The impact of therapeutic alliance in physical therapy for chronic musculoskeletal pain: A systematic review of the literature
Affiliations.
- 1 Outpatient Physical Therapy Department, BreakThrough Physical Therapy , Wake Forest, NC, USA.
- 2 Outpatient Physical Therapy Department, Select Physical Therapy , Arlington, VA, USA.
- 3 Department of Physical Therapy and Occupational Therapy, Adult Ambulatory Division, Duke University Health System , Durham, NC, USA.
- 4 Outpatient Physical Therapy Department, Back to Work Physical Therapy , Tampa, FL, USA.
- 5 Outpatient Physical Therapy Department, Korunda Medical LLC , Naples, FL, USA.
- 6 Doctor of Physical Therapy Division, Department of Orthopaedics, Duke University , Durham, NC, USA.
- PMID: 30265840
- DOI: 10.1080/09593985.2018.1516015
To systematically determine the specific impact of therapeutic alliance (TA) on chronic musculoskeletal pain, identify factors influencing TA between physical therapists and patients with chronic musculoskeletal pain, and determine the working definition of TA across studies. Data Sources : Databases, including PubMed, CINHAL, and Embase, were searched from inception to January 2017. Study Selection : The initial search resulted in 451 papers. After screening, seven studies were identified that examined the role of TA on chronic pain (> 12 weeks) management in physical therapy settings. Data Extraction : Authors extracted data into tables. Risk of bias was assessed using Cochrane Collaboration methodology. Data Synthesis : Three studies examined the influence of a strong TA coupled with physical therapy on pain outcomes. Four studies identified factors that positively and negatively influenced TA. The working definition of TA was identified in each study. Conclusions : Emerging evidence suggests that for individuals participating in physical therapy for chronic musculoskeletal pain, a strong TA may improve pain outcomes. In order to facilitate a strong TA, physical therapists must understand factors that positively and negatively influence the relationship. Studies demonstrate that the definition of TA remains consistent as it transitions to the physical therapy setting.
Keywords: Chronic Pain; Pain Management; Physical Therapy Specialty; Professional-Patient Relations; Therapeutic Alliance.

Publication types
- Systematic Review
- Musculoskeletal Pain / therapy*
- Physical Therapy Modalities*
- Therapeutic Alliance*
- University Home
- Library Home
- SOPHIA Home
Home > School of Health > Physical Therapy > DPT Research Papers
Doctor of Physical Therapy Research Papers
Research papers from 2017 2017.
A Systematic Mapping Review of Health Promotion and Well-being Concepts in Physical Therapy , Andrew Amundson, Jesse Klein, Bailey Ringold, and Aaron Theis
The Influence of Hip Strength and Core Endurance on Recurrent Patella Dislocations: A Pilot Study , Samuel Arnold, Emily Bradshaw, Anna Hansen, Jessica Knutson, and Mackenzie Newman
The Impact of Walker Style on Gait Characteristics in Non-assistive Device Dependent older Adults , Matthew Bennett, Taylor Hutchins, and Kaci Platz
The Impact of a Community based Exercise Program on Somali Immigrants Residing in Subsidized Housing in Minnesota , Kimberly Berggren, Meghan Gerardi, and Laura Mueller
Comparison of Three-Dimensional Motion of the Scapula during the Hawkins-Kennedy Test and the Sidelying Sleeper Stretch , Alyssa Buchner, Tami Buus, Brittany Evans, Kirsten Lambert, and Lisandra Scheevel
Influence of Fatigue and Anticipation on Knee Kinematics and Kinetics during a Jump-cut Maneuver , Sara Buermann, Erica Gloppen, Regan Kriechbaum, Dani Potter, and Nicole Sheehan
The Accuracy of Wireless Sensors in Detecting the leg Movements and Kicks of Young Typically Developing Infants: A Pilot Study , Bri Coulter, Julia Johnson, Molly Koch, and Christina Ramsdell
Research Papers from 2016 2016
The Effects of an On-Site Exercise Program on Health and Health Behaviors in Community Dwelling Adults Living in a Subsidized Apartment Building , Alexandra Anders, Chad McNutt, and Sarah Whitmore
Influence of Fatigue on Jump and Land Movement Patterns , Sarah Bard, Beth Anne Cooper, Kevin Kosel, Owen Runion, and Kristi Thorwick
Hip Strength and Core Endurance in Female Adolescent Runners With and Without Knee Pain , Brandon Boeck, Emily Kammerer, Lisa Kelley, Cody Misuraca, and Mitchell Peterson
Factors Impacting Adherence to a Multifactorial Fall Prevention Program - a Matter of Balance , Megan Dean, Justine Eggers, Brittany Stevens, and Gunther Wolff
Chemotherapy Induced Peripheral Neuropathy and Foot Posture in Pediatric Cancer Patients , Parker Deutz, Magdalena Hoelmer, Sarah Knilans, and Abigail Semlak
The Effect of Hip and Hamstring Pathology on Sacroiliac Joint Dysfunction: A Case Series , Sarah DuPlissis, Rachel Hedden, Nicholas Manning, Josh Patterson, and Luke Wahlstrom
Goal-directed Leg Movements and Kicks in Infants with Spina Bifida , Emily Goracke, Kelsey Jacobs, Elizabeth Pilney, and Katherine Shephard
The Role of the Physical Therapist in Health Promotion as Perceived by Patients with Neurological Pathologies: A Descriptive Study , Ariel Hansen, Gabrielle McGurran-Hanson, Kayla LeDuc, and Hannah Von Arb
Research Papers from 2015 2015
Proximal Strength and Functional Testing Applicable to Patellofemoral Instability: A Preliminary Study , Samantha Alschlager, Danielle Honnette, Katelyn Ley, Brianna Ludtke, and Kristen Reed
Recovery of Nerve Function after Treatment for Childhood Cancer , Allison Baker, Alison Bottke, Maria Leider, and Timothy Mann
The Effects of Electrical Stimulation on Chronic Wound Healing: A Systematic Review , Elena Campea, Alice Fasnacht, and Allison Kirkvold
Glenohumeral Osteoarthritis: Patient Profiles and Outcomes of Shoulder Arthroplasty , Lisa Carlson, Katie Kruger, Callie Larsen, and Kim Ruehlmann
The Effect of Conjugate Reinforcement on the Leg Movements of Infants with Spina Bifida , Sarah DeRosier, Jeremy Martin, Anna Payne, Kelly Swenson, and Elisabeth Wech
Recovery from Central Cord Syndrome: A Case Report , Katie Jacobson
Cerebral Vascular Accident Confounded by Parkinson's Disease: A Case Report , Jacqueline Moseman
Physical Therapy for Mobilization of a Patient with a Prolonged Intensive Care Unit Stay: A Case Report , Jennifer Pulscher
Physical Therapy Management of a Patient with Diffuse Pigmented Villonodular Synovitis: A Case Report , Christa Schutte
Research Papers from 2014 2014
Fairview Cancer Rehab Program Outcomes and Effectiveness: a Pilot Study , Kaeleigh Adami, Elizabeth Koch, Allie Meier, and Laura Vaughn
Core Strength Testing: Developing Normative Data for Three Clinical Tests , Alexis Anderson, Jessica Hoffman, Brent Johnson, Anna Simonson, and Laurel Urquhart
Hip Strength and Core Endurance Among Female Adolescent Runners , Jenna Batchelder, Angela Everson, Leah Paquin, and Heidi Sande
Effect of Lower Extremity Sensory Amplitude Electrical Stimulation on Motor Recovery and Function after Stroke: a Pilot Study , David Bowman, Rebecca Nelson, Kelsey Shearen, and Emily Wizykoski
Volunteering as an Occupation in African-American Women in a Rural Community , Kayla Clafton, Melissa Danielson, Danielle Glenn, and Samuel Vukov
The Influence of Age, Position, and Timing of Surgical Repair on the Kicks of Infants with Spina Bifida , Ann Engstrom, Shannon Lucken, Kayla Sis, and Sarah Wehrheim
Facilitators and Barriers to Health Promotion Perceived by Minnesota Physical Therapists Working in Outpatient Settings , Ashley Fisher, Marit Otterson, and Sarah Pitzen
Establishment of Normative Shoulder Internal Rotation Passive Range of Motion Values in the Sidelying and Semi-sidelying Positions , Alisse Indrelie, Shannon Kelly, Hugo Klaers, Tatia Nawrocki, and Michael Stelzmiller
Research Papers from 2013 2013
Core Strength Testing: Developing Normative Data for Three Clinical Tests , David Anderson, Lindsay Barthelemy, Rachel Gmach, and Breanna Posey
The Effects of Walking Poles and Training on Gait Characteristics and Fear of Falling in Community Dwelling Older Adults , Sarah Becker, Lisa Glad, Kelsie Nebelsick, and Katie Yernberg
Effects of a Therapeutic Dance Program on Balance and Quality of Life in Community Dwelling Older Adults , Krista Berger, Julie Kaminski, Lindsey Kolnik, and Jennifer Miller
Physical Therapists’ Role in Health Promotion as Perceived by the Patient: A Descriptive Study , Jessica Berglund and Erin Poepping
Findings of the Lower Extremity Dynamic Screen in Patients with Patellofemoral Pain Syndrome: A Pilot Study , Jake Foley, Meghan Grathen, Lindsey Johnson, and Elizabeth Volk
Prevention of Work-Related Shoulder and Neck Injuries: A Systematic Review , Daniel Frush, Kimberly Redlin, and Jacob Cruze
The Impact of Chemotherapy on the Neuromuscular Components of Gait , Kari Johnson, Britta Schwartzhoff, Sandy Silva, and Rina Terk
Reentry Home after Disaster Relief Work in Haiti: A Mixed Methods Study of the Reentry Process of Medical Professionals , Kelsey Leeman, Andrea Olson, Abby Rassat, and Rita White
Physical Therapy Interventions and Outcomes for a Patient Following Hospitalization for Viral Gastroenteritis and Resulting Hospital-Acquired Pneumonia: A Case Report , Rachel Lewis
Research Papers from 2012 2012
Comparison of the Proprioceptive and Motion Reduction Effects of Shoulder Braces in Individuals With and Without Anterior Shoulder Dislocations: A Pilot Study , Evan Boldt, Marci Burg, Leah Jackson, and Lana Prokop
Risk Factors for Patellofemoral Pain Syndrome , Scott Darling, Hannah Finsaas, Andrea Johnson, Ashley Takekawa, and Elizabeth Wallner
Experiences of Physical Therapists who Participate in Disaster Relief Work in Haiti , Erin Faanes, Andrea Guggenbuehl, Ellen Johnston, Katie Larsen, and Crystal Stien
The Sensitivity of Infants with Spina Bifida to Sensory Information , Katie Gulsvig, Christina Hawn, James Plummer, and Ann Schmitz
Physical Therapists' Knowledge, Beliefs, and Practices Pertaining to Health Promotion and Fitness Testing , Megan Johnson, Allison Fisher, Megan Wiemann, Jenna Laska, and Andrea Eckstrom
Clinical Decision Making and Physical Therapy Management of Knee Pain Following Total Hip Arthoplasty: A Case Report , Lisa Marais
Physical Therapy Management Following Femoroacetabular Impingment Correction and Acetabular Labral Repair: A Case Report , Jessica Walker
Unraveling the Mystery of Knee Pain: A Case Report , Nicole L. Zehnder
Research Papers from 2011 2011
3D Knee Kinematics and Kinetics With Visual Disruption in Subjects With ACL Reconstruction , Brittni Baune, Jennifer Henderson, Jenna Merchant, and Kristian Olson
Lower Extremity Functional Screen for Biomechanical Faults in Female Athletes , Jacqueline Carpenter, Ann Donner, Kristine Hoff, and Naomi Johnson
The Effect of Training on Novice Raters When Performing Radiographic Measurement of Humeral Retroversion: a Follow-up Study , Ryan Christensen, Danielle Grambo, Erin Ingram, and Lyna Menezes
The Effect of Walking Poles on Gait Characteristics and Fear of Falling in Community Dwelling, Four-Wheel Walker Dependent and Non-Assistive Device Dependent Older Adults , Jennifer Gonnerman, Ellen Guerin, Karen Koza, and Courtney Tofte
Physical Therapy Intervention for a Patient with Bilateral Achilles Tendinopathy Following Periods of Immobilization: a Case Report , Alyssa Hageman
An Outpatient Physical Therapy Intervention Program , Rebecca K. Henderson
Functional Recovery in a 67-Year-Old Male with Staphylococcus Aureus Spinal Cord Abscess: a Case Report , Andrea Hokanson
Lower Extremity Activity of Infants with Spina Bifida: Does Context Still Matter , Sarah Meissner, Megan Ogaard, Jeanna Shirley, and Kristin Warfield
Clinical Use of the Nintendo WII for Balance Rehabilitation: a Case Report , Jasey Olsen
Safety of Physical Therapy Using Symptomatic Blood Value Guidelines in Children Being Treated for Cancer , Katie Peters and Jessica Tice
Research Papers from 2010 2010
Political Participation in Physical Therapy: Attitudes and Perceptions Across the Practice Spectrum , Cole Kampen, Nicholas Schneider, Miranda Swensen, and Amy Thompson
Advanced Search
- Notify me via email or RSS
- Collections
- Disciplines
Author Corner
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
- Research article
- Open access
- Published: 16 November 2020
Exercise/physical activity and health outcomes: an overview of Cochrane systematic reviews
- Pawel Posadzki 1 , 2 ,
- Dawid Pieper ORCID: orcid.org/0000-0002-0715-5182 3 ,
- Ram Bajpai 4 ,
- Hubert Makaruk 5 ,
- Nadja Könsgen 3 ,
- Annika Lena Neuhaus 3 &
- Monika Semwal 6
BMC Public Health volume 20 , Article number: 1724 ( 2020 ) Cite this article
31k Accesses
131 Citations
132 Altmetric
Metrics details
Sedentary lifestyle is a major risk factor for noncommunicable diseases such as cardiovascular diseases, cancer and diabetes. It has been estimated that approximately 3.2 million deaths each year are attributable to insufficient levels of physical activity. We evaluated the available evidence from Cochrane systematic reviews (CSRs) on the effectiveness of exercise/physical activity for various health outcomes.
Overview and meta-analysis. The Cochrane Library was searched from 01.01.2000 to issue 1, 2019. No language restrictions were imposed. Only CSRs of randomised controlled trials (RCTs) were included. Both healthy individuals, those at risk of a disease, and medically compromised patients of any age and gender were eligible. We evaluated any type of exercise or physical activity interventions; against any types of controls; and measuring any type of health-related outcome measures. The AMSTAR-2 tool for assessing the methodological quality of the included studies was utilised.
Hundred and fifty CSRs met the inclusion criteria. There were 54 different conditions. Majority of CSRs were of high methodological quality. Hundred and thirty CSRs employed meta-analytic techniques and 20 did not. Limitations for studies were the most common reasons for downgrading the quality of the evidence. Based on 10 CSRs and 187 RCTs with 27,671 participants, there was a 13% reduction in mortality rates risk ratio (RR) 0.87 [95% confidence intervals (CI) 0.78 to 0.96]; I 2 = 26.6%, [prediction interval (PI) 0.70, 1.07], median effect size (MES) = 0.93 [interquartile range (IQR) 0.81, 1.00]. Data from 15 CSRs and 408 RCTs with 32,984 participants showed a small improvement in quality of life (QOL) standardised mean difference (SMD) 0.18 [95% CI 0.08, 0.28]; I 2 = 74.3%; PI -0.18, 0.53], MES = 0.20 [IQR 0.07, 0.39]. Subgroup analyses by the type of condition showed that the magnitude of effect size was the largest among patients with mental health conditions.
There is a plethora of CSRs evaluating the effectiveness of physical activity/exercise. The evidence suggests that physical activity/exercise reduces mortality rates and improves QOL with minimal or no safety concerns.
Trial registration
Registered in PROSPERO ( CRD42019120295 ) on 10th January 2019.
Peer Review reports
The World Health Organization (WHO) defines physical activity “as any bodily movement produced by skeletal muscles that requires energy expenditure” [ 1 ]. Therefore, physical activity is not only limited to sports but also includes walking, running, swimming, gymnastics, dance, ball games, and martial arts, for example. In the last years, several organizations have published or updated their guidelines on physical activity. For example, the Physical Activity Guidelines for Americans, 2nd edition, provides information and guidance on the types and amounts of physical activity that provide substantial health benefits [ 2 ]. The evidence about the health benefits of regular physical activity is well established and so are the risks of sedentary behaviour [ 2 ]. Exercise is dose dependent, meaning that people who achieve cumulative levels several times higher than the current recommended minimum level have a significant reduction in the risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events [ 3 ]. Benefits of physical activity have been reported for numerous outcomes such as mortality [ 4 , 5 ], cognitive and physical decline [ 5 , 6 , 7 ], glycaemic control [ 8 , 9 ], pain and disability [ 10 , 11 ], muscle and bone strength [ 12 ], depressive symptoms [ 13 ], and functional mobility and well-being [ 14 , 15 ]. Overall benefits of exercise apply to all bodily systems including immunological [ 16 ], musculoskeletal [ 17 ], respiratory [ 18 ], and hormonal [ 19 ]. Specifically for the cardiovascular system, exercise increases fatty acid oxidation, cardiac output, vascular smooth muscle relaxation, endothelial nitric oxide synthase expression and nitric oxide availability, improves plasma lipid profiles [ 15 ] while at the same time reducing resting heart rate and blood pressure, aortic valve calcification, and vascular resistance [ 20 ].
However, the degree of all the above-highlighted benefits vary considerably depending on individual fitness levels, types of populations, age groups and the intensity of different physical activities/exercises [ 21 ]. The majority of guidelines in different countries recommend a goal of 150 min/week of moderate-intensity aerobic physical activity (or equivalent of 75 min of vigorous-intensity) [ 22 ] with differences for cardiovascular disease [ 23 ] or obesity prevention [ 24 ] or age groups [ 25 ].
There is a plethora of systematic reviews published by the Cochrane Library critically evaluating the effectiveness of physical activity/exercise for various health outcomes. Cochrane systematic reviews (CSRs) are known to be a source of high-quality evidence. Thus, it is not only timely but relevant to evaluate the current knowledge, and determine the quality of the evidence-base, and the magnitude of the effect sizes given the negative lifestyle changes and rising physical inactivity-related burden of diseases. This overview will identify the breadth and scope to which CSRs have appraised the evidence for exercise on health outcomes; and this will help in directing future guidelines and identifying current gaps in the literature.
The objectives of this research were to a. answer the following research questions: in children, adolescents and adults (both healthy and medically compromised) what are the effects (and adverse effects) of exercise/physical activity in improving various health outcomes (e.g., pain, function, quality of life) reported in CSRs; b. estimate the magnitude of the effects by pooling the results quantitatively; c. evaluate the strength and quality of the existing evidence; and d. create recommendations for future researchers, patients, and clinicians.
Our overview was registered with PROSPERO (CRD42019120295) on 10th January 2019. The Cochrane Handbook for Systematic Reviews of interventions and Preferred Reporting Items for Overviews of Reviews were adhered to while writing and reporting this overview [ 26 , 27 ].
Search strategy and selection criteria
We followed the practical guidance for conducting overviews of reviews of health care interventions [ 28 ] and searched the Cochrane Database of Systematic Reviews (CDSR), 2019, Issue 1, on the Cochrane Library for relevant papers using the search strategy: (health) and (exercise or activity or physical). The decision to seek CSRs only was based on three main aspects. First, high quality (CSRs are considered to be the ‘gold methodological standard’) [ 29 , 30 , 31 ]. Second, data saturation (enough high-quality evidence to reach meaningful conclusions based on CSRs only). Third, including non-CSRs would have heavily increased the issue of overlapping reviews (also affecting data robustness and credibility of conclusions). One reviewer carried out the searches. The study screening and selection process were performed independently by two reviewers. We imported all identified references into reference manager software EndNote (X8). Any disagreements were resolved by discussion between the authors with third overview author acting as an arbiter, if necessary.
We included CSRs of randomised controlled trials (RCTs) involving both healthy individuals and medically compromised patients of any age and gender. Only CSRs assessing exercise or physical activity as a stand-alone intervention were included. This included interventions that could initially be taught by a professional or involve ongoing supervision (the WHO definition). Complex interventions e.g., assessing both exercise/physical activity and behavioural changes were excluded if the health effects of the interventions could not have been attributed to exercise distinctly.
