

Essay on Healthcare in India
Students are often asked to write an essay on Healthcare in India in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Healthcare in India
Introduction.
Healthcare in India is a critical sector. It includes public and private hospitals, clinics, and other medical facilities.
Public Healthcare
The government provides public healthcare. It’s often free or low-cost, making it accessible to many people.
Private Healthcare
Private healthcare, on the other hand, is usually more expensive. However, it tends to have better facilities and shorter wait times.
India faces challenges in healthcare, like inadequate facilities in rural areas and a shortage of trained medical professionals.
Despite these challenges, India is striving to improve its healthcare system for everyone.
250 Words Essay on Healthcare in India
Healthcare in India is a multifaceted system, encompassing public and private sectors, traditional and modern medicine, and urban and rural disparities. This essay explores the current state of healthcare in India, its challenges, and potential solutions.
Current State of Healthcare
India’s healthcare sector has made significant strides, with increased life expectancy and decreased infant mortality. However, it is riddled with disparities. While urban areas enjoy better healthcare facilities, rural regions grapple with inadequate infrastructure and lack of trained medical personnel.
The challenges are manifold. Accessibility and affordability remain major concerns. A large portion of the population lacks access to quality healthcare, while high out-of-pocket expenses push many into poverty. Furthermore, there is a significant shortage of healthcare professionals, particularly in rural areas.
Public-Private Partnership
A public-private partnership (PPP) is seen as a viable solution. The private sector’s resources and efficiency can supplement the public sector’s reach and affordability. However, the implementation of PPPs requires stringent regulations to prevent exploitation.
Role of Technology
Technology can bridge the urban-rural divide. Telemedicine, AI, and mobile health technologies can facilitate remote consultations, predictive diagnostics, and health monitoring, making healthcare more accessible and affordable.
While India’s healthcare system faces significant challenges, the combination of public-private partnerships and technology can pave the way for an efficient, inclusive, and affordable healthcare system. It is crucial for policymakers, healthcare providers, and technology companies to work together towards this common goal.
500 Words Essay on Healthcare in India
India’s healthcare sector is a study in contrasts, presenting a complex tapestry of cutting-edge advancements and systemic challenges. With an expansive population and diverse health needs, the healthcare system in India is a critical component of the nation’s development agenda.
The Landscape of Indian Healthcare
India’s healthcare infrastructure is a mix of public and private providers. The public system, under the aegis of the Ministry of Health and Family Welfare, provides primary, secondary, and tertiary care. However, it suffers from inadequate funding, lack of infrastructure, and a dearth of healthcare professionals. The private sector, on the other hand, is burgeoning. It is technologically advanced, offers high-quality services, but is often criticized for being expensive and inaccessible to the poor.
Healthcare Accessibility and Affordability
Access to quality healthcare is a significant issue in India. Rural areas, in particular, face a shortage of healthcare facilities and professionals. The urban-rural divide is stark, with the majority of quality healthcare services concentrated in cities. Affordability is another concern. High out-of-pocket expenses push many into poverty every year. The situation calls for a robust health insurance framework to protect citizens from catastrophic health expenditures.
Government Initiatives
Recognizing these challenges, the Indian government has launched various initiatives. The National Health Mission aims to improve health outcomes, particularly for the rural population. The Ayushman Bharat scheme, launched in 2018, provides health insurance coverage to the underprivileged, aiming to make healthcare more affordable. These initiatives, while commendable, need effective implementation and monitoring to ensure their success.
Technological Innovations
Technological innovations have the potential to revolutionize India’s healthcare landscape. Telemedicine, artificial intelligence, and digital health records can address the issues of accessibility and affordability. Telemedicine can bridge the urban-rural divide by providing remote consultations. AI can assist in disease prediction and management, while digital health records can streamline patient data, improving efficiency and patient care.
Challenges and Future Prospects
Despite these advancements, India’s healthcare system faces significant challenges. The COVID-19 pandemic has exposed the fragility of the healthcare infrastructure, with hospitals overwhelmed and resources stretched thin. India also grapples with a dual disease burden – communicable diseases like tuberculosis and non-communicable diseases like diabetes and heart disease.
The future of healthcare in India lies in adopting a holistic approach. This includes increasing public health expenditure, strengthening primary healthcare, improving health literacy, and leveraging technology.
India’s healthcare sector, while fraught with challenges, is teeming with potential. With the right mix of policy interventions, technology adoption, and a focus on equitable access, India can transform its healthcare landscape, ensuring a healthier future for its citizens. The journey is long and arduous, but with concerted efforts, a robust and inclusive healthcare system is achievable.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on Handloom and Indian Legacy
- Essay on Growth of Banking Sector in India
- Essay on Greatness of India
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Featured Topics
Featured series.
A series of random questions answered by Harvard experts.
Explore the Gazette
Read the latest.

How dating sites automate sexual racism
Forget ‘doomers.’ Warming can be stopped, top climate scientist says

Finding middle way out of Gaza war
Community nurse Swasthya Sakhi, who was trained by the host organization, during a routine day at work in Kaniguma village’s Swasthya Swaraj clinic.
Photos by Amrit Vatsa
Amid pandemic tragedy, an opportunity for change?
Alvin Powell
Harvard Staff Writer
Mittal Institute/Lancet commission to study universal care in India
With almost 11 million cases and more than 150,000 deaths, India is among the nations hardest-hit by the coronavirus pandemic. The Asian giant has also taken an economic hit, its gross domestic product expected to shrink 8 percent this year.
The figures have starkly highlighted the connection between a nation’s physical and economic health, and the Harvard chairs of a new panel seeking to overhaul and improve health care in India say today’s difficult times create a moment of opportunity because people who often tune each other out are now listening.
“For the first time the connection between health and economic outcomes has become transparent,” said Tarun Khanna , director of Harvard’s Lakshmi Mittal and Family South Asia Institute and one of four co-chairs of a new Lancet Citizens’ Commission to study how to bring universal health care to India. “The morality of universal health care has always been a driver of this urgency, but that’s not the new thing here. Rather, for the first time in 30 years GDP is expected to fall in response to a health crisis.”
The 21-member commission is a joint effort between The Lancet medical journal and Mittal Institute. The panel is chaired by Khanna; Vikram Patel , the Pershing Square Professor of Global Health at Harvard Medical School ; Professor Gagandeep Kang, vaccine researcher at Christian Medical College in Vellore, India; and Kiran Mazumdar-Shaw, executive chairperson of Indian biotech company Biocon Ltd and one of India’s top businesspeople. S.V. Subramanian , professor of population health and geography at the Harvard T.H. Chan School of Public Health , is a member of the commission.
The group’s charge is to report by August 2022 how India can achieve universal health care within a decade. The Mittal Institute is encouraging participation by the Harvard community and sponsoring an online panel discussion on Monday to introduce the effort.
Patel and Khanna said the commission has a challenging road ahead, one that has proven too difficult for an array of efforts studying the same question in the decades since India became independent in 1947.
Most of the nation’s 1.4 billion residents (a population second only to China) view the current publicly-funded system as so bad that even the poorest Indians would rather pay out-of-pocket for care in a network of private providers, itself sometimes seen as uncaring and untrustworthy. The end result is that more than 60 percent of Indian health care is paid for out-of-pocket, and a sudden illness can mean financial ruin for millions. Only the wealthy can afford regular, high-quality care.
Sandeep Praharsha (India Fellow) discussing preventive measures for malaria in Kerpai village in Thumul Rampur block of Kalahandi district in Odisha Swasthya Swaraj.
“Today, India’s health care system is routinely ranked as one of the worst in the world,” Patel said. “A few get expensive, world-class care, while a large part of the population doesn’t even get basic quality care.”
Where the current commission differs from prior efforts is that it is based on a consultative effort to seek input from an array of stakeholders, including representatives of the private health care sector, providers of traditional medicine, physicians, community health workers, and citizens from diverse communities across the country.
“It genuinely is a cross-section of society,” said Khanna, HBS’ Jorge Paulo Lemann Professor. “That makes consultation more complex, but the potential for achievement is large.”
The eventual report will focus on the “architecture” of a new system, according to an article by the initiative’s co-chairs and commissioners in The Lancet in December. It will include ways to provide preventive care for physical and mental health, offer financial protection for all health care costs, not just hospitalization, and ensure access to the same quality of care for all.
“We aspire for a health care system in which most people do not pay out-of-pocket for most health care needs,” Patel said. “The last thing a sick person needs is to have their care calibrated by how much they can afford to pay or to be impoverished by their medical bills.”
Resources are always a key issue in consideration of universal health care and India — whose proportion of GDP spent on health care is low compared with other middle-income countries — will likely have to spend more, Khanna said. But he also said that significant low-cost steps probably could be taken early in the process.
“I think we can improve outcomes with existing resources being better managed,” Khanna said. “We can get some victories in the next two to three years through optimization of existing structures.”
Share this article
You might like.
Sociologist’s new book finds algorithms that suggest partners often reflect stereotypes, biases
Michael Mann points to prehistoric catastrophes, modern environmental victories

