Social Determinants of Health: Call for Nursing Education Reform
- First Online: 11 February 2023

Cite this chapter

- Linda McCauley 4
970 Accesses
Nursing has long been at the forefront of understanding the importance of communities—places of work, prayer, and play, and the overall environment—in determining the health of individuals. These factors have gained prominence as we have become a more global community and seen the stark disparities in longevity, overall health, and flourishing among populations. This chapter outlines why the nursing profession must integrate social determinants of health into twenty-first century curricula. We review our historic roots in caring for people in their communities, and why SDOH is being newly conceptualized as a fundamental premise of all nursing care. Adequately preparing the nursing workforce of the future will require a systematic approach to integrating these concepts into all aspects of nursing curricula.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
World Health Organization (WHO). Closing the gap in a generation: health equity through action on the social determinants of health. Geneva: WHO Commission on Social Determinants of Health; 2008.
Google Scholar
Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014;129(Suppl 2):19–31.
Article Google Scholar
McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Aff (Millwood). 2002;21:78–93.
Galea S, Tracy M, Hoggatt KJ, Dimaggio C, Karpati A. Estimated deaths attributable to social factors in the United States. Am J Public Health. 2011;101:1456–65.
Fee E, Bu L. The origins of public health nursing: the Henry Street Visiting Nurse Service. Am J Public Health. 2010;100:1206–7.
American Nurses Association (ANA). About ANA. 2020. Nursingworld.org/ana/about-ana
Beck AJ, Boulton ML. The public health nurse workforce in U.S. state and local health departments, 2012. Public Health Rep. 2016;131:145–52.
Institute of Medicine (IOM). For the public’s health: investing in a healthier future. Washington, DC: Committee on Public Health Strategies to Improve Health; 2012.
National Academies of Sciences, Engineering, and Medicine (NASEM). The future of nursing 2020–2030: charting a path to achieve health equity. The National Academies Press; 2021.
Thornton RL, Glover CM, Cené CW, Glik DC, Henderson JA, Williams DR. Evaluating strategies for reducing health disparities by addressing the social determinants of health. Health Aff (Millwood). 2016;35:1416–23.
Frieden TR. A framework for public health action: the health impact pyramid. Am J Public Health. 2010;100:590–5.
Lathrop B. Nursing leadership in addressing the social determinants of health. Policy Polit Nurs Pract. 2013;14:41–7.
Dankwa-Mullan I, Rhee KB, Williams K, et al. The science of eliminating health disparities: summary and analysis of the NIH summit recommendations. Am J Public Health. 2010;100(Suppl 1):S12–8.
Chhabra M, Sorrentino AE, Cusack M, Dichter ME, Montgomery AE, True G. Screening for housing instability: providers’ reflections on addressing a social determinant of health. J Gen Intern Med. 2019;34:1213–9.
Higginbotham K, Davis Crutcher T, Karp SM. Screening for social determinants of health at well-child appointments: a quality improvement project. Nurs Clin North Am. 2019;54:141–8.
Morgenlander MA, Tyrrell H, Garfunkel LC, Serwint JR, Steiner MJ, Schilling S. Screening for social determinants of health in pediatric resident continuity clinic. Acad Pediatr. 2019;19:868–74.
Morone J. An integrative review of social determinants of health assessment and screening tools used in pediatrics. J Pediatr Nurs. 2017;37:22–8.
Walter LA, Schoenfeld EM, Smith CH, et al. Emergency department-based interventions affecting social determinants of health in the United States: a scoping review. Acad Emerg Med. 2021;28:666–74.
National Academies of Sciences, Engineering, and Medicine. Implementing high-quality primary care: rebuilding the foundation of health care. Washington, DC: The National Academies Press; 2021.
National Institute of Nursing Research (NINR). The National Institute of Nursing Research 2022–2026 strategic plan. 2022.
Porter K, Jackson G, Clark R, Waller M, Stanfill AG. Applying social determinants of health to nursing education using a concept-based approach. J Nurs Educ. 2020;59:293–6.
American Association of Colleges of Nursing (AACN). The essentials. AACN; 2021.
U.S Department of Health and Human Services. Healthy people 2030. 2022. https://health.gov/healthypeople/priority-areas/social-determinants-health . Accessed 3 Oct 2022.
Download references
Author information
Authors and affiliations.
Nell Hodgson Woodruff School of Nursing, Emory University, Atlanta, GA, USA
Linda McCauley
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Linda McCauley .
Editor information
Editors and affiliations.
Jill B. Hamilton
Emory Nursing Learning Center, Nell Hodgson Woodruff School of Nursing,, Emory University, Atlanta, GA, USA
Beth Ann Swan
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
McCauley, L. (2023). Social Determinants of Health: Call for Nursing Education Reform. In: Hamilton, J.B., Swan, B.A., McCauley, L. (eds) Integrating a Social Determinants of Health Framework into Nursing Education . Springer, Cham. https://doi.org/10.1007/978-3-031-21347-2_1
Download citation
DOI : https://doi.org/10.1007/978-3-031-21347-2_1
Published : 11 February 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-21346-5
Online ISBN : 978-3-031-21347-2
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Open access
- Published: 08 June 2022
The impact of social determinants of health on early childhood development: a qualitative context analysis in Iran
- Omolbanin Atashbahar 1 ,
- Ali Akbari Sari 2 , 3 ,
- Amirhossein Takian 2 , 4 , 5 ,
- Alireza Olyaeemanesh 5 ,
- Efat Mohamadi 5 &
- Sayyed Hamed Barakati 6
BMC Public Health volume 22 , Article number: 1149 ( 2022 ) Cite this article
10k Accesses
8 Citations
2 Altmetric
Metrics details
Social determinants have a significant impact on children’s development and their abilities and capacities, especially in early childhood. They can bring about inequity in living conditions of children and, as a result, lead to differences in various dimensions of development including the social, psychological, cognitive and emotional aspects. We aimed to identify and analyze the social determinants of Early Childhood Development (ECD) in Iran and provide policy implications to improve this social context.
In a qualitative study, data were collected through semi-structured interviews with 40 experts from October 2017 to June 2018. Based on Leichter’s (1979) framework and using the deductive approach, two independent researchers conducted the data analysis. We used MAXQDA.11 software for data management.
We identified challenges related to ECD context in the form of 8 themes and 22 subthemes in 4 analytical categories relevant to the social determinants of ECD including: Structural factors (economic factors: 6 subthemes, political factors: 2 subthemes), Socio-cultural factors (the socio-cultural setting of society: 6 subthemes, the socio-cultural setting of family: 4 subthemes), Environmental or International factors (the role of international organizations: 1 subtheme, political sanctions: 1 subtheme), and Situational factors (genetic factors: 1 subtheme, the phenomenon of air pollution: 1 subtheme). We could identify 24 policy recommendations to improve the existing ECD context from the interviews and literature.
With regard to the challenges related to the social determinants of ECD, such as increasing social harms, decreasing social capital, lack of public awareness, increasing socio-economic inequities, economic instability, which can lead to the abuse and neglect of children or unfair differences in their growth and development, the following policy-making options are proposed: focusing on equity from early years in policies and programs, creating integration between policies and programs from different sectors, prioritizing children in the welfare umbrella, empowering families, raising community awareness, and expanding services and support for families, specially the deprived families subject to special subsidies.
Peer Review reports
There is a lot of evidence that shows vital development in children begins before their birth and continues in the first 8 years of life [ 1 ]. In various literatures, this period is considered the most critical period in human life because it is the fastest period of brain development [ 2 ]. Also, it is the most cost-effective period of life to invest in the development of human capital [ 3 ]. However, an important consideration in this regard is that early childhood development (ECD) is not only affected by heredity but there are also numerous variables in the child’s living environment at the micro, meso, exo and macro levels which play an important role in ECD [ 4 ].
Among the factors that can affect ECD, the following can be mentioned: education of parents [ 5 ], maternal mental health [ 6 , 7 ], malnutrition, infectious diseases, exposure to environmental toxins [ 8 ], limitations of intrauterine growth [ 7 ], ethnicity [ 9 ], characteristics of family environment [ 10 ], quality of child care [ 7 , 11 ], parent-child interactions [ 12 ], socio-cultural context, biological factors, and genetic inheritance [ 5 ], child’s educational opportunities or cognitive motivators, and exposure to violence [ 7 ]. On the other hand, children’s failure to realize their developmental potential plays an important role in the intergenerational transmission of poverty [ 5 ]. The fact is that more than 200 million children in developing countries are failing to reach their developmental potential [ 13 ].
Given the nature of ECD, the issue of inequity has a particular importance, since unequal conditions and opportunities in society will have adverse effects on the development of children’s capacities and abilities in various social, psychological, emotional, and physical aspects [ 14 ]. Inadequate and unequal living conditions are the result of deeper structural factors that together shape the way societies are organized with inappropriate social programs and policies, unfair economic conditions, and inappropriate policies. In this regard, the new global agenda on health equity states that Our children have dramatically different opportunities to live, depending on where they are born. In Japan or Sweden, they can expect to live more than 80 years; in Brazil 72 years, in India it is 63 years and in one of several African countries, it is less than 50 years [ 15 ]. Between and inside the countries, there are huge differences in the chance of survival, and this can be seen all over the world. In many countries, at all income levels, the development of children and the outcomes of children and families follow a social gradient: the lower the socio-economic conditions are, the poorer the children’s pertaining conditions will be, and finally, the more unfavorable developmental status they will have. In this regard, and as reflected in a report by the World Health Organization’s Commission for Social Determinants of Health, (2008), entitled “Closing the Gap in a Generation”, ECD has been emphasized [ 16 ]. Also, in the sixth chapter of the Health in All Policies report entitled “ Seizing opportunities, implementing policies “ published by the Ministry of Social Affairs and Health of Finland in 2013, the promotion of equity from the start through the ECD and health has been focused on in all policies [ 17 ].
In Iran, after the setting up of a Committee for Social Determinants of Health and the selection of ECD as one of its highest priority subjects, it was proposed that a policy document on ECD be drawn up by the Ministry of Health, the Ministry of Education and the Welfare Organization in 2008. Nevertheless, this policy document has not been implemented at a national level [ 18 ]. As experts and policy makers in the field of children have reached a consensus, the current situation of Iranian society at all levels of ECD policy making is facing many challenges [ 19 ] such as the lack of integration and coordination between policies and programs in various sectors, the lack of focus on all aspects of ECD, and lack of emphasis on eliminating the existing inequities [ 20 ]. These problems regarding children’s development in the country have prevented them from fully achieving their rights [ 21 ].
In relation to child health, according to Iran’s Multiple Indicator Demographic and Health Survey (IrMIDHS, 2010), the rate of underweight and short stature in children has been reported to be 4.8 and 6.83%. Also, a heterogeneous distribution of child malnutrition at the national level with high prevalence in deprived provinces was seen [ 22 ]. The sampling method in this survey was multi-stage stratified cluster-random. The final sample size in this study was 31,350 households in the country. Information on sampling clusters was obtained from the Statistics Center of Iran [ 23 ]. Based on the national survey of anthropometric indices in children under 5, which was conducted in 2017, the percentage of underweight and short stature was reported to be 4.3 and 4.8% respectively and a significant difference was seen between urban and rural areas. In this study, the sample size is 600 children for each province and the data obtained from health ministry software (SIB software) were selected randomly [ 24 ]. Various studies have also shown a reduction in child mortality rates in Iran in recent decades [ 22 , 25 , 26 , 27 , 28 ]. In this regard, in the IrMIDHS survey (2010), the mortality rates of under-5 children, infants and neonates per thousand live births were reported to be 22.52, 20.32 and 15.29 respectively and there were differences among various provinces of the country [ 22 ]. Moreover, based on Hosseinpoor’s (2005 and 2006.) studies, a significant difference was seen in infant mortality rate between various provinces and the lowest and highest socioeconomic quintiles [ 25 , 26 ]. In these studies, data extracted from the Iran’s Demographic and Health Survey (DHS), which was conducted in 2000 [ 28 ]. The concentration index of infant mortality was used to measure the socioeconomic inequalities [ 25 , 26 ].
On the other hand, in relation to child education and according to the Educational Inequality Index (UNDP) (2014), Iran ranks 12th in the region with a score of 0.433 followed by Syria, Iraq, Pakistan and Afghanistan [ 29 ]. Based on the report from the Social Welfare Studies Office, some reasons for the increase of inequality in education include the neglect of the quality of manpower in education, non-compulsory and non-free preschool education, failure to provide statistical reports on indicators of educational inequality by the government, and no attention paid to the field of education by civil society [ 30 ]. Given that, no study has so far been conducted in Iran to examine the policy context of ECD. Also, with regards to the importance of the early years in human capital development and sustainable development of the society as well as the critical role of social determinants in ECD, the study aims to identify and clarify the contextual factors affecting ECD and its policy process in order to identify policy recommendations to improve the current situation. The context refers to the circumstances and settings in which children are born and raised. It includes systematic economic, political, social, and cultural factors at national and international levels which may influence the ECD [ 31 ]. This study answers the following questions: What factors (including structural, situational, social, economic, political, and international) affect ECD and policymaking in various levels of micro, meso, exo and macro in Iran? What works to decrease the existing inequities and improve the context for optimal ECD?
Conceptual framework
In this qualitative study, the researchers attempted to explore the ECD context of Iran. We used the Leichter (1979) conceptual framework for policy context analysis. This divided contextual factors into four categories including: situational factors (irregular and unstable events such as war), cultural factors (values of society or different groups in society), structural factors (more stable factors of social organizations such as economic-political system) and environmental factors (factors outside the national system of politics such as multinational corporations) [ 32 ]. To collect the data, the researchers made use of interviews with experts from different sectors related to children including health and nutrition, early care and education, and protection.
Data collection
Forty face-to-face, in-depth, semi-structured interviews were conducted from October 2017 to June 2018 using an interview guide (Appendix 1 ) in Tehran, Iran. Since no new data was added to our study during the last interviews, we concluded that the data has reached the saturation level. All interviews took place in the interviewees’ workplaces and each interview lasted for 30–90 minutes.
Sampling method
To select the participants, we used the purposive sampling approach with maximum variation in terms of scientific background, activity domain, employment status, gender, and executive experience. In addition, the snowball sampling method was used to identify more interviewees. The participants were divided into five groups including policymakers (PM), managers (M), academics and researchers (Aca), NGOs’ representatives (NGO-R), and children service providers (CSP) from different organizations related to ECD (Ministry of Health and Medical Education; State Welfare Organization; Ministry of Education; Ministry of Cooperatives, Labor, and Social Welfare; Ministry of Justice; Children’s Medical Center; The Islamic Consultative Assembly; Society for Protecting the Rights of the Child (SPRC); universities and research centers, etc.) (Appendix 2 ). The participants met at least one of the following criteria:
Specializing in majors related to children or neuroscience, social sciences, human sciences, and rehabilitation sciences
Having at least 3 years of professional experience with children in non-governmental or governmental sectors
Having a position related to children’s affairs in non-governmental or governmental sectors at the time of the study (Appendix 2 )
Data analysis
For data analysis, a deductive approach was used. In this regard, the interviews were transcribed verbatim, the codes were extracted from the summaries of the interviews, the open coding was carried out, and the extracted codes were finally categorized based on Leichter’s (1979) framework [ 32 ] using the thematic analysis approach. Coding and data categorization were done manually. MAXQDA.11 software was also used to assist data management. To ensure the accuracy of statements, transcripts were sent to the participants who were asked to confirm if necessary It should be noted that in the meantime, no changes were made to the transcripts. AA and OA also analyzed the data separately and then cross-checked the extracted themes and sub-themes, discussing the differences among some of the obtained themes and sub-themes and reaching a consensus. The consensus was then finalized by two team supervisors (AT, EM) and the confirmation was made by cheking these changes to ensure the validity of the qualitative analysis and the consistency of the findings among the authors.
Ethical considerations
Before the interviews, necessary information regarding the study and its objectives were given to the participants and informed consent was obtained from them verbally. Moreover, they were assured that their information would remain confidential and the data of the study would be analyzed anonymously. Also, the current study has been confirmed by the Ethical Committee of Tehran University of Medical Sciences (IR.TUMS.REC.1396.2694).
The results of this study are presented based on Leichter’s (1979) framework under analytical categories including structural, socio-cultural, environmental (international), and situational factors. In our study, 8 themes and 22 subthemes were identified (Tables 1 , 2 , 3 and 4 ). These categories are presented in the following:
Structural factors
In this analytical category, two themes and eight sub-themes were identified.
Economic factors
The participants stated that economic factors change the well-being of children through various ways. These factors can directly affect children’s well-being and development by increasing or decreasing family financial resources. Indirectly, these factors can affect government revenues and the sustainability of government resources to provide beneficial services to children. Although the living conditions of the family are affected by the macroeconomic status of the country, even in prosperous and developed countries, there are deprived and poor families. Therefore, it is necessary to consider the economic status of families separately. In this study, factors such as parents’ employment status, family income and housing status have been identified as indicators of family living conditions. Also, the concept of economic inequities was repeatedly cited by experts in the interviews as one of the most important factors influencing children’s opportunities for optimal development and ultimately the continuous vicious cycle of poverty.
