

What does the scholarly research say about the effect of gender transition on transgender well-being?
We conducted a systematic literature review of all peer-reviewed articles published in English between 1991 and June 2017 that assess the effect of gender transition on transgender well-being. We identified 55 studies that consist of primary research on this topic, of which 51 (93%) found that gender transition improves the overall well-being of transgender people, while 4 (7%) report mixed or null findings. We found no studies concluding that gender transition causes overall harm. As an added resource, we separately include 17 additional studies that consist of literature reviews and practitioner guidelines.
Bottom Line
This search found a robust international consensus in the peer-reviewed literature that gender transition, including medical treatments such as hormone therapy and surgeries, improves the overall well-being of transgender individuals. The literature also indicates that greater availability of medical and social support for gender transition contributes to better quality of life for those who identify as transgender.
Below are the 8 findings of our review, and links to the 72 studies on which they are based. Click here to view our methodology . Click here for a printer-friendly one-pager of this research analysis .
Suggested Citation : What We Know Project, Cornell University, “What Does the Scholarly Research Say about the Effect of Gender Transition on Transgender Well-Being?” (online literature review), 2018.
Research Findings
1. The scholarly literature makes clear that gender transition is effective in treating gender dysphoria and can significantly improve the well-being of transgender individuals.
2. Among the positive outcomes of gender transition and related medical treatments for transgender individuals are improved quality of life, greater relationship satisfaction, higher self-esteem and confidence, and reductions in anxiety, depression, suicidality, and substance use.
3. The positive impact of gender transition on transgender well-being has grown considerably in recent years, as both surgical techniques and social support have improved.
4. Regrets following gender transition are extremely rare and have become even rarer as both surgical techniques and social support have improved. Pooling data from numerous studies demonstrates a regret rate ranging from .3 percent to 3.8 percent. Regrets are most likely to result from a lack of social support after transition or poor surgical outcomes using older techniques.
5. Factors that are predictive of success in the treatment of gender dysphoria include adequate preparation and mental health support prior to treatment, proper follow-up care from knowledgeable providers, consistent family and social support, and high-quality surgical outcomes (when surgery is involved).
6. Transgender individuals, particularly those who cannot access treatment for gender dysphoria or who encounter unsupportive social environments, are more likely than the general population to experience health challenges such as depression, anxiety, suicidality and minority stress. While gender transition can mitigate these challenges, the health and well-being of transgender people can be harmed by stigmatizing and discriminatory treatment.
7. An inherent limitation in the field of transgender health research is that it is difficult to conduct prospective studies or randomized control trials of treatments for gender dysphoria because of the individualized nature of treatment, the varying and unequal circumstances of population members, the small size of the known transgender population, and the ethical issues involved in withholding an effective treatment from those who need it.
8. Transgender outcomes research is still evolving and has been limited by the historical stigma against conducting research in this field. More research is needed to adequately characterize and address the needs of the transgender population.
Below are 51 studies that found that gender transition improves the well-being of transgender people. Click here to jump to 4 studies that contain mixed or null findings on the effect of gender transition on transgender well-being. Click here to jump to 17 studies that consist of literature reviews or guidelines that help advance knowledge about the effect of gender transition on transgender well-being.
Ainsworth and spiegel, 2010.

Ainsworth, T., & Spiegel, J. (2010). Quality of life of individuals with and without facial feminization surgery or gender reassignment surgery. Quality of Life Research , 19 (7), 1019-1024.
Objectives: To determine the self-reported quality of life of male-to-female (MTF) transgendered individuals and how this quality of life is influenced by facial feminization and gender reassignment surgery. Methods: Facial Feminization Surgery outcomes evaluation survey and the SF-36v2 quality of life survey were administered to male-to-female transgender individuals via the Internet and on paper. A total of 247 MTF participants were enrolled in the study. Results: Mental health-related quality of life was statistically diminished (P < 0.05) in transgendered women without surgical intervention compared to the general female population and transwomen who had gender reassignment surgery (GRS), facial feminization surgery (FFS), or both. There was no statistically significant difference in the mental health-related quality of life among transgendered women who had GRS, FFS, or both. Participants who had FFS scored statistically higher (P < 0.01) than those who did not in the FFS outcomes evaluation. Conclusions: Transwomen have diminished mental health-related quality of life compared with the general female population. However, surgical treatments (e.g. FFS, GRS, or both) are associated with improved mental health-related quality of life.
Bailey, Ellis, & McNeil, 2014

Bailey, L., Ellis, S. J., & McNeil, J. (2014). Suicide risk in the UK trans population and the role of gender transition in decreasing suicidal ideation and suicide attempt. The Mental Health Review , 19 (4), 209-220.
Purpose: The purpose of this paper is to present findings from the Trans Mental Health Study (McNeil et al., 2012) – the largest survey of the UK trans population to date and the first to explore trans mental health and well-being within a UK context. Findings around suicidal ideation and suicide attempt are presented and the impact of gender dysphoria, minority stress and medical delay, in particular, are highlighted. Design/methodology/approach: This represents a narrative analysis of qualitative sections of a survey that utilised both open and closed questions. The study drew on a non-random sample (n 1⁄4 889), obtained via a range of UK-based support organisations and services. Findings: The study revealed high rates of suicidal ideation (84 per cent lifetime prevalence) and attempted suicide (48 per cent lifetime prevalence) within this sample. A supportive environment for social transition and timely access to gender reassignment, for those who required it, emerged as key protective factors. Subsequently, gender dysphoria, confusion/denial about gender, fears around transitioning, gender reassignment treatment delays and refusals, and social stigma increased suicide risk within this sample. Research limitations/implications: Due to the limitations of undertaking research with this population, the research is not demographically representative. Practical implications: The study found that trans people are most at risk prior to social and/or medical transition and that, in many cases, trans people who require access to hormones and surgery can be left unsupported for dangerously long periods of time. The paper highlights the devastating impact that delaying or denying gender reassignment treatment can have and urges commissioners and practitioners to prioritise timely intervention and support. Originality/value: The first exploration of suicidal ideation and suicide attempt within the UK trans population revealing key findings pertaining to social and medical transition, crucial for policy makers, commissioners and practitioners working across gender identity services, mental health services and suicide prevention.
Bar et al., 2016

Bar, M. A., Jarus, T., Wada, M., Rechtman, L., & Noy, E. (2016). Male-to-female transitions: Implications for occupational performance, health, and life satisfaction. The Canadian Journal of Occupational Therapy , 83 (2), 72-82.
Background. People who undergo a gender transition process experience changes in different everyday occupations. These changes may impact their health and life satisfaction. Purpose. This study examined the difference in the occupational performance history scales (occupational identity, competence, and settings) between male-to-female transgender women and cisgender women and the relation of these scales to health and life satisfaction. Method. Twenty-two transgender women and 22 matched cisgender women completed a demographic questionnaire and three reliable measures in this cross-sectional study. Data were analyzed using a two-way analysis of variance and multiple linear regressions. Findings. The results indicate lower performance scores for the transgender women. In addition, occupational settings and group membership (transgender and cisgender groups) were found to be predictors of life satisfaction. Implications. The present study supports the role of occupational therapy in promoting occupational identity and competence of transgender women and giving special attention to their social and physical environment.
Bodlund and Kullgren, 1996

Bodlund, O., & Kullgren, G. (1996). Transsexualism–general outcome and prognostic factors: A five-year follow-up study of nineteen transsexuals in the process of changing sex. Archives of Sexual Behavior , 25 (3), 303-316.
Nineteen transsexuals, approved for sex reassignement, were followed-up after 5 years. Outcome was evaluated as changes in seven areas of social, psychological, and psychiatric functioning. At baseline the patients were evaluated according to axis I, II, V (DSM-III-R), SCID screen, SASB (Structural Analysis of Social Behavior), and DMT (Defense Mechanism Test). At follow-up all but 1 were treated with contrary sex hormones, 12 had completed sex reassignment surgery, and 3 females were waiting for phalloplasty. One male transsexual regretted the decision to change sex and had quit the process. Two transsexuals had still not had any surgery due to older age or ambivalence. Overall, 68% (n = 13) had improved in at least two areas of functioning. In 3 cases (16%) outcome were judged as unsatisfactory and one of those regarded sex change as a failure. Another 3 patients were mainly unchanged after 5 years. Female transsexuals had a slightly better outcome, especially concerning establishing and maintaining partnerships and improvement in socio-economic status compared to male transsexuals. Baseline factors associated with negative outcome (unchanged or worsened) were presence of a personality disorder and high number of fulfilled axis II criteria. SCID screen assessments had high prognostic power. Negative self-image, according to SASB, predicted a negative outcome, whereas DMT variables were not correlated to outcome.
Bouman et al., 2016

Bouman, W. P., Claes, L., Marshall, E., Pinner, G. T., Longworth, J., et al. (2016). Sociodemographic variables, clinical features, and the role of preassessment cross-sex hormones in older trans people. The Journal of Sexual Medicine , 13 (4), 711-719.
Introduction: As referrals to gender identity clinics have increased dramatically over the last few years, no studies focusing on older trans people seeking treatment are available. Aims: The aim of this study was to investigate the sociodemographic and clinical characteristics of older trans people attending a national service and to investigate the influence of cross-sex hormones (CHT) on psychopathology. Methods: Individuals over the age of 50 years old referred to a national gender identity clinic during a 30-month period were invited to complete a battery of questionnaires to measure psychopathology and clinical characteristics. Individuals on cross-sex hormones prior to the assessment were compared with those not on treatment for different variables measuring psychopathology. Main Outcome Measures: Sociodemographic and clinical variables and measures of depression and anxiety (Hospital Anxiety and Depression Scale), self-esteem (Rosenberg Self-Esteem Scale), victimization (Experiences of Transphobia Scale), social support (Multidimensional Scale of Perceived Social Support), interpersonal functioning (Inventory of Interpersonal Problems), and nonsuicidal self-injury (Self-Injury Questionnaire). Results: The sex ratio of trans females aged 50 years and older compared to trans males was 23.7:1. Trans males were removed for the analysis due to their small number (n = 3). Participants included 71 trans females over the age of 50, of whom the vast majority were white, employed or retired, and divorced and had children. Trans females on CHT who came out as trans and transitioned at an earlier age were significantly less anxious, reported higher levels of self-esteem, and presented with fewer socialization problems. When controlling for socialization problems, differences in levels of anxiety but not self-esteem remained. Conclusion: The use of cross-sex hormones prior to seeking treatment is widespread among older trans females and appears to be associated with psychological benefits. Existing barriers to access CHT for older trans people may need to be re-examined.
Boza and Nicholson, 2014

Boza, C., & Nicholson Perry, K. (2014). Gender-related victimization, perceived social support, and predictors of depression among transgender Australians. International Journal Of Transgenderism , 15 (1), 35-52.
This study examined mental health outcomes, gender-related victimization, perceived social support, and predictors of depression among 243 transgender Australians (n= 83 assigned female at birth, n= 160 assigned male at birth). Overall, 69% reported at least 1 instance of victimization, 59% endorsed depressive symptoms, and 44% reported a previous suicide attempt. Social support emerged as the most significant predictor of depressive symptoms (p>.05), whereby persons endorsing higher levels of overall perceived social support tended to endorse lower levels of depressive symptoms. Second to social support, persons who endorsed having had some form of gender affirmative surgery were significantly more likely to present with lower symptoms of depression. Contrary to expectations, victimization did not reach significance as an independent risk factor of depression (p=.053). The pervasiveness of victimization, depression, and attempted suicide represents a major health concern and highlights the need to facilitate culturally sensitive health care provision.
Budge et al., 2013

Budge, S. L., Katz-Wise, S. L., Tebbe, E. N., Howard, K. A. S., Schneider, C. L., et al. (2013). Transgender emotional and coping processes: Facilitative and avoidant coping throughout gender transitioning. The Counseling Psychologist , 41 (4), 601-647.
Eighteen transgender-identified individuals participated in semi-structured interviews regarding emotional and coping processes throughout their gender transition. The authors used grounded theory to conceptualize and analyze the data. There were three distinct phases through which the participants described emotional and coping experiences: (a) pretransition, (b) during the transition, and (c) posttransition. Five separate themes emerged, including descriptions of coping mechanisms, emotional hardship, lack of support, positive social support, and affirmative emotional experiences. The authors developed a model to describe the role of coping mechanisms and support experienced throughout the transition process. As participants continued through their transitions, emotional hardships lessened and they used facilitative coping mechanisms that in turn led to affirmative emotional experiences. The results of this study are indicative of the importance of guiding transgender individuals through facilitative coping experiences and providing social support throughout the transition process. Implications for counselors and for future research are discussed.
Cardoso da Silva et al., 2016

Cardoso da Silva, D., Schwarz, K., Fontanari, A.M.V., Costa, A.B., Massuda, R., et al. (2016). WHOQOL-100 Before and after sex reassignment surgery in Brazilian male-to-female transsexual individuals. Journal of Sexual Medicine , 13 (6), 988-993.
Introduction: The 100-item World Health Organization Quality of Life Assessment (WHOQOL-100) evaluates quality of life as a subjective and multidimensional construct. Currently, particularly in Brazil, there are controversies concerning quality of life after sex reassignment surgery (SRS). Aim: To assess the impact of surgical interventions on quality of life of 47 Brazilian male-to-female transsexual individuals using the WHOQOL-100. Methods: This was a prospective cohort study using the WHOQOL-100 and sociodemographic questions for individuals diagnosed with gender identity disorder according to criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. The protocol was used when a transsexual person entered the ambulatory clinic and at least 12 months after SRS. Main Outcome Measures: Initially, improvement or worsening of quality of life was assessed using 6 domains and 24 facets. Subsequently, quality of life was assessed for individuals who underwent new surgical interventions and those who did not undergo these procedures 1 year after SRS. Results: The participants showed significant improvement after SRS in domains II (psychological) and IV (social relationships) of the WHOQOL-100. In contrast, domains I (physical health) and III (level of independence) were significantly worse after SRS. Individuals who underwent additional surgery had a decrease in quality of life reflected in domains II and IV. During statistical analysis, all results were controlled for variations in demographic characteristics, without significant results. Conclusion: The WHOQOL-100 is an important instrument to evaluate the quality of life of male-to-female transsexuals during different stages of treatment. SRS promotes the improvement of psychological aspects and social relationships. However, even 1 year after SRS, male-to-female transsexuals continue to report problems in physical health and difficulty in recovering their independence.
(Due to a citation error, this study was initially listed twice.)
Castellano et al., 2015

Castellano, E., Crespi, C., Dell’Aquila, R., Rosato, C., Catalano, V., et al. (2015). Quality of life and hormones after sex reassignment surgery. Journal of Endocrinological Investigation , 38 (12), 1373-1381.
Background: Transpeople often look for sex reassignment surgery (SRS) to improve their quality of life (QoL). The hormonal therapy has many positive effects before and after SRS. There are no studies about correlation between hormonal status and QoL after SRS. Aim: To gather information on QoL, quality of sexual life and body image in transpeople at least 2 years after SRS, to compare these results with a control group and to evaluate the relations between the chosen items and hormonal status. Subjects and methods: Data from 60 transsexuals and from 60 healthy matched controls were collected. Testosterone, estradiol, LH and World Health Organization Quality of Life (WHOQOL-100) self-reported questionnaire were evaluated. Student’s t test was applied to compare transsexuals and controls. Multiple regression model was applied to evaluate WHOQOL’s chosen items and LH. Results: The QoL and the quality of body image scores in transpeople were not statistically different from the matched control groups’ ones. In the sexual life subscale, transwomen’s scores were similar to biological women’s ones, whereas transmen’s scores were statistically lower than biological men’s ones (P = 0.003). The quality of sexual life scored statistically lower in transmen than in transwomen (P = 0.048). A significant inverse relationship between LH and body image and between LH and quality of sexual life was found. Conclusions: This study highlights general satisfaction after SRS. In particular, transpeople’s QoL turns out to be similar to Italian matched controls. LH resulted inversely correlated to body image and sexual life scores.
Colizzi, Costa, & Todarello, 2014

Colizzi, M., Costa, R. & Todarello, O. (2014). Transsexual patients’ psychiatric comorbidity and positive effect of cross-sex hormonal treatment on mental health: Results from a longitudinal study. Psychoneuroendocrinology , 39 , 65-73.
The aim of the present study was to evaluate the presence of psychiatric diseases/symptoms in transsexual patients and to compare psychiatric distress related to the hormonal intervention in a one year follow-up assessment. We investigated 118 patients before starting the hormonal therapy and after about 12 months. We used the SCID-I to determine major mental disorders and functional impairment. We used the Zung Self-Rating Anxiety Scale (SAS) and the Zung Self-Rating Depression Scale (SDS) for evaluating self-reported anxiety and depression. We used the Symptom Checklist 90-R (SCL-90-R) for assessing self-reported global psychological symptoms. Seventeen patients (14%) had a DSM-IV-TR axis I psychiatric comorbidity. At enrollment the mean SAS score was above the normal range. The mean SDS and SCL-90-R scores were on the normal range except for SCL-90-R anxiety subscale. When treated, patients reported lower SAS, SDS and SCL-90-R scores, with statistically significant differences. Psychiatric distress and functional impairment were present in a significantly higher percentage of patients before starting the hormonal treatment than after 12 months (50% vs. 17% for anxiety; 42% vs. 23% for depression; 24% vs. 11% for psychological symptoms; 23% vs. 10% for functional impairment). The results revealed that the majority of transsexual patients have no psychiatric comorbidity, suggesting that transsexualism is not necessarily associated with severe comorbid psychiatric findings. The condition, however, seemed to be associated with subthreshold anxiety/depression, psychological symptoms and functional impairment. Moreover, treated patients reported less psychiatric distress. Therefore, hormonal treatment seemed to have a positive effect on transsexual patients’ mental health.
Colizzi et al., 2013

Colizzi. M., Costa, R., Pace, V., & Todarello, O. (2013). Hormonal treatment reduces psychobiological distress in gender identity disorder, independently of the attachment style. The Journal of Sexual Medicine , 10 (12), 3049–3058.
Introduction: Gender identity disorder may be a stressful situation. Hormonal treatment seemed to improve the general health as it reduces psychological and social distress. The attachment style seemed to regulate distress in insecure individuals as they are more exposed to hypothalamic–pituitary–adrenal system dysregulation and subjective stress. Aim: The objectives of the study were to evaluate the presence of psychobiological distress and insecure attachment in transsexuals and to study their stress levels with reference to the hormonal treatment and the attachment pattern. Methods: We investigated 70 transsexual patients. We measured the cortisol levels and the perceived stress before starting the hormonal therapy and after about 12 months. We studied the representation of attachment in transsexuals by a backward investigation in the relations between them and their caregivers. Main Outcome Measures: We used blood samples for assessing cortisol awakening response (CAR); we used the Perceived Stress Scale for evaluating self‐reported perceived stress and the Adult Attachment Interview to determine attachment styles. Results: At enrollment, transsexuals reported elevated CAR; their values were out of normal. They expressed higher perceived stress and more attachment insecurity, with respect to normative sample data. When treated with hormone therapy, transsexuals reported significantly lower CAR (P < 0.001), falling within the normal range for cortisol levels. Treated transsexuals showed also lower perceived stress (P < 0.001), with levels similar to normative samples. The insecure attachment styles were associated with higher CAR and perceived stress in untreated transsexuals (P < 0.01). Treated transsexuals did not expressed significant differences in CAR and perceived stress by attachment. Conclusion: Our results suggested that untreated patients suffer from a higher degree of stress and that attachment insecurity negatively impacts the stress management. Initiating the hormonal treatment seemed to have a positive effect in reducing stress levels, whatever the attachment style may be.
Colton-Meier et al., 2011

Colton-Meier, S. L., Fitzgerald, K. M., Pardo, S. T., & Babcock, J. (2011). The effects of hormonal gender affirmation treatment on mental health in female-to-male transsexuals. Journal of Gay & Lesbian Mental Health , 15 (3), 281-299.
Hormonal interventions are an often-sought option for transgender individuals seeking to medically transition to an authentic gender. Current literature stresses that the effects and associated risks of hormone regimens should be monitored and well understood by health care providers (Feldman & Bockting, 2003). However, the positive psychological effects following hormone replacement therapy as a gender affirming treatment have not been adequately researched. This study examined the relationship of hormone replacement therapy, specifically testosterone, with various mental health outcomes in an Internet sample of more than 400 self-identified female-to-male transsexuals. Results of the study indicate that female-to-male transsexuals who receive testosterone have lower levels of depression, anxiety, and stress, and higher levels of social support and health related quality of life. Testosterone use was not related to problems with drugs, alcohol, or suicidality. Overall findings provide clear evidence that HRT is associated with improved mental health outcomes in female-to-male transsexuals.
Costantino et al., 2013

Costantino, A., Cerpolini, S., Alvisi, S., Morselli, P. G., Venturoli, S., & Meriggiola, M. C. (2013). A prospective study on sexual function and mood in female-to-male transsexuals during testosterone administration and after sex reassignment surgery. Journal of Sex & Marital Therapy , 39 (4), 321-335.
Testosterone administration in female-to-male transsexual subjects aims to develop and maintain the characteristics of the desired sex. Very little data exists on its effects on sexuality of female-to-male transsexuals. The aim of this study was to evaluate sexual function and mood of female-to-male transsexuals from their first visit, throughout testosterone administration and after sex reassignment surgery. Participants were 50 female-to-male transsexual subjects who completed questionnaires assessing sexual parameters and mood. The authors measured reproductive hormones and hematological parameters. The results suggest a positive effect of testosterone treatment on sexual function and mood in female-to-male transsexual subjects.
Davis and Meier, 2014

Davis, S. A. & Meier, S. C. (2014). Effects of testosterone treatment and chest reconstruction surgery on mental health and sexuality in female-to-male transgender people. International Journal of Sexual Health , 26 (2), 113-128.
Objectives: This study examined the effects of testosterone treatment with or without chest reconstruction surgery (CRS) on mental health in female-to-male transgender people (FTMs). Methods: More than 200 FTMs completed a written survey including quantitative scales to measure symptoms of anxiety and depression, feelings of anger, and body dissatisfaction, as well as qualitative questions assessing shifts in sexuality after the initiation of testosterone. Fifty-seven percent of participants were taking testosterone and 40% had undergone CRS. Results: Cross-sectional analysis using a between-subjects multivariate analysis of variance showed that participants who were receiving testosterone endorsed fewer symptoms of anxiety and depression as well as less anger than the untreated group. Participants who had CRS in addition to testosterone reported less body dissatisfaction than both the testosterone-only or the untreated groups. Furthermore, participants who were injecting testosterone on a weekly basis showed significantly less anger compared with those injecting every other week. In qualitative reports, more than 50% of participants described increased sexual attraction to nontransgender men after taking testosterone. Conclusions: Results indicate that testosterone treatment in FTMs is associated with a positive effect on mental health on measures of depression, anxiety, and anger, while CRS appears to be more important for the alleviation of body dissatisfaction. The findings have particular relevance for counselors and health care providers serving FTM and gender-variant people considering medical gender transition.
De Cuypere et al., 2006

De Cuypere, G., Elaut, E., Heylens, G., Maele, G. V., Selvaggi, G., et al. (2006). Long-term follow-up: Psychosocial outcome of Belgian transsexuals after sex reassignment surgery. Sexologies , 15 (2), 126-133.
Background: To establish the benefit of sex reassignment surgery (SRS) for persons with a gender identity disorder, follow-up studies comprising large numbers of operated transsexuals are still needed. Aims: The authors wanted to assess how the transsexuals who had been treated by the Ghent multidisciplinary gender team since 1985, were functioning psychologically, socially and professionally after a longer period. They also explored some prognostic factors with a view to refining the procedure. Method: From 107 Dutch-speaking transsexuals who had undergone SRS between 1986 and 2001, 62 (35 male-to-females and 27 female-to-males) completed various questionnaires and were personally interviewed by researchers, who had not been involved in the subjects’ initial assessment or treatment. Results: On the GAF (DSM-IV) scale the female-to-male transsexuals scored significantly higher than the male-to-females (85.2 versus 76.2). While no difference in psychological functioning (SCL-90) was observed between the study group and a normal population, subjects with a pre-existing psychopathology were found to have retained more psychological symptoms. The subjects proclaimed an overall positive change in their family and social life. None of them showed any regrets about the SRS. A homosexual orientation, a younger age when applying for SRS, and an attractive physical appearance were positive prognostic factors. Conclusion: While sex reassignment treatment is an effective therapy for transsexuals, also in the long term, the postoperative transsexual remains a fragile person in some respects.
Dhejne et al., 2014

Dhejne, C., Öberg, K., Arver, S., & Landén, M. (2014). An analysis of all applications for sex reassignment surgery in sweden, 1960-2010: Prevalence, incidence, and regrets. Archives of Sexual Behavior , 43 (8), 1535-1545.
Incidence and prevalence of applications in Sweden for legal and surgical sex reassignment were examined over a 50-year period (1960-2010), including the legal and surgical reversal applications. A total of 767 people (289 natal females and 478 natal males) applied for legal and surgical sex reassignment. Out of these, 89 % (252 female-to-males [FM] and 429 male-to-females [MF]) received a new legal gender and underwent sex reassignment surgery (SRS). A total of 25 individuals (7 natal females and 18 natal males), equaling 3.3 %, were denied a new legal gender and SRS. The remaining withdrew their application, were on a waiting list for surgery, or were granted partial treatment. The incidence of applications was calculated and stratified over four periods between 1972 and 2010. The incidence increased significantly from 0.16 to 0.42/100,000/year (FM) and from 0.23 to 0.73/100,000/year (MF). The most pronounced increase occurred after 2000. The proportion of FM individuals 30 years or older at the time of application remained stable around 30 %. In contrast, the proportion of MF individuals 30 years or older increased from 37 % in the first decade to 60 % in the latter three decades. The point prevalence at December 2010 for individuals who applied for a new legal gender was for FM 1:13,120 and for MF 1:7,750. The FM:MF sex ratio fluctuated but was 1:1.66 for the whole study period. There were 15 (5 MF and 10 MF) regret applications corresponding to a 2.2 % regret rate for both sexes. There was a significant decline of regrets over the time period.
Eldh, Berg, & Gustafsson, 1997

