The Hip Joint
Written by Oliver Jones
Last updated January 21, 2022 • 41 Revisions •
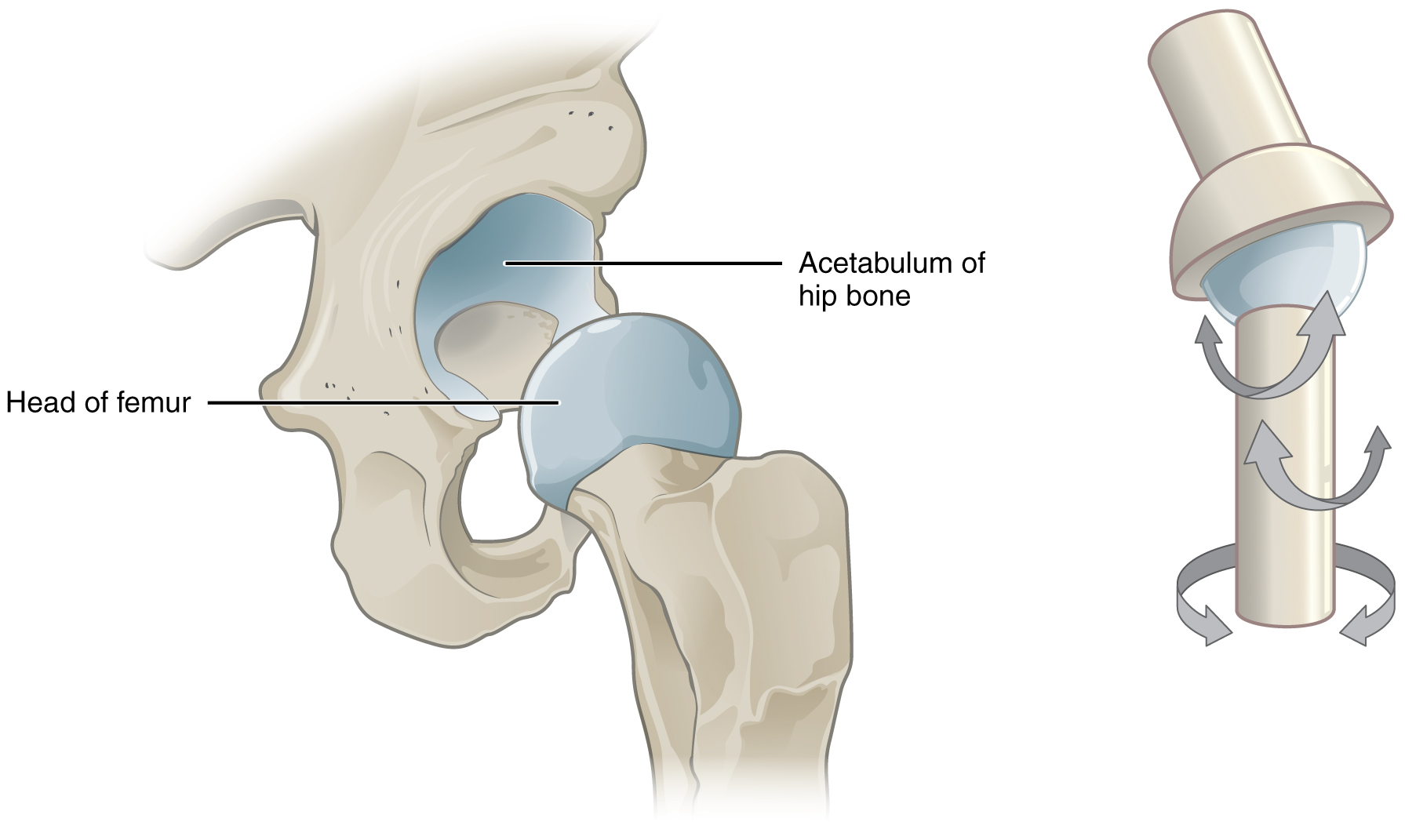
The hip joint is a ball and socket synovial joint, formed by an articulation between the pelvic acetabulum and the head of the femur.
It forms a connection from the lower limb to the pelvic girdle, and thus is designed for stability and weight-bearing – rather than a large range of movement.
In this article, we shall look at the anatomy of the hip joint – its articulating surfaces, ligaments and neurovascular supply.

Premium Feature
Structures of the hip joint, articulating surfaces.
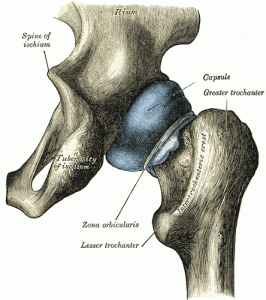
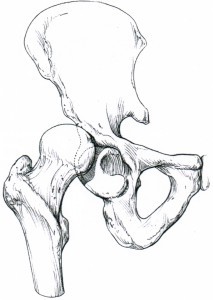
The hip joint consists of an articulation between the head of femur and acetabulum of the pelvis.
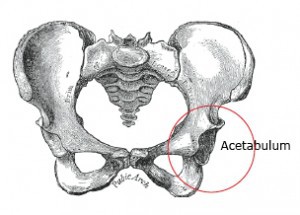
The acetabulum is a cup-like depression located on the inferolateral aspect of the pelvis. Its cavity is deepened by the presence of a fibrocartilaginous collar – the acetabular labrum . The head of femur is hemispherical, and fits completely into the concavity of the acetabulum.
Both the acetabulum and head of femur are covered in articular cartilage, which is thicker at the places of weight bearing.
The capsule of the hip joint attaches to the edge of the acetabulum proximally. Distally, it attaches to the intertrochanteric line anteriorly and the femoral neck posteriorly.
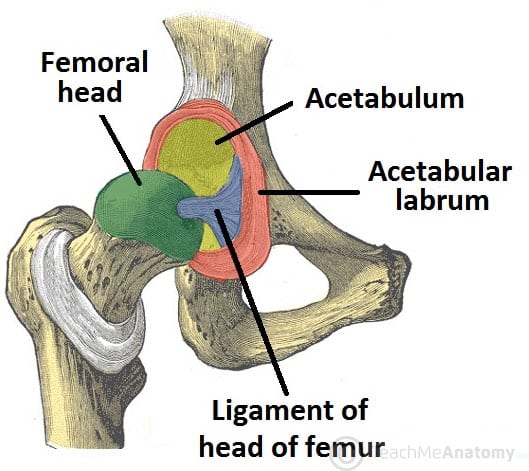
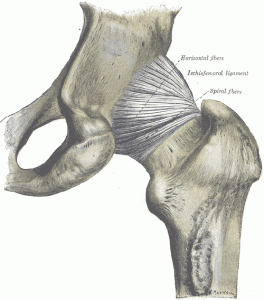
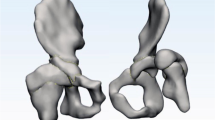
Fig 1 The articulating surfaces of the hip joint – pelvic acetabulum and head of the femur.
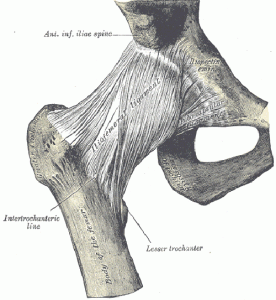
The ligaments of the hip joint act to increase stability. They can be divided into two groups – intracapsular and extracapsular:
Intracapsular
The only intracapsular ligament is the ligament of head of femur . It is a relatively small structure, which runs from the acetabular fossa to the fovea of the femur.
It encloses a branch of the obturator artery (artery to head of femur), a minor source of arterial supply to the hip joint.
Extracapsular
There are three main extracapsular ligaments, continuous with the outer surface of the hip joint capsule:
- It has a ‘Y’ shaped appearance, and prevents hyperextension of the hip joint. It is the strongest of the three ligaments.
- It has a triangular shape, and prevents excessive abduction and extension.
- It has a spiral orientation, and prevents hyperextension and holds the femoral head in the acetabulum.
Neurovascular Supply
The arterial supply to the hip joint is largely via the medial and lateral circumflex femoral arteries – branches of the profunda femoris artery (deep femoral artery). They anastomose at the base of the femoral neck to form a ring, from which smaller arteries arise to supply the hip joint itself.
The medial circumflex femoral artery is responsible for the majority of the arterial supply (the lateral circumflex femoral artery has to penetrate through the thick iliofemoral ligament). Damage to the medial circumflex femoral artery can result in avascular necrosis of the femoral head.
The artery to head of femur and the superior/inferior gluteal arteries provide some additional supply.
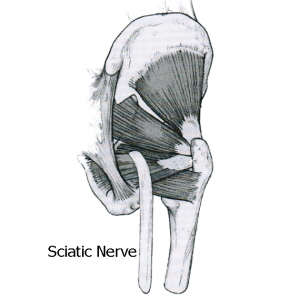
The hip joint is innervated primarily by the sciatic, femoral and obturator nerves. These same nerves innervate the knee, which explains why pain can be referred to the knee from the hip and vice versa.
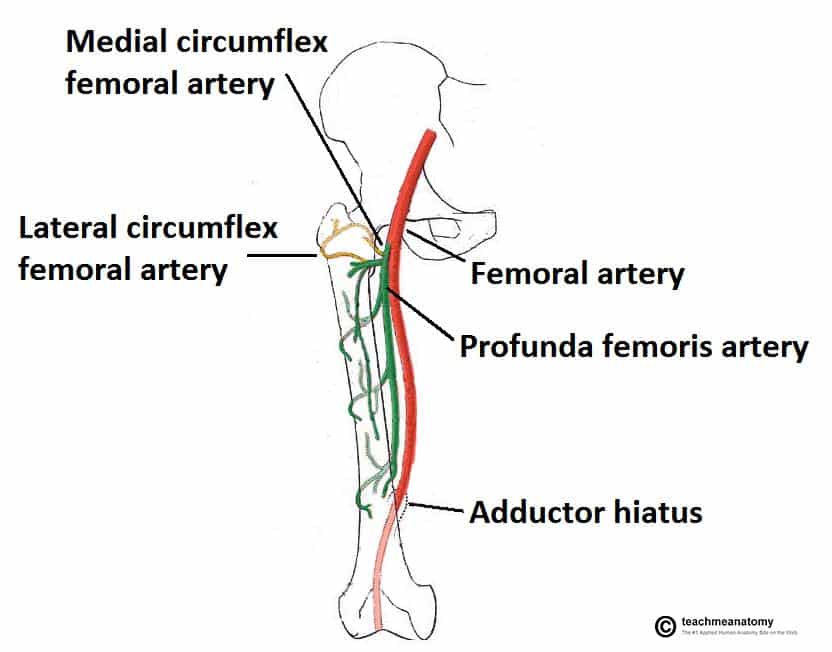
Fig 2 The medial and lateral circumflex femoral arteries are the major blood supply to the hip joint.
Stabilising Factors
The primary function of the hip joint is to weight-bear . There are a number of factors that act to increase stability of the joint.
The first structure is the acetabulum . It is deep, and encompasses nearly all of the head of the femur. This decreases the probability of the head slipping out of the acetabulum (dislocation).
There is a horseshoe shaped fibrocartilaginous ring around the acetabulum which increases its depth, known as the acetabular labrum . The increase in depth provides a larger articular surface, further improving the stability of the joint.
The iliofemoral, pubofemoral and ischiofemoral ligaments are very strong, and along with the thickened joint capsule, provide a large degree of stability. These ligaments have a unique spiral orientation ; this causes them to become tighter when the joint is extended.
In addition, the muscles and ligaments work in a reciprocal fashion at the hip joint:
- Anteriorly , where the ligaments are strongest, the medial flexors (located anteriorly) are fewer and weaker.
- Posteriorly , where the ligaments are weakest, the medial rotators are greater in number and stronger – they effectively ‘pull’ the head of the femur into the acetabulum.
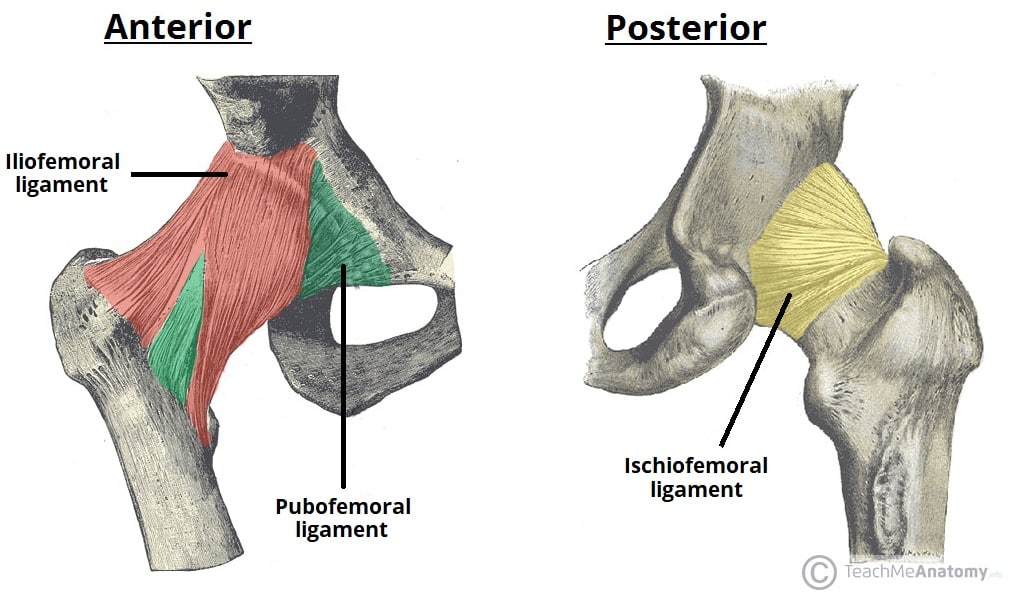
Fig 3 The extracapsular ligaments of the hip joint; ileofemoral, pubofemoral and ischiofemoral ligaments.
Movements and Muscles
The movements that can be carried out at the hip joint are listed below, along with the principle muscles responsible for each action:
- Flexion – iliopsoas, rectus femoris, sartorius, pectineus
- Extension – gluteus maximus; semimembranosus, semitendinosus and biceps femoris (the hamstrings)
- Abduction – gluteus medius, gluteus minimus, piriformis and tensor fascia latae
- Adduction – adductors longus, brevis and magnus, pectineus and gracilis
- Lateral rotation – biceps femoris, gluteus maximus, piriformis, assisted by the obturators, gemilli and quadratus femoris.
- Medial rotation – anterior fibres of gluteus medius and minimus, tensor fascia latae
The degree to which flexion at the hip can occur depends on whether the knee is flexed – this relaxes the hamstring muscles , and increases the range of flexion.
Extension at the hip joint is limited by the joint capsule and the iliofemoral ligament . These structures become taut during extension to limit further movement.
Clinical Relevance
Dislocation of the hip joint, congenital dislocation.
Congenital hip dislocation occurs as a result of developmental dysplasia of the hip (DDH). It occurs when the Acetabulum is shallow as a result of failure to develop properly in utero
Common clinical features include:
- Limited abduction at the hip joint
- Limb length discrepancy – the affected limb is shorter
- Asymmetrical gluteal or thigh skin folds
DDH is usually treated with a Pavlik harness . This holds the femoral head in the acetabular fossa and promotes normal development of the hip joint. Surgery is indicated in cases that do not respond to harness treatment.
Acquired Dislocation
Acquired dislocations of the hip joint are relatively uncommon, owing to the strength and stability of the joint. They usually occur as a result of trauma , but it can occur as a complication following Total Hip Replacement or hemiarthroplasty.
There are two main types of acquired hip dislocation; posterior and anterior:
- The affected limb becomes shortened and medially rotated.
- The sciatic nerve runs posteriorly to the hip joint, and is at risk of injury (occurs in 10-20% of cases). This is often associated with anterior femoral head and posterior wall fractures
- Anterior dislocation (rare) – occurs as a consequence of traumatic extension, abduction and lateral rotation. The femoral head is displaced anteriorly and (usually) inferiorly in relation to the acetabulum.

