25.3 Gross Anatomy of the Kidney
Learning objectives.
By the end of this section, you will be able to:
- Describe the external structure of the kidney, including its location, support structures, and covering
- Identify the major internal divisions and structures of the kidney
- Identify the major blood vessels associated with the kidney and trace the path of blood through the kidney
- Compare and contrast the cortical and juxtamedullary nephrons
- Name structures found in the cortex and medulla
- Describe the physiological characteristics of the cortex and medulla
The kidneys lie on either side of the spine in the retroperitoneal space between the parietal peritoneum and the posterior abdominal wall, well protected by muscle, fat, and ribs. They are roughly the size of your fist, and the male kidney is typically a bit larger than the female kidney. The kidneys are well vascularized, receiving about 25 percent of the cardiac output at rest.

Interactive Link
There have never been sufficient kidney donations to provide a kidney to each person needing one. Watch this video to learn about the TED (Technology, Entertainment, Design) Conference held in March 2011. In this video, Dr. Anthony Atala discusses a cutting-edge technique in which a new kidney is “printed.” The successful utilization of this technology is still several years in the future, but imagine a time when you can print a replacement organ or tissue on demand.
External Anatomy
The left kidney is located at about the T12 to L3 vertebrae, whereas the right is lower due to slight displacement by the liver. Upper portions of the kidneys are somewhat protected by the eleventh and twelfth ribs ( Figure 25.7 ). Each kidney weighs about 125–175 g in males and 115–155 g in females. They are about 11–14 cm in length, 6 cm wide, and 4 cm thick, and are directly covered by a fibrous capsule composed of dense, irregular connective tissue that helps to hold their shape and protect them. This capsule is covered by a shock-absorbing layer of adipose tissue called the renal fat pad , which in turn is encompassed by a tough renal fascia. The fascia and, to a lesser extent, the overlying peritoneum serve to firmly anchor the kidneys to the posterior abdominal wall in a retroperitoneal position.
On the superior aspect of each kidney is the adrenal gland. The adrenal cortex directly influences renal function through the production of the hormone aldosterone to stimulate sodium reabsorption.
Internal Anatomy
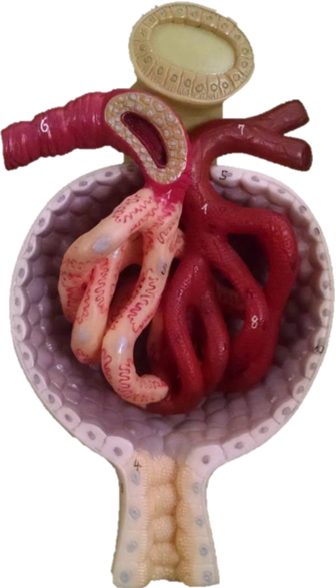
A frontal section through the kidney reveals an outer region called the renal cortex and an inner region called the medulla ( Figure 25.8 ). The renal columns are connective tissue extensions that radiate downward from the cortex through the medulla to separate the most characteristic features of the medulla, the renal pyramids and renal papillae . The papillae are bundles of collecting ducts that transport urine made by nephrons to the calyces of the kidney for excretion. The renal columns also serve to divide the kidney into 6–8 lobes and provide a supportive framework for vessels that enter and exit the cortex. The pyramids and renal columns taken together constitute the kidney lobes.
Renal Hilum
The renal hilum is the entry and exit site for structures servicing the kidneys: vessels, nerves, lymphatics, and ureters. The medial-facing hila are tucked into the sweeping convex outline of the cortex. Emerging from the hilum is the renal pelvis, which is formed from the major and minor calyxes in the kidney. The smooth muscle in the renal pelvis funnels urine via peristalsis into the ureter. The renal arteries form directly from the descending aorta, whereas the renal veins return cleansed blood directly to the inferior vena cava. The artery, vein, and renal pelvis are arranged in an anterior-to-posterior order.
Nephrons and Vessels
The renal artery first divides into segmental arteries, followed by further branching to form interlobar arteries that pass through the renal columns to reach the cortex ( Figure 25.9 ). The interlobar arteries, in turn, branch into arcuate arteries, cortical radiate arteries, and then into afferent arterioles. The afferent arterioles service about 1.3 million nephrons in each kidney.
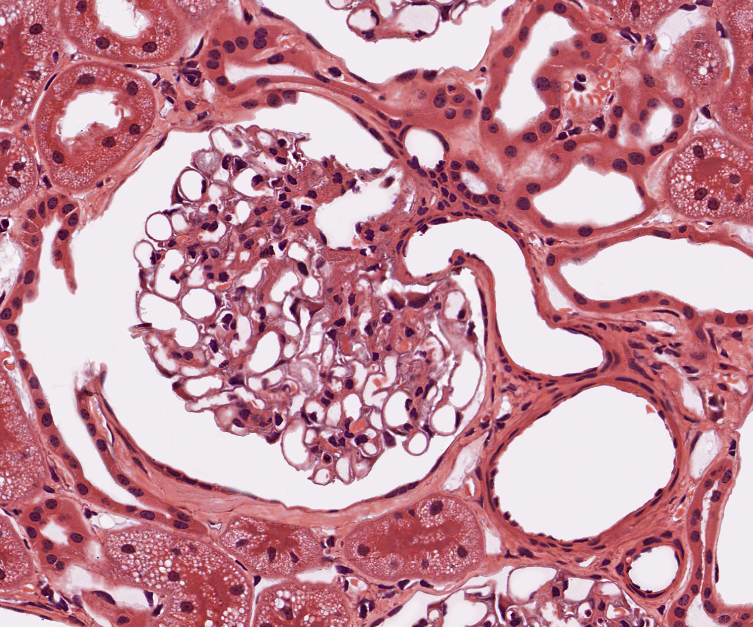
Nephrons are the “functional units” of the kidney; they cleanse the blood and balance the constituents of the circulation. The afferent arterioles form a tuft of high-pressure capillaries about 200 µm in diameter, the glomerulus . The rest of the nephron consists of a continuous sophisticated tubule whose proximal end surrounds the glomerulus in an intimate embrace—this is Bowman’s capsule . The glomerulus and Bowman’s capsule together form the renal corpuscle . As mentioned earlier, these glomerular capillaries filter the blood based on particle size. After passing through the renal corpuscle, the capillaries form a second arteriole, the efferent arteriole ( Figure 25.10 ). These will next form a capillary network around the more distal portions of the nephron tubule, the peritubular capillaries and vasa recta , before returning to the venous system. As the glomerular filtrate progresses through the nephron, these capillary networks recover most of the solutes and water, and return them to the circulation. Since a capillary bed (the glomerulus) drains into a vessel that in turn forms a second capillary bed, the definition of a portal system is met. This is the only portal system in which an arteriole is found between the first and second capillary beds. (Portal systems also link the hypothalamus to the anterior pituitary, and the blood vessels of the digestive viscera to the liver.)
Visit this link to view an interactive tutorial of the flow of blood through the kidney.
In a dissected kidney, it is easy to identify the cortex; it appears lighter in color compared to the rest of the kidney. All of the renal corpuscles as well as both the proximal convoluted tubules (PCTs) and distal convoluted tubules are found here. Some nephrons have a short loop of Henle that does not dip beyond the cortex. These nephrons are called cortical nephrons . About 15 percent of nephrons have long loops of Henle that extend deep into the medulla and are called juxtamedullary nephrons .
As an Amazon Associate we earn from qualifying purchases.
This book may not be used in the training of large language models or otherwise be ingested into large language models or generative AI offerings without OpenStax's permission.
Want to cite, share, or modify this book? This book uses the Creative Commons Attribution License and you must attribute OpenStax.
Access for free at https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction
- Authors: J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble, Peter DeSaix
- Publisher/website: OpenStax
- Book title: Anatomy and Physiology 2e
- Publication date: Apr 20, 2022
- Location: Houston, Texas
- Book URL: https://openstax.org/books/anatomy-and-physiology-2e/pages/1-introduction
- Section URL: https://openstax.org/books/anatomy-and-physiology-2e/pages/25-3-gross-anatomy-of-the-kidney
© Dec 19, 2023 OpenStax. Textbook content produced by OpenStax is licensed under a Creative Commons Attribution License . The OpenStax name, OpenStax logo, OpenStax book covers, OpenStax CNX name, and OpenStax CNX logo are not subject to the Creative Commons license and may not be reproduced without the prior and express written consent of Rice University.

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

21.7: Laboratory Activities and Assignment
- Last updated
- Save as PDF
- Page ID 53836