Eldh, J., Berg, A., Gustafsson, M. (1997). Long-term follow up after sex reassignment surgery. Scandinavian Journal of Plastic and Reconstructive Surgery and Hand Surgery , 27 (1), 39-45.
A long-term follow up of 136 patients operated on for sex reassignment was done to evaluate the surgical outcome. Social and psychological adjustments were also investigated by a questionnaire in 90 of these 136 patients. Optimal results of the operation are essential for a successful outcome. Personal and social instability before operation, unsuitable body build, and age over 30 years at operation correlated with unsatisfactory results. Adequate family and social support is important for postoperative functioning. Sex reassignment had no influence on the person’s ability to work.
Fisher et al., 2014

Fisher, A. D., Castellini, G., Bandini, E., Casale, H., Fanni, E., et al. (2014). Cross‐sex hormonal treatment and body uneasiness in individuals with gender dysphoria. The Journal of Sexual Medicine , 11 (3), 709–719.
Introduction: Cross‐sex hormonal treatment (CHT) used for gender dysphoria (GD) could by itself affect well‐being without the use of genital surgery; however, to date, there is a paucity of studies investigating the effects of CHT alone. Aims: This study aimed to assess differences in body uneasiness and psychiatric symptoms between GD clients taking CHT and those not taking hormones (no CHT). A second aim was to assess whether length of CHT treatment and daily dose provided an explanation for levels of body uneasiness and psychiatric symptoms. Methods: A consecutive series of 125 subjects meeting the criteria for GD who not had genital reassignment surgery were considered. Main Outcome Measures: Subjects were asked to complete the Body Uneasiness Test (BUT) to explore different areas of body‐related psychopathology and the Symptom Checklist‐90 Revised (SCL‐90‐R) to measure psychological state. In addition, data on daily hormone dose and length of hormonal treatment (androgens, estrogens, and/or antiandrogens) were collected through an analysis of medical records. Results: Among the male‐to‐female (MtF) individuals, those using CHT reported less body uneasiness compared with individuals in the no‐CHT group. No significant differences were observed between CHT and no‐CHT groups in the female‐to‐male (FtM) sample. Also, no significant differences in SCL score were observed with regard to gender (MtF vs. FtM), hormone treatment (CHT vs. no‐CHT), or the interaction of these two variables. Moreover, a two‐step hierarchical regression showed that cumulative dose of estradiol (daily dose of estradiol times days of treatment) and cumulative dose of androgen blockers (daily dose of androgen blockers times days of treatment) predicted BUT score even after controlling for age, gender role, cosmetic surgery, and BMI. Conclusions: The differences observed between MtF and FtM individuals suggest that body‐related uneasiness associated with GD may be effectively diminished with the administration of CHT even without the use of genital surgery for MtF clients. A discussion is provided on the importance of controlling both length and daily dose of treatment for the most effective impact on body uneasiness.
Glynn et al., 2016

Glynn, T. R., Gamarel, K. E., Kahler, C. W., Iwamoto, M., Operario, D., & Nemoto, T. (2016). The role of gender affirmation in psychological well-being among transgender women. Psychology Of Sexual Orientation And Gender Diversity , 3 (3), 336-344.
High prevalence of psychological distress, including greater depression, lower self-esteem, and suicidal ideation, has been documented across numerous samples of transgender women and has been attributed to high rates of discrimination and violence. According to the gender affirmation framework (Sevelius, 2013), access to sources of gender-affirmative support can offset such negative psychological effects of social oppression. However, critical questions remain unanswered in regards to how and which aspects of gender affirmation are related to psychological well-being. The aims of this study were to investigate the associations among 3 discrete areas of gender affirmation (psychological, medical, and social) and participants’ reports of psychological well-being. A community sample of 573 transgender women with a history of sex work completed a 1-time self-report survey that assessed demographic characteristics, gender affirmation, and mental health outcomes. In multivariate models, we found that social, psychological, and medical gender affirmation were significant predictors of lower depression and higher self-esteem whereas no domains of affirmation were significantly associated with suicidal ideation. Findings support the need for accessible and affordable transitioning resources for transgender women to promote better quality of life among an already vulnerable population. However, transgender individuals should not be portrayed simplistically as objects of vulnerability, and research identifying mechanisms to promote wellness and thriving is necessary for future intervention development. As the gender affirmation framework posits, the personal experience of feeling affirmed as a transgender person results from individuals’ subjective perceptions of need along multiple dimensions of gender affirmation. Thus, personalized assessment of gender affirmation may be a useful component of counseling and service provision for transgender women.
Gomez-Gil et al., 2012

Gomez-Gil, E., Zubiaurre-Elorz, L., Esteva, I., Guillamon, A., Godas, T., Cruz Almaraz, M., Halperin, I., Salamero, M. (2012). Hormone-treated transsexuals report less social distress, anxiety and depression. Psychoneuroendocrinology , 37 (5), 662-670.
Introduction: The aim of the present study was to evaluate the presence of symptoms of current social distress, anxiety and depression in transsexuals. Methods: We investigated a group of 187 transsexual patients attending a gender identity unit; 120 had undergone hormonal sex-reassignment (SR) treatment and 67 had not. We used the Social Anxiety and Distress Scale (SADS) for assessing social anxiety and the Hospital Anxiety and Depression Scale (HADS) for evaluating current depression and anxiety. Results: The mean SADS and HADS scores were in the normal range except for the HAD-Anxiety subscale (HAD-A) on the non-treated transsexual group. SADS, HAD-A, and HAD-Depression (HAD-D) mean scores were significantly higher among patients who had not begun cross-sex hormonal treatment compared with patients in hormonal treatment (F = 4.362, p = .038; F = 14.589, p = .001; F = 9.523, p = .002 respectively). Similarly, current symptoms of anxiety and depression were present in a significantly higher percentage of untreated patients than in treated patients (61% vs. 33% and 31% vs. 8% respectively). Conclusions: The results suggest that most transsexual patients attending a gender identity unit reported subclinical levels of social distress, anxiety, and depression. Moreover, patients under cross-sex hormonal treatment displayed a lower prevalence of these symptoms than patients who had not initiated hormonal therapy. Although the findings do not conclusively demonstrate a direct positive effect of hormone treatment in transsexuals, initiating this treatment may be associated with better mental health of these patients.
Gomez-Gil et al., 2014

Gómez-Gil, E., Zubiaurre-Elorza, L., de Antonio, E. D., Guillamon, A., & Salamero, M. (2014). Determinants of quality of life in Spanish transsexuals attending a gender unit before genital sex reassignment surgery. Quality of Life Research , 23 (2), 669-676.
Purpose: To evaluate the self-reported perceived quality of life (QoL) in transsexuals attending a Spanish gender identity unit before genital sex reassignment surgery, and to identify possible determinants that likely contribute to their QoL. Methods: A sample of 119 male-to-female (MF) and 74 female-to-male (FM) transsexuals were included in the study. The WHOQOL-BREF scale was used to evaluate self-reported QoL. Possible determinants included age, sex, education, employment, partnership status, undergoing cross-sex hormonal therapy, receiving at least one non-genital sex reassignment surgery, and family support (assessed with the family APGAR questionnaire). Results: Mean scores of all QoL domains ranged from 55.44 to 63.51. Linear regression analyses revealed that undergoing cross-sex hormonal treatment, having family support, and having an occupation were associated with a better QoL for all transsexuals. FM transsexuals have higher social domain QoL scores than MF transsexuals. The model accounts for 20.6 % of the variance in the physical, 32.5 % in the psychological, 21.9 % in the social, and 20.1 % in the environment domains, and 22.9 % in the global QoL factor. Conclusions: Cross-sex hormonal treatment, family support, and working or studying are linked to a better self-reported QoL in transsexuals. Healthcare providers should consider these factors when planning interventions to promote the health-related QoL of transsexuals.
Gorin-Lazard et al., 2012

Gorin‐Lazard, A., Baumstarck, K., Boyer, L., Maquigneau, A., Gebleux, S., Penochet, J., Pringuey, D., Albarel, F., Morange, I., Loundou, A., Berbis, J., Auquier, P., Lançon, C. and Bonierbale, M. (2012). Is hormonal therapy associated with better quality of life in transsexuals? A cross‐sectional study. The Journal of Sexual Medicine , 9 (2), 531–541.
Introduction: Although the impact of sex reassignment surgery on the self‐reported outcomes of transsexuals has been largely described, the data available regarding the impact of hormone therapy on the daily lives of these individuals are scarce. Aims: The objectives of this study were to assess the relationship between hormonal therapy and the self‐reported quality of life (QoL) in transsexuals while taking into account the key confounding factors and to compare the QoL levels between transsexuals who have, vs. those who have not, undergone cross‐sex hormone therapy as well as between transsexuals and the general population (French age‐ and sex‐matched controls). Methods: This study incorporated a cross‐sectional design that was conducted in three psychiatric departments of public university teaching hospitals in France. The inclusion criteria were as follows: 18 years or older, diagnosis of gender identity disorder (302.85) according to the Diagnostic and Statistical Manual, fourth edition text revision (DSM‐IV TR), inclusion in a standardized sex reassignment procedure following the agreement of a multidisciplinary team, and pre‐sex reassignment surgery. Main Outcome Measure. QoL was assessed using the Short Form 36 (SF‐36). Results: The mean age of the total sample was 34.7 years, and the sex ratio was 1:1. Forty‐four (72.1%) of the participants received hormonal therapy. Hormonal therapy and depression were independent predictive factors of the SF‐36 mental composite score. Hormonal therapy was significantly associated with a higher QoL, while depression was significantly associated with a lower QoL. Transsexuals’ QoL, independently of hormonal status, did not differ from the French age‐ and sex‐matched controls except for two subscales of the SF‐36 questionnaire: role physical (lower scores in transsexuals) and general health (lower scores in controls). Conclusion: The present study suggests a positive effect of hormone therapy on transsexuals’ QoL after accounting for confounding factors. These results will be useful for healthcare providers of transgender persons but should be confirmed with larger samples using a prospective study design.
Gorin-Lazard et al., 2013

Gorin-Lazard, A., Baumstarck, K., Boyer, L., Maquigneau, A., Penochet, J. C., et al. (2013). Hormonal therapy is associated with better self-esteem, mood, and quality of life in transsexuals. Journal of Nervous and Mental Disease , 201 (11), 996–1000.
Few studies have assessed the role of cross-sex hormones on psychological outcomes during the period of hormonal therapy preceding sex reassignment surgery in transsexuals. The objective of this study was to assess the relationship between hormonal therapy, self-esteem, depression, quality of life (QoL), and global functioning. This study incorporated a cross-sectional design. The inclusion criteria were diagnosis of gender identity disorder (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision) and inclusion in a standardized sex reassignment procedure. The outcome measures were self-esteem (Social Self-Esteem Inventory), mood (Beck Depression Inventory), QoL (Subjective Quality of Life Analysis), and global functioning (Global Assessment of Functioning). Sixty-seven consecutive individuals agreed to participate. Seventy-three percent received hormonal therapy. Hormonal therapy was an independent factor in greater self-esteem, less severe depression symptoms, and greater “psychological-like” dimensions of QoL. These findings should provide pertinent information for health care providers who consider this period as a crucial part of the global sex reassignment procedure.
Hess et al., 2014

Hess, J., Neto, R. R., Panic, L., Rübben, H., & Senf, W. (2014). Satisfaction with male-to-female gender reassignment surgery: Results of a retrospective analysis. Deutsches Ärzteblatt International , 111 (47), 795–801.
Background: The frequency of gender identity disorder is hard to determine; the number of gender reassignment operations and of court proceedings in accordance with the German Law on Transsexuality almost certainly do not fully reflect the underlying reality. There have been only a few studies on patient satisfaction with male-to-female gender reassignment surgery. Methods: 254 consecutive patients who had undergone male-to-female gender reassignment surgery at Essen University Hospital’s Department of Urology retrospectively filled out a questionnaire about their subjective postoperative satisfaction. Results: 119 (46.9%) of the patients filled out and returned the questionnaires, at a mean of 5.05 years after surgery (standard deviation 1.61 years, range 1–7 years). 90.2% said their expectations for life as a woman were fulfilled postoperatively. 85.4% saw themselves as women. 61.2% were satisfied, and 26.2% very satisfied, with their outward appearance as a woman; 37.6% were satisfied, and 34.4% very satisfied, with the functional outcome. 65.7% said they were satisfied with their life as it is now. Conclusion: The very high rates of subjective satisfaction and the surgical outcomes indicate that gender reassignment surgery is beneficial. These findings must be interpreted with caution, however, because fewer than half of the questionnaires were returned.
Heylens et al., 2014

Heylens, G., Verroken, C., De Cock, S., T’Sjoen, G., & De Cuypere, G. (2014). Effects of different steps in gender reassignment therapy on psychopathology: a prospective study of persons with a gender identity disorder. The Journal of Sexual Medicine , 11 (1), 119–126.
Introduction: At the start of gender reassignment therapy, persons with a gender identity disorder (GID) may deal with various forms of psychopathology. Until now, a limited number of publications focus on the effect of the different phases of treatment on this comorbidity and other psychosocial factors. Aims: The aim of this study was to investigate how gender reassignment therapy affects psychopathology and other psychosocial factors. Methods: This is a prospective study that assessed 57 individuals with GID by using the Symptom Checklist‐90 (SCL‐90) at three different points of time: at presentation, after the start of hormonal treatment, and after sex reassignment surgery (SRS). Questionnaires on psychosocial variables were used to evaluate the evolution between the presentation and the postoperative period. The data were statistically analyzed by using SPSS 19.0, with significance levels set at P < 0.05. Main Outcome Measures: The psychopathological parameters include overall psychoneurotic distress, anxiety, agoraphobia, depression, somatization, paranoid ideation/psychoticism, interpersonal sensitivity, hostility, and sleeping problems. The psychosocial parameters consist of relationship, living situation, employment, sexual contacts, social contacts, substance abuse, and suicide attempt. Results: A difference in SCL‐90 overall psychoneurotic distress was observed at the different points of assessments (P = 0.003), with the most prominent decrease occurring after the initiation of hormone therapy (P < 0.001). Significant decreases were found in the subscales such as anxiety, depression, interpersonal sensitivity, and hostility. Furthermore, the SCL‐90 scores resembled those of a general population after hormone therapy was initiated. Analysis of the psychosocial variables showed no significant differences between pre‐ and postoperative assessments. Conclusions: A marked reduction in psychopathology occurs during the process of sex reassignment therapy, especially after the initiation of hormone therapy.
Imbimbo et al., 2009

Imbimbo, C., Verze, P., Palmieri, A., Longo, N., Fusco, F., Arcaniolo, D., & Mirone, V. (2009). A report from a single institute’s 14-year experience in treatment of male-to-female transsexuals. The Journal of Sexual Medicine , 6 (10), 2736–2745.
Introduction: Gender identity disorder or transsexualism is a complex clinical condition, and prevailing social context strongly impacts the form of its manifestations. Sex reassignment surgery (SRS) is the crucial step of a long and complex therapeutic process starting with preliminary psychiatric evaluation and culminating in definitive gender identity conversion. Aim: The aim of our study is to arrive at a clinical and psychosocial profile of male-to-female transsexuals in Italy through analysis of their personal and clinical experience and evaluation of their postsurgical satisfaction levels SRS. Methods: From January 1992 to September 2006, 163 male patients who had undergone gender-transforming surgery at our institution were requested to complete a patient satisfaction questionnaire. Main Outcome Measures: The questionnaire consisted of 38 questions covering nine main topics: general data, employment status, family status, personal relationships, social and cultural aspects, presurgical preparation, surgical procedure, and postsurgical sex life and overall satisfaction. Results: Average age was 31 years old. Seventy-two percent had a high educational level, and 63% were steadily employed. Half of the patients had contemplated suicide at some time in their lives before surgery and 4% had actually attempted suicide. Family and colleague emotional support levels were satisfactory. All patients had been adequately informed of surgical procedure beforehand. Eighty-nine percent engaged in postsurgical sexual activities. Seventy-five percent had a more satisfactory sex life after SRS, with main complications being pain during intercourse and lack of lubrication. Seventy-eight percent were satisfied with their neovagina’s esthetic appearance, whereas only 56% were satisfied with depth. Almost all of the patients were satisfied with their new sexual status and expressed no regrets. Conclusions: Our patients’ high level of satisfaction was due to a combination of a well-conducted preoperative preparation program, competent surgical skills, and consistent postoperative follow-up.
Johansson et al., 2010

Johansson, A., Sundbom, E., Höjerback, T., & Bodlund, O. (2010). A five-year follow-up study of Swedish adults with gender identity disorder. Archives of Sexual Behavior , 39 (6), 1429-1437.
This follow-up study evaluated the outcome of sex reassignment as viewed by both clinicians and patients, with an additional focus on the outcome based on sex and subgroups. Of a total of 60 patients approved for sex reassignment, 42 (25 male-to-female [MF] and 17 female-to-male [FM]) transsexuals completed a follow-up assessment after 5 or more years in the process or 2 or more years after completed sex reassignment surgery. Twenty-six (62%) patients had an early onset and 16 (38%) patients had a late onset; 29 (69%) patients had a homosexual sexual orientation and 13 (31%) patients had a non-homosexual sexual orientation (relative to biological sex). At index and follow-up, a semi-structured interview was conducted. At follow-up, 32 patients had completed sex reassignment surgery, five were still in process, and five—following their own decision—had abstained from genital surgery. No one regretted their reassignment. The clinicians rated the global outcome as favorable in 62% of the cases, compared to 95% according to the patients themselves, with no differences between the subgroups. Based on the follow-up interview, more than 90% were stable or improved as regards work situation, partner relations, and sex life, but 5–15% were dissatisfied with the hormonal treatment, results of surgery, total sex reassignment procedure, or their present general health. Most outcome measures were rated positive and substantially equal for MF and FM. Late-onset transsexuals differed from those with early onset in some respects: these were mainly MF (88 vs. 42%), older when applying for sex reassignment (42 vs. 28 years), and non-homosexually oriented (56 vs. 15%). In conclusion, almost all patients were satisfied with the sex reassignment; 86% were assessed by clinicians at follow-up as stable or improved in global functioning.
Keo-Meier et al., 2015

Keo-Meier, C. L., Herman, L. I., Reisner, S. L., Pardo, S. T., Sharp, C., & Babcock, J. C. (2015). Testosterone treatment and MMPI-2 improvement in transgender men: A prospective controlled study. Journal of Consulting and Clinical Psychology, 83 , 143-156.
Objective: Most transgender men desire to receive testosterone treatment in order to masculinize their bodies. In this study, we aimed to investigate the short-term effects of testosterone treatment on psychological functioning in transgender men. This is the 1st controlled prospective follow-up study to examine such effects. Method: We examined a sample of transgender men (n = 48) and nontransgender male (n = 53) and female (n = 62) matched controls (mean age = 26.6 years; 74% White). We asked participants to complete the Minnesota Multiphasic Personality Inventory (2nd ed., or MMPI–2; Butcher, Graham, Tellegen, Dahlstrom, & Kaemmer, 2001) to assess psychological functioning at baseline and at the acute posttreatment follow-up (3 months after testosterone initiation). Regression models tested (a) Gender × Time interaction effects comparing divergent mean response profiles across measurements by gender identity; (b) changes in psychological functioning scores for acute postintervention measurements, adjusting for baseline measures, comparing transgender men with their matched nontransgender male and female controls and adjusting for baseline scores; and (c) changes in meeting clinical psychopathological thresholds. Results: Statistically significant changes in MMPI–2 scale scores were found at 3-month follow-up after initiating testosterone treatment relative to baseline for transgender men compared with female controls (female template): reductions in Hypochondria (p < .05), Depression (p < .05), Hysteria (p < .05), and Paranoia (p < .01); and increases in Masculinity–Femininity scores (p < .01). Gender × Time interaction effects were found for Hysteria (p < .05) and Paranoia (p < .01) relative to female controls (female template) and for Hypochondria (p < .05), Depression (p < .01), Hysteria (p < .01), Psychopathic Deviate (p < .05), Paranoia (p < .01), Psychasthenia (p < .01), and Schizophrenia (p < .01) compared with male controls (male template). In addition, the proportion of transgender men presenting with co-occurring psychopathology significantly decreased from baseline compared with 3-month follow-up relative to controls (p < .05). Conclusions: Findings suggest that testosterone treatment resulted in increased levels of psychological functioning on multiple domains in transgender men relative to nontransgender controls. These findings differed in comparisons of transgender men with female controls using the female template and with male controls using the male template. No iatrogenic effects of testosterone were found. These findings suggest a direct positive effect of 3 months of testosterone treatment on psychological functioning in transgender men.
Kraemer et al., 2008

Kraemer, B., Delsignore, A., Schnyder, U., & Hepp, U. (2008). Body image and transsexualism. Psychopathology , 41 (2), 96-100.
Background: To achieve a detailed view of the body image of transsexual patients, an assessment of perception, attitudes and experiences about one’s own body is necessary. To date, research on the body image of transsexual patients has mostly covered body dissatisfaction with respect to body perception. Sampling and Methods: We investigated 23 preoperative (16 male-to-female and 7 female-to-male transsexual patients) and 22 postoperative (14 male-to-female and 8 female-to-male) transsexual patients using a validated psychological measure for body image variables. Results: We found that preoperative transsexual patients were insecure and felt unattractive because of concerns about their body image. However, postoperative transsexual patients scored high on attractiveness and self-confidence. Furthermore, postoperative transsexual patients showed low scores for insecurity and concerns about their body. Conclusions: Our results indicate an improvement of body image concerns for transsexual patients following standards of care for gender identity disorder. Follow-up studies are recommended to confirm the assumed positive outcome of standards of care on body image.
Landen et al., 1998

Landén, M., Wålinder, J., Hambert, G., & Lundström, B. (1998). Factors predictive of regret in sex reassignment. Acta Psychiatrica Scandinavica , 97 (4), 284-289.
The objective of this study was to evaluate the features and calculate the frequency of sex-reassigned subjects who had applied for reversal to their biological sex, and to compare these with non-regretful subjects. An inception cohort was retrospectively identified consisting of all subjects with gender identity disorder who were approved for sex reassignment in Sweden during the period 1972-1992. The period of time that elapsed between the application and this evaluation ranged from 4 to 24 years. The total cohort consisted of 218 subjects. The results showed that 3.8% of the patients who were sex reassigned during 1972-1992 regretted the measures taken. The cohort was subdivided according to the presence or absence of regret of sex reassignment, and the two groups were compared. The results of logistic regression analysis indicated that two factors predicted regret of sex reassignment, namely lack of support from the patient’s family, and the patient belonging to the non-core group of transsexuals. In conclusion, the results show that the outcome of sex reassignment has improved over the years. However, the identified risk factors indicate the need for substantial efforts to support the families and close friends of candidates for sex reassignment.
Lawrence, 2003

Lawrence, A. A. (2003). Factors associated with satisfaction or regret following male-to-female sex reassignment surgery. Archives of Sexual Behavior , 32 (4), 299-315.
This study examined factors associated with satisfaction or regret following sex reassignment surgery (SRS) in 232 male-to-female transsexuals operated on between 1994 and 2000 by one surgeon using a consistent technique. Participants, all of whom were at least 1-year postoperative, completed a written questionnaire concerning their experiences and attitudes. Participants reported overwhelmingly that they were happy with their SRS results and that SRS had greatly improved the quality of their lives. None reported outright regret and only a few expressed even occasional regret. Dissatisfaction was most strongly associated with unsatisfactory physical and functional results of surgery. Most indicators of transsexual typology, such as age at surgery, previous marriage or parenthood, and sexual orientation, were not significantly associated with subjective outcomes. Compliance with minimum eligibility requirements for SRS specified by the Harry Benjamin International Gender Dysphoria Association was not associated with more favorable subjective outcomes. The physical results of SRS may be more important than preoperative factors such as transsexual typology or compliance with established treatment regimens in predicting postoperative satisfaction or regret.
Lawrence, 2006

Lawrence, A. A. (2006). Patient-reported complications and functional outcomes of male-to-female sex reassignment surgery. Archives of Sexual Behavior , 35 (6), 717-727.
This study examined preoperative preparations, complications, and physical and functional outcomes of male-to-female sex reassignment surgery (SRS), based on reports by 232 patients, all of whom underwent penile-inversion vaginoplasty and sensate clitoroplasty, performed by one surgeon using a consistent technique. Nearly all patients discontinued hormone therapy before SRS and most reported that doing so created no difficulties. Preoperative electrolysis to remove genital hair, undergone by most patients, was not associated with less serious vaginal hair problems. No patients reported rectal-vaginal fistula or deep-vein thrombosis and reports of other significant surgical complications were uncommon. One third of patients, however, reported urinary stream problems. No single complication was significantly associated with regretting SRS. Satisfaction with most physical and functional outcomes of SRS was high; participants were least satisfied with vaginal lubrication, vaginal touch sensation, and vaginal erotic sensation. Frequency of achieving orgasm after SRS was not significantly associated with most general measures of satisfaction. Later years of surgery, reflecting greater surgeon experience, were not associated with lower prevalence rates for most complications or with better ratings for most physical and functional outcomes of SRS.
Lobato et al., 2006

