Diagnosis. September 28, 2022
Administering High-Strength Insulin from a Pen Device in Hospital. September 14, 2022
Advancing Anticoagulation Stewardship: A Playbook. September 7, 2022
NAM Scholars in Diagnostic Excellence program. January 31, 2022
NCICLE Pathways to Excellence: Expectations for an Optimal Clinical Learning Environment to Achieve Safe and High-Quality Patient Care, 2021. November 24, 2021
Using performance improvement to enhance time-out compliance and prevent wrong-site surgery. August 11, 2021
Diagnostic Excellence Video Series December 2, 2020
Improving Diagnostic Quality and Safety/Reducing Diagnostic Error: Measurement Considerations. Final Report October 28, 2020
Association of current opioid use with serious adverse events among older adult survivors of breast cancer. October 14, 2020
Misdiagnosis, mistreatment, and harm - when medical care ignores social forces. April 8, 2020
Using incident reports to assess communication failures and patient outcomes. April 17, 2019
Formative evaluation of the video reflexive ethnography method, as applied to the physician–nurse dyad. February 6, 2019
Quality Improvement and Patient Safety Competencies Across the Learning Continuum. January 1, 2019
How communications issues between doctors and nurses can affect your health. September 19, 2018
Effective approaches to control non-actionable alarms and alarm fatigue. September 12, 2018
Quality and Safety Between Ward and Board: a Biography of Artefacts Study. August 29, 2018
The association between professional burnout and engagement with patient safety culture and outcomes: a systematic review. August 15, 2018
Master of Healthcare Quality and Safety. July 18, 2018
Diagnostic errors and the bedside clinical examination. June 27, 2018
Standardized Competencies for Parenteral Nutrition Administration: the ASPEN Model. June 20, 2018
Identifying quality markers of a safe surgical ward: an interview study of patients, clinical staff, and administrators. May 2, 2018
The first U.S. study on nurses' evidence-based practice competencies indicates major deficits that threaten healthcare quality, safety, and patient outcomes. April 25, 2018
White paper on recommendation for systems-based practice competency. December 6, 2017
The Role of Clinical Learning Environments in Preparing New Clinicians to Engage in Patient Safety. October 18, 2017
Addressing the Opioid Epidemic: Is There a Role for Physician Education? August 23, 2017

Connect With Us
Sign up for Email Updates
To sign up for updates or to access your subscriber preferences, please enter your email address below.
Agency for Healthcare Research and Quality
5600 Fishers Lane Rockville, MD 20857 Telephone: (301) 427-1364
- Accessibility
- Disclaimers
- Electronic Policies
- HHS Digital Strategy
- HHS Nondiscrimination Notice
- Inspector General
- Plain Writing Act
- Privacy Policy
- Viewers & Players
- U.S. Department of Health & Human Services
- The White House
- Don't have an account? Sign up to PSNet
Submit Your Innovations
Please select your preferred way to submit an innovation.
Continue as a Guest
Track and save your innovation
in My Innovations
Edit your innovation as a draft
Continue Logged In
Please select your preferred way to submit an innovation. Note that even if you have an account, you can still choose to submit an innovation as a guest.
Continue logged in
New users to the psnet site.
Access to quizzes and start earning
CME, CEU, or Trainee Certification.
Get email alerts when new content
matching your topics of interest
in My Innovations.
- Open access
- Published: 11 April 2024
Diagnostic delay of sarcoidosis: an integrated systematic review
- Tergel Namsrai 1 ,
- Christine Phillips 4 ,
- Anne Parkinson 1 ,
- Dianne Gregory 1 , 2 ,
- Elaine Kelly 1 , 2 ,
- Matthew Cook 3 &
- Jane Desborough ORCID: orcid.org/0000-0003-1406-4593 1
Orphanet Journal of Rare Diseases volume 19 , Article number: 156 ( 2024 ) Cite this article
10 Accesses
1 Altmetric
Metrics details
Sarcoidosis is a chronic inflammatory granulomatous disease of unknown cause. Delays in diagnosis can result in disease progression and poorer outcomes for patients. Our aim was to review the current literature to determine the overall diagnostic delay of sarcoidosis, factors associated with diagnostic delay, and the experiences of people with sarcoidosis of diagnostic delay.
Three databases (PubMed/Medline, Scopus, and ProQuest) and grey literature sources were searched. Random effects inverse variance meta-analysis was used to pool mean diagnostic delay in all types of sarcoidosis subgroup analysis. Diagnostic delay was defined as the time from reported onset of symptoms to diagnosis of sarcoidosis.
We identified 374 titles, of which 29 studies were included in the review, with an overall sample of 1531 (694 females, 837 males). The overall mean diagnostic delay in all types of sarcoidosis was 7.93 months (95% CI 1.21 to 14.64 months). Meta-aggregation of factors related to diagnostic delay in the included studies identified three categories: (1) the complex and rare features of sarcoidosis, (2) healthcare factors and (3) patient-centred factors. Meta-aggregation of outcomes reported in case studies revealed that the three most frequent outcomes associated with diagnostic delay were: (1) incorrect diagnosis, (2) incorrect treatment and (3) development of complications/disease progression. There was no significant difference in diagnostic delay between countries with gatekeeper health systems (where consumers are referred from a primary care clinician to specialist care) and countries with non-gatekeeper systems. No qualitative studies examining people’s experiences of diagnostic delay were identified.
The mean diagnostic delay for sarcoidosis is almost 8 months, which has objective consequences for patient management. On the other hand, there is a paucity of evidence about the experience of diagnostic delay in sarcoidosis and factors related to this. Gaining an understanding of people’s experiences while seeking a diagnosis of sarcoidosis is vital to gain insight into factors that may contribute to delays, and subsequently inform strategies, tools and training activities aimed at increasing clinician and public awareness about this rare condition.
Trial registration
PROSPERO Registration number: CRD42022307236.
Introduction
Sarcoidosis is a multisystem granulomatous inflammatory disease of unknown cause, which can affect any organ, but primarily affects the lungs. Sarcoidosis can present as acute or chronic disease - acute sarcoidosis, with joint pain, erythema nodosum and hilar adenopathy, that resolves spontaneously; or chronic sarcoidosis with insidious onset and slow progression that continues to invade multiple systems. In studies using national patient registers the incidence appears to be highest in northern Europe at 11.5 per 100,000 per year in Sweden [ 1 ] and 11.3–14.8 per 100,000 per year in Denmark [ 2 ], There are significant intra-country differences attributable to ethnicity in the USA where African Americans have significantly higher rates of disease [ 1 , 2 ], earlier peak age of onset [ 3 ] and higher mortality [ 4 ]. The patterns of organ involvement [ 5 , 6 , 7 ] and gender distribution [ 3 , 4 , 8 ] vary between countries and within countries.
The reported delay of diagnosis in sarcoidosis ranges from 6 months [ 2 ] to 24 months [ 9 ]. Its complex clinical features, acute or chronic presentation, spontaneous or treatment-induced remission in some cases, and the absence of a single simple diagnostic test all contribute to challenges in timely diagnosis. In many cases, diagnosis hinges on tissue diagnosis and therefore a firm diagnosis might be delayed even when the diagnosis is suspected. Some of the most consequential extrapulmonary manifestations of sarcoidosis – neurological, ophthalmic, and cardiac – are among the most difficult to diagnose [ 8 , 9 , 10 , 11 ]. Spontaneous remission occurs frequently in sarcoidosis [ 12 ]; some studies report remission in half of the cases [ 13 ]. Diagnostic delay can occur with both acute and chronic presentations of sarcoidosis, but particularly for chronic presentations marked by slow progression and complex features, mimicking other diseases. Failure to initiate treatment for progressive pulmonary sarcoidosis [ 14 ] and many extrapulmonary manifestations of sarcoidosis can result in permanent organ damage [ 11 , 15 , 16 ]. Since the pathogenesis of sarcoidosis remains unknown, it is a diagnosis of exclusion. The differential diagnosis includes other causes of granulomas, which encompass infections, including mycobacteria, fungi and bacteria, occupational exposures such as beryllium and silica, sterile granulomatous inflammation, and lymphoma.
There is a paucity of research examining the diagnostic delay of sarcoidosis, including factors associated with diagnostic delay and people’s experiences from the time of symptom onset to diagnosis. Our aim was to systematically review the current evidence regarding the diagnostic delay of sarcoidosis and people’s experiences of this. This evidence may help to inform the development of strategies to enhance awareness of rare manifestations of sarcoidosis, enabling timely intervention when warranted for chronic and progressive sarcoidosis.
