- Search Menu
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Urban Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Papyrology
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Evolution
- Language Reference
- Language Acquisition
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Media
- Music and Religion
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Science
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Lifestyle, Home, and Garden
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Clinical Neuroscience
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Ethics
- Business Strategy
- Business History
- Business and Technology
- Business and Government
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic History
- Economic Systems
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Behaviour
- Political Economy
- Political Institutions
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Theory
- Politics and Law
- Public Policy
- Public Administration
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Developmental and Physical Disabilities Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

- < Previous chapter
- Next chapter >

10 Conducting Mixed Methods Literature Reviews: Synthesizing the Evidence Needed to Develop and Implement Complex Social and Health Interventions
Jennifer Leeman, DrPH, MDiv, is an Assistant Professor at the University of North Carolina at Chapel Hill School of Nursing. Her research focuses on identifying, translating, and disseminating the evidence base for prevention interventions that target change at the levels of behavior, environments, and policy. Dr. Leeman is Co-Principal Investigator of the Centers for Disease Control and Prevention (CDC)-funded Center for Training and Research Translation in Obesity Prevention (2004-2014) and Principal Investigator of the Comprehensive Cancer Control Collaborative, NC (2009-2014), a National Cancer Institute/CDC-funded center that works with nine other centers nationwide to advance dissemination and implementation science in the area of cancer prevention and control. She has published numerous mixed-methods literature reviews and served as a co-investigator on two National Institutes of Health-funded mixed-methods literature synthesis studies.
Corrine I. Voils is Associate Professor, Durham Veterans Affairs Medical Center and Duke University Medical Center. Dr. Voils’ primary research interest is in developing and testing behavioral interventions to improve dietary intake, physical activity levels, and medication adherence for chronic disease prevention and management. She uses mixed methods for intervention development and evaluation as well as survey/measure development. Previously, she co-led with Dr. Margie Sandelowski a National Institutes of Health-funded methodology project to develop and evaluate methods for synthesizing qualitative and quantitative research.
Margarete Sandelowski has published widely in nursing, interdisciplinary health, and social science anthologies and journals in the areas of technology and gender, infertility and prenatal diagnosis, and of qualitative and mixed-methods primary research and research synthesis. Among her funded studies are three National Institutes of Health (NIH)/National Institute of Nursing Research (NINR) R01 grants for mixed-methods research projects. Most recently she completed a NIH/NINR-funded study to develop techniques to synthesize qualitative and quantitative research findings. She is currently multiple PI (with Kathleen Knafl) of the NIH/NINR-funded “Mixed-methods synthesis of research on childhood chronic conditions and family,” which is directed toward integrating the findings of empirical research addressing the intersection between family life and childhood chronic physical conditions. Her many publications in the mixed-methods research domain include Sandelowski, M. (2014). Unmixing mixed-methods research. Research in Nursing & Health, 37, 3-8; Sandelowski, M., Voils, C. I., & Knafl, G. (2009). On quantitizing. Journal of Mixed Methods Research, 3, 208-222; Song, M., Sandelowski, M., & Happ, M. B. (2010). Current practices and emerging trends in conducting mixed-methods intervention studies in the health sciences. In A. Tashakkori & C. Teddlie (Eds.), Sage handbook of mixed methods in social & behavioral research (2nd ed., pp. 725-747). Thousand Oaks, CA: Sage; and Sandelowski, M., Voils, C. I., Leeman, J., & Crandell, J. L. (2012). Mapping the mixed research synthesis terrain. Journal of Mixed Methods Research, 6, 317-331.
- Published: 19 January 2016
- Cite Icon Cite
- Permissions Icon Permissions
Systematic literature reviews serve the purpose of integrating findings from reports of multiple research studies and thereby build the evidence base for both research and practice. Mixed methods literature reviews (MMLRs) are distinct in that they summarize and integrate findings from qualitative, quantitative, and mixed methods studies via qualitative and/or quantitative methods. Although MMLRs encompass a range of approaches, the focus of this chapter is on their potential to contribute to the evidence base for complex social and health interventions. The chapter includes examples illustrating how MMLRs have been applied to synthesize evidence for complex interventions and concludes with a discussion of the challenges involved and suggestions for surmounting them.
Introduction
Systematic literature reviews serve the purpose of integrating findings from reports of multiple research studies and, thereby, build the evidence base for both research and practice. Like mono-method research reviews, mixed methods literature reviews (MMLRs) are systematic in that they follow specified research protocols for retrieving literature and extracting and synthesizing data from that literature. MMLRs are distinct in that they summarize and integrate findings from qualitative, quantitative, and mixed methods studies via qualitative and/or quantitative methods. In MMLRs “what is ‘mixed’ are both the object of synthesis (i.e., the findings appearing in written reports of primary qualitative, quantitative, and mixed methods studies) and the mode of synthesis (i.e., the qualitative and quantitative approaches to the integration of those findings)” ( Sandelowski, Voils, Leeman, & Crandell, 2012 , p. 317). Although MMLRs encompass a range of approaches (e.g., Harden & Thomas, 2010 ; Pope, Mays, & Popay, 2007 ), in this chapter, we focus on MMLRs used for the purpose of building the evidence base for practice. We focus, in particular, on the use of MMLR as an approach to developing and implementing complex social and health interventions, in other words, interventions that aim to improve the well-being of individuals and populations either directly (e.g., behavioral and education interventions) or indirectly via changes to policies, systems, and environments.
Although MMLRs constitute a relatively small percentage of published reviews of the literature, their numbers are increasing rapidly. Much of this growth is being driven by calls for greater use of research findings in practice coupled with the recognition that this will require greater understanding of the contexts and perspectives of the potential users of those findings ( Chalmers & Glasziou, 2009 ; Glasgow et al., 2012 ; Tunis, Stryer, & Clancy, 2003 ). Because MMLRs include methodologically diverse findings and multiple methods, they are well suited to the goal of capturing and analyzing the breadth of evidence needed to incorporate users’ contexts and perspectives into the understanding and use of interventions. The inclusion of diverse findings and use of multiple methods also present distinct challenges to those conducting MMLRs. Accordingly, in this chapter, we present an overview of MMLRs’ potential to contribute to the science and practice of complex interventions followed by illustrations of how MMLRs may be applied to build the evidence base. The chapter concludes with a summary of challenges involved in conducting MMLRs of complex interventions and suggestions for surmounting them.
Mixed Methods Literature Reviews’ Potential to Contribute to the Science and Practice of Complex Interventions
Interventions include programs, processes, policies, or guidelines that are intended to improve the well-being of individuals and populations. Historically, generating the evidence base for these interventions has been focused on assessing their effectiveness at achieving targeted outcomes via single-method “effectiveness reviews” of single-method findings. The Cochrane Collaboration, National Institute for Health and Clinical Excellence, and Campbell Collaboration are among the major producers of effectiveness reviews.
Effectiveness reviews involve the use of quantitative methods (e.g., meta-analysis) to summarize and synthesize quantitative findings of an intervention’s effects on outcomes ( Pope et al., 2007 ). For example, Ellis et al. (2004) systematically reviewed diabetes education interventions and applied meta-analysis to synthesize findings on the 28 identified interventions’ effectiveness at improving glycemic control. They identified diabetes education interventions as effective based on the finding that glycemic levels for participants in the intervention groups were .32% lower than for those in the control groups. In many cases, the studies testing an intervention are too few or too dissimilar to synthesize via meta-analyses. In such cases, vote counting can be used to quantify the number of studies in support versus not in support of an intervention’s effectiveness, frequently with additional weight given to studies deemed to have greater methodological rigor ( Cooper, 2010 ). Vote counting is illustrated in Goode, Reeves, and Eakin’s (2012) systematic review of telephone-delivered interventions to increase physical activity and/or improve dietary behavior, in which they counted the number of cases in which the intervention groups’ outcomes were significantly better than the comparison groups’ ( n = 20) versus the number in which they were not ( n = 7).
Although effectiveness reviews have made invaluable contributions to the evidence base for intervention effectiveness, they have been criticized for failing to provide the full range of evidence necessary to generalize findings to new contexts and implement them in real-world settings. As is described in greater detail later, effectiveness reviews have been critiqued for decontextualizing findings, excluding available evidence, and taking a largely atheoretical approach to the assessment of interventions and their effects. Thus they provide information on the net effectiveness of an intervention but fail to detail contextual factors or to build theory that might explain variations in effectiveness across different settings, populations, providers, and approaches to intervening.
The limitations of effectiveness reviews are especially evident for complex social and health interventions. Interventions are complex to the extent that they include multiple components, function at multiple levels, target multiple outcomes, and/or are designed to be tailored and individualized to recipients’ needs and preferences ( Craig et al., 2008 ). Complex interventions may include intervention programs, such as a multicomponent diabetes self-management intervention tailored to recipients’ self-management priorities. They may also include professional, organizational, and public policies such as a public policy requiring that elementary schools implement specific nutrition standards or guidelines specifying the optimal approach to depression screening. To further complicate the issue, complexity encompasses not only the intervention but also the systems within which interventions function ( Sterman, 2006 ). With few exceptions, social and health interventions function within complex systems comprised of numerous heterogeneous components and actors interrelating across multiple levels, such as cafeteria staff working in local schools that operate as part of school districts and food distribution systems or patient-care teams functioning within a medical center that is part of a larger healthcare system ( Hammond, 2009 ; Sterman, 2006 ).
Effectiveness reviews assess the evidence on “what works” by documenting the regularity of the relationship between an intervention and its outcomes ( Howe, 2012 ). In assessing effectiveness, reviewers apply a largely reductionist analytic approach that views interventions as something that can be extracted and understood independent from the broader contexts in which they function. This reductionist approach is consistent with the conventional approach to knowledge translation whereby interventions are viewed as something that can be identified, “commodified,” and then “rolled out across organizations” ( Greig, Entwistle, & Beech, 2012 , p. 305).
Complex interventions challenge a reductionist approach on multiple fronts. Because they involve multiple, flexible, and often interacting activities, complex interventions are difficult to standardize ( Ogilvie, Egan, Hamilton, & Petticrew, 2011 ), and reviewers are challenged to identify the configuration of activities that constituted “the intervention” and achieved the intended outcomes. Furthermore, intervention activities often affect intended outcomes through their effects on a chain of intermediate outcomes (i.e., mediators) that are essential to understanding why an intervention works ( Sidani & Braden, 1998 ).
The effects of intervention activities on intermediate and longer term outcomes are largely a function of how activities interact with contexts. The extent of this interaction is so integral to complex interventions as to trouble the legitimacy of trying to understand interventions separate from the contexts in which they occur ( Greig et al., 2012 ). Reviewers have attempted to capture the interaction between contextual factors and interventions by assessing the moderating effects of factors such as intervention setting or characteristics of inteveners or participants (e.g., race/ethnicity, literacy level). These reviewers often report that data are insufficient to assess variations in outcomes relative to different contextual factors (e.g., Rueda et al., 2006 ). Even when data are sufficient, this approach does not capture the interaction of interventions with the dynamics of complex systems ( Hawe, Shiell, & Riley, 2009 ). Therefore, the evidence base to guide interventions cannot be garnered solely, or even principally, via systematic reviews that take a reductionist approach. Developing the evidence base for intervening requires evidence on how intervention activities, contextual factors, and intermediate and longer term outcomes interact as part of complex systems. In other words, it requires evidence in the form of theories explaining “what works for whom in what circumstances and in what respects” ( Pawson, 2006 , p. 74).
Traditional effectiveness reviews offer conclusions about whether complex interventions have worked, but they do so by “establishing black box associations” between interventions and outcomes ( Howe, 2011 , p. 169). These reviews provide little guidance on how and why the interventions worked or how they functioned differently across contexts ( Pawson, 2006 ). For example, an effectiveness review may quantify the extent to which a problem-centered math intervention led to improvements in sixth graders’ ability to correctly answer word problems. The review typically does not, however, identify which intervention activities (or combination of activities) were effective (i.e., the intervention’s “active ingredients”; Miller, Druss, & Rohrbaugh, 2003 ). In other words, did students improve because the intervention included small work groups, didactic content, tailored practice problems, and/or peer coaching? The findings also will not address the mechanisms through which the intervention affected students’ performance (i.e., intermediate outcomes or mediators). Did students improve because they became more confident, developed new strategies, gained new knowledge, and/or became more motivated? The reviews also provide little evidence on how the effects of active ingredients on mediators and outcomes may have varied across differences in contextual factors (i.e., moderated mediation) such as subgroup and/or community cultures, teachers’ training and experience, students’ prior educational experiences, students’ math aptitudes, or class size. Review findings also do not provide guidance on how to navigate multiple levels and negotiate with diverse actors within the school system to promote widespread intervention adoption and implementation.
To build the evidence base for complex interventions, “the evidence for their effectiveness must be sufficiently comprehensive to encompass that complexity” ( Rychetnik, Frommer, Hawe, & Shiell, 2002 , p. 119). As detailed in the following section, MMLRs are well positioned to encompass complexity (i.e., multiple components, levels, or outcomes) by virtue of the fact that they capture more of the available data, apply and often integrate both inductive and deductive approaches, and prioritize the development of theories.
Mixed Methods Literature Reviews Include More of the Available Data
By design, effectiveness reviews include only a subset of the literature reporting the development and testing of an intervention, and they thereby exclude much of the available evidence. The exclusion of evidence is largely the result of the priority placed in effectiveness reviews on internal validity and resulting restrictions on the types of studies and publications included ( Glasgow et al., 2012 ). A Cochrane review, for example, “would typically seek all rigorous studies (e.g. randomized trials)” testing the effectiveness of an intervention ( Higgins & Green, 2011 , 5.1.2). Restrictive inclusion criteria may be appropriate for making claims about an intervention’s effect on outcomes, but these criteria limit the inclusion of evidence on how interventions work and how they vary across contexts ( Lewin et al., 2012 ). They may exclude data on participants’ and providers’ perceptions of the intervention or on contextual factors that impeded or facilitated intervention implementation, delivery, and receipt. MMLRs, however, have the potential to include a broader range of studies that provide additional evidence, including studies that are preliminary to controlled trials (e.g., pilot studies with quasi-experimental designs) or that, by design, prioritize a deep understanding of the interplay of contexts and effects, such as case studies or ethnographies. They also have the potential to capture more data from publications included in the review, such as data on intervention feasibility or acceptability or users’ experiences with an intervention. Broader inclusion criteria are particularly important in areas where most of the available evidence is from observational or quasi-experimental designs, such as public policy and health systems research ( Baxter, Killoran, Kelly, & Goyder, 2010 ; Kelly et al., 2010 ; Lewin et al., 2012 ; Rockers et al., 2012 ).
Mixed Methods Literature Reviews Apply and Often Integrate Inductive and Deductive Approaches
When developing research questions, reviewers determine the extent to which their review will be guided by questions and constructs that emerge during the course of the literature review (inductive) as opposed to those that are predefined (deductive). Conventional effectiveness reviews take a predominantly confirmatory or deductive approach. In fact, guidelines for conducting and critiquing these reviews specify that review questions, variables, and constructs be identified a priori (The Cochrane Collaboration, 2011; Shea et al., 2007 ). MMLRs, on the other hand, often apply an inductive approach, with reviewers identifying one or more broad research questions and then iteratively identifying and conceptualizing phenomena and their interrelationships as they emerge during the review ( Dixon-Woods, Agarwal, Jones, Young, & Sutton, 2005 ). The evidence base for many complex interventions is in the early stages of development, and, therefore, an inductive approach is critical to discovering unknown and therefore unanticipated phenomena and relationships. For example, Jagosh et al. (2012) conducted a MMLR of the benefits of participatory research, or research that involves an ongoing partnership between the researchers and the people affected by the problems being studied. Although previous reviewers had assessed the value of participatory research, their review methodologies “failed to embrace the complexity of programs or address mechanisms of change” (p. 313). In light of the limited knowledge of how participatory research works, Jagosh et al. took an inductive approach to their review. Rather than identifying variables and constructs a priori, they extracted data on any findings describing how any participatory research process led to an outcome, organized data into themes, and created visual maps of each partnership to depict the evolving relationships among contexts, mechanisms, and outcomes. They then sought patterns of relationships across the projects’ maps with the goal of developing theory to describe the outcomes of participatory research and explain how they occur and why they vary across projects.
Similar to primary mixed methods studies, MMLRs often incorporate inductive and deductive approaches over a series of stages by connecting the findings from an initial inductive analysis of data with findings from subsequent deductive analyses to confirm identifed relationships. Findings from one analysis can be placed beside, “sprinkled” onto, or “mixed” into the findings from a review of the other type of evidence, as when quotations are inserted into findings from a quantitative synthesis ( Bazeley & Kemp, 2012 , pp. 59–60). An analysis of one type of data (e.g., quantitative) may be used to confirm, explain, or explore findings from analysis of another type of data (e.g., qualitative; Creswell, Klassen, Plano Clark, & Clegg Smith, 2011 ). For example, Thomas et al. (2003) conducted a meta-analysis to assess the effects that healthy eating interventions had on children’s fruit and vegetable consumption. They also synthesized qualitative and quantitative findings on children’s views of healthy eating and then integrated findings from both analyses to explore whether interventions were more effective when they were consistent with children’s views. The ability to transition between types of evidence and synthesis methods allows MMLRs the flexibility to draw on the strengths of both qualitative and quantitative data and both inductive and deductive approaches.
Mixed Methods Literature Reviews Prioritize Theory Development
Greater use of theory has been recommended as a central approach to addressing the challenges introduced by the complexity of interventions and the systems in which they function ( Craig et al., 2008 ; Kelly et al., 2010 ; Ogilvie et al., 2011 ). MMLRs may be used to focus on refining or creating theories or conceptual frameworks. The inductive approach afforded by MMLRs offers the advantage of allowing for the discovery of new phenomena and relationships and thereby the development and refinement of theory. Reviewers contribute to theory development and testing via the configuration or aggregation of data, the two defining logics of MMLRs ( Sandelowski et al., 2012 ). Synthesis by configuration involves arranging thematically different phenomena into “a coherent theoretical rendering of them” ( Sandelowski et al., 2012 , p. 325). Reviewers applying logic of configuration explore interrelationships among phenomena with the goal of developing theory to explain why, how, and when they are related. Quantitative approaches to configuring mixed data include structural equation modeling and mediation meta-analyses. Qualitative approaches include meta-ethnography, framework-based synthesis, realist synthesis, meta-synthesis, and grounded theory ( Dixon-Woods, 2011 ; Harden & Thomas, 2010 ; Pawson, 2006 ; Sandelowski & Barroso, 2007 ). The Jagosh et al. (2012) review described earlier is an example of a review that applied logic of configuration to develop beginning theory to explain how participatory-research interventions work and why they vary across contexts.
Synthesis by aggregation, on the other hand, involves pooling or merging findings considered to address similar phenomena and relationships in order to quantify the extent and nature of those relationships ( Sandelowski et al., 2012 ). Aggregation methods may be used to test and refine theory by, for example, assessing the weight of evidence in support of relationships posited by existing or reviewer-developed theories and then modifying theory accordingly. Although inherently quantitative, the logic of aggregation may be applied to merge quantitative and qualitative data. Review methodologies that fall within this logic include meta-analysis, meta-summary, and vote counting ( Sandelowski et al., 2012 ). Meta-analysis is a method in which effect sizes (i.e., a statistic representing the difference between the intervention and control group or between two interventions) are pooled across studies. Bayesian meta-analysis is a specific type of meta-analysis in which the findings from prior studies are updated with new evidence as it is obtained. Meta-summary is a quantitatively oriented approach to synthesizing qualitative data whereby the prevalence of findings across reports indicates the extent of replication ( Sandelowski & Barroso, 2007 ). Vote counting is a method in which the proportion of studies reporting a statistically significant finding or reporting a finding of a minimum effect size is calculated.
How Mixed Methods Literature Reviews May be Applied to Build the Evidence Base for Complex Interventions
In the following section, we review a range of questions that MMLRs may address and illustrate how MMLRs may be applied to build the evidence base for complex interventions (see Table 10.1 for an overview). This section is organized around the conceptualization of complex interventions as the interaction of intervention and implementation activities, contextual factors, and intermediate and longer term outcomes within complex systems.
Mixed Methods Literature Reviews Contribute to Understanding Intervention and Implementation Activities
In the implementation science literature, a distinction typically is made between intervention and implementation activities, with intervention activities targeting change in the intervention’s intended outcomes and implementation targeting the adoption or integration of interventions within organizations or systems ( Dissemination and Implementation Research in Health , 2010 ). We maintain this distinction, recognizing that the line between intervention and implementation activities often is blurred for complex interventions, particularly those that target change at the level of policies, systems, and environments rather than at the level of individuals or populations. For example, creating a system to remind physicians to screen for colorectal cancer may be conceived as an intervention activity to improve rates of colorectal screening in the clinic’s population or as an implementation activity to increase physicians’ use of an intervention (colorectal screening guidelines) within a clinic system. Taxonomies have been created for use in systematically reviewing organization-level implementation activities, which include, among others, use of reminder systems and change agents, audit and feedback, technical assistance, coaching, and a range of quality improvement methods ( Effective Practice and Organisation of Care, 2002 ; Fixsen, Naoom, Blase, Friedman, & Wallace, 2005 ; Shojania et al., 2004 ). Michie et al. (2011) created a taxonomy of policy-level activities such as legislating, regulating, and environmental/social planning that may be applied to either intervention or implementation activities.
MMLRs may contribute to describing intervention components and identifying those intervention components (i.e., active ingredients) required to achieve intermediate or longer term outcomes. Abraham and Michie (2008) created a taxonomy of intervention components for use in systematic reviews of behavioral change interventions, which includes components such as providing information, encouraging, setting goals, and providing feedback. Identifying an intervention’s active ingredients will aid in determining those components that must be retained versus those that might be adapted when an intervention is transferred to new contexts ( Baker et al., 2008 ; McKleroy et al., 2006 ). What is referred to here as active ingredients may also be referred to as core elements ( Galbraith et al., 2011 ) or as causal mechanisms ( Pawson, 2006 ). Care should be taken with the term causal mechanism because its use often conflates components of the intervention (i.e., active ingredients) with intermediate outcomes that mediate the intervention’s effects on longer term outcomes.
