
- DNA Replication
- Active Transport
- Cellular Receptors
- Endocytosis and Exocytosis
- Enzyme Inhibition
- Enzyme Kinetics
- Protein Structure
- Transcription of DNA
- Translation of DNA
- Anaerobic Respiration
- Electron Transport Chain
- Gluconeogenesis
- Calcium Regulation
- External Balance of Potassium
- Internal Balance of Potassium
- Sodium Regulation
- Cell Membrane
- Endoplasmic Reticulum
- Golgi Apparatus
- Mitochondria
- Blood Vessels
- Cellular Adaptations
- Epithelial Cells
- Muscle Histology
- Structure of Glands
- Control of Stroke Volume
- Control of Heart Rate
- Cardiac Cycle
- Cardiac Pacemaker Cells
- Conduction System
- Contraction of Cardiac Muscle
- Ventricular Action Potentials
- Blood Flow in Vessels
- Control of Blood Pressure
- Capillary Exchange
- Flow In Peripheral Circulation
- Venous Return
- Cardiac Muscle
- Hepatic Circulation
- Skeletal Muscle
- Airway Resistance
- Lung Volumes
- Mechanics of Breathing
- Gas Exchange
- Oxygen Transport in The Blood
- Transport of Carbon Dioxide in the Blood
- Ventilation-Perfusion Matching
- Chemoreceptors
- Cough Reflex
- Neural Control of Ventilation
- Respiratory Regulation of Acid-Base Balance
- Responses of The Respiratory System to Stress
- Regulation of Saliva
- Secretion of Saliva
- Gastric Acid Production
- Gastric Mucus Production
- Digestion and Absorption
- Histology and Cellular Function of the Small Intestine
- Absorption in the Large Intestine
- Large Intestinal Motility
- Bilirubin Metabolism
- Carbohydrate Metabolism in the Liver
- Lipid Metabolism in the Liver
- Protein and Ammonia Metabolism in the Liver
- Storage Functions of the Liver
- Bile Production
- Function of The Spleen
- Exocrine Pancreas
- Somatostatin
- Proximal Convoluted Tubule
- Loop of Henle
- Distal Convoluted Tubule and Collecting Duct
- Storage Phase of Micturition
- Voiding Phase of Micturition
- Antidiuretic Hormone
- Renin-Angiotensin-Aldosterone System
- Urinary Regulation of Acid-Base Balance
- Water Filtration and Reabsorption
- Development of the Reproductive System
- Gametogenesis
- Gonadotropins and the Hypothalamic Pituitary Axis
- Menstrual Cycle
- Placental Development
- Fetal Circulation
- Maternal Adaptations in Pregnancy
- Cells of the Nervous System
- Central Nervous System
- Cerebrospinal Fluid
- Neurotransmitters
- Peripheral Nervous System
- Action Potential
- Excitatory and Inhibitory Synaptic Signalling
- Resting Membrane Potential
- Synaptic Plasticity
- Synaptic Transmission
- Ascending Tracts
- Auditory Pathway
- Consciousness and Sleep
- Modalities of Sensation
- Pain Pathways
- Sensory Acuity
- Visual Pathway
- Descending Tracts
- Lower Motor Neurones
- Muscle Stretch Reflex
- Upper Motor Neurones
- Aqueous Humour
- Ocular Accommodation
- Thyroid Gland
- Parathyroid Glands
- Adrenal Medulla
- Zona Glomerulosa
- Zona Fasciculata
- Zona Reticularis
- Endocrine Pancreas
- The Hypothalamus
- Anterior Pituitary
- Posterior Pituitary
- White Blood Cells – Summary
- Barriers to Infection
- Infection Recognition Molecules
- Phagocytosis
- The Complement System
- Antigen Processing and Presentation
- Primary and Secondary Immune Responses
- T Cell Memory
- Acute Inflammation
- Autoimmunity
- Chronic Inflammation
- Hypersensitivity Reactions
- Immunodeficiency
- Types of Immunity
- Antibiotics
- Viral Infection

Blood Groups
- Coagulation
- Erythropoiesis
- Iron Metabolism
- Mononuclear Phagocyte System
Original Author(s): Neera Chaudhary and Laurie Peters Last updated: 7th August 2023 Revisions: 16
- 1 ABO Grouping System
- 2 Rhesus Grouping System
- 3 Clinical Relevance – Blood Transfusion
- 4 Clinical Relevance – Haemolytic Disease of the Newborn (HDN)
- 5 Clinical Relevance – Blood typing and Cross-matching
- 6 Clinical Relevance – Antiglobulin Testing (Coombs’ Test)
Blood typing is a method of classifying blood into different blood groups depending on the presence of different antigens on the surface of red blood cells (RBCs). Understanding the different blood groups is vital in preventing complications from blood transfusion .
In this article, we will explore the most common blood grouping systems, blood transfusions, associated investigations, and clinical correlations.
ABO Grouping System
Erythrocytes (RBCs) have multiple glycoprotein antigens attached to their cell surface. The most important are ABO antigens , which determine a person’s ABO blood group. An individual inherits one ABO allele from each parent, with A and B alleles being codominant and producing the A and B antigens respectively.
- Group A – have antigen A attached to the erythrocyte cell surface
- Group B – have antigen B attached to the erythrocyte cell surface
- Group AB – have both antigen A and B attached to the erythrocyte cell surface
- Group O – have neither antigen attached to the erythrocyte cell surface
Each person also has ABO antibodies in their plasma, which will recognise and attack RBCs expressing foreign antigens . These antibodies develop over the first months and years of life . This is crucial in blood transfusion as giving someone an incompatible blood group can be potentially fatal. The A and B antibodies are predominantly IgM .
- Group A – have anti-B antibodies
- Group B – have anti-A antibodies
- Group AB – have neither antibody
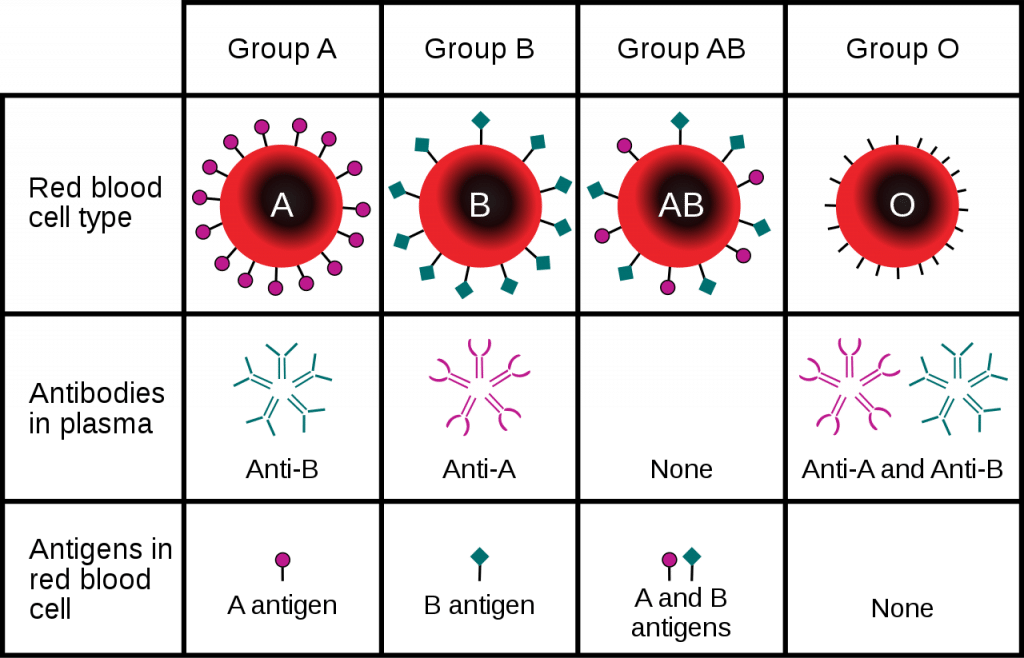
Fig 1 – Summary of blood types
Rhesus Grouping System
The second most important blood grouping system is based on Rhesus ( Rh ) antigens . There are many different Rh antigens but only 5 are clinically significant: D, C, c, E, and e.
Rh D is the most immunogenic (i.e. likely to produce an immune response) and therefore the most likely to precipitate a transfusion reaction . The presence or absence of Rh D antigen on the erythrocyte cell surface determines whether the person has Rh positive (Rh+) or Rh negative (Rh-) blood groups.
- Rh positive : have the Rh D antigen and can receive both Rh+ and Rh- blood
- Rh negative : lack the Rh D antigen and should only receive Rh- blood
Rh negativity is generally more prevalent in Caucasian populations (15%), than Afro-Caribbean (8%) and Asian (1%) populations but prevalence varies in different parts of the world.
Anti-D antibody is usually absent in Rh- patients (until they have been exposed to Rh+ erythrocytes). Rh- patients should not be transfused with Rh+ blood as this can cause them to develop anti-D antibodies. This may cause transfusion reactions in the future.
Alongside ABO and Rh blood groups, there are many other grouping systems based on other antigens. These antigens can also, more rarely, cause transfusion reactions.
Clinical Relevance – Blood Transfusion
A person should not receive blood products containing antigens for which they have the corresponding antibodies. Transfusing an incompatible blood type will precipitate a potentially fatal transfusion reaction as the recipient’s ABO antibodies attack the donor’s antigen (seen as foreign). Patients having blood transfusions need to be frequently monitored, particularly at the start of each unit.
People with blood type O- are universal donors – they can donate their blood to anyone. This is because their RBCs have no A, B, or RhD antigens which the recipient’s immune system could attack.
People with blood type AB+ are universal recipients – they can receive blood from anyone. This is because their plasma does not contain anti-A, anti-B, or anti-D antibodies, so they will usually not mount an immune response to the donor blood.
Fig 2 – Generic bag of packed red cells, labelled as group AB+
Clinical Relevance – Haemolytic Disease of the Newborn (HDN)
Anti-D antibodies cause the most severe type of HDN.
Exposure of a Rh- person to the Rh D antigen causes Rh D sensitisation . For instance, during a first pregnancy if the foetus is Rh+. The presence of Rh D antigens in the maternal circulation stimulates the production of anti-D antibodies.
Maternal anti-D antibodies recognise and destroy foetal Rh+ RBCs . Upon first exposure, the antibodies are IgM , which cannot cross the placenta and will not cause issues in the first pregnancy. However, future Rh+ pregnancies will result in the production of large amounts of IgG anti-D which can cross the placenta and cause haemolysis .
Thankfully the administration of anti-D Ig prophylaxis to unsensitised Rh- mothers has significantly reduced the incidence of HDN caused by anti-D antibodies. The prophylaxis works by destroying foetal RBCs that leak into the maternal circulation, reducing the chance of Rh D sensitisation.
Clinical Relevance – Blood typing and Cross-matching
Blood typing (also known as a “group and save”) followed by cross-matching helps avoid transfusion of incompatible blood types.
ABO typing tests the patient’s blood for the presence of A/B antigens, and A/B antibodies. This is followed by Rh typing. The lab will also screen the patient’s blood for atypical antibodies.
Cross-matching involves mixing the donor’s blood with the recipient’s blood to detect any immune reaction .
Clinical Relevance – Antiglobulin Testing (Coombs’ Test)
Direct Antiglobulin Testing (DAT) detects whether a patient’s RBCs have antibodies directly attached to them. Coombs’ reagent binds to specific immunoglobulins on the RBCs. It is added to the patient’s blood. A positive test results in the RBCs agglutinating (clumping together).
A positive DAT indicates that haemolysis has an immune aetiology, causes include autoimmune haemolytic anaemia, haemolytic transfusion reactions, and HDN.
Indirect Antiglobulin Testing (IAT) detects antibodies present in the patient’s plasma. This can be used in cross-matching or to detect maternal anti-D IgG. Donor’s RBCs and Coombs’ reagent is combined with the patient’s isolated plasma.
Again, the test is positive if agglutination occurs. This indicates the patient has antibodies against the antigens present on the donor’s RBCs.
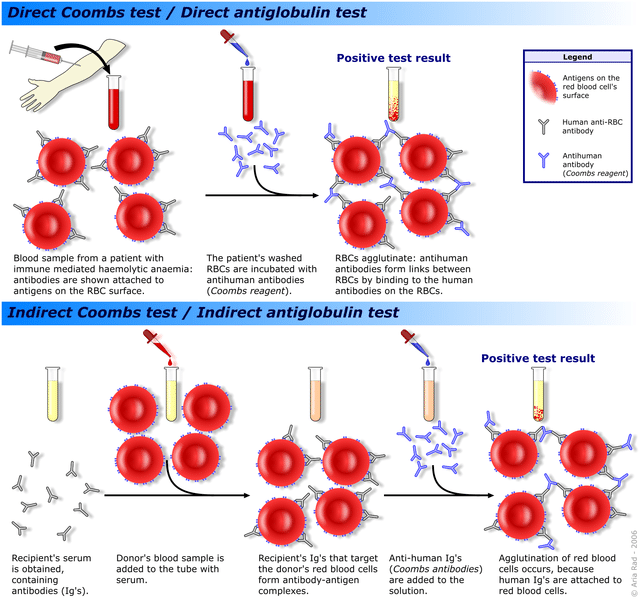
Fig 3 – Schematic of the direct and indirect Coombs test
[start-clinical]
Clinical Relevance - Blood Transfusion
A person should not receive blood products containing antigens for which they have the corresponding antibodies. Transfusing an incompatible blood type will precipitate a potentially fatal transfusion reaction as the recipient's ABO antibodies attack the donor's antigen (seen as foreign). Patients having blood transfusions need to be frequently monitored, particularly at the start of each unit.
Clinical Relevance - Haemolytic Disease of the Newborn (HDN)
Clinical relevance - blood typing and cross-matching, clinical relevance - antiglobulin testing (coombs’ test).
Indirect Antiglobulin Testing (IAT) detects antibodies present in the patient’s plasma. This can be used in cross-matching or to detect maternal anti-D IgG. Donor’s RBCs and Coombs’ reagent is combined with the patient's isolated plasma.
[end-clinical]
Found an error? Is our article missing some key information? Make the changes yourself here!
Once you've finished editing, click 'Submit for Review', and your changes will be reviewed by our team before publishing on the site.
We use cookies to improve your experience on our site and to show you relevant advertising. To find out more, read our privacy policy .
Privacy Overview
- Biology Article
- Blood Groups
Blood Groups-ABO Blood Group and Rh Group System
Blood is a fluid connective tissue and the most crucial component of the circulatory system. In a healthy person, approximately 5 liters (12 pints) of blood circulates throughout their body. In this article, blood groups and their types are explained in detail.

