- Open access
- Published: 05 August 2021

Family reported outcomes, an unmet need in the management of a patient's disease: appraisal of the literature
- R. Shah ORCID: orcid.org/0000-0001-8158-712X 1 ,
- F. M. Ali ORCID: orcid.org/0000-0002-4184-2023 1 ,
- A. Y. Finlay ORCID: orcid.org/0000-0003-2143-1646 1 &
- M. S. Salek ORCID: orcid.org/0000-0002-4612-5699 2 , 3
Health and Quality of Life Outcomes volume 19 , Article number: 194 ( 2021 ) Cite this article
4790 Accesses
16 Citations
9 Altmetric
Metrics details
A Correction to this article was published on 31 August 2021
This article has been updated
A person’s chronic health condition or disability can have a huge impact on the quality of life (QoL) of the whole family, but this important impact is often ignored. This literature review aims to understand the impact of patients' disease on family members across all medical specialities, and appraise existing generic and disease-specific family quality of life (QoL) measures.
The databases Medline, EMBASE, CINHAL, ASSIA, PsycINFO and Scopus were searched for original articles in English measuring the impact of health conditions on patients' family members/partner using a valid instrument.
Of 114 articles screened, 86 met the inclusion criteria. They explored the impact of a relative's disease on 14,661 family members, mostly 'parents' or 'mothers', using 50 different instruments across 18 specialities including neurology, oncology and dermatology, in 33 countries including the USA, China and Australia. These studies revealed a huge impact of patients' illness on family members. An appraisal of family QoL instruments identified 48 instruments, 42 disease/speciality specific and six generic measures. Five of the six generics are aimed at carers of children, people with disability or restricted to chronic disease. The only generic instrument that measures the impact of any condition on family members across all specialities is the Family Reported Outcome Measure (FROM-16). Although most instruments demonstrated good reliability and validity, only 11 reported responsiveness and only one reported the minimal clinically important difference.
Conclusions
Family members' QoL is greatly impacted by a relative's condition. To support family members, there is a need for a generic tool that offers flexibility and brevity for use in clinical settings across all areas of medicine. FROM-16 could be the tool of choice, provided its robustness is demonstrated with further validation of its psychometric properties.
A person’s chronic health condition or disability can have a huge impact on the quality of life (QoL) of the whole family. Sometimes this impact may be similar to or even greater than that experienced by the patient [ 1 , 2 , 3 ]. Although awareness of the impact of a person’s disease on family quality of life (FQoL) has recently been increasing, there is a need to measure this impact in the clinical setting to inform those providing support to the family. Turnbull et al. first proposed the term in 2000 and defined normal “family quality of life” as being "where the family's needs are met, and family members enjoy their life together as a family and have the chance to do things which are important to them" [ 4 ].
Golics et al.’s [ 5 ] detailed literature review of the impact of chronic disease on a patient's family revealed that various aspects of family life are affected by relative’s health condition. That review only identified information about a few disease areas and specialities [ 5 ] and concluded that there was no generic instrument at that time to measure disease impact on family members of patients.
The investigation of FQoL is a newly emerging field, with research now extending to many different areas of medicine. It is, therefore, timely to update the existing knowledge base on the family impact of disease and identify the development of new generic and disease-specific FQoL tools. This critical appraisal of the literature builds on the areas covered by Golics et al. [ 5 ] and summarises the greatly increased research activity over the last seven years. It aims to identify the impact of chronic disease on family members of patients across a range of medical specialities and appraise the characteristics and measurement properties of existing generic and disease-specific FQoL measures.
The definition of ‘family’ has changed over time and its use is no longer restricted to describing 'two parents and their children living under the same roof’. In this review, we use the term as defined by Poston et al. [ 6 ] as “People who think of themselves as part of the family, whether related by blood or marriage or not and who support and care for each other on a regular basis”. This review studies the impact of a patient's disease on all family members, including partners, whether or not they are also carers. Although the terms family caregivers, carers and informal caregivers are often used interchangeably, the only caregivers covered by this review are those unpaid carers (caregivers) who are family members or partners.
Search strategy
A search strategy was developed to identify studies published up to January 2020 that reported the impact of chronic disease on patients’ family members and partners. Six electronic databases were searched: Medline via OVIDSP; EMBASE via OVIDSP; CINHAL via EBSCO; ASSIA via ProQuest; PsycINFO Via OVIDSP; and Scopus using the PICO framework (Population: family members of chronic patients, Intervention: Patients chronic illness, Comparison: Non-applicable, Outcome: impact on family members) to identify and record the data (Additional file 1 : Table S1a and S1b). The PICO framework was developed by the lead author and agreed by the other authors. The reference lists of included articles were also examined to ensure that all relevant articles were captured.
The search to identify existing generic and disease-specific FQoL measures was extended by combining search terms such as ‘family*or caregiver’ and ‘quality of life’ with the terms scale, index, measure, instrument, assessment, surveys, questionnaires, inventory, tools, generic or disease-specific (Additional file 1 : Table S2). In addition, hand searches were carried out of the COnsensus-based Standards for the selection of health Measurement Instruments (COSMIN) [ 7 ] database and the reference lists of relevant articles. Google Scholar was searched for articles reporting development or psychometric properties of the instruments identified.
Eligibility criteria
Articles were included in the review if the source was an original paper, in the English language and measuring the impact of chronic illness or disability on patients' family members/partner using a valid tool. Studies were excluded if they were book chapters, congress abstracts, if they used qualitative methodology or if the caregiver was not a family member. This review paper is in two parts, the first part focuses on the impact of a patient’s disease on family members and the second part appraises the instruments available to measure this impact. As one of the inclusion criteria for the second part was only to include quantitative techniques, it was felt methodologically appropriate to align the two parts by including only quantitative studies in the first part. We recognize this could be considered as a limitation of the study.
In the first stage of article screening, duplicates were removed, and irrelevant titles and abstracts were discarded based on eligibility criteria. In the second stage, full-text articles of potentially relevant abstracts were read and assessed against eligibility criteria by RS to make a final decision about study selection agreed by MSS and AYF.
Data extraction
Data extraction was carried out by RS and was discussed using an iterative process with other members of the research team (MSS and AYF). The data extracted included authors, publication year, country of study, study design, sample size, patients’ chronic disease, family member gender, relationship to the patient, impact on the family members and tools used to measure this impact (Additional file 1 : Table S3).
A separate data extraction table was used for recording psychometric properties of identified family QoL instruments.
Synthesis of data
We used a thematic approach to synthesise findings. Selected papers were carefully read by RS: in case of ambiguity, papers were discussed with FMA, AYF and MSS to ensure accuracy of data extraction. The data on the impact of patients’ disease on family members were summarised as short notes for the 86 studies. These notes were then coded to capture their essence and finally, codes were sorted into potential themes.
Quality assessment and risk of bias
The quality of selected papers and assessment of risk of bias was evaluated using the Joanna Briggs quality assessment tool for cross-sectional and cohort studies, with the involvement of MSS and AYF [ 8 ]. The checklist consists of 8–11 questions with answers “yes”, “no” and “unclear”. When all answers were “yes”, the study was considered to have less chance of bias and if any answer was “no”’ the study was classified as having a risk of bias. The PRISMA principles were followed to ensure robustness of the review as well as minimising bias [ 9 ].
A total of 7,767 articles were identified. After removing duplicates and irrelevant titles, 558 abstracts were screened. The resultant 114 articles underwent full-text review, 86 articles met all inclusion criteria and were included in the final analysis (Fig. 1 ).
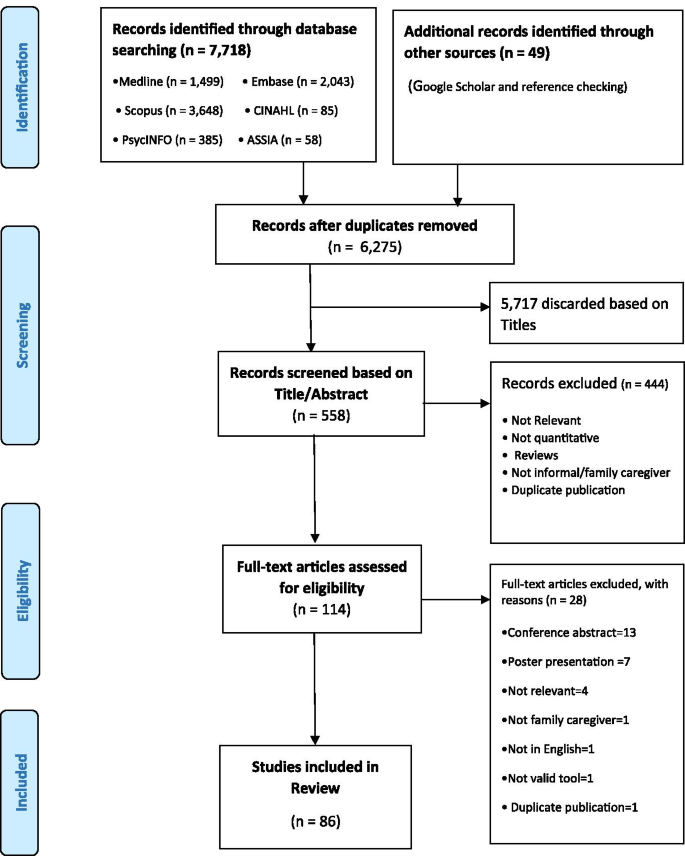
PRISMA flow diagram of article selection
Study characteristics
Eighty-one studies were cross-sectional, and five studies were longitudinal prospective cohort studies with follow-up ranging from one month to two years. The studies explored the impact of a relative's disease on a total of 14,661 family members, mostly 'parents' or 'mothers', using 50 different tools across 18 specialities including neurology, oncology and dermatology and covering 33 countries including the USA, China, and Australia (Figs. 2 and 3 ; Additional file 1 : Table S4 and S5). The most widely used tool to measure the impact of a patient's disease on a family member was the Zarit Caregiver Burden Scale (13 studies) followed by WHOQOL (11), SF-36 (11), SF-12 (nine), IOF (seven) and EQ-5D (six) (Fig. 2 ). While most of the articles reported the impact of a single chronic disease on family members, ten studies included more than one chronic condition, allowing comparison of the family impact of different diseases.
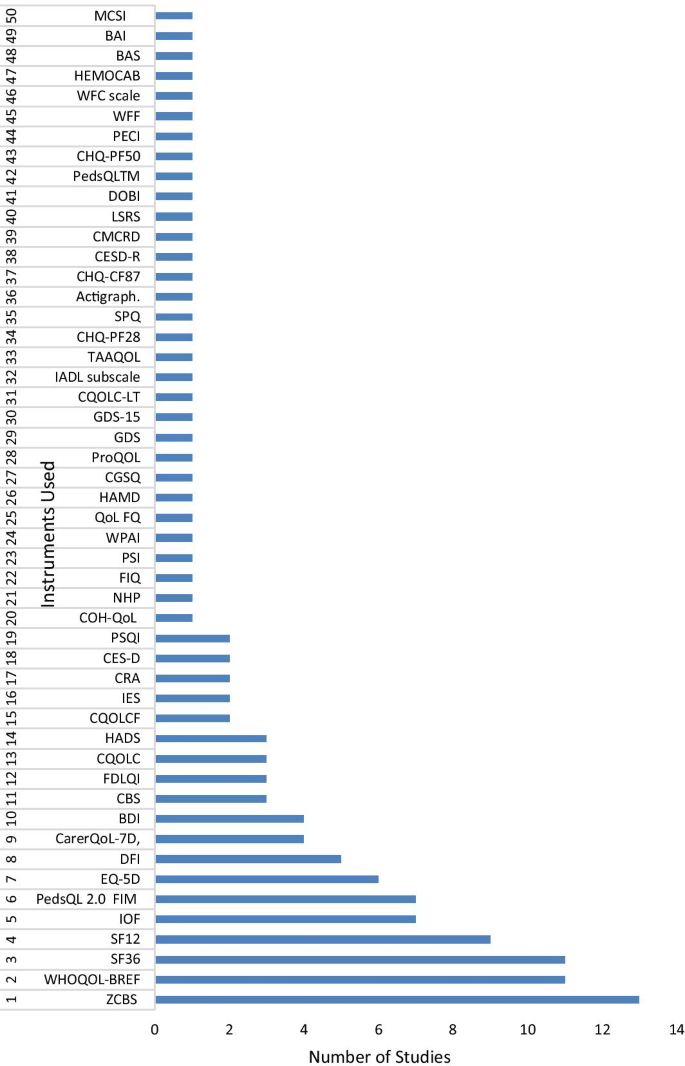
Instruments used in the reviewed studies to measure the impact of the disease on family members/partners. ZCBS : Zarit Caregiver Burden Scale; WHOQOL : The World Health Organization Quality of Life; SF36 : The Short Form (36) Health Survey; SF12 : 12-item Short Form Health Survey; IOF : Impact on Family Scale; EQ-5D : Euroqol- 5 Dimension; PedsQL 2.0 FIM : PedsQL TM 2.0 Family Impact Module; DFI : Dermatitis Family Impact questionnaire; CBS : Caregiver Burden Scale; CarerQoL-7D : Care-related Quality of Life instrument-7 Dimension; BDI : Beck Depression Inventory; FDLQI : Family Dermatology Life Quality Index; CQOLC : Caregiver Quality of Life Index-Cancer; HADS : Hospital Anxiety and Depression Scale; CQOLCF : Caregiver Quality of Life Cystic Fibrosis; IES : The Impact of Event Scale; CRA : The Caregivers Reaction Assessment Scale; CES-D : Centre for Epidemiologic Studies Depression Scale; COH-QOL : City of Hope Quality of life Questionnaire: NHP : The Nottingham Health profile questionnaire; FIQ : Family Impact Questionnaire; PSQI : Pittsburgh Sleep Quality Index; PSI : The Parenting Stress Index Questionnaire; WPAI-SHP : The Work Productivity and Activity Impairment-Specific Health Problem V2.0; QoLFQ : QoL Family Questionnaire; HAMD : Hamilton Depression Scale; CGSQ : the Caregiver Strain Questionnaire. ProQOL : Professional Quality of Life; GDS : Geriatric Depression Scale; GDS-15 : Geriatric Depression Scale-15; CQOLC-LT : Caregiver Quality of life index-Liver Transplantation; IADL subscale : Instrumental Activities of Daily Living; TAAQOL : TNO-AZL Questionnaire for Adult Health-Related Quality of life; CHQ-PF28 : Child Health Questionnaire-Parent Form-28; SPQ : Sibling Perception Questionnaire; CHQ-CF87 : Child Health Questionnaire-Child Form 87; CESD-R : Centre for Epidemiologic Studies Depression Scale (revised); CMCRD : Caring for my Child with a Juvenile Rheumatic Disease; LSRS : Lifespan Sibling Relationship scale; DOBI : Dutch Objective Burden Inventory; CHQ-PF50 : Child Health Questionnaire-Parent Form 50; PECI : Parent Experience of Child Illness; WFF : Work-Family Facilitation scale; WFC scale : Work-Family Conflict scale; PedsQLTM : Pediatric Quality of Life Inventory TM; HEMOCAB : Hemophilia Associated Caregiver Burden Scale; BAS : Burden assessment Scale; BAI : Becks Anxiety Inventory; MCSI : Modified version of Caregiver Strain Index
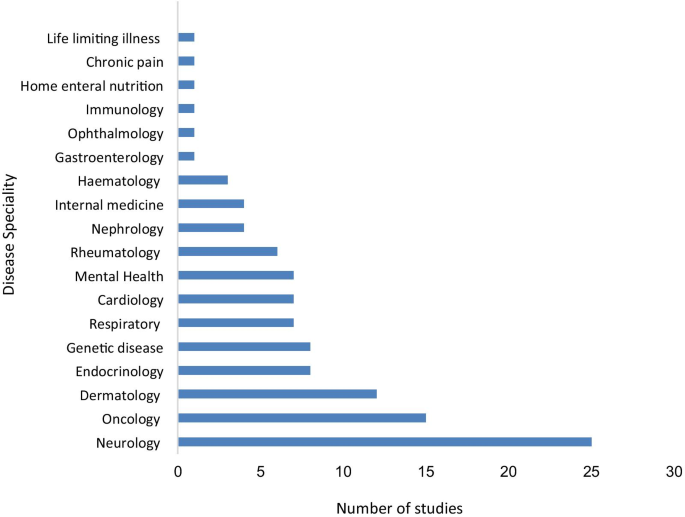
Disease speciality and number of studies included in this review
Thirteen cross-sectional studies and one cohort study did not mention confounders and strategies to address them while one cohort study did not mention reasons for loss of follow-ups. However, the remaining requirements were met for all of these studies, which all fulfilled the minimum criteria for quality. None of the 86 studies was rejected based on their quality or risk of bias. Overall, all studies were moderate to high quality (Additional file 1 : Table S6).
Synthesis of findings—key impact areas
This review revealed a huge impact of patients’ illness on family members’ QoL [ 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 ]. In general, relatives’ chronic diseases impacted family members in similar ways, with some conditions such as cancer having a bigger impact than others. Some common themes identified in this review are discussed below.
Emotional and psychological impact
Caring for a relative’s chronic disease affects family members’ lives in many ways, impacting their emotional and psychological wellbeing [ 19 ]. The family members caring for their relative with a chronic disease were at risk of themselves developing a mental health condition, with an adult offspring or spouse at higher risk than other family members [ 10 , 20 , 21 ], and suffered similar psychological distress, depression and anxiety levels to that of the patient [ 22 , 23 , 24 ]. The presence of anxiety and/or depression in the family member was the most consistent factor influencing family members’ burden and perceived health-related QoL (HRQoL) [ 25 , 26 ].
Nature of relationship and psychological impact
Mothers of children with chronic disease experienced high rates of stress, anxiety and depression [ 15 , 27 , 28 , 29 , 30 ]. Parenting stress was higher when a child was of pre-school age [ 31 , 32 ] and displaying disruptive behaviours and developmental disabilities [ 33 ] or showing flares due to increased severity of their condition [ 34 , 35 ]. Some parents perceived the increased caring demands of a sick child as 'intrusive' which led to higher levels of parental stress and psychological distress [ 36 ] affecting the perception of burden experienced by the mother [ 37 ]. However, this emotional distress did not result in mothers being less caring of the sick child [ 38 ]. The children of mothers with a chronic condition experienced more symptoms of hyperactivity and inattention, especially when the mothers had psychological problems [ 39 ]. Siblings of children with a more severe chronic condition and an unpredictable prognosis reported more internalising of problems and behavioural difficulties than siblings of children with a chronic condition that followed a daily routine treatment pattern [ 40 ]. However, poor emotional health of siblings of children with controlled asthma was not related to disease severity [ 41 ]. Moreover, what is worrying is that parents are sometimes unaware of the impact of their child’s disease on their other children [ 42 ].
Gender differences
Female family members, spouses and mothers, experienced significantly higher rates of depression and anxiety than male family members [ 15 , 21 , 25 , 28 , 29 , 43 ] and the impact was greater when patients suffered from a severe disease such as a long-term mental health condition [ 44 ]. However, two studies showed fathers experiencing more stress [ 45 ] and lower HRQoL [ 46 ] than mothers. Such paternal outcomes could be explained based on increased stressors arising from disease flares, such as additional medical visits and medical bills, both of which could be particularly distressing for fathers compared to mothers [ 46 ]. The reverse gender difference was found in siblings of a patient, with female siblings experiencing a lower QoL than male siblings [ 40 ].
Impact on physical health
Caring for a relative with a chronic disease can have an impact on family members’ physical health owing to the burden resulting from the relative’s functional disabilities, cognitive impairment [ 27 , 47 , 48 ], medication management [ 49 ] duration of care [ 43 , 50 ] and total daily hours spent on assisting patients with basic activities of daily living and medical tasks [ 12 , 50 , 51 , 52 ]. Caring for their relative can leave family members overwhelmed and physically exhausted [ 53 , 54 ], which may result in compassion fatigue. It is not the total number of years of caregiving that contributed to differences in compassion fatigue, but the number of hours per week [ 55 ], suggesting that intensity of caring rather than duration is the critical factor. Furthermore, family members of people with less severe chronic diseases reported only a moderate burden on QoL [ 56 , 57 ], indicating that caregiving burden is related to the severity of the patient's disease and the family member's perception of burden [ 35 , 58 ].
The physical health of family members caring for their relative was impacted by poor sleep quality [ 59 , 60 , 61 , 62 , 63 , 64 ]. Meltzer et al. [ 61 ] found that parents of ventilator-assisted children experienced shorter sleep duration and greater variability in sleep quality impacting their physical health compared to parents of healthy children. In the mothers of children with Duchenne muscular dystrophy, impaired sleep quality was related to the disease duration [ 62 ], while the sleep disturbance in the parents of children with atopic disease was related to the children’s sleep disruption [ 63 ]. The partners of cancer patients experienced poor sleep quality: there was a significant correlation between patients' and their partners' sleep quality and sleep onset latency [ 60 ]. Although partners used medication to minimise the negative impact of sleep problems, Chen et al. [ 60 ] argue that this could have affected their ability to respond to the needs of the patient, indicating that many family members may be hesitant to use drugs to aid sleep.
Impact on social, leisure and daily activities
Family members caring for a relative with a chronic condition experience a considerable impact on their social, leisure and daily activities [ 38 , 51 , 58 , 65 , 66 ], with women reporting greater disruption than men [ 67 ]. Most family members caring for their relative reported difficulties in combining caring tasks with daily activities [ 29 , 68 , 69 ].
Parents of children with chronic disease reported less opportunity for leisure and social activities [ 38 , 53 , 68 , 70 ]. The high caregiving demands of children with developmental disabilities, especially if outwardly visible, contributed to social isolation [ 33 ]. The parents of children with obsessive compulsive disorder experienced interruptions in social life such as postponing social activities [ 71 ]. Parents of children receiving palliative care felt little desire to go out, indicating that the severity of their child's disease led to a loss of interest in leisure activities [ 72 ].
There seems to be a cultural aspect to the impact of caregiving on social life. Japanese caregivers reported high social scores on the Zarit burden scale [ 73 ], even when their perception of general health was lower than that of the care recipient. This indicates that unlike Western caregivers, Japanese caregivers do not report their feelings about their social life being impacted by caregiving [ 73 ]. Arab mothers of children with disabilities experienced reduced social interactions and lower QoL due to the cultural beliefs and the stigma attached to having a child with a disability [ 48 ].
Impact on family relationships
A relative's chronic condition has an impact on the relationships among family members and between the patient and the family members [ 29 , 74 , 75 ]. Caring for a family member not only impacts the carer but also the whole family [ 16 , 76 ] and better family relationships improved QoL for both patient and family members [ 35 , 69 , 77 ].
Mothers caring for children with attention deficit hyperactivity disorder and oppositional developmental disorder (ODD) experienced negative feelings towards their affected child. Some mothers attributed their child’s ODD to increased conflicts between them and their partners [ 74 ]. However, having more children was seen as being protective against partner conflict and maternal hostility, as siblings could assist the mother by caring for the sick child, thereby reducing parental stress and negative feelings towards the child [ 74 ]. Conversely, siblings may internalise their emotional reactions to the situation, leading to behavioural problems [ 40 ]. Better alignment and coordination between parents and involving the siblings, however, could lead to family cohesion, tackling the problem together.
Partners of patients experienced poor sexual life and relationship quality because of the patient's symptoms [ 68 , 78 ], with a significant decrease in the partners’ ability to spend quality time with the patient [ 70 ], leading to marital conflicts [ 68 ]. For many, the caregiving role restricted them from having more children [ 72 ]. Knap et al. [ 72 ] reported that 48% of parents of children with life-limiting illnesses choose not to have more children because of their child's illness and associated caring responsibilities.
Financial impact
Caring for a relative with a chronic disease can necessitate increased expenditure [ 15 , 31 , 67 , 68 , 79 , 80 , 81 , 82 , 83 ]. In an Australian study, the annual personal cost for mild, moderate, and severe atopic dermatitis was calculated at Aus$330, 818, and 1255, respectively, with most being spent on medication, dressings and non-irritant clothing [ 64 ]. In a Swedish study, 20% of parents reported experiencing financial difficulties even after the cost of the chronic disease treatment was covered by the welfare system [ 84 ]. The family members reduced their working hours or left their jobs to take up their caring responsibilities. This and the expense of hospital visits contributed to their financial difficulties [ 64 , 84 , 85 ].
Impact on work
Work was seen to have a positive impact on the QoL of mothers, as it provided temporary relief from their caring role, time to socialise and offset the financial burden [ 47 , 71 ]. However, many family members caring for their relative suffered work impairment [ 75 , 86 ] and had to give up their jobs, change jobs, alter career choices or reduce their work hours to look after an ill family member and to manage hospital visits [ 64 , 70 , 87 , 88 ].
Positive aspect of caregiving
Despite the physical, social and psychological impact that a relative having a disease has on family members, many family members reported a positive experience of caregiving, with older family members reporting more satisfaction than younger ones [ 55 ]. Meriggi et al. [ 67 ] reported 93.5% family members caring for their relative were happy with their role. Son et al. [ 77 ] attribute positivity in family members caring for cancer patients to their spiritual upliftment. Awadalla et al. [ 89 ] attribute this positive impact to family cohesion, and an attitude of hopefulness. Adult siblings caring for their parents reported that they see caregiving as a way of giving something back to parents [ 90 ]. Although the health status of family members with caring experience was lower than that of non-carers in an Australian study, the difference in scores did not reach the minimal important difference (MID) magnitude for either the mental or physical domains of SF-12, suggesting that caregivers might be satisfied in their caring roles [ 91 ].
Existing family QoL instruments
The appraisal of the family QoL measures identified 48 instruments measuring the impact of a patient's disease on family members. Forty-two of the instruments are disease or speciality specific and are limited to that particular group of patients. The properties of these measures are summarised in Tables 1 and 2 .
The review also identified Six population-specific/generic measures: their properties are summarised in Tables 3 and 4 . Five of these measures (Impact on Family Scale, the Beach Centre Family Quality of Life, the PedsQL™ Family Impact Module, Family Quality of Life Survey and Care-related QoL), are aimed at specific populations of carers (parents of children, family members of people with disability, informal caregivers not necessarily family members of people with long term conditions). The only generic instrument that measures the impact of any condition on family members across all specialities is the FROM-16.
The HRQoL instruments, regardless of having been developed for patients or their family member/partner, should demonstrate essential psychometric properties such as validity, reliability and responsiveness to change [ 159 , 160 ]. Although most instruments demonstrated good internal consistency, reliability and construct validity, only 11 reported responsiveness and only one reported the MID. Thus, it is not known whether these instruments are sensitive to detecting change over time in family members' QoL.
This review has demonstrated that family members caring for relatives with various chronic diseases are impacted in similar ways in terms of physical, social and psychological wellbeing. The high number of FQoL instruments identified in this review demonstrates a growing interest in FQoL, though most research has focused on a few medical fields including neurology, oncology and dermatology, findings consistent with the previous review [ 5 ]. One key strength of this current review is that its findings are based on studies that have used valid tools to measure the impact of a patient's chronic disease on a family member/partner. The studies included have used many different instruments to measure the impact of chronic disease on family members, indicating a lack of consensus on the use of instruments: perhaps a clear consensus has not yet emerged because this field is still young. Furthermore, the heterogeneity of the instruments used prevents comparison of the impact of caregiving on family members across disease areas. Such comparison is important in identifying the most vulnerable family members and directing them to appropriate support. This is critical as a physically unhealthy family member would be less able to discharge their caregiving duties, thus having a negative impact on the patients' health [ 20 ]. While many studies in this review have used disease-specific instruments, most used generic health status or population instruments to measure the family impact of a person's chronic condition, indicating a strong need for a generic QoL measure specific to family members. Furthermore, most instruments used in this review have been designed keeping patients in mind and may not address issues relevant to family members. Using a measure designed to be family-specific should provide a better understanding of the needs of family members, including support services. Disease-specific FQoL instruments are used to assess QoL of family members of people with a specific disease and thus can detect changes in family member’s QoL following clinical interventions. Generic FQoL instruments on the other hand, can assess the effects of a wide range of diseases or treatment on the QoL of a partner or family member. Published research has shown that family members caring for relatives with different health conditions are impacted in similar ways [ 161 ]. Thus, generic FQoL instruments allow the comparison of QoL of individuals across different disease areas and identification of population-wide trends. While disease-specific instruments can help clinicians to understand the extent to which a partner or family member has been affected by a person’s disease and inform appropriate treatment decisions, they cannot be used to compare across conditions or between treatments. Moreover, generic instruments can measure the family impact of disease in areas where there are no disease-specific measures. Some research studies may use both generic and disease-specific instruments to capture the different patient/family member viewpoints or to validate the results of using each type of instrument. The FROM-16 could fill this gap as a generic family outcome measure since it has been developed directly from the experience of family members, for family members. One practical feature of FROM-16 is that it is a user-friendly and relatively simple questionnaire with an average completion time of 2–3 min, making it a practical tool for use in a clinical setting.
There are some limitations of this review. The review is not a systematic review. Although not a systematic review, it followed rigorous methodology and fulfilled 19 relevant PRISMA checklist items (Additional file 2 : Table S1) [ 8 ]. Besides, the review only included studies in the English language, thus limiting understanding of the impact of patients' disease on family members in different cultures. Nevertheless, most studies carried out in different cultures are usually published in English language scientific journals; this suggests the amount of missed information may be minimal. Most studies in this review were cross-sectional. Only five studies were longitudinal, revealing that greater carer burden was associated with poor physical and mental health and lower QoL of family members over time, with women being impacted more than men. Future research should focus on longitudinal studies to build understanding of the long-term family impact of disease. This is important as most acute and chronic diseases may influence major life-changing decisions, thus understanding long-term impacts may help clinicians in developing better management plans for patients and their family members [ 162 ]. In addition, the majority of family members caring for relatives in the studies reviewed were women, mostly mothers. There is a dearth of research on the impact of caregiving on fathers, although this review highlighted two studies where fathers were impacted more than mothers. The fact that fathers are mostly unavailable at the point of contact results in the impact on fathers being forgotten or difficult to obtain. Thus, future research should focus on the impact of children's diseases on fathers.