To illustrate the use of MMLR for identifying active ingredients, O’Campo, Kirst, Tsamis, Chambers, and Ahmad (2011) conducted a MMLR of intimate partner violence screening programs in healthcare settings with the goal of identifying the active ingredients responsible for screening programs’ success in increasing provider self-efficacy and rates of universal screening (program outcomes). They identified four active ingredients (institutional support, staff training, screening protocols, and access to on- and off-site support services) and created a conceptual model to configure the relationship of these ingredients to program outcomes.
MMLRs may also be used to describe components of implementation activities. For example, Rycroft-Malone et al. (2012) conducted a MMLR to configure a beginning theory of active ingredients of “change agents” as an approach to implementing change. The term change agents encompassed the roles of, among others, opinion leaders, facilitators, and knowledge brokers, and was used to refer to individuals who were successful in promoting the adoption and implementation of change (e.g., interventions). Rycroft-Malone et al. found, for example, that serving as a role model for a desired change in practice may be one of the active ingredients by which change agents promote implementation of change.
In addition to identifying the core components of intervention and implementation activities, MMLRs may contribute to providing practical guidance on how to deliver and implement specific interventions. Rogers (2003) described this as “how to” guidance, which may include training and oversight of those implementing and delivering the intervention, deviations between the intervention as planned and delivered, resources required, barriers encountered, how barriers were overcome, and other lessons learned from prior implementations of the intervention ( Baker et al., 2008 ; Leeman, Sommers, Leung, & Ammerman, 2011 ). Efforts to use MMLRs to identify implementation guidance have been limited by the lack of implementation data provided in published reports ( Arai et al., 2005 ; Egan et al., 2009 ; Roen et al., 2006 ).
Mixed Methods Literature Reviews Contribute to Understanding Intermediate Outcomes
MMLRs also may be used to identify the intermediate outcomes through which intervention activities both cause and contribute to intended outcomes, a central component of an intervention’s theory of change ( McKleroy et al., 2006 ; Michie, van Stralen, & West, 2011 ). Michie et al. (2005) developed a widely used taxonomy of the intermediate outcomes (i.e., mediators) through which interventions cause behaviors to change, such as knowledge, skills, and motivation. To illustrate how MMLRs may be applied to better understand mediators, Leeman, Chang, Voils, Crandell, & Sandelowski (2011) conducted an initial inductive review of qualitative and quantitative observational studies to identify potential mediators of individuals’ adherence to antiretroviral regimens. They then used the identified list of eight mediators (e.g., social support) to guide a deductive mediation meta-analysis of both quantitative observational and intervention studies to assess the strength of evidence in support of their potential role as mediators of intervention effects on individuals’ adherence.
Not all intermediate outcomes function as mediators in that they may not be directly linked into a causal chain between interventions and the intended outcomes. Many intermediate outcomes may best be conceived as one of multiple strands that contribute to or support intended outcomes without directly or indirectly “causing them.” For example, as Figure 10.1 illustrates, although intervening to create more sidewalks may not directly cause improvements in physical activity and health status among the population, it may contribute to and support those changes. Multiple other interventions will need to occur to achieve changes in population physical activity and health status. Lavis et al. (2012) developed a taxonomy of organizational and public policy changes generally supportive of longer term outcomes that include changes to governance (e.g., what entities set policies and how they are enforced), finances (e.g., how providers are remunerated, the fees consumers pay), and delivery arrangements (e.g., who delivers services, where and with what level of support). Supportive intermediate outcomes also include changes in environments and sociocultural mechanisms ( Baxter et al., 2010 ). Developing the evidence base for the value of supportive interventions is difficult because most research tends to “deal with end points and outcomes rather than the many and interrelated social and behavioural, structural and cultural intermediate points along the causal chain” ( Kelly et al., 2010 , p. 1060). MMLRs address this challenge by enabling the development of theories of change and synthesis of evidence in support of the intermediate, interrelated outcomes along the causal chain ( Baxter et al., 2010 ; Kelly et al., 2010 ). Identifying intermediate outcomes will also be helpful in identifying proxy measures of success for interventions ( Lewin et al., 2012 ). Using the example of sidewalks, successful enactment of policy and construction of more sidewalks are both measures of success on the road to increasing population-level physical activity.
Intermediate outcomes in a sidewalk intervention’s effects on health status
Mixed Methods Literature Reviews Incorporate the Perspectives of Intervention Decision Makers, Providers, and Recipients
The engagement of numerous actors is critical to the implementation and effectiveness of intervention activities. These actors include the formal and informal leaders who decide which interventions to promote and support; staff, community members, and teams who provide intervention services; and the individuals, social groups, and populations who participate in or are reached by the intervention. Understanding the perspectives of these actors is essential to developing interventions that address problems recognized as high priority and use approaches considered acceptable ( Chalmers & Glasziou, 2009 ; Glasgow et al., 2012 ; Tunis et al., 2003 ).
MMLRs may be used to incorporate qualitative research findings documenting actors’ perspectives with a range of other findings to derive a more complete understanding of problems that may be amendable to intervention. For example, Alderson, Foy, Glidewell, McLintock, and House (2012) conducted a sequential, mixed methods synthesis of patients’ beliefs about depression for the purpose of building the evidence base to better engage patients in depression screening. Using Leventhal’s Illness Representations as a guiding framework, these reviewers conducted a content analysis of interview data, during which they revised the framework to more fully capture findings. They then mapped quantitative findings onto the themes and summarized and explained findings specific to each identified theme.
MMLRs may be used to assess participants’ perspectives on the acceptability of different intervention options. Proctor and Brownson (2012) defined “acceptability” as the perception among potential users that an intervention is “agreeable, palatable, or satisfactory” (p. 265). An intervention’s acceptability will likely play a critical role in determining whether it is used in practice, which is critical to determining its potential effectiveness in improving health ( Bowen et al., 2009 ). To illustrate MMLRs’ use in advancing understanding of acceptability, Harden, Brunton, Fletcher, and Oakley (2009) reviewed reports of controlled trials of teenage pregnancy prevention interventions and then reviewed findings from research examining teenagers’ perceptions of the need and appropriateness of different approaches to intervening. They aligned the findings from the two reviews to assess the extent to which existing interventions addressed the needs and concerns of teenagers.
MMLRs may be applied to better understand individuals’ experience of receiving an intervention. To illustrate, Voils, Sandelowski, Barroso, and Hasselblad (2008) aggregated qualitative and quantitative findings on factors influencing HIV-positive women’s adherence to their antiretroviral therapies. They initially aggregated the qualitative data inductively to identify factors and their frequencies across studies. They then integrated the quantitative and qualitative data to ascertain their relationships, that is, whether findings confirmed, refuted, or extended each other. For example, from the review of qualitative findings, they found that women reported greater success with incorporating regimens into their routine schedules when the regimens were less complex, and this was confirmed by the finding from quantitative studies that having a regimen with less (as compared to more) complex dosing was associated with greater adherence.
Mixed Methods Literature Reviews Contribute to Understanding How Interventions Interact with Contexts to Affect Outcomes
Understanding how interventions interact with contexts to affect outcomes is essential to assessing an intervention’s generalizability. Understanding the interaction of interventions and contexts also is needed to determine when intervention, implementation, and/or context may need to be modified or adapted to enhance intervention/context fit and thereby achieve intended outcomes ( Glasgow, 2008 ). The effects of interventions vary across contexts because contextual factors modify (i.e., moderate) interactions among activities, mediators, and outcomes ( Ramsay, Thomas, Croal, Grimshaw, & Eccles, 2010 ). Contextual factors at the level of intervention recipients may include, for example, race, ethnicity, socioeconomic status, literacy levels, or readiness to change. Contextual factors also include the characteristics of the complex systems in which interventions occur, for example, multiple interacting social networks, organizational infrastructures, socioeconomic pressures, and incentives ( Damschroder et al., 2009 ). MMLRs can be used to synthesize evidence on how contextual factors interact with intervention and implementation activities, and intermediate and longer term outcomes. This evidence may be synthesized via aggregation or configuration to develop theory to explain how activities interact with contexts to affect intermediate and long-term outcomes.
Wong, Greenhalgh, and Pawson (2010) , for example, applied a configuration logic to develop theory to explain what types of Internet-medical education worked for whom under what circumstances. They then used vote counting to quantify the number of studies that either supported or refuted specific theoretical constructs. They determined that physician and medical student response to Internet courses was contingent on the fit between their needs and priorities and the technical attributes of the course.
Contandriopoulos, Lemire, Denis, and Tremblay (2010) conducted a MMLR to configure interrelationships among actors, contexts, and knowledge in interventions aimed at influencing behaviors or opinions through the communication of information at the organizational or policymaking level. They identified three central dimensions of context: the extent of polarization in actors’ perceptions of the problem and its potential solutions, the way intervention activity costs were distributed within the system, and characteristics of the social networks through which information was communicated. Based on review findings, they posited that the most effective approach to promoting knowledge use (i.e., implementation) would be contingent on the interaction between the extent of polarization and distribution of costs.
For an intervention to have an impact on a population’s health, it must not only be effective but also have broad reach, particularly to the populations at greatest risk and the providers and settings that serve those at-risk populations. To have maximal impact, interventions also need to be implemented with fidelity to their active ingredients and maintained over time ( Glasgow, Lichtenstein, & Marcus, 2003 ; Rychetnik et al., 2002 ). Therefore, to ensure population impact, evidence is needed on the contextual factors that influence whether providers, settings, and systems adopt an intervention, implement it with fidelity, and maintain it over time.
Leeman et al. (2010) conducted a MMLR to identify barriers and facilitators encountered in implementing antiretroviral therapy interventions. They configured implementation to include providers delivering the intervention and participants enrolling in, attending, and continuing the intervention over time. They then explored the effects that contextual factors had on each link in the implementation chain, with contextual factors including characteristics of the intervention, intervention participants and providers, and settings. Based on review findings, the researchers developed a beginning theory that posited that individuals with HIV would be more likely to enroll in interventions that protected their confidentiality and to attend when interventions were scheduled to meet their needs and when they facilitated a strong relationship with the intervener. Dropout rates were likely to be lower for individuals who had less (as opposed to more) prior experience with antiretroviral therapy and were likely to be higher when interventions were integrated into existing delivery systems than when offered as stand-alone interventions (Figure 10.2 ).
Mixed Methods Literature Reviews Contribute to the Identification of Promising Interventions
Numerous scholars have called for a shift from the prevailing approach of testing the internal validity of researcher-developed interventions and then attempting to translate them into real-world practice settings (e.g., Kessler & Glasgow, 2011 ). This approach has been critiqued not only for its limited attention to external validity but also its inattention to viability validity ( Chen, 2010 ). In designing interventions, researchers have often not attended to whether ordinary people, particularly those in greatest need of an intervention, will participate in or be reached by the intervention or whether busy clinicians, educators, and other practitioners will be able to implement it in their practice settings ( Klesges, Estabrooks, Dzewaltowski, Bull, & Glasgow, 2005 ). To identify more viable interventions, some scholars are advocating looking to identify and carry out interventions that have achieved high levels of reach, adoption, and implementation (i.e., have high viability validity) and then formally testing those interventions in studies ( Chen, 2010 ; Leviton, Khan, Rog, Dawkins, & Cotton, 2010 ). MMLRs may be used to identify promising interventions. For example, Brennan, Castro, Brownson, Claus, and Orleans (2011) reported on methods they were using in a systematic review of both research-tested and practice-based interventions for the purpose of identifying promising policy and environmental change interventions to prevent obesity in children.
Contextual factors influencing each step in an implementation chain
Challenges in Conducting Mixed Methods Literature Reviews to Develop the Evidence Base for Complex Interventions
Like other systematic reviews, MMLRs entail the formulation of purpose and research questions, search for and retrieval of relevant literature, extraction and evaluation of data from retrieved literature, and analysis and integration of extracted data ( Cooper, 2010 ). These activities are not sequential but rather cyclical in that one activity (e.g., searching for literature) often leads to revisions in a prior activity (formulation of purpose).
Multiple resources are available that provide guidance on how to conduct mono- and mixed methods systematic reviews of quantitative and/or qualitative research findings (e.g., Cooper 2010 ; Pope, Mays, & Popay, 2007 ; Sandelowski & Barroso, 2007 ; Sandelowski et al., 2012 ). In previous publications, we have addressed the challenges of conducting MMLRs such as managing data derived from different sampling (i.e., purposeful vs. probability) and data collection imperatives (open vs. closed ended), aggregating data at the study vs. subject level, and data that were adjusted versus unadjusted ( Crandell, Voils, & Sandelowski, 2012 ; Sandelowski, Voils, Crandell, & Leeman, 2013 ; Voils, Crandell, Chang, Leeman, & Sandelowski, 2011 ).
Accordingly, we highlight here only those issues distinctive to conducting MMLRs for the purpose of building the evidence base for complex interventions. Specifically, we address issues related to the extraction of findings from primary research reports and to aspects of MMLRs that have been the subject of critique, namely limitations in the way reviewers address the quality of included studies, describe their methods, and link review findings to their sources (Table 10.2 ).
Extracting Findings from Primary Research Reports
When conducting systematic reviews, reviewers typically separate contextual data from data on the intervention’s effects. In the predominant approach to data extraction, reviewers create, pilot, and then use an extraction form to standardize the collection of data on study sample, context, methods, and findings. In the typical extraction form, findings are separated from the information in other sections of the form that make those findings meaningful. Indeed, Pawson (2006) argued that the best way to avoid separating findings from context was to reject the data extraction process altogether. In his realist synthesis approach to MMLR, Pawson argued that rather than extracting data and then reintegrating it, reviewers should configure the findings from each study and then look for demi-regularities across the configurations created for included studies (e.g., Jagosh et al., 2012 ). Concerns have been raised, however, that this approach may be very time-consuming and the findings may not justify the resources required to generate them ( Sheldon, 2005 ).
Sandelowski et al. (2012) developed an approach to the extraction of primary study findings intended to preserve key aspects of the context of those findings in a comparable form regardless of whether they were produced in qualitative or quantitative studies. Findings from qualitative and quantitative studies are transformed into complete and portable statements that anchor those findings to features likely to be most relevant to understanding the context of their production. These include aspects of the sample, the source of the finding (e.g., mother-reported child depression vs. child-reported child depression), time, comparative reference point (e.g., mothers vs. fathers), magnitude and significance, and study-specific conceptualization of phenomena (e.g., family functioning defined as balance between cohesion and conflict). An example of such a statement of findings from a quantitative study is: In families with infants with a congenital heart defect, more mother-reported family cohesion immediately after diagnosis was significantly associated with more father-reported family cohesion one year after diagnosis; neither mother- nor father-reported family cohesion was related to marital satisfaction at any time. All statements addressing family cohesion—whether derived from qualitative or quantitative studies—might then be grouped together to ascertain their topical (e.g., about families with infants as opposed to older children, about congenital heart defect as opposed to other condition) and thematic (whether they confirm, refute, or otherwise modify each other) relationships to each other in preparation for synthesizing them on the basis of common relationships.
Applying Quality Criteria
Methodological problems within the primary studies included in a systematic review are a central threat to the validity of findings for all types of systematic literature reviews. Mono-method reviewers often minimize this potential for bias by excluding studies that fall below predetermined criteria for methodological quality. Yet this a priori, gate-keeping approach to research synthesis has recurrently been shown to be idiosyncratic, unreliable, and a major reason why reviews often cover only a fraction of the potentially relevant research literature available in a target domain ( Cooper, 2010 ; Ogilvie, Egan, Hamilton, & Petticrew, 2005 ; Pawson, 2008 ; Sandelowski & Barroso, 2007 ). Because the goal is to maximize the amount of data available, MMLR reviewers typically choose not to exclude studies a priori for quality reasons. With the goal of maximizing the available data, reviewers may include findings from pilot studies conducted preliminary to more rigorous tests of an intervention. By design, these studies may provide valuable information on intervention acceptability, feasibility, and approaches to increasing the fit between the intervention and variations in context ( Bowen et al., 2009 ). Reviewers may also include studies that employed quasi-experimental or case study designs to assess and explore relationships between interventions and outcomes and the range of contextual factors that may influence those relationships. Although the breadth of findings will contribute to the richness of the MMLR, the design and execution of included studies may fall short of meeting established criteria for methodological rigor in the varieties of qualitative and quantitative methods used. In their review of systematic literature reviews, Bouchard, Dubuisson, Simard, and Dorval (2011) found that authors of MMLRs were significantly less likely to account appropriately for the quality of included studies than were authors of mono-method quantitative reviews.
Yet there is no consensus on the best approach to judging the methodological quality of studies included in MMLRs ( Dixon-Woods et al., 2005 ). Efforts to establish quality criteria are challenged by the absence of widely agreed-on and reliable standards for evaluating qualitative studies ( Sandelowski, 2012 ). They are further challenged by the fact that MMLRs will require different criteria for different types of included studies and because the importance of different aspects of study design and execution varies depending on the purpose of the review ( Lewin et al., 2012 ; Pope et al., 2007 ). The problem of study quality becomes even greater when MMLRs include literature other than empirical research reports, such as theoretical papers and grey literature (e. g., unpublished or conference reports). Establishing a standardized approach to evaluating quality may not even be appropriate for MMLR, given the variety and breadth of study aims and methods at the level of both the MMLR and the included studies.
Reviewers have multiple options for addressing the quality of the studies included in a MMLR. First and foremost they need to consider the purpose of their reviews and the types of studies to be included and then select quality criteria that are most relevant to assessing validity within the distinct context of their MMLR. Different criteria will apply if the purpose of the review is to determine the weight of evidence in support of the relationship between two phenomena (e.g., gender and adherence) than if the purpose is to explore contextual factors that may explain differences in implementation. Next, reviewers need to identify criteria appropriate to their review and then justify the selected criteria in their reports of MMLR findings. A vast literature details characteristics of study design and execution that are most relevant to assessing the validity of study findings (e.g., Boeije, van Wesel, & Alisic, 2011 ; Higgins & Green, 2011 ; Pluye, Gagnon, Griffiths, & Johnson-Lafleur, 2009 ; Wong, Greenhalgh, Westhorp, Buckingham, & Pawson, 2013 ).
As with other types of systematic reviews, researchers conducting MMLRs may document concerns related to the quality of the primary literature included and then address those concerns during analysis ( Pawson, 2006 ) by addressing quality appraisal as a moderator of review findings or by giving greater weight to findings from studies that are methodologically stronger ( Pope et al., 2007 ). Reviewers also may include critical exploration of threats to validity as an integral part of the synthesis process. Dixon-Woods et al. (2006) incorporated a critical review of methods into an inductive synthesis of literature on vulnerable group’s access to healthcare and identified a concern with the predominant approach used to conceptualize and measure access. They then developed an alternative conceptualization of access they used to guide the subsequent phase of the review.
Explicating Mixed Methods Literature Reviews Methods
Of necessity, MMLRs of complex interventions often are methodologically and conceptually complicated. Reviewers retrieve a broad variety of literatures, use multiple synthesis methods, and employ an iterative approach to both retrieval and synthesis. The complexity of review methods challenges reviewers to explicate methods clearly and completely within the page limits allowed by most journals. Reviewers conducting effectiveness and other types of mono-method reviews often have the advantage of predetermined protocols that prescribe the overall design and methods for the review. The Cochrane Collaboration ( Higgins & Green, 2011 ), for example, provides reviewers with 22 chapters of guidance on how to structure their effectiveness reviews. In contrast, MMLR is a fairly new field with a growing menu of diverse and evolving designs and methods. MMLR by its very nature offers reviewers the opportunity and the challenge to select, revise, and shape their methods as the review progresses. This provides reviewers with the opportunity to select and develop approaches to fit the available literature, the data within that literature, and their evolving research purposes and questions. Although this flexibility enhances reviewers’ capacity to capture the evidence base for complex interventions, it may challenge their efforts explicitly to communicate the details of their methods.
The comprehensive and iterative nature of MMLRs mandates that reviewers take care to document and justify their methodological decisions in ways that are explicit but that accommodate journal word limits. Reviewers may make their methods more explicit by following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for documenting publication yields and exclusion decisions at each phase of the search and retrieval process ( Liberati et al., 2009 ; e.g., Alderson et al., 2012 ). Wong et al. (2013) proposed an approach similar to the PRISMA guidelines that reviewers conducting realist MMLRs may use to depict their iterative literature retrieval process within a single flow diagram (see Figure 10.3 ). Transparency also is enhanced by describing who extracted what data and from which parts of the reports, if and how data were transformed during the extraction process, and how discrepancies between extractors were reconciled.
Adapting the PRISMA approach to document an iterative MMLR search
Reviewers may also take advantage of opportunities to submit additional details of their methods in online journal supplements where available. Additional materials may include search criteria and strategy, extraction tools, and coding schemas. For example, Rycroft-Malone et al. (2012) provided a graphic summarizing the search and retrieval process and also included multiple tables within the text and as online supplements to describe the data extraction form, search terms and strategy, and stages of the synthesis process. Reviewers also may use graphics more thoroughly to describe methods; graphical approaches to methods presentations are especially useful in mixed methods reports of any kind ( Onwuegbuzie & Dickinson, 2008 ).
Linking Included Studies, Extracted Data, and Review Findings
In reporting their MMLRs, reviewers often fail to link their integrated findings to the primary sources of those findings. Linking findings to sources is particularly difficult in largely inductive studies where the findings emerge and evolve over the course of the review. To counter this critique, reviewers might link review findings to their sources in tables, text, graphics, and online supplements. For example, Hage, Roo, van Offenbeek, and Boonstra (2013) used tables to link the themes identified in an inductive review to the source documents that included each theme. Wong et al. (2010) provided supplementary documents providing examples of extracted text in support of their study findings.
