- Patient Care & Health Information
- Diseases & Conditions
Syphilis is an infection caused by bacteria. Most often, it spreads through sexual contact. The disease starts as a sore that's often painless and typically appears on the genitals, rectum or mouth. Syphilis spreads from person to person through direct contact with these sores. It also can be passed to a baby during pregnancy and childbirth and sometimes through breastfeeding.
After the infection happens, syphilis bacteria can stay in the body for many years without causing symptoms. But the infection can become active again. Without treatment, syphilis can damage the heart, brain or other organs. It can become life-threatening.
Early syphilis can be cured, sometimes with a single shot of medicine called penicillin. That's why it's key to get a health care checkup as soon as you notice any symptoms of syphilis. All pregnant people should get tested for syphilis at their first prenatal checkup too.

Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition

- Primary syphilis
Primary syphilis causes painless sores (chancres) on the genitals, rectum, tongue or lips. The disease can be present with the appearance of a single chancre (shown here on a penis) or many.
Syphilis develops in stages. The symptoms vary with each stage. But the stages may overlap. And the symptoms don't always happen in the same order. You may be infected with syphilis bacteria without noticing any symptoms for years.
The first symptom of syphilis is a small sore called a chancre (SHANG-kur). The sore is often painless. It appears at the spot where the bacteria entered your body. Most people with syphilis develop only one chancre. Some people get more than one.
The chancre often forms about three weeks after you come in contact with syphilis bacteria. Many people who have syphilis don't notice the chancre. That's because it's usually painless. It also may be hidden within the vagina or rectum. The chancre heals on its own within 3 to 6 weeks.
Secondary syphilis
You may get a rash while the first chancre heals or a few weeks after it heals.
A rash caused by syphilis:
- Often is not itchy.
- May look rough, red or reddish-brown.
- Might be so faint that it's hard to see.
The rash often starts on the trunk of the body. That includes the chest, stomach area, pelvis and back. In time, it also could appear on the limbs, the palms of the hands and the soles of the feet.
Along with the rash, you may have symptoms such as:
- Wartlike sores in the mouth or genital area.
- Muscle aches.
- Sore throat.
- Tiredness, also called fatigue.
- Weight loss.
- Swollen lymph nodes.
Symptoms of secondary syphilis may go away on their own. But without treatment, they could come and go for months or years.
Latent syphilis
If you aren't treated for syphilis, the disease moves from the secondary stage to the latent stage. This also is called the hidden stage because you have no symptoms. The latent stage can last for years. Your symptoms may never come back. But without treatment, the disease might lead to major health problems, also called complications.
Tertiary syphilis
After the latent stage, up to 30% to 40% of people with syphilis who don't get treatment have complications known as tertiary syphilis. Another name for it is late syphilis.
The disease may damage the:
- Blood vessels.
- Bones and joints.
These problems may happen many years after the original, untreated infection.
Syphilis that spreads
At any stage, untreated syphilis can affect the brain, spinal cord, eyes and other body parts. This can cause serious or life-threatening health problems.
Congenital syphilis
Pregnant people who have syphilis can pass the disease to their babies. Unborn babies can become infected through the organ that provides nutrients and oxygen in the womb, called the placenta. Infection also can happen during birth.
Newborns with congenital syphilis might have no symptoms. But without fast treatment, some babies might get:
- Sores and rashes on the skin.
- A type of discolored skin and eyes, called jaundice.
- Not enough red blood cells, called anemia.
- Swollen spleen and liver.
- Sneezing or stuffed, drippy nose, called rhinitis.
- Bone changes.
Later symptoms may include deafness, teeth problems and saddle nose, a condition in which the bridge of the nose collapses.
Babies with syphilis also can be born too early. They may die in the womb before birth. Or they could die after birth.
When to see a doctor
Call a member of your health care team if you or your child has any symptoms of syphilis. These could include any unusual discharge, a sore or a rash, especially in the groin area.
Also get tested for syphilis if you:
- Have had sexual contact with someone who might have the disease.
- Have another sexually transmitted disease such as HIV .
- Are pregnant.
- Regularly have sex with more than one partner.
- Have unprotected sex, meaning sex without a condom.
- Mayo Clinic Minute: Signs and symptoms of syphilis
Vivien Williams: Syphilis is a sexually transmitted infection caused by the bacterium Treponema pallidum. Dr. Stacey Rizza, an infectious diseases specialist at Mayo Clinic, says syphilis affects men and women and can present in various stages.
Stacey Rizza, M.D.: Primary syphilis causes an ulcer, and this sometimes isn't noticed because it's painless and can be inside the vagina or on the cervix…after a few weeks, two months, they can get secondary syphilis, which is a rash.
Vivien Williams: It may then progress to latent stage syphilis and, finally, the most serious stage: tertiary. Pregnant women are not immune to syphilis. Congenital syphilis can lead to miscarriage, stillbirth or infant deaths. That's why all pregnant women should be screened. Syphilis is preventable and treatable. As for prevention, Dr. Rizza recommends barrier protection during sex.
Dr. Rizza: And that's during oral sex, anal sex, vaginal sex — using condoms, dental dams and any other barrier protection.
Vivien Williams: For the Mayo Clinic News Network, I'm Vivien Williams.
More Information
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
The cause of syphilis is a bacterium called Treponema pallidum. The most common way syphilis spreads is through contact with an infected person's sore during vaginal, oral or anal sex.
The bacteria enter the body through minor cuts or scrapes in the skin or in the moist inner lining of some body parts.
Syphilis is contagious during its primary and secondary stages. Sometimes it's also contagious in the early latent period, which happens within a year of getting infected.
Less often, syphilis can spread by kissing or touching an active sore on the lips, tongue, mouth, breasts or genitals. It also can be passed to babies during pregnancy and childbirth and sometimes through breastfeeding.
Syphilis can't be spread through casual contact with objects that an infected person has touched.
So you can't catch it by using the same toilet, bathtub, clothing, eating utensils, doorknobs, swimming pools or hot tubs.
Once cured, syphilis doesn't come back on its own. But you can become infected again if you have contact with someone's syphilis sore.
Risk factors
The risk of catching syphilis is higher if you:
- Have unprotected sex.
- Have sex with more than one partner.
- Live with HIV , the virus that causes AIDS if untreated.
The chances of getting syphilis also are higher for men who have sex with men. The higher risk may be linked, in part, with less access to health care and less use of condoms among this group. Another risk factor for some people in this group includes recent sex with partners found through social media apps.
Complications
Without treatment, syphilis can lead to damage throughout the body. Syphilis also raises the risk of HIV infection and can cause problems during pregnancy. Treatment can help prevent damage. But it can't repair or reverse damage that's already happened.
Small bumps or tumors
Rarely in the late stage of syphilis, bumps called gummas can form on the skin, bones, liver or any other organ. Most often, gummas go away after treatment with medicine called antibiotics.
Neurological problems
Syphilis can cause many problems with the brain, its covering or the spinal cord. These issues include:
- Meningitis, a disease that inflames the protective layers of tissue around the brain and spinal cord.
- Confusion, personality changes or trouble focusing.
- Symptoms that mimic dementia, such as loss of memory, judgment and decision-making skills.
- Not being able to move certain body parts, called paralysis.
- Trouble getting or keeping an erection, called erectile dysfunction.
- Bladder problems.
Eye problems
Disease that spreads to the eye is called ocular syphilis. It can cause:
- Eye pain or redness.
- Vision changes.
Ear problems
Disease that spreads to the ear is called otosyphilis. Symptoms can include:
- Hearing loss.
- Ringing in the ears, called tinnitus.
- Feeling like you or the world around you is spinning, called vertigo.
Heart and blood vessel problems
These may include bulging and swelling of the aorta — the body's major artery — and other blood vessels. Syphilis also may damage heart valves.
HIV infection
Syphilis sores on the genitals raise the risk of catching or spreading HIV through sex. A syphilis sore can bleed easily. This provides an easy way for HIV to enter the bloodstream during sex.
Pregnancy and childbirth complications
If you're pregnant, you could pass syphilis to your unborn baby. Congenital syphilis greatly raises the risk of miscarriage, stillbirth or your newborn's death within a few days after birth.
There is no vaccine for syphilis. To help prevent the spread of syphilis, follow these tips:
- Have safe sex or no sex. The only certain way to avoid contact with syphilis bacteria is not to have sex. This is called abstinence. If a person is sexually active, safer sex means a long-term relationship in which you and your partner have sex only with each other, and neither of you is infected. Before you have sex with someone new, you should both get tested for syphilis and other sexually transmitted infections (STIs).
- Use a latex condom. Condoms can lower your risk of getting or spreading syphilis. But condoms work only if they cover an infected person's syphilis sores. Other types of birth control do not lower your risk of syphilis.
- Be careful with alcohol and stay away from street drugs. Drinking too much alcohol or taking drugs can get in the way of your judgment. Either can lead to unsafe sex.
- Do not douche. It can remove some of the healthy bacteria that's usually in the vagina. And that might raise your risk of getting STIs .
- Breastfeed with caution. Syphilis can pass from a parent to a baby during breastfeeding if sores are on one or both breasts. This can happen when the baby or pumping equipment touches a sore. To keep that from happening, pump or hand-express breastmilk from the breast with sores. Do so until the sores heal. If your pump touches a sore, get rid of the milk you just pumped.
Partner notification and preventive treatment
If tests show that you have syphilis, your sex partners need to know so that they can get tested. This includes your current partners and any others you've had over the last three months to 1 year. If they're infected, they can then get treatment.
After you learn you have syphilis, your local health department may contact you. A department employee talks with you about private ways to let your partners know that they've been exposed to syphilis. You can ask the department to do this for you without revealing your identity to your partners.
Or you can contact your partners along with a department employee or simply tell your partners yourself. This free service is called partner notification. It can help limit the spread of syphilis. The practice also steers those at risk toward counseling and the right treatment.
And since you can get syphilis more than once, partner notification lowers your risk of getting infected again.
Screening tests for pregnant people
You can be infected with syphilis and not know it. And the disease can have deadly effects on unborn babies. For this reason, health officials recommend that all pregnant people be tested for the disease.
- Syphilis — CDC detailed fact sheet. Centers for Disease Control and Prevention. https://www.cdc.gov/std/syphilis/stdfact-syphilis-detailed.htm. Accessed April 27, 2023.
- Sexually transmitted infections treatment guidelines, 2021: Syphilis. Centers for Disease Control and Prevention. https://www.cdc.gov/std/treatment-guidelines/syphilis.htm. Accessed April 27, 2023.
- Hicks CB, et al. Syphilis: epidemiology, pathophysiology, and clinical manifestations in patients without HIV. https://www.uptodate.com/contents/search. Accessed April 27, 2023.
- Syphilis. Merck Manual Professional Version. https://www.merckmanuals.com/professional/infectious-diseases/sexually-transmitted-diseases-stds/syphilis. Accessed April 27, 2023.
- Hicks CB, et al. Syphilis: Treatment and monitoring. https://www.uptodate.com/contents/search. Accessed April 27, 2023.
- Hicks CB, et al. Syphilis: Screening and diagnostic testing. https://www.uptodate.com/contents/search. Accessed April 27, 2023.
- Syphilis — CDC basic fact sheet. Centers for Disease Control and Prevention. https://www.cdc.gov/std/syphilis/stdfact-syphilis.htm. Accessed April 27, 2023.
- Loscalzo J, et al., eds. Syphilis. In: Harrison's Principles of Internal Medicine. 21st ed. McGraw Hill; 2022. https://accessmedicine.mhmedical.com. Accessed July 14, 2019.
- AskMayoExpert. Syphilis (adult). Mayo Clinic; 2021.
- Sexually transmitted infections. Office on Women's Health. http://womenshealth.gov/publications/our-publications/fact-sheet/sexually-transmitted-infections.html. Accessed April 27, 2023.
- Tosh PK (expert opinion). Mayo Clinic. May 1, 2023.
- Cáceres CF, et al. Syphilis in men who have sex with men: advancing research and human rights. The Lancet Global Health. 2021; doi:10.1016/S2214-109X(21)00269-2.
- How can partner services programs help me and my patients? Centers for Disease Control and Prevention. https://www.cdc.gov/hiv/clinicians/screening/partner-notification.html. Accessed April 28, 2023.
- Penicillin allergy FAQ. American Academy of Allergy, Asthma & Immunology. https://www.aaaai.org/tools-for-the-public/conditions-library/allergies/penicillin-allergy-faq. Accessed April 28, 2023.
- Just diagnosed? Next steps after testing positive for gonorrhea or chlamydia. Centers for Disease Control and Prevention. https://www.cdc.gov/std/prevention/NextSteps-GonorrheaOrChlamydia.htm. Accessed May 1, 2023.
News from Mayo Clinic
- Newborns diagnosed with syphilis at alarming rates Feb. 19, 2024, 03:30 p.m. CDT
- Mayo Clinic Minute: Syphilis surge is cause for concern Feb. 03, 2024, 12:00 p.m. CDT
- Syphilis: A rising community presence Aug. 01, 2022, 04:30 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Related content
- Peer review
This article has a correction. Please see:
- Syphilis - July 19, 2019
- Patrick O'Byrne , associate professor, nurse practitioner 1 2 ,
- Paul MacPherson , infectious disease specialist 3
- 1 School of Nursing, University of Ottawa, Ottawa, Ontario K1H 8M5, Canada
- 2 Sexual Health Clinic, Ottawa Public Health, Ottawa, Ontario K1N 5P9
- 3 Division of Infectious Diseases, Ottawa Hospital General Campus, Ottawa, Ontario
- Correspondence to: P O'Byrne patrick.obyrne{at}uottawa.ca
What you need to know
Incidence rates of syphilis have increased substantially around the world, mostly affecting men who have sex with men and people infected with HIV
Have a high index of suspicion for syphilis in any sexually active patient with genital lesions or rashes
Primary syphilis classically presents as a single, painless, indurated genital ulcer (chancre), but this presentation is only 31% sensitive; lesions can be painful, multiple, and extra-genital
Diagnosis is usually based on serology, using a combination of treponemal and non-treponemal tests. Syphilis remains sensitive to benzathine penicillin G
Staging syphilis is important because it is the basis of management (treatment, expected treatment response, follow-up periods, and partner follow-up)
Patients with syphilis should be screened for HIV, gonorrhoea, and chlamydia
Caused by the bacteria Treponema pallidum , 1 2 syphilis is transmitted through direct (usually sexual) contact with infected mucosal lesions. Other bodily fluids are also infectious when patients are bacteraemic. With infectivity up to 10-30% per sexual contact or 60% per relationship, 3 syphilis rates have risen 300% since 2000 in many Western countries. 4 5 6 7 While most infections involve men who have sex with men, infections among people with opposite sex partners also occur. 4 5 6 7 In addition to increasing rates, syphilis can cause early complications such as irreversible loss of vision, so awareness of the infection is important for primary care clinicians. 8 9 10
What symptoms should alert me to this diagnosis?
While syphilis causes protean symptoms ( box 1 ), the diagnosis should be considered in any sexually active patient with genital lesions or with rashes. 16 17 18
Symptoms of syphilis by stage of infection (see fig 1 )
Symptoms appear 10-90 days (mean 21 days) after exposure
Main symptom is a <2 cm chancre:
Progresses from a macule to papule to ulcer over 7 days
Painless, solitary, indurated, clean base (98% specific, 31% sensitive)
On glans, corona, labia, fourchette, or perineum
A third are extragenital in men who have sex with men and in women
Localised painless adenopathy
Symptoms appear 2 weeks to 6 months (mean 2-12 weeks) after exposure. Can be concurrent with, or up to 8 weeks after, chancre
Rash—Diffuse, symmetric, on trunk (often subtle or atypical)
Mucus lesions, condylomata lata
Patchy alopecia (4-11%)
Fever, headaches, generalised painless adenopathy
Neurologic symptoms—Cranial nerve palsies (II,VIII), eye redness or pain, meningitis, changes to mental status or memory
No symptoms
In early latent stage (<12 months* or <24 months† after exposure) 25% of subjects relapse to secondary syphilis (90% of these in first year, 94% within 2 years)
In late latent stage (>12* or 24† months after exposure), no relapse and not infectious
1-46 years after exposure
Neurologic—paresis, tabes dorsalis
Cardiovascular—aortitis
Gummatous—necrotic granulomatous lesions
*According to US, 11 UK, 12 and Canadian 13 guidelines
†According to World Health Organization 14 and European 15 guidelines
Primary syphilis— Patients with primary syphilis ( fig 1 ) have a chancre at the site of inoculation—classically a solitary, painless, indurated, non-exudative ulcer ( fig 2 ). 17 19 While often on the glans, corona, labia, fourchette, or perineum, it may occur in the mouth ( fig 3 ), rectum, or vagina. 17 Chancres can be inconspicuous ( fig 4 ) and resolve in 3-10 weeks, possibly explaining why 60% of patients do not recall this lesion. Chancres may be multiple, painful, or atypical due to coinfection with other bacteria or herpesvirus. 20 Depending on inoculum size, chancres appear 10-90 days after exposure (mean 21 days). 17 Localised painless adenopathy may occur. 17

Stages of syphilis
- Download figure
- Open in new tab
- Download powerpoint

Chancre (sore) on penis due to syphilis

Syphilis in the mouth

Inconspicuous syphilitic chancre on penis
Secondary syphilis— Secondary syphilis is a manifestation of bacterial dissemination and classically presents as a diffuse, symmetric, copper, maculopapular, possibly pruritic rash of any morphology except vesicular ( fig 5 ). 17 20 21 A rash on the palms or soles is common (11-70%, fig 6 ). Mucus lesions ( fig 7 ), patchy alopecia, fever, headaches, and generalised painless adenopathy may also occur. 17 18 19 20 21 Early neurosyphilis develops in 25-60% of people ( box 1 ). 9 17 18 19 20 21 22 Secondary symptoms appear 2-24 weeks after infection, concurrently with or up to eight weeks after chancres, and disappear spontaneously after several weeks with or without marking. 17 19

Rash associated with secondary syphilis

Secondary syphilis on palms of hands

Condylomata lata in secondary syphilis
Latent syphilis— Syphilis then becomes latent, although symptoms of secondary syphilis recur in 25% of people, mostly (90%) within one year of acquiring the infection. 17 Latent syphilis has early and late stages. 17 Early latent disease includes the period of potential symptom relapse, classified by the WHO 14 and European 15 guidelines as <2 years since inoculation and as <1 year by US, 11 UK, 12 and Canadian 13 guidelines. As symptom relapse indicates bacterial replication, early latent disease can be infectious. Late latent syphilis occurs >1-2 years after acquisition and is non-infectious (see fig 1 ).
Tertiary syphilis— Without treatment, 14-40% of people with syphilis progress to tertiary disease—irreversible damage to any organ—within 1-46 years. The damage is primarily neurologic, cardiovascular, or gummatous (necrotic granulomatous lesions pathognomonic of tertiary syphilis). 2 17
Which diagnostic test should be done ( table 1 )?
Diagnostic tests for syphilis 23 24 25
- View inline
Treponema pallidum may be visualised from lesions using dark field microscopy, direct fluorescent antibody testing, or polymerase chain reaction. 11 12 13 14 15 Because these tests are not widely available, diagnosis predominantly relies on serology. 17 26 27 While serologic tests and laboratory algorithms vary, testing usually begins with a screening treponemal test, such as an enzyme or chemiluminescence immunoassay (EIA or CLIA) to detect treponemal antibodies. A positive screening test should be followed by a confirmatory treponemal test, typically the T pallidum particle agglutination (TPPA). If both tests are positive, infection with syphilis is confirmed. Thereafter, the rapid plasma reagin (RPR) test (a quantitative non-treponemal test) should be used to measure disease activity and to track response to treatment (although 15-41% of patients remain reactive even after successful treatment). 28
Test timing
Screening treponemal tests (EIA or CLIA) usually become reactive first, often within two weeks of the chancre. However, patients with negative results who have syphilis-like symptoms or who report a high risk contact should be re-tested after a further two to four weeks. 13
The RPR test may remain non-reactive for up to four weeks after the chancre, so it is often negative in primary syphilis, but it is 98-100% sensitive in secondary syphilis. However, because the RPR is a test of non-specific tissue damage, it may be positive for reasons other than syphilis. 15
In the absence of treatment, a negative non-treponemal test three months after potential exposure effectively rules out a new syphilis infection.
Note that treponemal tests cannot distinguish active from treated infections and generally remain positive for life (see table 2 ).
Interpretation of results from diagnostic tests for syphilis
Staging of syphilis
Staging of syphilis cannot be done based on laboratory results alone, and requires history and examination. Primary and secondary syphilis are symptomatic; early and late latent syphilis are generally asymptomatic. Careful examination to identify any symptoms not noticed by the patient is important and should include thorough anogenital and dermatologic inspection. 21
The staging criteria for early latent syphilis are given in box 2 . Asymptomatic patients with positive serology who do not fulfil the criteria of early latent syphilis could be staged as latent syphilis or as having syphilis of unknown duration.
Staging criteria for early latent syphilis 11 12 13 14 15
Patients with early latent syphilis are asymptomatic, with one of the following:
New positive serology with a documented negative test within previous 12* or 24† months
≥4-fold increase in the RPR titre relative to a previous test done within 12* or 24† months
Unequivocal symptoms of primary or secondary syphilis within the previous 12* or 24† months
Only one possible exposure, which occurred within previous 12* or 24† months
What should I do with inconclusive results?
Generally, inconclusive results arise in early infection or from waning antibody levels in late infection. The most common combinations are:
A positive RPR with negative treponemal screening (EIA/CLIA) and confirmatory tests (TPPA) suggests the RPR result is a false positive
A positive screen (EIA/CLIA) with negative confirmatory test (TPPA) and negative RPR is likely a false positive but could indicate early infection
A positive screen (EIA/CLIA) with indeterminant confirmatory test (TPPA) and negative RPR could represent waning antibody levels after a previous, treated infection or a new infection.
When results are inconclusive, clinicians should inquire about previous syphilis infection and treatment, and, if early syphilis is possible, retest in two to four weeks. 13 If results are unchanged, interpretation is based on history—consider the possibility of late untreated infection, treated infection, or non-venereal treponemal disease in adults from endemic countries in South and Central America, South-East Asia, and Africa.
What are the recommended treatment options? ( box 3 )
Recommended treatments for syphilis, primary, secondary, and early latent disease.
First line treatment
Benzathine penicillin G 2.4×10 6 units, single intramuscular dose*†
Doxycycline 100 mg, taken orally twice daily for 14 days*†
Alternate treatments
Ceftriaxone 1 g, intravenous or intramuscular once daily for 10 days*
Procaine penicillin G 1.2×10 6 units, intramuscular once daily for 10 days†
Azithromycin 2 g, single oral dose†
Late latent disease
Benzathine penicillin G 2.4×10 6 units, intramuscular dose once weekly for 3 weeks*†
Doxycycline 100 mg, taken orally twice daily for 28 days*†
Procaine penicillin G 1.2×10 6 units, intramuscular once daily for 14-21 days†
†According to WHO, 14 UK, 12 and European 15 guidelines
For primary, secondary, and early latent syphilis, in the absence of neurologic findings, first-line treatment is benzathine penicillin G (BPG) 2.4×10 6 units as a single intramuscular injection. Late latent syphilis is treated with the same dose of BPG weekly for three weeks with no more than 14 days between doses (no more than 7 days for pregnant women). 11 12 13 14 15 Additional BPG doses do not improve treatment outcomes for patients with early syphilis, 28 29 30 although some guidelines suggest pregnant women with early syphilis can receive up to two doses. 13 BPG has not been evaluated in controlled trials, but remains the first-line treatment because it is long acting (so covering the long dividing time of T pallidum ) and because penicillin-resistant syphilis has not been documented in 60 years of the drug’s use. 28 30 31
Non-pregnant patients who are allergic to penicillin can be given doxycycline 100 mg by mouth twice daily for two weeks for primary, secondary, and early latent syphilis, or for four weeks for late latent syphilis, 11 12 13 14 15 although doxycycline, compared with BPG, may yield more treatment failures (defined according to the CDC as a fourfold or higher increase in RPR titre). 28 30 31 There is no alternative treatment to BPG for pregnant women.
Counsel patients about the possibility of Jarish-Herxheimer reactions, which start two to four hours after treatment and usually resolve within 24 hours. Symptoms include fever and systemic symptoms (such as chills, rigors, myalgias, arthralgias) with worsening rash or chancre. 17 While UK guidelines 12 state prednisolone can be used for symptom management, other guidelines 11 13 14 15 recommend only over-the-counter antipyretics.
What about follow-up?
Because syphilis has no test-of-cure, conversion to a non-reactive RPR is the best evidence of successful treatment. 28 Patients should be tested at the start of treatment and monitored at six and 12 months. No clinical data guide interpretation of RPR titres after treatment, and guidelines are based on expert opinion. See table 3 for recommendations from European, UK, US, Canadian, and WHO guidelines. 11 12 13 14 15
Recommendations for assessment of treatment of syphilis
When should I consider evaluation of cerebrospinal fluid?
Indications for lumbar puncture and evaluation of cerebrospinal fluid (CSF) include neurologic symptoms or tertiary disease ( table 3 ). 11 12 13 14 15 CSF evaluation can also be considered for the 10-20% of patients with earlier disease who do not achieve a fourfold decline in RPR titres by 6-12 months after treatment. 11 12 13 14 15
Because BPG poorly penetrates CSF, 11 neurosyphilis should be treated with aqueous penicillin G, 4×10 6 units intravenously every 4 hours for 10-14 days. If neurosyphilis is ruled out, optimal management is unclear. 11 Clinicians may monitor the RPR titre until it is low or non-reactive, or repeat the treatment for early or late latent syphilis. 11 Factors limiting post-treatment RPR declines in the absence of neurosyphilis include prior infection, longer duration of infection, older age, HIV co-infection, and low pre-treatment titres. 11 12 14 15
Referral to secondary care may be necessary for patients requiring CSF evaluation and should be considered for those with uncertain diagnoses or poor response to treatment.
Are there specific considerations for patients with HIV?
Syphilis and HIV infection often co-exist. 32 33 Patients with syphilis should be screened for HIV and, if negative, offered pre-exposure prophylaxis. 32 33 34 They should also be screened for gonorrhoea and chlamydia. HIV-positive patients have additional indications for CSF evaluation (see table 3 ). Otherwise, diagnosis and treatment are unchanged. 31 35 36 37
How should I manage contact tracing?
Contacts (people who have had sex with a person diagnosed with infectious (early) syphilis) within 90 days should receive treatment with one dose of BPG even if their serology results are is negative; asymptomatic contacts who had sex with an infected person more than 90 days ago could defer treatment until their serology results are available, but only if follow-up is assured. Discussions about contact tracing should be non-stigmatising and sensitive to patients’ concerns about confidentiality. Explain that contact tracing has important benefits for the individual concerned and their contacts. It helps to limit ongoing transmission of a serious infection and prevent re-infection. Patients need help and support to notify contacts confidentially.
How this article was created
This article was created based on a review of international guidelines, expert opinion (local public health unit, STI clinic, and infectious disease department), and through a review of Medline and CINAHL, using the search term “syphilis.” We also undertook a manual review of the reference lists of identified articles.
Education into practice
Do you consider syphilis as a differential diagnosis of genital lesions and rashes among sexually active patients?
How would you approach a conversation about contact tracing with a young man, recently diagnosed?
How patients were involved in this article
We reviewed the contents of this material with Max Ottawa, a local “community-based organisation that focuses on maximising the health and wellness of gay, bisexual, Two-spirit, queer, and other guys who are into guys, both cis and trans.”
Acknowledgments
PO’B holds a research chair in public health and HIV prevention from the Ontario HIV Treatment Network.
Competing interests: We have read and understood the BMJ policy on declaration of interests and have no relevant interests to declare.
Provenance and peer review: Commissioned; externally peer reviewed.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- Holmes KK ,
- Sparling PF ,
- Lukehard SA
- LaFond RE ,
- Lukehart SA
- Stoltey JE ,
- ↵ Centers of Disease Control and Prevention (CDC). Sexually transmitted disease surveillance 2017–Syphilis. https://www.cdc.gov/std/stats17/syphilis.htm .
- Choudhri Y ,
- ↵ European Centre for Disease Control and Prevention. Syphilis–Annual epidemiologic report for 2016. https://ecdc.europa.eu/en/publications-data/syphilis-annual-epidemiological-report-2016 .
- Golden MR ,
- Nyatsanza F ,
- ↵ Centers of Disease Control and Prevention. 2015 sexually transmitted diseases treatment guidelines–Syphilis. https://www.cdc.gov/std/tg2015/syphilis.htm .
- Kingston M ,
- Higgins S ,
- Members of the Syphilis guidelines revision group 2015
- ↵ Public Health Agency of Canada. Canadian guidelines on sexually transmitted infections: management and treatment of specific infections–syphilis. https://www.canada.ca/en/public-health/services/infectious-diseases/sexual-health-sexually-transmitted-infections/canadian-guidelines/sexually-transmitted-infections/canadian-guidelines-sexually-transmitted-infections-27.html .
- ↵ World Health Organization. WHO guidelines for the treatment of Treponema pallidum (syphilis). https://www.who.int/reproductivehealth/publications/rtis/syphilis-treatment-guidelines/en/ .
- ↵ Janier M, Hegyi V, Dupin N, et al. 2014 European guideline on the management of syphilis. https://www.iusti.org/regions/europe/pdf/2014/2014SyphilisguidelineEuropean.pdf .
- Swartz MN ,
- Musher DM ,
- Romanowski B
- Ballard RC ,
- Moreland AA
- ↵ Cherneskie T. An update and review of the diagnosis and management of syphilis. https://www.nycptc.org/x/Syphilis_Module_Online.pdf .
- Baughn RE ,
- Oliver SE ,
- ↵ Cantor A, Nelson HD, Daeges M, Pappas M. Screening for syphilis in nonpregnant adolescents and adults: systematic review to update the 2004 US Preventive Services Task Force recommendation. Evidence Synthesis No 136. Agency for Healthcare Research and Quality, 2016. https://www.ncbi.nlm.nih.gov/books/NBK368467/pdf/Bookshelf_NBK368467.pdf .
- Fakile YF ,
- Wheeler HL ,
- Agarwal S ,
- Morshed MG ,
- Levett PN ,
- Fonseca K ,
- Tsang RSW ,
- Clement ME ,
- Pathela P ,
- Braunstein SL ,
- Shepard C ,
- Schillinger JA
- Solomon MM ,
- Glidden DV ,
- iPrEx Study Team
- Biomedical HIV Prevention Working Group of the CIHR Canadian HIV Trials Network
- Larsen SA ,
- Clement MJ ,
- Bacchetti P ,
- Yinnon AM ,
- Coury-Doniger P ,
- Reichman RC