An appraisal of existing FQoL instruments identified a recent plethora of FQoL measures indicating the growing recognition of the importance of FQoL. Only a few instruments have published responsiveness and MID information, however evidence of responsiveness is essential for such questionnaires to be useful for clinical monitoring or as an outcome measure to assess the value of interventions. Information concerning MID is important for the clinician to be able to interpret change in scores over time. Most instruments reviewed were developed recently, and perhaps new studies underway might later report their further psychometric properties. Further psychometric testing of existing measures is required. Furthermore, all instruments identified in this review were created in developed countries, highlighting a need for cross-cultural validation in developing countries [ 163 ].
In conclusion, this review found that family members caring for their sick relative experience a huge but similar impact on their physical, social and psychological wellbeing across different disease areas. However, to translate this evidence into practice and support family members impacted by their relative's disease, there is a need for a generic family QoL measure which offers acceptable practicality and flexibility both to the relatives and to researchers as well as to clinicians. This review has identified FROM-16 as the only generic user-friendly instrument that can be implemented across all disease areas to measure the family impact of a person with a disease. However, to support the use of FROM-16 across all disciplines of medicine, there is a need for further examination of its psychometric properties. Furthermore, with greater digitalisation of healthcare, such information could be captured routinely and combined with that of the patient’s which would, no doubt, enhance the appropriateness of treatment decision-making. There are many reasons why the routine capture of quality of life information concerning patients may be helpful in enhancing the quality of clinical care [ 164 ]. Exactly similar potential advantages may be gained by the use of family quality of life measures. The final thought in this context is the utility of such instruments in meeting the aftermath challenges of the current pandemic crisis and impact of Long Covid on families of the survivors.
Availability of data and materials
All data are included within the article and supplemental material.
Change history
31 august 2021.
A Correction to this paper has been published: https://doi.org/10.1186/s12955-021-01839-0
Abbreviations
- Quality of life
- Family quality of life
Health-related quality of life
Preferred reporting items for systematic reviews and meta-analyses
Oppositional developmental disorder
Family reported outcome measure-16
Minimal important difference
Rees J, O’Boyle C, MacDonagh R. Quality of life: impact of chronic illness on the partner. J R Soc Med. 2001;94(11):563–6.
Article CAS PubMed PubMed Central Google Scholar
Weitzenkamp DA, Gerhart KA, Charlifue SW, Whiteneck GG, Savic G. Spouses of spinal cord injury survivors: the added impact of caregiving. Arch Phys Med Rehabil. 1997;78(8):822–7.
Article CAS PubMed Google Scholar
Basra M, Finlay AY. The family impact of skin diseases: the Greater Patient concept. Br J Dermatol. 2007;156(5):929–37.
Turnbull AP, Turnbull HR, Poston D, Beegle G, Blue-Banning M, Diehl K, Frankland C, Lord L, Marquis J, Park J, Matt S. Enhancing quality of life of families of children and youth with disabilities in the United States. 2000.
Golics CJ, Basra MKA, Finlay AY, Salek S. The impact of disease on family members: a critical aspect of medical care. J R Soc Med. 2013;106(10):399–407.
Article PubMed PubMed Central Google Scholar
Poston D, Turnbull A, Park J, Mannan H, Marquis J, Wang M. Family quality of life: a qualitative inquiry. Ment Retard. 2003;41(5):313–28.
Article PubMed Google Scholar
COnsensus-based Standards for the selection of health Measurement Instruments COSMIN. Database of systematic reviews of outcome measurement instruments 2021 [online] 2021. https://database.cosmin.nl/?utf8=%E2%9C%93&search_field=all_fields&q=family+caregivers .
Moola SMZ, Tufanaru C, Aromataris E, Sears K, Sfetcu R, Currie M, Qureshi R, Mattis P, Lisy K, Mu P-F. The Joanna Briggs Institute. . Chapter 7: Systematic reviews of etiology and risk. In: Aromataris E, Munn Z (Editors). Joanna Briggs Institute Reviewer's Manual. 2017. https://reviewersmanual.joannabriggs.org/ .
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Arora A, Gupta ID, Sharma P, Dudani K. A comparative study of family burden and quality of life of caregivers of patients with chronic psychiatric versus chronic medical disorders. Indian J Psychiatry. 2015;1:S32–S3.
Jirakova A, Vojackova N, Gopfertova D, Hercogova J. A comparative study of the impairment of quality of life in Czech children with atopic dermatitis of different age groups and their families. Int J Dermatol. 2012;51(6):688–92.
Karg N, Graessel E, Randzio O, Pendergrass A. Dementia as a predictor of care-related quality of life in informal caregivers: a cross-sectional study to investigate differences in health-related outcomes between dementia and non-dementia caregivers. BMC Geriatr. 2018;18(1):189.
Lazow MA, Jaser SS, Cobry EC, Garganta MD, Simmons JH. Stress, depression, and quality of life among caregivers of children with osteogenesis imperfecta. J Pediatr Health Care. 2019;33(4):437–45.
Mazzone L, Postorino V, De Peppo L, Della Corte C, Lofino G, Vassena L, et al. Paediatric non-alcoholic Fatty liver disease: impact on patients and mothers' quality of life. Hepat Mon. 2013;13(3):e7871.
Pustišek N, Vurnek Živkovic M, Šitum M. Quality of life in families with children with atopic dermatitis. Pediatr Dermatol. 2016;33(1):28–32.
Tadros A, Vergou T, Stratigos AJ, Tzavara C, Hletsos M, Katsambas A, et al. Psoriasis: is it the tip of the iceberg for the quality of life of patients and their families? J Eur Acad Dermatol Venereol. 2011;25(11):1282–7.
Wei L, Li J, Cao Y, Xu J, Qin W, Lu H. Quality of life and care burden in primary caregivers of liver transplantation recipients in China. Medicine. 2018;97(24).
Macchi ZA, Koljack CE, Miyasaki JM, Katz M, Galifianakis N, Prizer LP, et al. Patient and caregiver characteristics associated with caregiver burden in Parkinson’s disease: a palliative care approach. Ann Palliat Med. 2019:S24–S33.
Bruce DG, Paley GA, Nichols P, Roberts D, Underwood PJ, Schaper F. Physical disability contributes to caregiver stress in dementia caregivers. J Gerontol A Biol Sci Med Sci. 2005;60(3):345–9.
Sewitch MJ, McCusker J, Dendukuri N, Yaffe MJ. Depression in frail elders: impact on family caregivers. Int J Geriatr Psychiatry. 2004;19(7):655–65.
McCusker J, Latimer E, Cole M, Ciampi A, Sewitch M. Major depression among medically ill elders contributes to sustained poor mental health in their informal caregivers. Age Ageing. 2007;36(4):400–6.
Walsh JD, Blanchard EB, Kremer JM, Blanchard CG. The psychosocial effects of rheumatoid arthritis on the patient and the well partner. Behav Res Ther. 1999;37(3):259–71.
Yildirim SA, Ozer S, Yilmaz O, Duger T, Kilinc M. Depression, anxiety and health related quality of life in the caregivers of the persons with chronic neurological illness. Turkiye Klinikleri J Med Sci. 2009;29(6):1535–42.
Google Scholar
Rioux JP, Narayanan R, Chan CT. Caregiver burden among nocturnal home hemodialysis patients. Hemodial Int. 2012;16(2):214–9.
Carod-Artal FJ, Ferreira Coral L, Trizotto DS, Menezes MC. Burden and perceived health status among caregivers of stroke patients. Cerebrovasc Dis. 2009;28(5):472–80.
Ito E, Tadaka E. Quality of life among the family caregivers of patients with terminal cancer at home in Japan. Jpn J Nurs Sci. 2017;14(4):341–52.
Okurowska-Zawada B, Wojtkowski J, Kułak W. Quality of life of mothers of children with myelomeningocele. Pediatr Pol. 2013;88(3):241–6.
Article Google Scholar
Serin HM, Akinci A, Mermi O, Atmaca M, Yilmaz E. The depression and anxiety profiles of motherswho have children with epilepsy. Turk Klinikleri Pediatr. 2016;25(3):133–8.
Ten Hoopen LW, de Nijs PFA, Duvekot J, Greaves-Lord K, Hillegers MHJ, Brouwer WBF, et al. Children with an autism spectrum disorder and their caregivers: capturing health-related and care-related quality of life. J Autism Dev Disord. 2020;50(1):263–77.
Sharghi A, Karbakhsh M, Nabaei B, Meysamie A, Farrokhi A. Depression in mothers of children with thalassemia or blood malignancies: a study from Iran. Clin Pract Epidemiol Ment Health. 2006;2.
Chernyshov PV, Ho RC, Monti F, Jirakova A, Velitchko SS, Hercogova J, et al. An international multi-center study on self-assessed and family quality of life in children with atopic dermatitis. Acta Dermatovenerol Croat. 2015;23(4):247–53.
PubMed Google Scholar
Van Nimwegen KJM, Kievit W, van der Wilt GJ, Schieving JH, Willemsen MAAP, Donders ART, et al. Parental quality of life in complex paediatric neurologic disorders of unknown aetiology. Eur J Paediatr Neurol. 2016;20(5):723–31.
Gupta VB. Comparison of parenting stress in different developmental disabilities. J Dev Phys Disabil. 2007;19(4):417–25.
Grant M, Del Ferraro C, Williams AC, Sun V, Fujinami R, Ferrell B. Quality of life, preparedness, and perceived burden of family caregivers in lung cancer. Support Care in Cancer. 2012;1:S71.
Sikorová L, Bužgová R. Associations between the quality of life of children with chronic diseases, their parents’ quality of life and family coping strategies. Cent Eur J Nurs Midwifery. 2016;7(4):534–41.
Gamwell KL, Mullins AJ, Tackett AP, Suorsa KI, Mullins LL, Chaney JM. Caregiver demand and distress in parents of youth with juvenile rheumatic diseases: examining illness intrusiveness and parenting stress as mediators. J Dev Phys Disabil. 2016;28(6):889–904.
Calderón C, Gómez-López L, Martínez-Costa C, Borraz S, Moreno-Villares JM, Pedrón-Giner C. Feeling of burden, psychological distress, and anxiety among primary caregivers of children with home enteral nutrition. J Pediatr Psychol. 2011;36(2):188–95.
Ho RCM, Giam YC, Ng TP, Mak A, Goh D, Zhang MWB, et al. The influence of childhood atopic dermatitis on health of mothers, and its impact on Asian families. Pediatr Allergy Immunol. 2010;21(3):501–7.
Guo VY, Wong CK, Wong RS, Yu EY, Ip P, Lam CL. Spillover effects of maternal chronic disease on children’s quality of life and behaviors among low-income families. The Patient. 2018;11(6):625–35.
Havermans T, Croock ID, Vercruysse T, Goethals E, Diest IV. Belgian siblings of children with a chronic illness: is their quality of life different from their peers? J Child Health Care. 2015;19(2):154–66.
Yilmaz O, Turkeli A, Karaca O, Yuksel H. Does having an asthmatic sibling affect the quality of life in children? Turk J Pediatr. 2017;59(3):274–80.
Dinleyici M, Carman KB, Ozdemir C, Harmanci K, Eren M, Kirel B, et al. Quality-of-life evaluation of healthy siblings of children with chronic illness. Balkan Med J. 2019;37(1):34–42.
PubMed PubMed Central Google Scholar
Forbes A, While A, Mathes L. Informal carer activities, carer burden and health status in multiple sclerosis. Clin Rehabil. 2007;21(6):563–75.
Johansson A, Ewertzon M, Andershed B, Anderzen-Carlsson A, Nasic S, Ahlin A. Health-related quality of life—from the perspective of mothers and fathers of adult children suffering from long-term mental disorders. Arch Psychiatr Nurs. 2015;29(3):180–5.
Bonner MJ, Hardy KK, Willard VW, Hutchinson KC. Brief report: psychosocial functioning of fathers as primary caregivers of pediatric oncology patients. J Pediatr Psychol. 2007;32(7):851–6.
Kunz JH, Greenley RN, Howard M. Maternal, paternal, and family health-related quality of life in the context of pediatric inflammatory bowel disease. Qual Life Res. 2011;20(8):1197–204.
Farajzadeh A, Maroufizadeh S, Amini M. Factors associated with quality of life among mothers of children with cerebral palsy. 2020:e12811.
Manee F, Ateya Y, Rassafiani M. A comparison of the quality of life of Arab mothers of children with and without chronic disabilities. Phys Occup Ther Pediatr. 2016;36(3):260–71.
Luckett T, Agar M, DiGiacomo M, Lam L, Phillips J. Health status in South Australians caring for people with cancer: a population-based study. Psychooncology. 2019;28(11):2149–56.
Duimering A, Turner J, Chu K, Huang F, Severin D, Ghosh S, et al. Informal caregiver quality of life in a palliative oncology population. Support Care Cancer. 2020;28(4):1695–702.
Baji P, Golicki D, Prevolnik-Rupel V, Brouwer WBF, Zrubka Z, Gulacsi L, et al. The burden of informal caregiving in Hungary, Poland and Slovenia: results from national representative surveys. Eur J Health Econ. 2019;20(Suppl 1):5–16.
Blanes L, Carmagnani MIS, Ferreira LM. Health-related quality of life of primary caregivers of persons with paraplegia. Spinal Cord. 2007;45(6):399–403.
Arafa MA, Zaher SR, El-Dowaty AA, Moneeb DE. Quality of life among parents of children with heart disease. Health Qual Life Outcomes. 2008;6:91.
Lu L, Pan B, Sun W, Cheng L, Chi T, Wang L. Quality of life and related factors among cancer caregivers in China. Psychiatry Clin Neurosci. 2010;64(5):505–13.
Lynch SH, Shuster G, Lobo ML. The family caregiver experience—examining the positive and negative aspects of compassion satisfaction and compassion fatigue as caregiving outcomes. Aging Ment Health. 2018;22(11):1424–31.
Koşan Z, Yılmaz S, Bilge Yerli E, Köyceğiz E. Evaluation of the burden of care and the quality of life in the parents of turkish children with familial mediterranean fever. J Pediatr Nurs. 2019;48:e21–6.
McDonald L, Turnbull P, Chang L, Crabb DP. Taking the strain? Impact of glaucoma on patients’ informal caregivers. Eye. 2020;34(1):197–204.
Luttik ML, Jaarsma T, Veeger N, Tijssen J, Sanderman R, van Veldhuisen DJ. Caregiver burden in partners of Heart Failure patients; limited influence of disease severity. Eur J Heart Fail. 2007;9(6–7):695–701.
Al Robaee AA, Shahzad M. Impairment quality of life in families of children with atopic dermatitis. Acta Dermatovenerol Croat. 2010;18(4):243–7.
Chen Q, Terhorst L, Lowery-Allison A, Cheng H, Tsung A, Layshock M, et al. Sleep problems in advanced cancer patients and their caregivers: Who is disturbing whom? J Behav Med. 2019:1–9.
Meltzer LJ, Sanchez-Ortuno MM, Edinger JD, Avis KT. Sleep patterns, sleep instability, and health related quality of life in parents of ventilator-assisted children. J Clin Sleep Med. 2015;11(3):251–8.
Nozoe KT, Polesel DN, Moreira GA, Pires GN, Akamine RT, Tufik S, et al. Sleep quality of mother-caregivers of Duchenne muscular dystrophy patients. Sleep Breath. 2016;20(1):129–34.
Ridolo E, Caffarelli C, Olivieri E, Montagni M, Incorvaia C, Baiardini I, et al. Quality of sleep in allergic children and their parents. Allergol Immunopathol (Madr). 2015;43(2):180–4.
Article CAS Google Scholar
Su JC, Kemp AS, Varigos GA, Nolan TM. Atopic eczema: Its impact on the family and financial cost. Arch Dis Child. 1997;76(2):159–62.
Haverman L, van Oers HA, Maurice-Stam H, Kuijpers TW, Grootenhuis MA, van Rossum MA. Health related quality of life and parental perceptions of child vulnerability among parents of a child with juvenile idiopathic arthritis: results from a web-based survey. Pediatr Rheumatol. 2014;12:34.
Splinter K, Niemi A-K, Cox R, Platt J, Shah M, Enns GM, et al. Impaired health-related quality of life in children and families affected by methylmalonic acidemia. J Genet Couns. 2016;25(5):936–44.
Meriggi F, Andreis F, Premi V, Liborio N, Codignola C, Mazzocchi M, et al. Assessing cancer caregivers’ needs for an early targeted psychosocial support project: the experience of the oncology department of the Poliambulanza Foundation. Palliat Supportive Care. 2015;13(4):865–73.
Jafari H, Ebrahimi A, Aghaei A, Khatony A. The relationship between care burden and quality of life in caregivers of hemodialysis patients. BMC Nephrol. 2018;19(1):321.
O’Mahony J, Marrie RA, Laporte A, Bar-Or A, Yeh EA, Brown A, et al. Pediatric-onset multiple sclerosis is associated with reduced parental health-related quality of life and family functioning. Mult Scler J. 2019;25(12):1661–72.
Suthoff E, Mainz JG, Cox DW, Thorat T, Grossoehme DH, Fridman M, et al. Caregiver burden due to pulmonary exacerbations in patients with cystic fibrosis. J Pediatr. 2019;215:164-71.e2.
Suculluoglu Dikici D, Eser E, Cokmus FP, Demet MM. Quality of Life and associated risk factors in caregivers of patients with obsessive compulsive disorder. Psychiatry Clin Psychopharmacol. 2019;29(4):579–86.
Knapp CA, Madden VL, Curtis CM, Sloyer P, Shenkman EA. Family support in pediatric palliative care: How are families impacted by their children's illnesses? J Palliat Med. 2010; 13(4):421–426.
Morimoto T, Schreiner AS, Asano H. Caregiver burden and health-related quality of life among Japanese stroke caregivers. Age Ageing. 2003;32(2):218–23.
Fleck K, Jacob C, Philipsen A, Matthies S, Graf E, Hennighausen K, et al. Child impact on family functioning: a multivariate analysis in multiplex families with children and mothers both affected by attention-deficit/hyperactivity disorder (ADHD). ADHD. 2015;7(3):211–23.
Mowforth OD, Davies BM, Kotter MR. Quality of life among informal caregivers of patients with degenerative cervical myelopathy: cross-sectional questionnaire study. Interact J Med Res. 2019;8(4):e12381.
Hunfeld JA, Perquin CW, Duivenvoorden HJ, Hazebroek-Kampschreur AA, Passchier J, van Suijlekom-Smit LW, et al. Chronic pain and its impact on quality of life in adolescents and their families. J Pediatr Psychol. 2001;26(3):145–53.
Son KY, Lee CH, Park SM, Lee CH, Oh SI, Oh B, et al. The factors associated with the quality of life of the spouse caregivers of patients with cancer: a cross-sectional study. J Palliat Med. 2012;15(2):216–24.
Roy A, Minaya M, Monegro M, Fleming J, Wong RK, Lewis SK, et al. Partner burden in celiac disease. Gastroenterology. 2016;1:S179–S80.
Farzi S, Farzi S, Moladoost A, Ehsani M, Shahriari M, Moieni M. Caring burden and quality of life of family caregivers in patients undergoing hemodialysis: a descriptive-analytic study. Int J Community Based Nurs Midwifery. 2019;7(2):88–96.
Ab. Ghani A, Norhayati N, Muhamad R, Ismail Z. Atopic eczema in children: disease severity, quality of life and its impact on family. Int Med J (1994). 2012;20.
Khair K, Mackensen Sv. Caregiver burden in haemophilia: results from a single UK centre. J Haemoph Pract. 2017;4(1):40.
Al Qadire M, Aloush S, Alkhalaileh M, Qandeel H, Al-Sabbah A. Burden among parents of children with cancer in Jordan: prevalence and predictors. Cancer Nurs. 2020;43(5):396–401.
Włodarek K, Głowaczewska A, Matusiak Ł, Szepietowski JC. Psychosocial burden of Hidradenitis Suppurativa patients’ partners. J Eur Acad Dermatol Venereol. 2020;34(8):1822–7.
Hoven EI, Lannering B, Gustafsson G, Boman KK. Persistent impact of illness on families of adult survivors of childhood central nervous system tumors: a population-based cohort study. Psychooncology. 2013;22(1):160–7.
Aung L, Saw SM, Chan MY, Khaing T, Quah TC, Verkooijen HM. The hidden impact of childhood cancer on the family: a multi-institutional study from Singapore. Ann Acad Med Singap. 2012;41(4):170–5.
Chua CKT, Wu JT, Yeewong Y, Qu L, Tan YY, Neo PSH, et al. Caregiving and its resulting effects—the care study to evaluate the effects of caregiving on caregivers of patients with advanced cancer in Singapore. Cancers. 2016;8(11).
Khair K, Von Mackensen S. Caregiver burden of parents of children with haemophilia—results from a single UK centre. Haemophilia. 2016;22(Supplement 4):113.
Shalitin S, Hershtik E, Phillip M, Gavan M-Y, Cinamon RG. Impact of childhood type 1 diabetes on maternal work-family relations. J Pediatr Endocrinol Metab. 2018;31(5):569–76.
Awadalla AW, Ohaeri JU, Al-Awadi SA, Tawfiq AM. Diabetes mellitus patients’ family caregivers’ subjective quality of life. J Natl Med Assoc. 2006;98(5):727–36.
Ngangana PC, Davis BL, Burns DP, McGee ZT, Montgomery AJ. Intra-family stressors among adult siblings sharing caregiving for parents. J Adv Nurs. 2016;72(12):3169–81.
Luckett T, Agar M, DiGiacomo M, Ferguson C, Lam L, Phillips J. Health status of people who have provided informal care or support to an adult with chronic disease in the last 5 years: results from a population-based cross-sectional survey in South Australia. Aust Health Rev. 2019;43(4):408–14.
Basra MKA, Sue-Ho R, Finlay AY. The family dermatology life quality index: measuring the secondary impact of skin disease. Br J Dermatol. 2007;156(3):528–38.
Basra MKA, Edmunds O, Salek MS, Finlay AY. Measurement of family impact of skin disease: further validation of the Family Dermatology Life Quality Index (FDLQI). J Eur Acad Dermatol Venereol. 2008;22(7):813–21.
Lawson V, Lewis-Jones MS, Finlay AY, Reid P, Owens RG. The family impact of childhood atopic dermatitis: the Dermatitis Family Impact Questionnaire. Br J Dermatol. 1998;138(1):107–13.
Beattie PE, Lewis-Jones MS. An audit of the impact of a consultation with a paediatric dermatology team on quality of life in infants with atopic eczema and their families: further validation of the Infants’ Dermatitis Quality of Life Index and Dermatitis Family Impact score. Br J Dermatol. 2006;155(6):1249–55.
McKenna SP, Whalley D, Dewar AL, Erdman RAM, Kohlmann T, Niero M, et al. International development of the Parents’ Index of Quality of Life in Atopic Dermatitis (PIQoL-AD). Qual Life Res. 2005;14(1):231–41.
Meads DM, McKenna SP, Kahler K. The quality of life of parents of children with atopic dermatitis: interpretation of PIQoL-AD scores. Qual Life Res. 2005;14(10):2235.
Kondo-Endo K, Ohashi Y, Nakagawa H, Katsunuma T, Ohya Y, Kamibeppu K, et al. Development and validation of a questionnaire measuring quality of life in primary caregivers of children with atopic dermatitis (QPCAD). Br J Dermatol. 2009;161(3):617–25.
Katsunuma T, Tan A, Ohya Y. Short version of a quality-of-life questionnaire in primary caregivers of children with atopic dermatitis (QPCAD): development and validation of QP9. Arerugi=[Allergy]. 2013;62(1):33–46.
Chamlin SL, Cella D, Frieden IJ, Williams ML, Mancini AJ, Lai JS, et al. Development of the Childhood Atopic Dermatitis Impact Scale: initial validation of a quality-of-life measure for young children with atopic dermatitis and their families. J Invest Dermatol. 2005;125(6):1106–11.
Chamlin SL, Lai J-S, Cella D, Frieden IJ, Williams ML, Mancini AJ, et al. Childhood atopic dermatitis impact scale: reliability, discriminative and concurrent validity, and responsiveness. Arch Dermatol. 2007;143(6):768–72.
Eghlileb AM, Basra MK, Finlay AY. The psoriasis family index: preliminary results of validation of a quality of life instrument for family members of patients with psoriasis. Dermatology. 2009;219(1):63–70.
Basra MKA, Zammit AM, Kamudoni P, Eghlileb AM, Finlay AY, Salek MS. PFI-14©: a Rasch analysis refinement of the psoriasis family index. Dermatology. 2015;231(1):15–23.
Méni C, Bodemer C, Toulon A, Merhand S, Perez-Cullell N, Branchoux S, et al. Atopic dermatitis burden scale: creation of a specific burden questionnaire for families. J Eur Acad Dermatol Venereol. 2013;27(11):1426–32.
Boccara O, Méni C, Léauté-Labreze C, Bodemer C, Voisard JJ, Dufresne H, et al. Haemangioma family burden: creation of a specific questionnaire. Acta Derm Venereol. 2015;95(1):78–82.
Mrowietz U, Hartmann A, Weißmann W, Zschocke I. FamilyPso—a new questionnaire to assess the impact of psoriasis on partners and family of patients. J Eur Acad Dermatol Venereol. 2017;31(1):127–34.
Dufresne H, Hadj-Rabia S, Taieb C, Bodemer C. Development and validation of an epidermolysis bullosa family/parental burden score. Br J Dermatol. 2015;173(6):1405–10.
Dufresne H, Hadj-Rabia S, Méni C, Sibaud V, Bodemer C, Taïeb C. Family burden in inherited ichthyosis: creation of a specific questionnaire. Orphanet J Rare Dis. 2013;8(1):28.
Taieb C, Hadj-Rabia S, Monnet J, Bennani M, Bodemer C, the Filière Maladies Rares en D. Incontinentia pigmenti burden scale: designing a family burden questionnaire. Orphanet J Rare Dis. 2019;14(1):271.
Vandagriff JL, Marrero DG, Ingersoll GM, Fineberg NS. Parents of children with diabetes: what are they worried about? Diabetes Educ. 1992;18(4):299–302.
Spezia Faulkner M, Clark FS. Quality of life for parents of children and adolescents with type 1 diabetes. Diabetes Educ. 1998;24(6):721–7.
Cappelleri JC, Gerber RA, Quattrin T, Deutschmann R, Luo X, Arbuckle R, et al. Development and validation of the WEll-being and Satisfaction of CAREgivers of Children with Diabetes Questionnaire (WE-CARE). Health Qual Life Outcomes. 2008;6(1):3.
Katz M, Volkening L, Dougher C, Laffel L. Validation of the Diabetes Family Impact Scale: a new measure of diabetes-specific family impact. Diabet Med. 2015;32(9):1227–31.
Berdeaux G, Hervié C, Smajda C, Marquis P, The Rhinitis Survey G. Parental quality of life and recurrent ENT infections in their children: development of a questionnaire. Qual Life Res. 1998;7(6):501–12.
Cohen BL, Noone S, Muñoz-Furlong A, Sicherer SH. Development of a questionnaire to measure quality of life in families with a child with food allergy. J Allergy Clin Immunol. 2004;114(5):1159–63.
Boling W, Macrina DM, Clancy JP. The Caregiver Quality of Life Cystic Fibrosis (CQOLCF) scale: modification and validation of an instrument to measure quality of life in cystic fibrosis family caregivers. Qual Life Res. 2003;12(8):1119–26.
Coyne KS, Matza LS, Brewster-Jordan J, Thompson C, Bavendam T. The psychometric validation of the OAB family impact measure (OAB-FIM). Neurourol Urodyn. 2010;29(3):359–69.
Barnard D, Woloski M, Feeny D, McCusker P, Wu J, David M, et al. Development of disease-specific health-related quality-of-life instruments for children with immune thrombocytopenic purpura and their parents. J Pediatr Hematol Oncol. 2003;25:56–62.
Aubeeluck A, Buchanan H. The Huntington’s Disease quality of life battery for carers: reliability and validity. Clin Genet. 2007;71(5):434–45.
Aubeeluck A, Dorey J, Toomi M, Buchanan H. Huntington’s disease quality of life battery for carers-short form.(HDQoLC–SF). 2009.
Doward LC. The development of the Alzheimer's carers' quality of life instrument. Qual Life Res. 1997:639.
Benito-León J, Rivera-Navarro J, Guerrero A, Heras V, Balseiro J, Lorenzo E, et al. The CAREQOL-MS was a useful instrument to measure caregiver quality of life in multiple sclerosis. J Clin Epidemiol. 2010;64:675–86.
Jenkinson C, Dummett S, Kelly L, Peters M, Dawson J, Morley D, et al. The development and validation of a quality of life measure for the carers of people with Parkinson’s disease (the PDQ-Carer). Parkinsonism Relat Disord. 2012;18(5):483–7.
Morley D, Dummett S, Kelly L, Peters M, Dawson J, Fitzpatrick R, et al. The PDQ-Carer: development and validation of a summary index score. Parkinsonism Relat Disord. 2012;19.
Pillas M, Selai C, Quinn NP, Lees A, Litvan I, Lang A, et al. Development and validation of a carers quality-of-life questionnaire for parkinsonism (PQoL Carers). Qual Life Res. 2016;25(1):81–8.
