- Print this article

The State of Research in Veterans Studies: A Systematic Literature Review
- Janani Chandrasekar
- Janani Chandrasekar , San Jose State University, United States
New areas of research on veterans are emerging as the field of veterans studies develops and grows. Yet gaps remain in interdisciplinary research efforts on veterans. The research available across disciplines is still too fragmented to coalesce into a full-fledged field of veteran studies, as other categorical, area, and identity fields of study have done so. By surveying research literature of multiple disciplines used in the curricula of higher education-level veteran study programs, this article presents a thematic and integrative review of the state of research contributing to the growing field of veterans studies. Discussion follows about research emerging from within contributing disciplines, the themes across disciplines, and comments on the need for further research as the field of veterans studies continues to mature.
- Page/Article: 46–65
- DOI: 10.21061/jvs.v6i2.191
- Accepted on 13 Sep 2020
- Published on 12 Oct 2020
- Peer Reviewed
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 75, NO. 4 CURRENT ISSUE pp.307-398
- March 01, 2024 | VOL. 75, NO. 3 pp.203-304
- February 01, 2024 | VOL. 75, NO. 2 pp.107-201
- January 01, 2024 | VOL. 75, NO. 1 pp.1-71
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Mental Health Care Use Among U.S. Military Veterans: Results From the 2019–2020 National Health and Resilience in Veterans Study
- Alexander C. Kline , Ph.D. ,
- Kaitlyn E. Panza , Ph.D. ,
- Brandon Nichter , Ph.D. ,
- Jack Tsai , Ph.D. ,
- Ilan Harpaz-Rotem , Ph.D. ,
- Sonya B. Norman , Ph.D. ,
- Robert H. Pietrzak , Ph.D., M.P.H.
https://orcid.org/0000-0001-7420-7547
Search for more papers by this author
https://orcid.org/0000-0002-6066-9406
Psychiatric and substance use disorders are prevalent among U.S. military veterans, yet many veterans do not engage in treatment. The authors examined characteristics associated with use of mental health care in a nationally representative veteran sample.
Using 2019–2020 data from the National Health and Resilience in Veterans Study (N=4,069), the authors examined predisposing, enabling, and need factors and perceived barriers to care as correlates of mental health care utilization (psychotherapy, counseling, or pharmacotherapy). Hierarchical logistic regression and relative importance analyses were used.
Among all veterans, 433 (weighted prevalence, 12%) reported current use of mental health care. Among 924 (26%) veterans with a probable mental or substance use disorder, less than a third (weighted prevalence, 27%) reported care utilization. Mental dysfunction (24%), posttraumatic stress disorder symptom severity (18%), using the U.S. Department of Veterans Affairs as primary health care provider (14%), sleep disorder (12%), and grit (i.e., trait perseverance including decision and commitment to address one’s needs on one’s own; 7%) explained most of the variance in mental health care utilization in this subsample. Grit moderated the relationship between mental dysfunction and use of care; among veterans with high mental dysfunction, those with high grit (23%) were less likely to use services than were those with low grit (53%).
Conclusions:
A minority of U.S. veterans engaged in mental health care. Less stigmatized need factors (e.g., functioning and sleep difficulties) may facilitate engagement. The relationship between protective and need factors may help inform understanding of veterans’ decision making regarding treatment seeking and outreach efforts.
Only 12% of all veterans in the full sample and 27% of those who screened positive for mental or substance use disorder reported current mental health treatment utilization.
Need factors, such as mental and cognitive functioning, posttraumatic stress disorder symptoms, and sleep-related difficulties, were most predictive of utilization.
Perceived stigma and barriers to care explained minimal variance in use of mental health care but were endorsed by a meaningful number of veterans.
Among veterans with lower mental functioning, those with high grit were substantially less likely to use services than were those with low grit, suggesting that protective factors may influence the relationship between need factors and care utilization.
Among U.S. military veterans, mental and substance use disorders are prevalent, impairing, and often chronic without treatment ( 1 , 2 ). Although evidence-based interventions are often effective ( 3 – 6 ), up to one-third of veterans with mental disorders do not receive treatment ( 7 , 8 ). Further, even when veterans ultimately engage in services, delayed treatment initiation is common, with one nationally representative study estimating median times of 16 and 2.5 years for pre- and post-9/11 veterans, respectively, between onset of diagnosis and treatment for posttraumatic stress disorder (PTSD) ( 9 ). To engage more veterans in treatment in a timely manner, it is critical to identify determinants and correlates of mental health care utilization.
Treatment utilization research among veterans has primarily focused on psychotherapy for PTSD ( 10 ). Less is known about other disorders, such as depression, anxiety, and substance use disorders, which frequently co-occur with PTSD and each other ( 2 , 11 , 12 ). Additionally, research has primarily examined veterans in the Veterans Health Administration (VHA) ( 10 ), yet most veterans receive health care outside the VHA ( 13 ). Only one in five veterans use the U.S. Department of Veterans Affairs (VA) for primary health care ( 2 , 13 , 14 ), and many maintain other health care coverage ( 15 ). Consequently, the prevalence and correlates of mental health care utilization in the population of U.S. veterans remain unknown.
A widely used model to understand use of health care is the behavioral model of health service utilization (BMHSU) ( 16 ), positing that use is determined by predisposing, enabling, and need factors. Predisposing characteristics, such as nonminority ethnic-racial status ( 17 , 18 ) and trauma or combat exposure ( 18 , 19 ), have been linked to higher rates of health care utilization among veterans. Enabling factors, such as unemployment ( 19 ) or closer proximity to services ( 20 ), may also facilitate use. Need factors have been most robustly associated with use ( 19 , 20 ), particularly greater severity of PTSD or depressive symptoms ( 17 , 20 – 23 ), medical conditions ( 19 ), and screening positive for mental or substance use disorders and comorbid psychiatric conditions ( 20 , 24 , 25 ). Researchers have also frequently studied factors related to perceived barriers to care, such as stigma, pragmatic barriers, and treatment-related beliefs. Among veterans, more positive treatment beliefs ( 21 , 24 , 26 , 27 ) and lower perceived stigma ( 14 , 24 , 26 ) have been linked to greater likelihood of mental health care utilization.
Although studies of need factors have often emphasized psychological distress and impairment, we have also examined medical conditions and insomnia, given their associations with mental health ( 28 ), possible links to health care utilization ( 24 , 29 ), and the older age of the veteran population. Further, we have considered the role of protective psychosocial characteristics (e.g., grit, defined as trait perseverance that extends to one’s decision or commitment to address mental health needs on one’s own; dispositional optimism; and purpose in life) as possible need factors, because these factors could inhibit or facilitate use by affecting an individual’s perceived need for services. Given the links of these factors to lower psychological distress ( 30 ), individuals scoring higher on these characteristics may perceive an ability to manage distress on their own, in turn dissuading them from seeking care ( 21 ). Furthermore, these traits may moderate the relation between need-based correlates and mental health care utilization; for example, among individuals with high distress, those with higher grit may be less likely to engage in treatment.
In this study, we applied a BMHSU-informed model of health care utilization that included predisposing, enabling, and need factors and perceived barriers to care to examine the prevalence and correlates of current use of mental health care (i.e., counseling, psychotherapy, or medication) in a nationally representative sample of veterans and a subsample of those with a probable current mental disorder (e.g., PTSD, major depressive disorder, or generalized anxiety disorder [GAD]) or substance use disorder (e.g., alcohol use or drug use disorder). Veterans with a probable mental or substance use disorder were grouped together, given high diagnostic overlap among these disorders and because they frequently co-occur among U.S. veterans ( 28 , 31 ). We examined correlates of care utilization in the full sample given that functional impairment or distress occur in subclinical or subthreshold conditions ( 32 , 33 ) and to adhere to previous methods in utilization literature ( 24 ). We hypothesized that need factors ( 10 , 17 , 20 – 22 , 24 , 25 ) and fewer barriers to care ( 14 , 21 , 24 , 27 ) would be most strongly associated with use.
Participants, Procedures, and Variables
Data were drawn from the 2019–2020 National Health and Resilience Veterans Study, a nationally representative survey of 4,069 U.S. military veterans. The human subjects subcommittee of the VA Connecticut Healthcare System approved the study protocol, and all participants provided informed consent. Table S1 in an online supplement to this article describes the study variables, which included predisposing, enabling, and need characteristics and perceived barriers to care.
Data Analyses
Analyses proceeded in five steps. First, exploratory factor analyses combined variables assessing common constructs into one variable (e.g., functional difficulties). Second, in the full sample and a subsample of veterans with a probable mental or substance use disorder (N=924), independent-samples t tests and chi-square analyses compared characteristics of veterans who were engaged in mental health care with those of veterans who were not engaged. Third, hierarchical logistic regression analyses identified independent correlates of care utilization; we entered variables into sequential blocks by using the BMHSU-informed model of health care to determine specific variance explained by each variable cluster. After identifying significant correlates, we incorporated an interaction term to evaluate whether the strongest protective factor moderated the association between the strongest negative correlate and use of health care. Statistics from the final, comprehensive models with each block of variables are reported in Results. Fourth, post hoc analyses of multicomponent variables (e.g., psychological distress and functional difficulties) were conducted to specify features that drove associations with use. Fifth, relative importance analyses ( 34 ) determined relative contributions of each significant variable in predicting use after accounting for intercorrelations among independent variables.
The mean±SD age of the participants was 62±16 years (range 22–99), and 90% (N=3,564) were male (percentages were calculated with poststratification weighting). Most participants were non-Hispanic White (N=3,318, 78%), with 11% (N=296) being non-Hispanic Black, 7% (N=307) Hispanic, and 4% (N=148) other or mixed race. Veterans of all branches were represented (Army, 47% [N=2,707]; Navy, 20% [N=879]; Air Force, 19% [N=955]; Marines, 6% [N=260]; and National Guard, Reserves, or Coast Guard, 8% [N=409]). Overall, 35% (N=1,353) were combat veterans, and 36% (N=1,476) had served for ≥10 years. Nearly all (N=3,989, 98%) reported having health insurance such as Medicare (N=2,399, 47%) or through a current or former employer (N=1,447, 41%) or the VA (N=1,336, 33%); 21% (N=790) reported the VA as their primary source of health care. (Details regarding data collection are presented in the online supplement .)
In the full sample (N=4,069), 433 veterans (weighted prevalence, 12%, 95% confidence interval [CI]=11%–13%) reported current engagement in mental health care, including psychotherapy or counseling (N=243, weighted prevalence, 7%, 95% CI=6%–8%), pharmacotherapy (N=383, weighted prevalence, 10%, 95% CI=9%–11%), or both (N=193, weighted prevalence, 6%, 95% CI=5%–6%). In total, 924 (26%) veterans screened positive on one or more of the respective self-report measures of PTSD, major depressive disorder, GAD, alcohol use disorder, or drug use disorder. Most of these veterans (N=685, weighted prevalence, 73%, 95% CI=71%–76%) reported no current engagement in treatment, and 157 (weighted prevalence, 19%, 95% CI=17%–21%) reported receiving psychotherapy or counseling, 211 (weighted prevalence, 23%, 95% CI=21%–26%) pharmacotherapy, and 129 (weighted prevalence, 16%, 95% CI=13%–18%) both types of treatments.
In the full sample, 10% (N=359) had alcohol use disorder, 9% (N=291) major depressive disorder, 9% (N=313) drug use disorder, 8% (N=229) GAD, and 7% (N=214) PTSD. In the subsample of veterans with a probable mental or substance use disorder (N=924), 40% (N=360) had alcohol use disorder, 37% (N=314) drug use disorder, 33% (N=292) major depressive disorder, 30% (N=232) GAD, and 25% (N=217) PTSD; 62% (N=612) had one probable disorder, 21% (N=190) had two, 10% (N=81) had three, 6% (N=34) had four, and 1% (N=7) had all five.
Bivariate analyses for the two samples are shown in Tables S2 and S3 in the online supplement . Tables 1 and 2 present results of multivariable regression analyses examining correlates of current health care utilization in the full sample and in the subsample with a probable mental or substance use disorder, respectively. Collinearity diagnostics did not reveal multicollinearity in either model, with variance inflation factors for all variables <5. Results from parallel analyses in a subset of veterans (N=3,007, 74%) unlikely to have a mental or substance use disorder per screening measures are available in the online supplement .
a ACES, Adverse Childhood Experiences Scale; ADL, activities of daily living; IADL, instrumental activities of daily living; VA, U.S. Department of Veterans Affairs.
b Cumulative variance is explained in the full multivariable model (Nagelkerke R 2 =0.44).
c Post hoc analyses indicated that the association between psychological distress and mental health treatment use was driven by posttraumatic stress disorder symptoms (odds ratio [OR]=1.02, 95% confidence interval [CI]=1.01–1.04, p<0.001) but not by depression or generalized anxiety disorder symptoms (p>0.11).
d Post hoc analyses indicated that the association between medical conditions and mental health treatment use was driven by sleep disorder (OR=2.51, 95% CI=1.88–3.35, p<0.001), high cholesterol (OR=1.95, 95% CI=1.46–2.60, p<0.001), chronic pain (OR=1.61, 95% CI=1.22–2.14, p=0.001), hypertension (OR=1.38, 95% CI=1.02–1.86, p=0.037), and no previous heart attack (OR=0.36, 95% CI=0.19–0.68, p=0.002) but not by any other conditions (p>0.08).
e Post hoc analyses indicated that the association between functioning and mental health treatment use was driven by worse mental (OR=0.93, 95% CI=0.91–0.96, p<0.001) and cognitive (OR=0.89, 95% CI=0.97–0.99, p=0.009) functioning and better physical functioning (OR=1.02, 95% CI=1.01–1.03, p=0.044) but not by psychosocial functioning (p=0.20).
TABLE 1. Associations between current mental health care utilization and predisposing, enabling, and need factors and barriers to care among U.S. military veterans (N=4,069) a
a Veterans in his subgroup had screened positive for current posttraumatic stress, major depressive, generalized anxiety, alcohol use, or drug use disorder. ACES, Adverse Childhood Experiences Scale; ADL, activities of daily living; IADL, instrumental activities of daily living; VA, U.S. Department of Veterans Affairs.
c Post hoc analyses indicated that the association between psychological distress and mental health treatment utilization was driven by PTSD symptoms (odds ratio [OR]=1.01, 95% confidence interval [CI]=1.01–1.03, p=0.048) but not by depression or generalized anxiety disorder symptoms (p>0.06).
d Post hoc analyses indicated that the association between number of medical conditions and mental health treatment utilization was primarily driven by sleep disorder (OR=2.50, 95% CI=1.63–3.83, p<0.001), previous concussion or mild traumatic brain injury (OR=2.03, 95% CI=1.16–3.58, p<0.001), high cholesterol (OR=2.20, 95% CI=1.44–3.36, p<0.001), and no previous heart attack (OR=0.28, 95% CI=0.11–0.72, p=0.008) but not by any other conditions (p>0.10).
e Post hoc analyses indicated that the association between functioning and mental health treatment use was driven by worse mental functioning (OR=0.93, 95% CI=0.90–0.95, p<0.001) and better physical functioning (OR=1.02, 95% CI=1.01–1.05, p=0.030) but not by changes in cognitive or psychosocial functioning (p>0.19).
TABLE 2. Associations between current mental health care utilization and predisposing, enabling, and need factors and barriers to care among U.S. military veterans who screened positive for a mental or substance use disorder (N=924) a
Relative importance analysis in the full sample revealed that mental dysfunction (i.e., emotional difficulties, such as anxiety and depression and their impact on social and occupational functioning; 19% relative variance explained [RVE]) and cognitive dysfunction (12% RVE), PTSD symptom severity (12% RVE), chronic pain (9% RVE), and grit (6% RVE) accounted for most of the explained variance in health care utilization. In the subsample, mental dysfunction (24% RVE), PTSD symptom severity (18% RVE), the VA as primary source of health care (14% RVE), sleep disorder (12% RVE), grit (7% RVE), and history of suicide attempt (6% RVE) accounted for most of the explained variance (see Figures S1 and S2 in the online supplement ).
To examine whether the strongest protective correlate—grit—moderated the effect of the strongest need correlate—mental dysfunction—on use of care, we incorporated a mental functioning × grit interaction term into regression models. This interaction was statistically significant in both the full sample (Wald χ 2 =4.82, p=0.028; odds ratio [OR]=0.88, 95% CI=0.78–0.99) and the subsample (Wald χ 2 =7.94, p=0.005; OR=0.80, 95% CI=0.68–0.93). Among veterans with high mental dysfunction, those with high grit (23%) were significantly less likely to use services than were those with low grit (53%) ( Figure 1 ).
FIGURE 1. Probability of mental health treatment among veterans, by mental functioning tertile and level of grit a
a A: full sample of veterans (N=4,069); B: subsample of veterans screening positive for mental or substance use disorder (N=924). Mental functioning tertiles were computed with mental component summary scores from the Short Form–8 Health Survey. The score range for tertile 1 was 8–52 (median=46); tertile 2, 53–58 (median=55); and tertile 3, 59–68 (median=59). Possible scores range from 0 to 100, with higher scores indicating better functioning. A median split procedure was used to stratify groups into low- and high-grit groups; the score range was 1.1–3.7 (median=3.4) for the low-grit group and 3.9–5.0 (median=4.1) for the high-grit group. Error bars show 95% confidence intervals. −1 SD and +1 SD refer to one standard deviation below and above the mean for grit, respectively.
In line with literature indicating underuse of mental health care among veterans ( 24 ), we found that only 27% of U.S. veterans with a probable mental or substance use disorder and 12% of U.S. veterans in general were currently engaged in mental health treatment. A key implication of this finding is that available treatments—although often effective—may not be reaching most veterans who could benefit from them. Correlates were generally consistent with literature reporting that need factors are most robustly associated with mental health care utilization ( 10 , 17 , 19 – 22 , 24 , 25 ). However, previous studies have rarely examined need factors that may be protective. This study therefore extends this literature, showing that protective psychosocial factors and their interaction with more commonly studied need characteristics may shed additional light on veterans’ health services use and could help inform strategies to engage veterans in treatment.
As hypothesized, need factors emerged as the strongest correlates of mental health care utilization among veterans. Psychological distress—indexed with a composite variable of depressive, anxiety, and PTSD symptoms—was strongly associated with use of care, primarily driven by PTSD symptoms. Indices of cognitive dysfunction and mental dysfunction were also salient contributors, accounting for nearly a third of the explained variance in care utilization. Previous findings suggest that functional impairment accompanying psychological distress may motivate use of mental health services ( 35 ) and underscore the importance of assessing functioning in addition to psychiatric symptoms to most accurately gauge veterans’ mental health care needs. In the full sample, a diagnosis of a substance use disorder was not associated with mental health care utilization, suggesting that the reasons underlying treatment seeking may differ between individuals with mental or substance use disorders. It is also possible that individuals with a substance use disorder sought treatment through 12-step programs rather than psychotherapy, counseling, or medication.
