- Preferences


Case Presentation Obstructive Jaundice - PowerPoint PPT Presentation

Case Presentation Obstructive Jaundice
Case presentation obstructive jaundice dr. ravi madhusudhana professor dr. manjunath post graduate dept of anaesthesiology. sdumc, kolar. * * * * identification of ... – powerpoint ppt presentation.
- Dr. Ravi Madhusudhana
- Dr. Manjunath
- Post Graduate
- Dept of Anaesthesiology. SDUMC, Kolar.
- History- Relevant To Causes Of Jaundice Symptoms
- Abdominal Examination To Differentiate Liver/ Spleen/Kidney For Ascites
- Types Of Jaundice- LFT
- Problems Of Hyperbilirubinemia
- Relevance Of Child-pugh Score
- Accumulation of Bilirubin (yellow pigment)in the skin and other tissues
- Hemolytic Jaundice
- Hepatic Jaundice
- Obstructive Jaundice(Cholestasis)
- Congenital Jaundice
- It is due to intra- or extra hepatic obstruction of bile ducts
- Intra Hepatic Jaundice
- Primary Biliary Cirrhosis,
- Drugs (contact with DDT, heavy metals, beryllium )
- Extra Hepatic Biliary Obstruction
- Inflammation,
- Tumors, (Ampulla of Vater)
- Name kalyan,
- Age -50yrs ,
- occupation - Farmer
- Main complaints
- Pain in abdomen - 15 days
- Yellowish discoloration of urine - 12 days
- Yellowish discoloration of eye - 10 days
- pain at rt. Upper abdomen which is sudden in onset ,severe and colicky in nature ,increasing intensity for 2-3 min then relieved spontaneously after few minutes.
- Frequency of pain was initially 2-3 times a day, presently 4-6 times a day.
- Pain was non radiating in nature and increases on food intake and pt used to get mild relief on taking analgesic .
- Pain was associated with nausea and vomiting .
- Pain was not associated with body posture
- Pt. also noticed clay colored stool since 12 days with yellowish discoloration of urine which gradually increased in intensity
- No H/O of burning micturition
- Then he also noticed yellowish discoloration of eyes followed by nail and palm.
- Pt. is also giving h/o itching all over body since 8 days which was more in night .
- There is also H/O decreased appetite since 4 days
- Feeling better with less pain jaundice after an endoscopic stenting procedure done 3 days ago
- Negative H/O-
- no H/O fever
- no H/O weight loss
- no H/O similar illness previously
- no history suggestive of
- TB,DM ,HTN, any other chronic illness./ bleeding diathesis
- no H/O blood transfusion / tattoo
- pain, due to
- gallbladder disease,
- malignancy, or
- stretching of the liver capsule
- fever, due to ascending cholangitis
- palpable and / or tender gallbladder
- enlarged liver, usually smooth
- palmar creases, below the breast, on the neck.
- They indicate raised serum cholesterol of several months.
- Xanthomas on the tendon sheaths are uncommonly associated with cholestasis.
- xanthelasma -on the eyelids
- scratch marks excoriation
- finger clubbing
- loose, pale, bulky, offensive stools
- dark orange urine
- Age and sex
- Viral hepatitis is common in young adults.
- CBD stone neoplastic jaundice seen in middle aged or elderly individuals.
- Portal cirrhosis, primary cancer of liver pancreatic cancer predominates in males.
- CBD Stone , PBC, carcinoma gall bladder common in females.
- Any employment involving handling of hepatotoxic agents like
- DDT, heavy metals, beryllium etc should be
- Exposure to infection in medical paramedical workers ,there is a predisposition to leptospirosis among workers in rat infected premises.
- Contact with jaundiced patients, if recent , should suggest possibility of infective hepatitis.
- Family history
- Association with anemia, gall stones removal of spleen suggests hemolytic jaundice.
- Past history
- Recent biliary tract surgery
- History of alcohol intake in cirrhosis.
- Use of drugs such as chlorpromazine, testosterone.
- Sexual orientation
- Diseases associated with male homosexuality
- Onset of jaundice
- Sudden Viral hepatitis, gall stones
- Gradual more likely with cirrhosis,
- pancreatic carcinoma, metastasis.
- Progressive typical of malignant obstruction.
- Fluctuating Stone in CBD, carcinoma
- ampulla of vater or repeated
- hemolytic episodes.
- Strong colicky character suggests gall stones
- Severe boring pain passing through back
- suggests pancreatitis
- In older patients, painless but fluctuating jaundice suggests intermittent obstruction by gall stones or necrotising papillary carcinoma.
- Painless but progressive jaundice is usually due to
- malignant obstruction of CBD.
- Fever chills
- if associated with bacterial viral infection ascending cholangitis.
- Pruritus characteristic of cholestasis.
- Morning anorexia , nausea retching suggests
- alcoholism if symptoms are longstanding.
- Urine dark coloured indicates cholestasis.
- Stools pale stools indicate cholestatic jaundice.
- EXAMINATION
- Conscious cooperative and well oriented to T/P/P
- Avg. built / Avg.nutrition
- Hair normal
- yellowish sclera - tongue dry and yellowish
- Icterus present / no engorged neck vein / no enlarged lymph node / no pallor / no clubbing/no koilonychiya / no cyanosis / no edema
- No general signs of liver cell failure gynecomastia,
- loss axillary hair, spider naevi, clubbing, leukonychia,
- palmar erythema, hepatic flap
- RR- 14/min regular and abdominothoracic
- Pulse-84/min (rt radial pulse), regular ,normal volume ,
- no R-R delay no R-F delay , all peripheral pulses are palpable
- BP- 130/84 (supine) rt arm ,by auscultatory method
- Temp Afebrile
- airway MPII, mouth opening - adequate
- SYSTEMIC EXAMINATION
- No added sounds
- CVS-S1 S2 normal
- ABDOMEN EXAMINATION-
- INSPECTION- Contour normal flat abdomen
- Umbilicus normal in shape and centrally placed.
- scratch mark present on abdomen
- no visible peristalsis seen
- no any scar mark, no dilated vein
- no petechiae ,no ecchymosis
- no abdominal distension
- local temperature normal
- soft abdomen
- no tenderness
- no rebound tenderness
- no localized swelling
- no hepatomegaly
- no splenomegaly
- no palpable gall bladder
- no fluid thrill
- PERCUSSION-
- tympanic note all over abdomen
- liver dullness present and liver span is 13 cm in
- midclavicular line
- no shifting dullness
- AUSCULTATION-
- bowel sound present
- no added sound and bruit present
- No signs of portal hypertension
- SHIFTING DULLNESS
- Before ERCP
- -Total bilirubin level of 26 mg/dL with a conjugated bilirubin of 18 mg/dL (normal level lt 0.7 mg/dl)
- -Total bilirubin level of 8 mg/dL with a conjugated bilirubin of 6.85mg/dl
- Aspartate aminotransferase 220 IU/L
- Alanine aminotransferase 250 IU/L,
- Hemoglobin level of 9 g/dL.
- Albumin 3 g
- CBC Normal limits
- prothrombin time (secs) 45
- Urinalysis positive bilirubin, normal urobilinogen
- 50 yrs male with complaints of pain in right hypochondrium with yellowish discoloration of body associated with itching and clay colored stool without any history of weight loss, fever and chronic alcohol intake .
- Provisional diagnosis obstructive jaundice post- ERCP status
- D/D-choledocholithiasis
- periampullary growth which obstruct
- biliary tract.