“Well, when you compare countries, you certainly see countries that have high economic growth and their economic situation is better, the quality of life of their children is higher, and they receive the high-quality services (CSP 4) .”
“If the family is suffering from issues such as poverty and unemployment, this family will not be able to take positive actions in this regard, no matter how much you talk about the development of the children and increase the knowledge of that family (PM10) .”
“If you look at the investment curve of the country, it is a linear curve, which is the complete opposite of opportunity. We have the highest investments in the third, fourth and fifth decades of human life and the resources are spent there, while milestones of development are established in early years (PM9) .”
“ Inequities and gaps between the rich and the poor in the country and the problems caused by the poverty of families such as the phenomenon of working children, addiction, child abuse, etc. exacerbate the issue (PM 8) .”
Political factors
Political factors were one of the important issues which have a significant impact on ECD and the design of programs and policies in this regard. In this category, participants pointed to the politicization and policy-based decisions made by these streams of thought and politics.
“The fact is that our political and national discourse on children only goes back to school education. That means we do not have a very coherent, comprehensive discourse on children (PM 22) .”
“One of the main problems that we face in the field of children, which is perhaps less seen, is the contradictory political attitudes and thoughts that we have towards family, women and children (PM 12) .”
Socio-cultural factors
In this analytical category, two themes and ten sub-themes were identified.
The socio-cultural setting of society
Another point that was mentioned in the interviews as an important factor in ECD was the socio-cultural factors of society. According to the findings of this study, the socio-cultural context of society affects ECD directly and indirectly (by influencing the socio-cultural context of the family). In this study, the socio-cultural context of society has been identified by several concepts including social inequalities, uneven urban development, declining social capital, misconceptions and ignorance of society, development of communication technology and media, and issues in the national educational system. In several interviews, for instance, the uneven development of urbanization was mentioned as a social-cultural factor which has made cities an unsafe and unfriendly environment for children. Participants stated that the uneven development of urbanization is associated with many consequences, including increasing social harm, expanding marginalization, changing lifestyles, creating a harsh city, air pollution, noise pollution, etc., each of which will affect ECD in special ways. Another concept that was mentioned as an effective factor in children’s development was the social capital. In other words, the interviewees referred to the negative impacts of decreased social capital on children’s personality by decreasing public trust and weakening empathy, social responsibility, and identity.
“How many of us are marginalized now? Statistics say that we have twelve million marginalized people, some say eighteen million, right? What does marginalized mean? That is, those who do not receive education, care and health facilities that are necessary for the growth and development of their children? (CSP 18) .”
“Social capital in our society has decreased, distrust is too much; this affects how the child's personality is formed (M 17) . “
“Many parents, people and teachers still consider physical and verbal punishment as correct methods of nurturing while these are examples of child abuse (Aca 4) .”
The socio-cultural setting of family
The family plays an important role in the well-being and development of children. Parental behavior and family environment can promote or inhibit children’s development. In this study, factors such as socio-demographic variables of the family have been identified as effective factors in ECD in relation to the socio-cultural context of the family. For example, many participants referred to family harms including various types of domestic violence (such as physical, sexual, psychological, and verbal violence and indifference), mental problems of parents (such as stress, anxiety, depression), parental conflict, separation or loss of parents) as factors influencing children’s development. Another very important factor that was repeatedly mentioned in the interviews was the knowledge, attitude and practice of parents regarding parenting. In other words, parenting style was believed to have a tremendous impact on the formation of children’s personality and development. In several interviews, the weakness of families in nurturing their children has been mentioned. Issues which were mentioned in connection with the role of parenting included nurturing of dependent and non-capable children, children with inability to say no, those with inability to solve problems and those who lack social skills. Such issues also included nurturing children with emotional deficiencies and mental problems as well as children who will face academic failure and social harms in the future.
“I think we have some defects in parenting. With my experience in psychology, we do not have many independent children. Or we sometimes see that they do not have the ability to say no or their problem-solving abilities are weak. There are a number of nurturing problems (Aca 26) . “
“Domestic violence, from physical and verbal violence to other types of violence in our country, is at a high rate. Research has shown that children have this experience in terms of psychology (PM 13) .”
“Our children have little information about their rights. Families should provide some information and lessons to their children, but we see that families do not even educate their children about healthy behaviors (NGO-P 11) .”
Environmental (international) factors
In this analytical category, two themes and two sub-themes were identified.
The role of international organizations
Among the interviews, the role of international organizations including UNESCO, UNICEF, the World Bank, and the World Health Organization was mentioned. Interviewees stated that the political commitment of international organizations to ECD could play an important role in facilitating national political commitments to young children. Interviewees cited the financial and technical support of these international organizations to the countries.
“International programs also have an impact on the national context of countries, such as the Sustainable Development Goals, which include seventeen core programs, some of which are directly related to health and some are directly related to poverty alleviation.” “It can also have a positive effect on our country so that we can finally pay more attention to these programs (Aca 1) . ”
Political sanctions
Another issue raised by some interviewees was political sanctions as an external and international factor influencing the conditions and well-being of society, including the development of children.
“Well, now these sanctions that we are facing act as a lever of pressure and disturb the condition in the country, so that they can have many effects on different people in society and lead to the violation of the rights of people, including children (PM33) .”
Situational factors
In this analytical category, three themes and three sub-themes were identified.
Genetic factors
Genetic factors are mentioned as a situational factor in interviews with health policy makers and health service providers. They stated that development is the result of a combination of both environmental and genetic factors. Therefore, genetic factors can be the source of some developmental disorders and defects in children.
“Children's development is affected by various factors, including psychological, social, hereditary and environmental factors, so we can say that children's development is the result of a dynamic and continuous interaction of biological and acquired factors (CSP 18) .”
The phenomenon of air pollution
Air pollution in some regions of the country was another situational factor mentioned in our study. This phenomenon has adverse effects on the physical and mental development of children as one of the vulnerable and sensitive groups in the society. It has also been stated that children living in societies with low socioeconomic status are more likely to be exposed to toxic waste, air pollution, poor water quality, excessive noise, and poor housing quality.
“Well, look at the problem of air pollution and dust, which can have an impact on the health of society, especially pregnant women and children. Some of these problems manifest themselves in the short term, such as shortness of breath, allergies, asthma, and some manifest themselves in the long term. (PM 40) .”
“The effects of air pollution, noise pollution, and poor environmental quality are greater on poor children because they probably have very poor access to protective equipment and facilities (M14) .”
According to the results of this study, economic factors can make a significant difference in children’s life conditions and affect the financial space of governments and families to invest in ECD. This issue has been emphasized in many studies. According to the World Bank, OECD member countries spend about 1.6% of their gross domestic product (GDP) on family and preschool services for children aged 0 to 6, of which 0.43% is spent on kindergartens alone. By comparison, low-income countries such as Nepal, Kenya, and Tajikistan spend only 0.1% of their GDP on preschool services, compared with less than 0.002% in Nicaragua and Senegal [ 33 ]. Based on the results of PISA study (2012), the mathematical performance of 15-year-old students in countries such as Italy, Greece, Finland, Thailand, Spain, etc., as compared to their performance in 2003, shows an increase of 25 points, which is due to an increase in the enrollment rate in preschools in this period in the mentioned countries [ 34 ]. In Iran, privatization in public education and, at the same time, a significant (50%) reduction in the share of education in the public budget are the main reasons for the increase of educational inequalities [ 30 ] so that statistics from 2011 to 2012 shows that the government’s involvement in preschool education was only for licensing. According to statistics, the number of government-run preschool centers have dropped to zero in this year [ 35 ]. World Bank’s report (2003) it was stated that the positive impact of preschool on improving education and breaking the poverty cycle can be proven in the case of Iran [ 30 ].
Economic inequities were also emphasized in our study. This shows that economic growth alone is not enough, but the distribution and quality of this growth is very important. In this regard, Boyden has emphasized the nature and quality of economic growth for ECD in his study. He states that policies should be made to ensure the sustainability of investments, to focus on the most vital stage in childhood, and to bring about benefits for all children [ 36 ]. Another study by Bennett has shown that improvements in children’s access have been distributed differently among different socioeconomic groups, and different results have been achieved [ 6 ]. Abbasian and Mahmoudi, in their study, examined the situation of child poverty in Iran. The results showed that on average between 22 and 27% of children suffered from poverty during 1983–2013. This study also showed that rural children and girls have a higher poverty rate than urban children and boys [ 37 ]. Also, according to the Social Studies and Research Institute of Iran, 34.7% of street children are hungry [ 38 ]. In the area of education, the difference in preschool coverage rates between urban and rural areas has not changed in Iran during the 1980s and 1990s, and the gap between the two areas has always been 15 to 20% [ 29 ]. For example, the coverage rate for urban and rural preschools in 2006 was 56.7 and 34.7%, respectively [ 30 ].
Another issue mentioned in this study is the role of political factors in the form of various political and intellectual mainstreams which impact the design of appropriate programs and policies for children. Since the influence of attitudes, interests, expediencies and political decisions on phenomena at the level of community is quite evident, the role of the political context in ECD has been emphasized in several studies [ 39 , 40 , 41 ]. Vegas states that the political context influences a country’s investment in ECD and the type of policies and programs it finances [ 39 ]. Also, Moussa’s study shows that the political violence affects the children’s mental health [ 41 ].
In our study, the effect of socio-cultural factors on ECD, like economic factors, has been considered at both macro and micro levels. The essence and quality of the social environment affect the ECD and the performance of families [ 42 ]. Among these factors, social inequalities play a critical role. The increased risk of adverse health outcomes is not limited to the lowest levels of poverty and socioeconomic status, but many child health outcomes indicate that there is a social slope. For example, birth weight indicates a specific social slope that has profound effects not only on childhood and infancy but also on adulthood [ 43 ]. Vaida argues in his study that racial and ethnical inequalities play a significant role in birth outcomes in Wisconsin. A higher proportion of infants born to black/African American women than infants born to white women are low birth weight and premature, which is the leading cause of death for black/African American infants [ 44 ]. Participants also cited the consequences of uneven urban development as lifestyle changes, increased marginalization, and social harm, all of which have negative effects on children’s development, including obesity, increased violence against children, and the creation of an insecure environment for children. Based on Jalili Moayad’s results, Iranian working children experience a relatively high rate of abuse in their work environments. 77.6% of these children have experienced at least one type of abuse, of which emotional abuse is the highest at 70.4%, followed by negligence at 52% [ 45 ].
Also, the report on the kids in communities shows that neighborhoods marked with security concerns, garbage on the streets, and delinquency were associated with a number of adverse health behaviors and consequences, including overweight and childhood obesity, behavioral problems, and other negative consequences of child development [ 39 ]. Moreover, Powers et al. emphasized the role of social capital and stated that poor social cohesion, social capital, and social support are associated with increased maternal postpartum depression, child abuse, and alcohol drinking and smoking in pregnancy [ 46 ] and potentially play a role in the current health slope among children [ 47 ]. This finding is consistent with the results of our study. In addition to addressing the social and economic causes of childhood inequities, it is important to consider cultural factors as well. In this study, cultural factors that can affect the physical and psychological development of children are referred to. These factors appear in the form of misconceptions and lack of awareness in the society with regard to parenting methods such as the belief in physical punishment in child rearing or their beliefs about the unnecessity of child sexual education. Such misconceptions have also been addressed in other studies. For example, Moore states that one of the cultural misconceptions among Australians is that young children are passive in absorbing concepts and their lives are perceived to be so simple that will not be disturbed or disrupted by influential factors. He argues that these misconceptions can indirectly increase or maintain early childhood inequities by influencing public opinions in general, and the extent of governmental support and investments in reducing early childhood inequities [ 47 ]. In Iran, negative beliefs such as avoiding to feed the baby with colostrum to prevent neonatal jaundice are seen among some ethnicities, especially those living in rural areas [ 48 ] Based on Oveisi’s study, in general, the families believe that the use of physical punishment in raising children is sometimes necessary [ 49 ]. Also, according to IRMDIS study, 18.18% of parents considered the use of physical punishment appropriate for raising a child and 79.33% used verbal punishment to raise a child [ 22 ].
Based on our findings, Families play a critical role in the well-being and development of children. Parental behavior and family environment can promote or inhibit children’s development. Because families are the first environments in which children interact with others from birth, they play a very important role in preparing children with stimulation, support and kindness. These characteristics are, in turn, influenced by the resources that families have to devote to parenting (strongly influenced by income), which is the same as their parenting style. Such characteristics tend to provide a rich and responsive environment (strongly influenced by parents’ education levels) [ 39 , 50 , 51 , 52 ]. Hesterman states that Adverse Childhood Experiences (ACEs) such as abuse, neglect, domestic violence, discrimination, etc. and toxic stress (non- tolerable stress) threaten the physical and mental health of the child, impairing their brain development and emotional regulation. Moreover, their long-term effects are evident in adulthood [ 53 ]. In this regard, Hajnasiri in a meta-analysis study with a sample size of 15,514 on 31 articles from 2000 to 2014 estimated the prevalence of domestic violence at 66% in Iran [ 54 ] which could have adverse effects on children’s development. Still, there are not enough legislations or organizations to support these victims [ 55 ].
This study revealed that international factors, including the political commitment of international organizations to ECD, could play an important role in facilitating national political commitments to young children. Strong sponsors of ECD investment such as the UNESCO, the UNICEF, the World Bank, and the World Health Organization can provide financial support and technical advice to country leaders, including the latest evidence and the best practices. In addition, international development treaties can support national and social policies that focus on the needs of children. International policies, such as the Millennium Development Goals, offer developing countries a challenge and an opportunity. Millennium Development Goals are very child-centered, with a strong focus on children and synergies at the international and national levels that can be used to promote common child-friendly policies [ 40 ].
According to the results of our study, genetic factors are among the situational factors that can be the source of some developmental disorders and defects in children. The analysis of the effect of genes and the environment on the transmission of antisocial behaviors from parents to children, depression and hyperactivity shows that both genetics and family environment play a role in this regard [ 51 ]. The results of various studies have shown a vigorous relationship between early adverse conditions and epigenetic changes in genes related to stress responses, immunity, and the increase of mental disorders [ 56 ]. For example, based on the results of Roth’s study, early infant ill-treatment was associated with decreased expression of genes responsible for appropriate serotonin required to preserve mood balance [ 57 ]. In this regard, Vaida states that the integrated nature of growth and development is largely preserved through constant interactions between genes, hormones, nutrients, and other factors. Some of these factors that affect physical function are rooted in heredity. Factors such as season, dietary restrictions, and severe psychological stress are rooted in the environment. Other factors, such as the socioeconomic class, reflect a complex combination of hereditary and environmental effects which are likely to play a role throughout development [ 44 ]. Many studies have also emphasized the negative effects of air pollution as a situational factor on pregnant mothers and children. In this regard, Pem states in his study that fetuses that are exposed to lead and arsenic before birth may be born prematurely or at a low birth weight, and as a result, this can affect the development of the child [ 52 ].
ECD focuses on equity and reducing the gap between rich and poor from the early years. Inequity in socioeconomic conditions will adversely affect the integrated development of early childhood, and children ‘s lack of optimal development will lead to the continuation of this unfavorable cycle. This principle is very weak in the current policies and programs of the country. Fair promotion of economic, cultural and social conditions of the society and consequently of the families can be very helpful in ECD and achieving the sustainable development of the society. While the context of our country is facing many challenges such as increasing social harms, reducing social capital, lack of public awareness, increasing socio-economic inequities, reducing economic growth, economic instability, etc. this will provide conditions for the abuse and neglect of children or their unfair growth and development. We should, therefore, consider creating integration between policies and programs of different sectors, prioritizing children in the welfare umbrella, empowering families, raising community awareness, and expanding services and support for families, specially the deprived families subject to special subsidies. Finally, we recommend that further studies be conducted on ECD in Iran including a survey of developmental disorders and delays in children and their relationship with social determinants of health, designing and surveying indicators in early care and education and support areas of children such as quality of early care and education, play, children with special needs, poverty, abuse, neglect, domestic violence, discrimination, children street, toxic stress and etc., conducting an evaluation/review of progress in reducing inequalities in various aspects of ECD, assessing the knowledge, attitude and practice of parents in relation to ECD in rural and urban areas, and examining the pilot implementation of ECD policy and its consequences in order to provide policy solutions.
Strengths and limitations
This study was the first of its kind in conducting a deep and extensive analysis of social determinants of ECD in Iran. The results of the current study can improve the developmental conditions of children and lead to more attention to contextual factors in formulating policies related to ECD. However, our study has two main limitations; first, we have not presented the developmental status of children in various areas of ECD in the form of figures due to the lack of statistics and information in this field in our country. Second, some participants were not able to participate in the confirmation process because of their busy schedule and the lack of time.
