- Find My Rep

You are here
Qualitative Methods for Health Research
- Judith Green - Exeter University, UK
- Nicki Thorogood - Independent Academic
- Description
- Author(s) / Editor(s)
Packed with practical advice and research quick tips, this book is the perfect companion to your health research project. It not only explains the theory of qualitative health research so you can interpret the studies of others, but also showcases how to approach, start, maintain, and disseminate your own research.
It will help you:
- Understand the role of the researcher
- Develop an effective research proposal
- Seek ethical approval
- Conduct interviews, observational studies, mixed methods, and web-based designs
- Use secondary and digital sources
- Code, manage, and analyse data
- Write up your results
Whether you are studying public health, sports medicine, occupational therapy, nursing, midwifery, or another health discipline, the authors will be your surrogate supervisors and guide you through evaluating or undertaking any type of health research.
Supplements
This book is the clear and extensive introduction to qualitative health research. It is useful for all under and post graduate students, and even for PhDs with quantitative background.
A thoughtful, thorough and readable account of the history and current practice of qualitative research in health.
An enormously helpful resource for anyone interested in interpreting and conducting qualitative health research. In addition to describing complex social theory in an easily digestible style, it also provides a practical ‘how to’ guide for all the stages of qualitative data collection, analysis and dissemination. Filled with useful examples, it brings qualitative health research to life in a way that is both engaging and highly accessible. It is a must read for students and experienced scholars alike!
This new edition of Green and Thorogood’s excellent textbook should be required reading for health professionals considering undertaking qualitative research. Along with a practical introduction to the theory and methods of qualitative research, this revised edition expands on the importance of theory for qualitative research, the use of secondary sources and digital methods in data collection and the integration of methods, disciplines and designs within research. It continues to be a core text for any qualitative methods training for students in health and related disciplines.
Very good basic introduction, focus on ethnography and observation as essential qual. research designs/methods. Great book also for nursing science students.
This is an great resource for students undertaking qualitative methods for the first time. Additionally, it provides a great go-to for those further along in their use of these methods.
An informative introduction to qualitative research with practical advice and real-world examples.
An excellent resource for graduate and post graduate students in health research.
Added to my reading list for three modules-like the clear writing style, and 'how to' guides-useful for both undergraduate and post graduate students
I enjoyed reading this. Its an excellent practical book that helped organise and conduct qualitative research, safe in the knowledge that the project would be robust and credible. It also serves a s a useful reference for supervision.
Preview this book
Judith green.
Judith Green has degrees in anthropology and sociology, and a PhD in the sociology of heath. She has taught research methods to a wide range of students over the last 30 years, including undergraduate, postgraduate and doctoral students and health professionals from nursing, medicine, public health and sociology. She is currently Professor of Sociology of Health at King’s College London, and has held posts at the London School of Hygiene and Medicine and London South Bank University. Judith has broad substantive interests in the sociology of health and health services, and has researched and published on primary... More About Author
Nicki Thorogood
Nicki Thorogood’s first degree was in sociology and social anthropology, and she has a PhD in the sociology of health from the University of London. She has over 30 years experience of teaching undergraduate and postgraduate students. Before coming to LSHTM (London School of Hygiene and Tropical Medicine) in 1999 she held posts at Middlesex University and at Guy’s King’s and Thomas’s School of Medicine and Dentistry (GKT). Her research interests are primarily in qualitative research into aspects of ‘identity’, e.g. ethnicity, gender, disability and sexuality and in the sociology of the body. She is also interested in the intersection of... More About Author
Purchasing options
Please select a format:
Order from:
- Buy from SAGE
Related Products

(Stanford users can avoid this Captcha by logging in.)
- Send to text email RefWorks EndNote printer
The SAGE handbook of qualitative methods in health research [electronic resource]
Available online.
- Sage Research Methods
More options
- Find it at other libraries via WorldCat
- Contributors
Description
Creators/contributors, contents/summary.
- Introduction PART ONE: CONTRIBUTIONS OF QUALITATIVE RESEARCH There's More to Dying Than Death: Qualitative Research on the End-of-Life - Stefan Timmermans Healer-Patient Interaction: New Mediations in Clinical Relationships - Arthur W. Frank, Michael K. Corman, Jessica A. Gish and Paul Lawton Qualitative Contributions to the Study of Health Professions and Their Work - Johanne Collin Why Use Qualitative Methods to Study Health-Care Organizations? Insights from Multilevel Case Studies - Carol A. Caronna How Country Matters: Studying Health Policy in a Comparative Perspective - Sirpa Wrede Exploring Social Inequalities in Health: The Importance of Thinking Qualitatively - Gareth Williams and Eva Elliott PART TWO: THEORY Theory Matters in Qualitative Health Research - Mita Giacomini Ethnographic Approaches to Health and Development Research: The Contributions of Anthropology - Rebecca Prentice What Is Grounded Theory and Where Does It Come from? - Dorothy Pawluch and Elena Neiterman Qualitative Methods from Psychology - Helen Malson Conversation Analysis and Ethnomethodology: The Centrality of Interaction - Timothy Halkowski and Virginia Teas Gill Phenomenology - Carol L. McWilliam Studying Organizations: The Revival of Institutionalism - Karen Staniland History and Social Change in Health and Medicine - Claire Hooker PART THREE: COLLECTING AND ANALYZING DATA Qualitative Research Review and Synthesis - Jennie Popay and Sara Mallinson Qualitative Interviewing Techniques and Styles - Susan E. Kelly Focus Groups - Rosaline S. Barbour Fieldwork and Participant Observation - Davina Allen Video-Based Conversation Analysis - Ruth Parry Practising Discourse Analysis in Healthcare Settings - Srikant Sarangi Documents in Health Research - Lindsay Prior Participatory Action Research: Theoretical Perspectives on the Challenges of Researching Action - Louise Potvin, Sherri L. Bisset and Leah Walz Qualitative Research in Programme Evaluation - Isobel MacPherson and Linda McKie Auto-Ethnography: Making Sense of Personal Illness Journeys - Elizabeth Ettore Institutional Ethnography - Marie L. Campbell Visual Methods for Collecting and Analysing Data - Susan E. Bell Keyword Analysis: A New Tool for Qualitative Research - Clive Seale and Jonathan Charteris-Black PART FOUR: ISSUES IN QUALITATIVE HEALTH RESEARCH Recognizing Quality in Qualitative Research - Kath M. Melia Mixed Methods Involving Qualitative Research - Alicia O'Cathain A Practical Guide to Research Ethics - Laura Stark and Adam Hedgecoe Using Qualitative Research Methods to Inform Health Policy: The Case of Public Deliberation - Julia Abelson Cross National Qualitative Health Research - Carine Vassy and Richard Keller PART FIVE: APPLYING QUALITATIVE METHODS Researching Reproduction Qualitatively: Intersections of Personal and Political - Kereen Reiger and Pranee Liamputtong Understanding the Shaping, Incorporation and Co-Ordination of Health Technologies through Qualitative Research - Tiago Moreira and Tim Rapley Transgressive Pleasures: Undertaking Qualitative Research in the Radsex Domain - Dave Holmes, Patrick O'Byrne and Denise Gastaldo The Challenges and Opportunities of Qualitative Health Research with Children - Ilina Singh and Sinead Keenan The Dilemmas of Advocacy: The Paradox of Giving in Disability Research - Ruth Pinder Qualitative Approaches for Studying Environmental Health - Phil Brown.
- (source: Nielsen Book Data)
Bibliographic information
Browse related items.
- Stanford Home
- Maps & Directions
- Search Stanford
- Emergency Info
- Terms of Use
- Non-Discrimination
- Accessibility
© Stanford University , Stanford , California 94305 .
- Technical Support
- Find My Rep
You are here

Qualitative Research Methods for Health Professionals
- Janice M. Morse - University of Utah, USA
- Peggy Anne Field - University of Alberta - Edmonton, Canada
- Description
See what’s new to this edition by selecting the Features tab on this page. Should you need additional information or have questions regarding the HEOA information provided for this title, including what is new to this edition, please email [email protected] . Please include your name, contact information, and the name of the title for which you would like more information. For information on the HEOA, please go to http://ed.gov/policy/highered/leg/hea08/index.html .
For assistance with your order: Please email us at [email protected] or connect with your SAGE representative.
SAGE 2455 Teller Road Thousand Oaks, CA 91320 www.sagepub.com
Select a Purchasing Option
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Qualitative methods for health research

Choice Reviews Online
Related Papers
Catherine Pope
Online Journal of …
Kalaiselvan Ganapathy
Journal of Evaluation in Clinical Practice
Mary Boulton
It is increasingly argued that qualitative approaches have an important role in health care research. A wide range of methods are used to collect qualitative data, including in-depth interviews, focus groups and observational methods such as participant observation. The reliability and validity of qualitative studies can be addressed by a variety of techniques. Although there is less consensus about appropriate methods of analysing qualitative data, such analyses tend to be grounded in the data, and involve iterative procedures and the development and refinement of typologies, analogies and other forms of concept to make sense of data.
Douglas Ezzy
Australian and New Zealand Journal of Public Health
Objective: To provide an overview of qualitative methodologies for health researchers in order to inform better research practices.Approach: Different possible goals in health research are outlined: quantifying relationships between variables, identifying associations, exploring experience, understanding process, distinguishing representations, comprehending social practices and achieving change. Three important issues in understanding qualitative approaches to research are discussed: the partiality of our view of the world, deductive and inductive approaches to research, and the role of the researcher in the research process. The methodologies of phenomenology, grounded theory, discourse analysis, ethnography, ethnomethodology and action research are illustrated.Conclusion: In order to undertake high-quality qualitative research, it is important for researchers to consider their analytic focus and methodological position.
A hand search of the original papers in seven medical journals over 5 years was conducted in order to identify those reporting qualitative research. A total of 210 papers were initially identified, of which 70 used qualitative methods of both data collection and analysis. These papers were evaluated by the researchers using a checklist which specified the criteria of good practice. Overall, 2% of the original papers published in the journals reported qualitative studies. Papers were more frequently positively assessed in terms of having clear aims, reporting research for which a qualitative approach was appropriate and describing their methods of data collection. Papers were less frequently positively assessed in relation to issued of data analysis such as validity, reliability and providing representative supporting evidence. It is concluded that the full potential of qualitative research has yet to be realized in the field of health care.
