School of Nursing Advances Cardiovascular Health Through Research, Practices, Education
For almost a century, heart disease has been the leading cause of death and a leading cause of disability in the United States. Heart or cardiovascular disease covers several conditions. In the U.S., the most common of these is coronary artery disease. This condition affects how blood flows to the heart and can lead to a heart attack.
In 1963, President Lyndon Johnson proclaimed February American Heart Month to make Americans “aware of the medical, social, and economic aspects of the problem of cardiovascular diseases, and the measures being taken to combat them.” Later, the first Friday of February was proclaimed National Wear Red Day to highlight the impact of heart disease on U.S. women. Heart disease is the leading cause of death of women, particularly African American/Black and white women.
Because it affects people of any age, sex, race, and background, many organizations continue to research, prevent, and treat cardiovascular disease. Across the Duke University School of Nursing, students and faculty members are putting forth nurse-led models of care, extensive expertise, educational opportunities and clinical practice to advance cardiovascular health:
- Five faculty members are active cardiology practitioners and researchers, bringing nursing students real-world experience from the bedside and the bench. Learn more about these faculty members below.
- MSN and DNP students can pursue a cardiology specialty, one of only four in the country. Learn more about the Duke Nursing cardiology specialty .
- Relevant, cutting-edge, and patient-centered cardiologic content is included in all degree programs. The Center for Nursing Discovery , a state-of-the-art simulation center, provides a variety of instructional methodologies to support the program including EKG interpretation workshops, telemedicine for guideline-directed medical therapy titration, high-fidelity simulation for acute myocardial infarction, and practice with interprofessional consults.
- Several DNP and PhD candidates are engaged in research projects to study cardiovascular disease.
“Cardiovascular disease is still the number one cause of death in the country,” Margaret Midge Bowers, DNP, RN, FNP-BC, CHSE, AACC, FAANP, FAAN , associate professor, said. “When I started as a nurse practitioner 22 years ago, the mortality rate for heart failure was 50% at five years. It’s still close to that now.”
Bowers, who is the lead faculty for the Cardiovascular Specialty, acknowledges that nurses are vital to changing the trend.
“The more nurses that specialize in cardiology, the more impact we can have from advanced practitioners at the bedside, in outpatient clinics, in home health—all across the continuum of care. That's the best way to help people reduce their risk and improve their outcomes,” she said.

Faculty Spotlights

She/Her/Hers Associate Professor & Cardiovascular Specialty Lead Faculty Nurse Practitioner, Heart Failure Same-Day Access Clinic In the final semester of my nursing program, I worked on a cardiac telemetry unit and became fascinated with the physiology of the heart. In my career, I’ve cared for patients across the care continuum—in a Cardiac Intensive Care Unit, outpatient cardiac rehab, critical care air and ground transport, cardiology clinic, and skilled nursing facilities.
These settings allow cardiac nurses to learn about cardiovascular disease while caring for diverse patient populations in acute, primary, and long-term care settings. The dynamic nature of cardiology research and evolving clinical practice guidelines provide are one of the many reasons I see a future where the focus of my care is on health promotion and disease prevention rather than treatment.
Learn more about Dr. Bowers.

He/ Him/ His Assistant Clinical Professor CNIII 7 West Cardiothoacic ICU As a nursing student in 1988, I worked as a professional nursing assistant in cardiology under a dynamic nurse manager, Barry Hawthorn, who mentored me. I ended up staying on the unit as a new graduate nurse. Later in my career I went back to the bedside in Cardiothoracic Intensive Care Unit (CTICU) in Duke Heart while working on my MSN and PhD degrees. Once again, the dynamic nursing leadership of Drs. Jill Engel, associate vice president heart services, Mary Lindsay, Duke Heart Center associate chief nursing officer, and Kelly Kester, clinical operations director for heart services, cultivated my current success in becoming an assistant clinical professor here at DUSON.
I still enjoy the bedside experience in the CTICU and working with end-stage heart failure patients needing surgical interventions. Technology in this population has exponentially increased over the past decade with the advancement of ventricular assistant devices and extracorpeal membrane oxygenation. These devices have helped individuals with end-stage heart failure to achieve better patient outcomes including heart transplantation. Many nurses starting out will immediately discover the many opportunities for the bedside nurse in terms of clinical practice, education, and leadership. For me, it is the people, patients, family members, nurses and physicians, all collaborating to advance the quality of life for anyone suffering from advance heart disease. The Heart Center is where innovation is fostered and celebrated.
Learn more about Dr. Cadavero.

Professor Director, Duke Heart Center Nursing Research Program Core faculty, Duke-Margolis Center for Health Policy Bradi has extensive clinical experience in cardiovascular nursing and is an active member of organizations such as the American Heart Association. Her research scope in this area has included contributing to efforts on a palliative care in heart failure trial and to improve advanced practice provider knowledge and assessment of medication adherence in patients with cardiovascular disease.
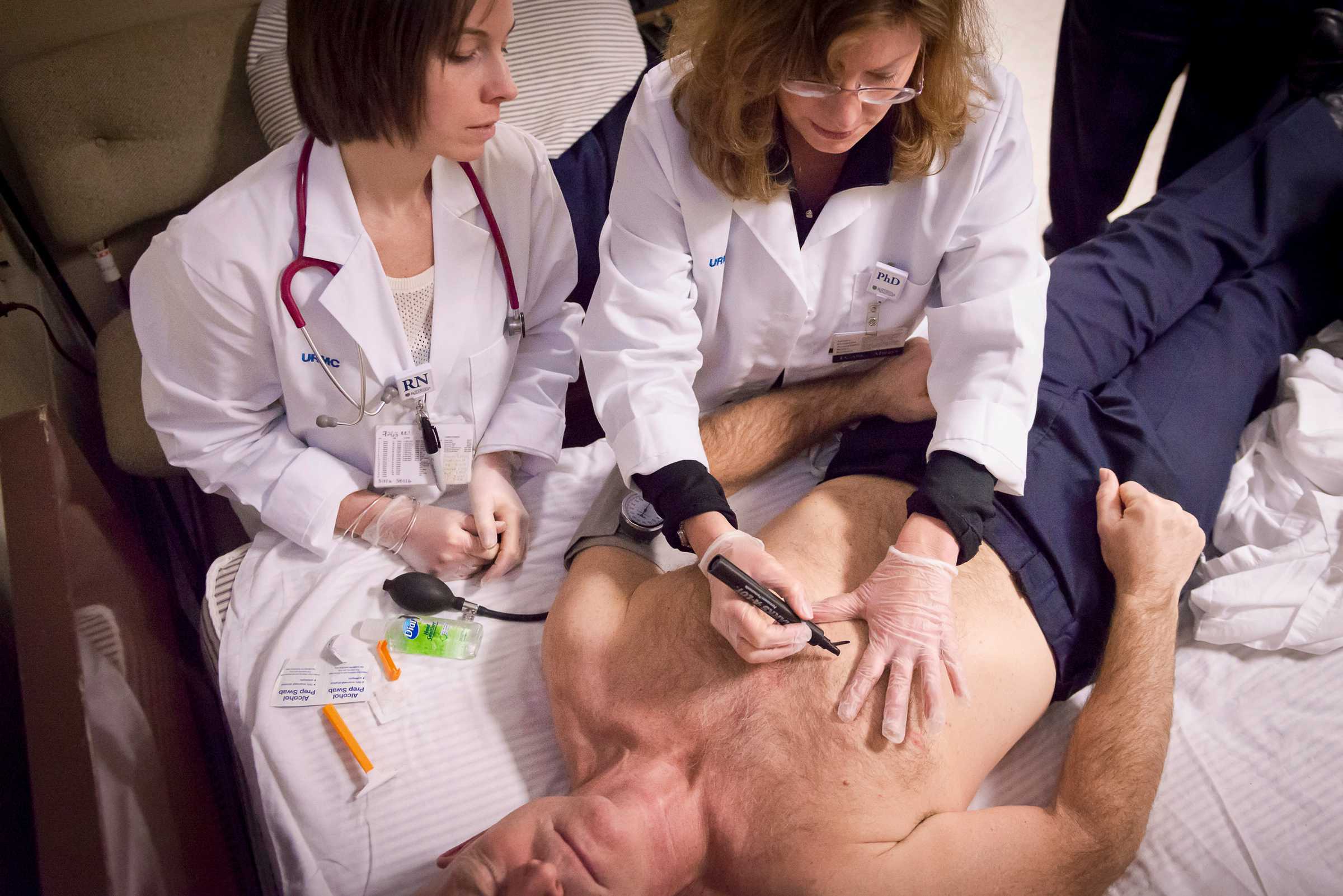
Currently, she is leading a project with Holly Biola, MD, of Lincoln Community Health Center, that is using community-based intervention to identify and reduce disparities and inequities among women with high blood pressure to help more women control their hypertension; the project is supported by the Alpha Phi Foundation’s generous Heart to Heart Grant.
Learn more about Dr. Granger.

She/Her/Hers Assistant Professor Cardiology has always been fascinating to me. I loved caring for patients with cardiac complaints as an emergency nurse when I first started my career. When I decided to expand my scope of practice and passed my nurse practitioner certification exam, I knew I wanted to pursue my clinical practice in the field of inpatient cardiology.
In addition to my love for cardiology, I also share a passion for interprofessional collaborative practice. I am so grateful to work with an amazing collaborative team of health care providers who strive to provide high-quality evidence-based cardiac care to patients. Patients with complex cardiology disorders benefit significantly from a team-based approach. I feel so fortunate that these passions intersect and allow me to advocate for and positively impact patients and their families.
Learn more about Dr. Leonard.

She/ Her/ Hers Assistant Professor Acute Care Nurse Practitioner, Duke Heart Center A personal diagnosis of Long QT Syndrome launched me into cardiology, first as a patient, then as a clinical nurse, and now as a nurse practitioner and educator. The nature of cardiology is that ailments are commonly multisystem disease processes. This requires care from clinicians who have a broad understanding of pathophysiology and the knowledge to address problems in a holistic way. It is challenging, complex, and chronic. It has never been more important for patients to have access to high-quality cardiology providers.
Nurses have a crucial role in teams that provide evidence-based cardiac care at both the acute and primary care levels. Heart disease is so prevalent and requires a holistic and patient-centered approach—an ideal place for nurses!
Learn more about Dr. Tennyson.

Create Free Account or
- Acute Coronary Syndromes
- Anticoagulation Management
- Arrhythmias and Clinical EP
- Cardiac Surgery
- Cardio-Oncology
- Cardiovascular Care Team
- Congenital Heart Disease and Pediatric Cardiology
- COVID-19 Hub
- Diabetes and Cardiometabolic Disease
- Dyslipidemia
- Geriatric Cardiology
- Heart Failure and Cardiomyopathies
- Invasive Cardiovascular Angiography and Intervention
- Noninvasive Imaging
- Pericardial Disease
- Pulmonary Hypertension and Venous Thromboembolism
- Sports and Exercise Cardiology
- Stable Ischemic Heart Disease
- Valvular Heart Disease
- Vascular Medicine
- Clinical Updates & Discoveries
- Advocacy & Policy
- Perspectives & Analysis
- Meeting Coverage
- ACC Member Publications
- ACC Podcasts
- View All Cardiology Updates
- Earn Credit
- View the Education Catalog
- ACC Anywhere: The Cardiology Video Library
- CardioSource Plus for Institutions and Practices
- ECG Drill and Practice
- Heart Songs
- Nuclear Cardiology
- Online Courses
- Collaborative Maintenance Pathway (CMP)
- Understanding MOC
- Image and Slide Gallery
- Annual Scientific Session and Related Events
- Chapter Meetings
- Live Meetings
- Live Meetings - International
- Webinars - Live
- Webinars - OnDemand
- Certificates and Certifications
- ACC Accreditation Services
- ACC Quality Improvement for Institutions Program
- CardioSmart
- National Cardiovascular Data Registry (NCDR)
- Advocacy at the ACC
- Cardiology as a Career Path
- Cardiology Careers
- Cardiovascular Buyers Guide
- Clinical Solutions
- Clinician Well-Being Portal
- Diversity and Inclusion
- Infographics
- Innovation Program
- Mobile and Web Apps
The Emerging Role of Advanced Practice Registered Nurses in Cardiology: Insights From the ACC APRN Survey
Cardiology Magazine