This systematic review was performed and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [ 17 ] and the Cochrane Handbook for Systematic Reviews [ 6 ]. It is registered with PROSPERO, an International prospective register of systematic reviews (registration number: CRD42022289830).
Literature search, study selection, and data extraction
A systematic electronic search of the literature was conducted using PubMed/Medline, Scopus, and ProQuest databases up to the 25th of May 2022, with no limitations. The search string was pre-developed and peer-reviewed using the PRESS checklist [ 18 ]. The final search string included “sarcoidosis” AND “delay in diagnosis” OR “diagnostic delay” OR “misdiagnosis” OR “time to diagnosis” OR “incorrect diagnosis” OR “missed diagnosis” OR “delayed diagnosis” without restrictions on study type, date, and language. A detailed search string and strategy are available in the published protocol [ 19 ]. Grey literature sources were searched up to the 25th of May 2022 in Open Access Theses and Dissertations ( https://oatd.org/ ), ProQuest thesis and dissertations, and the National Library of Australia. Manual reference searches were conducted on all review articles identified in the literature search.
There was no restriction on publication dates. All studies, both qualitative and quantitative, examining diagnostic delay, incorrect diagnosis, missed diagnosis or slow diagnosis of sarcoidosis in all age groups were included, except for review articles. Studies in languages other than English, German and Indonesian were excluded. Final search results were imported into a systematic review management software (Covidence) to facilitate reviewer collaboration [ 20 ].
Two authors conducted an independent screening of titles and abstracts followed by a full-text screening of articles using pre-developed PICOS eligibility criteria outlined in Table 1 . Articles that did not meet the eligibility criteria were excluded. Discrepancies were resolved in discussion with a third reviewer and through reaching a consensus. Included studies were quality appraised using the Mixed Methods Appraisal Tool (MMAT) [ 21 ]. A pre-developed and pre-piloted data extraction tool was used, and following further discussion after piloting, data describing the initial specialist and the presence/absence of gatekeeper health systems were also extracted.
Data analysis
General data preparation.
Diagnostic delay was defined in accordance with the included studies - from reported onset of symptoms to a diagnosis of sarcoidosis. In studies where mean diagnostic delay was presented in years or days, we converted it to months. For studies that did not report a standard deviation (SD) of mean diagnostic delay, we imputed the SD using the method recommended by Cochrane, which calculates SD using an upper limit, lower limit, and confidence interval [ 6 ]. In studies where the confidence interval was not reported, we calculated SD using the method improved by Wan and colleagues, incorporating the sample size or population [ 22 ].
Categorisation of studies was based on the location or organ involvement of sarcoidosis - pulmonary, extrapulmonary, and systemic. Where sarcoidosis involved only the lungs (defined as changes in hila, mediastina, and the lungs) the location was categorised as pulmonary; where sarcoidosis involved two or more organs the location was categorised as systemic. If only one organ other than the lungs was involved, the location was categorised as extrapulmonary. Health systems were categorised as either gatekeeper (where primary care physicians authorise access to specialist physicians) or non-gatekeeper health systems, based on the dominant health system in the country where the study was conducted. A country was classified as having a gatekeeper system if the system of health financing uniformly used primary care gatekeepers, without the option of self-funding to see specialists, or models of health funding that supported open access to specialists. In countries with diverse health insurance models which may include open access and gatekeepers, such as the USA, an assessment was made for each publication by two authors. Where we could not determine the gatekeeper system used by participants the paper was excluded. We calculated the missing mean age of the study sample when complete data of the study participants was available.
Analysis of diagnostic delay in sarcoidosis
We used an inverse variance weighted random effects model (Der-Simonian-Laird method) to pool mean diagnostic delay [ 6 ]. Sensitivity analyses between studies with estimated SDs and original SDs were conducted. Additionally, we conducted subgroup analyses based on healthcare system type and publication year to investigate possible group differences in diagnostic delay in sarcoidosis. We analysed quantitative data through a meta-synthesis. The alpha level was set at 0.05, and the heterogeneity of meta-analysis estimates was presented using the I 2 statistic. Funnel plots were used to assess the risk of publication bias.
We descriptively analysed and presented a narrative synthesis of the quantitative data from case reports that could not be pooled. Gender difference in diagnostic delay was calculated in case reports where data on sex and delay in diagnosis (months) was available. The distribution of delay in diagnosis in case reports was examined by density plot and Shapiro test ( p <.05), indicating non-normal distribution; thus, the Mann-Whitney-Wilcoxon test was used to analyse the group differences of delay in diagnosis by sex. All statistical analyses were performed using R version 4.6.2 [ 23 ] and the ‘meta’ package.
Analysis of symptoms, factors, outcomes and experiences associated with diagnostic delay
To investigate the factors associated with diagnostic delay, data on symptoms that changed the diagnosis, and factors related to and outcomes of diagnostic delay were extracted and synthesised using meta-aggregation, for which meanings from qualitative data are identified and aggregated into categories that can be synthesised and analysed [ 24 ]. The broader categorisation of the aggregated data was decided through peer discussion and referral back to the original papers when needed. Additionally, factors linked to pulmonary, extrapulmonary and systemic sarcoidosis were grouped and further analysed.
To our knowledge, none of the included studies reported data on experiences of diagnostic delay in sarcoidosis.
Out of 374 titles identified, we removed 100 duplicates, and screened 274 titles and abstracts. Of those, 67 articles were reviewed at full text and 29 studies were included in the review as shown in Fig. 1 .
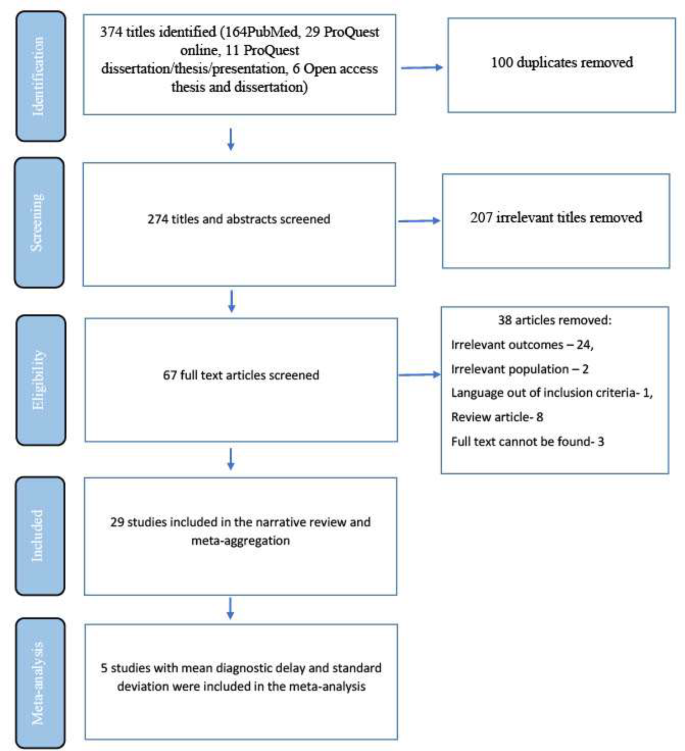
Selection flow chart of studies included in the systematic review
Description of included studies
Included studies are summarised in Table 2 and a full data extraction table is presented in Supplementary Table 1 . The 29 included studies comprised 24 non-comparative descriptive studies (including 15 case reports [ 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 ], five case series [ 40 , 41 , 42 , 43 , 44 ], two surveys [ 45 , 46 ], and two descriptive cross-sectional studies [ 2 , 47 ]), and five comparative studies (all analytical cross-sectional studies) [ 9 , 48 , 49 , 50 , 51 ]. Twenty-eight of the included studies used non-patient-reported data including clinical reports and retrospective patient registry data, while one used patient-reported data [ 45 ]. In total, there were eleven studies from Europe [ 2 , 9 , 25 , 26 , 33 , 35 , 38 , 42 , 45 , 47 , 48 ], nine from the United States or Canada [ 27 , 29 , 30 , 32 , 34 , 37 , 43 , 44 , 49 ], three from West Asia [ 41 , 46 , 50 ], four from East Asia [ 28 , 31 , 39 , 40 ], one from sub-Saharan Africa [ 36 ], and one from South America [ 51 ]. Various organ involvement of sarcoidosis was reported, including eyes [ 9 ], nasal passages [ 42 ], kidney [ 26 , 27 ], skin [ 28 , 34 ], heart [ 40 , 48 ], nervous system [ 30 , 38 , 44 ], lungs [ 35 , 36 , 37 , 43 ], skeletal muscle [ 33 ], subcutaneous tissue [ 39 ], and systemic or mixed [ 2 , 25 , 29 , 31 , 32 , 41 , 45 , 46 , 49 , 50 , 51 ]. Based on the manual categorisation, thirteen studies examined extrapulmonary sarcoidosis [ 26 , 27 , 28 , 29 , 30 , 32 , 33 , 34 , 39 , 40 , 44 , 47 , 48 ], five examined systemic sarcoidosis [ 9 , 25 , 31 , 38 , 42 ], and four examined pulmonary sarcoidosis [ 35 , 36 , 37 , 43 ]. In seven studies it was not possible to differentiate between pulmonary and non-pulmonary sarcoidosis [ 2 , 41 , 45 , 46 , 49 , 50 , 51 ]. Of the 29 included studies, 18 were from countries with non-gatekeeper health systems (2, 25, 27–33, 3537, 39, 40, 43, 44, 47, 49) and 11 were from countries with gatekeeper health systems [ 9 , 26 , 34 , 38 , 41 , 42 , 45 , 46 , 48 , 50 , 51 ]. Twelve studies reported data on ethnicity or race [ 2 , 25 , 29 , 30 , 31 , 32 , 33 , 36 , 42 , 43 , 49 , 51 ].