Kieron Ivan Gutierrez
This paper focuses on the question of sampling (or selection of cases) in qualitative research. Although the literature includes some very useful discussions of qualitative sampling strategies, the question of sampling often seems to receive less attention in methodological discussion than questions of how data is collected or is analysed. Decisions about sampling are likely to be important in many qualitative studies (although it may not be an issue in some research). There are varying accounts of the principles applicable to sampling or case selection. Those who espouse 'theoretical sampling', based on a 'grounded theory' approach, are in some ways opposed to those who promote forms of 'purposive sampling' suitable for research informed by an existing body of social theory. Diversity also results from the many different methods for drawing purposive samples which are applicable to qualitative research. We explore the value of a framework suggested by Miles and Huberman [Miles, M., Huberman,, A., 1994. Qualitative Data Analysis, Sage, London.], to evaluate the sampling strategies employed in three examples of research by the authors. Our examples comprise three studies which respectively involve selection of: 'healing places'; rural places which incorporated national anti-malarial policies; young male interviewees, identified as either chronically ill or disabled. The examples are used to show how in these three studies the (sometimes conflicting) requirements of the different criteria were resolved, as well as the potential and constraints placed on the research by the selection decisions which were made. We also consider how far the criteria Miles and Huberman suggest seem helpful for planning 'sample' selection in qualitative research. Abstract PURPOSE We wanted to review and synthesize published criteria for good qualitative research and develop a cogent set of evaluative criteria. METHODS We identified published journal articles discussing criteria for rigorous research using standard search strategies then examined reference sections of relevant journal articles to identify books and book chapters on this topic. A cross-publication content analysis allowed us to identify criteria and understand the beliefs that shape them. RESULTS Seven criteria for good qualitative research emerged: (1) carrying out ethical research; (2) importance of the research; (3) clarity and coherence of the research report; (4) use of appropriate and rigorous methods; (5) importance of reflexivity or attending to researcher bias; (6) importance of establishing validity or credibility; and (7) importance of verification or reliability. General agreement was observed across publications on the first 4 quality dimensions. On the last 3, important divergent perspectives were observed in how these criteria should be applied to qualitative research, with differences based on the paradigm embraced by the authors. CONCLUSION Qualitative research is not a unified field. Most manuscript and grant reviewers are not qualitative experts and are likely to embrace a generic set of criteria rather than those relevant to the particular qualitative approach proposed or reported. Reviewers and researchers need to be aware of this tendency and educate health care researchers about the criteria appropriate for evaluating qualitative research from within the theoretical and methodological framework from which it emerges.
Journal of General Internal Medicine
Sayeeda Rahman
Ciência & Saúde Coletiva
Vera L P Alves
Qualitative Health research procedures that are not always applied, mainly in the analysis phase. Our objective is to present a systematized technique of step-by-step procedures for qualitative content analysis in the health field: Clinical-Qualitative Content Analysis. Our proposal consider that the qualitative research applied to the field of health, can acquire a perspective analogous to clinical practice and aims to interpret meanings expressed in reports through individual interviews or statements. This analysis takes part of the Clinical-Qualitative Method. The literature review was realized through: a book chapter, eight original articles and three methodological articles. The Clinical-qualitative Content Analysis technique comprises seven steps: 1) Editing material for analysis; 2) Floating reading; 3) Construction of the units of analysis; 4) Construction of codes of meaning; 5) General refining of the codes and the Construction of categories; 6) Discussion; 7) Validity. Th...
RELATED PAPERS
Annals of Romanian Society of Cell Biology
YASIR H A I D E R AL-MAWLAH
Phys. Chem. Chem. Phys.
ABDESSELAM BELAARAJ
Schweizerische Ärztezeitung
Michel Romanens
Acta Neurologica Belgica
Kenou van Rijckevorsel
International Journal of Business and Development Studies
International Journal of Workplace Health Management
Johnny Dyreborg
Fisioterapia e Pesquisa
Guilherme Rodrigues
Universitas Humanística
Amurabi Oliveira
Jurnal Analis Medika Biosains (JAMBS)
erlin tatontos
Procedia Materials Science
KOLLI RAMUJEE
Nonlinearity
Changjiang Zhu
Iranian Journal of Chemistry & Chemical Engineering-international English Edition
Mohammad Reza Yaftian
Horacio Chiavazza
The journal of bone and joint surgery
Engineering Geology
Javier Martinez
Physica D: Nonlinear Phenomena
Thanos Manos
Journal of Fungi
Ayesha S Nair
Siti Munawaroh
hjhjgf frgtg
hjhfggf hjgfdf
Devoir surveillé N°2, Sciences mathématiques, Semestre 2, 2BAC PC, SVT, SM A et B, M. Karam Ouharou
Karam Ouharou
Maria Tsampra
Nucleation and Atmospheric Aerosols
Oria Farisi
Metafory polityki vol. 4
Michał Szczegielniak
SSRN Electronic Journal
Martin Cave
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
- Find My Rep
You are here
Sage online ordering services will be unavailable due to system maintenance on April 13th between 2:00 am and 8:00 am UK time If you need assistance, please contact Sage at [email protected] . Thank you for your patience and we apologise for the inconvenience.
Qualitative Health Research
Preview this book.
- Description
- Aims and Scope
- Editorial Board
- Abstracting / Indexing
- Submission Guidelines
Qualitative Health Research provides an international, interdisciplinary forum to enhance health and health care and further the development and understanding of qualitative health research. The journal is an invaluable resource for researchers and academics, administrators and others in the health and social service professions, and graduates, who seek examples of studies in which the authors used qualitative methodologies. Each issue of Qualitative Health Research provides readers with a wealth of information on conceptual, theoretical, methodological, and ethical issues pertaining to qualitative inquiry. A Variety of Perspectives We encourage submissions across all health-related areas and disciplines. Qualitative Health Research understands health in its broadest sense and values contributions from various traditions of qualitative inquiry. As a journal of SAGE Publishing, Qualitative Health Research aspires to disseminate high-quality research and engaged scholarship globally, and we are committed to diversity and inclusion in publishing. We encourage submissions from a diverse range of authors from across all countries and backgrounds. There are no fees payable to submit or publish in Qualitative Health Research .
Original, Timely, and Insightful Scholarship Qualitative Health Research aspires to publish articles addressing significant and contemporary health-related issues. Only manuscripts of sufficient originality and quality that align with the aims and scope of Qualitative Health Research will be reviewed. As part of the submission process authors are required to warrant that they are submitting original work, that they have the rights in the work, that they have obtained, and that can supply all necessary permissions for the reproduction of any copyright works not owned by them, and that they are submitting the work for first publication in the Journal and that it is not being considered for publication elsewhere and has not already been published elsewhere. Please note that Qualitative Health Research does not accept submissions of papers that have been published elsewhere. Sage requires authors to identify preprints upon submission (see https://us.sagepub.com/en-us/nam/preprintsfaq ). This Journal is a member of the Committee on Publication Ethics (COPE) .
This Journal recommends that authors follow the Recommendations for the Conduct, Reporting, Editing, and Publication of Scholarly Work in Medical Journals formulated by the International Committee of Medical Journal Editors (ICMJE).
Qualitative Health Research is an international, interdisciplinary, refereed journal for the enhancement of health care and to further the development and understanding of qualitative research methods in health care settings. We welcome manuscripts in the following areas: the description and analysis of the illness experience, health and health-seeking behaviors, the experiences of caregivers, the sociocultural organization of health care, health care policy, and related topics. We also seek critical reviews and commentaries addressing conceptual, theoretical, methodological, and ethical issues pertaining to qualitative enquiry.
- Applied Social Sciences Index & Abstracts (ASSIA)
- CAB Abstracts (Index Veterinarius, Veterinary Bulletin)
- CABI: Abstracts on Hygiene and Communicable Diseases
- CABI: CAB Abstracts
- CABI: Global Health
- CABI: Nutrition Abstracts and Reviews Series A
- CABI: Tropical Diseases Bulletin
- Clarivate Analytics: Current Contents - Physical, Chemical & Earth Sciences
- Combined Health Information Database (CHID)
- Corporate ResourceNET - Ebsco
- Current Citations Express
- EBSCO: Vocational & Career Collection
- EMBASE/Excerpta Medica
- Family & Society Studies Worldwide (NISC)
- Health Business FullTEXT
- Health Service Abstracts
- Health Source Plus
- MasterFILE - Ebsco
- ProQuest: Applied Social Science Index & Abstracts (ASSIA)
- ProQuest: CSA Sociological Abstracts
- Psychological Abstracts
- Rural Development Abstracts
- SRM Database of Social Research Methodology
- Social Sciences Citation Index (Web of Science)
- Social Services Abstracts
- Standard Periodical Directory (SPD)
- TOPICsearch - Ebsco
Manuscript submission guidelines:
Qualitative Health Research (QHR) has specific guidelines! While Sage Publishing has general guidelines , all manuscripts submitted to QHR must follow our specific guidelines (found below). Once you have reviewed these guidelines, please visit QHR ’s submission site to upload your manuscript. Please note that manuscripts not conforming to these guidelines will be returned and/or encounter delays in peer review. Remember you can log in to the submission site at any time to check on the progress of your manuscript throughout the peer review process.
1. Deciding whether to submit a manuscript to QHR
1.1 Aims & scope
1.2 Article types
2. Review criteria
2.1 Original research studies
2.2 Pearls, Piths, and Provocations
2.3 Common reasons for rejection
3. Preparing your manuscript
3.1 Title page
3.2 Abstract
3.3 Manuscript
3.4 Tables, Figures, Artwork, and other graphics
3.5 Supplemental material
4. Submitting your manuscript
5. Editorial Policies
5.1 Peer review policy
5.2 Authorship
5.3 Acknowledgments
5.4 Funding
5.5 Declaration of conflicting interests
5.6 Research ethics and participant consent
6. Publishing Policies
6.1 Publication ethics
6.2 Contribtor's publishing agreement
6.3 Open access and author archiving
1. Deciding whether to submit a manuscript to QHR
QHR provides an international, interdisciplinary forum to enhance health and health care and further the development and understanding of qualitative health research. The journal is an invaluable resource for researchers and academics, administrators and others in the health and social service professions, and graduates, who seek examples of studies in which the authors used qualitative methodologies. Each issue of QHR provides readers with a wealth of information on conceptual, theoretical, methodological, and ethical issues pertaining to qualitative inquiry.
Rather than send query letters to the Editor regarding article fit, QHR asks authors to make their own decision regarding the suitability of their manuscript for QHR by asking: Does your proposed submission make a meaningful and strong contribution to qualitative health research literature? Is it useful to readers and/or practitioners?
The following manuscript types are considered for publication.
- Original Research Studies : These are fully developed qualitative research studies. This may include mixed method studies in which the major focus/portion of the study is qualitative research. Please read Maintaining the Integrity of Qualitatively Driven Mixed Methods: Avoiding the “ This Work is Part of a Larger Study” Syndrome .
- Pearls, Piths, and Provocations : These manuscripts should foster discussion and debate about significant issues, enhance communication of methodological advances, promote and discuss issues related to the teaching of qualitative approaches in health contexts, and/or encourage the discussion of new and/or provocative ideas. They should also make clear what the manuscript adds to the existing body of knowledge in the area.
- Editorials : These are generally invited articles written by editors/editorial board members associated with QHR.
Please note, QHR does NOT publish pilot studies. We do not normally publish literature reviews unless they focus on qualitative research studies elaborating methodological issues and developments. Review articles should be submitted to the Pearls, Piths, and Provocations section. They are reviewed according to criteria in 2.2.
Back to top
2. Review criteria
2.1 Original research
Reviewers are asked to consider the following areas and questions when making recommendations about research manuscripts:
- Importance of submission : Does the manuscript make a significant contribution to qualitative health research literature? Is it original? Relevant? In depth? Insightful? Is it useful to the reader and/or practitioner?
- Methodological considerations : Is the overall study design clearly explained including why this design was an appropriate one? Are the methodology/methods/approaches used in keeping with that design? Are they appropriate given the research question and/or aims? Are they logically articulated? Clarity in design and presentation? Data adequacy and appropriateness? Evidence of rigor?
- Ethical Concerns : Are relevant ethical concerns discussed and acknowledged? Is enough detail given to enable the reader to understand how ethical issues were navigated? Has formal IRB approval (when needed) and consent from participants been obtained?
- Data analysis, findings, discussion : Does the analysis of data reflect depth and coherence? In-depth descriptive but also interpretive dimensions? Creative and insightful analysis? Are results linked to existing literature and theory, as appropriate? Is the contribution of the research clear including its relevance to health disciplines and their practice?
