Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.

Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.

Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.

Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.

If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.

- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Key Points |
Abnormal fetal lie or presentation may occur due to fetal size, fetal anomalies, uterine structural abnormalities, multiple gestation, or other factors. Diagnosis is by examination or ultrasonography. Management is with physical maneuvers to reposition the fetus, operative vaginal delivery , or cesarean delivery .
Terms that describe the fetus in relation to the uterus, cervix, and maternal pelvis are
Fetal presentation: Fetal part that overlies the maternal pelvic inlet; vertex (cephalic), face, brow, breech, shoulder, funic (umbilical cord), or compound (more than one part, eg, shoulder and hand)
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse
Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position.
Abnormal fetal lie, presentation, or position may occur with
Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal congenital anomalies
Uterine structural abnormalities (eg, fibroids, synechiae)
Multiple gestation
Several common types of abnormal lie or presentation are discussed here.

Transverse lie
Fetal position is transverse, with the fetal long axis oblique or perpendicular rather than parallel to the maternal long axis. Transverse lie is often accompanied by shoulder presentation, which requires cesarean delivery.
Breech presentation
There are several types of breech presentation.
Frank breech: The fetal hips are flexed, and the knees extended (pike position).
Complete breech: The fetus seems to be sitting with hips and knees flexed.
Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
Types of breech presentations
Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows. The head, which is the part with the largest diameter, can then be trapped during delivery.
Additionally, the trapped fetal head can compress the umbilical cord if the fetal umbilicus is visible at the introitus, particularly in primiparas whose pelvic tissues have not been dilated by previous deliveries. Umbilical cord compression may cause fetal hypoxemia.

Predisposing factors for breech presentation include
Preterm labor
Uterine abnormalities
Fetal anomalies
If delivery is vaginal, breech presentation may increase risk of
Umbilical cord prolapse
Birth trauma
Perinatal death

Face or brow presentation
In face presentation, the head is hyperextended, and position is designated by the position of the chin (mentum). When the chin is posterior, the head is less likely to rotate and less likely to deliver vaginally, necessitating cesarean delivery.
Brow presentation usually converts spontaneously to vertex or face presentation.
Occiput posterior position
The most common abnormal position is occiput posterior.
The fetal neck is usually somewhat deflexed; thus, a larger diameter of the head must pass through the pelvis.
Progress may arrest in the second phase of labor. Operative vaginal delivery or cesarean delivery is often required.
Position and Presentation of the Fetus
If a fetus is in the occiput posterior position, operative vaginal delivery or cesarean delivery is often required.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord.
For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Delivery, face and brow presentation.
Julija Makajeva ; Mohsina Ashraf .
Affiliations
Last Update: January 9, 2023 .
- Continuing Education Activity
Face and brow presentation is a malpresentation during labor when the presenting part is either the face or, in the case of brow presentation, it is the area between the orbital ridge and the anterior fontanelle. This activity reviews the evaluation and management of these two presentations and explains the role of the interprofessional team in managing delivery safely for both the mother and the baby.
- Describe the mechanism of labor in the face and brow presentation.
- Summarize potential maternal and fetal complications during the face and brow presentations.
- Review different management approaches for the face and brow presentation.
- Outline some interprofessional strategies that will improve patient outcomes in delivery cases with face and brow presentation issues.
- Introduction
The term presentation describes the leading part of the fetus or the anatomical structure closest to the maternal pelvic inlet during labor. The presentation can roughly be divided into the following classifications: cephalic, breech, shoulder, and compound. Cephalic presentation is the most common and can be further subclassified as vertex, sinciput, brow, face, and chin. The most common presentation in term labor is the vertex, where the fetal neck is flexed to the chin, minimizing the head circumference.
Face presentation – an abnormal form of cephalic presentation where the presenting part is mentum. This typically occurs because of hyperextension of the neck and the occiput touching the fetal back. Incidence of face presentation is rare, accounting for approximately 1 in 600 of all presentations. [1] [2] [3]
In brow presentation, the neck is not extended as much as in face presentation, and the leading part is the area between the anterior fontanelle and the orbital ridges. Brow presentation is considered the rarest of all malpresentation with a prevalence of 1 in 500 to 1 in 4000 deliveries. [3]
Both face and brow presentations occur due to extension of the fetal neck instead of flexion; therefore, conditions that would lead to hyperextension or prevent flexion of the fetal neck can all contribute to face or brow presentation. These risk factors may be related to either the mother or the fetus. Maternal risk factors are preterm delivery, contracted maternal pelvis, platypelloid pelvis, multiparity, previous cesarean section, black race. Fetal risk factors include anencephaly, multiple loops of cord around the neck, masses of the neck, macrosomia, polyhydramnios. [2] [4] [5]
These malpresentations are usually diagnosed during the second stage of labor when performing a digital examination. It is possible to palpate orbital ridges, nose, malar eminences, mentum, mouth, gums, and chin in face presentation. Based on the position of the chin, face presentation can be further divided into mentum anterior, posterior, or transverse. In brow presentation, anterior fontanelle and face can be palpated except for the mouth and the chin. Brow presentation can then be further described based on the position of the anterior fontanelle as frontal anterior, posterior, or transverse.
Diagnosing the exact presentation can be challenging, and face presentation may be misdiagnosed as frank breech. To avoid any confusion, a bedside ultrasound scan can be performed. [6] The ultrasound imaging can show a reduced angle between the occiput and the spine or, the chin is separated from the chest. However, ultrasound does not provide much predicting value in the outcome of the labor. [7]
- Anatomy and Physiology
Before discussing the mechanism of labor in the face or brow presentation, it is crucial to highlight some anatomical landmarks and their measurements.
Planes and Diameters of the Pelvis
The three most important planes in the female pelvis are the pelvic inlet, mid pelvis, and pelvic outlet.
Four diameters can describe the pelvic inlet: anteroposterior, transverse, and two obliques. Furthermore, based on the different landmarks on the pelvic inlet, there are three different anteroposterior diameters, named conjugates: true conjugate, obstetrical conjugate, and diagonal conjugate. Only the latter can be measured directly during the obstetric examination. The shortest of these three diameters is obstetrical conjugate, which measures approximately 10.5 cm and is a distance between the sacral promontory and 1 cm below the upper border of the symphysis pubis. This measurement is clinically significant as the fetal head must pass through this diameter during the engagement phase. The transverse diameter measures about 13.5cm and is the widest distance between the innominate line on both sides.
The shortest distance in the mid pelvis is the interspinous diameter and usually is only about 10 cm.
Fetal Skull Diameters
There are six distinguished longitudinal fetal skull diameters:
- Suboccipito-bregmatic: from the center of anterior fontanelle (bregma) to the occipital protuberance, measuring 9.5 cm. This is the presenting diameter in vertex presentation.
- Suboccipito-frontal: from the anterior part of bregma to the occipital protuberance, measuring 10 cm
- Occipito-frontal: from the root of the nose to the most prominent part of the occiput, measuring 11.5cm
- Submento-bregmatic: from the center of the bregma to the angle of the mandible, measuring 9.5 cm. This is the presenting diameter in face presentation where the neck is hyperextended.
- Submento-vertical: from the midpoint between fontanelles and the angle of the mandible, measuring 11.5cm
- Occipito-mental: from the midpoint between fontanelles and the tip of the chin, measuring 13.5 cm. It is the presenting diameter in brow presentation.
Cardinal Movements of Normal Labor
- Neck flexion
- Internal rotation
- Extension (delivers head)
- External rotation (Restitution)
- Expulsion (delivery of anterior and posterior shoulders)
Some of the key movements are not possible in the face or brow presentations.
Based on the information provided above, it is obvious that labor will be arrested in brow presentation unless it spontaneously changes to face or vertex, as the occipito-mental diameter of the fetal head is significantly wider than the smallest diameter of the female pelvis. Face presentation can, however, be delivered vaginally, and further mechanisms of face delivery will be explained in later sections.
- Indications
As mentioned previously, spontaneous vaginal delivery can be successful in face presentation. However, the main indication for vaginal delivery in such circumstances would be a maternal choice. It is crucial to have a thorough conversation with a mother, explaining the risks and benefits of vaginal delivery with face presentation and a cesarean section. Informed consent and creating a rapport with the mother is an essential aspect of safe and successful labor.
- Contraindications
Vaginal delivery of face presentation is contraindicated if the mentum is lying posteriorly or is in a transverse position. In such a scenario, the fetal brow is pressing against the maternal symphysis pubis, and the short fetal neck, which is already maximally extended, cannot span the surface of the maternal sacrum. In this position, the diameter of the head is larger than the maternal pelvis, and it cannot descend through the birth canal. Therefore the cesarean section is recommended as the safest mode of delivery for mentum posterior face presentations.
Attempts to manually convert face presentation to vertex, manual or forceps rotation of the persistent posterior chin to anterior are contraindicated as they can be dangerous.
Persistent brow presentation itself is a contraindication for vaginal delivery unless the fetus is significantly small or the maternal pelvis is large.
Continuous electronic fetal heart rate monitoring is recommended for face and brow presentations, as heart rate abnormalities are common in these scenarios. One study found that only 14% of the cases with face presentation had no abnormal traces on the cardiotocograph. [8] It is advised to use external transducer devices to prevent damage to the eyes. When internal monitoring is inevitable, it is suggested to place monitoring devices on bony parts carefully.
People who are usually involved in the delivery of face/ brow presentation are:
- Experienced midwife, preferably looking after laboring woman 1:1
- Senior obstetrician
- Neonatal team - in case of need for resuscitation
- Anesthetic team - to provide necessary pain control (e.g., epidural)
- Theatre team - in case of failure to progress and an emergency cesarean section will be required.
- Preparation
No specific preparation is required for face or brow presentation. However, it is essential to discuss the labor options with the mother and birthing partner and inform members of the neonatal, anesthetic, and theatre co-ordinating teams.
- Technique or Treatment
Mechanism of Labor in Face Presentation
During contractions, the pressure exerted by the fundus of the uterus on the fetus and pressure of amniotic fluid initiate descent. During this descent, the fetal neck extends instead of flexing. The internal rotation determines the outcome of delivery, if the fetal chin rotates posteriorly, vaginal delivery would not be possible, and cesarean section is permitted. The approach towards mentum-posterior delivery should be individualized, as the cases are rare. Expectant management is acceptable in multiparous women with small fetuses, as a spontaneous mentum-anterior rotation can occur. However, there should be a low threshold for cesarean section in primigravida women or women with large fetuses.
When the fetal chin is rotated towards maternal symphysis pubis as described as mentum-anterior; in these cases further descend through the vaginal canal continues with approximately 73% cases deliver spontaneously. [9] Fetal mentum presses on the maternal symphysis pubis, and the head is delivered by flexion. The occiput is pointing towards the maternal back, and external rotation happens. Shoulders are delivered in the same manner as in vertex delivery.
Mechanism of Labor in Brow Presentation
As this presentation is considered unstable, it is usually converted into a face or an occiput presentation. Due to the cephalic diameter being wider than the maternal pelvis, the fetal head cannot engage; thus, brow delivery cannot take place. Unless the fetus is small or the pelvis is very wide, the prognosis for vaginal delivery is poor. With persistent brow presentation, a cesarean section is required for safe delivery.
- Complications
As the cesarean section is becoming a more accessible mode of delivery in malpresentations, the incidence of maternal and fetal morbidity and mortality during face presentation has dropped significantly. [10]
However, there are still some complications associated with the nature of labor in face presentation. Due to the fetal head position, it is more challenging for the head to engage in the birth canal and descend, resulting in prolonged labor.
Prolonged labor itself can provoke foetal distress and arrhythmias. If the labor arrests or signs of fetal distress appear on CTG, the recommended next step in management is an emergency cesarean section, which in itself carries a myriad of operative and post-operative complications.
Finally, due to the nature of the fetal position and prolonged duration of labor in face presentation, neonates develop significant edema of the skull and face. Swelling of the fetal airway may also be present, resulting in respiratory distress after birth and possible intubation.
- Clinical Significance
During vertex presentation, the fetal head flexes, bringing the chin to the chest, forming the smallest possible fetal head diameter, measuring approximately 9.5cm. With face and brow presentation, the neck hyperextends, resulting in greater cephalic diameters. As a result, the fetal head will engage later, and labor will progress more slowly. Failure to progress in labor is also more common in both presentations compared to vertex presentation.
Furthermore, when the fetal chin is in a posterior position, this prevents further flexion of the fetal neck, as browns are pressing on the symphysis pubis. As a result, descend through the birth canal is impossible. Such presentation is considered undeliverable vaginally and requires an emergency cesarean section.
Manual attempts to change face presentation to vertex, manual or forceps rotation to mentum anterior are considered dangerous and are discouraged.
- Enhancing Healthcare Team Outcomes
A multidisciplinary team of healthcare experts supports the woman and her child during labor and the perinatal period. For a face or brow presentation to be appropriately diagnosed, an experienced midwife and obstetrician must be involved in the vaginal examination and labor monitoring. As fetal anomalies, such as anencephaly or goiter, can contribute to face presentation, sonographers experienced in antenatal scanning should also be involved in the care. It is advised to inform the anesthetic and neonatal teams in advance of the possible need for emergency cesarean section and resuscitation of the neonate. [11] [12]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Julija Makajeva declares no relevant financial relationships with ineligible companies.
Disclosure: Mohsina Ashraf declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Makajeva J, Ashraf M. Delivery, Face and Brow Presentation. [Updated 2023 Jan 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PubMed Links to PubMed
Similar articles in PubMed
- Sonographic diagnosis of fetal head deflexion and the risk of cesarean delivery. [Am J Obstet Gynecol MFM. 2020] Sonographic diagnosis of fetal head deflexion and the risk of cesarean delivery. Bellussi F, Livi A, Cataneo I, Salsi G, Lenzi J, Pilu G. Am J Obstet Gynecol MFM. 2020 Nov; 2(4):100217. Epub 2020 Aug 18.
- Review Sonographic evaluation of the fetal head position and attitude during labor. [Am J Obstet Gynecol. 2022] Review Sonographic evaluation of the fetal head position and attitude during labor. Ghi T, Dall'Asta A. Am J Obstet Gynecol. 2022 Jul 6; . Epub 2022 Jul 6.
- Stages of Labor. [StatPearls. 2024] Stages of Labor. Hutchison J, Mahdy H, Hutchison J. StatPearls. 2024 Jan
- Leopold Maneuvers. [StatPearls. 2024] Leopold Maneuvers. Superville SS, Siccardi MA. StatPearls. 2024 Jan
- Review Labor with abnormal presentation and position. [Obstet Gynecol Clin North Am. ...] Review Labor with abnormal presentation and position. Stitely ML, Gherman RB. Obstet Gynecol Clin North Am. 2005 Jun; 32(2):165-79.
Recent Activity
- Delivery, Face and Brow Presentation - StatPearls Delivery, Face and Brow Presentation - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Trying to Conceive
- Signs & Symptoms
- Pregnancy Tests
- Fertility Testing
- Fertility Treatment
- Weeks & Trimesters
- Staying Healthy
- Preparing for Baby
- Complications & Concerns
- Pregnancy Loss
- Breastfeeding
- School-Aged Kids
- Raising Kids
- Personal Stories
- Everyday Wellness
- Safety & First Aid
- Immunizations
- Food & Nutrition
- Active Play
- Pregnancy Products
- Nursery & Sleep Products
- Nursing & Feeding Products
- Clothing & Accessories
- Toys & Gifts
- Ovulation Calculator
- Pregnancy Due Date Calculator
- How to Talk About Postpartum Depression
- Editorial Process
- Meet Our Review Board
Fetal Positions for Labor and Birth
Knowing your baby's position can you help ease pain and speed up labor
In the last weeks of pregnancy , determining your baby's position can help you manage pain and discomfort. Knowing your baby's position during early labor can help you adjust your own position during labor and possibly even speed up the process.
Right or Left Occiput Anterior
Illustration by JR Bee, Verywell
Looking at where the baby's head is in the birth canal helps determine the fetal position.The front of a baby's head is referred to as the anterior portion and the back is the posterior portion. There are two different positions called occiput anterior (OA) positions that may occur.
The left occiput anterior (LOA) position is the most common in labor. In this position, the baby's head is slightly off-center in the pelvis with the back of the head toward the mother's left thigh.
The right occiput anterior (ROA) presentation is also common in labor. In this position, the back of the baby is slightly off-center in the pelvis with the back of the head toward the mother's right thigh.
In general, OA positions do not lead to problems or additional pain during labor or birth.
Right or Left Occiput Transverse
Illustration by JR Bee, Verywell
When facing out toward the mother's right thigh, the baby is said to be left occiput transverse (LOT). This position is halfway between a posterior and anterior position. If the baby was previously in a posterior position (in either direction), the LOT position indicates positive movement toward an anterior position.
When the baby is facing outward toward the mother's left thigh, the baby is said to be right occiput transverse (ROT). Like the previous presentation, ROT is halfway between a posterior and anterior position. If the baby was previously in a posterior position, ROT is a sign the baby is making a positive move toward an anterior position.
When a baby is in the left occiput transverse position (LOT) or right occiput transverse (ROT) position during labor, it may lead to more pain and a slower progression.
Tips to Reduce Discomfort
There are several labor positions a mother can try to alleviate pain and encourage the baby to continue rotating toward an anterior position, including:
- Pelvic tilts
- Standing and swaying
A doula , labor nurse, midwife , or doctor may have other suggestions for positions.
Right or Left Occiput Posterior
When facing forward, the baby is in the occiput posterior position. If the baby is facing forward and slightly to the left (looking toward the mother's right thigh) it is in the left occiput posterior (LOP) position. This presentation can lead to more back pain (sometimes referred to as " back labor ") and slow progression of labor.
In the right occiput posterior position (ROP), the baby is facing forward and slightly to the right (looking toward the mother's left thigh). This presentation may slow labor and cause more pain.
To help prevent or decrease pain during labor and encourage the baby to move into a better position for delivery, mothers can try a variety of positions, including:
- Hands and knees
- Pelvic rocking
Mothers may try other comfort measures, including:
- Bathtub or shower (water)
- Counter pressure
- Movement (swaying, dancing, sitting on a birth ball )
- Rice socks (heat packs)
How a Doctor Determines Baby's Position
Leopold's maneuvers are a series of hands-on examinations your doctor or midwife will use to help determine your baby's position. During the third trimester , the assessment will be done at most of your prenatal visits. Knowing the baby's position before labor begins can help you prepare for labor and delivery.
Once labor begins, a nurse, doctor, or midwife will be able to get a more accurate sense of your baby's position by performing a vaginal exam. When your cervix is dilated enough, the practitioner will insert their fingers into the vagina and feel for the suture lines of the baby's skull as it moves down in the birth canal. It's important to ensure the baby is head down and moving in the right direction.
Labor and delivery may be more complicated if the baby is not in a head-down position, such as in the case of a breech presentation.
How You Can Determine Baby's Position
While exams by health practitioners are an important part of your care, from the prenatal period through labor and delivery, often the best person to assess a baby's position in the pelvis is you. Mothers should pay close attention to how the baby moves and where different movements are felt.
A technique called belly mapping can help mothers ask questions of themselves to assess their baby's movement and get a sense of the position they are in as labor approaches.
For example, the position of your baby's legs can be determined by asking questions about the location and strength of the kicking you feel. The spots where you feel the strongest kicks are most likely where your baby's feet are.
Other landmarks you can feel for include a large, flat plane, which is most likely your baby's back. Sometimes you can feel the baby arching his or her back.
At the top or bottom of the flat plane, you may feel either a hard, round shape (most likely your baby's head) or a soft curve (most likely to be your baby's bottom).
Guittier M, Othenin-Girard V, de Gasquet B, Irion O, Boulvain M. Maternal positioning to correct occiput posterior fetal position during the first stage of labour: a randomised controlled trial . BJOG: An International Journal of Obstetrics & Gynaecology . 2016;123(13):2199-2207. doi:10.1111/1471-0528.13855
Gizzo S, Di Gangi S, Noventa M, Bacile V, Zambon A, Nardelli G. Women’s Choice of Positions during Labour: Return to the Past or a Modern Way to Give Birth? A Cohort Study in Italy . Biomed Res Int . 2014;2014:1-7. doi:10.1155/2014/638093
Ahmad A, Webb S, Early B, Sitch A, Khan K, MacArthur C. Association between fetal position at onset of labor and mode of delivery: a prospective cohort study . Ultrasound in Obstetrics & Gynecology . 2014;43(2):176-182. doi:10.1002/uog.13189
Nishikawa M, Sakakibara H. Effect of nursing intervention program using abdominal palpation of Leopold’s maneuvers on maternal-fetal attachment . Reprod Health . 2013;10(1). doi:10.1186/1742-4755-10-12
Choi S, Park Y, Lee D, Ko H, Park I, Shin J. Sonographic assessment of fetal occiput position during labor for the prediction of labor dystocia and perinatal outcomes . The Journal of Maternal-Fetal & Neonatal Medicine . 2016;29(24):3988-3992. doi:10.3109/14767058.2016.1152250
Bamberg C, Deprest J, Sindhwani N et al. Evaluating fetal head dimension changes during labor using open magnetic resonance imaging . J Perinat Med . 2017;45(3). doi:10.1515/jpm-2016-0005
Gabbe S, Niebyl J, Simpson J et al. Obstetrics . Philadelphia, Pa.: Elsevier; 2012.
By Robin Elise Weiss, PhD, MPH Robin Elise Weiss, PhD, MPH is a professor, author, childbirth and postpartum educator, certified doula, and lactation counselor.