The relationship between functioning and use of health care was further clarified when considered in the context of protective psychosocial factors. Specifically, grit was negatively associated with use and also moderated the relationship between mental functioning and utilization. Grit is positively correlated with constructs such as self-efficacy and conscientiousness ( 36 , 37 ), suggesting that this factor may reflect individuals’ self-efficacy and belief in their ability to handle mental health difficulties on their own. These traits are often considered assets or strengths (e.g., self-reliance and perseverance), but in the context of help seeking could also be a barrier (e.g., reluctance to seek help). Protective factors were included as need factors within the BMHSU framework, given that they may affect perceived need for services. Our results suggest nuanced relationships between service use and need and protective factors that merit attention.
Veterans who reported higher levels of mental dysfunction and scored lower on a measure of grit were particularly likely to be engaged in treatment, suggesting that these individuals may reflect a particularly distressed subgroup of veterans. Conversely, veterans reporting similar levels of mental dysfunction who scored highly on grit were less likely to be engaged in treatment. This pattern suggests that higher levels of grit among veterans may reduce their likelihood of seeking treatment, even in the presence of clinically meaningful distress. Clinically, our results highlight the potential utility of promoting grit once veterans begin treatment (i.e., leveraging grit to bolster treatment motivation and engagement and emphasizing goal setting). For veterans reporting greater functional impairment and lower protective factors, interventions designed to cultivate personal strengths ( 38 )—in addition to mitigating symptoms and functional difficulties—may be beneficial for boosting treatment engagement and response. Notably, of the four protective factors examined (i.e., resilience, purpose in life, grit, and optimism), only grit was strongly associated with mental health care utilization in the subsample. Our findings therefore need replication, and additional research is needed regarding protective factors, their links to distress, and how these factors affect treatment engagement.
Other need factors linked to greater likelihood of use in both samples included a history of attempted suicide, sleep-related difficulties, and medical burden. Although it is encouraging that veterans with suicide attempt histories were more likely to be engaged in treatment, continued efforts in suicide prevention ( 39 ) are critically needed. Suicide rates among veterans have increased in the past two decades ( 40 ), and 60% of veterans endorsing suicidal ideation are not engaged in mental health treatment ( 26 ). Regarding sleep-related difficulties and medical burden, screening veterans for mental health and substance use and connecting them with needed treatment via integration with primary care and nonmental health clinics are effective methods for increasing care access and boosting use ( 41 , 42 ) and have been increasingly adopted by the VA and other health care settings ( 43 , 44 ). Results suggest that health care systems should continue to leverage this overlap between medical, sleep, and mental health difficulties, because assessment of less stigmatized need factors (i.e., sleep and general medical health) may help identify veterans in need of mental health care. Insomnia treatment, for example, is preferred to PTSD or depression interventions among veterans ( 45 ) and has been theorized as a possible gateway for connecting veterans with needed mental health services ( 45 , 46 ). The broad array of need factors also highlights the significance of interdisciplinary, integrative care, which has been increasingly adopted within the VA and has effectively increased veterans’ mental health care utilization ( 47 ).
Enabling factors were generally unrelated to use of mental health care, a result that aligns with literature indicating that need factors are more consistent and stronger correlates of use. Aside from use of the VA as primary source of health care, only unemployment was linked to use in the full sample, and no other enabling characteristics emerged as correlates in the subsample of veterans with a probable current mental or substance use disorder. Employment was negatively associated with use, possibly because employed veterans have less functional or occupational impairment, have less distress due to financial problems, or have work schedules that interfere with treatment. In both samples, health care users were more likely than nonusers to report the VA as their primary source of health care. Veterans who use the VA tend to have higher rates of psychiatric symptoms, suicidality, trauma exposure, and functional impairment ( 13 ); however, the link between primary VA use and care utilization remained significant even when these factors were controlled for. Primary VA care may thus reflect an enabling factor that facilitates access to mental health care services and increases veterans’ likelihood of using them. Further research should examine specific facets of VA care that may promote mental health care engagement (e.g., no or minimal treatment cost, integrated primary and mental health care, routine mental health screenings, and increased telehealth availability), which may also promote mental health care engagement in non-VA systems.
Predisposing characteristics associated with health care utilization were female sex and deployments and, in the full sample, younger age. This finding highlights the potential importance of tailoring strategies to promote utilization among symptomatic veterans who are male, combat-exposed, and older. Outside the BMHSU framework, perceived stigma and barriers to care explained relatively little variance in utilization. Nevertheless, in the symptomatic subsample, endorsement of “it would be embarrassing to seek treatment” was associated with a highly reduced odds of use, whereas in the full sample, endorsements of “it would harm my reputation” and “mental health care does not work” also were associated with significantly reduced odds of use. Although stigma related to mental health treatment has decreased among U.S. military members in recent years ( 48 ), these findings suggest that continued efforts to combat stigma, such as psychoeducation and promotion of mental health literacy, may help motivate treatment engagement. Fortunately, beliefs regarding stigma are modifiable and unrelated to use once veterans have attended even a single mental health visit ( 22 ).
The results of this study should be interpreted in light of several limitations. First, its cross-sectional design precluded examining how changes in correlates over time may affect use of care. Second, screening instruments, rather than semistructured clinical interviews, were used to identify probable mental and substance use disorders. Although the results obtained with the scales we used are known to correlate strongly with results from gold-standard diagnostic interviews ( 49 , 50 ), screening via self-report measures may have inflated estimates of disorder prevalence. Third, because the sample comprised primarily older White male veterans, it is important to understand whether the results generalize to younger, more diverse veterans. Relatedly, although the sample was nationally representative, the participation rate from the larger panel of veterans was only 52%. Although poststratification weights enhanced generalizability of our results to the broader U.S. veteran population, it is possible that more symptomatic veterans may have been less represented in this sample, and homeless and institutionalized veterans were excluded altogether. Fourth, psychotherapy and medication categories were combined because only a small number of veterans engaged in psychotherapy only. This data handling may have limited the specificity of our findings, because correlates of medication and psychotherapy use may differ. Fifth, although we adhered to established theory and literature in classifying variables, some variables could have been placed in more than one cluster (e.g., activities of daily living could be an enabling or need factor). Finally, programs such as Alcoholics Anonymous and Narcotics Anonymous were not formally assessed and may affect utilization estimates.
Notwithstanding these limitations, strengths of this study included examination of a broad constellation of variables associated with mental health care utilization in a contemporary, nationally representative sample of U.S. veterans. Additionally, correlates examined in this study, including novel indicators of use (i.e., protective factors), explained 44%−50% of the variance in care utilization, thus providing insight into key correlates of use in this population.
Conclusions
Mental health treatments are often not reaching veterans who need them, a deficiency that may be especially pronounced among veterans who are distressed but also have high numbers of protective factors. Our findings underscore the importance for continued research on strategies to reduce stigma and negative beliefs and promote mental health literacy among veterans, particularly regarding the availability of evidence-based mental health interventions. Future work should also more precisely ascertain the impact of protective factors among veterans with mental and substance use disorders; specifically, our understanding of treatment seeking among veterans will be improved by deciphering whether protective factors reflect veterans’ self-reliance and capacity to manage distress on their own or whether they reflect a barrier to seeking help. Better understanding protective factors and their links to distress and impairment may help identify additional veterans who could benefit from care. Another future direction is to evaluate and disseminate self-help tools such as mobile apps and online programs (e.g., PTSD Coach, Virtual Hope Box, and VetChange), which may be treatment options ideal for veterans with high levels of both distress and protective factors and who want to manage mental health and substance use difficulties on their own.
The National Health and Resilience in Veterans Study is supported by the VA National Center for Posttraumatic Stress Disorder.
The authors report no financial relationships with commercial interests.
The authors thank the veterans who participated in the National Health and Resilience in Veterans Study and Steven M. Southwick, M.D., and John H. Krystal, M.D., for their critical input into the design of this study.
1 Fuehrlein BS, Mota N, Arias AJ, et al. : The burden of alcohol use disorders in US military veterans: results from the National Health and Resilience in Veterans Study . Addiction 2016 ; 111:1786–1794 Crossref , Medline , Google Scholar
2 Wisco BE, Marx BP, Wolf EJ, et al. : Posttraumatic stress disorder in the US veteran population: results from the National Health and Resilience in Veterans Study . J Clin Psychiatry 2014 ; 75:1338–1346 Crossref , Medline , Google Scholar
3 Olatunji BO, Cisler JM, Deacon BJ : Efficacy of cognitive behavioral therapy for anxiety disorders: a review of meta-analytic findings . Psychiatr Clin North Am 2010 ; 33:557–577 Crossref , Medline , Google Scholar
4 Karlin BE, Brown GK, Trockel M, et al. : National dissemination of cognitive behavioral therapy for depression in the Department of Veterans Affairs health care system: therapist and patient-level outcomes . J Consult Clin Psychol 2012 ; 80:707–718 Crossref , Medline , Google Scholar
5 Ray LA, Meredith LR, Kiluk BD, et al. : Combined pharmacotherapy and cognitive behavioral therapy for adults with alcohol or substance use disorders: a systematic review and meta-analysis . JAMA Netw Open 2020 ; 3:e208279 Crossref , Medline , Google Scholar
6 Lewis C, Roberts NP, Andrew M, et al. : Psychological therapies for post-traumatic stress disorder in adults: systematic review and meta-analysis . Eur J Psychotraumatol 2020 ; 11:1729633 Crossref , Medline , Google Scholar
7 Burnett-Zeigler I, Zivin K, Ilgen M, et al. : Depression treatment in older adult veterans . Am J Geriatr Psychiatry 2012 ; 20:228–238 Crossref , Medline , Google Scholar
8 Smith NB, Cook JM, Pietrzak R, et al. : Mental health treatment for older veterans newly diagnosed with PTSD: a national investigation . Am J Geriatr Psychiatry 2016 ; 24:201–212 Crossref , Medline , Google Scholar
9 Goldberg SB, Simpson TL, Lehavot K, et al. : Mental health treatment delay: a comparison among civilians and veterans of different service eras . Psychiatr Serv 2019 ; 70:358–366 Link , Google Scholar
10 Johnson EM, Possemato K : Correlates and predictors of mental health care utilization for veterans with PTSD: a systematic review . Psychol Trauma 2019 ; 11:851–860 Crossref , Medline , Google Scholar
11 Rytwinski NK, Scur MD, Feeny NC, et al. : The co-occurrence of major depressive disorder among individuals with posttraumatic stress disorder: a meta-analysis . J Trauma Stress 2013 ; 26:299–309 Crossref , Medline , Google Scholar
12 Seal KH, Cohen G, Waldrop A, et al. : Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: implications for screening, diagnosis and treatment . Drug Alcohol Depend 2011 ; 116:93–101 Crossref , Medline , Google Scholar
13 Meffert BN, Morabito DM, Sawicki DA, et al. : US veterans who do and do not utilize VA healthcare services: demographic, military, medical, and psychosocial characteristics . Prim Care Companion CNS Disord 2019 ; 21:18m02350 Crossref , Medline , Google Scholar
14 Tsai J, Mota NP, Pietrzak RH : US female veterans who do and do not rely on VA health care: needs and barriers to mental health treatment . Psychiatr Serv 2015 ; 66:1200–1206 Link , Google Scholar
15 Shen Y, Hendricks A, Zhang S, et al. : VHA enrollees’ health care coverage and use of care . Med Care Res Rev 2003 ; 60:253–267 Crossref , Medline , Google Scholar
16 Andersen RM : Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav 1995 ; 36:1–10 Crossref , Medline , Google Scholar
17 Doran JM, Pietrzak RH, Hoff R, et al. : Psychotherapy utilization and retention in a national sample of veterans with PTSD . J Clin Psychol 2017 ; 73:1259–1279 Crossref , Medline , Google Scholar
18 Hankin CS, Spiro A 3rd, Miller DR, et al. : Mental disorders and mental health treatment among US Department of Veterans Affairs outpatients: the Veterans Health Study . Am J Psychiatry 1999 ; 156:1924–1930 Abstract , Google Scholar
19 Elhai JD, Grubaugh AL, Richardson JD, et al. : Outpatient medical and mental healthcare utilization models among military veterans: results from the 2001 National Survey of Veterans . J Psychiatr Res 2008 ; 42:858–867 Crossref , Medline , Google Scholar
20 Hundt NE, Barrera TL, Mott JM, et al. : Predisposing, enabling, and need factors as predictors of low and high psychotherapy utilization in veterans . Psychol Serv 2014 ; 11:281–289 Crossref , Medline , Google Scholar
21 DeViva JC, Sheerin CM, Southwick SM, et al. : Correlates of VA mental health treatment utilization among OEF/OIF/OND veterans: resilience, stigma, social support, personality, and beliefs about treatment . Psychol Trauma 2016 ; 8:310–318 Crossref , Medline , Google Scholar
22 Harpaz-Rotem I, Rosenheck RA, Pietrzak RH, et al. : Determinants of prospective engagement in mental health treatment among symptomatic Iraq/Afghanistan veterans . J Nerv Ment Dis 2014 ; 202:97–104 Crossref , Medline , Google Scholar
23 Hoerster KD, Malte CA, Imel ZE, et al. : Association of perceived barriers with prospective use of VA mental health care among Iraq and Afghanistan veterans . Psychiatr Serv 2012 ; 63:380–382 Link , Google Scholar
24 Blais RK, Tsai J, Southwick SM, et al. : Barriers and facilitators related to mental health care use among older veterans in the United States . Psychiatr Serv 2015 ; 66:500–506 Link , Google Scholar
25 Fasoli DR, Glickman ME, Eisen SV : Predisposing characteristics, enabling resources and need as predictors of utilization and clinical outcomes for veterans receiving mental health services . Med Care 2010 ; 48:288–295 Crossref , Medline , Google Scholar
26 Nichter B, Hill M, Norman S, et al. : Mental health treatment utilization among US military veterans with suicidal ideation: results from the National Health and Resilience in Veterans Study . J Psychiatr Res 2020 ; 130:61–67 Crossref , Medline , Google Scholar
27 Pietrzak RH, Johnson DC, Goldstein MB, et al. : Perceived stigma and barriers to mental health care utilization among OEF-OIF veterans . Psychiatr Serv 2009 ; 60:1118–1122 Link , Google Scholar
28 Nichter B, Norman S, Haller M, et al. : Psychological burden of PTSD, depression, and their comorbidity in the US veteran population: suicidality, functioning, and service utilization . J Affect Disord 2019 ; 256:633–640 Crossref , Medline , Google Scholar
29 Lindsay Nour BM, Elhai JD, Ford JD, et al. : The role of physical health functioning, mental health, and sociodemographic factors in determining the intensity of mental health care use among primary care medical patients . Psychol Serv 2009 ; 6:243–252 Crossref , Google Scholar
30 Pietrzak RH, Cook JM : Psychological resilience in older US veterans: results from the national health and resilience in veterans study . Depress Anxiety 2013 ; 30:432–443 Crossref , Medline , Google Scholar
31 Seal KH, Bertenthal D, Miner CR, et al. : Bringing the war back home: mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities . Arch Intern Med 2007 ; 167:476–482 Crossref , Medline , Google Scholar
32 Cukor J, Wyka K, Jayasinghe N, et al. : The nature and course of subthreshold PTSD . J Anxiety Disord 2010 ; 24:918–923 Crossref , Medline , Google Scholar
33 Rucci P, Gherardi S, Tansella M, et al. : Subthreshold psychiatric disorders in primary care: prevalence and associated characteristics . J Affect Disord 2003 ; 76:171–181 Crossref , Medline , Google Scholar
34 Tonidaniel S, LeBreton JM : Relative importance analysis: a useful supplement to regression analysis . J Bus Psychol 2011 ; 26:1–9 Crossref , Google Scholar
35 McKibben JBA, Fullerton CS, Gray CL, et al. : Mental health service utilization in the US Army . Psychiatr Serv 2013 ; 64:347–353 Link , Google Scholar
36 Duckworth AL, Quinn PD : Development and validation of the Short Grit Scale (GRIT-S) . J Pers Assess 2009 ; 91:166–174 Crossref , Medline , Google Scholar
37 Duckworth AL, Peterson C, Matthews MD, et al. : Grit: perseverance and passion for long-term goals . J Pers Soc Psychol 2007 ; 92:1087–1101 Crossref , Medline , Google Scholar
38 Duckworth AL, Steen TA, Seligman MEP : Positive psychology in clinical practice . Annu Rev Clin Psychol 2005 ; 1:629–651 Crossref , Medline , Google Scholar
39 Tsai J, Snitkin M, Trevisan L, et al. : Awareness of suicide prevention programs among US military veterans . Adm Policy Ment Health 2020 ; 47:115–125 Crossref , Medline , Google Scholar
40 Department of Veterans Affairs : 2019 National Veteran Suicide Prevention Annual Report. Washington, DC, Office of Mental Health and Suicide Prevention, 2019 Google Scholar
41 Bartels SJ, Coakley EH, Zubritsky C, et al. : Improving access to geriatric mental health services: a randomized trial comparing treatment engagement with integrated versus enhanced referral care for depression, anxiety, and at-risk alcohol use . Am J Psychiatry 2004 ; 161:1455–1462 Link , Google Scholar
42 Pomerantz A, Cole BH, Watts BV, et al. : Improving efficiency and access to mental health care: combining integrated care and advanced access . Gen Hosp Psychiatry 2008 ; 30:546–551 Crossref , Medline , Google Scholar
43 Auxier A, Farley T, Seifert K : Establishing an integrated care practice in a community health center . Prof Psychol Res Pr 2011 ; 42:391–397 Crossref , Google Scholar
44 Zeiss AM, Karlin BE : Integrating mental health and primary care services in the Department of Veterans Affairs health care system . J Clin Psychol Med Settings 2008 ; 15:73–78 Crossref , Medline , Google Scholar
45 Gutner CA, Pedersen ER, Drummond SPA : Going direct to the consumer: examining treatment preferences for veterans with insomnia, PTSD, and depression . Psychiatry Res 2018 ; 263:108–114 Crossref , Medline , Google Scholar
46 Nappi CM, Drummond SPA, Hall JMH : Treating nightmares and insomnia in posttraumatic stress disorder: a review of current evidence . Neuropharmacology 2012 ; 62:576–585 Crossref , Medline , Google Scholar
47 Kearney LK, Post EP, Pomerantz AS, et al. : Applying the interprofessional patient aligned care team in the Department of Veterans Affairs: transforming primary care . Am Psychol 2014 ; 69:399–408 Crossref , Medline , Google Scholar
48 Quartana PJ, Wilk JE, Thomas JL, et al. : Trends in mental health services utilization and stigma in US soldiers from 2002 to 2011 . Am J Public Health 2014 ; 104:1671–1679 Crossref , Medline , Google Scholar
49 Kroenke K, Spitzer RL, Williams JB, et al. : An ultra-brief screening scale for anxiety and depression: the PHQ-4 . Psychosomatics 2009 ; 50:613–621 Crossref , Medline , Google Scholar
50 Weathers FW, Litz BT, Keane TM, et al. : The PTSD Checklist for DSM-5 (PCL-5) . Washington, DC, US Department of Veterans Affairs, 2013 . https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp. Accessed Sep 29 , 2021 Google Scholar
- Smaller rostral cingulate volume and psychosocial correlates in veterans at risk for suicide Psychiatry Research, Vol. 320
- Veterans issues
- Care utilization patterns
- Mental illness
- Alcohol abuse
- Substance use disorder
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
Key findings about America’s military veterans

