- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

What Is Breech?
When a fetus is delivered buttocks or feet first
- Types of Presentation
Risk Factors
Complications.
Breech concerns the position of the fetus before labor . Typically, the fetus comes out headfirst, but in a breech delivery, the buttocks or feet come out first. This type of delivery is risky for both the pregnant person and the fetus.
This article discusses the different types of breech presentations, risk factors that might make a breech presentation more likely, treatment options, and complications associated with a breech delivery.
Verywell / Jessica Olah
Types of Breech Presentation
During the last few weeks of pregnancy, a fetus usually rotates so that the head is positioned downward to come out of the vagina first. This is called the vertex position.
In a breech presentation, the fetus does not turn to lie in the correct position. Instead, the fetus’s buttocks or feet are positioned to come out of the vagina first.
At 28 weeks of gestation, approximately 20% of fetuses are in a breech position. However, the majority of these rotate to the proper vertex position. At full term, around 3%–4% of births are breech.
The different types of breech presentations include:
- Complete : The fetus’s knees are bent, and the buttocks are presenting first.
- Frank : The fetus’s legs are stretched upward toward the head, and the buttocks are presenting first.
- Footling : The fetus’s foot is showing first.
Signs of Breech
There are no specific symptoms associated with a breech presentation.
Diagnosing breech before the last few weeks of pregnancy is not helpful, since the fetus is likely to turn to the proper vertex position before 35 weeks gestation.
A healthcare provider may be able to tell which direction the fetus is facing by touching a pregnant person’s abdomen. However, an ultrasound examination is the best way to determine how the fetus is lying in the uterus.
Most breech presentations are not related to any specific risk factor. However, certain circumstances can increase the risk for breech presentation.
These can include:
- Previous pregnancies
- Multiple fetuses in the uterus
- An abnormally shaped uterus
- Uterine fibroids , which are noncancerous growths of the uterus that usually appear during the childbearing years
- Placenta previa, a condition in which the placenta covers the opening to the uterus
- Preterm labor or prematurity of the fetus
- Too much or too little amniotic fluid (the liquid that surrounds the fetus during pregnancy)
- Fetal congenital abnormalities
Most fetuses that are breech are born by cesarean delivery (cesarean section or C-section), a surgical procedure in which the baby is born through an incision in the pregnant person’s abdomen.
In rare instances, a healthcare provider may plan a vaginal birth of a breech fetus. However, there are more risks associated with this type of delivery than there are with cesarean delivery.
Before cesarean delivery, a healthcare provider might utilize the external cephalic version (ECV) procedure to turn the fetus so that the head is down and in the vertex position. This procedure involves pushing on the pregnant person’s belly to turn the fetus while viewing the maneuvers on an ultrasound. This can be an uncomfortable procedure, and it is usually done around 37 weeks gestation.
ECV reduces the risks associated with having a cesarean delivery. It is successful approximately 40%–60% of the time. The procedure cannot be done once a pregnant person is in active labor.
Complications related to ECV are low and include the placenta tearing away from the uterine lining, changes in the fetus’s heart rate, and preterm labor.
ECV is usually not recommended if the:
- Pregnant person is carrying more than one fetus
- Placenta is in the wrong place
- Healthcare provider has concerns about the health of the fetus
- Pregnant person has specific abnormalities of the reproductive system
Recommendations for Previous C-Sections
The American College of Obstetricians and Gynecologists (ACOG) says that ECV can be considered if a person has had a previous cesarean delivery.
During a breech delivery, the umbilical cord might come out first and be pinched by the exiting fetus. This is called cord prolapse and puts the fetus at risk for decreased oxygen and blood flow. There’s also a risk that the fetus’s head or shoulders will get stuck inside the mother’s pelvis, leading to suffocation.
Complications associated with cesarean delivery include infection, bleeding, injury to other internal organs, and problems with future pregnancies.
A healthcare provider needs to weigh the risks and benefits of ECV, delivering a breech fetus vaginally, and cesarean delivery.
In a breech delivery, the fetus comes out buttocks or feet first rather than headfirst (vertex), the preferred and usual method. This type of delivery can be more dangerous than a vertex delivery and lead to complications. If your baby is in breech, your healthcare provider will likely recommend a C-section.
A Word From Verywell
Knowing that your baby is in the wrong position and that you may be facing a breech delivery can be extremely stressful. However, most fetuses turn to have their head down before a person goes into labor. It is not a cause for concern if your fetus is breech before 36 weeks. It is common for the fetus to move around in many different positions before that time.
At the end of your pregnancy, if your fetus is in a breech position, your healthcare provider can perform maneuvers to turn the fetus around. If these maneuvers are unsuccessful or not appropriate for your situation, cesarean delivery is most often recommended. Discussing all of these options in advance can help you feel prepared should you be faced with a breech delivery.
American College of Obstetricians and Gynecologists. If your baby is breech .
TeachMeObGyn. Breech presentation .
MedlinePlus. Breech birth .