Fetal Presentation: Baby’s First Pose

Share this post

Occiput Anterior
Occiput posterior, transverse position, complete breech, frank breech, changing fetal presentation, baby positions.
The position in which your baby develops is called the “fetal presentation.” During most of your pregnancy, the baby will be curled up in a ball – that’s why we call it the “fetal position.” The baby might flip around over the course of development, which is why you can sometimes feel a foot poking into your side or an elbow prodding your bellybutton. As you get closer to delivery, the baby will change positions and move lower in your uterus in preparation. Over the last part of your pregnancy, your doctor or medical care provider will monitor the baby’s position to keep an eye out for any potential problems.
In the occiput anterior position, the baby is pointed headfirst toward the birth canal and is facing down – toward your back. This is the easiest possible position for delivery because it allows the crown of the baby’s head to pass through first, followed by the shoulders and the rest of the body. The crown of the head is the narrowest part, so it can lead the way for the rest of the head.
The baby’s head will move slowly downward as you get closer to delivery until it “engages” with your pelvis. At that point, the baby’s head will fit snugly and won’t be able to wobble around. That’s exactly where you want to be just before labor. The occiput anterior position causes the least stress on your little one and the easiest labor for you.
In the occiput posterior position, the baby is pointed headfirst toward the birth canal but is facing upward, toward your stomach. This can trap the baby’s head under your pubic bone, making it harder to get out through the birth canal. In most cases, a baby in the occiput posterior position will either turn around naturally during the course of labor or your doctor or midwife may help it along manually or with forceps.
In a transverse position, the baby is sideways across the birth canal rather than head- or feet-first. It’s rare for a baby to stay in this position all the way up to delivery, but your doctor may attempt to gently push on your abdomen until the baby is in a more favorable fetal presentation. If you go into labor while the baby is in a transverse position, your medical care provider will likely recommend a c-section to avoid stressing or injuring the baby.
Breech Presentation
If the baby’s legs or buttocks are leading the way instead of the head, it’s called a breech presentation. It’s much harder to deliver in this position – the baby’s limbs are unlikely to line up all in the right direction and the birth canal likely won’t be stretched enough to allow the head to pass. Breech presentation used to be extremely dangerous for mothers and children both, and it’s still not easy, but medical intervention can help.
Sometimes, the baby will turn around and you’ll be able to deliver vaginally. Most healthcare providers, however, recommend a cesarean section for all breech babies because of the risks of serious injury to both mother and child in a breech vaginal delivery.
A complete breech position refers to the baby being upside down for delivery – feet first and head up. The baby’s legs are folded up and the feet are near the buttocks.
In a frank breech position, the baby’s legs are extended and the baby’s buttocks are closest to the birth canal. This is the most common breech presentation .
By late in your pregnancy, your baby can already move around – you’re probably feeling those kicks! Unfortunately, your little one doesn’t necessarily know how to aim for the birth canal. If the baby isn’t in the occiput anterior position by about 32 weeks, your doctor or midwife will typically recommend trying adjust the fetal presentation. They’ll use monitors to keep an eye on the baby and watch for signs of stress as they push and lift on your belly to coax your little one into the right spot. Your doctor may also advise you to try certain exercises at home to encourage the baby to move into the proper position. For example, getting on your hands and knees for a few minutes every day can help bring the baby around. You can also put cushions on your chairs to make sure your hips are always elevated, which can help move things into the right place. It’s important to start working on the proper fetal position early, as it becomes much harder to adjust after about 37 weeks when there’s less room to move around.
In many cases, the baby will eventually line up properly before delivery. Sometimes, however, the baby is still in the wrong spot by the time you go into labor. Your doctor or midwife may be able to move the baby during labor using forceps or ventouse . If that’s not possible, it’s generally safer for you and the baby if you deliver by c-section.
Image Credit and License
Leave a Reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Stages of Pregnancy
- Foods to Avoid
- Medicines to Avoid
- Pregnancy Road Map
Birth Injuries
- Cerebral Palsy
- Brachial Plexus Injuries & Erb’s Palsy
- Brain Damage
- Meconium Aspiration
- Bone Fractures
- Nerve Damage
Newborn Care
- Baby Development
Legal Issues
- Birth Injury vs. Birth Defect
- Birth Injury Lawsuits
- Proving Your Case
- Elements Of A Case

- Email Address *
- Phone Number *
- Comments This field is for validation purposes and should be left unchanged.