This Veterans Day, Americans across the country will honor the service and sacrifice of U.S. military veterans. A recent Pew Research Center survey of veterans found that, for many who served in combat, their experiences strengthened them personally but also made the transition to civilian life difficult.
Here are key facts about veterans, drawn from that survey:
The experiences of post-9/11 veterans differ from those who served in previous eras. About one-in-five veterans today served on active duty after the terrorist attacks of Sept. 11, 2001. These post-9/11 veterans are more likely to have been deployed and to have served in combat, giving them a distinct set of experiences compared with those who served in previous eras.
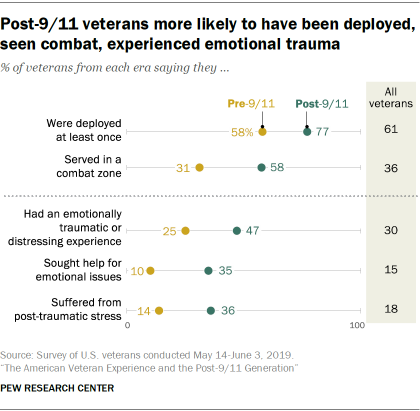
Post-9/11 veterans are also more likely than their predecessors to bear some of the physical and psychological scars of combat. Roughly half (47%) of post-9/11 veterans say they had emotionally traumatic or distressing experiences related to their military service, compared with one-quarter of pre-9/11 veterans. About a third (35%) of post-9/11 veterans say they sought professional help to deal with those experiences, and a similar share say that – regardless of whether they have sought help – they think they have suffered from post-traumatic stress (PTS).
A majority of veterans say they have felt proud of their service since leaving the military. Roughly two-thirds of all veterans (68%) say, in the first few years after leaving the military, they frequently felt proud of their military service. An additional 22% say they sometimes felt proud, and 9% say they seldom or never felt this way. Pre-9/11 veterans are more likely to say they frequently felt proud of their service than are post-9/11 veterans (70% vs. 58%).
Most veterans say they would endorse the military as a career choice. Roughly eight-in-ten (79%) say they would advise a young person close to them to join the military. This includes large majorities of post-9/11 veterans, combat veterans and those who say they had emotionally traumatic experiences in the military.
More veterans say the military did a good job preparing them for life in the service than it did in readying them for the transition to civilian life.
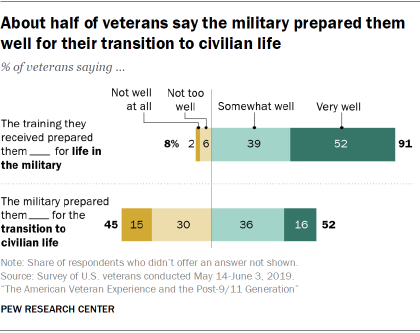
Veterans across eras offer similarly positive evaluations of the job the military did preparing them for military life, but less so when it comes to the return to civilian life. Roughly nine-in-ten veterans (91%) say the training they received when they first entered the military prepared them very or somewhat well for military life. By contrast, about half (52%) say the military prepared them very or somewhat well for the transition to civilian life.
About half of post-9/11 veterans say readjusting to civilian life was difficult. While about three-quarters of all veterans (73%) say readjusting to civilian life was very or somewhat easy, roughly one-in-four (26%) say it was at least somewhat difficult.
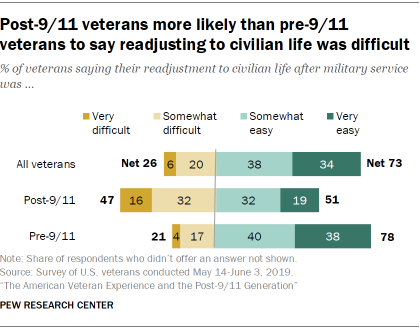
There is a significant gap between pre- and post-9/11 veterans in this regard. About half of post-9/11 veterans (47%) say it was very or somewhat difficult for them to readjust to civilian life after their military service. By comparison, only about one-in-five veterans whose service ended before 9/11 (21%) say their transition was very or somewhat difficult. A large majority of pre-9/11 veterans (78%) say it was easy for them to make the transition.
For many veterans, the imprints of war are felt beyond their tour of duty. The challenges some veterans face during the transition to civilian life can be financial, emotional and professional.
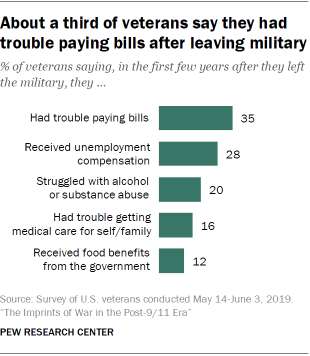
About a third of veterans (35%) say they had trouble paying their bills in their first few years after leaving the military, and roughly three-in-ten (28%) say they received unemployment compensation. One-in-five say they struggled with alcohol or substance abuse.
Veterans who say they have suffered from PTS are much more likely to report experiencing these things than those who did not. Roughly six-in-ten (61%) say they had trouble paying their bills, about four-in-ten (42%) say they had trouble getting medical care for themselves or their families, and a similar share (41%) say they struggled with alcohol or substance abuse.
When it comes to employment, a majority of veterans say their military service was useful in giving them the skills and training they needed for a civilian job. About one-in-three veterans (29%) say it was very useful, and another 29% say it was fairly useful. There are significant differences by rank: While 78% of veterans who served as commissioned officers say their military service was useful, smaller shares of those who were noncommissioned officers (59%) or enlisted (54%) say the same.
Most post-9/11 veterans say having served in the military was an advantage when it came to finding their first post-military job – 35% say this helped a lot and 26% say it helped a little. Only about one-in-ten (9%) say having served in the military hurt their ability to get a job. Among veterans who looked for a job after leaving the military, 57% say they found one in less than six months, and an additional 21% say they had a job in less than a year.
Veterans give the VA mixed reviews.
Most veterans (73%) say they have received benefits from the Department of Veterans Affairs. When asked to assess the job the VA is doing in meeting the needs of veterans, fewer than half (46%) of all veterans say the VA is doing an excellent or good job in this regard.
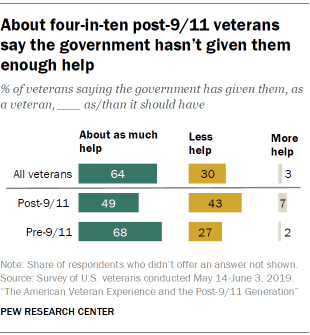
More broadly, 64% of veterans say the government has given them about as much help as it should have. Three-in-ten say the government has given them too little help. Post-9/11 veterans are more likely than those from previous eras to say the government has given them less help than it should have (43% vs. 27%).
Majorities of veterans say the wars in Iraq and Afghanistan were not worth fighting. Additional findings from the same survey show that about two-thirds of veterans (64%) say they think the war in Iraq was not worth fighting considering the costs versus the benefits to the United States, while 33% say it was. Similarly, a majority of veterans (58%) say the war in Afghanistan was not worth fighting. About four-in-ten (38%) say it was worth fighting.
Views differ significantly by party. Republican and Republican-leaning veterans are much more likely than veterans who identify with or lean toward the Democratic Party to say the wars in Iraq and Afghanistan were worth fighting: 45% of Republican veterans vs. 15% of Democratic veterans say the war in Iraq was worth fighting, while 46% of Republican veterans and 26% of Democratic veterans say the same about Afghanistan.
Views on U.S. military engagement in Syria are also more negative than positive. Among veterans, 42% say the campaign in Syria has been worth it, while 55% say it has not. (The survey was conducted entirely before President Donald Trump’s decision to remove U.S. troops from parts of Syria.)
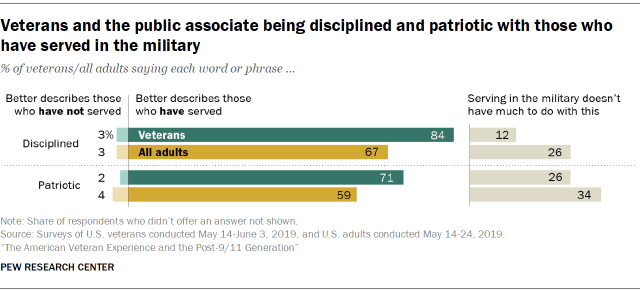
A majority of Americans and veterans associate discipline and patriotism with veterans. Majorities among veterans (61%) and the general public (64%) say most Americans look up to people who have served in the military. And veterans see themselves as more disciplined (84%) and patriotic (71%) than those who have not served in the military. Most Americans agree with this: 67% of all adults say being disciplined better describes veterans than non-veterans, and 59% say the same about being patriotic.
About a third or more among veterans and the public say veterans are more hard-working than those who haven’t served. Still, when it comes to things like being tolerant and open to all groups, the public is less likely to see this as a trait associated with military service than veterans are themselves.
Note: See full topline results and methodology .
- Military & Veterans