Advanced practice registered nurses (APRNs) continue to assume an increasing role in the care of individuals with cardiovascular disease. Although APRNs include nurse practitioners (NPs), clinical nurse specialists (CNSs), nurse anesthetists and nurse midwives, this article focuses on NPs and CNSs.
Depending on their scope of practice and role, APRNs function across the continuum of care, and provide care in acute care facilities, nursing homes, primary care clinics, outpatient clinics and offices, and other areas.
APRN Survey Results
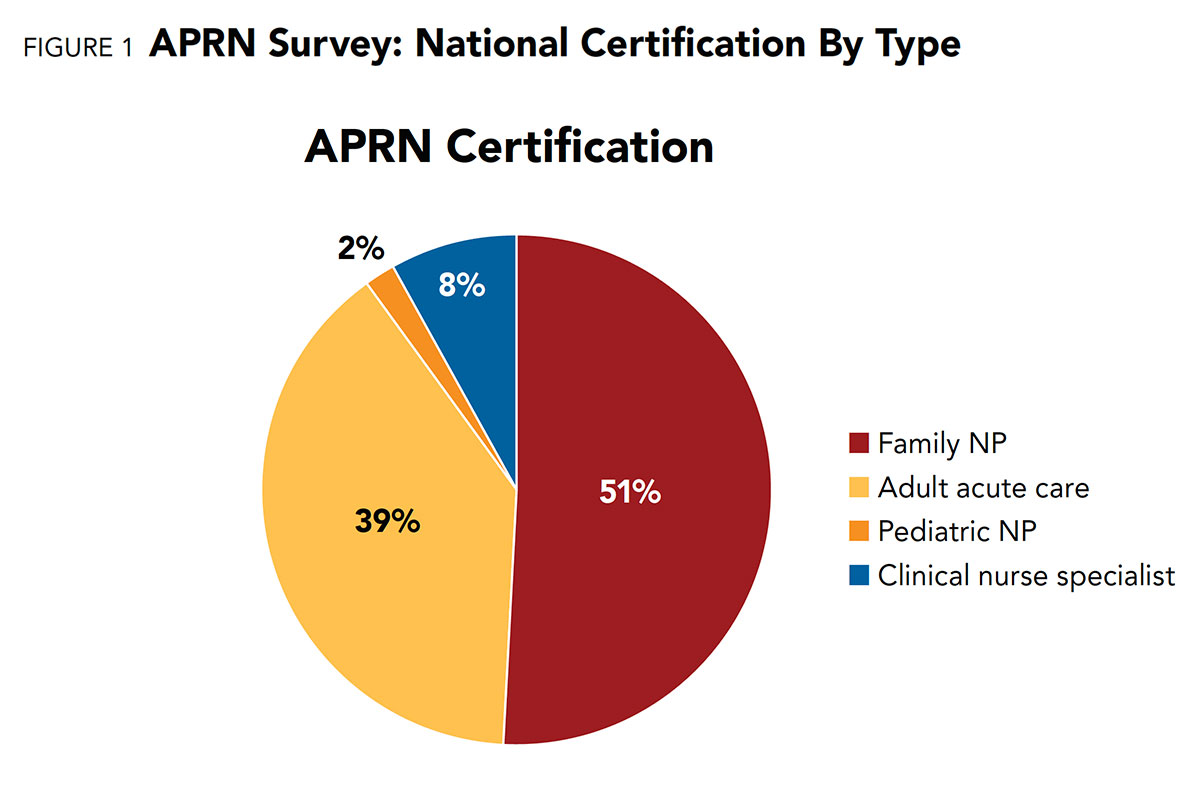
The majority of APRNs who responded to the survey were NPs with national certification as family nurse practitioners (43%) followed by adult acute care (29%). Only three respondents were certified as pediatric NPs. CNSs represented 7% of respondents (Figure 1).
The highest level of education achieved was a Master's degree for 76%, a Doctor of Nursing Practice (DNP) for 17% and PhD for 5%.
For respondents with a Master's degree, only 22% said they planned to further their education, although the reasons for this were not captured with the survey questionnaire.
Most of the APRNs ranged in age between 36 and 45 years (31%), with 24% over the age of 55. The greatest range for the number of years practicing in cardiology was over six years.
The vast majority (81%) worked full-time as direct patient care providers in hospital-based practices in urban areas.
Very few had administrative (16%) or research positions (6%). These demographics are consistent with data published by the American Association of Nurse Practitioners (AANP) in 2018. 1
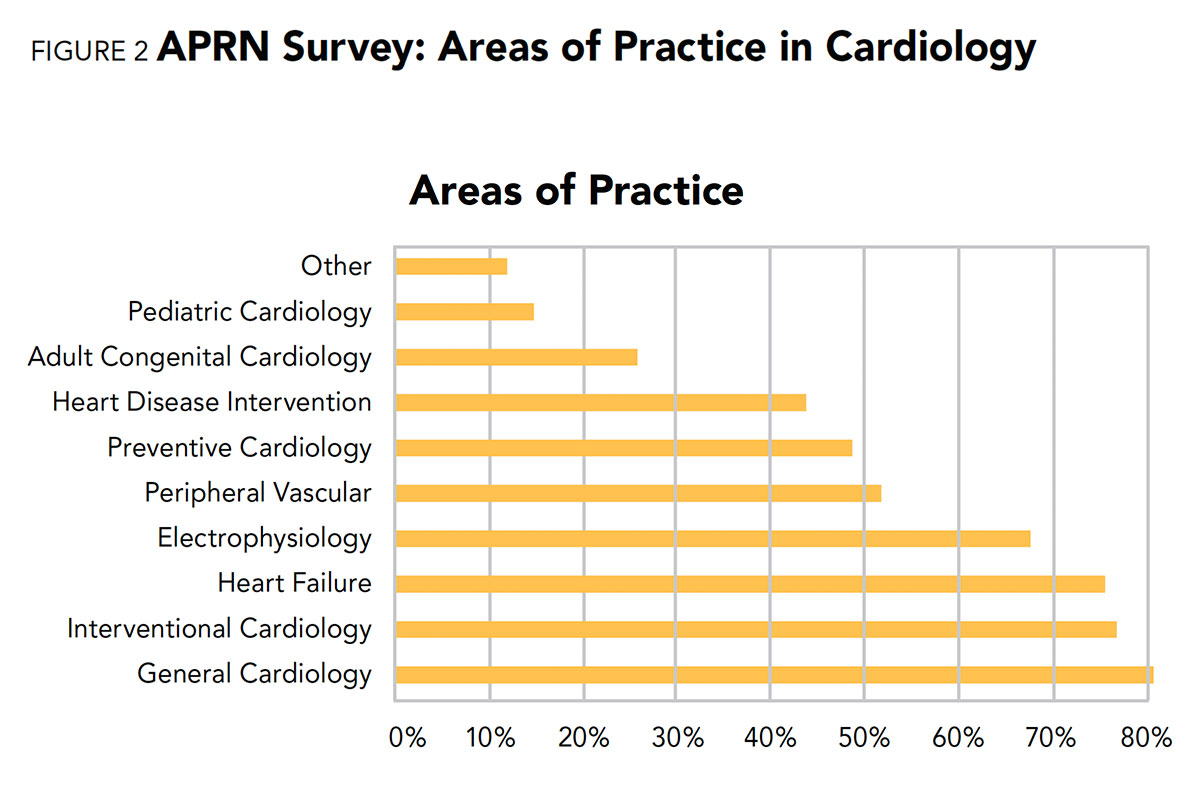
In our ACC study, the top three areas of practice of the respondents were general cardiology (81%), interventional cardiology (77%) and heart failure (76%) (Figure 2).
With respect to workload, the majority (35%) of respondents reported they had fewer than 25 inpatient encounters per week; 27% reported 26-50 encounters; 12% reported 51-75 encounters; and 3% more than 75 inpatient encounters. (Note that one patient seen on three separate days represents three encounters.)
For respondents who performed inpatient rounds, most (46%) reported a typical daily patient load of less than 10 patients; 39% reported 11-20 patients and 7% reported more than 21 patient encounters.
The primary responsibilities reported by the survey respondents were: patient education (67%), cardiology consults (65%), outpatient follow-ups (64%), hospital rounds (58%) and admission history and physicals (52%). (Note the percentages do not total 100 because more than one responsibility could be selected.)
A minority of respondents (less than 10%) performed procedures, such as elective cardioversion, catheter placement and/or endotracheal intubation.
APRN Survey Design
The APRN Work Group of ACC's CV Team Member Section developed and conducted a survey to better understand the roles and responsibilities of APRNs, as well as determine their potential education needs.
The 2019 Cardiology Advanced Practice Registered Nurses Workforce Survey was similar with one conducted the year before on the physician assistant workforce.
The APRN survey consisted of 34 questions that addressed demographics, place of employment, role and responsibilities, financial aspects and barriers to practice.
The survey was emailed to 2,600 APRN members of ACC and was promoted by six email invitations, the CV Team Section e-newsletter and CV Team State Liaisons, including information about deadline extensions.
As a result, 262 individuals (248 NPs; 14 CNSs) responded to the survey, corresponding to a 10% response rate that is consistent with response rates of other ACC surveys, which have averaged from 7-10%. Data are reported in aggregate based on response rates to each question.
Regarding role expectations, 56% of the APRN respondents reported being able to practice to the full level of their education and training, while 39% reported sometimes they were able to and 5% reported they never were able to practice to their full level.
This lack of autonomy may be related to the barriers reported in our survey. One of these barriers was state nurse practice acts (reported by 35%) which do not allow for full practice authority. Others reported barriers were state medical board rulings (24%), institution-wide lack of support for APRNs (29%), departmental lack of support for APRNs (20%), lack of support from direct supervisor (14%) and institutional bylaws (38%).
This provides insight into the majority of survey respondents stating they were only partly satisfied with their role. These barriers to practice are similar with those in an Institute of Medicine (IOM) report in 2011 on The Future of Nursing. 2
The IOM report notes that although APRNs are highly trained and able to provide a variety of services, they are unable to practice to the full scope of their education and training due to outdated insurance reimbursement models, institutional practices and culture, state laws and federal policies.
Turning to compensation, the average hourly base pay was between $50-55 (28%), with $35-40 (2%) the lowest and $115-120 the highest (1%). This is lower than the average hourly pay of $63 reported in the national NP survey. 1
Incentives reported in our ACC survey included education funds (82%), license reimbursement (71%), DEA registration (73%), medical staff dues reimbursement (31%) and bonuses (24%). The majority of salaries was paid by the department of cardiology (32%), and 9% came from the department of nursing.
Opportunities For APRNs in ACC
ACC Celebrates Nurses Appreciation Month
Nurses deserve our gratitude and appreciation for their commitment to delivering the highest standards of cardiovascular care.
The College is proud to stand by and support nurses – not just during the current pandemic – but always. The work you do is essential for transforming cardiovascular care and improving heart health. You have our heartfelt thanks for all you do.
ACC is offering free membership to new cardiovascular team members during the month of May as part of our support. Visit ACC.org/Join and use the code HereForYou . Applications are always welcome.
Discover all we have for you as a cardiovascular team member at ACC.org/CVT .
Currently, there are 2,971 APRN members in the CV Member Section, of which only 11 are international members. APRNs have become well recognized as valued members of team-based cardiology care, 3,4 and work in concert with other providers.
The ACC's Competency Management Committee is developing a competency statement that will describe the key experiences and skills of NPs and physician assistants (PAs) as members of the CV care team, including those in general cardiovascular practice and those working in focused areas of cardiovascular medicine.
The College offers several leadership opportunities for APRNs who wish to foster their professional commitment within cardiology and lend a voice for this discipline.
Other opportunities include joining ACC state chapters, participating in various committees within the CV Team Member Section, particularly the APRN Work Group, and participating in guideline development committees.
Another opportunity is to become an Associate of the American College of Cardiology (AACC). The AACC designation honors cardiology professionals who demonstrate a commitment to their discipline and to the College. Currently, 271 APRNs hold the AACC designation.
Another avenue of distinction for APRNs is to become a Fellow of the American College of Cardiology (FACC). Fellowship is conferred on members with outstanding contributions to cardiovascular medicine and is highly regarded amongst peers and the community. To date, three APRNs have achieved FACC designation.
The abundance of learning opportunities and avenues for professional development through the College, positions the ACC to serve as the professional home of APRNs who practice in cardiology.
Tweet #CardiologyMag
This article was authored by Kristine Anne Scordo, PhD, APRN, ACNP-BC, FAANP , from the Kettering Heart and Vascular Dayton, OH, and chair of the ACC's APRN Work Group of the CV Team Member Section, and Carla H. Weidner, DNP, FNP-BC, CLS, AACC , from St. Luke's University Health Network in Bethlehem, PA.
- Kleinpell R, Cook ML, Padden DL. J Am Assoc Nurse Pract 2018;30:140-9.
- Institute of Medicine. The future of nursing: Leading change, advancing health. The National Academies Press; 2011. Washington, DC. Available here . Accessed Jan. 30, 2019.
- Brush JE Jr, Handberg EM, Biga C, et al. J Am Coll Cardiol 2015;65:2118-36.
- Arnett DK, Blumenthal RS, Albert MA, et al. J Am Coll Cardiol 2019;74:1376–1414.
Clinical Topics: Arrhythmias and Clinical EP, Cardiovascular Care Team, EP Basic Science
Keywords: ACC Publications, Cardiology Magazine, Advanced Practice Nursing, Motivation, Nurse Clinicians, Institutional Practice, Fellowships and Scholarships, Leadership, Inpatients, Electric Countershock, Pandemics
You must be logged in to save to your library.
The Latest From Cardiology
Read the entire May issue by clicking the links below!
Guest Editorial | COVID in the U.S.: A Clear Dichotomy
Quick Reads | The Pulse of ACC: Two NCDR Registries Collecting COVID-19 Data; Understanding COVID-19 Impact on Health Care Workers and More!
Calling All Clinicians: Help With Understanding COVID-19 Impact on Health Care Workers
Cover Story | Cannabis and Cardiovascular Disease: Time For Education Deleterious Effects of Marijuana Becoming Clearer
SPECIAL FEATURES
Lessons from Wuhan: Insights From Our Colleague in China
COVID-19 Pandemic: A Fellow-in-Training Perspective
Challenges For the Cardiovascular Community During the COVID-19 Pandemic
FROM THE MEMBER SECTIONS
From Caregiver to Patient: My First-Hand Experience Surviving COVID-19
Pandemic-Driven Changes at the Front Lines of Medical Education: FITs Respond to COVID-19
From AIDS to COVID-19: A Lesson For the Present
Poem | And People Went to Work
For the FITs | Accelerating the Cardiovascular Subspecialist Training Pathway
Quality Improvement For Institutions | Congratulations to Hospitals Earning an ACC Accreditation!
Business of Medicine | Reinventing Cardiovascular Care in Two Weeks: An Industry Adapts to a Pandemic
Cutting Edge Structural Interventions | Nurse-led Sedation in TAVR: Optimizing Resources, Outcomes
Innovation at ACC | Future Hub to the FDA: Following HeartHero's Journey Since the ACC.19 Innovation Challenge Win
Heart of Health Policy | ACC, Others Offer Framework for Resuming CV Services
Heart of Health Policy | Advocacy in Action: Newest CMS COVID-19 Rule Includes Telehealth Measures Requested By ACC
Heart of Health Policy | Provided COVID-19 Testing or Treatment for Uninsured Patients?
Heart of Health Policy | CMS Reevaluates Accelerated Payment Program
Heart of Health Policy | FDA Update: Farxiga
Number Check | National Physical Fitness and Sports Month
On Balance | So... You're Thinking of Retiring?
JACC in a Flash
Journal Wrap
JACC Journals on ACC.org
- JACC: Advances
- JACC: Basic to Translational Science
- JACC: CardioOncology
- JACC: Cardiovascular Imaging
- JACC: Cardiovascular Interventions
- JACC: Case Reports
- JACC: Clinical Electrophysiology
- JACC: Heart Failure
- Current Members
- Campaign for the Future
- Become a Member
- Renew Your Membership
- Member Benefits and Resources
- Member Sections
- ACC Member Directory
- ACC Innovation Program
- Our Strategic Direction
- Our History
- Our Bylaws and Code of Ethics
- Leadership and Governance
- Annual Report
- Industry Relations
- Support the ACC
- Jobs at the ACC
- Press Releases
- Social Media
- Book Our Conference Center
Clinical Topics
- Chronic Angina
- Congenital Heart Disease and Pediatric Cardiology
- Diabetes and Cardiometabolic Disease
- Hypertriglyceridemia
- Invasive Cardiovascular Angiography and Intervention
- Pulmonary Hypertension and Venous Thromboembolism
Latest in Cardiology
Education and meetings.
- Online Learning Catalog
- Products and Resources
- Annual Scientific Session
Tools and Practice Support
- Quality Improvement for Institutions
- Accreditation Services
- Practice Solutions
Heart House
- 2400 N St. NW
- Washington , DC 20037
- Email: [email protected]
- Phone: 1-202-375-6000
- Toll Free: 1-800-253-4636
- Fax: 1-202-375-6842
- Media Center
- ACC.org Quick Start Guide
- Advertising & Sponsorship Policy
- Clinical Content Disclaimer
- Editorial Board
- Privacy Policy
- Registered User Agreement
- Terms of Service
- Cookie Policy
© 2024 American College of Cardiology Foundation. All rights reserved.
Helpful links:
- Tuition & Fees
- Course Schedules
- Academic Calendar
- Application System
Resources for:
- Prospective Students
- Current Students
- Faculty & Staff
Cardiovascular Nursing Research
About the Cardiovascular Nursing Research group
Cardiovascular disease is the leading cause of death across the U.S. among nearly every race and gender. Building on a history of excellence in cardiovascular science at the University of Rochester Medical Center, the School of Nursing’s cardiovascular nursing research group seeks to accelerate the pace at which new discoveries are implemented into patient care.
Driven by data science, emerging technologies, and investigators’ wealth of clinical experiences, this team of nurse scientists is working toward solutions to today’s most pressing issues in cardiac care. Our internationally recognized work has helped improve treatment and better predict outcomes among patients with heart conditions, and is shaping the future of nursing’s role in cardiac care.
Faculty & Student Members
Research projects, latest publications, news & stories.