Policy recommendations
Availability of data and materials.
The data of this study are raw data which were accessible to the researchers in the interviews and are reported in the paper. The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Avan BI, Kirkwood BR. Review of the theoretical frameworks for the study of child development within public health and epidemiology. J Epidemiol Community Health. 2010;64:388–93.
Article CAS PubMed Google Scholar
Busolo B, Agembo W. Access and equity in early childhood education: challenges and opportunities. Baraton Interdiscip Res J. 2017;7:1–7.
Google Scholar
Heckman JJ, Cunha F. Investing in our young people. The National Institutes of Health and the Committee for Economic DevelopmentChicago: University of Chicago; 2006. http://jenni.uchicago.edu
Woodhead M, Bolton L, Featherstone I, Robertson P. Early childhood development: delivering inter-sectoral policies, programmes and services in low-resource settings. In: The Health & Education Advice & Resource Team (HEART); 2014.
McGregor SG, Cheung YB, Cueto S, Glewwe P, Richter L, Strupp B, et al. Developmental potential in the first 5 years for children in developing countries. Lancet. 2007;369:60–70.
Article Google Scholar
Bennett IM, Schott W, Krutikova S, Behrman JR. Maternal mental health and child growth and development in four low-income and middle-income countries. J Epidemiol Community Health. 2016;70:168–73.
Article PubMed Google Scholar
Walker SP, Wachs TD, Gardner JM, Lozoff B, Wasserman GA, Pollitt E, et al. Child development: risk factors for adverse outcomes in developing countries. Lancet. 2007;369:145–57.
Walker SP, Wachs TD, Grantham-McGregor S, Black MM, Nelson CA, Huff man SL, et al. Inequality in early childhood: risk and protective factors for early child development. Lancet. 2011;378:1325–38.
Sacker A, J. Kelly Y. Ethnic differences in growth in early childhood: an investigation of two potential mechanisms. Eur J Pub Health. 2012;22(2):197–203.
Schoon I, Jones E, Cheng H, Maughan B. Family hardship, family instability and cognitive development. J Epidemiol Community Health. 2012;66:716–22.
Gialamas A, Mittinty MN, Sawyer MG, Zubrick SR, Lynch J. Social inequalities in childcare quality and their effects on children’s development at school entry: findings from the longitudinal study of Australian children. J Epidemiol Community Health. 2015;69:841–8.
De Falco S, Emer A, Martini L, Rigo P, Pruner S, Venuti P. Predictors of mother–child interaction quality and child attachment security in at-risk families. Front Psychol. 2014;5:898. https://doi.org/10.3389/fpsyg.2014.00898 .
Article PubMed PubMed Central Google Scholar
Engle P, Black M, Behrman J, Cabral de Mello M, Gertler P, Kapiriri L, et al. Strategies to avoid the loss of developmental potential in more than 200 million children in the developing world. Lancet. 2007;369:229–42.
Moore T, McDonald M, McHugh-Dillon H. Early childhood development and the social determinants of health inequities: a review of the evidence. Parkville: Centre for Community Child Health at the Murdoch Childrens Research Institute and the Royal Children’s Hospital; 2014.
WHO Commission on Social Determinants of Health, World Health Organization. Closing the gap in a generation: health equity through action on the social determinants of health: Commission on Social Determinants of Health final report. World Health Organization; 2008.
Marmot M, Friel S, Bell R, Houwelin TA, Taylor S. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372:1661–9.
Leppo K, Ollila E, Pen˜a S, Wismar M, Cook S. Health in all policies: seizing opportunities, implementing policies. In: Ministry of social affairs and health, Finland; 2013.
National Secretariat of the integrated of early childhood development. National policy document on integrated early child development. Tehran: Ministry of Health and Medical Education, Ministry of education and welfare organization; 2013. (origin persian).
Vameghi R, Marandi A, Sajedi F, Soleymani F, Shahshahanipour S, Hatamizadeh N. Strategic analysis of the situation in Iran regarding the development of young children (analysis swot) and proposed strategies and activities. J Soc Welf. 2010;9(35):379–412 ( origin persian).
Atashbahar O, Akbari Sari A, Takian A, Olyaeemanesh A, Mohamadi E, Barakat SH. Integrated early childhood development policy in Iran: a qualitative policy process analysis. BMC Public Health. 2021;21:649.
Rarani MA, Nosratabadi M, Moeeni M. Early childhood development in Iran and its provinces: Inequality versus average. Int J Health Plann Manage. 2018;33(4):1136–45.
Rashidian A, Khosravi A, Khabiri R, Khodayari-Moez E, Elahi E, Arab M, et al. Islamic Republic of Iran's multiple Indicator demographic and health survey (IrMIDHS) 2010. Tehran: Ministry of Health and Medical Education; 2012. (origin persian)
Rashidian A, Karimi-Shahanjarini A, Khosravi A, et al. Iran's multiple Indicator demographic and health survey - 2010: study protocol. Int J Prev Med. 2014;5(5):632–42.
PubMed PubMed Central Google Scholar
Ministry of Health and Medical Education. national survey of anthropometric status, nutritional and growth and development indicators, and some indicators of health services evaluation in children Under five years. Tehran: Ministry of Health and Medical Education; 2018. (origin persian).
Hosseinpoor AR, Mohammad K, Majdzadeh R, Naghavi M, Abolhassani F, Sousa A, et al. Socioeconomic inequality in infant mortality in Iran and across its provinces. Bull World Health Organ. 2005;83:837–44.
Hosseinpoor AR, Van Doorslaer E, Speybroeck N, Naghavi M, Mohammad K, Majdzadeh R, et al. Decomposing socioeconomic inequality in infant mortality in Iran. Int J Epidemiol. 2006;35(5):1211–9.
Khosravi A, Taylor R, Naghavi M, Lopez AD. Mortality in the Islamic Republic of Iran, 1964-2004. Bull World Health Organ. 2007;85:607–14.
Ministry of Health and Medical Education. Population and Health in the Islamic Republic of Iran: Iran Demographic and Health Survey (DHS) 2000. Tehran: Ministry of Health and Medical Education; 2000. (origin persian).
Abasi L, Bayat M. With the people's representatives in the tenth parliament, report 19. Introduction to the education sector. In: Office of Social Studies, Parliamentary Research Center, vol. 14870; 2016. https://rc.majlis.ir/fa/report/show/970064 . (origin Persian).
Karimian J. Collection of reports on poverty, inequality and conflict of interest: poverty and inequality in education: Ministry of Cooperatives, labor and social welfare, deputy of social welfare, Office of Social Welfare Studies; 2020. https://poverty-research.ir/blog/study-reports/5276/ .(origin Persian)
O'Brien GL, Sinnott SJ, Walshe V, Mulcahy M, Byrne S. Health policy triangle framework: narrative review of the recent literature. Health Policy Open. 2020;1:100016.
Buse K, Mays N, Walt G. Making health policy. UK: McGraw-hill Education; 2012.
Lake A. Early childhood development—global action is overdue. Lancet. 2011;378. https://doi.org/10.1016/S0140-6736(11)61450-5 .
OECD (2014) PISA in focus – 2014/06 (June) does pre-primary education reach those who need it most?
Abasi L, Pouzesh SH. Assessing the preschool situation with emphasis on legal documents and duties of the welfare organization and the Ministry of Education, vol. 13662: Office of Social Studies, Parliamentary Research Center; 2014. https://rc.majlis.ir/fa/report/show/887366 . (origin Persian)
Boyden J, Dercon S. Child development and economic development: lessons and future challenges: Young Lives; 2012. www.younglives.org.uk
Abasian E, Mahmoudi V. Multidimensional poverty of families with children in Kerman province using the generational approach: 1983–2013. Soc Dev Quarterly. 2016;11(1):35–52 origin Persian.
Vameghi M, Dejman M, Rafiei H, Roshanfekr P. Urgent assessment of children’s street situation in Tehran: causes and risk of working children on the street. Quarterly Soc Stud Res Iran Univ Tehran. 2013;4(1):34–53.
Goldfeld S, Villanueva K, Lee JL, Robinson R., Moriarty A, Peel D et al. Foundational community factors (FCFs) for Early Childhood Development: A report on the Kids in Communities Study; 2017.
Vegas E, Santibáñez L, Brière BL, Caballero A, Hautier JA, Devesa DR. The promise of early childhood development in Latin America and the Caribbean: The International Bank for Reconstruction and Development / the World Bank; 2010. https://doi.org/10.1596/978-0-8213-7759-8 .
Book Google Scholar
Moussa S, El Kholy M, Enaba D, Salem K, Ali A, Nasreldin M, et al. Impact of political violence on the mental health of school children in Egypt. J Ment Health. 2015;24(5):289–93. https://doi.org/10.3109/09638237.2015.1019047 .
Kawachi I, Berkman LF. Neighborhoods and health. New York: Oxford University Press; 2003.
Spencer N. Social, economic, and political determinants of child health. Pediatrics. 2003;112(3):704–6.
Vaida N. A study on various factors affecting growth during the first two years of life. Eur Sci J. 2003;8(29):16–37.
Jalili Moayad S, Mohaqeqi Kamal SH, Sajjadi H, Vameghi M, Ghaedamini Harouni Gh, Makki Alamdari S. Child labor in Tehran, Iran: Abuses experienced in work environments. Child Abuse Negl. 2021;117:105054. https://doi.org/10.1016/j.chiabu.2021.105054 .
Powers JR, McDermott LJ, Loxton DJ, Chojenta CL. A prospective study of prevalence and predictors of concurrent alcohol and tobacco use during pregnancy. Matern Child Health J. 2013;17:76–84.
Moore TG, McDonald M, Carlon L, O’Rourke K. Early childhood development and the social determinants of health inequities. Health Promot Int. 2015;30:S2 ii102–15. https://doi.org/10.1093/heapro/dav031 .
Keshavar Z, Abassi A-SMJ, Ebadi A, Alavi moghadam F, Salari E. Ethnic, cultures and reproductive behavior in North Khorasan. J North Khorasan Univ Med Sci. 2017;9(1):109–19 origin Persian.
Oveisi S, Eftekhare Ardabili H, Majdzadeh R, Mohammadkhani P, Jean AR, Loo J. Mothers’ attitudes toward corporal punishment of children in Qazvin- Iran. J Fam Violence. 2010;25(2):159–64.
Maggi S, Irwin LG, Siddiqi A, Poureslami I, Hertzman E, Hertzman C. Knowledge network for early child development. Analytic and Strategic Review Paper: International Perspectives on Early Child Development. World Health Organization’s Commission on the Social Determinants of Health; Human Early Learning Partnership; 2005. p. 6–9.
Ibberson CL. Environmental factors among young children contributing to the onset of behavior disorders. In: Culminating projects in Special Education, vol. 46; 2017. http://repository.stcloudstate.edu/sped.etds/46 .
Pem D. Factors Affecting early childhood growth and development: golden 1000 days. J Adv Pract Nurs. 2015;1(1). https://doi.org/10.4172/2573-0347.1000101 .
Hesterman M. The effects of adverse childhood experiences on long-term brain development and health development and health. Aisthesis. 2021;12(1).
Hajnasiri H, Gheshlagh Ghanei R, Sayehmiri K, Moafi F, Farajzadeh M. Domestic violence among Iranian women: a systematic review and meta-analysis. Iran Red Crescent Med J. 2016;18(6):e34971 (origin Persian).
Ghaffarihosseini F, Jalali Nadoushan AM, Alavi K, Bolhari J. Supporting the victims of domestic violence in Iran: two decades of effort. J Inj Violence Res. 2021;13(2):161–4. https://doi.org/10.5249/jivr.vo113i2.1638 .
Sokolowski MB, Boyce WT. Epigenetic embedding of early adversity and developmental risk. In: ENCYCLOPEDIA on Early Childhood Development (CEECD); 2017.
Roth TL, Lubin FD, Funk AJ, Sweatt JD. Lasting epigenetic influence of early-life adversity on the BDNF gene. Biol Psychiatry. 2009;65(9):760–9.
Article CAS PubMed PubMed Central Google Scholar
Download references
Acknowledgements
The authors acknowledge the Ministry of Health and Medical Education, Ministry of education, Welfare Organization of Iran and Tehran University of Medical sciences for their participation in the interviews.
This research was funded by Tehran University of Medical sciences.
Author information
Authors and affiliations.
Department of Public Health, Sirjan School of Medical Sciences, Sirjan, Iran
Omolbanin Atashbahar
Department of Health Management and Economics, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran
Ali Akbari Sari & Amirhossein Takian
National Institute for Health Research, Tehran University of Medical Sciences, Tehran, Iran
Ali Akbari Sari
Department of Global Health and Public Policy, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran
Amirhossein Takian
Health Equity Research Centre (HERC), Tehran University of Medical Sciences, No. 70, Bozorgmehr Ava., Vesal St., Keshavars Blvd, Tehran, 1416833481, Iran
Amirhossein Takian, Alireza Olyaeemanesh & Efat Mohamadi
Population, Family and School Health Office, Ministry of Health and Medical Education, Tehran, Iran
Sayyed Hamed Barakati
You can also search for this author in PubMed Google Scholar
Contributions
OA, AS, AT and AO designed this study and determined its methods. OA conducted the collection, analysis and interpretation of the data with assistance from AS and AT for revising the analytical approach. OA and HB carried out the analytical experiment. All authors discussed the results and contributed to the final manuscript. OA, AS and EM wrote the manuscript. All authors contributed to the development and approval of the final manuscript. AS is the guarantor.
Corresponding author
Correspondence to Efat Mohamadi .
Ethics declarations
Ethics and consent to participate.
In our study, before the interviews, necessary information regarding the study and its objectives were given to the participants and informed consent was obtained from them verbally and recorded audio. The current study is approved by the Ethical Committee of Tehran University of Medical Science (code: IR.TUMS.REC.1396.2694) and all the used methods were performed in accordance with the relevant guidelines and regulations. The verbal informed consent procedure was approved by the Ethical Committee of Tehran University of Medical Science that confirmed the present study (code: IR.TUMS.REC.1396.2694). It should also be noted that written consent was not necessary for this study because the names of the interviewees were not mentioned in the findings. Moreover, participants were assured that their information would remain confidential and the data of the study would be analyzed anonymously.
Consent for publication
Not Applicable.
Competing interests
There is no conflict of interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

Supplementary Information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Atashbahar, O., Sari, A.A., Takian, A. et al. The impact of social determinants of health on early childhood development: a qualitative context analysis in Iran. BMC Public Health 22 , 1149 (2022). https://doi.org/10.1186/s12889-022-13571-5
Download citation
Received : 08 October 2021
Accepted : 03 June 2022
Published : 08 June 2022
DOI : https://doi.org/10.1186/s12889-022-13571-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Early childhood development
- Social determinants
- Policy analysis
- Health policy
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Social Determinants of Health
What are social determinants of health.
Social determinants of health (SDOH) are the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.
SDOH can be grouped into 5 domains:
Suggested citation
Healthy People 2030, U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Retrieved [date graphic was accessed], from https://health.gov/healthypeople/objectives-and-data/social-determinants-health
Social determinants of health (SDOH) have a major impact on people’s health, well-being, and quality of life. Examples of SDOH include:
- Safe housing, transportation, and neighborhoods
- Racism, discrimination, and violence
- Education, job opportunities, and income
- Access to nutritious foods and physical activity opportunities
- Polluted air and water
- Language and literacy skills
SDOH also contribute to wide health disparities and inequities. For example, people who don't have access to grocery stores with healthy foods are less likely to have good nutrition. That raises their risk of health conditions like heart disease, diabetes, and obesity — and even lowers life expectancy relative to people who do have access to healthy foods.
Just promoting healthy choices won't eliminate these and other health disparities. Instead, public health organizations and their partners in sectors like education, transportation, and housing need to take action to improve the conditions in people's environments.
That's why Healthy People 2030 has an increased and overarching focus on SDOH.
How Does Healthy People 2030 Address SDOH?
One of Healthy People 2030’s 5 overarching goals is specifically related to SDOH: “Create social, physical, and economic environments that promote attaining the full potential for health and well-being for all.”
In line with this goal, Healthy People 2030 features many objectives related to SDOH. These objectives highlight the importance of "upstream" factors — usually unrelated to health care delivery — in improving health and reducing health disparities.
More than a dozen workgroups made up of subject matter experts with different backgrounds and areas of expertise developed these objectives. One of these groups, the Social Determinants of Health Workgroup , focuses solely on SDOH.
Explore Research Related to SDOH
Social determinants of health affect nearly everyone in one way or another. Our literature summaries provide a snapshot of the latest research related to specific SDOH.
View SDOH Infographics
Each SDOH infographic represents a single example from each of the 5 domains of the social determinants of health. You can download them, print them, and share them with your networks.