- Mammary Glands
- Fallopian Tubes
- Supporting Ligaments
- Reproductive System
- Gametogenesis
- Placental Development
- Maternal Adaptations
- Menstrual Cycle
- Antenatal Care
- Small for Gestational Age
- Large for Gestational Age
- RBC Isoimmunisation
- Prematurity
- Prolonged Pregnancy
- Multiple Pregnancy
- Miscarriage
- Recurrent Miscarriage
- Ectopic Pregnancy
- Hyperemesis Gravidarum
- Gestational Trophoblastic Disease
- Breech Presentation
- Abnormal lie, Malpresentation and Malposition
- Oligohydramnios
- Polyhydramnios
- Placenta Praevia
- Placental Abruption
- Pre-Eclampsia
- Gestational Diabetes
- Headaches in Pregnancy
- Haematological
- Obstetric Cholestasis
- Thyroid Disease in Pregnancy
- Epilepsy in Pregnancy
- Induction of Labour
- Operative Vaginal Delivery
- Prelabour Rupture of Membranes
- Caesarean Section
- Shoulder Dystocia
- Cord Prolapse
- Uterine Rupture
- Amniotic Fluid Embolism
- Primary PPH
- Secondary PPH
- Psychiatric Disease
- Postpartum Contraception
- Breastfeeding Problems
- Primary Dysmenorrhoea
- Amenorrhoea and Oligomenorrhoea
- Heavy Menstrual Bleeding
- Endometriosis
- Endometrial Cancer
- Adenomyosis
- Cervical Polyps
- Cervical Ectropion
- Cervical Intraepithelial Neoplasia + Cervical Screening
- Cervical Cancer
- Polycystic Ovary Syndrome (PCOS)
- Ovarian Cysts & Tumours
- Urinary Incontinence
- Genitourinary Prolapses
- Bartholin's Cyst
- Lichen Sclerosus
- Vulval Carcinoma
- Introduction to Infertility
- Female Factor Infertility
- Male Factor Infertility
- Female Genital Mutilation
- Barrier Contraception
- Combined Hormonal
- Progesterone Only Hormonal
- Intrauterine System & Device
- Emergency Contraception
- Pelvic Inflammatory Disease
- Genital Warts
- Genital Herpes
- Trichomonas Vaginalis
- Bacterial Vaginosis
- Vulvovaginal Candidiasis
- Obstetric History
- Gynaecological History
- Sexual History
- Obstetric Examination
- Speculum Examination
- Bimanual Examination
- Amniocentesis
- Chorionic Villus Sampling
- Hysterectomy
- Endometrial Ablation
- Tension-Free Vaginal Tape
- Contraceptive Implant
- Fitting an IUS or IUD
Abnormal Fetal lie, Malpresentation and Malposition
Original Author(s): Anna Mcclune Last updated: 1st December 2018 Revisions: 12
- 1 Definitions
- 2 Risk Factors
- 3.2 Presentation
- 3.3 Position
- 4 Investigations
- 5.1 Abnormal Fetal Lie
- 5.2 Malpresentation
- 5.3 Malposition
The lie, presentation and position of a fetus are important during labour and delivery.
In this article, we will look at the risk factors, examination and management of abnormal fetal lie, malpresentation and malposition.
Definitions
- Longitudinal, transverse or oblique
- Cephalic vertex presentation is the most common and is considered the safest
- Other presentations include breech, shoulder, face and brow
- Usually the fetal head engages in the occipito-anterior position (the fetal occiput facing anteriorly) – this is ideal for birth
- Other positions include occipito-posterior and occipito-transverse.
Note: Breech presentation is the most common malpresentation, and is covered in detail here .
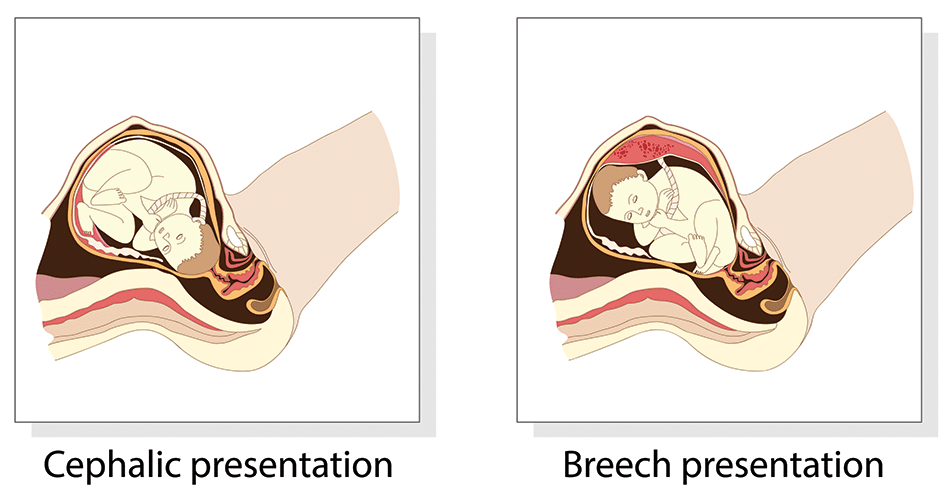
Fig 1 – The two most common fetal presentations: cephalic and breech.
Risk Factors
The risk factors for abnormal fetal lie, malpresentation and malposition include:
- Multiple pregnancy
- Uterine abnormalities (e.g fibroids, partial septate uterus)
- Fetal abnormalities
- Placenta praevia
- Primiparity
Identifying Fetal Lie, Presentation and Position
The fetal lie and presentation can usually be identified via abdominal examination. The fetal position is ascertained by vaginal examination.
For more information on the obstetric examination, see here .
- Face the patient’s head
- Place your hands on either side of the uterus and gently apply pressure; one side will feel fuller and firmer – this is the back, and fetal limbs may feel ‘knobbly’ on the opposite side
Presentation
- Palpate the lower uterus (above the symphysis pubis) with the fingers of both hands; the head feels hard and round (cephalic) and the bottom feels soft and triangular (breech)
- You may be able to gently push the fetal head from side to side
The fetal lie and presentation may not be possible to identify if the mother has a high BMI, if she has not emptied her bladder, if the fetus is small or if there is polyhydramnios .
During labour, vaginal examination is used to assess the position of the fetal head (in a cephalic vertex presentation). The landmarks of the fetal head, including the anterior and posterior fontanelles, indicate the position.
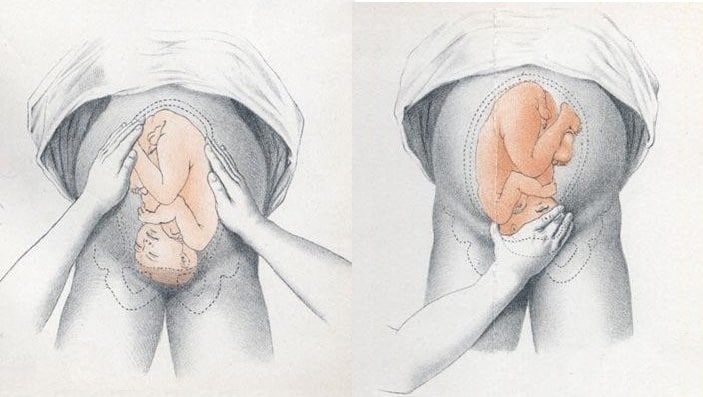
Fig 2 – Assessing fetal lie and presentation.
Investigations
Any suspected abnormal fetal lie or malpresentation should be confirmed by an ultrasound scan . This could also demonstrate predisposing uterine or fetal abnormalities.
Abnormal Fetal Lie
If the fetal lie is abnormal, an external cephalic version (ECV) can be attempted – ideally between 36 and 38 weeks gestation.
ECV is the manipulation of the fetus to a cephalic presentation through the maternal abdomen.
It has an approximate success rate of 50% in primiparous women and 60% in multiparous women. Only 8% of breech presentations will spontaneously revert to cephalic in primiparous women over 36 weeks gestation.
Complications of ECV are rare but include fetal distress , premature rupture of membranes, antepartum haemorrhage (APH) and placental abruption. The risk of an emergency caesarean section (C-section) within 24 hours is around 1 in 200.
ECV is contraindicated in women with a recent APH, ruptured membranes, uterine abnormalities or a previous C-section .
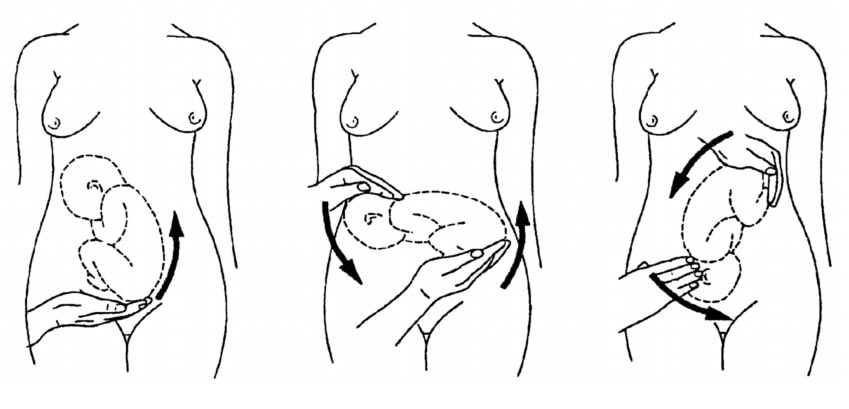
Fig 3 – External cephalic version.
Malpresentation
The management of malpresentation is dependent on the presentation.
- Breech – attempt ECV before labour, vaginal breech delivery or C-section
- Brow – a C-section is necessary
- If the chin is anterior (mento-anterior) a normal labour is possible; however, it is likely to be prolonged and there is an increased risk of a C-section being required
- If the chin is posterior (mento-posterior) then a C-section is necessary
- Shoulder – a C-section is necessary
Malposition
90% of malpositions spontaneously rotate to occipito-anterior as labour progresses. If the fetal head does not rotate, rotation and operative vaginal delivery can be attempted. Alternatively a C-section can be performed.
- Usually the fetal head engages in the occipito-anterior position (the fetal occiput facing anteriorly) - this is ideal for birth
If the fetal lie is abnormal, an external cephalic version (ECV) can be attempted - ideally between 36 and 38 weeks gestation.
- Breech - attempt ECV before labour, vaginal breech delivery or C-section
Found an error? Is our article missing some key information? Make the changes yourself here!
Once you've finished editing, click 'Submit for Review', and your changes will be reviewed by our team before publishing on the site.
We use cookies to improve your experience on our site and to show you relevant advertising. To find out more, read our privacy policy .
Privacy Overview

- About Merck
- Merck Careers
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Variations in Fetal Position and Presentation |
During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front. At first, the fetus can move around easily or shift position as the mother moves. Toward the end of the pregnancy the fetus is larger, has less room to move, and stays in one position. How the fetus is positioned has an important effect on delivery and, for certain positions, a cesarean delivery is necessary. There are medical terms that describe precisely how the fetus is positioned, and identifying the fetal position helps doctors to anticipate potential difficulties during labor and delivery.
Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way.
Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back).
Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique).
For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following:
Head first (called vertex or cephalic presentation)
Facing backward (occiput anterior position)
Spine parallel to mother's spine (longitudinal lie)
Neck bent forward with chin tucked
Arms folded across the chest
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible.
Variations in fetal presentation, position, or lie may occur when
The fetus is too large for the mother's pelvis (fetopelvic disproportion).
The uterus is abnormally shaped or contains growths such as fibroids .
The fetus has a birth defect .
There is more than one fetus (multiple gestation).

