

Improving Health in India
As the world’s second-most-populous country and one of its fastest-growing economies, India faces both unique challenges and unprecedented opportunities in the sphere of public health.
For more than a decade, India has experienced record-breaking economic growth that has been accompanied by significant reductions in poverty. According to the World Bank, infant mortality in India fell from 66 to 38 per 1,000 live births from 2000 to 2015. Life expectancy at birth has increased from 63 to 68 years, and the maternal mortality ratio has fallen from 374 to 174 per 100,000 live births over the same period.
India also has dynamic pharmaceutical and biotechnology industries; world-class scientists, including a burgeoning clinical trials industry; and leading hospitals that attract foreign patients and treat its better-off citizens.
Yet Indian government and public health officials agree that the country also faces persistent and daunting public health challenges, particularly for the poor. These include child undernutrition and low birth weights that often lead to premature death or lifelong health problems; high rates of neonatal and maternal mortality; growth in noncommunicable diseases such as obesity, diabetes, and tobacco use, leading to cancer and other diseases; and high rates of road traffic accidents that result in injuries and deaths.
As the Indian government strives to provide comprehensive health coverage for all, the country’s rapidly developing health system remains an area of concern. There are disparities in health and health care systems between poorer and richer states and underfunded health care systems that in many cases are inefficiently run and underregulated. New government-financed health insurance programs are increasing coverage, but insurance remains limited.
Public and private health systems are placing huge demands on the country’s capacity to train exceptional health leaders and professionals. Rising to meet these challenges, the people of India have an opportunity to have a major influence on their own future health and on the future of public health and medical efforts globally.
Supporting Development of India’s Health Workforce
The Harvard T.H. Chan School of Public Health is collaborating with partners across India to address those challenges. Together, the School and its partners are introducing educational innovations to India to expand skills training, degree programs, and leadership development at new schools and institutes of public health. We seek to leverage the School’s resources to help strengthen public health training and build capacity across the health sector in India.
Featured Topics
Featured series.
A series of random questions answered by Harvard experts.
Explore the Gazette
Read the latest.

Harvard stargazer whose humanity still burns bright

Taiwan sees warning signs in weakening congressional support for Ukraine

How dating sites automate racism
Community nurse Swasthya Sakhi, who was trained by the host organization, during a routine day at work in Kaniguma village’s Swasthya Swaraj clinic.
Photos by Amrit Vatsa
Amid pandemic tragedy, an opportunity for change?
Alvin Powell
Harvard Staff Writer
Mittal Institute/Lancet commission to study universal care in India
With almost 11 million cases and more than 150,000 deaths, India is among the nations hardest-hit by the coronavirus pandemic. The Asian giant has also taken an economic hit, its gross domestic product expected to shrink 8 percent this year.
The figures have starkly highlighted the connection between a nation’s physical and economic health, and the Harvard chairs of a new panel seeking to overhaul and improve health care in India say today’s difficult times create a moment of opportunity because people who often tune each other out are now listening.
“For the first time the connection between health and economic outcomes has become transparent,” said Tarun Khanna , director of Harvard’s Lakshmi Mittal and Family South Asia Institute and one of four co-chairs of a new Lancet Citizens’ Commission to study how to bring universal health care to India. “The morality of universal health care has always been a driver of this urgency, but that’s not the new thing here. Rather, for the first time in 30 years GDP is expected to fall in response to a health crisis.”
The 21-member commission is a joint effort between The Lancet medical journal and Mittal Institute. The panel is chaired by Khanna; Vikram Patel , the Pershing Square Professor of Global Health at Harvard Medical School ; Professor Gagandeep Kang, vaccine researcher at Christian Medical College in Vellore, India; and Kiran Mazumdar-Shaw, executive chairperson of Indian biotech company Biocon Ltd and one of India’s top businesspeople. S.V. Subramanian , professor of population health and geography at the Harvard T.H. Chan School of Public Health , is a member of the commission.
The group’s charge is to report by August 2022 how India can achieve universal health care within a decade. The Mittal Institute is encouraging participation by the Harvard community and sponsoring an online panel discussion on Monday to introduce the effort.
Patel and Khanna said the commission has a challenging road ahead, one that has proven too difficult for an array of efforts studying the same question in the decades since India became independent in 1947.
Most of the nation’s 1.4 billion residents (a population second only to China) view the current publicly-funded system as so bad that even the poorest Indians would rather pay out-of-pocket for care in a network of private providers, itself sometimes seen as uncaring and untrustworthy. The end result is that more than 60 percent of Indian health care is paid for out-of-pocket, and a sudden illness can mean financial ruin for millions. Only the wealthy can afford regular, high-quality care.
Sandeep Praharsha (India Fellow) discussing preventive measures for malaria in Kerpai village in Thumul Rampur block of Kalahandi district in Odisha Swasthya Swaraj.
“Today, India’s health care system is routinely ranked as one of the worst in the world,” Patel said. “A few get expensive, world-class care, while a large part of the population doesn’t even get basic quality care.”
Where the current commission differs from prior efforts is that it is based on a consultative effort to seek input from an array of stakeholders, including representatives of the private health care sector, providers of traditional medicine, physicians, community health workers, and citizens from diverse communities across the country.
“It genuinely is a cross-section of society,” said Khanna, HBS’ Jorge Paulo Lemann Professor. “That makes consultation more complex, but the potential for achievement is large.”
The eventual report will focus on the “architecture” of a new system, according to an article by the initiative’s co-chairs and commissioners in The Lancet in December. It will include ways to provide preventive care for physical and mental health, offer financial protection for all health care costs, not just hospitalization, and ensure access to the same quality of care for all.
“We aspire for a health care system in which most people do not pay out-of-pocket for most health care needs,” Patel said. “The last thing a sick person needs is to have their care calibrated by how much they can afford to pay or to be impoverished by their medical bills.”
Resources are always a key issue in consideration of universal health care and India — whose proportion of GDP spent on health care is low compared with other middle-income countries — will likely have to spend more, Khanna said. But he also said that significant low-cost steps probably could be taken early in the process.
“I think we can improve outcomes with existing resources being better managed,” Khanna said. “We can get some victories in the next two to three years through optimization of existing structures.”
Share this article
You might like.
Seminar foregrounds Harlow Shapley, who helped scholars escape Nazi rule

Ambassador says if Russia is allowed to take over sovereign nation, China may try to do same

Sociologist’s new book finds algorithms that suggest partners often reflect stereotypes, biases
Yes, it’s exciting. Just don’t look at the sun.
Lab, telescope specialist details Harvard eclipse-viewing party, offers safety tips
Forget ‘doomers.’ Warming can be stopped, top climate scientist says
Michael Mann points to prehistoric catastrophes, modern environmental victories