Lobato M. I., Koff, W. J., Manenti, C., da Fonseca Seger, D., Salvador, J., et al. (2006). Follow-up of sex reassignment surgery in transsexuals: a Brazilian cohort. Archives of Sexual Behavior, 35(6) , 711–715.
This study examined the impact of sex reassignment surgery on the satisfaction with sexual experience, partnerships, and relationship with family members in a cohort of Brazilian transsexual patients. A group of 19 patients who received sex reassignment between 2000 and 2004 (18 male- to-female, 1 female-to-male) after a two-year evaluation by a multidisciplinary team, and who agreed to participate in the study, completed a written questionnaire. Mean age at entry into the program was 31.21 ± 8.57 years and mean schooling was 9.2 ± 1.4 years. None of the patients reported regret for having undergone the surgery. Sexual experience was considered to have improved by 83.3% of the patients, and became more frequent for 64.7% of the patients. For 83.3% of the patients, sex was considered to be pleasurable with the neovagina/neopenis. In addition, 64.7% reported that initiating and maintaining a relationship had become easier. The number of patients with a partner increased from 52.6% to 73.7%. Family relationships improved in 26.3% of the cases, whereas 73.7% of the patients did not report a difference. None of the patients reported worse relationships
Manieri et al., 2014

Manieri, C., Castellano, E., Crespi, C., Di Bisceglie, C., Dell’Aquila, C., et al. (2014). Medical treatment of subjects with gender identity disorder: The experience in an Italian public health center. International Journal Of Transgenderism , 15 (2), 53-65.
Hormonal treatment is the main element during the transition program for transpeople. The aim of this paper is to describe the care and treatment of subjects, highlighting both the endocrine-metabolic effects of the hormonal therapy and the quality of life during the first year of cross-sex therapy in an Italian gender team. We studied 83 subjects (56 male-to-female [MtF], 27 female-to-male [FtM]) with hematological and hormonal evaluations every 3 months during the first year of hormonal therapy. MtF persons were treated with 17βestradiol and antiandrogens (cyproterone acetate, spironolactone, dutasteride); FtM persons were treated with transdermal or intramuscular testosterone. The WHO Quality of Life questionnaire was administered at the beginning and 1 year later. Hormonal changes paralleled phenotype modifications with wide variability. Most of both MtF and FtM subjects reported a statistically significant improvement in body image (p < 0.05). In particular, MtF subjects reported a statistically significant improvement in the quality of their sexual life and in the general quality of life (p < 0.05) 1 year after treatment initiation. Cross-sex therapy seems to be free of major risks in healthy subjects under clinical supervision during the first year. Selected subjects show an optimal adaptation to hormone-induced neuropsychological modifications and satisfaction regarding general and sexual life.
Megeri and Khoosal, 2007

Megeri, D., & Khoosal, D. (2007). Anxiety and depression in males experiencing gender dysphoria. Sexual & Relationship Therapy , 22 (1), 77-81.
Objective: The aim of the study was to compare anxiety and depression scores for the first 40 male to female people experiencing gender dysphoria attending the Leicester Gender Identity Clinic using the same sample as control pre and post gender realignment surgery. Hypothesis: There is an improvement in the scores of anxiety and depression following gender realignment surgery among people with gender dysphoria (male to female – transwomen). Results: There was no significant change in anxiety and depression scores in people with gender dysphoria (male to female) pre- and post-operatively.
Nelson, Whallett, & Mcgregor, 2009

Nelson, L., Whallett, E., & McGregor, J. (2009). Transgender patient satisfaction following reduction mammaplasty. Journal of Plastic, Reconstructive & Aesthetic Surgery , 62 (3), 331-334.
Aim: To evaluate the outcome of reduction mammaplasty in female-to-male transgender patients. Method: A 5-year retrospective review was conducted on all female-to-male transgender patients who underwent reduction mammaplasty. A postal questionnaire was devised to assess patient satisfaction, surgical outcome and psychological morbidity. Results: Seventeen patients were identified. The senior author performed bilateral reduction mammaplasties and free nipple grafts in 16 patients and one patient had a Benelli technique reduction. Complications included two haematomas, one wound infection, one wound dehiscence and three patients had hypertrophic scars. Secondary surgery was performed in seven patients and included scar revision, nipple reduction/realignment, dog-ear correction and nipple tattooing. The mean follow-up period after surgery was 10 months (range 2–23 months). Twelve postal questionnaires were completed (response rate 70%). All respondents expressed satisfaction with their result and no regret. Seven patients had nipple sensation and nine patients were satisfied with nipple position. All patients thought their scars were reasonable and felt that surgery had improved their self-confidence and social interactions. Conclusion: Reduction mammaplasty for female-to-male gender reassignment is associated with high patient satisfaction and a positive impact on the lives of these patients.
Newfield et al., 2006

Newfield, E., Hart, S., Dibble, S., & Kohler, L. (2006). Female-to-male transgender quality of life. Quality of Life Research , 15 (9), 1447-1457.
Objectives: We evaluated health-related quality of life in female-to-male (FTM) transgender individuals, using the Short-Form 36-Question Health Survey version 2 (SF-36v2). Methods: Using email, Internet bulletin boards, and postcards, we recruited individuals to an Internet site ( http://www.transurvey.org ), which contained a demographic survey and the SF36v2. We enrolled 446 FTM transgender and FTM transsexual participants, of which 384 were from the US. Results: Analysis of quality of life health concepts demonstrated statistically significant (p<0.0\) diminished quality of life among the FTM transgender participants as compared to the US male and female population, particularly in regard to mental health. FTM transgender participants who received testosterone (67%) reported statistically significant higher quality of life scores (/?<0.01) than those who had not received hormone therapy. Conclusions: FTM transgender participants reported significantly reduced mental health-related quality of life and
Padula, Heru, & Campbell, 2016

Padula, W. V., Heru, S. & Campbell, J. D. (2016). Societal implications of health insurance coverage for medically necessary services in the U.S. transgender population: A cost-effectiveness analysis. Journal of General Internal Medicine , 31 ( 4), 394-401.
Background: Recently, the Massachusetts Group Insurance Commission (GIC) prioritized research on the implications of a clause expressly prohibiting the denial of health insurance coverage for transgender-related services. These medically necessary services include primary and preventive care as well as transitional therapy. Objective: To analyze the cost-effectiveness of insurance coverage for medically necessary transgender-related services. Design: Markov model with 5- and 10-year time horizons from a U.S. societal perspective, discounted at 3 % (USD 2013). Data on outcomes were abstracted from the 2011 National Transgender Discrimination Survey (NTDS). Patients: U.S. transgender population starting before transitional therapy. Interventions: No health benefits compared to health insurance coverage for medically necessary services. This coverage can lead to hormone replacement therapy, sex reassignment surgery, or both. Main Measures: Cost per quality-adjusted life year (QALY) for successful transition or negative outcomes (e.g. HIV, depression, suicidality, drug abuse, mortality) dependent on insurance coverage or no health benefit at a willingness-to-pay threshold of $100,000/QALY. Budget impact interpreted as the U.S. per-member-per-month cost. Key Results: Compared to no health benefits for transgender patients ($23,619; 6.49 QALYs), insurance coverage for medically necessary services came at a greater cost and effectiveness ($31,816; 7.37 QALYs), with an incremental cost-effectiveness ratio (ICER) of $9314/QALY. The budget impact of this coverage is approximately $0.016 per member per month. Although the cost for transitions is $10,000–22,000 and the cost of provider coverage is $2175/year, these additional expenses hold good value for reducing the risk of negative endpoints —HIV, depression, suicidality, and drug abuse. Results were robust to uncertainty. The probabilistic sensitivity analysis showed that provider coverage was cost-effective in 85 % of simulations. Conclusions: Health insurance coverage for the U.S. transgender population is affordable and cost-effective, and has a low budget impact on U.S. society. Organizations such as the GIC should consider these results when examining policies regarding coverage exclusions.
Parola et al., 2010

Parola, N., Bonierbale, M., Lemaire, A., Aghababian, V., Michel, A., & Lançon, C. (2010). Study of quality of life for transsexuals after hormonal and surgical reassignment. Sexologies , 19 (1), 24-28.
Aim: The main objective of this work is to provide a more detailed assessment of the impact of surgical reassignment on the most important aspects of daily life for these patients. Our secondary objective was to establish the influence of various factors likely to have an impact on the quality of life (QoL), such as biological gender and the subject’s personality. Methods: A personality study was conducted using Eysenck Personality Inventory (EPI) so as to analyze two aspects of the personality (extraversion and neuroticism). Thirty-eight subjects who had undergone hormonal surgical reassignment were included in the study. Results: The results show that gender reassignment surgery improves the QoL for transsexuals in several different important areas: most are satisfied of their sexual reassignment (28/30), their social (21/30) and sexual QoL (25/30) are improved. However, there are differences between male-to-female (MtF) and female-to-male (FtM) transsexuals in terms of QoL: FtM have a better social, professional, friendly lifestyles than MtF. Finally, the results of this study did not evidence any influence by certain aspects of the personality, such as extraversion and neuroticism, on the QoL for reassigned subjects.
Pfäfflin, 1993

Pfäfflin, F. (1993). Regrets after sex reassignment surgery. Journal of Psychology & Human Sexuality , 5 (4), 69-85.
Using data draw from the follow-up literature covering the last 30 years, and the author’s clinical data on 295 men and women after SRS, an estimation of the number of patients who regretted the operations is made. Among female-to-male transsexuals after SRS, i.e., in men, no regrets were reported in the author’s sample, and in the literature they amount to less than 1%. Among male-to- female transsexuals after SRS, i.e., in women, regrets are reported in 1-1.5%. Poor differential diagnosis, failure to carry out the real-life- test, and poor surgical results seem to be the main reasons behind the regrets reported in the literature. According to three cases observed by the author in addition to personality traits the lack of proper care in treating the patients played a major role.
Pimenoff and Pfäfflin, 2011

Pimenoff, V., & Pfäfflin, F. (2011). Transsexualism: Treatment outcome of compliant and noncompliant patients. International Journal Of Transgenderism , 13 (1), 37-44.
The objective of the study was a follow-up of the treatment outcome of Finnish transsexuals who sought sex reassignment during the period 1970–2002 and a comparison of the results and duration of treatment of compliant and noncompliant patients. Fifteen male-to-female transsexuals and 17 female-to-male transsexuals who had undergone hormone and surgical treatment and legal sex reassignment in Finland completed a questionnaire on psychosocial data and on their experience with the different phases of clinical assessment and treatment. The changes in their vocational functioning and social and psychic adjustment were used as outcome indicators. The results and duration of the treatment of compliant and noncompliant patients were compared. The patients benefited significantly from treatment. The noncompliant patients achieved equally good results as the compliant ones, and did so in a shorter time. A good treatment outcome could be achieved even when the patient had told the assessing psychiatrist a falsified story of his life and sought hormone therapy, genital surgery, or legal sex reassignment on his own initiative without a recommendation from the psychiatrist. Based on these findings, it is recommended that the doctor-patient relationship be reconsidered and founded on frank cooperation.
Rakic et al., 1996

Rakic, Z., Starcevic, V., Maric, J., & Kelin, K. (1996). The outcome of sex reassignment surgery in Belgrade: 32 patients of both sexes. Archives of Sexual Behavior , 25 (5), 515-525.
Several aspects of the quality of life after sex reassignment surgery in 32 transsexuals of both sexes (22 men, 10 women) were examined. The Belgrade Team for Gender Identity Disorders designed a standardized questionnaire for this purpose. The follow-up period after operation was from 6 months to 4 years, and four aspects of the quality of life were examined: attitude towards the patients’ own body, relationships with other people, sexual activity, and occupational functioning. In most transsexuals, the quality of life was improved after surgery inasmuch as these four aspects are concerned. Only a few transsexuals were not satisfied with their life after surgery.
Rehman et al., 1999

Rehman, J., Lazer, S., Benet, A. E., Schaefer, L. C., & Melman, A. (1999). The reported sex and surgery satisfactions of 28 postoperative male-to-female transsexual patients. Archives of Sexual Behavior , 28 (1), 71-89.
From 1980 to July 1997 sixty-one male-to-female gender transformation surgeries were performed at our university center by one author (A.M.). Data were collected from patients who had surgery up to 1994 (n = 47) to obtain a minimum follow-up of 3 years; 28 patients were contacted. A mail questionnaire was supplemented by personal interviews with 11 patients and telephone interviews with remaining patients to obtain and clarify additional information. Physical and functional results of surgery were judged to be good, with few patients requiring additional corrective surgery. General satisfaction was expressed over the quality of cosmetic (normal appearing genitalia) and functional (ability to perceive orgasm) results. Follow-up showed satisfied who believed they had normal appearing genitalia and the ability to experience orgasm. Most patients were able to return to their jobs and live a more satisfactory social and personal life. One significant outcome was the importance of proper preparation of patients for surgery and especially the need for additional postoperative psychotherapy. None of the patients regretted having had surgery. However, some were, to a degree, disappointed because of difficulties experienced post operatively in adjusting satisfactorily as women both in their relationships with men and in living their lives generally as women. Findings of this study make a strong case for making a change in the Harry Benjamin Standards of Care to include a period of postoperative psychotherapy.
Rotondi et al., 2011

Rotondi, N. K., Bauer, G. R., Scanlon, K., Kaay, M., Travers, R., & Travers, A. (2011). Prevalence of and risk and protective factors for depression in female-to-male transgender Ontarians: Trans PULSE Project. Canadian Journal Of Community Mental Health , 30 (2), 135-155.
Although depression is understudied in transgender and transsexual communities, high prevalences have been reported. This paper presents original research from the Trans PULSE Project, an Ontario-wide, community-based initiative that surveyed 433 participants using respondent-driven sampling. The purpose of this analysis was to determine the prevalence of, and risk and protective factors for, depression among female-to-male (FTM) Ontarians (n = 207). We estimate that 66.4% of FTMs have symptomatology consistent with depression. In multivariable analyses, sexual satisfaction was a strong protective factor. Conversely, experiencing transphobia and being at the stage of planning but not having begun a medical transition (hormones and/or surgery) adversely affected mental health in FTMs.
Ruppin and Pfäfflin, 2015

Ruppin, U., & Pfäfflin, F. (2015). Long-term follow-up of adults with gender identity disorder. Archives of Sexual Behavior , 44 (5), 1321-1329.
The aim of this study was to re-examine individuals with gender identity disorder after as long a period of time as possible. To meet the inclusion criterion, the legal recognition of participants’ gender change via a legal name change had to date back at least 10 years. The sample comprised 71 participants (35 MtF and 36 FtM). The follow-up period was 10–24 years with a mean of 13.8 years (SD = 2.78). Instruments included a combination of qualitative and quantitative methods: Clinical interviews were conducted with the participants, and they completed a follow-up questionnaire as well as several standardized questionnaires they had already filled in when they first made contact with the clinic. Positive and desired changes were determined by all of the instruments: Participants reported high degrees of well-being and a good social integration. Very few participants were unemployed, most of them had a steady relationship, and they were also satisfied with their relationships with family and friends. Their overall evaluation of the treatment process for sex reassignment and its effectiveness in reducing gender dysphoria was positive. Regarding the results of the standardized questionnaires, participants showed significantly fewer psychological problems and interpersonal difficulties as well as a strongly increased life satisfaction at follow-up than at the time of the initial consultation. Despite these positive results, the treatment of transsexualism is far from being perfect.
Smith et al., 2005

Smith, Y. L. S., Van Goozen, S. H. M., Kuiper, A. J., & Cohen-Kettenis, P. (2005). Sex reassignment: Outcomes and predictors of treatment for adolescent and adult transsexuals. Psychological Medicine, 35 (1), 89-99.
Background: We prospectively studied outcomes of sex reassignment, potential differences between subgroups of transsexuals, and predictors of treatment course and outcome. Method: Altogether 325 consecutive adolescent and adult applicants for sex reassignment participated: 222 started hormone treatment, 103 did not; 188 completed and 34 dropped out of treatment. Only data of the 162 adults were used to evaluate treatment. Results between subgroups were compared to determine post-operative differences. Adults and adolescents were included to study predictors of treatment course and outcome. Results were statistically analysed with logistic regression and multiple linear regression analyses. Results: After treatment the group was no longer gender dysphoric. The vast majority functioned quite well psychologically, socially and sexually. Two non-homosexual male-to-female transsexuals expressed regrets. Post-operatively, female-to-male and homosexual transsexuals functioned better in many respects than male-to-female and non-homosexual transsexuals. Eligibility for treatment was largely based upon gender dysphoria, psychological stability, and physical appearance. Male-to-female transsexuals with more psychopathology and cross-gender symptoms in childhood, yet less gender dysphoria at application, were more likely to drop out prematurely. Non-homosexual applicants with much psychopathology and body dissatisfaction reported the worst post-operative outcomes. Conclusions: The results substantiate previous conclusions that sex reassignment is effective. Still, clinicians need to be alert for non-homosexual male-to-females with unfavourable psychological functioning and physical appearance and inconsistent gender dysphoria reports, as these are risk factors for dropping out and poor post-operative results. If they are considered eligible, they may require additional therapeutic guidance during or even after treatment.
van de Grift et al., 2017

van de Grift, T. C., Elaut, E., Cerwenka, S. C., Cohen-Kettenis, P. T., Cuypere, G. D., Richter-Appelt, H., & Kreukels, B. P. (2017). Effects of medical interventions on gender dysphoria and body image. Psychosomatic Medicine , 79 (7), 815-823.
Objective: The aim of this study from the European Network for the Investigation of Gender Incongruence is to investigate the status of all individuals who had applied for gender confirming interventions from 2007 to 2009, irrespective of whether they received treatment. The current article describes the study protocol, the effect of medical treatment on gender dysphoria and body image, and the predictive value of (pre)treatment factors on posttreatment outcomes. Methods: Data were collected on medical interventions, transition status, gender dysphoria (Utrecht Gender Dysphoria Scale), and body image (Body Image Scale for transsexuals). In total, 201 people participated in the study (37% of the original cohort). Results: At follow-up, 29 participants (14%) did not receive medical interventions, 36 hormones only (18%), and 136 hormones and surgery (68%). Most transwomen had undergone genital surgery, and most transmen chest surgery. Overall, the levels of gender dysphoria and body dissatisfaction were significantly lower at follow-up compared with clinical entry. Satisfaction with therapy responsive and unresponsive body characteristics both improved. High dissatisfaction at admission and lower psychological functioning at follow-up were associated with persistent body dissatisfaction. Conclusions: Hormone-based interventions and surgery were followed by improvements in body satisfaction. The level of psychological symptoms and the degree of body satisfaction at baseline were significantly associated with body satisfaction at follow-up.

van de Grift, T. C., Elaut, E., Cerwenka, S. C., Cohen-Kettenis, P. T., & Kreukels, B. P. (2017). Surgical satisfaction, quality of life, and their association after gender-affirming surgery: A follow-up study. Journal of Sex & Marital Therapy , 44 (2), 138-148.
We assessed the outcomes of gender-affirming surgery (GAS, or sex-reassignment surgery) 4 to 6 years after first clinical contact, and the associations between postoperative (dis)satisfaction and quality of life (QoL). Our multicenter, cross-sectional follow-up study involved persons diagnosed with gender dysphoria (DSM-IV-TR) who applied for medical interventions from 2007 until 2009. Of 546 eligible persons, 201 (37%) responded, of whom 136 had undergone GAS (genital, chest, facial, vocal cord and/or thyroid cartilage surgery). Main outcome measures were procedure performed, self-reported complications, and satisfaction with surgical outcomes (standardized questionnaires), QoL (Satisfaction With Life Scale, Subjective Happiness Scale, Cantril Ladder), gender dysphoria (Utrecht Gender Dysphoria Scale), and psychological symptoms (Symptom Checklist-90). Postoperative satisfaction was 94% to 100%, depending on the type of surgery performed. Eight (6%) of the participants reported dissatisfaction and/or regret, which was associated with preoperative psychological symptoms or self-reported surgical complications (OR= 6.07). Satisfied respondents’ QoL scores were similar to reference values; dissatisfied or regretful respondents’ scores were lower. Therefore, dissatisfaction after GAS may be viewed as indicator of unfavorable psychological and QoL outcomes.
Vujovic et al., 2009

Vujovic, S., Popovic, S., Sbutega-Milosevic, G., Djordjevic, M., & Gooren, L. (2009). Transsexualism in Serbia: A twenty-year follow-up study. The Journal of Sexual Medicine , 6 (4), 1018-1023.
Introduction: Gender dysphoria occurs in all societies and cultures. The prevailing social context has a strong impact on its manifestations as well as on applications by individuals with the condition for sex reassignment treatment. Aim: To describe a transsexual population seeking sex reassignment treatment in Serbia, part of former Yugoslavia. Methods: Data, collated over a period of 20 years, from subjects applying for sex reassignment to the only center in Serbia, were analyzed retrospectively. Main Outcome Measures: Age at the time of application, demographic data, family background, sex ratio, the prevalence of polycystic ovarian syndrome (PCOS) among female-to-male (FTM) transsexuals, and readiness to undergo surgical sex reassignment were tabulated. Results: Applicants for sex reassignment in Serbia are relatively young. The sex ratio is close to 1:1. They often come from single-child families. More than 10% do not wish to undergo surgical sex reassignment. The prevalence of PCOS among FTM transsexuals was higher than in the general population but considerably lower than that reported in the literature from other populations. Of those who had undergone sex reassignment, none expressed regret for their decision. Conclusions: Although transsexualism is a universal phenomenon, the relatively young age of those applying for sex reassignment and the sex ratio of 1:1 distinguish the population in Serbia from others reported in the literature.

Weigert et al., 2013

Weigert, R., Frison, E., Sessiecq, Q., Al Mutairi, K., & Casoli, V. (2013). Patient satisfaction with breasts and psychosocial, sexual, and physical well-being after breast augmentation in male-to-female transsexuals. Plastic and Reconstructive Surgery, 132 (6), 1421-1429.
Background: Satisfaction with breasts, sexual well-being, psychosocial well-being, and physical well-being are essential outcome factors following breast augmentation surgery in male-to-female transsexual patients. The aim of this study was to measure change in patient satisfaction with breasts and sexual, physical, and psychosocial well-being after breast augmentation in male-to-female transsexual patients. Methods: All consecutive male-to-female transsexual patients who underwent breast augmentation between 2008 and 2012 were asked to complete the BREAST-Q Augmentation module questionnaire before surgery, at 4 months, and later after surgery. A prospective cohort study was designed and postoperative scores were compared with baseline scores. Satisfaction with breasts and sexual, physical, and psychosocial outcomes assessment was based on the BREAST-Q. Results: Thirty-five male-to-female transsexual patients completed the questionnaires. BREAST-Q subscale median scores (satisfaction with breasts, +59 points; sexual well-being, +34 points; and psychosocial well-being, +48 points) improved significantly (p < 0.05) at 4 months postoperatively and later. No significant change was observed in physical well-being. Conclusions: In this prospective, noncomparative, cohort study, the current results suggest that the gains in breast satisfaction, psychosocial well-being, and sexual well-being after male-to-female transsexual patients undergo breast augmentation are statistically significant and clinically meaningful to the patient at 4 months after surgery and in the long term.
Weyers et al., 2009

Weyers, S., Elaut, E., De Sutter, P., Gerris, J., T’Sjoen, G., et al. (2009). Long-term assessment of the physical, mental, and sexual health among transsexual women. The Journal of Sexual Medicine , 6 (3), 752-760.
Introduction: Transsexualism is the most extreme form of gender identity disorder and most transsexuals eventually pursue sex reassignment surgery (SRS). In transsexual women, this comprises removal of the male reproductive organs, creation of a neovagina and clitoris, and often implantation of breast prostheses. Studies have shown good sexual satisfaction after transition. However, long-term follow-up data on physical, mental and sexual functioning are lacking. Aim: To gather information on physical, mental, and sexual well-being, health-promoting behavior and satisfaction with gender-related body features of transsexual women who had undergone SRS. Methods: Fifty transsexual women who had undergone SRS >or=6 months earlier were recruited. Main Outcome Measures: Self-reported physical and mental health using the Dutch version of the Short-Form-36 (SF-36) Health Survey; sexual functioning using the Dutch version of the Female Sexual Function Index (FSFI). Satisfaction with gender-related bodily features as well as with perceived female appearance; importance of sex, relationship quality, necessity and advisability of gynecological exams, as well as health concerns and feelings of regret concerning transition were scored. Results: Compared with reference populations, transsexual women scored good on physical and mental level (SF-36). Gender-related bodily features were shown to be of high value. Appreciation of their appearance as perceived by others, as well as their own satisfaction with their self-image as women obtained a good score (8 and 9, respectively). However, sexual functioning as assessed through FSFI was suboptimal when compared with biological women, especially the sublevels concerning arousal, lubrication, and pain. Superior scores concerning sexual function were obtained in those transsexual women who were in a relationship and in heterosexuals. Conclusions: Transsexual women function well on a physical, emotional, psychological and social level. With respect to sexuality, they suffer from specific difficulties, especially concerning arousal, lubrication, and pain.
Back to Top
Below are 4 studies that contain mixed or null findings on the effect of gender transition on transgender well-being. Click here to jump to the 17 studies that consist of literature reviews or guidelines that help advance knowledge about the effect of gender transition on transgender well-being . Click here to jump to the 51 studies that found that gender transition improves the well-being of transgender people .
Barrett, 1998.

