- Credit cards
- View all credit cards
- Banking guide
- Loans guide
- Insurance guide
- Personal finance
- View all personal finance
- Small business
- Small business guide
- View all taxes

You’re our first priority. Every time.
We believe everyone should be able to make financial decisions with confidence. And while our site doesn’t feature every company or financial product available on the market, we’re proud that the guidance we offer, the information we provide and the tools we create are objective, independent, straightforward — and free.
So how do we make money? Our partners compensate us. This may influence which products we review and write about (and where those products appear on the site), but it in no way affects our recommendations or advice, which are grounded in thousands of hours of research. Our partners cannot pay us to guarantee favorable reviews of their products or services. Here is a list of our partners .
How Much Does Gender-Affirming Surgery Cost?

Many or all of the products featured here are from our partners who compensate us. This influences which products we write about and where and how the product appears on a page. However, this does not influence our evaluations. Our opinions are our own. Here is a list of our partners and here's how we make money .
Gender-affirming care encompasses a broad range of psychological, behavioral and medical treatments for transgender, nonbinary and gender-nonconforming people.
The care is designed to “support and affirm an individual’s gender identity” when it is at odds with the sex they were assigned at birth, as defined by the World Health Organization.
What is gender-affirming surgery?
Gender-affirming surgery refers to the surgical and cosmetic procedures that give transgender and nonbinary people “the physical appearance and functional abilities of the gender they know themselves to be,” according to the American Society of Plastic Surgeons. It is sometimes called gender reassignment surgery.
There are three main types of gender-affirming surgeries, per the Cleveland Clinic:
Top surgery , in which a surgeon either removes a person’s breast tissue for a more traditionally masculine appearance or shapes a person’s breast tissue for a more traditionally feminine appearance.
Bottom surgery , or the reconstruction of the genitals to better align with a person’s gender identity.
Facial feminization or masculinization surgery , in which the bones and soft tissue of a person’s face are transformed for either a more traditionally masculine or feminine appearance.
Some people who undergo gender-affirming surgeries also use specific hormone therapies. A trans woman or nonbinary person on feminizing hormone therapy, for example, takes estrogen that’s paired with a substance that blocks testosterone. And a trans man or nonbinary person on masculinizing hormone therapy takes testosterone.
Gender-affirming surgeries and treatments are the recommended course of treatment for gender dysphoria by the American Medical Association. Gender dysphoria is defined as “clinically significant distress or impairment related to gender incongruence, which may include desire to change primary and/or secondary sex characteristics,” according to the American Psychiatric Association.
Some LGBTQ+ advocates and medical professionals feel that gender dysphoria shouldn't be treated as a mental disorder, and worry that gender dysphoria’s inclusion in the DSM-5 — the authoritative source on recognized mental health disorders for the psychiatric industry — stigmatizes trans and nonbinary people.
How much does gender-affirming surgery cost?
Gender-affirming surgery can cost between $6,900 and $63,400 depending on the precise procedure, according to a 2022 study published in The Journal of Law, Medicine and Ethics.
Out-of-pocket costs can vary dramatically, though, depending on whether you have insurance and whether your insurance company covers gender-affirming surgeries.
There are also costs associated with the surgery that may not be represented in these estimates. Additional costs may include:
Surgeons fees
Hospital fees
Consultation fees
Insurance copays
The cost of psychiatric care or therapy, as most insurance companies and surgeons require at least one referral letter prior to the surgery. An hour of therapy can cost between $65 and $250, according to Good Therapy, an online platform for therapists and counselors.
Time off work. After bottom surgery, you can expect to miss six weeks of work while recovering. Most people miss around two weeks of work after top surgery.
Miscellaneous goods that’ll help you recover. For example, after bottom surgery, you might need to invest in a shower stool, waterproof bed sheets, cheap underwear and sanitary towels. Top surgery patients may need, depending on the procedure, a mastectomy pillow, chest binder and baggy clothes.
Is gender-affirming surgery covered by insurance?
It’s illegal for any federally funded health insurance program to deny coverage on the basis of gender identity, sexual orientation or sexual characteristics, per Section 1557, a section of the Affordable Care Act. Section 1557 doesn’t apply to private insurance companies, though, and several U.S. states have passed laws banning gender-affirming care.
The following states have banned gender-affirming surgery for people under 18 years old, according to the Human Rights Campaign: Alabama, Arkansas, Florida, Georgia, Idaho, Indiana, Iowa, Kentucky, Louisiana, Mississippi, Missouri, Montana, Nebraska, North Carolina, North Dakota, Oklahoma, South Dakota, Tennessee, Texas, Utah, West Virginia. In four of these states — Alabama, Arkansas, Florida and Indiana — court injunctions are currently ensuring access to care.
And these states have either passed laws — or have governors who issued executive orders — protecting access to gender-affirming surgery, according to the Movement Advancement Project, a public policy nonprofit: California, Colorado, Connecticut, Illinois, Maryland, Massachusetts, Minnesota, New Jersey, New Mexico, New York, Oregon, Vermont and Washington, D.C.
But even if your state has enshrined protections for gender-affirming care, some private insurance companies may consider surgeries “cosmetic” and therefore “not medically necessary,” according to the Transgender Legal Defense and Education Fund. If you have private insurance or are insured through your employer, contact your insurance company and see if they cover gender-affirming care. Also, ask about any documentation the insurance company requires for coverage.
The Williams Institute estimates that 14% of trans Americans currently enrolled in Medicaid live in states where such coverage is banned, while another 27% of trans Americans live in states where coverage is “uncertain,” because their state laws are “silent or unclear on coverage for gender-affirming care.”
Because of Section 1557, Medicaid is federally banned from denying coverage on the basis of sex or gender; among the roughly 1.3 million transgender Americans, around 276,000 have Medicaid coverage, according to a 2022 report from the Williams Institute.
How to pay for gender-affirming surgery
If your private insurance company won’t cover gender-affirming care, and you’re unable to obtain coverage through the federal marketplace, consider these sources:
Online personal loan.
Credit union personal loan.
Credit card.
CareCredit.
Home equity line of credit.
Family loan.
There are also several nonprofits that offer financial assistance for gender-affirmation surgeries. Those organizations include:
Point of Pride , which offers grants and scholarships to trans and nonbinary people seeking gender-affirming surgery and care.
The Jim Collins Foundation , which raises money to fund gender-affirming surgeries.
Genderbands , which offers grants for gender-affirming surgeries and care.
Black Transmen Inc. , which funds gender-affirming surgeries for Black trans men.
On a similar note...
- Search Search Please fill out this field.
Does Insurance Cover Gender-Affirming Care?
How much does gender-affirming surgery cost, how much does gender-affirming medication cost, other ways to pay for gender-affirming care and surgery, tips for financing gender-affirming care and surgery, bottom line.
- Health Insurance
In many cases, health insurance in the U.S. covers gender-affirming care. However, whether or not your insurance plan covers a specific gender-affirming treatment depends on your state, employer, and the plan’s benefits.
Key Takeaways
- Health insurance generally covers gender-affirming care.
- Not all plans cover all procedures, or the process can be murky and require preauthorization and appeals.
- Gender-affirming care can cost tens of thousands of dollars.
Major insurance companies recognize transgender-related care as being medically necessary and have put policies in place outlining coverage criteria. However, at least 20 states have passed legislation limiting coverage of gender-affirming care for people up to age 18. And some transgender people may still be denied coverage of hormone treatments or transition-related surgery by an insurer.
An estimated 1.6 million Americans at least 13 years old identify as transgender, according to a June 2022 estimate.
Health insurers generally cover an array of medically necessary services that affirm gender or treat gender dysphoria, according to the American Medical Association. Gender dysphoria is a condition that occurs when someone feels a conflict between the sex they were assigned at birth and the gender they now identify with.
Gender-affirming care is the phrase used by most medical groups for dysphoria treatment. This care includes hormones, surgery, or counseling. The care aligns a person’s gender identity with gender expression in appearance, anatomy, and voice.
In 2010, the federal Affordable Care Act banned health insurance discrimination based on sexual orientation and gender identity. Before the law’s passage, medically necessary gender-affirming surgeries and hormones often weren’t covered by insurers.
A 2022 rule from the Biden Administration noted that “categorical coverage exclusions or limitations for all health services related to gender transition are discriminatory” and that a covered entity can’t deny or limit coverage or claims, or charge more in cost-sharing related to gender transition.
However, insurance is regulated at the federal and state level based on whether it is an ACA, public, or employer plan, so the rule doesn’t apply evenly to all insurers. Coverage and requirements vary based on state, employer, plan type, and more.
Investopedia / Candra Huff
Determining What Your Plan Covers
Plan members can generally find out what’s available in their member booklet. This should have been given to you when you got the policy or, if it’s an employee plan, when you joined the company. It may be called a certificate of coverage, a benefit plan, a summary plan description, a certificate of insurance, or something similar.
This document should describe the insurer’s clinical evidence criteria to qualify for gender dysphoria treatment claim coverage. Requirements might include:
- One or two letters from a therapist containing specific information
- Being on hormones for a year
- Being at least 18 years old to have surgery.
Some plans may still list exclusions for certain procedures. Even if an exclusion exists in the documentation, the next step is to apply for pre-authorization or pre-approval. This earns a plan’s approval in advance for claims and may even be successful if an exclusion is evident—as it allows an appeal.
"Many [patients] call their insurance carrier and are told services will not be covered, and on that basis never attempt to file a claim,” says an article on the San Francisco-based UCSF Gender Affirming Health Program’s website. “Transgender individuals and their health providers should be aware that unless a denial is in writing, it is not a denial and cannot be appealed.
Typically, documentation submitted to the health plan shows why the treatment is medically necessary or explains the legal problems with an exclusion. Not getting preauthorization can lead to a claim denial, even if a procedure is covered. For example, many plans routinely require preauthorization for all surgeries of any kind for anyone.
If denied a preauthorization request or a claim, an attorney, health care advocate, or your human resources department may be able to help with filing an appeal. Appeals should include individualized, extensive documentation of a service’s medical necessity and appropriateness, and a comprehensive overview of the transition process of gender transition.
Here, we list four types of health insurance and how they might cover gender-affirming care.
Employer-Provided Insurance
Altogether, 24 states and the District of Columbia prohibit transgender exclusions in private health insurance coverage, according to the nonprofit LGBTQ+ advocacy organization Movement Advance Project, leaving 26 states without such protections.
However, health coverage benefits that a private employer provides can vary based on whether the employer fully funds the plan. If funded by the employer, the plan is governed by the federal law ERISA, the Employee Retirement Income Security Act , which overrides any state nondiscrimination law. The employer decides what health care is or is not covered.
Employer-based plans are governed in the state where the plan was issued, not where you live.
Up to 91% of businesses on the 2022 Human Rights Campaign’s Corporate Equality Index-rated businesses offer at least one transgender-inclusive plan option, up from 0 in 2002.
Affordable Care Act Plan Coverage
Individuals can buy their own health insurance policies, often with the help of federal subsidies, through the Healthcare.gov marketplace. Most insurers are getting rid of transgender-specific exclusions, which ACA regulation explicitly banned.
Still, policies vary by state and in what they cover. Health insurance policies may feature exclusions for items such as “services related to sex change” or “sex reassignment surgery” to deny coverage.
Around 6% of Silver Marketplace plans specifically exclude coverage for exclusions for treatment of gender dysphoria, according to a survey by Out2Enroll, an organization connecting the LGBT+ community with health care coverage.
Check a policy’s terms of coverage for a full explanation of which procedures and services are covered or excluded. You can also use a state-based Trans Insurance Guide from Out2Enroll to find a plan with the coverage you want.
Medicare and Medicaid Coverage
Nearly 10,000 transgender Americans 65 and older are enrolled in Medicare or Medicare Advantage. Under these plans, medically necessary care—including some gender-affirming procedures—is covered. Coverage by Medicare Advantage plans may vary, so try to get preauthorization before accessing transition-related services, suggests the National Center for Transgender Equality.
On a state-by-state basis, Medicaid coverage is uneven for lower-income people seeking gender-affirming care. Medicaid programs cover transgender-related care in 26 states and the District of Columbia. Meanwhile, programs in nine states bar coverage of transgender-related care for people of all ages, and programs in two states prohibit coverage of transgender-related care for minors.
Military and Veteran Coverage
Active military members can access gender-affirming hormonal treatment and therapy for gender dysphoria. Tricare, the health benefits provider for military members, does not usually cover gender-affirming surgeries. However, a waiver may be requested and granted in some cases for medically necessary gender-affirming surgery.
The Veterans Health Administration offers gender-affirming health care, including hormones and prosthetics, mental health care, and other health care. Coverage for gender-affirming surgery has traditionally been denied but is currently undergoing a review.
For just one person, the cost of gender-affirming care might range from $25,000 to $75,000, according to estimates from the HRC Foundation.
Gender-affirming surgeries may include top surgery (breast removal or augmentation), bottom surgery, vocal surgery, and face and body surgeries such as browlifts, jawline contouring, Adam’s apple removal, and forehead reduction.
Bottom surgery may include:
- Phalloplasty : Creation of penis
- Metoidioplasty : Phallus created from existing genital region tissue.
- Hysterectomy : Uterus and cervix removal
- Nullification surgery : Creating a gender-neutral look in the groin
- Oophorectomy : Removal of one or both ovaries
- Vaginoplasty and vulvoplasty : Creation of vagina and vulva
- Orchiectomy : Testicle removal
Research published in 2022 by The Journal of Law, Medicine & Ethics detailed the costs of gender-affirming surgery from 1993 to 2019. The chart below shows the average costs of five of the most common gender-affirming procedures within a commercially insured population over the span of those years.
However, not all transgender people desire surgery. According to 2019 statistics, only 28% of transgender women get any type of surgery, and only 5%–13% receive genital surgery. Surgery is more common among transgender men, with 42%–54% getting some type of surgery; up to 50% get genital surgery.
Gender-affirming medication is far more common. Up to 65% of transgender people received gender-affirming hormone therapy in 2019, up from 17% in 2011, according to The Journal of Law, Medicine & Ethics. The study notes the costs of gender-affirming medication from 1993 to 2019.
Another 2022 study from Vanderbilt University found that masculinizing hormones run $29.76 to $463.54 per fill while feminizing hormones cost $12.95 to $180.98. Much of the cost depends on the delivery method, such as injection or gel. The authors note that “the most cost-effective hormone therapies were oral estrogen and injectable testosterone esters.”
One 2020 survey found that among insured respondents taking gender-affirming hormones, almost 21% reported that their claims were denied. This group (and those uninsured) were more likely to take non-prescription hormones from unlicensed sources, which may not be monitored for quality and potentially lead to health risks.
Other costs are involved as well. For example, at Planned Parenthood of South, East, and North Florida, gender-affirming hormone treatment costs between $95 to $105. Lab monitoring may need to be run to ensure health while taking hormones, which can average $26 to $142 per visit.
Aside from health insurance, how can you pay for gender-affirming care or surgery? Here are 10 options.
Payment Plans
Some healthcare providers offer payment plans directly or through lenders that let you pay off medical bills over time.
You might take out a personal loan or even a type of personal loan called a medical loan to cover expenses related to gender-affirming care or surgery. A medical loan is just a personal loan used to pay for medical expenses.
Credit Cards
Credit cards may be another avenue for covering the costs of gender-affirming care or surgery, although these tend to have higher interest rates. You may see promotional materials for the CareCredit credit card in your provider’s office, but other credit cards can pay for the same healthcare costs, often with a better interest rate and without the dangerous deferred interest feature that CareCredit cards have. You’re better off with a regular credit card that has a promotional 0% purchase rate offer.
Even with health insurance, hormone therapy may be less expensive if you comparison shop and use pharmacy programs, such as GoodRx.
Surgery Grants
Several organizations offer grants for people seeking gender-affirming care or surgery, such as the Darcy Jeda Crobitt Foundation and the Jim Collins Foundation.
Health Accounts
If you have a flexible spending account (FSA) or Health Savings Account (HSA) , consider allocating some account money for gendering-affirming care or surgery.
Health Reimbursement Agreement
A health reimbursement agreement (HRA) is an employer-funded group health plan that reimburses employees for qualified medical expenses, which might include gender-affirming care or surgery.
Home Equity Line of Credit (HELOC)
You could take out a home equity line of credit to cover the costs of gender-affirming care or surgery. With this type of loan, you typically can borrow up to a specific percentage of your home equity. Interest rates on HELOCs are generally lower than those on a personal loan, because your home serves as collateral. Just realize that if you can’t repay the loan, your could lose your home.
Friends-and-Family Loans
If you’ve got supportive friends or relatives, they might be willing to chip in money to pay for your gender-affirming care or surgery. Just make sure you have a written agreement and repayment plan.
Crowdfunding
You might consider setting up a crowdfunding campaign on a platform like GoFundMe to raise money from friends, relatives, colleagues or strangers.
When you’re financing gender-affirming care or surgery, follow these tips:
Shop Around
A number of online tools such as Hospital Cost Compare and Healthcare Bluebook allow you to compare costs for the same procedures and treatments offered by different healthcare providers. This homework could save you a lot of money.
Explore Your Options
Even if health insurance covers a procedure or treatment, you must cover some out-of-pocket costs. Therefore, consider looking into surgery grants, crowdfunding, friends-and-family loans or other methods to bridge the monetary gap.
Check the Interest Rate
Be sure to investigate how much you’ll pay to borrow money if you go down that road. With the CareCredit card, for example, the APR may be higher than a regular credit card or a personal loan.
Try Negotiating or a Payment Plan
You can negotiate with a healthcare provider to lower the costs of gender-affirming care or surgery. For instance, a healthcare provider might discount your services if you agree to pay off your medical bills quickly. If a healthcare provider isn’t willing to provide a discount, they might let you make interest-free payments as part of a payment plan.
Ask About Financial Assistance
Some nonprofit healthcare providers offer financial assistance programs that cover all or some of your medical expenses.
What Are the Different Types of Gender-Affirming Care?
Various types of gender-affirming care include puberty-blocking medication, hormone therapy, top surgery, bottom surgery, nullification surgery, laser hair removal, facial feminization surgery, speech therapy, and mental health services.
How Much Does Gender-affirming Care Cost in the U.S?
The cost of gendering-affirming care varies widely, depending on the type of procedure or treatment involved. For one person, gender-affirming care might cost anywhere from $25,000 to $75,000, according to estimates from the Human Rights Campaign Foundation. Health insurance may or may not cover these costs to varying degrees.
Does Insurance Cover Puberty Blockers?
According to one study, insurance companies cover puberty blockers 72% of the time. The estimated out-of-pocket cost for a 3-month supply ranges between $9,500 and $39,000.
The campaign for transgender rights in the U.S. has experienced victories and setbacks in recent years—in some cases affecting coverage of gender-affirming care. Even amid progress made, some people still encounter problems securing health insurance coverage for gender-affirming care or covering out-of-pocket costs. Getting coverage for care may require preauthorization, documentation of medical necessity, and an appeal. This may prompt use of alternative financing methods like crowdfunding, credit cards, loans, or grants.
U.S. Department of Health and Human Services. “ HHS Announces Prohibition on Sex Discrimination Includes Discrimination on the Basis of Sexual Orientation and Gender Identity .”
The Williams Institute at UCLA. " How Many Adults and Youth Identify as Transgender in the United States? "
American Medical Association. “ Transgender Coverage Issue Brief .”
First Report Managed Care. “ Transgender Patients: Calculating the Actual Cost .”
UCSF. " Health Insurance Coverage Issues for Transgender People in the United States .”
Transgender Health Insurance. " Health Insurance - Understanding Your Plan ."
HRC. " Corporate Equality Index 2022. "
Society for Evidence-Based Gender Medicine. “ Sweden’s Karolinska Ends All Use of Puberty Blockers and Cross-Sex Hormones for Minors Outside of Clinical Studies .”
BlueCross BlueShield of Tennessee. “ BlueCross BlueShield of Tennessee Medical Policy Manual .”
Movement Advancement Project. " Medicaid Coverage of Transgender-Related Health Care ."
HealthCare.gov. “ Transgender Health Care .”
U.S. Department of Veterans Affairs. "VHA LGBTQ+ Health Program. "
Williams Institute, UCLA School of Law. “ Medicaid Coverage for Gender-Affirming Care ,” Page 1.
National Center for Biotechnology Information. “ Health Insurance Coverage of Recommended Gender-Affirming Health Care Services for Transgender Youth: Shopping Online for Coverage Information .”
British Columbia Nurses’ Union. “ Position Statement: Gender-Affirming Care .”
Journal of General Internal Medicine. " Gender-Affirming Hormone Therapy Spending and Use in the USA, 2013–2019. "
Annals of Family Medicine. "Insurance Coverage and Use of Hormones Among Transgender Respondents to a National Survey ."
Aetna. “ Gender Affirming Surgery .”
Current Problems in Pediatric and Adolescent Health Care. " Gender Affirming Medical Care of Transgender Youth ."
- Guide to Finance for LGBTQ+ People 1 of 18
- LGBTQ+ Marriage and Personal Finance 2 of 18
- The Costs of LGBTQ+ Family Planning 3 of 18
- Mortgage Lending for LGBTQ+ People 4 of 18
- Banks that Support the LGBTQ+ Community 5 of 18
- LGBTQ+ Credit Barriers: Why They Exist and How to Avoid Them 6 of 18
- Top LGBTQ+ Financial Influencers to Learn From 7 of 18
- Paying for College as an LGBTQ+ Student 8 of 18
- LGBTQ+ Representation in the Workforce 9 of 18
- LGBTQ+ Pay Gap and Unemployment 10 of 18
- Health Insurance for LGBTQ+ People 11 of 18
- How Being Nonbinary Affects Getting Life Insurance 12 of 18
- Qualifying for Life Insurance When You're Transgender 13 of 18
- Does Insurance Cover Gender-Affirming Care? 14 of 18
- How to Invest in LGBTQ+-Friendly Companies 15 of 18
- Preparing for Retirement as an LGBTQ+ Person 16 of 18
- Social Security Benefits for for Same-Sex Couples: History and How Survivors Benefits Work 17 of 18
- Finding LGBTQ+ Friendly Retirement Options 18 of 18
:max_bytes(150000):strip_icc():format(webp)/GettyImages-451474560-78fbdb4302b749f488c4d2507157b712.jpg)
- Terms of Service
- Editorial Policy
- Privacy Policy
- Your Privacy Choices
An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Transgender health care
A transgender person’s assigned sex at birth doesn’t match their gender identity, expression, or behavior.
Refer to glossary for more details.
Applying for Marketplace coverage
Sex-specific preventive services.
A fixed amount ($20, for example) you pay for a covered health care service after you've paid your deductible.
The percentage of costs of a covered health care service you pay (20%, for example) after you've paid your deductible.
The amount you pay for covered health care services before your insurance plan starts to pay. With a $2,000 deductible, for example, you pay the first $2,000 of covered services yourself.
Plans with transgender exclusions
An easy-to-read summary that lets you make apples-to-apples comparisons of costs and coverage between health plans. You can compare options based on price, benefits, and other features that may be important to you. You'll get the "Summary of Benefits and Coverage" (SBC) when you shop for coverage on your own or through your job, renew or change coverage, or request an SBC from the health insurance company.
You are leaving HealthCare.gov
You're about to connect to a third-party site. Select Continue to proceed or Cancel to stay on this site.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Does Health Insurance Cover Transgender Health Care?
For transgender Americans, access to necessary health care can be fraught with challenges. Section 1557 of the Affordable Care Act (ACA) prohibits discrimination on a wide variety of grounds for any "health program or activity" that receives any sort of federal financial assistance.
But the specifics of how that section is interpreted and enforced are left up to the Department of Health and Human Services (HHS) and the Office for Civil Rights (OCR). Not surprisingly, the Obama and Trump administrations took very different approaches to ACA Section 1557. But the Biden administration has reverted to the Obama-era rules.
In 2020, the Trump administration finalized new rules that rolled back the Obama administration's rules. This came just days before the Supreme Court ruled that employers could not discriminate against employees based on sexual orientation or gender identity. The Trump administration's rule was subsequently challenged in various court cases.
And in May 2021, the Biden administration issued a notice clarifying that the Office of Civil Rights would once again prohibit discrimination by health care entities based on sexual orientation or gender identity.
The Biden administration subsequently issued a proposed rule in 2022 to update the implementation of Section 1557 and strengthen nondiscrimination rules for health care. The proposed rule " restores and strengthens civil rights protections for patients and consumers in certain federally funded health programs and HHS programs after the 2020 version of the rule limited its scope and power to cover fewer programs and services. "
Section 1557 of the ACA
ACA Section 1557 has been in effect since 2010, but it's only a couple of paragraphs long and very general in nature. It prohibits discrimination in health care based on existing guidelines—the Civil Rights Act, Title IX, the Age Act, and Section 504 of the Rehabilitation Act—that were already very familiar to most Americans (i.e., age, disability, race, color, national origin, and sex).
Section 1557 of the ACA applies those same non-discrimination rules to health plans and activities that receive federal funding.
Section 1557 applies to any organization that provides healthcare services or health insurance (including organizations that have self-insured health plans for their employees) if they receive any sort of federal financial assistance for the health insurance or health activities.
That includes hospitals and other medical facilities, Medicaid , Medicare (with the exception of Medicare Part B ), student health plans, Children's Health Insurance Program, and private insurers that receive federal funding.
For private insurers, federal funding includes subsidies for their individual market enrollees who purchase coverage in the exchange (marketplace). In that case, all of the insurer's plans must be compliant with Section 1557, not just their individual exchange plans.
(Note that self-insured employer-sponsored plans are not subject to Section 1557 unless they receive some type of federal funding related to health care activities. The majority of people with employer-sponsored health coverage are enrolled in self-insured plans.)
To clarify the nondiscrimination requirements, the Department of Health and Human Services (HHS) and the Office for Civil Rights (OCR) published a 362-page final rule for implementation of Section 1557 in May 2016.
At that point, HHS and OCR clarified that gender identity "may be male, female, neither, or a combination of male and female." The rule explicitly prohibited health plans and activities receiving federal funding from discrimination against individuals based on gender identity or sex stereotypes.
But the rule was subject to ongoing litigation, and the nondiscrimination protections for transgender people were vacated by a federal judge in late 2019.
And in 2020, the Trump administration finalized new rules which reversed much of the Obama administration's rule. The new rule was issued in June 2020, and took effect in August 2020. It eliminated the ban on discrimination based on gender identity, sexual orientation, and sex stereotyping, and reverted to a binary definition of sex as being either male or female.
Just a few days later, however, the Supreme Court ruled that it was illegal for a workplace to discriminate based on a person's gender identity or sexual orientation. The case hinged on the court's interpretation of what it means to discriminate on the basis of sex, which has long been prohibited under US law. The majority of the justices agreed that "it is impossible to discriminate against a person for being homosexual or transgender without discriminating against that individual based on sex."
The Biden administration announced in May 2020 that Section 1557's ban on sex discrimination by health care entities would once again include discrimination based on gender identity and sexual orientation.
And in 2022, the Biden administration published a new proposed rule for the implementation of Section 1557, rolling back the Trump-era rule changes and including a new focus on gender-affirming care (as opposed to just gender transition care).
Are Health Plans Required to Cover Gender Affirming Care?
Even before the Obama administration's rule was blocked by a judge and then rolled back by the Trump administration, it did not require health insurance policies to " cover any particular procedure or treatment for transition-related care ."
The rule also did not prevent a covered entity from " applying neutral standards that govern the circumstances in which it will offer coverage to all its enrollees in a nondiscriminatory manner ." In other words, medical and surgical procedures had to be offered in a non-discriminatory manner, but there was no specific requirement that insurers cover any specific transgender-related healthcare procedures, even when they're considered medically necessary.
Under the Obama administration's rule, OCR explained that if a covered entity performed or paid for a particular procedure for some of its members, it could not use gender identity or sex stereotyping to avoid providing that procedure to a transgender individual. So for example, if an insurer covers hysterectomies to prevent or treat cancer in cisgender women, it would have to use neutral, non-discriminatory criteria to determine whether it would cover hysterectomies to treat gender dysphoria.
And gender identity could not be used to deny medically necessary procedures, regardless of whether it affirmed the individual's gender. For example, a transgender man could not be denied treatment for ovarian cancer based on the fact that he identifies as a man.
But the issue remained complicated, and it's still complicated even with the Biden administration's proposed rule to strengthen Section 1557's nondiscrimination rules.
Under the 2016 rule, covered entities in every state were prohibited from using blanket exclusions to deny care for gender dysphoria and had to utilize non-discriminatory methods when determining whether a procedure will be covered. But that was vacated by a federal judge in 2019.
However, the new rules proposed in 2022 by the Biden administration " prohibit a covered entity from having or implementing a categorical coverage exclusion or limitation for all health services related to gender transition or other gender-affirming care. "
As of 2023, HealthCare.gov's page about transgender health care still states that " many health plans are still using exclusions such as “services related to sex change” or “sex reassignment surgery” to deny coverage to transgender people for certain health care services. Coverage varies by state. "
The page goes on to note that " transgender health insurance exclusions may be unlawful sex discrimination. The healthcare law prohibits discrimination on the basis of sex, among other bases, in certain health programs and activities ."
The page advises that " if you believe a plan unlawfully discriminates, you can file complaints of discrimination with your state’s Department of Insurance, or report the issue to the Centers for Medicare & Medicaid Services by email to [email protected] ." (note that this language existed on that page in 2020 as well.)
State Rules for Health Coverage of Gender Affirming Care
Prior to the 2016 guidance issued in the Section 1557 final rule, there were 17 states that specifically prevented state-regulated health insurers from including blanket exclusions for transgender-specific care and 10 states that prevented such blanket exclusions in their Medicaid programs. And as of 2023, the list of states that ban specific transgender exclusions in state-regulated private health plans has grown to 24, plus the District of Columbia.
Starting in 2023, Colorado became the first state to explicitly include gender-affirming care in its benchmark plan (used to define essential health benefits ), ensuring that all individual and small-group health plans in the state must provide that coverage.
While Section 1557 was initially a big step towards equality in health care for transgender Americans, it does not explicitly require coverage for sex reassignment surgery and related medical care. And the implementation of Section 1557 has been a convoluted process with various changes along the way. Most recently, the Biden administration has restored nondiscrimination protections based on gender identity.
Do Health Insurance Plans Cover Sex Reassignment?
It depends on the health insurance plan. This description from Aetna and this one from Blue Cross Blue Shield of Tennessee are good examples of how private health insurers might cover some—but not all—aspects of the gender transition process, and how medical necessity is considered in the context of gender-affirming care.
Since 2014, Medicare has covered medically necessary sex reassignment surgery , with coverage decisions made on a case-by-case basis depending on medical need. And the Department of Veterans Affairs (VA) has announced in June 2021 that it has eliminated its long-standing ban on paying for sex reassignment surgery for America's veterans.
But Medicaid programs differ from one state to another, and there are pending lawsuits over some states' refusals to cover gender transition services for Medicaid enrollees.
Over the last several years, many health plans and self-insured employers have opted to expand their coverage in order to cover sex reassignment surgery and other gender-affirming care. But although health coverage for transgender-specific services has become more available, it is still far from universal.
This issue is likely to face protracted legal debate over the coming years, and coverage will likely continue to vary from one state to another and from one employer or private health plan to another.
Many health plans in the U.S. are subject to ACA Section 1557, which prohibits discrimination based on gender. But this section is implemented via HHS rules, which have changed over time: The Obama administration issued rules to protect people from gender-related discrimination in health care, the Trump administration relaxed those rules, and the Biden administration has proposed changes to strengthen them once again.
A Word from Verywell
If you're in need of gender-affirming medical care, you'll want to carefully consider the specifics of the health policy you have or any that you may be considering. If you think that you're experiencing discrimination based on your gender identity, you can file a complaint with the Office of Civil Rights . But you may find that a different health plan simply covers your needs more comprehensively.
US Department of Health and Human Services. Section 1557 of the Patient Protection and Affordable Care Act .
Keith, Katie. Health Affairs. HHS Will Enforce Section 1557 To Protect LGBTQ People From Discrimination . May 11, 2021.
U.S. Department of Health and Human Services. HHS Announces Proposed Rule to Strengthen Nondiscrimination in Health Care . July 25, 2022.
United States DoJ. Overview of Title IX of the education amendments of 1972 . Updated August, 2015.
DHS. Nondiscrimination in health programs and activities . Effective July 18, 2016.
Keith, Katie. Health Affairs. Court Vacates Parts Of ACA Nondiscrimination Rule . October 16, 2019.
Department of Health and Human Services. Nondiscrimination in Health and Health Education Programs or Activities, Delegation of Authority . June 12, 2020.
SCOTUS Blog. R.G. & G.R. Harris Funeral Homes Inc. v. Equal Employment Opportunity Commission . Argued October 2019; Decision issued June 15, 2020.
U.S. Department of Health and Human Services. HHS Announces Prohibition on Sex Discrimination Includes Discrimination on the Basis of Sexual Orientation and Gender Identity . May 10, 2021.
National Center for Transgender Equality. Know your rights: medicare .
HealthCare.gov. Transgender Health Care .
Health Affairs. LGBT protections in affordable care act section 1557 . June 2016.
LGBT Map. Health Care Laws and Policies .
U.S. Department of Health and Human Services. Biden-Harris Administration Greenlights Coverage of LGBTQ+ Care as an Essential Health Benefit in Colorado . October 12, 2021.
Military Times. VA to Offer Gender Surgery to Transgender Vets for the First Time . June 19, 2021.
Fleig, Shelby. Des Moines Register. ACLU of Iowa Renews Effort to Overturn Law Restricting Public Funds for Trans Iowans' Transition-Related Care . April 22, 2021.
By Louise Norris Norris is a licensed health insurance agent, book author, and freelance writer. She graduated magna cum laude from Colorado State University.