Migliorini C, Callaway L, Moore S, Simpson GK. Family and TBI: an investigation using the Family Outcome Measure - FOM-40. Brain Inj. 2019;33(3):282–90.
Vickrey BG, Hays RD, Maines ML, Vassar SD, Fitten J, Strickland T. Development and preliminary evaluation of a quality of life measure targeted at dementia caregivers. Health Qual Life Outcomes. 2009;7(1):56.
Brown A, Page TE, Daley S, Farina N, Basset T, Livingston G, et al. Measuring the quality of life of family carers of people with dementia: development and validation of C-DEMQOL. Qual Life Res. 2019;28(8):2299–310.
Locker D, Jokovic A, Stephens M, Kenny D, Tompson B, Guyatt G. Family impact of child oral and oro-facial conditions. Commun Dent Oral Epidemiol. 2002;30(6):438–48.
Cohen R, Leis AM, Kuhl D, Charbonneau C, Ritvo P, Ashbury FD. QOLLTI-F: measuring family carer quality of life. Palliat Med. 2006;20(8):755–67.
Minaya P, Baumstarck K, Berbis J, Goncalves A, Barlesi F, Michel G, et al. The CareGiver Oncology Quality of Life questionnaire (CarGOQoL): development and validation of an instrument to measure the quality of life of the caregivers of patients with cancer. Eur J Cancer. 2012;48(6):904–11.
Weitzner MA, Jacobsen PB, Wagner H, Friedland J, Cox C. The Caregiver Quality of Life Index-Cancer (CQOLC) scale: development and validation of an instrument to measure quality of life of the family caregiver of patients with cancer. Qual Life Res. 1999;8(1):55–63.
Ferrell BR, Ferrell BA, Rhiner M, Grant M. Family factors influencing cancer pain management. Postgrad Med J. 1991;67(Suppl 2):S64–9.
City of Hope National Medical Center. QOL Scale - FAMILY. Copyright: City of Hope National Medical Center. Duarte, CA: City of Hope National Medical Center; 2020. https://prc.coh.org/QOL-Family.pdf .
Boruk M, Lee P, Faynzilbert Y, Rosenfeld RM. Caregiver well-being and child quality of life. Otolaryngol Head Neck Surg. 2007;136(2):159–68.
Dubé E, De Wals P, Ouakki M. Quality of life of children and their caregivers during an AOM episode: development and use of a telephone questionnaire. Health Qual Life Outcomes. 2010;8(1):75.
Juniper EF, Guyatt GH, Feeny DH, Ferrie PJ, Griffith LE, Townsend M. Measuring quality of life in the parents of children with asthma. Qual Life Res. 1996;5(1):27–34.
Minard JP, Thomas NJ, Olajos-Clow JG, Wasilewski NV, Jenkins B, Taite AK, et al. Assessing the burden of childhood asthma: validation of electronic versions of the Mini Pediatric and Pediatric Asthma Caregiver’s Quality of Life Questionnaires. Qual Life Res. 2016;25(1):63–9.
Chow MY, Morrow A, Heron L, Yin JK, Booy R, Leask J. Quality of life for parents of children with influenza-like illness: development and validation of Care-ILI-QoL. Qual Life Res. 2014;23(3):939–51.
Torres-Made MD, Peláez-Ballestas I, García-Rodríguez F, Villarreal-Treviño AV, Fortuna-Reyna BdJ, de la O-Cavazos ME, et al. Development and validation of the CAREGIVERS questionnaire: multi-assessing the impact of juvenile idiopathic arthritis on caregivers. Pediatric Rheumatol. 2020;18(1):3.
Abreu Paiva LM, Gandolfi L, Pratesi R, Harumi Uenishi R, Puppin Zandonadi R, Nakano EY, et al. Measuring quality of life in parents or caregivers of children and adolescents with celiac disease: development and content validation of the questionnaire. 2019.
Nauser JA, Bakas T, Welch JL. A new instrument to measure quality of life of heart failure family caregivers. J Cardiovasc Nurs. 2011;26(1):53–64.
Varni JW, Sherman SA, Burwinkle TM, Dickinson PE, Dixon P. The PedsQL Family Impact Module: preliminary reliability and validity. Health Qual Life Outcomes. 2004;2:55.
Stein RE, Jessop DJ. The impact on family scale revisited: further psychometric data. J Dev Behav Pediatr. 2003;24(1):9–16.
Williams AR, Piamjariyakul U, Williams PD, Bruggeman SK, Cabanela RL. Validity of the revised Impact on Family (IOF) scale. J Pediatr. 2006;149(2):257–61.
Jalil YF, Villarroel GS, Silva AA, Briceño LS, Ormeño VP, Ibáñez NS, et al. Reliability and validity of the revised impact on family scale (RIOFS) in the hospital context. J Patient Rep Outcomes. 2019;3(1):28.
Park J, Hoffman L, Marquis J, Turnbull AP, Poston D, Mannan H, et al. Toward assessing family outcomes of service delivery: validation of a family quality of life survey. J Intellect Disabil Res. 2003;47(Pt 4–5):367–84.
Brouwer WB, van Exel NJ, van Gorp B, Redekop WK. The CarerQol instrument: a new instrument to measure care-related quality of life of informal caregivers for use in economic evaluations. Qual Life Res. 2006;15(6):1005–21.
Isaacs BJ, Brown I, Brown RI, Baum N, Myerscough T, Neikrug S, et al. The international family quality of life project: goals and description of a survey tool. J Policy Pract Intellect Disabil. 2007;4(3):177–85.
Perry A, Isaacs B. Validity of the family quality of life survey-2006. J Appl Res Intellect Disabil. 2015;28(6):584–8.
Samuel PS, Tarraf W, Marsack C. Family Quality of Life Survey (FQOLS-2006): evaluation of internal consistency, construct, and criterion validity for socioeconomically disadvantaged families. Phys Occup Ther Pediatr. 2018;38(1):46–63.
Golics CJ, Basra MK, Finlay AY, Salek S. The development and validation of the Family Reported Outcome Measure (FROM-16)© to assess the impact of disease on the partner or family member. Quality life Res. 2014;23(1):317–26.
Scarpelli A, Paiva S, Pordeus I, Varni J, Viegas C, Allison P. The Pediatric Quality of Life Inventory™ (PedsQL™) family impact module: reliability and validity of the Brazilian version. Health Qual Life Outcomes. 2008;6:35.
Hoffman L, Marquis J, Poston D, Summers J, Turnbull A. Assessing family outcomes: psychometric evaluation of the beach center family quality of life scale. J Marriage Fam. 2006;68.
Waschl N, Xie H, Chen M, Poon KK. Construct, convergent, and discriminant validity of the beach center family quality of life scale for Singapore. Infants Young Child. 2019;32(3):201–14.
Rivard M, Mercier C, Mestari Z, Terroux A, Mello C, Bégin J. Psychometric Properties of the Beach Center Family Quality of Life in French-speaking families with a preschool-aged child diagnosed with autism spectrum disorder. Am J Intellect Dev Disabil. 2017;122(5):439–52.
Hoefman RJ, van Exel J, Brouwer WBF. Measuring the impact of caregiving on informal carers: a construct validation study of the CarerQol instrument. Health Qual Life Outcomes. 2013;11(1):173.
McCaffrey N, Bucholc J, Rand S, Hoefman R, Ugalde A, Muldowney A, et al. Head-to-head comparison of the psychometric properties of 3 carer-related preference-based instruments. Value in Health. 2020.
Guyatt G, Walter S, Norman G. Measuring change over time: assessing the usefulness of evaluative instruments. J Chronic Dis. 1987;40(2):171–8.
Guyatt GH, Osoba D, Wu AW, Wyrwich KW, Norman GR, Aaronson N, et al. Methods to explain the clinical significance of health status measures. Mayo Clin Proc. 2002;77(4):371–83.
Golics CJ, Basra MKA, Salek MS, Finlay AY. The impact of patients’ chronic disease on family quality of life: an experience from 26 specialties. Int J Gen Med. 2013;6:787–98.
Bhatti Z, Salek M, Finlay A. Chronic diseases influence major life changing decisions: a new domain in quality of life research. J R Soc Med. 2011;104(6):241–50.
Camfield L. Quality of Life in Developing Countries. In: Land KC, Michalos AC, Sirgy MJ, editors. Handbook of social indicators and quality of life research. Dordrecht: Springer Netherlands; 2012. p. 399–432.
Finlay AY, Salek MS, Abeni D, Tomás-Aragonés L, van Cranenburgh OD, Evers AW, et al. Why quality of life measurement is important in dermatology clinical practice: an expert-based opinion statement by the EADV Task Force on Quality of Life. J Eur Acad Dermatol Venereol. 2017;31(3):424–31.
Download references
Acknowledgements
There was no external funding for this Cardiff University study.
Author information
Authors and affiliations.
Division of Infection and Immunity, School of Medicine, Cardiff University, Cardiff, UK
R. Shah, F. M. Ali & A. Y. Finlay
School of Life and Medical Sciences, University of Hertfordshire, Hatfield, UK
M. S. Salek
Institute of Medicines Development, Cardiff, UK
You can also search for this author in PubMed Google Scholar
Contributions
RS carried out the literature review and wrote the first draft of the manuscript. AYF, FMA and MSS contributed equally to the extensive revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to R. Shah .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
RS and FMA declared no competing interest. AYF and MSS are joint copyright holders of FROM-16.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Supplementary tables-methods and results.
Additional file 2.
Supplementary table S1-PRISMA Checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Shah, R., Ali, F.M., Finlay, A.Y. et al. Family reported outcomes, an unmet need in the management of a patient's disease: appraisal of the literature. Health Qual Life Outcomes 19 , 194 (2021). https://doi.org/10.1186/s12955-021-01819-4
Download citation
Received : 07 April 2021
Accepted : 07 July 2021
Published : 05 August 2021
DOI : https://doi.org/10.1186/s12955-021-01819-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Family member
- Impact of illness
- Management of a patient's disease
Health and Quality of Life Outcomes
ISSN: 1477-7525
- Submission enquiries: [email protected]
- Search Menu
- Advance articles
- Author Guidelines
- Submission Site
- Open Access
- About Family Practice
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
- < Previous
Quality of Life —a Review of the Literature
- Article contents
- Figures & tables
- Supplementary Data
MIDGE FOWLIE, JOHN BERKELEY, Quality of Life —a Review of the Literature, Family Practice , Volume 4, Issue 3, September 1987, Pages 226–234, https://doi.org/10.1093/fampra/4.3.226
- Permissions Icon Permissions
This review of the literature looks at the meaning of the concept ‘quality of life’, the use to which it has been put in various branches of medicine, its meaning in particular in cancer patients, especially those for whom there is no longer expectation of cure, and the instruments already developed for its measurement and their relevance to terminal care. The review concentrates mainly on patients with terminal malignant disease as the quality of life of other patients is a much broader issue.
- terminal patient care
- quality of life
- concentrate dosage form
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1460-2229
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 24 April 2015
Haematological cancer and quality of life: a systematic literature review
- P Allart-Vorelli 1 ,
- B Porro 2 ,
- F Baguet 2 , 3 ,
- A Michel 2 , 4 &
- F Cousson-Gélie 2 , 3
Blood Cancer Journal volume 5 , page e305 ( 2015 ) Cite this article
10k Accesses
92 Citations
3 Altmetric
Metrics details
- Haematological cancer
- Haematological diseases
- Quality of life
The aim of this study is to examine the impact of haematological cancers on quality of life (QoL). A review of the international literature was conducted from the databases ‘PsycInfo' and 'Medline' using the keywords: 'haematological cancer', 'quality of life', 'physical', 'psychological', 'social', 'vocational', 'professional', 'economic', 'cognitive', and 'sexual'. Twenty-one reliable studies were analysed. Among these studies, 12 showed that haematological cancer altered overall QoL, 8 papers found a deterioration of physical dimension, 8 papers reported on functional and role dimensions, 11 papers reported on the psychological component and 9 on the social component. Moreover, one study and two manuscripts, respectively, reported deteriorated sexual and cognitive dimensions. Our review demonstrates that the different dimensions of QoL are deteriorated by haematological malignancies and, probably, by the side effects of treatment.
Similar content being viewed by others
Use of the European Organisation for Research and Treatment of Cancer multiple myeloma module (EORTC QLQ-MY20): a review of the literature 25 years after development
The quality of life index: a pilot study integrating treatment efficacy and quality of life in oncology

Temporal stability of quality of life assessments in cancer patients
Introduction.
Haematological cancers include various diseases (Hodgkin’s lymphoma, non-Hodgkin’s lymphoma, leukaemia and multiple myeloma. The term leukaemia comprises acute myeloid leukaemia, chronic myelogenous leukaemia, acute lymphoblastic leukaemia and chronic lymphoblastic leukaemia); they can affect children, young adults and the elderly, and their incidence increases with age. 1 As liquid tumours moving in the blood or lymph, acute or chronic diseases, with side effects induced by different treatments, are unique. Just as these diseases are distinct entities showing many differences from solid tumours, so too is the manner in which they are managed. 2 In 1999, leukaemias and lymphomas accounted for approximately 8% of all cancers in adults. 3 The 5-year survival rates vary from 47% to 95% depending on the malignancy. 4
Quality of life (QoL) is usually impaired in the elderly: the biological nature and course of treatment of haematological cancer differ among children and adults, 5 , 6 , 7 with long-term survival outcomes favouring young people diagnosed and treated as children. 3
Our paper also focuses on health-related QoL (QoL), a factor reflecting the individual’s assessment of his/her life at any one time relative to his/her previous state and prior experience. 8 Health-related QoL is multidimensional and temporal, relating to a state of functional, physical, psychological and social/family well-being. 9 Compared with the general population, the health-related QoL of cancer patients is worse in most dimensions. 10 , 11
This review describes the QoL and the different problems that patients with haematological malignancies encounter.
Materials and methods
Search strategy.
A review was conducted from databases ‘PsycInfo’ and ‘Medline’, searching for studies published between 1990 and 2011 with keywords: ‘haematological cancer’, ‘quality of life’, ‘physical’, ‘psychological’, ‘social’, ‘vocational’, ‘professional’, ‘economic’, ‘cognitive’, and ‘sexual’ appearing in the abstracts.
We used nine combinations for all databases: (1) ‘QoL and haematological cancer’, (2) ‘haematological cancer and physical’, (3) ‘haematological cancer and psychological’, (4) ‘haematological cancer and social’, (5) ‘haematological cancer and cognitive’, (6) ‘haematological cancer and economic’, (7) ‘haematological cancer and professional’, (8) ‘haematological cancer and vocational’, and (9) ‘haematological cancer and sexual’.
Criteria for inclusion/exclusion
Prospective, comparative, exploratory, longitudinal or cross-sectional studies, assessing the QoL or health-related QoL, were analysed. Papers focusing on lymphoma, leukaemia or myeloma patients with chemotherapy, radiotherapy or blood transfusion in periods of remission or relapse were included. However, retrospective studies with other forms of cancer and reviews of the literature were excluded.
Quality assessment and levels of evidence
The studies had to be based on reliable methodological procedure (large population study, standardized tools and relevant statistical methods) and meet the criteria of a table that describes five levels of evidence (Level I: high-quality prospective study (all patients were enrolled at the same point in their disease with 80% follow-up of patients); Level II: retrospective study, untreated controls from a randomized control trial, lesser prospective study (patients enrolled at different points in their disease or <80% follow-up); Level III: case control study; Level IV: case series; Level V: expert opinion) in prognostic studies (investigating the effect of a patient’s characteristic on the outcome of the disease). 12 We considered only level I and II studies.
Data synthesis
Studies were analyzed by dimensions of QoL and symptoms (description of QoL in Table 1 ).
Article identification
In total, 82 studies emerged: 73 studies for ‘PsycInfo’ and 9 studies for ‘Medline’. There were 21 studies for combination 1, 14 for combination 2, 14 for combination 3, 9 for combination 4, 11 for combination 5, 3 for the combination 6, 10 for the combination 7 and 0 for the combinations 8 and 9. By limiting inclusion to studies that provided evidence of the impact of cancer on QoL, we selected 21 studies.
Methodological characteristics
One paper presented the level of evidence I 13 and 20 level II. 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 Twelve were comparative, 14 , 15 , 16 , 17 , 18 , 20 , 23 , 24 , 26 , 28 , 30 , 32 , 34 5 were longitudinal, 14 , 19 , 20 , 22 , 33 5 were cross-sectional, 21 , 23 , 24 , 26 , 27 2 were descriptive, 16 , 17 2 were pilot, 25 , 29 1 was prospective, 23 1 was retrospective, 31 1 was international 28 and 1 was a web-based survey. 28
Patient population
In total, 7349 patients (3987 patients with lymphoma, 2303 with leukaemia, 711 with myeloma, 6 patients with amyloidosis and 1 with myelofibrosis; 341 no specified patients) were included in the studies (average age of 54.8 years).
One study focussed on the cognitive functioning of lymphoma patients by comparing two groups (test group and no-test group (diagnosis unknown). 15 Another paper examined the QoL, without specifying the number of patients per diagnosis. 33 The health-related QoL was studied in acute lymphoblastic leukaemia, myelofibrosis or unclassified leukaemia patients, but the authors did not specify the sample size of patients per diagnosis. 21 There were 1171 control groups with haematological patients and healthy subjects in 3 studies. 20 , 26 , 32
QoL and health-related QoL of haematological cancer patients
Overall qol.
Twelve papers showed that haematological cancer negatively affect overall QoL and health-related QoL. 13 , 14 , 16 , 18 , 20 , 22 , 24 , 25 , 27 , 28 , 30 , 31 We noted a strong association between anaemia and QoL in lymphoma patients before chemotherapy. 22 We found an impairment of QoL in multiple myeloma patients at diagnosis, 18 at the beginning of treatment 13 and during treatment, 27 in chronic lymphoblastic leukaemia patients with chemotherapy 16 and in multiple myeloma and acute lymphoblastic leukaemia patients at the start of chemotherapy. 25 The latter study found that QoL was more deteriorated in patients with relapses, in comparison to patients who had no relapse, even at the onset of treatment. Moreover, QoL was worse in patients with an advanced stage of disease. 28
Chronic lymphoblastic leukaemia patients had impaired health-related QoL compared with the general population. 16 Compared with healthy controls, chronic lymphoblastic leukaemia patients with chemotherapy reported a lower QoL. 20 Non-Hodgkin’s lymphoma survivors with active disease presented a worse QoL compared with short- or long-term survivors. 30 Moreover, one paper found a better QoL in Hodgkin’s lymphoma survivors diagnosed 10–15 years previously than patients diagnosed 5–9 years ago. 24
QoL improved after aerobic exercise training programme 14 and was better in non-Hodgkin’s lymphoma patients meeting public health exercise guidelines, compared with those who did not. 31 Nevertheless, one study found that QoL of chronic lymphoblastic leukaemia patients was similar to or better than published population. 28 However, one study demonstrated that QoL improved during and after chemotherapy in aggressive non-Hodgkin’s lymphoma patients. 22
General health
Five reports investigated the general health in haematological population. 14 , 17 , 22 , 23 , 24 For multiple myeloma and non-Hodgkin’s lymphoma patients, their physical health and mobility were the most frequent domains affected by the disease. 17 Two studies noted that non-Hodgkin’s lymphoma patients had a worse general health and that Hodgkin’s lymphoma survivors presented lower general health compared with the population. 23 , 24 In another study comparing general health in patients treated with usual care or aerobic exercise training programme, aerobic exercise training patients had better general health than the other patients. 14 However, after chemotherapy, general health improved in non-Hodgkin’s lymphoma patients in one study. 22
Physical dimension
Eight studies showed that haematological cancer deteriorates the physical component of QoL. 14 , 18 , 19 , 20 , 21 , 24 , 29 , 30 Some patients negatively perceived their physical well-being after bone marrow transplanation. 19 Four other studies showed that physical function was affected in multiple myeloma patients 17 , 18 , 21 , 29 and that older patients presented more reduced physical functioning than younger patients. 21 Non-Hodgkin’s lymphoma survivors with active disease demonstrated worse physical functioning compared with disease-free survivors and population. 30 Aerobic exercise training programme patients had better cardiovascular fitness than usual care patients. 14 Long-term Hodgkin’s lymphoma survivors diagnosed 10–15 years earlier reported better physical functioning than survivors diagnosed 5–9 years before. 24 For chronic lymphoblastic leukaemia patients, physical functioning was significantly deteriorated compared with the healthy controls. 20
Fatigue, lack of vitality and energy: Ten papers found that fatigue was one of the most prevalent symptoms experienced in haematological patients. 14 , 15 , 16 , 18 , 20 , 21 , 25 , 26 , 29 , 32 Compared with population, chronic lymphoblastic leukaemia patients had impaired health-related QoL for fatigue. 16 For 55% of haematological patients, fatigue was the main symptom with insomnia, 21 in particular in acute leukaemia and highly malignant lymphoma patients. 25 One paper reported that levels of fatigue in Hodgkin’s lymphoma and chronic lymphoblastic patients were higher than patients in healthy controls, even for years after treatment. 20 Having severe illnesses in Hodgkin’s lymphoma survivors was positively associated with fatigue. 26 Another study showed that lymphoma patients who reported concentration and memory difficulties demonstrated much fatigue; 15 symptom less pronounced in aerobic exercise training programme patients compared with usual care patients. 14 These findings are consistent with the results found in another report. 18 , 29
Three studies noted that patients with bone marrow transplanation, 19 Hodgkin’s lymphoma survivors treated by radiotherapy or chemotherapy 32 and Hodgkin’s lymphoma survivors 24 presented a lack of energy. For vitality, patients diagnosed 5–9 years before presented a greater lack of vitality than those diagnosed 10–15 years before. 24 Finally, non-Hodgkin’s lymphoma patients reported less vitality compared with population. 23
Pain: Painful sensations were frequent in haematological patients for five studies. 18 , 21 , 22 , 23 , 29 Pain was the most distressing problem for multiple myeloma, 18 monoclonal gammopathy of unknown significance (MGUS) 29 and leukaemia and lymphoma patients. 21 In the latter study, older patients had more pain than younger patients. Similar results were found in non-Hodgkin’s lymphoma patients who reported more bodily pain than the general population. 23 However, during chemotherapy, less pain was experienced by aggressive non-Hodgkin’s lymphoma patients in only one study. 22
Sleep disorders: Four studies found that sleep was affected by haematological cancer. 16 , 19 , 22 , 25 Sleep disorders were prevalent in acute leukaemia and highly malignant lymphoma patients at the start of treatment. 25 Compared with the general population, chronic lymphoblastic leukaemia patients presented more sleep disorders, 16 related to functional well-being. 19 An improvement was found in sleep disturbances during and after chemotherapy in aggressive non-Hodgkin’s lymphoma patients. 22
Digestive symptoms: Digestive symptoms may occur during haematological disease in four studies. 20 , 21 , 22 , 33 Among the most common problems in acute leukaemia patients, we found lack of appetite, weight loss, nausea and vomiting, 1 day after the end of chemotherapy or bone marrow transplanation. However, these symptoms had improved 10 and 21 days after the end of treatment. 33 Older and recently hospitalised patients had more constipation, nausea and loss of appetite than younger patients and outpatients. 21 Moreover, non-Hodgkin’s lymphoma patients presented diarrhoea during chemotherapy but showed constipation 1 month after the end of treatment. 22 Finally, chronic lymphoblastic leukaemia patients showed more nausea and vomiting, constipation and appetite loss than healthy controls. 20
Dyspnoea: In three studies, dyspnoea, predominant with chemotherapy, was one of the most common symptoms in acute leukaemia and highly malignant lymphoma patients 25 and in chronic lymphoblastic leukaemia patients. 16 , 20
Nutrition: In one study, nutritional deficits predominated in multiple myeloma and MGUS patients, treated with transplant. 29
Fever: Only one study mentioned the problem of fever in acute leukaemia during chemotherapy. 33
Functional and role dimensions
Two studies focussed on the functional dimension, 19 , 28 negatively affected after a bone marrow transplanation. However, in one study could most patients carry on with their daily activities without any help 1 year after bone marrow transplanation. 19 Moreover, some authors found that daily functioning was similar or better than the population norms. 28
Concerning role, six studies focussed on this dimension. 16 , 18 , 20 , 21 , 22 , 25 One study analysed the deterioration of role function in leukaemia, multiple myeloma or lymphoma patients. 21 Role was affected in leukaemia and lymphoma 25 and multiple myeloma patients, 18 essentially in older patients. Compared with the general population, chronic lymphoblastic lymphoma patients had impaired role functioning for two studies. 16 , 20 However, improvement of role was observed 1 month after the end of chemotherapy in non-Hodgkin’s lymphoma patients. 22
Psychological dimension
Eleven studies showed that haematological cancers affect psychological QoL. 14 , 15 , 19 , 20 , 23 , 24 , 28 , 29 , 30 , 32 , 33 One paper found that patients diagnosed 10–15 years earlier reported better psychological well-being than patients diagnosed 5–9 years ago. 23 Lymphoma patients with chemotherapy presented possible anxiety and depression 15 and we noted a high frequency of anxiety and depression in acute leukaemia patients, with a trend to improvement at the end of treatment. 33 One study suggested that patients experienced more anxiety and mood disturbance after bone marrow transplanation compared with those with a longer follow-up. 19 Hodgkin’s lymphoma or non-Hodgkin’s lymphoma patients receiving aerobic exercise training programme reported less depression and greater happiness compared with those who did not participate in the programme. 14 Individuals with active disease demonstrated worse mental health functioning compared with population and disease-free survivors. 30 Additional studies reported that emotional distress was present in multiple myeloma, MGUS, amyloid 29 and chronic lymphoblastic leukaemia patients. 20 Finally, chronic lymphoblastic leukaemia patients presented lower emotional well-being compared with the general population. 24 , 28 Moreover, Hodgkin’s lymphoma survivors presented a different and positive vision of life after disease. 32
Cognitive dimension
Two papers focussed on the cognitive functioning. 15 , 20 The cognitive area was significantly deteriorated in chronic lymphoblastic leukaemia patients, compared with healthy controls, 20 and lymphoma patients with memory problems had a lower QoL. 15
Social, professional and economic dimensions
Nine papers showed that social, professional and financial QoL were affected by haematological cancer. 17 , 19 , 20 , 21 , 23 , 24 , 25 , 28 , 32 One report found a deterioration of social functioning in leukaemia and lymphoma patients with chemotherapy. 25 Chronic lymphoblastic leukaemia patients presented a lower social QoL, mainly women. 20 Another study found the same finding in patients diagnosed 5–9 years earlier compared with patients diagnosed 10–15 years before. 24 In one study, the availability of, and satisfaction with, social support declined after bone marrow transplanation. 19 The domain of family was affected in 89% of haematological patients. 17 However, in one paper, the social functioning of chronic lymphoblastic leukaemia patients was similar to or better than that of the general population. 28
Furthermore, one paper showed that Hodgkin’s lymphoma survivors mentioned the topics of leisure and finance less frequently than controls. 32 Older patients had fewer financial difficulties than outpatients, and multiple myeloma patients had a worse social QoL compared with those with other haematological cancers. 21 Finally, most frequent domains mentioned were hobbies/pastimes, partnerships, profession and social life and friends 17 and difficulties to obtain health-care insurance and life insurance. 23
Sexual dimension
One study focussed on the sexual component 29 and found that multiple myeoloma or MGUS patients presented sexual difficulties associated with body image. 29 The problem of body image could be associated with hair loss mentioned in another paper. 33
The general findings show that the haematological disease negatively affects overall QoL. 13 , 14 , 16 , 18 , 20 , 22 , 24 , 25 , 27 , 28 , 30 , 31 Compared with the general population, fatigue, pain or vitality were the more exposed 35 , 36 aspects of QoL, which were specifically deteriorated during an advanced stage of haematological cancer. 28 Compared with the general population, haematological patients had an adverse general health. 23 These results confirm other findings concerning cancer populations. 37
Fatigue was the most prevalent physical symptom. 14 , 15 , 16 , 18 , 21 , 25 , 26 , 29 , 32 , 33 Most of the samples included elderly patients, and the progressive loss of autonomy in older people is not conducive to maintaining physical QoL. Haematological patients were more susceptible to fatigue than others because of the comorbidity and side effects due to treatment. 38 Moreover, the benefits of physical programme on physical well-being were demonstrated. 27 Similar data were found in Hodgkin’s lymphoma survivors, an improvement in physical functioning and cardiovascular fitness being observed after exercise. 39 The other physical symptoms were common to patients with other forms of cancers 40 as well as breast cancer patients. 41 , 42
Only one study found that haematological patients can manage acts of daily life without the need for support after bone marrow transplanation. 19 However, older and multiple myeloma patients experienced more reduced role function than younger patients and subjects with other diagnoses. 21 Indeed, the multiple myeloma patients were older than patients with other diagnoses, and advanced age proved to be a predictor of symptoms. Role was more affected in haematological patients than in the general population. 16 Because of physical disabilities, it is plausible that familial or social missions were disturbed.