Educators, activists explore peacebuilding based on shared desires for ‘freedom and equality and independence’ at Weatherhead panel
College accepts 1,937 to Class of 2028
Students represent 94 countries, all 50 states
Pushing back on DEI ‘orthodoxy’
Panelists support diversity efforts but worry that current model is too narrow, denying institutions the benefit of other voices, ideas

Improving Health in India
As the world’s second-most-populous country and one of its fastest-growing economies, India faces both unique challenges and unprecedented opportunities in the sphere of public health.
For more than a decade, India has experienced record-breaking economic growth that has been accompanied by significant reductions in poverty. According to the World Bank, infant mortality in India fell from 66 to 38 per 1,000 live births from 2000 to 2015. Life expectancy at birth has increased from 63 to 68 years, and the maternal mortality ratio has fallen from 374 to 174 per 100,000 live births over the same period.
India also has dynamic pharmaceutical and biotechnology industries; world-class scientists, including a burgeoning clinical trials industry; and leading hospitals that attract foreign patients and treat its better-off citizens.
Yet Indian government and public health officials agree that the country also faces persistent and daunting public health challenges, particularly for the poor. These include child undernutrition and low birth weights that often lead to premature death or lifelong health problems; high rates of neonatal and maternal mortality; growth in noncommunicable diseases such as obesity, diabetes, and tobacco use, leading to cancer and other diseases; and high rates of road traffic accidents that result in injuries and deaths.
As the Indian government strives to provide comprehensive health coverage for all, the country’s rapidly developing health system remains an area of concern. There are disparities in health and health care systems between poorer and richer states and underfunded health care systems that in many cases are inefficiently run and underregulated. New government-financed health insurance programs are increasing coverage, but insurance remains limited.
Public and private health systems are placing huge demands on the country’s capacity to train exceptional health leaders and professionals. Rising to meet these challenges, the people of India have an opportunity to have a major influence on their own future health and on the future of public health and medical efforts globally.
Supporting Development of India’s Health Workforce
The Harvard T.H. Chan School of Public Health is collaborating with partners across India to address those challenges. Together, the School and its partners are introducing educational innovations to India to expand skills training, degree programs, and leadership development at new schools and institutes of public health. We seek to leverage the School’s resources to help strengthen public health training and build capacity across the health sector in India.
Skip to content
Read the latest news stories about Mailman faculty, research, and events.
Departments
We integrate an innovative skills-based curriculum, research collaborations, and hands-on field experience to prepare students.
Learn more about our research centers, which focus on critical issues in public health.
Our Faculty
Meet the faculty of the Mailman School of Public Health.
Become a Student
Life and community, how to apply.
Learn how to apply to the Mailman School of Public Health.
Comparative Health Policy Library
India | summary.
- Population: 1.38 billion
- Housing: 33% Urban, 67% Rural
Health & Health system
Health indicators & demographics.
- Fertility Rate: 2.2 live births per woman
- Life Expectancy (Female, Male): 72, 69
- Infant Mortality Rate: 26.6 deaths per 1,000 live births
- Child Mortality Rate: 32.9 per 1,000 live births
- Maternal Mortality Rate: 113 deaths per 100,000 live births
- Prevalence of Obesity: 4%
- Indo-Aryan: 72%
- Dravidian (South Indian): 25%
- 0-14 years: 27%
- 15-24 years: 17.8%
- 25-54 years: 41.2%
- 55-64 years: 7.6%
- 65 years and over: 6.4%
1 The World Bank. India . Data. https://data.worldbank.org/country/india .
2 The World Bank. (2017). Current health expenditure (% of GDP). Data. https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS .
3 India Population 2020 (Live). India Population 2020 (Demographics, Maps, Graphs). (2020). https://worldpopulationreview.com/countries/india-population .
4 Mushtaq, M. (2009). Public health in British India: A brief account of the history of medical services and disease prevention in colonial India. Indian Journal of Community Medicine, 34(1), 6–14. https://doi.org/10.4103/0970-0218.45369
5 Mushtaq, M. (2009). Public health in British India: A brief account of the history of medical services and disease prevention in colonial India. Indian Journal of Community Medicine, 34(1), 6–14. https://doi.org/10.4103/0970-0218.45369
6 Healthcare System in India. International Student Insurance. https://www.internationalstudentinsurance.com/india-student-insurance/he... .
7 Tabish, S. A. Health Planning: Past, Present & Future. In Hospital & Health Services Administration: Principles & Practice. essay. https://www.researchgate.net/publication/290447383_Historical_Developmen... .
8 OVERVIEW OF INDIAN HEALING TRADITIONS: History and Science of Indian Systems of Knowledge. OVERVIEW OF INDIAN HEALING TRADITIONS | History and Science of Indian Systems of Knowledge. https://www.ncbs.res.in/HistoryScienceSociety/content/overview-indian-he... .
9 Ranjan, A. (2018, August 17). Healthcare System in Pre and Post Independence India. Medlife Blog: Health and Wellness Tips. https://www.medlife.com/blog/healthcare-system-pre-post-independence-india/ .
10 Alam, M., & Allchin, F. R. India. In Encyclopedia Britannica. essay. https://www.britannica.com/place/India/Health-and-welfare .
11 Tikkanen, R., Osborn, R., Mossialos, E., Djordjevic, A., & Wharton, G. A. (2020, June 5). India. Commonwealth Fund. https://www.commonwealthfund.org/international-health-policy-center/coun... .
12 Ehrenfeld , T. (2018, September 25). Comparing the Healthcare Systems in India and the United States. Healthline. https://www.healthline.com/health-news/comparing-healthcare-systems-indi... .
13 Brand India. IBEF. (2020, September 6). https://www.ibef.org/industry/healthcare-india.aspx .
14 Harvard T.H. Chan School of Public Health. (2018, March 7). Improving Health in India. India Research Center. https://www.hsph.harvard.edu/india-center/improving-health-in-india/ .
15 Healthcare System in India. International Student Insurance. https://www.internationalstudentinsurance.com/india-student-insurance/he... .
16 Geography Now! India. (2017). YouTube. https://www.youtube.com/watch?v=vEy6tcU6eLU .
17 India Population (LIVE). Worldometer. (2020). https://www.worldometers.info/world-population/india-population/ .
18 India Age structure. India Age structure - Demographics. (2020). https://www.indexmundi.com/india/age_structure.html .
Suggest Additional Subjects and Resources
Other topics or articles you'd like to see included in the Comparative Health Policy Library?
- Screen Reader
- Skip to main content
- Text Size A
- Language: English
Case Studies
- EXIM Procedure
Media & Events
- Image Gallery
- Media Coverage
Other Links
- GI of India
- Experience India
- Indian Trend Fair 2022
India Organic Biofach 2022
Gulfood dubai 2023, healthcare industry in india, the indian health-tech market is expected to grow at a cagr of 39% and touch us$ 50 billion by 2033., advantage india, strong demand.
* Healthcare market in India is expected to reach US$ 372 billion by 2022, driven by rising income, better health awareness, lifestyle diseases and increasing access to insurance.
* The healthcare sector is expected to generate 27 lakh jobs in India between 2017-22, over 5 Lakh jobs per year.
Attractive Opportunities
* India’s public expenditure on healthcare touched 2.1 % of GDP in FY23 and 2.2% in FY22, against 1.6% in FY21, as per the Economic Survey 2022-23.
* Two vaccines (Bharat Biotech's Covaxin and Oxford-AstraZeneca’s Covishield manufactured by SII) were instrumental in medically safeguarding the Indian population against COVID-19.
Rising Manpower
* Availability of a large pool of well-trained medical professionals in the country.
* The number of allopathic doctors with recognised medical qualifications (under the I.M.C Act) registered with state medical councils/national medical council increased to 1.3 million in November 2021, from 0.83 million in 2010.
Policy and government support
* In the Union Budget 2023-24, the government allocated Rs. 89,155 crore (US$ 10.76 billion) to the Ministry of Health and Family Welfare (MoHFW).
* The Indian government is planning to introduce a credit incentive programme worth Rs. 500 billion (US$ 6.8 billion) to boost the country’s healthcare infrastructure.
Healthcare Industry Report
Introduction.
Healthcare has become one of India’s largest sectors, both in terms of revenue and employment. Healthcare comprises hospitals, medical devices, clinical trials, outsourcing, telemedicine, medical tourism, health insurance and medical equipment. The Indian healthcare sector is growing at a brisk pace due to its strengthening coverage, services, and increasing expenditure by public as well as private players.
India’s healthcare delivery system is categorised into two major components - public and private. The government, i.e., the public healthcare system, comprises limited secondary and tertiary care institutions in key cities and focuses on providing basic healthcare facilities in the form of Primary Healthcare Centers (PHCs) in rural areas. The private sector provides the majority of secondary, tertiary, and quaternary care institutions with a major concentration in metros, tier-I, and tier-II cities.
India's competitive advantage lies in its large pool of well-trained medical professionals. India is also cost-competitive compared to its peers in Asia and Western countries. The cost of surgery in India is about one-tenth of that in the US or Western Europe. The low cost of medical services has resulted in a rise in the country’s medical tourism, attracting patients from across the world. Moreover, India has emerged as a hub for R&D activities for international players due to its relatively low cost of clinical research.