Conclusions
Tackling society’s most challenging social and health problems requires the development, evaluation, and implementation of complex interventions. The explicit reporting of methods and findings is essential to ensuring that MMLRs fully contribute to improvements in complex interventions. Yet reporting is often difficult due to the diversity of the included literature and review methods. To increase the clarity of reporting, reviewers are advised to use the PRISMA guidance to detail their literature search and retrieval methods. They also might employ tables, diagrams, and online supplements to facilitate reporting of their methods and the linkage of findings to their resources.
Those conducting MMLR often also have difficulty addressing differences in the quality of the studies included in their reviews. A seemingly endless array of evermore cumbersome checklists and standards (e.g., Pluye et al., 2009 ) have been, and continue to be, advanced whereby the quality of studies is judged with a view to excluding, or severely limiting the contribution of, studies found to be deficient for research synthesis projects. Yet the value of a study cannot be determined a priori without reference to specific purposes. Moreover, methodological deficiencies do not necessarily invalidate findings or make them unusable ( Pawson, 2006 , 2008 ; Sandelowski & Barroso, 2007 ). Therefore, additional research is needed to develop methods to identify and assess the aspects of study quality that are relevant to the varying aims of different syntheses projects and to then incorporate these aspects of quality assessment into the analysis of synthesis findings.
Because MMLRs include methodologically diverse findings and multiple methods, they are well suited to the task of capturing and analyzing the breadth and depth of evidence needed to understand the activities involved in intervening and implementing complex interventions. The incorporation of both inductive and deductive approaches makes MMLRs particularly well suited to the development of theory and the exploration of interactions among intervention activities, contextual factors, and outcomes. Thus MMLRs can be used to identify gaps in knowledge regarding the generalizability of complex interventions for various settings and populations. These gaps, in turn, can lead to informed decisions about whether to obtain additional effectiveness data prior to implementation in various settings. This information ultimately can facilitate the translation of effective interventions to improve population health and well-being.
Discussion Questions
In what ways do MMLRs diverge from mono-method reviews?
Compare the use of systematic reviews designed to synthesize evidence of effectiveness to those designed to synthesize evidence of their utility in real-world contexts.
What are the distinctive contributions of MMLRs to the science and practice of implementation?
What are the distinctive challenges for conducting MMLRs for the purpose of building the evidence base for complex interventions?
Suggested Websites
www.cochrane.org
The Cochrane Collaboration promotes systematic literature reviews with a primary focus on building the evidence base for the effectiveness of healthcare interventions. The site includes access to over 5,000 systematic reviews and to resources detailing Cochrane review methods and quality criteria.
www.joannabriggs.edu.au
The Joanna Briggs Institute promotes systematic literature reviews with a primary focus on building the evidence base for healthcare. The site includes access to systematic reviews and also to resources detailing methods for appraising and synthesizing the findings from qualitative research studies.
www.campbellcollaboration.org
The Campbell Collaboration is a sibling organization to the Cochrane Collaboration. The Campbell Collaboration promotes systematic literature reviews in areas such as education, criminal justice, and social policy, among others.
Abraham, C. , & Michie, S. ( 2008 ). A taxonomy of behavior change techniques used in interventions. Health Psychology , 27 , 379–387.
Google Scholar
Alderson, S. L. , Foy, R. , Glidewell, L. , McLintock, K. , & House, A. ( 2012 ). How patients understand depression associated with chronic physical disease: A systematic review. BMC Family Practice , 13 , 41. Retrieved from http://www.biomedcentral.com/1471-2296/13/41
Arai, L. , Roen, K. , Roberts, H. , & Popay, J. ( 2005 ). It might work in Oklahoma but will it work in Oakhampton? Context and implementation in the effectiveness literature on domestic smoke detectors. Injury Prevention , 11 , 148–151.
Baker, E. A. , Brennan Ramirez, L. K. , Claus, J. M. , & Land, G. ( 2008 ). Translating and disseminating research- and practice-based criteria to support evidence-based intervention planning. Journal of Public Health Management and Practice , 14 , 124–130.
Baxter, S. , Killoran, A. , Kelly, M. P. , & Goyder, E. ( 2010 ). Synthesizing diverse evidence: The use of primary qualitative data analysis methods and logic models in public health reviews. Public Health , 124 , 99–106.
Bazeley, P. , & Kemp, L. ( 2012 ). Mosaics, triangles, and DNA: Metaphors for integrated analysis in mixed methods research. Journal of Mixed Methods Research , 6 , 55–72.
Boeije, H. R. , van Wesel, F. , & Alisic, E. ( 2011 ). Making a difference: Towards a method for weighing the evidence in a qualitative synthesis. Journal of Evaluation in Clinical Practice , 17 , 657–663.
Bouchard, K. , Dubuisson, W. , Simard, J. , & Dorval, M. ( 2011 ). Systematic mixed-methods reviews are not ready to be assessed with the available rools. Journal of Clinical Epidemiology , 64 , 926–928.
Bowen, D. J. , Kreuter, M. , Spring, B. , Cofta-Woerpel, L. , Linnan, L. , Weiner, D. , . . . Fernandez, M. ( 2009 ). How we design feasibility studies. American Journal of Preventive Medicine , 36 , 452–457.
Brennan, L. , Castro, S. , Brownson, R. C. , Claus, J. , & Orleans, C. T. ( 2011 ). Accelerating evidence reviews and broadening evidence standards to identify effective, promising, and emerging policy and environmental strategies for childhood obesity prevention. Annual Review of Public Health , 32 , 199–223.
Chalmers, I. , & Glasziou, P. ( 2009 ). Avoidable waste in the production and reporting of research evidence. Lancet , 374 (9683), 86–89.
Chen, H. T. ( 2010 ). The bottom-up approach to integrative validity: A new perspective for program evaluation. Evaluation and Program Planning , 33 , 205–214.
Contandriopoulos, D. , Lemire, M. , Denis, J. L. , & Tremblay, E. ( 2010 ). Knowledge exchange processes in organizations and policy arenas: A narrative systematic review of the literature. Milbank Quarterly , 88 , 444–483.
Cooper, H. ( 2010 ). Research synthesis and meta-analysis: A step-by-step approach (4th ed.). Los Angeles, CA: Sage.
Google Preview
Craig, P. , Dieppe, P. , Macintyre, S. , Michie, S. , Nazareth, I. , & Petticrew, M. ( 2008 ). Developing and evaluating complex interventions: The new medical research council guidance. BMJ , 337 , a1655. Retrieved from http://www.bmj.com/content/337/bmj.a1655
Crandell, J. L. , Voils, C. I. , & Sandelowski, M. ( 2012 ). Bayesian approaches to the synthesis of qualitative and quantitative research findings. In K. Hannes & C. Lockwood (Eds.), Synthesizing qualitative research: Choosing the right approach (pp. 137–159). Oxford, UK: Wiley-Blackwell.
Creswell, J. W. , Klassen, A. C. , Plano Clark, V. L. , & Clegg Smith, K. ( 2011 ). Best practices for mixed methods research in the health sciences . Bethesda, MD: National Institutes of Health Office of Behavioral and Social Sciences Research.
Damschroder, L. J. , Aron, D. C. , Keith, R. E. , Kirsh, S. R. , Alexander, J. A. , & Lowery, J. C. ( 2009 ). Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science , 4 , 50. Retrieved from http://www.implementationscience.com/content/4/1/50
Dissemination and Implementation Research in Health (R01). (2010). Washington, DC: National Institutes of Health, Department of Health and Human Services. Retrieved from http://grants.nih.gov/grants/guide/pa-files/PAR-10-038.html
Dixon-Woods, M. ( 2011 ). Using framework-based synthesis for conducting reviews of qualitative studies. BMC Medicine , 9 , 39. Retrieved from http://www.biomedcentral.com/1741-7015/9/39
Dixon-Woods, M. , Agarwal, S. , Jones, D. , Young, B. , & Sutton, A. ( 2005 ). Synthesizing qualitative and quantitative evidence: A review of possible methods. Journal of Health Services Research & Policy , 10 , 45–53.
Dixon-Woods, M. , Cavers, D. , Agarwal, S. , Annandale, E. , Arthur, A. , Harvey, J. , . . Sutton, A. J. ( 2006 ). Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Medical Research Methodology , 6 , 35. Retrieved from http://www.biomedcentral.com/1471-2288/6/35
Effective Practice and Organisation of Care. ( 2002 ). EPOC taxonomy of professional and and organisational interventions. Ottawa:. Cochrane Effective Practice and Organisation of Care Group. Retrieved from http://epoc.cochrane.org/epoc-author-resources
Egan, M. , Bambra, C. , Petticrew, M. , & Whitehead, M. ( 2009 ). Reviewing evidence on complex social interventions: Appraising implementation in systematic reviews of the health effects of organisational-level workplace interventions. Journal of Epidemiology and Community Health , 63 , 4–11.
Ellis, S. E. , Speroff, T. , Dittus, R. S. , Brown, A. , Pichert, J. W. , & Elasy, T. A. ( 2004 ). Diabetes patient education: A meta-analysis and meta-regression. Patient Education and Counseling , 52 , 97–105.
Fixsen, D. L. , Naoom, S. F. , I, K. A. , Friedman, R. M. , & Wallace, F. ( 2005 ). Implementation research: A synthesis of the literature . Tampa, FL: National Implementation Research Network. Retrieved from http://ctndisseminationlibrary.org/PDF/nirnmonograph.pdf .
Galbraith, J. S. , Herbst, J. H. , Whittier, D. K. , Jones, P. L. , Smith, B. D. , Uhl, G. , & Fisher, H. H. ( 2011 ). Taxonomy for strengthening the identification of core elements for evidence-based behavioral interventions for HIV/AIDS prevention. Health Education Research , 26 , 872–885.
Glasgow, R. E. ( 2008 ). What types of evidence are most needed to advance behavioral medicine? Annals of Behavioral Medicine , 35 , 19–25.
Glasgow, R. E. , Green, L. W. , Taylor, M. V. , & Stange, K. C. ( 2012 ). An evidence integration triangle for aligning science with policy and practice. American Journal of Preventive Medicine , 42 , 646–654.
Glasgow, R. E. , Lichtenstein, E. , & Marcus, A. C. ( 2003 ). Why don’t we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. American Journal of Public Health , 93 , 1261–1267.
Goode, A. D. , Reeves, M. M. , & Eakin, E. G. ( 2012 ). Telephone-delivered interventions for physical activity and dietary behavior change: An updated systematic review. American Journal of Preventive Medicine , 42 , 81–88.
Greig, G. , Entwistle, V. A. , & Beech, N. ( 2012 ). Addressing complex healthcare problems in diverse settings: Insights from activity theory. Social Science & Medicine , 74 , 306–312.
Hage E. , Roo, J. P. , van Offenbeek, M. A. G. , & Boonstra, A. ( 2013 ). Implementation factors and their effect on e-health service adoption in rural communities: A systematic literature review. BMC Health Services Research , 13 , 19.
Hammond, R. A. ( 2009 ). Complex systems modeling for obesity research. Preventing Chronic Disease , 6 (3), A97. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2722404/
Harden, A. , Brunton, G. , Fletcher, A. , & Oakley, A. ( 2009 ). Teenage pregnancy and social disadvantage: Systematic review integrating controlled trials and qualitative studies. BMJ , 339 , b4254. Retrieved from http://www.bmj.com/content/339/bmj.b4254
Harden, A. , & Thomas, J. ( 2010 ). Mixed methods and systematic reviews: Examples and emerging issues. In A. Tashakkori & C. Teddlie (Eds.), The SAGE handbook of mixed methods in social & behavioral research (pp. 749–774). Los Angeles, CA: Sage.
Hawe, P. , Shiell, A. , & Riley, T. ( 2009 ). Theorising interventions as events in systems. American Journal of Community Psychology , 43 , 267–276.
Higgins, J. P. T. , & Green, S. (2011, March). Cochrane handbook for systematic reviews of interventions . Cochrane Collaboration Version 5.1.0. Retrieved from http://handbook.cochrane.org/
Howe, K. R. ( 2011 ). Mixed methods, mixed causes? Qualitative Inquiry , 17 , 166–171.
Howe, K. R. ( 2012 ). Mixed methods, triangulation, and causal explanation. Journal of Mixed Methods Research , 6 , 89–96.
Jagosh, J. , Macaulay, A. C. , Pluye, P. , Salsberg, J. , Bush, P. L. , Henderson, J. , . . . Greenhalgh, T. ( 2012 ). Uncovering the benefits of participatory research: Implications of a realist review for health research and practice. Milbank Quarterly , 90 , 311–346.
Kelly, M. , Morgan, A. , Ellis, S. , Younger, T. , Huntley, J. , & Swann, C. ( 2010 ). Evidence based public health: A review of the experience of the National Institute of Health and Clinical Excellence (NICE) of developing public health guidance in England. Social Science & Medicine , 71 , 1056–1062.
Kessler, R. , & Glasgow, R. E. ( 2011 ). A proposal to speed translation of healthcare research into practice: Dramatic change is needed. American Journal of Preventive Medicine , 40 , 637–644.
Klesges, L. M. , Estabrooks, P. A. , Dzewaltowski, D. A. , Bull, S. , & Glasgow, R. E. ( 2005 ). Beginning with the application in mind: Designing and planning health behavior change interventions to enhance dissemination. Annals of Behavioral Medicine , 29 , 66–75.
Lavis, J. N. , Rottingen, J. A. , Bosch-Capblanch, X. , Atun, R. , El-Jardali, F. , Gilson, L. , . . . Haines, A. ( 2012 ). Guidance for evidence-informed policies about health systems: Linking guidance development to policy development. PLoS Medicine , 9 (3), e1001186. Retrieved from http://www.plosmedicine.org/article/info%3Adoi%2F10.1371%2Fjournal.pmed.1001186
Leeman, J. , Chang, Y. K. , Lee, E. J. , Voils, C. I. , Crandell, J. , & Sandelowski, M. ( 2010 ). Implementation of antiretroviral therapy adherence interventions: A realist synthesis of evidence. Journal of Advanced Nursing , 66 , 1915–1930.
Leeman, J. , Chang, Y. K. , Voils, C. I. , Crandell, J. , & Sandelowski, M. ( 2011 ). A mixed-methods approach to synthesizing evidence on mediators of intervention effects. Western Journal of Nursing Research , 33 , 870–900.
Leeman, J. , Sommers, J. , Leung, M. M. , & Ammerman, A. ( 2011 ). Disseminating evidence from research and practice: A model for selecting evidence to guide obesity prevention. Journal of Public Health Management and Practice , 17 , 133–140.
Leviton, L. C. , Khan, L. K. , Rog, D. , Dawkins, N. , & Cotton, D. ( 2010 ). Evaluability assessment to improve public health policies, programs, and practices. Annual Review of Public Health , 31 , 213–233.
Lewin, S. , Bosch-Capblanch, X. , Oliver, S. , Akl, E. A. , Vist, G. E. , Lavis, J. N. , . . . Haines, A. ( 2012 ). Guidance for evidence-informed policies about health systems: Assessing how much confidence to place in the research evidence. PLoS Medicine , 9 (3), e1001187. Retrieved from http://www.plosmedicine.org/article/info%3Adoi%2F10.1371%2Fjournal.pmed.1001185
Liberati, A. , Altman, D. G. , Tetzlaff, J. , Mulrow, C. , Gotzsche, P. C. , Ioannidis, J. P. , . . . Moher, D. ( 2009 ). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ , 339 . Retrieved from http://www.bmj.com/content/339/bmj.b2700
McKleroy, V. S. , Galbraith, J. S. , Cummings, B. , Jones, P. , Harshbarger, C. , Collins, C. , . . . Carey, J.W. ( 2006 ). Adapting evidence-based behavioral interventions to new settings and target populations. AIDS Education and Prevention , 18 (4 Suppl. A), 59–73.
Michie, S. , Johnston, M. , Abraham, C. , Lawton, R. , Parker, D. , & Walker, A. ( 2005 ). Making psychological theory useful for implementing evidence based practice: A consensus approach. Quality and Safety in Health Care , 14 , 26–33.
Michie, S. , van Stralen, M. M. , & West, R. ( 2011 ). The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implementation Science , 6 , 42. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/21513547
Miller, C. L. , Druss, B. G. , & Rohrbaugh, R. M. ( 2003 ). Using qualitative methods to distill the active ingredients of a multifaceted intervention. Psychiatric Services , 54 , 568–571.
O’Campo, P. , Kirst, M. , Tsamis, C. , Chambers, C. , & Ahmad, F. ( 2011 ). Implementing successful intimate partner violence screening programs in health care settings: Evidence generated from a realist-informed systematic review. Social Science & Medicine , 72 , 855–866.
Ogilvie, D. , Cummins, S. , Petticrew, M. , White, M. , Jones, A. , & Wheeler, K. ( 2011 ). Assessing the evaluability of complex public health interventions: Five questions for researchers, funders, and policymakers. Milbank Quarterly , 89 , 206–225.
Ogilvie, D. , Egan, M. , Hamilton, V. , & Petticrew, M. ( 2005 ). Systematic reviews of health effects of social interventions: 2. Best available evidence: How low should you go? Journal of Epidemiology and Community Health , 59 , 886–892.
Onwuegbuzie, A. J. , & Dickinson, W. B. ( 2008 ). Mixed methods analysis and information visualization: Graphical display for effective communication of research results. The Qualitative Report , 13 , 204–225.
Pawson, R. ( 2006 ). Evidence-based policy: A realist perspective . London, England: Sage.
Pawson, R. ( 2008 ). Method mix, technical hex, and theory fix. In M. M. Bergman (Ed.), Advances in mixed methods research: Theories and applications (pp. 120–137). London, England: Sage.
Pluye, P. , Gagnon, M. P. , Griffiths, F. , & Johnson-Lafleur, J. ( 2009 ). A scoring system for appraising mixed methods research, and concomitantly appraising qualitative, quantitative and mixed methods primary studies in mixed studies reviews. International Journal of Nursing Studies , 46 , 529–546.
Pope, C. , Mays, N. , & Popay, J. ( 2007 ). Synthesizing qualitative and quantitative health evidence: A guide to methods . Berkshire, UK: Open University Press.
Proctor, E. K. , & Brownson, R. C. ( 2012 ). Measurement issues in dissemination and implementation research. In R. C. Brownson , G. A. Colditz , & E. K. Proctor (Eds.), Dissemination and implementation research in health (pp. 261–281). New York, NY: Oxford University Press.
Ramsay, C. R. , Thomas, R. E. , Croal, B. L. , Grimshaw, J. M. , & Eccles, M. P. ( 2010 ). Using the theory of planned behaviour as a process evaluation tool in randomised trials of knowledge translation strategies: A case study from UK primary care. Implementation Science , 5 , 71. Retrieved from http://www.implementationscience.com/content/5/1/71
Rockers, P. C. , Feigl, A. B. , Rottingen, J.A. , Fretheim, A. , de Ferranti, D. , Lavis, J. , & Barnighausen, T. ( 2012 ). Study-design selection criteria in systematic reviews of effectiveness of health systems interventions and reforms: A meta-review. Health Policy , 104 , 206–214.
Roen, K. , Arai, L. , Roberts, H. , & Popay, J. ( 2006 ). Extending sytematic reviews to include evidence on implementation: Methodological work on a review of community-based initiatives to prevent injuries. Social Science & Medicine , 63 , 1060–1071.
Rogers, E. M. ( 2003 ). Diffusion of innovations (5th ed.). New York, NY: Free Press.
Rueda, S. , Park-Wyllie, L. Y. , Bayoumi, A. M. , Tynan, A. M. , Antoniou, T. A. , Rourke, S. B. , & Glazier, R. H. ( 2006 ). Patient support and education for promoting adherence to highly active antiretroviral therapy for HIV/AIDS. Cochrane Database of Systematic Reviews , 3 , Art. No. CD001442. Retrieved from http://onlinelibrary.wiley.com.libproxy.lib.unc.edu/doi/10.1002/14651858.CD001442.pub2/pdf
Rychetnik, L. , Frommer, M. , Hawe, P. , & Shiell, A. ( 2002 ). Criteria for evaluating evidence on public health interventions. Journal of Epidemiology & Community Health , 56 , 119–127.
Rycroft-Malone, J. , McCormack, B. , Hutchinson, A. M , Decorby, K. , Bucknall, T. K. , Kent, B. , . . . Wilson, V. ( 2012 ). Realist synthesis: Illustrating the method for implementation research. Implementation Science , 7 , 33. Retrieved from http://www.implementationscience.com/content/7/1/33
Sandelowski, M. ( 2012 ). Metasynthesis of qualitative research. In H. Cooper (Ed.), APA handbook of research methods in psychology: Vol.2. Research designs: Quantitative, qualitative, neuropsychological, and biological (pp. 19–36). Washington, DC: American Psychological Association.
Sandelowski, M. , & Barroso, J. ( 2007 ). Handbook for synthesizing qualitative research . New York, NY: Springer.
Sandelowski, M. , Leeman, J. , Knafl, K. , & Crandell, J. L. ( 2013 ). Text-in-context: A method for extracting findings in mixed-methods mixed research synthesis studies. Journal of Advanced Nursing , 69 , 1428–1437.
Sandelowski, M. , Voils, C. I. , Crandell, J. , & Leeman, J. ( 2013 ). Synthesizing qualitative and quantitative research findings. In C. T. Beck (Ed.), Routledge international handbook of qualitative nursing research (pp. 347–356). New York, NY: Routledge.
Sandelowski, M. , Voils, C. I. , Leeman, J. , & Crandell, J. L. ( 2012 ). Mapping the mixed research synthesis terrain. Journal of Mixed Methods Research , 6 , 317–331.