- Detection of hepatocellular injury
- Aminotransferases
- Lactate dehydrogenase
- Glutathione-S-transferase
- Assessment of hepatic protein synthesis
- Serum albumin
- Serum globulin
- Prothrombin time
- Detection of cholestatic disorders
- (Indices of obstructed bile flow)
- Alkaline phosphatase
- 5 nucleotidase
- Gamma glutamyl transpeptidase
- Serum bilirubin(lt1mg/dl)
- Quantitative liver tests
- (Indices of hepatic blood flow metabolic capacity)
- Indocyanine green(ICG)
- Obstructive Jaundice
- Lab Findings
- Serum Bilirubin?
- Feceal urobilinogen? (incomplete obstruction)
- Feceal urobilinogen absence (complete obstruction)
- urobilinogenuria is absent in complete obstructive jaundice
- bilirubinuria ?
- cholesterol ?
- Urinary changes
- bilirubin increased
- urobilinogen reduced or absent
- Faecal changes
- stercobilinogen reduced or absent
- ALT/SGPT-cytoplasmic(5-45 IU/L)18 hrs
- AST/SGOT-cytoplasmic and mitochondrial(5-30 IU/L)36 hrs
- Mild(100-249IU/l)- non-specific
- Moderate(250-999IU/l)
- Large(1000-1999IU/l)
- Extreme(gt2000IU/l)
- Mild - steatosis,
- medications,
- alcohol consumption,
- cholestasis, chronic viral hepatitis,
- haemochromatosis, neoplasms, cirrhosis
- Moderate - acute viral hepatitis,
- drug-induced liver injury and
- flare-ups of chronic liver diseases
- Large - acute on chronic active liver disease
- Extreme - fulminant viral hepatitis,
- severe drug induced liver injury,
- shock liver,
- hypoxic hepatitis,
- autoimmune hepatitis,
- acute biliary obstruction
- gt4 wilsons disease
- 2-4 alcoholic liver disease
- lt1 non-alcoholic steatohepatitis
- 105-333 IU/L
- Elevated levels may reflect hepatocellular injury, extrahepatic disorders or both
- Extreme increases signify massive liver disease
- Prolonged concurrent elevations in LDH and AP-malignant infiltration of the liver
- Extrahepatic- hemolysis,
- rhabdomyolysis,
- tumour necrosis,
- renal infarction,
- acute cerebrovascular accident,
- myocardial infarction
- Hepatocellular injury- accompanied by AST/ALT
- Sensitive and specific test for drug induced liver injury
- Serial measurements can reveal the time course of hepatic injury
- In acinar zone 3
- More sensitive than AST or ALT as a marker of centrilobular necrosis in its incipient stages.
- To assess hepatocellular function
- To evaluate chronic liver disease
- Half life of nearly 3 weeks
- Procoagulants have short half life
- Factor VII 4 hrs, fibrinogen 4 days
- Levels descend shortly after liver begins to fail
- PT-measures factors II, V, VII and X
- Prolonged PT- low level of factor VIIa
- 20-140 IU/L(35-115 in males and 25-95 in females)
- Circulating half life 7 days
- To screen diseases of the liver or biliary tree- hepatitis, malignancies and cholestatic diseases
- Extreme increases indicate
- a) major block in biliary flow due to primary biliary
- cirrhosis and choledocholithiasis.
- b) hepatic malignancy compressing some
- intrahepatic bile ducts.
- 5nucleotidase-2-17U/L
- Gamma glutamyl transpeptidase 0-51IU/L(lt70 in males and lt40 in females)
- To distinguish between hepatic and extrahepatic sources of AP
- Changes in AP secondary to hepatobiliary disease usually followed by 5NT
- Serum AP and GGTP increase in tandem, whereas 5NT may not change for days
- Inducible microsomal enzyme( by alcohol, anticonvulsants and warfarin)
- Less specific than 5NT
- Bone contains very little GGTP-therefore distinguish between osseous and hepatobiliary sources.
- Most widely used test for hepatic excretory function
- Normally below 1mg/dl
- gt4mg/dl-yellowish discoloration of body tissues
- Serological testing- viral, microbial and autoimmune
- Genetic testing-heritable metabolic disorders
- Tumor marker assays- hepatic malignancies
- Total Hepatocellular mass- by measuring the clearance of a substance such as indocyanine green, bromsulphalein and rose Bengal
- Drug metabolizing capacity
- Caffeine clearance
- Galactose elimination capacity
- Aminopyrine breath test
- Antipyrine clearance
- Unconjugated bilirubin is toxic for neuronal cell whereas the conjugated bilirubin is responsible for renal dysfunction in patient with obstructive jaundice.
- Bilirubin value rarely exceeds 6mg/dl in Haemolytic anaemia.
- Intrahepatic cholestasis to cause rise in bilirubin, drainage of
- bile in gt75 parenchyma should be blocked
- Sepsis or renal failure should be excluded if the bilirubin exceeds 30mg/dl in patient with CBD stone.
- Serum bilirubin will take atleast 1-2 weeks to return to normal following the relief of obstruction ( half life of bilirubin is 2weeks).
- Negative inotropic effect by bile salt.
- Negative chronotropic effect by bile salt.
- Due to activation of RAS, intravascular interstitial volume expansion occurs, several types of shunts develop ,leading to hyderdynamic circulation.
- Decreased vascular resistance( peripheral vasodilation, increased arteriovenous shunting)
- Blood volume maintained or increased , but redistributed.(splanchnic hypervolaemia, central hypovolemia)
- Increased blood flow in splanchnic (extrahepatic), pulmonary, muscular and cutaneous tissues.
- Decreased total hepatic blood flow
- maintained hepatic arterial blood flow
- decreased portal venous blood flow
- Beta receptor density reactivity in the myocardium of cirrhotic patients diminished, thus ionotropic responses to sympathomimetic drugs reduced in liver disease.
- Intrapulmonary shunting caused by intrapulmonary vascular dilatations(precapillary or arteriovenous)
- triad of chronic liver disease ,increased alveolar
- arterial oxygen gradient and evidence of IPVD is
- defined as hepatopulmonary syndrome.
- Ventilation perfusion mismatch caused by impaired hypoxic pulmonary vasoconstriction, pleural effusions, ascites and diaphragm dysfunction.
- Decrease in pulmonary diffusion capacity secondary to increased extracelluar fluid, interstitial pneumonitis,and/or pulmonary hypertension.
- Haemodynamic instability caused by the bile salts
- endotoxin on the cardiovascular function.
- Three main functional abnormalities in cirrhosis are reduction in sodium excretion,
- reduction in free water clearance,
- decrease in renal perfusion and glomerular filtration.
- Direct nephrotoxic effect by bile salt and conjugated
- bilirubin .
- Renal tubule blockade of bilirubin cast may further
- potentiate the renal injury.
- Decreased production of coagulation and inhibitor factors
- Synthesis of dysfunctional clotting factors
- Quantitative and qualitative platelet defects
- Vitamin K deficiency
- Decreased clearance of activated factors
- Hyperfibrinolysis
- elevated serum bilirubin - in proportion to duration of cholestasis returns to normal once cholestasis is relieved
- raised serum alkaline phosphatase - to more than 3X upper limit of normal
- LFTs - aminotransferases mildly raised raised gamma GT
- increased urinary bilirubin
- urinary urinobilinogen is excreted in proportion to amount of bile reaching the duodenum i.e. absence of urinobilinogen indicates complete biliary obstruction
- The first diagnostic test to use in patients whose liver tests suggest cholestasis,
- To look for the presence of a dilated intrahepatic or extrahepatic biliary tree or to identify gallstones.
- In addition, it shows space-occupying lesions within the liver, enables the clinician to distinguish between cystic and solid masses.