Market Size
The Indian healthcare sector is expected to record a three-fold rise, growing at a CAGR of 22% between 2016–22 to reach US$ 372 billion in 2022 from US$ 110 billion in 2016. By FY22, Indian healthcare infrastructure is expected to reach US$ 349.1 billion. The healthcare sector is expected to generate 27 lakh jobs in India between 2017-22, over 5 Lakh jobs per year.
India’s public expenditure on healthcare touched 2.1 % of GDP in FY23 and 2.2% in FY22, against 1.6% in FY21, as per the Economic Survey 2022-23.
In FY22, premiums underwritten by health insurance companies grew to Rs. 73,582.13 crore (US$ 9.21 billion). The health segment has a 33.33% share in the total gross written premiums earned in the country.
The Indian medical tourism market was valued at US$ 2.89 billion in 2020 and is expected to reach US$ 13.42 billion by 2026. According to India Tourism Statistics at a Glance 2020 report, close to 697,300 foreign tourists came for medical treatment in India in FY19. India has been ranked tenth in the Medical Tourism Index (MTI) for 2020-21 out of 46 destinations by the Medical Tourism Association. With US$ 5-6 billion size of Medical value travel (MVT) and 500000 International patients annually, India is among the global leader destinations for international patients seeking advanced treatment.
The e-health market size is estimated to reach US$ 10.6 billion by 2025.
As per information provided to the Lok Sabha by the Minister of Health & Family Welfare, Dr. Bharati Pravin Pawar, the doctor population ratio in the country is 1:854, assuming 80% availability of 12.68 lakh registered allopathic doctors and 5.65 lakh AYUSH doctors.
Investments/ Developments
Between April 2000-September 2023, the FDI inflow for the drugs and pharmaceuticals sector stood at US$ 21.58 billion, according to the data released by Department for Promotion of Industry and Internal Trade (DPIIT). Inflows in sectors such as hospitals and diagnostic centres and medical and surgical appliances stood at US$ 9.48 billion and US$ 3.22 billion, respectively, between April 2000-September 2023.
During 2022-23 (up to December 2022) Foreign Direct Investment, (FDI) inflow in India stood at US$ 36,746 million. Some of the recent developments in the Indian healthcare industry are as follows:
- As of August 1, 2023, a total of 24.33 crore Ayushman cards have been created. To prevent, detect, and deter healthcare fraud and to ensure that eligible beneficiaries receive adequate treatment, the Government of India is using Artificial Intelligence (AI) and Machine Learning (ML). As on October, 2023, a total of 26 crore Ayushman cards have been created.
- As of February 20, 2023, more than 220.63 crore COVID-19 vaccine doses have been administered across the country. While as of May 11, 2023, more than 2.20 billion COVID-19 vaccine doses have been administered across the country.
- As of July 15, 2023, India has exported 30.12 crore vaccine doses.
- Multinational healthcare company Abbott has committed to converting 75 Primary Health Centers (PHCs) to Health and Wellness Centers (HWCs) in nine Indian States, in collaboration with Americares India Foundation, a nonprofit organisation dedicated to relief and development in the field of health. This will benefit over 2.5 million people from under-resourced communities every year.
- In November 2022, diabetes management app BeatO raised US$ 33 million in its Series B funding round led by impact investor Lightrock India.
- In August 2022, Edelweiss General Insurance partnered with the Ministry of Health, Government of India, to help Indians generate their Ayushman Bharat Health Account (ABHA) number.
- The healthcare and pharmaceutical sector in India had M&A activity worth US$ 4.32 billion in the first half of 2022.
- As of 2023, the number medical colleges in India stood at 706.
- In July 2022, the Indian Council of Medical Research (ICMR) released standard treatment guidelines for 51 common illnesses across 11 specialities to assist doctors, particularly in rural regions, in diagnosing, treating, or referring patients in time for improved treatment outcomes.
- In July 2022, the National Pharmaceutical Pricing Authority (NPPA) fixed the retail prices for 84 drug formulations, including those used for the treatment of diabetes, headache, and high blood pressure.
- In March 2022, Hyderabad-based pharmaceutical company Biological E applied for emergency use authorisation (EUA) for its Covid-19 vaccine Corbevax for the 5-12 years age group.
- In January 2022, Phase 3 trials commenced of India's first intranasal vaccine against COVID-19 which is being developed by Bharat Biotech, in conjunction with the Washington University School of Medicine in St Louis, the US.
- Startup HealthifyMe, with a total user base of 30 million people, is adding half a million new users every month and crossed US$ 40 million ARR in January 2022.
- The number of policies issued to women in FY21 stood at 93 lakh, with one out of every three life insurance policies in FY21 sold to a woman.
- In December 2021, Eka Care became the first CoWIN-approved organization in India, through which users could book their vaccination slot, download their certificate, and even create their Health IDs.
- As of November 18, 2021, 80,136 Ayushman Bharat Health and Wellness Centres (AB-HWCs) are operational in India.
- As of November 18, 2021, 638 e-Hospitals are established across India as part of the central government's ‘Digital India’ initiative.
- In November 2021, Aster DM Healthcare announced that it is planning Rs. 900 crore (US$ 120.97 million) capital expenditure over the next three years to expand its presence in India, as it looks at increasing the share of revenue from the country to 40% of the total revenue by 2025.
- In September 2021, a Russian-made COVID-19 vaccine, Sputnik Light received permission for Phase 3 trials in India.
- In September 2021, Biocon Biologics Limited, a subsidiary of Biocon, announced a strategic alliance with Serum Institute Life Sciences, a subsidiary of Serum Institute of India (SII). The alliance is expected to strengthen India's position as a global vaccine and biologics manufacturing powerhouse.
Government Initiatives
Some of the major initiatives taken by the Government of India to promote the Indian healthcare industry are as follows:
- PoshanAbhiyan is a Centrally Sponsored Scheme with the implementation of the scheme being done by States/UTs. To ensure that all Anganwadi Centres are equipped with Smartphones and Growth Monitoring devices (GMDs) such as Infantometer, Stadiometers, and Weighing Scale for Mothers and Infant, the Ministry has released revised guidelines for technical specifications and replacement of GMDs by the States.
- Under the Union Budget 2023-24, the Ministry of Health and Family Welfare has been allocated Rs. 89,155 crore (US$ 10.76 billion), an increase of 3.43% compared to Rs. 86,200.65 crore (US$ 10.4 billion) in 2021-22.
- Pradhan Mantri Swasthya Suraksha Yojana (PMSSY) was allocated Rs. 3,365 crore (US$ 0.41 billion)
- Human Resources for Health and Medical Education was allotted Rs. 6,500 crore (US$ 780 million).
- National Health Mission was allotted Rs. 29,085 crore (US$ 3.51 billion).
- Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana (AB-PMJAY) was allotted Rs. 7,200 crore (US$ 870 million).
- In July 2022, the World Bank approved a US$ 1 billion loan towards India's Pradhan Mantri-Ayushman Bharat Health Infrastructure Mission.
- To promote medical tourism in the country, the government of India is extending the e-medical visa facility to the citizens of 156 countries.
- In May 2022, the Union Government approved grants for five new medical colleges in Gujarat with a grant of Rs. 190 crore (US$ 23.78 million) each. These colleges will come up in Navsari, Porbandar, Rajpipla, Godhra and Morbi.
- In November 2021, the Government of India, the Government of Meghalaya, and the World Bank signed a US$ 40-million health project for the state of Meghalaya. The project will improve the quality of health services and strengthen the state’s capacity to handle future health emergencies, including the COVID-19 pandemic.
- In September 2021, Prime Minister Mr. Narendra Modi launched the Ayushman Bharat Digital Mission. The mission will connect the digital health solutions of hospitals across the country. Under this, every citizen will now get a digital health ID and their health record will be digitally protected.
- In September 2021, the Telangana government, in a joint initiative with World Economic Forum, NITI Aayog and HealthNet Global (Apollo Hospitals), launched the ‘Medicine from the Sky’ project. The project will pave the way for drone delivery of life-saving medicines and jabs in far-flung regions of the country.
- According to a spokesperson, the Indian government is planning to introduce a credit incentive programme worth Rs. 500 billion (US$ 6.8 billion) to boost the country’s healthcare infrastructure. The programme will allow firms to leverage the fund to expand hospital capacity or medical supplies with the government acting as a guarantor and strengthening COVID-19-related health infrastructure in smaller towns.
- In July 2021, the Ministry of Tourism established the ‘National Medical & Wellness Tourism Board’ to promote medical and wellness tourism in India.
- In July 2021, the Union Cabinet approved the continuation of the National Ayush Mission, responsible for the development of traditional medicines in India, as a centrally sponsored scheme until 2026.
- In July 2021, the Union Cabinet approved the MoU between India and Denmark on cooperation in health and medicine. The agreement will focus on joint initiatives and technology development in the health sector, to improve the public health status of the population of both countries.
- In June 2021, the Ministry of Health, and Family Welfare, in partnership with UNICEF, held a capacity-building workshop for media professionals and health correspondents in Northeastern states on the current COVID-19 situation in India, to bust myths regarding COVID-19 vaccines & vaccination and reinforce the importance of COVID-19 Appropriate Behaviour (CAB).
India’s healthcare sector is extremely diversified and is full of opportunities in every segment, which includes providers, payers, and medical technology. With the increase in the competition, businesses are looking to explore the latest dynamics and trends which will have a positive impact on their business. The hospital industry in India is forecast to increase to Rs. 8.6 trillion (US$ 132.84 billion) by FY22 from Rs. 4 trillion (US$ 61.79 billion) in FY17 at a CAGR of 16–17%.
India is a land full of opportunities for players in the medical devices industry. The country has also become one of the leading destinations for high-end diagnostic services with tremendous capital investment for advanced diagnostic facilities, thus catering to a greater proportion of the population. Besides, Indian medical service consumers have become more conscious towards their healthcare upkeep. Rising income levels, an ageing population, growing health awareness and a changing attitude towards preventive healthcare are expected to boost healthcare services demand in the future. Greater penetration of health insurance aided the rise in healthcare spending, a trend likely to intensify in the coming decade.
The Government aims to develop India as a global healthcare hub and is planning to increase public health spending to 2.5% of the country's GDP by 2025.
References: Department for Promotion of Industry and Internal Trade (DPIIT), RNCOS Reports, Media Reports, Press Information Bureau (PIB), Union Budget 2023-24
Related News
PwC India's report highlights GenAI's transformative impact on Indian healthcare, enhancing treatment efficiency and reshaping industry practices.
Female fresher recruitment by corporate entities notably escalated in 2023, particularly from tier 2 and 3 colleges, exhibiting a remarkable 116% year-on-year increase.
Health and Chemicals & Fertilisers Minister, Mr. Mansukh Mandaviya launches SIDBI credit scheme for Jan Aushadi Kendras, offering collateral-free loans with credit guarantee.
Prime Minister, Mr. Narendra Modi initiated the Nyaya Maha Abhiyan, a three-year mission with a project outlay of US$ 2.9 billion (Rs. 24,000 crore), and in the last three months, projects totalling over (Rs. 7000 crore) have been approved.
The healthcare infrastructure of a nation relies significantly on the pharmaceutical and medical device sectors, playing essential roles in preventive and curative healthcare systems.