Hofmeyr GJ, Kulier R, West HM. External cephalic version for breech presentation at term . Cochrane Database Syst Rev . 2015 Apr 1;2015(4):CD000083. doi:10.1002/14651858.CD000083.pub3
By Christine Zink, MD Dr. Zink is a board-certified emergency medicine physician with expertise in the wilderness and global medicine.
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
INTRODUCTION
This topic will provide an overview of major issues related to breech presentation, including choosing the best route for delivery. Techniques for breech delivery, with a focus on the technique for vaginal breech delivery, are discussed separately. (See "Delivery of the singleton fetus in breech presentation" .)
TYPES OF BREECH PRESENTATION
● Frank breech – Both hips are flexed and both knees are extended so that the feet are adjacent to the head ( figure 1 ); accounts for 50 to 70 percent of breech fetuses at term.
● Complete breech – Both hips and both knees are flexed ( figure 2 ); accounts for 5 to 10 percent of breech fetuses at term.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Breech - series—Types of breech presentation
- Go to slide 1 out of 7
- Go to slide 2 out of 7
- Go to slide 3 out of 7
- Go to slide 4 out of 7
- Go to slide 5 out of 7
- Go to slide 6 out of 7
- Go to slide 7 out of 7
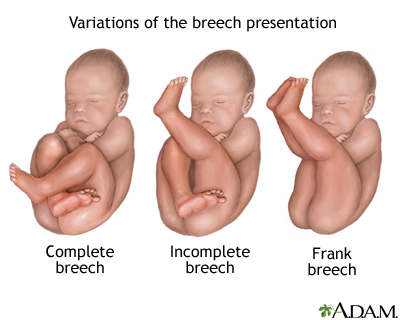
There are three types of breech presentation: complete, incomplete, and frank.
Complete breech is when both of the baby's knees are bent and his feet and bottom are closest to the birth canal.
Incomplete breech is when one of the baby's knees is bent and his foot and bottom are closest to the birth canal.
Frank breech is when the baby's legs are folded flat up against his head and his bottom is closest to the birth canal.
There is also footling breech where one or both feet are presenting.
Review Date 11/21/2022
Updated by: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Related MedlinePlus Health Topics
- Childbirth Problems

- Pregnancy Classes

Breech Births
In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby’s buttocks, feet, or both are positioned to come out first during birth. This happens in 3–4% of full-term births.
What are the different types of breech birth presentations?
- Complete breech: Here, the buttocks are pointing downward with the legs folded at the knees and feet near the buttocks.
- Frank breech: In this position, the baby’s buttocks are aimed at the birth canal with its legs sticking straight up in front of his or her body and the feet near the head.
- Footling breech: In this position, one or both of the baby’s feet point downward and will deliver before the rest of the body.
What causes a breech presentation?
The causes of breech presentations are not fully understood. However, the data show that breech birth is more common when:
- You have been pregnant before
- In pregnancies of multiples
- When there is a history of premature delivery
- When the uterus has too much or too little amniotic fluid
- When there is an abnormally shaped uterus or a uterus with abnormal growths, such as fibroids
- The placenta covers all or part of the opening of the uterus placenta previa
How is a breech presentation diagnosed?
A few weeks prior to the due date, the health care provider will place her hands on the mother’s lower abdomen to locate the baby’s head, back, and buttocks. If it appears that the baby might be in a breech position, they can use ultrasound or pelvic exam to confirm the position. Special x-rays can also be used to determine the baby’s position and the size of the pelvis to determine if a vaginal delivery of a breech baby can be safely attempted.
Can a breech presentation mean something is wrong?
Even though most breech babies are born healthy, there is a slightly elevated risk for certain problems. Birth defects are slightly more common in breech babies and the defect might be the reason that the baby failed to move into the right position prior to delivery.
Can a breech presentation be changed?
It is preferable to try to turn a breech baby between the 32nd and 37th weeks of pregnancy . The methods of turning a baby will vary and the success rate for each method can also vary. It is best to discuss the options with the health care provider to see which method she recommends.
Medical Techniques
External Cephalic Version (EVC) is a non-surgical technique to move the baby in the uterus. In this procedure, a medication is given to help relax the uterus. There might also be the use of an ultrasound to determine the position of the baby, the location of the placenta and the amount of amniotic fluid in the uterus.
Gentle pushing on the lower abdomen can turn the baby into the head-down position. Throughout the external version the baby’s heartbeat will be closely monitored so that if a problem develops, the health care provider will immediately stop the procedure. ECV usually is done near a delivery room so if a problem occurs, a cesarean delivery can be performed quickly. The external version has a high success rate and can be considered if you have had a previous cesarean delivery.
ECV will not be tried if:
- You are carrying more than one fetus
- There are concerns about the health of the fetus
- You have certain abnormalities of the reproductive system
- The placenta is in the wrong place
- The placenta has come away from the wall of the uterus ( placental abruption )
Complications of EVC include:
- Prelabor rupture of membranes
- Changes in the fetus’s heart rate
- Placental abruption
- Preterm labor
Vaginal delivery versus cesarean for breech birth?