- Ultrasound with Doppler imaging can detect the patency of the portal vein, hepatic artery, and hepatic veins and determine the direction of blood flow.
- Dilated ducts on ultrasound - percutaneous transhepatic cholangiograpy
- Undilated ducts on ultrasound - endoscopic retrograde cholangio-pancreatography
- Needle biopsy of the liver
- Pain, jaundice (charcot s triad)
- Hepatomegaly
- Spleenomegaly
- GI bleeding
- Once Jaundice is recognized, it is important to determine whether hyperbilirubinemia is predominantly Conjugated B or UnConjugated B?
- Differentiation of hemolytic from other type of Jaundice is usually not difficult.
- The laboratory findings are in constant in partial biliary obstruction and differentiation from intrahepatic cholestesis is particularly difficult.
- Jaundice- Differential diagnosis
- Differential Diagnosis
- Exclude UCB (e.g. hemolysis or Gilbert Synd.)
- Distinguish hepatocellular from obstructive
- Distinguish intrahepatic from extra hepatic cholestasis
- DIXON FREIDMAN RISK FACTORS
- S.Bilirubin gt 11mg/dl
- Malignant obstruction
- Haematocrit lt 30
- Renal failure
- Cholangitis
- Hypoalbuminemia
- If at least 3 of above mortality 60
- If none of above mortality 5
- Child A - Safely undergo elective surgery.
- Child B - may undergo elective surgery after
- optimisation with caution.
- Child C - Contraindication for elective surgery.
- Presence of infection
- WBC gt 10,000
- Treatment with gt 2 antibiotics
- PT gt 1.5 sec over control
- Presence of ascites
- Malnutrition
- Emergence surgery
PowerShow.com is a leading presentation sharing website. It has millions of presentations already uploaded and available with 1,000s more being uploaded by its users every day. Whatever your area of interest, here you’ll be able to find and view presentations you’ll love and possibly download. And, best of all, it is completely free and easy to use.
You might even have a presentation you’d like to share with others. If so, just upload it to PowerShow.com. We’ll convert it to an HTML5 slideshow that includes all the media types you’ve already added: audio, video, music, pictures, animations and transition effects. Then you can share it with your target audience as well as PowerShow.com’s millions of monthly visitors. And, again, it’s all free.
About the Developers
PowerShow.com is brought to you by CrystalGraphics , the award-winning developer and market-leading publisher of rich-media enhancement products for presentations. Our product offerings include millions of PowerPoint templates, diagrams, animated 3D characters and more.

OBSTRUCTIVE JAUNDICE
Sep 02, 2014
1.08k likes | 2.69k Views
OBSTRUCTIVE JAUNDICE. Presented by: MD. TANVIR MAJUMDER, Roll no.144 MD. MAHEDI HASAN, Roll no.150 MONIRUL HOQUE, Roll no.162 MD. SHAHADATH HOSSAIN, Roll no.163. CASE PRESENTATION ON: Obstructive jaundice. PARTICULARS OF THE PATIENT :.
Share Presentation
- obstructive jaundice
- thrill absent
- bowel sound
- added sound absent
- obstructive jaundice occurs due

Presentation Transcript
OBSTRUCTIVE JAUNDICE Presented by: MD. TANVIR MAJUMDER, Roll no.144 MD. MAHEDI HASAN, Roll no.150 MONIRUL HOQUE, Roll no.162 MD. SHAHADATH HOSSAIN, Roll no.163
CASE PRESENTATION ON: • Obstructive jaundice
PARTICULARSOFTHEPATIENT : Name : Mr. Kala Mohon Das Age : 65 years Fathers name :Late Nagar Baul Das Sex : Male Marital status: Married Religion : Sanatan Occupation: Garment worker Address: Gangabari, Pathorghata, Kotowalli, Ctg Bed no. : 18 Ward no.: 25 Date of admission :7-4-2013; 7pm Date of examination :25-4-2013;8pm
THE PRESENTING COMPLAINTS: • 1. recurrent pain in the right upper abdomen for last 1 year. • 2. yellow discoloration of eyes and skin for the same duration.
HISTORY OF PRESENT ILLNESS: According to the patient’s statement his presenting complaints started 1 year back. He developed severe pain in right upper abdomen which is colicky in nature, intermittent, radiating to the back on the tip of the scapula. The pain aggravated by taking food and relieved by medication, which was episodic occurring at an interval of 1 or 2 months. He had moderate grade, intermittent fever which was associated with chills and rigor. He also complained of vomiting after taking any food. Vomitus was non projectile, whitish in colour and contained both digested and undigested food particles. He had yellow discolouration of eyes and urine for the same duration. His bowel habit is normal. He has no history of pale colouration of stool. He has itching all over the body. He also has no history of weight loss, cough, hemoptysis, haematemesis, melaena or bone pain.
HISTORY OF PAST ILLNESS: • Patient gave no history of DM, HTN, TB, bronchial asthma.
PERSONAL AND SOCIO-ECONOMIC HISTORY: • Patient is non-smoker, non-alcoholic. • He comes from a lower-middle class family. He lives on average diet and uses sanitary latrine. FAMILY HISTORY: None of his family members is known to be suffering from the same or any other diseases.
DRUG HISTORY : He used to take analgesics and antipyretics for the last 3 months but could not mention the name of the drugs. ALLERGIC HISTORY: • He is not allergic to any drug or any particular food. TRANSFUSION HISTORY: • Patient has no history of blood transfusion.
General Examination
Appearance: Anxious • Body built: Average • Nutrition: Average • Co-operation: Cooperative • Decubitus: On choice • Anaemia: Absent • Jaundice: PRESENT (++) • Cyanosis: Absent • Clubbing: Absent • Edema: Absent • Dehydration: Absent • Pulse: 80 beats/minute • Blood pressure: 110/80 mm of Hg • Temperature: 100 degree F • Respiratory rate: 18 breaths/minute • Neck vein: Not engorged • Neck gland: Not enlarged • Peripheral lymph node: Not palpable • Hernial orifice: Intact
Abdomen examination • Abdomen is normal in shape. • Umbilicus is centrally placed, inverted, vertical slit. • No engorged vein. • No visible peristalsis. • No scar mark. • Hair distribution normal. • No visible pulsation. inspection
SUPERFICIAL PALPATION : • Hyperesthesia: absent • Tenderness: present in right hypochondriac region. • Temperature : raised • Muscle guard: absent DEEP PALPATION • Liver : not palpable • Gall Bladder: not palpable • Spleen: not palpable • Kidney: not palpable • Urinary bladder :not palpable. • Murphy’s sign: negative
Percussion • Note: Tympanic • Shifting dullness and fluid thrill absent
Auscultation • Shows no abnormality • Bowel sound present digital rectal examination
Cardiovuscular system: Peripheral pulses: All are present,symmetrical. Precordium: Apex beat: Left 5th ICS, 9 cm from midline Thrill: Absent Left parasternal heave: Absent Heart sound: Audible normally in all 4 areas Added sound: Absent
Respiratory system: Position of trachea and apex beat: Normal Chest expansion: Normal Percussion note: Resonant Breath sound: Normal Added sound: Absent
Nervous system Higher Mental function: Normal Cranial nerves: Intact Speech: Normal Signs of meningeal irritation: Absent Motor function: Intact Sensory function: Intact
SALIENT FEATURES: Mr. Kala Mohon Das, 65 years old, hailing from Kotowalli, Chittagong presented with the complaints of pain in the right upper abdomen for last 1 year, and yellow discoloration of eye and skin for the same duration. According to the patient’s statement, his presenting complaints started 1 years back when he developed pain in right upper abdomen which was severe, colicky in nature, intermittent, radiating to the back, aggravated by taking food and relieved after taking medication, which was episodic occurring at an interval of 1 or 2 months. He had moderate grade, intermittent fever which was associated with chills and rigor. He also complained of vomiting after taking any food. Vomitus was non projectile, whitish in colour and contained both digested and undigested food particles. He had yellow discolouration of eyes and urine for the same duration. His bowel habit is normal. He gives no history of pale colouration of stool. He has itching all over the body. He gave no history of weight loss, cough, chest pain, hemoptysis, haematemesis, melaena and bone pain. He has no history of blood transfusion. No member of his family is suffering from this disease. He is non-smoker, non-hypertensive, not diabetic.