Learn How SDOH Affect Older Adults
SDOH have a big impact on our chances of staying healthy as we age. Healthy People’s actionable scenarios highlight ways professionals can support older adults’ health and well-being.
The Office of Disease Prevention and Health Promotion (ODPHP) cannot attest to the accuracy of a non-federal website.
Linking to a non-federal website does not constitute an endorsement by ODPHP or any of its employees of the sponsors or the information and products presented on the website.
You will be subject to the destination website's privacy policy when you follow the link.
The independent source for health policy research, polling, and news.
Beyond Health Care: The Role of Social Determinants in Promoting Health and Health Equity
Samantha Artiga and Elizabeth Hinton Published: May 10, 2018
- Issue Brief
Introduction
Efforts to improve health in the U.S. have traditionally looked to the health care system as the key driver of health and health outcomes. However, there has been increased recognition that improving health and achieving health equity will require broader approaches that address social, economic, and environmental factors that influence health. This brief provides an overview of these social determinants of health and discusses emerging initiatives to address them.
What are Social Determinants of Health?
Social determinants of health are the conditions in which people are born, grow, live, work and age. 1 They include factors like socioeconomic status, education, neighborhood and physical environment, employment, and social support networks, as well as access to health care (Figure 1).
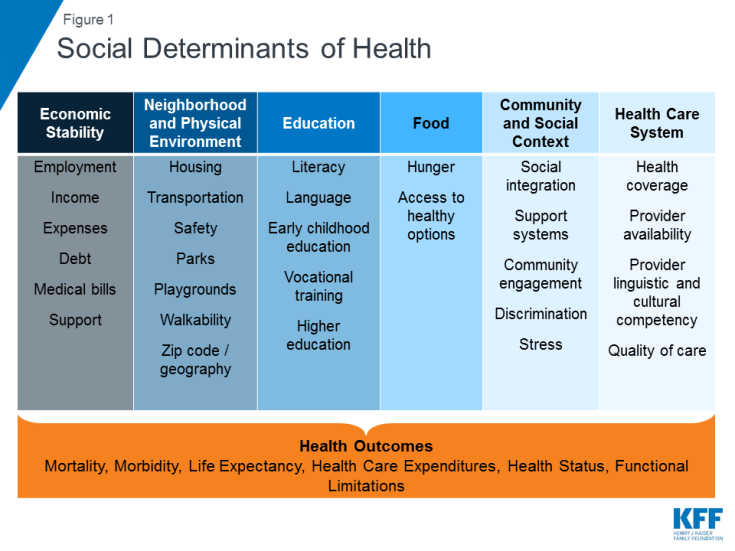
Figure 1: Social Determinants of Health
Addressing social determinants of health is important for improving health and reducing health disparities. 2 Though health care is essential to health, it is a relatively weak health determinant. 3 Research shows that health outcomes are driven by an array of factors, including underlying genetics, health behaviors, social and environmental factors, and health care. While there is currently no consensus in the research on the magnitude of the relative contributions of each of these factors to health, studies suggest that health behaviors, such as smoking, diet, and exercise, and social and economic factors are the primary drivers of health outcomes, and social and economic factors can shape individuals’ health behaviors. For example, children born to parents who have not completed high school are more likely to live in an environment that poses barriers to health such as lack of safety, exposed garbage, and substandard housing. They also are less likely to have access to sidewalks, parks or playgrounds, recreation centers, or a library. 4 Further, evidence shows that stress negatively affects health across the lifespan 5 and that environmental factors may have multi-generational impacts. 6 Addressing social determinants of health is not only important for improving overall health, but also for reducing health disparities that are often rooted in social and economic disadvantages.
Initiatives to Address Social Determinants of Health
A growing number of initiatives are emerging to address social determinants of health. Some of these initiatives seek to increase the focus on health in non-health sectors, while others focus on having the health care system address broader social and environmental factors that influence health.
Focus on Health in Non-Health Sectors
Policies and practices in non-health sectors have impacts on health and health equity. For example, the availability and accessibility of public transportation affects access to employment, affordable healthy foods, health care, and other important drivers of health and wellness. Nutrition programs and policies can also promote health, for example, by supporting healthier corner stores in low-income communities, 7 farm to school programs 8 and community and school gardens, and through broader efforts to support the production and consumption of healthy foods. 9 The provision of early childhood education to children in low-income families and communities of color helps to reduce achievement gaps, improve the health of low-income students, and promote health equity. 10
“Health in All Policies” is an approach that incorporates health considerations into decision making across sectors and policy areas. 11 A Health in All Policies approach identifies the ways in which decisions in multiple sectors affect health, and how improved health can support the goals of these multiple sectors. It engages diverse partners and stakeholders to work together to promote health, equity, and sustainability, and simultaneously advance other goals such as promoting job creation and economic stability, transportation access and mobility, a strong agricultural system, and improved educational attainment. States and localities are utilizing the Health in All Policies approach through task forces and workgroups focused on bringing together leaders across agencies and the community to collaborate and prioritize a focus on health and health equity. 12 At the federal level, the Affordable Care Act (ACA) established the National Prevention Council, which brings together senior leadership from 20 federal departments, agencies, and offices, who worked with the Prevention Advisory Group, stakeholders, and the pubic to develop the National Prevention Strategy.
Place-based initiatives focus on implementing cross-sector strategies to improve health in neighborhoods or communities with poor health outcomes. There continues to be growing recognition of the relationship between neighborhoods and health, with zip code understood to be a stronger predictor of a person’s health than their genetic code. 13 A number of initiatives focus on implementing coordinated strategies across different sectors in neighborhoods with social, economic, and environmental barriers that lead to poor health outcomes and health disparities. For example, the Harlem Children’s Zone (HCZ) project focuses on children within a 100-block area in Central Harlem that had chronic disease and infant mortality rates that exceeded rates for many other sections of the city as well as high rates of poverty and unemployment. HCZ seeks to improve the educational, economic, and health outcomes of the community through a broad range of family-based, social service, and health programs.
Addressing Social Determinants in the Health Care System
In addition to the growing movement to incorporate health impact/outcome considerations into non-health policy areas, there are also emerging efforts to address non-medical, social determinants of health within the context of the health care delivery system. These include multi-payer federal and state initiatives, Medicaid initiatives led by states or by health plans, as well as provider-level activities focused on identifying and addressing the non-medical, social needs of their patients.
Federal and State Initiatives
In 2016, Center for Medicare and Medicaid Innovation (CMMI), which was established by the ACA, announced a new “Accountable Health Communities” model focused on connecting Medicare and Medicaid beneficiaries with community services to address health-related social needs. The model provides funding to test whether systematically identifying and addressing the health-related social needs of Medicare and Medicaid beneficiaries through screening, referral, and community navigation services will affect health costs and reduce inpatient and outpatient utilization. In 2017, CMMI awarded 32 grants to organizations to participate in the model over a five-year period. Twelve awardees will provide navigation services to assist high-risk beneficiaries with accessing community services and 20 awardees will encourage partner alignment to ensure that community services are available and responsive to the needs of enrollees. 14
Through the CMMI State Innovation Models Initiative (SIM), a number of states are engaged in multi-payer delivery and payment reforms that include a focus on population health and recognize the role of social determinants. SIM is a CMMI initiative that provides financial and technical support to states for the development and testing of state-led, multi-payer health care payment and service delivery models that aim to improve health system performance, increase quality of care, and decrease costs. To date, the SIM initiative has awarded nearly $950 million in grants to over half of states to design and/or test innovative payment and delivery models. As part of the second round of SIM grant awards, states are required to develop a statewide plan to improve population health. States that received Round 2 grants are pursuing a variety of approaches to identify and prioritize population health needs; link clinical, public health, and community-based resources; and address social determinants of health.
- All 11 states that received Round 2 SIM testing grants plan to establish links between primary care and community-based organizations and social services. 15 For example, Ohio is using SIM funds, in part, to support a comprehensive primary care (CPC) program in which primary care providers connect patients with needed social services and community-based prevention programs. As of December 2017, 96 practices were participating in the CPC program. Connecticut’s SIM model seeks to promote an Advanced Medical Home model that will address the wide array of individuals’ needs, including environmental and socioeconomic factors that contribute to their ongoing health.
- A number of the states with Round 2 testing grants are creating local or regional entities to identify and address population health needs and establish links to community services. For example, Washington State established nine regional “Accountable Communities of Health,” which will bring together local stakeholders from multiple sectors to determine priorities for and implement regional health improvement projects. 16 Delaware plans to implement ten “Healthy Neighborhoods” across the state that will focus on priorities such as healthy lifestyles, maternal and child health, mental health and addiction, and chronic disease prevention and management. 17 Idaho is creating seven “Regional Health Collaboratives” through the state’s public health districts that will support local primary care practices in Patient-Centered Medical Home transformation and create formal referral and feedback protocols to link medical and social services providers. 18
- The Round 2 testing grant states also are pursuing a range of other activities focused on population health and social determinants. Some of these activities include using population health measures to qualify practices as medical homes or determine incentive payments, incorporating use of community health workers in care teams, and expanding data collection and analysis infrastructure focused on population health and social determinants of health. 19
Medicaid Initiatives
Delivery system and payment reform.
A number of delivery and payment reform initiatives within Medicaid include a focus on linking health care and social needs. In many cases, these efforts are part of the larger multi-payer SIM models noted above and may be part of Section 1115 Medicaid demonstration waivers. 20 For example, Colorado and Oregon are implementing Medicaid payment and delivery models that provide care through regional entities that focus on integration of physical, behavioral, and social services as well as community engagement and collaboration.
- In Oregon, each Coordinated Care Organization (or “CCO”) is required to establish a community advisory council and develop a community health needs assessment. 21 CCOs receive a global payment for each enrollee, providing flexibility for CCOs to offer “health-related services” – which supplement traditional covered Medicaid benefits and may target the social determinants of health. 22 Early experiences suggest that CCOs are connecting with community partners and beginning to address social factors that influence health through a range of projects. For example, one CCO has funded a community health worker to help link pregnant or parenting teens to health services and address other needs, such as housing, food, and income. 23 Another CCO worked with providers and the local Meals on Wheels program to deliver meals to Medicaid enrollees discharged from the hospital who need food assistance as part of their recovery. 24 An evaluation conducted by the Oregon Health & Science University’s Center for Health Systems Effectiveness released in 2017 found CCOs were associated with reductions in spending growth and improvement in some quality domains. 25 According to the evaluation, most CCOs believed health-related flexible services were effective at improving outcomes and reducing costs. 26
- Similarly, in Colorado, the Regional Collaborative Organizations (RCCOs), which are paid a per member per month payment for enrollees, help connect individuals to community services through referral systems as well as through targeted programs designed to address specific needs identified within the community. 27 A study published in 2017 comparing Oregon’s CCO program to Colorado’s RCCO program found that Colorado’s RCCO program generated comparable reductions in expenditures and inpatient care days. 28
Several other state Medicaid programs have launched Accountable Care Organization (ACO) models that often include population-based payments or total cost of care formulas, which may provide incentives for providers to address the broad needs of Medicaid beneficiaries, including the social determinants of health. 29
Some state Medicaid programs are supporting providers’ focus on social determinants of health through “Delivery System Reform Incentive Payment” (DSRIP) initiatives. DSRIP initiatives emerged under the Obama Administration as part of Section 1115 Medicaid demonstration waivers. DSRIP initiatives link Medicaid funding for eligible providers to process and performance metrics, which may involve addressing social needs and factors. For example, in New York, provider systems may implement DSRIP projects aimed at ensuring that people have supportive housing. The state also has invested significant state dollars outside of its DSRIP waiver in housing stock to ensure that a better supply of appropriate housing is available. 30 In Texas, some providers have used DSRIP funds to install refrigerators in homeless shelters to improve individuals’ access to insulin. 31 The California DSRIP waiver has increased the extent to which the public hospital systems focus on coordination with social services agencies and county-level welfare offices. 32 To date, data on the results of DSRIP programs are limited, but a final federal evaluation report is scheduled to for 2019. 33
Medicaid programs also are providing broader services to support health through the health homes option established by the ACA. Under this option, states can establish health homes to coordinate care for people who have chronic conditions. Health home services include comprehensive care management, care coordination, health promotion, comprehensive transitional care, patient and family support, as well as referrals to community and social support services. Health home providers can be a designated provider, a team of health professionals linked to a designated provider, or a community health team. A total of 21 states report that health homes were in place in fiscal year 2017. 34 A federally-funded evaluation of the health homes model found that most providers reported significant growth in their ability to connect patients to nonclinical social services and supports under the model, but that lack of stable housing and transportation were common problems for many enrollees that were difficult for providers to address with insufficient affordable housing and rent support resources. 35
Housing and Employment Supports
Some states are providing housing support to Medicaid enrollees through a range of optional state plan and waiver authorities. While states cannot use Medicaid funds to pay for room and board, Medicaid funds can support a range of housing-related activities, including referral, support services, and case management services that help connect and retain individuals in stable housing. 36 For example, the Louisiana Department of Health formed a partnership with the Louisiana Housing Authority to establish a Permanent Supportive Housing (PSH) program with the dual goals of preventing and reducing homelessness and unnecessary institutionalization among people with disabilities. Louisiana’s Medicaid program covers three phases of tenancy support services for Medicaid beneficiaries in permanent supportive housing: pre-tenancy services (housing search assistance, application assistance etc.), move-in services, and ongoing tenancy services. 37 Louisiana reports a 94% housing retention rate since the program began housing tenants in 2008. A preliminary analysis shows statistically significant reductions in hospitalizations and emergency department utilization after the PSH intervention, and an early independent analysis of the PSH program’s impact on Medicaid spending found a 24% reduction in Medicaid acute care costs after a person was housed. 38
Through a range of optional and waiver authorities, some states are providing voluntary supported employment services to Medicaid enrollees. Supported employment services may include pre-employment services (e.g., employment assessment, assistance with identifying and obtaining employment, and/or working with employer on job customization) as well as employment sustaining services (e.g., job coaching and/or consultation with employers). States often target these services to specific Medicaid populations, such as persons with serious mental illness or substance use disorders and individuals with intellectual or developmental disabilities. For example, under a Section 1115 waiver, Hawaii offers supportive employment services to Medicaid enrollees with serious mental illness (SMI), individuals with serious and persistent mental illness (SPMI), and individuals who require support for emotional and behavioral development (SEBD). 39
Medicaid Managed Care Organizations (MCOs)
Medicaid MCOs are increasingly engaging in activities to address social determinants of health. Data from the Kaiser Family Foundation’s 50-state Medicaid budget survey show that a growing number of states are requiring Medicaid MCOs to address social determinants of health as part of their contractual agreements (Box 1). In 2017, 19 states required Medicaid MCOs to screen beneficiaries for social needs and/or provide enrollees with referrals to social services and six states required MCOs to provide care coordination services to enrollees moving out of incarceration, with additional states planning to implement such requirements in 2018. 40 Other data from a 2017 Kaiser Family Foundation survey of Medicaid managed care plans show that almost all responding MCOs 41 (91%) reported activities to address social determinants of health, with housing and nutrition/food security as the top areas of focus. 42 The most common activities plans reported engaging in were working with community -based organizations to link members to social services (93%), assessing members’ social needs (91%), and maintaining community or social service resource databases (81%) (Figure 2). 43 Some plans also reported using community health workers (67%), using interdisciplinary community care teams (66%), offering application assistance and counseling referrals for social services (52%), and assisting justice-involved individuals with community reintegration (20%).
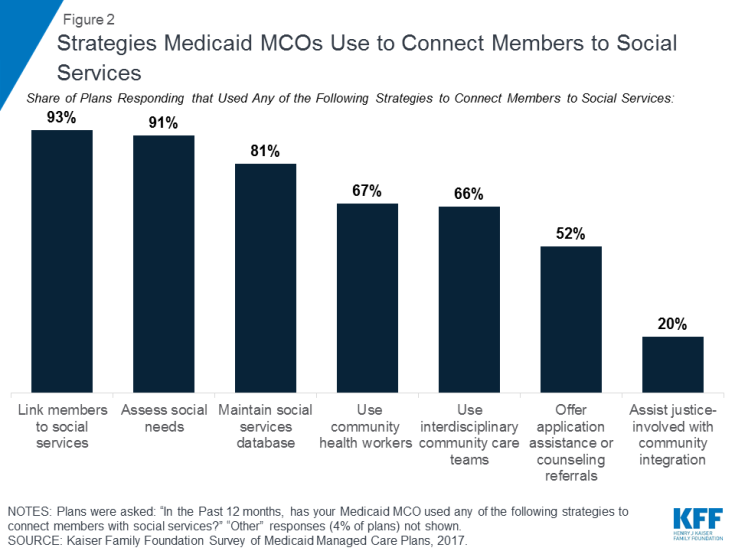
Figure 2: Strategies Medicaid MCOs Use to Connect Members to Social Services
PROVIDER ACTIVITIES
Under the ACA, not-for-profit hospitals are required to conduct a community health needs assessment (CHNA) once every three years and develop strategies to meet needs identified by the CHNA . The CDC defines a community health assessment as “the process of community engagement; collection, analysis, and interpretation of data on health outcomes and health determinants; identification of health disparities; and identification of resources that can be used to address priority needs.” 44 Under the ACA, the assessment must take into account input from people who represent the broad interests of the community being served, including those with public health knowledge or expertise.