Major Healthcare Centers in India

Industry Contacts
- Indian Medical Association
- Indian Healthcare Federation
- Indian Dental Association

OPEN YOUR EYES
With over 2.5 million operations performed and 20 million patients treated in the last 30 years, Aravind Eye Care System is the largest eye care provider in the world.
IBEF Campaigns

APEDA India Pavilion Gulfood February 20th-26th, 2022 | World Trade Centre,...

Ibef Organic Indian Pavilion BIOFACH2022 July 26th-29th, 2022 | Nuremberg, ...
India's White Revolution

The "White Revolution" in India refers to the successful implementation of Operation Flood, a dairy development program launched on January ...
The Growth of Ayurveda in India

Ayurveda, an ancient health system originating from India, has a longstanding history. It revolves around using plants and herbs to maintain health an...
The Success of Digital India

India's digital ecosystem has undergone an enormous change in recent years. The progressive integration of government services into digital platfo...
Unlocking India's Digital SME Credit Gap and Economic Potential
The Indian economy thrives on the contributions of the Micro, Small, and Me...

The Inevitable Emergence of Digital Engineering
Digital Engineering involves utilizing digital tools and technologies to de...
Introduction to Digital Payments- Unified Payments Interface (UPI) and RuPay credit cards in India
India's digital payment ecosystem has undergone a remarkable transforma...