On general examination, patient is anxious,co-operative,average built. He is icteric but not anaemic. Neck gland are not palpable, neck veins are not engorged, no ascites, no oedema is present. Hernial orifices are intact and all accessible peripheral lymph node are not palpable. His pulse, B.P., respiration was within normal limit and there was slight rise of body temperature. On abdominal examination, abdomen is normal in shape, umbilicus centrally placed,inverted,no scar mark, no engorged vein. Murphy’s sign is negative. There is tenderness in right hypochondriac region. Liver or other organs are not palpable. Bowel sound is present. Other systemic examination reveals no abnormality.
PROVISIONAL DIAGNOSIS: • OBSTRUCTIVE JAUNDICE due to choledocholithiasis
DIFFERENTIAL DIAGNOSIS: Obstructive jaundice due to: • carcinoma head of pancreas • Biliaryascariasis • Periampullary carcinoma • Cholangiocarcinoma
INVESTIGATIONS: 1.USG of whole abdomen with special attention to hepatobilliary system and pancreas: To visualize- -gall bladder -Liver -LN -Ascites 2.LIVER FUNCTION TEST: -serum bilirubin -SGOT -SGPT -Alkaline phosphatase -prothrombin time 3.FOR GENERAL ASSESSMENT: -CBC -urine R/E -RBS -serum creatinine -CXR -ECG
Confirmatory diagnosis: • Obstructive jaundice due to choledocholithiasis.
What is jaundice ? Jaundice may be defined as yellow discolouration of skin,sclera and mucous membrane due to an increase billirubin concentration in the body fluid above normal. Serum total bilirubin:(normal 0.3-1.2 mg/dl ) clinically detectable: >3.0 mg/dL
Anatomy of biliary system
BilLirubin Production & Metabolism:
Pathophysiologic classification of Jaundice • Hemolytic Jaundice • HepatocellularJaundice • Obstructive Jaundice
OBSTRUCTIVE JAUNDICE: • Obstructive jaundice occurs due to mechanical obstruction of the common bile duct.
CAUSES OF OBSTRUCTIVE JAUNDICE: 1.IN THE LUMEN: -gall stone -round worm 2.IN THE WALL: -congenital atresia -traumatic stricture -cholangitis -tumour of the bile duct 3.OUTSIDE THE WALL: -carcinoma head of the pancreas -carcinoma of ampulla of vater -pancreatitis -enlarged LN at portahepatis due to metastasis.
EXAMINATION FINDINGS OF OBSTRUCTIVE JAUNDICE: B.CARCINOMA HEAD OF PANCREAS: 1.Palpable liver 2.palpable mass 3.splenomegaly 4.palpable gall bladder. 5.weight loss. A.CHOLEDOCHOLITHIASIS: 1.patient-toxic,ill-looking 2.jaundice-long standing produce a deep green hue. 3.dehydrated 4.skin scratch mark all over the body. 5.increased temperature. 6.no lymphadenopathy. 7.tenderness in right hypochondriac region. 8.gall bladder is not palpable. 9.liver may be enlarged.
EXAMINATION FINDINGS OF OBSTRUCTIVE JAUNDICE: D.CHOLANGIOCARCINOMA: 1.patient is cachectic, anaemic 2.ichteric,dehydrated 3.hepatomegaly 4.palpable gall bladder-if lesion below cystic duct 5.ascitis-in advanced cases. C.PERIAMPULLARY CARCINOMA: 1.Fluctuating jaundice 2.palpable gall bladder 3.ascitis. 4.weight loss 5.palpable liver(may be)
COURVOISIER’S LAW: THE LAW STATES: 1)In case of obstructive jaundice due to stone in CBD,the gall bladder is not palpable/distended due to previous inflammatory fibrosis. 2)whereas,in obstruction of CBD due to pressure from outside(CA head of pancreas)the gall bladder become distended and palpable in an attempt to reduce the pressure in biliary system.
COMPLICATIONS OF OBSTRUCTIVE JAUNDICE: 1.Cholangitis 2.liver abscess 3.septicemia 4.hepatic failure 5.secondary biliary cirrhosis 6.acute pancreatitis 7.haemorrhage or haemobilia 8.acute renal failure. 9.gall stone ileus
Investigation
For diagnosis of obstructive jaundice: Liver function test: • Prothrombin time (markedly raised) • Serum Bilirubin (conjugated) • Fecealurobilinogen (incomplete obstruction) • Fecealurobilinogen absence (complete obstruction) • Bilirubinuria(conjugated) • ALP markedly • GGT & 5’ nucleosidase (most reliable)
For diagnosis of cause: • USG of whole abdomen with special attention to hepatobiliary system and pancreas (sensitivity 75-90%,specificity 80-100%) • ERCP • MRCP • CT scan • Radioisotope scanning • PTC • Endoscopic ultrasound • Routine investigation: For general anaesthesia: • CBC • Urine R/E • RBS • Serum creatinine • CXR • ECG
For staging • CXR • CT scan • MRI • PET-scan • Bone scan-if symptoms present
- More by User
Obstructive jaundice
Obstructive jaundice. I C Cameron. Acute on call. Deranged LFTs, esp Alk Ph and GGT Conjugated Bilirubin high Take a good history Onset, drugs, pain, previous attacks, alcohol, gallstones, pale stools, dark urine, wt loss Look for signs of liver failure USS - gallstones?
1.32k views • 14 slides
Jaundice. By Saud Al-Sultan Saud Al- Deghaither Abdullah Al- Masoud Supervised by Dr. Faisal Al- Saif. Jundice is an increased concentration of bilirubin in plasma . The normal upper limit is 17 mic mol/L
2.2k views • 58 slides
Frequent manifestationNormal Serum bilirubin 0.5-1.3 mg/dLJaundice: exceed 2mg/dLPre-hepatic: Hemolysis, Gilbert's, Crigler-Najjar.Hepatic: HepatoCellular or Cholestatic. Viral Hepatitis, Alcoholic cirrhosis, Primary biliary cirrhosis, toxic drugs, pregnancy, postoperative. Ext
928 views • 30 slides
JAUNDICE . UNIV VAN PTA Pretoria Academic Hospital GASTROENTEROLOGY Dr Obedy Mwantembe. JAUNDICE. Symptom. Three Causes. Prehepatic Hepatic Post Hepatic. HISTORY. Duration and onset Drug intake/history The Progression Associated Features Pruritus Colour of stool Anaemia.
671 views • 15 slides
Jaundice . http://thestandard.org.nz/wp-content/uploads/2010/09/Dr-Nick-Riviera.png. Steven Smith. Objectives. Bilirubin Physiology Jaundice Definitions Jaundice Presentation History and examination Investigations & Interpretation Differential Diagnosis Approach to differential
7.3k views • 19 slides
Jaundice. Bilirubin Metabolism. Pre-hepatic Hepatic Post-hepatic. Bilirubin Metabolism: Pre-Hepatic. Bilirubin is formed in reticuloendothelial system as breakdown product of hemaglobin. Heme group biliverdin bilirubin Bilirubin is insoluble in water, bound to albumin.