Essay on Healthcare in India
Students are often asked to write an essay on Healthcare in India in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Healthcare in India
Introduction.
Healthcare in India is a critical sector. It includes public and private hospitals, clinics, and other medical facilities.
Public Healthcare
The government provides public healthcare. It’s often free or low-cost, making it accessible to many people.
Private Healthcare
Private healthcare, on the other hand, is usually more expensive. However, it tends to have better facilities and shorter wait times.
India faces challenges in healthcare, like inadequate facilities in rural areas and a shortage of trained medical professionals.
Despite these challenges, India is striving to improve its healthcare system for everyone.
250 Words Essay on Healthcare in India
Healthcare in India is a multifaceted system, encompassing public and private sectors, traditional and modern medicine, and urban and rural disparities. This essay explores the current state of healthcare in India, its challenges, and potential solutions.
Current State of Healthcare
India’s healthcare sector has made significant strides, with increased life expectancy and decreased infant mortality. However, it is riddled with disparities. While urban areas enjoy better healthcare facilities, rural regions grapple with inadequate infrastructure and lack of trained medical personnel.
The challenges are manifold. Accessibility and affordability remain major concerns. A large portion of the population lacks access to quality healthcare, while high out-of-pocket expenses push many into poverty. Furthermore, there is a significant shortage of healthcare professionals, particularly in rural areas.
Public-Private Partnership
A public-private partnership (PPP) is seen as a viable solution. The private sector’s resources and efficiency can supplement the public sector’s reach and affordability. However, the implementation of PPPs requires stringent regulations to prevent exploitation.
Role of Technology
Technology can bridge the urban-rural divide. Telemedicine, AI, and mobile health technologies can facilitate remote consultations, predictive diagnostics, and health monitoring, making healthcare more accessible and affordable.
While India’s healthcare system faces significant challenges, the combination of public-private partnerships and technology can pave the way for an efficient, inclusive, and affordable healthcare system. It is crucial for policymakers, healthcare providers, and technology companies to work together towards this common goal.
500 Words Essay on Healthcare in India
India’s healthcare sector is a study in contrasts, presenting a complex tapestry of cutting-edge advancements and systemic challenges. With an expansive population and diverse health needs, the healthcare system in India is a critical component of the nation’s development agenda.
The Landscape of Indian Healthcare
India’s healthcare infrastructure is a mix of public and private providers. The public system, under the aegis of the Ministry of Health and Family Welfare, provides primary, secondary, and tertiary care. However, it suffers from inadequate funding, lack of infrastructure, and a dearth of healthcare professionals. The private sector, on the other hand, is burgeoning. It is technologically advanced, offers high-quality services, but is often criticized for being expensive and inaccessible to the poor.
Healthcare Accessibility and Affordability
Access to quality healthcare is a significant issue in India. Rural areas, in particular, face a shortage of healthcare facilities and professionals. The urban-rural divide is stark, with the majority of quality healthcare services concentrated in cities. Affordability is another concern. High out-of-pocket expenses push many into poverty every year. The situation calls for a robust health insurance framework to protect citizens from catastrophic health expenditures.
Government Initiatives
Recognizing these challenges, the Indian government has launched various initiatives. The National Health Mission aims to improve health outcomes, particularly for the rural population. The Ayushman Bharat scheme, launched in 2018, provides health insurance coverage to the underprivileged, aiming to make healthcare more affordable. These initiatives, while commendable, need effective implementation and monitoring to ensure their success.
Technological Innovations
Technological innovations have the potential to revolutionize India’s healthcare landscape. Telemedicine, artificial intelligence, and digital health records can address the issues of accessibility and affordability. Telemedicine can bridge the urban-rural divide by providing remote consultations. AI can assist in disease prediction and management, while digital health records can streamline patient data, improving efficiency and patient care.
Challenges and Future Prospects
Despite these advancements, India’s healthcare system faces significant challenges. The COVID-19 pandemic has exposed the fragility of the healthcare infrastructure, with hospitals overwhelmed and resources stretched thin. India also grapples with a dual disease burden – communicable diseases like tuberculosis and non-communicable diseases like diabetes and heart disease.
The future of healthcare in India lies in adopting a holistic approach. This includes increasing public health expenditure, strengthening primary healthcare, improving health literacy, and leveraging technology.
India’s healthcare sector, while fraught with challenges, is teeming with potential. With the right mix of policy interventions, technology adoption, and a focus on equitable access, India can transform its healthcare landscape, ensuring a healthier future for its citizens. The journey is long and arduous, but with concerted efforts, a robust and inclusive healthcare system is achievable.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on Handloom and Indian Legacy
- Essay on Growth of Banking Sector in India
- Essay on Greatness of India
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Skip to primary navigation
- Skip to main content
- Skip to primary sidebar
UPSC Coaching, Study Materials, and Mock Exams
Enroll in ClearIAS UPSC Coaching Join Now Log In
Call us: +91-9605741000
Healthcare Sector in India
Last updated on April 8, 2024 by ClearIAS Team
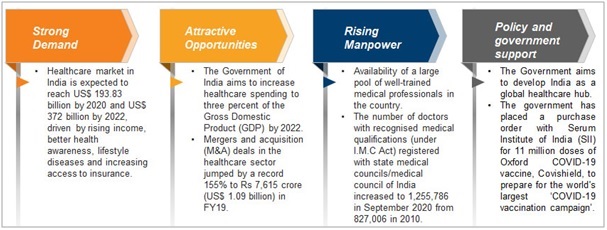
Healthcare sector in India has grown significantly in both employment and income. Over the past two years, technology and innovation in healthcare have become more prominent, and 80% of healthcare systems plan to increase their investment in digital healthcare technologies over the next five years. Read here to learn more about the Indian Healthcare sector.
The Healthcare sector in India comprises of hospitals, medical devices, clinical trials, outsourcing, telemedicine, medical tourism, health insurance, and medical equipment.
Due to improved services, coverage, and rising spending by both public and private entities, the Indian healthcare industry is expanding quickly.
Growing incidence of lifestyle diseases, rising demand for affordable healthcare delivery systems due to the increasing healthcare costs, technological advancements, the emergence of telemedicine, rapid health insurance penetration, and government initiatives like e-health together with tax benefits and incentives are driving the healthcare market in India.
Also read: National Medical Commission (NMC)
Table of Contents
Healthcare sector in India
The public and private sectors make up the two main components of India’s healthcare delivery system.
Join Now: UPSC Prelims cum Mains Course
- The government, or public healthcare system, concentrates on establishing primary healthcare centers (PHCs) in rural areas while maintaining a small number of secondary and tertiary care facilities in major cities.
- The bulk of secondary, tertiary, and quaternary care facilities are run by the private sector, with a focus on metropolises and tier-I and tier-II cities.
The abundance of highly qualified medical personnel in India is a competitive advantage. India’s costs are competitive with those of its neighbors in Asia and the West.
- Surgery in India costs roughly a tenth of what it does in the US or Western Europe.
- The low cost of healthcare has led to an increase in medical tourism in the nation, drawing people from all over the world.
- Further, due to its relatively low cost of clinical research, India has become a center for R&D activity for foreign businesses.
The Indian Medical Value Travel Market size is valued at $5-6 bn and is expected to grow to $13 bn by 2026.
- Over the years, India has become a premier and attractive destination for travelers from across the globe to attain best-in-class clinical treatment, recharge, and rejuvenate
- The high-end healthcare system in India is as good as the best in the world with complex surgical procedures being done in world-class global hospitals by acclaimed medical specialists at a much lower cost than what it normally takes in other countries
- India has also become a favored destination for Yoga and Wellness with its focus on traditional therapies through AYUSH.
- Indian hospitals are largely switching to AI for keeping health records & providing the best possible treatment to patients at the right time.
India is ranked 10th by the Medical Tourism Association on the Medical Tourism Index (MTI) for 2020-21 out of 46 destinations of the world, 12th in the top 20 wellness tourism markets globally, and 5th in wellness tourism markets in Asia-Pacific.
- India has a large number of accredited facilities, that provide care at par or above global standards.
- There are 40 Joint Commission International (JCI) accredited and 1400+ National Accreditation Board for Hospitals & Healthcare Providers (NABH) accredited hospitals that provide care of quality standards.
India offers the largest pool of doctors and paramedics with high-quality medical training received globally, along with fluency in English.
Also read: Palliative Care in India
Join Now: CSAT Course
Healthcare sector in numbers
The hospital industry in India, accounting for 80% of the total healthcare market, is witnessing a huge investor demand from both global as well as domestic investors.
- In 2020, India’s Medical Tourism market was estimated to be worth $5-6 Bn and is expected to grow to $13 Bn by 2026.
- The healthcare sector in India is expected to grow to reach a size of $50 bn by 2025.
- The digital healthcare market is expected to more than 20% by 2023.
- The Telemedicine market is the maximum potential eHealth segment in India, which is expected to touch $5.4 Bn by 2025
- In the Economic Survey of 2022, India’s public expenditure on healthcare stood at 2.1% of GDP in 2021-22 against 1.8% in 2020-21 and 1.3% in 2019-20.
- Over the next 10 years, National Digital Health Blueprint can unlock the incremental economic value of over $200 bn for the healthcare industry in India
- India has the world’s largest Health Insurance Scheme (Ayushman Bharat) supported by the government.
- 100% FDI is allowed under the automatic route for greenfield projects.
- For investments in brownfield projects, up to 100% FDI is permitted under the government route.
- To promote medical tourism in the country, the government of India is extending the e-medical visa facility to the citizens of 156 countries.
- India is emerging as a strong market for wearables, with approximately 2 million units sold in 2017, expected to reach 129 million units in 2030.
- India’s surgical robotics market is estimated to expand to hit the size of $350 mn by 2025.
Also read: Indian Health Sector Problems – Can the National Health Policy 2017 Make a Change?
The healthcare system still faces a variety of problems, such as inadequate budget, a scarcity of healthcare staff, and inadequate infrastructure, despite substantial advancements in recent years.
- India suffers from a hospital deficit, especially in rural areas, and many of the country’s current healthcare institutions need basic supplies and equipment.
- In India, the quality of healthcare varies greatly, with insufficient regulation leading to subpar care in some private healthcare facilities and rural areas with inadequate facilities and resources.
- Over 60% of all deaths in India are caused by non-communicable diseases (NCDs) , which also have high rates of chronic illnesses like diabetes , cancer , and heart disease.
- India is one of the countries with the least mental health specialists per person.
- The government spends very little money on mental health. Poor mental health outcomes and insufficient care for those with mental illnesses are the results of this.
- The imbalance in the doctor-patient ratio is one of the most important issues. The Indian Journal of Public Health estimates that India will require 20 lakh doctors by 2030.
Government initiatives for the healthcare sector
- Pradhan Mantri Swasthya Suraksha Yojana (PMSSY)
- National Health Mission
- Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana (AB-PMJAY)
- Pradhan Mantri-Ayushman Bharat Health Infrastructure Mission (PM-ABHIM) to strengthen India’s health infrastructure and improve the country’s primary, secondary and tertiary care services.
- Ayushman Bharat Digital Mission to connect the digital health solutions of hospitals across the country. Under this, every citizen will now get a digital health ID and their health record will be digitally protected.
- ‘National Medical & Wellness Tourism Board’ to promote medical and wellness tourism in India.
- National Ayush Mission, responsible for the development of traditional medicines in India, as a centrally sponsored scheme until 2026.
- MoU between India and Denmark on cooperation in health and medicine. The agreement will focus on joint initiatives and technology development in the health sector, to improve the public health status of the population of both countries.
Way forward
The healthcare industry in India is very diversified and offers numerous opportunities in each of the provider, payer, and medical technology segments.
Businesses are trying to investigate the newest dynamics and trends that will have a beneficial impact on their business as a result of the increased competition.
Join Now: UPSC Prelims Test Series
Medical device manufacturers have a lot of prospects in India.
- With significant capital expenditure for cutting-edge diagnostic facilities, the nation has also emerged as one of the top locations for high-end diagnostic services, serving a larger section of the populace.
- Additionally, Indian customers of medical services are more concerned with maintaining their health.
- Future demand for healthcare services is anticipated to increase due to factors such as advancing income levels, an aging population, rising health awareness, and shifting attitudes toward preventative healthcare.
- Healthcare spending increased as a result of more people having health insurance, and this trend is expected to continue over the next 10 years.
The Government aims to develop India as a global healthcare hub and is planning to increase public health spending to 2.5% of the country’s GDP by 2025.
Read: Climate Resilient Health Systems
-Article written by Swathi Satish

Take a Test: Analyse Your Progress
Aim IAS, IPS, or IFS?

