If you have any questions or concerns, please contact us at [email protected] or call in at 1-800-334-4245. We are open Monday-Friday 8am-5pm EST, USA.
NOTE: Sometimes our system emails get caught in SPAM. Please contact us if you are expecting a quote or other email and have not received it.

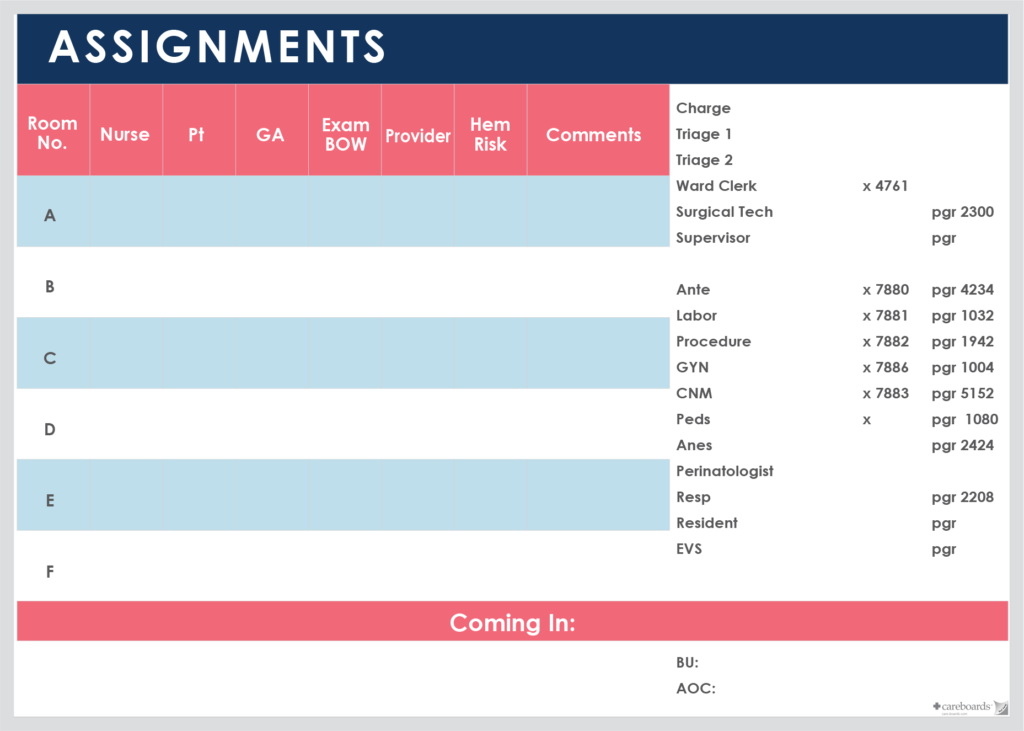
Hospital Rooms Coverage Whiteboard
Assign daily staff to patient rooms on a magnetic whiteboard.
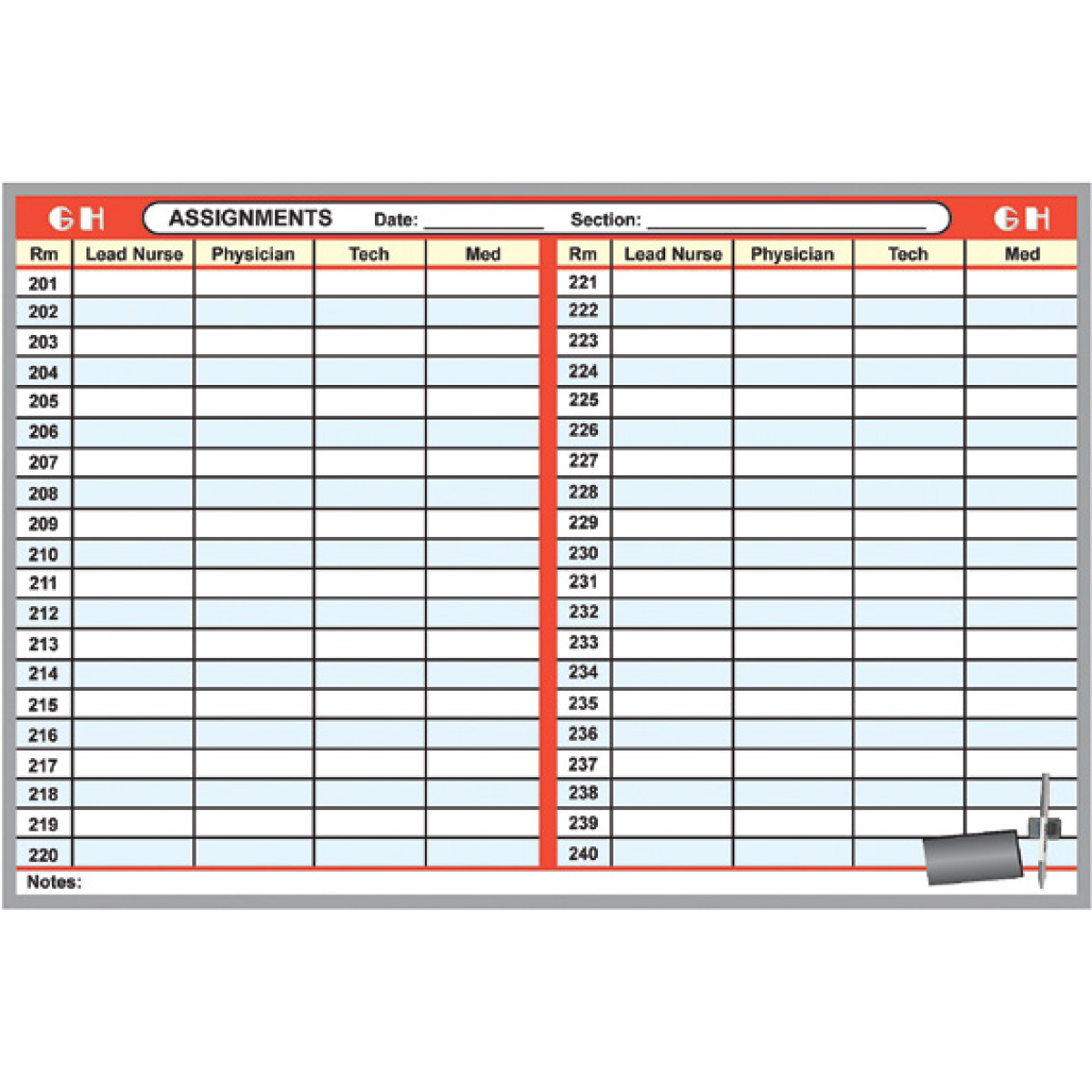
- Staff coverages can be quickly identified and assignments adjusted as needed
- Whiteboard to organize lead nurses, physicians, technicians and support staff for various units or hospital sections
- Helps patient ensure proper coverage and optimize personnel utilization
- We will customize the room assignment board to your staff and patient needs
- This staff scheduling system includes a FREE Supply Kit - see Detailed Description below
- Select the board size based upon the maximum number of rooms you need to assign per unit per shift
- Highly durable, dry-erase surface on which to write assignment data
- List all personnel assignments by room number
- FREE DESIGN CUSTOMIZATION to your specs
- Add or change the number of patient rooms
- Change the staff column headers
- Change border accent color(s) or add a department, floor or section name or the logo of your hospital, nursing home, clinic or healthcare facility
- We create the staff scheduling system to best address your staff to patient room coverage -- simply tell us (call, email or fax) what you would like when you order
- 2 Dry-Erase Markers - fine point black
- Magnetic Penholder
- Magnetic Eraser
- Hanging Hardware
- High quality magnetic whiteboard in an aluminum frame Intense heat permanently fuses your color graphics design with a sheet of solid steel to produce a highly durable, brilliant, dry-erase magnetic surface
- Our process produces a sturdy three-layer construction - the steel is laminated onto a rigid engineered wood foundation and backed with a sheet of aluminum foil as a protective moisture barrier
- WILL NOT STAIN, FADE, SHADOW OR CRACK
- No surface blemishes that are commonly seen on inferior whiteboards
- Our Polymer Fusion ™ Process creates a long lasting, custom magnetic surface
- Maintains its "like new" appearance throughout years and years of daily use
- This specialized process produces the most durable of any color printed whiteboard surface available in the market today!
- Construction is 0.022" coated sheet of solid steel laminated onto a rigid 3/8" MDF engineered wood foundation
- Service temperature range = -10F to +160F
- This staff scheduling system is made for indoor use
- Class C Fire rated
- Aluminum frame: Satin anodized extrusion of 6063 Aluminum-Magnesium-Silicon alloy which is extremely resistant to cracking and corrosion, framed board weighs 2.7 lbs per square foot, depth from board surface face to wall = 9/16" (14.3 mm)
- Wood frame: color stained and sealed ash, framed board weighs 3.1 lbs per square foot, depth from board surface face to wall = 15/16" (23.8 mm)
- Also available in a rolling whiteboard style - contact Customer Service for pricing
- Whiteboard cleaner, letter/number sets, markers - see Whiteboard Supplies
- Magnetic indicator symbols, chalktray, message clips - see Other Magnetic Accessories
- Additional sizes and custom designs - contact Customer Service for quote
Our Review of Your Design
- click on the desired blue part number above and complete your request. You will be then prompted to attach your file NOW or to receive an email to submit your file LATER .
- to confirm your design or data file is usable or for assistance in selecting the best size or style - Upload Your File Now for our review and acceptance. We will respond by the next business day.

Colored whiteboard markers for dry erase surfaces
Assign room numbers leave informative notes for nurses
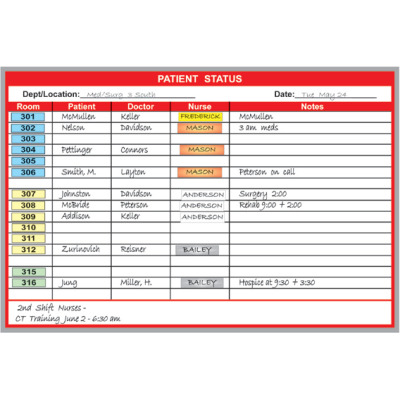
Communicate patient information to hospital staff
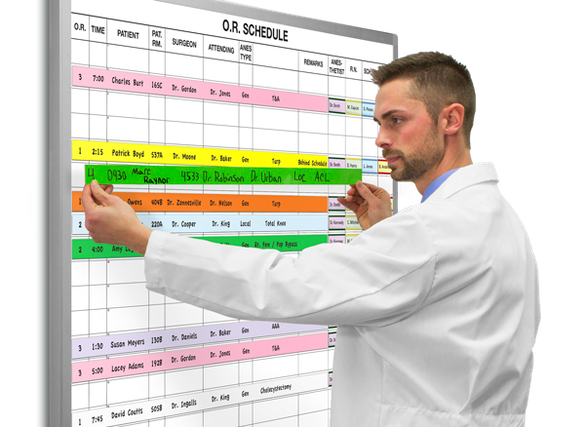
Magnetic Dry-Erase Whiteboard Systems for Hospitals
Magnatag ® hospital whiteboards are top-quality, designed to stay like new for lifetime of daily hospital use..
These are efficient, comprehensive and easy-to-use boards for managing hospital patient-staff communication, time, schedules, notes, patient-tracking and more.
We've designed and built them from daily dialogue with hospital management since 1967. Each board kit is ready-to-use with all the carefully-selected magnets and supplies needed to operate them.
To order custom-printed boards, please contact us or call one of our whiteboard specialists at 800 624 4154. No obligation. We ship factory-direct in 3 business days or less.
- SMB Technology
- Mobile Productivity
- Mobile Security
- Computing & Monitors
- Memory & Storage
- Digital Signage
- Trending Tech
- Hospitality
- Manufacturing
- Transportation
- Food & Beverage
- Live Events & Sports
- Spectaculars & DOOH
- Gaming & Esports
- White Papers
- Infographics
- Assessments & Calculators
- Case Studies
- About Samsung Insights
- Our Experts
Subscribe to Insights
Get the latest insights from Samsung delivered right to your inbox.
See our Privacy Policy
Samsung Business Insights

Featured posts in

4 mobile technology trends that are transforming patient engagement today

How health systems can support their clinical teams during staffing shortages

How to improve the patient experience with healthcare TVs
Key considerations when designing patient rooms for the future.
The digital transformation of healthcare has also transformed hospital design. At the heart of this transformation lies the patient room, the anchor of the hospital.
Like the modern medical complex, the modern patient room is streamlined with integrated and automated digital display solutions that enhance clinical workflows — while supporting patient engagement, satisfaction and safety.
Account for integration
Dry-erase boards have been included in hospital design plans for decades, and today, most patient rooms feature them. But these boards need to be updated manually each shift to include the names of everyone on the patient’s care team, as well as other pertinent information like dietary restrictions, medications and estimated discharge date. It’s easy for this handwritten information to become out of date or illegible. Besides, making these updates takes staff away from more involved clinical tasks.
The patient room of the future will include a digital whiteboard that updates automatically, drawing on information from the electronic health record (EHR) and shift assignment software. Patients, families and the care team will get the most current information at the point of care. And nurses don’t need to stop to update the display.
Reimagine healthcare facility design — brilliantly