In total, a population size of 1531 participants (694 females; 837 males) was included in the review. The mean age was 47.91 years (SD = 5.47), excluding case reports (see below). Overall, participant ages ranged from 9.3 years to 69 years (including case reports).
Results of the quality appraisal
Consensus on the quality appraisal of the included studies is shown in Supplementary Table 2 . After the double-quality appraisal, a consensus was reached by two authors regarding an overall low risk of bias for all studies; therefore, no study was excluded.
Case studies
Twenty case studies comprising 15 case reports (8 females; 7 males) [ 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 ] and five case series [ 40 , 41 , 42 , 43 , 44 ], with 29 participants (22 females, 7 males), were included. The mean age of participants in case report studies was 47.87 years (SD = 14.06 years), with individual age ranging between 26 years [ 25 ] and 69 years [ 27 ]. In the case series, mean age of individuals ranged from 9.3 years [ 41 ] to 44 years [ 42 ].
Of the 20 included case studies, 11 examined extrapulmonary sarcoidosis [ 26 , 27 , 28 , 29 , 30 , 32 , 33 , 34 , 39 , 40 , 44 ], and four each focused on pulmonary [ 35 , 36 , 37 , 43 ] and systemic sarcoidosis [ 25 , 31 , 38 , 42 ]. In the one remaining case study, it was not possible to determine the extent of organ involvement [ 41 ].
In the 15 included case reports, individual diagnostic delay ranged from 0.25 months (0.02 years) [ 39 ] to 96 months (8 years) [ 35 ] and the mean diagnostic delay was 21.73 months. In the five case series, the mean diagnostic delay ranged from 5 months [ 42 ] to 43.5 months [ 43 ].
There was no significant gender difference in delay in diagnosis in case reports ( n = 15, Mann-Whitney-Wilcoxon test: w = 21.5, p =.749).
Pooled diagnostic delay in sarcoidosis
The results of the pooled mean diagnostic delay of the five studies [ 2 , 9 , 23 , 41 , 42 ] with an overall sample size of 124 are presented in Fig. 2 . Individual study sample size of these studies ranged from 8 [ 41 , 42 ] to 67 [ 9 ], while the mean diagnostic delay ranged from 5 months [ 42 ] to 23 months [ 9 ]. The pooled diagnostic delay was 7.93 months (95% CI 1.21 to 14.64 months) ( Fig. 2 ) . A funnel plot of the pooled diagnostic delay is presented in Supplementary Fig. 1 . We conducted a sensitivity analysis on SD estimated studies and SD not estimated studies and found no significant difference (between groups difference = 1.06 months, P =.30) in mean diagnostic delay between the two groups as shown in Supplementary Fig. 2 .
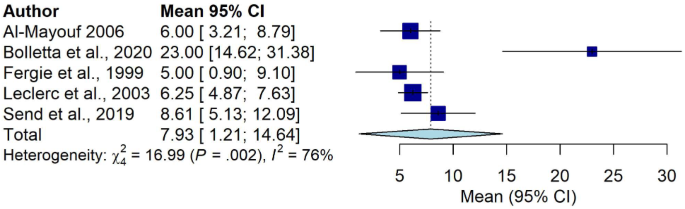
Pooled mean diagnostic delay in sarcoidosis
We could not conduct a subgroup analysis between pulmonary, extrapulmonary and systemic sarcoidosis due to the small number of studies with complete data (mean delay, total number of participants and SD of mean delay) in each group. However, in the included studies, systemic sarcoidosis had the longest mean diagnostic delay at 23.0 months [ 9 ] compared with extrapulmonary sarcoidosis, which had the shortest mean diagnostic delay of 5.0 months [ 42 ].
A subgroup analysis comparing studies ( n = 5) with different healthcare systems is presented in Supplementary Fig. 3 . There was no significant difference in mean diagnostic delay in countries with gatekeeper healthcare systems when compared with those with non-gatekeeper systems (between groups difference = 0.34 months, P = .56).
We conducted an additional subgroup analysis examining publication year of studies, which showed a significant inter-study difference in diagnostic delay in studies conducted (between groups difference = 16.99 months, P =.002) (see Supplementary Fig. 4 ). Further analysis examining publication year of the studies (e.g., before 2000 and after 2000) was not feasible due to the small number of studies.
Initial symptoms
Twenty-one studies comprising 15 case reports [ 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 ], three case series [ 40 , 42 , 43 ], two cross-sectional studies [ 47 , 49 ] and one survey [ 46 ] reported initial symptoms. Initial symptoms included weight loss [ 29 , 36 , 37 , 41 , 43 ], fatigue or generalised weakness [ 29 , 37 , 40 , 43 ], dyspnoea [ 36 , 40 , 43 ], muscle pain/muscle cramps/general body pain [ 32 , 37 , 40 ], headache [ 38 ], palpitations [ 40 ], nasal obstruction [ 42 ] and a subcutaneous mass [ 39 ] (refer to Supplementary Table 3 ). When aggregated, these symptoms could be categorised as: (1) general symptoms (fever, fatigue, weight loss), (2) organ-specific extrapulmonary symptoms (neurological- nausea, headache, vomiting; cardiac- palpitations; skin - rash, ulcers), and (3) pulmonary symptoms (cough, dyspnoea). Of the initial symptoms, 31.25% (25/80) were general; 55% (44/80) were organ specific and related to extrapulmonary symptoms, while 13.75% (11/80) were pulmonary (see Supplementary Table 3 ).
Initial specialist and treatment/diagnostic centre
Five of the included studies reported the cadre of specialist first consulted, one study each reporting general practitioner [ 29 ], emergency specialist [ 31 ], gynaecologist [ 38 ], oncologist [ 39 ], and neurologist [ 32 ] as the first specialist consulted. Twenty-one studies reported visits to treatment or diagnostic centres including secondary or tertiary hospitals, research centres and university hospitals [ 2 , 9 , 25 , 26 , 27 , 31 , 32 , 33 , 35 , 37 , 38 , 39 , 40 , 41 , 42 , 44 , 47 , 48 , 49 , 50 , 51 ]. Nineteen of these 21 studies reported treatment or diagnosis at multidisciplinary centres [ 2 , 9 , 25 , 26 , 27 , 31 , 32 , 33 , 35 , 37 , 38 , 41 , 42 , 44 , 47 , 48 , 50 , 51 ], and one study each at an institute of oncology [ 39 ] and a research centre [ 49 ].