Some providers have adopted screening tools within their practices to identify health-related social needs of patients. For example, according to a survey of nearly 300 hospitals and health systems conducted by the Deloitte Center for Health Solutions in 2017, nearly 9 in 10 (88%) hospitals screen patients to gauge their health-related social needs, though only 62% report screening target populations in a systematic or consistent way. 45 These hospitals are mostly screening inpatient and high-utilizer populations. 46 The National Association for Community Health Centers, in coordination with several other organizations, developed the Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE) tool to help health centers and other providers collect data to better understand and act on their patients’ social determinants of health. Other organizations and entities have created screening tools, including Health Leads, a non-profit organization funded by the Robert Wood Johnson Foundation, which has developed a social needs screening toolkit for providers and CMMI, which released an Accountable Health Communities screening tool to help providers identify unmet patient needs. 47
Looking Ahead
The ACA provided a key opportunity to help improve access to care and reduce longstanding disparities faced by historically underserved populations through both its coverage expansions and provisions to help bridge health care and community health. To date, millions of Americans have gained coverage through the coverage expansions, but coverage alone is not enough to improve health outcomes and achieve health equity. With growing recognition of the importance of social factors to health outcomes, an increasing number of initiatives have emerged to address social determinants of health by bringing a greater focus on health within non-health sectors and increasingly recognizing and addressing health-related social needs through the health care system.
Within the health care system, a broad range of initiatives have been launched at the federal and state level, including efforts within Medicaid. Many of these initiatives reflect new funding and demonstration authorities provided through the ACA to address social determinants of health and further health equity. They also reflect a broader system movement toward care integration and “whole-person” delivery models, which aim to address patients’ physical, mental, and social needs, as well as a shifts towards payments tied to value, quality, and/or outcomes.
Although there has been significant progress recognizing and addressing social determinants of health, many challenges remain. Notably, these efforts require working across siloed sectors with separate funding streams, where investments in one sector may accrue savings in another. Moreover, communities may not always have sufficient service capacity or supply to meet identified needs. Further, there remain gaps and inconsistencies in data on social determinants of health that limit the ability to aggregate data across settings or to use data to inform policy and operations, guide quality improvement, or evaluate interventions. 48 Within Medicaid, the growing focus on social determinants of health raises new questions about the appropriate role Medicaid should play in addressing non-medical determinants of health and how to incentivize and engage Medicaid MCOs in addressing social determinants of health. 49
The Trump Administration is pursuing policies that may limit individuals’ access to assistance programs to address health and other needs and reduce resources to address social determinants of health. The Administration has begun phasing out DSRIP programs, 50 is revising Medicaid managed care regulations, 51 and has signaled reductions in funding for prevention and public health. It has also announced plans to change the direction of models under the CMMI. 52 , 53 , 54 The Administration also is pursuing approaches to enforce and expand work requirements in public programs, 55 including Medicaid. 56 CMS asserts that this policy is designed to “improve Medicaid enrollee health and well-being through incentivizing work and community engagement” and that state efforts to make participation in work or other community engagement a requirement for Medicaid coverage may “help individuals and families rise out of poverty and attain independence.” 57 In guidance, CMS has specified that states implementing such programs will be required to describe strategies to assist enrollees in meeting work requirements (e.g., linking individuals to job training, childcare assistance, transportation, and other work supports), but that states may not use federal Medicaid funds for supportive services to help people overcome barriers to work. 58 Data show that most nonelderly Medicaid adults already are working or face significant barriers to work, leaving a small share of adults to whom these policies are directed. 59 However, eligible individuals could lose Medicaid coverage due to difficulty navigating documentation and administrative processes associated with these requirements. 60
- Racial Equity and Health Policy
- Access to Care
- Care Coordination
- Delivery System
- Managed Care
- ISSUE BRIEF
Also of Interest
- Medicaid Authorities and Options to Address Social Determinants of Health
- A Look at Recent Medicaid Guidance to Address Social Determinants of Health and Health-Related Social Needs
- 10 Things to Know About Medicaid Managed Care
What Are Social Determinants of Health? Essay
Different factors, medical and non-medical, influence the outcome of health systems. The social determinants of health (SDOH) include the non-medical factors that affect health outcomes. These factors include conditions that people interact with, live, grow, work and the conditions that make up their daily activities. Five main domains make up SDOH, namely education, community and social context, economic stability, health and healthcare, and neighborhood. In the evolving trends in healthcare, clinical records are being digitized by using electronic health records (EHRs). Integrating SDOH with EHRs helps in improving patient health outcomes. Healthcare facilities seek to extract SDOHs data from their electronic health records to address healthcare challenges (Reeves et al., 2021). SDOHs can be extracted from structured data collected by EHRs in structured and unstructured data. However, universally accepted formats and standards for extracting EHRs structured data have not been identified. Additionally, the collection of unstructured EHR data is time-consuming and requires complex methods, for example, chart reviews.
Structured data are non-medical factors that are demonstrated in elements like age, diagnosis codes, and race. EHRs capture patient information such as previous medical disorders, medical history, and lab tests. Advanced EHR systems can capture lifestyle trends of a patient like alcoholism, diet, smoking, and their preferred language in systematic and structured data. Unstructured data is data that is not defined or organized in a specific manner. The main sources of unstructured data in EHRs include clinical images and clinical texts. Clinical imaging contains data obtained from medical procedures, such as images produced by medical tools like x-rays and radiography. After capturing structured and unstructured information using EHRs, meaningful SDOH information can be extracted. The machine learning method has been employed by many institutions in extracting SDOH data from the captured EHRs data. The SDOH data collected is used as an essential tool in developing and improving the health outcome of a patient.
Reeves, R. M., Christensen, L., Brown, J. R., Conway, M., Levis, M., Gobbel, G. T., Shah, R. U., Goodrich, C., Ricket, I., Minter, F., Bohm, A., Bray, B. E., Matheny, M. E., & Chapman, W. (2021). Adaptation of an NLP system to a new healthcare environment to identify social determinants of health. Journal of Biomedical Informatics , 120 , 103851. Web.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, November 18). What Are Social Determinants of Health? https://ivypanda.com/essays/what-are-social-determinants-of-health/
"What Are Social Determinants of Health?" IvyPanda , 18 Nov. 2022, ivypanda.com/essays/what-are-social-determinants-of-health/.
IvyPanda . (2022) 'What Are Social Determinants of Health'. 18 November.
IvyPanda . 2022. "What Are Social Determinants of Health?" November 18, 2022. https://ivypanda.com/essays/what-are-social-determinants-of-health/.
1. IvyPanda . "What Are Social Determinants of Health?" November 18, 2022. https://ivypanda.com/essays/what-are-social-determinants-of-health/.
Bibliography
IvyPanda . "What Are Social Determinants of Health?" November 18, 2022. https://ivypanda.com/essays/what-are-social-determinants-of-health/.
- Social Determinates of Health of a Family
- Latino People and Type 2 Diabetes
- Social Determinants of Health and Their Impact
- Policies Affecting Nursing Homes
- Temporary Assistance for Needy Families and Nation’s Health
- Social Determinants of Health in the USA
- Concussion Occurring Among Football Athletes
- Radiography Stereotypes and Emotional Intelligence
- Medical Ethics in Radiography
- Radiology and Radiography: Research Paper
- How Smoking Is Harmful to Your Health
- Medicaid, American Governmental Health Insurance Program
- Interoperability, Data Dictionary, and Communications Draft
- The "Death Stalks a Continent" Article Review
- Importance of Marketing Program in Organizations
Essay On Social Determinants Of Health
There are many social determinants of health. Some of these include income, occupation, education, race, and gender. Each of these factors play a role in how healthy a person is.
Income is one of the most important social determinants of health. People who earn more money are generally healthier than those who earn less. This is because they can afford to buy better food and have better access to health care. They can also afford to live in safer neighborhoods with better schools and parks.
Occupation is another important social determinant of health. People who work in dangerous or unhealthy jobs are more likely to get sick than those who work in safe environments. This is because their jobs expose them to harmful chemicals or other hazards.
Education is another important social determinant of health. People who have more education are generally healthier than those who have less education. This is because they know more about how to stay healthy and prevent diseases. They also tend to have better jobs with higher incomes.
Race is another important social determinant of health. People of color are generally not as healthy as white people. This is partly because they often live in neighborhoods with fewer resources and worse schools and parks. They also face discrimination in the workplace and in the health care system.
Gender is another important social determinant of health. Women are not as healthy as men, on average, partly because they often earn less money and have fewer opportunities for good jobs. They also face discrimination in the workplace and in the health care system.
There are many other social determinants of health, including housing, food, transportation, and social support. All of these factors play a role in how healthy a person is.
It is important to remember that social determinants of health are not the only things that affect our health. Personal choices also play a role. People who eat unhealthy foods and don’t exercise are more likely to get sick than those who eat healthy foods and exercise regularly. But it is clear that social determinants of health play a major role in our overall well-being.
An explanation of the phrase “social determinants of health” The social determinants of health include settings, as well as organizational effects on them. Furthermore, they are influenced by currency distribution, influence, and resources at both local and global levels. They assess a person’s accurate social, personal, and physical assets in order to achieve his or her objectives, fulfill his or her requirements, and cope with changes in his or her circumstances.
The social determinants of health are significant because they reveal why some people are healthier than others and also help in understanding the health disparities that exist among different social groups. It is important to study the social determinants of health because they provide information on how different policies can be implemented in order to improve the overall health of the population.
Health is determined by a number of factors, including biology, environment, lifestyle and socioeconomic status. The social determinants of health are those factors that influence an individual’s health status within society.
There are a variety of social determinants of health, but some of the most important include:
– Income and Wealth: Low income and wealth are associated with poorer health outcomes. This is due to a variety of factors, including lack of access to health care, poor living conditions, and stress from economic insecurity.
– Education: Studies have shown that people with more education tend to have better health outcomes than those with less education. This is likely due to the fact that people with more education are more likely to have higher incomes and better jobs, and they are also more likely to have access to health information and resources.
– Employment Status: Unemployed people are more likely to have poorer health outcomes than those who are employed. This is likely due to the fact that unemployed people often have lower incomes and fewer resources, which can lead to stress and poorer living conditions.
– Race/Ethnicity: Health disparities exist among different racial and ethnic groups in the United States. Studies have shown that minority groups, such as African Americans and Hispanics, tend to have worse health outcomes than whites. This is likely due to a variety of factors, including socioeconomic status, access to health care, and exposure to stressors such as racism and discrimination.
– Gender: Women tend to have worse health outcomes than men. This is likely due to a number of factors, including biological differences, social roles, and access to health care.
– Sexual Orientation: Health disparities exist among different sexual orientations. Studies have shown that lesbian, gay, bisexual, and transgender (LGBT) individuals tend to have worse health outcomes than heterosexuals. This is likely due to a number of factors, including discrimination, lack of access to health care, and stress from hiding one’s sexual orientation.
Each of these social determinants of health can influence an individual’s health status in a variety of ways. For example, low income can lead to poor living conditions, which can in turn lead to health problems. Additionally, minority groups may have less access to health care and resources, which can also lead to poorer health outcomes.
The social determinants of health are important because they reveal why some people are healthier than others and also help in understanding the health disparities that exist among different social groups. By understanding the social determinants of health, we can develop policies and programs that aim to improve the overall health of the population.
Social determinants of health, as defined by the World Health Organization (WHO), are complex, interconnected, and comparable social and economic systems that account for most health disparities. Such social and economic structures include not just the social situation but also people’s physical surroundings, medical services, structural aspects as well as societal elements (WHO n.d.). The phrase “social determinants of health” refers to events such as where individuals are conceived, reared, lived their lives, worked, and sought oldness.
Health, in other words, is not merely a matter of personal responsibility; it is also shaped by the social and economic environments within which people live their lives. Health is determined by a complex interaction between people and their physical and social environment.
Health disparities among different social groups are shaped by the distribution of money, power, and resources in society. Health is not only about access to health services; it is also about the quality of the environment, education, employment, food, housing, and social support. The conditions in which people live their lives determine their health status.
More Essays
- Social Determinants Of Health Essay
- Advantages And Disadvantages Of The Biomedical Model Of Health Essay
- Disparity In Health Essay
- Seeking Health Care Case Study Essay
- Public Health Approach To Mental Health
- Public Health In The 19th Century Essay
- The Importance Of Health Promotion Essay
- Public Health Case Study Essay
- Health In The Elizabethan Era
Leave a Comment Cancel reply
Save my name, email, and website in this browser for the next time I comment.

An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Academy of Medicine; Alexander C, Murry VMB, Bogard K, editors. Perspectives on Health Equity and Social Determinants of Health. Washington (DC): National Academies Press (US); 2017.
Perspectives on Health Equity and Social Determinants of Health.
- Hardcopy Version at National Academies Press
1 HEALTH INEQUITIES, SOCIAL DETERMINANTS, AND INTERSECTIONALITY
Editors: NANCY LÓPEZ , PHD and VIVIAN L. GADSDEN , EDD.
In this essay, we focus on the potential and promise that intersectionality holds as a lens for studying the social determinants of health, reducing health disparities, and promoting health equity and social justice. Research that engages intersectionality as a guiding conceptual, methodological, and praxis-oriented framework is focused on power dynamics, specifically the relationships between oppression and privilege that are intrinsic to societal practices. Intersectional knowledge projects aimed at studying this interplay within and across systems challenge the status quo. Whether reframing existing conceptualizations of power, implementing empirical research studies, or working with community organizations and global social movements, intersectional inquiry and praxis are designed to excavate the ways a person's multiple identities and social positions are embedded within systems of inequality. Intersectionality also is attentive to the need to link individual, institutional, and structural levels of power in a given sociohistorical context for advancing health equity and social justice.
- HEALTH DISPARITIES, INEQUITY, AND SOCIAL DETERMINANTS: A BRIEF CONTEXT
The urgency to promote health, reduce health disparities, and address the social determinants of health is highlighted in countless reports ( Hankivsky and Christoffersen, 2008 ; World Health Organization, 2006 , 2015 ). In short, problems in health disrupt the human developmental process. They undermine the quality of life and opportunities for children, youth, and families, particularly those exposed to vulnerable circumstances. Despite incremental change within and across health-serving agencies and increased health education and scrutiny of patient care, we continue to see significant disparities in the quality of health and life options that children in racial and ethnic minority, low-income homes and neighborhoods experience ( Bloche, 2001 ). Research has uncovered several interconnections between health and environmental and social factors ( Chapman and Berggren, 2005 ; Thorpe and Kelley-Moore, 2013 ) but has not always shifted paradigms sufficiently to either disentangle intersecting inequalities or tease apart the ways social factors and structural barriers at once interlock to prevent meaningful and sustainable change.
In this essay, we focus on the potential and promise that intersectionality holds as a lens for studying the social determinants of health, reducing health disparities, and promoting health equity and social justice. Collins and Bilge (2016) describe intersectionality as follows:
A way of understanding and analyzing complexity in the word, in people, and in human experiences. The events and conditions of social and political life and the self can seldom be understood as shaped by one factor. They are shaped by many factors in diverse and mutually influencing ways. When it comes to social inequality, people's lives and the organization of power in a given society are better understood as being shaped not by a single axis of social division, be it race or gender or class, but by many axes that work together and influence each other. Intersectionality as an analytic tool gives people better access to the complexity of the world and of themselves . . . People use intersectionality as an analytic tool to solve problems that they or others around them face. (p. 2)
We ask: How do we engage in inquiry and praxis (action and reflection) that departs from the understanding that intersecting systems of oppression, including race/structural racism, class/capitalism, ethnicity/ethnocentrism, color/colorism, sex and gender/patriarchy, and sexual orientation/heterosexism, nationality and citizenship/nativism, disability/ableism, and other systemic oppressions intersect and interact to produce major differences in embodied, lived race-gender that shape the social determinants of health? How can we as scholars, researchers, and practitioners concerned with child and family well-being take seriously the reality of how intersecting systems of power produce lived race-gender-class and other social locations of disadvantage and develop an intersectionality health equity lens for advancing health equity inquiry, knowledge projects, and praxis?
