
- The Knee Prosthesis
- Mary’s Knee
- Board Certified
- Pre-op Medical Evaluation
- Stop Your NSAIDs/Herbals
- Both Knees at Once
- Hospital Stay
- Incentive Spirometer
- CPM Machine
- Home Health and Therapy
- In-Patient Rehabilitation
- Road to Recovery
- Home Exercise Program
- Acetaminophen Alert
- Knee Numbness
- Knee Motion
- Athletic Activity
- Dental Care
- Blood Clots
- Finding an Orthopaedic Surgeon
- Pre-op Questions
- Prepare Your Home
- Hospital Teaching Class
- Day Before Surgery Checklist
- Post-Op Visit Questions
- Lifestyle Changes
- Physical Therapy
- Cortisone Injections
- Hyaluronic Acid Injections
- Stories Homepage
- I decided to have my knee replaced when
- How my life changed after knee replacement
- Research Projects
- When To Have Replacement?
- Return To Work - Stories
- Return To Work - Timeline
- ProPublica Misleads Complications
- Joint Replacement Warranty

Sign Up for My Knee Guide to:
- Save Checklists and Notes
- Save Surgery Dates/Surgery Calendar
- Post Stories and Comment
- Access your My Knee Guide info from your mobile device.

Add Your Story

Add Your Comment

Written by: Brian Hatten, M.D. | Revised: May 20, 2016
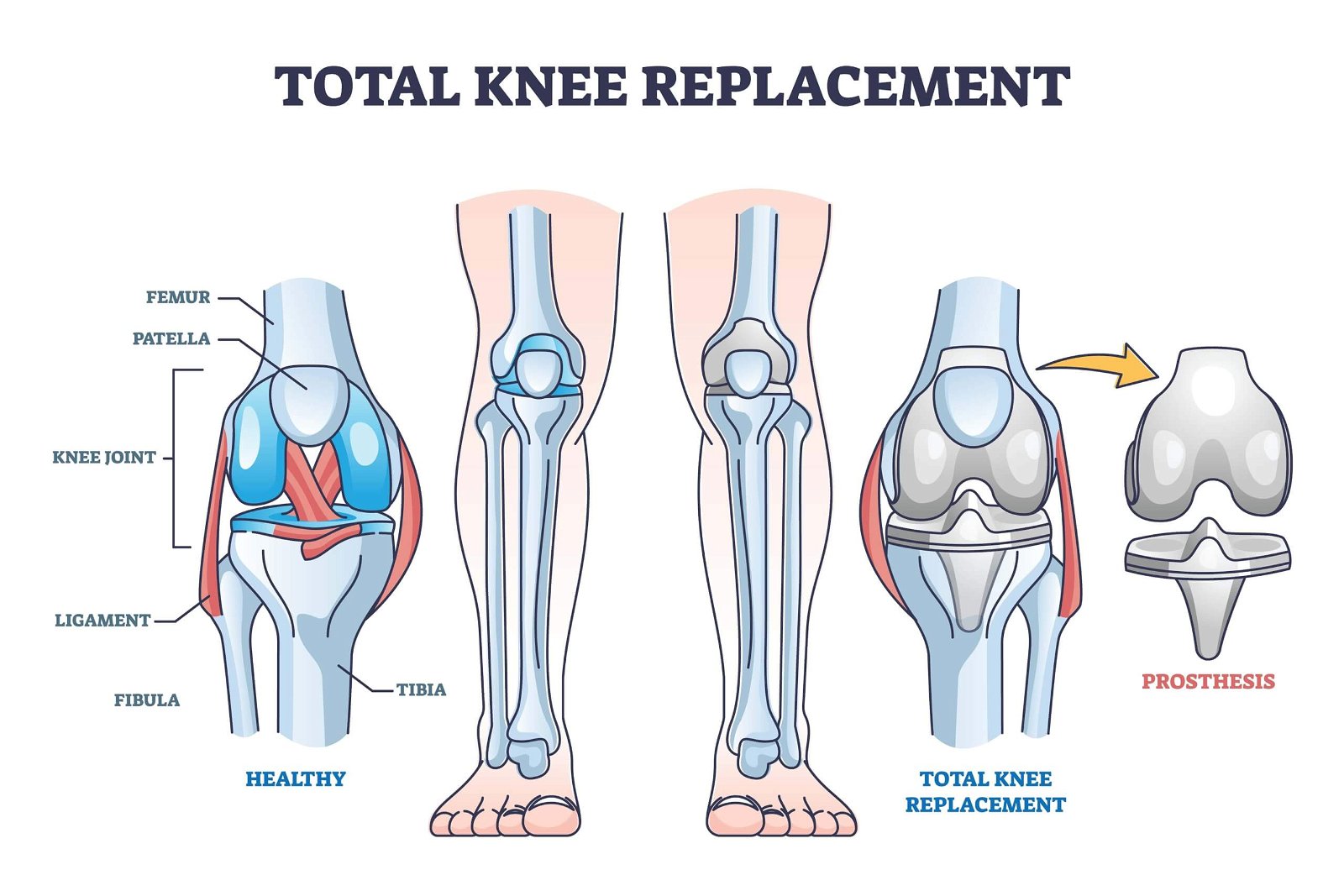
Total knee replacement surgery Total knee replacement consists of three main components: the femoral component, the tibial component, and the plastic spacer (polyethylene). The following model shows the components of a knee replacement. The model on the left shows the front view and the model on the right shows the side view.

There are several types of full knee replacements that are available to your surgeon. The decision for the type of knee replacement to be used may be based on several factors. These include your particular anatomy anatomy , amount of knee deformity knee deformity , ligament stability, quality of soft tissues, and the surgeon's experience surgeon's experience .
One way of categorizing knee replacement components involves whether the plastic (polyethylene) is fixed securely upon the underlying tibial component or whether it allows rotation upon the tibial component. These are respectively referred to as fixed bearing versus rotating platform (RP) knees. Tap on the below image to show how a rotating platform knee allows rotation of the plastic in relation to the tibia.

There are advantages to using each type of prosthesis. PS knees allow for the reliable restoration of knee kinematics, small improvements in motion compared to CR knees, and the theoretical reduction in polyethylene wear. PS knees are specifically indicated in patients with severe deformity, severe flexion contracture, previous removal of the knee cap, and during revision surgery. CR knees require less bone to be removed, decrease the chance of a “patella clunk” syndrome, and decrease the potential complications associated with having a polyethylene post.
When looking at an x-ray, there are defining characteristics that can be used to identify whether a posterior cruciate substituting (PS) or cruciate retaining (CR) knee was implanted. This is due to the “box” that is required to make the PS knee function correctly. On the side view of the x-ray, the difference can be seen on the metal component on the thigh bone (femur). Look at the following example: The blue arrow points to the “box” portion of the prosthesis of the PS knee. The red arrow points to CR knee. Notice how the CR knee requires less bone to be removed.

The last category has to do with how the metal components are fixed to the underlying bone. Most replacement systems use a special type of cement called methylmethacrylate to bond the metal component to the bones. This cement sets up in approximately 13 minutes (during the surgery) and allows the patient to walk without restricting the amount of weight bearing after the procedure. There are other ways to secure the prosthesis to the bone without cement such as using an “interference” fit or by augmenting with screws. Use of these techniques may also allow the patient to progress to immediate weight bearing.
Additionally, most surgeons in the United States will also resurface the underside of the knee cap. This is done with a plastic button. However, it is common for surgeons in the United Kingdom to not resurface the knee cap. There is slightly more anterior knee pain anterior knee pain associated with not resurfacing the knee cap, but lowers the small risk of complications from the resurfacing procedure.

Related Articles
When Should I Have My Knee Replaced? – A Surgeon's Perspective
Knee Replacement Surgery - The Truth and the Hype
Does your Joint Replacement have a Warranty?
Timeline for Recovery - What to Expect after Surgery
Knee Replacement Prosthesis Components

- Download the iPhone App
- Share with Facebook
- About My Knee Guide
- Medical Disclaimer Privacy Policy Terms of Use

Total endoprosthesis of the knee
Inserting an endoprosthesis of the knee is one of the most common orthopedic surgeries. The reasoning for undergoing the procedure is based on a progressed state of illness and a state where non-surgical methods and other reconstructive surgical procedures fail to improve treatment (15).
Medical science is ever evolving and improving. In endoprosthetics, by using modern materials and surgical techniques, in conjunction with appropriate presurgical preparation and quality rehabilitation , we can help the individuals regain their complete quality of life. That is, the individual whose severe pain, limited mobility, and instability while walking prevented them from completing everyday activities.
To some degree, non-surgical procedures can prove effective and are therefore the first choice of treatment – this includes all physiotherapeutic methods and a carefully planned exercise program. However, when all options are exhausted, the condition does not better and no further improvement can be expected, the only long-term solution is a total endoprosthesis of the knee .
The knee joint is complex and frequently injured
The knee joint is the most complex joint in the human body. Because of its structure, exposure to external forces, and great functional requirements it is the most frequently injured one. The bones to which it is connected are the femur, tibia, and patella.
The fibula, the thinner bone of the shin, connects to the tibia and, while not directly part of the knee joint, plays an important role in regard to the muscle’s insertion and knee ligaments. The stability of the knee joint is made possible by means of the cruciate ligaments, menisci, collateral ligaments, joint capsule and tendomuscular apparatus .
The joint allows movement in the direction of extension and flexion and, while the knee is bent, also facilitates slight medial and lateral rotations.

Osteoarthritis is the most common reason for inserting a total knee endoprosthesis
The number of procedures performed on the knee is increasing constantly, in Slovenia, as well as in the world (10). The indicator for surgical treatment is most frequently a progressed state of primary or secondary arthrosis.
Osteoarthrosis (OA) is a degenerative process that damages the articular cartilage, which is then after unable to absorb the forces caused by movement, consequently causing damage to the bone surface. This is evidenced by pain and limited mobility. Later on, these can be accompanied by grinding or creaking in the joint (crepitations), joint effusion caused by secondary inflammation, muscle weakness, contractures, ankylosis, and an enlarged or deformed joint (15).
In 2018, 90,4% of all surgical procedures in Slovenia were performed due to the diagnosis of OA (7) . Other diagnoses represented post-traumatic injuries, rheumatoid / psoriatic arthritis, aseptic necrosis and consequences of meniscus or ligament injuries (7). Statistically, they consist of a predominantly female population, in the ages of about 60-70, where the majority of patients is either overweight or morbidly obese (7).
The development of AO is greatly shaped by the lifestyle one lives from the viewpoint of physical activity and diet – habits that we can alter. Also contributing to its development are all previous injuries and surgeries of the knee, congenital malformations and other adjacent autoimmune diseases.
The primary reason for inserting a total endoprosthesis of the knee
As life expectancy increases so does the number of individuals with various degenerative knee joint diseases. The changes brought about by ageing are simply impossible to be averted, which is why a mere “bad x-ray” is insufficient reasoning to undergo the surgical procedure.
The primary reason for inserting a prosthetic joint is persistent, severe pain that is caused by a worn-out knee and which often does not even cease at night. The pain is frequently accompanied by limited mobility and instability while walking causing problems in everyday activities.
At the early onset of problems all conservation treatments with physiotherapy and kinesiotherapy need to be exhausted and only thereafter, if the pain management and improvement of the basic functionality prove unsuccessful, can the surgical procedure be considered.
Total knee arthroplasty is more complicated than hip replacement surgery
Why is the surgical procedure not carried out as soon as changes or pain in the knee appears? The knee has a complex flexibility along and around all three axes, which are constantly shifting during movement.
Biomechanically, the knee endoprosthesis is far more complicated than a hip prosthesis (10). Statistical data for Slovenia between the years 2002 and 2018, comparing knee and hip endoprostheses, shows greater incidence (14,4 %) of instability, poor placement and decreased range of motion after knee prosthesis surgery compared to hip prostheses (0%).
Revision surgeries and the occurrence of pain is also more prevalent among knee than among hip endoprostheses (7). Nevertheless, the only long-term solution for major issues remains solely a knee replacement surgery (total knee arthroplasty).
The total knee endoprosthesis is the most commonly used type of endoprosthesis
Total knee arthroplasty (TKA) serves as a bone surface replacement. The prosthesis is composed of metal and polyethylene inserts.
Both cemented and cementless techniques are used, the latter ones being used predominantly in younger patients with well-preserved bone mass, where the knee biomechanics are still relatively intact and good retention of the metal part of the prosthesis can be expected.
Considering the deformation and condition of the surrounding soft tissues, the surgeon can also choose between inserting an unconstrained or semiconstrained endoprosthesis with either the preservation or removal of the posterior cruciate ligament (10).
How to prepare for the operative procedure?
Various research studies suggest that preoperative exercise improves postoperative functional results. Patients who have gone through a preoperative exercise programme tend to have shorter inpatient hospital stays, quicker physical recovery (2), reduced pain and improved quality of life (13).
Increased stability during standing can also be achieved with proprioceptive (»balance«) training (5).

According to the latest clinical guidelines (2020) preoperative exercise is encouraged, as it reduces pain, improves balance, enhances the range of motion of the knee joint as well as the isometric force of the knee and hip muscles.
As a result of all above-mentioned parameters, improved quality of life can be achieved along with a faster and more successful treatment outcome (6).
Surgical procedure
The primary surgical procedure usually takes about 1 to 2 hours. During this time, the surgeon removes the damaged cartilage and bone tissue and inserts new metal and plastic inserts (3). It is common to feel pain immediately after the surgical procedure.
In the first days following the surgery, the pain can be treated by using analgesics and with the help of non-pharmacological approaches such as cooling and lifting of the operated leg (6).
Postoperative rehabilitation
The postoperative rehabilitation process is generally longer and more complex than after hip replacement surgery (10). With age natural neuromotor changes occur, which leads to decreased muscle strength, with the surgical procedure causing a further decrease of at least 24 % in muscle strength compared to the contralateral side (6).
This is why a complex rehabilitation process is necessary in order to achieve a positive treatment outcome which will help to eliminate any muscle deficits.
Phase I: From the surgical procedure up to 2-3 weeks after surgery
The most important objective in the first days following the surgery is to carefully manage and alleviate the pain and swelling, as well as to pay special attention to the surgical wound, ensuring its healing without getting infected (3). As the wound is healing, avoid bending the knee more than 90° in the first two weeks.
The extension in the knee joint is not restricted and should be encouraged in order to achieve the maximum range of motion. Some exercises that can be performed in the hospital bed include: active movement of the ankle joint in order to stimulate blood circulation, isometric exercises for the anterior thigh muscles, active bending and extending of the knee within the recommended range of movement and lifting of the extended leg (6).
In individuals found to have muscle activation deficits, neuromuscular electric stimulation (NMES) is advised. It should be started as soon as possible following the surgical procedure and should be performed for at least 3 weeks. The use of NMES will result in the improvement of the maximal voluntary muscle contraction (6).
Phase II: 4-6 weeks after surgery
The aim of the second phase is to achieve a normal walking pattern without limping as well as to regain the initial flexibility and strength .
The exercises are carried out twice a week, the frequency can be increased or decreased according to the individual progress of the patient. The exercises are targeted at gradually regaining the neuromuscular control and increasing the muscle strength of the operated leg (12).
Phase III: 6-8 weeks after surgery
In this phase we want to achieve good control when standing on one leg as well as incorporate various lateral movements into the exercise regime, such as taking lateral steps or step overs. Later more emphasis is placed on increasing muscle strength and endurance.
In this phase the individual should be able to walk without limping (12). Studies that incorporated sensorimotor exercises into the rehabilitation process have shown improved walking function (8). Participants self-evaluation showed better physical functionality and ability to engage in recreational activities in individuals who took part in balance improvement exercises (1).
Therefore, it is safe to assume that the incorporation of such exercises is beneficial.
Phase IV: 8-12 weeks after surgery
The emphasis of the fourth phase of the rehabilitation process is to gradually include specific exercises needed to allow the patient to return to daily activities such as household chores, work specific activities and sports .
Until the end of the 12th week the patient is encouraged to take part only in non-contact physical activities and advised against pivoting and rotating on the operated leg (12).
- Bruun-Olsen, V., Heiberg, K.E., Wahl, A.K. & Mengshoel, A.M., 2013. The immediate and long-term effects of a walking-skill program compared to usual physiotherapy care in patients who have undergone total knee arthroplasty (TKA): a randomized controlled trial. Disabil Rehabilm, 35, pp. 2008–2015.
- Calatayud, J., Casana, J., Ezzatvar, Y., Jakobsen, M.D., Sundstrup, E. & Andersen, L.L., 2017. High-intensity preoperative training improves physical and functional recovery in the early post-operative periods after total knee arthroplasty: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc, 25, pp. 2864–2872.
- Foran. J. Total Knee Replacement. OrthoInfo. Available at: https://orthoinfo.aaos.org/en/treatment/total-knee-replacement/ [29.8.2021].
- Groen, J.W., Stevens, M., Kersten, R.F., Reininga, I.H. & van den Akker-Scheek I., 2012. After total knee arthroplasty, many people are not active enough to maintain their health and fitnes. J Physiother, 58(2), pp. 113-6.
- Gstoettner, M., Raschner, C., Dirnberger, E., Leimser, H. & Krismer, M., 2011. Preoperative proprioceptive training in patients with total knee arthroplasty. Knee, 18, pp. 265–270.
- Jette, D.U., Hunter, S.J., Burkett, L., Langham, B., Logerstedt, D.S:, Piuzzi, N.S., et al, 2020. Physical Therapist Management of Total Knee Arthroplasty. Clinical Practice guidelines. Physical Therapy, 10, pp. 1-29.
- Levašič, V., Savarin, D. &Milošev, I., 2020. VALDOLTRA KNEE ARTHROPLASTY REGISTRY REPORT 2002-2019. Valdoltra Arthroplasty registry.
- Liao, C.D., Lin, L.F., Huang, Y.C, Huang, S.W., Chou, L.C. & Liou, T.H., 2015. Functional outcomes of outpatient balance training following total knee replacement in patients with knee osteoarthritis: a randomized controlled trial. Clin Rehabil, 29, pp. 855–867.
- Mikša, M., 2014. Funkcionalna anatomija kolenskega sklepa – razlike med odraščajočim in odraslim kolenom. Medicina športa, 1, pp. 4-6.
- Moličnik, A. & Merc, M., 2010. Endoprotetika kolenskega sklepa. In: VI. Mariborsko ortopedstko srečanje. Interdisciplinarno strokovno srečanje in učne delavnice. Artroza in endoprotetika sklepov. Zbornik vabljenih predavanj. Maribor, pp. 81-93.
- Shadyab, A.H., Eaton, C.B., Li, W. & LaCroix, A.Z., 2018. Association of Physical Activity with late-life mobility limitation among women with total joint replacement for knee or hip osteoarthritis. J Rheumatol, 45, pp. 1180–1187.
- The stone clinic. Total Knee Replacement Surgery Rehab Protocol & Recovery Time. Available at: https://www.stoneclinic.com/total-knee-replacement-rehab-protocol [29.8.2021].
- Tungtrongjit, Y., Weingkum, P. & Saunkool, P., 2012. The effect of preoperative quadriceps exercise on functional outcome after total knee arthroplasty. J Med Assoc Thai, 95(10), pp. 58–66.
- Valtonen, A., Poyhonen, T., Sipila, S. & Heinonen, A., 2010. Effects of aquatic resistance training on mobility limitation and lower-limb impairments after knee replacement. Arch Phys Med Rehabil, 91, pp. 833–839.
- Vogrin, M. & Naranđa, J., 2010. Osteoartroza: Epidemiologija, patogeneza in dejavniki tveganja. In: VI. Mariborsko ortopedstko srečanje. Interdisciplinarno strokovno srečanje in učne delavnice. Artroza in endoprotetika sklepov. Zbornik vabljenih predavanj. Maribor, pp. 9-21.
Importance of a well-defined rehabilitation process
A regular, guided and goal-oriented rehabilitation process allows for a better treatment outcome and a life with less limitations after a total knee arthroplasty procedure.
Physical activity has a number of beneficial effects on an individual’s quality of life (6). However, if a certain condition cannot be improved by way of physiotherapy or exercise programs, knee arthroplasty has proven to be a safe and effective procedure. It must be remembered that a knee prosthesis has a certain limited lifespan.
In younger individuals, the decision to opt for a knee arthroplasty is usually taken when due to severe joint impairment no other effective type of treatment is available. It should also be considered that because of the functional complexity of the knee joint it is still not possible to achieve a perfectly »normal« knee, despite all of the newly available techniques and implants (10).
Nevertheless, it has been shown that a regular, guided and goal-oriented rehabilitation process allows for a better treatment outcome, a life with fewer limitations, and promises positive results.
Provided that you decide to continue with a regular exercise regime even after the completed rehabilitation program, you can expect a higher quality of life, which means improved walking function, increased muscle strength and endurance, enhanced balance and mobility, alongside a better ability to care for yourself, as well as a quicker reintegration into your social and recreational life.

@medicofit_klinika
Medicofit articles

A sprained knee doesn’t necessarily imply a torn ligament

Physiotherapy during a waiting list? What do I need to know?

5 reasons for neck pain

What is ankle arthroscopy? How is it treated?

Hip pain - what can go wrong?

The role of exercise in the treatment of chronic lower back pain

Manual therapy techniques and their effects

Stiff neck - symptoms, causes and treatment

What is Osgood Schlatter syndrome?
All articles

- Privacy Overview
- Strictly Necessary Cookies
- 3rd Party Cookies
- Additional Cookies
- Cookie Policy
This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
This website uses Google Analytics to collect anonymous information such as the number of visitors to the site, and the most popular pages. Keeping this cookie enabled helps us to improve our website.
Please enable Strictly Necessary Cookies first so that we can save your preferences!
This website uses the following additional cookies:
(List the cookies that you are using on the website here.)
More information about our Cookie Policy

- Vision, Mission and Purpose
- Focus & Scope
- Editorial Info
- Open Access Policy
- Editing Services
- Article Outreach
- Why with us
- Focused Topics
- Manuscript Guidelines
- Ethics & Disclosures
- What happens next to your Submission
- Submission Link
- Special Issues
- Latest Articles
- All Articles
- Article Details
Endoprosthetic Reconstruction in Limb Salvage for Malignant Bone Tumours in Children
Sagar Tontanahal 1 , Gahukamble Abhay Deodas 1 , Deeptiman James 1 , Anand Kurian 2 , Thomas Palocaren 1* 1 Department of Paediatric Orthopaedics, Christian Medical College, Vellore, India 2 Department of Orthopaedics, Christian Medical College, Vellore, India
Background: The management of malignant bone tumors in children has come a long way in the past few decades. The transition from amputation to limb salvage has been made possible due to the rapid development in the diagnosis and the oncological management of these malignant tumors. However, there exist significant reservations regarding endoprosthetic reconstruction in children.
Material and methods: A mini-review was conducted of articles detailing the use of prosthetic reconstruction following tumor resection in children. The data regarding complications and functional outcomes following surgery were collected and presented.
Results: The studies reviewed reported a 5-year survival rate between 60 – 70 %. Uniform across the studies was the need for multiple surgeries when endoprosthesis was used for limb reconstruction, ranging between 2.8 – 3.5 surgeries. The most common complication noted across the studies was related to soft tissue problems such as joint instability followed by structural failure of the prosthesis. Infections were noted with a frequency of 10 – 15 %. Studies showed successful management of limb length discrepancy with expandible prosthesis. Musculoskeletal Tumor Society (MSTS) score used to evaluate the functional outcome showed satisfactory outcomes.
Conclusion: Limb salvage surgery, with recent advances in technique and prosthesis design, is an attractive option in children with extremity malignant bone tumors. In recent time, endoprosthetic reconstruction of extremities have yielded good functional results and are well accepted by the child and the parents. The purpose of this mini-review is to shed some light on the use of endoprosthetic reconstruction in children following tumor resection with its potential benefits and drawbacks.
Introduction
The treatment of extremity malignant tumors in children has evolved tremendously over the past few years. In the early part of the 20 th century, the only curative treatment modality was amputation, offering a 5-year survival rate between 12 and 23 % 1,2 . In children, however, the survival rates following amputation were consistently found to be low, with studies by Campannaci and Cervellati 3 showing 10-year survival rates as low as 11%.
In the late 20 th century, there was a tremendous improvement in the treatment of malignant tumors using chemotherapy and radiation therapy, as evidenced by improved 5-year survival rates of up to 70 % 4,5 . In 1979, the study of Copeland et al. 6 advocated the possible success of limb salvage surgery following wide en-bloc resection in selected cases of malignant bone tumors.;
The landmark study, which broadened the scope of limb salvage surgery, was published in 1986 by Simon and his colleagues 7 . In this study, they found no difference in the 5-year survival of patients with osteosarcoma who underwent amputation or limb-salvage surgery. Following this study, there has been a paradigm shift in the trend towards limb salvage with an assumption that limb salvage is a better option both functionally and psychologically for the child and the family.
In the pediatric population, the acceptability of amputation by the child, the higher rates of reported complications and the need for further procedures to manage limb length discrepancy following physeal resection, make limb salvage challenging.
Recent advances in endoprosthetic design coupled with developments in the field of cancer treatment makes limb salvage surgery with endoprosthesis a viable option for management of extremity malignant tumors in children.
History of metallic endoprosthesis
The idea of limb salvage surgery has undergone tremendous changes since its initiation. The idea of joint spanning with a fusion construct was the initial idea for limb salvage in children with the idea to preserve length and distal function. This concept gave way to prosthetic design intending to preserve joint function as well. It was Scales in 1976 8 , who revolutionized the use of endoprosthesis in limb salvage surgery in children. Scales and his colleagues from the division of Biomedical Engineering in Stanmore, UK, developed an extendible endoprosthesis which, in addition to preserving joint function, addressed the issue of limb length discrepancy following physeal excision.
Unwin and Walker 9 studied the outcomes of limb salvage surgery in children between 1976 and 1992. They noted 4 distinct designs of the expanding implants based on the growing mechanism. The first design used a worm drive screw for expanding the telescoping titanium components. This was later replaced by a ball bearing mechanism in 1982 after a growing number of mechanical failures were noted. In 1988, this design was replaced by a C collar mechanism, which required open dissection, manual traction, and placement of a C collar spacer.
All these prostheses required invasive surgical procedures to carry out lengthening. With improvement in manufacturing techniques, the design of the endoprosthesis reverted to a screw mechanism that could be controlled with an Allen wrench inserted percutaneously. This obliviated the need for open surgery thereby reducing the incidence of complications 10 .
The next advancement in the design of the expandable prosthesis came from the Stanmore group, described by Gupta and his colleagues in 2006 11 . This prosthesis has a magnetic disk within the prosthesis which is attached to a power screw through a gearbox. This prosthesis can be lengthened by a circular external drive unit, which induces a circular magnetic field, which in turn drives the power screw. This prosthesis came in three lengths which provide 50 mm, 70 mm, and 90 mm of lengthening. This offered the advantage of non-invasive, predictable, and reversible lengthening without the need for additional surgical procedures thereby reducing the complications associated with endoprosthetic reconstruction.
Alternative designs of non-invasive expanding endoprosthesis have also been developed and are being used like, the Repiphysis prosthesis 12 . The expansion mechanism rests in the tubular portion of the prosthesis and utilizes the stored energy from compressed springs for expansion. The expansion is brought about by an externally applied magnetic field that melts the polymer tube housing the coiled spring, which releases the spring producing the force needed to expand the tubular insert.
The MUTARS (Modular Universal Tumor and Revision System) with their Xpand prosthesis target growth of the prosthesis by both mechanical and biological means. The device uses a high-frequency transmitter to control the actuator within the prosthesis and for the biological aspect of growth, it uses an intramedullary rod system which is capable of distraction osteogenesis 13 .
Considerations in selecting a prosthesis in children
The primary goals of tumor management are of paramount importance when considering limb salvage surgery in children. These include accurate diagnosis and staging followed by appropriate chemotherapeutic management and radiation therapy if necessary. Another important aspect to consider in children while using endoprosthesis for reconstruction is the age at which the tumor resection is being done and the expected limb length discrepancy. The course of treatment with limb salvage surgery can be prolonged, requiring multiple surgical procedures in addition to the protracted course of multiagent chemotherapy.
When considering the choice of endoprosthesis for reconstruction, the growing child can be subdivided into three categories based on estimated growth remaining at the resected physis 13 . The first, nearing skeletal maturity with 2 cm or less of growth remaining. In this subset, normal adult implants can be used with the residual limb length discrepancy being managed by an external shoe raise. Alternatively, the operated limb can be lengthened to the expected limb length at skeletal maturity using a long implant. The extent of lengthening is limited by the potential to induce sciatic nerve damage or loss of knee range of motion.
The second group are the ones who are expected to have a limb length discrepancy between 2 and 6 cm. This group can be managed by one of two equally effective methods. The first, using a combination of ipsilateral lengthening using an adult implant and timely contralateral epiphysiodesis. The advantage of this being the use of adult prosthesis avoids the need for revision at skeletal maturity. The alternative being the use of a growing endoprosthesis. The advantage of this is that the ipsilateral limb can mirror the growth of the normal limb, the growth of which is affected by tumor treatment modalities. Additionally, this avoids operative intervention of the unaffected side, which may be a concern in some patients.
The final group is one far from skeletal maturity with growth of more than 8 cm remaining. The only option for endoprosthetic reconstruction is the use of growing endoprosthesis. The use of endoprosthesis in this subgroup has been reported in small case series and case reports. This group will require more than one growing prosthesis in addition to final conversion to an adult implant at skeletal maturity. This option is one requiring major commitment on behalf of the child, parents and the treating surgeon.
Complications and failures
The goals for surgical management of extremity sarcoma in children is get the child functioning at near normal levels. This can be achieved by restoring the range of motion and stability of the joint, maintaining distal functioning and also prevent local recurrence and infections. The five-year survival rates in various studies, which evaluated the use of endoprosthesis for limb reconstruction, was around 60 - 70 % 14,15,16 . This might not be an accurate estimation of the survival rates as almost all of the studies had a selection bias, restricting the choice of cases to be ones without metastasis and low volume tumors.
The course of treatment with endoprosthesis is a long one and involves multiple surgeries. Studies report anywhere between an average of 2.5 – 8.7 surgeries per child. This number has reduced with the improvement in surgical technique and implant design. Failure is defined as the need for revision of the prosthesis or surrounding soft tissue following the index surgery. Henderson and colleagues classified failures due to endoprosthetic reconstruction in adults into 5 groups which was later modified by the author to include complications specific to the pediatric population. It is also interesting to note that the different regions where the endoprosthesis were used showed different complication rates.
The Henderson type I complication, involving the soft tissues, was the most common observed. This complication included joint instability, tendon rupture and aseptic wound dehiscence. Studies by Schinhan et al. 16 and Dotan et al. 14 reported an incidence of 46 and 47 % respectively. A recent study by Tsuda et al. 17 , which reviewed 124 children who underwent extendable endoprosthetic reconstruction for malignant tumors showed the incidence of this complications of 27 %. The incidence of complications also varied on the site of use of the endoprosthesis. Higher rates were observed in the proximal femur, distal femur and proximal tibia. This could be attributed differential growth between the acetabulum and proximal femur at the hip joint and stiffness and the patellar maltracking at the knee joint respectively.
The next most frequently encountered complication was structural failure (type 3 failure). This encompassed periprosthetic and prosthetic fracture, stress shielding and failure of growing mechanism. Three studies by Schinhan et al. 16 , Dotan et al. 14 and Tsuda et al. 17 , which followed up a good number if patients for a significantly long-time frame, report an incidence of type 3 failure of 28 %, 23 % and 26 % respectively. Distal femoral endoprosthesis showed the greatest propensity for this type of complication. Infections (type 4 failure) were the next most common complication. The high rates of infection in these patients can be attributed to their immunodeficiency state as a consequence of the systemic chemotherapy they receive. The rates of infection as reported by various studies are in the range of 10 – 15 %. Several authors thereby recommend the use of systemic antibiotics during the post-operative period.
The incidence of aseptic loosening is relatively high as reported by various studies. This is attributed to the increase in canal diameter of the bone with growth of the child which thereby results in the loosening of the stem. The studies by Dotan et al. 14 , Tsuda et al. 17 and Zou et al. 18 report the incidence of aseptic loosening as 28 %, 26 % and 15.6 % respectively. The highest incidence, amongst the different sites of use of the endoprosthesis, was seen around the knee with almost similar incidence between the distal femur and proximal tibial implants. In a systematic review by Groundland and colleagues 19 , they compared the outcomes of endoprosthesis in children and adults, they found that children fared well. The study also found that only the children undergoing proximal femoral endoprosthetic reconstruction were at a higher risk of failure. They also noted significantly reduced rates of subsequent amputations compared to the adult population.
The expandible prosthesis provide an attractive option for the management of limb length discrepancy following physeal resection in children. Various studies have shown the effectiveness of the expanding endoprosthesis in this respect. In studies by Tsuda et al. 17 and Zou et al. 18 , the average lengthening carried out was 39.5 mm and 42 mm respectively. Study by Schinhan et al. 16 and Groundland et al. 19 reported greater extent of lengthening in their case series with an average lengthening of 70.5 mm and 84.8 mm respectively. In all these studies, the majority of the cases had a limb length discrepancy of less than 2 cm at final follow up, which can easily be managed by footwear modifications.
Studies report good functional outcomes following endoprosthesis reconstruction in children. The studies utilize the Musculoskeletal Tumor Society (MSTS) score to evaluate the functional outcome which encompass pain, emotional acceptance, function, use of ambulatory support, walking ability and gait. Studies report an average MSTS score of around 82 – 83 % 14,15,16,17,18,19 . The score varied minimally depending on the site of the endoprosthesis use, with best scores obtained for the proximal tibial prosthesis.