Fig 4 Radiograph showing dislocation of the left hip joint.
Do you think you’re ready? Take the quiz below
Question 1 of 3
Recommended Reading
Forgot password.
Please enter your username or email address below. You will receive a link to create a new password via emai and please check that the email hasn't been delivered into your spam folder.
We use cookies to improve your experience on our site and to show you relevant advertising. To find out more, read our privacy policy .
Privacy Overview
Report question, rate this article.
Forum Login
- Login with Facebook
- No, create an account now.
- Yes, my password is:

in all of BoneSmart.org in forum only ( options ) exclude forum
About the Hip Joint
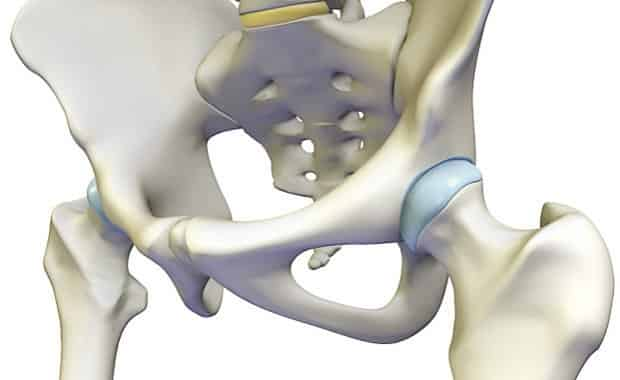
The hip is the body’s second largest weight-bearing joint (after the knee ). It is a ball and socket joint at the juncture of the leg and pelvis. The rounded head of the femur (thighbone) forms the ball, which fits into the acetabulum (a cup-shaped socket in the pelvis). Ligaments connect the ball to the socket and usually provide tremendous stability to the joint. The hip joint is normally very sturdy because of the fit between the femoral head and acetabulum as well as strong ligaments and muscles at the joint.
All of the various components of the hip mechanism assist in the mobility of the joint. Damage to any single component can negatively affect range of motion and ability to bear weight on the joint. Orthopedic degeneration or trauma – those conditions affecting the bones in the hip joint – can necessitate total hip replacement , partial hip replacement or hip resurfacing .
Bones of the hip joint
Normal Hip Joint vs. Arthritic Hip Joint
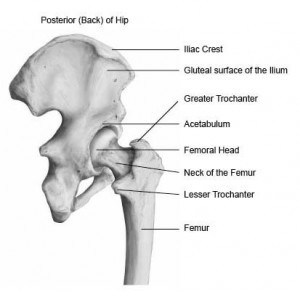
The femur is the upper leg bone or thigh. It is the largest bone in the body. At the top of the femur is a rounded protrusion which articulates with the pelvis. This portion is referred to as the head of the femur, or femoral head.
There are two other protrusions near the top of the femur, known as the greater and lesser trochanters. The muscles involved in hip motion are attached to the joint at these trochanters.
The acetabulum is a concave area in the pelvis, into which the femoral head fits. The pelvis is a girdle of bones, connected at the front by cartilage pad, called the pubis, and at the back by the lowest four fused vertebrae (the sacrum). The sacro-iliac joints are located where the sacrum meets the pelvis.
The bone surfaces of the femoral head and acetabulum have a smooth durable layer of articular cartilage that cushions the ends of the bones and allows for smooth movement.
Hip joint capsule or socket

Hip capsule (socket) illustration (image courtesy of: Smith & Nephew )
You may hear your hip surgeon refer to the capsule or socket, when describing the structure of the hip joint. The joint capsule is a thick ligamentous structure surrounding the entire joint.
Inside the capsule, the surfaces of the hip joint are covered by a thin tissue called the synovial membrane. This membrane nourishes and lubricates the joint.
As noted above, the stability of the hip joint is directly related to its muscles and ligaments. The most notable ligaments in the hip joint are:
- Iliofemoral ligament , which connects the pelvis to the femur at the front of the joint. It keeps the hip from hyper-extension
- Pubofemoral ligament , which attaches the most forward part of the pelvis known as the pubis to the femur
- Ischiofemoral ligament , which attaches to the ischium (the lowest part of the pelvis) and between the two trochanters of the femur.
The labrum is a circular layer of cartilage which surrounds the outer part of the acetabulum effectively making the socket deeper to provide more stability for the joint. Labrum tears are not an uncommon hip injury.
Muscle Groups
The various muscles which attach to or cover the hip joint generate the hip’s movement.
- Gluteals : The gluteals are the muscles in your buttocks. The gluteals (gluteus maximus, gluteus minimus and gluteus medius) are the three muscles attached to back of the pelvis and insert into the greater trochanter of the femur.
- Quadriceps : The four quadricep muscles (vastus lateralis, medialis, intermedius and rectus femoris) are located at the front of the femur. All four attach to the top of the tibia. The rectus femoris originates at the front of the ilium.The three other quads attach around the greater trochanter of the femur and just below it.
- Iliopsoas : This is the primary hip flexor muscle. The three parts of the iliopsoas attach the lower part of the spine and pelvis, then cross the joint and insert into the lesser trochanter of the femur.
- Hamstrings : The three muscles at the back of the thigh are called the hamstrings. All three attach to the lowest part of the pelvis.
- Groin muscles : The groin or adductor muscles attach to the pubis and run down the inside of the thigh.
Filed Under: Hip Replacement The Hip Joint
Related Articles & FAQs

More Hip Articles & FAQs
Recent Forum Discussions
- BILATERAL SIMULTANEOUS HIP REPLACEMENT SURGERY
- 2024 May Marvels - Are you having hip surgery in May?
- New to Forum
- Choosing a hip surgeon
- 2024 June Sunbeams - Are you having hip surgery in June?
More Hip Discussions

- Articles / FAQs
- Forum / Community
- Ask the Expert Webinar
- Minorities & Joint Replacement
- Orthopedic Companies
- Knee Replacement Articles
- Knee Replacement Forum
- Knee Patient Stories
- Hip Replacement Surgery
- Hip Replacement Forum
- Hip Patient Stories
- Shoulder Replacement Library
- Shoulder Replacement Forum
- Advertising Information
- Privacy Policy Disclaimer
- Terms of Use Disclaimer
- BoneSmart® News
Presented By
Hip Anatomy
By: marco funiciello, do, physiatrist.
Peer-Reviewed
The hip’s unique anatomy enables it to be both extremely strong and amazingly flexible, so it can bear weight and allow for a wide range of movement.