- Find a plan

- Health Insurance
- Data & Insights
- Resource Center
- For Carriers

Transgender health care: Does health insurance cover gender-affirming surgery?
By HealthSherpa
Share this post
For many trans folks, navigating the United States health care system can be complicated. Transgender individuals often struggle when it comes to finding health care providers who understand the nuances of trans health care. Not all providers are cognizant of the use of consistent and respectful pronoun usage.
Plus, it can be difficult to understand how health insurance does or does not cover care.
One important thing up front: Federal and state law prohibits most public and private health plans from discriminating against a person because they are transgender. And this means that, on the whole, it is illegal for your health insurance plan to refuse to cover medically necessary transition-related care .
This means that a health plan can’t have a categorical exclusion of transition-related care. And a health plan can’t have a categorical exclusion of a specific transition-related procedure either. Your health insurance company also can’t place limits on coverage for transition-related care if it covers the same procedure for non-transgender people. And thanks to the Affordable Care Act, health care plans also cannot refuse to enroll you in a plan, cancel your coverage, charge you higher rates, or deny you coverage because of your gender identity.
Trying to figure out how much gender-affirming surgery might cost you? Here’s what to know about how your health insurance may or may not cover that care.
Is gender-affirming surgery ever covered by health insurance?
Yes, sometimes health insurance coverage includes gender-affirming surgery.
It’s important to note that it’s not a requirement for a single health insurance plan to cover any specific kind of procedure.
For private insurers who do cover gender-affirming surgery, a patient must first prove that the procedure is medically necessary. While the details of this may vary from plan to plan, it often consists of getting one to two letters of referral from a qualified mental health professional, a “persistent, well-documented” case of gender dysphoria, and the proven ability to make fully informed decisions.
A 2018 study published in JAMA Surgery , the surgical journal of the American Medical Association, found that gender-affirming surgery accounted for just 11 percent of all encounters coded with gender identity disorder codes between 2000 and 2014, but that the number of individuals receiving gender-affirming surgery is on the rise. More than half of the individuals receiving gender-affirming surgery during that period did not have coverage by health insurance. But the amount of patients who identified as self-payers decreased over that time period. That means that the number of people who did not have insurance coverage for their gender-affirming surgery also decreased.
Medicare and Medicaid did start to provide coverage for this kind of care in 2014. Still, decisions are made on a case-by-case basis after medical necessity is evaluated. R esearchers also found that the coverage of gender-affirming surgery by private insurance has increased. It went from 25.6 percent between 2000 and 2011 to 45.2 percent in 2014.
Do Marketplace (aka Affordable Care Act or Obamacare) plans cover gender-affirming surgery?
Just like with private insurance, coverage of gender-affirming surgery by Marketplace plans varies by health insurance company and by state. According to HealthCare.gov, before enrolling in any Marketplace plan, you should check the complete terms of coverage included in the “evidence of coverage” or “certificate of coverage” that accompany a given plan. This document will give the full explanation of what’s covered and what’s excluded by a given plan.
To see Marketplace (Obamacare) health plans and prices, enter your zip code below.
If you need help applying for insurance or have questions, you can call our Consumer Advocates at (872) 228-2549 .
Some plans that exclude coverage for gender-affirming surgery use language like “all procedures related to being transgender are not covered.” They may have prohibitive language around words like “gender change,” “gender reassignment surgery,” “transsexual,” “gender identity disorder,” and “gender identity dysphoria.”
Don’t forget that your health plan should cover transition-related care, though. You may have to prove that gender-affirming surgery is medically necessary via additional documentation from providers. But, you should be able to access this care. Your insurance company may also require a preauthorization letter for your gender-affirming surgery; you can find a template for this here .
What should you do if your plan has transgender exclusions?
Again, coverage of transition-related care varies greatly between insurer and state. But is your right to receive a given service if it is covered for other people on your plan. Don’t forget that you always have the right to appeal a decision regarding coverage made by your insurance company if you believe you have been wrongly denied coverage. You can also check this list to see how various insurance plans cover and do not cover various forms of transgender-specific health services.
Denied coverage or your plan has an exclusion? You may need to work with your health plan to explain why such denials are illegal. And keep in mind that transgender health insurance exclusions may be unlawful sex discrimination. The health care law prohibits discrimination on the basis of sex, among other bases, in certain health programs and activities. If you believe a Marketplace plan is unlawfully discriminating, you should contact [email protected].
You can also file a civil rights complaint with the U.S. Department of Health and Human Services, Office for Civil Rights .
Leave a Comment Cancel Reply
Save my name, email, and website in this browser for the next time I comment.
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Have you experienced a major life event?
You may be eligible to enroll outside of the open enrollment period..
Looking to enroll in health insurance?
Click on the button below to shop and compare plans, 1 out of 2 people pay under $10/month, grab this free guide.
More Health Insurance Articles

MAY 9, 2022
New enrollment period for...
There is a new Special Enrollment Period (SEP) that enables qualifying consumers to...

NOVEMBER 7, 2021
How much does ACA health...
Uninsured right now and don’t want to be? Then you’re likely wondering how much...

OCTOBER 21, 2021
Your Quick Guide to the 2022...
The Affordable Care Act (ACA) ensures that all eligible Americans get an opportunity once...
Press Enter to Begin Search / Esc to close popup
Yes, please! I would love the free PDF
Enter your email below to download a PDF containing all of this plan's coverage details
Shop for Car Insurance
Other Insurance Products
Types of mortgages
Calculators
Find & Compare Credit Cards
Cards with Rewards
Cards for a Purpose
Cards for Building Credit
Credit Card Reviews
Understanding Credit & Score
Student Loans
Paying for College
Personal Finance for College Students
Life Events
Financing & Support for Gender Confirmation Surgery
Updated: December 5, 2023
Quality Verified
Featured Experts:
On This Page:
- Options and Average Costs
What Health Insurance Can Cover
- Ways to Navigate Health Insurance
Financing Options and Support
- Organizations Making a Change
- Expert Insight
- Additional Healthcare Resources
Advertising & Editorial Disclosure
Between 1.4 million and 1.65 million adults in the U.S. identify as transgender, according to the Williams Institute at UCLA's School of Law. For many transgender and gender non-conforming individuals, medical transition is a significant and empowering part of their journey. Transition may include hormonal treatment and/or surgery known as gender confirmation surgery or gender affirmation surgery.
Many transgender individuals go through the process of transition — which includes legal, psychological, social and medical experiences — to resolve gender incongruence between their internal sense of self and external anatomy. Gender identity refers to an individual's experienced gender and sense of self.
Not all transgender people want to undergo gender confirmation surgery. But for those who do, the process can help to alleviate gender dysphoria . Gender confirmation surgery also doesn’t change or “reassign” one’s gender or sex. Instead, it allows transgender and gender non-conforming people to change their bodies to reflect their gender identity more accurately.
While hormonal treatment and/or surgery is a deeply important step for many trans and gender non-conforming people, it can also be expensive. Learn more about the average costs of medical transition care options and find resources and ways to help fund procedures.
Medical Transition Care Options and Average Costs
Medical transition care options are diverse in terms of procedures, costs and outcomes. Each transgender person, along with their medical provider, should choose the options that make the most sense in terms of budget and desired results.
The main two medical transition care options are hormonal transition and gender confirmation surgery. Here’s a breakdown of the average costs of each kind of gender-confirming healthcare treatment.
Hormonal Transition
Average Cost: $20–350/month
The majority of transgender individuals who seek out medical transition choose to undergo hormonal transition, also known as hormone therapy. Because of its relative affordability and accessibility, hormone therapy can be a particularly effective option for those experiencing gender dysphoria or looking for an alternative to surgery. Hormone therapy can help trans men and women, as well as nonbinary and gender non-conforming individuals, achieve significant physical changes.
Patients who undergo masculinizing hormone therapy often take testosterone. Testosterone therapy can affect a patient’s fat distribution, facial characteristics, vocal cords, hair growth patterns, libido, menstrual cycles and more. Testosterone typically comes in the form of injections (approximately $80 per month), patches ($300 per month), and gels ($300–350 per month) .
Patients who go through feminizing hormone therapy often take estrogen or testosterone blockers such as spironolactone and/or progesterone. Like testosterone therapy, this can affect a patient’s voice, facial appearance, libido, fertility, emotions and fat distribution. It can also promote breast development. On average, oral estrogen costs about $20 per month, while estrogen injections can cost up to $200 per month and spironolactone up to $20 per month.
Gender Confirmation Surgeries
Average Cost: $5,000–$50,000
Gender confirmation surgery for transgender patients refers to reconstructive surgeries to bring patients' bodies into conformity with their experienced gender. Surgeries might include reconstruction of the chest and/or face. Depending on the type of surgery, patients may have a recovery period from about two weeks to several months after their initial hospitalization.
Like all surgeries, these procedures come with potential risks. But patients who seek out board-certified surgeons and follow all pre- and post-op guidelines are usually satisfied with their results.
Here are some of the most common gender confirmation surgeries that transgender and gender non-conforming patients seek out.
Types of Surgeries for Trans Men
For trans patients, gender confirmation surgery might include removing breast tissue and reconstructing the chest, facial masculinization surgery (FMS) to make their facial features appear more masculine, removing and reconstructing the external genitalia, and removing internal reproductive organs.
Here are the most common forms of gender confirmation surgery for trans men and nonbinary patients.
How much is facial masculinization surgery (FMS)?
Average Cost: $10,000–$50,000
Here is what FMS surgery may include:
- Thyroid cartilage enhancement: An “Adam’s apple” is made using a small incision in the chin area and an implant in the throat region.
- Cheek augmentation: Small incisions inside the mouth allow the surgeon to place implants in the cheek to create a more angular appearance.
- Forehead lengthening or augmentation: Forehead lengthening and augmentation procedures involve lengthening the area between the eyes and scalp, and sometimes placing an implant, to create a more masculine, angular forehead.
- Jaw and chin augmentation: Jaw and chin reshaping and implants can help to widen the face and contour the jawline for more masculine facial proportions.
- Nose reshaping: Rhinoplasty can help to widen the nose and masculinize the facial proportions.
How much does it cost to have surgery procedures for trans men and what are the procedures?
Surgery procedures could include:
- Facial masculinization surgery (FMS): FMS may include thyroid cartilage enhancement, cheek augmentation, forehead lengthening or augmentation, jaw and chin augmentation and nose reshaping.
- Periareolar procedure: The areolas and nipples are resized and repositioned during this surgery. Two circular incisions around the areolas allow the surgeon to remove the “ring” of chest tissue.
- Keyhole procedure: The keyhole procedure involves just one semi-circular incision below each of the nipples. Keyhole top surgery also allows most patients to keep the sensation in their nipple area.
- Double incision: In double incision top surgery, the surgeon makes two incisions at the top and bottom of the pectoral muscles. The nipples and areolas are removed and replaced with nipple grafts.
- Inverted-T top surgery: Inverted-T top surgery involves horizontal and vertical incisions and the removal of chest tissue but not nipples. Sensation is retained for most patients.
- Metoidioplasty: Metoidioplasty involves releasing the clitoris from the ligament attached to it and repositioning it to create a penis. With this procedure, patients can also choose to undergo urethral lengthening and remove vaginal tissue.
- Phalloplasty: Surgeons use skin grafts from other parts of the body (usually the thigh or forearm) to create a penis. A vaginectomy, or the closing of the opening in the front of the pelvis, as well as scrotoplasty, which creates a scrotum, can be included in some phalloplasty procedures. This is the most expensive of bottom surgery options for trans men, with price tags up to $150,000 in some cases.
- Hysterectomy: A hysterectomy includes the removal of the uterus and ovaries.