The optimal choice of surgical reconstruction following extremity tumor resection in pediatric population remains an enigma. However, the use of endoprosthesis shows good functional outcomes and patient acceptance in addition to reduced rates of amputation following the index surgery. They are associated with high rates of failure and multiple surgeries but these rates are similar to those in the adult population undergoing endoprosthetic reconstruction. The limited availability and high cost also limit the use of expanding endoprosthesis, particularly in low-income countries. In conclusion, endoprosthesis provide a good option for reconstruction in the pediatric population but the long course of follow up and multiple procedures required need to be well understood by the child, parents and the treating surgeon.
The authors state that they have not received any funding towards this.
Conflict of Interest
The authors state that there is no conflict of interest.
- Campanacci M, Bacci G, Bertoni F, et al. The treatment of osteosarcoma of the extremities: twenty year's experience at the Istituto Ortopedico Rizzoli. Cancer. 1981; 48(7): 1569-1581.
- Price CH, Zhuber K, Salzer-Kuntschik M, et al. Osteosarcoma in children. A study of 125 cases. J Bone Joint Surg Br. 1975; 57(3): 341-345.
- Campanacci M, Cervellati G. Osteosarcoma: A review of 345 cases. Ital J Orthop Traumatol. 1975; 1(1): 5-22.
- van Oosterom AT, Voûte PA, Taminiau AH, et al. Combination chemotherapy preceding surgery in osteogenic sarcoma. Prog Clin Biol Res. 1985; 201: 53-57.
- Rosen G, Caparros B, Nirenberg A, et al. Ewing's sarcoma: ten-year experience with adjuvant chemotherapy. Cancer. 1981; 47(9): 2204-2213.
- Copeland MM, Sutow WW. Osteogenic sarcoma: the past, present, and future. Int Adv Surg Oncol. 1979; 2: 177-200.
- Simon MA, Aschliman MA, Thomas N, et al. Limb-salvage treatment versus amputation for osteosarcoma of the distal end of the femur. J Bone Joint Surg Am. 1986; 68(9): 1331-1337.
- Scales JT. Bone and joint replacement for the preservation of limbs. Br J Hosp Med. 1983; 30(4): 220-232.
- Unwin PS, Walker PS. Extendible endoprostheses for the skeletally immature. Clin Orthop Relat Res. 1996; (322): 179-193.
- Schindler OS, Cannon SR, Briggs TW, et al. Stanmore custom-made extendible distal femoral replacements. Clinical experience in children with primary malignant bone tumours. J Bone Joint Surg Br. 1997; 79(6): 927-937.
- Gupta A, Meswania J, Pollock R, et al. Non-invasive distal femoral expandable endoprosthesis for limb-salvage surgery in paediatric tumours. J Bone Joint Surg Br. 2006; 88(5): 649-654.
- Wilkins RM, Soubeiran A. The Phenix expandable prosthesis: early American experience. Clin Orthop Relat Res. 2001; (382): 51-58.
- Groundland JS, Binitie O. Reconstruction After Tumor Resection in the Growing Child. Orthop Clin North Am. 2016; 47(1): 265-281.
- Dotan A, Dadia S, Bickels J, et al. Expandable endoprosthesis for limb-sparing surgery in children: long-term results. J Child Orthop. 2010; 4(5): 391-400.
- Ruggieri P, Mavrogenis AF, Pala E, et al. Outcome of expandable prostheses in children. J Pediatr Orthop. 2013; 33(3): 244-53.
- Schinhan M, Tiefenboeck T, Funovics P, et al. Extendible Prostheses for Children After Resection of Primary Malignant Bone Tumor: Twenty-seven Years of Experience. J Bone Joint Surg Am. 2015; 97(19): 1585-1591.
- Tsuda Y, Tsoi K, Stevenson JD, et al. Extendable Endoprostheses in Skeletally Immature Patients: A Study of 124 Children Surviving More Than 10 Years After Resection of Bone Sarcomas. J Bone Joint Surg Am.2020; 102(2): 151-162.
- Zou C, Zhao Z, Lin T, et al. Long-term outcomes of limb salvage treatment with custom-made extendible endoprosthesis for bone sarcoma around the knee in children. J Orthop Surg Res. 2020; 15(1): 14.
- Groundland JS, Ambler SB, Houskamp LD, et al. Surgical and Functional Outcomes After Limb-Preservation Surgery for Tumor in Pediatric Patients: A Systematic Review. JBJS Rev. 2016; 4(2): 01874474-201602000-00002.
Article Info
- Journal of Orthopedics and Orthopedic Surgery
- Article Type : Mini Review
- View/Download pdf
- DOI : 10.29245/2767-5130/2021/2.1135
Article Notes
- Published on: June 20, 2021
- Limb salvage
- Malignant tumors
*Correspondence:
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- EFORT Open Rev
- v.4(7); 2019 Jul

Advances in tumour endoprostheses: a systematic review
Maria a. smolle.
1 Department of Orthopaedics and Trauma, Medical University of Graz, Austria
Dimosthenis Andreou
2 Department of General Orthopaedics and Tumour Orthopaedics, University Hospital Muenster, Germany
Per-Ulf Tunn
3 Tumour Orthopaedics, HELIOS Klinikum Berlin-Buch, Germany
Andreas Leithner
- Tumour endoprostheses have facilitated limb-salvage procedures in primary bone and soft tissue sarcomas, and are increasingly being used in symptomatic metastases of the long bones.
- The objective of the present review was to analyse articles published over the last three years on tumour endoprostheses and to summarize current knowledge on this topic. The NCBI PubMed webpage was used to identify original articles published between January 2015 and April 2018 in journals with an impact factor in the top 25.9% of the respective category (orthopaedics, multidisciplinary sciences).
- The following search-terms were used: tumour endoprosthesis, advances tumour endoprosthesis, tumour megaprosthesis, prosthetic reconstruction AND tumour. We identified 347 original articles, of which 53 complied with the abovementioned criteria.
- Articles were categorized into (1) tumour endoprostheses in the shoulder girdle, (2) tumour endoprostheses in the proximal femur, (3) tumour endoprostheses of the knee region, (4) tumour endoprostheses in the pelvis, (5) (expandable) prostheses in children and (6) long-term results of tumour endoprostheses.
- The topics of interest covered by the selected studies largely matched with the main research questions stated at a consensus meeting, with survival outcome of orthopaedic implants being the most commonly raised research question.
- As many studies reported on the risk of deep infections, research in the future should also focus on potential preventive methods in endoprosthetic tumour reconstruction.
Cite this article: EFORT Open Rev 2019;4:445-459. DOI: 10.1302/2058-5241.4.180081
Introduction
Endoprosthetic reconstruction in orthopaedic oncology has evolved over the last 30 to 40 years, with novel endoprosthetic systems and solutions developed constantly. Endoprosthetic reconstruction has made limb-salvage surgery possible in many cases, leading to a steady decrease in the rate of amputations. 1 , 2 Long-term results of tumour endoprostheses are important to evaluate functional outcome for patients, possible complications and implant survival.
The main objective of the present review was to identify all major studies dealing with endoprosthetic reconstruction in tumour surgery published between January 2015 and 10 June 2018. The specific focus was on long-term results and functional outcome, complications as well as recent advances and novel concepts. Within the last three years, 53 studies have been published in top-ranking journals dealing with tumour endoprostheses in orthopaedic surgery. Most studies came from China ( n = 12), followed by the United States ( n = 10) and the United Kingdom ( n = 6). International Orthopedics was the journal with the most publications on the topic ‘advances in tumour endoprostheses’.
Materials and methods
All studies published in PubMed between January 2015 and 10 June 2018 were included in the study, after applying the specific search terms listed below. Original articles dealing with tumour endoprostheses published in English in PubMed-indexed journals with an impact factor ranking them in the top 25.9% in the categories multidisciplinary sciences or orthopaedics were considered to be eligible. This number was calculated by dividing the total number of publications in the respective categories through the rank of the journal of interest. Literature research was performed until 10 June 2018.
The following search-terms were used to identify studies on advances in tumour endoprostheses: advances tumour endoprostheses, tumour endoprosthesis, tumour megaprosthesis, prosthetic reconstruction AND tumour. Reviews, case reports, duplicates and meta-analyses were excluded manually. Altogether, 347 original studies were identified based on the four abovementioned search terms within the predefined time period. In a first step, 177 articles were excluded from further analyses with study titles not in the scope of the present review, leaving 170 articles potentially eligible. Following the review of the abstract, another 51 articles were excluded due to them not being in the scope of this review and 20 further articles due to duplication. From the remaining 100 articles, 53 had an impact factor ranking them in the top 25.9% either in the category ‘orthopaedics’ or ‘multidisciplinary sciences’ ( Fig. 1 ). All articles with ‘case report’ in the title were excluded in the first step of article selection.

Flow diagram showing selection of articles
From all articles finally eligible for this study, full-text articles were either downloaded from the respective journal’s website or requested via the author’s own online library. As all necessary information could be extracted from the full-text articles, authors from specific studies were not personally contacted. The majority of the studies were retrospective in design, with only one study with a clear prospective aim.
All articles finally eligible were grouped into six categories: (1) tumour endoprostheses in the shoulder girdle, (2) tumour endoprostheses of the proximal femur, (3) tumour endoprostheses in the knee region, (4) tumour endoprostheses in the pelvis, (5) (expandable) prostheses in children and (6) long-term results of tumour endoprostheses.
Primary literature research was performed by the first author of the study (MAS), including study selection over the three steps as mentioned above. Those studies finally eligible for the study were reviewed by both the first (MAS) and senior author (AL).
As case reports were excluded from the final analysis, very novel – but to date not well established – reconstructive methods using tumour endoprostheses may not be included in this review. Furthermore, we set the journal’s rating due to the impact factor to < 25.9%, thus potentially excluding studies in small patient cohorts. We only included journals ranking in the top 25.9% of their respective category (this cut-off also includes International Orthopaedics ) in order to report results of studies with a presumably high impact on readers (see Fig. 2 for the distribution of journals in the respective categories split by impact factor). No additional analyses were performed. The review protocol can be accessed by contacting the corresponding author (MAS).