Composition of blood is rather interesting. It consists of erythrocytes, leukocytes and platelets suspended in plasma along with the millions of different molecules with its own specific roles and functions.

Even though components of blood are the same for all humans, there are various blood types. In fact, there are more than 40 blood groups, but all of them are not clinically significant. The discovery of the ABO blood group created great excitement as until then, all blood had been assumed to be the same.
Blood Group System
Karl Landsteiner, an Austrian scientist discovered the ABO blood group system in the year 1900. In his experiments, he mixed different blood types and noted that the plasma from certain blood type produced agglutinates or formed clusters which were caused by the absence of molecules on red blood cells and resulting in antibodies to defeat that molecule. He then made a note of the agglutination and divided the blood types into 4 different groups. For the discovery of ABO blood group, he was awarded the Nobel Prize.
The blood grouping system is pivotal in blood transfusion. Our immune system recognizes another blood type as foreign and attacks it if introduced in the body causing a transfusion reaction . Any inappropriate match with the Rh and ABO blood types, causes the most serious and life-threatening transfusion reactions. Therefore, before blood transfusion, it is suggested to have a blood group checked.
What are ABO and Rh blood groups?
During the blood transfusion, the two most important group systems examined are the ABO-system and the Rhesus system .
The ABO blood group system consists of 4 types of blood group – A, B, AB, and O and is mainly based on the antigens and antibodies on red blood cells and in the plasma. Both antigens and antibodies are protein molecules in which antigens are present on the surface of Red Blood Cells and antibodies are present in the plasma which is involved in defending mechanisms.
On the other hand, the Rh blood group system consists of 50 defined blood group antigens. In the Rh system, the most important antigens are D, C, c, E, and e. The ABO and Rh blood systems are discussed in detail below.
1. ABO blood Group system
The basis of ABO grouping is of two antigens- Antigen A and Antigen B. The ABO grouping system is classified into four types based on the presence or absence of antigens on the red blood cells surface and plasma antibodies.
- Group A – contains antigen A and antibody B.
- Group B –contains antigen B and antibody A.
- Group AB –contains both A and B antigen and no antibodies (neither A nor B).
- Group O – contains neither A nor B antigen and both antibodies A and B.
The ABO group system is important during blood donation or blood transfusion as mismatching of blood group can lead to clumping of red blood cells with various disorders. It is important for the blood cells to match while transfusing i.e. donor-recipient compatibility is necessary. For example, a person of blood group A can receive blood either from group A or O as there are no antibodies for A and O in blood group A.
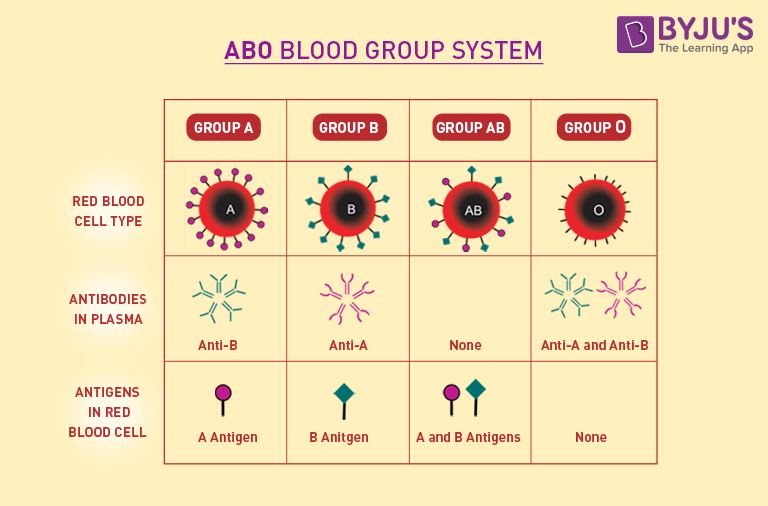
As shown in the above table, individuals of blood group O are called as universal donors , whereas individuals of blood group AB are universal recipients .
2. Rh Blood Group System
In addition to the ABO blood grouping system, the other prominent one is the Rh blood group system. About two-thirds of the population contains the third antigen on the surface of their red blood cells known as Rh factor or Rh antigen ; this decides whether the blood group is positive or negative. If the Rh factor is present, an individual is rhesus positive (Rh+ve); if an Rh factor is absent individual is rhesus negative (Rh-ve) as they produce Rh antibodies. Therefore, compatibility between donor and individual is crucial in this case as well.
Frequently Asked Questions
What are blood group antigens and antibodies.
The ABO system divides blood into four major blood groups:
- Blood type A contains anti-B antibodies and A antigens in the plasma.
- Blood group B contains anti-A antibodies and B antigens in the plasma.
- Blood type O has both anti-A and anti-B antibodies in the plasma but no antigens.
- Blood type AB lacks antibodies but possesses both A and B antigens.
How are blood antibodies formed?
The immune system uses antibodies white blood cells produce to recognise and combat foreign elements in the body. Red blood cells have blood type antigens on their surface, but the immune system does not recognise them. However, antibodies will recognise the antigens of a different blood type as foreign and attack them.
To learn more about Blood groups with interactive video lessons, keep visiting BYJU’S.
Put your understanding of this concept to test by answering a few MCQs. Click ‘Start Quiz’ to begin!
Select the correct answer and click on the “Finish” button Check your score and answers at the end of the quiz
Explore BYJU’S for more concepts on Biology
Your result is as below
Request OTP on Voice Call
Leave a Comment Cancel reply
Your Mobile number and Email id will not be published. Required fields are marked *
Post My Comment
Very helpful thanks Byju’s
- Share Share
Register with BYJU'S & Download Free PDFs
Register with byju's & watch live videos.