Types of Surgeries for Trans Women
Around half of trans patients choose to undergo breast augmentation, facial feminization surgery (FFS) (which involves a variety of procedures that make facial features appear more feminine) and the removal or reconstruction of genitalia.
How much is facial feminization surgery (FFS)?
Average Cost: $20,000–$50,000
Facial feminization surgery (FFS) may include:
- Genioplasty: Genioplasty uses surgical incisions inside the mouth to contour the chin for a softer, rounder shape.
- Cheek augmentation: Implants, fat transfers or fillers can soften the face to create a more feminine look.
- Brow lift: A brow lift raises the eyebrows for a shorter forehead, softer look, and enlarged appearance of the eyes.
- Tracheal shave: The neck bump created by thyroid cartilage is reduced in a tracheal shave.
- Lip lift or augmentation: Lip augmentation can be achieved with implants and fillers. A lip lift emphasizes the upper lip.
What are the surgery procedures for trans women and how much do they cost?
Here are some of the most common gender confirmation surgeries for trans women:
- Facial feminization surgery (FFS): This surgery may include genioplasty, cheek augmentation, brow lifts, tracheal shave and lip lift or augmentation.
- Breast augmentation/augmentation mammoplasty: Breast augmentation is one of the most common gender confirmation surgeries for trans women and nonbinary patients. It might involve saline or silicone implants or even fat transfers from other parts of the body.
- Vaginoplasty: In vaginoplasty, a surgeon uses skin grafts from another part of the body (usually the scrotum or abdomen) to create a vaginal canal. The surgeon also uses existing genital tissue to create a clitoris. This allows most patients to have penetrative intercourse.
- Orchiectomy: An orchiectomy is often a transfeminine patient ’s first gender affirmation surgery. It involves the removal of the testicles.
- Vulvoplasty: A vulvoplasty involves the external part of the vagina rather than the vaginal canal. Skin from the patient’s genitalia is used to create a vaginal opening, the inner and outer labia, a clitoris and an opening that allows the patient to urinate.
Additional Alternatives
Some trans women undergo voice feminizing therapy to adapt their voice to their gender identity. In voice feminizing therapy, vocal cords are surgically altered to raise the patient’s vocal pitch.
Some trans patients might also choose to undergo gender confirmation surgery in the form of body contouring procedures. These might include liposuction or abdominoplasty as well as implants in the calves, buttocks or other areas.
In the U.S., it is illegal for most public and private health insurance providers to discriminate against transgender patients or deny them transition-related care. However, trans patients may still face financial and logistical barriers. Here’s what you should know about health insurance coverage and gender confirmation surgery.
Type of Barriers
Transgender patients still sometimes face health disparities and barriers to medical care, including transition-related medical care. These are some of the obstacles that trans and gender non-conforming people might face when trying to access healthcare and insurance coverage.
- Differences in state-by-state health insurance coverage: Each U.S. state has different policies regarding health insurance and trans-related care. Some U.S. states legally require health insurance providers to cover transition-related care while others do not.
- Difficulty accessing up-to-date and accurate insurance information: The language in health insurance plan summaries can be out-of-date or vague. This can lead to discriminatory denials of care.
- Discrimination and stigma: Discrimination against the LGBTQ community remains widespread, and transgender people may face health disparities and stigma in the context of medical care as a result, as well as other financial challenges . A 2015 study by the National Center for Transgender Equality revealed that about one-third of transgender patients said they were denied medical care or harassed by a medical provider.
- Lack of training and cultural competency among health providers: Some healthcare providers haven’t had adequate training in healthcare for transgender patients, which can lead them to make questionable decisions.
Additional Insurance Considerations
Transgender patients might also have questions about Medicaid coverage and Medicare coverage for gender confirmation surgery and other transition-related care. Both Medicare and Medicaid are prohibited from denying coverage of trans-related care if it is medically necessary.
The Veterans Health Administration (VHA) provides some coverage for transition-related medical care to transgender veterans . However, there is still an exclusion when it comes to coverage of gender confirmation surgery.
If you have insurance through your employer, you might be able to save up for your out-of-pocket surgery costs with a non-taxed Flexible Spending Account (FSA).
Ways to Navigate Health Insurance for Gender-Confirming Surgeries
It can be challenging to navigate health insurance coverage for gender confirmation surgery, but it’s not impossible. It’s important to know your rights as a patient when interacting with providers and finding the best health insurance plan for your needs. Here are some tips to keep in mind.
Stay informed
Remember that your health insurance plan should cover your transition-related care. Make sure that you read your insurance provider’s member handbook. Ask for the medical policy and any specific documents about eligibility for trans-related medical care to determine if you qualify.
Find a plan with no exclusions
Look for a health insurance plan that doesn’t have exclusions for either all transition-related care or specific kinds of treatments. You can often find this information in the medical policy.
Ask your current or potential employer about coverage
If you’re in the negotiation phase of a job interview, don’t be afraid to ask your potential employer about transition-related health coverage. If your current company or school doesn’t cover transition-related care, you might want to advocate for coverage.
Understand informed consent vs. WPATH standards
Before choosing a plan and care provider, find out about your potential provider’s ethical approach. An informed consent model of care allows you to make your own transition-related decisions after being informed of the risks by a physician. The WPATH standards of care might require additional steps, such as letters of support from therapists and other providers.
Look into pre-authorization
You'll need to see your primary care physician before requesting pre-authorization for surgery. It is also known as prior authorization. You might need to gather documents such as letters from medical providers before applying. Depending on the plan you selected, your primary care physician can provide you with a referral. Keep in mind that the referral or pre-authorization may not guarantee the surgery or other procedures will be authorized. National Center for Transgender Equality addresses common health coverage questions related to pre-authorization that may be helpful. It may be a good idea to speak with your health coverage provider directly.
Appeal denials
If you are denied coverage for a transition-related procedure, do not be afraid to appeal your insurance provider’s decision. Some exclusions might be prohibited or deemed discriminatory.
Outside of partial or full health insurance coverage, there are several other options for financing gender confirmation surgery, such as loans, lines of credit, grants and scholarships and fundraising.
There are several different personal loans you can use to fund your transition-related care.
- Bank or credit union loans: To qualify for a loan from a bank or credit union, you’ll need a good credit score and history.
- Family loans: If a family member can extend you a personal loan, consider creating a promissory note so that you have a repayment schedule in writing.
- Online loans: If your credit history is less than ideal, an online personal loan could be a good option.
Grants and Scholarships
Several organizations offer grants and scholarships to cover some or all of the costs associated with gender-confirming surgeries. These can help you avoid or offset any potential medical debt .
- The Jim Collins Foundation : The Jim Collins Foundation is dedicated to funding gender-confirming surgeries for trans people who need them. Grants are awarded on an annual basis.
- Genderbands Transition Grants : Genderbands offers transition grants to offset the expense of gender confirmation surgery for trans and nonbinary recipients.
- Rizi Xavier Timane Trans Surgery Grant : Rizi Xavier Timane, DSW, established a grant program to aid in the costs of gender-confirming surgeries for trans and nonbinary individuals.
- TransMission : The Loft LGBTQ+ Community Center’s TransMission is a small scholarship fund that helps trans and nonbinary recipients with medical, surgical and legal expenses.
- Stealth Bros & Co. Surgery Support Fund : The Stealth Bros & Co. Support Fund offers financial aid to trans men and transmasculine people for surgery, hormone therapy and related expenses.
- Black Transmen, Inc. Surgery Scholarship : Black trans men in the U.S. who have already been approved for surgery by a surgeon can apply for up to $1,000 in financial assistance.
- Point of Pride : Point of Pride offers scholarship-like funding for gender-confirming surgeries on an annual basis with a competitive application process each November.
Fundraising
Many people may raise funds for their gender confirmation surgery. For example, some throw parties with suggested donation amounts so friends, family and other supporters come together. Others raise money for their procedures by selling original art and letting would-be buyers know that they’re supporting a good cause.
Line of Credit
A home equity line of credit (HELOC) is one option if you own your home. With a HELOC, you can borrow against your home’s appraised value and repay it over time.
Certain surgeons partner with medical financing companies to help gender confirmation surgery patients make payments over time. You may want to check your credit score with a free report . Other surgeons allow patients to make smaller payments in installments.
Advocacy Organizations Making a Change
Many LGBTQ advocacy organizations are making a difference in the lives of transgender and gender non-conforming people every day. Here are just a few of the LGBTQ charities , nonprofits and other organizations making positive changes.
- The Sylvia Rivera Law Project : In addition to impact litigation advocacy, the Sylvia Rivera Law Project offers legal services and resources to aid people in their journey toward gender self-determination.
- Transgender Legal Defense & Education Fund : The Transgender Legal Defense & Education Fund is a nonprofit that fights for trans rights and against discrimination. The organization’s Trans Health Project helps transgender people access trans-confirming health insurance.
- Transgender Law Center : The Transgender Law Center is a trans-led advocacy organization that offers educational materials and other resources around healthcare, immigration, incarceration and employment.
- National Center for Transgender Equality : The National Center for Transgender Equality offers educational materials, self-help guides and other resources for the trans community.
- SPARTA : SPARTA is a nonprofit organization dedicated to transgender, nonbinary and gender non-conforming people serving in the U.S. military.
Additional Resources for Trans-Related Healthcare and Support
If you are a transgender or gender non-conforming patient seeking funding or support for your gender confirmation surgery, various resources can help. Here are some of the best resources available for trans people, loved ones and allies who want to know more about gender confirmation surgery.
- National Center for Transgender Equality's Know Your Rights : The National Center for Transgender Equality regularly updates its guide to existing and expanding legal protections for trans people in the U.S.
- HealthCare.gov's Transgender Health Care : The website helps explain what to know about applying for Marketplace health insurance coverage as a trans or gender non-conforming patient.
- HRC's Corporate Equality Index : Human Rights Campaign (HRC) publishes an annual guide to workplace policies and benefits for LGBTQ employees, including a list of companies that offer trans-inclusive benefits.
- Transgender Law Center's Transgender Health Benefits Guide : The Transgender Law Center offers a guide to healthcare advocacy for trans and gender non-conforming patients, including advice on what to do if you face discriminatory denials of care.
- Out2Enroll : Out2Enroll helps members of the LGBTQ community find and enroll in health insurance plans.
- Trans-Health.com's Trans Health Clinics : The clinics in this list specialize in transition-related and trans-confirming care and mental health support.
Social Support
- Transbucket : Initially started in 2009, Transbucket is an online resource and peer-to-peer support group exclusively dedicated to trans participants, primarily discussing gender confirming surgeries and medical transition.
- Gender Spectrum : Gender Spectrum hosts online support groups for trans, nonbinary and gender non-conforming youth, as well as parents and educators.
- Sam & Devorah Foundation for Trans Youth : The Sam & Devorah Foundation for Trans Youth connects members of the trans community with mentors who can offer emotional support and advice as well as empowerment and "building the confidence and skills critical for self-agency and leadership."
Mental Health Support
- The Trevor Project : The Trevor Project provides a number of resources, including suicide prevention and crisis intervention services, to LGBTQ people under 25.
- Trans Lifeline : The Trans Lifeline is a hotline offering peer-to-peer support services for trans callers, as well as their family, friends and allies.
- The Tribe, LGBTribe : The LGBTribe offers mental health support and wellness tools to LGBTQ participants.
About Laura Dorwart

Laura Dorwart is a writer living in Oberlin, Ohio, with her family. She has bylines at VICE, The New York Times, The Guardian and many others. She has a Ph.D. from UCSD, an MFA in nonfiction writing from Antioch University Los Angeles and experience in UX writing and copywriting for brands such as KeyBank. Follow her work at www.lauradorwart.com.
- American Psychiatric Association . " What Is Gender Dysphoria ." Accessed May 27, 2021 .
- CostHelper . " How Much Does Sex Reassignment Surgery Cost ." Accessed May 30, 2021 .
- Current Opinion in Endocrinology, Diabetes and Obesity . " Barriers to Health Care for Transgender Individuals ." Accessed May 28, 2021 .
- European Association of Urology . " First accurate data showing that male to female transgender surgery can lead to a better life ." Accessed May 19, 2023 .
- First Report Managed Care . " Transgender Patients: Calculating the Actual Cost ." Accessed May 30, 2021 .
- Gender Confirmation Center . " Techniques, Incisions, & Surgery Options Facial For Feminization Surgery ." Accessed May 30, 2021 .
- Grand View Research . " U.S. Sex Reassignment Surgery Market Size, Share & Trends Analysis Report by Gender Transition ." Accessed May 29, 2021 .
- Jones, Jeffrey M. Gallup . " LGBT Identification Rises to 5.6% in Latest U.S. Estimate ." Accessed June 1, 2021 .
- Mount Sinai Center for Transgender Medicine and Surgery . " Trans-masculine (Female to Male) Surgeries ." Accessed May 30, 2021 .
- National Center for Transgender Equality . " U.S. Trans Survey ." Accessed May 26, 2021 .
- Planned Parenthood . " Sex and Gender Identity ." Accessed May 25, 2021 .
- The International Center for Transgender Care . " Facial Masculinization Surgery ." Accessed May 30, 2021 .
- UCSF Transgender Care . " Information on Estrogen Hormone Therapy ." Accessed May 29, 2021 .
- UCSF Transgender Care . " Information on Testosterone Hormone Therapy ." Accessed May 29, 2021 .
- University of Utah Healthcare . " Transfeminine Bottom Surgery ." Accessed May 30, 2021 .
- Williams Institute at UCLA School of Law . " How Many Adults Identify as Transgender in the United States ." Accessed May 27, 2021 .
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
Health Reporting in the States
Bill of the month: a plan for affordable gender-confirmation surgery goes awry.
Emmarie Huetteman

Wren Vetens was promised a significant discount on the cost of her gender-confirmation surgery if she paid in cash upfront, without using her health insurance. Yet afterward, Vetens received an explanation of benefits saying the hospital had billed her insurer nearly $92,000. Lauren Justice for KHN hide caption
Wren Vetens was promised a significant discount on the cost of her gender-confirmation surgery if she paid in cash upfront, without using her health insurance. Yet afterward, Vetens received an explanation of benefits saying the hospital had billed her insurer nearly $92,000.
Wren Vetens thought she'd done everything possible to prepare for her surgery.
She chose a doctoral program in physics at the University of Wisconsin-Madison, a school that not only embraced transgender students like her, but also granted insurance coverage for her gender-confirmation surgery when she enrolled in 2016. When uncertainty over the fate of an Obama-era anti-discrimination rule allowed the state to discontinue such coverage, Vetens and her mother, Kimberly Moreland, an OB-GYN, shopped for another plan.
Deducing the procedure would run from $19,000 to $25,000, based on prices posted online, they purchased insurance from Consolidated Health Plans. It would pay a maximum of $25,000 for the operation.
With that information in hand, Vetens planned ahead: She got her insurer's preapproval and scheduled surgery during winter break of her second year, allowing time for recovery before returning to her studies.
Tell Us Your Billing Story
Do you have a medical bill or explanation of benefits that you'd like us to see? Submit it here and tell us the story behind it .
We may use it, with your permission, in one of our monthly features.
So, she was shocked when a hospital representative called her a couple of months before the long-awaited surgery estimating the bill would be $100,000. That meant she would be on the hook for as much as $75,000 after her insurer's $25,000 payout.
With preparations for the surgery well underway, Vetens was feeling overwhelmed with stress. "There were days when I just couldn't get out of bed for a whole day," she said, describing two weeks of panic attacks.
After mother and daughter complained about the last-minute surprise, a hospital representative offered a solution: If they paid out of pocket and in full before Vetens' surgery — forgoing their use of insurance — the hospital would accept just $20,080, assuring them the hospital would charge nothing to Vetens' insurer. But if they did not decide and pay up right away, the surgery would be canceled.
"I certainly felt that I had no choice," Vetens said.
After Moreland gave the hospital her credit card number for payment, they thought the financial roller coaster was over and Vetens could focus on recovery.
Then the bill came.
Patient: Wren Vetens, then 23, a Ph.D. student at the University of Wisconsin-Madison
Total bill: $91,850.20
Insurance payment: $25,427.91
Vetens owed: $13,191.95 (after $20,080 that was counted as a deposit)
Service provider: University of Wisconsin Hospital in Madison
Medical treatment: Vetens underwent a procedure known as penile inversion vaginoplasty to address her diagnosis of gender dysphoria, a condition resulting from one's sex identified at birth being in conflict with one's gender identity.
The procedure, in which the patient's penile and scrotal tissue is used to create a vagina, generally takes about two to four hours and requires a short inpatient stay, according to Dr. Madeline Deutsch, the medical director for transgender care at the University of California, San Francisco.
Candidates for the procedure must live for at least one year in their identified gender role and undergo at least one year of hormone therapy, Deutsch said. Preparation also includes permanent hair removal.
What gives: Though gender dysphoria is relatively uncommon, many of the billing and insurance issues Vetens encountered are typical for patients planning major surgery. Much of her stress and frustration arose from the vast difference between online price estimates ($19,000-$25,000), the hospital's billed price to the insurer ($91,850) and what it was willing to accept as an upfront cash payment ($20,080).
Hospitals set list prices high because insurers with whom they have contracts typically negotiate them down. In exchange for charging an insurer's members a lower price, doctors and hospitals gain access to those customers, who have incentives to use these in-network providers. Hospitals may offer package deals for procedures to patients, if they pay cash upfront, in part because the hospital avoids the hassle of negotiation.
Officials at University of Wisconsin Hospital said they offered Vetens the option to pay $20,080 for these reasons: to secure extra experience and exposure for the hospital's programs for transgender patients, and to shield Vetens from an even bigger bill. "We were trying to protect the patient," said Dr. Katherine Gast, Vetens' surgeon.