Number of publications split by impact factor in the respective six categories
1) Tumour endoprostheses in the shoulder girdle
Seven studies were identified dealing with tumour endoprostheses around the shoulder girdle ( Table 1 ). In a study by Maclean et al, the outcome of eight patients receiving the Bayle Walker (Stanmore® Implants Worldwide Ltd, Elstree, England, United Kingdom) reversed polarity linked shoulder endoprosthesis was analysed. 3 In half of patients, a Trevira® tube was used to potentially enhance shoulder stability. 3 The mean Musculoskeletal Tumour Society (MSTS) score in this patient cohort was 60.0%. 3 This is comparable to a mean MSTS score of 66.7% reported by Schmolders et al in a study including 30 patients receiving a MUTARS® anatomical prosthesis (implantcast GmbH, Buxtehude, Germany) for intra-articular resections of the proximal humerus. 4 In this cohort, again half of patients received a Trevira® tube. 4 Of note, the authors discovered no difference between the Trevira® and non-Trevira® groups with regard to range of motion (ROM), being on average 38° flexion, 35° abduction and 15° external rotation. 4 This is comparable to the 36° abduction and 39° shoulder flexion as reported by Wang et al in a cohort of 18 patients treated with endoprosthesis (LDK, Co., Ltd, Haidian, Beijing, China) polypropylene mesh composite (PROLENE® light mesh, Ethicon) after bone tumour resection of the proximal humerus. 5 In that study, a mean MSTS score of 66.7% at last follow-up was reported. 5 In a similar study by Tang et al, mesh-suspended proximal humeral endoprostheses (LARS (Laboratoire d’Application et de Recherche Scientifique, Arc-sur-Tille, France) wrapped around the shaft of the endoprosthesis; n = 14) for malignant tumours were compared with proximal humeral endoprostheses with soft tissue reconstruction only ( n = 15). 6 Of note, a significantly better MSTS score was observed in patients with mesh reconstruction than in the soft tissue reconstruction only group (80.0% vs. 66.7%; p = 0.001). 6 Moreover, none of the patients in the mesh group showed proximal migration of the prosthesis, compared with five of 15 patients without mesh reconstruction (33.3%; p = 0.042). 6 This number is similar to the 33.3% of shoulder instability observed by Fujibuchi et al, although these patients had received a proximal humeral endoprosthesis wrapped in PMKM (Marlex mesh or Bard mesh, Warwick, RI, USA) fixed to soft tissues (4/12). 7 On the other hand, the same mesh fixed to bone resulted in less shoulder instability (0/9) and better shoulder flexion (65° vs. 35° in the soft tissue suspension group; no p-value provided by authors). 7
Tumour endoprostheses in the shoulder girdle
In another study by Min et al, the functional outcome of patients with scapular hemiarthroplasty following total scapulectomy for tumours was investigated. 8 The ROM, with average shoulder abduction of 45.3° and flexion of 65.7°, was relatively better than in the abovementioned studies on proximal humeral resections followed by endoprosthetic reconstruction. 8 Moreover, rotator-cuff reconstruction was associated with a better postoperative function and improved MSTS score. 8
Regarding complications of proximal humeral endoprostheses in tumour surgery, Schmolders et al observed six complications in 30 patients (20.0%) treated with a MUTARS® endoprosthesis, of which one was related to deep infection (3.3%). 4 This is less than the 12.0% infection rate reported by Meijer et al in a large study on 150 patients with proximal humeral reconstruction for tumours. 9 In their study, osteoarticular allografts ( n = 45) were not associated with a higher infection rate (11%) in comparison to endoprostheses ( n = 85; 14% infection rate) or allograft prosthetic composites ( n = 20; 10% infection rate). 9
To summarize, MSTS scores in tumour endoprostheses of the shoulder girdle range between 60.0% and 80.0%, depending on the type of reconstruction. A shoulder flexion up to 65° has been reported in one study where a synthetic mesh was fixed to the bone, thus improving shoulder stability.
2) Tumour endoprostheses in the proximal femur
Eight studies dealing with tumour endoprostheses of the proximal femur could be included in our review ( Table 2 ). The largest study was performed by Henderson et al, comprising 527 patients with proximal femoral arthroplasty for primary bone tumours (benign and malignant) as well as metastases. 10 The authors observed postoperative instability in 20 patients (4.0%), developing after a mean of 35 days. 10 Of note, no capsular repair was not associated with a reduced rate of instability, whilst advanced age, female gender and primary bone tumours were risk factors for instability. 10 The only protective factor against hip instability was a posterolateral approach. 10 Moreover, the authors concluded that a posterolateral approach, together with application of a synthetic device for reconstruction of the soft tissues and a hemiarthroplasty should be best chosen to reduce instability. 10 Corresponding to this, Du et al investigated hip instability in 58 patients with total femoral replacement for sarcoma. 11 In 12 patients, a LARS artificial ligament was additionally wrapped spirally around the proximal end of the prosthesis, resulting in a significantly lower hip dislocation rate as compared with conventional soft tissue reconstruction. 11 Moreover, the infection rates were comparable between LARS-augmented prostheses and conventional reconstruction (8.3% vs. 10.9%; p = 0.529). 11 These infection rates are less than the 20.0% observed by Gorter et al in 10 patients treated with push-through total femoral endoprostheses. 12 However, this system allows preservation of parts of the femur as well as its muscle attachments, thus potentially resulting in a better postoperative function. 12 Interestingly, though, a mean MSTS score of 64.0% was achieved in their cohort, in comparison to 72.3% in the group by Du et al, where additional reconstruction with a LARS band significantly increased the postoperative MSTS score from 70.4% to 80.0%. 11 , 12 Moreover, the authors observed that simple re-attachment of the gluteus maximus to the LARS band does not improve active ROM, whilst re-attachment of other external rotators (i.e. gemellus, obturator, piriformis, quadratus femoris) may improve external rotation. Of note, Li et al observed a mean MSTS score of 93.0% for patients treated with hemipelvic and proximal femoral endoprostheses, although significantly more structures had to be sacrificed in their procedures. 13
Tumour endoprostheses in the proximal femur
With regard to postoperative function, Hobusch et al investigated the functional outcome of 16 patients with proximal femoral reconstructions for bone sarcomas and a minimum follow-up of five years. 14 Prior to surgery, 14 of 16 patients (87.5%) were able to do sports. At the mean latest follow-up of 18 years (range 5–27 years), 11 of these patients had resumed sporting activities (68.8%). 14
Another question that arises when dealing with proximal femoral endoprostheses is the durability of hemiarthroplasty in view of chondro-osseous wear-off. With regard to this, Houdek et al investigated the outcome of hemiarthroplasty for pathological femoral fractures in 199 patients. 15 After a mean follow-up of four years, two patients required conversion to a total hip arthroplasty (1.0%). 15 Reasons for conversion may be prosthetic head protrusion, as observed by Drexler et al in nine out of 65 patients (13.8%) treated with bipolar proximal femoral endoprostheses for tumours. 16 In their cohort, three prostheses had to be converted to total hip replacement after a mean follow-up of 9.1 years (range: 2.0 to 11.8 years; 4.6%). 16 Interestingly, according to Stevenson et al, only eight out of 49 patients treated with unipolar ( n = 64) and bipolar ( n = 36) endoprostheses without acetabular resurfacing showed acetabular wear after a minimum follow-up of one year, not exceeding Baker Grade 2. 17
In tumours involving the hip joint, extra-articular resection may become necessary, as described by Li et al in a study involving 18 patients. 13 Modular hemipelvic prostheses and custom-made or modular proximal femoral endoprostheses were used for reconstruction. 13
Conclusively, the better the stability of a proximal femoral implant, the better the postoperative functional outcome can be expected. Moreover, bipolar reconstruction is justified in tumour patients, as acetabular wear can be expected to be minimal.
3) Tumour endoprostheses in the knee region
Nineteen articles were identified dealing with tumour endoprostheses around the distal femur and proximal tibia ( Table 3 ). The largest study identified was that of Pala et al, including 687 distal femoral modular tumour endoprostheses implanted between 1983 and 2010. 18 Of these, the majority were fixed hinge ( n = 491), whilst 196 implants were rotating hinge. 18 Altogether, 27.0% of patients ( n = 185) developed complications, with no difference between the rotating hinge and fixed hinge systems. 18 However, all component breakages occurred in prostheses with a rotating hinge system, whilst there was no difference in rate of aseptic loosening (5.9% vs. 2%; p = 0.55) or infection (8.9% vs. 6.6%, p = 0.237) between fixed-hinge vs. rotating-hinge. 18 Of note, patients with a rotating hinge system had a significantly better mean MSTS score (82.7% compared with 76.3%). 18 This MSTS score is comparable to the 76.3% reported by Zhang et al in a study investigating the outcome of 108 patients with endoprosthetic rotating hinge knee replacement for osteosarcoma. 19 Implant failures occurred in 21 patients (19.4%) after a mean follow-up of 4.4 years, most commonly due to infection. 19 Of note, though, an overall incidence rate of complications of 41.7% was observed in the entire cohort, including peroneal nerve palsy, local recurrences, periprosthetic fracture, joint instability, wound healing disorders, aseptic loosening, mechanical dysfunction, prosthetic infection and breakage of the prosthesis. 19 Moreover, the authors observed a slightly better functional outcome in patients with tumours located in the distal femur in comparison to the proximal tibia, which could be partly related to the fact that proximal tibial resection often necessitates reconstruction of the extensor mechanism, thus influencing postoperative function. 19 These results are contradictory to the observations made by Pala et al in a study on 247 rotating-hinge GMRS knee prostheses (Stryker Inc., Rutherford, NJ, USA) implanted for bone tumours, where there was no difference in MSTS score between distal femoral and proximal tibial tumours (mean MSTS score 84.0%). 20 An even better MSTS score was reported by Wang et al in a study on 41 patients reconstructed with allograft-prosthesis composites and rotating-hinge knee prostheses for tumours, being 93.4% on average. 21
Tumour endoprostheses of the knee region
The overall failure rate of the GMRS prosthesis as evaluated by Pala et al was 29.1% (72/247), with infections being most common ( n = 23), followed by soft tissue failure ( n = 21). 20 These rates are comparable with those reported by Bus et al in a study on 101 patients with 110 reconstructions with a MUTARS® implant of the distal femur or proximal tibia for malignancy. 22 Of 63 complications observed (57.3%), 14 were due to infection and 15 due to structural failure. 22 Also in the cohort of Holm et al, most complications observed in this study on 50 patients with megaprostheses of the knee joint and total femur were due to deep infection ( n = 19). 23 Additionally, in the cohort by Hardes et al, the most common complication in 98 patients treated with a MUTARS® endoprosthesis of the proximal tibia was due to infection ( n = 15). 24 Moreover, eight of these patients ultimately required an amputation. 24
Twenty-seven stem fractures (12.2%) were reported by Hauer et al in a study involving 221 patients treated with the Kotz Modular Femoral Tibial Reconstruction System (KMFTR®; Stryker Inc., Rutherford, NJ, USA). 25 Notably, stem fractures were associated with a significantly smaller stem diameter and a significantly longer extramedullary component. 25 Therefore, augmented systems with osteoarticular allografts may be used, as described by Qu et al in a study on 29 patients treated with cortical strut bone grafts combined with long-stem endoprosthetic reconstruction in the knee joint. 26 In their study, bone healing was observed in 23 of 29 patients reconstructed with cortical strut allografts in addition to tumour endoprostheses after a mean of 3.9 years. 26
In patients receiving endoprostheses or osteoarticular allografts in the proximal tibia, mean MSTS scores of 88.6% and 91.7% were observed by Albergo et al. 27 Interestingly, failure rates were higher in the osteoarticular allograft group as compared with the group of patients reconstructed with endoprostheses (18.0% vs. 27.0% at five years). Moreover, mechanical failure was the most common reason for revision in patients with endoprostheses, whilst infections were the main cause in the osteoarticular allograft group. 27
Regarding periprosthetic joint infections, the use of silver-coated implants in order to minimize infection risk is of interest. In the study by Hardes et al, the infection rate was lower in 56 silver-coated implants of the proximal tibia in comparison to 42 titanium-based implants in the same body region after a median follow-up of 8.2 years (8.9% vs. 16.7%). 28 Additionally, only one patient in the silver-coated implant group had to undergo an amputation, as compared with three patients in the titanium-based group. 28
With regard to osseointegration of tumour endoprostheses, Liang et al compared the functional and oncological outcomes of 62 cases with uncemented tibial fixation and 58 cases with cemented tibial fixation in distal femoral replacement for bone tumours. 29 Osseointegration was observed in 64.3% of patients with an uncemented system. Moreover, the surgical time was reduced by 26 minutes on average when implanting an uncemented system, prompting the conclusion that in tumour patients with a poor general condition uncemented systems are likewise suitable with the advantage of shortened surgery time. 29 There was no difference in revision rates between cemented and uncemented systems (9.6% vs. 5.4%, p = 0.399).
Another interesting finding regarding the postoperative function of tumour endoprostheses around the knee joint was reported by Etchebehere et al in a study involving 108 patients with distal femoral endoprosthetic replacement for tumoural ( n = 107) and non-tumoural reasons ( n = 1). 30 They investigated the relative patellar height by applying the Insall-Salvati ratio (ISR) as well as the Insall-Salvati patellar tendon insertion ratio (PTR) directly postoperatively and at last follow-up. 30 Of note, the patellar height was not associated with ROM, anterior knee pain or extension lag, but generally decreased significantly after the operation (from 1.45 to 1.4 for the PTR (ratio of two lines drawn on lateral radiographic images of the knee)). 30
Regarding patellar resurfacing, Etchebehere et al analysed the outcomes of 48 patients receiving tumour endoprostheses of the distal femur or proximal tibia with patellar resurfacing and 60 patients without patellar resurfacing. 31 There was no difference in anterior knee pain between the groups. 31 Moreover, anterior knee pain did not significantly alter extensor lag, range of motion, reoperation or complication rates. 31 Although complications in general were similar between the resurfaced and non-resurfaced groups, peripatellar calcifications were more frequently seen in the resurfaced group. 31 Nevertheless, mean MSTS scores of 81% and 71% were observed for the non-patellar resurfacing and patellar resurfacing-groups respectively, which was not statistically significant (p = 0.30). 31 Consequently, the decision in favour of or against patellar resurfacing should be made individually in each case.
Another interesting study investigated the postoperative mobility in patients receiving allografts ( n = 15) or megaprostheses ( n = 6) for malignant tumours of the knee region. 32 An allograft augmented with a fibula graft was implanted in cases where more than 2 cm above the knee joint could be kept. According to Pesenti et al, there was no difference in gait pattern between the groups, albeit in the megaprosthesis group, a decreased knee flexion during the load and stance phase was observed. 32 Moreover, the Gait Deviation Index (GDI), was significantly lower in both groups as compared to a control group. 32 Therefore, sparing of the epiphysis may not significantly increase the functional outcome in patients with tumours around the knee joint.
With regard to functional outcomes, Lang et al investigated the postoperative ability of patients to perform sports following reconstruction with modular tumour endoprostheses around the knee joint. 33 Prior to implantation, 24 of 27 (89.0%) patients were able to do sports, as were 24 patients at last follow-up (89.0%). Importantly, the rate of sporting activity increased steadily over the years, from 33.0% over 74.0% to the abovementioned 89.0% at an average follow-up of 11 years. 33 Even revision surgeries that became necessary in 14 patients had no influence on the patients’ activity levels. 33
One study elaborating the outcome of tumour patients with periprosthetic fractures was performed by Barut et al. 34 They investigated 17 patients with 18 periprosthetic fractures following endoprosthetic replacement for tumours around the knee joint. 34 Sixteen of these patients underwent surgery, with only one requiring another implant. Overall probability of failure following periprosthetic fracture for any reason was 55.0% at 10 years. 34
Another problem in reconstruction with (tumour) megaprostheses is the huge bone loss in case of failed treatment, limiting further reconstructions. With regard to this, Zimel et al have discovered low rates of mechanical failure in 27 patients treated with the Compress® Compliant Prestress Device (Zimmer Biomet, Warsaw, IN, USA) for failed reconstruction of the distal femur for tumoural ( n = 26) and non-tumoural ( n = 1) indications. 35 The cumulative incidence of mechanical failure was 11% at five years and did not increase thereafter. A median MSTS score of 90.0% was reported, which is surprisingly high. 35 Noteworthy, the Compress® Compliant Prestress Device requires few bone contacts in the shaft, but has a shallow learning curve.
Contrary to this, Goulding et al have investigated the outcome of a compressive osseointegration endoprosthesis (Compress® Compliant Prestress Device; Zimmer Biomet, Warsaw, IN, USA) coupled with modular prostheses in nine patients with a total of 13 endoprosthetic replacements and discovered a high complication rate. 36 The revision rate of 50% in 12 implants with a follow-up > 24 months was relatively high. 36
4) Tumour endoprostheses in the pelvis
Four studies were focused on tumour endoprostheses and prosthetic reconstruction in the pelvis ( Table 4 ). Two of these described the results of 3D-printed pelvic endoprostheses for large bone defects following wide tumour resection, whilst the third investigated the outcome with the Integra® ice-cream cone prosthesis (Lépine, Genay, France) and the fourth study reported the results on a custom-designed hemipelvic prosthesis.
Tumour endoprostheses in the pelvis
In the Integra® ice-cream cone study by Issa et al, 24 patients with periacetabular malignant tumours – necessitating Type II ± Type III resections – were followed-up for a mean of 4.1 years. 37 Mean MSTS score was 72.0% at last follow-up. 37 However, complications were observed in 14 patients (58.3%), with infections being most common ( n = 4). 37 In comparison to periacetabular resections, the mean MSTS scores for hemipelvic resections were relatively lower in the other studies, ranging from 53.9% to 64.0%. 38 , 39 The largest of the three studies by Liang et al investigating the outcome after hemipelvic resection involved 35 patients reconstructed with 3D-printed pelvic endoprostheses. 38 Nine patients (25.7%) developed complications (seven wound healing deficits, two hip dislocations), albeit no deep infection was observed, after a median of 20.5 months. 38 In another study by Wang et al, the outcomes of 11 patients receiving personalized 3D-printed hemipelvic endoprostheses were investigated. 39 Comparable to the study by Liang et al, one patient presented with delayed wound healing and two patients had hip dislocation. 40 The mean MSTS score at last follow-up was 64.0%, which is comparable with the 53.9% observed by Wang et al in six patients receiving hemipelvic prostheses for bone tumours. 39 The authors did not only investigate the subjective outcome, but also performed stress tests with patients sitting or standing on two feet. 39 Whilst stress distribution in the normal pelvis was mainly located around the acetabulum, arcuate line, sacroiliac joint and sacral midline both when sitting or standing, the stress distribution moved to the connecting rods of the acetabular component and the proximal segment of the pedicle rods in patients with reconstructions. 39 This highlights that peak stresses are generally higher in the reconstructed pelvis, which should be considered in the development of new implants.
5) (Expandable) prostheses in children
Seven original articles were identified dealing with expandable tumour endoprostheses in young patients ( Table 5 ). Gilg et al investigated 51 custom-made growing prostheses (Juvenile Tumour System, Stanmore® Implants Worldwide Ltd, Elstree, England, UK) used for reconstruction of primary bone sarcoma of the femur and proximal tibia in 50 children between 2003 and 2014. 41 Three- and five-year revision-free survival were 81.7% and 61.6%, with deep infections (Henderson Type IV) being most common ( n = 10). 41 In another study by Arteau et al, distal femoral growing prostheses in 23 children were investigated (Repiphysis® (Wright Medical Technology Inc., Arlington, TN, USA)) in 14 patients, custom Biomet® prosthesis (Zimmer Biomet, Warsaw, IN, USA) in eight, Juvenile Tumour System (Stanmore® Implants Worldwide Ltd, Elstree, England, UK) in one patient), with specific focus on leg-length discrepancy. 42 In 65% of patients, the proximal tibial epiphysis – although intact except for the insertion point of the tibial stem – grew less over time than the contralateral epiphysis. 42 Interestingly, in one patient an overgrowth of the proximal physis was observed. 42 Corresponding to this, Cipriano et al reported the outcomes of the Repiphysis® (Wright Medical Technology Inc., Arlington, TN, USA) expandable prosthesis in 10 young patients with osteosarcoma. 43 Altogether, they observed 37 implant-related complications (amounting to an average of 3.7 complications per patient), requiring 15 revision surgeries. 43 Slightly fewer complications were reported by Schinhan et al on the identical system, with a mean of 2.6 complications per patient. 44 Each patient in this cohort underwent a mean of 4.4 lengthening procedures (invasive, minimally invasive and non-invasive) with an average limb elongation of 70.8 mm. 44 This is more than the 42.7 mm reported by Gilg et al and the 39 mm observed in the study by Staals et al. 41 , 45
(Expandable) prostheses in children
Interestingly, mean MSTS scores of 88.3% and 87.8% were observed in the study by Gilg et al and Schinhan et al, 41 , 44 compared to 64.0% and 67% reported by Staals et al and Cipriano et al. 43 , 45 In the latter three studies, the Repiphysis ® system was used, where no clear tendency towards a poorer outcome can be observed.
Additionally, Torner et al reported on a mean lengthening of 36.4 mm in seven patients receiving a MUTARS® Xpand Growing Prosthesis (implantcast GmbH, Buxtehude, Germany) in the distal femur ( n = 6) and proximal femur ( n = 1), and a mean MSTS score of 87.7%. 46 Notably, none of the patients in this cohort developed any local recurrence and one deep infection was treated by arthroscopy and antibiotics. 46 On the other hand, seven out of 50 patients (14.0%) in the cohort by Gilg et al finally underwent amputation due to infection ( n = 4) or local recurrence ( n = 3). 41 A lower rate was observed by both Arteau et al, with two out of 23 patients undergoing amputation for local recurrence (8.7%), 42 and Schinhan et al, with 2 out of 71 patients (2.8%) undergoing amputation, again due to local recurrences. 44
Another technique that may be used in reconstruction of large bone defects, especially in children, are resurfaced allograft-prosthetic composites, as described in the study by Campanacci et al including 19 young patients treated with this method for bone tumours of the proximal tibia. 47 The mean implant survival was 68 months, with major complications including six allograft fractures, two non-unions and one infection. 47 The most common complication was leg-length discrepancy that could be lowered to a mean of 1.9 cm at latest follow-up following contralateral epiphysiodesis. The mean MSTS score was 73.3% in this cohort. 47
6) Long-term results of tumour endoprostheses
Altogether, six articles published between 2015 and 2018 meeting the abovementioned criteria were dealing with the long-term outcome of tumour endoprostheses in primary and metastatic bone disease as well as soft tissue sarcomas ( Table 6 ). Regarding very long-term complications, Grimer et al observed in their cohort of 230 patients treated with growing ( n = 46) and non-growing ( n = 184) tumour endoprostheses in the knee joint, hip, humerus and pelvis 2.7 further operations on average (equivalent to 610 additional surgeries), most commonly aseptic loosening ( n = 112), re-bushing ( n = 40) and deep infection ( n = 25) after a mean follow-up of 29.4 years. 48 On the other hand, Capanna et al observed in their cohort of 200 patients treated with the Megasystem C (Waldemar LINK® GmbH & Co. KG, Hamburg, Germany) for tumours of the hip and knee 71 failures in 58 implants, most commonly due to mechanical reasons (59.2% of all failures, including aseptic loosening, soft tissue failure and structural failure). 49
Long-term results of tumour endoprostheses
In order to minimize the risk of implant fractures, extra-cortical plates may be used for augmentation of short-stemmed endoprostheses, as described in the study by Stevenson et al. 50 In their cohort of 37 patients reconstructed with tumour endoprostheses augmented by extra-cortical plates for large resections exceeding > 70.0% of the bone’s original length, there was no difference in implant survival when compared to standard stemmed controls at any site (humerus, hip and knee). 50
Another important topic regarding long-term outcome of tumour endoprostheses is the postoperative mobility of patients. In the study by Bernthal et al, the postoperative mobility of 24 patients treated with tumour endoprostheses in the hip ( n = 7) and knee ( n = 17) was analysed using gait analysis and O2-consumption. 51 According to their results, the median O2-consumption was not significantly different in the tumour prosthesis group as compared with healthy controls. 51 Interestingly, patients with proximal tibial replacements had reduced knee extension (reduced by 84%) and flexion strength (reduced by 35%) in comparison to patients in the other reconstruction groups, which is comparable to the results of the study by Pesenti et al. 32
Very few studies were discovered in the present review dealing with smaller joints such as the ankle and the wrist. In the study by Wang et al, the outcome of 10 patients treated with unipolar prostheses after resection of Grade III giant cell tumours in the distal radius was investigated. 52 In their cohort, six out of 10 patients developed a complication, including two wrist subluxations and one aseptic loosening. 52 In two patients pain associated with the implant was still present at last follow-up.
The outcome of intracalary implants in the femur ( n = 21), humerus ( n = 18) and tibia ( n = 5) was reported by Benevenia et al. 53 In total, 13 complications were observed in 44 patients, most commonly due to structural failure ( n = 6). 53 Of note, the majority of complications were observed in implants of the femur. 53 A mean MSTS score of 77.0% was observed for all locations, with cemented implants being associated with a better score. 53
In summary, long-term outcomes following endoprosthetic reconstruction in tumour surgery are relatively good in terms of functionality. However, complications occur frequently and do not only pose a threat to the treating team but also significantly affect a single patient’s perspective on postoperative outcome.
In the studies compiled in the present review, the authors focused on functional outcomes, complications and long-term follow-up of tumour endoprostheses used in orthopaedic oncology. Regarding functional outcomes – usually evaluated with the MSTS score – these did not significantly differ between studies dealing with identical body regions. However, there was a tendency towards poorer functional outcomes the more aggressive the resections had been and the larger the used implants were. Moreover, the larger the implants, the more frequently complications were observed. Specifically, infections posed a major problem in endoprosthetic reconstruction with megaprostheses. Of note, only a few studies were identified dealing with preventive procedures to lower the risk of infection in tumour surgery, e.g. the use of silver-coated implants. In this field, further in-depth research should be performed in order to lower the risk of infection, which often leads to revision and implant explantation with major consequences for the patient. Another important issue in endoprosthetic reconstruction with large tumour endoprostheses is the fact that patients are getting older despite staying more active, wherefore the risk for periprosthetic fractures is raised. Of note, only one study was identified in the present review dealing exclusively with periprosthetic fractures around tumour endoprostheses. 34
There are some limitations in the present review. As we excluded studies journals with an impact factor ranking > 25.9% in the respective category, results on smaller patient cohorts or from small-volume centres may not have been discussed. Moreover, as we excluded all case reports, very novel advances in endoprosthetic reconstruction of tumour endoprostheses may not have been considered.
The long-term results of tumour endoprostheses used in orthopaedic oncology depend on several factors, including the postoperative functionality, patient satisfaction and the rate of complications.
Over the last three years, 53 studies have been published dealing with tumour endoprostheses. However, significant novelties were lacking amongst these studies. On the other hand, many studies focused on long-term results on already established reconstructive procedures, which is equally important with regard to clinical applicability of specific reconstructive techniques.
In the next few years, studies should also focus on prevention of frequently observed complications – especially deep infections of tumour endoprostheses and periprosthetic fractures, as these issues pose a major threat to orthopaedic surgeons and treated patients.
ICMJE Conflict of interest statement: DA reports honorarium and travel expenses for a lecture, unrelated to this study from Lilly and travel expenses for a meeting unrelated to this study from Implantcast GmbH.
AL reports grants/grants pending paid to his institution outside the submitted work from Metronic, Johnson & Johnson, Alphamed.
All other authors declare no conflict of interest.
Funding statement
Although none of the authors has received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article, benefits have been or will be received but will be directed solely to a research fund, foundation, educational institution, or other non-profit organization with which one or more of the authors are associated.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 29 July 2021
Recent trends in revision knee arthroplasty in Germany
- Markus Rupp 1 ,
- Nike Walter 1 ,
- Edmund Lau 2 ,
- Michael Worlicek 1 ,
- Steven M. Kurtz 3 &
- Volker Alt 1
Scientific Reports volume 11 , Article number: 15479 ( 2021 ) Cite this article
2968 Accesses
16 Citations
14 Altmetric
Metrics details
- Epidemiology
- Medical research
We aimed to answer the following questions: (1) How did numbers of revision knee arthroplasty procedures develop in Germany over the last decade compared to primary TKA? (2) How high was the percentage of septic interventions in knee prosthesis revisions? (3) Which treatment strategy was chosen for surgical treatment of knee PJI? Revision arthroplasty rates as a function of age, gender, infection and type of prosthesis were quantified based on Operation and Procedure Classification System codes using r evision knee arthroplasty data from 2008 to 2018, provided by the Federal Statistical Office of Germany (Destatis). In 2018, a total number 23,812 revision knee arthroplasties were performed in Germany, yielding an overall increase of 20.76% between 2008 and 2018. In comparison, primary TKA procedures increased by 23.8% from 152,551 performed procedures in 2008 to 188,866 procedures in 2018. Hence, 12.6% of knee arthroplasties required a revision in 2018. Septic interventions increased by 51.7% for all revisions . A trend towards higher numbers in younger patients was observed. Compared to 2008, 17.41% less DAIR procedures were performed, whereby single-stage and two- or multi-stage change increased by 38.76% and 42.76% in 2018, respectively. The increasing number of revision knee arthroplasty in Germany, especially in younger patients and due to infection, underlines the need for future efforts to improve treatment strategies to delay primary arthroplasty and avoid periprosthetic joint infection.
Similar content being viewed by others

A retrospective analysis of trends in primary knee arthroplasty in Germany from 2008 to 2018

Improvement in fast-track hip and knee arthroplasty: a prospective multicentre study of 36,935 procedures from 2010 to 2017
Older age increases the risk of revision and perioperative complications after high tibial osteotomy for unicompartmental knee osteoarthritis
Introduction.
The introduction of joint arthroplasty is one of the greatest achievements of modern medicine. Joint arthroplasty is one of the most efficacious and cost-effective surgical procedure. Since the 1960s, it has led to a significant reduction in pain and movement restrictions, thus significantly improving patients' quality of life 1 , 2 . This success and the demographic development in the industrialized nations have led to a significant increase in the number of total hip and total knee arthroplasties (TKA) which is predicted to continue in the next decades 3 , 4 , 5 , 6 . Especially an increasing number of primary knee arthroplasties in younger patients leads us to anticipate an increasing number of revision surgeries in the coming years. Recently, projections of revision knee arthroplasties based on numbers of past knee revision arthroplasties have been published 7 , 8 , 9 . For the U.S. an increase in revision TKA is predicted between 78 and 182% within the next 10 years 8 . Although these data suggest that the expected increase in revision arthroplasty is likely to occur due to the significant increase in primary TKAs, estimation of future data based on recent revision arthroplasty numbers is subject to significant limitations. For instance, the risk of periprosthetic joint infection (PJI) decreases with increasing prosthesis lifetime, while aseptic loosening increases 10 , 11 . In addition, the revision rate depends on the number of patients living with an endoprosthesis. Besides, patients´ mortality rate as well as prosthesis lifetime would have to be taken into account in order to make a reliable statement about future revision rates. Since these different aspects cannot be reconstructed with certainty while relying on a large number of registry data, a detailed analysis of recent numbers seems to be beneficial to estimate future demands and to foresee developments which could be influenced by adaption of prevention and therapeutic measures.
We have therefore aimed to answer the following questions for the Germany population: (1) How did numbers of revision knee arthroplasty procedures developed over the last decade compared to primary TKA? (2) How high was the percentage of septic interventions in knee prosthesis revisions? (3) Which therapy strategy (debridement antibiotics implant retention (DAIR), single-stage change or two- or multi-stage change) was chosen for surgical treatment of knee PJI?
Material and methods
Revision knee arthroplasty data from 2008 to 2018 was provided by the Federal Statistical Office of Germany (Destatis) consisting of annual surgical procedures performed in medical institutions of all 16 German federal states. Surgery and procedure keys (Operation and Procedure Classification System codes) were used to identify all revision knee arthroplasties in patients aged 20 years or older, regardless of the underlying disease or injury. In particular, the Operation and Procedure Classification System code “5-823, revision, exchange and removal of an knee joint endoprosthesis “ was used (Table 1 ). A detailed breakdown of these data by age group and gender was performed. Surgical strategies were retrieved by evaluating the Operation and Procedure Classification System codes in combination with ICD-10 diagnosis codes. In particular, the ICD-10 code “T84.5, infection and inflammatory reaction by a joint endoprosthesis” was used for septic cases and “T84.04, mechanical complication of a joint endoprosthesis” for aseptic cases. To compare revision rates to numbers of primary TKA, the Operation and Procedure Classification System code “5–822, implantation of an endoprothesis of the knee joint” was used. Prevalence rates were calculated based on Germany’s historical populationaged 20 years or older provided by Destatis. Data were analyzed using the statistical software SPSS Version 26.0 (IBM, SPSS Inc. Armonk, NY, USA).
In 2018, a total number 23,812 revision knee arthroplasties were performed in Germany, yielding an overall increase of 20.76% between 2008 and 2018 (Table 2 ). In comparison, primary TKA procedures increased by 23.8% from 152,551 performed procedures in 2008 to 188,866 procedures in 2018. Hence, 12.6% of knee arthroplasties required a revision in 2018 (− 0.3% change compared to 2008) (Fig. 1 ).
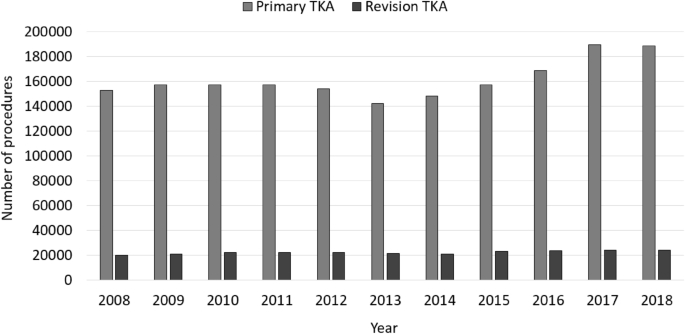
Performed revision knee arthroplasty procedures in comparison to performed primary knee arthroplasty procedures from 2008 through 2018.
In general, more female than male patients were affected, whereas the numbers of male patients increased between 2008 to 2018 (Fig. 2 ). Patients aged 65 years or older comprised the largest cohort with 71.83% of all revision cases in 2008. Over time, a shift of the age distribution could be observed. Compared to ten years earlier, 1964 more revision knee joint endoprosthetic surgeries were performed on patients younger than 65 years in 2018, which depicts an increase of 7.37%. Most of revision procedures were carried out in patients aged 70–79 years (34.66% of all male patients and 35.23% of all female patients in 2018) followed by patients aged 60–69 years (29.84% of all male patients and 26.06% of all female patients in 2018) and patients aged 50–59 years (16.57% of all male patients and 15.01% of all female patients in 2018) (Figs. 3 , 4 ). The rate of septic interventions in knee prosthesis revisions steadily increased by 51.7% over time from 3402 (17.25%) procedures in 2008 to 5161 (21.67%) procedures due to infection in 2018 (Fig. 5 ). In addition, the choice of treatment strategy changed over the years. In 2008, 20.28% of the PJI patients were treated with the debridement antibiotics implant retention (DAIR) approach (690 procedures), whereas 36.95% of the patients underwent a single-stage change (1257 procedures). 42.77% cases were managed with a two- or multi-stage change coded as “explantation” (1455 procedures). In 2018, however, DAIR procedures decreased to 11.41% (589 procedures), whereas the single-stage change as the chosen treatment strategy increased to 42.55% of all PJI cases (2196 procedures), and a two- or multi-stage change was performed in 46.04% of revisions due to infection (2376 procedures) (Fig. 6 ).
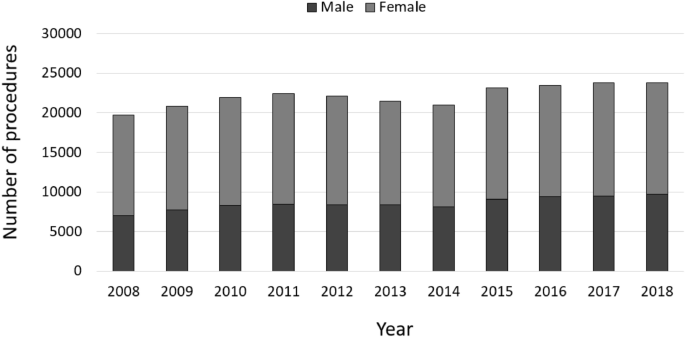
Performed revision knee arthroplasty procedures from 2008 through 2018 divided by gender.
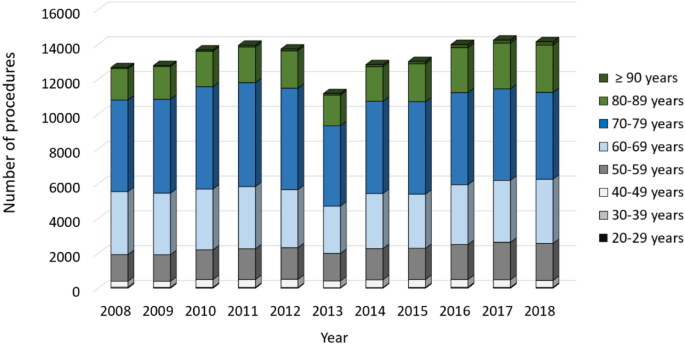
Revision knee arthroplasty procedures of female patients from 2008 through 2018 divided by age.
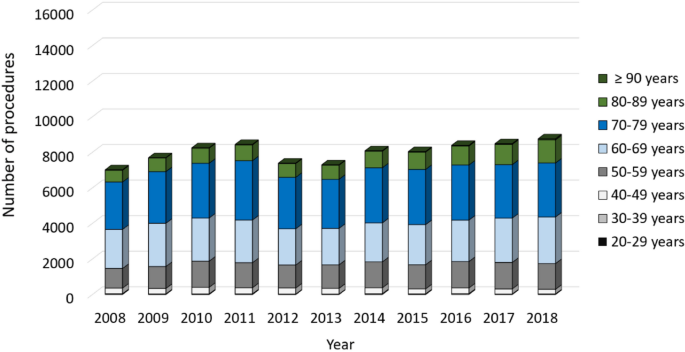
Revision knee arthroplasty procedures of male patients from 2008 through 2018 divided by age.
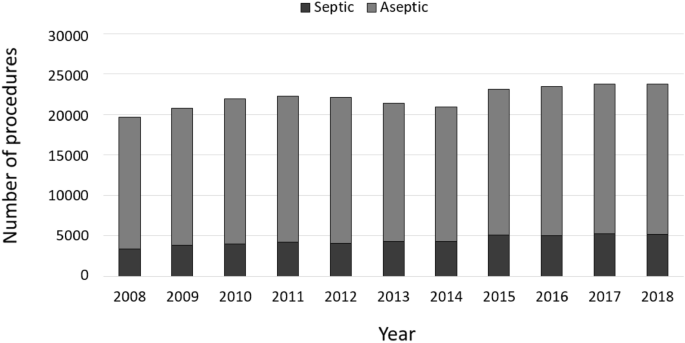
Performed revision knee arthroplasty procedures from 2008 through 2018 divided in septic and aseptic cases.
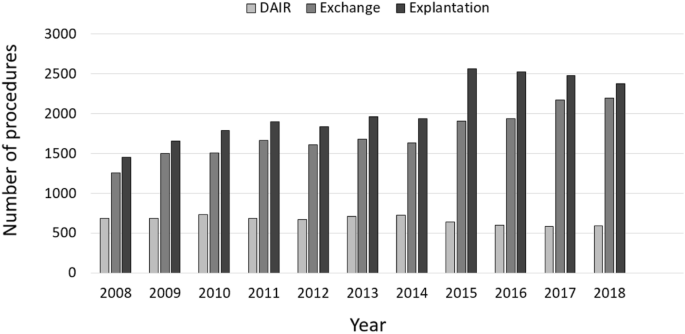
Performed surgical procedures in septic revision cases.
Our analysis outlines recent trends in revision knee arthroplasty from 2008 through 2018 in Germany. Total numbers of revision knee arthroplasty experienced a substantial overall increase during this period, similar to the increase of primary TKA numbers (+ 23.8% from 2008 through 2018). The revision burden (the quotient of revision and primary arthroplasty) in Germany (12.61% in 2018) compared to data reported for the US from 2005 through 2010 (9.1–9.6%, respectively) and comparisons between projected primary TKA numbers in the US and Germany make a detailed analysis of the revision knee arthroplasty numbers seem useful 3 , 4 , 12 .
Influence of age, gender and primary arthroplasty procedure on revision TKA
A reported increase in revision TKA (rTKA) procedures of about 102% as published by Schwartz and coworkers between 2002 and 2014 could not be observed in Germany over a similar time frame 8 . The same applies to the analysis of different age groups. Schwartz et al. reported the largest increase in rTKA numbers in patients aging 55–64 years (+ 195% change) and those aged 65–74 years (+ 119% change). Our analysis could demonstrate highest increase in rTKA numbers in patients aged 90 years or older (+ 94.2% change), followed by patients aged 80–89 years (+ 63.0% change), which is by far less than the observed increase in revision numbers reported for the US. Despite a lower increase in rTKA, strategies to avoid revision arthroplasty should be intensified. Especially in geriatric patients who are extremely challenged by necessary surgical revisions with reported higher mortality rates after rTKA due to infection and fracture, efforts to avoid the causes for surgical interventions should be intensified 13 , 14 .
Revision surgery for knee PJI accounts for about 20% of all cases
In accordance with formerly published analysis of revision TKA, revisions due to PJI account for about 20% of all cases. Bozic and coworkers analyzed reasons for rTKA in the US between 2005 and 2010 and reported PJI as reason for surgical revision to be 25% 12 . Other studies assessing reasons for reinterventions after primary TKA reported infection to be reason for rTKA in 30.3% 15 and 20.3% of the cases, respectively 16 . An analysis from two orthopedic centers in Germany reported PJI accounting for rTKA from 14.5% through 26.8%, depending on time after index total knee arthroplasty 17 , which corresponds with reported higher incidence rates of rTKA due to PJI compared to aseptic loosening early after index TKA 10 , 18 .
Septic revision TKA are increasingly managed by one-stage and two-stage exchange
Septic revision TKA are increasingly managed by one-stage and two-stage exchange (Fig. 6 ). Intriguingly, DAIR procedures did not show a substantial increase in numbers during the observation period. Analysis of operation and procedure codes for septic revision after TKA revealed a substantial increase of one-stage exchange as well as two-stage procedures. Reasons might be manifold. Since exchange arthroplasty should be performed in chronic PJI or acute PJI with implant loosening, DAIR procedures could be demonstrated to be reasonable in case of acute PJI either directly postoperative or in case of late hematogenous PJI 19 . Since our analysis allows not to distinguish between acute and chronic PJIs as rTKA reasons, a steady state in DAIR procedures would suggest chronic PJIs having increased over time or DAIR experienced less acceptance by the treating surgeons. A survey of 515 centers for primary and revision arthroplasty, however, revealed that DAIR is an established treatment alternative in 97.6% of the centers 20 . Thus, limited acceptance to DAIR might be due to factors associated with DAIR failure. Those are high numbers of patients´ comorbidities, infection with antibiotic resistant pathogens, duration of infection and previous revision surgeries 21 . In accordance with the increase of explantation procedures as a first step of a two-stage procedure, one-stage exchange experienced an increase in case numbers over the last 11 years. Defining recommendations for successful one-stage exchange arthroplasty might be a key driver for this trend 22 . Besides, favorable outcomes reported after one-stage exchange in chronic PJI might encourage orthopedic surgeons to save the patients a prosthesis-free interval with at least one more elaborate surgery 23 .
Limitations
The study has several limitations. Historical inpatient data provided by Destatis have been analyzed based on OPS codes, which only allow distinction between different surgical procedures. Inherent limitation of all such analysis is the unverifiable accuracy of coding and data input. Since DRG lump sum reimbursement relies on accurate coding and reimbursement is strictly controlled by the Medical Service of Health Funds, correct coding of diagnosis and procedures can be assumed, however. Prosthesis types explanted and implanted could not be investigated by this approach. In addition, reasons for rTKA could not be itemized beyond revision due to infection using the unspecific ICD code T84.5 (revision arthroplasty due to infection). These downsides had to be accepted when analyzing 243,476 rTKA procedures. Since rTKA is generally performed as an inpatient procedure being reported to the German federal statistical office (Destatis), it can be assumed that the analyzed data set comprises all rTKA patients in the set time frame. Although, the investigated rTKA sample can be regarded as complete data set, patient characteristics additionally to gender and age, in general, have not been reported to Destatis, which unfortunately did not allow to analyze factors associated with type of rTKA. Additionally, no information about hospitals and their volume of rTKA was available which would be of interest in investigating application of treatment strategies and resource utilization.
Although the increase in numbers of revision knee arthroplasty is smaller than observed for the US, increasing numbers of revision knee arthroplasty in younger patients and due to periprosthetic joint infection underlines the need for future efforts to improve treatment strategies to delay primary arthroplasty and avoid periprosthetic joint infection. Since other industrialized countries provide similar health care service and face similar demographic trends, the present analysis may help to adapt resource management for stakeholders in the health care systems worldwide.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Markatos, K. et al. Hallmarks in the history and development of total hip arthroplasty. Surg. Innov. 1553350620947209 (2020).
Saragaglia, D., Rubens-Duval, B., Gaillot, J., Lateur, G. & Pailhe, R. Total knee arthroplasties from the origin to navigation: history, rationale, indications. Int. Orthop. 43 , 597–604 (2019).
Article Google Scholar
Rupp, M., Lau, E., Kurtz, S. M. & Alt, V. Projections of primary TKA and THA in Germany From 2016 through 2040. Clin. Orthop. Relat. Res. https://doi.org/10.1097/CORR.0000000000001214 (2020).
Article PubMed PubMed Central Google Scholar
Kurtz, S., Ong, K., Lau, E., Mowat, F. & Halpern, M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J. Bone Joint Surg. Am. 89 , 780–785 (2007).
Culliford, D. et al. Future projections of total hip and knee arthroplasty in the UK: results from the UK clinical practice research datalink. Osteoarthr. Cartil. 23 , 594–600 (2015).
Article CAS Google Scholar
Romanini, E. et al. Total knee arthroplasty in Italy: reflections from the last fifteen years and projections for the next thirty. Int. Orthop. 43 , 133–138 (2019).
Klug, A. et al. The projected volume of primary and revision total knee arthroplasty will place an immense burden on future health care systems over the next 30 years. Knee Surg. Sports Traumatol. Arthrosc. 1–12 (2020).
Google Scholar
Schwartz, A. M., Farley, K. X., Guild, G. N. & Bradbury, T. L. Jr. Projections and epidemiology of revision hip and knee arthroplasty in the United States to 2030. J. Arthroplasty 35 , S79–S85 (2020).
Kim, T. W. et al. Current trends and projected burden of primary and revision total knee arthroplasty in korea between 2010 and 2030. J. Arthroplasty 36 , 93–101 (2020).
Article ADS Google Scholar
Kurtz, S. M. et al. Are we winning or losing the battle with periprosthetic joint infection: trends in periprosthetic joint infection and mortality risk for the medicare population. J. Arthroplasty 33 , 3238–3245 (2018).
Kurtz, S. M. et al. Prosthetic joint infection risk after TKA in the Medicare population. Clin. Orthop. Relat. Res. 468 , 52–56 (2010).
Bozic, K. J. et al. Comparative epidemiology of revision arthroplasty: failed THA poses greater clinical and economic burdens than failed TKA. Clin. Orthop. Relat. Res. 473 , 2131–2138 (2015).
Yao, J. J. et al. Long-term mortality trends after revision total knee arthroplasty. J. Arthroplasty 34 , 542–548 (2019).
Song, S. J., Kim, K. I., Bae, D. K. & Park, C. H. Mid-term lifetime survivals of octogenarians following primary and revision total knee arthroplasties were satisfactory: a retrospective single center study in contemporary period. Knee Surg. Relat. Res. 32 , 1–8 (2020).
Schmidt, A. et al. Why reintervention after total knee arthroplasty fails? A consecutive cohort of 1170 surgeries. J. Arthroplasty 35 , 2550–2560 (2020).
Delanois, R. E. et al. Current epidemiology of revision total knee arthroplasty in the United States. J. Arthroplasty 32 , 2663–2668 (2017).
Thiele, K. et al. Current failure mechanisms after knee arthroplasty have changed: polyethylene wear is less common in revision surgery. J. Bone Joint Surg. Am. 97 , 715–720 (2015).
Koh, C. K. et al. Periprosthetic joint infection is the main cause of failure for modern knee arthroplasty: an analysis of 11,134 knees. Clin. Orthop. Relat. Res. 475 , 2194–2201 (2017).
Izakovicova, P., Borens, O. & Trampuz, A. Periprosthetic joint infection: current concepts and outlook. EFORT Open Rev. 4 , 482–494 (2019).
Rimke, C. et al. Evaluation of the standard procedure for the treatment of periprosthetic joint infections (PJI) in Germany-results of a survey within the EndoCert initiative. BMC Musculoskel. Disord. 21 , 1–8 (2020).
Qasim, S. N., Swann, A. & Ashford, R. The DAIR (debridement, antibiotics and implant retention) procedure for infected total knee replacement—a literature review. Sicot-J 3 (2017).
Thakrar, R., Horriat, S., Kayani, B. & Haddad, F. Indications for a single-stage exchange arthroplasty for chronic prosthetic joint infection: a systematic review. Bone Joint J. 101 , 19–24 (2019).
Abdelaziz, H., von Förster, G., Kühn, K.-D., Gehrke, T. & Citak, M. Minimum 5 years’ follow-up after gentamicin-and clindamycin-loaded PMMA cement in total joint arthroplasty. J. Med. Microbiol. 68 , 475–479 (2019).
Download references
Acknowledgements
We thank the Federal Satistical Office of Germany (Destatis) for their support of this work.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
Department of Trauma Surgery, University Medical Center Regensburg, Franz-Josef-Strauß-Allee 11, 93053, Regensburg, Germany
Markus Rupp, Nike Walter, Michael Worlicek & Volker Alt
Exponent Inc, Menlo Park, CA, USA
Exponent Inc, Philadelphia, PA, USA
Steven M. Kurtz
You can also search for this author in PubMed Google Scholar
Contributions
M.R. designed the study, wrote the manuscript and analyzed the data. N.W., E.L. and M.W. and S.M.K. analyzed data and critically reviewed, performed the statistical analysis and revised the manuscript. V.A. designed the study, analyzed the data and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Markus Rupp .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Rupp, M., Walter, N., Lau, E. et al. Recent trends in revision knee arthroplasty in Germany. Sci Rep 11 , 15479 (2021). https://doi.org/10.1038/s41598-021-94988-7
Download citation
Received : 21 February 2021
Accepted : 13 July 2021
Published : 29 July 2021
DOI : https://doi.org/10.1038/s41598-021-94988-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Preparation and pet/ct imaging of implant directed 68ga-labeled magnetic nanoporous silica nanoparticles.
- Andras Polyak
- Heidi Harting
- Janin Reifenrath
Journal of Nanobiotechnology (2023)
Periprothetische Streckapparatruptur
- Dominik Szymski
- Philipp von Roth
Knie Journal (2023)
Revision arthroplasty after unicompartimental knee arthroplasty
- Nike Walter
- Johannes Weber
- Markus Rupp
Journal of Orthopaedic Surgery and Research (2021)