Show Transcript
The hip is located where the head of the femur, or thighbone, fits into a rounded socket of the pelvis. This ball-and-socket construction allows for three distinct types of flexibility:
- Hip flexion and extension - moving the leg back and forth;
- Hip abduction and adduction - moving the leg out to the side (abduction) and inward toward the other leg (adduction); and
- Rotation - pointing toes inward (internal rotation) or outward (external rotation) and then moving the straightened leg in the direction of the toes.
Also known as the acetabulofemoral joint, the hip joint is comprised of these basic components:
- Hip bones , including the femur and pelvic bones;
- Hip articular cartilage that decreases friction between the bones and allows for a smooth gliding motion;
- Hip muscles that both support the joint and enable movement;
- Hip ligaments and tendons , tough, fibrous tissues that bind bones to bones and muscles to bones; and
- Synovial membrane and fluid , which encapsulates the hip joint and lubricates it, respectively.
Hip problems occur when any one of these components starts to degenerate or is in some way compromised or irritated.
Structure of the Hip Joint
The hip joint is constructed and functions as follows:
- The hip is located where the top of the femur bone, or thighbone, fits into the pelvis.
- The femur bone is the longest bone in the body, extending from the knee to the hip. At the top of the femur bone is the greater trochanter, that boney knob that people often refer to as their hip, and the bulbous "femoral head" which makes contact with the pelvis and forms the ball of the ball and socket joint. It is covered with articular cartilage, which serves to decrease friction.
- The femoral head fits into the acetabulum, the round socket of the pelvic bone.
Hip articular cartilage
- Both the femoral head and the acetabulum are lined with articular cartilage.
- When the femoral head rotates in the acetabulum, the articular cartilage allows the two surfaces to glide against each other.
- Articular cartilage also acts as a shock absorber, cushioning bones against impacting each other (e.g. while jumping).
- When articular cartilage is damaged or thinned, its ability to protect against friction and impact are impeded.
Read more about What Is Cartilage?
- A strong piece of cartilage, called the labrum , rings the outer edge of the acetabulum. The labrum deepens the socket joint, making the joint more stable, but its elasticity allows for flexibility.
- Over time the smooth articular cartilage that makes up the surfaces of the hip joint may be damaged or blemished by normal wear and tear or from trauma. This process is referred to as arthritis.
Hip ligaments and tendons
- The hip has several ligaments connecting the femur to the pelvis and tendons connecting the bones to many surrounding muscles. Tightness of these ligaments and tendons can cause hip instability and pain.
- Strong and flexible ligaments and tendons provide structure to the hip, reducing strain on the joint, so most hip osteoarthritis therapies will including stretching and strengthening of these structures.
Synovial fluid
- A synovial membrane encapsulates the entire hip joint. This membrane produces synovial fluid, a viscous substance that lubricates and circulates nutrients to the joint.
- When the hip is at rest, the synovial fluid is stored in the cartilage, much like water in a sponge.
- When the hip rotates or bears weight the synovial fluid is squeezed out. Therefore, joint use is necessary to keep the hip joint lubricated and healthy.
See What Is a Synovial Joint?
Hip muscles The hip joint is surrounded by several muscles, including:
- Gluteal muscles, located on the back of the hip (buttocks);
- The adductor muscle on the inner thigh;
- The iliopsoas muscle, which extends from the lower back to upper femur;
- Quadriceps, a group of four muscles that comprise the front of the thigh; and
- Hamstrings, a group of muscles that comprise the back of the thigh and extend to just below the knee.
Together, these muscles support the hip joint, so exercises to relieve hip osteoarthritis symptoms will focus on these muscles as well as muscles of the core.
When the hip joint becomes inflamed and painful, the pain may be felt in the groin but may also be referred into the back, buttocks and down the front or back of the leg.
Hip Anatomy on X-Rays and Other Imaging Studies
It is important to note that the degree of anatomical problems (such as the degree of hip joint deterioration) that can be seen on a hip x-ray does not always correlate with the level of pain.
For example, a patient could have hip x-rays that show moderate right hip arthritis and mild arthritis on the left, but he or she may only have pain on the side showing mild hip arthritis.
This counterintuitive result is due to the fact that the pain felt from arthritis is usually due to inflammation in the joint and not the arthritis itself. This concept applies to all the joints in the body and is important to understand because treating the inflammation will often treat the pain and dysfunction and can often help someone put off surgery or avoid it all together.
Dr. Marco Funiciello is a physiatrist with Princeton Spine and Joint Center. He has a decade of clinical experience caring for spine and muscle conditions with non-surgical treatments. Dr. Funiciello specializes in interventional spine procedures, ultrasound-guided injections, osteopathic manipulative treatments, and electrodiagnostic testing. He is also certified to practice acupuncture.
- Hip Anatomy "> Share on Facebook
- Hip Anatomy "> Share on Pinterest
- Hip Anatomy "> Share on X
- Subscribe to our newsletter
- Print this article
- Hip Anatomy &body=https://www.arthritis-health.com/types/joint-anatomy/hip-anatomy&subject= Hip Anatomy "> Email this article
Editor’s Top Picks
Hip pain and arthritis, what is hip osteoarthritis, hip (trochanteric) bursitis, what is cartilage.
Hip Osteoarthritis Video
Hip Bursitis Video
Popular Videos

Rheumatoid Arthritis Overview Video

Knee Osteoarthritis Video

Ankylosing Spondylitis Video

Health Information (Sponsored)
- Take the Chronic Pain Quiz
- Learn How Bone Growth Stimulation Works
- Learn a Proven Effective Therapy to Stimulate Fracture Repair
- Schedule a Consultation With Cedars-Sinai’s Integrated Spine Team
Hip Anatomy, Function and Common Problems
The hip joint is a ball-and-socket type joint and is formed where the thigh bone (femur) meets the pelvis. The femur has a ball-shaped head on its end that fits into a socket formed in the pelvis, called the acetabulum. Large ligaments, tendons, and muscles around the hip joint hold the bones (ball and socket) in place and keep it from dislocating.

Normally, a smooth cushion of shiny white hyaline (or articular) cartilage about 1/4 inch thick covers the femoral head and the acetabulum. The articular cartilage is kept slick by fluid made in the synovial membrane (joint lining). Synovial fluid and articular cartilage are a very slippery combination—3 times more slippery than skating on ice and 4 to 10 times more slippery than a metal on plastic hip replacement. Synovial fluid is what allows us to flex our joints under great pressure without wear. Since the cartilage is smooth and slippery, the bones move against each other easily and without pain.
When the cartilage is damaged, whether secondary to osteoarthritis (wear-and-tear type arthritis) or trauma, joint motion can become painful and limited.
The hip joint is one of the largest joints in the body and is a major weight-bearing joint. Weight bearing stresses on the hip during walking can be 5 times a person’s body weight. A healthy hip can support your weight and allow you to move without pain. Changes in the hip from disease or injury will significantly affect your gait and place abnormal stress on joints above and below the hip.
It takes great force to seriously damage the hip because of the strong, large muscles of the thighs that support and move the hip.
Anatomical Terms
Anatomical terms allow us to describe the body and body motions more precisely. Instead of your doctor simply saying that “the patient knee hurts”, he or she can say that “the patient’s knee hurts anterolaterally”. Identifying specific areas of pain helps to guide the next steps in treatment or work-up. Below are some anatomic terms doctors use to describe location (applied to the hip):
- Anterior — the abdominal side (front) of the hip
- Posterior — the back side of the hip
- Medial — the side of the hip closest to the spine
- Lateral — the side of the hip farthest from the spine
- Abduction — move away from the body (raising the leg away from midline i.e. towards the side)
- Adduction — move toward the body (lowering the leg toward midline i.e. from the side)
- example: the knee is proximal to the ankle
- example: the ankle is distal to the knee
- Inferior — located beneath, under or below; under surface
Anatomy of the Hip
Like the shoulder , the hip is a ball-and-socket joint, but is much more stable. The stability in the hip begins with a deep socket—the acetabulum. Additional stability is provided by the surrounding muscles, hip capsule and associated ligaments. If you think of the hip joint in layers, the deepest layer is bone, then ligaments of the joint capsule, then muscles are on top. Various nerves and blood vessels supply the muscles and bones of the hip.
Bony Structures of the Hip
The hip is formed where the thigh bone (femur) meets the three bones that make up the pelvis: the ilium, the pubis (pubic bone) and the ischium. These three bones converge to form the acetabulum, a deep socket on the outer edge of the pelvis. By adulthood, these three bones are completely fused and the pelvis is effectively a single bone.
The femur is the longest bone in the body. The neck of the femur connects the femoral head with the shaft of the femur. The neck ends at the greater and lesser trochanters, which are bony prominences of the femur that various muscles attach to. The greater trochanter serves as the site of attachment for the abductor and external rotator muscles which are important stabilizers of the hip joint. This is the prominent part of your hip that you can actually feel on the outer aspect of your thigh. The lesser trochanter serves as the attachment site of the iliopsoas tendon, one of the muscles that allows you to bend your hip.
It is important to remember that the actual hip joint lies deep in the groin area. This is important, because true hip joint issues are typically associated with groin pain.
The Hip Joint
The hip joint is a ball and socket type joint. The femoral head (ball) fits into the acetabulum (socket) of the pelvis. The large round head of the femur rotates and glides within the acetabulum. The depth of the acetabulum is further increased by a fibrocartilagenous labrum that attaches to the outer rim of the acetabulum. It acts to deepen the socket and to add additional stability to the hip joint. The labrum can become torn and cause symptoms such as pain, weakness, clicking, and instability of the hip.
There are numerous structures that contribute stability to the hip:
- The ball and socket bony structure
- The capsule and its associated ligaments: e.g. iliofemoral ligament, pubofemoral ligament
- The surrounding muscles including the abductors (gluteus medius and minimus) and external rotators (gemelli muscles, piriformis, the obturators).
Hip Ligaments
The stability of the hip is increased by the strong ligaments that encircle the hip (the iliofemoral, pubofemoral, and ischiofemoral ligaments). These ligaments completely encompass the hip joint and form the joint capsule. The iliofemoral ligament is considered by most experts to be the strongest ligament in the body. The ligamentum teres is a small tubular structure that connects the head of the femur to the acetabulum. It contains the artery of the ligamentum teres. In infants, this serves as a relatively important source of blood supply to the head of the femur. In adults, the ligamentum teres is thought by most to be more of a vestigial structure that serves little function.
Muscles of the Hip
The muscles of the thigh and lower back work together to keep the hip stable, aligned and moving. It is the muscles of the hip that allow the movements of the hip:
- flexion – bend
- extension – straighten
- abduction – leg move away from midline
- adduction – leg moves back towards midline
- external rotation (allows for the foot to point outwards)
- internal rotation (allows for the foot to point inward)
The hip muscles are divided up into three basic groups based on their location: anterior muscles (front), posterior (back), and medial (inside). The muscles of the anterior thigh consist of the quadriceps (or quads): vastus medialis, intermedius, lateralis and rectus femoris muscles. The quads make up about 70% of the thigh’s muscle mass. The main functions of the quads are flexion (bending) of the hip and extension (straightening) of the knee.
The gluteal and hamstring muscles, as well as the external rotators of the hip are located in the buttocks and posterior thigh. The gluteal muscles consist of the gluteus maximum, gluteus medius, and gluteus minimus. The gluteus maximus is the main hip extensor and helps keep up the normal tone of the fascia lata or iliotibial (IT) band, which is the long, sheet-like tendon on the side of your thigh. It helps with motion of the hip, but perhaps more importantly, acts to help stabilize the knee joint.
Gluteus medius and minimus are the main abductors of the hip —that is, they move the leg away from the midline of the body (using the spine as a midline reference point). They also are the main internal rotators of the hip (i.e. turn the foot inwards). The gluteus medius and minimus are also important stabilizers of the hip joint and help to keep the pelvis level as we walk.
The tensor fascia lata (TFL) is another abductor of the hip, which, along with the gluteus maximus, attaches to the IT band. The IT band is a common cause of lateral (outside) hip, thigh, and knee pain.
The medial muscles of the hip are involved in the adduction of the leg i.e. bringing the leg back towards the midline. These muscles include the adductors (adductor magnus, adductor longus, adductor brevis, pectineus, gracilis). Obturator externus also helps to adduct the leg.
The external rotator muscles (piriformis, gemelli, obturator internus) of the hip are located in the buttock area and assist in lateral rotation of the hip (out-toeing). Lateral rotation is needed for crossing the legs.
Blood Vessels and Nerves of the Hip
Nerves carry signals from the brain to the muscles to move the hip and carry signals from the muscles back to the brain about pain, pressure and temperature. The main nerves of the hip that supply the muscles in the hip include the femoral, obturator, and sciatic nerves.
The sciatic nerve is the most commonly recognized nerve in the hip and thigh. The sciatic nerve is large—as big around as your thumb—and travels beneath the gluteus maximus down the back of the thigh where it branches to supply the muscles of the leg and foot. Hip dislocations can cause injury to the sciatic nerve.
The blood supply to the hip is extensive and comes from branches of the internal and external iliac arteries: the femoral, obturator, superior and inferior gluteal arteries. The femoral artery is well-known because of its use in cardiac catheterization. You can feel its pulse in your groin area. It travels from deep within the hip down the thigh and down to the knee. It is the continuation of the external iliac artery which lies within the pelvis. The main blood supply to the femoral head comes from vessels that branch off of the femoral artery: the lateral and medial femoral circumflex arteries. Disruption of these arteries can lead to osteonecrosis (bone death) of the femoral head. These arteries can become disrupted with hip fractures and hip dislocations.
Bursae are fluid filled sacs lined with a synovial membrane which produce synovial fluid. Bursae are often found near joints. Their function is to lessen the friction between tendon and bone, ligament and bone, tendons and ligaments, and between muscles. There are as many as 20 bursae around the hip. Inflammation or infection of the bursa called bursitis.
The trochanteric bursa is located between the greater trochanter (the bony prominence on the femur) and the muscles and tendons that cross over the greater trochanter. This bursa can get irritated if the IT band is too tight. This bursa is a common cause of lateral thigh (hip) pain. Two other bursa that can get inflamed are the iliopsoas bursa, located under the iliopsoas muscle and the bursa located over the ischial tuberosity (the bone you sit on).
Common Problems of the Hip
- Osteoarthritis
- Dislocation (see image above of simple dislocation)
- Femoroacetabular impingement
- Labral tear
- IT band syndrome
- Snapping hip syndrome
- Aseptic or Avascular necrosis
- Congenital Dislocation
- Acetabular dysplasia
- Legg-Perthes disease
Surgery of the Hip
- Hip Replacement
- Hip arthroscopy
- Hip fracture fixation
- Hip preservation surgery
The hip joint is largely responsible for mobility. So any injury, trauma, or disease that affects its function can significantly reduce a person’s independence.
Lastly, there are many conditions in and around the hip and even conditions of the spine, that can cause pain in the hip area. Therefore, if you suspect that you might be having a problem with your hip(s), don’t hesitate to visit a trusted doctor for further evaluation.
Note that the information in this article is purely informative and should never be used in place of the advice of professionals.