BBGuy Video
“blood groups overview”, (basic immunohematology, part 1), recorded december 2011.
This Blood Bank Guy video is the first in a series of four videos that I did on basic immunohematology. It contains lots of information about the major blood group systems. This video is, in fact, a modified and updated version of the blood groups lecture (Blood Bank 1) that I used to give at the Osler Institute Pathology Review Course. Please download the handout for this lecture at the link below.
NOTE that some things have changed since 2011 when I recorded this video! See disclaimer below the video.
Download the handout for this video.
BBGuy Videos
- Acquired B Phenotype
- Antibody ID Part 1
- Antibody ID Part 2
- Blood Groups Overview
- Fun with the Lewis System
- Kell Kills!
- Pretransfusion Testing
- RhIG Dosage
- Transfusion Reaction Workup
- Transfusion Reactions; Specifics
- Transfusion-transmitted Disease Testing
- Transfusion-transmitted Diseases
- Weak in the D’s
- What the H? (Bombay)
- Why Do We Irradiate?
- Why Do We Leukoreduce?
Pin It on Pinterest
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Rh blood group system.
Daniel Rosenkrans ; Muhammad Zubair ; Alexander Doyal .
Affiliations
Last Update: August 2, 2023 .
- Continuing Education Activity
The Rh blood group system has been extensively studied and remains clinically relevant. This highly polymorphic system comprises over 50 expressed antigens embedded in the red blood cell (RBC) membrane. The function of these highly immunogenic proteins is unknown. Patients with specific Rh phenotypes require special attention during transfusion and pregnancy to avoid potentially life-threatening complications. This activity reviews the evaluation and management of patients with various Rh blood group phenotypes and highlights the role of the interprofessional healthcare team in caring for these patients in various clinical settings.
- Correlate specific Rh complex genotypes with clinically relevant Rh phenotypes.
- Identify patients at increased risk for alloimmunization.
- Assess and manage a patient with a hemolytic transfusion reaction.
- Implement interprofessional team strategies for improving care coordination and communication to ensure safe transfusion processes.
- Introduction
The Rh blood group system has been extensively studied and remains clinically relevant to transfusion medicine. The system has over 50 antigens; the 5 most significant antigens are D, C, c, E, and e. [1] The Rh antigens are a part of proteins expressed on the surface of the red blood cell (RBC) membrane. The function of these antigens is unknown; they may play a role in membrane stability and ammonium transport. Importantly, the Rh antigens are highly immunogenic; exposure often leads to antibody formation. There are various expressions of Rh antigens with clinically significant phenotypes. The most significant phenotype is Rh negative, which has notable implications during pregnancy and for patients receiving blood transfusions. [2]
Rh blood group system International Society of Blood Transfusion (ISBT) symbol: Rh
ISBT Number: 004
- Etiology and Epidemiology
The first report of the Rh blood group was in 1939 when Levine and Stetson described a pregnant woman that developed postpartum hemorrhage requiring transfusion from her husband. Even though she and her husband were ABO compatible, she developed pain and discolored urine after the transfusion. Agglutination occurred when her blood was remixed with her husband's blood. Levine and Stetson tested her blood with multiple ABO-matched donors and noted agglutination with 80% of the donor samples. The authors concluded that the patient had been isoimmunized with an unknown antigen from her fetus resulting in the incompatible blood transfusion. [3]
Landsteiner and Wiener would describe the offending antigen as Rhesus (Rh) factor because of the agglutination in their experiments using rhesus monkey blood, assuming rhesus RBCs expressed the same antigens as humans. Their work would also describe the autosomal dominant inheritance pattern of the Rh factor. [4] Later, it was discovered that humans and rhesus monkeys do not share the same RBC antigens, though the name persists. The anti-Rh antibody produced from the Rh factor would subsequently be renamed anti-D. [5]
- Pathophysiology
The Rh blood group system comprises 56 antigens; the five most clinically significant antigens are D, C, c, E, and e. The Rh blood group is encoded by two tightly linked loci on chromosome 1p34-36. The RHD gene encodes the RhD antigen, and the RHCE gene encodes RhCE antigens. SMP1 , a sequence of unknown significance, separates RHD and RHCE . [6] RHD and RHCE encode eight haplotypes of the Rh antigens in various combinations. The Rh proteins are hydrophobic transmembrane proteins embedded in the RBC phospholipid bilayer with an extracellular expression of the antigens. Interestingly, the RhD and RhCE proteins are very similar, with the first 41 amino acids identical. [7]
Rh proteins require the presence of Rh-associated glycoprotein (RhAG) for proper assembly in the RBC membrane. [8] Though RhAG and the Rh proteins are similar in structure, the gene locus for RhAG is located on chromosome 6p12-21. The combination of the Rh proteins and RhAG is termed the Rh family. Various other accessory glycoproteins comprise the Rh structure, including LW glycoprotein, integrin-associated protein, glycophorin B, and band 3 glycoprotein, encoded on chromosomes 19, 3, 4, and 17, respectively. The Rh proteins, RhAG, and accessory proteins are collectively termed the Rh complex. [1] The function of the Rh complex is unclear. Studies of different Rh phenotypes indicate that the Rh complex plays a role in the RBC membrane integrity and may be involved with ammonium transport across the RBC membrane. [6]
Various Rh complex phenotypes exist due to point and nonsense mutations, rearrangements, and nucleotide deletions. Of these phenotypes, a lack of D antigen (D-negative), weak D, partial D, RhCE variants, and Rh null have clinical implications.
Lack of D Antigen
The lack of D antigen (D-negative) occurs for various reasons closely linked to ethnicity. Commonly identified in White populations, the deletion of RHD or mutations resulting in a premature stop codon produces the D-negative phenotype. In other people, the lack of D-antigen may be due to mutations preventing gene expression. For example, in African populations, the presence of a pseudogene leads to base pair duplication preventing gene expression. [6] Patients lacking D-antigen warrant special consideration to prevent alloimmunization; if exposed to D-antigen through transfusion or pregnancy, they may develop anti-D antibodies, as seen when a D-negative parturient has a D-positive fetus. [9]
Approximately 1% of D-positive individuals type as weak D (historically known as Du), characterized by weak or absent RBC agglutination by anti-D antibodies during routine serologic testing. In weak D individuals, the D antigen usually requires enhancement with anti-human globulin (AHG) owing to a quantitative decrease in RhD protein. The weak D phenotype is a quantitative change in the D-antigen epitope caused by a defect in transcribing the RHD gene. [1] Various weak D genotypes exist; Types 1, 2, and 3 are the most common and produce sufficient D antigen epitopes to be managed as D-positive. [10] Female patients of childbearing age who are positive for a weak D phenotype should undergo additional genotyping to determine if immunoprophylaxis during pregnancy is necessary. [11]
The partial D phenotype is a qualitative change to the D antigen epitope caused by RHD gene conversions, point mutations, or expression of a low-incidence antigen. [6] The majority of patients with partial D phenotype will type D-positive. Notably, these patients may form anti-D antibodies if exposed to D-positive RBCs and require special consideration for transfusion and during pregnancy. [10]
RhCE Variants
RhCE polymorphisms occur due to single or multiple nucleotide substitutions in RHCE . The E and e alleles differ only by a proline to alanine substitution. However, the C and c polymorphic alleles have four different amino acid substitutions. [12] The expression of these different alleles significantly impacts patients receiving chronic transfusions as they may develop alloantibodies more frequently. Notably, patients with sickle cell disease are at particular risk for alloimmunization. [13]
Rh null
Rh null phenotype contains two classifications, amorph and regulator. Amorph Rh null occurs from a mutation of RHCE, leading to nonfunctional proteins on a D-negative background. Regulator Rh-null is the most common phenotype due to an RHAG mutation that produces dysfunctional RhAG. [6] Clinically, Rh null patients have shortened RBC life spans, characteristic RBC morphology on a peripheral blood smear and compensated hemolytic anemias. Transfusion support can be challenging because Rh null individuals can become sensitized to multiple Rh antigens, including high-frequency antigens. Some alloimmunized Rh null patients can develop anti-RH29 antibodies; however, this antibody does not react with Rh null RBCs. [14]
- Specimen Requirements and Procedure
The blood sample collected in EDTA is called whole blood and is used for ABO and Rh typing. EDTA is the preferred anticoagulant for hematological testing because it allows the best preservation of cellular components and morphology of blood cells. [15] The minimum volume of blood required for Rh typing ranges from 0.5 to 4 mL of whole blood, depending on the laboratory and the age of the patient.
- Diagnostic Tests
The direct antiglobulin test (DAT) demonstrates the in vivo coating of RBC surfaces with immunoglobulin antibodies or complement protein C3. The DAT is most commonly utilized for the serologic investigation of potential antibody-mediated hemolysis. [16] Clinical situations warranting a DAT include acute or delayed hemolytic transfusion reactions due to antibody incompatibility, hemolytic disease of the fetus and newborn, and antibody-mediated drug-induced hemolysis. While a DAT is not routinely performed for otherwise uncomplicated pretransfusion testing, it may be informative in cases where the auto-control is reactive to confirm the presence of self-reactive antibodies. [17]
The DAT is performed by directly adding antihuman globulin (AHG) reagent to a sample of the patient’s RBCs and observing for agglutination with a positive reaction occurring if the RBCs are already coated such that AHG can bind. All positive DAT samples should be tested with an inert control such as saline or 6% albumin before concluding a DAT test is positive. [16] Various preparations of AHG sera are available for blood bank testing; the choice of AHG preparation is dictated by the application, direct or indirect, and whether testing is being performed to detect RBC sensitization by IgG, complement, or both. [18]
The indirect antiglobulin test (IAT) is performed to detect in vitro antibody binding to RBCs, regardless of the antibody’s ability to fix complement. Laboratory indications include antibody detection as in crossmatch and antibody screening, antibody identification, antibody titration, and RBC phenotyping. Antiglobulin testing may be performed using test tubes, capillary tubes, microtiter plates, or gel microtube techniques. [19] To standardize antiglobulin sera and confirm true-negative antiglobulin reactions, two types of quality control RBCs are customarily used, those coated with IgG and those coated with C3b, C3d, or both. Rh antibodies are usually used to sensitize RBCs with IgG. [17]
Quality control cells for the antiglobulin test are called check cells or Coombs control cells. In a true-negative test, free active antiglobulin reagent should remain. Control cells, sensitized with IgG or C3, are added to all negative tests and centrifuged. Hemagglutination of check cells confirms the presence and reactivity of the AHG reagent, thus validating a negative test result. If the control cells fail to agglutinate in any tube, the tests must be repeated because they are invalid and may have yielded false-negative results. [20]
Although the antiglobulin test is extremely sensitive, a negative test does not exclude the possible presence of antibodies on RBCs. A negative reaction can occur with small quantities of bound IgG and C3. [16] In addition, AHG sera may possess greater activity against some subclasses of IgG than others. Consequently, certain AHG sera may produce negative results with RBCs coated by a particular IgG subclass. [21]
- Testing Procedures
Rh typing detects the presence or absence of the D antigen on the surface of RBCs and is performed analogously to ABO forward typing. During Rh typing, the RBCs of the patient are combined with reagent anti-D antibodies, and the resulting presence or absence of agglutination confers the Rh “positive” or “negative” status, respectively. [22] While not routinely required for pretransfusion testing, serologic testing to detect weak D or partial D phenotypes should occur in cases of ambiguous Rh typing or discrepancies with a patient’s historical typing result. [23] In cases of an apparently negative Rh type, the serologic assessment for weak or partial D requires adding AHG reagent to enhance otherwise undetectable agglutination. Agglutination in this context suggests the presence of a weak or partial D phenotype; definitive distinction requires subsequent molecular genotyping to predict the true D antigen phenotype. [24]
Various methods for Rh blood group testing may be employed. Serological testing is most commonly based on hemagglutination reactions with RBC antigens against specific antibodies. [25] The hemagglutination process occurs in 2 stages. The first stage, often called RBC sensitization, combines paratope and epitope in a reversible reaction that follows the law of mass action and has an associated equilibrium constant. Noncovalent attractions hold together the antigen and antibody. During the second stage, multiple RBCs with bound antibodies form a stable latticework through antigen-antibody bridges formed between adjacent cells. This latticework is the basis of all visible agglutination reactions. [26]
Reagents that detect the D antigen in the slide, tube, microplate, automated, and gel tests often have different formulations and performance characteristics. Various anti-D reagents may contain different antibody clones, potentiators, additives, or diluents, and reagents that contain the same antibody clone may vary in antibody dilution or preservative. Hence, instructions for testing may differ and must be consulted and followed carefully for accurate testing. [27]
Slide Testing