Megaprothesen in der Knierevision
- M. Weißenberger
Der Orthopäde (2021)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Open access
- Published: 10 March 2022
Revision surgeries for tumor endoprostheses around the knee joint: a mid-long-term follow-up of 20 cases
- Pengfei Zan 1 ,
- Hongsheng Wang 1 ,
- Zhengdong Cai 1 ,
- Jiakang Shen 1 &
- Wei Sun 1
World Journal of Surgical Oncology volume 20 , Article number: 76 ( 2022 ) Cite this article
1587 Accesses
8 Citations
Metrics details
Tumor endoprostheses of the knee joint after limb salvage surgery is associated with high rates of complications, which has introduced great challenges to a delayed revision surgery. The aim of the study was to summarize the failures, functional outcomes and prosthetic survival in revision tumor endoprostheses of the knee joint.
The clinical data of 20 patients with malignant tumors who received prosthetic revisions after limb salvage surgery from January, 2000 until January, 2018 were retrospectively reviewed. The cohort was constituted of 11 male and 9 female patients with a mean age of 34.1 years (range, 16 to 66 years). Infection cases received two-stage revisions after removing prostheses initially, while all other cases received one-stage revisions. Revision reasons and complications were well documented and analyzed.
All patients received complete follow-up with a mean time of 64.7 months (range, 27 to 155 months). A total of 6 (6/20, 30.0%) patients experienced a second complication after revision surgery, of whom, one patient with deep infection experienced repeated infections after prosthetic revision and received amputation surgery; one patient revised of prosthetic fracture experienced an infection and received a second-stage infection revision; one case revised of prosthetic loosening had deep infection receiving anti-infective therapy with prostheses still in position; one case having wound complication healed after receiving two times of debridement surgery; one MBGCT patient experienced a second aseptic loosening 6 years after the initial loosening thus undergoing a second revision; a recurrent osteosarcoma patient died of pulmonary metastasis 3 years after revision surgery. Kaplan-Meier survival curve indicated a 5-year survival rate of initial prostheses was 75%. The Musculoskeletal Tumor Society (MSTS-93) score [20.9 (range, 15 to 27 scores)] at 1 year after revision surgeries was significantly improved ( p < 0.001) when compared with the score [17.2 (range, 13 to 21 scores)] before revisions.
Prosthetic mechanical problems, aseptic loosening and infections were primary reasons for revisions after tumor endoprostheses of the knee joint. Although revision surgeries were complicated while still associated with high risk of failure, which remains the remedy strategy for limb salvage and functional recovery in those patients.
Introduction
With recent advancements in imaging, design of the prostheses, surgical skills and adjuvant chemotherapy for primary malignant bone tumors, limb salvage surgery have become the main strategy for treating those tumors around the knee joint [ 1 ]. Various methods, such as autologous bone transplantation, inactive autografting, allografting, tumor endoprostheses, allograft prosthetic composite, and three-dimensional–printed custom-made components have been employed for the reconstruction of the affected limb, of which reconstruction with tumor endoprostheses is most widely used [ 2 , 3 , 4 , 5 , 6 , 7 ]. Tumor endoprostheses is advantageous at that it can provide early stability of the affected extremity, allowing a patient to better return social activities [ 4 , 8 , 9 ]. Despite the improvements in the materials used for implants and component designs, potentially serious complications such as prosthetic fracture, infection, mechanical aseptic loosening continue to limit the survival of these endoprosthetic replacements [ 10 ]. It was reported that the revision risk of tumor endoprostheses in the knee joint was 17% at 5 years, 33% at 10 years and even more than 50% in 20 years [ 11 ]. As a consequence, number of later period revision procedures due to prostheses failure is growing. Similar to the primary endoprostheses, revision surgeries were also associated with a series of complications, such as vascular and nerve injury, prosthetic fracture and loosening, infections, etc. [ 10 , 12 ]. Even so, revision surgery remains the main solution to preserve the affected extremity and restore functions to date [ 13 ]. However, failures, functional outcomes, possible revision strategies, and the survival of these revision implants have not been fully identified.
In a long term, we recruited 144 patients who were diagnosed with malignant tumor around the knee joint, most of these cases received tumor endoprostheses replacement. Synthesize treatments including neoadjuvant and postoperative chemotherapy or targeted therapy have prolonged survival period in those cases, making a revision surgery necessary in a growing number of patients. This study retrospectively analyzed a total of 20 patients admitted by our Bone and Soft Tissue Tumor Center from January 2000 until January 2018 who received revision surgeries due to failure of the primary tumor endoprostheses. Objectives were (1) to summarize different failure types of tumor endoprostheses around the knee joint; and (2) to follow the mid-long-term clinical results and prosthetic survival after revision surgeries.
Material and methods
A retrospective review was performed of all patients who had undergone a revision surgery due to primary failure of the tumor endoprostheses of knee joint at our Bone and Soft Tissue Tumor Center. Institutional review board approval was obtained before the initiation of the study and all patients consented to the use of their clinical information at the moment of revision. Using a prospectively maintained database, we identified a total of 20 patients with at least one component of prostheses removal during the period of 2000 and 2018. Of whom, 11 were males and 9 were female patients with a mean age of 34.1 years (range, 16 to 66 years) at the time of index revision. The average interval between initial endoprostheses and revision surgery was 101.3 months (range, 32 to 178 months), those patients were followed at least 2 years after revision surgery.
Oncologic diagnoses included 10 osteosarcomas, 5 malignant bone giant cell tumors (MBGCT), 2 Ewing’s sarcomas and 3 chondrosarcomas. 17 of those tumors were located at the distal femur and 3 cases were at proximal tibia. Preoperative examinations included routine X-ray radiographs, computed tomography (CT) scans and magnetic resonance imaging (MRI). Pulmonary CT scan was performed for all patients to exclude any pulmonary metastasis at the time of revision, and positron emission tomography-computed tomography (PET-CT) was conducted if necessary. Indications for a revision surgery would be that the patient was able to tolerate the procedure and had an expectancy of more than 6 months. Patients received routine outpatient follow-up visits at 6 weeks, 3 months, 6 months, 1 year, and every year thereafter postoperatively. Demographic data, operation time, blood loss of before and those after revision were recorded; interval between primary surgery and revision, follow-up time, reasons for revision, and any complications were documented in detail for final analysis. Full length X-ray of both lower extremities was performed to evaluate the mechanical alignment of the limb (center of hip to center of knee to center of ankle), the location and stability of the prostheses. Pulmonary CT scans were conducted to detect any possible metastasis. Local CT scan or systemic isotope bone scan was performed to assess local control of tumor when necessary. Functional outcomes were measured using the 1993 Musculoskeletal Tumor Society (MSTS-93) score [ 14 ] preoperatively and 1 year after revision. Reasons for revision were classified according to the system proposed by Henderson et al. [ 15 ], this system defines complications as those leading to a revision of the prostheses. They were categorized as mechanical failures: soft-tissue failures (Type 1), aseptic loosening (Type 2), structural failures such as implant fractures, breakage, and periprosthetic fracture (Type 3); and non-mechanical failures: periprosthetic infection (Type 4) and tumor progression (Type 5). Periprosthetic infection was diagnosed through clinical examination, radiographic images, laboratory values and bacterial culture.
When revision surgeries were required, either a one-stage or two-stage procedure was performed. One-stage revision procedure involves removal of the failed prosthetic components and polyethylene parts, debridement of all infected soft tissues; in the meanwhile, new prostheses and other components were implanted to reconstruct the defects. Two-stage revision procedure involves complete removal of all prosthetic components and replaced with antibiotic-loaded bone cement. Systemic antibiotics were administrated to those patients for at least 6 weeks based on the bacterial culture and laboratory values, a revision was performed until white blood cell count, C-reactive protein, and erythrocyte sedimentation rate were normal.
Statistical analysis
Data was recorded and analyzed using the standard statistical software (SPSS, version22.0, 2013, IBM Corp., Armonk, New York). Categorical variables are presented as numbers and percentages, continuous variables are shown in means and ranges. The Student’s t test was used to detect the differences between the preoperative outcomes and those after revision surgeries, including operation time, blood loss and MSTS-93 score. Kaplan-Meier curve analysis was performed to evaluate the prosthetic survival rate. Results were considered statistically significant if a p value < 0.05.
Demographic data are presented in Table 1 . Patients were followed at least 2 years with a mean of 64.7 months (range, 27 to 155 months), of whom 11 cases were followed more than 5 years. The mean operation time for primary prosthetic replacements was 163.0 min (range, 130.0 to 190.0 min) and 187.8 min (range, 135.0 to 250.0 min) in the revision surgeries; blood loss was 555.0 ml (range, 300 to 800 ml) and 805.0 ml (range, 400–1500 ml) in the primary surgeries and revisions, respectively, all showing statistically significant differences ( p < 0.05). Seven of them received preoperative chemotherapy and 11 patients had postoperative chemotherapy; no radiotherapy was performed in those patients. One recurrent osteosarcoma patient died of pulmonary metastasis at 3 years follow-up after revision surgery, and the remaining patients were all alive and free of disease at the most recent follow-up.
Types of failures were summarized in Table 2 and two revision cases were presented as Figs. 1 and 2 . Failed primary endoprostheses requiring revision included 5 cases of Type 2 failures (20.0%), 11 cases of Type 3 failures (55.0%), 3 cases of Type 4 failures (25.0%), and 1 case of Type 5 failure (5.0%); and there were no cases of Type 1 failures in this cohort. Type 2 failure (aseptic loosening) occurred at a mean of 115.4 months (range, 61 to 155 months). A total of 5 patients experienced this failure, and all received a one-stage revision procedure. Those patients were followed at a mean of 87.6 months (range, 55 to 155 months), of whom, one case experienced a second aseptic loosening 6 years after the initial revision and received a second revision; one case had postoperative early infection after revision and healed by debridement and antibiotics administration; another case experienced wound complication and treated with numbers of dressing changes. Other two cases were without any accident in the latest follow-up.

A 57-year-old male osteosarcoma patient, 14 years after initial endoprosthetic replacement. A Preoperative X-ray showed proximal femur prosthetic component loosening and breakout. B The shortened affected extremity, leg length discrepancy (LLD). C Allograft segment, two cables, plate, and screws were used to reconstruct and fix the proximal prostheses. D Proximal component was rebuilt. E , postoperative 1-year X-ray showed prostheses and other components in position