- Manuscript style and format : Is the manuscript organized in a clear and concise manner? Has sufficient attention been paid to word choice, spelling, grammar, and so forth? Did the author adhere to APA guidelines? Do diagrams/illustrations comply with guidelines? Is the overall manuscript aligned with QHR guidelines in relation to formatting?
- Scope: Does the article fit with QHR ’s publication mandate? Has the author cited the major work in the area, including those published in QHR ?
The purpose of papers in this section is to raise and discuss issues pertinent to the development and advancement of qualitative research in health-related arenas. As the name Pearls, Piths, and Provocations suggests, we are looking for manuscripts that make a significant contribution to areas of dialogue, development, experience sharing and debate relevant to the scope of QHR in this section of the journal. Reviewers are asked to consider the following questions when making recommendations about articles in the Pearls, Piths, and Provocations section.
- Significance : Does the paper highlight issues that have the potential to advance, develop, and/or challenge thinking in qualitative health related research?
- Clarity : Are the arguments clearly presented and well supported?
- Rigor : Is there the explicit use of/interaction with methodology and/or theory and/or empirical studies (depending on the focus of the paper) that grounds the work and is coherently carried throughout the arguments and/or analysis in the manuscript? Put another way, is there evidence of a rigorously constructed argument?
- Engagement : Does the paper have the potential to engage the reader to ‘think differently’ by raising questions, suggesting innovative directions for qualitative health research, and/or stimulating critical reflection? Are the implications of the paper for the practice of either qualitative research and/or health clear?
- Quality of the writing : Is the main argument of the paper clearly articulated and presented with few grammatical or typographical issues? Are terms and concepts key to the scholarship communicated clearly and in sufficient detail?
QHR most commonly turns away manuscripts that fall outside the journal’s scope, do not make a novel contribution to the literature, lack substantive and/or interpretative depth, require extensive revisions, and/or do not adequately address ethical issues that are fundamental to qualitative inquiry. Submissions of the supplementary component of mixed methods studies often are rejected as the findings are difficult to interpret without the findings of the primary study. For additional information on this policy, please read Maintaining the Integrity of Qualitatively Driven Mixed Methods: Avoiding the “ This Work is Part of a Larger Study” Syndrome .
3. Preparing your manuscript for submission
We strongly encourage all authors to review previously published articles in QHR for style prior to submission.
QHR journal practices include double anonymization. All identifying information MUST be removed completely from the Abstract, Manuscript, Acknowledgements, Tables, and Figure files prior to submission. ONLY the Title Page and Cover Letter may contain identifying information. See Sage’s general submission guidelines for additional guidance on making an anonymous submission.
Preferred formats for the text and tables of your manuscript are Word DOC or PDF. The text must be double-spaced throughout with standard 1-inch margins (APA formatting). Text should be standard font (i.e., Times New Roman) 12-point.
3.1 Title page
- The title page should be uploaded as a separate document containing the following information: Author names; Affiliations; Author contact information; Contribution list; Acknowledgements; Ethical statement; Funding Statement; Conflict of Interest Statements; and, Grant Number. Please know that the Title Page is NOT included in the materials sent out for Peer Review.
- Ethical statement: An ethical statement must include the following: the full name of the ethical board that approved your study; the approval number given by the ethical board; and, confirmation that all your participants gave informed consent. Authors are also required to state in the methods section whether participants provided informed consent, whether the consent was written or verbal, and how it was obtained and by whom. For example: “Our study was approved by The Mercy Health Research Ethics Committee (approval no. XYZ123). All participants provided written informed consent prior to enrollment in the study.” If your study did not need ethical approval (often manuscripts in the Pearls, Piths, and Provocations may not), we still need a statement that states that your study did not need approval and an explanation as to why. For example: “Ethical Statement: Our study did not require an ethical board approval because it did not directly involve humans or animals.”
3.2 Abstract and Keywords
- The Abstract should be unstructured, written in narrative form. Maximum of 250 words. This should be on its own page, appearing as the first page of the Main Manuscript file.
- The keywords should be included beneath the abstract on the Main Manuscript file.
- Length: 8,000 words or less excluding the abstract, list of references, and acknowledgements. Please note that text from Tables and Figures is included in the word count limits. On-line supplementary materials are not included in the word limit.
- Structure: While many authors will choose to use headings of Background, Methods, Results, and Discussion to organize their manuscript, it is up to authors to choose the most appropriate terms and structure for their submission. It is the expectation that manuscripts contain detailed reflections on methodological considerations.
- Ethics: In studies where data collection or other methods present ethical challenges, the authors should explicate how such issues were navigated including how consent was gained and by whom. An anonymized version of the ethical statement should be included in the manuscript (in addition to appearing on the title page).
- Participant identification: Generally, demographics should be described in narrative form or otherwise reported as a group. Quotations may be linked to particular participants and/or demographic features provided measures are taken to ensure anonymity of participants (e.g., use of pseudonyms).
- Use of checklists: Authors should not include qualitative research checklists, such as COREQ (COnsolidated criteria for REporting Qualitative research). Generally, authors should use a narrative approach to describe the processes used to enhance the rigor of their study. For additional information on this policy, please read Why the Qualitative Health Research (QHR) Review Process Does Not Use Checklists
- References: APA format. While there is no limit to the number of references, authors are recommended to use pertinent references only, including literature previously published in QHR . References should be on a separate page. QHR adheres to the APA 7 reference style. View the APA guidelines to ensure your manuscript conforms to this reference style. Please ensure you check carefully that both your in-text references and list of references are in the correct format.
- Authors are required to disclose the use of generative Artificial Intelligence (such as ChatGPT) and other technologies (such as NVivo, ATLAS. Ti, Quirkos, etc.), whether used to conceive ideas, develop study design, generate data, assist in analysis, present study findings, or other activities formative of qualitative research. We suggest authors provide both a description of the technology, when it was accessed, and how it was used (see https://uk.sagepub.com/en-gb/eur/chatgpt-and-generative-ai ).
- Manuscripts that receive favorable reviews will not be accepted until any formatting and copy-editing required has been done.
- Tables, Figures, Artwork, and other graphics should be submitted as separate files rather than incorporated into the main manuscript file. Within the manuscript, indicate where these items should appear (i.e. INSERT TABLE 1 HERE).
- TIFF, JPED, or common picture formats accepted. The preferred format for graphs and line art is EPS.
- Resolution: Rasterized based files (i.e. with .tiff or .jpeg extension) require a resolution of at least 300 dpi (dots per inch). Line art should be supplied with a minimum resolution of 800 dpi.
- Dimension: Check that the artworks supplied match or exceed the dimensions of the journal. Images cannot be scaled up after origination.
- Figures supplied in color will appear in color online regardless of whether or not these illustrations are reproduced in color in the printed version. For specifically requested color reproduction in print, you will receive information regarding the costs from Sage after receipt of your accepted article.
- Core elements of the manuscript should not be included as supplementary material.
- QHR is able to host additional materials online (e.g., datasets, podcasts, videos, images etc.) alongside the full-text of the article. For more information please refer to Sage’s general guidelines on submitting supplemental files .
4. Submitting your manuscript
QHR is hosted on Sage Track, a web based online submission and peer review system powered by ScholarOne™ Manuscripts. Visit https://mc.manuscriptcentral.com/QHR to login and submit your article online.
IMPORTANT: Please check whether you already have an account in the system before trying to create a new one. If you have reviewed or authored for the Journal in the past year it is likely that you will have had an account created. For further guidance on submitting your manuscript online please visit ScholarOne Online Help .
5. Editorial policies
QHR adheres to a rigorous double-anonymized reviewing policy in which the identities of both the reviewer and author are always concealed from both parties.
Sage does not permit the use of author-suggested (recommended) reviewers at any stage of the submission process, be that through the web-based submission system or other communication. Reviewers should be experts in their fields and should be able to provide an objective assessment of the manuscript. Our policy is that reviewers should not be assigned to a manuscript if:
• The reviewer is based at the same institution as any of the co-authors
• The reviewer is based at the funding body of the manuscript
• The author has recommended the reviewer
• The reviewer has provided a personal (e.g. Gmail/Yahoo/Hotmail) email account and an institutional email account cannot be found after performing a basic Google search (name, department and institution).
Qualitative Health Research is committed to delivering high quality, fast peer-review for your manuscript, and as such has partnered with Web of Science. Web of Science is a third-party service that seeks to track, verify and give credit for peer review. Reviewers for Qualitative Health Research can opt in to Web of Science in order to claim their reviews or have them automatically verified and added to their reviewer profile. Reviewers claiming credit for their review will be associated with the relevant journal, but the article name, reviewer’s decision, and the content of their review is not published on the site. For more information visit the Web of Science website.
The Editor or members of the Editorial Team or Board may occasionally submit their own manuscripts for possible publication in the Journal. In these cases, the peer review process will be managed by alternative members of the Editorial Team or Board and the submitting Editor Team/Board member will have no involvement in the decision-making process.
Manuscripts should only be submitted for consideration once consent is given by all contributing authors. Those submitting manuscripts should carefully check that all those whose work contributed to the manuscript are acknowledged as contributing authors. The list of authors should include all those who can legitimately claim authorship. This is all those who meet all of the following criteria:
(i) Made a substantial contribution to the design of the work or acquisition, analysis, interpretation, or presentation of data, (ii) Drafted the article or revised it critically for important intellectual content, (iii) Approved the version to be published, (iv) Each author should have participated sufficiently in the work to take public responsibility for appropriate portions of the content.
Acquisition of funding, collection of data, or general supervision of the research group alone does not constitute authorship, although all contributors who do not meet the criteria for authorship should be listed in the Acknowledgments section. Please refer to the International Committee of Medical Journal Editors (ICMJE) authorship guidelines for more information on authorship.
Authors are required to disclose the use of generative Artificial Intelligence (such as ChatGPT) and other technologies (such as NVivo, ATLAS. Ti, Quirkos, etc.), whether used to conceive ideas, develop study design, generate data, assist in analysis, present study findings, or other activities formative of qualitative research. We suggest authors provide both a description of the technology, when it was accessed, and how it was used. This needs to be clearly identified within the text and acknowledged within your Acknowledgements section. Please note that AI bots such as ChatGPT should not be listed as an author. For more details on this policy, please visit ChatGPT and Generative AI .
5.3 Acknowledgements
All contributors who do not meet the criteria for authorship should be listed in an Acknowledgements section. Examples of those who might be acknowledged include a person who provided purely technical help, or a department chair who provided only general support.
Please supply any personal acknowledgements separately to the main text to facilitate anonymous peer review.
Per ICMJE recommendations , it is best practice to obtain consent from non-author contributors who you are acknowledging in your manuscript.
1.3.1 Writing assistance
Individuals who provided writing assistance, e.g., from a specialist communications company, do not qualify as authors and so should be included in the Acknowledgements section. Authors must disclose any writing assistance – including the individual’s name, company and level of input – and identify the entity that paid for this assistance. It is not necessary to disclose use of language polishing services.
Qualitative Health Research requires all authors to acknowledge their funding in a consistent fashion under a separate heading. Please visit the Funding Acknowledgements page on the Sage Journal Author Gateway to confirm the format of the acknowledgment text in the event of funding, or state that: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
It is the policy of Qualitative Health Research to require a declaration of conflicting interests from all authors enabling a statement to be carried within the paginated pages of all published articles.
Please ensure that a ‘Declaration of Conflicting Interests’ statement is included at the end of your manuscript, after any acknowledgements and prior to the references. If no conflict exists, please state that ‘The Author(s) declare(s) that there is no conflict of interest’. For guidance on conflict of interest statements, please see the ICMJE recommendations here .