Discover how digital displays can empower caregivers, engage patients, and elevate health brands. Download Now
Similarly, a real-time location system (RTLS) ensures that patients and their loved ones know which staff member has entered the patient room at any given time. Each clinician and employee will wear a badge that communicates with the patient room TV , automatically displaying their name and care team role as they enter the room. An integrated RTLS also ensures that the right information goes to the right care team member at the right time.
Screens located above the bed behind the patient can simultaneously display information relevant to whichever team member is checking on them. Their nurse, for example, would see different information than the attending physician, the respiratory tech or the dietitian. Implementing these digital solutions will require not only adequate space but adequate outlets and connectivity, which hospital architects and engineers will need to account for as they consider the patient room design.
Plan for telepresence
Connected patient rooms will also include cameras for telehealth and remote patient monitoring (RPM). These will soon be as standard as hygiene stations and bed alarms. COVID-19 has proven how important RPM is : Clinicians who can monitor their patients remotely don’t have to “gown up” and use limited PPE resources each time they see a new patient, yet they’re still able to speak with the patient face to face. With connected diagnostics, remote visits allow clinicians to make accurate assessments over a video call. This flexible technology also makes it easier for patients and their care team to connect with outside specialists.
For patients who are fall risks, cameras can function as virtual bed rails, alerting the patient’s care team if they attempt to get out of bed alone. But in-room cameras and telehealth aren’t only for dire situations: They allow for virtual family visits, as well as language translation services. And the same tools can be used to offer real-time, interactive education sessions with patients and their caregivers before discharge.
Support patient engagement
A digitally streamlined patient room doesn’t just support clinical workflows; it also enhances the patient experience . The in-room TV, for example, can provide entertainment in addition to diagnostics and data. It offers a welcome distraction, helping to alleviate the pain, discomfort and anxiety many patients struggle with during a hospital stay. When patients are entertained and engaged, they’re also less likely to call the nurses station.
Patient rooms might also have bedside tablets , which they can use to view their records and prescriptions, see who’s on their care team and communicate with nurses, doctors and other hospital staff. Rather than pushing the call button to ask a nurse for something simple like another blanket, patients can request these services directly from their tablet, so the nurses station no longer needs to work like a switchboard. This reduces the nurses’ administrative burden, eases alarm fatigue and allows them to work at the top of their license.
On the same tablet, an automated message can ask patients if their room is quiet enough for them to sleep and make the appropriate changes. Patients can adjust the room’s temperature, lighting and window shades with the touch of a button — all to create a better, more comfortable experience for patients.
Think beyond the room
The patient room is just the beginning. Digital displays improve clinical efficiency across the entire facility, such as these use cases:
- Nurses stations: Equipping nursing stations with large, centralized USB-C monitors provides efficient, all-in-one information dashboards. Because they require fewer cables, these monitors easily fit on nursing carts.
- Outside the door: Smaller displays outside each patient room ensure that clinicians, staff and visitors are informed of the patient’s dietary restrictions, relevant allergies and preferred language, as well as all safety protocols required to enter the room.
- Waiting rooms: Visitors can track their loved one’s status on an updated waiting room monitor . Uncertainty leads to questions: Are they still in the operating room? For how much longer? When these questions are answered more quickly, the waiting room is a much less stressful place.
- Wayfinding: Touchscreen maps show patients and visitors exactly where they need to go, avoiding frustration and freeing up busy hospital staff from the need to provide repetitive directions.
- Marketing and development: Hospitals can install a microLED video wall to recognize donors and share brand stories.
Be mindful of budgets
Designers need to think about more than just design. Profit margins for hospitals are slim, around 1 to 2 percent. Designing the hospital of the future requires that every element work together seamlessly. And the design must be scalable, because technology is constantly evolving.
When digital displays are properly deployed and fully integrated, patients and their loved ones are more engaged and at ease. Hospitals get to use their resources as efficiently as possible, future-proofed to serve patients for years to come.
Learn more about how digital displays are easing pain points and transforming clinician and patient experiences in our free guide . And discover Samsung’s lineup of UL-listed healthcare TVs , built to support clinicians and improve the patient experience at a manageable price point.

Roxanna Guilford-Blake
Roxanna Guilford-Blake writes about health, healthcare and the business of healthcare. She began as a journalist, but for more than 25 years, she’s helped clients tell their stories and enlighten their audiences. She runs her own editorial business (Guilford-Blake Corp.) and previously served as director of strategic communications at a boutique healthcare communications firm. She’s especially interested in the intersection of digital tech and patient-centered care.
- IT Strategy
- Patient Engagement
- patient experience
- USB-C Monitors
Related Posts

Healthcare digital signage is the key to hospital transformation
Healthcare digital signage, including hospital patient whiteboards, is the key to hospital digital transformation.

7 benefits of digital signage in hospitals
Healthcare digital signage provides ready access to up-to-date information, improving efficiency, patient care and the clinical experience.

Meet them where they are: Waiting room signs for patients can improve the patient journey
Medical centers are places of high emotion and stress. The right signage, such as waiting room signs for patients, can improve the patient journey.
Featured Posts

Hospitals are using mobile technology to improve patient engagement across the care continuum and deliver connected, hybrid care. Here are the top trends.

Staffing shortages are becoming the norm in healthcare, but there are mobility solutions that can help.

Hospital patient TV systems provide more than entertainment. Properly deployed, hospital room TVs can become an all-in-one communications hub that transforms the patient experience.
How can we help you?
Shop special offers.
Find out about offers on the latest Samsung technology.
Speak to a solutions expert
Get expert advice from a solutions consultant.
Who are you buying for?
I'm buying for myself
I'm buying for a small business
I'm buying for a large enterprise
Our solutions architects are ready to collaborate with you to address your biggest business challenges.
- Mobile Phones
- Laptops/2-in-1
- Business Services
- Displays & Digital Signage
- Hospitality TVs
- Wireless Networks
- Public Safety

A member of our solutions architect team will be in touch with you soon.

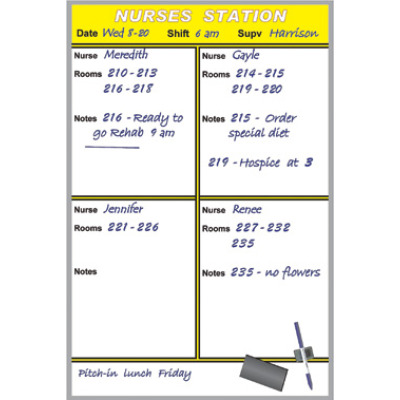
Nurse Station Communication Boards
Help your team stay on task.
Nurse station communication boards create operational efficiencies that streamline workflows for your nursing staff. Our nurse station boards allow your team to easily view schedules and room assignments. You can clearly display patient rooms, staff names, and any special notes. Since the board incorportes printed graphics there is no messy tape to apply or remove.
Board graphics can also be customized to include when rounds and medication are due, pain levels, and more.

All CareBoards patient room communication boards are built to your unique requirements. You have 15 colors to choose from and 5 standard sizes . Custom sizes can also be built.
As with all CareBoards products, all aspects of the design can be customized to reflect your hospital brand and your own unique communication needs. Board graphics can be customized to include when rounds and medication are due, pain levels, and more.
Here’s some examples of nurse station boards we’ve produced. Get some ideas and we’ll work with you to create a design customized for your unit.
View the Graphics Examples page to to see a variety of designs for other hospital units and healthcare applications.

An Easy-to-Follow Guide to Designing Hospital Whiteboards
Aug 31, 2018

You don’t have to be a professional designer or an expert in patient/provider communication to build your own custom whiteboards . While designing a whiteboard is a complex process, we have greatly simplified it with our Board Builder tool. It’s easy to use and will help you design and lay out a whiteboard that suits your healthcare facility.
There are a lot of options to choose from, but not to worry, we will walk you through each of the options in this guide. If you are ready to get started, head on over to build.vividboard.com .
Step #1: Choosing a Category

We’ll start off with an easy question: where will your whiteboard be placed? The two most basic options to choose from are “Patient Room” whiteboards and “Nurses’ Station” whiteboards. These two types of whiteboards serve very different purposes :
- Patient Room: hospitals use patient room boards to display everything from basic patient & provider information to meal & treatment schedules. They can be used in nearly every area of the hospital, from pediatrics to maternity, emergency and even behavioral health.
- Nurses’ Station: these whiteboards are great for listing nurse schedules, on-call information, room assignments and so much more. Nurses use them to coordinate their daily tasks and stay organized throughout the day.
Step #2: Choosing a Whiteboard Type

Before you get into design specifics, you can choose the type of whiteboard that you will be working with. “There’s more than one type of whiteboard,” you ask? That’s right, we offer multiple styles for the modern healthcare facility:
- Low Profile Glassboards: these low-profile whiteboards are frameless and feature no visible hanging hardware. They essentially “float” on the wall, adding a more modern, elegant look to any patient room.
- Changeable Glassboards: not your traditional glass whiteboards. These permanent fixtures feature interchangeable inserts that can be swapped out as needed. Use them to showcase information in different languages or change them out as rooms change over.
- Glassboards with Stand-Offs: frameless, borderless glassboards made of materials. These modern whiteboards are a permanent fixture that complement any room design.
- Custom Whiteboards: these boards offer the classic whiteboard look that comes complete with custom framing options, images, colors and more.
Many of these options can be used across the entire hospital, and the “right” one to choose is often a matter of preference, but some options can better serve you based on where they will be placed. For example, nurse’s stations and other small areas benefit from low profile Aria whiteboards, while behavioral health facilities may want to opt for frameless Classic Whiteboards that rest flat against the wall and cannot be tampered with.
Step #3: Choosing a Frame

Based on the whiteboard type you choose, you will have different frame options that come with it. Aria glassboards come standard with frameless edges and square corners, while InHarmony and MyHarmony whiteboards allow you to choose from square and rounded corners and standoffs. Classic Whiteboards offer the greatest variety of frame options:
- Silver Aluminum
- Black Powder Coated Steel
- Light Oak Wood
- Cherry Oak Wood
Step #4: Choosing Size and Orientation

Select your whiteboard size and choose between landscape and portrait options. Keep in mind that each board is made to order. If you need custom sizing, shapes or anything else, reach out to us and let us know how we can customize your whiteboard.
Step #5: Choosing a Background

Now that the physical build of your whiteboard is complete, it’s time to move onto the design phase, starting with your choice in background options. We have included some of the most popular options within our Board Builder, but these are by no means the extent of the pre-printed backgrounds we offer. Best of all, you can add a custom background by uploading an image or design of your own. Many hospitals choose images, logos or other designs based on their brand.
We have even partnered with Pattern Pod to bring even more custom designs to our whiteboards. Choose a background that best suits the design of your space.
Step #6: Choosing a Layout

How information is presented on a whiteboard is important to increasing patient understanding . We have several pre-designed layouts you can choose from. These are designed based on our expertise and experience with patient/provider communication, but you can have us lay out a board in any format you feel best serves your needs. You can choose to have a header and/or footer and incorporate columns and rows into the design, as well.
Step #7: Finalizing Your Design

This is where the real fun begins. It’s also the most important part of the design process. Choosing the right information fields to display is essential to the core functionality of your whiteboard. Not sure where to begin? Ask yourself, your care providers and your patients what they want to see on a whiteboard. The information you display should be used to address patient needs , help nurses and doctors during treatment , and even address the concerns of the patient’s loved ones who come to visit.
There are dozens of information fields to choose from, and you aren’t limited to the options we have in our Board Builder. You can upload your own information fields or work with us to create something new and unique. Running short on inspiration? Take a look at our IdeaBook to see how facilities like yours have designed their whiteboards.
What to Do When You’re Done
When you are finished with your whiteboard design, you can submit it to us for a free quote. And don’t worry, we won’t consider this a final design. We will reach out to you to discuss your needs and help you create a whiteboard that addresses every single one of them.
Ready to get started?
Start Building Your Whiteboard
Recent posts.
Custom Whiteboard Frames That Match Your Interiors Jan 06, 2022
Next Year’s Trends in Patient Room Design Dec 30, 2021
Glassboards in Hospital Rooms: From a Design Perspective Dec 20, 2021
Addressing HIPAA Concerns with Patient Whiteboards Dec 03, 2021
Sanitization of Boards Nov 26, 2021
Dave Fennema, HMC Architects
Hospital Room Design Strategies To Increase Staff Efficiency and Effectiveness
Hospital room design has a significant impact on patient care and recovery outcomes. Patients rely on staff to respond to emergency situations quickly, check in on them frequently, and ensure a full recovery. However, staff can only treat patients effectively when they can perform their tasks efficiently and have equipment and supplies that are easily accessible. By partnering with an architectural firm to design hospital rooms around staff workflows and make those spaces as comfortable as possible for patients and their visitors, hospital administrators can assure the highest level of care.
Hospital Room Design Challenges Architects Must Overcome
One of the greatest challenges that architects face when designing a hospital room is the need to accommodate three very different functions in the space. First, the room has to be comfortable and calming for the patient. Second, caregivers must be able to navigate the space quickly and efficiently. And finally, family and other visitors must have an area in which they can sit or sleep comfortably without disrupting attending staff workflow or the patient’s recovery. In a small hospital room, this is a serious challenge, as space is extremely limited.
Another challenge of hospital room design is providing clear lines of sight from the nurses’ station. Efficient hospital room design should also be adaptable, which can add an extra layer of complexity to the design process because every patient has different needs.
Architects have discovered innovative ways to meet these challenges and create efficient hospital rooms that support patients, staff, and visitors. By focusing on details such as equipment placement, flexible furniture, acoustics, and lighting, architects can dramatically improve staff efficiency and effectiveness.
Hospital Room Design Features That Foster Greater Efficiency
To create the most efficient hospital room design strategy, architects thoroughly research staff and patient needs in advance. By leading eco-charrettes, researching scientific studies, analyzing hospital-provided data , and following evidence-based design principles , HMC Architects has developed strategies for hospital room designs that can help staff perform their daily tasks more easily, while at the same time allowing for great patient and family experiences in the hospital. These strategies include the following:
Clear Lines of Sight
The following design concepts help nurses observe all patients:
- Room Layout. U and C patient room configurations work best in ICUs, as they better allow staff to observe and quickly access every patient room from a central station.
- Cockpit Stations. For large Nursing Units where nurses’ stations are located far apart, architects design smaller, decentralized “cockpit” nurses’ stations in between groups of two rooms, allowing for direct observation of the patient.
- Glazed Doors. Doors with glass panel windows allow staff visibility into patient rooms.
Improving the line of sight to hospital rooms is a best practice that architects prioritize to streamline staff workflows and offer excellent patient care.
Easily Accessible Supply and Equipment Locations
The placement of necessary tools and equipment also has an impact on staff efficiency. As such, architects consider:
- Lower Cabinet and Equipment Placement. When we designed Henderson Hospital in Nevada , we learned that some nurses had trouble reaching the top shelves in patient rooms and supply closets. So, we placed essential equipment and supplies lower in storage rooms to accommodate them.
- Supply Storage Where It’s Needed. Small supply drawers built into the patient room corridor wall can offer staff the supplies they need on-demand.
- Ceiling-Integrated Equipment. Supporting medical equipment like patient lifts and IV poles from the ceiling opens up floor space, allowing staff to move through the room more efficiently.
- Supporting Mobile Equipment for Care On-the-Go. A study published by JMIR Human Factors in 2017 found that more than 20 percent of nurses use their personal mobile devices to access important work-related medical information. By embedding outlets into furniture and offering more outlets, or USB charging stations in walls and on countertops, nurses and other staff members can keep their devices fully-charged at all times.
By placing supplies and tools within easier reach, staff can perform tasks much faster and more efficiently.
Room Layout and Furniture Placement
Furnishings in patient rooms are required for patient and visitor comfort, but they can also disrupt staff workflow. To cause the least disruption, room layout should be maximized, or right-sized. To create a more efficient hospital room design, architects can:
- Divide the Room into Three Zones: The staff zone should be at the entrance to the room to foster efficiency in performing their tasks, while providing the least impact on occupants. Patient amenities should be placed at the center of the room, and at the back of the room, place comfortable seating for visitors.
- Use Lightweight or Wheeled Furniture: Wheeled furniture and lightweight, modular ottomans can be quickly moved out of the way in an emergency. A sofa that can expand into a bed will serve a dual purpose.
- Design Bathrooms Based on Need: Front-located bathrooms leave room for a larger visitor area in the back of the room but may limit visibility to the patient. Rear-located bathrooms provide improved sight lines to the patient but sacrifice family space and expansive exterior views out of the room. Center-bar bathrooms represent a compromise between the front and back bathroom options, allowing both maximum visibility into the room and unobstructed views to the outside.
These patient room details allow architects to design with the patient experience in mind while also providing clear pathways for staff.
Room Flexibility
If a hospital doesn’t have enough rooms to accommodate patients and the treatments they need, active and latent failures can occur . A 2017 joint study by Ariadne Labs and MASS Design Group found that Caesarean deliveries are more common in hospitals that have fewer dedicated labor rooms and a greater number of operating rooms. The study suggests that doctors are less likely to choose specific treatment plans if the hospital lacks the resources to support them—even when those treatment plans are the best options for patients.
To reduce the chances of this occurring, architects create acuity-adaptable rooms that are designed to accommodate various types and levels of care. For example, in an Obstetrics Unit, patient rooms can be specifically designed for delivery, short-term surgical recovery, and antepartum care. Flexible furniture and wheeled equipment make these rooms adaptable to more situations. Moreover, patients won’t have to be transferred to other locations for treatment as often.
Acuity-adaptable Nursing Units can manage different levels of care if the room is right-sized for the most intensive use. As hospitals must manage varying occupancy rates and acuity levels, strategies that allow for Nursing Units to “flex” are in good part driven by bed room sizes.
Lighting, Ventilation, and Acoustics
Patients and staff need plenty of light and healthy ventilation. Nurses’ stations can often get loud, which can be distracting for patients. To solve these challenges, architects focus on the following features:
- Varied Lighting: The highest lighting levels are at the entrance to a patient room, where caregivers perform their tasks, as well as at nurse stations. Implementing dimming features and night lighting on the orange-red spectrum can reduce the risk of patient disruption while they’re trying to sleep.
- Quiet HVAC System: A super sound-insulating HVAC system or a white noise sound-masking system can reduce noise levels in rooms located near high traffic work areas.
- Ventilation for Comfort: Good ventilation improves patient and staff comfort, as well as patient health outcomes.
By considering all of these design details, architects can create a hospital room that fully supports the staff’s efforts while also offering a calm place for patients to recover.
Efficient Hospital Room Design Benefits Staff and Patients Alike
Hospital rooms should be safe spaces in which patients feel well cared for and staff can easily provide treatment. These design details not only streamline staff workflows but can also help improve patient recovery rates and lead to higher patient satisfaction . This, in turn, may even result in increased revenue at your facility—the Centers for Medicare & Medicaid Services reimburse hospitals for up to 2% of the total cost of treatment if a patient’s satisfaction rating is high.
When you partner with an experienced architecture firm that understands the needs of patients and staff, as well as the room design features that patients find calming, you can create a responsive healthcare facility that exceeds everyone’s highest expectations.
For more information about hospital room design strategies, contact HMC Architects today. Our team of experienced architects creates efficient patient rooms that are designed to improve staff workflows and help your healthcare facility run as smoothly as possible. If you have specific questions about our healthcare facility design process, email Christopher Naughton, AIA, ACHA Senior Healthcare Planner , directly.