A 22-year-old osteosarcoma male patient, underwent a revision surgery because of the prostheses loosening. A – C Preoperative X-ray, CT-scan, and MRI image showed a lesion at the distal femur. D Postoperative 1-year X-ray showed the prosthetic components at position. E , F Postoperative 3-year X-ray showed a prostheses loosening at the femur site. H , I , Prosthetic components at the femur site were removed. J , K The residual cement was removed and followed with allograft implanted. L A biological prosthetic component was implanted. M Postoperative full length film of double lower extremities showed the prostheses at position
Type 3 failures (structural failures) accounted for 55.0% (11/20) of all the revisions, and they happened at a mean of 97.9 months (range, 32 to 178 months) after the primary endoprostheses. Those patients were followed at a mean of 61.7 months (range, 45 to 93 months) after revisions, one patient experienced deep infection in the early postoperative period after the revision procedure and received a two-stage revision surgery; another case had wound complications and treated with debridement and antibiotics therapy.
Type 4 failures (periprosthetic infection) occurred in 3 patients at a mean time of 111.3 months (range, 93 to 145 months) and those patients were followed 47 months (range, 27 to 70 months) after the revisions. All the 3 cases received two-stage revision procedures with prostheses removal and antibiotic-loaded bone cement in occupation initially. One patient was cultured with Methicillin-resistant Staphylococcus aureus (MRSA); although a two-stage revision was performed, the patient experienced persistent infections after revision and received amputation procedure in the end. The other two cases were disease-free at the latest follow-up period.
Type 5 failures (tumor progression) occurred in one case in this cohort, and this patient experienced tumor recurrence 38 months after the primary endoprostheses and received a second tumor resection with prostheses reconstruction. In the following, the patient was diagnosed with pulmonary metastasis receiving multiple chemotherapies and died at 3 years after the revision surgery.
Kaplan-Meier survival curve was plotted, which indicated that 5-year survival rate of the initial prostheses in the revision cohort was 75% and 10-year survival rate was 40%. Functional MSTS-93 scores were obtained in all the cases before and 1 year after revision procedures. The average overall score was 17.2 (range, 13 to 21 scores) before revision and 20.9 (range, 15 to 27 scores) 1 year after revision, significant difference was detected in between ( p < 0.001).
The introduction of neoadjuvant and adjuvant chemotherapy allowed resection and reconstruction instead of amputation as surgical treatment in most cases of bone sarcomas [ 16 , 17 , 18 ]. Segmental metallic endoprostheses have been more frequently used and play an increasingly important role in limb reconstruction after resection of long bones around the knee joint [ 15 ]. However, failures such as infection, tumor progression, aseptic lessening, prosthetic breakage, and periprothestic fracture may occur during the follow-up period [ 4 , 10 , 19 , 20 ]. It was reported that failures of the endoprosthetic reconstruction range from 17 to 75% at 5 to 15 years [ 11 , 21 , 22 ]. Therefore, it will be of clinical significance to summarize the failures, clinical outcomes, and prosthetic survival of the tumor endoprosthses replacement around the knee joint.
Prosthetic mechanical problems after tumor endoprostheses reconstruction were the primary reasons for a revision surgery, followed by aseptic loosening and infection. Soft tissue failure did not occur in our cohort, and tumor progression was detected in one case, as prosthetic revision was rarely necessary in most cases of soft tissue failure and tumor progression. Overall, the reports in the literatures had similar results to our findings [ 15 , 23 , 24 ]. In Henderson’s report [ 15 ], the most common mode of failure was infection, followed by aseptic loosening and structural failures, soft tissue problem and tumor progression accounted less, whereas in their cohort different kinds of endoprostheses were included, such as proximal humeral replacements, total humeral replacement, distal humeral replacements, proximal femoral replacements, total femoral replacement, distal femoral replacement, combined distal femoral-proximal tibial replacements, and proximal tibial replacements. Biau and colleagues [ 23 ] reported a total of 91 cases of tumor endoprotheses around the knee joint, 36 received revision surgeries, of which 23 were mechanical problems, 7 were infection, and 6 were tumor recurrence. Wirganowicz et al. [ 24 ] reported in their 64 failure cases that aseptic loosening and mechanical failure accounted for most of the failures and they were revised successfully; a total of 9 patients experienced tumor recurrence, of whom 8 received amputation surgery.
The infection rate of distal femur tumor endoprostheses was reported in the literature as 5.5% and range from 3.6 to 40% in the proximal tibia [ 15 , 25 , 26 ]. Theoretically, the risk of infection in the proximal tibia had increased because of the relative lack of wound coverage and unreliable extensor mechanism reconstruction [ 27 ]. In our series 2 infection occurred in the distal femur and 1 was in the proximal tibia, a two-stage revision was performed with spacer implanted initially and new prostheses were implanted after infection control. Infections after revision surgeries remain a vital problem in those patients, and three cases experienced a second infection after revision surgery, a MRSA infection patient had continuous infection and received amputation in the end, another one received a two-stage revision and the last one healed by debridement. Most literatures suggested a two-stage revision instead of one-stage for those tumor endoprostheses replacements [ 25 , 28 , 29 ]. Although a literature reported the successful rate of early stage in a one-stage revision is high, it continues to decline to 14% in the long follow-up period [ 30 ]. The success rate in a two-stage revision for those infections in the tumor endoprostheses replacements was reported as high as 74% [ 25 ]. We conducted 4 cases of two-stage infection revisions, one case had infection uncontrolled and received amputation.
Our results showed that overall 13.9% of the patients required a revision of their initial prostheses, this rate was lower than those reported in literatures [ 11 , 15 , 31 ] as some failures failed to have the opportunity to revise in our cohort. Studies published reported that a survival rate of up to 87% at 3 years and 67 to 88% at 5 years, this decreased to 48 to 65% at 10 years and very limited data was available at 20 years [ 32 , 33 , 34 ]. In Wirganowicz’s report [ 24 ], the 5-year survival rate of the prostheses in their cohort was 81%, and another report showed a 5-year survival rate of the prostheses in their revision group of 79% and a 10-year survival rate of 65% [ 33 ]. In our cohort, the 5-year survival rate of initial prostheses in the revised cohort was 75%, and this decreased to 40% at 10-years, which was co-insistent with reports in the literatures. Tumor endoprostheses replacement around the knee joint mostly achieved better functions of the extremities. In Kawai’s report [ 33 ], range of motion of the knee joint after tumor endoprostheses reached to approximate 90° and MSTS-93 scores were 80% at an average. However, revised tumor endoprostheses experienced inferior functional results. Shin et al. [ 35 ] reported 19 revised cases of tumor endoprostheses replacements, a 10-year MSTS-93 score was only 57%. Reasons for revision may introduce major effect to postoperative functional outcomes, patients revised of mechanical failure mostly achieve better functions, whereas infection cases always had inferior functional recovery [ 36 ]. In our cohort, the MSTS-93 scores were significantly improved compared with the values before revision, which indicated a better functional recovery in these revision cases, especially for those patients with mechanical problems and aseptic loosening.
Several limitations of the present study should be addressed as follows. First, it is a retrospective, non-randomized case series with a small sample size which may have introduced potential selection bias. Second, the tumors of the included patients in the study are heterogeneous regarding biological behavior and stages, and the intervention of neoadjuvant and adjuvant chemotherapy may have affected the oncologic prognosis and results. Third, although comparisons were conducted in different type of prosthetic failures, primary and revision surgeries, this study lacked a true control group. Whereas, we opted to include all patients who received prosthetic revisions after limb salvage surgery in a long period to address failure types, functional outcomes, and prosthetic survival in revision tumor endoprostheses of the knee joint, even with limitations, our results may be of meaningful.
Tumor endoprostheses replacements of knee joint are associated with high rate of failures with mechanical problems, aseptic loosening, and infection as the primary reasons. Even revision surgery is challenging as well as accompanied with high rate of complications, it is still the main solution for those patients to preserve the affect limb and restore functions.
Availability of data and materials
The dataset supporting the conclusions of this article is available on request—please contact the corresponding author.
Abbreviations
Malignant bone giant cell tumor
Musculoskeletal Tumor Society 1993
Papakonstantinou E, Stamatopoulos A, Athanasiadis DI, et al. Limb-salvage surgery offers better five-year survival rate than amputation in patients with limb osteosarcoma treated with neoadjuvant chemotherapy. A systematic review and meta-analysis. J Bone Oncol. 2020;25:100319.
Article Google Scholar
Donati D, Colangeli M, Colangeli S, et al. Allograft-prosthetic composite in the proximal tibia after bone tumor resection. Clin Orthop Relat Res. 2008;466(2):459–65.
Xu M, Xu M, Zhang S, et al. Comparative efficacy of intraoperative extracorporeal irradiated and alcohol-inactivated autograft reimplantation for the management of osteosarcomas-a multicentre retrospective study. World J Surg Oncol. 2021;19(1):157.
Pala E, Trovarelli G, Angelini A, at al. Megaprosthesis of the knee in tumor and revision surgery. Acta Biomed. 2017;88(2S):129–38.
CAS PubMed PubMed Central Google Scholar
Sun W, Zan P, Ma X, at al. Surgical resection and reconstructive techniques using autologous femoral head bone-grafting in treating partial acetabular defects arising from primary pelvic malignant tumors. BMC Cancer. 2019;19(1):969.
Jud L, Müller DA, Fürnstahl P, at al. Joint-preserving tumour resection around the knee with allograft reconstruction using three-dimensional preoperative planning and patient-specific instruments. Knee. 2019;26(3):787–93.
Wang J, An J, Lu M, et al. Is three-dimensional-printed custom-made ultra-short stem with a porous structure an acceptable reconstructive alternative in peri-knee metaphysis for the tumorous bone defect? World J Surg Oncol. 2021;19(1):235.
Haijie L, Dasen L, Tao J, et al. Implant survival and complication profiles of endoprostheses for treating tumor around the knee in adults: a systematic review of the literature over the past 30 years. J Arthroplast. 2018;33(4):1275–1287.e3.
Chandrasekar CR, Grimer RJ, Carter SR, et al. Modular endoprosthetic replacement for tumours of the proximal femur. J Bone Joint Surg (Br). 2009;91(1):108–12.
Article CAS Google Scholar
Theil C, Röder J, Gosheger G, Andreou D, et al. What is the likelihood that tumor endoprostheses will experience a second complication after first revision in patients with primary malignant bone tumors and what are potential risk factors? Clin Orthop Relat Res. 2019;477(12):2705–14.
Myers GJ, Abudu AT, Carter SR, et al. Endoprosthetic replacement of the distal femur for bone tumours: long-term results. J Bone Joint Surg (Br). 2007;89(4):521–6.
Foo LS, Hardes J, Henrichs M, et al. Surgical difficulties encountered with use of modular endoprosthesis for limb preserving salvage of failed allograft reconstruction after malignant tumor resection. J Arthroplast. 2011;26(5):744–50.
Funovics PT, Hipfl C, Hofstaetter JG, et al. Management of septic complications following modular endoprosthetic reconstruction of the proximal femur. Int Orthop. 2011;35(10):1437–44.
Enneking WF, Dunham W, Gebhardt MC, et al. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993;286:241–6.
Henderson ER, Groundland JS, Pala E, et al. Failure mode classification for tumor endoprostheses: retrospective review of five institutions and a literature review. J Bone Joint Surg Am. 2011;93(5):418–29.
Simpson E, Brown HL. Understanding osteosarcomas. JAAPA. 2018;31(8):15–9.
Benjamin RS. Adjuvant and Neoadjuvant Chemotherapy for Osteosarcoma: A Historical Perspective. Adv Exp Med Biol. 2020;1257:1–10.
Harrison DJ, Geller DS, Gill JD, et al. Current and future therapeutic approaches for osteosarcoma. Expert Rev Anticancer Ther. 2018;18(1):39–50.
Thornley P, Vicente M, MacDonald A, et al. Causes and frequencies of reoperations after endoprosthetic reconstructions for extremity tumor surgery: a systematic review. Clin Orthop Relat Res. 2019;477(4):894–902.
Zhang C, Hu J, Zhu K, et al. Survival, complications and functional outcomes of cemented megaprostheses for high-grade osteosarcoma around the knee. Int Orthop. 2018;42(4):927–38.
Gosheger G, Gebert C, Ahrens H, et al. Endoprosthetic reconstruction in 250 patients with sarcoma. Clin Orthop Relat Res. 2006;450:164–71.
Zeegen EN, Aponte-Tinao LA, Hornicek FJ, et al. Survivorship analysis of 141 modular metallic endoprostheses at early followup. Clin Orthop Relat Res. 2004;420:239–50.
Biau D, Faure F, Katsahian S, et al. Survival of total knee replacement with a megaprosthesis after bone tumor resection. J Bone Joint Surg Am. 2006;88(6):1285–93.
Wirganowicz PZ, Eckardt JJ, Dorey FJ, et al. Etiology and results of tumor endoprosthesis revision surgery in 64 patients. Clin Orthop Relat Res. 1999;358:64–74.
Grimer RJ, Belthur M, Chandrasekar C, et al. Two-stage revision for infected endoprostheses used in tumor surgery. Clin Orthop Relat Res. 2002;395:193–203.
Unwin PS, Cannon SR, Grimer RJ, et al. Aseptic loosening in cemented custom-made prosthetic replacements for bone tumours of the lower limb. J Bone Joint Surg (Br). 1996;78(1):5–13.
Mavrogenis AF, Pala E, Angelini A, et al. Proximal tibial resections and reconstructions: clinical outcome of 225 patients. J Surg Oncol. 2013;107(4):335–42.
Rao K, Lahiri A, Peart FC. Role of staged endoprosthetic revision with flap cover for limb salvage in endoprosthetic failure. Int Orthop. 2006;30(6):473–7.
Jeys LM, Kulkarni A, Grimer RJ, et al. Endoprosthetic reconstruction for the treatment of musculoskeletal tumors of the appendicular skeleton and pelvis. J Bone Joint Surg Am. 2008;90(6):1265–71.
Hardes J, Gebert C, Schwappach A, et al. Characteristics and outcome of infections associated with tumor endoprostheses. Arch Orthop Trauma Surg. 2006;126(5):289–96.
Griffin AM, Parsons JA, Davis AM, et al. Uncemented tumor endoprostheses at the knee: root causes of failure. Clin Orthop Relat Res. 2005;438:71–9.
Unwin PS, Cobb JP, Walker PS. Distal femoral arthroplasty using custom-made prostheses. The first 218 cases. J Arthroplast. 1993;8(3):259–68.
Kawai A, Muschler GF, Lane JM, et al. Prosthetic knee replacement after resection of a malignant tumor of the distal part of the femur. Medium to long-term results. J Bone Joint Surg Am. 1998;80(5):636–47.
Kawai A, Healey JH, Boland PJ, et al. A rotating-hinge knee replacement for malignant tumors of the femur and tibia. J Arthroplast. 1999;14(2):187–96.
Shin DS, Weber KL, Chao EY, et al. Reoperation for failed prosthetic replacement used for limb salvage. Clin Orthop Relat Res. 1999;358:53–63 PMID: 9973976.
Guo W, Ji T, Yang R, et al. Endoprosthetic replacement for primary tumours around the knee: experience from Peking University. J Bone Joint Surg (Br). 2008;90(8):1084–9.
Download references
Acknowledgements
We thank Dr. Merel Mol (From University of Amsterdam, Netherlands) for language editing.
This work was funded by the National Natural Science Foundation of China (NSFC, No. 81772859, Dr. Wei Sun designed the study and completed the surgeries), (NSFC, No. 82000839, Dr. Pengfei Zan) and Natural Science Foundation of Zhejiang Province (No. LQ2H060009, Dr. Pengfei Zan designed the study and drafted the manuscript, assisted to complete the surgeries).
Author information
Authors and affiliations.
Department of Orthopedic Surgery, Shanghai General Hospital, Shanghai Jiao Tong University School of Medicine, No. 100 Haining Road, Hongkou District, Shanghai, China
Pengfei Zan, Hongsheng Wang, Zhengdong Cai, Jiakang Shen & Wei Sun
You can also search for this author in PubMed Google Scholar
Contributions
PZ, WS, and JS designed the study and drafted the manuscript. PZ, HW, and WS accumulated the data. WS, PZ, HW, and CZ analyzed the data. PZ and JS proofread the English language. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Jiakang Shen or Wei Sun .
Ethics declarations
Ethics approval and consent to participate.
The Ethics Committee of Shanghai General Hospital, Shanghai Jiao Tong University School of Medicine approved the study protocol. Written informed consent was obtained from all patients enrolled in the investigation.
Consent for publication
Consent for publication has been obtained from all participated patients in the study.
Competing interests
The authors declared that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Zan, P., Wang, H., Cai, Z. et al. Revision surgeries for tumor endoprostheses around the knee joint: a mid-long-term follow-up of 20 cases. World J Surg Onc 20 , 76 (2022). https://doi.org/10.1186/s12957-022-02542-0
Download citation
Received : 18 October 2021
Accepted : 27 February 2022
Published : 10 March 2022
DOI : https://doi.org/10.1186/s12957-022-02542-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Tumor endoprostheses
- Prosthetic fracture
- Aseptic loosening
World Journal of Surgical Oncology
ISSN: 1477-7819
- General enquiries: [email protected]
- Research article
- Open access
- Published: 03 September 2021
A novel tool for predicting the survival of endoprosthesis used for reconstruction of the knee following tumor resection: a retrospective cohort study
- Cheng-gang Pang 1 na1 ,
- Xiong-gang Yang 2 na1 ,
- Yun-long Zhao 1 ,
- Yan-cheng Liu 3 &
- Yong-cheng Hu 3
BMC Cancer volume 21 , Article number: 986 ( 2021 ) Cite this article
1289 Accesses
5 Citations
Metrics details
Prosthesis-related complications, after knee reconstruction with endoprosthesis during operation for tumors around the knee, remain an unresolved problem which necessitate a revision or even an amputational surgery. The purpose of the current study was to identify significant risk factors associated with implant failure, and establish a novel model to predict survival of the prosthesis in patients operated with endoprostheses for tumor around knee.
We retrospectively reviewed the clinical database of our institution for patients who underwent knee reconstruction due to tumors. A total of 203 patients were included, including 123 males (60.6%) and 80 (39.4%) females, ranging in age from 14 to 77 years (mean: 34.3 ± 17.3 years). The cohort was randomly divided into training ( n = 156) and validation ( n = 47) samples. Univariable COX analysis was used for initially identifying potential independent predictors of prosthesis survival with the training group ( p < 0.150). Multivariate COX proportional hazard model was selected to identify final significant prognostic factors. Using these significant predictors, a graphic nomogram, and an online dynamic nomogram were generated for predicting the prosthetic survival. C-index and calibration curve were used for evaluate the discrimination ability and accuracy of the novel model, both in the training and validation groups.
The 1-, 5-, and 10-year prosthetic survival rates were 94.0, 90.8, and 83.0% in training sample, and 96.7, 85.8, and 76.9% in validation sample, respectively. Anatomic sites, length of resection and length of prosthetic stem were independently associated with the prosthetic failure according to multivariate COX regression model (p<0.05). Using these three significant predictors, a graphical nomogram and an online dynamic nomogram model were generated. The C-indexes in training and validation groups were 0.717 and 0.726 respectively, demonstrating favourable discrimination ability of the novel model. And the calibration curve at each time point showed favorable consistency between the predicted and actual survival rates in training and validation samples.
Conclusions
The length of resection, anatomical location of tumor, and length of prosthetic stem were significantly associated with prosthetic survival in patients operated for tumor around knee. A user-friendly novel online model model, with favorable discrimination ability and accuracy, was generated to help surgeons predict the survival of the prosthesis.
Peer Review reports
The distal femur and the proximal tibia are common sites for primary and metastatic bone tumor [ 1 ]. Amputation was the traditional surgical treatment for musculoskeletal sarcomas of the extremities, with the aim of saving the patients’ life. With the simultaneous improvement on the understanding of the biology and staging of tumors, reconstructive techniques, and effective adjuvant chemotherapy, however, limb salvage surgery has replaced the amputation as the predominated treatment choice for more than 90% of patients with a primary malignancy on the knee [ 2 , 3 , 4 ].
Because of the unique biological inherent properties of the tumor, the complex anatomic features of the knee and problems associated with extensor reconstruction, tumors arising around the knee pose a unique set of challenges in the management of soft tissues and the restoration of limb length and joint kinetics. The options for reconstruction after resection of a tumor around the knee joint include implantation of a prosthesis, osteoarticular allograft, allograft-prosthesis composite, recycled autologous bone graft, arthrodesis with intercalary bone grafting or conversion to a rotationplasty [ 5 ]. Among these methods, tumor prosthesis offers the advantages of convenience, early mobilization, and weight bearing capability, and it allows the early introduction of postoperative adjuvant therapy. Furthermore, there are no differences in survival rates between limb-salvage and ablative surgery [ 6 , 7 , 8 ].
Although advances in materials and implant design have occurred over the past three decades, complications and failures of these devices remain high compared to other arthroplasty procedures [ 9 , 10 , 11 ]. Prosthesis-related complications, including infection, aseptic loosening, dislocation, recurrence of the tumor, joint stiffness or contracture, instability of components, and implant mechanical weaknesses, remain an unresolved problem which necessitate a revision or even an amputational surgery [ 12 , 13 , 14 ]. High rate of prosthesis-related failure indicates that tumor endoprostheses need to be further studied, and improvements in surgical technique and component design are required. To guide the treatments selection and decision making, it may be crucial to clarify the prognostic factors that significantly predict the survival of prosthesis used for reconstructing the knee operated for tumors. Until now few studies have analyzed the prognostic effect of patients’ and operation-related characteristics.
The nomogram is a type of easy-to-use predicting model, which transforms traditional statistical predictive models into visualized probability estimates tailored to each patient. Using this model, one could be provided with continuous survival probabilities at several time points that predicted for an individual patient. What is more, the nomogram could be further transformed into a webpage based predicting widget, easily providing a predicted Kaplan-Meier survival curve, and survival rate at each time point.
Thus, the purpose of this study was (1) to evaluate the clinical and functional outcomes of patients who underwent a limb salvage surgery for tumors around the knee, (2) to identify prognostic factors significantly associated with implant failure, (3) and to develop a validated nomogram model as well as a webpage based predicting tool.
This study was conducted according to the Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis (TRIPOD) statement [ 15 ], and reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement (Available in Additional file 1 ).
Patients inclusion
In accordance with the Declaration of Helsinki and upon the attained ethical approval from the hospital ethics committee, information of 297 consecutive patients with neoplastic disease around the knee who were treated with tumor resection and subsequent endoprosthetic reconstruction between April 1995 and August 2018 in two individual research centers were retrospectively reviewed for potential eligibility.
Patients would be included following the inclusion criteria: (1) age ≥ 14 years at the time of surgery; (2) bone tumors located around the knee; (3) limb-salvage or ablative surgery. The initial diagnosis was made based on pre-operative radiographs (X ray, magnetic resonance imaging [MRI] or computed tomography), and consequently confirmed by core needle biopsy or by open biopsy and pathological examination. Patients with reconstructed knee for medical conditions other than bone tumor, patients lost to follow-up, or patients with incomplete medical document were excluded.
Surgical treatment
All patients indicative for limb-salvage surgery were evaluated systemically on the lesion size, preoperative planning of the level and optimal types of prostheses. The dimensions of the tumor and boundaries were measured by a combination of total leg-length radiographs and cross-sectional imaging, including MRI or 3D Multi-Slice Computerized Tomography (3D MSCT). With the completion of imaging materials and histology diagnosis, patients were categorized to a surgical stage according to Musculoskeletal Tumor Society (MSTS) classification [ 16 ] and received neoadjuvant chemotherapy on protocol when applicable. After resection of the tumor, reconstruction was performed using a cemented metal endoprosthesis (custom/modular). During the early time of the surgery, custom implants (fixed/hinged) were used in 88 patients. Modular implants featuring a rotating hinge mechanism were subsequently implanted in the remaining 63 patients. The surgical resection and reconstruction were performed by two senior professors, whose members of the team were orthopedic surgeons with extensive experience in the field the knee arthroplasty procedures, following the generally accepted oncologic principles of obtaining a wide surgical margin. Excision was performed through a medial or lateral parapatellar approach. Frozen section analysis of the intramedullary canal contents at the resection site was performed intraoperatively to ensure a negative marrow margin. An intraoperative radiograph was also performed to confirm that the fine line force of the knee was obtained for all the patients. We then performed a soft tissue reconstruction for each individual to achieve muscular coverage of the implants and to restore function of the knee.
Post-operative management mainly focused on prophylaxis of incision infection and application of antithrombotics and analgesics. Intravenous antibiotic prophylaxis was maintained until the wound drains were removed. Mobilization commenced on the second day postoperatively with the assistance of a walker with the purpose of preventing thrombogenesis or development of a infection in the urinary systems.
Post-operative rehabilitation protocol
In order to obtain the maximum function of the knee postoperatively, detailed procedures were described as follows. Firstly, immediate weight bearing assisted with the hinged brace around the knee for all patients was permitted due to the stability of the cemented implants and the stability of reconstructed knee. A continuous passive motion (CPM) apparatus was used under professional rehabilitation therapist’s guidance and supervision on the first day post-operatively and continued until discharge. Extra attention was paid for patients with reconstructions of the extensor mechanism, whose motion was commenced from − 5° to 10° extension to 30° to 45° flexion and gradually increased to greater than 90° flexion before discharge. When rehabilitation was executed, patients were administrated appropriate anodyne, which allowed them an indolent restoration.
Recorded variables
The patients were required to be interviewed every 3 weeks for the first 3 months after surgery, then on a quarterly basis for 3 years, semiannually for an additional 2 years, and then annually. The medical records, radiographs and pathologic records, operation details, information about adjuvant oncological therapies, and oncologic outcomes were reviewed. We recorded the following variables as the potential prognostic factors: age at operation, sex, body mass index (BMI), tumor types (divided into borderline tumor, malignant primary tumor, and metastatic bone tumor), operation related complications within 6 months, adjuvant chemotherapy/ radiotherapy, pathological fracture, primary/ revision reconstruction, anatomical location (proximal tibia or distal femur), site of knee (left or right), bleeding volume, operation time, bone transplantation, prosthesis type (custom or modular), prosthesis motion mode (rotational or fixed), length of prosthetic stem, diameter of prosthetic stem, material of prosthesis (titanium or vatallium), and length of resection.
The outcome variable was prosthesis survival, which was defined as the time interval between operation and prosthesis failure (any cause that required replacement of the components of the prosthesis).
Statistical analysis
The included patients were randomly divided into training sample and validation sample with a ratio of 7:3. The training sample was used for model establishing and internal validation, while the validation sample was used for external validation. The continuous variables, including the age, BMI, length of prosthetic stem, diameter of prosthetic stem, length of osteotomy, operation time, and bleeding volume, were transformed into dichotomous variable using the cutoff point detected with the method of running log rank test [ 17 , 18 ]. The distribution of the patients according to each prognostic factor was described as mean ± SD or percentage. Kaplan-Meier survival curve was used to describe the overall patients’ survival and prosthetic survival, in training and validation samples.
Univariate analysis using COX proportional hazards model was performed to initially identify the potential significance of each prognostic variable on predicting the prosthetic survival. All of the variables demonstrated to be significantly or marginally significantly ( p < 0.15) associated with prosthetic survival were included in the multivariable COX analysis. Kaplan-Meier survival curves were generated for all prognostic factors involved in multivariable analysis. Hazard ratio (HR) and confidence interval (95%CI) were selected as the effect size for both univariate and multivariate COX model. A forest plot was generated to display the result of multivariate analysis.
Basing on the significant variables screened by multivariate COX model, a novel nomogram was plotted, to graphically provide continuous survival rates at several time points and the median survival time of prosthesis. C-index and calibration curve were used to evaluate the discrimination ability and accuracy of the nomogram respectively. Finally, after fitting of a new COX model using the variables involved in the graphical nomogram, a webpage-based dynamic nomogram, which could provide predicted survival curve and survival rate at any time point as wanted, was established.
All analyses have been performed with program of R language (Foundation for Statistical Computing, Vienna, Austria). The univariable and multivariable COX models were fitted using the R package “survival”. The graphical nomogram and the online dynamic nomogram were generated with the packages “rms” and “DynNom”. Level of statistical significance was set at P < 0.05.
Patients’ baseline characteristics
A total of 203 patients (156 divided into the training sample and 47 divide into the validation sample) were eligible for final inclusion according to the inclusion and exclusion criteria. The baseline characteristics is shown in the Table 1 . Among these patients, there were 99 males (63.46%) and 53 (36.54%) females, and 24 male (51.06%) and 23 female in the training and validation samples, respectively. The mean age was 35.31 ± 17.54 and 31.09 ± 16.17 years in the training and validation samples at the time of surgery. The distal femur ( n = 99, 63.46%) was more common than proximal tibia ( n = 57, 36.54%) concerning the involved anatomical location. The distribution of the tumor histology is presented in Fig. 1 , showing that malignant primary tumor (osteosarcoma, 72; malignant fibrous histiotoma, 9; chondrosarcoma, 6; leiomyosarcoma, 3; synoviosarcoma, 2) was the predominated tumor type, followed by borderline tumor (giant cell tumor of bone, 53; fibrous histiotoma, 3) and malignant metastatic tumor.
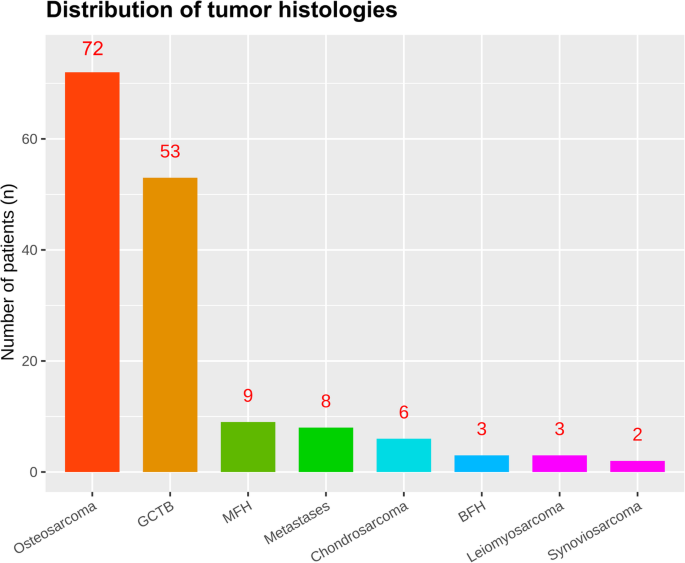
Distribution of the tumor histology. Abbreviations: GCTB, giant cell tumor of bone; MFH, malignant fibrous histiotoma; BFH, borderline fibrous histiotoma
Within 6 months post-operatively, a total of 26 (16.67%) and 7 (14.89%) patients were encountered with operation related complications, in the training and validation groups. The major complications leading to implant failure were aseptic loosening in 26 out of 20 patients (20/132, 15.1%), followed by superficial or periprosthetic infection (16), local recurrence or metastases or both (12), periprosthetic or prosthetic fracture (7), wound healing disorders (4), joint instability or flexion contracture in two (2), dislocation of the prosthesis in one patients (3). Four patients developed nonprosthesis-related complications include peroneal nerve palsy (2), others (3). Local relapse arose in 16 (10.26%) patients and 5 (10.64%) patients during the follow-up.
The Kaplan-Meier survival curves for the patients’ overall survival and prosthesis survival are shown in Fig. 2 . The overall patients’ survival at 12, 60, and 120 months were 94.0, 90.8 and 83.0%, and 95.7, 92.8 and 83.9% in training and validation groups, respectively. The prosthesis survival at 12, 60, 120, and 180 months were 96.7, 85.8, 76.9 and 44.0%, and 95.7, 82.9, 67.5 and 45.0% in training and validation groups, respectively.
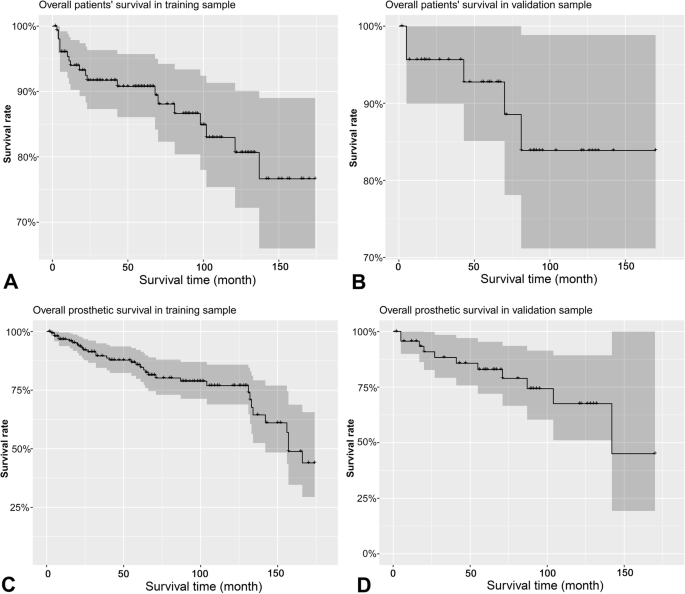
Kaplan-Meier survival curves for the patients’ overall survival and prosthetic survival in training and validation samples