Mostly, psychological QoL was found to be worse. 14 , 15 , 19 , 20 , 23 , 24 , 28 , 29 , 30 , 32 , 33 One study noted that aerobic exercise training programme helped maintain good mental QoL. 27 This may be due to the involvement of social interaction and a process of being distracted from one’s cancer and treatments, a finding already made in advanced cancer patients. 43 Moreover, emotional benefits occurred after patients with breast cancer followed a sports programme. 44
Furthermore, haematological cancer damaged social, professional and financial QoL. 17 , 19 , 20 , 21 , 23 , 24 , 25 , 28 , 32 Having cancer may improve social and familial relations by increasing the intensity of support and the availability of family caregivers. Conversely, emotional distress can affect the family sphere, and interpersonal relationships are likely to move towards the feeling of ambiguity or fear. Familial structure may be modified, leading to distress within the family. The deterioration of social well-being could be linked with self-image, including hair loss which increases after chemotherapy. 33 Otherwise, the time since diagnosis may also have an impact on social QoL: in two studies, patients diagnosed 10–15 years earlier presented a better social QoL than those diagnosed 5–9 years before. 23 , 24 These findings were similar among families of patients with a head and neck cancer. 45
Some studies found that professional life was negatively affected in patients. 23 , 39 , 41 , 46 Another study strengthened this finding by establishing that economic stress was negatively associated with QoL in gynaecological survivors. 47 Moreover, one paper showed an increase in disability days in patients with breast, lung and gastrointestinal cancers. 48 These consequences can lead to social isolation and frustration. 49
Sexual activity, related to body image, was also reduced. 29 Body image could be an important aspect of our criteria, with the fear of loss of masculinity or femininity and self-image. Other forms of cancer such as gynaecological malignancies also affected patients’ sex life. 50
With regard to cognitive functioning, haematological patients presented several memory and concentration disturbances. 28 Similar results were found in cancer patients, in whom cognitive deficits were observed after chemotherapy. 51
Physical, psychological, social and professional problems may be associated with the effects of treatment modalities. QoL was particularly affected in multiple myeloma and chronic lymphoblastic leukaemia patients, treated by chemotherapy or transplantation, in older patients, and in patients with active disease or an advanced stage of disease. Therefore, it would be interesting to conduct a further review with a synthesis of articles that highlight the impact on QoL of treatments recommended for a haematological malignancy.
The potential limitations of this review concern the literature search. Others involve the complexity in interpreting and measuring QoL, the heterogeneity of samples and the loss of subjects during research due to poor medical conditions, death or refusal.
The major strength of our review is the reliability of the selected studies. It shows that haematological cancer patients have a poor QoL or health-related QoL compared with the general population. These findings hold regardless of the type of disease, the treatment modality and the stage of the disease. Generally, we found similar outcomes in other cancers, such as fatigue, which was greater in haematological patients. In theoretical terms, QoL is a complex concept that encompasses various aspects of life and is similar to well-being, so the very meaning of the notion is debatable. Clinically, it is important to analyse QoL early in the course of care. Some types of intervention may prove helpful such as physical programmes, which may be considered as a form of functional care intervention, and other supportive actions, such as psychotherapy which can improve physical and mental functioning.
Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR et al . Proposals for the Classification of the Acute Leukaemias French-American-British (FAB) Co-operative Group. Brit J Haematol 1976; 33 : 451–458.
Article CAS Google Scholar
Ireland R . Haematological malignancies: the rationale for integrated haematopathology services, key elements of organization and wider contribution to patient care. Histopathology 2011; 58 : 145–154.
Article Google Scholar
Zebrack B . Quality of life of long-term survivors of leukemia and lymphoma. J Psychosoc Oncol 2000; 18 : 39–59.
Pulte D, Gondos A, Brenner H . Trends in survival after diagnosis with hematologic malignancy in adolescence or young adulthood in the United States, 1981-2005. Cancer 2009; 115 : 4973–4979.
Lesko LM . Hematological malignancies. Handbook of Psychooncology: Psychological Care of the Patient with Cancer . Oxford University Press: New York NY, USA, 1989, pp 218–231.
Google Scholar
Aaronson NK, Meyrowitz BE, Bard M, Bloom JR, Fawzy I, Feldstein M et al . Quality of life research in oncology. Past achievements and future priorities. Cancer 1991; 67 : 839–843.
van Den Beuken-van Everdingen MHJ, de Rijke JM, Kessels AG, Schouten HC, van Kleef M, Patijn J . Quality of life and non-pain symptoms in patients with cancer. J Pain Symptom Manag 2009; 38 : 216–233.
Chao NJ, Tierney DK, Bloom JR, Long GD, Barr TA, Stallbaum BA et al . Dynamic assessment of quality of life after autologous bone marrow transplantation. Blood 1992; 80 : 825–830.
CAS PubMed Google Scholar
Ferrell BR, Hassey Dow K, Grant M . Measurement of the quality of life in cancer survivors. Qual Life Res 1995; 4 : 523–531.
Baker F, Denniston M, Haffer SC, Liberatos P . Change in health-related quality of life of newly diagnosed cancer patients, cancer survivors, and controls. Cancer 2009; 115 : 3024–3033.
Baumann R, Pütz C, Röhrig B, Höffken K, Wedding U . Health-related quality of life in elderly cancer patients, elderly non-cancer patients and an elderly general population. Eur J Cancer Care 2009; 18 : 457–465.
Wright JG., Swiontkowski MF, Heckman JD . Introducing levels of evidence to the journal. J Bone Joint Surg 2003; 85 : 1–3.
Strasser-Weippl K, Ludwig H . Psychosocial QOL is an independent predictor of overall survival in newly diagnosed patients with multiple myeloma. Eur J Haematol 2008; 81 : 374–379.
PubMed Google Scholar
Courneya KS, Sellar CM, Stevinson C, McNeely ML, Peddle CJ, Friedenreich CM et al . Randomized controlled trial of the effects of aerobic exercise on physical functioning and quality of life in lymphoma patients. J Clin Oncol 2009; 27 : 4605–4612.
Cull A, Hay C, Love SB, Mackie M, Smets E, Stewart M . What do cancer patients mean when they complain of concentration and memory problems? Brit J Cancer 1996; 74 : 1674–1679.
Else M, Smith AG, Cocks K, Richards SM, Crofts S, Wade R et al . Patients' experience of chronic lymphocytic leukaemia: baseline health-related quality of life results from the LRF CLL4 trial. Brit J Haematol 2008; 143 : 690–697.
Frick E, Borasio GD, Zehentner H, Fischer N, Bumeder I . Individual quality of life of patients undergoing autologous peripheral blood stem cell transplantation. Psychooncol 2004; 13 : 116–124.
Gulbrandsen N, Hjermstad MJ, Wisløff F . Interpretation of quality of life scores in multiple myeloma by comparison with a reference population and assessment of the clinical importance of score differences. Eur J Haematol 2004; 72 : 172–180.
Heinonen H, Volin L, Uutela A, Zevon M, Barrick C, Ruutu T . Quality of life and factors related to perceived satisfaction with quality of life after allogeneic bone marrow transplantation. Ann Hematol 2001; 80 : 137–143.
Holzner B, Kemmler G, Kopp M, Nguyen-Van-Tam D, Sperner-Unterweger B, Greil R . Quality of life of patients with chronic lymphocytic leukemia: results of a longitudinal investigation over 1 yr. Eur J Haematol 2004; 72 : 381–389.
Johnsen AT, Tholstrup D, Petersen MA, Pedersen L, Groenvold M . Health related quality of life in a nationally representative sample of haematological patients. Eur J Haematol 2009; 83 : 139–148.
Merli F, Bertini M, Luminari S, Mozzana R, Berté R, Trottini M et al . Quality of life assessment in elderly patients with aggressive non-Hodgkin's Lymphoma treated with anthracycline-containing regimens. Report of a prospective study by the Intergruppo Italiano Linfomi. Haematologica 2004; 89 : 973–978.
Mols F, Aaronson NK, Vingerhoets AJJM, Coebergh JW, Vreugdenhil G, Lybeert MLM et al . Quality of life among long-term non-Hodgkin lymphoma survivors: a population-based study. Cancer 2007; 109 : 1659–1667.
Mols F, Vingerhoets AJJM, Coebergh JW, Vreugdenhil G, Aaronson NK, Lybeert MLM et al . Better quality of life among 10-15 year survivors of Hodgkin's lymphoma compared to 5-9 year survivors: a population-based study. Eur J Cancer 2006; 42 : 2794–2801.
Persson L, Larsson G, Ohlsson O, Hallberg IR . Acute leukaemia or highly malignant lymphoma patients' quality of life over two years: a pilot study. Eur J Cancer Care 2001; 10 : 36–47.
Rüffer JU, Flechtner H, Tralls P, Josting A, Sieber M, Lathan B et al German Hodgkin Lymphoma Study Group. Fatigue in long-term survivors of Hodgkin's lymphoma; a report from the German Hodgkin Lymphoma Study Group (GHSG). Eur J Cancer 2003; 39 : 2179–2186.
Santos FRM, Kozasa EH, Chauffaille Mde L, Colleoni GW, Leite JR . Psychosocial adaptation and quality of life among Brazilian patients with different haematological malignancies. J Psychosom Res 2006; 60 : 505–511.
Shanafelt TD, Bowen D, Venkat C, Slager SL, Zent CS, Kay NE et al . Quality of life in chronic lymphocytic leukaemia: an international survey of 1482 patients. Brit J Haematol 2007; 139 : 255–264.
Sherman AC, Coleman EA, Griffith K, Simonton S, Hine RJ, Cromer J et al . Use of a supportive care team for screening and preemptive intervention among multiple myeloma patients receiving stem cell transplantation. Support Care Cancer 2003; 11 : 568–574.
Smith SK, Zimmerman S, William CS, Zebrack BJ . Health status and quality of life among non-Hodgkin lymphoma survivors. Cancer 2009; 115 : 3312–3323.
Vallance JKH, Courneya KS, Jones LW, Reiman T . Differences in quality of life between non-Hodgkin's lymphoma survivors meeting and not meeting public health exercise guidelines. Psychooncol 2005; 14 : 979–991.
Wettergren L, Björkholm M, Axdorph U, Bowling A, Langius-Eklöf A . Individual quality of life in long-term survivors of Hodgkin's lymphoma - a comparative study. Qual Life Res 2003; 12 : 545–554.
Zittoun R, Achard S, Ruszniewski M . Assessment of quality of life during intensive chemotherapy or bone marrow transplantation. Psychooncol 1999; 8 : 64–73.
Shipp MA, Harrington DP, Anderson JR, Armitage JO, Bonadonna G, Brittinger G et al . A predictive model for aggressive non-Hodgkin's lymphoma. New Engl J Med 1993; 329 : 987–994.
Flechtner H, Rüffer JU, Henry-Amar M, Mellink WA, Sieber M, Fermé C et al . Quality of life assessment in Hodgkin's disease: a new comprehensive approach. First experiences from the EORTC/GELA and GHSG trials. EORTC Lymphoma Cooperative Group. Groupe D'Etude des Lymphomes de L'Adulte and German Hodgkin Study Group. Ann Oncol 1998; 9 : S147–S154.
Jones LW, Eves ND, Peterson BL, Garst J, Crawford J, West MJ et al . Safety and feasibility of aerobic training on cardiopulmonary function and quality of life in postsurgical nonsmall cell lung cancer patients: a pilot study. Cancer 2008; 113 : 3430–3439.
Steinsbekk A, Adams J, Sibbritt D, Johnsen R . Complementary and alternative medicine practitioner consultations among those who have or have had cancer in a Norwegian total population (Nord-Trøndelag Health Study): prevalence, socio-demographics and health perceptions. Eur J Cancer Care 2010; 19 : 346–351.
Miltényi Z, Magyari F, Simon Z, Illés Á . Quality of life and fatigue in Hodgkin's lymphoma patients. Tumori 2010; 96 : 594–600.
Oldervoll LM, Kaasa S, Knobel H, Loge JH . Exercise reduces fatigue in chronic fatigued Hodgkins disease survivors—results from a pilot study. Eur J Cancer 2003; 39 : 57–63.
Theobald DE . Cancer pain, fatigue, distress, and insomnia in cancer patients. Clin Cornerstone 2004; 6 : S15–S21.
Fortner BV, Stepanski EJ, Wang SC, Kasprowicz S, Durrence HH . Sleep and quality of life in breast cancer patients. J Pain Symptom Manag 2002; 24 : 471–480.
Ivanauskiene R, Kregzdyte R, Padaiga Z . Evaluation of health-related quality of life in patients with breast cancer. Medicina (Kaunas) 2010; 46 : 351–359.
Voogt E, van der Heide A, van Leeuwen AF, Visser AP, MPHD Cleiren, Passchier J et al . Positive and negative affect after diagnosis of advanced cancer. Psychooncol 2005; 14 : 262–273.
McNeely ML, Campbell KL, Rowe BH, Klassen TP, Mackey JR, Courneya KS . Effects of exercise on breast cancer patients and survivors: a systematic review and meta-analysis. Can Med Assoc J 2006; 175 : 34–41.
Kaplan BE, Hurley FL . Head and neck cancer: a threat to life and social functioning. Soc Work Health Care 1979; 5 : 51–58.
Miller JJ, Frost MH, Rummans TA, Huschka M, Atherton P, Brown P et al . Role of a medical social worker in improving quality of life for patients with advanced cancer with a structured multidisciplinary intervention. J Psychosoc Oncol 2007; 25 : 105–119.
Ell K, Xie B, Wells A, Nedjat-Haiem F, Lee PJ, Vourlekis B . Economic stress among low-income women with cancer: Effects on quality of life. Cancer 2008; 112 : 616–625.
Kroenke K, Theobald D, Wu J, Loza JK, Carpenter JS, Tu W . The association of depression and pain with health-related quality of life, disability, and health care use in cancer patients. J Pain Symptom Manag 2010; 40 : 327–341.
Persson L, Hallberg IR, Ohlsson O . Survivors of acute leukaemia and highly malignant lymphoma — retrospective views of daily life problems during treatment and when in remission. J Adv Nurs 1997; 25 : 68–78.
Dunberger G., Lind H, Steineck G, Waldenström AC, Nyberg T, Al-Abany M et al . Fecal incontinence affecting quality of life and social functioning among long-term gynecological cancer survivors. Int J Gynecol Cancer 2010; 20 : 449–460.
Schagen SB, Vardy J . Cognitive dysfunction in people with cancer. Lancet Oncol 2007; 8 : 852–853.
Download references
Author information
Authors and affiliations.
Laboratory of Psychology ‘Health and Quality of Life’ EA 4139, University Bordeaux Segalen, Bordeaux, France
P Allart-Vorelli
Department of Psychology, Epsylon EA 4556 Laboratory ‘Dynamics of Human Abilities and Health Behaviors’, University Paul Valéry Montpellier 3, Montpellier, France
B Porro, F Baguet, A Michel & F Cousson-Gélie
ICM, Institut Régional du Cancer de Montpellier, Epidaure Prevention Unit - Rue des Apothicaires, Montpellier Cedex 5, France
F Baguet & F Cousson-Gélie
MIS, Montpellier Institut du Sein – 25 rue de Clémentville, Montpellier, France
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to B Porro .
Ethics declarations
Competing interests.
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
Reprints and permissions
About this article
Cite this article.
Allart-Vorelli, P., Porro, B., Baguet, F. et al. Haematological cancer and quality of life: a systematic literature review. Blood Cancer Journal 5 , e305 (2015). https://doi.org/10.1038/bcj.2015.29
Download citation
Received : 21 January 2015
Accepted : 02 February 2015
Published : 24 April 2015
Issue Date : April 2015
DOI : https://doi.org/10.1038/bcj.2015.29
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Partnership, sexuality, and fertility-related communication: findings from a register-based study among long-term hematological cancer survivors.
- Britta Lohmann
- Katharina Kuba
- Peter Esser
Supportive Care in Cancer (2023)
Quality of life of patients with hematological malignancies and factors affecting health state utility values
- Keiichi Osaki
- Shinichiro Morishita
Supportive Care in Cancer (2022)
Patient-reported outcomes in patients with hematological relapse or progressive disease: a longitudinal observational study
- Lene Kongsgaard Nielsen
- Lone Jørgensen
Health and Quality of Life Outcomes (2021)
Retrospective and prospective measures of post-traumatic growth reflect different processes: longitudinal evidence of greater decline than growth following a hematopoietic stem-cell transplantation
- Maya Corman
- Marie-Thérèse Rubio
- Michaël Dambrun
BMC Psychiatry (2021)
Shared care follow-up of patients with B-cell neoplasms based on nurse-led telephone consultations and PRO-data: a feasibility study from the North Denmark Region
- Lone Frandsen
- Tarec Christoffer El-Galaly
BMC Health Services Research (2020)

Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Open access
- Published: 16 April 2024
Review on epidemiology, disease burden, and treatment patterns of IgA nephropathy in select APAC countries
- Omer Zaidi 1 ,
- Zhaoli Tang 2 ,
- Sandipan Bhattacharjee 3 &
- Kristin Pareja 3
BMC Nephrology volume 25 , Article number: 136 ( 2024 ) Cite this article
327 Accesses
Metrics details
Immunoglobulin type A (IgA) nephropathy is the most common primary glomerulonephritis (GN) worldwide with higher rates in East and Pacific Asia compared to North America and Europe. Despite high reported prevalence of IgAN in these countries, the overall disease prevalence across Asia is not available. Treatment patterns of IgAN patients across Asian countries have also not been summarized. The aim of this study was to review and summarize evidence on IgA nephropathy prevalence, treatment patterns, and humanistic and economic burden in mainland China, Taiwan, South Korea, Japan, and Australia.
A targeted literature review was conducted in PubMed and local databases in China (including Taiwan), South Korea, Japan, and Australia between January 2010-December 2021. Website literature searches were conducted using Google Scholar and Baidu.
Sixty-nine publications and 3 clinical guidelines were included. Incidence ranged from 0 to 10.7 per 100 000 people per year in Australia, Japan, and Taiwan, and ranged from 6.3 to 24.70% among patients who underwent renal biopsy in mainland China. Prevalence and diagnosis rates ranged from 0 to 72.1% in mainland China, South Korea, Taiwan, Japan, and Australia. Mortality rates in mainland China, South Korea, and Japan varied widely. The top 3 commonly used therapies were angiotensin-converting enzyme inhibitor/angiotensin receptor blockers (0.9-99.6%), corticosteroids (3.5-100%), and immunosuppressants (1.6-85.5%) in Japan, mainland China, and South Korea. Patient quality of life was measured by different tools, and annual hospitalization costs ranged from $1 284.73 to $2 252.12 (2015–2018) in China.
Conclusions
The prevalence of IgA nephropathy among the general population in select countries/regions is not commonly available, despite evidence from studies and clinical guidelines. In addition, it is observed across geographic regions that heterogeneity exists in prevalence rates, and large variations exist in treatment patterns. There is need to fill in these gaps to understand the contributing factors behind the differences through population-based, multi-center, and real-world studies.
Peer Review reports
Immunoglobulin type A nephropathy (IgAN), also known as Berger’s disease, is a kidney disease caused by kidney deposition of immunoglobulin type A (IgA) complexes involving galactose-deficient IgA [ 1 ] and resulting in inflammatory tissue damage [ 2 ]. IgAN affects the kidneys by attacking the glomeruli and is characterized by persistent urinary abnormalities including microscopic hematuria, gross hematuria, and/or proteinuria [ 2 , 3 ]. IgAN is the most common form of biopsy-proven primary glomerulonephritis (PGN) worldwide [ 3 ] and is one of the leading causes of chronic kidney disease (CKD) and end-stage renal disease (ESRD) [ 4 ].
Primary treatments for IgAN include angiotensin-converting enzyme inhibitor/angiotensin receptor blockers (ACEIs/ARBs), corticosteroids, and immunosuppressants [ 1 , 4 ]. These treatments aim to address symptoms and manifestations of IgAN but not the underlying cause. Nearly one-third of IgAN patients develop ESRD within 10 years [ 5 ]. On average, patients with IgAN die 6 years earlier than the general population [ 6 ]. In addition, patients’ quality of life (QoL) is greatly impacted due to pain, fatigue, and poor mental health [ 4 ], and indirect caregiver burden is high due to time spent caring for patients who progress to ESRD. Thus, caregivers’ QoL and psychological well-being can also be negatively impacted [ 7 ].
IgAN prevalence is highest in Asia, intermediate in Europe and the US, and lower in African countries [ 8 ]. The overall global incidence is approximately 2.5 per 100,000 people per year [ 2 ]. A higher prevalence of IgAN is seen in countries where routine screening is practiced [ 4 ]. While geographic variations of IgAN have been studied previously [ 3 , 9 ], few recent studies have focused on regional disease burden differences and treatment patterns in among IgAN patients across Asian countries/regions and Australia.
This review aimed to summarize the disease burden and treatment patterns of IgAN in select countries/regions in the Asia-Pacific region, specifically mainland China, Taiwan, South Korea, Japan, and Australia.
Data sources and search strategy
A targeted literature review (TLR) was conducted to identify relevant literature published from January 2010 to December 2021 for mainland China, Taiwan, South Korea, Australia, and Japan. The earliest year of publication was expanded from 2010 to 2001 to capture evidence more comprehensively on outcomes of interest. Medline and Embase were the primary databases for publications in English. For publications in local languages, WANFANG and China National Knowledge Infrastructure (CNKI) databases were searched for publications in Chinese, Korean Medical Database and Korean Information Service System (KISS) databases were searched for publications in Korean, and Scholarly and Academic Information Navigator (CiNii) was searched for publications in Japanese. Supplementary searches for clinical guidelines, conference proceedings, and websites of governmental and non-governmental organizations were conducted using Google, Baidu (for Chinese sources), and Naver (for Korean sources). Publications cited as references were also considered for screening.
Search terms included IgA nephropathy, Berger’s disease, incidence, prevalence, mortality, quality of life, cost, burden, and treatment. Observational studies, reviews, and registry studies were included in the search. Publications that reported prevalence, incidence, mortality, treatment patterns, guidelines, economic, and humanistic burden were included for data extraction. Search terms in English and local languages are listed in Supplementary Table S1 .
Study selection and data extraction
After the search was conducted and duplicates were removed, the title, abstract, and full texts of the remaining publications were screened. A second reviewer conducted the validation and finalization for publications to be included in the data extraction phase. During screening, the inclusion and exclusion criteria mainly focused on outcomes. Systematic reviews, observational studies including registry/database studies and other real-world studies, annual reports were considered for inclusion. Publications that reported evidence regarding epidemiology (incidence, prevalence, and mortality), humanistic and economic burden, and treatment patterns (treatment guidelines, duration, adherence, persistence, switching, and discontinuation) were included for data extraction. Studies that did not include outcomes of interest were excluded, as were studies with a small sample size (< 25). Strict predefined population, intervention, comparators, outcomes, and study design (PICOS) selection criteria and a Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram were not used in this study. Study characteristics, patient characteristics, epidemiological outcomes, disease burden, and treatment patterns were extracted.
Study quality assessment
All eligible studies went through a quality assessment (QA) using a recommended checklist, according to the Center for Reviews and Dissemination Guidance for Undertaking Reviews in Health Care recommendations [ 10 ]. Quality assessment was performed for all eligible articles by two reviewers. The checklist consisted of 9 items excluding basic information for the included studies. Because all publications included in this study were observational studies or reviews, only the non-randomized clinical trial checklist was used for observational studies.
Sixty-nine publications were included for this review, among which 38 were from mainland China (2015–2021) [ 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 ], 15 from Japan (2003–2021) [ 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 ], 10 from South Korea (2010–2020) [ 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 ], 3 from Taiwan (2014–2019) [ 74 , 75 , 76 ], and 3 from Australia (2001–2021) [ 77 , 78 , 79 ]; characteristics of the studies are shown in Supplementary Table S2 . Approximately 83% the publications reported a retrospective study design ( n = 57). For publications from mainland China, sample sizes ranged from 74 [ 37 ] to 4,367,829 [ 47 ], and male percentages ranged from 37.5% [ 17 ] to 97.3% [ 32 ]. For publications from Japan, sample sizes ranged from 52 [ 53 ] to 270,902 [ 63 ]; the male percentage ranged from 37.1% [ 58 ] to 56.96% [ 52 ]. For publications from South Korea, sample sizes ranged from 25 [ 64 ] to 5,114 [ 67 ]; the male percentage ranged from 36% [ 64 ] to 66.6% [ 73 ]. For publications from Taiwan, sample sizes ranged from 91 [ 75 ] to 7,073 [ 76 ]; the male percentage ranged from 45.9% [ 76 ] to 52.7% [ 75 ]. For publications from Australia, sample sizes ranged from 1,147 [ 78 ] to 2,457 [ 79 ]; the male percentage ranged from 60% [ 77 ] to 69.7% [ 79 ]. The Kidney Disease: Improving Global Outcomes (KDIGO) Clinical Practice Guideline [ 1 ] and 2 country-specific guidelines [ 80 , 81 ] were also included for evidence on treatment patterns.
Sixty-eight journal articles were assessed for study quality (all details of the quality assessment are shown in Supplementary Table S3 ); one white paper was not included in the study quality assessment. Approximately 75% (51/68 articles) were deemed to be of good quality (i.e., without inherent flaws). Few studies reported the incidence/prevalence of IgAN directly and percentage of IgAN were extracted from included studies. The appropriateness of the statistical analysis conducted was not clear or not specified in 5 studies, as they did not define P values and the level of significance for all observations. Across studies, outcome measures were generally considered reliable. However, 33 articles stated that the results could be generalized to routine practice. In one case-control study, the similarity of both groups at the outset of the study was not clear.
Six publications provided evidence on IgAN incidence [ 30 , 61 , 63 , 74 , 77 , 78 ] in Australia ( n = 2), Japan ( n = 2), mainland China ( n = 1), and Taiwan ( n = 1). Most were cross-sectional observational studies ( n = 4), and sample sizes ranged from 156 [ 74 ] to 270,902 [ 63 ].
In Australia, IgAN incidence was estimated to be 1.41–10.5 per 100,000 people per year [ 77 , 78 ]. According to Briganti 2001 [ 78 ], IgAN incidence in Australia was lowest (0.0 per 100,000 per year) among male children and highest (10.7 per 100,000 per year) among male adults [ 78 ]. In Japan, only 2 studies reporting incidence data among children were identified. Utsunomiya 2003 [ 63 ] reported an incidence rate of 4.5 per 100,000 per year among 270,902 junior high and elementary school students; Kajiwara 2020 [ 61 ] reported a rate of 3.3 per 100,000 per year among 60,816 junior high and elementary school students. Both publications collected urine samples through a school urinary screening system in students 6 to 15 years old. In mainland China, the incidence rate of IgAN was estimated to be 6.3% among elderly patients who underwent renal biopsy and 24.7% among non-elderly patients who underwent renal biopsy [ 30 ]. In Taiwan, IgAN incidence was estimated to be 5.5 per million per year among the general population (around 23.5 million between 2014 and 2016), based on 1,445 renal biopsy records from a registry database [ 74 ]. In general, IgAN incidence was higher in males (5.7 per 100,000 per year) compared with females (2.9 per 100,000 per year) [ 78 ]. IgAN incidence was not reported in Korean populations.
Prevalence and diagnosis rate
IgAN prevalence among the general population was not reported in the included publications. But one cross-sectional study ( n = 3,623) reported an IgAN prevalence rate of 0.03% among the general Chinese pediatric population [ 34 ]. Thirty-five publications were identified with diagnosis rates among 2 populations: patients who received renal biopsies and PGN patients [ 13 , 14 , 17 , 18 , 19 , 21 , 22 , 24 , 30 , 31 , 33 , 34 , 35 , 36 , 39 , 40 , 43 , 44 , 45 , 46 , 47 , 48 , 52 , 59 , 67 , 68 , 69 , 70 , 71 , 72 , 74 , 75 , 76 , 79 ]. Twenty-one publications were from mainland China [ 13 , 14 , 17 , 18 , 19 , 21 , 24 , 30 , 31 , 33 , 34 , 35 , 36 , 39 , 40 , 43 , 44 , 45 , 46 , 47 , 48 ], 6 from South Korea [ 67 , 68 , 69 , 70 , 71 , 72 ], 3 from Taiwan [ 74 , 75 , 76 ], 3 from Japan [ 52 , 55 , 59 ], and 1 from Australia [ 79 ]. The majority (88%) were cohort studies ( n = 17) [ 13 , 21 , 31 , 33 , 35 , 36 , 39 , 40 , 43 , 44 , 45 , 46 , 52 , 68 , 69 , 70 , 71 ] and cross-sectional studies ( n = 13) [ 14 , 17 , 18 , 19 , 21 , 24 , 34 , 37 , 47 , 59 , 67 , 72 , 74 , 79 ], with the remainder being an annual report [ 76 ], a registry study [ 55 ] and a chart review [ 75 ]. Sample sizes ranged from 33 [ 70 ] to 43,67,829 [ 47 ].
In mainland China, the mean diagnosis rate of IgAN was estimated to be 24.1% among patients undergoing renal biopsies (median: 23.0%; range: 6.3-40.9%) [ 13 , 19 , 21 , 22 , 24 , 30 , 46 ] and 27.3% (median: 27.9%; range: 0-72.1%) [ 14 , 19 , 21 , 33 , 36 , 40 , 43 , 44 , 45 , 48 ] among PGN patients (Fig. 1 a); The mean IgAN diagnosis rate was estimated to be 21.7% (median: 17.5%; 17-30.4%) among children who underwent renal biopsy [ 17 , 18 , 35 ]. In Taiwan, the mean diagnosis rate of IgAN was 12.1% (median: 12.2%; range: 10.8-13.2%) among patients undergoing renal biopsies [ 74 , 75 ] and was reported similar (26%) among PGN patients [ 74 , 76 ] (Fig. 1 b). In South Korea, the mean diagnosis rate was 41% (median: 38.1%; range: 25.8-61.9%) among patients undergoing renal biopsies [ 67 , 69 , 71 , 72 ] and around 51.6% (average of 51.3% and 51.9%) among PGN patients [ 68 , 70 ] (Fig. 1 c). In Japan, Hattori 2016 reported a mean estimated IgAN diagnosis rate of 23% (median: 22.9%) among CKD patients [ 59 ]. In addition, the reported IgAN diagnosis rate among patients who underwent renal biopsy was 31%, with 6.9% in patients aged 65 to 80 years old and 10.5% in patients aged 80 years or older [ 52 , 55 ]. In Australia, Lee 2020 reported an IgAN diagnosis rate of 13% among patients undergoing renal biopsy [ 79 ].