Any types of controls were admissible. Reviews evaluating any type of health-related outcome measures were deemed eligible. However, we excluded protocols or/and CSRs that have been withdrawn from the Cochrane Library as well as reviews with no included studies.
Data analysis
Three authors (HM, ALN, NK) independently extracted relevant information from all the included studies using a custom-made data collection form. The methodological quality of SRs included was independently evaluated by same reviewers using the AMSTAR-2 tool [ 32 ]. Any disagreements on data extraction or CSR quality were resolved by discussion. The entire dataset was validated by three authors (PP, MS, DP) and any discrepant opinions were settled through discussions.
The results of CSRs are presented in a narrative fashion using descriptive tables. Where feasible, we presented outcome measures across CSRs. Data from the subset of homogeneous outcomes were pooled quantitatively using the approach previously described by Bellou et al. and Posadzki et al. [ 33 , 34 ]. For mortality and quality of life (QOL) outcomes, the number of participants and RCTs involved in the meta-analysis, summary effect sizes [with 95% confidence intervals (CI)] using random-effects model were calculated. For binary outcomes, we considered relative risks (RRs) as surrogate measures of the corresponding odds ratio (OR) or risk ratio/hazard ratio (HR). To stabilise the variance and normalise the distributions, we transformed RRs into their natural logarithms before pooling the data (a variation was allowed, however, it did not change interpretation of results) [ 35 ]. The standard error (SE) of the natural logarithm of RR was derived from the corresponding CIs, which was either provided in the study or calculated with standard formulas [ 36 ]. Binary outcomes reported as risk difference (RD) were also meta-analysed if two more estimates were available. For continuous outcomes, we only meta-analysed estimates that were available as standardised mean difference (SMD), and estimates reported with mean differences (MD) for QOL were presented separately in a supplementary Table 9 . To estimate the overall effect size, each study was weighted by the reciprocal of its variance. Random-effects meta-analysis, using DerSimonian and Laird method [ 37 ] was applied to individual CSR estimates to obtain a pooled summary estimate for RR or SMD. The 95% prediction interval (PI) was also calculated (where ≥3 studies were available), which further accounts for between-study heterogeneity and estimates the uncertainty around the effect that would be anticipated in a new study evaluating that same association. I -squared statistic was used to measure between study heterogeneity; and its various thresholds (small, substantial and considerable) were interpreted considering the size and direction of effects and the p -value from Cochran’s Q test ( p < 0.1 considered as significance) [ 38 ]. Wherever possible, we calculated the median effect size (with interquartile range [IQR]) of each CSR to interpret the direction and magnitude of the effect size. Sub-group analyses are planned for type and intensity of the intervention; age group; gender; type and/or severity of the condition, risk of bias in RCTs, and the overall quality of the evidence (Grading of Recommendations Assessment, Development and Evaluation (GRADE) criteria). To assess overlap we calculated the corrected covered area (CCA) [ 39 ]. All statistical analyses were conducted on Stata statistical software version 15.2 (StataCorp LLC, College Station, Texas, USA).
The searches generated 280 potentially relevant CRSs. After removing of duplicates and screening, a total of 150 CSRs met our eligibility criteria [ 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 , 138 , 139 , 140 , 141 , 142 , 143 , 144 , 145 , 146 , 147 , 148 , 149 , 150 , 151 , 152 , 153 , 154 , 155 , 156 , 157 , 158 , 159 , 160 , 161 , 162 , 163 , 164 , 165 , 166 , 167 , 168 , 169 , 170 , 171 , 172 , 173 , 174 , 175 , 176 , 177 , 178 , 179 , 180 , 181 , 182 , 183 , 184 , 185 , 186 , 187 , 188 , 189 ] (Fig. 1 ). Reviews were published between September 2002 and December 2018. A total of 130 CSRs employed meta-analytic techniques and 20 did not. The total number of RCTs in the CSRs amounted to 2888; with 485,110 participants (mean = 3234, SD = 13,272). The age ranged from 3 to 87 and gender distribution was inestimable. The main characteristics of included reviews are summarised in supplementary Table 1 . Supplementary Table 2 summarises the effects of physical activity/exercise on health outcomes. Conclusions from CSRs are listed in supplementary Table 3 . Adverse effects are listed in supplementary Table 4 . Supplementary Table 5 presents summary of withdrawals/non-adherence. The methodological quality of CSRs is presented in supplementary Table 6 . Supplementary Table 7 summarises studies assessed at low risk of bias (by the authors of CSRs). GRADE-ings of the review’s main comparison are listed in supplementary Table 8 .
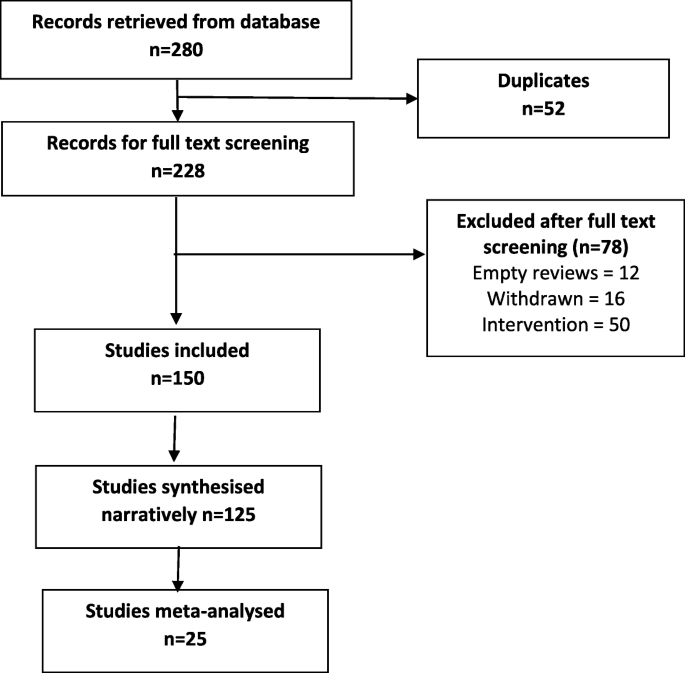
Study selection process
There were 54 separate populations/conditions, considerable range of interventions and comparators, co-interventions, and outcome measures. For detailed description of interventions, please refer to the supplementary tables . Most commonly measured outcomes were - function 112 (75%), QOL 83 (55%), AEs 70 (47%), pain 41 (27%), mortality 28 (19%), strength 30 (20%), costs 47 (31%), disability 14 (9%), and mental health in 35 (23%) CSRs.
There was a 13% reduction in mortality rates risk ratio (RR) 0.87 [95% CI 0.78 to 0.96]; I 2 = 26.6%, [PI 0.70, 1.07], median effect size (MES) = 0.93 [interquartile range (IQR) 0.81, 1.00]; 10 CSRs, 187 RCTs, 27,671 participants) following exercise when compared with various controls (Table 1 ). This reduction was smaller in ‘other groups’ of patients when compared to cardiovascular diseases (CVD) patients - RR 0.97 [95% CI 0.65, 1.45] versus 0.85 [0.76, 0.96] respectively. The effects of exercise were not intensity or frequency dependent. Sessions more than 3 times per week exerted a smaller reduction in mortality as compared with sessions of less than 3 times per week RR 0.87 [95% CI 0.78, 0.98] versus 0.63 [0.39, 1.00]. Subgroup analyses by risk of bias (ROB) in RCTs showed that RCTs at low ROB exerted smaller reductions in mortality when compared to RCTs at an unclear or high ROB, RR 0.90 [95% CI 0.78, 1.02] versus 0.72 [0.42, 1.22] versus 0.86 [0.69, 1.06] respectively. CSRs with moderate quality of evidence (GRADE), showed slightly smaller reductions in mortality when compared with CSRs that relied on very low to low quality evidence RR 0.88 [95% CI 0.79, 0.98] versus 0.70 [0.47, 1.04].
Exercise also showed an improvement in QOL, standardised mean difference (SMD) 0.18 [95% CI 0.08, 0.28]; I 2 = 74.3%; PI -0.18, 0.53], MES = 0.20 [IQR 0.07, 0.39]; 15 CSRs, 408 RCTs, 32,984 participants) when compared with various controls (Table 2 ). These improvements were greater observed for health related QOL when compared to overall QOL SMD 0.30 [95% CI 0.21, 0.39] vs 0.06 [− 0.08, 0.20] respectively. Again, the effects of exercise were duration and frequency dependent. For instance, sessions of more than 90 mins exerted a greater improvement in QOL as compared with sessions up to 90 min SMD 0.24 [95% CI 0.11, 0.37] versus 0.22 [− 0.30, 0.74]. Subgroup analyses by the type of condition showed that the magnitude of effect was the largest among patients with mental health conditions, followed by CVD and cancer. Physical activity exerted negative effects on QOL in patients with respiratory conditions (2 CSRs, 20 RCTs with 601 patients; SMD -0.97 [95% CI -1.43, 0.57]; I 2 = 87.8%; MES = -0.46 [IQR-0.97, 0.05]). Subgroup analyses by risk of bias (ROB) in RCTs showed that RCTs at low or unclear ROB exerted greater improvements in QOL when compared to RCTs at a high ROB SMD 0.21 [95% CI 0.10, 0.31] versus 0.17 [0.03, 0.31]. Analogically, CSRs with moderate to high quality of evidence showed slightly greater improvements in QOL when compared with CSRs that relied on very low to low quality evidence SMD 0.19 [95% CI 0.05, 0.33] versus 0.15 [− 0.02, 0.32]. Please also see supplementary Table 9 more studies reporting QOL outcomes as mean difference (not quantitatively synthesised herein).
Adverse events (AEs) were reported in 100 (66.6%) CSRs; and not reported in 50 (33.3%). The number of AEs ranged from 0 to 84 in the CSRs. The number was inestimable in 83 (55.3%) CSRs. Ten (6.6%) reported no occurrence of AEs. Mild AEs were reported in 28 (18.6%) CSRs, moderate in 9 (6%) and serious/severe in 20 (13.3%). There were 10 deaths and in majority of instances, the causality was not attributed to exercise. For this outcome, we were unable to pool the data as effect sizes were too heterogeneous (Table 3 ).
In 38 CSRs, the total number of trials reporting withdrawals/non-adherence was inestimable. There were different ways of reporting it such as adherence or attrition (high in 23.3% of CSRs) as well as various effect estimates including %, range, total numbers, MD, RD, RR, OR, mean and SD. The overall pooled estimates are reported in Table 3 .
Of all 16 domains of the AMSTAR-2 tool, 1876 (78.1%) scored ‘yes’, 76 (3.1%) ‘partial yes’; 375 (15.6%) ‘no’, and ‘not applicable’ in 25 (1%) CSRs. Ninety-six CSRs (64%) were scored as ‘no’ on reporting sources of funding for the studies followed by 88 (58.6%) failing to explain the selection of study designs for inclusion. One CSR (0.6%) each were judged as ‘no’ for reporting any potential sources of conflict of interest, including any funding for conducting the review as well for performing study selection in duplicate.
In 102 (68%) CSRs, there was predominantly a high risk of bias in RCTs. In 9 (6%) studies, this was reported as a range, e.g., low or unclear or low to high. Two CSRs used different terminology i.e., moderate methodological quality; and the risk of bias was inestimable in one CSR. Sixteen (10.6%) CSRs did not identify any studies (RCTs) at low risk of random sequence generation, 28 (18.6%) allocation concealment, 28 (18.6%) performance bias, 84 (54%) detection bias, 35 (23.3%) attrition bias, 18 (12%) reporting bias, and 29 (19.3%) other bias.
In 114 (76%) CSRs, limitation of studies was the main reason for downgrading the quality of the evidence followed by imprecision in 98 (65.3%) and inconsistency in 68 (45.3%). Publication bias was the least frequent reason for downgrading in 26 (17.3%) CSRs. Ninety-one (60.7%) CSRs reached equivocal conclusions, 49 (32.7%) reviews reached positive conclusions and 10 (6.7%) reached negative conclusions (as judged by the authors of CSRs).
In this systematic review of CSRs, we found a large body of evidence on the beneficial effects of physical activity/exercise on health outcomes in a wide range of heterogeneous populations. Our data shows a 13% reduction in mortality rates among 27,671 participants, and a small improvement in QOL and health-related QOL following various modes of physical activity/exercises. This means that both healthy individuals and medically compromised patients can significantly improve function, physical and mental health; or reduce pain and disability by exercising more [ 190 ]. In line with previous findings [ 191 , 192 , 193 , 194 ], where a dose-specific reduction in mortality has been found, our data shows a greater reduction in mortality in studies with longer follow-up (> 12 months) as compared to those with shorter follow-up (< 12 months). Interestingly, we found a consistent pattern in the findings, the higher the quality of evidence and the lower the risk of bias in primary studies, the smaller reductions in mortality. This pattern is observational in nature and cannot be over-generalised; however this might mean less certainty in the estimates measured. Furthermore, we found that the magnitude of the effect size was the largest among patients with mental health conditions. A possible mechanism of action may involve elevated levels of brain-derived neurotrophic factor or beta-endorphins [ 195 ].
We found the issue of poor reporting or underreporting of adherence/withdrawals in over a quarter of CSRs (25.3%). This is crucial both for improving the accuracy of the estimates at the RCT level as well as maintaining high levels of physical activity and associated health benefits at the population level.
Even the most promising interventions are not entirely risk-free; and some minor AEs such as post-exercise pain and soreness or discomfort related to physical activity/exercise have been reported. These were typically transient; resolved within a few days; and comparable between exercise and various control groups. However worryingly, the issue of poor reporting or underreporting of AEs has been observed in one third of the CSRs. Transparent reporting of AEs is crucial for identifying patients at risk and mitigating any potential negative or unintended consequences of the interventions.
High risk of bias of the RCTs evaluated was evident in more than two thirds of the CSRs. For example, more than half of reviews identified high risk of detection bias as a major source of bias suggesting that lack of blinding is still an issue in trials of behavioural interventions. Other shortcomings included insufficiently described randomisation and allocation concealment methods and often poor outcome reporting. This highlights the methodological challenges in RCTs of exercise and the need to counterbalance those with the underlying aim of strengthening internal and external validity of these trials.
Overall, high risk of bias in the primary trials was the main reason for downgrading the quality of the evidence using the GRADE criteria. Imprecision was frequently an issue, meaning the effective sample size was often small; studies were underpowered to detect the between-group differences. Pooling too heterogeneous results often resulted in inconsistent findings and inability to draw any meaningful conclusions. Indirectness and publication bias were lesser common reasons for downgrading. However, with regards to the latter, the generally accepted minimum number of 10 studies needed for quantitatively estimate the funnel plot asymmetry was not present in 69 (46%) CSRs.
Strengths of this research are the inclusion of large number of ‘gold standard’ systematic reviews, robust screening, data extractions and critical methodological appraisal. Nevertheless, some weaknesses need to be highlighted when interpreting findings of this overview. For instance, some of these CSRs analysed the same primary studies (RCTs) but, arrived at slightly different conclusions. Using, the Pieper et al. [ 39 ] formula, the amount of overlap ranged from 0.01% for AEs to 0.2% for adherence, which indicates slight overlap. All CSRs are vulnerable to publication bias [ 196 ] - hence the conclusions generated by them may be false-positive. Also, exercise was sometimes part of a complex intervention; and the effects of physical activity could not be distinguished from co-interventions. Often there were confounding effects of diet, educational, behavioural or lifestyle interventions; selection, and measurement bias were inevitably inherited in this overview too. Also, including CSRs only might lead to selection bias; and excluding reviews published before 2000 might limit the overall completeness and applicability of the evidence. A future update should consider these limitations, and in particular also including non-CSRs.
Conclusions
Trialists must improve the quality of primary studies. At the same time, strict compliance with the reporting standards should be enforced. Authors of CSRs should better explain eligibility criteria and report sources of funding for the primary studies. There are still insufficient physical activity trends worldwide amongst all age groups; and scalable interventions aimed at increasing physical activity levels should be prioritized [ 197 ]. Hence, policymakers and practitioners need to design and implement comprehensive and coordinated strategies aimed at targeting physical activity programs/interventions, health promotion and disease prevention campaigns at local, regional, national, and international levels [ 198 ].
Availability of data and materials
Data sharing is not applicable to this article as no raw data were analysed during the current study. All information in this article is based on published systematic reviews.
Abbreviations
Adverse events
Cardiovascular diseases
Cochrane Database of Systematic Reviews
Cochrane systematic reviews
Confidence interval
Grading of Recommendations Assessment, Development and Evaluation
Hazard ratio
Interquartile range
Mean difference
Prediction interval
Quality of life
Randomised controlled trials
Relative risk
Risk difference
Risk of bias
Standard error
Standardised mean difference
World Health Organization
https://www.who.int/dietphysicalactivity/pa/en/ . (Accessed 8 June 2020).
Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, George SM, Olson RD. The physical activity guidelines for AmericansPhysical activity guidelines for AmericansPhysical activity guidelines for Americans. Jama. 2018;320(19):2020–8.
PubMed Google Scholar
Kyu HH, Bachman VF, Alexander LT, Mumford JE, Afshin A, Estep K, Veerman JL, Delwiche K, Iannarone ML, Moyer ML, et al. Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the global burden of disease study 2013. BMJ. 2016;354:i3857.
PubMed PubMed Central Google Scholar
Abell B, Glasziou P, Hoffmann T. The contribution of individual exercise training components to clinical outcomes in randomised controlled trials of cardiac rehabilitation: a systematic review and meta-regression. Sports Med Open. 2017;3(1):19.
Anderson D, Seib C, Rasmussen L. Can physical activity prevent physical and cognitive decline in postmenopausal women? A systematic review of the literature. Maturitas. 2014;79(1):14–33.
Barbaric M, Brooks E, Moore L, Cheifetz O. Effects of physical activity on cancer survival: a systematic review. Physiother Can. 2010;62(1):25–34.
Barlow PA, Otahal P, Schultz MG, Shing CM, Sharman JE. Low exercise blood pressure and risk of cardiovascular events and all-cause mortality: systematic review and meta-analysis. Atherosclerosis. 2014;237(1):13–22.
CAS PubMed Google Scholar
Aljawarneh YM, Wardell DW, Wood GL, Rozmus CL. A systematic review of physical activity and exercise on physiological and biochemical outcomes in children and adolescents with type 1 diabetes. J Nurs Scholarsh. 2019.
Chastin SFM, De Craemer M, De Cocker K, Powell L, Van Cauwenberg J, Dall P, Hamer M, Stamatakis E. How does light-intensity physical activity associate with adult cardiometabolic health and mortality? Systematic review with meta-analysis of experimental and observational studies. Br J Sports Med. 2019;53(6):370–6.
Abdulla SY, Southerst D, Cote P, Shearer HM, Sutton D, Randhawa K, Varatharajan S, Wong JJ, Yu H, Marchand AA, et al. Is exercise effective for the management of subacromial impingement syndrome and other soft tissue injuries of the shoulder? A systematic review by the Ontario protocol for traffic injury management (OPTIMa) collaboration. Man Ther. 2015;20(5):646–56.
Alanazi MH, Parent EC, Dennett E. Effect of stabilization exercise on back pain, disability and quality of life in adults with scoliosis: a systematic review. Eur J Phys Rehabil Med. 2018;54(5):647–53.
Adsett JA, Mudge AM, Morris N, Kuys S, Paratz JD. Aquatic exercise training and stable heart failure: a systematic review and meta-analysis. Int J Cardiol. 2015;186:22–8.
Adamson BC, Ensari I, Motl RW. Effect of exercise on depressive symptoms in adults with neurologic disorders: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2015;96(7):1329–38.
Abdin S, Welch RK, Byron-Daniel J, Meyrick J. The effectiveness of physical activity interventions in improving well-being across office-based workplace settings: a systematic review. Public Health. 2018;160:70–6.
Albalawi H, Coulter E, Ghouri N, Paul L. The effectiveness of structured exercise in the south Asian population with type 2 diabetes: a systematic review. Phys Sportsmed. 2017;45(4):408–17.
Sellami M, Gasmi M, Denham J, Hayes LD, Stratton D, Padulo J, Bragazzi N. Effects of acute and chronic exercise on immunological parameters in the elderly aged: can physical activity counteract the effects of aging? Front Immunol. 2018;9:2187.