At HMC Architects, we believe a successful design is one that ultimately enriches the lives of patients, families, healthcare professionals, and communities.
To learn more or become part of our story, contact us today.
GET IN TOUCH
Media Inquiries
Contact Bruce Boul at (951) 382-0444 or [email protected]
HMC Architects
Related articles.
Building Compassion into Architecture: Harness the Power of Empathy in Healthcare Design
Rethinking Healthcare Design to Address Post-Pandemic Workforce Shortage
HMC and SBCCD Board of Trustees Visit San Bernardino Valley College Progress
An industry leading benefits package is just the beginning. A collaborative culture helps us thrive.

Our Results
We work to improve the health care continuum, based on our extensive research and experience.
Read Case Studies
% INCREASE IN PATIENT VOLUME
Clinical Locations
If you have a location in mind, use our Locations search to find clinical careers.
Search Locations by State
- For Patients
NEWS & RESOURCES
At USACS, we are always gathering – and sharing – information. It’s through the process of documenting best practices, reviewing metrics and adopting innovative solutions that we find success with our nationwide partners.
General News
Mar 7, 2024


USACS Announces Annual Clinical Excellence Award Winners
CANTON, Ohio, March 7, 2024 – US Acute Care Solutions (USACS), the nation’s largest physician-owned provider of hospital-based emergency and inpatient medicine, is pleased to announce eight clinicians who have been named recipients of the National Clinical Governance Board’s (NCGB) Clinical Excellence Award. These recipients were honored during USACS’ annual Assembly meeting held in Denver, CO, last month. The Clinical Excellence Award was created to recognize outstanding clinical care by individual physicians and advanced practice providers (APPs) who do not serve in leadership or management roles and represent each USACS service line. Nominations are submitted year-round by clinical colleagues and are reviewed at the beginning of each calendar year. Recipients are selected and notified before the annual spring Assembly meeting. Congratulations to the following recipients of the 2024 Clinical Excellence Award: Matthew Baltz, MD, Bon Secours Memorial Regional Medical Center— Mechanicsville, VA Calen Hart, MD, AdventHealth Tampa—Tampa, FL Waleed Hussein, MD, Hazel Hawkins Memorial Hospital—Hollister, CA Omar Naji, MD, StoneSprings Hospital Center—Dulles, VA Ryan Nguyen, PA-C, Dell Children's Medical Center of Central Texas—Austin, TX James (Ian) Richardson, DO, Bon Secours Memorial Regional Medical Center—Mechanicsville, VA Nathan Scherer, DO, AdventHealth ER and Urgent Care at Meridian—Parker, CO Melissa Volpe, PA-C, Sentara Martha Jefferson Hospital—Charlottesville, VA National Director of Clinical Education and Vice Chair of the NCGB, Roya Caloia, DO, MPH, FACEP, shared, “These are the people you work alongside who make you want to be a better physician or APP. Their efforts and commitment to high-quality patient care remind you of why you chose to go into medicine in the first place. Congratulations to each recipient, I am honored to call each of you colleagues!” About USACS Founded by emergency medicine and inpatient physicians across the country, USACS is solely owned by its physicians and hospital system partners. The group is a national leader in integrated acute care, including emergency medicine, hospitalist, and critical care services. USACS provides high-quality care to approximately ten million patients annually across more than 400 programs and is aligned with many of the leading health systems in the country. Visit usacs.com for more. ### Media Contact Marty Richmond Corporate Communications Department US Acute Care Solutions 330.493.4443 x1406 [email protected]
OWNERSHIP MATTERS
When physicians own the business, they’re empowered to make the best decisions.