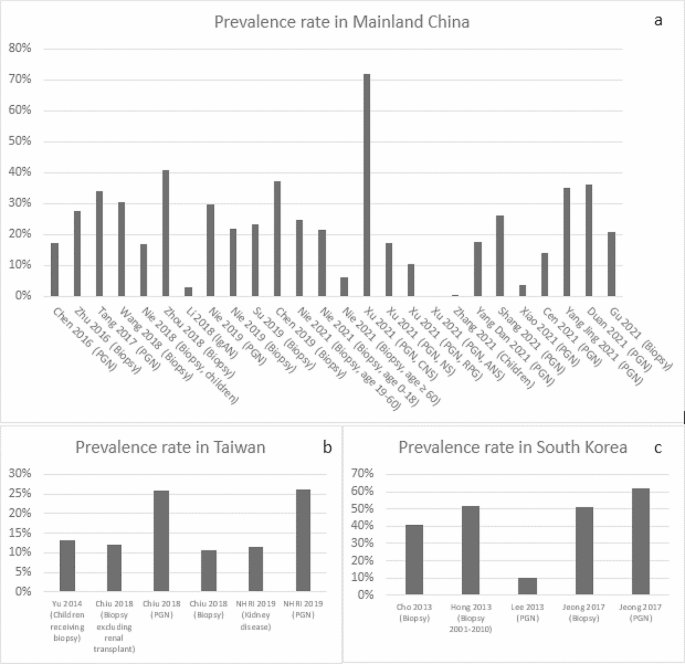
IgAN Prevalence in Mainland China, Taiwan and South Korea (Abbreviation: ANS, acute nephritic syndrome; CNS, chronic nephrotic syndrome; NHRI, National Health Research Institute & Taiwan Society of Nephrology; NS, nephritis syndrome(e; PGN, primary glomerulonephritis; RPG, rapidly progressive glomerulonephritis)
Disease progression and mortality
Among included studies, all-cause mortality was mainly reported as deaths due to ESRD. Seven publications from mainland China [ 23 , 26 , 27 , 28 , 29 , 41 , 42 ], 7 from Korea [ 64 , 65 , 66 , 68 , 70 , 71 , 73 ], 4 from Japan [ 50 , 51 , 57 , 62 ], and 1 from Taiwan [ 75 ] reported rate of progression to ESRD in IgAN. These studies varied in the definition of endpoint, patient characteristics, and follow-up duration. In China, the median rate of progression to ESRD was 4.1% [ 28 ] over 6 months, ranged from 1.3 to 15.8% (median: 1.3%) over 40–45 months [ 29 , 41 ], ranged from 6.6 to 15% (median: 8.3%) over 4–10 years [ 23 , 27 , 42 ], and 33% over 15 years [ 42 ]. In Korea, the median rate of progression to ESRD ranged from 2.5 to 39.7% (median: 19%) from 60 to 100 months [ 64 , 65 , 66 , 68 , 70 , 71 , 73 ].
Regarding direct reports on mortality, in mainland China, 0.7% of adult IgAN patients progressed to death according to 1 study of 944 patients from 2003 to 2014 with a median follow-up of 4.2 years [ 23 ]. In South Korea, the median death rate was 5.3% (range: 4.4-5.9%) [ 65 , 66 , 68 ] for 1,364 IgAN patients with a median follow-up of 100 months. In addition, 2 publications reported a standard mortality ratio (expressed as the ratio between the observed and the expected number of deaths in the general population) of 1.43 (95% confidence interval:1.04–1.92) among 1,364 IgAN patients in relation to the general population [ 65 , 68 ]. In Japan, IgAN mortality was estimated to be 0.3 per 100 person-years among non-smokers [ 51 ], 1.3 per 100 person-years among smokers [ 51 ] and 1.2 per 100 person-years among patients who received kidney replacement therapy [ 53 ] based on 2 retrospective studies [ 51 , 53 ]. No mortality data was found among IgAN patients in Taiwan or Australia.
- Treatment patterns
Twenty publications [ 1 , 11 , 15 , 26 , 27 , 29 , 42 , 49 , 50 , 54 , 56 , 57 , 58 , 60 , 62 , 64 , 68 , 71 , 73 , 81 ] and 3 clinical guidelines reported treatment patterns. Nine from mainland China [ 11 , 15 , 26 , 27 , 28 , 29 , 32 , 41 , 42 ], 8 from Japan [ 49 , 50 , 54 , 56 , 57 , 58 , 60 , 62 ], and 4 from South Korea [ 64 , 68 , 71 , 73 ]. 80% publications were retrospective studies ( n = 16) [ 11 , 15 , 26 , 27 , 29 , 42 , 49 , 56 , 57 , 58 , 60 , 62 , 64 , 68 , 71 , 73 ]. Sample sizes ranged from 25 [ 64 ] to 2,283 [ 50 ]. The KDIGO [ 1 ] and 2 country-specific treatment guidelines, 1 from mainland China [ 80 ] and 1 from Japan [ 81 ], were identified. No treatment guidelines were identified in Taiwan, South Korea, or Australia.
The KDIGO guidelines (2021 version) provide treatment recommendations for adults and children with IgAN [ 1 ]. The guidelines state that the management of IgAN should be multifaceted, optimized with supportive care, and include ACEIs/ARBs as tolerated or allowed, control blood pressure, minimize cardiovascular risk, and adherence to lifestyle changes including dietary counseling, smoking cessation, weight control, and exercise, as appropriate. The guidelines provide specific treatment recommendations according to the variant forms of IgAN, the level of proteinuria, and high-risk rate for progression after maximal supportive care. The main treatment regimens include ACEIs and ARBs, immunosuppressants, cyclophosphamide, tonsillectomy, and lifestyle modification [ 1 ]. Similar to the KDIGO guidelines, the primary treatment recommendations in the Chinese 2017 guidelines for children with IgAN were glucocorticoids, immunosuppressants, and ACEIs/ARBs [ 80 ]. Japanese 2020 guidelines covered children and adults, with different treatment recommendations based on symptoms and subtype of IgAN (the subgroup classification for adults was based on estimated glomerular filtration rate and proteinuria; symptoms among children were classified as mild or severe) [ 81 ].
In mainland China, 6 studies investigated adult populations [ 15 , 26 , 28 , 29 , 32 , 42 ] (Table 1 ) and 3 investigated pediatric populations [ 11 , 27 , 41 ] (Table 2 ). For drug usage among adult patients, ACEIs/ARBs had the largest median percentage at 66.7% (range: 38-90%) [ 15 , 26 , 28 , 29 , 32 , 42 ], followed by steroids, with median of 36% (corticosteroids/prednisone/intravenous methylprednisolone injection, range: 10-100%) [ 15 , 26 , 28 , 29 , 32 , 42 ] and immunosuppressants (including in combination with steroids), with median of 25.9% (cyclophosphamide, tacrolimus and tripterygium wilfordii, range: 1.6-72%) [ 15 , 26 , 28 , 29 , 32 , 42 ]. Among pediatric patients, immunosuppressants (cyclophosphamide/mycophenolate /Tripterygium wilfordii /leflunomide) were the common drugs recommended, with a median of 64% (range: 1.7–72.2%) [ 11 , 27 , 41 ], followed by ACEIs/ARBs, with a median of 49.5% (range: 2.5-70%) [ 11 , 27 , 41 ] and steroids with a median of 45% (range: 25.3-69.3% as sum of oral prednisone and intravenous methylprednisolone) [ 11 , 27 , 41 ].
In South Korea, 3 publications on adult IgAN patients [ 64 , 68 , 71 ] (Table 1 ) and 1 publication among pediatric patients [ 73 ] (Table 2 ) were identified. Among adults, ACEIs/ARBs were the most common treatments (27.7-83.4%) [ 68 , 71 , 73 ], followed by ACEIs/ARBs and corticosteroid combinations (33.9%) [ 64 ] and corticosteroids alone (12.4-28.8%) [ 68 , 71 , 73 ]. Among pediatric patients, the frequency of immunosuppressant use was 50.2% [ 73 ].
In Japan, 7 publications reported IgAN treatment patterns among adults [ 50 , 54 , 56 , 57 , 58 , 60 , 62 ] (Table 1 ) and 2 publications [ 49 , 54 ] among pediatric patients (Table 2 ). Among adults, ACEIs/ARBs were the most common treatment (25-99.6%) [ 50 , 54 , 56 , 57 , 58 , 60 , 62 ], followed by antiplatelet agents (58.1-96.8%) [ 54 ] and corticosteroid-immunosuppressant combination therapy (1.5-74%) [ 62 ]. Notably, the rate of administering steroid-immunosuppressant combination was only 1.5% in a retrospective cohort study that sampled 1,012 IgAN patients with a mean age of 32.96 ± 12 years [ 56 ]. Among pediatric patients, ACEIs/ARBs were the most frequently administered treatments (0.9-95.7%) [ 49 , 54 ], followed by antiplatelet agents (range: 1.2-82.6%) [ 49 , 54 ] and immunosuppressants (range: 4.6-68.5%) [ 49 ]. The frequency of administering treatments varied greatly across different subgroups. For example, the frequency of administering ACEIs/ARBs ranged from 0.9% for the diffuse mesangial proliferation subgroup ( n = 108) to 50.9% for the focal mesangial proliferation subgroup ( n = 173) in 1 retrospective study in Japanese children with IgAN from 1990 to 2004 [ 49 ]. Tonsillectomy or tonsillectomy combined with steroid was mostly reported in Japanese studies, with frequencies ranging from 1 to 66.2% across publications (Table 1 ). This is in accordance with the KDIGO 2021 guidelines’ evidence that supports the routine use of tonsillectomy in Japanese high-risk patients with IgAN [ 1 ]. No publications reporting IgAN treatment patterns were identified for Taiwan or Australia.
Humanistic burden
Four publications in China reported QoL, measured by the 36-Item Short Form Health Survey (SF-36) [ 16 , 25 ], Daily Living Ability Rating Scale (DLARS) [ 37 ], and QoL scale (QOLs) combined with Self-Rating Anxiety Scale (SAS) and Self-Rating Depression Scale (SDS) [ 38 ]. SF-36 scores reflect physical and mental health based on 8 health concepts, including physical and social functioning, role limitations due to physical and emotional problems, mental health, vitality, bodily pain, and general health (GH) perception [ 82 ]. Two publications evaluated the effects of individualized nursing intervention (INI, one improved nursing intervention which costs more time than routine nursing intervention [RNI]) on the psychological mood and QoL among IgAN patients [ 16 , 25 ]. There were two subgroups, the patients in the control group received RNI and patients in the intervention group received INI [ 16 , 25 ]. The mean GH score was 32.16 [ 16 ] among total IgAN patients ( n = 98; mean age: 32.74 years; male percentage: 50%) in 2017 and 80.15 increasing from 69.93 at baseline [ 25 ] after intervention among total IgAN patients ( n = 84; mean age: 33.57 years; male percentage: 60.7%) in 2019. In both publications, the intervention groups had higher mean GH scores than that in the control groups (39.47 vs. 24.84 [ 16 ] and 85.73 vs. 74.56 [ 25 ], respectively). Two other prospective studies assessed the effect of INI for IgAN patients [ 37 , 38 ]. Results showed that both mean DLARS and QOLs scores were higher among the intervention group compared to the control group (88.5 vs. 75.7 and 39.5 vs. 24.8, respectively) [ 37 , 38 ]. SAS and SDS scores were also evaluated by Qi 2021 [ 38 ], the mean SAS score decreased more in the intervention group (49.2 ± 6.3 decreased from 62.1 ± 5.8) than that in the control group (57 ± 4.9 decreased from 62.4 ± 6.1) from baseline. Similarly, the mean SDS score decreased more in the intervention group (43.3 ± 5.2 decreased from 56.2 ± 6) than in the control group (52.6 ± 6.4 decreased from 57 ± 6.2) from baseline [ 38 ].
Economic burden
No publications reported indirect costs, but 3 retrospective studies reported hospitalization costs for IgAN patients in China (see Supplementary Figure S1 ) [ 12 , 20 , 47 ]. Hospitalization cost per patient per year is ¥14,900 ($2,252.12; exchange rate of Chinese Yuan [CNY] and US dollar in 2018 was 6.616 [ 83 ]) as reported by Zheng 2018 [ 20 ], and between ¥9,618 ($1,532.26; exchange rate of CNY and US dollar in 2015 is 6.227 [ 83 ]) and ¥10,019 ($1,608.96) as reported by Peng 2015 [ 12 ]. One large database study covering 54.1% of tertiary hospitals in 31 Chinese provinces from 2010 to 2015 reported a hospitalization cost of ¥8,000/$1,284.73 (¥6,000-¥12,000) [ 47 ]. Drug costs accounted for 28.39% of total hospitalization costs, followed by diagnostic testing costs [ 12 ]. Length of stay per patient per year in China ranged from 10 to 14.3 days across 3 publications [ 12 , 20 , 47 ].
To our knowledge, this is the first TLR to summarize the evidence on IgAN disease burden and treatment patterns in mainland China, Taiwan, South Korea, Japan, and Australia. The findings of this review revealed evidence gaps in IgAN epidemiology and humanistic and economic burden. No incidence data was identified in South Korea; no mortality data was identified in Taiwan and Australia; no country/region-specific treatment guidelines were found for Taiwan, South Korea, or Australia; no evidence on treatment patterns from the publications was identified for Taiwan or Australia; and no humanistic burden or economic data was identified except for mainland China.
The IgAN incidence rates among Japanese, Taiwanese, and Australian populations ranged from 0 to 10.7 per 100,000 people per year, higher than the incidence rate reported in a recent systematic literature review (SLR) by Kwon 2021 [ 84 ] (1.29 per 100,000 people per year). Kwon 2021 [ 84 ] is an SLR focusing on US epidemiology, health-related QoL, and the economic burden of IgAN (the included studies were published from January 2010 to June 2020), similar to our study’s objective. Incidence rates among children and teenagers (0-4.5 per 100,000 per year) were similar to the incidence rate in Venezuela (0.03 per 100,000 per year) [ 85 ] and in Italy (0.31 per 100,000 per year) [ 86 ]. The overall prevalence and diagnosis rates of IgAN were similar across selected countries/regions. The diagnosis rates in this review differed from those found in PGN patients and patients who received renal biopsy in Kwon 2021 [ 84 ]; diagnosis rates of IgAN from our results were higher in PGN patients compared with patients who received renal biopsies since renal biopsies were often performed on PGN patients before diagnosis. This applied to both adult and pediatric populations. Compared to the US population in Kwon 2021 [ 84 ], the diagnosis rate among PGN populations in this review was higher (26-72.1% vs. 9.4-19.7%). The diagnosis rate among populations with renal biopsies was also higher (6.3-61.9% vs. 6.3-14.3%). Notably, though not covered by this review, the pathological profile such as Oxford Classification/MEST classification could also shed light upon disease burden, which could be further explored by future studies.
IgAN treatments primarily consisted of ACEIs/ARBs, and high utilization of steroids was found despite mixed evidence on their benefits and safety. There is limited data on IgAN treatment patterns from Taiwan and Australia. Among the publications that reported treatment patterns, few specified drugs’ generic names. The primary treatment patterns reported among select countries/regions in this study are similar to those in US as reported by Kwon 2021 (frequently used therapies were immunosuppressives, corticosteroids, and ACEIs/ARBs) [ 84 ]. Immunosuppressives were used more by children than adults based on data from mainland China, South Korea, and Japan. According to the KDIGO guideline regarding glomerular diseases, the immunosuppressive therapies including azathioprine, cyclophosphamide, calcineurin inhibitors, and rituximab are not recommended for treating IgAN. Mycophenolate mofetil is recommended in Chinese patients and tonsillectomy is recommended to be used in Japanese IgAN patients [ 1 ]. Only Chinese studies reporting SF-36 scores and other metrics were identified. Therefore, more studies on QoL in IgAN patients and caregivers in other regions are warranted.
Evidence of economic burden was identified only from studies in mainland China; Li 2018 was one retrospective national inpatient database study, which included the major hospitals that covers multiple geographic locations [ 47 ], other two studies used the data from one hospital. The mean cost per patient per year reported by Li 2018 is $1,284.73, while one Canadian retrospective study for costs and healthcare resource utilization reported a mean outpatient medication cost per patient per year of Canadian dollar (CAD) $221 in 2016 [ 87 ]. To control medical costs, hospitals in China are undergoing clinical pathway optimization programs [ 12 ].
Publications reported heterogeneous sample populations where IgAN prevalence/diagnosis rates were evaluated. Among 22 publications that reported IgAN prevalence/diagnosis rates, 15 measured IgAN prevalence for patients who underwent renal biopsy and 9 measured IgAN prevalence for patients diagnosed with PGN. Heterogeneity in IgAN prevalence/diagnosis rates may be attributed to differences in study years, patient race/ethnicity, patient age, treatment method, risk factors, diagnosis, and follow-up duration. Other study design–related factors that could introduce bias include sample size and gender composition.
Finally, differences in IgAN prevalence across regions should be noted. County/region-specific healthcare infrastructure and policies influence the epidemiological evidence of IgAN. systematic urine screening programs among individuals with asymptomatic, persistent microscopic hematuria with/without mild proteinuria are commonly implemented in certain countries/regions. These programs facilitate detection of IgAN patients who would otherwise receive a delayed diagnosis or none at all. Countries/regions where screening programs are performed may therefore have higher reported IgAN prevalence. Screening programs play a crucial role in early diagnosis and early treatment [ 88 ].
To our knowledge, this is the first TLR for IgAN in mainland China, Taiwan, South Korea, Japan, and Australia. However, several limitations should be noted. Due to the targeted nature of this review, the search focused on the most relevant literature, and the publications included in this study were prioritized, which potentially have led to an incomplete picture of IgAN-related epidemiology, treatment patterns and disease burden. Across included publications, the sample sizes varied widely and were not always reported. Additionally, this TLR did not weigh the data from included publications; therefore, biases should be considered when comparing outcomes. Studies came from primarily single institutions, and national-level data was not always available for the selected countries/regions. Moreover, this review only covered select Asia-Pacific countries/regions; future reviews and studies in other countries and regions within Asia-Pacific are therefore warranted. Despite these limitations, the evidence gathered in this literature review may help provide a preliminary understanding of the disease burden of IgAN in the Asia-Pacific region.
This TLR summarized evidence on Immunoglobulin type A nephropathy (IgAN) prevalence, treatment patterns, and humanistic and economic burden. Our results suggest that despite the overall scarcity of information in general, evidence on disease burden and treatment patterns has been reported by some studies and several clinical guidelines. The prevalence of IgAN among the general population is not commonly available, while that among patients receiving renal biopsies and diagnosed with PGN is more frequently reported. Heterogeneity in prevalence rates across geographic regions might be explained by differences in initial diagnosis in some regions due to variation in local screening policy and disease management. There is a need to understand how the disease progression differs by those practices. Treatment patterns have been reported mainly in studies from some Asia areas, but geographic variations are noticeable. There is also a need to generate more evidence to shed light upon the possible explanation to the differences in the treatment patterns across geographic regions. In sum, more real-world studies at national levels across select countries/regions are warranted to fill the evidence gaps, particularly regarding incidence, humanistic burden, and economic burden.
The prevalence of IgA nephropathy among the general population in select APAC countries/regions is not commonly available, despite evidence from studies and clinical guidelines. In addition, it is observed across geographic regions that heterogeneity exists in prevalence rates, and large variations exist in treatment patterns. Future studies are needed to fill in these gaps to understand the contributing factors behind the differences through population-based, multi-center, and real-world studies.
Data availability
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Abbreviations
Angiotensin-converting enzyme inhibitor
Acute nephritic syndrome
Asia Pacific
Angiotensin receptor blockers
Canadian dollar
Chronic kidney disease
China National Knowledge Infrastructure
Chronic nephrotic syndrome
Chinese Yuan
Cyclophosphamide
Daily Living Ability Rating Scale
Diffuse mesangial proliferation
Excerpta Medica Database
End-stage kidney failure
Focal mesangial proliferation
General health
Individualized nursing intervention
The Kidney Disease: Improving Global Outcomes
Korean Information Service System
Mycophenolate mofetil
Not reported
Nephritis syndrome
Primary glomerulonephritis
Population, intervention, comparators, outcomes, and study design
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Quality assessment
Routine nursing intervention
Rapidly progressive glomerulonephritis
Self-Rating Anxiety Scale
Standard deviation
Self-Rating Depression Scale
36-Item Short Form Health Survey
Systematic literature review
Targeted literature review
Taiwan Society of Nephrology
Working Group for National Survey on Status of Diagnosis and Treatment of Childhood Renal Diseases
Kidney Disease. Improving global outcomes (KDIGO) Glomerular Diseases Work Group. KDIGO 2021 clinical practice guideline for the management of glomerular diseases. Kidney Int. 2021;100(4S):S1–276.
Google Scholar
National Institute of Diabetes and Digestive and Kidney Diseases. IgA nephropathy [Available from: https://www.niddk.nih.gov/health-information/kidney-disease/iga-nephropathy .
Schena FP, Nistor I. Epidemiology of IgA nephropathy: a global perspective. Semin Nephrol. 2018;38(5):435–42.
Article PubMed Google Scholar
Hassler JR. IgA nephropathy: a brief review. Semin Diagn Pathol. 2020;37(3):143–7.
Zhang H. KDIGO Zhinan Jiedu: IgA shenbing zhiliao[KDIGO guideline interpretation: treatment of IgA nephropathy. Chin J Practical Intern Medicine]. 2012;32(12):925–7.
CAS Google Scholar
Jarrick S, Lundberg S, Welander A, Carrero JJ, Hoijer J, Bottai M, et al. Mortality in IgA nephropathy: a nationwide population-based cohort study. J Am Soc Nephrol. 2019;30(5):866–76.
Article PubMed PubMed Central Google Scholar
Adejumo OA, Iyawe IO, Akinbodewa AA, Abolarin OS, Alli EO. Burden, psychological well-being and quality of life of caregivers of end stage renal disease patients. Ghana Med J. 2019;53(3):190–6.
Woo KT, Chan CM, Mooi CY, LC H, Tan HK, Foo M, et al. The changing pattern of primary glomerulonephritis in Singapore and other countries over the past 3 decades. Clin Nephrol. 2010;74(5):372–83.
Coppo R. Pediatric IgA Nephropathy in Europe. Kidney Dis (Basel). 2019;5(3):182–8.
Centre for Reviews and Dissemination. University of York. Systematic Reviews: CRD’s guidance for undertaking reviews in health care. 2009.
Working Group for National Survey on Status Diagnosis and Treatment of Childhood Renal Diseases. [Multicenter investigation of therapeutic status of children with IgA nephropathy in China]. Zhonghua Er Ke Za Zhi. 2013;51(7):486–90.
Peng Q, Xu G, Zhang C, Fang P. Wuhan Mou sanjia Yiyuan IgA shenbing Shen Chuanci huojian huanzhe linchuang lujing shishi xiaoguo pingjia[Evaluation of clinical pathway implementation effect in patients with IgA nephropathy renal puncture biopsy in a tertiary hospital in Wuhan]. Med Soc. 2015;28(10):18–20.
Zhu Z, Zou Q, Chen Y, Hu F, Bai J, Chao Q, et al. 224 Li Shen Huoti Zuzhi Jiancha De Linchuang lujing Yu Bingli fenxi[Analysis of the clinical pathway and pathologic features of 224 cases of renal biopsy]. Huaxi Med. 2016;31(5):845–9.
Tang L, Yao J, Kong X, Sun Q, Wang Z, Zhang Y, et al. Increasing prevalence of membranous nephropathy in patients with primary glomerular diseases: a cross-sectional study in China. Nephrol (Carlton). 2017;22(2):168–73.
Article Google Scholar
Zhou S, Fu J, Liu M, Yang S, Zhou Q, Yu X, et al. The prevalence and risk factors of abnormal circadian blood pressure in patients with IgA nephropathy. Clin Nephrol. 2017;88(12):344–53.
Article CAS PubMed Google Scholar
Lu H, Xiao L, Lu X, Liang J. Gexinghua huli moshi dui IgA shenbing huanzhe qingxu ji shenghuo zhiliang yingxiang de yanjiu [The effect of personalized nursing mode on the emotion and quality of life of patients with IgA nephropathy]. Contemp Med. 2017;23(5):30–3.
Wang N, Zhu T, Tao Y. Clinicopathological features of pediatric renal biopsies in the plateau regions of China. J Int Med Res. 2018;46(11):4539–46.
Nie S, He W, Huang T, Liu D, Wang G, Geng J, et al. The spectrum of biopsy-proven glomerular diseases among children in China: a national, cross-sectional survey. Clin J Am Soc Nephrol. 2018;13(7):1047–54.
Zhou Q, Yang X, Wang M, Wang H, Zhao J, Bi Y, et al. Changes in the diagnosis of glomerular diseases in east China: a 15-year renal biopsy study. Ren Fail. 2018;40(1):657–64.
Article CAS PubMed PubMed Central Google Scholar
Zheng X, Zhang J, Lu C. Xinjiang Weiwuerzu Zizhiqu renmin Yiyuan 2012 ~ 2017nian manxing shenzangbing huanzhe de jibing goucheng ji yiliao feiyong de hengduanmian diaocha [Disease composition and medical expenses of chronic kidney disease in people’s hospital of Xinjiang Uygur Autonomous Region from 2012 to 2017: a cross-sectional survey]. Chin J Evid-Based Med. 2018;18(9):903–6.
Nie P, Chen R, Luo M, Dong C, Chen L, Liu J et al. Clinical and pathological analysis of 4910 patients who received renal biopsies at a single center in Northeast China. Biomed Res Int 26 Mar 2019;2019:6869179.
Su S, Yu J, Wang Y, Wang Y, Li J, Xu Z. Clinicopathologic correlations of renal biopsy findings from northeast China: a 10-year retrospective study. Med (Baltim). 2019;98(23):e15880.
Cai Q, Shi S, Wang S, Ren Y, Hou W, Liu L, et al. Microangiopathic lesions in IgA nephropathy: a cohort study. Am J Kidney Dis. 2019;74(5):629–39.
Chen L, Luodelete M, Dong C, Li B, Zhang W, Nie P, et al. Pathological spectrum of glomerular disease in patients with renal insufficiency: a single-center study in northeastern China. Ren Fail. 2019;41(1):473–80.
Huang L. Tanjiu dui huanyou butong dengji IgAshenbing de huanzhe yuyi gexinghua huli ganyu duiyu xinli qingxu ji shenghuo zhiliang de yingxiang [Investigation of the effect of personalized nursing interventions on psychological, emotional and quality of life in patients with different grades of IgA nephropathy (IgAN)]. J Gen Pract Dentistry (Electronic Version). 2019;6(25):110–4.
Tian S, Yang X, Luo J, Guo H. Clinical and prognostic significance of C1q deposition in IgAN patients-a retrospective study. Int Immunopharmacol. 2020;88:106896.
Wu H, Xia Z, Gao C, Zhang P, Yang X, Wang R, et al. The correlation analysis between the Oxford classification of Chinese IgA nephropathy children and renal outcome– a retrospective cohort study. BMC Nephrol. 2020;21(1):247.
Liu Y, Wei W, Yu C, Xing L, Wang M, Liu R, et al. Epidemiology and risk factors for progression in Chinese patients with IgA nephropathy. Med Clin (Barc). 2021;157(6):267–73.
Wen D, Tang Y, Tan L, Tan J, Chen D, Zhang Y, et al. Sex disparities in IgA nephropathy: a retrospective study in Chinese patients. Int Urol Nephrol. 2021;53(2):315–23.
Nie P, Lou Y, Wang Y, Bai X, Zhang L, Jiang S, et al. Clinical and pathological analysis of renal biopsies of elderly patients in Northeast China: a single-center study. Ren Fail. 2021;43(1):851–9.
Feng S, Wang L, Liu X, Luo W, Xie M, Yang Q. 1002 li manxing shenzangbing huaner linchuang Ji Bingli fenxi[Clinical and pathological analysis of 1002 children with chronic kidney disease]. J Clin Pediatr. 2021;39(02):87–90.
Zhu L, Huang X, Zhang J, Li W, Chen E, Guo N. 102 Li Yizhishen IgA shenbing de huli tihui [Nursing experience of 102 cases of IgA nephropathy in transplanted kidneys]. Gen Pract Nurs. 2021;19(04):513–5.
Xu Z, Xiong Z. 3554 li shenzang bingli yu linchuang xiangguanxing fenxi [Analysis of renal pathology and clinical correlation in 3554 cases] [Shuoshi, https://doi.org/10.26921/d.cnki.ganyu.2021.001127] : M.S., Anhui Medical University; 2021.
Zhang P, Chen Z, Liu M. Huizhoushi dayawan diqu xuelingqian ertong niaoye shaicha fenxi [Analysis of urine screening in preschool children in Dayawan, Huizhou]. World’s Newest Med Inform Digest. 2021;21(84).
Yang D, Xie Y, He Z, Li Y, Li C. Qinhuangdaoshi 1459 Li xueling ertong shenzang jibing linchuang Yu Bingli fenxi [Clinical and pathological analysis of 1459 cases of renal disease in school-age children in Qinhuangdao]. Chin Healing Med. 2021;30(06):640–3.
Shang R, Zhu Y, Lin Z, Ma D, Ma Y, Ji M, et al. Yu Qiong liangdi yuanfaxing shenxiaoqiubing bingli leixing de bianqian duibi ji linchuang fenxi[Comparison and clinical analysis of pathological types of primary glomerular diseases in North Henan and Hainan]. J Clin Nephrol. 2021;21(2):111–8.