Dr. Andrew Chung is a Spine Surgeon at Sonoran Spine in Tempe, Arizona. He is a graduate of the Philadelphia College of Osteopathic Medicine and was formerly Spine Surgeon Clinical Fellow at Cedars-Sinai, Spine Surgery Fellow at Keck Hospital, University of Southern California and Chief Resident and an Instructor of Orthopedic Surgery in the Department of Orthopedic Surgery at the Mayo Clinic in Arizona. Dr. Chung's research .
134k followers
13k followers
290k followers
826k followers
Hip Assessment

- Extremity Online Course
The Hip Joint
The hip joint is a deep ball and socket joint comprised of the convex femoral head and the concave acetabulum of the pelvis. Similar to the glenohumeral joint, the acetabulum has a glenoidal lip or labrum around its edges for extra stability.

Epidemiology
It is estimated that around 10% of the general population suffers from some sort of hip complaint ( Birrel et al. 2005 ). In the athletic population (mainly club football) hip/groin injuries accounted for 4-19% of all injuries ( Weir et al. 2015 ). The most common conditions, which we will cover in more detail in this course are osteoarthritis, labral tears due to femoroacetabular impingement (FAI), and greater trochanteric pain syndrome (GTPS) also known as gluteal tendinopathy.
According to the Dutch study by Picavet et al. (2003) , around 28% of people with hip or knee pain have continuous mild pain and mild pain is recurrent in 46% of people with either a hip or knee complaint.
Lievense et al. (2007) followed 224 patients age ≥50 with hip pain over a period of six years and assessed disease progression and incidence of total hip replacement at three and six years. After three years, 15% of patients showed disease progression and 12% underwent hip replacement surgery. Disease progression almost doubled at the second follow-up (28%) and 22% had received a hip replacement.
The individual prognosis for the specific pathologies is discussed in the next units.
Prognostic factors
According to a review by Artus et al. (2017) the following factors are related, but not limited to, the course of hip pain:
- widespread pain
- high functional disability
- somatization
- high pain intensity
- presence of previous pain episodes
Next to the general red flags that should be asked in any case, specific red flags in the hip joint can be:
1) Region-specific red flags:
- Again fractures. This is especially important in the elderly population where hip fractures accounted for up to 14% of all fractures ( Burge et al. 2007 , Ensrud et al. 2013 )
- Avascular femoral head necrosis, which manifests as intermittent groin pain that increases with activity. Usually the case in prolonged use of corticosteroids ( Barille et al. 2014 )
2) Tract anamnesis:
- Gastrointestinal tract: this visceral pain is mostly deep aching, gnawing, vague, or deep grinding. Conditions include GI bleeding, epigastric pain, constipation, obturator or psoas abscess, appendicitis.
Furthermore, you should not forget to rule out SI Joint or lumbar spine involvement in case of a hip complaint. This is because the hip receives innervation from spinal segments L2-S2. Therefore it is a common site for referred pain from these structures. Check the “further reading” section and the bottom for literature on the topic.
LEVEL UP YOUR DIFFERENTIAL DIAGNOSIS IN RUNNING RELATED HIP PAIN – FOR FREE!

Basic Assessment
Depending on the outcome, your basic assessment can give you the following info: 1) Limitations in range of motion and their end-feel can guide structural assessment (e.g. bone to bone=osteoarthritis, empty=tendinopathy due to pain)
It’s best to start with Active Range of Motion Assessment:
Standard values for the range of motion in different directions are as follows:

AROM assessment is then typically followed by Passive Range of Motion Assessment (PROM). PROM assessment in the hip joint is also used as part of the diagnostic criteria for hip osteoarthritis, where a marked decrease increases the likelihood of OA.
During PROM assessment, it’s important to compare the range of motion as well as the end-feel of the affected hip with the unaffected side.
Muscle strains or sprains are common in the hip and groin region, especially in athletic populations. In the following two videos, you will see how you can stress the muscles around the hip joint to possibly identify them as a source of nociception as well as a video on the differentiation of groin pain in athletes.
Specific Pathologies in the Hip
There are several pathologies that are commonly seen in the hip area. For more information, click on the respective pathology (content will be added in the near future):
- Muscle Contractures
- Leg Length Difference
- Hip Microinstability
- Femoroacetabular Impingement (FAI) / Labrum Tears
- Tendinopathy
- Deep Gluteal Syndrome
- Ischiofemoral Impingement
- Osteoarthritis of the Hip
Artus, Majid et al. “Generic Prognostic Factors for Musculoskeletal Pain in Primary Care: A Systematic Review.” BMJ Open 7.1 (2017): e012901. PMC . Web. 6 Sept. 2018.
Birrell F, Croft P, Cooper C, Hosie G, Macfarlane GJ & Silman A. (2000) Radiographic change is common in new presenters in primary care with hip pain. Rheumatology. 2000;39:772–5.
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A & Tosteson A. (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465–475.
Barille MF, Wu JS & McMahon CJ. (2014) Femoral head avascular necrosis: a frequently missed incidental finding on multidetector CT. Clin Radiol. 2014 Mar;69(3):280–5.
Ensrud KE. (2013) Epidemiology of fracture risk with advanced age. Gerontol A Biol Sci Med Sci 2013;68(10):1236–1242
Lievense, Annet M., et al. “Prognosis of hip pain in general practice: a prospective followup study.” Arthritis Care & Research 57.8 (2007): 1368-1374.
Picavet, H. S. J., and J. S. A. G. Schouten. “Musculoskeletal pain in the Netherlands: prevalences, consequences and risk groups, the DMC3-study.” Pain 102.1-2 (2003): 167-178.
Weir, Adam, et al. “Doha agreement meeting on terminology and definitions in groin pain in athletes.” Br J Sports Med 49.12 (2015): 768-774.
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
How to Boost Your Knowledge about the 23 Most Common Orthopedic Pathologies in Just 40 Hours

What customers have to say about this online course

Create your free account to gain access to this exclusive content and more!
To provide the best experiences, we and our partners use technologies like cookies to store and/or access device information. Consenting to these technologies will allow us and our partners to process personal data such as browsing behavior or unique IDs on this site and show (non-) personalized ads. Not consenting or withdrawing consent, may adversely affect certain features and functions.
Click below to consent to the above or make granular choices. Your choices will be applied to this site only. You can change your settings at any time, including withdrawing your consent, by using the toggles on the Cookie Policy, or by clicking on the manage consent button at the bottom of the screen.
Download our free physiotherapy app with all the knowledge you need.

Select a Community
- MB 1 Preclinical Medical Students
- MB 2/3 Clinical Medical Students
- ORTHO Orthopaedic Surgery
Are you sure you want to trigger topic in your Anconeus AI algorithm?
You are done for today with this topic.
Would you like to start learning session with this topic items scheduled for future?
Hip Physical Exam - Adult

- Discoloration, wounds, or gross deformity
- Length - compare to contralateral side
- Position - internally or externally rotated; flexion contractures
- Gross deformity
- Observe the stride length, foot rotation, pelvic rotation, stance phase
- shortened stance phase on affected side
- secondary to abductor weakness
- weight bearing on the affected hip leads to a contralateral hip drop
- Pain can be attributable to bursitis, tendonitis, infection, or fracture
- ITB can snap over GT and cause pain
- pain with sartorius avulsions / injuries
- pain with hamstring avulsions / tendinopathy
- pain with oblique avulsions / hip pointers
- Iliotibial band / TFL
- hip adduction - obturator nerve
- thigh abduction - superior gluteal nerve
- hip flexion - femoral nerve
- hip extension - inferior gluteal nerve
- proximal anteromedial thigh - genitofemoral nerve
- inferomedial thigh - obturator nerve
- lateral thigh - lateral femoral cutaneous nerve
- anteromedial thigh - femoral nerve
- posterior thigh - posterior femoral cutaneous nerve
- 120-135 deg
- evaluates hip flexion contractures
- hip F lexed to 90 deg, AD ducted and I nternally R otated
- positive test if patient has hip or groin pain
- can suggest possible labral tear or FAI
- hip F lexed to 90 deg, AB ducted and E xternally R otated
- positive test if patient has hip or back pain or ROM is limited
- can suggest intra-articular hip lesions, iliopsoas pain, or sacroiliac disease (posteriorly located pain)
- passive maximal internal and external rotation of lower extremity while supine
- clicking or popping suggest acetabular labral tear
- increased total ROM compared to contralateral side suggests ligament or capsular laxity
- with patient supine, fully flex one hip.
- if contralateral hip lifts off table, there is likely a fixed flexion deformity
- patient placed in lateral position with affected side up
- with hip in slight extension, abduct the leg then allow it to drop into adduction
- if unable to adduct leg, suspect tight ITB
- with patient supine and extended knee, examiner resists active hip flexion past 30-45 deg
- a positive test ellicits pain which is likely to be associated with an intraarticular hip pathology
- - Hip Physical Exam - Adult
Please Login to add comment