- Email Address Subscribe
- Featured (1)
- For Residents (57)
- Future of Healthcare (69)
- General (24)
- Great Patient Saves (3)
- Honoring our Heroes (8)
- Hospital Partnership (35)
- Hospitalist Medicine (11)
- Leadership (42)
- Life in the ER (96)
- Location! Location! Location! (13)
- Observation Care (15)
- Patient Satisfaction (10)
- Physician Wellness (47)
- Quality Efficiency Utilization (65)
- Questions of the Job Search (1)
- Servant's Heart (6)
- Skilled Nursing (4)
- The Shift (18)
- Transition Care (3)
- Uncategorized (20)
- Where We Work (7)
- Search Search
Four Rules for Bed Assignment In An Efficient Hospital
Editor’s Note: the following is an excerpt from Dr. Robbin Dick’s forthcoming book on Hospital Capacity Management. Dr. Dick is MEP’s Director of Observation Services. He will be speaking on hospital capacity management and other subjects at MEP’s third annual observation medicine conference, Observation Care ’15 .
Bed assignment often sets the pulse for the entire hospital, affecting every patient and every department from minute to minute, yet is often poorly managed.
I have been amazed over the years at how many people desire the position of bed assigner. Nurses, Surgeons, Private internists, Hospitalists, ED providers and even Hospital Administrators at some point in time want to assign beds to patients. They often have no idea, however, how their decisions will affect ED wait times, operating room and cath lab needs, and the flow of non-ED patients throughout the hospital, to name just a few factors that need to be considered. Yet bed assignment has far reaching effects.
Many think that bed assignment is a simple task. In theory it should be. A bed is available and the patient gets assigned. There are certain constraints—sex, semi-private versus private, isolation issues, acuity, telemetry and specialty needs. All need to be taken into account to ensure that each patient goes to the right place and receives the proper care. But good capacity management demands that bed assignment be carefully considered and executed.
Centralize bed assignment authority. All beds need to be assigned by a centralized authority – and no one else. Patients cannot be moved without a reason. Patients cannot be assigned by others. All discharges must quickly and accurately be handed over to environmental services for bed cleaning then immediately handed back to bed assignment.
I can recall an analysis of environmental services staffing on the evening shift. Beds vacated by discharged patients at 5 p.m. weren’t being cleaned until 1 or 2 a.m. All the data said that there was sufficient staffing. Drilling down we discovered that nursing staff had decided to transfer patients from bed to bed, for multiple reasons, without contacting bed assignment. This was being done so frequently that it consumed 1/3 of the environmental staff that was allocated to clean beds for discharged patients. Thus the need for rule 1.
Use Non-clinical staff to do bed assignment. Set the rules and parameters on when and where patients can go and let them do their job. Nurses tend to look through clinical content to assign just the right bed. This wastes time and energy while producing no better results than non-clinical staff. The main reason clinical staff are involved at all is that there is an idea that bed assignment provides a report to the accepting unit. This is not only inappropriate but dangerous since the true clinical status of a patient can rarely be gleaned from reviewing the chart not to mention that care handoffs need to be done by the current care provider (where they are) and the receiving care provider. Bed assignment simply provides the proper location based on specific patient attributes like sex, isolation, telemetry, acuity and specialty needs.
Provide a mechanism of escalation. When problems arise the bed assignment staff need help. Assistance with inadequate telemetry availability, limits on private room use, prevention of patient movement within the hospital all can have a significant impact on bed assignment and timely patient placement.
Provide priorities and establish mechanisms to maintain them. Priorities for bed assignment need to be linked to the needs of the sickest patients in the organization wherever they may be. Those patients requiring ICU level of care whether in the ED, PACU, Floor or another facility needing to transfer the patient would have the highest priority. It has been demonstrated that patients requiring this level of care have a lower mortality rate and suffer the fewest complications the quicker they are placed in the intensive care unit.
- Share on Facebook:
- Share on Twitter:
- Share on LinkedIn:
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Exploring the spatial arrangement of patient rooms for minimum nurse travel in hospital nursing units in Korea
a Department of Interior Architecture and Built Environment, Yonsei University, Seoul 03722, Republic of Korea
b Department of Design and Environmental Analysis, Cornell University, Ithaca, NY 14853, USA
Hyunsoo Lee
Mardelle mccuskey shepley.
With increasing demands on medical care services, one of the trends is the mixed patient room arrangement of single/double-bed and multi-bed rooms in a nursing unit on the same floor. This influences nurse-to-patient assignment and often causes an unbalanced workload and longer travel distances for nurses. The objective of this study was to investigate how floor configuration and room density influence nurse travel in the hospital's medical surgical units in Korea. This study presented a novel approach to measure nurse travel distances in eight existing nursing units. The agent-based simulation was conducted to model nurses' walking trails, and the distance of one nurse travel to assigned patient rooms was measured for each nurse. With revisions in the spatial arrangement of patient rooms, locating multi-bed rooms near the nurse station, symmetric room layout centering the nurse station, and planning both single/double-bed and multi-bed rooms on one side of corridors, nurse travel distance decreased more than 15%. This study contributed to the knowledge of agent-based simulation as an evaluation framework for spatial analysis. Apart from application to Korea, these results are particularly of interest in countries where private patient rooms are not commonly economically feasible.
1. Introduction
Nurses are one of the most valuable resources in the healthcare industry, and they are responsible for direct patient care. Nurses' roles and responsibilities are essential in meeting the high demands of patient care and advancing improved patient outcomes ( Institute of Medicine, 2011 ). However, the healthcare industry is facing a growing shortage of nursing staff and a high staff turnover rate, while the high demand for quality care services persists ( Health Resources and Services Administration, 2013 ). The primary reason nurses leave their jobs is a highly demanding workload ( Mazurenko et al., 2015 ; Tao et al., 2015 ). Their work is physically and emotionally intense with heavy daily duties, high emotional exhaustion, and physical burnout, which results in nurse dissatisfaction with their jobs ( Aiken et al., 2002 ; Faller et al., 2011 ). Factors such as extended working hours, continuous working shifts, lack of rest breaks, and long walking distances contribute to nurse fatigue and stress ( Hendrich and Chow, 2008 ; Pati et al., 2008 ; Witkoski and Dickson, 2010 ). Poor environments result in nurse stress and a reduced sense of well-being ( Hendrich and Chow, 2008 ; Ulrich et al., 2004 , 2008 ; Zimring et al., 2004 ). In a nursing unit, long travel distance has been one of the most critical issues that impact nurse fatigue and stress ( Chaudhury et al., 2009 ; Zborowsky et al., 2010 ). Nurse travel is also directly related to the time spent on patient care. The literature indicates that nurses who spend more time walking spend less time at patients' bedsides ( Hendrich et al., 2008 ; Shepley and Davies, 2003 ; Trites et al., 1970 ; Ulrich et al., 2004 ). Researchers have tried to evaluate how much walking distance can be shortened and how much time saved, which can potentially be directed to patient care ( Gurascio-Howard and Malloch, 2007 ; Lu and Zimring, 2012 ; Pati et al., 2012 , 2015 ). Improving the environment to support a well-balanced patient load and reduce walking distance is necessary for the nurses’ well-being as well as secured time for patient care.
This study examined the effects of spatial features on nurse walking distance (NWD), particularly focusing on the arrangement of patient rooms. The patient room locations need to facilitate effective access from the center of the ward, i.e., the nurse station, and other assigned patient rooms for minimum nurse travel ( Nazarian et al., 2018 ). Over the last two decades, trends in patient room types have moved towards the preference for single-occupancy patient rooms. Single-occupancy rooms have been considered to be more appropriate than multi-occupancy rooms because they enhance privacy, prevent infections, reduce noise, and incorporate space for families ( Chaudhury et al., 2005 , 2006 ). However, the majority of patient room types differ by country depending on the level of medical service demands and cultural and financial structures. Multi-occupancy rooms are still in the majority in many countries, including the UK, Germany, and Korea ( Choi et al., 2017 ; Maben, 2009 ; Scott et al., 2012 ; Wagenaar and Mens, 2018 ). In Korea, with high medical demands and limited land property, most general hospitals consist of a mix of single, double, and multi-bed rooms in one nursing unit. Experts report staff challenges with single room-only hospitals ( Stephenson, 2015 ), and argue for a flexible mix of room types for varied preferences and clinical goals ( Pennington and Isles, 2013 ; Trant, 2010 ) Notably, in an epidemic condition like COVID-19, flexible patient room occupancy levels are needed. Healthcare facilities with single rooms only did not meet the demand, and patient beds were placed in corridors. In the mixed arrangement, both single/double-bed and multi-bed rooms are assigned to each nurse for balanced workload ( Choi et al., 2014 , 2017 ; Shin and Kang, 2016 ). In the racetrack type units where single/double-bed and multi-bed rooms are located on the opposite sides of the floor (with the service core in the middle), nurses have to travel along both sides to care assigned patients. However, studies on the relationship between patient room types and nurse travel distance are lacking.
Nurses' movement patterns relate to nurse experience, patient care mix reflecting patient condition and patient load, and most of all, the location of assigned patient rooms ( Choudhary et al., 2010 ; Heo et al., 2009 ; Nanda et al., 2015 ). The distance between assigned rooms and patient room to patient room circulation are major contributors to nurse walking ( Pati et al., 2008 ). In this paper, an ‘assignment’ refers to a set of rooms assigned to a nurse. Current healthcare models represent proximity between spaces, typically reflecting a simple path for an effective sequence of activities. This is adequate in cases where the patient and staff movement are explicitly determined, such as the outpatient unit, emergency department, and operation room. However, for predicting and simulating movement in inpatient units, the simple approach of point-to-point distance is limited, because nurses move continuously during a shift, rarely following the same pattern. In this study, a novel approach of agent-based modeling is applied as a process-oriented analysis methodology to reflect a sequence of nurse activities. This study evaluates the effect of different layouts of hospital nursing units on nurse movement patterns, and also contributes to the field of agent-based simulations. In this study, a simulation-specific approach is taken to provide strong evidence to healthcare providers regarding the location of patient rooms in a nursing unit.
2. Literature review
2.1. spatial features, nurse-patient assignment, and nurse travel distance.
The spatial relation between the nurse station and patient rooms is one of the most critical elements influencing nurse travel ( Cai and Zimring, 2012 ; Gurascio-Howard and Malloch, 2007 ). The literature reports that the most traveled paths of nurses are between the nurse station and patient rooms ( Acar and Butt, 2016 ; Nazarian et al., 2018 ). In an observational study, the travel between the nurse station and patient rooms took 34.5% of total nurses’ travel during a 12-h shift ( Acar and Butt, 2016 ). An individual nurse walks an average of 2.4–3.4 miles per daytime shift ( Hendrich et al., 2008 ; Shepley and Davies, 2003 ), and this distance can be as much as 6 miles ( Pati et al., 2012 ). Hendrich et al. (2008) described how nurse travel distance, time with patients, and workload varied between different unit layouts in 36 medical-surgical units: 19 racetrack type units, 12 double-loaded units, single corridor, and five radial type units. It was obvious that the travel distance and patient time among nurses varied more within the same unit than between units. They found no statistically significant correlation between unit type, travel distance, and patient time; however, the difference in nurse travel distance between spatially contiguous patient assignment and non-contiguous room assignment was significant ( Hendrich et al., 2008 ). Nurse managers and directors even walk longer than the average nurses walk, and long walking distances are a challenge for care coordination and overall management ( Nanda et al., 2015 ). The variability of distance traveled between individual nurses on the same unit is often greater than the variance across different hospital units ( Hendrich et al., 2008 ).
One of the causes of the large variability in distances traveled among individual nurses on the same unit is the spatial properties of room assignments. The associated spatial properties affect nurse travel patterns and distance traveled. Nurses travel between assigned patient rooms, nurse stations, and supply rooms ( Butt et al., 2004 ). The nurse-to-patient assignment involves a time-consuming and complicated process with many considerations, such as patient acuity, patient preference, continuity of care, and nurse experience. The patient's location in the unit is one of the primary factors to consider for patient assignments and often more critical than nurse experience and expertise ( van Oostveen et al., 2014 ). Patient rooms that lie outside the main circulation of a nursing unit contribute to added walking distance to and from the patient rooms to nurses' areas ( Pati et al., 2008 ), and patient assignments in two corridors result in additional walking ( Gurascio-Howard and Malloch, 2007 ). The travel from the center of the ward, i.e., the nurse station, and other assigned patient rooms impacts walking distance ( Nazarian et al., 2018 ).
In nursing units with a flexible mix of room types for varied preferences and clinical goals, the arrangement of room types is one of the causes for scattered patient assignments. Even though patient assignments are complicated, for balanced workload, assigning both single/double-bed and multi-bed rooms is prevalent in Korea where most hospitals consist of a mix of room types within the same unit ( Choi et al., 2014 , 2017 ; Shin and Kang, 2016 ). Patient room assignments are a basis for nurse travel, and a nurse is required to establish movement pattern strategies according to the spatial relationship between patient rooms and nurses’ areas ( Heo et al., 2009 ). Also, the number of visits to patients is correlated with spatial properties ( Choudhary et al., 2010 ; Hendrich et al., 2008 ; Heo et al., 2009 ).
2.2. Agent-based modeling for pedestrian walking simulation
Agent-based simulations have been widely applied to simulate pedestrian walking behaviors in architecture from a building to an urban scale. They are often employed to generate realistic and autonomous pedestrian walking behavior. Using simple rules to simulate the decision-making processes while interacting with environments, agent-based models perform high levels of correlation to human behavior. Various successful models, such as the cellular automata ( Dijkstra and Timmermans, 2002 ), social force ( Helbing and Molnar, 1995 ), boids-type behavior ( Reynold, 1987 ), shortest path ( Hoogendoorn and Bovy, 2004 ), and exosomatic visual architecture ( Turner and Penn, 2002 ) have been described in the literature.
Previous case studies find strong correlations between agent-based models with human pedestrian behavior in comparison to real-world observations and computing movement models ( Batty, 2001 ; Helbing et al., 2002 ; Turner and Penn, 2002 ; Turner, 2007 ; Torrens, 2012 ; Yang et al., 2011 ; Vizzari et al., 2015 ). Due to the similarity of agent-based models and human movement behavior, evacuation modeling and wayfinding are the most common consolidated areas in which agent-based models are employed ( Najian and Dean, 2017 ; Orellana and Alsayed, 2013 ; Raubal, 2001a , 2001b ; Vizzari et al., 2020). Although many researchers have conducted agent-based models using aggregated data, some researchers focus on individual human movement level. Orellana and Alsayed (2013) carried out research covering on-site observations and virtual simulations of pedestrian walking and demonstrated a strong relation between observed and virtual pedestrian movement at an individual level. Traditionally, in nursing unit studies, walking distances have been estimated based on point-to-point linear proximity between key areas ( Hendrich et al., 2008 ; Shepley and Davies, 2003 ; Pati et al., 2012 ; Yi and Seo, 2012 ). Among Korean inpatient unit case studies, Shin and Kang (2016) assessed nurse walking distances using traditional point-to-point linear measurement based on field interviews of nurses’ patient room assignments. However, human walking behavior typically does not follow the centerline and makes a curve at corners to move along the shortest path to a destination point ( Helbing et al., 2001 ). Agent-based modeling can accommodate multiple path options of every nurse and, at the same time, reflect more realistic human behavior patterns.
2.3. Nurse travel assessment
Most studies on nurse travel assessment are based on field observations (e.g., Choudhary et al., 2010 ; Hendrich et al., 2008 ; Seo et al., 2011 ; Shepley and Davies, 2003 ; Shin and Kang, 2016 ; Sturdavant, 1960 ; Yi and Seo, 2012 ), and few employ simulation-based experiments ( Nanda et al., 2015 ; Pati et al., 2015 ). For visualizing and measuring walking distances within buildings using a computational method, Dym et al. (1988) suggested travel-distance algorithms that examine a hospital floor plan via defining the shortest path between each wall's midpoints. Lee et al. (2010) employed a metric graph structure to represent building circulation and calculated walking distances with the shortest path and interpreted the building shape with a buffered space-boundary polygon reflecting half the width of a person's shoulder from a wall as minimum buffer distance. Nanda et al. (2015) combined field research and spatial parametric modeling tools in their study on assessing nurse walking distance in a medical-surgical unit. A Rhino/Grasshopper model was developed to assess nurse walking distance from every patient room to the support areas.
Observation studies on nurse walking distance reveal the complexity of their travel. The variations between the sequence of activities, frequencies of visits, unexpected interruptions for minor tasks during patient visits are variable. However, the literature agrees that the most frequently visited areas are patient rooms ( Acar and Butt, 2016 ; Hendrich et al., 2008 ; Nanda et al., 2015 ; Nazarian et al., 2018 ; Pati et al., 2012 ) and the proximity between the nurse station and the patient room is critical ( Cai and Zimring, 2012 ; Gurascio-Howard and Malloch, 2007 ). Also, studies predicting and computing nurses’ movement suggest that nurse walking routes are more relevant when based on a sequence of activities rather than simple proximity measures ( Choudhary et al., 2010 ; Heo et al., 2009 ; Nanda et al., 2015 ; Shin and Kang, 2016 ).
A novel spatial analysis tool was implemented to visualize nurse walking behavior and spatial data on the current environment of hospital inpatient units. Using a parametric model in Rhino/Grasshopper, an agent-based simulation was conducted to assess each nurse's walking distance. The agent-based simulation generated virtual nurses' walking trails, and the parametric algorithm measured the distance (NWD) of each walking trail. A visualized nurse walking trail reflected one patient visit “round” of each nurse, which was regularly taken for activities such as doctor visits, shift handover, or medication during a shift. Those were paths from the nurse station toward assigned patient rooms, stopping by a clean supply/medication room, and returning to the nurse station. The selected cases included typical medical-surgical inpatient units of eight general hospitals ( Fig. 4 ). This article represented partial findings of a doctoral dissertation ( Lee, 2019 ), which applied mixed methods of data collection: literature review, case studies, and simulations.

Hospital ward floor plans: four in triangular shapes and four in rectangular shapes, and two nursing units located on each floor except Unit 6.
3.1. Agent-based modeling
In the agent-based simulation, virtual agents represent nurses. Nurses' walking trails were generated and measured in a Rhino modeling space of each unit. The Grasshopper plug-in program “PedSim” is used to model nurse walking behavior. PedSim has been used to simulate walking paths in healthcare facilities for evaluating accumulated walking trails of patients ( Lee and Lee, 2020 ). Fig. 1 demonstrates how the possible routes where agents can move within a given environment are analyzed in PedSim. In the simulation, the building components, such as walls and fixed furniture, are set as obstacles, i.e., a series of closed polygons that form a space boundary. The edges and vertices are automatically generated at a buffered distance from the building polygons, and the edges become the possible routes that agents can choose. The buffered distance is a half-width of a shoulder and reflects the distance humans offset from walls to avoid collisions while walking in indoor space. PedSim also employs multiple forces for agents’ walking behavior. It is based on the social force model ( Helbing and Molnar, 1995 ) with agents driven by multiple forces, namely a target force, person repulsion, and obstacle repulsion for their basic movement mechanism, and an anticipatory collision avoidance force to make agents aware of potential collisions and take actions earlier ( Wang, 2019 ). In the simulation, an agent chooses the shortest path among the possible routes within the given environment and moves to a target point, avoiding collisions with multiple forces ( Wang, 2019 ).

Example of the environment setting. Agents move from starting to destination points, and edges and vertices of space boundary at a buffered distance from building polygons are possible routes that agents can choose ( Wang, 2019 ).
In the agent-based modeling, nurse travel is set with a sequence of movements per patient assignment. The movement sequence is programmed by a set of parameters: visit locations, number of visits, and a flow of the assignment. The methodology is process oriented. When the movement path is visualized on the layout following the key sequence of movement, the distance is measured automatically by the parametric components. The agents also have a vision, and they move to the target point in possible visible routes.
This study simulates nurse travel based on the most obvious sequence of visits during a shift, which is a patient visit round. Each nurse movement path reflects a set of patient assignments. Four or five different patient rooms, which are assigned to one nurse, are visited in each round, and four or five sets of assignments cover all the unit's rooms. The simulation process ( Fig. 2 ) for a patient visit round is as follows: (1) the agent finds the shortest path to the destination point, (2) it visits points of interest if it sees those and avoids obstacles and other agents on its way, and (3) goes to the destination point. In the simulation, an agent, which is a nurse, (1) travels from a starting point: the nurse station, (2) visits points of interest: the supply/medication room and assigned patient rooms of each nurse, and (3) goes to a destination point: the nurse station, avoiding obstacles such as walls and furniture in the plans ( Fig. 3 ).

Nurse movement process for NWD calculation in the simulation ( Wang, 2019 ).