Dr. Kimberly Moreland (left) helped her daughter shop for an insurance plan that would cover Vetens' gender-confirmation surgery. Yet mother and daughter still found themselves caught between the hospital and the insurer. Courtesy of Richard Malatesta/Kimberly Moreland hide caption
Dr. Kimberly Moreland (left) helped her daughter shop for an insurance plan that would cover Vetens' gender-confirmation surgery. Yet mother and daughter still found themselves caught between the hospital and the insurer.
As both parties hedged their bets in trying to determine what a penile inversion vaginoplasty was worth, Vetens was stuck in the middle with the prospect of hugely varying payments.
Lisa Brunette, a hospital spokeswoman, said that, despite having provided Vetens an estimate of $100,000, the hospital really did not know how much it would charge for the procedure because it did not know how much it would be reimbursed by the insurance company. Vetens was the second person to have the procedure at the hospital.
The spokeswoman for the hospital said its contract with Vetens' insurer "relies on a complex formula."
And in an apparent chicken-and-egg quandary, Drew DiGiorgio, president and chief executive of Consolidated Health Plans, said the insurer did not know how much it would reimburse because it did not know how much the hospital would charge.
When Moreland called the hospital to pay the $20,080 price — an option she acknowledged many simply could not afford — she asked for an itemized bill.
The next day, she received a brief letter outlining some of the general services included for the price, such as "physician's fee" and "post surgery labs." Then it simply said: "Penile Inversion Vaginoplasty — $20,080.00."
"How in the world did you come up with a number if you have no idea what it covers?" she asked.
Had Vetens chosen a hospital that did not contract with her insurer, the family could have been reimbursed 60 percent, or about $12,000 of the money paid, since her insurance pays a portion of out-of-network care.
But since Consolidated Health Plans has a contract with the University of Wisconsin Hospital, it said it would not reimburse anything at all. Contracts between insurers and providers discourage such sideline cash transactions, since hospitals can make more money when patients use insurance, as evidenced by Vetens' bill.
Vetens and Moreland appealed to Consolidated Health Plans, feeling that they had been "the victims of a bait-and-switch scam."
The surprises didn't end there. Though multiple hospital representatives reassured Vetens that they wouldn't charge her insurance after her cash payment, Vetens received an explanation of benefits saying the hospital had billed her insurer nearly $92,000.
A hospital bill followed, identifying their $20,080 as "pre-payment," treating it like a partial deposit. Vetens owed more than $13,000, it said.
Studies have shown that more than half of hospital bills contain errors , a problem made worse by the fact that medical bills — with codes and jargon — can be nearly impossible for even savvy patients to understand.
"That was not supposed to happen. That was an error," said Abby Abongwa, a hospital billing official. "That was absolutely an error on our part."
Resolution: After the bill for $91,850 arrived, an alarmed Vetens showed it to her surgeon. The hospital quickly apologized and repaid her insurance company.
Within a few weeks of receiving the appeal — which noted that Vetens and Moreland had contacted a national media outlet — Consolidated Health Plans reimbursed Vetens nearly $18,000, offering her no explanation for why the company had ultimately decided to reverse its earlier judgement that it would not pay anything toward her care.
With their reimbursement, Vetens and Moreland paid about $2,100 for the surgery, all told.
The Takeaway: Be mindful that online pricing estimates frequently represent cash prices, which are often far lower than the price hospitals will bill your insurance.
Ask about a cash price — you may get a better deal. But if you forgo insurance, you're on your own. Your insurer is under no obligation to pay you back for any part of the bill or help you troubleshoot billing, and any payment you make likely will not count toward your deductible.
Enlist your doctor's help. Gast, Vetens' surgeon, proved a powerful advocate for her patient when disputes arose about billing and pricing. Billing representatives might not always be responsive to patients, but it's in the hospital executives' interest to keep staff surgeons happy.
Some of these issues can be settled only through legislation. Right now, there is no legal requirement for hospitals to provide itemized bills to patients. Hospital bills are fraught with errors, and there is little accountability for providers who bill erroneously.
In the meantime, don't be afraid to ask questions and fight back.
Bram Sable-Smith, who contributed to the audio story, is part of NPR's reporting partnership with Side Effects Public Media, member station KBIA and Kaiser Health News.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
You can follow Emmarie Huetteman on Twitter: @emmarieDC .
- bill of the month
- gender dysphoria
- gender identity
- transgender
- Health Insurance
- Plastic surgery