- Rosanna Hartline
- West Hills College Lemoore
Laboratory Activities and Assignment
Part 1: review of the urinary system.
1. On the diagram below, label the following structures:
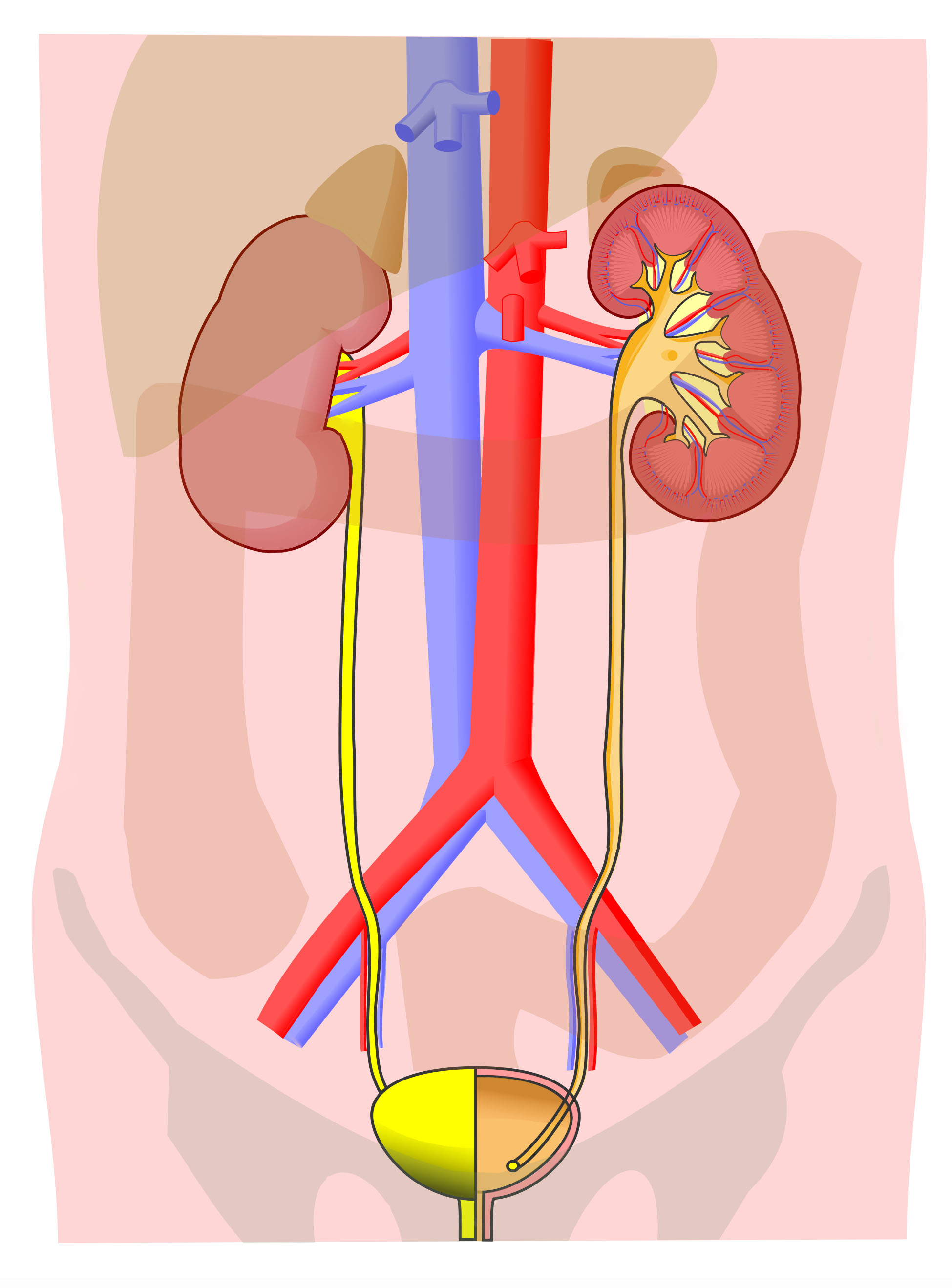
2. On the diagram below, match the numbers on the diagram with the following structures (not all numbers will be used):
3. On the diagram below, label the following structures:
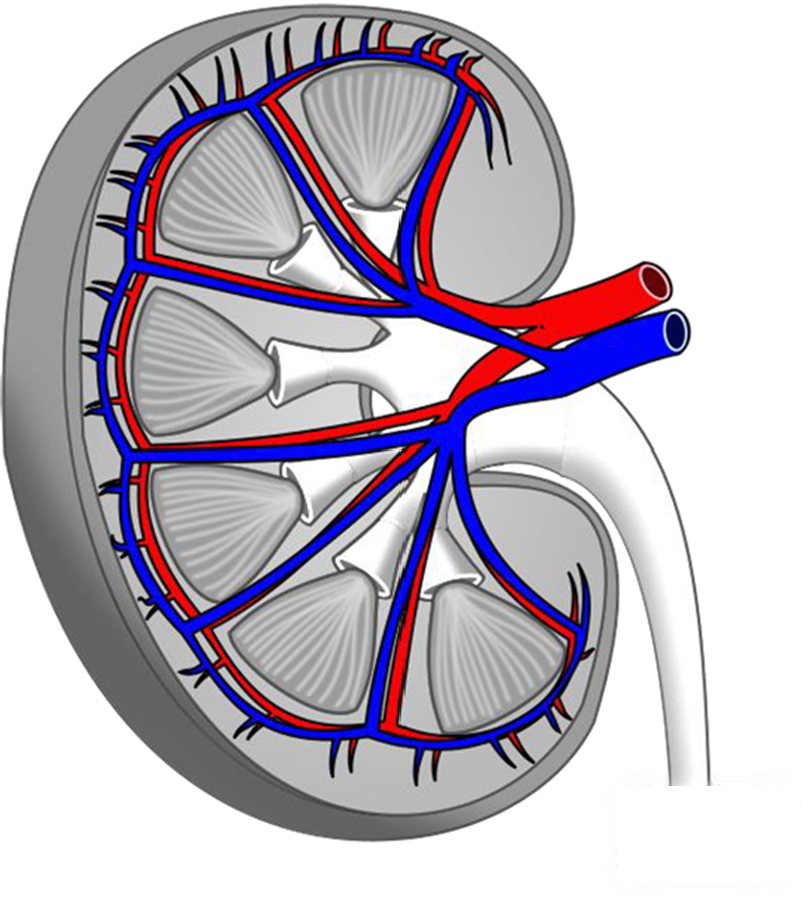
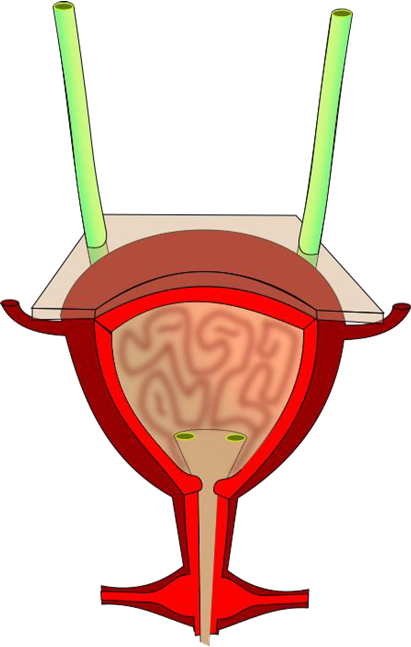
4. On the diagram below, label the following structures:
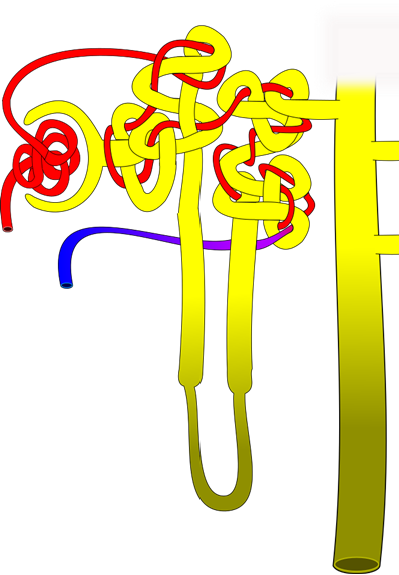
5. On the diagram below, number the path of filtrate through the nephron, beginning with the location where it is created (#1) and follow its path as it becomes urine and is transported toward the ureter (you will have 6-8 steps total, depending on how you label the figure).
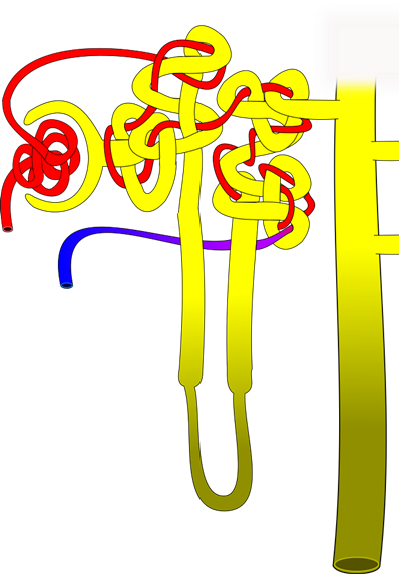
6. On the diagram below, number the path of blood through the nephron, beginning with the blood vessel bringing blood to the nephron (#1) and follow its path until it exits the nephron and moves back toward the heart (you should have 6 steps total and include cortical radiate blood vessels).
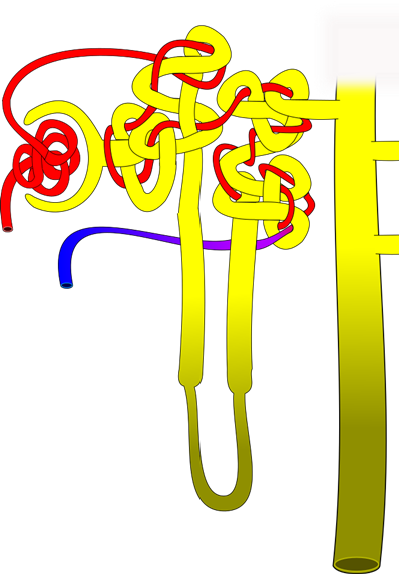
7. On the diagram below, label the following structures:
8. On the microscopic image of cortical tissue of the kidney, label the following structures:
9. On the diagram below, label the following structures:
Part 2: Histology of the Urinary System
Make one illustration at a low magnification and another at a higher magnification to view structures of the nephron.
Label the tissue with: cortex, medulla, renal column, pyramid, glomerulus, Bowman's capsule, Bowman's space, parietal layer, podocytes, afferent arteriole, efferent arteriole, macula densa, juxtaglomerular cells (if possible), proximal convoluted tubule, distal convoluted tubule, simple cuboidal epithelium lining kidney tubules
Label the tissue with: lumen, transitional epithelium, connective tissue, muscularis externa, adventitia
Urinary Bladder
Label the tissue with: lumen, transitional epithelium, lamina propria, muscularis externa, adventitia/serosa
Part 3: Sheep Kidney Dissection
- Patient Care & Health Information
- Diseases & Conditions
- Chronic kidney disease
- What is kidney disease? An expert explains
Learn more from kidney doctor Andrew Bentall, M.D.
I'm Dr. Andrew Bentall, a kidney doctor at Mayo Clinic. I look after patients with kidney disease, either in the early stages, or with more advanced kidney disease considering dialysis and transplantation as treatment options. In this video, we'll cover the basics of chronic kidney disease. What is it? Who gets it? The symptoms, diagnosis and treatment. Whether you are looking for answers for yourself or for someone you love, we're here to give you the best information available.
Chronic kidney disease is a disease characterized by progressive damage and loss of function in the kidneys. It's estimated that chronic kidney disease affects about one in seven American adults. And most of those don't know they have it. Before we get into the disease itself, let's talk a little bit about the kidneys and what they do. Our kidneys play many important roles keeping our bodies in balance. They remove waste and toxins, excess water from the bloodstream, which is carried out of the body in urine. They helped to make hormones to produce red blood cells, and they turn vitamin D into its active form, so it's usable in the body.
There are quite a few things that can cause or put you at higher risk for chronic kidney disease. Some of them are not things that can be avoided. Your risk is simply higher if you have a family history of certain genetic conditions like polycystic kidney disease or some autoimmune diseases like lupus or IgA nephropathy. Defects in the kidney structure can also cause your kidneys to fail, and you have an increased risk as you get older. Sometimes, other common medical conditions can increase your risk. Diabetes is the most common cause of kidney disease. Both type 1 and type 2 diabetes. But also heart disease and obesity can contribute to the damage that causes kidneys to fail. Urinary tract issues and inflammation in different parts of the kidney can also lead to long-term functional decline. There are things that are more under our control: Heavy or long-term use of certain medications, even those that are common over-the-counter. Smoking can also be a contributing factor to chronic kidney disease.
Often there are no outward signs in the earlier stages of chronic kidney disease, which is grouped into stages 1 through 5. Generally, earlier stages are known as 1 to 3. And as kidney disease progresses, you may notice the following symptoms. Nausea and vomiting, muscle cramps, loss of appetite, swelling via feet and ankles, dry, itchy skin, shortness of breath, trouble sleeping, urinating either too much or too little. However, these are usually in the later stages, but they can also happen in other disorders. So don't automatically interpret this as having kidney disease. But if you're experiencing anything that concerns you, you should make an appointment with your doctor.
Even before any symptoms appear, routine blood work can indicate that you might be in the early stages of chronic kidney disease. And the earlier it's detected, the easier it is to treat. This is why regular checkups with your doctor are important. If your doctor suspects the onset of chronic kidney disease, they may schedule a variety of other tests. They may also refer you to a kidney specialist, a nephrologist like myself. Urine tests can reveal abnormalities and give clues to the underlying cause of the chronic kidney disease. And this can also help to determine the underlying issues. Various imaging tests like ultrasounds or CT scans can be done to help your doctor assess the size, the structure, as well as evaluate the visible damage, inflammation or stones of your kidneys. And in some cases, a kidney biopsy may be necessary. And a small amount of tissue is taken with a needle and sent to the pathologist for further analysis.
Treatment is determined by what is causing your kidneys to not function normally. Treating the cause is key, leading to reduced complications and slowing progression of kidney disease. For example, getting better blood pressure control, improved sugar control and diabetes, and reducing weight are often key interventions. However, existing damage is not usually reversible. In some conditions, treatment can reverse the cause of the disease. So seeking medical review is really important. Individual complications vary, but treatment might include high blood pressure medication, diuretics to reduce fluid and swelling, supplements to relieve anemia, statins to lower cholesterol, or medications to protect your bones and prevent blood vessel calcification. A lower-protein diet may also be recommended. It reduces the amount of waste your kidneys need to filter from your blood. These can not only slow the damage of kidney disease, but make you feel better as well. When the damage has progressed to the point that 85 to 90 percent of your kidney function is gone, and they no longer work well enough to keep you alive, it's called end-stage kidney failure. But there are still options. There's dialysis, which uses a machine to filter the toxins and remove water from your body as your kidneys are no longer able to do this. Where possible, the preferred therapy is a kidney transplant. While an organ transplant can sound daunting, it's actually often the better alternative, and the closest thing to a cure, if you qualify for a kidney transplant.
If you have kidney disease, there are lifestyle choices. Namely quit smoking. Consuming alcohol in moderation. If you're overweight or obese, then try to lose weight. Staying active and getting exercise can help not only with your weight, but fatigue and stress. If your condition allows, keep up with your routine, whether that's working, hobbies, social activities, or other things you enjoy. It can be helpful to talk to someone you trust, a friend or relative who's good at listening. Or your doctor could also refer you to a therapist or social worker. It can also be helpful to find a support group and connect with people going through the same thing. Learning you have chronic kidney disease and learning how to live with it can be a challenge. But there are lots of ways to help you to be more comfortable for longer before more drastic measures are needed. And even then, there is plenty of hope. If you'd like to learn even more about chronic kidney disease, watch our other related videos or visit mayoclinic.org. We wish you well.
Chronic kidney disease, also called chronic kidney failure, involves a gradual loss of kidney function. Your kidneys filter wastes and excess fluids from your blood, which are then removed in your urine. Advanced chronic kidney disease can cause dangerous levels of fluid, electrolytes and wastes to build up in your body.
In the early stages of chronic kidney disease, you might have few signs or symptoms. You might not realize that you have kidney disease until the condition is advanced.
Treatment for chronic kidney disease focuses on slowing the progression of kidney damage, usually by controlling the cause. But, even controlling the cause might not keep kidney damage from progressing. Chronic kidney disease can progress to end-stage kidney failure, which is fatal without artificial filtering (dialysis) or a kidney transplant.
- How kidneys work
One of the important jobs of the kidneys is to clean the blood. As blood moves through the body, it picks up extra fluid, chemicals and waste. The kidneys separate this material from the blood. It's carried out of the body in urine. If the kidneys are unable to do this and the condition is untreated, serious health problems result, with eventual loss of life.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- A Book: The Body's Keepers
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Signs and symptoms of chronic kidney disease develop over time if kidney damage progresses slowly. Loss of kidney function can cause a buildup of fluid or body waste or electrolyte problems. Depending on how severe it is, loss of kidney function can cause:
- Loss of appetite
- Fatigue and weakness
- Sleep problems
- Urinating more or less
- Decreased mental sharpness
- Muscle cramps
- Swelling of feet and ankles
- Dry, itchy skin
- High blood pressure (hypertension) that's difficult to control
- Shortness of breath, if fluid builds up in the lungs
- Chest pain, if fluid builds up around the lining of the heart
Signs and symptoms of kidney disease are often nonspecific. This means they can also be caused by other illnesses. Because your kidneys are able to make up for lost function, you might not develop signs and symptoms until irreversible damage has occurred.
When to see a doctor
Make an appointment with your doctor if you have signs or symptoms of kidney disease. Early detection might help prevent kidney disease from progressing to kidney failure.
If you have a medical condition that increases your risk of kidney disease, your doctor may monitor your blood pressure and kidney function with urine and blood tests during office visits. Ask your doctor whether these tests are necessary for you.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
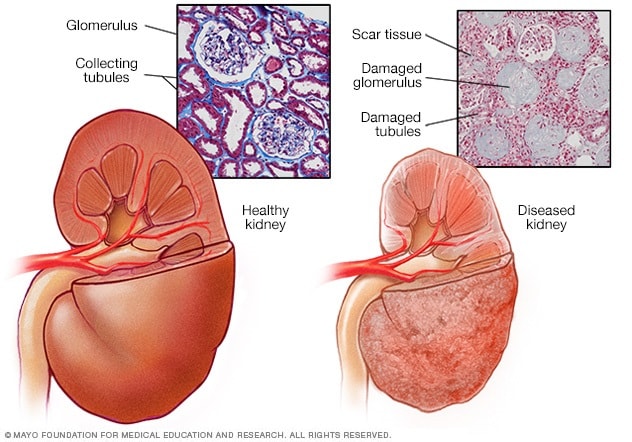
- Healthy kidney vs. diseased kidney
A typical kidney has about 1 million filtering units. Each unit, called a glomerulus, joins a tubule. The tubule collects urine. Conditions such as high blood pressure and diabetes harm kidney function by damaging these filtering units and tubules. The damage causes scarring.
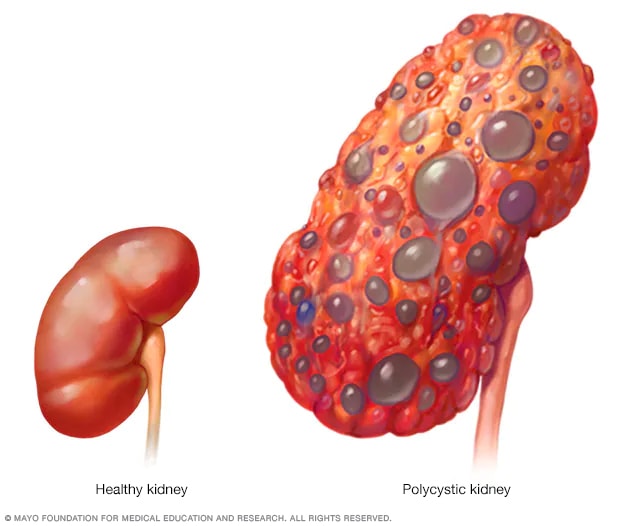
- Polycystic kidney
A healthy kidney (left) eliminates waste from the blood and maintains the body's chemical balance. With polycystic kidney disease (right), fluid-filled sacs called cysts develop in the kidneys. The kidneys grow larger and gradually lose the ability to function as they should.
Chronic kidney disease occurs when a disease or condition impairs kidney function, causing kidney damage to worsen over several months or years.
Diseases and conditions that cause chronic kidney disease include:
- Type 1 or type 2 diabetes
- High blood pressure
- Glomerulonephritis (gloe-mer-u-low-nuh-FRY-tis), an inflammation of the kidney's filtering units (glomeruli)
- Interstitial nephritis (in-tur-STISH-ul nuh-FRY-tis), an inflammation of the kidney's tubules and surrounding structures
- Polycystic kidney disease or other inherited kidney diseases
- Prolonged obstruction of the urinary tract, from conditions such as enlarged prostate, kidney stones and some cancers
- Vesicoureteral (ves-ih-koe-yoo-REE-tur-ul) reflux, a condition that causes urine to back up into your kidneys
- Recurrent kidney infection, also called pyelonephritis (pie-uh-low-nuh-FRY-tis)
Risk factors
Factors that can increase your risk of chronic kidney disease include:
- Heart (cardiovascular) disease
- Being Black, Native American or Asian American
- Family history of kidney disease
- Abnormal kidney structure
- Frequent use of medications that can damage the kidneys
Complications
Chronic kidney disease can affect almost every part of your body. Potential complications include:
- Fluid retention, which could lead to swelling in your arms and legs, high blood pressure, or fluid in your lungs (pulmonary edema)
- A sudden rise in potassium levels in your blood (hyperkalemia), which could impair your heart's function and can be life-threatening
- Heart disease
- Weak bones and an increased risk of bone fractures
- Decreased sex drive, erectile dysfunction or reduced fertility
- Damage to your central nervous system, which can cause difficulty concentrating, personality changes or seizures
- Decreased immune response, which makes you more vulnerable to infection
- Pericarditis, an inflammation of the saclike membrane that envelops your heart (pericardium)
- Pregnancy complications that carry risks for the mother and the developing fetus
- Irreversible damage to your kidneys (end-stage kidney disease), eventually requiring either dialysis or a kidney transplant for survival
To reduce your risk of developing kidney disease:
- Follow instructions on over-the-counter medications. When using nonprescription pain relievers, such as aspirin, ibuprofen (Advil, Motrin IB, others) and acetaminophen (Tylenol, others), follow the instructions on the package. Taking too many pain relievers for a long time could lead to kidney damage.
- Maintain a healthy weight. If you're at a healthy weight, maintain it by being physically active most days of the week. If you need to lose weight, talk with your doctor about strategies for healthy weight loss.
- Don't smoke. Cigarette smoking can damage your kidneys and make existing kidney damage worse. If you're a smoker, talk to your doctor about strategies for quitting. Support groups, counseling and medications can all help you to stop.
- Manage your medical conditions with your doctor's help. If you have diseases or conditions that increase your risk of kidney disease, work with your doctor to control them. Ask your doctor about tests to look for signs of kidney damage.
Chronic kidney disease care at Mayo Clinic
Living with chronic kidney disease?
Connect with others like you for support and answers to your questions in the Transplants support group on Mayo Clinic Connect, a patient community.
Transplants Discussions

