These are the 10 biggest global health threats of the decade

Global warming and conflict zones are among the main obstacles. Image: REUTERS/Goran Tomasevic - RC186A78C7A0

.chakra .wef-1c7l3mo{-webkit-transition:all 0.15s ease-out;transition:all 0.15s ease-out;cursor:pointer;-webkit-text-decoration:none;text-decoration:none;outline:none;color:inherit;}.chakra .wef-1c7l3mo:hover,.chakra .wef-1c7l3mo[data-hover]{-webkit-text-decoration:underline;text-decoration:underline;}.chakra .wef-1c7l3mo:focus,.chakra .wef-1c7l3mo[data-focus]{box-shadow:0 0 0 3px rgba(168,203,251,0.5);} Johnny Wood

.chakra .wef-9dduvl{margin-top:16px;margin-bottom:16px;line-height:1.388;font-size:1.25rem;}@media screen and (min-width:56.5rem){.chakra .wef-9dduvl{font-size:1.125rem;}} Explore and monitor how .chakra .wef-15eoq1r{margin-top:16px;margin-bottom:16px;line-height:1.388;font-size:1.25rem;color:#F7DB5E;}@media screen and (min-width:56.5rem){.chakra .wef-15eoq1r{font-size:1.125rem;}} Global Health is affecting economies, industries and global issues

.chakra .wef-1nk5u5d{margin-top:16px;margin-bottom:16px;line-height:1.388;color:#2846F8;font-size:1.25rem;}@media screen and (min-width:56.5rem){.chakra .wef-1nk5u5d{font-size:1.125rem;}} Get involved with our crowdsourced digital platform to deliver impact at scale
Stay up to date:, global health.
- The WHO released the top 10 global healthcare challenges in the coming decade.
- Global warming, conflict zones and unfair healthcare provision are among the main obstacles.
- Many healthcare challenges are interconnected and will require a coordinated international effort to overcome.
- Experts are concerned governments around the world are failing to invest sufficient funds in overcoming these issues.
The world can’t afford to do nothing – that's the World Health Organization’s message on the release of its report listing the most urgent health challenges for the coming decade.
All of the health challenges on the WHO list are urgent – and many are linked. And each challenge requires a coordinated effort from the global health sector, policymakers, international agencies and communities, the organization says. However, there is concern global leaders are failing to invest enough resources in core health priorities and systems.
Have you read?
Why the 21st century's biggest health challenge is our shared responsibility, here are 3 ways ai will change healthcare by 2030, to bring universal healthcare to africa, the private sector must get involved.

These are the main challenges on the list.
1. Elevating health in the climate debate The climate crisis poses one of the biggest threats to both the planet and the health of the people who live on it.
Emissions kill around 7 million people each year, and are responsible for more than a quarter of deaths from diseases including heart attacks, stroke and lung cancer. At the same time, more – and more intense – extreme weather events like drought and floods increase malnutrition rates and help spread infectious diseases like malaria.
2. Delivering health in conflict and crisis

The already difficult task of containing disease outbreaks is made more challenging in countries rife with conflict.
Nearly 1,000 attacks on healthcare workers and medical facilities in 11 countries were recorded in 2019, leaving 193 medical staff dead. Despite stricter surveillance, many healthcare workers remain vulnerable.
For the tens of millions of people forced to flee their homes, there is often little or no access to healthcare.
3. Making healthcare fairer
The gap between the haves and have-nots is growing, especially in terms of access to healthcare.
People in wealthy nations can expect to live 18 years longer than their poorer neighbours, and wealth can determine access to healthcare within countries and individual cities, as well. Rising global rates of diseases like cancer, diabetes and chronic respiratory conditions have a greater impact on low- and middle-income countries, where medical bills can quickly deplete the limited resources of poorer families.
4. Expanding access to medicines Although many in the world take access to medication for granted, medicines and vaccines are not an option for almost one-third of the global population.
The challenge of expanding access to medicines in areas where few, if any, healthcare products are available includes combatting substandard and imitation medical products . In addition to putting lives at risk by failing to treat the patient’s condition, these products can undermine confidence in medicines and healthcare providers.
5. Stopping infectious diseases
Infectious diseases continue to kill millions of people, most of them poor. This picture looks unlikely to change in the near future.
Preventing the spread of diseases like HIV, tuberculosis and malaria depends on sufficient levels of funding and robust healthcare systems. But in some areas where they are most needed, these resources are in short supply.
Greater funding and political will is required to develop immunization programmes, share data on disease outbreaks and reduce the effects of drug resistance.
6. Preparing for epidemics

Airborne viruses or diseases transferred by mosquito bite can spread quickly, with potentially devastating consequences.
Currently, more time and resources are spent reacting to a new strain of influenza or an outbreak of yellow fever, rather than preparing for future outbreaks. But it’s not a question of if a dangerous virus will come about – but when.
Epidemics are a huge threat to health and the economy: the vast spread of disease can literally destroy societies.
In 2017, at our Annual Meeting, the Coalition for Epidemic Preparedness Innovations (CEPI) was launched – bringing together experts from government, business, health, academia and civil society to accelerate the development of vaccines against emerging infectious diseases and to enable access to them during outbreaks.
Our world needs stronger, unified responses to major health threats. By creating alliances and coalitions like CEPI, which involve expertise, funding and other support, we are able to collectively address the most pressing global health challenges.
Is your organisation interested in working with the World Economic Forum to tackle global health issues? Find out more here .
7. Protecting people from dangerous products
Many poorer parts of the world face malnutrition and food insecurity, while at the same time, global obesity levels and diet-related problems are on the rise. We need to rethink what we eat, reduce the consumption of food and drinks high in sugar, salt and harmful fats, and promote healthy, sustainable diets. To this end, the WHO is working with countries to develop policies that reduce our reliance on harmful foodstuffs.
Health workers are in short supply the world over. Sustainable health and social care systems depend on well-paid and properly trained staff who can deliver quality care. WHO research predicts that by 2030, there will be a shortfall of 18 million health workers, mostly in low- and middle-income countries.
New investment is needed to properly train health workers and provide decent salaries for people in the profession, it says.
9. Keeping adolescents safe
Every year, more than 1 million adolescents – aged between 10 and 19 – die. The main causes include road accidents, suicides, domestic violence and diseases like HIV or lower respiratory conditions. But many of these premature deaths are preventable. Policymakers, educators and health practitioners need to promote positive mental health among adolescents, to prevent illicit drug use, alcohol abuse and self harm. Programmes that raise awareness of things like contraception, sexually transmitted infections and pregnancy care help address some of the underlying causes of adolescent fatalities.
10. Earning public trust Delivering safe, reliable healthcare to patients involves first gaining their confidence and trust; a trust which can be undermined by the rapid spread of misinformation on social media. For example, the anti-vaccination movement has led to an increase in deaths from preventable diseases. But social media can also be used to spread reliable information and build public trust in healthcare. Community programmes are another way to boost confidence in healthcare provision and practices that prevent the spread of diseases, such as vaccinations or condom use.
Don't miss any update on this topic
Create a free account and access your personalized content collection with our latest publications and analyses.
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
The views expressed in this article are those of the author alone and not the World Economic Forum.
The Agenda .chakra .wef-n7bacu{margin-top:16px;margin-bottom:16px;line-height:1.388;font-weight:400;} Weekly
A weekly update of the most important issues driving the global agenda
.chakra .wef-1dtnjt5{display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;-webkit-flex-wrap:wrap;-ms-flex-wrap:wrap;flex-wrap:wrap;} More on Health and Healthcare Systems .chakra .wef-17xejub{-webkit-flex:1;-ms-flex:1;flex:1;justify-self:stretch;-webkit-align-self:stretch;-ms-flex-item-align:stretch;align-self:stretch;} .chakra .wef-nr1rr4{display:-webkit-inline-box;display:-webkit-inline-flex;display:-ms-inline-flexbox;display:inline-flex;white-space:normal;vertical-align:middle;text-transform:uppercase;font-size:0.75rem;border-radius:0.25rem;font-weight:700;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;line-height:1.2;-webkit-letter-spacing:1.25px;-moz-letter-spacing:1.25px;-ms-letter-spacing:1.25px;letter-spacing:1.25px;background:none;padding:0px;color:#B3B3B3;-webkit-box-decoration-break:clone;box-decoration-break:clone;-webkit-box-decoration-break:clone;}@media screen and (min-width:37.5rem){.chakra .wef-nr1rr4{font-size:0.875rem;}}@media screen and (min-width:56.5rem){.chakra .wef-nr1rr4{font-size:1rem;}} See all

How midwife mentors are making it safer for women to give birth in remote, fragile areas
Anna Cecilia Frellsen
May 9, 2024

From Athens to Dhaka: how chief heat officers are battling the heat
Angeli Mehta
May 8, 2024