Position and Presentation of the Fetus
Variations in fetal position and presentation.
Some variations in position and presentation that make delivery difficult occur frequently.
Occiput posterior position
In occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back).
When a fetus faces up, the neck is often straightened rather than bent,which requires more room for the head to pass through the birth canal. Delivery assisted by a vacuum device or forceps or cesarean delivery may be necessary.
Breech presentation
In breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head).
When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first.
In a first delivery, these problems may occur more frequently because a woman’s tissues have not been stretched by previous deliveries. Because of risk of injury or even death to the baby, cesarean delivery is preferred when the fetus is in breech presentation, unless the doctor is very experienced with and skilled at delivering breech babies or there is not an adequate facility or equipment to safely perform a cesarean delivery.
Breech presentation is more likely to occur in the following circumstances:
Labor starts too soon (preterm labor).
The uterus is abnormally shaped or contains abnormal growths such as fibroids .
Other presentations
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.
In brow presentation, the neck is moderately arched so that the brow presents first.
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended.
In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Wednesday, April 17, 2024
- Nursing Article
4 Key Steps of the Leopold Maneuver for Accurate Fetal Positioning
The Leopold Maneuver is a fundamental examination technique used to assess fetal presentation, position, and size during pregnancy . It has been widely employed as a routine prenatal assessment tool by obstetricians and midwives for over a century. The technique involves a series of four maneuvers that allow the examiner to palpate the maternal abdomen and identify the fetal presentation and position.
In this article, we will explore the history, purpose, benefits, and limitations of the Leopold Maneuver , as well as provide a step-by-step guide on how to perform the examination. We will also discuss the importance of the Leopold Maneuver in prenatal care, common issues that may arise during the examination , and the role of the procedure in diagnosing fetal position.
Table of Contents
Definition of the Leopold Maneuver
The Leopold maneuver is a four-step procedure used by healthcare professionals to assess the fetal presentation, fetal lie, and fetal position . This technique involves feeling the abdomen, identifying the location of the fetal back, and palpating the fetal head, buttocks, and limbs to determine their position within the uterus .
History of the Leopold Maneuver
The Leopold maneuver was first described in 1899 by Christian Gerhard Leopold , a German obstetrician. Since then, it has become a standard procedure in obstetrics worldwide. Over the years, the technique has undergone several modifications to make it more accurate and reliable.
Importance of Leopold Maneuver in Obstetrics
The Leopold maneuver is a vital tool in assessing fetal presentation, lie, and position. The information obtained from this technique helps healthcare professionals determine the best mode of delivery and anticipate potential complications during labor and delivery. It also assists in identifying multiple gestations and abnormal fetal presentations , ensuring the safe delivery of the baby.
Purpose and Benefits of the Leopold Maneuver
Assessment of fetal presentation.
The Leopold maneuver is used to determine fetal presentation, which refers to the part of the fetus that enters the maternal pelvis first. The most common fetal presentation is the cephalic presentation, where the baby is head-down. However, other presentations, such as breech or transverse, require special attention during labor and delivery. The Leopold maneuver helps healthcare professionals determine the fetal presentation to prepare for the most optimal delivery for both the mother and baby.
Estimating Fetal Weight
During the Leopold maneuver, healthcare professionals can estimate fetal weight by palpating the mother’s abdomen. This information is crucial in assessing fetal growth and development and determining the need for intervention or delivery in cases where the fetus is too large or too small.
Identifying Fetal Lie and Attitude
The Leopold maneuver also helps healthcare professionals identify fetal lie and attitudes. Fetal lie refers to the orientation of the fetus in the uterus , while fetal attitude refers to the position of the fetus’s head and limbs in relation to its body . Accurate identification of fetal lie and attitudes is essential in preparing for safe and successful delivery.
Step-by-Step Guide on Performing the Leopold Maneuver
Preparing the Patient for the Examination
Before beginning the Leopold maneuver, the mother should empty her bladder, lie down, and relax her abdominal muscles. The healthcare professional should wash their hands and warm them before beginning the examination.
Step 1: Identification of the Fundus

Palpation of the fundus: The first maneuver is also called Fundal Grip . The healthcare professional palpates the uppermost part of the uterus (fundus) to determine the fetal lie, presentation, and engagement . The healthcare professional should identify the position of the fundus, which is the top of the uterus, by palpating the abdomen with both hands. The fundus is usually located near the navel.
Your Findings Should Be Recorded as, Head : round, more mobile Breach : Large, nodular mass
Step 2: Identification of the Fetal Back

Palpation of the sides of the uterus : The second maneuver is also called Umbilical Grip . The healthcare professional palpates the sides of the uterus to determine the fetal presentation and position . The healthcare professional should identify the location of the fetal back by feeling a smooth, firm, and long surface on one side of the uterus.
Your Findings Should Be Recorded as,
Back : Hard, resistant structure, directed anteriorly, posteriorly, or transversely Fetal Extremities : Numerous small irregular mobile parts

Step 3: Identification of the Fetal Part occupying the Pelvic Inlet

Palpation of the fetal parts : This maneuver is also known as the first Pawlik Grip . The healthcare professional palpates the fetal parts to determine the fetal position and engagement . The healthcare professional should identify the fetal part occupying the pelvic inlet by palpating the lower abdomen . Depending on the fetal presentation, this could be the fetal head or buttocks.
When the head has descended, can feel the anterior shoulder or the space created by the neck from the head.
- Palpate the lower abdomen to identify the presenting part of the fetus (e.g., “The fetal buttocks are presenting at the inlet.”)
- Note the position of the presenting part in relation to the mother’s pelvis (e.g., “The presenting part is in a transverse lie.”)
Step 4: Identification of the Fetal Part in the Pelvic Cavity

Palpation of the pelvic inlet : This maneuver is also known as the second Pawlik Grip . The healthcare professional palpates the pelvic inlet to determine fetal engagement . Finally, the healthcare professional should identify the fetal part in the pelvic cavity . This could be the fetal head, buttocks, or limbs.
Not engaged: Movable mass is felt
Engaged : Fixed mass is felt
Importance of the Leopold Maneuver in Prenatal Care
Identification of abnormal fetal presentation.
The Leopold maneuver is crucial in identifying abnormal fetal presentations , such as breech or transverse, which require special attention during labor and delivery to ensure the safety of both the mother and baby.
Assessment of Fetal Growth and Development
The Leopold maneuver provides healthcare professionals with vital information about fetal growth and development and helps them anticipate potential complications during labor and delivery.
Identification of Multiple Gestations
The Leopold maneuver is an essential tool in identifying multiple gestations to ensure appropriate prenatal care and delivery planning for mothers carrying more than one baby.
Common Issues and Solutions During the Leopold Maneuver
The Leopold maneuver is an obstetric examination technique used to assess fetal presentation, position, and engagement. However, performing this maneuver can be challenging due to various factors. Here are some common issues and solutions during the Leopold maneuver.
Difficulty in Assessing the Fetal Presentation
One common issue during the Leopold maneuver is difficulty in identifying fetal presentation . This can happen when the fetal presentation is not well defined or when there are multiple fetuses. To solve this issue, the examiner should carefully palpate the abdomen and try to differentiate between the fetal parts.
Difficulties in Identifying the Fetal Parts
Another common issue during the Leopold maneuver is difficulty in identifying fetal parts . This can happen when the fetus is in an atypical position or when there are fetal anomalies. To solve this issue, the examiner should use various techniques such as ultrasound or auscultation to guide them in identifying the fetal parts.
Confounding Factors that May Affect the Examination
There are confounding factors that may affect the accuracy of the Leopold maneuver, including obesity, polyhydramnios, fetal anomalies, and fetal movements . These factors can make it more challenging to perform the Leopold maneuver accurately. To solve this issue, examiners should try to minimize these factors or use additional examination techniques to confirm fetal presentation and position.
The Role of the Leopold Maneuver in Diagnosing Fetal Position
The Leopold maneuver is a crucial examination technique for diagnosing fetal position, and it plays a significant role in obstetric care. Here are some important factors to consider when using the Leopold maneuver to diagnose fetal position.
Importance of Diagnosing Fetal Position
Diagnosing fetal position is essential for obstetricians and midwives to ensure safe delivery. By knowing the fetal position, they can anticipate any potential complications during delivery and prepare accordingly. This can help minimize the risk of fetal distress, maternal injury, and other delivery-related complications .
Accuracy of Leopold Maneuver in Diagnosing Fetal Position
The Leopold maneuver is an accurate technique for diagnosing fetal position, with a sensitivity of up to 84%. It is a non-invasive and cost-effective method that can be performed by most healthcare providers. Therefore, it is widely used in obstetric care to diagnose fetal position.
Limitations of the Leopold Maneuver in Diagnosing Fetal Position
However, the Leopold maneuver has some limitations in diagnosing fetal position. It may not be accurate in identifying fetal presentation in cases of multiple pregnancies, fetal anomalies, or when the fetus is in an atypical position . Additionally, the examiner’s experience and skill level can also affect the accuracy of the Leopold maneuver.
Complications
The Leopold maneuver is generally considered a safe and non-invasive examination, but as with any medical procedure, there are potential complications that can occur. Some possible complications of the Leopold maneuver include:
- Discomfort: The Leopold maneuver can cause some discomfort or mild pain for the patient, especially if the examiner is pressing too hard or manipulating the fetus in a way that causes discomfort.
- False results: In some cases, the Leopold maneuver can produce false results, which can lead to incorrect decisions about delivery options or interventions. This can occur if the fetus is in an unusual position or if the examiner is inexperienced or unable to accurately interpret the results of the exam.
- Fetal distress: In rare cases, the Leopold maneuver can cause fetal distress or other complications, such as premature labor or rupture of the amniotic sac. This can occur if the examiner is too forceful or aggressive during the exam or if the fetus is in a vulnerable position.
- Infection: While the Leopold maneuver is a non-invasive exam, there is still a small risk of infection if the examiner does not follow proper hygiene protocols, such as washing their hands before and after the exam.
Nurse’s Responsibilities
The Leopold maneuver is a technique used by healthcare professionals, including nurses, to assess the position of a fetus in the mother’s uterus. As a nurse, your responsibilities during Leopold maneuvers include:
- Explaining the procedure to the patient: Before performing the Leopold maneuver, it is important to explain the procedure to the patient and ensure that they understand what will happen during the exam. This can help reduce anxiety and improve the patient’s overall experience.
- Preparing the patient: Before performing the exam, you will need to ensure that the patient is positioned correctly and that their clothing is adjusted to allow access to their abdomen. You may also need to provide a drape or cover for modesty.
- Assisting the healthcare provider: During the Leopold maneuver, you may be asked to assist the healthcare provider by holding the patient’s abdomen or providing support as needed. You may also need to help position the patient to allow for optimal access to the uterus.
- Monitoring the patient: As the Leopold maneuver can cause some discomfort or pain for the patient, it is important to monitor their vital signs and overall comfort level throughout the exam. If the patient experiences any discomfort or pain, you may need to provide comfort measures, such as adjusting their position or providing pain relief medication.
- Documenting the exam: After the Leopold maneuver, it is important to document the results of the exam in the patient’s medical record. This includes noting the fetal presentation, position, and engagement, as well as any other relevant information.
- Providing patient education: Following the exam, you may need to provide the patient with education about the results of the exam, as well as any next steps that may be needed. This can include discussing delivery options, potential complications, and follow-up appointments.
What is the Leopold Maneuver?
The Leopold Maneuver is a manual examination technique used by obstetricians and midwives to assess the fetal presentation, position, and size during pregnancy. The technique involves a series of four maneuvers that allow the examiner to palpate the maternal abdomen and identify the fetal presentation and position.
How is the Leopold Maneuver performed?
The Leopold Maneuver involves four maneuvers, which are performed in sequence. The first maneuver involves palpating the fundus to determine the location of the fetal head or buttocks. The second maneuver involves identifying the location of the fetal back. The third maneuver involves palpating the lower abdomen to identify the presenting part of the fetus. The fourth maneuver involves determining fetal descent and engagement.
What is the purpose of the Leopold Maneuver?
The purpose of the Leopold Maneuver is to assess the fetal presentation, position, and size during pregnancy. The examination can provide valuable information to obstetricians and midwives to ensure the health and safety of both the mother and the baby. The Leopold Maneuver can help identify abnormal fetal presentation, and multiple gestations, and estimate fetal weight.
Can the Leopold Maneuver be performed at home?
No, the Leopold Maneuver is a medical examination technique that should only be performed by trained healthcare professionals, such as obstetricians or midwives. It requires specialized knowledge, training, and experience to perform the examination accurately.
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
How your twins’ fetal positions affect labor and delivery