9.1 Classification of Joints
Learning objectives.
By the end of this section, you will be able to:
Discuss both functional and structural classifications for body joints
- Distinguish between the functional and structural classifications for joints
- Describe the three functional types of joints and give an example of each
- Describe the three structural types of joints and give an example of each
- Describe the planes of movement possible in diarthrodial joints
A joint , also called an articulation , is any place where adjacent bones or bone and cartilage come together (articulate with each other) to form a connection. Joints are classified both structurally and functionally. Structural classifications of joints take into account whether the adjacent bones are strongly anchored to each other by fibrous connective tissue or cartilage, or whether the adjacent bones articulate with each other within a fluid-filled space called a joint cavity . Functional classifications describe the degree of movement available between the bones, ranging from immobile, to slightly mobile, to freely moveable joints. The amount of movement available at a particular joint of the body is related to the functional requirements for that joint. Thus immobile or slightly moveable joints serve to protect internal organs, give stability to the body, and allow for limited body movement. In contrast, freely moveable joints allow for much more extensive movements of the body and limbs.
Structural Classification of Joints
The structural classification of joints is based on whether the articulating surfaces of the adjacent bones are directly connected by fibrous connective tissue or cartilage, or whether the articulating surfaces contact each other within a fluid-filled joint cavity. These differences serve to divide the joints of the body into three structural classifications. A fibrous joint is where the adjacent bones are united by fibrous connective tissue. At a cartilaginous joint , the bones are joined by hyaline cartilage or fibrocartilage. At a synovial joint , the articulating surfaces of the bones are not directly connected, but instead come into contact with each other within a joint cavity that is filled with a lubricating fluid. Synovial joints allow for free movement between the bones and are the most common joints of the body.
Functional Classification of Joints
The functional classification of joints is determined by the amount of mobility found between the adjacent bones. Joints are thus functionally classified as a synarthrosis or immobile joint, an amphiarthrosis or slightly moveable joint, or as a diarthrosis, which is a freely moveable joint (arthroun = “to fasten by a joint”). Depending on their location, fibrous joints may be functionally classified as a synarthrosis (immobile joint) or an amphiarthrosis (slightly mobile joint). Cartilaginous joints are also functionally classified as either a synarthrosis or an amphiarthrosis joint. All synovial joints are functionally classified as a diarthrosis joint.
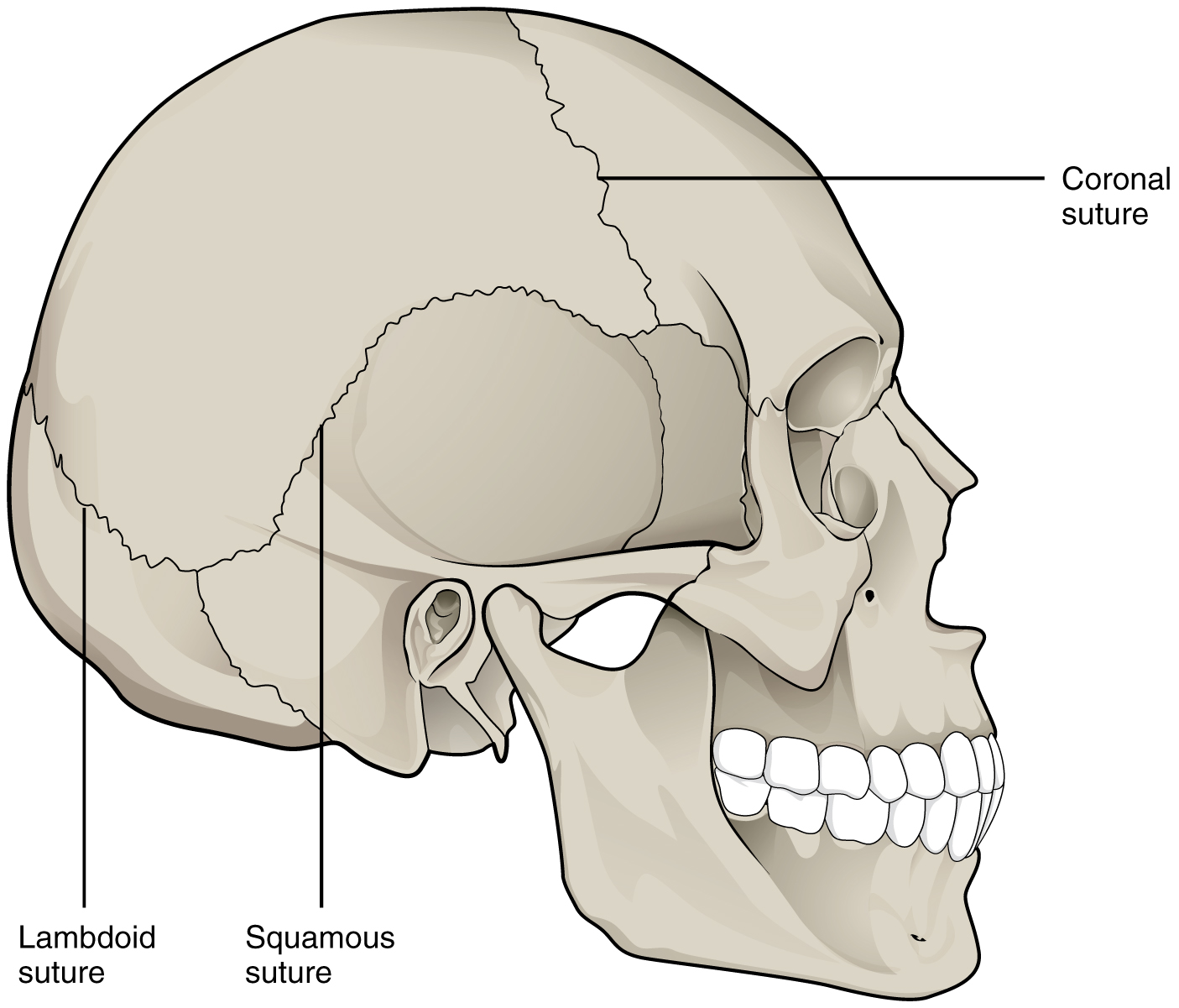
Synarthrosis
An immobile or nearly immobile joint is called a synarthrosis (plural = synarthroses). The immobile nature of these joints provide for a strong union between the articulating bones. This is important at locations where the bones provide protection for internal organs. Examples include sutures, the fibrous joints between the bones of the skull that surround and protect the brain ( Figure 9.1.1 ), and the epiphyseal growth plate, a cartilaginous joint that unites the epiphyses and diaphysis of a growing long bone like the femur.