A glass slide containing a drop of 40% to 50% serum or plasma suspension of RBCs and a drop of anti-D is mixed and placed on a heated Rh viewing box tilted continuously for 2 minutes to observe for agglutination. To rapidly warm the materials on the slide at 37°C, the Rh viewing box is kept at a temperature between 40°C and 50°C. The result is positive when the patient sample shows agglutination and the control shows suspension. [28] The sensitivity of this method is low and can be easily affected by multiple factors, thus making standardization difficult. [29]
Tube Testing
The test tube method can be utilized for emergency and first-time blood group typing. The test tube method is quicker, more sensitive, and uses fewer reagants than the slide method. [28] In the test tube method, a patient’s antibody-containing plasma and reagent RBCs known to express specific antigens are combined in a test tube. Alternatively, a patient’s RBCs may be combined with reagent antibodies of known specificity. The mixture undergoes a series of centrifugation and incubation steps with stepwise quantitation of agglutination. The strongest agglutination, a 4+ reaction, results in an effectively nondissociable single clump of RBCs when the tube is gently agitated, whereas the weakest agglutination, a negative reaction, results in complete dissociation into individual RBCs by the same assessment. The intermediate strength reactions fall in a spectrum in between these extremes. [30]
Gel Testing
The gel testing method is a widely available alternative serologic testing method that utilizes dextran acrylamide gel-containing microtube columns built into small plastic cards. [31] Antibodies containing plasma and reagent RBCs are combined in a chamber above the columns, and the card is subsequently centrifuged to force the RBCs down through the permeable gel, which acts like a size-selective sieve. The gel is typically impregnated with AHG to facilitate agglutination. Depending on the degree of agglutination, the RBCs have varying mobility as they travel down the column, and their visible stopping point quantifies the reaction. Gel method testing can be automated and has the advantage of a more objective scale for quantifying results than tube testing. [25]
Microplate Agglutination Testing
The microplate technology uses automated platforms to detect serum antibodies and RBC surface antigens. [26] The reactants are centrifuged and incubated in microplates, and the ABO/RH(D) blood type is read through an automated system. The antiserum must indicate that it is formulated for automation or microplate Rh testing and may require the blood to be collected in a specific anticoagulant. [25]
- Interfering Factors
False positive or negative results can be caused by improper technique, contaminated materials, omission of reagents or antisera, delays in reading tests, inadequate incubation time and temperature, inappropriate centrifugation, inappropriate or prolonged storage of red cells, and autoantibodies. [32]
- Results, Reporting, and Critical Findings
A patient or donor RBC sample previously found to be positive but now determined to be negative, or vice versa, should always be investigated to rule out identification, clerical, or recording errors. [32] A new sample should be obtained and tested. If the discrepancy is between current and historical test results, the difference may be due to the testing method employed, phase of testing (DAT or IAT), type of reagent (polyclonal vs. monoclonal), or manufacturer. [33] Different reagents often contain different antibody clones that may demonstrate varying reactions with RBCs with weak or partial Rh antigens. Knowledge of the ethnicity of the donor or patient can be helpful when investigating a typing discrepancy because some partial and weak phenotypes are more common in a specific ethnic group. Typing with several reagents from different manufacturers may be helpful. [34]
- Clinical Significance
Hemolytic Disease of the Newborn
Hemolytic disease of the newborn (HDN), or erythroblastosis fetalis, is a clinically important and potentially life-threatening condition where antibodies from an Rh-negative gravida attack an Rh-positive fetus. [35] Despite being described by a French midwife in 1609, HDN was not understood until the 1950s. [36] Before the onset of immunoprophylactic therapies, 1% of all pregnancies resulted in fetal death from HDN. HDN is currently estimated to affect 3 to 8 of every 100,000 pregnancies.
HDN results from maternal antibodies attacking fetal red blood cells. Typically, it is the second Rh-positive fetus that is affected. The first fetus inherits the paternal D antigen following an autosomal dominant pattern, and maternal and fetal blood mixing occurs during the pregnancy. This mixing most commonly happens during labor and delivery but can theoretically occur at any time during the pregnancy. Once mixing occurs, the gravida begins producing anti-D antibodies. This constitutes alloimmunization, as the gravida is D-negative.
The initial antibodies produced are IgM, which cannot cross the placental barrier. However, when isotype switching occurs, IgG antibodies are produced. The general absence of maternal and fetal blood mixing during the first pregnancy and the delay of IgG antibody production make it unlikely that the first D-negative pregnancy is affected. However, in the subsequent D-negative pregnancy, IgG antibodies cross the placenta and attack the D antigens on fetal RBCs. This leads to hemolysis that may result in jaundice, anemia, kernicterus, and hydrops fetalis. Intrauterine death may occur without intrauterine blood transfusion, and any surviving fetus may have developmental delays, hearing loss, and hypotonia. [35]
Hemolytic Transfusion Reactions
One of the more serious complications of autologous blood transfusion is a hemolytic transfusion reaction (HTR). HTR is rare, with an incidence of 1:70,000 per unit transfused. [37] [38]
HTRs are caused when there is an immunological mismatch between the RBCs from the blood donor and the transfusion recipient, resulting in extravascular or intravascular immune-mediated hemolysis. [37] An intravascular HTR is typically more clinically severe than extravascular hemolysis. [39]
HTRs are classified by their severity and onset time, early or late. HTRs greatly vary in severity from mild, clinically insignificant hemolysis presenting weeks after the transfusion to very sudden and life-threatening intravascular hemolysis leading to shock, renal failure, disseminated intravascular coagulation, and death. The main determining factor of the reaction's onset and severity is the antibody's class, such as IgG, IgM, IgG subclass, or complement binding, the antigens targeted, and their titer concentration. [40]
The most severe type of HTR occurs during an ABO mismatch, typically due to clerical error. Patients who create AB antigens do so because of molecular mimicry to antigen presentation of gastrointestinal bacteria. These antibodies are typically IgM but may also be IgG. Severe reactions occur when IgM binds to ABO-typed antigens on RBCs and subsequently fixes complement, creating a sudden, massive intravascular rupture of RBCs. Hemolysis releases large amounts of hemoglobin, resulting in shock, renal failure, and DIC leading to hemorrhage and hypercoagulability with thrombosis.
Extravascular HTRs occur when the antibody targeting the RBCs results in opsonization. Opsonized cells are sequestered by the macrophages of the reticuloendothelial system, primarily in the liver and spleen. Extravascular hemolysis is a comparatively slower and more progressive process, as each RBC may make several passes through the reticuloendothelial system before being phagocytosed. Unlike intravascular hemolysis, the hemoglobin is released inside the sequestering macrophage, where it is processed normally. The clinical manifestations of extravascular hemolysis are typically milder, resulting in hyperbilirubinemia and fever. However, more severe complications, such as kidney failure, may also occur. [39]
Immune-mediated Hemolytic Anemia
Immune-mediated hemolytic anemia occurs when autoantibodies bind to RBCs, resulting in hemolysis and possible anemia. The autoantibodies are generally IgG, although IgM and IgA have also been reported. [41] Particular subclasses of antibodies are more destructive than others; IgG1 and IgG3 can fix complement at a high rate and are very destructive. The RBCs are mainly cleared through the reticuloendothelial system, but intravascular hemolysis may occur in severe cases.
Like many autoimmune disorders, most immune-mediated hemolytic anemias are associated with an underlying or triggering condition. Common triggering conditions are viral infections, autoimmune disorders, immunodeficiency, or pregnancy. Rarer instances of medication interactions, spider bites, sickle cell disease, babesiosis, and organ transplants have been documented. [42]
- Quality Control and Lab Safety
All blood centers, hospital blood banks, and collection centers must establish and implement a quality management system guided by requirements of established standards, guidelines, and principles. It is the responsibility of the management to ensure that each personnel has a clear job description which includes lines of authority and responsibility. [43] Each personnel must be adequately trained and assessed to be competent in the specified task before being allowed to carry out the task independently. Records of training and assessment of competency are established and systematically maintained. [44]
All critical equipment that impacts the quality of tests or blood components prepared must be operated within their defined specifications. Materials used in laboratory tests and processing must be appropriately validated. All reagents shall be used and controlled according to the manufacturer's instructions. All anti-sera must be visually inspected for contamination, such as discoloration, cloudiness, turbidity, or particulate matter. The visual inspection results, reagent lot number, expiry date, inspection date, and the individual performing the inspection must be documented. The expiry date should be checked on each reagent used. [45] Do not use reagents beyond the expiry date. The reactivity of blood grouping reagents shall be confirmed daily by control tests with known antigen-positive and negative red cells. [46]
Under CLIA regulations, all laboratories that perform non-waived testing must enroll in and perform proficiency testing (PT) using one of the CMS-approved PT providers. The PT programs are required to provide a minimum of 5 samples per testing event, with 3 testing events per year. The minimum acceptable score for satisfactory participation in immunohematology PT is 100% for each analyte and overall testing event score for the ABO group and Rh(D) typing. [47]
The blood centers, hospital blood banks, and collection centers must establish policies and procedures on safety and security. Relevant committees should maintain and continually improve safety and security in the organization. [48] Access to the laboratory area must be restricted to authorized personnel only. Staff must wear white coats on entering the laboratory and remove them before leaving the laboratory. Keep the laboratory clean and tidy and retain only necessary items. Do not store food or personal items in the laboratory, especially in the main area of the laboratory. Wash hands with soap and water before leaving the laboratory. Eating, drinking, smoking, and applying cosmetics are strictly prohibited in the laboratory. Prevent the formation of aerosols or splashing of materials. Consider all specimens as potentially infectious. Any spillage, waste, or reusable materials must be appropriately decontaminated by bleach solution before disposal. Dispose of all needles and lancets into secured, puncture-proof containers located as close as possible to where they are to be used, and then handle them as infected materials. [45]
- Enhancing Healthcare Team Outcomes
Patients with known Rh antibodies require additional testing to receive transfusions safely. This includes knowledge of transfusion reactions, compatibility testing, and, in some cases, genotyping. Healthcare practitioners should be attuned to the possibility of patients developing new and rare antibodies, especially those undergoing chronic transfusion. There should be established protocols and guidelines to ensure safe transfusion practices for patients with different Rh blood group phenotypes. This may involve additional consultation with a hematologist. Clinicians must ensure that transfusions are necessary as each transfusion may lead to the alloimmunization of Rh antigens.
Communication is essential for ensuring safe transfusion practices. Healthcare team members must confirm that the correct blood product is administered to the correct patient at the correct time. Likewise, all healthcare team members should know the patient's transfusion history, allergies, and other relevant medical information.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Daniel Rosenkrans declares no relevant financial relationships with ineligible companies.
Disclosure: Muhammad Zubair declares no relevant financial relationships with ineligible companies.
Disclosure: Alexander Doyal declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Rosenkrans D, Zubair M, Doyal A. Rh Blood Group System. [Updated 2023 Aug 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Duffy Blood Group System. [StatPearls. 2024] Duffy Blood Group System. Maheshwari A, Killeen RB. StatPearls. 2024 Jan
- Sensitization to multiple rh antigens by transfusion of random donor platelet concentrates in a -D- phenotype patient. [Ann Lab Med. 2012] Sensitization to multiple rh antigens by transfusion of random donor platelet concentrates in a -D- phenotype patient. Yun JW, Kang ES, Ki CS, Koh KC, Kim DW. Ann Lab Med. 2012 Nov; 32(6):429-32. Epub 2012 Oct 17.
- Effects of prophylactic red blood cell (RBC) transfusion with extended antigen matching on alloimmunization in patients with Sickle Cell Disease (SCD). [Transfus Apher Sci. 2023] Effects of prophylactic red blood cell (RBC) transfusion with extended antigen matching on alloimmunization in patients with Sickle Cell Disease (SCD). Leal I, Dos Santos TD, Gilli S, Castilho L. Transfus Apher Sci. 2023 Dec; 62(6):103813. Epub 2023 Sep 14.
- Review Basic principles of the ABO and Rh blood group systems for hemapheresis practitioners. [J Clin Apher. 1992] Review Basic principles of the ABO and Rh blood group systems for hemapheresis practitioners. Sigmon JM. J Clin Apher. 1992; 7(3):158-62.
- Review Rh proteins: key structural and functional components of the red cell membrane. [Blood Rev. 2006] Review Rh proteins: key structural and functional components of the red cell membrane. Van Kim CL, Colin Y, Cartron JP. Blood Rev. 2006 Mar; 20(2):93-110. Epub 2005 Jun 14.
Recent Activity
- Rh Blood Group System - StatPearls Rh Blood Group System - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Preferences