Research involving participants must be conducted according to the World Medical Association Declaration of Helsinki
Submitted manuscripts should conform to the ICMJE Recommendations for the Conduct, Reporting, Editing, and Publication of Scholarly Work in Medical Journals :
All manuscripts must state that the relevant Ethics Committee or Institutional Review Board provided (or waived) approval. Please ensure that you blind the name and institution of the review committee until such time as your article has been accepted. The Editor will request authors to replace the name and add the approval number once the article review has been completed. Please note that in itself, simply stating that Ethics Committee or Institutional Review was obtained is not sufficient. Authors are also required to state in the methods section whether participants provided informed consent, whether the consent was written or verbal, and how it was obtained and by whom.
Please do not submit the participant’s informed consent documents with your article, as this in itself breaches the participant’s confidentiality. The Journal requests that you confirm to us, in writing, that you have obtained informed consent recognizing the documentation of consent itself should be held by the authors/investigators themselves (for example, in a participant’s hospital record or an author’s institution’s archives).
Please also refer to the ICMJE Recommendations for the Protection of Research Participants .
6. Publishing Policies
Sage is committed to upholding the integrity of the academic record. We encourage authors to refer to the Committee on Publication Ethics’ International Standards for Authors and view the Publication Ethics page on the Sage Author Gateway .
6.1.1 Plagiarism
Qualitative Health Research and Sage take issues of copyright infringement, plagiarism or other breaches of best practice in publication very seriously. The Committee on Publication Ethics (COPE) defines plagiarism as: “When somebody presents the work of others (data, words or theories) as if they were his/her own and without proper acknowledgment.” We seek to protect the rights of our authors and we always investigate claims of plagiarism or misuse of published articles. Equally, we seek to protect the reputation of the journal against malpractice. Submitted articles may be checked with duplication-checking software. Where an article, for example, is found to have plagiarised other work or included third-party copyright material without permission or with insufficient acknowledgement, or where the authorship of the article is contested, we reserve the right to take action including, but not limited to: publishing an erratum or corrigendum (correction); retracting the article; taking up the matter with the head of department or dean of the author's institution and/or relevant academic bodies or societies; or taking appropriate legal action.
6.1.2 Prior publication
If material has been previously published it is not generally acceptable for publication in a Sage journal. However, there are certain circumstances where previously published material can be considered for publication. Please refer to the guidance on the Sage Author Gateway or if in doubt, contact the Editor at the address given below.
6.2 Contributor's publishing agreement
Before publication, Sage requires the author as the rights holder to sign a Journal Contributor’s Publishing Agreement. Sage’s Journal Contributor’s Publishing Agreement is an exclusive licence agreement which means that the author retains copyright of the work but grants Sage the sole and exclusive right and licence to publish for the full legal term of copyright. Exceptions may exist where an assignment of copyright is required or preferred by a proprietor other than Sage. In this case copyright in the work will be assigned from the author to the society. For more information please visit the Sage Author Gateway .
Qualitative Health Research offers optional open access publishing via the Sage Choice programme and Open Access agreements, where authors can publish open access either discounted or free of charge depending on the agreement with Sage. Find out if your institution is participating by visiting Open Access Agreements at Sage . For more information on Open Access publishing options at Sage please visit Sage Open Access . For information on funding body compliance, and depositing your article in repositories, please visit Sage’s Author Archiving and Re-Use Guidelines and Publishing Policies .
- Read Online
- Sample Issues
- Current Issue
- Email Alert
- Permissions
- Foreign rights
- Reprints and sponsorship
- Advertising
Individual Subscription, E-access
Individual Subscription, Print Only
Institutional Backfile Purchase, E-access (Content through 1998)
Institutional Subscription, E-access
Institutional Subscription & Backfile Lease, E-access Plus Backfile (All Online Content)
Institutional Subscription, Print Only
Institutional Subscription, Combined (Print & E-access)
Institutional Subscription & Backfile Lease, Combined Plus Backfile (Current Volume Print & All Online Content)
Individual, Single Print Issue
Institutional, Single Print Issue
Subscription Information
To purchase a non-standard subscription or a back issue, please contact SAGE Customer Services for availability.
[email protected] +44 (0) 20 7324 8701
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Patient Cent Res Rev
- v.11(1); Spring 2024
- PMC11000705

Research Frameworks: Critical Components for Reporting Qualitative Health Care Research
Qualitative health care research can provide insights into health care practices that quantitative studies cannot. However, the potential of qualitative research to improve health care is undermined by reporting that does not explain or justify the research questions and design. The vital role of research frameworks for designing and conducting quality research is widely accepted, but despite many articles and books on the topic, confusion persists about what constitutes an adequate underpinning framework, what to call it, and how to use one. This editorial clarifies some of the terminology and reinforces why research frameworks are essential for good-quality reporting of all research, especially qualitative research.
Qualitative research provides valuable insights into health care interactions and decision-making processes – for example, why and how a clinician may ignore prevailing evidence and continue making clinical decisions the way they always have. 1 The perception of qualitative health care research has improved since a 2016 article by Greenhalgh et al. highlighted the higher contributions and citation rates of qualitative research than those of contemporaneous quantitative research. 2 The Greenhalgh et al. article was subsequently supported by an open letter from 76 senior academics spanning 11 countries to the editors of the British Medical Journal . 3 Despite greater recognition and acceptance, qualitative research continues to have an “uneasy relationship with theory,” 4 which contributes to poor reporting.
As an editor for the Journal of Patient-Centered Research and Reviews , as well as Human Resources for Health , I have seen several exemplary qualitative articles with clear and coherent reporting. On the other hand, I have often been concerned by a lack of rigorous reporting, which may reflect and reinforce the outdated perception of qualitative research as the “soft option.” 5 Qualitative research is more than conducting a few semi-structured interviews, transcribing the audio recordings verbatim, coding the transcripts, and developing and reporting themes, including a few quotes. Qualitative research that benefits health care is time-consuming and labor-intensive, requires robust design, and is rooted in theory, along with comprehensive reporting. 6
What Is “Theory”?
So fundamental is theory to qualitative research that I initially toyed with titling this editorial, “ Theory: the missing link in qualitative health care research articles ,” before deeming that focus too broad. As far back as 1967, Merton 6 warned that “the word theory threatens to become meaningless.” While it cannot be overstated that “atheoretical” studies lack the underlying logic that justifies researchers’ design choices, the word theory is so overused that it is difficult to understand what constitutes an adequate theoretical foundation and what to call it.
Theory, as used in the term theoretical foundation , refers to the existing body of knowledge. 7 , 8 The existing body of knowledge consists of more than formal theories , with their explanatory and predictive characteristics, so theory implies more than just theories . Box 1 9 – 12 defines the “building blocks of formal theories.” 9 Theorizing or theory-building starts with concepts at the most concrete, experiential level, becoming progressively more abstract until a higher-level theory is developed that explains the relationships between the building blocks. 9 Grand theories are broad, representing the most abstract level of theorizing. Middle-range and explanatory theories are progressively less abstract, more specific to particular phenomena or cases (middle-range) or variables (explanatory), and testable.
The Building Blocks of Formal Theories 9
The importance of research frameworks.
Researchers may draw on several elements to frame their research. Generally, a framework is regarded as “a set of ideas that you use when you are forming your decisions and judgements” 13 or “a system of rules, ideas, or beliefs that is used to plan or decide something.” 14 Research frameworks may consist of a single formal theory or part thereof, any combination of several theories or relevant constructs from different theories, models (as simplified representations of formal theories), concepts from the literature and researchers’ experiences.
Although Merriam 15 was of the view that every study has a framework, whether explicit or not, there are advantages to using an explicit framework. Research frameworks map “the territory being investigated,” 8 thus helping researchers to be explicit about what informed their research design, from developing research questions and choosing appropriate methods to data analysis and interpretation. Using a framework makes research findings more meaningful 12 and promotes generalizability by situating the study and interpreting data in more general terms than the study itself. 16
Theoretical and Conceptual Frameworks
The variation in how the terms theoretical and conceptual frameworks are used may be confusing. Some researchers refer to only theoretical frameworks 17 , 18 or conceptual frameworks, 19 – 21 while others use the terms interchangeably. 7 Other researchers distinguish between the two. For example, Miles, Huberman & Saldana 8 see theoretical frameworks as based on formal theories and conceptual frameworks derived inductively from locally relevant concepts and variables, although they may include theoretical aspects. Conversely, some researchers believe that theoretical frameworks include formal theories and concepts. 18 Others argue that any differences between the two types of frameworks are semantic and, instead, emphasize using a research framework to provide coherence across the research questions, methods and interpretation of the results, irrespective of what that framework is called.
Like Ravitch and Riggan, 22 I regard conceptual frameworks (CFs) as the broader term. Including researchers’ perspectives and experiences in CFs provides valuable sources of originality. Novel perspectives guard against research repeating what has already been stated. 23 The term theoretical framework (TF) may be appropriate where formal published and identifiable theories or parts of such theories are used. 24 However, existing formal theories alone may not provide the current state of relevant concepts essential to understanding the motivation for and logic underlying a study. Some researchers may argue that relevant concepts may be covered in the literature review, but what is the point of literature reviews and prior findings unless authors connect them to the research questions and design? Indeed, Sutton & Straw 25 exclude literature reviews and lists of prior findings as an adequate foundation for a study, along with individual lists of variables or constructs (even when the constructs are defined), predictions or hypotheses, and diagrams that do not propose relationships. One or more of these aspects could be used in a research framework (eg, in a TF), and the literature review could (and should) focus on the theories or parts of theories (constructs), offer some critique of the theory and point out how they intend to use the theory. This would be more meaningful than merely describing the theory as the “background” to the study, without explicitly stating why and how it is being used. Similarly, a CF may include a discussion of the theories being used (basically, a TF) and a literature review of the current understanding of any relevant concepts that are not regarded as formal theory.
It may be helpful for authors to specify whether they are using a theoretical or a conceptual framework, but more importantly, authors should make explicit how they constructed and used their research framework. Some studies start with research frameworks of one type and end up with another type, 8 , 22 underscoring the need for authors to clarify the type of framework used and how it informed their research. Accepting the sheer complexity surrounding research frameworks and lamenting the difficulty of reducing the confusion around these terms, Box 2 26 – 31 and Box 3 offer examples highlighting the fundamental elements of theoretical and conceptual frameworks while acknowledging that they share a common purpose.

Examples of How Theoretical Frameworks May Be Used
Examples of how conceptual frameworks may be used, misconceptions about qualitative research.
Qualitative research’s “uneasy relationship with theory” 4 may be due to several misconceptions. One possible misconception is that qualitative research aims to build theory and thus does not need theoretical grounding. The reality is that all qualitative research methods, not just Grounded Theory studies focused on theory building, may lead to theory construction. 16 Similarly, all types of qualitative research, including Grounded Theory studies, should be guided by research frameworks. 16
Not using a research framework may also be due to misconceptions that qualitative research aims to understand people’s perspectives and experiences without examining them from a particular theoretical perspective or that theoretical foundations may influence researchers’ interpretations of participants’ meanings. In fact, in the same way that participants’ meanings vary, qualitative researchers’ interpretations (as opposed to descriptions) of participants’ meaning-making will differ. 32 , 33 Research frameworks thus provide a frame of reference for “making sense of the data.” 34
Studies informed by well-defined research frameworks can make a world of difference in alleviating misconceptions. Good qualitative reporting requires research frameworks that make explicit the combination of relevant theories, theoretical constructs and concepts that will permeate every aspect of the research. Irrespective of the term used, research frameworks are critical components of reporting not only qualitative but also all types of research.