Ruth Igielnik is a former senior researcher at Pew Research Center
The changing face of America’s veteran population
A look back at how fear and false beliefs bolstered u.s. public support for war in iraq, new congress will have a few more veterans, but their share of lawmakers is still near a record low, around one-in-five candidates for congress or governor this year are veterans, americans’ trust in scientists, other groups declines, most popular.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Age & Generations
- Coronavirus (COVID-19)
- Economy & Work
- Family & Relationships
- Gender & LGBTQ
- Immigration & Migration
- International Affairs
- Internet & Technology
- Methodological Research
- News Habits & Media
- Non-U.S. Governments
- Other Topics
- Politics & Policy
- Race & Ethnicity
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Terms & Conditions
Privacy Policy
Cookie Settings
Reprints, Permissions & Use Policy
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Subst Abuse Rehabil
Substance use disorders in military veterans: prevalence and treatment challenges
Jenni b teeters.
1 Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina, Charleston, SC, USA
2 Ralph H Johnson Veterans Affairs (VA) Medical Center, Charleston, SC, USA
Cynthia L Lancaster
Delisa g brown.
3 Department of Human Development and Psychoeducation, Howard University, Washington, DC, USA
Sudie E Back
Substance use disorders (SUDs) are a significant problem among our nation’s military veterans. In the following overview, we provide information on the prevalence of SUDs among military veterans, clinical characteristics of SUDs, options for screening and evidence-based treatment, as well as relevant treatment challenges. Among psychotherapeutic approaches, behavioral interventions for the management of SUDs typically involve short-term, cognitive-behavioral therapy interventions. These interventions focus on the identification and modification of maladaptive thoughts and behaviors associated with increased craving, use, or relapse to substances. Additionally, client-centered motivational interviewing approaches focus on increasing motivation to engage in treatment and reduce substance use. A variety of pharmacotherapies have received some support in the management of SUDs, primarily to help with the reduction of craving or withdrawal symptoms. Currently approved medications as well as treatment challenges are discussed.
Introduction
Substance use disorders (SUDs) are a significant problem among military veterans and are associated with numerous deleterious effects. 1 – 3 There are a number of services and interventions available to help reduce SUDs among veterans, including both behavioral and pharmacological treatments. The aims of this review are to provide information on the epidemiology of SUDs among military veterans, clinical characteristics of SUDs, and options for screening and treatment. Challenges and barriers to treatment are also discussed. For the purposes of this review, the focus is primarily on veterans who previously served in the military (i.e., are now retired or separated from the military). Additionally, much of the available research on SUDs among military veterans focuses on Department of Veterans Affairs (VA) services and patients. Notably, some of the features of VA care, such as integration and relatively easy access to specialty mental health care and/or treatment for SUDs, which are discussed in this review, may not be present in non-VA treatment settings.
Despite numerous attempts by the VA and other agencies over the past two decades to reduce problematic substance use, rates of SUDs in veterans continue to rise. SUDs are associated with substantial negative correlates, including medical problems, other psychiatric disorders (e.g., depression and anxiety), interpersonal and vocational impairment, and increased rates of suicidal ideation and attempts. 2 , 4 One study of military personnel found that ~30% of completed suicides were preceded by alcohol or drug use, and an estimated 20% of high-risk behavior deaths were attributed to alcohol or drug overdose. 5 , 6 Given the deleterious associations with SUDs, greater attention to the identification of effective, evidence-based treatment is critically needed. In this paper, we review the prevalence of SUDs among veterans as well as options for treatment. Articles selected for inclusion in this overview were chosen following an extensive literature search in PubMed using relevant key words (e.g., military substance use disorders, veteran substance use disorders, and veteran addiction). Preference for inclusion was given to articles published in the past 10 years.
Diagnostic criteria
SUDs are defined in the Fifth Edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) 7 as a pattern of use that results in marked distress and/or impairment, with two or more symptoms occurring in the past year (see Box 1 for DSM-5 diagnostic criteria). The DSM-5 marked the transition of SUD from a categorical model of severity (previously defined as “abuse” or “dependence”) to a more dimensional model in which SUDs are qualified as mild, moderate, or severe, based on the number of symptoms endorsed by the patient. 7
Prevalence rates
Prior to presenting epidemiological data, it is important to note that many VA-based studies published prior to the release of DSM-5 in May 2013 used The International Classification of Diseases, Ninth Revision (ICD-9) diagnosis codes (which roughly correspond to the DSM-4 criteria). Differences in diagnostic criteria may lead to some important differences in rates of SUDs among those utilizing VA care. For example, previous studies have concluded that prevalence rates of SUDs differ based on the specific criteria used, with studies using diagnostic criteria (i.e., DSM ) reporting higher rates of SUDs when compared to studies using administrative data (i.e., ICD-9). 8 Additionally, because not all veterans choose to utilize VA health care services and only a percentage of patients receive mental health care through the VA and receive a diagnosis, VA diagnostic rates may not reflect true prevalence rates, even among VA patients. Furthermore, studies presenting data solely from veterans that utilize the VA do not capture substance use rates among all military veterans and may have a selection bias, as not all veterans receive care through VA hospitals. 9
The most prevalent types of substance use problems among male and female veterans include heavy episodic drinking and cigarette smoking. 9 Among veterans presenting for first-time care within the VA health care system, ~11% meet criteria for a diagnosis of SUD. 3 Consistent with the general population, alcohol and drug use disorder diagnoses are more common among male than female veterans (10.5% current alcohol use disorders and 4.8% current drug use disorders among male veterans; 4.8% current alcohol use disorders and 2.4% current drug use disorders among female veterans) and are more common among non-married and younger veterans (i.e., <25 years old). 3 Demographics associated with higher rates of SUDs (e.g., young, male) in the general civilian population make up a greater proportion of the military population, which could contribute to an increased risk of certain SUDs relative to civilians. 2 , 3 , 10 A number of environmental stressors specific to military personnel have been linked to increased risk of the development of SUDs among military personnel and veterans, including deployment, combat exposure, and post-deployment civilian/reintegration challenges. 3 , 11 Onset of SUDs can also emerge secondary to other mental health problems associated with these stressors, such as post-traumatic stress disorder (PTSD) and depression. 12 , 13 Additionally, interpersonal traumas (e.g., histories of child physical or sexual abuse) have been shown to mediate the risk of developing an SUD among military veterans, and some individuals join the military to escape adverse home environments. 14 , 15 Furthermore, age is an important predictor of SUD prevalence, with higher rates of SUDs associated with younger age. It is important to keep in mind that many estimates lump together all age groups despite significant variation by age. For example, a recent epidemiological study found that among male veterans, the overall prevalence of substance abuse was lower than rates of civilian substance use when all ages were examined together. 9 However, when looking at the pattern for male veterans aged 18–25 years only, the rates of substance abuse were higher in veterans compared with civilians.
DSM-5 diagnostic criteria for substance use disorders
Substance use disorders are defined as a pattern of use that results in marked distress and/or impairment, with two or more of the following symptoms over the course of a 12-month period:
- Using the substance in larger amounts or over a longer period of time than intended
- Unsuccessful attempts or persistent desire to reduce use
- Too much time spent on obtaining, using, and/or recovering from the effects of the substance
- A strong craving for the substance
- Significant interference with roles at work, school, or home
- Continued use despite recurrent social or interpersonal consequences
- Reducing or giving up important social, occupational, or recreational activities because of the substance use
- Substance use in situations in which it may be physically hazardous
- Substance use despite recurrent or persistent physical or psychological consequences
- Tolerance of the substance
- Withdrawal from the substance
Note: Adapted from American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5 ® ) . Washington, DC: American Psychiatric Publishing; 2013. 7
Specific substances
Despite strict US military policies implemented in 1986 to reduce problematic alcohol consumption, heavy drinking and alcohol use disorders are common among military personnel. 2 , 16 Policies tend to be enforced with inconsistency, and heavy alcohol consumption has long been a cultural norm used for recreation, stress relief, and socializing among military personnel. 1 , 2 Alcohol use disorders are the most prevalent form of SUD among military personnel. 3 , 17 A study examining data collected as part of the National Survey on Drug Use and Health found that, compared to their non-veteran counterparts, veterans were more likely to use alcohol (56.6% vs 50.8% in a 1-month period), and to report heavy use of alcohol (7.5% vs 6.5% in a 1-month period). 18 Furthermore, negative consequences from alcohol use (e.g., interpersonal, legal, and professional) are about twice as likely among binge drinkers relative to non-binge drinkers (9% vs 4%), and among heavy drinkers relative to binge drinkers (9% vs 19%). 19 High levels of combat exposure confer greater risk of problematic alcohol use; those with high levels of combat exposure are more likely to engage in heavy (26.8%) and binge (54.8%) drinking relative to other military personnel (17% and 45%, respectively). 19 These increasing rates of problematic drinking are particularly concerning, given that alcohol is the fourth leading cause of preventable death in the general US population, and that alcohol-impaired driving accounts for 31% of all driving-related fatalities. 20 , 21 Among veterans, specifically, studies demonstrate that alcohol use increases risk of interpersonal violence, poorer health, and mortality. 22 , 23
Misuse of prescription drugs, such as opioids, is on the rise among veterans. 16 Opioids, which are one of the most addicting prescription drugs available, 25 are being prescribed at increasing rates to veterans to address issues such as migraine headaches and chronic pain. 26 From 2001 to 2009, the percent of veterans in the VA health care system receiving an opioid prescription increased from 17% to 24%, and the number of prescriptions written for pain medication by military physicians has more than quadrupled. 27 , 28 From 2003 to 2007, chronic opioid use (i.e., 6 months or longer) among young veterans in the VA health care system increased from 3.0% to 4.5%. 29 On average, patients were prescribed two different opioids and had three different prescribers. 29 Of these opioid prescriptions, the majority were for oxycodone (46.9%), hydrocodone (39.5%), or codeine (6.8%). 30 Mental health diagnoses increase the likelihood of receiving an opioid prescription. Specifically, veterans with a diagnosis of PTSD (17.8%) or another mental health disorder (11.7%) were more likely to receive an opioid prescription than those without mental health diagnoses (6.5%). 31 As compared to veterans without a mental health diagnosis, those with a diagnosis of PTSD receive higher doses of opioid medications, are more likely to receive a simultaneous prescription for additional opioids or for a sedative hypnotic, and are more likely to receive an early refill. 31 Unfortunately, research suggests that those with mental health disorders are also more likely to develop opioid use disorders and to experience a number of adverse clinical outcomes (e.g., inpatient or emergency room admissions, opioid-related accidents and overdoses, and violence-related injuries). 27 , 31
Illicit drug use among veterans is roughly equivalent to their civilian counterparts (4% in the past month reporting use of any illicit drug). 18 Marijuana accounts for the vast majority of illicit drug use among veterans (3.5% report marijuana use, 1.7% report use of illicit drugs other than marijuana in a 1-month period). 18 From 2002 to 2009, cannabis use disorders increased >50% among veterans in the VA health care system. 32 Finally, data suggest that veterans are more likely to be smokers, and age-adjusted prevalence of smoking is higher among veterans than matched civilian groups (27% vs 21%). 33 Of concern for medical outcomes, more veterans than civilians with coronary heart disease are smokers. 33 Furthermore, cigarette smoking accounts for 23% of cancer-related deaths among veterans who are former smokers, and 50% of cancer-related deaths among current smokers. 34
There are a number of services and interventions available to help reduce SUDs among veterans. These include both behavioral and pharmacological treatments, and range on a spectrum from preventive screening to residential treatment programs. SUD treatment services are available to veterans connected with VA Medical Centers (VAMC) across the country. However, many veterans are not connected with a local VAMC and even when they are, access to care can be challenging. This is especially true for rural veterans who may not have a qualified provider in the area (see “Treatment challenges” section for more discussion on these issues). 35
The sections below focus on psychotherapies and pharmacotherapies typically utilized to treat SUDs among veterans. In addition to these behavioral and pharmacological interventions reviewed below, however, veterans with SUDs are encouraged to try self-help groups, such as Alcoholics Anonymous (AA) and Narcotics Anonymous (NA), which are free of charge and available in most cities. Participation in AA/NA can be particularly helpful as part of “aftercare” and ongoing engagement with services to help manage SUDs. Providers are encouraged to consult the recently updated VA/Department of Defense Clinical Practice Guidelines for SUDs for more detailed treatment recommendations. 81
Psychotherapy
In response to high rates of alcohol use among veterans, the VA has implemented system-wide alcohol screening. The goal of Screening, Brief Intervention, and Referral to Treatment (SBIRT) is to intervene upon risky and unhealthy drinking habits prior to progression to an alcohol use disorder, or to provide immediate treatment to those with alcohol use disorders. 24 According to the VA/Department of Defense Clinical Practice Guidelines for SUDs, if treatment or further evaluation is indicated and acceptable to a patient after receiving a brief intervention, the patient should be offered a specialty referral or management in primary care. The guidelines state that if there is “an indication for and a willingness to seek treatment” a biopsychosocial assessment should be completed followed by the development and implementation of a comprehensive treatment plan. Following the collaborative development of the treatment plan, SUD-focused pharmacotherapy should be offered, if indicated, for alcohol use disorders and opioid use disorders, and all patients should be offered SUD-focused psychosocial interventions. Evidence-based psychotherapies and behavioral interventions for the management of SUDs typically involve short-term, cognitive-behavioral therapy (CBT) interventions. These interventions focus on the identification and modification of maladaptive thoughts and behaviors associated with increased craving, use, or relapse to substances. In addition, they may help reduce SUDs by helping incentivize individuals to achieve and maintain abstinence (e.g., contingency management therapies), or increase their ability to successfully manage stress without substances. Behavioral interventions can be delivered in person, via telehealth, and/or via the Internet. 36 – 40
Client-centered motivational interviewing approaches focus on helping increase motivation to engage in treatment and reduce or abstain from substances. 41 Walker et al conducted a randomized controlled trial of motivational interviewing among 242 Army personnel. Participants received one session of motivational interviewing plus feedback or a psychoeducation control. The findings showed that the intervention resulted in significantly fewer drinks per week and lower rates of alcohol dependence diagnosis. 42
Recognizing that young veterans are often unlikely to seek care at traditional VAMCs, researchers have begun to develop alternative, novel methods of treatment engagement and delivery. For example, Pedersen et al developed a web-based, single-session intervention to reduce alcohol use among young veterans. 43 In just 2 weeks, using Facebook as a recruitment site, they recruited a sample of 784 veterans. The intervention uses personalized normative feedback (PNF) and was found to reduce number of drinks per week as well as binge drinking 1 month later. The advantages of an intervention like this one include the fact that it requires no clinician time or patient travel to a VAMC. In addition, web-based interventions reduce other barriers to care such as stigma.
Pharmacotherapy
In addition to behavioral interventions, pharmacotherapy can play an important role in the treatment and management of SUDs. 44 Medications can help reduce withdrawal symptoms which may serve as a trigger or reason for relapse, if untreated. In addition, medications can be helpful in decreasing craving, which is also a potent trigger for increased substance use or relapse following treatment. There are three medications that are approved by the US Food and Drug Administration (FDA) for alcohol use disorders: naltrexone, acamprosate, and disulfiram. Methadone, buprenorphine, naltrexone, and extended-release injectable naltrexone are approved by the FDA for the treatment of opioid use disorders. There are no FDA-approved medications for the treatment of cocaine or marijuana use disorders.
Recently, exploratory use of off-label medications for SUDs has also been the interest of much attention (e.g., oxytocin and N -acetylcysteine). 45 , 46 Investigators have also begun to explore the use of medications to treat SUDs and commonly co-morbid mental health disorders. Rarely does a veteran present with only an SUD. Oftentimes, veterans with an SUD also have co-occurring psychiatric conditions such as PTSD or depression. Recent studies have investigated several medications to help identify effective pharmacologic interventions for SUD and PTSD. For example, studies have investigated the use of prazosin, topiramate, and N -acetylcysteine with mixed results. 47 – 49
Treatment challenges
Rural locations.
According to the VA Office of Rural Health, there are ~3.4 million rural veterans (41%) that comprise the total number of veterans enrolled in VA health care system. 50 Access to care, particularly mental health services, is problematic for veterans residing in rural areas. Increased access to mental health care via telemental health (TMH) modalities may improve quality of life for veterans living in rural areas. 51 Feasibility and efficacy have been shown in the utilization of TMH in home-based settings and remote locations among veterans and civilian populations. 52 – 56 Though literature directly pertaining to the delivery of TMH services for SUDs is limited, the small body of research that specifically investigates substance use TMH treatments has demonstrated favorable results. 53 , 57 Frueh et al examined relapse prevention in veterans with alcohol use disorder using telehealth from a remote site to a local clinic. Results showed that abstinence was retained in 13 of 14 treatment completers and there was high participant satisfaction for the services delivered. 57 It is also worth noting that this study delivered TMH in a group format. Similar findings were demonstrated among veterans receiving individual home-based TMH (HBTMH) services. Veterans living in rural areas who received HBTMH reported that they prefer to receive their mental health treatment using TMH, they would recommend TMH services to other veterans, and they felt safe and less subjected to perceived stigma associated with mental illness, including SUD. 54
Clinicians have also cited advantages of TMH services for rural veterans including low no-show rates, reduced stigma felt by patients, reduced costs and travel burden, and social connection. 58 While the benefits of TMH are promising, the delivery of TMH is not without disadvantages. Limitations include issues with connectivity (e.g., slow bandwidth, problems connecting via satellite internet providers, and availability of internet connection in very rural areas), issues regarding how user savvy the clinician and patient are, and confidentiality and privacy issues, though continuous advancements made in telecommunications have lessened the severity of these issues. Specific to SUD treatment, limitations of TMH include reduced ability to identify when a patient is intoxicated (e.g., inability to smell alcohol or other substance) or conduct unplanned drug testing. 53 Telehealth can play a considerable role in increasing mental health access for veterans residing in rural communities. TMH overcomes geographic, financial, and stigma-related barriers while yielding high patient satisfaction and perceived safety to veterans who would likely not otherwise receive it. Additionally, telehealth could have a transformative impact on the VA health care system and significantly improve quality of life for veterans.
Female veterans
In recent years, rates of problematic substance use among female veterans have been increasing. 38 SUD diagnoses among female veterans utilizing VA services have increased by 81% from 2005 to 2010. 59 Some female veterans may feel uncomfortable seeking SUD treatment within the VA. Female veterans may find it difficult to disclose substance use to providers due to perceived stigma and shame associated with being a female substance user. 60 Additionally, female veterans with SUDs have higher rates of childhood sexual abuse, military sexual trauma, and domestic violence than female veterans without SUDs, and women with PTSD are particularly at risk of developing substance-related problems. 61 , 62 SUD treatments are often provided in groups made up primarily of male veterans. 62 Understandably, female veterans may feel uncomfortable discussing traumatic experiences in a male-dominated treatment setting. Female veterans may also be more likely to have childcare needs that may interfere with treatment utilization and engagement. 63 It is important for providers to remain conscious of women’s minority status within the military and the VA and to handle hesitancy to disclose with compassion and sensitivity. Female veterans are likely to benefit from specialized SUD treatment and gender-tailored treatment, which may increase treatment utilization, attendance, and comfort. 61 Female veterans receiving care at VAMCs offering specialized services for women were more likely to engage in treatment and were more receptive to SUD treatment when gender-specific care options were accessible. 64 , 65
Dual diagnoses
Veterans with SUDs commonly meet criteria for co-occurring mental health disorders, such as PTSD, depression, anxiety, and adjustment disorder. 3 Among Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) veterans diagnosed with an SUD, 82%–93% were diagnosed with another comorbid mental health disorder. 3 Notably, veterans with an SUD diagnosis were three to four times more likely to receive a PTSD or depression diagnosis and <1% of veterans received an isolated diagnosis of SUD without any diagnosis of a co-occurring disorder. 3 Prevalence rates of SUDs and co-occurring disorders among OEF/OIF veterans echo findings from studies on Vietnam-era veterans, although post-Vietnam veterans are more likely to be dually diagnosed. 66 , 67 Notably, individuals presenting with multiple diagnoses of SUDs and comorbid disorders demonstrate greater symptom severity and poorer treatment outcomes. 17 Dually diagnosed veterans are also more likely to have experienced homelessness and to receive VA disability benefits. 68 Psychiatric symptoms, such as symptoms associated with depression and PTSD, can precede or exacerbate drug and alcohol misuse and psychological distress can increase substance craving. 3 , 69 Thus, there is an urgent need for efficacious treatments aimed at treating not only the SUD but also the co-occurring disorder.
Additionally, veterans with SUDs often have co-occurring medical conditions, such as obesity, sleep disturbance, physical injury, and chronic pain as well as other complicating issues such as lower overall quality of life, poorer quality relationships, and higher levels of aggression compared to veterans with a mental health diagnosis but no substance use diagnosis. 70 – 72 Female veterans with an SUD diagnosis are more likely to have reproductive and urinary problems than female veterans without an SUD diagnosis while male veterans with an SUD diagnosis are more likely to be diagnosed with circulatory and digestive system diseases than male veterans without an SUD diagnosis. 73 Though not typically addressed in SUD treatment manuals, these issues are likely to impact treatment and should be addressed during treatment.
Among OEF/OIF veterans, 63% diagnosed with an SUD also met criteria for PTSD. 3 Veterans dually diagnosed with PTSD and SUDs are more likely to have additional co-occurring psychiatric and medical conditions, such as seizures, liver disease, HIV, schizophrenia, anxiety disorders, and bipolar disorder. 68 Due to the high rates of comorbid PTSD and SUDs, the VA has attempted to integrate treatment by funding PTSD/SUD specialist positions and research efforts aimed at identifying efficacious evidence-based PTSD/SUD treatments. 74 However, services are often underutilized with only about 10% of SUD positive veterans receiving any type of SUD treatment in the past year. 75 Though psychotherapy is an important part of treatment for PTSD and SUD, the majority of patients with PTSD and comorbid SUD receive treatment for the SUD only. 76 , 77 There remains a prevailing belief that the SUD should be treated first or that a patient must achieve abstinence before beginning treatment, leaving many active substance using clients unable to obtain treatment. 77 Additionally, patients are not always referred to PTSD treatment after completing SUD treatment. 78 This may lead to greater likelihood of a relapse in the future due to untreated PTSD symptomology and the chronic nature of addictive disorders. “Integrated” treatment models, in which both the SUD and PTSD are simultaneously addressed in therapy, have been developed over the past decade. The findings from studies of integrated treatments show that substance use typically decreases significantly and does not increase with the addition of trauma-focused interventions. 79 , 80 Multiple randomized controlled trials of integrated interventions have been conducted, demonstrating improvements in both PTSD and SUD outcomes. 76 , 79 , 80 However, there is insufficient evidence to conclude that integrated treatments are superior to SUD-only or PTSD-only singular treatments. 80 Further research is needed to determine whether integrated treatments outperform evidence-based SUD and PTSD treatments. Additionally, research on treatments designed to target other mental health disorders that often co-occur with SUDs, such as depression, anxiety, and adjustment disorders, is greatly needed as the vast majority of veterans with SUDs are dually diagnosed.
Another challenge to treatment that is sometimes encountered by veterans is the stigma associated with seeking SUD treatment. Efforts to integrate SUD care within the context of other mental health care would be helpful. So, instead of having to seek care at the “addiction clinic,” veterans could be seen at a general “mental health clinic” that would address a myriad of issues (e.g., anxiety, depression, bereavement, PTSD, couples and family therapy). Furthermore, integrating SUD care into primary care would take it another step further in reducing stigma and increasing access to care. 2
Additionally, the hypermasculine military culture often places importance and value on self-reliance. Therefore, military veterans may be more likely to strive to solve mental health issues on their own and view getting professional mental health treatment as a sign of “weakness”. Additionally, they may feel the need to help “protect” family or friends by not talking about their symptoms or struggles. It is important that providers are aware of these issues so that they can choose to address and normalize these in a sensitive manner early on in treatment.
In summary, veterans demonstrate high rates of SUDs. There is a clear need for the development of novel, more effective, evidence-based interventions to address the health care needs of our veterans and their family members struggling with SUDs. Efforts to overcome barriers to those seeking treatment are needed so that veterans in need of services are able to access treatment and experience long-term recovery.
Acknowledgments
The authors would like to acknowledge support from National Institute on Drug Abuse grant K02 DA039229 (Back SE) and resources at the Ralph H. Johnson VAMC. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of NIDA, the Department of Veterans Affairs, or the USA government.
The authors report no conflicts of interest in this work.
- - K-town Now
- Asia-Pacific
- - Storm Tracker
- Middle East
- Map of Memorials
- Entertainment
- - Video Games
- Europe Travel
- - Quick Trips
- - After Hours
- Pacific Travel
- The Meat and Potatoes of Life
- U.S. Travel
- Storm Tracker
- Rewards for readers
- Get Stripes
- Stripes Lite
- Archives/Library
- Special Publications
- Mobile Apps
- Email Newsletters
- Digital Access
- Home Delivery
- Marine Corps
- Coast Guard
- Space Force
- Archive photo of the day
- - Schedules Europe
- - Scoreboards Europe
- - Schedules Pacific
- - Scoreboards Pacific
- - Pacific Sports Blog
- - Military Matters
- - Force for Hire
- Out of Uniform
- Communities
- Stripes Europe
- Stripes Guam
- Stripes Japan
- Stripes Korea
- Stripes Okinawa
- Our Other Websites
- In Memoriam
- Month of the Military Child
- Best of Germany
- Best of the Pacific
- Letters to Santa
Elevated health risks from burn pits could affect millions of veterans, latest study finds