Barrett J. (1998). Psychological and social function before and after phalloplasty. The International Journal of Transgenderism , 2 (1), 1-8.
There are no quantitative assessments of the benefits of phalloplasty in a female transsexual population. The study addresses this question, comparing transsexuals accepted for such surgery with transsexuals after such surgery has been performed. A population of 23 transsexuals accepted for phalloplasty was compared to a population of 40 who had undergone such surgery between six and one hundred and sixty months previously. The General Health Questionnaire (GHQ), Symptom Checklist 90 (SCL-90), Bem Sex Role Inventory and Social Role Performance Schedule (SRPS) were employed. Additionally, a questionnaire assessing satisfaction with cosmetic appearance, sexual function, relationship and urinary function was used, along with a semi-structured interview quantifying alcohol, cigarette and drug usage, and current sexual practice. There were significant differences between the populations. The post operative group showed higher depression ratings on the depression subscale of the GHQ. The masculine pre-operative Bem scores were neutral post-operatively as feminine sub-scores increased. There was improved satisfaction with genital appearance post-operatively, but satisfaction with relationships fell, although to a non-significant extent. Most other changes were in the expected direction but did not achieve significance. Transsexuals accepted for phalloplasty have very good psychological health. Tendency to further improvement is the case after phalloplasty. Depression is commoner, however, and quality of relationships declines somewhat, perhaps in consequence. Surgeons might advise partners as well as patients of realistic expectations from such surgery.
Lindqvist et al., 2017

Lindqvist, E. K., Sigurjonsson, H., Möllermark, C., Rinder, J., Farnebo, F., et al. (2017). Quality of life improves early after gender reassignment surgery in transgender women. European Journal of Plastic Surgery , 40 (3), 223-226.
Background: Few studies have examined the long-term quality of life (QoL) of individuals with gender dysphoria, or how it is affected by treatment. Our aim was to examine the QoL of transgender women undergoing gender reassignment surgery (GRS). Methods: We performed a prospective cohort study on 190 patients undergoing male-to-female GRS at Karolinska University Hospital between 2003 and 2015. We used the Swedish version of the Short Form-36 Health Survey (SF-36), which measures QoL across eight domains. The questionnaire was distributed to patients pre-operatively, as well as 1, 3, and 5 years post-operatively. The results were compared between the different measure points, as well as between the study group and the general population. Results: On most dimensions of the SF-36 questionnaire, transgender women reported a lower QoL than the general population. The scores of SF-36 showed a non-significant trend to be lower 5 years post-GRS compared to pre-operatively, a decline consistent with that of the general population. Self-perceived health compared to 1 year previously rose in the first post-operative year, after which it declined. Conclusions: To our knowledge, this is the largest prospective study to follow a group of transgender patients with regards to QoL over continuous temporal measure points. Our results show that transgender women generally have a lower QoL compared to the general population. GRS leads to an improvement in general well-being as a trend but over the long-term, QoL decreases slightly in line with that of the comparison group. Level of evidence: Level III, therapeutic study.
Simonsen et al., 2016

Simonsen, R. K., Giraldi, A., Kristensen, E., & Hald, G. M. (2016). Long-term follow-up of individuals undergoing sex reassignment surgery: Psychiatric morbidity and mortality. Nordic Journal Of Psychiatry , 70 (4), 241-247.
Background: There is a lack of long-term register-based follow-up studies of sex-reassigned individuals concerning mortality and psychiatric morbidity. Accordingly, the present study investigated both mortality and psychiatric morbidity using a sample of individuals with transsexualism which comprised 98% (n = 104) of all individuals in Denmark. Aims: (1) To investigate psychiatric morbidity before and after sex reassignment surgery (SRS) among Danish individuals who underwent SRS during the period of 1978–2010. (2) To investigate mortality among Danish individuals who underwent SRS during the period of 1978–2010.Method: Psychiatric morbidity and mortality were identified by data from the Danish Psychiatric Central Research Register and the Cause of Death Register through a retrospective register study of 104 sex-reassigned individuals. Results: Overall, 27.9% of the sample were registered with psychiatric morbidity before SRS and 22.1% after SRS (p = not significant). A total of 6.7% of the sample were registered with psychiatric morbidity both before and after SRS. Significantly more psychiatric diagnoses were found before SRS for those assigned as female at birth. Ten individuals were registered as deceased post-SRS with an average age of death of 53.5 years. Conclusions: No significant difference in psychiatric morbidity or mortality was found between male to female and female to male (FtM) save for the total number of psychiatric diagnoses where FtM held a significantly higher number of psychiatric diagnoses overall. Despite the over-representation of psychiatric diagnoses both pre- and post-SRS the study found that only a relatively limited number of individuals had received diagnoses both prior to and after SRS. This suggests that generally SRS may reduce psychological morbidity for some individuals while increasing it for others.
Udeze, 2008

Udeze, B., Abdelmawla, N., Khoosal, D., & Terry, T. (2008). Psychological functions in male-to-female transsexual people before and after surgery. Sexual & Relationship Therapy , 23 (2), 141-145.
Patients with gender dysphoria (GD) suffer from a constant feeling of psychological discomfort related to their anatomical sex. Gender reassignment surgery (GRS) attempts to release this discomfort. The aim of this study was to compare the functioning of a cohort or patients with GD before and after GRS. We hypothesized that there would be an improvement in the scores of the self-administered SCL-90R following gender reassignment surgery among male-to-female people with gender dysphoria. We studied 40 patients with a DSM-IV diagnosis of Gender Identity Disorder (GID) who attended Leicester Gender Identity Clinic. We compared their functioning as measured by Symptom Check List-90R (SCL-90R) which was administered to 40 randomly selected male-to-female patients before and within six months after GRS using the same sample as control pre-and post-surgery. There was no significant change in the different sub-scales of the SCL-90R scores in patients with male-to-female GID pre- and within six months post-surgery. The results of the study showed that GRS had no significant effect on functioning as measured by SCL-90R within six months of surgery. Our study has the advantage of reducing inter-subject variability by using the same patients as their own control. This study may be limited by the duration of reassessment post-surgery. Further studies with larger sample size and using other psychosocial scales are needed to elucidate on the effectiveness of surgical intervention on psychosocial parameters in patients with GD.
Below are 17 studies that consist of literature reviews or guidelines that help advance knowledge about the effect of gender transition on transgender well-being. Click here to jump to the 4 studies that contain mixed or null findings on the effect of gender transition on transgender well-being. Click here Click here to jump to the 51 studies that found that gender transition improves the well-being of transgender people .
American psychological, 2015.

Guidelines for psychological practice with transgender and gender nonconforming people. (2015). American Psychologist, 70 (9), 832-864.
In 2015, the American Psychological Association adopted Guidelines for Psychological Practice with Transgender and Gender Nonconforming Clients in order to describe affirmative psychological practice with transgender and gender nonconforming (TGNC) clients. There are 16 guidelines in this document that guide TGNC-affirmative psychological practice across the lifespan, from TGNC children to older adults. The Guidelines are organized into five clusters: (a) foundational knowledge and awareness; (b) stigma, discrimination, and barriers to care; (c) lifespan development; (d) assessment, therapy, and intervention; and (e) research, education, and training. In addition, the guidelines provide attention to TGNC people across a range of gender and racial/ethnic identities. The psychological practice guidelines also attend to issues of research and how psychologists may address the many social inequities TGNC people experience.
Bockting et al., 2016

Bockting, W., Coleman, E., Deutsch, M. B., Guillamon, A., Meyer, W., et al. (2016). Adult development and quality of life of transgender and gender nonconforming people. Current Opinion in Endocrinology & Diabetes and Obesity , 23 (2), 188–197.
Purpose of review: Research on the health of transgender and gender nonconforming people has been limited with most of the work focusing on transition-related care and HIV. The present review summarizes research to date on the overall development and quality of life of transgender and gender nonconforming adults, and makes recommendations for future research. Recent findings: Pervasive stigma and discrimination attached to gender nonconformity affect the health of transgender people across the lifespan, particularly when it comes to mental health and well-being. Despite the related challenges, transgender and gender nonconforming people may develop resilience over time. Social support and affirmation of gender identity play herein a critical role. Although there is a growing awareness of diversity in gender identity and expression among this population, a comprehensive understanding of biopsychosocial development beyond the gender binary and beyond transition is lacking. Summary: Greater visibility of transgender people in society has revealed the need to understand and promote their health and quality of life broadly, including but not limited to gender dysphoria and HIV. This means addressing their needs in context of their families and communities, sexual and reproductive health, and successful aging. Research is needed to better understand what factors are associated with resilience and how it can be effectively promoted.
Byne et al., 2012

Byne, W., Bradley, S.J., Coleman, E., et al. (2012). Report of the American Psychiatric Association task force on treatment of gender identity disorder. Archives of Sexual Behavior, 41 (4): 759–796.
Both the diagnosis and treatment of Gender Identity Disorder (GID) are controversial. Although linked, they are separate issues and the DSM does not evaluate treatments. The Board of Trustees (BOT) of the American Psychiatric Association (APA), therefore, formed a Task Force charged to perform a critical review of the literature on the treatment of GID at different ages, to assess the quality of evidence pertaining to treatment, and to prepare a report that included an opinion as to whether or not sufficient credible literature exists for development of treatment recommendations by the APA. The literature on treatment of gender dysphoria in individuals with disorders of sex development was also assessed. The completed report was accepted by the BOT on September 11, 2011. The quality of evidence pertaining to most aspects of treatment in all subgroups was determined to be low; however, areas of broad clinical consensus were identified and were deemed sufficient to support recommendations for treatment in all subgroups. With subjective improvement as the primary outcome measure, current evidence was judged sufficient to support recommendations for adults in the form of an evidence-based APA Practice Guideline with gaps in the empirical data supplemented by clinical consensus. The report recommends that the APA take steps beyond drafting treatment recommendations. These include issuing position statements to clarify the APA’s position regarding the medical necessity of treatments for GID, the ethical bounds of treatments of gender variant minors, and the rights of persons of any age who are gender variant, transgender or transsexual.
Carroll, 1999

Carroll, R. A. (1999). Outcomes of treatment for gender dysphoria. Journal of Sex Education and Therapy , 24 (3), 128–136.
This paper reviews the empirical research on the psychosocial outcomes of treatment for gender dysphoria. Recent research has highlighted the heterogeneity of transgendered experiences. There are four possible outcomes for patients who present with the dilemma of gender dysphoria: an unresolved outcome, acceptance of one’s given gender, engaging in a cross-gender role on a part-time basis, and making a full-time transition to the other gender role. Clinical work, but not empirical research, suggests that some individuals with gender dysphoria may come to accept their given gender role through psychological treatment. Many individuals find that it is psychologically sufficient to express the transgendered part of themselves through such activities as cross-dressing or gender blending. The large body of research on the outcome of gender reassignment surgery indicates that, for the majority of those who undergo this process, the outcome is positive. Predictors of a good outcome include good pre-reassignment psychological adjustment, family support, at least 1 year of living in the desired role, consistent use of hormones, psychological treatment, and good surgical outcomes. The outcome literature provides strong support for adherence to the Standards of Care of the Harry Benjamin International Gender Dysphoria Association. Implications to be drawn from this research include an appreciation of the diversity of transgendered experience, the need for more research on non-reassignment resolutions to gender dysphoria, and the importance of assisting the transgendered individual to identify the resolution that best suits him or her.
Cohen-Kettenis and Gooren, 1999

Cohen-Kettenis, P. T., & Gooren, L. J. G. (1999). Transsexualism: A review of etiology, diagnosis and treatment. Journal of Psychosomatic Research , 46 (4), 315-333.
Transsexualism is considered to be the extreme end of the spectrum of gender identity disorders characterized by, among other things, a pursuit of sex reassignment surgery (SRS). The origins of transsexualism are still largely unclear. A first indication of anatomic brain differences between transsexuals and nontranssexuals has been found. Also, certain parental (rearing) factors seem to be associated with transsexualism. Some contradictory findings regarding etiology, psychopathology and success of SRS seem to be related to the fact that certain subtypes of transsexuals follow different developmental routes. The observations that psychotherapy is not helpful in altering a crystallized cross-gender identity and that certain transsexuals do not show severe psychopathology has led clinicians to adopt sex reassignment as a treatment option. In many countries, transsexuals are now treated according to the Standards of Care of the Harry Benjamin International Gender Dysphoria Association, a professional organization in the field of transsexualism. Research on postoperative functioning of transsexuals does not allow for unequivocal conclusions, but there is little doubt that sex reassignment substantially alleviates the suffering of transsexuals. However, SRS is no panacea. Psychotherapy may be needed to help transsexuals in adapting to the new situation or in dealing with issues that could not be addressed before treatment.
Coleman et al., 2012

Coleman, E., Bockting, W., Botzer, M., Cohen-Kettenis, P., DeCuypere, G., et al. (2012). Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. International Journal of Transgenderism , 13 (4), 165-232.
The Standards of Care (SOC) for the Health of Transsexual, Transgender, and Gender Nonconforming People is a publication of the World Professional Association for Transgender Health (WPATH). The overall goal of the SOC is to provide clinical guidance for health professionals to assist transsexual, transgender, and gender nonconforming people with safe and effective pathways to achieving lasting personal comfort with their gendered selves, in order to maximize their overall health, psychological well-being, and self-fulfillment. This assistance may include primary care, gynecologic and urologic care, reproductive options, voice and communication therapy, mental health services (e.g., assessment, counseling, psychotherapy), and hormonal and surgical treatments. The SOC are based on the best available science and expert professional consensus. Because most of the research and experience in this field comes from a North American and Western European perspective, adaptations of the SOC to other parts of the world are necessary. The SOC articulate standards of care while acknowledging the role of making informed choices and the value of harm reduction approaches. In addition, this version of the SOC recognizes that treatment for gender dysphoria i.e., discomfort or distress that is caused by a discrepancy between persons gender identity and that persons sex assigned at birth (and the associated gender role and/or primary and secondary sex characteristics) has become more individualized. Some individuals who present for care will have made significant self-directed progress towards gender role changes or other resolutions regarding their gender identity or gender dysphoria. Other individuals will require more intensive services. Health professionals can use the SOC to help patients consider the full range of health services open to them, in accordance with their clinical needs and goals for gender expression.
Committee on Health Care for Underserved, 2011

Committee Opinion No. 512: Health Care for Transgender Individuals. (2011). Obstetrics & Gynecology , 118 (6), 1454–1458.
Transgender individuals face harassment, discrimination, and rejection within our society. Lack of awareness, knowledge, and sensitivity in health care communities eventually leads to inadequate access to, underutilization of, and disparities within the health care system for this population. Although the care for these patients is often managed by a specialty team, obstetrician–gynecologists should be prepared to assist or refer transgender individuals with routine treatment and screening as well as hormonal and surgical therapies. The American College of Obstetricians and Gynecologists opposes discrimination on the basis of gender identity and urges public and private health insurance plans to cover the treatment of gender identity disorder.
Costa and Colizzi, 2016

Costa, R., & Colizzi, M. (2016). The effect of cross-sex hormonal treatment on gender dysphoria individuals’ mental health: A systematic review. Neuropsychiatric Disease and Treatment , 12 , 1953-1966.
Cross-sex hormonal treatment represents a main aspect of gender dysphoria health care pathway. However, it is still debated whether this intervention translates into a better mental well-being for the individual and which mechanisms may underlie this association. Although sex reassignment surgery has been the subject of extensive investigation, few studies have specifically focused on hormonal treatment in recent years. Here, we systematically review all studies examining the effect of cross-sex hormonal treatment on mental health and well-being in gender dysphoria. Research tends to support the evidence that hormone therapy reduces symptoms of anxiety and dissociation, lowering perceived and social distress and improving quality of life and self-esteem in both male-to-female and female-to-male individuals. Instead, compared to female-to-male individuals, hormone-treated male-to-female individuals seem to benefit more in terms of a reduction in their body uneasiness and personality-related psychopathology and an amelioration of their emotional functioning. Less consistent findings support an association between hormonal treatment and other mental health-related dimensions. In particular, depression, global psychopathology, and psychosocial functioning difficulties appear to reduce only in some studies, while others do not suggest any improvement in these domains. Results from longitudinal studies support more consistently the association between hormonal treatment and improved mental health. On the contrary, a number of cross-sectional studies do not support this evidence. This review provides possible biological explanation vs psychological explanation (direct effect vs indirect effect) for the hormonal treatment-induced better mental well-being. In conclusion, this review indicates that gender dysphoria-related mental distress may benefit from hormonal treatment intervention, suggesting a transient reaction to the nonsatisfaction connected to the incongruent body image rather than a stable psychiatric comorbidity. In this perspective, timely hormonal treatment intervention represents a crucial issue in gender dysphoria individuals’ mental health-related outcome.
Dhejne et al., 2016

Dhejne, C., Van Vlerken, R., Heylens, G., & Arcelus, J. (2016). Mental health and gender dysphoria: A review of the literature. International Review Of Psychiatry , 28 (1), 44-57.
Studies investigating the prevalence of psychiatric disorders among trans individuals have identified elevated rates of psychopathology. Research has also provided conflicting psychiatric outcomes following gender-confirming medical interventions. This review identifies 38 cross-sectional and longitudinal studies describing prevalence rates of psychiatric disorders and psychiatric outcomes, pre- and post-gender-confirming medical interventions, for people with gender dysphoria. It indicates that, although the levels of psychopathology and psychiatric disorders in trans people attending services at the time of assessment are higher than in the cis population, they do improve following gender-confirming medical intervention, in many cases reaching normative values. The main Axis I psychiatric disorders were found to be depression and anxiety disorder. Other major psychiatric disorders, such as schizophrenia and bipolar disorder, were rare and were no more prevalent than in the general population. There was conflicting evidence regarding gender differences: some studies found higher psychopathology in trans women, while others found no differences between gender groups. Although many studies were methodologically weak, and included people at different stages of transition within the same cohort of patients, overall this review indicates that trans people attending transgender health-care services appear to have a higher risk of psychiatric morbidity (that improves following treatment), and thus confirms the vulnerability of this population.
Gijs and Brewaeys, 2007

Gijs, L., & Brewaeys, A. (2007). Surgical treatment of gender dysphoria in adults and adolescents: Recent developments, effectiveness, and challenges. Annual Review of Sex Research , 18 (1), 178-224.
In 1990 Green and Fleming concluded that sex reassignment surgery (SRS) is an effective treatment for transsexuality because it reduced gender dysphoria drastically. Since 1990, many new outcome studies have been published, raising the question as to whether the conclusion of Green and Fleming still holds. After describing terminological and conceptual developments related to the treatment of gender identity disorder (GID), follow-up studies, including both adults and adolescents, of the outcomes of SRS are reviewed. Special attention is paid to the effects of SRS on gender dysphoria, sexuality, and regret. Despite methodological shortcomings of many of the studies, we conclude that SRS is an effective treatment for transsexualism and the only treatment that has been evaluated empirically with large clinical case series.
Gooren, 2011

Gooren, L. J. (2011). Care of transsexual persons. New England Journal of Medicine , 364 (13), 1251–1257.
This Journal feature begins with a case vignette highlighting a common clinical problem. Evidence supporting various strategies is then presented, followed by a review of formal guidelines, when they exist. The article ends with the author’s clinical recommendations. A healthy and successful 40-year-old man finds it increasingly difficult to live as a male. In childhood he preferred playing with girls and recalls feeling that he should have been one. Over time he has come to regard himself more and more as a female personality inhabiting a male body. After much agonizing, he has concluded that only sex reassignment can offer the peace of mind he craves. What would you advise? A healthy and successful 40-year-old man finds it increasingly difficult to live as a male. In childhood he preferred playing with girls and recalls feeling that he should have been one. Over time he has come to regard himself more and more as a female personality inhabiting a male body. After much agonizing, he has concluded that only sex reassignment can offer the peace of mind he craves. What would you advise?
Hembree et al., 2009

Hembree, W. C., Cohen-Kettenis, P., Delemarre-van de Waal, H. A., Gooren, L. J., Meyer, W., et al. (2009). Endocrine treatment of transsexual persons: An endocrine society clinical practice guideline. The Journal of Clinical Endocrinology & Metabolism, 94 (9), 3132–3154.
Objective: The aim was to formulate practice guidelines for endocrine treatment of transsexual persons. Evidence: This evidence-based guideline was developed using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) system to describe the strength of recommendations and the quality of evidence, which was low or very low. Consensus Process: Committees and members of The Endocrine Society, European Society of Endocrinology, European Society for Paediatric Endocrinology, Lawson Wilkins Pediatric Endocrine Society, and World Professional Association for Transgender Health commented on preliminary drafts of these guidelines. Conclusions: Transsexual persons seeking to develop the physical characteristics of the desired gender require a safe, effective hormone regimen that will 1) suppress endogenous hormone secretion determined by the person’s genetic/biologic sex and 2) maintain sex hormone levels within the normal range for the person’s desired gender. A mental health professional (MHP) must recommend endocrine treatment and participate in ongoing care throughout the endocrine transition and decision for surgical sex reassignment. The endocrinologist must confirm the diagnostic criteria the MHP used to make these recommendations. Because a diagnosis of transsexualism in a prepubertal child cannot be made with certainty, we do not recommend endocrine treatment of prepubertal children. We recommend treating transsexual adolescents (Tanner stage 2) by suppressing puberty with GnRH analogues until age 16 years old, after which cross-sex hormones may be given. We suggest suppressing endogenous sex hormones, maintaining physiologic levels of gender-appropriate sex hormones and monitoring for known risks in adult transsexual persons. Endocrine treatment of transsexual persons should include suppression of endogenous sex hormones, physiologic levels of gender-appropriate sex hormones, and suppression of puberty in adolescents (Tanner stage 2).
Michel et al., 2002

Michel, A., Ansseau, M., Legros, J., Pitchot, W., & Mormont, C. (2002). The transsexual: What about the future? European Psychiatry , 17 (6), 353-362.
Since the 1950s, sexual surgical reassignments have been frequently carried out. As this surgical therapeutic procedure is controversial, it seems important to explore the actual consequences of such an intervention and objectively evaluate its relevance. In this context, we have carried out a review of the literature. After looking at the methodological limitations of follow-up studies, the psychological, sexual, social, and professional futures of the individuals subject to a transsexual operation are presented. Finally, prognostic aspects are considered. In the literature, follow-up studies tend to show that surgical transformations have positive consequences for the subjects. In the majority of cases, transsexuals are very satisfied with their intervention and any difficulties experienced are often temporary and disappear within a year after the surgical transformation. Studies show that there is less than 1% of regrets, and a little more than 1% of suicides among operated subjects. The empirical research does not confirm the opinion that suicide is strongly associated with surgical transformation.
Murad et al., 2010

Murad, M. H., Elamin, M. B., Garcia, M. Z., Mullan, R. J., Murad, A., Erwin, P. J., & Montori, V. M. (2010). Hormonal therapy and sex reassignment: A systematic review and meta-analysis of quality of life and psychosocial outcomes. Clinical Endocrinology , 72 (2), 214-231.
Objective: To assess the prognosis of individuals with gender identity disorder (GID) receiving hormonal therapy as a part of sex reassignment in terms of quality of life and other self‐reported psychosocial outcomes. Methods: We searched electronic databases, bibliography of included studies and expert files. All study designs were included with no language restrictions. Reviewers working independently and in pairs selected studies using predetermined inclusion and exclusion criteria, extracted outcome and quality data. We used a random‐effects meta‐analysis to pool proportions and estimate the 95% confidence intervals (CIs). We estimated the proportion of between‐study heterogeneity not attributable to chance using the I2 statistic. Results: We identified 28 eligible studies. These studies enrolled 1833 participants with GID (1093 male‐to‐female, 801 female‐to‐male) who underwent sex reassignment that included hormonal therapies. All the studies were observational and most lacked controls. Pooling across studies shows that after sex reassignment, 80% of individuals with GID reported significant improvement in gender dysphoria (95% CI = 68–89%; 8 studies; I2 = 82%); 78% reported significant improvement in psychological symptoms (95% CI = 56–94%; 7 studies; I2 = 86%); 80% reported significant improvement in quality of life (95% CI = 72–88%; 16 studies; I2 = 78%); and 72% reported significant improvement in sexual function (95% CI = 60–81%; 15 studies; I2 = 78%). Conclusions: Very low quality evidence suggests that sex reassignment that includes hormonal interventions in individuals with GID likely improves gender dysphoria, psychological functioning and comorbidities, sexual function and overall quality of life.
Reisner et al., 2016

Reisner, S. L., Poteat, T., Keatley, J., Cabral, M., Mothopeng, T., et al. (2016). Global health burden and needs of transgender populations: A review. The Lancet , 388 (10042), 412-436.
Transgender people are a diverse population affected by a range of negative health indicators across high-income, middle-income, and low-income settings. Studies consistently document a high prevalence of adverse health outcomes in this population, including HIV and other sexually transmitted infections, mental health distress, and substance use and abuse. However, many other health areas remain understudied, population-based representative samples and longitudinal studies are few, and routine surveillance efforts for transgender population health are scarce. The absence of survey items with which to identify transgender respondents in general surveys often restricts the availability of data with which to estimate the magnitude of health inequities and characterise the population-level health of transgender people globally. Despite the limitations, there are sufficient data highlighting the unique biological, behavioural, social, and structural contextual factors surrounding health risks and resiliencies for transgender people. To mitigate these risks and foster resilience, a comprehensive approach is needed that includes gender affirmation as a public health framework, improved health systems and access to health care informed by high quality data, and effective partnerships with local transgender communities to ensure responsiveness of and cultural specificity in programming. Consideration of transgender health underscores the need to explicitly consider sex and gender pathways in epidemiological research and public health surveillance more broadly.
Schmidt and Levine, 2015

Schmidt, L., & Levine, R. (2015). Psychological Outcomes and Reproductive Issues Among Gender Dysphoric Individuals. Endocrinology and Metabolism Clinics of North America , 44 (4), 773-785.
Gender dysphoria is a condition in which a person experiences discrepancy between the natal anatomic sex and the gender he or she identifies with, resulting in internal distress and a desire to live as the preferred gender. There is increasing demand for treatment, which includes suppression of puberty, cross-sex hormone therapy, and sex reassignment surgery. This article reviews longitudinal outcome data evaluating psychological well-being and quality of life among transgender individuals who have undergone cross-sex hormone treatment or sex reassignment surgery. Proposed methodologies for diagnosis and initiation of treatment are discussed, and the effects of cross-sex hormones and sex reassignment surgery on future reproductive potential.
White Hughto and Reisner, 2016

White Hughto, J. M., & Reisner, S. L. (2016). A systematic review of the effects of hormone therapy on psychological functioning and quality of life in transgender individuals. Transgender Health , 1 (1), 21–31.
Objectives: To review evidence from prospective cohort studies of the relationship between hormone therapy and changes in psychological functioning and quality of life in transgender individuals accessing hormone therapy over time. Data Sources: MEDLINE, PsycINFO, and PubMed were searched for relevant studies from inception to November 2014. Reference lists of included studies were hand searched. Results: Three uncontrolled prospective cohort studies, enrolling 247 transgender adults (180 male-to-female [MTF], 67 female-to-male [FTM]) initiating hormone therapy for the treatment of gender identity disorder (prior diagnostic term for gender dysphoria), were identified. The studies measured exposure to hormone therapy and subsequent changes in mental health (e.g., depression, anxiety) and quality of life outcomes at follow-up. Two studies showed a significant improvement in psychological functioning at 3–6 months and 12 months compared with baseline after initiating hormone therapy. The third study showed improvements in quality of life outcomes 12 months after initiating hormone therapy for FTM and MTF participants; however, only MTF participants showed a statistically significant increase in general quality of life after initiating hormone therapy. Conclusions: Hormone therapy interventions to improve the mental health and quality of life in transgender people with gender dysphoria have not been evaluated in controlled trials. Low quality evidence suggests that hormone therapy may lead to improvements in psychological functioning. Prospective controlled trials are needed to investigate the effects of hormone therapy on the mental health of transgender people.
Share this:
- Reference Manager
- Simple TEXT file
People also looked at
Original research article, male-to-female gender-affirming surgery: 20-year review of technique and surgical results.