- HIV Clinical Guidelines: Adult and Adolescent Opportunistic Infections
Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV
Search guidelines.
- Archived Guidelines (1)
- Guidance for COVID-19 and People with HIV (2)
- Guidelines for Caring for Persons with HIV in Disaster Areas (4)
- HIV Clinical Guidelines: Adult and Adolescent ARV (19)
- HIV Clinical Guidelines: Adult and Adolescent Opportunistic Infections (34)
- HIV Clinical Guidelines: Pediatric ARV (19)
- HIV Clinical Guidelines: Pediatric Opportunistic Infections (28)
- Perinatal HIV Clinical Guidelines (18)
NOTE: Update in Progress
Epidemiology.
Syphilis, caused by Treponema pallidum , is associated with an increased risk of sexual acquisition and transmission of HIV. 1-8 In the United States, the national rate of primary and secondary syphilis has increased since 2001. 9-12 Although HIV infection, particularly in the advanced stages, may modify the diagnosis, natural history, or management of T. pallidum infection, the principles of syphilis management remain the same for people with and without HIV. 13-18
Clinical Manifestations
The effects of HIV on the protean manifestations of syphilis have been documented in multiple case reports and small case series, and in a limited number of large studies. In most people with HIV and syphilis, the clinical manifestations of syphilis are similar to those observed in people without HIV. Some studies suggest that infection with HIV may affect the clinical presentation of syphilis, as atypical or multiple genital lesions are more apparent, and accelerated progression of syphilis may be seen in people with advanced immunosuppression. 16,17,19-22 Primary or secondary syphilis also may cause a transient decrease in CD4 T lymphocyte (CD4) cell count and increase in HIV viral load that improves with recommended syphilis treatment regimens. 13,23-27 Independent of HIV, previous syphilis can attenuate the clinical and laboratory manifestations of incident infection with T. pallidum . 28-30
Primary syphilis commonly presents as a single painless nodule at the site of contact that rapidly ulcerates to form a classic chancre; however, multiple or atypical painful chancres may occur, and primary lesions may be absent or missed in people with HIV. 16,21,31 Progression to secondary syphilis typically follows 2 to 8 weeks after primary syphilis, but an overlap in primary and secondary manifestations can occur, especially in people with HIV. The most common manifestations of secondary syphilis are mucocutaneous lesions that are macular, maculopapular, papulosquamous, or pustular. These lesions can involve the palms and soles and are often accompanied by generalized lymphadenopathy, fever, malaise, anorexia, arthralgias, and headache. 13,17,18 Mpox (formerly known as monkeypox) lesions can have a similar appearance and can occur simultaneously with early syphilis. 32 Condylomata lata (moist, flat, papular lesions in warm intertriginous regions) can occur and may resemble condylomata acuminata caused by human papillomavirus. Lues maligna is a rare manifestation of secondary syphilis, characterized by papulopustular skin lesions that can evolve into ulcerative lesions with sharp borders and a dark central crust. 33-35 Manifestations of secondary syphilis involving other locations can occur (e.g., ocular and otic syphilis, meningoencephalitis, hepatitis, nephrotic syndrome, gastritis, pneumonia). In people with secondary syphilis, non-focal central nervous system (CNS) symptoms and cerebrospinal fluid (CSF) abnormalities, such as lymphocytic pleocytosis with a mildly elevated CSF protein, can occur. 19,22,31,36-40 Signs and symptoms of primary and secondary syphilis can overlap or persist from a few days to several weeks before resolving. In some instances, recrudescence of symptoms may occur after secondary infection with subsequent evolution to latent stages.
Latent syphilis is defined as serologic reactivity without clinical signs and symptoms of infection. Latent syphilis can be categorized as early latent syphilis if ≤1 year duration, late latent syphilis if >1 year duration, or latent syphilis of unknown duration if there is insufficient information to determine the duration of infection. Tertiary syphilis refers to gumma, cardiovascular syphilis, psychiatric manifestations (e.g., memory loss, personality changes), or late neurosyphilis that can develop 10 to 30 years after untreated infection.
Neurosyphilis, similar to ocular and otic syphilis, can occur at any stage of syphilis with different clinical presentations, including cranial nerve dysfunction, meningitis, stroke, acute or chronic change in mental status, and loss of vibration sense. Manifestations of neurosyphilis in people with HIV are similar to those in individuals who do not have HIV. However, clinical manifestations of neurosyphilis, such as concomitant ocular syphilis (including uveitis) or meningitis, may be more common in people with HIV. 19,22,40-46
Syphilitic uveitis or other ocular syphilis manifestations (e.g., neuroretinitis and optic neuritis) can occur during any stage of syphilis and can manifest as isolated abnormalities or can be associated with neurosyphilis. Syphilis can involve almost any ocular structure, but posterior uveitis and panuveitis are the most common presentations. Other common manifestations can include interstitial keratitis, recurrent anterior uveitis, retinal vasculitis, and optic neuropathy. 47
All people with ocular symptoms and reactive syphilis serology need a full ocular examination, including cranial nerve evaluation. If cranial nerve dysfunction is present, a CSF evaluation is needed. Among people with isolated ocular symptoms (no cranial nerve dysfunction or other neurologic abnormalities), reactive syphilis serology, and confirmed ocular abnormalities on examination, CSF examination is unnecessary before treatment. CSF analysis might be helpful in evaluating people with ocular symptoms and reactive syphilis serology who do not have ocular findings on examination. If ocular syphilis is suspected, immediate referral to and management in collaboration with an ophthalmologist is crucial. Ocular syphilis should be treated similarly to neurosyphilis, even if a CSF examination is normal.
Isolated hearing loss or other otologic symptoms can occur at any stage of syphilis or can be associated with neurosyphilis. Among people with isolated auditory abnormalities and reactive syphilis serology, CSF evaluation is likely to be normal and is not necessary before treatment. 48
Direct Detection
Darkfield microscopy and molecular tests to detect T. pallidum in lesion exudates or tissue (e.g., biopsy with silver stain) are definitive for diagnosing early syphilis. 49 Although T. pallidum direct antigen detection tests are no longer commercially available, some laboratories provide locally developed and validated polymerase chain reaction (PCR) tests for the direct detection of T. pallidum .
Serologic Testing
Serologic diagnosis of syphilis traditionally has involved screening for nontreponemal antibodies with confirmation of reactive tests by treponemal-based assays. 13,50,51 A serologic diagnosis of syphilis is based on nontreponemal tests (i.e., Venereal Disease Research Laboratory [VDRL] and rapid plasma reagin [RPR]), followed by confirmation with treponemal tests (i.e., T. pallidum particle agglutination [TP-PA], enzyme immunoassays [EIAs], chemiluminescence immunoassays [CIAs], fluorescent treponemal antibody absorbed [FTA-ABS], or immunoblots). Rapid treponemal assays are also available to screen for syphilis; however, these tests can not differentiate recent or past infection, so testing with a nontreponemal test is indicated to inform further patient management. 50-52 Use of only one type of serologic test (nontreponemal or treponemal) is insufficient for diagnosis and can result in false-negative results among people tested during primary syphilis and false-positive results among people without syphilis or previously treated syphilis.
Traditional Algorithm
False-positive nontreponemal test results can be associated with medical conditions and other factors unrelated to syphilis, including HIV, autoimmune disease, vaccinations, injection drug use, pregnancy, and older age. 50 Individuals with a reactive nontreponemal test should always receive a treponemal test to confirm the syphilis diagnosis. Nontreponemal test antibody titers can correlate with disease activity and are used for monitoring treatment response. Sequential serologic tests should be performed using the same testing method (VDRL or RPR), preferably by the same laboratory. VDRL and RPR are equally valid assays; however, quantitative results from the two tests cannot be compared directly with each other because the methods are different, and RPR titers frequently are slightly higher than VDRL titers.
Nontreponemal test titers usually decrease after treatment and can become nonreactive with time. However, in some instances nontreponemal antibodies might decrease less than fourfold after treatment (i.e., inadequate serologic response) or might decline appropriately but fail to serorevert and persist for a long period. Atypical nontreponemal serologic test results (e.g., unusually high, unusually low, or fluctuating titers) might occur regardless of HIV status. When serologic tests do not correspond with clinical findings indicative of primary, secondary, or latent syphilis, presumptive treatment is recommended for people with risk factors for syphilis, and use of other tests (e.g., biopsy for histology and immunostaining and PCR of lesion) should be considered. For most people with HIV, serologic tests are accurate and reliable for diagnosing syphilis and evaluating response to treatment. 28
Reverse-Sequence Algorithm
Most people who have reactive treponemal tests will have reactive tests for the remainder of their lives, regardless of adequate treatment or disease activity and do not predict treatment response.
Some laboratories have initiated a reverse-sequence screening algorithm using treponemal EIA or CIA as a screening test, followed by a reflex-quantitative, nontreponemal test if the EIA or CIA is positive.
This reverse-sequence algorithm can identify people previously treated for syphilis, those with untreated or incompletely treated syphilis, and those with false-positive results that can occur with a low likelihood of infection. 13,53 Persons with a positive treponemal screening test should have a standard quantitative nontreponemal test with titer performed reflexively by the laboratory to guide patient management decisions.
In the reverse-sequence screening strategy, a positive treponemal EIA or CIA and a negative reflex-quantitative nontreponemal test requires a second treponemal test (based on different antigens from the initial test) to confirm the results of the positive initial treponemal test. If a second treponemal test is positive, people who have been treated appropriately for their stage of syphilis will require no further treatment unless sexual risk history suggests likelihood of re-exposure, or there is a sustained fourfold increase in nontreponemal antibody titers. In this instance, a repeat nontreponemal test 2 to 4 weeks after the most recent possible exposure is recommended to evaluate for early infection. Those without a history of treatment for syphilis should be offered treatment. Unless history or results of a physical examination suggest a recent infection (e.g., early-stage syphilis), previously untreated people should be treated for late latent syphilis. If the second treponemal test is negative and the risk of syphilis is low, no treatment is indicated. 13,54 However, if the risk of syphilis is high, treatment should be considered. Multiple studies demonstrate that high quantitative index values or high signal-to-cutoff ratio from treponemal EIA or CIA tests correlate with TP-PA positivity, which might eliminate the need for additional confirmatory testing; however, the range of index values varies among different treponemal immunoassays, and the values that correspond to high levels of reactivity with confirmatory testing might differ by immunoassay. 51,55,56
In the absence of neurologic signs or symptoms, risk of neurosyphilis is low in people with a reactive treponemal test and a nonreactive nontreponemal test 55,57 ; examination of CSF is not recommended.
Early-stage disease (i.e., primary, secondary, and early latent syphilis) is identified using the same diagnostic tests used in people without HIV: standard serologic tests and darkfield microscopy of mucocutaneous lesions, if available. VDRL and RPR titers may be higher, lower (in rare instances), or delayed in people with HIV with early-stage syphilis. 58-62 No data indicate that treponemal tests perform differently among people with HIV 51 ; although uncommon, false-negative serologic tests for syphilis can occur with documented T. pallidum infection. 61,62 When serologic tests do not correspond with clinical findings indicative of primary or secondary syphilis, presumptive treatment is recommended for people with risk factors for syphilis, and dilution of the sample for prozone phenomenon should be considered. For most people with HIV, serologic tests are accurate and reliable for diagnosing syphilis and for determining response to treatment.
By definition, people with latent syphilis have serological evidence of syphilis (nontreponemal and treponemal testing) in the absence of clinical manifestations. Early latent syphilis may occur in the interval between the primary and secondary stage of infection or following resolution of secondary manifestations and is defined by evidence of infection during the preceding year by—
- A documented seroconversion or fourfold or greater increase in nontreponemal titer; or
- Symptoms of primary or secondary syphilis; or
- A sex partner with documented primary, secondary, or early latent syphilis. 13
Late latent syphilis is defined as syphilis in a person who does not have evidence of acquiring infection in the preceding year.
All people with syphilis and signs or symptoms suggesting neurologic disease (e.g., cranial nerve dysfunction, meningitis, stroke, altered mental status) warrant evaluation for neurosyphilis.
CSF abnormalities (i.e., elevated protein and mononuclear pleocytosis) are common in early-stage syphilis 36 and in people with HIV, even those with no neurologic symptoms. The clinical and prognostic significance of CSF laboratory abnormalities with early-stage syphilis in people without neurologic symptoms is unknown. Several studies have demonstrated that in people with syphilis and HIV, CSF laboratory abnormalities are associated with CD4 counts ≤350 cells/mm 3 or in combination with RPR titers ≥1:32. 39,40,63,64 However, unless neurologic signs and symptoms are present, a CSF examination has not been associated with improved clinical outcomes. Although laboratory testing is helpful in supporting the diagnosis of neurosyphilis, no single test can be used to diagnose neurosyphilis. The diagnosis of neurosyphilis depends on a combination of CSF tests (CSF cell count, CSF protein, and CSF-VDRL) in the setting of reactive serologic test results and neurologic signs and symptoms. CSF examination may indicate mononuclear pleocytosis (6–200 cells/mm 3 ), mildly elevated protein concentration, or a reactive CSF-VDRL. Among people with HIV, the CSF leukocyte count can be elevated (>5 white blood cell count [WBC]/mm 3 ); using a higher cutoff (>20 WBC/mm 3 ) may improve the specificity of neurosyphilis diagnosis. 39 In people with neurologic signs or symptoms, a reactive CSF-VDRL (in a specimen not contaminated with blood) is considered diagnostic of neurosyphilis; however, it is thought to have a very low sensitivity and therefore may miss true disease. Therefore, in people with neurologic signs or symptoms, reactive serologic test results, lymphocytic pleocytosis, or elevated protein, neurosyphilis should be considered even when the CSF-VDRL is negative. In that instance, additional evaluation by using FTA-ABS or TP-PA testing on CSF might be warranted. 13 The CSF FTA-ABS test is less specific for neurosyphilis than the CSF-VDRL but is highly sensitive. Fewer data are available regarding CSF TP-PA; however, the sensitivity and specificity appears similar to the CSF FTA-ABS. 65,66 Neurosyphilis is highly unlikely with a negative CSF FTA-ABS or TP-PA test, especially among people with nonspecific neurologic signs and symptoms.
RPR tests of the CSF have been associated with a high false-negative rate and are not recommended. 67 PCR-based diagnostic methods are not currently recommended as diagnostic tests for neurosyphilis.
Preventing Disease
The resurgence of syphilis and other sexually transmitted infections (STIs), as well as the emergence of mpox, in men who have sex with men (MSM) with HIV underscores the importance of primary prevention of syphilis in this population, which should begin with a behavioral risk assessment and routine discussion of sexual behaviors. Health care providers should discuss patient-centered risk reduction messages and advise specific actions that can reduce the risk of acquiring STIs and of transmitting HIV. 13,68-72 Routine serologic screening for syphilis is recommended at least annually for all people with HIV who are sexually active, with more frequent screening (every 3–6 months) for those who have multiple or anonymous partners. 13,73-75 The occurrence of syphilis or any other STI in a person with HIV is an indication of risk behaviors that should prompt intensified risk assessment and counseling messages about the manifestations of syphilis, risk of HIV transmission, and prevention strategies with strong consideration for behavioral intervention. 76,77 People undergoing screening or treatment for syphilis also should be evaluated for other STIs, including mpox, chlamydia, and gonorrhea at anatomic sites of exposure in men and chlamydia, gonorrhea, and trichomonas infections in women. 13,78
Frequent serologic screening can identify people with recent infection and, in some instances, before infectious lesions develop. Treatment can prevent disease progression in the individual and transmission to their partners. Studies in the pre-HIV era demonstrated that approximately one-third of the sexual partners of persons who have primary syphilis will develop syphilis within 30 days of exposure; empiric treatment of sexual partners exposed to syphilis will prevent the development of disease and onward syphilis transmission. 79-82 Individuals with recent sexual contact with a person with syphilis in any stage should be evaluated clinically and serologically and treated presumptively. People who have had sexual contact with an individual diagnosed with primary, secondary, or early latent syphilis during the 90 days preceding the diagnosis should be treated presumptively for early syphilis, even if serologic test results are negative (AII).
People who have had sexual contact with a person who receives a diagnosis of primary, secondary, or early latent syphilis >90 days before the diagnosis should be treated presumptively for early syphilis if serologic test results are not immediately available and the opportunity for follow-up is uncertain (AIII). If serologic tests are negative, no treatment is needed. If serologic tests are positive, treatment should be based on clinical and serologic evaluation and the stage of syphilis. Long-term sexual partners of people who have late latent syphilis should be evaluated clinically and serologically for syphilis and treated on the basis of the evaluation’s findings. Sexual partners of people with syphilis should be notified of their exposure and the importance of evaluation for testing and empiric therapy. 13 The following sex partners of people with syphilis are considered at risk for infection and should be confidentially notified of the exposure and need for evaluation: partners who have had sexual contact within (1) 3 months plus the duration of symptoms for people who receive a diagnosis of primary syphilis, (2) 6 months plus the duration of symptoms for those diagnosed with secondary syphilis, and (3) 1 year for people diagnosed with early latent syphilis.
Pre-Exposure Prophylaxis and Post-Exposure Prophylaxis for Prevention
Doxycycline pre-exposure prophylaxis (PrEP) has been examined for prevention of bacterial STIs. In a pilot study, 30 MSM with HIV with previous syphilis were randomly assigned to doxycycline 100 mg daily for 48 weeks versus a financial incentive–based behavioral intervention; doxycycline was associated with a lower incidence of syphilis, but this did not reach statistical significance due to small sample size. 83
Post-exposure prophylaxis (doxycycline 200 mg after unprotected anal sex) has been studied among MSM and transgender women, with a reduction in incident syphilis by 73%. 84 Several recent randomized open-label clinical trials have found that doxycycline 200 mg after condomless sex among MSM or transgender women with HIV or on HIV PrEP significantly reduced chlamydia, gonorrhea, and syphilis acquisition; a randomized trial of cisgender women on HIV PrEP administered doxycycline 200 mg within 72 hours after sex did not reduce chlamydia, gonorrhea, or syphilis acquisition. 85 There is ongoing evaluation regarding the potential impact of STI postexposure prophylaxis on antimicrobial resistance and the microbiome. Other studies are underway or in development regarding doxycycline prophylaxis for bacterial STIs. 86,87
Targeted mass treatment of high-risk populations with azithromycin has not been demonstrated to be effective. 88 Azithromycin is not recommended as secondary prevention because of azithromycin treatment failures reported in people with HIV and reports of chromosomal mutations associated with macrolide-resistant T. pallidum. 89-93
Treatment regimens for syphilis demonstrate that most people with HIV respond appropriately to single dose benzathine penicillin G after exposure to syphilis and for primary, secondary, and early latent syphilis (within the previous 12 months). 13,59,94,95 However, in people with HIV, more frequent clinical and serologic evaluation is recommended—at least every 3 months rather than every 6 months—because serologic nonresponse and neurologic complications may be more frequent. 19,96,97 Use of antiretroviral therapy (ART) in people with syphilis has also been associated with a reduced risk of serologic failure of syphilis treatment 22 and a lower risk of developing neurosyphilis. 22
Benzathine penicillin G remains the treatment of choice for syphilis. People with HIV with early-stage (primary, secondary, or early latent) syphilis should receive a single intramuscular (IM) injection of 2.4 million units of benzathine penicillin G (AII). 13 High-dose amoxicillin given with probenecid in addition to benzathine penicillin G in early syphilis is not associated with improved clinical outcomes. 59 Persons with a penicillin allergy whose compliance or follow-up cannot be ensured should be desensitized and treated with benzathine penicillin G (AIII).
The efficacy of alternative non-penicillin regimens in people with HIV and early syphilis has not been well studied. The use of any alternative penicillin treatment regimen should be undertaken only with close clinical and serologic monitoring. The Panel on Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV (the Panel) supports the use of doxycycline, 100 mg orally twice daily for 14 days, to treat early syphilis (BII). 98,99 Based on limited clinical studies in people with and without HIV, ceftriaxone (1 g daily either IM or intravenously [IV] for 10–14 days) is also recommended for treating early-stage syphilis (BII), but the optimal dose and duration of therapy have not been defined. 100-102 There are limited data suggesting a single 2-g oral dose of oral azithromycin can be effective for treating early syphilis 103-105 ; however T. pallidum chromosomal mutations associated with azithromycin resistance and treatment failures have been reported most commonly in MSM. 89-93,106 Azithromycin has not been well studied in people with HIV or among pregnant people. Therefore, azithromycin should not be used as treatment for syphilis (AII).
In people with HIV who have late latent syphilis, treatment with three weekly IM injections of 2.4 million units of benzathine penicillin G is recommended (AII). Alternative therapy is doxycycline, 100 mg orally twice daily for 28 days; however, it has not been sufficiently evaluated in people with HIV (BIII). Limited clinical studies and biologic and pharmacologic evidence suggest that ceftriaxone may be effective, but the optimal dose and duration of therapy have not been determined. 107,108 If the clinical situation requires use of an alternative to penicillin, treatment should be undertaken with close clinical and serologic monitoring.
People with HIV who have clinical evidence of tertiary syphilis (cardiovascular or gummatous disease) should have CSF examination to rule out CSF abnormalities before therapy is initiated. If the CSF evaluation is normal, the recommended treatment of late-stage syphilis is three weekly IM injections of 2.4 million units of benzathine penicillin G (AII). 13 However, due to the complexity of tertiary syphilis management, especially cardiovascular syphilis, health care providers are advised to consult an infectious disease specialist.
People with HIV diagnosed with neurosyphilis or ocular or otic syphilis should receive IV aqueous crystalline penicillin G, 18 to 24 million units daily, administered 3 to 4 million units IV every 4 hours or by continuous infusion for 10 to 14 days (AII), or procaine penicillin, 2.4 million units IM once daily plus probenecid 500 mg orally four times a day for 10 to 14 days (BII). 13 However, procaine penicillin has been recently discontinued by the manufacturer. 109
People with HIV who are allergic to sulfa-containing medications should not be given probenecid because of potential allergic reaction; therefore, IV penicillin is recommended (AIII). Although systemic steroids are used frequently as adjunctive therapy for otic syphilis, such therapy has not been proven beneficial.
Because neurosyphilis treatment regimens are of shorter duration than those used in late latent syphilis, 2.4 million units of benzathine penicillin IM once after completion of IV penicillin G can be considered to provide a comparable duration of therapy (CIII) . 13
People who have a history of immunoglobulin E mediated penicillin hypersensitivity may lose their sensitivity after 10 years, 110,111 and a subsequent negative skin test evaluation followed by oral challenge can be considered. Among people for whom the only option is penicillin (e.g., syphilis in pregnancy) and among those with a positive skin test, desensitization to penicillin is the preferred approach. However, based on limited data, ceftriaxone (2 g daily IV for 10–14 days) is recommended as an acceptable alternative regimen (BII). 100,101,108 Other alternative regimens for neurosyphilis have not been evaluated adequately. Syphilis treatment recommendations are available in the 2021 Centers for Disease Control and Prevention STI Treatment Guidelines . 13
Special Considerations with Regard to Starting Antiretroviral Therapy
There are no special considerations regarding the initiation of ART in patients with syphilis. Specifically, there is no evidence that treatment with ART needs to be delayed until treatment for syphilis has been completed. Immune reconstitution inflammatory syndrome in association with syphilis following treatment with ART in people with HIV is uncommon. 112,113
Monitoring and Adverse Events
Clinical and serologic responses (fourfold decrease from the nontreponemal titer at the time of treatment) to treatment of early-stage (primary, secondary, and early latent) disease should be performed at 3, 6, 9, 12, and 24 months after therapy to ensure resolution of signs and symptoms within 3 to 6 months and seroreversion or a fourfold decline in nontreponemal titers within 24 months. Clinical and serologic responses to treatment are similar in people with HIV; subtle variations can occur, however, including a slower temporal pattern of serologic response in people with HIV. 13,59,79,94,95 Factors associated with the serologic response to treatment in people without HIV include younger age, earlier syphilis stage, and higher RPR titer. 114-116 If clinical signs and symptoms persist, treatment failure should be considered. If clinical signs or symptoms recur or there is a sustained fourfold increase in nontreponemal titers of greater than 2 weeks, treatment failure or reinfection should be considered and managed per recommendations (see Managing Possible Treatment Failure or Reinfection ). The potential for reinfection should be based on the sexual history and risk assessment. Clinical trial data have demonstrated that 15% to 20% of people (including people with HIV) treated with recommended therapy for early-stage syphilis will not achieve the fourfold decline in nontreponemal titer used to define treatment response at 1 year. 13,59 Serum nontreponemal test titers may remain reactive, usually ≤1:8, although can be higher, for prolonged periods. In addition, people treated for early-stage syphilis who have a fourfold decline in titer may not serorevert to a negative nontreponemal test, which does not represent treatment failure but an inadequate serologic response. 117
Response to therapy for late latent syphilis should be monitored using nontreponemal serologic tests at 6, 12, 18, and 24 months to ensure at least a fourfold decline in titer, if initially high (≥1:32), within 24 months of therapy. However, data to define the precise time intervals for adequate serologic responses are limited. Many people with low titers and late latent syphilis do not have a fourfold decline in the initial titer. If clinical symptoms develop or a fourfold increase in nontreponemal titers is sustained over 2 weeks, then treatment failure or reinfection should be considered and managed per recommendations (see Managing Possible Treatment Failure or Reinfection ). The potential for reinfection should be based on sexual history and risk assessment. 13
The earliest CSF indicator of response to neurosyphilis treatment is a decline in CSF lymphocytosis. The CSF-VDRL may respond more slowly. Limited data suggest that changes in CSF parameters may occur more slowly in people with HIV, especially with advanced immunosuppression. 22,39 Among people with HIV who are on effective ART and people without HIV, normalization of the serum RPR titer predicts normalization of abnormal CSF parameters after neurosyphilis treatment. 118,119 Therefore, repeated CSF examinations are unnecessary for people without HIV or among people with HIV who are on ART and who exhibit serologic and clinical responses to treatment. 13
The Jarisch-Herxheimer reaction is an acute febrile reaction frequently accompanied by headache, rigors, transient worsening of rash, myalgia, and sometimes even a sepsis-like syndrome, that can occur within the first 24 hours after initiation of treatment for syphilis. Antipyretics can be used to manage symptoms but have not been proven to prevent this reaction. The Jarisch-Herxheimer reaction occurs most frequently in people with early syphilis, high nontreponemal antibody titers, and prior penicillin treatment. 120 People with syphilis should be warned about this reaction, instructed how to manage it, and informed that it is not an allergic reaction to penicillin.
Managing Possible Treatment Failure or Reinfection
Retreatment should be considered for people with early-stage syphilis who have persistent or recurring clinical signs or symptoms of disease, or a sustained fourfold increase in serum nontreponemal titers after an initial fourfold decrease following treatment. The assessment for potential reinfection should be informed by a sexual history and syphilis risk assessment including information about a recent sexual partner with signs or symptoms or recent treatment for syphilis. People who have had syphilis are at increased risk for reinfection. One study showed that 6% of MSM had a repeat early-stage syphilis infection within 2 years of initial infection; HIV infection and multiple sexual partners were associated with increased risk of reinfection. 11 Serologic response should be compared to the titer at the time of treatment. However, assessing serologic response to treatment can be difficult, as definitive criteria for cure or failure have not been well established. People with HIV may be at increased risk of treatment failure, but the magnitude of these risks is not precisely defined and is likely low. 13,38,97
People who meet the criteria for treatment failure (i.e., signs or symptoms that persist or recur, or a fourfold increase or greater in titer sustained for more than 2 weeks) and who are at low risk for reinfection should be managed for possible treatment failure. If neurologic symptoms or signs are identified, a CSF evaluation is recommended, with findings guiding management. People with nontreponemal titers that do not decrease fourfold within 12 to 24 months of therapy should also be managed as a possible treatment failure. Management should include neurologic examination and retreatment with benzathine penicillin G, 2.4 million units at 1-week intervals for 3 weeks (BIII). If titers do not respond appropriately after retreatment, the value of repeated CSF examination or additional therapy is unclear, but it is generally not recommended. The Panel supports benzathine penicillin treatment (2.4 million units IM) without a CSF examination (unless signs or symptoms of neurosyphilis are present) and close clinical follow-up in people with recurrent signs and symptoms of primary or secondary syphilis or a fourfold increase in nontreponemal titers within the past year who are at high risk of syphilis reinfection (CIII).
People treated for late latent syphilis should have a CSF examination and be re-treated if they develop clinical signs or symptoms of syphilis or have a sustained fourfold increase in serum nontreponemal test titer and are at low risk for reinfection; this can also be considered if they experience an inadequate serologic response (i.e., less than fourfold decline in an initially high [ ≥1:32 ] nontreponemal test titer) within 12 months for early syphilis and 24 months for late latent syphilis. If CSF examination is consistent with CNS involvement, retreatment should follow the recommendations for treatment of neurosyphilis. People with a normal CSF examination or without ocular or otic symptoms should be treated with benzathine penicillin 2.4 million units IM weekly for three doses (BIII). The Panel supports benzathine penicillin treatment (2.4 million units IM) without a CSF examination (unless signs or symptoms of neurosyphilis are present) and close clinical follow-up in people with signs or symptoms of primary or secondary syphilis or a fourfold increase in nontreponemal titers within the past year who are at high risk of reinfection (CIII) .
Among people with HIV who are on effective ART and people without HIV, normalization of the serum RPR titer predicts normalization of abnormal CSF parameters after neurosyphilis treatment. 118,119 Therefore, repeated CSF examinations are unnecessary for people with HIV who are on ART and who exhibit serologic and clinical responses after treatment.
Special Considerations During Pregnancy
In recent years, there has been a resurgence in neonatal syphilis in the United States. Syphilis in pregnancy is associated with increased risk of several adverse outcomes, including pregnancy loss, preterm birth, stillbirth, impaired fetal growth, neonatal mortality, and congenital infection, which can cause abnormalities in multiple organ systems. The clinical manifestations of syphilis in pregnancy are similar in people with and without HIV.
Serologic screening for syphilis should be conducted at the first prenatal visit and at 28 weeks. In communities and populations in which the prevalence of syphilis is high and in people at increased risk of infection (i.e., sex with multiple partners or new partner, sex in conjunction with drug use or transactional sex, late entry or no prenatal care, methamphetamine or heroin use, hepatitis C, alcohol misuse, 121 incarceration, STI in pregnancy or partner with STI, unstable housing or homelessness), 122 serologic testing should also be performed at delivery. 13 Providers should consider offering screening for syphilis to sexual partners of pregnant people.
Screening for syphilis during pregnancy should be offered at sites providing episodic care, including emergency departments, jails, and prisons. 123 Antepartum screening with nontreponemal testing is typical but treponemal screening is being used in some settings. If a treponemal EIA or CIA test is used for antepartum syphilis screening, all positive EIA or CIA tests should be confirmed with a quantitative, nontreponemal test (RPR or VDRL), as titers are essential to monitoring treatment response. If the nontreponemal test is negative and the prozone reaction is ruled out (false-negative nontreponemal test that results from high antibody titer) then the results are discordant; a second treponemal test should be performed, preferably on the same specimen (see Diagnosis section above). 124 If the second treponemal test is negative (i.e., EIA positive, RPR negative, and TP-PA negative), the positive EIA or CIA is more likely to represent a false-positive test result for people who are living in communities with low rates of syphilis, have a partner who is uninfected, and have no history of treated syphilis. 55,124 During pregnancy, if there is a low risk for syphilis, there are no signs or symptoms of primary syphilis, the partner has no clinical or serologic evidence of syphilis, and the pregnant person is likely to follow up with clinical care, repeat serologic testing within 4 weeks can be considered to determine whether the EIA or CIA remains positive or whether the RPR, VDRL, or TP-PA result becomes positive. If both the RPR and TP-PA remain negative, no further treatment is necessary. If follow-up is not likely, treatment appropriate for the stage of syphilis is recommended for people with an isolated reactive treponemal test without a history of syphilis treatment.
No postpartum individual or neonate should leave the hospital without documentation of maternal syphilis serologic status determined at least once during pregnancy. 13 All individuals who have a fetal death after 20 weeks of gestation also should be tested for syphilis.
Rates of transmission to the fetus and adverse pregnancy outcomes for untreated syphilis are highest with primary, secondary, and early latent syphilis and decrease with increasing duration of infection. Pregnancy does not appear to alter the clinical course, manifestations, or diagnostic test results for syphilis infection in adults. Concurrent syphilis infection has been associated with increased risk of perinatal transmission of HIV to the infant. 125-131
Syphilis infection during pregnancy should be considered in those with reactive syphilis serology unless an adequate treatment history is documented clearly in the medical records and sequential serologic antibody titers have declined appropriately for the stage of syphilis. In general, the risk of antepartum fetal infection or congenital syphilis at delivery is related to the quantitative maternal nontreponemal titer, especially if ≥1:8. However, risk for fetal infection is still substantial among pregnant people with late latent syphilis and low titers. All neonates born to people with syphilis should be evaluated for congenital syphilis regardless of maternal treatment or response.