The burn pit at Balad Air Base, Iraq, in 2008. Long deployments to military bases with open-air burn pits put veterans of the wars in Iraq and Afghanistan at higher risk for certain respiratory ailments, according to new research that used recently declassified deployment data. (Stars and Stripes)
Prolonged deployments to bases with burn pits put veterans of the wars in Iraq and Afghanistan at slightly higher risk for certain respiratory ailments, according to new research that used recently declassified deployment data.
The study, published Thursday by JAMA Network Open looked at the records of 459,381 military veterans receiving health care from the Veterans Administration to determine the health effects of exposure to burn pits.
Longer deployment to military bases with open burn pits was associated with small increases in risk of asthma, chronic obstructive pulmonary disease and hypertension, said the report, authored by a collection of researchers from numerous universities.
The study “is an important milestone in conducting research on health outcomes associated with exposures occurring during military service,” the researchers said.
While the associations were modest in magnitude, several million veterans could be affected by the findings, the report said.
For years, many in the military community have believed that burn pits, which were commonplace at scores of combat outposts in Iraq and Afghanistan, put the health of troops in danger.
But for a long time, Defense Department and Department of Veterans Affairs officials denied any connection between illness and burn pits.
The situation remained a hot button issue in Washington, where for years hearings have been held on what should be done to better care for veterans with ailments believed to have stemmed from burn pit exposure.
A big turning point came in 2022, when Congress passed a law that expanded health care and disability benefits for millions of veterans exposed to toxic burn pits during their careers.
But to date, research on the long-term health consequences of exposure to open burn pits has been limited despite public concern, the JAMA study said.
While deployments to Afghanistan and Iraq have been associated with a higher risk of respiratory disease, a research challenge has been determining whether exposure to something other than burn pits could account for the ailments, the study said.
To carry out a more precise analysis required a large sample of veterans and the ability to isolate any burn pit exposure from other environmental hazards during a deployment.
The researchers were able to do that by reconstructing veterans’ histories of deployment to bases with and without burn pits, using recently declassified military deployment records and VA health data.
The study is perhaps the most extensive look at long-term health outcomes associated with burn pit exposures, given that it considers a much larger number of veterans than past reviews, researchers said.
previous coverage
- More than 400,000 veterans signed up for VA health care in a year
- VA health coverage will expand to all veterans exposed to toxins from Vietnam War through post-9/11 conflicts
- Veterans claims for benefits surge since PACT Act became law
- VA secretary says providing care to vets suffering from toxic exposure is an obligation
related stories
- VA secretary: ‘We’re at a critical moment for shaping and securing veteran health care’
Sign Up for Daily Headlines
Sign up to receive a daily email of today's top military news stories from Stars and Stripes and top news outlets from around the world.
Sign Up Now
- Open access
- Published: 26 April 2024
Clinician and staff experiences with frustrated patients during an electronic health record transition: a qualitative case study
- Sherry L. Ball 1 ,
- Bo Kim 2 , 3 ,
- Sarah L. Cutrona 4 , 5 ,
- Brianne K. Molloy-Paolillo 4 ,
- Ellen Ahlness 6 ,
- Megan Moldestad 6 ,
- George Sayre 6 , 7 &
- Seppo T. Rinne 2 , 8
BMC Health Services Research volume 24 , Article number: 535 ( 2024 ) Cite this article
36 Accesses
Metrics details
Electronic health record (EHR) transitions are known to be highly disruptive, can drastically impact clinician and staff experiences, and may influence patients’ experiences using the electronic patient portal. Clinicians and staff can gain insights into patient experiences and be influenced by what they see and hear from patients. Through the lens of an emergency preparedness framework, we examined clinician and staff reactions to and perceptions of their patients’ experiences with the portal during an EHR transition at the Department of Veterans Affairs (VA).
This qualitative case study was situated within a larger multi-methods evaluation of the EHR transition. We conducted a total of 122 interviews with 30 clinicians and staff across disciplines at the initial VA EHR transition site before, immediately after, and up to 12 months after go-live (September 2020-November 2021). Interview transcripts were coded using a priori and emergent codes. The coded text segments relevant to patient experience and clinician interactions with patients were extracted and analyzed to identify themes. For each theme, recommendations were defined based on each stage of an emergency preparedness framework (mitigate, prepare, respond, recover).
In post-go-live interviews participants expressed concerns about the reliability of communicating with their patients via secure messaging within the new EHR portal. Participants felt ill-equipped to field patients’ questions and frustrations navigating the new portal. Participants learned that patients experienced difficulties learning to use and accessing the portal; when unsuccessful, some had difficulties obtaining medication refills via the portal and used the call center as an alternative. However, long telephone wait times provoked patients to walk into the clinic for care, often frustrated and without an appointment. Patients needing increased in-person attention heightened participants’ daily workload and their concern for patients’ well-being. Recommendations for each theme fit within a stage of the emergency preparedness framework.
Conclusions
Application of an emergency preparedness framework to EHR transitions could help address the concerns raised by the participants, (1) mitigating disruptions by identifying at-risk patients before the transition, (2) preparing end-users by disseminating patient-centered informational resources, (3) responding by building capacity for disrupted services, and (4) recovering by monitoring integrity of the new portal function.
Peer Review reports
Electronic health record (EHR) transitions present significant challenges for healthcare clinicians and staff. These transitions require adjustments in care delivery and may threaten care quality and value. It is critical that healthcare organizations undergoing these changes learn from others who have undergone similar transitions [ 1 , 2 ]. However, the current literature lacks adequate guidance on navigating EHR transitions, especially as they relate to how clinicians and staff interact with patients [ 3 ].
Embedded within EHRs, patient portals facilitate complete, accurate, timely, and unambiguous exchange of information between patients and healthcare workers [ 4 , 5 ]. These portals have become indispensable for completing routine out-of-office-visit tasks, such as medication refills, communicating laboratory results, and addressing patient questions [ 6 ]. In 2003, the VA launched their version of a patient portal, myHealtheVet [ 7 ] and by 2017 69% of Veterans enrolled in healthcare at the VA had registered to access the patient portal [ 8 ]. Similar to other electronic portals, this system allows Veterans to review test results, see upcoming appointments, and communicate privately and securely with their healthcare providers.
EHR transitions can introduce disruptions to patient portal communication that may compromise portal reliability, impacting patient and clinician satisfaction, patients’ active involvement in self-management, and ultimately health outcomes [ 9 ]. During an EHR transition, patients can expect reductions in access to care even when clinician capacity and IT support are increased. Patients will likely need for more assistance navigating the patient portal including and using the portal to communicate with their providers [ 10 ]. Staff must be prepared and understand how the changes in the EHR will affect patients and safeguards must be in place to monitor systems for potential risks to patient safety. Building the capacity to respond to emerging system glitches and identified changes must be included in any transition plan. Although portal disruptions are likely to occur when a new EHR is implemented, we know little about how these disruptions impact healthcare workers’ interactions and care delivery to patients [ 11 , 12 ].
Due to an urgency to raise awareness and promote resolution of these patient portal issues,, we utilized existing data from the first EHR transition site for the Department of Veterans Affairs (VA)’s enterprise-wide transition. We focused on end users’ responses to the question “How Veterans were affected by the transition?”. We used qualitative methods to begin to understand how provider and patient interactions were affected during and by the EHR transition. We explored the impact of the EHR transition on patients through healthcare workers’ vicarious and direct experiences with patients. Due to the high level of disruption in care delivery we draw on insights from an emergency preparedness framework [ 13 ] to generate a set of recommendations to improve healthcare workers’ experiences during EHR transitions. The emergency preparedness framework includes 4 phases of an iterative cycle that include: (1) building capacity to mitigate issues, (2) preparing for the inevitable onset of issues, (3) responding to issues as they emerge, and (4) strategies to recover from any damage incurred.
In early 2020, the VA embarked on an EHR transition from a homegrown, legacy EHR system, developed by VA clinicians and used since the 1990s, to a new commercial system by the Oracle-Cerner Corporation. The primary objectives of this transition were to standardize care and improve interoperability between VA Medical Centers nationwide and the Department of Defense (DoD). Spanning over a decade, this transition plan is scheduled to roll out to all VA medical centers and outpatient clinics.
In this manuscript, we present data from the Mann-Grandstaff VA Medical Center in Spokane, WA, VA’s first EHR transition site. The study uses qualitative methods with clinician and staff interviews as part of a larger multi-method evaluation of the EHR transition. Our overarching goal is to identify and share recommendations to improve VA’s EHR transition efforts; rather than be guided by a theoretical framework our study design including the interview guides [ 14 , 15 ] were based primarily on what was being experienced. An experienced team of ten qualitative methodologists and analysts conducted the study.
This evaluation was designated as non-research/quality improvement work by the VA Bedford Healthcare System Institutional Review Board deeming it exempt from needing an informed consent. Study materials, including interview guides with verbal consent procedures, were reviewed and approved by labor unions and by the VA Bedford Healthcare System Institutional Review Board; all methods were carried out in accordance with local and national VA guidelines and regulations.
Interview guides and an outline of the data collection plans were reviewed and approved by relevant national unions before beginning recruitment.
Recruitment
Recruitment began in July 2020, before the first site implemented the new EHR. Prior to collecting data, we met with site leadership to get buy-in and support for the study, understand local context, determine how the site was approaching the transition, and to obtain the names of clinicians and staff for potential interviews. All potential participants were invited by email to participate in a one-hour voluntary interview conducted on Microsoft Teams® about their experiences with this transition; we used snowball sampling during interviews to expand the pool of interviewees. Verbal permission for audio recording of interviews was obtained immediately prior to the interview. Interview participants were informed that they could skip any questions, pause or stop the recording, and stop the interview at any time and were invited to ask questions before beginning the interview.
Most participants were interviewed at multiple timepoints; these included pre-implementation interviews, brief check-ins, and post-implementation interviews (Table 1 ). At the end of the pre-implementation interview, participants were invited to participate in 3–4 additional, shorter (15–20 min), check-in interviews where information about any changes in the transition process, context, or experience could be discussed. Most initial interviewees, in addition to three new participants, participated in post-implementation interviews (35–60 min; approximately 2–3 months and 10–12 months after the implementation) to reflect on the entire transition process.
Data collection
Experienced qualitative interviewers included PhD trained qualitative methodologist and masters level qualitative analysts (JB, SB, AC, EK, MM, GS) conducted individual interviews with clinicians and staff, aligning to a semi-structured interview guide with follow-up probes using the participant’s words to elicit rich responses grounded in the data [ 16 ]. The guide was designed to inform ongoing efforts to improve the rollout of the new EHR. Six main categories were covered in our interview guides, including (1) attitudes toward the new software, (2) information communicated about the transition, (3) training and education, (4) resources, (5) prior experience with EHRs, and (6) prior experiences with EHR transitions. After piloting the interview guide with a clinician, initial interviews were completed between September and October 2020 and averaged ∼ 45 min in duration. Two-month and one-year post-implementation interview guides included an additional question, “Has the Cerner transition affected Vets?”; data presented here largely draw from responses to this question. Check-ins (October 2020– December 2020) took ∼ 15 min; two-month post-implementation interviews (December 2020– January 2021) and one-year post-implementation interviews (October 2020 - November 2021) took ∼ 45 min. Audio recordings of all interviews were professionally transcribed. To ensure consistency and relationship building, participants were scheduled with the same interviewer for the initial and subsequent interviews whenever feasible (i.e., check-ins and post-implementation interviews). Immediately following each interview, interviewers completed a debrief form where highlights and general reflections were noted.
Throughout the data collection process, interviewers met weekly with the entire qualitative team and the project principal investigators to discuss the recruitment process, interview guide development, and reflections on data collection. To provide timely feedback to leadership within the VA, a matrix analysis [ 17 ] was conducted concurrently with data collection using the following domains: training, roles, barriers, and facilitators. Based on these domains, the team developed categories and subcategories, which formed the foundation of an extensive codebook.
Data analysis
All interviewers also coded the data. We used inductive and deductive content analysis [ 18 ]. Interview transcripts were coded in ATLAS.ti qualitative data analysis software (version 9). A priori codes and categories (based on the overall larger project aims and interview guide questions) and emergent codes and categories were developed to capture concepts that did not fit existing codes or categories [ 18 ]. Codes related to patient experience and clinician interactions with patients were extracted and analyzed using qualitative content analysis to identify themes [ 18 ]. Themes were organized according to their fit within the discrete stages of an emergency preparedness framework to generate recommendations for future rollout. In total, we examined data from 111 interviews with 24 VA clinicians and staff (excluding the initial 11 stakeholder meetings (from the 122 total interviews) that were primarily for stakeholder engagement). We focused on participants’ responses related to their experiences interacting with patients during the EHR transition.
Exemplar quotes primarily came from participants’ responses to the question, “Has the Cerner transition affected Vets?” and addressed issues stemming from use of the patient portal. This included both clinicians’ direct experiences with the portal and indirect experiences when they heard from patients about disruptions when using the portal. We identified four themes related to clinicians’ and staff members’ reported experiences: (1) stress associated with the unreliability of routine portal functions and inaccurate migrated information; (2) concern about patients’ ability to learn to use a new portal (especially older patients and special populations); (3) frustration with apparent inadequate dissemination of patient informational materials along with their own lack of time and resources to educate patients on use of the new portal; and (4) burden of additional tasks on top of their daily workload when patients needed increased in-person attention due to issues with the portal.
Stress associated with the unreliability of routine portal functions and inaccurate migrated information
One participant described the portal changes as, “It’s our biggest stress, it’s the patients’ biggest stress… the vets are definitely frustrated; the clinicians are; so I would hope that would mean that behind the scenes somebody is working on it” (P5, check-in).
Participants expressed significant frustration when they encountered veterans who were suddenly unable to communicate with them using routine secure messaging. These experiences left them wondering whether messages sent to patients were received.
Those that use our secure messaging, which has now changed to My VA Health, or whatever it’s called, [have] difficulty navigating that. Some are able to get in and send the message. When we reply to them, they may or may not get the reply. Which I’ve actually asked one of our patients, ‘Did you get the reply that we took care of this?’ And he was like, ‘No, I did not (P11, 2-months post)
Participants learned that some patients were unable to send secure messages to their care team because the portal contained inaccurate or outdated appointment and primary site information.
I’ve heard people say that the appointments aren’t accurate in there… veterans who have said, ‘yeah, it shows I’m registered,’ and when they go into the new messaging system, it says they are part of a VA that they haven’t gone to in years, and that’s the only area they can message to, they can’t message to the [site] VA, even though that’s where they’ve actively being seen for a while now. (P20, 2-months post)
After the EHR transition, participants noted that obtaining medications through the portal, which was once a routine task, became unreliable. They expressed concern around patients’ ability to obtain their medications through the portal, primarily due to challenges with portal usability and incomplete migration of medication lists from the former to the new EHR.
I think it’s been negative, unfortunately. I try to stay optimistic when I talk to [patients], but they all seem to be all having continued difficulty with their medications, trying to properly reorder and get medications seems to still be a real hassle for them. (P17, one-year post) …the medications, their med list just didn’t transfer over into that list [preventing their ability to refill their medications]. (P13, 2-months post)
Concern about patients’ ability to learn to use a new portal
Clinicians and staff expressed concerns around veterans’ ability to access, learn, and navigate a new portal system. Clinicians noted that even veterans who were adept at using the prior electronic portal or other technologies also faced difficulties using the new portal.
They can’t figure out [the new portal], 99% of them that used to use our [old] portal, the electronic secure messaging or emailing between the team, they just can’t use [the new one]. It’s not functioning. (P13, one-year post) Apparently, there’s a link they have to click on to make the new format work for them, and that’s been confusing for them. But I still am having a lot of them tell me, I had somebody recently, who’s very tech savvy, and he couldn’t figure it out, just how to message us. I know they’re still really struggling with that. (P5, 2-months post) And it does seem like the My Vet [my VA Health, new portal], that used to be MyHealtheVet [prior portal], logging on and getting onto that still remains really challenging for a large number of veterans. Like they’re still just unable to do it. So, I do think that, I mean I want to say that there’s positive things, but really, I struggle (P17, one-year post)
Participants recognized difficulties with the new system and expressed empathy for the veterans struggling to access the portal.
I think that a lot of us, individually, that work here, I think we have more compassion for our veterans, because they’re coming in and they can’t even get onto their portal website. (P24, one-year post)
Participants acknowledged that learning a new system may be especially difficult for older veterans or those with less technology experience.
But, you know, veterans, the general population of them are older, in general. So, their technologic skills are limited, and they got used to a system and now they have to change to a new one. (P13, 2-months post) So, for our more elderly veterans who barely turn on the computer, they’re not getting to this new portal. (P8, check in) And you know, I do keep in mind that this is a group of people who aren’t always technologically advanced, so small things, when it’s not normal to them, stymie them.(P13, one-year post)
Concerns were heightened for veterans who were more dependent on the portal as a key element in their care due to specific challenges. One participant pointed out that there may be populations of patients with special circumstances who depend more heavily on the prior portal, MyHealtheVet.
I have veterans from [specific region], that’s the way they communicate. Hearing impaired people can’t hear on the phone, the robocall thing, it doesn’t work, so they use MyHealtheVet. Well, if that goes away, how is that being communicated to the veteran? Ok? (P18, Check-in)
Frustration with inadequate dissemination of information to veterans about EHR transition and use of new portal
Participants were concerned about poor information dissemination to patients about how to access the new portal. During medical encounters, participants often heard from patients about their frustrations accessing the new portal. Participants noted that they could only give their patients a phone number to call for help using the new system but otherwise lacked the knowledge and the time to help them resolve new portal issues. Some clinicians specifically mentioned feeling ill-equipped to handle their patients’ needs for assistance with the new portal. These experiences exacerbated clinician stress during the transition.
Our veterans were using the MyHealtheVet messaging portal, and when our new system went up, it transitioned to My VA Health, but that wasn’t really communicated to the veterans very well. So, what happened was they would go into their MyHealtheVet like they had been doing for all of these years, to go in and request their medications, and when they pulled it up it’d show that they were assigned to a clinician in [a different state], that they have no active medications. Everything was just messed up. And they didn’t know why because there was no alert or notification that things would be changing. (P8, check in) I field all-day frustration from the veterans. And I love my job, I’m not leaving here even as frustrated as I am, because I’m here for them, not to, I’m here to serve the veterans and I have to advocate for them, and I know it will get better, it can’t stay like this. But I constantly field their frustrations.… So, I give them the 1-800 number to a Cerner help desk that helps with that, and I’ve had multiple [instances of] feedback that it didn’t help. (P13, one-year post) And [the patients are] frequently asking me things about their medication [within the portal], when, you know, I can’t help them with that. So, I have to send them back up to the front desk to try to figure out their medications. (P17, one-year post)
Veteran frustration and the burden of additional tasks due to issues with the portal
Clinicians reported that veterans expressed frustration with alternatives to the portal, including long call center wait times. Some veterans chose to walk into the clinic without an appointment rather than wait on the phone. Clinicians noted an increase in walk-ins by frustrated veterans, which placed added workload on clinics that were not staffed to handle the increase in walk-ins.
It’s been kind of clunky also with trying to get that [new portal] transitioned. And then that’s created more walk-ins here, because one, the vets get frustrated with the phone part of it, and then MyHealtheVet (prior portal) not [working], so they end up walking [into the clinic without an appointment]. (P19, check-in) In terms of messages, they can’t necessarily find the clinician they want to message. We had a veteran who came in recently who wanted to talk to their Rheumatologist, and it’s like, yeah, I typed in their name, and nothing came up. So, they have to try calling or coming in. (P20, 2-months post)
In summary, participants described the new patient portal as a source of stress for both themselves and their patients.
In addition to their own direct experience using a new EHR to communicate with their patients, clinicians and staff can be affected by perceptions of their patients’ experiences during an EHR transition [ 19 ]. At this first VA site to transition to the new EHR, clinicians and staff shared their concerns about their patients’ experiences using the portal. They were particularly troubled by unreliability of the secure messaging system and challenges patients faced learning to use the new system without proper instruction. Moreover, clinicians were alarmed to hear about patients having to make in-person visits– especially unplanned (i.e., walk in) ones– due to challenges with the new portal. Each of these issues needs to be addressed to ensure veteran satisfaction. However, the only solution participants could offer to frustrated patients was the telephone number to the help desk, leaving them with no clear knowledge of a solution strategy or a timeline for resolution of the issues.
We propose applying emergency preparedness actions to future EHR rollouts: mitigate, prepare, respond, and recover (Fig. 1 ) [ 13 ]. By applying these actions, patient portal disruptions may be alleviated and patients’ communication with their clinicians and access to care can be maintained. For example, issues stemming from a disruption in the portal may be mitigated by first identifying and understanding which patients typically use the portal and how they use it. Sites can use this information to prepare for the transition by disseminating instructional materials to staff and patients on how to access the new portal, targeting the most common and critical portal uses. Sites can respond to any expected and emerging portal disruptions by increasing access to alternative mechanisms for tasks disrupted by and typically completed within the portal. After the transition, recovery can begin by testing and demonstrating the accuracy and reliability of functions in the new portal. These actions directly address reported clinician concerns and can help maintain patient-clinician communication, and access to care.
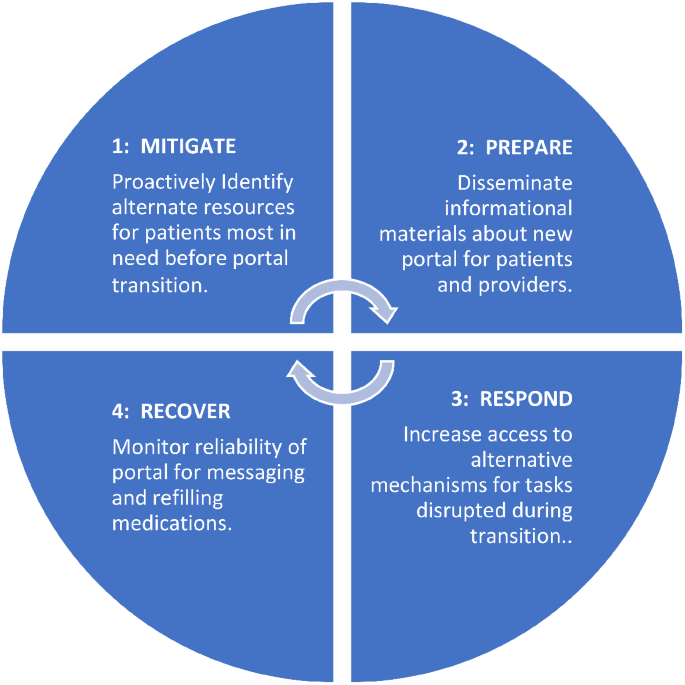
The emergency preparedness framework was applied. This framework includes 4 actions: (1) mitigate, (2) prepare, (3) respond, and (4) recover. These actions can be repeated. Recommendations for how each action (1–4) can be applied to a portal transition are included in each blue quadrant of the circle
Sites could mitigate issues by first understanding which patients will be most affected by the transition, such as those who rely heavily on secure messaging. Reliable use of secure messaging within the VA facilitates positive patient-clinician relationships by providing a mechanism for efficient between-visit communication [ 20 , 21 , 22 , 23 ]. During the EHR transition, clinicians and staff became concerned about the well-being of patients from whom they weren’t receiving messages and those who depended on the portal to complete certain tasks. Since secure messaging is often initiated by patients to clinicians [ 23 ], clinicians will likely be unaware that messages are being missed. Understanding how and which patients currently use the portal and anticipating potential portal needs is a first step toward mitigating potential issues.
Despite efforts to inform Veterans of the EHR transition and patient portal [ 24 ] including information sent to a Veteran by email, direct mail, postings on VA websites, and a town hall, our findings agree with those of Fix and colleagues [ 10 ] and suggest that many Veterans were unprepared for the transition. Our findings suggest that end users heard that more is needed to improve the dissemination of knowledge about the transition and how to navigate the new patient portal to both VA employees and the patients they serve.
Preparations for the transition should prioritize providing VA clinicians and staff with updated information and resources on how to access and use the new portal [ 25 ]. VA clinicians deliver quality care to veterans and many VA employees are proud to serve the nation’s veterans and willing to go the extra mile to support their patients’ needs [ 26 ]. In this study, participants expressed feeling unprepared to assist or even respond to their patients’ questions and concerns about using the new portal. This unpreparedness contributed to increased clinician and staff stress, as they felt ill-equipped to help their patients with portal issues. Such experiences can negatively affect the patient-clinician relationship. Preparing clinicians and patients about an upcoming transition, including technical support for clinicians and patients, may help minimize these potential issues [ 10 , 27 ]. Specialized training about an impending transition, along with detailed instructions on how to gain access to the new system, and a dedicated portal helpline may be necessary to help patients better navigate the transition [ 23 , 28 ].
In addition to a dedicated helpline, our recommendations include responding to potential changes in needed veteran services during the transition. In our study, participants observed more veteran walk-ins due to challenges with the patient portal. Health systems need to anticipate and address this demand by expanding access to in-person services and fortifying other communication channels. For example, sites could use nurses to staff a walk-in clinic to handle increases in walk-in traffic and increase call center capacity to handle increases in telephone calls [ 29 ]. Increased use of walk-in clinics have received heightened attention as a promising strategy for meeting healthcare demands during the COVID-19 pandemic [ 30 ] and can potentially be adapted for meeting care-related needs during an EHR transition. These strategies can fill a gap in communication between clinicians and their patients while patients are learning to access and navigate a new electronic portal.
Finally, there is a need for a recovery mechanism to restore confidence in the reliability of the EHR and the well-being of clinicians and staff. Healthcare workers are experiencing unprecedented levels of stress [ 31 ]. A plan must be in place to improve and monitor the accuracy of data migrated, populated, and processed within the new system [ 2 ]. Knowing that portal function is monitored could help ease clinician and staff concerns and mitigate stress related to the transition.
Limitations
This study has several limitations. First, data collection relied on voluntary participation, which may introduce self-selection response bias. Second, this work was completed at one VA medical center that was the first site in the larger enterprise-wide transition, and experiences at other VAs or healthcare systems might differ substantially. Third, we did not interview veterans and relied entirely on secondhand accounts of patient experiences with the patient portal. Future research should include interviews with veterans during the transition and compare veteran and VA employee experiences.
Despite a current delay in the deployment of the new EHR at additional VA medical centers, findings from this study offer timely lessons that can ensure clinicians and staff are equipped to navigate challenges during the transition. The strategies presented in this paper could help maintain patient-clinician communication and improve veteran experience. Guided by the emergency preparedness framework, recommended strategies to address issues presented here include alerting those patients most affected by the EHR transition, being prepared to address patients’ concerns, increasing staffing for the help desk and walk-in care clinics, and monitoring the accuracy and reliability of the portal to provide assurance to healthcare workers that patients’ needs are being met. These strategies can inform change management at other VA medical centers that will soon undergo EHR transition and may have implications for other healthcare systems undergoing patient portal changes. Further work is needed to directly examine the perspectives of veterans using the portals, as well as the perspectives of both staff and patients in the growing number of healthcare systems beyond VA that are preparing for an EHR-to-EHR transition.
Data availability
Deidentified data analyzed for this study are available from the corresponding author on reasonable request.
Abbreviations
Electronic health record
Department of Veterans Affairs
VA Medical Centers
Department of Defense
Huang C, Koppel R, McGreevey JD 3rd, Craven CK, Schreiber R. Transitions from one Electronic Health record to another: challenges, pitfalls, and recommendations. Appl Clin Inf. 2020;11(5):742–54.
Article Google Scholar
Penrod LE. Electronic Health Record Transition considerations. PM R. 2017;9(5S):S13–8.
Article PubMed Google Scholar
Cogan AM, Haltom TM, Shimada SL, Davila JA, McGinn BP, Fix GM. Understanding patients’ experiences during transitions from one electronic health record to another: a scoping review. PEC Innov. 2024;4:100258. https://doi.org/10.1016/j.pecinn.2024.100258 . PMID: 38327990; PMCID: PMC10847675.
Article PubMed PubMed Central Google Scholar
Powell KR. Patient-perceived facilitators of and barriers to Electronic Portal Use: a systematic review. Comput Inf Nurs. 2017;35(11):565–73.
Google Scholar
Wilson-Stronks A, Lee KK, Cordero CL, et al. One size does not fit all: meeting the Health Care needs of diverse populations. Oakbrook Terrace, IL: The Joint Commission; 2008.
Carini E, Villani L, Pezzullo AM, Gentili A, Barbara A, Ricciardi W, Boccia S. The Impact of Digital Patient Portals on Health outcomes, System Efficiency, and patient attitudes: updated systematic literature review. J Med Internet Res. 2021;23(9):e26189.
Home -. My HealtheVet - My HealtheVet (va.gov).
Nazi KM, Turvey CL, Klein DM, Hogan TP. A decade of veteran voices: examining patient Portal Enhancements through the Lens of user-centered design. J Med Internet Res. 2018;20(7):e10413. https://doi.org/10.2196/10413 .
Tapuria A, Porat T, Kalra D, Dsouza G, Xiaohui S, Curcin V. Impact of patient access to their electronic health record: systematic review. Inf Health Soc Care. 2021;46:2.
Fix GM, Haltom TM, Cogan AM, et al. Understanding patients’ preferences and experiences during an Electronic Health Record Transition. J GEN INTERN MED. 2023. https://doi.org/10.1007/s11606-023-08338-6 .
Monturo C, Brockway C, Ginev A. Electronic Health Record Transition: the patient experience. CIN: Computers Inf Nurs. 2022;40:1.
Tian D, Hoehner CM, Woeltje KF, Luong L, Lane MA. Disrupted and restored patient experience with transition to New Electronic Health Record System. J Patient Exp. 2021;18:8.
Emergency management programs for healthcare facilities. the four phases of emergency management. US Department of Homeland Security website: https://www.hsdl.org/?view&did=765520 . Accessed 28 Aug 2023.
Ahlness EA, Orlander J, Brunner J, Cutrona SL, Kim B, Molloy-Paolillo BK, Rinne ST, Rucci J, Sayre G, Anderson E. Everything’s so Role-Specific: VA Employee Perspectives’ on Electronic Health Record (EHR) transition implications for roles and responsibilities. J Gen Intern Med. 2023;38(Suppl 4):991–8. Epub 2023 Oct 5. PMID: 37798577; PMCID: PMC10593626.
Rucci JM, Ball S, Brunner J, Moldestad M, Cutrona SL, Sayre G, Rinne S. Like one long battle: employee perspectives of the simultaneous impact of COVID-19 and an Electronic Health Record Transition. J Gen Intern Med. 2023;38(Suppl 4):1040–8. https://doi.org/10.1007/s11606-023-08284-3 . Epub 2023 Oct 5. PMID: 37798583; PMCID: PMC10593661.
Sayre G, Young J. Beyond open-ended questions: purposeful interview guide development to elicit rich, trustworthy data [videorecording]. Seattle (WA): VA Health Services Research & Development HSR&D Cyberseminars; 2018.
Averill JB. Matrix analysis as a complementary analytic strategy in qualitative inquiry. Qual Health Res. 2002;12:6855–66.
Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62:1107–15.
Haun JN, Lind JD, Shimada SL, Simon SR. Evaluating Secure Messaging from the veteran perspective: informing the adoption and sustained use of a patient-driven communication platform. Ann Anthropol Pract. 2013;372:57–74.
Kittler AF, Carlson GL, Harris C, Lippincott M, Pizziferri L, Volk LA, et al. Primary care physician attitudes toward using a secure web-based portal designed to facilitate electronic communication with patients. Inf Prim Care. 2004;123:129–38.
Shimada SL, Petrakis BA, Rothendler JA, Zirkle M, Zhao S, Feng H, Fix GM, Ozkaynak M, Martin T, Johnson SA, Tulu B, Gordon HS, Simon SR, Woods SS. An analysis of patient-provider secure messaging at two Veterans Health Administration medical centers: message content and resolution through secure messaging. J Am Med Inf Assoc. 2017;24:5.
Jha AK, Perlin JB, Kizer KW, Dudley RA. Effect of the transformation of the Veterans Affairs Health Care System on the quality of care. N Engl J Med. 2003;348:22.
McAlearney AS, Walker DM, Gaughan A, Moffatt-Bruce S, Huerta TR. Helping patients be better patients: a qualitative study of perceptions about Inpatient Portal Use. Telemed J E Health. 2020;26:9.
https://www.myhealth.va.gov/mhv-portal-web/transitioning-to-my-va-health-learn-more .
Beagley L. Educating patients: understanding barriers, learning styles, and teaching techniques. J Perianesth Nurs. 2011;26:5.
Moldestad M, Stryczek KC, Haverhals L, Kenney R, Lee M, Ball S, et al. Competing demands: Scheduling challenges in being veteran-centric in the setting of Health System initiatives to Improve Access. Mil Med. 2021;186:11–2.
Adusumalli J, Bhagra A, Vitek S, Clark SD, Chon TY. Stress management in staff supporting electronic health record transitions: a novel approach. Explore (NY). 2021;17:6.
Heponiemi T, Gluschkoff K, Vehko T, Kaihlanen AM, Saranto K, Nissinen S, et al. Electronic Health Record implementations and Insufficient Training Endanger nurses’ Well-being: cross-sectional survey study. J Med Internet Res. 2021;23:12e27096.
Laurant M, van der Biezen M, Wijers N, Watananirun K, Kontopantelis E, van Vught AJ. Nurses as substitutes for doctors in primary care. Cochrane Database Syst Rev. 201;7(7):CD001271.
Elnahal S, Kadakia KT, Gondi S, How, U.S. Health systems Can Build Capacity to Handle Demand Surges. Harvard Business Review. 2021. https://hbr.org/2021/10/how-u-s-health-systems-can-build-capacity-to-handle-demand-surges/ Accessed 25 Nov 2022.
George RE, Lowe WA. Well-being and uncertainty in health care practice. Clin Teach. 2019;16:4.
Download references