(a) Simulation view of agent movements in the Rhino modeling space. (b) Start/destination points in the simulation setting (▲: nurse station, ■: clean supply/medication room, ●: patient room; B refers to the number of beds).
3.2. Case description
3.2.1. unit characteristics.
The typical double-loaded corridor type nursing unit was the standard design for many years from the early design of hospital wards, because of the need for cross-ventilation and natural lighting. With an increase in the demands for hospitals, planners have tried various plan configurations to achieve efficient activity patterns. The more compact plans, such as radial (Valley Presbyterian Hospital in California and Brigham And Women's Hospital in Boston), L-shaped (Aspirus Wausau Hospital in Wisconsin), square (Providence Hospital in Alaska), and triangular-shaped (Jacobs Medical Center in San Diego) nursing units have been developed with groupings of concentric support areas in inpatient units ( Kobus et al., 2008 ). Valley Presbyterian Hospital in California (1956) developed the first compact radial type unit, and recently Brigham And Women's Hospital in Boston developed radial intensive care units. Recent trends have shown a shift toward the racetrack type. Racetrack type design maximizes the perimeter wall of the unit while providing moderate visibility and accessibility from the nurse working area to patient rooms. Another trend is toward pod configuration, which provides better patient monitoring opportunities ( Cama, 2009 ; Hamilton and Shepley, 2010 ; Thompson et al., 2012 ). However, in Korea, with its enormous scale and high land prices, high-rise hospitals with a racetrack or triangular shape units are the most common.
This study included four rectangular and one triangular-shaped inpatient unit layouts of the most highly ranked hospitals among 42 tertiary care hospitals in Korea ( Ministry of Health and Welfare, 2018 ) and three representative triangular layouts from secondary care hospitals ( Fig. 4 ). Among the selected medical-surgical inpatient units of eight hospitals, four are in Seoul and four in other cities. The typical floor plans of the units follow the criteria: 40 to 50 beds per unit, 500 to 1000 inpatient beds in total, and being built after 2000. Each ward floor has two nursing units and two centralized nurse stations, two medication and clean supply rooms, one nourishment room, two soiled linen rooms, and two equipment rooms at the center of each unit. Each nursing unit had a double-corridor design with a triangular or rectangular shape, and mixed arrangement of patient room types: single, double, or multi-occupancy ( Table 1 , Table 2 ). The characteristics of the units were categorized by (1) unit shape - triangular or rectangular and (2) location of the nurse station - near the elevator core or center of the unit.
Building description of selected hospital cases.
Number of rooms (beds) in each unit by room occupancy type.
3.2.2. Nurse-patient ratio
A nursing unit refers to the number of beds the nurses in a group are accountable to take care of, and the units of general hospitals in Korea have 40–60 beds per nursing unit due to a large number of patients. The staff to patient ratio ranges from 1:7 to 1:12 for registered nurses ( National Health Insurance Service, 2019 ). The nurse-patient assignments of selected units are based on Shin and Kang's (2016) research on the nurse-patient assignments. The nurse-room ratio of the eight units was set with respect to three criteria: (a) nurse-patient ratio was 10–12 patients per nurse, (b) both single/double-bed patient rooms and multi-bed patient rooms were assigned to one nurse for workload balance, and (c) all patients in a single room assigned to the same nurse ( Table 3 ).
Nurse-to-patient room assignments of each unit. Number in parentheses refers to number of rooms of that room occupancy (for example 4B[2] means two rooms with four patients).
3.2.3. Nurse movement setting
To compare the nurse travel distance between units, one patient visit “round” of each nurse was measured in the simulation. In the delivery of patient care and related activities, the locations nurses visit may vary based on urgent medication and patient requests. According to empirical studies on the traveled paths of nurses ( Acar and Butt, 2016 ; Kim and Chai, 2018 ; Nanda et al., 2015 ), the most frequently visited paths during both day and night shifts are between: (i) patient rooms and nurse station; (ii) nurse station and clean supply/medication room; and (iii) patient rooms and clean supply/medication room, in this order. In this study, the simulation setting was limited to one patient visit round of each nurse to the assigned patient room visits at each shift change, excluding irregular travel. The distance to the patient room doors was calculated, and the movement inside the patient room was excluded from the measured distance.
The movement process for a round is shown in Fig. 5 :
- (1) Starting from the centralized nurse station, a nurse (an agent) visits a clean supply/medication room for preparation prior to an assigned patient room round.
- (2) The nurse (agent) moves to the assigned patient rooms.
- (3) After visiting the assigned patient rooms, the nurse returns to the nurse station.

Nursing activity movement process for one patient visit round in the simulation.
4.1. Nurse walking distance
Nurse walking trails for one round of each nurse (N = 33) were simulated, and the distance of each round path was measured ( Fig. 6 and Table 4 ). The shortest average NWD of each unit was measured in Unit 4, and the longest in Unit 7 (41.56 and 68.97). Units 1, 2, and 4 showed relatively short average NWD. The shortest NWD of one nurse was captured in N-1 of Unit 2, and the longest in N-1 of Units 8 (26.06 and 82.51). The variations of NWD among nurses were in a broader range within a layout than between other units. Considering nurses travel between the nurse station and assigned patient rooms approximately fourteen times during a shift ( Kim and Chai, 2018 ), the variations will be even more substantial. Unit 4 shows the most equivalent distances among nurses within a unit. Units 3 and 7 show lower SD than the average; however, Unit 7 had the longest average NWD, which indicated that nurses in Unit 7 walked more than nurses in other units. The NWD in Unit 6 varied in the largest differences among nurses, and the variations of NWD among nurses in Units 1, 2 were also larger than other units. Units 7 and 8 had long average NWD, and variations of NWD within the units were at the average level.

Nursing unit layouts with simulated nurse walking trails. Nurse-to-patient assignment marked in each room.
Nurse walking distance (m) for one patient visit round from nurse station to assigned patient rooms.
Note. (N: Nurse-patient assignment, SD: Standard deviation, P: Perimeter of patient room walls on the door side, NS to EU: Longer distance from the center of nurse station (NS) to end of the unit (EU).
Although the triangular units showed shorter NWD than the rectangular units, unit typology may not be the most fundamental reason for the short walking distance. The simulation results presented strong evidence that the average NWD was shorter in the units with a nurse station located at the center of the unit ( Table 5 ), and the locations of nurse stations were closer to the center of the units in the triangular units ( Fig. 6 ). Therefore, the distance to the patient rooms from the nurse station was shorter in the triangular units than the rectangular units. In rectangular units, the nurse station was closer to the unit entrance rather than the center of the units.
Comparison between units grouped according to unit shape, NS location, and patient assignments.
With a categorized comparison of two groups of ‘contiguous’ and ‘non-contiguous’ patient room assignments, the average NWD was 46.34 and 59.98 m ( Table 5 ). This study defined the nurse-patient assignments between immediately adjacent patient rooms as “contiguous”, and with nearby but not contiguously neighboring patient rooms as “non-contiguous”. Obviously, the units with geographically contiguous patient room assignments had shorter NWD than the units with non-contiguous patient room assignments. Unit 3, a triangular unit with a non-contiguous patient room assignment, had a longer NWD than other triangular units. Unit 6 was the only rectangular unit with a contiguous patient assignment, and it had a shorter NWD than other rectangular units. Unit 6 had the lounges located in the middle of the patient room sections, which increased the distance between the nurse station and patient rooms.
4.2. Distance from nurse station to end of unit and perimeter of patient rooms
The simulation results revealed that these measures did not consequently result in longer NWD. The units of the long distances from nurse station to end of the unit (NS to EU) were Units 1, 6, and 8, and of the long perimeter (length of patient room walls on door side) were Units 3, 6, and 8, compared to the average ( Fig. 7 and Table 4 ). However, Unit 1 showed a short NWD with a long NS to EU distance, while Unit 7 showed the longest NWD with one of the shortest NS to EU distance. The average ranges of NWD were captured in Units 3 and 6 despite the long perimeter length. Unit 6 showed an average range of NWD with a long NS to EU distance and perimeter length.

Comparisons of NWD of each unit: average, longest, shortest NWD, and SD measures. The x -axis represents the unit number and y -axis the distance in meters.
4.3. Patient room arrangement
One of the critical spatial attributes influencing nurse travel distance was the patient room arrangement. In the cases where single/double-bed patient rooms and multi-bed rooms were planned in the same unit, an equivalent number of single/double-bed and multi-bed patient rooms were to be assigned to each nurse for balanced workload distribution. In Units 5, 7, and 8, where single/double-bed and multi-bed rooms were located in separate two hallways, the nurses had to move up and down across the center support areas to visit patients in two corridors. These geographically non-contiguous patient assignments caused long travel distances. Among the rectangular units, Unit 6 presented an average level of NWD despite the lounges located in between patient rooms, the long perimeter of patient rooms, and long NS to EU distance. Unit 6 had the patient room arrangement, which supported a contiguous patient assignment plan, locating a mixed arrangement of patient rooms along the same corridor, as nurses get assigned for patient rooms of both single/double-bed and multi-bed rooms. However, in Unit 3, even though both room types were located along the same corridor, they were placed in distant locations. Consequently, Unit 3 presented non-contiguous patient assignments with longer NWD than others among the triangular units. The patient room arrangement contributed to the geographical continuity of the nurse-patient assignment, and non-contiguous patient assignments often caused inefficient travel distances for nurses. Therefore, the spatial arrangement of patient room types was one of the critical features for nurse walking efficiency, as this was highly related to the patient assignment plan.
4.4. Revised patient room arrangements to reduce nurse travel distance
The frequency of nurse visits to patient rooms from the nurse station was higher in double-bed rooms than single-bed rooms ( Nazarian et al., 2018 ), which means locating multi-bed patient rooms closer to the nurse station would reduce nurse walking. To explore the effects of patient room arrangement on NWD, the room arrangements of three rectangular units, Units 5, 7, and 8, were revised to support geographically contiguous nurse-patient room assignment through the following modifications:
- 1) Symmetric room layout centering the nurse station,
- 2) Mixed planning of single/double-bed and multi-bed patient rooms on one side of the corridor, and
- 3) Multi-bed rooms as near as possible to the main nurse station to shorten nurse travel.
In Unit 5, two multi-bed patient rooms on the upper corridor were moved to the lower corridor for nurses to care for patients in a single corridor. In Units 7 and 8, similar changes to the layouts were made. One patient visit round was simulated for each nurse, and the travel distance was measured ( Table 6 , Table 7 ). A notable reduction in NWD was evident for all three units, with around 15% decrease in the revised layouts. Of the three units, Unit 7 had the largest difference. In Unit 7, the average NWD decreased from 68.97 to 55.95 m for one round, with an 18.88% reduction in distance. Also, SD decreased from 10.21 to 3.84, which is a noticeable improvement for equivalent NWD among nurses within Unit 7. In Units 5 and 8, the reduction was also evident: the averages of NWD decreased by 14.64% and 16.31%, respectively. However, SD slightly increased as the shortest NWD further decreased. Considering this was based on a single trip, the reduction of NWD would be more substantial with multiple trips in real situations. Based on the results, mixed planning of single/double-bed rooms with multi-bed rooms on one side of the corridor with consideration of contiguous nurse-patient room assignment influenced shorter nurses’ travel distance.
Nurse walking trails on existing layouts and modified patient room arrangements.