Not a member
- State of International EM
- Open access
- Published: 04 August 2010
Emergency care in India: the building blocks
- Imron Subhan 1 &
- Anunaya Jain 2
International Journal of Emergency Medicine volume 3 , pages 207–211 ( 2010 ) Cite this article
4147 Accesses
23 Citations
Metrics details
The Republic of India, the world’s most populous democracy, has struggled with establishing Emergency Medical Care. However, with the recent recognition of Emergency Medicine as a formal specialty in medical training, there has been renewed vigor in the developments in the field.
Method and Results
We outline here the building blocks of the health care system in India, and the contribution each has made and is capable of making to the growth of emergency medical services. We also provide an account of the current situation of emergency medicine education in the country.
Conclusions
As we trace the development and status of emergency medicine in India, we offer insight into the current state of the field, what the future holds for the emergency medical community, and how we can get there.
Introduction
The Republic of India is the seventh largest country in the world and is home to nearly 1.2 billion people. With 28 states and 7 union territories (Fig. 1 ) spread over a vast geographic area with varying economic resources and infrastructure, India is the world’s most populous democracy.
Political map of India
The India of today is a young nation, finding its roots in socioeconomic development, and is plagued by challenges in health care created by its overwhelming population density of 943.9/mile², its limited ability to expand health care, the persistent burden of communicable diseases, and the rising liability of diseases of affluence [ 1 , 2 ].
Health care provision
Health care provision in India is multi-pronged, including a tiered national health system, private hospitals, and a multitude of alternative medicine practitioners.
The National Health Policy (NHP) was first formulated in 1983 [ 3 ]. This policy-guided government effort aims to provide health for all by outlining a time-bound phased setup of comprehensive primary health care services throughout the country. Under its aegis, health care services in centralized hospitals were made free for people below the poverty line, and numerous preventive programs were initiatied. The first review of the NHP in 2002 focused on the new objective of achieving an acceptable standard of good health among the general population of the country by advocating higher expenditure on health care with equitable access to health care services [ 4 ].
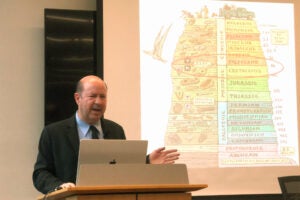
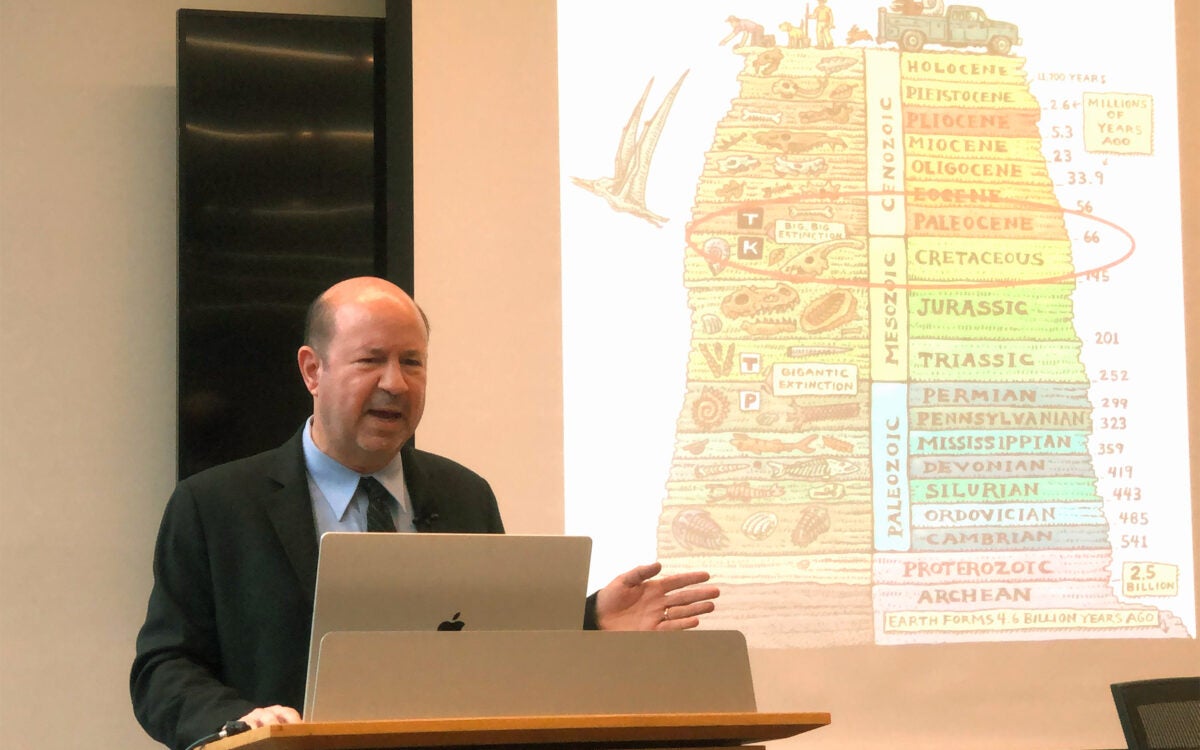
The tiered system of public health care is highlighted in Fig. 2 . It serves as the front line of emergency medical care for the masses. The system has remained plagued by a lack of accountability and staffing. According to the 2004 WHO statistics, the number of PHCs in India is 23,109, which is far below the required number. The lack of organized pre-hospital care coupled with the lack of resources and the high volume of patients that throng the government-run tertiary care hospitals further compound problems [ 7 ].
Tiered health care system
This system is further complicated by the unregulated expansion of private health care facilities in the country. The average person today considers expenditure in these private hospitals to receive health care far more acceptable than submitting to the unprofessionalism rampant in many of the public health care delivery areas. This has prompted an anarchy of sorts, with the private hospitals dictating costs.
The lack of universal medical insurance only compounds this issue, as do the limited economic resources. The federal expenditure on health care in India was 8.8% of the GDP in 2003. The public expenditure was only 25%, whereas the private expenditure was 75%, a practice very different from developed nations like the USA [ 5 ]. The WHO also estimated that the share of social insurance in India was only about 4.2% [ 6 ].
Emergency care in India
Although emergency physicians and emergency medicine have remained a realized need in the country, the practice of emergent care has remained centralized, with traditionally few private hospitals admitting emergency cases [ 11 ] as they prefer to avoid dealing with medico-legal formalities during emergencies (Supreme Court of India; Parmanand Katara vs. Union of India AIR1989SC 2039) [ 8 ]. This problem was mitigated to some extent when the judicial system mandated the delivery of care by any and every hospital regardless of a patient's paying and medico-legal status in times of emergency [ 9 ]. Failure on the part of any hospital to provide timely medical treatment to a person in need of such treatment results in a violation of the patient's "Right to Life,” which is guaranteed under Article 21 of the Constitution of India [ 10 ]. This is the closest India has come to enacting laws similar to The EMTALA (Emergency Medical Treatment and Labor Act) and the COBRA (Consolidated Omnibus Budget Reconciliation Act), which are well recognized in the USA.
Most emergency departments in centrally run university and government hospitals do not match up to the “Emergency Department Categorization Standards” proposed by the Society of Academic Emergency Medicine (SAEM) [ 14 ]. Emergency care is offered in areas designated as ‘ casualties’ that are often manned by junior specialty residents with little overview and are mere ‘referral points’ for specialized care. Triage, something that is instrumental to good emergency care, is rarely practiced. Problems are worse in rural areas, where even the most basic emergency obstetric care has been found to be lacking [ 12 ].
On a completely different level, however, is the defense sector in India, in which command hospitals, paramedics, and nurses trained in emergency medicine have long been functioning.
The first privatized emergency department (ED), modeled on the American Community Hospital Emergency system, was established at the Sundaram Medical Foundation, Chennai, with help and support from emergency physicians from the Long Island Jewish Medical Center, USA, in the late 1990s [ 13 ]. This marked a landmark change in the psyche of the private hospitals in the country. Today, well-equipped EDs have cropped up in private medical centers all over the country, and many of these centers are headed by physicians who have formally trained in emergency medicine in other countries.
EMS in India
The EMS system in India is best described as ‘fragmented .’ The basic fundamental principal behind EMS systems worldwide is to have a common emergency communication number connected to responsive agencies. Although India has the emergency number 102 for calling ambulances, the responsiveness of the system has always been doubted. In 2007, Ramanujam et al. reported that nearly 50% of trauma victims admitted to a premier hospital in an urban Indian city had received no pre-hospital care [ 15 ].
The first of its kind, the CATS (Centralized Accident and Trauma Services) ambulance system was conceptualized in 1984 [ 16 ]. The service was expanded nationally, but lack of a driving force behind the initiative made it fall by the side. Today, NGOs (non-governmental organizations) and private hospitals in cities and states have constructed their own EMS setups. Principal among these are the National Network of Emergency Services (NNES), Ahmedabad, Delhi, Pune, Hyderabad, Chennai, Raipur, Ranchi, and Kolkata [ 17 ]; Emergency Management and Research Institute (EMRI), Haryana, Chandigarh, Uttaranchal, Rajasthan, Gujarat, Madhya Pradesh, Andhra Pradesh, Goa, Karnataka, Tamil Nadu, Meghalaya, and Assam [ 18 ]; Life Support Ambulance Service (LSAS), Kerala, Mumbai [ 19 ]; Operation Sanjeevani, Bengaluru; Ambulance Access for All (AAA), Mumbai; Indian Institute of Emergency Medical Services (IIEMS), Kerela, etc.
Lack of a uniform EMS access number across the country and the lack of awareness among commuters about the existing numbers makes access and egress from emergencies difficult [ 20 ]. The lack of trained professionals manning ambulances makes quality of care heterogeneous. EMS services have remained unaccountable, and this has led to failure to introduce corrective measures for improving EMS in India.
However, steps are being taken in the right direction. The Gujarat state government set up the Gujarat Emergency Medical Services Authority (GEMSA). This was the first state to actually pass an Emergency Services Regulation in the country. By bringing together government, NGOs and other private agencies, a statewide system of emergency care has been set up, which could signal a tide of vital change in EMS.
Collaborations with internationally acclaimed institutes like Stanford University, CA (EMRI) and the American Association of Physicians of Indian Origin (AAPI) have provided several breakthroughs in technical and educational expertise.
There is palpable vigor among the bureaucratic brass and political leadership regarding re-initiating the process for allotting a unique emergency response number. How successful this push will be remains to be seen!
Emergency medicine education
One of the shining beacons in Indian emergency medicine has been the evolution of academic training for physicians. Medical colleges have always emphasized a minimum of 2 weeks spent in ‘casualties’ of hospitals during the mandatory year of internship training prior to obtaining the baccalaureate in medicine and surgery.
The lack of specialist training in the field was one of the principal issues highlighted by the white paper on Indian emergency medicine published by the INDUS collaboration [ 21 ]. David et al., in their landmark article, suggested that one of the three important prongs essential for the development of emergency medicine in India was the development of formal education in emergency medicine with its recognition as a specialty by the Medical Council of India [ 22 ].
Since then, several institutes have instituted formal training in emergency medicine. Most of these have been developed in collaboration with international agencies, including RCGP UK (Royal College of General Practitioners, UK), CEM UK (College of Emergency Medicine, UK), GWU USA (George Washington University, USA), etc. Others have formulated locally modulated curricula for training in emergency medicine.
The recognition of Emergency Medicine as the 30th specialty in medical training by the medical council of India in July 2009 brought about a welcome change. There is now a move to increase the number of eligible seats for training in emergency medicine throughout the country. The FACET program started by the INDUS collaboration in 2009 is a future faculty development program that will give rise to local champions for emergency medicine education [ 23 ].
There has also been a surge in training programs for emergency medicine nursing and paramedic training. Spearheading this effort are the WHO-recognized Emergency Nursing course at CMC Vellore and the collaboration with Stanford University at EMRI. Several other private institutes and hospitals have also initiated diploma courses towards the same goal. The EMRI Emergency Nurses Award (EENA), initiated in 2005 to recognize nurses’ excellence in Emergency Medicine, is a step towards recognition of these important pieces of the puzzle [ 24 ]. However, the absence of a regulatory body puts the uniformity of training into question.
There has also been a move towards making emergency medicine a trainable specialty under the National Board of Examination (NBE) training programs run at private and public sector hospitals within the country. The parallel introduction of simulation facilities and a variety of training programs in emergency ultrasound and resuscitation throughout the country will further interest in the field among young physicians [ 25 ].
Emergency medicine interest groups
Several interest groups have been instrumental in the development of emergency medicine. SEMI, the Society of Emergency Medicine in India, was started in 1999 [ 26 ] and has served as an important forum not only for national emergency physicians to brainstorm the steps for the development of emergency medicine in the country, but they have also served as an important focal point of contact with other international agencies like the ACEP (American College of Emergency Physicians). AAEMI, the American Academy for Emergency Medicine in India, was established in 2001 and has partnered with SEMI in order to bring attention and recognition to Indian Emergency Medicine [ 27 ]. The more recent Indo-US Emergency and Trauma Collaborative (INDUS) has furthered the cause of nationalized emergency medicine education in India [ 28 ]. NEPI, the Network of Emergency Physicians in India, is a virtual network of emergency physicians and aspirants in the field that provides a venue to engage in academic, administrative, and research-related discussions about emergency medicine in India [ 29 ].
A collaborative effort is needed not only by the medical community, but also by other agencies to reform the emergency response system in India. With India burdened by the most traffic accidents in the world, it is important to fight this problem with awareness drives among the general population. What is needed is a championed effort to bring everyone together towards the greater common good. Private-public partnership, which is lacking today, seems to be the most viable way to proceed if we want to develop a system that not only works, but also avoids the mistakes of the past.
As a country of over a billion people, our needs and resources differ from most other countries in the world. We cannot simply hope to copy the established systems, but we can surely hope to learn from them. By collaborating with agencies worldwide, we can bring in the essential technical expertise to truly reform the system.
Perhaps what is most essential to develop Indian Emergency Medicine is to stimulate the young minds of graduating physicians, nurses, and paramedics to see Emergency Medicine as a career opportunity and to influence decision makers to formulate policy conducive to fair practice and training in emergency medicine.
Krishnaswami S, Joseph G, Richard J (1991) Demands on tertiary care for cardiovascular diseases in India: analysis of data for 1960–1989. Bull World Health Organ 69:325–330
PubMed CAS PubMed Central Google Scholar
Reddy KS (2007) India wakes up to the threat of cardiovascular diseases. J Am Coll Cardiol 50:1370–1372
Article PubMed Google Scholar
Ministry of Health and Family Welfare ND, India. National Health Policy (1983) http://www.mohfw.nic.in/kk/95/ii/95ii0101.htm .
Ministry of Health and Family Welfare ND, India. NATIONAL HEALTH POLICY 2002 (India). 2002; http://www.mohfw.nic.in/NRHM/Documents/National_Health_policy_2002.pdf .
India: New Directions in Health Sector Development at the State Level (1997) The World Bank.
WHO. National Health System Profile : India (2007).
PoSaw LL, Aggarwal P, Bernstein SL (1998) Emergency medicine in the New Delhi area, India. Ann Emerg Med 32:609–615
Article PubMed CAS Google Scholar
Rao JJ (2006) The Law Commission of India. http://lawcommissionofindia.nic.in/reports/rep201.pdf .
Mathiharan K (2003) The fundamental right to health care. Issues Med Ethics 11:123
PubMed CAS Google Scholar
Constitution I. Article 21. http://rshrc.nic.in/07%20Human%20Right%20Article-21.pdf .
Aggarwal P, Banga A, Kurukumbi M, Gupta M (2001) Emergency physicians and emergency medicine: an imminent need in India. Natl Med J India 14:257–259
Mavalankar DV (2002) Policy and management constraints on access to and use of life-saving emergency obstetric care in India. J Am Med Womens Assoc;57:165-6, 8
Google Scholar
Alagappan K, Cherukuri K, Narang V, Kwiatkowski T, Rajagopalan A (1998) Early development of emergency medicine in Chennai (Madras), India. Ann Emerg Med 32:604–608
Goldfrank L, Henneman PL, Ling LJ, Prescott JE, Rosen C, Sama A (1999) Emergency center categorization standards. Acad Emerg Med 6:638–655
Ramanujam P, Aschkenasy M (2007) Identifying the need for pre-hospital and emergency care in the developing world: a case study in Chennai, India. J Assoc Physicians India 55:491–495
Government of Delhi I. Centralized Accident & Trauma Services (CATS). http://health.delhigovt.nic.in/Cats/content.html .
Apollo Hospitals I. National Network of Emergency Services. http://www.apollohospitals.com/component/content/article/332.html .
GVK-EMRI. Emergency Medicine Research Institute. http://www.emri.in/ .
1298. Life Support Ambulance Service. http://www.1298.in/ .
David SS (1997) Strategy for the development of emergency medical services in India. J Indian Med Assoc;95:17, 26.
Das AK, Gupta SB, Joshi SR et al (2008) White paper on academic emergency medicine in India: INDO-US Joint Working Group (JWG). J Assoc Physicians India 56:789–798
David SS, Vasnaik M (2007) T VR. Emergency medicine in India: why are we unable to 'walk the talk'? Emerg Med Australas 19:289–295
FACET-INDIA. http://www.facetindia.org/ .
Jampala A (2006) Celebrating emergency nurses in India. J Emerg Nurs 32:122–123
Gupta A, Peckler B, Schoken D (2008) Introduction of hi-fidelity simulation techniques as an ideal teaching tool for upcoming emergency medicine and trauma residency programs in India. J Emerg Trauma Shock 1:15–18
Article PubMed PubMed Central Google Scholar
SEMI - Society for Emergency Medicine in India. http://www.semi.org.in/index.php .
American Academy for Emergency Medicine in India. http://www.aaemi.org/aaemi/aaemi_born.htm .
Indo-US Emergency and Trauma Collaborative. http://www.indusem.com/ .
Network of Emergency Physicians India. http://nepi.emergencymedicine.in/ .
Download references
Conflicts of Interest
Author information, authors and affiliations.
Department of Emergency Medicine, Apollo Health City, Jubillee Hills, Hyderabad, Andhra Pradesh, India,, 500033
Imron Subhan
Department of Emergency Medicine, University of Rochester, 601 Elmwood Ave, 655A, Rochester, NY, 14620, USA
Anunaya Jain
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Anunaya Jain .
Additional information
The views expressed in this paper are those of the author(s) and not those of the editors, editorial board or publisher.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Subhan, I., Jain, A. Emergency care in India: the building blocks. Int J Emerg Med 3 , 207–211 (2010). https://doi.org/10.1007/s12245-010-0223-7
Download citation
Received : 25 February 2010
Accepted : 11 July 2010
Published : 04 August 2010
Issue Date : December 2010
DOI : https://doi.org/10.1007/s12245-010-0223-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Emergency medicine
- Emergency medical services
- Medical education
- International
- Development
- Current status
International Journal of Emergency Medicine
ISSN: 1865-1380
- General enquiries: [email protected]
- Education News
KCET 2024 Admit Card OUT at cetonline.karnataka.gov.in; direct link to download
How to check and download KCET 2024 Admit Card?
Visual stories.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Public Health Res
- v.12(3); 2023 Jul
- PMC10345816