Shea, B. J. , Grimshaw, J. M. , Wells, G. A. , Boers, M. , Andersson, N. , Hamel, C. , . . . Bouter. L. M. ( 2007 ). Development of AMSTAR: A measurement tool to assess the methodological quality of systematic reviews. BMC Medical Research Methodology , 7 , 10. Retrieved from http://www.biomedcentral.com/1471-2288/7/10
Sheldon, T. ( 2005 ). Making evidence synthesis more useful for management and policy-making [Editorial]. Journal of Health Services Research & Policy , 10 (Suppl. 1), 1–5.
Shojania, K. G. , Ranji, S. R. , Shaw, L. K. , Charo, L. N. , Lai, J. C. , Rushakoff, R. J. , . . . Owens, D. K. ( 2004 ). Closing the quality gap: A critical analysis of quality improvement strategies: Vol. 2: Diabetes care . Technical review 9. Rockville, MD: Agency for Healthcare Research and Quality. Retrieved from http://www.ahrq.gov/downloads/pub/evidence/pdf/qualgap2/qualgap2.pdf
Sidani, S. , & Braden, C. J. ( 1998 ). Evaluating nursing interventions: A theory-driven approach . Thoursand Oaks, CA: Sage.
Sterman, J. D. ( 2006 ). Learning from evidence in a complex world. American Journal of Public Health , 96 , 505–514.
Thomas, J. , Sutcliffe, K. , Harden, A. , Oakley, A. , Oliver, S. , Rees, R. , . . . Kavanagh, J. ( 2003 ). Children and healthy eating: A systematic review of barriers and facilitators . London: EPPI Centre, Social Science Research Unit, Institute of Education, University of London. Retrieved from http://eppi.ioe.ac.uk/EPPIWebContent/hp/reports/healthy_eating02/Final_report_web.pdf
Tunis, S. R. , Stryer, D. B. , & Clancy, C. M. ( 2003 ). Practical clinical trials: Increasing the value of clinical research for decision making in clinical and health policy. JAMA: Journal of the American Medical Association , 290 , 1624–1632.
Voils, C. I. , Crandell, J. L. , Chang, Y. , Leeman, J. , & Sandelowski, M. ( 2011 ). Combining adjusted and unadjusted findings in mixed research synthesis studies. Journal of Evaluation in Clinical Practice , 17 , 429–434.
Voils, C. I. , Sandelowski, M. , Barroso, J. , & Hasselblad, V. ( 2008 ). Making sense of qualitative and quantitative findings in mixed research synthesis studies. Field Methods , 20 , 3–25.
Wong, G. , Greenhalgh, T. , & Pawson, R. ( 2010 ). Internet- based medical education: a realist review of what works, for whom and in what circumstances. BMC Medical Education , 10 , 12.
Wong, G. , Greenhalgh, T. , Westhorp, G. , Buckingham, J. , & Pawson, R. ( 2013 ). RAMESES publication standards: Meta-narrative reviews. BMC Medicine , 11 , 20. Retrieved from http://www.biomedcentral.com/1741-7015/11/20/
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Methodological guidance for the conduct of mixed methods systematic reviews
Affiliations.
- 1 JBI, Faculty of Health and Medical Sciences, The University of Adelaide, Adelaide, SA, Australia.
- 2 School of Healthcare Sciences, Cardiff University, Cardiff, Wales.
- 3 The Wales Centre For Evidence Based Care: A JBI Centre of Excellence, Cardiff, Wales.
- 4 School of Nursing, Queen's University, Kingston, ON, Canada.
- 5 Queen's Collaboration for Health Care Quality: A JBI Centre of Excellence, Kingston, ON, Canada.
- 6 College of Nursing, University of Manitoba, Winnipeg, MB, Canada.
- 7 School of Nursing, Rutgers, The State University of New Jersey, New Brunswick, NJ, USA.
- 8 The Northeast Institute for Evidence Synthesis and Translation (NEST): A JBI Centre of Excellence, Newark, NJ, USA.
- 9 Escola Superior de Enfermagem de Coimbra, Coimbra, Portugal.
- 10 Portugal Centre for Evidence Based Practice: A JBI Centre of Excellence, Coimbra, Portugal.
- 11 The Institute for Health and Wellbeing Research, Robert Gordon University, Aberdeen, Scotland.
- 12 The Scottish Centre for Evidence-based, Multi-professional Practice: A JBI Centre of Excellence, Aberdeen, Scotland.
- 13 College of Nursing, Midwifery and Healthcare, University of West London, London, England.
- 14 The University of West London Centre for Evidence-Based Healthcare: A JBI Affiliated Group, London, UK.
- PMID: 32813460
- DOI: 10.11124/JBISRIR-D-19-00169
Objective: The objective of this paper is to outline the updated methodological approach for conducting a JBI mixed methods systematic review with a focus on data synthesis; specifically, methods related to how data are combined and the overall integration of the quantitative and qualitative evidence.
Introduction: Mixed methods systematic reviews provide a more complete basis for complex decision-making than that currently offered by single method reviews, thereby maximizing their usefulness to clinical and policy decision-makers. Although mixed methods systematic reviews are gaining traction, guidance regarding the methodology of combining quantitative and qualitative data is limited. In 2014, the JBI Mixed Methods Review Methodology Group developed guidance for mixed methods systematic reviews; however, since the introduction of this guidance, there have been significant developments in mixed methods synthesis. As such, the methodology group recognized the need to revise the guidance to align it with the current state of knowledge on evidence synthesis methodology METHODS:: Between 2015 and 2019, the JBI Mixed Methods Review Methodology Group undertook an extensive review of the literature, held annual face-to-face meetings (which were supplemented by teleconferences and regular email correspondence), sought advice from experts in the field, and presented at scientific conferences. This process led to the development of guidance in the form of a chapter in the JBI Manual for Evidence Synthesis, the official guidance for conducting JBI systematic reviews. In 2019, the guidance was ratified by the JBI International Scientific Committee.
Results: The updated JBI methodological guidance for conducting a mixed methods systematic review recommends that reviewers take a convergent approach to synthesis and integration whereby the specific method utilized is dependent on the nature/type of questions that are posed in the systematic review. The JBI guidance is primarily based on Hong et al. and Sandelowski's typology on mixed methods systematic reviews. If the review question can be addressed by both quantitative and qualitative research designs, the convergent integrated approach should be followed, which involves data transformation and allows reviewers to combine quantitative and qualitative data. If the focus of the review is on different aspects or dimensions of a particular phenomenon of interest, the convergent segregated approach is undertaken, which involves independent synthesis of quantitative and qualitative data leading to the generation of quantitative and qualitative evidence, which are then integrated together.
Conclusions: The updated guidance on JBI mixed methods systematic reviews provides foundational work to a rapidly evolving methodology and aligns with other seminal work undertaken in the field of mixed methods synthesis. Limitations to the current guidance are acknowledged, and a series of methodological projects identified by the JBI Mixed Methods Review Methodology Group to further refine the methodology are proposed. Mixed methods reviews offer an innovative framework for generating unique insights related to the complexities associated with health care quality and safety.
- Data Accuracy*
USF Libraries Hours by campus
Libraries locations.
- Libraries Hours
- Outages & Maintenance Alerts
RESEARCH TOOLS
- Subject & Course Guides
- USF Libraries Catalog
- Quicksearch All-in-one-search
- Citing Sources
- Find my Librarian
GUIDES / HOW-TO
- Tutorials & Workshops
- Finding Books and Articles
- Finding Reserves
- Checking Out & Renewing
- Reserve a Study Room
- Additional Help Topics
- star Other Services
- For Faculty
- For Graduate Students
- For Undergrads
- Requesting Books & Articles (ILL)
- Textbook Affordability (TAP)
- Library Instruction
- Laptop Checkout
- Schedule Research Help
- Geographic Information Systems
- Data Management Planning
- Copyright & Intellectual Property
- Scholarly Publishing
- Other Services
COLLECTIONS
- What are Collections?
- Special Collections
- Digital Collections
- Digital Heritage & Humanities
- Digital Commons @ USF
- Oral Histories
- Online Exhibitions
- Printing in the Library
- IT Help Desk
- Digital Media Commons (DMC)
- Writing Studio
- Office of Development
- Office for Undergraduate Research
- Directions to the Library
- Library Info & Floor Maps
- Connect From Off Campus
- Renew Materials Online
- Check UBorrow Status
- Printing Help
- Report a Problem
- About the USF Libraries
Systematic Reviews for Social Sciences
- Systematic Reviews
- Mapping Review
Mixed Methods Review
- Rapid Review
- Scoping Review
- Develop the Question
- Define Inclusion/Exclusion Criteria
- Develop A Review Protocol
- Create Search Strategies
- Select Studies
- Extract Data
- Assess the Quality of Studies
- Synthesize Data and Write the Report
- Review Tools
- Librarian Involvement
- Grey Literature
A comprehensive syntheses of two or more types of data (e.g. quantitative and qualitative) are conducted and then aggregated into a final, combined synthesis
Mixed Methods Reviews are best designed for:
- Multidisciplinary topics or topics with a body of literature that includes quantitative, qualitative, and mixed methods studies.
- To determine not only the effects of interventions but also their appropriateness.
- To identify research gaps.
- To provide an explanation for possible heterogeneity between trials.
- To answer multiple questions in one systematic review.
Limitations:
- May result in a larger number of citations.
- Requires more search time to create multiple searches for varying outcomes.
- There are no universally adopted methods for conducting Mixed Methods Reviews.
- Requires significant methodological skill.
- Resource intensive--may take time to engage with the evidence and develop theory.
- Not inherently reproducible or transparent because of the highly iterative nature of the interpretative process
(Source: M. Petticrew et al, 2013)
Outline of Stages
Timeframe: 12-18+ months. Same as a systematic review or longer.
Question: Addresses 2 or more review framework criteria, "Mixed methods reviews should pose a question that specifically requires the inclusion of two or more syntheses that are grounded in different approaches". A priori review protocol is recommended.
Examples of and clearly articulated questions that may be posed by one mixed methods systematic review are:
1. What is the effectiveness of educational strategies associated with insulin pump therapy?
2. What is the appropriateness of educational strategies associated with insulin pump therapy
Sources and searches: Types of studies and their findings are mixed. This requires a very broad search or multiple structured searches. "This should address each of the syntheses included in the review...[and] aims to find both published and unpublished studies."
Selection: Based upon inclusion criteria.
- Quantitative component - consider any experimental study design before and after studies for inclusion
- Qualitative component - consider studies that focus on qualitative data including, but not limited to, designs such as phenomenology, grounded theory, ethnography, action research and feminist research. In the absence of research studies, other text such as opinion papers and reports should be considered.
- Textual component - consider expert opinion, discussion papers, position papers and other text
- Economic component - consider cost effectiveness, cost benefit, cost minimization, cost utility
Appraisal: Address each of the syntheses included in the review
Example: Quantitative, Qualitative, Textual or Economic papers
The appropriate critical appraisal tool or method should be applied by study type or there should be one general tool used that will represent all study designs.
Synthesis: Depends on findings and included studies, applying mixed synthesis methods (qualitative: thematic synthesis/meta-ethnography & quantitative: statistical meta-analysis). “The results of each single method synthesis included in the mixed method review will be extracted in numerical, tabular or textual format."
(Source: Joanna Briggs Institute 2014)
- JBI Manual: Mixed Methods Review
- Toolkit for Mixed Studies Reviews
- Using mixed methods research synthesis for literature reviews
- Conducting Mixed Methods Research Systematic Methodological Reviews: A Review of Practice and Recommendations
- Text-in-context: a method for extracting findings in mixed-methods mixed research synthesis studies
- Mixed-Methods Systematic Reviews: Integrating Quantitative and Qualitative Findings
- Mixed Methods Appraisal Tool (MMAT)
- Mixed Methods Studies in Environmental Management Research: Prevalence, Purposes and Designs
- Help seeking by male victims of domestic violence and abuse: an example of an integrated mixed methods synthesis of systematic review evidence defining methodological terms
- Community-Led Total Sanitation: A Mixed-Methods Systematic Review of Evidence and Its Quality
- << Previous: Mapping Review
- Next: Rapid Review >>
- Last Updated: Aug 31, 2023 4:34 PM
- URL: https://guides.lib.usf.edu/systematicreviews
- Open access
- Published: 15 December 2015
Qualitative and mixed methods in systematic reviews
- David Gough 1
Systematic Reviews volume 4 , Article number: 181 ( 2015 ) Cite this article
22k Accesses
46 Citations
23 Altmetric
Metrics details
Expanding the range of methods of systematic review
The logic of systematic reviews is very simple. We use transparent rigorous approaches to undertake primary research, and so we should do the same in bringing together studies to describe what has been studied (a research map) or to integrate the findings of the different studies to answer a research question (a research synthesis). We should not really need to use the term ‘systematic’ as it should be assumed that researchers are using and reporting systematic methods in all of their research, whether primary or secondary. Despite the universality of this logic, systematic reviews (maps and syntheses) are much better known in health research and for answering questions of the effectiveness of interventions (what works). Systematic reviews addressing other sorts of questions have been around for many years, as in, for example, meta ethnography [ 1 ] and other forms of conceptual synthesis [ 2 ], but only recently has there been a major increase in the use of systematic review approaches to answer other sorts of research questions.
There are probably several reasons for this broadening of approach. One may be that the increased awareness of systematic reviews has made people consider the possibilities for all areas of research. A second related factor may be that more training and funding resources have become available and increased the capacity to undertake such varied review work.
A third reason could be that some of the initial anxieties about systematic reviews have subsided. Initially, there were concerns that their use was being promoted by a new managerialism where reviews, particularly effectiveness reviews, were being used to promote particular ideological and theoretical assumptions and to indirectly control research agendas. However, others like me believe that explicit methods should be used to enable transparency of perspectives driving research and to open up access to and participation in research agendas and priority setting [ 3 ] as illustrated, for example, by the James Lind Alliance (see http://www.jla.nihr.ac.uk/ ).
A fourth possible reason for the development of new approaches is that effectiveness reviews have themselves broadened. Some ‘what works’ reviews can be open to criticism for only testing a ‘black box’ hypothesis of what works with little theorizing or any logic model about why any such hypothesis should be true and the mechanisms involved in such processes. There is now more concern to develop theory and to test how variables combine and interact. In primary research, qualitative strategies are advised prior to undertaking experimental trials [ 4 , 5 ] and similar approaches are being advocated to address complexity in reviews [ 6 ], in order to ask questions and use methods that address theories and processes that enable an understanding of both impact and context.
This Special Issue of Systematic Reviews Journal is providing a focus for these new methods of review whether these use qualitative review methods on their own or mixed together with more quantitative approaches. We are linking together with the sister journal Trials for this Special Issue as there is a similar interest in what qualitative approaches can and should contribute to primary research using experimentally controlled trials (see Trials Special Issue editorial by Claire Snowdon).
Dimensions of difference in reviews
Developing the range of methods to address different questions for review creates a challenge in describing and understanding such methods. There are many names and brands for the new methods which may or may not withstand the changes of historical time, but another way to comprehend the changes and new developments is to consider the dimensions on which the approaches to review differ [ 7 , 8 ].
One important distinction is the research question being asked and the associated paradigm underlying the method used to address this question. Research assumes a particular theoretical position and then gathers data within this conceptual lens. In some cases, this is a very specific hypothesis that is then tested empirically, and sometimes, the research is more exploratory and iterative with concepts being emergent and constructed during the research process. This distinction is often labelled as quantitative or positivist versus qualitative or constructionist. However, this can be confusing as much research taking a ‘quantitative’ perspective does not have the necessary numeric data to analyse. Even if it does have such data, this might be explored for emergent properties. Similarly, research taking a ‘qualitative’ perspective may include implicit quantitative themes in terms of the extent of different qualitative findings reported by a study.
Sandelowski and colleagues’ solution is to consider the analytic activity and whether this aggregates (adds up) or configures (arranges) the data [ 9 ]. In a randomized controlled trial and an effectiveness review of such studies, the main analysis is the aggregation of data using a priori non-emergent strategies with little iteration. However, there may also be post hoc analysis that is more exploratory in arranging (configuring) data to identify patterns as in, for example, meta regression or qualitative comparative analysis aiming to identify the active ingredients of effective interventions [ 10 ]. Similarly, qualitative primary research or reviews of such research are predominantly exploring emergent patterns and developing concepts iteratively, yet there may be some aggregation of data to make statements of generalizations of extent.
Even where the analysis is predominantly configuration, there can be a wide variation in the dimensions of difference of iteration of theories and concepts. In thematic synthesis [ 11 ], there may be few presumptions about the concepts that will be configured. In meta ethnography which can be richer in theory, there may be theoretical assumptions underlying the review question framing the analysis. In framework synthesis, there is an explicit conceptual framework that is iteratively developed and changed through the review process [ 12 , 13 ].
In addition to the variation in question, degree of configuration, complexity of theory, and iteration are many other dimensions of difference between reviews. Some of these differences follow on from the research questions being asked and the research paradigm being used such as in the approach to searching (exhaustive or based on exploration or saturation) and the appraisal of the quality and relevance of included studies (based more on risk of bias or more on meaning). Others include the extent that reviews have a broad question, depth of analysis, and the extent of resultant ‘work done’ in terms of progressing a field of inquiry [ 7 , 8 ].
Mixed methods reviews
As one reason for the growth in qualitative synthesis is what they can add to quantitative reviews, it is not surprising that there is also growing interest in mixed methods reviews. This reflects similar developments in primary research in mixing methods to examine the relationship between theory and empirical data which is of course the cornerstone of much research. But, both primary and secondary mixed methods research also face similar challenges in examining complex questions at different levels of analysis and of combining research findings investigated in different ways and may be based on very different epistemological assumptions [ 14 , 15 ].
Some mixed methods approaches are convergent in that they integrate different data and methods of analysis together at the same time [ 16 , 17 ]. Convergent systematic reviews could be described as having broad inclusion criteria (or two or more different sets of criteria) for methods of primary studies and have special methods for the synthesis of the resultant variation in data. Other reviews (and also primary mixed methods studies) are sequences of sub-reviews in that one sub-study using one research paradigm is followed by another sub-study with a different research paradigm. In other words, a qualitative synthesis might be used to explore the findings of a prior quantitative synthesis or vice versa [ 16 , 17 ].
An example of a predominantly aggregative sub-review followed by a configuring sub-review is the EPPI-Centre’s mixed methods review of barriers to healthy eating [ 18 ]. A sub-review on the effectiveness of public health interventions showed a modest effect size. A configuring review of studies of children and young people’s understanding and views about eating provided evidence that the public health interventions did not take good account of such user views research, and that the interventions most closely aligned to the user views were the most effective. The already mentioned qualitative comparative analysis to identify the active ingredients within interventions leading to impact could also be considered a qualitative configuring investigation of an existing quantitative aggregative review [ 10 ].
An example of a predominantly configurative review followed by an aggregative review is realist synthesis. Realist reviews examine the evidence in support of mid-range theories [ 19 ] with a first stage of a configuring review of what is proposed by the theory or proposal (what would need to be in place and what casual pathways would have to be effective for the outcomes proposed by the theory to be supported?) and a second stage searching for empirical evidence to test for those necessary conditions and effectiveness of the pathways. The empirical testing does not however use a standard ‘what works’ a priori methods approach but rather a more iterative seeking out of evidence that confirms or undermines the theory being evaluated [ 20 ].
Although sequential mixed methods approaches are considered to be sub-parts of one larger study, they could be separate studies as part of a long-term strategic approach to studying an issue. We tend to see both primary studies and reviews as one-off events, yet reviews are a way of examining what we know and what more we want to know as a strategic approach to studying an issue over time. If we are in favour of mixing paradigms of research to enable multiple levels and perspectives and mixing of theory development and empirical evaluation, then we are really seeking mixed methods research strategies rather than simply mixed methods studies and reviews.
Noblit G. Hare RD: meta-ethnography: synthesizing qualitative studies. Newbury Park NY: Sage Publications; 1988.
Google Scholar
Barnett-Page E, Thomas J. Methods for the synthesis of qualitative research: a critical review. BMC Med Res Methodol. 2009;9:59.
Article PubMed PubMed Central Google Scholar
Gough D, Elbourne D. Systematic research synthesis to inform policy, practice and democratic debate. Soc Pol Soc. 2002;2002:1.
Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance 2015. BMJ. 2015;350:h1258
Candy B, Jone L, King M, Oliver S. Using qualitative evidence to help understand complex palliative care interventions: a novel evidence synthesis approach. BMJ Support Palliat Care. 2014;4:Supp A41–A42.
Article Google Scholar
Noyes J, Gough D, Lewin S, Mayhew A, Michie S, Pantoja T, et al. A research and development agenda for systematic reviews that ask complex questions about complex interventions. J Clin Epidemiol. 2013;66:11.
Gough D, Oliver S, Thomas J. Introduction to systematic reviews. London: Sage; 2012.
Gough D, Thomas J, Oliver S. Clarifying differences between review designs and methods. Syst Rev. 2012;1:28.
Sandelowski M, Voils CJ, Leeman J, Crandlee JL. Mapping the mixed methods-mixed research synthesis terrain. J Mix Methods Res. 2012;6:4.
Thomas J, O’Mara-Eves A, Brunton G. Using qualitative comparative analysis (QCA) in systematic reviews of complex interventions: a worked example. Syst Rev. 2014;3:67.
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8:45.
Oliver S, Rees R, Clarke-Jones L, Milne R, Oakley AR, Gabbay J, et al. A multidimensional conceptual framework for analysing public involvement in health services research. Health Exp. 2008;11:72–84.
Booth A, Carroll C. How to build up the actionable knowledge base: the role of ‘best fit’ framework synthesis for studies of improvement in healthcare. BMJ Qual Saf. 2015. 2014-003642.