Sustained low nontreponemal titers after documented treatment for the appropriate stage of infection might not require additional treatment; however, rising or persistently high antibody titers may indicate reinfection or treatment failure, and retreatment should be considered. 13
Benzathine penicillin G is recommended for the treatment of syphilis during pregnancy. Penicillin is the only known effective antimicrobial for preventing transmission to the fetus and for treatment of fetal infection; however evidence is insufficient to determine the optimal penicillin regimen. 132 For management of early syphilis during pregnancy, limited evidence indicates a second dose of benzathine penicillin G 2.4 million units IM 1 week after the single dose treatment may be of benefit for congenital syphilis prevention. 13,129,133-135 If a second dose of benzathine penicillin is administered, it should be provided no later than 9 days after the first dose. 13 Sexual partners of pregnant individuals with syphilis should be referred for evaluation and treatment.
Since no alternatives to penicillin have been proven effective and safe for prevention of fetal infection, desensitization and treatment with penicillin should be performed in pregnancy for those who have a history of penicillin allergy (AIII). 13 Erythromycin and azithromycin should not be used because these regimens do not reliably cure infection in the pregnant individual or the fetus (AII) 132 ; tetracyclines should be avoided in the second and third trimesters of pregnancy (AII). 129,136 Data are insufficient to recommend ceftriaxone 137,138 for treatment of antenatal infection and prevention of congenital syphilis (BIII).
Treatment of syphilis during the second half of pregnancy may precipitate preterm labor or fetal distress if a Jarisch-Herxheimer reaction occurs. 139,140 Obstetric attention is advised if contractions develop or a decrease in fetal movement is noted after treatment. During the second half of pregnancy, syphilis management can be facilitated with sonographic fetal evaluation for congenital syphilis, but this evaluation should not delay therapy. Sonographic signs of fetal or placental syphilis (e.g., hepatomegaly, ascites, fetal hydrops, thickened placenta) indicate a greater risk of fetal treatment failure. 141 Such cases should be managed in consultation with high-risk obstetric specialists. After 20 weeks of gestation, fetal and contraction monitoring for 24 hours after initiation of treatment for early syphilis should be considered when sonographic findings indicate fetal infection.
Coordinated prenatal care and treatment are vital because providers should document that treatment is adequate for the syphilis stage and ensure that the clinical and antibody responses are appropriate for the patient’s disease stage. Maternal serologic response during pregnancy after adequate therapy varies by stage of disease and timing of treatment. 142 If syphilis is diagnosed and treated at or before 24 weeks’ gestation, serologic titers should not be repeated before 8 weeks after treatment but should be repeated again at delivery. Titers should be repeated sooner if reinfection or treatment failure is suspected. For syphilis diagnosed and treated after 24 weeks’ gestation, serologic titers should be repeated at delivery. 13 A majority of women will not achieve a fourfold decrease in titers before delivery, although this does not indicate treatment failure. Inadequate antenatal treatment is likely if delivery occurs within 30 days of therapy, clinical signs of infection are present at delivery, or the maternal nontreponemal titer at delivery is fourfold higher than the pre-treatment titer. There is no evidence that pregnant women with syphilis and HIV are at increased risk for delayed syphilis treatment response compared with women without HIV. 143
- Dennis AM, Cressman A, Pasquale D, et al. Intersection of syphilis and HIV networks to identify opportunities to enhance HIV prevention. Clin Infect Dis . 2021. Available at: https://pubmed.ncbi.nlm.nih.gov/33978757 .
- Wu MY, Gong HZ, Hu KR, Zheng HY, Wan X, Li J. Effect of syphilis infection on HIV acquisition: a systematic review and meta-analysis. Sex Transm Infect . 2021;97(7):525-533. Available at: https://pubmed.ncbi.nlm.nih.gov/33219164 .
- Hart-Malloy R, Rosenthal M, Patterson W, Currenti S, O'Donnell T, Gunn JK. Syphilis among adult males with a history of male-to-male sexual contact living with diagnosed HIV in New York State (excluding New York City): the challenge of intersecting epidemics. PLoS One . 2019;14(12):e0226614. Available at: https://pubmed.ncbi.nlm.nih.gov/31851719 .
- Pathela P, Braunstein SL, Schillinger JA, Shepard C, Sweeney M, Blank S. Men who have sex with men have a 140-fold higher risk for newly diagnosed HIV and syphilis compared with heterosexual men in New York City. J Acquir Immune Defic Syndr . 2011;58(4):408-416. Available at: https://pubmed.ncbi.nlm.nih.gov/21857351 .
- Fleming DT, Wasserheit JN. From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm Infect . 1999;75(1):3-17. Available at: https://pubmed.ncbi.nlm.nih.gov/10448335 .
- Rottingen JA, Cameron DW, Garnett GP. A systematic review of the epidemiologic interactions between classic sexually transmitted diseases and HIV: how much really is known? Sex Transm Dis . 2001;28(10):579-597. Available at: https://pubmed.ncbi.nlm.nih.gov/11689757 .
- Peterman TA, Newman DR, Maddox L, Schmitt K, Shiver S. High risk for HIV following syphilis diagnosis among men in Florida, 2000–2011. Public Health Rep . 2014;129(2):164-169. Available at: https://pubmed.ncbi.nlm.nih.gov/24587551 .
- Solomon MM, Mayer KH, Glidden DV, et al. Syphilis predicts HIV incidence among men and transgender women who have sex with men in a preexposure prophylaxis trial. Clin Infect Dis . 2014;59(7):1020-1026. Available at: https://pubmed.ncbi.nlm.nih.gov/24928295 .
- Centers for Disease Control and Prevention. Outbreak of syphilis among men who have sex with men--Southern California, 2000. MMWR Morb Mortal Wkly Rep . 2001;50(7):117-120. Available at: https://pubmed.ncbi.nlm.nih.gov/11393490 .
- Spicknall IH, Kreisel KM, Weinstock HS. Estimates of the prevalence and incidence of syphilis in the United States, 2018. Sex Transm Dis . 2021;48(4):247-252. Available at: https://pubmed.ncbi.nlm.nih.gov/33492091 .
- Cohen SE, Chew Ng RA, Katz KA, et al. Repeat syphilis among men who have sex with men in California, 2002—2006: implications for syphilis elimination efforts. Am J Public Health . 2012;102(1):e1-8. Available at: https://pubmed.ncbi.nlm.nih.gov/22095364 .
- Centers for Disease Control and Prevention. Syphilis surveillance supplemental slides, 2016–2020. 2022. Available at: https://www.cdc.gov/std/statistics/syphilis-supplement/default.htm .
- Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep . 2021;70(4):1-187. Available at: https://pubmed.ncbi.nlm.nih.gov/34292926 .
- Rasoldier V, Gueudry J, Chapuzet C, et al. Early symptomatic neurosyphilis and ocular syphilis: a comparative study between HIV-positive and HIV-negative patients. Infect Dis Now . 2021;51(4):351-356. Available at: https://pubmed.ncbi.nlm.nih.gov/33239175 .
- Calza L, Manfredi R, Marinacci G, Tadolini M, Fortunato L, Chiodo F. Efficacy of penicillin G benzathine as antimicrobial treatment of cutaneous secondary syphilis in patients with HIV infection. J Chemother . 2002;14(5):533-534. Available at: https://pubmed.ncbi.nlm.nih.gov/12462435 .
- Rompalo AM, Lawlor J, Seaman P, Quinn TC, Zenilman JM, Hook EW, 3rd. Modification of syphilitic genital ulcer manifestations by coexistent HIV infection. Sex Transm Dis . 2001;28(8):448-454. Available at: https://pubmed.ncbi.nlm.nih.gov/11473216 .
- Musher DM, Hamill RJ, Baughn RE. Effect of human immunodeficiency virus (HIV) infection on the course of syphilis and on the response to treatment. Ann Intern Med . 1990;113(11):872-881. Available at: https://pubmed.ncbi.nlm.nih.gov/2240901 .
- Radolf JD, Kaplan RP. Unusual manifestations of secondary syphilis and abnormal humoral immune response to Treponema pallidum antigens in a homosexual man with asymptomatic human immunodeficiency virus infection. J Am Acad Dermatol . 1988;18(2 Pt 2):423-428. Available at: https://pubmed.ncbi.nlm.nih.gov/2963840 .
- Centers for Disease Control and Prevention. Symptomatic early neurosyphilis among HIV-positive men who have sex with men--four cities, United States, January 2002-June 2004. MMWR Morb Mortal Wkly Rep . 2007;56(25):625-628. Available at: https://pubmed.ncbi.nlm.nih.gov/17597693 .
- Nieuwenburg SA, Sprenger RJ, Schim van der Loeff MF, de Vries HJC. Clinical outcomes of syphilis in HIV-negative and HIV-positive MSM: occurrence of repeat syphilis episodes and non-treponemal serology responses. Sex Transm Infect . 2021. Available at: https://pubmed.ncbi.nlm.nih.gov/33608479 .
- Towns JM, Leslie DE, Denham I, Azzato F, Fairley CK, Chen M. Painful and multiple anogenital lesions are common in men with Treponema pallidum PCR-positive primary syphilis without herpes simplex virus coinfection: a cross-sectional clinic-based study. Sex Transm Infect . 2016;92(2):110-115. Available at: https://pubmed.ncbi.nlm.nih.gov/26378262 .
- Ghanem KG, Moore RD, Rompalo AM, Erbelding EJ, Zenilman JM, Gebo KA. Neurosyphilis in a clinical cohort of HIV-1-infected patients. AIDS . 2008;22(10):1145-1151. Available at: https://pubmed.ncbi.nlm.nih.gov/18525260 .
- Muccini C, Crowell TA, Pinyakorn S, et al. Brief report: syphilis incidence and effect on viral load, CD4, and CD4/CD8 ratio in a Thai cohort of predominantly men who have sex with men living with HIV. J Acquir Immune Defic Syndr . 2021;86(2):219-223. Available at: https://pubmed.ncbi.nlm.nih.gov/33433124 .
- Buchacz K, Patel P, Taylor M, et al. Syphilis increases HIV viral load and decreases CD4 cell counts in HIV-infected patients with new syphilis infections. AIDS . 2004;18(15):2075-2079. Available at: https://pubmed.ncbi.nlm.nih.gov/15577629 .
- Modjarrad K, Vermund SH. Effect of treating co-infections on HIV-1 viral load: a systematic review. Lancet Infect Dis . 2010;10(7):455-463. Available at: https://pubmed.ncbi.nlm.nih.gov/20610327 .
- Palacios R, Jimenez-Onate F, Aguilar M, et al. Impact of syphilis infection on HIV viral load and CD4 cell counts in HIV-infected patients. J Acquir Immune Defic Syndr . 2007;44(3):356-359. Available at: https://pubmed.ncbi.nlm.nih.gov/17159654 .
- Kofoed K, Gerstoft J, Mathiesen LR, Benfield T. Syphilis and human immunodeficiency virus (HIV)-1 coinfection: influence on CD4 T-cell count, HIV-1 viral load, and treatment response. Sex Transm Dis . 2006;33(3):143-148. Available at: https://pubmed.ncbi.nlm.nih.gov/16505739 .
- Tuddenham S, Ghanem KG. Management of adult syphilis: key questions to inform the 2021 Centers for Disease Control and Prevention Sexually Transmitted Infections Treatment Guidelines. Clin Infect Dis . 2022;74(Suppl_2):S127-S133. Available at: https://pubmed.ncbi.nlm.nih.gov/35416969 .
- Marra CM, Maxwell CL, Sahi SK, Tantalo LC, Dunaway SB, Lukehart SA. Previous syphilis alters the course of subsequent episodes of syphilis. Clin Infect Dis . 2020;71(5):1243-1247. Available at: https://pubmed.ncbi.nlm.nih.gov/31560366 .
- N’Gom PT, Jaffar S, Ricard D, et al. Immune stimulation by syphilis and malaria in HIV-2-infected and uninfected villagers in West Africa. Br J Biomed Sci . 1997;54(4):251-255. Available at: https://pubmed.ncbi.nlm.nih.gov/9624734 .
- Rompalo AM, Joesoef MR, O’Donnell JA, et al. Clinical manifestations of early syphilis by HIV status and gender: results of the syphilis and HIV study. Sex Transm Dis . 2001;28(3):158-165. Available at: https://pubmed.ncbi.nlm.nih.gov/11289198 .
- Hussain A, Kaler J, Lau G, Maxwell T. Clinical conundrums: differentiating monkeypox from similarly presenting infections. Cureus . 2022;14(10):e29929. Available at: https://pubmed.ncbi.nlm.nih.gov/36348880 .
- Tambe S, Zambare U, Nayak C. Nodulo-ulcerative and erythrodermic secondary syphilis in human immunodeficiency virus-infected individuals. Int J STD AIDS . 2019;30(5):505-508. Available at: https://pubmed.ncbi.nlm.nih.gov/30630397 .
- Wang H, Wang X, Li S. A case of lues maligna in an AIDS patient. Int J STD AIDS . 2012;23(8):599-600. Available at: https://pubmed.ncbi.nlm.nih.gov/22930302 .
- Tucker JD, Shah S, Jarell AD, Tsai KY, Zembowicz A, Kroshinsky D. Lues maligna in early HIV infection case report and review of the literature. Sex Transm Dis . 2009;36(8):512-514. Available at: https://pubmed.ncbi.nlm.nih.gov/19455078 .
- Lukehart SA, Hook EW, 3rd, Baker-Zander SA, Collier AC, Critchlow CW, Handsfield HH. Invasion of the central nervous system by Treponema pallidum: implications for diagnosis and treatment. Ann Intern Med . 1988;109(11):855-862. Available at: https://pubmed.ncbi.nlm.nih.gov/3056164 .
- Bayne LL, Schmidley JW, Goodin DS. Acute syphilitic meningitis. Its occurrence after clinical and serologic cure of secondary syphilis with penicillin G. Arch Neurol . 1986;43(2):137-138. Available at: https://pubmed.ncbi.nlm.nih.gov/3947251 .
- Berry CD, Hooton TM, Collier AC, Lukehart SA. Neurologic relapse after benzathine penicillin therapy for secondary syphilis in a patient with HIV infection. N Engl J Med . 1987;316(25):1587-1589. Available at: https://pubmed.ncbi.nlm.nih.gov/3587291 .
- Marra CM, Maxwell CL, Smith SL, et al. Cerebrospinal fluid abnormalities in patients with syphilis: association with clinical and laboratory features. J Infect Dis . 2004;189(3):369-376. Available at: https://pubmed.ncbi.nlm.nih.gov/14745693 .
- Marra CM, Maxwell CL, Tantalo L, et al. Normalization of cerebrospinal fluid abnormalities after neurosyphilis therapy: does HIV status matter? Clin Infect Dis . 2004;38(7):1001-1006. Available at: https://pubmed.ncbi.nlm.nih.gov/15034833 .
- Biotti D, Bidot S, Mahy S, et al. Ocular syphilis and HIV infection. Sex Transm Dis . 2010;37(1):41-43. Available at: https://pubmed.ncbi.nlm.nih.gov/20118676 .
- Tucker JD, Li JZ, Robbins GK, et al. Ocular syphilis among HIV-infected patients: a systematic analysis of the literature. Sex Transm Infect . 2011;87(1):4-8. Available at: https://pubmed.ncbi.nlm.nih.gov/20798396 .
- Wagner LF, Lanzl I, Rothe K, et al. Clinical and ophthalmological characteristics of ocular syphilis in a retrospective tertiary hospital cohort. Sex Transm Dis . 2021;48(6):436-442. Available at: https://pubmed.ncbi.nlm.nih.gov/33156290 .
- Oliver SE, Aubin M, Atwell L, et al. Ocular syphilis – eight jurisdictions, United States, 2014–2015. MMWR Morb Mortal Wkly Rep . 2016;65(43):1185-1188. Available at: https://pubmed.ncbi.nlm.nih.gov/27811837 .
- Cope AB, Mobley VL, Oliver SE, et al. Ocular syphilis and human immunodeficiency virus coinfection among syphilis patients in North Carolina, 2014–2016. Sex Transm Dis . 2019;46(2):80-85. Available at: https://pubmed.ncbi.nlm.nih.gov/30169474 .
- Woolston S, Cohen SE, Fanfair RN, Lewis SC, Marra CM, Golden MR. A Cluster of Ocular Syphilis Cases – Seattle, Washington, and San Francisco, California, 2014–2015. MMWR Morb Mortal Wkly Rep . 2015;64(40):1150-1151. Available at: https://pubmed.ncbi.nlm.nih.gov/26469141 .
- Furtado JM, Simoes M, Vasconcelos-Santos D, et al. Ocular syphilis. Surv Ophthalmol . 2022;67(2):440-462. Available at: https://pubmed.ncbi.nlm.nih.gov/34147542 .
- Ramchandani MS, Litvack JR, Marra CM. Otosyphilis: a review of the literature. Sex Transm Dis . 2020;47(5):296-300. Available at: https://pubmed.ncbi.nlm.nih.gov/32149965 .
- Theel ES, Katz SS, Pillay A. Molecular and direct detection tests for treponema pallidum subspecies pallidum: a review of the literature, 1964–2017. Clin Infect Dis . 2020;71(Suppl 1):S4-S12. Available at: https://pubmed.ncbi.nlm.nih.gov/32578865 .
- Tuddenham S, Katz SS, Ghanem KG. Syphilis laboratory guidelines: performance characteristics of nontreponemal antibody tests. Clin Infect Dis . 2020;71(Suppl 1):S21-S42. Available at: https://pubmed.ncbi.nlm.nih.gov/32578862 .
- Park IU, Tran A, Pereira L, Fakile Y. Sensitivity and specificity of treponemal-specific tests for the diagnosis of syphilis. Clin Infect Dis . 2020;71(Suppl 1):S13-S20. Available at: https://pubmed.ncbi.nlm.nih.gov/32578866 .
- Bristow CC, Klausner JD, Tran A. Clinical test performance of a rapid point-of-care syphilis treponemal antibody test: a systematic review and meta-analysis. Clin Infect Dis . 2020;71(Suppl 1):S52-S57. Available at: https://pubmed.ncbi.nlm.nih.gov/32578863 .
- Ortiz DA, Shukla MR, Loeffelholz MJ. The traditional or reverse algorithm for diagnosis of syphilis: pros and cons. Clin Infect Dis . 2020;71(Suppl 1):S43-S51. Available at: https://pubmed.ncbi.nlm.nih.gov/32578864 .
- Centers for Disease Control and Prevention. Syphilis testing algorithms using treponemal tests for initial screening--four laboratories, New York City, 2005-2006. MMWR Morb Mortal Wkly Rep . 2008;57(32):872-875. Available at: https://pubmed.ncbi.nlm.nih.gov/18701877 .
- Park IU, Chow JM, Bolan G, Stanley M, Shieh J, Schapiro JM. Screening for syphilis with the treponemal immunoassay: analysis of discordant serology results and implications for clinical management. J Infect Dis . 2011;204(9):1297-1304. Available at: https://pubmed.ncbi.nlm.nih.gov/21930610 .
- Wong EH, Klausner JD, Caguin-Grygiel G, et al. Evaluation of an IgM/IgG sensitive enzyme immunoassay and the utility of index values for the screening of syphilis infection in a high-risk population. Sex Transm Dis . 2011;38(6):528-532. Available at: https://pubmed.ncbi.nlm.nih.gov/21233789 .
- Wohrl S, Geusau A. Neurosyphilis is unlikely in patients with late latent syphilis and a negative blood VDRL-test. Acta Derm Venereol . 2006;86(4):335-339. Available at: https://pubmed.ncbi.nlm.nih.gov/16874420 .
- Rompalo AM, Cannon RO, Quinn TC, Hook EW, 3rd. Association of biologic false-positive reactions for syphilis with human immunodeficiency virus infection. J Infect Dis . 1992;165(6):1124-1126. Available at: https://pubmed.ncbi.nlm.nih.gov/1583332 .
- Rolfs RT, Joesoef MR, Hendershot EF, et al. A randomized trial of enhanced therapy for early syphilis in patients with and without human immunodeficiency virus infection. The Syphilis and HIV Study Group. N Engl J Med . 1997;337(5):307-314. Available at: https://pubmed.ncbi.nlm.nih.gov/9235493 .
- Augenbraun MH, DeHovitz JA, Feldman J, Clarke L, Landesman S, Minkoff HM. Biological false-positive syphilis test results for women infected with human immunodeficiency virus. Clin Infect Dis . 1994;19(6):1040-1044. Available at: https://pubmed.ncbi.nlm.nih.gov/7888531 .
- Hicks CB, Benson PM, Lupton GP, Tramont EC. Seronegative secondary syphilis in a patient infected with the human immunodeficiency virus (HIV) with Kaposi sarcoma. A diagnostic dilemma. Ann Intern Med . 1987;107(4):492-495. Available at: https://pubmed.ncbi.nlm.nih.gov/3307583 .
- Kingston AA, Vujevich J, Shapiro M, et al. Seronegative secondary syphilis in 2 patients coinfected with human immunodeficiency virus. Arch Dermatol . 2005;141(4):431-433. Available at: https://pubmed.ncbi.nlm.nih.gov/15837859 .
- Libois A, De Wit S, Poll B, et al. HIV and syphilis: when to perform a lumbar puncture. Sex Transm Dis . 2007;34(3):141-144. Available at: https://pubmed.ncbi.nlm.nih.gov/16865051 .
- Ghanem KG. Sensitivity and specificity of lumbar puncture in HIV-infected patients with syphilis and no neurologic symptoms reply. Clin Infect Dis . 2009;49:162-163. Available at: https://pubmed.ncbi.nlm.nih.gov/19187028 .
- Jaffe HW, Larsen SA, Peters M, Jove DF, Lopez B, Schroeter AL. Tests for treponemal antibody in CSF. Arch Intern Med . 1978;138(2):252-255. Available at: https://pubmed.ncbi.nlm.nih.gov/343742 .
- Harding AS, Ghanem KG. The performance of cerebrospinal fluid treponemal-specific antibody tests in neurosyphilis: a systematic review. Sex Transm Dis . 2012;39(4):291-297. Available at: https://pubmed.ncbi.nlm.nih.gov/22421696 .
- Marra CM, Tantalo LC, Maxwell CL, Ho EL, Sahi SK, Jones T. The rapid plasma reagin test cannot replace the venereal disease research laboratory test for neurosyphilis diagnosis. Sex Transm Dis . 2012;39(6):453-457. Available at: https://pubmed.ncbi.nlm.nih.gov/22592831 .
- Kamb ML, Fishbein M, Douglas JM, Jr., et al. Efficacy of risk-reduction counseling to prevent human immunodeficiency virus and sexually transmitted diseases: a randomized controlled trial. Project RESPECT Study Group. JAMA . 1998;280(13):1161-1167. Available at: https://pubmed.ncbi.nlm.nih.gov/9777816 .
- U.S. Preventive Services Task Force, Krist AH, Davidson KW, et al. Behavioral counseling interventions to prevent sexually transmitted infections: U.S. Preventive Services Task Force recommendation statement. JAMA . 2020;324(7):674-681. Available at: https://pubmed.ncbi.nlm.nih.gov/32809008 .
- Metsch LR, Feaster DJ, Gooden L, et al. Effect of risk-reduction counseling with rapid HIV testing on risk of acquiring sexually transmitted infections: the AWARE randomized clinical trial. JAMA . 2013;310(16):1701-1710. Available at: https://pubmed.ncbi.nlm.nih.gov/24150466 .
- Brookmeyer KA, Hogben M, Kinsey J. The role of behavioral counseling in sexually transmitted disease prevention program settings. Sex Transm Dis . 2016;43(2 Suppl 1):S102-112. Available at: https://pubmed.ncbi.nlm.nih.gov/26779681 .
- Patel P, Bush T, Mayer K, et al. Routine brief risk-reduction counseling with biannual STD testing reduces STD incidence among HIV-infected men who have sex with men in care. Sex Transm Dis . 2012;39(6):470-474. Available at: https://pubmed.ncbi.nlm.nih.gov/22592834 .
- Tuite AR, Shaw S, Reimer JN, Ross CP, Fisman DN, Mishra S. Can enhanced screening of men with a history of prior syphilis infection stem the epidemic in men who have sex with men? A mathematical modelling study. Sex Transm Infect . 2018;94(2):105-110. Available at: https://pubmed.ncbi.nlm.nih.gov/28705938 .
- de Voux A, Bernstein KT, Bradley H, et al. Syphilis testing among sexually active men who have sex with men and who are receiving medical care for human immunodeficiency virus in the United States: Medical Monitoring Project, 2013–2014. Clin Infect Dis . 2019;68(6):934-939. Available at: https://pubmed.ncbi.nlm.nih.gov/29985985 .
- Thompson MA, Horberg MA, Agwu AL, et al. Primary care guidance for persons with human immunodeficiency virus: 2020 update by the HIV Medicine Association of the Infectious Diseases Society of America. Clin Infect Dis . 2021;73(11):e3572-e3605. Available at: https://pubmed.ncbi.nlm.nih.gov/33225349 .
- Kidd SE, Grey JA, Torrone EA, Weinstock HS. Increased methamphetamine, injection drug, and heroin use among women and heterosexual men with primary and secondary syphilis - United States, 2013–2017. MMWR Morb Mortal Wkly Rep . 2019;68(6):144-148. Available at: https://pubmed.ncbi.nlm.nih.gov/30763294 .
- Copen CE, Brookmeyer KA, Haderxhanaj LT, Hogben M, Torrone EA. Sexual risk behaviors among persons diagnosed with primary and secondary syphilis who reported high-risk substance use: data from the National Notifiable Diseases Surveillance System, 2018. Sex Transm Dis . 2022;49(2):99-104. Available at: https://pubmed.ncbi.nlm.nih.gov/34475356 .
- Centers for Disease Control and Prevention. Recommendations for partner services programs for HIV infection, syphilis, gonorrhea, and chlamydial infection. MMWR Recomm Rep . 2008;57(RR-9):1-83; quiz CE81-84. Available at: https://pubmed.ncbi.nlm.nih.gov/18987617 .
- Ghanem KG, Ram S, Rice PA. The modern epidemic of syphilis. N Engl J Med . 2020;382(9):845-854. Available at: https://pubmed.ncbi.nlm.nih.gov/32101666 .
- Moore MB, Jr., Price EV, Knox JM, Elgin LW. Epidemiologic treatment of contacts to infectious syphilis. Public Health Rep . 1963;78:966-970. Available at: https://pubmed.ncbi.nlm.nih.gov/14084872 .
- Schroeter AL, Turner RH, Lucas JB, Brown WJ. Therapy for incubating syphilis. Effectiveness of gonorrhea treatment. JAMA . 1971;218(5):711-713. Available at: https://pubmed.ncbi.nlm.nih.gov/5171497 .
- Schober PC, Gabriel G, White P, Felton WF, Thin RN. How infectious is syphilis? Br J Vener Dis . 1983;59(4):217-219. Available at: https://pubmed.ncbi.nlm.nih.gov/6871650 .
- Bolan RK, Beymer MR, Weiss RE, Flynn RP, Leibowitz AA, Klausner JD. Doxycycline prophylaxis to reduce incident syphilis among HIV-infected men who have sex with men who continue to engage in high-risk sex: a randomized, controlled pilot study. Sex Transm Dis . 2015;42(2):98-103. Available at: https://pubmed.ncbi.nlm.nih.gov/25585069 .
- Molina JM, Charreau I, Chidiac C, et al. Post-exposure prophylaxis with doxycycline to prevent sexually transmitted infections in men who have sex with men: an open-label randomised substudy of the ANRS IPERGAY trial. Lancet Infect Dis . 2018;18(3):308-317. Available at: https://pubmed.ncbi.nlm.nih.gov/29229440 .
- Stewart J, Oware K, Donnell D, et al. Doxycycline postexposure prophylaxis for prevention of STIs among cisgender women. Presented at: Conference on Retroviruses and Opportunistic Infections; 2023. Seattle, WA. Available at: https://www.natap.org/2023/CROI/croi_04.htm .
- Grant JS, Stafylis C, Celum C, et al. Doxycycline prophylaxis for bacterial sexually transmitted infections. Clin Infect Dis . 2020;70(6):1247-1253. Available at: https://pubmed.ncbi.nlm.nih.gov/31504345 .
- Luetkemeyer AF, Donnell D, Dombrowski J, et al. Doxy-PEP and antimicrobial resistance in S. aureus, N. gonorrhoeae, and commensal Neisseria. Presented at: Conference on Retroviruses and Opportunistic Infections; 2023. Seattle, WA. Available at: https://www.natap.org/2023/CROI/croi_11.htm .
- Rekart ML, Patrick DM, Chakraborty B, et al. Targeted mass treatment for syphilis with oral azithromycin. Lancet . 2003;361(9354):313-314. Available at: https://pubmed.ncbi.nlm.nih.gov/12559870 .
- Mitchell SJ, Engelman J, Kent CK, Lukehart SA, Godornes C, Klausner JD. Azithromycin-resistant syphilis infection: San Francisco, California, 2000–2004. Clin Infect Dis . 2006;42(3):337-345. Available at: https://pubmed.ncbi.nlm.nih.gov/16392078 .
- Wu H, Chang SY, Lee NY, et al. Evaluation of macrolide resistance and enhanced molecular typing of Treponema pallidum in patients with syphilis in Taiwan: a prospective multicenter study. J Clin Microbiol . 2012;50(7):2299-2304. Available at: https://pubmed.ncbi.nlm.nih.gov/22518868 .
- Chen CY, Chi KH, Pillay A, Nachamkin E, Su JR, Ballard RC. Detection of the A2058G and A2059G 23S rRNA gene point mutations associated with azithromycin resistance in treponema pallidum by use of a TaqMan real-time multiplex PCR assay. J Clin Microbiol . 2013;51(3):908-913. Available at: https://pubmed.ncbi.nlm.nih.gov/23284026 .
- Lukehart SA, Godornes C, Molini BJ, et al. Macrolide resistance in Treponema pallidum in the United States and Ireland. N Engl J Med . 2004;351(2):154-158. Available at: https://pubmed.ncbi.nlm.nih.gov/15247355 .
- Centers for Disease Control and Prevention. Azithromycin treatment failures in syphilis infections--San Francisco, California, 2002-2003. MMWR Morb Mortal Wkly Rep . 2004;53(9):197-198. Available at: https://pubmed.ncbi.nlm.nih.gov/15017376 .
- Ganesan A, Mesner O, Okulicz JF, et al. A single dose of benzathine penicillin G is as effective as multiple doses of benzathine penicillin G for the treatment of HIV-infected persons with early syphilis. Clin Infect Dis . 2015;60(4):653-660. Available at: https://pubmed.ncbi.nlm.nih.gov/25389249 .
- Yang CJ, Lee NY, Chen TC, et al. One dose versus three weekly doses of benzathine penicillin G for patients co-infected with HIV and early syphilis: a multicenter, prospective observational study. PLoS One . 2014;9(10):e109667. Available at: https://pubmed.ncbi.nlm.nih.gov/25286091 .
- Malone JL, Wallace MR, Hendrick BB, et al. Syphilis and neurosyphilis in a human immunodeficiency virus type-1 seropositive population: evidence for frequent serologic relapse after therapy. Am J Med . 1995;99(1):55-63. Available at: https://pubmed.ncbi.nlm.nih.gov/7598143 .
- Walter T, Lebouche B, Miailhes P, et al. Symptomatic relapse of neurologic syphilis after benzathine penicillin G therapy for primary or secondary syphilis in HIV-infected patients. Clin Infect Dis . 2006;43(6):787-790. Available at: https://pubmed.ncbi.nlm.nih.gov/16912958 .
- Ghanem KG, Erbelding EJ, Cheng WW, Rompalo AM. Doxycycline compared with benzathine penicillin for the treatment of early syphilis. Clin Infect Dis . 2006;42(6):e45-49. Available at: https://pubmed.ncbi.nlm.nih.gov/16477545 .
- Wong T, Singh AE, De P. Primary syphilis: serological treatment response to doxycycline/tetracycline versus benzathine penicillin. Am J Med . 2008;121(10):903-908. Available at: https://pubmed.ncbi.nlm.nih.gov/18823862 .
- Bettuzzi T, Jourdes A, Robineau O, et al. Ceftriaxone compared with benzylpenicillin in the treatment of neurosyphilis in France: a retrospective multicentre study. Lancet Infect Dis . 2021;21(10):1441-1447. Available at: https://pubmed.ncbi.nlm.nih.gov/34051142 .
- Cao Y, Su X, Wang Q, et al. A multicenter study evaluating ceftriaxone and benzathine penicillin G as treatment agents for early syphilis in Jiangsu, China. Clin Infect Dis . 2017;65(10):1683-1688. Available at: https://pubmed.ncbi.nlm.nih.gov/29020150 .
- Hook EW, 3rd, Roddy RE, Handsfield HH. Ceftriaxone therapy for incubating and early syphilis. J Infect Dis . 1988;158(4):881-884. Available at: https://pubmed.ncbi.nlm.nih.gov/3171231 .
- Kiddugavu MG, Kiwanuka N, Wawer MJ, et al. Effectiveness of syphilis treatment using azithromycin and/or benzathine penicillin in Rakai, Uganda. Sex Transm Dis . 2005;32(1):1-6. Available at: https://pubmed.ncbi.nlm.nih.gov/15614114 .
- Riedner G, Rusizoka M, Todd J, et al. Single-dose azithromycin versus penicillin G benzathine for the treatment of early syphilis. N Engl J Med . 2005;353(12):1236-1244. Available at: https://pubmed.ncbi.nlm.nih.gov/16177249 .
- Hook EW, 3rd, Behets F, Van Damme K, et al. A phase III equivalence trial of azithromycin versus benzathine penicillin for treatment of early syphilis. J Infect Dis . 2010;201(11):1729-1735. Available at: https://pubmed.ncbi.nlm.nih.gov/20402591 .
- Martin IE, Tsang RS, Sutherland K, et al. Molecular characterization of syphilis in patients in Canada: azithromycin resistance and detection of Treponema pallidum DNA in whole-blood samples versus ulcerative swabs. J Clin Microbiol . 2009;47(6):1668-1673. Available at: https://pubmed.ncbi.nlm.nih.gov/19339468 .
- Dowell ME, Ross PG, Musher DM, Cate TR, Baughn RE. Response of latent syphilis or neurosyphilis to ceftriaxone therapy in persons infected with human immunodeficiency virus. Am J Med . 1992;93(5):481-488. Available at: https://pubmed.ncbi.nlm.nih.gov/1442850 .
- Smith NH, Musher DM, Huang DB, et al. Response of HIV-infected patients with asymptomatic syphilis to intensive intramuscular therapy with ceftriaxone or procaine penicillin. Int J STD AIDS . 2004;15(5):328-332. Available at: https://pubmed.ncbi.nlm.nih.gov/15117503 .
- U. S. Food and Drug Administration. Current and resolved drug shortages and discontinuations reported to FDA. 2023. Available at: https://www.accessdata.fda.gov/scripts/drugshortages/dsp_ActiveIngredientDetails.cfm?AI=Penicillin%20G%20Procaine%20Injectable%20Suspension&st=d .
- Shenoy ES, Macy E, Rowe T, Blumenthal KG. Evaluation and management of penicillin allergy: a review. JAMA . 2019;321(2):188-199. Available at: https://pubmed.ncbi.nlm.nih.gov/30644987 .
- Pham MN, Ho HE, Desai M. Penicillin desensitization: treatment of syphilis in pregnancy in penicillin-allergic patients. Ann Allergy Asthma Immunol . 2017;118(5):537-541. Available at: https://pubmed.ncbi.nlm.nih.gov/28477786 .
- Frunza-Stefan S, Acharya G, Kazlouskaya V, Vukasinov P, Chiou Y, Thet Z. Immune reconstitution inflammatory syndrome associated with secondary syphilis. Int J STD AIDS . 2017;28(3):302-305. Available at: https://pubmed.ncbi.nlm.nih.gov/27566775 .
- Bernal E, Munoz A, Ortiz Mdel M, Cano A. [Syphilitic panuveitis in an HIV-infected patient after immune restoration]. Enferm Infecc Microbiol Clin . 2009;27(8):487-489. Available at: https://pubmed.ncbi.nlm.nih.gov/19406524 .
- Sena AC, Wolff M, Behets F, et al. Response to therapy following retreatment of serofast early syphilis patients with benzathine penicillin. Clin Infect Dis . 2013;56(3):420-422. Available at: https://pubmed.ncbi.nlm.nih.gov/23118269 .
- Sena AC, Wolff M, Martin DH, et al. Predictors of serological cure and Serofast State after treatment in HIV-negative persons with early syphilis. Clin Infect Dis . 2011;53(11):1092-1099. Available at: https://pubmed.ncbi.nlm.nih.gov/21998287 .
- Jinno S, Anker B, Kaur P, Bristow CC, Klausner JD. Predictors of serological failure after treatment in HIV-infected patients with early syphilis in the emerging era of universal antiretroviral therapy use. BMC Infect Dis . 2013;13:605. Available at: https://pubmed.ncbi.nlm.nih.gov/24369955 .
- Ghanem KG, Hook EW, 3rd. The terms “serofast” and “serological nonresponse” in the modern syphilis era. Sex Transm Dis . 2021;48(6):451-452. Available at: https://pubmed.ncbi.nlm.nih.gov/33534408 .
- Marra CM, Maxwell CL, Tantalo LC, Sahi SK, Lukehart SA. Normalization of serum rapid plasma reagin titer predicts normalization of cerebrospinal fluid and clinical abnormalities after treatment of neurosyphilis. Clin Infect Dis . 2008;47(7):893-899. Available at: https://pubmed.ncbi.nlm.nih.gov/18715154 .
- Xiao Y, Tong ML, Lin LR, et al. Serological response predicts normalization of cerebrospinal fluid abnormalities at six months after treatment in HIV-negative neurosyphilis patients. Sci Rep . 2017;7(1):9911. Available at: https://pubmed.ncbi.nlm.nih.gov/28855625 .
- Yang CJ, Lee NY, Lin YH, et al. Jarisch-Herxheimer reaction after penicillin therapy among patients with syphilis in the era of the hiv infection epidemic: incidence and risk factors. Clin Infect Dis . 2010;51(8):976-979. Available at: https://pubmed.ncbi.nlm.nih.gov/20825309 .
- Aaron KJ, Brill I, Causey-Pruitt Z, et al. Factors associated with syphilis seroprevalence in women with and at-risk for HIV infection in the Women’s Interagency HIV Study (1994–2015). Sex Transm Infect . 2022;98(1):4-10. Available at: https://pubmed.ncbi.nlm.nih.gov/33408096 .
- Trivedi S, Williams C, Torrone E, Kidd S. National trends and reported risk factors among pregnant women with syphilis in the United States, 2012–2016. Obstet Gynecol . 2019;133(1):27-32. Available at: https://pubmed.ncbi.nlm.nih.gov/30531570 .
- U.S. Preventive Services Task Force, Curry SJ, Krist AH, et al. Screening for syphilis infection in pregnant women: U.S. Preventive Services Task Force reaffirmation recommendation statement. JAMA . 2018;320(9):911-917. Available at: https://pubmed.ncbi.nlm.nih.gov/30193283 .
- Mmeje O, Chow JM, Davidson L, Shieh J, Schapiro JM, Park IU. Discordant syphilis immunoassays in pregnancy: perinatal outcomes and implications for clinical management. Clin Infect Dis . 2015;61(7):1049-1053. Available at: https://pubmed.ncbi.nlm.nih.gov/26063719 .
- Adachi K, Xu J, Yeganeh N, et al. Combined evaluation of sexually transmitted infections in HIV-infected pregnant women and infant HIV transmission. PLoS One . 2018;13(1):e0189851. Available at: https://pubmed.ncbi.nlm.nih.gov/29304083 .
- Berman SM. Maternal syphilis: pathophysiology and treatment. Bull World Health Organ . 2004;82(6):433-438. Available at: https://pubmed.ncbi.nlm.nih.gov/15356936 .
- Tess BH, Rodrigues LC, Newell ML, Dunn DT, Lago TD. Breastfeeding, genetic, obstetric and other risk factors associated with mother-to-child transmission of HIV-1 in Sao Paulo State, Brazil. Sao Paulo Collaborative Study for Vertical Transmission of HIV-1. AIDS . 1998;12(5):513-520. Available at: https://pubmed.ncbi.nlm.nih.gov/9543450 .
- Lee MJ, Hallmark RJ, Frenkel LM, Del Priore G. Maternal syphilis and vertical perinatal transmission of human immunodeficiency virus type-1 infection. Int J Gynaecol Obstet . 1998;63(3):247-252. Available at: https://pubmed.ncbi.nlm.nih.gov/9989893 .
- Wendel GD, Jr., Sheffield JS, Hollier LM, Hill JB, Ramsey PS, Sanchez PJ. Treatment of syphilis in pregnancy and prevention of congenital syphilis. Clin Infect Dis . 2002;35(Suppl 2):S200-209. Available at: https://pubmed.ncbi.nlm.nih.gov/12353207 .
- Kreitchmann R, Fuchs SC, Suffert T, Preussler G. Perinatal HIV-1 transmission among low income women participants in the HIV/AIDS Control Program in Southern Brazil: a cohort study. BJOG . 2004;111(6):579-584. Available at: https://pubmed.ncbi.nlm.nih.gov/15198786 .
- Mwapasa V, Rogerson SJ, Kwiek JJ, et al. Maternal syphilis infection is associated with increased risk of mother-to-child transmission of HIV in Malawi. AIDS . 2006;20(14):1869-1877. Available at: https://pubmed.ncbi.nlm.nih.gov/16954728 .
- Walker GJ. Antibiotics for syphilis diagnosed during pregnancy. Cochrane Database Syst Rev . 2001(3):CD001143. Available at: https://pubmed.ncbi.nlm.nih.gov/11686978 .
- Donders GG, Desmyter J, Hooft P, Dewet GH. Apparent failure of one injection of benzathine penicillin G for syphilis during pregnancy in human immunodeficiency virus-seronegative African women. Sex Transm Dis . 1997;24(2):94-101. Available at: https://pubmed.ncbi.nlm.nih.gov/9111755 .
- Sheffield JS, Sanchez PJ, Morris G, et al. Congenital syphilis after maternal treatment for syphilis during pregnancy. Am J Obstet Gynecol . 2002;186(3):569-573. Available at: https://pubmed.ncbi.nlm.nih.gov/11904625 .
- Zhu L, Qin M, Du L, Xie RH, Wong T, Wen SW. Maternal and congenital syphilis in Shanghai, China, 2002 to 2006. Int J Infect Dis . 2010;14 Suppl 3:e45-48. Available at: https://pubmed.ncbi.nlm.nih.gov/20137991 .
- Ramsey PS, Vaules MB, Vasdev GM, Andrews WW, Ramin KD. Maternal and transplacental pharmacokinetics of azithromycin. Am J Obstet Gynecol . 2003;188(3):714-718. Available at: https://pubmed.ncbi.nlm.nih.gov/12634646 .
- Zhou P, Gu Z, Xu J, Wang X, Liao K. A study evaluating ceftriaxone as a treatment agent for primary and secondary syphilis in pregnancy. Sex Transm Dis . 2005;32(8):495-498. Available at: https://pubmed.ncbi.nlm.nih.gov/16041252 .
- Katanami Y, Hashimoto T, Takaya S, et al. Amoxicillin and ceftriaxone as treatment alternatives to penicillin for maternal syphilis. Emerg Infect Dis . 2017;23(5):827-829. Available at: https://pubmed.ncbi.nlm.nih.gov/28418316 .
- Klein VR, Cox SM, Mitchell MD, Wendel GD, Jr. The Jarisch-Herxheimer reaction complicating syphilotherapy in pregnancy. Obstet Gynecol . 1990;75(3 Pt 1):375-380. Available at: https://pubmed.ncbi.nlm.nih.gov/2304710 .
- Butler T. The Jarisch-Herxheimer reaction after antibiotic treatment of spirochetal infections: a review of recent cases and our understanding of pathogenesis. Am J Trop Med Hyg . 2017;96(1):46-52. Available at: https://pubmed.ncbi.nlm.nih.gov/28077740 .
- Hollier LM, Harstad TW, Sanchez PJ, Twickler DM, Wendel GD, Jr. Fetal syphilis: clinical and laboratory characteristics. Obstet Gynecol . 2001;97(6):947-953. Available at: https://pubmed.ncbi.nlm.nih.gov/11384701 .
- Rac MW, Bryant SN, Cantey JB, McIntire DD, Wendel GD, Jr., Sheffield JS. Maternal titers after adequate syphilotherapy during pregnancy. Clin Infect Dis . 2015;60(5):686-690. Available at: https://pubmed.ncbi.nlm.nih.gov/25414264 .
- Webster CM, Kasaro MP, Price JT, et al. Seroreduction of syphilis non-treponemal titers during pregnancy for women with and without HIV co-infection. Int J Gynaecol Obstet . 2022. Available at: https://pubmed.ncbi.nlm.nih.gov/35122676 .
Download Guidelines
- Section Only PDF (309.18 KB)
- Full Guideline PDF (5.39 MB)
- Tables Only PDF (869.15 KB)
Related Content
- CDC | 2021 STI Treatment Guidelines
- HCV Guidance: Recommendations for Testing, Managing, and Treating Hepatitis C
- HIVinfo Fact Sheets: What is an Opportunistic Infection?
- HIV Source | HIV-Related Conditions
- AETC National HIV Curriculum
- How to Cite These Guidelines
- Adult and Adolescent Opportunistic Infection Archived Guidelines
Syphilis – CDC Basic Fact Sheet
Retrospective detection of asymptomatic monkeypox virus infections among male sexual health clinic attendees in Belgium
Irith De Baetselier, Christophe Van Dijck, … for the ITM Monkeypox study group