We argue that the potential power of intersectionality as a transformational paradigm lies in two domains relevant to understanding social determinants. First, it is a critical knowledge project that questions the status quo and raises questions about the meaning and relationship between different social categories and intersecting systems of privilege and oppression ( Bowleg, 2008 ; Collins, 2008 , 2015 ; Collins and Bilge, 2016 ; Hancock, 2016 ; McCall, 2001 ; Yuval-Davis, 2011 ). It also pushes against the idea of “blaming the victim”—the simplicity of explaining health or educational outcomes by attributing problems to individuals' genetics or cultural and social behaviors alone. Second, by focusing on power relations at the individual, institutional, and global levels and the convergence of experiences in a given sociohistorical context and situational landscape, it serves as an anchor to advance equity and social justice aims for marginalized communities that have experienced and continue to experience structural inequalities ( Collins, 2008 , 2009 , 2015 ; Crenshaw, 1993 ; Weber, 2010 ). In both instances, researchers and practitioners cross traditional academic, sectoral, and disciplinary boundaries to reconceptualize a problem and combine methods from different disciplines (e.g., in interdisciplinary research), or they apply conceptualizations and methods from one discipline to closely examine issues in another (e.g., in transdisciplinary research, epistemologies, and methodologies).
There is growing evidence and professional wisdom to suggest that health disparities do not exist in isolation, but are part of a reciprocal and complex web of problems associated with inequality and inequity in education, housing, and employment ( LaVeist and Isaac, 2013 ; Schultz and Mullings, 2006 ; Weber, 2010 ; Williams and Mohammed, 2013 ). These disparities affect the unborn child through social-emotional challenges such as maternal stress and diagnosed and undiagnosed medical problems, including higher prevalence of gestational and preexisting diabetes in some pregnant populations. In other cases, they are observable at birth, particularly pronounced when prenatal care is unavailable, when the importance of care is not understood fully, and when young children are not exposed to the cognitive and social-emotional stimulation needed to thrive. These and other problems are manifested in parental stress, for example, in mother-headed and two-parent, low-income, and immigrant households alike. Parent and family adversity may reduce the number and quality of resources available and life experiences for children and families in the early years and throughout the life course. Such adversity is exacerbated by structural barriers that limit employment opportunities, increase housing instability, and contribute to homelessness, and that constrain efforts by families to effect positive change.
Over the past 20 years, two major shifts in discussions of health disparities and inequity have spurred interest and research. One shift is the growth in and opportunities presented by interdisciplinary and transdisciplinary research (e.g., work extending from sociology and psychology to economics, among other fields) and cross-domain practice (e.g., medicine, education, and social work) (see Gadsden et al., 2015b ; LaVeist and Isaac, 2013 ). The reach of interests in these issues can be found not only in the social and medical sciences but also in contemporary ethical, moral, and political philosophy, such as Sen et al.'s (2009) linking of health equity and agency, and their commentaries on the implications for social justice. A second shift has been the heightened attention to health determinants, more frequently called social determinants of health, instead of a biomedical model that solely focuses on the individual-level makeup and behaviors of patients as the source of health disparity. The report of the Commission on the Social Determinants of Health ( CSDH, 2008 ) points to the importance of being attentive to the overlapping effects and simultaneity of intersecting inequalities and their implications for social determinants:
The poor health of the poor, the social gradient in health within countries, and the marked health inequities between countries are caused by the unequal distribution of power, income, goods, and services, globally and nationally, the consequent unfairness in the immediate, visible circumstances of people's lives—their access to health care, schools, and education, their conditions of work and leisure, their homes, communities, towns, or cities—and their chances of leading a flourishing life. This unequal distribution of health-damaging experiences is not in any sense a “natural” phenomenon, but is the result of a toxic combination of poor social policies and programmes, unfair economic arrangements, and bad politics. Together, the structural determinants and conditions of daily life constitute the social determinants of health and are responsible for a major part of health inequities between and within countries. (p. 1)
In emerging conceptualizations of these social determinants, racism and discrimination are overwhelmingly significant factors, but are not the only critical dimensions related to identity to be considered ( Williams and Mohammed, 2013 ). They are tied inextricably to multiple identities and social locations that children, youth, and adults assume, and define a context for health (Bauer et al., 2016; Brown et al., 2016 ). One might argue that there is no issue more important than ensuring health. How a person understands this point and is able to act upon it is determined by more than her or his cognitive ability to engage the idea. It is influenced as well by a range of dynamic and situational identities and social positions that are biological, cultural, and epigenetic; by social determinants (i.e., where people are born, grow up, work, and age, and interact with their changing environments); and by a person's social experiences and encounters, rather than solely her or his self-agency across a variety of social settings. Even individuals with the strongest work ethic and sense of agency, when faced with daily problems associated with intersectionality across any combination of racial, class, gender, sexual orientation, language, or disability systemic oppressions and discrimination, may find fighting against these inequalities daunting.
Several researchers have advocated for a new way of combining the insights and perspectives used in intersectional knowledge projects in order to move away from decontextualized, biomedical frameworks that often fetishize “cultural competence” as the panacea for structural intersecting inequalities ( Viruell-Fuentes et al., 2012 ). Instead of getting distracted by the alleged “deficits” or “individual behaviors” of marginalized communities, they call for what Chapman and Berggren (2005) refer to as a “radical contextualization of the social determinants of health perspectives.” Sen and colleagues (2009) acknowledge this shift:
In addition to the obvious benefit of deepening our insights into social inequalities and how they interact, the study of intersectionality . . . has the potential to provide critical guidance for policies and programmes. By giving precise insights into who is affected and how, in different settings, it provides a scalpel for policies rather than the current hatchet. It enables policies and programmes to identify whom to focus on, whom to protect, what exactly to promote and why. It also provides a simple way to monitor and evaluate the impact of policies and programmes on different subgroups from the most disadvantaged through the middle layers to those with particular advantages. (p. 412)
Our objective in the remainder of this essay is to provide a discussion of the possibilities for innovation in conceptualization, methodologies, and practices that can promote human development and health equity through an “intersectionality health equity lens.” We employ Jones's (2016) definition of health equity. Jones defines health equity as “the [active] assurance of optimal conditions for all people.” Jones explains that we can get there by “valuing everyone equally, rectifying historic inequities and distributing resources according to need.” Jones invites us to think deeply and critically about equity as a never-ending process that requires constant and ongoing vigilance and not just an outcome that once accomplished can be forgotten. Building on Jones's (2016) and Collins and Bilge's (2016) ideas about equity and intersectionality we define an intersectionality health equity lens as ongoing critical knowledge projects, inquiry, and praxis that can include research, teaching, and practice approaches that are attentive to the ways systems of inequality interlock to create conditions for either health equity or health inequities ( Collins, 2008 , 2015 ; Collins and Bilge, 2016 ; Crenshaw, 1993 ).
We also embrace Collins and Bilge's (2016) core ideas of intersectionality, namely a focus on inequality, relationality and connectedness, power, social context, complexity, and social justice. They use the analogy of “domains of power” to paint a picture of the way that power is visible at the “interpersonal” or individual level in terms of who is advantaged or disadvantaged at the level of social interactions. For example, individuals may experience privilege or disadvantages when searching for a job, housing, interacting with law enforcement, or even when accessing a voting booth. Collins and Bilge (2016) assert
Using intersectionality as an analytic lens highlights the multiple nature of individual identities and how varying combinations of class, gender, race, sexuality, and citizenship categories differentially position every individual. (p. 8)
Collins and Bilge (2016) also underscore that we must always be attentive to the “disciplinary” level as a domain of power that organizes and regulates the lives of people in ways that echo our distinct social positions with regard to systems of oppression. For example, rules about who will or will not be seen at a medical office because of the ability to pay a copay, who will or will not be admitted to a domestic violence shelter based on their English proficiency, and who has access to a gifted classroom, based on IQ test scores that are rooted in eugenicist origins, will inevitably impact the conditions for the advancement of health equity (see also Crenshaw, 1993 ; Zuberi, 2001 ).
Collins and Bilge also invite us to reflect on how power is visible at the “cultural” level or in the realm of ideas, norms, and narratives. For Collins and Bilge (2016) , ideas matter and how messages are manufactured creates explanations, justifications, or challenges to the status quo vis-à-vis inequalities. For instance, if the idea that racialized health inequalities are simply a matter of individual behavior, food ways, and choice, and that we live in a meritocracy, where your station in life is simply a matter of individual effort, then we are subscribing to what Bonilla-Silva refers to as “colorblind” racism or the belief that present-day realities of race gaps in health only mirror individual deficits of individuals or defective cultures.
The last arena where Collins and Bilge interrogate the dynamic of power includes the “structural” level or at the level of institutional arrangements, which interrogates how intersecting systems of institutionalized power, whether in the economy and labor market in terms of whose labor is valued and who is exploited, or at the political level in who is granted substantive citizenship rights and privileges and who is not, as well as at the level of who has access to structures of political power and influence, shapes the institutionalization of the conditions for health equity. For example, the struggle for sovereignty of indigenous people, as evidenced in the Standing Rock movement to protect indigenous land and water for generations in South Dakota provides a snapshot of the structural location of indigenous nations and capitalist neoliberal actors that are in a struggle to define the environmental context for current and future generations, which will have grave consequences for health justice for marginalized indigenous communities.
While an intersectionality health equity lens may inform or drive interdisciplinary or transdisciplinary research, it must also be considered as part of both the process of conceptualizing the problem and the product of research on the problem. Throughout this essay, readers should consider the potential applications of an intersectionality health equity lens, how its use enhances (or disrupts) our understanding of salient and longstanding issues, what might be learned from its use that will inform and deepen research and practice with children and families who are among the marginalized in society, and what types of intersectionality-focused approaches might lead to health access and equity. In the next section, we focus on the contributions of an intersectionality health equity lens for research and for promoting health equity.
AN “INTERSECTIONALITY HEALTH EQUITY LENS” FOR SOCIAL JUSTICE
When developing or applying an intersectionality health equity lens, the researcher engages in deep self-reflection that contextualizes and recognizes the ways race, gender, class, sexual orientation, disability, and other axes of inequality constitute intersecting systems of oppression. Such systems produce very different lived experiences for entire categories of people who are embedded within complex webs and social networks at different levels (e.g., family, neighborhood, and community as well as institutional and structural). These lived experiences can either enhance or challenge the developmental pathways of children through adulthood and the ability of parents and families to ensure a positive trajectory for their children. They affect both the individual child and the networks and communities in which children live and grow and that define their access to resources.
An intersectionality health equity lens for the purposes of our discussion takes on the broader, philosophical meaning attached to praxis as a process involving health, educational, and social service researchers and practitioners in not only self-reflection but also action. Critical self-reflection allows researchers and practitioners to continually and closely examine their own race, gender, class, sexual orientation, disability, language, nativity/citizenship and social position, and their relationship to systems of inequality as part of intersecting systems of oppression and privilege. It argues for researchers and practitioners to draw upon their own experiences with health inequities and discrimination, and to understand and respond to new or subtle forms of inequities and discrimination. These subtle forms of inequity and discrimination are sometimes so deeply embedded in and accepted as societal practices that they may be difficult to uncover, yet render many children and families hopeless. The interplay between and among relevant systems and the statuses accompanying power attributed to different ethnic, racial, cultural, and socioeconomic groups affect both individuals and their social networks (e.g., family, neighborhood, and community). They are tied directly to and within institutional and structural hierarchies.
Crenshaw (1993) points to the entrenched nature of inequity, underscoring the need for a useful paradigm in which to locate the issues faced by African American women and other racially stigmatized, visible minority women of color. Credited with creating a systematic analysis of the concept of intersectionality, Crenshaw (1993) urged readers to “map the margins” by focusing on those social locations that remain invisible. She argues that such invisibility results from a reliance on a mythical, universal “black experience” (e.g., when we assume that the default category is the “black male experience” and by the same token when we speak about “‘women's experiences” and assume that all women's experiences are represented in white women's experience). In each of these dominant conceptualizations of the black [male] and [white] woman's experience, heteronormativity is the invisible structure.
Crenshaw (1993) also illustrates how language, and potentially nativity and citizenship status, can serve as other axes of stratification that have received less attention than race and class. To illustrate her point, Crenshaw flexes her intersectional lens to bring into sharp relief the effects of “good intentions” on the real lives of women. She demonstrates that, despite their good intentions, some domestic violence shelters may operate in ways that ignore the plight of immigrant women with children who may not speak English and are unable to access domestic violence shelters. It goes without saying that this would structurally exclude immigrant (both documented and undocumented) women and their children who do not speak English. “Nativism, English Only” categories are the invisible, yet real, structural barriers to addressing domestic violence in the aforementioned situation. By the same token, members of lesbian, gay, bisexual, transgender, queer, and in-transition (LGBTQI) communities may not face explicit rules about being barred from these services because of their gender identity, but if counselors and other providers assume that their clients are in heterosexual, gender-conforming relationships, heteronormativity can operate as another type of an informal barrier.
One might well ask, given the complex relationships in addressing identity, whether it is possible to create intersectionality-grounded projects that integrate the issues of race, class, gender, disability, and other identities, statuses, and social locations in research on health and well-being for the range of issues facing marginalized children, youth, and families. Although we do not have a simple response, we highlight the need to address the real or perceived complexity of creating such projects and allowing time and resources for them to be developed well and to be refined ( Cacari-Stone et al., 2017 ; López et al., 2017a , 2018 ; Van Hattum et al., 2017 ). We similarly understand the limitations of relying on one-dimensional categories that are, at best, additive, for example, first race, then maybe class, then maybe gender, depending on the focus of the research. As the World Health Organization (2015) and several health researchers before (e.g., LaVeist and Isaac, 2013 ; Williams and Mohammed, 2013 ) suggest, understanding the social determinants of health requires a broad reach to identify, and respond to, the embedded and entrenched inequities of policies that are situated in place and context.
Intersectionality health equity lenses help us understand that every person's experience is fundamentally different than the experience of others, based on their unique identity and structural positions within systems of inequality and structural impediments ( Feagin and Sikes, 1994 ; López, 2003 , Nakano Glenn, 2002 , 2015 ; Weber, 2010 ). More than just a theory or framework to be used selectively, it is a commitment to developing a relentlessly critical and self-reflective lens that begins with the premise that race, class, gender, and other axes of social identities are intertwined and mutually constitutive, and that such a lens can help advance health disparities research, practice, and leadership by making the invisible visible ( López et al., 2017b ; López, 2018 ).
- INTEGRATING RACE, GENDER, CLASS, AND SEXUALITY AS LIVED EXPERIENCES: A CASE EXAMPLE
In considering intersectionality projects, we must be aware of the overwhelming inequities associated with longstanding problems of race and gender and the added problems of poverty and class—problems that have narrowed in some cases over time but where inequality persists. It should come as no surprise that an intersectionality-focused project might appear opaque or obscure initially, despite its potential to uncover the breadth of issues faced in ensuring health and well-being.
Imagine the year 2050, and all institutional data are derived from the critical insight offered by Bowleg (2008) :
It is the analysis and interpretation of research findings within the sociohistorical context of structural inequality for groups positioned in social hierarchies of unequal power . . . . that best defines intersectionality research. (p. 323)
López (2013) proposes the “racialized-gendered social determinant of health” as a heuristic device or framework for centering the lives of marginalized communities. This framework consists of two major concepts: (1) “lived race-gender” and (2) “racialized-gendered pathways of embodiment.” López (2003) offers an example of the enactment of these concepts in the minds and experiences of both the observer and the observed. For example, she makes explicit the ways race-gender disparities are enacted and experienced in school and society by young Dominican and Caribbean men and women in what she calls “New York Immigration and Racialization.” Consider Orfelia's narrative on the public's perceptions of blacks, Hispanics, and whites and the differential result of their identities on these perceptions:
If you put on the news, anyone who does anything bad, if he's not Black, he's Hispanic . . . . You watch the news and you see that when any white guy does something, you won't see their face. They might just say it, and that's all. But if it's a Dominican, a Hispanic, a Black, they put him on for about two minutes, so that you can know him. (p. 23)
Orfelia points to the ways she has internalized race and gender stigma as dominant identity markers and their intersections with place (Queens in New York) and other intersectional identities such as immigrant and Spanish speaker. The mental health costs of feeling racially stigmatized may become embodied by many youth who also feel what sociologist W. E. B. DuBois coined in 1903 as the “double consciousness” experienced by blacks in the U.S. context or the sense of always being seen with contempt, pity, or disdain because of one's stigmatized status ( DuBois, 1999 ; Vidal-Ortiz, 2005 ). 1
López also underscores the dominance of race and gender identities, along with other identities (e.g., social class, sexual orientation, age, ethnicity and nativity, and legal status) that form the basis for education and health frameworks. She draws upon a personal example to demonstrate connections among race, gender, sexuality, and social class and the significance attached to heteronormativity ( Box 1-1 ).
BOX 1–1
Contextualizing Lived Race-Gender and the Racialized-Gendered Social Determinants of Health.