ABO BLOOD GROUP SYSTEM - PowerPoint PPT Presentation

ABO BLOOD GROUP SYSTEM
Dr amina tariq biochemistry the abo blood group system is the most important blood type system (or blood group system) in human blood transfusion. – powerpoint ppt presentation.
- DR AMINA TARIQ
- BIOCHEMISTRY
- The ABO blood group system is the most important blood type system (or blood group system) in human blood transfusion.
- The ABO blood group system wasdiscovered by the Austrian scientist Karl Landsteiner, who found three different blood types in 1900,he was awarded the Nobel Prize in Physiology or Medicine in 1930 for his work.
- Blood has two main components serum and cells. Karl Landsteiner, a physician at the University of Vienna, Austria, noted that the sera of some individuals caused the red cells of others to agglutinate.
- Two years later, two of his students discovered the fourth and rarest type, namely AB.
- ABO substances are oligosaccharides present in most cells of the body and in certain secretions.
- On membranes of red cells the oligosaccharides that determine the specific nature of ABO substances are present in glycosphingolipids.
- In secretions the oligosaccharides are present in glycoproteins.
- Alleles at a locus independent of the ABO blood group locus, known as the secretor locus, determine an individual's ability to secrete the ABO blood group substances in saliva and other body fluids.
- There are two genes, Se and se, where Se is dominant to se. In other words, an individual with at least one Se gene is a secretor.
- The antigens expressed on the red blood cell determine an individual's blood group. The main two blood groups are called ABO (with blood types A, B, AB, and O) and Rh (with Rh D-positive or Rh D-negative blood types).
- Blood type O is the most common worldwide, followed by group A. Group B is less common, and group AB is the least common.
- People with blood type O are said to be "universal donors" because their blood is compatible with all ABO blood types.
- Blood type AB individuals are known as "universal receivers" because they can receive blood from any ABO type.
- The H antigen is precursor to the ABO blood group antigens. The H locus is located on chromosome 19.
- All humans contain enzymes which catalyze the synthesis of the O antigen.
- The ABO blood group substances are glycoproteins, the basic molecule of which is known as the H substance. This H substance is present in unmodified form in individuals with blood type O. Adding extra sugar molecules to the H substance produces the A and B substances.
- H- substance itself is formed by the action of a fucosyltransferase.
- It catalyzes the transfer of fucose onto the terminal galactose residue in a1-2 linkage.
- Humans with A-type blood also contain an additional enzyme which adds N-Acetylgalactosamine to the O antigen.
- Humans with B-type blood contain another enzyme which adds Galactose to the O antigen.
- GalNAc transferase
- A substance
- Gal transferase
- B substance
- Humans with AB-type blood contain both A-type and B-type enzymes.
- While humans with O-type blood lack both types of enzymes.
- An antigen is a substance, usually a protein or a glycoprotein, which, when injected into a human (or other organism) that does not have the antigen, will cause an antibody to be produced..
- Antibodies are a specific type of immune-system proteins known as immunoglobulins, whose role is to fight infections by binding themselves to antigens.
- In the case of the ABO blood groups, the antigens are present on the surface of the red blood cell, while the antibodies are in the serum.
- Individuals with type A blood can receive blood from donors of type A and type O blood.
- Individuals with type B blood can receive blood from donors of type B and type O blood.
- Individuals with type AB blood can receive blood from donors of type A, type B, type AB, or type O blood.
- Individuals with type O blood can receive blood from donors of only type O.
- Individuals of type A, B, AB and O blood can receive blood from donors of type O blood. Type O blood is called the universal donor.
- The second most important blood group in humans is the Rhesus (Rh) system. Landsteiner and Wiener discovered the Rh blood group in 1940. They found that when they injected rabbits with Rhesus monkey blood the rabbits produced antibodies against the Rhesus red cells.
- The Rh blood group system is the major cause of hemolytic anemia in the newborn.
- A fetus who is Rh and whose mother is Rh- is at high risk for this disorder, because the mother will produce antibodies against the fetal antigen.
- Anti-Rh antibody is injected into the mother soon after her first delivery. This antibody coats the fetal Rh cells in the mother's circulation, which prevents them from causing antibody production in the mother and, therefore, her next child will not be at risk for hemolytic anemia.
- Harpers Biochemistry
- Teachers Notes
PowerShow.com is a leading presentation sharing website. It has millions of presentations already uploaded and available with 1,000s more being uploaded by its users every day. Whatever your area of interest, here you’ll be able to find and view presentations you’ll love and possibly download. And, best of all, it is completely free and easy to use.
You might even have a presentation you’d like to share with others. If so, just upload it to PowerShow.com. We’ll convert it to an HTML5 slideshow that includes all the media types you’ve already added: audio, video, music, pictures, animations and transition effects. Then you can share it with your target audience as well as PowerShow.com’s millions of monthly visitors. And, again, it’s all free.
About the Developers
PowerShow.com is brought to you by CrystalGraphics , the award-winning developer and market-leading publisher of rich-media enhancement products for presentations. Our product offerings include millions of PowerPoint templates, diagrams, animated 3D characters and more.


- My presentations
Auth with social network:
Download presentation
We think you have liked this presentation. If you wish to download it, please recommend it to your friends in any social system. Share buttons are a little bit lower. Thank you!
Presentation is loading. Please wait.
ABO/Rh Blood Group System A . Amirzargar
Published by Madeleine Allison Modified over 8 years ago
Similar presentations
Presentation on theme: "ABO/Rh Blood Group System A . Amirzargar"— Presentation transcript:
Terry Kotrla, MS, MT(ASCP)BB 2010
Dr. MH Saiemaldahr Blood Bank
Hemolytic Disease of the Newborn Case #3
District 1 ACOG Medical Student Education Module 2008
BLOOD GROUPS & TYPING. Blood Groups RBCs contain antigens (glycoproteins) for cell recognition (identification tags) The immune system has cells and chemicals.
ALLOIMMUNIZATION IN PREGNANCY
Rh/D y grupos débiles de D, de notas de internet Notas amables, sencillas, claras de apoyo en el estudio del tema.
Hemolytic disease of newborn
1. ABO blood group System By : Mr. Waggas Ela’as, M.Sc; MLT.
DR. MOHAMMED H SAIEMALDAHR Faculty of Applied Medical Science
Drmsaiem Rh Blood Group System DR. MOHAMMED H SAIEMALDAHR BB Faculty of Applied Medical Sciences MED TECH DEP.
The Rh System Immunohematology.
The Rhesus (Rh) Blood Group system

ABO & Rh Discrepancies.