NWD of existing and revised layouts with patient room arrangement changes.
Note. (DA: the difference between the average NWD of the existing and revised layouts).
5. Discussion
5.1. patient assignment and nurse travel distance.
The results of this study indicated that changes in spatial features, such as nurse station location, patient room arrangement, affect nurses' walking distances, and the size of the units, may not merely increase nurse travel with supportive spatial planning. Also, this study discussed the relationship between nurse-patient room assignment and nurse travel distance. Nurse travel is based on the patient assignment during a shift, and the assignment frequently involves geographically non-contiguous patient rooms ( Pati et al., 2008 ). Non-contiguous patient room assignments often increase walking for nurses ( Hendrich et al., 2008 ). Although it is assumed that nurses are assigned to a set of contiguous patient rooms, actual patient assignments vary in regard to other factors, such as the acuity level of a patient, competency of a nurse, and a nurse-to-patient ratio ( Pati et al., 2008 ). This study emphasized that patient assignment is one of the critical factors to consider in the design stage for reducing nurses’ walking, even though it is an operational issue and not a spatial issue.
With an understanding that the actual patient assignment may vary and not result in contiguous rooms, depending on the balance between criteria, this study explored the optimal layout that healthcare designers could provide to support contiguous room assignments, initially. In a mix of single/double and multi-bed patient rooms in one nursing unit, this study demonstrated two spatial factors impacting minimum nurse travel distance: 1) locating multi-bed patient rooms near the nurse station and 2) planning both single/double-bed and multi-bed rooms on one side of corridors instead of separating single/double-bed and multi-bed patient rooms on two different corridors.
5.2. Patient room arrangement, visibility, and noise level
The critical design factors in a nursing unit design are space layout that supports efficient nursing activities, reduced walking distances, organized supply areas, controlled noise level, and visibility with ease of supervision ( Zborowsky et al., 2010 ). This study has focused on the issue of walking distances, and the results demonstrated that planning multi-occupancy patient rooms near the nurse station were more effective in reducing nurse travel distance. This approach can also impact patient visibility and noise level. More patients are easily visible and accessible from the nurse station when locating multi-bed patient rooms near the nurse station ( Lee, 2019 ). A high noise level is often reported around the nurse station, and patients who prefer single-occupancy rooms would benefit from being at a quieter location than around the nurse station.
5.3. Patient visibility versus visual control over the entrance
The nurse station is a central hub for nursing activities in a hospital unit and the primary work area of each unit. The location and distance of the nurse station to the patient room has been considered as a critical influence on nurse walking distance. Planning the nurse station closer to the center of the units is a convincing design strategy to keep nurse travel distance to a minimum, especially in a linear and less concentric rectangular unit. However, one of the reasons for positioning the nurse station close to the entrance would be the high need for visual control over the entrance. Even though it is out of the scope of this study, planning both the entrance and nurse station at the center could be a robust design strategy to keep nurse travel distance to a minimum and gain sufficient visibility to the entrance. Among the cases of this study, Unit 5 has the nurse station close to both entrance and center of the unit. However, patient visibility was low due to the orientation of the nurse station, which was facing the entrance rather than patient rooms. In Unit 5, despite the long perimeter length, the NWD was at the average level. It could be a good strategy to develop this unit into a hybrid nursing station model to improve patient visibility. It will also satisfy visual control to the entrance and patients, as well as achieving moderate NWD.
5.4. Other implications of agent-based modeling
Representing the process of how nurses' movements are made, this study attempted to contribute to the field of agent-based simulations. While classic population-level modeling has been limited in its ability to integrate individuals’ decision-making, this study expanded the application areas of agent-based modeling to an individual level. Even though this study has limited the application strategy to minimum nurse travel, agents can be set as patients, physicians, staff, visitors, and caregivers within the facilities as an expanded approach. In this sense, an agent can also be set with any spatial factors in the simulation, such as noise level, visibility, and patient preferences. Planners can develop a simulation model with a mixed approach for optimized layout planning. Simulation of healthcare in the design process is useful because it allows designers and planners to analyze the performance of the facilities at an organizational level and also enables relative comparisons among design options.
6. Conclusions
This study investigated how floor configuration and room density influenced nurse walking distance in the hospital's medical-surgical units with the intent of reducing staff fatigue and securing more time for nurses to spend on direct patient care. The effects of the unit typology, nurse station location, and spatial arrangement of patient rooms on nurse travel were evaluated. In units with a nurse station placed at the center of the unit, shorter nurse walking distances were measured. In triangular units, the nurse stations were placed closer to the center of the units, compared to the rectangular units. Also, a contiguous patient assignment contributed to shorter nurse travel.
A well-planned patient room arrangement was one of the spatial features that influenced the contiguous patient assignment. With increasing demands on medical care services, nursing units in Korea have tended to consist of mixed patient room arrangements of single/double-bed and multi-bed patient rooms in the same unit. In units with a mixed arrangement, nurses were often assigned to patients in scattered locations, which resulted in more walking. Rearranging spatial layout of patient rooms such as, locating multi-bed patient rooms near the nurse station and mixed planning of single/double-bed rooms and multi-bed rooms on one side of the corridor, helped to reduce nurse walking.
One of the limitations of this study was that the patient assignment model was limited to one scenario. The study did not address patient acuity or unit specialization (maternity, oncology, etc.). Despite other constraints of patient room assignments such as patient case mix and nurse experience, this study limited the model to a balanced distribution of patient rooms of single/double or multi-occupancy, which was a major distribution criterion in selected cases. Other limitations were that this was a simulation and not a real observation study, and all nurse walking behaviors were not taken into account. Another limitation is that the shapes of units in this research have been limited to two types, racetrack or triangular types. This was appropriate for the geographic region in which this research took place. In Korea, these are the most common configurations for an inpatient unit design due to the need for large-scale hospitals and high land prices.
Methodologically, this study presented a novel application of agent-based simulation to simulate and measure nurse walking models, enabling automatic distance measuring via setting the start and destinations. This study aimed to help healthcare providers to test their design options and make improvements with evidence in decision-making. For future studies, decentralized and hybrid nursing station models in long linear units will be further explored in relation to the spatial arrangement of patient rooms to facilitate efficient nurse walking and sufficient patient visibility. Achieving equivalent nurse walking distances for nurses remains a challenge for both designers and healthcare providers.
This work was supported by the BK 21 Plus funded by the Ministry of Education of Korea.
Conflict of interest
The authors have no conflicts of interest to report.
Peer review under responsibility of Southeast University.
- Acar I., Butt S.E. Modeling nurse-patient assignments considering patient acuity and travel distance metrics. J. Biomed. Inf. 2016; 64 :192–206. [ PubMed ] [ Google Scholar ]
- Aiken L.H., Clarke S.P., Sloane D.M., Sochalski J., Silber J.H. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002; 288 (16):1987–1993. [ PubMed ] [ Google Scholar ]
- Batty M. Exploring isovist fields: space and shape in architectural and urban morphology. Environ. Plann. Plann. Des. 2001; 28 (1):123–150. [ Google Scholar ]
- Butt S., Fredericks T., Kumar A., Wahl J., Harrelson K., Means S., Dumasius A., Brown E. Proceedings of the XVIII Annual International Occupational Ergonomics and Safety Conference (ISOES). Houston, TX, USA. 2004. An evaluation of physiological work demands on registered nurses over a 12-hour shift. [ Google Scholar ]
- Cai H., Zimring C. Proceedings of the 8th International Space Syntax Symposium. Santiago, Chile. 2012. Out of Sight, Out of Reach: correlating spatial metrics of nurse station typology with nurses' communication and co-awareness in an intensive care unit. [ Google Scholar ]
- Cama R. first ed. John Wiley & Sons; New Jersey: 2009. Evidence-Based Healthcare Design. [ Google Scholar ]
- Chaudhury H., Mahmood A., Valente M. Advantages and disadvantages of single-versus multiple-occupancy rooms in acute care environments: a review and analysis of the literature. Environ. Behav. 2005; 37 (6):760–786. [ Google Scholar ]
- Chaudhury H., Mahmood A., Valente M. Nurses' perception of single-occupancy versus multi-occupancy rooms in acute care environments: an exploratory comparative assessment. Appl. Nurs. Res. 2006; 19 (3):118–125. [ PubMed ] [ Google Scholar ]
- Chaudhury H., Mahmood A., Valente M. The effect of environmental design on reducing nursing errors and increasing efficiency in acute care settings: a review and analysis of the literature. Environ. Behav. 2009; 41 (6):755–786. [ Google Scholar ]
- Choi K., Chai C.G., Kwon S.J. vol. 21. Korea Institute of Healthcare Architecture; 2014. pp. 15–26. (A Study on the Architectural Planning Guidelines of the Wards in Central Public Hospitals of the Communities). 1. [ Google Scholar ]
- Choi K., Lee H., Kim C., Shin Y.S., Jung T.W., Kwon S.J. Vol. 8. 2017. A Study on the facility guidelines of the ward in hospitals; pp. 13–20. (Proceedings of the Annual Conference of Korea Institute of Healthcare Architecture). 1. [ Google Scholar ]
- Choudhary R., Bafna S., Heo Y., Hendrich A., Chow M. A predictive model for computing the influence of space layouts on nurses' movement in hospital units. J. Build. Perform. Simulat. 2010; 3 (3):171–184. [ Google Scholar ]
- Dijkstra J., Timmermans H. Towards a multi-agent model for visualizing simulated user behavior to support the assessment of design performance. Autom. ConStruct. 2002; 11 (2):135–145. [ Google Scholar ]
- Dym C.L., Henchey R.P., Delis E.A., Gonick S. A knowledge-based system for automated architectural code checking. Comput. Aided Des. 1988; 20 (3):137–145. [ Google Scholar ]
- Faller M.S., Gates M.G., Georges J.M., Connelly C.D. Work-related burnout, job satisfaction, intent to leave, and nurse-assessed quality of care among travel nurses. JONA: J. Nurs. Adm. 2011; 41 (2):71–77. [ PubMed ] [ Google Scholar ]
- Gurascio-Howard L., Malloch K. Centralized and decentralized nurse station design: an examination of caregiver communication, work activities, and technology. Health Environ. Res. Des. J. 2007; 1 (1):44–57. [ PubMed ] [ Google Scholar ]
- Hamilton D.K., Shepley M.M. Elsevier/Architectural Press; Netherlands: 2010. Design for Critical Care: an Evidence-Based Approach. [ Google Scholar ]
- Health Resources and Services Administration . U.S. Department of Health and Human Services; Rockville, Maryland: 2013. National Center for Health Workforce Analysis. Projecting the Supply and Demand for Primary Care Practitioners through 2020. [ Google Scholar ]
- Helbing D., Molnar P. Social force model for pedestrian dynamics. Phys. Rev. 1995; 51 (5):4282. [ PubMed ] [ Google Scholar ]
- Helbing D., Molnár P., Farkas I.J., Bolay K. Self-organizing pedestrian movement. Environ. Plann. Plann. Des. 2001; 28 (3):361–383. [ Google Scholar ]
- Helbing D., Farkas I.J., Molnar P., Vicsek T. Simulation of pedestrian crowds in normal and evacuation situations. Pedestrian Evacuation Dynamics. 2002; 21 (2):21–58. [ Google Scholar ]
- Hendrich A., Chow M. The Center for Health Design; 2008. Healthcare Leadership: Maximizing the Impact of Nursing Care Quality: a Closer Look at the Hospital Work Environment and the Nurse's Impact on Patient Care Quality; pp. 1–21. [ Google Scholar ]
- Hendrich A., Chow M.P., Skierczynski B.A., Lu Z. A 36-hospital time and motion study: how do medical-surgical nurses spend their time? Perm. J. 2008; 12 :25–34. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Heo Y., Choudhary R., Bafna S., Hendrich A., Chow M.P. vol. 1. 2009. A modeling approach for estimating the impact of spatial configuration on nurses' movement; p. 41. (Proceedings of the 7th International Space Syntax Symposium). 1. [ Google Scholar ]
- Hoogendoorn S.P., Bovy P.H. Pedestrian route-choice and activity scheduling theory and models. Transp. Res. Part B Methodol. 2004; 38 (2):169–190. [ Google Scholar ]
- Institute of Medicine . National Academies Press; Washington, DC: 2011. The Future of Nursing: Leading Change, Advancing Health. [ PubMed ] [ Google Scholar ]
- Kim M.Y., Chai C.G. A study on the change of physical environment in Seoul Medical Center by providing comprehensive nursing service. Korea Ins. Healthc. Architect. J. 2018; 24 (1):15–24. [ Google Scholar ]
- Kobus R.L., Skaggs R.L., Bobrow M., Thomas J., Payette T.M., Kliment S.A. second ed. John Wiley & Sons; New Jersey: 2008. Building Type Basics for Healthcare Facilities. [ Google Scholar ]
- Lee J. Yonsei University; Seoul, Republic of Korea: 2019. Visibility and Circulation Efficiency in Hospital Nursing Units: Visibility and Accessibility Analysis Using Agent-Based Simulation. (Doctoral dissertation) [ Google Scholar ]
- Lee J., Lee H. Employing visibility and agent-based accessibility analysis to enhance social interactions in older adult care facilities. Architect. Sci. Rev. 2020:1–11. [ Google Scholar ]
- Lee J.K., Eastman C.M., Lee J., Kannala M., Jeong Y.S. Computing walking distances within buildings using the universal circulation network. Environ. Plann. Plann. Des. 2010; 37 (4):628–645. [ Google Scholar ]
- Lu Y., Zimring C. Can intensive care staff see their patients? An improved visibility analysis methodology. Environ. Behav. 2012; 44 (6):861–876. [ Google Scholar ]
- Maben J. Splendid isolation? The pros and cons of single rooms for the NHS. Nurs. Manag. UK. 2009; 16 (2) [ PubMed ] [ Google Scholar ]
- Mazurenko O., Gupte G., Shan G. Analyzing US nurse turnover: are nurses leaving their jobs or the profession itself. J. Hosp. Adm. 2015; 4 (4):48–56. [ Google Scholar ]
- Ministry of Health and Welfare . Ministry of Health and Welfare; 2018. The Tertiary Care Hospital List. http://www.mohw.go.kr [ Google Scholar ]
- Najian A., Dean D.J. Advances in Geocomputation. Springer; Cham: 2017. Simulation of human wayfinding uncertainties: operationalizing a wandering disutility function. [ Google Scholar ]
- Nanda U., Pati S., Nejati A. Field research and parametric analysis in a medical–surgical unit. Health Environ. Res. Des. J. 2015; 8 (4):41–57. [ PubMed ] [ Google Scholar ]
- National Health Insurance Service . Ministry of Health and Welfare; 2019. Policy Direction of Comprehensive Nursing Care. https://www.nhis.or.kr/ [ Google Scholar ]
- Nazarian M., Price A., Demian P., Malekzadeh M. Design lessons from the analysis of nurse journeys in a hospital ward. Health Environ. Res. Des. J. 2018; 11 (4):116–129. [ PubMed ] [ Google Scholar ]
- Orellana N., Alsayed K. Proceedings of the Ninth International Space Syntax Symposium. Sejong University; Seoul: 2013. On Spatial Wayfinding: agent and human navigation patterns in virtual and real worlds; p. 79. [ Google Scholar ]
- Pati D., Harvey T., Cason C. Inpatient unit flexibility: design characteristics of a successful flexible unit. Environ. Behav. 2008; 40 (2):205–232. [ Google Scholar ]
- Pati D., Harvey T., Thurston T. Estimating design impact on waste reduction: examining decentralized nursing. J. Nurs. Adm. 2012; 42 :513–518. [ PubMed ] [ Google Scholar ]
- Pati D., Harvey T.E., Jr., Redden P., Summers B., Pati S. An empirical examination of the impacts of decentralized nursing unit design. Health Environ. Res. Des. J. 2015; 8 (2):56–70. [ PubMed ] [ Google Scholar ]
- Pennington H., Isles C. Should hospitals provide all patients with single rooms? BMJ. 2013; 347 :5695. [ PubMed ] [ Google Scholar ]
- Raubal M. Human wayfinding in unfamiliar buildings: a simulation with a cognizing agent. Cognit. Process. 2001; 2 (3):363–388. [ Google Scholar ]
- Raubal M. Ontology and epistemology for agent-based wayfinding simulation. Int. J. Geogr. Inf. Sci. 2001; 15 (7):653–665. [ Google Scholar ]
- Reynolds C.W. Proceedings of the 14th Annual Conference on Computer Graphics and Interactive Techniques. 1987. Flocks, herds and schools: a distributed behavioral model; pp. 25–34. [ Google Scholar ]
- Scott A., Stevenson T., Chua V. Finance. The profitability of private patients. Health Serv. J. 2012; 122 (6322):25. [ PubMed ] [ Google Scholar ]
- Seo H.B., Choi Y.S., Zimring C. Impact of hospital unit design for patient-centered care on nurses' behavior. Environ. Behav. 2011; 43 (4):443–468. [ Google Scholar ]
- Shepley M.M., Davies K. Nursing unit configuration and its relationship to noise and nurse walking behavior: an AIDS/HIV unit case study. AIA Acad. J. 2003; 6 :12–14. [ Google Scholar ]
- Shin D., Kang M. A study improving a nurse's walking path and staff visibility in general hospital wards. J. Architect. Inst. Korea Plann. Des. 2016; 32 (1):41–50. [ Google Scholar ]
- Stephenson J. Single rooms in hospitals “increase anxiety” among nursing staff. Nurs. Times. 2015; 47 [ Google Scholar ]
- Sturdavant M. American Hospital Association; Rochester, Minn: 1960. Comparisons of Intensive Nursing Service in a Circular and a Rectangular Unit: Rochester Methodist Hospital. (No.8) [ Google Scholar ]
- Tao H., Ellenbecker C.H., Wang Y., Li Y. Examining perception of job satisfaction and intention to leave among ICU nurses in China. Int. J. Nurs. Sci. 2015; 2 (2):140–148. [ Google Scholar ]
- Thompson D.R., Hamilton D.K., Cadenhead C.D., Swoboda S.M., Schwindel S.M., Anderson D.C., Schmitz E.V., St Andre A.C., Axon D.C., Harrell J.W., Harvey M.A., Howard A., Kaufman D.C., Petersen C. Guidelines for intensive care unit design. Crit. Care Med. 2012; 40 (5):1586–1600. [ PubMed ] [ Google Scholar ]
- Torrens P.M. Moving agent pedestrians through space and time. Ann. Assoc. Am. Geogr. 2012; 102 (1):35–66. [ Google Scholar ]
- Trant K. Ward design must not be restricted to single rooms. Nurs. Times. 2010; 106 (26):24. [ PubMed ] [ Google Scholar ]
- Trites D.K., Galbraith F.D., Sturdavant M., Leckwart J. Influence of nursing unit design on the activities and subjective feelings of nursing personnel. Environ. Behav. 1970; 2 (3):303–334. [ Google Scholar ]
- Turner A. From axial to road-centre lines: a new representation for space syntax and a new model of route choice for transport network analysis. Environ. Plann. Plann. Des. 2007; 34 (3):539–555. [ Google Scholar ]
- Turner A., Penn A. Encoding natural movement as an agent-based system: an investigation into human pedestrian behaviour in the built environment. Environ. Plann. Plann. Des. 2002; 29 (4):473–490. [ Google Scholar ]
- Ulrich R., Zimring C., Joseph A., Choudhary R. The Center for Health Design; Concord, CA: 2004. The Role of the Physical Environment in the Hospital of the 21st Century: a Once-In-a-Lifetime Opportunity. [ Google Scholar ]
- Ulrich R.S., Zimring C., Zhu X., DuBose J., Seo H.B., Choi Y.S., Quan X., Joseph A. A review of the research literature on evidence-based healthcare design. Health Environ. Res. Des. J. 2008; 1 (3):61–125. [ PubMed ] [ Google Scholar ]