Building public engagement and access to palliative care and advance care planning: a qualitative study
- Rachel Black ORCID: orcid.org/0000-0001-8952-0501 1 ,
- Felicity Hasson ORCID: orcid.org/0000-0002-8200-9732 2 ,
- Paul Slater ORCID: orcid.org/0000-0003-2318-0705 3 ,
- Esther Beck ORCID: orcid.org/0000-0002-8783-7625 4 &
- Sonja McIlfatrick ORCID: orcid.org/0000-0002-1010-4300 5
BMC Palliative Care volume 23 , Article number: 98 ( 2024 ) Cite this article
33 Accesses
2 Altmetric
Metrics details
Research evidence suggests that a lack of engagement with palliative care and advance care planning could be attributed to a lack of knowledge, presence of misconceptions and stigma within the general public. However, the importance of how death, dying and bereavement are viewed and experienced has been highlighted as an important aspect in enabling public health approaches to palliative care. Therefore, research which explores the public views on strategies to facilitate engagement with palliative care and advance care planning is required.
Exploratory, qualitative design, utilising purposive random sampling from a database of participants involved in a larger mixed methods study. Online semi-structured interviews were conducted ( n = 28) and analysed using reflexive thematic analysis. Thematic findings were mapped to the social-ecological model framework to provide a holistic understanding of public behaviours in relation to palliative care and advance care planning engagement.
Three themes were generated from the data: “Visibility and relatability”; “Embedding opportunities for engagement into everyday life”; “Societal and cultural barriers to open discussion”. Evidence of interaction across all five social ecological model levels was identified across the themes, suggesting a multi-level public health approach incorporating individual, social, structural and cultural aspects is required for effective public engagement.
Conclusions
Public views around potential strategies for effective engagement in palliative care and advance care planning services were found to be multifaceted. Participants suggested an increase in visibility within the public domain to be a significant area of consideration. Additionally, enhancing opportunities for the public to engage in palliative care and advance care planning within everyday life, such as education within schools, is suggested to improve death literacy and reduce stigma. For effective communication, socio-cultural aspects need to be explored when developing strategies for engagement with all members of society.
Peer Review reports
It is estimated that globally only 14% of patients who require palliative support receive it [ 1 ]. The World Health Organisation (WHO) advocates for palliative care (PC) to be considered a public health issue and suggests earlier integration of PC services within the wider healthcare system is required [ 2 ]. However, research has shown that a lack of public knowledge and misconceptions about PC may deter people from accessing integrative PC services early in a disease trajectory [ 3 ]. Integral to good PC is the facilitation of choice and decision-making, which can be facilitated via advance care planning (ACP). Evidence suggests that ACP can positively impact the quality of end of life care and increase the uptake of palliative care services [ 4 ]. While ACP is commonly associated with end of life (EOL) care, it provides the opportunity for adults of any age to consider their wishes for future care and other financial and personal planning. However, there is evidence of a lack of active engagement in advance care planning (ACP) [ 5 ]. Recent research exploring knowledge and public attitudes towards ACP found just 28.5% of participants had heard the term and only 7% had engaged in ACP [ 6 ]. Barriers to engagement in ACP discussions have been found to include topics such as death and dying are considered a social taboo, posing an increased risk of distress for loved ones; and [ 6 ] a misconception that ACP is only for those at the end of life rather than future planning [ 7 ]. Therefore, there is a need for a public health approach to ACP, to enable and support individuals to engage in conversations about their wishes and make decisions surrounding their future care.
The need for a public health approach to PC, to tackle the challenges of equity and access for diverse populations, was noted in a recent Lancet paper [ 8 ]. This is further supported in a recent review, exploring inequalities in hospice care in the UK, Australia, New Zealand, and Canada which reported that disadvantaged groups such as those with non-cancer illnesses, people living in rural locations and homeless individuals had unequal access to palliative care [ 9 ]. They postulated that differing levels of public awareness in what hospice care provides, and to whom, was an influencing factor with variations in health literacy and knowledge of health services being present in both minority and socioeconomic groups [ 9 ].
Changes in how we experience death and dying have resulted in a shift away from family and community settings into healthcare settings. The Lancet commission exploring the ‘Value of Death’, suggests it has created an imbalance where the value of death is no longer recognised [ 10 ]. The commission’s report posits the need to rebalance death, dying and grieving, where changes across all death systems are required. This needs to consider how the social, cultural, economic, religious, and political factors that determine how death, dying, and bereavement are understood, experienced, and managed [ 10 ].
New public health approaches that aim to strengthen community action and improve death literacy, through increased community responsibility are reflected in initiatives, such as ‘Compassionate Communities’ and ‘Last Aid’ [ 11 , 12 ]. However, a suggested challenge is the management of potential tensions that are present when attempting to conceptualise death in a way that mobilises a whole community [ 13 ]. Whilst palliative care education (PCE) can be effective in improving knowledge and reducing misconceptions, many PCE intervention studies, have focused on carers and healthcare professionals [ 14 ]. Initiatives such as ‘Last Aid’ attempt to bridge this gap by focusing on delivering PCE to the public, however, they are not embedded into the wider social networks of communities. It can be argued that public health campaigns, such as these are falling short by neglecting to use the full range of mass media to suit different ages, cultures, genders and religious beliefs [ 15 ]. Consequently, to understand what is required to engage the public successfully, the voice of the public must lead this conversation. Therefore, this study sought to explore public views on strategies and approaches to enable engagement with palliative care and advance care planning to help share future debate and decision making.
Within the last decades the delivery of PC and ACP have been increasingly medicalised and viewed as a specialist territory, however in reality, the care of those with life-limiting conditions occurs not only within clinical settings but within a social structure that affects the family and an entire community [ 16 ]. Therefore, death, dying and bereavement involve a combination of social, physical, psychological and spiritual events, therefore, to frame PC and ACP within a public health approach the response requires a shift from the individual to understanding the systems and culture within which we live. The Social Ecological Model (SEM) recognises the complex interplay between individual behaviours, and organisational, community, and societal factors that shape our acceptance and engagement. SEM provides a framework to understand the influences affecting engagement with PC and ACP and has been utilised as a lens through which the data in this study is explored.
Qualitative research, using semi-structured interviews were adopted as this enabled an in-depth understanding of public views on strategies to enable engagement with PC. This research was part of a larger mixed-methods study [ 17 ]. Comprehensive Consolidated Criteria for Reporting Qualitative research (COREQ) were used [ 18 ](See Supplementary file 1 ).
A purposive random sampling method, using a random number generator, was adopted to recruit participants who consented to be contacted during data collection of a larger mixed methods study. Selected individuals were contacted by telephone and email to invite them to participate. Inclusion and exclusion criteria are outlined in Table 1 . Interested individuals were provided with a participant information sheet detailing the aims of the study and asked to complete a consent form and demographic questionnaire.
A total of 159 participants were contacted, 105 did not respond, 21 declined and three were ineligible to participate. A total of thirty participants consented, however, two subsequently opted to withdraw prior to the interview.
Data collection
Data was collected from December 2022 to March 2023 by RB. The qualitative interview schedule comprised four broad topic areas: (1) participants’ knowledge of PC and ACP; (2) sources of information on PC and ACP and current awareness of local initiatives for public awareness; (3) knowledge of accessibility to PC and ACP and (4) future strategies for promoting public awareness of PC and ACP, with a consideration of supporting and inhibiting factors. The interview schedule was adapted from a previous study on palliative care to incorporate the topic of ACP [ 3 ] (See Supplementary file 2 ). This paper reports on future strategies.
Participants were asked to complete a short demographic questionnaire prior to the interview to enable the research team to describe the characteristics of those who participated. These questions included variables such as age, gender, religion, marital status, behaviour relating to ACP and experience of PC.
Data was collected via online interviews conducted using the videoconferencing platform Microsoft Teams. Interviews lasted between 20 and 60 min and were recorded with participant consent. Data were stored on a secure server and managed through NVivo 12 Software.
Data analysis
Qualitative data were transcribed verbatim automatically by Microsoft Teams and the transcripts were reviewed and mistakes corrected by the interviewer. All identifying information was removed. Transcripts were analysed using reflexive thematic analysis which involved a six-step process: familiarisation, coding, generating initial themes, developing and reviewing themes, refining, defining and naming themes, and writing up [ 19 ]. Themes were derived by exploring patterns, similarities and differences within and across the data in relation to participant’s views on the promotion of PC and ACP and the best ways to engage the public in open discussions.
The study explored the data through a SEM lens to provide a holistic framework for understanding the influences surrounding health behaviour change in relation to palliative care and advance care planning by mapping the findings to each of the SEM constructs.
The SEM for public health was conceptualised by McLeroy et al. [ 20 ]., and was based on previous work by Bronfenbrenner’s ecological systems theory [ 21 ]. The SEM looks to identify social-level determinants of health behaviours [ 22 ]. Five factor levels have been identified within the SEM; (1) Intrapersonal factors (2) Interpersonal processes (3) Institutional factors (4) Community factors and (5) Public policy [ 20 ]. In short, the SEM suggests that the social factors that influence health behaviours on an individual level are nestled within a wider complex system of higher levels. Current research literature has explored SEM as a model for understanding barriers and facilitators to the delivery of PC, adults’ preferences for EOL care and older adults’ knowledge and attitudes of ACP within differing socioeconomic backgrounds [ 23 , 24 , 25 ]. It has demonstrated the importance of a multilevel approach within these populations. However, there is a scarcity of research exploring strategies for public engagement with PC and/or ACP which are underpinned by SEM theory.
To ensure rigour in the analysis four members of the research team (RB, SM, FH, EB) independently reviewed the transcripts and were involved in the analysis and development of themes as a method of confirmability [ 26 ].
Ethical approval was gained from the University Research Ethics Filter Committee prior to commencing data collection. Participants provided written informed consent prior to the commencement of the interviews. They were advised of their right to withdraw, and the confidentiality and anonymity of all data were confirmed. All data was kept in accordance with the Data Protection Act (2018) [ 27 ].
All participants were white; 70% were female (n-19) and 70% were either married or cohabiting (n-19). The largest proportion of the sample 44% was aged under 50 years (n-12), with 22% aged between 50 and 59 (n-6) and 33% (n-9) aged between 60 and 84. Over half of the sample was employed (n-15), 15% were self-employed [ 4 ] whilst 26% were retired (n-7). Demographic data were missing for one of the included participants (see Table 2 ).
Responses to questions relating to ACP knowledge and behaviours found just 12 participants had heard of the term ACP prior to completing the Northern Ireland Life and Times Survey. Furthermore, none of the participants had been offered the opportunity to discuss ACP and none had prepared a plan of their wishes and preferences.
Main findings
Three overarching themes were generated from the data: ‘Visibility and relatability’; ‘Embedding opportunities for engagement into everyday life’; ‘Societal and cultural barriers. These findings were then mapped to the five social ecological model (SEM) levels ( individual; interpersonal; institutional; community; and policy ) to demonstrate the importance of a multilevel approach when seeking to engage the public around PC and ACP. See Fig. 1 for SEM construct mapping.
Theme 1: visibility and relatability
This theme relates to the suggestion that social taboo was a barrier to awareness and the mechanism to ameliorate this was visibility – in turn promoting reduction of stereotypes and promoting understanding and engagement. This posits the idea that the lack of understanding of PC is the root cause of much of the stigma surrounding it. The SEM construct mapping suggests a multilevel approach is required with intrapersonal (increased individual understanding), interpersonal (openness in discussion with friends and family through media normalisation) and institutional (health service policies for promotion and support) levels being identified.