Hagen KB, Dagfinrud H, Moe RH, Østerås N, Kjeken I, Grotle M, Smedslund G. Exercise therapy for bone and muscle health: an overview of systematic reviews. BMC Med. 2012;10(1):167.
Burton DA, Stokes K, Hall GM. Physiological effects of exercise. Contin Educ Anaesth Crit Care Pain. 2004;4(6):185–8.
Google Scholar
Kraemer WJ, Ratamess NA. Hormonal responses and adaptations to resistance exercise and training. Sports Med. 2005;35(4):339–61.
Nystoriak MA, Bhatnagar A. Cardiovascular effects and benefits of exercise. Front Cardiovasc Med. 2018;5:135.
CAS PubMed PubMed Central Google Scholar
Vina J, Sanchis-Gomar F, Martinez-Bello V, Gomez-Cabrera MC. Exercise acts as a drug; the pharmacological benefits of exercise. Br J Pharmacol. 2012;167(1):1–12.
Warburton DER, Bredin SSD. Health benefits of physical activity: a systematic review of current systematic reviews. Curr Opin Cardiol. 2017;32(5):541–56.
Excellence NIfHaC: Cardiovascular disease prevention public health guideline [PH25] Published date: June 2010. Available at: https://www.nice.org.uk/guidance/ph25/resources/cardiovascular-disease-prevention-pdf-1996238687173 .
Excellence NIfHaC: Obesity prevention clinical guideline [CG43] published date: December 2006 Last updated: March 2015. Available at: https://www.nice.org.uk/guidance/cg43/resources/obesity-prevention-pdf-975445344709 .
Excellence NIfHaC: Physical activity for children and young people public health guideline [PH17] Published date: January 2009. Available at: https://www.nice.org.uk/guidance/ph17/resources/physical-activity-for-children-and-young-people-pdf-1996181580229 .
Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Version 6 [updated September 2018] edition. Available from www.cochrane-handbook.org : The Cochrane Collaboration, 2011. 2011.
Bougioukas KI, Liakos A, Tsapas A, Ntzani E, Haidich A-B. Preferred reporting items for overviews of systematic reviews including harms checklist: a pilot tool to be used for balanced reporting of benefits and harms. J Clin Epidemiol. 2018;93:9–24.
Pollock M, Fernandes RM, Newton AS, Scott SD, Hartling L. The impact of different inclusion decisions on the comprehensiveness and complexity of overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):18.
Handoll H, Madhok R. Quality of Cochrane reviews. Another study found that most Cochrane reviews are of a good standard. BMJ. 2002;324(7336):545.
Petticrew M, Wilson P, Wright K, Song F. Quality of Cochrane reviews. Quality of Cochrane reviews is better than that of non-Cochrane reviews. BMJ. 2002;324(7336):545.
Shea B, Moher D, Graham I, Pham B, Tugwell P. A comparison of the quality of Cochrane reviews and systematic reviews published in paper-based journals. Eval Health Prof. 2002;25(1):116–29.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Posadzki PP, Bajpai R, Kyaw BM, Roberts NJ, Brzezinski A, Christopoulos GI, Divakar U, Bajpai S, Soljak M, Dunleavy G, et al. Melatonin and health: an umbrella review of health outcomes and biological mechanisms of action. BMC Med. 2018;16(1):18.
Bellou V, Belbasis L, Tzoulaki I, Evangelou E, Ioannidis JP. Environmental risk factors and Parkinson's disease: an umbrella review of meta-analyses. Parkinsonism Relat Disord. 2016;23:1–9.
Walter SD, Cook RJ. A comparison of several point estimators of the odds ratio in a single 2 x 2 contingency table. Biometrics. 1991;47(3):795–811.
Khan H, Sempos CT. Statistical methods in epidemiology. New York: Oxford University Press; 1989.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
CAS Google Scholar
Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019): Cochrane; 2019. Available from www.training.cochrane.org/handbook .
Pieper D, Antoine SL, Mathes T, Neugebauer EA, Eikermann M. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol. 2014;67(4):368–75.
Adeniyi FB, Young T. Weight loss interventions for chronic asthma. Cochrane Database Syst Rev. 2012;7.
Al-Khudairy L, Loveman E, Colquitt JL, Mead E, Johnson RE, Fraser H, Olajide J, Murphy M, Velho RM, O'Malley C, et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese adolescents aged 12 to 17 years. Cochrane Database Syst Rev. 2017;6.
Amorim Adegboye AR, Linne YM. Diet or exercise, or both, for weight reduction in women after childbirth. Cochrane Database Syst Rev. 2013;7.
Anderson L, Nguyen TT, Dall CH, Burgess L, Bridges C, Taylor RS. Exercise-based cardiac rehabilitation in heart transplant recipients. Cochrane Database Syst Rev. 2017;4.
Anderson L, Thompson DR, Oldridge N, Zwisler AD, Rees K, Martin N, Taylor RS. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2016;1.
Andriolo RB, El Dib RP, Ramos L, Atallah Á, da Silva EMK. Aerobic exercise training programmes for improving physical and psychosocial health in adults with Down syndrome. Cochrane Database Syst Rev. 2010;5.
Araujo DN, Ribeiro CTD, Maciel ACC, Bruno SS, Fregonezi GAF, Dias FAL. Physical exercise for the treatment of non-ulcerated chronic venous insufficiency. Cochrane Database Syst Rev. 2016;12.
Ashworth NL, Chad KE, Harrison EL, Reeder BA, Marshall SC. Home versus center based physical activity programs in older adults. Cochrane Database Syst Rev. 2005;1.
Bartels EM, Juhl CB, Christensen R, Hagen KB, Danneskiold-Samsøe B, Dagfinrud H, Lund H. Aquatic exercise for the treatment of knee and hip osteoarthritis. Cochrane Database Syst Rev. 2016;3.
Beggs S, Foong YC, Le HCT, Noor D, Wood-Baker R, Walters JAE. Swimming training for asthma in children and adolescents aged 18 years and under. Cochrane Database Syst Rev. 2013;4.
Bergenthal N, Will A, Streckmann F, Wolkewitz KD, Monsef I, Engert A, Elter T, Skoetz N. Aerobic physical exercise for adult patients with haematological malignancies. Cochrane Database Syst Rev. 2014;11.
Bidonde J, Busch AJ, Schachter CL, Overend TJ, Kim SY, Góes SM, Boden C, Foulds HJA. Aerobic exercise training for adults with fibromyalgia. Cochrane Database Syst Rev. 2017;6.
Bidonde J, Busch AJ, van der Spuy I, Tupper S, Kim SY, Boden C. Whole body vibration exercise training for fibromyalgia. Cochrane Database Syst Rev. 2017;9.
Bidonde J, Busch AJ, Webber SC, Schachter CL, Danyliw A, Overend TJ, Richards RS, Rader T. Aquatic exercise training for fibromyalgia. Cochrane Database Syst Rev. 2014;10.
Braam KI, van der Torre P, Takken T, Veening MA, van Dulmen-den Broeder E, Kaspers GJL. Physical exercise training interventions for children and young adults during and after treatment for childhood cancer. Cochrane Database Syst Rev. 2016;3.
Bradt J, Shim M, Goodill SW. Dance/movement therapy for improving psychological and physical outcomes in cancer patients. Cochrane Database Syst Rev. 2015;1.
Broderick J, Crumlish N, Waugh A, Vancampfort D. Yoga versus non-standard care for schizophrenia. Cochrane Database Syst Rev. 2017;9.
Broderick J, Knowles A, Chadwick J, Vancampfort D. Yoga versus standard care for schizophrenia. Cochrane Database Syst Rev. 2015;10.
Broderick J, Vancampfort D. Yoga as part of a package of care versus standard care for schizophrenia. Cochrane Database Syst Rev. 2017;9.
Brown J, Ceysens G, Boulvain M. Exercise for pregnant women with gestational diabetes for improving maternal and fetal outcomes. Cochrane Database Syst Rev. 2017;6.
Busch AJ, Barber KA, Overend TJ, Peloso PMJ, Schachter CL. Exercise for treating fibromyalgia syndrome. Cochrane Database Syst Rev. 2007;4.
Busch AJ, Webber SC, Richards RS, Bidonde J, Schachter CL, Schafer LA, Danyliw A, Sawant A, Dal Bello-Haas V, Rader T, et al. Resistance exercise training for fibromyalgia. Cochrane Database Syst Rev. 2013;12.
Cameron ID, Dyer SM, Panagoda CE, Murray GR, Hill KD, Cumming RG, Kerse N. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev. 2018;9.
Carson KV, Chandratilleke MG, Picot J, Brinn MP, Esterman AJ, Smith BJ. Physical training for asthma. Cochrane Database Syst Rev. 2013;9.
Carvalho APV, Vital FMR, Soares BGO. Exercise interventions for shoulder dysfunction in patients treated for head and neck cancer. Cochrane Database Syst Rev. 2012;4.
Cavalheri V, Granger C. Preoperative exercise training for patients with non-small cell lung cancer. Cochrane Database Syst Rev. 2017;6.
Cavalheri V, Tahirah F, Nonoyama ML, Jenkins S, Hill K. Exercise training undertaken by people within 12 months of lung resection for non-small cell lung cancer. Cochrane Database Syst Rev. 2013;7.
Ceysens G, Rouiller D, Boulvain M. Exercise for diabetic pregnant women. Cochrane Database Syst Rev. 2006;3.
Choi BKL, Verbeek JH, Tam WWS, Jiang JY. Exercises for prevention of recurrences of low-back pain. Cochrane Database Syst Rev. 2010;1.
Colquitt JL, Loveman E, O'Malley C, Azevedo LB, Mead E, Al-Khudairy L, Ells LJ, Metzendorf MI, Rees K. Diet, physical activity, and behavioural interventions for the treatment of overweight or obesity in preschool children up to the age of 6 years. Cochrane Database Syst Rev. 2016;3.
Connolly B, Salisbury L, O'Neill B, Geneen LJ, Douiri A, Grocott MPW, Hart N, Walsh TS, Blackwood B. Exercise rehabilitation following intensive care unit discharge for recovery from critical illness. Cochrane Database Syst Rev. 2015;6.
Cooney GM, Dwan K, Greig CA, Lawlor DA, Rimer J, Waugh FR, McMurdo M, Mead GE. Exercise for depression. Cochrane Database Syst Rev. 2013;9.
Corbetta D, Sirtori V, Castellini G, Moja L, Gatti R. Constraint-induced movement therapy for upper extremities in people with stroke. Cochrane Database Syst Rev. 2015;10.
Cramer H, Lauche R, Klose P, Lange S, Langhorst J, Dobos GJ. Yoga for improving health-related quality of life, mental health and cancer-related symptoms in women diagnosed with breast cancer. Cochrane Database Syst Rev. 2017;1.
Cramp F, Byron-Daniel J. Exercise for the management of cancer-related fatigue in adults. Cochrane Database Syst Rev. 2012;11.
Dal Bello-Haas V, Florence JM. Therapeutic exercise for people with amyotrophic lateral sclerosis or motor neuron disease. Cochrane Database Syst Rev. 2013;5.
Dale MT, McKeough ZJ, Troosters T, Bye P, Alison JA. Exercise training to improve exercise capacity and quality of life in people with non-malignant dust-related respiratory diseases. Cochrane Database Syst Rev. 2015;11.
Daley A, Stokes-Lampard H, Thomas A, MacArthur C. Exercise for vasomotor menopausal symptoms. Cochrane Database Syst Rev. 2014;11.
de Morton N, Keating JL, Jeffs K. Exercise for acutely hospitalised older medical patients. Cochrane Database Syst Rev. 2007;1.
Dobbins M, Husson H, DeCorby K, LaRocca RL. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst Rev. 2013;2.
Doiron KA, Hoffmann TC, Beller EM. Early intervention (mobilization or active exercise) for critically ill adults in the intensive care unit. Cochrane Database Syst Rev. 2018;3.
Ekeland E, Heian F, Hagen KB, Abbott JM, Nordheim L. Exercise to improve self-esteem in children and young people. Cochrane Database Syst Rev. 2004;1.
Elbers RG, Verhoef J, van Wegen EEH, Berendse HW, Kwakkel G. Interventions for fatigue in Parkinson's disease. Cochrane Database Syst Rev. 2015;10.
Felbel S, Meerpohl JJ, Monsef I, Engert A, Skoetz N. Yoga in addition to standard care for patients with haematological malignancies. Cochrane Database Syst Rev. 2014;6.
Forbes D, Forbes SC, Blake CM, Thiessen EJ, Forbes S. Exercise programs for people with dementia. Cochrane Database Syst Rev. 2015;4.
Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev. 2015;1.
Fransen M, McConnell S, Hernandez-Molina G, Reichenbach S. Exercise for osteoarthritis of the hip. Cochrane Database Syst Rev. 2014;4.
Freitas DA, Holloway EA, Bruno SS, Chaves GSS, Fregonezi GAF, Mendonça K. Breathing exercises for adults with asthma. Cochrane Database Syst Rev. 2013;10.
Furmaniak AC, Menig M, Markes MH. Exercise for women receiving adjuvant therapy for breast cancer. Cochrane Database Syst Rev. 2016;9.
Giangregorio LM, MacIntyre NJ, Thabane L, Skidmore CJ, Papaioannou A. Exercise for improving outcomes after osteoporotic vertebral fracture. Cochrane Database Syst Rev. 2013;1.
Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, Lamb SE. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9.
Gorczynski P, Faulkner G. Exercise therapy for schizophrenia. Cochrane Database Syst Rev. 2010;5.
Grande AJ, Keogh J, Hoffmann TC, Beller EM, Del Mar CB. Exercise versus no exercise for the occurrence, severity and duration of acute respiratory infections. Cochrane Database Syst Rev. 2015;6.
Grande AJ, Reid H, Thomas EE, Nunan D, Foster C. Exercise prior to influenza vaccination for limiting influenza incidence and its related complications in adults. Cochrane Database Syst Rev. 2016;8.
Grande AJ, Silva V, Andriolo BNG, Riera R, Parra SA, Peccin MS. Water-based exercise for adults with asthma. Cochrane Database Syst Rev. 2014;7.
Gross A, Kay TM, Paquin JP, Blanchette S, Lalonde P, Christie T, Dupont G, Graham N, Burnie SJ, Gelley G, et al. Exercises for mechanical neck disorders. Cochrane Database Syst Rev. 2015;1.
Hageman D, Fokkenrood HJP, Gommans LNM, van den Houten MML, Teijink JAW. Supervised exercise therapy versus home-based exercise therapy versus walking advice for intermittent claudication. Cochrane Database Syst Rev. 2018;4.
Han A, Judd M, Welch V, Wu T, Tugwell P, Wells GA. Tai chi for treating rheumatoid arthritis. Cochrane Database Syst Rev. 2004;3.
Han S, Middleton P, Crowther CA. Exercise for pregnant women for preventing gestational diabetes mellitus. Cochrane Database Syst Rev. 2012;7.
Hartley L, Dyakova M, Holmes J, Clarke A, Lee MS, Ernst E, Rees K. Yoga for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2014;5.
Hartley L, Flowers N, Lee MS, Ernst E, Rees K. Tai chi for primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2014;4.
Hartley L, Lee MS, Kwong JSW, Flowers N, Todkill D, Ernst E, Rees K. Qigong for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2015;6.
Hassett L, Moseley AM, Harmer AR. Fitness training for cardiorespiratory conditioning after traumatic brain injury. Cochrane Database Syst Rev. 2017;12.
Hayden J, van Tulder MW, Malmivaara A, Koes BW. Exercise therapy for treatment of non-specific low back pain. Cochrane Database Syst Rev. 2005;3.
Hay-Smith EJC, Herderschee R, Dumoulin C, Herbison GP. Comparisons of approaches to pelvic floor muscle training for urinary incontinence in women. Cochrane Database Syst Rev. 2011;12.
Heine M, van de Port I, Rietberg MB, van Wegen EEH, Kwakkel G. Exercise therapy for fatigue in multiple sclerosis. Cochrane Database Syst Rev. 2015;9.
Heiwe S, Jacobson SH. Exercise training for adults with chronic kidney disease. Cochrane Database Syst Rev. 2011;10.
Hemmingsen B, Gimenez-Perez G, Mauricio D, Roqué i Figuls M, Metzendorf MI, Richter B. Diet, physical activity or both for prevention or delay of type 2 diabetes mellitus and its associated complications in people at increased risk of developing type 2 diabetes mellitus. Cochrane Database Syst Rev. 2017;12.
Herbert RD, de Noronha M, Kamper SJ. Stretching to prevent or reduce muscle soreness after exercise. Cochrane Database Syst Rev. 2011;7.
Heymans MW, van Tulder MW, Esmail R, Bombardier C, Koes BW. Back schools for non-specific low-back pain. Cochrane Database Syst Rev. 2004;4.
Holland AE, Hill CJ, Jones AY, McDonald CF. Breathing exercises for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012;10.
Howe TE, Rochester L, Neil F, Skelton DA, Ballinger C. Exercise for improving balance in older people. Cochrane Database Syst Rev. 2011;11.
Howe TE, Shea B, Dawson LJ, Downie F, Murray A, Ross C, Harbour RT, Caldwell LM, Creed G. Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst Rev. 2011;7.
Hurkmans E, van der Giesen FJ, Vliet Vlieland TPM, Schoones J, Van den Ende E. Dynamic exercise programs (aerobic capacity and/or muscle strength training) in patients with rheumatoid arthritis. Cochrane Database Syst Rev. 2009;4.
Hurley M, Dickson K, Hallett R, Grant R, Hauari H, Walsh N, Stansfield C, Oliver S. Exercise interventions and patient beliefs for people with hip, knee or hip and knee osteoarthritis: a mixed methods review. Cochrane Database Syst Rev. 2018;4.
Jones M, Harvey A, Marston L, O'Connell NE. Breathing exercises for dysfunctional breathing/hyperventilation syndrome in adults. Cochrane Database Syst Rev. 2013;5.
Katsura M, Kuriyama A, Takeshima T, Fukuhara S, Furukawa TA. Preoperative inspiratory muscle training for postoperative pulmonary complications in adults undergoing cardiac and major abdominal surgery. Cochrane Database Syst Rev. 2015;10.
Kendrick D, Kumar A, Carpenter H, Zijlstra GAR, Skelton DA, Cook JR, Stevens Z, Belcher CM, Haworth D, Gawler SJ, et al. Exercise for reducing fear of falling in older people living in the community. Cochrane Database Syst Rev. 2014;11.
Kramer MS, McDonald SW. Aerobic exercise for women during pregnancy. Cochrane Database Syst Rev. 2006;3.
Lahart IM, Metsios GS, Nevill AM, Carmichael AR. Physical activity for women with breast cancer after adjuvant therapy. Cochrane Database Syst Rev. 2018;1.
Lane R, Harwood A, Watson L, Leng GC. Exercise for intermittent claudication. Cochrane Database Syst Rev. 2017;12.
Larun L, Brurberg KG, Odgaard-Jensen J, Price JR. Exercise therapy for chronic fatigue syndrome. Cochrane Database Syst Rev. 2017;4.
Larun L, Nordheim LV, Ekeland E, Hagen KB, Heian F. Exercise in prevention and treatment of anxiety and depression among children and young people. Cochrane Database Syst Rev. 2006;3.
Lauret GJ, Fakhry F, Fokkenrood HJP, Hunink MGM, Teijink JAW, Spronk S. Modes of exercise training for intermittent claudication. Cochrane Database Syst Rev. 2014;7.
Lawrence M, Celestino Junior FT, Matozinho HHS, Govan L, Booth J, Beecher J. Yoga for stroke rehabilitation. Cochrane Database Syst Rev. 2017;12.
Lin CWC, Donkers NAJ, Refshauge KM, Beckenkamp PR, Khera K, Moseley AM. Rehabilitation for ankle fractures in adults. Cochrane Database Syst Rev. 2012;11.
Liu CJ, Latham NK. Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst Rev. 2009;3.
Long L, Anderson L, Dewhirst AM, He J, Bridges C, Gandhi M, Taylor RS. Exercise-based cardiac rehabilitation for adults with stable angina. Cochrane Database Syst Rev. 2018;2.