Acknowledgments
We acknowledge and thank members of the EMPIRIC Evaluation qualitative and supporting team for their contributions to this work including Ellen Ahlness, PhD, Julian Brunner, PhD, Adena Cohen-Bearak, MPH, M.Ed, Leah Cubanski, BA, Christine Firestone, Bo Kim, PhD, Megan Moldestad, MS, and Rachel Smith. We greatly appreciate the staff at the Mann-Grandstaff VA Medical Center and associated community-based outpatient clinics for generously sharing of their time and experiences participating in this study during this challenging time.
The “EHRM Partnership Integrating Rapid Cycle Evaluation to Improve Cerner Implementation (EMPIRIC)” (PEC 20–168) work was supported by funding from the US Department of Veterans Affairs, Veterans Health Administration, Health Services Research & Development Quality Enhancement Research Initiative (QUERI) (PEC 20–168). The findings and conclusions in this article are those of the authors and do not necessarily reflect the views of the Veterans Health Administration, Veterans Affairs, or any participating health agency or funder.
Author information
Authors and affiliations.
VA Northeast Ohio Healthcare System, 10701 East Blvd., Research Service 151, 44106, Cleveland, OH, USA
Sherry L. Ball
Center for Healthcare Organization and Implementation Research, VA Boston Healthcare System, Boston, MA, USA
Bo Kim & Seppo T. Rinne
Department of Psychiatry, Harvard Medical School, Boston, MA, USA
Center for Healthcare Organization and Implementation Research, VA Bedford Healthcare System, Bedford, MA, USA
Sarah L. Cutrona & Brianne K. Molloy-Paolillo
Division of Health Informatics & Implementation Science, Department of Population and Quantitative Health Sciences, University of Massachusetts Chan Medical School, Worcester, MA, USA
Sarah L. Cutrona
Seattle-Denver Center of Innovation for Veteran-Centered and Value-Driven Care, VHA Puget Sound Health Care System, Seattle, WA, USA
Ellen Ahlness, Megan Moldestad & George Sayre
University of Washington School of Public Health, Seattle, WA, USA
George Sayre
Geisel School of Medicine at Dartmouth, Hannover, NH, USA
Seppo T. Rinne
You can also search for this author in PubMed Google Scholar
Contributions
S.R. designed the larger study. G.S. was the qualitative methodologist who led the qualitative team. S.B., E.A., and M.M. created the interview guides and completed the interviews; Data analysis, data interpretation, and the initial manuscript draft were completed by S.B. and B.K. S.C. and B.M. worked with the qualitative team to finalize the analysis and edit and finalize the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Sherry L. Ball .
Ethics declarations
Ethics approval and consent to participate.
This evaluation was designated as non-research/quality improvement by the VA Bedford Healthcare System Institutional Review Board. All methods were carried out in accordance with local and national VA guidelines and regulations for quality improvement activities. This study included virtual interviews with participants via MS Teams. Employees volunteered to participate in interviews and verbal consent was obtained to record interviews. Study materials, including interview guides with verbal consent procedures, were reviewed and approved by labor unions and determined as non-research by the VA Bedford Healthcare System Institutional Review Board.
Consent for publication
Not applicable.
The findings and conclusions in this paper are those of the authors and do not necessarily represent the official position of the Department of Veterans Affairs.
Prior presentations
Ball S, Kim B, Moldestad M, Molloy-Paolillo B, Cubanski L, Cutrona S, Sayre G, and Rinne S. (2022, June). Electronic Health Record Transition: Providers’ Experiences with Frustrated Patients. Poster presentation at the 2022 AcademyHealth Annual Research Meeting. June 2022.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ball, S.L., Kim, B., Cutrona, S.L. et al. Clinician and staff experiences with frustrated patients during an electronic health record transition: a qualitative case study. BMC Health Serv Res 24 , 535 (2024). https://doi.org/10.1186/s12913-024-10974-5
Download citation
Received : 29 August 2023
Accepted : 09 April 2024
Published : 26 April 2024
DOI : https://doi.org/10.1186/s12913-024-10974-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- EHR transition
- Patient experience
- Clinician experience
- Qualitative analysis
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Online First
- Postsurgical opioid prescribing among veterans using community care for orthopedic surgery at non-VA hospitals compared to a VA hospital with a transitional pain service: a retrospective cohort study
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0001-8222-1461 Michael Jacob Buys 1 , 2 ,
- Zachary Anderson 2 ,
- Kimberlee Bayless 2 ,
- Chong Zhang 3 ,
- Angela P Presson 3 ,
- Julie Hales 4 and
- http://orcid.org/0000-0002-3521-3749 Benjamin Sands Brooke 5
- 1 Department of Anesthesiology , University of Utah Health Hospitals and Clinics , Salt Lake City , Utah , USA
- 2 Anesthesiology , George E Wahlen Department of Veterans Affairs Medical Center , Salt Lake City , Utah , USA
- 3 Internal Medicine-Epidemiology , University of Utah Health Sciences Center , Salt Lake City , Utah , USA
- 4 Department of Surgery , University of Utah Health , Salt Lake City , Utah , USA
- 5 Surgery , University of Utah School of Medicine , Salt Lake City , Utah , USA
- Correspondence to Dr Michael Jacob Buys, Department of Anesthesiology, University of Utah Health Hospitals and Clinics, Salt Lake City, UT, 84132, USA; michael.buys{at}hsc.utah.edu
Background The USA provides medical services to its military veterans through Veterans Health Administration (VHA) medical centers. Passage of recent legislation has increased the number of veterans having VHA-paid orthopedic surgery at non-VHA facilities.
Methods We conducted a retrospective cohort study among veterans who underwent orthopedic joint surgery paid for by the VHA either at the Salt Lake City VHA Medical Center (VAMC) or at non-VHA hospitals between January 2018 and December 2021. 562 patients were included in the study, of which 323 used a non-VHA hospital and 239 patients the VAMC. The number of opioid tablets prescribed at discharge, the total number prescribed by postdischarge day 90, and the number of patients still filling opioid prescriptions between 90 and 120 days after surgery were compared between groups.
Results Veterans who underwent orthopedic surgery at a non-VHA hospital were prescribed more opioid tablets at discharge (median (IQR)); (40 (30–60) non-VHA vs 30 (20–47.5) VAMC, p<0.001) and in the first 90 days after surgery than patients who had surgery at the Salt Lake City VAMC (60 (40–120) vs 35 (20–60), p<0.001). Patients who had surgery at Salt Lake City VAMC were also significantly less likely to fill opioid prescriptions past 90 days after hospital discharge (OR (95% CI) 0.06 (0.01 to 0.48), p=0.007).
Conclusion These results suggest that veterans who have surgery at a veterans affairs hospital with a transitional pain service are at lower risk for larger opioid prescriptions both at discharge and within 90 days after surgery as well as persistent opioid use beyond 90 days after discharge than if they have surgery at a community hospital.
- Analgesics, Opioid
- Opioid-Related Disorders
Data availability statement
Data are available upon reasonable request.
https://doi.org/10.1136/rapm-2023-105162
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
WHAT IS ALREADY KNOWN ON THIS TOPIC
The US government spends billions of dollars each year paying for veteran care in non-veterans affairs (VA) hospitals.
WHAT THIS STUDY ADDS
Veterans having orthopedic surgery at non-VA hospitals received a higher number of opioids prescribed both at discharge and in the first 90 days after discharge and were also more likely to continue to receive opioids past 90 days after surgery than veterans having surgery at a VA hospital with a transitional pain service.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
This information may be important for policymakers when allocating funds for veteran surgical care and for veterans when choosing where to receive their surgical care.
Introduction
The Veterans Health Administration (VHA) is part of the Department of Veterans Affairs (VA) and is responsible for providing care to eligible veterans who have served in the United States Military. The VHA maintains a large infrastructure of government-run healthcare facilities to serve these veterans. In 2014, the United States Congress passed the Veterans Choice Act, which established the VA Community Care program that eligible veterans could use to receive VHA-paid care in community hospitals and clinics. This legislation aimed to improve access to care for veterans, particularly those living in rural areas with a long travel distance to the nearest VA healthcare facility. Subsequently, in 2018, the United States congress passed the VA MISSION (Maintaining Internal Systems and Strengthening Integrated Outside Networks) Act which expanded the eligibility criteria for receiving VHA-funded care in the community. 1 As a result of these bills, many veterans have the option and have chosen to receive their medical care at non-VHA hospitals in the community rather than at a VA medical center (VAMC). A Congressional Budget Office report states that 2.3 million veterans (~30% of enrolled veterans) were authorized to use community care in 2021 and that VHA’s costs for community care grew from US$7.9 billion in 2014 to US$17.6 billion in 2021 (expressed in 2021 dollars). 2
Despite the large increase in utilization and cost of delivering community care to the VHA, it is not clear that undergoing surgery using the community care program results in improved veteran outcomes. Limited data available support shorter wait times at VHA facilities compared with community care 3–5 and either similar, 6 7 or improved, 8 9 surgical outcomes compared with community care surgery. We found no publicly available data comparing opioid prescribing for veterans having surgery in the community versus at VHA facilities.
Since inception of the VA Community Care Program, one of the most common specialty referrals to non-VA providers has been for orthopedic joint surgery. This study was designed to evaluate if there is a difference in opioid-prescribing practices among veterans not on chronic opioid therapy who underwent orthopedic joint procedures using community care at non-VHA hospitals as opposed to the major VAMC in the same geographical referral region. To achieve this goal, we compared postoperative opioid prescriptions among veterans undergoing knee, hip or shoulder joint replacement surgery or rotator cuff or arthroscopic shoulder surgery at the Salt Lake City VAMC and using VA Community Care in the Salt Lake City catchment area (Utah, Eastern Nevada, Southern Idaho, Western Colorado) during the same time period.
We conducted a retrospective cohort study of veterans who had orthopedic joint surgery either at the Salt Lake City VAMC (Group VAMC), which uses a transitional pain service to assist with pain management and opioid reduction, or at a community hospital (Group Community Care) in the Salt Lake City VA referral region (Utah, Southern Idaho, Eastern Nevada, Western Colorado) under the VHA Community Care Program between January 2018 and December 2021.
All patients who received primary or revision total hip, knee, or shoulder arthroplasty as well as those receiving rotator cuff repair or arthroscopic shoulder surgery either at the Salt Lake City VAMC or from community hospitals in the Salt Lake City VA region and paid for by the VHA were included. We excluded patients who had an additional surgery within 90 days of the index surgery, patients who died within 90 days of the index surgery, patients who were discharged to an extended care facility after surgery, or who were taking chronic opioid therapy prior to surgery. Chronic opioid use was defined as receiving a prescription of opioids for either 60 continuous days prior to surgery or if they had filled 3 or more prescriptions of at least 28 days duration within 180 days prior to surgery as determined by controlled substance database records and review of the medical record.
Demographic data and baseline characteristics were collected on all patients including sex, age at discharge, body mass index (BMI), history of anxiety, depression, post-traumatic stress disorder, or other mental health diagnoses, and history of substance abuse were collected from VA medical records and the VA Corporate Data Warehouse. Rural residence of the patient was also collected from VA records and was determined using the Rural-Urban Commuting Areas system. We used the Program Integrity Tool tables within the VA Corporate Data Warehouse to identify veterans within the Salt Lake City VA catchment area who had undergone surgery at a non-VHA hospital using the VHA Community Care Program. CPT codes 29827, 23334, 23335, 23410, 23412, 23420, 23470, 23472, 23473, 27054, 27090, 27091, 27125, 27130, 27132, 27134, 27137, 27138, 27437, 27440, 27441, 27442, 27443, 27445, 27446, 27447, 27486, 27487, 27488, 27570, 29806, 29807, 29819, 29820, 29821, 29822, 29823, 29824, 29825, 29827, and 29828 were used to identify veterans who underwent primary and revision total knee, hip, and shoulder arthroplasty, rotator cuff repair, and arthroscopic shoulder surgery. Veterans who had surgery at the Salt Lake City VAMC were identified using the transitional pain service database and the same CPT codes as above.
Data on the type of surgery, the number of days spent in the hospital after surgery, the name of the surgeon, the name of the hospital, the number of opioid tablets prescribed at discharge, the number of opioid refills between discharge and 90 days after discharge, the total number of opioid tablets prescribed in the first 90 days after discharge, and whether or not patients received an opioid prescription between 90 and 120 days from discharge were collected from the medical record, VA payment records, and from controlled substance database records. Persistent postsurgical opioid use was defined as at least one refill of opioids within 90 days after discharge and the filling of another opioid prescription between 90 and 120 days after discharge.
Data analysis
Patient demographics and clinical measures were summarized descriptively stratified by whether veterans underwent orthopedic joint surgery at a non-VHA hospital versus the VAMC. Continuous variables were skewed and as a result were summarized as median and IQR and compared between groups using Wilcoxon rank sum tests. Categorical variables were summarized as frequency and percent and compared using χ 2 tests or Fisher’s exact test if expected counts in either group were fewer than 5.
Total opioid tabs prescribed by day 90 were compared between patients who underwent orthopedic joint surgery at a non-VHA hospital versus the VAMC using a negative binomial regression model accounting for the random effects of surgeons. We examined goodness of fit by comparing model residuals to simulated residuals using the R package DHARMa. All regression coefficients were exponentiated to represent incident rate ratios. Results from both univariable and multivariable models were reported with 95% CI and p values. Covariates that were adjusted for in the model included: age, sex, BMI, rural residence, number of days in the hospital after surgery, surgery type, any mental health diagnosis, and any substance use disorder diagnosis. Surgeon random effects were visualized using a caterpillar plot. To evaluate for potential differences in 90-day opioid prescribing based on the size of the hospital, hospitals were stratified into small (<100 beds), medium (100–199 beds), and large (200+ beds). We then compared the total number of opioid tablets prescribed in 90 days in a mixed effects negative binomial regression model. Covariates that were adjusted for in the model included: age, sex, BMI, rural residence, number of days in the hospital after surgery, surgery type, any mental health diagnosis, and any substance use disorder diagnosis.
‘Persistent post-surgical opioid use’ as an outcome was compared between Community Care and VAMC groups using logistic regressions. ORs were reported with 95% CI and p values. Due to the rarity of this outcome, only univariable analyses were performed.
Analyses were conducted using R V.4.1.2. 10 Statistical significance was assessed at p=0.05 level, and all tests were two sided.
We identified 434 veterans who underwent orthopedic joint surgery in the community (Group Community Care) during the study time period along with 403 veterans who had similar procedures at the Salt Lake City VAMC (Group VAMC). After exclusions ( figure 1 ), a total of 323 veterans from community care and 239 veterans from VAMC were included in the final analysis. Veterans from group community care had surgery from 136 unique surgeons and 50 unique hospitals. Veterans from group VAMC all had surgery in the same hospital with 17 unique surgeons.
- Download figure
- Open in new tab
- Download powerpoint
Consolidated Standards of Reporting Trials flow diagram.
Veterans who used community care for orthopedic surgery were younger, had a higher BMI, were more likely to have a rural residence, and had a shorter median (IQR) hospital stay than patients who underwent surgery at the VAMC. Veterans from the community care group were also more likely than veterans in the VAMC cohort to have a mental health diagnosis and less likely to have a history of a substance use disorder. Further, veterans who used community care had a higher percentage of rotator cuff repair/shoulder arthroscopy procedures, whereas patients at the VAMC had a higher percentage of knee replacement surgery ( table 1 ).
- View inline
Patient characteristics and clinical outcomes comparing VA medical center (VAMC) and community care
Veterans from the VAMC cohort on average were prescribed fewer opioid tablets at hospital discharge (median (IQR)) (30 (20–47.5) VAMC versus 40 (30–60) community care, p<0.001) and fewer opioid tablets in the first 90 days after discharge (35 (20–60) VAMC vs 60 (40–120) community care, p<0.001) than the community care cohort ( figure 2 ).
Density curve plot showing total number of opioid tablets prescribed within 90 days after discharge. Vertical dashed lines represent medians. VAMC, VA medical center.
A multivariable regression model demonstrated that the number of opioid tablets prescribed in the first 90 days after joint surgery was less in the VAMC group than in the community (ratio=0.45, 95% CI 0.36 to 0.55, p<0.001). Type of procedure was also independently associated with the number of opioid tablets prescribed, with knee surgery patients receiving significantly more tablets than shoulder or hip surgery patients ( table 2 ). The number of tablets prescribed at discharge and in 90 days stratified by type of surgery and study group is shown in online supplemental table 4 . Online supplemental figure 3 shows the variability in prescribing practices at the surgeon level for both VAMC and community hospital surgeons.
Supplemental material
Results of negative binomial regression analysis for 90-day total opioid tablets prescribed
There was considerable variation in opioid-prescribing patterns among surgeons, with SD in the surgeon random effect varied between −23% and 31% when exponentiated. Without accounting for the random effects of surgeons, the model explains 31.1% of total variance in the number of tablets prescribed in the first 90 days (Nakagawa’s marginal R2=0.311). With the random effects of surgeons included, the model explains 41.2% of the total variance (Nakagawa’s conditional R2=0.412).
Veterans that underwent orthopedic surgery at the VAMC were significantly less likely to meet the criteria for persistent postsurgical opioid use than patients using community care (OR (95% CI), 0.06 (0.01 to 0.48), p=0.007) ( table 3 ). Online supplemental table 5 shows persistent postsurgical opioid use stratified by type of surgery. A closer review of the subjects who met criteria for persistent postsurgical opioid use revealed one subject from each group who had sporadic, intermittent opioid prescriptions prior to surgery but did not meet the defined criteria for chronic opioid use. The subject from group community care filled an opioid prescription every 4–5 months prior to his surgery without filling one within 3 months of surgery. The subject received another of the same prescription from the same non-surgeon prescriber at around 90 days after surgery and then again 4 months after that. The subject from Group SLC VAMC had a similar presurgical sporadic opioid prescription fill and then filled a similar prescription from the same non-surgeon prescriber between 90 and 120 days after his surgery. For both of these subjects, they received a single opioid refill shortly after surgery by the surgeon and then nothing until receiving their usual sporadic opioid refill. Removing both of these subjects did not change the statistically significant difference between cohorts for persistent opioid use >90 days (p<0.001). Univariate logistic regression analysis could not be done after removing both subjects as the SLC VAMC cohort would not have anyone who met criteria for persistent use.
Mixed effects logistic regression results for opioid prescriptions beyond 90 days
A negative binomial regression model assessing the effect of hospital size on the total number of tablets prescribed within 90 days to group community care showed that veterans who had surgery at small hospitals received 34% more opioid tablets than veterans who had surgery at medium-sized hospitals (ratio=1.35, 95% CI 1.01 to 1.80, p=0.044) and no difference between medium and large hospitals ( online supplemental table 6 ).
Passage of the MISSION Act by the US Congress has resulted in an increasing number of veterans having VHA-paid surgery in the community and the expenditure of many of billions of dollars in addition to what is used to operate VHA facilites. 2 In this study, we compared opioid outcomes among veterans not on chronic opioid therapy who either had a VHA-funded orthopedic joint surgery at the Salt Lake City VAMC facility or at non-VHA hospitals located in the same geographical referral region. The results demonstrated that undergoing orthopedic surgery at a non-VHA hospital in the community is an independent risk factor for being prescribed more opioids both at discharge and in the first 90 days after surgery. This remained true even though group VAMC were more likely to have knee replacement surgery than the community care group, with knee surgery also being an independent risk for larger 90-day opioid prescribing totals. After controlling for possible confounding variables, veterans having surgery at the Salt Lake City VAMC were prescribed 44% fewer opioids than veterans who underwent surgery in the community during the first 90 days after surgery. In addition, having surgery in the community was also associated with a higher likelihood of filling opioid prescriptions beyond 90 days, with only 1 (0.4%) veteran from the Salt Lake City VAMC group having that outcome compared with 20 (6.2%) from the community care group (OR 0.06, 95% CI 0.01 to 0.48, p=0.007). These results are important since long-term opioid use is associated with risks such as opioid overdose, opioid abuse, falls, fractures, myocardial infarction, depression, sexual dysfunction, adrenal insufficiency, and a generally poorer quality of life. 11–19 Interestingly, veterans who had surgery in the community at small hospitals were more likely to receive more opioids in the first 90 days than those who had surgery at moderate or large hospitals (ratio=1.33, 95% CI 1.01 to 1.80, p=0.044). It is not clear why this difference would exist but it raises the question of whether larger hospitals are more likely to have protocolized opioid-prescribing practices or are more likely to use non-opioid modalities (eg, nerve blocks, non-steroidal anti-inflammatory medications) than small hospitals.
While it was not within the scope of this study to evaluate the reasons for the observed differences in opioid prescribing, there are likely many contributory factors that include individual (surgeon) preferences as well as systemic and policy influences. Surgeons in the USA have historically used liberal opioid prescribing for postsurgical pain management compared with the rest of the world. 20 Reluctance by an individual surgeon to change their usual and customary approach to managing postsurgical pain may be an important barrier to reducing opioid prescribing. Additionally, lack of familiarity with current data and recommendations for opioid prescribing after surgery may contribute to failure to change prescribing practices. Lastly, an absence of hospital policies and/or support for implementing proven concepts 21–28 such as enhanced recovery after surgery protocols and transitional pain services likely influence whether opioid-prescribing practices change. The transitional pain service at the SLC VAMC has been shown previously to have an effect on reducing opioid prescriptions 24 26 27 and likely contributed to the difference seen between groups as it is unlikely that other hospitals use similar services. All providers involved in postsurgical pain management should become familiar with current data and recommendations for opioid prescribing after surgery.
The results of this study have a number of potential policy implications. As the VHA (and the American taxpayer) is allocating many billions of additional dollars to pay for veterans to have surgery in the community, an effort should be made to evaluate and compare all relevant outcomes between VHA facilities and the non-VHA community facilities where veterans are receiving care. This information can be used for policymakers to determine whether the high additional cost of community care is a worthwhile investment. In addition, veterans should be presented with relevant outcomes between VHA and non-VHA facilities in the community in order to make an informed decision regarding where they would prefer to receive their care. Lastly, as the payer for services, the VHA has a responsibility to ensure that community care providers maintain high-quality veteran care consistent with current best practices.
There are several limitations of this study to discuss. First, this study is a retrospective analysis and outcomes may have been confounded by unmeasured risk factors. While an effort was made to control for potential confounding in our regression models, opioid prescribing and refills may have been impacted by covariates that were not analyzed, such as the use or non-use of non-opioid pain therapies. Second, our study only evaluated postoperative opioid prescribing among patients undergoing orthopedic surgery procedures. This may have introduced a selection bias, and study findings may not be generalizable to different surgical populations. Third, we only evaluated opioid prescribing and outcomes from a single VA. The Salt Lake City VA has a transitional pain service dedicated to optimizing non-opioid pain therapy and minimizing opioid use and may not be representative of other VHA facilities across the USA. Fourth, while protocols for opioid prescribing and tapering are standardized among patients having orthopedic surgery at the Salt Lake City VA, protocols for pain management may have varied significantly among veterans having surgery by different community surgeons. Specific variations in opioid prescribing among community care surgeons were not evaluated as part of this study. Fifth, while it is not unreasonable to assume that multiple refills of opioid medications would correlate with the patient continuing to take opioids, this study evaluates only opioid prescriptions filled, which does not provide data on actual opioid usage and it cannot be known how or when opioids were taken and precisely when opioid use ceased. Lastly, this study only focused on opioid prescribing as an outcome. Other outcomes such as functional recovery and surgical complications were not part of this study but are important factors in comparing meaningful differences between VHA and community surgical outcomes. Future studies focusing on surgical complication rates, functional recovery outcomes, pain management outcomes, and opioid outcomes will be important to compare community care to VHA surgery for veterans.
Conclusions
Veterans who underwent orthopedic joint surgery at the Salt Lake City VAMC were prescribed significantly fewer opioids at discharge and in the first 90 days after surgery compared with veterans having VHA-funded orthopedic joint surgery at non-VHA community hospitals in the same geographical referral region. In addition, veterans who had surgery at non-VHA community hospitals were at significantly higher risk to continue to fill opioid prescriptions 90 days after surgery than veterans who had surgery at the Salt Lake City VAMC. The presence of a transitional pain service at the Salt Lake City VAMC likely contributed significantly to this difference. This information is important for veterans to consider when choosing between using the VA community care program for surgery or undergoing surgery at a VHA facility. In addition, it is important for policymakers and VHA hospital leadership to understand differences in clinical outcomes when evaluating resource allocation for veteran care. Lastly, all providers managing postsurgical pain should be familiar with current evidence and guidelines for postsurgical pain management and opioid prescribing.
Ethics statements
Patient consent for publication.
Not applicable.
Acknowledgments
We would like to acknowledge the contributions of the members of the transitional pain service at the Salt Lake City VA Medical Center whose clinical work was essential to being able to complete this study: Jennifer Blue MSN, Justin Carrell BSN, Christian DeGrey APRN, Tania Knight BSN, Alysia Martinez BSN, David Merrill BSN, and Ray Walsh-Thacker BSN.
- Congressional Budget Office
- Gurewich D ,
- Shwartz M ,
- Beilstein-Wedel E , et al
- Hickok A , et al
- Vanneman ME ,
- O’Brien WJ , et al
- Beilstein-Wedel EE ,
- Shwartz M , et al
- Harris AHS , et al
- Harris AHS ,
- Rosen AK , et al
- R Core Team
- Ashworth J , et al
- Edgerton L ,
- Donegan D ,
- Fountas A ,
- Van Uum S ,
- Karavitaki N
- Johnston L ,
- O’Malley PM , et al
- Coluzzi F ,
- Billeci D ,
- Maggi M , et al
- Khodneva Y ,
- Muntner P ,
- Kertesz S , et al
- Scherrer JF ,
- Copeland LA , et al
- Campbell G ,
- Nielsen S ,
- Bruno R , et al
- Kaafarani HMA ,
- El Moheb M , et al
- Anderson M ,
- Hallway A ,
- Brummett C , et al
- Argentieri DM ,
- Gutierrez CA , et al
- Silver JA ,
- Mora AN , et al
- Featherall J ,
- Anderson JT ,
- Anderson LA , et al
- Segal S , et al
- Bayless K ,
- Romesser J , et al
- Bleicher J ,
- Brooke BS ,
- Bayless K , et al
- Vetter TR ,
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
- Data supplement 2
X @DrKimBaylessNP, @BenjaminSBrooke
Contributors Study concept and design; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content: all authors. Acquisition of data: MJB and ZA. MJB is responsible for the overall content as the guarantor.
Funding This work was supported by the Veterans Health Administration Office of Rural Health (ORH Contract #14434) and the University of Utah Population Health Research (PHR) Foundation, with funding in part from the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Numbers UL1TR002538 and KL2TR002539.
Disclaimer The content is solely the responsibility of the authors and does not necessarily represent the official views of the Federal Government or the National Institutes of Health.
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
ORIGINAL RESEARCH article
This article is part of the research topic.
How Animals Affect Us: Examining the Influence of Human-Animal Interactions on Human’s Health
The Feasibility of Wildlife Immersion Activities for Veterans with PTSD Provisionally Accepted