1.38k views • 15 slides
OBSTRUCTIVE JAUNDICE. DR.JAMIL SAWAKED. DEFITION OF JAUNDICE. YELLOW DISCOLOURATION OF SKIN AND MUCOUS MEMBRANE. TYPES. HAEMOLYSIS. PREHEPATIC. A. HEPATIC . POSTHEPATIC. OBSTRUCTIVE OR SURGICAL. ANATOMY. ANATOMY. A. BILIRUBIN CYCLE. BROKEN DOWN RED CELLS ARE
2.52k views • 62 slides
Jaundice. Tad Kim, M.D. UF Surgery [email protected] (c) 682-3793; (p) 413-3222. Overview. Normal Physiology Pathophysiology Broad Differential Diagnosis DDx of Obstructive Jaundice Work-up for “Medical” Jaundice Work-up if Obstructive Jaundice Treatment of Obstructive Jaundice.
933 views • 16 slides
OBSTRUCTIVE JAUNDICE. PROF P DARWIN PROF AND HEAD DEPT OF GENERAL SURGERY STANLEY MEDICAL COLLEGE. WHAT IS JAUNDICE ?. Yellowish pigmentation of the conjunctival membranes over the sclerae and other mucous membranes caused by increased levels of bilirubin in the blood >2 mg/dl.
22.99k views • 51 slides
Obstructive jaundice for 3 mon with itching & wt.loss
Obstructive jaundice for 3 mon with itching & wt.loss.
207 views • 6 slides

Anaesthetic management of obstructive jaundice
Anaesthetic management of obstructive jaundice. Dr. S. Parthasarathy MD., DA., DNB, MD ( Acu ), Dip. Diab.DCA, Dip. Software statistics PhD ( physio ) Mahatma Gandhi Medical college and research institute , puducherry - India. Anatomy . Functions of liver . The liver is vital for
1.64k views • 50 slides
Obstructive Jaundice: A rare cause
Obstructive Jaundice: A rare cause. A-65-year-old male. Three weeks of jaundice. Upper abdominal pain. Biliary papillomatosis . Forlano I1, Fersini A, Tartaglia N, Ambrosi A, Neri V. Abstract
452 views • 21 slides
Jaundice. Mohammad Mobasheri SpR General Surgery. Jaundice. Definition: yellow discolouration of skin and sclera as a result of hyperbilirubinaemia Bilirubin >35mmol/L for jaundice to be visible on examination Sclera first place to become jaundiced. Haemoglobin Metabolism.
2.5k views • 22 slides
Jaundice. Dr. Ahmed Kensarah. Introduction.
814 views • 37 slides

Obstructive Jaundice – Whipple’s Operation Anesthetic Management
Obstructive Jaundice – Whipple’s Operation Anesthetic Management. Munisha Agarwal Professor Deptt. of Anaesthesiology & Intensive Care L N Hospital & Maulana Azad Medical College Delhi. www.anaesthesia.co.in [email protected]. Obstructive Jaundice.
5.26k views • 58 slides
Jaundice. Definition Accumulation of yellow pigment in the skin and other tissues (Bilirubin). Bilirubin Metabolism Bilirubin formation Transport of bilirubin in plasma Hepatic bilirubin transport Hepatic uptake Conjugation Biliary excretion Enterohepatic circulation. Iron hemoglobin
3.27k views • 65 slides
JAUNDICE. By Anfal Gadour. Objectives. Definition of Jaundice Bilirubin Metabolism Investigations Categories Common causes and management. What do you already know?. How would you define jaundice?
1.32k views • 17 slides
JAUNDICE. Ultrasound Obstructive Hepatocellular. Obstructive Jaundice. Gallstones Pancreatic Cancer Cholangiocarcinoma Ampullary tumour Benign Biliary stricture Metastatic-Liver, Portal Primary sclerosing cholangitis IgG 4 disease Surgical trauma. ERCP or PTC.
580 views • 15 slides
Obstructive Jaundice
Obstructive Jaundice. Michael Richardson 8/20/04. Obstructive jaundice. LC is a 57 yo male who presents with painless jaundice Differential diagnosis (highest on list) Pancreatic carcinoma Ampullary adenoma Gallstones Liver disease Initial imaging – U/S followed by CT. Labs.
1.31k views • 11 slides
RT.hypochondrial pain , obstructive jaundice and vomting 2 wk duration.
272 views • 5 slides
BIOCHEMISTRY
640 views • 22 slides
Approach to Obstructive Jaundice & Pancreatic Cancer
Approach to Obstructive Jaundice & Pancreatic Cancer. MO TEACHING – JULY 21, 2015. Learning Points . Obstructive Jaundice Definition of Jaundice Bilirubin Cycle Anatomy Causes Investigations Management Pancreatic Cancer Incidence Risk Factors, Clinical Signs & Symptoms
1.62k views • 64 slides
- Search Menu
- Volume 2024, Issue 5, May 2024 (In Progress)
- Volume 2024, Issue 4, April 2024
- Bariatric Surgery
- Breast Surgery
- Cardiothoracic Surgery
- Colorectal Surgery
- Colorectal Surgery, Upper GI Surgery
- Gynaecology
- Hepatobiliary Surgery
- Interventional Radiology
- Neurosurgery
- Ophthalmology
- Oral and Maxillofacial Surgery
- Otorhinolaryngology - Head & Neck Surgery
- Paediatric Surgery
- Plastic Surgery
- Transplant Surgery
- Trauma & Orthopaedic Surgery
- Upper GI Surgery
- Vascular Surgery
- Author Guidelines
- Submission Site
- Open Access
- Reasons to Submit
- About Journal of Surgical Case Reports
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, case presentation, removal of a large symptomatic retrocardiac mediastinal lipoma.
- Article contents
- Figures & tables
- Supplementary Data
Martina Wollheim, Lily F S Willatt, Jonas P Ehrsam, Priska Cerncic, Mario L Lachat, Othmar Schöb, Ilhan Inci, Removal of a large symptomatic retrocardiac mediastinal lipoma, Journal of Surgical Case Reports , Volume 2024, Issue 5, May 2024, rjae273, https://doi.org/10.1093/jscr/rjae273
- Permissions Icon Permissions
Large mediastinal lipomas are rare. Complete surgical resection can be difficult due to the intricate anatomy in the mediastinum. We report the case of a 75-year-old man with worsened retrosternal pressure, decline in performance and syncope episodes. Computed tomography revealed a large retrocardiac low-attenuated mediastinal lesion measuring 10 × 8 cm, compressing the left atrium and pulmonary veins bilaterally. Surgical exploration was achieved through a right anterolateral thoracotomy with a successful en bloc resection without any intraoperative complications. The total operation time was 185 min with a total blood loss of <250 ml. Stand-by extracorporeal life support was present throughout the procedure, but its use was not required. The postoperative course was uneventful. The pathological examination revealed a mature mediastinal lipoma without any evidence of malignancy. In the 12-month control the patient was completely free of symptoms and in a good general condition.
Lipomas are well-demarcated, slow-growing mesenchymal tumors originating from adipose tissue, predominantly manifesting a benign entity. Mediastinal location is rare and are mostly incidental findings. They rarely produce mediastinal compartment syndrome even at considerable sizes and can grow undetected for years. Surgical excision is usually postponed until symptomatic, leading to an increased morbidity associated with surgery, generally requiring cardiopulmonary support. Successful tumor resection is associated with a good prognosis. This case-report illustrates a safe-approach for removal of a large symptomatic retrocardiac mediastinal lipoma, not requiring extracorporeal life support (ECLS) despite cardiac manipulation. This work has been reported in line with the SCARE criteria [ 1 ].