Results of univariate and multivariate COX analyses
Figure 3 shows the results of running log-rank test for the continuous predictors, presenting the optimal cut-off points to convert these factors into categorical variables. The results of univariate COX analysis are shown in Table 2 , and the Kaplan-Meier survival curves for the significant and marginally significant ( p < 0.15) prognostic factors are presented in Fig. 4 . As a result, anatomical location at distal femur (HR = 0.412, 95%CI: 0.180 ~ 0.945, P = 0.036), fixed prosthetic motion mode (HR = 2.336, 95%CI: 1.134 ~ 4.812, P = 0.021), and length of resection (> = 10.4 cm; HR = 8.959, 95%CI: 3.767 ~ 21.310, P < 0.001) were significantly associated with increased implant failure, while BMI (HR = 2.555, 95%CI: 0.715 ~ 9.135, P = 0.149), operation related complications (HR = 1.877, 95%CI: 0.918 ~ 3.840, P = 0.085), custom/ modular prosthesis (HR = 2.244, 95%CI: 0.957 ~ 5.257, P = 0.063), and length of prosthetic stem (HR = 0.578, 95%CI: 0.287 ~ 1.165, P = 0.125) were demonstrated to be marginally associated with the survival of implant.
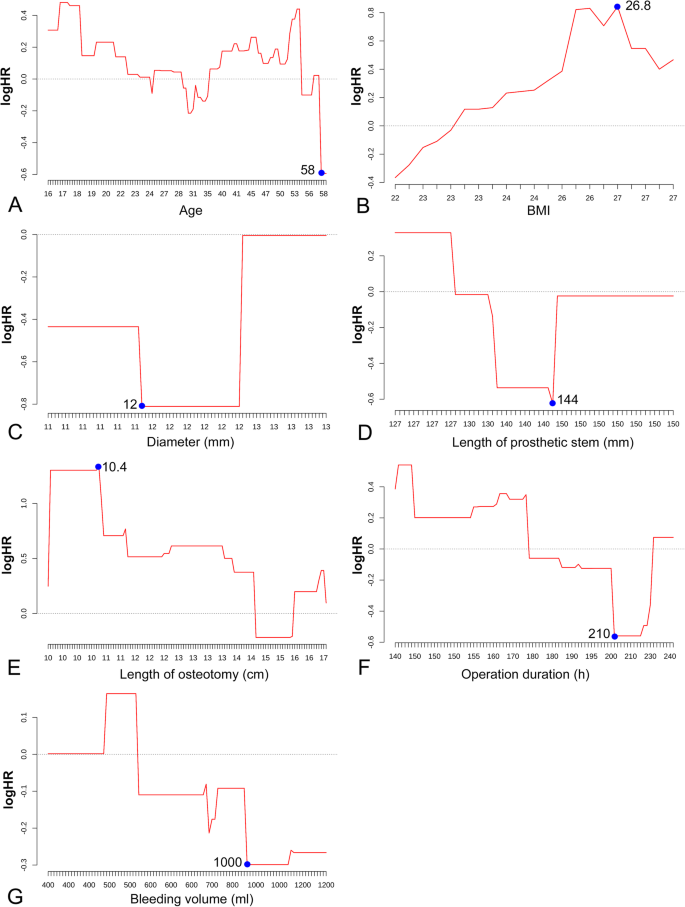
Results of running log-rank tests to detect the optimal cutoff points for continuous prognostic factors of implant survival, including age ( A ), BMI ( B ), stem diameter ( C ), stem length ( D ), length of osteotomy ( E ), operation duration ( F ) and bleeding volume ( G )
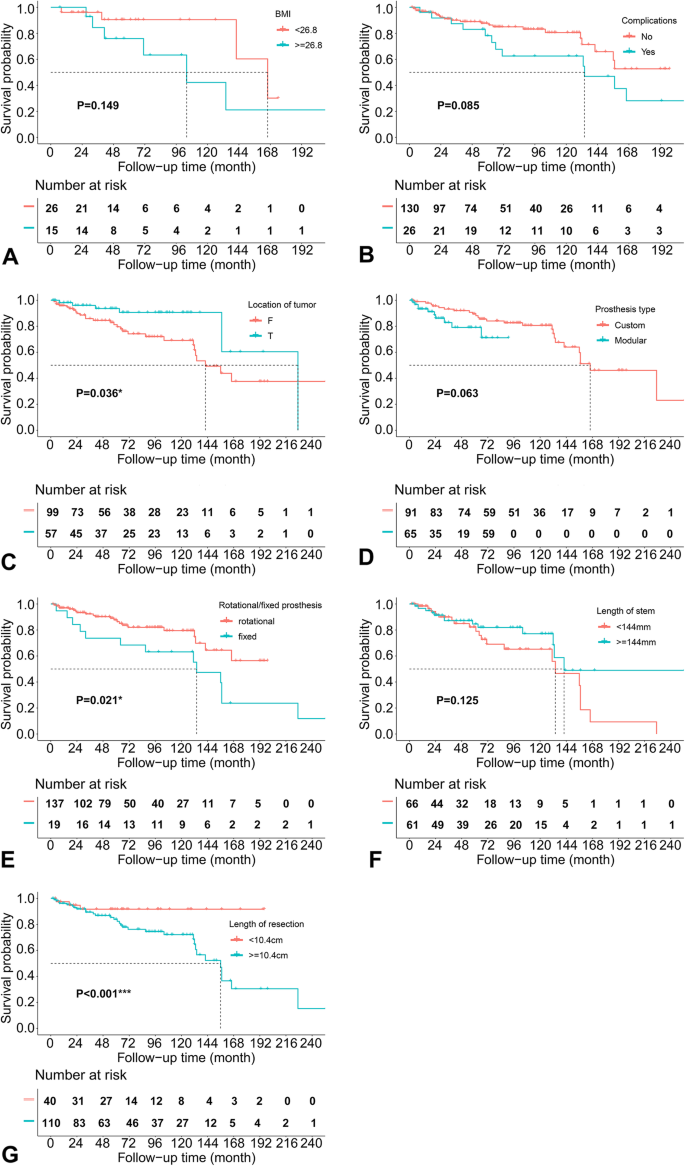
Kaplan-Meier survival curves for prognostic factors significantly associated with prosthetic survival, according to univariate COX analysis
The forest plot in Fig. 5 shows the effect sizes of multivariate analysis, presenting that anatomical location (HR = 0.42, 95%CI: 0.20 ~ 0.89, P = 0.024), length of prosthetic stem (HR = 0.44, 95%CI: 0.19 ~ 0.99, P = 0.048) and length of bone resection (HR = 11.08, 95%CI: 3.34 ~ 36.78, P < 0.001) remained to be statistically significant prognostic factors for prosthetic survival.
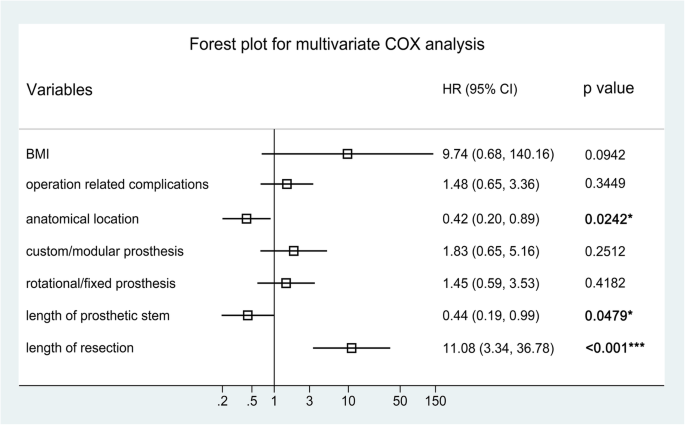
Forest plot displaying the effect sizes of prognostic factors involved in multivariate COX analysis
Establishing and validation of nomogram model
Basing on the significant prognostic factors screened by multivariate COX model, a graphical predicting nomogram model was developed, to calculate the predicted prosthetic survival probabilities at 1, 5, and 10 years post-operatively, as well as the median survival time (Fig. 6 ).
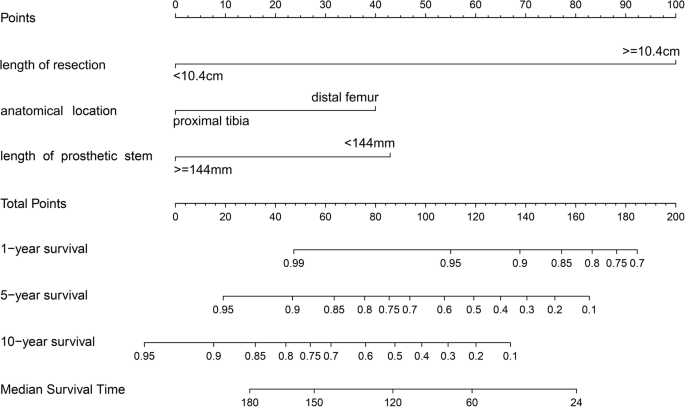
Graphical nomogram established for predicting the prosthetic survival at 1, 5 and 10 years, and the median prosthetic survival
The C-indexes were 0.717 (95%CI: 0.497 ~ 0.937) and 0.726 (95%CI: 0.244 ~ 1.208) for the training and validation samples respectively, demonstrating that the newly established nomogram possesses favorable discrimination ability. The calibration curves at 12, 60 and 120 months for the two samples are displayed in Fig. 7 . Generally, favorable consistencies between the predicted and actual survival were presented, indicating satisfactory accuracy of the novel predicting model.
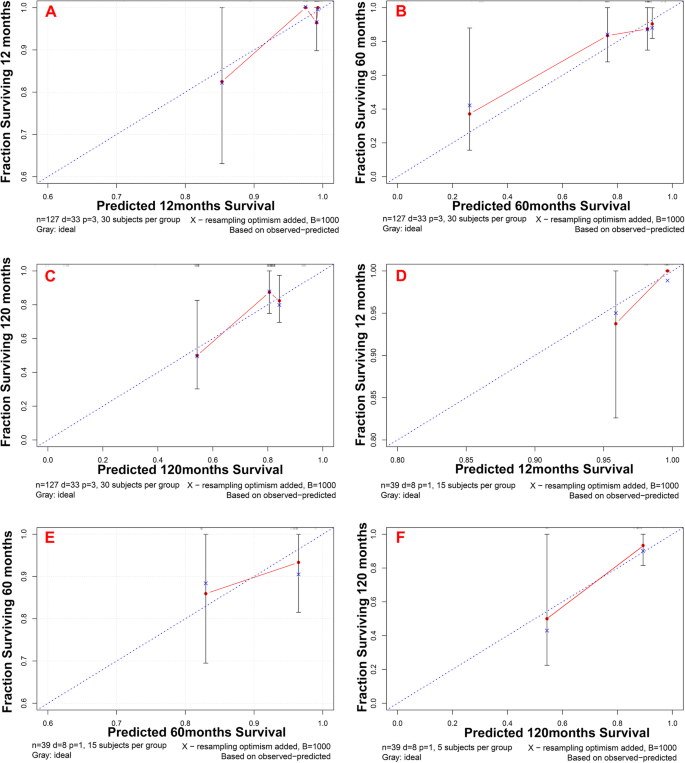
Calibration curves for evaluating the consistency between the predicted and actual survival probabilities, both in training and validation samples, at time points of 1, 5 and 10 years. Generally, satisfactory consistencies between predicted and actual survival rates were demonstrated
To facilitate the usage of our novel predicting model, a web link ( https://hellonihao.shinyapps.io/PangCG_DynNomapp/ ) was generated to automatically calculate the prosthetic survival online for each individual patient. The predicted survival curve, forest plot presenting survival probability, and numeric summary table would be output, after selecting of the patients’ characteristics and clicking on the button “Predict”. The survival probability at any time point could be obtained by dragging the sliderbar “time”.
Case presentation
Figure 8 and Fig. 9 show a case of patient who was operated for bone tumor locates at distal femur and reconstructed with a prosthesis that was more than 14.4 cm on length of stem, and more than 10.4 cm of bone was resected during tumorectomy. Using the graphical nomogram, only approximate survival rates could be read on the plot by drawing a vertical line through the total point. While, through the webpage-based dynamic nomogram, the detailed prosthetic survival probabilities at 12, 60 and 120 months could be automatically calculated, which is shown to be 0.890, 0.305 and 0.068, respectively.
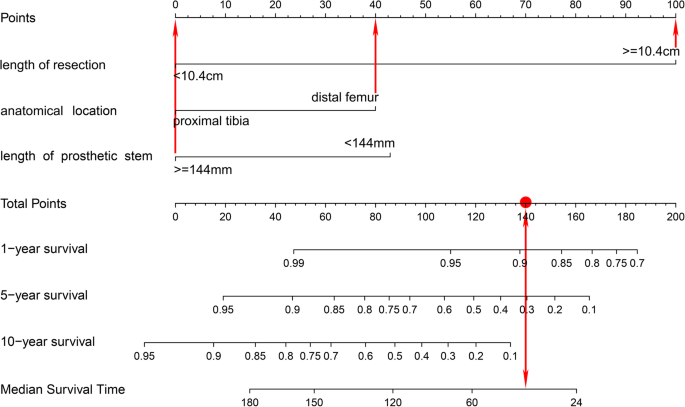
A case of patient who was operated for bone tumor locates at distal femur and reconstructed with a prosthesis that was more than 14.4 cm on length of stem, and more than 10.4 cm of bone was resected during tumorectomy. Using the graphical nomogram, survival rates could be read on the plot by drawing a vertical line through the total point
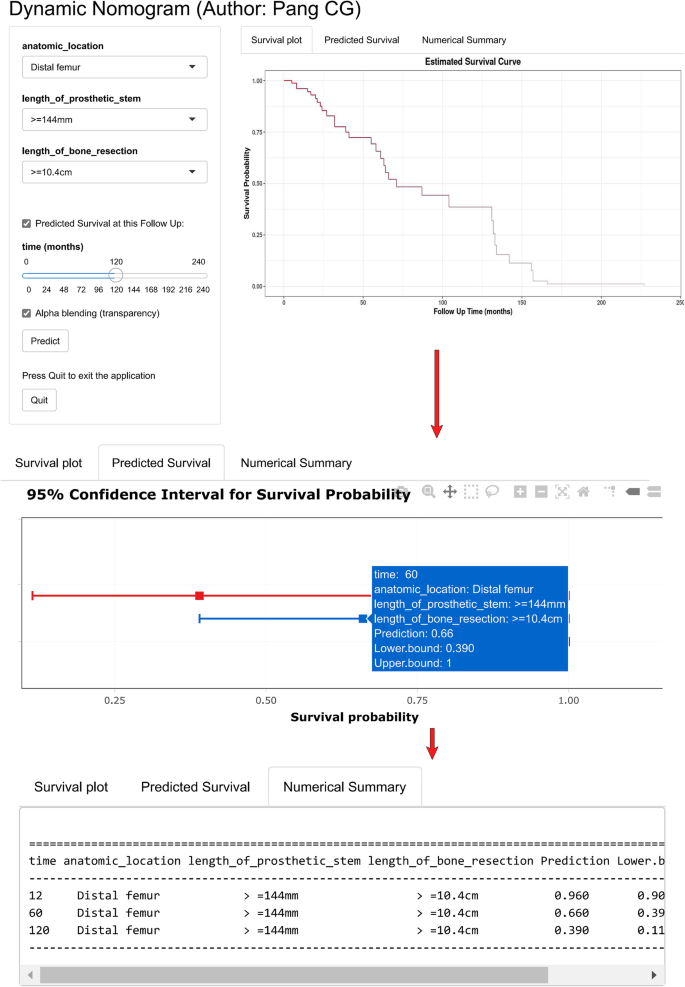
A case of patient who was operated for bone tumor locates at distal femur and reconstructed with a prosthesis that was more than 14.4 cm on length of stem, and more than 10.4 cm of bone was resected during tumorectomy. Through the webpage-based dynamic nomogram, the detailed prosthetic survival probabilities at 12, 60 and 120 months could be automatically calculated, which is shown to be 0.890, 0.305 and 0.068, respectively
Multimodality limb salvage therapy has replaced amputation as the preferred form of treatment for primary musculoskeletal tumors primarily owing to improvements in adjuvant and neo-adjuvant therapy, as well as advances in imaging and diagnostic modalities [ 2 , 3 , 4 ]. After the resection of bone and soft tissue tumors, reconstruction of the resulting defects was challenging because of the unique anatomic features of the knee. Limb-salvage surgery for malignant bone tumors must be successful in three different respects, that is, the cure of oncology, the durability of prostheses and the satisfactory of the function in the limbs. Following reconstruction of the operated knee, arising of complications in implants was not uncommon, and the prosthetic failure has always been regarded as a major event causing serious adverse effect on the patients’ overall survival, lower limb function and the quality of life, for these tumor patients. Thus, it is necessary to figure out the significant prognostic factors for prosthetic survival in patients operated for tumor around the knee. In the current study, we identified that the anatomical location of tumor, length of prosthetic stem, and length of bone resection during operation were significantly associated with the prosthetic survival. Basing on these factors, we also generated a graphic nomogram and a web predicting tool, which could easily applied for predicting survival probabilities of the implant at several time points.
Until now there are only a few predicting models that have been developed to help estimate the prosthetic survival probability, using independent prognostic factors. In the studies of Zhang et al. [ 19 ], they identified the significant factors associated with the incidence of aseptic loosening after tumor prosthetic replacement around the knee, demonstrating that tumor anatomical location (proximal tibia vs. distal femur), length of prosthetic stem (< 14 cm vs. > = 14 cm), and prosthetic motion mode (fixed hinge vs. rotation hinge) were independent predictors. After that, they established a graphical nomogram to help predict the risk of aseptic loosening at the time points of 5 and 10 years. This model, however, could only provide approximate risks of aseptic loosening at two points, and the applying of the model is not convenient as one need to calculate the sub-scores of the prognostic factors and the total score, and to gain the predicted survival by drawing vertical line. In the current study, we also developed a web-page based dynamic nomogram, to output a continuous survival curve, a forest plot of predicted survival and a numeric table online, being easier-to-use for clinicians and patients.
Regarding to the prognostic factors involved in our novel model, they have been widely analyzed in the previous researches [ 5 , 20 , 21 , 22 , 23 ]. The anatomical location of the tumor at proximal tibia has been demonstrated to be associated with increased risk of implant failure compared to the tumor at distal femur in many former studies [ 5 , 21 , 22 , 23 ]. In the study of Pala et al. [ 20 ], they reported that the failure rates of distal femoral and proximal tibia replacements were 26.7 and 36.7%, but the difference was non-significant between two groups. Hu et al. [ 5 ] also reported that the anatomical site of tumor was associated with the implant survival of tumor prosthesis around knee. Zhang et al. [ 21 ] investigated the prognosis value of site of the implant, and they reported a slight difference on the 5-year prosthetic survival (86.1% at distal femur and 66.9% at proximal tibia, p = 0.09). Guo et al. [ 22 ] identified the independent risk factors for implant failure in patients operated for tumor around the knee, and the result of multivariate COX analysis presented that the prosthesis implanted at the proximal tibia was associated with increased failure risk, when compared to that of the distal femur. Mazaleyrat et al. [ 23 ] reported that the 5-year and 10-year survival rates of implant were 84 and 70% for tumor located at distal femur, while 74 and 43% for tumor located at proximal tibia, being significantly different between the two groups by log-rank test ( p = 0.02). Our result about the prognostic effect of anatomical location of tumor was in accordance with these previous researches. It could be speculated that the poor soft tissue coverage, difficulties with anchoring the patellar tendon and possible injuries to the neurovascular system are the most likely causes for this difference.
Length of prosthetic stem was another important predictor for the implant failure, in several published articles [ 19 , 24 , 25 ]. Bergin et al. [ 24 ] evaluated the influences of the diameter of prosthetic stem and length ratio of bone:stem on the incidence of aseptic loosening in distal femoral endoprostheses, and they found that patients with stable implants had significantly larger stem sizes and lower bone:stem ratios than those with loose implants. Zhang et al. [ 19 ] established a predicting nomogram for aseptic loosening after tumor prosthetic replacement around the knee, and they identified that the length of the prosthetic stem was independent prognostic factor, being included in their novel prediction model. This suggests that longer stem of the endoprostheses may have a mechanical advantage by obtain more osteointergration between the bone and the endoprosthesis, to prevent the early failures.
Resection length during tumorectomy was also recognized as an independent prognostic factor for prosthetic survival in former studies [ 5 , 22 , 24 , 26 , 27 ]. Guo et al. [ 22 ] found that a resection length of 14 cm or more was significant negative prognostic factor for endopristhetic replacement for primary tumors around the knee. Hu et al. [ 5 ] reviewed the published articles about application of artificial prosthesis reconstruction techniques in malignant tumors around the knee joint, showing that the longer the neoplastic bone resected, the worse the prosthetic survival rate is. Wu et al. [ 26 ] identified the prognostic effect of several factors, including the patient age, surgical stage, design of implant (custom vs. modular), stem diameter, and resection length, through multivariate COX analysis, demonstrating that design of prosthesis and length of resection were significantly associated with prosthetic survival. Kawai et al. [ 27 ] reported 82 cases of artificial prosthesis reconstruction after resection of distal femur malignant bone tumors. The prosthetic survival rate of the group in whom < 40% of the distal femur length was resected was considerably higher than that of the group with resection lengthmore than 40%, according to multivariate analysis. In our study, we divided the patients into two group by the cutoff point detected with running log-rank test, and found that patients with more than 10.4 cm of resection length was associated with increased implant failure. The influence of the extent of bone resections on the development of implant failure may be contributed by the increased torque production out of the line of prosthesis and/or impairment of quadriceps contraction. Changes in biomechanical stresses after extensive resections of bone and adjacent muscles probably are the reasons for the increased failure incidence of these implants.
This study, nevertheless, is of several limitations. Firstly, this study was designed as a retrospective cohort study, causing inevitable risk of bias on collection of the data. Thus, some more prospective and long-term cohort studies or randomized controlled trials should be conducted to clarified the prognostic effect of the predicting factors identified in this study. Secondly, as only a few patients were provided with uncemented prostheses in our institutions, it was impossible to take full assessment on the prognostic effect of the fixation method for the endoprostheses. Thus, we excluded patients reconstructed by implants without cement fixation to minimize the risk of bias caused by fixation methods. Thirdly, the patients used for external validation was sampled from the same cohort as the training sample used for model developing. Hence, further external validation using sample from different clinical centers or even different countries is necessary. Finally, it is difficult to collect large sample size in this topic due to the low frequency of tumor resection and endoprosthetic reconstruction for tumor around knee. Thus, to ensure the statistical power in the regression analysis and model developing, most participants were put in the training sample, causing the relative small size of validation sample.
The anatomical location of the endoprostheses, length of the prosthetic stem and the length of the bone resection were demonstrated to be significantly associated with the risk of implant failure in patients reconstructed for tumors around the knee. A graphical nomogram and a user-interactive online dynamic nomogram were developed to help clinicians and patients easily predict the survival probabilities of implant at any time point post-operatively.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
continuous passive motion
body mass index
confidence interval
hazard ratio
magnetic resonance imaging
Multi Slice Computerized Tomography
Musculoskeletal Tumor Society
Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis
Zhang X, Wang Z. A statistic analysis of 3409 cases of tumors and tumorlike lesions of bones and joints. Chinese J Bone Tumor Bone Dis. 2010;9(3):189–95.
Google Scholar
Henderson ER, Groundland JS, Pala E, Dennis JA, Wooten R, Cheong D, et al. Failure mode classification for tumor endoprostheses: retrospective review of five institutions and a literature review. J Bone Joint Surg Am. 2011;93(5):418–29. https://doi.org/10.2106/JBJS.J.00834 .
Article PubMed Google Scholar
Allison DC, Carney SC, Ahlmann ER, Hendifar A, Chawla S, Fedenko A, et al. A meta-analysis of osteosarcoma outcomes in the modern medical era. Sarcoma. 2012;2012:704872.
Article PubMed PubMed Central Google Scholar
Kotz RI. Progress in musculoskeletal oncology from 1922–2012. Int Orthop 2014;38(5):1113–1122, Progress in musculoskeletal oncology from 1922 – 2012, DOI: https://doi.org/10.1007/s00264-014-2315-0 .
Hu YC, Lun DX. Application of artificial prosthesis reconstruction techniques in malignant tumors around the knee joint. Orthop Surg. 2012;4(1):1–10. https://doi.org/10.1111/j.1757-7861.2011.00161.x .
Article CAS PubMed PubMed Central Google Scholar
Ahlmann ER, Menendez LR, Kermani C, Gotha H. Survivorship and clinical outcome of modular endoprosthetic reconstruction for neoplastic disease of the lower limb. J Bone Joint Surg Br. 2006;88:790–5.
Article CAS PubMed Google Scholar
Mirra JM, Picci P, Gold RH, eds. Bone Tumors: Clinical, Radiologic and Pathologic Correlations. Vol. 1. Philadelphia: Lea & Febiger; 1989:248–62.
Ruggieri P, Bosco G, Pala E, Errani C, Mercuri M. Local recurrence, survival and function after total femur resection and megaprosthetic reconstruction for bone sarcomas. Clin Orthop Relat Res. 2010;468(11):2860–6. https://doi.org/10.1007/s11999-010-1476-4 .
Gaur AH, Liu T, Knapp KM, Daw NC, Rao BN, Neel MD, et al. Infections in children and young adults with bone malignancies undergoing limb-sparing surgery. Cancer. 2005;104(3):602–10. https://doi.org/10.1002/cncr.21212 .
Gitelis S, Yergler J, Sawlani N, Schiff A, Shott S. Short and long term failure of the modular oncology knee prosthesis. Orthopedics. 2008;31:362.
Sim IW, Tse LF, Ek ET, Powell GJ, Choong PF. Salvaging the limb salvage: management of complications following endoprosthetic reconstruction for tumors around the knee. Eur J Surg Oncol. 2007;33(6):796–802. https://doi.org/10.1016/j.ejso.2006.10.007 .
Shehadeh A, Noveau J, Malawer M, Henshaw R. Late complications and survival of endoprosthetic reconstruction after resection of bone tumors. Clin Orthop Relat Res. 2010;468(11):2885–95. https://doi.org/10.1007/s11999-010-1454-x .
Unwin PS, Cannon SR, Grimer RJ, Kemp HB, Sneath RS, Walker PS. Aseptic loosening in cemented custom-made prosthetic replacements for bone tumours of the lower limb. J Bone Joint Surg Br. 1996;78:5–13.
Wirganowicz PZ, Eckardt JJ, Dorey FJ, Eilber FR, Kabo JM. Etiology and results of tumor endoprosthesis revision surgery in 64 patients. Clin Orthop Relat Res. 1999;358:64–74.
Article Google Scholar
Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD State-13; 2015.
Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993;286:241–6.
Facciorusso A, Prete VD, Crucinio D, Serviddio G, Vendemiale G, Muscatiello N. Lymphocyte-to-monocyte ratio predicts survival after radiofrequency ablation for colorectal liver metastases. World J Gastroenterol. 2016;22(16):4211–8. https://doi.org/10.3748/wjg.v22.i16.4211 .
Facciorusso A, Prete VD, Antonino M, Neve V, Crucinio N, Di Leo A, et al. Serum ferritin as a new prognostic factor in hepatocellular carcinoma patients treated with radiofrequency ablation. J Gastroenterol Hepatol. 2014;29(11):1905–10. https://doi.org/10.1111/jgh.12618 .
Zhang HR, Zhao YL, Wang F, Yang XG, Xu MY, Qiao RQ, et al. Establishment and validation of a nomogram model for periprosthetic infection after megaprosthetic replacement around the knee following bone tumor resection: a retrospective analysis. Orthop Traumatol Surg Res. 2020;106(3):421–7. https://doi.org/10.1016/j.otsr.2019.10.023 .
Pala E, Trovarelli G, Calabrò T, Angelini A, Abati CN, Ruggieri P. Survival of modern knee tumor Megaprostheses: failures, functional results, and a comparative statistical analysis. Clin Orthop Relat Res. 2015;473(3):891–9. https://doi.org/10.1007/s11999-014-3699-2 .
Zhang C, Hu J, Zhu K, Cai T, Ma X. Survival, complications and functional outcomes of cemented megaprostheses for high-grade osteosarcoma around the knee. Int Orthop. 2018;42(4):927–38. https://doi.org/10.1007/s00264-018-3770-9 .
Guo W, Ji T, Yang R, Tang X, Yang Y. Endoprosthetic replacement for primary tumours around the knee: experience from Peking University. J Bone Joint Surg Br. 2008;90:1084–9.
Mazaleyrat M, Nail LL, Auberger G, Biau D, Rosset P, Waast D, et al. Survival and complications in hinged knee reconstruction prostheses after distal femoral or proximal tibial tumor resection: a retrospective study of 161 cases. Orthop Traumatol Surg Res. 2020;106(3):403–7. https://doi.org/10.1016/j.otsr.2019.11.027 .
Bergin PF, Noveau JB, Jelinek JS, Henshaw RM. Aseptic loosening rates in distal femoral Endoprostheses: does stem size matter? Clin Orthop Relat Res. 2012;470(3):743–50. https://doi.org/10.1007/s11999-011-2081-x .
Bus MA, van de Sande MAJ, Fiocco M, Schaap GR, Bramer JAM, Dijkstra PDS. What are the long-term results of MUTARS modular Endoprostheses for reconstruction of tumor resection of the distal femur and proximal tibia? Clin Orthop Relat Res. 2017;475(3):708–18. https://doi.org/10.1007/s11999-015-4644-8 .
Wu CC, Henshaw RW, Pritsch T, Squires MH, Malawer MM. Implant design and resection length affect cemented Endoprosthesis survival in proximal Tibial reconstruction. J Arthroplast. 2008;23(6):886–93. https://doi.org/10.1016/j.arth.2007.07.007 .
Kawai A, Lin PP, Boland PJ, Athanasian EA, Healey JH. Relationship between magnitude of resection, complication, and prosthetic survival after prosthetic knee reconstructions for distal femoral tumors. J Surg Oncol. 1999;70(2):109–15. https://doi.org/10.1002/(SICI)1096-9098(199902)70:2<109::AID-JSO9>3.0.CO;2-X .
Download references
Acknowledgements
Not applicable.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Cheng-gang Pang and Xiong-gang Yang contributed equally to this work.
Authors and Affiliations
Graduate School, Tianjin Medical University, Tianjin, 300070, China
Cheng-gang Pang & Yun-long Zhao
Department of Orthopedic Surgery, Huashan Hospital, Fudan University, No. 12 Wulumuqi Road, Shanghai, 200040, China
Xiong-gang Yang
Department of Bone Tumor of Tianjin Hospital, Tianjin, 300211, China
Yan-cheng Liu & Yong-cheng Hu
You can also search for this author in PubMed Google Scholar
Contributions
PCG and HYC conceived of and designed the study, performed the analysis, interpreted the results and wrote the manuscript. YXG performed the revision and validation of the manuscript. ZYL and LYC performed the data collection and analysis. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Yong-cheng Hu .
Ethics declarations
Ethics approval and consent to participate.
This study was performed according to the “Declaration of Helsinki” (as revised in 2013) and was approved by the ethics committee of Tianjin Hospital. Informed consent was waived by the Institutional Ethics Committee of Tianjin Hospital because of the retrospective nature of this study.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Pang, Cg., Yang, Xg., Zhao, Yl. et al. A novel tool for predicting the survival of endoprosthesis used for reconstruction of the knee following tumor resection: a retrospective cohort study. BMC Cancer 21 , 986 (2021). https://doi.org/10.1186/s12885-021-08710-x
Download citation
Received : 23 October 2020
Accepted : 18 August 2021
Published : 03 September 2021
DOI : https://doi.org/10.1186/s12885-021-08710-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Limb salvage
- Prognostic factor
- Tumor endoprostheses
ISSN: 1471-2407
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Research article
- Open access
- Published: 29 November 2023
A comparative study of reconstruction modalities after knee joint-preserving tumor resection: reconstruction with a custom-made endoprosthesis versus reconstruction with a liquid nitrogen-inactivated autologous bone graft
- Yuan Li 1 ,
- Hairong Xu 1 ,
- Huachao Shan 1 ,
- Weifeng Liu 1 &
- Xiaohui Niu 1
Journal of Orthopaedic Surgery and Research volume 18 , Article number: 908 ( 2023 ) Cite this article
511 Accesses
Metrics details
This study evaluated the feasibility, complications, graft survival rate, and clinical outcomes of joint-preserving resection using a custom-made endoprosthesis and liquid nitrogen-inactivated autologous bone graft reconstruction in patients with malignant bone tumors around the knee joint.
We retrospectively analyzed 23 consecutive patients who underwent joint preservation surgery between 2008 and 2018 at our center. The study cohort included 13 patients who underwent custom-made endoprosthesis reconstruction and 10 who underwent liquid nitrogen-inactivated autologous bone graft reconstruction. The resected bone length, distance between the resection line and the joint, intraoperative blood loss, operation time, complications, and MSTS were compared between the two groups.
The median follow-up time was 68.5 months in the endoprosthesis group and 65.3 months in the inactivated autograft group. There were no significant differences in baseline characteristics, resected bone length, distance between the resection line and the joint, or intraoperative blood loss between the two groups. The operative time was longer in the inactivated bone graft group than in the endoprosthesis group ( p < 0.001). The endoprosthesis group had more complications (six patients) and reoperations due to complications (five) than the inactivated autograft group (one), but there was no significant difference in the incidence of complications between the two groups ( p = 0.158). The inactivated autograft group had one patient with type 1b complications, while the endoprosthesis group had one with type 1b complications, one with type 2b complications, and one with type 4a complications. One patient in the endoprosthesis group with type 5a complications experienced two soft tissue recurrences. The overall 5-year survival rate was 86.5% and the graft survival and final limb salvage rates were 100% in both groups. After the follow-up period, the mean MSTS scores were 91% ± 7% in the endoprosthesis group and 94% ± 6% in the inactivated autograft group, with no significant difference ( p = 0.280).
Joint-preserving resection is a reliable and effective tumor resection method that can achieve good postoperative function. There were no significant differences in the incidence of complications, overall survival rate, or graft survival rate between the two groups.
Malignant bone tumors preferentially develop at the metaphyses that surround the knee joint, and surgery usually involves the removal of the entire metaphysis followed by reconstruction. Currently, the most common surgical approach is reconstruction of the resected bone defect and contralateral articular surface using an endoprosthesis [ 1 , 2 ]. However, for some patients, if tumor resection is performed based on preoperative imaging assessment, it is possible to obtain a safe surgical margin while preserving the articular surface, resulting in greater postoperative function. Preservation of the joints and periarticular ligaments allows for better proprioception [ 3 ]. Furthermore, the absence of a polyethylene spacer and rotatable shaft of the endoprosthesis shaft at the joint can reduce abrasive debris and mechanical complications. In pediatric patients, preservation of the epiphysis preserves the potential growth capacity of the diseased bone. The absence of a contralateral endoprosthesis also preserves the growth capacity of the epiphysis on the contralateral side of the joint [ 4 ]. For these patients, many physicians attempt to preserve the joint and use various modalities to reconstruct bone defect [ 4 , 5 , 6 , 7 ].
To date, the most commonly used reconstruction modalities for knee joint preservation surgeries include custom-made endoprostheses (traditional customized endoprosthesis or three-dimensional (3D) printed endoprosthesis), bone allografts, inactivated bone autografts, and allografts or inactivated autografts coupled with a free vascularized fibular graft [ 5 , 6 , 7 , 8 , 9 ]. Regardless of the type of reconstruction, when the thickness of the residual articular bone is small (less than 3 cm), its connection with the reconstructed part and its long-term stability are challenges for orthopedic surgeons [ 10 ]. Currently used fixation methods include screws, conventional steel plates, customized steel plates, and 3D-printed endoprostheses [ 4 , 6 , 11 ]. However, because only a small number of patients are suitable for this type of surgery, most published reports have small sample sizes and apply only a single method. To our knowledge, no studies have compared the results of different reconstruction modalities to date.
Our institution adopted reconstruction using both custom-made endoprosthesis and liquid nitrogen-inactivated autologous bone graft for knee joint-preserving tumor resection, and we have obtained satisfactory clinical prognosis and complication rates. However, no specific study has compared the complications, survival rate, and long-term function of these two reconstruction modalities, and there is no standardized reconstruction protocol for preserving the knee joint in specific patients. This study compared reconstruction using a customized prosthesis and a liquid nitrogen-inactivated autologous bone graft in patients who underwent knee joint-preserving tumor resection and investigated differences in (1) oncologic safety, (2) rate of complications, and (3) 5-year graft survival rate and patient limb salvage rate between the two reconstruction modalities.
Materials and methods
Study subjects.
This study was approved by the Ethics Committee of the Beijing Jishuitan Hospital, Capital Medical University. This study retrospectively analyzed the clinical data of 23 consecutive patients with malignant bone tumors around the knees who were admitted to our hospital between November 2008 and November 2018. The inclusion criteria were as follows: (1) primary malignant bone tumors around the knee joint, (2) patients who underwent tumor resection with preservation of the knee joint, (3) residual host bone adjacent to the knee joint of ≤ 3 cm after tumor resection, and (4) reconstruction with a custom-made endoprosthesis or a liquid nitrogen-inactivated autologous bone graft. The exclusion criteria were as follows: (1) bone metastases, (2) non-first-time surgical patients, (3) patients who underwent reconstruction for non-tumor factors, and (4) patients who underwent reconstruction using a liquid nitrogen-inactivated autologous bone graft together with an autologous iliac or fibular graft. According to the above inclusion and exclusion criteria, 23 patients were included in this study cohort. They were then divided based on the reconstruction modality into a custom-made endoprosthesis group and a liquid nitrogen-inactivated autologous bone graft group.
There were 13 patients in the group with a custom-made endoprosthesis (referred to as the endoprosthesis group), including seven males and six females, with an average age of 26.3 ± 12.9 years (range: 13–49 years). There were eight patients with classic osteosarcoma, three with chondrosarcoma, one with undifferentiated high-grade pleomorphic sarcoma, and one with spindle cell sarcoma. There were 11 patients with tumors located in the distal femur and two with tumors located in the proximal tibia.
There were ten patients in the liquid nitrogen-inactivated autologous bone graft group (referred to as the inactivated autograft group), including five males and five females, with an average age of 18.74 ± 9.6 years. There were seven patients with classic osteosarcoma, one with high-grade surface osteosarcoma, one with chondrosarcoma, and one with Ewing’s sarcoma. There were five patients with tumors located at the distal femur and five with tumors located at the proximal tibia.
The difference in age between the two groups was insignificant (nonparametric Mann–Whitney U test: Z = − 1.833, p = 0.067). There was also no significant differences in sex ( X 2 = 0.034, p = 1.000) nor the classification of diseases ( X 2 = 4.756, p = 0.446) between the two groups.
Prior to this study, we did not use a standardized method to choose between the two reconstruction modalities. Before 2015, we used only custom-made endoprostheses for reconstruction, whereas we began using liquid nitrogen-inactivated autologous bone grafts to perform reconstruction after 2015. Therefore, the patients included in this study were not randomly selected between the two reconstruction modalities. However, we analyzed the demographic characteristics of the patients and found no significant differences in patient characteristics between the two study groups.
Preoperative preparation
All patients underwent preoperative histological testing to confirm diagnosis. Patients with osteosarcoma, undifferentiated high-grade pleomorphic sarcoma, and Ewing sarcoma received four courses of neoadjuvant chemotherapy and underwent surgery after completion of chemotherapy. The remaining patients underwent direct surgery. All patients underwent preoperative radiography, enhanced computed tomography (CT), magnetic resonance imaging (MRI), and bone scan. Both the response to neoadjuvant chemotherapy and extent of the tumor were determined based on the imaging results. If the resection was performed more than 1 cm outside the extent of the tumor and a residual bone of 10 mm could be preserved on the tibial side, or a residual bone of 20 mm could be preserved on the femoral side, knee joint-preserving tumor resection was performed.
The patients in the endoprosthesis group were treated by the attending physicians who determined the position of resection by importing the preoperative imaging data into a medical image processing software (Mimics 15.0, Mimics®; Materialize, Leuven, Belgium), followed by transmitting the Mimics data to the endoprosthetics engineers (LDK Co., Ltd., Beijing, China) for designing the prostheses. The prosthesis surface adjacent to the resection surface on the articular side must completely match the host bone resection surface. Auxiliary steel plates were designed on both sides of the prosthesis to fix the residual bone in place, and the direction and length of the screws were designed according to the size and shape of the residual bone so that there were three screws on each side. Each prosthesis was fabricated using a subtractive manufacturing method after the design was approved by the surgeon.
Surgical procedure
Each patient underwent surgery in the supine position with an anteromedial incision at the knee joint, and the knee joint was separated and exposed outside the reaction zone following the principles of a tumor-free operation. A tracker was fixed to a safe portion of the diseased bone, and the tracker and various tools were registered at the workstation of the navigation system. Intraoperative data on the surgical area were acquired using ISO-C (Siremobil ISO-C 3D; Siemens Medical Solutions, Erlangen, Germany) and imported into the navigation system, to determine the actual resection position during surgery based on the preoperatively planned resection position. The bone was resected using a Gigli saw, and a small amount of tissue was removed from the medullary cavity of the resected end for pathological examination to determine whether a safe surgical margin had been reached.
In the endoprosthesis group, the defect was reconstructed using a customized endoprosthesis. The residual bone was fixed using an extracortical fixation plate after completely fitting the resection surface close to the articular side of the customized prosthesis. Intraoperative fluoroscopy was used to verify whether the direction and length of the screws matched those in the preoperative design. An intramedullary stem fixed with bone cement was placed at the other end of the prosthesis. For patients with tibial tumors, the patellar tendon was fixed to the prosthesis, and a gastrocnemius muscle flap was used to cover the anterior part of the prosthesis, whereas the wound was directly closed for the remaining patients (Fig. 1 ).
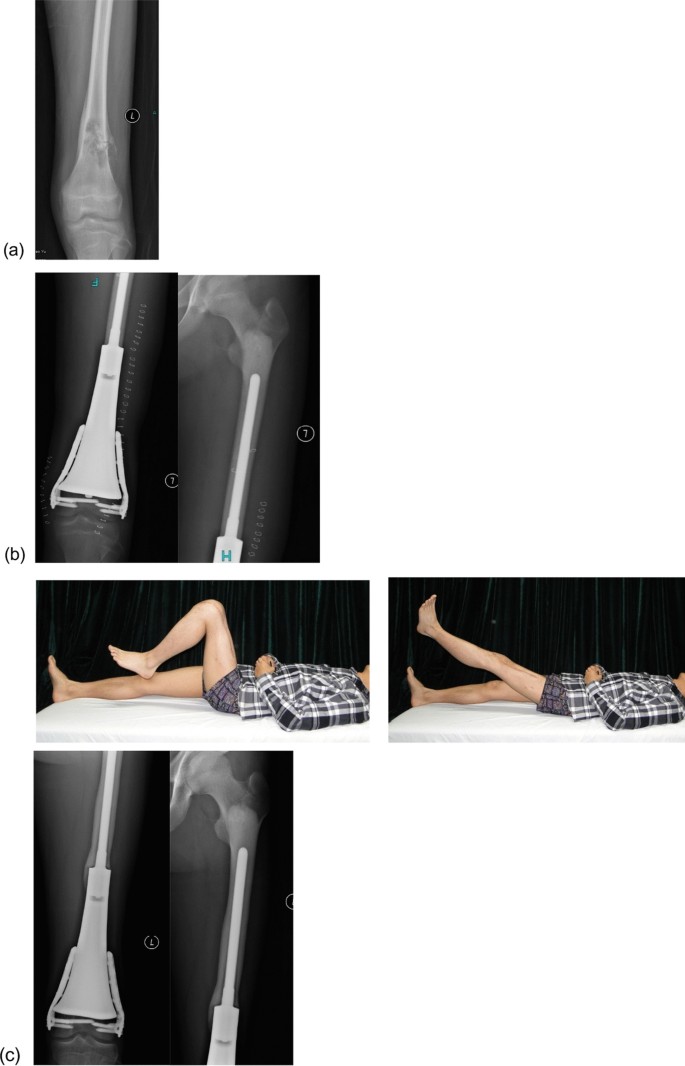