About ClearIAS Team
ClearIAS is one of the most trusted learning platforms in India for UPSC preparation. Around 1 million aspirants learn from the ClearIAS every month.
Our courses and training methods are different from traditional coaching. We give special emphasis on smart work and personal mentorship. Many UPSC toppers thank ClearIAS for our role in their success.
Download the ClearIAS mobile apps now to supplement your self-study efforts with ClearIAS smart-study training.
Reader Interactions
August 8, 2023 at 9:47 pm
Difference between positive aspects and negative aspects of healthcare issue in india….
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Don’t lose out without playing the right game!
Follow the ClearIAS Prelims cum Mains (PCM) Integrated Approach.
Join ClearIAS PCM Course Now
UPSC Online Preparation
- Union Public Service Commission (UPSC)
- Indian Administrative Service (IAS)
- Indian Police Service (IPS)
- IAS Exam Eligibility
- UPSC Free Study Materials
- UPSC Exam Guidance
- UPSC Prelims Test Series
- UPSC Syllabus
- UPSC Online
- UPSC Prelims
- UPSC Interview
- UPSC Toppers
- UPSC Previous Year Qns
- UPSC Age Calculator
- UPSC Calendar 2024
- About ClearIAS
- ClearIAS Programs
- ClearIAS Fee Structure
- IAS Coaching
- UPSC Coaching
- UPSC Online Coaching
- ClearIAS Blog
- Important Updates
- Announcements
- Book Review
- ClearIAS App
- Work with us
- Advertise with us
- Privacy Policy
- Terms and Conditions
- Talk to Your Mentor
Featured on

and many more...
- Our Centers Delhi Bhubaneswar Lucknow
Current Affairs for UPSC IAS
Indian health sector: opportunities and challenges.
- Category Economy
- Published 13th Apr, 2021
In Budget 2021 health sector is focused on by Government, which was severely hit by the unprecedented pandemic. The focus has been laid on healthcare and infrastructure with an eye on achieving the vision of Atmanirbhar Bharat.
- The unprecedented COVID-19 pandemic has completely changed the situation no one could ever imagine. Almost all aspects of society have witnessed disruptions.
- However, every challenge comes with various opportunities, so does this pandemic.
- It has opened a wide window of opportunities to restructure and reform the Indian health industry which has been in a bad state of repair.
- Underscoring the significant importance of health and wellbeing for the growth and development of the country, the Budget allocation for the same was increased to ?2,23,846 crore in 2021-22 as against this year's ?94,452 crores, according to an official release.
- This manifests into an increase of 137%.
Assessing Indian Healthcare Industry
- In India, the Health care sector is one of the largest sectors in terms of both revenue and employment.
- Public health care hospitals comprise secondary and tertiary care institutions in urban areas while primary basic facilities are focused in rural areas.
- Private health care sectors provide secondary, tertiary, and quaternary services in metro cities.
Healthcare Industry in India
What are the issues and concerns of the Sector?
India’s health care sector has achieved some positive achievements on the health indicators but suffers some serious shortcomings in care delivery.
- Inadequate reach: The inadequate reach of basic healthcare services, shortage of medical personnel, quality assurance, the inadequate outlay for health, and most importantly insufficient impetus to research.
- Inadequate Fund: The inadequate fund allocation by the administrations is one of the grave concerns.
- Optimal Insurance: The concept of health insurance is still not clear in India and the market is still virgin.
- No focus on Preventive Care : In India, there is a very low emphasis on preventive care, which can be proved very effective in solving a lot of problems for the patient in terms of misery or financial losses.
- Less emphasis on Medical Research: In India, there is no much impetus is being given to R&D and cutting-edge technology-led new initiatives. Such technologies could be useful in an unprecedented situation like Covid-19.
- Issue of Policymaking: For providing effective and efficient healthcare services policymaking is certainly an important aspect. In India, the problem is fundamental of supply than demand, where policymaking can be effective.
- Shortage of Medical Workforce: In India, there is a shortage of doctors, nurses, and other staff in the health sector. As per a report laid down by a minister in Parliament, there is a shortage of 600,000 doctors in India.
- Inadequate outlay for health: As per National Health Policy 2002, India contributes only 0.9 percent of its GDP to the Health care sector.
- Lack of structure: Private hospitals are expensive and public hospitals are either not enough for the Indian Population or lack the basic facilities.
Opportunities in Health Care Sector
- Indian health care sector is expected to increase to Rs. 8.6 trillion (US$ 133.44 billion) by 2022. It is almost three times which is what it’s now in present.
- Data Analytics: With the arrival of the National Digital Health Mission (NDHM), the digital Health ID will come which will store the data of patients. It would help in effective policymaking and private players can get an edge in introducing the new technologies in the market.
- Employment opportunity: As we know Indian health care sector lacks a workforce, there is a space for thousands of employees.
- Start-ups: With the help of Government and private players an environment of start-ups and entrepreneurship can be created in this field.
- Medical Tourism: India is already one of the favorite medical Tourism Destinations in the world and in the upcoming years this sector can be harnessed efficiently.
What measures are required in the sector?
- Improving infrastructure: There is a need of improvising the infrastructure of public hospitals which have a lot of burden due to the high population in India.
- Focus on private hospitals: Private hospitals must be encouraged by the government because their contribution is important. Private sector also needs to participate because the challenges are significant and these cannot be resolved only by the government alone.
- Efficiency enhancement: More medical personnel must be recruited to enhance the capabilities and efficiency of the sector.
- Technology utilisation: Technologies must be used to connect the dots in the health system. Medical devices in hospitals/ clinics, mobile care applications, wearables, and sensors are some forms of technology that should be added in this sector.
- Awareness: People should be made aware of early detection and preventive care. It would help them in saving pocket expenditure also.
The year 2021 could be the year when India consolidates and expands on its social determinants of health (SDH) approach. India now needs to sustain its current interest in strategic health policy as a key pillar of the economy.
Related Articles
State’s Borrowing Limits and Challenges(Special)
The evolution of Neuroscience & Concerns
US-UK Partnership on AI
PRATUSH - India's Moon based Telescope
Cyber Slavery
Russia’s war limits ability to track Arctic climate

Verifying, please be patient.
Our Centers
DELHI (Karol Bagh)
GS SCORE, 1B, Second Floor, Pusa Road, Karol Bagh, New Delhi - 110005 (Beside Karol Bagh Metro Station Gate No. 8)
Get directions on Google Maps
BHUBANESWAR (Jaydev Vihar)
GS SCORE, Plot No.2298, Jaydev Vihar Square, Near HCG Day Care, BBSR - 751013
LUCKNOW (Aliganj)
GS SCORE, 2nd Floor, B-33, Sangam Chauraha, Sector H, Aliganj, Lucknow, UP - 226024

© 2024 IAS SCORE. All Rights Reserved
Welcome to our secure login portal. Access your account with ease.

- Using Password
Not registered yet? register here!
Welcome to our secure register portal. For a brighter future, register now and unlock endless learning opportunities.
User Register
Already have an account? Login
Oops, forgot your password? Don't worry, we've got you covered. Reset it here
Lost your login details? No problem! forgot your password in just a few clicks
Forgot Password
Verify your mobile number, you have successfully logged in.
Join Us on WhatsApp
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Equity Health