Brannen J. Mixed methods research: a discussion paper. NCRM Methods Review Papers, 2006. NCRM/005.
Creswell J. Mapping the developing landscape of mixed methods research. In: Teddlie C, Tashakkori A, editors. SAGE handbook of mixed methods in social & behavioral research. New York: Sage; 2011.
Morse JM. Principles of mixed method and multi-method research design. In: Teddlie C, Tashakkori A, editors. Handbook of mixed methods in social and behavioural research. London: Sage; 2003.
Pluye P, Hong QN. Combining the power of stories and the power of numbers: mixed methods research and mixed studies reviews. Annu Rev Public Health. 2014;35:29–45.
Harden A, Thomas J. Mixed methods and systematic reviews: examples and emerging issues. In: Tashakkori A, Teddlie C, editors. Handbook of mixed methods in the social and behavioral sciences. 2nd ed. London: Sage; 2010. p. 749–74.
Chapter Google Scholar
Pawson R. Evidenced-based policy: a realist perspective. London: Sage; 2006.
Book Google Scholar
Gough D. Meta-narrative and realist reviews: guidance, rules, publication standards and quality appraisal. BMC Med. 2013;11:22.
Download references
Author information
Authors and affiliations.
EPPI-Centre, Social Science Research Unit, University College London, London, WC1H 0NR, UK
David Gough
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to David Gough .
Additional information
Competing interests.
The author is a writer and researcher in this area. The author declares that he has no other competing interests.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Gough, D. Qualitative and mixed methods in systematic reviews. Syst Rev 4 , 181 (2015). https://doi.org/10.1186/s13643-015-0151-y
Download citation
Received : 13 October 2015
Accepted : 29 October 2015
Published : 15 December 2015
DOI : https://doi.org/10.1186/s13643-015-0151-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Technical Support
- Find My Rep
You are here
Using Mixed Methods Research Synthesis for Literature Reviews
- Mieke Heyvaert - KU Leuven—University of Leuven
- Karin Hannes - KU Leuven—University of Leuven
- Patrick Onghena - KU Leuven, Belgium
- Description
This practical guide provides step-by-step instruction for conducting a mixed methods research synthesis (MMRS) that integrates both qualitative and quantitative evidence. The book progresses through a systematic, comprehensive approach to conducting an MMRS literature review to analyze and summarize the empirical evidence regarding a particular review question. Readers will benefit from discussion of the potential advantages of MMRS and guidance on how to avoid its potential pitfalls.
Using Mixed Methods Research Synthesis for Literature Reviews is Volume 4 in the SAGE Mixed Methods Research Series. To learn more about each text in the series, please visit www.sagepub.com/mmrs .
See what’s new to this edition by selecting the Features tab on this page. Should you need additional information or have questions regarding the HEOA information provided for this title, including what is new to this edition, please email [email protected] . Please include your name, contact information, and the name of the title for which you would like more information. For information on the HEOA, please go to http://ed.gov/policy/highered/leg/hea08/index.html .
For assistance with your order: Please email us at [email protected] or connect with your SAGE representative.
SAGE 2455 Teller Road Thousand Oaks, CA 91320 www.sagepub.com
“This text absolutely offers an avenue for introducing new ways of getting at information in the literature and combining it for effective explanations of results using a chosen methodology.”
“Each step of the MMRS process is given adequate coverage…This is a great tool for students and novice researchers.”
“The consistent format of each chapter would provide students with a clear and ‘comforting’ process for learning the material.”
“[The practical tips] are very useful and demonstrate how the information can be utilized in a manner beyond the theoretical discussion of the process.”
“‘Using Mixed Methods Research Synthesis for Literature Review’ is a book whose time has come. It provides a thoughtful overview of research synthesis techniques that have been developed from different epistemological traditions. The authors show these traditions complement, rather than compete, with one another. They integrate and present these methods in a practical manner while keeping front and center the importance of the theories underlying the synthesis’ constituent research. They argue convincingly that we need to know not only if social policies and practices work but also why and how they work. The ability of social science to contribute to social policy and practice will benefit greatly from the approach to research synthesis contained herein.”
“Here Heyvaert, Hannes and Onghena unpack literature syntheses—both qualitative and quantitative—detailing ways to synthesize, segregate, integrate and even to convert qual findings to quan, or quan to qual. An excellent resource and the next step in moving mixed methods forward!”
KEY FEATURES :
- Theoretical guidelines and practical strategies show readers how to conduct each step of an MMRS literature review process.
- Several worked examples of MMRS literature reviews published in diverse research fields showcase how to put the theory on the MMRS process into practice.
- Each chapter sets the stage with an outline and ends with summary points , challenges , questions for thought , and suggestions for further reading to enhance reader mastery.
- Numerous boxes contain concrete research examples and illustrations to further clarify important points.
- Practical Tip boxes in every chapter include “how-to” guidelines that demonstrate how information can be utilized in a manner beyond the theoretical discussion of the MMRS process.
- Exercises provide concrete activities related to conducting each step of the MMRS process for hands-on practice.
Sample Materials & Chapters
For instructors, select a purchasing option, related products.

This title is also available on SAGE Research Methods , the ultimate digital methods library. If your library doesn’t have access, ask your librarian to start a trial .
Addressing quality in mixed methods research: a review and recommendations for a future agenda
- Published: 21 October 2016
- Volume 51 , pages 2847–2863, ( 2017 )
Cite this article

- Sergi Fàbregues 1 &
- José F. Molina-Azorín 2
5257 Accesses
53 Citations
10 Altmetric
Explore all metrics
Quality is one of the most debated topics in the recent history of mixed methods research. A growing number of authors are currently discussing how the quality of mixed methods research should be conceptualised and operationalised, with the ultimate aim of promoting well designed and properly implemented mixed methods studies. These authors argue that mixed methods research has a number of unique features with respect to monomethod research and, as such, should be appraised according to its own set of quality criteria. Based on a systematic search of the literature, this review (1) examines the features and trends of the literature on the quality of mixed methods research published until February 2016; (2) provides a metasummary of the most prevalent quality criteria suggested in this literature; and (3) proposes a number of recommendations for future discussion and research on this topic. The review concludes that (1) publications on the quality of mixed methods research are increasingly more prevalent and elaborated; (2) a shared set of core quality criteria for appraising mixed methods research can be identified across publications; and (3) future work on this topic should focus on increasing the number of empirical publications on quality, achieving greater consistency in quality terminology, and reaching an agreement on core quality criteria.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

What is Qualitative in Qualitative Research
Criteria for Good Qualitative Research: A Comprehensive Review
Reporting reliability, convergent and discriminant validity with structural equation modeling: a review and best-practice recommendations.
Brown, K.M., Elliott, S.J., Leatherdale, S.T., Robertson-Wilson, J.: Searching for rigour in the reporting of mixed methods population health research: a methodological review. Health Educ. Res. 30 (6), 811–839 (2015)
Article Google Scholar
Bryman, A.: Integrating quantitative and qualitative research: how is it done? Qual. Res. 6 (1), 97–113 (2006a)
Bryman, A.: Paradigm peace and implications for quality. Int. J. Soc. Res. Method 9 (2), 111–126 (2006b)
Bryman, A.: The research question in social research: what is its role? Int. J. Soc. Res. Method 10 (1), 5–20 (2007)
Bryman, A.: June 1989 and beyond: Julia Brannen’s contribution to mixed methods research. Int. J. Soc. Res. Method 17 (2), 121–131 (2014)
Bryman, A., Becker, S., Sempik, J.: Quality criteria for quantitative, qualitative and mixed methods research: a view from social policy. Int. J. Soc. Res. Method 11 (4), 261–276 (2008)
Burrows, T.J.: A preliminary rubric design to evaluate mixed methods research. Doctoral Dissertation, Virginia Tech (2013)
Canales, G.: Transformative, mixed methods checklist for psychological research with mexican americans. J. Mixed Method Res. 7 (1), 6–21 (2013)
Caracelli, V.J., Riggin, L.J.C.: Mixed-method evaluation: developing quality criteria through concept mapping. Eval. Pract. 15 (2), 139–152 (1994)
Cheek, J.: It depends: possible impacts of moving the field of mixed methods research toward best practice guidelines. In: Hesse-Biber, S., Johnson, R.B. (eds.) The Oxford Handbook of Multimethod and Mixed Methods Research Inquiry, pp. 624–636. Oxford University Press, New York (2015)
Google Scholar
Collins, K.M.T.: Validity in multimethod and mixed research. In: Hesse-Biber, S., Johnson, R.B. (eds.) The Oxford Handbook of Multimethod and Mixed Methods Research Inquiry, pp. 240–256. Oxford University Press, New York (2015)
Collins, K.M.T., Onwuegbuzie, A.J., Jiao, Q.G.: A mixed methods investigation of mixed methods sampling designs in social and health science research. J. Mixed Method Res. 1 (3), 267–294 (2007)
Collins, K.M.T., Onwuegbuzie, A.J., Johnson, B.: Securing a place at the table: a review and extension of legitimation criteria for the conduct of mixed research. Am. Behav. Sci. 56 (6), 849–865 (2012)
Creswell, J.W.: A Concise Introduction to Mixed Methods Research. Sage, Thousand Oaks (2015a)
Creswell, J.W.: Revisiting mixed methods and advancing scientific practices. In: Hesse-Biber, S., Johnson, R.B. (eds.) The Oxford Handbook of Multimethod and Mixed Methods Research Inquiry, pp. 57–71. Oxford University Press, New York (2015b)
Creswell, J.W., Plano-Clark, V.L.: Designing and Conducting Mixed Methods Research, 2nd edn. Sage, Thousand Oaks (2011)
Creswell, J.W., Tashakkori, A.: Editorial: developing publishable mixed methods manuscripts. J. Mixed Method Res. 1 (2), 107–111 (2007)
Creswell, J.W., Klassen, A.C., Plano Clark, V.L., Smith, K.C.: Best Practices for Mixed Methods Research in the Health Sciences. National Institutes of Health, Washington, DC (2011)
Book Google Scholar
Curry, L.A., Nunez-Smith, M.: Mixed Methods in Health Sciences Research: A Practical Primer. Sage, Thousand Oaks (2015)
Dahlberg, B., Wittink, M.N., Gallo, J.J.: Funding and publishing integrated studies: Writing effective mixed methods manuscripts and grant proposals. In: Tashakkori, A., Teddlie, C. (eds.) The SAGE Handbook of Mixed Methods in Social and Behavioral Research, pp. 775–802. Sage, Thousand Oaks (2010)
Chapter Google Scholar
Dellinger, A.B., Leech, N.L.: Toward a unified validation framework in mixed methods research. J. Mixed Method Res. 1 (4), 309–332 (2007)
Giddings, L.S., Grant, B.M.: From rigour to trustworthiness: validating mixed methods. In: Andrew, S., Halcomb, E.J. (eds.) Mixed Methods Research for Nursing and the Health Sciences, pp. 119–134. Wiley-Blackwell, Oxford (2009)
Greene, J.C.: Mixed Methods in Social Inquiry. Jossey-Bass, San Francisco (2007)
Hadi, M.A., Alldred, D.P., Closs, S.J., Briggs, M.: Mixed-methods research in pharmacy practice: recommendations for quality reporting (part 2). Int. J. Pharm. Pract. 22 (1), 96–100 (2014)
Halcomb, E.J., Hickman, L.: Mixed methods research. Nurs. Stand. 29 (32), 41–47 (2015)
Hammersley, M.: The issue of quality in qualitative research. Int. J. Res. Method Educ. 30 (3), 287–305 (2007)
Hesse-Biber, S., Johnson, R.B.: Editorial: coming at things differently: future directions of possible engagement with mixed methods research. J. Mixed Method Res. 7 (2), 103–109 (2013)
Heyvaert, M., Hannes, K., Maes, B., Onghena, P.: Critical appraisal of mixed methods studies. J. Mixed Method Res. 7 (4), 302–327 (2013)
Ihantola, E.-M., Kihn, L.-A.: Threats to validity and reliability in mixed methods accounting research. Qual. Res. Acc. Manag. 8 (1), 39–58 (2011)
Ivankova, N.V.: Implementing quality criteria in designing and conducting a sequential QUAN → QUAL mixed methods study of student engagement with learning applied research methods online. J. Mixed Method Res. 8 (1), 25–51 (2014)
Ivankova, N.V.: Mixed Methods Applications in Action Research. Sage, Thousand Oaks (2015)
Ivankova, N.V., Kawamura, Y.: Emerging trends in the utilization of integrated designs in the social, behavioral, and health sciences. In: Tashakkori, A., Teddlie, C. (eds.) The SAGE Handbook of Mixed Methods in Social and Behavioral Research, pp. 581–612. Sage, Thousand Oaks (2010)
Johnson, R.B., Onwuegbuzie, A.J., Turner, L.A.: Towards a definition of mixed methods research. J. Mixed Method Res. 1 (2), 112–133 (2007)
Lavelle, E., Vuk, J., Barber, C.: Twelve tips for getting started using mixed methods in medical education research. Med. Teach. 35 (4), 272–276 (2013)
Leech, N.L.: Interviews with the early developers of mixed methods research. In: Tashakkori, A., Teddlie, C. (eds.) The SAGE Handbook of Mixed Methods in Social and Behavioral Research, pp. 253–272. Sage, Thousand Oaks (2010)
Leech, N.L.: Writing mixed research reports. Am. Behav. Sci. 56 (6), 866–881 (2012)
Leech, N.L., Dellinger, A.B.: Validity: Mixed methods. In: Chapelle, C.A. (ed.) The Encyclopedia of Applied Linguistics, pp. 1–7. Wiley-Blackwell, Oxford (2013)
Leech, N.L., Onwuegbuzie, A.J.: A typology of mixed methods research designs. Qual. Quant. 43 (2), 265–275 (2009)
Mertens, D.M.: Editorial: publishing mixed methods research. J. Mixed Method Res. 5 (1), 3–6 (2011)
Mertens, D.M.: Mixed methods. In: Trainor, A.A., Graue, E. (eds.) Reviewing Qualitative Research in the Social Sciences, pp. 139–150. Routledge, New York (2013)
Mertens, D.M.: Research and Evaluation in Education and Psychology, 4th edn. Sage, Thousand Oaks (2015)
Mertens, D.M., Bazeley, P., Bowleg, L., Fielding, N., Maxwell, J., Molina-Azorin, J.F., Niglas, K.: The future of mixed methods: a five year projection to 2020. MMIRA (2016). https://mmira.wildapricot.org/resources/Documents/MMIRAtaskforcereportJan2016final.pdf
Molina-Azorin, J.F.: The use and added value of mixed methods in management research. J. Mixed Method Res. 5 (1), 7–24 (2011)
Morse, J.M., Niehaus, L.: Mixed Method Design: Principles and Procedures. Left Coast Press, Walnut Creek (2009)
Nastasi, B.K., Hitchcock, J.H., Brown, L.M.: An inclusive framework for conceptualizing mixed methods design typologies: Moving toward fully integrated synergistic research models. In: Tashakkori, A., Teddlie, C. (eds.) The SAGE Handbook of Mixed Methods in Social and Behavioral Research, pp. 305–338. Sage, Thousand Oaks (2010)
O’Cathain, A.: Assessing the quality of mixed methods research: Toward a comprehensive framework. In: Tashakkori, A., Teddlie, C. (eds.) The SAGE Handbook of Mixed Methods in Social and Behavioral Research, pp. 531–555. Sage, Thousand Oaks (2010)
O’Cathain, A., Murphy, E., Nicholl, J.: The quality of mixed methods studies in health services research. J. Health Serv. Res. Policy 13 (2), 92–98 (2008)
Onwuegbuzie, A.J., Corrigan, J.A.: Improving the quality of mixed research reports in the field of human resource development and beyond: a call for rigor as an ethical practice. Hum. Resour. Dev. Q. 25 (3), 273–299 (2014)
Onwuegbuzie, A.J., Johnson, R.K.: The validity issue in mixed research. Res. Sch. 13 (1), 48–63 (2006)
Onwuegbuzie, A.J., Poth, C.: Editors’ afterword: toward evidence-based guidelines for reviewing mixed methods research manuscripts submitted to journals. Int. J. Qual. Method 15 (1), 1–13 (2016)
Onwuegbuzie, A.J., Johnson, R.B., Collins, K.M.T.: Assessing legitimation in mixed research: a new framework. Qual. Quant. 45 (6), 1253–1271 (2011)
Papadimitriou, A., Ivankova, N.V., Hurtado, S.: Addressing challenges of conducting quality mixed methods studies in higher education. In: Tight, M. (ed.) Theory and Method in Higher Education Research, pp. 133–153. Bingley, Emerald (2013)
Plano-Clark, V.L., Ivankova, N.V.: Mixed Methods Research: A Guide to the Field. Sage, Thousand Oaks (2016)
Plano-Clark, V.L., Huddleston-Casas, C.A., Churchill, S.L., Green, D.O., Garrett, A.L.: Mixed methods approaches in family science research. J. Fam. Issues 29 (11), 1543–1566 (2008)
Pluye, P., Gagnon, M.-P., Griffiths, F., Johnson-Lafleur, J.: A scoring system for appraising mixed methods research, and concomitantly appraising qualitative, quantitative and mixed methods primary studies in Mixed Studies Reviews. Int. J. Nurs. Stud. 46 (4), 529–546 (2009)
Ridenour, C.S., Newman, I.: Mixed methods research: exploring the interactive continuum. Southern Illinois University Press, Illinois (2008)
Ritchie, J., Spencer, L., O’Connor, W.: Carrying out qualitative analysis. In: Ritchie, J., Lewis, J. (eds.) Qualitative Research Practice: A Guide for Social Science Students and Researchers, pp. 219–262. Sage, London (2003)
Sale, J.E.M., Brazil, K.: A strategy to identify critical appraisal criteria for primary mixed-method studies. Qual. Quant. 38 (4), 351–365 (2004)
Sandelowski, M., Barroso, J.: Handbook for Synthesizing Qualitative Research. Springer, New York (2007)
Schifferdecker, K.E., Reed, V.A.: Using mixed methods research in medical education: basic guidelines for researchers. Med. Educ. 43 (7), 637–644 (2009)
Seale, C.: The Quality of Qualitative Research. Sage, London (1999)
Tashakkori, A., Teddlie, C.: Quality of inferences in mixed methods research: calling for an integrative framework. In: Bergman, M.M. (ed.) Advances in Mixed Methods Research, pp. 101–119. Sage, London (2008)
Tashakkori, A., Teddlie, C.: Epilogue: Current developments and emerging trends in integrated research methodology. In: Tashakkori, A., Teddlie, C. (eds.) The SAGE Handbook of Mixed Methods in Social and Behavioral Research, pp. 803–826. Sage, Thousand Oaks (2010)
Teddlie, C., Tashakkori, A.: Major issues and controversies in the use of mixed methods in the social and behavioral sciences. In: Tashakkori, A., Teddlie, C. (eds.) Handbook of Mixed Methods in Social and Behavioral Research, pp. 3–50. Sage, Thousand Oaks (2003)
Teddlie, C., Tashakkori, A.: Foundations of Mixed Methods Research: Integrating Quantitative and Qualitative Approaches in the Social and Behavioral Sciences. Sage, Thousand Oaks (2009)
Teddlie, C., Tashakkori, A.: Overview of contemporary issues in mixed methods research. In: Tashakkori, A., Teddlie, C. (eds.) The SAGE Handbook of Mixed Methods in Social and Behavioral Research, pp. 1–41. Sage, Thousand Oaks (2010)
Venkatesh, V., Brown, S.A., Bala, H.: Bridging the qualitative-quantitative divide: guidelines for conducting mixed methods research in Information Systems. MIS Q. 37 (1), 21–54 (2013)
Wisdom, J.P., Cavaleri, M.A., Onwuegbuzie, A.J., Green, C.A.: Methodological reporting in qualitative, quantitative, and mixed methods health services research articles. Health Serv. Res. 47 (2), 721–745 (2012)
Download references
Acknowledgments
The authors would like to thank Marie-Hélène Paré for her valuable comments on the manuscript.
Author information
Authors and affiliations.
Department of Psychology and Education, Universitat Oberta de Catalunya, Rambla del Poblenou, 156, 08018, Barcelona, Spain
Sergi Fàbregues
Department of Management, University of Alicante, Campus de San Vicente, Ap. 99, 03080, Alicante, Spain
José F. Molina-Azorín
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Sergi Fàbregues .
Rights and permissions
Reprints and permissions
About this article
Fàbregues, S., Molina-Azorín, J.F. Addressing quality in mixed methods research: a review and recommendations for a future agenda. Qual Quant 51 , 2847–2863 (2017). https://doi.org/10.1007/s11135-016-0449-4
Download citation
Published : 21 October 2016
Issue Date : November 2017
DOI : https://doi.org/10.1007/s11135-016-0449-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mixed methods research
- Quality issues
- Quality criteria
- Find a journal
- Publish with us
- Track your research

Systematic Reviews & Other Review Types
- What is a Systematic Review?
- What is a Scoping Review?
- What is a literature review?
- What is a Rapid Review?
What is a Mixed Methods Review?
- What is a Network Meta-Analysis?
- What is an Overview of Reviews?
- What is a Meta-Syntheses?
- What is an Integrative Review?
- What is a Diagnostic Test Accuracy Review?
- What is a Living Systematic Review?
A comprehensive syntheses of two or more types of data (e.g. quantitative and qualitative) are conducted and then aggregated into a final, combined synthesis
Qualitative and quantitative data are combined and synthesized in a single primary synthesis.
(The Joanna Briggs Institute 2014 Reviewers Manual)
Mixed Methods Reviews are best designed for:
- Multidisciplinary topics or topics with a body of literature that includes quantitative, qualitative, and mixed methods studies.
- To determine not only the effects of interventions but also their appropriateness.
- To identify research gaps.
- To provide an explanation for possible heterogeneity between trials.