Symptoms that changed the diagnostic approach
Twelve case studies, containing a total of 13 cases/participants, reported 24 symptoms that changed the diagnostic approach [ 27 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 40 , 43 ]. These symptoms ranged from no response to treatment [ 31 , 36 , 43 ], persistent or increasing shortness of breath/dyspnoea [ 35 , 40 , 43 ], persistent cough [ 35 , 37 ] to worsening hypertension [ 27 ], renal function decline and hypercalcemia [ 27 ] (Supplementary Table 4 ). None of the cross-sectional studies and surveys reported symptoms that changed the diagnostic approach. When aggregated, symptoms that changed the diagnostic approach were categorised into: (1) persistent symptoms (7/24, 29.2%) [ 33 , 35 , 40 , 43 ], (2) new symptoms or signs (7/24, 29.2%) [ 31 , 32 , 38 ], (3) worsening of symptoms (6/24, 25%) [ 27 , 34 , 40 ] and (4) no response to treatment (4/24, 16.6%) [ 31 , 36 , 43 ], as shown in Supplementary Tables 4 and Supplementary Fig. 5 .
Factors related to diagnostic delay
Fifteen case reports [ 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 ], three case series [ 40 , 42 , 44 ], two analytical cross-sectional studies [ 9 , 48 ], one survey [ 45 ] and one descriptive cross-sectional study [ 47 ] reported factors that might influence diagnostic delay in sarcoidosis (see Supplementary Table 5 ). Two analytical cross-sectional studies examined association between several factors and diagnostic delay [ 49 , 51 ]. In one study, the presence of pulmonary symptoms was associated with a longer time to diagnosis, whereas the presence of skin symptoms was associated with a shorter time to diagnosis [ 49 ]. People assessed as being at a higher stage on the Scadding scale (radiological scale to measure lung changes; higher stage correlates to greater structural damage in lungs) had a longer time-to-diagnosis compared to people with lower stage features (stage IV vs. stage II, stage III vs. stage 0 or I on chest radiographs) [ 49 ]. One study in Brazil found that misdiagnosis of and treatment for tuberculosis was more likely to be reported among those with a time-to-diagnosis of more than 6 months [ 51 ].
The factors mentioned in the 22 studies were meta-aggregated and the results are shown in Fig. 3 . We categorised these factors into: (1) complex and rare features of sarcoidosis (27/35, 77.1%), (2) healthcare factors (7/35, 20%) and (3) patient-centred factors (1/35, 2.9%). Of these, 77.1% (27/35 factors) were related to complex and rare features of sarcoidosis (category 1), including broad clinical features and differential diagnosis [ 9 , 25 , 26 , 27 , 28 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 40 , 42 , 44 , 47 , 48 ], rare presentation [ 28 , 32 , 34 , 36 , 37 , 38 , 42 ], lack of awareness and rarity of sarcoidosis [ 29 , 30 , 32 , 33 , 40 ], and coexisting disease or comorbidities [ 35 , 38 ]. The 20% (7/35 factors) pertaining to healthcare factors (category 2) included exclusion diagnosis [ 39 ], lack of standard procedure to distinguish sarcoidosis [ 47 ], not using appropriate diagnostic techniques/ relying on chest x-ray [ 45 , 48 ], challenges with biopsy [ 9 , 40 ], and challenges with making a definitive diagnosis in sarcoidosis [ 32 ]. The remaining 2.9% of factors were patient-centred (category 3), which referred to refusal of biopsy (1/35 factors) [ 35 ].
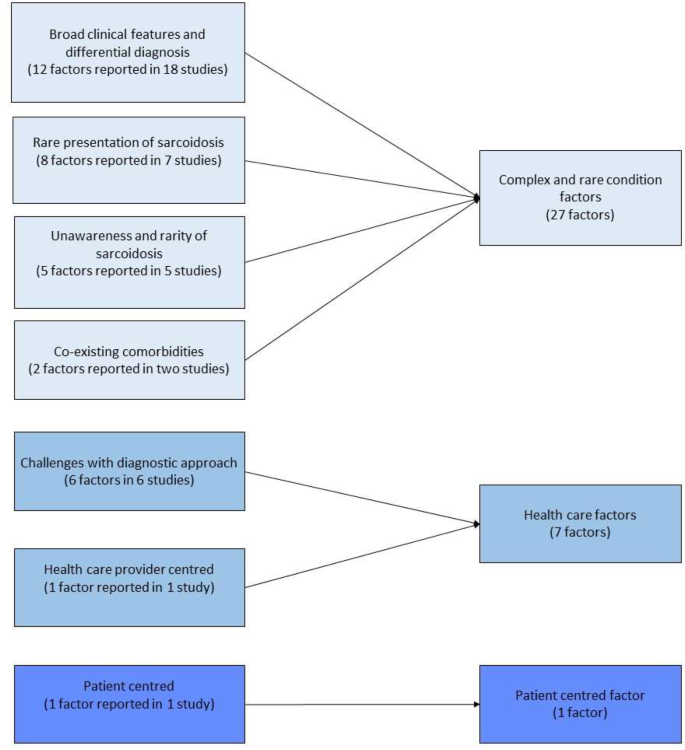
Meta-aggregation results of factors related to diagnostic delay in sarcoidosis
We further analysed these factors by sarcoidosis type (Supplementary Table 6 ). Twenty-two studies reported types of sarcoidosis; of these, 21 studies [ 9 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 42 , 44 , 47 , 48 ] reported factors related to diagnostic delay. Three studies reported five factors of diagnostic delay in pulmonary sarcoidosis. Of these, 80% were categorised as complex and rare features of sarcoidosis (category 1), which included co-existing disease and comorbidities [ 35 ], rare presentations [ 36 , 37 ] and broad clinical features [ 37 ]. The remaining 20% were patient-centred factors, referring to patient’s refusal of a biopsy (category 3) [ 35 ]. Thirteen studies reported twenty factors related to diagnostic delay in extrapulmonary sarcoidosis [ 26 , 27 , 28 , 29 , 30 , 32 , 33 , 34 , 39 , 40 , 44 , 47 , 48 ]. Of these, 75% were linked to complex and rare features of sarcoidosis (category 1), including broad clinical features and differential diagnosis [ 26 , 27 , 28 , 40 , 44 , 47 , 48 ], rare presentation [ 28 , 32 , 34 ] and lack of awareness of sarcoidosis [ 29 , 30 , 32 , 33 , 40 ]. The remaining 25% were categorised as healthcare related (category 2), which included factors relating to healthcare providers [ 48 ] and challenges with diagnostic approach or tools [ 32 , 39 , 40 , 47 ]. Nine factors were mentioned to be linked to diagnostic delay in systemic sarcoidosis [ 9 , 25 , 31 , 38 , 42 ]; eight of these were linked to the complex and rare features of sarcoidosis (category 1); broad clinical features [ 25 , 31 , 38 , 42 ], rare presentation [ 9 , 38 , 42 ], and co-existing disease [ 38 ]. One factor was linked to healthcare (category 2): challenges with diagnostic approach and tool, described by the authors of the paper as limited number of patients amenable to lymph node biopsy [ 9 ].
Outcomes related to diagnostic delay
Sixteen studies described the outcomes of diagnostic delay, including 11 case reports [ 26 , 27 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 ], two case series [ 40 , 44 ], two analytical cross-sectional studies [ 48 , 51 ], and one survey [ 45 ]. The survey and analytical cross-sectional studies did not use statistical methods to examine the relationship between independent variables and diagnostic delay; however, they reported descriptive or comparative results of the outcomes of diagnostic delay. One study described incorrect diagnoses that were provided instead of sarcoidosis, including tuberculosis, lung cancer, rheumatic fever, Hodgkin’s lymphoma, pneumonia, and patients simulating the symptoms [ 45 ]. One study reported irreversible deterioration of cardiac function (6/10 cases) and high mortality (5/10 cases) in people with a late diagnosis of sarcoidosis [ 48 ], and another study reported poor lung function in people with a late diagnosis [ 51 ].