A large screen identifies beta-lactam antibiotics which can be repurposed to target the syphilis agent
Kathryn A. Hayes, Jules M. Dressler, … Brandon L. Jutras

Evaluating congenital syphilis in a reverse sequence testing environment
May W. Chen, Ibukunoluwa C. Akinboyo, … W. Christopher Golden
Introduction
Syphilis is a sexually transmitted infection (STI) that can also be transmitted vertically. It is caused by the spirochaete Treponema pallidum subspecies pallidum (order Spirochaetales) ( Fig. 1 ). Three other organisms within this genus are causes of nonvenereal or endemic treponematoses. T. pallidum subspecies pertenue is the causative agent of yaws, T. pallidum subspecies endemicum causes endemic (nonvenereal) syphilis and T. carateum causes pinta. These pathogens are morphologically and antigenically indistinguishable. However, they can be differentiated by their age at acquisition, principal mode of transmission, clinical manifestations, capacity for invasion of the central nervous system (CNS) and placenta, and genomic sequences, although the accuracy of these differences remains a subject of debate 1 . Analyses based on the mutation rates of genomic sequences suggest that the causative agents of yaws and venereal syphilis diverged several thousand years ago from a common progenitor originating in Africa 2 . These estimates argue against the so-called Columbian hypothesis — the notion that shipmates of Christopher Columbus imported a newly evolved spirochaete causing venereal syphilis from the New World into western Europe in the late 15th century 3 .
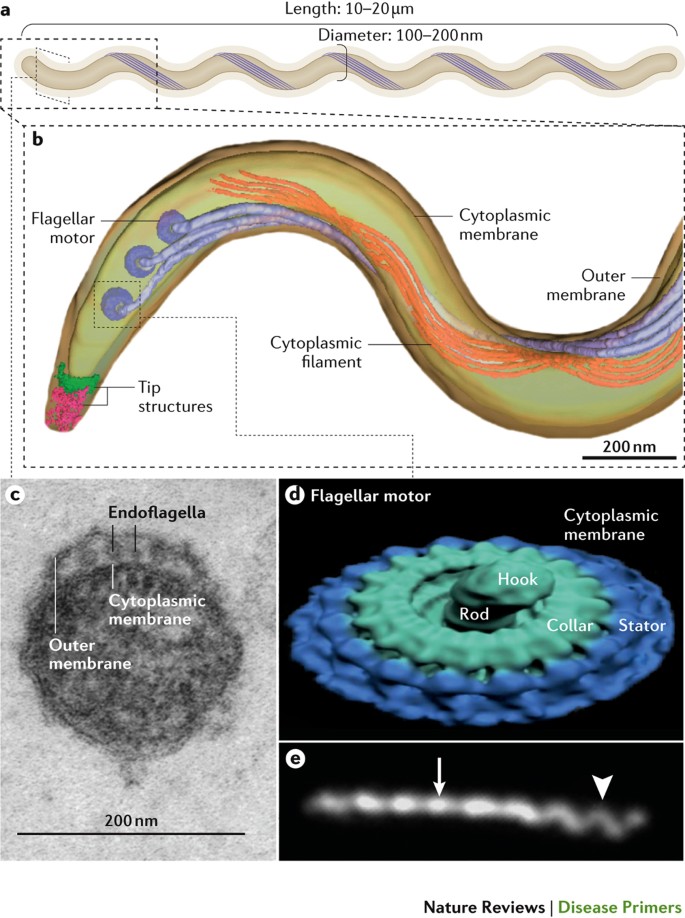
a | Like all spirochaetes, Treponema pallidum consists of a protoplasmic cylinder and cytoplasmic membrane bounded by a thin peptidoglycan sacculus and outer membrane 239 , 240 . Usually described as spiral-shaped, T. pallidum is actually a thin planar wave similar to Borrelia burgdorferi , the agent that causes Lyme borreliosis 239 . The bacterium replicates slowly and poorly tolerates desiccation, elevated temperatures and high oxygen tensions 55 . b | Periplasmic flagellar filaments, a defining morphological feature of spirochaetes, originate from nanomotors situated at each pole and wind around the cylinder atop the peptidoglycan, overlapping at the middle of the cell. Force exerted by the rigid filaments against the elastic peptidoglycans deforms the sacculus to create the flat-wave morphology of the spirochaete 100 . Panel b is reproduced with permission from American Society for Microbiology (Ref. 239 ): Journal of Bacteriology, volume 191, 7566–7580, doi: 10.1128/JB.01031-09. c | Ultrathin section of T. pallidum showing the outer and cytoplasmic membranes and flagellar filaments (endoflagella) within the periplasmic space 9 . d | Surface rendering of a flagellar motor based on cryo-electron tomograms. Panel d is reproduced with permission from Ref. 240 , Elsevier. e | Darkfield micrograph showing the flat-wave morphology of T. pallidum . The arrow and arrowhead indicate segments that are oriented 90° from each other. The different appearances of the helical wave at 90° to the viewer can be explained only by a flat-wave morphology; a corkscrew shape would appear the same from any angle. Panel e is reproduced with permission from American Society for Microbiology (Ref. 239 ): Journal of Bacteriology, volume 191, 7566–7580, doi: 10.1128/JB.01031-09.
PowerPoint slide
T. pallidum is an obligate human pathogen renowned for its invasiveness and immune-evasiveness 4 – 7 ; clinical manifestations result from the local inflammatory response elicited by spirochaetes replicating within tissues 8 – 10 . Infected individuals typically follow a disease course divided into primary, secondary, latent and tertiary stages over a period of ≥10 years. Different guidelines define early latency as starting 1–2 years after exposure. Typically, ‘early syphilis’ refers to infections that can be transmitted sexually (including primary, secondary and early latent infections) and is synonymous with active (infectious) syphilis; the WHO defines ‘early syphilis’ as an infection of <2 years duration 11 , whereas the guidelines from the United States 12 and Europe 13 define it as an infection <1 year in duration. These differences in definition can affect the interpretation of results and the prescription of therapeutic regimens used in some circumstances.
Owing to its varied and often subtle manifestations, which can mimic other infections, syphilis has earned the names the Great Imitator and Great Mimicker 14 . Patients with primary syphilis present with a single ulcer (chancre) or multiple lesions on the genitals or other body sites involved in sexual contact and present regional lymphadenopathy ∼ 3 weeks after infection; these are typically painless and resolve spontaneously. Resolution of primary lesions is followed 6–8 weeks later by secondary manifestations, which can include fever, headache and a maculopapular rash on the flank, shoulders, arm, chest or back and that often involves the palms of the hands and soles of the feet. As signs and symptoms subside, patients enter a latent phase, which can last many years. A patient in the first 1–2 years of latency is still considered infectious owing to a 25% risk of secondary syphilis-like relapses 15 . Historical literature suggests that 15–40% of untreated individuals will develop tertiary syphilis, which can manifest as destructive cardiac or neurological conditions, severe skin or visceral lesions (gummas) or bony involvement 9 . Recent data suggest that tertiary syphilis is less common today, perhaps owing to the wide use of antibiotics. Numerous case reports and small series suggest that HIV infection increases the risk of neuro-ophthalmological complications in those with syphilis 16 . Importantly, neurosyphilis is typically described as a late manifestation but can occur in early syphilis. Indeed, T. pallidum can be frequently identified in the cerebral spinal fluid (CSF) of patients with early disease 9 , 15 , 17 . However, the majority of patients with early syphilis who have CSF abnormalities do not demonstrate CNS symptoms and do not require therapy for neurosyphilis 12 . Symptomatic manifestations of neurosyphilis include chronic meningitis, meningovascular stroke-like syndromes and manifestations common in the neurological forms of tertiary syphilis (namely, tabes dorsalis and general paresis, a progressive dementia mimicking a variety of psychotic syndromes) 9 . Numerous case reports and small series suggest that HIV infection predisposes individuals with syphilis to neuro-ophthalmological complications 16 . Cardiovascular syphilis, typically involving the aortic arch and leading to aneurysmal dilatation, usually occurs 10–30 years after the initial infection 9 .
Sexual transmission of syphilis occurs during the first 1–2 years after infection (that is, during primary, secondary and early latent stages of infection) 9 . The risk of mother-to-child transmission (MTCT) is highest in primary and secondary stages, followed by the early latent stage. However, transmission risk continues during the first 4 years after exposure, after which the risk of vertical transmission declines over time 18 . The rate of fetal infection depends on the stage of maternal infection, with ∼ 30% of pregnancies resulting in fetal death in utero , stillbirth (late second and third trimester fetal death) or death shortly after delivery 19 – 21 . Infants born to infected mothers are often preterm, of low birthweight or have clinical signs that mimic neonatal sepsis (that is, poor feeding, lethargy, rash, jaundice, hepatosplenomegaly and anaemia).
Given that T. pallidum has a long generation time of 30–33 hours 22 , long-acting penicillin preparations (such as benzathine penicillin G) are the preferred therapies for most patients with syphilis. Since the 1940s (when penicillin became widely available), syphilis prevalence has continued to decline in regions able to appropriately test for and treat the infection. However, syphilis outbreaks continue to occur throughout the world. In particular, with declining AIDS-related mortality related to effective HIV treatment over the past two decades, syphilis has re-emerged in urban settings among men who have sex with men (MSM). High-income and middle-income countries have observed rises in syphilis case rates as well as increased neurosyphilis case rates (such as ocular syphilis) and, in some countries, congenital syphilis. In low-income countries where syphilis prevalence has remained high, MTCT of syphilis continues to be the most common cause of STI-related mortality outside HIV 23 , 24 , with perinatal deaths owing to untreated syphilis exceeding those due to HIV or malaria 25 . Following malaria, syphilis is now the second-leading cause of preventable stillbirths worldwide 25 .
Syphilis should be an ideal disease for elimination as it has no known animal reservoir, can usually be diagnosed with simple and inexpensive tests and can be cured 9 , 16 . Nevertheless, syphilis remains a continuing public health challenge globally 26 . In this Primer, we describe recent discoveries that have improved our understanding of the biological and genetic structure of the pathogen, novel diagnostic tests and testing approaches that can improve disease detection and current, evidence-based management recommendations. We also draw attention to the call for the global elimination of MTCT of syphilis and HIV, as well as recent successes in eliminating syphilis in low-income and middle-income countries (LMICs), particularly through fundamental public health strategies such as ensuring quality antenatal care that includes testing for syphilis early in pregnancy and providing prompt treatment of women and their partners. We also report on the rising numbers of syphilis cases in MSM and ongoing work supporting improved interventions against syphilis in marginalized populations and, ultimately, the development of an effective vaccine.
Epidemiology
According to the most recent estimation of the WHO, ∼ 17.7 million individuals globally 15–49 years of age had syphilis in 2012, with an estimated 5.6 million new cases every year 27 ( Fig. 2 ). The estimated prevalence and incidence of syphilis varies substantially by region or country, with the highest prevalence in Africa and >60% of new cases occurring in LMICs 27 . The greatest burden of maternal syphilis occurs in Africa, representing >60% of the global estimate 23 , 24 .
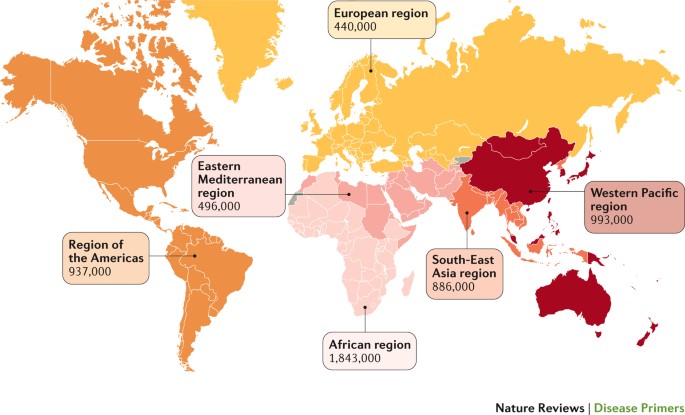
The WHO estimates of incident cases of syphilis by region in 2012 are shown for the different geographical regions. Data from Ref. 27 .
Prevalence and incidence
In LMICs, the heterosexual spread of syphilis has declined in the general population but remains problematic in some high-risk subpopulations, such as female sex workers (FSWs) and their male clients. A recent study of FSWs in Johannesburg, South Africa, showed that 21% of participating women had antibodies suggestive of past or current infection, and 3% had an active (infectious) infection 28 . Another study of FSWs in 14 zones in Sudan showed a high seroprevalence (median 4.1%), with the highest value (8.9%) in the eastern zone of the country 29 . A large study of >1,000 FSWs in Kampala, Uganda, showed that 21% were seropositive for syphilis and 10% had an active infection 30 . Studies in emerging economies, such as China, indicate that syphilis is increasing among ‘mobile men with money’ (Ref. 31 ). Although syphilis case rates are low in the general population in China, syphilis prevalence is ∼ 5% among FSWs and ∼ 3% among their male clients 31 , 32 . The risk of infection varies among FSWs working in different venues, with the highest prevalence ( ∼ 10%) among street-based FSWs and the lowest prevalence ( ∼ 2%) among venue-based FSWs 33 .
By contrast, higher-income countries have had declining syphilis prevalence among heterosexual men and women. However, a resurgence of syphilis that disproportionately affects MSM has been noted. Syphilis is associated with high-risk sexual behaviours and infection substantially increases in association with HIV transmission and acquisition. Indeed, the numbers and rates of reported cases of syphilis among MSM in the United States and western Europe have been increasing since 1998 (Ref. 34 ). In 2015, the case rate for primary and secondary syphilis among MSM (309 per 100,000) in the United States was 221-fold the rate for women (1.4 per 100,000) and 106-fold the rate for heterosexual men (2.9 per 100,000) 35 . In Canada, the incidence of syphilis was 300-fold greater among MSM positive for HIV than the reported case rate in the general male population 36 . Syphilis infection has been associated with certain behavioural and other factors, including incarceration, multiple or anonymous sex partners, sexual activity connected with illicit drug use, seeking sex partners on the Internet and other high-risk sexual network dynamics 37 – 41 . Risk factors for syphilis are frequently overlapping 40 . Reports of unusual presentations and rapid progression of syphilis in patients with concurrent HIV infection have led to the hypothesis that infection with or treatment for HIV alters the natural history of syphilis 42 .
Adverse birth outcomes caused by fetal exposure to syphilis are preventable if women are screened for syphilis and treated before the end of the second trimester of pregnancy 21 . However, MTCT of syphilis caused such a high rate of perinatal and infant mortality that, in 2007, the WHO and partners launched a global initiative to eliminate it as a public health problem 43 – 45 . At the time of the campaign launch, ∼ 1.4 million pregnant women had active syphilis infections, of whom 80% had attended at least one antenatal visit, suggesting missed opportunities for testing and treatment 23 . At that time, untreated maternal syphilis infections were estimated to have resulted in >500,000 adverse pregnancy outcomes, including >300,000 perinatal deaths (stillbirths and early neonatal deaths).
Syphilis testing and treatment during pregnancy are highly effective and were included in the Lives Saved Tool for effective maternal–child health interventions 46 . Furthermore, studies have shown that prenatal syphilis screening, testing to support treatment and treatment during pregnancy are highly cost-effective in most countries regardless of disease prevalence or the availability of resources and can even be cost-saving in LMICs with a syphilis prevalence ≥3% in pregnant women 47 – 50 . In China, where syphilis and HIV prevalence in pregnant women are low but increasing, the integration of prenatal syphilis and HIV screening was shown to be highly cost-effective 51 .
Since 2007, an increasing number of countries have implemented regional and national initiatives to prevent MTCT of syphilis 52 , improving guidance documents, using point-of-care (POC) tests as a means of improving access to testing and treatment and integrating behavioural and medical interventions into HIV prevention and control programmes 53 . By 2012, these efforts had contributed to a reduction in the global number of adverse pregnancy outcomes due to MTCT of syphilis to 350,000, including 210,000 perinatal deaths, and had decreased the rates of maternal and congenital syphilis by 38% and 39%, respectively 23 , 24 . In 2015, Cuba became the first country to be validated for having achieved the elimination of MTCT of HIV and syphilis 54 . Subsequently, Thailand, Belarus and four United Kingdom Overseas Territories (Bermuda, the Cayman Islands, Montserrat and Antigua) were validated for the elimination of MTCT of HIV and syphilis, Moldova was validated for the elimination of MTCT of syphilis and Armenia was validated for the elimination of MTCT of HIV. However, these gains were mostly in Asia and the Americas — the maternal prevalence in Africa has remained largely unchanged 23 , 24 .
Mechanisms/pathophysiology
Although a local inflammatory response elicited by spirochaetes is thought to be the root cause of all clinical manifestations of syphilis 9 , the mechanisms that cause tissue damage, as well as the host defences that eventually gain a measure of control over the bacterium, are ill-defined. The recalcitrance of T. pallidum to in vitro culture and the consequent inability to harness genetic techniques to delineate its virulence determinants remain the primary obstacles to progress 55 . Additionally, the fragility and low protein content of its outer membrane have confounded efforts to characterize surface-exposed molecules 56 , 57 . Finally, facile murine models to dissect the host response and the components of protective immunity are also lacking 58 . Outbred rabbits are essential for isolating T. pallidum strains from clinical specimens 59 and for routine propagation in the laboratory 60 . Because rabbits are highly susceptible to T. pallidum infection, develop lesions grossly and histopathologically resembling chancres following intradermal inoculation and generate antibody responses similar to those in humans, the rabbit is the model organism of choice for studying endogenous and exogenous protective immunity 61 , 62 . However, the rabbit model poorly recapitulates some clinical and immunological facets of the human disease 63 . Not surprisingly, even in the post-genomics era, our understanding of the pathogenic mechanisms in syphilis lags well behind that of other common bacterial diseases 63 .
Molecular features
The morphological features of T. pallidum are described in Fig. 1 . Because of its double-membrane structure, the spirochaete is often described as a Gram-negative bacterium. However, this analogy is phylogenetically, biochemically and ultrastructurally inaccurate 63 , 64 . The T. pallidum outer membrane lacks lipopolysaccharides 65 and has a markedly different phospholipid composition than the outer membranes of typical Gram-negative bacteria 66 . Although T. pallidum expresses abundant lipoproteins, these molecules reside predominantly below the surface 5 , 63 , 67 . Accordingly, this paucity of surface-exposed pathogen-associated molecular patterns (PAMPs) enables the spirochaete to avoid triggering host innate surveillance mechanisms, facilitating local replication and early dissemination. Its limited surface antigenicity promotes the evasion of adaptive immune responses (that is, antibody recognition), facilitating persistence 5 , 56 , 68 , 69 . Collectively, these attributes have earned T. pallidum its designation as ‘the stealth pathogen’ (Refs 63 , 69 ). Understanding events unfolding at the host–pathogen interface requires a detailed knowledge of the T. pallidum repertoire of surface-exposed proteins. However, characterization of the protein constituents of the outer membrane has been, and continues to be, daunting 8 , 55 , 57 , 63 .
Lipoproteins . In the 1980s, investigators screened E. coli recombinant libraries with syphilitic sera and murine monoclonal antibodies based upon the unproven (and, as it turned out, immunologically incorrect) assumption that immunoreactive proteins ought to be surface-exposed in T. pallidum 57 . Biochemical and genetic analyses subsequently revealed that most of the antigens identified by these screens are lipoproteins 70 – 72 tethered by their N-terminal lipids to the cytoplasmic membrane (hence, the protein moieties are in the periplasmic space) 67 , 73 – 75 . However, convincing evidence now shows that the spirochaete displays small amounts of lipoproteins on its surface that have the potential to enhance infectivity ( Fig. 3 ). For example, TP0751 (also known as pallilysin) is a laminin-binding lipoprotein and zinc-dependent metalloproteinase capable of degrading clots and the extracellular matrix 76 – 78 . Although expressed by T. pallidum in minute quantities, surface exposure of TP0751 has been demonstrated by knock-in experiments in Borrelia burgdorferi (the spirochaete that causes Lyme borreliosis 79 ) and the cultivatable commensal treponeme Treponema phagedenis 80 , in opsonophagocytosis assays in T. pallidum 77 and, most recently, in the protection of immunized rabbits against the dissemination of spirochaetes following intradermal challenge 81 . The X-ray structure of TP0751, which demonstrates an unusual lipocalin fold, should inform efforts to clarify its multifunctionality 79 . Additionally, the lipoprotein Tpp17 (also known as TP0435) has been shown to be at least partially surface-exposed and can function as a cytadhesin 82 . The structurally characterized lipoprotein TP0453 attaches to the inner leaflet of the outer membrane via its N-terminal lipids and two amphipathic helices within its protein moiety 83 .
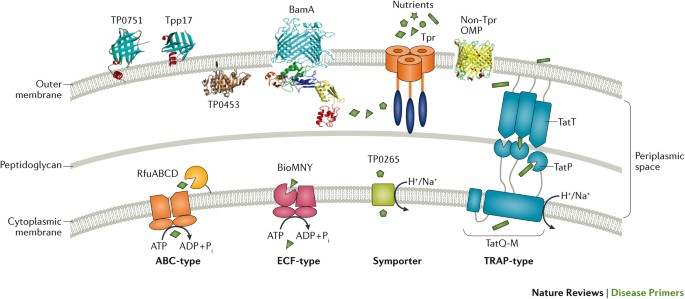
Shown in the outer membrane are TP0751 (as known as pallilysin) 79 , 81 and Tpp17 (also known as TP0435) 82 , 241 , two surface-exposed lipoproteins; TP0453, a lipoprotein attached to the inner leaflet of the outer membrane 83 ; β-barrel assembly machinery A (BamA, also known as TP0326) 84 , 94 ; a full-length T. pallidum repeat (Tpr) attached by its N-terminal portion to the peptidoglycan 93 , 94 ; and a generic β-barrel that represents other non-Tpr outer membrane proteins (OMPs) identified by computational mining of the T. pallidum genome 112 . Substrates and nutrients present in high concentration in the extracellular milieu (such as glucose) traverse the outer membrane through porins, such as TprC. At the cytoplasmic membrane, prototypic ABC-like transporters (such as RfuABCD, a riboflavin transporter) use a periplasmic substrate-binding protein (SBP), usually lipoproteins, and components with transmembrane and ATP-binding domains to bind nutrients that have traversed the outer membrane for transport across the cytoplasmic membrane. The energy coupling factor (ECF)-type ABC transporters use a transmembrane ligand-binding protein in place of a separate periplasmic SBP for binding of ligands (BioMNY is thought to transport biotin) 242 . Symporter permeases (for example, TP0265) use the chemiosmotic or electrochemical gradient across the cytoplasmic membrane to drive substrate transport 243 . The tripartite ATP-independent periplasmic (TRAP)-type transporters also use transmembrane electrochemical gradients to drive substrate transport; the periplasmic component protein TatT (also known as TP0956) likely associates with the SBP TatP (also known as TP0957), which binds ligands (perhaps hydrophobic molecules, such as long chain fatty acids), the uptake of which is probably facilitated by the permease TatQ-M (also known as TP0958) 244 , 245 . Figure adapted from Ref. 63 , Macmillan Publishers Limited.
BamA . With the publication of the T. pallidum genome in 1998 (Ref. 65 ), only one protein with sequence relatedness to an outer membrane protein of Gram-negative bacteria was identified: β-barrel assembly machinery A (BamA, also known as TP0326) 84 , 85 . BamA has a dual domain architecture consisting of a 16-stranded, outer membrane-inserted, C-terminal β-barrel and five tandem polypeptide transport-associated repeats within the periplasm 84 , 85 . The opening of the channel is covered by a ‘dome’ comprising three extracellular loops, one of which contains an opsonic target that is sequence-variable among T. pallidum strains 85 . BamA is the essential central component of the molecular machine that catalyses the insertion of newly exported outer membrane proteins to the outer membrane 86 .
Tpr proteins . The T. pallidum repeat (Tpr) proteins, a 12-member paralogous family with sequence homology to the major outer sheath protein of the oral commensal Treponema denticola , were also identified in the T. pallidum genomic sequence 65 . Of these, TprK (TP0897) has received the most attention because of its presumed role in immune evasion by the spirochaete 87 , 88 ; it has been shown to undergo antigenic variation in seven regions believed to be extracellular loops harbouring B cell epitopes 89 – 92 . DNA sequence cassettes that correspond to V-region sequences in an area of the T. pallidum chromosome located away from the tprK gene have been proposed to serve as unidirectional donor sites for the generation of variable regions by nonreciprocal gene conversion 89 . Two other Tpr proteins, TprC and TprI, have met stringent experimental criteria for being classified as rare outer membrane proteins. They form trimeric β-barrels when refolded in vitro , cause large increases in permeability upon insertion into liposomes and are surface-exposed opsonic targets in T. pallidum 93 , 94 . Unlike classic porins, for which the entire polypeptide forms a β-barrel, TprC and TprI are bipartite. As with BamA, the C-terminal domain forms the surface-exposed β-barrel, whereas the N-terminal half anchors the barrel to the peptidoglycan sacculus. These results collectively imply that Tprs serve as functional orthologues of Gram-negative porins, using variations in the substrate specificities of their channel-forming β-barrels, probably along with differential expression, to import the nutritional requirements of the spirochaete into the periplasmic space from blood and body fluids 95 , 96 . These proteins also furnish a topological template for efforts to understand how antibody responses to Tprs promote bacterial clearance.
Biosynthetic machinery . T. pallidum has evolved to dispense with a vast amount of the biosynthetic machinery found in other bacterial pathogens 55 , 63 – 65 . T. pallidum relies on an optimized conventional glycolytic pathway as its primary means for generating ATP. By dispensing with oxidative phosphorylation, the spirochaete has no need for cytochromes and the iron required to synthesize them. Accordingly, the spirochaete maintains a complex, yet parsimonious, assortment of ABC transporters and symporters (totalling ∼ 5% of its 1.14 Mb circular genome) to transfer essential molecules from the periplasmic space to the cytosol ( Fig. 3 ). Whereas many pathogens have highly redundant systems for the uptake of transition metals across the cytoplasmic membrane, T. pallidum accomplishes this task with just two ABC transporters (Tro, which imports zinc, manganese and iron, and Znu, which is zinc-specific). A small but powerful arsenal of enzymes neutralizes superoxides and peroxides to fend off host responses to infection. Lastly, the spirochaete possesses novel and surprisingly intricate mechanisms ostensibly to redirect transcription and fine-tune metabolism in response to environmental cues and nutrient flux 63 .
Transmission and dissemination
Transmission of venereal syphilis occurs during sexual contact with an actively infectious partner; exudate containing as few as ten organisms can transmit the disease 8 , 68 . Spirochaetes directly penetrate mucous membranes or enter through abrasions in skin, which is less heavily keratinized in perigenital and perianal areas than skin elsewhere 8 , 68 . To establish infection, T. pallidum must adhere to epithelial cells and the extracellular matrix components; in vitro binding studies suggest that fibronectin and laminin are key substrates for these interactions 76 , 97 – 99 . Once below the epithelium, organisms multiply locally and begin to disseminate through the lymphatic system and bloodstream. Spirochaetes penetrate the extracellular matrix and intercellular junctions via ‘stop and go’ movements that coordinate adherence with motility and are powered by front-to-back undulating waves generated by flagellar rotation and presumably assisted by the proteolytic activity of TP0751 (Refs 77 , 100 ). Ex vivo studies using cultured human umbilical vein endothelial cells ( Fig. 4a ) suggest that spirochaetes invade tissues using motility to negotiate their way through intercellular junctions: so-called ‘interjunctional’ penetration 7 , 101 . The infection rapidly becomes systemic 9 , 16 , 100 . Profuse spirochaetes within the epidermis and superficial dermis in secondary syphilitic lesions ( Fig. 4b ) enable tiny abrasions created during sexual activity to transmit infection 10 , 102 . Penetration of the blood–brain barrier, occurring in as many as 40% of individuals with untreated early syphilis, can cause devastating neurological complications 9 , 16 .
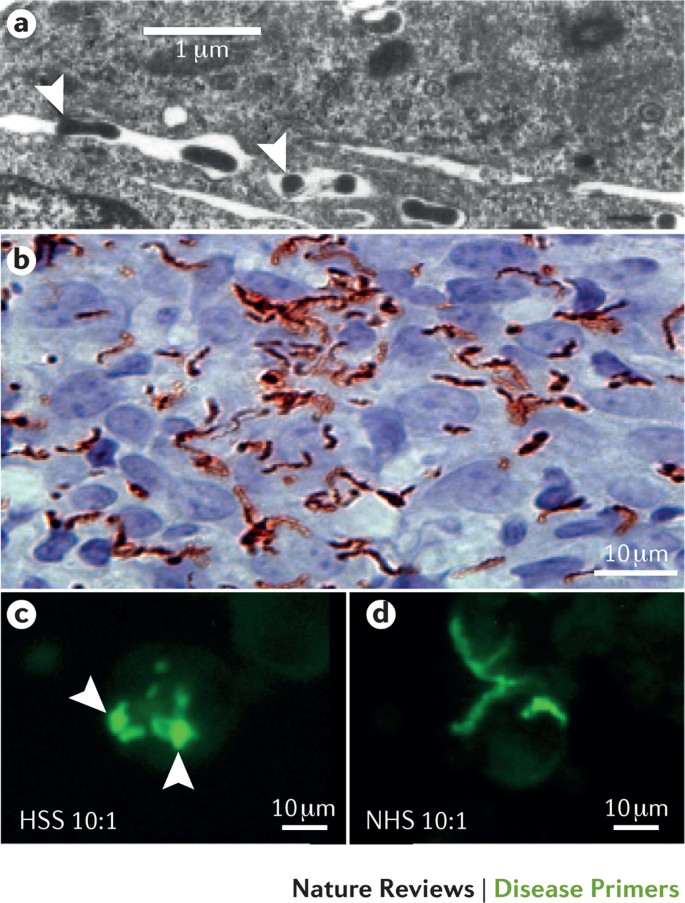
a | Transmission electron micrograph of Treponema pallidum (arrowheads) penetrating the junctions between cultured umbilical vein endothelial cells. ‘Interjunctional invasion’ following attachment to the vascular endothelium is thought to provide T. pallidum access to tissue parenchyma during haematogenous dissemination. Part a is reproduced by permission of Oxford University Press (Ref. 101 ): Riley, B.S. et al ., Virulent Treponema pallidum activates human vascular endothelial cells, The Journal of infectious diseases, 1992, 165, 3, 484–493. b | Immunohistochemical staining (using commercial anti- T. pallidum antibodies) of a secondary syphilitic skin lesion reveals abundant spirochaetes embedded within a mixed cellular inflammatory infiltrate in the papillary dermis. The inflammatory response elicited by spirochaetes replicating in tissues is widely thought to be the cause of clinical manifestations at all stages of syphilis. Reproduced from Ref. 10 . c | Fluorescence microscopy images showing that human syphilitic serum (HSS) dramatically enhances opsonophagocytosis of T. pallidum by purified human peripheral blood monocytes compared with part d , which shows normal human serum (NHS). Arrowheads indicate treponemes being degraded within phagolysosomes.
Adaptive immune response and inflammation
Although the paucity of PAMPs in the T. pallidum outer membrane enables the bacterium to replicate locally and undergo repeated bouts of dissemination, pathogen sensing in the host is eventually triggered. The organisms are taken up by dendritic cells 103 , which then traffic to draining lymph nodes to present cognate treponemal antigens to naive B cells and T cells. The production of opsonic antibodies markedly enhances the uptake and degradation of spirochaetes by phagocytes ( Fig. 4c,d ), liberating lipopeptides and other PAMPs for binding to Toll-like receptors lining the interior of the phagosome and antigenic peptides for presentation to locally recruited T cells 62 , 104 , 105 . Activated lesional T cells secrete IFNγ, promoting clearance by macrophages but also bolstering the production of tissue-damaging cytokines, such as tumour necrosis factor and IL-6 (Refs 10 , 106 , 107 ). Immunohistochemical analysis has identified CD4 + and CD8 + T cells 10 , 106 , 108 , 109 , natural killer cells 10 and activated macrophages in early syphilitic lesions 10 , 109 . Perivascular infiltration of lymphocytes, histiocytes (phagocytic cells in connective tissues) and plasma cells with endothelial cell swelling and proliferation are characteristic histopathological findings in all stages of syphilis and can progress to frank endarteritis obliterans (leading to the occlusion of arteries and severe clinical manifestations, such as the stroke syndromes of meningovascular syphilis) 9 , 110 .
Antibody avoidance
T. pallidum is widely regarded as an extracellular bacterium 61 . Thus, a question of paramount importance is why, unlike ‘classic’ extracellular pathogens, syphilis-causing spirochaetes not only fail to be cleared rapidly but can also replicate and circulate in the midst of a prolific antibody response 8 , 68 , 69 . Immunolabelling, opsonophagocytosis and complement-dependent neutralization assays have shown that T. pallidum populations consist of antibody-binding and nonbinding subpopulations; the minority of organisms that bind antibodies do so in minute amounts and with delayed kinetics 10 , 111 – 114 . Accordingly, one can envision a scenario whereby nonbinders replenish the spirochaetes that bind and are cleared 63 .
Understanding the basis for the heterogeneity of T. pallidum 's surface antigenicity is critical to unravelling its strategy for antibody avoidance. The picture emerging from our evolving understanding of the molecular architecture of the spirochaete is multifactorial and probably involves the copious production of antibodies against subsurface lipoprotein ‘decoys’ (Refs 57 , 110 ); poor target availability due to low copy numbers of outer membrane proteins and surface-exposed lipoproteins 67 , 77 , 82 , 84 , 93 ; in the case of bipartite outer membrane proteins, limited production of antibodies against surface-exposed epitopes along with the skewed production of antibodies against periplasmic domains 84 , 93 ; organism-to-organism variation in the levels of expression of outer membrane proteins and outer surface lipoproteins through a variety of mechanisms, including phase variation 82 , 92 , 115 , 116 ; and, in the case of TprK, antigenic variation as a result of intra-genomic recombination 89 , 92 , 117 . Additionally, the ability of motile spirochaetes to ‘outrun’ infiltrating phagocytes and reach sequestered locations, including the epidermis, could be an under-appreciated aspect of immune evasion 10 , 102 . As infection proceeds, the antibody repertoire possibly broadens and intensifies to the point where the antigen-poor surface of the spirochaete is overwhelmed and its capacity for antigenic variation is exhausted, ushering in the asymptomatic period called latency. Once in the latent state, the organism can survive for years in untreated individuals, establishing niduses of inflammation in skin, bones, the thoracic aorta, the posterior uveal tract and the CNS that set the stage for recrudescent disease — collectively referred to as tertiary syphilis. How immune containment mechanisms decline and enable the balance to shift back in favour of the pathogen in tertiary syphilis is unclear 9 , although a hyper-intense cellular response to the spirochaete is generally believed to be the cause of the highly destructive lesions of tertiary syphilis 9 .
Congenital infection
Although MTCT of syphilis can occur at the time of delivery, the overwhelming majority of cases are caused by in utero transmission. Studies have shown spirochaetes in placental and umbilical cord samples, supporting the transplacental passage of the organism to the fetus, as early as 9–10 weeks of gestation 118 . Although fetal syphilis infections were thought to not occur before the second trimester, the fetus can indeed be infected very early in pregnancy but may be unable to mount a characteristic immune response until the development of the embryonic immune system at 18–20 weeks of gestation.
Transmission risk is directly related to the stage of syphilis in the pregnant woman (that is, the extent and duration of fetal exposure to spirochetes). Small case series have found the highest MTCT risk in primary and secondary stages, during which transmission probability may be ≥80%. Systematic reviews assessing women with predominantly asymptomatic infections are consistent in showing that delayed or inadequate treatment results in stillbirth, early neonatal death, prematurity, low birthweight or congenital infection in infants (more than half of syphilis-exposed fetuses); syphilitic stillbirth was the most commonly observed adverse outcome 21 , 45 , 119 .
Diagnosis, screening and prevention
Syphilis has varied and often subtle manifestations that make clinical diagnosis difficult and can lead to many infections being unrecognized. The classically painless lesions of primary syphilis can be missed, especially in hidden sites of exposure such as the cervix or rectum. The rash ( Fig. 5 ) and other symptoms of secondary syphilis can be faint or mistaken for other conditions. A syphilis diagnosis is often based on a suggestive clinical history and supportive laboratory 9 , 16 (that is, serodiagnostic) test results. Serological testing has become the most common means to diagnose syphilis, whether in people with symptoms of syphilis or in those who have no symptoms but are identified through screening. A limitation of all syphilis serological tests is their inability to distinguish between infection with T. pallidum subspecies pallidum and the T. pallidum subspecies that cause (nonvenereal) yaws, pinta or bejel.
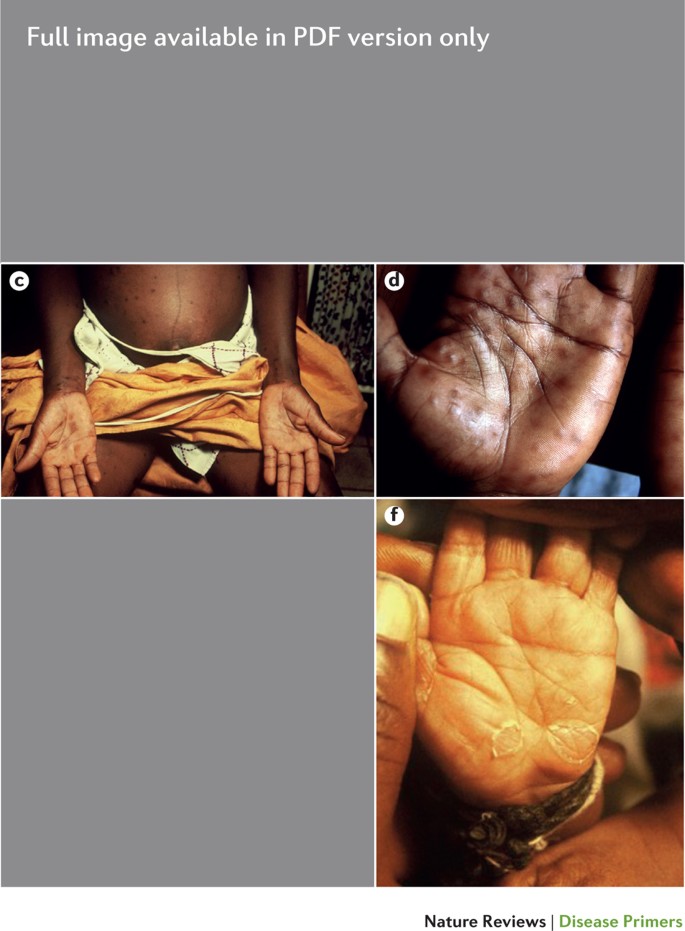
a | Primary chancre. b | Primary chancre with rash in secondary syphilis. c | Secondary syphilis in a pregnant woman who has a palmar rash. d | Palmar rash in secondary syphilis. e | 3-month-old baby with congenital syphilis showing hepatosplenomegaly and a desquamating rash. The child also presented with nasal discharge. f | Typical palmar desquamating rash in a baby with congenital syphilis.
Ensuring the accuracy and reliability of syphilis testing is important, especially in nonspecialized laboratories, where most patient samples are tested 120 . Syphilis-specific quality assurance strategies include the training of technologists on specific techniques as well as implementation of internal quality control systems, test evaluation and interassay standardization of commercially available test kits on a regular basis 37 , 120 . It is especially important to provide adequate training and regular external quality assessment or proficiency testing with corrective action to ensure the quality of tests and testing for health care providers who perform rapid tests in clinic-based or outreach settings 121 – 124 . Because many parts of the world lack laboratory capacity for making an accurate diagnosis, the requirement for laboratory testing has greatly constrained the control of syphilis and the elimination of congenital syphilis. However, the development of inexpensive, rapid tests that can be performed at the POC has greatly increased access to prenatal screening and diagnosis, even in under-resourced and remote settings.
Definitive diagnosis by direct detection
The choice of method for diagnosing syphilis depends on the stage of disease and the clinical presentation 125 . In patients presenting with primary syphilitic ulcers, condyloma lata (genital lesions of secondary syphilis) or lesions of congenital syphilis, direct detection methods — which include darkfield microscopy, fluorescent antibody staining, immunohistochemistry and PCR — can be used to make a microbiological diagnosis. However, with the exception of PCR, these methods are insensitive and require fresh lesions from which swab or biopsy material can be collected, as well as experienced technologists ( Table 1 ).
Microscopy had been used for direct detection and diagnosis since 1920 but is now used infrequently. A 2014 survey of national reference and large clinical laboratories in Latin America and the Caribbean showed that only two of 69 participating facilities, of which half were reference laboratories, still performed darkfield or direct fluorescent antibody staining for T. pallidum (DFA-TP) 126 . The most recent European guidelines recommended against DFA-TP testing in clinical settings, and the reagents are no longer available 13 . PCR techniques are increasingly used; however, there is as yet no commercially available or internationally approved PCR test for T. pallidum 13 . Species-specific and subspecies-specific T. pallidum PCR testing is a developing technology that is still primarily available only in research laboratories 127 , 128 , although these tests are anticipated to be more widely available in the near future. A systematic review and meta-analysis concluded that T. pallidum PCR testing was more efficient for confirming a diagnosis of syphilis than for excluding a diagnosis in samples from lesions 129 . Recent research indicates that this technology might be helpful for the diagnosis of neurosyphilis via the detection of T. pallidum DNA in the CSF of patients with syphilis, particularly among individuals infected with HIV 130 , 131 .
Diagnosis using serology
Serodiagnostic tests are the only means for screening asymptomatic individuals and are the most commonly used methods to diagnose patients presenting with signs and symptoms suggestive of syphilis. Serodiagnostic tests for syphilis can be broadly categorized into nontreponemal tests (NTTs) and treponemal tests (TTs).
NTTs . NTTs measure immunoglobulins (IgM and IgG) produced in response to lipoidal material released from the bacterium and/or dying host cells. The most commonly used NTTs — the rapid plasma reagin (RPR) test, the toluidine red unheated serum test (TRUST) and the Venereal Disease Research Laboratory (VDRL) test — are flocculation (precipitation) tests that detect antibodies to a suspension of lecithin (including phosphatidylcholine and phosphatidylethanolamine), cholesterol and cardiolipin. NTTs are useful in detecting active syphilis. However, because individuals with an infection do not become positive until 10–15 days after the onset of the primary lesion, 25–30% of primary syphilis cases may be missed 132 , 133 ( Fig. 6 ). Although simple and inexpensive, NTTs must be performed manually on serum, and they rely on a subjective interpretation ( Table 2 ). These tests also require trained laboratory personnel and specialized reagents and equipment and, therefore, do not fulfil the ASSURED (affordable, sensitive, specific, user-friendly, rapid and robust, equipment-free and deliverable to those who need them) criteria for tests that can be used at the POC 134 .