72 Replies Tue, Apr 30, 2024

362 Replies Tue, Apr 30, 2024

1564 Replies Mon, Apr 29, 2024
- Goldman L, et al., eds. Chronic kidney disease. In: Goldman-Cecil Medicine. 26th ed. Elsevier; 2020. http://www.clinicalkey.com. Accessed April 27, 2021.
- Chronic kidney disease (CKD). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/kidney-disease/chronic-kidney-disease-ckd#:~:text=Chronic kidney disease (CKD) means,family history of kidney failure. Accessed April 26, 2021.
- Rosenberg M. Overview of the management of chronic kidney disease in adults. https://www.uptodate.com/contents/search. Accessed April 26, 2021.
- Chronic kidney disease (CKD) symptoms and causes. National Kidney Foundation. https://www.kidney.org/atoz/content/about-chronic-kidney-disease. Accessed April 26, 2021.
- Chronic kidney disease. Merck Manual Professional Version. https://www.merckmanuals.com/professional/genitourinary-disorders/chronic-kidney-disease/chronic-kidney-disease?query=Chronic kidney disease. Accessed April 26, 2021.
- Ammirati AL. Chronic kidney disease. Revista da Associação Médica Brasileira. 2020; doi:10.1590/1806-9282.66.S1.3.
- Chronic kidney disease basics. Centers for Disease Control and Prevention. https://www.cdc.gov/kidneydisease/basics.html. Accessed April 26, 2021.
- Warner KJ. Allscripts EPSi. Mayo Clinic; April 21, 2021.
- Office of Patient Education. Chronic kidney disease treatment options. Mayo Clinic; 2020.
- Chronic kidney disease: Is a clinical trial right for me?
- Eating right for chronic kidney disease
- Effectively managing chronic kidney disease
- Kidney biopsy
- Kidney disease FAQs
- Low-phosphorus diet: Helpful for kidney disease?
- MRI: Is gadolinium safe for people with kidney problems?
- Renal diet for vegetarians
Associated Procedures
- Deceased-donor kidney transplant
- Hemodialysis
- Kidney transplant
- Living-donor kidney transplant
- Nondirected living-donor transplant
- Peritoneal dialysis
- Preemptive kidney transplant
News from Mayo Clinic
- Mayo Clinic Minute: Why Black Americans are at higher risk of chronic kidney disease March 05, 2024, 05:00 p.m. CDT
- Mayo Clinic Minute: Can extra salt hurt your kidneys? Feb. 16, 2024, 04:00 p.m. CDT
- Mayo Clinic Minute: Using AI to predict kidney failure in patients with polycystic kidney disease April 06, 2023, 04:00 p.m. CDT
- Mayo Clinic Q and A: Understanding chronic kidney disease March 23, 2023, 12:35 p.m. CDT
- Mayo Clinic Minute: Game-changing treatment for chronic kidney disease could slow down progression of the disease March 06, 2023, 04:01 p.m. CDT
- Science Saturday: Seeking a cellular therapy for chronic kidney disease Nov. 12, 2022, 12:00 p.m. CDT
- Science Saturday: Mayo Clinic researchers integrate genomics into kidney disease diagnosis, care Sept. 17, 2022, 11:00 a.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Chronic kidney disease: assessment and management
NICE Guideline, No. 203
- Copyright and Permissions
This guideline replaces CG157, CG182 and NG8.
This guideline is the basis of QS5.
This guideline covers care and treatment for people with, or at risk of, chronic kidney disease (CKD). It aims to prevent or delay the progression, and reduce the risk of complications and cardiovascular disease. It also covers managing anaemia and hyperphosphataemia associated with CKD.
NICE has produced a COVID-19 rapid guideline on chronic kidney disease . It recommends changes to usual practice to maximise the safety of patients and protect staff from infection during the COVID-19 pandemic.
Who is it for?
- Healthcare professionals
- Commissioners and providers
- People with CKD, their families and carers
- Recommendations
People have the right to be involved in discussions and make informed decisions about their care, as described in NICE’s information on making decisions about your care .
Making decisions using NICE guidelines explains how we use words to show the strength (or certainty) of our recommendations, and has information about prescribing medicines (including off-label use), professional guidelines, standards and laws (including on consent and mental capacity), and safeguarding.
Adults, children and young people
Some recommendations in this guideline apply to adults only, and we have specified ‘adults’ in these individual recommendations. When a recommendation applies to children and young people only, we have also specified this in the recommendation. When recommendations apply to adults, children and young people we have specified this in recommendations at the beginning of a section. But for brevity, we have used ‘people’ for later recommendations. When a recommendation refers to ‘people’, this means adults, children and young people.
1.1. Investigations for chronic kidney disease
Measuring kidney function, creatinine-based estimate of glomerular filtration rate.
Whenever a request for serum creatinine measurement is made, clinical laboratories should report an estimate of (eGFRcreatinine) using a prediction equation (see recommendation 1.1.2 ) in addition to reporting the serum creatinine result.
eGFRcreatinine may be less reliable in certain situations (for example, acute kidney injury, pregnancy, oedematous states, muscle wasting disorders, and in adults who are malnourished, who have higher muscle mass or use protein supplements, or who have had an amputation) and has not been well validated in certain ethnic groups (for example, black, Asian and other minority ethnic groups with CKD living in the UK). [2014]
- use the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) creatinine equation to estimate GFRcreatinine for adults, using creatinine assays with calibration traceable to standardised reference material
- use creatinine assays that are specific (for example, enzymatic assays) and zero-biased compared with isotope dilution mass spectrometry (IDMS)
- participate in a UK national external quality assessment scheme for creatinine. [2014]
The committee reviewed the evidence on creatinine-based estimation of glomerular filtration rate (GFR) in 2021. For a short explanation of why they did not make new recommendations, see the rationale and impact section on creatinine-based estimate of GFR .
Full details of the evidence and the committee’s discussion are in evidence review A: diagnostic accuracy of eGFR calculations in adults, children, and young people from black, Asian and other minority ethnic groups with CKD .
Interpret eGFRcreatinine with caution in adults with extremes of muscle mass, for example, in bodybuilders, people who have had an amputation or people with muscle wasting disorders. (Reduced muscle mass will lead to overestimation and increased muscle mass to underestimation of the GFR.) [2008]
Advise adults not to eat any meat in the 12 hours before having a blood test for eGFRcreatinine. Avoid delaying the despatch of blood samples to ensure that they are received and processed by the laboratory within 12 hours of venepuncture. [2008]
Reporting and interpreting GFR values
Clinical laboratories should report eGFR either as a whole number if it is 90 ml/min/1.73 m 2 or less, or as ‘greater than 90 ml/min/1.73 m 2 ’. [2014]
If eGFR is greater than 90 ml/min/1.73 m 2 , use an increase in serum creatinine concentration of more than 20% to infer significant reduction in kidney function. [2014]
Interpret eGFR values of 60 ml/min/1.73 m 2 or more with caution, bearing in mind that estimates of GFR become less accurate as the true GFR increases. [2014]
Confirm an eGFR result of less than 60 ml/min/1.73 m 2 in an adult not previously tested by repeating the test within 2 weeks. Allow for biological and analytical variability of serum creatinine (±5%) when interpreting changes in eGFR. [2008]
When highly accurate measures of GFR are needed
If a highly accurate measure of GFR is needed, for example, during monitoring of chemotherapy and in the evaluation of kidney function in potential living donors, consider a reference standard measure (inulin, 51Cr-EDTA, 125I-iothalamate or iohexol). [2008]
Investigations for proteinuria
Do not use reagent strips to identify proteinuria in children and young people. [2021]
Do not use reagent strips to identify proteinuria in adults unless they are capable of specifically measuring albumin at low concentrations and expressing the result as an albumin:creatinine ratio (ACR). [2008]
- use urine ACR rather than protein:creatinine ratio (PCR) because of the greater sensitivity for low levels of proteinuria
- check an ACR between 3 mg/mmol and 70 mg/mmol in a subsequent early morning sample to confirm the result. A repeat sample is not needed if the initial ACR is 70 mg/mmol or more. [2021]
Regard a confirmed ACR of 3 mg/mmol or more as clinically important proteinuria. [2021]
- adults, children and young people with diabetes (type 1 or type 2)
- adults with an eGFR of less than 60 ml/min/1.73 m 2
- adults with an eGFR of 60 ml/min/1.73 m 2 or more if there is a strong suspicion of CKD
- children and young people without diabetes and with creatinine above the upper limit of the age-appropriate reference range. When ACR is 70 mg/mmol or more, PCR can be used as an alternative to ACR. [2021]
For a short explanation of why the committee made these recommendations and how they might affect practice, see the rationale and impact section on investigations for proteinuria .
Full details of the evidence and the committee’s discussion are in evidence review B: accuracy of albumin:creatinine ratio versus protein:creatinine ratio measurements to quantify proteinuria in children and young people with CKD .
Incidental finding of proteinuria on reagent strips
If unexplained proteinuria is an incidental finding on a reagent strip, offer testing for CKD using eGFRcreatinine and ACR. [2021]
- Evaluate further for results of 1+ or higher.
- Do not use urine microscopy to confirm a positive result. [2021]
For a short explanation of why the committee made these recommendations and how they might affect practice, see the rationale and impact section on reagent strips for proteinuria and haematuria .
Full details of the evidence and the committee’s discussion are in evidence review C: accuracy of reagent strips for detecting protein and blood in urine in children and young people with CKD .
Managing isolated invisible haematuria
When there is the need to differentiate persistent invisible haematuria in the absence of proteinuria from transient haematuria, regard 2 out of 3 positive reagent strip tests as confirmation of persistent invisible haematuria. [2008]
Persistent invisible haematuria, with or without proteinuria, should prompt investigation for urinary tract malignancy in appropriate age groups (see NICE’s guideline on suspected cancer: recognition and referral ). [2008]
Persistent invisible haematuria in the absence of proteinuria should be followed up annually with repeat testing for haematuria (see recommendations 1.1.17 and 1.1.18 ), proteinuria or albuminuria, GFR and blood pressure monitoring as long as the haematuria persists. [2008]
Who should be tested for CKD
Monitor GFR at least annually in adults, children and young people who are taking medicines that can adversely affect kidney function, such as calcineurin inhibitors (for example, ciclosporin or tacrolimus), lithium or non-steroidal anti-inflammatory drugs (long-term chronic use of NSAIDs). [2021]
- hypertension
- previous episode of acute kidney injury
- cardiovascular disease (ischaemic heart disease, chronic heart failure, peripheral vascular disease or cerebral vascular disease)
- structural renal tract disease, recurrent renal calculi or prostatic hypertrophy
- multisystem diseases with potential kidney involvement, for example, systemic lupus erythematosus
- family history of end-stage renal disease (GFR category G5) or hereditary kidney disease
- incidental detection of haematuria or proteinuria. [2021]
- solitary functioning kidney. [2021]
- low birth weight (2,500 g or lower)
- cardiac disease
- structural renal tract disease or recurrent renal calculi
- obesity in the absence of metabolic syndrome, diabetes or hypertension. [2021]
Monitor adults, children and young people for the development or progression of CKD for at least 3 years after acute kidney injury (longer for people with acute kidney injury stage 3) even if eGFR has returned to baseline. [2021]
- monitoring for complications and associated conditions of type 1 diabetes
- monitoring for complications and associated conditions of type 2 diabetes . [2021]
For a short explanation of why the committee made these recommendations and how they might affect practice, see the rationale and impact section on who should be tested for CKD .
Full details of the evidence and the committee’s discussion are in evidence review D: children and young people who should be tested for CKD .
1.2. Classification of CKD in adults
- increased ACR is associated with increased risk of adverse outcomes
- decreased GFR is associated with increased risk of adverse outcomes
- increased ACR and decreased GFR in combination multiply the risk of adverse outcomes. [2014]
Do not determine management of CKD solely by age. [2014]
Risk of adverse outcomes in adults by GFR and ACR category.
Investigating the cause of CKD and determining the risk of adverse outcomes
Agree a plan to establish the cause of CKD during an informed discussion with the person with CKD, particularly if the cause may be treatable (for example, urinary tract obstruction, medicines that can adversely affect kidney function or glomerular disease). [2014]
Use the person’s GFR and ACR categories (see table 1 ) to indicate their risk of adverse outcomes (for example, CKD progression, acute kidney injury, all-cause mortality and cardiovascular events) and discuss this with them. [2014]
Indications for renal ultrasound in adults
- have accelerated progression of CKD (see recommendation 1.3.5 )
- have visible or persistent invisible haematuria
- have symptoms of urinary tract obstruction
- have a family history of polycystic kidney disease and are older than 20
- have a GFR of less than 30 ml/min/1.73 m 2 (GFR category G4 or G5)
- are considered by a nephrologist to need a renal biopsy. [2008, amended 2014]
Advise adults with a family history of hereditary kidney disease about the implications of an abnormal result before a renal ultrasound scan is arranged for them. [2008]
1.3. Frequency of monitoring
If an adult, child or young person has CKD, or is at risk of it, agree the frequency of monitoring (eGFRcreatinine and ACR) with them (and their family members or carers, as appropriate), bearing in mind that CKD is not progressive in many people. [2021]
the recommendations on patient views and preferences in NICE’s guideline on patient experience in adult NHS services
- NICE’s guideline on shared decision making . [2021]
See the recommendations on when to refer adults ( recommendation 1.5.5 ) and children and young people ( recommendation 1.5.6 ) for specialist assessment. [2021]
- the underlying cause of CKD
- the rate of decline in eGFR or increase in ACR (but be aware that CKD progression is often non-linear)
- other risk factors, including heart failure, diabetes and hypertension
- changes to their treatment (such as renin–angiotensin–aldosterone system [RAAS] antagonists , NSAIDs and diuretics)
- intercurrent illness (for example acute kidney injury)
- whether they have chosen conservative management of CKD. [2021]
Minimum number of monitoring checks (eGFRcreatinine) per year for adults, children and young people with or at risk of chronic kidney disease. Note: ACR monitoring should be individualised based on a person’s individual characteristics, risk of (more...)
For a short explanation of why the committee made these recommendations and how they might affect practice, see the rationale and impact section on frequency of monitoring .
Full details of the evidence and the committee’s discussion are in evidence review E: optimal monitoring frequency and evidence review N: defining clinically significant decline in eGFR in terms of risk of kidney disease progression .
Defining progression in adults
- a sustained decrease in GFR of 25% or more and a change in GFR category within 12 months or
- a sustained decrease in GFR of 15 ml/min/1.73 m 2 per year. [2014]
- Obtain a minimum of 3 GFR estimations over a period of not less than 90 days.
- In adults with a new finding of reduced GFR, repeat the GFR within 2 weeks to exclude causes of acute deterioration of GFR. For example, acute kidney injury or starting renin–angiotensin system antagonist therapy. [2008, amended 2014]
- a sustained decrease in GFR of 25% or more over 12 months or
- a sustained decrease in GFR of 15 ml/min/1.73 m 2 or more over 12 months. [2008, amended 2014]
When assessing CKD progression, extrapolate the current rate of decline of GFR and take this into account when planning intervention strategies, particularly if it suggests that the person might need renal replacement therapy in their lifetime. [2008, amended 2014]
Risk factors associated with CKD progression in adults
- cardiovascular disease
- proteinuria
- African, African-Caribbean or Asian family origin
- chronic use of NSAIDs
- untreated urinary outflow tract obstruction. [2014]
In adults with CKD the chronic use of NSAIDs may be associated with progression and acute use is associated with a reversible decrease in GFR. Exercise caution when giving NSAIDs to people with CKD over prolonged periods of time. Monitor the effects on GFR, particularly in people with a low baseline GFR and/or in the presence of other risks for progression. [2008]
1.4. Information and education for people with CKD
- the information on enabling patients to actively participate in their care in NICE’s guideline on patient experience in adult NHS services
- NICE’s guideline on shared decision making
- the section on shared decision making in NICE’s guideline on babies, children and young people’s experience of healthcare . [2008]
- What is CKD and how does it affect people?
- What questions should people ask about their kidneys?
- What treatments are available for CKD, what are their advantages and disadvantages, and what complications or side effects may occur as a result of treatment or medication?
- What can people do to manage and influence their own condition?
- In what ways could CKD and its treatment affect people’s daily life, social activities, work opportunities and financial situation, including benefits and allowances available?
- How can people cope with and adjust to CKD and what sources of psychological support are available?
- Information about renal replacement therapy (such as the frequency and length of time of dialysis treatment sessions or exchanges and pre-emptive transplantation) and the preparation needed (such as having a fistula or peritoneal catheter), if appropriate for the person. See NICE’s guideline on renal replacement therapy and conservative management .
- Conservative management and when it may be considered. [2008]
Offer adults with CKD (and their family members or carers, as appropriate) high-quality information or education programmes as appropriate to the severity of their condition to allow time for them to fully understand and make informed choices about their treatment. [2008]
Ensure healthcare professionals providing information and education programmes have specialist knowledge about CKD and the necessary skills to facilitate learning. [2008]
Take account of the psychological aspects of coping with CKD and offer adults with CKD access to support, for example, support groups, counselling or a specialist nurse. [2008]
Lifestyle advice
Encourage adults with CKD to take exercise, achieve a healthy weight and stop smoking. [2008]
Dietary interventions
Offer dietary advice about potassium, phosphate, calorie and salt intake appropriate to the severity of CKD. [2008, amended 2014]
If dietary intervention is agreed, provide it alongside education, detailed dietary assessment and supervision to ensure malnutrition is prevented. [2008]
Low-protein diets
Do not offer low-protein diets (dietary protein intake less than 0.6 to 0.8 g/kg/day) to adults with CKD. [2014]
Self-management
- inform adults with CKD (and their family members or carers, as appropriate) of their diagnosis
- enable adults with CKD (and their family members or carers, as appropriate) to share in decision making about their care
- support self-management (this includes providing information about blood pressure, smoking cessation, exercise, diet and medicines) and enable adults with CKD to make informed choices. [2014]
Give adults access to their medical data (including diagnosis, comorbidities, test results, treatments and correspondence) through information systems, such as Renal PatientView , to encourage and help them to self-manage their CKD. [2014]
1.5. Risk assessment, referral criteria and shared care
Risk assessment.
Give adults with CKD and their family members or carers (as appropriate) information about their 5-year risk of needing renal replacement therapy (measured using the 4-variable Kidney Failure Risk Equation ).
Follow NICE’s guideline on shared decision making when communicating risk. [2021]
Use every day, jargon-free language to communicate information on risk. If technical and medical terms are used, explain them clearly. [2021]
Set aside enough time during the consultation to give information on risk assessment and to answer any questions. Arrange another appointment for more discussion if this is needed. [2021]
Document the discussion on risk assessment and any decisions the person makes. [2021]
Referral criteria
- a 5-year risk of needing renal replacement therapy of greater than 5% (measured using the 4-variable Kidney Failure Risk Equation)
- an ACR of 70 mg/mmol or more, unless known to be caused by diabetes and already appropriately treated (see recommendations 1.6.6 and 1.6.7 )
- an ACR of more than 30 mg/mmol (ACR category A3), together with haematuria
- a sustained decrease in eGFR of 25% or more and a change in eGFR category within 12 months
- a sustained decrease in eGFR of 15 ml/min/1.73 m 2 or more per year
- hypertension that remains poorly controlled (above the person’s individual target) despite the use of at least 4 antihypertensive medicines at therapeutic doses (see also NICE’s guideline on hypertension in adults )
- known or suspected rare or genetic causes of CKD
- suspected renal artery stenosis. [2021]
- an ACR of 3 mg/mmol or more, confirmed on a repeat early morning urine sample
- any decrease in eGFR
- suspected renal artery stenosis
- renal outflow obstruction. [2021]
Consider discussing management with a specialist by letter, email, telephone, or virtual meeting, if there are concerns but the person with CKD does not need to see a specialist. [2021]
Refer people with CKD and renal outflow obstruction to urological services, unless urgent treatment is needed (for example, for hyperkalaemia, severe uraemia, acidosis or fluid overload). [2021]
Shared care
NICE’s guideline on shared decision making .
- Consider routine follow up at the GP surgery or with a paediatrician rather than in a specialist clinic.
- Specify criteria for future referral and re-referral if GP follow up is agreed. For children and young people, these criteria should be agreed between the GP and secondary care services. [2021]
For a short explanation of why the committee made these recommendations and how they might affect practice, see the rationale and impact section on risk assessment, referral criteria and shared care .
Full details of the evidence and the committee’s discussion are in evidence review F: the best combination of measures to identify increased risk of progression in adults, children and young people .
1.6. Pharmacotherapy
Blood pressure control.
See NICE’s guideline on hypertension in adults for advice on blood pressure control in people with frailty and multimorbidity.
NICE’s guideline on hypertension in adults recommends using clinic blood pressure for monitoring response to lifestyle changes or medical treatment (see recommendation 1.4.15).
In adults with CKD and an ACR under 70 mg/mmol, aim for a clinic systolic blood pressure below 140 mmHg (target range 120 to 139 mmHg) and a clinic diastolic blood pressure below 90 mmHg. [2021]
In adults with CKD and an ACR of 70 mg/mmol or more, aim for a clinic systolic blood pressure below 130 mmHg (target range 120 to 129 mmHg) and a clinic diastolic blood pressure below 80 mmHg. [2021]
In children and young people with CKD and an ACR of 70 mg/mol or more, aim for a clinic systolic blood pressure below the 50th percentile for height. [2021]
For a short explanation of why the committee made these recommendations and how they might affect practice, see the rationale and impact section on pharmacotherapy for blood pressure control .
Full details of the evidence and the committee’s discussion are in evidence review G: optimal blood pressure targets
Pharmacotherapy for hypertension
Follow the recommendations on treating hypertension in NICE’s guideline on hypertension in adults for adults with CKD, hypertension and an ACR of 30 mg/mmol or less (ACR categories A1 and A2). [2014, amended 2021]
Offer an angiotensin-receptor blocker (ARB) or an angiotensin-converting enzyme (ACE) inhibitor (titrated to the highest licensed dose that the person can tolerate) to adults, children and young people with CKD who have hypertension and an ACR over 30 mg/mmol (ACR category A3 or above). [2021]
Pharmacotherapy for CKD in adults, children, and young people with related persistent proteinuria
- NICE’s guideline on type 1 diabetes in adults
- NICE’s guideline on type 2 diabetes in adults
- NICE’s guideline on type 1 and type 2 diabetes in children and young people .
For adults with CKD and diabetes (type 1 or type 2) offer an ARB or an ACE inhibitor (titrated to the highest licensed dose that the person can tolerate) if ACR is 3 mg/mmol or more. [2021]
For guidance on SGLT2 inhibitors for adults with CKD and type 2 diabetes, see chronic kidney disease in NICE’s guideline on type 2 diabetes in adults . [2021]
For children and young people with CKD and diabetes (type 1 or 2), offer an ARB or an ACE inhibitor (titrated to the highest licensed dose that they can tolerate) if ACR is 3 mg/mmol or more. [2021]
- refer for nephrology assessment and offer an ARB or an ACE inhibitor (titrated to the highest licensed dose that they can tolerate), if ACR is 70 mg/mmol or more
- monitor in line with recommendations 1.3.1 and 1.3.4 if ACR is above 30 but below 70 mg/mmol; consider discussing with a nephrologist if eGFR declines or ACR increases. [2021]
- offer an ARB or an ACE inhibitor if ACR (titrated to the highest licensed dose that they can tolerate) is 70 mg/mol or more