Loughney LA, West MA, Kemp GJ, Grocott MPW, Jack S. Exercise interventions for people undergoing multimodal cancer treatment that includes surgery. Cochrane Database Syst Rev. 2018;12.
Macedo LG, Saragiotto BT, Yamato TP, Costa LOP, Menezes Costa LC, Ostelo R, Maher CG. Motor control exercise for acute non-specific low back pain. Cochrane Database Syst Rev. 2016;2.
Macêdo TMF, Freitas DA, Chaves GSS, Holloway EA, Mendonça K. Breathing exercises for children with asthma. Cochrane Database Syst Rev. 2016;4.
Martin A, Booth JN, Laird Y, Sproule J, Reilly JJ, Saunders DH. Physical activity, diet and other behavioural interventions for improving cognition and school achievement in children and adolescents with obesity or overweight. Cochrane Database Syst Rev. 2018;3.
McKeough ZJ, Velloso M, Lima VP, Alison JA. Upper limb exercise training for COPD. Cochrane Database Syst Rev. 2016;11.
McNamara RJ, McKeough ZJ, McKenzie DK, Alison JA. Water-based exercise training for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2013;12.
McNeely ML, Campbell K, Ospina M, Rowe BH, Dabbs K, Klassen TP, Mackey J, Courneya K. Exercise interventions for upper-limb dysfunction due to breast cancer treatment. Cochrane Database Syst Rev. 2010;6.
Mead E, Brown T, Rees K, Azevedo LB, Whittaker V, Jones D, Olajide J, Mainardi GM, Corpeleijn E, O'Malley C, et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese children from the age of 6 to 11 years. Cochrane Database Syst Rev. 2017;6.
Meekums B, Karkou V, Nelson EA. Dance movement therapy for depression. Cochrane Database Syst Rev. 2015;2.
Meher S, Duley L. Exercise or other physical activity for preventing pre-eclampsia and its complications. Cochrane Database Syst Rev. 2006;2.
Mehrholz J, Kugler J, Pohl M. Water-based exercises for improving activities of daily living after stroke. Cochrane Database Syst Rev. 2011;1.
Mehrholz J, Kugler J, Pohl M. Locomotor training for walking after spinal cord injury. Cochrane Database Syst Rev. 2012;11.
Mehrholz J, Thomas S, Elsner B. Treadmill training and body weight support for walking after stroke. Cochrane Database Syst Rev. 2017;8.
Mishra SI, Scherer RW, Geigle PM, Berlanstein DR, Topaloglu O, Gotay CC, Snyder C. Exercise interventions on health-related quality of life for cancer survivors. Cochrane Database Syst Rev. 2012;8.
Mishra SI, Scherer RW, Snyder C, Geigle PM, Berlanstein DR, Topaloglu O. Exercise interventions on health-related quality of life for people with cancer during active treatment. Cochrane Database Syst Rev. 2012;8.
Montgomery P, Dennis JA. Physical exercise for sleep problems in adults aged 60+. Cochrane Database Syst Rev. 2002;4.
Morris NR, Kermeen FD, Holland AE. Exercise-based rehabilitation programmes for pulmonary hypertension. Cochrane Database Syst Rev. 2017;1.
Muktabhant B, Lawrie TA, Lumbiganon P, Laopaiboon M. Diet or exercise, or both, for preventing excessive weight gain in pregnancy. Cochrane Database Syst Rev. 2015;6.
Ngai SPC, Jones AYM, Tam WWS. Tai chi for chronic obstructive pulmonary disease (COPD). Cochrane Database Syst Rev. 2016;6.
Norton C, Cody JD. Biofeedback and/or sphincter exercises for the treatment of faecal incontinence in adults. Cochrane Database Syst Rev. 2012;7.
O'Brien K, Nixon S, Glazier R, Tynan AM. Progressive resistive exercise interventions for adults living with HIV/AIDS. Cochrane Database Syst Rev. 2004;4.
O'Brien K, Nixon S, Tynan AM, Glazier R. Aerobic exercise interventions for adults living with HIV/AIDS. Cochrane Database Syst Rev. 2010;8.
Østerås N, Kjeken I, Smedslund G, Moe RH, Slatkowsky-Christensen B, Uhlig T, Hagen KB. Exercise for hand osteoarthritis. Cochrane Database Syst Rev. 2017;1.
Page MJ, Green S, Kramer S, Johnston RV, McBain B, Chau M, Buchbinder R. Manual therapy and exercise for adhesive capsulitis (frozen shoulder). Cochrane Database Syst Rev. 2014;8.
Page MJ, Green S, McBain B, Surace SJ, Deitch J, Lyttle N, Mrocki MA, Buchbinder R. Manual therapy and exercise for rotator cuff disease. Cochrane Database Syst Rev. 2016;6.
Page MJ, O'Connor D, Pitt V, Massy-Westropp N. Exercise and mobilisation interventions for carpal tunnel syndrome. Cochrane Database Syst Rev. 2012;6.
Panebianco M, Sridharan K, Ramaratnam S. Yoga for epilepsy. Cochrane Database Syst Rev. 2017;10.
Perry A, Lee SH, Cotton S, Kennedy C. Therapeutic exercises for affecting post-treatment swallowing in people treated for advanced-stage head and neck cancers. Cochrane Database Syst Rev. 2016;8.
Radtke T, Nevitt SJ, Hebestreit H, Kriemler S. Physical exercise training for cystic fibrosis. Cochrane Database Syst Rev. 2017;11.
Regnaux JP, Lefevre-Colau MM, Trinquart L, Nguyen C, Boutron I, Brosseau L, Ravaud P. High-intensity versus low-intensity physical activity or exercise in people with hip or knee osteoarthritis. Cochrane Database Syst Rev. 2015;10.
Ren J, Xia J. Dance therapy for schizophrenia. Cochrane Database Syst Rev. 2013;10.
Rietberg MB, Brooks D, Uitdehaag BMJ, Kwakkel G. Exercise therapy for multiple sclerosis. Cochrane Database Syst Rev. 2005;1.
Risom SS, Zwisler AD, Johansen PP, Sibilitz KL, Lindschou J, Gluud C, Taylor RS, Svendsen JH, Berg SK. Exercise-based cardiac rehabilitation for adults with atrial fibrillation. Cochrane Database Syst Rev. 2017;2.
Romano M, Minozzi S, Bettany-Saltikov J, Zaina F, Chockalingam N, Kotwicki T, Maier-Hennes A, Negrini S. Exercises for adolescent idiopathic scoliosis. Cochrane Database Syst Rev. 2012;8.
Ryan JM, Cassidy EE, Noorduyn SG, O'Connell NE. Exercise interventions for cerebral palsy. Cochrane Database Syst Rev. 2017;6.
Saragiotto BT, Maher CG, Yamato TP, Costa LOP, Menezes Costa LC, Ostelo R, Macedo LG. Motor control exercise for chronic non-specific low-back pain. Cochrane Database Syst Rev. 2016;1.
Saunders DH, Sanderson M, Hayes S, Kilrane M, Greig CA, Brazzelli M, Mead GE. Physical fitness training for stroke patients. Cochrane Database Syst Rev. 2016;3.
Schulzke SM, Kaempfen S, Trachsel D, Patole SK. Physical activity programs for promoting bone mineralization and growth in preterm infants. Cochrane Database Syst Rev. 2014;4.
Seron P, Lanas F, Pardo Hernandez H, Bonfill Cosp X. Exercise for people with high cardiovascular risk. Cochrane Database Syst Rev. 2014;8.
Shaw KA, Gennat HC, O'Rourke P, Del Mar C. Exercise for overweight or obesity. Cochrane Database Syst Rev. 2006;4.
Shepherd E, Gomersall JC, Tieu J, Han S, Crowther CA, Middleton P. Combined diet and exercise interventions for preventing gestational diabetes mellitus. Cochrane Database Syst Rev. 2017;11.
Sibilitz KL, Berg SK, Tang LH, Risom SS, Gluud C, Lindschou J, Kober L, Hassager C, Taylor RS, Zwisler AD. Exercise-based cardiac rehabilitation for adults after heart valve surgery. Cochrane Database Syst Rev. 2016;3.
Silva IS, Fregonezi GAF, Dias FAL, Ribeiro CTD, Guerra RO, Ferreira GMH. Inspiratory muscle training for asthma. Cochrane Database Syst Rev. 2013;9.
States RA, Pappas E, Salem Y. Overground physical therapy gait training for chronic stroke patients with mobility deficits. Cochrane Database Syst Rev. 2009;3.
Strike K, Mulder K, Michael R. Exercise for haemophilia. Cochrane Database Syst Rev. 2016;12.
Takken T, Van Brussel M, Engelbert RH, van der Net JJ, Kuis W, Helders P. Exercise therapy in juvenile idiopathic arthritis. Cochrane Database Syst Rev. 2008;2.
Taylor RS, Sagar VA, Davies EJ, Briscoe S, Coats AJS, Dalal H, Lough F, Rees K, Singh SJ, Mordi IR. Exercise-based rehabilitation for heart failure. Cochrane Database Syst Rev. 2014;4.
Thomas D, Elliott EJ, Naughton GA. Exercise for type 2 diabetes mellitus. Cochrane Database Syst Rev. 2006;3.
Ussher MH, Taylor AH, Faulkner GEJ. Exercise interventions for smoking cessation. Cochrane Database Syst Rev. 2014;8.
Valentín-Gudiol M, Mattern-Baxter K, Girabent-Farrés M, Bagur-Calafat C, Hadders-Algra M, Angulo-Barroso RM. Treadmill interventions in children under six years of age at risk of neuromotor delay. Cochrane Database Syst Rev. 2017;7.
van der Heijden RA, Lankhorst NE, van Linschoten R, Bierma-Zeinstra SMA, van Middelkoop M. Exercise for treating patellofemoral pain syndrome. Cochrane Database Syst Rev. 2015;1.
Vloothuis JDM, Mulder M, Veerbeek JM, Konijnenbelt M, Visser-Meily JMA, Ket JCF, Kwakkel G, van Wegen EEH. Caregiver-mediated exercises for improving outcomes after stroke. Cochrane Database Syst Rev. 2016;12.
Voet NBM, van der Kooi EL. Riphagen, II, Lindeman E, van Engelen BGM, Geurts ACH: strength training and aerobic exercise training for muscle disease. Cochrane Database Syst Rev. 2013;7.
White CM, Pritchard J, Turner-Stokes L. Exercise for people with peripheral neuropathy. Cochrane Database Syst Rev. 2004;4.
Wieland LS, Skoetz N, Pilkington K, Vempati R, D'Adamo CR, Berman BM. Yoga treatment for chronic non-specific low back pain. Cochrane Database Syst Rev. 2017;1.
Williams AD, Bird ML, Hardcastle SGK, Kirschbaum M, Ogden KJ, Walters JAE. Exercise for reducing falls in people living with and beyond cancer. Cochrane Database Syst Rev. 2018;10.
Williams MA, Srikesavan C, Heine PJ, Bruce J, Brosseau L, Hoxey-Thomas N, Lamb SE. Exercise for rheumatoid arthritis of the hand. Cochrane Database Syst Rev. 2018;7.
Yamamoto S, Hotta K, Ota E, Matsunaga A, Mori R. Exercise-based cardiac rehabilitation for people with implantable ventricular assist devices. Cochrane Database Syst Rev. 2018;9.
Yamato TP, Maher CG, Saragiotto BT, Hancock MJ, Ostelo R, Cabral CMN, Menezes Costa LC, Costa LOP. Pilates for low back pain. Cochrane Database Syst Rev. 2015;7.
Yang ZY, Zhong HB, Mao C, Yuan JQ, Huang YF, Wu XY, Gao YM, Tang JL. Yoga for asthma. Cochrane Database Syst Rev. 2016;4.
Young J, Angevaren M, Rusted J, Tabet N. Aerobic exercise to improve cognitive function in older people without known cognitive impairment. Cochrane Database Syst Rev. 2015;4.
Zainuldin R, Mackey MG, Alison JA. Optimal intensity and type of leg exercise training for people with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2011;11.
Mok A, Khaw K-T, Luben R, Wareham N, Brage S. Physical activity trajectories and mortality: population based cohort study. Bmj. 2019;365:l2323.
Ekelund U, Brown WJ, Steene-Johannessen J, Fagerland MW, Owen N, Powell KE, Bauman AE, Lee IM. Do the associations of sedentary behaviour with cardiovascular disease mortality and cancer mortality differ by physical activity level? A systematic review and harmonised meta-analysis of data from 850 060 participants. Br J Sports Med. 2019;53(14):886–94. https://doi.org/10.1136/bjsports-2017-098963 . Epub 2018 Jul 10.
Article PubMed Google Scholar
Ekelund U, Steene-Johannessen J, Brown WJ, Fagerland MW, Owen N, Powell KE, Bauman A, Lee IM. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016;388(10051):1302–10.
Lear SA, Hu W, Rangarajan S, Gasevic D, Leong D, Iqbal R, Casanova A, Swaminathan S, Anjana RM, Kumar R, et al. The effect of physical activity on mortality and cardiovascular disease in 130000 people from 17 high-income, middle-income, and low-income countries: the PURE study. Lancet. 2017;390(10113):2643–54.
Sattelmair J, Pertman J, Ding EL, Kohl HW 3rd, Haskell W, Lee IM. Dose response between physical activity and risk of coronary heart disease: a meta-analysis. Circulation. 2011;124(7):789–95.
Heyman E, Gamelin FX, Goekint M, Piscitelli F, Roelands B, Leclair E, Di Marzo V, Meeusen R. Intense exercise increases circulating endocannabinoid and BDNF levels in humans--possible implications for reward and depression. Psychoneuroendocrinology. 2012;37(6):844–51.
Horton R. Offline: the gravy train of systematic reviews. Lancet. 2019;394(10211):1790.
Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1.9 million participants. Lancet Glob Health. 2018;6(10):e1077–86.
Fletcher GF, Landolfo C, Niebauer J, Ozemek C, Arena R, Lavie CJ. Promoting physical activity and exercise: JACC health promotion series. J Am Coll Cardiol. 2018;72(14):1622–39.
Download references
Acknowledgements
Not applicable.
There was no funding source for this study. Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
Kleijnen Systematic Reviews Ltd., York, UK
Pawel Posadzki
Nanyang Technological University, Singapore, Singapore
Institute for Research in Operative Medicine, Witten/Herdecke University, Witten, Germany
Dawid Pieper, Nadja Könsgen & Annika Lena Neuhaus
School of Medicine, Keele University, Staffordshire, UK
Jozef Pilsudski University of Physical Education in Warsaw, Faculty Physical Education and Health, Biala Podlaska, Poland
Hubert Makaruk
Health Outcomes Division, University of Texas at Austin College of Pharmacy, Austin, USA
Monika Semwal
You can also search for this author in PubMed Google Scholar
Contributions
PP wrote the protocol, ran the searches, validated, analysed and synthesised data, wrote and revised the drafts. HM, NK and ALN screened and extracted data. MS and DP validated and analysed the data. RB ran statistical analyses. All authors contributed to writing and reviewing the manuscript. PP is the guarantor. The authors read and approved the final manuscript.
Corresponding author
Correspondence to Dawid Pieper .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:.
Supplementary Table 1. Main characteristics of included Cochrane systematic reviews evaluating the effects of physical activity/exercise on health outcomes ( n = 150). Supplementary Table 2. Additional information from Cochrane systematic reviews of the effects of physical activity/exercise on health outcomes ( n = 150). Supplementary Table 3. Conclusions from Cochrane systematic reviews “quote”. Supplementary Table 4 . AEs reported in Cochrane systematic reviews. Supplementary Table 5. Summary of withdrawals/non-adherence. Supplementary Table 6. Methodological quality assessment of the included Cochrane reviews with AMSTAR-2. Supplementary Table 7. Number of studies assessed as low risk of bias per domain. Supplementary Table 8. GRADE for the review’s main comparison. Supplementary Table 9. Studies reporting quality of life outcomes as mean difference.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Posadzki, P., Pieper, D., Bajpai, R. et al. Exercise/physical activity and health outcomes: an overview of Cochrane systematic reviews. BMC Public Health 20 , 1724 (2020). https://doi.org/10.1186/s12889-020-09855-3
Download citation
Received : 01 April 2020
Accepted : 08 November 2020
Published : 16 November 2020
DOI : https://doi.org/10.1186/s12889-020-09855-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Effectiveness
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
TheScholarsRepository@LLU: Digital Archive of Research, Scholarship & Creative Works
Home > SAHP > PT > ETD-PT
Theses, Dissertations and Projects - Physical Therapy
Theses/dissertations from 2022 2022.