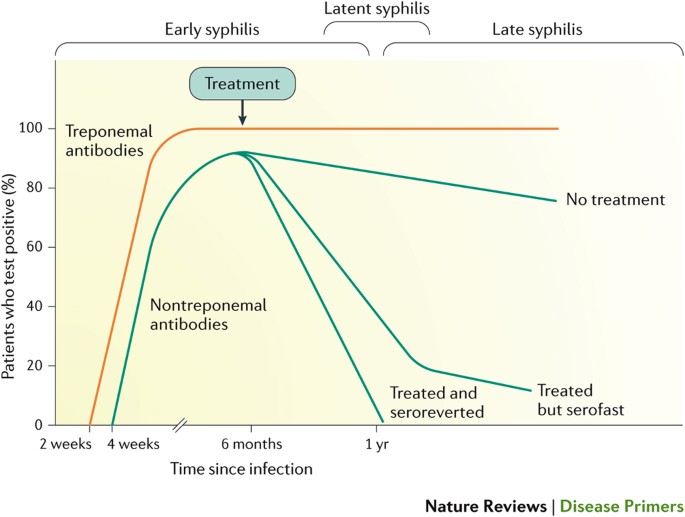
Diagnosis of syphilis can be made by measuring a patient's serological response to infection. IgM antibodies against Treponema pallidum proteins are the first to appear, followed a few weeks later by IgG antibodies. Both IgM and IgG antibodies can be measured using treponemal tests such as the T. pallidum haemagglutination assay (TPHA), T. pallidum particle assay (TPPA), fluorescent treponemal antibody absorption assay (FTA-ABS), enzyme immunoassays (EIAs) and chemiluminescence immunoassays (CIAs). IgM and IgG antibodies against proteins that are not specific to T. pallidum (nontreponemal antibodies) can be detected using the rapid plasma reagin (RPR) Venereal Disease Research Laboratory (VDRL) or toluidine red unheated serum (TRUST) tests and usually appear 2–3 weeks after treponemal antibodies are detected. With effective treatment (which is arbitrarily shown here as occurring at 6 months), the nontreponemal antibody levels decline, whereas the treponemal antibodies remain high for many years. In ∼ 20% of patients, nontreponemal antibodies persist 6 months after treatment; these individuals are labelled as having a serofast status. Despite repeated treatment, ∼ 11% of patients remain serofast 187 . Here, we show early syphilis (including primary, secondary and early latent infections; infectious syphilis) and late syphilis (including late latent and tertiary infections) as being ≤1 year in duration and >1 year in duration, respectively, in line with US and European guidelines. However, the WHO guidelines place this demarcation at 2 years. Beyond primary and secondary syphilis, the pattern of serological response over time is less well defined and is accordingly not shown.
Without treatment, titres peak at 1–2 years after infection and remain positive even in late disease (usually at a low titre). After treatment, titres generally decline and in most immunocompetent individuals become nonreactive within 6 months. However, up to 20% of individuals infected with syphilis show persistently reactive (albeit low-titre) NTT results even after treatment, possibly related to a less-robust pro-inflammatory immune response 135 . These patients are labelled as having a serofast status, which is observed more commonly with treatment for late latent than for early syphilis 37 , 136 . Biological false-positive results can occur in ∼ 2–5% of the population, regardless of the NTT test used, although the proportion is difficult to estimate with certainty because it is influenced by the population studied 137 . These low-titre reactions might be of limited duration if related to acute factors (such as febrile illness, immunization or pregnancy) or longer duration if related to chronic conditions (such as autoimmune diseases, hepatitis C infection or leprosy) 136 , 138 . By contrast, false-negative results can occur in sera with very high titres (such as sera from patients with secondary syphilis) that are not diluted before testing, a phenomenon known as a prozone effect. Pre-dilution of sera re-establishes the concentration needed for optimal antibody–antigen interaction and avoids this problem.
TTs . In contrast to NTTs, TTs detect antibodies directed against T. pallidum proteins and are theoretically highly specific. However, as most individuals infected with syphilis develop treponemal antibodies that persist throughout life, TTs cannot be used to distinguish an active from a past or previously treated infection and are not useful in evaluating treatment effectiveness. TTs are used as confirmatory assays following a positive NTT result.
TT results become positive 6–14 days after the primary chancre appears ( ∼ 5 weeks after infection) and, therefore, may be useful to detect early syphilis missed by NTT testing. These tests are usually laboratory-based and include the fluorescent treponemal antibody absorbed (FTA-ABS) test, the microhaemagglutination assay for antibodies to T. pallidum (MHA-TP), the T. pallidum passive particle agglutination (TPPA) and T. pallidum haemagglutination (TPHA) assays ( Table 2 ). These tests also require trained personnel in a laboratory setting, are more expensive and technically complex than NTTs and involve specialized reagents and equipment. For these reasons, in the developing world, laboratory-based TTs are not widely available in primary care settings, hence limiting their utility as assays for confirming NTT results.
In recent years, TTs using recombinant T. pallidum antigens in enzyme and chemiluminescence immunoassays (EIA and CIA, respectively) have been commercialized. These assays are useful for large-scale screening as they are automated or semi-automated and, because they are read spectrophotometrically, are not subjective 13 , 139 – 142 . In higher-income countries, many health care institutions depend on high-throughput screening and have adopted ‘reverse’ algorithms that screen with an automated treponemal EIA or CIA and confirm results with an NTT rather than the opposite, traditional approach ( Fig. 7 ). Few studies as yet have addressed the accuracy of these ‘reverse testing’ algorithms 40 , 143 . The traditional and reverse approaches should theoretically produce the same result. However, the reverse algorithm results in the detection of patients with early syphilis (TT-positive, NTT-negative) who would not be detected by the conventional approach 144 . As this pattern of serological reactivity occurs in very early primary syphilis, in previously treated disease and late infection, considerable attention should be given to a thorough physical examination of the patient and assessment of previous history and recent sexual risk factors before initiating any treatment and partner notification activities.
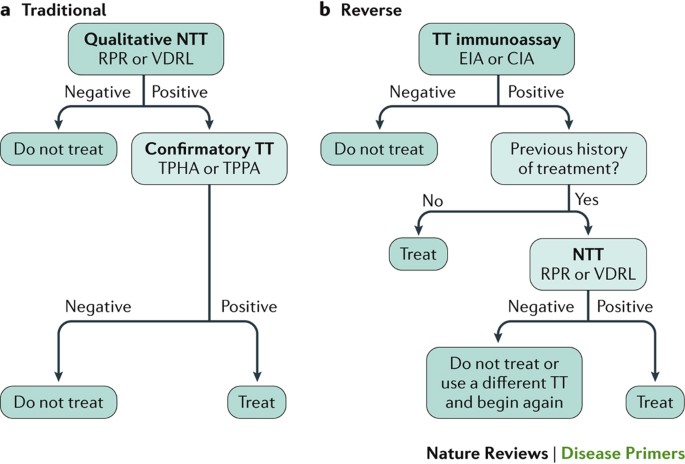
a | The traditional algorithm begins with a qualitative nontreponemal test (NTT) that is confirmed with a treponemal test (TT). This algorithm has a high positive predictive value when both tests are reactive, although early primary and previously treated infections can be missed owing to the lower sensitivity of NTTs 136 . Importantly, this algorithm is less costly than reverse screening algorithms and does not require highly specialized laboratory equipment, but it is limited by the subjective interpretation of the technologist. Additionally, false-negative NTT results can arise from the prozone effect (when there is an excess of antibody). Finally, because the traditional algorithm is not always followed by a confirmatory TT, previously treated, early untreated and late latent patients can be missed, and biologically false-positive patients can be overtreated. b | The reverse screening algorithm uses a TT with recombinant T. pallidum antigens in enzyme immunoassay (EIA) or chemiluminescence immunoassay (CIA) formats that, when reactive, is followed by an NTT. This approach is associated with higher initial setup costs and ongoing operational costs than the traditional algorithm, but the algorithm permits treatment of 99% of patients with syphilis, which is higher than the percentage treated on the basis of the traditional algorithm in a low-prevalence setting 246 . However, this approach is at the expense of serodiagnosis in patients without risk factors and, therefore, who are unlikely to have syphilis, leading to potential overtreatment and any psychosocial consequences associated with a false positive result. Additionally, because TTs are not flocculation assays, false-negative test results due to the prozone effect do not occur. However, in high-risk populations, screening with a TT can result in a high rate of positive results due to previously treated infections, leading to an increase in the clinician workload needed to review cases and determine appropriate management. Some guidelines recommend further evaluation of reactive TT results with a quantitative NTT and, if results of the latter are nonreactive, a second (different) TT to help resolve the discordant results 143 , 247 , 248 . The European Centre for Disease Prevention and Control uses a variation of this approach: a reactive TT immunoassay is followed by a second (different) TT of any kind (that is, not followed by an NTT) 249 . Ideally, a positive TT result should be supplemented by another TT or an NTT. However, in most developing countries, particularly given the serious consequences of syphilis during pregnancy, treatment is recommended for a patient with a positive TT result. RPR, rapid plasma reagin test; TPHA, T. pallidum haemagglutination assay; TPPA, T. pallidum particle assay; VDRL, Venereal Disease Research Laboratory test.
Rapid tests . Rapid POC TTs are a recent technology that enable onsite screening and treatment and are particularly useful in settings with limited laboratory capacity. Rapid syphilis tests use a finger-prick whole blood sample and are typically immuno-chromatographic strip-based TT assays using components that can be stored at room temperature, require no equipment and minimal training and give a result in <20 minutes 145 ( Table 2 ). Various rapid tests have been evaluated in a range of clinical and community settings and shown to fulfil the ASSURED criteria 134 , 146 – 154 . Like other TTs, most POC diagnostics have the limitation of being unable to distinguish between recent and previously treated syphilis infections and, therefore, could lead to overtreatment. Ideally, patients who test positive to a POC TT would be further evaluated with an NTT to support management decisions; however, this is often not possible in settings with limited laboratory capacity as is the case in many antenatal care clinics and outreach programmes for high-risk populations. Rapid POC tests play an important part when delayed diagnosis is problematic, such as in pregnant women in whom delayed or no treatment poses substantial risks to the fetus that far outweigh the risks of overtreatment for the mother 45 , 155 . In nonpregnant individuals who test positive, the recommendations are treatment for those who have no prior history of treatment and referral to have an NTT for those with a prior history 11 .
At least one test has been developed that enables the simultaneous detection of nontreponemal and treponemal antibodies in a single POC device 156 – 158 . Additionally, rapid, dual syphilis and HIV tests are available to screen for HIV and treponemal antibodies using a single lateral-flow immuno-chromatographic strip. These tests are increasingly important tools for the global elimination of MTCT of HIV and syphilis in settings in which laboratory capacity is limited 159 .
Tests useful in special situations
Neurosyphilis . The diagnosis of neurosyphilis is challenging. The CSF is frequently abnormal in patients with neurosyphilis, with both pleocytosis (lymphocyte accumulation) and an increased protein concentration. The VDRL assay performed on CSF is considered the gold standard for specificity but is recognized to have limited sensitivity 160 , 161 . Other CSF tests, including serological assays, such as the RPR 162 , FTA-ABS 163 and TPHA tests 164 , and molecular assays, such as PCR 165 , have all been assessed and show differences in their specificity and sensitivity for the diagnosis of neurosyphilis. Difficulties in the interpretation of CSF pleocytosis in individuals co-infected with HIV and syphilis make it challenging to evaluate the relationship between the two diseases. CSF pleocytosis occurs in individuals with either infection alone 37 , 165 ; thus, discerning the cause of pleocytosis in individuals with co-infections is not always possible.
Congenital syphilis . Diagnosing congenital syphilis in exposed, asymptomatic infants is another area of testing that can be improved. Because maternal nontreponemal and treponemal IgG antibodies can be transferred from mother to child, treponemal testing of infant serum is difficult to interpret and is not recommended 37 . An infant with a reactive RPR or VDRL serum titre that is at least fourfold that of the mother is highly suggestive of congenital syphilis, but its absence does not exclude a diagnosis. A clinical examination, reactive infant CSF VDRL assay results, abnormal complete blood count or liver function test results or suggestive long-bone radiographs (that, for example, show retarded ossification or dislocation of epiphyses and radiolucencies (low-density areas)) can support a diagnosis of congenital syphilis. Use of IgM immunoblots is controversial due to the limited availability of tests and inconclusive data thus far on their sensitivity; their use in diagnosing congenital syphilis is recommended in some guidelines 11 , 13 but not others 37 . Maternal syphilis infection is highly correlated with fetal loss; thus, the evaluation of a stillborn infant should include an evaluation of maternal test results for syphilis 11 .
The wide availability of effective treatments and resulting decline in syphilis prevalence has led to a low yield of screening in low-prevalence settings; thus, screening in low-risk adults (for example, premarital adults or those admitted to hospital) has been abandoned in most places. However, systematic reviews provide convincing evidence in favour of syphilis screening for pregnant women 13 , 166 , adults and adolescents at increased risk of infection 13 , 40 and individuals donating blood, blood products or solid organs 13 , 167 – 169 . Several countries also recommend syphilis testing in people with unexplained sudden visual loss, deafness or meningitis as these may be manifestations of early neurosyphilis 13 , 37 .
Prenatal screening . Syphilis screening is universally recommended for pregnant women, regardless of previous exposure, because of the high risk of MTCT during pregnancy and the availability of a highly effective preventive intervention against adverse pregnancy outcomes 11 , 37 , 41 , 46 . Global normative authorities and most national guidelines recommend syphilis screening at the first prenatal visit, ideally during the first trimester 11 , 37 , 41 , 170 . Some countries recommend that women at high risk have repeat screening in the third trimester and again at delivery to identify new infections 37 . Women should be tested during each pregnancy, even if they tested negative in a previous pregnancy. When access to prenatal care is not optimal or laboratory capacity is limited, rapid tests have been shown to be beneficial in detecting and treating syphilis in pregnant women 148 . Guidelines recommend that after delivery, neonates should not be discharged from the health facility unless the serological status of the mother had been determined at least once during pregnancy and preferably again at delivery 11 , 37 .
The importance of universal syphilis screening in pregnancy to prevent perinatal and infant morbidity and mortality is highlighted in the current WHO global initiative to eliminate congenital syphilis 43 , 44 and is justified by the continuing high global burden of congenital syphilis, availability of an effective and affordable preventive intervention and wider availability of low cost rapid POC tests that can be used when laboratory capacity is lacking 23 , 43 , 44 , 46 , 145 . A systematic review of studies (most of which were conducted in low-income countries) reporting on antenatal programmes initiating or expanding syphilis screening, compared with various local control conditions, found that enhanced screening reduced syphilis-associated adverse birth outcomes by >50% 171 . Integration of syphilis testing with other prenatal interventions, including HIV testing, has been shown to be cost-effective across settings, even when syphilis prevalence is low 48 – 51 . Strategies that enhance screening coverage, such as increased use of rapid POC testing and integrating syphilis and HIV screening, will further support the global elimination of congenital syphilis 145 , 172 – 174 .
Screening at-risk populations . Increased risks of infection can be related to personal or partner behaviours leading to syphilis infection or living in a community with a high syphilis prevalence 37 , 40 . In many countries, syphilis testing is recommended for all attendees at STI or sexual health centres and as part of integrated services targeted to high-risk groups (such as HIV testing centres or drug treatment centres) 13 , 37 . The optimal screening interval for individuals at an increased risk of infection is not well established; however, some guidelines suggest that MSM or people with HIV show a greater benefit from more frequent screening than others at risk of syphilis infection (for example, testing every 3 months rather than a single annual screening) 37 , 40 , 175 , 176 .
At-risk communities are often marginalized from care and experience discrimination and stigma when using traditional STI services 177 . Innovations in promoting the uptake of testing and developing user-friendly services are important in the control of syphilis in these communities to reduce transmission. Social entrepreneurship and crowdsourcing approaches have been shown as innovative approaches to improve HIV and syphilis testing coverage rates and accelerate linkage to care, two fundamental elements within the cascade of STI service delivery 178 , 179 . Studies evaluating other interventions, such as pre-exposure prophylaxis for syphilis, are also underway 180 . One future option might be to administer pre-exposure prophylaxis simultaneously for syphilis and HIV 181 .
Blood-bank screening . Although syphilis was among the first identified infectious risks for blood donation and syphilis transmission through blood has been documented 182 – 184 , reports of transfusion-transmitted syphilis have become exceedingly rare over the past 60 years as more countries adopt donor selection processes, universal serological screening of donors and the use of refrigerated products rather than fresh blood components 183 , 185 . The survival of T. pallidum in different blood components has been shown to vary according to storage conditions, with fresh blood or blood components stored for <5 days being more infectious than blood stored for longer periods 183 . Screening of blood, blood components and solid organs for syphilis remains a recommendation in many countries 13 , 169 . Occasional cases of transfusion-transmitted syphilis are still reported in settings with high syphilis prevalence, particularly with the transfusion of fresh blood 167 .
There is as yet no vaccine against syphilis; the most effective mode of prevention is prompt treatment to avoid continued sexual transmission or MTCT, and the treatment of all sex partners to avoid reinfection. Other prevention modalities against the sexual transmission of syphilis are latex condom use, male circumcision and avoiding sex with infected partners 37 . Treating exposed sex partners is important to avoid reinfection 37 .
Important factors in managing syphilis are early detection, prompt treatment with an effective antibiotic regimen and treating sex partners of a person with infectious syphilis (primary, secondary or early latent infections). The WHO guidelines 11 ( Box 1 ) and European guidelines 13 for the management of early syphilis in adults are the same. The US Centers for Disease Control and Prevention (CDC) guidelines do not suggest procaine penicillin as a treatment but are otherwise identical 12 . Patients with late syphilis are no longer infectious. Thus, the objective of treatment is to prevent complications in persons who are asymptomatic (that is, those who have late latent syphilis) or arrest disease development if the patient has manifestations of tertiary disease. Treating late syphilis requires longer courses of antimicrobial therapy than treating early syphilis.
Penicillin has been the mainstay of treatment for syphilis since it first became widely available in the late 1940s. Although its efficacy was never demonstrated in a randomized controlled trial, it was clearly far superior to all previous treatments, and T. pallidum resistance to penicillin has never been reported. As T. pallidum divides slower than most bacteria, it is necessary to maintain penicillin levels in the blood above the minimum inhibitory concentration for ≥10 days; this can be achieved by giving a single intramuscular injection of long-acting benzathine penicillin G (which benefits from not requiring patient adherence to a long-term drug regimen). The first-line treatments for early syphilis recommended by the CDC and European (authored by the International Union Against Sexually Transmitted Infections) guidelines are very similar 12 , 13 , as are recommendations for treating exposed sex partners. Patients with late syphilis, or with syphilis of unknown duration, should receive longer courses of treatment ( Box 1 ). Those with symptoms suggestive of neurosyphilis or ocular involvement should undergo lumbar puncture to confirm or rule out the presence of neurosyphilis, which requires more-intensive treatment. However, CDC and European guidelines define latent syphilis as occurring beginning at 1 year after infection, whereas the WHO defines latent syphilis to occur beginning at 2 years, resulting in some differences in management; that is, a longer treatment duration is recommended for some patients in the United States and Europe.
Given that confirmation or exclusion of the presence of viable T. pallidum after treatment is not possible, treatment efficacy is measured indirectly using serology. Being cured is usually defined as reversion to a negative serostatus or a fourfold reduction in the titre from an NTT. However, as noted earlier, a minority of patients remain seropositive, with a less than fourfold reduction in their NTT titre, in spite of almost certainly having been cured and with no evidence of progressive disease — the so-called serofast state 186 . The management of these patients depends on taking a careful sexual history to exclude the possibility of reinfection, which can be challenging as patients may not recognize new infections. The serofast state more commonly occurs in patients with late syphilis and low NTT titres and in patients positive for HIV who are not on antiretroviral treatment 187 . Because few data are available on long-term clinical outcomes in serofast patients, CDC guidelines recommend continuing clinical follow-up and retreatment if follow-up cannot be ensured 12 .
Second-line treatments
Patients who are allergic to penicillin should be treated with doxycycline or ceftriaxone (although an allergy to cephalosporins is more common in those who are allergic to penicillin) with repeat NTT serology as a follow-up. Doxycycline is contraindicated during pregnancy. Two treatment trials of early syphilis in Africa showed that a single oral dose of azithromycin was equivalent to treatment with benzathine penicillin G (Refs 188 , 189 ). Unfortunately, strains of T. pallidum with a mutation that confers resistance to azithromycin and other macrolide antibiotics are common in the United States, Europe, China and Australia 190 – 194 . A study of HIV-positive patients with syphilis showed that administering azithromycin to prevent opportunistic infections led to better serological outcomes 195 . The WHO recommends the use of azithromycin for the treatment of syphilis only in settings where the prevalence of macrolide-resistant T. pallidum is known to be very low.
HIV co-infection
In patients with early syphilis, an increased cell count and protein concentration are found more frequently in the CSF of patients with an HIV infection than in patients without an HIV infection, and there is some evidence that early symptomatic neurosyphilis is more common in patients positive for HIV 196 , 197 . As single-dose benzathine penicillin G treatment does not reliably lead to treponemicidal levels in the CSF, some experts have suggested that HIV co-infected patients with early syphilis should receive enhanced treatment 198 . However, a randomized controlled trial ( n = 541) showed no significant difference in clinical outcomes between patients receiving a standard or enhanced treatment 15 . Notably, the 101 patients infected with HIV enrolled in the trial responded less well serologically, but due to loss at follow-up, the study was underpowered to detect a twofold difference in the standard versus enhanced treatment in patients co-infected with HIV. Furthermore, a large ( n = 573) prospective observational study in Taiwan found no difference between single-dose benzathine penicillin G and enhanced treatments in a per-protocol analysis 199 . However, using a last-observed-carried-forward analysis to account for missing data, the authors concluded that 67.1% of those who received one dose responded serologically compared with the 74.8% response rate in those who received the enhanced treatment, a statistically significant difference ( P = 0.044) 199 . Finally, a retrospective study ( n = 478) showed no difference in serological response rates at 13 months between those receiving a single-dose of benzathine penicillin G or enhanced treatment 200 . Given the inconclusive results of these studies, many clinicians continue to offer enhanced therapy to patients with early syphilis and HIV co-infection.
Treatment during pregnancy
Adverse pregnancy outcomes are common in women with syphilis 45 , 119 . A study in Tanzania found that of women with latent syphilis who had RPR titres ≥1:8, 25% delivered a stillborn infant, and 33% delivered a live but preterm infant 21 . A second study showed that adverse pregnancy outcomes due to syphilis can be prevented with a single dose of benzathine penicillin G given before 28 weeks of gestation 201 and that, in this setting in which 5–6% of pregnant women had syphilis, this was one of the most cost-effective interventions available in terms of cost per disability-adjusted life years saved 202 .
Penicillin is the only antibiotic known to be effective in treating syphilis during pregnancy and preventing adverse birth outcomes. Given that doxycycline is contraindicated during pregnancy, and macrolides such as azithromycin and erythromycin do not cross the placenta effectively, there are few alternatives to penicillin for the treatment of pregnant women with syphilis who are allergic to penicillin. The CDC recommends desensitization for those who are allergic to penicillin 12 .
Congenital syphilis
The WHO recommends that infants with suspected congenital syphilis, including infants who are born to mothers who are seropositive for syphilis and not treated with penicillin >30 days before delivery, should be treated with aqueous benzyl penicillin or procaine penicillin ( Box 1 ). All infants exposed to syphilis, including infants without signs or symptoms at birth, should be followed closely, ideally with NTT titres. Titres should decline by 3 months of age and be nonreactive by 6 months 12 . TTs are not useful in infants due to persistent maternal antibodies.
Neurosyphilis and ocular syphilis
Involvement of the CNS can occur during any stage of syphilis, but there is no evidence supporting a need to deviate from recommended syphilis regimens without the presence of clinical neurological findings (such as ophthalmic or auditory symptoms, cranial nerve palsies, cognitive dysfunction, motor or sensory deficits or signs of meningitis or stroke) 203 . With symptoms and tests indicating neurosyphilis, or any suggestion of ocular syphilis regardless of CSF testing, more-intensive treatment is recommended. For example, the CDC recommends that adults with neurosyphilis or ocular syphilis should be treated with high-dose intravenous aqueous crystalline penicillin, or intramuscular procaine penicillin plus probenecid, for 10–14 days 204 .
Box 1: WHO guidelines for the treatment of syphilis
Early syphilis
Intramuscular benzathine penicillin G (single dose)
Or intramuscular procaine penicillin (daily doses for 10–14 days)
If penicillin-based treatment cannot be used, oral doxycycline (two doses daily for 10–14 days)* or intramuscular ceftriaxone (daily doses for 10–14 days)
Late syphilis
Intramuscular benzathine penicillin G (weekly doses for 3 weeks)
Or intramuscular procaine penicillin (daily doses for 20 days)
If penicillin-based treatment cannot be used, oral doxycycline (daily doses for 30 days)*
Intravenous aqueous benzyl penicillin (daily doses for 10–15 days)
Or intramuscular procaine penicillin (daily doses for 10–15 days)
*Contraindicated during pregnancy. From Ref. 11
Quality of life
Historical reports dating from the 15th century indicate that syphilis was perceived as a dangerous infection and a source of public alarm via fear of contagion and dread of its manifestations, as well as anxiety around its highly toxic ‘cures’ (heavy metal therapy with mercury, arsenic or bismuth) 205 – 207 . Case reports through the 19th century, as well as modern re-evaluations of skeletal remains, support the fact that the disease could cause severe physical stigmata, with individuals having disfiguring rashes, nonhealing ulcerations, painful bony lesions that often involved destruction of the nose and palate, visceral involvement, dementia and other incapacitating neurological complications and early death 208 . Stigmatization associated with syphilis was also evident, with symptomatic patients quarantined to specialized hospitals, and affected people hiding their symptoms, perhaps fearing societal shunning or the dubiously effective treatment regimens even more than they feared the disease 209 . Reductions in syphilis prevalence were documented after the introduction of penicillin 210 , and since that time, the most virulent manifestations of the disease have almost vanished; today it is rare to find a patient with tertiary disease 211 . Nevertheless, continuing reports emphasize that complications of late syphilis, particularly those involving the eyes, CNS and cardiovascular system, can cause lifelong disability and even death 9 . For example, the number of cases of ocular syphilis has increased with rising syphilis incidence in many communities 212 , with delayed treatment associated with permanently diminished visual acuity 213 . Thus, caregivers must be cognizant of the need to screen at-risk patients for latent infection and administer therapy if previous treatment has not been documented.
Few modern studies have addressed quality of life in men and women with syphilis, whether in social, psychological or economic contexts. One study ( n = 250) showed only a minor effect on patient-reported quality of life at time of treatment and essentially no effect 1 month after treatment 214 . The currently high case rates of syphilis infection and reinfection among MSM in urban centres throughout the world might lend support to the notion that syphilis in the modern era poses a limited impact on quality of life as long as it is detected and treated. However, partner notification studies suggest that STI diagnoses can lead to substantial social stigma, intense embarrassment and fear of retaliation, domestic violence or loss of relationships 177 . Public health experts have posited that syphilis is the source of more stigma than other STI diagnoses, although this is difficult to measure with certainty because STI programmes tend to focus contact tracing efforts more strongly on syphilis than on other curable STIs owing to its serious consequences 215 . In one study measuring the level of shame associated with several stigmatizing skin diseases, patients assigned the greatest shame to syphilis — more than to HIV/AIDS, other STIs or several disfiguring skin conditions 216 .
Untreated maternal syphilis results in severe adverse perinatal outcomes, most prominently stillbirth, in at least half of affected pregnant women 45 . Although MTCT of syphilis is clearly linked to a lack of prenatal care, WHO data indicate that globally, whether in wealthy or poor nations, most adverse pregnancy outcomes caused by maternal syphilis are in women who attended prenatal care but were not adequately tested or treated 24 . This suggests that other factors, such as ineffective health systems, gender inequality, lack of political will to support quality STI and reproductive health services or other structural influences associated with a lack of screening might be at play 217 . Increasing research supports the conclusion that, as for infant loss, a stillbirth can lead to poor mental and other health outcomes for both parents and the wider family, even extending to health care providers. For example, experiencing a stillbirth has been linked to ‘unspoken grief’ and a variety of psychosocial consequences such as depression, blame, shame, social isolation, problems in future pregnancies and relationship dissolution 218 – 220 . In Haiti, pregnancy loss associated with syphilis is so common (maternal prevalence of 6%) that a myth about a werewolf sucking the blood out of the unborn fetus has developed to help women with their loss and suffering 221 . Economic research suggests that a stillbirth results in substantial direct and indirect costs and can sometimes require more resources than a livebirth 219 .
With syphilis continuing to be the leading cause of preventable stillbirths in the developing world and re-emerging as a public health threat in developed nations, particularly in MSM co-infected with HIV, the demand for improved diagnostics, prevention strategies and treatments is growing. Here, we describe the most pressing issues and propose a call to action ( Box 2 ).
Elimination of MTCT of syphilis
The WHO campaign to eradicate yaws, which treated >50 million people with penicillin and reduced the number of cases by ≥95% worldwide between 1952 and 1964, was ultimately unsuccessful. What can we learn from this heroic failure? The yaws eradication campaign was based on clinical examination and serological testing to determine prevalence by community and on mass treatment or selective mass treatment (patients and contacts) of communities with penicillin depending on prevalence. Unfortunately, as the prevalence of yaws fell, it was no longer perceived as an important public health problem worthy of an expensive vertical programme; resources were diverted to other programmes, yaws was forgotten, and it re-emerged 222 . To some extent the same is true of syphilis; once penicillin became available, its incidence and prevalence declined in many parts of the world, and it was no longer seen as a public health priority. Although screening of all pregnant women for syphilis has continued to be recommended in most countries, coverage has been low in many regions; for example, WHO estimates that approximately 50% of antenatal clinic attendees in Africa are not currently screened for syphilis 24 . This low coverage has resulted in a high burden of entirely preventable stillbirths and neonatal deaths 23 . Exacerbating this situation, the WHO has received reports of depleted stocks and shortages of injectable benzathine penicillin G in multiple countries, many with a high burden of maternal and congenital syphilis. In collaboration with international partners, the WHO has spearheaded an initiative to assess the global supply, current and projected demand and production capacity for benzathine penicillin G (Ref. 223 ).
Strong advocacy will be needed to ensure that the control and elimination of syphilis is given a high priority on the global health agenda. Policy makers and funders need to be made aware that syphilis is a leading cause of preventable stillbirths and neonatal death, that these deaths can be prevented with a single dose of penicillin given to the mother before 28 weeks of gestation and that this is one of the most cost-effective health interventions available 51 , 202 . Perhaps with this awareness and political will, syphilis MTCT elimination programmes, which have failed to progress in the past 10 years 224 , will witness the same success achieved in the MTCT of HIV programmes in Africa. Other developments are occurring that are forging change. For example, the availability of POC tests has led to increased coverage of antenatal screening and treatment for syphilis in many settings 148 , and the WHO campaign for the elimination of MTCT of HIV and syphilis has increased the visibility of syphilis on the global health agenda. In 2014, the WHO target for the elimination of MTCT of syphilis was ≤50 cases of congenital syphilis per 100,000 live births. The targeted processes are antenatal care coverage (at least one visit) of ≥95% of pregnant women, syphilis testing coverage for ≥95% of pregnant women and treatment of ≥95% of pregnant women seropositive for syphilis WHO http://apps.who.int/iris/bitstream/10665/112858/1/9789241505888_eng.pdf (2014)." href="/articles/nrdp201773#ref-CR225" id="ref-link-section-d184586964e3628">225 . Additionally, the WHO has conducted a systematic review of the performance of rapid, dual HIV and syphilis tests and issued an information note on testing algorithms for dual HIV and syphilis tests 226 .
The huge reduction in the number of infants positive for HIV in Africa in recent years, a more difficult undertaking than reducing MTCT of syphilis, is proof of concept that congenital syphilis elimination is achievable. Given that Cuba, Thailand, Belarus, Moldova and Armenia have eliminated MTCT of HIV, syphilis or both, elimination can be achieved with political will and a well-organized health care system. Indeed, inclusion of syphilis and HIV screening with tests for anaemia, diabetes and pre-eclampsia as a package of essential diagnostics for prenatal care should be implemented as a minimum standard to ensure safe and healthy pregnancies worldwide.
The use of POC testing has greatly increased access to screening for pregnant women and has the potential to increase access to screening for high-risk groups such as MSM and FSWs through outreach programmes. However, the quality of testing must be assured given that these tests are conducted outside the laboratory. Strategies to ensure the reliability of POC tests include the use of electronic readers 227 and microfluidic assays powered by smart phones 228 for real-time monitoring of progress 229 and the routine provision of proficiency testing panels 121 , 122 . For example, one study in the Amazon region of Brazil showed that proficiency panels consisting of dried serum tubes that were assessed by each health care worker could be used to monitor the performance of health care workers in remote settings 123 .
HIV and syphilis co-infection in MSM
In developed countries, the incidence of syphilis in MSM is several hundred times higher than in the general population. Furthermore, the incidence continues to increase as condom use has fallen with increasing use of pre-exposure prophylactic antiretroviral medications for HIV 42 , 230 . Indeed, with wider HIV treatment coverage in recent years and HIV no longer considered a ‘death sentence’, safe sex practices have declined and risk-taking behaviours have increased 231 . However, the alarming increase in the incidence of syphilis, compared with that of other STIs, in HIV-infected MSM cannot be explained by behavioural factors alone. The frequent co-infection of HIV and syphilis in MSM in many countries has led researchers and policy makers to consider the hypothesis that treatment for HIV may be a double-edged sword that contributes to increased susceptibility to syphilis through impairment of the innate or acquired immunity to T. pallidum 42 , 232 .
Accordingly, research is urgently needed to understand the underlying causes of this twin epidemic. The involvement of the MSM community is critical in the design and implementation of innovative approaches to promote the uptake of testing and linkage to care, particularly as this community is still stigmatized and marginalized from care in many societies. Although self-testing for HIV and hepatitis C virus infection is now possible using highly sensitive and specific oral tests that are commercially available, syphilis does not elicit sufficient antibody levels for an oral test. Thus, implementation science is needed to integrate and optimize the delivery of a package of HIV, syphilis, hepatitis and other STI screening and treatment strategies and partner notification systems for MSM in different cultural, socioeconomic and political settings.