- 1 Tan Chingfen Graduate School of Nursing, University of Massachusetts Medical School, United States
- 2 Other, United States
- 3 Department of Psychiatry, University of Massachusetts Medical School, United States
The final, formatted version of the article will be published soon.
Introduction: Animal-assisted interventions (AAI) offer potential physical and psychological health benefits that may assist Veterans with post-traumatic stress disorder. However, more feasibility studies are needed regarding intervention details, adverse events, reasons for study withdrawal, and animal welfare. Methods: This mixed methods feasibility trial involved a modified crossover study in which Veterans with PTSD/ PTSD symptoms were provided a series of 8 nature and wildlife immersion experiences to evaluate feasibility and preliminary efficacy. The sample included 19 Veterans with PTSD/ PTSD symptoms who were followed for a mean of 15.1 weeks. The intervention was comprised of a baseline forest walk, assisting with wildlife rehabilitation, observation in a wildlife sanctuary, and bird watching. Post study bird feeders were provided for sustainability. The theory of transcendent pluralism, which is grounded in mutual human-ecological dignity, guided the study.Results: This AAI nature/ wildlife immersion intervention was feasible, acceptable, and safe to administer to Veterans with PTSD/ PTSD symptoms with appropriate support. Logistical and relational facilitators were identified that supported the wildlife immersion activities. Participants reported greatly enjoying the activities. Attention to animal welfare and care was an important ethical foundation that also contributed to feasibility. Discussion: AAI immersion experiences with wildlife are feasible and can safely be administered to Veterans with PTSD/ PTSD symptoms. Logistical and relational facilitators are important to support nature and wildlife immersion activities.
Keywords: feasibility, human-animal interaction, human-wildlife interaction, animal-assisted intervention, Veterans, PTSD, transcendent pluralism, wildlife immersion
Received: 07 Sep 2023; Accepted: 23 Apr 2024.
Copyright: © 2024 Perry, Crawford, Mackin, Averka and Smelson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Dr. Donna J. Perry, University of Massachusetts Medical School, Tan Chingfen Graduate School of Nursing, Worcester, United States
People also looked at
Military Burn Pits Associated with Increased Health Risk
April 29, 2024
Can deployment to military bases with open burn pits lead to an increased risk of chronic respiratory and cardiovascular conditions? In a recent cohort study, “Deployment to Military Bases With Open Burn Pits and Respiratory and Cardiovascular Disease,” researchers assess the potential association between the length of deployment to military bases with open burn pits and the risk of adverse health outcomes. Westat’s Joseph Gasper, PhD, was a co-investigator on the study.
Published in JAMA Network Open , the study analyzed medical records and declassified deployment records of over 450,000 veterans who were deployed between 2001 and 2011 and received care from the Veterans Health Administration, with a follow-up through December 2020. The findings suggest that extended exposure to open burn pits may increase the risk of developing asthma, congestive heart failure, and other chronic illnesses.
“This study provides new information about the health outcomes associated with burn pit exposure because of its large population size, ability to reconstruct detailed histories of deployment to bases with burn pits, and long-term follow-up using VHA medical records,” says Gasper.
Focus Areas
Capabilities
Featured Expert
Joseph Gasper
Associate Vice President
Deep Dive with Our Experts
Agency for Healthcare Research and Quality (AHRQ)
Washington State Department of Corrections
How can we help?
We welcome messages from job seekers, collaborators, and potential clients and partners.
Want to work with us?
You’ll be in great company.
- Privacy Overview
- Strictly Necessary Cookies
- 3rd Party Cookies
- Additional Cookies