How a pair of reading glasses could increase your income
Emma Charlton

Nigeria is rolling out Men5CV, a ‘revolutionary’ meningitis vaccine

5 conditions that highlight the women’s health gap
Kate Whiting
May 3, 2024

How philanthropy is empowering India's mental health sector
Kiran Mazumdar-Shaw
May 2, 2024
- Search Menu
- Advance articles
- Editor's Choice
- Supplement Archive
- Cover Archive
- IDSA Guidelines
- IDSA Journals
- The Journal of Infectious Diseases
- Open Forum Infectious Diseases
- Photo Quizzes
- State-of-the-Art Reviews
- Voices of ID
- Author Guidelines
- Open Access
- Why Publish
- Advertising and Corporate Services
- Advertising
- Journals Career Network
- Reprints and ePrints
- Sponsored Supplements
- Branded Books
- About Clinical Infectious Diseases
- About the Infectious Diseases Society of America
- About the HIV Medicine Association
- IDSA COI Policy
- Editorial Board
- Self-Archiving Policy
- For Reviewers
- For Press Offices
- Journals on Oxford Academic
- Books on Oxford Academic
Article Contents
The scope of the problem, emerging and reemerging infections, infectious causes of chronic diseases, bioterrorism, the science base for infectious diseases in the 21st century, vaccinology in the 21st century, global health, acknowledgment, infectious diseases: considerations for the 21st century.
This article is a shortened and edited version of an address delivered at the 38th annual meeting of the Infectious Diseases Society of America, held in New Orleans on 7–10 September 2000.
- Article contents
- Figures & tables
- Supplementary Data
Anthony S. Fauci, Infectious Diseases: Considerations for the 21st Century, Clinical Infectious Diseases , Volume 32, Issue 5, 1 March 2001, Pages 675–685, https://doi.org/10.1086/319235
- Permissions Icon Permissions
The discipline of infectious diseases will assume added prominence in the 21st century in both developed and developing nations. To an unprecedented extent, issues related to infectious diseases in the context of global health are on the agendas of world leaders, health policymakers, and philanthropies. This attention has focused both on scientific challenges such as vaccine development and on the deleterious effects of infectious diseases on economic development and political stability. Interest in global health has led to increasing levels of financial support, which, combined with recent technological advances, provide extraordinary opportunities for infectious disease research in the 21st century. The sequencing of human and microbial genomes and advances in functional genomics will underpin significant progress in many areas, including understanding human predisposition and susceptibility to disease, microbial pathogenesis, and the development new diagnostics, vaccines, and therapies. Increasingly, infectious disease research will be linked to the development of the medical infrastructure and training needed in developing countries to translate scientific advances into operational reality.
The history of the medical discipline of infectious diseases is rich in extraordinary accomplishments that have had a major impact on humankind [ 1 ]. The successful diagnosis, prevention, and treatment of a wide array of infectious diseases has altered the very fabric of society, providing important social, economic and political benefits.
In considering the importance of infectious diseases globally as well as in the United States in these first years of the 21st century, I reflect back to December 1967, when then-Surgeon General William H. Stewart, contemplating the benefits realized from antibiotics and vaccines, declared victory against the threat of infectious diseases and suggested that our nation turn its attention and resources to the more important threat of chronic diseases [ 2 ]. At the time, I was completing my residency training in internal medicine at New York Hospital-Cornell Medical Center and anticipating my move to Bethesda, Maryland, to begin my infectious diseases fellowship at the National Institutes of Health. I became concerned that I was entering a subspecialty of clinical medicine and an area of biomedical research that was disappearing at the same time that I was training for it. However, the history of infectious diseases from that time in my training until the present day has proven quite the opposite. At the dawn of the 21st century, the future of infectious diseases and its impact on societies throughout the world is strikingly apparent. It is this future that I will address herein.
Infectious diseases are the second leading cause of death and the leading cause of disability-adjusted life years worldwide (1 disability-adjusted life year is 1 lost year of healthy life) and the third leading cause of death in the United States [ 3 , 4 ]. Among these infectious diseases causing death worldwide, acute lower respiratory tract infections, HIV/AIDS, diarrheal diseases, tuberculosis, and malaria predominate ( table 1 ). Clearly, despite earlier predictions to the contrary [ 2 ], infectious diseases remain a dominant feature of domestic and international public health considerations for the 21st century. In fact, the continual evolution of emerging and reemerging diseases, particularly the acceleration of the HIV/AIDS pandemic in developing countries, will heighten the global impact of infectious diseases in this century.
Leading infectious causes of death worldwide, 1999.
The extent of the global burden of infectious diseases depends on the already established incidences and prevalences of known infections together with the constant, but uneven, flow of emerging and reemerging infections [ 5–8 ]. Emerging infections are those that have not been previously recognized. The AIDS pandemic is a prototypical example of a truly new and emerging infectious disease whose public health impact had not been previously experienced. Reemerging infections have been experienced previously but have reappeared in a more virulent form or in a new epidemiological setting. The influenza A pandemics of 1918, 1957, and 1968 are prototypical examples of reemerging infections [ 9 ].
HIV/AIDS . Despite the fact that the HIV/AIDS pandemic exacted a terrible toll in deaths and human suffering in the last 2 decades of the 20th century, the full impact of this disease will be realized in the 21st century. As of the end of 2000, there were 36 million people worldwide living with HIV infection; >90% of them live in developing countries, and 70% live in southern Africa [ 6 ]. There have been ∼22 million cumulative deaths due to AIDS. In certain countries in Africa, such as Botswana, Zimbabwe, and Swaziland, 25%–35% of the adult population (ages 15–49 years) are infected with HIV [ 10 ]. In South Africa, it is estimated that there are >4 million people infected with HIV, ∼10% of the entire population and 20% of the adult population. The life expectancy in several southern African countries has decreased dramatically because of the HIV/AIDS pandemic, negating the impressive gains that had been made over the previous few decades.
India and other southern and southeastern Asian countries will be the next epicenters of the HIV/AIDS pandemic; the cultural and socioeconomic conditions in those countries are unfortunately well-suited to explosive spread of this infection [ 10 ]. Indeed, it is estimated that ∼4 million people in India are already infected with HIV. The potential for catastrophic spread in this country of >1 billion people is enormous, as it is for China, the most populous nation in the world. Aggressive and sustained AIDS prevention programs are critical to contain the epidemic in these Asian countries.
The continual evolution of infectious diseases . In addition to HIV/AIDS and pandemic influenza [ 10 ], which have had an extraordinary impact on global health, there is a continual evolution of a wide range of emerging and reemerging infectious diseases with varying potentials for global spread. Figure 1 illustrates some salient examples of emerging and reemerging infections throughout the world in recent years. Some, such as Ebola virus and Nipah virus, have been highly virulent but have involved relatively small numbers of people, have remained tightly restricted in their spread, and so have been more medical curiosities than global public health threats. Others, such as multidrug-resistant malaria, have involved large numbers of people but have, because of the demography of the infection, remained for the most part geographically restricted. This has resulted in a serious situation in the region involved but not a global public health threat. Multidrug-resistant tuberculosis and vancomycin-resistant Staphylococcus aureus and enterococci are examples of emerging infections that do not immediately involve large numbers of persons but that will ultimately have a serious impact on public health throughout the world [ 8 ].
Range and recognized site(s) of origin of variety of emerging and reemerging infections. v-CJD, variant Creutzfeldt-Jakob disease; E. coli, Escherichia coli .
Two examples of recently reemerging infections that are currently causing considerable concern in the United States are dengue and West Nile fever. Dengue has posed an extraordinary problem in Brazil, with >530,000 cases reported in 1998 [ 11 ]. In addition, other nations in South and Central America and the Caribbean have varying degrees of problems with dengue. Dengue has appeared infrequently in the United States since the 1940s. However, it remains a threat because the mosquito vectors for dengue are widely dispersed in the United States, particularly in the states bordering the Gulf of Mexico. Indeed, in 1999, 17 locally acquired cases of dengue were reported in Texas (Gubler D, Centers for Disease Control and Prevention, personal communication). In contrast, West Nile fever had never been seen in the United States before 1999, when there were 62 cases and 7 deaths identified in the New York City area [ 12 ]. West Nile fever is caused by a flavivirus that is transmitted by mosquitoes, with a variety of birds serving as intermediate hosts. It is indigenous to the region of the West Nile River (hence its name) and is seen commonly in Middle Eastern countries such as Israel. The virus survived the winter of 1999–2000 in the United States; in 2000, 18 human cases (including 1 death) and numerous infections in various avian and mammalian species were reported in the summer and early fall. Infected birds were identified along the eastern seaboard as far south as North Carolina [ 13 ]. Here again, the major vector for this virus (the Culex pipiens mosquito) is widely dispersed throughout the eastern part of the country. It is unclear how serious West Nile fever will turn out to be in the United States; however, it is clearly a new infectious diseases problem that must be dealt with, and it illustrates the constant threat of reemergence of old diseases in new epidemiological settings.
No discussion of the threat of reemerging infectious diseases in the 21st century would be complete without mention of the threat of yet another catastrophic influenza A epidemic. In an average year, influenza A is responsible for ∼20,000 excess deaths in the United States [ 14 ]. During the influenza A pandemic of 1918, there were at least 20 million deaths worldwide and >500,000 deaths in the United States. In 1957, the second most deadly influenza A epidemic occurred, accounting for ∼70,000 deaths in the United States. In 1968, the third most important influenza epidemic occurred, accounting for ∼35,000–40,000 deaths. Thus, serious influenza epidemics occur about every 20–40 years. The appearance of bird-to-human transmission of H5N1 influenza A virus in Hong Kong in the winter of 1997–1998 [ 15 ] was a cogent reminder of the ever-present threat of a new strain of influenza A virus entering a population that is relatively naïve for the microbe in question. Most public heath experts agree that it is only a matter of time before another catastrophic influenza epidemic occurs, and it certainly will occur in the 21st century.
Antimicrobial resistance . The development of resistance of microbes to antimicrobial drugs has been a problem in medicine since the use of the very first antimicrobial agents. Unfortunately, this problem has worsened, in part because of the widespread and often inappropriate use of antimicrobials [ 16 ]. In this first decade of the 21st century, we are faced with this continuing threat on a wider scale than ever before, with the emergence of resistant strains of a number of important microbes, including pneumococci, enterococci, staphylococci, Plasmodium falciparum, and Mycobacterium tuberculosis . Furthermore, despite the extraordinary success of antiretroviral drugs in the treatment of HIV/AIDS, the development of viral resistance is a major problem in the management of HIV-infected persons. Strategies to contain antimicrobial resistance in these early years of the 21st century should include heightened surveillance; appropriate infection control programs, particularly in hospitals; promotion of the rational use of antimicrobials; and accelerated basic and applied research in the areas of microbial pathogenesis, improved diagnostics, and vaccine and drug development. The recent sequencing of the genomes of important pathogens (see below, “The pathogens”) will provide novel opportunities to delineate more precisely the genetic basis for resistance, as has been accomplished with P. falciparum and chloroquine resistance [ 17 ]. Such information will greatly facilitate the development of alternative therapies against resistant strains of microbes.
During the second half of the 20th century, a number of chronic diseases not thought to be associated with microbial infections were shown to be directly caused by or indirectly resulting from infectious microbes [ 18–20 ]. Table 2 provides a partial list of chronic diseases whose etiologies have proven to be infectious. Perhaps the most dramatic example has been the recent proof that Helicobacter pylori is directly responsible for most peptic ulcer disease as well as gastric carcinoma. Also of considerable interest and importance is the relationship between hepatitis B and/or C virus and hepatocellular carcinoma, as well as the strong association of certain strains of human papillomavirus with cervical, vulvar, and anal carcinoma. These associations have potentially important implications for the use of vaccination to prevent microbe-associated cancers. In this regard, the successful use of hepatitis B vaccine has already resulted in a decrease in the incidence of hepatic cancers in certain populations [ 21 ]. Indeed, the association of infectious diseases with cancer is striking; it is estimated that ∼16% of all cancers are directly or indirectly associated with a microbial agent ( figure 2 ) [ 22 ].
Examples of chronic diseases that have infectious etiologies.
Infectious causes of cancer, based on data from [ 22 ]. EBV, Epstein-Barr virus; HHV, human herpesvirus; HTLV, human T lymphotropic virus.
A bioterrorism attack against the civilian population in the United States is inevitable in the 21st century [ 23 , 24 ]. The only question is which agent(s) will be used and under what circumstances will the attack(s) occur.
The threat of bioterrorism underscores the importance of pathogen genome sequencing projects, because rapid diagnostics will be critical to an adequate response to an attack. The availability of genomic sequences of microbes likely to be used in a bioterrorism attack will allow for the development of gene chips for sensitive, rapid, and accurate diagnosis [ 24 , 25 ]. In addition, it is likely that microbes used for bioterrorism will be genetically modified for antimicrobial resistance. Understanding the genetic basis of resistance will greatly facilitate the development of alternative antimicrobials. Depending on the microorganism used in the bioterrorism attack, vaccines may be effective in protecting substantial numbers of the population after initiation of the attack, as would be the case with an agent such as smallpox. Hence, the development of new and improved vaccines against smallpox and similar agents, as well as the stockpiling of antimicrobials against such agents, will be important components of the effort against bioterrorism in the coming decades.
Critical to our ability to meet the challenges of infectious diseases in the 21st century is the continual and rapid evolution of the scientific and technological advances that serve as the foundation for the response of the public health enterprise to established, emerging, and reemerging diseases ( table 3 ) [ 26 ]. For the discipline of infectious diseases, the application of functional genomics and proteomics will be a critical component of this science base and will draw from the sequencing not only of the human genome but also of a wide array of microbial pathogens. The areas of synthetic chemistry and robotics will greatly facilitate drug design and high-throughput screening of potential antimicrobial candidates. Computer and mathematical modeling likewise will prove useful in drug design and will also provide predictive models of microbial transmission. The field of molecular epidemiology will allow more precise delineation of microbial transmission and virulence patterns. Genetic epidemiology will lead to greater insights into host susceptibility at the individual and population levels. Finally, the rapidly advancing field of information technology will have a great impact on the field of infectious diseases in the 21st century, because rapid access and exchange of information among developed and developing nations will be critical to the overall success of any global health program.
Science base for infectious diseases research in 21st century.
The pathogens . Although we have entered the 21st century armed with an ever-expanding array of technological advances to meet the current and future challenges of microbial pathogens, the microbial world is extraordinarily diverse and possesses an adaptive capacity that in many respects matches our technological capabilities [ 5–8 , 27–29 ]. Microbes are an important part of the external and internal environment of the human species. Indeed, microbial species constitute ∼60% of the Earth's biomass, but <0.5% of the estimated 2–3 billion microbial species have been identified [ 27–29 ]. Microbes preceded animals and plants on Earth by >3 billion years, and although only a minute fraction of all microbial species are real or potential pathogens for the human host, these pathogens continue to emerge and reemerge.
One of the most important recent technological advances in infectious diseases research has been the ability to rapidly sequence the entire genome of microbial pathogens [ 29 ]. This capability will be a critical component of 21st century strategies for the development of diagnostics, therapeutics, and vaccines against currently recognized as well as emerging pathogens. Indeed, the microbial genome sequencing project will likely have as great an impact on the field of infectious diseases as the human genome project will on the entire field of medicine, including infectious diseases.
The first sequence of a human pathogen was obtained for Haemophilus influenzae in 1995 [ 30 ]. Subsequently, the pace of microbial genome sequencing has been extraordinary. As of January 2001, the sequencing of ∼50 microbial genomes had been completed [ 31 ]. It is projected that within 2–4 years, the complete sequencing of an additional 100 microbial species will be available. Table 4 provides a partial list of some of the important human pathogenic microbial species for which genomic sequences have been published. The ability to sequence and perform sequence analysis rapidly on microbial species has resulted from the development and application of novel sequencing and computational techniques. The bold and successful application of the whole-genome “shotgun” sequencing technique used to determine the complete genome sequence of H. influenzae has revolutionized the field of genome sequencing ( figure 3 ) [ 29 ].
Examples of important human pathogens for which complete genomic sequences have been published.
Steps in a whole-genome sequencing project. A “shotgun” sequencing strategy for whole-genome analysis is based on construction of a random cloned DNA library from the microbe in question, followed by sequencing of DNA clones, followed by the assembly of sequences, closing of gaps, editing of sequences, and finally annotation or assignment of function. Adapted from [ 29 ] (with permission).
The real and potential advantages of a microbial genomics approach to diagnostics, therapeutics, and vaccines are already being realized despite the fact that only ∼50% of the genes of already sequenced microbes have tentatively assigned functions [ 29 ]. When the functions of the remaining 50% of genes of these microbes become known, it is likely that some proportion of these will provide medically applicable insights. Determination of the function of these genes should assume a high priority in the post-sequencing, functional genomics era of the first decade of the 21st century.
The host: the human genome project and infectious diseases . The discipline of infectious diseases is centered around the study of the microbes, the host, or the interaction between the two. The completion of a working draft of the sequence of the entire human genome [ 32 , 33 ] and the subsequent assignment of function to the 30,000–40,000 human genes, which is projected to occur over a period of several years, will have an enormous impact on the entire field of medicine [ 34 ]. This will clearly be the case in the discipline of infectious diseases, as well as that of immunology, a large component of which represents the host response to invading microbes. The ability to examine across the entire human genome the expression of the full menu of host factors involved in the response to a microbial pathogen will provide unprecedented opportunities to understand disease pathogenesis. The cascade of gene expressions involved in the response of the innate immune system and the adaptive immune system [ 35 ] to an invading microbe will clarify the important relationship between these two essential components of host defenses. The feasibility of identifying and assigning function to the entire array of soluble factors (cytokines) and their receptors, together with the relevant signal transduction pathways associated with the host response to pathogens, will truly revolutionize the field of host defense mechanisms.
Before the availability of the sequence of the human genome and the continuing assignment of specific functions to all genes, the recognition of the association of identifiable phenotypes with genetic polymorphisms was often a chance event and was relatively restricted in its scope. In the future, the study of gene polymorphisms and their role in host-microbe interactions will assume a new dimension in the era of human genomics. Polymorphisms are variations in DNA sequence, and most are single-nucleotide polymorphisms [ 36 ]. Certainly, only a small fraction of single-nucleotide polymorphisms might be relevant to host defenses; however, this small degree of difference would still play a potential role in the susceptibility to certain infectious agents at the individual and population levels. In addition, genetic polymorphisms will be identified that determine responses to certain drugs, including antibiotics [ 36 ]. The availability of gene chips or microarrays will enable us to scan the entire human genome for relevant polymorphisms.
The availability of sequences of the entire genomes of non-human species that have a considerable degree of homology with humans will greatly facilitate the task of assigning function to the human genes as they are identified. Species such as the mouse, rat, zebrafish, Caenorhabditis elegans, Drosophila melanogaster, and Saccharomyces cerevisiae, among others, whose genomes have and will be sequenced will serve as invaluable tools for experimentation on the function of a wide array of genes [ 37 , 38 ]. Among these will surely be a variety of genes whose expression is directly or indirectly involved in host defense mechanisms against pathogenic microbes. Thus, the era of genomics will affect the study of infectious diseases from a number of standpoints, including the availability of the genomic sequences of the microbes in question, the human host species, and a variety of animal species that will serve as models for experimentation and delineation of pathogenic processes associated with infection by microbial pathogens.
The impact of vaccinology on the public health in the 20th century has been enormous. Without question, vaccines have been our most powerful tools for preventing disease, disability, and death and controlling health care costs [ 39–42 ]. The evolution of the field of vaccinology has been driven by the development of enabling technologies, such as detoxification methodologies, the use of a variety of tissue culture systems to propagate microbes, and the new biotechnology of the last quarter of the 20th century, particularly that of recombinant DNA. The use of the currently available and future technologies in the 21st century promises to provide a renaissance in an already vital field. As mentioned above, the availability of the annotated sequences of the entire genomes of virtually all of the microbial pathogens will allow for the identification of a wide array of new antigens for vaccine targets. In the 21st century, vaccines derived from microbial genome-based expression of candidate antigens will be widely used. In addition to the traditional live attenuated and whole killed vaccines, concepts that are currently being actively pursued are recombinant proteins, conjugated vaccines, pseudovirions, replicons, vectored vaccines, “naked” DNA vaccines, microencapsulated vaccines, and edible vaccines [ 43 ].
One of the important challenges for the 21st century is the development of safe and effective vaccines for the 3 greatest microbial killers worldwide: HIV/AIDS, malaria, and tuberculosis. These 3 diseases account for one-third to one-half of healthy years lost in less developed countries [ 3 ]. They have become the target of a proposed Millennium Vaccine Initiative [ 44 ] and were addressed in the communiqué from a summit of 8 major industrialized nations (G8) held in Okinawa in July 2000, which stated the goal of substantially reducing the burden of these 3 diseases by the year 2010 [ 45 ] (see below).
Despite the enormous successes of vaccines in decreasing the burden of morbidity and mortality caused by a variety of pathogens worldwide, continual frustration has resulted from the fact there are still millions of deaths from vaccine-preventable diseases worldwide ( table 5 ) [ 46 ]. This is largely caused by the failure to implement vaccine delivery programs in a number of developing countries. As advanced technologies allow for the development of new vaccines against microbes for which no vaccines currently exist and improved vaccines against microbes for which a vaccine currently does exist, it is imperative that a vigorous effort is mounted to assure the delivery of such vaccines for the populations at risk.
Global mortality from major vaccine-preventable diseases.
Global health has long been a subject of intense interest and an area of commitment for a relatively small proportion of the biomedical research and public health communities in the United States. Over the past decade, this interest has become more universal and will become even more intensified in the 21st century. Although humanitarian concerns alone should have spurred such an interest, it was other factors that precipitated an acceleration of involvement in global health issues. The globalization of our economy has led to an unprecedented dependence on the economic and political stability of our trading partners [ 47 , 48 ]. The economic and political stability of a nation is heavily influenced by the general health of that nation. The AIDS epidemic in less developed countries, particularly in sub-Saharan Africa, is a cogent example of this tenet; the same can be said for countries with a high prevalence of endemic malaria, tuberculosis, diarrheal diseases, and a wide range of parasitic diseases [ 47 , 48 ].
The globalization of health problems and their relevance to the United States have been brought emphatically to the attention of the American public with the HIV/AIDS epidemic. Although first recognized in the United States, HIV/AIDS is now predominantly a disease of developing countries [ 9 ]. The scientific and public health response to HIV/AIDS in the United Sates, to which I will refer as “the AIDS model,” provides important scientific and policy lessons that should be considered in our approach to other diseases of high global health impact.
The AIDS model . There have been >750,000 reported cases of AIDS in the United States and >430,000 deaths [ 49 ]. Despite dramatic decreases in the infection rate, the number of new infections has plateaued at an unacceptably high level of 40,000 per year since the early 1990s [ 50 ]. Nonetheless, the importance and speed of research advances that have been made since the disease was first recognized in the summer of 1981 have been breathtaking and unprecedented [ 51 ]. Within 3 years of recognition of this new disease, the etiologic agent was identified and causality proven. A simple and accurate diagnostic test was available for screening blood donors and populations in general. Pathogenic mechanisms of HIV disease have been extensively delineated. There are currently 17 antiretroviral drugs available for the treatment of HIV disease, and these together with earlier and better treatment and prophylaxis of opportunistic diseases has led to a striking decrease in the AIDS-related death rate over the past 5 years [ 52 , 53 ] ( figure 4 ). Many of these drugs were approved by the US Food and Drug Administration with unprecedented speed. Furthermore, a number of vaccine candidates are in various stages of clinical trials [ 54 ]. Government and private organizations mobilized quickly and effectively for the care of HIV-infected persons. Education and behavioral modification efforts have contributed to considerable progress in the prevention of HIV infection, although continued and heightened vigilance is essential, because the successes with therapy have led to an unfortunate increase in risky behavior among certain groups, such as young men who have sex with men [ 55 ].
Death rates from leading causes of death in persons aged 25–44 years, United States, 1983–1998 [ 53 ]
These striking advances would not have occurred without the extraordinary investment in resources for biomedical research at the National Institutes of Health ( figure 5 ). In addition, major investments have been made in the public health arenas of education, behavioral modification, prevention measures, and care of HIV-infected persons. In fiscal year 2000, US Department of Health and Human Services funding for AIDS research and services exceeded $8.5 billion [ 56 ]. These investments were made possible only by the consistent bipartisan commitment of several administrations and congresses to support such endeavors. The paradigm was highly successful: a major domestic public health problem was met with a major investment of public resources, and the results in the United States and other industrialized nations were striking. However, in the last few years of the 20th century, it became apparent that the toll in suffering and death from HIV/AIDS in developing nations was enormous and dwarfed that in the United States. HIV/AIDS had evolved into a true global health catastrophe. Furthermore, the global impact of AIDS began to call greater attention to the fact that other diseases, such as malaria and tuberculosis ( table 6 ), had been having a similar impact in developing nations for centuries. Indeed, in certain countries in sub-Saharan Africa, the “big three” of HIV/AIDS, malaria, and tuberculosis account for ⩾50% of all deaths [ 3 ]. Compared with HIV/AIDS, relatively few research and public health resources were committed to these latter diseases by the United States and other developed nations. The question arises whether we can accomplish in malaria and tuberculosis research what has been accomplished in AIDS research. Almost certainly an infusion of dollars into malaria and tuberculosis research, analogous to the “AIDS model,” would yield advances similar to those associated with HIV/AIDS research. Obviously, effective vaccines for all 3 of these diseases would be the ultimate accomplishment of a heightened research effort and would have an enormous impact on global health. However, implementation of such advances would be extremely problematic in many developing nations under the current economic conditions and with the lack of adequate health care infrastructure. In a different era, this would have been seen as an insurmountable problem, or at least someone else's problem. Today, however, global health problems, particularly those related to infectious diseases, are beginning to be perceived by political leaders in the United States and in other nations as a threat to destabilize the world [ 57 ].
Funding at National Institutes of Health for HIV/AIDS research. Est., estimated (Office of Financial Management, National Institutes of Health, personal communication).
Global burden of 3 diseases.
Global health as a foreign policy issue . For the first time in the history of the United States, global infectious diseases are being viewed in the context of foreign policy. In January 2000, HIV/AIDS was discussed by the Security Council of the United Nations [ 57 ], and in April 2000, the White House formally designated HIV/AIDS as a threat to the national security of the United States in that it could potentially contribute to the fall of foreign governments, touch off ethnic wars, and undo decades of work in building free-market democracies abroad [ 58 ]. As noted above, a Millennium Vaccine Initiative targeting HIV/AIDS, malaria, and tuberculosis for vaccine development and delivery has been proposed [ 44 ]. In addition, a number of legislative proposals have been put forth in the US Congress relating to varying forms of assistance in the development and delivery of vaccines and therapeutics that would benefit developing nations [ 57 ]. Other developed nations are also expressing renewed awareness of the implication of global health issues. At a meeting of the G8 nations in Okinawa in July 2000, a communiqué was issued stating that “infectious and parasitic diseases, most notably HIV/AIDS, tuberculosis, and malaria, as well as childhood diseases and common infections, threaten to reverse decades of development and to rob an entire generation of hope for a better future.” It also established goals to reduce the number of infections and deaths caused by HIV/AIDS, malaria, and tuberculosis by 25%–50% by the year 2010 [ 45 ]. Philanthropic organizations are investing billions of dollars to assist developing countries in the promotion of health [ 59 ].
It is noteworthy that the area of science that contributed most obviously to foreign policy in the 20th century was the physical sciences related to nuclear weapons, the cold war, and the race for space exploration [ 60 ]. It appears that the growing forces of globalization together with the fact that the health of nations is critical for economic and political stability will lead to an increasing appreciation in the 21st century of the role of biological sciences and global health, particularly with regard to infectious diseases, in the development and execution of foreign policy.
The 21st century will see an ever-increasing emphasis on infectious diseases, both because of the certainty that emerging and reemerging diseases will continue to challenge us and because globalization has led to an increased awareness of and commitment to addressing the terrible burden of infectious diseases in developing nations. Indeed, global health with an emphasis on infectious diseases is gradually assuming an important role in the foreign policy agenda of the United States and other developed nations. Clearly, the anxiety that I felt in 1968 as I traveled to the NIH for my infectious diseases fellowship because of the proclamation by the then-Surgeon General of the United States, that infectious diseases were no longer a problem, has been replaced by a realization of the enormity of the infectious diseases challenges that lie ahead in the 21st century and beyond.
I thank Gregory Folkers for helpful discussions and for invaluable assistance in collecting materials.
Google Scholar
Google Preview
Author notes
- communicable diseases
- developing countries
- world health
Email alerts
More on this topic, related articles in pubmed, citing articles via, looking for your next opportunity.
- Recommend to your Library
Affiliations
- Online ISSN 1537-6591
- Print ISSN 1058-4838
- Copyright © 2024 Infectious Diseases Society of America
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