Better diagnostic tests
Research is needed to identify biomarkers that can more accurately distinguish between past, treated syphilis infections and active infections requiring treatment, can identify patients who have become reinfected and can provide a test of cure. Using current serological tools, a high proportion of patients have been shown to remain serofast after treatment in some settings, and the optimal management of these individuals is uncertain. Additionally, more-accurate diagnostic tests are needed to confirm the diagnosis of congenital syphilis, as serological tests based on IgG antibodies cannot distinguish between infected infants and those with passively acquired maternal antibodies. IgM tests can be highly sensitive in symptomatic infants but have suboptimal sensitivity in infants who are infected but not symptomatic at birth 12 .
The diagnosis of neurosyphilis also remains a challenge, particularly in patients co-infected with HIV, in whom an increased CSF protein concentration or cell count does not necessarily indicate that the patient has neurosyphilis. Promisingly, a rapid POC test has been adapted for the diagnosis of neurosyphilis using CSF 233 ; the performance of this test is better in cell-free specimens, requiring the use of a centrifuge. Another promising assay might be the measurement of macrophage migration factor (MIF); measurement of CSF levels of MIF alone was shown to have a sensitivity of 74.42% and a specificity of 67.74% for the diagnosis of neurosyphilis in one study ( n = 43) 234 . By integrating all CSF parameters (pleocytosis, increased protein concentrations and MIF), the sensitivity and specificity would be improved. Additionally, assays of B cell attractant chemokine CXCL13 in the CSF could be used to distinguish the pleocytosis caused by HIV from that caused by neurosyphilis in patients infected with HIV 235 .
Better use of existing drugs
With the use of penicillin, many countries still struggle with the fear of injections on the part of patients and the management of anaphylactic shock on the part of the health care providers. Oral regimens that are safe for use during pregnancy and effective in preventing the transmission of syphilis to the fetus are urgently needed. Furthermore, macrolide resistance is correlated with treatment failure in patients with primary syphilis 191 , lending further urgency to the need to find alternative oral therapies. Incentives for a drug discovery programme for syphilis need to be established and, in the meantime, evaluation of existing drug combinations might be useful as alternatives to reduce the threat of developing resistance.
Vaccine development
Human-challenge studies have shown that people with late latent syphilis are resistant to symptomatic reinfection with heterologous strains of T. pallidum , and protective immunity has been induced in rabbits by repeated inoculation with γ-irradiated T. pallidum 236 , 237 . Accordingly, it should be possible to develop protective vaccines. However, research on virulence determinants of T. pallidum and our understanding of protective immunity against T. pallidum have been hindered by our inability to culture the bacteria in vitro . Genome sequencing of T. pallidum directly from clinical samples is now possible, which can overcome this limitation 92 , 238 . This advance should enable the understanding of strain variation on a global scale and help to identify outer membrane proteins and other surface antigens as possible vaccine candidates 81 . A recent study showed that the immunization of rabbits with the lipoprotein TP0751 prevented the dissemination of T. pallidum and, hence, has become a promising vaccine candidate 81 . Integrating potential vaccine targets with diagnostic targets in discovery programmes also holds promise in accelerating progress towards the development of improved tools for the control, prevention and, ultimately, elimination of this disease.
Box 2: Major challenges and a call to action wish list
Eliminate mother-to-child transmission of syphilis
Requires political commitment
Prenatal syphilis screening to be integrated into mother-to-child transmission elimination programmes for HIV or as a component of an essential diagnostic package for prenatal care
Develop point-of-care tests with data connectivity or data transmission capability to facilitate automated surveillance and to improve the efficiency of health systems
Address HIV and syphilis co-infection in MSM
Requires research into potential synergies between the two infections
Implement scientific and community involvement to reach at-risk populations
Integrate programmes for HIV, syphilis, hepatitis and other sexually transmitted infections
Develop tests for active infection, neurosyphilis and congenital syphilis
Identify and validate biomarkers for test development
Develop a network of clinical sites for rapid validation of new tests
Develop new oral drugs to prevent transmission to fetus and to sex partners
Provide incentives for drug discovery programmes
Provide incentives to evaluate drug combinations
Develop vaccines
Requires research to better understand syphilis pathogenesis
Requires research to identify vaccine targets and methods for validation
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
How to cite this Primer
Peeling, R. W. et al . Syphilis. Nat. Rev. Dis. Primers 3 , 17073 (2017).
Giacani, L. & Lukehart, S. A. The endemic treponematoses. Clin. Microbiol. Rev. 27 , 89–115 (2014).
Google Scholar
Smajs, D., Norris, S. J. & Weinstock, G. M. Genetic diversity in Treponema pallidum : implications for pathogenesis, evolution and molecular diagnostics of syphilis and yaws. Infect. Genet. Evol. 12 , 191–202 (2012).
de Melo, F. L., de Mello, J. C. M., Fraga, A. M., Nunes, K. & Eggers, S. Syphilis at the crossroad of phylogenetics and paleopathology. PLoS Negl. Trop. Dis. 4 , e575 (2010).
Penn, C. W. Avoidance of host defences by Treponema pallidum in situ and on extraction from infected rabbit testes. J. Gen. Microbiol. 126 , 69–75 (1981).
Stamm, L. V., Hodinka, R. L., Wyrick, P. B. & Bassford, P. J. Changes in the cell surface properties of Treponema pallidum that occur during in vitro incubation of freshly extracted organisms. Infect. Immun. 55 , 2255–2261 (1987).
Salazar, J. C., Rathi, A., Michael, N. L., Radolf, J. D. & Jagodzinski, L. L. Assessment of the kinetics of Treponema pallidum dissemination into blood and tissues in experimental syphilis by real-time quantitative PCR. Infect. Immun. 75 , 2954–2958 (2007).
Thomas, D. D. et al . Treponema pallidum invades intercellular junctions of endothelial cell monolayers. Proc. Natl Acad. Sci. USA 85 , 3608–3612 (1988).
LaFond, R. E. & Lukehart, S. A. Biological basis for syphilis. Clin. Microbiol. Rev. 19 , 29–49 (2006).
Radolf, J. D., Tramont, E. C. & Salazar, J. C. in Mandell, Douglas and Bennett's Principles and Practice of Infectious Diseases 8 th edn (eds Bennett, J. E., Dolin, R. & Blaser, M. J. ) 2684–2709 (Saunders, 2014).
Cruz, A. R. et al . Immune evasion and recognition of the syphilis spirochete in blood and skin of secondary syphilis patients: two immunologically distinct compartments. PLoS Negl. Trop. Dis. 6 , e1717 (2012).
World Health Organisation. WHO guidelines for the treatment of Treponema pallidum (syphilis). WHO http://www.who.int/reproductivehealth/publications/rtis/syphilis-treatment-guidelines/en/ (2016).
Workowski, K. A. & Bolan, G. A. & Centers for Disease Control & Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recommen. Rep. 64 , 1–137 (2015).
Janier, M. et al . 2014 European guideline on the management of syphilis. J. Eur. Acad. Dermatol. Venereol. 28 , 1581–1593 (2014).
Peeling, R. W. & Hook, E. W. The pathogenesis of syphilis: the Great Mimicker, revisited. J. Pathol. 208 , 224–232 (2005).
Rolfs, R. T. et al . A randomized trial of enhanced therapy for early syphilis in patients with and without human immunodeficiency virus infection. N. Engl. J. Med. 337 , 307–314 (1997).
Golden, M. R., Marra, C. M. & Holmes, K. K. Update on syphilis. JAMA 290 , 1510 (2003).
Lukehart, S. A. et al . Invasion of the central nervous system by Treponema pallidum : implications for diagnosis and treatment. Ann. Intern. Med. 109 , 855–862 (1988).
Shaffi, T., Radolf, J. D., Sanchez, P. J., Schulz, K. F. & Murphy, F. K. in Sexually Transmitted Diseases 4th edn (eds Holmes, K. K. et al . ) 1577 –1609 (McGraw-Hill Medical, 2008).
Sánchez, P. J. et al . Evaluation of molecular methodologies and rabbit infectivity testing for the diagnosis of congenital syphilis and neonatal central nervous system invasion by Treponema pallidum. J. Infect. Dis. 167 , 148–157 (1993).
Fiurmara, N. J. Congenital syphilis in Massachusetts. N. Engl. J. Med. 245 , 634–640 (1951).
Watson-Jones, D. et al . Syphilis in pregnancy in Tanzania. I. Impact maternal syphilis outcome pregnancy. J. Infect. Dis. 186 , 940–947 (2002). A comprehensive and well-designed study that showed the outcomes of syphilis during pregnancy.
Magnuson, H. J., Eagle, H. & Fleischman, R. The minimal infectious inoculum of Spirochaeta pallida (Nichols strain) and a consideration of its rate of multiplication in vivo. Am. J. Syph. Gonorrhea Vener. Dis. 32 , 1–18 (1948).
Newman, L. et al . Global estimates of syphilis in pregnancy and associated adverse outcomes: analysis of multinational antenatal surveillance data. PLoS Med. 10 , e1001396 (2013).
Wijesooriya, N. S. et al . Global burden of maternal and congenital syphilis in 2008 and 2012: a health systems modelling study. Lancet Glob. Health 4 , e525–e533 (2016). This paper is one of three WHO studies that have provided the backbone of our data on the global burden of syphilis; it provided updated global estimates in pregnant women and of adverse pregnancy outcomes 5 years into the global programme for congenital syphilis elimination (that is, monitoring progress).
Lawn, J. E. et al . Stillbirths: rates, risk factors, and acceleration towards 2030. Lancet 387 , 587–603 (2016). The first paper that showed that syphilis has emerged as the leading cause of preventable stillbirths.
Hook, E. W. & Peeling, R. W. Syphilis control — a continuing challenge. N. Engl. J. Med. 351 , 122–124 (2004).
Newman, L. et al . Global estimates of the prevalence and incidence of four curable sexually transmitted infections in 2012 based on systematic review and global reporting. PLoS ONE 10 , e0143304 (2015).
Black, V. et al . Field evaluation of Standard Diagnostics’ Bioline HIV/Syphilis Duo test among female sex workers in Johannesburg, South Africa. Sex. Transm. Infect. 92 , 495–498 (2016).
Elhadi, M. et al . Integrated bio-behavioural HIV surveillance surveys among female sex workers in Sudan, 2011–2012. Sex. Transm. Infect. 89 , S17–S22 (2013).
Vandepitte, J. et al . HIV and other sexually transmitted infections in a cohort of women involved in high-risk sexual behavior in Kampala, Uganda. Sex. Transm. Dis. 38 , 316–323 (2011).
McLaughlin, M. M. et al . Sexually transmitted infections among heterosexual male clients of female sex workers in China: a systematic review and meta-analysis. PLoS ONE 8 , e71394 (2013).
Su, S. et al . Sustained high prevalence of viral hepatitis and sexually transmissible infections among female sex workers in China: a systematic review and meta-analysis. BMC Infect. Dis. 16 , 2 (2015).
Chen, X.-S. et al . Prevalence of syphilis infection in different tiers of female sex workers in China: implications for surveillance and interventions. BMC Infect. Dis. 12 , 84 (2012).
Abara, W. E., Hess, K. L., Neblett Fanfair, R., Bernstein, K. T. & Paz-Bailey, G. Syphilis trends among men who have sex with men in the United States and western Europe: a systematic review of trend studies published between 2004 and 2015. PLoS ONE 11 , e0159309 (2016). A good review that described the alarming increase of syphilis in MSM in the developed world.
de Voux, A. et al . State-specific rates of primary and secondary syphilis among men who have sex with men - United States, 2015. MMWR. Morb. Mortal. Wkly Rep. 66 , 349–354 (2017).
Burchell, A. N. et al . High incidence of diagnosis with syphilis co-infection among men who have sex with men in an HIV cohort in Ontario, Canada. BMC Infect. Dis. 15 , 356 (2015).
Centers for Disease Control and Prevention. Syphilis treatment and care. Centers for Disease Control and Prevention https://www.cdc.gov/std/syphilis/treatment.htm (2015).
Brodsky, J. L. et al . Syphilis outbreak at a California men's prison, 2007-2008: propagation by lapses in clinical management, case management, and public health surveillance. J. Correct. Health Care 19 , 54–64 (2012).
Van Wagoner, N. J., Harbison, H. S., Drewry, J., Turnipseed, E. & Hook, E. W. Characteristics of women reporting multiple recent sex partners presenting to a sexually transmitted disease clinic for care. Sex. Transm. Dis. 38 , 210–215 (2011).
Bibbins-Domingo, K. et al . Screening for syphilis infection in nonpregnant adults and adolescents. JAMA 315 , 2321 (2016).
European Centre for Disease Prevention and Control. Antenatal screening for HIV, hepatitis B, syphilis and rubella susceptibility in the EU/EEA. European Centre for Disease Prevention and Control http://ecdc.europa.eu/en/publications/Publications/antenatal-screening-sci-advice-2017.pdf (2017).
Rekart, M. L. et al . A double-edged sword: does highly active antiretroviral therapy contribute to syphilis incidence by impairing immunity to Treponema pallidum ? Sex. Transm. Infect. 93 , 374–378 (2017). This paper presented an interesting hypothesis to explain the twin epidemics of HIV and syphilis in MSM.
Schmid, G. P., Stoner, B. P., Hawkes, S. & Broutet, N. The need and plan for global elimination of congenital syphilis. Sex. Transm. Dis. 34 , S5–S10 (2007).
World Health Organisation. The global elimination of congenital syphilis: rationale and strategy for action. WHO http://www.who.int/reproductivehealth/publications/rtis/9789241595858/en/ (2007).
Gomez, G. B. et al . Untreated maternal syphilis and adverse outcomes of pregnancy: a systematic review and meta-analysis. Bull. World Health Organ. 91 , 217–226 (2013).
Blencowe, H., Cousens, S., Kamb, M., Berman, S. & Lawn, J. E. Lives Saved Tool supplement detection and treatment of syphilis in pregnancy to reduce syphilis related stillbirths and neonatal mortality. BMC Public Health 11 , S9 (2011).
WHO. Investment case for eliminating mother-to-child transmission of syphilis. WHO http://apps.who.int/iris/bitstream/10665/75480/1/9789241504348_eng.pdf?ua=1 (2012).
Kahn, J. G. et al . The cost and cost-effectiveness of scaling up screening and treatment of syphilis in pregnancy: a model. PLoS ONE 9 , e87510 (2014).
Kuznik, A., Lamorde, M., Nyabigambo, A. & Manabe, Y. C. Antenatal syphilis screening using point-of-care testing in sub-Saharan African countries: a cost-effectiveness analysis. PLoS Med. 10 , e1001545 (2013).
Kuznik, A., Muhumuza, C., Komakech, H., Marques, E. M. R. & Lamorde, M. Antenatal syphilis screening using point-of-care testing in low- and middle-income countries in Asia and Latin America: a cost-effectiveness analysis. PLoS ONE 10 , e0127379 (2015).
Owusu-Edusei, K. et al . Cost-effectiveness of integrated routine offering of prenatal HIV and syphilis screening in China. Sex. Transm. Dis. 41 , 103–110 (2014).
Pan American Health Organization. Regional initiative for the elimination of mother-to-child transmission of HIV and congenital syphilis in Latin America and the Caribbean. Concept document for the Caribbean. Pan American Health Organization http://www.paho.org/clap/index.php?option=com_content&view=article&id=104:iniciativa-regional-para-la-eliminacion-de-la-transmision-maternoinfantil-de-vih-y-de-la-sifilis&Itemid=234&lang=en (2009).
Chen, X., Yin, Y., Wang, Q. & Wang, B. Historical perspective of syphilis in the past 60 years in China: eliminated, forgotten, on the return. Chin. Med. J. (Engl.). 126 , 2774–2779 (2013). Many lessons can be learnt from this account of the history of syphilis in China, which was once eliminated but has now come back with a vengeance.
Taylor, M. et al . Elimination of mother-to-child transmission of HIV and Syphilis (EMTCT): process, progress, and program integration. PLoS Med. 14 , e1002329 (2017). This paper described a success story of syphilis control and elimination, and highlighted how continuing global efforts can achieve an AIDS-free and syphilis-free generation.
Norris, S. J., Cox, D. L. & Weinstock, G. M. Biology of Treponema pallidum : correlation of functional activities with genome sequence data. J. Mol. Microbiol. Biotechnol. 3 , 37–62 (2001).
Penn, C. W., Cockayne, A. & Bailey, M. J. The outer membrane of Treponema pallidum : biological significance and biochemical properties. J. Gen. Microbiol. 131 , 2349–2357 (1985).
Radolf, J. D. Treponema pallidum and the quest for outer membrane proteins. Mol. Microbiol. 16 , 1067–1073 (1995).
Silver, A. C. et al . MyD88 deficiency markedly worsens tissue inflammation and bacterial clearance in mice infected with Treponema pallidum , the agent of syphilis. PLoS ONE 8 , e71388 (2013).
Turner, T. B., Hardy, P. H. & Newman, B. Infectivity tests in syphilis. Sex. Transm. Infect. 45 , 183–195 (1969).
Lukehart, S. A. & Marra, C. M. Current Protocols in Microbiology (John Wiley and Sons, Inc., 2007).
Sell, S. & Norris, S. J. The biology, pathology, and immunology of syphilis. Int. Rev. Exp. Pathol. 24 , 203–276 (1983).
Lukehart, S. A. Scientific monogamy: thirty years dancing with the same bug. Sex. Transm. Dis. 35 , 2–7 (2008).
Radolf, J. D. et al . Treponema pallidum , the syphilis spirochete: making a living as a stealth pathogen. Nat. Rev. Microbiol. 14 , 744–759 (2016). The review provided a very informative summary of the interaction of T. pallidum and its human hosts.
Paster, B. J. & Dewhirst, F. in Pathogenic Treponema: Molecular and Cellular Biology (eds Radolf, J. D. & Lukehart, S. A. ) 9–18 (Horizon Scientific Press, 2006).
Fraser, C. M. Complete genome sequence of Treponema pallidum , the syphilis spirochete. Science 281 , 375–388 (1998).
Radolf, J. D. et al . Characterization of outer membranes isolated from Treponema pallidum , the syphilis spirochete. Infect. Immun. 63 , 4244–4252 (1995).
Cox, D. L., Akins, D. R., Porcella, S. F., Norgard, M. V. & Radolf, J. D. Treponema pallidum in gel microdroplets: a novel strategy for investigation of treponemal molecular architecture. Mol. Microbiol. 15 , 1151–1164 (1995).
Radolf, J. D., Hazlett, K. R. O. & Lukehart, S. A. in Pathogenic Treponemes: Cellular and Molecular Biology (eds Radolf, J. D. & Lukehart, S. A. ) 197–236 (Horizon Scientific Press, 2006).
Salazar, J. C., Hazlett, K. R. O. & Radolf, J. D. The immune response to infection with Treponema pallidum , the stealth pathogen. Microbes Infect. 4 , 1133–1140 (2002).
Chamberlain, N. R., Brandt, M. E., Erwin, A. L., Radolf, J. D. & Norgard, M. V. Major integral membrane protein immunogens of Treponema pallidum are proteolipids. Infect. Immun. 57 , 2872–2877 (1989).
Purcell, B. K., Swancutt, M. A. & Radolf, J. D. Lipid modification of the 15 kiloDalton major membrane immunogen of Treponema pallidum . Mol. Microbiol. 4 , 1371–1379 (1990).
Akins, D. R., Purcell, B. K., Mitra, M. M., Norgard, M. V. & Radolf, J. D. Lipid modification of the 17-kilodalton membrane immunogen of Treponema pallidum determines macrophage activation as well as amphiphilicity. Infect. Immun. 61 , 1202–1210 (1993).
Radolf, J. D., Chamberlain, N. R., Clausell, A. & Norgard, M. V. Identification and localization of integral membrane proteins of virulent Treponema pallidum subsp. pallidum by phase partitioning with the nonionic detergent triton X-114. Infect. Immun. 56 , 490–498 (1988).
Cox, D. L., Chang, P., McDowall, A. W. & Radolf, J. D. The outer membrane, not a coat of host proteins, limits antigenicity of virulent Treponema pallidum . Infect. Immun. 60 , 1076–1083 (1992).
Deka, R. K. et al . Crystal structure of the Tp34 (TP0971) lipoprotein of Treponema pallidum : implications of its metal-bound state and affinity for human lactoferrin. J. Biol. Chem. 282 , 5944–5958 (2006).
Cameron, C. E., Brouwer, N. L., Tisch, L. M. & Kuroiwa, J. M. Y. Defining the interaction of the Treponema pallidum adhesin Tp0751 with laminin. Infect. Immun. 73 , 7485–7494 (2005).
Houston, S., Hof, R., Honeyman, L., Hassler, J. & Cameron, C. E. Activation and proteolytic activity of the Treponema pallidum metalloprotease, pallilysin. PLoS Pathog. 8 , e1002822 (2012).
Houston, S. et al . The multifunctional role of the pallilysin-associated Treponema pallidum protein, Tp0750, in promoting fibrinolysis and extracellular matrix component degradation. Mol. Microbiol. 91 , 618–634 (2014).
Parker, M. L. et al . The structure of Treponema pallidum Tp0751 (pallilysin) reveals a non-canonical lipocalin fold that mediates adhesion to extracellular matrix components and interactions with host cells. PLOS Pathog. 12 , e1005919 (2016).
Cameron, C. E. et al . Heterologous expression of the Treponema pallidum laminin-binding adhesin Tp0751 in the culturable spirochete Treponema phagedenis . J. Bacteriol. 190 , 2565–2571 (2008).
Lithgow, K. V. et al . A defined syphilis vaccine candidate inhibits dissemination of Treponema pallidum subspecies pallidum. Nat. Commun. 8 , 14273 (2017).
Chan, K. et al . Treponema pallidum lipoprotein TP0435 expressed in Borrelia burgdorferi produces multiple surface/periplasmic isoforms and mediates adherence. Sci. Rep. 6 , 25593 (2016).
Luthra, A. et al . The transition from closed to open conformation of Treponema pallidum outer membrane-associated lipoprotein TP0453 involves membrane sensing and integration by two amphipathic helices. J. Biol. Chem. 286 , 41656–41668 (2011).
Desrosiers, D. C. et al . TP0326, a Treponema pallidum β-barrel assembly machinery A (BamA) orthologue and rare outer membrane protein. Mol. Microbiol. 80 , 1496–1515 (2011).
Luthra, A. et al . A homology model reveals novel structural features and an immunodominant surface loop/opsonic target in the Treponema pallidum BamA ortholog TP_0326. J. Bacteriol. 197 , 1906–1920 (2015).
Rollauer, S. E., Sooreshjani, M. A., Noinaj, N. & Buchanan, S. K. Outer membrane protein biogenesis in Gram-negative bacteria. Phil. Trans. R. Soc. B Biol. Sci. 370 , 20150023 (2015).
Centurion-Lara, A. et al . Treponema pallidum major sheath protein homologue Tpr K is a target of opsonic antibody and the protective immune response. J. Exp. Med. 189 , 647–656 (1999).
Hazlett, K. R. O. et al . The Tprk protein of Treponema pallidum is periplasmic and is not a target of opsonic antibody or protective immunity. J. Exp. Med. 193 , 1015–1026 (2001).
Centurion-Lara, A. et al . Gene conversion: a mechanism for generation of heterogeneity in the tprK gene of Treponema pallidum during infection. Mol. Microbiol. 52 , 1579–1596 (2004).
LaFond, R. E., Centurion-Lara, A., Godornes, C., Van Voorhis, W. C. & Lukehart, S. A. TprK sequence diversity accumulates during infection of rabbits with Treponema pallidum subsp. pallidum Nichols strain. Infect. Immun. 74 , 1896–1906 (2006).
Giacani, L. et al . Antigenic variation in Treponema pallidum : TprK sequence diversity accumulates in response to immune pressure during experimental syphilis. J. Immunol. 184 , 3822–3829 (2010).
Pinto, M. et al . Genome-scale analysis of the non-cultivable Treponema pallidum reveals extensive within-patient genetic variation. Nat. Microbiol. 2 , 16190 (2016).
Anand, A. et al . TprC/D (Tp0117/131), a trimeric, pore-forming rare outer membrane protein of Treponema pallidum , has a bipartite domain structure. J. Bacteriol. 194 , 2321–2333 (2012).
Anand, A. et al . Bipartite topology of Treponema pallidum repeat proteins C/D and I: outer membrane insertion, trimerization, and porin function require a C-terminal β-barrel domain. J. Biol. Chem. 290 , 12313–12331 (2015).
Giacani, L. et al . TP0262 is a modulator of promoter activity of tpr subfamily II genes of Treponema pallidum ssp. pallidum. Mol. Microbiol. 72 , 1087–1099 (2009).
Radolf, J. D. & Desrosiers, D. C. Treponema pallidum , the stealth pathogen, changes, but how? Mol. Microbiol. 72 , 1081–1086 (2009).
Brinkman, M. B. et al . A novel Treponema pallidum antigen, TP0136, is an outer membrane protein that binds human fibronectin. Infect. Immun. 76 , 1848–1857 (2008).
Cameron, C. E., Brown, E. L., Kuroiwa, J. M. Y., Schnapp, L. M. & Brouwer, N. L. Treponema pallidum fibronectin-binding proteins. J. Bacteriol. 186 , 7019–7022 (2004).
Ke, W., Molini, B. J., Lukehart, S. A. & Giacani, L. Treponema pallidum subsp. pallidum TP0136 protein is heterogeneous among isolates and binds cellular and plasma fibronectin via its NH2-terminal end. PLoS Negl. Trop. Dis. 9 , e0003662 (2015).
Harman, M., Vig, D. K., Radolf, J. D. & Wolgemuth, C. W. Viscous dynamics of Lyme disease and syphilis spirochetes reveal flagellar torque and drag. Biophys. J. 105 , 2273–2280 (2013).
Riley, B. S., Oppenheimer-Marks, N., Hansen, E. J., Radolf, J. D. & Norgard, M. V. Virulent Treponema pallidum activates human vascular endothelial cells. J. Infect. Dis. 165 , 484–493 (1992).
Quatresooz, P. & Piérard, G. E. Skin homing of Treponema pallidum in early syphilis: an immunohistochemical study. Appl. Immunohistochem. Mol. Morphol. 17 , 47–50 (2009).
Bouis, D. A., Popova, T. G., Takashima, A. & Norgard, M. V. Dendritic cells phagocytose and are activated by Treponema pallidum . Infect. Immun. 69 , 518–528 (2001).
Moore, M. W. et al . Phagocytosis of Borrelia burgdorferi and Treponema pallidum potentiates innate immune activation and induces gamma interferon production. Infect. Immun. 75 , 2046–2062 (2007).
Salazar, J. C. et al . Treponema pallidum elicits innate and adaptive cellular immune responses in skin and blood during secondary syphilis: a flow-cytometric analysis. J. Infect. Dis. 195 , 879–887 (2007).
Stary, G. et al . Host defense mechanisms in secondary syphilitic lesions. Am. J. Pathol. 177 , 2421–2432 (2010).
Van Voorhis, W. C. et al . Primary and secondary syphilis lesions contain mRNA for Th1 cytokines. J. Infect. Dis. 173 , 491–495 (1996).
Van Voorhis, W. C., Barrett, L. K., Nasio, J. M., Plummer, F. A. & Lukehart, S. A. Lesions of primary and secondary syphilis contain activated cytolytic T cells. Infect. Immun. 64 , 1048–1050 (1996).
McBroom, R. L. et al . Secondary syphilis in persons infected with and not infected with HIV-1: a comparative immunohistologic study. Am. J. Dermatopathol. 21 , 432 (1999).
Radolf, J. D. & Lukehart, S. A. in Pathogenic Treponemes: Cellular and Molecular Biology (eds Radolf, J. D. & Lukehart, S. A. ) 285–322 (Horizon Scientific Press, 2006).
Lukehart, S. A. L., Shaffer, J. M. & Baker-Zander, S. A. Subpopulation of Treponema pallidum is resistant to phagocytosis: possible mechanism of persistence. J. Infect. Dis. 166 , 1449–1453 (1992).
Cox, D. L. et al . Surface immunolabeling and consensus computational framework to identify candidate rare outer membrane proteins of Treponema pallidum . Infect. Immun. 78 , 5178–5194 (2010).
Nelson, R. A. Jr. & Mayer, M. M. Immobilization of Treponema pallidum in vitro by antibody produced in syphilitic infection. J. Exp. Med. 89 , 369–393 (1949).
Bishop, N. H. & Miller, J. N. Humoral immunity in experimental syphilis. II. The relationship of neutralizing factors in immune serum to acquired resistance. J. Immunol. 117 , 197–207 (1976).
Giacani, L., Lukehart, S. & Centurion-Lara, A. Length of guanosine homopolymeric repeats modulates promoter activity of subfamily II tpr genes of Treponema pallidum ssp. pallidum. FEMS Immunol. Med. Microbiol. 51 , 289–301 (2007).
Giacani, L. et al . Transcription of TP0126, Treponema pallidum putative OmpW Homolog, is regulated by the length of a homopolymeric guanosine repeat. Infect. Immun. 83 , 2275–2289 (2015).
Deitsch, K. W., Lukehart, S. A. & Stringer, J. R. Common strategies for antigenic variation by bacterial, fungal and protozoan pathogens. Nat. Rev. Microbiol. 7 , 493–503 (2009).
Harter, C. & Benirschke, K. Fetal syphilis in the first trimester. Am. J. Obstet. Gynecol. 124 , 705–711 (1976).
Qin, J. et al . Reported estimates of adverse pregnancy outcomes among women with and without syphilis: a systematic review and meta-analysis. PLoS ONE 9 , e102203 (2014). Together with Ref. 45, these two large systematic reviews estimated the extent of adverse pregnancy outcomes caused by untreated maternal syphilis and provided our best evidence on adverse pregnancy outcomes associated with syphilis.
Muller, I. et al . Is serological testing a reliable tool in laboratory diagnosis of syphilis? Meta-analysis of eight external quality control surveys performed by the German Infection Serology Proficiency Testing Program. J. Clin. Microbiol. 44 , 1335–1341 (2006).
Parekh, B. S. et al . Dried tube specimens: a simple and cost-effective method for preparation of HIV proficiency testing panels and quality control materials for use in resource-limited settings. J. Virol. Methods 163 , 295–300 (2010).
Beber, A. M. B., Sabidó, M., Vieira, J. M. R., Bazzo, M. L. & Benzaken, A. S. External quality assessment in the voluntary counseling and testing centers in the Brazilian Amazon using dried tube specimens: results of an effectiveness evaluation. Rev. Soc. Bras. Med. Trop. 48 , 87–97 (2015).
Benzaken, A. S. et al . External quality assurance with dried tube specimens (DTS) for point-of-care syphilis and HIV tests: experience in an indigenous populations screening programme in the Brazilian Amazon. Sex. Transm. Infect. 90 , 14–18 (2013).
Smit, P. W. et al . The development and validation of dried blood spots for external quality assurance of syphilis serology. BMC Infect. Dis. 13 , 102 (2013).
Sparling, P. F. in Sexually Transmitted Diseases 3rd edn (eds Holmes, K. K., Sparling, P. F. & Mardh, P. A. ) 473–478 (McGraw-Hill Medical, 1999).
Centre for Disease Control and Prevention & Pan American Health Organization. Syphilis testing practices in the Americas region: results of the 2014 survey. Pan American Health Organization http://www2.paho.org/hq/index.php?option=com_docman&task=doc_view&Itemid=270&gid=37676&lang=en (2016).
Chi, K.-H. et al . Molecular differentiation of Treponema pallidum subspecies in skin ulceration clinically suspected as yaws in Vanuatu using real-time multiplex PCR and serological methods. Am. J. Trop. Med. Hyg. 92 , 134–138 (2014).
Liu, H., Rodes, B., Chen, C.-Y. & Steiner, B. New tests for syphilis: rational design of a PCR method for detection of Treponema pallidum in clinical specimens using unique regions of the DNA polymerase I Gene. J. Clin. Microbiol. 39 , 1941–1946 (2001).
Gayet-Ageron, A., Lautenschlager, S., Ninet, B., Perneger, T. V. & Combescure, C. Sensitivity, specificity and likelihood ratios of PCR in the diagnosis of syphilis: a systematic review and meta-analysis. Sex. Transm. Infect. 89 , 251–256 (2013).
Castro, R. et al . Detection of Treponema pallidum sp. pallidum DNA in cerebrospinal fluid (CSF) by two PCR techniques. J. Clin. Lab. Anal. 30 , 628–632 (2016).
Fraga, D. et al . Detection of Treponema pallidum by semi-nested PCR in the cerebrospinal fluid of asymptomatic HIV-infected patients with latent syphilis. Clin. Lab. 60 , 2051–2054 (2014).
Creegan, L. et al . An evaluation of the relative sensitivities of the venereal disease research laboratory test and the Treponema pallidum particle agglutination test among patients diagnosed with primary syphilis. Sex. Transm. Dis. 34 , 1016–1018 (2007).
Wende, R. D., Mudd, R. L., Know, J. M. & Holder, W. R. The VDRL slide test in 322 cases of darkfield positive primary syphilis. South. Med. J. 64 , 633–634 (1971).
Peeling, R. W., Holmes, K. K., Mabey, D. & Ronald, A. Rapid tests for sexually transmitted infections (STIs): the way forward. Sex. Transm. Infect. 82 (Suppl. 5), 1–6 (2006).
Pastuszczak, M. et al . Robust pro-inflammatory immune response is associated with serological cure in patients with syphilis: an observational study. Sex. Transm. Infect. 93 , 11–14 (2016).
Larsen, S. A. & Johnson, R. E. A Manual of Tests for Syphilis: Diagnostic Tests 9th edn https://www.cdc.gov/std/syphilis/manual-1998/chapt1.pdf (1998).
Sparling, P. F. Diagnosis and treatment of syphilis. N. Engl. J. Med. 284 , 642–653 (1971).
Fiumara, N. J. Posttreatment serological response of biologic false-positive reactors. JAMA 247 , 817–818 (1982).
Donkers, A., Levy, H. R. & Letens-van Vliet, A. Syphilis detection using the Siemens ADVIA Centaur Syphilis treponemal assay. Clin. Chim. Acta 433 , 84–87 (2014).
Gomez, E., Jespersen, D. J., Harring, J. A. & Binnicker, M. J. Evaluation of the Bio-Rad BioPlex 2200 syphilis multiplex flow immunoassay for the detection of IgM- and IgG-class antitreponemal antibodies. Clin. Vaccine Immunol. 17 , 966–968 (2010).
Sambri, V. et al . Western immunoblotting with five Treponema pallidum recombinant antigens for serologic diagnosis of syphilis. Clin. Vaccine Immunol. 8 , 534–539 (2001).
Wong, E. H. et al . Evaluation of an IgM/IgG sensitive enzyme immunoassay and the utility of index values for the screening of syphilis infection in a high-risk population. Sex. Transm. Dis. 38 , 528–532 (2011).
Centers for Disease Control and Prevention (CDC). Discordant results from reverse sequence syphilis screening — five laboratories, United States, 2006–2010. MMWR Morb. Mortal. Wkly Rep. 60 , 133–137 (2011).
Centers for Disease Control and Prevention (CDC). Syphilis testing algorithms using treponemal tests for initial screening — four laboratories, New York City, 2005–2006. MMWR Morb. Mortal. Wkly Rep. 57 , 872–875 (2008).
Peeling, R. W. & Ye, H. Diagnostic tools for preventing and managing maternal and congenital syphilis: an overview. Bull. World Health Organ. 82 , 439–446 (2004).
Benzaken, A. S. et al . Field performance of a rapid point-of-care diagnostic test for antenatal syphilis screening in the Amazon region. Int. J. STD AIDS 22 , 15–18 (2011).
Mabey, D. et al . Prospective, multi-centre clinic-based evaluation of four rapid diagnostic tests for syphilis. Sex. Transm. Infect. 82 (Suppl. 5), 13–16 (2006).
Mabey, D. C. et al . Point-of-care tests to strengthen health systems and save newborn lives: the case of syphilis. PLoS Med. 9 , e1001233 (2012).
Siedner, M., Zapitz, V., Ishida, M., De La Roca, R. & Klausner, J. D. Performance of rapid syphilis tests in venous and fingerstick whole blood specimens. Sex. Transm. Dis. 31 , 557–560 (2004).
Tinajeros, F. et al . Diagnostic accuracy of a point-of-care syphilis test when used among pregnant women in Bolivia. Sex. Transm. Infect. 82 (Suppl. 5), 17–21 (2006).
West, B. Performance of the rapid plasma reagin and the rapid syphilis screening tests in the diagnosis of syphilis in field conditions in rural Africa. Sex. Transm. Infect. 78 , 282–285 (2002).
Gianino, M. M. et al . Performance and costs of a rapid syphilis test in an urban population at high risk for sexually transmitted infections. J. Prev. Med. Hyg. 48 , 118–122 (2007).
Hernández-Trejo, M., Hernández-Prado, B., Uribe-Salas, F., Juárez-Figueroa, L. & Conde-González, C. J. Maternal and congenital syphilis in two Mexican hospitals: evaluation of a rapid diagnostic test [Spanish]. Rev. Invest. Clin. 58 , 119–125 (2006).
Lien, T. X. et al . Evaluation of rapid diagnostic tests for the detection of human immunodeficiency virus types 1 and 2, hepatitis B surface antigen, and syphilis in Ho Chi Minh City. Am. J. Trop. Med. Hyg. 62 , 301–309 (2000).
Galvao, T. F. et al . Safety of benzathine penicillin for preventing congenital syphilis: a systematic review. PLoS ONE 8 , e56463 (2013).
Castro, A. R. et al . Novel point-of-care test for simultaneous detection of nontreponemal and treponemal antibodies in patients with syphilis. J. Clin. Microbiol. 48 , 4615–4619 (2010).
Yin, Y.-P. et al . A dual point-of-care test shows good performance in simultaneously detecting nontreponemal and treponemal antibodies in patients with syphilis: a multisite evaluation study in China. Clin. Infect. Dis. 56 , 659–665 (2012).
Causer, L. M. et al . An evaluation of a novel dual treponemal/nontreponemal point-of-care test for syphilis as a tool to distinguish active from past treated infection. Clin. Infect. Dis. 61 , 184–191 (2015).
Gliddon, H. D. et al . A systematic review and meta-analysis of studies evaluating the performance and operational characteristics of dual point-of-care tests for HIV and syphilis. Sex. Transm. Infect. http://dx.doi.org/10.1136/sextrans-2016-053069 (2017).
Ghanem, K. G. & Workowski, K. A. Management of adult syphilis. Clin. Infect. Dis. 53 (Suppl. 3), 110–128 (2011).
Kingston, M. et al . UK national guidelines on the management of syphilis 2015. Int. J. STD AIDS 27 , 421–446 (2016).
Marra, C. M. et al . The rapid plasma reagin test cannot replace the venereal disease research laboratory test for neurosyphilis diagnosis. Sex. Transm. Dis. 39 , 453–457 (2012).
Marra, C. M., Tantalo, L. C., Maxwell, C. L., Dougherty, K. & Wood, B. Alternative cerebrospinal fluid tests to diagnose neurosyphilis in HIV-infected individuals. Neurology 63 , 85–88 (2004).
Marra, C. M., Maxwell, C. L., Dunaway, S. B., Sahi, S. K. & Tantalo, L. C. Cerebrospinal Fluid Treponema pallidum particle agglutination assay for neurosyphilis diagnosis. J. Clin. Microbiol. 55 , 1865–1870 (2017).
Marra, C. M. et al . Cerebrospinal fluid abnormalities in patients with syphilis: association with clinical and laboratory features. J. Infect. Dis. 189 , 369–376 (2004).
Meyers, D. et al . USPSTF recommendations for STI screening. Am. Fam. Physician 77 , 819–824 (2008).
Owusu-Ofori, A., Parry, C. & Bates, I. Transfusion-transmitted syphilis in teaching hospital. Emerg. Infect. Dis. 17 , 2080–2082 (2011).
Food and Drug Administration. Requirements for blood and blood components intended for transfusion or for further manufacturing use; Federal Register, Rules and Regulations. Government Publishing Office https://www.gpo.gov/fdsys/pkg/FR-2015-05-22/pdf/2015-12228.pdf (2015).
Tapko, J. B., Toure, B. & Sambo, L. G. Status of blood safety in the WHO African region: report of the 2010 survey. World Health Organization http://www.afro.who.int/index.php?option=com_docman&task=doc_download&gid=9135&Itemid=2593 (2014).
Hossain, M., Broutet, N. & Hawkes, S. The elimination of congenital syphilis: a comparison of the proposed World Health Organization action plan for the elimination of congenital syphilis with existing national maternal and congenital syphilis policies. Sex. Transm. Dis. 34 , S22–S30 (2007).
Hawkes, S., Matin, N., Broutet, N. & Low, N. Effectiveness of interventions to improve screening for syphilis in pregnancy: a systematic review and meta-analysis. Lancet Infect. Dis. 11 , 684–691 (2011). This systematic review of 10 studies showed that interventions to improve the coverage and effect of screening programmes for antenatal syphilis could reduce the syphilis-attributable incidence of stillbirth and perinatal death by 50%.
Swartzendruber, A., Steiner, R. J., Adler, M. R., Kamb, M. L. & Newman, L. M. Introduction of rapid syphilis testing in antenatal care: a systematic review of the impact on HIV and syphilis testing uptake and coverage. Int. J. Gynecol. Obstet. 130 , S15–S21 (2015).
Valderrama, J., Zacarías, F. & Mazin, R. Sífilis materna y sífilis congénita en América Latina: un problema grave de solución sencilla [Spanish]. Rev. Panam. Salud Pública 16 , 211–217 (2004).
Pan American Health Organization. Update 2014: elimination of mother-to-child transmission of HIV and syphilis in the Americas. Pan American Health Organization http://iris.paho.org/xmlui/handle/123456789/31357 (2014).
Cantor, A. G., Pappas, M., Daeges, M. & Nelson, H. D. Screening for syphilis. JAMA 315 , 2328 (2016).
Tuite, A. & Fisman, D. Go big or go home: impact of screening coverage on syphilis infection dynamics. Sex. Transm. Infect. 92 , 49–54 (2015).
Reed, J. L. et al . Adolescent patient preferences surrounding partner notification and treatment for sexually transmitted infections. Acad. Emerg. Med. 22 , 61–66 (2014).
Tucker, J. D. et al . Organizational characteristics of HIV/syphilis testing services for men who have sex with men in South China: a social entrepreneurship analysis and implications for creating sustainable service models. BMC Infect. Dis. http://dx.doi.org/10.1186/s12879-014-0601-5 (2014).
Tucker, J. D., Fenton, K. A., Peckham, R. & Peeling, R. W. Social Entrepreneurship for Sexual Health (SESH): a new approach for enabling delivery of sexual health services among most-at-risk populations. PLoS Med. 9 , e1001266 (2012).
Dubourg, G. & Raoult, D. The challenges of preexposure prophylaxis for bacterial sexually transmitted infections. Clin. Microbiol. Infect. 22 , 753–756 (2016).
Molina, J.-M. et al . On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N. Engl. J. Med. 373 , 2237–2246 (2015).
NIH Consensus Development Panel on Infectious Disease Testing for Blood Transfusions et al . Infectious disease testing for blood transfusions. JAMA 274 , 1374–1379 (1995).
Gardella, C., Marfin, A. A., Kahn, R. H., Swint, E. & Markowitz, L. E. Persons with early syphilis identified through blood or plasma donation screening in the United States. J. Infect. Dis. 185 , 545–549 (2002).
Marfin, A. A. et al . Amplification of the DNA polymerase I gene of Treponema pallidum from whole blood of persons with syphilis. Diagn. Microbiol. Infect. Dis. 40 , 163–166 (2001).
Chambers, R. W., Foley, H. T. & Schmidt, P. J. Transmission of syphilis by fresh blood components. Transfusion 9 , 32–34 (1969).
Seña, A. C. et al . A systematic review of syphilis serological treatment outcomes in HIV-infected and HIV-uninfected persons: rethinking the significance of serological non-responsiveness and the serofast state after therapy. BMC Infect. Dis. 15 , 479 (2015).
Seña, A. C. et al . Predictors of serological cure and serofast state after treatment in HIV-negative persons with early syphilis. Clin. Infect. Dis. 53 , 1092–1099 (2011).
Riedner, G. et al . Single-dose azithromycin versus penicillin G benzathine for the treatment of early syphilis. N. Engl. J. Med. 353 , 1236–1244 (2005).
Hook III, E. W. et al . A phase III equivalence trial of azithromycin versus benzathine penicillin for treatment of early syphilis. J. Infect. Dis. 201 , 1729–1735 (2010).
Lukehart, S. A. et al . Macrolide resistance in Treponema pallidum in the United States and Ireland. N. Engl. J. Med. 351 , 154–158 (2004).
Zhou, P. et al . Azithromycin treatment failure among primary and secondary syphilis patients in Shanghai. Sex. Transm. Dis. 37 , 726–729 (2010).
Read, P. et al . Azithromycin-resistant syphilis-causing strains in Sydney, Australia: prevalence and risk factors. J. Clin. Microbiol. 52 , 2776–2781 (2014).
Stamm, L. V. Global challenge of antibiotic-resistant Treponema pallidum . Antimicrob. Agents Chemother. 54 , 583–589 (2010).
Grillová, L. et al . Molecular typing of Treponema pallidum in the Czech Republic during 2011 to 2013: increased prevalence of identified genotypes and of isolates with macrolide resistance. J. Clin. Microbiol. 52 , 3693–3700 (2014).
Ghanem, K. G. et al . Antiretroviral therapy is associated with reduced serologic failure rates for syphilis among HIV-infected patients. Clin. Infect. Dis. 47 , 258–265 (2008).
Ghanem, K. G. et al . Neurosyphilis in a clinical cohort of HIV-1-infected patients. AIDS 22 , 1145–1151 (2008).
Tuddenham, S. & Ghanem, K. G. Emerging trends and persistent challenges in the management of adult syphilis. BMC Infect. Dis. 15 , 351 (2015).
Zetola, N. M. & Klausner, J. D. Syphilis and HIV infection: an update. Clin. Infect. Dis. 44 , 1222–1228 (2007).
Yang, C.-J. et al . One dose versus three weekly doses of benzathine penicillin G for patients co-infected with HIV and early syphilis: a multicenter, prospective observational study. PLoS ONE 9 , e109667 (2014).
Ganesan, A. et al . A single dose of benzathine penicillin G is as effective as multiple doses of benzathine penicillin G for the treatment of hiv-infected persons with early syphilis. Clin. Infect. Dis. 60 , 653–660 (2014).
Watson-Jones, D. et al . Syphilis in pregnancy in Tanzania. II. The effectiveness of antenatal syphilis screening and single-dose benzathine penicillin treatment for the prevention of adverse pregnancy outcomes. J. Infect. Dis. 186 , 948–957 (2002).
Terris-Prestholt, F. Is antenatal syphilis screening still cost effective in sub-Saharan Africa. Sex. Transm. Infect. 79 , 375–381 (2003).
Singh, A. E. & Romanowski, B. Syphilis: review with emphasis on clinical, epidemiologic, and some biologic features. Clin. Microbiol. Rev. 12 , 187–209 (1999). An excellent review that covered all aspects of syphilis.
Centers for Disease Control and Prevention. 2015 Sexually Transmitted Diseases Treatment Guidelines: Syphilis. Centers for Disease Control and Prevention https://www.cdc.gov/std/tg2015/syphilis.htm (2015).
Harman, N. B. in Venereal Disease 33–44 (Methuen & Company, Limited 1917).
Frith, J. Syphilis — its early history and treatment until penicillin and the debate on its origins. J. Mil. Veterans Health 20 , 49–28 (2012).
Sartin, J. S. & Perry, H. O. From mercury to malaria to penicillin: the history of the treatment of syphilis at the Mayo Clinic — 1916–1955. J. Am. Acad. Dermatol. 32 , 255–261 (1995).
Lopes, C., Powell, M. L. & Santos, A. L. Syphilis and cirrhosis: a lethal combination in a XIX century individual identified from the Medical Schools Collection at the University of Coimbra (Portugal). Mem. Inst. Oswaldo Cruz 105 , 1050–1053 (2010).
Bjarne, B. The “rade” disease--a Norwegian tragedy [Norwegian]. Tidsskr. Nor. Laegeforen. 24 , 3557–3558 (2003).
Division of STD Prevention et al . Sexually Transmitted Diseases Surveillance 2015. Centers for Disease Control and Prevention https://www.cdc.gov/std/stats15/ (2015).
Ropper, A. H. Two centuries of neurology and psychiatry in the journal. N. Engl. J. Med. 367 , 58–65 (2012).
Oliver, S. E. et al . Ocular syphilis — eight jurisdictions, United States, 2014–2015. MMWR. Morb. Mortal. Wkly. Rep. 65 , 1185–1188 (2016).
Moradi, A. et al . Clinical features and incidence rates of ocular complications in patients with ocular syphilis. Am. J. Ophthalmol. 159 , 334–343.e1 (2015).
Andreyev, S. V., Setko, N. P. & Voronina, L. G. Assessment of quality of life of patients with syphilis. Prakt. Med. Infect. Dis. 7 , 1 (2014).
Ferreira, A., Young, T., Mathews, C., Zunza, M. & Low, N. Strategies for partner notification for sexually transmitted infections, including HIV. Cochrane Database Syst. Rev. 3 , CD002843 (2013).
Rzepa, T., Jakubowicz, O., Witmanowski, H. & Zaba, R. Disease-induced level of shame in patients with acne, psoriasis and syphilis. Postepy Dermatol. Alergol. 30 , 233–236 (2013).
Wu, D. & Hawkes, S. Eliminating mother-to-child transmission of syphilis: the need for more consistent political commitment. J. Publ. Health Emerg. 1 , 41 (2016).
Burden, C. et al . From grief, guilt pain and stigma to hope and pride — a systematic review and meta-analysis of mixed-method research of the psychosocial impact of stillbirth. BMC Pregnancy Childbirth http://dx.doi.org/10.1186/s12884-016-0800-8 (2016).
Heazell, A. E. P. et al . Stillbirths: economic and psychosocial consequences. Lancet 387 , 604–616 (2016).
Kiguli, J. et al . Stillbirths in sub-Saharan Africa: unspoken grief. Lancet 387 , e16–e18 (2016).
Fitzgerald, D. W. & Behets, F. M. A piece of my mind. Beyond folklore. JAMA 288 , 2791–2792 (2002).
Meheus, A. & Antal, G. M. The endemic treponematoses: not yet eradicated. World Health Stat. Q. 45 , 228–237 (1992).
Taylor, M. M. et al . Estimating benzathine penicillin need for the treatment of pregnant women diagnosed with syphilis during antenatal care in high-morbidity countries. PLoS ONE 11 , e0159483 (2016).
Peeling, R. W. & Mabey, D. Celebrating the decline in syphilis in pregnancy: a sobering reminder of what's left to do. Lancet. Glob. Health 4 , e503–e504 (2016).
World Health Organization. Global guidance on criteria and processes for validation: elimination of mother-to-child transmission of HIV and syphilis. >WHO http://apps.who.int/iris/bitstream/10665/112858/1/9789241505888_eng.pdf (2014).
World Health Organization. WHO information note on the use of dual HIV/Syphilis rapid diagnostic tests (RDT). WHO http://www.who.int/reproductivehealth/publications/rtis/dual-hiv-syphilis-diagnostic-tests/en/ (2017).
Wedderburn, C. J., Murtagh, M., Toskin, I. & Peeling, R. W. Using electronic readers to monitor progress toward elimination of mother-to-child transmission of HIV and syphilis: an opinion piece. Int. J. Gynecol. Obstet. 130 , S81–S83 (2015).
Guo, T., Patnaik, R., Kuhlmann, K., Rai, A. J. & Sia, S. K. Smartphone dongle for simultaneous measurement of hemoglobin concentration and detection of HIV antibodies. Lab Chip 15 , 3514–3520 (2015).
Peeling, R. W. Diagnostics in a digital age: an opportunity to strengthen health systems and improve health outcomes. Int. Health 7 , 384–389 (2015).
Hook, E. W. Syphilis. Lancet 389 , 1550–1557 (2017).
Lewnard, J. A. & Berrang-Ford, L. Internet-based partner selection and risk for unprotected anal intercourse in sexual encounters among men who have sex with men: a meta-analysis of observational studies. Sex. Transm. Infect. 90 , 290–296 (2014).
Tuddenham, S., Shah, M. & Ghanem, K. G. Syphilis and HIV: is HAART at the heart of this epidemic? Sex. Transm. Infect. 93 , 311–312 (2017).
Ho, E. L., Tantalo, L. C., Jones, T., Sahi, S. K. & Marra, C. M. Point-of-care treponemal tests for neurosyphilis diagnosis. Sex. Transm. Dis. 42 , 48–52 (2015).
Lin, L.-R. et al . Macrophage migration inhibitory factor as a novel cerebrospinal fluid marker for neurosyphilis among HIV-negative patients. Clin. Chim. Acta 463 , 103–108 (2016).
Marra, C. M., Tantalo, L. C., Sahi, S. K., Maxwell, C. L. & Lukehart, S. A. CXCL13 as a cerebrospinal fluid marker for neurosyphilis in HIV-infected patients with syphilis. Sex. Transm. Dis. 37 , 283–287 (2010).
Cameron, C. E. & Lukehart, S. A. Current status of syphilis vaccine development: need, challenges, prospects. Vaccine 32 , 1602–1609 (2014). This review described the progress in vaccine development for syphilis and all the challenges that need to be overcome.
Miller, J. N. Immunity in experimental syphilis. VI. Successful vaccination of rabbits with Treponema pallidum , Nichols strain, attenuated by -irradiation. J. Immunol. 110 , 1206–1215 (1973).
Arora, N. et al . Origin of modern syphilis and emergence of a pandemic Treponema pallidum cluster. Nat. Microbiol. 2 , 16245 (2016).
Izard, J. et al . Cryo-electron tomography elucidates the molecular architecture of Treponema pallidum , the syphilis spirochete. J. Bacteriol. 191 , 7566–7580 (2009).
Liu, J. et al . Cellular architecture of Treponema pallidum : novel flagellum, periplasmic cone, and cell envelope as revealed by cryo electron tomography. J. Mol. Biol. 403 , 546–561 (2010).
Brautigam, C. A., Deka, R. K., Liu, W. Z. & Norgard, M. V. Insights into the potential function and membrane organization of the TP0435 (Tp17) lipoprotein from Treponema pallidum derived from structural and biophysical analyses. Protein Sci. 24 , 11–19 (2014).
Erkens, G. B., Majsnerowska, M., ter Beek, J. & Slotboom, D. J. Energy coupling factor-type ABC transporters for vitamin uptake in prokaryotes. Biochemistry 51 , 4390–4396 (2012).
Boudker, O., Ryan, R. M., Yernool, D., Shimamoto, K. & Gouaux, E. Coupling substrate and ion binding to extracellular gate of a sodium-dependent aspartate transporter. Nature 445 , 387–393 (2007).
Brautigam, C. A., Deka, R. K., Schuck, P., Tomchick, D. R. & Norgard, M. V. Structural and thermodynamic characterization of the interaction between two periplasmic Treponema pallidum lipoproteins that are components of a TPR-protein-associated TRAP transporter (TPAT). J. Mol. Biol. 420 , 70–86 (2012).
Deka, R. K. et al . Structural, bioinformatic, and in vivo analyses of two Treponema pallidum lipoproteins reveal a unique TRAP transporter. J. Mol. Biol. 416 , 678–696 (2012).
Park, I. U. et al . Screening for syphilis with the treponemal immunoassay: analysis of discordant serology results and implications for clinical management. J. Infect. Dis. 204 , 1297–1304 (2011).
Binnicker, M. J., Yao, J. D. & Cockerill, F. R. Non-treponemal serologic tests: a supplemental, not confirmatory testing approach. Clin. Infect. Dis. 52 , 274–275 (2010).
Lipinsky, D., Schreiber, L., Kopel, V. & Shainberg, B. Validation of reverse sequence screening for syphilis. J. Clin. Microbiol. 50 , 1501 (2012).
Tong, M.-L. et al . Analysis of 3 algorithms for syphilis serodiagnosis and implications for clinical management. Clin. Infect. Dis. 58 , 1116–1124 (2014).
Tucker, J. D. et al . Accelerating worldwide syphilis screening through rapid testing: a systematic review. Lancet Infect. Dis. 10 , 381–386 (2010).
Jafari, Y. et al . Are Treponema pallidum specific rapid and point-of-care tests for syphilis accurate enough for screening in resource limited settings? Evidence from a meta-analysis. PLoS ONE 8 , e54695 (2013).
World Health Organization. Laboratory diagnosis of sexually transmitted infections, including human immunodeficiency virus. WHO http://who.int/reproductivehealth/publications/rtis/9789241505840/en/ (2013).
Download references
Acknowledgements
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the US Centers for Disease Control and Prevention.
Author information
Authors and affiliations.
London School of Hygiene & Tropical Medicine, Keppel Street, London, WC1E 7HT, UK
Rosanna W. Peeling & David Mabey
Division of STD Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD and TB Prevention, Centers for Disease Control and Prevention, Atlanta, Georgia, USA
Mary L. Kamb
National Center for STD Control, Chinese Academy of Medical Sciences and Peking Union Medical College Institute of Dermatology, Nanjing, China
Xiang-Sheng Chen
Department of Medicine, UConn Health, Farmington, Connecticut, USA
Justin D. Radolf
Department of Surveillance, Prevention and Control of STI, HIV/AIDS and Viral Hepatitis, Ministry of Health, Brasília, Brazil
Adele S. Benzaken
You can also search for this author in PubMed Google Scholar
Contributions
Introduction (R.W.P. and D.M.); Epidemiology (D.M. and X.-S.C.); Mechanisms/pathophysiology (J.D.R.); Diagnosis, screening and prevention (R.W.P., M.L.K., X.-S.C. and A.S.B.); Management (D.M.); Quality of life (M.K. and A.S.B.); Outlook (all authors); overview of the Primer (R.W.P.).
Corresponding author
Correspondence to Rosanna W. Peeling .
Ethics declarations
Competing interests.
J.D.R. receives royalties for licensing of syphilis diagnostics reagents. The other authors declare no competing interests.
PowerPoint slides
Powerpoint slide for fig. 1, powerpoint slide for fig. 2, powerpoint slide for fig. 3, powerpoint slide for fig. 4, powerpoint slide for fig. 5, powerpoint slide for fig. 6, powerpoint slide for fig. 7, rights and permissions.
Reprints and permissions
About this article
Cite this article.
Peeling, R., Mabey, D., Kamb, M. et al. Syphilis. Nat Rev Dis Primers 3 , 17073 (2017). https://doi.org/10.1038/nrdp.2017.73
Download citation
Published : 12 October 2017
DOI : https://doi.org/10.1038/nrdp.2017.73
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Ocular syphilis masquerading as refractory retinal diseases.
- Sung Who Park
- Kye-Hyung Kim
- Quan Dong Nguyen
BMC Infectious Diseases (2024)
A multi-country comparative study of two treponemal tests for the serodiagnosis of syphilis amongst men who have sex with men (MSM): Chemo-luminescent assay vs Treponema pallidum particle agglutination assay
- Lorenzo Gios
- Massimo Mirandola
- Igor Toskin
Social and individual vulnerability factors associated with syphilis among populations living on islands in the Brazilian Amazon
- Ellen Christiane Correa Pinho
- José Jorge da Silva Galvão
- Glenda Roberta Oliveira Naiff Ferreira
An observational prospective study based on a large cohort of HIV-negative neurosyphilis patients with particular reference to the Jarisch-Herxheimer reaction
- Rui-Rui Peng
- Pingyu Zhou
European Journal of Clinical Microbiology & Infectious Diseases (2024)
An unusual cardiac magnetic resonance finding in a patient with syphilis presenting with heart block
- Akshay Nandagopal
- Babu Peter Sathyanathan
Egyptian Journal of Radiology and Nuclear Medicine (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Help & Feedback
- About epocrates
Syphilis infection
Highlights & basics, diagnostic approach, risk factors, history & exam, differential diagnosis.
- Tx Approach
Emerging Tx
Complications.
PATIENT RESOURCES
Patient Instructions
Syphilis is a common sexually transmitted infection. An estimated 6 million new infections occurred worldwide in 2016. Incidence of congenital, primary, and secondary syphilis is increasing.
Caused by the spirochetal bacterium Treponema pallidum , subspecies pallidum .
Clinical presentation is often asymptomatic, but can manifest in a number of ways.
A painless ulcer (chancre) in the anogenital region is a hallmark of primary infection.
Diagnosis is usually straightforward after clinical exam and serologic tests.
Syphilis infection is treated with penicillin.
Untreated syphilis facilitates HIV transmission and causes considerable morbidity, such as cardiovascular and neurologic disease, as well as a congenital syndrome in the newborn.
Syphilis in pregnancy is a major cause of miscarriage, stillbirth, and perinatal morbidity and mortality in some parts of the world.
Quick Reference
Key Factors
anogenital ulcer
Lymphadenopathy, diffuse rash, constitutional symptoms, rhinitis (congenital syphilis), hepatosplenomegaly (congenital syphilis), patchy alopecia, condylomata lata, memory impairment, altered mood, confusion, or dementia, visual changes, argyll-robertson pupils, loss of sense of vibration, proprioception, and position sense, loss of anal and bladder sphincter control, positive romberg sign, diastolic murmur, rubbery lesions/nodules with a necrotic center, miscarriage, stillbirth, or neonatal death (congenital syphilis), premature labor and intrauterine growth retardation (congenital syphilis), neonatal skin rash (congenital syphilis), tibial bowing (congenital syphilis), craniofacial malformation (congenital syphilis), tooth abnormalities (congenital syphilis), necrotizing funisitis (congenital syphilis).
Other Factors
mouth ulcer
Asymptomatic with positive serology (latent syphilis), meningismus, hearing loss, peripheral edema, peripheral neuropathy, organomegaly, skin or visceral organ perforation or collapse of structure, neonatal neurologic abnormalities (congenital syphilis).
Diagnostics Tests
1st Tests to Order
dark-field microscopy of swab from lesion
Serum treponemal enzyme immunoassay (eia), serum treponema pallidum particle agglutination (tppa), serum treponema pallidum hemagglutination (tpha), serum fluorescent treponemal antibody absorption (fta-abs) test, immunocapture assay, line immunoassay (lia) serologic test, serum rapid plasma reagin (rpr) test, serum venereal disease research laboratory (vdrl) test.
Other Tests to consider
lumbar puncture, cerebrospinal fluid (CSF) analysis
Chest x-ray, echocardiogram, computed tomography brain, magnetic resonance imaging brain, fetal ultrasound scan, complete blood count, long-bone x-rays, liver enzymes (aspartate aminotransferase, alanine aminotransferase and alkaline phosphatase) and bilirubin, auditory brainstem response, fetal skeletal survey.
Emerging Tests
Treponema pallidum polymerase chain reaction (PCR) (sample taken directly from ulcerative lesions)
Point of care (poc) testing with either treponemal or combination treponemal/nontreponemal antibody, treatment options.
presumptive
adults with suspected early infection or sexual contacts of patients with confirmed infection
consideration of empiric antibiotics
adults without neurosyphilis
without penicillin allergy
with penicillin allergy: nonpregnant
with penicillin allergy: pregnant
Classifications
Classification according to transmission
Transmission through direct person-to-person sexual contact with an individual who has early (primary or secondary) syphilis.
Transmission from mother to fetus during pregnancy
May result in miscarriage, stillbirth, or neonatal death [ 3 ]
Early (clinical manifestations occur from birth to 2 years of age)
Late (clinical manifestations occur >2 years of age).
Acquired syphilis, classified according to stage of infection
Initial inoculation of Treponema pallidum into tiny abrasions caused by sexual trauma results in local infection [ 5 ]
A single macule develops, which changes into a papule and then ulcerates, forming a chancre 9-90 days after exposure (usually 14-21 days after exposure). [ 5 ]
Clinical features develop 4 to 8 weeks after primary syphilis infection
Later presentation can occur up to 6 months after primary infection [ 6 ]
Characterized by spirochetemia and widespread dissemination of T pallidum to the skin and other tissues.
Asymptomatic infection diagnosed on the basis of positive serology alone, acquired <1 year previously (according to Centers for Disease Control and Prevention [CDC] criteria) or <2 years previously (according to World Health Organization [WHO] criteria). [ 7 ] [ 8 ]
Relapse to secondary syphilis may occur during the early latent stage.
Asymptomatic infection acquired >1 year previously (according to CDC criteria) or >2 years previously (according to WHO criteria) [ 7 ] [ 8 ]
The patient is not known to have been seronegative within the past year (according to CDC criteria) or past 2 years (according to WHO criteria). [ 7 ] [ 8 ]
It is estimated that 14% to 40% of patients with untreated syphilis progress to tertiary syphilis (late symptomatic disease) [ 6 ]
Characterized by chronic end-organ complications, often many years after initial infection
Includes cardiovascular syphilis, neurosyphilis, and gummatous syphilis.
Congenital syphilis, classified according to likelihood of infection
An abnormal physical exam that is consistent with congenital syphilis
A serum quantitative nontreponemal serologic titer that is fourfold (or greater) higher than the mother's titer at delivery (e.g., maternal titer = 1:2, neonatal titer ≥1:8 or maternal titer = 1:8, neonatal titer ≥1:32); or
A positive darkfield test or polymerase chain reaction of placenta, cord, lesions, or body fluids or a positive silver stain of the placenta or cord.
The mother was not treated, was inadequately treated, or has no documentation of having received treatment
The mother was treated with erythromycin or a regimen other than those recommended by the CDC (i.e., a nonpenicillin G regimen)
The mother received the recommended regimen but treatment was initiated <30 days before delivery.
The mother was treated during pregnancy, treatment was appropriate for the infection stage, and the treatment regimen was initiated ≥30 days before delivery
The mother has no evidence of reinfection or relapse.
The mother's treatment was adequate before pregnancy
The mother's nontreponemal serologic titer remained low and stable (i.e., serofast) before and during pregnancy and at delivery (e.g., Venereal Disease Research Laboratory test ≤1:2 or rapid plasma reagin test ≤1:4).
Common Vignette 1
Common Vignette 2
Other Presentations
Epidemiology
Pathophysiology.
- Juan C. Salazar, MD, MPH, FAAP
- Acknowledgements
- Robert A. Larsen, MD
- William Rodriguez, MD
- Jennifer Handforth, MB ChB, MRCPCH, DTM&H