Impact of COVID-19 on healthcare system in India: A systematic review
Megha kapoor.
1 Laboratory of Disease Dynamics & Molecular Epidemiology, Amity Institute of Public Health, Amity University, Noida, Uttar Pradesh, India
Karuna Nidhi Kaur
Shazina saeed.
2 Amity Institute of Public Health, Amity University, Uttar Pradesh, Noida, India
Mohd Shannawaz
Amrish chandra.
Despite an extensive healthcare system in India, the COVID-19 Pandemic created havoc upon the existing Indian healthcare system by disrupting the supply of essential healthcare services to patients. It has also highlighted the significant-quality discrepancies of healthcare facilities between the rural-urban areas and between public and private healthcare providers. The not so advanced healthcare system of India was exposed through the lack of oxygen and essential drugs required for the treatment of COVID-19. Additionally, during the pandemic period there was a drastic decline in seeking non-COVID-19 disease related healthcare services. The objective of this systematic review is to determine whether COVID-19 has impacted the healthcare system in India.
Introduction
India, the second most populous country in the world has been severely impacted by the ongoing COVID-19 pandemic since it’s emergence. COVID-19 has impacted every sector in the country including healthcare. Indian healthcare system crumbled under the massive burden of the global pandemic highlighting the gaps and challenges in the existing health delivery system.
COVID-19 or Coronavirus is an upper respiratory tract infection of high virulence. It was formerly known as ‘2019-nCoV’ and is caused by the SARS-CoV-2 virus. 1 It first originated from Wuhan city, Central Hubei province of China in December 2019. Several clusters of patients with viral pneumonia of unknown origin were reported to be epidemiologically associated with the Hunan seafood market, Wuhan, China. 2 Soon, cases of pneumonia were reported in other parts of the world as it spread rapidly crossing the borders of China. A massive number of people started losing their lives in China and following its spread to other countries; it was declared a public health emergency of international concern on 30th January 2020 by World Health Organization (WHO). After more than 118,000 cases in 114 countries, and 4291 people lost their lives, COVID-19 was declared as a pandemic by World Health Organization (WHO) on 11th march 2020. 3 As the countries continued to struggle with a lack of resources and capacity the viral outbreak spread rapidly worldwide, infecting millions of people all across the globe including India.
Those infected with Coronavirus disease (COVID-19) exhibit a varying range of symptoms ranging from mild to moderate. It affects people of all ages; however, the risk of serious infection increases with advancing age. Patients infected with coronavirus disease and presenting with pre-existing co-morbidities such as diabetes, asthma and cardiovascular diseases (CVDs) are more vulnerable to experiencing unfavourable outcomes or experiencing death.
A healthy individual can acquire COVID-19 infection directly by coming in close contact with an infected individual through the droplets emitted during sneezing or coughing. It can also be transmitted indirectly after coming in contact with contaminated surfaces such as door knobs. It affects every individual differently with cough, fever, sore throat, tiredness and lethargy being the most common symptoms of the illness. Individuals can also develop few lesser common symptoms such as loss of taste, diarrhoea, irritation of the eyes and rash on the skin among others. An individual can develop shortness of breath or experience difficulty in breathing and requires urgent medical attention. These symptoms may take 4–5 days to appear after coming in contact with a virus or as long as 14 days and can also be asymptomatic.
The first wave
In India, the first case of COVID-19 infection was reported on 27TH January 2020, when a 20 year old female with a travel history of China presented with a sore throat and dry cough in the emergency department of General Hospital, Thrissur, Kerala. 4 Since then, COVID-19 has taken a serious toll in India and worldwide. To prevent the spread of COVID-19 infection, the Government of India announced a nationwide lockdown for 21 days on 24 March 2020, which was further extended. It was not until 30th May, that the government uplifted the restrictions in an ‘unlock’ phase-wise manner. Throughout, national advisories were generated and the norm of ‘social distancing’ and ‘work from home was introduced. People were advised to practise social distancing, wear masks and avoid going out unnecessarily and only people of ‘essential services such as doctors, nurses, police and home services were exempted. These preventive measures allowed the Indian Healthcare delivery system to prepare for the pandemic. These measures stopped the further spread of COVID-19 infection and the efforts of the Indian Government to contain the viral spread were applauded internationally. India has experienced three COVID-19 pandemic waves till now with a massive surge during the second wave in March 2021. 5
The second wave and Indian healthcare system
The first wave had a low infectivity rate since the lockdown was imposed and individuals practised social distancing. Therefore, it largely affected the economy and livelihoods of Indians without any serious implications on the healthcare system. However, during march 2021, the country witnessed the most dangerous second wave that created havoc as individuals started taking preventive measures more casually due to ‘pandemic fatigue’. This was characterized by an increasing number of cases between 25 and 50 years of age, a shortage of essential medicine and equipment, and medical professionals. 6 Indian healthcare system failed to meet daily oxygen demand, Intensive Care Units (ICU) beds and oxygen beds due to which many hospitals had to turn the patients away, resulting in higher mortality rates. This lead to the disruption of routine immunization procedures, and treatment of Non-communicable and communicable diseases. 7 This revealed the overstretched and overburdened existing Indian Healthcare system. This also highlighted the failing healthcare management system and lacking public health system and efficient healthcare models in India. The Indian government failed to respond to the second wave effectively unlike the first wave.
The third wave of COVID-19 in India
With the emergence of the new Omicron variant of SARS-CoV2, the cases increased in January 2022. 8 The majority of the cases were asymptomatic or mildly symptomatic. With increased administration of the COVID-19 vaccine, the patients admitted in ICU were mostly unvaccinated or with pre-existing co-morbidities. The demand for hospital beds, oxygen beds and ventilators were low and mostly remained unoccupied.
The third wave was different from the first two waves due to various factors such as low virulence of the omicron variant despite high transmissibility and administration of either single or both doses of COVID—19 vaccine to the adult population, authenticating the effectiveness of the vaccine.
Therefore, the COVID-19 pandemic has significantly disrupted the healthcare systems in India. Hence, this review aims to describe the impact of COVID-19 on the healthcare system concerning the patient visit and reception of treatment, diagnostic tests done and referral services in India. It is necessary to conduct this review as it will aid in developing new healthcare models in order to manage the COVID-19 pandemic at present and prevent any further waves from arising in the future.
Health care system in India
A sound and effective healthcare system enable the country to respond to a pandemic efficiently by overcoming the challenges and barriers encountered in providing healthcare.
The Indian healthcare system is a mixed framework, including both public and private healthcare service providers. However, a large proportion of private healthcare providers are present in urban India, providing, secondary and tertiary healthcare services. 9
The objective of this systematic review is to determine the impact of the COVID-19 pandemic on the healthcare system in India.
Rationale: The rationale for this study is to investigate the impact of the COVID-19 pandemic on the healthcare system in India, considering the challenges, gaps and disruptions experienced during this global health crisis.
Material and methods
Study design.
This systematic review was conducted on the available online published studies in high-quality journals related to COVID-19 impact on healthcare services in India.
Search strategy
A thorough extensive literature search was conducted between 14 February 2022 and 20 February 2022 on the electronic database ‘PubMed’ for quality studies published between time period 2019 and 2022 using the search strategy (impact) AND (COVID-19) AND (healthcare system) OR (Primary Health centre)) OR (secondary health centre)) OR (community health centre)) OR (tertiary health centre))) OR (hospital)) OR (government)) OR (private)) AND (India).
The following keywords and Medical Subject Headings (MeSH) entries were used:
COVID-19, healthcare system, India.
Studies that met the eligibility criteria were selected based on the inclusion and exclusion criteria after screening the database for this systematic review.
Inclusion and exclusion criteria
This systematic review included the studies conducted in the English language during the COVID-19 Pandemic assessing the healthcare system in India. Studies involving outpatient clinics visit, hospital admissions, diagnostic tests done, minor and major surgeries and case referrals were also included.
Studies which were conducted in private clinics & not involving government, primary, secondary and tertiary centres, along with the studies conducted on the physical & mental health status of healthcare providers through surveys were excluded as shown in Table 1 .
Summary of excluded studies.
Data extraction
After completion of the initial screening process, a total of seven articles were selected to be included in this systematic review. The study selection process is illustrated in Figure 1 , representing the PRISMA (Preferred reporting items for systematic reviews and meta-analysis) flow diagram for this systematic review.