Most health care providers do not believe in attempting a vaginal delivery for a breech position. However, some will delay making a final decision until the woman is in labor. The following conditions are considered necessary in order to attempt a vaginal birth:
- The baby is full-term and in the frank breech presentation
- The baby does not show signs of distress while its heart rate is closely monitored.
- The process of labor is smooth and steady with the cervix widening as the baby descends.
- The health care provider estimates that the baby is not too big or the mother’s pelvis too narrow for the baby to pass safely through the birth canal.
- Anesthesia is available and a cesarean delivery possible on short notice
What are the risks and complications of a vaginal delivery?
In a breech birth, the baby’s head is the last part of its body to emerge making it more difficult to ease it through the birth canal. Sometimes forceps are used to guide the baby’s head out of the birth canal. Another potential problem is cord prolapse . In this situation the umbilical cord is squeezed as the baby moves toward the birth canal, thus slowing the baby’s supply of oxygen and blood. In a vaginal breech delivery, electronic fetal monitoring will be used to monitor the baby’s heartbeat throughout the course of labor. Cesarean delivery may be an option if signs develop that the baby may be in distress.
When is a cesarean delivery used with a breech presentation?
Most health care providers recommend a cesarean delivery for all babies in a breech position, especially babies that are premature. Since premature babies are small and more fragile, and because the head of a premature baby is relatively larger in proportion to its body, the baby is unlikely to stretch the cervix as much as a full-term baby. This means that there might be less room for the head to emerge.
Want to Know More?
- Creating Your Birth Plan
- Labor & Birth Terms to Know
- Cesarean Birth After Care
Compiled using information from the following sources:
- ACOG: If Your Baby is Breech
- William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 24.
- Danforth’s Obstetrics and Gynecology Ninth Ed. Scott, James R., et al, Ch. 21.
BLOG CATEGORIES
- Can I get pregnant if… ? 3
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Breastfeeding 29
- Changes In Your Body 5
- Cord Blood 4
- Genetic Disorders & Birth Defects 17
- Health & Nutrition 2
- Is it Safe While Pregnant 54
- Labor and Birth 65
- Multiple Births 10
- Planning and Preparing 24
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Pregnancy Health and Wellness 149
- Pregnancy Products & Tests 8
- Pregnancy Supplements & Medications 14
- The First Year 41
- Week by Week Newsletter 40
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Paternity Tests 2
- Pregnancy Symptoms 5
- Prenatal Testing 16
- The Bumpy Truth Blog 7
- Uncategorized 4
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Women's Health 34
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
Share this post:
Similar post.

Episiotomy: Advantages & Complications

Retained Placenta

What is Dilation in Pregnancy?
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.
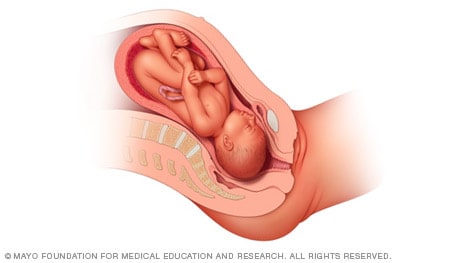
Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

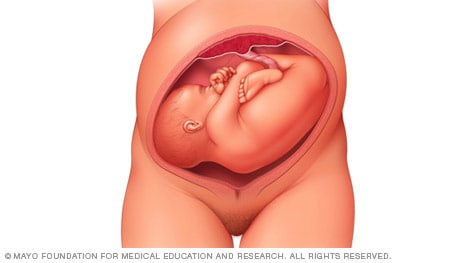
Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.
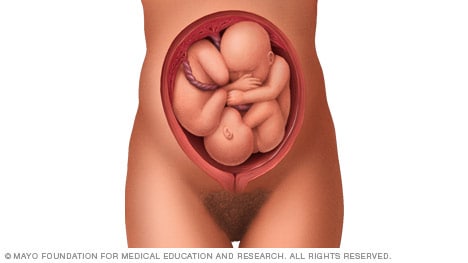
If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.
- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Make twice the impact
Your gift can go twice as far to advance cancer research and care!

- about Merck
- Merck Careers
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Key Points |
Abnormal fetal lie or presentation may occur due to fetal size, fetal anomalies, uterine structural abnormalities, multiple gestation, or other factors. Diagnosis is by examination or ultrasonography. Management is with physical maneuvers to reposition the fetus, operative vaginal delivery , or cesarean delivery .
Terms that describe the fetus in relation to the uterus, cervix, and maternal pelvis are
Fetal presentation: Fetal part that overlies the maternal pelvic inlet; vertex (cephalic), face, brow, breech, shoulder, funic (umbilical cord), or compound (more than one part, eg, shoulder and hand)
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse
Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position.
Abnormal fetal lie, presentation, or position may occur with
Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal congenital anomalies
Uterine structural abnormalities (eg, fibroids, synechiae)
Multiple gestation
Several common types of abnormal lie or presentation are discussed here.