Gender Affirming Surgery
- Clinical Policy Bulletins
- Medical Clinical Policy Bulletins
Number: 0615
Table Of Contents
The International Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) and the Diagnostic and Statistical Manual of Mental Disorders, (DSM-5-TR) are the diagnostic classifications and criteria manuals used in the United States. Notwithstanding, the World Professional Association of Transgender Health Standard of Care 8th edition (WPATH SOC8) states: “While Gender Dysphoria (GD) is still considered a mental health condition in the Diagnostic and Statistical Manual of Mental Disorders, (DSM-5-TR) of the American Psychiatric Association. Gender incongruence is no longer seen as pathological or a mental disorder in the world health community. Gender Incongruence is recognized as a condition in the International Classification of Diseases and Related Health Problems, 11th Version of the World Health Organization (ICD-11). Because of historical and current stigma, TGD people can experience distress or dysphoria that may be addressed with various gender-affirming treatment options. While nomenclature is subject to change and new terminology and classifications may be adopted by various health organizations or administrative bodies, the medical necessity of treatment and care is clearly recognized for the many people who experience dissonance between their sex assigned at birth and their gender identity.”
Gender dysphoria refers to discomfort or distress that is caused by a discrepancy between an individual’s gender identity and the gender assigned at birth (and the associated gender role and/or primary and secondary sex characteristics). A diagnosis of gender dysphoria requires a marked difference between the individual’s expressed/experienced gender and the gender others would assign him or her, and it must continue for at least six months. This condition may cause clinically significant distress or impairment in social, occupational or other important areas of functioning.
Gender affirming surgery is performed to change primary and/or secondary sex characteristics. For transfeminine (assigned male at birth) gender transition, surgical procedures may include genital reconstruction (vaginoplasty, penectomy, orchidectomy, clitoroplasty), breast augmentation (implants, lipofilling), and cosmetic surgery (facial reshaping, rhinoplasty, abdominoplasty, thyroid chondroplasty (laryngeal shaving), voice modification surgery (vocal cord shortening), hair transplants) (Day, 2002). For transmasculine (assigned female at birth) gender transition, surgical procedures may include mastectomy, genital reconstruction (phalloplasty, genitoplasty, hysterectomy, bilateral oophorectomy), mastectomy, and cosmetic procedures to enhance male features such as pectoral implants and chest wall recontouring (Day, 2002).
The criterion noted above for some types of genital surgeries is based on expert clinical consensus that this experience provides ample opportunity for patients to experience and socially adjust in their desired gender role, before undergoing irreversible surgery (Coleman, et al., 2022).
It is recommended that transfeminine persons undergo feminizing hormone therapy (minimum 6 months) prior to breast augmentation surgery. The purpose is to maximize breast growth in order to obtain better surgical (aesthetic) results.
In addition to hormone therapy and gender affirming surgery, psychological adjustments are necessary in affirming sex. Treatment should focus on psychological adjustment, with hormone therapy and gender affirming surgery being viewed as confirmatory procedures dependent on adequate psychological adjustment. Mental health care may need to be continued after gender affirming surgery. The overall success of treatment depends partly on the technical success of the surgery, but more crucially on the psychological adjustment of the trans identified person and the support from family, friends, employers and the medical profession.
Nakatsuka (2012) noted that the third versions of the guideline for treatment of people with gender dysphoria (GD) of the Japanese Society of Psychiatry and Neurology recommends that feminizing/masculinizing hormone therapy and genital surgery should not be carried out until 18 years old and 20 years old, respectively. On the other hand, the sixth (2001) and the seventh (2011) versions of the standards of care for the health of transsexual, transgender, and gender non-conforming people of World Professional Association for Transgender Health (WPATH) recommend that transgender adolescents (Tanner stage 2, [mainly 12 to 13 years of age]) are treated by the endocrinologists to suppress puberty with gonadotropin-releasing hormone (GnRH) agonists until age 16 years old, after which gender-affirming hormones may be given. A questionnaire on 181 people with GID diagnosed in the Okayama University Hospital (Japan) showed that female to male (FTM) trans identified individuals hoped to begin masculinizing hormone therapy at age of 15.6 +/- 4.0 (mean +/- S.D.) whereas male to female (MTF) trans identified individuals hoped to begin feminizing hormone therapy as early as age 12.5 +/- 4.0, before presenting secondary sex characters. After confirmation of strong and persistent trans gender identification, adolescents with GD should be treated with gender-affirming hormone or puberty-delaying hormone to prevent developing undesired sex characters. These treatments may prevent transgender adolescents from attempting suicide, suffering from depression, and refusing to attend school.
Spack (2013) stated that GD is poorly understood from both mechanistic and clinical standpoints. Awareness of the condition appears to be increasing, probably because of greater societal acceptance and available hormonal treatment. Therapeutic options include hormone and surgical treatments but may be limited by insurance coverage because costs are high. For patients seeking MTF affirmation, hormone treatment includes estrogens, finasteride, spironolactone, and GnRH analogs. Surgical options include feminizing genital and facial surgery, breast augmentation, and various fat transplantations. For patients seeking a FTM gender affirmation, medical therapy includes testosterone and GnRH analogs and surgical therapy includes mammoplasty and phalloplasty. Medical therapy for both FTM and MTF can be started in early puberty, although long-term effects are not known. All patients considering treatment need counseling and medical monitoring.
Leinung and colleagues (2013) noted that the Endocrine Society's recently published clinical practice guidelines for the treatment of transgender persons acknowledged the need for further information on transgender health. These investigators reported the experience of one provider with the endocrine treatment of transgender persons over the past 2 decades. Data on demographics, clinical response to treatment, and psychosocial status were collected on all transgender persons receiving gender-affirming hormone therapy since 1991 at the endocrinology clinic at Albany Medical Center, a tertiary care referral center serving upstate New York. Through 2009, a total 192 MTF and 50 FTM transgender persons were seen. These patients had a high prevalence of mental health and psychiatric problems (over 50 %), with low rates of employment and high levels of disability. Mental health and psychiatric problems were inversely correlated with age at presentation. The prevalence of gender affirming surgery was low (31 % for MTF). The number of persons seeking treatment has increased substantially in recent years. Gender-affirming hormone therapy achieves very good results in FTM persons and is most successful in MTF persons when initiated at younger ages. The authors concluded that transgender persons seeking hormonal therapy are being seen with increasing frequency. The dysphoria present in many transgender persons is associated with significant mood disorders that interfere with successful careers. They stated that starting therapy at an earlier age may lessen the negative impact on mental health and lead to improved social outcomes.
Meyer-Bahlburg (2013) summarized for the practicing endocrinologist the current literature on the psychobiology of the development of gender identity and its variants in individuals with disorders of sex development or with transgenderism. Gender reassignment remains the treatment of choice for strong and persistent gender dysphoria in both categories, but more research is needed on the short-term and long-term effects of puberty-suppressing medications and cross-sex hormones on brain and behavior.
Note on Breast Reduction/Mastectomy and Nipple Reconstruction
The CPT codes for mastectomy (CPT codes 19303) are for breast cancer, and are not appropriate to bill for reduction mammaplasty for female to male (transmasculine) gender affirmation surgery. CPT 2020 states that “Mastectomy procedures (with the exception of gynecomastia [19300]) are performed either for treatment or prevention of breast cancer.” CPT 2020 also states that "Code 19303 describes total removal of ipsilateral breast tissue with or without removal of skin and/or nipples (eg, nipple-sparing), for treatment or prevention of breast cancer.” There are important differences between a mastectomy for breast cancer and a mastectomy for gender reassignment. The former requires careful attention to removal of all breast tissue to reduce the risk of cancer. By contrast, careful removal of all breast tissue is not essential in mastectomy for gender reassignment. In mastectomy for gender reassignment, the nipple areola complex typically can be preserved.
Some have tried to justify routinely billing CPT code 19350 for nipple reconstruction at the time of mastectomy for gender reassignment based upon the frequent need to reduce the size of the areola to give it a male appearance. However, the nipple reconstruction as defined by CPT code 19350 describes a much more involved procedure than areola reduction. The typical patient vignette for CPT code 19350, according to the AMA, is as follows: “The patient is measured in the standing position to ensure even balanced position for a location of the nipple and areola graft on the right breast. Under local anesthesia, a Skate flap is elevated at the site selected for the nipple reconstruction and constructed. A full-thickness skin graft is taken from the right groin to reconstruct the areola. The right groin donor site is closed primarily in layers.”
The AMA vignette for CPT code 19318 (reduction mammaplasty) clarifies that this CPT code includes the work that is necessary to reposition and reshape the nipple to create an aesthetically pleasing result, as is necessary in female to male breast reduction. "The physician reduces the size of the breast, removing wedges of skin and breast tissue from a female patient. The physician makes a circular skin incision above the nipple, in the position to which the nipple will be elevated. Another skin incision is made around the circumference of the nipple. Two incisions are made from the circular cut above the nipple to the fold beneath the breast, one on either side of the nipple, creating a keyhole shaped skin and breast incision. Wedges of skin and breast tissue are removed until the desired size is achieved. Bleeding vessels may be ligated or cauterized. The physician elevates the nipple and its pedicle of subcutaneous tissue to its new position and sutures the nipple pedicle with layered closure. The remaining incision is repaired with layered closure" (EncoderPro, 2019). CPT code 19350 does not describe the work that that is being done, because that code describes the actual construction of a new nipple. Code 19350 is a CCI “incidental to” edit to code 19318, and, accordingly, the services of code 19350 are included in code 19318. Similarly, graft codes, such as code 15200 (full thickness skin graft) and 15877 (liposuction), are CCI “incidental to” edits to code 19318, and, accordingly, the services of graft codes, such as 15200, and liposuction codes, such as 15877, are included in code 19318.
Vulvoplasty Versus Vaginoplasty as Gender-Affirming Genital Surgery for Transgender Women
Jiang and colleagues (2018) noted that gender-affirming vaginoplasty aims to create the external female genitalia (vulva) as well as the internal vaginal canal; however, not all patients desire nor can safely undergo vaginal canal creation. These investigators described the factors influencing patient choice or surgeon recommendation of vulvoplasty (creation of the external appearance of female genitalia without creation of a neovaginal canal) and evaluated the patient's satisfaction with this choice. Gender-affirming genital surgery consults were reviewed from March 2015 until December 2017, and patients scheduled for or who had completed vulvoplasty were interviewed by telephone. These investigators reported demographic data and the reasons for choosing vulvoplasty as gender-affirming surgery for patients who either completed or were scheduled for surgery, in addition to patient reports of satisfaction with choice of surgery, satisfaction with the surgery itself, and sexual activity after surgery. A total of 486 patients were seen in consultation for trans-feminine gender-affirming genital surgery: 396 requested vaginoplasty and 39 patients requested vulvoplasty; 30 Patients either completed or are scheduled for vulvoplasty. Vulvoplasty patients were older and had higher body mass index (BMI) than those seeking vaginoplasty. The majority (63 %) of the patients seeking vulvoplasty chose this surgery despite no contraindications to vaginoplasty. The remaining patients had risk factors leading the surgeon to recommend vulvoplasty. Of those who completed surgery, 93 % were satisfied with the surgery and their decision for vulvoplasty. The authors concluded that this was the first study of factors impacting a patient's choice of or a surgeon's recommendation for vulvoplasty over vaginoplasty as gender-affirming genital surgery; it also was the first reported series of patients undergoing vulvoplasty only.
Drawbacks of this study included its retrospective nature, non-validated questions, short-term follow-up, and selection bias in how vulvoplasty was offered. Vulvoplasty is a form of gender-affirming feminizing surgery that does not involve creation of a neovagina, and it is associated with high satisfaction and low decision regret.
Autologous Fibroblast-Seeded Amnion for Reconstruction of Neo-vagina in Transfeminine Reassignment Surgery
Seyed-Forootan and colleagues (2018) stated that plastic surgeons have used several methods for the construction of neo-vaginas, including the utilization of penile skin, free skin grafts, small bowel or recto-sigmoid grafts, an amnion graft, and cultured cells. These researchers compared the results of amnion grafts with amnion seeded with autograft fibroblasts. Over 8 years, these investigators compared the results of 24 male-to-female transsexual patients retrospectively based on their complications and levels of satisfaction; 16 patients in group A received amnion grafts with fibroblasts, and the patients in group B received only amnion grafts without any additional cellular lining. The depths, sizes, secretions, and sensations of the vaginas were evaluated. The patients were monitored for any complications, including over-secretion, stenosis, stricture, fistula formation, infection, and bleeding. The mean age of group A was 28 ± 4 years and group B was 32 ± 3 years. Patients were followed-up from 30 months to 8 years (mean of 36 ± 4) after surgery. The depth of the vaginas for group A was 14 to 16 and 13 to 16 cm for group B. There was no stenosis in neither group. The diameter of the vaginal opening was 34 to 38 mm in group A and 33 to 38 cm in group B. These researchers only had 2 cases of stricture in the neo-vagina in group B, but no stricture was recorded for group A. All of the patients had good and acceptable sensation in the neo-vagina; 75 % of patients had sexual experience and of those, 93.7 % in group A and 87.5% in group B expressed satisfaction. The authors concluded that the creation of a neo-vaginal canal and its lining with allograft amnion and seeded autologous fibroblasts is an effective method for imitating a normal vagina. The size of neo-vagina, secretion, sensation, and orgasm was good and proper. More than 93.7 % of patients had satisfaction with sexual intercourse. They stated that amnion seeded with fibroblasts extracted from the patient's own cells will result in a vagina with the proper size and moisture that can eliminate the need for long-term dilatation. The constructed vagina has a 2-layer structure and is much more resistant to trauma and laceration. No cases of stenosis or stricture were recorded. Level of Evidence = IV. These preliminary findings need to be validated by well-designed studies.
Pitch-Raising Surgery in Transfeminine Persons
Van Damme and colleagues (2017) reviewed the evidence of the effectiveness of pitch-raising surgery performed in male-to-female transsexuals. These investigators carried out a search for studies in PubMed, Web of Science, Science Direct, EBSCOhost, Google Scholar, and the references in retrieved manuscripts, using as keywords "transsexual" or "transgender" combined with terms related to voice surgery. They included 8 studies using cricothyroid approximation, 6 studies using anterior glottal web formation, and 6 studies using other surgery types or a combination of surgical techniques, leading to 20 studies in total. Objectively, a substantial rise in post-operative fundamental frequency was identified. Perceptually, mainly laryngeal web formation appeared risky for decreasing voice quality. The majority of patients appeared satisfied with the outcome. However, none of the studies used a control group and randomization process. The authors concluded that future research needs to investigate long-term effects of pitch-raising surgery using a stronger study design.
Azul and associates (2017) evaluated the currently available discursive and empirical data relating to those aspects of trans-masculine people's vocal situations that are not primarily gender-related, and identified restrictions to voice function that have been observed in this population, and made suggestions for future voice research and clinical practice. These researchers conducted a comprehensive review of the voice literature. Publications were identified by searching 6 electronic databases and bibliographies of relevant articles. A total of 22 publications met inclusion criteria. Discourses and empirical data were analyzed for factors and practices that impact on voice function and for indications of voice function-related problems in trans-masculine people. The quality of the evidence was appraised. The extent and quality of studies investigating trans-masculine people's voice function was found to be limited. There was mixed evidence to suggest that trans-masculine people might experience restrictions to a range of domains of voice function, including vocal power, vocal control/stability, glottal function, pitch range/variability, vocal endurance, and voice quality. The authors concluded that more research into the different factors and practices affecting trans-masculine people's voice function that took account of a range of parameters of voice function and considered participants' self-evaluations is needed to establish how functional voice production can be best supported in this population.
Facial Feminization Surgery
Raffaini and colleagues (2016) stated that gender dysphoria refers to the discomfort and distress that arise from a discrepancy between a person's gender identity and sex assigned at birth. The treatment plan for gender dysphoria varies and can include psychotherapy, hormone treatment, and gender affirmation surgery, which is, in part, an irreversible change of sexual identity. Procedures for transformation to the female sex include facial feminization surgery, vaginoplasty, clitoroplasty, and breast augmentation. Facial feminization surgery can include forehead re-modeling, rhinoplasty, mentoplasty, thyroid chondroplasty, and voice alteration procedures. These investigators reported patient satisfaction following facial feminization surgery, including outcome measurements after forehead slippage and chin re-modeling. A total of 33 patients between 19 and 40 years of age were referred for facial feminization surgery between January of 2003 and December of 2013, for a total of 180 procedures. Surgical outcome was analyzed both subjectively through questionnaires administered to patients and objectively by serial photographs. Most facial feminization surgery procedures could be safely completed in 6 months, barring complications. All patients showed excellent cosmetic results and were satisfied with their procedures. Both frontal and profile views achieved a loss of masculine features. The authors concluded that patient satisfaction following facial feminization surgery was high; they stated that the reduction of gender dysphoria had psychological and social benefits and significantly affected patient outcome. The level of evidence of this study was IV.
Morrison and associates (2018) noted that facial feminization surgery encompasses a broad range of cranio-maxillofacial surgical procedures designed to change masculine facial features into feminine features. The surgical principles of facial feminization surgery could be applied to male-to-female transsexuals and anyone desiring feminization of the face. Although the prevalence of these procedures is difficult to quantify, because of the rising prevalence of transgenderism (approximately 1 in 14,000 men) along with improved insurance coverage for gender-confirming surgery, surgeons versed in techniques, outcomes, and challenges of facial feminization surgery are needed. These researchers appraised the current facial feminization surgery literature. They carried out a comprehensive literature search of the Medline, PubMed, and Embase databases was conducted for studies published through October 2014 with multiple search terms related to facial feminization. Data on techniques, outcomes, complications, and patient satisfaction were collected. A total of 15 articles were selected and reviewed from the 24 identified, all of which were either retrospective or case series/reports. Articles covered a variety of facial feminization procedures. A total of 1,121 patients underwent facial feminization surgery, with 7 complications reported, although many articles did not explicitly comment on complications. Satisfaction was high, although most studies did not use validated or quantified approaches to address satisfaction. The authors concluded that facial feminization surgery appeared to be safe and satisfactory for patients. These researchers stated that further studies are needed to better compare different techniques to more robustly establish best practices; prospective studies and patient-reported outcomes are needed to establish quality-of-life (QOL) outcomes for patients.
In a systematic review, Gorbea et al (2021) provided a portrait of gender affirmation surgery (GAS) insurance coverage across the U.S., with attention to procedures of the head and neck. State policies on transgender care for Medicaid insurance providers were collected for all 50 states. Each state's policy on GAS and facial gender affirmation surgery (FGAS) was examined. The largest medical insurance companies in the U.S. were identified using the National Association of Insurance Commissioners Market Share report. Policies of the top 49 primary commercial medical insurance companies were examined. Medicaid policy reviews found that 18 states offer some level of gender-affirming coverage for their patients, but only 3 include FGAS (17 %); 13 states prohibit Medicaid coverage of all transgender surgery, and 19 states have no published gender-affirming medical care coverage policy; 92 % of commercial medical insurance providers had a published policy on GAS coverage. Genital reconstruction was described as a medically necessary aspect of transgender care in 100 % of the commercial policies reviewed; 93 % discussed coverage of FGAS, but 51 % considered these procedures cosmetic. Thyroid chondroplasty (20 %) was the most commonly covered FGAS procedure. Mandibular and frontal bone contouring, rhinoplasty, blepharoplasty, and facial rhytidectomy were each covered by 13 % of the medical policies reviewed. The authors concluded that while certain surgical aspects of gender-affirming medical care are nearly ubiquitously covered by commercial insurance providers, FGAS is considered cosmetic by most Medicaid and commercial insurance providers. Level of Evidence = V.
Hohman and Teixeira (2022) stated that with respect to gender affirmation procedures for the face, the majority of interventions will occur in patients transitioning from male to female, i.e., transgender women. While there are slightly more transgender women than transgender men in the population (33 % transgender women, 29 % transgender men, 35 % non-binary, 3 % cross-dressers, according to the USTS), the reason that more females require surgery than males is that testosterone therapy typically produces enough changes in secondary sex characteristics of the face (growth of facial hair, thickening of the skin, increase in frontal bossing, lowering of the voice, etc.) that surgery is not necessary . In some cases, placement of implants or fat transfer can increase volume in the lower 1/3 of the face and contribute to masculinization. Still, the primary area of focus for facial feminization is generally the upper 1/3. Feminization of the upper 1/3 of the face often requires several techniques to be applied in combination: The advancement of the hairline, hair transplantation, brow-lifting, and reduction of frontal bossing or "frontal cranioplasty". While the advancement of a scalp flap, hair transplant, and pretrichial brow-lifting are commonly employed cosmetic surgery interventions, frontal cranioplasty bears special consideration. Several methods of reducing the brow's prominence are often described as type 1, 2, and 3 frontal cranioplasties. Type 1 cranioplasty reduces the supra-orbital ridge's protrusion, usually using a drill, including decreasing the thickness of the anterior table of the frontal sinus. This technique is the simplest, but it is only effective in patients with either a very thick anterior frontal sinus table or an absent pneumatized frontal sinus. Type 2 cranioplasty involves augmentation of the forehead's convexity using bone cement or methyl methacrylate in addition to a reduction of the supra-orbital ridge with a drill. Type 3 cranioplasty is advocated by many prominent facial feminization surgeons and consists of removal of the anterior table of the frontal sinus, thinning of the bone flap, and replacement of that bone onto the frontal sinus but in a more recessed position, in addition to a reduction of the remainder of the supra-orbital ridge. An alternative to removal and recession of the frontal sinus's anterior table is to thin the bone with a drill and then fracture it in a controlled fashion to produce the desired contour, which is also performed routinely by some authors.
Forehead Feminization Cranioplasty
Eggerstedt and colleagues (2020) stated that forehead feminization cranioplasty (FFC) is an important component of gender-affirming surgery and has become increasingly popular in recent years. However, there is little objective evidence for the procedure's safety and clinical impact via patient-reported outcome measures (PROMs). In a systematic review, these researchers determined what complications are observed following FFC, the relative frequency of complications by surgical technique, and what impact the procedure has on patient's QOL. They carried out database searches in PubMed/Medline, Scopus, CINAHL, Cochrane CENTRAL, Cochrane Database of Systematic Reviews, and PsycINFO. The search terms included variations of forehead setback/FFC. Both controlled vocabularies (i.e., MeSH and CINAHL's Suggested Subject Terms) and keywords in the title or abstract fields were searched. Two independent reviewers screened the titles and abstracts of all articles; and 2 independent surgeon reviewers examined the full text of all included articles, and relevant data points were extracted. Main outcomes and measures included complications and complication rate observed following FFC. Additional outcome measures were the approach used, concurrent procedures carried out, and the use and findings of a PROM. A total of 10 articles describing FFC were included, entailing 673 patients. The overall pooled complication rate was 1.3 %; PROMs were used in 50 % of studies, with no standardization among studies. The authors concluded that complications following FFC were rare and infrequently required reoperation. Moreover, these researchers stated that further studies into standardized and validated PROMs in facial feminization patients are needed. Level of Evidence = III.
Hand Feminization and Masculinization
Lee and colleagues (2021) noted that anatomical characteristics that are incongruent with an individual's gender identity can cause significant gender dysphoria. Hands exhibit prominent dimorphic sexual features, but despite their visibility, there are limited studies examining gender affirming procedures for the hands. These researchers examined the anatomical features that define feminine and masculine hands, the surgical and non-surgical approaches for feminization and masculinization of the hand; and adapted established aesthetic hand techniques for gender affirming care. They carried out a comprehensive database search of PubMed, Embase OVID and SCOPUS to identify articles on the characterization of feminine or masculine hands, hand treatments related to gender affirmation, and articles related to techniques for hand feminization and masculinization in the non-transgender population. From 656 possibly relevant articles, 42 met the inclusion criteria for the current literature search. There is currently no medical literature specifically examining the surgical or non-surgical options for hand gender affirmation. The available techniques for gender affirming procedures discussed in this paper were appropriated from those more commonly used for hand rejuvenation. The authors concluded that there is very little evidence addressing the options for transgender individuals seeking gender affirming procedures of the hand. These researchers stated that although established procedures used for hand rejuvenation may be employed in gender affirming care, further study is needed to determine relative salience of various hand features to gender dysphoria in transgender patients of various identities, as well as development of novel techniques to meet these needs. Level of Evidence = III.
Peritoneal Pull-Through Technique Vaginoplasty in Neovagina Construction in Gender-Affirming Surgery
Tay and Lo (2022) reviewed the application, effectiveness and outcomes of a novel surgical technique, peritoneal pull-through technique vaginoplasty, in gender-affirming surgery. Specific outcome parameters included healing time, depth of cavity achieved,) alleviation of dysphoria, and morbidity of the surgery. These researchers carried out a systematic review according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement and PROSPERO registration obtained before commencement. A search was performed in OVID Medline, Embase, Willey Online Library and PubMed. Specialty-related journals, grey literature and reference lists of relevant articles were manually searched. From 476 potentially relevant articles, 12 articles were analyzed; and the publications were all level 4 or level 5 evidence. Healing times were poorly reported or often not mentioned. A total of 8 authors reported neovagina cavity depth of at least 13 cm and good patient satisfaction. Alleviation of dysphoria was not discussed by any of the publications and only 6reported complications. Average follow-up ranged from 6 weeks to 14.8 months. The authors concluded that the use of peritoneal pull-through vaginoplasty in gender-affirming surgery is promising and novel; however, there is a paucity of data. These investigators stated that further research and longer-term data are needed to examine the safety and effectiveness of this technique including stabilization of vaginal depth, later morbidity and complications. Patients seeking this surgery overseas should be informed of the potential difficulties they may face.
Urethral Complications and Outcomes in Transgender Men
Hu et al (2022) noted that urologic problems, such as urethral fistulas and strictures, are among the most frequent complications following phalloplasty. Although many studies have reported successful phalloplasty and urethral reconstruction with reliable outcomes in transgender men; so far, no method has become standardized. These researchers examined the reports on urological complications and outcomes in transgender men with respect to various types of urethral reconstruction. They carried out a comprehensive literature search of PubMed, Scopus, and Google Scholar databases for studies related to phalloplasty in transsexuals. Data on various phallic urethral techniques, urethral complications, and outcomes were collected and analyzed using the random-effects model. A total of 21 studies (1,566 patients) were included: 8 studies (1,061 patients) on "tube-in-tube", 9 studies (273 patients) on "prelaminated flap, and 6 studies (221 patients) on "second flap". Compared with the tube-in-tube technique, the pre-laminated flap was associated with a significantly higher urethral stricture/stenosis rate; however, there was no difference between the pre-laminated flap and the 2nd flap techniques. For all phalloplasty patients, the pooled rate of urethral fistula or stenosis was 48.9 %, the rate of the ability to void while standing was 91.5 %, occurrence rate of tactile or erogenous sensation was 88 %, the prosthesis complication rate was 27.9 %, and patient-reported satisfactory outcome rate was 90.5 %. The authors concluded that urethral reconstruction with a pre-laminated flap was associated with a significantly higher urethral stricture rate and increased need of revision surgery compared with that observed using a skin flap. Overall, most patients were able to void while standing and were satisfied with the outcomes.
DSM 5 Criteria for Gender Dysphoria in Adults and Adolescents
A marked incongruence between one’s experienced/expressed gender and assigned gender, of at least 6 months duration, as manifested by two or more of the following:
- A marked incongruence between one’s experienced/expressed gender and primary and/or secondary sex characteristics (or, in young adolescents, the anticipated secondary sex characteristics)
- A strong desire to be rid of one’s primary and/or secondary sex characteristics because of a marked incongruence with one’s experienced/expressed gender (or, in young adolescents, a desire to prevent the development of the anticipated secondary sex characteristics)
- A strong desire for the primary and/or secondary sex characteristics of the other gender
- A strong desire to be of the other gender (or some alternative gender different from one’s assigned gender)
- A strong desire to be treated as the other gender (or some alternative gender different from one’s assigned gender)
- A strong conviction that one has the typical feelings and reactions of the other gender (or some alternative gender different from one’s assigned gender).
The condition is associated with clinically significant distress or impairment in social, occupational, or other important areas of functioning.
There is no minimum duration of relationship required with mental health professional. It is the professional’s judgment as to the appropriate length of time before a referral letter can appropriately be written. A common period of time is three months, but there is significant variation in both directions.
Evaluation of candidacy for gender affirmation surgery by a mental health professional is covered under the member’s medical benefit, unless the services of a mental health professional are necessary to evaluate and treat a mental health problem, in which case the mental health professional’s services are covered under the member’s behavioral health benefit. Please check benefit plan descriptions.
Characteristics of a Qualified Health Professionals (From SOC-8)
Qualifications of Mental Health Professional for assessing transgender and gender diverse adults for physical treatments (from WPATH SOC-8):
- Are licensed by their statutory body and hold, at a minimum, a master’s degree or equivalent training in a clinical field relevant to this role and granted by a nationally accredited statutory institution.
- Are able to identify co-existing mental health or other psychosocial concerns and distinguish these from gender dysphoria, incongruence, and diversity.
- Are able to assess capacity to consent for treatment.
- Have experience or be qualified to assess clinical aspects of gender dysphoria, incongruence, and diversity.
- Undergo continuing education in health care relating to gender dysphoria, incongruence, and diversity.
- Liaise with professionals from different disciplines within the field of transgender health for consultation and referral on behalf of gender diverse adults seeking gender-affirming treatment, if required.
Credentials of surgeons who perform gender-affirming surgical procedures (fromWPATH SOC-8):
- Training and documented supervision in gender-affirming procedures;
- Maintenance of an active practice in gender-affirming surgical procedures;
- Knowledge about gender diverse identities and expressions;
- Continuing education in the field of gender-affirmation surgery;
- Tracking of surgical outcomes.
Characteristics of health care professionals working with gender diverse adolescents:
- Are licensed by their statutory body and hold a postgraduate degree or its equivalent in a clinical field relevant to this role granted by a nationally accredited statutory institution.
- Receive theoretical and evidenced-based training and develop expertise in general child, adolescent, and family mental health across the developmental spectrum.
- Receive training and have expertise in gender identity development, gender diversity in children and adolescents, have the ability to assess capacity to assent/consent, and possess general knowledge of gender diversity across the life span.
- Receive training and develop expertise in autism spectrum disorders and other neurodevelopmental presentations or collaborate with a developmental disability expert when working with autistic/neurodivergent gender diverse adolescents.
- Continue engaging in professional development in all areas relevant to gender diverse children, adolescents, and families.
The above policy is based on the following references:
- Almazan AN, Boskey ER, Labow B, Ganor O. Insurance policy trends for breast surgery in cisgender women, cisgender men, and transgender men. Plast Reconstr Surg. 2019;144(2):334e-336e.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013.
- Azul D, Nygren U, Södersten M, Neuschaefer-Rube C. Transmasculine people's voice function: A review of the currently available evidence. J Voice. 2017;31(2):261.e9-261.e23.
- Boczar D, Huayllani MT, Saleem HY, et al. Surgical techniques of phalloplasty in transgender patients: A systematic review. Ann Transl Med. 2021;9(7):607.
- Bowman C, Goldberg J. Care of the Patient Undergoing Sex Reassignment Surgery. Vancouver, BC: Vancouver Coastal Health, Transcend Transgender Support & Education Society, and the Canadian Rainbow Health Coalition; January 2006.
- Buncamper ME, Honselaar JS, Bouman MB, et al. Aesthetic and functional outcomes of neovaginoplasty using penile skin in male-to-female transsexuals. J Sex Med. 2015;12(7):1626-1634.
- Byne W, Bradley SJ, Coleman E, et al.; American Psychiatric Association Task Force on Treatment of Gender Identity Disorder. Report of the American Psychiatric Association Task Force on Treatment of Gender Identity Disorder. Arch Sex Behav. 2012;41(4):759-796.
- Claes KEY, D'Arpa S, Monstrey SJ. Chest surgery for transgender and gender nonconforming individuals. Clin Plast Surg. 2018;45(3):369-380.
- Colebunders B, Brondeel S, D'Arpa S, et al. An update on the surgical treatment for transgender patients. Sex Med Rev. 2017;5(1):103-109.
- Coleman E, Radix AE, Bouman WP, et al. Standards of Care for the Health of Transgender and Gender Diverse People, Version 8. Int J Transgend. 2022; 23 sup1:S1-S259.
- Coleman E, Adler R, Bockting W, et al. Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People. Version 7. Minneapolis, MN: World Professional Association for Transgender Health (WPATH); 2011.
- Coleman E, Bockting W, Botzer M, et al. Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People, Version 7. Int J Transgend. 2011;13:165-232.
- Day P. Trans-gender reassignment surgery. NZHTA Tech Brief Series. Christchurch, New Zealand: New Zealand Health Technology Assessment (NZHTA); 2002;1(1).
- Djordjevic ML, Bizic MR, Duisin D, et al. Reversal surgery in regretful male-to-female transsexuals after sex reassignment surgery. J Sex Med. 2016;13(6):1000-1007.
- Eggerstedt M, Hong YS, Wakefield CJ, et al. Setbacks in forehead feminization cranioplasty: A systematic review of complications and patient-reported outcomes. Aesthetic Plast Surg. 2020;44(3):743-749.
- Falcone M, Preto M, Timpano M, et al. The surgical outcomes of radial artery forearm free-flap phalloplasty in transgender men: Single-centre experience and systematic review of the current literature. Int J Impot Res. 2021;33(7):737-745.
- Gooren LJG, Tangpricha V. Treatment of transsexualism. UpToDate [serial online]. Waltham, MA: UpToDate; reviewed April 2014.
- Gorbea E, Gidumal S, Kozato A, et al. Insurance coverage of facial gender affirmation surgery: A review of Medicaid and commercial insurance. Otolaryngol Head Neck Surg. 2021;165(6):791-797.
- Guan X, Bardawil E, Liu J, Kho R. Transvaginal natural orifice transluminal endoscopic surgery as a rescue for total vaginal hysterectomy. J Minim Invasive Gynecol. 2018;25(7):1135-1136.
- Hembree et al. Endocrine Treatment of Transsexual Persons: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2009; 94(9):3132-3154.
- Hohman MH, Teixeira J. Transgender surgery of the head and neck. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; February 27, 2022.
- Horbach SE, Bouman MB, Smit JM, et al. Outcome of vaginoplasty in male-to-female transgenders: A systematic review of surgical techniques. J Sex Med. 2015;12(6):1499-1512.
- Hu C-H, Chang C-J, Wang S-W, Chang K-V. A systematic review and meta-analysis of urethral complications and outcomes in transgender men. J Plast Reconstr Aesthet Surg. 2022;75(1):10-24.
- Jiang D, Witten J, Berli J, Dugi D 3rd. Does depth matter? Factors affecting choice of vulvoplasty over vaginoplasty as gender-affirming genital surgery for transgender women. J Sex Med. 2018;15(6):902-906.
- Jolly D, Wu CA, Boskey ER, et al. Is clitoral release another term for metoidioplasty? A systematic review and meta-analysis of metoidioplasty surgical technique and outcomes. Sex Med. 2021;9(1):100294.
- Kaariainen M, Salonen K, Helminen M, Karhunen-Enckell U. Chest-wall contouring surgery in female-to-male transgender patients: A one-center retrospective analysis of applied surgical techniques and results. Scand J Surg. 2016;106 (1):74-79.
- Lawrence AA, Latty EM, Chivers ML, Bailey JM. Measurement of sexual arousal in postoperative male-to-female transsexuals using vaginal photoplethysmography. Arch Sex Behav. 2005;34(2):135-145.
- Lawrence AA. Factors associated with satisfaction or regret following male-to-female sex reassignment surgery. Arch Sex Behav. 2003;32(4):299-315.
- Lee J, Nolan IT, Swanson M, et al. A review of hand feminization and masculinization techniques in gender affirming therapy. Aesthetic Plast Surg. 2021;45(2):589-601.
- Lee YL, Hsu TF, Jiang LY, et al. Transvaginal natural orifice transluminal endoscopic surgery for female-to-male transgender men. J Minim Invasive Gynecol. 2019;26(1):135-142.
- Leinung MC, Urizar MF, Patel N, Sood SC. Endocrine treatment of transsexual persons: Extensive personal experience. Endocr Pract. 2013;19(4):644-650.
- Meriggiola MC, Jannini EA, Lenzi A, et al. Endocrine treatment of transsexual persons: An Endocrine Society Clinical Practice Guideline: Commentary from a European perspective. Eur J Endocrinol. 2010;162(5):831-833.
- Meyer-Bahlburg HF. Sex steroids and variants of gender identity. Endocrinol Metab Clin North Am. 2013;42(3):435-452.
- Miller TJ, Wilson SC, Massie JP, et al. Breast augmentation in male-to-female transgender patients: Technical considerations and outcomes. JPRAS Open. 2019;21:63-74.
- Morrison SD, Vyas KS, Motakef S, et al. Facial feminization: Systematic review of the literature. Plast Reconstr Surg. 2016;137(6):1759-1770.
- Nakatsuka M. [Adolescents with gender identity disorder: Reconsideration of the age limits for endocrine treatment and surgery]. Seishin Shinkeigaku Zasshi. 2012;114(6):647-653.
- Ngaage LM, Knighton BJ, McGlone KL, et al. Health insurance coverage of gender-affirming top surgery in the United States. Plast Reconstr Surg. 2019;144(4):824-833.
- Oles N, Darrach H, Landford W, et al. Gender affirming surgery: A comprehensive, systematic review of all peer-reviewed literature and methods of assessing patient-centered outcomes (Part 1: Breast/chest, face, and voice). Ann Surg. 2022;275(1):e52-e66.
- Oles N, Darrach H, Landford W, et al. Gender affirming surgery: A comprehensive, systematic review of all peer-reviewed literature and methods of assessing patient-centered outcomes (Part 2: Genital reconstruction). Ann Surg. 2022;275(1):e67-e74.
- Olson-Kennedy J, Warus J, Okonta V, et al. Chest reconstruction and chest dysphoria in transmasculine minors and young adults: Comparisons of nonsurgical and postsurgical cohorts. JAMA Pediatr. 2018;172(5):431-436.
- Patel H, Arruarana V, Yao L, et al. Effects of hormones and hormone therapy on breast tissue in transgender patients: A concise review. Endocrine. 2020;68(1):6-15.
- Raffaini M, Magri AS, Agostini T. Full facial feminization surgery: Patient satisfaction assessment based on 180 procedures involving 33 consecutive patients. Plast Reconstr Surg. 2016;137(2):438-448..
- Rafferty J; Committee on Psychosocial Aspects of Child and Family Health; Committee on Adolescence; Section on Lesbian, Gay, Bisexual, and Transgender Health and Wellness. Ensuring comprehensive care and support for transgender and gender-diverse children and adolescents. Pediatrics. 2018;142(4).
- Salgado CJ, Fein LA. Breast augmentation in transgender women and the lack of adherence amongst plastic surgeons to professional standards of care. J Plast Reconstr Aesthet Surg. 2015;68(10):1471-1472.
- Sarıkaya S, Ralph DJ. Mystery and realities of phalloplasty: A systematic review. Turk J Urol. 2017;43(3):229-236.
- Schechter LS. Gender confirmation surgery: An update for the primary care provider. Transgender Health. 2016;1.1:32-40.
- Seyed-Forootan K, Karimi H, Seyed-Forootan NS. Autologous fibroblast-seeded amnion for reconstruction of neo-vagina in male-to-female reassignment surgery. Aesthetic Plast Surg. 2018;42(2):491-497.
- Smith YL, Cohen L, Cohen-Kettenis PT. Postoperative psychological functioning of adolescent transsexuals: A Rorschach study. Arch Sex Behav. 2002;31(3):255-261.
- Spack NP. Management of transgenderism. JAMA. 2013;309(5):478-484.
- Sutcliffe PA, Dixon S, Akehurst RL, et al. Evaluation of surgical procedures for sex reassignment: A systematic review. J Plast Reconstr Aesthet Surg. 2009;62(3):294-306; discussion 306-308.
- Tay YT, Lo CH. Use of peritoneum in neovagina construction in gender-affirming surgery: A systematic review. ANZ J Surg. 2022;92(3):373-378.
- Tonseth KA, Bjark T, Kratz G, et al. Sex reassignment surgery in transsexuals. Tidsskr Nor Laegeforen. 2010;130(4):376-379.
- Tugnet N, Goddard JC, Vickery RM, et al. Current management of male-to-female gender identity disorder in the UK. Postgrad Med J. 2007;83(984):638-642.
- UK National Health Service (NHS), Oxfordshire Primary Care Trust, South Central Priorities Committee. Treatments for gender dysphoria. Policy Statement 18c. Ref TV63. Oxford, UK: NHS; updated September 2009.
- Van Damme S, Cosyns M, Deman S, et al. The effectiveness of pitch-raising surgery in male-to-female transsexuals: A systematic review. J Voice. 2017;31(2):244.e1-244.e5.
- Wesp LM, Deutsch MB. Hormonal and surgical treatment options for transgender women and transfeminine spectrum persons. Psychiatr Clin North Am. 2017;40(1):99-111.
Policy History