PRISMA flow diagram of the systematic search.
From the selected articles following data was extracted by preparing an MS Excel spreadsheet: title of the study, study objectives, study methodology and conclusion.
Table 2 shows the summary of all the included articles in this systematic review.
Summary of included studies.
According to the objective of this systematic review the results described based upon the Impact of the COVID-19 Pandemic on the health care system in India on various parameters – number of outpatients, number of inpatients, number of patients undergoing minor and major surgeries, emergency trauma cases, patients undergoing nonurgent elective procedures.
Impact of COVID-19 on cancer care in India
From the seven included articles in this review, two articles described the disrupted oncology services in India by comparing these before and during the pandemic. A cohort study to describe the impact of COVID-19 on cancer care in India compared the oncology services provisions by cancer patients between 01 March 2020 and 01 March 2020 with similar duration for 2019 and concluded that there was a 54% reduction in new patient registration, 46% reduction in patient follow-up visit, 36% reduction in hospital admissions, 37% reduction in outpatient chemotherapy, 49% reduction in number of major surgeries, 52% reduction in minor surgeries, 23% reduction in patients accessing radiotherapy, 38% reduction in pathological diagnostic testing, 43% reduction in radiological diagnostic tests and 29% reduction in palliative care referrals. It also found that there was more reduction of oncology services for larger metro cities than smaller cities. 10 Another study, A retrospective analysis from western India determining the impact of the COVID-19 lockdown on Cancer care stated reduced patient visits and number of treatments received during the lockdown with chemotherapy being the most common treatment received. 11
Impact of COVID-19 on nephrology services in India
Only one study out of the seven included studies described the impact of the COVID-19 pandemic on nephrology and transplant services at a tertiary care centre, in Ahmedabad, India. The study concluded that there was significant reduction in a number of outpatients and inpatients between April 2020 and June 2020 when compared with a similar duration in 2019 almost by 50%. There was also a reduction in donor transplants, haemodialysis and nonelective procedures such as renal biopsies and arteriovenous fistulas during March 2020. 12
Impact of COVID-19 on ophthalmic care in India
Three out of seven included studies reported the impact of COVID-19 on ophthalmic care in India. A study conducted at a tertiary care ophthalmic institute in India reported a decrease of 97.14% in the routine patient visit, a decline of 35.25% in emergency outpatient visits, a decrease in routine and emergency ward admissions by 95.18% and 61.66% respectively, a reduction of elective surgeries by 98.18%, decrease of 58.81% in emergency surgeries, reduction of 99.61% in the number of donor corneas collected between 25 March 2020 and 15 July 2020 with comparison on previous year data of the same duration. 13 A study conducted in rural eye centres of Southern India reported that between 23 March 2020 and 19 April 2020, the total number of patients reduced during the lockdown-I period versus pre-lockdown. Only essential procedures were performed and most of the patients were treated for conjunctivitis. 14 A third study, which was conducted in a tertiary eye care Institute reported that there was a reduction in the number of patients presenting with ocular trauma in their emergency department during the lockdown as compared to the previous year. 15
Impact of the COVID-19 pandemic on the clinical practice of trauma and orthopaedics
A single epidemiology study out of seven studies included in this article, which was conducted at a tertiary care centre in New Delhi, explained various outcomes of the COVID-19 pandemic on the practice of orthopaedics and trauma through comparison between the pandemic period and pre-lockdown. It stated a reduction by 71.93% in outpatient attendance, a reduction of 59.35% in inpatient admissions, 55.78% reduction in surgical procedures including arthroplasty surgery, trauma and arthroscopic surgery during the pandemic period. 16
This study is being conducted to investigate the impact of the COVID-19 pandemic on the health care system in India by a systematic review approach based upon the eligibility criteria, seven articles related to the purpose of the study were screened after inclusion and the final analysis was prepared. The included studies defined various parameters – number of outpatients, number of inpatients, number of patients undergoing minor and major surgeries, emergency trauma cases, patients undergoing nonurgent elective procedures, follow-up visits for assessment of the impact of the COVID-19 pandemic on overstretched and overburdened health care system Of India. The studies included in this article reported that the COVID-19 pandemic has sharply affected the health care services in India including cancer care, nephrology services, ophthalmic care, trauma practice and orthopaedics care.
The COVID-19 Pandemic has led to a disrupted healthcare system which has subsequently impacted non-COVID disease conditions. The observed reduction in the number of new patient registrations, hospital registrations, major and minor surgeries, and transplant procedures as summarized in various studies during March 2020–April 2020 could be due to fear of infection among patients. The patients residing in rural parts of India found it difficult to access health services in metro cities due to travel restrictions during the lockdown period and this has led to delays in early screening, correct diagnosis and appropriate treatment which is of grave concern. These patients may present with advanced stages of the disease and create a backlog of patients by overloading the healthcare system.
Hospitals faced certain challenges that inhibited them from providing appropriate care to the patient such as- many hospitals being converted to COVID-19 dedicated treatment facilities and as result, they faced a widespread shortage of Personal Protective Equipment (PPE) supplies. Hospitals reported a shortage of adequate staff as they were themselves exposed to the virus. Various hospitals reported lack of necessary medical equipments such as ICU beds and Ventilators which was a major threat.
Despite the lockdown and various challenges encountered, hospitals realized the need of improving the accessibility of healthcare through teleconsultation along with in-person visits during these challenging times. In the absence of direct consultations to the patients, telemedicine was conducted to address the concerns of outpatients and therefore, reduce their need to visit the hospital.
In general, the COVID-19 Pandemic has posed a serious threat to all aspects of the healthcare system in India by affecting the activities of hospitals that provide treatment services to patients for non-COVID-19 diseases.
The results of this study show that Indian Healthcare System during the COVID-19 pandemic has suffered serious challenges, which can be a wake-up call because due to delayed diagnosis, a large number of patients will present with advanced stages of the non- covid-19 disease such as cancers, which may require emergency treatment. Strengthening of the Indian healthcare system is required so that it does not crumble under future pandemics if any. Need of the hour is a robust healthcare model and effective healthcare policies with regular updates to manage the current pandemic along with more emphasis on telemedicine as this is not the last pandemic that India will face. In conclusion, the COVID-19 pandemic has significantly impacted the healthcare system in India.
Limitations of the study: This study has limitation regarding language inclusion, as the researchers’ proficiency was limited to English, resulting in the exclusion of articles written in other languages. Another major limitation is the bias as the he papers relies on available online published studies in high-quality journals, which may introduce a bias towards studies that have been published and accessible. There may be relevant studies that have not been included in the review, potentially leading to a skewed representation of the impact of COVID-19 on the healthcare system in India.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical statement: No Ethical approval is needed.