Transverse lie
Fetal position is transverse, with the fetal long axis oblique or perpendicular rather than parallel to the maternal long axis. Transverse lie is often accompanied by shoulder presentation, which requires cesarean delivery.
Breech presentation
There are several types of breech presentation.
Frank breech: The fetal hips are flexed, and the knees extended (pike position).
Complete breech: The fetus seems to be sitting with hips and knees flexed.
Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
Types of breech presentations
Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows. The head, which is the part with the largest diameter, can then be trapped during delivery.
Additionally, the trapped fetal head can compress the umbilical cord if the fetal umbilicus is visible at the introitus, particularly in primiparas whose pelvic tissues have not been dilated by previous deliveries. Umbilical cord compression may cause fetal hypoxemia.
Predisposing factors for breech presentation include
Preterm labor
Uterine abnormalities
Fetal anomalies
If delivery is vaginal, breech presentation may increase risk of
Umbilical cord prolapse
Birth trauma
Perinatal death

Face or brow presentation
In face presentation, the head is hyperextended, and position is designated by the position of the chin (mentum). When the chin is posterior, the head is less likely to rotate and less likely to deliver vaginally, necessitating cesarean delivery.
Brow presentation usually converts spontaneously to vertex or face presentation.
Occiput posterior position
The most common abnormal position is occiput posterior.
The fetal neck is usually somewhat deflexed; thus, a larger diameter of the head must pass through the pelvis.
Progress may arrest in the second phase of labor. Operative vaginal delivery or cesarean delivery is often required.
Position and Presentation of the Fetus
If a fetus is in the occiput posterior position, operative vaginal delivery or cesarean delivery is often required.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord.
For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Key Points |
Abnormal fetal lie or presentation may occur due to fetal size, fetal anomalies, uterine structural abnormalities, multiple gestation, or other factors. Diagnosis is by examination or ultrasonography. Management is with physical maneuvers to reposition the fetus, operative vaginal delivery , or cesarean delivery .
Terms that describe the fetus in relation to the uterus, cervix, and maternal pelvis are
Fetal presentation: Fetal part that overlies the maternal pelvic inlet; vertex (cephalic), face, brow, breech, shoulder, funic (umbilical cord), or compound (more than one part, eg, shoulder and hand)
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse
Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position.
Abnormal fetal lie, presentation, or position may occur with
Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal congenital anomalies
Uterine structural abnormalities (eg, fibroids, synechiae)
Multiple gestation
Several common types of abnormal lie or presentation are discussed here.
Transverse lie
Fetal position is transverse, with the fetal long axis oblique or perpendicular rather than parallel to the maternal long axis. Transverse lie is often accompanied by shoulder presentation, which requires cesarean delivery.
Breech presentation
There are several types of breech presentation.
Frank breech: The fetal hips are flexed, and the knees extended (pike position).
Complete breech: The fetus seems to be sitting with hips and knees flexed.
Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
Types of breech presentations
Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows. The head, which is the part with the largest diameter, can then be trapped during delivery.
Additionally, the trapped fetal head can compress the umbilical cord if the fetal umbilicus is visible at the introitus, particularly in primiparas whose pelvic tissues have not been dilated by previous deliveries. Umbilical cord compression may cause fetal hypoxemia.
Predisposing factors for breech presentation include
Preterm labor
Uterine abnormalities
Fetal anomalies
If delivery is vaginal, breech presentation may increase risk of
Umbilical cord prolapse
Birth trauma
Perinatal death
Face or brow presentation
In face presentation, the head is hyperextended, and position is designated by the position of the chin (mentum). When the chin is posterior, the head is less likely to rotate and less likely to deliver vaginally, necessitating cesarean delivery.
Brow presentation usually converts spontaneously to vertex or face presentation.
Occiput posterior position
The most common abnormal position is occiput posterior.
The fetal neck is usually somewhat deflexed; thus, a larger diameter of the head must pass through the pelvis.
Progress may arrest in the second phase of labor. Operative vaginal delivery or cesarean delivery is often required.
Position and Presentation of the Fetus
If a fetus is in the occiput posterior position, operative vaginal delivery or cesarean delivery is often required.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord.
For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Breech Presentation
Affiliations.
- 1 Creighton University School of Medicine
- 2 Creighton University
- PMID: 28846227
- Bookshelf ID: NBK448063
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. The complete breech has the fetus sitting with flexion of both hips and both legs in a tuck position. Finally, the incomplete breech can have any combination of one or both hips extended, also known as footling (one leg extended) breech, or double footling breech (both legs extended).
Copyright © 2024, StatPearls Publishing LLC.
- Continuing Education Activity
- Introduction
- Epidemiology
- Pathophysiology
- History and Physical
- Treatment / Management
- Differential Diagnosis
- Pearls and Other Issues
- Enhancing Healthcare Team Outcomes
- Review Questions
Publication types
- Study Guide
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
- Identification of breech presentation
Evidence review L
NICE Guideline, No. 201
National Guideline Alliance (UK) .
- Copyright and Permissions
Review question
What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation?