Health inequalities research in India: a review of trends and themes in the literature since the 1990s
Nandita bhan.
1 Public Health Foundation of India, New Delhi, India
Krishna Dipankar Rao
2 Johns Hopkins University, Baltimore, USA
Shivani Kachwaha
3 The Graduate Institute of International and Development Studies Geneva, Geneva, Switzerland
Associated Data
All data associated with this study are freely available and can be requested from the authors as needed.
Research on health inequalities can be instrumental in drawing attention to the health of socioeconomically vulnerable groups in India in the context of rapid economic growth. It can shape the dialogue for public health action, emphasizing the need for greater investments in health, and monitor effectiveness of health programs. Our objective was to examine trends in studies on health inequalities in the last 25 years.
We conducted a systematic literature review of studies on health inequalities published from 1990. The year, 1990, marked the beginning of economic reforms and liberalization in India. We searched PubMED using key terms to identify 8800 articles between 1990 and 2016; we identified 1,312 final studies for review. Key domains of analysis included measures of equity, health outcomes, populations studied, year of publication, study methodology, study focus (descriptive versus analytical), and location of main author.
We found an increase in studies on health inequalities after 2005. About 88 % of the studies utilized quantitative methods for analysis. About 8 % of the studies related to health interventions or programs; the number of intervention studies have been increasing since 2010. A majority of studies were led by authors based in India. Early studies focused on mortality, communicable and non-communicable diseases, and nutrition, while later studies have focused on non-communicable diseases, mental health, risk factors, and injuries. Studies on women and children comprised nearly half of the literature; studies on the youth (15–24 years or as defined by the study) and elderly have been rising. Wealth and income were the most common measures of equity, followed by education and gender. The proportion of studies on wealth, education, region and caste have stayed consistent over time, while studies on gender disparities have been rising.
In a country as diverse as India with large social inequalities combined with rapid economic growth, research on health inequalities has a special significance for policy. We recommend that studies on health inequalities in the future focus on evaluations of policy and health programs, and on underrepresented health outcomes and populations.
Research on health inequalities has been instrumental in drawing attention to the health of socially and economically vulnerable groups in India. It has shaped the dialogue for public health action, emphasized the need for greater and targeted investments in health, and can be an important marker for the effectiveness of public health services [ 1 – 5 ]. Importantly, health inequalities research enriches our understanding of societal disparities in health and healthcare, moving away from a narrow focus on income to include markers of deprivation like gender, caste, religion and occupation that afflict health and the quality of life. Research on health inequalities has now become one of the central pillars of the development dialogue [ 6 – 9 ]. This research profoundly influences health policy; the recent call for universal health coverage (UHC) represents the latest effort to reduce health disparities globally and in India [ 8 , 10 – 12 ].
Prior to the 1980s, few studies investigated health inequalities. There may be several reasons for this. Post-independence, the focus of health policy was increasing the coverage of health services and hence, research focused on the delivery of basic health services. Philosophical debates on nation-building and the role of modern medicine also led to a shift from investigations of the role of caste, religion and ethnicity [ 13 , 14 ]. Socioeconomic stratifiers were considered ‘shackles’, holding India back from modernization [ 15 , 16 ]. This vision and the recommendations of the Bhore Committee led to a number of clinical research studies [ 17 ]. The Bhore committee was set up in 1943 under Sir Joseph Bhore to make recommendations on improving public health system in India. The report envisioned a national health system that was tax funded and publicly run along the lines of the Beveridge model adopted in the United Kingdom. At the other end, social science studies were mainly investigating micro-perspectives and health practices of specific cultural groups leading to village studies, anthropological assessments and historical analyses [ 18 – 24 ].
In 1964, the Indian Journal for Medical Research (IJMR), a bi-annual journal of the ICMR, was turned to a monthly publication, increasing the scope for publishing more studies. Until then, few research journals published health studies and research and training in public health was the domain of physicians and departments of community medicine within medical colleges [ 25 ]. However, most published studies were clinical and the objective was to identify new clinical conditions and issues in different parts of India. Few studies focused on assessing health inequalities. The policy sphere was also devoid of discussion on health inequalities. Different governmental committees were engaged in evaluating health service delivery and improving coverage of health services [ 26 – 28 ].
A series of global and national events brought health inequalities on the policy radar. The Alma Ata ‘Health for All’ declaration emphasized the significance of primary health care for reducing health disparities [ 29 ]. People’s movements for health highlighted multiple deprivations faced by vulnerable groups globally. In Brazil, for instance, after 20 years of political dictatorship, movements for health as a fundamental right led to a constitutional amendment in 1988, based on the principle of reducing health disparities through a responsive public health infrastructure [ 30 ]. In India, the focus of research in the 1980s was on family planning, reproductive health and child survival [ 31 – 34 ]. Policy emphasis on the role of women in reducing health disparities in reproductive and child health led to mainstreaming of gender in research [ 35 , 36 ]. Gender and poverty were considered the structural determinants of health inequalities in maternal and child health. Health inequalities research also received a push with the WHO Commission on Social Determinants of Health (CSDH) [ 37 , 38 ]. This commission emphasized the importance of systematically investigating the role of social inequalities, particularly living conditions, for health.
Social and political movements also played an important role in highlighting inequalities. The landmark report on gender, ‘Towards Equality’, highlighted socioeconomic challenges faced by women in diverse domains of life [ 39 ]. Poverty and education have been central to Indian public policy and health [ 40 – 50 ]. Low rates of education among women was considered a major barrier in achieving health goals [ 2 , 31 ]. Movements related to caste, region and religion have also contributed to improving our understanding of inequalities [ 51 – 53 ].
Developments in health education, particularly the setting up of departments of preventive and social medicine in medical schools and health electives in other courses such as in social work built capacity for research on health inequalities in India [ 25 ]. Training and course development in these streams improved capacity for conducting field epidemiological studies. Early studies on the health burden emerged from surveillance sites set up by independent research groups affiliated to universities. The Indian Association of Preventive and Social Medicine (IAPSM) (1974) and launch of the Indian Journal of Community Medicine (IJCM) enhanced avenues for discussion and publication of research on health issues and the scope of training and research in these institutes.
A paradigm shift for research on health inequalities in India was seen with public availability of survey data. A Ministry for Statistics and Program Implementation had been set up shortly after independence to plan and conduct decennial census, population surveys and surveillance studies. However, for decades only few statistics were available in the public domain and raw data could not be acquired. The National Sample Survey Organization (NSSO) provided the first national level assessments of self-reported health and health care data on a cross-section of social and policy themes. Nutrition surveys conducted by the National Institute of Nutrition (NIN) gathered data on food and nutrition; this data remains underutilized. In the 1990s, the USAID funded the Demographic Health Surveys (DHS), a multi country cross-sectional survey focused on reproductive health and family planning [ 54 ]. In India, this was referred to as the National Family Health Survey and data are now available for three rounds (1992–93, 1999–2000 and 2005–06). In the 1980s, the national government also released the National Sample Surveys (NSS) which collect data from households on consumption, labor force participation and other key development themes [ 55 ]. Both these surveys led to a flurry of studies on health inequalities as data became available to both international and national researchers [ 56 , 57 ]. These research studies have added depth and richness to the understanding of health inequalities in India. While research on social inequalities including gender, caste, poverty and education is conducted by social scientists, research on health inequalities has been driven by cross-disciplinary groups of epidemiologists and social science scholars.
The main objective of this study was to examine the direction of health inequalities research in India over the last three decades to understand key patterns, themes and trends. With this research question , we conducted a review of published peer-reviewed studies on health inequalities in India to understand the issues examined and key gaps in present research.
In this study, we reviewed published studies to examine trends in health inequalities research in India since 1990, which marked the onset of economic reforms in India. We describe the populations in focus, main methods utilized, health outcomes studied and measures of equity used in the research on health inequalities in India.
We conducted a systematic literature search on PubMED, the database of the US National Library of Medicine for research on health inequalities published between 1990 and 2016. PubMED is a widely used online bibliographic database for public health and medicine and indexes a large number of international and national journals. We considered publications from 1990 onwards for two reasons. Firstly, 1990 marked the beginning of economic reforms in in India which has implications for equity in health and healthcare. Additionally, the period from 1990 to 2016 covers a time period of more than 25 years of research publications. Databases were searched using the terms: ‘ India ’, ‘ health status disparities ’, ‘ healthcare disparities ’, ‘ health services needs and demand ’, ‘ social justice ’, ‘ social marginalization ’, ‘ poverty ’, ‘ socioeconomic factor ’, ‘ social class ’, ‘ ethnic groups ’, and ‘ minority health ’. We followed relevant aspects of the PRISMA guidelines for the literature search, for defining key aspects of the study methodology and in drafting the manuscript.
Study selection
We used search terms to review and identify relevant study abstracts. We included studies that reported single or multiple types of health inequalities, studies on the burden of diseases reporting stratification by socioeconomic factors, studies showing gender differences, multi country studies that reported disparities for India and any other studies of studies that included data on health inequalities. We excluded duplicates, clinical studies, studies on the burden of diseases that did not stratify by any socioeconomic or demographic factors, reviews, editorials or any other studies of articles, studies on Indian populations in other countries and studies showing differences in health outcomes by age groups only.
Data extraction
Following this, information was extracted from identified abstracts and full text studies. Domains of data extraction included information on year of publication, study methodology, study focus (descriptive versus analytical), location of main author, health outcomes of focus, population group and measures of socioeconomic disparity.
Summary measures
In particular, we examined population groups, health outcomes and measures of disparity in focus. Extracted data was summarized into spreadsheet templates and results were synthesized quantitatively.
Data items and synthesis of results
We classified studies into nine thematic sub-groups. These included studies on mortality, communicable diseases, non-communicable diseases, mental health, injuries, health services, risk factors, malnutrition and others. Key population groups considered by the study included men, women, adults (i.e. men and women), child (including adolescents), youth (age group of 15–24 years or as defined by the study), elderly and all populations (for studies that did not specify a population group). We classified measures of socioeconomic disparities into geographical markers (rural, urban or states), income or wealth, occupation, education, religion, caste/tribe, gender and access to water/sanitation. If studies reported multiple socioeconomic markers, all of them were recorded in the analysis.
A review of research published on health inequalities between 1990 and 2016 yielded 8,800 abstracts of which 1,312 studies were relevant to this review (Fig. 1 ).