While case reports or case studies are not designed to assess the association between two variables, we analysed their data using meta-aggregation as shown in Supplementary Tables 7 and Fig. 4 . Thirteen case studies, including 11 case reports [ 26 , 27 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 ] and two case series [ 40 , 44 ], described outcomes from 26 cases. We aggregated the outcomes into: (1) incorrect diagnosis, (2) incorrect treatment and (3) complications/progression of the condition. Incorrect diagnosis (category 1) was reported in 38.5% (10/26 cases), including xanthogranulomatous pyelonephritis [ 26 ], monoclonal gammopathy of undetermined significance [ 27 ], tuberculosis [ 31 , 36 ], deep tissue infection [ 34 ], bronchitis [ 35 ], respiratory infection [ 37 ], tachycardia and heart block [ 40 ], and multiple sclerosis [ 44 ]. Incorrect treatment (category 2) was reported in 34.6% (9/10 cases), consisting of nephrectomy [ 26 ], anti-tuberculosis agents [ 31 , 36 ], antibiotics [ 34 , 35 , 37 ] and excision of mass [ 39 ]. Complications/progression of symptoms or the condition (category 3) was reported in 26.9% (7/10 cases) of the cases. These included renal failure [ 27 ], seizure [ 32 ], weakness of the extremities [ 33 ], infection [ 34 ], dyspnoea and oxygen therapy [ 35 ], headache, vomiting and blurred vision [ 38 ], dyspnoea and haemoptysis [ 40 ].
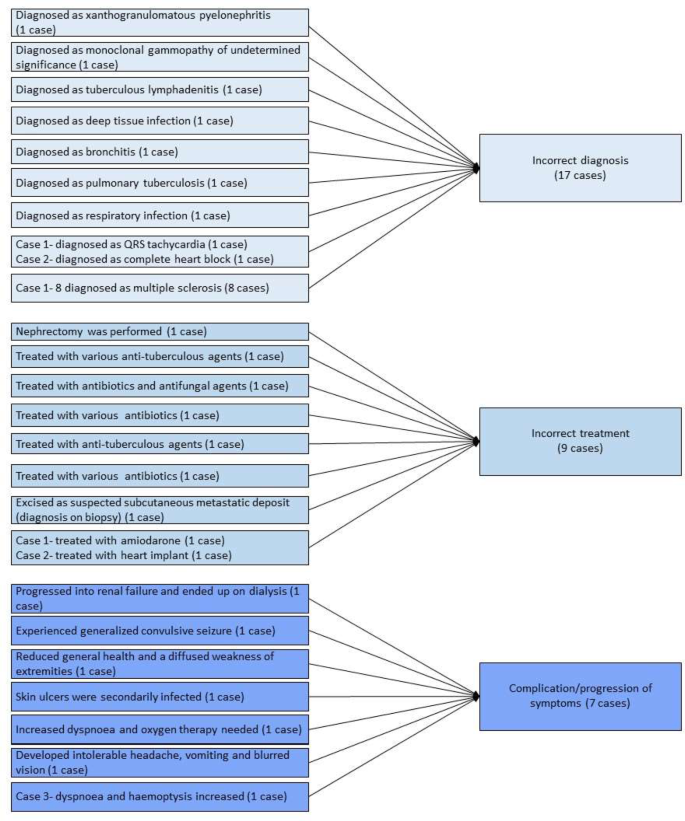
Meta-aggregation of outcomes of diagnostic delay in case studies
People’s experiences related to diagnostic delay
We did not identify any studies, including qualitative, that examined people’s experiences of diagnostic delay in our systematic search.
Using data from the 29 studies included in this review, we were able to present a pooled analysis of diagnostic delay in all types of sarcoidosis to describe factors that are related to and associated with diagnostic delay, and the outcomes for people living with sarcoidosis. Pooled mean diagnostic delay for all types of sarcoidosis was 7.93 months (95% CI 1.21 to 14.64 months), a similar range to delays described for other chronic inflammatory diseases, including inflammatory bowel disease [ 52 ]. The overall sample pool of this study consisted of more males than females (54.7% vs. 45.3%). No difference in delay in diagnosis was found between males and females based on the analysis conducted on case reports. The high number of single-person case studies on misdiagnosis attests to the size of the diagnostic challenge for the clinician. Several factors may influence diagnostic delay of sarcoidosis, including the clinical characteristics of the condition, prevalence, different types/presentation of the condition, clinicians’ and patients’ awareness of the condition, and the availability of diagnostic tests.
The present review found complex and rare features of sarcoidosis, healthcare factors, and patient-centred factors may contribute to diagnostic delay in all types of sarcoidosis. In some studies included in the review, associations were found between pulmonary symptoms and higher Scadding scores, and prolonged diagnostic delay of sarcoidosis. The presence of pulmonary symptoms that may be attributable to various health conditions (common flu, pneumonia, bronchitis, asthma, emphysema, and lung cancer) create challenges for healthcare providers working to narrow down the health condition and differentiate between possible causes of pulmonary symptoms. In these cases, healthcare providers may first choose to investigate more common causes of pulmonary symptoms and pursue a diagnostic approach that excludes the most common causes through minimal testing, which is cost effective.
The review also revealed healthcare factors (exclusion diagnosis, challenges with obtaining a biopsy and lack of standard procedure to distinguish sarcoidosis) may lead to diagnostic delay. Difficulties with access to medical resources needed to conduct a biopsy (availability of clinicians and medical facilities) may cause delay in the definitive diagnosis of sarcoidosis through extending the time between suspicion and confirmation of diagnosis. Identifying the difference between suspicion and confirmation of diagnosis can provide further insights into the depth of the impact on diagnostic delay associated with healthcare factors.
Diagnostic delay due to misdiagnosis of tuberculosis was also identified in this review, highlighting the similarity of the two conditions and that differentiating between them is crucial for initiating the correct treatment, as treatment of sarcoidosis involves immunosuppression. In countries with a high prevalence of tuberculosis, it is understandable that clinicians may initially suspect tuberculosis. A misdiagnosis of tuberculosis has implications for the individual, their families and carers, and the use of medical resources, signalling the need for a careful and methodical approach in diagnosis. Once a clinician has made a diagnosis, it is natural to attribute the constellation of symptoms and signs of a rare disease to the identified cause (misdiagnosed condition), until clear evidence arises to disprove the current diagnosis.
Both acute and chronic presentation of sarcoidosis may influence the diagnostic delay. Acute sarcoidosis may follow acute onset with more typical features and radiological findings (hilar adenopathy in chest x-ray). Chronic sarcoidosis has insidious onset and may mimic other disorders (signs and symptoms from multiple systems); therefore, chronic sarcoidosis may present additional challenges for diagnosis of sarcoidosis. The present review did not study the difference in diagnostic delay between acute and chronic sarcoidosis due to limited data. Analyses of sarcoidosis location and factors related to diagnostic delay revealed similar findings, in which most reported factors were linked to complex and rare features, regardless of the location of sarcoidosis. Raising clinicians’ awareness of the complex clinical presentations of all types of sarcoidosis, including rare presentations, may assist in expediting diagnosis.
While none of the included studies used quantitative methods to examine outcomes of diagnostic delay, we used meta-aggregation to extract and examine outcomes described in case reports and case series which revealed incorrect diagnosis, incorrect treatment, and complications/progression of the condition as outcomes of diagnostic delay of sarcoidosis. This accords with findings from a recent review of diagnostic delay in myositis where outcomes including misdiagnoses, progression of symptoms, incorrect treatment, and early discharge were reported [ 53 ]. These outcomes align with people’s experiences of diagnostic delay recently described [ 54 ], signalling the need for improved awareness of sarcoidosis and a better understanding of its diagnosis and treatment.
As in our previous study examining diagnostic delay of myositis, where we did not find any studies examining people’s experiences of diagnostic delay [ 53 ], we did not find research examining experiences of diagnostic delay of sarcoidosis. We believe that further exploration of people’s experiences from symptom onset until diagnosis may assist in understanding these experiences and factors that may impact and influence diagnosis and its delay in sarcoidosis. This information may then be used to inform strategies aimed at reducing the undiagnosed period, including raising awareness and the development of clinical reasoning tools to distinguish when clinicians might consider re-evaluation of an existing diagnosis and the presence of a rare disease.
Despite the lack of studies examining people with sarcoidosis’ experiences of diagnostic delay, a recent commentary describes people with sarcoidosis’ experiences of misdiagnoses [ 54 ]. One person described frustration at ‘being dismissed’ and not listened to by their clinician, an experience that has also been described by people with multiple sclerosis seeking a diagnosis [ 55 ]. All of those interviewed for the article highlighted ongoing pain and discomfort from symptoms pre- and post-diagnosis as greatly impacting their lives, aligning with evidence of the negative impact that sarcoidosis has on people’s quality of life [ 56 ].