- Chronicle Conversations
- Article archives
- Issue archives

Global Health: Priority Agenda for the 21st Century
About the author, haile t. debas.
At the core of the United Nations Millennium Declaration of 2000 are the Millennium Development Goals (MDGs) for 2015, which recognize that global health is a priority agenda for the twenty-first century. Achieving the MDGs is essential for world peace and economic stability, and for addressing the critical issues of human rights, equality, and equity. Never in human history have people of different national and geographic origins been as interdependent as in the twenty-first century. Globalization and the degree and speed of human mobility have created circumstances under which the health concerns of poor countries are de facto concerns of rich countries. These considerations, and others to be discussed below, emphasize the centrality of the MDGs in an interdependent world. Global health and the global economy are intricately linked. In its 1995 report, the Commission of Global Governance stated: "As economies become more interdependent, it is not only the opportunity for wealth creation that is multiplied, but also the opportunity for destabilizing shocks to be transmitted from one country to another." Pandemics are a perfect example of such "destabilizing shocks". The Severe Acute Respiratory Syndrome epidemic of 2003 brought the vibrant Hong Kong economy rapidly to its knees, reducing consumption of goods, tourism, and air travel.1 It is expected that an avian influenza pandemic would cause much worse economic and social dislocation worldwide, with a potential impact of $2 trillion to $3 trillion on the world economy and the loss of tens of millions of lives.2 But the linkage between global health and the global economy goes beyond the effect of pandemics. The global market economy is increasingly dependent on a healthy, productive global workforce, especially since the thirty member nations of the Organisation for Economic Co-operation and Development move much of their manufacturing and service industries to low- and middle-income countries. Even as we strive to achieve the MDGs by 2015, the heightened attention and greater public and private investment in global health in recent years is paying dividends. As documented by the Living Proof Project of the Bill and Melinda Gates Foundation, child mortality decreased by 27 per cent between 1990 and 2007.3, 4 Despite earlier gloomy assumptions, maternal mortality has dropped by 35 per cent over the past twenty-eight years -- an encouraging progress towards achieving MDG 55 on improving maternal health. The immunization programme of the Global Alliance for Vaccines and Immunisation is credited with preventing an estimated 3.4 million deaths in the past decade.6 The United States President's Emergency Plan for AIDS Relief is estimated to have saved 1.2 million lives.7 By 2008, about 3 million people were receiving anti-retroviral drugs.8 Similarly, thanks to the combined efforts of the Global Fund and the US President's Malaria Initiative, malaria prevention and treatment services have been significantly expanded. Since 2000, reported malaria cases and/or deaths have declined by at least half in twenty-five countries around the world.9 This is all good news -- and there is more of it. Nevertheless, global health faces several great challenges. Most sub-Saharan countries will not achieve the MDGs. One important reason for this is the lack of functional health systems due to a shortage in the health workforce, management incompetence, inadequate infrastructure, and health care financing. The World Health Report 2006 estimates a global deficit of 2.3 million doctors, nurses, and midwives. Critical health workforce shortages exist in fifty-seven countries, of which thirty-seven are in sub-Saharan Africa. It is hard to see how these countries can possibly achieve those MDGs relating to health. Emphasis on vertical or disease-specific programmes such as HIV/AIDS, malaria, and tuberculosis may have further weakened the already fractured health systems, thus making delivery of general health care in low-income countries that much more difficult. Unfortunately, neither the governments of these countries nor the global donor community have invested adequately in capacity building. There are more challenges facing global health. Prominent among these are the development of microbial resistance to antibiotics and disinfectants, along with the prevalence, in epidemic proportions, of non-communicable diseases and injuries in low- and middle-income countries. Tackling these challenges is also a priority agenda for global health in the twenty-first century. Several important questions beg for answers: Is the generous aid given by the donor community to poor countries optimally utilized? How do we balance investment in technological solutions with those in capacity building? Have we adequately engaged all the available talent pool to solve the complex problems in global health? In response to the last question, I believe the expertise of academic institutions in both poor and rich countries has been inadequately tapped. Effective collaborations among governments, non-governmental agencies, and academia will be key to addressing the health workforce crisis and to training the leadership that health care requires. An important global health priority agenda for the twenty-first century is achieving the MDGs. Unfortunately, many of the low-income countries are unlikely to achieve these goals, primarily because of critical shortages of health workers and weak health care systems. Beyond the achievement of the MDGs, other priority agenda items are developing effective vaccines and drugs for HIV/AIDS, malaria, tuberculosis, and other infectious diseases, addressing microbial resistance, and preparing a worldwide coordinated response to inevitable pandemics. A balanced funding strategy for vaccine and drug discovery on the one hand, and capacity building on the other, will determine how well and how fast we will achieve the MDGs and address the other global health priorities for the twenty-first century.
1 A.K.F. Siu, Y.C.R. Wong, "Economic Impact of SARS: The Case of Hong Kong", Asian Economic Papers 3:1, MIT Press, (2004): pp.62-83. 2 M.T. Osterholm, "Preparing for the next pandemic". N Engl J Med. (2005) May 5;352(18): 1839-42 3 United Nations Population Division: http://esa.un.org/unpp/ 4 D. You, T. Wardlaw, P. Salama, G. Jones, "Levels and trends in under-5 mortality, 1990 -- 2008". The Lancet, Published online September 10, 2009, DOI:10.1016/S0140-6736(09)61601-9 5 M. C Hogan, K. J Foreman, M. Naghavi, S. Y. Ahn, M. Wang, S. M. Makela, A. D. Lopez, R. Lozano, C. J. L. Murray, "Maternal mortality for 181 countries, 1980-2008: a systematic analysis of progress towards Millennium Development Goal 5", The Lancet, Early Online Publication, April 12, 2010,DOI:10.1016/S0140-6736(10)60518-1 6 GAVI Alliance Global Results: http://www.gavialliance.org/performance/global_results/index.php 7 E. Bendavid, J. Bhattacharya, "The President's Emergency Plan for AIDS Relief in Africa: An Evaluation of Outcomes", Annals of Internal Medicine, May 19 (2009), vol. 150 no. 10 688-695 8 Celebrating Life: The U.S. President's Emergency Plan for AIDS Relief 2009 Annual Report to Congress. http://www.pepfar.gov/documents/organization/113827.pdf 9 WHO, World Malaria Report, September 2008: http://whqlibdoc.who.int/publications/2008/9789241563697_eng.pdf
The UN Chronicle is not an official record. It is privileged to host senior United Nations officials as well as distinguished contributors from outside the United Nations system whose views are not necessarily those of the United Nations. Similarly, the boundaries and names shown, and the designations used, in maps or articles do not necessarily imply endorsement or acceptance by the United Nations.

Thirty Years On, Leaders Need to Recommit to the International Conference on Population and Development Agenda
With the gains from the Cairo conference now in peril, the population and development framework is more relevant than ever. At the end of April 2024, countries will convene to review the progress made on the ICPD agenda during the annual session of the Commission on Population and Development.

The LDC Future Forum: Accelerating the Attainment of the Sustainable Development Goals in the Least Developed Countries
The desired outcome of the LDC Future Forums is the dissemination of practical and evidence-based case studies, solutions and policy recommendations for achieving sustainable development.

From Local Moments to Global Movement: Reparation Mechanisms and a Development Framework
For two centuries, emancipated Black people have been calling for reparations for the crimes committed against them.
Documents and publications
- Yearbook of the United Nations
- Basic Facts About the United Nations
- Journal of the United Nations
- Meetings Coverage and Press Releases
- United Nations Official Document System (ODS)
- Africa Renewal
Libraries and Archives
- Dag Hammarskjöld Library
- UN Audiovisual Library
- UN Archives and Records Management
- Audiovisual Library of International Law
- UN iLibrary
News and media
- UN News Centre
- UN Chronicle on Twitter
- UN Chronicle on Facebook
The UN at Work
- 17 Goals to Transform Our World
- Official observances
- United Nations Academic Impact (UNAI)
- Protecting Human Rights
- Maintaining International Peace and Security
- The Office of the Secretary-General’s Envoy on Youth
- United Nations Careers
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Perspective
- Open access
- Published: 15 November 2022
Medicine and health of 21st Century: Not just a high biotech-driven solution
- Mourad Assidi ORCID: orcid.org/0000-0003-2750-1764 1 , 2 ,
- Abdelbaset Buhmeida 1 &
- Bruce Budowle ORCID: orcid.org/0000-0003-4116-2930 3
npj Genomic Medicine volume 7 , Article number: 67 ( 2022 ) Cite this article
5703 Accesses
3 Citations
Metrics details
- Molecular medicine
- Quality of life
Many biotechnological innovations have shaped the contemporary healthcare system (CHS) with significant progress to treat or cure several acute conditions and diseases of known causes (particularly infectious, trauma). Some have been successful while others have created additional health care challenges. For example, a reliance on drugs has not been a panacea to meet the challenges related to multifactorial noncommunicable diseases (NCDs)—the main health burden of the 21st century. In contrast, the advent of omics-based and big data technologies has raised global hope to predict, treat, and/or cure NCDs, effectively fight even the current COVID-19 pandemic, and improve overall healthcare outcomes. Although this digital revolution has introduced extensive changes on all aspects of contemporary society, economy, firms, job market, and healthcare management, it is facing and will face several intrinsic and extrinsic challenges, impacting precision medicine implementation, costs, possible outcomes, and managing expectations. With all of biotechnology’s exciting promises, biological systems’ complexity, unfortunately, continues to be underestimated since it cannot readily be compartmentalized as an independent and segregated set of problems, and therefore is, in a number of situations, not readily mimicable by the current algorithm-building proficiency tools. Although the potential of biotechnology is motivating, we should not lose sight of approaches that may not seem as glamorous but can have large impacts on the healthcare of many and across disparate population groups. A balanced approach of “omics and big data” solution in CHS along with a large scale, simpler, and suitable strategies should be defined with expectations properly managed.
Similar content being viewed by others

Axes of a revolution: challenges and promises of big data in healthcare
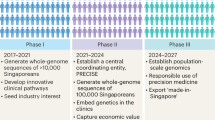
The Singapore National Precision Medicine Strategy

Strategic vision for improving human health at The Forefront of Genomics
Historical context of over-reliance on biotechnology-driven treatments.
The contemporary healthcare system (CHS) has been shaped by century-long innovations and discoveries made notably in the late 1800s and early 1900s 1 . To achieve the ultimate goal of allowing people to live longer and healthier, scientists and clinicians, among others, have made remarkable efforts to continuously enhance the CHS, which has improved the lives of nearly every person on the planet, although not necessarily equally (i.e., there are disparity issues that need to be addressed). While preventive healthcare is practiced by some, CHS is mainly a reactive approach strategy that often waits until the person becomes ill with acute symptoms to undertake a specific surgical intervention and/or a drug-based corrective action.
The “magic bullet” era
Drug therapy began centuries ago with the use of plant extracts and progressively evolved into the development of purified and targeted materials for a wide range of health-related applications, such as morphine (1803), anesthetics (1840s), antipyretics, and analgesics (1870s) in the 19th century. At the beginning of the 20th century, Ehrlich’s research laid the foundations for drug screening and discovery by bridging the gap between chemistry, biology, and medicine. His research discovered one of the first “magic bullets”—the antisyphilitic drug Arsphenamine. Other treatments for other diseases were subsequently discovered, including insulin, penicillin, and chemotherapy 2 , 3 . Pharmacological research expanded significantly to develop new cures and ameliorative approaches for various diseases with many noted successes. Consequently, the proportion of patents and newly-developed pharmaceutical products increased from 25% of all pharmacy remedies in the 1940s to nearly 90% at the end of 20th century 2 . Based on the realized health benefits of drug therapy, there has become an enormous reliance on drug prescriptions and unprecedented levels of use 4 . With the rapid economic development and enhanced living standards since the end of World War II, the use of drugs has steadily increased, boosted in part by the support of insurance and social security systems.
Through marketing and lobbying adopted by pharmaceutical companies to continuously expand their markets and benefits 5 , a major bias has taken root in the public and healthcare providers’ mindset and culture: treatment of disease primarily is achieved through prescription of drugs with a concomitant (and unfortunate) lower reliance on prevention and health promotion 6 , 7 . This reliance on drug therapies has made their use varied and commonplace 4 , although some treatments have become cost prohibitive for the majority of the population contributing to healthcare disparity. The pushing of drug therapy without an appreciation of the human factor has seen a concomitant increase in patients suffering medication (ab)use and/or iatrogenic effects. Many individuals over 65 years of age in the Western world take anywhere between 5 to more than 20 drugs per day 4 , 8 , 9 . Moreover, most of these drugs are palliative treatments; for example, in the USA, 9 out of 10 prescribed drugs are pain killers and symptom relievers 10 . This drug reliance strategy has been associated with unprecedented waste in annual global healthcare expenditures due to overspending, unnecessary prescriptions, mistakes, and corruption costing upwards of USD 300 billion (according to the European Healthcare Fraud and Corruption Network) 11 . The epidemic opioids crisis in the USA is an example of drug (ab)use due to the underestimation of the neurobiological harm and the potential addiction effects mainly on individuals/groups with particular social vulnerabilities 12 , 13 . This crisis is a heavy public health burden that begets severe health, socioeconomic and legal consequences 12 .
Other challenges of the “drug-only” solution
This “drug solution” problem, in turn, is exacerbated with new challenges related to availability, accessibility, affordability, safety and effectiveness 11 . Beyond the heavy financial burden of healthcare commodification and, more importantly, drug interactions and side effects—due to both polypharmacy and inappropriate prescriptions—have led to frailty, severe comorbidities, higher hospital admissions, and increased mortality 14 . Similar issues can be seen with other hopeful cures such as vaccine access to immunize the population suffering from the current pandemic. While rather elegant biotechnology-based solutions have been undertaken to rapidly develop SARS-CoV-2 vaccines (experiencing the fastest development of an approved vaccine(s) in history), the roll out and access to the vaccine to all population groups, as well as willingness by some to receive it, has been far more challenging 15 , 16 , 17 . One would have thought that the logistics for dissemination could have been planned better 18 , 19 . Innovation and cost of vaccine purchase were not impediments but instead, a more basic distribution strategy(ies) and information dissemination should have been implemented. A well-planned distribution strategy reduces the virus reservoir, impacts the greater population, and reduces health disparities.
Despite the considerable budget allocated to drug discovery, pharmacogenomics, and high biotechnology, these fields have substantial bottlenecks in CHS, as they have high rates of failure. These failures were in part due to instrumentation, methods, statistics, computational power, machine learning, etc. that were not able to accommodate, organize, and process the information needed to provide more precise solutions. In the USA, 90% of new drug applications to the FDA are rejected because of a lack of efficacy and/or toxicity 20 . Moreover, among the most prescribed drugs in the USA, the most successful one was reported to be effective in only 25% of patients 21 . This “imprecision medicine” is mostly due to the complexity of human biology systems, inappropriate or limited settings during, for example, the drug development process, and/or the inability of a specific drug to fix multi-level molecular perturbations. Omics solutions will help in predicting those patients in which a positive effect will occur and which patients who will have no effect or adverse reactions to the treatment. Because one can foresee drug development will be targeted to only those individuals with a positive effect, the cost will continue to rise, and likely health disparity will be further exacerbated.
Advancements in biotechnology to improve human health
The promise of omics and big data sciences.
At the beginning of the 21st century, the completion of the human genome project (HGP) provided a blueprint map towards precision medicine (PM) with a promise to improve quality of life. The first deciphered blueprint in itself had little impact. However, the HGP fostered biotechnology innovation and advances in bioinformatics, such as exquisite massively parallel sequencing technologies turning the herculean effort of sequencing an entire human genome into a reasonable cost and trivial exercise today. Boosted by digital analytics, the HGP has metamorphosed the way life science research is conceived and applied. Subsequently, several new disciplines have emerged, such as biobanking, bioinformatics, comparative genomics, pharmacogenomics, clinical genomics, and projects such as the human proteome project, the human microbiome project, the cancer genome atlas project, and the illuminating druggable genome program, to name a few. Furthermore, the emergence of the digital revolution has been progressively introducing extensive changes on all aspects of contemporary society, economy, firms, and job market 22 . This huge impact has also encompassed the way science and research are conducted in every discipline 23 . In medicine, mega sets of sequence and metagenomic data, super-libraries of medical images, and complex drug databases are generated on a massive scale. These huge data sets are clear illustrations of a new complex, automated and data-driven trend to gain insights about both the clinical profiles and molecular signatures in health and disease statuses 24 , 25 , 26 . Experts estimate that innovations, such as omics biotechnologies mainly integrative personal omics profile (iPOP) 27 , connected health systems, wireless wearable devices, blockchain technology, the Internet of Things (IoT), health tokens, artificial intelligence (AI), and machine learning (ML) are promising ways to address CHS’s challenges 28 , 29 , 30 (Table 1 ).
With the advent of these omics-based biotechnologies (e.g., genomics, transcriptomics, epigenomics, proteomics, and metabolomics) and big data science, a new wave of hope has spread over the scientific and clinical communities as well as the general public, in search of instant, individualized, and accurate theranostics 31 . There are and will be CHS improvements at both the individual and population levels in NCDs and infectious diseases. While omics undoubtedly will impact positively precision medicine 32 , it is important not to lose focus that individualized solutions that can be leveraged to affect population level challenges still will provide the greatest improvement in CHS. One of the main outcomes of deciphering cancer using omics technologies was targeted therapies. In fact, targeted anticancer therapy (TAT) is an expanding area that revolutionized cancer treatment modalities and significantly improved prognosis, treatment, and prediction of several malignancies 33 , 34 . Furthermore, TATs have played a major role in converting several cancers from fatal diseases to manageable chronic conditions 35 , 36 , 37 , 38 . However, these TATs-induced improvements were lacking enough specificity and effectiveness. The wide genomic instability and tumor heterogeneity marked by myriad possible multi-mutations precludes any hope for precision treatments 33 . Therefore, TATs were often combined with the other treatment modalities as surgery, chemo, radio, hormonal therapy, and even other targeted therapies. So far, the developed TATs were not able to overcome the toxicity, and cross-reactivity on nontarget tissues, relapse, and drug resistance 37 . Notably, only a small proportion of the population benefits from TATs at a higher cost. Therefore, it is obvious that a “magic bullet” solution for cancer treatment is still unreachable.
Noteworthy, of five health determinants (genome and biology, lifestyle choices, social circumstances, environment, and healthcare system), medical care’s contribution does not exceed 11% of each individual’s health 39 , 40 . This means that 89% of one’s health is impacted by determinants outside of the CHS realm. Thus, more emphasis on the remaining health determinants will substantially improve CHS’s performance. A tendency to marginalize prevention and health promotion—perhaps due to its unprofitability character or its lack of glamour or lack of insurance support—has impeded more focus on implementation of health quality pillars and adequate prevention strategies.
For instance, half of all deaths in the U.S. were due to behavioral causes 41 and therefore may be preventable. These health-related behaviors, which are only part of the problem, were mainly driven/influenced by social determinants as education, employment, and income 41 , 42 . Another illustration of the cost-effective and global impact of the health determinants outside the healthcare realm were the findings of McKeown who demonstrated that the sharp increases in life expectancy at the 19th century in the UK was mainly triggered by the improved living conditions, such as nutrition, sanitation, and potable water availability, decades ahead of the discovery of antibiotics, vaccines, and intensive care units 41 , 43 . Strikingly, more than 75% of healthcare spending in rich countries is dedicated to managing lifestyle-induced conditions. However, it is estimated that 80% of these NCDs are preventable by readily and cost-effective lifestyle choices improvements 44 . Taken together, these findings highlight that CHS effectiveness could not be enhanced by high-tech-driven inputs only but must consider the other health determinants as the foundation of any future reform.
Although better insights and resolution about diseases’ diagnoses and stratification, as well as healthcare management, can be observed given their descriptive character 45 , the digital revolution impact on precision therapeutics may not be realized readily, except for applications such as rapid vaccine development, robotic surgery, detection of unknown pathogens, disease monitoring and predicting adverse drug reactions to name a few. The new and unprecedented challenges are related to big data and biospecimens’ collection, storage, sharing, analysis, reliability, reproducibility, interpretation, governance, and bioethics that have emerged, with accompanying logistics requirements and considerations 46 , 47 , 48 , 49 . The PM concept at this post-genomic era—although inspirational—remains costly with limited success for population level impact at least in the short and medium term 50 . We are not advocating a reduced effort in this regard but managing expectations should become part of the strategy and more so not to lose sight of alternate not as “newsworthy” strategies that may have greater outreach to improving healthcare disparity and quality.
Biology: inconceivable complexity nevertheless user-friendly
Human biology is a multi-layered complexity of dynamic and interactive networks at the single-cell, multicellular, tissue, organ, system, organismal, environmental as well as social levels. In this context, NCDs are a series of perturbations of afore described complex networks that are deeply rooted in the biology, lifestyle choices, and the engineered/devised environment in which we live today. Given its appearance as user-friendly, biology complexity continues to be, unfortunately, underestimated. While the HGP and the ensuing development of omics solutions have lofty goals, the problem of molecular complexity has been underestimated, and deciphering the genotype-phenotype relationship continues to plague reaching the “magic bullet” goal 51 . For example, Singh and Gupta point out that the unanticipated necessary and unnecessary complexity of molecular machinery and systems in conjunction with evolutionary processes make it extremely difficult, currently, to apply PM effectively. An organism’s genetic redundancy and multiple molecular pathways are complex, related, and integrated and they also affect traits and thus complicate interpretation. It should not be surprising that individuals with similar risk factors for a disease may have different phenotypes 52 , 53 . Genetic backgrounds, gene interaction networks, environments, and histories impact PM making it “uncertain, chance-ridden, and probabilistic” 52 .
The scientific community should be aware that these biological systems could not be compartmentalized as independent and segregated problems in the digital and molecular realm, and therefore are very challenging to be mimicable by the current digital tools. Although impressive strides have been made with the advent of customized artificial intelligence (AI) and machine learning (ML) algorithms that analyze the complexity of these still poorly understood biological networks, they likely will not achieve the status of the “magic bullet” solution in the near future. There is a need for education and training of algorithm-building proficiency experts—a fundamental part of the roll out of advance technological solutions that has not been a major focus of national or global strategies. Perhaps computer science or better yet bioinformatics should become a requisite course in the secondary school system or at least part of an undergraduate curriculum for all students.
It is noticeable that the development of technology and data-driven applications is significantly faster than the progress of the scientific understanding of the complex interactions in biology (e.g., assessing differences between association and causality) and related fields. The realization of AI, ML and big data promises to deliver accurate clinical decisions and robust therapeutic predictions will require first overcoming the major intrinsic challenges related to their origin and cause such as the 4 Vs (volume, velocity, variety, and veracity) 49 , 54 , 55 . The combination of complexity and limitations of big data and omics-based sciences, confounded with health disparities, has revealed that what we dream of as “precision medicine” is still “imprecision medicine” 56 . Beyond these complexities that will be challenges for the foreseeable future is the impediment of the rapidly developing, rapidly changing technology and bioinformatics. These dynamic changes are welcomed because they bring bigger and better ways to identify and use diagnostic and prognostic bioindicators. However, the swift change that is occurring is an indication that the -omics biotechnologies are far from mature and obviously not stable. Technology will have to become somewhat standardized (or stabilized) to differentiate variation in assay performance and noise from -omics contributions and to be able to compare data effectively among the multitude of studies. Moreover, unstable biotechnologies are challenging to implement into operation-oriented diagnostic laboratories as it is costly to invest, requires ever changing quality assurance practices, can create a chaotic environment and the staff in such facilities are users, not innovators of new technologies and will not be able to adjust and troubleshoot as problems arise. While there no doubt will be successes in healthcare developed in the post-genomic era, the belief that “omics and big data” are poised to become routine parts of the HCS may be premature.
Population health and prevention: Simpler solutions matter
This high reliance on drugs has been a landmark that shaped the CHS. Unfortunately, this drug-only strategy was strongly applied to be the cure of multifactorial NCDs (e.g., cardiovascular diseases, cancer, chronic obstructive pulmonary diseases, diabetes, obesity, etc.), the current main global health burden. However, NCDs have complex causes. Their vectors are embedded in multi-generic effects as patients’ genetics (to include genetic imprinting), socio-economic environment, biology, and lifestyle choices 57 , 58 . Socio-economic vectors, a large and often under considered set of factors, for instance, encompass the complex interactions and disparities between economic growth, urbanization, aging, education, globalization, and the pervasiveness of unhealthy products on the market 59 , 60 , 61 . Given such inherent complexity, trying to develop drugs for NCDs using a reductionist approach likely will have limited positive results which at best will serve subcomponents of the population and may not have the global impact desired. The treatment concept for these diseases should move from a drug only strategy carapace to a more comprehensive approach of positive change/intervention in the individual/population socio-economic environment and lifestyle choices following a more holistic approach.
History is replete of simpler solutions with large impact (Fig. 1 ). For example, during the Crimean war in 1854 where there was a shortage of medicines’ supply, the famous British nurse Florence Nightingale significantly reduced the death rates of wounded soldiers from 42 to 2%, and prevented mass infections mainly through improving the hygiene through hand washing, proper ventilation, reducing crowdedness, and sewage evacuation 62 (Fig. 1 ). Also, and following three successive and unexplained tragic outbreaks of Cholera in London, the sewage system proposed by civil engineer Joseph Bazalgette in 1859, suggested by some historians as a “hero of London”, was able to stop the water-borne transmission of disease. The role of the implemented sewage system was to pump the effluent through several interconnecting pipes beyond the metropolitan city 63 , 64 . These examples, among others, clearly pinpoint that simpler and affordable measures outside the realm of HCS and advanced biotechnologies could have significant and sustainable impact on human quality of life, wellbeing, and sustainability.
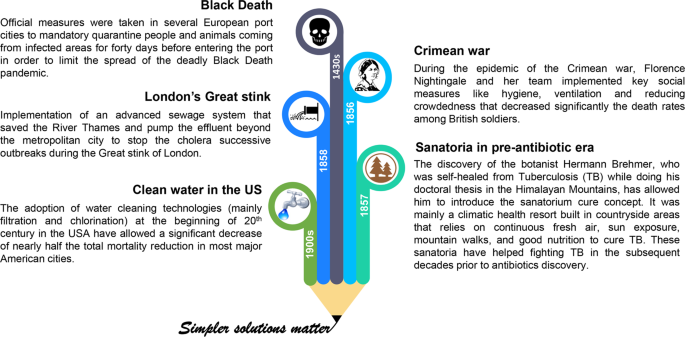
These measures included quarantine during Black Death epidemic 95 , hygiene and social distancing in the Crimean war 62 , the building of mountain sanatoria to cure TB 96 , 97 , 98 , the implementation of a sewage system to overcome London’s Great stink 63 , 64 , and the introduction of water filtration and chlorination systems/technologies to clean potable water in the USA 99 .
COVID-19 and Socio-Economic Disparities
Currently, for instance, the world is facing successive waves of the life-threatening COVID-19 pandemic. Sadly, this coronavirus has affected about a half billion people and killed over 6 million according to WHO 65 . Indeed, humanity is expressing a deep need for science to develop a “cure” with drugs/vaccines and the power of big data more than ever before to overcome this global health issue 32 . This public health crisis has been aggravated by concomitant economic, humanitarian crises, and notable social and health disparity effects 66 , 67 . Now more than two years since the declaration of this pandemic and despite unprecedented planetary networks/initiatives, dedicated mega scale budgets, the intensive use of big data in drug/vaccines development, and the waves of seemingly effective vaccine, the ready access to vaccines is still a struggle in many parts of the world 17 . As mentioned above government dissemination strategies faltered still leaving today large portions of the population to be immunized and some countries of the world lagging well behind others. A balanced strategy of high biotechnology solutions and those other areas that affect socio-economic determinants that impact healthcare of the general population would have been well-served to meet the challenge of combatting this pandemic. Given the rapid mutation rate of SARS-CoV-2, the slow and not well-planned dissemination strategy may contribute to extending the pandemic as opposed to being the hopeful cure to end it. In contrast to individual-level management of the COVID-19 pandemic, it is noteworthy that population-level interventions mainly those targeting the socio-economic determinants of health would have the most impactful and cost-effective outcomes on flattening the pandemic curve 41 , 68 . In the interim, governments and societies have immediately sought refuge in social and lifestyle choices to alleviate the burden of the pandemic and to flatten the uprising infection curves until herd immunity of some sort is reached, i.e., a population-based approach to alleviate the impact. Lockdown, isolation of confirmed cases, quarantine of suspected infected and/or contacted individuals, social distancing, and the simple practice of wearing masks have been among the most effective social measures. Indeed, surges have been related to relaxing of these practices. These actions, together with lifestyle commitments as facemask wearing, frequent hand washing, healthy diet, exercise, and adequate sleep are considered as key tools to reduce the virus’ spread and flatten the epidemiological curve (Fig. 2 ).