A 75-year-old Caucasian man presented with worsened retrosternal pressure, decline in performance and syncope episodes. The patient was investigated 2-years earlier for performance intolerance, revealing a 9 × 8.5 cm mediastinal retrocardiac lesion in a computed tomography (CT)-scan, initially classified as oligosymptomatic. The progredient symptomatology prompted a new CT-scan showing a slight increase in size of the lesion to 8 × 10 cm, compression of the left atrium and pulmonary veins bilaterally ( Fig. 1A–C ). An echocardiography performed at rest demonstrated a regular cardiac output with no obstruction of flow in the pulmonary veins or arteries. A pre-operative diagnosis of a benign lipoma was suspected. Interdisciplinary concerns about a potentially abrupt and fatal insufficiency during increased exercise led to the referral to surgery.
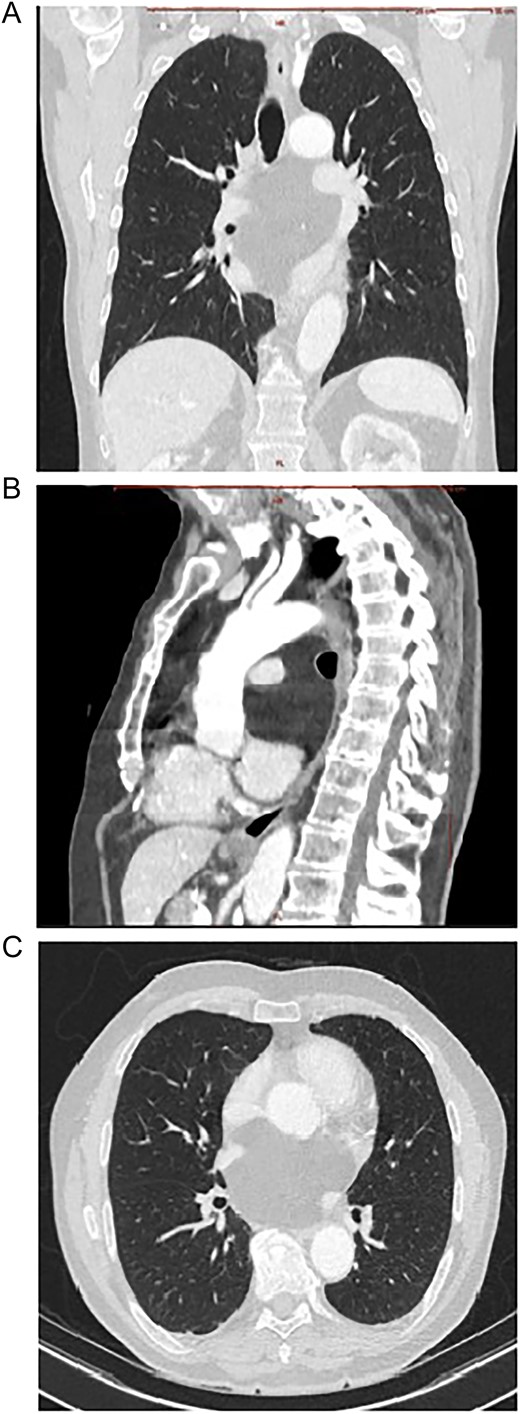
Contrast enhanced CT scan of mediastinum demonstrating the well-defined focal fat-attenuated homogenous lesion. (A) Coronal view, (B) sagittal view, (C)axial view.
The surgical exploration was achieved through a right lateral thoracotomy with a retro- and trans-pericardial approach. The thoracotomy was performed in the fifth intercostal space with division of the fifth rib in the cartilaginous portion with subsequent severing of the pulmonary ligament ( Fig. 2A ). Following circumferential dissection of the posterior pulmonary hilum the encapsulated soft tumor, reminiscent of a lipoma, became visible in the posterior mediastinum. The inferior pulmonary vein and the left atrium were intricately grown together with the tumor capsule, spanning from an extra- to intrapericardial location which required a meticulous dissection ( Fig. 2B, C ). Additionally, a 5-cm-long pericardial opening lateral to the phrenic nerve was necessary for complete resection ( Fig. 3A ). Free dissection of the superior vena cava (SVC) and azygos vein in a dorsal direction was performed to detach the tumor capsule from the retrocaval space and right atrium. An additional 8 cm long longitudinal opening of the pericardium up to the level of the anonymous vein was required. Dissection of the aperture between the SVC and aorta generated a supplementary window to further dissect the tumor capsule dorsally from these structures, the pulmonary artery and the remaining retro-pericardial area. Finally, with ventral mobilization of the heart the tumor resection could be completed ( Fig. 3B, C ). Upon re-ventilation, the lungs promptly expanded to optimal capacity.
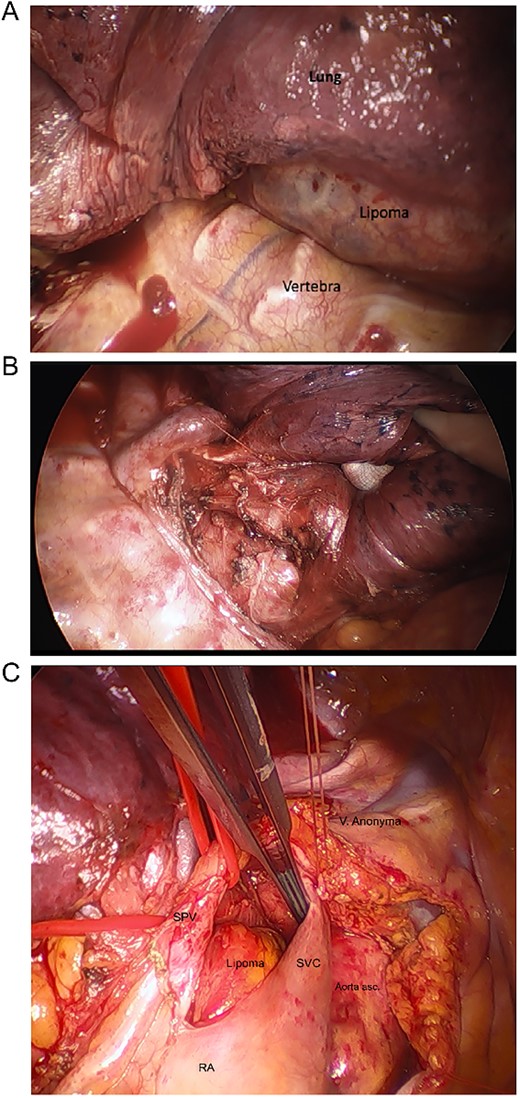
Intraoperative images. (A) After thoracotomy giving access to mediastinum, (B) incision in posterior mediastinal pleura giving access to posterior mediastinum, (C) separating lipoma around SVC, superior pulmonary vein (SPV), ascending aorta, right atrium (RA), hidden pulmonary truncus, and right pulmonary artery.