Amphiarthrosis
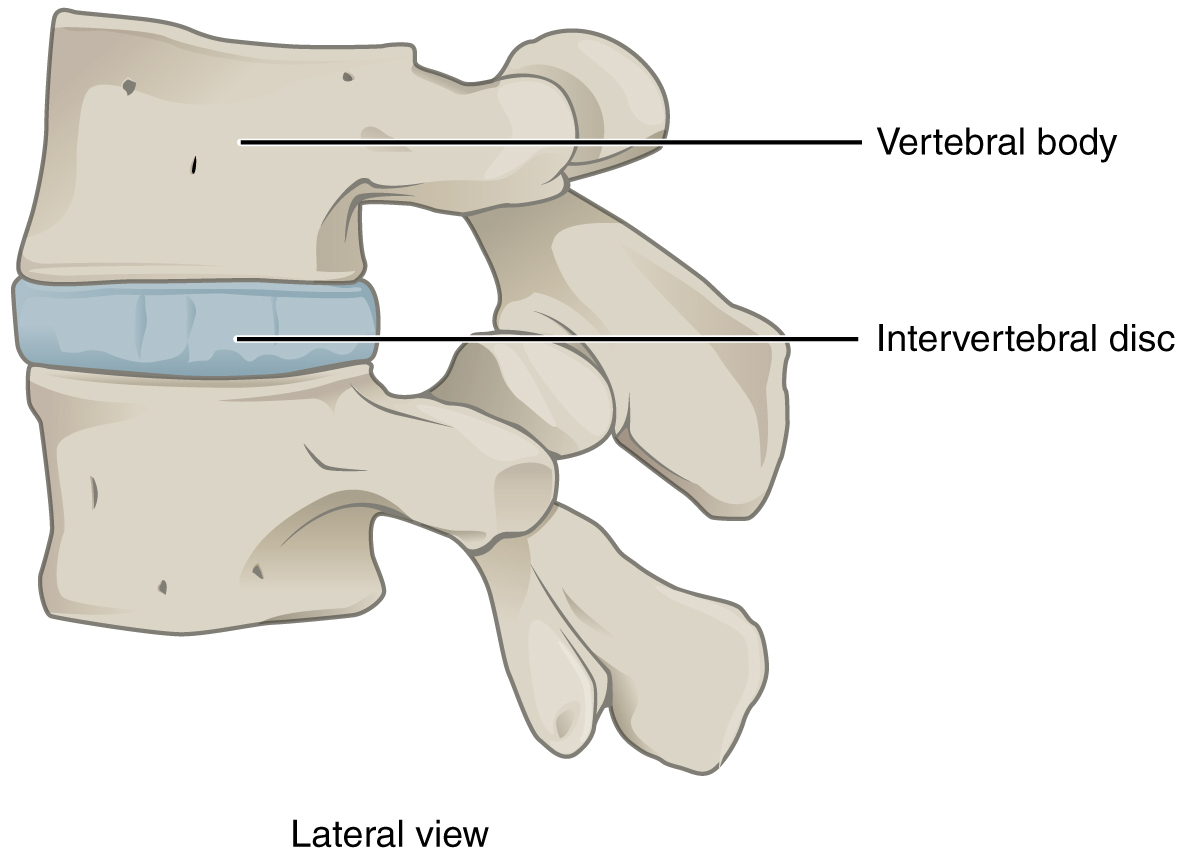
An amphiarthrosis (plural = amphiarthroses) is a joint that has limited mobility. An example of this type of joint is the cartilaginous joint that unites the bodies of adjacent vertebrae. Filling the gap between the vertebrae is a thick pad of fibrocartilage called an intervertebral disc ( Figure 9.1.2 ). Each intervertebral disc strongly unites the vertebrae but still allows for a limited amount of movement between them. However, the small movements available between adjacent vertebrae can sum together along the length of the vertebral column to provide for large ranges of body movements.
Another example of an amphiarthrosis is the pubic symphysis of the pelvis. This is a cartilaginous joint in which the pubic regions of the right and left hip bones are strongly anchored to each other by fibrocartilage. This joint normally has very little mobility. The strength of the pubic symphysis is important in conferring weight-bearing stability to the pelvis. During pregnancy, increased levels of the hormone relaxin lead to increased mobility at the pubic symphysis which allows for expansion of the pelvic cavity during childbirth.
Diarthrosis
A freely mobile joint is classified as a diarthrosis (plural = diarthroses). This functional classification of joints describes all synovial joints of the body, which provide the majority of body movements. Most diarthrotic joints are found in the appendicular skeleton and give the limbs a wide range of motion. These joints are divided into three categories, based on the number of axes of motion provided by each. An axis in anatomy is described as the movements in reference to the three anatomical planes: transverse, frontal, and sagittal. Thus, diarthroses are classified as uniaxial, biaxial, or multiaxial joints.
A uniaxial joint only allows for a motion in a single plane (around a single axis). The elbow joint, which only allows for bending or straightening, is an example of a uniaxial joint. A biaxial joint allows for motions within two planes. An example of a biaxial joint is a metacarpophalangeal joint (knuckle joint) of the hand. The joint allows for movement along one axis to produce bending or straightening of the finger, and movement along a second axis, which allows for spreading of the fingers away from each other and bringing them together. A joint that allows for the several directions of movement is called a multiaxial joint (sometimes called polyaxial or triaxial joint). This type of diarthrotic joint allows for movement along three axes ( Figure 9.1.3 ). The shoulder and hip joints are multiaxial joints. They allow the upper or lower limb to move in an anterior-posterior direction and a medial-lateral direction. In addition, the limb can also be rotated around its long axis. This third movement results in rotation of the limb so that its anterior surface is moved either toward or away from the midline of the body.
Chapter Review
Structural classifications of the body joints are based on how the bones are held together and articulate with each other. At fibrous joints, the adjacent bones are directly united to each other by fibrous connective tissue. Similarly, at a cartilaginous joint, the adjacent bones are united by cartilage. In contrast, at a synovial joint, the articulating bone surfaces are not directly united to each other, but come together at a fluid-filled joint cavity.
The functional classification of body joints is based on the degree of movement found at each joint. A synarthrosis is a joint that is essentially immobile. This type of joint provides for a strong connection between the adjacent bones, which serves to protect internal structures such as the brain or heart. Examples include the fibrous joints of the skull sutures and the cartilaginous epiphyseal plate. A joint that allows for limited movement is an amphiarthrosis. An example is the pubic symphysis of the pelvis, the cartilaginous joint that strongly unites the right and left hip bones of the pelvis. The cartilaginous joints in which vertebrae are united by intervertebral discs provide for small movements between the adjacent vertebrae and are also amphiarthrotic joints. Thus, based on their movement ability, some fibrous and cartilaginous joints are functionally classified as synarthroses while others are amphiarthroses.
The most common type of joint is the diarthrosis, which is a freely moveable joint. All synovial joints are functionally classified as diarthroses. A uniaxial diarthrosis, such as the elbow, is a joint that only allows for movement within a single anatomical plane. Joints that allow for movements in two planes are biaxial joints, such as the metacarpophalangeal joints of the fingers. A multiaxial joint, such as the shoulder or hip joint, allows for three planes of motions.
Review Questions
Critical thinking questions.
1. Define how joints are classified based on function. Describe and give an example for each functional type of joint.
2. Explain how degree of mobility is related to joint strength.
Answers for Critical Thinking Questions
- Functional classification of joints is based on the degree of mobility exhibited by the joint. A synarthrosis is an immobile or nearly immobile joint. An example is the epiphyseal plate or the joints between the skull bones surrounding the brain. An amphiarthrosis is a slightly moveable joint, such as the pubic symphysis or an intervertebral cartilaginous joint. A diarthrosis is a freely moveable joint. These are subdivided into three categories. A uniaxial diarthrosis allows movement within a single anatomical plane or axis of motion. The elbow joint is an example. A biaxial diarthrosis, such as the metacarpophalangeal joint, allows for movement along two planes or axes. The hip and shoulder joints are examples of a multiaxial diarthrosis. These allow movements along three planes or axes.
- Joint mobility is inversely related to joint strength. A synarthrosis, which is an immobile joint, serves to strongly connect bones thus protecting internal organs such as the heart or brain. A slightly moveable amphiarthrosis provides for small movements while maintaining stability between adjacent bones as in the vertebral column. The freedom of movement provided by a diarthrosis can allow for large movements, such as is seen with most joints of the limbs. However, these joints are the most frequently injured due to their looser articulations at the joint cavity.
This work, Anatomy & Physiology, is adapted from Anatomy & Physiology by OpenStax , licensed under CC BY . This edition, with revised content and artwork, is licensed under CC BY-SA except where otherwise noted.
Images, from Anatomy & Physiology by OpenStax , are licensed under CC BY except where otherwise noted.
Access the original for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction .
Anatomy & Physiology Copyright © 2019 by Lindsay M. Biga, Staci Bronson, Sierra Dawson, Amy Harwell, Robin Hopkins, Joel Kaufmann, Mike LeMaster, Philip Matern, Katie Morrison-Graham, Kristen Oja, Devon Quick, Jon Runyeon, OSU OERU, and OpenStax is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License , except where otherwise noted.
Please Enable JavaScript in your Browser to Visit this Site.
We are there to help you, click on any available representative to contact 🌸
Morphological Changes and Concentricity of the Hip Joint During Gradual Reduction in Infants with Late-Detected Developmental Dysplasia of the Hip: A Retrospective Study
- Original Article
- Published: 15 May 2024
Cite this article

- Yaichiro Okuzu ORCID: orcid.org/0000-0003-2706-3725 1 , 2 ,
- Masako Tsukanaka 2 ,
- Koji Goto 3 ,
- Yutaka Kuroda 1 ,
- Toshiyuki Kawai 1 ,
- Yugo Morita 1 ,
- Tohru Futami 2 &
- Shuichi Matsuda 1
Explore all metrics
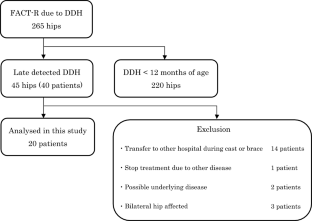
The relationship between hip morphological changes and joint concentricity in infants with late-detected developmental dysplasia of the hip (DDH) treated with gradual reduction remains unclear. Therefore, we investigated hip morphological changes and concentricity in infants with late-detected unilateral DDH using magnetic resonance imaging (MRI) during gradual reduction.
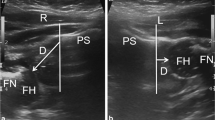
We enrolled 20 infants aged ≥ 12 months with unilateral DDH. Treatment comprised continuous traction, a hip-spica cast, and an abduction brace. MRI was performed before treatment, immediately after hip-spica cast placement, after cast removal, and at the end of the brace. We evaluated the acetabulum and femoral head morphology and joint concentricity.
The mean age was 25 months, and female sex and the left side were predominant. Before treatment, the acetabulum was small and shallow and the femoral head was spherically flat on the affected side. Immediately after the continuous traction, the affected acetabulum and femoral head were still smaller than the healthy/contralateral one. However, they improved to a deeper acetabulum and round femoral head. Intra-articular soft tissue (IAST) and femoral–acetabular distance (FAD) continuously decreased, indicating gradual improvement in joint concentricity. Deeper formation of the acetabulum and round shaping of the femoral head had occurred even in non-concentric reduction.
The shape and concentricity of the hip joint improved after treatment; however, the acetabulum and femoral head remained small. The deeper acetabulum and round femoral head were observed the non-concentric reduction before the concentric reduction was achieved. The continuous decrease in IAST and FAD indicates effective post-traction therapy.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others
Evaluation of the short-term curative effect of closed reduction in the treatment of developmental dysplasia of the hip based on three-dimensional magnetic resonance imaging finite element analysis
Use of ultrasonography to evaluate early outcomes of reduction in developmental dysplasia of the hip
The pubo-femoral distance decreases with pavlik harness treatment for developmental dysplasia of the hip in newborns, data availability.
The datasets analyzed in this study are available from the corresponding author on reasonable request.
Code Availability
Not applicable.
Vaquero-Picado, A., González-Morán, G., Garay, E. G., & Moraleda, L. (2019). Developmental dysplasia of the hip: Update of management. EFORT Open Reviews, 2019 (4), 548–556.
Article Google Scholar
Studer, K., Williams, N., Studer, P., Baker, M., Glynn, A., Foster, B. K., & Cundy, P. J. (2017). Obstacles to reduction in infantile developmental dysplasia of the hip. Journal of Children’s Orthopaedics, 2017 (11), 358–366.
Glorion, C. (2018). Surgical reduction of congenital hip dislocation. Orthopaedics and Traumatology, Surgery and Research, 2018 (104), S147–S157.
Meng, X., Yang, J., & Wang, Z. (2021). Magnetic resonance imaging follow-up can screen for soft tissue changes and evaluate the short-term prognosis of patients with developmental dysplasia of the hip after closed reduction. BMC Pediatrics, 21 (115), 2021.
Google Scholar
Rosenbaum, D. G., Servaes, S., Bogner, E. A., Jaramillo, D., & Mintz, D. N. (2016). MR imaging in postreduction assessment of developmental dysplasia of the hip: Goals and obstacles. Radiographics, 2016 (36), 840–854.
Kaneko, H., Kitoh, H., Kitamura, A., Sawamura, K., & Hattori, T. (2021). Docking phenomenon and subsequent acetabular development after gradual reduction using overhead traction for developmental dysplasia of the hip over six months of age. Journal of Children’s Orthopaedics, 2021 (15), 554–563.
Talathi, N. S., Chauvin, N. A., & Sankar, W. N. (2018). Docking of the femoral head following closed reduction for DDH: Does it really occur? Journal of Pediatric Orthopedics, 2018 (38), e440–e445.
Fukiage, K., Fukuda, A., Harada, Y., Suzuki, S., & Futami, T. (2015). Femoral head volume indicates the severity of developmental dysplasia of the hip by a method using three-dimensional magnetic resonance imaging. Journal of Pediatric Orthopedics, Part B, 2015 (24), 286–290.
Sankar, W. N., Neubuerger, C. O., & Moseley, C. F. (2010). Femoral head sphericity in untreated developmental dislocation of the hip. Journal of Pediatric Orthopedics, 2010 (30), 558–561.
Rosenberg, M. R., Walton, R., Rae, E. A., Bailey, S., & Nicol, R. O. (2017). Intra-articular dysplasia of the femoral head in developmental dysplasia of the hip. Journal of Pediatric Orthopedics, Part B, 2017 (26), 298–302.
Crowe, J. F., Mani, V. J., & Ranawat, C. S. (1979). Total hip replacement in congenital dislocation and dysplasia of the hip. Journal of Bone and Joint Surgery, American Volume, 1979 (61), 15–23.
Okuzu, Y., Goto, K., Kawata, T., So, K., Kuroda, Y., & Matsuda, S. (2017). The relationship between subluxation percentage of the femoroacetabular joint and acetabular width in Asian women with developmental dysplasia of the hip. Journal of Bone and Joint Surgery, American Volume, 99 (e31), 2017.
Fukiage, K., Futami, T., Ogi, Y., Harada, Y., Shimozono, F., Kashiwagi, N., Takase, T., & Suzuki, S. (2015). Ultrasound-guided gradual reduction using flexion and abduction continuous traction for developmental dysplasia of the hip: A new method of treatment. The Bone and Joint Journal, 2015 (97-B), 405–411.
Suzuki, S., & Yamamuro, T. (1990). Avascular necrosis in patients treated with the Pavlik harness for congenital dislocation of the hip. Journal of Bone and Joint Surgery, American Volume, 72 (1048), 1990.
Yamamuro, T., Chene, S. H., & Ito, T. (1975). A radiological study on the developmental of the hip joint in normal infants. The Japanese Orthopaedic Association, 49 , 421–439 ( in Japanese ).
Home—International Hip Dysplasia Institute. https://hipdysplasia.org/
Steppacher, S. D., Tannast, M., Werlen, S., & Siebenrock, K. A. (2008). Femoral morphology differs between deficient and excessive acetabular coverage. Clinical Orthopaedics and Related Research, 466 (782), 2008.
Zhou, W., Sankar, W. N., Zhang, F., Li, L., Zhang, L., & Zhao, Q. (2020). Evolution of concentricity after closed reduction in developmental dysplasia of the hip. The Bone and Joint Journal, 102-B , 618.
PubMed Google Scholar
Okano, K., Yamaguchi, K., Ninomiya, Y., Matsubayashi, S., Osaki, M., & Takahashi, K. (2013). Femoral head deformity and severity of acetabular dysplasia of the hip. The Bone and Joint Journal, 95-B , 1192.
CAS PubMed Google Scholar
Clohisy, J. C., Nunley, R. M., Carlisle, J. C., & Schoenecker, P. L. (2009). Incidence and characteristics of femoral deformities in the dysplastic hip. Clinical Orthopaedics and Related Research, 2009 (467), 128–134.
Chen, C., Doyle, S., Green, D., Blanco, J., Scher, D., Sink, E., & Dodwell, E. R. (2017). Presence of the Ossific nucleus and risk of osteonecrosis in the treatment of developmental dysplasia of the hip: A meta-analysis of cohort and case–control studies. Journal of Bone and Joint Surgery, American Volume, 2017 (99), 760–767.
Gardner, R. O., Bradley, C. S., Howard, A., Narayanan, U. G., Wedge, J. H., & Kelley, S. P. (2014). The incidence of avascular necrosis and the radiographic outcome following medial open reduction in children with developmental dysplasia of the hip: A systematic review. The Bone and Joint Journal, 2014 (96-B), 279–286.
Ogden, J. A. (1975). Treatment positions for congenital dysplasia of the hip. Journal of Pediatrics, 1975 (86), 732–734.
Slullitel, P. A., Coutu, D., Buttaro, M. A., Beaule, P. E., & Grammatopoulos, G. (2020). Hip preservation surgery and the acetabular fossa. Bone and Joint Research, 2020 (9), 857–869.
Download references
Author information
Authors and affiliations.
Department of Orthopaedic Surgery, Kyoto University Graduate School of Medicine, 54 Shogoin-Kawahara-cho, Sakyo-ku, Kyoto, 606-8507, Japan
Yaichiro Okuzu, Yutaka Kuroda, Toshiyuki Kawai, Yugo Morita & Shuichi Matsuda
Department of Paediatric Orthopaedics, Shiga Medical Center for Children, 5-7-30, Moriyama, Moriyama-City, Shiga Pref., 524-0022, Japan
Yaichiro Okuzu, Masako Tsukanaka & Tohru Futami
Department of Orthopaedic Surgery, Kindai University Hospital, 377-2 Ohno-Higashi, Osakasayama City, Osaka, 589-8511, Japan
You can also search for this author in PubMed Google Scholar
Contributions
YO, MT, TF were involved in conceptualization, data curation, formal analysis, investigation, and methodology. KG, YK, TK, YM, and SM were involved in project administration, supervision, validation. YO and MT were major contributors in the writing the original draft. KG, YK, TK, YM, TF, and SM reviewed and edited the original draft. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Yaichiro Okuzu .
Ethics declarations
Conflict of interest.
The authors declare that they have no relevant conflicts of interest.
Ethical Standards
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed Consent in Studies with Human Subjects
This retrospective study was approved by the local institutional review board and conducted in accordance with the World Medical Association Declaration of Helsinki. Written informed consent was waived in this study.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Okuzu, Y., Tsukanaka, M., Goto, K. et al. Morphological Changes and Concentricity of the Hip Joint During Gradual Reduction in Infants with Late-Detected Developmental Dysplasia of the Hip: A Retrospective Study. JOIO (2024). https://doi.org/10.1007/s43465-024-01184-6
Download citation
Received : 20 January 2024
Accepted : 06 May 2024
Published : 15 May 2024
DOI : https://doi.org/10.1007/s43465-024-01184-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Developmental dysplasia of the hip
- Joint concentricity
- Closed reduction
- Find a journal
- Publish with us
- Track your research