Lu X. Zhendui butong fenji IgA shenbing huanzhe kaizhan gexinghua huli moshi de linchuang xiaoguo guancha [Clinical effects of personalized care model for patients with different grades of IgA nephropathy]. Essent Health Readings. 2021;8:125.
Qi S. Zhendui butong fenji IgA shenbing kaizhan gexinghua huli moshi de linchuang xiaoguo guancha [Clinical effects of personalized care model for patients with different grades of IgA nephropathy]. Diet Health Care. 2021;8.
Pan Q, Ye Z, Zeng C, Ning W. Feishenbingxing tefaxing moxing shenbing Yu feishenbingxing IgA shenbing de linchuang tedian bijiao [Clinical comparative analysis of non-nephrotic idiopathic membranous nephropathy and non-nephrotic IgA nephropathy]. Anhui Med. 2021;25(2):268–70.
Xiao L, Wang J, Zhang M, He X, Gao J, Xi C. Yufangxing kangning zai budui guanbing shenbing zonghezheng zhiliao zhong de yingyong xiaoguo yanjiu [Study on the effect of preventive anticoagulation in the treatment of nephrotic syndrome in army officers and soldiers]. Northwest J De?F Med. 2021;42(01):30–6.
Zhao JL, Wang JJ, Huang GP, Feng CY. Primary IgA nephropathy with nephrotic-range proteinuria in Chinese children. Med (Baltim). 2021;100(21):e26050.
Article CAS Google Scholar
Le W, Liang S, Deng K, Hu Y, Zeng C, Liu D. 1126 li zhongguo hanzu chengren IgA shenbing huanzhe de changqi yuhou ji weixian yinsu fenxi [Long-term prognosis and risk factor analysis of 1126 Chinese Han adult patients with IgA nephropathy]. J Nephrol Dialysis Ren Transplantation. 2011;20(02):101–8.
Cen J, Hu H, Cheng Y, Liu Y, Wu S, Qin W, et al. Guangxi duominzu juju diqu dan zhongxin shenhuojian bingli ziliao ji minzu tedian fenxi [Pathological data of single-center kidney biopsy and analysis of ethnic characteristics in a multi-ethnic area of Guangxi]. J Chengdu Med Coll. 2021;16(04):482–5.
Yang J, Zhang L, Wang Y. Manxing Shenzangbing Shen Chuanci huojian bingli tezheng fenxi [Analysis of pathological features of renal puncture biopsy in chronic kidney disease]. Tibetan Med. 2021;42(05):49–51.
Duan Y, Lie C, Zhang L, AYiJiaKen K, Guo W, Li Y, et al. Xinjiang Weiwuer Zizhiqu 10 684 Li Shen huojian bingli ziliao Yu Liuxingbingxue tedian fenxi [Analysis of pathological data and epidemiological characteristics of 10 684 kidney biopsies in Xinjiang Uygur Autonomous Region]. Chin J Nephrol. 2021;37(06):490–8.
Gu C, Li Q, Liang W, Bi H, Xie M, Wu D. Guilin he jining liangsuo yiyuan 1370 Li Shen huojian jibing fenbu tezheng [Characteristics of disease distribution in 1370 kidney biopsies from two hospitals in Guilin and Jining]. J Cent South Univ (Medical Edition). 2021;46(09):974–82.
Li J, Cui Z, Long J, Huang W, Wang J, Zhang H, et al. Primary glomerular nephropathy among hospitalized patients in a national database in China. Nephrology, Dialysis, transplantation: Official Publication of the European Dialysis and Transplant Association -. Eur Ren Association. 2018;33(12):2173–81.
Chen S, Tang Z, Xiang H, Li X, Chen H, Zhang H, et al. Etiology and outcome of crescentic glomerulonephritis from a single center in China: a 10-year review. Am J Kidney Dis. 2016;67(3):376–83.
Yata N, Nakanishi K, Shima Y, Togawa H, Obana M, Sako M, et al. Improved renal survival in Japanese children with IgA nephropathy. Pediatr Nephrol. 2008;23(6):905–12.
Goto M, Wakai K, Kawamura T, Ando M, Endoh M, Tomino Y. A scoring system to predict renal outcome in IgA nephropathy: a nationwide 10-year prospective cohort study. Nephrology, Dialysis, transplantation: Official Publication of the European Dialysis and Transplant Association -. Eur Ren Association. 2009;24(10):3068–74.
Yamamoto R, Nagasawa Y, Shoji T, Iwatani H, Hamano T, Kawada N, et al. Cigarette smoking and progression of IgA nephropathy. Am J Kidney Dis. 2010;56(2):313–24.
Yokoyama H, Sugiyama H, Sato H, Taguchi T, Nagata M, Matsuo S, et al. Renal disease in the elderly and the very elderly Japanese: analysis of the Japan Renal Biopsy Registry (J-RBR). Clin Exp Nephrol. 2012;16(6):903–20.
Komatsu H, Kikuchi M, Nakagawa H, Fukuda A, Iwakiri T, Toida T, et al. Long-term survival of patients with IgA nephropathy after dialysis therapy. Kidney Blood Press Res. 2013;37(6):649–56.
Matsuzaki K, Suzuki Y, Nakata J, Sakamoto N, Horikoshi S, Kawamura T, et al. Nationwide survey on current treatments for IgA nephropathy in Japan. Clin Exp Nephrol. 2013;17(6):827–33.
Sugiyama H, Yokoyama H, Sato H, Saito T, Kohda Y, Nishi S, et al. Japan Renal Biopsy Registry and Japan kidney Disease Registry: Committee Report for 2009 and 2010. Clin Exp Nephrol. 2013;17(2):155–73.
Moriyama T, Tanaka K, Iwasaki C, Oshima Y, Ochi A, Kataoka H, et al. Prognosis in IgA nephropathy: 30-year analysis of 1,012 patients at a single center in Japan. PLoS ONE. 2014;9(3):e91756.
Sato R, Joh K, Komatsuda A, Ohtani H, Okuyama S, Togashi M, et al. Validation of the Japanese histologic classification 2013 of immunoglobulin A nephropathy for prediction of long-term prognosis in a Japanese single-center cohort. Clin Exp Nephrol. 2015;19(3):411–8.
Oshima Y, Moriyama T, Itabashi M, Takei T, Nitta K. Characteristics of IgA nephropathy in advanced-age patients. Int Urol Nephrol. 2015;47(1):137–45.
Hattori M, Iwano M, Sako M, Honda M, Okada H, Akioka Y, et al. Transition of adolescent and young adult patients with childhood-onset chronic kidney disease from pediatric to adult renal services: a nationwide survey in Japan. Clin Exp Nephrol. 2016;20(6):918–25.
Kaihan AB, Yasuda Y, Katsuno T, Kato S, Imaizumi T, Ozeki T, et al. The Japanese histologic classification and T-score in the Oxford classification system could predict renal outcome in Japanese IgA nephropathy patients. Clin Exp Nephrol. 2017;21(6):986–94.
Kajiwara N, Hayashi K, Fujiwara M, Nakayama H, Ozaki Y. Identification of children with chronic kidney disease through school urinary screening using urinary protein/creatinine ratio measurement: an observational study. Clin Exp Nephrol. 2020;24(5):450–7.
Miyabe Y, Karasawa K, Akiyama K, Ogura S, Takabe T, Sugiura N, et al. Grading system utilising the total score of Oxford classification for predicting renal prognosis in IgA nephropathy. Sci Rep. 2021;11(1):3584.
Utsunomiya Y, Koda T, Kado T, Okada S, Hayashi A, Kanzaki S, et al. Incidence of pediatric IgA nephropathy. Pediatr Nephrol. 2003;18(6):511–5.
Lee S, Choi S, Se-bin S, Kyunghwan J, Taewon L. Relative risk factors of prognosis in IgA nephropathy patients with depressed renal functions. Korean J Nephrol. 2010;29(2):198–207.
Lee H, Kim DK, Oh KH, Joo KW, Kim YS, Chae DW, et al. Mortality of IgA nephropathy patients: a single center experience over 30 years. PLoS ONE. 2012;7(12):e51225.
Lee Ha-Jung. Long-term patient and renal survivals and their predictable factor analyses in IgA nephropathy patients [Thesis]: College of Medicine, Seoul National University; 2012.
Cho BS, Hahn WH, Cheong HI, Lim I, Ko CW, Kim SY, et al. A nationwide study of mass urine screening tests on Korean school children and implications for chronic kidney disease management. Clin Exp Nephrol. 2013;17(2):205–10.
Lee H, Kim DK, Oh KH, Joo KW, Kim YS, Chae DW, et al. Mortality and renal outcome of primary glomerulonephritis in Korea: observation in 1,943 biopsied cases. Am J Nephrol. 2013;37(1):74–83.
Bae HJ, Moon KR, Kim YJ, Choi DE, Na KR, Lee KW, et al. Clinical and histopathological analysis of the kidney biopsies of 2,450 patients seen over 30 years at Chungnam National University Hospital. Korean J Med. 2015;84(3):379–88.
Jeong EG, Hyoun S, Lee SM, An WS, Kim SE, Son YK. Clinical outcomes of nephrotic syndrome in immunoglobulin a nephropathy. Saudi J Kidney Dis Transplantation. 2017;28(6):1314–20.
Kee YK, Yoon CY, Kim SJ, Moon SJ, Kim CH, Park JT, et al. Determination of the optimal target level of proteinuria in the management of patients with glomerular diseases by using different definitions of proteinuria. Med (Baltim). 2017;96(44):e8154.
Shin HS, Cho DH, Kang SK, Kim HJ, Kim SY, Yang JW, et al. Patterns of renal disease in South Korea: a 20-year review of a single-center renal biopsy database. Ren Fail. 2017;39(1):540–6.
Suh JS, Jang KM, Hyun H, Cho MH, Lee JH, Park YS, et al. Remission of proteinuria may protect against progression to chronic kidney disease in pediatric-onset IgA nephropathy. J Clin Med. 2020;9(7):2058.
Chiu HF, Chen HC, Lu KC, Shu KH. Taiwan Society of Nephrology. Distribution of glomerular diseases in Taiwan: preliminary report of National Renal Biopsy Registry-publication on behalf of Taiwan Society of Nephrology. BMC Nephrol. 2018;19(1):6.
Yu MC, Lee F, Huang WH, Hsueh S. Percutaneous ultrasound-guided renal biopsy in children: the need for renal biopsy in pediatric patients with persistent asymptomatic microscopic hematuria. Biomedical J. 2014;37(6):391–7.
National Health Research Institute & Taiwan Society of Nephrology. 2019 Annual Report on Kidney Disease in Taiwan.
Jegatheesan D, Nath K, Reyaldeen R, Sivasuthan G, John GT, Francis L, et al. Epidemiology of biopsy-proven glomerulonephritis in Queensland adults. Nephrol (Carlton). 2016;21(1):28–34.
Briganti EM, Dowling J, Finlay M, Hill PA, Jones CL, Kincaid-Smith PS, et al. The incidence of biopsy-proven glomerulonephritis in Australia. Nephrology, Dialysis, transplantation: Official Publication of the European Dialysis and Transplant Association. - Eur Ren Association. 2001;16(7):1364–7.
Lee AYS, Lin M-W. Do IgA nephropathy presentations display any seasonality? J Nephropathology. 2021;10(3):e33–e.
Subspecialty Group of Renal Diseases of the Society of Pediatrics Chinese Medical Association. [Evidence-based guidelines for diagnosis and treatment of primary IgA nephropathy (2016)]. Zhonghua Er Ke Za Zhi. 2017;55(9):643–6.
[Health, Labor and Welfare Scientific Research Grant Policy Research Project for Intractable Diseases. (Intractable Disease Policy Research Project)].[IgA Nephropathy 2020 Clinical Practice Guidelines].[Tokyo Igakusha]. 2021.
LoMartire R, Ang BO, Gerdle B, Vixner L. Psychometric properties of short Form-36 Health Survey, EuroQol 5-dimensions, and hospital anxiety and Depression Scale in patients with chronic pain. Pain. 2020;161(1):83–95.
OECD. Conversion rates - Exchange rates - OECD Data [Available from: http://data.oecd.org/conversion/exchange-rates.htm .
Kwon CS, Daniele P, Forsythe A, Ngai C. A systematic literature review of the epidemiology, health-related quality of life impact, and economic burden of immunoglobulin A nephropathy. J Health Econ Outcomes Res. 2021;8(2):36–45.
Orta-Sibu N, Lopez M, Moriyon JC, Chavez JB. Renal diseases in children in Venezuela, South America. Pediatr Nephrol. 2002;17(7):566–9.
Coppo R, Gianoglio B, Porcellini MG, Maringhini S. Frequency of renal diseases and clinical indications for renal biopsy in children (report of the Italian National Registry of Renal biopsies in Children). Group of Renal Immunopathology of the Italian Society of Pediatric Nephrology and Group of Renal Immunopathology of the Italian Society of Nephrology. Nephrology, Dialysis, transplantation: Official Publication of the European Dialysis and Transplant Association -. Eur Ren Association. 1998;13(2):293–7.
Barbour S, Lo C, Espino-Hernandez G, Sajjadi S, Feehally J, Klarenbach S, et al. The population-level costs of immunosuppression medications for the treatment of glomerulonephritis are increasing over time due to changing patterns of practice. Nephrology, Dialysis, transplantation: Official Publication of the European Dialysis and Transplant Association -. Eur Ren Association. 2018;33(4):626–34.
Shen P, He L, Li Y, Wang Y, Chan M. Natural history and prognostic factors of IgA nephropathy presented with isolated microscopic hematuria in Chinese patients. Nephron Clin Pract. 2007;106(4):c157–61.
Download references
Acknowledgements
This work was presented as an abstract at the ISN World Congress of Nephrology 2022 meeting.
This work was supported by Otsuka Pharmaceutical Development & Commercialization, Inc., Princeton, NJ.
Author information
Authors and affiliations.
OPEN Health, Boston, MA, USA
OPEN Health, Shanghai, China
Fen Du & Zhaoli Tang
Otsuka Pharmaceutical Development & Commercialization, Inc., NJ, Princeton, USA
Sandipan Bhattacharjee & Kristin Pareja
You can also search for this author in PubMed Google Scholar
Contributions
Research conception and/or design: Kristin Pareja, Sandipan Bhattacharjee, Omer Zaidi, Fen Du, and Zhaoli Tang; Literature searching strategy: Omer Zaidi, Fen Du, and Zhaoli Tang; literature screening and data extraction and analysis: Fen Du and Zhaoli Tang; All authors were involved in the drafting and /or substantial revision of manuscript; All authors accept accountability for their contributions and agree as a condition of authorship to ensure resolution of questions about the work. All authors approved the submitted version.
Corresponding author
Correspondence to Kristin Pareja .
Ethics declarations
Competing interests.
Kristin Pareja and Sandipan Bhattacharjee are employees of Otsuka Pharmaceutical Development & Commercialization, Inc., Princeton, NJ, United States. Omer Zaidi, Fen Du, and Zhaoli Tang are employees of OPEN Health and were paid consultants by Otsuka.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Zaidi, O., Du, F., Tang, Z. et al. Review on epidemiology, disease burden, and treatment patterns of IgA nephropathy in select APAC countries. BMC Nephrol 25 , 136 (2024). https://doi.org/10.1186/s12882-024-03555-5
Download citation
Received : 21 April 2023
Accepted : 21 March 2024
Published : 16 April 2024
DOI : https://doi.org/10.1186/s12882-024-03555-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- IgA nephropathy
- Epidemiology
- Disease burden
BMC Nephrology
ISSN: 1471-2369
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Modifiable risk factors that may be addressed in routine care to prevent progression to and extension of multimorbidity in people with COPD: a systematic literature review
Affiliations.
- 1 Health Economics Unit, London, UK [email protected].
- 2 Department of Primary Care and Public Health, Imperial College London, London, UK.
- 3 Health Economics Unit, London, UK.
- PMID: 38653506
- DOI: 10.1136/bmjresp-2023-002272
Chronic obstructive pulmonary disease (COPD) is a multisystem disease, and many patients have multiple conditions. We explored multimorbidity patterns that might inform intervention planning to reduce health-care costs while preserving quality of life for patients. Literature searches up to February 2022 revealed 4419 clinical observational and comparative studies of risk factors for multimorbidity in people with COPD, pulmonary emphysema, or chronic bronchitis at baseline. Of these, 29 met the inclusion criteria for this review. Eight studies were cluster and network analyses, five were regression analyses, and 17 (in 16 papers) were other studies of specific conditions, physical activity and treatment. People with COPD more frequently had multimorbidity and had up to ten times the number of disorders of those without COPD. Disease combinations prominently featured cardiovascular and metabolic diseases, asthma, musculoskeletal and psychiatric disorders. An important risk factor for multimorbidity was low socioeconomic status. One study showed that many patients were receiving multiple drugs and had increased risk of adverse events, and that 10% of medications prescribed were inappropriate. Many patients with COPD have mainly preventable or modifiable multimorbidity. A proactive multidisciplinary approach to prevention and management could reduce the burden of care.
Keywords: COPD epidemiology.
© Author(s) (or their employer(s)) 2024. Re-use permitted under CC BY-NC. No commercial re-use. See rights and permissions. Published by BMJ.
Publication types
- Systematic Review
- Research Support, Non-U.S. Gov't
- Disease Progression*
- Multimorbidity*
- Pulmonary Disease, Chronic Obstructive* / epidemiology
- Pulmonary Disease, Chronic Obstructive* / therapy
- Quality of Life
- Risk Factors
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley-Blackwell Online Open

Quality of life versus length of life considerations in cancer patients: A systematic literature review
Anne shrestha.
1 Department of Oncology and Metabolism, University of Sheffield, Sheffield
Charlene Martin
Maria burton.
2 Faculty of Health and Wellbeing, Sheffield Hallam University, Sheffield
Stephen Walters
3 School of Health and Related Research, University of Sheffield, Sheffield
Karen Collins
Associated data.
Patients with cancer face difficult decisions regarding treatment and the possibility of trading quality of life (QoL) for length of life (LoL). Little information is available regarding patients' preferences and attitudes toward their cancer treatment and the personal costs they are prepared to exchange to extend their life. The aim of this review is to determine the complex trade‐offs and underpinning factors that make patients with cancer choose quality over quantity of life.
A systematic review of the literature was conducted using MeSH terms: cancer, longevity or LoL, QoL, decision making, trade‐off, and health utility. Articles retrieved were published between 1942 and October 2018.
Out of 4393 articles, 30 were included in this review. Older age, which may be linked to declining physical status, was associated with a preference for QoL over LoL. Younger patients were more likely to undergo aggressive treatment to increase survival years. Preference for QoL and LoL was not influenced by gender, education, religion, having children, marital status, or type of cancer. Patients with better health valued LoL and inversely those with poorer physical status preferred QoL.
Baseline QoL and future expectations of life seem to be key determinants of preference for QoL versus LoL in cancer patients. In‐depth studies are required to understand these trade‐offs and the compromises patients are willing to make regarding QoL or LoL, especially in older patients with naturally limited life expectancy.
1. BACKGROUND
A diagnosis of cancer can be devastating, and deciding on the appropriate treatment can be complicated and daunting. Patients are asked to consider factors that include mortality from the disease and the potential for acute and chronic morbidity from the treatment. Appropriate decision making requires satisfactory patient understanding of these treatment choices, which includes the potential benefits and harms. 1 The primary focus of cancer treatment has always been to increase overall and disease free survival; however, quality of life (QoL) has been increasingly recognized as an important end point. 2
Although there is an instinctive understanding of the term “quality of life,” there are multiple definitions, which gives testimony to the fact that it is a complex concept with many diverse facets and components. The standard dimensions used in QoL questionnaires measure the presence or absence of specific symptoms or overall general health. They do not measure patients' beliefs or attitudes toward treatment and intervention outcomes. 3 Decision making in a cancer setting can be a difficult process due to its multifaceted nature. The patients' outlook and beliefs are paramount, but this is heavily influenced by their own experiences and those of friends and family. 4 In addition, current QoL and physical status can affect subsequent decisions.
Most cancer trials primarily focus on the standard oncology end points relating to survival, but it is possible to derive composite measures, which assess the impact of QoL on the final outcome of different therapies. These are called quality adjusted survival metrics or health utility metrics, and a wide range of them have been developed over the past 30 years. Utility measures allow patients a chance to value a different perspective on treatment and outcomes. Two methods of utility measurement that may be used to calculate quality adjusted life years (QALY) or quality adjusted survival are standard gamble and time trade‐off (TTO). 5 In standard gamble, patients are asked to choose between staying in a state of ill health for a specified time period or choosing a treatment that may either cause their death or restore perfect health. In the case of TTO, the individual expresses a preference between two choices, usually between LoL or a better health status. 4 These methods have been increasingly adapted in cost‐utility analyses of pharmaceuticals and various health‐care interventions. In reality, scenarios are often more complex with disease and treatment effects impacting variably on QoL over a prolonged time course. There may be a significant drop in QoL after an intervention but an overall better long‐term QoL and increased life expectancy. QoL measurement should not just focus on a single time point when assessing an intervention.
In cancer treatment, patients are often required to make trade‐offs between QoL and length of life (LoL). 6 Tumor‐specific therapy can potentially prolong life; however, this may reduce QoL significantly. Some patients are willing to endure toxicities associated with treatment in order to increase their LoL, while others value QoL more and are reluctant to spend their remaining years in a compromised state. 7 This involves weighing the risks and benefits of treatment and managing the patients' concerns and expectations. There may be personal reasons associated with their health, the effect on their family and friends, and the consequences of the treatment itself. A trade‐off for potential gain in life expectancy may involve short‐term debility from treatment (postsurgical pain, chemotherapy‐induced nausea and alopecia, and etc) or permanent side effects (stoma, disfigurement, physical dependency, and etc). Moreover, the compromise is not always related to health but instead may be about financial burdens and increased dependency on friends and family.
To understand cancer treatment choices concerning trade‐off, various questionnaires and methodologies have been devised to understand patient preferences and priorities toward cancer treatment. Quality‐adjusted time without symptoms or toxicity (Q‐Twist) allows the combination of both quality and quantity of survival time. 8 , 9 The principle hypothesis of this method is that patients without disease symptoms or treatment toxicity have a better health‐related quality of life (HrQoL) than those who have disease‐specific symptoms and toxicity. Q‐TWiST was initially used to assess adjuvant therapy for breast cancer and has now been adapted in other cancers. 10 , 11 , 12 The Quality/Quantity Questionnaire designed by Stiggelbout and colleagues was created to assess patients' preferences toward either QoL or LoL when deciding about cancer treatments. 7 Other methods include discrete choice experiments and various bespoke questionnaires tailored to a specific study. 13 , 14 , 15
The aim of this review was to determine the factors influencing patient preferences for either QoL or LoL and how these impacts on cancer treatment choices.
2.1. Search strategy and selection criteria
A systematic literature search was performed according to PRISMA guidelines (see supporting information ) using five databases between 1942 and October 2018. The databases included MEDLINE, SCOPUS, Cumulative Index to Nursing and Allied Health Literature (CINAHL), PsychINFO, and Web of Science. A pilot search on MEDLINE, was performed to identify the relevant keywords contained in the title, abstract, and subject descriptors. Five broad categories of concepts were searched: “quality of life,” “cancer,” “length of life,” “health utilities,” and “decision making.” The search terms included (cancer* OR neoplasm* OR oncolog* or tumo?r*) AND (quality of life OR QoL) AND (Longevity OR Length of Life) AND (decision making OR patient participation OR patient preference OR patient participation OR treatment choice) AND (health state utilit* OR standard gambl* OR trade‐off). See Appendix S1 for the search strategy as used in Ovid Medline. The literature search was carried out by two authors (A.S. and C.M.).
A study was only included if there was reference made to preference for QoL or LoL with or without determinants that may influence treatment choice. These factors could be either demographic influences, health status, or personal factors. Study designs could be qualitative, quantitative, or of mixed methods. Studies included were limited to adults with cancer and published in English. A PRISMA format was used to filter through articles. Editorials, reviews, and expert opinions were excluded. Hypothetical studies with healthy volunteers were also excluded as it was felt that these studies were unrealistic in their assessment of whether LoL or QoL would be favored in a cancer setting. Health status utilities were included in the search to include any trade‐off papers suitable for review. Time trade‐off studies may indicate treatment preferences, however not necessarily in the context of a preference for QoL versus LoL. Only those focusing on QoL versus LoL preferences were included.
Study selection was by a two‐step process by two independent reviewers (A.S. and C.M.), at titles and abstract stage with arbitration for articles with uncertainty. In the second stage, full‐text articles were independently reviewed (Figure 1 ). Reference lists of all selected articles were reviewed to identify any additional relevant articles, identifying five further articles. When an article referred to additional publications for more details concerning study methods and design, those publications were also acquired.

PRISMA flow chart of study selection
2.2. Data abstraction
Data extraction was performed by two independent reviewers (A.S. and C.M.). The information collected included study design, aim of study, location of study, sample size and response rate, age of the sample, type of cancer, any research tools used in the form of questionnaires and the findings of the study relating to QoL versus LoL preferences.
2.3. Quality assessment
The Mixed Methods Appraisal Tool (MMAT) was used to quality assess the articles that were included in the study. The 2011 MMAT tool encompasses five types of mixed methods study components or primary studies: qualitative, quantitative randomized controlled trials, quantitative nonrandomized, quantitative descriptive, and mixed methods, each with its own set of methodological quality criteria. For each item the response categories were “yes,” “no,” or “can't tell” followed by comments. 16 Higher quality is denoted by the number of stars (*) in the tables. Quality assessment was independently scored by two reviewers (A.S. and C.M.). No study was excluded based on quality assessment, as all were of acceptable quality.
The literature search revealed 4388 articles. A total of 843 abstracts were excluded because of duplication, and 3494 articles were declined as they were either reviews, expert opinions/editorials, or not suitable for the topic under review. A total of 56 articles were reviewed fully, and only 30 deemed suitable for inclusion. The 26 rejected papers were not suitable as they were either reviews or not relevant (Figure 1 ). Included studies are summarized in Tables 1 (quantitative), 2 (mixed methods), and 3 (purely qualitative) (Tables 2 and and3 3 ).
Details of quantitative studies included in this review, associated with the trade‐offs related to length of life (LoL) and quality of life (QoL) (NR—not reported)
Details of mixed method studies included in this review, associated with the trade‐offs related to length of life (LoL) and quality of life (QoL) (NR—not reported)
Details of purely qualitative studies included in this review, associated with the trade‐offs related to LoL and QoL (NR – not reported)
The majority of studies identified in this review were quantitative. Generic questionnaires (EORTC‐QLQ‐C30 and FACT‐G) and disease specific questionnaires (EORTC‐QLQ‐H&N) were used to assess QoL. The studies were mainly conducted to understand the decision‐making process in the advanced cancer setting. The studies had wide focus that included understanding the role of the doctor and the attitude the patient has toward their treatment, among other themes. Understanding QoL and LoL trade‐offs as part of the decision‐making process, usually formed a limited part of many of these studies.
3.1. QoL versus LoL
Meropol and colleagues (2008) suggested that QoL and LoL are both equally important; however, the majority of patients with advanced cancer in this study prioritized QoL over LoL. 41 This was also reflected by the study of Jenkins and associates. 36 Silvestri and associates noted although there were some patients who would endure treatment and associated toxicities just to live a single day longer, there were also patients who would decline all treatments. These latter patients would rather maintain their QoL and having to withstand the adverse effects of treatment would not be a worthwhile trade‐off. 20 The authors postulated that patients may opt for enhanced QoL only if the chance of survival was less than 50% relative to baseline survival (without treatment). 42
Many patients in the study by Brom and colleagues felt that they ought to have some sort of intervention for their cancer and found it difficult to accept the concept of LoL and QoL. Although some patients opted for treatment initially, they expressed the view that if it was affecting their QoL, they would cease treatment. 39 Marta and colleagues noted that the majority of patients in their study wanted to undergo a treatment that would prolong life but not compromise their QoL. 43 In a qualitative study by Gerber and colleagues, patients stated that they were keen to maintain their activities and not be a burden on family, and therefore not undergo chemotherapy if those factors were compromised, indicating the importance of QoL. 38
3.2. Survival and baseline QoL
Survival seemed to be a key feature in the decision‐making process and patients were found to opt for treatment if they felt that their prognosis was likely to improve. 15 , 19 , 28 , 40 Their current health status also affected their choice. Perez and associates found that those who wanted to trade time, scored lower in many of the domains of the baseline HRQoL questionnaires. 3 Patients in better health were found to rate LoL more highly, whereas those who were in poorer health strived to maintain their QoL. 7 , 22 , 32 , 44 Kiebert and associates noted that issues patients felt were important were baseline QoL and the probability of survival. 17
3.3. Demographic factors
Kiebert and associates assessed factors affecting decision making for cancer treatment and noted that important factors were age, marital status, children, inability to work due to side effects, disease related life expectancy, and baseline QoL. No significant associations were found between the various determinants; however, patients did rate having children and marital status as somewhat important in decision making. 17
Other studies have shown different results, with gender, children, education, religion, and cancer type not influencing treatment choices. 3 , 6 , 23 , 35 Those with strong family links preferred survival. Unemployed patients prioritized QoL. 6 Wong and colleagues concluded that those who were able to pay for their treatment chose to have treatment to prolong their life. 45 These latter findings are only relevant in self paying health care systems.