When offering medicines to lower proteinuria to people with frailty, comorbidities or who are taking many other prescribed medicines, follow the recommendations in NICE’s guideline on medicines optimisation to ensure the best possible outcomes. Seek specialist advice if needed, for example from a consultant in care of the elderly, or from a kidney physician if the person asks about contraception. [2021]
For a short explanation of why the committee made the 2021 recommendations and how they might affect practice, see the rationale and impact section on pharmacotherapy for proteinuria and choice of antihypertensive agent .
Full details of the evidence and the committee’s discussion are in evidence review H: interventions to lower proteinuria .
Renin–angiotensin system antagonists
Do not offer a combination of renin–angiotensin system antagonists to adults with CKD. [2014]
- achieving the optimal tolerated dose of renin–angiotensin system antagonists and
- monitoring eGFR and serum potassium in achieving this safely. [2008]
Measure serum potassium concentrations and estimate the GFR before starting renin–angiotensin system antagonists in people with CKD. Repeat these measurements between 1 and 2 weeks after starting renin–angiotensin system antagonists and after each dose increase. [2008]
Do not routinely offer a renin–angiotensin system antagonist to adults with CKD if their pretreatment serum potassium concentration is greater than 5.0 mmol/litre. [2008, amended 2014]
- assess for and treat any other factors that promote hyperkalaemia and
- recheck serum potassium concentration. [2008]
Be aware that more frequent monitoring of serum potassium concentration may be needed if medicines known to promote hyperkalaemia are prescribed for use in people alongside renin–angiotensin system antagonists. [2008]
Stop renin–angiotensin system antagonists in adults if the serum potassium concentration increases to 6.0 mmol/litre or more and other medicines known to promote hyperkalaemia have been discontinued. [2008]
For recommendations on hyperkalaemia treatment in adults with categories G3b to G5 chronic kidney disease, see NICE’s technology appraisals on sodium zirconium cyclosilicate and patiromer . [2021]
- the GFR decrease from pretreatment baseline is less than 25% or
- the serum creatinine increase from baseline is less than 30%. [2008]
If there is a decrease in eGFR or increase in serum creatinine after starting or increasing the dose of renin–angiotensin system antagonists, but it is less than 25% (eGFR) or 30% (serum creatinine) of baseline, repeat the test in 1 to 2 weeks. Do not modify the renin–angiotensin system antagonist dose if the change in eGFR is less than 25% or the change in serum creatinine is less than 30%. [2008]
- investigate other causes of a deterioration in kidney function, such as volume depletion or concurrent medication (for example, NSAIDs)
- if no other cause for the deterioration in kidney function is found, stop the renin–angiotensin system antagonist or reduce the dose to a previously tolerated lower dose, and add an alternative antihypertensive medication if needed. [2008]
Statins for adults
Follow the recommendations in NICE’s guideline on cardiovascular disease: risk assessment and reduction, including lipid modification for the use of statins in adults with CKD. [2014]
Oral antiplatelets and anticoagulants for adults
Offer antiplatelet medicines to adults with CKD for the secondary prevention of cardiovascular disease, but be aware of the increased risk of bleeding. [2014]
For guidance on oral anticoagulants for people with CKD, see NICE’s guidelines on atrial fibrillation and venous thromboembolic diseases . [2014, amended 2021]
1.7. Diagnosing and assessing anaemia
Diagnostic role of haemoglobin levels.
- their haemoglobin (Hb) level falls to 110 g/litre or less (or 105 g/litre or less if younger than 2 years) or
- they develop symptoms attributable to anaemia (such as tiredness, shortness of breath, lethargy and palpitations). [2011]
Diagnostic role of glomerular filtration rate
- If eGFR is above 60 ml/min/1.73 m 2 , investigate other causes of anaemia as it is unlikely to be caused by CKD.
investigate other causes of anaemia, but
use clinical judgement to decide how extensive this investigation should be, because the anaemia may be caused by CKD.
- If eGFR is below 30 ml/min/1.73 m 2 , think about other causes of anaemia but note that anaemia is often caused by CKD. [2021]
For a short explanation of why the committee made the 2021 recommendation and how it might affect practice, see the rationale and impact section on diagnostic role of glomerular filtration rate .
Full details of the evidence and the committee’s discussion are in evidence review I: eGFR threshold for the investigation of anaemia due to CKD .
Diagnostic tests to determine iron status and predict response to iron therapy
- Use percentage of hypochromic red blood cells (% HRC; more than 6%), but only if processing of blood sample is possible within 6 hours.
- If using percentage of hypochromic red blood cells is not possible, use reticulocyte Hb content (CHr; less than 29 pg) or equivalent tests – for example, reticulocyte Hb equivalent.
- If these tests are not available or the person has thalassaemia or thalassaemia trait, use a combination of transferrin saturation (less than 20%) and serum ferritin measurement (less than 100 micrograms/litre). [2015]
Do not request transferrin saturation or serum ferritin measurement alone to assess iron deficiency status in people with anaemia of CKD. [2015]
Do not routinely measure erythropoietin levels for the diagnosis or management of anaemia in people with anaemia of CKD. [2006]
1.8. Managing anaemia
Starting erythropoietic stimulating agent therapy in iron-deficiency.
ESA (erythropoietic stimulating agent) therapy should not be started in the presence of absolute iron deficiency without also managing the iron deficiency. [2006]
Maximum iron levels in people with anaemia of CKD
In adults, children and young people treated with iron, serum ferritin levels should not rise above 800 micrograms/litre. In order to prevent this, review the dose of iron when serum ferritin levels reach 500 micrograms/litre. [2006]
Clinical utility of ESA therapy in people with sufficient iron
Discuss the pros and cons of a trial of anaemia management with the person with anaemia of CKD, and their families and carers if agreed. [2006]
ESAs need not be administered if the presence of comorbidities, or the prognosis, is likely to negate the benefits of correcting the anaemia. [2006]
Start a trial of anaemia correction when there is uncertainty over whether the presence of comorbidities, or the prognosis, would negate benefit from correcting the anaemia with ESAs. [2006]
If a trial of ESA therapy is carried out, assess the effectiveness of the trial after an agreed interval. Agree with the person with anaemia of CKD (and their families and carers, if appropriate) whether or not to continue ESA therapy. [2006]
Review treatment in all people started on ESA therapy after an agreed interval to decide whether or not to continue using ESAs. [2006]
Nutritional supplements
Do not prescribe supplements of vitamin C, folic acid or carnitine as adjuvants specifically for the treatment of anaemia of CKD. [2006]
Do not use androgens to treat anaemia in people with anaemia of CKD. [2006]
Hyperparathyroidism
Treat clinically relevant hyperparathyroidism in adults, children and young people with CKD to improve the management of the anaemia. [2006]
Person-centred care and ESAs
Give adults, children and young people offered ESA therapy and their GPs information about why ESA therapy is needed, how it works and what benefits and side effects may be experienced. [2006]
When managing the treatment of anaemia of CKD, there should be agreed protocols defining roles and responsibilities of healthcare professionals in primary and secondary care. [2006]
Explain to people receiving ESA therapy about the importance of concordance with therapy and the consequences of poor adherence. [2006]
When prescribing ESA therapy, take into account the person’s preferences about supervised- or self-administration, dose frequency, pain on injection, method of supplying ESA and storage. [2006]
In order for people to self-administer their ESA in a way that is clinically effective and safe, make arrangements to provide ready, reasonable and uninterrupted access to supplies. [2006]
Patient education programmes
- Practical information about how anaemia of CKD is managed.
- Knowledge (for example, about symptoms, iron management, causes of anaemia, associated medications, phases of treatment).
- Professional support (for example, contact information, community services, continuity of care, monitoring, feedback on progress of results).
- Lifestyle (for example, diet, physical exercise, maintaining normality, meeting other people with the condition).
- Adaptation to chronic disease (for example, previous information and expectations, resolution of symptoms). [2006]
1.9. Assessing and optimising erythropoiesis in people with anaemia
Benefits of treatment with esas.
Offer treatment with ESAs to adults, children and young people with anaemia of CKD who are likely to benefit in terms of quality of life and physical function. [2006]
Blood transfusions
Avoid blood transfusions if possible in people with anaemia of CKD in whom kidney transplant is a treatment option. [2006]
If a transfusion is indicated clinically in a person with anaemia of CKD, follow NICE’s guideline on blood transfusion . [2006, amended 2015]
Comparisons of ESAs
- the person’s dialysis status
- the route of administration
- the local availability of ESAs
- the lack of evidence comparing the efficacy of ESAs. [2006]
Coordinating care
- Monitoring and managing a caseload in line with locally agreed protocols.
- Providing information, education and support to empower people and their families and carers to participate in their care.
- Coordinating an anaemia service for people with CKD, working between secondary and primary care and providing a single point of contact, to ensure people receive a seamless service of the highest standard.
- Prescribing medicines related to anaemia management and monitoring their effectiveness. [2006]
Providing ESAs
- continuity of medicine supply
- flexibility of where the medicine is delivered and administered
- the person’s lifestyle and preferences
- cost of medicine supply
- desire for self-care if appropriate
- regular review of the plan in light of changing needs. [2006]
ESAs: optimal route of administration
- patient population (for example, people having haemodialysis)
- pain of injection
- frequency of administration
- efficacy (for example, subcutaneous compared with intravenous administration, or long-acting compared with short-acting preparations)
- cost of medicine supply. [2006]
The prescriber should take into account that when using short-acting ESAs, subcutaneous injection allows the use of lower doses of medicines than intravenous administration. [2006]
ESAs: dose and frequency
- determined by the duration of action and route of administration of the ESA
- adjusted to keep the rate of Hb increase between 10 and 20 g/litre/month. [2006]
Optimal Hb levels
- their preferences
- symptoms and comorbidities
- the necessary treatment. [2011]
- Typically maintain the aspirational Hb range between 100 and 120 g/litre for adults, young people and children aged 2 years and over, and between 95 and 115 g/litre for children under 2 years, reflecting the lower normal range in that age group.
- To keep the Hb level within the aspirational range, do not wait until Hb levels are outside the aspirational range before adjusting treatment (for example, take action when Hb levels are within 5 g/litre of the range’s limits). Follow the MHRA safety advice on recombinant human erythropoietins , particularly the advice to avoid Hb levels above 120 g/litre because of the increased risk of death and serious adverse cardiovascular events in people with CKD. People should have close monitoring to ensure that the lowest approved dose of ESA is used to provide adequate control of the anaemia symptoms. [2021]
For a short explanation of why the committee made the 2021 recommendation and how it might affect practice, see the rationale and impact section on optimal Hb levels .
Full details of the evidence and the committee’s discussion are in evidence review J: aspirational haemoglobin target range for children and young people with CKD .
- high doses of ESAs are needed to achieve the aspirational range or
- the aspirational range is not achieved despite escalating ESA doses. High doses are more than 175 IU/kg per week for people having haemodialysis; more than 125 IU/kg per week for people having peritoneal dialysis; more than 100 IU/kg per week for people not having dialysis. [2011]
Do not use age alone to determine treatment of anaemia of CKD. [2006]
Adjusting ESA treatment
Optimise iron status before or at the same time as starting ESAs and during maintenance treatment with ESAs. [2006, amended 2011]
Use of ACE inhibitors or angiotensin type II receptor antagonists is not precluded, but if they are used, an increase in ESA therapy should be considered. [2006]
- Investigate the cause of an unexpected change in Hb level (that is, intercurrent illness or bleeding) to enable intervention and optimise iron status.
- Increase or decrease ESA dose and/or frequency when Hb measurements fall outside action thresholds (usually below 105 g/litre or above 115 g/litre), or for example when the rate of change of Hb suggests an established trend (for example, greater than 10 g/litre/month). [2006, amended 2011]
Correcting iron deficiency
- percentage of hypochromic red blood cells less than 6% (unless ferritin is greater than 800 micrograms/litre)
- reticulocyte Hb count or equivalent tests above 29 pg (unless serum ferritin is greater than 800 micrograms/litre). If these tests are not available or the person has thalassaemia or thalassaemia trait, iron therapy should maintain transferrin saturation greater than 20% and serum ferritin level greater than 100 micrograms/litre (unless serum ferritin is greater than 800 micrograms/litre). Most adults will need 500 to 1,000 mg of iron (equivalent doses for children) in a single or divided dose depending on the preparation. Intravenous iron should be administered in a setting with facilities for resuscitation. [2015] In August 2021, this was an off-label use of intravenous iron products for some ages of children and young people. See NICE’s information on prescribing medicines .
Offer a high-dose intravenous iron regimen to adults, children and young people with stage 5 CKD on in-centre (hospital or satellite unit) haemodialysis, if they have iron deficiency (see recommendation 1.7.3 ).
See table 3 for an example of a high-dose intravenous iron regimen for adults or use a bioequivalent dose of iron. For children and young people, use the maximum dosing regimen in the British National Formulary for Children (BNFc) unless serum ferritin is greater than 800 micrograms/litre when the dose should be withheld.
In August 2021, this was an off-label use of intravenous iron products for some children and young people. See NICE’s information on prescribing medicines . [2021]
Example of high-dose intravenous iron regimen for adults.
For a short explanation of why the committee made the 2021 recommendation and how it might affect practice, see the rationale and impact section on correcting iron deficiency .
Full details of the evidence and the committee’s discussion are in evidence review K: anaemia – IV iron .
Maintaining iron levels after a deficiency is corrected
Once the percentage of hypochromic red blood cells is less than 6%, reticulocyte Hb count or equivalent tests are above 29 pg, or transferrin saturation is greater than 20% and serum ferritin level is greater than 100 micrograms/litre, offer maintenance iron to people with anaemia of CKD who are receiving ESAs.
The dosing regimen will depend on modality, for example people having haemodialysis will need the equivalent of 50 to 60 mg intravenous iron per week (or an equivalent dose in children of 1 mg/kg/week). [2015]
In August 2021, this was an off-label use of intravenous iron products for some ages of children and young people. See NICE’s information on prescribing medicines .
Monitoring iron status during ESA treatment
- percentage of hypochromic red blood cells less than 6% (unless serum ferritin is greater than 800 micrograms/litre)
- reticulocyte Hb count or equivalent tests above 29 pg (unless serum ferritin is greater than 800 micrograms/litre)
- transferrin saturation level above 20% and serum ferritin level above 100 micrograms/litre (unless serum ferritin is greater than 800 micrograms/litre). The marker of iron status should be monitored every 1 to 3 months in people having haemodialysis. In people who are pre-dialysis or receiving peritoneal dialysis, levels are typically monitored every 3 months. If these people have a normal full blood count there is little benefit in checking iron status. [2015] In August 2021, this was an off-label use of intravenous iron products for some ages of children and young people. See NICE’s information on prescribing medicines .
Iron therapy for people who are iron deficient and not on ESA therapy
- Discuss the risks and benefits of treatment options. Take into account the person’s choice.
- For people who are not having haemodialysis, consider a trial of oral iron before offering intravenous iron therapy. If they are intolerant of oral iron or target Hb levels are not reached within 3 months (see recommendation 1.9.11 ), offer intravenous iron therapy.
- intravenous iron therapy is contraindicated or
- the person chooses not to have intravenous iron therapy after discussing the relative efficacy and side effects of oral and intravenous iron therapy. [2015]
Discuss the results of the iron therapy with the person or, if appropriate, with their family or carers and offer ESA therapy if needed (see recommendation 1.9.1 ). [2015]
Iron therapy for people who are iron deficient and receiving ESA therapy
- For adults and young people, offer intravenous iron therapy.
- For children who are having haemodialysis, offer intravenous iron therapy.
- For children who are not having haemodialysis, consider oral iron. If the child is intolerant of oral iron or target Hb levels are not reached within 3 months (see recommendation 1.9.11 ), offer intravenous iron therapy. [2015]
- preferences of the person with anaemia of CKD or, if appropriate, their family or carers
- nursing and administration costs
- cost of local medicine supply
- provision of resuscitation facilities. High-dose and low-frequency iron is a maximum of 2 infusions, with a minimum of 500 mg of iron in each infusion for adults. Low dose and high frequency is more than 2 infusions with 100 mg to 200 mg of iron in each infusion for adults. [2015] In August 2021, this was an off-label use of intravenous iron products for some ages of children and young people. See NICE’s information on prescribing medicines .
1.10. Monitoring anaemia treatment
Monitoring iron status.
Do not check iron levels earlier than 1 week after administering intravenous iron in adults, children and young people with anaemia of CKD. The length of time to monitoring of iron status is dependent on the product used and the amount of iron given. [2006]
Carry out routine monitoring of iron stores to prevent iron overload using serum ferritin at intervals of 1 to 3 months. [2006, amended 2015]
Monitoring Hb levels
- every 2 to 4 weeks in the induction phase of ESA therapy
- every 1 to 3 months in the maintenance phase of ESA therapy
- more frequently after an ESA dose adjustment
- in a clinical setting chosen in discussion with the person, taking into account their convenience and local healthcare systems. [2006]
Detecting ESA resistance
- an aspirational Hb range is not achieved despite treatment with 300 IU/kg/week or more of subcutaneous epoetin or 450 IU/kg/week or more of intravenous epoetin or 1.5 micrograms/kg/week of darbepoetin or
- there is a continued need for the administration of high doses of ESAs to maintain the aspirational Hb range. [2006]
In people with CKD, pure red cell aplasia (PRCA) is indicated by a low reticulocyte count, together with anaemia and the presence of neutralising antibodies. Confirm PRCA by the presence of anti-erythropoietin antibodies together with a lack of pro-erythroid progenitor cells in the bone marrow. [2006]
In people with anaemia of CKD, aluminium toxicity should be considered as a potential cause of a reduced response to ESAs after other causes, such as intercurrent illness and chronic blood loss, have been excluded. [2006]
Managing ESA resistance
If aluminium toxicity is suspected in an adult, child or young person with anaemia of CKD having haemodialysis, perform a desferrioxamine test and review the management of their condition accordingly. [2006]
Consider specialist referral for people with ESA-induced PRCA. [2006, amended 2011]
Role of blood transfusion in managing ESA resistance
Consider referring adults, children and young people with ESA resistance to a haematology service, particularly if an underlying haematological disorder is suspected. [2015]
Evaluate and discuss the risks and benefits of red cell transfusion with the person or, if appropriate, with their family or carers. [2015]
Take into account the person’s symptoms, quality of life, underlying conditions and the chance of a future successful kidney transplant, in addition to Hb levels, when thinking about the need for red cell transfusion. [2015]
- all reversible causes of ESA resistance have been taken into account and excluded and
- the person’s condition is otherwise stable (without intercurrent illness such as infection) and
- the person is receiving adequate dialysis. Review the rate of red cell transfusion between 1 and 3 months after stopping ESA therapy. If the rate of transfusion has increased, consider restarting ESA therapy. [2015]
1.11. Hyperphosphataemia in people with CKD stage 4 or 5
Dietary management for adults, children and young people.
A specialist renal dietitian, supported by healthcare professionals with the necessary skills and competencies, should carry out a dietary assessment and give individualised information and advice on dietary phosphate management. [2013]
Tailor advice on dietary phosphate management to the person’s learning needs and preferences, rather than using a generalised or complex multicomponent programme of delivery. [2013]
Give information about controlling intake of phosphate-rich foods (in particular, foods with a high phosphate content per gram of protein, as well as food and drinks with high levels of phosphate additives) to control serum phosphate, while avoiding malnutrition by maintaining a protein intake at or above the minimum recommended level. For people on dialysis, take into account possible dialysate protein losses. [2013]
If a nutritional supplement is needed to maintain protein intake in children and young people with hyperphosphataemia, offer a supplement with a lower phosphate content, taking into account the person’s preference and other nutritional requirements. [2013]
Before starting phosphate binders for adults, children and young people
- diet (see recommendations 1.4.7 to 1.4.9 for adults)
- dialysis, for people who are having this. [2021]
- the reason for offering phosphate binders
- the risks if they are not taken
- the side effects linked to phosphate binders
- when and how they have to be taken (depending on the type of binder), including the exact timing (before, with or after food) and the need to take them with food containing phosphate (including, for example, high-protein snacks). [2021]
Take into account the person’s preferences on phosphate binders. [2021]
If the person has problems taking the first phosphate binder offered, consider switching to the next recommended one (see recommendations 1.11.9 to 1.11.15 ). [2021]
Phosphate binders for children and young people
Offer children and young people with CKD stage 4 or 5 and hyperphosphataemia a calcium-based phosphate binder to control serum phosphate levels. [2021]
In August 2021, this was an off-label use of some calcium-based phosphate binders in people not on dialysis. See NICE’s information on prescribing medicines .
- investigate possible causes other than the phosphate binder
- consider reducing the dose of the calcium-based phosphate binder and adding sevelamer carbonate or switching to sevelamer carbonate alone. [2021] In August 2021, this was an off-label use of sevelamer carbonate. See NICE’s information on prescribing medicines .
For all children and young people who are taking more than 1 phosphate binder, titrate the dosage to achieve the best possible control of serum phosphate while keeping serum calcium levels below the upper normal limit. [2021]
Phosphate binders for adults
First phosphate binder for adults.
Offer adults with CKD stage 4 or 5 and hyperphosphataemia calcium acetate to control serum phosphate levels. [2021]
In August 2021, this was an off-label use of calcium acetate in people not on dialysis. See NICE’s information on prescribing medicines .
Offer sevelamer carbonate if calcium acetate is not indicated (for example, because of hypercalcaemia or low serum parathyroid hormone levels) or not tolerated. [2021]
In August 2021, this was an off-label use of sevelamer carbonate. See NICE’s information on prescribing medicines .
- sucroferric oxyhydroxide, for adults on dialysis if a calcium-based phosphate binder is not needed or
- calcium carbonate, if a calcium-based phosphate binder is needed. In August 2021, this was an off-label use of these phosphate binders in people not on dialysis. See NICE’s information on prescribing medicines . [2021]
Only consider lanthanum carbonate for adults with CKD stage 4 or 5 if other phosphate binders cannot be used.
In August 2021, this was an off-label use of lanthanum carbonate phosphate binders in people not on dialysis and with serum phosphate levels less than 1.78 mmol/l. See NICE’s information on prescribing medicines . [2021]
Combinations of phosphate binders for adults
- check they are taking it as prescribed
- consider combining a calcium-based phosphate binder with a non-calcium-based phosphate binder. [2021]
For all adults who are taking more than 1 phosphate binder, titrate the dosage to achieve the best possible control of serum phosphate while keeping serum calcium levels below the upper normal limit. [2021]