Review of Literature on Health Inequalities
Publication trends over time
We found an increase in the research published on health inequalities, especially after 2005 (Fig. 2 ). Our review shows that of the studies published, more than 9 % were published between 1990 and 2000, and 90 % were published between 2001 and 2016. Among the studies published, a majority (75 %) were led by authors based in Indian institutions. The share of lead authors based at international institutions was small but growing (Fig. 2 ). Studies led by international researchers originated in developed nations such as the United States of America (USA), United Kingdom (UK), European Union (EU) countries (Germany, France, Denmark, Sweden and Ireland) and Australia.

Published studies on health inequalities between 1990 and 2016 by country of lead author. *Note: Data for the year 2016 is till July only
Research methods
More than 88 % of the studies identified by the review used quantitative methods, with 4.1 % using qualitative methods and 4.5 % using mixed methods. Over time, we noted a decline in the proportion of qualitative and mixed methods studies from 6.7 and 5.8 % respectively in the 1990s to 3.8 and 4.4 % respectively between 2000 and 2016. The proportion of quantitative studies increased from 84 % in the 1990s to 89 % between 2000 and 2016. Nearly 92 % of the studies were descriptive or comparative in nature, with 7.9 % investigating the impact of health interventions and programs. Since 2010, intervention studies are on the rise.
Health outcomes
Communicable and non-communicable diseases and malnutrition comprised the largest proportion of the research literature (Fig. 3 ). Of the studies reviewed, 10.1 % examined disparities in communicable diseases, 16.2 % in non-communicable diseases and 13.8 % focused on nutrition. Studies on health services comprised 11.7 % of the total studies reviewed and the category ‘Other’ comprised 12.2 %. Studies on risk factors comprised 8.8 % of the reviewed studies. About 5.7 % of the studies focused on mortality, 4.5 % on mental health and 4.6 % on maternal health.

Distribution of Study Outcomes in the Health inequalities Research (1990–2016)
Studies prior to 2000 focused on mortality, communicable and non-communicable diseases. Studies on mortality declined after 2000 and studies on non-communicable diseases started increasing between 2000 and 2016. We did not find any studies on injuries or accidents prior to 2000, but between 2000 and 2016, 3 % of the studies examined injuries. Studies on mental health doubled from 2.5 % (1990–2000) to 5.2 % (2000–2016), while the proportion of studies on health services declined. The number of studies on risk factors and nutrition increased between 2000 and 2016. Research on sexual health and dental health emerged as defined areas from 2000 onwards comprising 3 % each of the total literature respectively.
Population groups
Nearly half of the published studies focused on women and children (Fig. 4 ). About 20.3 % of the studies focused exclusively on women, 24.6 % focused exclusively on children and 3.5 % examined outcomes for both women and children. Studies on men comprised only 2.9 % of the total studies and youth and elderly comprised 3.4 % and 3.2 % of the literature respectively.

Distribution of Population Groups in the Health inequalities research (1990–2016)
We noted three trends in the population groups studied by the research literature. Firstly, we found a decline in the proportion of studies on children from 41.7 % (1990–2000) to 21.3 % (2010–2016). Secondly, we found that the proportion of studies focused on all populations increased from 5.1 % in 1990–2000 to 20.2 % in 2000–2016. This may be attributed to diversification of study themes that were earlier focused on maternal and child health. Finally, we noted an increase in studies on youth and elderly. Studies on elderly increased from none in the 1990s to 3.5 % in 2000–16. Studies on the youth populations increased from none in 1990s to 3.8 % in 2010–16.
Measures of equity
Income (including wealth) (61.2 %) was the most common measure of equity for health disparities, followed by education (45.4 %) and gender (36.1 %) (Table 1 ). A substantial number of studies considered disparities based on region, occupation and caste/tribe status. The importance of wealth or income stayed consistent over time. The proportion of studies on education, income, region, caste and religion also stayed consistent over time. Studies on gender disparities in health increased over time from 33.3 % (1990–2000) to 38.1 % (2011 onwards).
Trends in Equity Measures Used in Health Inequalities Research in India (1990–2016)
Note: Multiple measures of equity were present in many studies
In a country as diverse as India with large social inequalities combined with rapid economic growth, research on health inequalities has a special significance for policy. The rapidly growing literature on health inequalities further attests that. While health inequalities as a research domain emerged from disciplines like demography, economics and sociology, today it represents a large and interdisciplinary field of study in health research. Studies that show socioeconomic gradients have firmly established health inequalities in the development discourses both internationally and in India [ 46 , 47 , 56 – 60 ]. However, to an extent research on health inequalities in India follows international trends with local flavor.
We found that despite their gaps, research on health inequalities has systematically highlighted the large disparities across health outcomes that exist in India [ 56 , 57 , 61 – 65 ]. Outcomes have extended beyond documented differences in health outcomes across groups, to research on the distribution of public subsidies and out of pocket payments for health and impoverishment across socioeconomic groups [ 61 – 65 ]. These studies have been widely used to inform health policy and programs. We also found that studies on interventions have also contributed to measuring how successful health programs have been in reaching disadvantaged groups (and reducing health disparities) [ 46 ]. Hence, health inequalities research has also moved beyond documentation to become an important policy tool.
Our review of the literature on health inequalities in the last 25 years provides insight into how the field of research has evolved in India. The number of studies has grown over time and this research has been led by researchers based in India. A majority of studies conducted are quantitative, which shows the important role of quantitative disciplines like epidemiology and economics in this research. The contribution of qualitative studies at present remains largely untapped. We found that a majority of studies were situational analyses with few studies on health programs and interventions. Even as the latter have played an important role for policy, their potential for health inequalities research in evaluation of programs and policies remains underutilized.
The themes investigated in the literature on health inequalities also indicate the changing politics of health issues in public health. We found that studies in the 1990s focused on mortality, communicable and non-communicable diseases and nutrition. However, in the latter period, non-communicable diseases, health risk factors, mental health and injuries acquired increasing importance. These patterns broadly reflect shifts in public health priorities, globally and in India. Studies on women and children have dominated this research in India, attributed to policy focus on reproductive and child health in public health programs. Wealth has been the main socioeconomic marker studied followed by education and gender. This resonates largely with global practice. In the Indian context, caste/tribe status and religion occupy an important position as they capture sociocultural aspects of disadvantage. However, in health inequalities studies, their proportion remains low.
In a country as diverse as India with large social inequalities, research on health inequalities has a special significance for monitoring effectiveness of health policies and programs. We recommend that future research in this area focuses on evaluations of policies and health programs in order to ensure improved targeting towards underserved populations. We also recommend that future research focuses on underrepresented health areas and populations.
Acknowledgements
The authors would like to thank Arshima Dost, Radhika Arora, and Aasim Khan for their help with the literature review.
The authors received no specific funding for this research and were not funded under any fellowships at the time of the study.
Availability of data and materials
Authors’ contributions.
KDR conceptualized the paper. NB and KDR jointly designed and analyzed the study. NB and KDR contributed to different sections of the manuscript. SK assisted with additional data analysis. NB drafted the final manuscript and KDR and SK edited and provided comments. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
No issues anticipated.
Ethics approval and consent to participate
Not applicable.
Abbreviations
Contributor information.
Nandita Bhan, Phone: +91-124-4781400, Email: [email protected] .
Krishna Dipankar Rao, Email: ude.uhj@oardk .
Shivani Kachwaha, Email: [email protected] .
25,000 Health Facilities Across India are Transforming Public Health Systems to address Growing Critical Climate Issues
April 7, 2023.

An IKEA Foundation and SELCO Foundation partnership embarks upon the world’s largest public health infrastructure program to sustainably upgrade health facilities with solar energy
- 25,000 health care facilities in 12 states in India will be powered by sustainable energy, and upgraded with energy efficient medical equipments by 2026.
- According to the 2023 IPCC Report, power generation, buildings, industry, and transport are responsible for close to 80% of global emissions, therefore, investing in clean energy & efficiency is one of the key solutions to mitigate climate change.
- The initiative, in collaboration with the Ministry of Health and Family Welfare, Government of India, State Health Missions and SELCO Foundation, has received initial funding of €48 million from the IKEA Foundation.
NEW DELHI. 7th April 2023 . In 2021, WHO identified climate change as the biggest global health threat of the 21st century. While half of the world’s population continue to lack access to essential health services, according to a 2019 Health care climate footprint report, if the healthcare sector were a country, it would be the fifth largest greenhouse gas emitter on the planet .
In a significant step towards transforming the public health infrastructure for improved sustainability, SELCO Foundation and IKEA Foundation, in partnership with India’s Ministry of Health and Family Welfare (MOHFW) and various State Health Missions, have launched a groundbreaking initiative ‘Energy for Health’. The program recognises climate adaptation and mitigation at the center to all efforts to upgrade the public health facilities across the world.
Speaking about the significance of this program globally, Dr. Maria Neira, Assistant Director-General a.i., Division of Healthier Populations, and Director, Department of Environment, Climate Change and Health, at the World Health Organization said, “Reliable electricity in health-care facilities is essential to save lives and to provide quality health care. And yet, one billion people around the world are still served by health-care facilities without reliable electricity or with no electricity access at all. Decentralized renewable energies represent a key opportunity to accelerate electrification of health-care facilities, including in remote areas. I congratulate the Government of India and our partners from Selco Foundation and Ikea Foundation for this critical program, which will have a transformative impact on strengthening the health system”.
The first-of-a-kind initiative will bring solar energy solutions with efficient medical and electrical equipment to 25,000 healthcare facilities in 12 states by 2026. Across the 12 states under this program, there is a diversity in terms of topography, socio-economic vulnerabilities, disease burden and climate. This diversity across selected geographies will contribute to this programme serving as a showcase globally- innovating on approaches, models and processes relevant for similar contexts in other parts of the world.
Mr. Per Heggenes, CEO of IKEA Foundation said, “‘At the IKEA Foundation, we strongly believe caring for the health of people and our planet must go hand-in-hand. This initiative will improve healthcare outcomes and reduce emissions, by providing reliable and renewable energy to thousands of clinics. Our hope is that the success of this programme can serve as a model for building effective and efficient health systems globally.’
Reflecting on India’s leadership in the effort, Dr. Harish Hande, CEO of SELCO Foundation said, “Affordable and equitable access to healthcare is a function of two aspects- one, resources required to deliver health care, and two, cost of accessing health care. Through this program, SELCO Foundation and IKEA Foundation, along with India’s Ministry of Health and Family Welfare (MOHFW) and various State Health Missions, will showcase at scale how sustainable energy can be used to make health services affordable at the doorstep of the poor.”
‘Energy for Health’ initiative brings with it positive impacts across the spectrum of stakeholders- for last mile communities in their access to timely healthcare; for health facility staff in ensuring a conducive work environment to provide quality services; for health sector in reducing energy and equipment-related costs as well as avoiding wastage of vaccines and other critical resources; reinforcing climate resilience building and carbon mitigation efforts while ensuring positive health outcomes for all citizens.
Supported by IKEA Foundation, through this initiative, SELCO Foundation along with Government of India will create systems and processes that demonstrate ownership, management, and regular maintenance of the energy systems and appliances. Together, through the 25,000 public health facilities, technical knowledge and capacity, as well as guidelines and policies that enable health staff at different levels to plan for public health infrastructure in a sustainable manner will be improved. The program will also improve the local technical network for solar energy, which could potentially also have indirect impacts on local economies and boost adoption of solar energy across other sectors as well.
The initiative aims to reach over 170 million people across the 12 states and improve working conditions for over 160,000 front line health staff at these health facilities. Across the 25,000 public health facilities, this will add ~100MW of solar energy capacity in the country, and mitigate over 3 million tonnes of CO2e emissions over a 20 year period. These will directly contribute to India’s Net Zero targets, while also creating a paradigm shift on how health targets can be achieved for resource constrained communities across the world in an efficient manner.
About the partners:
SELCO Foundation:
Established in 2010, SELCO Foundation’s mission is to develop holistic solutions that use sustainable energy as a catalyst to address poverty alleviation alongside ensuring environmental sustainability. SELCO’s interventions lead to the sustainable delivery of essential services such as healthcare, and enable improvements in livelihoods productivity and till date more than 7 million people have been impacted. The foundation does this by also developing enabling conditions, i.e the ecosystem for sustainable energy solutions to be locally developed, adopted, scaled and institutionalized through stakeholders including government agencies, financiers, local NGOs and enterprises.
For more information, visit www.selco foundation.org , and follow them on Twitter (@SELCOFoundation) and LinkedIn.
IKEA Foundation:
The IKEA Foundation is a strategic philanthropy that focuses its grant making efforts on tackling the two biggest threats to children’s futures: poverty and climate change. It currently grants more than €200 million per year to help improve family incomes and quality of life while protecting the planet from climate change. Since 2009, the IKEA Foundation has granted more than €1.5 billion to create a better future for children and their families.
In 2021 the Board of the IKEA Foundation decided to make an additional €1 billion available over the next five years to accelerate the reduction of Greenhouse Gas emissions.
Press Contact: Lotika Mehta, [email protected]
- Share this article on 25,000 Health Facilities Across India are Transforming Public Health Systems to address Growing Critical Climate Issues
- Share article "25,000 Health Facilities Across India are Transforming Public Health Systems to address Growing Critical Climate Issues" on Facebook
- Share article "25,000 Health Facilities Across India are Transforming Public Health Systems to address Growing Critical Climate Issues" on LinkedIn
Media contact
Related articles

This site uses functional cookies and external scripts to improve your experience.
Privacy settings
Privacy Settings
This site uses functional cookies and external scripts to improve your experience. Which cookies and scripts are used and how they impact your visit is specified on the left. You may change your settings at any time. Your choices will not impact your visit.
NOTE: These settings will only apply to the browser and device you are currently using.
Google Analytics
Google Analytics is a web analytics service offered by Google that tracks and reports website traffic, currently as a platform inside the Google Marketing Platform brand.
Google Tag Manager
Google Tag Manager measures the number of visits to a website and the parts of the website that are the most popular among the website’s visitors. This information is used to provide information on the use of the website and enhance the user’s experience.
- Skip to main content
- Skip to secondary menu
- Skip to primary sidebar
- Skip to footer
Study Today
Largest Compilation of Structured Essays and Exams
Essay on Health Care in India
December 16, 2017 by Study Mentor Leave a Comment
Health is wealth . It is more important than the wealth we have. Only when we have a proper health we will able to get the necessary wealth in our life. If we do not have a proper health, whatever wealth we have also goes into waste. We will not be able to use even the available wealth without a proper health.
This is the reason one should take important care of their health. We should focus more on our health. Then, automatically we will be able to work hard and earn according to the work we have been able to do. Thus, health is very important in our life.
First, people should learn to take care of their health and then focus on other areas of life. But we taking care of ourselves alone does not matter. We should have the facilities in order to take proper care of our health. We should have easy access to all the health facilities.
In order for people to maintain a proper health, they should have proper health care systems. Only then people will be able to take care of their health and get treatment when they are suffering from any sort of sickness.
But do we have access to proper health care. Many of us have easy access to the health care. But for those who have problem to access these health care ultimately lose their life.
Table of Contents
What do you mean by health care?
Health care means the process or way in which one is taking different procedures or medical measures to make a person’s health better. With proper health care a person’s health can become better. This will include dong the right treatment, taking medicine and altering one’s own life habits.
A proper health care will help to save so many people’s lives. These days because of unhealthy lifestyle people are getting prone to many sickness and diseases. Due to these reasons, treatment is on the light. But when a person does not get the right treatment there are chances of losing the life.
Health care system should be improved and regularly updated. In the previous years, very outdated machines and treatments were used. They are not still used in the present-day time because diseases these days have taken another turn compared to before. So obviously the treatment should also be changed.
There should be proper health care system so that everyone gets the treatment when needed. They will not have to run helter skelter when they need the treatment in emergency. There are still many places all over the world where there are no health care systems and people have lost their lives.
Why is health care important?
In order to remain healthy and be free or get treated from different sickness and diseases one needs to have access to health care. With time, new diseases are coming into action. More people are getting ill every single day of the life. In order to get diagnosed and treated, health care is needed for the people.

If people will have access to health care and more hospitals or health care systems are made, there will be growth in the medical sector.
Moreover, the medical sector contributes a lot to the GDP (Gross Domestic Product) of the country. Proper health care will help people to be free from sickness and their lives will be saved.
If the number of lives saved by proper treatment is increased, the death rate will start reducing. The production of the country will increase which will further improve the economy.
Health Care in India
The number of health care systems in India has increased from the past years. Facilities have also improved. More primary health centers have been opened in the rural areas as well. In the urban areas the hospitals have also increased with many advanced facilities. Many medical colleges have also been opened so that there are many aspiring doctors to treat the sick people.
We can see medical colleges and hospitals almost everywhere. But just opening medical colleges and hospitals alone is not enough. There should be proper treatment in the health care centers and hospitals. The doctors and staff should be dedicated to treat the people. They should not only focus on their benefit. In many hospitals we see that the doctors come late and leave early from their work.
They take leave very often. This does not happen. This will not only lead to reduction in the growth of the medical sector but also many people will be left untreated. It is also seen that in many places the staff are not good. They do not take proper care of the patients.
They behave rudely with the patients and their family members. No matter how many new centers and hospitals are made, there are still many people who do not get treatment. They are left untreated and ultimately they lose their life.
Another reason why everyone is not able to get proper treatment is because of high population. Fertility rate is increasing every year and every single day someone gets sick. As there are too many people getting sick there is not enough place in the centers and hospital to diagnose and treat everyone.
In private hospitals there will be rush because everything is according to the numbers and there is limitation. But one should go and visit the government hospitals and centers.
There is a huge rush everywhere. There is not even a single proper place to get fresh air. There almost same things are used for every patient. Cleanliness is not maintained properly. Every place is crowded like a fish market. Some of the staff members are very lazy to work while others are strict for everything.
Personal experience on health care
It was the month of March, 2007 I had got abscess on my chest. It could not be self treated so I visited a known doctor in a private hospital. The doctor examined the abscess and told us that operation would have to be done that day. So, I was admitted in the hospital.
I was kept in the female common ward till the operation time. I was given saline water till my operation was started and I was not allowed to eat anything. As I was in the common ward, too many patients were admitted there. The air smelled so foul that I could not even breathe properly. My father came to visit me. As I was in the common ward, he could see me every time he wanted.
So, they asked the staff to shift me to a private room. I realized the private rooms were cleaner than the common wards. Also the staff was more dedicated and caring for the private room patients. Some of them used to take their own sweet to finish their work. Well, this should not be done. They should not be bias to anyone. Soon, my operation time came and I was taken to the operation room.
After that I do not remember anything about the room. I only realized after I was being shifted to my room. I was kept in the hospital for one week. In this week I used to walk around the hospital when I used to get fed up resting in the room. I realized the hospital needs more doctors and staff.
There was no discipline maintained in the hospital. The staff should be taking care of all patients. One day some other nurse came to give me an injection. She gave me injection in such a way that she is giving it to some non living thing. It was very painful.
I did not like to see such conditions of the hospital. I just wished to be discharged from the hospital and go back home soon. After I went back home, I had to go to the hospital once a week to change the dressing in the operated area. The nurses who would come to change my dressing used to behave rudely with me.
Reader Interactions
Leave a reply cancel reply.
Your email address will not be published. Required fields are marked *
Top Trending Essays in March 2021
- Essay on Pollution
- Essay on my School
- Summer Season
- My favourite teacher
- World heritage day quotes
- my family speech
- importance of trees essay
- autobiography of a pen
- honesty is the best policy essay
- essay on building a great india
- my favourite book essay
- essay on caa
- my favourite player
- autobiography of a river
- farewell speech for class 10 by class 9
- essay my favourite teacher 200 words
- internet influence on kids essay
- my favourite cartoon character
Brilliantly
Content & links.
Verified by Sur.ly
Essay for Students
- Essay for Class 1 to 5 Students
Scholarships for Students
- Class 1 Students Scholarship
- Class 2 Students Scholarship
- Class 3 Students Scholarship
- Class 4 Students Scholarship
- Class 5 students Scholarship
- Class 6 Students Scholarship
- Class 7 students Scholarship
- Class 8 Students Scholarship
- Class 9 Students Scholarship
- Class 10 Students Scholarship
- Class 11 Students Scholarship
- Class 12 Students Scholarship
STAY CONNECTED
- About Study Today
- Privacy Policy
- Terms & Conditions
Scholarships
- Apj Abdul Kalam Scholarship
- Ashirwad Scholarship
- Bihar Scholarship
- Canara Bank Scholarship
- Colgate Scholarship
- Dr Ambedkar Scholarship
- E District Scholarship
- Epass Karnataka Scholarship
- Fair And Lovely Scholarship
- Floridas John Mckay Scholarship
- Inspire Scholarship
- Jio Scholarship
- Karnataka Minority Scholarship
- Lic Scholarship
- Maulana Azad Scholarship
- Medhavi Scholarship
- Minority Scholarship
- Moma Scholarship
- Mp Scholarship
- Muslim Minority Scholarship
- Nsp Scholarship
- Oasis Scholarship
- Obc Scholarship
- Odisha Scholarship
- Pfms Scholarship
- Post Matric Scholarship
- Pre Matric Scholarship
- Prerana Scholarship
- Prime Minister Scholarship
- Rajasthan Scholarship
- Santoor Scholarship
- Sitaram Jindal Scholarship
- Ssp Scholarship
- Swami Vivekananda Scholarship
- Ts Epass Scholarship
- Up Scholarship
- Vidhyasaarathi Scholarship
- Wbmdfc Scholarship
- West Bengal Minority Scholarship
- Click Here Now!!
Mobile Number
Have you Burn Crackers this Diwali ? Yes No

- Publications
- Virtual Health Library
- Virtual Campus for Public Health
- PAHO/WHO Collaborating Centres
- Track your shipment
- Regional Revolving Funds
- The Decade of Healthy Aging
- Elimination Initiative
- Migration and Health in the Americas
- HEARTS in the Americas
- Sustainable Health Agenda for the Americas 2018-2030
- Alerts and Epidemiologic Updates
- Technical and Scientific Products
- Resources for Journalists
- News Releases
- Country News
- Technical Unit News
- Infographics
- Champions of Health
- Public Health Heroes
- Collaborators
- Past campaigns
- PAHO/WHO Newsletters
- PAHO Calendars
- History of PAHO
- PAHO's Former Directors
- Organizational Chart
- Statement of Assessed Contributions due from Member States
- Communicable Disease Prevention, Control, and Elimination
- Comprehensive Immunization
- Evidence and Intelligence for Action in Health
- Innovation, Access to Medicines and Health Technologies
Social and Environmental Determinants for Health Equity
- Health Emergencies
- Health Systems and Services
- Noncommunicable Diseases and Mental Health
- Pan American Sanitary Conference
- Directing Council
- Executive Committee
- Subcommittee on Program, Budget and Administration
- Internships
- Partnerships
- Office of Internal Audit
World Health Day 2024 - 'My health, my right’

April 7, 2024
Around the world, the right to health of millions is increasingly coming under threat.
Diseases and disasters loom large as causes of death and disability.
Conflicts are devastating lives, causing death, pain, hunger and psychological distress.
The burning of fossil fuels is simultaneously driving the climate crisis and taking away our right to breathe clean air, with indoor and outdoor air pollution claiming a life every 5 seconds.
The WHO Council on the Economics of Health for All has found that at least 140 countries recognize health as a human right in their constitution. Yet countries are not passing and putting into practice laws to ensure their populations are entitled to access health services. This underpins the fact that at least 4.5 billion people — more than half of the world’s population — were not fully covered by essential health services in 2021.
To address these types of challenges, the theme for World Health Day 2024 is 'My health, my right’.
This year’s theme was chosen to champion the right of everyone, everywhere to have access to quality health services, education, and information, as well as safe drinking water, clean air, good nutrition, quality housing, decent working and environmental conditions, and freedom from discrimination.
Key messages
Human rights factsheet (WHO)
Communication material - PAHO | WHO

Human Rights and Health

Universal Health

Air Quality

Health Equity
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
Mental health care is hard to find, especially for people with Medicare or Medicaid
Rhitu Chatterjee

With rates of suicide and opioid deaths rising in the past decade and children's mental health declared a national emergency , the United States faces an unprecedented mental health crisis. But access to mental health care for a significant portion of Americans — including some of the most vulnerable populations — is extremely limited, according to a new government report released Wednesday.
The report, from the Department of Health and Human Services' Office of Inspector General, finds that Medicare and Medicaid have a dire shortage of mental health care providers.
The report looked at 20 counties with people on Medicaid, traditional Medicare and Medicare Advantage plans, which together serve more than 130 million enrollees — more than 40% of the U.S. population, says Meridith Seife , the deputy regional inspector general and the lead author of the report.
Medicaid serves people on low incomes, and Medicare is mainly for people 65 years or older and those who are younger with chronic disabilities.
The report found fewer than five active mental health care providers for every 1,000 enrollees. On average, Medicare Advantage has 4.7 providers per 1,000 enrollees, whereas traditional Medicare has 2.9 providers and Medicaid has 3.1 providers for the same number of enrollees. Some counties fare even worse, with not even a single provider for every 1,000 enrollees.
"When you have so few providers available to see this many enrollees, patients start running into significant problems finding care," says Seife.
The findings are especially troubling given the level of need for mental health care in this population, she says.
"On Medicare, you have 1 in 4 Medicare enrollees who are living with a mental illness," she says. "Yet less than half of those people are receiving treatment."
Among people on Medicaid, 1 in 3 have a mental illness, and 1 in 5 have a substance use disorder. "So the need is tremendous."
The results are "scary" but "not very surprising," says Deborah Steinberg , senior health policy attorney at the nonprofit Legal Action Center. "We know that people in Medicare and Medicaid are often underserved populations, and this is especially true for mental health and substance use disorder care."
Among those individuals able to find and connect with a provider, many see their provider several times a year, according to the report. And many have to drive a long way for their appointments.
"We have roughly 1 in 4 patients that had to travel more than an hour to their appointments, and 1 in 10 had to travel more than an hour and a half each way," notes Seife. Some patients traveled two hours each way for mental health care, she says.
Mental illnesses and substance use disorders are chronic conditions that people need ongoing care for, says Steinberg. "And when they have to travel an hour, more than an hour, for an appointment throughout the year, that becomes unreasonable. It becomes untenable."
"We know that behavioral health workforce shortages are widespread," says Heather Saunders , a senior research manager on the Medicaid team at KFF, the health policy research organization. "This is across all payers, all populations, with about half of the U.S. population living in a workforce shortage."
But as the report found, that's not the whole story for Medicare and Medicaid. Only about a third of mental health care providers in the counties studied see Medicare and Medicaid patients. That means a majority of the workforce doesn't participate in these programs.
This has been well documented in Medicaid, notes Saunders. "Only a fraction" of providers in provider directories see Medicaid patients, she says. "And when they do see Medicaid patients, they often only see a few."
Lower reimbursement rates and a high administrative burden prevent more providers from participating in Medicaid and Medicare, the report notes.
"In the Medicare program, they set a physician fee rate," explains Steinberg. "Then for certain providers, which includes clinical social workers, mental health counselors and marriage and family therapists, they get reimbursed at 75% of that rate."
Medicaid reimbursements for psychiatric services are even lower when compared with Medicare , says Ellen Weber , senior vice president for health initiatives at the Legal Action Center.
"They're baking in those discriminatory standards when they are setting those rates," says Steinberg.
The new report recommends that the Centers for Medicare & Medicaid Services (CMS) take steps to increase payments to providers and lower administrative requirements. In a statement, CMS said it has responded to those recommendations within the report.
According to research by Saunders and her colleagues at KFF, many states have already started to take action on these fronts to improve participation in Medicaid.
Several have upped their payments to mental health providers. "But the scale of those increases ranged widely across states," says Saunders, "with some states limiting the increase to one provider type or one type of service, but other states having rate increases that were more across the board."
Some states have also tried to simplify and streamline paperwork, she adds. "Making it less complex, making it easier to understand," says Saunders.
But it's too soon to know whether those efforts have made a significant impact on improving access to providers.
CMS has also taken steps to address provider shortages, says Steinberg.
"CMS has tried to increase some of the reimbursement rates without actually fixing that structural problem," says Steinberg. "Trying to add a little bit here and there, but it's not enough, especially when they're only adding a percent to the total rate. It's a really small increase."
The agency has also started covering treatments and providers it didn't use to cover before.
"In 2020, Medicare started covering opioid treatment programs, which is where a lot of folks can go to get medications for their substance use disorder," says Steinberg.
And starting this year, Medicare also covers "mental health counselors, which includes addiction counselors, as well as marriage and family therapists," she adds.
While noteworthy and important, a lot more needs to be done, says Steinberg. "For example, in the substance use disorder space, a lot of addiction counselors do not have a master's degree. And that's one of their requirements to be a counselor in the Medicare program right now."
Removing those stringent requirements and adding other kinds of providers, like peer support specialists, is key to improving access. And the cost of not accessing care is high, she adds.
"Over the past two decades, [in] the older adult population, the number of overdose deaths has increased fourfold — quadrupled," says Steinberg. "So this is affecting people. It is causing deaths. It is causing people to go to the hospital. It increases [health care] costs."
- Centers for Medicare & Medicaid Services
- mental health

IMAGES
VIDEO
COMMENTS
India has made significant improvements in the health outcomes of its people. Life expectancy at birth increased to 69.6 years in 2020, from expected 47.7years in 1970. MMR declined from 301 to 130 per 100 000 live births between 2003 and 2014-16, and IMR declined from 68 in the year 2000 to 24 per 1000 live births in 2016.
India's health care sector provides a wide range of quality of care, from globally acclaimed hospitals to facilities that deliver care of unacceptably low quality. Efforts to improve the quality ...
The Scenario of the Health Care Sector in India. Let us look at an overview of the current healthcare sector in India. Health Infrastructure. The government, or public healthcare system, concentrates on establishing primary healthcare centres (PHCs) in rural areas while maintaining a small number of secondary and tertiary care facilities in major cities.
National Health Policy. The National Health Policy was endorsed by the Parliament of India in 1983 and updated in 2002, and then again updated in 2017. The recent four main updates in 2017 mention the need to focus on the growing burden of non-communicable diseases, the emergence of the robust healthcare industry, growing incidences of unsustainable expenditure due to healthcare costs, and ...
While the National (Rural) Health Mission has done much to improve the infrastructure in the Indian Government healthcare system, a 2012 study of six states in India revealed that many of the primary health centers (PHCs) lacked basic infrastructural facilities such as beds, wards, toilets, drinking water facility, clean labor rooms for ...
According to the World Bank, infant mortality in India fell from 66 to 38 per 1,000 live births from 2000 to 2015. Life expectancy at birth has increased from 63 to 68 years, and the maternal mortality ratio has fallen from 374 to 174 per 100,000 live births over the same period. India also has dynamic pharmaceutical and biotechnology ...
India Health System Review Health Systems in Transition Health Sy Vol. 11 No. 1 2022 s t ems in T r ansition Vol. 11 No. 1 2022 India Health System Review The Asia Pacific Observatory on Health Systems and Policies (the APO) is a collaborative partnership of interested governments, international agencies, foundations, and researchers that promotes
By Indrani Gupta, Institute of Economic Growth, Delhi In collaboration with Nishali Patel, Policy Fellow, International Health Systems, London School of Economics All Indian citizens can get free outpatient and inpatient care at government facilities. Under India's decentralized approach to health care delivery, the states are primarily responsible for organizing health services.
The group's charge is to report by August 2022 how India can achieve universal health care within a decade. The Mittal Institute is encouraging participation by the Harvard community and sponsoring an online panel discussion on Monday to introduce the effort. Patel and Khanna said the commission has a challenging road ahead, one that has ...
India's health equity issues require a comprehensive approach that go beyond improvements in health-care facilities. April 08, 2024 01:36 am | Updated 09:18 pm IST
Abstract. After reviewing health outcomes and policy in India, this paper concludes that there are at least six sets of issues to be addressed about improving the quantity and quality of health services, and ipso facto improving health outcomes, in India. First, the amount of resources earmarked for health needs to increase.
The government has been working to improve the healthcare system through various initiatives to strengthen primary, secondary, and tertiary healthcare services. The Indian government spent two percent of India's gross domestic product (GDP) on healthcare in financial year 2022 and is forecast to reach over 2.5% of the GDP by 2025.
Indian states are in different phases of epidemiological transition, resulting in large variations in disease burden across the states.1 However, the public health priorities across the country remain similar. Addressing the availability of relevant and robust data for meaningful planning of programmes and policies is a gap that needs urgent consideration to improve population health and the ...
978-93-80449-15-9. Health care is the prevention, treatment, and management of illness and the preservation of. mental and physical well being through the services offered by the medical, nursing ...
and may kindly be communicated with CBHI, Directorate General of Health Services, Government of India. (ul Goel)at Room No. 446, A, Nirman Bhavan, New Delhi-110108 ... General of health services Ministry of health and Family Welfare nirman Bhawah, new Delhi-110108 Tele/Fax : 91 (11) 23063175 e-mail : [email protected]
India's National Health Policy, 2017 envisions the goal of attaining highest possible level of health and well-being for all and for all ages through a preventive and promotive health care orientation in all developmental policies and universal access to good quality health care services without financial hardship to the citizens.
India is rapidly becoming urbanised. By 2030, around 40% of the country's population will live in urban areas. The extent to which India's health system can provide for this large and growing city-based population will determine the country's success in achieving universal health coverage and improved national health indices. In The Lancet Global Health, Sundeep Salvi and colleagues1 offer a ...
500 Words Essay on Healthcare in India Introduction. India's healthcare sector is a study in contrasts, presenting a complex tapestry of cutting-edge advancements and systemic challenges. With an expansive population and diverse health needs, the healthcare system in India is a critical component of the nation's development agenda.
The healthcare sector in India is expected to grow to reach a size of $50 bn by 2025. The digital healthcare market is expected to more than 20% by 2023. The Telemedicine market is the maximum potential eHealth segment in India, which is expected to touch $5.4 Bn by 2025. In the Economic Survey of 2022, India's public expenditure on ...
In India, the Health care sector is one of the largest sectors in terms of both revenue and employment. In India, the health care sector can be categorized into public and private . Public health care hospitals comprise secondary and tertiary care institutions in urban areas while primary basic facilities are focused in rural areas.
Post-independence, the focus of health policy was increasing the coverage of health services and hence, research focused on the delivery of basic health services. Philosophical debates on nation-building and the role of modern medicine also led to a shift from investigations of the role of caste, religion and ethnicity [ 13 , 14 ].
An IKEA Foundation and SELCO Foundation partnership embarks upon the world's largest public health infrastructure program to sustainably upgrade health facilities with solar energy NEW DELHI. 7th April 2023. In 2021, WHO identified climate change as the biggest global health threat of the 21st century. While half of the world's population continue to lack access […]
Health care means the process or way in which one is taking different procedures or medical measures to make a person's health better. With proper health care a person's health can become better. This will include dong the right treatment, taking medicine and altering one's own life habits.
World Health Day 2024 is 'My health, my right'. This year's theme was chosen to champion the right of everyone, everywhere to have access to quality health services, education, and information, as well as safe drinking water, clean air, good nutrition, quality housing, decent working and environmental conditions, and freedom from discrimination.
These guidelines summarize the approach proposed by WHO to collect, analyse, report, disseminate and use strategic information on viral hepatitis. They strengthen person-centred monitoring - with a priority for indicators that support person-centred health services, the core prevention, diagnosis and treatment interventions.
A significant rural-urban disparity in unsafe child stool disposal practices exists in India, yet existing research falls short in identifying the contributing factors to this gap. This study addresses the research gap by contextualizing the rural-urban divide in unsafe child stool disposal using data from the fifth round of the National Family Health Survey (NFHS-5, 2019-21).
A report from the Department of Health and Human Services' inspector general finds a dire shortage of mental health care providers in Medicaid and Medicare, which together serve some 40% of Americans.