Diagnostic delay can create a sense of uncertainty and, in many cases, escalating symptoms, as found in research examining people’s experiences with multiple sclerosis [ 55 ], placing them in a stressful state of ‘not knowing”. Delayed diagnosis of childhood illnesses has consequences for both children and their families, including anxiety, frustration and stress, and fear of future reproduction due to ill-defined genetic risk [ 57 ]. Hospitalisation and surgical interventions related to rare diseases are more frequent among people who experience a delayed diagnosis [ 58 ]. Research examining experiences of hereditary angioedema found that inappropriate treatments were ineffective and at times, exacerbated the underlying condition [ 59 ]. For some patients, symptoms were attributed to psychological reasons and due to this, some stopped seeking medical care despite experiencing severe symptoms [ 59 ]. Attribution of rare disease symptoms to psychological or psychiatric reasons, and treatment in line with this is not uncommon; [ 57 , 58 , 59 ] however the impact of a rare disease on individuals’ mental health has important implications for the treatment and care of people with these health conditions [ 59 ].
Delay in diagnosis of sarcoidosis can cause impaired physical function, pain, reduced capacity to work, and strain on personal relationships, leading to a reduction in quality of life and the ability to engage in pleasurable activities, which in turn can have negative emotional consequences that impact wellbeing [ 60 ]. A survey of the treatment priorities of people with sarcoidosis found that they most valued quality of life and functionality and concluded that psychological support was key to their wellbeing [ 61 ]. Unfortunately, being able to discuss issues and concerns about sarcoidosis with clinician(s) cannot be realised until a diagnosis is received.
There is a paucity of evidence about the patient experience of diagnostic delay in sarcoidosis and factors related to this. Diagnosis of sarcoidosis can take a long time, during which the impacts on the lives of people living with sarcoidosis can be substantial, including receiving incorrect diagnoses and treatment, and suffering unfavourable outcomes. Further studies examining factors that contribute to diagnostic delay in sarcoidosis, and people’s experiences from symptom onset to diagnosis, are crucial in determining target areas for clinicians, policy-makers and consumer advocacy groups. With this further knowledge, we may develop strategies, training activities and awareness-raising programs that expedite diagnosis and improve outcomes for people living with sarcoidosis.
Strengths and limitation
The main strength of this review is inclusion of the current evidence of diagnostic delay in all types of studies (including qualitative and quantitative studies) which provided clear insight into the status of diagnostic delay, its factors, and consequences. This systematic review identified a lack of qualitative studies examining patients’ experience of diagnostic delay in sarcoidosis. The main limitation of the present systematic review is the low number of study samples used in pooling of the diagnostic delay ( n = 124 over 5 studies). The lack of available data on health specialists, clinics, acute or chronic presentation of sarcoidosis, and the period between suspected and confirmed diagnosis limited the possibility of analysing the difference in diagnostic delay in various settings. Lastly, the analysis of case reports may reflect features of chronic sarcoidosis with complex features due to publication bias- tendency to publish rare and interesting cases.
Data availability
All data relevant to the study is available in the supplementary materials. A detailed extracted data table can be accessed via figtree repository (via DOI: https://doi.org/10.6084/m9.figshare.24431275 ).
Baughman RP, Field S, Costabel U, Crystal RG, Culver DA, Drent M, et al. Sarcoidosis in America. Analysis based on Health Care Use. Ann Am Thorac Soc. 2016;13(8):1244–52.
Article PubMed Google Scholar
Leclerc S, Myers RP, Moussalli J, Herson S, Poynard T, Benveniste O. Sarcoidosis and interferon therapy: report of five cases and review of the literature. Eur J Intern Med. 2003;14(4):237–43.
Article CAS PubMed Google Scholar
Rybicki BA, Major M, Popovich J Jr., Maliarik MJ, Iannuzzi MC. Racial differences in sarcoidosis incidence: a 5-year study in a health maintenance organization. Am J Epidemiol. 1997;145(3):234–41.
Mirsaeidi M, Machado RF, Schraufnagel D, Sweiss NJ, Baughman RP. Racial difference in sarcoidosis mortality in the United States. Chest. 2015;147(2):438–49.
Perlman DM, Sudheendra MT, Furuya Y, Shenoy C, Kalra R, Roukoz H, et al. Clinical presentation and treatment of high-risk Sarcoidosis. Annals Am Thorac Soc. 2021;18(12):1935–47.
Article Google Scholar
Higgins JPTTJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane Handbook for Systematic Reviews of Interventions version 6.2 2021.
Pasadhika S, Rosenbaum JT. Ocular Sarcoidosis. Clin Chest Med. 2015;36(4):669–83.
Article PubMed PubMed Central Google Scholar
Kidd DP. Neurosarcoidosis: clinical manifestations, investigation and treatment. Pract Neurol. 2020;20(3):199–212.
Bolletta E, Mastrofilippo V, Invernizzi A, Aldigeri R, Spaggiari L, Besutti G et al. Clinical relevance of Subcentimetric Lymph Node Biopsy in the diagnosis of ocular sarcoidosis. Ocul Immunol Inflamm. 2020:1–4.
Kusano KF, Satomi K. Diagnosis and treatment of cardiac sarcoidosis. Heart. 2016;102(3):184–90.
Ungprasert P, Tooley AA, Crowson CS, Matteson EL, Smith WM. Clinical characteristics of ocular sarcoidosis: a Population-based study 1976–2013. Ocul Immunol Inflamm. 2019;27(3):389–95.
Johns CJ, Michele TM. The clinical management of sarcoidosis. A 50-year experience at the Johns Hopkins Hospital. Med (Baltim). 1999;78(2):65–111.
Article CAS Google Scholar
Hillerdal G, Nöu E, Osterman K, Schmekel B, Sarcoidosis. Epidemiology and prognosis. Am Rev Respir Dis. 1984;130(1):29–32.
CAS PubMed Google Scholar
Belperio JA, Shaikh F, Abtin FG, Fishbein MC, Weigt SS, Saggar R, et al. Diagnosis and treatment of pulmonary sarcoidosis: a review. JAMA. 2022;327(9):856–67.
Ungprasert P, Crowson CS, Matteson EL. Characteristics and long-term outcome of neurosarcoidosis: a Population-based study from 1976–2013. Neuroepidemiology. 2017;48(3–4):87–94.
Hunninghake GW, Costabel U, Ando M, Baughman R, Cordier JF, du Bois R, et al. ATS/ERS/WASOG statement on sarcoidosis. American Thoracic Society/European Respiratory Society/World Association of Sarcoidosis and other Granulomatous disorders. Sarcoidosis Vasc Diffuse Lung Dis. 1999;16(2):149–73.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Reviews. 2015;4(1):1.
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 Guideline Statement. J Clin Epidemiol. 2016;75:40–6.
Namsrai T, Phillips C, Desborough J, Gregory D, Kelly E, Cook M et al. December,. Diagnostic delay of sarcoidosis: protocol for an integrated systematic review. PLoS ONE Accepted on 7 2022.
Veritas Health Innovation. Covidence systematic review software Melbourne, Australia [Available from: Available at www.covidence.org.
Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The mixed methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ Inform. 2018;34:285–91.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135.
RStudio Team. RStudio: Integrated Development for R. PBC, Boston MA. RStudio; 2020. http://www.rstudio.com/ .
Florczak KL. Meta-aggregation: just what is it? Nurs Sci Q. 2018;32(1):11.
Darugar A, Mathian A, Lehoang P, Bodaghi B. Acute posterior multifocal placoid pigment epitheliopathy as the initial manifestation of sarcoidosis. J Ophthalmic Vis Res. 2011;6(4):338–43.
PubMed PubMed Central Google Scholar
Froehner M, Meinhardt M, Parmentier S, Hugo C, Wirth MP. Renal Sarcoidosis Mimicking Xanthogranulomatous Pyelonephritis. Urology. 2016;97:e19–20.
Ghafoor A, Almakki A. Renal confined sarcoidosis: natural history and diagnostic challenge. Avicenna J Med. 2014;4(2):44–7.
Ghorpade A, Ramanan C. Cutaneous sarcoidosis. Indian J Dermatol Venereol Leprol. 1996;62(3):171–2.
Ho B, Choi KS, Ochoa W, Torralba KD, Sandhu VK, Pakbaz Z. Atypical manifestations of sarcoidosis in a hispanic male. J Community Hosp Intern Med Perspect. 2019;9(3):271–4.