Participants discussed how there is a lack of knowledge on what PC is, with many assuming that it was for people in the latter stages of life or facing end of life care. This highlighted the lack of individual education with participants suggesting that there should be more visibility and promotion on PC and ACP so that individuals are better informed.
“So, it’s really um there needs to be more education, maybe, I think around it. So that people can view it maybe differently or you know talk about it a bit more. Yeah, probably demystifying what it is. This is this is what it is. This isn’t what it is. You know, this isn’t about um, ending your life for you, you know. And this is about giving you choices and ensuring that you know, you know people are here looking after you”(P37538F45) .
However, there was a recognition that individual differences play a part in whether people engage in discussions. A number of participants explored the idea that some people just don’t want to talk about death and that for some it was not a subject that they want to approach. Despite this, there was a sense that increasing visibility was considered important as there will still be many people who are willing to increase their knowledge and understanding of PC and ACP.
“I can talk about it, for example, with one of my sisters, but not with my mom and not with my other sister or my brothers. They just refuse point blank to talk about it…. some of them have done and the others have started crying and just shut me. Shut me off. And just. No, we don’t want to talk about that. So, it just depends on the personality, I suppose” (P14876F59) .
The lack of knowledge and awareness of PC and ACP was suggested to be the attributed to the scarcity of information being made available at a more institutional level. For some participant’s, this was felt to be the responsibility of the health service to ensure the knowledge is out there and being promoted.
“I think people are naive and they know they’re not at that stage and they don’t know what palliative care is, you know. It’s all like it’s ignorance. But our health service is not promoting this. Well in my eyes, they’re not promoting it whatsoever. And they should, they should, because it would help a hell of a lot of people ” (P37172M61). “I and I think it needs to be promoted by the point of contact, whether it’s a GP, National Health, whatever it might be, I think when they’re there, there needs to be a bit more encouragement to have that conversation” (P26495M43) .
The lack of visibility within the general practice was discussed by several participants who said that leaflets and posters would be helpful in increasing visibility. One participant went as far as to say that a member of staff within a GP surgery would be beneficial.
“I suppose the palliative care because it is a bit more personal. There should be even maybe a professional that you could talk to in your GP practice, or you know, like they have mental health practitioners now in GP practices. Maybe there are I don’t know if there is or not, but there should be maybe a palliative health practitioner that talks to people when they are at that stage of their life” (P21647F29).
Participants also noted how there were generational differences in how people accessed health information. Many of the participants suggested that they would turn to the internet and ‘google’ for information, however, the suggestion was made that care should be taken to target awareness campaigns to different age groups via different methods to reduce disparities in technology skills such as those with less computer literacy.
“ I think a certain proportion of society need the visibility because they’re not always going to be self-sufficient enough to jump on the Internet even though you know we’re getting to the point now where the generational thing is. The generation have been brought up with the Internet and they’re obviously they go to it as the first point of call. But we still got the generation at the moment that don’t”. (P25046F-)
One of the participants talked about ways to increase visibility via the use of the media, including social media, and the utilisation of famous faces.
“Yeah, I think you know, they need to discuss it on Loose Women. You know, morning TV need to get on the bandwagon….But you know. It only takes like that one celebrity to mention it and then the whole media is jumping on the bandwagon.” (P19874F-) .
The UK media coverage of other successful campaigns such as those highlighting mental health and bowel cancer were noted to have been particularly helpful in raising awareness.
“if I think myself about the whole exposure that we have and as a society at the minute about mental health in general, you know a lot of the work on that has been done via social media. You know, celebrities hash tagging and talked about their experience. It’s OK to not be OK etcetera. And I feel like that is responsible for a lot of people who are now discussing their mental health” (P21647F29) .
The sentiment expressed in the above quotes regarding increased visibility in the media also suggests that unless a topic seems relevant to an individual then they won’t engage with health promotion. This concept of relatability pertains to those aspects of human empathy where they can place themselves within a situation leading it to become more relevant to them.
Many participants discussed that using real-life stories on television and in campaigns would be an effective way to connect with the public and it would make PC and ACP more relatable and highlight the importance of thinking about it.
“I think always what tends to be most effective is when it’s somebody that we could all relate to telling their own story (…)……I’m not too sure I know enough about what it involves, but really, like the consequences, that the consequences that people have suffered from not having done that. Not knowing what the wishes were, not having planned for it”. (P32288F62)
Several participants discussed how the topics of PC and ACP were not something they would identify with as being relevant to them. The suggestion was that without it being an immediate concern, for example, if they were not approaching a certain age, then they would assume that they did not need to increase their knowledge about what PC or ACP involves.
“You have to be able to relate to it in order to think, oh, yeah, that applies to me. You need to have something in which you identify with”. (P13697F51)
Theme 2: embedding opportunities for engagement into everyday life
Throughout the discussions, there was evidence that participants felt that death literacy could be increased by providing more opportunities to gain knowledge about planning for future care and what PC involves. Education was highlighted as a potential pathway to engaging the public by targeting appropriate age groups and professions with relevant knowledge and skills. For some, this was thought to be best achieved through educating the youth and for others, the importance of educating those who are working in the healthcare profession was particularly salient. In addition, almost half of the participants suggested they would approach charity organisations for information, with participants advocating for education within secondary and tertiary levels and within community organisations. This data reflects an institutional-level construct within the SEM framework.
Educating younger generations on the topics of PC and ACP through open discussions in schools, and providing skills on how to have difficult conversations with loved ones were seen to be a valuable strategies.
“ young people don’t have that ability to accept and admit and bring it out into the open and I think they need to be perhaps encouraged more to do that through some kind of teaching in the school environment when they’re at a young and impressionable age ”. (P25046F-)
Due to the difficulties around having conversations about death, it was suggested that different healthcare professionals should be trained to have conversations with their patients.
“Yeah, it’s like you think the discussions are difficult to broach for maybe health care professionals that you know, a difficult topic even for them to bring up. Well, if you’re working with someone who’s you know with a family and where things are quite distressed and very often it can be either, it can be the stress can cause a lot of friction and you know, decision making can be very difficult for people…., but just at every level, there’s, you know, possibility to be having conversations like that with people.”(P37538F45) . “I suppose you could think about training some care professionals (…) there may be some way that as a second part of the person’s job or whatever that they’re trained so that people could go along and discuss ” (P19265F76) .
Further to education for young people and healthcare professionals, there was the recognition that community organisations are perfectly positioned to educate the public in PC and ACP. One participant highlighted the missed opportunity to educate family members and carers through an existing programme on dementia. This is particularly pertinent to ACP due to the impact of cognitive decline on decision-making.
“I went to zoom meetings for four weeks in a row with the Alzheimer’s Society. Umm regarding things to do with dementia. And you know, there was a week about your finances and things like that. I suppose. They never really talked about end of life care you know that sort of thing. Um I suppose it would have been useful had they you know, broached that subject as well. But it wasn’t, you know, there was more about looking after yourself, looking after the person. The symptoms of dementia and all this sort of thing, Alzheimer’s and then you know, um the financial and the help available to you. You know, but they didn’t mention about the end-of-life care and like the end result of dementia, I guess, is death. So, you know that that subject, you know, I was, I suppose to just those organizations that deal with um the issues of, like dementia or, as you say, all the rest for, you know, the rest of the diseases and that. You know to be up front and honest and say you know where this can lead and to make people you know, make people aware that there is a palliative care process that can be gone through.” (P19874F-) .
Furthermore, the option of a helpline was suggested with reference made to other successful charity helplines such as the National Society for the Prevention of Cruelty to Children (NSPCC) and The Samaritans. Whilst it was acknowledged there were specialist support services available for people living with a terminal diagnosis, there was a sense that a generic information support helpline would be helpful.
“You know, people need to be (aware)… they’re not alone. There is help out there. You know, you see your helpline, your children, NSPCC, your Samaritans. All on all these helplines, I have to think, I’ve never seen a helpline for palliative care or who you can contact. You don’t see things like that.” (P22964F52) .
In addition to education, the suggestion that embedding ACP discussions into other more common aspects of future planning such as will making, and organ donation was postulated as a potential way to engage the public. This demonstrated clear links to the policy and institutional level constructs within SEM. Changes within organisational policies and public law to support individuals to consider future planning would promote better engagement on a wider societal level.
Participants suggested that they would like to see some of the conversations surrounding ACP introduced into workplace policies and guidelines, as well as through other legal discussions. They noted that conversations surrounding future planning already occur when discussing legal wills and workplace pensions. The potential to expand these discussions to include ACP with solicitors and in workplaces was seen to be a missed opportunity.
“So maybe um around people who are making their wills and you know, you get will making services advertised and things like that. And I think once you get into your 30s and 40s, people start thinking about a will and things like that. So maybe aligned to something like that, you know would get younger people.” (P13790F67) . “when people talk about the pension, you know so retirement, you know, to make people aware about this as well. You know, I would say that’s probably good ways to reach people” (P21263M54) .
Current legislation and promotion regarding organ donation were discussed as being successful in engaging the public and therefore implied that the government should take a more active role in the promotion of ACP.
“If you look at the way, sort of, government have been promoting like organ donation and that. You know that sort of thing. And then people have really bought into it and you know, and there’s a lot of positivity around it. So, I think that’s sort of similar approach would be good”. (P29453F40) “You know, people talking about pension, pension plans and so on and it’s part of the natural life circle, you know. So, if it’s in connection with this, you know, so think about your future, make your plans …so probably in connection with organ donation and so on, you know, so I think they could be trigger points, you know,, people talking about this.” (P21263M54) .
Theme 3: societal and cultural barriers to open discussion
In conversations surrounding why there was a lack of openness in discussion, participants postulated that a potential factor was the influence of cultural and societal norms. This was found to overlap in the SEM levels of intrapersonal, interpersonal and community.
Rural farming communities were highlighted as potentially being more isolated and traditional in their views around death and dying, whilst those with strong religious beliefs were seen to be less likely to engage in discussions.
“You know, and there is a, I’m out in the countryside. Well, it’s (place name). So it’s a relatively rural sort of conservative place and it and it’s that… you know you’re tied to the land, you’re tied to the farm. This is your home and sending you away from it early it is seen as a bit of a shameful thing. So yeah, to try and educate folk and to try and speak into that I think would be really helpful because again, I’ve seen situations where probably the individual’s life, the end of life, has been made tougher because the family have fought to keep that person at home.…. We’re going to try and do it ourselves” (P26495M43) . “I think it’s probably a lot to do with religion more than likely because people just like to hear, because we still are very much, you know, a lot is dictated by religion. So, people just want to leave stuff in God’s hands so they don’t want to have like…that would be the kind of where my mom and dad are coming from, you know, don’t interfere with it, blah blah blah. So, it’s a very gentle like kind of reminding them, you know, well, I think we do need to think about it. And I think people are afraid that they’ll make again that um it’s kind of euthanasia you know what I mean” (P37538F45) .
Cultural differences between countries were also considered with some seeing other global communities approaching death as a celebration rather than something to shy away from.
“I think in Northern Ireland we are, and the UK and probably the world in general. We are really poor at talking about, about death, and it has to be a positive thing to be able to talk more about death. You look at other cultures where you know. Death is treated differently, you know, even in Africa things where, you know, it’s a real celebration, whereas it’s seen so differently in in Northern Ireland” (P31154F35) .
Furthermore, regions and countries that have experienced war and conflict were perceived by one participant as a potential barrier to engaging in subject matters which involve death.