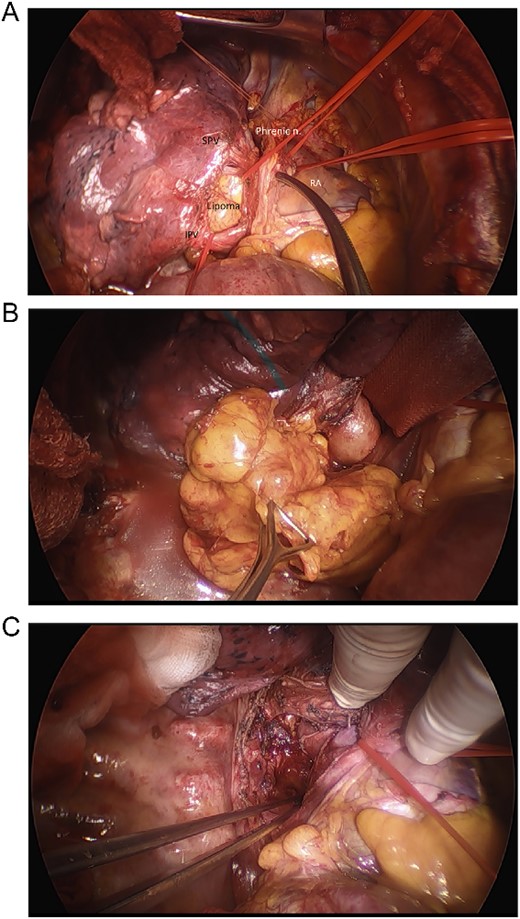
Intraoperative images. (A) Intraoperative view of inferior pulmonary vein (IPV), SPV, phrenic nerve, right atrium, and the lipoma, (B) final removal of the Lipoma from the right incision of the dorsal mediastinum, (C) resection site after removal of lipoma before closure.
The tumor was successfully resected en bloc in its capsule without any intraoperative complications. The total operation time was 185 min with a total blood loss of <250 ml. Stand-by ECLS was present throughout the procedure in case of hemodynamic insufficiency during cardiac manipulations or bleeding, but its use was not required at any point. The postoperative course was uneventful and 4-h after the operation the patient could be extubated in the intensive-care unit (ICU). 24-h post-surgery the patient could be transferred from the ICU to a regular ward and the chest-drain could be removed after 4 days. The subsequent x-ray revealed distended lungs bilaterally with an unremarkable mediastinal silhouette and the patient was discharged from the hospital in a good general condition on Day 7 post-op. The following day, the patient experienced an episode of atrial fibrillation for which he sought medical attention in his local hospital. In the 12-month control the patient was completely free of symptoms and in a good general condition.
Gross appearance showed a lobulated lesion with distinct yellow-fatty-tissue resembling a lipoma. It had a soft texture with a smooth surface covered by a thin shiny membrane. The tumor measured 10 × 8.5 cm and had a formalin-fixed weight of 172 g ( Fig. 4A ). The microscopic examination showed an encapsulated tumor composed of abundant mature adipose cells with adipocytes that exhibited uniformity in both size and shape ( Fig. 4B ). There was no detection of lipoblasts, increased mitotic rate, or zones of necrosis indicating malignancy. The definitive pathological examination was a mature retrocardiac mediastinal lipoma without any evidence of malignancy.
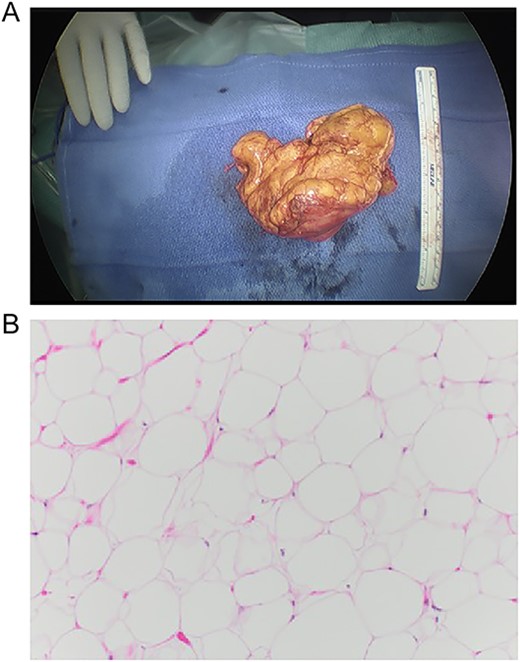
Macro- and microscopic findings. (A) Gross appearance of the lesion, (B) histological examination of the lesion, composed of abundant mature adipose cells with adipocytes exhibiting uniformity in both size and shape. 10× magnification, H&E stain.
Lipomas are the most frequently encountered soft-tissue neoplasm in adults and are rarely situated in the mediastinum [ 2 ]. In this case, large mediastinal tumors occur mostly in the anterior portion and represent 1.6–2.3% of all primary mediastinal tumors [ 3 ]. A lipomatous lesion of the mediastinum tends to grow slowly and is always classified as benign except those causing mediastinal compartment syndrome. These lesions should be regarded as clinically malignant and treated with en bloc excision [ 4 ].
Liposarcomas are a diverse group of malignant soft-tissue tumors. Well-differentiated liposarcomas (WDLS) can be difficult to discern from a benign lipoma on imaging. In a study [O’Donnell et al .], experienced musculoskeletal-radiologists and orthopedic-oncologists were able to differentiate between lipomas and WDLS in imaging in 69% of cases [ 5 ]. WDLS are associated with amplification of chromosome segment 12q13-15, which carries the oncogenes MDM 2 , CDK 4 , and HMGA 2 [ 6 ]. These amplifications are not seen in lipomas and its presence helps to differentiate them from WDLS [ 7 ]. A histological exploration is therefore recommended in the pre-operative phase to differentiate these, especially in surgeries where an en bloc resection can’t be guaranteed. In our case, the suspected pre-operative diagnosis of lipoma was based on imaging in conjunction with the slow progression of the lesion over time. A fluorescence in situ hybridization to detect genetic abnormalities involving MDM 2 to rule out a malignant WDLS should have been performed.
Local recurrence of intrathoracic and mediastinal lipomas is uncommon following complete resection [ 7 ]. Generally, surgery is delayed until the lipoma is large, probably because of the morbidity associated with surgery under cardiopulmonary support. This case illustrated an original interdisciplinary, less invasive and safe approach with a good patient outcome. Such an approach allows to treat patients earlier before they develop life-threatening symptoms. Stand-by ECLS is an important pre-cautionary to have available during surgery, but may not be required.
Sohrabi C , Mathew G , Maria N , et al. The SCARE 2023 guideline: updating consensus surgical case report (SCARE) guidelines . Int J Surg 2023 ; 109 : 1136 – 40 . https://doi.org/10.1097/js9.0000000000000373 .
Google Scholar
Salam GA . Lipoma excision . Am Fam Physician 2002 ; 65 : 901 – 4 .
Gaerte SC , Meyer CA , Winer-Muram HT , et al. Fat-containing lesions of the chest . Radiographics 2002 ; 22 : S61 – 78 . https://doi.org/10.1148/radiographics.22.suppl_1.g02oc08s61 .
Kandakure PR , Kambhampati S , Katta Y , et al. Giant bilateral posterior mediastinal liposarcoma excision . Indian J Thorac Cardiovasc Surg 2018 ; 35 : 91 – 3 . https://doi.org/10.1007/s12055-018-0703-6 .
O’Donnell PW , Griffin AM , Eward WC , et al. Can experienced observers differentiate between lipoma and well-differentiated liposarcoma using only MRI? Sarcoma 2013 ; 2013 : 1 – 6 . https://doi.org/10.1155/2013/982784 .
Crago AM , Dickson MA . Liposarcoma . Surg Oncol Clin N Am 2016 ; 25 : 761 – 73 . https://doi.org/10.1016/j.soc.2016.05.007 .
Rizer M , Singer AD , Edgar M , et al. The histological variants of liposarcoma: predictive MRI findings with prognostic implications, management, follow-up, and differential diagnosis . Skeletal Radiol 2016 ; 45 : 1193 – 204 . https://doi.org/10.1007/s00256-016-2409-4 .