Twin fetal presentation – also known as the position of your babies in the womb – dictates whether you'll have a vaginal or c-section birth. Toward the end of pregnancy, most twins will move in the head-down position (vertex), but there's a risk that the second twin will change position after the first twin is born. While there are options to change the second twin's position, this can increase the risk of c-section and other health issues. Learn about the six possible twin fetal presentations: vertex-vertex, vertex-breech, breech-breech, vertex-transverse, breech-transverse, and transverse-transverse – and how they'll impact your delivery and risks for complications.
What is fetal presentation and what does it mean for your twins?
As your due date approaches, you might be wondering how your twins are currently positioned in the womb, also known as the fetal presentation, and what that means for your delivery. Throughout your pregnancy, your twin babies will move in the uterus, but sometime during the third trimester – usually between 32 and 36 weeks – their fetal presentation changes as they prepare to go down the birth canal.
The good news is that at most twin births, both babies are head-down (vertex), which means you can have a vaginal delivery. In fact, nearly 40 percent of twins are delivered vaginally.
But if one baby has feet or bottom first (breech) or is sideways (transverse), your doctor might deliver the lower twin vaginally and then try to rotate the other twin so that they face head-down (also called external cephalic version or internal podalic version) and can be delivered vaginally. But if that doesn't work, there's still a chance that your doctor will be able to deliver the second twin feet first vaginally via breech extraction (delivering the breech baby feet or butt first through the vagina).
That said, a breech extraction depends on a variety of factors – including how experienced your doctor is in the procedure and how much the second twin weighs. Studies show that the higher rate of vaginal births among nonvertex second twins is associated with labor induction and more experienced doctors, suggesting that proper delivery planning may increase your chances of a vaginal birth .
That said, you shouldn't totally rule out a Cesarean delivery with twins . If the first twin is breech or neither of the twins are head-down, then you'll most likely have a Cesarean delivery.
Research also shows that twin babies who are born at less than 34 weeks and have moms with multiple children are associated with intrapartum presentation change (when the fetal presentation of the second twin changes from head-down to feet first after the delivery of the first twin) of the second twin. Women who have intrapartum presentation change are more likely to undergo a Cesarean delivery for their second twin.
Here's a breakdown of the different fetal presentations for twin births and how they will affect your delivery.
Head down, head down (vertex, vertex)
This fetal presentation is the most promising for a vaginal delivery because both twins are head-down. Twins can change positions, but if they're head-down at 28 weeks, they're likely to stay that way.
When delivering twins vaginally, there is a risk that the second twin will change position after the delivery of the first. Research shows that second twins change positions in 20 percent of planned vaginal deliveries. If this happens, your doctor may try to rotate the second twin so it faces head-down or consider a breech extraction. But if neither of these work or are an option, then a Cesarean delivery is likely.
In vertex-vertex pairs, the rate of Cesarean delivery for the second twin after a vaginal delivery of the first one is 16.9 percent.
Like all vaginal deliveries, there's also a chance you'll have an assisted birth, where forceps or a vacuum are needed to help deliver your twins.
Head down, bottom down (vertex, breech)
When the first twin's (the lower one) head is down, but the second twin isn't, your doctor may attempt a vaginal delivery by changing the baby's position or doing breech extraction, which isn't possible if the second twin weighs much more than the first twin.
The rates of emergency C-section deliveries for the second twin after a vaginal delivery of the first twin are higher in second twins who have a very low birth weight. Small babies may not tolerate labor as well.
Head down, sideways (vertex, transverse)
If one twin is lying sideways or diagonally (oblique), there's a chance the baby may shift position as your labor progresses, or your doctor may try to turn the baby head-down via external cephalic version or internal podalic version (changing position in the uterus), which means you may be able to deliver both vaginally.
Bottom down, bottom down (breech, breech)
When both twins are breech, a planned C-section is recommended because your doctor isn't able to turn the fetuses. Studies also show that there are fewer negative neonatal outcomes for planned C-sections than planned vaginal births in breech babies.
As with any C-section, the risks for a planned one with twins include infection, loss of blood, blood clots, injury to the bowel or bladder, a weak uterine wall, placenta abnormalities in future pregnancies and fetal injury.
Bottom down, sideways (breech, transverse)
When the twin lowest in your uterus is breech or transverse (which happens in 25 percent of cases), you'll need to have a c-section.
Sideways, sideways (transverse, transverse)
This fetal presentation is rare with less than 1 percent of cases. If both babies are lying horizontally, you'll almost definitely have a C-section.
Learn more:
- Twin fetal development month by month
- Your likelihood of having twins or more
- When and how to find out if you’re carrying twins or more
Was this article helpful?
32 weeks pregnant with twins

28 weeks pregnant with twins

36 weeks pregnant with twins

24 weeks pregnant with twins

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
Cleveland Clinic. Fetal Positions for Birth: https://my.clevelandclinic.org/health/articles/9677-fetal-positions-for-birth Opens a new window [Accessed July 2021]
Mayo Clinic. Fetal Presentation Before Birth: https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/multimedia/fetal-positions/sls-20076615?s=7 Opens a new window [Accessed July 2021]
NHS. Giving Birth to Twins or More: https://pubmed.ncbi.nlm.nih.gov/29016498/ Opens a new window [Accessed July 2021]
Science Direct. Breech Extraction: https://www.sciencedirect.com/topics/medicine-and-dentistry/breech-extraction Opens a new window [Accessed July 2021]
Obstetrics & Gynecology. Clinical Factors Associated With Presentation Change of the Second Twin After Vaginal Delivery of the First Twin https://pubmed.ncbi.nlm.nih.gov/29016498/ Opens a new window [Accessed July 2021]
American Journal of Obstetrics and Gynecology. Fetal presentation and successful twin vaginal delivery: https://www.ajog.org/article/S0002-9378(04)00482-X/fulltext [Accessed July 2021]
The Journal of Maternal-Fetal & Neonatal Medicine. Changes in fetal presentation in twin pregnancies https://www.tandfonline.com/doi/abs/10.1080/14767050400028592 Opens a new window [Accessed July 2021]
Reviews in Obstetrics & Gynecology. An Evidence-Based Approach to Determining Route of Delivery for Twin Gestations https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3252881/ Opens a new window [Accessed July 2021]
Nature. Neonatal mortality and morbidity in vertex–vertex second twins according to mode of delivery and birth weight: https://www.nature.com/articles/7211408 Opens a new window [Accessed July 2021]
Cochrane. Planned cesarean for a twin pregnancy: https://www.cochrane.org/CD006553/PREG_planned-caesarean-section-twin-pregnancy Opens a new window [Accessed July 2021]
Kids Health. What Is the Apgar Score?: https://www.kidshealth.org/Nemours/en/parents/apgar0.html Opens a new window [Accessed July 2021]
American Journal of Obstetrics & Gynecology. Neonatal mortality in second twin according to cause of death, gestational age, and mode of delivery https://pubmed.ncbi.nlm.nih.gov/15467540/ Opens a new window [Accessed July 2021]
Lancet. Planned cesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. Term Breech Trial Collaborative Group https://pubmed.ncbi.nlm.nih.gov/11052579/ Opens a new window [Accessed July 2021]
Cleveland Clinic. Cesarean Birth (C-Section): https://my.clevelandclinic.org/health/treatments/7246-cesarean-birth-c-section Opens a new window [Accessed July 2021]
St. Jude Medical Staff. Delivery of Twin Gestation: http://www.sjmedstaff.org/documents/Delivery-of-twins.pdf Opens a new window [Accessed July 2021]

Where to go next

Lecturio Nursing
Cheat Sheets
Nursing Knowledge
5 Ps of Labor: Overview
Table of contents, what are the 5 ps of labor .
“The 5 Ps of labor” is a mnemonic used to remember the key aspects of the labor process. Each of the Ps stands for an element of labor that contributes to the progress and will need to be assessed and monitored to make sure labor is progressing safely.
Related videos
#1: passenger (fetal presentation and position) .
The first P, “Passenger,” refers to the position of the fetus.
Fetal attitude
Fetal attitude describes the relationship of the fetal parts to each other. The amount of flexion in the fetal body, specifically the head (how close the chin is to the chest).
The more flexed the fetal head, the smaller the diameter as it passes through the pelvis → the easier.
The fetal lie describes the relationship of the fetal spine to the maternal spine. It can be
- Vertical (both spines are in the same direction, could be breech or head-first)
- Oblique (fetal spine is at an angle to the maternal spine)
- Horizontal (fetal spine perpendicular to the maternal spine; vaginal birth not possible)
Fetal presentation
Fetal presentation is the relationship of the presenting part of the fetus to the quadrants of the maternal pelvis.
Types:
- Vertex (head coming first, most ideal)
- Breech (bottom coming first)
- Shoulder (shoulder coming first)
#2: Passageway: pelvic shape
The passageway includes the bony pelvis, the soft structures of the cervix, the vagina, and the introitus (vaginal opening).
The pelvic shapes are:
- Platypelloid
Gynecoid is the most common and most favorable for vaginal birth.

Download: Pelvis Types Cheat Sheet
The different types of pelvis shapes and their implications for labor and delivery
This refers to the contraction of the uterus and the maternal effort that moves the fetus out of the uterus.
Ideally, contractions are close together and regular. Excessive contractions can lead to tachysystole, such as 5 contractions within 10 minutes.
Primary powers
Primary powers are the uterine contractions, which are responsible for cervical dilation, effacement, and descent.
Secondary powers
Secondary powers refers to the maternal pushing efforts.
#4: Position
Position refers to the maternal position during labor and birth.
Tip: Help the client move. Maternal movement helps promote vaginal birth. Upright positions help internal fetal rotation.
Labor positions chart
Labor positions with epidural
Epidurals limit mobility but still allow for several labor positions, including lying on the back, side, on hands and knees, and being semi-seated. Even with an epidural, frequent position changes and movement as possible can help with labor progression.
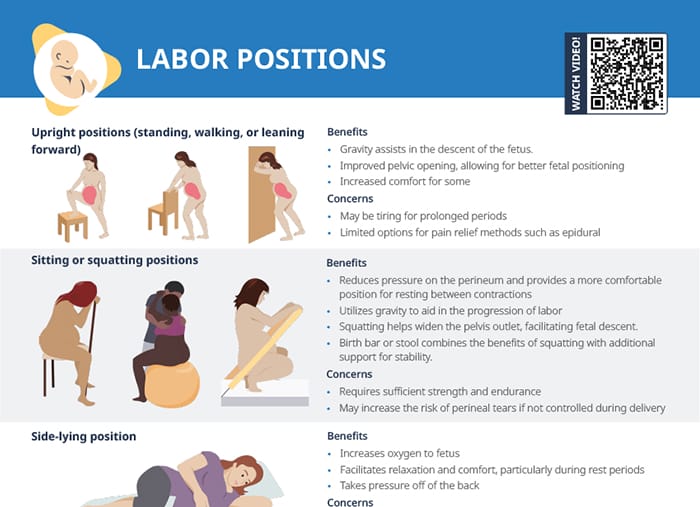
Download: Labor Positions Cheat Sheet
Overview of the primary labor positions with a summary of their benefits and risks
#5: Psyche
This aspect refers to supporting the pregnant client’s psychological adaptation to labor.
Ways to support birthing clients with their frame of mind during labor include:
- Education: childbirth classes, anticipatory guidance during labor
- Labor support: Continuous labor support increases vaginal birth rate. Build trust, frame labor pain as meaningful and productive, guide clients to their own decisions.
- Client-centered support: Respect cultural differences, respect client autonomy, and communicate effectively.
RELATED TOPIC:
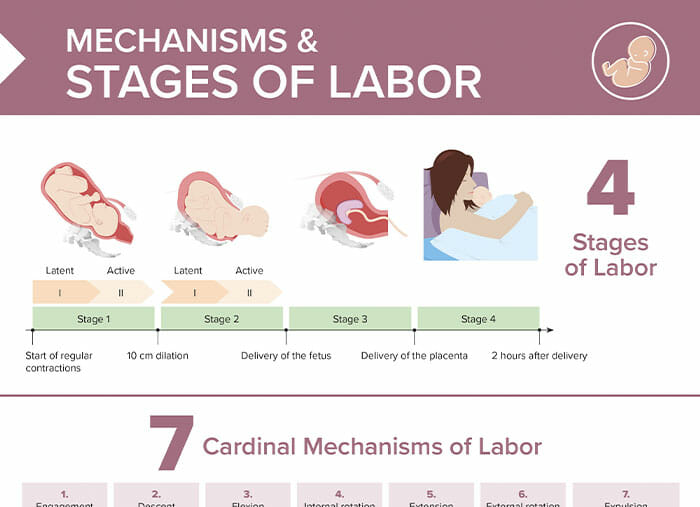
Stages of Labor
FREE CHEAT SHEET
Free Download
Nursing Cheat Sheet
Master the topic with a unique study combination of a concise summary paired with video lectures.
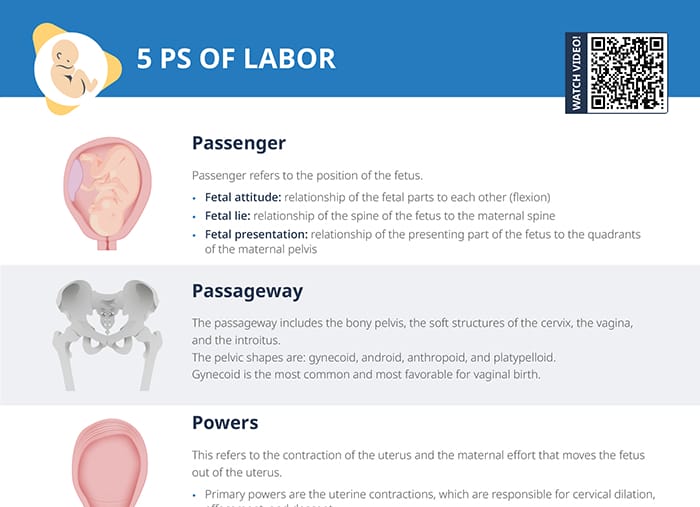
- Data Privacy
- Terms and Conditions
- Legal Information
USMLE™ is a joint program of the Federation of State Medical Boards (FSMB®) and National Board of Medical Examiners (NBME®). MCAT is a registered trademark of the Association of American Medical Colleges (AAMC). NCLEX®, NCLEX-RN®, and NCLEX-PN® are registered trademarks of the National Council of State Boards of Nursing, Inc (NCSBN®). None of the trademark holders are endorsed by nor affiliated with Lecturio.
User Reviews
Get premium to test your knowledge.
Lecturio Premium gives you full access to all content & features
Get Premium to watch all videos
Verify your email now to get a free trial.
Create a free account to test your knowledge
Lecturio Premium gives you full access to all contents and features—including Lecturio’s Qbank with up-to-date board-style questions.