Electron micrograph of Treponema pallidum on cultures of cotton-tail rabbit epithelium cells

A primary vulvar syphilitic chancre due to Treponema pallidum bacteria

A penile chancre located on the proximal penile shaft: primary syphilitic infection

Gummatous lesions on the dorsal surface of the left hand

Secondary syphilitic papulosquamous rash on the torso and upper body

Secondary syphilitic lesions on the face

Secondary syphilis presenting pigmented macules and papules on the skin

Secondary syphilitic lesions of vagina

This was a case of congenital syphilis resulting in the death of this newborn infant

This newborn presented with symptoms of congenital syphilis that included lesions on the soles of both feet

Interstitial keratitis

Peg-shaped, notched central incisors (Hutchinson teeth)

Osteoperiostitis of the tibia ("saber shins")

Clutton joints
Signs and symptoms of primary syphilis
Signs and symptoms of secondary syphilis, latent syphilis, signs and symptoms of tertiary syphilis.
Loss of anal and bladder sphincter control
Dorsal column loss (loss of vibration and proprioception/position sense)
Romberg sign.
Behavioral changes
Memory impairment
Altered mood
Argyll-Robertson pupils.
HIV coinfection
Primary syphilis: larger, painful multiple ulcers.
Secondary syphilis: genital ulcers more common and higher titers with rapid plasma reagin (RPR) testing and Venereal Disease Research Laboratory (VDRL) testing.
Possibly more rapid progression to neurosyphilis. [ 18 ]
Serologic responses to infection may be atypical. [ 34 ]
Signs and symptoms of congenital syphilis
Identification of syphilis in the mother
Adequacy of maternal treatment
Presence of clinical, laboratory, or radiographic evidence of syphilis in the infant (testing should include paired maternal and neonatal nontreponemal serologic titers using the same test, preferably conducted at the same laboratory).
Peg-shaped central incisors, notched at the apex (Hutchinson teeth)
Eighth cranial nerve deafness
Frontal bossing of the skull
Anterior bowing of the shins (Saber shins)
Saddle nose deformity
Clutton joints (symmetric painless knee swelling).
Initial investigations for acquired syphilis
Treponemal enzyme immunoassay (EIA)
T pallidum particle agglutination assay (TPPA)
T pallidum haemagglutination assay (TPHA)
Fluorescent antibody absorption (FTA-ABS)
Immunocapture assay (ICA).
EIA: 3 weeks
TPPA: 4-6 weeks
TPHA: 4-6 weeks.
RPR: 4 weeks
VDRL: 4 weeks.
Other initial investigations for acquired syphilis
Emerging investigations, further investigations for acquired syphilis.
CSF white blood cell (WBC) count >10 cells/mm³ (10 × 10⁶ cells/L)
CSF protein >50 mg/dL (0.50 g/L)
A positive CSF VDRL test.
Initial investigations for congenital syphilis
Further investigations for congenital syphilis.
An abnormal physical exam that is consistent with congenital syphilis (e.g., nonimmune hydrops, conjugated or direct hyperbilirubinemia or cholestatic jaundice or cholestasis, hepatosplenomegaly, rhinitis, skin rash, or pseudoparalysis of an extremity) or
A serum quantitative nontreponemal serologic titer that is fourfold higher than the mother's titer (e.g., maternal titer = 1:2, neonatal titer ≥1:8 or maternal titer = 1:8, neonatal titer ≥1:32) or
A positive dark-field test or PCR of placenta, cord, lesions or body fluids, or a positive silver stain of the placenta or cord.
The mother was not treated, was inadequately treated, or has no documentation of having received treatment or
The mother was treated with erythromycin or other nonpenicillin regimen or
The mother received treatment <4 weeks before delivery.
Infants and children ages ≥1 month with reactive serologic tests for syphilis.
sexual contact with an infected person
The risk of acquiring syphilis after sex with someone with primary or secondary syphilis is between 30% and 60%. [ 17 ]
men who have sex with men (MSM)
At higher risk, particularly if they are also HIV coinfected, use illicit drugs such as methamphetamine, or have multiple, casual sexual partners. [ 21 ] [ 22 ]
In 2021, almost half (46.5%) of all reported cases of primary and secondary syphilis in the US occurred in MSM. [ 12 ]
illicit drug use
Association due to the exchange of sex for money or drugs, particularly crack cocaine. [ 23 ]
commercial sex workers
Multiple sexual partners.
A risk factor for all STIs.
Important in syphilis epidemiology. [ 21 ]
people with HIV or other STIs
Suggests unprotected sexual intercourse, which increases the risk of STIs.
All patients who have an STI should have syphilis screening, as should patients at higher risk of STIs, irrespective of where they are seen.
syphilis during pregnancy (risk for congenital syphilis)
The fetus acquires the infection from the infected mother. Inadequate treatment of maternal syphilis accounts for up to one-third of congenital syphilis cases. [ 24 ]
This may result in miscarriage, stillbirth, or neonatal death. [ 3 ]
Screening for syphilis at the first prenatal visit aims to identify and treat asymptomatic infected women, thus preventing transplacental transmission. [ 25 ] The Centers for Disease Control and Prevention recommends repeating syphilis screening at 28 weeks' gestation and at delivery for women at high risk of syphilis infection. Risk factors for syphilis infection during pregnancy include commercial sex work, a history of substance misuse, sex with multiple partners, late entry into prenatal care (i.e., first visit during the second trimester or later) or no prenatal care, unstable housing or homelessness, and imprisonment of the woman or her partner. [ 8 ]
Initially a macule, developing into a papule and then ulcerating to form a chancre. Image
Classically appears in the anogenital area 14 to 21 days after exposure (primary infection).
Usually indurated, solitary, and painless. Image
May not always be noticed by the patient and examining physician, and it heals spontaneously.
Atypically may be multiple and painful. Coinfection with genital herpes or chancroid may cause painful ulceration. HIV coinfection may be associated with multiple ulcers.
Erosions on the genitalia may also occur in secondary syphilis. Image
Moderately enlarged, rubbery regional lymphadenopathy associated with the classical syphilitic ulcer (chancre) in primary infection.
Generalized lymphadenopathy may occur with secondary syphilis.
Symmetric macular, papular, or maculopapular rash in secondary syphilis. Image
Often widespread with mucous membrane involvement. Image
May desquamate.
Usually nonitchy, over the trunk, palms, soles, and scalp.
In dark-skinned patients may cause pruritus.
May accompany a history of constitutional symptoms such as fever and malaise.
Onset is usually 6 to 12 weeks after exposure.
Up to 25% of people who have untreated secondary syphilis develop relapsing episodes of rash and fever. [ 9 ] [ 17 ]
Rash also occurs in congenital syphilis.
Such as fever, malaise, myalgia, fatigue, and arthralgia with secondary syphilis.
May be mistaken for primary HIV infection or another intercurrent viral illness.
As a result of cardiovascular syphilis (tertiary disease), which may lead to heart failure.
May also be a constitutional symptom in secondary syphilis.
A sign of early congenital syphilis (occurring <2 years of age).
Discharge may be purulent and bloody.
Usually associated with other signs of disseminated infection (rash, mucous membrane ulceration).
May develop in secondary syphilis.
Slightly raised, or flat, round, or oval papules covered by gray exudates.
A sign of secondary syphilis.
May be present within moist areas of the perineum.
May be mistaken for genital warts.
Possible signs of neurosyphilis. [ 66 ]
Brain involvement in tertiary syphilis causes a range of syndromes, including cognitive and motor impairment, which are sometimes grouped under the broad term "general paresis".
Visual impairment may be a presenting feature of syphilitic iritis or uveitis, occurring in secondary infection.
Bilaterally small, irregular pupils, which do not constrict when exposed to bright light, but do constrict in response to accommodation.
A feature of tabes dorsalis occurring in tertiary syphilis.
Dorsal column loss is a feature of tabes dorsalis, occurring in tertiary syphilis.
Possible sign of cardiovascular syphilis (tertiary disease).
Diastolic murmur at the left sternal edge indicates aortic regurgitation, which may be due to aortitis caused by cardiovascular syphilis.
A sign of gummatous syphilis (also known as benign tertiary syphilis).
Affects skin and visceral organs.
The destructive gumma may gradually replace normal tissue.
Signs of congenital syphilis. [ 67 ]
Signs of early congenital syphilis.
May occur in early congenital syphilis (occurring <2 years of age).
This rash may be similar to the rash of secondary syphilis in adults. It may also be more widespread, bullous or papulonecrotic, or desquamating.
Initially the rash may be a vesicular rash with small blisters appearing on the palms and plantar surfaces of the feet. An erythematous or maculopapular rash, which is often copper-colored, may subsequently appear on the face, palms, and plantar surfaces of the feet. The rash may also affect the mouth, genitalia, and anus. Images
A sign of late congenital syphilis (occurring >2 years of age).
Due to neonatal osteochondritis in congenital syphilis. Image
Including frontal bossing, high cranium, and saddle nose.
Hutchinson teeth (peg-shaped incisors, notched at the apex), mulberry molars dome-shaped with small cusps at the apex.
Poorly mineralized teeth. Image
Necrotizing funisitis (inflammation of the umbilical cord) is virtually diagnostic of congenital syphilis. Usually found in preterm infants who are stillborn, or die within a few weeks of birth.
The umbilical cord has a specific appearance known as the "barberpole" cord as a result of inflammation of the matrix of the umbilical cord. [ 37 ]
May coexist with genital ulceration.
Occurs in both primary and secondary infection.
In secondary infection the mouth ulcers (snail track ulcers) will usually be coexistent with other symptoms or signs, such as rash, fever.
Latent syphilis is defined as positive serology in the absence of clinical features of syphilis.
Ulcers in primary syphilis may not be noticed by the patient and examining physician.
Possible sign of tertiary disease with brain involvement.
May indicate neurologic involvement.
May occur with neck stiffness.
May be a presenting feature of syphilitic iritis or uveitis, occurring in secondary infection.
The eighth cranial nerve is the most commonly affected cranial nerve in neurosyphilis.
Hearing loss may be a symptom and a sign of both early and late neurosyphilis.
Deafness may also occur as a result of late congenital syphilis (occurring >2 years of age).
Suggest neurologic involvement.
Occurs with nephrotic syndrome that may develop due to vasculitis in secondary syphilis.
May indicate hepatitis, due to vasculitis in secondary syphilis.
Sign of neurosyphilis.
Usually affecting lower limbs.
May occur in all forms of neurosyphilis.
As a result of cardiovascular syphilis (tertiary disease).
Aortic aneurysm caused by syphilis almost always affects the thoracic aorta (usually the ascending part of the thoracic aorta), resulting in heart failure.
Lesions in gummatous syphilis may cause organomegaly, and become infiltrative or destructive.
May occur as a result of gummatous syphilis.
May include a wide range of problems such as seizures, meningitis, obstructive hydrocephalus, and cranial nerve palsies.
coiled spirochete bacterium with a corkscrew appearance and motility
Performed to identify Treponema pallidum .
Can provide a definitive diagnosis of syphilis, but is not usually available outside specialist settings.
The lesion is cleansed and abraded with a gauze pad until serous exudates appear, which are collected onto a glass slide for microscopic analysis.
A single negative result does not exclude infection; ideally 3 negative examinations on different days are required.
Primary syphilis: sensitivity of dark-field microscopy is 74% to 86%, specificity is 85% to 100%. [ 5 ] [ 6 ] [ 39 ]
Secondary syphilis: dark-field microscopy may be positive from ulcerative anogenital lesions.
Gummata in tertiary syphilis have few, if any, identifiable T pallidum organisms.
Congenital syphilis: test suspicious lesions (e.g., bullous rash or nasal discharge). [ 8 ]
A treponemal serology test.
A patient with a positive treponemal test result will remain positive for life. Therefore, a positive result alone cannot distinguish between an active infection or past (treated) infection.
The most common approach is to use a treponemal test as the initial serologic test, followed by a nontreponemal test to confirm diagnosis and provide evidence of active disease or reinfection (i.e., a "reverse sequence screening algorithm"). [ 40 ]
False-positive results may occur with other nonsexually transmitted treponemal infection (e.g., yaws, pinta, bejel).
False-negative results may occur in incubating and early primary syphilis. It usually takes 3 weeks for an EIA IgG/IgM test to become positive after infection with Treponema pallidum .
EIA is the test generally used for screening. [ 10 ]
Primary syphilis: EIA sensitivity 82% to 100%, and specificity 97% to 100%. [ 68 ]
Secondary syphilis: EIA sensitivity is 100%. [ 68 ]
Late latent syphilis: EIA sensitivity is 98% to 100%. [ 68 ]
A patient with a positive treponemal test result will remain positive for life. Therefore, a positive result alone cannot distinguish between an active or past (treated) infection.
Primary syphilis: TPPA sensitivity is 85% to 100%, and specificity is 98% to 100%. [ 69 ] [ 70 ]
Secondary and late latent syphilis: TPPA sensitivity is 98% to 100%. [ 70 ]
FTA-ABS is used less often than TPHA and TPPA because it is less specific.
LIA serologic tests (e.g., INNO-LIA syphilis test) can be used to confirm syphilis infection following initial serologic treponemal testing. A single LIA test can confirm infection, making it more convenient than traditional methods of serologic confirmation (which usually require multiple assays). Studies evaluating the performance of LIA tests for syphilis infection have demonstrated higher sensitivity and specificity compared with FTA-ABS and TPHA serology tests. [ 49 ] [ 50 ]
A nontreponemal serology test.
Provides a quantitative measure of disease activity and can be used to monitor treatment response (RPR titers decrease or become nonreactive with effective treatment).
Despite adequate treatment, some patients maintain a persisting low level positive antibody titer (known as a serofast reaction). [ 44 ]
False positives may occur due to the presence of a variety of medical conditions (e.g., pregnancy, autoimmune disorders, and infections).
A false-negative test may occasionally occur in an undiluted specimen (the prozone phenomenon).
Primary syphilis: RPR sensitivity is 70% to 73%. [ 5 ] [ 71 ]
Secondary syphilis: RPR sensitivity is 100%. [ 71 ]
Preferred test over the serum Venereal Disease Research Laboratory test.
Congenital syphilis: include paired maternal and neonatal nontreponemal serologic titers using the same test, preferably conducted at the same laboratory. [ 8 ]
The Food and Drug Administration (FDA) has issued a warning of false-positive RPR results linked to COVID-19 vaccination. RPR false reactivity has been observed in some individuals for at least 5 months following the vaccine. The issue has been identified in the Bio-Rad BioPlex 2200 Syphilis Total & RPR test kit. It is not yet known if other RPR tests are affected similarly. For healthcare professionals who use the Bio-Rad BioPlex 2200 Syphilis Total & RPR test kit, the FDA recommends performing confirmatory testing for all reactive results. In patients previously treated for syphilis who received a COVID-19 vaccine, and whose clinical presentation and epidemiologic considerations do not support syphilis reinfection, reactive RPR results obtained from the BioPlex 2200 Syphilis Total & RPR test kit should be confirmed using an RPR test from a different manufacturer. [ 45 ]
Provides a quantitative measure of disease activity and can be used to monitor treatment response (VDRL titers decrease or become nonreactive with effective treatment).
Primary syphilis: VDRL sensitivity is 44% to 76%. [ 5 ]
VDRL is positive in 77% of cases of late latent syphilis. [ 5 ]
VDRL sensitivity in secondary syphilis is 100%. [ 71 ]
WBC count >10 cells/mm³; CSF protein >50 mg/dL; CSF VDRL positive; CSF TPHA/TPPA/FTA-ABS positive
Indicated for any patient with clinical evidence of neurologic involvement (e.g., cranial nerve dysfunction, meningitis, stroke, acute or chronic altered mental status, or loss of vibration sense).
Indicated if syphilis of unknown duration exists in the presence of HIV coinfection.
Indicated in any child with congenital syphilis and neurologic symptoms or signs. [ 8 ]
An elevated CSF WBC count and positive CSF Venereal Disease Research Laboratory (VDRL) suggests neurologic involvement. [ 31 ]
Some patients with neurosyphilis have an isolated elevated CSF WBC count and negative rapid plasma reagin/VDRL.
Neurosyphilis is unlikely at CSF Treponema pallidum hemagglutination assay (TPHA)/ T pallidum particle agglutination assay (TPPA) titers <1:320.
A nonreactive CSF-TPHA test result usually excludes neurosyphilis.
possible widened thoracic aorta, aortic calcification
May detect possible thoracic aortic aneurysm or aortic calcification.
Required in people with symptoms or signs of aortic regurgitation, heart failure, or aortic aneurysm.
may show evidence of heart failure, aortic regurgitation, or thoracic aortic aneurysm
Required if cardiovascular syphilis is strongly suspected (e.g., a patient has symptoms or signs of aortic regurgitation, heart failure, or aortic aneurysm).
usually normal
Performed before lumbar puncture to exclude elevated intracranial pressure, to ensure that a lumbar puncture procedure will be safe.
Elevated intracranial pressure is rarely caused by syphilis itself.
positive or negative
All patients with syphilis should be tested for HIV.
In geographic areas in which the prevalence of HIV is high, patients who have syphilis should be retested for HIV after 3 months, even if the first HIV test result is negative, and be offered HIV pre-exposure prophylaxis (PrEP). [ 8 ]
All infants and children at risk for congenital syphilis should be tested for HIV. [ 8 ]
may show hepatomegaly, ascites, hydrops fetalis, intrauterine growth retardation
Should be performed on all pregnant women with syphilis or suspected of having syphilis.
Presence of fetal or placental syphilis indicates a greater risk of treatment failure for congenital syphilis. [ 65 ]
may show anemia, thrombocytopenia, leukopenia, possible neutrophilia
Performed in infants with possible congenital syphilis.
may demonstrate osteochondritis
May be indicated in infants with suspected congenital syphilis. [ 8 ]
Performed if osteochondritis suspected.
aspartate aminotransferase and alanine aminotransferase may be elevated
Performed if clinical findings suggestive of liver involvement (e.g., hepatomegaly).
may detect deafness
Performed if clinically indicated.
may detect hearing deficit
Neurosyphilis may involve cranial nerves (particularly the 8th cranial nerve).
osseous lesions
Might aid diagnosis of congenital syphilis in stillborn infants. [ 8 ]
T pallidum PCR has been shown to have moderate sensitivity (70% to 80%) and high specificity >90% in the diagnosis of primary or secondary syphilis, when compared with adequate reference tests (e.g., serology, dark-field microscopy). [ 51 ]
The Centers for Disease Control and Prevention considers PCR testing a valid method for diagnosing primary, secondary, and congenital syphilis, and its use is likely to increase. [ 8 ] [ 52 ]
positive; however, a positive result for treponemal antibodies alone does not distinguish between current, past, or treated infection
POC syphilis testing has been assessed in the setting of high-risk regions, where rapid and early diagnosis may be more important than accuracy. Several clinical trials have shown promise and POC testing has been recommended as part of the Pan American Health Organization strategy to diagnose and treat syphilis. [ 53 ] [ 54 ]
Genital herpes
Differentiating Signs/Symptoms
There may be a history of fever, genital blisters or sores, and lymphadenopathy with first episode herpes simplex.
The patient may describe previous episodes of genital ulceration.
On physical exam there are typically multiple, painful vesicular or ulcerative lesions on or around the genitals or rectum.
Differentiating Tests
If lesions are present, clinical diagnosis should be confirmed by swabbing lesions for herpes simplex virus (HSV) culture or HSV polymerase chain reaction (PCR). [ 8 ]
Because of the higher sensitivity of PCR, this is the preferred test when available. [ 8 ]
Glycoprotein G-based type-specific serology may be indicated in certain patient groups and can differentiate between infection with HSV-1 and HSV-2. [ 8 ]
Characterized by painful genital ulcers and painful inguinal lymphadenopathy. Lesions of primary syphilis are typically not painful.
Usually occurs in discrete outbreaks.
On physical exam there may be an erythematous papule, pustule, or painful ulcer, as well as painful unilateral inguinal lymphadenopathy (bubo formation), which may rupture.
Haemophilus ducreyi is identified on specialist culture medium, which is not widely commercially available and has a sensitivity of <80%. [ 72 ]
Polymerase chain reaction testing is up to 100% sensitive but is not universally approved. [ 72 ] [ 73 ]
Therefore a positive diagnosis of chancroid is suggested by the presence of one or more painful genital ulcers with no evidence of syphilis or herpes simplex virus. [ 8 ] Regional lymphadenopathy is also confirmatory, if present. [ 8 ]
Primary HIV infection
Not preceded by genital ulceration.
However, genital ulceration may be present at the same time as primary HIV infection and the rash associated with the ulceration.
Laboratory tests positive for HIV, including antigen (P24 antigen) tests.
Other acute viral exanthems
Laboratory tests positive for specific virus.
Skin lesions are usually pruritic.
Typical distribution: interdigital, wrists, nipples, ankles, buttocks.
Diagnosis is usually clinical, but skin scrapings and microscopy for Sarcoptes scabiei may be performed.
Skin lesions are usually absent on palms and plantar aspects of feet.
Not associated with signs of systemic infection.
Diagnosis is usually clinical.
Skin biopsy can be undertaken to confirm diagnosis.
Lichen planus
Skin lesions are usually absent on palms and plantar aspect of feet.
Genital warts
Pink lumps, in genital and/or perianal skin and mucous membranes. Not necessarily confined to opposing membranes.
Not associated with other signs of secondary syphilis (rash, constitutional symptoms, generalized lymphadenopathy).
Exclusion of syphilis (negative syphilis serology).
Alzheimer dementia
Progressive dementia.
No specific differentiating symptoms and signs compared with neurosyphilis.
Less likely to have a history of possible signs and symptoms of earlier stages of syphilis infection.
Vascular dementia
Multi-infarct dementia often associated with other evidence of arteriopathy.
Syphilis infection is often asymptomatic but highly transmissible
If untreated, it causes in-utero mortality and considerable morbidity many years after initial infection
Treatment of syphilis in the early stage of infection is curative and aims to halt disease progression and eliminate further transmission of infection
Syphilis is an important facilitator of HIV transmission.
Asymptomatic patients who are at risk of syphilis infection [ 1 ] [ 74 ]
Pregnant women [ 8 ] [ 29 ] [ 62 ] [ 63 ] [ 75 ]
Blood donors. [ 76 ]
Screening tests
Screening in sti clinic, prenatal screening, screening low-risk asymptomatic population, screening for hiv and other stis, treatment approach, without neurosyphilis, neurosyphilis, infection in pregnancy, coinfection with hiv, congenital syphilis.
Presence of clinical, laboratory, or radiographic evidence of syphilis in the infant (testing should include paired maternal and neonatal non-treponemal serological titres using the same test, preferably conducted at the same laboratory).
Potential adverse effects of therapy
Primary Options
penicillin G benzathine
2.4 million units intramuscularly as a single dose
Secondary Options
100 mg orally twice daily for 14 days
Empiric therapy may be considered in those with suspected early infection (a rash or ulceration) before results of serology are available. Empiric therapy may be appropriate if there are concerns regarding re-attendance. The benefits of empiric therapy (prompt therapy) and risks (potentially unnecessary treatment) should be discussed with the patient.
Intramuscular benzathine penicillin G as a single dose is given. If the patient is allergic to penicillin and is not pregnant, oral doxycycline may be offered.
Sexual contacts of patients with confirmed syphilis should be screened and offered presumptive treatment if follow-up may be problematic.
intramuscular benzathine penicillin G
primary/secondary/early latent syphilis (nonpregnant): 2.4 million units intramuscularly as a single dose; primary/secondary/early latent syphilis (pregnant): 2.4 million units intramuscularly as a single dose, may repeat in 1 week; late-latent/tertiary syphilis with normal cerebrospinal fluid examination: 2.4 million units intramuscularly once weekly for 3 weeks
The first-line treatment for primary, secondary, and early latent syphilis (without neurosyphilis) is intramuscular benzathine penicillin G as a single dose. [ 8 ] Note that the dose may be split and administered at two discrete injection sites.
The first-line treatment of late latent and tertiary (gummatous, cardiovascular, psychiatric manifestations, late neurosyphilis) syphilis with normal cerebrospinal fluid (CSF) examination is intramuscular benzathine penicillin G (once weekly for 3 weeks).
All patients who have tertiary syphilis should undergo cerebrospinal fluid examination before treatment is started. Patients with abnormal CSF findings should be treated with a neurosyphilis regimen. [ 8 ]
Pregnant women should receive penicillin-based treatment according to their stage of syphilis. For pregnant women with primary, secondary, or early latent syphilis, certain evidence suggests that administering two injections of intramuscular benzathine penicillin G, rather than one, can help prevent congenital syphilis. Pregnant women with late latent or tertiary syphilis with normal CSF examination should receive three injections of intramuscular benzathine penicillin G, as per the guidance for nonpregnant individuals. [ 8 ]
Most clinicians treat HIV-positive and HIV-negative individuals with the same penicillin regimens, according to the stage of syphilis. [ 8 ]
Antibiotic therapy for cardiovascular syphilis does not reverse cardiovascular disease, which may continue to progress after treatment. Discussion with a cardiologist is advised.
40-60 mg orally once daily for 3 days; start 24 hours before penicillin
Corticosteroid therapy may be considered to minimize the risk of Jarisch-Herxheimer reaction in nonpregnant patients with neurosyphilis. [ 10 ] However, evidence of effectiveness is unclear and it is not routinely recommended in the US.
Jarisch-Herxheimer reaction is an acute febrile illness that can occur within the first 24 hours after initiation of antibiotic treatment for syphilis. Symptoms include acute fever, headache, and myalgia, usually occurring in patients with early syphilis. [ 8 ]
oral doxycycline
100 mg orally twice daily for 14 days (primary/secondary/early latent syphilis) or 28 days (late latent/tertiary syphilis with normal cerebrospinal fluid examination)
If the patient is allergic to penicillin, the first-line treatment in nonpregnant patients is oral doxycycline.
Adherence and patient compliance may influence treatment outcome if oral therapy is administered.
Patients who are allergic to penicillin, with primary or secondary syphilis and HIV coinfection, should receive antibiotic therapy as recommended for penicillin-allergic, HIV-negative patients. [ 8 ]
40-60 mg orally once daily for 3 days; start 24 hours before doxycycline
Corticosteroid therapy may be considered to minimize the risk of Jarisch-Herxheimer reaction in nonpregnant patients with neurosyphilis. [ 10 ] However, evidence of effectiveness is unclear and it is not routinely recommended in the US.
desensitization
Penicillin desensitization is recommended for all patients with penicillin hypersensitivity in pregnancy. The evidence for the use of nonpenicillin regimens is relatively weak. [ 8 ]
Penicillin allergy skin testing identifies patients at high risk for penicillin reactions. Skin reagents used should include major and minor allergens. [ 97 ] Those who are skin-test negative can receive penicillin therapy. However, some clinicians perform desensitization without skin testing, particularly if the skin reagents for both minor and major determinants of penicillin allergy are not available.
Acute desensitization can be performed in patients who have a positive skin test to one of the penicillin determinants, and should be performed in a hospital setting. Oral or intravenous desensitization can be performed, and is usually completed in 4 hours, following which the first dose of penicillin is administered. [ 98 ]
postdesensitization intramuscular benzathine penicillin G
primary/secondary/early latent syphilis: 2.4 million units intramuscularly as a single dose, may repeat in 1 week; late-latent/tertiary syphilis with normal cerebrospinal fluid examination: 2.4 million units intramuscularly once weekly for 3 weeks
Desensitization is usually completed in 4 hours, following which the first dose of penicillin is administered. [ 98 ]
Pregnant women should receive penicillin-based treatment according to their stage of syphilis. For pregnant women with primary, secondary, or early latent syphilis, certain evidence suggests that administering two injections of intramuscular benzathine penicillin G, rather than one, can help prevent congenital syphilis. Pregnant women with late latent or tertiary syphilis with normal cerebrospinal fluid examination should receive three injections of intramuscular benzathine penicillin G, as per the guidance for nonpregnant individuals. [ 8 ]
adults with neurosyphilis
intravenous aqueous penicillin G
penicillin G sodium
18-24 million units/day intravenously given in divided doses every 4 hours (or by continuous infusion) for 10-14 days
Central nervous system involvement can occur at any stage of syphilis and can range from asymptomatic meningeal involvement to dementia and sensory neuropathy. [ 18 ] First-line treatment for neurosyphilis is intravenous aqueous penicillin G. [ 8 ]
Pregnant women should receive penicillin-based treatment according to their stage of syphilis.
Most clinicians treat HIV-positive and HIV-negative patients with the same penicillin regimens, according to the stage of syphilis. [ 8 ]
subsequent intramuscular benzathine penicillin G
2.4 million units intramuscularly once weekly for 1-3 weeks
Some specialists administer benzathine penicillin G once weekly for up to 3 weeks after the intravenous aqueous penicillin G regimen for neurosyphilis has been completed.
This ensures the duration of treatment is comparable with that of late syphilis in the absence of neurosyphilis. [ 8 ]
intramuscular procaine penicillin G plus oral probenecid
penicillin G procaine
2.4 million units intramuscularly once daily for 10-14 days
500 mg orally four times daily for 10-14 days
Second-line treatment for neurosyphilis is intramuscular procaine penicillin G plus oral probenecid.
Most clinicians treat HIV-positive and HIV-negative patients with the same penicillin regimens according to the stage of syphilis.
Pregnant women should receive penicillin-based treatment according to their stage of syphilis. [ 8 ]
with penicillin allergy
Penicillin desensitization is recommended for all patients with neurosyphilis who have penicillin hypersensitivity. The evidence for the use of nonpenicillin regimens is relatively weak. [ 8 ]
postdesensitization penicillin G
subsequent postdesensitization intramuscular benzathine penicillin G
Some specialists administer benzathine penicillin G once weekly for up to 3 weeks after the treatment regimen for neurosyphilis has been completed (only if first-line intravenous therapy was chosen as the initial therapy).
high-dose oral doxycycline
200 mg orally twice daily for 28 days
The evidence for the use of nonpenicillin regimens is relatively weak. However, high-dose doxycycline is used by some clinicians in this situation. [ 7 ] [ 18 ]
congenital syphilis
neonate: confirmed proven or highly probable congenital syphilis
intravenous aqueous penicillin G or intramuscular procaine penicillin G
100,000 to 150,000 units/kg/day intravenously, administered as 50,000 units/kg/dose every 12 hours during the first 7 days of life and then every 8 hours thereafter for a total of 10 days
50,000 units/kg intramuscularly once daily for 10 days
All neonates born to mothers who have reactive nontreponemal and treponemal tests results should be evaluated with a quantitative nontreponemal serologic test (rapid plasma reagin tests [RPR] or Venereal Disease Research Laboratory [VDRL]) performed on the neonate's serum. The nontreponemal test performed on the neonate should be the same type of nontreponemal test performed on the mother. [ 8 ]
Confirmed proven or highly probable syphilis includes any neonate with: an abnormal physical exam that is consistent with congenital syphilis (e.g., nonimmune hydrops, conjugated or direct hyperbilirubinemia or cholestatic jaundice or cholestasis, hepatosplenomegaly, rhinitis, skin rash, or pseudoparalysis of an extremity); a serum quantitative nontreponemal serologic titer that is fourfold (or greater) higher than the mother's titer at delivery (e.g., maternal titer = 1:2, neonatal titer ≥1:8 or maternal titer = 1:8, neonatal titer ≥1:32); or a positive darkfield test or polymerase chain reaction (PCR) of placenta, cord, lesions, or body fluids or a positive silver stain of the placenta or cord. [ 8 ]
First-line treatment of confirmed proven or highly probable congenital syphilis is intravenous aqueous penicillin G or intramuscular procaine penicillin G. [ 8 ] [ 100 ]
Discussion with an obstetric specialist and neonatologist is recommended. Subsequently, close clinical and serologic follow-up by a pediatric specialist is recommended.
Neonates with reactive nontreponemal tests should be followed up to ensure that the nontreponemal test returns to negative. [ 8 ]
Neonates with a penicillin allergy or those who develop an allergic reaction presumed secondary to penicillin should be desensitized and treated with penicillin. [ 8 ] The evidence for the use of nonpenicillin regimens is relatively weak.
Skin testing is not possible in neonates with congenital syphilis as the procedure has not been standardized in this age group. [ 8 ]
neonate: possible congenital syphilis
intravenous aqueous penicillin G or intramuscular procaine penicillin G or intramuscular benzathine penicillin G
50,000 units/kg intramuscularly as a single dose
All neonates born to mothers who have reactive nontreponemal and treponemal test results should be evaluated with a quantitative nontreponemal serologic test (rapid plasma reagin [RPR] or Venereal Disease Research Laboratory [VDRL]) performed on the neonate's serum. The nontreponemal test performed on the neonate should be the same type of nontreponemal test performed on the mother.
Possible congenital syphilis includes any neonate who has a normal physical exam and a serum quantitative nontreponemal serologic titer equal to or less than fourfold of the maternal titer at delivery (e.g., maternal titer = 1:8, neonatal titer ≤1:16) and one of the following: the mother was not treated, was inadequately treated, or has no documentation of having received treatment; the mother was treated with erythromycin or a regimen other than those recommended by the Centers for Disease Control and Prevention (i.e., a nonpenicillin G regimen); the mother received the recommended regimen but treatment was initiated <30 days before delivery. [ 8 ]
Treatment of possible congenital syphilis is intravenous aqueous penicillin G, intramuscular procaine penicillin G, or intramuscular benzathine penicillin G. [ 8 ] [ 100 ]
Single-dose benzathine penicillin G may be used if follow up is certain and the following investigations are normal: cerebrospinal fluid analysis for VDRL test, cell count, and protein; complete blood count including differential and platelet count; and long-bone radiographs. [ 8 ] Single-dose benzathine penicillin G may also be considered if the risk of untreated maternal syphilis is considered low and the neonate's nontreponemal test is nonreactive. If the mother had untreated early syphilis at the time of delivery, the neonate is at increased risk for congenital syphilis and the 10-day course of aqueous penicillin G should be considered, even if investigations are normal, nontreponemal test is nonreactive, and follow-up is assured. [ 8 ]
neonate: congenital syphilis less likely
Congenital syphilis is less likely in any neonate who has a normal physical exam and a serum quantitative nontreponemal serologic titer equal or less than fourfold of the maternal titer at delivery (e.g., maternal titer = 1:8, neonatal titer ≤1:16) and both of the following are true: the mother was treated during pregnancy, treatment was appropriate for the infection stage, and the treatment regimen was initiated ≥30 days before delivery; the mother has no evidence of reinfection or relapse. [ 8 ]
Recommended treatment is with intramuscular benzathine penicillin G. [ 8 ]
If the mother's nontreponemal titers decreased at least fourfold after therapy for early syphilis, or remained stable for low-titer, latent syphilis (e.g., VDRL test <1:2 or RPR <1:4), an alternative approach is to provide close serologic follow-up every 2-3 months for 6 months. [ 8 ]
neonate: congenital syphilis unlikely
observation
Congenital syphilis is unlikely if the neonate has a normal physical exam and a serum quantitative nontreponemal serologic titer equal to or less than fourfold of the maternal titer at delivery and both of the following are true: the mother's treatment was adequate before pregnancy; and the mother's nontreponemal serologic titer remained low and stable (i.e., serofast) before and during pregnancy and at delivery (e.g., VDRL test ≤1:2 or RPR ≤1:4). [ 8 ]
No treatment is required. However, neonates with reactive nontreponemal tests should be followed up to ensure that the nontreponemal test returns to negative. [ 8 ]
Intramuscular benzathine penicillin G may be considered, particularly if the neonate has a reactive nontreponemal test and follow up is not certain. [ 8 ]
infant or child
intravenous aqueous penicillin G or intramuscular benzathine penicillin G
200,000 to 300,000 units/kg/day intravenously, administered as 50,000 units/kg/dose every 4-6 hours for 10 days
50,000 units/kg intramuscularly once weekly for up to 3 weeks, maximum 2.4 million units/dose
Infants and children ages ≥1 month who have reactive serologic tests for syphilis (e.g., serum rapid plasma reagin reactive, serum treponemal enzyme immunoassay reactive, or serum Treponema pallidum particle agglutination reactive) should be examined thoroughly for clinical manifestations of congenital syphilis. [ 8 ] Maternal records should be reviewed for evidence of maternal infection. Maternal serologic tests may have been negative in cases of extremely early or incubating syphilis. [ 8 ]
Evaluation should include: cerebrospinal fluid analysis for Venereal Disease Research Laboratory test, cell count, and protein; complete blood count, including differential and platelet count; and other tests if clinically indicated (e.g., long-bone x-rays, chest x-ray, liver enzymes, neuroimaging, auditory brain-stem response). [ 8 ]
Infants and children with clinical manifestations of congenital syphilis or abnormal evaluation should be treated with intravenous aqueous penicillin G. A single dose of intramuscular benzathine penicillin G may be considered after the 10-day treatment course of intravenous aqueous penicillin G to provide a more comparable duration as treatment for late syphilis. [ 8 ]
Infants and children with no clinical manifestations of congenital syphilis and normal evaluation (including normal cerebrospinal fluid evaluation) may be treated with up to 3 weekly doses of intramuscular benzathine penicillin G. [ 8 ]
Infants and children ages >1 month with acquired primary or secondary syphilis should be managed by a pediatric infectious disease specialist and evaluated for sexual abuse. [ 8 ] See Sexual abuse and assault .
Infants and children with a penicillin allergy or those who develop an allergic reaction presumed secondary to penicillin should be desensitized and treated with penicillin. [ 8 ] Skin testing may be used in children ages ≥2 years. The evidence for the use of nonpenicillin regimens is relatively weak.
Azithromycin
Ceftriaxone, primary prevention, secondary prevention.
People exposed within 90 days preceding diagnosis of primary, secondary, or early latent syphilis in a sexual partner should be treated presumptively, on the basis that they may be infected even if seronegative. It is estimated that 30% to 60% of sexual partners of people with early syphilis will develop the infection. [ 17 ]
People exposed more than 90 days before diagnosis of primary, secondary, or early latent syphilis in a sexual partner should be treated presumptively if syphilis serology is not available immediately and if follow-up may be problematic.
Treatment of long-term sexual partners of patients with latent syphilis is dependent on clinical evaluation and serology results.
For primary syphilis: exposure 3 months before treatment, plus duration of symptoms.
For secondary syphilis: 6 months plus duration of symptoms.
For early latent syphilis: 1 year.
Follow-Up Overview
Natural course of infection
Serology test results
Jarisch-Herxheimer reaction
Occurs within the first 24 hours after antibiotic therapy due to the rapid killing of treponemes.
Characterized by acute fever, headache, and myalgia, usually in patients with early syphilis. [ 8 ]
The likelihood of reaction is high in early syphilis but low in late syphilis. However, all patients should be advised of a possible reaction prior to receiving antibiotic treatment.
In pregnant women, Jarisch-Herxheimer reaction may cause fetal distress and premature labor. [ 8 ]
Treatment is supportive with oral fluids, acetaminophen, and nonsteroidal anti-inflammatory drugs.
Corticosteroid therapy may be considered to minimize the risk of a Jarisch-Herxheimer reaction in nonpregnant patients with cardiovascular syphilis or neurosyphilis. [ 10 ] However, the evidence of effectiveness is unclear and it is not routinely recommended in the US.
allergic reaction to penicillin
May arise in patients not previously known to be allergic.
In patients with penicillin allergy, alternative treatment options may be offered, dependent on the stage of syphilis.
Penicillin allergy skin testing and desensitization may be required (e.g., in the treatment of pregnant women).
Penicillin-allergic responses may include urticaria, angioedema, and anaphylaxis.
Treatment of allergic reaction is determined by the severity of the reaction.
asymptomatic progression of disease
Organ-specific complications can occur in untreated infection of unknown duration.
Specialist opinion should be sought depending on the nature of the complication (e.g., ophthalmology specialist opinion for ocular infection, cardiovascular specialist opinion for aortic regurgitation).
HIV infection
Syphilis facilitates the acquisition of HIV. [ 17 ]
iatrogenic procaine reaction
Occurs when intramuscular procaine penicillin G (e.g., used to treat neurosyphilis) is mistakenly administered intravenously.
Patients may develop penicillin allergic responses, including anaphylactic shock. [ 23 ]
Key Articles
Stoltey JE, Cohen SE. Syphilis transmission: a review of the current evidence. Sex Health. 2015 Apr;12(2):103-9. [Abstract] [Full Text]
British Association for Sexual Health and HIV (BASHH). UK national guidelines on the management of syphilis. December 2015 [internet publication]. [Full Text]
World Health Organization. Guidelines for the treatment of Treponema pallidum (syphilis). 2016 [internet publication]. [Full Text]
Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. MMWR Recomm Rep. 2021 Jul 23;70(4):1-187. [Abstract] [Full Text]
World Health Organization. WHO guideline on syphilis screening and treatment for pregnant women. 2017 [internet publication]. [Full Text]
Referenced Articles
1. Stoltey JE, Cohen SE. Syphilis transmission: a review of the current evidence. Sex Health. 2015 Apr;12(2):103-9. [Abstract] [Full Text]
2. Baughn RE, Musher DM. Secondary syphilitic lesions. Clin Microbiol Rev. 2005 Jan;18(1):205-16. [Abstract] [Full Text]
3. Newman L, Kamb M, Hawkes S, et al. Global estimates of syphilis in pregnancy and associated adverse outcomes: analysis of multinational antenatal surveillance data. PLoS Med. 2013;10(2):e1001396. [Abstract] [Full Text]
4. British Association for Sexual Health and HIV (BASHH). UK national guidelines on the management of syphilis. December 2015 [internet publication]. [Full Text]
5. Goh BT. Syphilis in adults. Sex Transm Infect. 2005 Dec;81(6):448-52. [Abstract] [Full Text]
6. O'Byrne P, MacPherson P. Syphilis. BMJ. 2019 Jun 28;365:l4159. [Erratum in: Syphilis. BMJ. 2019 Jul 19;366:l4746.] [Abstract] [Full Text]
7. World Health Organization. Guidelines for the treatment of Treponema pallidum (syphilis). 2016 [internet publication]. [Full Text]
8. Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. MMWR Recomm Rep. 2021 Jul 23;70(4):1-187. [Abstract] [Full Text]
9. Ghanem KG, Ram S, Rice PA. The modern epidemic of syphilis. N Engl J Med. 2020 Feb 27;382(9):845-54. [Abstract]
10. British Association for Sexual Health and HIV (BASHH). UK national guidelines on the management of syphilis. December 2015 [internet publication]. [Full Text]
11. World Health Organization. Report on global sexually transmitted infection surveillance, 2018. 2018 [internet publication]. [Full Text]
12. Centers for Disease Control and Prevention. Sexually transmitted disease surveillance, 2021. Apr 2023 [internet publication]. [Abstract] [Full Text]
13. Edmondson DG, Hu B, Norris SJ. Long-term in vitro culture of the syphilis spirochete Treponema pallidum subsp. pallidum. mBio. 2018 Jun 26;9(3). [Abstract] [Full Text]
14. Lee V, Kinghorn G. Syphilis: an update. Clin Med (Lond). 2008 Jun;8(3):330-3. [Abstract] [Full Text]
15. Stoltey JE, Cohen SE. Syphilis transmission: a review of the current evidence. Sex Health. 2015 Apr;12(2):103-9. [Abstract] [Full Text]
16. Centers for Disease Control and Prevention. Transmission of primary and secondary syphilis by oral sex - Chicago, Illinois, 1998-2002. MMWR Morb Mortal Wkly Rep. 2004 Oct 22;53(41):966-8. [Abstract] [Full Text]
17. French P. Syphilis. BMJ. 2007 Jan 20;334(7585):143-7. [Abstract]
18. Ropper AH. Neurosyphilis. N Engl J Med. 2019 Oct 3;381(14):1358-63. [Abstract]
19. Clark EG, Danbolt N. The Oslo study of the natural course of untreated syphilis. Med Clin North Am. 1964;48:613-21.
20. Chaudhary PM, Roninson IB. Activation of MDR1 (P-glycoprotein) gene expression in human cells by protein kinase C agonists. Oncol Res. 1992;4(7):281-90. [Abstract]
21. Peterman TA, Heffelfinger JD, Swint EB, et al. The changing epidemiology of syphilis. Sex Transm Dis. 2005 Oct;32(10 suppl):S4-10. [Abstract]
22. Centers for Disease Control and Prevention. Outbreak of syphilis among men who have sex with men - Southern California, 2000. MMWR Morb Mortal Wkly Rep. 2001 Feb 23;50(7):117-20. [Abstract]
23. Janier M, Unemo M, Dupin N, et al. 2020 European guideline on the management of syphilis. J Eur Acad Dermatol Venereol. 2021 Mar;35(3):574-88. [Abstract]
24. Keuning MW, Kamp GA, Schonenberg-Meinema D, et al. Congenital syphilis, the great imitator-case report and review. Lancet Infect Dis. 2020 Jul;20(7):e173-9. [Abstract]
25. Saloojee H, Velaphi S, Goga Y, et al. The prevention and management of congenital syphilis: an overview and recommendations. Bull World Health Organ. 2004 Jun;82(6):424-30. [Abstract] [Full Text]
26. National Institute for Health and Care Excellence. Recommendations on reducing sexually transmitted infections. Jun 2022 [internet publication]. [Full Text]
27. Holmes KK, Levine R, Weaver M. Effectiveness of condoms in preventing sexually transmitted infections. Bull World Health Organ. 2004 Jun;82(6):454-61. [Abstract]
28. Tobian AA, Serwadda D, Quinn TC, et al. Male circumcision for the prevention of HSV-2 and HPV infections and syphilis. N Engl J Med. 2009 Mar 26;360(13):1298-309. [Abstract] [Full Text]
29. US Preventive Services Task Force. Syphilis infection in pregnant women: screening. Sept 2018 [internet publication]. [Full Text]
30. Molina JM, Charreau I, Chidiac C, et al. Post-exposure prophylaxis with doxycycline to prevent sexually transmitted infections in men who have sex with men: an open-label randomised substudy of the ANRS IPERGAY trial. Lancet Infect Dis. 2018 Mar;18(3):308-17. [Abstract] [Full Text]
31. Brown DL, Frank JE. Diagnosis and management of syphilis. Am Fam Physician. 2003 Jul 15;68(2):283-90. [Abstract]
32. Rompalo AM, Lawlor J, Seaman P, et al. Modification of syphilitic genital ulcer manifestations by coexistent HIV infection. Sex Transm Dis. 2001 Aug;28(8):448-54. [Abstract] [Full Text]
33. Lafond RE, Lukehart SA. Biological basis for syphilis. Clin Microbiol Rev. 2006 Jan;19(1):29-49. [Abstract] [Full Text]
34. Tucker JD, Li JZ, Robbins GK, et al. Ocular syphilis among HIV-infected patients: a systematic analysis of the literature. Sex Trans Infect. 2011 Feb;87(1):4-8. [Abstract]
35. Rottingen JA, Cameron DW, Garnett GP. A systematic review of the epidemiologic interactions between classic sexually transmitted diseases and HIV: how much is really known? Sex Transm Dis. 2001 Oct;28(10):579-97. [Abstract]
36. Centers for Disease Control and Prevention. Sexually transmitted disease (STDs): syphilis & MSM fact sheet. 22 July 2021 [internet publication]. [Full Text]
37. Fojaco RM, Hensley GT, Moskowitz L. Congenital syphilis and necrotizing funisitis. JAMA. 1989 Mar 24-31;261(12):1788-90. [Abstract]
38. Hammerschlag MR, Guillén CD. Medical and legal implications of testing for sexually transmitted infections in children. Clin Microbiol Rev. 2010 Jul;23(3):493-506. [Abstract] [Full Text]
39. Wheeler HL, Agarwal S, Goh BT. Dark ground microscopy and treponemal serological tests in the diagnosis of early syphilis. Sex Transm Infect. 2004 Oct;80(5):411-4. [Abstract]
40. Centers for Disease Control and Prevention. Sexually transmitted diseases: syphilis. CDC fact sheet (detailed). 10 August 2021 [internet publication]. [Full Text]
41. Centers for Disease Control and Prevention (CDC). Discordant results from reverse sequence syphilis screening - five laboratories, United States, 2006-2010. MMWR Morb Mortal Wkly Rep. 2011 Feb 11;60(5):133-7. [Abstract] [Full Text]
42. Park IU, Fakile YF, Chow JM, et al. Performance of treponemal tests for the diagnosis of syphilis. Clin Infect Dis. 2019 Mar 5;68(6):913-18. [Abstract] [Full Text]
43. Pope V. Use of treponemal tests to screen for syphilis. Infect Med. 2004;21:399-402.
44. Seña AC, Wolff M, Behets F, et al. Rate of decline in nontreponemal antibody titers and seroreversion after treatment of early syphilis. Sex Transm Dis. 2017 Jan;44(1):6-10. [Abstract] [Full Text]
45. US Food and Drug Administration. Possible false RPR reactivity with BioPlex 2200 Syphilis Total & RPR test kit following a COVID-19 vaccine - letter to clinical laboratory staff and health care providers. Dec 2021 [internet publication]. [Full Text]
46. Smith G, Holman RP. The prozone phenomenon with syphilis and HIV-1 co-infection. South Med J. 2004 Apr;97(4):379-82. [Abstract]
47. Kingston AA, Vujevich J, Shapiro M, et al. Seronegative secondary syphilis in 2 patients coinfected with human immunodeficiency virus. Arch Dermatol. 2005 Apr;141(4):431-3. [Abstract]
48. British Association for Sexual Health and HIV (BASHH). BASHH national guideline on the management of sexually transmitted infections and related conditions in children and young people 2021. 2021 [internet publication]. [Full Text]
49. Lam TK, Lau HY, Lee YP, et al. Comparative evaluation of the INNO-LIA syphilis score and the MarDx Treponema pallidum immunoglobulin G Marblot test assays for the serological diagnosis of syphilis. Int J STD AIDS. 2010 Feb;21(2):110-3. [Abstract]
50. Hagedorn HJ, Kraminer-Hagedorn A, de Bosschere K, et al. Evaluation of INNO-LIA syphilis assay as a confirmatory test for syphilis. J Clin Microbiol. 2002 Mar;40(3):973-8. [Abstract] [Full Text]
51. Gayet-Ageron A, Lautenschlager S, Ninet B, et al. Sensitivity, specificity and likelihood ratios of PCR in the diagnosis of syphilis: a systematic review and meta-analysis. Sex Transm Infect. 2013 May;89(3):251-6. [Abstract]
52. Gayet-Ageron A, Sednaoui P, Lautenschlager S, et al. Use of Treponema pallidum PCR in testing of ulcers for diagnosis of primary syphilis. Emerg Infect Dis. 2015 Jan;21(1):127-9. [Abstract] [Full Text]
53. Shahrook S, Mori R, Ochirbat T, et al. Strategies of testing for syphilis during pregnancy. Cochrane Database Syst Rev. 2014 Oct 29;(10):CD010385. [Abstract] [Full Text]
54. Pan American Health Organization (PAHO). Guidance on syphilis testing in Latin America and the Caribbean: improving uptake, interpretation, and quality of testing in different clinical settings. 2015. 2015 [internet publication]. [Full Text]
55. Luger AF, Schmidt BL, Kaulich M. Significance of laboratory findings for the diagnosis of neurosyphilis. Int J STD AIDS. 2000 Apr;11(4):224-34. [Abstract]
56. Lavi R, Yarnitsky D, Rowe JM, et al. Standard vs atraumatic Whitacre needle for diagnostic lumbar puncture: a randomized trial. Neurology. 2006 Oct 24;67(8):1492-4. [Abstract]
57. Arendt K, Demaerschalk BM, Wingerchuk DM, et al. Atraumatic lumbar puncture needles: after all these years, are we still missing the point? Neurologist. 2009 Jan;15(1):17-20. [Abstract]
58. Nath S, Koziarz A, Badhiwala JH, et al. Atraumatic versus conventional lumbar puncture needles: a systematic review and meta-analysis. Lancet. 2018 Mar 24;391(10126):1197-204. [Abstract]
59. Rochwerg B, Almenawer SA, Siemieniuk RAC, et al. Atraumatic (pencil-point) versus conventional needles for lumbar puncture: a clinical practice guideline. BMJ. 2018 May 22;361:k1920. [Abstract] [Full Text]
60. Ahmed SV, Jayawarna C, Jude E. Post lumbar puncture headache: diagnosis and management. Postgrad Med J. 2006 Nov;82(973):713-6. [Abstract] [Full Text]
61. Arevalo-Rodriguez I, Ciapponi A, Roqué i Figuls M, et al. Posture and fluids for preventing post-dural puncture headache. Cochrane Database Syst Rev. 2016 Mar 7;(3):CD009199. [Abstract] [Full Text]
62. American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 752: prenatal and perinatal human immunodeficiency virus testing. Obstet Gynecol. 2018 Sep;132(3):e138-42. [Abstract] [Full Text]
63. National Institute for Health and Care Excellence (UK). Antenatal care. 19 August 2021 [internet publication]. [Full Text]
64. Simundic AM, Bölenius K, Cadamuro J, et al. Joint EFLM-COLABIOCLI recommendation for venous blood sampling. Clin Chem Lab Med. 2018;56(12):2015-38. [Abstract]
65. Hollier LM, Harstad TW, Sanchez PJ, et al. Fetal syphilis: clinical and laboratory characteristics. Obstet Gynecol. 2001 Jun;97(6):947-53. [Abstract]
66. Ropper AH. Neurosyphilis. N Engl J Med. 2019 Oct 3;381(14):1358-63. [Abstract]
67. Arnesen L, Serruya S, Duran P. Gestational syphilis and stillbirth in the Americas: a systematic review and meta-analysis. Rev Panam Salud Publica. 2015 Jun;37(6):422-9. [Abstract] [Full Text]
68. Cole M, Perry K. MHRA 04109: ten syphilis EIAs. UK: HSMO; 2004.
69. Creegan L, Bauer HM, Samuel MC, et al. An evaluation of the relative sensitivities of the venereal disease research laboratory test and the Treponema Pallidum particle agglutination test among patients diagnosed with primary syphilis. Sex Transm Dis. 2007 Dec;34(12):1016-18. [Abstract]
70. Manavi K, Young H, McMillan A. The sensitivity of syphilis assays in detecting different stages of early syphilis. Int J STD AIDS. 2006 Nov;17(11):768-71. [Abstract]
71. Cantor A, Nelson HD, Daeges M, et al. Screening for syphilis in nonpregnant adolescents and adults: systematic review to update the 2004 US Preventive Services Task Force recommendation [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2016 Jun. Report No: 14-05213-EF-1. [Abstract] [Full Text]
72. Lewis DA. Chancroid: clinical manifestations, diagnosis, and management. Sex Transm Infect. 2003 Feb;79(1):68-71. [Abstract] [Full Text]
73. Patterson K, Olsen B, Thomas C, et al. Development of a rapid immunodiagnostic test for Haemophilus ducreyi. J Clin Microbiol. 2002 Oct;40(10):3694-702. [Abstract] [Full Text]
74. US Preventive Services Task Force. Syphilis infection in nonpregnant adults and adolescents: screening. Sep 2022 [internet publication] [Full Text]
75. World Health Organization. WHO guideline on syphilis screening and treatment for pregnant women. 2017 [internet publication]. [Full Text]
76. World Health Organization. Screening donated blood for transfusion-transmissible infections: recommendations. 2009 [internet publication]. [Abstract] [Full Text]
77. Tucker JD, Bu J, Brown LB, et al. Accelerating worldwide syphilis screening through rapid testing: a systematic review. Lancet Infect Dis. 2010 Jun;10(6):381-6. [Abstract]
78. World Health Organization. The use of rapid syphilis tests. 2006 [internet publication]. [Full Text]
79. Young H. Guidelines for serological testing for syphilis. Sex Transm Infect. 2000 Oct;76(5):403-5. [Abstract]
80. Centers for Disease Control and Prevention. Recommendations for partner services programs for HIV infection, syphilis, gonorrhea, and chlamydial infection. MMWR Recomm Rep. 2008 Nov 7;57(RR-9):1-83;quiz CE1-4. [Abstract] [Full Text]
81. World Health Organization. WHO guideline on self-care interventions for health and well-being, 2022 revision. Jun 2022 [internet publication]. [Full Text]
82. Lin JS, Eder ML, Bean SI. Screening for syphilis infection in pregnant women: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2018 Sep 4;320(9):918-25. [Abstract] [Full Text]
83. World Health Organization, Department of Reproductive Health and Research. The global elimination of congenital syphilis: rationale and strategy for action. 2007 [internet publication]. [Full Text]
84. Menezes EV, Yakoob MY, Soomro T, et al. Reducing stillbirths: prevention and management of medical disorders and infections during pregnancy. BMC Pregnancy Childbirth. 2009 May 7;9(suppl 1):S4. [Abstract] [Full Text]
85. Hawkes SJ, Gomez GB, Broutet N. Early antenatal care: does it make a difference to outcomes of pregnancy associated with syphilis? A systematic review and meta-analysis. PLoS One. 2013;8(2):e56713. [Abstract] [Full Text]
86. Blencowe H, Cousens S, Kamb M, et al. Lives Saved Tool supplement detection and treatment of syphilis in pregnancy to reduce syphilis related stillbirths and neonatal mortality. BMC Public Health. 2011 Apr 13;11(suppl 3):S9. [Abstract] [Full Text]
87. Chen XS, Peeling RW, Yin YP, Mabey D. Improving antenatal care to prevent adverse pregnancy outcomes caused by syphilis. Future Microbiol. 2011 Oct;6(10):1131-4. [Abstract]
88. Hawkes S, Matin N, Broutet N, et al. Effectiveness of interventions to improve screening for syphilis in pregnancy: a systematic review and meta-analysis. Lancet Infect Dis. 2011 Sep;11(9):684-91. [Abstract]
89. Munkhuu B, Liabsuetrakul T, Chongsuvivatwong V, et al. One-stop service for antenatal syphilis screening and prevention of congenital syphilis in Ulaanbaatar, Mongolia: a cluster randomized trial. Sex Transm Dis. 2009 Nov;36(11):714-20. [Abstract]
90. World Health Organization. WHO guideline on syphilis screening and treatment for pregnant women. 2017 [internet publication]. [Full Text]
91. Stoner BP. Current controversies in the management of adult syphilis. Clin Infect Dis. 2007 Apr 1;44(suppl 3):S130-46. [Abstract] [Full Text]
92. Parkes R, Renton A, Meheus A, et al. Review of current evidence and comparison for effective syphilis treatment in Europe. Int J STD AIDS. 2004 Feb;15(2):73-88. [Abstract]
93. Hook EW 3rd, Martin DH, Stephens J, et al. A randomized, comparative pilot study of azithromycin versus benzathine penicillin G for treatment of early syphilis. Sex Transm Dis. 2002 Aug;29(8):486-90. [Abstract]
94. Riedner G, Rusizoka M, Todd J, et al. Single-dose azithromycin versus penicillin G benzathine for the treatment of early syphilis. N Engl J Med. 2005 Sep 22;353(12):1236-44. [Abstract] [Full Text]
95. Lukehart SA, Godornes C, Molini BJ, et al. Macrolide resistance in Treponema pallidum in the United States and Ireland. N Engl J Med. 2004 Jul 8;351(2):154-8. [Abstract] [Full Text]
96. World Health Organization. Guidelines for the treatment of Treponema pallidum (syphilis). 2016 [internet publication]. [Full Text]
97. Ansotegui IJ, Melioli G, Canonica GW, et al. IgE allergy diagnostics and other relevant tests in allergy, a World Allergy Organization position paper. World Allergy Organ J. 2020 Feb;13(2):100080. [Abstract] [Full Text]
98. Chastain DB, Hutzley VJ, Parekh J, et al. Antimicrobial desensitization: a review of published protocols. Pharmacy (Basel). 2019 Aug 9;7(3):112. [Abstract] [Full Text]
99. World Health Organization. WHO guideline on syphilis screening and treatment for pregnant women. 2017 [internet publication]. [Full Text]
100. Walker GJ, Walker D, Molano Franco D, et al. Antibiotic treatment for newborns with congenital syphilis. Cochrane Database Syst Rev. 2019 Feb 15;(2):CD012071. [Abstract] [Full Text]
101. Liang Z, Chen YP, Yang CS, et al. Meta-analysis of ceftriaxone compared with penicillin for the treatment of syphilis. Int J Antimicrob Agents. 2016 Jan;47(1):6-11. [Abstract]
102. Liu HY, Han Y, Chen XS, et al. Comparison of efficacy of treatments for early syphilis: A systematic review and network meta-analysis of randomized controlled trials and observational studies. PLoS One. 2017 Jun 28;12(6):e0180001. [Abstract] [Full Text]
103. Faculty of Sexual and Reproductive Healthcare. Barrier methods for contraception and STI prevention. August 2015 [internet publication]. [Full Text]
104. Ng BE, Butler LM, Horvath T, et al. Population-based biomedical sexually transmitted infection control interventions for reducing HIV infection. Cochrane Database Syst Rev. 2011 Mar 16;(3):CD001220. [Abstract] [Full Text]
105. de Walque D, Dow WH, Nathan R, et al. Incentivising safe sex: a randomised trial of conditional cash transfers for HIV and sexually transmitted infection prevention in rural Tanzania. BMJ Open. 2012 Feb 8;2(1):e000747. [Abstract] [Full Text]
106. British Association for Sexual Health and HIV (BASHH). BASHH National Guideline on the Management of Sexually Transmitted Infections and Related Conditions in Children and Young People 2021. 2021 [internet publication]. [Full Text]
Published by
Centers for Disease Control and Prevention
World Health Organization
International Union against Sexually Transmitted Infections
British Association for Sexual Health and HIV
International Union against Sexually Transmitted Infections
National Institute for Health and Care Excellence (UK)
Faculty of Sexual and Reproductive Healthcare (UK)
Topic last updated: 2023-12-11
Juan C. Salazar , MD, MPH, FAAP
Professor and Chair
Department of Pediatrics
University of Connecticut School of Medicine
Physician in Chief
Connecticut Children's
Acknowledgements :
Dr Juan C. Salazar would like to gratefully acknowledge Adriana R. Cruz, Jairo M. Montezuma-Rusca, Nicholas Bennett, Patrick French, and Nooshin Barmania, previous contributors to this topic. We would also like to acknowledge our infectious diseases expert panel member, Dr Elisabeth Adderson, for her contribution to this topic.
Peer Reviewers
Robert A. Larsen , MD
Associate Professor of Medicine
University of Southern California
Keck School of Medicine
Los Angeles
William Rodriguez , MD
Assistant Professor of Medicine
Harvard Medical School
Director of Research
Global Health Delivery Project
Harvard School of Public Health
Jennifer Handforth , MB ChB, MRCPCH, DTM&H
Consultant Paediatrician
Croydon University Hospital
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