(1: quarantine/lockdown/curfew; 2: healthy and balanced diet; 3: adequate sleeping; 4: frequent hand washing; 5: cleaning and disinfection of both surfaces and the air; 6: regular domestic exercise; 7: facemask wearing; and 8: social distancing).
Despite big data and digital technologies’ intensive use during this global health crisis, they were quite helpful in the pandemic management (monitoring, surveillance, detection, prediction) and prevention measures 69 , 70 , 71 , 72 . Although some laudable initiatives have developed vaccines against SARS-CoV-2 73 , there is still speculation about their time frame, safety, and effectiveness of future remedies. It seems overly ambitious of the expectations (time frame, levels) for omics and big data to achieve their full potential in health and life sciences in general. Therefore, the current “omics and big data” solution in CHS, which undeniably offers potential benefits, should only be part of a larger and more comprehensive strategy. There needs to be more effort on holistic approaches that include health disparities, social determinants, and lifestyle choices to improve the quality of life. Social and economic systems should rethink cost/benefit analyses to determine the most effective ways to improve healthcare. While omics and digital technologies will have a substantial impact in healthcare and should be pursued, interventions, such as socio-economic determinants, that impact the greater population still will likely have more impact on CHS and must be part of our 21st century healthcare system.
Reporting Summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
No datasets were generated or analyzed during the current study.
Chew, M. & Sharrock, K. Medical Milestones: Celebrating Key Advances Since 1840 (British Medical Association, 2007).
Laporte, J., Baksaas, I. & Lunde, P. Drug Utilization Studies . Methods and Uses 5–22 (1993).
Strebhardt, K. & Ullrich, A. Paul Ehrlich’s magic bullet concept: 100 years of progress. Nat. Rev. Cancer 8 , 473–480 (2008).
Article CAS PubMed Google Scholar
Cullis, P. The Personalized Medicine Revolution: How Diagnosing and Treating Disease are About to Change Forever (Geystones Books LTD., 2015).
Dukes, M. N. G. & Organization, W. H. Drug Utilization Studies: Methods and Uses (World Health Organization. Regional Office for Europe, 1993).
Fani Marvasti, F. & Stafford, R. S. From sick care to health care–reengineering prevention into the U.S. system. N. Engl. J. Med. 367 , 889–891 (2012).
Article PubMed Google Scholar
Clark, J. Do the solutions for global health lie in healthcare? BMJ 349 , g5457 (2014).
Stuckler, D. et al. Comprehensive strategies to reduce the burden of chronic diseases. Management 2 , 1 (2011).
Google Scholar
Gu, Q. Prescription Drug Use Continues to Increase: US Prescription Drug Data for 2007 – 2008 (US Department of Health and Human Services, Centers for Disease Control and …, 2010).
Pizzorno, J. & Stephenson, S. Health care system and addressing the determinants of health. Integr. Med. 16 , 16–18 (2017).
WHO. Chapter 4: More health for the money. Report No. 9241564024, World Health Organization. Regional Office for Europe, WHO Regional Publications, European Series, 45. Retrieved on 20th July, 2020 at: https://www.who.int/whr/2010/en/ (2010).
Volkow, N. D. & Blanco, C. The changing opioid crisis: development, challenges, and opportunities. Mol. Psychiatry https://doi.org/10.1038/s41380-020-0661-4 (2020).
Perry, B. L., Pescosolido, B. A. & Krendl, A. C. The unique nature of public stigma toward non-medical prescription opioid use and dependence: A national study. Addiction https://doi.org/10.1111/add.15069 (2020).
Monaco, A. et al. Integrated care for the management of ageing-related non-communicable diseases: current gaps and future directions. Aging Clin. Exp. Res. 32 , 1353–1358 (2020).
Article PubMed PubMed Central Google Scholar
Jecker, N. S. Vaccine passports and health disparities: A perilous journey. J. Med. Ethics https://doi.org/10.1136/medethics-2021-107491 (2021).
Fitzpatrick, C. M. Social disparities in COVID-19 prevention. Nat. Rev. Cardiol. 18 , 542–542 (2021).
Article CAS PubMed PubMed Central Google Scholar
Nana-Sinkam, P. et al. Health disparities and equity in the era of COVID-19. J. Clin. Transl. Sci. 5 , e99 (2021).
Chowkwanyun, M. & Reed, A. L. Racial health disparities and Covid-19—Caution and context. N. Engl. J. Med. 383 , 201–203 (2020).
Duan, Y. et al. Disparities in COVID-19 vaccination among low-, middle-, and high-income countries: The mediating role of vaccination policy. Vaccines 9 , 905 (2021).
Feng, X. & Xie, H.-G. Applying Pharmacogenomics in Therapeutics (CRC Press, 2016).
Schork, N. J. Personalized medicine: time for one-person trials. Nature 520 , 609–611 (2015).
Makridakis, S. The forthcoming Artificial Intelligence (AI) revolution: Its impact on society and firms. Futures 90 , 46–60 (2017).
Article Google Scholar
Mayer-Schönberger, V. & Cukier, K. Big Data: A Revolution that Will Transform How We Live, Work, and Think (Houghton Mifflin Harcourt, 2013).
Filipp, F. V. Opportunities for artificial intelligence in advancing precision medicine. Curr. Genet. Med. Rep. 7 , 208–213 (2019).
Shilo, S., Rossman, H. & Segal, E. Axes of a revolution: Challenges and promises of big data in healthcare. Nat. Med. 26 , 29–38 (2020).
Yu, K.-H., Beam, A. L. & Kohane, I. S. Artificial intelligence in healthcare. Nat. Biomed. Eng. 2 , 719–731 (2018).
Stanford Medicine. Integrated Personal Omics Profiling https://med.stanford.edu/ipop.html (2022).
Rathbone, A. L. & Prescott, J. The use of mobile apps and SMS messaging as physical and mental health interventions: Systematic review. J. Med. Internet Res. 19 , e295 (2017).
Ahmad, S. S., Khan, S. & Kamal, M. A. What is blockchain technology and its significance in the current healthcare system? A brief insight. Curr. Pharm. Des. 25 , 1402–1408 (2019).
Cell Editorial Team. Embracing the landscape of therapeutics. Cell 181 , 1–3 (2020).
Field, D. et al. Megascience.‘Omics data sharing. Science 326 , 234–236 (2009).
Green, E. D. et al. Strategic vision for improving human health at The Forefront of Genomics. Nature 586 , 683–692 (2020).
Keefe, D. M. K. & Bateman, E. H. Potential successes and challenges of targeted cancer therapies. J. Natl Cancer Institute Monographs https://doi.org/10.1093/jncimonographs/lgz008 (2019).
Casali, P. G. Successes and limitations of targeted cancer therapy in gastrointestinal stromal tumors. Successes Limit. Target. Cancer Ther. 41 , 51–61 (2014).
Spaans, J. N. & Goss, G. D. Epidermal growth factor receptor tyrosine kinase inhibitors in early-stage nonsmall cell lung cancer. Curr. Opin. Oncol. 27 , 102–107 (2015).
Wen, Y. & Grandis, J. R. Emerging drugs for head and neck cancer. Expert Opin. Emerg. Drugs 20 , 313–329 (2015).
Arteaga, C. L. et al. Treatment of HER2-positive breast cancer: Current status and future perspectives. Nat. Rev. Clin. Oncol. 9 , 16–32 (2012).
Article CAS Google Scholar
Tang, J. et al. Trial watch: The clinical trial landscape for PD1/PDL1 immune checkpoint inhibitors. Nat. Rev. Drug Discov. 17 , 854–856 (2018).
Booske, B. C., Athens, J. K., Kindig, D. A., Park, H. & Remington, P. L. Different perspectives for assigning weights to determinants of health. University of Wisconsin: Population Health Institute , https://www.countyhealthrankings.org/sites/default/files/differentPerspectivesForAssigningWeightsToDeterminantsOfHealth.pdf (2010).
McGovern, L., Miller, G. & Hughes-Cromwick, P. The relative contribution of multiple determinants to health. Health Affairs Health Policy Briefs. Published August 21 , https://www.healthaffairs.org/do/10.1377/hpb20140821.404487/full/healthpolicybrief_123.pdf (2014).
Braveman, P. & Gottlieb, L. The social determinants of health: It’s time to consider the causes of the causes. Public Health Rep. 129 , 19–31 (2014).
Stringhini, S. et al. Association of socioeconomic position with health behaviors and mortality. JAMA: J. Am. Med. Assoc. 303 , 1159–1166 (2010).
McKeown, T., Record, R. & Turner, R. An interpretation of the decline of mortality in England and Wales during the twentieth century. Popul. Stud. 29 , 391–422 (1975).
Patwardhan, B., Mutalik, G. & Tillu, G. Integrative Approaches for Health (eds Patwardhan, B., Mutalik, G. & Tillu, G.) 53–78 (Academic Press, 2015).
Hodson, R. Digital health. Nature 573 , S97–S97 (2019).
Hey, S. P. & Kesselheim, A. S. Countering imprecision in precision medicine. Science 353 , 448 (2016).
Househ, M. S., Aldosari, B., Alanazi, A., Kushniruk, A. W. & Borycki, E. M. Big data, big problems: A healthcare perspective. Stud. Health Technol. Inform. 238 , 36–39 (2017).
PubMed Google Scholar
Seeman, N. Embrace data anonymity, not ‘digital consent’. Nature 573 , 34 (2019).
Feero, W. G. Bioinformatics, sequencing accuracy, and the credibility of clinical genomics. JAMA: J. Am. Med. Assoc. 324 , 1945–1947 (2020).
Prasad, V. Perspective: The precision-oncology illusion. Nature 537 , S63–S63 (2016).
Ritchie, M. D., Holzinger, E. R., Li, R., Pendergrass, S. A. & Kim, D. Methods of integrating data to uncover genotype–phenotype interactions. Nat. Rev. Genet. 16 , 85–97 (2015).
Singh, R. S. & Gupta, B. P. Genes and genomes and unnecessary complexity in precision medicine. NPJ Genom. Med. 5 , 1–9 (2020).
Singh, R. S. Decoding ‘unnecessary complexity’: A law of complexity and a concept of hidden variation behind “missing heritability” in precision medicine. J. Mol. Evolution 89 , 513–526 (2021).
L’Heureux, A., Grolinger, K., Elyamany, H. F. & Capretz, M. A. M. Machine learning with big data: Challenges and approaches. IEEE Access 5 , 7776–7797 (2017).
Ohlhorst, F. J. Big Data Analytics: Turning Big Data into Big Money Vol. 65 (John Wiley & Sons, 2012).
Hutchinson, L. & Romero, D. Precision or imprecision medicine? Nat. Rev. Clin. Oncol. 13 , 713–713 (2016).
Olsen, L., Saunders, R. S. & Yong, P. L. The Healthcare Imperative: Lowering Costs and Improving Outcomes: Workshop Series Summary (National Academies Press, 2010).
Hodges, K. & Jackson, J. Pandemics and the global environment. Sci. Adv. 6 , eabd1325 (2020).
Clark, J. Medicalization of global health 3: The medicalization of the non-communicable diseases agenda. Glob. Health Action 7 , 24002 (2014).
Allen, L. Are we facing a noncommunicable disease pandemic? J. Epidemiol. Glob. Health 7 , 5–9 (2017).
WHO, W. H. O. WHO Methods and Data Sources for Global Burden of Disease Estimates 2000–2015 . https://cdn.who.int/media/docs/default-source/gho-documents/global-health-estimates/ghe2019_daly-methods.pdf?sfvrsn=31b25009_7 (2017).
Nightingale, F. Notes on Hospitals (Longman, Green, Longman, Roberts, and Green, 1863).
Halliday, S. The great stink of London: Sir Joseph Bazalgette and the cleansing of the Victorian capital. Trans. Med. Soc. Lond. 124 , 137–138 (2007).
Porter, D. H. Review of The Great Stink of London: Sir Joseph Bazalgette and the Cleansing of the Victorian Metropolis. (Project MUSE). Victorian Studies 43 , 530–531 (2001).
WHO. WHO Coronavirus Disease (COVID-19) Dashboard https://covid19.who.int/ . Accessed on November 2020 (2020).
Miller, G. Social distancing prevents infections but it can have unintended consequences. Science . https://www.science.org/content/article/we-are-social-species-how-will-social-distancing-affect-us (2020).
Ahmad, K. et al. Association of poor housing conditions with COVID-19 incidence and mortality across US counties. PloS one 15 , e0241327 (2020).
Frieden, T. R. A framework for public health action: the health impact pyramid. Am. J. Public Health 100 , 590–595 (2010).
Ting, D. S. W., Carin, L., Dzau, V. & Wong, T. Y. Digital technology and COVID-19. Nat. Med. 26 , 459–461 (2020).
Keesara, S., Jonas, A. & Schulman, K. Covid-19 and Health Care’s Digital Revolution. N. Engl. J. Med. 382 , e82 (2020).
Riba, M., Sala, C., Toniolo, D. & Tonon, G. Big data in medicine, the present and hopefully the future. Front. Med. 6 , 263–263 (2019).
Dong, E., Du, H. & Gardner, L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 20 , 533–534 (2020).
Al-Kassmy, J., Pedersen, J. & Kobinger, G. Vaccine Candidates against Coronavirus Infections. Where Does COVID-19 Stand? Viruses https://doi.org/10.3390/v12080861 (2020).
Johnson, I. S. Human insulin from recombinant DNA technology. Science 219 , 632–637 (1983).
Khan, S. et al. Role of Recombinant DNA Technology to Improve Life. Int. J. Genomics 2016 , 2405954 (2016).
Singh, S. et al. Monoclonal antibodies: A review. Curr. Clin. Pharmacol. 13 , 85–99 (2018).
Breedveld, F. C. Therapeutic monoclonal antibodies. Lancet 355 , 735–740 (2000).
Agrawal, N. et al. RNA interference: Biology, mechanism, and applications. Microbiol. Mol. Biol. Rev. 67 , 657–685 (2003).
Sen, G. L. & Blau, H. M. A brief history of RNAi: the silence of the genes. FASEB J. 20 , 1293–1299 (2006).
Mello, C. C. & Conte, D. Revealing the world of RNA interference. Nature 431 , 338–342 (2004).
Collins, F. S., Green, E. D., Guttmacher, A. E. & Guyer, M. S. A vision for the future of genomics research. Nature 422 , 835–847 (2003).
Gibbs, R. A. The Human Genome Project changed everything. Nat. Rev. Genet. 21 , 575–576 (2020).
Green, E. D., Watson, J. D. & Collins, F. S. Human Genome Project: Twenty-five years of big biology. Nature 526 , 29–31 (2015).
Bentley, D. R. Whole-genome re-sequencing. Curr. Opin. Genet. Dev. 16 , 545–552 (2006).
von Bubnoff, A. Next-generation sequencing: The race is on. Cell 132 , 721–723 (2008).
Shendure, J. & Ji, H. Next-generation DNA sequencing. Nat. Biotechnol. 26 , 1135–1145 (2008).
Zhao, J. et al. Induced pluripotent stem cells: Origins, applications, and future perspectives. J. Zhejiang Univ. Science B 14 , 1059–1069 (2013).
Yamanaka, S. Pluripotent stem cell-based cell therapy-promise and challenges. Cell Stem Cell 27 , 523–531 (2020).
Beam, A. L. & Kohane, I. S. Big data and machine learning in health care. JAMA: J. Am. Med. Assoc. 319 , 1317–1318 (2018).
Panch, T., Szolovits, P. & Atun, R. Artificial intelligence, machine learning and health systems. J. Glob. Health 8 , 020303 (2018).
Russell, S. & Norvig, P. AI a modern approach. Learning 2 , 4 (2005).
Peter, S. et al. Artificial Intelligence and life in 2030: The one hundred year study on artificial intelligence. https://doi.org/APO-210721 (2016).
Jiang, F. & Doudna, J. A. CRISPR-Cas9 structures and mechanisms. Annu. Rev. Biophys. 46 , 505–529 (2017).
Doudna, J. A. & Charpentier, E. Genome editing. The new frontier of genome engineering with CRISPR-Cas9. Science 346 , 1258096 (2014).
Paliga, R. E. Quarantine as a tool of epidemic fight. Prz. Epidemiologiczny 74 , 180–195 (2020).
Frith, J. History of tuberculosis. Part 2-the sanatoria and the discoveries of the tubercle bacillus. J. Mil. Veterans Health 22 , 36–41 (2014).
McCarthy, O. R. The key to the sanatoria. J. R. Soc. Med. 94 , 413–417 (2001).
Daniel, T. M. Hermann Brehmer and the origins of tuberculosis sanatoria [Founders of our knowledge]. Int. J. Tuberculosis Lung Dis. 15 , 161–162 (2011).
CAS Google Scholar
Cutler, D. & Miller, G. The role of public health improvements in health advances: The twentieth-century United States. Demography 42 , 1–22 (2005).
Download references
Acknowledgements
This research work was funded by Institutional Fund Projects under grant no. (IFPIP: 498-117-1443). Therefore, the authors gratefully acknowledge technical and financial support from the Ministry of Education and King Abdulaziz University, Jeddah, Saudi Arabia.
Author information
Authors and affiliations.
Center of Excellence in Genomic Medicine Research, King Abdulaziz University, Jeddah, Saudi Arabia
Mourad Assidi & Abdelbaset Buhmeida
Medical Laboratory Department, Faculty of Applied Medical Sciences, King Abdulaziz University, Jeddah, Saudi Arabia
Mourad Assidi
Department of Forensic Medicine, University of Helsinki, Helsinki, Finland
Bruce Budowle
You can also search for this author in PubMed Google Scholar
Contributions
M.A., A.B., and B.B. conceived the concept of the paper, contributed equally to the content and writing of the paper, and are accountable for its content.
Corresponding author
Correspondence to Bruce Budowle .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Reporting summary checklist, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Assidi, M., Buhmeida, A. & Budowle, B. Medicine and health of 21st Century: Not just a high biotech-driven solution. npj Genom. Med. 7 , 67 (2022). https://doi.org/10.1038/s41525-022-00336-7
Download citation
Received : 31 May 2022
Accepted : 27 October 2022
Published : 15 November 2022
DOI : https://doi.org/10.1038/s41525-022-00336-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
You are using an outdated browser. Please upgrade your browser to improve your experience.