BRIAN OSTLER, MD, SOUMYA CHOUDHURY, MD, AMANDA KIM, MD, MPH, AND JON O. NEHER, MD, Valley Family Medicine, Renton, Washington
SARAH SAFRANEK, MLIS, University of Washington, Seattle, Washington
Am Fam Physician. 2024;109(4):367-368
Author disclosure: No relevant financial relationships.
Clinical Question
Does the use of a peanut ball in pregnant patients with an epidural improve labor outcomes?
Evidence-Based Answer
In pregnant patients laboring with epidural anesthesia, the use of a peanut ball with regular position changes decreases the duration of first-stage labor by 87 minutes compared with usual care ( Figure 1 ) . (Strength of Recommendation [SOR]: A, meta-analysis of randomized controlled trials [RCTs].) The effect may be more pronounced in primiparous patients. (SOR: B, single RCT.) A patient safety bundle that includes several improvements in labor support, including the use of a peanut ball, is associated with a reduction in cesarean deliveries. (SOR: B, cross-sectional cohort study.)

Evidence Summary
A 2022 systematic review and meta-analysis of four randomized or quasirandomized clinical trials (n = 818) compared the effect of using a peanut ball with usual care for laboring patients with epidural analgesia. 1 In the intervention groups, researchers encouraged primiparous and multiparous patients 18 to 35 years of age with a singleton fetus in vertex position to use a peanut ball soon after epidural placement for at least 15 minutes every hour until reaching full cervical dilation. Patients changed position every 0.5 to 2 hours while using the peanut ball. Compared with patients receiving usual care, those laboring with a peanut ball had a shorter first stage of labor (two trials; n = 272; mean difference [MD] = 87.5 minutes; 95% CI, 80.3 to 94.5; high-certainty evidence based on the GRADE system) and a shorter second stage of labor (one trial; n = 201; MD = 22.2 minutes; 95% CI, 20.8 to 23.5; moderate-certainty evidence). The use of a peanut ball as a single intervention did not significantly change the risk of cesarean delivery (three trials; n = 669; relative risk = 0.75; 95% CI, 0.57 to 1.00; low-certainty evidence).
The two RCTs used in this meta-analysis did not consistently demonstrate a decrease in the duration of first stage of labor for all patients. The larger of the two trials, a 2015 RCT (n = 201) conducted at an inner-city teaching hospital, analyzed the effects of a peanut ball vs. position changes (deemed usual care) in patients who received an epidural. 2 Researchers defined the primary outcomes as the length of labor and vaginal delivery rates. The control group changed position every 1 to 2 hours, whereas the intervention group received a peanut ball to use after epidural administration and then made position changes. Researchers enrolled patients with a mean age of 27 years; 56% were nulliparous, and an equal number of Hispanic and non-Hispanic White patients participated. In the raw data, the group using the peanut ball in addition to position changes had a shorter first stage (269 vs. 356 minutes; P < .01) and second stage (21 vs. 44minutes; P < .001) of labor and a lower cesarean delivery rate (10% vs. 21%; P < .05) than patients in the usual care group. However, after the authors controlled for differences in parity and cervical dilation between the groups, there was no difference in the duration of the first stage of labor (MD = 29 minutes; P = .053), but the second stage of labor was significantly shorter (MD = 11 minutes; P < .001). After parity adjustment, use of the peanut ball was associated with fewer cesarean deliveries (odds ratio = 0.41; P = .04). Researchers identified no harms from use of the peanut ball.
A 2016 RCT (n = 149) from the previous systematic review (but not part of the meta-analysis due to incomplete outcome reporting) sought to determine whether the peanut ball would decrease the duration of labor in patients with epidurals. 3 Patients had a mean age of 31 years, 30% were primiparous, and 76% were White. Patients assigned to the intervention group had a peanut ball placed between their knees within 30 minutes after epidural administration with lateral position rotation every 30 minutes. Patients in the control group used one pillow between their knees (if desired) and followed a similar rotation protocol. Overall, no decrease was shown for multiparous patients. However, in a subanalysis of patients given oxytocin, the peanut ball shortened the first-stage of labor for primiparous patients by 177 minutes and lengthened it by 32 minutes in multiparous patients (between groups; P = .018). There was no difference in either group in the duration of second-stage labor. This study's small number of primiparous patients limited its certainty (n = 45). Researchers did not track cesarean delivery rates.
A pre- and postguideline implementation study compared cesarean delivery rates among nulliparous women with term, singleton, and vertex presentation pregnancies at three hospitals before (n = 434) and after (n = 401) initiating a system-wide patient safety bundle that included peanut ball use as part of standardized labor support. 4 Use of the safety bundle resulted in increased use of peanut balls (16% to 45% of labors; P < .001) and maternal position changes (79% to 88% of labors; P = .001). Although the duration of labor was not measured and the protocol used many interventions in addition to peanut balls, the overall cesarean delivery rate in the health system significantly decreased (28% to 20%; P = .006).
Recommendations From Others
In 2018, the Council on Patient Safety in Women's Health Care (which included representatives from the American Academy of Family Physicians and the American College of Obstetricians and Gynecologists) recommended implementing maternity safety bundles to decrease the number of primary cesarean deliveries. 5 The Council referenced a toolkit recommending that all maternity care units provide education to support “freedom of movement in labor, upright and ambulatory positioning, techniques and tools (such as the peanut ball) that facilitate fetal rotation, flexion, and descent for women with epidural anesthesia, and maternal exercises and positioning that facilitate fetal rotation in women with and without epidural anesthesia.” 6
Copyright © Family Physicians Inquiries Network. Used with permission.
Delgado A, Katz L, Melo RS, et al. Effectiveness of the peanut ball use for women with epidural analgesia in labour: a systematic review and meta-analysis. J Obstet Gynaecol. 2022;42(5):726-733.
Tussey CM, Botsios E, Gerkin RD, et al. Reducing length of labor and cesarean surgery rate using a peanut ball for women laboring with an epidural. J Perinat Educ. 2015;24(1):16-24.
Roth C, Dent SA, Parfitt SE, et al. Randomized controlled trial of use of the peanut ball during labor. MCN Am J Matern Child Nurs. 2016;41(3):140-146.
Bell AD, Joy S, Gullo S, et al. Implementing a systematic approach to reduce cesarean birth rates in nulliparous women. Obstet Gynecol. 2017;130(5):1082-1089.
Lagrew DC, Low LK, Brennan R, et al. National Partnership for Maternal Safety: consensus bundle on safe reduction of primary cesarean births–supporting intended vaginal births [published correction appears in Obstet Gynecol . 2019; 133(6): 1288]. Obstet Gynecol. 2018;131(3):503-513.
California Maternal Quality Care Collaborative. Toolkit to support vaginal birth and reduce primary cesareans. Accessed March 9, 2024. https://www.cmqcc.org/sites/default/files/Vbirth-Toolkit-with-Supplement_Final_11.30.22_2.pdf
Clinical Inquiries provides answers to questions submitted by practicing family physicians to the Family Physicians Inquiries Network (FPIN). Members of the network select questions based on their relevance to family medicine. Answers are drawn from an approved set of evidence-based resources and undergo peer review. The strength of recommendations and the level of evidence for individual studies are rated using criteria developed by the Evidence-Based Medicine Working Group ( https://www.cebm.net ).
The complete database of evidence-based questions and answers is copyrighted by FPIN. If interested in submitting questions or writing answers for this series, go to https://www.fpin.org or email: [email protected] .
This series is coordinated by John E. Delzell Jr., MD, MSPH, associate medical editor.
A collection of FPIN’s Clinical Inquiries published in AFP is available at https://www.aafp.org/afp/fpin .
Continue Reading

More in AFP
Copyright © 2024 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Recently Viewed
Listening...
Johnson & Johnson Reports Q1 2024 Results
2024 first-quarter reported sales growth of 2.3% to $21.4 billion with operational growth of 3.9%* and adjusted operational growth of 4.0%* · adjusted operational growth excluding covid-19 vaccine of 7.7%* 2024 first-quarter earnings per share (eps) increased to $2.20 and adjusted eps increased to $2.71 or 12.4%* company increasing the midpoint for full-year 2024 operational sales 5 and adjusted operational eps guidance.
- Copy link Link copied
New Brunswick, N.J. (April 16, 2024) – Johnson & Johnson (NYSE: JNJ) today announced results for first-quarter 2024. “Johnson & Johnson’s solid first quarter performance reflects our sharpened focus and the progress in our portfolio and pipeline,” said Joaquin Duato, Chairman and Chief Executive Officer. “Our impact across the full spectrum of healthcare is unique in our industry, and the milestones achieved this quarter reinforce our position as an innovation powerhouse.”
Unless otherwise noted, the financial results and earnings guidance included below reflect the continuing operations of Johnson & Johnson.
Overall Financial Results
1 Non-GAAP financial measure; refer to reconciliations of non-GAAP financial measures included in accompanying schedules 2 Excludes the impact of translational currency 3 Excludes the net impact of acquisitions and divestitures and translational currency 4 Excludes intangible amortization expense and special items 5 Excludes COVID-19 Vaccine 6 Basic shares are used to calculate loss per share in the first quarter of 2023 as use of diluted shares when in a loss position would be anti-dilutive Note: Values may have been rounded
Regional Sales Results
1 Non-GAAP financial measure; refer to reconciliations of non-GAAP financial measures included in accompanying schedules 2 Excludes the impact of translational currency 3 Excludes the net impact of acquisitions and divestitures and translational currency Note: Values may have been rounded
Segment Sales Results
1 Non-GAAP financial measure; refer to reconciliations of non-GAAP financial measures included in accompanying schedules 2 Excludes the impact of translational currency 3 Excludes the net impact of acquisitions and divestitures and translational currency Values may have been rounded
First Quarter 2024 Segment Commentary: Operational sales* reflected below excludes the impact of translational currency. Adjusted operational sales* reflected below excludes the net impact of acquisitions and divestitures and translational currency.
Innovative Medicine Innovative Medicine worldwide operational sales, excluding the COVID-19 Vaccine, grew 8.3%*. Growth was driven by DARZALEX (daratumumab), ERLEADA (apalutamide), CARVYKTI (ciltacabtagene autoleucel), TECVAYLI (teclistamab-cqyv) and Other Oncology in Oncology, UPTRAVI (selexipag) and OPSUMIT (macitentan) in Pulmonary Hypertension, TREMFYA (guselkumab) in Immunology, and SPRAVATO (esketamine) in Neuroscience. Including the COVID-19 Vaccine, Innovative Medicine worldwide operational sales grew 2.5%*.
MedTech MedTech worldwide operational sales grew 6.3%* driven primarily by electrophysiology products and Abiomed in Cardiovascular, previously referred to as Interventional Solutions, and wound closure products in General Surgery.
Notable New Announcements in the Quarter: The information contained in this section should be read together with Johnson & Johnson’s other disclosures filed with the Securities and Exchange Commission, including its Current Reports on Form 8-K, Quarterly Reports on Form 10-Q and Annual Reports on Form 10-K. Copies of these filings are available online at www.sec.gov , www.jnj.com or on request from Johnson & Johnson. The reader is also encouraged to review all other news releases and information available in the Investor Relations section of the company’s website at News Releases , as well as Innovative Medicine News Center , MedTech News & Events , www.factsabouttalc.com , and www.LLTManagementInformation.com.
1 Subsequent to the quarter
Full-Year 2024 Guidance: Johnson & Johnson does not provide GAAP financial measures on a forward-looking basis because the company is unable to predict with reasonable certainty the ultimate outcome of legal proceedings, unusual gains and losses, acquisition-related expenses, and purchase accounting fair value adjustments without unreasonable effort. These items are uncertain, depend on various factors, and could be material to Johnson & Johnson’s results computed in accordance with GAAP.
1 Non-GAAP financial measure; excludes the net impact of acquisitions and divestitures 2 Non-GAAP financial measure; excludes the impact of translational currency 3 Calculated using Euro Average Rate: April 2024 = $1.08 and January 2024 = $1.09 (Illustrative purposes only) 4 Non-GAAP financial measure; excludes intangible amortization expense and special items 5 Excludes COVID-19 Vaccine
Note: Percentages may have been rounded
Other modeling considerations will be provided on the webcast .
Webcast Information: Johnson & Johnson will conduct a conference call with investors to discuss this earnings release today at 8:30 a.m., Eastern Time. A simultaneous webcast of the call for investors and other interested parties may be accessed by visiting the Johnson & Johnson website . A replay and podcast will be available approximately two hours after the live webcast in the Investor Relations section of the company’s website at events-and-presentations .
About Johnson & Johnson: At Johnson & Johnson, we believe health is everything. Our strength in healthcare innovation empowers us to build a world where complex diseases are prevented, treated, and cured, where treatments are smarter and less invasive, and solutions are personal. Through our expertise in Innovative Medicine and MedTech, we are uniquely positioned to innovate across the full spectrum of healthcare solutions today to deliver the breakthroughs of tomorrow, and profoundly impact health for humanity. Learn more at https://www.jnj.com/ .
Non-GAAP Financial Measures: * “Operational sales growth” excluding the impact of translational currency, “adjusted operational sales growth” excluding the net impact of acquisitions and divestitures and translational currency, as well as “adjusted net earnings”, “adjusted diluted earnings per share” and “adjusted operational diluted earnings per share” excluding after-tax intangible amortization expense and special items, are non-GAAP financial measures and should not be considered replacements for, and should be read together with, the most comparable GAAP financial measures. Except for guidance measures, reconciliations of these non-GAAP financial measures to the most directly comparable GAAP financial measures can be found in the accompanying financial schedules of the earnings release and the Investor Relations section of the company’s website at quarterly results .
Copies of the financial schedules accompanying this earnings release are available on the company’s website at quarterly results . These schedules include supplementary sales data, a condensed consolidated statement of earnings, reconciliations of non-GAAP financial measures, and sales of key products/franchises. Additional information on Johnson & Johnson, including adjusted income before tax by segment, an Innovative Medicine pipeline of selected compounds in late stage development and a copy of today’s earnings call presentation can also be found in the Investor Relations section of the company’s website at quarterly results .
Note to Investors Concerning Forward-Looking Statements: This press release contains “forward-looking statements” as defined in the Private Securities Litigation Reform Act of 1995 regarding, among other things: future operating and financial performance, product development, and market position and business strategy. The reader is cautioned not to rely on these forward-looking statements. These statements are based on current expectations of future events. If underlying assumptions prove inaccurate or known or unknown risks or uncertainties materialize, actual results could vary materially from the expectations and projections of Johnson & Johnson. Risks and uncertainties include, but are not limited to: economic factors, such as interest rate and currency exchange rate fluctuations; competition, including technological advances, new products and patents attained by competitors; challenges inherent in new product research and development, including uncertainty of clinical success and obtaining regulatory approvals; uncertainty of commercial success for new and existing products; challenges to patents; the impact of patent expirations; the ability of the Company to successfully execute strategic plans, including restructuring plans; the impact of business combinations and divestitures; manufacturing difficulties or delays, internally or within the supply chain; product efficacy or safety concerns resulting in product recalls or regulatory action; significant adverse litigation or government action, including related to product liability claims; changes to applicable laws and regulations, including tax laws and global health care reforms; trends toward health care cost containment; changes in behavior and spending patterns of purchasers of health care products and services; financial instability of international economies and legal systems and sovereign risk; increased scrutiny of the health care industry by government agencies; the Company’s ability to realize the anticipated benefits from the separation of Kenvue Inc; and Kenvue’s ability to succeed as a standalone publicly traded company. A further list and descriptions of these risks, uncertainties and other factors can be found in Johnson & Johnson’s Annual Report on Form 10-K for the fiscal year ended December 31, 2023, including in the sections captioned “Cautionary Note Regarding Forward-Looking Statements” and “Item 1A. Risk Factors,” and in Johnson & Johnson’s subsequent Quarterly Reports on Form 10-Q and other filings with the Securities and Exchange Commission. Copies of these filings are available online at www.sec.gov , www.jnj.com or on request from Johnson & Johnson. Any forward-looking statement made in this release speaks only as of the date of this release. Johnson & Johnson does not undertake to update any forward-looking statement as a result of new information or future events or developments.
Media contact: Tesia Williams [email protected]
Investor contact: Jessica Moore [email protected]
Inside the GOP reckoning over Arizona’s 1864 abortion ban
As the legislature considers repealing a civil war-era abortion ban, the state gop — like the party nationally — is deeply divided over abortion ahead of the presidential election.
PHOENIX — A Republican state legislator proclaimed on the floor of the Arizona Senate two months ago that “abortion is the ending of an innocent human life.”
Another includes a declaration on his website that he will always “fight for the unborn.”
And a third championed a law to allow pregnant women to use the carpool lane, arguing that a “pre-born baby” should be treated “as the human they are.”
Now all three state lawmakers say they are likely to vote to repeal a Civil War-era law that would soon ban abortion across the state. A vote could happen as early as Wednesday.
Like many of their fellow conservatives around the country, the lawmakers had long expressed a seemingly unshakable moral view that abortion was an abomination that should be stopped. But then came the national uproar over a decision by the Arizona Supreme Court last week upholding an 1864 abortion ban that punishes providers with prison time — coupled with a sense that the backlash could hurt Donald Trump’s presidential campaign in a state he narrowly lost four years ago.
The shift by state Sen. Shawnna Bolick and Reps. Tim Dunn and Matt Gress — as well as Arizona U.S. Senate candidate Kari Lake — lays bare a larger crisis within the Republican party over how to handle the abortion issue ahead of November. The U.S. Supreme Court’s 2022 ruling to overturn Roe v. Wade passed the practical decision of whether to allow access to abortion to state lawmakers, and many Republicans are now caught between long-held, often religiously rooted views that have defined the GOP for generations and a more practical desire to win elections.
In recent days, Lake, who once described the 160-year-old measure as a “great law,” has been personally lobbying some Republicans to repeal the ban, highlighting the political stakes of the looming vote. According to one lawmaker who received such a call and spoke on the condition of anonymity to describe private conversations, Lake made it clear that she “understands [the pre-Roe ban] will be bad for her and for Trump.” They discussed how Arizona is essential for Trump to secure the presidency, the lawmaker said. Trump lost the state to President Biden in 2020 by only 10,457 votes .
The dilemma facing Republicans on abortion has grown even more acute since last Wednesday, when Trump said Arizona’s abortion ban goes too far and promised it would be “straightened out” by “the governor and everybody else.” Trump, the presumptive Republican presidential nominee who has bragged about his role in the overturning of Roe, made a similar promise about a pending six-week abortion ban in Florida , even as he has argued the abortion issue should be left to the states .
Two Republicans in the Arizona House of Representatives and two in the Senate would have to join all of both chambers’ Democrats to repeal the ban, which could take effect as early as June 8 without legislative action. If the legislature agrees to repeal the 1864 ban, the current law banning abortion after 15 weeks of pregnancy prevails, legislative staffers and lawmakers said. On the eve of the legislature taking up the issue, people on both sides said they could not predict the outcome.
As they weighed their votes, many Republicans in Arizona described agonizing over the decision — reckoning with core beliefs as they texted colleagues, talked to constituents, pastors and priests, and prayed for wisdom. One received what they described as “threats” from a leading state antiabortion advocate.
“This is the most difficult decision that I’ve made in the eight years that I’ve been there,” said Rep. David Cook (R), a longtime abortion foe who, as of Tuesday, said he had not decided how he would vote. “You’re faced with the personal convictions of protecting … an innocent life.”
Sen. Ken Bennett (R), who represents a red area and once presided over the chamber as president and also served as secretary of state, predicted that several Republicans would not “have a chance” of getting reelected if the pre-Roe ban is allowed to stand.
“I’m expecting Wednesday to be one of the hardest days the Arizona legislature has ever had,” he said.
The question of the 1864 law has deeply divided the caucus, with some staunch antiabortion advocates urging their colleagues to hold firm against repeal — and lobbing personal attacks at those who are considering voting for it.
“Anybody who would allow innocent people to be killed to preserve their political career to win an election does not deserve to win,” said Rep. Alex Kolodin (R), who sees the 1864 law as a victory for the party’s core ideological position as well as a major humanitarian triumph.
Several GOP lawmakers and operatives said Trump’s comments could ease the decision to vote for a repeal for some Republicans who were on the fence, granting them permission to go against their values for a better chance at securing victory in November.
“It gave them cover,” said one prominent Arizona Republican who supports the repeal and spoke on the condition of anonymity to candidly discuss internal party dynamics. Trump’s statements would have been even more helpful, the person added, if some antiabortion members were not “virtue signaling” about the pre-Roe ban and “trying to force everybody to be pilloried for representing their constituents.”
Some Republican resistance to the state Supreme Court ruling emerged almost immediately. Soon after the court made its decision on April 9, several GOP lawmakers issued statements condemning the move, including Gress, Bolick and Sen. T.J. Shope — who all hail from districts that could be competitive in November.
Bolick, who is married to an Arizona Supreme Court justice, urged fellow Republicans to “find common ground of common sense” and “repeal the territorial law.”
Gress made a similar argument on the House floor last Wednesday, after he moved to suspend the chamber’s rules to bring forward the motion to repeal the law — a maneuver that surprised and angered many of his Republican colleagues. When he was shut down by the GOP majority, the Democrats erupted into chants of “Shame, Shame, Shame!”
(Bolick did not respond to a request for comment. Gress declined to comment.)
Almost all of the GOP lawmakers who are now considering a repeal voted in the spring of 2022 — before Roe was overturned — for a law that banned abortions after 15 weeks of pregnancy and included an explicit endorsement of the 1864 ban, specifying that the new 15-week law would not preclude the near-total abortion ban from taking effect if the U.S. Supreme Court acted. The leaders of the Arizona House and Senate went even further, submitting an amicus brief in May 2023 to the state’s highest court arguing that the pre-Roe ban should be allowed to stand.
In an interview, Arizona Gov. Katie Hobbs (D) stressed that Republicans in the legislature “asked for this.”
“They own this. They voted for a bill that had this explicit language in it,” she said. “They had the ability to not vote for this law in the first place.”
Hobbs and her team have talked to key GOP lawmakers about the repeal effort, assuring them she would sign repeal legislation if it passes, according to people familiar with the discussions who spoke on the condition of anonymity to disclose private deliberations.
Some Republicans started to recognize the shifting political winds soon after Roe was overturned — especially after voters in conservative Kansas voted overwhelmingly to protect abortion rights in August 2022. In Arizona, Gress sent out mailers ahead of the midterms that year saying he opposed the pre-Roe ban, despite sponsoring several bills during his time in the legislature designed to recognize a fetus as a person.
Some Republicans maintain that a vote to repeal the 1864 law would not be at odds with their antiabortion beliefs because they are trying to be strategic about choosing a path forward that would prevent the most abortions. Democrats are trying to get an initiative on the November ballot that would enshrine abortion rights in the state constitution and allow the procedure to the point of fetal viability, or about 24 weeks. These Republicans argue that supporting the repeal could demonstrate they are attuned to voter sentiments while lending credibility to GOP opposition to the ballot measure.
“What’s going to save the most lives? That’s what Republicans are struggling with,” said Dunn, the GOP representative. “You do not want to vote for something that moves it from a zero ban to … 15 weeks. … But if we don’t remove it, you’re going to force this ballot measure that’s going to be almost guaranteed to win.”
The Democratic-led ballot initiative is a major concern for Arizona Republicans.
On Monday, the House GOP general counsel circulated a PowerPoint presentation outlining the party’s strategy to combat the abortion referendum likely to appear on the Arizona ballot in November, provided the measure is backed by the necessary number of signatures and clears all possible challenges from antiabortion advocates.
The presentation was sent to all House members — not just Republicans — and was promptly shared with reporters.
It outlined a plan to add another abortion referendum to the ballot that would allow the procedure only up until six weeks of pregnancy, before many people know they’re pregnant, or 15 weeks. The goal, according to the presentation, would be to “pull votes” from the Democrats’ referendum.
The presentation ended with a meme of comedian Seth Meyers, with the words, “Boom. Easy as That.”
Abortion rights advocates have triumphed around the country each of the seven times abortion has appeared on the ballot since Roe was overturned.
Although he wants the 160-year-old law repealed, Sen. Brian Fernandez, a Democrat from Yuma, is wary about the GOP’s next move. By joining forces with Republicans to try to eliminate that law, he warned his Democratic colleagues during an emotional meeting last week, they would usher in another big fight with the GOP on abortion.
Fernandez suspects Republicans would try to get their own initiative on the November ballot that is more restrictive than the Democratic-favored abortion access measure, as indicated in the PowerPoint presentation. Such a move could compete with the Democratic measure or confuse voters, said lawmakers and political consultants in the state.
“Now all the sudden, Matt Gress is the savior for women’s rights?” Fernandez asked, referring to the Republican who pushed last week for a vote to repeal.
“I don’t buy it. Maybe I’m just cynical, maybe I’m stupid, I don’t know, but I don’t buy that these guys are somehow going to be the savior for us,” he said.


An internal document shows Arizona Republicans are considering new abortion ballot measures
H ouse Republicans may refer several new measures to the November ballot that would compete with the citizen initiative to enshrine abortion rights in the Arizona Constitution, per a leaked internal document.
The big picture: Republican lawmakers are trying to figure out a path forward after last week's Arizona Supreme Court ruling that reinstated an 1864 ban on all abortions except those necessary to save the mother's life.
- GOP leadership in both chambers blocked votes to repeal the ban last Wednesday, which would have allowed a 2022 15-week ban to go into effect.
- Legislative Democrats plan to try again this week.
Zoom in: A presentation drafted by House Republicans' legal counsel, obtained by Axios and other outlets, proposes three ballot measures across a two-pronged strategy, the first of which it described as "complementary" to the abortion rights initiative.
- However, that proposal would ask voters to preserve the legislature's ability to regulate abortion, which would be taken out of lawmakers' hands by the abortion rights measure.
- It would also codify existing laws such as a prohibition on abortions based on a baby's race or sex and so-called "partial-birth abortions."
- It wouldn't limit abortions to a specific time period or establish a right to one.
Secondly, the presentation proposes lawmakers refer two other measures to the ballot, which would conflict with the existing initiative.
- The move would effectively offer voters three different abortion regulation options in November.
- One of these Republican proposals would limit abortions to the first day of the 15th week of pregnancy (which the presentation described as "a 14-week law disguised as a 15-week law"), with exceptions for health of the mother or fatal fetal abnormalities.
- The second, dubbed the "Heartbeat Protection Act," would limit abortions to six weeks, except those considered medically necessary or in cases of rape or incest.
Flashback: The abortion rights initiative proposes permitting abortions to the point of fetal viability, generally around 24 weeks.
- Abortions would, however, be allowed past that point to "protect the life or physical or mental health" of the mother.
Between the lines: The GOP lawyer argues these new measures would change the narrative and show Republicans have a plan on abortion.
- It could also pull votes from the abortion initiative and put Democrats "in a defensive position to argue against partial-birth abortions, discriminatory abortions and other basic protections," per the presentation.
What they're saying: In a statement to Axios, House Speaker Ben Toma (R-Glendale) said the document outlines ideas for internal caucus discussion.
- "I've publicly stated that we are looking at options to address this subject, and this is simply part of that," he said.
- Toma opposes repealing the 1864 ban and said last week that lawmakers shouldn't rush to vote on it.
The other side: "Arizona for Abortion Access," the abortion rights initiative campaign, called the Republicans' proposals a "dishonest attempt to refer multiple competing abortion bans to the November ballot."
- "This shows yet again why Arizonans can't leave our most basic and personal rights in the hands of politicians," the campaign said in a press statement.
- Co-House Minority Whip Nancy Gutierrez (D-Tucson) said Republicans are trying to "muddy the water" and confuse voters, and the leaked document shows why the legislature should vote for a clean repeal of the ban.
What we're watching: The House and Senate reconvene Wednesday.
- Senate President Warren Petersen told the Arizona Mirror his caucus had not met to discuss the plan.
The intrigue: The proposal leaked after the attorney who drafted it accidentally sent it to every member of the chamber rather than just Republicans, according to the Mirror.
Get more local stories in your inbox with Axios Phoenix.

Advertisement
Under Pressure From Trump, Arizona Republicans Weigh Response to 1864 Abortion Ban
Liberal activists are proposing a ballot measure that would enshrine the right to an abortion in the state Constitution. Republicans in the State Legislature are considering plans to undermine it.
- Share full article

By Chris Cameron
Reporting from Washington
- April 15, 2024
Facing mounting pressure to strike down a near-total abortion ban revived last week by Arizona’s Supreme Court, Republican state legislators are considering efforts to undermine a planned ballot measure this fall that would enshrine abortion rights in the Arizona Constitution, according to a presentation obtained by The New York Times.
The 1864 law that is set to take effect in the coming weeks bans nearly all abortions and mandates prison sentences of two to five years for providing abortion care. The proposed ballot measure on abortion rights, known as the Arizona Abortion Access Act, would enshrine the right to an abortion before viability , or about 24 weeks. Supporters of the measure say they have already gathered enough signatures to put the question on the ballot ahead of a July 3 filing deadline.
Republicans in the Legislature are under tremendous pressure to overturn, or at least amend, the 1864 ban. Former President Donald J. Trump, the national standard-bearer of the Republican Party, directly intervened on Friday, calling on Republican legislators, in a frantically worded post online, to “act immediately” to change the law. A top Trump ally in Arizona who is running for the Senate, Kari Lake, has also called for the overturning of the 1864 law , which she had once praised.
Abortion rights have been a winning message for Democrats since the Supreme Court, with three justices appointed by Mr. Trump, overturned Roe v. Wade in 2022. And even though it is an objectively unpopular aspect of his White House legacy, Mr. Trump has repeatedly bragged that he is personally responsible for overturning Roe.
Republicans in Arizona, however, have already resisted efforts to repeal the 160-year-old law and are bracing for the potential for another floor battle on the ban that is looming for the Legislature, which is set to convene on Wednesday. The plans that circulated among Republican legislators suggest the caucus is considering other measures that would turn attention away from the 1864 law.
The presentation to Republican state legislators, written by Linley Wilson, the general counsel for the Republican majority in the Arizona State Legislature, proposed several ways in which the Republican-controlled Legislature could undermine the ballot measure, known as A.A.A., by placing competing constitutional amendments on the ballot that would limit the right to abortion even if the proposed ballot measure succeeded.
The plan, the document said, “Changes narrative — Republicans have a plan!” adding that the plan “puts Democrats in a defensive position to argue against partial birth abortions, discriminatory abortions, and other basic protections.”
One proposal would have the Legislature send to voters two other ballot initiatives that would “conflict with” and “pull votes from” the A.A.A. ballot measure. Ballot measures for a constitutional amendment can be proposed through a petition, as with the A.A.A. ballot measure, or through the State Legislature , and the document suggests that voters could read the Republican ballot measures first on the ballot if they are filed before the A.A.A. ballot measure.
One of the Republican ballot initiatives outlined in the presentation would enact an abortion ban after the fifth week of pregnancy, with exceptions for rape, incest and medical necessity. The other ballot option would propose a ban after the 14th week of pregnancy. The language of the measures would be intentionally written to mislead voters on when exactly an abortion would become illegal, according to the presentation.
The second option, for example, would be known as the “Fifteen Week Reproductive Care and Abortion Act.” But “in reality,” according to the presentation, “It’s a 14-week law disguised as a 15-week law because it would only allow abortion until the beginning of the 15th week.” Similarly, the wording of the five-week abortion ban would make abortion illegal “after the sixth week of pregnancy begins.”
An alternative to those two options would be to put forward a ballot measure that would take effect only if the A.A.A. ballot measure also passes. That plan, known as “conditional enactment,” would insert language in the state Constitution declaring that the right to an abortion in the A.A.A. ballot measure “is not absolute and shall not be interpreted to prevent the Legislature from” regulating abortion in the future. It would also include language used by anti-abortion activists, referring to “the preservation of prenatal life” and “mitigation of fetal pain.”
Ben Toma, the speaker of the Arizona House of Representatives, confirmed the authenticity of the document and said in a statement that it “presents ideas drafted for internal discussion and consideration within the caucus. I’ve publicly stated that we are looking at options to address this subject, and this is simply part of that.”
State Senator Anna Hernandez said in a statement that she and fellow Democrats would continue to push to repeal the 1864 law and that the Republicans’ proposals were “intentionally drafted to confuse voters” with policies “based in arbitrary numbers of weeks that have no factual grounding in science or health care.”
Dawn Penich, a spokeswoman for Arizona for Abortion Access, the liberal coalition organizing the A.A.A. ballot measure, said in a statement that the Republican presentation “shows yet again why Arizonans can’t leave our most basic and personal rights in the hands of politicians.”
Kate Zernike contributed reporting from New York.
Chris Cameron covers politics for The Times, focusing on breaking news and the 2024 campaign. More about Chris Cameron

COMMENTS
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
Toward the end of pregnancy, the fetus moves into position for delivery. Normally, the presentation is vertex (head first), and the position is occiput anterior (facing toward the pregnant person's spine) and with the face and body angled to one side and the neck flexed. Variations in fetal presentations include face, brow, breech, and shoulder.
Possible fetal positions can include: Occiput or cephalic anterior: This is the best fetal position for childbirth. It means the fetus is head down, facing the birth parent's spine (facing backward). Its chin is tucked towards its chest. The fetus will also be slightly off-center, with the back of its head facing the right or left.
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse. Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position. Abnormal fetal lie, presentation, or position may occur with. Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal position refers to whether the baby is facing your spine (anterior position) or facing your belly (posterior position). Fetal position can change often: Your baby may be face up at the beginning of labor and face down at delivery. Here are the many possibilities for fetal presentation and position in the womb.
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse
As a result, the fetal head will engage later, and labor will progress more slowly. Failure to progress in labor is also more common in both presentations compared to vertex presentation. Furthermore, when the fetal chin is in a posterior position, this prevents further flexion of the fetal neck, as browns are pressing on the symphysis pubis.
Vertex Presentation. A vertex presentation is the ideal position for a fetus to be in for a vaginal delivery. It means the fetus is head down, headfirst and facing your spine with its chin tucked to its chest. Vertex presentation describes a fetus being head-first or head down in the birth canal.
The left occiput anterior (LOA) position is the most common in labor. In this position, the baby's head is slightly off-center in the pelvis with the back of the head toward the mother's left thigh. The right occiput anterior (ROA) presentation is also common in labor.
The position in which your baby develops is called the "fetal presentation.". During most of your pregnancy, the baby will be curled up in a ball - that's why we call it the "fetal position.". The baby might flip around over the course of development, which is why you can sometimes feel a foot poking into your side or an elbow ...
Fetal position reflects the orientation of the fetal head or butt within the birth canal. Anterior Fontanel. The bones of the fetal scalp are soft and meet at "suture lines." Over the forehead, where the bones meet, is a gap, called the "anterior fontanel," or "soft spot." This will close as the baby grows during the 1st year of life, but at ...
👉I know OB-Maternity can be overwhelming. Let me help YOU!👉Fetal Positioning, Presentation, and Station can be complex concepts that I tried to break down ...
During pregnancy and when preparing for childbirth, there are exercises moms can do when the baby is active to get it in the optimal fetal position, which is known as baby spinning.Starting at the 35th week of pregnancy, talk to your doctor about maternal positioning. Occiput anterior (OA) or vertex presentation. This is the optimal fetal positioning for childbirth.
compound presentation—when any other part presents along with the fetal head; Related obstetrical terms Attitude. Definition: Relationship of fetal head to spine: flexed, (this is the normal situation) neutral ("military"), extended. hyperextended; Position. Relationship of presenting part to maternal pelvis based on presentation.
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse. Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position. Abnormal fetal lie, presentation, or position may occur with. Fetopelvic disproportion (fetus too large for the pelvic inlet)
Abnormal Fetal Lie. If the fetal lie is abnormal, an external cephalic version (ECV) can be attempted - ideally between 36 and 38 weeks gestation. ECV is the manipulation of the fetus to a cephalic presentation through the maternal abdomen. It has an approximate success rate of 50% in primiparous women and 60% in multiparous women.
Variations in fetal presentation, position, or lie may occur when. The fetus is too large for the mother's pelvis (fetopelvic disproportion). The uterus is abnormally shaped or contains growths such as fibroids Uterine Fibroids A fibroid is a noncancerous tumor of the uterus that is composed of muscle and fibrous tissue. Uterine fibroids are ...
🍼🧸 Fetal Positions, Presentation, and Station 🧸🍼👉What is a Fetal Presentation vs. Position vs. Station?👶 Presentation: Fetal Presentation is the part o...
The Leopold Maneuver is a fundamental examination technique used to assess fetal presentation, position, and size during pregnancy.It has been widely employed as a routine prenatal assessment tool by obstetricians and midwives for over a century. The technique involves a series of four maneuvers that allow the examiner to palpate the maternal abdomen and identify the fetal presentation and ...
This fetal presentation is the most promising for a vaginal delivery because both twins are head-down. Twins can change positions, but if they're head-down at 28 weeks, they're likely to stay that way. When delivering twins vaginally, there is a risk that the second twin will change position after the delivery of the first.
#1: Passenger (fetal presentation and position) The first P, "Passenger," refers to the position of the fetus. Fetal attitude. Fetal attitude describes the relationship of the fetal parts to each other. The amount of flexion in the fetal body, specifically the head (how close the chin is to the chest).
FETAL POSITION: • Document fetal position. FETAL SITUS: • With a dual screen, image demonstrating fetal situs. In a transverse view, show side by side images of the fetal stomach and 4-Chamber heart on the left side of the fetus' body. • If the fetus has changed position since presentation first documented, show
In the raw data, the group using the peanut ball in addition to position changes had a shorter first stage (269 vs. 356 minutes; P < .01) and second stage (21 vs. 44minutes; P < .001) of labor and ...
Investor contact: Jessica Moore. [email protected]. 2024 First-Quarter reported sales growth of 2.3% to $21.4 Billion with operational growth of 3.9%* and adjusted operational growth of 4.0%* · Adjusted operational growth excluding COVID-19 Vaccine of 7.7%* 2024 First-Quarter Earnings per share (EPS) increased to $2.20 and ...
On Monday, the House GOP general counsel circulated a PowerPoint presentation outlining the party's strategy to combat the abortion referendum likely to appear on the Arizona ballot in November ...
One of these Republican proposals would limit abortions to the first day of the 15th week of pregnancy (which the presentation described as "a 14-week law disguised as a 15-week law"), with ...
A presentation drafted by House Republicans' legal counsel, obtained by Axios, leaked Monday. ... The abortion rights initiative proposes permitting abortions to the point of fetal viability, generally around 24 ... It could also pull votes from the abortion rights initiative and put Democrats "in a defensive position to argue against partial ...
The second option, for example, would be known as the "Fifteen Week Reproductive Care and Abortion Act." But "in reality," according to the presentation, "It's a 14-week law disguised ...