Firefighters Face High Risk of Cardiac Events. AI Can Predict Them, With Help from UR Nursing Research
Jan 15, 2024

UR Nursing Researchers Recognized at American Heart Association Scientific Sessions
Nov 21, 2023

UR Nursing Researchers Earn AACN “All of Us” Grant For Postpartum Depression Study
Oct 2, 2023

Mary Carey, PhD, RN, FAHA, FAAN
Director of Clinical Nursing Research Center Professor of Nursing
A critical care nurse by training, Mary Carey, PhD, RN, FAHA, FAAN, is a highly respected researcher, educator, and mentor whose work has made significant contributions to the understanding of ECG monitoring to help detect cardiac arrhythmias and myocardial ischemia and infarction, and on the ECG's use in predicting cardiac events and sudden cardiac death. With funding from the National Institutes of Health, she has improved the detection of myocardial ischemia in patients with and without heart disease.
“No matter what discipline you work in as a nurse, every patient has a heart. It’s very important for all nurses to have a high level of competence in cardiac care.” Mary Carey, PhD, RN, FAHA, FAAN
Interested in pursuing research at the University of Rochester School of Nursing? Connect with us to discuss postdoctoral and tenure-track faculty opportunities.
Email UR Nursing Research
See Research Opportunities
Follow the School of Nursing at the University of Rochester

- Search Menu
- Advance Articles
- Editor's Choice
- Supplements
- Patient Perspectives
- Methods Corner
- ESC Content Collections
- Author Guidelines
- Instructions for reviewers
- Submission Site
- Open Access Options
- Self-Archiving Policy
- Read & Publish
- About European Journal of Cardiovascular Nursing
- About ACNAP
- About European Society of Cardiology
- ESC Publications
- Editorial Board
- Advertising & Corporate Services
- Journals on Oxford Academic
- Books on Oxford Academic
Article Contents
Cardiovascular nursing research: challenges and opportunities.
- Article contents
- Figures & tables
- Supplementary Data
Chantal F Ski, David R Thompson, Cardiovascular Nursing Research: Challenges and Opportunities, European Journal of Cardiovascular Nursing , Volume 10, Issue 1, 1 March 2011, Pages 1–2, https://doi.org/10.1016/j.ejcnurse.2010.09.002
- Permissions Icon Permissions
Cardiovascular nursing has developed markedly in recent decades and research is now being seen as a legitimate activity. Cardiovascular nurses and nursing have made significant research contributions in key areas, notably in the design and evaluation of cardiac rehabilitation [ 1 , 2 ], secondary prevention [ 3 , 4 ] and heart failure disease management programmes [ 5 , 6 ]. This work has informed not only the evidence base for interventions and outcomes but also for guidelines and policies. However, there remain important and pressing research questions regarding why some of these programmes vary, for example in terms of design and outcomes [ 7 , 8 ], and these need to be acknowledged.
Many of these cardiovascular disease management programmes are multi-faceted and diverse in design with a multitude of contextual factors. They are essentially complex interventions and new approaches may be needed to seek explanations regarding their appropriateness, feasibility and effectiveness. Three major challenges appear to face nursing about such programmes: what is the strength of evidence; what works for who, when and why; and how best to evaluate complex interventions? [ 9 ]. It is therefore essential to establish reliable and robust evidence on prevention and management of cardiovascular disease. By doing so, this will provide a solid foundation on which to progress a systematic approach to nursing research into cardiovascular disease.
If nurses are to engage fully in this research enterprise they need to rapidly shift their focus and efforts. There remain significant challenges not only in terms of research capacity and capability but also sustainability. Nurses need to think bigger about research [ 10 ] with appropriate vision, strategy, focus, energy and confidence. What is needed is a ‘paradigm shift’ to harness the expertise and capacity that currently exists and apply these efforts to large-scale, multi-centre, team-led, thematic programmes of research [ 11 ]. This should not only apply to nursing but in collaboration with other disciplines to be truly inter-/multi/trans-disciplinary.
Local collaboration is all well and good but to have real significance and impact it needs to move to a national and international level to conceive, design, conduct and disseminate original research. There are some good examples of international networking and research collaboration in cardiovascular nursing, including the UNITE (Undertaking Nursing Interventions Throughout Europe) research group of the European Society of Cardiology Council on Cardiovascular Nursing and Allied Professions [ 12 , 13 ]. However, if it is to be truly collaborative and to have ‘reach’, nursing research should be strongly linked with medicine, the basic sciences and the social sciences.
Such an enterprise is likely to yield improved productivity in terms of generating and addressing key research questions that span bench to bedside (translational research), outputs (including publications, grants, and research training) and succession planning (training and development of the next generation of researchers).
Research is now indeed a global enterprise and international collaboration is not only desirable but necessary [ 14 ]. The advent of the World Wide Web and the Internet make this mission all the more attainable. Groups have greater stores of knowledge and research capacity than individuals. Nurses have an important role to play in the advancement of cardiovascular research. Nurses are appositely placed within cardiovascular health services to initiate, engage and lead collaborative research projects that will lead to rapid clinical changes and improved patient outcomes. If they truly wish to be seen as equal partners now is the time to seize the opportunity and rise to the occasion of the new generation of nursing scholars who are engaging in assiduous interdisciplinary cardiovascular health research.
[1] Thompson D R Cardiac rehabilitation: adding years to life and life to years J Res Nurs 14 2009 207 – 219
Google Scholar
[2] Thompson D R , Clark A M Cardiac rehabilitation: into the future Heart 95 2009 1897 – 1900
[3] Clark A M , Hartling L , Vandermeer B , McAlister F A Meta-analysis: secondary prevention programs for coronary artery disease Ann Intern Med 143 2005 659 – 672
[4] Wood DA et al Wood DA, Kotseva K, Connolly S, Jennings C, Mead A, Jones J, Holden A, De Bacquer D, Collier T, De Backer G, Faergeman O, on behalf of EUROACTION Study Group. Nurse-coordinated multidisciplinary, family-based cardiovascular disease prevention programme (EUROACTION) for patients with coronary heart disease and asymptomatic individuals at high risk of cardiovascular disease: a paired, cluster-randomised controlled trial. Lancet 2008;371:1999–2012
[5] Stewart S , Pearson S , Horowitz J D Effects of a home-based intervention among patients with chronic congestive heart failure Arch Intern Med 158 1998 1067 – 1072
[6] Jaarsma T , van der Wal M , Lesman-Leegte I , Luttik M , Hogenhuis J , Veeger N et al. Effect of moderate or intensive disease management program on outcome in patients with heart failure coordinating study evaluating outcomes of advising and counseling in heart failure (COACH) Arch Intern Med 168 2008 316 – 324
[7] Clark A M , Thompson D R The future of heart failure disease management programs Lancet 372 2008 784 – 786
[8] Clark A M , Savard L A , Thompson D R What is the strength of evidence for heart failure disease management programs? J Am Coll Cardiol 54 2009 397 – 401
[9] Clark A M , Thompson D R Deepening evidence into heart failure management programs: insights from complexity science Eur J Heart Fail 2010
[10] Thompson D R Thinking bigger about research J Adv Nurs 43 2003 1 – 2
[11] Thompson D R Research partnerships and collaboration in cardiovascular nursing Eur J Cardiovasc Nurs 3 2004 261 – 262
[12] Jaarsma T , Strömberg A , Fridlund B , de Geest S , Mårtensson J , Moons P et al. On behalf of the UNITE research group. Sexual counselling of cardiac patients: nurses' perception of practice, responsibility and confidence Eur J Cardiovasc Nurs 9 2010 24 – 29
[13] Axelsson ÅB , Fridlund B , Moons P , Mårtensson J , Norekvål T M , Scholte op Reimer WJ M The Undertaking Nursing Interventions Throughout Europe (UNITE) Study Group. European cardiovascular nurses' experiences of and attitudes towards having family members present in the resuscitation room Eur J Cardiovasc Nurs 9 2010 15 – 23
[14] Thompson D R International collaboration and sharing lessons learned J Res Nurs 11 2006 285 – 287
Email alerts
Citing articles via.
- Recommend to Your Librarian
- Advertising and Corporate Services
- Journals Career Network
Affiliations
- Online ISSN 1873-1953
- Print ISSN 1474-5151
- Copyright © 2024 European Society of Cardiology
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Cookie Notice
This website uses cookies. Contact us for questions or requests.