“I don’t I don’t know about other countries, but those that grew up maybe during the conflict here, maybe it’s just something that, you know it’s it’s a completely different mindset to them” (P23609M39) .
Whilst it is unclear from the data why the participant felt the conflict might inhibit engagement with the subject of dying, it could be interpreted that the participant was suggesting that death is too morbid to engage with following a conflict period which saw numerous deaths. An alternative interpretation could be that people are desensitised to death and do not see death as something that an individual has autonomy over.
It was noted that in many modern societies communities are changing. People no longer interact with their neighbours in the way they used to which results in a reduced sense of community responsibility.
“I don’t know that everyone is as neighbourly as they used to be. Northern Ireland I always perceived as being open door policy and everybody looked out for everyone else. But I think as a society has changed and it has changed in Northern Ireland, and it’s become becoming more closed (…) So I think we need to try and encourage that community um experience back again so that people are mindful of their neighbours and share that responsibility and making sure that everyone’s OK” (P25046F) .
This sense of social isolation was discussed by one participant who referred to homeless people. They reflected on how current social structures may not be providing the information and support to this minority group and therefore should be considered when developing public health approaches to engaging them in PC and ACP education.
“And if you look at homeless people on the streets, where do they get the information from? Where do they get the care, the information, the attention. I know there are Street workers that work, but I don’t know again to what extent in Northern Ireland compared with the likes of London” (P25046F) .
Mapping the findings to a social ecological model framework
Following thematic analysis each of the resulting themes were mapped to the five socioecological levels identified by McLeroy et al. (1988) for health promotion programmes. Construct mapping can be found in Fig. 1 below.
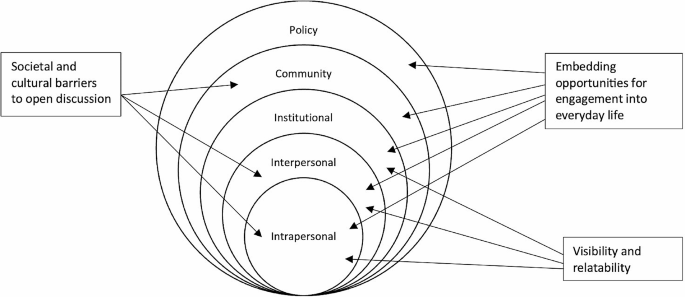
Thematic interaction within the Social Ecological Model levels
The findings from this study highlight the complexity of current public perceptions of palliative care and their views on effective engagement with PC and ACP. Within medicalised western culture there is a tendency to focus on the preservation of life, with conversations about death avoided. This has resulted in death becoming a taboo, raising fear and stigma where death is equated with failure. These social taboos that exist around death, dying and bereavement are posited to stem from the lack of awareness and understanding of PC and ACP and the resulting stigma of approaching these discussions. There was evidence of influencing factors on all SEM levels, which demonstrates the need for a multifaceted public health approach that uses not only behaviour change communication but also social change communication, social mobilisation and advocacy. It can be argued this reflects the key aspects outlined in Lancet Commission report on ‘Valuing Death’, which advocated for a ‘systems approach’ [ 10 ]. This systems approach is aligned to differing levels within the SEM and the different approaches the public have identified when seeking to build public engagement and access to palliative care. Three key aspects were noted: visibility, embedding opportunities for engagement in everyday life and societal and cultural influences.
It was clear from the analysis that a major factor associated with poor public engagement was the lack of visibility within the public domain, which was hindering both the normalisation of death and understanding that PC was more than just end of life care. The findings demonstrated different ways to address the lack of visibility, such as the use of targeted social media and wider publicity campaigns. Research to date has demonstrated that palliative care education is a useful tool in improving knowledge of, confidence in and attitudes towards palliative care amongst healthcare professionals and carers [ 14 ]. Similar results have been noted for the public when exploring the potential to promote palliative care through various media challenges such as YouTube and social media [ 28 ]. This does, however, raise questions around the quality and accuracy of information offered via the media, taking cognisance of whether some of the messaging may inadvertently be adding to misunderstanding, and thus a lack of public engagement.
Secondly, the findings indicated that experience at the individual level within a social context was noted as an important element when seeking ways to increase public engagement with PC and ACP. The experience of illness, dying and loss is often overlooked, therefore, this points to the potential value of community-based education approaches, with peers enabling experience-based exchange. Such interventions have been noted in the literature on the role of volunteers and education [ 29 ]. This reflects the need for an overall public health palliative care approach that seeks to empower individuals, families and communities to draw on their own resources and community supports to adapt and cope with death and dying [ 6 , 30 ].
Thirdly, the findings from this study indicated the need for enhancing opportunities for engagement in PC and ACP within everyday life. Research indicates there is an appetite for people to talk about death, for example, in the UK, a recent YouGov ‘daily question’ survey reported 67% of adults who responded think the subject of death and dying should be talked about in schools [ 31 ]. This speaks to the need to consider schools, workplaces and key trigger points in life as times to consider engagement with PC and ACP. This reflects the overall need for death literacy in society to improve experiences at the end of life [ 10 ].
Finally, the importance of socio-cultural aspects for the public cannot be underestimated. Therefore, effective communication strategies need to be tailored to individuals, and communities and be culturally appropriate. This has been noted as an important aspect for specific communities, such as the Chinese diaspora, for example, but nuances around this for specific ethnic, political, religious, and geographical aspects need further consideration [ 32 ]. Cultural competence, defined as an understanding of how culture affects an individual’s beliefs, values and behaviour, is an important consideration [ 33 ]. A meta-analysis of 19 review articles, concluded that interventions to increase cultural competence in healthcare were effective in enhancing the knowledge, skills and attitudes of healthcare providers, leading to clinical benefits for patients/clients through improved access and utilization of healthcare [ 34 ]. The translation of such reviews for public engagement in PC and ACP warrants further exploration. It has been advocated that elements of cultural systems should be analysed with a socio-ecological framework [ 35 ]. Such consideration and integration of salient contextual cultural factors could assist public messaging and cultural communication, which would enhance more effective and sustainable public engagement in PC and ACP.
Limitations
When considering potential limitations, it is pertinent to note that due to the sensitive nature of the topic the exclusion criteria restricted the sample to those who had not experienced a recent bereavement. This may have limited the ability to gain a wider perspective, as the views of the recently bereaved may have provided further nuanced insights into how best to engage the public. Furthermore, the participant sample was limited to those involved in a larger mixed-methods study. This may have introduced bias in relation to true knowledge and attitudes due to the participants having completed the survey questionnaire prior to the interviews.
In conclusion, this qualitative study has provided insights into how the public would like to be engaged in PC and ACP. The findings highlighted that to build public engagement and access to palliative care and advance care planning a multifaceted public health approach is required. Discussions of death and dying remain difficult for many members of society, therefore, an increase in death literacy across all systems to reduce misperceptions surrounding PC and APC is needed, by increasing visibility and providing opportunities for the public to engage with PC and ACP within everyday life. Finally, socio-cultural aspects need consideration when developing strategies to ensure effective communication and engagement with all members of the community.
Data availability
The datasets analysed are not publicly available but are available from the corresponding author upon reasonable request.
Abbreviations
Advance care plan
- Palliative care
Palliative care education
Social ecological model
World Health Organization. Newsroom Palliative Care Fact Sheet. 2020. https://www.who.int/news-room/fact-sheets/detail/palliative-care .
World Health Assembly 67. Strengthening of palliative care as a component of comprehensive care throughout the life course [Internet]. 2014. https://apps.who.int/iris/handle/10665/162863 .
McIlfatrick S, Slater P, Beck E, Bamidele O, McCloskey S, Carr K, et al. Examining public knowledge, attitudes and perceptions towards palliative care: a mixed method sequential study. BMC Palliat Care. 2021;20(1):44.
Article PubMed PubMed Central Google Scholar
Brinkman-Stoppelenburg A, Rietjens JA, Van Der Heide A. The effects of advance care planning on end-of-life care: a systematic review. Palliat Med. 2014;28(8):1000–25.
Article PubMed Google Scholar
Grant MS, Back AL, Dettmar NS. Public perceptions of Advance Care Planning, Palliative Care, and Hospice: a scoping review. J Palliat Med. 2021;24(1):46–52.
McIlfatrick S, Slater P, Bamidele O, Muldrew D, Beck E, Hasson F. ‘ It’s almost superstition: If I don’t think about it, it won’t happen ’. Public knowledge and attitudes towards advance care planning: A sequential mixed methods study. Palliat Med. 2021;35(7):1356–65.
Canny A, Mason B, Boyd K. Public perceptions of advance care planning (ACP) from an international perspective: a scoping review. BMC Palliat Care. 2023;22(1):107.
Mills J, Abel J, Kellehear A, Patel M. Access to palliative care: the primacy of public health partnerships and community participation. Lancet Public Health. 2021;6(11):e791–2.
Tobin J, Rogers A, Winterburn I, Tullie S, Kalyanasundaram A, Kuhn I, et al. Hospice care access inequalities: a systematic review and narrative synthesis. BMJ Support Palliat Care. 2022;12(2):142–51.
Sallnow L, Smith R, Ahmedzai SH, Bhadelia A, Chamberlain C, Cong Y, et al. Report of the Lancet Commission on the value of death: bringing death back into life. Lancet. 2022;399(10327):837–84.
Kellehear A. Compassionate communities: end-of-life care as everyone’s responsibility. QJM. 2013;106(12):1071–5.
Last Aid. Last Aid [Internet]. 2023. https://www.letztehilfe.info/project/ .
Sawyer JM, Higgs P, Porter JDH, Sampson EL. New public health approaches to palliative care, a brave new horizon or an impractical ideal? An integrative literature review with thematic synthesis. Palliat Care Soc Pract. 2021;15:263235242110329.
Article Google Scholar
Li WW, Chhabra J, Singh S. Palliative care education and its effectiveness: a systematic review. Public Health. 2021;194:96–108.
Article CAS PubMed Google Scholar
Seymour J. The Impact of Public Health Awareness Campaigns on the awareness and quality of Palliative Care. J Palliat Med. 2018;21(S1):S–30.
Seymour JE. Revisiting medicalisation and ‘natural’ death. Soc Sci Med. 1999;49(5):691–704.
McIlfatrick S, Slater PF, Beck E, Hasson F, Black R. NI Life and Times Survey: palliative care and Advance Care Planning. Ulster University; 2023.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Braun V, Clarke V. Thematic analysis: a practical guide. 1st ed. SAGE; 2022. p. 338.
McLeroy KR, Bibeau D, Steckler A, Glanz K. An Ecological Perspective on Health Promotion Programs. Health Educ Q. 1988;15(4):351–77.
Bronfenbrenner U. Toward an experimental ecology of human development. Am Psychol. 1977;32(7):513–31.
Sutton S. Determinants of Health-Related Behaviours: Theoretical and Methodological Issues. In: The SAGE Handbook of Health Psychology [Internet]. 1 Oliver’s Yard, 55 City Road, London EC1Y 1SP United Kingdom: SAGE Publications Ltd; 2008 [cited 2023 Jun 21]. pp. 94–126. https://sk.sagepub.com/reference/hdbk_sagehealthpsych/n4.xml .
Tripken JL, Elrod C, Bills S. Factors influencing Advance Care Planning among older adults in two socioeconomically diverse Living communities. Am J Hosp Palliat Med. 2018;35(1):69–74.
Chen Y, Zhang R, Lou Y, Li W, Yang H. Facilitators and barriers to the delivery of palliative care to patients with Parkinson’s disease: a qualitative study of the perceptions and experiences of stakeholders using the socio-ecological model. BMC Health Serv Res. 2023;23(1):215.