Review of treatments in adults, children and young people
- whether they are taking the phosphate binders as prescribed
- other relevant factors, such as vitamin D levels, serum parathyroid hormone levels, alkaline phosphatase, serum calcium, medications that might affect serum phosphate, or dialysis. [2021]
For a short explanation of why the committee made these 2021 recommendations and how they might affect practice, see the rationale and impact section on hyperphosphataemia in people with CKD stage 4 or 5 .
Full details of the evidence and the committee’s discussion are in evidence review L: use of phosphate binders .
1.12. Other complications in adults
Bone metabolism and osteoporosis.
Do not routinely measure calcium, phosphate, parathyroid hormone and vitamin D levels in adults with a GFR of 30 ml/min/1.73 m 2 or more (GFR category G1, G2 or G3). [2008]
Measure serum calcium, phosphate and parathyroid hormone concentrations in adults with a GFR of less than 30 ml/min/1.73 m 2 (GFR category G4 or G5). Determine the subsequent frequency of testing by the measured values and the clinical circumstances. If doubt exists, seek specialist opinion. [2008]
Offer bisphosphonates if indicated for the prevention and treatment of osteoporosis in adults with a GFR of 30 ml/min/1.73 m 2 or more (GFR category G1, G2 or G3). [2008]
Vitamin D supplements in the management of CKD–mineral and bone disorders
Detailed advice on the management of CKD–mineral and bone disorders is beyond the scope of this guideline. If uncertain, seek advice from your local renal service.
Do not routinely offer vitamin D supplementation to manage or prevent CKD–mineral and bone disorders. [2014]
Offer colecalciferol or ergocalciferol to treat vitamin D deficiency in people with CKD and vitamin D deficiency. [2014]
If vitamin D deficiency has been corrected and symptoms of CKD–mineral and bone disorders persist, offer alfacalcidol (1-alpha-hydroxycholecalciferol) or calcitriol (1-25-dihydroxycholecalciferol) to people with a GFR of less than 30 ml/min/1.73 m 2 (GFR category G4 or G5). [2014]
Monitor serum calcium and phosphate concentrations in people receiving alfacalcidol or calcitriol supplements. [2014]
Oral bicarbonate supplements in the management of metabolic acidosis
Detailed advice on the management of metabolic acidosis is beyond the scope of this guideline. If uncertain, seek advice from your local renal service.
- a GFR less than 30 ml/min/1.73 m 2 (GFR category G4 or G5) and
- a serum bicarbonate concentration of less than 20 mmol/litre. [2014]
Terms used in this guideline
This section defines terms that have been used in a particular way for this guideline. For other definitions see the NICE glossary .
Abnormalities of kidney function or structure present for more than 3 months, with implications for health. This includes all people with markers of kidney damage and those with a glomerular filtration rate (GFR) of less than 60 ml/min/1.73 m 2 on at least 2 occasions separated by a period of at least 90 days (with or without markers of kidney damage).
- A person with an eGFR of 25 ml/min/1.73 m 2 and an ACR of 15 mg/mmol has CKD G4A2.
- A person with an eGFR of 50 ml/min/1.73 m 2 and an ACR of 35 mg/mmol has CKD G3aA3.
- An eGFR of less than 15 ml/min/1.73 m 2 (GFR category G5) is referred to as kidney failure.
- GFR: either a measured or an estimated GFR
- eGFR: estimated GFR (without indicating the method of estimation)
- eGFRcreatinine: an estimation of GFR using serum creatinine
A person’s 5-year risk of needing renal replacement therapy (defined as the need for dialysis or transplant) is estimated, as in Major 2019 , as: 1 − 0.9570 exp ( β sum ) β sum = − 0.2201 × age 10 − 7.036 + [ 0.2467 × ( male − 0.5642 ) ] − 0.5567 × e G F R 5 − 7.222 + [ 0.4510 × ( log ( A C R / 0.113 ) − 5.137 ) ] In the above, eGFR is reported in ml/min/1.73 m 2 and ACR in mg/mmol. Where the term ‘male’ is used, this should be replaced by a 1 if the person being assessed is male, and a 0 if they are female. This equation and its coefficients are validated in a UK population, and it is important to use this version, and not a version validated in another country.
These include albuminuria (ACR more than 3 mg/mmol), urine sediment abnormalities, electrolyte and other abnormalities due to tubular disorders, abnormalities detected by histology, structural abnormalities detected by imaging, and a history of kidney transplantation.
Usually regarded to be CKD stages 4 and 5, although there is no accepted definition. Pre-dialysis includes people with a failing transplant and people having conservative management.
Life-supporting treatments for severe acute kidney injury or stage 5 CKD. This includes haemodialysis, haemofiltration, haemodiafiltration, peritoneal dialysis and kidney transplantation.
A medicine that blocks or inhibits the renin–angiotensin–aldosterone system, including angiotensin-converting enzyme (ACE) inhibitors, angiotensin-receptor blockers (ARBs), direct renin inhibitors and aldosterone antagonists.
A medicine that blocks or inhibits the renin–angiotensin system, including ACE inhibitors, ARBs and direct renin inhibitors. This group of medicines does not include aldosterone antagonists.
- Recommendations for research
As part of the 2021 update, the guideline committee made 18 recommendations for research on chronic kidney disease (CKD). They prioritised 5 key recommendations for research. They also retained some recommendations for research from previous guidelines.
Key recommendations for research
1. creatinine-based estimate of egfr – existing calculations.
In adults, children and young people from black, Asian and other minority ethnic groups with CKD living in the UK, which existing eGFR calculations are the most accurate? [2021]
2. Creatinine-based estimate of eGFR – improving accuracy of calculations
In adults, children and young people from black, Asian and other minority ethnic groups with CKD living in the UK, what biomarkers or factors, other than ethnicity, improve the diagnostic accuracy of eGFR calculations? [2021]
For a short explanation of why the committee made these recommendations for research, see the rationale on creatinine-based estimate of GFR .
3. Risk assessment for black, Asian and minority ethnic groups
What is the accuracy of the 4-variable Kidney Failure Risk Equation in adults, children and young people with CKD from black, Asian and minority ethnic groups living in the UK? [2021]
For a short explanation of why the committee made this recommendation for research, see the rationale on risk assessment, referral criteria and shared care .
4. Managing anaemia – optimal Hb levels for children and young people
What is the efficacy and safety of different aspirational haemoglobin (Hb) targets for children and young people with CKD undergoing treatment for anaemia? [2021]
For a short explanation of why the committee made this recommendation for research, see the rationale on optimal Hb levels .
5. Hyperphosphatemia in people with CKD stage 4 or 5
What are people with CKD and their family members and carers views and beliefs about taking oral phosphate binders? [2021]
For a short explanation of why the committee made this recommendation for research, see the rationale on hyperphosphataemia in people with CKD stage 4 or 5 .
Other recommendations for research
Cystatin-c equations.
What is the diagnostic accuracy of cystatin-C equations to estimate GFR as a measurement of kidney function in adults, young people and children in the UK? [2021]
In children and young people, what is the accuracy of reagent strips for detecting albumin in urine? [2021]
What is the effect of measuring proteinuria with albumin:creatinine ratio compared with protein:creatinine ratio on the timing of treatment changes in children and young people with CKD? [2021]
Frequency of monitoring
For adults, children and young people with CKD, what is the optimal monitoring frequency for albumin:creatinine ratio? [2021]
Risk assessment, referral criteria and shared care
What is the association between risk factors and CKD outcomes in children and young people? [2021]
What is the accuracy of the 4-variable Kidney Failure Risk Equation in children and young people living in the UK? [2021]
Frequency of review
What is the most clinical and cost-effective frequency of review for children and young people with CKD? [2021]
Managing anaemia
For adults, children and young people with CKD and anaemia, what is the diagnostic accuracy of eGFR thresholds of 60, 45, and 30 ml/min/1.73 m 2 for determining whether the anaemia is due to CKD? [2021]
For adults, children and young people with CKD and anaemia who are on peritoneal dialysis, what amount of intravenous (IV) iron is most clinically and cost effective in managing anaemia and its associated outcomes (including quality of life)? [2021]
What are the long-term consequences of high ferritin levels (above 800 micrograms/litre) in children and young people with CKD? [2021]
Phosphate binders
Which binders are the most clinically and cost effective in controlling serum phosphate in adults, children and young people with stage 4 or 5 CKD who are not on dialysis? [2021]
In adults with stage 4 or 5 CKD, including those on dialysis, what is the clinical and cost effectiveness and safety of long-term calcium acetate combined with magnesium carbonate for controlling serum phosphate? [2021]
Self-management of CKD
Does the provision of educational and supportive interventions to people with CKD by healthcare professionals increase the person’s skills and confidence in managing their conditions and improve clinical outcomes? [2014]
Antiplatelet therapy
For people with CKD at the highest risk of cardiovascular disease, what is the clinical effectiveness of low-dose aspirin compared with placebo for primary prevention of cardiovascular disease? [2014]
Renin–angiotensin–aldosterone system antagonists
For people aged over 75 years with CKD, what is the clinical effectiveness of renin–angiotensin–aldosterone system (RAAS) antagonists ? [2014]
In people with hyperparathyroidism secondary to CKD, does treatment with vitamin D or vitamin D analogues improve patient-related outcomes? [2014]
Management of anaemia of CKD with concurrent illness
What is the optimal management (in terms of clinical and cost effectiveness) of anaemia of CKD in people who are receiving erythropoietic stimulating agents (ESAs) and have a significant concurrent acute infectious illness? [2015]
Treatment of ESA resistance in people on haemodialysis
What is the most effective type of intervention to treat people on haemodialysis with ESA-resistant anaemia? [2015]
- Rationale and impact
These sections briefly explain why the committee made the recommendations and how they might affect practice.
Creatinine-based estimate of glomerular filtration rate (GFR)
Why the committee did not make recommendations.
Evidence on the specific eGFR equations or ethnicity adjustments seen by the committee was not from UK studies so may not be applicable to UK black, Asian and minority ethnic groups. None of the studies included children and young people. The committee was also concerned about the value of P30 as a measure of accuracy (P30 is the probability that the measured value is within 30% of the true value), the broad range of P30 values found across equations and the relative value or accuracy of ethnicity adjustments to eGFR equations in different ethnic groups. The committee agreed that adding an ethnicity adjustment to eGFR equations for different ethnicities may not be valid or accurate. Categorisations based on ethnicity lump together people with a diverse range of family backgrounds and differences in eGFR across ethnicities are likely to at least partly arise because of differences in average muscle mass between ethnic groups. However, muscle mass also differs from person to person within the same ethnicity and so making an adjustment based on ethnicity may be inaccurate for some people. Therefore, the committee agreed to remove the 2014 recommendation on how to adjust the CKD-EPI creatinine equation for adults of African-Caribbean or African family origin. The committee highlighted the 2008 recommendation, which states that caution should be used when interpreting eGFR and in adults with extremes of muscle mass and on those who consume protein supplements (this was added to recommendation 1.1.1 ). The committee made recommendations for research on appropriate eGFR equations for black, Asian and minority ethnic groups (adults, children and young people) in the UK (see recommendations for research 1 and 2 ). They agreed that factors other than ethnicity should also be explored as biomarkers.
The committee agreed that in the absence of good evidence for their accuracy, the 2014 recommendations that cystatin-c equations should be considered during diagnosis in certain circumstances, should be removed. In particular, they noted that although using cystatin-c equations may reduce false-positive results, it is likely to also increase false-negative results. This will avoid potentially misleading tests being conducted and the costs associated with these. They made a recommendation for research for a large study using UK data to evaluate the accuracy of cystatin-c equations (see other recommendations for research ).
Impact on practice
There will be an impact on practice, as the adjustment of the CKD-EPI creatinine equation for adults of African-Caribbean or African family origin has been removed from the guideline. Only a small number of centres in the UK currently use cystatin-c equations regularly, so most should not be affected by the removal of the cystatin-c recommendations.
Return to recommendations
Recommendations 1.1.10 to 1.1.14
Why the committee made the recommendations
For children and young people with CKD, there was no evidence for the accuracy of measuring albumin:creatinine ratio (ACR) compared with protein:creatinine ratio (PCR) to quantify proteinuria. The committee discussed the recommendations for adults and agreed that, overall, these fit well with current practice and can be recommended for children and young people as well.
The committee discussed the eGFR threshold recommended for quantifying urinary albumin or urinary protein loss in adults without diabetes. They agreed that this threshold is not appropriate for children and young people because any reduction in GFR in this population would prompt measuring proteinuria. Therefore, for children and young people they set the threshold for creatinine as above the upper limit of the age-appropriate reference range.
The committee agreed to make a recommendation for research to identify the effect of measuring proteinuria with ACR compared with PCR on the timing of treatment changes in children and young people with CKD and the consequences of the delay in treatment changes on different levels of proteinuria. (See other recommendations for research .)
How the recommendations might affect practice
The recommendations are in line with current practice, so no additional resources should be needed.
Reagent strips for proteinuria and haematuria
Recommendations 1.1.15 to 1.1.16
The evidence showed that reagent strips were less useful to rule out than to rule in proteinuria. The committee highlighted that ruling out proteinuria with confidence was the main goal when using reagent strips. Therefore, they agreed that reagent strips should not be used to identify proteinuria in children and young people. The evidence was not reviewed for adults and so the committee agreed to retain the 2014 recommendation not to use reagent strips to identify proteinuria in adults unless the strips are capable of specifically measuring albumin at low concentrations and expressing the result as an ACR. The committee also highlighted that these tests are commonly used in clinical practice and agreed to make a further recommendation for further investigations in adults, children and young people with an incidental finding of unexplained proteinuria on reagent strips. Further testing is needed to confirm CKD by identifying other markers of kidney damage (such as ACR or glomerular filtration rate).
There was limited evidence on the accuracy of reagent strips for albuminuria, so the committee did not feel able to make recommendations. There were only 2 studies, and only 1 showed that reagent strips could be useful.
There was no evidence on the accuracy of reagent strips for haematuria in children and young people. The 2014 guideline (which did not cover children and young people) recommended reagent strips for detecting haematuria in adults. The committee agreed to extend this recommendation to children and young people, because the evidence for adults is likely to be applicable to this population.
The recommendations are in line with current practice, so no additional resources should be needed. The committee noted that if all dipstick tests are confirmed by laboratory testing anyway, there would be extra costs attached to using dipsticks as a first step, which were not justified by the benefits.
Recommendations 1.1.20 to 1.1.25
For children and young people, the evidence showed that acute kidney injury and solitary functioning kidney were clinically significant risk factors for developing CKD. The committee highlighted that solitary functioning kidney was not due to kidney donation but to nephrectomy secondary to congenital anomalies of the kidney and urinary tract or to a lack of a kidney at birth or a non-functioning kidney.
The committee highlighted that there were other important risk factors for developing CKD in children and young people, but that no evidence was found for these. Based on their clinical knowledge and experience, they added ‘gout’ as a risk factor for adults and ‘low birth weight’ as a risk factor for children and young people.
The committee agreed that the frequency of monitoring (for developing CKD or progression) should be individualised for adults, children and young people. This is to address the different characteristics and risks that each person will have.
The committee agreed that more research on risk factors for developing CKD in children and young people would help to strengthen current guidance, so they made a recommendation for research. (See other recommendations for research .)
Recommendations 1.3.1 to 1.3.4
Most of the evidence showed that with eGFR decline, the risk of kidney disease progression and mortality increases, and this risk increases with the rate of eGFR decline. The committee agreed this is observed in clinical practice and any person presenting with an increase in eGFR decline would be monitored more frequently. The committee reviewed the recommendations and agreed that they are consistent with the evidence and clinical practice. They agreed to clarify monitoring by stating that repeat assessment is to be agreed with each person with or at risk of CKD.
The committee agreed that the frequency of monitoring they recommended was a minimum level and that more frequent monitoring would be appropriate for some patients. This should also be guided by rate of change in eGFR or ACR and specific comorbidities, including diabetes. ACR monitoring should be individualised. For example, ACR might be monitored more frequently in people with high ACR (categories A2 or A3), or if a change in ACR would affect management.
The committee made a recommendation for research to identify the optimal frequency of ACR monitoring in adults, children and young people with CKD. (See other recommendations for research .)
The committee discussed whether specific recommendations are needed for children and young people with CKD and decline in eGFR, but agreed that this population would be referred to specialist care.
The committee noted that no changes had been made to the previous suggested monitoring schedule, and they believed it was relatively well implemented in clinical practice. Therefore, they were confident there should not be a substantial impact on practice from the new recommendations.
Recommendation 1.5.1 to 1.5.9
New evidence found a UK validation of the 4-variable Kidney Failure Risk Equation for adults, which can be used as one of the referral criteria (5-year risk of needing renal replacement therapy greater than 5%). The results of both the validation study and cost-effectiveness modelling undertaken for the guideline showed using this equation and threshold as a referral criteria (rather than an eGFR threshold) was likely to be both more sensitive and more specific than the criteria in the 2014 NICE guideline, meaning people who will progress to needing renal replacement therapy are identified earlier, and there are fewer unnecessary referrals to secondary care.
The benefits of this approach over using an eGFR threshold (as in the 2014 NICE guideline) were not large, but the committee agreed they were meaningful. They also agreed there were additional potential benefits of using the 4-variable Kidney Failure Risk Equation, including the ability to provide people with an individual risk assessment, which could help them to proactively manage their own risk, and inform the management plans in secondary care.
However, validation of the risk equation was only in adults, so the committee made a separate recommendation for children and young people. Black people were under-represented in the study and, although there was a sizeable proportion of people of Asian family origin, the location of the study suggests that people of east Asian family origin were likely to be under-represented. Therefore, the committee agreed to make recommendation for research 3 for validation of the risk equation in adults, children and young people from black, Asian and other minority ethnic groups living in the UK.
The committee agreed that it is important to discuss with a person with CKD what risk means. They added additional recommendations on providing information about risk, using jargon-free language, allowing enough time for discussions and documenting any decisions made.
If the 4-variable Kidney Failure Risk Equation can be built into laboratory computer systems, as part of how eGFR and ACR results are returned to GPs, there should be no difficulty in implementing the recommendations. Because the calculation requires both an eGFR and ACR value, it can only be produced if the GP requests both those measurements. These recommendations are intended to provide additional information to supplement eGFR and ACR values, rather than changing how often these values are requested by GPs.
There may be particular difficulties for laboratories that store eGFR and ACR values on separate systems that cannot automatically communicate. In this situation, calculations may have to be done manually. However, this is still likely to be a more efficient system than calculations being carried out routinely by GPs. Overall, the referral criteria are predicted to slightly reduce monitoring costs but, excluding costs associated with dialysis, overall there should be no substantial impact on resource use.
There may be an implementation period before the risk equation results are available to all GPs. Until then, some GPs may have to continue to base referral decisions on eGFR and ACR values independently, as is currently done, without providing patients with a quantitative assessment of their risk of needing renal replacement therapy. The faster these recommendations can be routinely adopted the less time it will be necessary for these 2 parallel approaches to both be in use.
Pharmacotherapy for blood pressure control
Recommendations 1.6.1 to 1.6.3
Results from a meta-analysis (including the SPRINT trial) showed no meaningful difference between standard and more intensive blood pressure targets for adults with CKD. The 2014 guideline recommended maintaining systolic blood pressure below 140 mmHg and diastolic blood pressure below 90 mmHg. This is consistent with clinical practice and with the NICE guideline on managing hypertension. The committee noted that although there is limited evidence on blood pressure targets in people with CKD and proteinuria, it is important to maintain a systolic blood pressure below 130 mmHg and a diastolic pressure below 80 mmHg.
The committee agreed that none of the evidence they had seen warranted changing the recommendations. They also noted that intensive blood pressure targets only result in a marginal reduction in stroke and kidney failure, but put a large burden on patients in terms of polypharmacy and associated risks and side effects (such as falls).
The committee agreed that a useful target for blood pressure in children and young people with CKD and proteinuria is a systolic blood pressure below the 50th percentile for height.
The committee agreed that particular care had to be taken with people who were frail or who had multiple morbidities. However, the NICE guideline on hypertension already covers this group, so the committee did not make new recommendations.
The recommendations for adults are consistent with current practice and should not have an impact on resources. The recommendation for blood pressure targets in children and young people may have some cost implications, although the committee did not think they would be significant.
Pharmacotherapy for proteinuria and choice of antihypertensive agent
Recommendations 1.6.5 to 1.6.11
The interventions recommended are intended to improve a range of outcomes, including rates of progression to end-stage renal disease. There was evidence for adults, but not for children and young people. Paediatric experts on the committee agreed that the evidence for adults was also applicable to children and young people. Therefore, the committee did not make separate recommendations for different age groups.