This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognizing you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
This website uses Google Analytics to collect anonymous information such as the number of visitors to the site, and the most popular pages.
Keeping this cookie enabled helps us to improve our website.
Please enable Strictly Necessary Cookies first so that we can save your preferences!
This website uses the following additional cookies:
- Google Analytics
- Google Tag Manager
- Google Search Console
- Google Sitekit
Study record managers: refer to the Data Element Definitions if submitting registration or results information.
Search for terms

- Advanced Search
- See Studies by Topic
- See Studies on Map
- How to Search
- How to Use Search Results
- How to Find Results of Studies
- How to Read a Study Record

- Learn About Studies
- Other Sites About Studies
- Glossary of Common Site Terms

- Submit Studies to ClinicalTrials.gov PRS
- Why Should I Register and Submit Results?
- FDAAA 801 and the Final Rule
- How to Apply for a PRS Account
- How to Register Your Study
- How to Edit Your Study Record
- How to Submit Your Results
- Frequently Asked Questions
- Support Materials
- Training Materials

- Selected Publications
- Clinical Alerts and Advisories
- Trends, Charts, and Maps
- Downloading Content for Analysis

- ClinicalTrials.gov Background
- About the Results Database
- History, Policies, and Laws
- ClinicalTrials.gov Modernization
- Media/Press Resources
- Linking to This Site
- Terms and Conditions
- Search Results
- Study Record Detail

A Study to Evaluate SHR-1210 in Combination With Apatinib as First-Line Therapy in Patients With Advanced HCC
- Study Details
- Tabular View
- Study Results

Inclusion Criteria:
- Histopathologically or cytologically confirmed advanced HCC
- No previous systematic treatment for HCC
- Have at least one measurable lesion (in accordance with RECIST v1.1)
- BCLC stage B or C, and not suitable for surgical or local therapy, or has progressed following surgical and/or local therapy
- ECOG-PS score 0 or 1
- Child-Pugh Class: Grade A
- Life Expectancy of at least 12 weeks
- Subjects with HBV infection: HBV DNA<500 IU/ml or < 2500 copy/mL, and have received anti-HBV therapy for at least 14 days prior to enrollment in the study
- Subjects with HCV-RNA(+) must receive antiviral therapy
- Adequate organ function
Exclusion Criteria:
- Known hepatocholangiocarcinoma, sarcomatoid HCC, mixed cell carcinoma and lamellar cell carcinoma; other active malignant tumor except HCC within 5 years or simultaneously
- Moderate-to-severe ascites with clinical symptoms
- History of gastrointestinal hemorrhage within 6 months prior to the start of study treatment or clear tendency of gastrointestinal hemorrhage
- Abdominal fistula, gastrointestinal perforation or intraperitoneal abscess within 6 months prior to the start of study treatment
- Known genetic or acquired hemorrhage or thrombotic tendency
- Thrombosis or thromboembolic event within 6 months prior to the start of study treatment
- Cardiac clinical symptom or disease that is not well controlled
- Hypertension that can not be well controlled through antihypertensive drugs
- Factors to affect oral administration
- History of hepatic encephalopathy
- Previous or current presence of metastasis to central nervous system
- HIV infection
- Combined hepatitis B and hepatitis C co-infection
- Be ready for or previously received organ or allogenic bone marrow transplantation
- Interstitial lung disease that is symptomatic or may interfere with the detection and management of suspected drug-related pulmonary toxicity
- Active known, or suspected autoimmune disease
- Subjects with a condition requiring systemic treatment with either corticosteroids or other immunosuppressive medications within 14 days of first administration of study treatment
- Use of potent CYP3A4 inducers or inhibitors within 2 weeks prior to the signature of ICF
- Known history of serious allergy to any monoclonal antibody or targeted anti-angiogenic drug
- Severe infection within 4 weeks prior to the start of study treatment
- Palliative radiotherapy for non-target lesions to control symptoms is allowed, but it must be completed at least 2 weeks prior to the start of study treatment
- Treatment of other investigational product(s) within 28 days prior to the start of study treatment

- For Patients and Families
- For Researchers
- For Study Record Managers
- Customer Support
- Accessibility
- Viewers and Players
- Freedom of Information Act
- HHS Vulnerability Disclosure
- U.S. National Library of Medicine
- U.S. National Institutes of Health
- U.S. Department of Health and Human Services
WELCOME TO THE FAMILY! Please check your email for confirmation from us.
Racial discrimination lawsuit against VA could be watershed moment for Black veterans
Conley Monk Jr., a Vietnam War veteran accusing the Department of Veterans Affairs of denying benefits for decades, hopes other Black veterans will join him in a potential class-action lawsuit.
- Share on Facebook
- Share on Twitter
- Share via Email
- Copy Link Link Copied

A first-of-its-kind racial discrimination lawsuit against the U.S. Department of Veterans Affairs has the potential to set the course of justice for generations of Black veterans.
Last month, a federal judge in Connecticut ruled against the federal government in its attempt to dismiss the suit filed by Marine Corps veteran Conley Monk Jr., who accused the VA of denying him and his deceased father, Conley Monk Sr., benefits based on their race after they served in the Vietnam War and World War II, respectively.
The lawsuit argues that the Monks were denied unemployment compensation, along with education, home loan, and disability benefits, including for PTSD, as a result of the VA’s engaging in “systemic racial discrimination against Black veterans for decades.”
“It’s truly a blessing. I’ve been waiting for a long time for this,” Monk told theGrio after Judge Stefan R. Underhill’s consequential ruling. “I’m so glad that the courts decided to move forward with this case. It would truly bless me and my family and also other veterans.
Monk, who is suing on behalf of himself and the National Veterans Council for Legal Redress, a veterans services organization he founded in 1982, is bringing three claims against the VA under the Federal Torts Claims Act: negligence, negligent infliction of emotional distress, and negligent supervision. The suit alleges the Department of Veterans Affairs engaged in “tortious” conduct that caused “stigma, emotional distress [and] …. psychological, and dignitary harms.”
Monk told theGrio that navigating the VA for benefits has been a “nightmare” since he first attempted to access benefits in 1971, the year after he was discharged.
“I had to struggle to work two jobs in order to bring in income to support my family,” he said. “I’ve been totally discriminated against … I fought. I did what I was told to do. Then I came home and I was deprived.”
The legal complaint filed against the VA notes that while serving in the Marines, Monk experienced two PTSD “altercations” and was told he “could not depart until he agreed to an undesirable discharge.”

The complaint also points out that PTSD was not formally recognized by the American Psychiatric Association until 1980. Monk’s dishonorable discharge resulted in his denial of veteran benefits, including unemployment benefits from the state of Connecticut, because individuals with a dishonorable discharge are not considered veterans and, therefore, are ineligible.
Members of Monk’s legal team connect his case to a broader and systemic occurrence among Black veterans. They point out that in the 1970s, the Department of Defense determined that Black service members were “substantially more likely to face military disciplinary action.” Similar data was backed up by the Army and Equal Employment Opportunity Commission, according to the complaint.
Despite Monk’s repeated appeals to the VA to revise its 1971 discharge determination, he was denied.
The Monks’ historic case is a result of years-long efforts, including requests for the public release of government information and documents, led by the Black Veterans Project, a Black veterans advocacy group founded by Richard Brookshire, Zella Vanie and Daniele Anderson, in partnership with the Yale Law School Veterans Legal Services Clinic.
“We built basically a huge FOIA project that took about over a year to put together, and then we litigated it for almost two years,” Brookshire told theGrio, referring to the Freedom of Information Act. “We took all that data and those legal documents and internal VA documents and built a legal case for Monk v. United States.” FOIA requests from the Black Veterans Project and Yale Law School produced data from an internal 2017 study conducted by the VA concluded that “[n]on-Hispanic Blacks have the lowest grant rate at 43% and are largest outlier in terms of grant rate.”
“The evidence that we’ve already put forward shows pretty compellingly decades of discrimination at VA,” Jared Hirschfield, a student with the Yale Law Veterans Legal Services Clinic, told theGrio.
Hirschfield said the Yale group will continue to file FOIA requests in order to gather data to build Monk’s case, which, with the Connecticut court’s ruling, can enter the discovery phase. The discovery process is expected to go on for as long as a year. Hirschfield called the facts of the case thus far “damning.” “Unfortunately, I don’t think that his story is unique,” he said. “I think [Monk] deserves a ton of credit for putting his story out there and being the face of this, and hopefully in the process fixing this program for all Black veterans.”

Brookshire of the Black Veterans Project said the Monk case and its potential to reach class-action status is, at its core, a case for reparations.
“It provides an opportunity for the country to reckon with what is done to Black vets,” he told theGrio. “There hasn’t been an opportunity in a court of law for us to bring the history of benefit obstruction to the table and have it adjudicated on its merits, and in the case for reparations to be adjudicated on its merit.”
Experts say it would take more than $10 trillion to close the racial wealth gap. Brookshire said a “piece of that puzzle has been in accessibility to veteran benefits.” He argued that had Black veterans not been discriminated against for decades, “you would see more Black families in the middle class … with higher homeownership rates [and] the ability to pass those homes down to their children.”
He added, “You wouldn’t see the kind of statistics that you see affecting Black vets, [who are] twice as likely to live in poverty [and] represent a full 1/3 of the homeless veteran population.” Monk told theGrio that it would be a “rewarding” feeling if his civil case allowed other Black veterans to access benefits and receive compensation for what they’ve lost over the years.
“We would like to let the Black veterans know that they have a voice. They need to get involved,” Monk told theGrio. “We’re going to continue to fight to make sure this gets out.”
Recommended Stories

Gerren Keith Gaynor

Meet Veterans Affairs’ highest-ranking woman, Tanya Bradsher

Family of Black veteran buried at overgrown cemetery calls for cleanup
TheGrio Staff
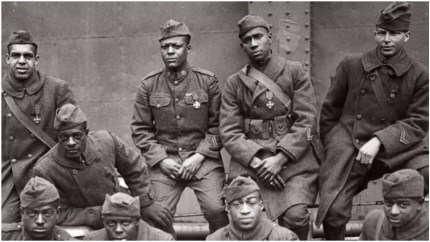
House Democrats reintroduce G.I. bill to help Black veterans and descendants receive overdue benefits
Ashlee Banks
A Black man who served as a Green Beret will receive the Medal of Honor after a nearly six-decade wait

Black disabled veteran files suit against the VA, claiming racial discrimination

Black veterans received lower benefits because of racism, study says

Black veterans honored with first-of-its-kind, 12-pillared monument
- Share on Facebook Facebook
- Share on Twitter Twitter
- Share via Email Email
- Copy Link Copy Link Link Copied

STREAM FREE MOVIES, LIFESTYLE AND NEWS CONTENT ON OUR NEW APP

IMAGES
COMMENTS
VA Office of Research and Development (ORD) supports health research at more than 115 VA facilities nationwide. Specially designated VA research centers conduct basic and clinical studies that support concentrated efforts by groups of scientists studying diseases such as AIDS, alcoholism, schizophrenia, and rehabilitation efforts. Other research programs foster additional multidisciplinary ...
Biomedical Laboratory Research and Development conducts preclinical research to understand life processes from the molecular, genomic, and physiological level in regard to diseases affecting Veterans. Clinical Science Research and Development focuses on clinical trials and other research involving human volunteers to study new treatments ...
Office of Research & Development. Find VA-sponsored clinical trials near you. Follow these steps to find recruiting clinical trials. The screenshots below show where to enter information: Visit https://clinicaltrials.gov by clicking the link or typing it into your web browser. Type a search term (for example, cancer) into the box under ...
A follow-up to a study that assessed the odds of unsheltered status among veterans (Byrne, Montgomery, and Fargo 2016) found that being unsheltered at the time of a veteran's initial response to the HSCR is associated with almost three times the odds of experiencing ongoing or persistent housing instability; while only 11 percent of veterans ...
The NHRVS is a large, nationally representative prospective study which consists of two separate cohorts of 3,157 and 1,484 U.S. military veterans. Additionally, the NHRVS utilizes well-validated measures to examine longitudinal changes of mental and physical health outcomes in this population.
VA's VA Health Systems Research (HSR), works to identify and evaluate innovative strategies that lead to accessible, high quality, cost-effective care for veterans and the nation. One of four research services within VA's Office of Research and Development, HSR is an intramural research program funding eligible VA clinicians and investigators to address VA health care priorities.
Families with complex needs face significant challenges accessing and navigating health and social services. For veteran families, these challenges are exacerbated by interactions between military and civilian systems of care, and the density of the veterans' non-profit sector. This qualitative study was designed to gather rich, detailed information on complex needs in veteran families; and ...
The Veterans Studies Association (VSA) is seeking applications for an Editor in Chief of the Journal of Veterans Studies (JVS). This is a paid position that requires 5-10 hours a week on average, with benefits to be paid in a stronger sense of community, pride, a vita line, and a modest annual stipend. Read more. Published on 3 Apr 2024.
New areas of research on veterans are emerging as the field of veterans studies develops and grows. Yet gaps remain in interdisciplinary research efforts on veterans. The research available across disciplines is still too fragmented to coalesce into a full-fledged field of veteran studies, as other categorical, area, and identity fields of study have done so. By surveying research literature ...
Objective: Psychiatric and substance use disorders are prevalent among U.S. military veterans, yet many veterans do not engage in treatment. The authors examined characteristics associated with use of mental health care in a nationally representative veteran sample. Methods: Using 2019-2020 data from the National Health and Resilience in Veterans Study (N=4,069), the authors examined ...
Mental health or behavioral adjustment disorders. Medical records of veterans reveal "that one in three patients was diagnosed with at least one mental health disorder - 41% were diagnosed with either a mental health or a behavioral adjustment disorder". 3 In compensation or in combination with military-related diseases, many veterans develop substance use disorders (SUDs) and a large ...
Research projects have significantly contributed to advancements in health care for Veterans and all Americans from every walk of life. VA researchers wouldn't be able to make the advancements they do without the volunteers who take part in our clinical studies. Clinical Research is focused on moving ideas along the translational pathway from scientific discovery to clinical application in ...
Advancing knowledge for veterans, citizens, educators & advocates. Join our scholarly community. Nonprofit scholarly association that encourages rigorous scholarship about interactions between military veterans and their families with civilian societies in order to inform understanding, teaching, service, and advocacy. We embrace research that ...
Stigmas surrounding mental illness in the military have steadily decreased over time but remain high (Acosta et al., 2014).Reducing the stigmas associated with mental health within military populations is a current priority as research has shown that these stigmas may serve as a barrier to treatment for those returning from combat (Acosta et al., 2014; Blais et al., 2014).
An additional 22% say they sometimes felt proud, and 9% say they seldom or never felt this way. Pre-9/11 veterans are more likely to say they frequently felt proud of their service than are post-9/11 veterans (70% vs. 58%). Most veterans say they would endorse the military as a career choice. Roughly eight-in-ten (79%) say they would advise a ...
Introduction. Substance use disorders (SUDs) are a significant problem among military veterans and are associated with numerous deleterious effects.1-3 There are a number of services and interventions available to help reduce SUDs among veterans, including both behavioral and pharmacological treatments. The aims of this review are to provide information on the epidemiology of SUDs among ...
Million Veteran Program (MVP) About. VA's Million Veteran Program (MVP) is a national research program looking at how genes, lifestyle, military experiences, and exposures affect health and wellness in Veterans. Since launching in 2011, 1 million Veterans have joined MVP. It's the largest research effort at VA to improve health care for Veterans and one of the largest research programs in the ...
A VA Boston researcher was approved for $6 million in funding Tuesday, April 23, 2024, by the Patient-Centered Outcomes Research Institute to study a comprehensive, personalized intervention for patients who have experienced intimate partner violence, commonly known as IPV. ... "IPV is more common among military Veterans, so there's a ...
The study, published Thursday by JAMA Network Open looked at the records of 459,381 military veterans receiving health care from the Veterans Administration to determine the health effects of ...
Future research should include interviews with veterans during the transition and compare veteran and VA employee experiences. Conclusion Despite a current delay in the deployment of the new EHR at additional VA medical centers, findings from this study offer timely lessons that can ensure clinicians and staff are equipped to navigate ...
The study included 459,381 Air Force and Army veterans deployed to OIF or OEF between 2001 and 2011. Follow-up data were collected from the VHA until the end of 2020.
Methods We conducted a retrospective cohort study among veterans who underwent orthopedic joint surgery paid for by the VHA either at the Salt Lake City VHA Medical Center (VAMC) or at non-VHA hospitals between January 2018 and December 2021. 562 patients were included in the study, of which 323 used a non-VHA hospital and 239 patients the VAMC. The number of opioid tablets prescribed at ...
Introduction: Animal-assisted interventions (AAI) offer potential physical and psychological health benefits that may assist Veterans with post-traumatic stress disorder. However, more feasibility studies are needed regarding intervention details, adverse events, reasons for study withdrawal, and animal welfare. Methods: This mixed methods feasibility trial involved a modified crossover study ...
The study has already received regulatory approval from an Institutional Review Board and the Department of Defense's Office of Human Research Oversight. OSU researchers are currently looking to recruit 150 more U.S. military personnel and veterans for this study.
The Cooperative Studies Program (CSP) is a division within the Clinical Science Research & Development Service of the U.S. Department of Veterans Affairs (VA) Office of Research and Development. Using its expertise in clinical research, the CSP conducts multi-site clinical trials and epidemiological research on key diseases that impact our nation's veterans.
Westat's Joseph Gasper, PhD, was a co-investigator on the study. Published in JAMA Network Open, the study analyzed medical records and declassified deployment records of over 450,000 veterans who were deployed between 2001 and 2011 and received care from the Veterans Health Administration, with a follow-up through December 2020. The findings ...
Pregnancy or breastfeeding, or intention of becoming pregnant during study treatment or within 5 months after the last dose of study treatment Patients who have received a non-FDA or non-EMA approved anti-EGFR agent or any other non-FDA or non-EMA, approved agent as part of definitive local therapy, unless the unapproved agent was given in ...
The purpose of this extension study is to provide continued treatment with Roche investigational medicinal product (IMP[s]) monotherapy or Roche IMP(s) combined with other agent(s) or comparator agent(s) for eligible participants with cancer who are still on study treatment at the time of roll-over from the parent study and who do not have access to the study treatment locally.
Choosing to participate in a study is an important personal decision. Talk with your doctor and family members or friends about deciding to join a study. To learn more about this study, you or your doctor may contact the study research staff using the contacts provided below. For general information, Learn About Clinical Studies.
FOIA requests from the Black Veterans Project and Yale Law School produced data from an internal 2017 study conducted by the VA concluded that "[n]on-Hispanic Blacks have the lowest grant rate ...