Effective: 05/14/2002
Next Review: 07/11/2024
Review History
Definitions
Additional Information
Clinical Policy Bulletin Notes
State Information
You are now leaving the aetna website ..
Links to various non-Aetna sites are provided for your convenience only. Aetna Inc. and its subsidiary companies are not responsible or liable for the content, accuracy, or privacy practices of linked sites, or for products or services described on these sites.

TLDEF's Trans Health Project
Gender affirmation surgery.
Policy: Gender Affirmation Surgery Policy Number: HUM-0518-020 Last Update: 2023-09-28
Please ctrl + F to find the correct document titled "gender affirmation surgery" and download the pdf.
Back to top
Updated on Nov 27, 2023
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Cambridge Open

Utilization and Costs of Gender-Affirming Care in a Commercially Insured Transgender Population
Kellan baker.
1: WHITMAN-WALKER INSTITUTE, WASHINGTON, DC, USA
2: JOHNS HOPKINS BLOOMBERG SCHOOL OF PUBLIC HEALTH, BALTIMORE, MD, USA
Arjee Restar
3: CENTER FOR APPLIED TRANSGENDER STUDIES, CHICAGO, IL, USA
4: UNIVERSITY OF WASHINGTON, SEATTLE, WA, USA.
Associated Data
For supplementary material accompanying this paper visit https://doi.org/10.1017/jme.2022.87.
Many transgender people need specific medical services to affirm their gender. Gender-affirming health care services may include mental health support, hormone therapy, and reconstructive surgeries. Scant information is available about the utilization or costs of these services among transgender people, which hinders the ability of insurance regulators, health plans, and other health care organizations to plan and budget for the health care needs of this population and to ensure that transgender people can access medically necessary gender-affirming care. This study used almost three decades of commercial insurance claims from a proprietary database containing data on more than 200 million people to identify temporal trends in the provision of gender-affirming hormone therapy and surgeries and to quantify the costs of these services.
Introduction
Transgender people have a gender identity that is different from the sex they were assigned at birth, and many seek multiple ways to access and attain gender affirmation across their lifetime. 1 Gender affirmation refers to the multifaceted ways in which one may attain recognition of their gender socially (by publicly expressing their gender), psychologically (by rejecting internalized transphobia), legally (by correcting their gender marker and name on identification documents and records), and medically (by pursuing medical interventions like hormones or surgery). 2 Gender affirmation is a non-linear, non-prescriptive pathway that is tailored to individual goals and affirmation needs, and it has been linked to multiple positive health outcomes such as better quality of life; 3 lower rates of mental health conditions such as depression, anxiety, and psychological distress; 4 decrease in or elimination of distress associated with gender dysphoria; and mitigation of stigma. 5
In the context of medical interventions, the Standards of Care for Transgender and Gender Diverse People maintained by the World Professional Association for Transgender Health (WPATH) have established categories of health services and procedures that are recognized as gender-affirming medical care. These services include psychological support, hormone therapy, and reconstructive surgeries. 6 Hormone therapy typically involves estrogens and anti-androgens for transgender women and other transfeminine people and testosterone for transgender men and other transmasculine people. Surgeries that may be part of gender affirmation for transgender people include genital surgeries, such as phalloplasty or vaginoplasty; gonadectomy; chest surgeries, including mastectomy or mammoplasty; and facial surgeries, particularly for transgender women.
There are multiple structural and economic barriers that transgender people face when seeking gender-affirming medical services and procedures. Compared to the general US population, transgender people are more likely to be uninsured (14% vs. 11%), unemployed (15% vs. 5%), and living in poverty (29% vs. 12%). 7 Even for people with insurance, reports of insurance denials are common, 8 and many people report that deductibles and other out-of-pocket costs like copays and coinsurance for hormones and surgeries are a major economic barrier to pursuing gender-affirmation care. 9 One study using Centers for Medicare and Medicaid Services prescription drug plan formulary files found that out-of-pocket costs for gender-affirming hormone therapy can be substantial, ranging between $84 to $2,716 in 2010 and from $72 to $3,792 in 2018. 10 Moreover, insurers often require proof of referral letters for hormone initiation as well as surgical procedures from mental health professionals, which can also serve as a limiting factor given the inadequate workforce capacity of gender-affirming therapists, counselors, social workers, primary care providers, and surgeons, particularly in geographical areas that are prone to insurance network inadequacy issues and policy restrictions in the US. 11
The objective of the present study was to investigate temporal trends in coding, utilization, and costs of gender-affirming hormone therapy and surgeries using a proprietary commercial insurance claims database that captures all encounters for enrolled beneficiaries.
As a step to providing coverage of gender-affirming care, one imperfect approach has been to characterize a need for gender-affirming care using diagnoses such as gender dysphoria, which replaced gender identity disorder in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). 12 This change, like the revision to the International Classification of Diseases , 11th Revision (ICD-11) to create a new diagnosis of gender incongruence (codes: HA60, HA61, HA6Z), clarifies that the target of gender-affirming medical interventions is not the person’s gender identity itself but rather the clinically significant distress that can accompany a lack of alignment between gender identity and sex assigned at birth. 13
Over the last decade, interest among insurance carriers, regulators, and medical coders about trends in gender-affirming care has grown as nondiscrimination laws and private employer practices have evolved toward ensuring coverage for and broadening the availability of these services. 14 Because no national health survey consistently asks questions about gender identity, efforts to track trends and measure the effects of coverage changes have focused on alternative sources of data, such as insurance claims. 15 The objective of the present study was to investigate temporal trends in coding, utilization, and costs of gender-affirming hormone therapy and surgeries using a proprietary commercial insurance claims database that captures all encounters for enrolled beneficiaries. We anticipated that transgender people in this database would be identified in all geographic regions and that claims for hormone therapy and gender-affirming surgeries would come from diverse clinical specialties and would increase over time, particularly in the period after 2010, when the Affordable Care Act (ACA) made private health insurance broadly more accessible and both public and private payers began to remove coverage exclusions of gender-affirming care. 16 We also expected that the age at which transgender people were first identified in the database would drop over time in parallel with general U.S. population trends, which have shown increasing numbers of people identifying as transgender at younger ages. 17 Finally, we anticipated that the system-wide costs of gender-affirming care would increase over time as insurance coverage of these services became more common, but that the impact of covering gender-affirming care on payers’ budgets would be small.
We accessed the OptumLabs Data Warehouse (OLDW), which contains insurance claims data for more than 200 million people covered by commercial and Medicare Advantage plans. The OLDW Unified View provides nationwide de-identified physician, facility, and pharmacy claims, as well as person-level enrollment and demographic information. Claims include ICD-9 and ICD-10 diagnostic codes (up to five codes for physician claims and up to nine codes plus any admitting diagnosis, if present, for facility claims), Healthcare Common Procedure Coding System (HCPCS) and Current Procedural Terminology (CPT) codes, health plan and patient paid amounts, type of facility, provider type, and an internal provider identification number. OLDW is a closed system that captures complete records of health service utilization during periods of enrollment. Claims data are refreshed monthly and are accessible for research after a six-month lag. The demographic information in the Unified View is year of birth, recorded sex, census region, and race/ethnicity. Race/ethnicity is imputed through a proprietary process by a third party and provided to OLDW for use in analyses. Most fields are 100 percent populated, with the exception of imputed race/ethnicity, which is approximately 70 percent complete. Individuals receive a unique identifier and can be followed over time whenever they are enrolled in coverage.
Study Population
Using an approach developed by researchers at the Veterans Administration (VA) and elsewhere, 18 we identified transgender people by searching OLDW for transgender-specific diagnostic codes in all physician and facility claims of people with simultaneous commercial medical and pharmacy coverage. Medicare Advantage enrollees were not included. Before the U.S. conversion to ICD-10 in mid-2015, we searched for the following ICD-9 codes in any diagnosis position: transsexualism (302.5x), gender identity disorder in children (302.6), and gender identity disorder in adolescents and adults (302.85). In 2015 and later, we added the following ICD-10 codes in any position: transsexualism (F64.0); gender identity disorder in adolescence or adulthood (F64.1); gender identity disorder in childhood (F64.2); other gender identity disorders (F64.8); gender identity disorder, unspecified (F64.9); and personal history of sex reassignment (Z87.890). 19 To improve specificity, we required two instances of at least one code separated by 30 days in the claims history. 20 The first appearance of any transgender-specific diagnosis code in a person’s claims history was designated as their index date of diagnosis, which was used to assess trends in the age at which people received their first transgender-specific code in the OLDW database. Research indicates that a child’s sense of gender identity typically develops around the age of three, so we excluded children who were younger than three on their index date. 21
To assess trends in prescribing patterns, we extracted the transgender-specific diagnostic codes assigned on each person’s index date, along with the demographic variables of year of birth, race/ethnicity, region, and recorded sex. We categorized age in 2021 as 4-17, 18-29, 30-39, 40-49, 50-59, 60-69, and 70+; race/ethnicity as white, Black, Asian, Hispanic, or unknown; and location by census region (Northeast, South, Midwest, West). Recorded sex was either male or female; OLDW contains very few instances of sex being recorded as “unknown,” so we dropped those rare cases. It was impossible to know whether this variable referred to gender identity or to sex assigned at birth, so while it was included as a covariate, it should not be interpreted as a true estimate of the proportions of transmasculine and transfeminine people in the database. To assess patterns in use of transgender-specific diagnostic codes by specialty, we also extracted the internal OLDW identification number and specialty of clinicians who assigned these codes in any encounter, regardless of whether it was the index diagnosis.
Outcome Measures
Following published guidelines for hormone therapy in transgender people, 22 we characterized gender-affirming testosterone therapy as at least one pharmacy claim for any formulation of testosterone without any claim for an estrogen formulation; for transgender women and other transfeminine people, gender-affirming hormone therapy was at least one claim for an estrogen formulation with at least one claim for an anti-androgen such as spironolactone or bicalutamide. Dutasteride and finasteride, which may be used by transfeminine people for purposes of gender affirmation but also by transmasculine people to prevent hair loss associated with testosterone use, were not included. 23 We classified people with claims for both testosterone and estrogen formulations as transmasculine because of the potential use of estrogen formulations for birth control among people assigned female at birth, regardless of gender identity. We did not use recorded sex data to classify hormone therapy because it was impossible to determine whether the sex variable in the database referred to current gender identity or to assigned sex at birth. Gonadotropin-releasing hormone (GnRH) analogs, which may be prescribed to transgender adolescents of any gender to delay the onset of puberty as a precursor to eventual hormone replacement therapy with testosterone or estrogens, were included as a separate category. For each gender-affirming hormone therapy claim, we extracted the generic and brand names, dosage, out-of-pocket and health plan paid amounts, and the prescribing provider’s specialty and internal OLDW identification number (Appendix A, Table A.1).
To identify gender-affirming surgeries, we first extracted all physician and facility claims that included a transgender-specific ICD-9 or ICD-10 diagnostic code in any position. We then used published coverage protocols 24 to identify claims with ICD-9 or ICD-10 procedure codes or CPT codes that can be used to bill for the following categories of gender-affirming surgical procedures: phalloplasty or metoidioplasty, hysterectomy, and mastectomy for transgender men and other transmasculine people and vaginoplasty, orchiectomy, mammoplasty, and facial feminization for transgender women and other transfeminine people (Appendix A, Table A.2). Codes that could not be readily associated with a specific gender were grouped as “unspecified top surgery” (i.e., mastectomy or mammoplasty) or “unspecified genital surgery” (i.e., phalloplasty/metoidioplasty or vaginoplasty). We confirmed the composition of this code list with a surgeon who performs high volumes of these procedures (Loren Schecter, personal communication, August 20, 2019).
Descriptive Analyses
We calculated the incidence by year of transgender people newly identified in OLDW using their index date. The denominator for both annual incidence and the total number of transgender people with coverage by year was the count of all people with commercial coverage in OLDW in that year. We explored trends in coding by calculating the mean age at index diagnosis for people with index dates between 1993 to 2000, 2001 to 2010, and 2011 to 2020, as well as by assessing the relative proportions of transgender-specific diagnostic codes assigned by each clinical specialty. We used χ 2 tests to compare index codes by demographics.
The assessment of gender-affirming health services utilization consisted of annual counts of individual hormone therapy prescriptions in each category (testosterone, estrogens plus anti-androgens, and GnRH analogs), annual counts of the number of people receiving any gender-affirming hormone therapy prescription, counts of episodes of individual surgical procedures in each category of surgeries by year, and annual counts of transgender people who underwent any gender-affirming surgical procedure. Procedures that occurred within 14 days of each other were counted as a single episode. We calculated the percentage of people who received hormone therapy or a surgical procedure among all individuals identified as transgender in the database who were enrolled in coverage for any part of each year. We used multivariable logistic regression models to identify demographic characteristics associated with receipt of hormone therapy or gender-affirming surgery. Statistical significance was set at α = 0.05, and analyses were conducted in R (version 4.0.2).
Annual costs for each category of hormone therapy were calculated from a payer perspective by summing the health plan paid costs; we also calculated average annual health plan paid costs per person for each category. Average and annual costs for each type of surgery were similarly calculated from a payer perspective, and all costs incurred during the 14-day window after each procedure were included. We calculated the annual budget impact of the overall cost of gender-affirming care, including all types of hormone therapy and surgical procedures, using the total OLDW population with commercial coverage in each year as the denominator. All costs were estimated in 2019 dollars.
We identified 16,619 people who had physician or facility claims and met our inclusion criteria between 1993 and 2019. Of this group, 15,790 also had pharmacy claims. The annual incidence of index codes, meaning the appearance of an individual’s first transgender-specific code in the database, rose from 4 per million enrollees in 1993 to 149 per million in 2019, with more than 80 percent of that growth occurring between 2011 and 2019. Between 1993 and 2000 and between 2001 and 2010, an average of 18 and 166 people, respectively, received a transgender-specific code for the first time each year; between 2011 and 2019, an average of 1,646 people were newly identified as transgender in OLDW each year. The number of people in OLDW with transgender codes in each year similarly increased slowly through the first two decades before beginning an exponential rise around 2011 ( Figure 2.1 ). In 1993, the number of transgender people with coverage in OLDW was 71 per million enrollees; this number rose slowly to 178 per million in 2010 before climbing rapidly to 411 per million by 2019. The mean age at index diagnosis declined from 33.9 years in 1993 to 26.3 years in 2019 ( Figure 2.2 ). The transgender population was young, with the largest proportion (46%) in the age group between 18 and 29 as of 2019. The majority were identified in the database as female (53%) and white (67%), and most (35%) lived in the South, where OLDW has large representation ( Table 2.1 ).

Annual New Identifications and Total Count of Transgender People in the OptumLabs Data Warehouse, 1993-2019

Age Distribution of Newly Identified Transgender People by Index Year, 1993-2019
Demographics of Transgender People Identified in the OptumLabs Data Warehouse, 1993-2019
The most common index code during the ICD-9 period was the non-specific code 302.85 (Gender Identity Disorder in Adolescents or Adults). Codes with sexual orientation subclassification (e.g., 302.53; Transsexualism, Heterosexual Sexual History) became less common throughout the ICD-9 period; these codes were phased out in the conversion to ICD-10 in mid-2015 (Appendix A, Figure A.1 ). Immediately following the conversion, there was a temporary spike in the use of F64.1 (Dual-Role Transvestism). There was no increase over time in the use of codes specific to children (e.g., F64.2, Gender Identity Disorder in Childhood). While transgender-specific diagnostic codes typically appeared in claims for services that could be part of gender affirmation, including mental health counseling as well as hormone therapy and surgeries, the use of these codes was not confined to gender-affirming care: these codes were also identified in claims for encounters such as arthroscopic knee surgeries and influenza vaccines. The provider specialties that used these codes most often were social work, family practice, and psychology (Appendix A, Figure A.2 ).
Seventy-two percent of transgender people had at least one encounter for gender-affirming hormone therapy. The clinical specialties most likely to write prescriptions for hormone therapy were family practice (28%) and endocrinology (18%) (Appendix A, Table A.3 ). Many individual providers were represented, and no single provider wrote more than 1.6 percent of all the prescriptions in the claims database. Hormone therapy by gender was roughly even between transmasculine and transfeminine regimens: 46 and 54 percent of people on hormone therapy were classified as transmasculine or transfeminine, respectively. Only 0.4 percent of those on hormone therapy were observed to have received GnRH treatment, and 78 percent of those who had been on GnRH treatment subsequently received prescriptions for estrogens or testosterone. While the number of people on GnRH treatment remained consistently low, the number of people receiving hormone therapy with estrogen or testosterone increased rapidly beginning around 2011 ( Figures 2.3 and 2.4 ). In 2011, 17 percent of transgender people identified in this database were receiving gender-affirming hormone therapy, and by 2019 this proportion had increased almost 4-fold, to 65 percent. The average payer costs of gender-affirming hormones were consistently low for both testosterone and estrogen therapy, at $121 and $153 per year; GnRH therapy cost an average of $2,410 per person per year ( Table 2.2 ). As a proportion of total costs, out-of-pocket spending per year was 38 percent for estrogens, 25 percent for testosterone, and 8 percent for GnRH.

Number of People with Claims for Gender-Affirming Hormone Therapy by Year and Medication Type, 1993-2019

Annual Health Plan Paid Cost by Gender-Affirming Hormone Therapy Type, 1993-2019
Frequency and Costs of Claims for Gender-Affirming Hormone Therapy, 1993-2019
GnRH = gonadotropin-releasing hormone
* Average weighted by proportion of people with prescriptions for each type of therapy; denominator is the total number of transgender people identified in OLDW (N = 16,619)
Temporal trends in the frequency of gender-affirming surgeries paralleled those of hormone therapy. Throughout the first two decades of claims, gender-affirming surgeries were performed infrequently, if at all, but the annual number of procedures performed began to increase around 2011: in 2011, 21 people (0.5% of all transgender people with coverage that year) underwent a gender-affirming surgery, and by 2019, that number had risen to 794 (8%) ( Figures 2.5 and 2.6 ). Overall, 14 percent of the transgender people identified for this analysis had ever undergone a gender-affirming surgery while enrolled in OLDW, of which mastectomy was the most common procedure. The per-episode payer costs of gender-affirming surgeries ranged from $6,927 for orchiectomy to $45,080 for vaginoplasty and $63,432 for phalloplasty ( Table 2.3 ). As vaginoplasty and phalloplasty were frequently multi-episode procedures, the total average cost of these procedures per person was $53,645 and $133,911, respectively. There were substantially lower odds of having undergone surgery among people living in the South (adjusted odds ratio [OR]: 0.74, 95% confidence interval [CI]: 0.63, 0.88), although there were no differences by imputed race (Appendix A, Table A.4 ). No single provider was responsible for more than 6.6 percent of surgeries.