Introduction
Breech presentation in late pregnancy may result in prolonged or obstructed labour for the woman. There are interventions that can correct or assist breech presentation which are important for the woman’s and the baby’s health. This review aims to determine the most effective way of identifying a breech presentation in late pregnancy.
Summary of the protocol
Please see Table 1 for a summary of the Population, Intervention, Comparison and Outcome (PICO) characteristics of this review.
Summary of the protocol (PICO table).
For further details see the review protocol in appendix A .
Methods and process
This evidence review was developed using the methods and process described in Developing NICE guidelines: the manual 2014 . Methods specific to this review question are described in the review protocol in appendix A .
Declarations of interest were recorded according to NICE’s conflicts of interest policy .
Clinical evidence
Included studies.
One single centre randomised controlled trial (RCT) was included in this review ( McKenna 2003 ). The study was carried out in Northern Ireland, UK. The study compared ultrasound examination at 30-32 and 36-37 weeks with maternal abdomen palpation during the same gestation period. The intervention group in the study had the ultrasound scans in addition to the abdomen palpation, while the control group had only the abdomen palpation. Clinical management options reported in the study based on the ultrasound scan or the abdomen palpation include referral for full biophysical assessment which included umbilical artery Doppler ultrasound, early antenatal review, admission to antenatal ward, and induction of labour.
The included study is summarised in Table 2 .
See the literature search strategy in appendix B and study selection flow chart in appendix C .
Excluded studies
Studies not included in this review are listed, and reasons for their exclusion are provided in appendix K .
Summary of clinical studies included in the evidence review
Summaries of the studies that were included in this review are presented in Table 2 .
Summary of included studies.
See the full evidence tables in appendix D . No meta-analysis was conducted (and so there are no forest plots in appendix E ).
Quality assessment of clinical outcomes included in the evidence review
See the evidence profiles in appendix F .
Economic evidence
One study, a cost utility analysis was included ( Wastlund 2019 ).
See the literature search strategy in appendix B and economic study selection flow chart in appendix G .
Studies not included in this review with reasons for their exclusions are provided in appendix K .
Summary of studies included in the economic evidence review
For full details of the economic evidence, see the economic evidence tables in appendix H and economic evidence profiles in appendix I .
Wastlund (2019) assessed the cost effectiveness of universal ultrasound scanning for breech presentation at 36 weeks’ gestational age in nulliparous woman (N=3879). The comparator was selective ultrasound scanning which was reported as current practice. In this instance, fetal presentation was assessed by palpation of the abdomen by a midwife, obstetrician or general practitioner. The sensitivity of this method ranges between 57%-70% whereas ultrasound scanning is detected with 100% sensitivity and 100% specificity. Women in the selective ultrasound scan arm only received an ultrasound scan after detection of a breech presentation by abdominal palpation. Where a breech was detected, a woman was offered external cephalic version (ECV). The structure of the model undertook a decision tree, with end states being the mode of birth; either vaginal, elective or emergency caesarean section. Long term health outcomes were modelled based on the mortality risk associated with each mode of birth. Average lifetime quality-adjusted life years (QALYs) were estimated from Euroqol general UK population values.
Only the probabilistic results (n=100000 simulations) were reported which showed that on average, universal ultrasound resulted in an absolute decrease in breech deliveries by 0.39% compared with selective ultrasound scanning. The expected cost per person with breech presentation of universal ultrasound was £2957 (95% Credibility Interval [CrI]: £2922 to £2991), compared to £2,949 (95%CrI: £2915 to £2984) from selective ultrasound. The expected QALYs per person was 24.27615 in the universal ultrasound cohort and 24.27582 in the selective ultrasound cohort. The incremental cost effectiveness ratio (ICER) from the probabilistic analysis was £23611 (95%CrI: £8184 to £44851).
A series of one-way sensitivity analysis were conducted which showed that the most important cost parameter was the unit cost of a universal ultrasound scan. This parameter is particularly noteworthy as the study costed this scan at a much lower value than the ‘standard antenatal ultrasound’ scan in NHS reference costs on the basis that such a scan can be performed by a midwife during a routine antenatal care visit in primary care. According to the NICE guideline manual economic evaluation checklist this model was assessed as being directly applicable with potentially severe limitations. The limitations were mostly attributable to the limitations of the clinical inputs.
Economic model
No economic modelling was undertaken for this review because the committee agreed that other topics were higher priorities for economic evaluation.
Evidence statements
Clinical evidence statements, comparison 1. routine ultrasound scan versus selective ultrasound scan, critical outcomes, unexpected breech presentation in labour.
No evidence was identified to inform this outcome.
Mode of birth
- Moderate quality evidence from 1 RCT (N=1993) showed that there is no clinically important difference between routine ultrasound scan at 36-37 weeks and selective ultrasound scan on the number of women who had elective caesarean section: RR 1.22 (95% CI 0.91 to 1.63).
- Moderate quality evidence from 1 RCT (N=1993) showed that there is no clinically important difference between routine ultrasound scan at 36-37 weeks and selective ultrasound scan on number of women who had emergency caesarean section: RR 1.20 (95% CI 0.90 to 1.60).