Information for:
- Current Students
- Faculty & Staff
- Degrees & Programs
- Campus Maps
- Jobs & Careers
- Campus Shuttles
- Student Life
- Giving
- Augusta University
- The Graduate School
Doctor of Philosophy with a Major in Nursing
Key highlights.
- Opportunities to engage in ground-breaking research in such vital areas as health disparities, cardiovascular risk reduction, cancer treatment/prevention, diabetes treatment/prevention and epigenetics.
- Access to a wide range of service to support their research interests through our Center for Nursing Research.
- Avenues to advance their research interests through our Interdisciplinary Simulation Center and through Augusta University's centers and institutes, such as the new Cancer Research Center
- Excellent opportunities to collaborate with world-class researchers in a dynamic, resource-rich health sciences university environment.
- Research mentoring, assistantship opportunities, and an exceptional financial package.
- The latest in classroom technology in a state-of-the-art facility.
Admission Criteria
Program website, tuition and fees, apply now - nursingcas application.
Your future starts now!
Questions? Contact Us
Beth NeSmith, PhD, MSN, RN Program Director [email protected]
ASK A QUESTION
ABOUT THE PROGRAM
The PhD in Nursing Program prepares nurse scientists for research-intensive academic careers.
The program emphasizes interdisciplinary knowledge development and dissemination through Biobehavioral nursing research. Our faculty are involved in ground-breaking research in such vital areas as health disparities, cancer prevention and control, cardiovascular risk reduction, and epigenetics.
Health Outcomes - Emphasizes clinical outcomes research with a focus on the development of evidence-based knowledge explicating the behavioral and biological outcomes of nursing interventions for vulnerable populations.
Health Disparities - Addresses genetic, biological, social, psychological, and environmental determinants of health disparities with a special focus on populations in the Southeastern U.S.
Health Provider Performance and Patient Safety - Promotes patient safety through an increased understanding of the interaction between heath care providers and their environment.
APPLICANT PROFILE
Our PhD program is designed for advanced students interested in working closely with faculty mentors in nursing and related disciplines within the context of established programs of research.
The program prepares graduates to:
- Critically evaluate behavioral and biological theories of health and illness
- Generate, test, and extend knowledge of linkages between behavioral and biological dimensions of health and illness
- Design basic and clinical nursing studies to investigate behavioral and biological phenomena within a selected area
- Participate in interdisciplinary approaches to generate and apply scientific knowledge
- Apply leadership strategies to address ethical, political, economic, and socio-cultural issues in nursing
Student Profile
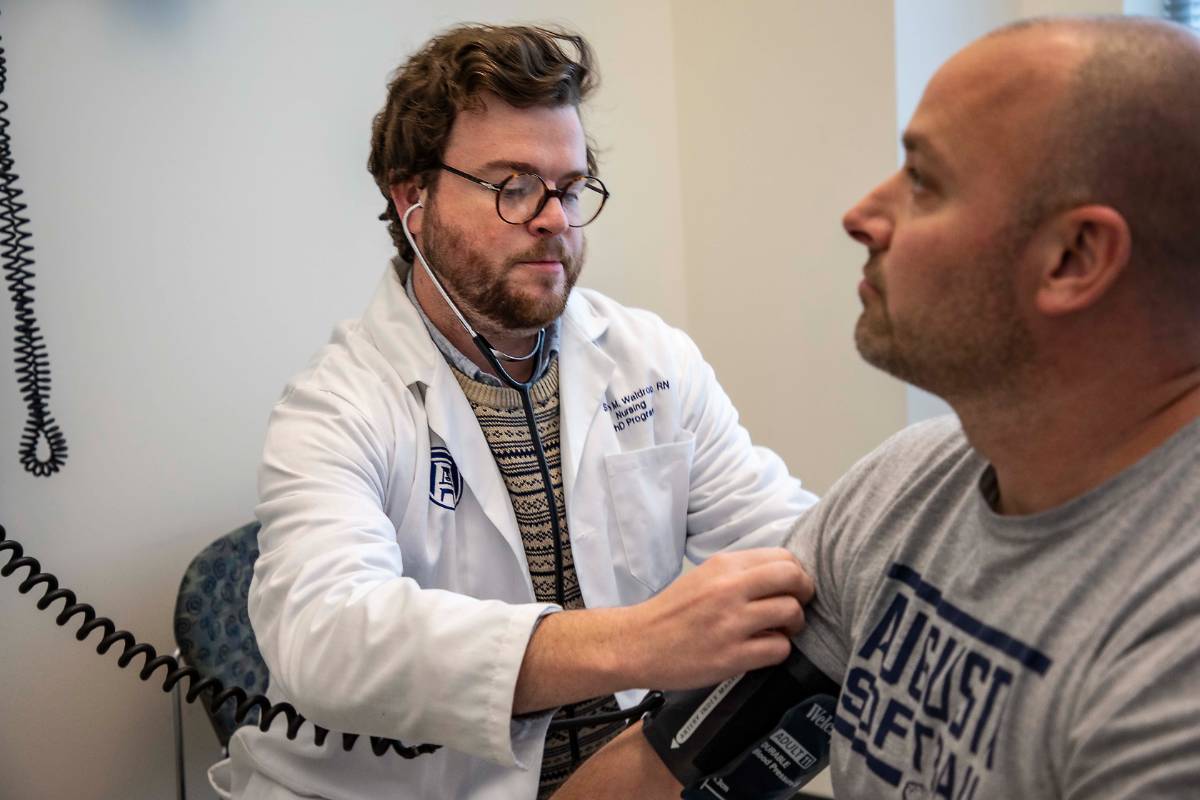
" As the healthcare environment rapidly changes, PhD prepared nurses are uniquely prepared to generate knowledge leading to vital clinical change. "
Steven Waldrop >>
What do you do with a PhD in nursing?

- North America

This site uses cookies to keep track of your information. Learn more here . Accept and close .
Truckers on the Road to Better Cardiovascular Health

Everyone enjoys treats that aren’t so healthy. But imagine if most days you couldn’t get a good night’s sleep, or eat a home-cooked meal, or even go for a walk.
“Truck drivers spend about two-thirds of their nights away from their homes each year,” says Kuo. “If you pack your lunch, it’s in your truck for at least six hours.”
“Truckers tend to drive at night, because there’s less traffic,” she explains. “Their salaries are dictated by how many miles they drive. They always mention that time is money. Often, they take a break on the road because they can sleep in the truck, but that’s lower quality rest.”
Kuo’s research program seeks to help truck drivers and other industrial workers prevent cardiovascular disease.
“Truckers are only one type of industrial worker, but it’s a large group that moves our economy and our society,” says Kuo. “Unfortunately, they experience a lot of cardiometabolic risk and health disparities.”
“We cannot just ask them to stay healthy,” she adds. “No matter how hard individual workers try, if the environment is not supportive, how can you eat healthy? How can you sleep better? When you identify so many problems as a scientist and nurse, you want to see what you can do.”
One of Kuo’s current studies seeks to better understand truck drivers’ daily routines. During virtual visits, study participants talk with interviewers and fill out surveys. On their own, participants record their sleep, physical activity, dietary, and other health behaviors.
The last part of the study is the toughest for busy truck drivers: an in-person visit.
“We need the in-person visit to collect physiological data like lung function, cardiovascular function, and mobility and cognitive tests,” says Kuo. “But in-person visits are challenging. We can’t ask them to go to a community center, because there’s no place to park their truck. We’re working with their employers to figure out how we can go to their workplace.”
Kuo knows her research team needs to meet truck drivers where they’re at.
“How can we build that relationship without interrupting their work?” she asks. “This is very important.”
Based on the observational data her team is collecting, Kuo will work with colleagues to design an intervention that supports truck drivers’ health.
“We are working with industrial engineers, civil and environmental engineers, and surgeons in the VA Hospital,” she says. “We want our intervention to have a person-centered approach, but what does that look like? You cannot ask truckers to come to your clinic every other week. So, we are thinking about telehealth. How can you use a telehealth model that’s effective, feasible and acceptable with this group, and provides a good user experience?”

Kuo and her research team, including students, jump at the opportunity to attend award lunches and other events for truck drivers.
“Students really like to talk to truck drivers and listen to their perspectives,” she says. She wants students to learn that “researchers cannot just collect data and then go back and analyze and publish. Then you never solve the problem.”
“We can’t do this work without many people helping,” Kuo adds. “We thank the truck drivers, the employers, the Wisconsin Motor Carriers Association, and all the community partners involved.”
In addition to her observational study and intervention plans, Kuo is working on an assessment to tease out how an individual’s occupational environment shapes their health. She’s also interested in how policies could reduce the risk of cardiovascular disease. As an example, she points to loan programs that help truck drivers afford newer and less polluting vehicles.
“My hope is that in the future, healthy behaviors are the default setting,” she says. “So, we don’t even need to pay attention and a healthy environment naturally occurs for everyone.”
–Diane Farsetta
- News & Events
- Faculty & Staff

A world-class city filled with art and culture and an incredible campus that offers cutting edge resources–that’s what students receive at Penn Nursing. And that’s just the start. Penn Nursing and the wider university offer something for everyone, as well as a lifelong community.

Penn Nursing is globally known for educating dynamic nurses—because our School values evidence-based science and health equity. That’s where our expertise lies, whether in research, practice, community health, or beyond. Everything we do upholds a through-line of innovation, encouraging our exceptional students, alumni, and faculty share their knowledge and skills to reshape health care.

Penn Nursing students are bold and unafraid, ready to embrace any challenge that comes their way. Whether you are exploring a career in nursing or interested in advancing your nursing career, a Penn Nursing education will help you meet your goals and become an innovative leader, prepared to change the face of health and wellness.

Penn Nursing is the #1-ranked nursing school in the world. Its highly-ranked programs help develop highly-skilled leaders in health care who are prepared to work alongside communities to tackle issues of health equity and social justice to improve health and wellness for everyone.

Penn Nursing’s rigorous academic curricula are taught by world renowned experts, ensuring that students at every level receive an exceptional Ivy League education . From augmented reality classrooms and clinical simulations to coursework that includes experiential global travel to clinical placements in top notch facilities, a Penn Nursing education prepares our graduates to lead.

Director of Harvard Global Nursing Leadership Program to be 2024 Penn Nursing Commencement Speaker
Stephanie Ferguson, PhD, RN, FAAN , the Director of the Harvard Global Nursing Leadership Program and Professor of the Practice of Health Policy and Management at the Harvard T.H. Chan School of Public Health , will serve as the 2024 Penn Nursing commencement speaker. The event will take place at 3:00 PM EST on Monday, May 20, 2024, at the Kimmel Center for the Performing Arts .

Dr. Ferguson is a global health care leader who has worked in more than 100 nations as a technical advisor, consultant, and facilitator for organizations including the World Health Organization (WHO), the Pan American Health Organization (PAHO), the International Council of Nurses (ICN), and the National Council of State Boards of Nursing (NCSBN).
“Dr. Ferguson’s exemplary career as a global health leader has influenced policy at the highest levels, both nationally and internationally. She is a great inspiration as our students look ahead to their careers in nursing,” said Penn Nursing Dean Antonia M. Villarruel . “Penn Nursing develops innovative leaders who are prepared to address looming challenges as opportunities to promote health, wherever they practice. Having Dr. Ferguson address our graduating class this year speaks to the drive I see in our students to expand the boundaries of what society typically thinks nurses do.”
For more than 20 years at WHO’s headquarters, regional offices, and PAHO, Ferguson developed strategic plans and initiatives to strengthen and evaluate health care delivery systems, human resources for health and regulations, population health outcomes, and nursing and other health professional education, leadership programs and services. During her ten-plus years at ICN, she directed the ICN Leadership for Change Programä, the ICN-Burdett Global Nursing Leadership Instituteä, and served as an ICN Consultant for Nursing and Health Policy.
Ferguson is an elected member of the National Academy of Medicine (NAM) and served on the NAM Nominating Committee. She was an appointed member on the NAM’s recent Consensus Study on Global Health and the Future Role of the USA. She is an elected Fellow of the American Academy of Nursing (AAN) and chaired the AAN’s International Task Force. She is a former chair of the Advisory Council for the AAN’s Institute for Nursing Leadership. Ferguson is a Distinguished Practitioner and Fellow in the National Academies of Practice and was a White House Fellow in 1996-97 in President Clinton’s Administration and served at the US Department of Health and Human Services in the Office of the Secretary.
Her many board appointments, honors and awards include the 2014 HRH Princess Muna Al Hussein Award from the American Nurses Credentialing Center, which recognized her significant contributions to health care across borders and exceptional dedication to nursing. She is also the recipient of the American Academy of Nursing’s 2020 Civitas Award for her extraordinary dedication to excellence in promoting quality care in nursing worldwide.
Dr. Ferguson received her PhD in 1996 and her BSN in 1985 from the University of Virginia in Charlottesville, VA. Her MS/Nursing degree in 1987 is from the Virginia Commonwealth University, Medical College of Virginia, in Richmond, VA.
More Stories
New leadership appointment for penn nursing professor, congratulations to the 2024 penn nursing faculty award recipients, national appointment for penn nursing professor, media contact, see yourself here.

An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, editors. Nursing Skills [Internet]. Eau Claire (WI): Chippewa Valley Technical College; 2021.

Nursing Skills [Internet].
- About Open RN
Chapter 9 Cardiovascular Assessment
9.1. cardiovascular assessment introduction, learning objectives.
- Perform a cardiovascular assessment, including heart sounds; apical and peripheral pulses for rate, rhythm, and amplitude; and skin perfusion (color, temperature, sensation, and capillary refill time)
- Identify S1 and S2 heart sounds
- Differentiate between normal and abnormal heart sounds
- Modify assessment techniques to reflect variations across the life span
- Document actions and observations
- Recognize and report significant deviations from norms
The evaluation of the cardiovascular system includes a thorough medical history and a detailed examination of the heart and peripheral vascular system. [ 1 ] Nurses must incorporate subjective statements and objective findings to elicit clues of potential signs of dysfunction. Symptoms like fatigue, indigestion, and leg swelling may be benign or may indicate something more ominous. As a result, nurses must be vigilant when collecting comprehensive information to utilize their best clinical judgment when providing care for the patient.
9.2. CARDIOVASCULAR BASIC CONCEPTS
While the cardiovascular assessment most often focuses on the function of the heart, it is important for nurses to have an understanding of the underlying structures of the cardiovascular system to best understand the meaning of their assessment findings.
For more information on the cardiovascular system, visit the “ Cardiovascular and Renal System ” chapter in Open RN Nursing Pharmacology .
Specific sections include the following topics:
- Review of Basic Concepts for more about that anatomy and physiology of the cardiovascular system
- Common Cardiac Disorders for more about cardiovascular medical conditions
- Cardiovascular Medication Classes for more about medications used to treat common cardiovascular conditions
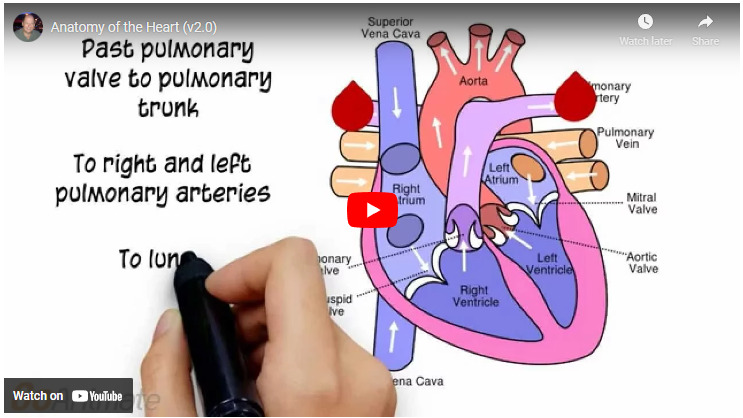
Video Review of Anatomy and Physiology of the Heart [ 1 ]
9.3. CARDIOVASCULAR ASSESSMENT
A thorough assessment of the heart provides valuable information about the function of a patient’s cardiovascular system. Understanding how to properly assess the cardiovascular system and identifying both normal and abnormal assessment findings will allow the nurse to provide quality, safe care to the patient.
Before assessing a patient’s cardiovascular system, it is important to understand the various functions of the cardiovascular system. In addition to the information provided in the “Review of Cardiac Basics” section, the following images provide an overview of the cardiovascular system. Figure 9.1 [ 1 ] provides an overview of the structure of the heart. Note the main cardiac structures are the atria, ventricles, and heart valves. Figure 9.2 [ 2 ] demonstrates blood flow through the heart. Notice the flow of deoxygenated blood from the posterior and superior vena cava into the right atria and ventricle during diastole (indicated by blue coloring of these structures). The right ventricle then pumps deoxygenated blood to the lungs via the pulmonary artery during systole. At the same time, oxygenated blood from the lungs returns to the left atria and ventricle via the pulmonary veins during diastole (indicated by red coloring of these structures) and then is pumped out to the body via the aorta during systole. Figure 9.3 [ 3 ] demonstrates the conduction system of the heart. This image depicts the conduction pathway through the heart as the tissue responds to electrical stimulation. Figure 9.4 [ 4 ] illustrates the arteries of the circulatory system, and Figure 9.5 [ 5 ] depicts the veins of the circulatory system. The purpose of these figures is to facilitate understanding of the electrical and mechanical function of the heart within the cardiovascular system.
Structure of the Heart
Blood Flow Through the Heart
Conduction System of the Heart
Circulatory System: Arteries
Figure 9.5.
Circulatory System: Veins
Assessing the cardiovascular system includes performing several subjective and objective assessments. At times, assessment findings are modified according to life span considerations.