A 2021 Update on Syphilis: Taking Stock from Pathogenesis to Vaccines
Giorgio tiecco.
1 Unit of Infectious and Tropical Diseases, Department of Clinical and Experimental Sciences, ASST Spedali di Brescia, University of Brescia, 25123 Brescia, Italy; [email protected] (G.T.); [email protected] (M.D.A.); [email protected] (S.S.); [email protected] (V.M.); [email protected] (E.F.); [email protected] (F.C.)
Melania Degli Antoni
Samuele storti, valentina marchese, emanuele focà, carlo torti.
2 Infectious and Tropical Disease Unit, Department of Medical and Surgical Sciences, “Magna Graecia” University of Catanzaro, 88100 Catanzaro, Italy; ti.zcinu@itrot
Francesco Castelli
Eugenia quiros-roldan, associated data.
Not applicable.
In 2021 the scientific community’s efforts have been focused on solving the back-breaking challenge of the COVID-19 pandemic, but sexually transmitted infections (STI) are still one of the most common global health problems. Syphilis is a systemic disease caused by the spirochaete Treponema pallidum (TP) and is one of the oldest known diseases. Its incidence has increased in the last few years and syphilis still remains a contemporary plague that continues to afflict millions of people worldwide. Despite research improvements, syphilis pathogenesis is not completely clear; clinical presentation is very heterogeneous and the diagnosis can sometimes be difficult. Furthermore, few therapeutic options are available, and a vaccine has not been found yet. In this review, we describe the most recent evidence concerning the clinical manifestation, diagnosis, treatment and vaccine prospectives for this disease.
1. Introduction
In 2021 the scientific community’s efforts have been focused on solving the back-breaking challenge of the COVID-19 pandemic, but sexually transmitted infections (STI) are still one of the most common global health problems.
Syphilis is a systemic disease caused by the spirochaete Treponema pallidum (TP) and is one of the oldest known diseases for which curative and inexpensive treatment is available. Without animal reservoirs, theoretically, syphilis should be an eradicable disease, but to date, multiple concerted efforts to eliminate syphilis have failed, such as the Syphilis Elimination Effort launched by United States Center for Disease Control and Prevention (CDC) in 1999 [ 1 ].
The complex natural history of syphilis reflects the invasiveness and immune evasiveness of TP. The infection does not lead to immunity against reinfection and repeated episodes of syphilis occur, predominantly in men who have sex with men (MSM) with a high rate of partner change [ 2 ]. Moreover, HIV infection may modulate the clinical presentation and the clinical and serologic response to syphilis treatment [ 3 , 4 , 5 , 6 ].
In 2017, the annual rate of primary and secondary syphilis in the United States was 11% higher than in 2016: more than 60% of infected individuals were MSM, of whom 46% were people living with HIV infection (PLWH) [ 7 ]. The rate continued to rise consecutively through 2019 [ 8 ], and recent data estimates a global pooled syphilis prevalence among MSM of 7.5% (95% CI 7.0–8.0%) over the last 20 years [ 9 ]. Preliminary 2020 data suggest that this trend continued in 2020, despite the COVID-19 pandemic and the decrease of syphilis testing and treatment during this period [ 10 ].
Syphilis facilitates both HIV transmission and HIV acquisition. The impact of syphilis infection on the risk of HIV-RNA elevation and decline in CD4+ reflects the complex interplay between these two diseases [ 11 ].
Although syphilis is a very old disease, its pathogenesis is not fully understood, diagnosis may be difficult and, lastly, few therapeutic or prophylactic options are available at the moment.
2. Etiology and Pathogenesis
TP is a member of the family Spirochaetaceae , and genus Treponema , which includes four human pathogens ( T. pallidum pallidum , T. pallidum endemicum , T. pallidum pertenue and T. pallidum carateum ) and at least six human nonpathogens.
TP is characterized by a rare outer membrane and a slow replication rate (about 33 h) with a dynamic regulation of TP genes, which is important for its successful colonization, dissemination, and invasion in hosts [ 12 , 13 ]. TP repeat genes ( Tpr ) encode proteins that mediate attachment to host tissue and function as porins. Tpr proteins are immunogenic and one of them, Tpr K , has been described as being a target for opsonic antibodies. Tpr K differs in seven discrete variable regions and antibodies to these variable regions offer only homologous protection and not against heterologous strains. Antigenic variation through gene conversion during infection seems to be the mechanism by which TP avoids the host immune response, allowing for prolonged infection and persistence even in the case of a robust host response [ 14 ]. TP is rich in transport proteins, and this may have a central role in antibiotic penetration through the bacterial membrane [ 15 ].
TP is presumed to penetrate through small skin lesions, but the exact mechanisms by which TP enters cells is not known. The invasion of endothelial cell monolayers and intact membranes are the main virulence features of the bacteria [ 16 ].
TP is one of the few pathogens capable of crossing specialized endothelial barriers such as the retinal, placental, and blood-brain barriers. This seems to occur through the TP protein Tp0751, a host-binding vascular adhesin, also referred to as pallilysin , that interacts with microvascular and macrovascular endothelial cells (including cerebral endothelial cells) through an endothelial receptor named LamR [ 16 ].
Although widely discussed, neuroinvasive strains are hypothesized: TP 14a/a and 14d/f. Those strains have been described as possessing a greater potential of neuroinvasion, and they may be better able at evading the host immune responses in the central nervous system (CNS) when compared to other strains in both humans and rabbits [ 17 ].
Whether HIV infection alters the natural history of syphilis or vice-versa remains controversial. TP can induce the expression of CCR5 (the major co-receptor for HIV entry) on monocytes in syphilitic lesions, enhancing the transmission of macrophage-tropic HIV-1 [ 18 ]. However, the impact of syphilis on CD4+ cells or HIV viremia seems marginal [ 19 ].
3. Clinical Manifestation
Syphilis clinical manifestations are so wide and heterogeneous that a classification based on clinical stages, chronologically beginning with the onset of a chancre, was needed. Nevertheless, stages might overlap (especially in PLWH) and the definition of early and late syphilis is still debated:
- ⮚ According to the Centre for Disease Prevention and Control (CDC), early syphilis is defined as syphilis acquired <1 year previously, otherwise it is considered late syphilis.
- ⮚ According to the World Health Organization (WHO), early syphilis is defined as syphilis acquired <2 years previously, otherwise it is considered late syphilis.
Early syphilis includes:
- ⮚ Primary syphilis: A chancre is a solitary skin indurated, non-exudative, painless ulcer that follows the acquisition of TP. Multiple and painful chancres, deeper and slower to resolve, have been described more commonly in PLWH [ 20 , 21 ].
Signs and symptoms of secondary syphilis.
- ▪ Malignant lues , a severe cutaneous ulcero-nodular form, has also been described more frequently in PLWH and has been related to a defective cell-mediated immune response [ 25 ].
- ▪ Ocular syphilis may occur without other CNS manifestations and has been documented to affect almost every structure of the eye, resulting in blindness, especially in PLWH with a CD4+ count < 200 cells/microL [ 29 ].
- ▪ Otosyphilis can manifest with a variety of audiovestibular symptoms (hearing loss is the main one). TP may also affect the eighth cranial nerve, the cochleovestibular apparatus, or the temporal bone [ 30 ].
- ⮚ Early latent syphilis refers to the asymptomatic period between primary and secondary or late syphilis. Up to 24% of untreated patients suffer from secondary lesion relapses (more frequently among PLWH) during the first year of infection [ 28 ]. For this reason, a 1-year cut-off period is frequently used to classify early and late syphilis [ 28 ].
Repeated episodes of syphilis in PLWH are mostly asymptomatic [ 4 ]. Patients with > 3 episodes of syphilis were more likely to have early latent syphilis than primary or secondary syphilis at the index visit compared to those with < 2 episodes [ 31 ].
Late syphilis occurs in 25% to 40% of patients with untreated syphilis. Clinical events may appear at any time, 1 to 30 years after the primary infection [ 6 ].
- ⮚ Tertiary syphilis includes patients with late syphilis that show symptomatic manifestations. PLWH may progress to tertiary syphilis more rapidly than HIV-uninfected patients [ 32 ]. The more frequent forms are:
- ▪ Cardiovas cular syphilis classically involves the ascending thoracic aorta, resulting in a dilated aorta and aortic valve regurgitation. It is thought to be a consequence of vasculitis in the vasa vasorum. Many diagnoses of syphilitic aortitis are invariably obtained or suspected on histopathological examination [ 33 ]. Syphilis may also involve coronary arteries, resulting in coronary artery narrowing and thrombosis [ 34 ].
- ▪ Gummatous syphilis presents as ulcers or heaped up granulomatous lesions ( gummas ). Several cases of gummas involving internal organs ( visceral gummas ), including the CNS, have been reported in PLWH [ 35 ].
- ▪ Meningovascular neurosyphilis results from inflammation of large- to medium-sized arteries of the brain or spinal cord [ 36 ]. Neurosyphilis and HIV should be investigated in young patients with cerebral infarction.
- ▪ Parenchymatous neurosyphilis is characterized by the destruction of cortical CNS parenchyma, clinically mimicking a mental disorder or dementia. When the infection involves the posterior column and nerve roots, it is known as Tabes dorsalis . It is estimated that 1.5–9% of cases of syphilis are complicated by Tabes dorsalis and is more commonly observed in MSM and Black people [ 37 ].
- ▪ Late Neurosyphilis , includes a paucisymptomatic form (with alterations in cerebrospinal fluid) that is present in about 15% of patients originally diagnosed as having latent syphilis and in 12% of those with cardiovascular syphilis. In one study of 117 PLWH diagnosed with neurosyphilis, approximately 33% were asymptomatic [ 38 ]. Without treatment, it evolves into symptomatic neurosyphilis in 5% of cases [ 28 ].
Latent late syphilis refers to the period when a patient infected for >1 year with TP (as demonstrated by serologic testing) has no symptoms.
4. Diagnosis
Diagnostic testing for syphilis should be performed on both symptomatic and asymptomatic patients at high risk of acquiring the disease or transmitting it to others. CDC suggests annual screening for sexually active MSM, although testing as often as every three months may increase the early detection of syphilis [ 6 , 39 ].
In PLWH, guideline panels recommend screening at the initial visit, and then annually for those who are sexually active [ 40 ]. More frequent screening (every three to six months) is recommended for those with multiple sex partners and those who engage in unprotected intercourse or have sex in conjunction with illicit drug use [ 36 ].
4.1. Indirect Methods
Serologic testing is the primary tool for diagnosing syphilis [ 40 ]. Two types of serologic tests are required for diagnosis.
▪ Nontreponemal tests (NTT) (also known as reagin tests ) are based upon the reactivity of serum from infected patients to a cardiolipin-cholesterol-lecithin antigen . Traditionally, they have been used for initial syphilis screening ( traditional algorithm ) ( Table 2 ) and include RPR ( Rapid Plasma Reagin ), VDRL ( Venereal Disease Research Laboratory ) and TRUST ( Toluidine Red Unheated Serum Test ). The results are quantitative and reported as a titer of antibodies. According to the traditional approach, a negative result excludes the diagnosis of active syphilis and no further testing is needed. These tests show a 62–78% sensitivity for primary syphilis, 97–100% for secondary and 80–100% for early latent syphilis [ 38 ]. The sensitivity of NNT is lower for late syphilis whereas, in early syphilis, a false negative might present in 30% of cases as a consequence of testing before the development of antibodies [ 41 ].
Differences between the traditional approach and reverse approach for syphilis diagnosis.
- Biological false positive, although uncommon, must be considered during pregnancy or autoimmune illnesses as well as other infectious diseases. Currently, NTT are manually performed and several attempts to automate these tests have been described [ 42 ].
Monitoring of nontreponemal test titer should be done using the same test and it is indicated to:
Syphilis: serological definitions after treatment.
Titer tends to wane over time even without treatment, but successful therapy accelerates the pace of antibody decline.
A serological cure is defined as a seroconversion (from positive to negative) or as a 4-fold (or two dilutions) decline in NNT antibody titer 6 to 12 months after therapy for early syphilis and 12 to 24 months for late syphilis [ 44 ]. A 4-fold or greater titer decline is generally associated with younger age, higher baseline nontreponemal titers, and earlier syphilis stage. Treatment failure is defined as a ≥4-fold rise in nontreponemal titers after treatment in the absence of reinfection [ 44 ]. Patients correctly treated, with a ≤4-fold titer decrease and unlikely to have a new infection, are known as serological non-responders . Serofast status concerns patients with a persistently reactive NTT despite adequate treatment without seroconversion after an initial ≥4-fold decline [ 44 , 45 ].
An individual with a previous serological cure might be considered as “re-infected” if a new seroconversion (from negative to positive) or a 4-fold or greater increase in antibody titer occurs ( Table 3 and Table 4 ).
Serological tools for syphilis diagnosis.
The choice of screening test depends on resource availability, either economical or human, since some TT are automatized, such as ELISA/EIA/CLIA. Moreover, disease prevalence should also be considered, as in low prevalence settings, TT may result in very low positive predictive value [ 40 ].
In PLWH, serologic testing for syphilis can be interpreted in the same manner regardless of HIV status. However, clinicians should be aware of the unusual serologic responses in PLWH who have syphilis [ 46 ]. In primary and, less commonly, in secondary syphilis, a delayed appearance of sero-reactivity is common and false-negative tests might be associated both with the Prozone Effect as well as with the advanced immunodeficiency of the patient (it is thought to reflect B-cell failure during late-stage HIV infection) [ 46 , 47 ].
4.2. Direct Methods
Since TP has always been taught to be non-culturable, currently the organism must be identified through direct visualization or detection in clinical specimens. Darkfield microscopy and direct fluorescent antibody testing can be used to detect the organism; however, neither of these tests are routinely available in clinical settings [ 40 ]. A recent study achieved a reproducible multiplication of TP subsp. pallidum using a long-term in vitro culture. Although the potential diagnostic implications are currently limited, this may lead to a better understanding of TP physiology, structure, gene expression, regulatory pathways, pathogenesis, immunologic properties, and antimicrobial susceptibility [ 48 ].
Some laboratories have developed polymerase chain reaction (PCR) tests to detect TP DNA from clinical specimens ( tpp47 and polA are the more frequently amplified targets) with variable sensitivity and specificity depending on specimens (lower in blood and cerebrospinal fluid) [ 49 ]. Currently, they are not approved by the Food and Drug Administration (FDA), but PCR is becoming widely used in some jurisdictions thanks to the encouraging results in detecting early primary syphilis lesions before the development of any serological marker [ 50 ]. Moreover, a recent study states that DNA tests with oral and anal swabs, also in the absence of oral or anal lesions, may reduce the time to diagnosis, preventing progression to the secondary stage and improving syphilis control [ 51 ].
Point-of-care (POC) tests, which can be performed at clinical visits, have been hypothesized to have a positive effect on shortening the duration of the infection, because patients can be treated before they leave the clinical encounter. Those tests should be highly sensitive and specific and inexpensive. Most of the available syphilis POC tests detect antibodies specific to TP, and they perform reasonably well in either whole blood or serum specimens, with sensitivities ranging from 74% to 99% and specificities ranging from 94% to 99%, but the main challenge is their inability to differentiate prior treated infections from current infections.
4.3. Neurosyphilis Diagnosis
There is no consensus for neurosyphilis diagnosis but if the diagnosis of neurosyphilis is being considered, additional testing on cerebrospinal fluid (CSF) should be performed [ 52 , 53 ]:
- ▪ CSF Analysis : Elevated white blood cells and proteins in CSF are often seen in neurosyphilis but are usually considered nonspecific findings. A CSF cell count >5 cells/microL is suggestive of neurosyphilis. The threshold is higher in PLWH since those may have a CSF pleocytosis due to HIV itself. For this reason, a CSF cell count >20 cells/microL is suggestive of neurosyphilis in PLWH [ 54 ].
- ▪ Non-Treponemal Test : RPR and VDRL in CSF are 100% specific for diagnosis of neurosyphilis but their sensitivity is poor (CSF VDRL is 49–87% sensitive and RPR 51–82%) [ 41 ].
- ▪ Treponemal Test : CSF FTA-ABS test has been suggested to have a strong negative predictive value and neurosyphilis is highly unlikely if negative [ 55 ].
The definition of asymptomatic neurosyphilis is quite contentious. Whether or not lumbar puncture should be carried out in patients with no neurological involvement remains controversial. CSF examination might be warranted in serological non responders and serofast patients [ 40 ]. Many experts believe that most patients with HIV and syphilis deserve CSF examination regardless of symptoms, especially those with a CD4+ cell count < 350 cells/microL and an RPR > 1:32 [ 54 , 56 ].
4.4. Syphilis Reinfections Diagnosis
It is difficult to distinguish syphilis reinfection from disease relapse since the diagnosis depends on clinical findings of syphilis and a 4-fold increase in NTT titre ( Table 4 ).
Syphilis infection leads only to partial immunity to reinfection. Thus, subsequent episodes of syphilis may not present in the same way as the initial episodes [ 57 ]. Moreover, in settings where syphilis is regularly screened for high-risk persons, syphilis is more likely to be diagnosed before the development of clinical symptoms, simply because of changes in titres of non-treponemal tests [ 58 ].
Data regarding serological response in patients with repeated episodes are discordant. Patients with syphilis reinfection had higher VDRL/RPR and TPPA serum titres but lower IgM serum titres than patients with one syphilis episode [ 59 ]. Additionally, each additional episode of syphilis results in a slightly attenuated immune response [ 3 ]. As a result, the diagnosis of repeat syphilis may be both under- and over-diagnosed. In the very near future, the routine use of PCR tests for TP DNA might be the solution for this issue.
5. Treatment
No controlled clinical trials are available to optimize the treatment of syphilis. Recommendations are mainly based on laboratory results, expert opinions, clinical cases and experience. Penicillin G benzathine (PGB) is the treatment of choice for syphilis and is preferred to short-acting penicillin. However, the dosage, formulation, and duration of treatment depend upon the stage of disease and whether the infection involves “ protected sites ” that “hide” T. pallidum (ocular structures or CNS). Scarce data are available for alternative treatments ( Table 5 ).
Recommended regimen for syphilis treatment [ 6 , 28 , 40 ].
Acronyms: MIU (Million International Units); IM (intramuscular injection); IV (intravenous injection); po (per os); qd (quaque die).
A nontreponemal serologic test should be obtained just before initiating therapy (ideally, on the first day of treatment) to establish the pre-treatment titre. This test is critical to establish the adequacy of the post-treatment serologic response [ 60 ].
The standard therapy based on a single intramuscular (IM) dose of PGB (2.4 million UI) maintains this serum concentration up to 21 days. Increasing the dose does not clear treponemes more quickly.
Alternative regimens are typically administered to patients who are unable to take penicillin or when it is unavailable. Doxycycline or Tetracycline are both employed, with a serologic response in 82.9% of patients [ 61 ].
Ceftriaxone is a promising alternative to PGB with a good CNS penetration, long half-life that enables once-daily dosing and efficacy similar to PGB, but there are limited clinical data and the optimal dose and duration of treatment have not been defined yet [ 62 , 63 ]. Azithromycin is an alternative, although generally not recommended due to the rapid emergence of macrolide resistance in TP.
The molecular basis for macrolide resistance is mediated by point mutations in the TP 23S ribosomal RNA gene at nucleotide positions 2058 and 2059 in both copies of the 23S rRNA genes. A2058G mutations conferring macrolide resistance are more common than A2059G [ 64 , 65 ]. To date, there have been no reports of strains possessing both mutations. Macrolide-resistant TP with the A2058G mutation is now present in several areas of the USA, Canada, Europe, and China, with a wide range of prevalence (from 16% in Canada, 85% in France and >90% in China) [ 66 , 67 , 68 ].
PLWH with syphilis should be treated as HIV-uninfected patients, although they may be at increased risk for treatment failure and may be more likely to progress to neurosyphilis [ 69 , 70 ]. Several studies have evaluated enhanced therapy with additional doses of PGB and found no additional benefit [ 71 , 72 ]. There are limited data on the efficacy of alternative regimens in PLWH; therefore, close monitoring of these patients must be carried out [ 73 ].
Extended treatment is needed as the duration of the infection increases (more relapses have been seen in later stages after short courses of treatment). During late syphilis, a cerebrospinal fluid examination before initiation of therapy is necessary to investigate neurosyphilis.
If neurosyphilis is excluded, the “ treponemicidal” level of PGB must be maintained for 21 days and 2.4 million UI IM once weekly for 3 weeks is the standard therapy. If a patient misses a dose or more than 14 days have elapsed since the prior dose, the course should be reinitiated. For those with cardiovascular disease, antibiotic therapy does not reverse the clinical manifestations of syphilis, but it may halt the progression of the disease.
Patients with neurosyphilis should generally be treated with intravenous (IV) therapy, because the dose of IM PGB that is administered for other stages of syphilis does not produce measurable CSF levels of the drug. IV therapy should be administered also to patients strongly suspected of having CNS syphilis, even if they have a nonreactive CSF-VDRL. Alternatives to these therapeutic regimens are poorly studied in this setting. Treatment based upon CSF results, in the absence of neurological involvement, has not been associated with improved clinical outcomes, but may mitigate subsequent cognitive decline [ 27 ].
There is no consensus on the management of serofast or serological non-responders ; a recent study among HIV-uninfected patients with a poor serological response after an appropriate treatment shows no additional benefit in retreatment [ 74 ].
Jarisch Herxheimer reaction (JHR) is a transient clinical phenomenon that occurs in patients infected by spirochetes, including TP, within 24 h of antibiotic therapy. It usually manifests as fever, rigors, nausea and vomiting, headache, tachycardia, hypotension, and exacerbation of skin lesions and it is important to distinguish it from antibiotic allergic reactions. Antibiotics mostly associated with the development of JHR are penicillins, tetracyclines and erythromycin, and rarely with cephalosporins and fluoroquinolones. This reaction can be expected in 55% to 95% of primary or secondary syphilis [ 75 ]. It is, however, very rare in late syphilis, but often unrecognized and underreported [ 75 ]. In PLWH, JHR occurs in 35–56% of treated patients, and for each 2-fold increase in RPR titer, the risk of JHR grows by 19%, suggesting that a higher load of spirochetes in the early stages of syphilis increases the risk of JHR [ 76 ]. In patients with neurosyphilis and HIV encephalitis, JHR has been described to be more severe and prophylaxis with anti-inflammatory agents could be employed [ 76 , 77 ].
Follow Up after Treatment
Patients should be monitored both clinically and with laboratory testing to ensure an appropriate response to therapy.
Clinical follow-up post treatment is recommended in patients with early syphilis to assess the resolution of symptoms. However, for patients with late-stage cardiovascular or noncutaneous gummatous disease, a significant change in symptoms is unlikely. For individuals with symptomatic neurosyphilis, serial neurological examinations should be performed every six months after treatment [ 54 ].
Serological follow-up with Nontreponemal titers every six months (every three months in PLWH) after treatment is recommended until serological cure . PLWH have a slower decline of NTT and seroreversion is observed in about half of treated patients, although it might take years to occur [ 46 ].
Additional treatments do not provide short-term serological benefits beyond watchful waiting. In cases of neurosyphilis with the presence of CSF pleocytosis or a positive CSF serologic test before treatment, CSF examinations should be repeated every six months until the cell count becomes normal. Resolution of the CSF pleocytosis is the most sensitive indicator of effective treatment in neurosyphilis.
Many studies have evaluated the association between HIV infection and poor serologic response following syphilis treatment: this seems to be less frequent in patients with high CD4+ cell counts, confirming the importance of those cells for an appropriate serological response [ 46 ]. Both clinical and serological follow up in reinfections are more difficult because multiple episodes of syphilis seem to attenuate clinical and laboratory manifestations of TP infection. Furthermore, the detection of TP DNA in blood samples was significantly lower in those with previous syphilis [ 31 ]. However, further studies are needed.
6. Syphilis Prevention and Vaccines
The high incidence of syphilis worldwide, despite available and inexpensive treatment, emphasizes the need to seek an alternative approach for syphilis control. Combined strategies of public health (i.e., implementation of screening and treatment campaigns) and vaccine development should be encouraged.
There are few studies regarding the use of chemoprophylaxis for syphilis. A randomized pilot study showed the effectiveness of a potential post-exposure prophylaxis (PEP) with daily doxycycline for syphilis in MSM [ 78 ], revealing a potential benefit for this population. More recently, the ANRS IPERGAY trial confirmed the efficacy and safety of PEP with a single 200 mg dose of doxycycline (taken within 24 h after sex) in MSM taking pre-exposure prophylaxis (PrEP) for HIV prevention. The occurrence of a first episode of syphilis in participants taking PEP was lower than in those not taking PEP (HR 0.27; 95% CI 0.07–0.98; p = 0.047) [ 79 ]. Although the undoubted benefits of this practice, it is reasonable to be aware of the risks for the onset of antimicrobial-resistant strains.
Notwithstanding this, vaccines might be the ideal tool of prevention because of their long-lasting protection, but syphilis vaccine development presents several challenges. The limited availability of long-term culture systems [ 48 ] and the TP surface-exposed antigen shortage are the main reasons why a viable candidate is still unavailable and probably years away from discovery.
Several syphilis candidates have been investigated over the past few years, including whole-cell inactivated, live attenuated or genetically engineered vaccines [ 80 ].
Among them, members of the TP repeat ( TPr ) family of paralogs, such as TprK (TP0897), have emerged as promising candidates in vaccine development studies. Although TprK is antigenically unreliable and known to play a role in immune evasion, the structural model of the protein predicts three conserved surface-exposed loops in the TprK NH2-terminus. Immunization of rabbits with a recombinant NH2-terminal fragment of TprK purified under denaturing conditions attenuated cutaneous lesion development and progression to ulceration. Additionally, the treponemal burden challenge sites were significantly reduced compared to controls [ 81 , 82 ].
A whole-cell bacterial vaccine might be more effective than a recombinant antigen-based vaccine and, accordingly, a group of scientists decided to employ this approach to present TP antigens in their native conformation within a spirochete membrane compartment similar to that of the syphilis pathogen. This heterologous antigen presentation system used Borrelia burgdorferi engineered to express TP genes. A limited amount of the TP Tp0435 lipoprotein, previously believed to be exclusively periplasmic, was considered to also possibly gain surface exposure in both B. burgdorferi strains—this was then confirmed in TP. Partial protection was observed in rabbits immunized with B. burgdorferi expressing Tp0435 and immunity was not protective [ 83 ].
Lastly, a plasmid DNA encoding TP flagellin FlaB3 emerged as a candidate for vaccine development, evaluation of immunogenicity and protection against dissemination, showing a significant reduction in the bacterial burden in the blood, liver, spleen and testicles of immunized rabbits [ 84 ].
Further studies are needed to assess the proper means of immunization, the type of immune response elicited, and the duration of immunity [ 85 ].
7. Conclusions
The resurgence of syphilis has revived interest both in developing and developed countries—especially in PLWH. Syphilis still presents several challenges: identifying reinfections, monitoring therapy appropriately with serological tests and developing a correct approach to asymptomatic neurosyphilis. Biomedical interventions such as PrEP, PEP and vaccines for syphilis are not available and condom use remains the cornerstone of prevention for syphilis.
Future priorities include validating rapid and direct detection methods for syphilis ( point of care test ), finding alternative treatment regimens, and developing more effective means of prevention.
8. Research Strategy and Selection Criteria
References for this review were identified from PubMed, Embase and Cochrane with the research terms: “ syphilis ”, “Treponema”, “ HIV ”, “ treatment ”, “ diagnosis ” and “ vaccine ” with several combinations. Only papers in English were included. The final reference list was generated based on timeline, originality and relevance to the scope of this Review.
Author Contributions
Conceptualization, G.T. and E.Q.-R.; original draft preparation, G.T. and E.Q.-R.; methodology, software, validation, investigation, resources, data curation, writing, writing—review and editing, visualization, supervision, G.T., E.Q.-R., M.D.A., S.S., V.M., E.F., C.T. and F.C. All authors have read and agreed to the published version of the manuscript.
This research received no external funding.
Institutional Review Board Statement
Informed consent statement, data availability statement, conflicts of interest.
Authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- Case Report
- Open access
- Published: 01 April 2024
Secondary syphilis presenting with alopecia and leukoderma in a stable HIV-positive patient in a resource-limited setting: a case report
- Sukoluhle Khumalo 1 ,
- Yves Mafulu 1 ,
- Victor Williams 2 ,
- Normusa Musarapasi 2 ,
- Samson Haumba 2 &
- Nkululeko Dube 1
AIDS Research and Therapy volume 21 , Article number: 19 ( 2024 ) Cite this article
95 Accesses
2 Altmetric
Metrics details
Syphilis is an infection caused by the bacteria T reponema pallidum . It is mainly transmitted through oral, vaginal and anal sex, in pregnancy and through blood transfusion. Syphilis develops in primary, secondary, latent and tertiary stages and presents with different clinical features at each stage. Infected patients can remain asymptomatic for several years and, without treatment, can, in extreme cases, manifest as damage in several organs and tissues, including the brain, nervous tissue, eyes, ear and soft tissues. In countries with a high human immunodeficiency virus (HIV) burden, syphilis increases the risk of HIV infections. We report the case of a young HIV-positive black woman who presented with alopecia and hypopigmentation as features of secondary syphilis.
Case presentation
A virologically suppressed 29-year-old woman on Anti-retroviral Therapy (ART) presented with a short history of generalized hair loss associated with a non-itchy maculopapular rash and skin depigmentation on the feet. Limited laboratory testing confirmed a diagnosis of secondary syphilis. She was treated with Benzathine Penicillin 2.4MU. After receiving three doses of the recommended treatment, the presenting features cleared, and the patient recovered fully.
This case demonstrates the importance of a high index of clinical suspicion and testing for syphilis in patients presenting with atypical clinical features of secondary syphilis, such as hair loss and hypopigmentation. It also highlights the challenges in diagnosing and clinically managing syphilis in a resource-limited setting.
Syphilis remains a public health threat, with an estimated seven million new cases in 2020 [ 1 ]. The disease burden is heavy in low- and middle-income countries, with a review of sexually transmitted infections (STIs) among pregnant women reporting a syphilis prevalence of 6.5% in Southern Africa [ 2 ]. A study conducted in Swaziland among 655 women aged 15 to 49 years reported the prevalence of syphilis to be 2.0% [ 3 ]. Morbidity from syphilis is related not only to the impact of the disease on individuals but also its role as a contributor to HIV acquisition, together with the morbidity and mortality associated with neonatal infections [ 4 ]. HIV – syphilis coinfection is considered a dangerous combination since HIV makes the failure of syphilis treatment more likely, and coinfection leads to more profound neurocognitive impairment [ 5 , 6 ]. Conversely, syphilis increases susceptibility to HIV infection due to its negative impact on the immune system [ 4 ].
Syphilis’s natural history evolves with alternating episodes of clinical and immunologic stages [ 7 ]. It progresses in three classical stages – primary, secondary and latent [ 5 , 8 ]. However, many presentations vary and do not follow the classical stages. A chancre characterises primary syphilis, extensive mucocutaneous lesions occur in secondary syphilis and latent syphilis is diagnosed on serologic testing with no symptoms [ 8 , 9 ]. Secondary syphilis is characterised by generalised mucocutaneous lesions affecting the skin, mucous membranes, and, characteristically, the palms and soles [ 4 ]. The symptoms and signs of secondary syphilis spontaneously resolve within 3 to 12 weeks, even without treatment, and if left untreated, the patient enters the latent stage. An estimated 25% of untreated secondary syphilis cases symptomatically recur, mostly within 12 months [ 5 , 10 ]. In this article, we report the case of a 29-year-old HIV-positive patient who presented with two distinctive features of secondary syphilis and how the condition was managed.
A case report was compiled using information retrospectively collected from the patient’s electronic and physical medical records. Pictures were taken at different stages of the illness, with the patient’s verbal and written consent.
The patient is a 29-year-old HIV-positive female on a first-line dolutegravir (DTG)-based ART regimen. She is single and works in a clothing factory. She presented on March 23 2022, with a 2-week history of hair loss. She initially noted her braids falling off and then progressive hair loss on her scalp, eyebrows, eyelashes, axilla, and groin. There was mild associated itching with no scaling on the head. The patient was not on any new medications. She also complained of a non-itchy rash on the limbs, mainly on the hands, rough looking and brownish. She reported no contact with anyone with similar symptoms and has not been pregnant before.
On review of systems, she reported a painless pustule on the groin, which has been there for about a year, not growing, with no associated discomfort. She had not reported it before, as it was not causing any issues. She reported no other genitourinary symptoms.
The patient was diagnosed with HIV and commenced ART in 2014. She is still on first-line ART, initially initiated on TDF/3TC/EFV, and later transitioned to TDF/3TC/DTG on 30/12/2021 per HIV program recommendations, three months before presentation. Her latest laboratory results at presentation were a lower-than-detectable viral load (4/8/2021) and serum creatinine of 50 μm/L (4/8/2021).
Examination
On physical examination, the patient looked well and stable; her temperature was 36.5 0 C, her blood pressure was 120/50mmHg, her heart rate was 80b/min, and her respiratory rate was 18c/min. She was pink, well hydrated, and had no jaundice or oedema. Her oral cavity was clear.
She had extensive scalp alopecia, with patchy areas with hair, but no scaling was noted. There was also hair loss on the eyebrows, eyelashes, axilla and groin regions (Fig. 1 ). She also had hyperpigmented papules on the palmar aspect of both hands extending to the wrist, also called Buschke Ollendorf sign when there is tenderness on the application of blunt pressure on the papules [ 11 ] (Fig. 2A ) and asymmetrical, homogenous, clearly demarcated hypopigmentation on the anterior of both feet (Fig. 2B ). On examination of her genitourinary system, she had a painless lump measuring about 0.5 cm x 0.5 cm on the left peri vulval region. There were no palpable lymph nodes in the groin on either side. Examination of her chest, cardiovascular system and abdomen were normal.

Extensive alopecia, with “moth-eaten appearance”, noted on the scalp, with patchy areas with hair. Hair loss is noted on the eyebrows.

A Hypopigmentation of the anterior half of both feet, with a mottled appearance, consistent with Leukoderma syphilliticum , also called syphilis vitiligo. B Hyperpigmented maculopapular lesions in the palms of both hands also known as Buschke Ollendorf sign.
Laboratory investigation and management
The investigations done for the patient at presentation included a full blood count (FBC) and a syphilis determine rapid tests. The full blood count showed a haemoglobin of 10.7 g/dl, mean corpuscular volume (MCV) of 90.3 fl., a white cell count of 4.1 × 10 9 cells/litre and a platelet count of 309 × 10 9 /litre. The syphilis determine rapid test (for antibodies) was positive. The titre was not estimated due to the limited laboratory capacity.
The patient was treated with benzathine penicillin 2.4MU stat per World Health Organization (WHO) guidelines for secondary syphilis [ 12 ]. At review after two weeks, some improvement was observed in the maculopapular rash on the palms, and the genital lump had disappeared completely. However, there was no change in hair growth and skin depigmentation. The patient missed her review two weeks later and only returned after three months for her ART refill. At this visit, she was attended to by another clinician and given another three-month supply of ART medication. Since her contacts were not updated in the database, she could not be reached for further review and evaluation until September 21 2022. The patient was given three doses of benzathine penicillin at this time, and a rapid plasma reagin (RPR) titre done in October 2022 was less than 1:8.
The patient reported that hair started growing three months after treatment, and the hypopigmentation cleared earlier than the hair growth (Figs. 3 , 4 and 5 ).

The hair, eyelashes and eyebrows grew back three months after therapy with benzathine Penicillin (pictured here six months after therapy)
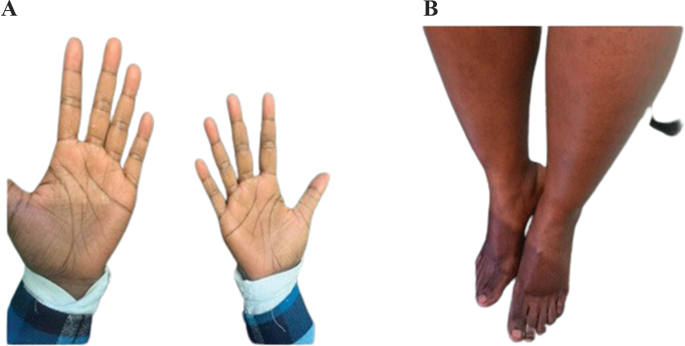
( A ) The maculopapular lesions disappeared from the palmar surface of both hands within two weeks. ( B ) The hypopigmentation on both feet cleared within three months (pictured here after six months of therapy)
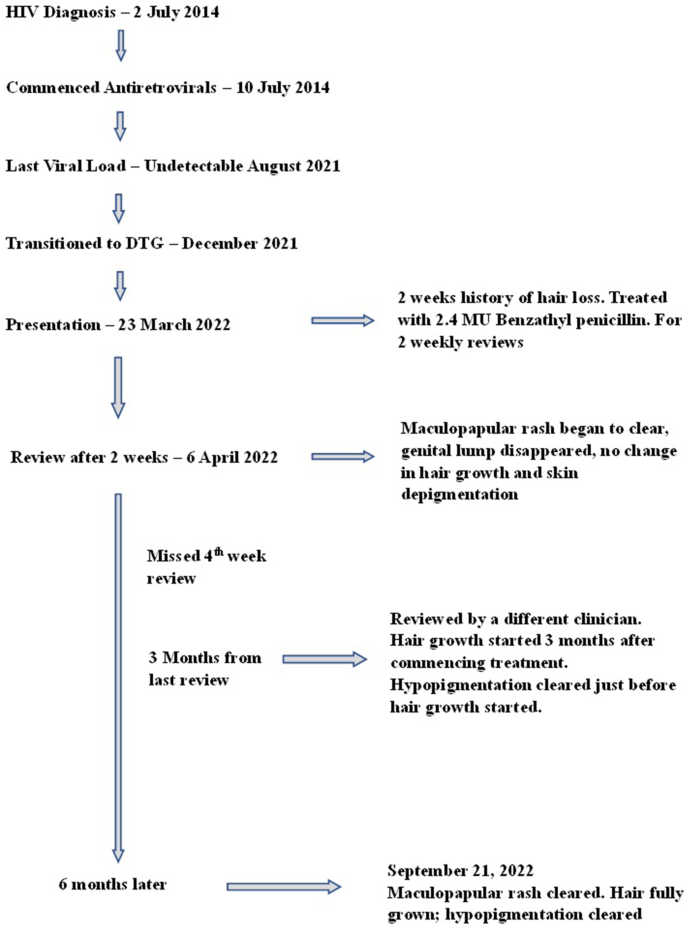
Timelines in patient care from HIV diagnosis to diagnosis of syphilis and treatment
Latest patient update
The patient had a viral load taken in August 2022, and it showed that her viral load was elevated at 13,187 copies/ml, and the CD4 count was 675 cells/microlitre. She subsequently admitted that she had struggled to take her treatment since May 2022 due to psychosocial issues. For this, she received stepped-up adherence counselling. By October 2022, she was diagnosed with drug-sensitive TB and had completed treatment. She was further referred to the cardiologist for further review and is being reviewed every six months for symptoms of relapse. In this case, we monitored variables such as RPR titers, clinical symptoms disappearance/relapse, time from treatment to recovery (disappearance of symptoms), and time to relapse, if ever relapse had to reoccur.
The patient gave written informed consent for the pictures to be taken, used for this study, and for reporting clinical details. The Eswatini Health and Human Research Review Board (EHHRB) has approved this case report’s public presentation and dissemination.
Discussion and conclusions
Our case scenario combines classical features of secondary syphilis with two uncommon features – alopecia and vitiligo, in a client receiving ART. Alopecia syphillitica, also described as “moth-eaten appearance”, is an unusual manifestation of secondary syphilis in 2.9–7% of individuals. It is a non-inflammatory, non-cicatrial hair loss that can present in a diffuse pattern with a classic patchy moth-eaten appearance or a combination of both [ 13 ]. The moth-eaten pattern is the most common presentation, as was seen in this case, which also had generalised, patchy hair loss. Two types of syphilis-associated alopecia have been described: symptomatic syphilis alopecia with other cutaneous lesions and the essential type, where no other cutaneous manifestations are noted [ 14 ]. The essential type would be complex to diagnose due to the absence of pointers, as seen in our patient with the palmar rash. Histologically, alopecia syphillitica can be differentiated from alopecia areata by the presence of peribulbar eosinophils [ 15 ].
Leukoderma syphilliticum, also known as syphilis vitiligo, manifests as hypopigmented patches, usually located in the neck, face and extremities [ 16 ]. Very few cases have been reported in the literature, with one previous case reported in an HIV-positive individual [ 16 ]. The published cases are heterogeneous in appearance [ 16 ]. The original description by Hardy in 1868 pointed to a mottled appearance. Leucoderma syphiliticum encompasses a spectrum of dyschromic lesions that emerge during syphilis [ 16 ]. The classic appearance is of small, clear or achromic spots surrounded by pigmented meshes in the early secondary phase [ 17 ]. Histologically, there is evidence of melanin absence from the epidermis [ 18 ]. In our case, the lesion did affect the extremities (feet), as previously described. However, the quasi-homogeneous presentation of the leukoderma syphilliticum, symmetrically affecting the anterior half of both feet, is particularly unique and could have been vitiligo, pityriasis alba, tinea versicolor, or post-inflammatory hyperpigmentation. However, distinct systemic signs of syphilis, non-atopic dermatological history, and lesion resolution post-treatment seen in our patient increased the odds for syphilis [ 19 ]. Acquired epidermodysplasia verruciformis, presenting with erythematous to skin-colored macules, should be considered in HIV-positive patients, as noted in our case, although its persistence and potential for malignant transformation makes it unlikely. Histological examination remains the most reliable diagnostic method for these conditions [ 19 , 20 ].
The pathogenesis of both leukoderma and syphilitic alopecia is based on an immune response to Treponema Pallidum , with resulting loss of terminal hairs, stoppage of the hair cycle and hair bending in the case of alopecia, and melanin loss in the leukoderma [ 21 ].
Our client was diagnosed using a syphilis determine test after clinical suspicion. The titres were not measured as the equipment was unavailable. Due to their cost, we did not have access to histology, skin biopsy or other tests that can rule out any cause of alopecia and leukoderma, such as thyroid hormone and auto-immune tests. Therefore, a high level of clinical suspicion is required to avoid incorrect or delayed diagnosis.
The therapeutic approach was based on the WHO guidelines for clients with secondary syphilis, consisting of a stat dose of 2.4 million IU of benzathine penicillin [ 12 ]. In the absence of the titres, whether a single dose of benzathine penicillin was sufficient or if the client should receive three doses given as one dose weekly is debatable. The client’s hair started growing 12 weeks post-treatment. Hernández-Bel et al. found in their report of five cases that alopecia disappeared completely within 8 to 12 weeks from treatment [ 22 ]. Their population comprised HIV-negative ( n = 3) and HIV-positive ( n = 2) clients.
Moreover, their HIV-positive patients received three doses of benzathine penicillin 2.4 million IU, while the HIV-negative clients received a single dose of penicillin. We are uncertain if there is a difference in the time to recovery between our HIV-positive case, who received a single dose of Benzathine Penicillin, and those of Hernández-Bel et al., who received three doses [ 22 ]. A larger study would be required to make a definitive conclusion. HIV infection can cause larger or more chancres, accelerated ulcerating secondary Syphilis, frequent ocular Syphilis, and faster progression to late syphilis like neurosyphilis and gummatous syphilis. The former has been reported mostly in those treated for early syphilis with single-dose benzathine penicillin [ 8 ]. Within a few weeks or months, leucoderma syphiliticum macules may repigment following therapy with penicillin [ 16 ]. In our case, leukoderma had disappeared within three months following Benzathine Penicillin administration. Based on literature and available evidence, the medical team decided the patient should receive two additional doses six months after initiation. Given the numerous reports of neurosyphilis progression after a single dosage of benzathine penicillin, Goh et al. thought in their study that it might be advisable to treat with three doses of benzathine penicillin 2.4 mega units at weekly intervals to avoid such development [ 8 ].
This case combined two rare presentations of secondary syphilis in a stable HIV-positive patient. The syphilitic alopecia followed a clinical course that has been commonly reported, but the leukoderma syphilliticum presented with homogeneous lesions in the affected area, contrary to the heterogenous presentation that has been previously described. This observation prompts the need for a high index of suspicion and syphilis investigation for patients with unusual clinical presentations such as vitiligo and alopecia.
Data availability
Data used in this case report is available upon a reasonable request to the corresponding author.
Abbreviations
Anti–retroviral therapy
Dolutegravir
Eswatini Health and Human Research Review Board
Full Blood Count
Human Immunodeficiency Virus
Rapid Plasma Reagin
Sexually Transmitted Infections
World Health Organisation
World Health Organisation. Sexually transmitted infections (STIs): Key Facts [Internet], Geneva. WHO; 2022 Aug [cited 2023 Oct 15]. Available from: https://www.who.int/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis ).
Kojima N, Klausner JD. An update on the Global Epidemiology of Syphilis. Curr Epidemiol Rep. 2018;5(1):24–38.
Article PubMed PubMed Central Google Scholar
Ginindza TG, Stefan CD, Tsoka-Gwegweni JM, Dlamini X, Jolly PE, Weiderpass E, et al. Prevalence and risk factors associated with sexually transmitted infections (STIs) among women of reproductive age in Swaziland. Infect Agent Cancer. 2017;12:29.
Peeling RW, Hook EW. The pathogenesis of syphilis: the great mimicker, revisited. J Pathol. 2006;208(2):224–32.
Article CAS PubMed Google Scholar
New South Wales Ministry of Health. Syphilis Control Guideline [Internet]. Sydney: NSW Health; 2023 [cited 2023 Oct 15]. Available from: https://www.health.nsw.gov.au/Infectious/controlguideline/Pages/syphilis.aspx .
Marra CM, Deutsch R, Collier AC, Morgello S, Letendre S, Clifford D, et al. Neurocognitive impairment in HIV-infected individuals with previous syphilis. Int J STD AIDS. 2013;24(5):351–5.
Article CAS PubMed PubMed Central Google Scholar
Carlson JA, Dabiri G, Cribier B, Sell S. The immunopathobiology of syphilis: the manifestations and course of syphilis are determined by the level of delayed-type hypersensitivity. Am J Dermatopathol. 2011;33(5):433–60.
Goh BT. Syphilis in adults. Sex Transm Infect. 2005;81(6):448–52.
Lee V, Kinghorn G. Syphilis: an update. Clin Med. 2008;8(3):330–330.
Article Google Scholar
Wojas-Pelc A, Pastuszczak M, Jaworek A, Syphilis. McMaster Textbook of Internal Medicine. [Internet]. Kraków: Medycyna Praktyczna; 2022 [cited 2023 Nov 28]. Available from: https://empendium.com/mcmtextbook/social/chapter/B31.II.18.96.6.4 .
Amrani A, Sil A, Das A. Cutaneous signs in infectious diseases. Indian J Dermatol Venereol Leprol. 2022;88(4):569–75.
Article PubMed Google Scholar
World Health Organisation. WHO guidelines for the treatment of Treponema pallidum (syphilis) [Internet]. Geneva: WHO. 2016 [cited 2023 Oct 15]. Available from: https://apps.who.int/iris/bitstream/handle/10665/249572/?sequence=1 .
Jordaan HF, Louw M. The moth-eaten alopecia of secondary syphilis. A histopathological study of 12 patients. Am J Dermatopathol. 1995;17(2):158–62.
Cuozzo DW, Benson PM, Sperling LC, Skelton HG. Essential syphilitic alopecia revisited. J Am Acad Dermatol. 1995;32(5 Pt 2):840–3.
Lee JYY, Hsu ML. Alopecia Syphilitica, a simulator of Alopecia Areata: histopathology and differential diagnosis. J Cutan Pathol. 1991;18(2):87–92.
Eyer-Silva W, de Martins A, Silva CJ, Acakpovi GAR. G, Pinto JF da C. Secondary syphilis presenting as leucoderma syphiliticum: case report and review. Rev Inst Med Trop Sao Paulo. 2017;59:e74.
de Miranda MFR, Bittencourt M, de JS, Lopes I, da Cumino C. S do SM. Leucoderma syphiliticum: a rare expression of the secondary stage diagnosed by histopathology. An Bras Dermatol. 2010;85:512–5.
Pandhi RK, Bedi TR, Bhutani LK. Leucoderma in early syphilis. Br J Vener Dis. 1977;53(1):19–22.
CAS PubMed PubMed Central Google Scholar
Sil A, Bhanja DB, Panigrahi A, Biswas SK. Acquired Epidermodysplasia Verruciformis during highly active antiretroviral therapy. Indian J Dermatol. 2022;67(3):316.
Rao M, Young K, Jackson-Cowan L, Kourosh A, Theodosakis N. Post-inflammatory Hypopigmentation: review of the etiology, clinical manifestations, and Treatment options. J Clin Med. 2023;12(3):1243.
Ciupińska M, Skibińska J, Sikora M, Blicharz L, Kotowska M, Rudnicka L. Nonscarring Alopecia and Hypopigmented lesions May be unusual signs of secondary Syphilis. Skin Appendage Disord. 2021;7(3):203–5.
Hernández-Bel P, Unamuno B, Sánchez-Carazo JL, Febrer I, Alegre V. Syphilitic alopecia: a report of 5 cases and a review of the literature. Actas Dermosifiliogr. 2013;104(6):512–7.
Download references
Acknowledgements
We thank the patient for permitting the documentation and publication of this case report. We also thank the clinical and support staff at the AIDS Healthcare Foundation (AHF) Lamvelase Clinic, Manzini, Eswatini, for providing care for the patient and assisting with retrieving the patient’s record to enable the write-up of this case report.
The write-up of this case report did not receive any specific funding. The AIDS Healthcare Foundation (AHF) LaMvelase Clinic, Manzini, Eswatini receives technical assistance from the Support Eswatini Achieve and Sustain HIV Epidemic Control (SEASEC) Program funded by the US President’s Emergency Plan for AIDS Relief (PEPFAR) through the Centers for Disease Control and Prevention (CDC) (Co-operative Agreement No.: NU2GGH002294), implemented by Georgetown University in collaboration with the Government of the Kingdom of Eswatini.
Author information
Authors and affiliations.
AIDS Healthcare Foundation, Manzini, Eswatini
Sukoluhle Khumalo, Yves Mafulu & Nkululeko Dube
Centre for Global Health Practice and Impact, Georgetown University, Mbabane, Eswatini
Victor Williams, Normusa Musarapasi & Samson Haumba
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualisation: SK, YM, VW, ND. Patient care and data extraction: SK, YM, NM, SH, ND. First draft: SK, YM, VW. Review of first draft: NM, SH, ND. Ethical clearance: SK, Review and approval of final draft: All authors.
Corresponding author
Correspondence to Victor Williams .
Ethics declarations
Ethical approval.
The Eswatini Health and Human Research Review Board (EHHRB) approved this case report’s documentation, public presentation, and publication (EHHRRB 053/2023). The patient also gave written informed consent for the pictures to be taken, used for this study, and for reporting clinical details.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Khumalo, S., Mafulu, Y., Williams, V. et al. Secondary syphilis presenting with alopecia and leukoderma in a stable HIV-positive patient in a resource-limited setting: a case report. AIDS Res Ther 21 , 19 (2024). https://doi.org/10.1186/s12981-024-00603-w
Download citation
Received : 12 November 2023
Accepted : 13 March 2024
Published : 01 April 2024
DOI : https://doi.org/10.1186/s12981-024-00603-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Secondary syphilis
- Leukoderma syphilliticum
- Human immuno-deficiency virus.
AIDS Research and Therapy
ISSN: 1742-6405
- Submission enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
The classic primary syphilis presentation is a solitary non-tender genital chancre in response to invasion by the T. pallidum. However, patients can have multiple non-genital chancres, such as digits, nipples, tonsils, and oral mucosa. ... If there are no clinical manifestations of syphilis and the evaluation is otherwise normal (VDRL of the ...
Primary syphilis occurs 10-90 days after contact with an infected individual. It manifests mainly on the glans penis in males and on the vulva or cervix in females. Ten percent of syphilitic lesions are found on the anus, fingers, oropharynx, tongue, nipples, or other extragenital sites. Regional nontender lymphadenopathy follows invasion.
The most common way syphilis spreads is through contact with an infected person's sore during vaginal, oral or anal sex. The bacteria enter the body through minor cuts or scrapes in the skin or in the moist inner lining of some body parts. Syphilis is contagious during its primary and secondary stages.
Primary syphilis classically presents as a single, painless, indurated genital ulcer (chancre), but this presentation is only 31% sensitive; lesions can be painful, multiple, and extra-genital. Diagnosis is usually based on serology, using a combination of treponemal and non-treponemal tests.
Some studies suggest that infection with HIV may affect the clinical presentation of syphilis, as atypical or multiple genital lesions are more apparent, and accelerated progression of syphilis may be seen in people with advanced immunosuppression. 16,17,19-22 Primary or secondary syphilis also may cause a transient decrease in CD4 T lymphocyte ...
Syphilis is an infectious disease caused by the spirochete bacterium treponema pallidum. Syphilis has a wide and varied presentation, so if it is not considered as a diagnosis, it can be easily missed. Syphilis has primary, secondary, and tertiary presentations. Diagnosis is predominantly by serological testing.
Clinical presentation. The clinical course of syphilis is one of overlapping clinical stages which begin 9-90 (median 21) days following direct contact with an infectious lesion (Fig 1). ... Primary syphilis is characterised by a papule at the point of entry of the bacterium that breaks down into an ulcer (chancre). Although classically ...
Clinical presentation, signs, and symptoms. After an incubation period of 10-70 days (median 21 days) a primary chancre develops at the site of inoculation (figure 1). 7,24. The chancre is typically a painless, single, non-tender, indurated ulcer, with a raised edge and a clean base. The primary presentation of syphilis has also
Clinical presentation 10 Laboratory diagnosis 11 1.2 Rationale for new recommendations 13 1.3 Objectives 14 1.4 Target audience 14 1.5 Structure of the guidelines 14 ... Primary syphilis classically presents as a solitary, painless chancre at the site of inoculation. However, the primary chancre may go unnoticed
There are four stages of syphilis (primary, secondary, latent, and tertiary). Each stage has different signs and symptoms. Primary Stage. During the first (primary) stage of syphilis, you may notice a single sore or multiple sores. The sore is the location where syphilis entered your body. These sores usually occur in, on, or around the. penis ...
The past decade has seen a sharp rise in syphilis cases among men, driven mostly by the MSM community. Males with primary and secondary syphilis outnumber females 10 to 1. Among women, the reported primary and secondary syphilis rate increased from 0.9 to 1.5 per 100,000 population per year during 2005- 2008 and decreased to 0.9 in 2013.
The choice of method for diagnosing syphilis depends on the stage of disease and the clinical presentation 125. In patients presenting with primary syphilitic ulcers, condyloma lata (genital ...
The clinical presentation of untreated syphilis varies according to its stage. These 4 stages are primary, secondary, latent, and tertiary. In primary syphilis, the spirochete causes a firm, ulcerative, painless lesion, called a chancre, at the site of entry. The chancre (or chancres) can appear on or around the external genitalia—in or ...
Primary syphilis is usually characterized by a chancre, ... The clinical presentation varies and is determined by the structures involved and duration of infection. The absence of gold-standard tests and the broad clinical features contribute to difficulties in diagnosis. The laboratory diagnosis of neurosyphilis requires serum and CSF ...
Primary syphilis. Primary syphilis is characterized by a nontender papule at the site of inoculation that quickly erodes, leaving an ulcer (the chancre). The base of the ulcer is smooth, without exudate, and the borders are raised and firm. Painless nonsuppurative enlargement of local lymph nodes accompanies the chancre and can persist for months.
The clinical presentation of syphilis does not differ between pregnant and nonpregnant women. Primary syphilis is characterized by one or more indurated chancres at the site of inoculation, which ...
Clinical features of secondary syphilis typically appear 4 to 8 weeks after primary syphilis infection, but they may also occur up to 6 months later. The presentation of secondary syphilis is diverse. Hematogenous dissemination in secondary syphilis affects different organs.
The clinical presentation of syphilis does not dif- ... Primary syphilis is characterized by one or more indurated chancres at the site of inoculation, which
Moreover, HIV infection may modulate the clinical presentation and the clinical and serologic response to syphilis treatment [3,4,5,6]. ... These tests show a 62-78% sensitivity for primary syphilis, 97-100% for secondary and 80-100% for early latent syphilis . The sensitivity of NNT is lower for late syphilis whereas, ...
Syphilis is an infection caused by the bacteria Treponema pallidum. It is mainly transmitted through oral, vaginal and anal sex, in pregnancy and through blood transfusion. Syphilis develops in primary, secondary, latent and tertiary stages and presents with different clinical features at each stage. Infected patients can remain asymptomatic for several years and, without treatment, can, in ...