- High quality evidence from 1 RCT (N=1993) showed that there is no clinically important difference between routine ultrasound scan at 36-37 weeks and selective ultrasound scan on number of women who had vaginal birth: RR 0.95 (95% CI 0.89 to 1.01).
Important outcomes
Maternal anxiety, women’s experience and satisfaction of care, gestational age at birth.
- High quality evidence from 1 RCT (N=1993) showed that there is no clinically important difference between routine ultrasound scan at 36-37 weeks and selective ultrasound scan on the number of babies’ born between 39-42 gestational weeks: RR 0.98 (95% CI 0.94 to 1.02).
Admission to neonatal unit
- Low quality evidence from 1 RCT (N=1993) showed that there is no clinically important difference between routine ultrasound scan at 36-37 weeks and selective ultrasound scan on the number of babies admitted into the neonatal unit: RR 0.83 (95% CI 0.51 to 1.35).
Economic evidence statements
One directly applicable cost-utility analysis from the UK with potentially serious limitations compared universal ultrasound scanning for breech presentation at 36 weeks’ gestational age with selective ultrasound scanning, stated as current practice. Universal ultrasound scanning was found to be borderline cost effective; the incremental cost-effectiveness ratio was £23611 per QALY gained. The cost of the scan was seen to be a key driver in the cost effectiveness result.
The committee’s discussion of the evidence
Interpreting the evidence, the outcomes that matter most.
Unexpected breech presentation in labour and mode of birth were prioritised as critical outcomes by the committee. This reflects the different options available to women with a known breech presentation in pregnancy and the different choices that women make. There are some women and/or clinicians who may feel uncomfortable with the risks of aiming for vaginal breech birth, and for these women and/or clinicians avoiding an unexpected breech presentation in labour would be the preferred option.
As existing evidence suggests that aiming for vaginal breech birth carries greater risk to the fetus than planned caesarean birth, it is important to consider whether earlier detection of the breech presentation would reduce the risk of these outcomes.
The committee agreed that maternal anxiety and women’s experience and satisfaction of care were important outcomes to consider as the introduction of an additional routine scan during pregnancy could have a treatment burden for women. Gestational age at birth and admission to neonatal unit were also chosen as important outcomes as the committee wanted to find out whether earlier detection of breech presentation would have an impact on whether the baby was born preterm, and as a consequence admitted to the neonatal unit. These outcomes were agreed to be important rather than critical as they are indirect outcomes of earlier detection of breech presentation.
The quality of the evidence
The quality of the evidence ranged from low to high. Most of the evidence was rated high or moderate, with only 1 outcome rated as low. The quality of the evidence was downgraded due to imprecision around the effect estimates for emergency caesarean section, elective caesarean section and admissions to neonatal unit.
No evidence was identified for the following outcomes: unexpected breech presentation in labour, maternal anxiety, women’s experiences and satisfaction of care.
The committee had hoped to find evidence that would inform whether early identification of breech presentation had an impact on preterm births, and although the review reported evidence for gestational age as birth, the available evidence was for births 39-42 weeks of gestation.
Benefits and harms
The available evidence compared routine ultrasound scanning with selective ultrasound scanning, and found no clinically important differences for mode of birth, gestational age at birth, or admissions to the neonatal unit. However, the committee discussed that it was important to note that the study did not focus on identifying breech presentation. The committee discussed the differences between the intervention in the study, which was an ultrasound scan to assess placental maturity, liquor volume, and fetal weight, to an ultrasound scan used to detect breech presentation. Whilst the ultrasound scan in the study has the ability to determine breech presentation, there are additional and costlier training required for the assessment of the other criteria. As such, it is important to separate the interventions. The committee also highlighted that the study did not look at whether an identification of breech presentation had an impact on the outcomes which were selected for this review.
In light of this, the committee felt that they were unable to reach a conclusion as to whether routine scanning to identify breech presentation, was associated with any benefits or harms. The committee agreed that while this review suggests routine ultrasound scanning to be no more effective than selective scanning, it does not definitively establish equivalence. Therefore, the committee agreed to recommend a continuation of the current practice with selective scanning and make a research recommendation to compare the clinical and cost effectiveness of routine ultrasound scanning versus selective ultrasound scanning from 36 weeks to identify fetal breech presentation.
Cost effectiveness and resource use
The committee acknowledged that there was included economic evidence on the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation.
The 1 included study suggested that offering a routine scan for breech is borderline cost effective. A key driver of cost effectiveness was the cost of the scan, which was substantially lower in the economic model than the figure quoted in NHS reference costs for routine ultrasound scanning. The committee noted that a scan for breech presentation only is a simpler technique and uses a cheaper machine. The committee agreed that the other costing assumptions presented in the study seemed appropriate.