The evidence for adults covered people with proteinuria or albuminuria, and included people with diabetes. This allowed the committee to make separate recommendations for people with and without diabetes. In the committee’s experience, many people with diabetes and CKD are frail, or are taking a lot of medicines, so they made a recommendation to address this.
People without diabetes
The evidence showed that, compared with placebo, ACE inhibitors reduced the risk of end-stage renal disease in people without diabetes. ARBs did not show the same effect. However, the committee did not believe the evidence was sufficiently robust to show that ACE inhibitors were better than ARBs. In addition, for people with type 2 diabetes, ARBs did reduce the risk of end-stage renal disease and heart failure. Based on the limitations of the evidence and the evidence available for people with type 2 diabetes, the committee recommended both ACE inhibitors and ARBs.
People with type 2 diabetes
- reduction of proteinuria
- end-stage renal disease
- all-cause mortality
- cardiovascular mortality
- non-fatal cardiovascular events
- adverse events (hypotension)
- hospitalisation.
There was no evidence comparing ACE inhibitors with placebo in people with type 2 diabetes. The evidence for people without diabetes did show that ACE inhibitors reduced the risk of end-stage renal disease, compared with placebo. The committee used this evidence to make the recommendation for people with diabetes.
The recommendations reflect current practice, so no additional resources should be needed.
Recommendation 1.7.2
Why the committee made the recommendation
There was limited evidence showing that eGFR thresholds below 60 ml/min/1.73 m 2 could be used to identify anaemia as being due to CKD. The committee questioned the applicability of this evidence because the studies did not rule out other causes of anaemia (which is usually done in practice).
The limited evidence meant that the committee was unable to recommend specific thresholds or probabilities. Instead, they used the available evidence and their expertise to specify ranges of GFR indicating that anaemia is more or less likely to be caused by CKD.
When anaemia may have other causes (such as gastrointestinal bleeding and certain cancers), investigating further will increase the chance of the real cause being identified and treated.
- putting people through extensive and unnecessary investigations when their anaemia is caused by CKD
- missing the real cause of their anaemia by assuming it is caused by CKD.
The committee agreed that when eGFR is below 30 ml/min/1.73 m 2 , anaemia is more likely to be caused by CKD. However, healthcare professionals should still use their clinical judgement and think about people’s circumstances when deciding whether further assessment is needed.
Only 1 study included people with diabetes, and no studies included children and young people. However, the recommendations still apply to these populations, because other causes of anaemia would be ruled out before attributing the anaemia to CKD.
The committee noted a need for further research on the diagnostic test accuracy of different eGFR thresholds, particularly for eGFR thresholds of 30 and 60 ml/min/1.73 m 2 . They highlighted that in clinical practice, an eGFR threshold of 45 ml/min/1.73 m 2 can also trigger investigation into anaemia due to CKD, but limited evidence was identified for the diagnostic accuracy of this threshold. The committee made a recommendation for research on the diagnostic accuracy of these specific eGFR thresholds for determining the likelihood of anaemia being CKD related. (See other recommendations for research .)
These recommendations should not increase the cost to primary care, because they reflect current practice and act as cautions for healthcare professionals to explore the cause of anaemia. They may reduce costs by ensuring that the correct cause of anaemia is identified more quickly with appropriate investigations.
Recommendation 1.9.11
In the 2015 guideline, an aspirational Hb range between 100 and 120 g/litre was recommended for adults, young people and children aged 2 years and over. For children under 2 years, the Hb range was between 95 and 115 g/litre. These were based on evidence for adults. In 2020, the committee reviewed the evidence specifically for children and young people. The only evidence for this population came from a single small low-quality study, comparing the effects of a high and low Hb target on left ventricular mass index. No difference in effect was found. Given the lack of evidence, the committee agreed that the recommendations made in 2015 should not be changed.
The 2015 guideline recommended using the same target Hb range as adults for children and young people over 2 years, and a slightly lower level in children under 2. However, children and young people have different coagulation risks than adults, and are more prone to reductions in Hb from blood loss in haemodialysis circuits. In practice, higher Hb targets (up to 130 g/litre) are often used for children and young people. Because of the lack of evidence in this age group, the committee agreed that research is needed to inform future guidance (see recommendation for research 4 ).
Recommendation 1.9.18
For people with stage 5 CKD who are on in-centre haemodialysis, the evidence showed that high-dose intravenous iron was better than a low-dose regimen at increasing levels of serum ferritin and haemoglobin as well as increasing the haematocrit. The committee agreed that the type of intravenous iron was not relevant and that there was no reason to recommend a specific preparation. They also highlighted that there are differences between iron preparations that affect their bioequivalence. Therefore, pharmacist advice is likely to be needed when choosing iron preparations. An example regimen for adults using iron sucrose was taken from the evidence to help guide practice. Ultimately, the choice of preparation should be based on local availability and policies. The committee agreed that children and young people should be given a high dose as set out in the BNFc, although they noted that use of intravenous iron preparations in children under 14 years was off label.
The committee was aware of a MHRA alert on intravenous iron and serious hypersensitivity reactions . The alert states that ‘intravenous iron products should only be administered when staff trained to evaluate and manage anaphylactic or anaphylactoid reactions – as well as resuscitation facilities – are immediately available.’ The committee agreed that intravenous iron should not be administered at home but recognised that this has a significant impact on people on home dialysis.
Most of the evidence was from studies with participants on haemodialysis. The committee agreed that more research would help to inform future guidance on intravenous iron for people with stage 5 CKD who are on peritoneal dialysis.
The recommendations are unlikely to lead to a substantial change in costs, as intravenous iron is relatively inexpensive, and there was evidence found in adults that use of high-dose iron leads to lower doses of erythropoiesis-stimulating agents being used, thereby offsetting any extra costs.
Hyperphosphataemia in people with CKD stage 4 or 5
Recommendations 1.11.5 to 1.11.18
There was a significant amount of evidence (of varying quality) for adults with stage 5 CKD who are having dialysis. However, evidence was limited for adults not on dialysis, and for children and young people. The committee agreed to extrapolate from the evidence for adults with stage 5 CKD on dialysis, so they could make recommendations for the other groups.
People’s preferences need to be taken into account when offering phosphate binders, because this could have an impact on adherence. The differences in phosphate binder formulations (for example, chewable and non-chewable) and the effect this has on how they are taken (before, with or after food) mean that people will often prefer one phosphate binder over the others. Oral phosphate binders are also unpleasant to take, and this might affect adherence as well. It is important to involve people in the choice of phosphate binder as far as possible, to ensure they are prescribed one they are happy with and can take as recommended.
The committee highlighted several factors that renal physicians assess at clinical reviews for people who are taking phosphate binders (including parathyroid hormone, vitamin D and serum calcium).
Which phosphate binders to use for children and young people
The committee reviewed the recommendations from the 2013 guideline in the light of limited new evidence. For children and young people with high serum calcium, they agreed to recommend sevelamer carbonate instead of sevelamer hydrochloride. This is because sevelamer carbonate offers a better balance of benefits and costs. The committee highlighted that in growing children and young people, calcium is often maintained close to, but not above the upper limit of the age-related reference range. Calcium is essential for bone development in children.
Which phosphate binders to use for adults
The committee reviewed the evidence for phosphate binders both in adults on dialysis and adults not having dialysis. Although the evidence for those not on dialysis was limited, it did reflect the evidence for adults on dialysis in every area apart from sucroferric oxyhydroxide. As there was no evidence on sucroferric oxyhydroxide in adults not on dialysis, the committee did not recommend it for this group.
- calcium acetate as a first-line treatment provides the best balance of benefits, harms and costs
- calcium carbonate is cheaper than calcium acetate, but is more likely to cause high serum calcium levels and associated adverse outcomes
- sevelamer carbonate and sevelamer hydrochloride are more expensive than calcium acetate, and do not provide enough benefit as a first-line treatment to justify the extra expense
- when people have high serum calcium levels and cannot take calcium acetate, sevelamer carbonate is the best alternative; it is cheaper than sevelamer hydrochloride, and provides similar benefits, however, it still costs more than calcium acetate and, for first-line treatment, it does not provide enough benefit to justify this extra expense
- sucroferric oxyhydroxide is not cost effective as a first-line treatment, but is a reasonable choice for people who cannot take calcium acetate or sevelamer carbonate
- lanthanum carbonate is much more expensive than calcium acetate and sevelamer carbonate and may provide less benefit than other non-calcium-based phosphate binders.
Based on this evidence, the committee recommended a treatment sequence and alternatives for different situations.
The committee also agreed that diet and dialysis (when appropriate) had a large impact on serum phosphate levels. Therefore, before offering phosphate binders it is important to provide dietary advice and ensure people are on the dialysis regime that works best for them.
The committee made recommendation for research 5 to address the lack of evidence in adults not on dialysis.
Replacing sevelamer hydrochloride with sevelamer carbonate may result in lower resource use, because there is a cheap generic version of sevelamer carbonate available.
There is currently variation across the UK in use of sucroferric oxyhydroxide. The recommendation on this phosphate binder may increase costs. However, this increase is unlikely to be substantial, because sucroferric oxyhydroxide is only recommended as a third-line option.
Chronic kidney disease (CKD) describes abnormal kidney function or structure. It is common and often occurs with other conditions (such as cardiovascular disease and diabetes). Moderate to severe CKD is also associated with an increased risk of acute kidney injury, falls, frailty and mortality. The risk of developing CKD increases with age.
CKD is usually asymptomatic, but it is detectable, and tests for CKD are simple and available. There is evidence that treatment can prevent or delay the progression of CKD, reduce or prevent the development of complications, and reduce the risk of cardiovascular disease. However, CKD is often unrecognised or diagnosed at an advanced stage. Late presentation of people with kidney failure increases morbidity, mortality and associated healthcare costs.
As kidney disease progresses, some coexisting conditions become more common and increase in severity. Hyperphosphataemia is an example of this, occurring because of insufficient filtering of phosphate from the blood by poorly functioning kidneys. This means that a certain amount of the phosphate does not leave the body in the urine, instead remaining in the blood at abnormally high levels.
High serum phosphate levels can directly and indirectly increase parathyroid hormone secretion, leading to the development of secondary hyperparathyroidism. Left untreated, secondary hyperparathyroidism increases morbidity and mortality and may lead to renal bone disease, with people experiencing bone and muscular pain, fracture, bone and joint abnormalities, and vascular and soft tissue calcification.
Many people with CKD or established renal failure also develop associated anaemia. The prevalence of anaemia associated with CKD increases progressively with the stage of CKD, especially when the person reaches stage 4 or 5. Anaemia of CKD contributes significantly to the burden of CKD. However, it is potentially reversible and manageable with appropriate identification and treatment.
The Health Survey for England (2016) found that 13% of adults (16 years and over) had any CKD (stages 1 to 5). The prevalence of stages 3 to 5 was 5% for all adults, rising to 34% in people aged 75 and over. At the end of 2018 there were 826 children and young people and 66,612 adults receiving renal replacement therapy in the UK according to the UK Renal Registry annual report .
- investigations for CKD
- classification of CKD
- frequency of monitoring for CKD
- blood pressure control for people with CKD
- phosphate binders to manage mineral and bone disorder in CKD
- glomerular filtration rate for diagnosing anaemia associated with CKD
- intravenous iron for treating anaemia associated with CKD.
- Finding more information and committee details
You can see everything NICE says on this topic in the NICE Pathway on chronic kidney disease .
To find NICE guidance on related topics, including guidance in development, see the NICE webpage on chronic kidney disease .
For full details of the evidence and the guideline committee’s discussions, see the evidence reviews . You can also find information about how the guideline was developed , including details of the committee .
NICE has produced tools and resources to help you put this guideline into practice . For general help and advice on putting our guidelines into practice, see resources to help you put NICE guidance into practice .
- Update information
November 2021 : We reviewed the evidence on SGLT2 inhibitors for adults with type 2 diabetes and chronic kidney disease. We made new recommendations, and removed the original recommendation 1.6.7 from this guideline. See the new recommendations on chronic kidney disease in the NICE guideline on type 2 diabetes in adults . We also clarified the use of the term ‘male’ in the 4-variable Kidney Failure Risk Equation .
August 2021 : This guideline is an update of NICE guideline CG182 (published July 2014), NICE guideline CG157 (published March 2013) and NICE guideline NG8 (published June 2015) and will replace them.
We have reviewed the evidence and made new recommendations on the assessment and management of CKD, management of hyperphosphataemia in people with CKD and the management of anaemia for people with CKD. These recommendations are marked [2021] .
- We have updated some wording to bring the language and style up to date, without changing the meaning.
- We have updated some recommendations to bring them in line with current terminology and practice.
- We have combined, clarified or reworded some recommendations to make them clearer and to improve ease of reading.
In recommendations ending [2006] , [2006, amended 2011] , [2006, amended 2015] , [2008] , [2008, amended 2014] , or [2014] , we have not reviewed the evidence. In some cases minor changes have been made – for example, to update links, or bring the language and style up to date – without changing the intent of the recommendation.
Your responsibility : The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals and practitioners are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or the people using their service. It is not mandatory to apply the recommendations, and the guideline does not override the responsibility to make decisions appropriate to the circumstances of the individual, in consultation with them and their families and carers or guardian.
Local commissioners and providers of healthcare have a responsibility to enable the guideline to be applied when individual professionals and people using services wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Nothing in this guideline should be interpreted in a way that would be inconsistent with complying with those duties.
Commissioners and providers have a responsibility to promote an environmentally sustainable health and care system and should assess and reduce the environmental impact of implementing NICE recommendations wherever possible.
Created: August 25, 2021; Last Update: November 24, 2021.
- Cite this Page Chronic kidney disease: assessment and management. London: National Institute for Health and Care Excellence (NICE); 2021 Nov 24. (NICE Guideline, No. 203.)
- PDF version of this title (354K)
In this Page
Other titles in this collection.
- National Institute for Health and Care Excellence: Guidelines
Related NICE guidance and evidence
- NICE Guideline 8: Anaemia Management in Chronic Kidney Disease: Partial Update 2015
- NICE Clinical Guideline 182: Chronic kidney disease in adults: assessment and management
- NICE Clinical Guideline 157: Hyperphosphataemia in Chronic Kidney Disease: Management of Hyperphosphataemia in Patients with Stage 4 or 5 Chronic Kidney Disease
- Evidence reviews for the diagnostic accuracy of eGFR calculations in adults, children, and young people from black, Asian and other minority ethnic groups with CKD: Chronic kidney disease: Evidence review A
- Evidence review for the accuracy of albumin: creatinine ratio versus protein creatinine ratio measurements to quantify proteinuria in children and young people with CKD: Chronic kidney disease: Evidence review B
- Evidence reviews for accuracy of reagent strips for detecting protein and blood in urine in children and young people with CKD: Chronic kidney disease: Evidence review C
- Evidence reviews for children and young people who should be tested for CKD: Chronic kidney disease: Evidence review D
- Evidence review for optimal monitoring frequency: Chronic kidney disease: Evidence review E
- Evidence review for the best combination of measures to identify increased risk of progression in adults, children and young people: Chronic kidney disease: Evidence review F
- Evidence review for optimal blood pressure targets for adults, children and young people with CKD: Chronic kidney disease: Evidence review G
- Evidence reviews for interventions to lower proteinuria: Chronic kidney disease: Evidence review H
- Evidence reviews for eGFR threshold for the investigation of anaemia due to chronic kidney disease: Chronic kidney disease: Evidence review I
- Evidence reviews for aspirational haemoglobin target range for children and young people with CKD: Chronic kidney disease: Evidence review J
- Evidence reviews for managing anaemia with IV iron in people with GFR category G5 who are on dialysis: Chronic kidney disease: Evidence review K
- Evidence reviews for the use of phosphate binders: Chronic kidney disease: Evidence review L
- Evidence reviews for cystatin C based equations to estimate GFR in adults, children and young people: Chronic kidney disease: Evidence review M
- Evidence review for defining clinically significant decline in eGFR in terms of risk of kidney disease progression: Chronic kidney disease: Evidence review N
- 2021 exceptional surveillance of chronic kidney disease (NICE guideline NG203)
- 2021 exceptional surveillance of HIV indicator conditions (NICE guidelines NG52, CG153, NG122 and NG203)
Supplemental NICE documents
- NICE Pathway: Chronic kidney disease overview (PDF)
- NICE Pathway: Acute kidney injury overview (PDF)
- NICE Quality Standard QS5: Chronic kidney disease in adults (PDF)
Related information
- NLM Catalog Related NLM Catalog Entries
Similar articles in PubMed
- Review Chronic kidney disease in adults: assessment and management [ 2015] Review Chronic kidney disease in adults: assessment and management . 2015 Jan
- Review Hypertension in adults: diagnosis and management [ 2023] Review Hypertension in adults: diagnosis and management . 2023 Nov 21
- Review Chronic obstructive pulmonary disease in over 16s: diagnosis and management [ 2019] Review Chronic obstructive pulmonary disease in over 16s: diagnosis and management . 2019 Jul
- Review COVID-19 rapid guideline: chronic kidney disease [ 2020] Review COVID-19 rapid guideline: chronic kidney disease . 2020 May 15
- Review Chronic pain (primary and secondary) in over 16s: assessment of all chronic pain and management of chronic primary pain [ 2021] Review Chronic pain (primary and secondary) in over 16s: assessment of all chronic pain and management of chronic primary pain . 2021 Apr 7
Recent Activity
- Chronic kidney disease: assessment and management Chronic kidney disease: assessment and management
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Kidney: Structure, Function and Related Diseases
The structure of human kidney can be seen as two reddish bean-shaped organs that are located below the rib cage on each side of the spine. They are almost a fistful in size, measuring around 10-12cm. Kidneys are the main organs in the human excretory system, which takes part in the filtration of the blood before the urine is formed. Let us look at the structure of the organ for a better understanding.
External and Internal Features of Kidney
- It has a convex and concave border.
- Towards the inner concave side, a notch called the hilum is present through which the renal artery enters the kidney and the renal vein and ureter leave.
- The outer layer of the kidney is a tough capsule.
- On the inside, the kidney is divided into an outer renal cortex and an inner renal medulla.
- The hilum extends inside the kidney into a funnel-like space called the renal pelvis.
- The renal pelvis has projections called calyces(sing: calyx).
- The medulla is divided into medullary pyramids, which project into the calyces.
- Between the medullary pyramids, the cortex extends as renal columns called Columns of Bertini.
- The kidney is made up of millions of smaller units called nephrons which are also the functional units.
Read: Nephrons
A simple structure of kidney can be understood by the following diagram:
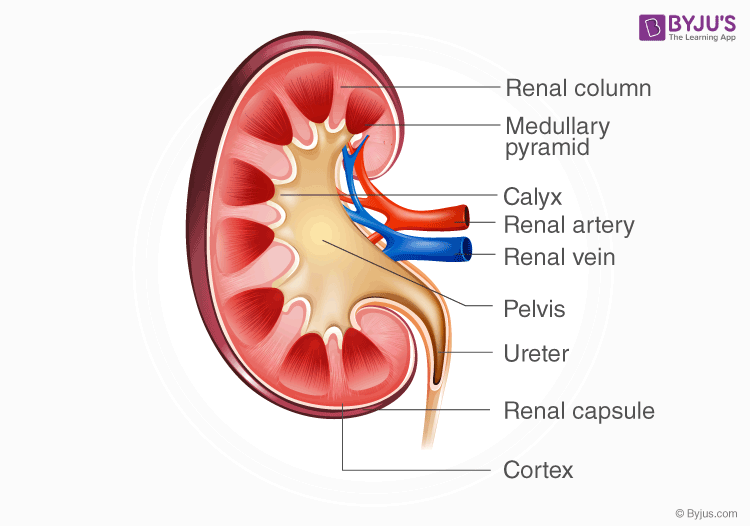
- The most important function of the kidney is to filter the blood for urine formation.
- It excretes metabolic wastes like urea and uric into the urine.
- Erythropoietin: It is released in response to hypoxia
- Renin: It controls blood pressure by regulation of angiotensin and aldosterone
- Calcitriol: It helps in the absorption of calcium in the intestines
- It maintains the acid-base balance of the body by reabsorbing bicarbonate from urine and excreting hydrogen ions and acid ions into the urine.
- It also maintains the water and salt levels of the body by working together with the pituitary gland .
Read: Urine Formation
Diseases related to Kidneys
In uremia, the kidneys are damaged, and there is a buildup of urea and other toxins in the blood, which is fatal and can cause kidney failure. Patients may experience fatigue, itching, muscle twitching, and loss of mental concentration. The urea can be removed by the process of hemodialysis.
2. Renal Calculi
Commonly called kidney stones, these are deposits of salt and minerals in our body. Symptoms include severe abdominal pain and nausea. The stones can be dissolved with medicines, or it passes with urine by improving diet and water intake.
3. Glomerulonephritis
It is the inflammation of the glomerulus. Symptoms include pink urine, oedema or swelling on the face and high blood pressure. It requires medical attention for prevention.
Note: Any person with high blood pressure and diabetes is more prone to kidney related diseases.
Explore BYJU’S Biology to learn more.
- Facts about Kidneys
- Regulation Of Kidney Function
- Kidney Function Test
- Kidney Failure Symptoms
- Difference Between Left and Right Kidney
What are the first signs of kidney problems?
You can see blood in your urine and it is also foamy. You will have a problem concentrating on things and will face swelling and dryness on your skin.
Can you live without a kidney?
It is not possible to live without a kidney. But since we have two of them, it is possible to survive with one kidney.
What causes kidney problems?
People with diseases like diabetes and high blood pressure have a high chance of developing kidney problems.
Leave a Comment Cancel reply
Your Mobile number and Email id will not be published. Required fields are marked *
Request OTP on Voice Call
Post My Comment
Thanking you Team Biju’s for this knowledge free of cost 😊
- Share Share
Register with BYJU'S & Download Free PDFs
Register with byju's & watch live videos.