Huang Y, Yates P, Thorberg FA, Wu C (Jo), editors. Influence of social interactions, professional supports and fear of death on adults’ preferences for life-sustaining treatments and palliative care. Int J Nurs Pract [Internet]. 2022 Aug [cited 2023 Jun 21];28(4). https://onlinelibrary.wiley.com/doi/ https://doi.org/10.1111/ijn.12940 .
Korstjens I, Moser A, Series. Practical guidance to qualitative research. Part 4: trustworthiness and publishing. Eur J Gen Pract. 2018;24(1):120–4.
Data Protection Act. (2018) [Internet]. https://www.legislation.gov.uk/ukpga/2018/12/contents/enacted .
Liu M, Cardenas V, Zhu Y, Enguidanos S. YouTube Videos as a Source of Palliative Care Education: a review. J Palliat Med. 2019;22(12):1568–73.
Buonocore S, Sussman-Skalka C, Project, insights: An evaluation of a community vision education project for older adults. Educ Gerontol. 2002;28(4):289–99.
McIlfatrick S, Hasson F, Slater PF, Beck E, Hanna-Trainor L, Muldrew D. Where are we now? - Examining public knowedge and attitudes towards palliative care and advance care planning in Northern Ireland [Internet]. 2021. https://www.ulster.ac.uk/__data/assets/pdf_file/0012/819678/Where-are-we-now-Examining-public-knowledge-and-attitudes-towards-palliative-care-and-advance-care-planning-in-NI.pdf .
YouGov. Daily question. Do you think the subject of death, and issues around dying, should or should not be taught in schools? https://yougov.co.uk/topics/philosophy/survey-results/daily/2021/03/16/d5536/2 .
Li Z, Beck ER, McIlfatrick S, Hasson F. Chinese Diaspora communities’ knowledge of and Engagement with Advance Care Planning: a systematic integrative review. J Palliat Care. 2023;38(3):381–97.
Balcazar FE, Suarez-Balcazar Y, Taylor-Ritzler T. Cultural competence: development of a conceptual framework. Disabil Rehabil. 2009;31(14):1153–60.
Truong M, Paradies Y, Priest N. Interventions to improve cultural competency in healthcare: a systematic review of reviews. BMC Health Serv Res. 2014;14(1):99.
Cain CL, Surbone A, Elk R, Kagawa-Singer M. Culture and Palliative Care: preferences, communication, meaning, and mutual decision making. J Pain Symptom Manage. 2018;55(5):1408–19.
Download references
Acknowledgements
The authors would like to thank all interviewees for their participation in the research.
This study was funded by HSC R&D Division of Public Health Agency in Northern Ireland.
Author information
Authors and affiliations.
Institute of Nursing and Health Research, Ulster University, Belfast, BT15 1AD, Northern Ireland
Rachel Black
Felicity Hasson
Institute of Nursing and Health Research, Ulster University, Belfast, BT15 1ED, Northern Ireland
Paul Slater
Esther Beck
Sonja McIlfatrick
You can also search for this author in PubMed Google Scholar
Contributions
SMcI is principal investigator responsible for study design, project management, analysis and manuscript review and dissemination. FH, PS, EB were responsible for study design, analysis, manuscript review and dissemination. RB was responsible for qualitative data collection, analysis, manuscript drafting and dissemination. All authors reviewed and approved the final manuscript.
Corresponding author
Correspondence to Sonja McIlfatrick .
Ethics declarations
Conflicts of interest.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics approval and consent to participate
Ethical approval was granted from the Ulster University Nursing and Health Sciences Ethics Filter Committee (FCNUR-22-063 Sept 2022). Participants provided written informed consent prior to the commencement of the interviews. They were advised of their right to withdraw, and the confidentiality and anonymity of all data was confirmed. All data was kept in accordance with the Data protection act (2018).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Black, R., Hasson, F., Slater, P. et al. Building public engagement and access to palliative care and advance care planning: a qualitative study. BMC Palliat Care 23 , 98 (2024). https://doi.org/10.1186/s12904-024-01420-8
Download citation
Received : 08 September 2023
Accepted : 25 March 2024
Published : 12 April 2024
DOI : https://doi.org/10.1186/s12904-024-01420-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Advance care planning
- Social Ecological Model
- Death literacy
- Public engagement
- Public health
- Death and dying.
BMC Palliative Care
ISSN: 1472-684X
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Qualitative Methods for Health Research. Packed with practical advice and research quick tips, this book is the perfect companion to your health research project. It not only explains the theory of qualitative health research so you can interpret the studies of others, but also showcases how to approach, start, maintain, and disseminate your ...
Qualitative Methods for Health Research. Packed with practical advice and research quick tips, this book is the perfect companion to your health research project. It not only explains the theory of qualitative health research so you can interpret the studies of others, but also showcases how to approach, start, maintain, and disseminate your ...
Qualitative Methods for Health Research. Judith Green, Nicki Thorogood. SAGE Publications, Feb 26, 2018 - Medical - 440 pages. Packed with practical advice and research quick tips, this book is the perfect companion to your health research project. It not only explains the theory of qualitative health research so you can interpret the studies ...
A section exploring issues relevant to the strategic place of qualitative research in health care environments. The Sage Handbook of Qualitative Methods in Health Research is an invaluable source of reference for all students, researchers, and practitioners with a background in the health professions or health sciences. Available Formats.
Qualitative Health Research is an international, interdisciplinary, refereed journal for the enhancement of health care and to further the development and understanding of qualitative research methods in health care settings.We welcome manuscripts in the following areas: the description and analysis of the illness experience, health and health-seeking behaviors, the experiences of caregivers ...
Preview. The Sage Handbook of Qualitative Methods in Health Research is a comprehensive and authoritative source on qualitative research methods. The Handbook compiles accessible yet vigorous academic contributions by respected academics from the fast-growing field of qualitative methods in health research and consists of: - A series of case ...
Qualitative Methods for Health Research. Packed with practical advice and research quick tips, this book is the perfect companion to your health research project. It not only explains the theory of qualitative health research so you can interpret the studies of others, but also showcases how to approach, start, maintain, and disseminate your ...
SAGE, Aug 19, 2010 - Social Science - 786 pages. The Sage Handbook of Qualitative Methods in Health Research is a comprehensive and authoritative source on qualitative research methods. The Handbook compiles accessible yet vigorous academic contributions by respected academics from the fast-growing field of qualitative methods in health ...
Revised and updated for a third edition, Green and Thorogood's excellent textbook provides a solid grounding for health professionals in the theory and practice of qualitative research methods. This new edition, with an increased focus on data management and analysis, will remain the core qualitative methods textbook for our Master in Public ...
Qualitative Methods for Health Research. Judith Green, Nicki Thorogood. SAGE, Oct 15, 2013 - Business & Economics - 360 pages. The Third Edition of this bestselling title is packed full of real-world advice for researchers and students. It is an invaluable introduction to the theoretical and practical essentials needed to design, conduct and ...
The Sage Handbook of Qualitative Methods in Health Research is a comprehensive and authoritative source on qualitative research methods. The Handbook compiles accessible yet vigorous academic contributions by respected academics from the fast-growing field of qualitative methods in health research and consists of: - A series of case studies in ...
The greatest strength of the qualitative research approach lies in the richness and depth of the healthcare exploration and description it makes. In health research, these methods are considered as the most humanistic and person-centered way of discovering and uncovering thoughts and actions of human beings. Table 1.
Qualitative Research Methods for Health Professionals . Janice M. Morse - University of Utah, USA; Peggy Anne Field - University of Alberta - Edmonton, Canada; June 1995 | 272 pages | SAGE Publications, Inc ... Please email us at [email protected] or connect with your SAGE representative. SAGE 2455 Teller Road
Qualitative research methods are increasingly recognized for their importance in healthcare-related research, particularly in contextualizing social and cultural realities that impact human behavior (Al-Busaidi et al., 2008; Renjith et al., 2021).There is a growing interest in and acceptance of qualitative research approaches in the health sciences, both as stand-alone methodologies and ...
Kirsi Lumme-Sandt. An enormously helpful resource for anyone interested in interpreting and conducting qualitative health research. In addition to describing complex social theory in an easily digestible style, it also provides a practical 'how to' guide for all the stages of qualitative data collection, analysis and dissemination.
Qualitative Health Research is an international, interdisciplinary, refereed journal for the enhancement of health care and to further the development and understanding of qualitative research methods in health care settings.We welcome manuscripts in the following areas: the description and analysis of the illness experience, health and health-seeking behaviors, the experiences of caregivers ...
Qualitative Methods for Health Research. Judith Green, Nicki Thorogood. SAGE Publications, Feb 4, 2014 - Business & Economics - 360 pages. The Third Edition of this bestselling title is packed full of real-world advice for researchers and students. It is an invaluable introduction to the theoretical and practical essentials needed to design ...
The growing interest in qualitative methods in health research, and their increasing acceptance in clinical and biomedical arenas, in the 10 years since the book was first published, suggest that such misunderstandings may be diminishing. ... Further reading Green J & Thorogood N. Qualitative Methods for Health Research. SAGE, London, 2004 ...
Qualitative Health Research is an international, interdisciplinary, refereed journal for the enhancement of health care and to further the development and understanding of qualitative research methods in health care settings.We welcome manuscripts in the following areas: the description and analysis of the illness experience, health and health-seeking behaviors, the experiences of caregivers ...
Qualitative health research consists of the systematic investigation of personal health, health services, and public health by means of qualitative methods (Green & Thorogood, 2018). The aim of the spring school was to foster an exchange of best practice examples in addressing challenges in the ethics review and practice of qualitative health ...
Let's study a case: "Understanding Online Discussions of Key Public Health Issues Using a Mixed-Methods Approach" Abstract. There has been a growing movement against vaccination in the United States. The extent to which misinformation and fear fuel decision making has been established by researchers yet needs further empirical understanding.
Qualitative research provides valuable insights into health care interactions and decision-making processes - for example, why and how a clinician may ignore prevailing evidence and continue making clinical decisions the way they always have.1 The perception of qualitative health care research has improved since a 2016 article by Greenhalgh et al. highlighted the higher contributions and ...
Ivy Bourgeault, Robert Dingwall, Ray de Vries. SAGE, Aug 19, 2010 - Social Science - 786 pages. The Sage Handbook of Qualitative Methods in Health Research is a comprehensive and authoritative source on qualitative research methods. The Handbook compiles accessible yet vigorous academic contributions by respected academics from the fast-growing ...
To investigate current methods for health promotion work for mental health in elementary school and to develop a professional model for interventions related to mental health through the use of an action research process. ... Step 1 involved choosing the area to be investigated and whether a qualitative method is suitable for investigating the ...
In this article, we expand the recommendations for cross-language research for multilingual researchers and health studies, through an examination of literature and processes from a Community-Engaged Qualitative Photovoice project. We present adapted cross-language research methods for future cross-language research studies.
Qualitative research, using semi-structured interviews were adopted as this enabled an in-depth understanding of public views on strategies to enable engagement with PC. ... This research was part of a larger mixed-methods study . ... The SAGE Handbook of Health Psychology [Internet]. 1 Oliver's Yard, 55 City Road, London EC1Y 1SP United ...
Background . The goal of qualitative research is to learn more about the opinions and experiences of the subjects being studied in relation to a particular question. There is a paucity of information on opportunities and challenges encountered to conduct qualitative research among the academic staffs in the health sciences. The purpose of this study was to examine the opportunities and ...