Health & Nursing
Courses and certificates.
- Bachelor's Degrees
- View all Business Bachelor's Degrees
- Business Management – B.S. Business Administration
- Healthcare Administration – B.S.
- Human Resource Management – B.S. Business Administration
- Information Technology Management – B.S. Business Administration
- Marketing – B.S. Business Administration
- Accounting – B.S. Business Administration
- Finance – B.S.
- Supply Chain and Operations Management – B.S.
- Accelerated Information Technology Bachelor's and Master's Degree (from the School of Technology)
- Health Information Management – B.S. (from the Leavitt School of Health)
Master's Degrees
- View all Business Master's Degrees
- Master of Business Administration (MBA)
- MBA Information Technology Management
- MBA Healthcare Management
- Management and Leadership – M.S.
- Accounting – M.S.
- Marketing – M.S.
- Human Resource Management – M.S.
- Master of Healthcare Administration (from the Leavitt School of Health)
- Data Analytics – M.S. (from the School of Technology)
- Information Technology Management – M.S. (from the School of Technology)
- Education Technology and Instructional Design – M.Ed. (from the School of Education)
Certificates
- View all Business Degrees
Bachelor's Preparing For Licensure
- View all Education Bachelor's Degrees
- Elementary Education – B.A.
- Special Education and Elementary Education (Dual Licensure) – B.A.
- Special Education (Mild-to-Moderate) – B.A.
- Mathematics Education (Middle Grades) – B.S.
- Mathematics Education (Secondary)– B.S.
- Science Education (Middle Grades) – B.S.
- Science Education (Secondary Chemistry) – B.S.
- Science Education (Secondary Physics) – B.S.
- Science Education (Secondary Biological Sciences) – B.S.
- Science Education (Secondary Earth Science)– B.S.
- View all Education Degrees
Bachelor of Arts in Education Degrees
- Educational Studies – B.A.
Master of Science in Education Degrees
- View all Education Master's Degrees
- Curriculum and Instruction – M.S.
- Educational Leadership – M.S.
- Education Technology and Instructional Design – M.Ed.
Master's Preparing for Licensure
- Teaching, Elementary Education – M.A.
- Teaching, English Education (Secondary) – M.A.
- Teaching, Mathematics Education (Middle Grades) – M.A.
- Teaching, Mathematics Education (Secondary) – M.A.
- Teaching, Science Education (Secondary) – M.A.
- Teaching, Special Education (K-12) – M.A.
Licensure Information
- State Teaching Licensure Information
Master's Degrees for Teachers
- Mathematics Education (K-6) – M.A.
- Mathematics Education (Middle Grade) – M.A.
- Mathematics Education (Secondary) – M.A.
- English Language Learning (PreK-12) – M.A.
- Endorsement Preparation Program, English Language Learning (PreK-12)
- Science Education (Middle Grades) – M.A.
- Science Education (Secondary Chemistry) – M.A.
- Science Education (Secondary Physics) – M.A.
- Science Education (Secondary Biological Sciences) – M.A.
- Science Education (Secondary Earth Science)– M.A.
- View all Technology Bachelor's Degrees
- Cloud Computing – B.S.
- Computer Science – B.S.
- Cybersecurity and Information Assurance – B.S.
- Data Analytics – B.S.
- Information Technology – B.S.
- Network Engineering and Security – B.S.
- Software Engineering – B.S.
- Accelerated Information Technology Bachelor's and Master's Degree
- Information Technology Management – B.S. Business Administration (from the School of Business)
- View all Technology Master's Degrees
- Cybersecurity and Information Assurance – M.S.
- Data Analytics – M.S.
- Information Technology Management – M.S.
- MBA Information Technology Management (from the School of Business)
- Full Stack Engineering
- Web Application Deployment and Support
- Front End Web Development
- Back End Web Development
3rd Party Certifications
- IT Certifications Included in WGU Degrees
- View all Technology Degrees
- View all Health & Nursing Bachelor's Degrees
- Nursing (RN-to-BSN online) – B.S.
- Nursing (Prelicensure) – B.S. (Available in select states)
- Health Information Management – B.S.
- Health and Human Services – B.S.
- Psychology – B.S.
- Health Science – B.S.
- Healthcare Administration – B.S. (from the School of Business)
- View all Nursing Post-Master's Certificates
- Nursing Education—Post-Master's Certificate
- Nursing Leadership and Management—Post-Master's Certificate
- Family Nurse Practitioner—Post-Master's Certificate
- Psychiatric Mental Health Nurse Practitioner —Post-Master's Certificate
- View all Health & Nursing Degrees
- View all Nursing & Health Master's Degrees
- Nursing – Education (BSN-to-MSN Program) – M.S.
- Nursing – Leadership and Management (BSN-to-MSN Program) – M.S.
- Nursing – Nursing Informatics (BSN-to-MSN Program) – M.S.
- Nursing – Family Nurse Practitioner (BSN-to-MSN Program) – M.S. (Available in select states)
- Nursing – Psychiatric Mental Health Nurse Practitioner (BSN-to-MSN Program) – M.S. (Available in select states)
- Nursing – Education (RN-to-MSN Program) – M.S.
- Nursing – Leadership and Management (RN-to-MSN Program) – M.S.
- Nursing – Nursing Informatics (RN-to-MSN Program) – M.S.
- Master of Healthcare Administration
- MBA Healthcare Management (from the School of Business)
- Business Leadership (with the School of Business)
- Supply Chain (with the School of Business)
- Back End Web Development (with the School of Technology)
- Front End Web Development (with the School of Technology)
- Web Application Deployment and Support (with the School of Technology)
- Full Stack Engineering (with the School of Technology)
- Single Courses
- Course Bundles
Apply for Admission
Admission requirements.
- New Students
- WGU Returning Graduates
- WGU Readmission
- Enrollment Checklist
- Accessibility
- Accommodation Request
- School of Education Admission Requirements
- School of Business Admission Requirements
- School of Technology Admission Requirements
- Leavitt School of Health Admission Requirements
Additional Requirements
- Computer Requirements
- No Standardized Testing
- Clinical and Student Teaching Information

Transferring
- FAQs about Transferring
- Transfer to WGU
- Transferrable Certifications
- Request WGU Transcripts
- International Transfer Credit
- Tuition and Fees
- Financial Aid
- Scholarships
Other Ways to Pay for School
- Tuition—School of Business
- Tuition—School of Education
- Tuition—School of Technology
- Tuition—Leavitt School of Health
- Your Financial Obligations
- Tuition Comparison
- Applying for Financial Aid
- State Grants
- Consumer Information Guide
- Responsible Borrowing Initiative
- Higher Education Relief Fund
FAFSA Support
- Net Price Calculator
- FAFSA Simplification
- See All Scholarships
- Military Scholarships
- State Scholarships
- Scholarship FAQs
Payment Options
- Payment Plans
- Corporate Reimbursement
- Current Student Hardship Assistance
- Military Tuition Assistance
WGU Experience
- How You'll Learn
- Scheduling/Assessments
- Accreditation
- Student Support/Faculty
- Military Students
- Part-Time Options
- Virtual Military Education Resource Center
- Student Outcomes
- Return on Investment
- Students and Gradutes
- Career Growth
- Student Resources
- Communities
- Testimonials
- Career Guides
- Skills Guides
- Online Degrees
- All Degrees
- Explore Your Options
Admissions & Transfers
- Admissions Overview
Tuition & Financial Aid
Student Success
- Prospective Students
- Current Students
- Military and Veterans
- Commencement
- Careers at WGU
- Advancement & Giving
- Partnering with WGU
21st Century Healthcare Challenges: Medical Trends
- See More Tags

The changes in our world are having a direct impact on the medical industry. The 21st century has the most advanced medical technology compared to any previous century, but it also has unique problems that make it necessary for healthcare to adapt.
From nursing shortages to changes in healthcare technology statistics , hospitals and clinics are working hard to be prepared for the changing needs in the medical community.
Qualified and trained healthcare leadership is crucial to ensuring that hospitals and clinics are able to keep up with changing needs for the industry. As more individuals become qualified to lead in the healthcare field, more minds will be at work to help tackle challenges and problems.
See what problems are facing 21st century healthcare, and what is currently being done to prepare and fight these issues.
Healthcare for an aging population.

By the year 2030, the number of people over 60 years of age will increase by 56 percent, from 900 million to 1.5 billion . In the United States alone, the number of Americans over the age of 65 is expected to double from roughly 50 million today to nearly 100 million by 2060.
What does this aging population mean for healthcare? Organizations will need to continuously learn and update their practices and routines.
From patient care to insurance, changes will need to be made on both the industry and governmental levels to accommodate.
More cost effective ways to care for the elderly will also need to be investigated. Working to remove some of the financial burden from elderly patient care will help ensure that as the population continues to age, they are still well-cared for.
Hospitals and clinics are investing in advanced technology, assembling a workforce, and trying to make healthcare jobs more flexible and appealing to workers. All these things will help the industry be more prepared for the demands of the aging population.
New minds in healthcare leadership and administration will help come up with solutions to these problems. Becoming qualified to work in the healthcare field and help come up with creative solutions is a great goal for your career.
Healthcare in the age of climate change.

Climate change is a public health concern that continues to escalate: UN scientists estimate we have only 12 years left to keep global temperatures from rising above 1.5 degrees celsius.
This is a crucial number. If we don’t hit that goal, we’ll see drought, food scarcity, and an increase in extreme weather that will cause injuries and deaths.
Climate change can bring hotter days and heat-related injuries. Additionally, it can cause food and water scarcity, which means hospitals and clinics would need to be prepared for patients suffering from nutritional deficiency.
Organizations are also calling for healthcare organizations to be more energy-efficient and eco-friendly to help with climate change problems.
As health leaders work to find ways to cut down their carbon footprint and prepare for what will follow climate changes, they will be prepared to serve patients and help create a safer community for them.
Healthcare and multimorbidity.
Research shows that nearly ⅓ of all Americans suffer from multiple chronic conditions. This is called multimorbidity, and is growing increasingly prevalent across the world.
Multimorbidity also increases with age, and as more of the population ages and lives longer than before, multiple chronic conditions won’t be far behind.
Multimorbidity is a health issue as doctors and nurses work to treat many conditions, at the same time. This requires new levels of skill and technique to avoid mixing medicines that could be problematic, and is more difficult on patients physically and financially.
It is also a financial burden on the healthcare industry, as multiple conditions prove intricate and expensive to treat.
The Chronic Care Model is an important redesign for chronic disease and multimorbidity. This model helps care for and educate patients in the most effective way possible. Many Accountable Care Organizations have built the Chronic Care Model into their system redesign for this purpose.
Today's nursing leaders need to assure nurses are knowledgeable about these concepts and able to lead or co-lead these efforts at system redesign.
Minimally disruptive medicine is an element of the Chronic Care Model, and seeks to reduce the burden currently placed upon patients/clients in today's health system design through provider reorientation and self-management programs.
The healthcare industry is also constantly learning new techniques for medical and patient management when it comes to multiple chronic conditions. From technology that helps regulate treatments, to research constantly being done on new options, there is always work being done to help with this issue.
Healthcare leadership needs to make specific decisions about financial and medical options for treating those with chronic conditions. As the population continues to age, as people live longer, and as more chronic conditions have treatments, the healthcare industry will have to be prepared to keep up with the demand to fight multimorbidity.
Healthcare for those suffering from mental illness.