While race, gender, and class were overriding identities in the short narrative in Box 1-1 , heteronormativity was the silent but overpowering lens for López and her cousin. 3 As López notes, the nature and type of her cousin's experiences in and out of school, within family and community contexts, and with stressors that were unnamed distinguished the two cousins. As she suggests through this anecdote, sexuality played only a small though apparently significant part in the everyday encounters that her cousin faced. What remains unanswered are questions about the ways race and gender (male and Dominican) played in her cousin's schooling, and the ways that gender nonconformance (what we now refer to as transgender identity) produced barriers to health access, care, prevention, and maintenance; to employment; to housing; and to the daily acceptances that allow individuals to maintain not just a healthy personal racial, gendered, class, ethnic, or sexual identity but also an identity that can be embraced in full in all social domains and situations that López's cousin traversed throughout their short life.
Focusing on López's cousin's experiences from a health equity perspective, several additional questions are raised: Did the health system fail her cousin, or was it the larger social system that did not accept their intersectional identities? To what degree do our current systems of data collection make her cousin's intersecting lived oppressions vis-à-vis race, national origin, class, sexuality, gender identity, and nativity invisible? If we collect data only on gender identity and not class, nativity, citizenship, ethnicity, language, and/or national origin, do we make some social locations invisible? Do we ignore the temporal element of identities across the life course? How would López's cousin's life experiences have been different if her cousin had been from an LGBTQI middle class, Dominican immigrant family that was light skinned, white-looking Latinx and not a visible minority? All of these data challenges are opportunities for establishing communities of practice committed to intersectionality praxis (action and reflection). 4 Bowleg (2008) provides us with critical epistemological, ontological, and methodological insights on advancing intersectional inquiry and praxis:
I argue that a key dilemma for intersectionality researchers is that the additive (e.g., Black + Lesbian + Woman) versus intersectional (e.g., Black Lesbian Woman) assumption inherent in measurement and qualitative and quantitative data analyses contradicts the central tenet of intersectionality: social identities and inequality are interdependent for groups such as Black lesbians, not mutually exclusive. In light of this, interpretation becomes one of the most substantial tools in the intersectionality researcher's methodological toolbox. (p. 312)
In studying these and other questions related to health access and equity, drawing upon broad conceptualizations and nuanced analyses is important as is drawing upon conceptually complementary methodological approaches. The efficacy of rigorous quasi-experimental studies and of large, integrated datasets, including administrative data, in identifying and addressing multiple problems facing differing communities is clear. For example, Brown and colleagues (2016) examine the influence of the intersecting consequences of race-ethnicity, gender, socioeconomics status (SES), and age on health inequality with almost 13,000 ( n = 12,976) whites, blacks, and Mexican Americans, based on panel data from the Health and Retirement Study. Drawing upon multiple-hierarchy stratification and life-course perspectives, they focus on (1) the variation of racial/ethnic stratification of health by gender and/or SES and (2) the decrease, stability, or increase of combined inequality in health between middle and late life. Analyses of the data indicated that the effects of racial/ethnic, gender, and SES stratification were interactive, resulting in the greatest racial/ethnic inequalities in health among women and those with higher SES.
Although improving our quantitative data infrastructure is of paramount importance, Chapman and Berggren (2005) also call upon health disparities researchers to take advantage of the benefits of qualitative data methods that “radically contextualize” the sociohistoric contexts that fuel the social determinants of health. They argue that qualitative methodologies such as participant observation, ethnography, and interviews can serve to demystify the link between structural, institutional, community, and individual processes that contribute to health inequities by shedding light on the social practices, interactions, policies, mechanisms, and processes that undergird manufactured health inequities. Rather than committing to one or the other, this focus on intersectionality will require the use of multiple methods, strategically layered to identify the problem and provide responsive interventions and equitable policies ( Minkler and Wallerstein, 2011 ).
An intersectional paradigm or conceptual universe takes identity categories embedded within systems of inequality as a starting point to understanding the interactions between individuals and systems and among individual identities, systems, and social locations across the life course. The categories are fluid and must be examined in combination with each other. Metzl and Hansen's (2014) concept of “structural competency” offers a useful example. It begins with the assumption that “inequalities in health [education, employment, housing, voting, law enforcement, nativity, etc.] must be conceptualized in relation to the institutions and social conditions that determine . . . resources” (p. 127). Discussions of intersectionality address Metzl and Hansen's concerns, described earlier, and emphasize the importance of examining the simultaneity of racism, sexism, heterosexism, classicism, and other axes of inequality for mapping and interrupting the sedimentation of health inequities in health care access and the social determinants of health. This perspective is moving slowly into mainstream health disparities research, as health focuses more directly on the social bases for health determinants ( WHO, 2015 ). Intersectionality considers the multiplicity of policies and practices constructed for different groups. At the same time, it acknowledges the ways these historically situated policies and practices reinscribe positions of power, dominance, and oppression that contribute to the social determinants of health, education, and well-being.
- DEVELOPING AN INTERSECTIONALITY HEALTH EQUITY LENS: CHANGING THE NARRATIVE FOR SOCIAL JUSTICE
What happens when health research takes an intersectional stance in producing and using knowledge to effect positive practice and social change and advance equity? In what ways do our personal and professional positionalities contribute to this intersectional stance, our research, and the opportunities afforded by our ways of seeing and knowing the world? How do we address the health inequalities and inequities that reduce these opportunities for children, youth, and families and redirect them to promote social justice?
We are aware that the answers to these questions require time, depth of inquiry, and breadth of analysis, and that they contribute to, rather than outline, a social justice framework. Throughout this essay, we argue that a critical, self-reflexive intersectionality health equity lens and praxis depend upon a visceral commitment to uncovering the workings of the multiple systems of inequality in unpacking the social determinants of health. Such a lens might be expanded to become an “intersectionality equity” lens that questions further how our research, teaching, and practice can enact Crenshaw's (1993) idea of “mapping the margins.” To achieve this, Crenshaw argues, we must center the lives of groups that remain often invisible when we talk about the generic working class “women” or “men” or “Latinos” or “LGBTQ” communities.
In moving forward, we also must be committed to enlarging and diversifying the pool of research scientists who study the issues. By diversity within an intersectionality health equity lens, we are referring to research scientists whose own awareness of their intersectional identities—that is, ethnicity, race, gender, class, sexuality, nativity, and disability—pushes them to design research that produces greater knowledge and clarity about the conceptualization of sound intersectionality-grounded studies and the range of methods to ensure new knowledge, better applications of knowledge, and effective uses of knowledge to guide our understanding of human development and health.
Initiatives focused on advancing social cohesion through intentional efforts to increase the diversity and number of research scientists with lived experiences that reflect multiple intersecting systems of oppression may take different forms. For example, in April 2011, the Institute for the Study of “Race” and Social Justice at the University of New Mexico, with support from a National Institutes of Health workshop grant, convened a group of scholars from the health and biological sciences and social sciences who embodied the intersecting race, gender, sexual orientation, class, age, disability status, religious, ethnic, citizenship, and national origin backgrounds that form the rich tapestry of our diverse union ( Figure 1-1 ).
FIGURE 1–1 |
National Institutes of Health (NIH) R21 Workshop. This gathering convened diverse multidisciplinary scholars for a workshop entitled, “Mapping ‘Race’ & Inequality: Best Practices for Conceptualizing and Operationalizing (more...)
Other activities may include opportunities for interdisciplinary conferences and collaborative research, teaching, and writing. For example, at the University of Pennsylvania, one health disparities course is cofacilitated with tenure-track and clinical faculty within education and across the social sciences, medicine, and nursing. Bringing together all of the insights from health sciences, psychology, anthropology, art history, American studies, and law can actually generate new knowledge and new ways of doing research and developing equity-based policy. It is tremendously powerful to build on interdisciplinary knowledge. It is not the case that any one discipline has all the answers. We need all of us working together, harmoniously, to continue to make advancements and these insights should be reflected in what is considered required coursework for all disciplines interested in health equity.
An intersectionality health equity lens offers enormous possibilities for research projects that take seriously the multiple identities of children, youth, and families in the study of health and human development. One might argue that a relationship exists between social-ecological models of human development and health that highlight the intersections and interactions between and across contexts and discussions of intersectionality that consider social statuses.
In supporting an “intersectionality health equity lens” for research, we accept the limitations of implementation and of ways of looking at problems that children, youth, and families face. In our examples, drawn from our personal and research experiences, we suggest that there is little to no likelihood that a clean, one-size-fits-all approach exists to uncover the multiple intersectional identities in a given situation or sociopolitical and historical context. We also argue that to reveal the full expanse of complex intersecting factors that create social determinants of health and well-being, the discomforts associated with linking the different identities, the tendency to focus on one over another, and the difficulty of determining and building appropriate methodologies will have to be addressed (see Gadsden et al., 2014 , 2015a ). Palència and colleagues (2014) , referring to their research and practice in Barcelona, remind us that “the development of research designs and methods that capture effectively all of the tenets of intersectionality theory remains underexplored” (p. 8). While intersectional analyses have relied heavily on ethnographic approaches, the authors note that “quantitative researchers have acknowledged the tensions between conventional research designs, intended to test for independent effects, and intersectionality principles” (p. 8).
The social sciences and health sciences are making progress toward considering the range of factors outside of simple genetics and social environments that affect health and health interventions. Intersectionality knowledge projects draw upon and have the potential to create innovative research and policy paradigms that can lead to practical measures and solutions for advancing health equity. Such measures map and interrupt inequality among racially stigmatized and other marginalized communities in local, municipal, state, and national contexts. At a minimum, they suggest a revisioning of policies that cut across relevant areas of health, education, social services, and law.
In developing our focus on intersectionality and social determinants of health, we attach our analysis to the goals of advancing social justice, where commitments to equality and equity reside and power is shared. A list of resources focused on intersectionality appears in Box 1-2 and demonstrates the range of efforts. As these efforts suggest, for all health and health policy researchers, scholars, practitioners, and community leaders who embrace a social justice framework, an intersectionality health equity lens could help to illuminate the often stifled issues that affect the health, development, and well-being of children and families in marginalized communities. This would mean that they would take seriously the ways institutional rights and duties allow people to participate and receive resources such as health, education, and social services in ways that are fundamentally shaped by intersecting inequalities. That would also mean promoting equal access to the fair distribution of wealth, equal opportunity, and equality of outcome by making the invisible visible through interrogating how race and class systems of oppression work together in shaping the social determinants of health.
Partial List of Intersectionality-Focused Resources.
Organizations such as the NAM can serve as convergence spaces where intersectionality knowledge projects centering on the lives of multiple and diverse marginalized groups in a given sociohistorical context can be incubated and developed to advance health justice. How specialists see, treat, and understand the human experiences of children and families and the potential for their well-being will be revised. As a result, we begin to address the multiplicity of identities, social positions, and systems of intersecting inequalities that contribute to the social determinants of health for diverse populations of children, youth, and families and move closer to effecting sustainable change and equity.
- Bauer G. Incorporating intersectionality theory into population health research methodology: Challenges and the potential to advance health equity. Social Science and Medicine. 2014; 110 :10–17. [ PubMed : 24704889 ]
- Bloche MG. Race and discretion in American medicine. Yale Journal of Health Policy, Law, and Ethics. 2001; 1 (1):5. [ PubMed : 12669322 ]
- Bowleg L. The methodological challenges of qualitative and quantitative intersectionality research. Sex Roles. 2008; 59 :312–325.
- Brown TH, Richardson LJ, Hargrove TW, Thomas CS. Using multiple-hierarchy stratification and life course approaches to understand health inequalities: The intersecting consequences of race, gender, SES, and age. Journal of Health and Social Behavior. 2016; 57 (2):200–222. [ PMC free article : PMC4905600 ] [ PubMed : 27284076 ]
- Cacari-Stone L, Diaz Fuentes C, López N, Raj Joshi F, Lauvidaus M. The heart of gender justice in New Mexico: Intersectionality, economic security, and health equity (Part 2: Quantitative data analysis). Santa Fe, NM: NewMexicoWomen.org; 2017.
- Chapman R, Berggren J. Radical contextualization: Contributions to an anthropology of racial/ethnic health disparities. Health: An Interdisciplinary Journal for the Social Study of Health, Illness, and Medicine. 2005; 9 (2):145–167. [ PubMed : 15788431 ]
- Collins PH. Black feminist thought: Knowledge, consciousness, and the politics of empowerment. New York: Routledge; 2008.
- Collins PH. Another kind of public education: Race, schools, the media and democratic possibilities. Boston, MA: Beacon Press; 2009.
- Collins PH. Intersectionality's definitional dilemmas. Annual Review of Sociology. 2015; 41 :1–20.
- Collins PH, Bilge S. Intersectionality. Malden, MA: Polity Press; 2016.
- Crenshaw K. Mapping the margins: Intersectionality, identity politics, and violence against women of color. In: Crenshaw K, Gotanda N, Peller G, Thomas K, editors. Critical race theory: The key writings that formed the movement. New York: New Press; 1993. pp. 357–383.
- CSDH (Commission on Social Determinants of Health). Building a global movement for health equity. World Health Organization; 2007. http://www .who.int/social_determinants /resources /csdh_media/csdh _interim_statement_07.pdf .
- CSDH. Closing the gap in a generation: Health equity through action on the social determinants of health. Geneva: World Health Organization; 2008. Final Report.
- Cuevas A, Ortiz K, López N, Williams D. Ethnicity and Health. forthcoming. Assessing racial differences in lifetime and current smoking status & menthol consumption among Latinos in a nationally representative sample. [ PMC free article : PMC6179942 ] [ PubMed : 29540075 ]
- DuBois WEB. On spiritual strivings. In: Gates HL, Oliver TH, editors. The souls of black folk. New York: W. W. Norton and Company; 1999.
- Feagin JR, Sikes MP. Living with racism: The black middle-class experience. Boston, MA: Beacon Press; 1994.
- Gadsden V, Gioia D, Mostafa K. Shifting the conversation: Emotional labor as learning in a pedagogy of discomfort; Poster presented at the 2014 American Educational Research Association Annual Meeting; Philadelphia, PA. 2014.
- Gadsden V, Jacobs KB, Peterman N. Emotion, knowledge, and inquiry: Students' comforts and discomforts in studying race, culture, and equity; Paper presented at the American Educational Research Association Annual Meeting; Chicago, IL. 2015a.
- Gadsden VL, Peterman N, Maton R, Yee M, Johnston M. University-community health partnerships: An inquiry into family and community health beliefs and practices; Paper presented at the American Educational Research Association Annual Meeting; Chicago, IL. 2015b.
- Glenn E. Unequal freedom: How race and gender shaped American citizenship and labor. Boston, MA: Harvard University Press; 2002.
- Glenn EN. Settler colonialism as structure: A framework for comparative studies of US race and gender formation. Sociology of Race and Ethnicity. 2015; 1 (1):52–72.
- Gómez LE. Law and Society Review. 2000. Race, colonialism, and criminal law: Mexicans and the American criminal justice system in territorial New Mexico; pp. 1129–1202.
- Gómez LE, López N, editors. Mapping “race”: Critical approaches to health disparities research. New Brunswick, NJ: Rutgers University Press; 2013.
- Gravlee C. How race becomes biology: Embodiment of social inequality. American Journal of Physical Anthropology. 2009; 139 :47–57. [ PubMed : 19226645 ]
- Hancock AM. Intersectionality: An intellectual history. Oxford University Press; 2016.
- Hankivsky O, Christoffersen A. Intersectionality and the determinants of health: A Canadian perspective. Critical Public Health. 2008; 18 (3):271–283.
- Hunter M. The persistent problem of colorism: Skin tone, status, and inequality. Sociology Compass. 2007; 1 (1):237–254.
- Johnson III RG, Rivera M, López N. Social movements and the need for a trans ethics approach to LGBTQ homeless youth. Public Integrity. 2017; 19 :1–14.
- Jones C. Closing General Session, “Creating the Healthiest Nation: Ensuring the Right to Health”; American Public Health Association Annual Meeting; Denver, CO. 2016.
- LaVeist TA, Isaac L, editors. Race, ethnicity, and health. 2nd ed. San Francisco, CA: Jossey-Bass; 2013.
- López N. Hopeful girls, troubled boys: Race and gender disparity in urban education. New York: Routledge; 2003.
- López N. Contextualizing lived race-gender and the racialized gendered social determinants of health. In: Gómez L, López N, editors. Mapping “race”: Critical approaches to health disparities research. New Brunswick, NJ: Rutgers University Press; 2013. pp. 179–211.
- López N. Scholars Strategy Network. 2017b. Why the 2020 Census should keep longstanding separate questions about Hispanic origin and race. http://www .scholarsstrategynetwork .org/brief /why-2020-census-should-keep-longstanding-separate-questions-about-hispanic-origin-and-race .
- López N. The Conversation. Feb 28, 2018. The US Census Bureau keeps confusing race and ethnicity. https: //theconversation .com/the-us-census-bureau-keeps-confusing-race-and-ethnicity-89649 .