Chronic Renal Failure
Learn about the nursing care management of patients with chronic renal failure in this nursing study guide .
Table of Contents
- What is Chronic Renal Failure?
Pathophysiology
Clinical manifestations, complications, assessment and diagnostic findings, medical management, nursing assessment, planning & goals, nursing priorities, nursing interventions, discharge and home care guidelines, documentation guidelines.
- Practice Quiz: Chronic Renal Failure
What is Chronic Renal Failure?
When the patient has sustained enough kidney damage to require renal replacement therapy on a permanent basis, the patient has moved into the fifth or final stage of CKD, also referred to as chronic renal failure.
- Chronic renal failure (CRF) is the end result of a gradual, progressive loss of kidney function.
- Causes include chronic infections ( glomerulonephritis , pyelonephritis ), vascular diseases ( hypertension , nephrosclerosis), obstructive processes (renal calculi), collagen diseases (systemic lupus ), nephrotoxic agents (drugs, such as aminoglycosides ), and endocrine diseases ( diabetes , hyperparathyroidism).
- This syndrome is generally progressive and produces major changes in all body systems.
- The final stage of renal dysfunction, end-stage renal disease (ESRD), is demonstrated by a glomerular filtration rate (GFR) of 15%–20% of normal or less.
- Renal failure results when the kidneys cannot remove the body’s metabolic wastes or perform their regulatory functions.
- The substances normally eliminated in the urine accumulate in the body fluids as a result of impaired renal excretion, affecting endocrine and metabolic functions as well as fluid, electrolyte, and acid-base disturbances.
- Renal failure is a systemic disease and is a final common pathway of many different kidney and urinary tract diseases.
- Accumulation. As renal function declines, the end products of protein metabolism (normally excreted in urine) accumulate in the blood .
- Adverse effects. Uremia develops and adversely affects every system in the body.
- Progression. The disease tends to progress more rapidly in patients who excrete significant amounts of protein or have elevated blood pressure than those without these conditions
There are many diseases that cause chronic renal disease; each has its own pathophysiology. However, there are common mechanisms for disease progression.
- Pathologic features include fibrosis, loss of renal cells, and infiltration of renal tissue by monocytes and macrophages .
- Proteinuria , hypoxia, and extensive angiotensin II production all contribute to the pathophysiology. In an attempt to maintain GFR, the glomerular hyperfiltration; this results in endothelial injury .
- Proteinuria results from increased glomerular permeability and increased capillary pressure.
- Hypoxia also contributes to disease progression. Angiotensin II increases glomerular hypertension , which further damages the kidney.
Predisposing Factors
- Diabetes , which is the most common risk factor for chronic kidney failure in the United States
- Age 60 or older
- Kidney disease present at birth (congenital)
- Family history of kidney disease
- Autoimmune Disorder (Lupus erythematosus)
- Bladder outlet obstruction (BPH and Prostatitis)
- Race (Sickle cell disease)
Precipitating Factors
- Occupational Hazard (overexposure to toxins and to some medications)
- Sedentary Lifestyle ( hypertension , atherosclerosis )
- Diet (High residue diet)
Schematic Diagram
Here’s a schematic diagram or concept map for Chronic Kidney Disease:
- Chronic Kidney Disease Pathophysiology and Schematic Diagram (via Scribd)
Because virtually every body system is affected in ESRD, patients exhibit a number of signs and symptoms.
- Peripheral neuropathy. Peripheral neuropathy, a disorder of the peripheral nervous system , is present in some patients.
- Severe pain . Patients complain of severe pain and discomfort.
- Restless leg syndrome. Restless leg syndrome and burning feet can occur in the early stage of uremic peripheral neuropathy.
Potential complications of chronic renal failure that concern the nurse and necessitate a collaborative approach to care include the following:
- Hyperkalemia. Hyperkalemia due to decreased excretion, metabolic acidosis, catabolism, and excessive intake (diet, medications, fluids).
- Pericarditis. Pericarditis due to retention of uremic waste products and inadequate dialysis.
- Hypertension. Hypertension due to sodium and water retention and the malfunction of the renin-angiotensin-aldosterone system.
- Anemia . Anemia due to decreased erythropoietin production decreased RBC lifespan, bleeding in the GI tract from irritating toxins and ulcer formation, and blood loss during hemodialysis.
- Bone disease. Bone disease and metastatic and vascular calcifications due to retention of phosphorus, low serum calcium levels, abnormal vitamin D metabolism, and elevated aluminum levels.
Laboratory studies required to establish the diagnosis of CRF include:
- Glomerular filtration rate . GFR and creatinine clearance decrease while serum creatinine (more sensitive indicator of renal function) and BUN levels increase.
- Sodium and water retention. Some patients retain sodium and water, increasing the risk for edema, heart failure , and hypertension.
- Acidosis. Metabolic acidosis occurs in ESRD because the kidneys are unable to excrete increased loads of acid.
- Anemia. In ESRD, erythropoietin production decreases and profound anemia results, producing fatigue, angina , and shortness of breath .
- Volume: Usually less than 400 mL/24 hr (oliguria) or urine is absent (anuria).
- Color: Abnormally cloudy urine may be caused by pus, bacteria, fat, colloidal particles, phosphates, or urates. Dirty, brown sediment indicates presence of RBCs, hemoglobin, myoglobin, porphyrins.
- Specific gravity: Less than 1.015 (fixed at 1.010 reflects severe renal damage).
- Osmolality: Less than 350 mOsm/kg is indicative of tubular damage, and urine/serum ratio is often 1:1.
- Creatinine clearance: May be significantly decreased (less than 80 mL/min in early failure; less than 10 mL/min in ESRD).
- Sodium: More than 40 mEq/L because the kidney is not able to reabsorb sodium.
- Protein: High-grade proteinuria (3–4+) strongly indicates glomerular damage when RBCs and casts are also present.
- BUN/Cr: Elevated, usually in proportion. A creatinine level of 12 mg/dL suggests ESRD. A BUN of >25 mg/dL is indicative of renal damage.
- CBC: Hb decreased because of anemia, usually less than 7–8 g/dL.
- RBCs: Life span decreased because of erythropoietin deficiency, and azotemia.
- ABGs : pH decreased. Metabolic acidosis (less than 7.2) occurs because of the loss of renal ability to excrete hydrogen and ammonia or end products of protein catabolism. Bicarbonate and PCO2 Decreased.
- Serum sodium: May be low (if the kidney “wastes sodium”) or normal (reflecting the dilutional state of hypernatremia ).
- Potassium : Elevated related to retention and cellular shifts (acidosis) or tissue release (RBC hemolysis). In ESRD, ECG changes may not occur until potassium is 6.5 mEq or higher. Potassium may also be decreased if the patient is on potassium-wasting diuretics or when the patient is receiving dialysis treatment.
- Magnesium, phosphorus: Elevated.
- Calcium/phosphorus: Decreased.
- Proteins (especially albumin): Decreased serum level may reflect protein loss via urine, fluid shifts, decreased intake, or decreased synthesis because of a lack of essential amino acids.
- Serum osmolality: Higher than 285 mOsm/kg; often equal to urine.
- KUB x-rays: Demonstrates size of kidneys/ureters/bladder and presence of obstruction (stones).
- Retrograde pyelogram: Outlines abnormalities of the renal pelvis and ureters.
- Renal arteriogram: Assesses renal circulation and identifies extravascularities, and masses.
- Voiding cystourethrogram: Shows bladder size, reflux into ureters, and retention.
- Renal ultrasound: Determines kidney size and presence of masses, cysts, and obstruction in the upper urinary tract.
- Renal biopsy : May be done endoscopically to examine tissue cells for histological diagnosis.
- Renal endoscopy, nephroscopy: Done to examine renal pelvis; flush out calculi, and hematuria; and remove selected tumors.
- ECG : This may be abnormal, reflecting electrolyte and acid-base imbalances.
- X-rays of feet, skull , spinal column, and hands: May reveal demineralization/calcifications resulting from electrolyte shifts associated with CRF.
The goal of management is to maintain kidney function and homeostasis for as long as possible.
- Calcium and phosphorus binders treat hyperphosphatemia and hypocalcemia ;
- Antihypertensive and cardiovascular agents ( digoxin and dobutamine ) manage hypertension;
- Anti- seizure agents (IV diazepam or phenytoin ) are used for seizures, and;
- Erythropoietin (Epogen) is used to treat anemia-associated ESRD.
- Nutritional therapy. Dietary intervention includes careful regulation of protein intake, fluid intake to balance fluid losses, sodium intake to balance sodium losses, and some restriction of potassium.
- Dialysis. Dialysis is usually initiated if the patient cannot maintain a reasonable lifestyle with conservative treatment.
Nursing Management
The patient with ESRD requires astute nursing care to avoid the complications of reduced renal function and the stresses and anxieties of dealing with a life-threatening illness.
Assessment of a patient with ESRD includes the following:
- Assess fluid status (daily weight, intake and output , skin turgor , distention of neck veins, vital signs, and respiratory effort).
- Assess nutritional dietary patterns (diet history, food preference, and calorie counts).
- Assess nutritional status (weight changes, laboratory values).
- Assess understanding of the cause of renal failure, its consequences, and its treatment.
- Assess patient’s and family’s responses and reactions to illness and treatment.
- Assess for signs of hyperkalemia.
Based on the assessment data, the following nursing diagnoses for a patient with chronic renal failure were developed:
- Excess fluid volume related to decreased urine output, dietary excesses, and retention of sodium and water.
- Imbalanced nutrition less than body requirements related to anorexia , nausea , vomiting , dietary restrictions, and altered oral mucous membranes.
- Activity intolerance related to fatigue, anemia, retention of waste products, and dialysis procedure.
- Risk for situational low self-esteem related to dependency, role changes, changes in body image , and changes in sexual function.
Main Article: 6 Chronic Renal Failure Nursing Care Plans
The goals for a patient with chronic renal failure include:
- Maintenance of ideal body weight without excess fluid.
- Maintenance of adequate nutritional intake.
- Participation in activity within tolerance.
- Improve self-esteem.
- Maintain homeostasis.
- Prevent complications.
- Provide information about disease process/prognosis and treatment needs.
- Support adjustment to lifestyle changes.
Nursing care is directed toward the following:
- Fluid status. Assess fluid status and identify potential sources of imbalance.
- Nutritional intake. Implement a dietary program to ensure proper nutritional intake within the limits of the treatment regimen.
- Independence. Promote positive feelings by encouraging increased self-care and greater independence.
- Protein. Promote intake of high–biologic–value protein foods: eggs, dairy products, and meats.
- Medications. Alter the schedule of medications so that they are not given immediately before meals.
- Rest. Encourage alternating activity with rest.
A successful nursing care plan has achieved the following:
- Maintained ideal body weight without excess fluid.
- Maintained adequate nutritional intake.
- Participated in activity within tolerance.
- Improved self-esteem.
The nurse should promote home and self-care to increase the esteem of the patient.
- Vascular access care. The patient should be taught how to check the vascular access device for patency and appropriate precautions, such as avoiding venipuncture and blood pressure measurements on the arm with the access device.
- Problems to report. The patient and the family need to know what problems to report: nausea, vomiting, change in usual urine output, ammonia odor on breath, muscle weakness , diarrhea , abdominal cramps, clotted fistula or graft, and signs of infection .
- Follow-up. The importance of follow-up examinations and treatment is stressed to the patient and family because of changing physical status, renal function, and dialysis requirements.
- Home care referral. Referral for home care gives the nurse an opportunity to assess the patient’s environment and emotional status and the coping strategies used by the patient and family.
The documentation of a patient with chronic renal failure should focus on the following:
- Existing conditions contribute to and degree of fluid retention.
- I&O and fluid balance .
- Results of laboratory tests.
- Caloric intake.
- Individual cultural or religious restrictions and personal preferences.
- Level of activity.
- Plan of care.
- Teaching plan.
- Response to interventions, teaching, and actions performed.
- Attainment or progress toward desired outcomes.
- Modifications to plan of care.
- Long-term needs.
Practice Quiz: Chronic Renal Failure
Here’s a 5-item practice quiz for this Chronic Renal Failure Study Guide. Please visit our nursing test bank for more NCLEX practice questions .
1. A major sensitive indicator of kidney disease is:
A. BUN level. B. Creatinine clearance level. C. Serum potassium level. D. Uric acid level.
2. Significant nursing assessment data relevant to renal function should include information about:
A. Any voiding disorders. B. The patient’s occupation. C. The presence of hypertension or diabetes . D. All of the above.
3. Decreased levels of erythropoietin, a substance normally secreted by the kidneys, leads to which serious complication of chronic renal failure?
A. Anemia. B. Acidosis. C. Hyperkalemia. D. Pericarditis.
4. Dietary intervention for renal deterioration includes limiting the intake of:
A. Fluid. B. Protein. C. Sodium and potassium. D. All of the above.
5. In chronic renal failure (end-stage renal disease), decreased glomerular filtration leads to:
A. Increased pH. B. Decreased creatinine clearance. C. Increased BUN. D. All of the above.
Answers and Rationale
1. Answer: B. Creatinine clearance level.
- B: Creatinine clearance is a major sensitive indicator of kidney disease.
- A: BUN level could also detect kidney disease but it is not as sensitive as creatinine clearance.
- C: Serum potassium level may indicate presence of kidney disease.
- D: Uric acid level may indicate presence of kidney disease.
2. Answer: D. All of the above.
- D: All of the answers listed above are relevant data to renal function.
- A: Voiding disorders are signs of impending or presence of kidney disease.
- B: The patient’s occupation could predispose him or her to kidney disease.
- C: The presence of hypertension or diabetes could predispose the patient to kidney disease.
3. Answer: A. Anemia.
- A: Anemia due to decreased erythropoietin production could occur in patients with chronic renal failure.
- B: Metabolic acidosis occurs in ESRD because the kidneys are unable to excrete increased loads of acid.
- C: Hyperkalemia occurs due to decreased excretion, metabolic acidosis, catabolism, and excessive intake (diet, medications, fluids).
- D: Pericarditis occurs due to retention of uremic waste products and inadequate dialysis.
4. Answer: D. All of the above.
- D: All of those mentioned above should be restricted in patients with chronic renal failure.
- A: Fluid should be restricted because the patient may result to excess fluid volume.
- B: Protein is restricted because its end products may accumulate in the blood stream.
- C: Sodium and potassium is restricted because they can aggravate the disease.
5. Answer: D. All of the above.
- D: The abovementioned laboratory results occur in patients with decreased GFR.
- A: Increased pH occurs due to decreased GFR.
- B: Decreased creatinine clearance occurs due to decreased GFR.
- C: Increased BUN occurs due to decreased GFR.
Posts related to Chronic Renal Failure:
- 6 Chronic Renal Failure Nursing Care Plans
- 6 Acute Renal Failure Nursing Care Plans
- Renal Disorders Nursing Management NCLEX Practice Quiz 1 (50 Items)
- Renal Disorders Nursing Management NCLEX Practice Quiz 2 (60 Items)
- Renal Disorders Nursing Management NCLEX Practice Quiz 3 (45 Items)
5 thoughts on “Chronic Renal Failure”
The website is very educative.
So helpful, educational and analyzing those can easily picture out how the disease damage physiologically! Thank you so much!
So educative and very much helpful. clearly summarized. Thanks a lot.
Easy to understand and educative.
Love this site! On question #5 in the quiz, shouldn’t choice A read “decreased Ph” since metabolic acidosis would be a lower number on the Ph scale?
Leave a Comment Cancel reply
Kidney in Detail
The aim of this lecture is to present on Kidney in Detail. The kidneys are two bean-shaped organs that extract waste from blood, balance body fluids, form urine, and aid in other important functions of the body. This lecture briefly present various important parts of kidney. Nephron: structure in the kidney that acts as a microscopic filtration unit; Glomerulus: dense mass of very fine blood capillaries at the nephron that act as a filter; and Glomerular filtrate: liquid removed from the blood by filtration in the kidney.
Lecture on Symbiosis and Homeostasis
Risks of using drugs, infectious diseases, 9am.health launches with $3.7m to tackle virtual diabetes care, significance of paper shredding services, exercise addiction, job application for the post of training officer, electrostatic precipitator (esp), analysis of sme loans in bbl, latest post, power optimizer – a dc to dc converter technology, dc-to-dc converter, coal train pollution exacerbates health risks and inequities, archaeological research demonstrates that humans can boost biodiversity, new uv broadband spectrometer transforms air pollutant analysis, atmospheric circulation.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
April 30, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
reputable news agency
Survival gains seen with assignment to experimental group in cancer trials
by Elana Gotkine