Number of Gender-Affirming Surgical Procedures by Year, 2010-2019

Annual Health Plan Paid Cost by Gender-Affirming Procedure Type, 2010-2019
Frequency and Costs of Claims for Gender-Affirming Surgeries, 1993-2019
Over the time period covered by this study, the annual frequency of gender-affirming hormone therapy and surgeries increased both in absolute terms and as a proportion of the number of transgender people identified in the database, and costs changed accordingly. In 2019, each covered transgender person incurred an average of $1,776 in costs for gender-affirming hormone therapy and surgeries combined. Considered on a per-member basis across the entire commercially insured population in OLDW, the budget impact of gender-affirming care in 2019 was $0.73 per year, or $0.06 per member per month (PMPM).
To our knowledge, this is the first study to evaluate temporal trends in coding, utilization, and costs for both gender-affirming hormone therapy and surgeries. We found that the number of people receiving transgender-specific diagnostic codes and accessing gender-affirming care in this privately insured population has increased rapidly over the decade between 2011 and 2019. Even as coverage of gender-affirming care has expanded, its budget impact remains small: the PMPM estimate of providing gender-affirming care in 2019 was $0.06 when distributed across all people with commercial coverage in OLDW. This is in line with estimates from a cost-effectiveness study that estimated the costs of coverage for gender-affirming care at $0.016 when spread across the entire U.S. population. 25
These trends in utilization of gender-affirming health services align with broader societal trends in the visibility of transgender people. The time frame of this increase coincides with policy reforms over the last decade lifting several barriers that previously limited both the use of transgender-specific codes and the provision of gender-affirming care. In 2010, the ACA introduced new guaranteed-issue protections in private insurance that were interpreted by the U.S. Department of Health and Human Services (HHS) to prohibit the designation of a transgender identity as a pre-existing condition for which insurance coverage could be restricted or denied. 34 Between 2010 and 2014, HHS promulgated several regulations that codified nondiscrimination protections on the basis of gender identity in insurance marketing, benefit design, and coverage determinations. 26 Around the same time, individual states began to adopt or strengthen similar protections by interpreting existing law to prohibit unfair discrimination against transgender people in both state-regulated health insurance markets and state Medicaid programs. 27 These reforms included the 2014 rescission of Medicare’s ban on coverage for gender-affirming surgeries and a 2016 HHS regulation that prohibited blanket exclusions of gender-affirming care in both public and private coverage. 28 Though the Trump administration revised that regulation in 2020 and future activity by the Biden administration remains unknown, state and federal courts have consistently found that discrimination against transgender people on the basis of gender identity is a form of sex discrimination. 29 As of early 2021, 24 states and territories prohibited blanket transgender coverage exclusions in state-regulated private coverage, up from one in the pre-2010 period. 30 The biggest increase in the number of people being identified as transgender in OLDW in the decade between 2010 and 2020 occurred in the South, where no states apart from Virginia, Maryland, and Delaware have state-specific protections. This pattern is consistent with the hypothesis that the 2016 national regulation played a substantial role in removing barriers to private coverage for transgender people, though more research is needed to explore this possibility.
The findings of this study indicate that the impact of gender-affirming care on payer budgets has remained nominal even as national trends in coverage policies have made this care more accessible to transgender people. Future directions for research include assessing the health outcomes associated with access to gender-affirming care, improving methods for identifying transgender people in insurance claims databases, and investigating opportunities to link different data sources to provide a more complete picture of the health needs and experiences of transgender people.
As restrictions on coverage for gender-affirming care have receded, other studies using data sources such as the National Inpatient Sample have identified increases in the number of gender-affirming surgeries performed in the U.S. 31 The present study expands this evidence base by analyzing the frequency of individual procedures and assessing trends in hormone therapy use as well; a better understanding of the availability and uptake of both gender-affirming surgeries and hormone therapy is important for insurance carriers seeking to ensure the adequacy of their coverage and provider networks for these services and for hospitals and other health service organizations identifying trends in patient care needs. These data may also help federal and state insurance regulators establish baseline estimates of service availability and utilization, which can be used to monitor market conduct and identify potential concerns related to inadequacy of benefit designs or inappropriate use of utilization management tools. For instance, this study found that utilization of GnRH treatment remained low, even as the number of people identified in the 4-17 age group increased. This pattern is consistent with reports that barriers in insurance coverage of GnRH treatment for transgender adolescents remain high. 32 Some regulators are beginning to explore the degree to which restrictions on coverage of GnRH treatment for this population may violate nondiscrimination requirements on the basis of gender identity and age. 33
Limitations
This study has several limitations, many of which relate to the difficulty of using diagnoses in insurance claims as proxies for gender identity, which is a complex aspect of personal identity that has social, legal, and medical components. Because this insurance claims database does not currently include any self-reported data on gender identity, it was not possible to determine how many people in the database would self-identify as transgender but are not captured by the algorithm based on transgender-specific diagnostic codes. The proportion of the population in this database that was identified as transgender was 411 per million in 2019 (0.04%), which is comparable to other estimates from clinical records but much less than estimates from more representative population surveys that use self-report, which range between 0.1 percent and 2.0 percent. 34 It was also impossible to definitively identify claims for gender-affirming care, as the assessment of coding practices indicated that these codes may be applied to services provided to transgender people that do not have any relation to gender affirmation. We thus may have incorrectly categorized unrelated services as gender-affirming care; this was a particular concern with services that may be more commonly needed for other indications, such as hysterectomy and estrogen therapy.
At the same time, we may have missed services and procedures that were provided for purposes of gender affirmation but were not submitted with transgender-specific diagnostic codes. The number of claims with procedure codes that might indicate a gender-affirming service but that were not coded with relevant diagnostic codes was very small among the group of people identified as transgender, but it was not possible to know how many such procedures for purposes of gender affirmation were performed for people who were not included in the transgender group. The routine capture of self-reported gender identity data in clinical records, including both medical records and claims, would aid in assessments of transgender population size and health services costs and use. Similarly, more consistent coding standards guiding the application of both diagnostic codes related to a need for gender-affirming care and procedure codes describing the provision of this care would improve estimates of the frequency and costs of these procedures.
The number of people with transgender-specific diagnostic codes in this commercial insurance claims database has increased sharply over the last decade, in tandem with law and policy changes that seek to remove barriers to coverage for this population. In 2019, almost 10,000 people were identified as transgender in this database, representing 0.04 percent of people with commercial coverage in OLDW. In the same year, 65 percent of people identified as transgender were receiving gender-affirming hormone therapy, and 8 percent had some gender-affirming surgical procedure. The annual cost of providing gender-affirming care for this population was $1,776 per person, or $0.06 per member per month. The findings of this study indicate that the impact of gender-affirming care on payer budgets has remained nominal even as national trends in coverage policies have made this care more accessible to transgender people. Future directions for research include assessing the health outcomes associated with access to gender-affirming care, improving methods for identifying transgender people in insurance claims databases, and investigating opportunities to link different data sources to provide a more complete picture of the health needs and experiences of transgender people.
The authors have no conflicts to disclose.
Acknowledgments
Our gratitude goes out to Jodi B. Segal, M.D., M.P.H. of the Johns Hopkins Bloomberg School of Public Health, Department of Health Policy and Management, and Helene Hedian, M.D. of the Johns Hopkins School of Medicine. We would also like to thank Optum Labs and the Robert Wood Johnson Foundation Health Policy Research Scholar Program.
Biographies
Kellan Baker, Ph.D., M.P.H., M.A., is affiliated with the Whitman-Walker Institute, Washington, DC, USA and the Department of Health Policy and Management, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA.
Arjee Restar, Ph.D., M.P.H., is affiliated with the Center for Applied Transgender Studies, Chicago, IL, USA and the Department of Epidemiology, University of Washington School of Public Health, Seattle, WA, USA.
Appendix A: Supplementary Material
Hormone Therapy Prescriptions by Provider Specialty
Associations Between Demographic Characteristics and Gender-Affirming Medical Services
OR = odds ratio, CI = confidence interval, Ref = reference category

Index Codes by Year, 1993-2019

Use of Transgender-Specific Codes by Provider Specialty
Supplementary material

Critics blast NY’s proposed ‘Equal Rights Amendment’ they say strips parents of their rights over kids’ transgender surgery
C ritics are raging against New York’s proposed “Equal Rights Amendment,” claiming the Nov. 5 ballot measure could curb the rights of parents when it comes to allowing minors to undergo gender reassignment surgery.
New York voters don’t yet know much about the particulars of the ERA, which could codify abortion rights in the state constitution — advanced by Gov. Kathy Hochul and Democrats who run the state legislature.
The broad language of the proposal — dubbed Proposition One — has sparked a fierce debate over what could happen if it gets passed, with opponents claiming it’ll lead to kids possibly being able to get serious medical procedures without their parents’ OK and allow transgender females to compete in women’s sports.
“Proposition One would strip the legal rights of parents with school age children to know about crucially important things happening with their kids, including controversial gender transformation procedures” the Coalition to Protect Kids said in a statement.
“Schools would be required to permit biological males to compete on girls’ sports teams if voters approve this amendment.”
The proposal asks voters whether they support or oppose adding language to the constitution that people cannot be denied rights based on their “ethnicity, national origin, age, and disability” or “sex, including sexual orientation, gender identity, gender expression, pregnancy, pregnancy outcomes, and reproductive healthcare and autonomy.”
Coalition to Protect Kids NY Executive Director Greg Garvey said the ERA should instead be called “The Parent Replacement Act,” because it “opens the floodgates” for the government wielding more authority over children than their parents on some of the most important decisions of their lives.
“Any decent lawyer will take one look at the Proposition One language and say, ‘you’ve got to be kidding me,’” said Garvey.
“This ballot initiative is written so broadly and so poorly that it could cause irreparable harm to children and families,” he added.
“Governor Hochul and her woke Albany colleagues have a lot of explaining to do.”
The group’s website includes a video saying a school could help a 7-year-old girl “try life as a boy” and help her transition without her mother “ever knowing” under the amendment, adding, “Do you think that’s OK?”
The Coalition to Protect Kids also claims that laws that determine the legal age to purchase and/or consume alcohol or cannabis, elder abuse and statutory rape could all be weakened because they might arguably “‘discriminate’ based on age.”
The group New Yorkers for Equal Rights denied that the amendment strips parents of their rights.
“These claims simply aren’t true. This amendment is about making sure our fundamental rights and reproductive freedoms are protected and never at risk of becoming a political football,” said Sasha Ahuja, campaign director of New Yorkers for Equal Rights.
The pro-amendment group, in a statement Monday, also said, “If passed, the NY ERA would provide the most comprehensive list of protected categories of any state in the country — safeguarding New Yorkers’ rights, as well as serving as a model for other states.”
Members of the pro-ERA group include 1199SEIU United Healthcare Workers East, Planned Parenthood, North Star, New York Immigration Coalition, the Civil Liberties Union, NEW Pride Agenda, National Institute for Reproductive Health Action Fund, NAACP, Make the Road New York and New York State United Teachers.
New York already has among the strongest abortion laws in the country and long been a pro-choice, with critics questioning whether such a controversial issue belongs in the constitution.
“It’s an ‘anything goes’ amendment,” said state Conservative Party chairman Gerard Kassar, whose party will campaign against the ERA.
He also said Democrats are looking to “change the conversation” away from problems they own — such as the migrant crisis and crime.
A lawsuit has been filed in Livingston County Supreme Court claiming that the legislature approved the proposed amendment going to the voters before getting a legal opinion from state Attorney General Letitia James’ Office.
There’s also been a recent public backlash in New York against permitting trans females from competing in women’s sports, leading to a controversial ban in some sporting venues in Nassau County.
Even one of the world’s most famous transgender females — Caitlyn Jenner — the former 1976 Olympic decathlon champion as Bruce Jenner — is opposed.
Additional reporting by Vaughn Golden
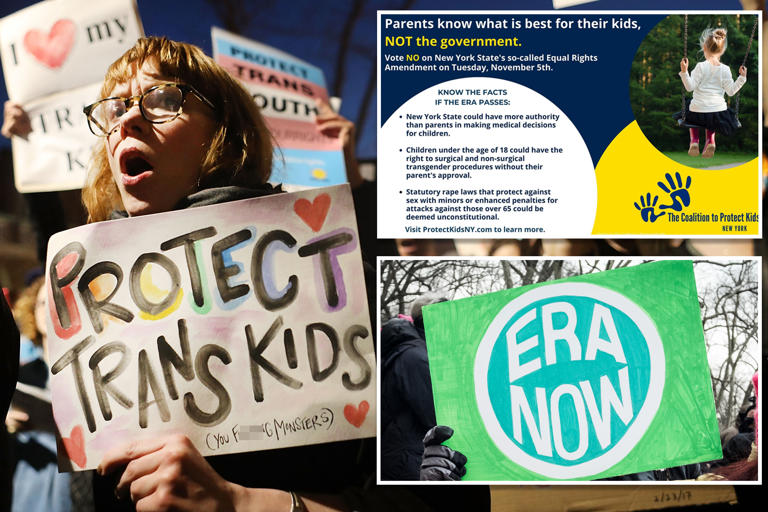
- Share full article
Advertisement
Supported by
Insurers Reap Hidden Fees by Slashing Payments. You May Get the Bill.
A little-known data firm helps health insurers make more when less of an out-of-network claim gets paid. Patients can be on the hook for the difference.