- Pet Supplies
- Health Supplies
- Hip & Joint Care

Enjoy fast, free delivery, exclusive deals, and award-winning movies & TV shows with Prime Try Prime and start saving today with fast, free delivery
Amazon Prime includes:
Fast, FREE Delivery is available to Prime members. To join, select "Try Amazon Prime and start saving today with Fast, FREE Delivery" below the Add to Cart button.
- Cardmembers earn 5% Back at Amazon.com with a Prime Credit Card.
- Unlimited Free Two-Day Delivery
- Streaming of thousands of movies and TV shows with limited ads on Prime Video.
- A Kindle book to borrow for free each month - with no due dates
- Listen to over 2 million songs and hundreds of playlists
- Unlimited photo storage with anywhere access
Important: Your credit card will NOT be charged when you start your free trial or if you cancel during the trial period. If you're happy with Amazon Prime, do nothing. At the end of the free trial, your membership will automatically upgrade to a monthly membership.
Image Unavailable

- To view this video download Flash Player

Senior Advanced Glucosamine Joint Supplement for Dogs - Hip & Joint Pain Relief - Small + Large Breeds -Omega-3 Fish Oil - Chondroitin, MSM- Mobility Soft Chews for Older Dogs - Bacon Flavor - 120Ct
Hemp + Lamb
120 Hemp + Glucosamine Chews
120 Hemp+Glucosamine Chews
120 Senior Advanced Treats (Pack of 1)
180 Senior Advanced Treats (Pack of 1)
(Value Pack) 240 Senior Advanced Treats
(Value Pack) 360 Senior Advanced Treats
Purchase options and add-ons
- Enhanced Senior Formula: This joint supplement for dogs is perfect for seniors, offering increased glucosamine and hyaluronic acid to promote your pet's active lifestyle and smooth movements. Our formula is a top choice among senior dog supplements.
- American Quality Assurance: Our glucosamine for dogs is proudly made in the USA, ensuring top-quality care for your pets with 24/7 customer support. Rescue your puppy's joints with our tasty bites: the ideal old dog supplement for healthier joints.
- Natural Joint Health for All: Ideal for every size, our senior dog joint supplement for large breed is just 2 grams, making it also perfect for small and medium pups, of all ages from adult to senior, older doggies.
- Vet-Approved Blend: This hip and joint supplement dogs love is full of glucosamine chondroitin MSM sulfate & vitamins for nutritional support that extends beyond typical dog treats. Ensure good mobility with our tasty hip and joint chews for dogs.
- Pain Relief Aid: Our glucosamine chondroitin for dogs formula provides max anti-inflammatory relief from joint pain in every chew. Give consistent joint health support for your puppy with our nutritious chewables, doubling as senior dog treats.
- Deliciously Healthy Chews: No more hassle with pills, tablets, or capsules; our dog hip and joint supplement is a soft, tasty, chewable treat every doggie loves, providing complete and advanced care in every tasty bite.
- Proven Excellence: For years, our dog glucosamine and chondroitin supplement for large dog has been advancing canine wellness. Leading as one of the best hips & joints supplements to help with joint pain relief and extend active years for old paws.
- Lasting Joint Care: Regular use of our joint support supplement for dogs ensures enduring bone strength & joint health for your pup. Plus, these dog glucosamine chews offer an extra boost to your furry buddy's daily routine.
Additional Details

Customer ratings by feature
Similar item to consider.

Frequently bought together

Top rated similar items

From the brand

Human Grade Pet Supplements
From skin and coat care to joint supplements, we at StrellaLab make no compromise when it comes to our buddies wellbeing.

Dogs are more than man’s best friend. They’re with us when we need them most, brringing a smile to our faces. So when it comes to caring for them, it’s only natural that we want only the best.
We launched StrellaLab to help our customers care for their dogs that bring them so much joy.
And in doing so, it is our way of saying "thank you" to all the dogs who’ve made us smile. They do so much for us, it’s our turn to give back to them.

Shop Functional Chews and more
Visit the Store

Shop Allergy, Skin&Coat Supps

Shop other treats and more
Product description.

Keep your Dog in Good Health, Active and Super Energetic with this Advanced Glucosamine Hip and Joint Supplement, formulated with max potency ingredients with adult and senior pets in mind.
This natural chewables is formulated with combination of all essential ingredients to provide extend care for joints: Double Glucosamine, MSM, Chondroitin Sulfate, Yucca Schidigera Extract, Omeg-3 Fish Oil, Calcium, Vitamins and Hyaluronic Acid
When used regularly, joints treatibles for dogs will effectively provide
- JOINT PAIN RELIEF : helps with inflammation, stiffness and pain releaf.
- SUPPORT FOR JOINTS AND HIPS : helps cushion and lubricate joints, promotes healthy joint structure and functioning, improves bones strength.
- INCREASE MOBILITY FOR SENIORS DOGS : helps with joint pain, improves general mobility and energy.
- POST-SURGERY RECOVERY: anti-inflammatory properties help with swelling, pain, stiffness, recovers from sprains, strains and broken bones.
- SYNERGISTIC BENEFITS : can be used in conjunction with regular medications with no interactions.
- NO SIDE EFFECTS: does not damage the liver, kidney or GI tract.
This dietary supplement can be administered daily as part of your doggie's diet. Soft chews for dogs are Made in USA, following strict quality standards, with all natural component for best possible product, to ensure the wellness of your pup from paw and tail to nose and ears. Our formula doesn't contain any soy, corn, dairy, sugar, hormones, artificial flavoring or preservatives. Joint chews for dogs are suitable for all ages, sizes of any breed from yorkies to large labs.
Product details
- Package Dimensions : 5.79 x 3.66 x 3.5 inches; 15.2 ounces
- Item model number : SL47ADVANCED
- Date First Available : June 27, 2022
- Manufacturer : STRELLALAB
- ASIN : B0B56G9DX7
- #23 in Dog Hip & Joint Care
Videos for this product