Faculty of Applied Medical Sciences BLOOD BANK MEDICAL TECNOLOGY KAAU
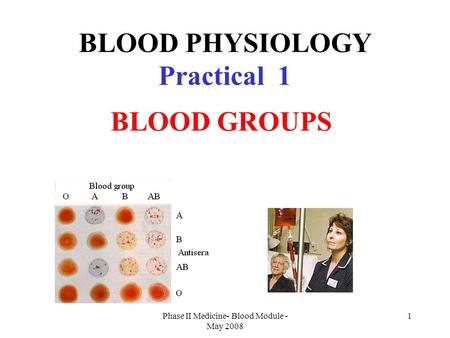
BLOOD PHYSIOLOGY Practical 1
1 BLOOD PHYSIOLOGY Practical 1 BLOOD GROUPS By: khulood Hussein.
Nada Mohamed Ahmed , MD, MT (ASCP)i
ABO Blood Group System.
About project
© 2024 SlidePlayer.com Inc. All rights reserved.

- Upload Ppt Presentation
- Upload Pdf Presentation
- Upload Infographics
- User Presentation
- Related Presentations

Blood Group
By: sunu7868 Views: 3555

Case-Child with Left Forearm Mass
By: Walaaawni Views: 624

Bleeding Disorders
By: FrankMarco Views: 395

Lab interpretation Hemoglobin abnormalitiess
By: drmedo2009 Views: 2367

By: brunomtn Views: 1409

By: staciazoghbi Views: 1215

- Occupation :
- Specialty :
HEALTH A TO Z
- Eye Disease
- Heart Attack
- Medications
Unit 7 Rh BLOOD GROUP SYSTEM
Jul 20, 2013
800 likes | 2.55k Views
Unit 7 Rh BLOOD GROUP SYSTEM. Terry Kotrla, MS, MT(ASCP)BB. Introduction. Rh is the most important blood group system after ABO in transfusion medicine. One of the most complex of all RBC blood group systems with more than 50 different Rh antigens.
Share Presentation
- d antigen do
- compatible blood
- routine testing
- allelic gene controls presence
- severe jaundice
- d pos blood