- 1 Serviço de Urologia, Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil
- 2 Serviço de Psiquiatria, Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil
- 3 Serviço de Psiquiatria, Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, Brazil
Purpose: Gender dysphoria (GD) is an incompatibility between biological sex and personal gender identity; individuals harbor an unalterable conviction that they were born in the wrong body, which causes personal suffering. In this context, surgery is imperative to achieve a successful gender transition and plays a key role in alleviating the associated psychological discomfort. In the current study, a retrospective cohort, we report the 20-years outcomes of the gender-affirming surgery performed at a single Brazilian university center, examining demographic data, intra and postoperative complications. During this period, 214 patients underwent penile inversion vaginoplasty.
Results: Results demonstrate that the average age at the time of surgery was 32.2 years (range, 18–61 years); the average of operative time was 3.3 h (range 2–5 h); the average duration of hormone therapy before surgery was 12 years (range 1–39). The most commons minor postoperative complications were granulation tissue (20.5 percent) and introital stricture of the neovagina (15.4 percent) and the major complications included urethral meatus stenosis (20.5 percent) and hematoma/excessive bleeding (8.9 percent). A total of 36 patients (16.8 percent) underwent some form of reoperation. One hundred eighty-one (85 percent) patients in our series were able to have regular sexual intercourse, and no individual regretted having undergone GAS.
Conclusions: Findings confirm that it is a safety procedure, with a low incidence of serious complications. Otherwise, in our series, there were a high level of functionality of the neovagina, as well as subjective personal satisfaction.
Introduction
Transsexualism (ICD-10) or Gender Dysphoria (GD) (DSM-5) is characterized by intense and persistent cross-gender identification which influences several aspects of behavior ( 1 ). The terms describe a situation where an individual's gender identity differs from external sexual anatomy at birth ( 1 ). Gender identity-affirming care, for those who desire, can include hormone therapy and affirming surgeries, as well as other procedures such as hair removal or speech therapy ( 1 ).
Since 1998, the Gender Identity Program (PROTIG) of the Hospital de Clínicas de Porto Alegre (HCPA), Universidade Federal do Rio Grande do Sul, Brazil has provided public assistance to transsexual people, is the first one in Brazil and one of the pioneers in South America. Our program offers psychosocial support, health care, and guidance to families, and refers individuals for gender-affirming surgery (GAS) when indicated. To be eligible for this surgery, transsexual individuals must have been adherent to multidisciplinary follow-up for at least 2 years, have a minimum age of 21 years (required for surgical procedures of this nature), have a positive psychiatric or psychological report, and have a diagnosis of GD.
Gender-affirming surgery (GAS) is increasingly recognized as a therapeutic intervention and a medical necessity, with growing societal acceptance ( 2 ). At our institution, we perform the classic penile inversion vaginoplasty (PIV), with an inverted penis skin flap used as the lining for the neovagina. Studies have demonstrated that GAS for the management of GD can promote improvements in mental health and social relationships for these patients ( 2 – 5 ). It is therefore imperative to understand and establish best practice techniques for this patient population ( 2 ). Although there are several studies reporting the safety and efficacy of gender-affirming surgery by penile inversion vaginoplasty, we present the largest South-American cohort to date, examining demographic data, intra and postoperative complications.
Patients and Methods
Subjects and study setup.
This is a retrospective cohort study of Brazilian transgender women who underwent penile inversion vaginoplasty between January of 2000 and March of 2020 at the Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil. The study was approved by our institutional medical and research ethics committee.
At our institution, gender-affirming surgery is indicated for transgender women who are under assistance by our program for transsexual individuals. All transsexual women included in this study had at least 2 years of experience as a woman and met WPATH standards for GAS ( 1 ). Patients were submitted to biweekly group meetings and monthly individual therapy.
Between January of 2000 and March of 2020, a total of 214 patients underwent penile inversion vaginoplasty. The surgical procedures were performed by two separate staff members, mostly assisted by residents. A retrospective chart review was conducted recording patient demographics, intraoperative and postoperative complications, reoperations, and secondary surgical procedures. Informed consent was obtained from all individual participants included in the study.
Hormonal Therapy
The goal of feminizing hormone therapy is the development of female secondary sex characteristics, and suppression/minimization of male secondary sex characteristics.
Our general therapy approach is to combine an estrogen with an androgen blocker. The usual estrogen is the oral preparation of estradiol (17-beta estradiol), starting at a dose of 2 mg/day until the maximum dosage of 8 mg/day. The preferred androgen blocker is spironolactone at a dose of 200 mg twice a day.
Operative Technique
At our institution, we perform the classic penile inversion vaginoplasty, with an inverted penis skin flap used as the lining for the neovagina. For more details, we have previously published our technique with a step-by-step procedure video ( 6 ). All individuals underwent intestinal cleansing the evening before the surgery. A first-generation cephalosporin was used as preoperative prophylaxis. The procedure was performed with the patient in a dorsal lithotomy position. A Foley catheter was placed for bladder catheterization. A inverted-V incision was made 4 cm above the anus and a flap was created. A neovaginal cavity was created between the prostate and the rectum with blunt dissection, in the Denonvilliers space, until the peritoneal fold, usually measuring 12 cm in extension and 6 cm in width. The incision was then extended vertically to expose the testicles and the spermatic cords, which were removed at the level of the external inguinal rings. A circumferential subcoronal incision was made ( Figure 1 ), the penis was de-gloved and a skin flap was created, with the de-gloved penis being passed through the scrotal opening ( Figure 2 ). The dorsal part of the glans and its neurovascular bundle were bluntly dissected away from the penile shaft ( Figure 3 ) as well as the urethra, which included a portion of the bulbospongious muscle ( Figure 4 ). The corpora cavernosa was excised up to their attachments at the symphysis pubis and ligated. The neoclitoris was shaped and positioned in the midline at the level of the symphysis pubis and sutured using interrupted 5-0 absorbable suture. The corpus spongiosum was reduced and the urethra was shortened, spatulated, and placed 1 cm below the neoclitoris in the midline and sutured using interrupted 4-0 absorbable suture. The penile skin flap was inverted and pulled into the neovaginal cavity to become its walls ( Figure 5 ). The excess of skin was then removed, and the subcutaneous tissue and the skin were closed using continuous 3-0 non-absorbable suture ( Figure 6 ). A neo mons pubis was created using a 0 absorbable suture between the skin and the pubic bone. The skin flap was fixed to the pubic bone using a 0 absorbable suture. A gauze impregnated with Vaseline and antibiotic ointment was left inside the neovagina, and a customized compressive bandage was applied ( Figure 7 —shows the final appearance after the completion of the procedures).

Figure 1 . The initial circumferential subcoronal incision.

Figure 2 . The de-gloved penis being passed through the scrotal opening.

Figure 3 . The dorsal part of the glans and its neurovascular bundle dissected away from the penile shaft.
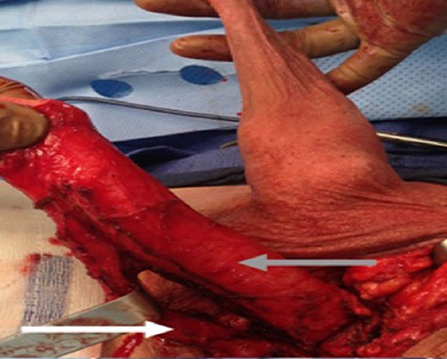
Figure 4 . The urethra dissected including a portion of the bulbospongious muscle. The grey arrow shows the penile shaft and the white arrow shows the dissected urethra.

Figure 5 . The inverted penile skin flap.
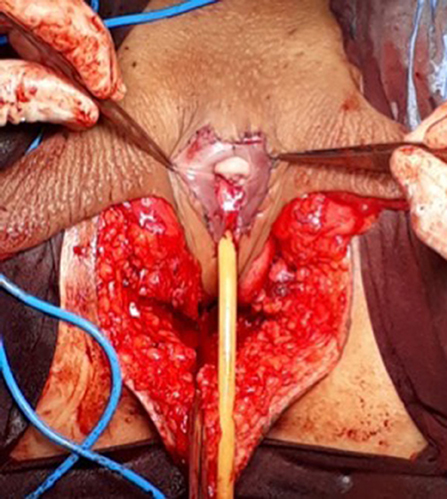
Figure 6 . The neoclitoris and the urethra sutured in the midline and the neovaginal cavity.
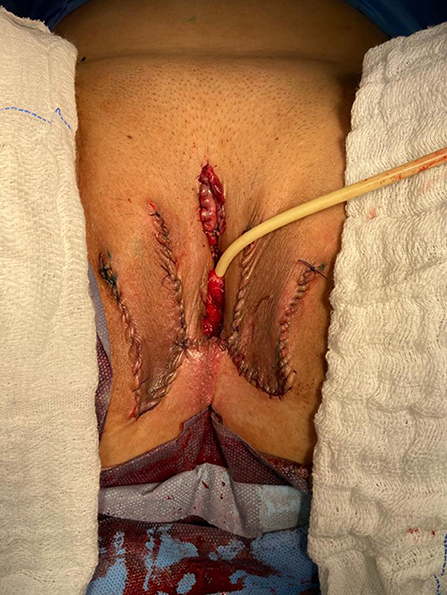
Figure 7 . The final appearance after the completion of the procedures.
Postoperative Care and Follow-Up
The patients were usually discharged within 2 days after surgery with the Foley catheter and vaginal gauze packing in place, which were removed after 7 days in an ambulatorial attendance.
Our vaginal dilation protocol starts seven days after surgery: a kit of 6 silicone dilators with progressive diameter (1.1–4 cm) and length (6.5–14.5 cm) is used; dilation is done progressively from the smallest dilator; each size should be kept in place for 5 min until the largest possible size, which is kept for 3 h during the day and during the night (sleep), if possible. The process is performed daily for the first 3 months and continued until the patient has regular sexual intercourse.
The follow-up visits were performed 7 days, 1, 2, 3, 6, and 12 months after surgery ( Figure 8 ), and included physical examination and a quality-of-life questionnaire.

Figure 8 . Appearance after 1 month of the procedure.
Statistical Analysis
The statistical analysis was conducted using Statistical Product and Service Solutions Version 18.0 (SPSS). Outcome measures were intra-operative and postoperative complications, re-operations. Descriptive statistics were used to evaluate the study outcomes. Mean values and standard deviations or median values and ranges are presented as continuous variables. Frequencies and percentages are reported for dichotomous and ordinal variables.
Patient Demographics
During the period of the study, 214 patients underwent penile inversion vaginoplasty, performed by two staff surgeons, mostly assisted by residents ( Table 1 ). The average age at the time of surgery was 32.2 years (range 18–61 years). There was no significant increase or decrease in the ages of patients who underwent SRS over the study period (Fisher's exact test: P = 0.065; chi-square test: X 2 = 5.15; GL = 6; P = 0.525). The average of operative time was 3.3 h (range 2–5 h). The average duration of hormone therapy before surgery was 12 years (range 1–39). The majority of patients were white (88.3 percent). The most prevalent patient comorbidities were history of tobacco use (15 percent), human immunodeficiency virus infection (13 percent) and hypertension (10.7 percent). Other comorbidities are listed in Table 1 .
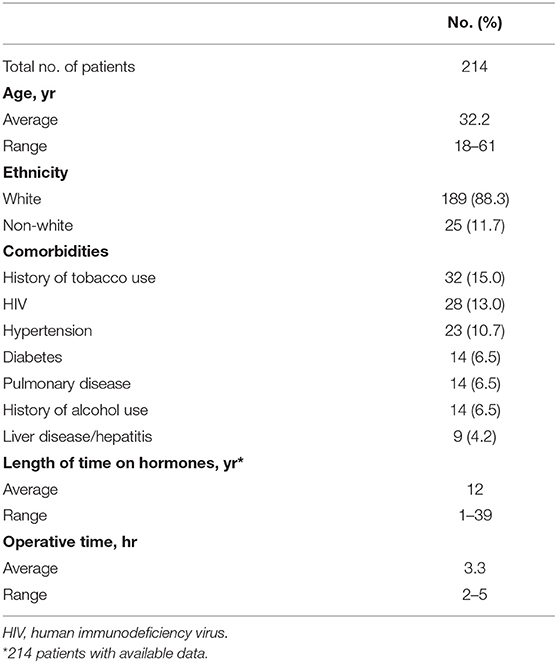
Table 1 . Patient demographics.
Multidisciplinary follow-up was comprised of 93.45% of patients following up with a urologist and 59.06% of patients continuing psychiatric follow-up, median follow-up time of 16 and 9.3 months after surgery, respectively.
Postoperative Results
The complications were classified according to the Clavien-Dindo score ( Table 2 ). The most common minor postoperative complications (Grade I) were granulation tissue (20.5 percent), introital stricture of the neovagina (15.4 percent) and wound dehiscence (12.6 percent). The major complications (Grade III-IV) included urethral stenosis (20.5 percent), urethral fistula (1.9 percent), intraoperative rectal injury (1.9 percent), necrosis (primarily along the wound edges) (1.4 percent), and rectovaginal fistula (0.9 percent). A total of 17 patients required blood transfusion (7.9 percent).
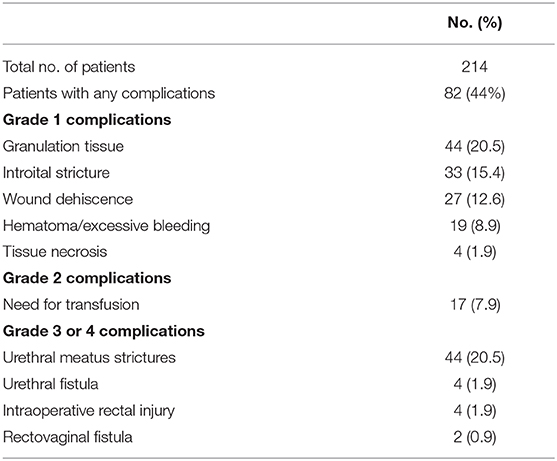
Table 2 . Complications after penile inversion vaginoplasty.
A total of 36 patients (16.8 percent) underwent some form of reoperation.
One hundred eighty-one (85 percent) patients in our series were able to have regular sexual vaginal intercourse, and no individual regretted having undergone GAS.
Penile inversion vaginoplasty is the gold-standard in gender-affirming surgery. It has good functional outcomes, and studies have demonstrated adequate vaginal depths ( 3 ). It is recognized not only as a cosmetic procedure, but as a therapeutic intervention and a medical necessity ( 2 ). We present the largest South-American cohort to date, examining demographic data, intra and postoperative complications.
The mean age of transsexual women who underwent GAS in our study was 32.2 years (range 18–61 years), which is lower than the mean age of patients in studies found in the literature. Two studies indicated that the mean ages of patients at time of GAS were 36.7 years and 41 years, respectively ( 4 , 5 ). Another study reported a mean age at time of GAS of 36 years and found there was a significant decrease in age at the time of GAS from 41 years in 1994 to 35 years in 2015 ( 7 ). According to the authors, this decrease in age is associated with greater tolerance and societal approval regarding individuals with GD ( 7 ).
There was no grade IV or grade V complications. Excessive bleeding noticed postoperatively occurred in 19 patients (8.9 percent) and blood transfusion was required in 17 cases (7.9 percent); all patients who required blood transfusions were operated until July 2011, and the reason for this rate of blood transfusion was not identified.
The most common intraoperative complication was rectal injury, occurring in 4 patients (1.9 percent); in all patients the lesion was promptly identified and corrected in 2 layers absorbable sutures. In 2 of these patients, a rectovaginal fistula became evident, requiring fistulectomy and colonic transit deviation. This is consistent with current literature, in which rectal injury is reported in 0.4–4.5 percent of patients ( 4 , 5 , 8 – 13 ). Goddard et al. suggested carefully checking for enterotomy after prostate and bladder mobilization by digital rectal examination ( 4 ). Gaither et al. ( 14 ) commented that careful dissection that closely follows the urethra along its track from the central tendon of the perineum up through the lower pole of the prostate is critical and only blunt dissection is encouraged after Denonvilliers' fascia is reached. Alternatively, a robotic-assisted approach to penile inversion vaginoplasty may aid in minimizing these complications. The proposed advantages of a robotic-assisted vaginoplasty include safer dissection to minimize the risk of rectal injury and better proximal vaginal fixation. Dy et al. ( 15 ) has had no rectal injuries or fistulae to date in his series of 15 patients, with a mean follow-up of 12 months.
In our series, we observed 44 cases (20.5 percent) of urethral meatus strictures. We credit this complication to the technique used in the initial 5 years of our experience, in which the urethra was shortened and sutured in a circular fashion without spatulation. All cases were treated with meatal dilatation and 11 patients required surgical correction, being performed a Y-V plastic reconstruction of the urethral meatus. In the literature, meatal strictures are relatively rare in male-to-female (MtF) GAS due to the spatulation of the urethra and a simple anastomosis to the external genitalia. Recent systematic reviews show an incidence of five percent in this complication ( 16 , 17 ). Other studies report a wide incidence of meatal stenosis ranging from 1.1 to 39.8 percent ( 4 , 8 , 11 ).
Neovagina introital stricture was observed in 33 patients (15.4 percent) in our study and impedes the possibility of neovaginal penetration and/or adversely affects sexual life quality. In the literature, the reported incidence of introital stenosis range from 6.7 to 14.5 percent ( 4 , 5 , 8 , 9 , 11 – 13 ). According to Hadj-Moussa et al. ( 18 ) a regimen of postoperative prophylactic dilation is crucial to minimize the development of this outcome. At our institution, our protocol for vaginal dilation started seven days after surgery and was performed three to four times a day during the first 3 months and was continued until the individual had regular sexual intercourse. We treated stenosis initially with dilation. In case of no response, we propose a surgical revision with diamond-shaped introitoplasty with relaxing incisions. In recalcitrant cases, we proposed to the patient a secondary vaginoplasty using a full-thickness skin graft of the lower abdomen.
One hundred eighty-one (85 percent) patients were classified as having a “functional vagina,” characterized as the capacity to maintain satisfactory sexual vaginal intercourse, since the mean neovaginal depth was not measured. In a review article, the mean neovaginal depth ranged from 10 to 13.5 cm, with the shallowest neovagina depth at 2.5 cm and the deepest at 18 cm ( 17 ). According to Salim et al. ( 19 ), in terms of postoperative functional outcomes after penile inversion vaginoplasty, a mean percentage of 75 percent (range from 33 to 87 percent) patients were having vaginal intercourse. Hess et al. found that 91.4% of patients who responded to a questionnaire were very satisfied (34.4%), satisfied (37.6%), or mostly satisfied (19.4%) with their sexual function after penile inversion vaginoplasty ( 20 ).
Poor cosmetic appearance of the vulva is common. Amend et al. reported that the most common reason for reoperation was cosmetic correction in the form of mons pubis and mucosa reduction in 50% of patients ( 16 ). We had no patient regrets about performing GAS, although 36 patients (16.8 percent) were reoperated due to cosmetic issues. Gaither et al. propose in order to minimize scarring to use a one-stage surgical approach and the lateralization of surgical scars to the groin ( 14 ). Frequently, cosmetic issues outcomes are often patient driven and preoperative patient education is necessary ( 14 ).
Analyzing the quality of life, in 2016, our health care group (PROTIG) published a study assessing quality of life before and after gender-affirming surgery in 47 patients using the diagnostic tool 100-item WHO Quality of Life Assessment (WHOQOL-100) ( 21 ). The authors found that GAS promotes the improvement of psychological aspects and social relations. However, even 1 year after GAS, MtF persons continue to report problems in physical and difficulty in recovering their independence. In a systematic review and meta-analysis of QOL and psychosocial outcomes in transsexual people, researchers verified that sex reassignment with hormonal interventions more likely corrects gender dysphoria, psychological functioning and comorbidities, sexual function, and overall QOL compared with sex reassignment without hormonal interventions, although there is a low level of evidence for this ( 22 ). Recently, Castellano et al. assessed QOL in 60 Italian transsexuals (46 transwomen and 14 transmen) at least 2 years after SRS using the WHOQOL-100 (general QOL score and quality of sexual life and quality of body image scores) to focus on the effects of hormonal therapy. Overall satisfaction improved after SRS, and QOL was similar to the controls ( 23 ). Bartolucci et al. evaluated the perception of quality of sexual life using four questions evaluating the sexual facet in individuals with gender dysphoria before SRS and the possible factors associated with this perception. The study showed that approximately half the subjects with gender dysphoria perceived their sexual life as “poor/dissatisfied” or “very poor/very dissatisfied” before SRS ( 24 ).
Our study has some limitations. The total number of operated patients is restricted within the long follow-up period. This is due to a limitation in our health system, which allows only 1 sexual reassignment surgery to be performed per month at our institution. Neovagin depth measurement was not performed routinely in the follow-up of operated patients.
Conclusions
The definitive treatment for patients with gender dysphoria is gender-affirming surgery. Our series demonstrates that GAS is a feasible surgery with low rates of serious complications. We emphasize the high level of functionality of the vagina after the procedure, as well as subjective personal satisfaction. Complications, especially minor ones, are probably underestimated due to the nature of the study, and since this is a surgical population, the results may not be generalizable for all transgender MTF individuals.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Hospital de Clínicas de Porto Alegre. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
GM: conception and design, data acquisition, data analysis, interpretation, drafting the manuscript, review of the literature, critical revision of the manuscript and factual content, and statistical analysis. ML and TR: conception and design, data interpretation, drafting the manuscript, critical revision of the manuscript and factual content, and statistical analysis. DS, KS, AF, AC, PT, AG, and RC: conception and design, data acquisition and data analysis, interpretation, drafting the manuscript, and review of the literature. All authors contributed to the article and approved the submitted version.
This study was supported by the Fundo de Incentivo à Pesquisa e Eventos (FIPE - Fundo de Incentivo à Pesquisa e Eventos) of Hospital de Clínicas de Porto Alegre.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Coleman E, Bockting W, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J, et al. Standards of care for the health of transsexual, transgender, and gender-non-conforming people, version 7. Int J Transgend. (2012) 13:165–232. doi: 10.1080/15532739.2011.700873
CrossRef Full Text | Google Scholar
2. Massie JP, Morrison SD, Maasdam JV, Satterwhite T. Predictors of patient satisfaction and postoperative complications in penile inversion vaginoplasty. Plast Reconstruct Surg. (2018) 141:911–921. doi: 10.1097/PRS.0000000000004427
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Pan S, Honig SC. Gender-affirming surgery: current concepts. Curr Urol Rep . (2018) 19:62. doi: 10.1007/s11934-018-0809-9
4. Goddard JC, Vickery RM, Qureshi A, Summerton DJ, Khoosal D, Terry TR. Feminizing genitoplasty in adult transsexuals: early and long-term surgical results. BJU Int . (2007) 100:607–13. doi: 10.1111/j.1464-410X.2007.07017.x
5. Rossi NR, Hintz F, Krege S, Rübben H, Vom DF, Hess J. Gender reassignment surgery – a 13 year review of surgical outcomes. Eur Urol Suppl . (2013) 12:e559. doi: 10.1016/S1569-9056(13)61042-8
6. Silva RUM, Abreu FJS, Silva GMV, Santos JVQV, Batezini NSS, Silva Neto B, et al. Step by step male to female transsexual surgery. Int Braz J Urol. (2018) 44:407–8. doi: 10.1590/s1677-5538.ibju.2017.0044
7. Aydin D, Buk LJ, Partoft S, Bonde C, Thomsen MV, Tos T. Transgender surgery in Denmark from 1994 to 2015: 20-year follow-up study. J Sex Med. (2016) 13:720–5. doi: 10.1016/j.jsxm.2016.01.012
8. Perovic SV, Stanojevic DS, Djordjevic MLJ. Vaginoplasty in male transsexuals using penile skin and a urethral flap. BJU Int. (2001) 86:843–50. doi: 10.1046/j.1464-410x.2000.00934.x
9. Krege S, Bex A, Lümmen G, Rübben H. Male-to-female transsexualism: a technique, results and long-term follow-up in 66 patients. BJU Int. (2001) 88:396–402. doi: 10.1046/j.1464-410X.2001.02323.x
10. Wagner S, Greco F, Hoda MR, Inferrera A, Lupo A, Hamza A, et al. Male-to-female transsexualism: technique, results and 3-year follow-up in 50 patients. Urol International. (2010) 84:330–3. doi: 10.1159/000288238
11. Reed H. Aesthetic and functional male to female genital and perineal surgery: feminizing vaginoplasty. Semin PlasticSurg. (2011) 25:163–74. doi: 10.1055/s-0031-1281486
12. Raigosa M, Avvedimento S, Yoon TS, Cruz-Gimeno J, Rodriguez G, Fontdevila J. Male-to-female genital reassignment surgery: a retrospective review of surgical technique and complications in 60 patients. J Sex Med. (2015) 12:1837–45. doi: 10.1111/jsm.12936
13. Sigurjonsson H, Rinder J, Möllermark C, Farnebo F, Lundgren TK. Male to female gender reassignment surgery: surgical outcomes of consecutive patients during 14 years. JPRAS Open. (2015) 6:69–73. doi: 10.1016/j.jpra.2015.09.003
14. Gaither TW, Awad MA, Osterberg EC, Murphy GP, Romero A, Bowers ML, et al. Postoperative complications following primary penile inversion vaginoplasty among 330 male-to-female transgender patients. J Urol. (2018) 199:760–5. doi: 10.1016/j.juro.2017.10.013
15. Dy GW, Sun J, Granieri MA, Zhao LC. Reconstructive management pearls for the transgender patient. Curr. Urol. Rep. (2018) 19:36. doi: 10.1007/s11934-018-0795-y
16. Amend B, Seibold J, Toomey P, Stenzl A, Sievert KD. Surgical reconstruction for male-to-female sex reassignment. Eur Urol. (2013) 64:141–9. doi: 10.1016/j.eururo.2012.12.030
17. Horbach SER, Bouman MB, Smit JM, Özer M, Buncamper ME, Mullender MG. Outcome of vaginoplasty in male-to-female transgenders: a systematic review of surgical techniques. J Sex Med . (2015) 12:1499–512. doi: 10.1111/jsm.12868
18. Hadj-Moussa M, Ohl DA, Kuzon WM. Feminizing genital gender-confirmation surgery. Sex Med Rev. (2018) 6:457–68.e2. doi: 10.1016/j.sxmr.2017.11.005
19. Salim A, Poh M. Gender-affirming penile inversion vaginoplasty. Clin Plast Surg. (2018) 45:343–50. doi: 10.1016/j.cps.2018.04.001
20. Hess J, Rossi NR, Panic L, Rubben H, Senf W. Satisfaction with male-to-female gender reassignment surgery. DtschArztebl Int. (2014) 111:795–801. doi: 10.3238/arztebl.2014.0795
21. Silva DC, Schwarz K, Fontanari AMV, Costa AB, Massuda R, Henriques AA, et al. WHOQOL-100 before and after sex reassignment surgery in brazilian male-to-female transsexual individuals. J Sex Med. (2016) 13:988–93. doi: 10.1016/j.jsxm.2016.03.370
22. Murad MH, Elamin MB, Garcia MZ, Mullan RJ, Murad A, Erwin PJ, et al. Hormonal therapy and sex reassignment: a systematic review and meta-analysis of quality of life and psychosocial outcomes. Clin Endocrinol . (2010) 72:214–31. doi: 10.1111/j.1365-2265.2009.03625.x
23. Castellano E, Crespi C, Dell'Aquila C, Rosato R, Catalano C, Mineccia V, et al. Quality of life and hormones after sex reassignment surgery. J Endocrinol Invest . (2015) 38:1373–81. doi: 10.1007/s40618-015-0398-0
24. Bartolucci C, Gómez-Gil E, Salamero M, Esteva I, Guillamón A, Zubiaurre L, et al. Sexual quality of life in gender-dysphoric adults before genital sex reassignment surgery. J Sex Med . (2015) 12:180–8. doi: 10.1111/jsm.12758
Keywords: transsexualism, gender dysphoria, gender-affirming genital surgery, penile inversion vaginoplasty, surgical outcome
Citation: Moisés da Silva GV, Lobato MIR, Silva DC, Schwarz K, Fontanari AMV, Costa AB, Tavares PM, Gorgen ARH, Cabral RD and Rosito TE (2021) Male-to-Female Gender-Affirming Surgery: 20-Year Review of Technique and Surgical Results. Front. Surg. 8:639430. doi: 10.3389/fsurg.2021.639430
Received: 17 December 2020; Accepted: 22 March 2021; Published: 05 May 2021.
Reviewed by:
Copyright © 2021 Moisés da Silva, Lobato, Silva, Schwarz, Fontanari, Costa, Tavares, Gorgen, Cabral and Rosito. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gabriel Veber Moisés da Silva, veber.gabriel@gmail.com
This article is part of the Research Topic
Gender Dysphoria: Diagnostic Issues, Clinical Aspects and Health Promotion
Sex-reassignment surgery yields long-term mental health benefits, study finds
When transgender people undergo sex-reassignment surgery, the beneficial effect on their mental health is still evident — and increasing — years later, a Swedish study suggests.
Overall, people in the study with gender incongruence — that is, their biological gender doesn’t match the gender with which they identify — were six times more likely than people in the general population to visit a doctor for mood and anxiety disorders. They were also three times more likely to be prescribed antidepressants, and six times more likely to be hospitalized after a suicide attempt, researchers found.
But among trans people who had undergone gender-affirming surgery, the longer ago their surgery, the less likely they were to suffer anxiety, depression or suicidal behavior during the study period, researchers reported in The American Journal of Psychiatry.