- López N, Vargas E, Juarez M, Cacari-Stone L, Bettez S. Sociology of Race and Ethnicity. 2017a. What's your “street race”? Leveraging multidimensional measures of race and intersectionality for examining physical and mental health status among Latinx. 10.1177/2332649217708798. [ PMC free article : PMC5800755 ] [ PubMed : 29423428 ]
- López N, Erwin C, Binder M, Chavez M. Making the invisible visible through critical race theory and intersectionality: Race-gender-class gaps at a public university in the southwest 1980–2015. Race, Ethnicity and Education. 2018a; 21 :180–207.
- McCall L. Complex inequality: Gender, class, and race in the new economy. New York: Routledge; 2001.
- Metzl J, Hansen H. Structural competency: Theorizing a new medical engagement with stigma and inequality. Social Science & Medicine. 2014; 103 :126–133. [ PMC free article : PMC4269606 ] [ PubMed : 24507917 ]
- Minkler M, Wallerstein N, editors. Community-based participatory research for health: From process to outcomes. New York: John Wiley & Sons; 2011.
- Morgen A. Movement-grounded theory: Intersectional analysis of health inequalities in the U.S. In: Schultz A, Mullings L, editors. Gender, race, class and health: Intersectional approaches. San Francisco, CA: Jossey-Bass; 2006. pp. 394–423.
- Monk E. The cost of color: Skin color, discrimination, and health among African-Americans. American Journal of Sociology. 2015; 121 (2):1–49. [ PubMed : 26594713 ]
- NBER (National Bureau of Economic Research). A summary overview of Moving to Oppportunity: A random assignment housing mobility study in five U.S. cities. Department of Housing and Urban Development; 2012. Moving to Opportunity for Fair Housing Program. http://www .nber.org/mtopublic /MTO%20Overview%20Summary.pdf .
- Ortiz KS, Duncan DT, Blosnich JR, Salloum RG, Battle J. Smoking among sexual minorities: Are there racial differences? Nicotine & Tobacco Research. 2015; 17 (11):1362–1368. [ PubMed : 25589679 ]
- Palència L, Malmusi D, Borrell C. Incorporating intersectionality in evaluation of policy impacts on health equity: A quick guide. Agencia de Salut Publica de Barcelona; 2014. CIBERESP. Available from http://www .sophieproject .eu/pdf/Guide_intersectionality _SOPHIE.pdf .
- Román MJ, Flores J, editors. The Afro-Latin@ reader: History and culture in the United States. Durham, NC: Duke University Press; 2010.
- Saenz R, Morales MC. Latinos in the United States: Diversity and change. John Wiley & Sons; 2015.
- Schultz A, Mullings L. Intersectionality and health: An introduction. In: Schultz A, Mullings L, editors. Gender, race, class and health: Intersectional approaches. San Francisco, CA: Jossey-Bass; 2006. pp. 3–20.
- Sen G, Iyer A, Mukherjee C. A methodology to analyse the intersections of social inequalities in health. Journal of Human Development and Capabilities. 2009; 10 (3):397–415.
- Thorpe R, Kelley-Moore J. Life course theories of race disparities: A comparison of cumulative dis/advantage perspective and the weathering hypothesis. In: LaVeist TA, Isaac L, editors. Race, ethnicity, and health. San Francisco, CA: Jossey-Bass; 2013. pp. 355–375.
- Van Hattum F, Ghiorse S, Villamil A. The heart of gender justice in New Mexico: Intersectionality, economic security, and health equity (Part 1: Community dialogues). Santa Fe, NM: NewMexicoWomen.Org; 2017.
- Vidal-Ortiz S. On being a white person of color: Using autoethnography to understand Puerto Ricans' racialization. Qualitative Sociology. 2004; 27 (2):179–203.
- Vidal-Ortiz S. Sexuality and gender in Santería: LGBT identities at the crossroads of Santería religious practices and beliefs. In: Thumma S, Gray E, editors. Gay religion. Walnut Creek, CA: Altamira Press; 2005. pp. 115–138.
- Viruell-Fuentes EA, Miranda PY, Abdulrahim S. More than culture: Structural racism, intersectionality theory, and immigrant health. Social Science & Medicine. 2012; 75 (12):2099–2106. [ PubMed : 22386617 ]
- Weber L. Understanding race, class, gender and sexuality: A conceptual framework. New York: Oxford University Press; 2010. Defining contested concepts; pp. 23–43.
- WHO (World Health Organization). Constitution of the World Health Organization. Basic Documents. 45th ed. 2006. Supplement. Available from http://www .who.int/governance /eb/who_constitution_en.pdf .
- WHO. Health systems equity update. 2015. http://www .who.int/healthsystems /topics/equity/en .
- Williams D, Mohammed S. Racism and health, I: Pathways & scientific evidence. American Behavioral Scientist. 2013; 57 (8):1152–1173. [ PMC free article : PMC3863357 ] [ PubMed : 24347666 ]
- Yuval-Davis N. The politics of belonging: Intersected contestations. London, UK: Sage; 2011.
- Zuberi T. Thicker than blood: How racial statistics lie. Minneapolis, MN: University of Minnesota Press; 2001.
See also Gravlee (2009) on when race becomes embodied.
“They” or “their” is used to denote the gender history of the transgender person.
For more information on providing equitable health care services for diverse LGBTQI communities, see Vidal-Ortiz (2005) , NBER (2012) , and Johnson et al. (2017) . For information on the difference between ethical accuracy for civil rights and aesthetic accuracy for compliance only and the value added for having a separate question on Hispanic origin and race for the 2020 Consensus, please see Johnson et al. (2017) .
For more on the AfroLatin@ experience in the United States, see Román and Flores (2010) ; for more information on providing equitable health care services for diverse LGBTQI communities, see Ortiz et al. (2015) ; for more on segregation, see Vidal-Ortiz (2004) , NBER (2012) , and Saenz and Morales (2015) .
- Cite this Page LÓPEZ NANCY, GADSDEN VIVIANL, editors. HEALTH INEQUITIES, SOCIAL DETERMINANTS, AND INTERSECTIONALITY. In: National Academy of Medicine; Alexander C, Murry VMB, Bogard K, editors. Perspectives on Health Equity and Social Determinants of Health. Washington (DC): National Academies Press (US); 2017. 1.
- PDF version of this title (3.4M)
In this Page
- AN “INTERSECTIONALITY HEALTH EQUITY LENS” FOR SOCIAL JUSTICE
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- HEALTH INEQUITIES, SOCIAL DETERMINANTS, AND INTERSECTIONALITY - Perspectives on ... HEALTH INEQUITIES, SOCIAL DETERMINANTS, AND INTERSECTIONALITY - Perspectives on Health Equity and Social Determinants of Health
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
My Internship Experience at the South Central Family Health Center
This essay about my internship experience at the South Central Family Health Center (SCFHC) explores the vital role of community health centers in providing care in underserved areas. Throughout my internship, I engaged in various tasks, from patient intake to supporting chronic disease management programs, gaining a comprehensive view of the day-to-day challenges and successes in a community health setting. I interacted with a diverse patient population facing multiple challenges, including economic hardships and access to care, which highlighted the importance of holistic and preventive health measures. The dedicated staff at SCFHC demonstrated a commitment to not only medical care but also to addressing broader social determinants of health through education and local partnerships. This experience deepened my understanding of community health dynamics and reinforced my passion for pursuing a career in this essential field, underscoring the profound impact of compassionate healthcare on community well-being.
How it works
My internship at the South Central Family Health Center (SCFHC) provided me with an invaluable firsthand experience of working in a community health center. Located in an underserved area, SCFHC offers a critical insight into the challenges and rewards associated with providing healthcare in a community where resources are often limited but the demand for medical care is high.
From the first day, my role was hands-on, immersing me directly into the daily operations of the health center. I was tasked with a variety of responsibilities, ranging from patient intake and data entry to assisting with health outreach programs.
This diversity of tasks helped me understand the multifaceted nature of healthcare management in a community setting.
One of the most impactful aspects of my internship was the interaction with the patients who visited the center. South Central Los Angeles is a melting pot of cultures and backgrounds, and the patient demographic at SCFHC reflected this diversity. Many of the patients I met faced a myriad of challenges, including language barriers, economic hardships, and limited access to preventive care. Despite these obstacles, the resilience and community spirit they demonstrated were profoundly inspiring.
Another significant part of my experience was observing and occasionally assisting in the management of chronic illnesses, which are prevalent in the community SCFHC serves. Conditions such as diabetes, hypertension, and cardiovascular disease were common, and managing these chronic issues is a central focus of the center. I learned about the importance of holistic treatment approaches that address not just the physical aspects of chronic disease but also the social determinants of health such as diet, lifestyle, and environmental factors.
The staff at SCFHC were exemplary in their dedication and compassion. The doctors, nurses, and administrative staff worked as a cohesive unit to provide the best possible care under often challenging circumstances. Their commitment to the community went beyond mere medical treatment; they were deeply involved in health education and preventive measures, striving to empower their patients with the knowledge and tools necessary for managing their health.
This internship also highlighted the critical role of community health centers in providing accessible healthcare. SCFHC not only offers medical services but also partners with local organizations to address social issues that affect health, such as homelessness, unemployment, and nutrition. The integrated approach to health and well-being I observed has reshaped my understanding of what it means to be a healthcare provider in a community context.
Reflecting on my time at SCFHC, I am left with a deep appreciation for the complex dynamics of community health and a renewed passion for pursuing a career in this vital field. The challenges are undeniable, but the impact of providing compassionate and comprehensive healthcare in underserved areas is immeasurable. I am grateful for the opportunity to have been a part of SCFHC and for the lessons I will carry forward in my professional life.
Cite this page
My Internship Experience At The South Central Family Health Center. (2024, Apr 29). Retrieved from https://papersowl.com/examples/my-internship-experience-at-the-south-central-family-health-center/
"My Internship Experience At The South Central Family Health Center." PapersOwl.com , 29 Apr 2024, https://papersowl.com/examples/my-internship-experience-at-the-south-central-family-health-center/
PapersOwl.com. (2024). My Internship Experience At The South Central Family Health Center . [Online]. Available at: https://papersowl.com/examples/my-internship-experience-at-the-south-central-family-health-center/ [Accessed: 2 May. 2024]
"My Internship Experience At The South Central Family Health Center." PapersOwl.com, Apr 29, 2024. Accessed May 2, 2024. https://papersowl.com/examples/my-internship-experience-at-the-south-central-family-health-center/
"My Internship Experience At The South Central Family Health Center," PapersOwl.com , 29-Apr-2024. [Online]. Available: https://papersowl.com/examples/my-internship-experience-at-the-south-central-family-health-center/. [Accessed: 2-May-2024]
PapersOwl.com. (2024). My Internship Experience At The South Central Family Health Center . [Online]. Available at: https://papersowl.com/examples/my-internship-experience-at-the-south-central-family-health-center/ [Accessed: 2-May-2024]
Don't let plagiarism ruin your grade
Hire a writer to get a unique paper crafted to your needs.

Our writers will help you fix any mistakes and get an A+!
Please check your inbox.
You can order an original essay written according to your instructions.
Trusted by over 1 million students worldwide
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers

IMAGES
VIDEO
COMMENTS
Education as a Social Determinant of Health. January 27, 2021. Eating healthy, getting regular medical check-ups, exercising and sleeping sufficiently are all behaviors well-known to influence health quality. However, studies suggest one unexpected factor that can predict how long people will live: education.
Social Determinants of Health and Health Education Essay. The notion of health care cannot exist in isolation from a variety of external influencers that surround human beings in terms of their day-to-day existence. Thus, to comprehend the extent to which social paradigm impacts human health, the US Department of Health and Human Services ...
Education and health and wellbeing are intrinsically linked. The evidence behind the importance of education as a determinant of health is amongst the most compelling. Education is strongly associated with life expectancy, morbidity, health behaviours, and educational attainment plays an important role in health by shaping opportunities ...
Education and health and wellbeing are intrinsically linked. The evidence behind the importance of education as a determinant of health is amongst the most compelling. Education is strongly associated with life expectancy, morbidity, health behaviours, and educational attainment plays an important role in health by shaping opportunities, employment, and income.
1. Introduction. The World Health Organization's Commission on the Social Determinants of Health has presented overwhelming evidence that health and quality of life are socially determined and that entrenched health inequities among people originate not so much from lack of hospital or community based services as from the failure of Governments to address the "social determinants of health
The objective of this essay is to clarify the understanding and use of Social Determinants of Health (SDOH) by exploring basic characteristics of 'determinants' and 'fundamental causes,' the 'social,' 'structure,' and 'modifiability,' and to consider theoretical and practical implications of this reconceptualization for public health.
The social determinants of health that typically make up this field of study are social class, sex, age, race, and ethnicity. In this essay I focus mainly on social class but note that there is a ...
The following list provides examples of the social determinants of health, which can influence health equity in positive and negative ways: Income and social protection. Education. Unemployment and job insecurity. Working life conditions. Food insecurity. Housing, basic amenities and the environment. Early childhood development.
Purpose. The purpose of this teaching guide is to provide educators with a basic overview of social determinants of health in order to help students understand the causes of health inequities observed between groups. The guide is part of a teaching pack on "Social Determinants of Health.".
The social determinants of health contribute to wide health disparities and inequities in areas such as economic stability, education quality and access, healthcare quality and access, neighborhood and built environment, and social and community context [ 23 ]. Nursing practices such as assessment, health promotion, access to care, and patient ...
Background Social determinants have a significant impact on children's development and their abilities and capacities, especially in early childhood. They can bring about inequity in living conditions of children and, as a result, lead to differences in various dimensions of development including the social, psychological, cognitive and emotional aspects. We aimed to identify and analyze the ...
Many people assume individual risk factors are the only conditions relevant to their wellbeing of physical and mental health but in fact, education, along with age, gender, income and many others, has been identified as one of the most important health promoting factors since people begin to acknowledge the social determinants of health. Higher ...
Understanding and addressing social determinants is crucial for promoting health equity and improving the overall well-being of communities. Discover the world's research 25+ million members
Social determinants of health (SDOH) are the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks. SDOH can be grouped into 5 domains: Economic Stability. Education Access and Quality. Health Care Access and Quality.
Introduction and background. According to the World Health Organization (WHO), social determinants of health (SDH) are defined as the circumstances in which humans are born, develop, live, earn, and age. At the international, regional, and state or local levels, the distribution of money, power, and resources shapes these circumstances [ 1 ].
Social determinants of health are the conditions in which people are born, grow, live, work and age.1 They include factors like socioeconomic status, education, neighborhood and physical ...
The social determinants of health (SDOH) include the non-medical factors that affect health outcomes. These factors include conditions that people interact with, live, grow, work and the conditions that make up their daily activities. Five main domains make up SDOH, namely education, community and social context, economic stability, health and ...
essay grishma rana magar 17103015 how do social determinants of health lead to poorer health outcomes for disadvantaged youth in australia? health is one of the ... above, a way to economical, and secure housing and health service can help to reduce the risks of physical and mental health. Education attainment can influence socioeconomic status ...
Share this: Facebook Twitter Reddit LinkedIn WhatsApp. Q1. The Social determinants of health is the observed social, economic, mental and environmental health factors that affect the quality of life of society or its people. The basic formation of these factors have been separated and placed into 10 different categories social gradients, stress ...
The social determinants of health are those factors that influence an individual's health status within society. There are a variety of social determinants of health, but some of the most important include: - Income and Wealth: Low income and wealth are associated with poorer health outcomes. This is due to a variety of factors, including ...
Based on its review of the literature and multiple calls for action, the committee concludes that there is a need and a demand for a holistic, consistent, coherent structure that aligns education, health, and other sectors to better meet local needs in partnership with communities. This conclusion informed the committee's vision for inspiring health professionals to engage in action on the ...
Social Determinants of Health Project Instructions The goal of this project is allow you to explore how your community is addressing a community health concern. Completing this project and presenting at poster session satisfies the Community/Experiential/Clinical component for one year. Through a stepwise
6073. The determinants of health are economic and social conditions that affect people's health status. These influence the living and working conditions that impacts people's everyday living condition. Factors such as the place and the environment we live in, genetics, educational level or work status and income, as well as friends and ...
In this essay, we focus on the potential and promise that intersectionality holds as a lens for studying the social determinants of health, reducing health disparities, and promoting health equity and social justice. Research that engages intersectionality as a guiding conceptual, methodological, and praxis-oriented framework is focused on power dynamics, specifically the relationships between ...
The dedicated staff at SCFHC demonstrated a commitment to not only medical care but also to addressing broader social determinants of health through education and local partnerships. This experience deepened my understanding of community health dynamics and reinforced my passion for pursuing a career in this essential field, underscoring the ...
ABSTRACT This article explores the role of affect in addressing the advantage conventionally accorded to high socio-economic status (SES) in higher education (HE) and how this advantage plays out for…