Email alerts
Citing articles via, affiliations.
- Online ISSN 2042-8812
- Copyright © 2024 Oxford University Press and JSCR Publishing Ltd
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

IMAGES
VIDEO
COMMENTS
It defines obstructive jaundice as a failure of bile to reach the intestine due to mechanical obstruction. Pathophysiological changes include bile duct dilation, hepatic fibrosis, and portal hypertension. Causes include gallstones, strictures, tumors, and congenital anomalies. A thorough history, physical exam, and lab tests can localize the ...
25. Add a cup of barley to about three liters of water and simmer for a couple of hours. Drink this frequently during the day for relief from jaundice. Add some pepper and salt to fresh tomato juice and drink every morning. Lycopene from tomatoes can help to reduce damage to the liver and even facilitate recovery.
Herein, we present a case of cholangiocarcinoma in which obstructive jaundice was caused by inflammatory jelly like contents. 2 Case presentation. A 66-year-old female visited our hospital due to body weakness and jaundice. The patient suffered from gradually worsening complaints of generalized body weakness, jaundice, and anorexia for the last ...
ERCP: internal stenting. The Mirizzi syndrome refers to common hepatic duct obstruction caused by an extrinsic compression from an impacted stone in the cystic duct or Hartmann's pouch of the gallbladder. 1 The majority of the patients present the clinical triad of jaundice, fever, and right upper quadrant pain, showing in the laboratory ...
19. PATHOPHYSIOLOGY OF OBSTRUCTIVE JAUNDICE Obstructive jaundice is a condition in which there is blockage of the flow of bile out of the liver. This results in an overflow of bile and its by-products into the blood, and bile excretion from the body is incomplete Hepatic functions Protein synthesis, Reticulo-endothelial function Hepatic metabolism Coagulation defect..increased prothrombin time ...
Cholangiocarcinoma is a common cause of obstructive jaundice but is mainly associated with solid mass and not semisolid secretion. In this report, the patient was admitted to the hospital with obstructive jaundice; however, no solid mass was found to lead to jaundice. ... Case presentation. A 66-year-old female visited our hospital due to body ...
Case presentation. A 36-year-old Hispanic male presented to the Emergency Room twice with abdominal pain, nausea, and vomiting. The physical exam was remarkable for scleral icterus and abdominal tenderness. ... Although obstructive jaundice could be explained by numerous conditions, biliary tract disease is one of the most common causes of ...
The White Army Comprehensive Clinical Class Case Presentation on Obstructive Jaundice by Dr. Kaviprabha, 3rd year M.S. General Surgery, Coimbatore Government...
A 48 year old woman presents to the emergency department with jaundice. Work through the case to reach a diagnosis. UK Medical Licensing Assessment (UKMLA) This clinical case maps to the following UKMLA presentations: Jaundice; ... Obstructive jaundice can be caused by direct extrinsic compression by the stone or from fibrosis caused by chronic ...
ULTRASOUND IN OBSTRUCTIVE JAUNDICE • Sensitivity 70-95% • Specificity 87% • Limitations Fails to detect CBD Stones at ampulla in75-85 % of cases. OBESE patients. CT SCAN IN OBSTRUCTIVE JAUNDICE • Sensitivity and specificity similar to good quality Ultrasound. • Useful in Obese patients or Excessive bowel Gas.
Jaundice is the yellowish pigmentation of the skin, the conjunctival membranes over the sclerae, and other mucous membranes caused by hyperbilirubinemia. • Total serum bilirubin values are normally 0.2-1.2 mg/dL. Jaundice may not be clinically recognizable until levels are at least 3 mg/dL. DEFINITION.
Case Presentation Obstructive Jaundice Dr. Ravi Madhusudhana Professor Dr. Manjunath Post Graduate Dept of Anaesthesiology. SDUMC, Kolar. * * * * Identification of ... - A free PowerPoint PPT presentation (displayed as an HTML5 slide show) on PowerShow.com - id: 465c18-NWFmY
The patient was asymptomatic, and the diagnosis of jaundice was made accidentally when he presented to his dentist for a routine checkup. Previously, only one such case presentation has been reported, in which the patient presented with obstructive jaundice due to diffuse metastatic disease that developed because of small-cell lung cancer .
#ComprehensiveClinicalClass Obstructive Jaundice Case Presentation by Dr.Vinay, 3rd year MS General Surgery, AJIMS, Mangalore. Mentor: Dr.Kishan Rao, MBBS (B...
Obstructive Jaundice Case Discussion. Sep 7, 2013 • Download as PPTX, PDF •. 315 likes • 28,948 views. AI-enhanced title and description. Dr.S.N.Bhagirath .. This document presents the case of a 68-year-old male with obstructive jaundice. He presents with pain in the right upper abdomen, itching, and fever for the past few weeks.
Obstructive Jaundice clinical case presentation by Mr. Hriday Das, 4th year MBBS, Agartala Government Medical College.Mentors:Prof.K Rajgopal Shenoy,Author o...
Abstract. Introduction: Obstructive jaundice caused by metastases to the distal common bile duct or the ampulla of Vater is often observed in patients with various advanced cancers; however, metastasis of lung cancer to the ampulla of Vater with subsequent development of jaundice is rare. Case presentation: The patient was a 41-year-old Chinese ...
CASE PRESENTATION ON: • Obstructive jaundice PARTICULARSOFTHEPATIENT : Name : Mr. Kala Mohon Das Age : 65 years Fathers name :Late Nagar Baul Das Sex : Male Marital status: Married Religion : Sanatan Occupation: Garment worker Address: Gangabari, Pathorghata, Kotowalli, Ctg Bed no. : 18 Ward no.: 25 Date of admission :7-4-2013; 7pm Date of ...
Endoscopic and surgical techniques are the mainstay of treatment for LBS. We present this case of choledocholithiasis complicated by limy bile as an addition to the limited literature concerning this rare condition. Case report. A man aged in his 50s was referred to the emergency department with painful obstructive jaundice.
About Press Copyright Contact us Creators Advertise Developers Terms Privacy Policy & Safety How YouTube works Test new features NFL Sunday Ticket Press Copyright ...
Health & Medicine. 1 of 10. Download now. CASE PRESENTATION ON JAUNDICE. CASE PRESENTATION BY RAHMAN KHAN. DEMOGRAPHIC DETAILS • NAME. SUBJECTIVE EVIDENCE• PRESENT. OBJECTIVE EVIDENCE PHYSICAL EXAMINATIN: B.P: INVESTIGATION HAEMOLYTIC EVALUTION: • HEMOGLOBIN.
Our case highlights the diagnostic challenges of autoimmune pancreatitis, especially when it presents obstructive jaundice and radiological features that mimic pancreatic cancer. The patient's initial clinical presentation of jaundice, pruritus, weight loss, and an elevated CA 19-9 level raised suspicion for malignancy.
Download RAAONLINE App:Android: https://play.google.com/store/apps/details?id=com.sushrutha.appiOS: https://apps.apple.com/in/app/raaonline/id1564409258Cont...
Case presentation A 75-year-old Caucasian man presented with worsened retrosternal pressure, decline in performance and syncope episodes. The patient was investigated 2-years earlier for performance intolerance, revealing a 9 × 8.5 cm mediastinal retrocardiac lesion in a computed tomography (CT)-scan, initially classified as oligosymptomatic.
Case Presentation-Obstructive Jaundice-Dr.Sneha Raveendra Das, DNB Resident, Baby Memorial Hospital, Kozhikode