NBC OUT Baylor professor apologizes after guest speaker promotes conversion therapy
Surgery to modify a person’s sex characteristics “is often the last and the most considered step in the treatment process for gender dysphoria,” according to the World Professional Association for Transgender Health.
Many transgender and gender-nonconforming individuals "find comfort with their gender identity, role, and expression without surgery," but for others, "surgery is essential and medically necessary to alleviate their gender dysphoria," according to the organization.
While the new study confirms that transgender individuals are more likely to use mental health treatments, it also shows that gender-affirming therapy might reduce this risk, coauthor Richard Branstrom of the Karolinska Institutet in Stockholm told Reuters Health by email.

NBC OUT Protests, arrests and injuries as Georgians protest gay film's debut
Branstrom and colleague John Pachankis of the Yale School of Public Health in New Haven, Connecticut found that as of 2015, 2,679 people in Sweden had a diagnosis of gender incongruence, out of the total population of 9.7 million.
That year, 9.3 percent of people with gender incongruence visited a doctor for mood disorders, 7.4 percent saw a doctor for anxiety disorders and 29 percent were on antidepressants. In the general population, those percentages were 1 percent, 0.6 percent and 9.4 percent, respectively.
Just over 70 percent of people with gender incongruence were receiving feminizing or masculinizing hormones to modify outward sexual features such as breasts, body fat distribution and facial hair, and 48 percent had undergone gender-affirming surgery. Nearly all of those who had surgery also received hormone therapy.
The benefit of hormone treatment did not increase with time. But “increased time since last gender-affirming surgery was associated with fewer mental health treatments,” the authors report.
In fact, they note, “The likelihood of being treated for a mood or anxiety disorder was reduced by 8 percent for each year since the last gender-affirming surgery,” for up to 10 years.

NBC OUT LGBTQ advocates applaud judges' rejections of Trump health care rule
Transgender individuals’ use of mental health care still exceeded that of the general Swedish population, which the research team suggests is due at least partly to stigma, economic inequality and victimization.
“We need greater visibility and knowledge about challenges people are confronted with while breaking gender and identity norms,” Branstrom said.
Dr. Joshua Safer, executive director at Mount Sinai Center for Transgender Medicine and Surgery in New York City, told Reuters Health by email, “If anything, the study likely under-reports mental health benefits of medical and surgical care for transgender individuals.”
Safer, who was not involved in the study, said the fact that mental health continued to improve for years after surgery “suggests (surgery provides) extended and ongoing benefit to patients living according to gender identity.”
Follow NBC Out on Twitter , Facebook & Instagram

The Gender Reassignment Controversy
When people opt for surgery, are they satisfied with the outcome.
Posted March 16, 2018 | Reviewed by Ekua Hagan
In an age of increasing gender fluidity, it is surprising that so many find it difficult to accept the gender of their birth and take the drastic step of changing it through surgery. What are their motives? Are they satisfied with the outcome?
Gender may be the most important dimension of human variation, whether that is either desirable, or inevitable. In every society, male and female children are raised differently and acquire different expectations, and aspirations, for their work lives, emotional experiences, and leisure pursuits.
These differences may be shaped by how children are raised but gender reassignment, even early in life, is difficult, and problematic. Reassignment in adulthood is even more difficult.
Such efforts are of interest not just for medical reasons but also for the light they shed on gender differences.
The first effort at reassignment, by John Money, involved David Reimer whose penis was accidentally damaged at eight months due to a botched circumcision.
The Money Perspective
Money believed that while children are mostly born with unambiguous genitalia, their gender identity is neutral. He felt that which gender a child identifies with is determined primarily by how parents treat it and that parental views are shaped by the appearance of the genitals.
Accordingly, Money advised the parents to have the child surgically altered to resemble a female and raise it as “Brenda.” For many years, Money claimed that the reassignment had been a complete success. Such was his influence as a well-known Johns Hopkins gender researcher that his views came to be widely accepted by scholars and the general public.
Unfortunately for Brenda, the outcome was far from happy. When he was 14, Reimer began the process of reassignment to being a male. As an adult, he married a woman but depression and drug abuse ensued, culminating in suicide at the age of 38 (1).
Money's ideas about gender identity were forcefully challenged by Paul McHugh (2), a leading psychiatrist at the same institution as Money. The brunt of this challenge came from an analysis of gender reassignment cases in terms of both motivation and outcomes.
Adult Reassignment Surgery Motivation
Why do people (predominantly men) seek surgical reassignment (as a woman)? In a controversial take, McHugh argued that there are two main motives.
In one category fall homosexual men who are morally uncomfortable about their orientation and see reassignment as a way of solving the problem. If they are actually women, sexual interactions with men get redefined as heterosexual.
McHugh argued that many of the others seeking reassignment are cross-dressers. These are heterosexual men who derive sexual pleasure from wearing women's clothing. According to McHugh, surgery is the logical extreme of identifying with a female identity through cross-dressing.
If his thesis is correct, McHugh denies that reassignment surgery is ever either medically necessary or ethically defensible. He feels that the surgeon is merely cooperating with delusional thinking. It is analogous to providing liposuction treatment for an anorexic who is extremely slender but believes themselves to be overweight.
To bolster his case, McHugh looked at the clinical outcomes for gender reassignment surgeries.
Adult Reassignment Results
Anecdotally, the first hurdle for reassignment is how the result is perceived by others. This problem is familiar to anyone who looked at Dustin Hoffman's depiction of a woman ( Tootsie ). Diligent as the actor was in his preparation, his character looked masculine.
For male-to-female transsexuals, the toughest audience to convince is women. As McHugh reported, one of his female colleagues said: “Gals know gals, and that's a guy.”
According to McHugh, although transsexuals did not regret their surgery, there were little or no psychological benefits:
“They had much the same problems with relationships, work, and emotions, as before. The hope that they would emerge now from their emotional difficulties to flourish psychologically had not been fulfilled (2)”.

Thanks to McHugh's influence, gender reassignment surgeries were halted at Johns Hopkins. The surgeries were resumed, however, and are now carried out in many hospitals here and around the world.
What changed? One likely influence was the rise of the gay rights movement that now includes transgender people under its umbrella and has made many political strides in work and family.
McHugh's views are associated with the religious right-wing that has lost ground in this area.
Transgender surgery is now covered by medical insurance reflecting more positive views of the psychological benefits.
Aspirational Surgery
Why do people who are born as males want to be women? Why do females want to be men? There seems to be no easy biological explanation for the transgender phenomenon (2).
Transgender people commonly report a lifelong sense that they feel different from their biological category and express satisfaction after surgery (now called gender affirmation) that permits them to be who they really are.
The motivation for surgical change is thus aspirational rather than medical, as is true of most cosmetic surgery also. Following surgery, patients report lower gender dysphoria and improved sexual relationships (3).
All surgeries have potential costs, however. According to a Swedish study of 324 patients (3, 41 percent of whom were born female) surgery was associated with “considerably higher risks for mortality, suicidal behavior, and psychiatric morbidity than the general population.”
1 Blumberg, M. S. (2005). Basic instinct: The genesis of behavior. New York: Thunder's Mouth Press.
2 McHugh, P. R. (1995). Witches, multiple personalities, and other psychiatric artifacts. Nature Medicine, 1, 110-114.
3 Dhejne, S., Lichtenstein, P., Boman, M., et al. (2011). Long-term follow-up of transsexual persons undergoing sex reassignment surgery: Cohort study of Sweden . Plos One.

Nigel Barber, Ph.D., is an evolutionary psychologist as well as the author of Why Parents Matter and The Science of Romance , among other books.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Long-Term Regret and Satisfaction With Decision Following Gender-Affirming Mastectomy
- 1 University of Michigan Medical School, Ann Arbor
- 2 Section of Plastic Surgery, University of Michigan, Ann Arbor
- 3 Michigan Institute for Clinical Health Research, Ann Arbor, Michigan
- 4 Institute for Healthcare Policy and Innovation, Ann Arbor
- 5 Seattle Children’s Hospital, Seattle, Washington
- Invited Commentary Low Rate of Regret After Gender-Affirming Mastectomy Ian T. Nolan, MD; Brielle Weinstein, MD; Loren Schechter, MD JAMA Surgery
Question What is the rate of regret and satisfaction with decision after 2 years or more following gender-affirming mastectomy?
Findings In this cross-sectional study of 139 survey respondents who underwent gender-affirming mastectomy, the median satisfaction score was 5 on a 5-point scale, with higher scores indicating higher satisfaction. The median decisional regret score was 0 on a 100-point scale, with lower scores indicating lower levels of regret.
Meaning This study’s findings indicate low patient-reported long-term rates of regret and high satisfaction with the decision to undergo gender-affirming mastectomy, although the need exists for condition-specific instruments to assess satisfaction with decision and decisional regret for gender-affirming surgery.
Importance There has been increasing legislative interest in regulating gender-affirming surgery, in part due to the concern about decisional regret. The regret rate following gender-affirming surgery is thought to be approximately 1%; however, previous studies relied heavily on ad hoc instruments.
Objective To evaluate long-term decisional regret and satisfaction with decision using validated instruments following gender-affirming mastectomy.
Design, Setting, and Participants For this cross-sectional study, a survey of patient-reported outcomes was sent between February 1 and July 31, 2022, to patients who had undergone gender-affirming mastectomy at a US tertiary referral center between January 1, 1990, and February 29, 2020.
Exposure Decisional regret and satisfaction with decision to undergo gender-affirming mastectomy.
Main Outcomes and Measures Long-term patient-reported outcomes, including the Holmes-Rovner Satisfaction With Decision scale, the Decision Regret Scale, and demographic characteristics, were collected. Additional information was collected via medical record review. Descriptive statistics and univariable analysis using Fisher exact and Wilcoxon rank sum tests were performed to compare responders and nonresponders.
Results A total of 235 patients were deemed eligible for the study, and 139 responded (59.1% response rate). Median age at the time of surgery was 27.1 (IQR, 23.0-33.4) years for responders and 26.4 (IQR, 23.1-32.7) years for nonresponders. Nonresponders (n = 96) had a longer postoperative follow-up period than responders (median follow-up, 4.6 [IQR, 3.1-8.6] vs 3.6 [IQR, 2.7-5.3] years, respectively; P = .002). Nonresponders vs responders also had lower rates of depression (42 [44%] vs 94 [68%]; P < .001) and anxiety (42 [44%] vs 97 [70%]; P < .001). No responders or nonresponders requested or underwent a reversal procedure. The median Satisfaction With Decision Scale score was 5.0 (IQR, 5.0-5.0) on a 5-point scale, with higher scores noting higher satisfaction. The median Decision Regret Scale score was 0.0 (IQR, 0.0-0.0) on a 100-point scale, with lower scores noting lower levels of regret. A univariable regression analysis could not be performed to identify characteristics associated with low satisfaction with decision or high decisional regret due to the lack of variation in these responses.
Conclusions and Relevance In this cross-sectional survey study, the results of validated survey instruments indicated low rates of decisional regret and high levels of satisfaction with decision following gender-affirming mastectomy. The lack of dissatisfaction and regret impeded the ability to perform a more complex statistical analysis, highlighting the need for condition-specific instruments to assess decisional regret and satisfaction with decision following gender-affirming surgery.
- Invited Commentary Low Rate of Regret After Gender-Affirming Mastectomy JAMA Surgery
Read More About
Bruce L , Khouri AN , Bolze A, et al. Long-Term Regret and Satisfaction With Decision Following Gender-Affirming Mastectomy. JAMA Surg. 2023;158(10):1070–1077. doi:10.1001/jamasurg.2023.3352
Manage citations:
© 2024
Artificial Intelligence Resource Center
Surgery in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
May 12, 2022
What the Science on Gender-Affirming Care for Transgender Kids Really Shows
Laws that ban gender-affirming treatment ignore the wealth of research demonstrating its benefits for trans people’s health
By Heather Boerner