High-Intensity Interval Training and Biological Age , Trevor Lohman
Theses/Dissertations from 2021 2021
The Impact of Intraneural Facilitation Therapy on Diabetic Peripheral Neuropathy , Kyan Zhra-Sahba Alnajafi
The Influence of Strength and Mobility on Lumbar Biomechanics During Lifting , Christopher S. Patterson
Theses/Dissertations from 2019 2019
Spine Kinematics and Muscle Activities in Non-specific Chronic Low Back Pain Subgroups in Sitting , Mansoor Ahmed Alameri
Relationship between Balance and Physical Activity in Subjects with Non-Specific Chronic Low Back Pain , Muhsen B. Alsufiany
Does self-evaluation and education in students change attitudes and beliefs towards Weight Stigma? , Henry A. Garcia
Effects of Head Motion on Balance in Middle-Aged and Young Adults with Chronic Motion Sensitivity , Ammar E. Hafiz
Effect of Pediatric Ear Infections on Postural Stability , Ohud A. Sabir
Biomechanics and Postural Control Characteristics in Low Back Pain Subgroups During Dynamic Task , Amjad Shallan
Theses/Dissertations from 2018 2018
Effect of Adding Stretching Techniques to Standardized Intervention on Nonspecific Mechanical Neck Pain , Saad S. Alfawaz
Theses/Dissertations from 2017 2017
Effects of Head Motion on Postural Stability in Participants with Chronic Motion Sensitivity , Abdulaziz A. Albalwi
Relationship between Vestibular System, Vision, Anxiety, and Chronic Motion Sensitivity , Ahmad A. Alharbi
The Effects of Frequent Smartphone Use on Children’s Upper Posture and Pulmonary Function , Asma Alonazi
The Effects of Wearing Headscarves on Cervical Spine Proprioception and Range of Motion , Samiah Alqabbani
A Comparison of Neuromuscular Control between Subjects with and without Chronic Ankle Instability , Hatem Jaber
Theses/Dissertations from 2016 2016
Effects of Adjustments to Wheelchair Seat to Back Support Angle on Head, Neck, and Shoulder Postures , Afnan M. Alkhateeb
Effect of Jet Lag on Postural Stability , Faisal M. Al Mubarak
Effect of Heavy Lifting with a Head Strap on the Pelvic Floor across the Menstrual Cycle , Yvonne Biswokarma
Theses/Dissertations from 2015 2015
Physical Therapy after Triangular Fibrocartilage Injuries and Ulnar Wrist Pain , Mohamed A. Abdelmegeed
The Effect of Cervical Muscle Fatigue on Postural Stability during Immersion Virtual Reality , Mazen M. Alqahtani
The Effects of a Novel Therapeutic Intervention in Diabetic Peripheral Neuropathy Patients , Adel M. Alshahrani
Cross-cultural Adaption and Psychometric Properties Testing of The Arabic Anterior Knee Pain Scale , Abdullah S. Alshehri
Effect of Tai Chi Exercise Combined with Mental Imagery in Improving Balance , Abdulrahman Alsubiheen
Effect of Vestibular Adaptation Exercises on Chronic Motion Sensitivity , Danah Alyahya
Muscle Dynamics as the Result of Whole Body Vibration and Plyometrics , Richard Jeremy Hubbard
Theses/Dissertations from 2014 2014
Effect of Monophasic Pulsed Current on the Treatment of Plantar Fasciitis , Abdullah Alotaibi
Screening for Torticollis and Plagiocephaly: The Role of the Pediatrician , Lisa Ann Change-Yee Hwang
Effect of 17β Estradiol & Foot Strike Patterns on Physiological & Biomechanical Changes in Runners , Iman Akef Khowailed
Theses/Dissertations from 2013 2013
Inter-rater Reliability of Lumbar Segmental Instability Tests and the Subclassification , Faisal Mohammad Alyazedi
Sleep-wake Cycle Assessment in Type 2 Diabetes and Salivary Melatonin Correlates , Paula Regina Aguiar Cavalcanti
Anterior Cruciate Ligament Elasticity and Force for Knee Flexion during the Menstrual Cycle in Women , Haneul Lee
Effect of Passive Vibration on Skin Blood Flow in Good Glycemic Control and Poor Glycemic Control Type 2 Diabetics , Kanikkai Steni Balan Sackiriyas
Theses/Dissertations from 2012 2012
Co-diagnosis Frequency of Peripheral Vestibular Disorders and Physical Therapy , Summer M. San Lucas
Postural Sway, EEG and EMG Analysis of Hip and Ankle Muscles during Eight Balance Training Tasks , Yuen Yi Florence Tse
Effect of a Single High-Fat Meal and Vitamins on the Circulatory Response to Local Heat in Koreans and Caucasians , JongEun Yim
Theses/Dissertations from 2011 2011
Virtual Reality Gaming as a Tool for Rehabilitation in Physical Therapy , Abel A. Rendon
Theses/Dissertations from 2010 2010
Aerobic Exercise and Bone Turnover in Trained and Untrained Premenopausal Women , Michelle Prowse
Theses/Dissertations from 2005 2005
The Effect of Posterior Versus Anterior Glide Joint Mobilization on External Rotation Range of Motion of Patients with Shoulder Adhesive Capsulitis , Andrea J. Johnson
Isokinetic Knee Strength in Females with Fibromyalgia , Flora F. Shafiee
Difference in Transverse Plane Scapular Position of Professional Baseball Players Relative to Baseball Field Position , James M. Syms
The Effect of Positioning on Pelvic Floor Muscle Activity as Evaluated with Surface Electromyography in Normals , Karen R. Whitter-Brandon
Theses/Dissertations from 2004 2004
Orthopedic Treatment Outcomes and Physical Therapists' Orthopedic Clinical Specialist Status , Karin Granberg
The Effectiveness of a Physical Therapy Intervention for Children with Hypotonia and Flatfeet , Charmayne G. Ross

Theses/Dissertations from 2003 2003
The Role of Health Promotion in Physical Therapy , Brenda L. Rea
Predicting Sacroiliac Syndrome: The Association Between Noninvasive Sacroiliac Joint Tests and Sacroiliac Joint Injections , Lorraine D. Webb
Theses/Dissertations from 2002 2002
Effect of Electrode Size, Shape, and Placement on Electrical Current and Subject Comfort During Electrical Stimulation , Bonnie J. Forrester
Patterns of Scholarly Productivity in Physical Therapy Faculty , Ardith L. Williams-Meyer
Theses/Dissertations from 2001 2001
The Effects of Education on Fear-Avoidance Behavior of Subjects with Work-Related Low Back Pain , Marie A. Anger
Toward the Optimal Waveform for Electrical Stimulation , Scott Douglas Bennie
Factors in Predicting the Number of Home Care Physical Visits , Bruce D. Bradley
A Practice Analysis Survey: Defining the Clinical Practice of Primary Care Physical Therapy , Edsen Bermudez Donato
Disability Self-Assessment and Upper Quarter Muscle Balance in Females , Eric Glenn Johnson
Theses/Dissertations from 2000 2000
Comparison of Elderly Non-Fallers and Fallers on Performance Measures of Functional Reach, Sensory Organizations, and Limits of Stability , Harvey W. Wallmann
Theses/Dissertations from 1999 1999
Patient participation in physical therapy goal-setting , Susan M. Baker
Theses/Dissertations from 1998 1998
Prediction of Discharge Destination from Initial Physical Therapy Assessment using the Physical Assessment Key (PAK) , Wendy L. Chung and Kimberly A. Vieten
Does the Oswestry or SF-36 Help a Therapist to Predict Treatment Classification , Amy Crawford and Denese D. Kaufeldt-Soliz
Reliability and Validity of Assessing Student Performance of Psychomotor Skills in Entry Level Physical Therapy Curricula , Nancy Sue Darr
Theses/Dissertations from 1997 1997
Discharge Outcomes : An Evaluation of a Functional Index of Physical Assistance , Jan R. Snell
Theses/Dissertations from 1985 1985
A Comparison of Strength Improvement on Free Weights and the Universal Centurion , David J. Davies
Theses/Dissertations from 1984 1984
The effect of dextrose ingestion on cardiovascular endurance , Judith M. Axford
Theses/Dissertations from 1980 1980
The Ingestion of Garlic and its Effect on Cardiovascular Endurance , Thomas G. Blackwelder
- Collections
- Disciplines
Advanced Search
- Notify me via email or RSS
Author Corner
- Faculty Research (Pure)
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
- Search Menu
- Animal Research
- Cardiovascular/Pulmonary
- Health Services
- Health Policy
- Health Promotion
- History of Physical Therapy
- Implementation Science
- Integumentary
- Musculoskeletal
- Orthopedics
- Pain Management
- Pelvic Health
- Pharmacology
- Population Health
- Professional Issues
- Psychosocial
- Advance Articles
- COVID-19 Collection
- Featured Collections
- Special Issues
- PTJ Peer Review Academies
- Author Guidelines
- Submission Site
- Why Publish With PTJ?
- Open Access
- Call for Papers
- Self-Archiving Policy
- Promote your Article
- About Physical Therapy
- Editorial Board
- Advertising & Corporate Services
- Permissions
- Journals on Oxford Academic
- Books on Oxford Academic
Article Contents
Author contributions and acknowledgments, ethics approval, clinical trial registration, disclosures, a.1 appendix 1., b. appendix 2..
- < Previous
Effectiveness of an Evidence-Based Amputee Rehabilitation Program: A Pilot Randomized Controlled Trial
- Article contents
- Figures & tables
- Supplementary Data
Robert Gailey, Ignacio Gaunaurd, Michele Raya, Neva Kirk-Sanchez, Luz M Prieto-Sanchez, Kathryn Roach, Effectiveness of an Evidence-Based Amputee Rehabilitation Program: A Pilot Randomized Controlled Trial, Physical Therapy , Volume 100, Issue 5, May 2020, Pages 773–787, https://doi.org/10.1093/ptj/pzaa008
- Permissions Icon Permissions
Despite the prevalence of lower limb amputation (LLA), only a small percentage of people with LLA actually receive physical therapy post amputation and are rehabilitated to their full potential level of function. There is a need for the development of a rehabilitation program that targets impairments and limitations specific to people with LLA.
The objective of this study was to determine whether the Evidence-Based Amputee Rehabilitation program would improve functional mobility of people with unilateral transtibial amputation (TTA) who have already completed physical therapy and prosthetic training.
This study was a randomized, wait-list control, single-blinded pilot clinical trial.
This study researched participants who had received postamputation rehabilitation to varying degrees, either in an inpatient and/or outpatient settings.
The participants in this study included veterans and nonveterans with unilateral TTA due to dysvascular disease and trauma.
This study included a prescription-based rehabilitation program for people with amputations.
Results were measured with The Amputee Mobility Predictor with (AMPPro) and without a prosthesis (AMPnoPro) and 6-Minute Walk Test (6MWT) at baseline and at the end of the 8-week intervention.
The intervention group improved on the AMPPro scores (36.4 to 41.7), AMPnoro scores (23.2 to 27.1), and 6MWT distance (313.6 to 387.7 m). The effect size for the intervention was very large (1.32). In contrast, the wait-list control group demonstrated no change in AMPPro scores (35.3 to 35.6), AMPnoPro scores (24.7 to 25.0), and 6MWT distance (262.6 m to 268.8 m).
The sample size was small. A total 326 potential candidates were screened with 306 unable to meet inclusion criteria or unwilling to participate.
People with unilateral TTA who received Evidence-Based Amputee Rehabilitation program demonstrated significant improvement in functional mobility, with most participants (66.7%) improved at least 1 K-level (58.3%) and greater than the minimal detectable change (66.7%).
Physical therapist services after lower limb amputation (LLA) can have a meaningful impact on physical function and quality of life. People with LLA receiving physical therapy are more likely to have better prosthetic weight-bearing and mobility, musculoskeletal endurance, walking speed, and prosthetic fit, as well as an increased 1-year survival rate, compared with those who do not receive physical therapy. 1-4 Unfortunately, physical therapist services are only received by a few people after amputation. 5 , 6 A review of 12,599 veterans with LLA found that only 55% received rehabilitation services postoperatively, with physical therapy being the most common service. 7 Furthermore, there is a concern that many people receiving postamputation physical therapy are not rehabilitated to their full potential level of function. In a cohort of 42 people with unilateral LLA who received physical therapy, the majority remained at a high risk for falls at discharge. 3 Miller et al reported on a cohort of men with dysvascular disease and transtibial amputation (TTA) that impairments and limitations persisted even after completing rehabilitation. 8 The impairments and activity limitations that persist can manifest into asymmetrical lower limb use when performing everyday activities such as rising from a chair, standing, walking, and negotiating environmental obstacles such as inclines, declines, or stairs. 9-11 These mobility limitations may place the person at risk for increased secondary health effects such as osteoarthritis, low back pain, cardiovascular disease, obesity, and risk for future amputation. 12 , 13 A physical therapy rehabilitation program for people with LLA where exercise prescription is determined by performance-based functional assessment does not exist. Because of the importance of postamputation physical therapy, there is a need for the development of a rehabilitation program that targets impairments and limitations specific to people with LLA.
The Amputee Mobility Predictor (AMP) is a reliable performance-based outcome measure (PBOM) that has been validated for use in people with LLA as a measure of functional capabilities and mobility without a prosthesis (AMPnoPro) or with a prosthesis (AMPPro). 14 The AMPPro score has been used as an activity limitations outcome measure and has a minimal detectable change (MDC) value of 3.4 points. 15 , 16 The AMPnoPro and AMPPro scores can differentiate between the Medicare Functional Classification Level (MFCL) or K-Levels as defined by Centers for Medicare/Medicaid Services (CMS). 14 , 17 , 18 The AMP was developed as a measure for people with LLA that could discriminate the functional capabilities between the MFCLs, assist with identifying limitations in functional capabilities, and assess prosthetic mobility. 14 The AMP has demonstrated the ability to discriminate functional capabilities and mobility in higher functioning 19-21 and lower functioning 22-24 people with LLA as well as people with bilateral amputations. 19 , 25 The Comparative Effectiveness Review committee for the Agency for Healthcare and Research Quality identified the AMP as 1 of 12 outcome measures for people with LLA that are generalizable to the Medicare population. 26 , 27 The AMP has been found to correlate with other measures such as walking speed 14 , 16 , 28-30 and Time-up and Go, as well as self-report measures of prosthetic mobility. 17 It has also been found to have good outcome prediction capabilities. 14 , 22 , 28 The AMP does have better discrimination between levels of amputation than other performance-based measures 24 and is also easily administered by a variety of clinicians. 31 , 32 The AMP also has the ability to quantify change over time after rehabilitation. 16 , 29 , 33
The AMP can also be used to guide exercise prescription for limb loss and prosthetic rehabilitation. Each AMP task is designed to assess a person’s ability to perform specific physical skills at the activity level (general tasks/demands and mobility); in addition, each AMP task is also comprised of a number of components (neuromusculoskeletal and movement-related functions) within the body function domain as defined by the International Classification of Functioning. 15 , 34 To successfully complete the task at the activity level, the components at the body function level must be performed correctly. For example, AMP task number 4 assesses the activity of rising from a chair. This task involves several body function components, including organizational skills, postural control, momentum strategies, and dynamic postural stability. The neuromusculoskeletal and movement-related functions can be further itemized to specific body function impairments for each component of the task where limitations in strength, power, coordination, balance, and speed can be defined. Once the limitations at the impairment level are identified, specific exercises can be prescribed to address the possible deficits associated with each AMP task. If the exercises are effective in improving the components at the body function level, then the activity level performance will be enhanced, thus improving the quality of the sit-to-stand task and producing a higher score on the AMP task and AMP test. By using the AMP, the physical therapist can quantify at the activity level the specific task limitations for the person with LLA and prescribe specific exercises at the body function component level that will address those impairments that limit functional capabilities.
The concept of Evidenced-Based Amputee Rehabilitation (EBAR) is relatively consistent with traditional physical therapist practice models where the physical therapist assesses the patient, prescribes treatment, treats the patient, and reassesses. What may differ with this program is that, after the patient completes the AMP, the tasks that received a less than a satisfactory score are identified and exercises designed to address the impairment or limitation are prescribed. The rehabilitation principles and exercises for people with amputation chosen for EBAR have gained widespread acceptance in the clinical community worldwide. 35-47 After a predetermined period of time, the patient is reassessed to determine the change in function and if any modification to the exercise program is necessary. An EBAR program that uses PBOM like the AMP to assist with clinical decision-making and the prescription of effective rehabilitation interventions in people with LLAs has not been previously described in the literature.
The primary purpose of this study was to determine if an EBAR program will improve the functional mobility of people with unilateral TTA who have previously completed a traditional prosthetic rehabilitation program. We hypothesized that the mobility of people with TTA receiving the EBAR intervention would improve over an 8-week period of time, while the wait list control participants would remain unchanged. The secondary purposes of this study were to determine the trajectory of mobility change over the course of the 8-week intervention and to document pre-post intervention changes in individual AMPPro tasks.
Study Design
This randomized, wait-list control, single blinded pilot clinical trial was conducted at the Miami Veterans Affairs Healthcare System (Miami VAHS), Miami, Florida, in cooperation with the University of Miami Miller School of Medicine, Department of Physical Therapy. Participants were recruited from clinician referral and clinics by the research and clinical teams from Miami VAHS, Jackson Memorial Hospital, and local South Florida prosthetic and physical therapy clinics. Every candidate contact was logged and screened by the lead research physical therapist to explain the study commitment and determine eligibility based on predetermined inclusion criteria and subsequently enrolled with the Miami VAHS institutional review board-approved consent form.
Appendix 1 illustrates the study design. Participants were male and female between 55 and 80 years of age with unilateral TTA due to traumatic or dysvascular etiology, at least 1 year postamputation, fitted with their current prosthesis for at least 6 months, and had completed traditional postamputation rehabilitation and prosthetic training. All participants had received postamputation rehabilitation to varying degrees either in an inpatient and/or outpatient setting. Participants were excluded if they presented with severe cardiac or pulmonary disease, poorly controlled metabolic disease, nonhealing wounds, limiting musculoskeletal diagnoses, neurological disorders, or prosthetic fit issues. Participants were excluded if they scored a 43 or higher on the AMPPro, indicating that they were functioning at the MFCL K4-level (43–47pts) and not requiring the EBAR program, which focused on basic mobility skills. Estimated AMP score ranges were used to classify participants to the respective MFCLs: K1 (15–26 points), K2 (27–36 points), and K3 (37–42 points).
Study Procedures
Each participant received a physical examination for medical clearance by the study physician. The study prosthetist evaluated the prosthesis for fit, comfort, and alignment. All necessary adjustments to the prosthesis were made prior to the start of the intervention. Two research physical therapists assumed different roles and were blinded from each other throughout the study. One physical therapist who administered the AMPPro, AMPnoPro, and 6MWT at baseline and at the end of the 8-week intervention was blinded to group assignment (intervention vs wait-list control) and all intervention data.
At the conclusion of baseline testing, participants were randomly assigned to either the 8-week intervention or wait-list control for 8 weeks. The other physical therapist implemented the EBAR program for all participants. The EBAR program was administered for 60 minutes, 3 times per week for 8 weeks. The AMP and 6-MWT were also administered at the conclusion of weeks 2, 4, and 6 to assess change in function and modify the exercise prescription as outlined in the EBAR program. After repeating baseline testing, participants assigned to the wait-list control group were eligible to begin the EBAR program.
EBAR Program
The EBAR program consisted of 5 primary components: (1) cardiopulmonary endurance and flexibility, (2) trunk and lower limb strengthening, (3) balance and coordination, (4) weight-bearing and stance control, and (5) prosthetic gait training.
A combination of cardiopulmonary aerobic and warm-up exercises was performed for a maximum of 15 minutes at the onset of each treatment session. To avoid any residual limb issues, regular skin checks were conducted before and after warm-up as participants progressed from non-weight–bearing to partial and then full weight-bearing with the prosthesis using the following sequence over the 8 weeks: upper limb ergometry for weeks 1–2, progressing from sitting to standing; Nu-Step (TRS 4000 Nu-Step Recumbent Cross Trainer) for weeks 3–4, which incorporates both upper and lower limb movement and trunk rotation; elliptical machine for weeks 5–6; and treadmill walking for weeks 7–8, progressing from self-selected to moderate walking speed or as tolerated for 15 minutes. The participant’s heart rate and perceived exertion were monitored by the physical therapist. Flexibility exercises were performed for the lower limbs, pelvis, and trunk. Participants received from the physical therapist a manual stretching program for weeks 1–2 and then progressed to a 10-minute self-stretching program.
The remaining 35 minutes of the physical therapist session followed the exercise program outlined in the EBAR program (trunk and lower limb strengthening, balance and coordination, weight-bearing and stance control, and prosthetic gait training), which were guided by the performance on each AMP task. If the participant scored either a 0 (inability to perform the task) or 1 point (minimal level of achievement or with some assistance) out of 2 points (independence or mastery of task) on an AMP task, specific exercises that address the impairment were prescribed. 18 Exercises corresponding to tasks with scores of 0 points would take priority over scores of 1 point during exercise selection; however, the treating physical therapist could select the exercises from the task menu that in their professional judgement would best serve the participant ( Appendix 2 ).
For example, if at baseline testing a participant scored 0 points (unable to vary walking cadence in a controlled manner) or 1 (asymmetrical increase in cadence in a controlled manner) on AMP Task #18 (Variable Cadence), they present with impairments related to single limb balance, prosthetic gait control (transverse pelvic rotation), and dynamic postural stability. The treating physical therapist would choose from the exercises that corresponded with AMP Task #18 that are designed to address and improve those impairments: stool stepping, trunk rotation, resisted walking, and speed training to increase step frequency. 18 Stool stepping promotes stability within the stump socket interface and weight-bearing through the prosthesis, controlled displacement of center of mass over the base of support, and speed of contraction for hip and knee musculature. Trunk rotation in opposition to pelvic rotation promotes balance and momentum during gait. Resisted walking promotes power and balance over the prosthetic foot to facilitate equal stride length. Speed training focused on equal step length between limbs with improved single limb balance helps promote the ability for increased cadence and, as a result, fast walking speed or the ability for variable cadence.
All exercises designed to address impairments identified at baseline testing were prescribed during weeks 1 and 2. The exercises were progressed by increasing the repetitions or changing the surface (noncompliant to compliant to dynamic), direction of movement (uni-planar to bi-planar to multi-planar), speed (slow to fast), position (supine to sitting to standing), and/or resistance (no resistance to manual resistance to weighted resistance or resistance bands). Participants were retested on the AMPPro and AMPnoPro after the conclusion of week 2. If their scores improved but did not achieve a maximal score on an AMP task, those exercises were continued and progressed for the next 2 weeks. If they demonstrated a maximum score on the AMP task, then those exercises were discontinued and alternate exercises were prescribed based on their performance with other AMP tasks. Several AMP tasks assess related components within a body function domain; as a result, 1 exercise could be prescribed to address impairments related to 2 or more AMP tasks. The previously described exercise program enables the clinician to address multiple AMP tasks with similar exercises and facilitated the progression of exercises as function improved without overwhelming the participants with too many different exercises.
Outcome Measures
AMP is a measure of functional capability of a person with amputation to ambulate with (AMPPro) or without a prosthesis (AMPnoPro). 14 As previously described, the AMP can be easily administered (10–15 minutes) and requires standard equipment typically found in a clinical setting.
The 6MWT is considered a measure of overall mobility, endurance, and physical functioning in the adult and geriatric population as well as for people with LLA. 33 , 48 Administration of the 6MWT was consistent with recommendations by the American Thoracic Society. 49 The rectangular course dimensions were 60 feet (18.28 m) by 30 feet (9.14 m) for a total distance of 180 feet. At the completion of the 6MWT, the distance walked was recorded in meters. The MDC for the 6MWT for those with LLA is 45 m. 16
Statistical Analysis
Descriptive statistics were calculated to describe the intervention and wait-list control groups. Student’s t tests and chi-square statistics were calculated to compare the baseline characteristics between the 2 groups. A 2-group repeated-measures analysis of variance was used to compare the change in AMPPro and AMPnoPro scores and 6MWT distance of the intervention and wait-list control groups. Effect sizes were calculated for change in AMPPro, AMPnoPro, and 6MWT separately for the intervention group and wait-list control groups.