For patients with solid tumors, assignment to an experimental group in trials of investigational drugs yields significant survival gains, according to a review published online April 30 in the Annuals of Internal Medicine .
Renata Iskander, from McGill University in Montreal, and colleagues estimated progression-free survival and overall survival advantage of assignment to experimental groups in randomized trials of investigational drugs for six solid tumors . A total of 128 trials with 141 comparisons of a new drug and comparator were included in the sample, with 47,050 patients.
The researchers found that the pooled hazard ratio was 0.80 for progression-free survival, indicating significant benefit for patients in experimental groups and corresponding to a median progression-free survival advantage of 1.25 months. For overall survival, the pooled hazard ratio was 0.92, corresponding to a 1.18-month increase in survival. The absolute risk for a serious adverse event was 29.56 percent for comparator group patients compared with a 7.40 percent increase in risk for patients in experimental groups .
"Our findings provide a reassuring picture of current practices in drug regulation and research and can also help inform decisions about patient referral to trials, research policy, and consent discussions," the authors write.
Copyright © 2024 HealthDay . All rights reserved.
Explore further
Feedback to editors

Researcher discusses mechanism behind a birth defect affecting brain size

Study indicates that cancer patients gain important benefits from genome-matched treatments

Machine learning tool identifies rare, undiagnosed immune disorders through patients' electronic health records
2 hours ago

New technique improves T cell-based immunotherapies for solid tumors

Unraveling the roles of non-coding DNA explains childhood cancer's resistance to chemotherapy
3 hours ago

Conscious memories of childhood maltreatment strongly associated with psychopathology

Study finds private equity expanding to mental health facilities

Organ transplant drug may slow Alzheimer's disease progression

A sum greater than its parts: Time-restricted eating and high-intensity exercise work together to improve health
4 hours ago

Experimental vaccine targets portions of the flu virus that don't change
Related stories.

AACR: Cadonilimab plus chemo beneficial for gastric adenocarcinoma
Apr 8, 2024

Adding dostarlimab improves progression-free survival in endometrial cancer
Apr 4, 2023

Progression-free survival increased with zanubrutinib in leukemia
Jan 3, 2023

Study: Pembrolizumab + chemo, trastuzumab beneficial in gastroesophageal cancer
Oct 25, 2023

Drug combo doesn't lengthen glioblastoma survival
Nov 17, 2017

Survival advantage seen for A+ADV in advanced Hodgkin lymphoma
Jul 14, 2022
Recommended for you

New mRNA cancer vaccine triggers fierce immune response to fight malignant brain tumor
7 hours ago

Research on how dietary choline travels through the blood-brain barrier reveals pathway for treating brain disorders

Father's gut microbes affect the next generation in mouse study
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
- Share full article
Advertisement
Supported by
Walnuts Recalled From Natural Food Stores After E. Coli Outbreak
The outbreak linked to shelled organic walnuts distributed by Gibson Farms has sickened 12 people and hospitalized seven in California and Washington State, federal officials said.

By Johnny Diaz
A California company is recalling organic walnuts that were sold at natural food stores and coop retailers in 19 states because of an E. coli outbreak that has sickened 12 people and hospitalized seven, federal officials said.
Gibson Farms, the company based in Hollister, Calif., is voluntarily recalling its shelled walnuts branded as Organic Light Halves and Pieces after discovering that the nuts could carry the E. coli strain 0157: H7 that “causes a diarrheal illness often with bloody stools,” the Food and Drug Administration said in a notice on Tuesday .
The recall came after the Centers for Disease Control and Prevention notified the company of 12 recorded illnesses that were linked to the walnuts. They were distributed at more than 300 food retailers, including Whole Foods Market, New Seasons Market and Rosauers Supermarkets, the F.D.A. said.
An investigation is underway to determine the potential source of the contamination, the F.D.A. said. The company did not immediately respond to inquiries on Wednesday.
E. coli symptoms can vary from person to person and may include cramping, diarrhea or gastrointestinal distress. Other common symptoms include vomiting and fever. People begin to feel symptoms three to four days after ingesting food or drinks containing the E. coli bacteria, according to the C.D.C.
A Whole Foods spokesman said the recalled walnuts were shipped to 10 of their Whole Foods Market stores across Arkansas, Louisiana and Texas and used only as an ingredient in a salad offered on salad bars in those stores. The salad item was removed from the salad bars and the recalled walnuts were destroyed immediately, the spokesman said.
A spokesman for New Seasons Market said the grocery store chain “promptly removed the affected product” from its shelves, adding it also “placed signage in the relevant sections to alert consumers who may have bought it.”
This particular strain of E. coli is associated with a toxin called Shiga that can cause bloody diarrhea and “for a small number of people, can cause severe disease,” Dr. Richard Ellison, an epidemiologist at UMass Memorial Medical Center in Worcester, Mass., said on Wednesday.
Although most healthy adults would fully recover within a week, some people may develop a form of kidney failure called hemolytic uremic syndrome, which is most likely to occur in young children and older adults, the F.D.A. said in its notice.
Dr. Ellison said that about 90 percent of people will get better on their own without requiring antibiotics, and about 10 percent will develop the illness that can cause anemia and kidney damage.
“Generally, we recommend providing supportive care and keeping people well hydrated,” he added.
Consumers who have symptoms should contact their health care providers to receive care, the F.D.A. said.
So far, the people who were sickened in the outbreak have been in California and Washington State. No deaths have been reported.
The Organic Light Halves and Pieces were sold in bulk bins of 25-pound quantities, according to the F.D.A. The expiration dates for the affected product are between May 21, 2025, and June 7, 2025, the agency said.
A list of store locations where the walnuts were sold can be found on the F.D.A.’s website .
Consumers who bought the walnuts from bulk containers should check their pantries, refrigerators and freezers, and “not eat or use them,” the F.D.A. said. They should also “clean and sanitize surfaces” that came in contact with the product, the agency said.
Retailers that received the recalled products should discard the walnuts and sanitize bins before refilling them, the F.D.A. said.
Johnny Diaz is a general assignment reporter covering breaking news. He previously worked for the South Florida Sun Sentinel and The Boston Globe. More about Johnny Diaz
Food Safety Issues and How to Avoid Them
Norovirus: The virus, which leads to nausea and vomiting, is spreading and extremely contagious. Here’s what to know about norovirus , and how to protect yourself.
Salmonella: People often get sick with salmonellosis, the infection caused by the bacteria, after eating undercooked meat or other contaminated foods. Here is how to protect yourself .
Listeria: Most people who ingest listeria, bacteria naturally found in the soil, don’t get very sick, if they develop symptoms at all. But certain high-risk individuals can fall seriously ill .
Raw Milk: A growing number of states have allowed the sale of raw milk. Its proponents argue that it has several health benefits, but is it really safe ?
Expiration Dates: When is the right time to throw something out? J. Kenji López-Alt explains why many pantry items remain safe well past their expiration dates .
Washing Produce: To minimize the risk of food poisoning, you really do need to wash your fruit and vegetables before eating them. Luckily, no special produce washes are required .

IMAGES
VIDEO
COMMENTS
The kidneys have their anterior and posterior surfaces. The anterior surface faces towards the anterior abdominal wall, whereas the posterior surface is facing the posterior abdominal wall.These surfaces are separated by the edges of the kidney, which are the major convexity laterally, and minor concavity medially. The center of the minor concavity is marked as the hilum of the kidney where ...
The left kidney is located at about the T12 to L3 vertebrae, whereas the right is lower due to slight displacement by the liver. Upper portions of the kidneys are somewhat protected by the eleventh and twelfth ribs (Figure 25.7). Each kidney weighs about 125-175 g in males and 115-155 g in females.
Created by Raja Narayan.Watch the next lesson: https://www.khanacademy.org/test-prep/nclex-rn/rn-renal-system/rn-the-renal-system/v/glomerular-filtration-in-...
This Osmosis High-Yield Note provides an overview of Anatomy and Physiology of the Renal System essentials. All Osmosis Notes are clearly laid-out and contain striking images, tables, and diagrams to help visual learners understand complex topics quickly and efficiently. Find more information about Anatomy and Physiology of the Renal System:
Anatomy of the Urinary System. The urinary system consists of two kidneys, two ureters, a urinary bladder, and a urethra. The kidneys alone perform the functions just described and manufacture urine in the process, while the other organs of the urinary system provide temporary storage reservoirs for urine or serve as transportation channels to ...
Chronic kidney disease (CKD) is a common condition associated with significant amenable morbidity and mortality, primarily related to the substantially increased risk of cardiovascular disease (CVD) in this population. Early detection of people with CKD is important so that treatment can be initiated to prevent or delay kidney disease progression, reduce or prevent the development of ...
Part 1: Review of the Urinary System. 1. On the diagram below, label the following structures: inferior vena cava. descending thoracic aorta. external urethral orifice. internal urethral orifice. left adrenal gland. left kidney.
Diabetes. • Diabetes is the most common cause of kidney disease. • Diabetes is a chronic disease where the body cannot control sugar. A high sugar level in the blood damages the small filters (glomeruli) in the kidneys. • In people with diabetes, kidneys do not filter as well.
The urinary system consists of 4 major organs; the kidneys, ureters, urinary bladder and the urethra.Together these organs act to filter blood, remove waste products, create urine and transport urine out from the body. The urinary system is also called the excretory system, because held within the urine are the various excreted products, including by-products such as urea and uric acid, drugs ...
Blood that is about to be filtered enters a glomerulus, which is a tuft of blood capillaries (the smallest of blood vessels). The glomerulus is nestled inside a cup-like sac located at the end of each nephron, called a glomerular capsule. Glomerular capillaries have small pores in their walls, just like a very fine mesh sieve.
Chronic kidney disease is a condition that gradually damages your kidneys and affects their ability to filter waste and fluid from your blood. Learn about the symptoms, causes, risk factors and complications of this serious health problem, and how to prevent or delay its progression. Visit Mayo Clinic's website for more information and expert advice.
Overview. This guideline covers care and treatment for people with, or at risk of, chronic kidney disease (CKD). It aims to prevent or delay the progression, and reduce the risk of complications and cardiovascular disease. It also covers managing anaemia and hyperphosphataemia associated with CKD. NICE has produced a COVID-19 rapid guideline on ...
Diseases related to Kidneys. 1. Uremia. In uremia, the kidneys are damaged, and there is a buildup of urea and other toxins in the blood, which is fatal and can cause kidney failure. Patients may experience fatigue, itching, muscle twitching, and loss of mental concentration. The urea can be removed by the process of hemodialysis.
Kidney Lesson Plan. Adrianne has a master's degree in cancer biology and has taught high school and college biology. The organs in our body are important, but some, such as the kidneys, are ...
BIO102 Unit 8 The Urinary System Assignment 1 1. Characterize the roles of each of the parts of the urinary system. (Kidneys, nephrons, ureters, urinary bladder, and urethra) Kidneys: Excretes unwanted substances, such as cellular metabolic waste, excess salts, toxins, and urea, water balance, pH balance, blood pressure regulation, and regulation of RBC production.
In this chapter we explain: The basic anatomy and physiology of the kidney How kidney function changes through life. Nephons and their blood supply. Left : a short looped-and a long looped-nephron ...
The kidneys are two bean-shaped organs, each about the size of a fist. They are located just below the rib cage, one on each side of the spine. Every day, the two kidneys filter about 120 to 150 quarts of blood to produce about 1 to 2 quarts of urine, composed of wastes and extra fluid. The kidneys' function are to filter the blood.
The urinary system has four main components: - Kidneys: Two bean-shaped organs filter the blood and make up the central part of the urinary system. Adult kidneys are about 5 inches long, 2.5 inches wide, and an inch thick. - Glomerulus in the nephrons of the kidneys: where filtration occurs. - Ureters: Tube-like structures that transport urine ...
Share free summaries, lecture notes, exam prep and more!!
Renal failure is a systemic disease and is a final common pathway of many different kidney and urinary tract diseases. Accumulation. As renal function declines, the end products of protein metabolism (normally excreted in urine) accumulate in the blood. Adverse effects. Uremia develops and adversely affects every system in the body.
The aim of this lecture is to present on Kidney in Detail. The kidneys are two bean-shaped organs that extract waste from blood, balance body fluids, form urine, and aid in other important functions of the body. This lecture briefly present various important parts of kidney. Nephron: structure in the kidney that acts as a microscopic filtration ...
Kidney Injury Journal Assignment. I learned that there is a lot involved in living with kidney disease, especially when it becomes chronic. I watched a video of a woman who had acute renal reflux as an infant and, even though it was found and treated, she was diagnosed with chronic kidney disease at age 21, had a transplant that lasted 15 years, and was about to have another transplant.
View Assignment on kidneys (2).docx from BMS 310 at Colorado State University, Fort Collins. A). How does the body maintain acid-base balance? Similar to many life forms, the human body thrives at a
For patients with solid tumors, assignment to an experimental group in trials of investigational drugs yields significant survival gains, according to a review published online April 30 in the ...
Dr. Ellison said that about 90 percent of people will get better on their own without requiring antibiotics, and about 10 percent will develop the illness that can cause anemia and kidney damage.