As attacks against transgender kids increase in the U.S., Minnesotans hold a rally at the state’s capitol in Saint Paul in March 2022 to support trans kids in Minnesota and Texas and around the country.
Michael Siluk/UCG/Universal Images Group via Getty Images
Editor’s Note (3/30/23): This article from May 2022 is being republished to highlight the ways that ongoing anti-trans legislation is harmful and unscientific.
For the first 40 years of their life, Texas resident Kelly Fleming spent a portion of most years in a deep depression. As an adult, Fleming—who uses they/them pronouns and who asked to use a pseudonym to protect their safety—would shave their face in the shower with the lights off so neither they nor their wife would have to confront the reality of their body.
What Fleming was experiencing, although they did not know it at the time, was gender dysphoria : the acute and chronic distress of living in a body that does not reflect one’s gender and the desire to have bodily characteristics of that gender. While in therapy, Fleming discovered research linking access to gender-affirming hormone therapy with reduced depression in transgender people. They started a very low dose of estradiol, and the depression episodes became shorter, less frequent and less intense. Now they look at their body with joy.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
So when Fleming sees what authorities in Texas , Alabama , Florida and other states are doing to bar transgender teens and children from receiving gender-affirming medical care, it infuriates them. And they are worried for their children, ages 12 and 14, both of whom are agender—a identity on the transgender spectrum that is neither masculine nor feminine.
“I’m just so excited to see them being able to present themselves in a way that makes them happy,” Fleming says. “They are living their best life regardless of what others think, and that’s a privilege that I did not get to have as a younger person.”
Laws Based on “Completely Wrong” Information
Currently more than a dozen state legislatures or administrations are considering—or have already passed—laws banning health care for transgender young people. On April 20 the Florida Department of Health issued guidance to withhold such gender-affirming care. This includes social gender transitioning—acknowledging that a young person is trans, using their correct pronouns and name, and supporting their desire to live publicly as the gender of their experience rather than their sex assigned at birth. This comes nearly two months after Texas Governor Greg Abbott issued an order for the Texas Department of Family and Protective Services to investigate for child abuse parents who allow their transgender preteens and teenagers to receive medical care. Alabama recently passed SB 184 , which would make it a felony to provide gender-affirming medical care to transgender minors. In Alabama, a “minor” is defined as anyone 19 or younger.
If such laws go ahead, 58,200 teens in the U.S. could lose access to or never receive gender-affirming care, according to the Williams Institute at the University of California, Los Angeles. A decade of research shows such treatment reduces depression, suicidality and other devastating consequences of trans preteens and teens being forced to undergo puberty in the sex they were assigned at birth).
The bills are based on “information that’s completely wrong,” says Michelle Forcier, a pediatrician and professor of pediatrics at Brown University. Forcier literally helped write the book on how to provide evidence-based gender care to young people. She is also an assistant dean of admissions at the Warren Alpert Medical School of Brown University. Those laws “are absolutely, absolutely incorrect” about the science of gender-affirming care for young people, she says. “[Inaccurate information] is there to create drama. It’s there to make people take a side.”
The truth is that data from more than a dozen studies of more than 30,000 transgender and gender-diverse young people consistently show that access to gender-affirming care is associated with better mental health outcomes—and that lack of access to such care is associated with higher rates of suicidality, depression and self-harming behavior. (Gender diversity refers to the extent to which a person’s gendered behaviors, appearance and identities are culturally incongruent with the sex they were assigned at birth. Gender-diverse people can identify along the transgender spectrum, but not all do.) Major medical organizations, including the American Academy of Pediatrics (AAP) , the American Academy of Child and Adolescent Psychiatry , the Endocrine Society , the American Medical Association , the American Psychological Association and the American Psychiatric Association , have published policy statements and guidelines on how to provide age-appropriate gender-affirming care. All of those medical societies find such care to be evidence-based and medically necessary.
AAP and Endocrine Society guidelines call for developmentally appropriate care, and that means no puberty blockers or hormones until young people are already undergoing puberty for their sex assigned at birth. For one thing, “there are no hormonal differences among prepubertal children,” says Joshua Safer, executive director of the Mount Sinai Center for Transgender Medicine and Surgery in New York City and co-author of the Endocrine Society’s guidelines. Those guidelines provide the option of gonadotropin-releasing hormone analogues (GnRHas), which block the release of sex hormones, once young people are already into the second of five puberty stages—marked by breast budding and pubic hair. These are offered only if a teen is not ready to make decisions about puberty. Access to gender-affirming hormones and potential access to gender-affirming surgery is available at age 16—and then, in the case of transmasculine youth, only mastectomy, also known as top surgery. The Endocrine Society does not recommend genital surgery for minors.
Before puberty, gender-affirming care is about supporting the process of gender development rather than directing children through a specific course of gender transition or maintenance of cisgender presentation, says Jason Rafferty, co-author of AAP’s policy statement on gender-affirming care and a pediatrician and psychiatrist at Hasbro Children’s Hospital in Rhode Island. “The current research suggests that, rather than predicting or preventing who a child might become, it’s better to value them for who they are now—even at a young age,” Rafferty says.
A Safe Environment to Explore Gender
A 2021 systematic review of 44 peer-reviewed studies found that parent connectedness, measured by a six-question scale asking about such things as how safe young people feel confiding in their guardians or how cared for they feel in the family, is associated with greater resilience among teens and young adults who are transgender or gender-diverse. Rafferty says he sees his role with regard to prepubertal children as offering a safe environment for the child to explore their gender and for parents to ask questions. “The gender-affirming approach is not some railroad of people to hormones and surgery,” Safer says. “It is talking and watching and being conservative.”
Only once children are older, and if the incongruence between the sex assigned to them at birth and their experienced gender has persisted, does discussion of medical transition occur. First a gender therapist has to diagnose the young person with gender dysphoria .
After a gender dysphoria diagnosis—and only if earlier conversations suggest that hormones are indicated—guidelines call for discussion of fertility, puberty suppression and hormones. Puberty-suppressing medications have been used for decades for cisgender children who start puberty early, but they are not meant to be used indefinitely. The Endocrine Society guidelines recommend a maximum of two years on GnRHa therapy to allow more time for children to form their gender identity before undergoing puberty for their sex assigned at birth, the effects of which are irreversible.
“[Puberty blockers] are part of the process of ‘do no harm,’” Forcier says, referencing a popular phrase that describes the Hippocratic Oath, which many physicians recite a version of before they begin to practice.
Hormone blocker treatment may have side effects. A 2015 longitudinal observational cohort study of 34 transgender young people found that, by the time the participants were 22 years old, trans women experienced a decrease in bone mineral density. A 2020 study of puberty suppression in gender-diverse and transgender young people found that those who started puberty blockers in early puberty had lower bone mineral density before the start of treatment than the public at large. This suggests, the authors wrote, that GnRHa use may not be the cause of low bone mineral density for these young people. Instead they found that lack of exercise was a primary factor in low bone-mineral density, especially among transgender girls.
Other side effects of GnRHa therapy include weight gain, hot flashes and mood swings. But studies have found that these side effects—and puberty delay itself—are reversible , Safer says.
Gender-affirming hormone therapy often involves taking an androgen blocker (a chemical that blocks the release of testosterone and other androgenic hormones) and estrogen in transfeminine teens, and testosterone supplementation in transmasculine teens. Such hormones may be associated with some physiological changes for adult transgender people. For instance, transfeminine people taking estrogen see their so-called “good” cholesterol increase. By contrast, transmasculine people taking testosterone see their good cholesterol decrease. Some studies have hinted at effects on bone mineral density, but these are complicated and also depend on personal, family history, exercise, and many other factors in addition to hormones.”
And while some critics point to decade-old study and older studies suggesting very few young people persist in transgender identity into late adolescence and adulthood, Forcier says the data are “misleading and not accurate.” A recent review detailed methodological problems with some of these studies . New research in 17,151 people who had ever socially transitioned found that 86.9 percent persisted in their gender identity. Of the 2,242 people who reported that they reverted to living as the gender associated with the sex they were assigned at birth, just 15.9 percent said they did so because of internal factors such as questioning their experienced gender but also because of fear, mental health issues and suicide attempts. The rest reported the cause was social, economic and familial stigma and discrimination. A third reported that they ceased living openly as a trans person because doing so was “just too hard for me.”
The Harms of Denying Care
Data suggest the effects of denying that care are worse than whatever side effects result from delaying sex-assigned-at-birth puberty. And medical society guidelines conclude that the benefits of gender-affirming care outweigh the risks. Without gender-affirming hormone therapy, cisgender hormones take over, forcing body changes that can be permanent and distressing.
A 2020 study of 300 gender-incongruent young people found that mental distress—including self-harm, suicidal thoughts and depression— increased as the children were made to proceed with puberty according to their assigned sex. By the time 184 older teens (with a median age of 16) reached the stage in which transgender boys began their periods and grew breasts and transgender girls’ voice dropped and facial hair began to appear, 46 percent had been diagnosed with depression, 40 percent had self-harmed, 52 percent had considered suicide, and 17 percent had attempted it—rates significantly higher than those of gender-incongruent children who were a median of 13.9 years old or of cisgender kids their own age.
Conversely, access to gender-affirming hormones in adolescence appears to have a protective effect. In one study, researchers followed 104 teens and young adults for a year and asked them about their depression, anxiety and suicidality at the time they started receiving hormones or puberty blockers and again at the three-month, six-month and one-year mark. At the beginning of the study, which was published in JAMA Network Open in February 2022, more than half of the respondents reported moderate to severe depression, half reported moderate to severe anxiety, and 43.3 percent reported thoughts of self-harm or suicide in the past two weeks.
But when the researchers analyzed the results based on the kind of gender-affirming care the teens had received, they found that those who had access to puberty blockers or gender-affirming hormones were 60 percent less likely to experience moderate to severe depression. And those with access to the medical treatments were 73 percent less likely to contemplate self-harm or suicide.
“Delays in prescribing puberty blockers and hormones may in fact worsen mental health symptoms for trans youth,” says Diana Tordoff, an epidemiology graduate student at the University of Washington and co-author of the study.
That effect may be lifelong. A 2022 study of more than 21,000 transgender adults showed that just 41 percent of adults who wanted hormone therapy received it, and just 2.3 percent had access to it in adolescence. When researchers looked at rates of suicidal thinking over the past year in these same adults, they found that access to hormone therapy in early adolescence was associated with a 60 percent reduction in suicidality in the past year and that access in late adolescence was associated with a 50 percent reduction.
For Fleming’s kids in Texas, gender-affirming hormones are not currently part of the discussion; not all trans people desire hormones or surgery to feel affirmed in their gender. But Fleming is already looking at jobs in other states to protect their children’s access to such care, should they change their mind. “Getting your body closer to the gender [you] identify with—that is what helps the dysphoria,” Fleming says. “And not giving people the opportunity to do that, making it harder for them to do that, is what has made the suicide rate among transgender people so high. We just—trans people are just trying to survive.”
IF YOU NEED HELP If you or someone you know is struggling or having thoughts of suicide, help is available. Call the National Suicide Prevention Lifeline at 1-800-273-8255 (TALK), use the online Lifeline Chat or contact the Crisis Text Line by texting TALK to 741741.
Postoperative complications of male to female sex reassignment surgery: A 10-year French retrospective study
Affiliations.
- 1 Department of plastic, reconstructive and aesthetic surgery, Saint-Louis hospital, avenue Claude-Vellefaux, 75475 Paris cedex 10, France; Paris Diderot university, Sorbonne Paris, Paris, France; Plastic and aesthetic surgery department, hôpital Tenon, Paris, France.
- 2 Plastic and reconstructive surgery, Conception hospital, 147, boulevard Baille, 13005 Marseille, France.
- 3 Department of plastic, reconstructive and aesthetic surgery, Saint-Louis hospital, avenue Claude-Vellefaux, 75475 Paris cedex 10, France.
- 4 Department of plastic, reconstructive and aesthetic surgery, Saint-Louis hospital, avenue Claude-Vellefaux, 75475 Paris cedex 10, France; Paris Diderot university, Sorbonne Paris, Paris, France.
- 5 Plastic and aesthetic surgery department, hôpital Tenon, Paris, France.
- 6 Department of plastic, reconstructive and aesthetic surgery, Saint-Louis hospital, avenue Claude-Vellefaux, 75475 Paris cedex 10, France; Plastic and reconstructive surgery, François-Mitterand hospital, 14, rue Paul-Gaffarel, 21079 Dijon, France. Electronic address: [email protected].
- PMID: 30269882
- DOI: 10.1016/j.anplas.2018.08.002
In primary male to female (MTF) sex reassignment surgery (SRS), the most frequent postoperative functional complications using the penoscrotal skin technique remain neovaginal stenosis, urinary meatal stenosis and secondary revision surgery. We aimed to retrospectively analyze postoperative functional and anatomical complications, as well as secondary procedures required after MTF SRS by penile skin inversion. All patients operated on for MTF SRS, using the inverted technique, from June 2006 to July 2016, were retrospectively reviewed. The minimum follow-up was one year (five-years maximum follow-up). Soft postoperative dilationprotocol was prescribed until complete healing of the vagina. We did not prescribe long-term hard dilation systematically. Possible short-depth neovaginas were primarily treated with further temporary dilation using a hard bougie. Among the 189 included patients, we reported a 2.6% of rectovaginal wall perforations. In 37% of patients we had repeated compressive dressings and 15% of them required blood transfusions. Eighteen percent of patients presented with hematoma and 27% with early infectious complications. Delayed short-depth neovagina occurred in 21% of patients, requiring additional hard dilatation, with a 95.5% success rate. Total secondary vaginoplasty rate was 6.3% (4.7% skin graft and 3.7% bowel plasty). Secondary functional meatoplasty occurred in 1% of cases. Other secondary cosmetic surgery rates ranged between 3 to 20%. A low rate of secondary functional meatoplasty was showed after MTF SRS by penile skin inversion. Hard dilation was prescribed in case of healed short-depth vagina, with good efficiency in most of cases. Secondary vaginoplasty was required in cases of neovagina stenosis or persisting short-depth neovagina after failure of hard dilation protocol.
Keywords: Chirurgie de changement de sexe; Complications postopératoires; Follow-up; Postoperative complications; Sex reassignment surgery; Suivi.
Copyright © 2018 Elsevier Masson SAS. All rights reserved.
- Blood Transfusion / statistics & numerical data
- Middle Aged
- Postoperative Complications
- Retrospective Studies
- Sex Reassignment Surgery / adverse effects*
- Young Adult
- Election Integrity
- Immigration
Political Thought
- American History
- Conservatism
- Progressivism
International
- Global Politics
- Middle East
Government Spending
- Budget and Spending
Energy & Environment
- Environment
Legal and Judicial
- Crime and Justice
- Second Amendment
- The Constitution
National Security
- Cybersecurity
Domestic Policy
- Government Regulation
- Health Care Reform
- Marriage and Family
- Religious Liberty
- International Economies
- Markets and Finance
Sex Reassignment Doesn’t Work. Here Is the Evidence.

Ryan T. Anderson, Ph.D.
Former Visiting Fellow, DeVos Center

Key Takeaways
McHugh points to the reality that because sex change is physically impossible, it frequently does not provide the long-term wholeness and happiness that people seek.
Unfortunately, many professionals now view health care—including mental health care—primarily as a means of fulfilling patients’ desires, whatever those are.
Our brains and senses are designed to bring us into contact with reality, connecting us with the outside world and with the reality of ourselves.
Sex “reassignment” doesn’t work. It’s impossible to “reassign” someone’s sex physically, and attempting to do so doesn’t produce good outcomes psychosocially.
As I demonstrate in my book, “ When Harry Became Sally: Responding to the Transgender Moment ,” the medical evidence suggests that sex reassignment does not adequately address the psychosocial difficulties faced by people who identify as transgender. Even when the procedures are successful technically and cosmetically, and even in cultures that are relatively “trans-friendly,” transitioners still face poor outcomes.
Dr. Paul McHugh, the university distinguished service professor of psychiatry at the Johns Hopkins University School of Medicine, explains :
Transgendered men do not become women, nor do transgendered women become men. All (including Bruce Jenner) become feminized men or masculinized women, counterfeits or impersonators of the sex with which they ‘identify.’ In that lies their problematic future.
When ‘the tumult and shouting dies,’ it proves not easy nor wise to live in a counterfeit sexual garb. The most thorough follow-up of sex-reassigned people —extending over 30 years and conducted in Sweden, where the culture is strongly supportive of the transgendered—documents their lifelong mental unrest. Ten to 15 years after surgical reassignment, the suicide rate of those who had undergone sex-reassignment surgery rose to 20 times that of comparable peers.
Indeed, the best scientific research supports McHugh’s caution and concern.
Here’s how The Guardian summarized the results of a review of “more than 100 follow-up studies of post-operative transsexuals” by Birmingham University’s Aggressive Research Intelligence Facility:
[The Aggressive Research Intelligence Facility], which conducts reviews of health care treatments for the [National Health Service], concludes that none of the studies provides conclusive evidence that gender reassignment is beneficial for patients. It found that most research was poorly designed, which skewed the results in favor of physically changing sex. There was no evaluation of whether other treatments, such as long-term counseling, might help transsexuals, or whether their gender confusion might lessen over time.
“There is huge uncertainty over whether changing someone’s sex is a good or a bad thing,” said Chris Hyde, the director of the facility . Even if doctors are careful to perform these procedures only on “appropriate patients,” Hyde continued, “there’s still a large number of people who have the surgery but remain traumatized—often to the point of committing suicide.”
Of particular concern are the people these studies “lost track of.” As The Guardian noted, “the results of many gender reassignment studies are unsound because researchers lost track of more than half of the participants.” Indeed, “Dr. Hyde said the high drop-out rate could reflect high levels of dissatisfaction or even suicide among post-operative transsexuals.”
Hyde concluded: “The bottom line is that although it’s clear that some people do well with gender reassignment surgery, the available research does little to reassure about how many patients do badly and, if so, how badly.”
The facility conducted its review back in 2004, so perhaps things have changed in the past decade?
Not so. In 2014, a new review of the scientific literature was done by Hayes, Inc., a research and consulting firm that evaluates the safety and health outcomes of medical technologies. Hayes found that the evidence on long-term results of sex reassignment was too sparse to support meaningful conclusions and gave these studies its lowest rating for quality:
Statistically significant improvements have not been consistently demonstrated by multiple studies for most outcomes. … Evidence regarding quality of life and function in male-to-female adults was very sparse. Evidence for less comprehensive measures of well-being in adult recipients of cross-sex hormone therapy was directly applicable to [gender dysphoric] patients but was sparse and/or conflicting. The study designs do not permit conclusions of causality and studies generally had weaknesses associated with study execution as well. There are potentially long-term safety risks associated with hormone therapy but none have been proven or conclusively ruled out.
The Obama administration came to similar conclusions. In 2016, the Centers for Medicare and Medicaid Services revisited the question of whether sex reassignment surgery would have to be covered by Medicare plans. Despite receiving a request that its coverage be mandated, it refused, on the ground that we lack evidence that it benefits patients.
Here’s how the June 2016 “ Proposed Decision Memo for Gender Dysphoria and Gender Reassignment Surgery ” put it:
Based on a thorough review of the clinical evidence available at this time, there is not enough evidence to determine whether gender reassignment surgery improves health outcomes for Medicare beneficiaries with gender dysphoria. There were conflicting (inconsistent) study results—of the best designed studies, some reported benefits while others reported harms. The quality and strength of evidence were low due to the mostly observational study designs with no comparison groups, potential confounding, and small sample sizes. Many studies that reported positive outcomes were exploratory type studies (case-series and case-control) with no confirmatory follow-up.
The final August 2016 memo was even more blunt. It pointed out:
Overall, the quality and strength of evidence were low due to mostly observational study designs with no comparison groups, subjective endpoints, potential confounding (a situation where the association between the intervention and outcome is influenced by another factor such as a co-intervention), small sample sizes, lack of validated assessment tools, and considerable lost to follow-up.
That “lost to follow-up,” remember, could be pointing to people who committed suicide.
And when it comes to the best studies, there is no evidence of “clinically significant changes” after sex reassignment:
The majority of studies were non-longitudinal, exploratory type studies (i.e., in a preliminary state of investigation or hypothesis generating), or did not include concurrent controls or testing prior to and after surgery. Several reported positive results but the potential issues noted above reduced strength and confidence. After careful assessment, we identified six studies that could provide useful information. Of these, the four best designed and conducted studies that assessed quality of life before and after surgery using validated (albeit non-specific) psychometric studies did not demonstrate clinically significant changes or differences in psychometric test results after [gender reassignment surgery].
In a discussion of the largest and most robust study—the study from Sweden that McHugh mentioned in the quote above—the Obama Centers for Medicare and Medicaid Services pointed out the 19-times-greater likelihood for death by suicide, and a host of other poor outcomes:
The study identified increased mortality and psychiatric hospitalization compared to the matched controls. The mortality was primarily due to completed suicides (19.1-fold greater than in control Swedes), but death due to neoplasm and cardiovascular disease was increased 2 to 2.5 times as well. We note, mortality from this patient population did not become apparent until after 10 years. The risk for psychiatric hospitalization was 2.8 times greater than in controls even after adjustment for prior psychiatric disease (18 percent). The risk for attempted suicide was greater in male-to-female patients regardless of the gender of the control. Further, we cannot exclude therapeutic interventions as a cause of the observed excess morbidity and mortality. The study, however, was not constructed to assess the impact of gender reassignment surgery per se.
These results are tragic. And they directly contradict the most popular media narratives, as well as many of the snapshot studies that do not track people over time. As the Obama Centers for Medicare and Medicaid pointed out, “mortality from this patient population did not become apparent until after 10 years.”
So when the media tout studies that only track outcomes for a few years, and claim that reassignment is a stunning success, there are good grounds for skepticism.
As I explain in my book , these outcomes should be enough to stop the headlong rush into sex reassignment procedures. They should prompt us to develop better therapies for helping people who struggle with their gender identity.
And none of this even begins to address the radical, entirely experimental therapies that are being directed at the bodies of children to transition them.
Sex Change Is Physically Impossible
We’ve seen some of the evidence that sex reassignment doesn’t produce good outcomes psychosocially. And as McHugh suggested above, part of the reason why is because sex change is impossible and “it proves not easy nor wise to live in a counterfeit sexual garb.”
But what is the basis for the conclusion that sex change is impossible?
Contrary to the claims of activists , sex isn’t “assigned” at birth—and that’s why it can’t be “reassigned.” As I explain in “When Harry Became Sally,” sex is a bodily reality that can be recognized well before birth with ultrasound imaging. The sex of an organism is defined and identified by the way in which it (he or she) is organized for sexual reproduction.
This is just one manifestation of the fact that natural organization is “the defining feature of an organism,” as neuroscientist Maureen Condic and her philosopher brother Samuel Condic explain. In organisms, “the various parts … are organized to cooperatively interact for the welfare of the entity as a whole. Organisms can exist at various levels, from microscopic single cells to sperm whales weighing many tons, yet they are all characterized by the integrated function of parts for the sake of the whole.”
Male and female organisms have different parts that are functionally integrated for the sake of their whole, and for the sake of a larger whole—their sexual union and reproduction. So an organism’s sex—as male or female—is identified by its organization for sexually reproductive acts. Sex as a status—male or female—is a recognition of the organization of a body that can engage in sex as an act.
That organization isn’t just the best way to figure out which sex you are. It’s the only way to make sense of the concepts of male and female at all. What else could “maleness” or “femaleness” even refer to, if not your basic physical capacity for one of two functions in sexual reproduction?
The conceptual distinction between male and female based on reproductive organization provides the only coherent way to classify the two sexes. Apart from that, all we have are stereotypes.
This shouldn’t be controversial. Sex is understood this way across sexually reproducing species. No one finds it particularly difficult—let alone controversial—to identify male and female members of the bovine species or the canine species. Farmers and breeders rely on this easy distinction for their livelihoods. It’s only recently, and only with respect to the human species, that the very concept of sex has become controversial.
And yet, in an expert declaration to a federal district court in North Carolina concerning H.B. 2 (a state law governing access to sex-specific restrooms), Dr. Deanna Adkins stated, “From a medical perspective, the appropriate determinant of sex is gender identity.” Adkins is a professor at Duke University School of Medicine and the director of the Duke Center for Child and Adolescent Gender Care (which opened in 2015).
Adkins argues that gender identity is not only the preferred basis for determining sex, but “the only medically supported determinant of sex.” Every other method is bad science, she claims: “It is counter to medical science to use chromosomes, hormones, internal reproductive organs, external genitalia, or secondary sex characteristics to override gender identity for purposes of classifying someone as male or female.”
In her sworn declaration to the federal court, Adkins called the standard account of sex—an organism’s sexual organization—“an extremely outdated view of biological sex.”
Dr. Lawrence Mayer responded in his rebuttal declaration: “This statement is stunning. I have searched dozens of references in biology, medicine and genetics—even Wiki!—and can find no alternative scientific definition. In fact, the only references to a more fluid definition of biological sex are in the social policy literature.”
Just so. Mayer is a scholar in residence in the Department of Psychiatry at the Johns Hopkins University School of Medicine and a professor of statistics and biostatistics at Arizona State University.
Modern science shows that our sexual organization begins with our DNA and development in the womb, and that sex differences manifest themselves in many bodily systems and organs, all the way down to the molecular level. In other words, our physical organization for one of two functions in reproduction shapes us organically, from the beginning of life, at every level of our being.
Cosmetic surgery and cross-sex hormones can’t change us into the opposite sex. They can affect appearances. They can stunt or damage some outward expressions of our reproductive organization. But they can’t transform it. They can’t turn us from one sex into the other.
“Scientifically speaking, transgender men are not biological men and transgender women are not biological women. The claims to the contrary are not supported by a scintilla of scientific evidence,” explains Mayer.
Or, as Princeton philosopher Robert P. George put it, “Changing sexes is a metaphysical impossibility because it is a biological impossibility.”
The Purpose of Medicine, Emotions, and the Mind
Behind the debates over therapies for people with gender dysphoria are two related questions: How do we define mental health and human flourishing? And what is the purpose of medicine, particularly psychiatry?
Those general questions encompass more specific ones: If a man has an internal sense that he is a woman, is that just a variety of normal human functioning, or is it a psychopathology? Should we be concerned about the disconnection between feeling and reality, or only about the emotional distress or functional difficulties it may cause?
What is the best way to help people with gender dysphoria manage their symptoms: by accepting their insistence that they are the opposite sex and supporting a surgical transition, or by encouraging them to recognize that their feelings are out of line with reality and learn how to identify with their bodies?
All of these questions require philosophical analysis and worldview judgments about what “normal human functioning” looks like and what the purpose of medicine is.
Settling the debates over the proper response to gender dysphoria requires more than scientific and medical evidence. Medical science alone cannot tell us what the purpose of medicine is.
Science cannot answer questions about meaning or purpose in a moral sense. It can tell us about the function of this or that bodily system, but it can’t tell us what to do with that knowledge. It cannot tell us how human beings ought to act. Those are philosophical questions, as I explain in “ When Harry Became Sally .”
While medical science does not answer philosophical questions, every medical practitioner has a philosophical worldview, explicit or not. Some doctors may regard feelings and beliefs that are disconnected from reality as a part of normal human functioning and not a source of concern unless they cause distress. Other doctors will regard those feelings and beliefs as dysfunctional in themselves, even if the patient does not find them distressing, because they indicate a defect in mental processes.
But the assumptions made by this or that psychiatrist for purposes of diagnosis and treatment cannot settle the philosophical questions: Is it good or bad or neutral to harbor feelings and beliefs that are at odds with reality? Should we accept them as the last word, or try to understand their causes and correct them, or at least mitigate their effects?
While the current findings of medical science, as shown above, reveal poor psychosocial outcomes for people who have had sex reassignment therapies, that conclusion should not be where we stop. We must also look deeper for philosophical wisdom, starting with some basic truths about human well-being and healthy functioning.
We should begin by recognizing that sex reassignment is physically impossible. Our minds and senses function properly when they reveal reality to us and lead us to knowledge of truth. And we flourish as human beings when we embrace the truth and live in accordance with it. A person might find some emotional relief in embracing a falsehood, but doing so would not make him or her objectively better off. Living by a falsehood keeps us from flourishing fully, whether or not it also causes distress.
This philosophical view of human well-being is the foundation of a sound medical practice. Dr. Michelle Cretella, the president of the American College of Pediatricians—a group of doctors who formed their own professional guild in response to the politicization of the American Academy of Pediatrics—emphasizes that mental health care should be guided by norms grounded in reality, including the reality of the bodily self.
“The norm for human development is for one’s thoughts to align with physical reality, and for one’s gender identity to align with one’s biologic sex,” she says. For human beings to flourish, they need to feel comfortable in their own bodies, readily identify with their sex, and believe that they are who they actually are. For children especially, normal development and functioning require accepting their physical being and understanding their embodied selves as male or female.
Unfortunately, many professionals now view health care—including mental health care—primarily as a means of fulfilling patients’ desires, whatever those are. In the words of Leon Kass, a professor emeritus at the University of Chicago, today a doctor is often seen as nothing more than “a highly competent hired syringe”:
The implicit (and sometimes explicit) model of the doctor-patient relationship is one of contract: the physician—a highly competent hired syringe, as it were—sells his services on demand, restrained only by the law (though he is free to refuse his services if the patient is unwilling or unable to meet his fee). Here’s the deal: for the patient, autonomy and service; for the doctor, money, graced by the pleasure of giving the patient what he wants. If a patient wants to fix her nose or change his gender, determine the sex of unborn children, or take euphoriant drugs just for kicks, the physician can and will go to work—provided that the price is right and that the contract is explicit about what happens if the customer isn’t satisfied.
This modern vision of medicine and medical professionals gets it wrong, says Kass. Professionals ought to profess their devotion to the purposes and ideals they serve. Teachers should be devoted to learning, lawyers to justice, clergy to things divine, and physicians to “healing the sick, looking up to health and wholeness.” Healing is “the central core of medicine,” Kass writes—“to heal, to make whole, is the doctor’s primary business.”
To provide the best possible care, serving the patient’s medical interests requires an understanding of human wholeness and well-being. Mental health care must be guided by a sound concept of human flourishing. The minimal standard of care should begin with a standard of normality. Cretella explains how this standard applies to mental health:
One of the chief functions of the brain is to perceive physical reality. Thoughts that are in accordance with physical reality are normal. Thoughts that deviate from physical reality are abnormal—as well as potentially harmful to the individual or to others. This is true whether or not the individual who possesses the abnormal thoughts feels distress.
Our brains and senses are designed to bring us into contact with reality, connecting us with the outside world and with the reality of ourselves. Thoughts that disguise or distort reality are misguided—and can cause harm. In “ When Harry Became Sally ,” I argue that we need to do a better job of helping people who face these struggles.
This piece originally appeared in The Daily Signal
Neither federal lawmakers nor courts should have the power to redefine what it is to be a man or a woman for all Americans. Learn more about policies that curb government overreach with Solutions .
COMMENTARY 2 min read
COMMENTARY 3 min read
Subscribe to email updates
© 2024, The Heritage Foundation
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Plast Reconstr Surg Glob Open
- v.9(3); 2021 Mar
Complications and Patient-reported Outcomes in Transfemale Vaginoplasty: An Updated Systematic Review and Meta-analysis
Samyd s. bustos.
From the * Department of Plastic Surgery, University of Pittsburgh, Pittsburgh, Pa.
Valeria P. Bustos
† Division of Plastic and Reconstructive Surgery, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Mass.
Andres Mascaro
‡ Department of Plastic and Reconstructive Surgery, Cleveland Clinic, Weston, Fla.
Pedro Ciudad
§ Department of Plastic, Reconstructive and Burn Surgery, Arzobispo Loayza National Hospital, Lima, Peru
Antonio J. Forte
¶ Division of Plastic and Reconstructive Surgery, Mayo Clinic, Jacksonville, Fla.
Gabriel Del Corral
∥ Department of Plastic and Reconstructive Surgery, MedStar Georgetown University Hospital, Washington, D.C.
Oscar Javier Manrique
** Division of Plastic and Reconstructive Surgery, University of Rochester Medical Center, Strong Memorial Hospital, Rochester, N.Y.
Associated Data
Supplemental Digital Content is available in the text.
Background:
Vaginoplasty aims to create a functional feminine vagina, sensate clitoris, and labia minora and majora with acceptable cosmesis. The upward trend in the number of transfemale vaginoplasties has impacted the number of published articles on this topic. Herein, we conducted an updated systematic review on complications and patient-reported outcomes.
A update on our previous systematic review was conducted. Several databases including MEDLINE, EMBASE, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, and Scopus were assessed. Random effects meta-analysis and subgroup analyses were performed.
After compiling the results of the update with the previous systematic review, a total of 57 studies pooling 4680 cases were included in the systematic review, and 52 studies were used in the meta-analysis. Overall pooled data including any surgical technique showed rates of 1% [95% confidence interval (CI) <0.1%–2%] of fistula, 11% (95% CI 8%–14%) of stenosis and/or strictures, 4% (95% CI 1%–9%) of tissue necrosis, and 3% (95% CI 1%–4%) of prolapse. Overall satisfaction was 91% (81%–98%). Regret rate was 2% (95% CI <1%–3%). Average neovaginal depth was 9.4 cm (7.9–10.9 cm) for the penile skin inversion and 15.3 cm (13.8–16.7 cm) for the intestinal vaginoplasty.
Conclusions:
Transfemale vaginoplasty is a key component of the comprehensive surgical treatment of transfemale patients with gender dysphoria. Over time, we will see an increased demand for these procedures, so adequate surgical training, clinical/surgical experience, and research outcomes are required, as we continue to strive to provide the best care possible for a population in need.
INTRODUCTION
Transgender is a term that includes the many ways that people’s gender identities can differ from the sex they were assigned at birth. Unfortunately, the transgender population has largely suffered from transgender-related discrimination in healthcare and employment, and from high rates of mental illness, particularly anxiety and depression, in addition to violence and health-related problems. 1 , 2 This population expresses their gender identity in many different ways. Some use their dress or behavior (gender expressions) to live as the gender that feels appropriate for them, and many undergo medical or surgical treatment to change their body, so that it matches their gender identity. Surgical treatment, particularly genital or bottom surgery, is often the last and most considered step for transgender patients. 3 The role of surgery has shown to be essential and medically necessary to alleviate patients’ gender dysphoria, which is the distress caused by the discrepancy between a person’s gender identity and the sex assigned at birth. 4 – 10
For transgender women, genital surgery involves vaginoplasty, which entails the surgical reconstruction of all the anatomical structures of the female external genitalia and the creation of a functional vaginal canal. The Standards of Care from the World Professional Association for Transgender Health clearly defines the criteria for vaginoplasty in transfemale patients, which includes the following: persistent, well-documented gender dysphoria, capacity to make a fully informed decision and to consent for treatment, age of majority, control of significant medical or mental health concerns, 12 continuous months of hormonal therapy as appropriate, and 12 continuous months of living in a gender role that is congruent with their gender identity. 3
In general, vaginoplasty aims to create a functional feminine vulva, a deep and wide enough vagina, a hooded sensate clitoris, and labia minora and majora with acceptable cosmesis and sexual sensation. A number of surgical techniques have been described; however, the most commonly used technique is still the penile skin inversion with or without skin graft. Although less common, intestinal-based techniques, including colon or small bowel conduits, have also been reported. These may have specific indications; for instance, patients with micropenis, penile hypoplasia (<8 cm), or poor skin quality or elasticity due to prolonged hormonal treatment may not be suitable for penile skin inversion and other options such as intestinal conduits may be more appropriate. 11 , 12
Although there are still financial and social barriers to healthcare access for this particular population worldwide, the need for surgical gender-affirming care is increasing remarkably. This may be explained due to increased awareness of the needs of transgender and gender-nonbinary (TGNB) patients, and availability and accessibility to gender care centers. In 2015, the US Transgender Surgery sampled over 27,000 TGNB Americans and found that one fourth had undergone one or more gender affirmation surgeries (GAS). 13 , 14 A total of 12% of respondents had undergone vaginoplasty and/or labiaplasty, and 54% responded they wanted to have it someday. Therefore, both academic and private centers are facing an increased demand for transfemale vaginoplasty.
The need of a state-of-the-art review on surgical and patient-reported outcomes has been previously addressed by Manrique et al. 5 However, this upward trend in gender affirmation surgeries has also impacted the number of published articles on this topic over the past years about this surgical procedure. In this study, we aim to conduct an updated, comprehensive systematic review of the literature of papers in transfemale vaginoplasty with meta-analysis of complications and patient-reported outcomes.
Search Methodology
Based on the PRISMA guidelines, a comprehensive research of several databases from each database’s inception was conducted on July 15, 2020. 15 The databases included PubMed, Ovid MEDLINE Epub Ahead of Print, Ovid Medline In-Process and Other Non-Indexed Citations, Ovid MEDLINE, Ovid EMBASE, Web of Science, and Ovid Cochrane Central Register of Controlled Trials. A comprehensive research strategy using the same strategy from our previous study was conducted. 5 This was previously designed and conducted by experienced librarians with input from the study’s principal investigator. Controlled vocabulary with keywords was conducted to update the previous search and include studies from 2017 to 2020 of vaginoplasty in transgender and nonbinary population who reported our outcomes of interest.
The search terms were formulated using the PICO structure. Participants included transfemale patients. The intervention was vaginoplasty, bottom male-to-female surgery, or transfemale genital surgery. Comparisons addressed the specific technique used. Outcomes included complications, functional or aesthetic patient-reported outcomes. The strategy is available in Supplemental Digital Content 1 . (See pdf, Supplemental Digital Content 1, which displays the s earch strategies, http://links.lww.com/PRSGO/B611 .) All search results were combined in EndNote, a bibliographic management tool, and duplicates were removed.
Study Selection
We conducted a 2-stage screening process with the help of the online software Covidence. 16 Search strategy results were exported from EndNote into XML format and uploaded to Covidence. 16 Two researchers (S.S.B and V.P.B) conducted the first screening by reviewing titles and abstracts, and selected the ones relevant to the research question. Then, the second screening was conducted by the same researchers reviewing the full-text form of the remained articles. The studies included were those that met the inclusion and exclusion criteria. Conflicts in this stage were solved by a third reviewer (O.J.M.), who moderated a discussion and made final decision. Eligible criteria were based on our previous systematic review and meta-analysis by Manrique et al. 5 Inclusion criteria were all articles that included studies with sample size more than 5 patients, only transfemale vaginoplasty procedures studied, publication year 1985 or more, articles reporting at least 1 outcome measurement, and a follow-up time of at least 1 year. The exclusion criteria were all studies with surgical techniques for partial reconstruction of the vagina or vaginoplasty corrections, surgical techniques only for the creation of neoclitoris or labiaplasty, and unspecified surgical technique, non-English publications, cancer-related publications, trauma-related publications, and congenital-related publications.
Data Extraction and Synthesis
The included studies were analyzed in detail. We extracted information regarding the name of the first author, year of publication, and follow-ups time (minimum, maximum, and SDs variables). Major complications categorized as fistulas, vaginal and urethral stenosis and strictures, tissue necrosis, and prolapse were identified. For fistulas outcomes, vaginorectal and vesicovaginal fistulas were included. Stenosis and strictures outcomes included introital, stroma, urethral, and vaginal. Both partial and complete strictures were taken into account. The tissue necrosis outcome included necrosis of the urethra, glans, clitoris, and labia. Rectocele, urethral, or mucosal prolapse was included in the prolapse outcome.
Patient-reported outcomes were analyzed as proportions and percentages. Overall results, function, and aesthetic satisfaction outcomes were identified as the number of patients who reported such variables. Aesthetic outcome included perception of vaginal appearance as feminine. Satisfied included “very satisfied” and “mostly satisfied” in the included studies.
The ability to have orgasm, regret rate, and the patient-reported outcomes were analyzed as proportions and percentages. In addition, we extracted information about the vaginal cavity length, its mean, minimum and maximum values, and SD.
Quality Assessment
The Newcastle-Ottawa Scale was used to assess quality of nonrandomized studies in meta-analyses was used to assess the risk of bias in the included studies. A nonrandomized study can be ranked 9 stars on items related to: the selection of the study groups (4 points), comparability of the exposed and unexposed groups (2 points), and the ascertainment of outcomes of interest (3 points).
Statistical Analysis
The data were analyzed, and outcome estimations in this meta-analysis were conducted in Stata Software/IC (version 16.1). 17 We divided the studies in 2 major groups of interest: penile inversion technique and intestinal vaginoplasty. Given the heterogeneity between studies, we conducted a logistic-normal-random-effect model. The study-specific proportions with 95% exact confidence intervals (CIs) and overall pooled estimates with 95% Wald CIs with Freeman–Turkey double arcsine transformation were performed. The effect size and percentage of weight were presented for each individual study. To evaluate heterogeneity, I 2 statistics was used. If P value <0.05 or I 2 >50% significant heterogeneity was considered.
A total of 154 articles were identified in the updated search. The first screening process generated 36 articles, and the second screening yielded 11 articles, which were included in the systematic review and meta-analysis. We compiled these data to the one of the previous systematic review and meta-analysis of Manrique et al 5 as shown in Figure Figure1. 1 . A total of 57 studies were included in the systematic review and 52 in the meta-analysis. All included studies were assigned either a low- or moderate-quality design. (See pdf, Supplemental Digital Content 2, which displays the quality assessment of included studies, http://links.lww.com/PRSGO/B612 .)