However, the committee expressed concerns about the cohort study which underpinned the economic analysis which had a high risk of bias. The committee noted that a number of assumptions in the model which were key drivers of cost effectiveness, including the palpation diagnosis rates and prevalence of breech position, were from this 1 cohort study. This increased the uncertainty around the cost effectiveness of the routine scan. The committee also noted that, whilst the cost of the scan was fairly inexpensive, the resource impact would be substantial if a routine scan for breech presentation was offered to all pregnant women.
Overall, the committee felt that the clinical and cost effectiveness evidence presented was not strong enough to recommend offering a routine ultrasound scan given the potential for a significant resource impact. The recommendation to offer abdominal palpation to all pregnant women, and to offer an ultrasound scan where breech is suspected reflects current practice and so no substantial resource impact is anticipated.
McKenna 2003
Wastlund 2019
Appendix A. Review protocols
Review protocol for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 244K)
Appendix B. Literature search strategies
Literature search strategies for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 370K)
Appendix C. Clinical evidence study selection
Clinical study selection for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 117K)
Appendix D. Clinical evidence tables
Clinical evidence tables for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 213K)
Appendix E. Forest plots
Forest plots for review question: what is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation.
This section includes forest plots only for outcomes that are meta-analysed. Outcomes from single studies are not presented here, but the quality assessment for these outcomes is provided in the GRADE profiles in appendix F .
Appendix F. GRADE tables
GRADE tables for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 196K)
Appendix G. Economic evidence study selection
Economic evidence study selection for review question: what is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation.
A single economic search was undertaken for all topics included in the scope of this guideline. One economic study was identified which was applicable to this review question. See supplementary material 2 for details.
Appendix H. Economic evidence tables
Economic evidence tables for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 143K)
Appendix I. Economic evidence profiles
Economic evidence profiles for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 129K)
Appendix J. Economic analysis
Economic evidence analysis for review question: what is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation.
No economic analysis was conducted for this review question.
Appendix K. Excluded studies
Excluded clinical and economic studies for review question: what is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation, clinical studies, table 8 excluded studies and reasons for their exclusion.
View in own window
Economic studies
A single economic search was undertaken for all topics included in the scope of this guideline. No economic studies were identified which were applicable to this review question. See supplementary material 2 for details.
Appendix L. Research recommendations
Research recommendations for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 164K)
Evidence reviews underpinning recommendations 1.2.36 to 1.2.37
These evidence reviews were developed by the National Guideline Alliance, which is a part of the Royal College of Obstetricians and Gynaecologists
Disclaimer : The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or service users. The recommendations in this guideline are not mandatory and the guideline does not override the responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or their carer or guardian.
Local commissioners and/or providers have a responsibility to enable the guideline to be applied when individual health professionals and their patients or service users wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Nothing in this guideline should be interpreted in a way that would be inconsistent with compliance with those duties.
NICE guidelines cover health and care in England. Decisions on how they apply in other UK countries are made by ministers in the Welsh Government , Scottish Government , and Northern Ireland Executive . All NICE guidance is subject to regular review and may be updated or withdrawn.
- Cite this Page National Guideline Alliance (UK). Identification of breech presentation: Antenatal care: Evidence review L. London: National Institute for Health and Care Excellence (NICE); 2021 Aug. (NICE Guideline, No. 201.)
- PDF version of this title (518K)
In this Page
Other titles in this collection.
- NICE Evidence Reviews Collection
Related NICE guidance and evidence
- NICE Guideline 201: Antenatal care
Supplemental NICE documents
- Supplement 1: Methods (PDF)
- Supplement 2: Health economics (PDF)
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Management of breech presentation: Antenatal care: Evidence review M [ 2021] Review Management of breech presentation: Antenatal care: Evidence review M National Guideline Alliance (UK). 2021 Aug
- Vaginal delivery of breech presentation. [J Obstet Gynaecol Can. 2009] Vaginal delivery of breech presentation. Kotaska A, Menticoglou S, Gagnon R, MATERNAL FETAL MEDICINE COMMITTEE. J Obstet Gynaecol Can. 2009 Jun; 31(6):557-566.
- [The effect of the woman's age on the course of pregnancy and labor in breech presentation]. [Akush Ginekol (Sofiia). 1996] [The effect of the woman's age on the course of pregnancy and labor in breech presentation]. Dimitrov A, Borisov S, Nalbanski B, Kovacheva M, Chintolova G, Dzherov L. Akush Ginekol (Sofiia). 1996; 35(1-2):7-9.
- Review Cephalic version by moxibustion for breech presentation. [Cochrane Database Syst Rev. 2005] Review Cephalic version by moxibustion for breech presentation. Coyle ME, Smith CA, Peat B. Cochrane Database Syst Rev. 2005 Apr 18; (2):CD003928. Epub 2005 Apr 18.
- Review Hands and knees posture in late pregnancy or labour for fetal malposition (lateral or posterior). [Cochrane Database Syst Rev. 2005] Review Hands and knees posture in late pregnancy or labour for fetal malposition (lateral or posterior). Hofmeyr GJ, Kulier R. Cochrane Database Syst Rev. 2005 Apr 18; (2):CD001063. Epub 2005 Apr 18.