a A 17-year-old male with classical osteosarcoma of the distal femur. b Postoperative radiograph at 2 weeks. c Radiograph and function at 80 months postoperatively, showing the satisfactory function of the patient
In the inactivated autograft group, after tumor resection, the soft tissues and muscle attachments on the surface of the bone with the tumor were removed, followed by removal of the tissues in the medullary cavity and preservation of only the cortical bone. The bones were frozen for 20 min in liquid nitrogen, rewarmed at room temperature for 15 min, and then rewarmed in saline for 15 min. The medullary cavity was then filled with bone cement. Bilateral plate fixation was performed with at least four screws bilaterally passing through the host cortical bone at the diaphysis and at least two screws on each side close to the articular side to fix the residual bone. If no suitable plate is available, the residual bone can be fixed longitudinally by using screws to avoid the weight-bearing part of the articular surface during fixation. In patients with tibial tumors, the medial head of the gastrocnemius muscle flap was used to cover the grafted bone, whereas the wound was directly closed in the remaining patients (Fig. 2 ).
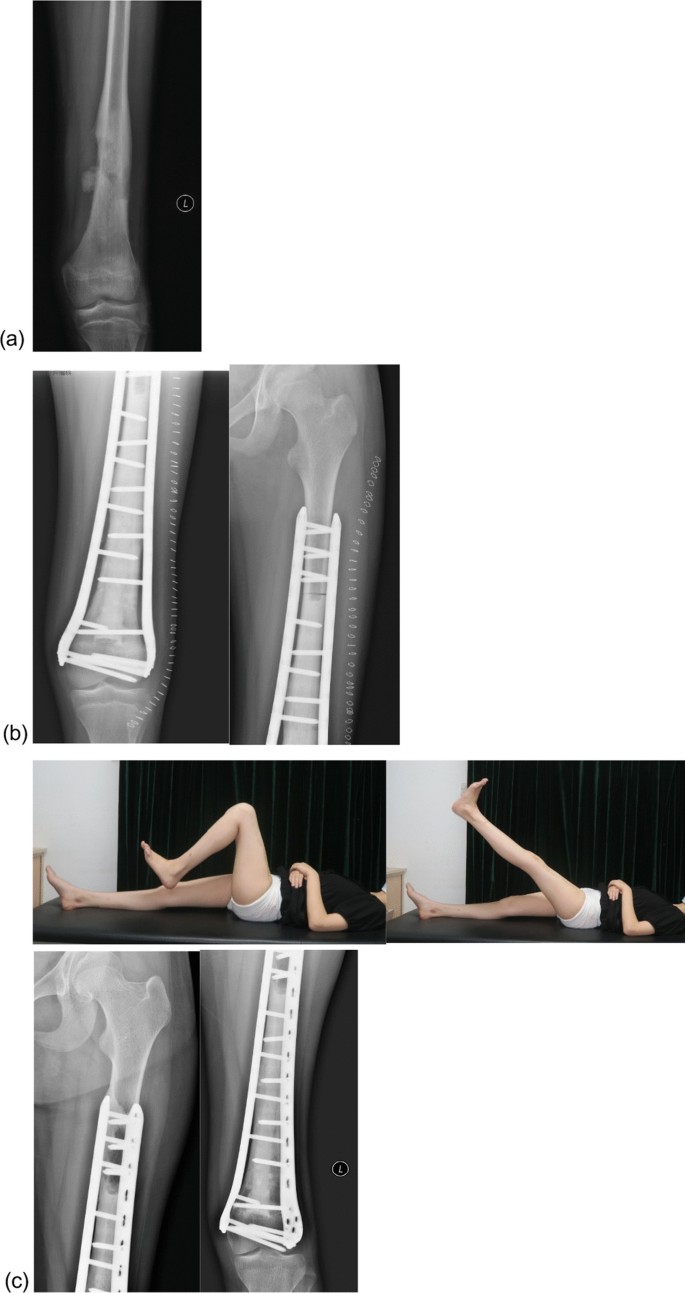
a A 13-year-old female with classical osteosarcoma of the distal femur. b Postoperative radiograph at 2 weeks. c Radiograph and function at 55 months postoperatively, showing satisfactory function of the patient
Postoperative rehabilitation
The surgical drain was removed when the drainage volume was less than 50 mL per day. Isometric muscle contractions were performed in the early postoperative period and joint exercises were started two weeks after surgery. Partial weight-bearing exercises were initiated six weeks after surgery. Finally, full weight-bearing exercises were started three months after surgery for patients in the prosthesis group but were started after bone healing for patients in the inactivated autograft group. Patients with osteosarcoma and Ewing sarcoma continue to receive adjuvant chemotherapy after wound healing.
Follow-up and indicators for evaluation
Perioperative complications were documented, and outpatient follow-up visit were conducted every three months for three years after surgery and every six months thereafter. Clinical and imaging evaluations were performed at each follow-up visit to document complications and Musculoskeletal Tumor Society (MSTS) scores. The International Society of Limb Salvage (ISOLS) assessment system was used to assess graft-related complications related to the grafts [ 12 ].
In the inactivated autograft group, bone healing was assessed using the ISOLS allograft radiographic evaluation system [ 13 ]. This evaluation system was initially designed for allograft transplantation, but there have been many reports of its practical applications in imaging evaluation after autograft transplantation [ 14 , 15 ]. Two senior orthopedic oncologists performed separate assessments. Any discrepancies in the results were resolved after a joint discussion.
Statistical analysis
Statistical analyses were performed using SPSS software package (version 22.0; SPSS, Chicago, IL, USA). The categorical variables were reported using frequency and percentage, whereas the continuous variables were reported using mean ± standard deviation. Kaplan–Meier curves were used to analyze the patient and graft survival rates. The chi-square test was used to compare categorical variables, whereas a nonparametric test was used to compare continuous variables between the two groups. Statistical significance was set at p < 0.05.
General results
All the patients successfully completed the surgery. For the 13 patients in the endoprosthesis group, the length of the resected bone was 91–356 mm, with an average of 188.8 ± 73.6 mm, and the distance between the resection line and the joint was 16–30 mm, with an average of 25.1 ± 4.4 mm. The duration of surgery was 180–390 min (average, 258.5 ± 54.7 min. The volume of intraoperative bleeding ranged from 150 to 1000 mL, with an average of 634.6 ± 296.8 mL. The median postoperative follow-up time was 68.5 months (20.9–177.3 months), with an average of 83.5 ± 44.7 months (Table 1 ).
For the ten patients in the inactivated autograft group, the length of resected bone was 125–283 mm, with an average of 193.8 ± 55.6 mm, and the distance between the resection line and the joint was 10–30 mm, with an average of 22.9 ± 7.8 mm. The duration of the operation was 295–600 min, with an average of 40.0 ± 93.4 min. The volume of intraoperative bleeding was 200–1000 mL, with an average of 660.0 ± 298.9 mL. The median postoperative follow-up time was 65.3 months (13.4–86.7 months), with an average duration of 60.5 ± 21.4 months.
There was no significant difference in the length of the resected end ( Z = − 0.310, p = 0.756), distance between the resection line and the joint ( Z = − 0.347, p = 0.729), and volume of intraoperative bleeding ( Z = − 0.190, p = 0.850) between the two groups. However, the duration of operation for the inactivated autograft group was significantly higher than that of the prosthesis group ( Z = − 3.578, p < 0.001).
Oncological results
Among the 23 patients, 46 resected ends were pathologically examined separately, and all resected ends were safe. There was no recurrence at the end of resection after surgery.
There was only one patients with local recurrence in the prosthesis group. The patient had stage III chondrosarcoma of the distal femur accompanied by pulmonary metastasis. The patient presented with two local soft tissue recurrences at 8 and 24 months postoperatively and underwent local tumor resection. Eventually, the patient died of pulmonary metastasis 30.5 months after the surgery.
Two deaths occurred in the inactivated autograft group; both patients had classic osteosarcoma of the distal femur. The patients died of lung metastases 13 and 33 months after surgery.
The 5-year survival rates were 86.5% for all patients, 91.7% in the prosthesis group, and 80% in the inactivated autograft group (Fig. 3 ). The difference in the survival rate between the two groups was insignificant ( X 2 = 0.639, p = 0.424).
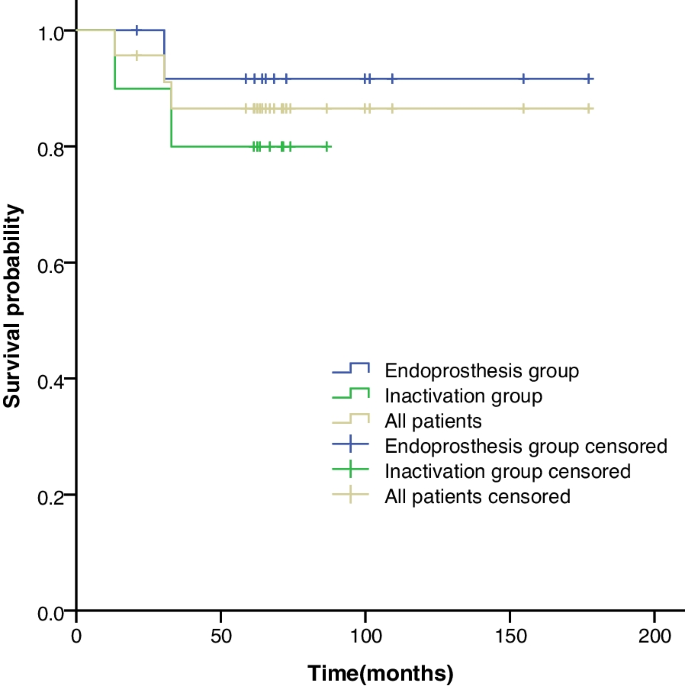
Kaplan–Meier curves showing the five-year survival rates for all the patients, the endoprosthesis group, and the inactivated autograft group. The graph shows an insignificant difference in the five-year survival rates between the endoprosthesis group and the inactivated autograft group, which were 91.7% and 80%, respectively
Complications
According to the ISOLS criteria for the evaluation of complications, there were six complications (26.1%) and five reoperations due to complications in the prosthesis group, whereas there was one complication and no reoperation due to complications in the inactivated autograft group. However, there was no significant difference in the incidence of complications between the two groups ( X 2 = 3.489, p = 0.158).
There were three patients with type 1b complications in the study cohort: two in the endoprosthesis group (one with a tumor at the distal femur and one with a tumor at the proximal tibia) and one in the inactivated autograft group (tibial tumor). All three patients developed necrosis at the skin edge due to high postoperative skin tension, which healed after debridement.
One case of aseptic loosening (type 2b) occurred in a patient in the endoprosthesis group who had an osteosarcoma at the distal femur. At the follow-up visit 52 months after surgery, imaging revealed loosening of the proximal prosthetic shaft end. Owing to the fact that the patient was asymptomatic, the patient continued using the prosthesis. No aseptic loosening of the prosthetic shaft was observed in any of the remaining patients during the follow-up.
Among the 13 patients in the endoprosthesis group, fixation of the residual bone close to the articular side of the knee joint remained stable during the follow-up period, and none of the patients had displacement of the residual bone from the prosthesis. Among the 10 patients in the inactivated autograft group, the resected end close to the knee joint side healed 6–16 months after surgery, with an average healing time of 8.0 ± 3.5 months, whereas the resected end close to the diaphysis side healed 6–26 months after surgery, with an average healing time of 13.7 ± 6.4 months. No type 2 or 3 complications related to mechanical strength were observed during follow-up.
During the follow-up period, one case of deep infection (type 4a) occurred in a patient from the prosthesis group who had osteosarcoma at the proximal tibia. A sinus tract appeared next to the anterolateral tibial incision 45 months after surgery, which healed after debridement and reappeared 53 months after surgery. The sinus tract was followed-up with intermittent changes in medication for up to 62 months.
One patient in the endoprosthesis group had two soft tissue recurrences (type 5a), and the recurrent foci were surgically resected on two separate occasions (see Oncological Results for details).
Final graft results
No patients in either group underwent endoprosthesis or bone graft removal due to complications, and the graft survival rate was 100%. Moreover, none of the patients in either group underwent amputation due to complications, and the final limb salvage rate was 100%.
At the end of the follow-up period, the MSTS scores ranged from 80 to 100% for the prosthesis group, with an average of 91% ± 7%, whereas the MSTS scores ranged from 87 to 100% for the inactivated autograft group, with an average of 94% ± 6%. There was no significant difference between the two groups ( Z = − 1.081, p = 0.280).
Knee joint-preserving tumor resection for malignant bone tumors around the knee allows better function and helps reduce leg length discrepancy in minor patients in the distant future by preserving the growth capacity of the epiphysis [ 16 , 17 ]. However, no standard reconstruction modality exists because of the rarity of cases that qualify for joint preservation. To provide a reference for the future selection of treatment modalities for knee joint preservation surgery, we retrospectively analyzed reconstruction using a customized prosthesis and reconstruction using a liquid nitrogen-inactivated autologous bone graft in terms of surgical difficulty, complications, and MSTS score.
Safety is the most important indicator of limb salvage surgery for bone malignancies [ 18 ]. The resection area that reaches a safe surgical margin is of utmost importance in reducing local tumor recurrence. According to Kawaguchi, the surgical margin of high-grade sarcomas must be greater than 3 cm in the absence of neoadjuvant therapy or when neoadjuvant therapy is ineffective, whereas it must be 2 cm when neoadjuvant therapy is effective [ 19 ]. All patients in this study, except for three patients with chondrosarcoma, underwent standardized neoadjuvant chemotherapy. Therefore, the resection site was designed to be > 2 cm from the tumor at the end and distal to the articular side. However, on the articular side, the minimum distance between the resection site and tumor was designed to be only 1 cm to preserve the thicker residual bone. Deng reported that in knee preservation limb salvage surgery for osteosarcoma, the difference between the resection position and the preoperatively planned position was 8.3 ± 6.0 mm when the resection was performed with bare hands, whereas the error was only 2.0 ± 1.6 mm when the resection was performed with positioning using a computerized navigation system [ 20 ]. Studies on pelvic resection and special resection surfaces have also confirmed that the accuracy of resection with computerized navigation systems is much higher than that of bare-handed resection [ 21 , 22 ]. Wong also reported the use of computer-assisted positioning in joint preservation surgery for resection 1 cm from the tumor to obtain safe margins [ 6 ]. To ensure the safety of the resected bone on the articular side, all patients in this study underwent preoperative radiography, enhanced CT, enhanced MRI, and electroconvulsive therapy. The tumor margins were determined by combining the results of all examinations. During the surgery, a computer-assisted navigation positioning system was used to determine the resection position. After the intraoperative resection, the resected ends were observed to be safe with the naked eye. Tissues of the resected ends were obtained during surgery for pathological examination, and the results were all negative. There were no cases of recurrence at the end of resection during the follow-up period. There was only one case (4.3%) of soft tissue recurrence, which is comparable to the recurrence rates reported for other tumor resections around the knee (2.4–10.5%) [ 23 , 24 , 25 , 26 ]. Based on our experience, within a median follow-up period > 60 months, joint preservation tumor resection is a safe and acceptable approach from the perspective of oncology.
In addition to tumor safety, the precise resection position is associated with reconstruction. The two reconstruction modalities do not have the same requirements for resection position accuracy. For reconstruction with a custom-made endoprosthesis, the resection surface close to the joint affects the position and orientation of the endoprosthesis, position of the lateral steel plate, and orientation and length of the fixation screws. Therefore, the resection position must be sufficiently accurate to perfectly match the endoprosthesis. In contrast, the only requirement for the inactivation technique is that the resection position exceeds the designed safety range, making surgical resection much easier.
For joint preservation surgery, it is challenging to stabilize and fix the residual bone close to the joint to an endoprosthesis or inactivated bone and to achieve long-term stability. Reconstruction with a short-stem interpositional endoprosthesis can be used in cases of long residual bone on the articular side. Tsuda et al. reported that a custom-made endoprosthesis with a short intramedullary stem and lateral steel plate can be used for reconstruction when the resected bone is 5 cm away from the joint, and a hydroxyapatite (HA) coating is used on the surface of the endoprosthetic stem and steel plate to minimize the risk of aseptic loosening [ 27 ]. Kong reported the use of a customized prosthesis and lateral plate to fix the residual bone, and HA coating was used to enhance osseointegration at the bone-prosthesis interface [ 17 ]. Zhao et al. treated five patients with an average residual bone of 2.65 cm at the proximal or distal tibia after tumor resection with a 3D-printed porous endoprosthesis. All patients achieved early biological fixation, with an average time to clinical osseointegration of three months at the bone-prosthesis interface of 3.2 months [ 11 ]. In this study, HA coating and 3D printing technology were not used on the customized prostheses, residual bone contact surfaces, or extracortical steel plates, but there was no displacement of the residual bone from the prosthesis and no fixation failure during the follow-up period, and the five-year survival rate of the prostheses was 100%. This may be attributed to the precise design and manufacturing of the prosthesis after the surgeon has determined the resection position based on preoperative imaging, and the position and length of the internal fixation screws were determined before surgery. Moreover, a computerized navigation system was used to determine the resection position during surgery so that the endoprosthesis perfectly matched the residual bone. Six screws on both sides also provided immediate postoperative stabilization. If endoprosthesis manufacturing companies offer HA coatings for resection surfaces or 3D-printed porous structures for contact surfaces in the future, better early- and long-term stability may be achieved.
Long-term survival of liquid nitrogen-inactivated autologous bone grafts requires healing of the host bone. Commonly used inactivation methods include freezing, pasteurization, and irradiation [ 14 , 28 , 29 , 30 ]. The liquid nitrogen inactivation method used in this study is simple, inexpensive, and does not rely on special equipment, such as radiotherapy or strict thermal control. Inactivated bone retains good biomechanical strength [ 31 ], preserves bone morphogenetic protein (BMP) [ 32 ], and retains osteoinductive capacity; however, the healing time of inactivated bone remains much longer than that of normal fractures. Wu reported that 84 patients who underwent surgery using the liquid nitrogen inactivation method achieved 79.8% healing at 18 months after surgery [ 14 ]. Araki reported that the healing time of 37 patients after surgery using the liquid nitrogen inactivation method was 3–24 months [ 30 ]. In the inactivated autograft group, the longest healing time was 16 months on the articular side and 26 months on the diaphyseal side. Therefore, it is necessary to provide an internal fixation with sufficient strength before healing. Frisoni‘s study [ 33 ] of reconstruction of backbone defect with bone allograft suggested that steel plate fixation was superior to intramedullary fixation for increasing the strength of reconstruction, which is supported by the findings of Chen et al. using inactivated bone grafts [ 34 ]. In order to provide stronger internal fixation, for all the patients in the inactivated autograft group in this study, the inactivated bone marrow cavity was filled with bone cement and then fixed with steel plates on both sides. No type 2 or 3 complications due to insufficient bone strength occurred during the follow-up.
In this study, there was no significant difference in the MSTS scores at the final follow-up visit between the two groups, which were 91% and 94% higher than the MSTS scores for conventional prostheses (71–88.6%) [ 9 , 24 , 35 , 36 ]. Previous reports on joint preservation surgery have shown that higher MSTS scores (90–96.7%) are associated with maximum intraoperative preservation of the cruciate ligaments, medial and lateral collateral ligaments, and contralateral articular surfaces [ 4 , 6 , 37 ].
Based on our clinical experience, we have become familiar with the advantages and disadvantages of using custom-made endoprostheses and liquid nitrogen-inactivated autologous bone grafts for the reconstruction of preserved joints. The endoprosthesis group was not limited by the degree of osteolysis and had a shorter operation time, faster postoperative recovery, early weight bearing, and good postoperative function. However, the design and manufacturing of prostheses requires professional skills, specialized equipment, and good medical–industrial integration. Bone cement is currently used to fix prosthetic stems, which have a high long-term risk of loosening. Inactivated bone grafts require simple equipment, have a high healing rate, function well, have a low complication rate, and can be restored using an endoprosthesis after failure. However, they are not suitable for patients with severe osteolysis or pathological fractures. Moreover, there are many steps for inactivation, rewarming, and fixation of the graft during surgery, resulting in a long duration of surgery, which might increase surgical complications. Inactivated bone grafts also have slow postoperative recovery and can only bear weight after complete healing. Therefore, liquid nitrogen-inactivated autologous bone grafts are preferred for patients suitable for joint preservation surgery. Reconstruction with a custom-made endoprosthesis was performed if 50% of the cortical bone was lysed or a pathological fracture was present.
This study had some limitations. First, this was a retrospective study with a small sample size, and the two patient groups were not randomized. Second, as the liquid nitrogen inactivation method started in 2015 at our institution, all patients underwent reconstruction with a custom-made endoprosthesis before that. Third, reconstruction with a bone allograft is another possible treatment modality for joint preservation in addition to endoprosthesis and inactivated autologous bone grafts for joint preservation surgery. However, as there is no bone bank in our medical institution, matching bone allografts were difficult to obtain; therefore, reconstruction using bone allografts was not included in this comparative study. Fourth, aseptic loosening of the endoprosthesis and fracture of the inactivated bone graft increase with time, which may result in reconstruction failure [ 38 ]. The current follow-up period is still relatively short, but we will continue to follow-up and obtain 10-year survival data for patients and grafts.
For future studies, we have three main directions: (1) a multi-center collaboration to increase the allograft group for comparative analysis; (2) the use of 3D printed porous interfaces for cases using endoprosthesis to further increase their stability; and (3) longer follow-up to obtain data on graft survival and complications in long-term follow-up.
Conclusions
This comparative study of different reconstruction modalities after knee joint-preserving tumor resection demonstrated its feasibility and safety. The use of a custom-made endoprosthesis and liquid nitrogen-inactivated autologous bone graft resulted in successful joint preservation and improved postoperative function. Although the endoprosthesis group had slightly better MSTS scores, the difference was not statistically significant. While complications during follow-up were less frequent in the inactivated autograft group, this difference was also not statistically significant.
Although this study has limitations, such as its retrospective design and small sample size, it provides valuable insights into the benefits and limitations of different reconstruction modalities. Further studies with larger sample sizes and longer follow-up periods are needed to confirm these findings and evaluate long-term patient and graft survival. This study also provides clinicians with directions for further research to optimize surgical techniques and improve patient outcomes.
Availability of data and materials
The datasets used and/or analyzed in the current study are available from the corresponding author upon reasonable request.
Abbreviations
Musculoskeletal Tumor Society
The International Society of Limb Salvage
Sadek WMS, Ebeid WA, Ghoneimy AE, Ebeid E, Senna WGA. Functional and oncological outcome of patients with distal femoral osteosarcoma managed by limb salvage using modular endoprosthesis. Ann Surg Oncol. 2023;30(8):5150–8.
Article PubMed PubMed Central Google Scholar
Li Y, Sun Y, Shan HC, Niu XH. Comparative analysis of early follow-up of biologic fixation and cemented stem fixation for femoral tumor prosthesis. Orthop Surg. 2019;11(3):451–9.
Article CAS PubMed PubMed Central Google Scholar
Kumta SM, Chow TC, Griffith J, Li CK, Kew J, Leung PC. Classifying the location of osteosarcoma with reference to the epiphyseal plate helps determine the optimal skeletal resection in limb salvage procedure. Arch Orthop Trauma Surg. 1999;119(5–6):327–31.
Article CAS PubMed Google Scholar
Takeuchi A, Yamamoto N, Hayashi K, Matsubara H, Kimura H, Miwa S, et al. Growth of epiphysis after epiphyseal-preservation surgery for childhood osteosarcoma around the knee joint. BMC Musculoskelet Disord. 2018;19(1):185.
Xu LH, Zhang Q, Zhao HT, Yu F, Niu XH. Computer navigation-aided joint-preserving resection and custom-made endoprosthesis reconstruction for bone sarcomas: long-term outcomes. Chin Med J (Engl). 2021;134(21):2597–602.
Article PubMed Google Scholar
Wong KC, Sze LKY, Kumta SM. Complex joint-preserving bone tumor resection and reconstruction using computer navigation and 3D-printed patient-specific guides: a technical note of three cases. J Orthop Translat. 2021;24(29):152–62.
Article Google Scholar
Muscolo DL, Ayerza MA, Aponte-Tinao LA, Ranalletta M. Partial epiphyseal preservation and intercalary allograft reconstruction in high-grade metaphyseal osteosarcoma of the knee. J Bone Joint Surg Am. 2005;87 Suppl 1(Pt 2):226–36.
PubMed Google Scholar
Li J, Guo Z, Yang Q, Ji C, Wang Z. Adjuvant argon-based cryoablation for joint-preserving tumor resection in patients with juxta-articular osteosarcoma around the knee. Cryobiology. 2015;71(2):236–43.
Albergo JI, Gaston LC, Farfalli GL, Laitinen M, Parry M, Ayerza MA, et al. Failure rates and functional results for intercalary femur reconstructions after tumour resection. Musculoskelet Surg. 2020;104(1):59–65.
Agarwal M, Puri A, Gulia A, Reddy K. Joint-sparing or physeal-sparing diaphyseal resections: the challenge of holding small fragments. Clin Orthop Relat Res. 2010;468(11):2924–32.
Zhao D, Tang F, Min L, Lu M, Wang J, Zhang Y, et al. Intercalary reconstruction of the “ultra-critical sized bone defect” by 3D-printed porous prosthesis after resection of tibial malignant tumor. Cancer Manag Res. 2020;8(12):2503–12.
Henderson ER, O’Connor MI, Ruggieri P, Windhager R, Funovics PT, Gibbons CL, et al. Classification of failure of limb salvage after reconstructive surgery for bone tumours: a modified system Including biological and expandable reconstructions. Bone Joint J. 2014;96(11):1436–40.
Ahmed AR, Manabe J, Kawaguchi N, Matsumoto S, Matsushita Y. Radiographic analysis of pasteurized autologous bone graft. Skeletal Radiol. 2003;32(8):454–61.
Wu PK, Chen CF, Chen CM, Cheng YC, Tsai SW, Chen TH, et al. Intraoperative extracorporeal irradiation and frozen treatment on tumor-bearing autografts show equivalent outcomes for biologic reconstruction. Clin Orthop Relat Res. 2018;476(4):877–89.
Poffyn B, Sys G, Van Maele G, Van Hoorebeke L, Forsyth R, Verstraete K, et al. Radiographic analysis of extracorporeally irradiated autografts. Skeletal Radiol. 2010;39(10):999–1008.
Huang M, Ma Z, Yu J, Lu Y, Chen G, Fan J, et al. Does joint-sparing tumor resection jeopardize oncologic and functional outcomes in non-metastatic high-grade osteosarcoma around the knee? World J Surg Oncol. 2023;21(1):185.
Wong KC, Kumta SM. Joint-preserving tumor resection and reconstruction using image-guided computer navigation. Clin Orthop Relat Res. 2013;471(3):762–73.
Enneking WF, Spanier SS, Goodman MA. A system for the surgical staging of musculoskeletal sarcoma. Clin Orthop Relat Res. 1980;153:106–20.
Kawaguchi N, Ahmed AR, Matsumoto S, Manabe J, Matsushita Y. The concept of curative margin in surgery for bone and soft tissue sarcoma. Clin Orthop Relat Res. 2004;419:165–72.
Deng Z, Zhang Q, Hao L, Ding Y, Niu X, Liu W. Accuracy of bony resection under computer-assisted navigation for bone sarcomas around the knee. World J Surg Oncol. 2023;21(1):187.
Sallent A, Vicente M, Reverté MM, Lopez A, Rodríguez-Baeza A, Pérez-Domínguez M, et al. How 3D patient-specific instruments improve accuracy of pelvic bone tumour resection in a cadaveric study. Bone Joint Res. 2017;6(10):577–83.
Bosma SE, Wong KC, Paul L, Gerbers JG, Jutte PC. A cadaveric comparative study on the surgical accuracy of freehand, computer navigation, and patient-specific instruments in joint-preserving bone tumor resections. Sarcoma. 2018;13(2018):4065846.
Google Scholar
Benevenia J, Kirchner R, Patterson F, Beebe K, Wirtz DC, Rivero S, et al. Outcomes of a modular intercalary endoprosthesis as treatment for segmental defects of the femur, tibia, and humerus. Clin Orthop Relat Res. 2016;474(2):539–48.
Pala E, Trovarelli G, Calabrò T, Angelini A, Abati CN, Ruggieri P. Survival of modern knee tumor megaprostheses: failures, functional results, and a comparative statistical analysis. Clin Orthop Relat Res. 2015;473(3):891–9.
Ji T, Yang Y, Li DS, Tang XD, Guo W. Limb salvage using non-hinged endoprosthesis and staged correction of leg-length discrepancy for children with distal femoral malignant tumors. Orthop Surg. 2019;11(5):819–25.
Albergo JI, Gaston CL, Aponte-Tinao LA, Ayerza MA, Muscolo DL, Farfalli GL, et al. Proximal tibia reconstruction after bone tumor resection: are survivorship and outcomes of endoprosthetic replacement and osteoarticular allograft similar? Clin Orthop Relat Res. 2017;475(3):676–82.
Tsuda Y, Fujiwara T, Sree D, Stevenson JD, Evans S, Abudu A. Physeal-preserving endoprosthetic replacement with short segment fixation in children with bone sarcomas. Bone Joint J. 2019;101-B(9):1144–50.
Outani H, Takenaka S, Hamada K, Imura Y, Kakunaga S, Tamiya H, et al. A long-term follow-up study of extracorporeal irradiated autografts in limb salvage surgery for malignant bone and soft tissue tumors: a minimum follow-up of 10 years after surgery. J Surg Oncol. 2020;121(8):1276–82.
Lee SY, Jeon DG, Cho WH, Song WS, Kim BS. Are pasteurized autografts durable for reconstructions after bone tumor resections? Clin Orthop Relat Res. 2018;476(9):1728–37.
Araki Y, Yamamoto N, Hayashi K, Takeuchi A, Miwa S, Igarashi K, et al. Clinical outcomes of frozen autograft reconstruction for the treatment of primary bone sarcoma in adolescents and young adults. Sci Rep. 2021;11(1):17291.
Yamamoto N, Tsuchiya H, Tomita K. Effects of liquid nitrogen treatment on the proliferation of osteosarcoma and the biomechanical properties of normal bone. J Orthop Sci. 2003;8(3):374–80.
Chen CM, Chen CF, Wang JY, Madda R, Tsai SW, Wu PK, et al. Bone morphogenetic protein activity preservation with extracorporeal irradiation- and liquid nitrogen freezing-treated recycled autografts for biological reconstruction in malignant bone tumor. Cryobiology. 2019;89:82–9.
Frisoni T, Cevolani L, Giorgini A, Dozza B, Donati DM. Factors affecting outcome of massive intercalary bone allografts in the treatment of tumours of the femur. J Bone Joint Surg Br. 2012;94(6):836–41.
Chen Y, Yu XC. Efficacy of a modified scoring system to facilitate surgical decision-making for diaphyseal malignancies: when is devitalized tumor-bearing autograft of value? Orthop Surg. 2019;11(4):586–94.
Holm CE, Bardram C, Riecke AF, Horstmann P, Petersen MM. Implant and limb survival after resection of primary bone tumors of the lower extremities and reconstruction with mega-prostheses fifty patients followed for a mean of forteen years. Int Orthop. 2018;42(5):1175–81.
Erol B, Saglam F. Are cemented endoprosthetic reconstructions superior to uncemented endoprostheses in terms of postoperative outcomes and complications in patients with extremity-located bone metastasis scheduled for adjuvant radiotherapy? J Arthroplasty. 2021;36(3):1160–7.
Muratori F, Totti F, D’Arienzo A, Scorianz M, Scoccianti G, Beltrami G, et al. Biological intercalary reconstruction with bone grafts after joint-sparing resection of the lower limb: is this an effective and durable solution for joint preservation? Surg Technol Int. 2018;1(32):346–345.
Igarashi K, Yamamoto N, Shirai T, Hayashi K, Nishida H, Kimura H, et al. The long-term outcome following the use of frozen autograft treated with liquid nitrogen in the management of bone and soft-tissue sarcomas. Bone Joint J. 2014;96-B(4):555–61.
Download references
Acknowledgements
Not applicable.
This study did not receive any specific grants from funding agencies in the public, commercial, or non-profit sectors.
Author information
Authors and affiliations.
Department of Orthopedic Oncology Surgery, Beijing Jishuitan Hospital, Capital Medical University, No.31 Xin Jie Kou East Street, Xi Cheng District, Beijing, 100035, China
Yuan Li, Hairong Xu, Huachao Shan, Ke Ma, Weifeng Liu & Xiaohui Niu
You can also search for this author in PubMed Google Scholar
Contributions
YL, HRX and XHN conceived the study and drafted the manuscript. YL, HRX, HCS, KM, and WFL were involved in the methodology, validation, investigation, and data curation, and XHN contributed to the project administration. All the authors have read and approved the final version of the manuscript.
Corresponding author
Correspondence to Xiaohui Niu .
Ethics declarations
Ethics approval and consent to participate.
This study was performed in accordance with the “Declaration of Helsinki” and approved by the Ethics Committee of Beijing Jishuitan Hospital. Approval No. of Ethics Committee: 积伦[K2023]第[249]号-00.
Consent for publication
Written informed consent for publication was obtained from each participant included in this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Li, Y., Xu, H., Shan, H. et al. A comparative study of reconstruction modalities after knee joint-preserving tumor resection: reconstruction with a custom-made endoprosthesis versus reconstruction with a liquid nitrogen-inactivated autologous bone graft. J Orthop Surg Res 18 , 908 (2023). https://doi.org/10.1186/s13018-023-04402-3
Download citation
Received : 05 October 2023
Accepted : 21 November 2023
Published : 29 November 2023
DOI : https://doi.org/10.1186/s13018-023-04402-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Malignant bone tumor
- Joint-preserving resection
- Custom-made endoprosthesis
- Liquid nitrogen-inactivated autologous bone graft
Journal of Orthopaedic Surgery and Research
ISSN: 1749-799X
- Submission enquiries: [email protected]
[Knee endoprosthesis: selection and requirements of materials]
Affiliation.
- 1 Orthopädische Klinik und Poliklinik, Ludwig-Maximilians-Universität München, Klinikum Grosshadern.
- PMID: 11013916
- DOI: 10.1007/s001320050518
The possibilities of using different material combinations for the replacement of knee joint endoprostheses are very limited. Therefore, cobalt-chromium-molybdenum alloys are currently being used for femoral components and ultra-high molecular weight polyethylene for tribologically stressed tibial components. Titanium alloys can be considered for the tibial component only. For tribological reasons, it is not possible to use a femoral component made of titanium unless it has a corresponding coating. As far as the design is concerned, problems arise from the fact that, on the one hand, there is a demand for the smallest possible size or resection height. On the other hand, however, the forces and strains are rather high and therefore a certain material thickness is necessary in order to avoid fatigue fracture. Regarding polyethylene, the same known principle must be taken into consideration here--not to avoid using the so-called floating design, i.e., the polyethylene components should always have a supporting limitation, or cold flow might occur. The tribological behaviour of polyethylene is restricted in cases of constrained tibia plateaus in so far as the linear or punctual contact of the initial run-in phase leads to correspondingly high surface pressure consequently overstressing the polyethylene. In order to improve this, mobile meniscal bearings are used and the surface pressures achieved here can be endured by the polyethylene even over a long-term. The extent to which the new so-called cross-linked polyethylene can be used in knee joint endoprosthetics is currently being tested, and the simulator results in this respect have been promising so far.
Publication types
- Comparative Study
- English Abstract
- Arthroplasty, Replacement, Knee / instrumentation*
- Biocompatible Materials*
- Bone Substitutes
- Follow-Up Studies
- Knee Prosthesis*
- Materials Testing*
- Polyethylenes
- Prosthesis Design
- Time Factors
- Biocompatible Materials