- To answer multiple questions in one systematic review.
- "Integrate quantitative estimates of benefit and harm with more qualitative understanding from people's lives."
(Harden A. 2010)
How a Mixed Methods Review differs from a Systematic Review
Timeframe: 12-18+ months. Same as a systematic review or longer.
Question: Addresses 2 or more specific PICO criteria, "Mixed methods reviews should pose a question that specifically requires the inclusion of two or more syntheses that are grounded in different approaches". A priori review protocol is recommended.
Examples of and clearly articulated PICO questions that may be posed by one mixed methods systematic review are:
1. What is the effectiveness of educational strategies associated with insulin pump therapy?
2. What is the appropriateness of educational strategies associated with insulin pump therapy”
Sources and searches: Types of studies and their findings are mixed. This requires a very broad search or multiple structured searches. "This should address each of the syntheses included in the review...[and] aims to find both published and unpublished studies."
Selection: Based upon inclusion criteria.
- "The quantitative component of the review will consider any experimental study design including randomized controlled trials, non-randomised controlled trials, quasi-experimental, before and after studies for inclusion."
- The qualitative component The textual component of the review will consider expert opinion, discussion papers, position papers and other text.
Appraisal: "This should address each of the syntheses included in the review." The appropriate critical appraisal tool or method should be applied by study type or there should be one general tool used that will represent all study designs.
Synthesis: Depends on findings and included studies, applying mixed synthesis methods (qualitative:thematic synthesis/meta-ethnography & quantitative:statistical meta-analysis). “The results of each single method synthesis included in the mixed method review will be extracted in numerical, tabular or textual format."
(Source: Joanna Briggs Institute 2014)
Mixed Methods Resources
- Mixed-Methods Systematic Reviews: Integrating Quantitative and Qualitative Findings
- Synthesizing evidence on complex interventions: how meta-analytical, qualitative, and mixed-method approaches can contribute
- Methodology for JBI Mixed Methods Systematic Reviews
Limitations of a Mixed Methods Review
- May result in a larger number of citations.
- Requires more search time to create multiple searches for varying outcomes.
- There are no universally adopted methods for conducting Mixed Methods Reviews.
- Requires significant methodological skill.
- Resource intensive--may take time to engage with the evidence and develop theory.
- Not inherently reproducible or transparent because of the highly iterative nature of the interpretative process.
(Source: M. Petticrew et al (2013)
Other names for a Mixed Methods Review
Mixed Research Synthesis, Mixed Methods Synthesis, Mixed Methods Systematic Review, Mixed Studies Review, Qualitative & Quantitative Systematic Review
Temple Attribution
Adapted with permission from Temple University Libraries. https://guides.temple.edu/systematicreviews
- Last Updated: Mar 13, 2024 4:27 PM
- URL: https://touromed.libguides.com/review_types
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 33, Issue 5
- Equitable and accessible informed healthcare consent process for people with intellectual disability: a systematic literature review
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-8498-7329 Manjekah Dunn 1 , 2 ,
- Iva Strnadová 3 , 4 , 5 ,
- Jackie Leach Scully 4 ,
- Jennifer Hansen 3 ,
- Julie Loblinzk 3 , 5 ,
- Skie Sarfaraz 5 ,
- Chloe Molnar 1 ,
- Elizabeth Emma Palmer 1 , 2
- 1 Faculty of Medicine & Health , University of New South Wales , Sydney , New South Wales , Australia
- 2 The Sydney Children's Hospitals Network , Sydney , New South Wales , Australia
- 3 School of Education , University of New South Wales , Sydney , New South Wales , Australia
- 4 Disability Innovation Institute , University of New South Wales , Sydney , New South Wales , Australia
- 5 Self Advocacy Sydney , Sydney , New South Wales , Australia
- Correspondence to Dr Manjekah Dunn, Paediatrics & Child Health, University of New South Wales Medicine & Health, Sydney, New South Wales, Australia; manjekah.dunn{at}unsw.edu.au
Objective To identify factors acting as barriers or enablers to the process of healthcare consent for people with intellectual disability and to understand how to make this process equitable and accessible.
Data sources Databases: Embase, MEDLINE, PsychINFO, PubMed, SCOPUS, Web of Science and CINAHL. Additional articles were obtained from an ancestral search and hand-searching three journals.
Eligibility criteria Peer-reviewed original research about the consent process for healthcare interventions, published after 1990, involving adult participants with intellectual disability.
Synthesis of results Inductive thematic analysis was used to identify factors affecting informed consent. The findings were reviewed by co-researchers with intellectual disability to ensure they reflected lived experiences, and an easy read summary was created.
Results Twenty-three studies were included (1999 to 2020), with a mix of qualitative (n=14), quantitative (n=6) and mixed-methods (n=3) studies. Participant numbers ranged from 9 to 604 people (median 21) and included people with intellectual disability, health professionals, carers and support people, and others working with people with intellectual disability. Six themes were identified: (1) health professionals’ attitudes and lack of education, (2) inadequate accessible health information, (3) involvement of support people, (4) systemic constraints, (5) person-centred informed consent and (6) effective communication between health professionals and patients. Themes were barriers (themes 1, 2 and 4), enablers (themes 5 and 6) or both (theme 3).
Conclusions Multiple reasons contribute to poor consent practices for people with intellectual disability in current health systems. Recommendations include addressing health professionals’ attitudes and lack of education in informed consent with clinician training, the co-production of accessible information resources and further inclusive research into informed consent for people with intellectual disability.
PROSPERO registration CRD42021290548.
- Decision making
- Healthcare quality improvement
- Patient-centred care
- Quality improvement
- Standards of care
Data availability statement
Data are available upon reasonable request. Additional data and materials such as data collection forms, data extraction and analysis templates and QualSyst assessment data can be obtained by contacting the corresponding author.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjqs-2023-016113
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
What is already known on this topic
People with intellectual disability are frequently excluded from decision-making processes and not provided equal opportunity for informed consent, despite protections outlined in the United Nations Convention on the Rights of Persons with Disabilities.
People with intellectual disability have the capacity and desire to make informed medical decisions, which can improve their well-being, health satisfaction and health outcomes.
What this review study adds
Health professionals lack adequate training in valid informed consent and making reasonable adjustments for people with intellectual disability, and continue to perpetuate assumptions of incapacity.
Health information provided to people with intellectual disability is often inaccessible and insufficient for them to make informed decisions about healthcare.
The role of support people, systemic constraints, a person-centred approach and ineffective healthcare communication also affect informed consent.
How this review might affect research, practice or policy
Health professionals need additional training on how to provide a valid informed consent process for people with intellectual disability, specifically in using accessible health information, making reasonable adjustments (e.g., longer/multiple appointments, options of a support person attending or not, using plain English), involving the individual in discussions, and communicating effectively with them.
Inclusive research is needed to hear the voices and opinions of people with intellectual disability about healthcare decision-making and about informed consent practices in specific healthcare settings.
Introduction
Approximately 1% of the world’s population have intellectual disability. 1 Intellectual disability is medically defined as a group of neurodevelopmental conditions beginning in childhood, with below average cognitive functioning and adaptive behaviour, including limitations in conceptual, social and practical skills. 2 People with intellectual disability prefer an alternative strength-based definition, reflected in the comment by Robert Strike OAM (Order of Australia Medal): ‘We can learn if the way of teaching matches how the person learns’, 3 reinforcing the importance of providing information tailored to the needs of a person with intellectual disability. A diagnosis of intellectual disability is associated with significant disparities in health outcomes. 4–7 Person-centred decision-making and better communication have been shown to improve patient satisfaction, 8 9 the physician–patient relationship 10 and overall health outcomes 11 for the wider population. Ensuring people with intellectual disability experience informed decision-making and accessible healthcare can help address the ongoing health disparities and facilitate equal access to healthcare.
Bodily autonomy is an individual’s power and agency to make decisions about their own body. 12 Informed consent for healthcare enables a person to practice bodily autonomy and is protected, for example, by the National Safety and Quality Health Service Standards (Australia), 13 Mental Capacity Act (UK) 14 and the Joint Commission Standards (USA). 15 In this article, we define informed consent according to three requirements: (1) the person is provided with information they understand, (2) the decision is free of coercion and (3) the person must have capacity. 16 For informed consent to be valid, this process must be suited to the individual’s needs so that they can understand and communicate effectively. Capacity is the ability to give informed consent for a medical intervention, 17 18 and the Mental Capacity Act outlines that ‘a person must be assumed to have capacity unless it is established that he lacks capacity’ and that incapacity can only be established if ‘all practicable steps’ to support capacity have been attempted without success. 14 These assumptions of capacity are also decision-specific, meaning an individual’s ability to consent can change depending on the situation, the choice itself and other factors. 17
Systemic issues with healthcare delivery systems have resulted in access barriers for people with intellectual disability, 19 despite the disability discrimination legislation in many countries who are signatories to the United Nations (UN) Convention on the Rights of Persons with Disabilities. 20 Patients with intellectual disability are not provided the reasonable adjustments that would enable them to give informed consent for medical procedures or interventions, 21 22 despite evidence that many people with intellectual disability have both the capacity and the desire to make their own healthcare decisions. 21 23
To support people with intellectual disability to make independent health decisions, an equitable and accessible informed consent process is needed. 24 However, current health systems have consistently failed to provide this. 21 25 To address this gap, we must first understand the factors that contribute to inequitable and inaccessible consent. To the best of our knowledge, the only current review of informed consent for people with intellectual disability is an integrative review by Goldsmith et al . 26 Many of the included articles focused on assessment of capacity 27–29 and research consent. 30–32 The review’s conclusion supported the functional approach to assess capacity, with minimal focus on how the informed consent processes can be improved. More recently, there has been a move towards ensuring that the consent process is accessible for all individuals, including elderly patients 33 and people with aphasia. 34 However, there remains a paucity of literature about the informed consent process for people with intellectual disability, with no systematic reviews summarising the factors influencing the healthcare consent process for people with intellectual disability.
To identify barriers to and enablers of the informed healthcare consent process for people with intellectual disability, and to understand how this can be made equitable and accessible.
A systematic literature review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols (PRISMA-P) systematic literature review protocol. 35 The PRISMA 2020 checklist 36 and ENhancing Transparency in REporting the synthesis of Qualitative research (ENTREQ) reporting guidelines were also followed. 37 The full study protocol is included in online supplemental appendix 1 .
Supplemental material
No patients or members of the public were involved in this research for this manuscript.
Search strategy
A search strategy was developed to identify articles about intellectual disability, consent and healthcare interventions, described in online supplemental appendix 2 . Multiple databases were searched for articles published between January 1990 to January 2022 (Embase, MEDLINE, PsychINFO, PubMed, SCOPUS, Web of Science and CINAHL). These databases include healthcare and psychology databases that best capture relevant literature on this topic, including medical, nursing, social sciences and bioethical literature. The search was limited to studies published from 1990 as understandings of consent have changed since then. 38 39 This yielded 4853 unique papers which were imported into Covidence, a specialised programme for conducting systematic reviews. 40
Study selection
Citation screening by abstract and titles was completed by two independent researchers (MD and EEP). Included articles had to:
Examine the informed consent process for a healthcare intervention for people with intellectual disability.
Have collected more than 50% of its data from relevant stakeholders, including adults with intellectual disability, families or carers of a person with intellectual disability, and professionals who engage with people with intellectual disability.
Report empirical data from primary research methodology.
Be published in a peer-reviewed journal after January 1990.
Be available in English.
Full text screening was completed by two independent researchers (MD and EEP). Articles were excluded if consent was only briefly discussed or if it focused on consent for research, capacity assessment, or participant knowledge or comprehension. Any conflicts were resolved through discussion with an independent third researcher (IS).
Additional studies were identified through an ancestral search and by hand-searching three major journals relevant to intellectual disability research. Journals were selected if they had published more than one included article for this review or in previous literature reviews conducted by the research team.
Quality assessment
Two independent researchers (MD and IS) assessed study quality with the QualSyst tool, 41 which can assess both qualitative and quantitative research papers. After evaluating the distribution of scores, a threshold value of 55% was used, as suggested by QualSyst 41 to exclude poor-quality studies but capture enough studies overall. Any conflicts between the quality assessment scores were resolved by a third researcher (EEP). For mixed-method studies, both qualitative and quantitative quality scores were calculated, and the higher value used.
Data collection
Two independent researchers (MD and JH) reviewed each study and extracted relevant details, including study size, participant demographics, year, country of publication, study design, data analysis and major outcomes reported. Researchers used standardised data collection forms designed, with input from senior researchers with expertise in qualitative research (IS and EEP), to extract data relevant to the review’s research aims. The form was piloted on one study, and a second iteration made based on feedback. These forms captured data on study design, methods, participants, any factors affecting the process of informed consent and study limitations. Data included descriptions and paragraphs outlining key findings, the healthcare context, verbatim participant quotes and any quantitative analyses or statistics. Missing or unclear data were noted.
Data analysis
A pilot literature search showed significant heterogeneity in methodology of studies, limiting the applicability of traditional quantitative analysis (ie, meta-analysis). Instead, inductive thematic analysis was chosen as an alternative methodology 42 43 that has been used in recent systematic reviews examining barriers and enablers of other health processes. 44 45 The six-phase approach described by Braun and Clarke was used. 46 47 A researcher (MD) independently coded the extracted data of each study line-by-line, with subsequent data grouped into pre-existing codes or new concepts when necessary. Codes were reviewed iteratively and grouped into categories, subthemes and themes framed around the research question. Another independent researcher (JH) collated and analysed the data on study demographics, methods and limitations. The themes were reviewed by two senior researchers (EEP and IS).
Qualitative methods of effect size calculations have been described in the literature, 48 49 which was captured in this review by the number of studies that identified each subtheme, with an assigned frequency rating to compare their relative significance. Subthemes were given a frequency rating of A, B, C or D if they were identified by >10, 7–9, 4–6 or <3 articles, respectively. The overall significance of each theme was estimated by the number of studies that mentioned it and the GRADE framework, a stepwise approach to quality assessment using a four-tier rating system. Each study was evaluated for risk of bias, inconsistency, indirectness, imprecision and publication bias. 50 51 Study sensitivity was assessed by counting the number of distinct subthemes included. 52 The quality of findings was designated high, moderate or low depending on the frequency ratings, the QualSyst score and the GRADE scores of studies supporting the finding. Finally, the relative contributions of each study were evaluated by the number of subthemes described, guided by previously reported methods for qualitative reviews. 52
Co-research
The findings were reviewed by two co-researchers with intellectual disability (JL and SS), with over 30 years combined experience as members and employees of a self-advocacy organisation. Guidance on the findings and an easy read summary was produced in line with best-practice inclusive research 53 54 over multiple discussions. Input from two health professional researchers (MD and EEP) provided data triangulation and sense-checking of findings.
Twenty-three articles were identified ( figure 1 ): 14 qualitative, 6 quantitative and 3 mixed-methods. Two papers included the same population of study participants: McCarthy 55 and McCarthy, 56 but had different research questions. Fovargue et al 57 was excluded due to a quality score of 35%. Common quality limitations were a lack of verification procedures to establish credibility and limited researcher reflexivity. No studies were excluded due to language requirements (as all were in English) or age restrictions (all studies had majority adult participants).
- Download figure
- Open in new tab
- Download powerpoint
PRISMA 2020 flowchart for the systematic review. 36
Studies were published from 1999 to 2020 and involved participant populations from the UK (n=18), USA (n=3), Sweden (n=1) and Ireland (n=1). Participant numbers ranged from 9 to 604 (median 21), and participants included people with intellectual disability (n=817), health professionals (n=272), carers and support people (n=48), and other professionals that work with people with intellectual disability (n=137, community service agency directors, social workers, administrative staff and care home staff). Ages of participants ranged from 8 to 84 years, though only Aman et al 58 included participants <18 years of age. This study was included as the article states very few children were included. Studies examined consent in different contexts, including contraception and sexual health (6/23 articles), 58–60 medications (5/23 articles), 58–62 emergency healthcare, 63 cervical screening, 64 community referrals, 58–61 65 mental health, 66 hydrotherapy, 64 blood collection 67 and broad decision-making consent without a specific context. 65 68–71 A detailed breakdown of each study is included in online supplemental appendix 3 .
Six major themes were identified from the studies, summarised in figure 2 . An overview of included studies showing study sensitivity, effect size, QualSyst and GRADE scores is given in online supplemental appendix 4 . Studies with higher QualSyst and GRADE scores contributed more to this review’s findings and tended to include more subthemes; specifically, Rogers et al , 66 Sowney and Barr, 63 Höglund and Larsson, 72 and McCarthy 55 and McCarthy. 56 Figure 3 gives the easy read version of theme 1, with the full easy read summary in online supplemental appendix 5 .
Summary of the identified six themes and subthemes.
Theme 1 of the easy read summary.
Theme 1—Health professionals’ attitudes and lack of education about informed consent
Health professionals’ attitudes and practices were frequently (18/21) identified as factors affecting the informed consent process, with substantial evidence supporting this theme. Studies noted the lack of training for health professionals in supporting informed consent for people with intellectual disability, their desire for further education, and stereotypes and discrimination perpetuated by health professionals.
Lack of health professional education on informed consent and disability discrimination legislation
Multiple studies reported inconsistent informed consent practices, for various reasons: some reported that health professionals ‘forgot’ to or ‘did not realise consent was necessary’, 63 73 but inconsistent consent practices were also attributed to healthcare providers’ unfamiliarity with consent guidelines and poor education on this topic. Carlson et al 73 reported that only 44% of general practitioners (GPs) were aware of consent guidelines, and there was the misconception that consent was unnecessary for people with intellectual disability. Similarly, studies of psychologists 66 and nurses 63 found that many were unfamiliar with their obligations to obtain consent, despite the existence of anti-discrimination legislation. People with intellectual disability describe feeling discriminated against by health professionals, reflected in comments such as ‘I can tell, my doctor just thinks I’m stupid – I'm nothing to him’. 74 Poor consent practices by health professionals were observed in Goldsmith et al , 67 while health professionals surveyed by McCarthy 56 were unaware of their responsibility to provide accessible health information to women with intellectual disability. Improving health professional education and training was suggested by multiple studies as a way to remove this barrier. 63 65–67 69 73
Lack of training on best practices for health professions caring for people with intellectual disability
A lack of training in caring for and communicating with people with intellectual disability was also described by midwives, 72 psychologists, 66 nurses, 63 pharmacists 61 and GPs. 56 72 75 Health professionals lacked knowledge about best practice approaches to providing equitable healthcare consent processes through reasonable adjustments such as accessible health information, 56 60 66 longer appointments times, 60 72 simple English 62 67 and flexible approaches to patient needs. 63 72
Health professionals’ stereotyping and assumptions of incapacity
Underlying stereotypes contributed to some health professionals’ (including nurses, 63 GPs 56 and physiotherapists 64 ) belief that people with intellectual disability lack capacity and therefore, do not require opportunities for informed consent. 56 64 In a survey of professionals referring people with intellectual disability to a disability service, the second most common reason for not obtaining consent was ‘patient unable to understand’. 73
Proxy consent as an inappropriate alternative
People with intellectual disability are rarely the final decision-maker in their medical choices, with many health providers seeking proxy consent from carers, support workers and family members, despite its legal invalidity. In McCarthy’s study (2010), 18/23 women with intellectual disability said the decision to start contraception was made by someone else. Many GPs appeared unaware that proxy consent is invalid in the UK. 56 Similar reports came from people with intellectual disability, 55 56 60 64 69 76 health professionals (nurses, doctors, allied health, psychologists), 56 63 64 66 77 support people 64 77 and non-medical professionals, 65 73 and capacity was rarely documented. 56 62 77
Exclusion of people with intellectual disability from decision-making discussions
Studies described instances where health professionals made decisions for their patients with intellectual disability or coerced patients into a choice. 55 72 74 76 77 In Ledger et al 77 , only 62% of women with intellectual disability were involved in the discussion about contraception, and only 38% made the final decision, and others stated in Wiseman and Ferrie 74 : ‘I was not given the opportunity to explore the different options. I was told what one I should take’. Three papers outlined instances where the choices of people with intellectual disability were ignored despite possessing capacity 65 66 69 and when a procedure continued despite them withdrawing consent. 69
Theme 2—Inadequate accessible health information
Lack of accessible health information.
The lack of accessible health information was the most frequently identified subtheme (16/23 studies). Some studies reported that health professionals provided information to carers instead, 60 avoided providing easy read information due to concerns about ‘offending’ patients 75 or only provided verbal information. 56 67 Informed consent was supported when health professionals recognised the importance of providing medical information 64 and when it was provided in an accessible format. 60 Alternative approaches to health information were explored, including virtual reality 68 and in-person education sessions, 59 with varying results. Overall, the need to provide information in different formats tailored to an individual’s communication needs, rather than a ‘one size fits all’ approach, was emphasised by both people with intellectual disability 60 and health professionals. 66
Insufficient information provided
Studies described situations where insufficient information was provided to people with intellectual disability to make informed decisions. For example, some people felt the information from their GP was often too basic to be helpful (Fish et al 60 ) and wanted additional information on consent forms (Rose et al 78 ).
Theme 3—The involvement of support people
Support people (including carers, family members and group home staff) were identified in 11 articles as both enablers of and barriers to informed consent. The antagonistic nature of these findings and lower frequency of subthemes are reflected in the lower quality assessments of evidence.
Support people facilitated communication with health professionals
Some studies reported carers bridging communication barriers with health to support informed consent. 63 64 McCarthy 56 found 21/23 of women with intellectual disability preferred to see doctors with a support person due to perceived benefits: ‘Sometimes I don’t understand it, so they have to explain it to my carer, so they can explain it to me easier’. Most GPs in this study (93%) also agreed that support people aided communication.