Jaster JH, Dohan FC Jr., Bertorini TE, Bass JE, Mönkemüller KE, Handorf CR, et al. Solitary spinal cord sarcoidosis without other manifestations of systemic sarcoidosis. Clin Imaging. 1997;21(1):17–22.
Lee CH, Jung YS, Lee SH. Hydrocephalus as a presenting manifestation of neurosarcoidosis: easy to misdiagnose as tuberculosis. J Korean Neurosurg Soc. 2010;48(1):79–81.
Mehta A, Khan F, Wagner C, Hashemzadeh T, Stemer A, Sloan EA, et al. A case of Neurosarcoid presenting as multiple intraparenchymal hemorrhages. Neurohospitalist. 2022;12(1):162–6.
Meyer N, Sutter R, Schirp U, Gutzeit A. Extensive intramuscular manifestation of sarcoidosis with initially missed diagnosis and delayed therapy: a case report. J Med Case Rep. 2017;11(1):246.
Noiles K, Beleznay K, Crawford RI, Au S. Sarcoidosis can present with necrotizing granulomas histologically: two cases of ulcerated sarcoidosis and review of the literature. J Cutan Med Surg. 2013;17(6):377–83.
Papaetis GS, Pefanis A, Solomon S, Tsangarakis I, Orphanidou D, Achimastos A. Asymptomatic stage I sarcoidosis complicated by pulmonary tuberculosis: a case report. J Med Case Rep. 2008;2:226.
Plit ML, Miller GB. Cavitating pulmonary sarcoidosis. S Afr Med J. 1983;64(2):67–8.
Thomas PM, Mabrouk T, Li Y, Wallach SL. Delayed diagnosis in a Rare Case of Pulmonary Sarcoidosis presenting as unilateral Hilar Lymphadenopathy and Fever of unknown origin. Cureus. 2021;13(6):e15792.
van Rooijen JM, Mijnhout GS, Aalders TT, de Bondt RB. Hydrocephalus, a rare manifestation of sarcoidosis. Clin Pract. 2011;1(3):e66.
Viswanath L, Pallade S, Krishnamurthy B, Naveen T, Preethi BL, Pramod KP, et al. Darier-Roussy Sarcoidosis mimicking metastatic breast Cancer. Case Rep Oncol. 2009;2(3):251–4.
Guleria R, Sharma R, Mohan A, Das C. Cardiac sarcoidosis: an uncommon presentation of sarcoidosis in India. Indian J Chest Dis Allied Sci. 2006;48(2):133–7.
Al-Mayouf SM, Al-Sonbul A, Al Jumaah S, Al-Hemidan A. Sarcoidosis: a delayed or missed diagnosis in children. Ann Saudi Med. 2006;26(3):220–3.
Fergie N, Jones NS, Havlat MF. The nasal manifestations of sarcoidosis: a review and report of eight cases. J Laryngol Otol. 1999;113(10):893–8.
Judson MA, Vincent B, Huggins T, Silvestri GA, Sahn SA. Unusual presentations of pulmonary sarcoidosis: cases from the medical university of South Carolina. Semin Respir Crit Care Med. 2007;28(1):75–82.
Scott TF, Yandora K, Kunschner LJ, Schramke C. Neurosarcoidosis mimicry of multiple sclerosis: clinical, laboratory, and imaging characteristics. Neurologist. 2010;16(6):386–9.
Kirsten D. [Sarcoidosis in Germany. Analysis of a questionnaire survey in 1992 of patients of the German Sarcoidosis Group]. Pneumologie. 1995;49(6):378–82.
Okumus G, Musellim B, Cetinkaya E, Turker H, Uzaslan E, Yenturk E, et al. Extrapulmonary involvement in patients with sarcoidosis in Turkey. Respirology. 2011;16(3):446–50.
Send T, Tuleta I, Koppen T, Thiesler T, Eichhorn KW, Bertlich M, et al. Sarcoidosis of the paranasal sinuses. Eur Arch Otorhinolaryngol. 2019;276(7):1969–74.
Hoogendoorn JC, Ninaber MK, Piers SRD, de Riva M, Grauss RW, Bogun FM, et al. The harm of delayed diagnosis of arrhythmogenic cardiac sarcoidosis: a case series. Europace. 2020;22(9):1376–83.
Judson MA, Thompson BW, Rabin DL, Steimel J, Knattereud GL, Lackland DT, et al. The diagnostic pathway to sarcoidosis. Chest. 2003;123(2):406–12.
Kobak S, Yildiz F, Semiz H, Orman M. Elderly-onset sarcoidosis: a single center comparative study. Reumatol Clin (Engl Ed). 2020;16(3):235–8.
Rodrigues MM, Coletta EN, Ferreira RG, Pereira CA. Delayed diagnosis of sarcoidosis is common in Brazil. J Bras Pneumol. 2013;39(5):539–46.
Sulkanen E, Repo M, Huhtala H, Hiltunen P, Kurppa K. Impact of diagnostic delay to the clinical presentation and associated factors in pediatric inflammatory bowel disease: a retrospective study. BMC Gastroenterol. 2021;21(1).
Namsrai T, Parkinson A, Chalmers A, Lowe C, Cook M, Phillips C, et al. Diagnostic delay of myositis: an integrated systematic review. Orphanet J Rare Dis. 2022;17(1):420.
Morgan J. Misdiagnosis of sarcoidosis. Lancet Respir Med. 2021;9(7):696–8.
Desborough J, Brunoro C, Parkinson A, Chisholm K, Elisha M, Drew J, et al. It struck at the heart of who I thought I was’: a meta-synthesis of the qualitative literature examining the experiences of people with multiple sclerosis. Health Expect. 2020;23(5):1007–27.
Voortman M, Hendriks CMR, Lodder P, Drent M, De Vries J. Quality of life of couples living with Sarcoidosis. Respiration. 2019;98(5):373–82.
Zurynski Y, Deverell M, Dalkeith T et al. Australian children living with rare diseases: experiences of diagnosis and perceived consequences of diagnostic delays. Orphanet J Rare Dis. 2017/04/11 2017;12(1):68. https://doi.org/10.1186/s13023-017-0622-4 .
Benito-Lozano J, Arias-Merino G, Gómez-Martínez M, Ancochea-Díaz A, Aparicio-García A, de la Posada M et al. Diagnostic process in Rare diseases: determinants Associated with Diagnostic Delay. Int J Environ Res Public Health. 2022;19(11).
Isono M, Kokado M, Kato K. Why does it take so long for rare disease patients to get an accurate diagnosis?—A qualitative investigation of patient experiences of hereditary angioedema. PLoS ONE. 2022;17(3):e0265847.
Article CAS PubMed PubMed Central Google Scholar
Saketkoo LA, Russell AM, Jensen K, Mandizha J, Tavee J, Newton J et al. Health-Related Quality of Life (HRQoL) in Sarcoidosis: diagnosis, management, and Health outcomes. Diagnostics (Basel). 2021;11(6).
Baughman RP, Barriuso R, Beyer K, Boyd J, Hochreiter J, Knoet C, et al. Sarcoidosis: patient treatment priorities. ERJ Open Res. 2018;4(4):00141–2018.
Download references
Acknowledgements
Not applicable.
This work was supported by “Missed opportunities in clinical practice: Tools to enhance healthcare providers’ awareness and diagnosis of rare diseases in Australia” a project funded by the Commonwealth represented by Department of Health Australia [ID 4-G5ZN0T7]. Sponsors or funding officials were not involved in any part of the review including protocol development, data selection, synthesis, reporting and publishing of the results.
Author information
Authors and affiliations.
National Centre for Epidemiology and Population Health, The Australian National University, 63, Eggleston Road, Acton ACT, Canberra, 2601, Australia
Tergel Namsrai, Anne Parkinson, Dianne Gregory, Elaine Kelly & Jane Desborough
Sarcoidosis Lyme Australia, Camden, Australia
Dianne Gregory & Elaine Kelly
John Curtin School of Medical Research, The Australian National University, Canberra, Australia
Matthew Cook
School of Medicine and Psychology, The Australian National University, Canberra, Australia
Christine Phillips
You can also search for this author in PubMed Google Scholar
Contributions
AP, CP, JD, EK, DG, and MC conceptualised the study and supported the study methodology. TN, CP, AP, and JD conducted the data collection and analysis. TN drafted the original manuscript. JD, AP, CP, MC, DG, and EK reviewed and edited the manuscript.
Corresponding author
Correspondence to Jane Desborough .
Ethics declarations
Ethics approval and consent to participate.
As this was a systematic review, no human was involved or participated in the study, with no necessity for ethical approval and consent to participate.
Consent for publication
As this was a systematic review, no human was involved or participated in the study, with no necessity for consent for publication.
Competing interests
The authors have declared no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, supplementary material 4, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Namsrai, T., Phillips, C., Parkinson, A. et al. Diagnostic delay of sarcoidosis: an integrated systematic review. Orphanet J Rare Dis 19 , 156 (2024). https://doi.org/10.1186/s13023-024-03152-7
Download citation
Received : 23 March 2023
Accepted : 28 March 2024
Published : 11 April 2024
DOI : https://doi.org/10.1186/s13023-024-03152-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Sarcoidosis
- Diagnostic delay
- Misdiagnosis
- Systematic review
- Meta-analysis
- Meta-aggregation
- Rare disease
Orphanet Journal of Rare Diseases
ISSN: 1750-1172
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Fixing America's hospitals. This report presents ten case studies to illustrate interventions that address prominent and targeted areas for patient safety improvement. The five areas of focus include promoting an organizational safety culture, improving teamwork and communication, enhancing rapid response to inpatient crises, preventing health ...
Case Examples. Based on a composite of a number of real sentinel event reports to The Joint Commission, Case Examples can be used for educational purposes to identify lapses in patient safety and missed opportunities for developing a safety culture. This learning resource highlights safety actions and strategies to have a better result.
C. Sample of documentation q shift X 72 hours or until stable using both SOAP and occurrence based documentation. 4/2/04 11pm. Example 1-SOAP. S: Mrs. P has no evidence of injury resulting from her two falls on 4/1/04 at this time.
With this in mind, we conducted case studies of ten potentially promising examples of safety improvement programs in health care institutions around the country. This article briefly reports the characteristics and lessons of six of these ongoing natural experiments in health care safety (see Table 1 for an overview of the cases).
Citation. D. McCarthy and D. Blumenthal, Committed to Safety: Ten Case Studies on Reducing Harm to Patients, The Commonwealth Fund, April 2006. Every year, thousands of Americans die in hospitals from oversights or mistakes in their medical care. A new Fund report describes innovative changes made by 10 organizations to improve patient care and ...
WebM&M: Case Studies. WebM&M (Morbidity & Mortality Rounds on the Web) features expert analysis of medical errors reported anonymously by our readers. Spotlight Cases include interactive learning modules available for CME. Commentaries are written by patient safety experts and published monthly.
Visiting Professor College of Medicine University College Cork Cork, Ireland. Jones & Bartlett Learning books and products are available through most bookstores and online booksellers. To contact Jones & Bartlett Learning directly, call 800-832-0034, fax 978-443-8000, or visit our website, www.jblearning.com.
In recognition of Canadian Patient Safety Week 2022, we are pleased to share these case studies featuring diverse examples of how our healthcare partners are applying the Canadian Quality and Patient Safety Framework in their settings. We hope you find them useful. Access the Canadian Quality and Patient Safety Framework Evaluation here.
This collection of case studies highlights AHRQ-funded patient safety tools, including the Comprehensive Unit-based Safety Program, Re-Engineered Discharge Toolkit , and patient safety culture surveys, to document their successful use in the field. Agency for Healthcare Research and Quality. 2019-2023.
Patient safety review and response case studies by clinical specialty. This page shows case studies, listed by clinical specialty, of where the National Patient Safety Team worked with partners to address issues identified through its review of recorded patient safety events. Urgent/emergency care. General medicine.
The development of a Safety Case for a defined clinical pathway was a centrepiece of the programme. We base our analysis on 143 interviews covering all aspects of the programme and on analysis of 13 Safety Cases produced by clinical teams. Results The principles behind a proactive, systematic approach to identifying and controlling risk that ...
Case Studies. 1. I-Pass Nurse Handoffs. Hawai'i Pacific Health recognized that communication amongst nurses at shift change in the neonatal intensive care unit was a patient safety improvement opportunity for the high volume, high acuity unit. In order to address this, they aimed to apply high reliability techniques and leverage EHR-based ...
The research design is a case study approach [16- 18] within a regional Norwegian hospital with the objective of gaining in-depth knowledge of the sta-tus and influencing factors concerning patient safety. Data has been collected using a combination of qualitative (interviews and document analysis) and quantitative (patient safety ...
1.1. Background. Research indicates that there is a potential for patients to improve safety (Davis, Jacklin, Sevdalis, & Vincent, 2007; Vincent & Coulter, 2002) and that patients are willing and able to be involved in safety‐related work (Waterman et al., 2006 Wright et al., 2016).However, several barriers to involving patients in improving patient safety has been identified and organized ...
Study design, sample, and setting. A case study methodology [] using surveys and interviews was employed and is described according to the Standards for Reporting Qualitative Research Checklist (Supplementary Appendix 1).Case study approaches are appropriate to generate an in-depth, multifaceted understanding of a complex issue such as patient safety interventions and governance in its real ...
Patient stories can help illustrate the impact of medical harm on patients and their families as well as uncover areas for improvement. This book offers a collection of 24 patient accounts of medical errors with further information from the editors including context, learning objectives, and a case discussion to guide understanding of key health professional competencies and how to integrate ...
Case studies are a form of storytelling that often includes learning objectives, reflection and analysis. This book by Julie K. Johnson, Helen W. Haskell and Paul R. Barach uses storytelling to explore medical cases from the viewpoints of surviving family members. The amount of effort to collect such stories must have been astounding, but the ...
We would like to show you a description here but the site won't allow us.
Methods Data are drawn from a mixed- methods evaluation of the Safer Clinical Systems programme. The development of a Safety Case for a defined clinical pathway was a centrepiece of the programme. We base our analysis on 143 interviews covering all aspects of the programme and on analysis of 13 Safety Cases produced by clinical teams.
The anesthesiologist received training on the equipment and has used it in six surgical cases to date. The equipment is being used in this surgical case. Two units of blood have been administered during the case using the equipment. As the anesthesiologist administers the last unit of blood, the patient suddenly experiences cardiopulmonary arrest.
WHO fact sheet on patient safety, including key facts, common sources of patient harm, factors leading to patient harm, system approach to patient safety, and WHO response. ... and more importantly better patient outcomes (5). An example of a good return on investment is patient engagement, which, if done well, can reduce the burden of harm by ...
Patient safety research is growing, spanning across more healthcare settings, and considers a wide array of contextual factors. The combination of emerging patient safety threats and the growing amount of published patient safety research, patient safety resources, and accrediting body standards makes it increasingly difficult to prioritize ...
"Safety cases" are used in healthcare and other industries to communicate the safety of a product, system, or service. In this study, researchers use the "safety case" approach to evaluate the safety of the Safer Clinical Systems program, which is designed to improve the safety and reliability of clinical pathways.
Purpose: Errors and incidents may occur at any point within radiotherapy (RT). The aim of the present retrospective analysis is to evaluate the impact of a customized ARIA Visual Care Path (VCP) on quality assurance (QA) for the RT process. Materials and Methods: The ARIA VCP was implemented in June 2019. The following tasks were customized and independently verified (by independent checks ...
The case studies presented in this paper demonstrate increasing alignment with the Society of Toxicologic Pathology recommendations (2013) towards (1) excluding recovery phase cohorts by default (include only when scientifically justified), (2) minimizing the number of recovery groups (e.g., control and one dose level), and (3) excluding ...
Essay Example: Suicide is a critical public health issue that necessitates comprehensive understanding and sensitive intervention, particularly within the healthcare setting. This analysis delves into a poignant nursing case study centered around Jessica, a young patient who tragically ended
This publication describes and analyzes clinical cases to illustrate patient safety concepts and types of medical errors to engage clinicians in improvement work. The second edition includes chapters devoted to safety challenges that emerged in prominence due to the COVID-19 pandemic (health disparities, inequities and nursing home care failures), as well as core topics such as high ...
Background Sarcoidosis is a chronic inflammatory granulomatous disease of unknown cause. Delays in diagnosis can result in disease progression and poorer outcomes for patients. Our aim was to review the current literature to determine the overall diagnostic delay of sarcoidosis, factors associated with diagnostic delay, and the experiences of people with sarcoidosis of diagnostic delay ...