By Chris Hamby
Chris Hamby reviewed more than 50,000 pages of documents and interviewed more than 100 people for this article. The New York Times also petitioned two federal courts for materials under seal.
Weeks after undergoing heart surgery, Gail Lawson found herself back in an operating room. Her incision wasn’t healing, and an infection was spreading.
At a hospital in Ridgewood, N.J., Dr. Sidney Rabinowitz performed a complex, hourslong procedure to repair tissue and close the wound. While recuperating, Ms. Lawson phoned the doctor’s office in a panic. He returned the call himself and squeezed her in for an appointment the next day.
“He was just so good with me, so patient, so kind,” she said.
But the doctor was not in her insurance plan’s network of providers, leaving his bill open to negotiation by her insurer. Once back on her feet, Ms. Lawson received a letter from the insurer, UnitedHealthcare, advising that Dr. Rabinowitz would be paid $5,449.27 — a small fraction of what he had billed the insurance company. That left Ms. Lawson with a bill of more than $100,000.
“I’m thinking to myself, ‘But this is why I had insurance,’” said Ms. Lawson, who is fighting UnitedHealthcare over the balance. “They take out, what, $300 or $400 a month? Well, why aren’t you people paying these bills?”
The answer is a little-known data analytics firm called MultiPlan. It works with UnitedHealthcare, Cigna, Aetna and other big insurers to decide how much so-called out-of-network medical providers should be paid. It promises to help contain medical costs using fair and independent analysis.
But a New York Times investigation, based on interviews and confidential documents, shows that MultiPlan and the insurance companies have a large and mostly hidden financial incentive to cut those reimbursements as much as possible, even if it means saddling patients with large bills. The formula for MultiPlan and the insurance companies is simple: The smaller the reimbursement, the larger their fee.
Here’s how it works: The most common way Americans get health coverage is through employers that “self-fund,” meaning they pay for their workers’ medical care with their own money. The employers contract with insurance companies to administer the plans and process claims. Most medical visits are with providers in a plan’s network, with rates set in advance.
But when employees see a provider outside the network, as Ms. Lawson did, many insurance companies consult with MultiPlan, which typically recommends that the employer pay less than the provider billed. The difference between the bill and the sum actually paid amounts to a savings for the employer. But, The Times found, it means big money for MultiPlan and the insurer, since both companies often charge the employer a percentage of the savings as a processing fee.
How MultiPlan and Insurers Make Money on Fees
MultiPlan and health insurers typically receive a percentage of the “savings” on each claim, creating an incentive to recommend lower payments.
MULTIPLAN ADVISES A 20% PAYMENT
MULTIPLAN ADVISES A 50% PAYMENT
A lower payment
means bigger fees for
the insurer and MultiPlan, but also a bigger potential bill for the patient.
The patient is potentially on the hook for this amount.
To MultiPlan
share of the
(paid by insurer)
(paid by employer)
For a doctor’s bill of $1,000:
20% PAYMENT
50% PAYMENT
A lower payment means bigger fees for the insurer and MultiPlan, but also a bigger potential bill for the patient.
Based on a share of the difference
Fee percentages vary based on negotiated contracts.
By The New York Times
In recent years, the nation’s largest insurer by revenue, UnitedHealthcare, has reaped an annual windfall of about $1 billion in fees from out-of-network savings programs, including its work with MultiPlan, according to testimony by two of its executives. Last year alone, MultiPlan told investors, it identified nearly $23 billion in bills from various insurers that it recommended not be paid.
MultiPlan and the insurers say they are combating rampant overbilling by some doctors and hospitals, a chronic problem that research has linked to rising health care costs and regulators are examining . Yet the little-understood financial incentive for insurers and MultiPlan has left patients across the country with unexpectedly large bills, as they are sometimes asked to pick up what their plans didn’t pay, The Times found. In addition, providers have seen their pay slashed, and employers have been hit with high fees, records and interviews show.
In some instances, the fees paid to an insurance company and MultiPlan for processing a claim far exceeded the amount paid to providers who treated the patient. Court records show, for example, that Cigna took in nearly $4.47 million from employers for processing claims from eight addiction treatment centers in California, while the centers received $2.56 million. MultiPlan pocketed $1.22 million.
Confidential Pricing and Fee Data
Itemized payments and fees for thousands of claims were made public in a lawsuit against Cigna after The Times petitioned the court. The insurer and MultiPlan opposed the release, calling the data “highly confidential.”
Payment amount
For providing outpatient
substance abuse treatment,
the facility received $134.13 .
Fee for Cigna
For processing the claim,
Cigna received $658.75 ,
nearly five times as much
as the treatment center.
Fee for MultiPlan
For recommending a payment
amount, MultiPlan received
$167.48 , slightly more than
the treatment center.
For providing outpatient substance abuse
treatment, the facility received $134.13 .
For processing the claim, Cigna received
$658.75 , nearly five times as much as the
treatment center.
For recommending a payment amount,
MultiPlan received $167.48 , slightly more
than the treatment center.
View the PDF .
MultiPlan, which makes nearly all its revenue from such fees, markets its calculations as “defensible, repeatable and completely transparent” and independent of insurance company influence. The firm estimates that its reach extends to more than 100,000 health plans covering more than 60 million people. Patients have encountered its pricing recommendations after a variety of treatments, including spine surgeries, physical therapy appointments and ambulance rides.
The company did not respond to detailed questions from The Times. In a statement, it said it uses “well-recognized and widely accepted solutions” to promote “affordability, efficiency and fairness,” by recommending a “reimbursement that is fair and that providers are willing to accept in lieu of billing plan members for the balance.”
In examining MultiPlan’s dominant role in this secretive world, The Times reviewed more than 50,000 pages of confidential corporate records, legal filings, claims information and other documents. The Times also interviewed more than 100 patients, doctors, billing specialists, advisers to employer health plans and former MultiPlan employees.
The Times found:
Patients hit with unexpectedly large bills sometimes forgo care or cease long-term treatment, and complain that appeals are fruitless. “They basically took away the mental health care I was getting,” said Olivia Henderson, who stopped her therapy sessions in New York when the cost spiked.
MultiPlan’s recommended payments not only push back against known overbillers, but can also squeeze smaller practices. Kelsey Toney, who provides behavioral therapy for children with autism from a clinic in rural Virginia, saw her pay cut in half for two patients. “I don’t want to say, ‘I’m sorry I can no longer accept you,’ especially when I’m the only provider within an hour,” she said.
Insurers pitch MultiPlan to employers as a way to control costs, but the fees can be onerous and unpredictable. New England Motor Freight, a New Jersey trucking company, was charged $50,650 by UnitedHealthcare for processing a single hospital bill.
Insurers can influence MultiPlan’s purportedly independent payment recommendations, according to MultiPlan documents made public by a federal judge after a petition from The Times. That generally means paying even less to doctors and making more in fees.
Former employees at MultiPlan, which has annual revenues of about a billion dollars, described a numbers-driven culture that encouraged locking in unreasonably low payments and tied their bonuses to the reductions. “I knew they were not fair,” said one former MultiPlan negotiator, Kajuana Young.
Regulators rarely intervene. The administration of employer-funded health plans is mostly exempt from state regulations. Enforcement primarily falls to an agency within the federal Department of Labor, which says it has one investigator for every 8,800 health plans.
In separate statements, UnitedHealthcare, Cigna and Aetna said MultiPlan helps them control costs for employers. A UnitedHealthcare spokesman said employers negotiate and accept contract terms, including the fee, and described the arrangement as “an industry-standard approach.” A Cigna spokeswoman also said the fee “aligns with industry standards,” adding that “it is fully transparent to our client” and has no influence on payouts to medical providers.
As to the issue of patients being billed for unpaid balances, Aetna said it offered employers “various options and strategies” to minimize the risk of unexpected charges. Cigna said that payment decisions could be appealed, and that it collected no fee if the patient was ultimately billed the balance. UnitedHealthcare blamed “egregious” charges by out-of-network providers and suggested that criticism of its work with MultiPlan had been stoked by a private-equity-backed medical staffing firm that is suing the insurer.
Determining what to pay when a patient goes out of network has long been a contentious issue. While such claims represent a small portion of all medical visits, they can be expensive, little understood by patients and difficult to avoid. Legislation that took effect in 2022 now protects patients from certain kinds of surprise bills but does not cover a vast majority of the claims directed to MultiPlan.
Insurers say that the traditional approach — paying a portion of what providers typically charge — no longer works because of dramatic price hikes. Cigna, in its statement, said some out-of-network providers last year tried to charge “up to 1,904 percent of what they charge Medicare.” Providers, meanwhile, argue that insurers and MultiPlan can’t be trusted to set fair rates.
The situation echoes a past scandal. Fifteen years ago, the New York attorney general broke up a pricing system that his office’s investigation concluded was “rigged.” The central player, UnitedHealth, agreed to pay $350 million to patients and medical professionals who said they had been shortchanged, and along with other major insurers, it agreed to reforms meant to ensure this wouldn’t happen again.
But the settlement left an opening.
An Industrywide Investigation
In 2009, a woman from Yonkers, N.Y., became a symbol of patients’ outrage and the promise of change.
Mary Reinbold Jerome had been diagnosed with ovarian cancer at age 62 and received treatment at Memorial Sloan Kettering. Because the hospital was outside her plan’s network, she was billed tens of thousands of dollars.
A tenacious woman who taught English to nonnative speakers at Columbia University, Dr. Jerome lodged a complaint with the state attorney general’s office, helping to prompt an industrywide investigation .
She stood beside Andrew M. Cuomo, then the attorney general, as he announced his office’s blistering conclusions : A payment system riddled with conflicts of interest had been shortchanging patients, and at its core was a data company called Ingenix. Insurers used the company, a UnitedHealth subsidiary, to unfairly lower their payments and shift costs to patients, the probe found.
UnitedHealthcare, Cigna, Aetna and other major insurers agreed to replace Ingenix with a nonprofit that would provide independent pricing data. Dr. Jerome was featured on news programs and hailed as an agent of change, while senators held hearings and blasted insurers for cheating patients.
In 2010, Dr. Jerome died.
“She was thinking beyond her own situation,” her daughter, Eva Jerome, said in an interview. “She was hoping it would have a broader impact.”
But amid the triumph, a key detail in the attorney general’s agreements with insurers largely escaped notice: The companies were required to use the nonprofit database for only five years.
When that term expired in 2014, MultiPlan was well positioned to capitalize.
‘All for Naught’
For decades, the company, founded in 1980, offered a traditional approach to managing out-of-network claims by negotiating rates with doctors. Insurers got discounts and assurances that patients would not have to make up the difference.
But after MultiPlan’s founder sold it to private equity investors in 2006, the company pursued a more aggressive approach. It embraced pricing tools that used algorithms to recommend lower payments, and no longer protected patients from having to pay the difference, documents show.
Meanwhile, private equity ramped up investments in physician groups and hospitals and, in some instances, began billing for extraordinary sums. Once insurers were no longer obligated to use the nonprofit database, FAIR Health, they began looking for ways to combat that billing and other charges they considered egregious. Because FAIR Health’s data was based on what doctors typically charged, insurers contended that overbilling would skew payments too high.
Cigna was particularly concerned with what it considered overbilling and fraud by substance abuse treatment centers. It halted some payments, opened investigations and met with a public relations firm “to precondition public support for any next steps we may need to take,” internal documents show.
In a 2015 email, unsealed after The Times’s request and over Cigna’s objection, a Cigna executive reminded colleagues of a key consideration.
“We cannot develop these charges internally (think of when Ingenix was sued for creating out-of-network reimbursements),” wrote Eva Borden, a chief risk officer at Cigna. “We need someone (external to Cigna) to develop acceptable” rates, she wrote.
UnitedHealthcare developed talking points to “position UnitedHealthcare as an advocate that is helping consumers push back on excessively high physician and facility bills,” a 2016 internal memo said.
Both insurers increasingly turned to MultiPlan. Internal documents show that UnitedHealthcare began a campaign to persuade employers to switch from FAIR Health. In a 2019 email, a UnitedHealthcare senior vice president emphasized creating a “sense of urgency” and helping companies still using FAIR Health “understand they don’t want to be on that program anymore.”
UnitedHealthcare had a big incentive to encourage this change. When it processed claims from employer plans using FAIR Health, the insurer collected no additional fee, according to legal testimony. But when it used MultiPlan, documents show, it typically charged employers 30 to 35 percent of the difference between the billed amount and the portion paid.
MultiPlan, too, charged a percentage of the savings, meaning it could make more by recommending lower payments. (FAIR Health charged a flat fee.)
While UnitedHealthcare was MultiPlan’s largest customer, Cigna and Aetna also embraced its tools and fee model, records show. Other insurers that work with MultiPlan include Kaiser Permanente, Humana and some Blue Cross Blue Shield plans.
Employers with self-funded plans administered by insurers include large companies like Coca-Cola and AstraZeneca and smaller organizations like school districts and union locals. (New York Times Company plans also operate this way.)
FAIR Health has expanded the types of data it offers and made it available online . Numerous states use the nonprofit when setting payments for government programs. Big commercial insurers still license its data, but they have largely shifted to other approaches, according to interviews, documents and statements from UnitedHealthcare and Cigna.
“If they’re able to go back to their old ways,” Eva Jerome said, “then it was all for naught.”
‘I’m Being Ripped Off’
When claims go through MultiPlan, some patients receive statements highlighting what their insurer calls discounts or savings — even as doctors or hospitals bill them for those amounts.
Cari Campbell, who received fertility treatment in Minnesota, was charged thousands of dollars that her insurer had labeled “you saved.” In Kansas City, Kan., Paul Haddix paid the amounts labeled “your discount” for his daughter’s occupational and speech therapy. In New Jersey, Jonathan Menjivar paid upfront for therapy appointments and saw his reimbursements plunge.
“I took a closer look at the explanation of benefits,” Mr. Menjivar said, “and noticed for the first time this column labeled ‘your discount,’ which is an interesting way of putting it.”
The supposed savings and discounts were the portions MultiPlan had recommended the employers not pay. Patients could still be on the hook.
Fact Check: An Explanation of Benefits
Insurance statements often identify savings or discounts. But sometimes patients can still be billed for that amount, as in this case involving the UnitedHealth subsidiary UMR.
Your discount: $871.78
Your plan negotiates discounts with providers and facilities to help save you money.
You saved: $1,293.74
82% of your service was covered by your
plan discounts, your employer-sponsored benefits plan, or other amounts for which you are not responsible.
82% of your service was
covered by your plan discounts, your employer-sponsored
benefits plan, or other amounts for which you are not responsible.
The burden can fall hardest on people with chronic or complex conditions who see out-of-network specialists. Justin Dynlacht, who has Crohn’s disease, paid extra for a plan that covered such visits. After seeing two in-network doctors about persistent abdominal pain, he went to an outside specialist who discovered a hernia containing abdominal tissue.
Aetna sent the specialist’s claims to MultiPlan, and Mr. Dynlacht was left with thousands of dollars in bills.
“I’m being ripped off,” he said. “It’s not right.”
Staying in-network can be especially difficult for mental health or substance abuse treatment.
A California woman whose teenage son was battling opioid addiction found only one treatment center that would accept him, and it was out of network. “When your kid has hit rock bottom, they’re dying, you get them in wherever you can,” she said, speaking on the condition that she not be named to protect her son’s privacy.
They had the most expensive health plan her employer offered, but her insurer, citing MultiPlan, left the family with tens of thousands of dollars in bills.
“I expected there would be some payment that wasn’t covered,” she said. “What I didn’t expect was the deceit that caused an even higher payment, an amount I never dreamed.”
Insurers sometimes suggest that a medical provider agreed to a lower payment, even when it’s not so. This patient was billed the amount that Cigna identified as savings.
You saved $370.62 . CIGNA negotiates discounts with health care professionals and facilities to help save you money.
Source: Read the PDF.
Some providers said they had begun requiring payment upfront or stopped accepting patients with certain insurance plans because appealing for higher payments can be time-consuming, infuriating and futile. Others have tried to sue insurers or MultiPlan. Dr. Rabinowitz, who repaired Ms. Lawson’s incision, hopes to collect the remaining balance from UnitedHealthcare in an ongoing case.
Surprise bills for some types of care are no longer an issue, insurers said, thanks to the law that went into effect in 2022 . Brittany Perritt didn’t realize the anesthesiologists at her 3-year-old’s brain tumor treatments in 2020 were out-of-network until the claims went to MultiPlan. If that care occurred today, she likely would be spared the calls from debt collectors, because she didn’t go out of network by choice.
But MultiPlan assured investors shortly before the law’s passage that it was likely to have “limited impact” on the company. In fact, MultiPlan said, 90 percent of its revenue involved out-of-network claims that wouldn’t be affected.
‘Lining Their Pockets’
Debra Margraf, a trustee for a union health plan covering about 1,500 Phoenix-area electricians, was stunned when she and her colleagues asked Cigna what they had paid for “cost-containment” services.
The answer: The fees had risen from just over $550,000 in 2016 to $2.6 million in 2019, according to a lawsuit the trustees filed.
“It’s very frustrating to go out and have someone pitch us that they’re going to save us money and then end up lining their pockets,” Ms. Margraf said.
Cigna did not respond to questions from The Times about specific employer plans.
Other employers have also questioned increased fees and complained about being kept in the dark. A UnitedHealthcare account executive emailed colleagues for help explaining the $50,650 fee charged to New England Motor Freight. The fee grew out of a $152,594 bill, of which just $7,879 was covered.
The trucking company “thinks these are a money tree for us in fees and we are milking them,” the account executive wrote.
One UnitedHealthcare executive suggested a partial refund and an annual cap on fees, but a colleague countered, “We have to be concerned about setting precedent.”
Inside an Insurer’s Debate About Fees
Internal emails show UnitedHealthcare employees grappling with complaints about high fees. When one executive suggested limiting the amount charged New England Motor Freight, a colleague resisted.
As a company we have been unwilling to enter into one-off agreements that cap our revenue, so we have to be very careful.
The way the fees were calculated was particularly galling: How could MultiPlan and insurers tie their own fees to bills they deemed unreasonable? It made no sense, one consultant for the trucking company wrote, to charge a 35 percent fee “if a hospital were to bill $20,000 for a flu shot.”
UnitedHealthcare did not respond to questions from The Times about the trucking company. In a statement, the insurer said it also offers fee arrangements not tied to billed amounts.
Cigna’s statement defended its fee, saying that “it enables us to administer the program, negotiate with providers and absorb the long-term risk associated with any challenging negotiation.”
Even verifying the accuracy of fees was difficult when UnitedHealthcare initially refused to provide the trucking company with the full underlying data. Cigna refused a similar request from auditors for Arlington County, Va., which it had charged $261,000 in one year. “There is no process for verifying the accuracy of any of these amounts,” the auditors wrote.
Large employers also have trouble getting data from insurers, said James Gelfand, head of the ERISA Industry Committee, which represents big companies with employee benefit plans.
Cost-containment programs can be a “revenue center” for insurers, Mr. Gelfand said, but are “extremely difficult for employers to police.”
‘In a Lot of Pain’
Patients have limited recourse. If they want to sue, they usually must first complete an administrative appeals process; even then, they stand to collect relatively modest amounts.
Regulators are unlikely to step in. Self-funded employer plans are largely exempt from state oversight. And federal regulators have limited resources and legal authority to police them.
Even when patients figured out where to direct complaints — the Employee Benefits Security Administration — they described the process as draining and mostly fruitless.
Patti Sietz-Honig, a video editor at Fox 5 in New York, filed a complaint in 2022. The cost of seeing a specialist for chronic back pain had spiked, and she faced roughly $60,000 in bills.
Ms. Sietz-Honig pressed for updates about her complaint and sent articles critical of MultiPlan from Capitol Forum, a site focused on antitrust and regulatory news. Last March, the agency emailed her that her employer and her insurer, Aetna, had agreed to a “temporary exception” and made additional payments.
“Unfortunately,” the agency wrote, the law “does not prohibit the use of third-party vendors” to calculate payments.
Meanwhile, her longtime pain specialist started requiring payment upfront. To save money, Ms. Sietz-Honig spaced out her appointments.
“I’ve been in a lot of pain lately,” she said, “so I’ve been going — and paying.”
‘Not a Real Negotiation’
As MultiPlan became deeply embedded with major insurers, it pitched new tools and techniques that yielded even higher fees, and in some instances told insurers what unnamed competitors were doing, documents and interviews show.
After meeting in 2019 with a MultiPlan executive, a UnitedHealthcare senior vice president wrote in an internal email that other insurers were using MultiPlan’s aggressive pricing options more broadly, and that UnitedHealthcare could catch up.
“Dale did not specifically name competitors but from what he did say we were able to glean who was who,” the executive, Lisa McDonnel, wrote, referring to Dale White, then an executive vice president at MultiPlan. She described how Cigna, Aetna and some Blue Cross Blue Shield plans were apparently using MultiPlan.
In recent years, MultiPlan’s top revenue generator has been an algorithm-based tool called Data iSight that consistently produces the lowest payment recommendations. Some insurers have used it as part of strategy MultiPlan calls “target pricing” or “meet-or-beat”: Insurers set a maximum price they will pay, and MultiPlan collects a fee only if its recommendation is lower.
In theory, many of MultiPlan’s recommendations are negotiable. But documents and interviews revealed tactics meant to pressure medical practices to accept low payments. Some offers came with all-caps admonitions and deadlines just hours away. Accept and receive prompt payment; refuse and risk an even lower payout. Practices and billing specialists said this often wasn’t an empty threat.
“It’s not a real negotiation,” said Tammie Farkas, who handles billing for her husband’s small New York-area practice focused on repairing blood vessels in the brain.
Insurers can set negotiation parameters for MultiPlan, including not negotiating at all, records and interviews show. Multiple providers and billing specialists said that in recent years they had increasingly been told their claims weren’t eligible for negotiation.
“It wasn’t this bad before,” said Tiffany Letosky, who oversees a small practice specializing in surgeries for endometriosis and gynecologic cancers.
Former MultiPlan negotiators said their bonuses had been linked to their success at reducing payments, incentivizing a hard-line approach.
Ms. Young, the former negotiator critical of the process, said she had occasionally called a provider from a cellphone — knowing that her work line was recorded — and advised against accepting her own offer.
Another former negotiator said the pressure to get bigger discounts had made her physically ill. “It was just a game,” she said. “It’s sad.”
Jennifer Pittinger, also a former negotiator, said she saw nothing wrong with the hard-driving approach because she believed she was combating overbilling.
“I was a bit of a viper,” she said. “Sometimes I just wanted to go in as hard as I could because my bonus is affected. If I can get a provider to accept 50 percent off, that’s great for me.”
But tools rolled out to combat price-gouging hospitals and private-equity profiteers, The Times found, have also been directed at people like Ms. Toney, the therapist in rural Virginia who treats children with autism.
She charges the rates that Virginia pays for people on Medicaid. But last year, she said, Meritain Health, an Aetna subsidiary, informed her that fair payment for her services was less than half what Medicaid paid, based on calculations by MultiPlan.
Ms. Toney has not billed the parents of her two patients covered by Meritain, but going forward she will not accept patients with similar insurance.
“It puts me in a tough position,” she said. “Do I want to pay myself a salary or be able to help people?”
Julie Tate contributed research. Produced by Guilbert Gates and Rumsey Taylor .
Chris Hamby is an investigative reporter for The Times, based in Washington. More about Chris Hamby

IMAGES
VIDEO
COMMENTS
Scenario 1: The insurance plan covers the surgery. If people have a health insurance plan that covers gender affirmation surgery, people will need to take steps to ensure they meet certain ...
Gender-affirming surgery can cost between $6,900 and $63,400 depending on the precise procedure, according to a 2022 study published in The Journal of Law, Medicine and Ethics. Out-of-pocket costs ...
Medicare. Medicare is federal health insurance for people 65 or older and some younger people with disabilities. Original Medicare (Part A and Part B) will cover gender-affirmation surgery when it is considered medically necessary. Prior to 2014, no coverage was offered.
The cost of transgender surgery can vary by provider and the type of surgery you choose to get. For a female-to-male transition, masculinization chest surgery (also known as top surgery) might ...
Hormone therapy can cost anywhere from $25 to $200 a month. That's between $300 and $2,400 a year. What's more, the counseling involved in preparing for a gender transition (and required by many doctors and insurance companies), can cost between $50 and $200 a session. In short, transitioning is expensive.
How Much Does Gender-Affirming Surgery Cost? For just one person, the cost of gender-affirming care might range from $25,000 to $75,000, according to estimates from the HRC Foundation.
The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed. A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019. Insurance Coverage for Sex Reassignment Surgery.
The standard premium for Medicare Part B in 2020 is $144.60 each month, and there is a $198 annual deductible cost. After a person pays the deductible, Medicare pays 80% of the allowable costs ...
Research consistently shows that people who choose gender affirmation surgery experience reduced gender incongruence and improved quality of life. Depending on the procedure, 94% to 100% of people report satisfaction with their surgery results. Gender-affirming surgery provides long-term mental health benefits, too.
Plans with transgender exclusions. Many health plans are still using exclusions such as "services related to sex change" or "sex reassignment surgery" to deny coverage to transgender people for certain health care services. Coverage varies by state. Before you enroll in a plan, you should always look at the complete terms of coverage ...
While Section 1557 was initially a big step towards equality in health care for transgender Americans, it does not explicitly require coverage for sex reassignment surgery and related medical care. And the implementation of Section 1557 has been a convoluted process with various changes along the way. Most recently, the Biden administration has ...
If you need help applying for insurance or have questions, you can call our Consumer Advocates at (872) 228-2549. Some plans that exclude coverage for gender-affirming surgery use language like "all procedures related to being transgender are not covered.". They may have prohibitive language around words like "gender change," "gender ...
Gender Confirmation Surgeries. Average Cost: $5,000-$50,000. Gender confirmation surgery for transgender patients refers to reconstructive surgeries to bring patients' bodies into conformity with their experienced gender. Surgeries might include reconstruction of the chest and/or face.
What gives: Though gender dysphoria is relatively uncommon, many of the billing and insurance issues Vetens encountered are typical for patients planning major surgery. Much of her stress and ...
Gender affirming chest surgery ( augmentation, mastectomy, or reduction) is considered reconstructive when all of the following criteria have been met: The individual is at least 18 years of age (see Further Considerations section below for individuals under 18 years of age); and. The individual has capacity to make fully informed decisions and ...
In a systematic review, Gorbea et al (2021) provided a portrait of gender affirmation surgery (GAS) insurance coverage across the U.S., with attention to procedures of the head and neck. State policies on transgender care for Medicaid insurance providers were collected for all 50 states. ... Tonseth KA, Bjark T, Kratz G, et al. Sex reassignment ...
Trans Health Insurance Tutorial. Choosing a Plan; Understanding Your Plan; Applying for Coverage; ... Prev Index Gender Dysphoria/Reassignment [99 of 162] Next. Humana Gender Affirmation Surgery. Policy: Gender Affirmation Surgery Policy Number: HUM-0518-020 Last Update: 2023-09-28 ...
Of the total 150 insurance companies identified, policies related to gender- affirming surgery were found for 124. Coverage for gender-affirming surgery varies by insurance company, state, and procedure. Most insurance companies, 122 of 124 (98%), covered chest masculinization, but only 25 of 124 (20%) of insurance companies covered nipple ...
Sarah Huny Young for The New York Times. Allison Escolastico, a 30-year-old transgender woman, has wanted breast augmentation surgery for a decade. By 2019, she finally thought her insurance ...
Compared to the general US population, transgender people are more likely to be uninsured (14% vs. 11%), unemployed (15% vs. 5%), and living in poverty (29% vs. 12%). 7 Even for people with insurance, reports of insurance denials are common, 8 and many people report that deductibles and other out-of-pocket costs like copays and coinsurance for ...
Critics are raging against New York's proposed "Equal Rights Amendment," claiming the Nov. 5 ballot measure could curb the rights of parents when it comes to allowing minors to undergo ...
Your gender identity typically doesn't affect your eligibility for life insurance or the amount and type of coverage you need, says Rikin Shah, CEO of GetSure, a life insurance brokerage based ...
Weeks after undergoing heart surgery, Gail Lawson found herself back in an operating room. ... Gail Lawson faced more than $100,000 in bills after a complex surgery. Her insurance paid out $5,449.27.