IMAGES
VIDEO
COMMENTS
India's health care sector provides a wide range of quality of care, from globally acclaimed hospitals to facilities that deliver care of unacceptably low quality. Efforts to improve the quality ...
500 Words Essay on Healthcare in India Introduction. India's healthcare sector is a study in contrasts, presenting a complex tapestry of cutting-edge advancements and systemic challenges. With an expansive population and diverse health needs, the healthcare system in India is a critical component of the nation's development agenda.
Physical reach is one of the basic determinants of access, defined as " the ability to enter a healthcare facility within 5 km from the place of residence or work" Using this definition, a study in India in 2012 found that in rural areas, only 37% of people were able to access IP facilities within a 5 km distance, and 68% were able to ...
The government has been working to improve the healthcare system through various initiatives to strengthen primary, secondary, and tertiary healthcare services. The Indian government spent two percent of India's gross domestic product (GDP) on healthcare in financial year 2022 and is forecast to reach over 2.5% of the GDP by 2025.
India has made significant improvements in the health outcomes of its people. Life expectancy at birth increased to 69.6 years in 2020, from expected 47.7years in 1970. MMR declined from 301 to 130 per 100 000 live births between 2003 and 2014-16, and IMR declined from 68 in the year 2000 to 24 per 1000 live births in 2016.
The group's charge is to report by August 2022 how India can achieve universal health care within a decade. The Mittal Institute is encouraging participation by the Harvard community and sponsoring an online panel discussion on Monday to introduce the effort. Patel and Khanna said the commission has a challenging road ahead, one that has ...
National Health Policy. The National Health Policy was endorsed by the Parliament of India in 1983 and updated in 2002, and then again updated in 2017. The recent four main updates in 2017 mention the need to focus on the growing burden of non-communicable diseases, the emergence of the robust healthcare industry, growing incidences of unsustainable expenditure due to healthcare costs, and ...
Abstract. After reviewing health outcomes and policy in India, this paper concludes that there are at least six sets of issues to be addressed about improving the quantity and quality of health services, and ipso facto improving health outcomes, in India. First, the amount of resources earmarked for health needs to increase.
According to the World Bank, infant mortality in India fell from 66 to 38 per 1,000 live births from 2000 to 2015. Life expectancy at birth has increased from 63 to 68 years, and the maternal mortality ratio has fallen from 374 to 174 per 100,000 live births over the same period. India also has dynamic pharmaceutical and biotechnology ...
arnt especially for developing economies like India where public healthcare system is grossly inadequate to take care of health needs of citizens. World Health Organization's framework of six health system building blocks was utilized to study the lessons learnt and actionable points in the post pandemic period. Participation in Global Health Security Alliance has to be stepped up with ...
Over 95% of facilities function with less than five workers, and only 195 hospitals in the entire nation operate with quality certifications. Essential diagnostics such as mammograms have scant coverage of only 1%. Second, the complacency of the medical staff in discharging their duties is a universal reality in the nation.
India Health System Review Health Systems in Transition Vol. 11 No. 1 2022 Written by: Sakthivel Selvaraj, Public Health Foundation of India, Delhi, India Anup K Karan, Indian Institute of Public Health, Delhi, India Swati Srivastava, Medical Faculty and University Hospital, Heidelberg University, Germany Nandita Bhan, Center on Gender Equity and Health, India
The latest official data on this comes from the 71st round of India's National Sample Survey (NSS), which was done between January and June 2014. Financial constraint was the reason most often cited for seeking treatment without medical advice. Next on the list was "no medical facility available in neighbourhood".
India is rapidly becoming urbanised. By 2030, around 40% of the country's population will live in urban areas. The extent to which India's health system can provide for this large and growing city-based population will determine the country's success in achieving universal health coverage and improved national health indices. In The Lancet Global Health, Sundeep Salvi and colleagues1 offer a ...
By Indrani Gupta, Institute of Economic Growth, Delhi In collaboration with Nishali Patel, Policy Fellow, International Health Systems, London School of Economics All Indian citizens can get free outpatient and inpatient care at government facilities. Under India's decentralized approach to health care delivery, the states are primarily responsible for organizing health services.
B). Dismal Number of Healthcare Centers: There are 1,45,894 Sub Centers, 23,391 Primary Health Centers and 4,510 Community Health Centers in India as on March 2009 (Latest). These figures are insufficient keeping in mind the model of 2005 National Commission on Macroeconomics and Health, which recommended a Sub Centre for
Western medicine has existed in India since the 1600s starting with early Portuguese influence 5 but it wasn't until 1664 that the French established the first hospital, followed by a British hospital in 1668. British rule over the country expanded healthcare facilities such as dispensaries at the local and sub-division levels.
Public health-care infrastructure in India. India has a mixed health-care system, inclusive of public and private health-care service providers. 6 However, most of the private health-care providers are concentrated in urban India, providing secondary and tertiary care health-care services. The public health-care infrastructure in rural areas has been developed as a three-tier system based on ...
By FY22, Indian healthcare ...
Approximately 86% of medical visits in India are from individuals living in rural areas, with a majority traveling over 100 km to reach available healthcare facilities, and where 70-80% of the cost is paid out-of-pocket. 16 Although poverty already has a negative effect on health, poverty in rural areas has been shown to have even greater negative effects than poverty in urban areas. 17 ...
According to World Health Statistics of 2018 India ranks 145 out of 194 countries. According to NITI Aayog India has a scarcity of 6 lakh doctors, 20 lakh nurses and 2 lakh dental surgeons. Though ...
The Republic of India, the world's most populous democracy, has struggled with establishing Emergency Medical Care. However, with the recent recognition of Emergency Medicine as a formal specialty in medical training, there has been renewed vigor in the developments in the field. We outline here the building blocks of the health care system in India, and the contribution each has made and is ...
Click on the link to proceed. Step 3: Enter your login credentials such as Application Number, Date of Birth, and any other details as required. Make sure to input accurate information. Step 4 ...
The first wave. In India, the first case of COVID-19 infection was reported on 27TH January 2020, when a 20 year old female with a travel history of China presented with a sore throat and dry cough in the emergency department of General Hospital, Thrissur, Kerala. 4 Since then, COVID-19 has taken a serious toll in India and worldwide. To prevent the spread of COVID-19 infection, the Government ...