Support people helped people with intellectual disability make decisions
By advocating for people with intellectual disability, carers encouraged decision-making, 64 74 provided health information, 74 77 emotional support 76 and assisted with reading or remembering health information. 55 58 76 Some people with intellectual disability explicitly appreciated their support person’s involvement, 60 such as in McCarthy’s 55 study where 18/23 participants felt supported and safer when a support person was involved.
Support people impeded individual autonomy
The study by Wiseman and Ferrie 74 found that while younger participants with intellectual disability felt family members empowered their decision-making, older women felt family members impaired their ability to give informed consent. This was reflected in interviews with carers who questioned the capacity of the person with intellectual disability they supported and stated they would guide them to pick the ‘best choice’ or even over-ride their choices. 64 Studies of psychologists and community service directors described instances where the decision of family or carers was prioritised over the wishes of the person with intellectual disability. 65 66 Some women with intellectual disability in McCarthy’s studies (2010, 2009) 55 56 appeared to have been coerced into using contraception by parental pressures or fear of losing group home support.
Theme 4—Systemic constraints within healthcare systems
Time restraints affect informed consent and accessible healthcare.
Resource limitations create time constraints that impair the consent process and have been identified as a barrier by psychologists, 66 GPs, 56 hospital nurses 63 and community disability workers. 73 Rogers et al 66 highlighted that a personalised approach that could improve informed decision-making is restricted by inflexible medical models. Only two studies described flexible patient-centred approaches to consent. 60 72 A survey of primary care practices in 2007 reported that most did not modify their cervical screening information for patients with intellectual disability because it was not practical. 75
Inflexible models of consent
Both people with intellectual disability 76 and health professionals 66 recognised that consent is traditionally obtained through one-off interactions prior to an intervention. Yet, for people with intellectual disability, consent should ideally be an ongoing process that begins before an appointment and continues between subsequent ones. Other studies have tended to describe one-off interactions where decision-making was not revisited at subsequent appointments. 56 60 72 76
Lack of systemic supports
In one survey, self-advocates highlighted a lack of information on medication for people with intellectual disability and suggested a telephone helpline and a centralised source of information to support consent. 60 Health professionals also want greater systemic support, such as a health professional specialised in intellectual disability care to support other staff, 72 or a pharmacist specifically to help patients with intellectual disability. 61 Studies highlighted a lack of guidelines about healthcare needs of people with intellectual disabilities such as contraceptive counselling 72 or primary care. 75
Theme 5—Person-centred informed consent
Ten studies identified factors related to a person-centred approach to informed consent, grouped below into three subthemes. Health professionals should tailor their practice when obtaining informed consent from people with intellectual disability by considering how these subthemes relate to the individual. Each subtheme was described five times in the literature with a relative frequency rating of ‘C’, contributing to overall lower quality scores.
Previous experience with decision-making
Arscott et al 71 found that the ability of people with intellectual disability to consent changed with their verbal and memory skills and in different clinical vignettes, supporting the view of ‘functional’ capacity specific to the context of the medical decision. Although previous experiences with decision-making did not influence informed consent in this paper, other studies suggest that people with intellectual disability accustomed to independent decision-making were more able to make informed medical decisions, 66 70 and those who live independently were more likely to make independent healthcare decisions. 56 Health professionals should be aware that their patients with intellectual disability will have variable experience with decision-making and provide individualised support to meet their needs.
Variable awareness about healthcare rights
Consent processes should be tailored to the health literacy of patients, including emphasising available choices and the option to refuse treatment. In some studies, medical decisions were not presented to people with intellectual disability as a choice, 64 and people with intellectual disability were not informed of their legal right to accessible health information. 56
Power differences and acquiescence
Acquiescence by people with intellectual disability due to common and repeated experiences of trauma—that is, their tendency to agree with suggestions made by carers and health professionals, often to avoid upsetting others—was identified as an ongoing barrier. In McCarthy’s (2009) interviews with women with intellectual disability, some participants implicitly rejected the idea that they might make their own healthcare decisions: ‘They’re the carers, they have responsibility for me’. Others appeared to have made decisions to appease their carers: ‘I have the jab (contraceptive injection) so I can’t be blamed for getting pregnant’. 55 Two studies highlighted that health professionals need to be mindful of power imbalances when discussing consent with people with intellectual disability to ensure the choices are truly autonomous. 61 66
Theme 6—Effective communication between health professionals and patients
Implementation of reasonable adjustments for verbal and written information.
Simple language was always preferred by people with intellectual disability. 60 67 Other communication aids used in decision-making included repetition, short sentences, models, pictures and easy read brochures. 72 Another reasonable adjustment is providing the opportunity to ask questions, which women with intellectual disability in McCarthy’s (2009) study reported did not occur. 55
Tailored communication methods including non-verbal communication
Midwives noted that continuity of care allows them to develop rapport and understand the communication preferences of people with intellectual disability. 72 This is not always possible; for emergency nurses, the lack of background information about patients with intellectual disability made it challenging to understand their communication preferences. 63 The use of non-verbal communication, such as body language, was noted as underutilised 62 66 and people with intellectual disability supported the use of hearing loops, braille and sign language. 60
To the best of our knowledge, this is the first systematic review investigating the barriers and enablers of the informed consent process for healthcare procedures for people with intellectual disability. The integrative review by Goldsmith et al 26 examined capacity assessment and shares only three articles with this systematic review. 69 71 73 Since the 2000s, there has been a paradigm shift in which capacity is no longer considered a fixed ability that only some individuals possess 38 39 but instead as ‘functional’: a flexible ability that changes over time and in different contexts, 79 reflected in Goldsmith’s review. An individual’s capacity can be supported through various measures, including how information is communicated and how the decision-making process is approached. 18 80 By recognising the barriers and enablers identified in this review, physicians can help ensure the consent process for their patients with intellectual disability is both valid and truly informed. This review has highlighted the problems of inaccessible health information, insufficient clinical education on how to make reasonable adjustments and lack of person-centred trauma-informed care.
Recommendations
Health professionals require training in the informed consent process for people with intellectual disability, particularly in effective and respectful communication, reasonable adjustments and trauma-informed care. Reasonable adjustments include offering longer or multiple appointments, using accessible resources (such as easy read information or shared decision-making tools) and allowing patient choices (such as to record a consultation or involve a support person). Co-researchers reported that many people with intellectual disability prefer to go without a support person because they find it difficult to challenge their decisions and feel ignored if the health professional only talks to the support person. People with intellectual disability also feel they cannot seek second opinions before making medical decisions or feel pressured to provide consent, raising the possibility of coercion. These experiences contribute to healthcare trauma. Co-researchers raised the importance of building rapport with the person with intellectual disability and of making reasonable adjustments, such as actively advocating for the person’s autonomy, clearly stating all options including the choice to refuse treatment, providing opportunities to contribute to discussions and multiple appointments to ask questions and understand information. They felt that without these efforts to support consent, health professionals can reinforce traumatic healthcare experiences for people with intellectual disability. Co-researchers noted instances where choices were made by doctors without discussion and where they were only given a choice after requesting one and expressed concern that these barriers are greater for those with higher support needs.
Co-researchers showed how these experiences contributed to mistrust of health professionals and poorer health outcomes. In one situation, a co-researcher was not informed of a medication’s withdrawal effects, resulting in significant side-effects when it was ceased. Many people with intellectual disability describe a poor relationship with their health professionals, finding it difficult to trust health information provided due to previous traumatic experiences of disrespect, coercion, lack of choice and inadequate support. Many feel they cannot speak up due to the power imbalance and fear of retaliation. Poor consent practices and lack of reasonable adjustments directly harm therapeutic alliances by reducing trust, contribute to healthcare trauma and lead to poorer health outcomes for people with intellectual disability.
Additional education and training for health professionals is urgently needed in the areas of informed consent, reasonable adjustments and effective communication with people with intellectual disability. The experiences of health professionals within the research team confirmed that there is limited training in providing high-quality healthcare for people with intellectual disability, including reasonable adjustments and accessible health information. Co-researchers also suggested that education should be provided to carers and support people to help them better advocate for people with intellectual disability.
Health information should be provided in a multimodal format, including written easy read information. Many countries have regulation protecting the right to accessible health information and communication support to make an informed choice, such as UK’s Accessible Information Standard, 81 and Australia’s Charter of Health Care Rights, 24 yet these are rarely observed. Steps to facilitate this include routinely asking patients about information requirements, system alerts for an individual’s needs or routinely providing reasonable adjustments. 82 Co-researchers agreed that there is a lack of accessible health information, particularly about medications, and that diagrams and illustrations are underutilised. There is a critical need for more inclusive and accessible resources to help health professionals support informed consent in a safe and high-quality health system. These resources should be created through methods of inclusive research, such as co-production, actively involving people with intellectual disability in the planning, creation, and feedback process. 53
Strengths and limitations
This systematic review involved two co-researchers with intellectual disability in sense-checking findings and co-creating the easy read summary. Two co-authors who are health professionals provided additional sense-checking of findings from a different stakeholder perspective. In future research, this could be extended by involving people with intellectual disability in the design and planning of the study as per recommendations for best-practice inclusive research. 53 83
The current literature is limited by low use of inclusive research practices in research involving people with intellectual disability, increasing vulnerability to external biases (eg, inaccessible questionnaires, involvement of carers in data collection, overcompliance or acquiescence and absence of researcher reflexivity). Advisory groups or co-research with people with intellectual disability were only used in five studies. 58 60 68 74 76 Other limitations include unclear selection criteria, low sample sizes, missing data, using gatekeepers in patient selection and predominance of UK-based studies—increasing the risk of bias and reducing transferability. Nine studies (out of 15 involving people with intellectual disability) explicitly excluded those with severe or profound intellectual disability, reflecting a selection bias; only one study specifically focused on people with intellectual disability with higher support needs. Studies were limited to a few healthcare contexts, with a focus on consent about sexual health, contraception and medications.
The heterogeneity and qualitative nature of studies made it challenging to apply traditional meta-analysis. However, to promote consistency in qualitative research, the PRISMA and ENTREQ guidelines were followed. 36 37 Although no meta-analyses occurred, the duplication of study populations in McCarthy 2009 and 2010 likely contributed to increased significance of findings reported in both studies. Most included studies (13/23) were published over 10 years ago, reducing the current relevance of this review’s findings. Nonetheless, the major findings reflect underlying systemic issues within the health system, which are unlikely to have been resolved since the articles were published, as the just-released final report of the Australian Royal Commission into Violence, Abuse, Neglect and Exploitation of People with Disability highlights. 84 There is an urgent need for more inclusive studies to explore the recommendations and preferences of people with intellectual disability about healthcare choices.
Informed consent processes for people with intellectual disability should include accessible information and reasonable adjustments, be tailored to individuals’ needs and comply with consent and disability legislation. Resources, guidelines and healthcare education are needed and should cover how to involve carers and support people, address systemic healthcare problems, promote a person-centred approach and ensure effective communication. These resources and future research must use principles of inclusive co-production—involving people with intellectual disability at all stages. Additionally, research is needed on people with higher support needs and in specific contexts where informed consent is vital but under-researched, such as cancer screening, palliative care, prenatal and newborn screening, surgical procedures, genetic medicine and advanced therapeutics such as gene-based therapies.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
- Maulik PK ,
- Mascarenhas MN ,
- Mathers CD , et al
- World Health Organisation
- Council for Intellectual Disability
- Emerson E ,
- Shogren KA ,
- Wehmeyer ML ,
- Reese RM , et al
- Cordasco KM
- Hallock JL ,
- Jordens CFC ,
- McGrath C , et al
- Brenner LH ,
- Brenner AT ,
- United Nations Population Fund
- Australian Commission on Safety and Quality in Health Care
- The Joint Commission
- Beauchamp TL ,
- Childress JF
- New South Wales Attorney General
- United Nations General Assembly
- Strnadová I ,
- Loblinzk J ,
- Scully JL , et al
- MacPhail C ,
- McKay K , et al
- Keywood K ,
- Fovargue S ,
- Goldsmith L ,
- Skirton H ,
- Cash J , et al
- Morris CD ,
- Niederbuhl JM ,
- Arscott K ,
- Fisher CB ,
- Davidson PW , et al
- Giampieri M
- Shamseer L ,
- Clarke M , et al
- McKenzie JE ,
- Bossuyt PM , et al
- Flemming K ,
- McInnes E , et al
- Appelbaum PS
- ↵ Covidence systematic review software . Melbourne, Australia ,
- Proudfoot K
- Papadopoulos I ,
- Koulouglioti C ,
- Lazzarino R , et al
- Onwuegbuzie AJ
- BMJ Best Practice
- Guyatt GH ,
- Vist GE , et al
- Garcia-Lee B
- Brimblecombe J , et al
- Benson BA ,
- Farmer CA , et al
- Ferguson L ,
- Graham YNH ,
- Gerrard D ,
- Laight S , et al
- Huneke NTM ,
- Halder N , et al
- Ferguson M ,
- Jarrett D ,
- McGuire BE , et al
- Woodward V ,
- Jackson L , et al
- Conboy-Hill S ,
- Leafman J ,
- Nehrenz GM , et al
- Höglund B ,
- Carlson T ,
- English S , et al
- Wiseman P ,
- Walmsley J ,
- Tilley E , et al
- Khatkar HS , et al
- Holland AJ , et al
- Beauchamp TL
- England National Health Service
- National Health Service England
- Royal Commission into Violence, Abuse, Neglect and Exploitation of People with Disability
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
- Data supplement 2
- Data supplement 3
- Data supplement 4
- Data supplement 5
Contributors MD, EEP and IS conceived the idea for the systematic review. MD drafted the search strategy which was refined by EEP and IS. MD and EEP completed article screening. MD and IS completed quality assessments of included articles. MD and JH completed data extraction. MD drafted the original manuscript. JL and SS were co-researchers who sense-checked findings and were consulted to formulate dissemination plans. JL and SS co-produced the easy read summary with MD, CM, JH, EEP and IS. MD, JLS, EEP and IS reviewed manuscript wording. All authors critically reviewed the manuscript and approved it for publication. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. MD is the guarantor responsible for the overall content of this manuscript.
Funding This systematic literature review was funded by the National Health & Medical Research Council (NHMRC), Targeted Call for Research (TCR) into Improving health of people with intellectual disability. Research grant title "GeneEQUAL: equitable and accessible genomic healthcare for people with intellectual disability". NHMRC application ID: 2022/GNT2015753.
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Linked Articles
- Editorial It is up to healthcare professionals to talk to us in a way that we can understand: informed consent processes in people with an intellectual disability Jonathon Ding Richard Keagan-Bull Irene Tuffrey-Wijne BMJ Quality & Safety 2024; 33 277-279 Published Online First: 30 Jan 2024. doi: 10.1136/bmjqs-2023-016830
Read the full text or download the PDF:
- Open access
- Published: 29 April 2024
Exploring patients’ perspectives: a mixed methods study on Outpatient Parenteral Antimicrobial Therapy (OPAT) experiences
- Sophie Peter 1 , 2 ,
- Charlotte Oberröhrmann 2 ,
- Holger Pfaff 3 , 4 ,
- Clara Lehmann 5 , 6 , 7 ,
- Kirsten Schmidt-Hellerau 5 ,
- Vanessa Brandes 5 ,
- Charlotte Leisse 5 ,
- Christoph Heinrich Lindemann 8 ,
- Peter Ihle 9 ,
- Jutta Küpper-Nybelen 9 ,
- Anna Hagemeier 10 &
- Nadine Scholten 2
BMC Health Services Research volume 24 , Article number: 544 ( 2024 ) Cite this article
Metrics details
Outpatient Parenteral Antimicrobial Therapy (OPAT), an alternative to inpatient intravenous antibiotic therapy, has shown benefits in international studies such as increased patient satisfaction. Because OPAT has been used only sporadically in Germany so far, no structured results on patients’ experiences and concerns regarding OPAT have yet been available. This study therefore aims to explore the experiences of OPAT patients in a pilot region in Germany.
This is an observational study in a German pilot region, including a survey of 58 patients on their experiences with OPAT, and in-depth interviews with 12 patients (explanatory-sequential mixed-methods design).
Patients reported that they were satisfied with OPAT. That a hospital discharge was possible and anti-infective therapy could be continued in the home environment was rated as being particularly positive. In the beginning, many patients in the interviews were unsure about being able to administer the antibiotic therapy at home on their own. However, healthcare providers (doctors and pharmacy service provider staff) were able to allay these concerns. Patients appreciated regular contact with care providers. There were suggestions for improvement, particularly concerning the organization of the weekly check-up appointments and the provision of information about OPAT.
Conclusions
Patients were generally satisfied with OPAT. However, the treatment structures in Germany still need to be expanded to ensure comprehensive and high-quality OPAT care.
Trial registration
NCT04002453, https://www.clinicaltrials.gov/ , (registration date: 2019–06-21).
Peer Review reports
When hospitalisation is required solely to administer intravenous antibiotic therapy to treat an infectious disease, Outpatient Parenteral Antimicrobial Therapy (OPAT) offers a means to entirely circumvent hospitalisation or at least significantly reduce its duration [ 1 , 2 ]. OPAT involves the delivery of approved parenteral antibiotic therapy outside of an inpatient hospital setting. Typically, a secure vascular catheter is inserted, allowing for the administration of the anti-infective therapy via infusion. OPAT can be carried out in various settings, including a general practitioner’s office, a specialised outpatient facility, or even the patient's own home [ 2 ]. Patients may self-administer or receive assistance from an informal caregiver or professional caregiver [ 2 , 3 ]. Typical indications for OPAT include skin and soft tissue infection, bone infection, and endocarditis, which are often associated with the need for prolonged intravenous antibiotic therapy [ 2 , 4 ]. Offering comparable efficacy to inpatient care, OPAT presents numerous advantages, including a lower risk of nosocomial infections [ 5 , 6 ]. At the same time, costs can be saved by preventing or shortening hospital stays [ 4 , 7 , 8 , 9 ]. OPAT is therefore an efficacious and safe alternative to inpatient treatment [ 10 , 11 ]. Research on OPAT consistently underscores the high levels of patient satisfaction attributable to its seamless integration into their daily routines [ 8 , 12 , 13 , 14 , 15 , 16 ]. OPAT is a standard care practice in many countries [ 3 , 17 , 18 ]. However, in Germany, there is a lack of healthcare infrastructure, regulations, and recommendations to support OPAT [ 1 ]. As a result, OPAT is only offered by few specialised centres or practices [ 2 , 19 ]. There has been little research about patients’ experiences with OPAT in Germany, despite the fundamental and active role of patients in this mode of treatment. In the spirit of patient-centred outcome measurement, this article aims to answer the question: How is OPAT experienced and accepted by patients in an urban pilot region of Germany (Cologne metropolitan region)? In a nationwide comparison, Cologne has an advantage in the developement of an OPAT structures: an infectiological network (consisting, for example, of hospitals and outpatient infectiological practices) dedicated to patient care, education and training and also research, e.g. for OPAT [ 1 ].
A prospective observational study as part of the K-APAT study (“outpatient parenteral antibiotic treatment in the metropolitan region of Cologne”), which scientifically evaluated the implementation of OPAT in a German pilot region (the Cologne metropolitan region), was conducted. Clinical data is published separately [ 20 ]. A detailed description of the study design can be found in the study protocol [ 21 ]. The study has been approved by the Institutional Review Board of the University of Cologne, Germany (19–1284-1). The study is a multi-centre study consisting of 5 hospitals and 5 outpatient practices with a focus on infectiology. All study centres were allowed to include patients in the study [ 21 ]. Patients who were considered suitable for OPAT by the infectious disease service were also enrolled in the patient satisfaction survey study after giving informed consent to OPAT. Inclusion criteria were therefore admission as an OPAT patient; a minimum age of 18 years; and written informed consent to the survey study. As the survey documents could only be provided in German, sufficient knowledge of German was mandatory. Data collection was carried out using an explanatory mixed-methods design between November 2019 and September 2021 [ 22 ]. The explanatory mixed-methods design allows a broad yet thorough understanding of the patient perspective [ 22 ]. Patients were invited to answer up to three surveys delivered by mail about their OPAT experience at three timepoints: T0 (before starting OPAT, 48 items), T1 (two weeks after starting OPAT, 51 items) and T2 (one week after finishing OPAT, 42 items). Most of the items were likert scaled. All questionnaires included one open ended question (“If you have any comments, please note them here:”). After the patients were enrolled in the study, a written questionnaire was sent to their homes if they had given their consent. The data was collected pseudonymously in returning the questionnaire to the research institute, which was not involved in the treatment of the patients. The questionnaires were developed based on the current literature [ 2 , 11 , 13 , 23 , 24 , 25 , 26 , 27 , 28 , 29 ] and critically reviewed by the study team consisting of social scientists, healthcare researchers, and clinicians with expertise in infectious diseases. The questionnaires used in the K-APAT study were developed specifically for this research. A German version is available in the project's final report [ 30 ]. Both self-developed questions and validated instruments were used in the questionnaires. The final report also contains information on validated and self-developed items [ 30 ]. The questionnaires were tested for comprehensibility and adapted within the framework of ten cognitive pretests with healthy adult persons of different age groups (19 to 70 years old). Topics of the questionnaires are shown in Table 1 (Tab. 1 ). See the appendix for the English version of the questionnaire items used for this publication (Additional file 1 ). Data were analysed descriptively using Stata 17 software.
After the quantitative data collection, in-depth interviews were conducted with selected patients who answered the questionnaires beforehand. These patients had indicated in the written declaration of consent for the study that they would be interested in taking part in in-depth interviews once the questionnaire survey had been completed. The patients were selected for the interviews by the researchers using the pseudonymised data set. The researchers were not involved in the patients' medical care and were only familiar with the patients’ T0, T1 and T2 questionnaires. The researchers wanted to map the greatest possible variability of the patients, especially with regard to their experiences and satisfaction with OPAT. Patients were also selected for a balance in gender, age, duration of OPAT treatment, and overall satisfaction with OPAT. All 12 interviews took place in person (mostly at patients' homes) or by telephone, due to contact restrictions during the COVID-19 pandemic.