The secondary analyses used data from the 9 intervention group participants and 3 wait-list control group participants who had successfully completed the entire 8-week intervention. In addition to the blinded information collected at baseline and 8 weeks, the AMPPRO, AMPnoPro, and 6MWT data collected at weeks 2, 4, and 6 to guide exercise prescription were analyzed. Single-group repeated-measures ANOVAs were calculated to examine intervention-related changes across the 5 time periods in AMPPRO, AMPnoPro, and 6MWT performance. Where the ANOVAs were significant, paired t tests were used to examine change between 2 relevant time periods. A frequency table was generated to examine pre-post intervention change at the item level.
Role of the Funding Source
This study was supported by the Department of Veterans Affairs and Rehabilitation Research and Development Services, which played no role in the design, conduct, or reporting of the study.
Eighteen people with TTA were enrolled in the study, with 2 participants in the wait-list control group withdrawing for medical conditions unrelated to the study. Nine of the 18 participants completed the EBAR intervention and 7 completed the wait-list period. Two participants randomized to the wait-list control group voluntarily withdrew from the study. The mean age was 63.25 years, mean time since amputation was 8.1 years, 81.2% were male, and 75% lost their limb because of peripheral vascular disease or diabetes mellitus. Participants in the intervention and wait-list control groups did not differ in their demographic characteristics or PBOM baseline measures ( Tab. 1 ). The mean number of PT treatments per week was 2.5 sessions.
Participant Baseline Characteristics and Self-Report and Performance-Based Outcome Measures for Those Randomized to the Intervention and Wait-List Control Group a
ABC = Activities Balance Confidence Scale; AMPnoPro = Amputee Mobility Predictor without a prosthesis; AMPPro = Amputee Mobility Predictor with a prosthesis; DM = diabetes mellitus; 6MWT = 6-Minute Walk Test; PVD = peripheral vascular disease.
Table 2 presents the repeated-measures ANOVA group × time interaction between the intervention group and the waitlist-control group at baseline and 8 weeks. The intervention group’s mean AMPPro score increased from 36.4 to 41.7 while the wait-list control group’s score remained unchanged from 35.3 to 35.6 ( P = .004) ( Tab. 2 ). The mean change in AMPPro of 5.3 points for the intervention group exceeds the AMPPro MDC (3.4 points). 16 Similarly, the AMPnoPro mean score of the intervention group improved from 23.2 to 27.1, while the wait-list control group score also remained unchanged (24.7 to 25.0; P = .04). The 6MWT distance of the intervention group improved from a mean of 313.6 m to 387.7 m ( P = .04), while the wait-list control group again demonstrated virtually no change (262.6 m to 268.8 m). The mean change in 6MWT distance of 74.1 m exceeds the 6MWT MDC (45 m). 16 The effect size of the EBAR program for the intervention group was very large (1.32) for change in AMPPro scores. The AMPnoPro score and 6MWT distance had a moderate to large effect size (0.68 and 0.53, respectively).
Seven participants (58.33%) improved at least 1 MFCL K-level, with 2 of those participants improving 2 MFCL K-levels (K2-level to K4-level). Seventy-five percent of the participants who completed the EBAR program demonstrated improvement in AMPPro greater than the MDC (3.4 pts). 16
Only 3 of the 7 participants who were randomized to the wait-list period completed the 8-week EBAR program. Two were lost to follow-up and 2 could not complete the intervention due to medical complications not related to the EBAR program participation ( Fig. 1 ). The 9 participants in the intervention group and the 3 participants in the wait-list group who crossed over and completed the intervention were part of a secondary analysis examining the effects of the EBAR intervention over time. Table 3 describes the significant improvement in AMPPro and AMPnoPro scores ( P .0001, respectively) and 6MWT distance ( P = .0006) across the 5 intervention time periods ( Tab. 3 ; Fig. 1 ). Table 4 describes the pairwise comparison of the AMPPro, AMPnoPro, and 6MWT distance across the 5 intervention time periods. No change occurred within the first 2 weeks. After 4 weeks, significant change occurred with the AMPPro score. Both significant statistical and clinical change in AMPPro and AMPnoPro scores, and 6MWT distance occurred between baseline and weeks 6 and 8 ( Tab. 4 ), where mean change exceeded MDC for the measures. 16 Missing data from Tables 3 and 4 were the result of participants’ noncompliance and not completing all testing intervals.
Comparison Between Intervention and Wait-list Control Groups on Pre-post Intervention Change a
a AMPPro = Amputee Mobility Predictor with a prosthesis; AMPnoPro = Amputee Mobility Predictor without a prosthesis; 6MWT = Six-Minute Walk Test.
b Repeated-measures ANOVA group × time interaction.
c Individual group pre-post intervention effect size.
The item level analysis ( Fig. 2 ) revealed participants demonstrated deficits in 21 of the 25 total tasks. A large proportion of the participants initially demonstrated deficits in the more challenging AMP tasks. Post intervention, participants improved in performance in up to 9 tasks with the mean improvement of 5 tasks. For the entire cohort (n = 12), there was an improvement of 58 points and only a 5-point decline.
Even though the participants enrolled in this study were many years postamputation and post rehabilitation, those who received the 8-week EBAR program demonstrated clinically significant improvement in mobility as measured by the AMPPro, AMPnoPro, and 6MWT. The wait-list control group participants remained unchanged during the wait period and those who completed the EBAR intervention also demonstrated significant improvement. The intervention group pre-post intervention effect size for the AMPPro (1.32) was twice that for the AMPnoPro. This suggests that the physical therapy exercises focused on prosthetic training are effective for improving prosthetic mobility and function. The AMPPro tasks with greatest improvement were step length prosthetic limb (3 points/25%), step length sound limb (5 points/42%), foot clearance sound limb (3 points/25%), variable cadence (7 points/58%), stepping over an obstacle (6 points/50%), ascending stairs (6 points/50%), and descending stairs (4 pts/33%). Because the majority of participants in this study had moderate to high functional capabilities, the targeted exercises were designed to improve strength, muscular endurance, balance, and coordination with both lower limbs that would improve prosthetic control and function. These findings suggest that people with LLA have the potential to benefit from an EBAR program with a more targeted exercise approach after they have recovered from surgery and completed postamputation rehabilitation. The absence of change in the wait-list control participants indicates that simply walking with the prosthesis is not sufficient for continued improvement of functional mobility and that skilled physical therapy is required to facilitate prosthetic mobility skills.
The secondary analysis of the cohort who completed the EBAR intervention suggests that significant improvement in prosthetic mobility as measured by the AMPPro occurred by week 4 with the greatest change occurring by week 6 and significant improvement found in both AMP tests. By week 8, all 3 measures demonstrated significant improvement. As expected, the 6MWT distance increased steadily over the course of treatment as strength, muscular endurance, and aerobic capacity improved, as did the distance walked, reaching a statistically significant improvement of 16% at week 8 (332 m progressing to 396 m). The change in walking speed and distance is consistent with other randomized controlled trial studies that used a specific exercise program in people with LLA. 50 Interestingly, previous work suggests that the estimated mean 6MWT distance for the K2-level is 190 m, 300 m for K3-level, and 400 m for K4-level. 14 This small cohort did have some participants with greater than expected mean distances for the 6MWT; however, the median distance for the entire group was 274 m at baseline progressing to 419 m at week 8.
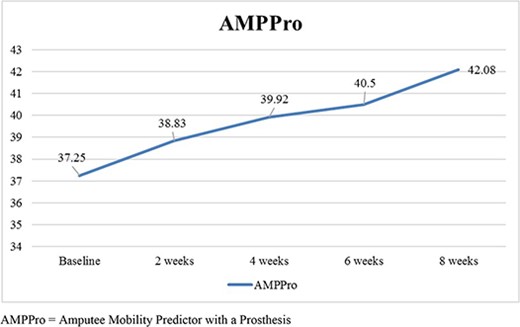
Mean change in AMPPro scores across the intervention intervals.
Change Across the Intervention Intervals in the Combined Intervention and Wait-List Groups a
AMPnoPro = Amputee Mobility Predictor without a prosthesis; AMPPro = Amputee Mobility Predictor with a prosthesis; 6MWT = 6-Minute Walk Test.
There were 5 participants who were K2-level and 7 K3-level participants at baseline, with 7 of the 12 (58%) progressing 1 or 2 K-level(s) with a mean AMPPro increase of 6.3 points by week 8 and an average increase in 6MWT distance of 48.9 m. One K2-level and 3 K3-level participants remained within their MFCL; however, all participants improved with their AMPPro scores and 6MWT distance an average of 3 points and 104.3 m, respectively. The EBAR program identifies physical impairments related to lower body strength, muscular endurance, coordination, balance, postural control, and speed of movement that are assessed at the activity level with sitting and standing balance activities, transfers, walking, and ascending and descending stairs. Target exercises at the impairment level can help to improve many different functional activities beyond just walking.
The participants in this study were able to perform sitting activities and transfers and could ambulate with adequate foot clearance, step length, and step continuity. If a cohort of people with LLA who had lower level functional capabilities (K1-level and K2-level) had enrolled in this study, it would be interesting to see where the improvement in function occurred and how much improvement would take place over time. The AMPPro tasks that presented the greatest difficulty were single limb balance, variable cadence, stepping over an obstacle, and stairs. These tasks have been found by previous investigators to be predictors of function in people with LLAs. 23 , 51 Although some participants did improve with these tasks, for example 58% improved cadence variance, single limb balance on either limb was not improved. It was not possible to determine if participants had reached their maximal potential or if alternative treatment strategies would have yielded greater improvements. Postamputation rehabilitation is inconsistent across the various treatment settings with many clinicians using standard treatment protocols focused on discharge criteria rather than using information based in evidence, such as using PBOM to determine physical impairments and limitations. Prosthetic gait training, typically administered a few weeks after surgery, is often insufficient for proficiency with a prosthesis. Many factors contribute to the person not reaching their prosthetic potential during the first bout of physical therapy, including, residual limb healing, pain, physical deconditioning, psychosocial adjustment to the loss of the limb, and simply the need for time to heal. 52–54 In addition, the rehabilitation goals and expectations can be low, resulting in the prescription of basic prosthetic componentry and limited access to the appropriate physical therapy. Evidence also suggests most people with amputations do not progress beyond the level of function achieved at discharge from acute rehabilitation. 55
Pairwise Comparison of Change in AMPPro, AMPnoPro, and 6MWT by Intervention Intervals a
6MWT = 6-Minute Walk Test; AMPnoPro = Amputee Mobility Predictor without a prosthesis; AMPPro = Amputee Mobility Predictor with a Prosthesis; n = number of participants.
Statistically significant difference.
For these reasons, the investigators believed that the majority of secondary issues would be resolved, allowing participants to focus on improved prosthetic mobility, if they were given additional physical therapy 1 year postamputation. Approximately one-half of participants enrolled in this study were people with K2-level function defined as household ambulators/limited community ambulators; however, the EBAR program progressed the majority of participants to K3-level community ambulators. Rehabilitating people to an activity level that permits community participation is the long-term goal of most rehabilitation programs because it can positively influence a person’s quality of life. This study demonstrates that a targeted rehabilitation program posttraditional rehabilitation period can significantly improve prosthetic mobility.
Limitations and Future Studies
The sample size for this study was small. The investigators approached 326 potential candidates for this intervention study, offering a comprehensive preenrollment medical evaluation, an 8-week PT intervention program, financial compensation for transportation to and from the study site, and any required therapies at the conclusion of the study. A total of 306 people were unable or declined to participate in the study. Because those who were asked to enroll chose to decline, no informed consent was signed, data concerning reasons for nonparticipation were not obtained, and participants who enrolled introduced self-selection bias to the study. Wong’s (2016) systematic review of 8 randomized controlled trial studies using exercise interventions in people with LLA found all other studies had similar enrollment with a range of 4 to 58 participants, illustrating the relatively low participation in these types of studies and the need for intervention research with larger populations. 50 As described in the introduction, the issue of low research rehabilitation participation by people with LLA is consistent with the literature and requires further understanding and investigation with respect to the motivation and reasons for participation or nonparticipation in physical therapy rehabilitation. Although the primary analyses achieved statistical significance, some aspects of the secondary analyses did not. This may be attributed to low statistical power. Sample size was affected by the inability of 2 of the wait-list control group participants to complete the EBAR program due to decline in medical status and 2 participants who withdrew for unknown reasons.
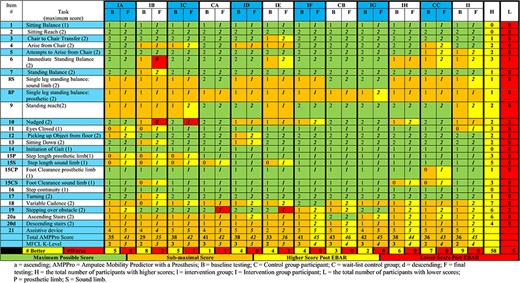
Pre-post intervention by AMPPro task.
This pilot intervention study produced questions by investigators for future work. For instance: when is the best time after amputation surgery to administer specific exercises, what is the appropriate duration for physical therapy, how do we know when a patient has reached their maximum potential, and should alternate exercises be added to the EBAR program? Moreover, the impact of the EBAR program during the acute phase of rehabilitation—when sitting balance, transfers, and standing with or without a prosthesis is the focus of physical therapy—is not known. Because there was so much improvement with this cohort, people with LLA should return to physical therapy regularly to receive EBAR over a lifetime for each new replacement prosthesis to maintain function or to reduce the risk of secondary health effects associated with age and long-term prosthetic use.
The EBAR program and targeted exercise prescription can significantly improve the efficacy of PT rehabilitation for people with TTA with the potential application for other patient populations. Future EBAR research should include a multi-site study at Veteran Affairs facilities and private sector hospitals that care for people with LLA. This study demonstrated that people with unilateral TTA can improve their prosthetic mobility after participating in an EBAR program when targeted exercises are prescribed based on the objective findings of the AMP. Physical therapy rehabilitation designed to address impairment level limitations can improve activity level tasks and mobility over 8 weeks of physical therapy administered 2 to 3 sessions per week. Most people who completed the EBAR program improved their AMP score, 6MWT distance, and functional K-level.
Concept/idea/research design: R. Gailey, M. Raya, N. Kirk-Sanchez, K. Roach
Writing: R. Gailey, I. Gaunaurd, M. Raya, N. Kirk-Sanchez, K. Roach
Data collection: R. Gailey, I. Gaunaurd, M. Raya, L.M. Prieto-Sanchez
Data analysis: R. Gailey, I. Gaunaurd, N. Kirk-Sanchez, K. Roach
Project management: R. Gailey, I. Gaunaurd
Fund procurement: R. Gailey, K. Roach
Providing participants: R. Gailey, I. Gaunaurd
Providing facilities/equipment: R. Gailey
Providing institutional liaisons: R. Gailey
Consultation (including review of manuscript before submitting): M. Raya, K. Roach
The authors thank John Bowker, MD, Curtis Clark, PT, Steve Decida, CPO, Rafael Hernandez, PT, MSPT, Thomas Dowell, CPO, Richard Ward, MD, and Ronald Tolchin, MD, for their dedication and countless hours of work contributed to make this project a success. The authors also thank the staff at the Miami Veterans Affairs Healthcare System Research, Physical Medicine and Rehabilitation and Prosthetics Departments, the University of Miami Miller School of Medicine Department of Physical Therapy, and Jackson Memorial Hospital for their generous support of this research project.
This study was approved by the Human Studies Subcommittee and Institutional Review Board at the Miami Veterans Affairs Healthcare System.
This study was supported by the Department of Veterans Affairs and Rehabilitation Research and Development Services (grant number A3381R), which played no role in the design, conduct, or reporting of the study.
The clinical trials registration number for this study is NCT00126126.
The authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest and reported no conflicts of interest.
Geertzen J , van der Linde H , Rosenbrand K , et al. Dutch evidence-based guidelines for amputation and prosthetics of the lower extremity: rehabilitation process and prosthetics. Part 2 . Prosthetics and Orthot Int. 2015 ; 39 : 361 – 371 .
Google Scholar
Kahle JT , Highsmith MJ , Schaepper H , Johannesson A , Orendurff MS , Kaufman K . Predicting walking ability following lower limb amputation: an updated systematic literature review . Technol Innov. 2016 ; 18 : 125 – 137 .
Christiansen CL , Fields T , Lev G , Stephenson RO , Stevens-Lapsley JE . Functional outcomes after the prosthetic training phase of rehabilitation after dysvascular lower extremity amputation . PM R. 2015 ; 7 : 1118 – 1126 .
Madsen UR , Baath C , Berthelsen CB , Hommel A . A prospective study of short-term functional outcome after dysvascular major lower limb amputation . Int J Orthop Trauma Nurs. 2018 ; 28 : 22 – 29 .
Dillingham TR , Pezzin LE , Mackenzie EJ . Discharge destination after dysvascular lower-limb amputations . Arch Phys Med Rehabil. 2003 ; 84 : 1662 – 1668 .
Dillingham TR , Pezzin LE . Rehabilitation setting and associated mortality and medical stability among persons with amputations . Arch Phys Med Rehabil. 2008 ; 89 : 1038 – 1045 .
Resnik LJ , Borgia ML . Factors associated with utilization of preoperative and postoperative rehabilitation services by patients with amputation in the VA system: an observational study . Phys Ther. 2013 ; 93 : 1197 – 1210 .
Miller MJ , Magnusson DM , Lev G , et al. Relationships among perceived functional capacity, self-efficacy, and disability after Dysvascular amputation . PM R. 2018 ; 10 : 1056 – 1061 .
Agrawal V , Gailey R , O'Toole C , Gaunaurd I , Dowell T . Weight distribution symmetry during the sit-to-stand movement of unilateral transtibial amputees . Ergonomics. 2011 ; 54 : 656 – 664 .
Agrawal V , Gailey RS , Gaunaurd IA , O'Toole C , Finnieston A , Tolchin R . Comparison of four different categories of prosthetic feet during ramp ambulation in unilateral transtibial amputees . Prosthetics Orthot Int. 2015 ; 39 : 380 – 389 .
Agrawal V , Gailey RS , Gaunaurd IA , O'Toole C , Finnieston AA . Comparison between microprocessor-controlled ankle/foot and conventional prosthetic feet during stair negotiation in people with unilateral transtibial amputation . J Rehabil Res Dev. 2013 ; 50 : 941 – 950 .
Robbins CB , Vreeman DJ , Sothmann MS , Wilson SL , Oldridge NB . A review of the long-term health outcomes associated with war-related amputation . Mil Med. 2009 ; 174 : 588 – 592 .
Gailey R , Allen K , Castles J , Kucharik J , Roeder M . Review of secondary physical conditions associated with lower-limb amputation and long-term prosthesis use . J Rehabil Res Dev. 2008 ; 45 : 15 – 29 .
Gailey R , Roach K , Applegate B , et al. The amputee mobility predictor: an instrument to assess determinants of the lower limb amputee’s ability to ambulate . Arch Phys Med Rehabil. 2002 ; 83 : 13 – 27 .
Kohler F , Cieza A , Stucki G , et al. Developing core sets for persons following amputation based on the international classification of functioning, disability and health as a way to specify functioning . Prosthet Orthot Int. 2009 ; 33 : 117 – 129 .
Resnik L , Borgia M . Reliability of outcome measures for people with lower-limb amputations: distinguishing true change from statistical error . Phys Ther. 2011 ; 91 : 555 – 565 .
Hafner BJ , Gaunaurd IA , Morgan SJ , Amtmann D , Salem R , Gailey RS . Construct validity of the prosthetic limb users survey of mobility (PLUS-M) in adults with lower limb amputation . Arch Phys Med Rehabil. 2017 ; 98 : 277 – 285 .
Samuelsen BT , Andrews KL , Houdek MT , Terry M , Shives TC , Sim FH . The impact of the immediate postoperative prosthesis on patient mobility and quality of life after transtibial amputation . Am J Phys Med Rehabil. 2016 ; 96 : 116 – 119 .
Li WS , Chan SY , Chau WW , Law SW , KM C . Mobility, prosthesis use and health-related quality of life of bilateral lower limb amputees from the 2008 Sichuan earthquake . Prosthet Orthot Int. 2019 ; 43 : 104 – 111 .
Esfandiari E , Yavari A , Karimi A , Masoumi M , Soroush M , Saeedi H . Long-term symptoms and function after war-related lower limb amputation: a national cross-sectional study . Acta Orthop Traumatol Turc. 2018 ; 52 : 348 – 351 .
Sions JM , Beisheim EH , Manal TJ , Smith SC , Horne JR , Sarlo FB . Differences in physical performance measures among patients with unilateral lower-limb amputations classified as functional level K3 versus K4 . Arch Phys Med Rehabil. 2018 ; 99 : 1333 – 1341 .
Dillon MP , Major MJ , Kaluf B , Balasanov Y , Fatone S . Predict the Medicare functional classification level (K-level) using the amputee mobility predictor in people with unilateral transfemoral and transtibial amputation: a pilot study . Prosthet Orthot Int. 2018 ; 42 : 191 – 197 .
Spaan MH , Vrieling AH , van de Berg P , Dijkstra PU , van Keeken HG . Predicting mobility outcome in lower limb amputees with motor ability tests used in early rehabilitation . Prosthet Orthot Int. 2017 ; 41 : 171 – 177 .
Seker A , Kara A , Camur S , Malkoc M , Sonmez MM , Mahirogullari M . Comparison of mortality rates and functional results after transtibial and transfemoral amputations due to diabetes in elderly patients-a retrospective study . Int J Surg. 2016 ; 33 : 78 – 82 .
Raya MA , Gailey RS , Gaunaurd IA , et al. Amputee mobility predictor-bilateral: a performance-based measure of mobility for people with bilateral lower-limb loss . J Rehabil Res Dev. 2013 ; 50 : 961 – 968 .
Balk EM , Gazula A , Markozannes G , et al. Lower limb prostheses: measurement instruments, comparison of component effects by subgroups, and long-term outcomes. Comparative Effectiveness Review. Agency for Healthcare Research and Quality; 2018;EHC017-EF.
Balk EM , Gazula A , Markozannes G , et al. Psychometric properties of functional, ambulatory, and quality of life instruments in lower limb amputees: a systematic review . Arch Phys Med Rehabil. 2019 ; 12 : 2354 – 2370 .
Batten HR , McPhail SM , Mandrusiak AM , Varghese PN , Kuys SS . Gait speed as an indicator of prosthetic walking potential following lower limb amputation . Prosthet Orthot Int. 2019 ; 43 : 196 – 203 .
Muderis MA , Tetsworth K , Khemka A , et al. The Osseointegration Group of Australia Accelerated Protocol (OGAAP-1) for two-stage osseointegrated reconstruction of amputated limbs . Bone Joint J . 2016 ; 98–B : 952 – 960 .
Gailey RS , Scoville C , Gaunaurd IA , et al. Construct validity of comprehensive high-level activity mobility predictor (CHAMP) for male servicemembers with traumatic lower-limb loss . J Rehabil Res Dev. 2013 ; 50 : 919 – 930 .
Gaunaurd I , Spaulding SE , Amtmann D , et al. Use of and confidence in administering outcome measures among clinical prosthetists: results from a national survey and mixed-methods training program . Prosthet Orthot Int. 2015 ; 39 : 314 – 321 .
Hafner BJ , Spaulding SE , Salem R , Morgan SJ , Gaunaurd I , Gailey R . Prosthetists' perceptions and use of outcome measures in clinical practice: long-term effects of focused continuing education . Prosthet Orthot Int. 2017 ; 41 : 266 – 273 .
Gailey RS , Gaunaurd I , Agrawal V , Finnieston A , O'Toole C , Tolchin R . Application of self-report and performance-based outcome measures to determine functional differences between four categories of prosthetic feet . J Rehabil Res Dev. 2012 ; 49 : 597 – 612 .
Kohler F , Xu J , Silva-Withmory C , Arockiam J . Feasibility of using a checklist based on the international classification of functioning, disability and health as an outcome measure in individuals following lower limb amputation . Prosthet Orthot Int. 2011 ; 35 : 294 – 301 .
Gailey R , Gaunaurd I , Laferrier J . Physical therapy management of adult lower-limb amputees. In: Krajbich JI , Pinzur MS , Potter BK , PM S , eds., Atlas of Amputations and Limb Deficiencies: Surgical, Prosthetic, and Rehabilitation Principles 4 . Rosemont, IL : American Academy of Orthopaedic Surgeons ; 2016 : 597 – 620 .
Google Preview
Gailey RS , Clark CR , Gaunaurd IA. Rehabilitation of the diabetic amputee. In: Bowker JH , MA P , eds. Levin and O’Neal’s The Diabetic Foot . 7 . Philadelphia, PA : Mosby Elsevier ; 2007 541 – 61 .
Gailey RS , Springer BA , Scherer M . Physical therapy for the polytrauma casualty with lower limb loss. In: MK Lenhart , ed., Combat Care of the Amputee 1 . Washington, DC : U.S. Government Printing Office ; 2009 : 451 – 492 .
Gailey RS , Clark CR . Physical therapy management of adult lower-limb amputees. In: Smith DG , Bowker JH , Michael JW , eds., Academy of Orthopaedic Surgeons, Atlas of Prosthetics: Surgical, Prosthetic, and Rehabilitation Principles 3 . Rosemont, IL : Mosby Co ; 2004 : 589 – 619 .
Gailey RS , Clark CR . Rehabilitation of the diabetic amputee. In: Bowker JH , MA Pfeifer , eds., The Diabetic Foot . Philadelphia PA : Mosby Co ; 2001 : 6 .
Gailey RS . Prosthetics. In: ML V, editor. Rehabilitation Techniques in Physical Therapy . In: New York, NY, USA: McGraw-Hill Companies . 2001 : 715 – 744 .
Gailey RS . Prosthetic gait assessment. In: J Van Deusen and D Brunt editor. Assessment in Occupational and Physical Therapy . Ann Arbor, Michigan, USA : W.B., Saunders ; 1996 : 199 – 246 .
Gailey RS , McKenzie A . Home Exercise Guide for Lower Extremity Amputees . Miami, FL : Advanced Rehabilitation Therapy, Inc ; 1995 .
Gailey RS , McKenzie A . Stretching and Strengthening for Lower Extremity Amputees . RS Gailey, editor. Advanced Rehabilitation Therapy, Inc : Miami, FL ; 1994 .
Gailey RS , McKenzie A . Balance, Agility, Coordination and Endurance for Lower Extremity Amputees . RS Gailey, editor. Miami, FL : Advanced Rehabilitation Therapy, Inc. ; 1994 .
Gailey RS , Gailey AM . Prosthetic Gait Training Program for Lower Extremity Amputees. AM G, editor. Miami, FL : Advanced Rehabilitation Therapy, Inc. ; 1989.
Gailey R . Rehabilitation of a traumatic lower limb amputee . Physiother Res Int. 1998 ; 3 : 239 – 243 .
Michael JW , Gailey RS , Bowker JH . New developments in recreational prostheses and adaptive devices for the amputee . Clin Orthop Relat Res. 1990 ; 64 – 75 .
Wurdeman SR , Schmid KK , Myers SA , Jacobsen AL , Stergiou N . Step activity and 6-minute walk test outcomes when wearing low-activity or high-activity prosthetic feet . Am J Phys Med Rehabil. 2017 ; 96 : 294 – 300 .
Linberg AA , Roach KE , Campbell SM , et al. Comparison of 6-minute walk test performance between male active duty soldiers and servicemembers with and without traumatic lower-limb loss . J Rehabil Res Dev. 2013 ; 50 : 931 – 940 .
Wong CK , Ehrlich JE , Ersing JC , et al. Exercise programs to improve gait performance in people with lower limb amputation: a systematic review . Prosthet orthot int. 2016 ; 40 : 8 – 17 .
Schoppen T , Boonstra A , Groothoff JW , de Vries J , Goeken LN , Eisma WH . Physical, mental, and social predictors of functional outcome in unilateral lower-limb amputees . Arch Phys Med Rehabil. 2003 ; 84 : 803 – 811 .
Bates B , Stineman MG , Reker DM , Kurichi JE , Kwong PL . Risk factors associated with mortality in veteran population following transtibial or transfemoral amputation . J Rehabil Res Dev. 2006 ; 43 : 917 – 928 .
Stineman MG , Kwong PL , Kurichi JE , et al. The effectiveness of inpatient rehabilitation in the acute postoperative phase of care after transtibial or transfemoral amputation: study of an integrated health care delivery system . Arch Phys Med Rehabil. 2008 ; 89 : 1863 – 1872 .
Chen MC , Lee SS , Hsieh YL , Wu SJ , Lai CS , Lin SD . Influencing factors of outcome after lower-limb amputation: a five-year review in a plastic surgical department . Ann Plast Surg. 2008 ; 61 : 314 – 318 .
Beekman CE , Axtell LA . Prosthetic use in elderly patients with dysvascular above-knee and through-knee amputations . Phys Ther. 1987 ; 67 : 1510 – 1516 .
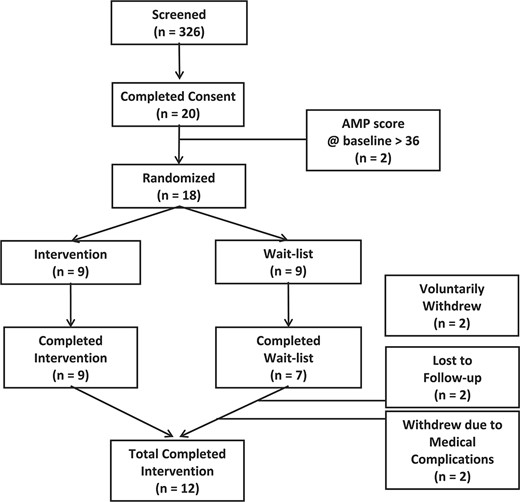
Constructs/Systems Being Assessed for Each Amputee Mobility Predictor Task and Exercises Choice
Amputee Mobility Predictor Evidence-Based Amputee Rehabilitation Exercise Guide a
(Continued)
Courtesy Advanced Rehabilitation Therapy, Inc. Miami, Florida Copyright © 2016. AMP = Amputee Mobility Predictor, BoS = base of support; COM = center of mass.
Email alerts
Citing articles via.
- Recommend to Your Librarian
- Advertising and Corporate Services
- Journals Career Network
Affiliations
- Online ISSN 1538-6724
- Copyright © 2024 American Physical Therapy Association
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Sports Phys Ther
- v.7(5); 2012 Oct
RESEARCH DESIGNS IN SPORTS PHYSICAL THERAPY
1 Baton Rouge, Louisiana, USA [email protected]
Research is designed to answer a question or to describe a phenomenon in a scientific process. Sports physical therapists must understand the different research methods, types, and designs in order to implement evidence‐based practice. The purpose of this article is to describe the most common research designs used in sports physical therapy research and practice. Both experimental and non‐experimental methods will be discussed.
INTRODUCTION
Evidence‐based practice requires that physical therapists are able to analyze and interpret scientific research. When performing or evaluating research for clinical practice, sports physical therapists must first be able to identify the appropriate study design. Research begins by identifying a specific aim or purpose; researchers should always attempt to use a methodologically superior design when performing a study. Research design is one of the most important factors to understand because:
- 1. Research design provides validity to the study;
- 2. The design must be appropriate to answer the research question; and
- 3. The design provides a “level of evidence” used in making clinical decisions.
Research study designs must have appropriate validity, both internally and externally. Internal validity refers to the design itself, while external validity refers to the study's applicability in the real world. While a study may have internal validity, it may not have external validity; however, a study without internal validity is not useful at all.
Most clinical research suffers from a conflict between internal and external validity. Internally valid studies are well‐controlled with appropriate designs to ensure that changes in the dependent variable result from manipulation of an independent variable. Well‐designed research provides controls for managing or addressing extraneous variables that may influence changes in the dependent variable. This is often accomplished by ensuring a homogenous population; however, clinical populations are rarely homogenous. An internally‐valid study with control of extraneous variables may not represent a more heterogeneous clinical population; therefore, clinicians should always consider the conflict between internal and external validity both when choosing a research design and when applying the results of research on order to make evidence‐based clinical decisions.
Furthermore, research can be basic or applied. Basic science research is often done on animals or in a controlled laboratory setting using tissue samples, for example. Applied research involves humans, including patient populations; therefore, applied research provides more clinical relevance and clinical application (i.e., external validity) than basic science research.
One of the most important considerations in research design for internal validity is to minimize bias. Bias represents the intentional or unintentional favoring of something in the research process. Within research designs, there are 5 important features to consider in establishing the validity of a study: sample, perspective, randomization, control, and blinding.
- Sample size and representation is very important for both internal and external validity. Sample size is important for statistical power, but also increases the representativeness of the target population. Unfortunately, some studies use a ‘convenience sample’, often consisting of college students, which may not represent a typical clinical population. Obviously, a representative clinical population can provide a higher level of external validity than a convenience sample.
- In terms of perspective, a study can be prospective (before the fact) or retrospective (after the fact). A prospective study has more validity because of more control of the variables at the beginning of and throughout the study, whereas a retrospective study has less control since it is performed after the end of an event. A prospective design provides a higher level of evidence to support cause‐and‐effect relationships, while retrospective studies are often associated with confounding variables and bias.
- Random assignment to an experimental or control group is performed to represent a ‘normal distribution’ of the population. Randomization reduces selection bias to ensure one group doesn't have an advantage over the other. Sometimes groups, rather than individual subjects, are randomly assigned to an experimental or control group; this is referred to as “block randomization.” Sample bias can also occur when a “convenience sample” is used that might not be representative of the target population. This is often seen when healthy, college‐aged students are included, rather than a representative sample of the population.
- A control group helps ensure that changes in the dependent variable are due to changes in the independent variable, and not due to chance. A control group receives no intervention, while the experimental group receives some type of intervention. In some situations, a true control group is not possible or ethical; therefore, “quasi‐experimental” designs are often used in clinical research where the control group receives a “standard treatment.” Sometimes, the experimental group can be used as it's “own control” by testing different conditions over time.
- Blinding (also known as “masking”) is performed to minimize bias. Ideally, both the subjects and the investigator should be blinded to group assignment and intervention. For example, a “double‐blind” study is one in which the subjects are not aware if they are receiving the experimental intervention or a placebo and at the same time, and the examiner is not aware which intervention the subjects received.
While considering these 5 features, a large sample size of patients, prospective, randomized, controlled, double‐blinded clinical outcome study would likely provide the best design to assure very high internal and external validity.
Most research follows the “scientific method”. The scientific method progresses through four steps:
- 1. Identification of the question or problem;
- 2. Formulation of a hypothesis (or hypotheses);
- 3. Collection of data; and
- 4. Analysis and interpretation of data.
Different research designs applying apply are used to answer a question or address a problem. Different authors provide different classifications of research designs. 1 ‐ 4
Within the scientific method, there are 2 main classifications of research methodology: experimental and non‐experimental. Both employ systematic collection of data. Experimental research is used to determine cause‐and‐effect relationships, while non‐experimental is used to describe observations or relationships in a systematic manner. Both experimental and non‐experimental research consist of several types and designs. ( Table 1 )
Research Designs.
Experimental Methods
Experimental methods follow the scientific method in order to examine changes in one variable by manipulating other variables to attempt to establish cause‐and‐effect. The dependent variable is measured under controlled conditions while controlling for confounding variables. It is important to remember that statistics do not establish cause‐and‐effect; rather, the design of the study does. Experimental statistics can only reject a null hypothesis and identify variance accounted for by the independent variable. Thomas et al. 4 provide three criteria to establish cause‐and‐effect:
- 1. Cause must precede effect in time;
- 2. Cause and effect must be correlated with each other; and
- 3. Relationship cannot be explained by another variable.
There are 3 elements of research to consider when evaluating experimental designs: groups, measures, and factors. Subjects in experimental research are generally classified into groups such as an experimental (those receiving treatment) or control group. Technically speaking, however, “groups” refers to the treatment of the data, not how the treatment is administered 2 . Groups are sometimes called “treatment arms” in order to denote subjects receiving different treatments. True experimental designs generally use randomized assignment to groups, while quasi‐experimental research may not.
Next, the order of measurements and treatments should be considered. “Time” refers to the course of the study from start to finish. Observations, or measurements of the dependent variables, can be performed one or several times throughout a study. The term, “repeated measures” denotes any measurement that is repeated on a group of subjects in the study. Repeated measures are often used in pseudo‐experimental research when the subjects act as their own control in one group, while true experimental research can use repeated measurements of the dependent variable as a single factor (“time”).
Since experimental designs are used to identify changes in a dependent variable by manipulating an independent variable, “factors” are used. Factors are essentially the independent variables. Individual factors can also have several levels. Single‐factor designs are referred to as “one‐way” designs with one independent variable and any number of levels. One‐way designs may have multiple dependent variables (measurements), but only one independent variable (treatment). Studies involving more than one independent variable are considered “multi‐factorial” and are referred to as “two‐way” or “three‐way” (and so on) designs. Multi‐factorial designs are used to investigate interactions within and between different variables. A “mixed design” factorial study includes 2 more independent variables with one repeated across all subjects and the other randomized to independent groups. Figure 1 is an example of a 2‐way repeated measures design including a true control group.

Two‐way repeated measures experimental design to determine interactions within and between groups.
Factorial designs are denoted with numbers representing the number of levels of each factor. A two‐way factorial (2 independent variables) with 2 levels of each factor is designated by “2 × 2”. The total number of groups in a factorial design can be determined by multiplying the factors together; for example, a 2×2 factorial has 4 groups while a 2×3×2 factorial has 12. Table 2 describes the differences in factorial designs using an example of 3 studies examining strength gains of the biceps during exercise. Each factor has multiple levels. In the 1‐way study, strength of the biceps is examined after performing flexion or extension with standard isotonic resistance. In the 2‐way study, a 3‐level factor is added by comparing different types of resistance during the same movements. In the 3‐way study, 2 different intensity levels are added to the design.
Examples of progressive factorial designs.
Statistical analysis of a factorial design begins by determining a main effect, which is an overall effect of a single independent variable on dependent variables. If a main effect is found, post‐hoc analysis examines the interaction between independent variables (factors) to identify the variance in the dependent variable.
As described in Table 1 previously, there are 2 types of experimental designs: true experimental and quasi‐experimental.
True Experimental Designs
True experimental designs are used to determine cause‐and‐effect by manipulating an independent variable and measuring its effect on a dependent variable. These designs always have at least 2 groups for comparison.
In a true experimental design, subjects are randomized into at least 2 independent, separate groups, including an experimental and “true” control. This provides the strongest internal validity to establish a cause‐and‐effect relationship within a population. A true control group consists of subjects that receive no treatment while the experimental group receives treatment. The randomized, controlled trial design is the “gold standard” in experimental designs, but may not be the best choice for every project.
Table 3 provides common true experimental designs that include 2 independent, randomly assigned groups and a true control group. Notation is often used to illustrate research designs:
Common true experimental designs.
n = subjects in a group (n 1 refers to experimental group while n 0 refers to control group)
T = treatment (T 1 . refers to sequential treatments)
0 = observation (O 0 refers to baseline, O 1 refers to sequential observations)
Quasi‐Experimental Designs
Clinical researchers often find it difficult to use true experimental designs with a ‘true’ control because it may be unethical and sometimes illegal to withhold treatment within a patient population. In addition, clinical trials are often affected by a conflict between internal and external validity. Internal validity requires rigorous control of variables; however, that control does not support real‐world generalizability (external validity). As previously described, clinical researchers must seek balance between internal and external validity.
Quasi‐experimental designs are those that do not include a true control group or randomization of subjects. While these types of designs may reduce the internal validity of a study, they are often used to maximize a study's external validity. Quasi‐experimental designs are used when true randomization or a true control group is unethical or difficult. For example, a ‘pseudo‐control’ group may include a group of patients receiving traditional treatment rather than a true control group receiving nothing.
Block‐randomization or cluster grouping may also be more practical when examining groups, rather than individual randomization. Subjects are grouped by similar variables (age, gender, etc) to help control for extraneous factors that may influence differences between groups. The block factor must be related to dependent variable (i.e., the factor affecting response to treatment).
A cross‐over or counterbalanced design may also be used in a quasi‐experimental study. This design is often used when only 2 levels of an independent variable are repeated to control for order effects. 3 A cross‐over study may require twice as long since both groups must undergo the intervention at different times. During the cross‐over, both groups usually go through a ‘washout’ period of no intervention to be sure prolonged effects are not a factor in the outcome.
Examples of quasi‐experimental designs can include both single and multiple groups ( Table 4 ). Quasi‐experimental designs generally do not randomize group assignment or use true control groups. (Note: One‐group pre‐post test designs are sometimes classified as “pre‐experimental” designs.)
Quasi-Experimental designs.
T = treatment (T 1 refers to sequential treatments)
O = observation (O 0 refers to baseline, O 1 refers to sequential observations
Single‐subject designs are also considered quasi‐experimental as they draw conclusions about the effects of a treatment based on responses of single patients under controlled conditions. 3 These designs are used when withholding treatment is considered unethical or when random assignment is not possible or when it is difficult to recruit subjects as is commonly seen in rare diseases or conditions. Single subject designs have 2 essential elements: design phases and repeated measures. 3 Design phases include baseline and intervention phases. The baseline measure serves as a ‘pseudo‐control.” Repeated measurement over time (for example, during each treatment session) can occur during the baseline and intervention phases. Common single‐subject designs are commonly denoted by the letters ‘A’ ‘(baseline phases) and ‘B’ (intervention phases): A‐B; A‐B‐A; and A‐B‐A‐B. Other single‐subject designs include withdrawal, multiple baselines, alternating treatment, multiple treatment, and interactive design. For more detailed descriptions on single subject designs, see Portney and Watkins. 3
Non‐Experimental Methods
Studies involving non‐experimental methods include descriptive, exploratory, and analytic designs. These designs do not infer cause‐and‐effect by manipulating variables; rather, they are designed to describe or explain phenomena. Non‐experimental designs help provide an early understanding about clinical conditions or situations, without a full clinical study through systematic collection of data.
Descriptive Designs
Descriptive designs are used to describe populations or phenomena, and can help identify groups and variables for new research questions. 3 Descriptive designs can be prospective or retrospective, and may use longitudinal or cross‐sectional methods. Phenomena can be evaluated in subjects either over a period time (longitudinal studies) or through sampling different age‐grouped subjects (cross‐sectional studies). Descriptive research designs are used to describe results of surveys, provide norms or descriptions of populations, and to describe cases. Descriptive designs generally focus on describing one group of subjects, rather than comparing different groups.
Surveys are one of the most common descriptive designs. 4 They can be in the form of questionnaires or interviews. The most important component of an effective survey is to have an appropriate sample that is representative of the population of interest. There are generally 2 types of survey questions: open‐ended and closed‐ended. Open‐ended questions have no fixed answer, while closed‐ended questions have definitive answers including rank, scale, or category. Investigators should be careful not to lead answers of subjects one way or another, and to keep true to the objectives of the study. Surveys are limited by the sample and the questions asked. External validity is threatened, for example, if the sample was not representative of the research question and design.
A special type of survey is the Delphi technique that uses expert opinions to make decisions about practices, needs, and goals. 4 The Delphi technique uses a series of questionnaires in successive stages called “rounds.” The first round of the survey focuses on opinions of the respondents, and the second round of questions is based on the results of the first round, where respondents are asked to reconsider their answers in context of other's responses. Delphi surveys are common in establishing expert guidelines where consensus around an issue is needed.
Observational
A descriptive observational study evaluates specific behaviors or variables in a specific group of subjects. The frequency and duration of the observations are noted by the researcher. An investigator observing a classroom for specific behaviors from students or teachers would use an observational design.
Normative research describes typical or standard values of characteristics within a specific population. 3 These “norms” are usually determined by averaging the values of large samples and providing an acceptable range of values. For example, goniometric measures of joint range of motion are reported with an accepted range of degrees, which may be recorded as “within normal limits.” Samples for normative studies must be large, random, and representative of the population heterogeneity. 3 The larger the target population, the larger sample required to establish norms; however, sample sizes of at least 100 are often used in normative research. Normative data is extremely useful in clinical practice because it serves as a basis for determining the need for an intervention, as well as an expected outcome or goal.
Developmental
Developmental research helps describe the developmental change and the sequencing of human behavior over time. 3 This type of research is particularly useful in describing the natural course of human development. For example, understanding the normal developmental sequencing of motor skills can be useful in both the evaluation and treatment of young athletes. Developmental designs are classified by the method used to collect data; they can be either cross‐sectional or longitudinal.
Case Designs
Case designs offer thoughtful descriptions and analysis of clinical information; 2 they include case reports, case studies, and case series. A case report is an in‐depth understanding of a unique patient, while a case study focuses on a unique situation. These cases may involve a series of patients or situations, which is referred to as a ‘case series’ design. Case designs are often useful in developing new hypotheses and contributing to theory and practice. They also provide a springboard for moving toward more quasi‐experimental or experimental designs in order to investigate cause and effect.
Qualitative
Research measures can also be classified as quantitative or quantitative. Quantitative measures explain differences, determines causal relationships, or describes relationships; these designs include those previously discussed. Qualitative research, on the other hand, emphasizes attempting to discern process and meaning without measuring quantity. Qualitative studies focus on analysis in trying to describe a phenomenon. Qualitative research examines beliefs, understanding, and attitudes through skillful interview and content analysis. 5 These designs are used to describe specific situations, cultures, or everyday activities. Table 5 provides a comparison between qualitative and quantitative designs.
Comparison of quantitative and qualitative designs (Adapted from Thomas et al4 and Carter et al 2 ).
Exploratory Designs
Exploratory designs establish relationships without manipulating variables while using non‐experimental methods. These designs include cohort studies, case control studies, epidemiological research, correlational studies, and methodological research. Exploratory research usually involves comparison of 2 or more groups.
Cohort Studies
A cohort is a group of subjects being studied. Cohort studies may evaluate single groups or differences between specific groups. These observations may be made in subjects one time, or over periods of time, using either cross‐sectional or longitudinal methods.
In contrast to experimental designs, non‐experimentally designed cohort studies do not manipulate the independent variable, and lack randomization and blinding. A prospective analysis of differences in cohort groups is similar to an experimental design, but the independent variable is not manipulated. For example, outcomes after 2 different surgeries in 2 different groups can be followed without randomization of subjects using a prospective cohort design.
Some authors 2 have classified “Outcomes Research” as a retrospective, non‐experimental cohort design, where differences in groups are evaluated ‘after the fact’ without random allocation to groups or manipulation of an independent variable. This design would include chart reviews examining outcomes of specific interventions.
Case Control Studies
Case control studies are similar to cohort studies comparing groups of subjects with a particular condition to a group without the condition. Both groups are observed over the same period of time, therefore requiring a shorter timeframe compared to cohort studies. Case control studies are better for investigations of rare disease or conditions because the sample size required is less than a cohort study. The control group (injury/disease‐free) is generally matched to the injury/disease group by confounding variables consistent in both groups such as age, gender, and ethnicity.
Case control studies sometimes use “odds ratios” in order to estimate the relative risk if a cohort study would have been done. 4 An odds ratio greater than 1 suggests an increased risk, while a ratio less than 1 suggests reduced risk.
Epidemiological Research
Studies that evaluate the exposure, incidence rates, and risk factors for disease, injury, or mortality are descriptive studies of epidemiology. According to Thomas et al, 4 epidemiological studies evaluate “naturally occurring differences in a population.” Epidemiological studies are used to identify a variety of measures in populations ( Table 6 ).
Measurement terminology used in epidemiological research.
“Relative risk,” (RR) which is associated with exposure and incidence rates. Portney and Watkins 3 use a “contingency table” ( Table 7 ) to determine the relative risk and odds ratio. Usually, incidence rates are compared between 2 groups by dividing the incidence of one group by the other.
Contingency Table to determine risk (Adapted from Portney and Watkins 3 ).
Using Table 7 ,
With these formulas, the “null value” is 1.0. A risk or odds ratio less than 1.0 suggests reduced risk or odds, while a value greater than 1.0 suggests increased risk or odds. For example, if the risk is 1.5 in a group, there is a 1.5 times greater risk of suffering an injury in that group. Relative risk should be reported with a confidence interval, typically 95%.
Epidemiological studies can also be used to test a hypothesis of the effectiveness of an intervention on on injury prevention by using incidence as a dependent variable. These studies help link exposures and outcomes with observations, and can include case control and cohort studies mentioned previously.
Correlational Studies
Correlations studies examine relationships among variables. Correlations are expressed using the Pearson's “r” value that can range from −1 to +1. A Pearson's “r” value of +1 indicates a perfect linear correlation, noting the increase in one variable is directly dependent on the other. In contrast, an “r” value of −1 indicates a perfect inverse relationship. An “r” value of 0 indicates that the variables are independent of each other. The most important thing to remember is that correlation does not infer causation; in other words, correlational studies can't be used to establish cause‐and‐effect. In addition, 2 variables may have a high correlation (r>.80), but lack statistical significance if the p‐value is not sufficient. Finally, be aware that correlational studies must have a representative sample in order to establish external validity.
Methodological
The usefulness of clinical research and decision‐making heavily depends on the validity and reliability of measurements. 3 Methodological research is used to develop and test measuring instruments and methods used in practice and research. Methodological studies are important because they provide the reliability and validity of other studies. First, the reliability of the rater (inter‐rater and intra‐rater reliability) must be established when administering a test in order to support the accuracy of measurements. Inter‐rater reliability supports consistent measurements between different raters, while intra‐rater reliability supports consistent measures for the same individual rater. Reliability can also be established for instruments by demonstrating consistent measurements over time. Reliability is related to the ability to control error, and thus associated with internal validity.
Methodological studies are also used to establish validity for a measurement, which may include clinical diagnostic tests, performance batteries, or measurement devices. Measurement validity establishes the extent to which an instrument measures what it intends to measure. Different types of validity can be measured, including face validity, content validity, criterion‐related validity and construct validity ( Table 8 ).
Different types of validity in scientifi c research.
Sports physical therapists may also be interested in the sensitivity and specificity of clinical tests. Sensitivity refers to the ability of a test to correctly identify those with a condition, while specificity refers to the ability to correctly identify those without the condition. Unfortunately, few clinical tests possess both high sensitivity and specificity. 6
Analytical Designs
Analytical research designs are not just a review or summary, but a method of evaluating the existing research to reach a conclusion. These designs provide a synthesis of the literature for empirical and theoretical conclusions. 4 Analytical designs explain phenomena and analyze existing data using systematic reviews and meta‐analysis techniques. In contrast to systematic reviews, meta‐analyses include statistical analysis of data.
Systematic Reviews
Systematic reviews most commonly examine the effectiveness of interventions, but may also examine the accuracy of diagnostic tools. 3 Systematic reviews of randomized controlled trials provide the highest level of evidence possible. 7 Systematic reviews should describe their methodology in detail, including inclusion and exclusion criteria for studies reviewed, study designs, and outcomes measures. In addition, the method of literature search should be detailed including databases, dates, and keywords used.
Meta‐Analysis
Systematic reviews can be extended into meta‐analysis if multiple studies contain necessary information and data. Meta‐analysis techniques are particularly useful when trying to analyze and interpret smaller studies and studies with inconsistent outcomes. Meta‐analysis of randomized controlled trials provides a high level of evidence, but may suffer in quality from heterogeneous samples, bias, outliers, and methodological differences.
Meta‐analysis quantifies the results of various studies into a standard metric that allows for statistical analysis to calculate effect sizes. The effect size, calculated by “Cohen's d value,” is defined as a standardized value of the relationship between two variables. Effect size provides magnitude and direction of the effect of a treatment, and is determined by the difference in means divided by the standard deviation (ΔM / SD). A Cohen's d value of .2 is considered small; .5 is considered moderate, and .8 and greater is a large effect size. Confidence intervals are then reported to provide an interval of certainty.
Levels of Evidence
Research designs are often viewed in a hierarchy of evidence. These designs have been discussed in this paper, but bear repeating in the context of evidence‐based practice. “Levels of Evidence” have been established by the Center for Evidence‐Based Medicine in Oxford, England ( Table 9 ) as well as other research consortiums. Each level is based on controlling as many factors (variables) as possible to confidently make conclusions without bias, the highest of which is cause‐and‐effect. In addition, “grades” of evidence have been established based on the quality and number of various levels of evidence to make recommendations in reviews and guidelines ( Table 10 ). Thus, a research publication could be described and labeled using a combination of a level and a grade, such as “Level II‐A” or “Level II‐B”.
Levels of Evidence (Adapted from the Center for Evidence-Based Medicine 7 ).
Grades of Evidence (Adapted from the Center for Evidence-Based Medicine 7 ).
In conclusion, it is important for sports physical therapists to understand different research designs not only to support evidence‐based practice, but also to contribute to the body of knowledge by using appropriate research designs. Clinicians should be aware of appropriate research design, validity, and levels of evidence in order to make informed clinical decisions. This commentary described the most common and relevant experimental and non‐experimental designs used and encountered by sports physical therapists who contribute to and utilize evidence‐based practice.

IMAGES
VIDEO
COMMENTS
The official journal of the American Physical Therapy Association. Publishes content for an international readership on topics related to physical therapy. ... Call for Papers Self-Archiving Policy Promote your Article ... Objectives The objective of this study was to conduct a systematic and comprehensive review of qualitative research to ...
The physical therapy was administered to the waist region by the physiotherapist, for a total of 10 sessions, five days per week, with a single session per day. The sessions included a hot pack, ultrasound, and TENS treatment. ... The authors received no financial support for the research and/or authorship of this article. References. 1.
The aim of this paper is to highlight new technology currently being used in Physical Therapy for orthopedic conditions ranging from sports medicine to joint arthroplasty to trauma. ... Future research utilizing instrumented insoles will most likely expand into additional orthopedic populations that typically demonstrate compensatory movement ...
Introduction. Physical therapy is a profession with a theoretical and scientific base that is dynamically evolving. Physical therapists are health professionals who diagnose and manage movement dysfunction to restore, maintain, and promote optimal physical function for the health and well-being of individuals, families, and communities. 1 Physical therapist assistants assist a physical ...
Call for Papers Self-Archiving Policy ... National Benchmarks to Understand how Doctor of Physical Therapy Learners from Minoritized Race and Ethnicity Groups Perceive their Physical Therapist Education Program. ... It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide.
PTJ 's stated vision is "To become the preeminent international journal in physical therapy and rehabilitation by publishing and promoting original research and relevant information that advance clinical practice, inform policy, and engender a powerful and sustained impact on the health of individuals and communities.".
Objectives To investigate the completeness of reporting of physical therapy interventions in randomized controlled trials before and after publication of the Template for Intervention Description and Replication (TIDieR) checklist (a reporting guideline for interventions). Design Meta-research. Methods We searched 6 journals for trials using physical therapy interventions that were published ...
OBJECTIVE: To quantify the proportion attributable to contextual effects of physical therapy interventions for musculoskeletal pain. DESIGN: Intervention systematic review with meta-analysis. LITERATURE SEARCH: We searched Ovid, MEDLINE, EMBASE, CINAHL, Scopus, PEDro, Cochrane Controlled Trials Registry, and SPORTDiscus databases from inception to April 2023. STUDY SELECTION CRITERIA ...
2. Utilization and cost: Explore the financial benefits for physical therapy. Compare utilization and costs (outcomes/ costs) of the numerous practice areas for physical therapists (identifying where physical therapists add value to the system, where physical therapists add additional cost, where physical therapy services add redundancy, etc.). 3.
High-Impact Research from PTJ. The latest Journal Citation Reports (Journal Citation Reports™, from Clarivate, 2022) have now been released, and I am pleased to announce that PTJ continues to grow its impact within the physical therapy and rehabilitation communities. To mark PTJ's continued growth, this selection of highly cited articles has been made free to read.
Physical Therapy in Sport covers topics dealing with the diagnosis, treatment, and prevention of injuries, as well as more general areas of sports and exercise medicine and those related to exercise rehabilitation. The journal publishes original research, case studies, reviews, masterclasses, papers on clinical approaches, and book reviews, as ...
The Research Agenda for Physical Therapy expands on our profession's continued advancement and considers current issues, new innovations, and forward-thinking viewpoints. The research agenda outlines research priorities that are vital to advancing physical therapist practice and the profession. The development of the research agenda included ...
2 Physiotherapy in Motion, Multi-Specialty Research Group (PTinMOTION), Department of Physiotherapy, University of Valencia, Valencia, Spain. ... The proportion of physical therapy interventions effect that is explained by contextual effects was calculated, and a quantitative summary of the data from the studies was conducted using the random ...
3 Department of Physical Therapy and Occupational Therapy, Adult Ambulatory Division, Duke University Health System , Durham, NC, USA. ... Study Selection: The initial search resulted in 451 papers. After screening, seven studies were identified that examined the role of TA on chronic pain (> 12 weeks) management in physical therapy settings. ...
This paper describes the PEDro scale, PEDro contents, who uses PEDro, searching, browsing the latest content, and developing skills in evidence-based physical therapy. ... PEDro will continue to be developed to facilitate the use of high-quality clinical research by physical therapy clinicians, educators, students, and researchers. In October ...
This review paper selected samples based on PRISMA 2020, and three researchers were involved in the selection and extraction process. ... Supervised physical therapy + Segmental muscle vibration (SPT-SMV) Duration: 30 min ... Research related to tele-rehabilitation is increasing, but studies examining the effects of timing are insufficient ...
Research Papers from 2017. A Systematic Mapping Review of Health Promotion and Well-being Concepts in Physical Therapy, Andrew Amundson, Jesse Klein, Bailey Ringold, and Aaron Theis. The Influence of Hip Strength and Core Endurance on Recurrent Patella Dislocations: A Pilot Study, Samuel Arnold, Emily Bradshaw, Anna Hansen, Jessica Knutson, and ...
Background Sedentary lifestyle is a major risk factor for noncommunicable diseases such as cardiovascular diseases, cancer and diabetes. It has been estimated that approximately 3.2 million deaths each year are attributable to insufficient levels of physical activity. We evaluated the available evidence from Cochrane systematic reviews (CSRs) on the effectiveness of exercise/physical activity ...
Theses/Dissertations from 2015. Physical Therapy after Triangular Fibrocartilage Injuries and Ulnar Wrist Pain, Mohamed A. Abdelmegeed. The Effect of Cervical Muscle Fatigue on Postural Stability during Immersion Virtual Reality, Mazen M. Alqahtani. The Effects of a Novel Therapeutic Intervention in Diabetic Peripheral Neuropathy Patients, Adel ...
Methods. Scoping review methodology was chosen to provide an overview of the published academic research on mental health and physical therapy, including key topics, types of evidence, and main sources. Scoping reviews can map and establish the scope of the existing literature in areas of emerging evidence in physical therapy, taking a broad ...
The Journal of Neurologic Physical Therapy (JNPT) is an indexed resource for dissemination of research-based evidence related to neurologic physical therapy intervention. High standards of quality are maintained through a rigorous, double-blinded, peer-review process and adherence to standards recommended by the International Committee of Medical Journal Editors.
These include tai chi, yoga, massage, and spinal manipulation. Public health programs should educate the public on the prevention of low back pain. In chronic low back pain, the physical therapy exercise approach remains a first-line treatment, and should routinely be used. Keywords: Disability prevention, Improved function, Low back pain ...
Physical therapist services after lower limb amputation (LLA) can have a meaningful impact on physical function and quality of life. People with LLA receiving physical therapy are more likely to have better prosthetic weight-bearing and mobility, musculoskeletal endurance, walking speed, and prosthetic fit, as well as an increased 1-year survival rate, compared with those who do not receive ...
Comparison of Two Thoracic Kinesio-Taping Techniques on Pulmonary Function, Oxygen Saturation, and Exercise Capacity in COPD Patients: A Randomized Clinical Trial. Ganesh, B. R.; Praneetha, N.; Naik, Varun. Indian Journal of Physical Therapy and Research. 5 (1):32-36, Jan-Jun 2023. Abstract.
Research design is one of the most important factors to understand because: 1. Research design provides validity to the study; 2. The design must be appropriate to answer the research question; and. 3. The design provides a "level of evidence" used in making clinical decisions.