Increasing numbers and understanding about mental illness also has a direct impact on current medical trends.
Around the world mental illness is causing injury and death for millions of people. It is also costly and difficult to diagnose and treat.
Similarly, the opioid crisis is attributable for the highest death, suicide, and overdose death rates in the United States. Many individuals with substance use disorders have co-occurring mental health conditions that are untreated.
Additionally, stigmas associated with mental health by providers and patients alike interfere with proper diagnosis and treatment.
Hospitals and health leaders need to work together to navigate ways to work with mentally ill patients, and researchers, to continue to find ways to help provide relief. There are many options for ways to increase help and treatment for those with mental illness.
For example, the use of telepsychiatry in an emergency department can decrease waiting time for a psychiatric consult, decrease cost of care, and increase linkage to outpatient mental health services.
Other options including education, self-management programs, and programs to end the opioid epidemic are all ways health leaders are currently working to tackle mental illness.
As health leaders work to help find cures, make space for mental health patients, and create dialogue about the issues, patients will be able to find help when they most need it.
Getting an education in health leadership can help you be qualified to help solve these 21st century medical issues. As more trained professionals enter the field, more patients will be able to be helped and solutions will be found for these health concerns.
Ready to Start Your Journey?
HEALTH & NURSING
Recommended Articles
Take a look at other articles from WGU. Our articles feature information on a wide variety of subjects, written with the help of subject matter experts and researchers who are well-versed in their industries. This allows us to provide articles with interesting, relevant, and accurate information.
{{item.date}}
{{item.preTitleTag}}
{{item.title}}
The university, for students.
- Student Portal
- Alumni Services
Most Visited Links
- Business Programs
- Student Experience
- Diversity, Equity, and Inclusion
- Student Communities
- COP Climate Change
- Coronavirus (COVID-19)
- Cancer Research
- Diseases & Conditions
- Mental Health
- Women’s Health
- Circular Economy
- Sustainable Development
- Agriculture
- Research & Innovation
- Digital Transformation
- Publications
- Academic Articles
- Health & Social Care
- Environment
- HR & Training
- Health Research
- North America Analysis
- Asia Analysis
- Our Audience
- Marketing Information Pack
- Prestige Contributors
- Testimonials

- North America
- Open Access News
- Health & Social Care News
New challenges for public health in the 21st century

Dineke Zeegers Paget, Executive Director of the European Public Health Association (EUPHA) provides a fascinating glimpse of the new challenges for public health in the 21st century
As Europe enters the third decade of the 21st century, we have never been healthier and advances in knowledge and technology have enormously improved our ability to prevent and treat current diseases. Yet there are warnings of developments that could, ultimately, threaten the future of humanity. For this article, I will be focusing on five challenges for public health in the coming decades.
1.) Changing demographics in Europe
The first challenge is the changing demographics in Europe. Climate change, urbanisation, migration and an ageing population are transforming our demographics at the speed of light. For instance, global warming has an increasing impact on migration and we can expect a move to Northern Europe because of economic reasons (e.g. less fertile agricultural land in the South). It is estimated that by 2030, 80% of our citizens will live in urban areas (1) and this may have serious consequences for health if we don’t act now.
In addition, the population in Europe is ageing rapidly and we expect the proportion of people aged 65 and older to increase to 25% in 2050. (2) People will live longer, but not necessarily in good health and well-being, thereby, increasing the burden on health care systems to treat multimorbidity and chronic diseases. We need to address these changing demographics to mitigate their impact.
2.) Technological and digital revolution
The second challenge is the technological and digital revolution. The benefits of technology in health care is clear, developing medical equipment (robot surgery for instance) and better and faster diagnostics (e.g. genetic mapping) are beneficial to prevention and treatment.
On the other hand, there is a real risk in digitalisation. For instance, genetic information can be used in a more discriminative manner for health insurances or mortgage requests. And even though the digital revolution has given us access to all health information on the internet, the quality of information available is not always in our best interests (fake news).
Finally, technology has also led to new ‘diseases’, such as gaming addiction, which was included in the 11th International Classification of Diseases of the WHO. (3) We should be aware of the advantages and disadvantages of technology and digitalisation.
3.) Political influence on public health
The third challenge is the political influence on public health, as public health can only be achieved by concerted action at all levels. And to achieve that, we need politics. We need an understanding of the political system and should be willing to work with politicians. (4)
Especially now where politics are changing rapidly, populism is on the rise and we see a shift in public opinion on the value of scientific evidence. We need to invest in collaborating and coordinating with politicians to make sure our evidence-based voice is heard.
4.) Influence of vested interests
The fourth challenge is the influence of vested interests. In an era of globalisation, big companies have the power to influence politics as well as research. For instance, the Foundation for a Smoke-Free World describes itself as an independent, private foundation, but is funded by Philip Morris International. (5) Another example is the financial support for numerous health organisations in Spain by Coca-Cola. (6) But it does not stop there (e.g. food and petrol industry) and we need to find ways to make the collaboration with industry transparent and beneficial to the public’s health.
5.) New ethical issues of the 21st century
The fifth challenge is the new ethical issues that arise in the 21st century. The right to health, as described in the World Health Organization (WHO) constitution adopted in 1948, includes the right to housing, employment, living standards. But in an era of urbanisation, the right to adequate housing may be nearly impossible to implement. In an ageing population, the discussion between the right to life and quality of life needs to be put on the table, including the right not to live any longer, if the quality of life is decreasing. We need lawyers and ethicists to sit around the table with public health professionals to openly discuss these issues.
It seems clear that the public health network needs to adapt to 21st century challenges. The 21st century public health professional needs to be smart, persistent and creative, be able to be a diplomat and a negotiator at the same time. The approach of health in all policies is essential and the recently published manifesto: ‘All policies for a healthy Europe’ (7) is a step in the right direction.
To overcome all the challenges, old and new, we need to:
- Be deliberately collaborative by forging broad alliances in and outside the field of public health to get our message across;
- Be open-minded to engage with partners, including politicians, to jointly come to solutions that have a broad support base;
- Tell compelling narratives, which address the concerns that people have in a way that people understand; and
- Be transparent and open about potential uncertainties surrounding the evidence-base.
(1) https://www.eea.europa.eu/media/speeches/urbanisation-in-europe-limits-to-spatial-growth (2) http://www.euro.who.int/en/health-topics/Life-stages/healthy-ageing last accessed 12 May 2019. (3) https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/1448597234 , last accessed 10 May 2019. (4) https://academic.oup.com/eurpub/article/28/suppl_3/1/5149575 last accessed 12 May 2019. (5) https://www.smokefreeworld.org/our-vision/funding 2 May 2019. (6) https://academic.oup.com/eurpub/advance-article-abstract/doi/10.1093/eurpub/cky175/5086412?redirectedFrom=fulltext Last accessed 10 May 2019. (7) http://healthyeurope.eu/wp-content/uploads/2019/04/Summary-Manifesto-for-Website-smaller.pdf last accessed 12 May 2019
Dineke Zeegers Paget
Executive Director
European Public Health Association (EUPHA) Director of the EPH Conference Office Tel: +31 30 2729 709 [email protected] https://eupha.org/ www.twitter.com/EUPHActs
Editor's Recommended Articles

RELATED ARTICLES MORE FROM AUTHOR

Being sober curious: What, why and how

Towards a European strategy for older persons

Bridging the gap between evidence and action for health promotion – shifting the public narrative

A guide to nourishing your mind: The link between diet and brain health

Cells possess a rapid decision-making system beyond DNA

Prescribing solutions for the NHS staff shortage crisis
Leave a reply cancel reply.
Save my name, email, and website in this browser for the next time I comment.
Related Academic Articles

Treating neuropathic pain and nicotine dependence: Epibatidine derivatives as potential therapeutics

Flipons: The discovery of Z-DNA and soft-wired genomes
Assessing blood clot risk in venous catheter selection for patients with...
Follow open access government, latest publication.

Open Access Government April 2024
- Terms & Conditions
- Privacy Policy
- GDPR Privacy Policy
- Marketing Info Pack
- Fee Schedule

What Are Some of the Most Critical Health Concerns We Face in the 21st Century and Why?

The 21st century is full of progress, scientific discovery, and innovation. As the pace of modern development is so rapid that it’s easy to lose sight of the fact that increased convenience sometimes comes with new risks to people’s health, which may be overlooked for the time being but won’t go away permanently.
The implications of convenience are so detrimental to our well-being that suffering has become our immediate neighbour out of which mental health problems are at the forefront of the list, leading to a crisis in a person’s life.
Mental health issues such as anxiety, depression, and chronic stress are affecting and plaguing humans day by day. In one word, the reason is our lifestyle and the growing competition to survive and thrive. Some call it the hustle culture , and others call it a productive life, but all these terms are just ruining the natural essence of living because not eating a healthy meal the whole day and completing three projects a day may sound like a productive life, but it cannot be considered as a healthy life in respect to physical and mental aspects.
Therefore, it’s important to continually prioritise mindful living despite one’s many responsibilities. Healthy habits like going for a walk in nature, meditating for five minutes, and eating three balanced meals a day will help you to be more fulfilled, happy, and powerful throughout the day in the long run.
Now, advocating that people should practise mindful living and having them actually do so are two very different things, and from my own personal experience, I have found that consistency is the key to creating a mindful life. So, it’s not possible to adopt a healthy lifestyle in a single day or even a week, but you may do it by taking baby steps and staying the course.
Begin by meditating for five minutes a day and then continue for a week and then extend that to one month. Once you’ve been meditating regularly for 30 days, you won’t need any external motivation to do so. Since now it’s second nature to you, you’ll be able to start another good habit with a clearer head and more energy.
As rising mental health issues are a major concern for the modern world and people are well aware of this, putting this knowledge into action is essential for a sustainable life, and I am underlining this again because mental health issues affect not only our minds, but also our bodies, and following the Covid pandemic , it is much more prevalent among the public as they suffer from various life stressors. Also, the stigma around mental health is still very much present among the general population, making it difficult for those in need to seek adequate treatment and care. So, it’s important to let people know that they can talk to mental health professionals for help if they need it.
Keep in mind the old adage, ‘Health is wealth.’ Therefore, handle it like you would your other material assets. You’d never risk damaging your car, so there’s no reason to jeopardise the health that allows you to operate one. It is crucial that you learn to alter your way of life and reprogram your thoughts about healthy living because as you age, you will lose strength and flexibility, but if you take good care of your mental and physical well-being from the start, you will benefit greatly even as you become older.
Taking care of one’s body and carrying out one’s responsibilities is essential to savouring life’s journey. I hope that this article may inspire everyone who is beginning a healthy lifestyle or preparing to do so.
Avni Mishra is a counselling psychologist from Swindon, England.
Related Articles
Study shows no genetic link between mir-146a and wilms tumour in chinese kids, enhancing yoga and flexibility with the right supplements, quick trick to check if your disposable vape brand is genuine or not, amid growing concerns over illicit products, getting to know the services of an endoscopy center, enhancing posture and alignment: the transformative power of yoga, accelerating recovery: strategies to speed up healing with physiotherapy treatments, occupational therapist reveals top 5 tips to maintaining muscle as we age, cancer support uk to be championed by top interiors writer and style influencer lisa dawson, the impact of your sleep position on health and longevity, growing strong: how hipp follow-on formula supports your baby’s nutritional needs, essential paediatric first aid techniques every parent should know, 5 approaches for treating scoliosis in teenagers, charity urges people to be vocal about viral meningitis for awareness week, sublingual treatment improves stroke outcomes, sinus treatments: how a sinus specialist can help with chronic sinusitis, how orthodontics can literally change your face, “national walking month” with u3a, fitness app development company: top 7 choices in 2024, nhs trust awards fellowship to further addiction research, swim your stress away: exploring the mental health benefits of swim spas, decoding health insurance waiting periods and finding the best health insurance plans for young adults, international study could help shape great midwife leaders around the globe, performance fuel: exploring the potential of popular supplements, beyond beauty: the versatility of trusculpt in body contouring.

Psychreg is a digital media company and not a clinical company. Our content does not constitute a medical or psychological consultation. See a certified medical or mental health professional for diagnosis.
- Privacy Policy
© Copyright 2014–2034 Psychreg Ltd
- PSYCHREG JOURNAL
- MEET OUR WRITERS
- MEET THE TEAM
- Share full article
Advertisement
The Morning
A fresh approach to a crisis.
A group of researchers posited another explanation for the youth mental health crisis: too much discussion.

By Ellen Barry
She covers mental illness.
For years now, policymakers have sought an explanation for the mental health crisis among young people. Suicide attempts and psychiatric hospitalizations were rising even before the pandemic. Then the rates of anxiety and depression doubled worldwide.
Why is this happening? The social psychologist Jonathan Haidt points to smartphones, and the algorithms that draw kids away from healthy play and into dangerous, addictive thought loops. No, his critics say. The real problem is a grim social landscape of school shootings, poverty and global warming. Or academic pressure. Or insufficient health care.
A group of researchers in Britain now propose another, at least partial, explanation: We talk about mental disorders so much. I cover this notion in a story The Times published today .
This hypothesis is called “prevalence inflation.” It holds that our society has become so saturated with discussion of mental health that young people may interpret mild, transient suffering as symptoms of a medical disorder.
This is a problem, they say, because identifying with a psychiatric diagnosis may not be helpful. Students who self-label as anxious or depressed are more likely than similar students who don’t self-label to view themselves as powerless over the disorder, recent studies have shown. They may respond by avoiding stressful situations like parties or public speaking, which could make their problems worse.
One of the psychologists behind the prevalence inflation theory, Lucy Foulkes of the University of Oxford, traces her skepticism back to 2018, when she began teaching undergraduates. They were “bombarded” with messages warning that they might be in crisis, she said. “It seemed like the more we were trying to raise awareness about it, it wasn’t getting better, and in fact, it only seemed to be getting worse.”
She grew critical of curricula that teach children to recognize and manage their emotions, sometimes referred to as social emotional learning. Schools have introduced an array of programs, teaching children the basics of techniques like mindfulness and cognitive behavioral therapy, which have proved beneficial in adults.
Several recent studies have found lackluster or negative effects for students who received trainings, especially those who started out with more severe symptoms. That evidence has done little to dampen their popularity, Foulkes said.
An urgent need
Many experts in the field of adolescent mental health defend awareness campaigns and school-based trainings. “Especially with teens, we need more universal interventions, not less,” said Zachary Blumkin, a child psychologist at Columbia University Irving Medical Center.
The main reason, they say, is that traditional, one-on-one therapy and psychiatric care is not easily available. Teenagers in crisis can wait months to see a clinician. They often land in emergency rooms as a last resort.
For that reason, the field has gravitated toward preventive models. These teach all students — not just the troubled ones — to manage distressing emotions. A 2023 meta-analysis of 252 such programs concluded that, generally, children benefit from them. There is also promise in a more tailored approach , one that lets schools focus on kids with the most acute needs.
Some experts also disagree that over-diagnosis is a problem.
Andrew Gerber, a child psychiatrist, says we should think of mental illness as a spectrum: Disorders like anxiety or depression occur in a bell curve distribution, so they’re more like hypertension than appendicitis. And like hypertension, he said, they’re worth treating early in their progression, with medication and therapy. “Anyone who tries to define a sharp line between ‘real’ illness and what is not real, no matter where they put the line, is doomed to get it wrong and do damage in the process,” said Gerber, the president and medical director at Silver Hill Hospital in New Canaan, Conn.
Foulkes disagrees. Even when we have good treatments, we’re bad at identifying whose disorder is likely to deteriorate, she said. And some children struggle because something is wrong at home, like domestic abuse or poverty or bullying. Mindfulness trainings are unlikely to help these kids.
“A lot of the time, what’s causing the problem is not something that’s going to improve with medication or therapy,” she said. “You’re running the risk of just telling people they have a problem without helping alleviate it.”
A generation is growing up fluent in the language of mental health, something that will benefit teens who badly need treatment. But others may apply medical diagnoses to the painful, normal adversity of growing up.
The “prevalence inflation” hypothesis asks us to keep an eye on those excesses. People hurt after breakups and struggle to adjust to new schools; negative feelings aren’t always a sign of mental illness. They can even teach us resilience.
Rates of mental health disorders are rising among American adolescents. Read one 13-year-old’s story .
There aren’t always enough resources to support teenagers’ mental health. As schools search for solutions, some student-led clubs step in .
Are smartphones driving teenagers to depression? It’s complicated , writes David Wallace-Wells in Times Opinion.
THE LATEST NEWS
Israel-hamas war.
The Israeli military said it was asking tens of thousands of Gazans sheltering in eastern Rafah to temporarily evacuate to what it described as a humanitarian zone.
Hamas claimed responsibility for a rocket attack that Israeli officials said killed three soldiers and left three more critically wounded.
Israel moved to shut down local operations of Al Jazeera , a Qatar-based news outlet.
Cease-fire talks between Israel and Hamas are at an impasse. The main obstacle is the duration of a pause.
Four children from Gaza arrived in the U.S. to receive urgent medical treatment . They were greeted at Kennedy Airport with toys and balloons.
Campus Protests
U.C.L.A. said that it would resume in-person classes today and that it had created a new campus security office .
New York Magazine and the Columbia student newspaper surveyed the campus about the protests . More than 60 percent of respondents said they had views on the conflict they avoided saying publicly.
More college professors — many of whom came of age during the era of Vietnam War protests — are joining student demonstrations , The Wall Street Journal reports.
More International News
Around Shanghai, women gather in bars and bookstores to debate their place in a country ruled by men.
Panamanians elected José Raúl Mulino, a former public security minister, as their next president .
Paris committed to making the Olympics more accessible for people with disabilities. Advocacy groups are concerned that the city remains unprepared .
In the 19th century, Belgian troops decapitated a Congolese leader and took his skull as a trophy. The leader’s descendants are struggling to have his remains returned .
Kim Godwin, the first Black woman to run a broadcast news division, said she would step down as president of ABC News after a tumultuous tenure.
Sony and the private equity firm Apollo are in talks to acquire Paramount .
Other Big Stories
New York City’s congestion pricing program aims to generate $15 billion for the mass transit system, but lawsuits threaten that windfall .
In Florida, Chinese residents expressed frustration with a new law that prohibits many Chinese citizens from buying homes in the state because of national security concerns.
We should welcome the emergence of this year’s cicadas with wonder, Margaret Renkl writes.
Ross Douthat suggests books and essays that could improve the intellectual diversity of university curricula.
Gail Collins and Bret Stephens discuss campus protests and Donald Trump .
Here are columns by Maureen Dowd on the three faces of Trump and Thomas Friedman on Israel and Saudi Arabia .
MORNING READS
Community: For generations of immigrants, Sunday soccer in a park in Queens is more than a game .
Health: Ultraprocessed foods are linked to poor health. But what are they exactly?
Loneliness: Social connection experts offer advice on cultivating a sense of belonging .
Ask Vanessa: “How do I know if my untucked shirt is too long?”
Kocktails: As nonalcoholic cocktails become a staple on American menus, some children have begun to partake .
Metropolitan Diary: A necklace rescue in Midtown .
Lives Lived: Bernard Hill was a British actor who incarnated humble masculine leadership as Capt. Edward J. Smith in “Titanic” and as Théoden, the king of Rohan, in two “Lord of the Rings” films. He died at 79 .
Formula One: McLaren’s Lando Norris secured his first victory at the Miami Grand Prix .
No punches pulled: At a live Netflix comedy roast, former Patriots players and Kevin Hart among others roasted Tom Brady about his divorce and Deflategate.
N.H.L.: The Dallas Stars eliminated the defending Stanley Cup champion Las Vegas Golden Knights in a thrilling 2-1 Game 7 win .
N.B.A.: Donovan Mitchell’s 24 second-half points led the Cleveland Cavaliers to a comeback win in their own Game 7 against the Orlando Magic.
ARTS AND IDEAS
The artist Frank Stella, who helped usher in the Minimalist movement of the 1960s, died on Saturday at 87. His career began during the Eisenhower era, when artistic tendencies — much like ideas about gender and sexuality — fell into fixed categories: one was either a figurative artist or an abstract one. Things changed, the critic Deborah Solomon writes, but Stella did not. “He never stopped insisting on the inherent superiority of abstract painting,” she adds. Read her full appraisal of Stella .
More on culture
Madonna ended her retrospective Celebration Tour with a free show in Rio de Janeiro, which was attended by an estimated 1.6 million people .
Trying to find your own song of the summer? Vulture has published a bracket to sort through this year’s pop deluge.
The HBO series “The Sympathizer” is a rebuttal to a Hollywood staple. It is its own Vietnam War movie and a detailed work of film criticism , James Poniewozik writes.
Over the weekend, “The Fall Guy,” starring Ryan Gosling, earned only $28.5 million . It is Hollywood’s lowest start to the summer box office season since 1995.
THE MORNING RECOMMENDS …
Make Dolester Miles’s famous coconut pecan cake .
Watch the Met Gala red carpet tonight.
Stargaze with a telescope for beginners .
Clear your phone’s camera roll .
Take our news quiz .
Here is today’s Spelling Bee . Yesterday’s pangram was maypole .
And here are today’s Mini Crossword , Wordle , Sudoku , Connections and Strands .
Thanks for spending part of your morning with The Times. See you tomorrow.
Correction: Yesterday’s newsletter named two different Kentucky Derby winners. The winner was Mystik Dan, not Sierra Leone.
Sign up here to get this newsletter in your inbox . Reach our team at [email protected] .
Ellen Barry is a reporter covering mental health for The Times. More about Ellen Barry
- Reference Manager
- Simple TEXT file
People also looked at
Opinion article, transforming agricultural research and development systems to meet 21st century needs for climate action.