Click to play video

Strella Lab Or Paws A Day Glucosamine MSM?
Ashley Murray

Honest review of Paws A Day Glucosamine for Dogs Hip & Joint

Paws a Day vs. Strella Lab?
Chrystal Shiarla

Customer Review: One week using it
Customer Review: A pep in her step
amythecrafter
Looking for specific info?
Product information, important information, ingredients.
Glucosamine, Chondroitin, MSM, Omega-3, Omega-6, Yucca, Calcium Ascorbate (Vitamin C), Vitamin E, Hyaluronic Acid
Serve daily based on the dog's weight: up to 10lbs - 1 chews, 11-39lbs - 2chews, 40-79lbs - 3 chews, over 80lbs - 4chews. Please, strictly follow recommended servings, do not allow overfeeding. Consult with your veterinarian specialist if your pet has any medical conditions.
Legal Disclaimer
Up to 5% of the pets may not respond to the formula.
Compare with similar items
Customer reviews.
Customer Reviews, including Product Star Ratings help customers to learn more about the product and decide whether it is the right product for them.
To calculate the overall star rating and percentage breakdown by star, we don’t use a simple average. Instead, our system considers things like how recent a review is and if the reviewer bought the item on Amazon. It also analyzed reviews to verify trustworthiness.
Customers say
Customers like the pain relief, quality and performance of the animal nutritional supplement. For example, they mention it reduces discomfort, is highly effective and worth a try. They also appreciate the activeness, and ingredients. However, some complain about the smell.
AI-generated from the text of customer reviews
Customers like the quality of the animal nutritional supplement. They say it's highly effective, seems beneficial, and worth a try. Some customers also mention that the flavor smells really strong.
"...The 2 nuggets seems to work perfectly . I was also super happy that this hasn't upset his system since giving him these...." Read more
"...Much better energy levels and seems a lot happier . I most highly recommend!" Read more
"...Overall, I would say this supplement is worth a try if you want something to support your dog's joint health, but don't expect immediate miracles." Read more
" Really promising but the flavor smells really strong and our old dog started to flatly reject it after a couple of days...." Read more
Customers find the pain relief of the hemp chews to be great. They say it reduces discomfort, helps with arthritis, and allows their pet to walk more comfortably. They also say it has no upset stomach, itching, or other side effects.
"...There's been no upset tummy , itching or other side effects that you can sometimes see with supplements...." Read more
"...She started walking visibly better within 3 days . She is almost done with her first jar so ordering more." Read more
"...Look at that pain-free energy & excitement !..." Read more
"...separately, due to his other issues, but this does seem to reduce his discomfort at the end of the day, and he stays active." Read more
Customers are satisfied with the performance of the animal nutritional supplement. They mention that it helps improve mobility, and that their pets seem to struggle less with mobility.
"... Her mobility has greatly improved ." Read more
"...The price is great and our dog limps much less and has more energy. Will continue to order. I bought the bacon flavor and Diego likes it." Read more
"...to these TWO Products, I can see the change in her walk; Much Better with less stiffness " Read more
"...These really help with his daily movement ." Read more
Customers like the taste of the chews. They mention that their dogs love the taste and have no trouble eating them. They also like that it's chowder friendly and easy to crumble up into food.
"...I've been really happy with this one so far. I like that it's Chowder friendly while still pocket book friendly too...." Read more
"...My furry friend seems to enjoy the taste , making it easier for me to give it to him...." Read more
" My dog loved the flavor , extremely moist, my dog seems to be limping less and in a better mood.." Read more
"...I love how much this has helped him and he enjoys the little treat . They do not smell great but he inhales them when given to him...." Read more
Customers are satisfied with the ingredients in the animal nutritional supplement. They mention that it contains great, anti-inflammatory, and standard ingredients for pets and humans. They also appreciate the combination of Glucosamine and Hemp seed Oil, which is a very healthy product.
"I initially bought these treats because of the great ingredients . My problem is my dog absolutely hates them...." Read more
"...been getting the medicated bone treats but these have a higher dose of medicine in them . Hope she shows improvement in the next two weeks." Read more
"...The best part is that there is no medicine involved …it’s a healthy way to make him feel better!! And it worked fast too!..." Read more
"...take to have full benefit in pets, but so far the supplement seems harmless and is helping , clearly helped the neighbors dog...." Read more
Customers are satisfied with the activeness of the animal nutritional supplement. They mention that it gives them more energy and that it makes them more playful. Some say that the product has made a good change in their energy level.
"... Much better energy levels and seems a lot happier. I most highly recommend!" Read more
"...The price is great and our dog limps much less and has more energy . Will continue to order. I bought the bacon flavor and Diego likes it." Read more
" Great product made him way more energetic !!!" Read more
"...does seem to reduce his discomfort at the end of the day, and he stays active ." Read more
Customers are mixed about the value of the animal nutritional supplement. Some mention it's a great product for a good price, and well worth it. However, others say that it'd be a waste of money and doesn't work.
"...I've tried various types of supplements and this option provides the best bang for your buck in terms of number of nuggets...." Read more
"...up a lot, but like I said compared to other brands these are reasonably priced ...." Read more
"My babies love, love, love these! They're a bit pricey for the quantity , but it's worth it if they love them...." Read more
Customers are dissatisfied with the smell of the animal nutritional supplement. They mention that the flavor is really strong and the product stinks.
"Really promising but the flavor smells really strong and our old dog started to flatly reject it after a couple of days...." Read more
"...Yes, the smell isn’t my favorite , but he doesn’t seem to mind. And he’s a picky dog!!" Read more
"...These things also smell disgusting - my youngest child says they smell like broccoli farts and that seems pretty accurate. Lol" Read more
"... It doesn't have a hemp smell to me, but I think he picked up a bit of a smell that was something different then what he's known before...." Read more
Reviews with images

- Sort reviews by Top reviews Most recent Top reviews
Top reviews from the United States
There was a problem filtering reviews right now. please try again later..
Top reviews from other countries
- Amazon Newsletter
- About Amazon
- Accessibility
- Sustainability
- Press Center
- Investor Relations
- Amazon Devices
- Amazon Science
- Sell on Amazon
- Sell apps on Amazon
- Supply to Amazon
- Protect & Build Your Brand
- Become an Affiliate
- Become a Delivery Driver
- Start a Package Delivery Business
- Advertise Your Products
- Self-Publish with Us
- Become an Amazon Hub Partner
- › See More Ways to Make Money
- Amazon Visa
- Amazon Store Card
- Amazon Secured Card
- Amazon Business Card
- Shop with Points
- Credit Card Marketplace
- Reload Your Balance
- Amazon Currency Converter
- Your Account
- Your Orders
- Shipping Rates & Policies
- Amazon Prime
- Returns & Replacements
- Manage Your Content and Devices
- Recalls and Product Safety Alerts
- Conditions of Use
- Privacy Notice
- Consumer Health Data Privacy Disclosure
- Your Ads Privacy Choices

IMAGES
VIDEO
COMMENTS
Hip joint (Articulatio coxae) The hip joint is a ball and socket type of synovial joint that connects the pelvic girdle to the lower limb. In this joint, the head of the femur articulates with the acetabulum of the pelvic (hip) bone.. The hip joint is a multiaxial joint and permits a wide range of motion; flexion, extension, abduction, adduction, external rotation, internal rotation and ...
The hip joint is a ball and socket synovial joint, formed by an articulation between the pelvic acetabulum and the head of the femur.. It forms a connection from the lower limb to the pelvic girdle, and thus is designed for stability and weight-bearing - rather than a large range of movement.. In this article, we shall look at the anatomy of the hip joint - its articulating surfaces ...
Ligaments, Blood supply, Relations, Nerve supply, Movements, Muscles associated with movements and Clinical anatomy of the Hip joint.To get the notes of anat...
Your hip joint connects your torso (axial skeleton) to your lower legs. The function of your hip joint is to: Provide balance and support for your upper body. Move your upper leg. Hold your body weight. The ball-and-socket joint lets your upper leg move at 3 degrees so you can do the following movements: Flex. Extend.
The hip joint is normally very sturdy because of the fit between the femoral head and acetabulum as well as strong ligaments and muscles at the joint. All of the various components of the hip mechanism assist in the mobility of the joint. Damage to any single component can negatively affect range of motion and ability to bear weight on the joint.
The hip joint is surrounded by a large number of muscles. According to their function these are divided into six groups: (1) flexors, (2) extensors, (3) abductors, (4) adductors, (5) lateral rotators, (6) medial rotators. In this chapter the ana-tomical and kinesiological aspects of particular importance in orthopaedic medicine are discussed.
The hip joint is constructed and functions as follows: Hip bones. The hip is located where the top of the femur bone, or thighbone, fits into the pelvis. The femur bone is the longest bone in the body, extending from the knee to the hip. At the top of the femur bone is the greater trochanter, that boney knob that people often refer to as their ...
The hip joint is a ball-and-socket type joint and is formed where the thigh bone (femur) meets the pelvis. The femur has a ball-shaped head on its end that fits into a socket formed in the pelvis, called the acetabulum. Large ligaments, tendons, and muscles around the hip joint hold the bones (ball and socket) in place and keep it from dislocating.
PROM assessment in the hip joint is also used as part of the diagnostic criteria for hip osteoarthritis, where a marked decrease increases the likelihood of OA. During PROM assessment, it's important to compare the range of motion as well as the end-feel of the affected hip with the unaffected side. Muscle strains or sprains are common in the ...
FADIR test. hip Flexed to 90 deg, ADducted and Internally Rotated. positive test if patient has hip or groin pain. can suggest possible labral tear or FAI. FABER test (aka Patrick's test) hip Flexed to 90 deg, ABducted and Externally Rotated. positive test if patient has hip or back pain or ROM is limited.
The joint with the greatest range of motion is the ball-and-socket joint. At these joints, the rounded head of one bone (the ball) fits into the concave articulation (the socket) of the adjacent bone (see Figure 9.4.3f). The hip joint and the glenohumeral (shoulder) joint are the only ball-and-socket joints of the body.
Stair Machine. Pushing down phase (extension) GSSB. Gluteus maximus, Biceps femoris, semimembranosus, Semitendinosus (concentric) Return phase (flexion) GSSB. Biceps femoris, Semimembranosus, Semitendinosus, Gluteus maximus (eccentric) Study with Quizlet and memorize flashcards containing terms like Push up, Squat, Dead lift and more.
A multiaxial joint, such as the shoulder or hip joint, allows for three planes of motions. Review Questions . Critical Thinking Questions. 1. Define how joints are classified based on function. Describe and give an example for each functional type of joint. 2. Explain how degree of mobility is related to joint strength.
Perform any technique of your choice showed in the hip joint chapters given above and record a video of yourself doing the technique. The video should not be more than 40-60 seconds. So, prepare your model/patient and your position before starting the recording. Make sure the angle of recording is appropriate for instructor to understand […]
Study with Quizlet and memorize flashcards containing terms like Proximal hamstring release., Partial hip replacement with bipolar arthroplasty to treat right hip fracture., Removal of a foreign body deep in the left thigh. and more.
Running head: Written Assignment Unit 2 (Jones, 2019). The hip joint is a ball-and-socket synovial type of joint, wherein the ball is the femoral head of the femur and the socket, which is acetabulum of the pelvis (Jones, 2019). It is the articulation of the pelvis with the femur where the axial skeleton is connected with the lower extremity. Adult coxae or hip bone is fusio of three (3) bones ...
KINES 3092 Assignment 5: Hip joint exercise movement analysis -After analyzing each of the exercises in the hip joint movement analysis chart, break each into two primary movement phases such as a lifting phase and lowering phase. -For each phase, determine which hip joint movements occur, and then list the hip joint muscles responsible for ...
Perform any technique of your choice showed in the hip joint chapters given above and record a video of yourself doing the technique. The video should not be more than 40-60 seconds. So, prepare your model/patient and your position before starting the recording. Make sure the angle of recording is appropriate for instructor to understand […]
Background The relationship between hip morphological changes and joint concentricity in infants with late-detected developmental dysplasia of the hip (DDH) treated with gradual reduction remains unclear. Therefore, we investigated hip morphological changes and concentricity in infants with late-detected unilateral DDH using magnetic resonance imaging (MRI) during gradual reduction. Methods We ...
Vet-Approved Blend: This hip and joint supplement dogs love is full of glucosamine chondroitin MSM sulfate & vitamins for nutritional support that extends beyond typical dog treats. Ensure good mobility with our tasty hip and joint chews for dogs. Pain Relief Aid: Our glucosamine chondroitin for dogs formula provides max anti-inflammatory ...