- van Oostveen C.J., Braaksma A., Vermeulen H. Developing and testing a computerized decision support system for nurse-to-patient assignment: a multimethod study. Comput. Inf. Nurs. 2014; 32 (6):276–285. [ PubMed ] [ Google Scholar ]
- Vizzari G., Manenti L., Ohtsuka K., Shimura K. An agent-based pedestrian and group dynamics model applied to experimental and real-world scenarios. J. Intell. Transport. Syst. 2015; 19 (1):32–45. [ Google Scholar ]
- Wagenaar C., Mens N. Birkhäuser; Berlin, Germany: 2018. Hospitals: a Design Manual. [ Google Scholar ]
- Wang P. 2019. PedSim. https://www.food4rhino.com/app/pedsim Available online at: [ Google Scholar ]
- Witkoski A., Dickson V.V. Hospital staff nurses' work hours, meal periods, and rest breaks: a review from an occupational health nurse perspective. AAOHN J. 2010; 58 (11):489–497. [ PubMed ] [ Google Scholar ]
- Yang Y., Roux A.V.D., Auchincloss A.H., Rodriguez D.A., Brown D.G. A spatial agent-based model for the simulation of adults' daily walking within a city. Am. J. Prev. Med. 2011; 40 (3):353–361. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Yi L., Seo H.B. The effect of hospital unit layout on nurse walking behavior. Health Environ. Res. Des. J. 2012; 6 (1):66–82. [ PubMed ] [ Google Scholar ]
- Zborowsky T., Bunker-Hellmich L., Morelli A., O'Neill M. Centralized vs. decentralized nurse stations: effects on nurses' functional use of space and work environment. Health Environ. Res. Des. J. 2010; 3 (4):19–42. [ PubMed ] [ Google Scholar ]
- Zimring C., Joseph A., Choudhary R. The Center for Health Design; Concord, CA: 2004. The Role of the Physical Environment in the Hospital of the 21st Century: A Once-In-a-Lifetime Opportunity. [ Google Scholar ]
- All Services A-Z
- Markey Cancer Center
- Gill Heart & Vascular Institute
- Barnstable Brown Diabetes Center
- Kentucky Children's Hospital
- Kentucky Neuroscience Institute
- Orthopaedic Surgery & Sports Medicine
- Digestive Health
- Primary Care
- Emergency Department
- Appointments
- Tests & Exams
- Find a Doctor
- Schedule an Appointment
- For Patients
- Amenities & Resources A-Z
- Appointment request online form
- Appointment reminders
- Patient Notice of Privacy Practices
- Become a Patient
- Clinical Trials
- Don and Cathy Jacobs Health Education Center
- Interpreter Services
- In-Network Insurance Plans
- Visit MyChart
- Maps & Directions
- Pastoral Care
- Office of Patient Experience
- Pharmacy Locations
- About Advance Directives
- Privacy Policy
- Notice of Nondiscrimination for UK Health Programs & Activities
- Subscribe to HealthMatters
- Wellness & Community
- For Visitors
- Food & Lodging
- Pay your bill
- Patient's Condition & Phone Number
- Tobacco Free Policy
- Authorizations & agreements
- Autorizaciones y Convenios
- Mail & eGreetings
- Thank a Great Provider
- Refer a Patient
- Request a Login
- Corporate Compliance
- Information Technology
- Manage Your Profile
- Brand Strategy
- Employee Health
- Enterprise Learning
- UK Human Resources
- Department Phone Directory
- Quality & Safety
- Cancer Clinical Trials
- Emergency Transport
- Physician Liaison Program
- UK•MDs Medical Contact Center
- Mission/Vision
- Employment at Eastern State Hospital
- Nurse Residency Program
- Continuing Nursing Education
- Nursing Faculty Orientation
- Nursing Staff Development
- Registered Nurse (RN) Internships
- Nursing Scholarships
- Student Nurse Academic Practicum (SNAP)
- Tuition Reimbursement
- Acute Care Nursing
- Behavioral Health Nurse Services
- Central Monitoring System
- Critical Care Nursing
- Emergency Services
- Maternal Care Area Nursing
- Markey Cancer Center Nursing
- Nursing at Kentucky Children's Hospital
- Per Diem Nursing Pool
- Perioperative Nursing Services
- Rapid Response Nursing Teams
- Nursing Special Services
- Ambulatory Care Nursing Services
- Advanced Practice
- Care Delivery Model
- Certifications
- Career Center
- Clinical Nurse Expert
- Community Outreach
- Professional Advancement
- Professional Practice Model
- Service Line Triads
- UK HealthCare Research
- Genomics Core Laboratory
- Sanders-Brown Center on Aging
- Cancer Researcher Directory
- Making a Difference
- Awards & Recognitions
- Strategic Plan
- Visual Arts
- Performing Arts
- Learn about volunteering
- Office of Observation and Learning Experience
- Diversity, Equity & Inclusion
- Healthcare Jumpstart Program
- Application Process
- How to become a RD
- Accreditation
- Tour facility
- Patient Stories
- Request an Appointment
- Medical Records
- Daisy Award Nomination Form
- Community Commitment
- Cooperative Extension Service
- Community Resources
- Office of Opioid Safety
- Safe Kids Fayette County
- UKHC Digital Platforms
- Learn about MyChart
- Log in to MyChart
- Request a MyChart account
- Proxy accounts
Appointment
- UK TeleCare FAQs
Your Inpatient Stay
- In-network insurance plans
- Financial Assistance
- Patient Meals
- Health Education Center
- Advisory Councils
- Compliments & Complaints
- Decedent Affairs
- Notice of Nondiscrimination
- How to get a second opinion
- Patient Mail, Flowers & Gifts
- Food and lodging
- Clinical Pastoral Education Internship and Residency
- SOAR (Supporting One Another to Rise)
- My UK HealthCare proxy accounts
About Your Hospital Room
Your room assignment will depend on room availability and your medical needs at the time of admission. In Pavilions H and HA, private rooms are assigned to patients whose medical conditions require that they be in a private room for their safety or the safety of others. We make every attempt to make your stay as comfortable as possible. If you have a roommate, please be considerate and discontinue television use between 9 p.m. and 7 a.m.
Safety drills: Safety drills are held periodically to enable staff to practice response procedures for emergency situations. Please do not be alarmed if the automatic doors begin to close and announcements are made on the overhead paging system. In the unlikely event there is a true emergency, your healthcare team will assist you.
Tobacco use: Smoking and all other forms of tobacco use, including electronic cigarettes, are prohibited anywhere on UK HealthCare grounds inside and out, including parking garages and personal vehicles. Information on options for patients and visitors who use tobacco is available at any of the information desks located throughout the enterprise. If you want help quitting tobacco, please ask your nurse or physician. Nicotine gum and patches are available at very low cost to visitors at campus gifts shops and pharmacies. Contact our Tobacco Treatment Specialist at 859-323-4222 for assistance. Go here for a map of UK’s boundaries and to learn more about nicotine replacement products. Join us in making our campus a healthy place to get well, visit and work.
Telephones: For your convenience, a bedside phone is provided. Callers may call your room directly, bypassing the hospital operator. Ask your nurse for the phone number to your room. Phones will not ring in patient rooms after 9 p.m. Long distance calls may be placed collect, charged to a third party or made with a calling card. You may use your cell phone; reception is available throughout most of the hospital. Courtesy phones are located at the information desks. Please remember to be courteous to other patients and visitors. Tell your nurse if you need TDD (telecommunication devices for the deaf) assistance.
Television: Free cable TV is offered in patient rooms.
Quiet time: Some nursing units observe a period of quiet time during the day to provide patients uninterrupted rest and sleep to promote healing. During quiet time, family members and visitors are encouraged to take a break as well. Any family member who chooses to stay with the patient during quiet time is asked to ensure there are no unnecessary interruptions to the patient’s rest.
Wi-Fi access: Free wireless Internet access is available throughout the UK HealthCare main campus. For assistance, call our Information Technology help desk at 859-323-8586 .
Hourly rounds: A member of your care team will be around every hour during the day, and every two hours at night, to check on you and answer any questions or concerns you may have. Please feel free to use the call light for any assistance needed outside of hourly rounding.
Know Your Care Team
Attending physicians are responsible for leading and supervising the care team. These physicians have a medical degree and at least three years of post-medical school training in a specialty area and are licensed to practice medicine.
Fellows are specialists who have completed three or more years of post-medical school training and are pursuing additional training in a specialized area of practice. Fellows are licensed to practice medicine, and they work under the direction of the attending physician.
Resident physicians have completed medical school and are pursuing initial training in a specialty area. They are licensed and work under the direction of the fellow and/or the attending physician.
Interns are licensed physicians in the first year of resident training.
Medical students have completed their undergraduate education and are in training to become physicians. Medical students may be involved in your care under the direction of the attending physician, although their involvement will be limited.
Physician assistants (PAs) and nurse practitioners (NPs) are health professionals who are certified by their professional organization. They may be involved in your care under the direction of the attending physician.
Nurses (who wear galaxy-blue scrubs) are the primary point of contact between you and your healthcare team both at the bedside and in outpatient settings. They perform frequent patient evaluations, including monitoring and tracking vital signs and performing procedures such as IV placement, drawing blood and administering medications.
Registered dietitians provide patients and family members with information on special diets and discuss any nutritional concerns. Dietitians are available from 8 a.m. to 5 p.m. Monday through Friday at 859-323-6987 .
Pharmacists work closely with your healthcare team to determine the best plan of care for you using the most appropriate medications. If you would like to speak with a pharmacist to clarify medication-related issues, please ask your nurse to arrange a consultation.
Physical and occupational therapists provide specialty care intended to help you return to your former state of physical mobility and function.
Certified nursing care technicians (who wear turquoise scrubs), sometimes called nursing assistants, provide assistance with your activities of daily living under the direction of the registered nurse.
Housekeepers play an important role in your care by keeping your room clean. If you have any concerns or comments about the cleanliness of your room, tell your nurse. You may also contact Environmental Services at 859-323-5133 .
Radiologists are medical doctors (MDs) or doctors of osteopathic medicine (DOs) who specialize in diagnosing and treating diseases and injuries using medical imaging techniques, such as X-rays, computed tomography (CT), magnetic resonance imaging (MRI), nuclear medicine, positron emission tomography (PET) and ultrasound.
Radiology imaging technologists (who wear black scrubs) are licensed healthcare professionals who specialize in the imaging of the human body for diagnosis and treatment purposes.
Infection Prevention
Wash your hands frequently. Hand hygiene is the single most important factor for preventing the spread of infection.
It is also very important that family and visitors wash their hands frequently using proper techniques or make frequent use of alcohol hand sanitizer.
Alcohol hand gel is available to everyone. Dispensers are in every patient care room and outside the door of the patient room.
Patient Safety
What you as a patient can do:
- Make sure you know your allergies and what medicines you take and share this information with your nurse.
- Speak up! if something does not seem right. Do not assume anything.
- Never forget that your opinion matters and that you have a right to feel respected.
- Become educated by your care providers about your illness and treatment options.
- Prepare a list of questions to ask your doctor during their daily rounding time.
- Ask your nurse to help you if you are concerned about falling.
- Tell your caregiver immediately if you have loss of vision or hearing or other sensory problems such as loss of smell, taste, difficulty swallowing or altered sense of touch.
- Tell your healthcare team if you have problems with standing, walking or moving from your bed to a chair.
- It is an important part of your recovery process to maintain as much independence as possible. However, please tell your caregiver if you need assistance with bathing, toileting, dressing, grooming, eating or other activities. We are here to help you.
What your care team can do for you:
- Every hospital employee involved in your care is expected to introduce themselves by name and to wear a hospital identification badge. If you are not sure who a person is or what their role is in your care, ask them.
- Your caregiver will check your wrist identification bracelet and ask your name and birthdate before administering any medication or treatment. Speak up if you think he or she has you confused with another patient.
- A member of your healthcare team will be around hourly to check on you.
- All healthcare team members are expected to wash their hands before touching patients and also as they are leaving the room. Please feel free to ask staff if they have done so.
- Your healthcare team is there to help you. If there are any questions or concerns, feel free to ask any member of your healthcare team.
Knowing Your Medications
While you are hospitalized, your doctor may prescribe medications for you. Be sure that you understand exactly what they are and why they are being prescribed. Use this checklist to help you get the information you need from your doctor:
- What is the name of the medicine?
- What is its generic name?
- Why am I taking this medicine?
- What dose will I be taking? How often, and for how long?
- When will the medicine begin to work?
- What are the possible side effects?
- Can I take this medicine while taking my other medications or dietary supplements?
- Are there any foods, drinks or activities I should avoid while taking this medicine?
- Should I take this medicine at meal time or between meals?
- Do I need to take the medicine on an empty stomach or with food or a whole glass of water?
- What should I do if I miss a dose?
Pain Management
Keeping pain at a minimum is important to your healing and overall well-being. To ensure that you receive the best care possible, you are encouraged to:
- Ask about proper pain management.
- Ask your doctor, nurse or pharmacist what to expect from efforts to manage your pain.
- Provide accurate information regarding your medical history, including any prescription and over-the-counter (non-prescription) medicines you may be taking.
- Describe how your pain interferes with your daily activities and/or sleep patterns. Tell your doctor or nurse what has helped in the past to manage your pain.
- Question any instructions or information you do not understand, and make sure you know whom to contact if your pain is not controlled.
Preparing for Discharge
Once your doctor determines it is medically safe for you to be released from the hospital, he or she will tell the rest of your care team. Each member of the team has responsibilities that must be completed before you can leave. This may take some time, so please be patient.
When your doctor tells you that you are ready for discharge, ask your nurse to estimate when you will be leaving. Make sure you collect all of your personal belongings. When all of the necessary arrangements have been made and you are ready to go, someone with Patient Transport or a nurse will come to your room to escort you to the front of the hospital to be picked up.
Meds-to-Beds: UK Pharmacy Services provides a Meds-to-Beds service for UK Chandler and Kentucky Children’s hospitals. The Chandler Retail Pharmacy staff coordinates with the patient care teams to deliver discharge medications to the patient’s bedside during the discharge process. Instead of sending the patient to the pharmacy, the pharmacy comes to the patient. Any copayments are collected upon delivery. All patients are eligible for this program unless they are transitioning to a facility that does not allow personal medications. If you would like to use this service, ask your nurse.
Before going home , be sure you know the answer to these questions:
- What is my diagnosis?
- When should I see my doctor?
- When should I call my doctor after being discharged?
- How do I contact my doctor?
- What are my medications? (Refer to medications chart located in the back of this patient guide.)
- Should I take the medicines I was taking before I was hospitalized?
- What should I be eating? c How do I take care of my incision? (for surgery patients)
- When can I shower or take a bath? c Are there any restrictions to my activity?
- When will it be safe for me to drive a car?
- When will I be able to return to work or school?
For the Caregiver
While your loved one is in the hospital, you may have to be the one to speak up for him or her. You can do this by being your loved one’s patient advocate, who will help the patient work with doctors, nurses and hospital staff. To help your loved one make the best decisions about their care and treatment, take a look at the advice in the caregiver checklist shown below.
While you are making sure that your loved one’s needs are being met either at the hospital or at home, don’t neglect your own. This can be a stressful and time-consuming job. You may neglect your diet, your normal exercise routine and your sleep needs. You may find that you have little or no time to relax, to be yourself, or to spend time with friends or other loved ones. Downtime is important, so don’t be reluctant to ask for help in caring for your loved one.
Caregiver checklist:
- Know what condition your loved one is being treated for.
- Know your patient’s rights and responsibilities.
- Know whether your loved one has advance directives and, if so, what they specify.
- Ask questions; if your loved one is too ill or reluctant to ask questions, make note of their concerns and any you may have, and please don’t be afraid to Speak Up! c Help your loved one track medications. The patient may be prescribed medications while in the hospital and may be seen by several different doctors.
If you have any questions regarding your loved one’s post-discharge plan , please contact Case Management by calling 859-323-5501 Monday − Friday, 8 a.m. − 4:30 p.m.
Going Home & Follow-Up Care
From the time your doctor feels you are close to leaving the hospital, plans will be made for your safe discharge. Your doctor and nurse will review with you any special instructions needed for follow-up care. Be sure to take copies of your written discharge instructions and your medicines to your regular doctor and to your specialists the first time you visit them after your hospitalization.
Information will be provided about what medicines you should be taking, and prescriptions will be provided for you to have filled. If you have questions about the new medicines or about whether you should continue to take medicines you were on prior to your hospital stay, please ask your doctor. If you would like to have your discharge prescriptions filled by UK HealthCare pharmacies before you leave the hospital, ask your nurse about our Meds-to-Beds service.
Follow-up care: Most UK HealthCare follow-up is provided on the main medical campus, which includes the Kentucky Clinic, Gill Heart & Vascular Institute and Markey Cancer Center, in collaboration with your primary doctor and the specialist who sent you to UK HealthCare. To schedule an appointment, call UK Health Connection at 859-257-1000 or toll-free 800-333-8874 .
Let us know how we did: Your opinion is important to us. Please expect a patient satisfaction survey in the mail soon. This provides us with valuable insight into how we may improve our patients’ experience.
- Acute care hospitals
- Cancer centers
- Children’s hospitals
- Rehabilitation hospitals
- Senior living facilities
- Technology platform
- Interactive TV
- Digital whiteboard
- Digital door sign
- Mobile / BYOD
- Digital signs & wayfinding
- Entertainment
- Proven outcomes
- Patient experience
- Patient education
- Quality & safety
- Administrative outcomes & ROI
- Seamless integrations
- Integration partners
- Analytics & insights
- People you can trust
- Featured resources
- Quality & safety
- Outcomes & ROI
- Case studies
Hospital smart rooms: What to consider