- 1 International Rice Research Institute (IRRI), Los Baños, Philippines
- 2 Nordic Africa Institute, Uppsala, Sweden
- 3 Leibniz Center for Agricultural Landscape Research (ZALF), Müncheberg, Germany
- 4 Department of Agricultural Economics, Humboldt University of Berlin, Berlin, Germany
Introduction
Climate shocks to agriculture threaten food security, especially in the Global South. Poverty and malnutrition are rising and there are dire warnings of what is to come. Agricultural research and development systems need to generate multiple game-changing innovations in order to transform our agricultural systems and ensure that they are climate-resilient, productive, sustainable, and equitable. The challenge is immense and there are no shortages of sound advice on required directions for research. This is particularly the case for CGIAR, a global partnership that unites international organizations engaged in research to reduce rural poverty, increase food security, and improve human health and nutrition, while fostering sustainable management of natural resources.
At the 2022 Conference of the Parties (COP26) in Glasgow, 45 world leaders launched “ The Breakthrough Agenda Report ” as part of a commitment to make clean technologies and sustainable practices more attractive, affordable and accessible by 2030. The Report argues that for the agriculture sector, the breakthrough goal is that “ Climate-resilient, sustainable agriculture is the most attractive and widely adopted option for farmers everywhere by 2030 ” ( IEA et al., 2023 , p. 141). Merrey et al. (2023 , p. 4) report that there is no single transformative agricultural innovation to realize this goal, but rather “ synergistic interactions among multiple game-changing innovations in hundreds of national and local agricultural systems ” that cumulatively lead to the transformation of global agriculture. A transformation which is urgently needed to address climate challenges.
For agricultural researchers the challenge of food systems transformation is immense, but so are the opportunities. The journal Food Policy has published a number of viewpoints that detail the type of research that CGIAR should focus on ( Coffman et al., 2020 ; Haddad, 2020 ; Nelson, 2020 ; Thornton et al., 2022 ). Lynam et al. (2024) outline organization changes required specifically for CGIAR, while Conti et al. (2024) address this issue more broadly for agricultural research organizations. Simultaneously, CGIAR has not escaped criticism. Some question its ability to respond to the challenge of ensuring food security under climate change ( McIntire and Dobermann, 2023 ).
As agricultural researchers, we relate to the multifarious suggested priority research areas, recommendations and critiques of CGIAR and other agricultural research organizations. We believe, however, that discussions to date obscure fundamental and wider aspects about how research is done to ensure that it contributes to the needed radical transformation of food, land and water systems to meet 21st Century needs. We recognize the huge contribution that a plethora of agricultural research and development systems have made and continue to make toward meeting these needs. It is not our intention to question the raison d'être of legions of committed professionals. On the contrary, we seek to make constructive suggestions and provoke discussions that we believe will render these systems even more effective, efficient and impactful. A fundamental first step is an urgent and radical transformation in the way that we conceptualize the research process and undertake research.
Research paradigms that were suitable for 20th Century challenges—e.g., the Green Revolution, an innovation system which CGIAR played a pivotal role in terms of both the science and practice—need to give way to those better suited to 21st Century challenges. The Green Revolution relied heavily on technology transfer and undoubtedly contributed to significant increases in food production and reductions in poverty. However, it tended to benefit men rather than women, large-scale farmers rather than small-scale ones, and it had less beneficial impact in marginal production environments ( Pingali, 2012 ).
The International Science Council (2023) in its report Flipping the Science Model: A Roadmap to Science Missions for Sustainability captures an example of the paradigm shift required. A change from a traditional science model, which is characterized often by siloed science funding, intense competition and a lack of trust among stakeholders, to a model “ that encourages science to cater directly to societal needs. This can be achieved by co-creating actionable knowledge and finding solutions tailored to the intricate sustainability issues identified by both local and global stakeholders ( International Science Council, 2023 , p. 6). Additional paradigms guiding agricultural research must also address social justice, environmental stewardship, and indigenous knowledge ( Pretty et al., 2010 ).
A fundamental point that may or may not be self-evident when considering the need for game-changing innovations to transform agriculture is that agricultural innovation systems are embedded within societal contexts. Hence, to encourage science to cater more to societal needs, social scientists need to play a more prominent role in building a global transdisciplinary research process that fosters the co-design and co-production of research and action, and encourages more inclusive collaboration among science, policy-makers and civil society ( Dolinska et al., 2023 ). At present, as we elaborate below, the role of social scientists is all-too-often peripheral to agricultural research.
We, hence, focus our opinion piece on two themes: (i) the urgent need to engage social (together with natural) scientists in transdisciplinary research processes; (ii) the importance of the co-creation of knowledge via more democratic partnerships that genuinely address power asymmetries, as well as different stakeholders' roles (and responsibilities). We highlight discrepancies in the mix of social and natural science agricultural research, and also what may come across as a tepid commitment to partnerships despite the best intentions of many researchers. The short-termism of research projects stymies the establishment of genuine partnerships and there may be an inherent power imbalance because of who holds the purse strings and the structure of research funding. Such partnerships are often further stymied by a lack of consensus on the roles, responsibilities and modus operandi of key stakeholders, ones that include public research and extension institutions, universities, private firms, producers, donors, and consumers ( Hellin et al., 2020 ).
A greater role for social science in transdisciplinary research
The need to tackle climate change will require major adjustments in a number of sectors, including research. The way many organizations do agricultural research needs to change substantially in order to meet the climate challenge. While technical challenges abound, the game-changing innovations referred to by Merrey et al. (2023) , are embedded in society and it is notoriously difficult to bring about deliberate societal change. The funding of climate research still appears to be largely based on the assumption that (natural) scientists need to focus on the causes, impacts, and technological answers to climate change, and then when exposed to solutions, targeted stakeholders (including farmers) will change their behavior. The assumption is flawed. Climate change has less to do with technology and more to do with society and political economy ( Vermeulen et al., 2018 ; Davidson, 2022 ). Innovation is shaped by people, and they are also the drivers of climate action ( Devine-Wright et al., 2022 ). Insights on societal change and dynamics from the social sciences are critical when it comes to transforming climate change research into action ( Weaver et al., 2014 ). The social sciences (and humanities) contribute critical and invaluable perspectives that provide context, framings, approaches, reflection and impacts on societal transformation ( Fisher et al., 2022 ).
Despite its importance, social science is still hugely underrepresented in climate change research. Overland and Sovacool (2020) , for example, analyzed a dataset of research grants from 333 donors worldwide and with a cumulative value of USD 1.3 trillion from 1950 to 2021. On issues related to climate change, the natural and technical sciences received 770% more funding than the social sciences. The preponderance of funding for natural as opposed to social science climate research can encourage ‘climate reductionism' whereby science removes climate change from its environmental and social contexts ( Rigg and Mason, 2018 ). The salutary reality is that “ the questions and challenges in climate science are at once political, moral, socioeconomic, cultural, psychological and historical—in addition to scientific and technical. Yet, it is the predictive natural sciences (earth, environmental, meteorological, atmospheric sciences), not the critical and interpretative social sciences and humanities, that set the terms of the climate change debate, leading to disciplinary reductionism” ( Rigg and Mason, 2018 ).
It is time we overturn business as usual and embrace business unusual in order to stimulate the opposite of ‘climate reductionism'. In the words of The International Science Council (2023) , we need more ‘mission-led science' that will “ require continued investments in basic, social, and natural sciences, both as disciplinary and interdisciplinary approaches and with a focus on ensuring practical outcomes .” We believe that organizations dedicated to agricultural research for development (AR4D) need to employ a larger cadre of social scientists from diverse disciplinary backgrounds. Others have made similar calls (e.g., Venot et al., 2015 ), but there is still some way to go especially in terms of the diversity of social science disciplines.
Among the social scientists in many AR4D organizations, agricultural economists predominate. There is very often a dearth of other social science disciplines that are critical to mission-led science. These include sociologists ( Davidson, 2022 ), anthropologists, psychologists ( Shah, 2020 ) geographers ( Castree, 2015 ), political scientists, development studies and gender specialists, plus those best positioned to communicate climate change research to policy makers and the public ( Nature Climate Change, 2019 ) and work with local communities to identify pathways to achieving the changes in behavior needed. Furthermore, social scientists are often perceived to be service providers to those engaged in biophysical research ( Cullen et al., 2023 ).
Working across the natural and social sciences is not easy; some may feel that their entire raison d'être is challenged, while others may find it difficult to embrace different ways of analyzing a similar problem. We struggle, for example, with the notion that Randomized Control Trials (RCTs) are a gold standard for evaluating the effectiveness of agricultural interventions such as climate-smart agriculture. Similar concerns are shared by others e.g., Glover et al. (2016) and Kabeer (2020) . A call for inter-disciplinary approaches does not require all researchers to modify their approach. We fully recognize the need for continued strong disciplinary research, be it from the natural or social sciences. Agricultural research and development systems still need specialists but they also require an open mindset and ability to engage outside disciplinary boundaries.
The payoffs of agricultural research giving more attention to social dimensions are often substantial. Examples include a better match between crop improvement and farmers' realities in terms of crop breeders recognizing the significance of traits such as taste, color and nutritional value rather than an undue focus on yields ( Cullen et al., 2023 ). Another example is the need to understand gender and social norms to foster equitable agricultural development ( Badstue et al., 2020 ).
There is also a need for more generalists who can support integration ( Grace et al., 2021 ). As Castree et al. (2014) wrote in the context of Geography's contribution to climate change research, we need more scientists who can play the role of a “weaver” in contrast to those working in specialist subjects who tend to be “spinners.” Brown et al. (2015) use the term “T-shaped” researchers, those able to flourish in their own discipline and also look beyond it and embrace others.
What emerges from accommodating different disciplinary perspectives is a “ messier intellectual landscape of climate understanding ” ( Schipper et al., 2021a ), one that lends itself to identifying global environmental challenges and opportunities for transformation while also recognizing the relevance of people's varied agency and capacity for change ( Fisher et al., 2022 ). This is something that many researchers may find discomforting, but it is critical to encourage a systems approach to climate research. Holistic inter-disciplinary thinking helps create the conditions for systems transformation and a paradigm shift that enables a transition to sustainability ( Voulvoulis et al., 2022 ).
Roles, responsibilities and power asymmetries in transdisciplinary partnerships
Another bottleneck to agricultural research and development systems being more impactful is that too often the importance of developing genuine partnerships, and the time that trust-building takes, is over-looked. Cundill et al. (2019a) note that climate change research funds are shifting toward large collaborative research networks and pose significant challenges (we would add also significant opportunities) for researchers. Researchers increasingly need to forge transdisciplinary networks and participatory process with other stakeholders. The ensuing climate action requires “ integrated and multiscale research that is simultaneously cutting edge, problem-oriented, and that creates space for other ways of knowing, beyond western science alone ” ( Cundill et al., 2019b ).
A transformative climate response requires actionable interdisciplinary science and strong partnerships among researchers and broader society ( Hernandez-Aguilera et al., 2021 ). This requires doing research differently, embracing both qualitative and quantitative research approaches ( Schipper et al., 2021b ) and placing more emphasis on action research, stakeholder engagement and social learning ( Miller et al., 2010 ). A concerted effort is need to shift from output-directed to process-oriented research during which diverse stakeholders with different cultural backgrounds, including researchers and policy-makers, co-produce knowledge ( Miller et al., 2010 ). Collaborative knowledge generation can encounter obstacles, particularly when participants from the Global South and North work together. The distinction between “co-creation” and traditional participatory approaches is currently unclear, leading to questions about what is a co-creation process, and how to avoid it being a means of scientific exploitation ( Keikelame and Swartz, 2019 ) and/or perpetuating coloniality ( Fúnez-Flores, 2023 ).
Building trustful partnerships takes time ( Newig et al., 2019 ; Thornton et al., 2024 ) often far longer than the 3-to-5 year lifetimes of many agricultural research projects. There are often power and finance asymmetries with insufficient ownership by Southern partners compared to their Northern colleagues ( Cundill et al., 2019a ; Schneider et al., 2019 ; Cullen et al., 2023 ). The pressure to articulate and develop research proposals and realize outcomes very often does not allow for the establishment and nourishment of (research) partnerships. There is a danger that short-termism (dictated by truncated funding cycles) gives the impression that research organizations are not a reliable partner. The impression is often an erroneous one but we should not forget that perception is reality. Power asymmetries also manifest themselves in terms of whose knowledge counts. Local and indigenous knowledge is still under-represented in climate change research although the situation is changing ( Head, 2020 ; Kassam et al., 2023 ).
As Reed and Fazey (2021) note, the “publish or perish” mantra has been coupled with an additional one: “impact or implode.” Too often the understandable pressure from donors and policy-makers to demonstrate impact means that there is a tendency for researchers to focus on “quick wins” rather than the longer-term and more obdurate transformations that are needed ( Hainzelin et al., 2017 ). In the words of Leeuwis et al. (2018) , “ there is an urgency to demonstrate how today's research activities will contribute to tomorrow's development .” There is pressure to report high numbers of farmers who have adopted certain technologies, or received training. Whilst important, these numbers are only one aspect of the development story. They reveal little about human development, the dangers of trade-offs and maladaptation ( Schipper, 2020 ) and the sustainability of any innovation (there are numerous examples of farmers abandoning agricultural innovations once external support is withdrawn).
As researchers ourselves, we totally empathize with the pressures to demonstrate rapid results that we all find ourselves under. We argue for more honest conversations about the contribution of agricultural research to game-changing innovations, and critically the time, trust, and relationship building it takes to realize impact. The required transformations of land, water and food systems take far longer than the life-times of the majority of agricultural research projects ( Hainzelin et al., 2017 ). Many stakeholders have roles and responsibilities in and along an impact pathway (or rather a web of impact pathways) that connects research activities, research outputs, impacts and outcomes ( Blundo-Canto et al., 2018 ).
Researchers should be held accountable for the delivery of “outputs”; this is in their sphere of control. It is also incumbent on them to embrace working with non-researchers, and to identify suitable mechanisms and changes to the policy, institutional and governance environments that drive the transformation process. Realizing impact, however, largely falls outside the control of researchers and within the operating spaces of governments, civil society and private sector. It is these stakeholders who are better best placed to nurture the organizational and institutional processes that underpin transformative change ( Hellin et al., 2020 ).
The design and use of more comprehensive theories of change e.g., Brown (2020) would allow for greater transparency and understanding about stakeholders' roles and responsibilities while also capturing learnings from what has not worked in the research process. Too often, so-called “failures” during the research process are under-reported; a technology that did not work; a research partnership that never got off the ground or disintegrated in acrimony. There are few incentives to report these failures or setbacks in agricultural research. Failure is not failure if one can learn from what did not work as we had hoped. In agricultural research, failures (or should we call them opportunities for learning?) are inevitable on the road to success. There are, however, few incentives within research organizations to learn from mistakes. One way forward could be journal sections specifically geared to publications that focus on what did not work, why and what can we learn going forward.
Lessons from history
Agricultural research and development systems need to generate multiple game-changing innovations in order to transform our agricultural systems and ensure that they are climate-resilient, productive, sustainable, and equitable. Social scientists can provide urgently needed insights on societal dynamics that are critical when it comes to transforming climate change research into action. Transdisciplinary partnerships are the foundation of transforming research into action; partnerships characterized by trust, accountability, a heavy dose of “intellectual humility” on the part of all stakeholders, including researchers ( Palmer, 2023 ), and integrating the different needs of the global North and South ( Schneider et al., 2022 ).
Co-creation in transdisciplinary research signifies a more profound dedication among the parties involved, who must collaborate to conceptualize, plan, and generate knowledge that benefits everyone, drawing on transformative learning in critical and dialogical research ( Freire, 2005 ). For global agricultural research and development systems to be truly fit-for-purpose and contribute to the needed radical transformation of food, land and water systems to meet 21st Century needs, greater numbers of ‘T-shaped' researchers i.e., weavers, are needed. This part depends on changed incentive schemes at universities and research centers.
History can provide some of the answers. In an essay entitled Humboldt for the Anthropocene , Jackson (2019) cites the example of Alexander von Humboldt, the German geographer who fused science and humanism, and whose “ combination of empathy, humility, confidence, and rigor can serve as a model for engaging the public on matters of urgent concern .” Climate action is one of these urgent concerns. A big (and realistic step) would, perhaps, be for research organizations to employ more von Humboldts as part of a radical transformation in the way that we conceptualize and do research. In this way can come genuine breakthroughs in transformative action to address climate challenges through sustainable agriculture, without the threat of breakdowns in the very agricultural systems that sustain life.
Author contributions
JH: Conceptualization, Writing—original draft, Writing—review & editing. EF: Conceptualization, Writing—original draft, Writing—review & editing. MB: Conceptualization, Writing—original draft.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was carried out with support from the CGIAR Research Initiative on Climate Resilience (ClimBeR). We would like to thank all funders who supported this research through their contributions to the CGIAR Trust Fund: https://www.cgiar.org/funders/ .
Acknowledgments
The authors are very grateful to one of the Topic Editors and reviewer for comments on an earlier version of the manuscript. EF acknowledges support by the Nordic Africa Institute.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The opinions expressed in this publication are those of the authors and not necessarily the views of their employer.
Badstue, L., Elias, M., Kommerell, V., Petesch, P., Prain, G., Pyburn, R., et al. (2020). Making room for manoeuvre: addressing gender norms to strengthen the enabling environment for agricultural innovation. Dev. Pract. 30, 541–547. doi: 10.1080/09614524.2020.1757624
PubMed Abstract | Crossref Full Text | Google Scholar
Blundo-Canto, G., Triomphe, B., Faure, G., Barret, D., de Romemont, A., Hainzelin, E., et al. (2018). Building a culture of impact in an international agricultural research organization: process and reflective learning. Res. Eval . 28, 136–144. doi: 10.1093/reseval/rvy033
Crossref Full Text | Google Scholar
Brown, B. Y. M. (2020). Unpacking the Theory of Change . The Stanford Center on Philanthropy and Civil Society at Stanford University.
Google Scholar
Brown, R., Deletic, A., and Wong, T. (2015). How to catalyse collaboration. Nature 525:315. doi: 10.1038/525315a
Castree, N. (2015). Geography and global change science: relationships necessary, absent, and possible. Geogr. Res . 53, 1–15. doi: 10.1111/1745-5871.12100
Castree, N., Adams, W. M., Barry, J., Brockington, D., Buscher, B., Corbera, E., et al. (2014). Changing the intellectual climate. Nat. Clim. Change 4, 763–768. doi: 10.1038/nclimate2339
Coffman, W. R., Acevedo, M., Davidson Evanega, S., Porciello, J., Tufan, H. A., McCandless, L., et al. (2020). Viewpoint: five recommendations for an inclusive and collaborative One CGIAR. Food Policy 91:101831. doi: 10.1016/j.foodpol.2020.101831
Conti, C., Hall, A., Percy, H., Stone-Jovicic, S., Turner, J., McMillan, L., et al. (2024). What does the agri-food systems transformation agenda mean for agricultural research organisations? Exploring organisational prototypes for uncertain futures. Glob. Food Secur . 40:100733. doi: 10.1016/j.gfs.2023.100733
Cullen, B., Snyder, K. A., Rubin, D., and Tufan, H. A. (2023). ‘They think we are delaying their outputs'. The challenges of interdisciplinary research: understanding power dynamics between social and biophysical scientists in international crop breeding teams. Front. Sustain. Food Syst . 7, 1–16. doi: 10.3389/fsufs.2023.1250709
Cundill, G., Currie-Alder, B., and Leone, M. (2019a). The future is collaborative. Nat. Clim. Change 9, 343–345. doi: 10.1038/s41558-019-0447-3
Cundill, G., Harvey, B., Tebboth, M., Cochrane, L., Currie-Alder, B., Vincent, K., et al. (2019b). Large-scale transdisciplinary collaboration for adaptation research: challenges and insights. Glob. Challenges 3:1700132. doi: 10.1002/gch2.201700132
Davidson, D. J. (2022). Climate change sociology: past contributions and future research needs. PLOS Clim . 1:e0000055. doi: 10.1371/journal.pclm.0000055
Devine-Wright, P., Whitmarsh, L., Gatersleben, B., O'Neill, S., Hartley, S., Burningham, K., et al. (2022). Placing people at the heart of climate action. PLOS Clim . 1:e0000035. doi: 10.1371/journal.pclm.0000035
Dolinska, A., Hassenforder, E., Loboguerrero, A. M., Sultan, B., Bossuet, J., Cottenceau, J., et al. (2023). Co-production opportunities seized and missed in decision-support frameworks for climate-change adaptation in agriculture – how do we practice the “best practice”? Agric. Syst. 212:103775. doi: 10.1016/j.agsy.2023.103775
Fisher, E., Brondizio, E., and Boyd, E. (2022). Critical social science perspectives on transformations to sustainability. Curr. Opin. Environ. Sustain . 55:101160. doi: 10.1016/j.cosust.2022.101160
Freire, P. (2005). Freire Paulo Pedagogy of the Oppressed . New York, NY: Continuum International Publishing Group Inc.
Fúnez-Flores, J. I. (2023). Anibal quijano: (dis)entangling the geopolitics and coloniality of curriculum. Curric J . 35, 288–306. doi: 10.1002/curj.219
Glover, D., Sumberg, J., and Andersson, J. A. (2016). The adoption problem; or why we still understand so little about technological change in African agriculture. Outlook Agric. 45, 3–6. doi: 10.5367/oa.2016.0235
Grace, K., Siddiqui, S., and Zaitchik, B. F. (2021). A framework for interdisciplinary research in food systems. Nat. Food 2, 1–3. doi: 10.1038/s43016-020-00212-6
Haddad, L. (2020). A view on the key research issues that the CGIAR should lead on 2020–2030. Food Policy 91:101824. doi: 10.1016/j.foodpol.2020.101824
Hainzelin, E., Barret, D., Faure, G., Dabat, M.-H., and Riomphe, B. (2017). Agricultural research in the Global South: steering research beyond impact promises. Perspective 42, 1–4. doi: 10.19182/agritrop/00009
Head, L. (2020). Transformative change requires resisting a new normal. Nat. Clim. Change 10, 173–174. doi: 10.1038/s41558-020-0712-5
Hellin, J., Balié, J., Fisher, E., Blundo-Carto, G., Meah, N., Kohli, A., et al. (2020). Sustainable agriculture for health and prosperity: stakeholders' roles, legitimacy and modus operandi. Dev. Pract. 30, 965–971. doi: 10.1080/09614524.2020.1798357
Hernandez-Aguilera, J. N., Anderson, W., Bridges, A. L., Hansen, W. D., Maurer, M. L., Ilboudo Nébié, E. K., et al. (2021). Supporting interdisciplinary careers for sustainability. Nat. Sustain . 4, 374–375. doi: 10.1038/s41893-020-00679-y
IEA, IRENA, and UN Climate Change High-Level Champions. (2023). Breakthrough Agenda Report 2023 . Paris: IEA (International Energy Agency).
International Science Council (2023). Flipping the Science Model: A Roadmap to Science Missions for Sustainability . Paris: International Science Council.
Jackson, S. T. (2019). Humboldt for the Anthropocene. Science 365, 1074–1076. doi: 10.1126/science.aax7212
Kabeer, N. (2020). Women's empowerment and economic development: a feminist critique of storytelling practices in “randomista” economics. Fem. Econ. 26, 1–26. doi: 10.1080/13545701.2020.1743338
Kassam, K.-A. S., Charles, M. T., and Johnson, S. M. (2023). Significance of different ways of knowing in responding to the climate crisis: the necessity for Indigenous knowledge. PLOS Clim . 2:e0000237. doi: 10.1371/journal.pclm.0000237
Keikelame, M. J., and Swartz, L. (2019). Decolonising research methodologies: lessons from a qualitative research project, Cape Town, South Africa. Glob. Health Action 12:1561175. doi: 10.1080/16549716.2018.1561175
Leeuwis, C., Klerkx, L., and Schut, M. (2018). Reforming the research policy and impact culture in the CGIAR: integrating science and systemic capacity development. Glob. Food Secur. 16, 17–21. doi: 10.1016/j.gfs.2017.06.002
Lynam, J., Byerlee, D., and Moock, J. L. (2024). The organizational challenge of international agricultural research: the fifty-year odyssey of the CGIAR. Food Policy 124:102617. doi: 10.1016/j.foodpol.2024.102617
McIntire, J., and Dobermann, A. (2023). The CGIAR needs a revolution. Glob. Food Sec ur . 38:100712. doi: 10.1016/j.gfs.2023.100712
Merrey, D. J., Loboguerrero, A. M., and Zeppenfeldt, L. (2023). An Enabling Innovation Ecosystem to Accelerate Agriculture Breakthroughs . Utrecht: Clim-Eat.
Miller, F., Osbahr, H., Boyd, E., Thomalla, F., Bharwani, S., Ziervogel, G., et al. (2010). Resilience and vulnerability : complementary or conflicting concepts? Ecol. Soc . 15:11. doi: 10.5751/ES-03378-150311
Nature Climate Change (2019). Scientific uncertainty. Nat. Clim. Change 9:797. doi: 10.1038/s41558-019-0627-1
Nelson, R. (2020). Viewpoint: international agriculture's needed shift from energy intensification to agroecological intensification. Food Policy 91:101815. doi: 10.1016/j.foodpol.2019.101815
Newig, J., Jahn, S., Lang, D. J., Kahle, J., and Bergmann, M. (2019). Linking modes of research to their scientific and societal outcomes. Evidence from 81 sustainability-oriented research projects. Environ. Sci. Policy 101, 147–155. doi: 10.1016/j.envsci.2019.08.008
Overland, I., and Sovacool, B. K. (2020). The misallocation of climate research funding. Energy Res. Soc. Sci . 62:101349. doi: 10.1016/j.erss.2019.101349
Palmer, J. (2023). Try a touch of intellectual humility. Nature 622, 2020–2022. doi: 10.1038/d41586-023-03063-w
Pingali, P. (2012). Green revolution: impacts, limits, and the path ahead. Proc. Natl. Acad. Sci. USA 109, 12302–12308. doi: 10.1073/pnas.0912953109
Pretty, J., Sutherland, W. J., Ashby, J., Auburn, J., Baulcombe, D., Bell, M., et al. (2010). The top 100 questions of importance to the future of global agriculture. Int. J. Agric. Sustain 8, 219–236. doi: 10.3763/ijas.2010.0534
Reed, M. S., and Fazey, I. (2021). Impact culture: transforming how universities tackle twenty first century challenges. Front. Sustain 2:662296. doi: 10.3389/frsus.2021.662296
Rigg, J., and Mason, L. R. (2018). Five dimensions of climate science reductionism. Nat. Clim. Change 8, 1030–1032. doi: 10.1038/s41558-018-0352-1
Schipper, E. L. F. (2020). Maladaptation: when adaptation to climate change goes very wrong. One Earth 3, 409–414. doi: 10.1016/j.oneear.2020.09.014
Schipper, E. L. F., Dubash, N. K., and Mulugetta, Y. (2021a). Climate change research and the search for solutions: rethinking interdisciplinarity. Clim. Change 168:18. doi: 10.1007/s10584-021-03237-3
Schipper, E. L. F., Eriksen, S. E., Fernandez Carril, L., Glavovic, B., and Shawoo, Z. (2021b). Turbulent transformation: abrupt societal disruption and climate resilient development. Clim. Dev . 13, 467–474. doi: 10.1080/17565529.2020.1799738
Schneider, F., Giger, M., Harari, N., Moser, S., Oberlack, C., Providoli, I., et al. (2019). Transdisciplinary co-production of knowledge and sustainability transformations: three generic mechanisms of impact generation. Environ. Sci. Policy 102, 26–35. doi: 10.1016/j.envsci.2019.08.017
Schneider, F., Llanque-Zonta, A., Andriamihaja, O. R., Andriatsitohaina, R. N. N., Tun, A. M., Boniface, K., et al. (2022). How context affects transdisciplinary research: insights from Asia, Africa and Latin America. Sustain. Sci . 17, 2331–2345. doi: 10.1007/s11625-022-01201-3
Shah, H. (2020). Global problems need social science. Nature 577:295. doi: 10.1038/d41586-020-00064-x
Thornton, P., Dijkman, J., Herrero, M., Szilagyi, L., and Cramer, L. (2022). Viewpoint: aligning vision and reality in publicly funded agricultural research for development: a case study of CGIAR. Food Policy 107:102196. doi: 10.1016/j.foodpol.2021.102196
Thornton, P., Mason D'Croz, D., Kugler, C., Remans, R., Zornetzer, H., and Herrero, M. (2024). Enabling food system innovation: accelerators for change. Glob. Food Sec ur . 40:100738. doi: 10.1016/j.gfs.2023.100738
Venot, J. P., Giordano, M., and Merrey, D. J. (2015). On the sidelines: social sciences and interdisciplinarity in an international research centre. Water Altern . 8, 415–432.
Vermeulen, S. J., Dinesh, D., Howden, S. M., Cramer, L., and Thornton, P. K. (2018). Transformation in practice: a review of empirical cases of transformational adaptation in agriculture under climate change. Front. Sustain. Food Syst . 2:65. doi: 10.3389/fsufs.2018.00065
Voulvoulis, N., Giakoumis, T., Hunt, C., Kioupi, V., Petrou, K. N., Souliotis, I., et al. (2022). Systems thinking as a paradigm shift for sustainability transformation. Glob. Environ. Chang e 75:102544. doi: 10.1016/j.gloenvcha.2022.102544
Weaver, C. P., Mooney, S., Allen, D., Beller-Simms, N., Fish, T., Grambsch, A. E., et al. (2014). From global change science to action with social sciences. Nat. Clim. Chang. 4, 656–659. doi: 10.1038/nclimate2319
Keywords: social science, transdisciplinary partnerships, climate action, agricultural research and development, impact
Citation: Hellin J, Fisher E and Bonatti M (2024) Transforming agricultural research and development systems to meet 21st Century needs for climate action. Front. Sustain. Food Syst. 8:1398079. doi: 10.3389/fsufs.2024.1398079
Received: 08 March 2024; Accepted: 23 April 2024; Published: 07 May 2024.
Reviewed by:
Copyright © 2024 Hellin, Fisher and Bonatti. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jon Hellin, j.hellin@irri.org
This article is part of the Research Topic
Reforming Agri-food Research And Development Systems To Meet 21st-Century Needs