Many of the studies carried out have not been age specific; therefore, it has been difficult to make inferences about the influence of age on LoL/QoL preferences. The studies in this review show a mixed picture. Older patients have a preference for QoL, which is not surprising considering natural limitations to life expectancy and the often reduced QoL associated with advanced age. 34 Younger cancer patients were more likely to tolerate aggressive treatments to increase survival years. 30 , 35 , 46 A study by Pisu and colleagues involving 170 ovarian cancer patients, showed that maintaining QoL and living as long as possible were both important. In women less than 65 years old, 96.9% felt longevity was important, and 95.9% felt that preserving QoL was important, compared with 87.5% and 90.3%, respectively, in the greater than 65‐year‐old age group. 33 Stiggelbout and associates noted that when age was adjusted for in their statistical calculations, those in relationships and with children preferred longevity. 7 Derks and colleagues found that older patients were less likely to receive standard treatment, an effect that was more evident in those above the age of 80 years old. Reasons behind this included lack of social support and being widowed. Patients who did not receive standard treatment also prioritized QoL more strongly. 27
3.4. Symptom trade‐off
When looking at symptom tradeoffs against longevity, patients were prepared to tolerate certain treatment side effects to live longer. Patients were willing to prioritize survival over intact sexual function in prostate cancer for instance. 18 , 44 When patients with advanced cancer reached the end of their lives and had to endure pain and discomfort, 47% of patients chose to have palliative surgery to maintain or enhance their current health status and independence. 37
3.5. Cancer‐specific trade‐off
Patients suffering from cancers with a good prognosis such as breast and testicular cancers, compared with recurrent colorectal or lung cancer had similar thoughts regarding QoL and LoL. 7 Despite the type of cancer, patients felt that QoL and LoL were equally important when considering treatment. 41 In the study by Pisu and colleagues involving ovarian cancer, more than 90% stated that QoL and LoL were equally important. 33 Another study by Jenkins and associates, involving participants with ovarian cancer showed that 57% felt LoL and QoL were equally important, 9% prioritized LoL, and 33% favored QoL. 36 However, Donovan and colleagues demonstrated that women who had recurrent ovarian cancer, would opt for LoL, and choose to receive aggressive treatment, QoL was a secondary issue. 23 Patients with a shorter history of cancer preferred LoL; however, those with poorer prognosis and closer to their predicted time of death valued QoL more. 35 In contrast, Meropol and colleagues found that there was no association between time since diagnosis and QoL/LoL preference. 41
4. DISCUSSION
This study presents the first comprehensive review of studies looking at trade‐offs between QoL and LoL in a cancer setting. The aim of this review was to highlight whether patients prioritize QoL or Lol and the determining factors that influence the decision‐making process for cancer treatment. In fact, the findings indicate that many of the studies do not directly test determinants. The QQ questionnaire has been designed specifically to quantify the patient's choice of QoL or LoL and also to what extent patients would be inclined toward either. The questionnaire does not capture the psychological reasoning behind the preference however. It is also perhaps more suited for patients with advanced cancers where the cancer will inevitably cause death regardless of whether it was treated or not. 7 For some patients, where curative treatments may be available, albeit with a high cost (for example, mutilating operations leading to disfigurement, ie, head and neck resections, mastectomy, and amputations) or where death due to old age or other, noncancer comorbidities is imminent; this trade‐off may also be relevant and the QQ tool is not designed to explore these scenarios.
This review highlights the importance of carrying out baseline QoL assessments prior to treatment and evaluating the impact of life expectancy. The importance of performing age specific studies is also noted as priorities between younger and older patients are different. The preferences for QoL or LoL by younger patients, may be influenced by their desire to spend time with their partner or children. Older patients are more likely to suffer from multiple comorbidities and be frailer, and discussions may need to include whether a treatment will be tolerated less well because of these limitations, or result in an increased risk of harm. Considerations should include patient intolerance to certain chemotherapy agents or surgery, as well as an understanding that they may never reach their preoperative baseline physical fitness again after treatment. This “step down” in function tends to be more prominent in the older age group, 47 , 48 an effect that is widely recognized across many medical interventions in older patients. They may feel that time spent receiving treatment may not be worth the extension of life for a relatively short period. Older individuals have a good overall understanding that they have lived their lives and are more accepting of the inevitability of death and of their physical limitations. Studies suggest that a good QoL in older people is often based around the following: independence, a strong social circle, and an ability to retain their “inner selves.” 49 These values may be compromised by having treatment. Other studies have shown that the most consistent factor influencing treatment decision making in older patients is a recommendation from doctors. 50 In breast cancer, undertreatment is well‐documented in older patients. 51 This has led to avoidable disease‐specific deaths. 52 Exploring the patients' views regarding treatment at an early stage would help reduce the impact of age‐related clinician bias, which is well recognized. 53
5. CONCLUSIONS
Decision making in cancer treatment is difficult as there are multiple components to consider aside from the purely medical aspects. Likewise, the compromises the patient is willing to make can vary greatly depending on many factors including patient age, personal family dynamics, social structures, and, patients' likely survival and baseline QoL. This may subsequently impact on whether the patient is more inclined towards longevity or QoL. Although there are studies trying to understand the factors influencing the final decision, there is limited information on preferences between QoL and LoL and the trade‐off the patient is willing to make. Clinicians have influence over the final decision, and therefore it is vital for the patient to have a full understanding of their treatment and the impact it may have on their life.
5.1. Study limitations
This study is the first to use a rigorous and systematic approach to review studies based on patient preferences regarding QoL or LoL in a cancer treatment setting. Despite a comprehensive database search strategy, it is possible that some relevant articles may have been missed and despite the various methodologies, all papers included were of an acceptable design and standard for inclusion. However, the main findings of the review are likely to be robust to missing studies. On the basis of our interpretation and weighting of the evidence, we are confident in the conclusions that have been drawn from findings across several studies rather than be based on isolated studies. None of the studies in this review has looked at the impact of preexisting, noncancer‐related limitations to life expectancy as part of this trade‐off, such as is seen in the oldest age groups and the impact of acceptance of impending age‐related mortality. With the aging of Western populations, this is an important gap in the literature.
The studies included in this review are exploratory cohort studies carried out in a retrospective manner, whereby patients have already made their decision regarding treatment. There may be a source of bias influencing their responses, as many issues may not have been considered prior to treatment or the decision‐making process.
Many of these studies have mainly focused on advanced cancers of all types. For patients who are facing mortality imminently, the decision to prioritize QoL and LoL is pertinent. In the case of slow growing cancers such as prostate and breast cancers, where conservative management is widely accepted, the choice between QoL and LoL can be more complicated. Patients often die from other causes rather than the cancer itself. 54 As the majority of the articles identified in this search did not involve early stage cancer, it is difficult to know what patients envisage from their treatment and what trade‐offs they were willing to make as well as how these factors may change with the course of the natural disease process. This is where patients' age and comorbidities may play a larger role in whether the patient opts for QoL or LoL.
5.2. Clinical implications
This review has several important clinical and research implications. With treatment and care now becoming more patient centered, it has become more pertinent to understand the impact of the cancer diagnosis on the patient and the motivations behind their treatment choices. The impact of treatment of certain cancers may be extreme and may involve a great deal of compromise and acceptance of change in circumstances. Factoring the likely impact of treatments on QoL relative to that at baseline should be discussed with every patient. This would ensure that patients have a full understanding of what their treatment entails and that they are aware of the consequences of treatment and nontreatment. Further in‐depth studies are required to understand the emotional and physical considerations and personal priorities the patients may have during the decision‐making process. This may go a long way in elucidating what aspects of their life they are willing to trade to maintain their QoL or increase LoL. Older age specific issues and cancer specific decision‐making processes also need exploring.
CONFLICTS OF INTEREST
The authors have declared no conflicts of interest. The views expressed are those of the authors and not those of the NHS, the NIHR, or the Department of Health.
Supporting information
Data S1. PRISMA checklist.
Appendix S1. Search Strategy used in Ovid (Medline).
ACKNOWLEDGEMENTS
This paper presents independent research funded by the National Institute for Health Research under its Programme Grants for Applied Research Programme (Grant Reference Number RP‐PG‐1209‐10071).
Shrestha A, Martin C, Burton M, Walters S, Collins K, Wyld L. Quality of life versus length of life considerations in cancer patients: A systematic literature review . Psycho‐Oncology . 2019; 28 :1367–1380. 10.1002/pon.5054 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Understanding the influence of different proxy perspectives in explaining the difference between self-rated and proxy-rated quality of life in people living with dementia: a systematic literature review and meta-analysis
- Open access
- Published: 24 April 2024
Cite this article
You have full access to this open access article

- Lidia Engel ORCID: orcid.org/0000-0002-7959-3149 1 ,
- Valeriia Sokolova 1 ,
- Ekaterina Bogatyreva 2 &
- Anna Leuenberger 2
Proxy assessment can be elicited via the proxy-patient perspective (i.e., asking proxies to assess the patient’s quality of life (QoL) as they think the patient would respond) or proxy-proxy perspective (i.e., asking proxies to provide their own perspective on the patient’s QoL). This review aimed to identify the role of the proxy perspective in explaining the differences between self-rated and proxy-rated QoL in people living with dementia.
A systematic literate review was conducted by sourcing articles from a previously published review, supplemented by an update of the review in four bibliographic databases. Peer-reviewed studies that reported both self-reported and proxy-reported mean QoL estimates using the same standardized QoL instrument, published in English, and focused on the QoL of people with dementia were included. A meta-analysis was conducted to synthesize the mean differences between self- and proxy-report across different proxy perspectives.
The review included 96 articles from which 635 observations were extracted. Most observations extracted used the proxy-proxy perspective (79%) compared with the proxy-patient perspective (10%); with 11% of the studies not stating the perspective. The QOL-AD was the most commonly used measure, followed by the EQ-5D and DEMQOL. The standardized mean difference (SMD) between the self- and proxy-report was lower for the proxy-patient perspective (SMD: 0.250; 95% CI 0.116; 0.384) compared to the proxy-proxy perspective (SMD: 0.532; 95% CI 0.456; 0.609).
Different proxy perspectives affect the ratings of QoL, whereby adopting a proxy-proxy QoL perspective has a higher inter-rater gap in comparison with the proxy-patient perspective.
Avoid common mistakes on your manuscript.
Quality of life (QoL) has become an important outcome for research and practice but obtaining reliable and valid estimates remains a challenge in people living with dementia [ 1 ]. According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) criteria [ 2 ], dementia, termed as Major Neurocognitive Disorder (MND), involves a significant decline in at least one cognitive domain (executive function, complex attention, language, learning, memory, perceptual-motor, or social cognition), where the decline represents a change from a patient's prior level of cognitive ability, is persistent and progressive over time, is not associated exclusively with an episode of delirium, and reduces a person’s ability to perform everyday activities. Since dementia is one of the most pressing challenges for healthcare systems nowadays [ 3 ], it is critical to study its impact on QoL. The World Health Organization defines the concept of QoL as “individuals' perceptions of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards, and concerns” [ 4 ]. It is a broad ranging concept incorporating in a complex way the persons' physical health, psychological state, level of independence, social relationships, personal beliefs, and their relationships to salient features of the environment.
Although there is evidence that people with mild to moderate dementia can reliably rate their own QoL [ 5 ], as the disease progresses, there is typically a decline in memory, attention, judgment, insight, and communication that may compromise self-reporting of QoL [ 6 ]. Additionally, behavioral symptoms, such as agitation, and affective symptoms, such as depression, may present another challenge in obtaining self-reported QoL ratings due to emotional shifts and unwillingness to complete the assessment [ 7 ]. Although QoL is subjective and should ideally be assessed from an individual’s own perspective [ 8 ], the decline in cognitive function emphasizes the need for proxy-reporting by family members, health professionals, or care staff who are asked to report on behalf of the person with dementia. However, proxy-reports are not substitutable for self-reports from people with dementia, as they offer supplementary insights, reflecting the perceptions and viewpoints of people surrounding the person with dementia [ 9 ].
Previous research has consistently highlighted a disagreement between self-rated and proxy-rated QoL in people living with dementia, with proxies generally providing lower ratings (indicating poorer QoL) compared with person’s own ratings [ 8 , 10 , 11 , 12 ]. Impairment in cognition associated with greater dementia severity has been found to be associated with larger difference between self-rating and proxy-rating obtained from family caregivers, as it becomes increasingly difficult for severely cognitively impaired individuals to respond to questions that require contemplation, introspection, and sustained attention [ 13 , 14 ]. Moreover, non-cognitive factors, such as awareness of disease and depressive symptoms play an important role when comparing QoL ratings between individuals with dementia and their proxies [ 15 ]. Qualitative evidence has also shown that people with dementia tend to compare themselves with their peers, whereas carers make comparisons with how the person used to be in the past [ 9 ]. The disagreement between self-reported QoL and carer proxy-rated QoL could be modulated by some personal, cognitive or relational factors, for example, the type of relationship or the frequency of contact maintained, person’s cognitive status, carer’s own feeling about dementia, carer’s mood, and perceived burden of caregiving [ 14 , 16 ]. Disagreement may also arise from the person with dementia’s problems to communicate symptoms, and proxies’ inability to recognize certain symptoms, like pain [ 17 ], or be impacted by the amount of time spent with the person with dementia [ 18 ]. This may also prevent proxies to rate accurately certain domains of QoL, with previous evidence showing higher level of agreement for observable domains, such as mobility, compared with less observable domains like emotional wellbeing [ 8 ]. Finally, agreement also depends on the type of proxy (i.e., informal/family carers or professional staff) and the nature of their relationship, for instance, proxy QoL scores provided by formal carers tend to be higher (reflecting better QoL) compared to the scores supplied by family members [ 19 , 20 ]. Staff members might associate residents’ QoL with the quality of care delivered or the stage of their cognitive impairment, whereas relatives often focus on comparison with the person’s QoL when they were younger, lived in their own home and did not have dementia [ 20 ].
What has been not been fully examined to date is the role of different proxy perspectives employed in QoL questionnaires in explaining disagreement between self-rated and proxy-rated scores in people with dementia. Pickard et al. (2005) have proposed a conceptual framework for proxy assessments that distinguish between the proxy-patient perspective (i.e., asking proxies to assess the patient’s QoL as they think the patient would respond) or proxy-proxy perspective (i.e., asking proxies to provide their own perspective on the patient’s QoL) [ 21 ]. In this context, the intra-proxy gap describes the differences between proxy-patient and proxy-proxy perspective, whereas the inter-rater gap is the difference between self-report and proxy-report [ 21 ].
Existing generic and dementia-specific QoL instruments specify the perspective explicitly in their instructions or imply the perspective indirectly in their wording. For example, the instructions of the Dementia Quality of Life Measure (DEMQOL) asks proxies to give the answer they think their relative would give (i.e., proxy-patient perspective) [ 22 ], whereas the family version of the Quality of Life in Alzheimer’s Disease (QOL-AD) instructs the proxies to rate their relative’s current situation as they (the proxy) see it (i.e., proxy-proxy perspective) [ 7 ]. Some instruments, like the EQ-5D measures, have two proxy versions for each respective perspective [ 23 , 24 ]. The Adult Social Care Outcome Toolkit (ASCOT) proxy version, on the other hand, asks proxies to complete the questions from both perspectives, from their own opinion and how they think the person would answer [ 25 ].
QoL scores generated using different perspectives are expected to differ, with qualitative evidence showing that carers rate the person with dementia’s QoL lower (worse) when instructed to comment from their own perspective than from the perspective of the person with dementia [ 26 ]. However, to our knowledge, no previous review has fully synthesized existing evidence in this area. Therefore, we aimed to undertake a systematic literature review to examine the role of different proxy-assessment perspectives in explaining differences between self-rated and proxy-rated QoL in people living with dementia. The review was conducted under the hypothesis that the difference in QoL estimates will be larger when adopting the proxy-proxy perspective compared with proxy-patient perspective.
The review was registered with the International Prospective Register of Systematic Reviews (CRD42022333542) and followed the Preferred Reporting Items System for Systematic Reviews and Meta-Analysis (PRISMA) guidelines (see Appendix 1 ) [ 27 ].
Search strategy
This review used two approaches to obtain literature. First, primary articles from an existing review by Roydhouse et al. were retrieved [ 28 ]. The review included studies published from inception to February 2018 that compared self- and proxy-reports. Studies that focused explicitly on Alzheimer’s Disease or dementia were retrieved for the current review. Two reviewers conducted a full-text review to assess whether the eligibility criteria listed below for the respective study were met. An update of the Roydhouse et al. review was undertaken to capture more recent studies. The search strategy by Roydhouse et al. was amended and covered studies published after January 1, 2018, and was limited to studies within the context of dementia. The original search was undertaken over a three-week period (17/11/2021–9/12/2021) and then updated on July 3, 2023. Peer-reviewed literature was sourced from MEDLINE, CINAHL, and PsycINFO databases via EBSCOHost as well as EMBASE. Four main search term categories were used: (1) proxy terms (i.e., care*-report*), (2) QoL/ outcome terms (i.e., ‘quality of life’), (3) disease terms (i.e., ‘dementia’), and (4) pediatric terms (i.e., ‘pediatric*’) (for exclusion). Keywords were limited to appear in titles and abstracts only, and MeSH terms were included for all databases. A list of search strategy can be found in Appendix 2 . The first three search term categories were searched with AND, and the NOT function was used to exclude pediatric terms. A limiter was applied in all database searches to only include studies with human participants and articles published in English.
Selection criteria
Studies from all geographical locations were included in the review if they (1) were published in English in a peer-reviewed journal (conference abstracts, dissertations, a gray literature were excluded); (2) were primary studies (reviews were excluded); (3) clearly defined the disease of participants, which were limited to Alzheimer’s disease or dementia; (4) reported separate QoL scores for people with dementia (studies that included mixed populations had to report a separate QoL score for people with dementia to be considered); (5) were using a standardized and existing QoL instrument for assessment; and (6) provided a mean self-reported and proxy-reported QoL score for the same dyads sample (studies that reported means for non-matched samples were excluded) using the same QoL instrument.
Four reviewers (LE, VS, KB, AL) were grouped into two groups who independently screened the 179 full texts from the Roydhouse et. al (2022) study that included Alzheimer’s disease or dementia patients. If a discrepancy within the inclusion selection occurred, articles were discussed among all the reviewers until a consensus was reached. Studies identified from the database search were imported into EndNote [ 29 ]. Duplicates were removed through EndNote and then uploaded to Rayyan [ 30 ]. Each abstract was reviewed by two independent reviewers (any two from four reviewers). Disagreements regarding study inclusions were discussed between all reviewers until a consensus was reached. Full-text screening of each eligible article was completed by two independent reviewers (any two from four reviewers). Again, a discussion between all reviewers was used in case of disagreements.
Data extraction
A data extraction template was created in Microsoft Excel. The following information were extracted if available: country, study design, study sample, study setting, dementia type, disease severity, Mini-Mental Health State Exam (MMSE) score details, proxy type, perspective, living arrangements, QoL assessment measure/instrument, self-reported scores (mean, SD), proxy-reported scores (mean, SD), and agreement statistics. If a study reported the mean (SD) for the total score as well as for specific QoL domains of the measure, we extracted both. If studies reported multiple scores across different time points or subgroups, we extracted all scores. For interventional studies, scores from both the intervention group and the control group were recorded. In determining the proxy perspective, we relied on authors’ description in the article. If the perspective was not explicitly stated, we adopted the perspective of the instrument developers; where more perspectives were possible (e.g., in the case of the EQ-5D measures) and the perspective was not explicitly stated, it was categorized as ‘undefined.’ For agreement, we extracted the Intraclass Correlation Coefficient (ICC), a reliability index that reflects both degree of correlation and agreement between measurements of continuous variables. While there are different forms of ICC based on the model (1-way random effects, 2-wy random effects, or 2-way fixed effects), the type (single rater/measurement or the mean k raters/measurements), and definition of relationship [ 31 ], this level of information was not extracted due to insufficient information provided in the original studies. Values for ICC range between 0 and 1, with values interpreted as poor (less than 0.5), moderate (0.5–0.75), good (0.75–0.9), and excellent (greater than 0.9) reliability between raters [ 31 ].
Data synthesis and analysis
Characteristics of studies were summarized descriptively. Self-reported and proxy-reported means and SD were extracted from the full texts and the mean difference was calculated (or extracted if available) for each pair. Studies that reported median values instead of mean values were converted using the approach outlined by Wan et al. (2014) [ 32 ]. Missing SDs (5 studies, 20 observations) were obtained from standard errors or confidence intervals reported following the Cochrane guidelines [ 33 ]. Missing SDs (6 studies, 29 observations) in studies that only presented the mean value without any additional summary statistics were imputed using the prognostic method [ 34 ]. Thereby, we predicted the missing SDs by calculating the average SDs of observed studies with full information by the respective measure and source (self-report versus proxy-report).
A meta-analysis was performed in Stata (17.1 Stata Corp LLC, College Station, TX) to synthesize mean differences between self- and proxy-reported scores across different proxy perspectives. First, the pooled raw mean differences were calculated for each QoL measure separately, given differences in scales between measures. Secondly, we calculated the pooled standardized mean difference (SMD) for all studies stratified by proxy type (family carer, formal carers, mixed), dementia severity (mild, moderate, severe), and living arrangement (residential/institutional care, mixed). SMD accounts for the use of different measurement scales, where effect sizes were estimated using Cohen’s d. Random-effects models were used to allow for unexplained between-study variability based on the restricted maximum-likelihood (REML) estimator. The percentage of variability attributed to heterogeneity between the studies was assessed using the I 2 statistic; an I 2 of 0%-40% represents possibly unimportant heterogeneity, 30–60% moderate heterogeneity, 50–90% substantial heterogeneity, and 75%-100% considerable heterogeneity [ 35 ]. Chi-squared statistics (χ 2 ) provided evidence of heterogeneity, where a p -value of 0.1 was used as significance level. For studies that reported agreement statistics, based on ICC, we also ran a forest plot stratified by the study perspective. We also calculated Q statistic (Cochran’s test of homogeneity), which assesses whether observed differences in results are compatible with chance alone.
Risk of bias and quality assessment
The quality of studies was assessed using the using a checklist for assessing the quality of quantitative studies developed by Kmet et al. (2004) [ 36 ]. The checklist consists of 14 items and items are scored as ‘2’ (yes, item sufficiently addressed), ‘1’ (item partially addressed), ‘0’ (no, not addressed), or ‘not applicable.’ A summary score was calculated for each study by summing the total score obtained across relevant items and dividing by the total possible score. Scores were adjusted by excluding items that were not applicable from the total score. Quality assessment was undertaken by one reviewer, with 25% of the papers assessed independently by a second reviewer.
The PRISMA diagram in Fig. 1 shows that after the abstract and full-text screening, 38 studies from the database search and 58 studies from the Roydhouse et al. (2022) review were included in this review—a total of 96 studies. A list of all studies included and their characteristics can be found in Appendix 3.
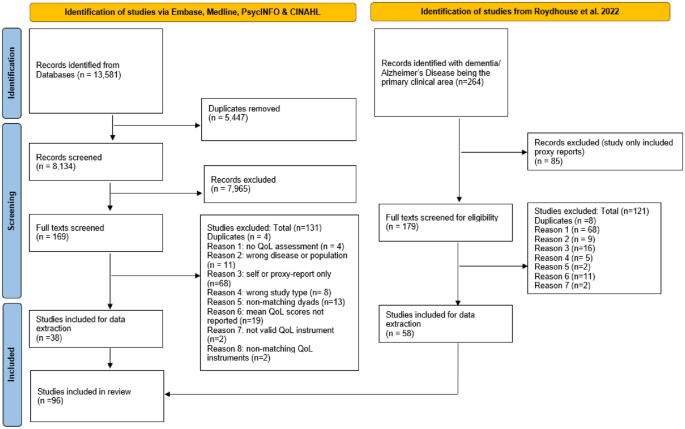
PRISMA 2020 flow diagram
General study characteristics
The 96 articles included in the review were published between 1999 and 2023 from across the globe; most studies (36%) were conducted in Europe. People with dementia in these studies were living in the community (67%), residential/institutional care (15%), as well as mixed dwelling settings (18%). Most proxy-reports were provided by family carers (85%) and only 8 studies (8%) included formal carers. The mean MMSE score for dementia and Alzheimer’s participants was 18.77 (SD = 4.34; N = 85 studies), which corresponds to moderate cognitive impairment [ 37 ]. Further characteristics of studies included are provided in Table 1 . The quality of studies included (see Appendix 4) was generally very good, scoring on average 91% (SD: 9.1) with scores ranging from 50 to 100%.
Quality of life measure and proxy perspective used
A total of 635 observations were recorded from the 96 studies. The majority of studies and observations extracted assumed the proxy-proxy perspective (77 studies, 501 observations), followed by the proxy-patient perspective (18 studies, 62 observations), with 18 studies (72 observations) not clearly defining the perspective. Table 2 provides a detailed overview of number of studies and observations across the respective QoL measures and proxy perspectives. Two studies (14 observations) adopted both perspectives within the same study design: one using the QOL-AD measure [ 5 ] and the second study exploring the EQ-5D-3L and EQ VAS [ 38 ]. Overall, the QOL-AD was the most often used QoL measure, followed by the EQ-5D and DEMQOL. Mean scores for specific QoL domains were accessible for the DEMQOL and QOL-AD. However, only the QOL-AD provided domain-specific mean scores from both proxy perspectives.
Mean scores and mean differences by proxy perspective and QoL measure
The raw mean scores for self-reported and proxy-reported QoL scores are provided in the Supplementary file 2. The pooled raw mean difference by proxy perspective and measure is shown in Table 3 . Regardless of the perspective adopted and the QoL instrument used, self-reported scores were higher (indicating better QoL) compared with proxy-reported scores, except for the DEMQOL, where proxies reported better QoL than people with dementia themselves. Most instruments were explored from one perspective, except for the EQ-5D-3L, EQ VAS, and QOL-AD, for which mean differences were available for both perspectives. For these three measures, mean differences were smaller when adopting the proxy-patient perspective compared with proxy-proxy perspective, although mean scores for the QOL-AD were slightly lower from the proxy-proxy perspective. I 2 statistics indicate considerable heterogeneity (I 2 > 75%) between studies. Mean differences by specific QoL domains are provided in Appendix 5, but only for the QOL-AD measure that was explored from both perspectives. Generally, mean differences appeared to be smaller for the proxy-proxy perspective than the proxy-patient perspective across all domains, except for ‘physical health’ and ‘doing chores around the house.’ However, results need to be interpreted carefully as proxy-patient perspective scores were derived from only one study.
Standardized mean differences by proxy perspective, stratified by proxy type, dementia severity, and living arrangement
Table 4 provides the SMD by proxy perspective, which adjusts for the different QoL measurement scales. Findings suggest that adopting the proxy-patient perspective results in lower SMDs (SMD: 0.250; 95% CI 0.116; 0.384) compared with the proxy-proxy perspective (SMD: 0.532; 95% CI 0.456; 0.609). The largest SMD was recorded for studies that did not define the study perspective (SMD: 0.594; 95% CI 0.469; 0.718). A comparison by different proxy types (formal carers, family carers, and mixed proxies) revealed some mixed results. When adopting the proxy-proxy perspective, the largest SMD was found for family carers (SMD: 0.556; 95% CI 0.465; 0.646) compared with formal carers (SMD: 0.446; 95% CI 0.305; 0.586) or mixed proxies (SMD: 0.335; 95% CI 0.211; 0.459). However, the opposite relationship was found when the proxy-patient perspective was used, where the smallest SMD was found for family carers compared with formal carers and mixed proxies. The SMD increased with greater level of dementia severity, suggesting a greater disagreement. However, compared with the proxy-proxy perspective, where self-reported scores were greater (i.e., better QoL) than proxy-reported scores across all dementia severity levels, the opposite was found when adopting the proxy-patient perspective, where proxies reported better QoL than people with dementia themselves, except for the severe subgroup. No clear trend was observed for different living settings, although the SMD appeared to be smaller for people with dementia living in residential care compared with those living in the community.
Direct proxy perspectives comparison studies
Two studies assessed both proxy perspectives within the same study design. Bosboom et al. (2012) found that compared with self-reported scores (mean: 34.7; SD: 5.3) using the QOL-AD, proxy scores using the proxy-patient perspective were closer to the self-reported scores (mean: 32.1; SD: 6.1) compared with the proxy-proxy perspective (mean: 29.5; SD: 5.4) [ 5 ]. Similar findings were reported by Leontjevas et al. (2016) using the EQ-5D-3L, including the EQ VAS, showing that the inter-proxy gap between self-report (EQ-5D-3L: 0.609; EQ VAS: 65.37) and proxy-report was smaller when adopting the proxy-patient perspective (EQ-5D-3L: 0.555; EQ VAS: 65.15) compared with the proxy-proxy perspective (EQ-5D-3L: 0.492; EQ VAS: 64.42) [ 38 ].
Inter-rater agreement (ICC) statistics
Six studies reported agreement statistics based on ICC, from which we extracted 17 observations that were included in the meta-analysis. Figure 2 shows the study-specific and overall estimates of ICC by the respective study perspective. The heterogeneity between studies was high ( I 2 = 88.20%), with a Q test score of 135.49 ( p < 0.001). While the overall ICC for the 17 observations was 0.3 (95% CI 0.22; 0.38), indicating low agreement, the level of agreement was slightly better when adopting a proxy-patient perspective (ICC: 0.36, 95% CI 0.23; 0.49) than a proxy-proxy perspective (ICC: 0.26, 95% CI 0.17; 0.35).