PRISMA flowchart.
Study Characteristics
A total of 4680 cases were represented in this systematic review. A total of 39 (75%) studies used the penile skin inversion technique with or without scrotal flap 18 – 54 and 11 (21.2%) studies used bowel pedicle flaps, of which 7 (13.5%) used sigmoid or rectosigmoid, 3 (5.8%) used ileal, and 1 (1.9%) used transverse colon as conduit. 55 – 67 One study (1.9%) reported both techniques, 68 and another study (1.9%) reported outcomes using amnion grafts with and without fibroblasts. 69 A total of 3930 (84.0%) cases used the penile skin inversion technique with or without scrotal graft or skin graft, whereas 726 (15.5%) cases used bowel pedicle flaps. One study reported 24 (0.5%) vaginoplasty cases using amnion grafts. The average number of cases per study was 90 with the smallest study including 7 cases and the largest study including 475. Table Table2 2 shows the differences between the findings of our previous meta-analysis and the current study.
Differences between the Previous and Current Metanalysis
Data shown as pooled value and 95% confidence interval.
IBV, intestinal-based vaginoplasty; PSI, penile skin inversion; =, no change.
N, no; NS, not specified; Y, yes.
Complications
Overall pooled data including both surgical techniques showed the following complication rates: 1% (95% CI <0.1%–2%, I 2 = 65.8%) of fistula, 11% (95% CI 8%–14%, I 2 = 87.3%) of stenosis and/or strictures, 4% (95% CI 1%–9%, I 2 = 94.3%) of tissue necrosis, and 3% (95% CI 1%–4%, I 2 = 77.2%) of prolapse (Fig. (Fig.2 2 ).

Meta-analyses of different types of complications. Fistula (A), tissue necrosis (B), stenosis and strictures (C), and prolapse (D) are depicted.
Subgroup meta-analysis showed the following outcome complications for the penile skin inversion technique with or with our scrotal flaps: 1% (<0.1%–2%, I 2 = 57.5%) of fistula, 10% (8%–14%, I 2 = 85.5%) of stenosis and strictures, 5% (1%–10%, I 2 = 93.9.0%) of tissue necrosis, and 2% (1%–4%, I 2 = 78.1%) of prolapse. Complications for intestinal vaginoplasty were as follows: 2% (<0.1%–9%, I 2 = 83.3%) of fistula, 14% (5%–26%, I 2 = 91.7%) of stenosis and strictures, 1% (<0.1%–2%) of tissue necrosis in 1 study, and 6% (1%–14%, I 2 = 76.4%) for prolapse. Complications reported for the 2 surgical techniques had an I 2 value greater than 50% representing considerable heterogeneity.
Patient-reported Outcomes
Satisfaction rates were 91% (81%–98%, I 2 = 94.8%), 87% (77%–94%, I 2 = 88.6%), and 90% (84%–94%, I 2 = 69.4%) for overall, functional, and aesthetic outcomes, respectively (Fig. (Fig.3). 3 ). For the penile skin inversion technique, patient-reported outcomes showed a satisfaction rate of 87% (78%–94%, I 2 = 88.3%) for overall satisfaction, 87% (74%–96%, I 2 = 90.9%) for functional outcomes, and 90% (84%–95%, I 2 = 71.0%) for aesthetical outcomes. For the intestinal vaginoplasty technique, patient-reported outcomes showed a satisfaction rate of 99% (97%–100%) for overall satisfaction, 86% (75%–95%, I 2 = 55.3%) for functional outcomes, and 86% (69%–94%) for aesthetic outcomes.

Meta-analyses of different types of patient-reported outcomes. Overall satisfaction (A), functional outcomes (B), and aesthetic outcomes (C) are depicted.
Overall, the ability to achieve orgasm was 76% (64%–86%, I 2 = 93.1%). In the subgroup analysis, the ability to achieve orgasm was 73% (60%–84%, I 2 = 92.8) for the penile skin inversion technique and 95% (88%–99%) for intestinal vaginoplasty (Fig. (Fig.4 4 ).

Meta-analysis of ability to achieve orgasm.
The overall regret rate was 2% (95% CI <1%–3%, I 2 = 0%). The regret rate was 2% (95% CI <1%–4%, I 2 = 0%) for the penile inversion technique and <1% (95% CI <1%–20%) for the intestinal-based vaginoplasty group (Fig. (Fig.5 5 ).

Meta-analysis of regret rates.
Vaginal Cavity Dimensions
Fifteen studies reported vaginal cavity length (Fig. (Fig.6). 6 ). The average neovaginal length for both surgical techniques was 10.9 cm (9.2–12.8 cm, I 2 = 93.5%). In the subgroup analysis, the average length was 9.4 cm (7.9–10.9 cm, I 2 = 84.6%) for the penile skin inversion technique and 15.3 cm (13.8–16.7 cm, I 2 = 0.0%) for the intestinal vaginoplasty group.

Meta-analysis of depth of neovagina. Weights are from random effects analysis.
The gender confirmation process involves a comprehensive treatment program including endocrine therapy, psychological treatment, breast surgery, facial surgery, and genital confirmation surgery. 5 Of all treatment modalities, genital surgery is generally the final stage of the gender confirmation process and is associated with significant improvement in both mental and sexual quality of life. 5
Various techniques have been described for transfemale vaginoplasty; most of these techniques have been adapted from procedures designed to treat vaginal agenesis 70 An optimal or ideal technique has not yet been determined due to the lack of sufficiently large comparative studies. However, penile inversion using a pedicle penoscrotal skin flap seems to be the first-line approach, as it is technically less complex and invasive when compared to other techniques while providing great cosmetic and functional results. Nevertheless, patients with penile hypoplasia (penile shaft less than 8 cm) pose a challenge to the surgeon, as they usually do not have sufficient penile skin to create the neovaginal cavity. In such cases, skin grafts from the lower abdomen or thighs are necessary. Additionally, intestinal transposition vaginoplasty emerges as a reasonable option, in which rectosigmoid or ileal segments are isolated (through open or minimally invasive approach) and transferred into the neovaginal space. The advantage of using an intestinal conduit is its length, texture, lubrication, and appearance similar to a natural vagina. However, it should be noted that an abdominal surgery is required, and there is a risk of colitis, peritonitis, intestinal obstruction, junctional neuroma, introital stenosis, mucocele, and constipation. 71 Furthermore, colonic mucosa is more vulnerable to sexually transmitted diseases and further screening for colon cancer is required. 71 , 72
Various grafts such as pedicle genital or nongenital skin flaps have also been described. 11 , 12 , 70 , 72 – 74 Skin graft vaginoplasty is not limited by a vascular pedicle. This ensures that there can be significantly more skin harvested if required to line the neovaginal cavity. Nonetheless, a circumferential skin graft tends to scar and contract leading to neovaginal stenosis in 33%–45% of cases, representing a real disadvantage of this technique. 72 , 73 In addition, undesirable scarring and hypopigmentation of donor sites are also major drawbacks. Hence, this approach is less likely to be utilized in current surgical practice. However, skin grafting may be used as an adjunct of other approaches, for instance when there is not enough tissue for the creation of the neovagina from penile skin alone. 70 Other options for reconstructing a neovagina are emerging, and include, but are not limited to the use of buccal mucosa, amnion grafts, or decellularized tissue. 11
In our analysis, the vast majority of studies included penile skin inversion with or without scrotal flaps. However, with the updated search, we included 2 studies reporting intestinal-based vaginoplasties, one of which was the largest retrospective study among this group including a total of 386 sigma-lead rectosigmoid colon vaginoplasties in India. 67 Only 1 study with amnion grafts was identified but not included in the meta-analysis. In general, quality of the studies was either low or moderate. Most of them were retrospective studies with no control group.
The largest study within the intestinal-based vaginoplasty group was conducted by Kaushik et al 67 in India and included a total of 386 sigma-lead rectosigmoid vaginoplasty. They reported a 20.2% complication rate of which the majority were minor complications (97.4%). A total of 11.4% required reoperations: 2.6% due to introital stricture and mucosal prolapse and 8.8% for elective minor aesthetic enhancement. Satisfaction was reported as 4.7 over a 5-point scale.
Slight changes were identified in this updated meta-analysis as compared with the previous meta-analysis. The differences between studies in complication rates and in patient-reported outcomes including overall, functional, and aesthetic outcomes, ranged from 1 to 4 percentage points. This reflects a stable prevalence among these outcomes, which may be translated as neither an improvement nor a decline in surgical quality standards. From all the complications of interest, fistula had the lowest rate with only 1% (<0.1%–2%), whereas stenosis and strictures had the highest rate with 11% (8%–14%). For stenosis and strictures, intestinal-based vaginoplasty had the highest complication rate with 14% (5%–26%) compared with the penile skin inversion technique with 10% (8%–14%). However, stenosis rates were lower compared with the previous meta-analysis.
Interestingly, the ability to achieve orgasm after both vaginoplasty techniques increased compared with the previous meta-analysis: from 70% (54%–84%) to 76% (64%–86%), respectively. The intestinal-based vaginoplasty technique reported the highest ability to achieve orgasm with 95% (88%–99%) compared with the penile skin inversion technique with 73% (60%–84%). This may be translated as an improvement in surgical techniques in preserving genital sensation.
Very low regret rates have been a common denominator among transfemale patients who undergo vaginoplasty. The prevalence of regret was almost the same as our previous meta-analysis, with only 1 point of difference: 1% (<1%–3%) and 2% (<1%–3%), respectively. For vaginal length, there was a 1.3 cm of difference compared with our previous report. Hence, no important changes were presented with regard to these 2 outcomes.
Gender confirmation surgery, and genital surgery particularly, does not fall within a single specialty’s scope of practice. 74 A multidisciplinary approach is typically required, involving endocrinology and psychology. It is essential to integrate mental health professionals, who are knowledgeable about the assessment and treatment of gender dysphoria and physical and sexual health in the preoperative and postoperative setting. The overall focus is to help maximize the patient´s psychological and physical state to improve quality of life. 3 , 75
CONCLUSIONS
Transfemale vaginoplasty is a key component of the comprehensive surgical treatment of TGNB patients with gender dysphoria. To improve quality of care, a multidisciplinary approach is always necessary. Over the next several years, we will see an increase demand for these procedures, so adequate surgical training, clinical/surgical experience and research outcomes are very much needed, as we continue to strive to provide the best care possible for a population in need.
ACKNOWLEDGMENT
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Supplementary Material
Published online 19 March 2021
This is an invited article for the transgender mini-series.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. All authors have completed the ICMJE uniform disclosure form.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com .

IMAGES
VIDEO
COMMENTS
A US study showed that from 2000 to 2011, the rate of surgical sex reassignment measures among trans persons rose from 72% to 83.9% ().These data move the question of the effectiveness of such operations increasingly into the focus of clinical attention and awareness (8- 11).In the context of evidence-based medicine, the consensus is now that the success of medical procedures should not be ...
However, limitations such as significant heterogeneity among studies and among instruments used to assess regret rates, and moderate-to-high risk of bias in some studies represent a big barrier for generalization of the results of this study. ... Adolescents with gender identity disorder who were accepted or rejected for sex reassignment ...
Effects of different steps in gender reassignment therapy on psychopathology: a prospective study of persons with a gender identity disorder. The Journal of Sexual Medicine, 11(1), 119-126. Introduction: At the start of gender reassignment therapy, persons with a gender identity disorder (GID) may deal with various forms of psychopathology.
Gender surgery improves quality of life. Dr. Hess and colleagues surveyed 156 people who had all had gender reassignment surgery 6.61 years prior to the study, on average. The survey included open ...
Results confirm previous results showing the procedures to be generally successful. More than 4,680 cases are now part of the meta-analysis. "Penile inversion makes up about 80% of the procedures and pedicle intestine techniques are about 12% to 14%," Dr. Mascaro says. "There are other clinical flaps that can be used as well.".
Studies of mortality and somatic well-being after sex-reassignment surgery (SRS) of transsexual individuals are equivocal. Accordingly, the present study investigated mortality and somatic morbidity using a sample of transsexual individuals who comprised 98% (n = 104) of all surgically reassigned transsexual individuals in Denmark.
Purpose: Gender dysphoria (GD) is an incompatibility between biological sex and personal gender identity; individuals harbor an unalterable conviction that they were born in the wrong body, which causes personal suffering. In this context, surgery is imperative to achieve a successful gender transition and plays a key role in alleviating the associated psychological discomfort. In the current ...
That year, 9.3 percent of people with gender incongruence visited a doctor for mood disorders, 7.4 percent saw a doctor for anxiety disorders and 29 percent were on antidepressants.
We assessed the outcomes of gender-affirming surgery (GAS, or sex-reassignment surgery) 4 to 6 years after first clinical contact, and the associations between postoperative (dis)satisfaction and quality of life (QoL). ... With a response rate of 37%, similar to the attrition rates of most follow-up studies ...
Research consistently shows that people who choose gender affirmation surgery experience reduced gender incongruence and improved quality of life. Depending on the procedure, 94% to 100% of people report satisfaction with their surgery results. Gender-affirming surgery provides long-term mental health benefits, too.
We assessed the outcomes of gender-affirming surgery (GAS, or sex-reassignment surgery) 4 to 6 years after first clinical contact, and the associations between postoperative (dis)satisfaction and quality of life (QoL). Our multicenter, cross-sectional follow-up study involved persons diagnosed with gender dysphoria (DSM-IV-TR) who applied for ...
Key Points. Question What are the temporal trends in gender-affirming surgery (GAS) in the US?. Findings In this cohort study of 48 019 patients, GAS increased significantly, nearly tripling from 2016 to 2019. Breast and chest surgery was the most common class of procedures performed overall; genital reconstructive procedures were more common among older individuals.
When he was 14, Reimer began the process of reassignment to being a male. As an adult, he married a woman but depression and drug abuse ensued, culminating in suicide at the age of 38 (1). Money's ...
119 (46.9%) of the patients filled out and returned the questionnaires, at a mean of 5.05 years after surgery (standard deviation 1.61 years, range 1-7 years). 90.2% said their expectations for life as a woman were fulfilled postoperatively. 85.4% saw themselves as women. 61.2% were satisfied, and 26.2% very satisfied, with their outward ...
Key Points. Question What is the rate of regret and satisfaction with decision after 2 years or more following gender-affirming mastectomy?. Findings In this cross-sectional study of 139 survey respondents who underwent gender-affirming mastectomy, the median satisfaction score was 5 on a 5-point scale, with higher scores indicating higher satisfaction.
Access to gender-affirming hormones and potential access to gender-affirming surgery is available at age 16—and then, in the case of transmasculine youth, only mastectomy, also known as top surgery.
Delayed short-depth neovagina occurred in 21% of patients, requiring additional hard dilatation, with a 95.5% success rate. Total secondary vaginoplasty rate was 6.3% (4.7% skin graft and 3.7% bowel plasty). Secondary functional meatoplasty occurred in 1% of cases. Other secondary cosmetic surgery rates ranged between 3 to 20%.
Sex "reassignment" doesn't work. ... Ten to 15 years after surgical reassignment, the suicide rate of those who had undergone sex-reassignment surgery rose to 20 times that of comparable ...
Gender reassignment surgeries are expensive. Male-to-female procedures cost between $7,000 and $24,000, and the cost of female-to-male procedures can reach $50,000. The complications and the ...
A 2022 study notes that complications from gender-affirming mastectomy procedures are low, and satisfaction rates are incredibly high. Removal of the uterus, ovaries, and fallopian tubes
Unfortunately, the transgender population has largely suffered from transgender-related discrimination in healthcare and employment, and from high rates of mental illness, particularly anxiety and depression, in addition to violence and health-related problems. 1,2 This population expresses their gender identity in many different ways. Some use ...
What the Equality Act says about gender reassignment discrimination. The Equality Act 2010 says that you must not be discriminated against because of gender reassignment. In the Equality Act, gender reassignment means proposing to undergo, undergoing or having undergone a process to reassign your sex. To be protected from gender reassignment ...
The study, published in 2011, estimated the "mortality, morbidity, and criminal rate after surgical sex reassignment of transsexual persons" of "324 "sex-reassigned persons" in Sweden for 30 years.
reasonably may constitute sex discrimination, including sexual violence and other forms of sex-based harassment. These regulations also require that schools train employees about the school's obligation to address sex discrimination, as well as employees' obligations to notify or provide contact information for the Title IX Coordinator.