Presentation Transcript
Unit 7 Rh BLOOD GROUP SYSTEM Terry Kotrla, MS, MT(ASCP)BB
Introduction • Rh is the most important blood group system after ABO in transfusion medicine. • One of the most complex of all RBC blood group systems with more than 50 different Rh antigens. • The genetics, nomenclature and antigenic interactions are unsettled. • This unit will concentrate on the most COMMONLY encountered observations, problems and solutions.
Antigens of Rh System • Terms “D positive” and “D negative” refer only to presence or absence of the Rh antigen D on the red blood cell. • Terms “Rh pos” and “Rhneg” are old terms, although blood products still labeled as such. • Early name “Rho” less frequently used. • Four additional antigens: C, c, E, e. • Named by Fisher for next letters of alphabet according to precedent set by naming A and B blood groups. • Major alleles are C/c and E/e. • MANY variations and combinations of the 5 principle genes and their products, antigens, have been recognized. • The Rh antigens and corresponding antibodies account for majority of unexpected antibodies encountered. • Rh antibodies stimulated as a result of transfusion or pregnancy, they are immune.
HISTORY • Key observation by Levine and Stetson in 1939 that delivery of stillborn fetus and adverse reaction in mom to blood transfusion from father were related. • Syndrome in fetus is now referred to as hemolytic disease of the fetus and newborn (HDFN). • Syndrome had complicated pregnancies for decades causing severe jaundice and fetal death, “erythroblastosisfetalis”. • Erythroblastosisfetalis (HDN) linked with Anti-Rh by Levine in 1941. • Rh system IDENTIFIED by Landsteiner and Wiener in 1940. • Immunized animals to Rhesus macaque monkey RBCs. • Antibody agglutinated 100% of Rhesus and 85% of human RBCs. • Reactivity paralleled reactivity of sera in women who delivered infant suffering from hemolytic disease. • Later antigen detected by rhesus antibody and human antibody established to be dissimilar but system already named.
Clinical Significance • D antigen, after A and B, is the most important RBC antigen in transfusion practice. • Individuals who lack D antigen DO NOT have anti-D. • Antibody produced through exposure to D antigen through transfusion or pregnancy. • Immunogenicity of D greater than that of all other RBC antigens studied. • Has been reported that 80%> of D neg individuals who receive single unit of D pos blood can be expected to develop immune anti-D. • Testing for D is routinely performed so D neg will be transfused with D neg.
Inheritance and Nomenclature • Two systems of nomenclature developed prior to advances in molecular genetics. • Reflect serologic observations and inheritance theories based on family studies. • Because these are used interchangeably it is necessary to understand the theories well enough to translate from one to the other. • Two additional systems developed so universal language available for use with computers.
Fisher-Race: CDE Terminology • Fisher Race • Suggested that antigens are determined by 3 pairs of genes which occupy closely linked loci. • Each gene complex carries D or its absence (d), C or c, E or e. • Each gene (except d, which is an amorph) causes production of an antigen. • The order of loci on the gene appears to be “DCE” but many authors prefer to use “CDE” to follow alphabet. • Inherited from parents in linked fashion as haplotypes • The gene d is assumed to be present when D is absent.
Fisher-Race • Three loci carry the Rh genes are so closely linked that they never separate but are passed from generation to generation as a unit or gene complex.
Fisher-Race • Below an offspring of the Dce/dce individual will inherit EITHER Dce or dce from the parent, never dCe as this would indicate crossing over which does not occur in Rh system in man.
Fisher-Race • With the exception of d each allelic gene controls presence of respective antigen on RBC. • The gene complex DCe would cause production of the D, C and e antigens on the red cells. • If the same gene complex were on both paired chromsomes (DCe/DCe) then only D, C and e would be present on the cells. • If one chromsome carried DCe and the other was DcE this would cause D, C, c, E and e antigens to be present on red blood cells. • Each antigen except d is recognizable by testing red cells with specific antiserum.
Wiener • Postulated that TWO genes, one on each chromosome pair, controls the entire express of Rh system. • Each gene produces a structure on the red cell called an agglutinogen (antigen). • Eight (8) major alleles (agglutinogens): R0, R1, R2, Rz, r, r’, r” and ry. • Each agglutinogen has 3 factors (antigens or epitopes) • The three factors are the antigens expressed on the cell. • For example the agglutinogen R0= Rh0 (D), hr’ (c), hr’ (e) • Each agglutinogen can be identified by its parts or factors that react with specific antibodies (antiserums).
Weiner’s Theory
Weiner and Fisher-Race • The two theories are the basis for the two notations currently used for the Rh system. • Immunohematologists use combinations of both systems when recording most probable genotypes. • You MUST be able to convert a Fisher-Race notation into Wiener shorthand, i.e., Dce (Fisher-Race) is written R0. • Given an individual’s phenotype you MUST determine all probable genotypes and write them in both Fisher-Race and Wiener notations. • R1r is the most common D positive genotype. • rr is the most common D negative genotype.
Comparison of Weiner and Fisher-Race
Weiner and Fisher-Race D = R 1 ( C) Z (both C & E ) 2 ( E ) 0 (neither C or E ) D c e D C E D C D c E d = r ‘( C) y (both C & E ) ‘’ ( E ) (neither C or E ) d c e d C E d C e d cE
Differentiating Superscript from Subscript Superscripts (Rh1) refer to genes Subscripts (Rh1) refer to the agglutinogen (complex of antigens) For example, the Rh1 gene codes for the Rh1 agglutinogen made of D, C, e Usually, this can be written in shorthand, leaving out the “h” DCe is written as R1
Converting Wiener into Fisher-Race or Vice Versa R D r no D 1 and ‘ C 2 and “ E Example: DcE R2 r” dcE Written in shorthand
Rosenfield • In 1962 proposed a nomenclature based ONLY on serologic (agglutination) reactions. • Antigens are numbered in the order of their discovery and recognition as belonging to the Rh system. • No genetic assumptions made • The phenotype of a given cell is expressed by the base symbol of “Rh” followed by a colon and a list of the numbers of the specific antisera used. • If listed alone, the Antigen is present (Rh:1 = D Ag) • If listed with a “-”, antigen is not present (Rh:1, -2, 3 = DcE) • If not listed, the antigen status was not determined • Adapts well to computer entry
Comparison of Three Systems
International Society of Blood Transfusion • Abbreviated ISBT • International organization created to standardize blood group system nomenclature. • Assigned 6 digit number for each antigen. • First 3 numbers indicate the blood group system, eg., 004 = Rh • Last 3 numbers indicates the specific antigen, eg., 004001 = D antigen. • For recording of phenotypes, the system adopts the Rosenfield approach
Phenotype versus Genotype The phenotype is the result of the reaction between the red cells and antisera The genotype is the genetic makeup and can be predicted using the phenotype and by considering the race of an individual Only family studies can determine the true genotype
Five reagent antisera available. Only anti-D required for routine testing. Other typing sera used for typing rbcs to resolve antibody problems or conduct family studies. Agglutination reactions (positive and negative) will represent the phenotype. No anti-d since d is an amorph. Use statistical probability to determine most probable genotype. Phenotyping and Genotyping
Rh Phenotyping • Uses • Parentage testing • Predicting hemolytic disease of the fetus and newborn (HDFN) • Confirmation of Rh antibody specificity • Locating compatible blood for recipients with Rh antibodies. • Protocol • Mix unknown RBCs with Rh antisera • Agglutination indicates presence of antigen on cell and determines phenotype. • Use published frequencies and subject information to determine genotype.
Phenotyping and Genotyping Molecular testing becoming more popular: Cannot use anti-sera on recently transfused individuals, molecular testing can differentiate. Anti-sera not available for some antigens, molecular testing being developed for all blood group genes. D zygosity can be determined. Fetal genotyping for D can be done on fetal DNA present in maternal plasma. Monoclonal reagents from different manufacturers react differently with variant D antigens, molecular test specific. Typing sera continue to be the “gold standard” but this will change in the future.
Genotype Frequencies • Refer to textbook. • Genotypes are listed as “presumptive” or “most probable”. • Genotypes will vary in frequency in different racial groups.
Weak Expression of D Not all D positive cells react equally well with anti-D. RBCs not immediately agglutinated by anti-D must be tested for weak D. Incubate cells with anti-D at 37C, coating of D antigens will occur if present. Wash X3 add AHG AHG will bind to anti-D coating cells if present. If negative, individual is D negative If positive, individual is D positive w
Three Mechanisms for Weak D Genetic Position effect Mosaic Results in differences from normal D expression Quantitative (inherited weak D or position effects) Qualitative (mosaic D; could produce Anti-D)
Weak D - Genetic Inheritance of D genes which result in lowered densities of D Antigens on RBC membranes, gene codes for less D.
Weak D - Genetic RBC with normal amounts of D antigen Weak D (Du)
Position Effect C trans - position effect; The D gene is in trans to the C gene, eg., C and D are on OPPOSITE sides: Dce/dCe C and D antigen arrangement causes steric hindrance which results in weakening or suppression of D expression.
Position Effect C in trans position to D: D c e / d C e Weak D C in cis position to D: D C e / d c e NOweak D
Partial D Absence of a portion or portions of the total material that comprises the D antigen. Known as “partial D” (old term “D mosaic”).
D Mosaic/Partial D If the patient is transfused with D positive red cells, they may develop an anti-Dalloantibody* to the part of the antigen (epitope) that is missing Missing portion RBC RBC *alloantibody- antibody produced with specificity other than self
Significance of Weak D Donors Labeled as D positive Weak D substantially less immunogenic than normal D Weak D has caused severe HTR in patient with anti-D Patients If weak D due to partial D can make antibody to portion they lack. If weak D due to suppression or genetic expression theoretically could give D positive Standard practice to transfuse with D negative Weak D testing on donors by transfusion service not required. Weak D testing on patients not required except in certain situations.
Compound Antigens Compound antigens are epitopes which occur due to presence of two Rh genes on the same chromosome, cis position. Gene products include not only products of single gene but also a combined gene that is also antigenic. (f, rh1, etc) f antigens occur when c and e are found in cis (Example: dce/dce) r(cde) gene makes c and e but also makes f (ce). ONLY OCCURS when c and e are in the CIS position. f antigen will NOT be present in trans position. rh1 or Ce antigens occur when C and e are in cis (example: dCe/dce) Antibodies rarely encountered but if individual had anti-f would only react with f positive cells, not cells positive for c or e in trans only. f cells clearly marked on antigram of screen and panel cells.
G Antigen Genes that code for C or D also code for G G almost invariably present on RBCs possessing C or D Anti-G mimics anti-C and anti-D. Anti-G activity cannot be separated into anti-C and anti-D.
D Deletion Very rare Individuals inherit Rh gene complex lacking alleles. May be at Ee or Cc Must be homozygous for rare deletion to be detected. No reaction when RBCs are tested with anti-E, anti-e, anti-C or anti-c Requires transfusion of other D-deletion red cells, because these individuals may produce antibodies with single or separate specificities. Written as D- - or -D-
Rh Null Red cells have no Rh antigen sites Genotype written ---/--- The lack of antigens causes the red cell membrane to appear abnormal leading to: Stomatocytosis Hemolytic anemia 2 Rh null phenotypes: Regulator type – gene inherited, but not expressed Amorph type – RHD gene is absent, no expression of RHCE gene Complex antibodies may be produced requiring use of rare, autologous or compatible blood from siblings.
LW Discovered at same time as Rh antigen. LW detected on cells of Rhesus monkeys and human rbcs in same proportion as D antigen. Thought was the same antigen but discovered differences. Named LW in honor of Landsteiner and Wiener. Rare individuals lack LW yet have normal Rh antigens. Can form allo anti-LW. Reacts more strongly with D pos than D neg cells. Keep in mind when D pos individual appears to have anti-D
Cw Variant Rh antigen Low frequency antigen found in only 1-2% of Whites and rare in Blacks Most individuals who are C+ are Cw+ Antibodies to these antigens can be naturally occuring and may play a role in HFDN and HTR
Rh Antibodies Except for rare examples of anti-E and anti-Cw which may be naturally occurring, most occur from immunization due to transfusion or pregnancy. Associated with HTR and HDFN. Characteristics IgG but may have MINOR IgM component so will NOT react in saline suspended cells (IS). May be detected at 37C but most frequently detected by IAT. Enhanced by testing with enzyme treated cells. Order of immunogenicity: D > c > E > C > e Do not bind complement, extravascular destruction.
Rh Antibodies Anti-E most frequently encountered antibody followed by anti-c. Anti-C rare as single antibody. Anti-e rarely encountered as only 2% of the population is antigen negative. Detectable antibody persists for many years and sometimes for life. Anti-D may react more strongly with R2R2 cells than R1R1 due to higher density of D antigen on cells.
Concomitant Rh Antibodies Antibodies which often occur TOGETHER. Sera containing anti-D may contain anti-G (anti-C + -D) Anti-C rarely occurs only, most often with anti-D. Anti-ce (-f) often seen in combinatiion with anti-c. MOST IMPORTANT is R1R1 who make anti-E frequently make anti-c. Patients with anti-E should be phenotyped for c antigen. If patient appears to be R1R1 should be transfused with R1R1 blood. Anti-c frequently falls below detectable levels.
Detection of D Antigens • Four types of anti-D reagents • High Protein - Faster, increased frequency of false positives; requires use of Rh control tube, converts to weak D testing • IgM (Low protein/Saline reacting) - Low protein (fewer false positives); long incubation times; cannot convert to weak D testing • Chemically modified - “Relaxed” form of IgG Anti-D in low protein medium; few false positives; saline control performed; converts to weak D testing • Monoclonal source, low protein, blends of mAbs • Must know the preparation, use, advantages and limitations of each.
High Protein Anti-D IgG anti-D potentiated with high protein and other macromolecules to ensure agglutination at IS. May cause false positives with rbcs coated with antibody. Diluent control REQUIRED. False positives due to autoagglutinins, abnormal serum proteins, antibodies to additives and using unwashed rbcs. Can be used for weak D test.
IgM Anti-D (low protein/saline) Prepared from predominantly IgM antibodies, scarce due to difficulty obtaining raw material. Reserved for individuals giving false positive with high protein anti-seras. Newer saline anti-sera require incubation at 37. No negative control required unless AB positive. CANNOT be used by slide test OR weak D test.
Chemically Modified IgG converted to saline agglutinin by weakining disulfide bonds at hinge region, greater flexibility, increases span distance. Stronger reactivity than IgM antibodies. Can be used for slide, tube and weak D test. Negative control unnecessary unless AB positive.
Monoclonal Anti-D Prepared from blend of moncolonal IgM and polyclonal IgG. IgM reacts at IS IgG reacts at AHG (weak D test) Most frequently utilized reagent. Used for tube, slide and weak D test. Negative control unnecessary unless AB positive.
Control for Low Protein Reagents Diluent used has protein concentration equaling human serum. False positives due to immunoglobulin coating of test rbcs occurs no more frequently than with other saline reactive anti-sera. False positives do occur, patient will appear to be AB positive on forward type. Must run saline or manufacturer’s control to verify.
Precautions for Rh Typing MUST follow manufacturer’s instructions as testing protocols vary. Cannot use IAT unless explicitly instructed by manufacturer. Positive and negative controls must be tested in parallel with test rbcs. QC performed daily for anti-D QC for other anti-seras performed in parallel with test since these are usually not tested each day, only when necessary.
- More by User
ABO Blood Group System
ABO Blood Group System. History: Karl Landsteiner. Discovered the ABO Blood Group System in 1901 He and his five co-workers began mixing each others red cells and serum together and inadvertently performed the first forward and reverse ABO groupings. Why is it important?.
2.51k views • 53 slides
History ABO System Phenotype ABO System Genotype Rh system Other Blood Groups Blood Group detection and incompatibility
2.06k views • 91 slides
Importance of ABO system. ABO compatibility between donor cell and patient serum is the essential foundation of pre-transfusion testingIt is the only system with expected antibodiesWhether they are IgG or IgM, ABO antibodies can activate complement readilyThis means that incompatibilities can cau
1.26k views • 29 slides
The Rh Blood Group
The Rh Blood Group. Brian Poirier, MD UCDavis Medical Center. Topics. Terminology systems Rh antibodies Consequences of Rh incompatibility Unusual phenotypes. Objectives. Explain the derivation of the term Rh Differentiate Rh from LW
1.62k views • 41 slides
The Rh System
The Rh System. Immunohematology. Objectives. Compare the three theories of inheritance of the Rh antigens. List the antigens and antibodies of the system using both Wiener and Fisher-Race nomenclature. Convert haplotype from Fisher-Race nomenclature into Wiener, and vice versa. Objectives.
1.06k views • 40 slides

ABO/ Rh Blood Typing
ABO/ Rh Blood Typing . Activity. ABO and Rh Blood Typing. ABO/ Rh is the most commonly used system for classifying blood type. It was developed in the late 1800’s by Austrian physician Karl Landsteiner.
866 views • 10 slides
MATERNAL-FETAL INTERACTIONS AND THE Rh BLOOD GROUP
MATERNAL-FETAL INTERACTIONS AND THE Rh BLOOD GROUP. Victoire N. Ndong Biology 327: Immunology. THE PLACENTA. HOW DOES THE FETUS STAY IMPLANTED IN THE UTERUS WITHOUT BEING REJECTED?. MEDAWAR’S THEORIES. The uterus is an “immunologically privileged site”
310 views • 14 slides
Rh factor & Blood Donation
Rh factor & Blood Donation. December 2, 2009. Catalyst. Entrance ticket! (collected) Make a table showing blood type, the antigen associated with that type and the antibody associated with that type. Really important! . So, you know how we say “has antibody for“
637 views • 49 slides
The Blood Group System s
The Blood Group System s. Inheritance and Genetics . History of Blood Groups and Blood Transfusions.
648 views • 34 slides
ABO and Rh Blood Group Systems
ABO and Rh Blood Group Systems. Teaching Aim. Understanding inheritance, synthesis, various antigens and antibodies and their clinical significance in ABO & Rh blood group systems Understanding practical aspects of ABO & Rh blood grouping. Human Blood Groups.
2.06k views • 73 slides
History ABO System Phenotype ABO System Genotype Rh system Other Blood Groups
IMMUNOHEMATOLOGY By E. Salehi Ph.D. Assistant prof. Department of Immunology. History ABO System Phenotype ABO System Genotype Rh system Other Blood Groups Blood Group detection and incompatibility Hereditary Newborn Disease HDN Blood Transfusion. Karl Landsteiner (1868-1943).
1.94k views • 91 slides
The Rhesus (Rh) Blood Group system
The Rhesus (Rh) Blood Group system. The Rh(D) Antigen. Rh is the most complex system, with over 45 antigens The complexity of the Rh blood group Ags is due to the highly polymorphic genes that encode them. Discovered in 1940 after work on Rhesus monkeys
2.47k views • 44 slides