It takes more than buying pieces of technology to make smart rooms that are truly smart.
Patient rooms that incorporate connected smart technology can improve your hospital’s operations, your staff’s efficiencies, and your patients’ experience.
But there are some basic considerations to factor in before you purchase or install new technology.
When weighing if smart rooms are worth it for your hospital, consider the wide-reaching benefits of:
- Improved clinical outcomes thanks to dynamic communications channels, on-demand education about health conditions, and easy access to individualized care plans
- Enhanced patient experience thanks to personalized displays, autonomous bedside and mobile controls, and soothing comforts when they need it most
- Higher efficiency and fewer unnecessary in-room visits thanks to integrated virtual care solutions and systems that have patient-driven features and requests
- Greener practices thanks to automations tied to occupancy status or time of day, energy-efficient displays, and control ranges for room environment selections
- Better planning for future initiatives based on patient feedback about preferences and usage of features

Deciding you want your patient rooms to have smart technology comes with a lot of options. Here are 10 considerations to keep in mind as your hospital creates smart rooms:
1. What are your goals?
First determine what you want to accomplish before focusing on how to accomplish it. Selecting technology that fits your goals will help make sure your decisions bring value and fit cohesively with your organization’s priorities.
2. Do you have the right team?
Find consultants who know these technology systems and infrastructures inside and out. They can help you architect how the smart room tech is going to fit within your world — making sure it’s easy to use, reliable, beneficial and seamlessly integrated .
3. What do the end users want?
Any technology you’re considering should improve patient experience and staff satisfaction. Think about:
- Will the new tech add to staff workloads, or help make them more efficient?
- What options can you give to patients that can make them feel at ease and connected to their care team?
- Are there room controls that patients can adjust from the bedside (saving a nurse call and preventing falls)?
4. What input devices will you have?
Think about where and how you’ll offer smart room features. Consider the in-room TVs , bedside tablets, pillow speakers, voice assistants , telehealth solutions, patient mobile devices (BYOD), automatic feeds based on ADT or real-time location system (RTLS), and more.

5. What’s the full potential?
A lot of decisions are made without enough information or input about how to maximize the value of the technology.
For example, many hospitals think of integrating temperature controls for patients, when they should also consider integrating controls for lights and window blinds as well.
Other didn’t consider that lighting controls aren’t just “on” and “off.” Smart controls can be put in place to adjust light levels, and to separate zone configurations in various parts of the room.
6. Do you have the right systems and wiring?
Make sure you choose the correct technology for your needs, and wire it appropriately.
For example, I’ve worked with customers who bought smart blinds but didn’t run the right wires to control them — or didn’t buy smart blinds at all, assuming they could be wired to be remotely controlled.
The room controls for temperature, lights and blinds can all be integrated with your Building Automation System (BAS) to offer the best capabilities for you and your patients.
7. What are the infrastructure needs?
For each technology system, factor in:
- Power: Does the display need 120VAC, DC or PoE (Power over Ethernet)?
- Wiring: Will existing RF coax or IP cabling support the technology, or is an upgrade required? Is there wiring where additional digital displays will be added? Does the wiring connect correctly to your BAS?
- Connectivity: Does the system need to be connected via wired Ethernet, or can it work off Wi-Fi? Do you have a unified or segregated LAN? How will BYOD functions be handled on your Wi-Fi? Would a private LTE or 5G network be best for your system needs?
- Retrofitting: Is there cabling already in the room that can be converted and connected to new devices? Are there switch ports or unused data ports in the room you can leverage?

8. Are your systems connected?
Think about how smart room technology can tie different systems together to really provide an extraordinary experience for your patients.
For example, your goals can inform if you should incorporate:
- Interfaces driven by EHR and ADT information to personalize displays
- Mobile or voice-activated controls for the TV to offer familiar and contactless control
- RTLS and Active Directory features on digital whiteboards and digital door signs to improve care team coordination and connections
- BAS integrations with ADT to remotely reset and regulate temperature, lights and shades
9. What’s the TCO?
Don’t just compare upfront costs when deciding what smart technology to add to patient rooms. Consider the total cost of ownership (TCO).
Factor in the impact of more efficient LED display models, the cost and support requirements for in-room hardware, how many separate devices need to be maintained, and how extensively the installation, implementation and ongoing usage of smart technology will affect your hospital’s operations.
10. What’s the long-term plan?
We know technology will evolve, and the demands being placed on your hospital will change over time.
If your organization strategically designs and architects smart room technology , it will be easier to evolve in the future, and to efficiently adapt the same strategy in additional locations.
Smart rooms are really complex. There’s a lot of considerations to factor in, from the display make and model, to the handheld devices, to the wiring and infrastructure in each room, to new construction or retrofitting, to the integrations needed to create connected experiences.
The good news is you don’t have to make these decisions all on your own.
Focus on what you want to accomplish, not what technology is available. What experience do you want to give to patients and staff? Let technology partners like SONIFI Health craft how that actually implements and connects on a cohesive system for your hospital.
Whether you’re renovating, building or upgrading, set yourself up for success by making smart decisions about smart rooms.
Additional resources
Why smart rooms are a smart choice.

The hospitality effect in healthcare
Sonifi health’s partnerships with leading healthcare providers pave the way for ‘smart’ hospital rooms.
Get exclusive insights delivered to your inbox from our experts.

IMAGES
VIDEO
COMMENTS
Staff coverages can be quickly identified and assignments adjusted as needed. Whiteboard to organize lead nurses, physicians, technicians and support staff for various units or hospital sections. Helps patient ensure proper coverage and optimize personnel utilization. We will customize the room assignment board to your staff and patient needs.
It has clues to the information you need. It provides the framework for the assignment-making process, including staff constraints, additional duties that must be covered, and patient factors most impor-tant on your unit. Use the electronic health record (EHR) to generate various useful pieces of patient in-formation.
We've designed and built them from daily dialogue with hospital management since 1967. Each board kit is ready-to-use with all the carefully-selected magnets and supplies needed to operate them. To order custom-printed boards, please contact us or call one of our whiteboard specialists at 800 624 4154. No obligation.
The patient room of the future will include a digital whiteboard that updates automatically, drawing on information from the electronic health record (EHR) and shift assignment software. Patients, families and the care team will get the most current information at the point of care.
Our nurse station boards allow your team to easily view schedules and room assignments. You can clearly display patient rooms, staff names, and any special notes. ... View the Graphics Examples page to to see a variety of designs for other hospital units and healthcare applications. CareBoards 5000 N. Basin Ave. Portland, OR 97217 503-850-9094 ...
DIGITAL DESIGNED SOLUTIONS, LLC. Manufacturer of Murerase® custom printed whiteboards. Offering a variety of wall mounted custom dry erase boards, whiteboard rail systems, mobile whiteboard stands, cubes and much more! Phone: 800-620-3073. Email: [email protected].
They can be used in nearly every area of the hospital, from pediatrics to maternity, emergency and even behavioral health. Nurses' Station: these whiteboards are great for listing nurse schedules, on-call information, room assignments and so much more. Nurses use them to coordinate their daily tasks and stay organized throughout the day.
OVERALL ASSESSMENT. The pod design for patient care assignments has improved patient satisfaction by increasing the visibility and accessibility of nurses and has enhanced nurses' ability to provide safe and reliable care. This care assignment design has also improved staff vitality by reducing the number of unnecessary steps nurses take during ...
Hospital Room Design Challenges Architects Must Overcome. One of the greatest challenges that architects face when designing a hospital room is the need to accommodate three very different functions in the space. First, the room has to be comfortable and calming for the patient. Second, caregivers must be able to navigate the space quickly and ...
Early assignment of patients to specific treatment teams improves length of stay, rate of patients leaving without being seen, patient satisfaction, and resident education. Multiple variations of patient assignment systems exist, including provider-in-triage/team triage, fast-tracks/vertical pathways, and rotational patient assignment. The authors discuss the theory behind patient assignment ...
Provide a mechanism of escalation. When problems arise the bed assignment staff need help. Assistance with inadequate telemetry availability, limits on private room use, prevention of patient movement within the hospital all can have a significant impact on bed assignment and timely patient placement. Rule 4
The nurse assigned to provide care to patient(s) in a mixed gender room will: ensure patient's privacy, dignity and safety is maintained during provision of care. provide a daily update to patient(s) and family (when appropriate) on efforts to resolve situation. inform manager/PCC or In-Charge nurse of any concerns raised by patient(s) and ...
2.1. Spatial features, nurse-patient assignment, and nurse travel distance. The spatial relation between the nurse station and patient rooms is one of the most critical elements influencing nurse travel (Cai and Zimring, 2012; Gurascio-Howard and Malloch, 2007).The literature reports that the most traveled paths of nurses are between the nurse station and patient rooms (Acar and Butt, 2016 ...
The hospital will provide safe and appropriate room assignments to all patients irrespective of race, ethnicity, religion, age, sex, sexual orientation, gender identity or expression, disability or any other basis prohibited by Federal, State or Local Law. PROCEDURE:
1. Room and bed assignments are based on individual patient care needs. Unit assignments are based on the Physician's order for level of care. Assignments are coordinated by the Admitting Department, HS, attending physician, and unit LN/CNs. Unit and room assignments should be focused on directing patients to appropriate specialized nursing ...
About Your Hospital Room. Your room assignment will depend on room availability and your medical needs at the time of admission. In Pavilions H and HA, private rooms are assigned to patients whose medical conditions require that they be in a private room for their safety or the safety of others. We make every attempt to make your stay as ...
Think about where and how you'll offer smart room features. Consider the in-room TVs, bedside tablets, pillow speakers, voice assistants, telehealth solutions, patient mobile devices (BYOD), automatic feeds based on ADT or real-time location system (RTLS), and more. 5. What's the full potential?
A New Level of Acceptance in Assigning Hospital Beds to Transgender Patients. June 28, 2021. ... The policy stipulates that the system's commitment is "to identifying gender-affirming room assignments when hospitalization is indicated . . . transgender patients will be assigned to rooms based on their self-identified gender, regardless of ...
The third room is vascular surgery room; the fourth one is neurosurgery room. If necessary, each room can be transformed for any surgical intervention," explains Fyodor Basov, the head of the operating unit of the Veresaev State Clinical Hospital flagship center. There is also a unique hybrid operating room.
How to access hospital treatment in Russia. To access hospital treatment in Russia as a foreign resident, you will need either public health insurance through your employment in Russia or private insurance, giving you access to private facilities.Some nationals can access medical treatment in Russia thanks to their home country's reciprocal healthcare agreement with the Russian government.
Intensive care unit. Online consultations with doctors. Available online consultations with doctors. Additional services. Facilities. Information about 41 hospitals located in Moscow, Russia. Here you can find prices , photos, addresses and specializations of clinics, etc. Also available to book online-consutation.