Recent Activity
- Identification of breech presentation Identification of breech presentation
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. The complete breech has the ...
At full term, around 3%-4% of births are breech. The different types of breech presentations include: Complete: The fetus's knees are bent, and the buttocks are presenting first. Frank: The fetus's legs are stretched upward toward the head, and the buttocks are presenting first. Footling: The fetus's foot is showing first.
The main types of breech presentation are: Frank breech - Both hips are flexed and both knees are extended so that the feet are adjacent to the head ( figure 1 ); accounts for 50 to 70 percent of breech fetuses at term. Complete breech - Both hips and both knees are flexed ( figure 2 ); accounts for 5 to 10 percent of breech fetuses at term.
Overview. There are three types of breech presentation: complete, incomplete, and frank. Complete breech is when both of the baby's knees are bent and his feet and bottom are closest to the birth canal. Incomplete breech is when one of the baby's knees is bent and his foot and bottom are closest to the birth canal.
There are several types of breech presentation. Frank breech: The fetal hips are flexed, and the knees extended (pike position). Complete breech: The fetus seems to be sitting with hips and knees flexed. Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
A breech presentation occurs when the baby's buttocks, feet, or both are positioned to come out first during birth. This happens in 3-4% of full-term births. What are the different types of breech birth presentations? Complete breech: Here, the buttocks are pointing downward with the legs folded at the knees and feet near the buttocks.
A complete breech is the least common type of breech presentation. Other Types of Mal Presentations The baby can also be in a transverse position, meaning that they're sideways in the uterus.
Breech presentation is defined as a fetus in a longitudinal lie with the buttocks or feet closest to the cervix. This occurs in 3-4% of all deliveries. ... This incidence varies with the type of breech: 0-2% with frank breech, 5-10% with complete breech, and 10-25% with footling breech.
Breech presentation of the fetus in late pregnancy may result in prolonged or obstructed labour with resulting risks to both woman and fetus. Interventions to correct breech presentation (to cephalic) before labour and birth are important for the woman's and the baby's health. The aim of this review is to determine the most effective way of ...
Recommended to determine type of breech, assess fetal growth and attitude of the fetal head/neck (1c, 2c, 3c, 4c). ... This pamphlet explains what a breech presentation is, the different types of breech presentation, discusses ECV and provides balanced information related to birth mode options along with visual representations of statistics ...
Breech delivery is the single most common abnormal presentation. The incidence is highly dependent on the gestational age. At 20 weeks, about one in four pregnancies are breech presentation. By full term, the incidence is about 4%. Other contributing factors include: Abnormal shape of the pelvis, uterus, or abdominal wall,
Breech presentation is a type of malpresentation and occurs when the fetal head lies over the uterine fundus and fetal buttocks or feet present over the maternal pelvis (instead of cephalic/head presentation). The incidence in the United Kingdom of breech presentation is 3-4% of all fetuses. 1.
A breech baby, or breech birth, is when your baby's feet or buttocks are positioned to come out of your vagina first. Your baby's head is up closest to your chest and its bottom is closest to your vagina. Most babies will naturally move so their head is positioned to come out of the vagina first during birth. Breech is common in early ...
This is the most common type of breech presentation. If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health ...
Types of breech presentations Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows.
There are several types of breech presentation. Frank breech: The fetal hips are flexed, and the knees extended (pike position). Complete breech: The fetus seems to be sitting with hips and knees flexed. Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
This pamphlet explains what a breech presentation is, the different types of breech presentation, discusses ECV and provides balanced information related to birth mode options along with visual representations of statistics comparing the perinatal mortality rate between cephalic vaginal birth, VBB and C/S. This pamphlet was also developed in ...
Three types of breech presentation are established concerning fetal attitude: complete, frank, and incomplete, which is sometimes referred to as footling breech. In complete breech, the fetal pelvis engages with the maternal pelvic inlet, and the fetal hips and knees are flexed. In frank breech, the fetal pelvis engages with the maternal pelvic ...
Breech birth happens when a baby doesn't move into a head-first position before birth and instead stays in a bottom-down position. The cause of a breech presentation isn't fully understood, but various situations make it more likely. There are three types of breech baby positions, depending on the position of the baby in your uterus ...
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face ...
Term breech presentation is a condition for which personalized obstetrical care is particularly needed. The best way is likely to be as follows: first, efficiently screen for breech presentation at 36-37 weeks of gestation; second, thoroughly evaluate the maternal/foetal condition, foetal weight and growth potential, and the type (frank ...
Some guidelines include the type of breech presentation among these conditions [4, 7], while others do not [2, 3, 5, 6]. Different types of breech are described: frank breech and incomplete or complete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face. The complete breech ...
The expected cost per person with breech presentation of universal ultrasound was £2957 (95% Credibility Interval [CrI]: £2922 to £2991), compared to £2,949 (95%CrI: £2915 to £2984) from selective ultrasound. ... data reported according to type of presentation rather than type of intervention received. WladimiroffJW, LaarJ, Ultrasonic ...