ABO blood group System
ABO blood group System. By : Mr. Waggas Ela’as , M.Sc ; MLT. ABO BLOOD GROUP SYSTEM. Discovered by Karl Landsteiner ; locus on chromosome 9 Single most important blood group for the selection and transfusion of blood
862 views • 25 slides
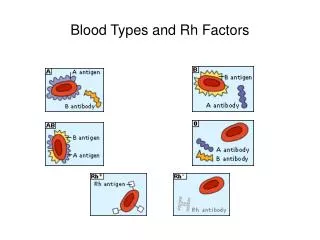
Blood Types and Rh Factors
Blood Types and Rh Factors. White Blood Cell Types.
235 views • 2 slides
ABO Blood Group System. Importance of ABO system. ABO compatibility between donor cell and patient serum is the essential foundation of pre-transfusion testing It is the only system with expected antibodies Whether they are IgG or IgM, ABO antibodies can activate complement readily
813 views • 28 slides
The ABO Blood Group System
The ABO Blood Group System. Laboratory Determination of the ABO System. Blood Types. Antigens : proteins located on the surface of the RBCs Antibodies : proteins in the blood plasma. Individuals have different types and combinations of these antigens and antibodies. .
608 views • 9 slides
Rh System. Antibody Identification. Rh System. Most important blood group system in blood transfusion medicine. (after ABO). Rh Discovery. 1939 – Levine and Stetson 1 st discovered antibody 1940 – Landsteiner and Weiner discovered
866 views • 32 slides
Rh blood system
Rh blood system. Difference between ABO and Rh blood types Six Rh antigens, each is called Rh factor. C,D,E,c,d,e Type D antigen is most prevalent and more antigenic Persons having D antigen--- Rh positive Persons not having D antigen--- Rh negative
264 views • 6 slides
Rh BLOOD GROUP SYSTEM
Rh BLOOD GROUP SYSTEM. AHLS 311. HISTORY. Ab in serum of mother of stillborn child; responsible for the death of fetus? (1939, Levine and Stetson) Rb-derived Ab to Rhesus monkey RBCs reacts with 85% of human subjects; same Ab as reported by Levine? (1940, Landsteiner and Weiner)
629 views • 25 slides
The Blood Group System s. Inheritance and Genetics. History of Blood Groups and Blood Transfusions.
484 views • 34 slides
ABO Blood Group System. Importance of ABO system. ABO compatibility between donor cell and patient serum is the essential foundation of pretransfusion testing It is the only system with expected antibodies Whether they are IgG or IgM, ABO antibodies can activate complement readily
1.03k views • 44 slides
Unit 7: Circulatory System
Unit 7: Circulatory System. Absorption & Circulation. A. Absorption 1. Where in the body are nutrients and materials absorbed by the body? a. Lungs – O 2. b. Small Intestine - nutrients = amino acids, glucose, lipids. B. Circulation Distribution of materials
340 views • 25 slides

IMAGES
VIDEO
COMMENTS
The ABO blood group system is the most important in transfusion medicine. This presentation covers basic ABO inheritance, antigen production and expression, and weak subgroups. ... After this presentation, participants will be able to: Describe the biochemistry and production of the A, B, and H antigens. ...
The ABO blood group system was first discovered in the early 1900s, and since that time, our understanding of the ABO blood group system has increased significantly. These discoveries have led to safer transfusion practices.[1][2] The ABO blood group system spans beyond transfusion medicine and has been used in the study of populations by anthropologists, police in forensic science, and ...
The most important are ABO antigens, which determine a person's ABO blood group. An individual inherits one ABO allele from each parent, with A and B alleles being codominant and producing the A and B antigens respectively. Group A - have antigen A attached to the erythrocyte cell surface. Group B - have antigen B attached to the ...
In the Rh system, the most important antigens are D, C, c, E, and e. The ABO and Rh blood systems are discussed in detail below. 1. ABO blood Group system. The basis of ABO grouping is of two antigens- Antigen A and Antigen B. The ABO grouping system is classified into four types based on the presence or absence of antigens on the red blood ...
BLOOD GROUPING SYSTEM. Major blood group system - based on Agglutinogens on cell membrane, present widely & causes severe transfusion reaction ABO Rh system Minor blood group system - based on Agglutinogens but present in few populations & causes mild transfusion reaction. MNS P Familial blood group system - found in few families KELL ...
Recorded December 2011. This Blood Bank Guy video is the first in a series of four videos that I did on basic immunohematology. It contains lots of information about the major blood group systems. This video is, in fact, a modified and updated version of the blood groups lecture (Blood Bank 1) that I used to give at the Osler Institute ...
The Rh blood group system has been extensively studied and remains clinically relevant to transfusion medicine. The system has over 50 antigens; the 5 most significant antigens are D, C, c, E, and e.[1] The Rh antigens are a part of proteins expressed on the surface of the red blood cell (RBC) membrane. The function of these antigens is unknown; they may play a role in membrane stability and ...
4 ABO Blood Groups Most well known & clinically important blood group system. Discovered by Karl Landsteiner in 1900 It was the first to be identified and is the most significant for transfusion practice It is the ONLY system that the reciprocal antibodies are consistently and predictably present in the sera of people who have had no exposure to human red cells ABO blood group consist of two ...
Blood groups are determined by the presence or absence of certain antigens on the surface of red blood cells. The most important blood group system is the ABO system, which is determined by the presence or absence of two antigens: A and B. People with blood group A have antibodies against the antigen B, people with blood group B have antibodies against the antigen A.
Presentation Transcript. The ABO Blood Group System Laboratory Determination of the ABO System. Blood Types • Antigens: proteins located on the surface of the RBCs • Antibodies: proteins in the blood plasma. • Individuals have different types and combinations of these antigens and antibodies. Blood group AA antigens on the surface of RBCs ...
Blood grouping : also called blood typing, is a test performed to define the individual blood group and it is performed by mixing anti-ABO and anti-Rh agglutinins (antibodies, anti-sera) with the. RBCs . The erythrocytes of a person contain blood group antigens on the surface of the membrane. When these antigens are allowed to treat with ...
About This Presentation. Title: ABO BLOOD GROUP SYSTEM. Description: DR AMINA TARIQ BIOCHEMISTRY The ABO blood group system is the most important blood type system (or blood group system) in human blood transfusion. - PowerPoint PPT presentation. Number of Views: 4499. Avg rating:3.0/5.0. Slides: 31.
Blood group ppt. Blood group ppt Nabiha_Khalid ... Rh GROUPING • It is the most important blood group system after ABO. • All Rh antigens are controlled by 2 genes - RHD gene- determines expression of D , RHCE - encodes for C,c and E,e. • RhD is a strong antigen (immunogenic) and other antigen are less antigenic than D and are of ...
Download ppt "ABO/Rh Blood Group System A . Amirzargar". History Carl Landsteiner: Discovered the ABO Blood Group System in 1901 He and five co-workers began mixing each others red blood cells and serum together and inadvertently performed the first forward and reverse ABO groupings. Landsteiners Rule: If an antigen is present on a patients red ...
Blood Group Antigens Antibodies Can give blood to Can receive blood from AB A and B None AB AB, A, B, O A A B A and AB A and O B B A B and AB B and O O None A and B AB, A, B, O O. The Blood Group System s. Inheritance and Genetics. History of Blood Groups and Blood Transfusions. Slideshow 6593944 by elijah-mcdaniel.
6. • ABO blood group system is the most important blood type system (or blood group system) in human blood transfusion. • ABO blood types are also present in some other animals for example rodents and apes such as chimpanzees, bonobos and gorillas • Determination of ABO blood groups depends upon the immunological reaction between antigen and antibody.
An Image/Link below is provided (as is) to download presentation Download Policy: ... The Kell blood group system was discovered in 1946. Number of Kell antigens: > 20 These antigens are the third most potent, after those of the ABO and Rh blood groups, at triggering an immune reaction. 1.99k views • 40 slides. Other Blood Group Systems.
ABO Blood Group System PPT - Free download as Powerpoint Presentation (.ppt / .pptx), PDF File (.pdf), Text File (.txt) or view presentation slides online.
Blood Group ppt presentation by mbbs 1st yr ... This law is only applicable to ABO blood grouping system. Slide 10-Agglutinins Anti-Rh antibodies (IgG) develop only in Rh- blood type and only with exposure to the antigen: transfusion of positive blood. during a pregnancy with a positive blood type fetus. Anti-Rh antibodies are not spontaneously ...
ABO Blood Group System. Importance of ABO system. ABO compatibility between donor cell and patient serum is the essential foundation of pretransfusion testing It is the only system with expected antibodies Whether they are IgG or IgM, ABO antibodies can activate complement readily. Download Presentation. abo.
Presentation Transcript. Blood grouping Biology 106. Two blood type system (or blood group system) in human blood transfusion • ABO system • The ABO blood group system is the most important blood typesystem. • The associated anti-A and anti-B antibodies are usuallyIgMantibodies. • Rh system • Clinically, it is the most important blood ...
Presentation Transcript. Unit 7 Rh BLOOD GROUP SYSTEM Terry Kotrla, MS, MT (ASCP)BB. Introduction • Rh is the most important blood group system after ABO in transfusion medicine. • One of the most complex of all RBC blood group systems with more than 50 different Rh antigens. • The genetics, nomenclature and antigenic interactions are ...