IMAGES
VIDEO
COMMENTS
Health policy is a critical component of health system strengthening to respond to the burden of MSK diseases and persistent pain. The priorities for health systems in the 21st century have evolved from the 20th century, particularly in the context of challenges associated with ageing and NCDs and also, currently, the COVID19 pandemic.
The world has lived through an extraordinary global health threat, the COVID-19 pandemic, leading to nearly 20 million deaths, staggering economic losses, a generational decline in human capital, and the first decline in global life expectancy since 1950 (the first year when UN estimates were published).1-4 Another major threat, climate change, now has broad scientific, political, and social ...
Most health systems around the world are designed around a single condition or body system, with ever-increasing sub-specialization by health professionals in recent decades.
Shobana Kamineni. Non-communicable diseases (NCDs) are one of the 21st century's major health and development challenges, both in terms of human suffering and the damage they cause to a country's socioeconomic fabric. NCDs carry a huge cost that extends beyond health, creating enormous disparities in terms of opportunity, wealth and power. NCDs ...
At the same time, more - and more intense - extreme weather events like drought and floods increase malnutrition rates and help spread infectious diseases like malaria. 2. Delivering health in conflict and crisis. WHO records show attacks on medical staff led to 193 deaths in 2019.
Global Health Threats of the 21st Century. Finance & Development, December 2014, Vol. 51, No. 4. PDF version. The world is a healthier place today but major issues continue to confront humanity. The world's health greatly improved in the past century. Major killers such as smallpox and polio have been eliminated or contained. A large part of ...
Countries worldwide are facing complex and diverse health challenges in 21st century, and usually there is one national health system for individual and population health outcomes. The COVID-19 pandemic and other emerging health challenges have exposed gaps and fragmentation in health systems with limited public health capacities and governance. In this context, "essential public health ...
10 global health issues to track in 2021. 2020 was a devastating year for global health. A previously unknown virus raced around the world, rapidly emerging as one of its top killers, laying bare the inadequacies of health systems. Today, health services in all regions are struggling to both tackle COVID-19, and provide people with vital care.
The Science Base for Infectious Diseases in the 21st Century. Critical to our ability to meet the challenges of infectious diseases in the 21st century is the continual and rapid evolution of the scientific and technological advances that serve as the foundation for the response of the public health enterprise to established, emerging, and ...
An important global health priority agenda for the twenty-first century is achieving the MDGs. Unfortunately, many of the low-income countries are unlikely to achieve these goals, primarily ...
The "magic bullet" era. Drug therapy began centuries ago with the use of plant extracts and progressively evolved into the development of purified and targeted materials for a wide range of ...
As the year 2022 winds down, what is next on the horizon for global health? We turned to our IHME experts for their takes on the most critical health issues to watch in 2023. Entering our fourth year grappling with COVID-19, most of our experts pointed to issues that were impacted in some way by the pandemic, like long COVID and mental health.
The challenge in adults is to combat the emergence of chronic diseases. We have to work to ensure health in middle-aged populations and to limit the impact of cancer, heart disease, mental health problems, and so on. It is estimated that climate change will cause an additional 250,000 deaths a year between 2030 and 2050.
One of the critical heal th concerns that are preval ent these days is the lack of a c cess to. better healthcare. As someone living in a third-world country, I am not privileged enough to. experience quality health care m os t especially becau se I do not have the m eans to pay for a bette r. service.
Mar 5, 2019. The changes in our world are having a direct impact on the medical industry. The 21st century has the most advanced medical technology compared to any previous century, but it also has unique problems that make it necessary for healthcare to adapt. From nursing shortages to changes in healthcare technology statistics, hospitals and ...
For this article, I will be focusing on five challenges for public health in the coming decades. 1.) Changing demographics in Europe. The first challenge is the changing demographics in Europe. Climate change, urbanisation, migration and an ageing population are transforming our demographics at the speed of light.
455 Reading Time: 3 minutes. The 21st century is full of progress, scientific discovery, and innovation. As the pace of modern development is so rapid that it's easy to lose sight of the fact that increased convenience sometimes comes with new risks to people's health, which may be overlooked for the time being but won't go away permanently.
Abstract. The progress of science and medicine is unabating and moves with a rapidity that threatens to outstrip our current ethical models and legal protections. Topics which were once confined to the realms of science fiction are now becoming integral to modern scientific practice. This article will examine three such topics: genetic testing ...
What are some of the Most Critical Health Concerns We Face in the 21st Century and Why? The progressions in our world are directly affecting the medical industry. The 21st century has the most developed clinical technology compared to any earlier century, however it additionally has sole issues that make it important for health care to modify.
May 6, 2024. By Ellen Barry. She covers mental illness. For years now, policymakers have sought an explanation for the mental health crisis among young people. Suicide attempts and psychiatric ...
Climate shocks to agriculture threaten food security, especially in the Global South. Poverty and malnutrition are rising rapidly and there are dire warnings of what is to come. Agricultural research and development systems need to generate multiple game-changing innovations in order to transform our agricultural systems and ensure that they are climate-resilient, productive, sustainable, and ...