Topics of the interview guide are shown in Fig. 1 (Fig. 1 ). The English version of the interview guide is available as a Supplementary file (Additional file 2 ). Dimensions of the semi-structured interview guide were developed from the literature [ 11 , 23 , 24 , 25 , 26 , 27 , 28 , 29 ] and expert feedback. The interview guide utilised in the K-APAT study was specifically developed for this research. The German version can be found in the final report [ 30 ].
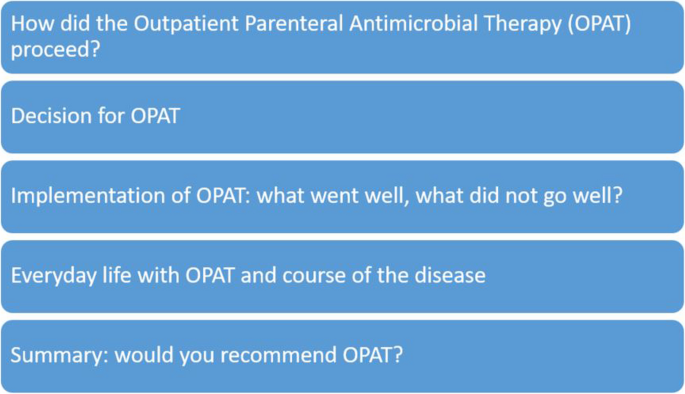
Topics of the interview guide
The qualitative data were interpreted by means of a content analysis (inductive and deductive categories), which was carried out iteratively by SP and CO [ 31 ].
The participants received a financial incentive for completing the questionnaires and participating in the interviews.
Patients’ characteristics can be found in Table 2 (Tab. 2).
As stated in the publication on the projects’ clinical data, the most frequently treated infections were joint and bone infections (26% of the patients) and vertebral osteomyelitis (14% of the patients) [ 20 ]. All results (including the overall results of the three questionnaires and the interviews) and all items of the survey instruments are included in the final report of the K-APAT project [ 30 ].
Results from the questionnaires
All 77 patients included in the study returned their questionnaires (response rate: 100%). 19 respondents did not answer at least one item of the questionnaire which are reported here. These patients were therefore excluded from the following analyses.
In the first and second questionnaire (T0 and T1) patients were asked about their experiences with OPAT subdivided in e.g. therapy confidence, experiences with intravenous antbiotic therapy and patient education (all topics are summarised in Table 1 ). In T2, all patients were asked to summarise their OPAT treatment. The aim was to obtain a final evaluation of their entire OPAT treatment. All respondents had a positive opinion on OPAT (Fig. 2 ).
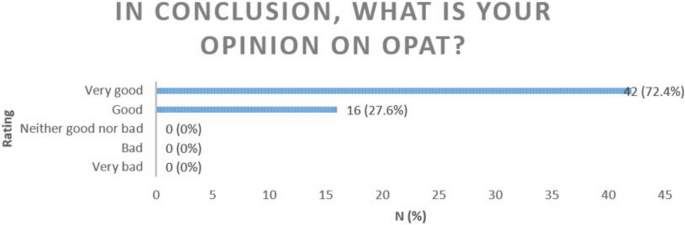
Opinions on OPAT
Also as part of the final conclusion to their OPAT most patients rated the organisation of their treatment as good (29.3%) or very good (70.7%) (Fig. 3 ).
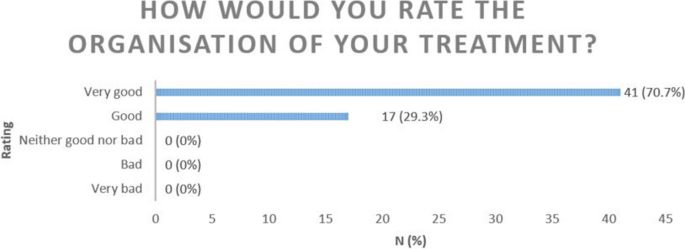
Rating of treatment organisation
The majority of patients (98.28%) would choose OPAT again if required. A similarly high proportion (96.55%) would recommend OPAT (Figs. 4 & 5 ).
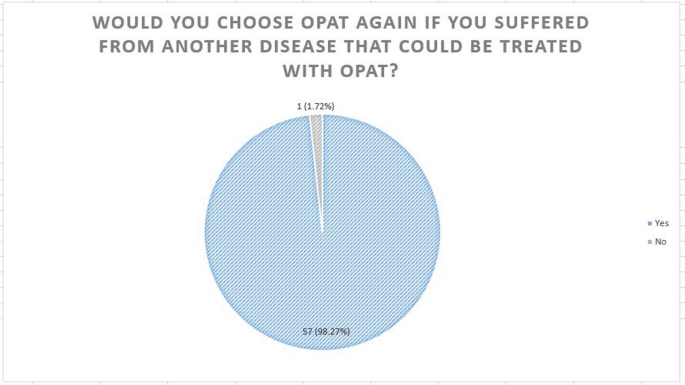
“Would you choose OPAT again if you suffered from another disease that could be treated with OPAT?”
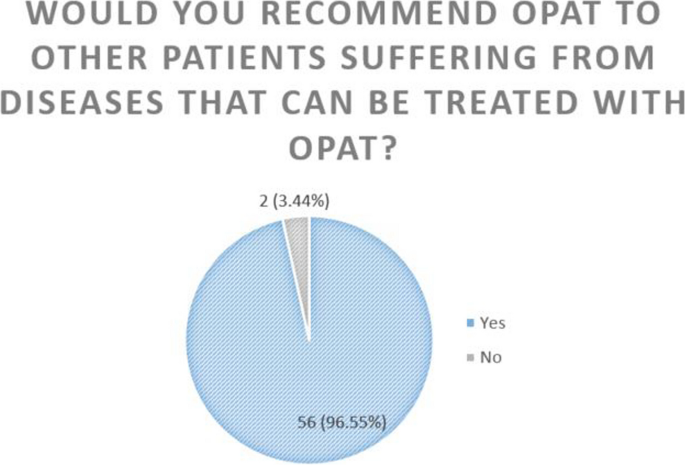
“Would you recommend OPAT to other patients suffering from diseases that can be treated with OPAT?”
Patients were asked to indicate their problems with OPAT using a Likert scale (strongly disagree, rather disagree, rather agree, strongly agree): Problems with material storage were infrequently reported, with only 10.34% strongly agreeing and 3.45% rather agreeing. A small number of individuals (1.72% strongly agree, 8.62% rather agree) reported feeling uncomfortable with the vascular catheter, while 13.9% tended to agree that the vascular catheter affected how they were perceived in public. Additionally, 12.07% strongly agreed and 18.97% rather agreed that they deliberately hid their vascular catheter in public. Eight people (3.45% strongly agree, 10.34% rather agree) reported complications during their treatment. None of the respondents reported any mistakes made by the medical staff, or that OPAT was an inappropriate treatment option for them (Table 3 ).
Results from the interviews
The results of the interviews are summarised in the Table 4 (Tab. 4).
The interviews lasted between 20 and 58 min (mean length: 39 min).
Despite the overall positive evaluation of OPAT, some difficulties were identified during the interviews following explicit enquiries. Eight of the interviewees reported anxiety or uncertainty, especially at the beginning of their therapy (e.g., fear of making mistakes when administering antibiotics; fear of venous catheter management because of the “at heart” location). One patient commented: “This [OPAT] is excellent. Painless and great. However, it is a strange feeling considering the access is in the heart [sic]. (…) You do have a queasy feeling. (…) But it is great. I always thought: Well, what if it slips? But how is it supposed to slip? Slipping is not possible.” (patient 4). However, most fears quickly subsided after the start of therapy. One patient reported severe mechanical problems due to blockage of the catheter, which led to her being switched to oral medication for the last 3 days of her treatment: "Overall it went well and only few problems occurred. Sometimes it happened that, [patient paused and reformulated] So once I had difficulty taking it [the pump system] off again. We then had to use a pipe wrench.” (patient 8). However, most patients had no problems with the OPAT at all. One interviewee said: “And, yes, here at home I had no problems at all. Even the first application, I did it a bit more carefully, of course, just to not forget anything, to do everything right, and very quickly routine comes in.” (patient 5). Another patient summarised: “There were no problems of any kind. There was no pain. There were no incidents.” (patient 9). Motor and cognitive limitations were mentioned as possible barriers to handling infusions.
The interviewees reported numerous benefits of the OPAT. They could be discharged from the hospital early, which they associated with greater self-determination and higher quality of life than in the hospital. One patient stated: “So that [the OPAT] has already given me a lot of freedom.” (patient 11) and another patient mentioned: “As I said, I’m at home, I have my familiar surroundings, and then I feel like I’m back to a normal life and I have the disease under control. So it [the OPAT] was a good way to not have to keep going back to the doctor again and again.” (patient 6). All interviewees emphasised how important it was for their well-being to be at home. One patient explained: “That I can be at home. That’s important for me because I feel most comfortable at home. I have 100 TV channels, and at the hospital, I have five that I don’t really watch at home. Or I can eat whatever I feel like. Home is home.” (patient 7). Freedom and independence in a homecare setting were highly valued compared to the lack of freedom and dependence in inpatient care. A lot of patients explained that OPAT at home was easy to perform and helpful for recovery. In addition, the treatment was predictable: “That was ritualised. I then took a book at some point and read, sat down in the corner and read. I didn't move wildly, right?” (patient 3). Patients did not feel that OPAT interfered with their daily life. In the words of one interviewee:”So everything I do here at home, I’ve been able to do with the [venous catheter].” (patient 10). One patient added: “I would say top-notch. I can only recommend it to everyone. So who is fit enough: definitely. Yes. Although I was also in the hospital [patient paused and started a new sentence] They were all super nice, doctors, nurses, everyone. They really did their best, but home is home, right? And if you really have the opportunity, (…) immediately. So I would do that again immediately. Yes. I hope not that I need it again, but let’s just say I would do it in a heartbeat.” (patient 12). In addition, three patients who work in healthcare themselves stated that OPAT is associated with cost savings for the healthcare system. They emphasised that no hospitalisation or nursing service is required for this treatment. From their experience, the venous catheter can stay in place for longer and does not need to be constantly replaced compared to peripheral catheters, and they heal well.
The interviewees reported some restrictions in everyday life due to OPAT: e.g., sleeping on the side with the catheter is uncomfortable, financial challenges (e.g., co-payment for those with statutory insurance was not explained and cost coverage for those with private insurance was initially unclear, both should be communicated more clearly), insecurity in handling, and suspected side effects (e.g., fatigue, eczema, exhaustion that patients attributed to their OPAT) were also reported by the patients. Most patients did not describe any side effects: “And I didn’t have any side effects or anything. So not that I felt anything bad, that I felt bad, that I felt dizzy or anything. It went wonderfully.” (patient 1).
The interviewees also reported their experiences with healthcare providers. Often patients mentioned a lack of awareness of OPAT among healthcare providers in the hospital and organisational barriers such as waiting times. The venous catheter placement and removal took place in the hospital for all patients. Weekly check-ups were also primarily performed in a hospital outpatient clinic. One patient reported on her hospital stay as: “I already noticed that the doctor was a bit worried […] and then [he] told me to make sure that I observe the hygiene measures, that would be very important. I think there is a bit of fear when you hand things over to the patient: let's see what the patient does with it himself? Surely there are differences there, right?” (patient 8). The interviewed patients evaluated the support by the pharmacy service providers as well-organised. The deliveries of the material (e.g. bandages, material for cleaning catheters, disinfectant) were organised well and without problems. The study participants received a high quantity of material, often more than was required. The OPAT briefing was good and adapted to the patients' needs. Nevertheless, the interviewees reported that the information they got from their healthcare providers was partially incomprehensible (e.g. the step-by-step instruction of the OPAT is very complex with preparation of the material, cleaning of the skin and the catheter and connecting the pumps). One patient felt that she had generally received too little information about OPAT from her physicians. The patients liked the check-ups and the option to contact the healthcare providers by phone: “Yes, she [the pharmacy employee] also called me again herself, I think on the fourth day, which I thought was very nice, and asked if everything was okay, if I was getting along, if I needed anything else.” (patient 2). Outpatient providers such as General Practitioners and other outpatient care services played a minor role among respondents and were only sporadically involved in treatment. Overall, the patients rated the organisation of the OPAT as good.
Main findings
In the K-APAT study, a prospective observational study, we aimed to investigate medical care with OPAT, focusing on the model region of Cologne. The goal was to assess the feasibility and success of implementing OPAT within the German healthcare system. The sub-study we presented here aimed to find out more about patient views on OPAT, their satisfaction, and their experience within the framework of a mixed-methods study.
In our study, OPAT had high levels of patient satisfaction, with nearly all patients expressing contentment. Other studies found comparable satisfaction with OPAT treatment with similar rates of recommendation and reporting that they would opt for OPAT again if necessary [ 13 , 26 ]. Saillen et al. (2017) concluded that OPAT patients were “happy to take over some responsibility for their treatment” [ 26 ]. In general, patient satisfaction with OPAT is comparably high internationally [ 8 , 12 , 13 , 14 , 15 , 16 ]. Quintens et al. (2020) also reported that all respondents were very satisfied with their OPAT treatment [ 32 ]. However, some patients in their study as well as in Berrevoets et al. (2018) also wanted more information about the OPAT and reported side effects attibuted to the OPAT [ 11 , 32 ] as the patients in our interviews did too. Similarly as can be seen in our data, Saillen et al. (2017) reported that patients initially had concerns about the self-application of and reported on mechanical problems in handling the pump system [ 26 ].
Notably, the most satisfying aspect was that this form of treatment allowed patients to be discharged from the hospital. This effect does not only apply to the OPAT patients reported here: As hospitalisation is often perceived as a burden [ 33 , 34 ], a lot of patients express satisfaction upon discharge from the hospital. The organisation of OPAT was largely perceived to be good. In particular, patients appreciated regular contact with healthcare providers (physicians and pharmacy service providers). It is important for the success of the therapy that patients feel comfortable and well cared for [ 11 ].
In countries where OPAT is well established, the number of patients participating in OPAT studies is significantly higher [ 35 ]. One Italian study showed that the COVID-19 pandemic supported the use of OPAT [ 10 ]. The number of participants in our study fell during the pandemic. We suspect that this is due to the heavy burden on hospital staff and outpatient practices.
Strengths and limitations
It is important to consider limitations when interpreting the results of this study. It was conducted in the densely populated metropolitan region of Cologne: the findings may therefore not be fully representative of other regions in Germany (e.g. rural areas, regions without infectiological networks). But the region was well suited to conducting a feasibility study on OPAT due to the already established expertise of the regional, infectiological network. In addition, most of the study was conducted during the COVID-19 pandemic, which could have led to a number of limitations. For example, our participant number ( N = 58) is low. Although all 77 patients we included in the study returned their questionnaires (response rate: 100%), due to missing values, we had to remove 19 patients from the dataset. We attempted to improve recruitment by having multiple study sites and conducting the study in a region that has a good OPAT care structure by national standards. Nevertheless, the case number limits the generalisability of the data. However, other international studies have reported similarly low participation rates [ 32 , 36 , 37 , 38 ].
Compared to other studies our patient population was mostly younger (mean of survey patients: 55.2 years) except for the study presented by Al Shareef et al. (2022) with the same median age as in our study [ 38 ]: Chambers et al. (2019) reported on patients with a median age of 61 years [ 35 ]. Saillen et al. (2017), Staples et al. (2022) and Berrevoets et al. (2018) also reported a higher median age of 59 years, 62 years and even 68 years [ 11 , 14 , 26 ]. Treatment periods in our population (survey data: mean: 15 days, interview data: mean: 27 days) were higher than in other studies. Wolter et al. (2004) reported about 11 days, Hase et al. (2020) reported 13 days and Saillen et al. (2017) 8.5.days [ 8 , 26 , 36 ]. As is common in many other OPAT studies, our survey data also has a high proportion of male participants. [ 11 , 14 , 32 , 36 , 38 ].
It is particularly interesting that in the survey, OPAT was described as good or very good. More detailed insights from the interviews showed that, despite the overall good rating, patients had minor problems with OPAT. Thus, the mixed-methods design and the extensive interview data complement the quantitative data well, e.g. patients were able to report on their experiences in more detail and more individually than it was possible in the questionnaires. Thus, the mixed-methods design supported the breadth and depth of data [ 39 ] on patients' OPAT experiences.
We tried to include a wide range of patient experiences with OPAT in the in-depth interviews and have made efforts to achieve a gender and age balance of the interviewees. But as you can see in Table 2 the interviewees were a little older and had a longer treatment period of OPAT compared to the survey population. In addition, the proportion of men in the survey was higher than in the interviews. Despricption on the underlying diseases can be found in the publication on the clinical data [ 20 ]. Unfortunately, patients who would not recommend OPAT ( N = 2) to others or tended to be less satisfied than average either did not consent to be contacted for an interview or were unwilling to be interviewed when asked to do so.
A professional proofreading service performed proofreading of this publication.
Implications
In the long term, OPAT can be a suitable option for standard care.
OPAT not only increases patient satisfaction through cross-sector, indication-based and patient-oriented care, but also relieves the burden on hospitals by reducing inpatient bed days [ 1 ]. Moreover, the inpatient sector is facing mounting pressures arising from a scarcity of specialists, demographic shifts, and soaring costs. In response, healthcare policy is advocating for the expansion of the outpatient care model, guided by the principle of “outpatient care before inpatient care” [ 40 ].
The data has shown that the OPAT programme can be improved in the following ways to further increase patient satisfaction: Some patients reported they did not know about potential co-payments, which should be communicated more clearly. Waiting times for check-ups in hospitals or doctors' offices should also be reduced. Patients have expressed the wish for flyers or information material explaining the OPAT procedure as well as the handling of the intravenous access in more detail. This improvement has already been introduced into care at the study sites: Flyers and videos describing the OPAT procedure have been developed.
This study shows a high level of patient satisfaction with OPAT. The preference for home-based treatment over hospital care is a key contributing factor. OPAT is still a relatively uncommon procedure in Germany, which is why there are still no nationwide structures for this treatment option. However, our studie shows that patients are satisfied with the care they received and that an expansion of the OPAT structures should therefore be considered. In the studied region, a quality infrastructure for OPAT exists, marked by specialists in specialised and interconnected outpatient clinics. Due to all of these advantages, it is important to further promote the use of OPAT and broaden these prerequisites by establishing adequate OPAT structures [ 41 ].
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Outpatient parenteral antibiotic treatment in the metropolitan region of Cologne
- Outpatient Parenteral Antimicrobial Therapy
Terhalle E, Jung N, Stegemann MS, Priesner V, Lehmann C, Schmiedel S. Neue Entwicklungen in der ambulanten parenteralen Antibiotikatherapie (APAT). [New developments in outpatient parenteral antibiotic therapy (OPAT)]. Dtsch Med Wochenschr. 2020;145:1688–94. https://doi.org/10.1055/a-1114-3990 .
Article CAS PubMed Google Scholar
Stegemann M, Hagel S, Lehmann C. Antibiotikatherapie (2): Ambulante parenterale Gabe. Deutsches Ärzteblatt Online. 2019. https://doi.org/10.3238/PersInfek.2019.07.22.03 .
Article Google Scholar
Norris AH, Shrestha NK, Allison GM, Keller SC, Bhavan KP, Zurlo JJ, et al. 2018 infectious diseases society of America clinical practice guideline for the management of outpatient parenteral antimicrobial therapy. Clin Infect Dis. 2019;68:e1–35. https://doi.org/10.1093/cid/ciy745 .
Article PubMed Google Scholar
Petrak RM, Skorodin NC, Fliegelman RM, Hines DW, Chundi VV, Harting BP. Value and clinical impact of an infectious disease-supervised outpatient parenteral antibiotic therapy program. Open Forum Infect Dis. 2016;3:ofw193. https://doi.org/10.1093/ofid/ofw193 .
Article PubMed PubMed Central Google Scholar
Rentala M, Andrews S, Tiberio A, Alagappan K, Tavdy T, Sheppard P, Silverman R. Intravenous home infusion therapy instituted from a 24-hour clinical decision unit for patients with cellulitis. Am J Emerg Med. 2016;34:1273–5. https://doi.org/10.1016/j.ajem.2016.04.022 .
Kayley J, Berendt AR, Snelling MJ, Moore H, Hamilton HC, Peto TE, et al. Safe intravenous antibiotic therapy at home: experience of a UK based programme. J Antimicrob Chemother. 1996;37:1023–9. https://doi.org/10.1093/jac/37.5.1023 .
Dalovisio JR, Juneau J, Baumgarten K, Kateiva J. Financial impact of a home intravenous antibiotic program on a medicare managed care program. Clin Infect Dis. 2000;30:639–42. https://doi.org/10.1086/313755 .
Wolter JM, Cagney RA, McCormack JG. A randomized trial of home vs hospital intravenous antibiotic therapy in adults with infectious diseases. J Infect. 2004;48:263–8. https://doi.org/10.1016/S0163-4453(03)00135-X .
Dimitrova M, Gilchrist M, Seaton RA. Outpatient parenteral antimicrobial therapy (OPAT) versus inpatient care in the UK: a health economic assessment for six key diagnoses. BMJ Open. 2021;11:e049733. https://doi.org/10.1136/bmjopen-2021-049733
Giuliano G, Raffaelli F, Faliero D, Tamburrini E, Tarantino D, Nurchis MC, Scoppettuolo G. Outpatient parenteral antimicrobial therapy (OPAT) from an emergency model applied during the COVID-19 pandemic to standard of care: preliminary lessons from our experience. Infect Dis Now. 2023;53;104642. https://doi.org/10.1016/j.idnow.2023.01.002
Article CAS PubMed PubMed Central Google Scholar
Berrevoets MAH, