- Search Search for:

How to study in first year MBBS? The Complete Guide
Even though all MBBS years are important, the first year is especially important because it sorts out early thinking problems, introduces new concepts, tests the basics, and helps students develop a solid understanding of the basics. As a result, the new topics and concepts in the first year may bore you or even scare you. Despite the fact that this time of year is typical, your seniors have also been through it, and having a better understanding of the first year can help you plan your study schedules.
To help you get around the boat more quickly, easily, and simply, here is a quick guide:
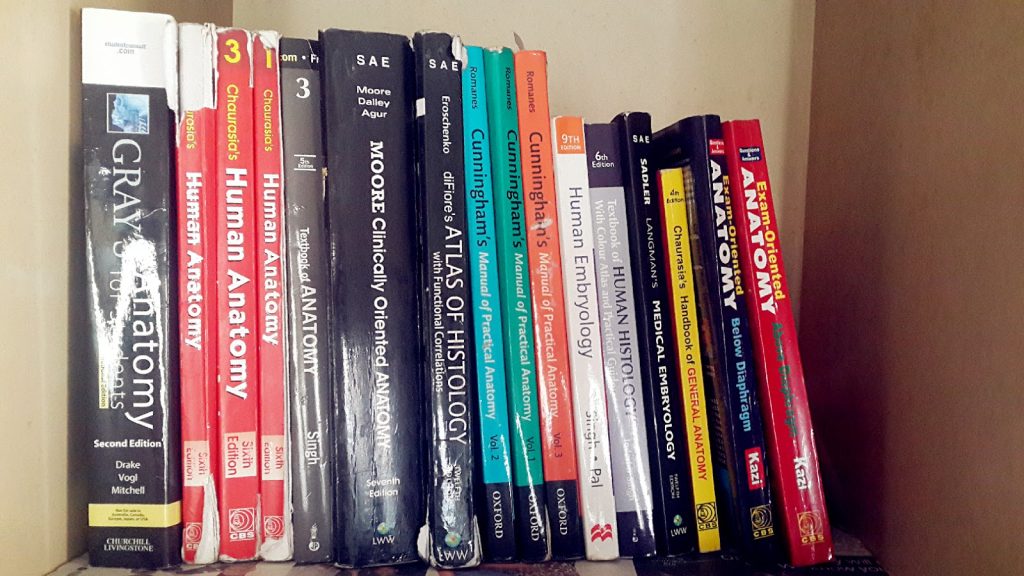
MBBS Subjects
In order to prepare for the tests, a first-year MBBS student should aim to devote six hours per day to studying. There are in fact five subjects, but the amount of time you devote to each depends on your knowledge and ability. Therefore, don’t waste time planning. Even though you need six hours, divide them up well so you can focus on your studies effectively during those hours.
How to get a high grade in first year subjects:
- Take your regular lectures and any course you subscribed to every day. Refer to the professors’ lectures and notes to make sure you understand the material.
- Practice drawing as many diagrams as you can for the exams.
- Make use of the online videos to get started on the subject. Also, check out the anatomy atlas from time to time.
- Complete all questions from the past ten years. NOTES : Elite Anatomy notes
- Take your regular lectures and any course you subscribed to every day.
- Create your own flowcharts and make as many as you can for your theory exams.
- Flowcharts are nicely provided in the 20th notebook
- Hard work and complete dedication to the subject are required.

Biochemistry:
- Take your regular lectures and any course you subscribed to every day. Refer to the professors’ lectures and refer to notes to learn about each metabolism cycle and the enzymes involved.
- Draw as many cycles as you can, as they all have equal weight in practice. Hard work and total dedication to the subject are required.
- Complete all questions from the past ten years.
Time Management:
The best way to study is to set aside sufficient time for each subject. Thinking about it for six hours a day is definitely a good idea. However, don’t worry too much about the timing. In times of difficulty, it is acceptable to cut short at times but whatever time you dedicate, your concentration level should be at peak. In addition, it’s a good idea to set ambitious goals so you can always push yourself to do more. However, you should try to be practical.
For instance, don’t limit your goal setting to thirty minutes if it takes you two hours to read just one part of a subject. You could start with one hour and thirty minutes and finish most of the topics in two hours. Instead of setting too lofty goals and failing to meet them, work on timings one step at a time.
A successful MBBS student understands the concepts in the prospectus well enough to be able to treat patients after earning their degree. Therefore, try to do your best. Keep learning!
Leave a Comment Cancel Reply
You must be logged in to post a comment.
Notespaedia App is live
Now you can read notes on your device with Notespaedia app. We are giving out all Previous Year Recall notes for free, check out other amazing features in app.
WhatsApp us
Insert/edit link
Enter the destination URL
Or link to existing content
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.15(1); 2023 Jan


Prevalence of Depression Among Undergraduate Medical Students in India: A Systemic Review and Meta-Analysis
Gitashree dutta.
1 Community Medicine and Family Medicine, All India Institute of Medical Sciences, Jodhpur, IND
Navin Rajendran
2 Paediatrics, Dr. Sampurnanand (SN) Medical College, Jodhpur, IND
Tarun Kumar
3 Pharmacology, All India Institute of Medical Sciences, Jodhpur, IND
Shoban B Varthya
Vinoth rajendran.
Background: Systematic reviews have proved that there is a high rate of depression among medical students when compared with their age-matched peers. Very few studies have evaluated the pooled prevalence of depression among medical students in India.
Objectives: To determine the pooled prevalence of depression among medical students in India.
Materials and methods: This review was done by searching databases like PubMed, Google Scholar, and Scopus for available original articles published between 2019 and 2022 on depression among Indian medical (MBBS) undergraduate students using PRISMA guidelines.
Results: A total of 19 original research articles were included in this review, involving students at different medical colleges from various regions of India. The pooled prevalence of depression among 5944 medical students was 50.0% (95% CI: (31%-70%)) based on the random effect model. This meta-analysis also found that the pooled prevalence of depression among females (pooled prevalence: 38.0%, 95% CI: 20.0 to 58.0) was slightly higher than among males (pooled prevalence: 34.0%, 95% CI: 15.0 to 55.0).
Conclusion: The high prevalence of depression among medical students demands regular screening for depression along with counselling services. It shows that there is a need to raise awareness among students and other stakeholders, such as parents and medical educators, concerning symptoms and signs of depression among medical students.
Introduction and background
The World Health Organization (WHO) defined health as "a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity", a definition relevant today [ 1 ]. Further, it is stated that "not depressed" is not the end goal as there is a spectrum of well-being, with the disease at one end and optimal well-being at the other. The World Health Organization recognizes mental health disorders as important causes of morbidity and disability, with depression as one of the leading causes of mental health disorders.
In 2016, the age-standardized prevalence of depressive disorders in South Asia was 3.9% (95% UI: 3.6 - 4.2%), 3.7% (95% uncertainty interval (UI): 3.4-4.1%) in Bhutan, 3.9% (95% UI: 3.6-4.2%) in India, 4.4% (95% UI: 4.4-4.8%) in Bangladesh, 3.0% (95% UI: 2.8-3.3%) in Pakistan, and 4.0% (95% UI: 3.7-4.3%) in Nepal [ 2 ]. Systematic reviews have proved that there is a high rate of depression or depressive symptoms (27.2%) among medical students when compared with their age-matched peers before the COVID-19 pandemic [ 3 , 4 ]. All people, including medical students, would benefit from being aware of where they are on the well-being spectrum and what they can do to climb up the spectrum. Students who experience depression also experience additional mental health issues like anxiety, burnout, substance abuse, and suicidal thoughts. Undergraduate students' mental health is a significant public health issue on a global scale [ 5 - 8 ].
The COVID-19 pandemic has taken a toll on the mental health of different individuals worldwide for various containment measures and the disease itself [ 9 ]. During the COVID-19 pandemic, college students are more prone to mental health disorders along with COVID-19 patients and medical personnel. Compared to other training programmes, medical education has the highest academic and emotional requirements. A systematic review and meta-analysis with research works published globally show depression prevalence of 37.9% among medical students [ 10 ].
The pooled prevalence of depression based on standard screening instruments among medical students in India was 40% before the COVID pandemic [ 11 ]. However, no studies have been conducted to date evaluating the effect of this healthcare crisis on medical trainees in India during the pandemic. This meta-analysis includes cross-sectional studies on depression among medical students in India to determine the pooled prevalence of depression among medical students in India.
Materials and methods
This study was completed following the PRISMA checklist [ 12 ], and it was registered in PROSPERO (CRD42022331012) [ 13 ]. Before beginning the literature search, the study's framework was created using PRISMA criteria; after that, no changes were made.
Literature search
A systematic search was undertaken in three databases, namely PubMed, Google Scholar and Scopus, for all the available articles published in the English language during 2019-2021 on the prevalence of depression amongst undergraduate medical students in India by two independent investigators. (Appendices 1) Based on the "PICOS" principle for formulating the search strategy, the search terms include "Depression", "Undergraduate students", "medical students", "undergraduate medical students", and "MBBS students". We have added relevant articles identified by several databases to the search using Rayyan software. It was also attempted to contact the authors of articles whose full texts were unavailable in the databases. Appendices 1 presents a comprehensive search strategy.
Inclusion and exclusion criteria
The inclusion criteria were 1) Cross-sectional study design, 2) The study population was undergraduate medical students from India, 3) Assessing the prevalence of depression using a standardized instrument, and 4) The study period was from January 2019 to April 2022. The articles which did not state the information on the prevalence of depression or outcome data among the undergraduate medical students were excluded.
Study selection and data extraction
The studies were retrieved based on the search strategy discussed a priori. Multiple publications of the same study were identified and collated. Two independent reviewers screened titles and abstracts to identify the studies that meet the inclusion and exclusion criteria. Any disagreements were resolved by discussion or by a third reviewer. Data were extracted using a pre-designed spreadsheet from the studies which included the first author name, year of publication, study period, study setting, sample size, the instrument used for assessing depression, the total number of medical students, number of females, number of males, age (mean) of the student, prevalence of depression overall, and among male students and female students.
Quality assessment/risk of bias (ROB)
Using the Joanna Briggs Institute's (JBI) Critical Appraisal tool for systematic reviews of prevalence studies, we evaluated the study's methodology which was shown in Table Table1 1 [ 14 , 15 ]. The reviewers independently assessed the ROB using the Modified JBI criteria. In case of a mismatch of results, the discrepancies or disputes have been checked, and the reviewers came to a common opinion by discussing it with a third investigator. The evaluated articles were divided into three categories: high ROB (JBI score 49%), moderate ROB (JBI score between 50% and 69%), and low ROB (JBI score >70%) [ 16 ].
NA- Not available, ROB- Risk of bias
Data synthesis and analysis
In this meta-analysis, to determine the prevalence of depression among medical students, the pooled estimates with 95% confidence intervals (95% CI) were calculated using the random-effects model (DerSimonian-Laird method) due to high heterogeneity [ 17 ]. The forest plots have been used to determine the prevalence of pooled estimates. The estimation was calculated using MetaXL version 5.3 and an Excel spreadsheet. A P-value less than 0.05 was considered significant. The Q and I 2 statistics were used as tests for heterogeneity. Q test with P < 0.10 was considered statistically significant heterogeneity and I 2 >75% was labelled as high heterogeneity [ 18 ]. This review used the Doi plot and the LFK index for publication bias. The double arcsine prevalence was taken as the x-axis for the funnel plot. Arcsine transformation was required with data with extreme values like 0 or 1. Otherwise, the confidence interval for the proportion could include values outside the range of 0 and 1, representing 0% and 100%. The y-axis of the graphic was set to the precision obtained from the inverse of Standard Error (SE). Doi plot and the LFK index for publication bias were used to validate the funnel plot's asymmetries. Values describe the publication bias over ±1 of the LFK index [ 19 ]. Sensitivity analysis was done to indicate the major determinant for the pooled prevalence of depression.
Study Characteristics
The initial search from PubMed, Scopus, and Google Scholar yielded 3297 studies. Only 56 pertinent papers were reviewed for eligibility after removing duplicates based on the screening of titles and abstracts. Out of 56 papers, 19 articles were included in the quantitative synthesis after various publications were excluded for multiple reasons (Figure 1 ).

Table 1 shows the study characteristics of the included studies comprising study population, study setting, study tool, study period, sample size and number of depressed undergraduate students along with ROB [ 20 - 38 ].
The Pooled Prevalence of Depression
All the selected studies reported the prevalence of depression among medical students using different instruments for assessing depression. The prevalence of depression in the nineteen studies ranged from 16.0% to 100.0%. The pooled prevalence of nineteen studies, [ 20 - 38 ] 50.0% (95% CI: 31.0 to 70.0), was shown in Figure Figure2 2 .

Minimal depression was seen in only four studies, [ 20 , 24 , 28 , 31 ] with a pooled prevalence of 28.0% (95% CI: 20.0 to 37.0) whereas mild depression was found in six studies, [ 24 , 27 - 30 , 34 ] with pooled prevalence of 14.0% (95% CI: 4.0 to 28.0). The pooled prevalence of thirteen studies that have found moderate depression was found to be 15.0% (95% CI: 11.0 to 19.0) [ 20 , 21 , 24 , 25 , 27 - 31 , 33 - 35 , 37 ]. The pooled prevalence of three studies that have found moderately severe depression was found to be 7.0% (95% CI: 3.0 to 12.0) [ 20 , 24 , 31 ]. Severe depression was seen in eleven studies [ 21 , 24 , 25 , 27 - 29 , 31 , 33 - 35 , 37 ] with a pooled prevalence of 5.0% (95% CI: 3.0 to 7.0), and extremely severe depression was found in five studies [ 21 , 25 , 34 , 35 , 37 ] with a pooled prevalence of 5.0% (95% CI: 2.0 to 11.0). Seven studies have seen the depression of undergraduate medical students among males and females. The pooled estimate of depression among the females (pooled prevalence: 38.0%, 95% CI: 20.0 to 58.0) was slightly higher when compared to males (pooled prevalence: 34.0%, 95% CI: 15.0 to 55.0). Subgroup analysis was calculated for the pooled prevalence of depression based on the instruments used for screening depression. It was found that the pooled prevalence of depression was 27.0% (95% CI: 23.0 to 31.0), 99.0% (95% CI: 96.0 to 100.0), and 37.0% (95% CI: 29.0 to 46.0) in Depression Inventory Scale, Patient Health Questionnaire, and Depression Anxiety Stress Scale respectively.
Heterogeneity and Publication Bias
The nineteen included studies were analyzed for heterogeneity and publication bias [ 20 - 38 ]. High heterogeneity was found in the analysis with the Q test (p <0.001) and I 2 statistics (I 2 = 99.6%). For publication bias, the Doi plot showed no asymmetry confirming the absence of bias (LFK index = 0.15) (Figure (Figure3 3 .)

Sensitivity Analysis
The effect of each study (i.e. nineteen studies) [ 20 - 41 ] on the pooled prevalence of depression has been analysed by excluding each study step by step using sensitivity analysis (Table (Table2). 2 ). It showed that in eight studies, [ 21 , 23 , 26 - 29 , 36 , 38 ] comparatively the prime determinants of the pooled prevalence of depression among undergraduate medical students and the major source of heterogeneity come from five studies [ 25 , 30 , 34 , 35 , 37 ].
Although it is of global public health concern, depression among medical students is still under-recognized and the associated discrimination and stigma deter most of the students from seeking help. Research done among medical students even before the pandemic were showing higher rates of depression and physical distress in comparison to the general population [ 3 - 9 ]. COVID pandemic may have further declined the mental health of all individuals, especially medical students.
This is one of the few systematic reviews and meta-analyses on medical trainees which has ventured into exploring the prevalence of depression amidst the COVID pandemic. It has incorporated 19 original articles published from 2019 to 2022 from medical colleges situated in different regions of India. These articles used various standard screening instruments such as Patient Health Questionnaire (PHQ-9), Depression Anxiety Stress Scale (DASS 21), Beck Depression Inventory (BDI) Scale, Centre for Epidemiologic Studies Depression Scale and Hospital Anxiety and Depression Scale (HADS) for screening depression. The pooled prevalence of depression among medical students (n=5944) was found to be 50.0% [95% CI: (31%-70%] based on a random effect model pertaining to high heterogeneity [Q test (p <0.001) and I2 = 99.6%]; the depression calculated in the various studies ranged from 16.0% to 100.0%. This pooled prevalence is higher than the pooled prevalence value of 40%, which was done before the COVID pandemic, as mentioned in a meta-analysis conducted by Dwivedi N et al. [ 11 ] In Jia Q et al. study, a meta-analysis done in 41 studies among medical students from different countries showed a high pooled prevalence of depression of 37.9% among the students. Comparatively, this meta-analysis has shown a higher prevalence among Indian medical undergraduates, slightly higher in female students [ 10 ]. This variation of the depression may reflect the trend of higher rates of depression in females in the general population [ 42 ]. The severity of depression has also been measured in various studies, though it is not uniform throughout the studies as different screening tools had different cut off for measuring depression. The pooled prevalence of depression in this review varied from 27.0% to 99.0% when stratified based on the study tools. Depression Anxiety Stress Scale was the most commonly used scale among the studies, followed by Patient Health Questionnaire and Beck Depression Inventory.
According to this meta-analysis, one out of two students was found to have some degree of depression which is a concerning number. The prevalence has increased during the COVID pandemic compared to the prevalence before the pandemic since the pandemic itself may have a negative impact on the mental health of the students [ 11 ]. Further, it was also stated that it would increase the burden of depression in South Asian populations and healthcare systems [ 2 ]. There have been multiple explanations behind depression among medical students such as the challenging medical curriculum, lack of sleep and recreational activities due to vast academic tasks given, transition from a familiar to a non-familiar situation, lack of communication skills, etc. Several strategies can be implemented at different levels like changing the grading system, setting clear learning objectives to decrease academic burden, incorporating team-based learning and group activities rather than following traditional didactic lectures, self-directed learning so that students are aware of their shortcomings and promoting professionalism and communication skills for dealing patients properly. This pandemic had led to online teaching of medical students, [ 43 ] further, the effects of social distancing and self-isolation could have made the students more vulnerable to depression and anxiety [ 44 ]. This global health concern can also be taken care of using evidence-based structured programmes for mental upliftment like mindfulness therapy, life skill training, and counselling sessions can be kept for the students [ 45 , 46 ].
Strengths and limitations
The strengths of this study are that it has no asymmetry in the doi plot and is one of the few meta-analyses which has investigated the pooled prevalence of depression among the undergraduate students in India. Despite the strengths, this study has a few limitations like high heterogeneity and there might be a possibility of overestimation of the prevalence of depression because pooled prevalence has been calculated based on screening instruments and in various studies which are self-reporting and does not involve any clinical diagnosis.
Conclusions
The high prevalence of depression among medical students demands regular screening for depression along with counselling services. It shows that there is a need to raise awareness among students and other stakeholders, such as parents and medical educators, concerning symptoms and signs of depression among medical students. Further, effective strategies with health education programs and interventions may be given at individual, family, and community levels for providing mental health services to undergraduate medical students. Research with large sample sizes and multicentric longitudinal research is needed to determine the prevalence and risk factors for depression among medical students in India.
Acknowledgments
The authors are thankful to Dr. Radhika Rajendran, B.tech, PhD., Assistant Professor, Madhav Institute of Science and Technology, Gwalior, Madhya Pradesh, for her valuable inputs.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.

IMAGES
VIDEO
COMMENTS
Materials and Methods. This cross-sectional study was conducted among 1 st year MBBS students (2019-2020 batch), between February and March 2020 after obtaining the Institutional Ethics Committee clearance. A semi-structured questionnaire (including both open- and closed-ended questions), eliciting the learners' perception on various facets of new curriculum was developed.
M ATERIALS AND M ETHODS. Our institution started formal training of UGs in research as a part of the community medicine curriculum in 2002. The MBBS students undergo training in community medicine during their 1 st-year MBBS (1 st and 2 nd semesters), 2 nd-year MBBS (3 rd and 4 th semesters), and 3 rd-year MBBS (6 th and 7 th semesters). The students undergo the mandatory research methodology ...
It is a 40-item questionnaire assessing stress over 6 domains. It is a validated instrument to study stressors among medical undergraduates in India. Stress score is scored as mild (0-1), moderate (1.01-2), high (2.01-3), and severe (3.01-4). 9. Burnout was studied by using Maslach burnout inventory-student survey, a 15-item ...
Results: A total of 104 students participated in the study. Among them, 68 (65.39%) were males and 36 (34.61%) females. The maximum percentage of students was of the age group of 20 years i.e. 26 ...
www.ejpmr.com Srabani et al.European Journal of Pharmaceutical and Medical Research 490 EARLY CLINICAL EXPOSURE FOR FIRST-YEAR MBBS STUDENTS Gajare Rupali1, Bhattacharya Srabani2* and Sundaram Kartikeyan3 1Assistant Professor, Anatomy Department, Rajiv Gandhi Medical College, Kalwa, Thane-400 605, Maharashtra, India. 2Professor and Head, Physiology Department, Rajiv Gandhi Medical College ...
Hence, the present observational study was carried out among 150 first MBBS students to sensitize them for a clinical set-up, to appreciate the finer aspect of human behavior while dealing with ...
Explore the latest full-text research PDFs, articles, conference papers, preprints and more on MBBS. ... MBBS - Science topic. ... All 200 medical students of 1st year MBBS were invited to ...
2. ). To truly make an impact on students, mastery of the subject material may be insufficient. One cannot expect an audience to be enthusiastic about learning if the presenter is monotonous and disinterested. Changing the speed, tone, and inflection of one's voice keeps the presentation fresh (. 3. , 4.
Study Guide for 1st Year MBBS Sharif Medical & Dental College, ... Presentations of the ongoing topic will be conducted throughout the year periodically by the students so as to cover the topic of discussion precisely according to course work designed by UHS and emphasizing its clinical relevance and research relationship. Preferably topics ...
Online resources: There are several online resources that MBBS first year students can use to improve their studies. Websites such as Khan Academy and Medscape provide free medical education material.
The top 16 academically best students of semester two were asked to participate in this project of creating a SPA (Student Projects in Anatomy). Materials and Methods Study settings and participants: Top 16 students (based on the marks scored in Anatomy in the first two blocks) of MBBS batch 32 (March 2013 admission) were chosen for this study.
Keep pace with your studies. Slow and steady wins the race. The same is true for studying for 1st-year MBBS. Break up your topic to be learned into small chunks and make a habit of reviewing it ...
Here are some steps to create a study schedule for your MBBS 1st year: 1. Assess Your Available Time: Start by assessing the amount of time you have available for studying each day. Consider your classes, practical sessions, and other commitments to determine the number of hours you can dedicate to studying. 2.
A total of 80 willing participants of first-year MBBS were included in the study. Informed consent was obtained duly from all participants. A standard questionnaire was given to students to answer ...
Download MBBS (Bachelor of Medicine, Bachelor of Surgery) Important Topics and materials for MBBS 1st Year Important Topics, MBBS 2nd Year Important Topics, MBBS 3rd Year Important Topics & MBBS Final Year Important Topics. MBBS LECTURE NOTES FOR ALL SUBJECTS (UPDATED FOR 2021 SYLLABUS) - ALL UNIVERSITIES Rajiv Gandhi University of Health Sciences (RGUHS) MBBS Last 10 year Question Papers ...
The feedback of students showed that 49.48% of students strongly agreed that contents discussed in the workshop were adequate, 61.85% agreed about better understanding of the topics of the workshop, 60.80% agreed that their queries and doubts are cleared, 53.6% agreed that the workshop motivates them to do research, and 44.3% agreed that they ...
videos to replace exposure to cadavers for students is a topic of debate and most of studies do prefer cadaveric dissection in first year of MBBS.7 any one Aim and Objectives 1. To detect the problems faced by first MBBS students invarious subdivisions of Anatomy with the help of questionnaire. 2.
MBBS Subjects. In order to prepare for the tests, a first-year MBBS student should aim to devote six hours per day to studying. There are in fact five subjects, but the amount of time you devote to each depends on your knowledge and ability. Therefore, don't waste time planning. Even though you need six hours, divide them up well so you can ...
The study was conducted on 177 first year MBBS students and 15 resource faculties involved in delivering various sessions of Foundation course.A statistically significant difference was obtained ...
Table 2: Feed Back Questionnaire 5 - 2020 - 2021 MBBS First Year Batch Question Agree Strongly agree ECE helped me to remember the topic better. 72% 28% Table 3: Feed Back Questionnaire 5 - 2021-2022 MBBS First Year Batch Question Agree Strongly agree ECE helped me to remember the topic better. 45% 55% Table 4: Feed Back Questionnaire 6-10
1st, 2nd, 3rd, and 4th year MBBS students Sikkim Manipal Institute of Medical Sciences, Gangtok. hospital anxiety and depression scale (HADS) January 2020 to January 2021 382 86 Low risk Rana S et al., 2021 18 years to 22 years First year MBBS students Government Medical College, Ner Chowk, Mandi, Himachal Pradesh
A medical student's first year of MBBS is an important time since it lays the groundwork for their future medical education. Students spend this time studying the foundational topics that make up medical knowledge. We shall examine the topics normally addressed about the MBBS 1st Year Books in this blog article.
Materials and Methods: Three-day long orientation program and foundation course were organized by the MEU, GAIMS for the incoming first-year MBBS students of 2016-2017 batch. 112 students ...