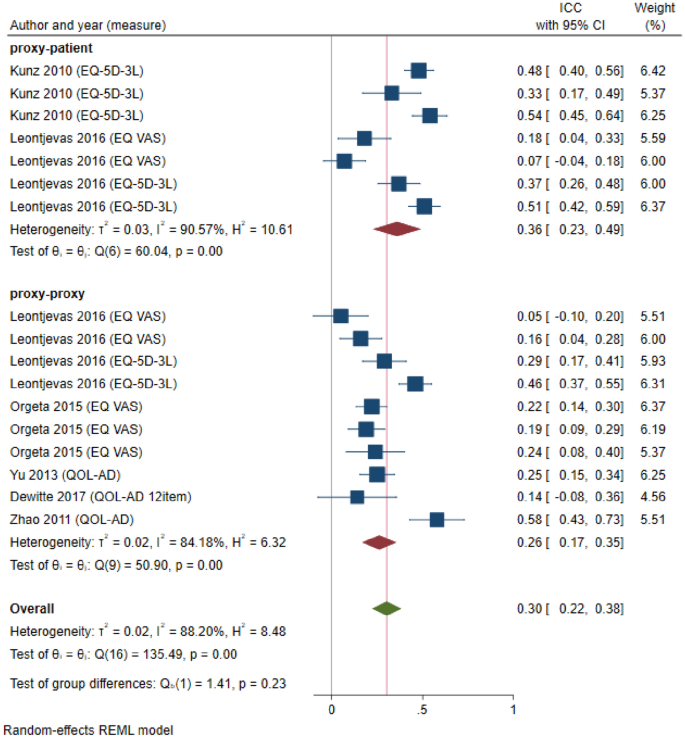
Forest plot depicting study-specific and overall ICC estimates by study perspective
While previous studies highlighted a disagreement between self-rated and proxy-rated QoL in people living with dementia, this review, for the first time, assessed the role of different proxy perspectives in explaining the inter-rater gap. Our findings align with the baseline hypothesis and indicate that QoL scores reported from the proxy-patient perspective are closer to self-reported QoL scores than the proxy-proxy perspective, suggesting that the proxy perspective does impact the inter-rater gap and should not be ignored. This finding was observed across different analyses conducted in this review (i.e., pooled raw mean difference, SMD, ICC analysis), which also confirms the results of two previous primary studies that adopted both proxy perspectives within the same study design [ 5 , 38 ]. Our findings emphasize the need for transparency in reporting the proxy perspective used in future studies, as it can impact results and interpretation. This was also noted by the recent ISPOR Proxy Task Force that developed a checklist of considerations when using proxy-reporting [ 39 ]. While consistency in proxy-reports is desirable, it is crucial to acknowledge that each proxy perspective holds significance in future research, depending on study objectives. It is evident that both proxy perspectives offer distinct insights—one encapsulating the perspectives of people with dementia, and the other reflecting the viewpoints of proxies. Therefore, in situations where self-report is unattainable due to advanced disease severity and the person’s perspective on their own QoL assessment is sought, it is recommended to use the proxy-patient perspective. Conversely, if the objective of future research is to encompass the viewpoints of proxies, opting for the proxy-proxy perspective is advisable. However, it is important to note that proxies may deviate from instructed perspectives, requiring future qualitative research to examine the adherence to proxy perspectives. Additionally, others have argued that proxy-reports should not substitute self-reports, and only serve as supplementary sources alongside patient self-reports whenever possible [ 9 ].
This review considered various QoL instruments, but most instruments adopted one specific proxy perspective, limiting detailed analyses. QoL instruments differ in their scope (generic versus disease-specific) as well as coverage of QoL domains. The QOL-AD, an Alzheimer's Disease-specific measure, was commonly used. Surprisingly, for this measure, the mean differences between self-reported and proxy-reported scores were smaller using the proxy-proxy perspective, contrary to the patterns observed with all other instruments. This may be due to the lack of studies reporting QOL-AD proxy scores from the proxy-patient perspective, as the study by Bosboom et al. (2012) found the opposite [ 5 ]. Previous research has also suggested that the inter-rater gap is dependent on the QoL domains and that the risk of bias is greater for more ‘subjective’ (less observable) domains such as emotions, feelings, and moods in comparison with observable, objective areas such as physical domains [ 8 , 40 ]. However, this review lacks sufficient observations for definitive results on QoL dimensions and their impact on self-proxy differences, emphasizing the need for future research in this area.
With regard to proxy type, there is an observable trend suggesting a wider inter-rater gap when family proxies are employed using the proxy-proxy perspective, in contrast to formal proxies. This variance might be attributed to the use of distinct anchoring points; family proxies tend to assess the individual's QoL in relation to their past self before having dementia, while formal caregivers may draw comparisons with other individuals with dementia under their care [ 41 ]. However, the opposite was found when the proxy-patient perspective was used, where family proxies scores seemed to align more closely with self-reported scores, resulting in lower SMD scores. This suggests that family proxies might possess a better ability to empathize with the perspective of the person with dementia compared to formal proxies. Nonetheless, it is important to interpret these findings cautiously, given the relatively small number of observations for formal caregiver reports. Additionally, other factors such as emotional connection, caregiver burden, and caregiver QoL may also impact proxy-reports by family proxies [ 14 , 16 ] that have not been explored in this review.
Our review found that the SMD between proxy and self-report increased with greater level of dementia severity, contrasting a previous study, which showed that cognitive impairment was not the primary factor that accounted for the differences in the QoL assessments between family proxies and the person with dementia [ 15 ]. However, it is noteworthy that different interpretations and classifications were used across studies to define mild, moderate, and severe dementia, which needs to be considered. Most studies used MMSE to define dementia severity levels. Given the MMSE’s role as a standard measure of cognitive function, the study findings are considered generalizable and clinically relevant for people with dementia across different dementia severity levels. When examining the role of the proxy perspective by level of severity, we found that compared with the proxy-proxy perspective, where self-reported scores were greater than proxy-reported scores across all dementia severity levels, the proxy-patient perspective yielded the opposite results, and proxies reported better QoL than people with dementia themselves, except for the severe subgroup. It is possible that in the early stages of dementia, the person with dementia has a greater awareness of increasing deficits, coupled with denial and lack of acceptance, leading to a more critical view of their own QoL than how proxies think they would rate their QoL. However, future studies are warranted, given the small number of observations adopting the proxy-patient perspective in our review.
The heterogeneity observed in the studies included was high, supporting the use of random-effects meta-analysis. This is not surprising given the diverse nature of studies included (i.e., RCTs, cross-sectional studies), differences in the population (i.e., people living in residential care versus community-dwelling people), mixed levels of dementia severity, and differences between instruments. While similar heterogeneity was observed in another review on a similar topic [ 42 ], our presentation of findings stratified by proxy type, dementia severity, and living arrangement attempted to account for such differences across studies.
Limitations and recommendations for future studies
Our review has some limitations. Firstly, proxy perspectives were categorized based on the authors' descriptions, but many papers did not explicitly state the perspective, which led to the use of assumptions based on instrument developers. Some studies may have modified the perspective's wording without reporting it. Due to lack of resources, we did not contact the authors of the original studies directly to seek clarification around the proxy perspective adopted. Regarding studies using the EQ-5D, which has two proxy perspectives, some studies did not specify which proxy version was used, suggesting the potential use of self-reported versions for proxies. In such cases, the proxy perspective was categorized as undefined. Despite accounting for factors like QoL measure, proxy type, setting, and dementia severity, we could not assess the impact of proxy characteristics (e.g., carer burden) or dementia type due to limited information provided in the studies. We also faced limitations in exploring the proxy perspective by QoL domains due to limited information. Further, not all studies outlined the data collection process in full detail. For example, it is possible that the proxy also assisted the person with dementia with their self-report, which could have resulted in biased estimates and the need for future studies applying blinding. Although we assessed the risk of bias of included studies, the checklist was not directly reflecting the purpose of our study that looked into inter-rater agreement. No checklist for this purpose currently exists. Finally, quality appraisal by a second reviewer was only conducted for the first 25% of the studies due to resource constraints and a low rate of disagreement between the two assessors. However, an agreement index between reviewers regarding the concordance in selecting full texts for inclusion and conducting risk of bias assessments was not calculated.
This review demonstrates that the choice of proxy perspective impacts the inter-rater gap. QoL scores from the proxy-patient perspective align more closely with self-reported scores than the proxy-proxy perspective. These findings contribute to the broader literature investigating factors influencing differences in QoL scores between proxies and individuals with dementia. While self-reported QoL is the gold standard, proxy-reports should be viewed as complements rather than substitutes. Both proxy perspectives offer unique insights, yet QoL assessments in people with dementia are complex. The difference in self- and proxy-reports can be influenced by various factors, necessitating further research before presenting definitive results that inform care provision and policy.
Data availability
All data associated with the systematic literature review are available in the supplementary file.
Moyle, W., & Murfield, J. E. (2013). Health-related quality of life in older people with severe dementia: Challenges for measurement and management. Expert Review of Pharmacoeconomics & Outcomes, 13 (1), 109–122. https://doi.org/10.1586/erp.12.84
Article Google Scholar
Sachdev, P. S., Blacker, D., Blazer, D. G., Ganguli, M., Jeste, D. V., Paulsen, J. S., & Petersen, R. C. (2014). Classifying neurocognitive disorders: The DSM-5 approach. Nature reviews Neurology, 10 (11), 634–642. https://doi.org/10.1038/nrneurol.2014.181
Article PubMed Google Scholar
Health, The Lancet Regional., & – Europe. (2022). Challenges for addressing dementia. The Lancet Regional Health . https://doi.org/10.1016/j.lanepe.2022.100504
The WHOQOL Group. (1995). The World Health Organization quality of life assessment (WHOQOL): Position paper from the World Health Organization. Social Science & Medicine, 41 (10), 1403–1409. https://doi.org/10.1016/0277-9536(95)00112-K
Bosboom, P. R., Alfonso, H., Eaton, J., & Almeida, O. P. (2012). Quality of life in Alzheimer’s disease: Different factors associated with complementary ratings by patients and family carers. International Psychogeriatrics, 24 (5), 708–721. https://doi.org/10.1017/S1041610211002493
Scholzel-Dorenbos, C. J., Rikkert, M. G., Adang, E. M., & Krabbe, P. F. (2009). The challenges of accurate measurement of health-related quality of life in frail elderly people and dementia. Journal of the American Geriatrics Society, 57 (12), 2356–2357. https://doi.org/10.1111/j.1532-5415.2009.02586.x
Logsdon, R. G., Gibbons, L. E., McCurry, S. M., & Teri, L. (2002). Assessing quality of life in older adults with cognitive impairment. Psychosomatic Medicine, 64 (3), 510–519. https://doi.org/10.1097/00006842-200205000-00016
Hutchinson, C., Worley, A., Khadka, J., Milte, R., Cleland, J., & Ratcliffe, J. (2022). Do we agree or disagree? A systematic review of the application of preference-based instruments in self and proxy reporting of quality of life in older people. Social Science & Medicine, 305 , 115046. https://doi.org/10.1016/j.socscimed.2022.115046
Smith, S. C., Hendriks, A. A. J., Cano, S. J., & Black, N. (2020). Proxy reporting of health-related quality of life for people with dementia: A psychometric solution. Health and Quality of Life Outcomes, 18 (1), 148. https://doi.org/10.1186/s12955-020-01396-y
Article CAS PubMed PubMed Central Google Scholar
Andrieu, S., Coley, N., Rolland, Y., Cantet, C., Arnaud, C., Guyonnet, S., Nourhashemi, F., Grand, A., Vellas, B., & group, P. (2016). Assessing Alzheimer’s disease patients’ quality of life: Discrepancies between patient and caregiver perspectives. Alzheimer’s & Dementia, 12 (4), 427–437. https://doi.org/10.1016/j.jalz.2015.09.003
Jönsson, L., Andreasen, N., Kilander, L., Soininen, H., Waldemar, G., Nygaard, H., Winblad, B., Jonhagen, M. E., Hallikainen, M., & Wimo, A. (2006). Patient- and proxy-reported utility in Alzheimer disease using the EuroQoL. Alzheimer Disease & Associated Disorders, 20 (1), 49–55. https://doi.org/10.1097/01.wad.0000201851.52707.c9
Zucchella, C., Bartolo, M., Bernini, S., Picascia, M., & Sinforiani, E. (2015). Quality of life in Alzheimer disease: A comparison of patients’ and caregivers’ points of view. Alzheimer Disease & Associated Disorders, 29 (1), 50–54. https://doi.org/10.1097/WAD.0000000000000050
Article CAS Google Scholar
Buckley, T., Fauth, E. B., Morrison, A., Tschanz, J., Rabins, P. V., Piercy, K. W., Norton, M., & Lyketsos, C. G. (2012). Predictors of quality of life ratings for persons with dementia simultaneously reported by patients and their caregivers: The Cache County (Utah) study. International Psychogeriatrics, 24 (7), 1094–1102. https://doi.org/10.1017/S1041610212000063
Article PubMed PubMed Central Google Scholar
Schiffczyk, C., Romero, B., Jonas, C., Lahmeyer, C., Muller, F., & Riepe, M. W. (2010). Generic quality of life assessment in dementia patients: A prospective cohort study. BMC Neurology, 10 , 48. https://doi.org/10.1186/1471-2377-10-48
Sousa, M. F., Santos, R. L., Arcoverde, C., Simoes, P., Belfort, T., Adler, I., Leal, C., & Dourado, M. C. (2013). Quality of life in dementia: The role of non-cognitive factors in the ratings of people with dementia and family caregivers. International Psychogeriatrics, 25 (7), 1097–1105. https://doi.org/10.1017/S1041610213000410
Arons, A. M., Krabbe, P. F., Scholzel-Dorenbos, C. J., van der Wilt, G. J., & Rikkert, M. G. (2013). Quality of life in dementia: A study on proxy bias. BMC Medical Research Methodology, 13 , 110. https://doi.org/10.1186/1471-2288-13-110
Gomez-Gallego, M., Gomez-Garcia, J., & Ato-Lozano, E. (2015). Addressing the bias problem in the assessment of the quality of life of patients with dementia: Determinants of the accuracy and precision of the proxy ratings. The Journal of Nutrition, Health & Aging, 19 (3), 365–372. https://doi.org/10.1007/s12603-014-0564-7
Moon, H., Townsend, A. L., Dilworth-Anderson, P., & Whitlatch, C. J. (2016). Predictors of discrepancy between care recipients with mild-to-moderate dementia and their caregivers on perceptions of the care recipients’ quality of life. American Journal of Alzheimer’s Disease & Other Dementias, 31 (6), 508–515. https://doi.org/10.1177/1533317516653819
Crespo, M., Bernaldo de Quiros, M., Gomez, M. M., & Hornillos, C. (2012). Quality of life of nursing home residents with dementia: A comparison of perspectives of residents, family, and staff. The Gerontologist, 52 (1), 56–65. https://doi.org/10.1093/geront/gnr080
Griffiths, A. W., Smith, S. J., Martin, A., Meads, D., Kelley, R., & Surr, C. A. (2020). Exploring self-report and proxy-report quality-of-life measures for people living with dementia in care homes. Quality of Life Research, 29 (2), 463–472. https://doi.org/10.1007/s11136-019-02333-3
Pickard, A. S., & Knight, S. J. (2005). Proxy evaluation of health-related quality of life: A conceptual framework for understanding multiple proxy perspectives. Medical Care, 43 (5), 493–499. https://doi.org/10.1097/01.mlr.0000160419.27642.a8
Smith, S. C., Lamping, D. L., Banerjee, S., Harwood, R. H., Foley, B., Smith, P., Cook, J. C., Murray, J., Prince, M., Levin, E., Mann, A., & Knapp, M. (2007). Development of a new measure of health-related quality of life for people with dementia: DEMQOL. Psychological Medicine, 37 (5), 737–746. https://doi.org/10.1017/S0033291706009469
Article CAS PubMed Google Scholar
Brooks, R. (1996). EuroQol: The current state of play. Health Policy, 37 (1), 53–72. https://doi.org/10.1016/0168-8510(96)00822-6
Herdman, M., Gudex, C., Lloyd, A., Janssen, M., Kind, P., Parkin, D., Bonsel, G., & Badia, X. (2011). Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Quality of Life Research, 20 (10), 1727–1736. https://doi.org/10.1007/s11136-011-9903-x
Rand, S., Caiels, J., Collins, G., & Forder, J. (2017). Developing a proxy version of the adult social care outcome toolkit (ASCOT). Health and Quality of Life Outcomes, 15 (1), 108. https://doi.org/10.1186/s12955-017-0682-0
Engel, L., Bucholc, J., Mihalopoulos, C., Mulhern, B., Ratcliffe, J., Yates, M., & Hanna, L. (2020). A qualitative exploration of the content and face validity of preference-based measures within the context of dementia. Health and Quality of Life Outcomes, 18 (1), 178. https://doi.org/10.1186/s12955-020-01425-w
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hrobjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. British Medical Journal, 372 , n71. https://doi.org/10.1136/bmj.n71
Roydhouse, J. K., Cohen, M. L., Eshoj, H. R., Corsini, N., Yucel, E., Rutherford, C., Wac, K., Berrocal, A., Lanzi, A., Nowinski, C., Roberts, N., Kassianos, A. P., Sebille, V., King, M. T., Mercieca-Bebber, R., Force, I. P. T., & the, I. B. o. D. (2022). The use of proxies and proxy-reported measures: A report of the international society for quality of life research (ISOQOL) proxy task force. Quality of Life Research, 31 (2), 317–327. https://doi.org/10.1007/s11136-021-02937-8
The EndNote Team. (2013). EndNote (Version EndNote X9) [64 bit]. Philadelphia, PA: Clarivate.
Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan—A web and mobile app for systematic reviews. Systematic Reviews, 5 (1), 210. https://doi.org/10.1186/s13643-016-0384-4
Koo, T. K., & Li, M. Y. (2016). A guideline of selecting and reporting intraclass correlation coefficients for reliability research. Journal of Chiropractic Medicine, 15 (2), 155–163. https://doi.org/10.1016/j.jcm.2016.02.012
Wan, X., Wang, W., Liu, J., & Tong, T. (2014). Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Medical Research Methodology, 14 , 135. https://doi.org/10.1186/1471-2288-14-135
Higgins JPT and Green S (editors). (2011). Cochrane handbook for systematic reviews of interventions.Version 5.1.0 [updated March 2011]. Retrieved 20 Jan 2023, from https://handbook-5-1.cochrane.org/chapter_7/7_7_3_2_obtaining_standard_deviations_from_standard_errors_and.htm
Ma, J., Liu, W., Hunter, A., & Zhang, W. (2008). Performing meta-analysis with incomplete statistical information in clinical trials. BMC Medical Research Methodology, 8 , 56. https://doi.org/10.1186/1471-2288-8-56
Deeks, J. J., Higgins, J. P. T., Altman, D. G., & on behalf of the Cochrane Statistical Methods Group. (2023). Chapter 10: Analysing data and undertaking meta-analyses. In J. Higgins & J. Thomas (Eds.), Cochrane Handbook for Systematic Reviews of Interventions. Version 6.4.
Kmet, L. M., Cook, L. S., & Lee, R. C. (2004). Standard quality assessment criteria for evaluating primary research papers from a variety of fields: Health and technology assessment unit. Alberta Heritage Foundation for Medical Research.
Lewis, T. J., & Trempe, C. L. (2017). Diagnosis of Alzheimer’s: Standard-of-care . USA: Elsevier Science & Technology.
Google Scholar
Leontjevas, R., Teerenstra, S., Smalbrugge, M., Koopmans, R. T., & Gerritsen, D. L. (2016). Quality of life assessments in nursing homes revealed a tendency of proxies to moderate patients’ self-reports. Journal of Clinical Epidemiology, 80 , 123–133. https://doi.org/10.1016/j.jclinepi.2016.07.009
Lapin, B., Cohen, M. L., Corsini, N., Lanzi, A., Smith, S. C., Bennett, A. V., Mayo, N., Mercieca-Bebber, R., Mitchell, S. A., Rutherford, C., & Roydhouse, J. (2023). Development of consensus-based considerations for use of adult proxy reporting: An ISOQOL task force initiative. Journal of Patient-Reported Outcomes, 7 (1), 52. https://doi.org/10.1186/s41687-023-00588-6
Li, M., Harris, I., & Lu, Z. K. (2015). Differences in proxy-reported and patient-reported outcomes: assessing health and functional status among medicare beneficiaries. BMC Medical Research Methodology . https://doi.org/10.1186/s12874-015-0053-7
Robertson, S., Cooper, C., Hoe, J., Lord, K., Rapaport, P., Marston, L., Cousins, S., Lyketsos, C. G., & Livingston, G. (2020). Comparing proxy rated quality of life of people living with dementia in care homes. Psychological Medicine, 50 (1), 86–95. https://doi.org/10.1017/S0033291718003987
Khanna, D., Khadka, J., Mpundu-Kaambwa, C., Lay, K., Russo, R., Ratcliffe, J., & Quality of Life in Kids: Key Evidence to Strengthen Decisions in Australia Project, T. (2022). Are We Agreed? Self- versus proxy-reporting of paediatric health-related quality of life (HRQoL) Using generic preference-based measures: A systematic review and meta-analysis. PharmacoEconomics, 40 (11), 1043–1067. https://doi.org/10.1007/s40273-022-01177-z
Download references
Open Access funding enabled and organized by CAUL and its Member Institutions. This study was conducted without financial support.
Author information
Authors and affiliations.
Monash University Health Economics Group, School of Public Health and Preventive Medicine, Monash University, Level 4, 553 St. Kilda Road, Melbourne, VIC, 3004, Australia
Lidia Engel & Valeriia Sokolova
School of Health and Social Development, Deakin University, Burwood, VIC, Australia
Ekaterina Bogatyreva & Anna Leuenberger
You can also search for this author in PubMed Google Scholar
Contributions
LE contributed to the study conception and design. The original database search was performed by AL and later updated by VS. All authors were involved in the screening process, data extraction, and data analyses. Quality assessment was conducted by VS and LE. The first draft of the manuscript was written by LE and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Lidia Engel .
Ethics declarations
Competing interests.
Lidia Engel is a member of the EuroQol Group.
Ethical approval
Not applicable.
Consent to participate
Consent to publish, additional information, publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (XLSX 67 KB)
Supplementary file2 (docx 234 kb), rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Engel, L., Sokolova, V., Bogatyreva, E. et al. Understanding the influence of different proxy perspectives in explaining the difference between self-rated and proxy-rated quality of life in people living with dementia: a systematic literature review and meta-analysis. Qual Life Res (2024). https://doi.org/10.1007/s11136-024-03660-w
Download citation
Accepted : 27 March 2024
Published : 24 April 2024
DOI : https://doi.org/10.1007/s11136-024-03660-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Quality of Life
- Outcome measurement
- Find a journal
- Publish with us
- Track your research

IMAGES
VIDEO
COMMENTS
"Quality of life (QoL) is being considered as one of the fundamental concepts in contemporary era. It tries to assess the level of general welfare of the communities." Bhatti et al. (2017, pp. 1193-1194) "The quality of life (QOL) is a measure of social wellbeing and life satisfaction of individuals in an area…
Purpose. Quality of life (QOL) is an important concept in the field of health and medicine. QOL is a complex concept that is interpreted and defined differently within and between disciplines, including the fields of health and medicine. The aims of this study were to systematically review the literature on QOL in medicine and health research ...
Purpose Quality of life (QOL) is an important concept in the field of health and medicine. QOL is a complex concept that is interpreted and defined differently within and between disciplines, including the fields of health and medicine. The aims of this study were to systematically review the literature on QOL in medicine and health research and to describe the country of origin, target groups ...
A review of literature from inception to May 2016 for all prospective English language articles on QOL in patients with KSD was done. QOL studies post urological procedures or ureteric stents were excluded. Nine studies (1570 patients) were included of which most (n = 6) used the SF-36 QOL tool. Overall, seven of the nine studies demonstrated a ...
As quality of life (QoL) is a highly interdisciplinary topic with a multitude of related research areas, it is beneficial to avail researchers of an overview of the different streams explored in the field. Furthermore, knowledge of prominent sub-domains helps researchers identify links and overlaps between QoL and their fields of interest. To meet these needs, a text-mining-based computational ...
Methods A systematic review was conducted to identify research studies on QOL and health-related quality of life (HRQOL). The databases Scopus, which includes Embase and MEDLINE, CINAHL, and ...
The concept of quality of life (QOL) is generally used to measure, and sometimes describes, the structures and the evolution patterns of world societies (Costanza et al., 2007 ). Social policies aimed at increasing people's living standards need to be constantly evaluated and, eventually, improved.
A systematic literature review was conducted to (a) identify the most frequently used health-related quality of life (HRQOL) models and (b) critique those models. Online search engines were queried using pre-determined inclusion and exclusion criteria. We reviewed titles, abstracts, and then full-text articles for their relevance to this review.
As quality of life (QoL) is a highly interdisciplinary topic with a multitude of related research areas, it is beneficial to avail researchers of an overview of the different streams explored in the field. ... To meet these needs, a text-mining-based computational literature review (CLR) of the journal of Applied Research in Quality of Life ...
A person's chronic health condition or disability can have a huge impact on the quality of life (QoL) of the whole family, but this important impact is often ignored. This literature review aims to understand the impact of patients' disease on family members across all medical specialities, and appraise existing generic and disease-specific family quality of life (QoL) measures.
Multimorbidity is typically defined as the co-existence of two or more chronic diseases within an individual. Its prevalence is highest among the elderly, with poor quality of life (QoL) being one of the major consequences. This study aims to: (1) understand the relationship between multimorbidity and QoL or health-related quality of life ...
Quality of life is a multidimensional construct composed of functional, physical, emotional, social and spiritual well-being (Peterman et al 2002). Several definitions and models of quality of ...
Purpose of review: The purpose of this study was to review the current evidence for quality of life (QOL) in patients with kidney stone disease (KSD). Recent findings: A review of literature from inception to May 2016 for all prospective English language articles on QOL in patients with KSD was done. QOL studies post urological procedures or ureteric stents were excluded.
Paloma V, Escobar-Ballesta M, Galván-Vega B, Díaz-Bautista JD, Benítez I. Determinants of life satisfaction of economic migrants coming from developing countries to countries with very high human development: A systematic review. Applied Research in Quality of Life. 2020 doi: 10.1007/s11482-020-09832-3.
Abstract. This review of the literature looks at the meaning of the concept 'quality of life', the use to which it has been put in various branches of medicine, its meaning in particular in cancer patients, especially those for whom there is no longer expectation of cure, and the instruments already developed for its measurement and their ...
BMC Health Services Research (2020) The aim of this study is to examine the impact of haematological cancers on quality of life (QoL). A review of the international literature was conducted from ...
Overview. Quality of Life Research is an international, multidisciplinary journal devoted to the rapid communication of original research, theoretical articles and methodological reports related to the field of quality of life, in all the health sciences. The journal also offers editorials, literature, book and software reviews, correspondence ...
Its prevalence is highest among the elderly, with poor quality of life (QoL) being one of the major consequences. This study aims to: (1) understand the relationship between multimorbidity and QoL or health-related quality of life (HRQoL) through systematic literature review; (2) explore the strength of this association by conducting the first ...
Quality of life (QoL) is a broad concept that has different definitions across diverse bodies of knowledge. The social-cultural environment and the characteristics of the built environment ...
A systematic review of physical activity and quality of life and well-being. David X Marquez, 1 Susan Aguiñaga, 2 Priscilla M Vásquez, 3 David E Conroy, 4 Kirk I Erickson, 5 Charles Hillman, 6 Chelsea M Stillman, 5 Rachel M Ballard, 8 Bonny Bloodgood Sheppard, 9 Steven J Petruzzello, 10 Abby C King, 11 and Kenneth E Powell 12.
Purpose of Review The purpose of this study was to review the current evidence for quality of life (QOL) in patients with kidney stone disease (KSD). Recent Findings A review of literature from inception to May 2016 for all prospective English language articles on QOL in patients with KSD was done. QOL studies post urological procedures or ureteric stents were excluded. Nine studies (1570 ...
Kwon CS, Daniele P, Forsythe A, Ngai C. A systematic literature review of the epidemiology, health-related quality of life impact, and economic burden of immunoglobulin A nephropathy. J Health Econ Outcomes Res. 2021;8(2):36-45. Article PubMed PubMed Central Google Scholar
Quality of life (QoL) is a broad concept that has different definitions across diverse bodies of knowledge. The social-cultural environment and the characteristics of the built environment influence people's perception of QoL. This study aims to identify and analyse the factors that impact QoL and sustainable development in the urban context.
Quality of life (QoL) is a concept which aims to capture the well-being, whether of a population or individual, regarding both positive and negative elements within the entirety of their existence at a specific point in time. For example, common facets of QoL include personal health (physical, mental, and spiritual), relationships, education status, work environment, social status, wealth, a ...
We explored multimorbidity patterns that might inform intervention planning to reduce health-care costs while preserving quality of life for patients. Literature searches up to February 2022 revealed 4419 clinical observational and comparative studies of risk factors for multimorbidity in people with COPD, pulmonary emphysema, or chronic ...
The purpose of this narrative review of the recent literature is to analyze the outcomes, complications, and implant survival of total knee arthroplasty (TKA) carried out on people with hemophilia (PWH). It has been shown that TKA substantially alleviates preoperative pain and improves knee function and the patient's quality of life. However, the complication rates of TKA range between 8.5% ...
When properly done it provides acceptable long time survival and good quality of life to patients. Renal cell carcinomas are the most common form of kidney cancer in adults. In addition to metastasizing in lungs, soft tissues, bones, and the liver, it also spreads locally. ... a case report and review of the literature. J Med Case Reports 18 ...
Quality of life versus length of life considerations in cancer patients: A systematic literature review. ... A systematic review of the literature was conducted using MeSH terms: cancer, longevity or LoL, QoL, decision making, trade‐off, and health utility. Articles retrieved were published between 1942 and October 2018.
Purpose Proxy assessment can be elicited via the proxy-patient perspective (i.e., asking proxies to assess the patient's quality of life (QoL) as they think the patient would respond) or proxy-proxy perspective (i.e., asking proxies to provide their own perspective on the patient's QoL). This review aimed to identify the role of the proxy perspective in explaining the differences between ...