Subjective Assessment
The subjective assessment of the cardiovascular and peripheral vascular system is vital for uncovering signs of potential dysfunction. To complete the subjective cardiovascular assessment, the nurse begins with a focused interview. The focused interview explores past medical and family history, medications, cardiac risk factors, and reported symptoms. Symptoms related to the cardiovascular system include chest pain, peripheral edema, unexplained sudden weight gain, shortness of breath (dyspnea), irregular pulse rate or rhythm, dizziness, or poor peripheral circulation. Any new or worsening symptoms should be documented and reported to the health care provider.
Table 9.3a outlines questions used to assess symptoms related to the cardiovascular and peripheral vascular systems. Table 9.3b outlines questions used to assess medical history, medications, and risk factors related to the cardiovascular system. Information obtained from the interview process is used to tailor future patient education by the nurse. [ 6 ] , [ 7 ] , [ 8 ]
Interview Questions for Cardiovascular and Peripheral Vascular Systems [ 9 ]
View in own window
Interview Questions Exploring Cardiovascular Medical History, Medications, and Cardiac Risk Factors
Objective Assessment
The physical examination of the cardiovascular system involves the interpretation of vital signs, inspection, palpation, and auscultation of heart sounds as the nurse evaluates for sufficient perfusion and cardiac output.
For more information about assessing a patient’s oxygenation status as it relates to their cardiac output, visit the “ Oxygenation ” chapter in Open RN Nursing Fundamentals .
Equipment needed for a cardiovascular assessment includes a stethoscope, penlight, centimeter ruler or tape measure, and sphygmomanometer . [ 10 ]
Evaluate Vital Signs and Level of Consciousness
Interpret the blood pressure and pulse readings to verify the patient is stable before proceeding with the physical exam. Assess the level of consciousness; the patient should be alert and cooperative.
As a general rule of thumb, findings of systolic blood pressure in adults less than 100,or a pulse rate less than 60 or greater than 100,require immediate follow-up. For more information on obtaining and interpreting vital signs, see the “General Survey” chapter . Keep in mind that excessive drowsiness, restlessness, or irritability can be symptoms of hypoxia.
- Skin color to assess perfusion. Inspect the face, lips, and fingertips for cyanosis or pallor. Cyanosis is a bluish discoloration of the skin, lips, and nail beds and indicates decreased perfusion and oxygenation. Pallor is the loss of color, or paleness of the skin or mucous membranes, as a result of reduced blood flow, oxygenation, or decreased number of red blood cells. Patients with light skin tones should be pink in color. For those with darker skin tones, assess for pallor on the palms, conjunctiva, or inner aspect of the lower lip.
- Jugular Vein Distension (JVD). Inspect the neck for JVD that occurs when the increased pressure of the superior vena cava causes the jugular vein to bulge, making it most visible on the right side of a person’s neck. JVD should not be present in the upright position or when the head of bed is at 30-45 degrees.
- Precordium for abnormalities. Inspect the chest area over the heart (also called precordium ) for deformities, scars, or any abnormal pulsations the underlying cardiac chambers and great vessels may produce.
- Upper Extremities: Inspect the fingers, arms, and hands bilaterally noting Color, Warmth, Movement, Sensation (CWMS). Alterations or bilateral inconsistency in CWMS may indicate underlying conditions or injury. Assess capillary refill by compressing the nail bed until it blanches and record the time taken for the color to return to the nail bed. Normal capillary refill is less than 3 seconds. [ 11 ]
- Edema: Note any presence of edema. Peripheral edema is swelling that can be caused by infection, thrombosis, or venous insufficiency due to an accumulation of fluid in the tissues. (See Figure 9.6 [ 12 ] for an image of pedal edema.) [ 13 ]
- Deep Vein Thrombosis (DVT): A deep vein thrombosis (DVT) is a blood clot that forms in a vein deep in the body. DVT requires emergency notification of the health care provider and immediate follow-up because of the risk of developing a life-threatening pulmonary embolism . [ 14 ] Inspect the lower extremities bilaterally. Assess for size, color, temperature, and for presence of pain in the calves. Unilateral warmth, redness, tenderness, swelling in the calf, or sudden onset of intense, sharp muscle pain that increases with dorsiflexion of the foot is an indication of a deep vein thrombosis (DVT). [ 15 ] See Figure 9.7 [ 16 ] for an image of a DVT in the patient’s right leg, indicated by unilateral redness and edema.
Peripheral Edema
Signs of a DVT
Auscultation
Heart sounds.
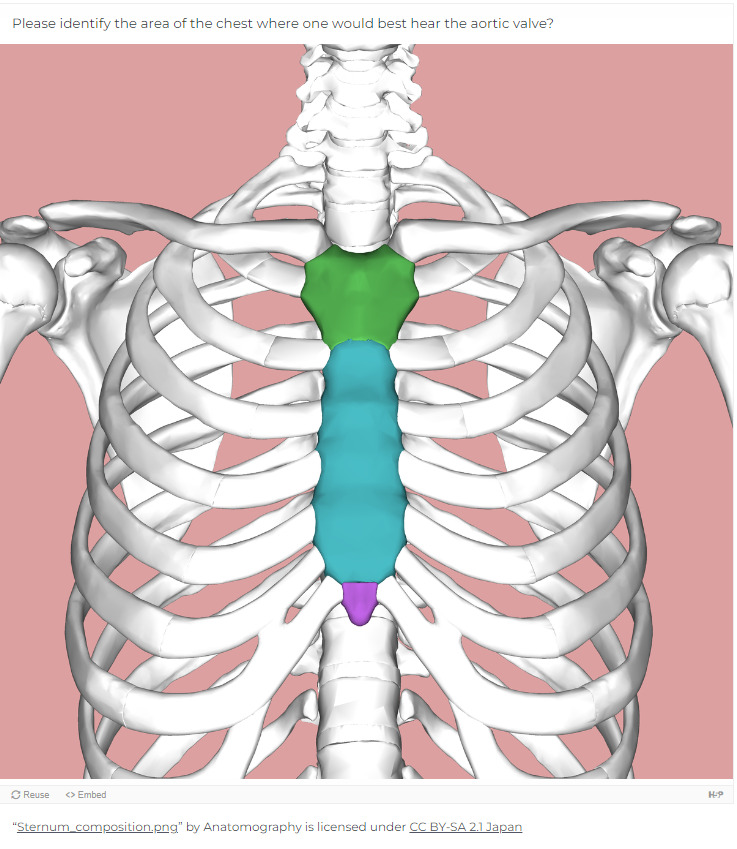
Auscultation is routinely performed over five specific areas of the heart to listen for corresponding valvular sounds. These auscultation sites are often referred to by the mnemonic “APE To Man,” referring to Aortic, Pulmonic, Erb’s point, Tricuspid, and Mitral areas (see Figure 9.8 [ 17 ] for an illustration of cardiac auscultation areas). The aortic area is the second intercostal space to the right of the sternum. The pulmonary area is the second intercostal space to the left of the sternum. Erb’s point is directly below the aortic area and located at the third intercostal space to the left of the sternum. The tricuspid (or parasternal) area is at the fourth intercostal space to the left of the sternum. The mitral (also called apical or left ventricular area) is the fifth intercostal space at the midclavicular line.
Cardiac Auscultation Areas
Auscultation usually begins at the aortic area (upper right sternal edge). Use the diaphragm of the stethoscope to carefully identify the S1 and S2 sounds. They will make a “lub-dub” sound. Note that when listening over the area of the aortic and pulmonic valves, the “dub” (S2) will sound louder than the “lub” (S1). Move the stethoscope sequentially to the pulmonic area (upper left sternal edge), Erb’s point (left third intercostal space at the sternal border), and tricuspid area (fourth intercostal space. When assessing the mitral area for female patients, it is often helpful to ask them to lift up their breast tissue so the stethoscope can be placed directly on the chest wall. Repeat this process with the bell of the stethoscope. The apical pulse should be counted over a 60-second period. For an adult, the heart rate should be between 60 and 100 with a regular rhythm to be considered within normal range. The apical pulse is an important assessment to obtain before the administration of many cardiac medications.
The first heart sound (S1) identifies the onset of systole, when the atrioventricular (AV) valves (mitral and tricuspid) close and the ventricles contract and eject the blood out of the heart. The second heart sound (S2) identifies the end of systole and the onset of diastole when the semilunar valves close, the AV valves open, and the ventricles fill with blood. When auscultating, it is important to identify the S1 (“lub”) and S2 (“dub”) sounds, evaluate the rate and rhythm of the heart, and listen for any extra heart sounds.
Listen to a normal S1/S2 sound. It may be helpful to use earbuds or a headphone:
https://wtcs.pressbooks.pub/app/uploads/sites/29/h5p/content/37/audios/files-5f999f8f37d98.mp3
Auscultating Heart Sounds
- To effectively auscultate heart sounds, patient repositioning may be required. Ask the patient to lean forward if able, or position them to lie on their left side.
- It is common to hear lung sounds when auscultating the heart sounds. It may be helpful to ask the patient to briefly hold their breath if lung sounds impede adequate heart auscultation. Limit the holding of breath to 10 seconds or as tolerated by the patient.
- Environmental noise can cause difficulty in auscultating heart sounds. Removing environmental noise by turning down the television volume or shutting the door may be required for an accurate assessment.
- Patients may try to talk to you as you are assessing their heart sounds. It is often helpful to explain the procedure such as, “I am going to take a few minutes to listen carefully to the sounds of blood flow going through your heart. Please try not to speak while I am listening, so I can hear the sounds better.”
EXTRA HEART SOUNDS
Extra heart sounds include clicks, murmurs, S3 and S4 sounds, and pleural friction rubs. These extra sounds can be difficult for a novice to distinguish, so if you notice any new or different sounds, consult an advanced practitioner or notify the provider. A midsystolic click , associated with mitral valve prolapse, may be heard with the diaphragm at the apex or left lower sternal border.
A click may be followed by a murmur. A murmur is a blowing or whooshing sound that signifies turbulent blood flow often caused by a valvular defect. New murmurs not previously recorded should be immediately communicated to the health care provider. In the aortic area, listen for possible murmurs of aortic stenosis and aortic regurgitation with the diaphragm of the stethoscope. In the pulmonic area, listen for potential murmurs of pulmonic stenosis and pulmonary and aortic regurgitation. In the tricuspid area, at the fourth and fifth intercostal spaces along the left sternal border, listen for the potential murmurs of tricuspid regurgitation, tricuspid stenosis, or ventricular septal defect.
Listen to a heart murmur caused by mitral valve regurgitation:
https://wtcs.pressbooks.pub/app/uploads/sites/29/h5p/content/33/audios/files-5f99a09a22700.mp3
S3 and S4 sounds, if present, are often heard best by asking the patient to lie on their left side and listening over the apex with the bell of the stethoscope. An S3 sound, also called a ventricular gallop , occurs with fluid overload or heart failure when the ventricles are filling. It occurs after the S2 and sounds like “lub-dub-dah,” or a sound similar to a horse galloping. The S4 sound, also called atrial gallop , occurs immediately before the S1 and sounds like “ta-lub-dub.” An S4 sound can occur with decreased ventricular compliance or coronary artery disease. [ 18 ]
Listen to a S3 ventricular gallop:
https://wtcs.pressbooks.pub/app/uploads/sites/29/h5p/content/36/audios/files-5f999f527ffd5.mp3
Listen to a S4 atrial gallop:
https://wtcs.pressbooks.pub/app/uploads/sites/29/h5p/content/35/audios/files-5f999fefa1774.mp3
A pleural friction rub is caused by inflammation of the pericardium and sounds like sandpaper being rubbed together. It is best heard at the apex or left lower sternal border with the diaphragm as the patient sits up, leans forward, and holds their breath.
CAROTID SOUNDS
The carotid artery may be auscultated for bruits . Bruits are a swishing sound due to turbulence in the blood vessel and may be heard due to atherosclerotic changes.
Palpation is used to evaluate peripheral pulses, capillary refill, and for the presence of edema. When palpating these areas, also pay attention to the temperature and moisture of the skin.
Compare the rate, rhythm, and quality of arterial pulses bilaterally, including the carotid, radial, brachial, posterior tibialis, and dorsalis pedis pulses. Review additional information about obtaining pulses in the “ General Survey ” chapter. Bilateral comparison for all pulses (except the carotid) is important for determining subtle variations in pulse strength. Carotid pulses should be palpated on one side at a time to avoid decreasing perfusion of the brain. The posterior tibial artery is located just behind the medial malleolus. It can be palpated by scooping the patient’s heel in your hand and wrapping your fingers around so that the tips come to rest on the appropriate area just below the medial malleolus. The dorsalis pedis artery is located just lateral to the extensor tendon of the big toe and can be identified by asking the patient to flex their toe while you provide resistance to this movement. Gently place the tips of your second, third, and fourth fingers adjacent to the tendon, and try to feel the pulse.
The quality of the pulse is graded on a scale of 0 to 3, with 0 being absent pulses, 1 being decreased pulses, 2 is within normal range, and 3 being increased (also referred to as “bounding”). If unable to palpate a pulse, additional assessment is needed. First, determine if this is a new or chronic finding. Second, if available, use a doppler ultrasound to determine the presence or absence of the pulse. Many agencies use doppler ultrasound to document if a nonpalpable pulse is present. If the pulse is not found, this could be a sign of an emergent condition requiring immediate follow-up and provider notification. See Figure 9.9 [ 19 ] and Figure 9.10 [ 20 ] for images of assessing pedal pulses.
Assessing Tibial Pedal Pulses
Figure 9.10
Assessing Dorsalis Pedis Pulses
CAPILLARY REFILL
The capillary refill test is performed on the nail beds to monitor perfusion , the amount of blood flow to tissue. Pressure is applied to a fingernail or toenail until it pales, indicating that the blood has been forced from the tissue under the nail. This paleness is called blanching . Once the tissue has blanched, pressure is removed. Capillary refill time is defined as the time it takes for the color to return after pressure is removed. If there is sufficient blood flow to the area, a pink color should return within 2 to 3 seconds after the pressure is removed. [ 21 ]
Edema occurs when one can visualize visible swelling caused by a buildup of fluid within the tissues. If edema is present on inspection, palpate the area to determine if the edema is pitting or nonpitting. Press on the skin to assess for indentation, ideally over a bony structure, such as the tibia. If no indentation occurs, it is referred to as nonpitting edema. If indentation occurs, it is referred to as pitting edema . See Figure 9.11 [ 22 ] for images demonstrating pitting edema.
Figure 9.11
Assessing Lower Extremity Edema
Note the depth of the indention and how long it takes for the skin to rebound back to its original position. The indentation and time required to rebound to the original position are graded on a scale from 1 to 4. Edema rated at 1+ indicates a barely detectable depression with immediate rebound, and 4+ indicates a deep depression with a time lapse of over 20 seconds required to rebound. See Figure 9.12 [ 23 ] for an illustration of grading edema. Additionally, it is helpful to note edema may be difficult to observe in larger patients. It is also important to monitor for sudden changes in weight, which is considered a probable sign of fluid volume overload.
Figure 9.12
Grading of Edema
HEAVES OR THRILLS
You may observe advanced practice nurses and other health care providers palpating the anterior chest wall to detect any abnormal pulsations the underlying cardiac chambers and great vessels may produce. Precordial movements should be evaluated at the apex (mitral area). It is best to examine the precordium with the patient supine because if the patient is turned on the left side, the apical region of the heart is displaced against the lateral chest wall, distorting the chest movements. [ 24 ] A heave or lift is a palpable lifting sensation under the sternum and anterior chest wall to the left of the sternum that suggests severe right ventricular hypertrophy. A thrill is a vibration felt on the skin of the precordium or over an area of turbulence, such as an arteriovenous fistula or graft.
Life Span Considerations
The cardiovascular assessment and expected findings should be modified according to common variations across the life span.
INFANTS AND CHILDREN
A murmur may be heard in a newborn in the first few days of life until the ductus arteriosus closes.
When assessing the cardiovascular system in children, it is important to assess the apical pulse. Parameters for expected findings vary according to age group. After a child reaches adolescence, a radial pulse may be assessed. Table 9.3c outlines the expected apical pulse rate by age.
Expected Apical Pulse by Age
Listen to pediatric heart tones:
https://wtcs.pressbooks.pub/app/uploads/sites/29/h5p/content/32/audios/files-5f99a0d8457d5.wav
OLDER ADULTS
In adults over age 65, irregular heart rhythms and extra sounds are more likely. An “irregularly irregular” rhythm suggests atrial fibrillation , and further investigation is required if this is a new finding. See the hyperlink in the box below for more information about atrial fibrillation.
Listen to atrial fibrillation:
https://wtcs.pressbooks.pub/app/uploads/sites/29/h5p/content/34/audios/files-5f99a05768bbf.wav
For more information on atrial fibrillation, visit the following web page: CDC Atrial Fibrillation .
Expected versus unexpected findings.
After completing a cardiovascular assessment, it is important for the nurse to use critical thinking to determine if any findings require follow-up. Depending on the urgency of the findings, follow-up can range from calling the health care provider to calling the rapid response team. Table 9.3d compares examples of expected findings, meaning those considered within normal limits, to unexpected findings, which require follow-up. Critical conditions are those that should be reported immediately and may require notification of a rapid response team.
Expected Versus Unexpected Findings on Cardiac Assessment
See Table 9.3e for a comparison of expected versus unexpected findings when assessing the peripheral vascular system.
Expected Versus Unexpected Peripheral Vascular Assessment Findings
9.4. SAMPLE DOCUMENTATION
Sample documentation of expected cardiac & peripheral vascular findings.
Patient denies chest pain or shortness of breath. Vital signs are within normal limits. Point of maximum impulse palpable at the fifth intercostal space of the midclavicular line. No lifts, heaves, or thrills identified on inspection or palpation. JVD absent. S1 and S2 heart sounds in regular rhythm with no murmurs or extra sounds . Skin is warm, pink, and dry. Capillary refill is less than two seconds. Color, movement, and sensation are intact in upper and lower extremities. Peripheral pulses are present (+2) and equal bilaterally. No peripheral edema is noted. Hair is distributed evenly on lower extremities.
Sample Documentation of Unexpected Cardiac & Peripheral Vascular Findings
Patient reports increase in breathing difficulty and increased swelling of bilateral lower extremities over the last three days. Diminished pulses (+1) bilaterally and pitting edema (+2) in the bilateral lower extremities. Upon auscultation, an S3 heart sound is noted and the patient has bilateral crackles in the posterior bases of the lungs. Skin is pink, warm, and dry with capillary refill of < 2 seconds. All other pulses are present (+2), and no other areas of edema are noted. JVD is absent.
9.5. CHECKLIST FOR CARDIOVASCULAR ASSESSMENT
Use the checklist below to review the steps for completion of a “Cardiovascular Assessment.” [ 1 ]
Disclaimer: Always review and follow agency policy regarding this specific skill.
Gather supplies: stethoscope and watch with a second hand.
Perform safety steps:
Perform hand hygiene.
- Check the room for transmission-based precautions.
- Introduce yourself, your role, the purpose of your visit, and an estimate of the time it will take.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain the process to the patient and ask if they have any questions.
- Be organized and systematic.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure the patient’s privacy and dignity.
- Assess ABCs.
Conduct a focused interview related to cardiovascular and peripheral vascular disease.
- Ask relevant focused questions based on patient status. See Tables 9.3a and 9.3b for example questions.
- Face, lips, and extremities for pallor or cyanosis
- Neck for jugular vein distension (JVD) in upright position or with head of bed at 30-45 degree angle
- Chest for deformities and wounds/scars on chest
- Bilateral arms/hands, noting color, warmth, movement, sensation (CWMS), edema, and color of nail beds
- Bilateral legs, noting CWMS, edema to lower legs and feet, presence of superficial distended veins, and color of nail beds
Auscultate with both the bell and the diaphragm of the stethoscope over five auscultation areas of the heart. Auscultate the apical pulse at the fifth intercostal space, midclavicular line for one minute. Note the rate and rhythm. Identify the S1 and S2 sounds and follow up on any unexpected findings (e.g., extra sounds or irregular rhythm).
Palpate the radial, brachial, dorsalis pedis, and posterior tibialis pulses bilaterally. Palpate the carotid pulse one side at a time. Note presence/amplitude of pulse and any unexpected findings requiring follow-up.
Palpate the nail beds for capillary refill. Document the capillary refill time as less than or greater than 2 seconds.
Assist the patient to a comfortable position, ask if they have any questions, and thank them for their time.
Ensure safety measures when leaving the room:
- CALL LIGHT: Within reach
- BED: Low and locked (in lowest position and brakes on)
- SIDE RAILS: Secured
- TABLE: Within reach
- ROOM: Risk-free for falls (scan room and clear any obstacles)
Document the assessment findings. Report any concerns according to agency policy.
9.6. SUPPLEMENTARY VIDEOS ON CARDIOVASCULAR ASSESSMENT
Video reviews for assessing the heart and lungs and the apical pulse:.
Chest Assessment – Heart and Lungs [ 1 ]
Assessing the Apical Pulse [ 2 ]
9.7. LEARNING ACTIVITIES
Learning activities.
(Answers to “Learning Activities” can be found in the “Answer Key” at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
As you walk into your patient’s room, you notice the patient appears to be short of breath. Your patient states “I have been short of breath and tired for the past week.” Upon assessment of your patient, you notice JVD, labored breathing, lung sounds with crackles in the posterior bases, and +2 edema to the lower extremities bilaterally.
From your assessment findings, determine the most likely disease state that is being described.
Hypertension
Pulmonary Embolism
Heart Failure
Your patient puts on the call light. You enter the room and notice the patient appears to be in distress. The patient states, “I cannot catch my breath and my heart feels like it is going to explode.” The patient’s vital signs are T 98, P 148, BP 112/68, and pulse oximetry 88% on room air. You apply oxygen at 2 liters/minute via nasal cannula and notify the health care provider (HCP). The HCP orders a stat ECG. The patient’s pulse oximetry increases to 94% with the oxygen, and the patient states, “I feel less short of breath but my heart is still racing.” Upon assessment of heart sounds, the apical pulse is 134 and irregular. The ECG results indicate atrial fibrillation.
What would be your next action?
Leave the room and see your other patients.
Stay with the patient and notify the HCP of the ECG results.
Have the CNA stay with your patient as you take a break.
Stay with the patient and wait for them to calm down.
- IX. GLOSSARY
An irregular heartbeat that is often fast and increases the risk of heart attack or stroke.
The whiteness that occurs when pressure is placed on tissue or a nail bed, causing blood to leave the area.
A swishing sound when auscultating the carotid arteries. This indicates turbulence in the blood vessel due to atherosclerotic changes.
The time it takes for color to return after pressure is applied to tissue causing blanching.
Clicking sound heard on auscultation of the precordium; often heard in patients with heart valve abnormalities.
A bluish discoloration of the skin, lips, and nail beds. It is an indication of decreased perfusion and oxygenation.
A blood clot that forms in a vein deep in the body.
Shunt that connects the pulmonary artery and aorta in the developing fetus.
A feeling of shortness of breath.
Swelling in tissues caused by fluid retention.
Palpable lifting sensation under the sternum and anterior chest wall to the left of the sternum; it suggests severe right ventricular hypertrophy.
Occurs when the increased pressure of the superior vena cava causes the jugular vein to bulge, making it most visible on the right side of a person’s neck.
A blowing or whooshing sound heard on auscultation of the precordium that signifies turbulent blood flow in the heart often caused by a valvular defect.
A feeling of shortness of breath when lying flat.
A reduced amount of oxyhemoglobin in the skin or mucous membranes. Skin and mucous membranes present with a pale skin color.
An attack of severe shortness of breath that generally occurs at night.
The amount of blood flow to tissue.
Swelling due to an accumulation of fluid in tissues perfused by the peripheral vascular system.
An accumulation of fluid in tissue and causes an indentation when the area is pressed.
Uncommon heart sounds produced when the parietal and visceral pericardium become inflamed, generating a creaky-scratchy noise as they rub together.
The region of the thorax in front of the heart.
A blood clot that lodges in one of the arteries that go from the heart to the lung.
An instrument for measuring blood pressure typically consisting of an inflatable rubber cuff.
A temporary loss of consciousness usually related to insufficient blood flow to the brain.
A vibration felt with palpation of the precordium.
Licensed under a Creative Commons Attribution 4.0 International License. To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/ .
- Cite this Page Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, editors. Nursing Skills [Internet]. Eau Claire (WI): Chippewa Valley Technical College; 2021. Chapter 9 Cardiovascular Assessment.
- PDF version of this title (449M)
In this Page
- CARDIOVASCULAR ASSESSMENT INTRODUCTION
- CARDIOVASCULAR BASIC CONCEPTS
- CARDIOVASCULAR ASSESSMENT
- SAMPLE DOCUMENTATION
- CHECKLIST FOR CARDIOVASCULAR ASSESSMENT
- SUPPLEMENTARY VIDEOS ON CARDIOVASCULAR ASSESSMENT
- LEARNING ACTIVITIES
Other titles in this collection
- Open RN OER Textbooks
Related Items in Bookshelf
- All Textbooks
Bulk Download
- Bulk download content from FTP
Related information
- PubMed Links to PubMed
Recent Activity
- Chapter 9 Cardiovascular Assessment - Nursing Skills Chapter 9 Cardiovascular Assessment - Nursing Skills
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

‘Total Disgrace’: Anger, Frustration as Mass Heating Failures Across Russia Leave Thousands in the Cold
P ODOLSK, Moscow region – Residents throughout Russia affected by unprecedented winter heating outages in recent days have expressed their frustration and urged local authorities to restore heating in their homes.
In Podolsk, a town some 30 kilometers south of the capital Moscow, at least 149,000 residents — nearly half of its population — were left without heating when a heating main burst at a nearby private ammunition plant.
“It’s a total disgrace. There is no heating and no hot water. We have to sleep in sleeping bags,” Yuri, a local resident, told The Moscow Times.
“I have no words to describe how bad the situation is," said Yuri, who declined to provide his surname. "We have had no heating for almost six days."
Heating issues have affected residents in the Moscow region, where temperatures have plunged to as low as minus 20 degrees Celsius in the past week, as well as people in the Far East Primorye region , the cities of Moscow and St. Petersburg , Penza , the southern Voronezh and Volgograd regions and more.
In the Tver region, a group of residents filmed an appeal to President Vladimir Putin, saying that they “are freezing from the cold” in the village of Novozavidovsky.
“We're literally being killed by the cold,” a woman in the video said, adding that they have been sending requests to local authorities since September after their houses were connected to a boiler room whose power was reportedly insufficient.
“This is some kind of torture and extermination of the population 100 kilometers from Moscow,” she added.
Residents of the Moscow region town of Elektrostal lit a fire in the street to draw the authorities’ attention to the heating problem.
“It’s impossible to stay in our houses. We're freezing!” a group of women in the video said.
Suffering from subzero temperatures, residents are placing the blame on local authorities and utility services for failing to take necessary precautions and not taking action to resolve the situation.
“We are sending complaints everywhere but no one listens to us. We have portable heaters working in every room, but the temperature inside is still 10 degrees Celsius,” Yelena from Podolsk said.
“There is a clinic and a hospital, as well as kindergartens, where there is no heating. And we have no answers, no assistance, no explanation,” Yelena added.
Podolsk authorities opened temporary heating centers and declared a state of emergency.
Local authorities linked the heating problems to the fact that the town is heated by a boiler plant owned by the Klimovsk Specialized Ammunition Plant, a private ammunition factory and one of the largest weapon cartridge production enterprises in the country.
“The facility is under tight security conditions, which limits our ability to oversee winter preparations,” the Moscow region’s Vice Governor Yevgeny Khromushin said last week. “We were unaware of the problem for nearly a day.”
An unidentified Moscow region official and two senior executives at the plant were arrested on suspicion of providing unsafe services, Russia’s Investigative Committee, which probes major crimes, said in a statement Tuesday.
Investigators said that Podolsk’s deputy mayor was accused of misusing authority by issuing a readiness certificate for the boiler house at the plant.
In the neighboring Tver region, the authorities opened a criminal case over the laundering of over 84 million rubles ($938,993) in heating bills paid by residents, the Astra Telegram channel reported this week, citing unidentified sources. According to investigators, the heads of the local water intake and boiler house misappropriated the heating payments for personal use.
Reacting to the heating failures, Putin on Tuesday asked Emergency Situations Minister Alexander Kurenkov to provide heat and electricity to the affected residents.
The outages appear to be the latest effect of several decades of crumbling infrastructure in Russia which have been linked to endemic corruption and mismanagement.
The overall decay of Russia's municipal infrastructure surpassed 70% in 2022, the pro-Kremlin newspaper Izvestia reported .
According to Sergei Pakhomov, head of the State Duma’s Construction, Housing and Utilities Committee, water pipes that were 90 years old or even older were still in use as recently as two years ago in some cases.
Housing, utilities and communal services are a common source of problems for Russians during the winter.
In St. Petersburg, residents regularly complain about extensive ice coverage on city streets and sidewalks, with many people ending up in the hospital over the years due to slipping and falling accidents.
In the Siberian republic of Khakassia, two villages were left without electricity last month due to apparent issues with outdated communication systems.
In the winter of 2020, five people in the Perm region were killed after a pipe burst.
When asked about the latest heating outages, Kremlin spokesman Dmitry Peskov acknowledged the problems and linked them to poor municipal infrastructure, saying that people “had to endure a lot of inconvenience in the cold and without electricity.”
"Despite all the titanic efforts to update all housing and communal services systems, there's still a certain part that remains considerably deteriorated. These programs will continue, but it is impossible to update all pipes and all housing and communal services systems in 10-15 years,” Peskov said.
As for now, residents affected by heating issues appear to lack optimism that the problems will be solved efficiently.
"It's been a week since we've had heating, and the temperature in my apartment is around 11 degrees Celsius,” Podolsk resident Lidiya told The Moscow Times.
“Unfortunately, no one knows when it will be repaired,” she added.


Russia establishes special site to fabricate fuel for China’s CFR-600
!{Model.Description}
A special production site to fabricate fuel for China’s CFR-600 fast reactor under construction has been established at Russia’s Mashinostroitelny Zavod (MSZ - Machine-Building Plant) in Elektrostal (Moscow region), part of Rosatom’s TVEL Fuel Company.
As part of the project, MSZ had upgraded existing facilities fo the production of fuel for fast reactors, TVEL said on 3 March. Unique equipment has been created and installed, and dummy CFR-600 fuel assemblies have already been manufactured for testing.
The new production site was set up to service an export contract between TVEL and the Chinese company CNLY (part of China National Nuclear Corporation - CNNC) for the supply of uranium fuel for CFR-600 reactors. Construction of the first CFR-600 unit started in Xiapu County, in China's Fujian province in late 2017 followed by the second unit in December 2020. The contract is for the start-up fuel load, as well as refuelling for the first seven years. The start of deliveries is scheduled for 2023.
“The Russian nuclear industry has a unique 40 years of experience in operating fast reactors, as well as in the production of fuel for such facilities,” said TVEL President Natalya Nikipelova. “The Fuel Division of Rosatom is fulfilling its obligations within the framework of Russian-Chinese cooperation in the development of fast reactor technologies. These are unique projects when foreign design fuel is produced in Russia. Since 2010, the first Chinese fast neutron reactor CEFR has been operating on fuel manufactured at the Machine-Building Plant, and for the supply of CFR-600 fuel, a team of specialists from MSZ and TVEL has successfully completed a complex high-tech project to modernise production,” she explained.
A special feature of the new section is its versatility: this equipment will be used to produce fuel intended for both the Chinese CFR-600 and CEFR reactors and the Russian BN-600 reactor of the Beloyarsk NPP. In the near future, the production of standard products for the BN-600 will begin.
The contract for the supply of fuel for the CFR-600 was signed in December 2018 as part of a governmental agreement between Russia and China on cooperation in the construction and operation of a demonstration fast neutron reactor in China. This is part of a wider comprehensive programme of cooperation in the nuclear energy sector over the coming decades. This includes serial construction of the latest Russian NPP power units with generation 3+ VVER-1200 reactors at two sites in China (Tianwan and Xudabao NPPs). A package of intergovernmental documents and framework contracts for these projects was signed in 2018 during a meeting between Russian President Vladimir Putin and Chinese President Xi Jinping.
- Terms and conditions
- Privacy Policy
- Newsletter sign up
- Digital Edition
- Editorial Standards

pediatric speech therapy travel jobs
Travel ot pediatrics jobs.
Browse nationwide ot pediatrics jobs now (tons exclusive only to aya)..
We don’t have anything that matches your search right now — but we update our jobs daily, so check back soon! Or register now , update your profile and save job searches to be notified when a job that matches your parameters becomes available!
We're currently updating our jobs so please check back soon!
Log in with Aya
Looks like you already have an account with Aya. Log in and access pay and facility information.
Register with Aya
Get instant access to pay and facility information.
- At least 8 characters
- 1 lowercase letter
- 1 uppercase letter
- 1 symbol/special character
*File types allowed: TXT, PDF, DOC *Maximum file size: 20MB
Already have an account? Log in here .
Aya delivers:
- The most jobs in the industry. We have the largest and most reliable job database, which means the jobs you see are open, updated in real time and ready for you!
- Competitive advantage over other agencies. Front-of-the-line access through our direct facility relationships — many with quick (even same-day) offers, giving you the best chance of securing your ideal opportunity.
- Expedited licensing and streamlined compliance. An industry-leading on-time start rate and strong relationships with boards of nursing across the country to accelerate the process in all 50 states.
- Expert career guidance. A dedicated recruiter to help you achieve your dream career. Travel, per diem, permanent — we have the reach and access to get you the jobs you want, and the expertise to help you realize your long-term goals.
- A best-in-class support system and an exceptional experience. Enjoy accurate, weekly pay, and an entire team dedicated to your happiness on assignment, 24/7.
Plus, you get everything you expect from the largest healthcare staffing company in the industry:
- Exceptional benefits, including premium medical, dental, vision and life insurance beginning day one of your assignment. Want to take time off? Keep insurance coverage for up to 24 days between assignments.
- A generous 401(k) match.
- Paid company housing (we'll help you bring your pets along, too!) or a generous housing stipend.
- Paid sick time in accordance with all applicable state, federal, and local laws. Aya's general sick leave policy is that employees accrue one hour of paid sick leave for every 30 hours worked. However, to the extent any provisions of the statement above conflict with any applicable paid sick leave laws, the applicable paid sick leave laws are controlling.
- The industry's only clinical ladder program for RNs on assignment.
- Access to unlimited continuing education units online.
- Licensure, relocation and other reimbursements, when applicable.
- Pay listed above includes taxable wages and tax-free expense reimbursements.
For all employees and employee applicants, Aya is an Equal Employment Opportunity ("EEO") Employer, including Disability/Vets, and welcomes all to apply. Please click here for our EEO policy.
- Bi-weekly weekend travel home.
- A rental car and paid housing.
With Aya Locums you get:
- Access to top hospitals and healthcare systems in diverse care settings.
- Highly competitive, transparent locum tenens pay.
- Dedicated application and assignment support.
- In-house credentialing and licensing teams.
- Full coverage of licensing costs.
- Travel and lodging coverage.
- Easy timekeeping and streamlined management of documents.
- Malpractice coverage and risk management support.
- Premium medical, dental, vision and life insurance beginning day one of your assignment.
- Paid sick time. Aya provides paid sick leave in accordance with all applicable state, federal, and local laws. Aya's general sick leave policy is that employees accrue one hour of paid sick leave for every 30 hours worked. However, to the extent any provisions of the statement above conflict with any applicable paid sick leave laws, the applicable paid sick leave laws are controlling.
- Generous 401k match.
- Aya may provide other benefits where required by applicable law, including but not limited to reimbursements.
- Aya coordinates all travel and lodging accommodations.
- Travel information is received the evening prior to your scheduled departure.
- Airfare is covered and, if driving to the assignment, reimbursement is available.
- Once notice is received, communication from our team is sent via email and text to ensure you are kept in the loop as soon as information becomes available.
- Your safety is Aya's top priority. We work closely with the facility to ensure additional security measures are taken onsite so you can focus on what really matters: patient care.
- Licensure, relocation and other reimbursements.
Experience the Aya difference today
- A dedicated recruiter who advocates for you every step of the way.
- We'll ensure the hiring manager prioritizes your interest and schedules an interview quickly.
- A streamlined hiring process means offers are often presented within 24-48 hours after an interview with a hiring leader.
- Flexible start dates that work around your availability.
- We make it simple with one point of contact the entire time.
- University of Washington (UW) offers a wide range of benefits as part of your total compensation package. Choose from top medical and dental insurance programs; plan for your future with tax-deferred investing through the UW retirement options; enjoy generous vacation and sick leave policies; and protect yourself and your family with life and long-term disability insurance. For more information, follow the links shown below or explore the Benefits website at http://hr.uw.edu/benefits/
With Aya, you get:
- Higher compensation - we negotiate on your behalf.
- Work-life balance - contracts are up to 40 hours per week, with workdays ending mid-late afternoon and weekends off!
- An employee advocate - our team ensures you have the support needed to be successful in your role.
- Options post contract - extend, convert to a permanent employee or find a new job.
- Paid company housing (pets are welcome to tag along) or a generous housing stipend.
- If qualified, continued insurance coverage over the summer.
- A generous 401k match.
- A robust team to support you every step of the way.
- A credentialing specialist to streamline the entire compliance process.
- Freedom and flexibility around your current schedule.
- The easy-to-use Shifts app. Select shifts anytime, anywhere.
- Premium medical, dental, vision and life insurance.
- Front-of-the-line access to exclusive jobs at thousands of healthcare facilities nationwide.
- A robust team to support you every step of the way to ensure you start on time, have accurate payroll and an exceptional experience.
- Certification and other reimbursements, when applicable.
Privacy Overview

275 Travel Pediatric Speech Language Pathologist jobs available on Indeed.com. Apply to Travel Speech Language Pathologist, Speech Language Pathologist, Speech Therapist and more! ... Looking for a speech language therapist (SLP) for 13 weeks.
2,650 Travel Pediatric Speech Therapy jobs available on Indeed.com. Apply to Speech Language Pathologist and more!
1,491 Pediatric Travel Speech Therapist jobs available on Indeed.com. Apply to Speech Therapist, Speech Language Pathologist, Travel Speech Language Pathologist and more!
379 pediatric travel slp jobs available. See salaries, compare reviews, easily apply, and get hired. New pediatric travel slp careers are added daily on SimplyHired.com. ... & Speech Therapy Independent (1099) Providers to serve infants & toddlers birth to three years old in Escambia, Okaloosa, Walton & Santa Rosa Counties.
A Speech language pathologist's travel job allows you to embrace your love for speech therapy and your passion for traveling. Professionally, travel speech-language pathologists have the largest database of travel jobs to choose from, and SLPs working in a school setting are in high demand!
Travel Contract Travel Speech Language Pathologist Sitka, AK Access Healthcare 5x8 hrs, Days $2,890/week. Days. 5x8. Above Average Pay. Apply now. Posted Today. Verified. Travel Contract Travel Speech Language Pathologist Grand Forks, ND GLC On-The-Go 4x10 hrs, Days Referral Bonus $2,801/week. Days.
For the latest job listings, be sure to call your recruiter at 800-884-8788. We offer many jobs that are not posted online — and we receive new openings around the clock! Employment of speech-language pathologists is projected to grow faster than the average for other healthcare occupations.
Browse nationwide OT Pediatrics jobs now (tons exclusive only to Aya). Therapy/Rehabilitation: OT Pediatrics. Select Locations. *Log in to access the map view, additional filters, and job details. Cookie.
Quick Apply $36.50 to $49.75 Hourly Estimated pay Full-Time Job Description: Any traveler not currently inpossession of an active State of HI license must ... Speech Therapist General Certifications:, General Certifications (BLS/BCLS) ; Rehabilitation ... Speech Therapist Rosewood Retirement Community Killeen, TX Quick Apply $40 to $46 Hourly
76 Traveling speech pathologist jobs in United States. Most relevant. Inspire Rehabilitation. Traveling Speech Language Pathologist. Nebraska. $75K - $100K (Employer est.) Easy Apply. Experience the adventure of a traveling speech language pathology position combined with the stability of joining an established company.…. 10d.
2,831 Speech Pediatric Travel jobs available on Indeed.com. Apply to Speech Language Pathologist, Speech Therapist, Speech Pathologist and more!
Floating Pediatric Speech Therapist (SLP) - Charlotte, NC Area - Local TravelExciting opportunity to join the team at th... See this and similar jobs on Glassdoor
Search and apply for Pediatric PT travel jobs with top pay and free benefits at American Traveler.
Job ... Allied - Speech Therapist - Travel Protouch Staffing Grand Forks, ND Quick Apply $2,702 Weekly Full-Time Gross Pay (weekly): $2702.0 Taxable Pay (weekly): 1540.0 Non-taxable Pay (weekly): 1162.0 Allied - Speech Therapist - Travel Shift: M-F, Days-flexible hours but generally 8-5. Would be open to 4-10 ...
January 26, 2024 Travel SLP Guide to Peds The field of pediatric speech therapy is both challenging and rewarding, particularly for Travel Speech-Language Pathologists (SLPs). These professionals play a vital role in addressing communication and swallowing disorders in children.
$32-$75/hr Pediatric Speech Therapist Jobs (NOW HIRING) Get fresh pediatric speech therapist jobs daily straight to your inbox! Create Alert Pediatric speech therapist jobs 10,623 Pediatric Speech Therapist Jobs Jobs within 5000 miles of Chicago, IL Change location Pediatric Speech Language Pathologist Milestone Therapy Harvey, IL Quick Apply
526 Travel Pediatric Speech Therapy Assistant jobs available on Indeed.com. Apply to Speech Language Pathologist, Speech Therapist, Occupational Therapist and more!
Pediatric OT Travel Jobs Pediatric occupational therapists can help children and teens regain independence that may have been lost after serious illness or injury. Plus, they have the amazing opportunity to travel the United States with American Traveler. About Pediatric OT Jobs
Job: Type: Part-Time, Contract. We have an immediate need for a Connecticut based pediatric Speech Language Pathologist (CCC-SLP) to join our referral network as an independent contractor. You will be able to set your own schedule, travel radius, as well as caseload requirements. We'll work to pair you with your ideal clients.
Speech Therapy Travel jobs Sort by: relevance - date 44 jobs Speech-Language Pathologists - SLP THER - Travel New Travel Nurse Across America 4.1 Sitka, AK $2,830.51 a week Easily apply We are looking for Speech-Language Pathologists (SLP) for an immediate travel opening in Sitka, AK. The right SLP should have 1 year of experience. Read below…
Today's 10 jobs in Elektrostal, Moscow, Russia. Leverage your professional network, and get hired. New Elektrostal, Moscow, Russia jobs added daily.
Rome2Rio is a door-to-door travel information and booking engine, helping you get to and from any location in the world. Find all the transport options for your trip from Kazanskiy Vokzal to Elektrostal right here. Rome2Rio displays up to date schedules, route maps, journey times and estimated fares from relevant transport operators, ensuring ...
34 Pediatric Travel Placement Speech Therapist jobs available on Indeed.com. Apply to Speech Language Pathologist, Assistant, School Psychologist and more!

IMAGES
VIDEO
COMMENTS
Several DNP and PhD candidates are engaged in research projects to study cardiovascular disease. ... As a nursing student in 1988, I worked as a professional nursing assistant in cardiology under a dynamic nurse manager, Barry Hawthorn, who mentored me. I ended up staying on the unit as a new graduate nurse.
The highest level of education achieved was a Master's degree for 76%, a Doctor of Nursing Practice (DNP) for 17% and PhD for 5%. For respondents with a Master's degree, only 22% said they planned to further their education, although the reasons for this were not captured with the survey questionnaire. ... The 2019 Cardiology Advanced Practice ...
A critical care nurse by training, Mary Carey, PhD, RN, FAHA, FAAN, is a highly respected researcher, educator, and mentor whose work has made significant contributions to the understanding of ECG monitoring to help detect cardiac arrhythmias and myocardial ischemia and infarction, and on the ECG's use in predicting cardiac events and sudden cardiac death.
This program will provide you with the knowledge and skills in theoretical, methodological, and analytical approaches that will enable you to conduct research to discover and apply knowledge in nursing science and health care. Most full-time Johns Hopkins Nursing PhD students are 100% funded with a stipend for the first three years of study.
Cardiovascular nursing has developed markedly in recent decades and research is now being seen as a legitimate activity. Cardiovascular nurses and nursing have made significant research contributions in key areas, notably in the design and evaluation of cardiac rehabilitation [1, 2], secondary prevention [3, 4] and heart failure disease management programmes [5, 6].
The Editors of The Journal of Cardiovascular Nursing plan to feature a heart failure section comprised of multiple articles about heart failure in each issue of the journal. We also plan several special issues on important heart failure topics. Our purpose with the inaugural special issue, Advances in the Science of Heart Failure Self-Care, is to present research that advances our ...
Nursing PhD students and emerging nurse scientists need this knowledge if they are truly to follow a path of generating impactful nursing knowledge. ... European journal of cardiovascular nursing : journal of the Working Group on Cardiovascular Nursing of the European Society of Cardiology, 19 (3), 190-191. doi: 10.1177/1474515119894215 ...
The PhD in Nursing is a hybrid program. The program features excellent mentoring and teaching by faculty, extensive research experiences, and committed peers. The PhD in Nursing program emphasizes interdisciplinary knowledge development and dissemination. The College of Nursing offers two campuses: in Augusta and in Athens, Georgia.
Journal of Cardiovascular Nursing is one of the leading journals for advanced practice nurses in cardiovascular care, providing thorough coverage of timely topics and information that is extremely practical for daily, on-the-job use. ... Debra K. Moser, PhD, RN, FAHA, FAAN Professor and Gill Chair of Cardiovascular Nursing College of Nursing ...
ABOUT THE PROGRAM. The PhD in Nursing Program prepares nurse scientists for research-intensive academic careers. The program emphasizes interdisciplinary knowledge development and dissemination through Biobehavioral nursing research. Our faculty are involved in ground-breaking research in such vital areas as health disparities, cancer ...
Cardiology (nursing) PhD Projects, Programmes & Scholarships We have 1 Cardiology (nursing) PhD Projects, Programmes & Scholarships. Show more Show all . More Details . Exercise, cardiovascular physiology and healthy ageing research scholarship. University of the Sunshine Coast School of Health.
Considering the scope of nursing practice, high level of expertise and invaluable insights of nurses to the care team, in-depth understanding of psychosocial and physical wellbeing of people with cardiovascular disease, and the internationally recognised research track records of our cardiovascular nurse members, inclusiveness and partnering ...
The Journal of Continuing Education in Nursing, 40(1), 28-32. > Link Google Scholar; Hong W.-H.S. (2010). Evidence-based nursing practice for health promotion in adults with hypertension: A literature review. Asian Nursing Research, 4(4), 227-245. > Crossref Medline Google Scholar
Goals and Mission. The goal of our program is to provide the highest quality training in Cardiovascular Medicine. Our program strives to uphold the Hopkins tradition of clinical excellence, teaching and research. We have a strong history of preparing leaders in the field of academic cardiology, providing them with the tools to become skilled ...
A nurse who has attained a PhD can practically work anywhere that research, education, or program evaluation takes place. The important thing to remember is that graduation from a reputable PhD program ensures that a nurse has received proper research training. Tiffany M. Montgomery, MSN, RNC-OB, C-EFM, a women's health nurse since 2005 ...
Comprehensive data on research undertaken in cardiovascular medicine can inform the scientific community and can support policy building. We used the publication output from 2004 to 2013 and the 2014 references to these documents, to identify research topics and trends in the field of cardiovascular disease. ... D.G. had a PhD Fellowship ...
Kuo's research program seeks to help truck drivers and other industrial workers prevent cardiovascular disease. "Truckers are only one type of industrial worker, but it's a large group that moves our economy and our society," says Kuo. "Unfortunately, they experience a lot of cardiometabolic risk and health disparities."
Best Doctorate in Nursing Education Online Programs. Regis University. Walsh University. Bryan College of Health Sciences. Ohio University-Main Campus. East Carolina University. Western ...
She is also the recipient of the American Academy of Nursing's 2020 Civitas Award for her extraordinary dedication to excellence in promoting quality care in nursing worldwide. Dr. Ferguson received her PhD in 1996 and her BSN in 1985 from the University of Virginia in Charlottesville, VA.
The evaluation of the cardiovascular system includes a thorough medical history and a detailed examination of the heart and peripheral vascular system.[1] Nurses must incorporate subjective statements and objective findings to elicit clues of potential signs of dysfunction. Symptoms like fatigue, indigestion, and leg swelling may be benign or may indicate something more ominous. As a result ...
PODOLSK, Moscow region - Residents throughout Russia affected by unprecedented winter heating outages in recent days have expressed their frustration and urged local authorities to restore ...
A special production site to fabricate fuel for China's CFR-600 fast reactor under construction has been established at Russia's Mashinostroitelny Zavod (MSZ - Machine-Building Plant) in Elektrostal (Moscow region), part of Rosatom's TVEL Fuel Company.
1,048 Sociology PhD jobs available on Indeed.com. Apply to Senior Researcher, User Experience Researcher, Researcher and more!... Careers with a Sociology PhD People with a doctorate in sociology can apply their skills in a variety of jobs, inside and outside academia. The traditional career path for sociology PhDs involves a position on the faculty of a college or university, with a focus on ...
275 Travel Pediatric Speech Language Pathologist jobs available on Indeed.com. Apply to Travel Speech Language Pathologist, Speech Language Pathologist, Speech Therapist and more! ... Looking for a speech language therapist (SLP) for 13 weeks.... 2,650 Travel Pediatric Speech Therapy jobs available on Indeed.com. Apply to Speech Language Pathologist and more!... 1,491 Pediatric Travel Speech ...