IMAGES
VIDEO
COMMENTS
In a unicompartmental (partial) knee replacement, only the damaged part of the knee is replaced. To Top. During knee replacement surgery, an orthopaedic surgeon will resurface your damaged knee with artificial components, called implants. The specific type of implant your surgeon uses will depend on many factors, including your knee condition ...
Total knee arthroplasty (TKA) is one of the most cost-effective and consistently successful surgeries performed in orthopedics. Patient-reported outcomes are shown to improve dramatically with respect to pain relief, functional restoration, and improved quality of life. TKA provides reliable outcomes for patients suffering from end-stage, tri-compartmental, degenerative osteoarthritis (OA).
The Total Knee Replacement Prosthesis. Various types are reviewed. Total knee replacement consists of three main components: the femoral component, the tibial component, and the plastic spacer (polyethylene). The following model shows the components of a knee replacement. The model on the left shows the front view and the model on the right ...
Endoprosthesis of the knee. This is an operation to replace a damaged knee joint with an artificial one. The most common reason for surgery is severe knee arthritis, rheumatoid arthritis or a previous injury to the joint. The goal of the surgery is to relieve pain, swelling and restore mobility in the knee.
Joint replacement surgery is a safe and effective procedure to relieve pain, correct leg deformity, and help you resume normal activities. Total knee replacement surgery was first performed in 1968. Since then, improvements in surgical materials and techniques have greatly increased its effectiveness.
12 min. Inserting an endoprosthesis of the knee is one of the most common orthopedic surgeries. The reasoning for undergoing the procedure is based on a progressed state of illness and a state where non-surgical methods and other reconstructive surgical procedures fail to improve treatment (15). Medical science is ever evolving and improving.
Knee endoprosthesis: 1: 110 (70-150) 4.0 (1.5-5.0) 85 (11.3) 7.1(1.8) 450 (47.5) Open in a separate window. ... Knee resection entails a wide loss of bone and muscle structures resulting in a marked sensory-motor shock that has severe repercussions on the neuromotor control of the knee and balance, ...
The highest incidence, amongst the different sites of use of the endoprosthesis, was seen around the knee with almost similar incidence between the distal femur and proximal tibial implants. In a systematic review by Groundland and colleagues 19, they compared the outcomes of endoprosthesis in children and adults, they found that children fared ...
This physical therapy protocol applies to primary total knee arthroplasty. In a revision total knee arthroplasty, or in cases where there is more connective tissue involvement, Phase I and II should be progressed with more caution to ensure adequate healing. Progression to the next phase is based on Clinical Criteria and/or Time Frames as ...
The following search-terms were used: tumour endoprosthesis, advances tumour endoprosthesis, tumour megaprosthesis, prosthetic reconstruction AND tumour. ... - 17 patients with 18 periprosthetic fractures following implantation of a tumour endoprosthesis in hip or knee were included - 12 fractures occurred after femoral resection (67%) and ...
To develop a more durable knee endoprosthesis, efforts should be focused on reducing loosening and infection, which would demand improved understanding of the biomechanics of knee endoprostheses, the evolution of new fixation methods, tests of new materials, and well-conducted clinical trials.
Knee endoprosthesis is the mainstream treatment of tumors around the knee and allows limb salvaging as an alternative to amputation [1], [2], [3]. Due to constraints on the hinges, the increase in the length of bone resection, and damage of the soft tissues, overall implant survival is worse over time compared to standard total knee replacement ...
Background: Endoprosthetic replacement has become the mainstream method of reconstruction after tumor resection around the knee for decades, but there is a lack of comprehensive review evaluating the implant outcomes. We performed a systematic review to analyze the implant survival and complication profiles of distal femoral replacement (DFR) and proximal tibial replacement (PTR) in adults ...
Figure 2 Alumina ceramic total knee endoprosthesis first implanted by Oonishi et al.14 The femoral and tibial ceramic component was combined with an ultra-high molecular weight polyethylene (UHMWPE) insert. Figure 3 The Multigen Plus Ceramic Knee consisting of a symmetric, cruciate-retaining (CR), cemented ceramic femoral component and a metal ...
Total knee arthroplasty (TKA) is one of the most frequent surgical procedures in orthopaedic surgery. ... [The S2k guideline: Indications for knee endoprosthesis : Evidence and consent-based indications for total knee arthroplasty] Orthopade. 2018 Sep;47(9):777-781. doi: 10.1007/s00132-018-3612-x. [Article in German] Authors J ...
Results. In 2018, a total number 23,812 revision knee arthroplasties were performed in Germany, yielding an overall increase of 20.76% between 2008 and 2018 (Table 2 ). In comparison, primary TKA ...
Of major importance in knee alloarthoplasty are restitution of the correct limb axis, sufficient lateral ligaments and the restoration of the patellofemoral joint. Therefore particularly in cases with deformities an extensive soft tissue release is mandatory. A meticulous operative technique and versatile implants lead to good clinical outcome.
Alumina ceramic total knee endoprosthesis first implanted by Oonishi et al. 14 The femoral and tibial ceramic component was combined with an ultra-high molecular weight polyethylene (UHMWPE) insert. ... and chromium. Total knee designs with a ceramic femoral component combined with a titanium tibial tray are an option in these cases. However ...
Tumor endoprostheses of the knee joint after limb salvage surgery is associated with high rates of complications, which has introduced great challenges to a delayed revision surgery. The aim of the study was to summarize the failures, functional outcomes and prosthetic survival in revision tumor endoprostheses of the knee joint. The clinical data of 20 patients with malignant tumors who ...
Prosthesis-related complications, after knee reconstruction with endoprosthesis during operation for tumors around the knee, remain an unresolved problem which necessitate a revision or even an amputational surgery. The purpose of the current study was to identify significant risk factors associated with implant failure, and establish a novel model to predict survival of the prosthesis in ...
This study evaluated the feasibility, complications, graft survival rate, and clinical outcomes of joint-preserving resection using a custom-made endoprosthesis and liquid nitrogen-inactivated autologous bone graft reconstruction in patients with malignant bone tumors around the knee joint. We retrospectively analyzed 23 consecutive patients who underwent joint preservation surgery between ...
Abstract. This paper deals with a knee joint endoprosthesis finite element analysis. Based on a three dimensional geometric model of a lower extremity, a mechanical axis of the limb was designed. This axis is important for several reasons. Firstly, the endoprosthesis was positioned due to its direction, secondly, boundary conditions was defined ...
Biocompatible Materials. Bone Substitutes. Polyethylenes. Vitallium. Titanium. The possibilities of using different material combinations for the replacement of knee joint endoprostheses are very limited. Therefore, cobalt-chromium-molybdenum alloys are currently being used for femoral components and ultra-high molecular weight polyethylene for ...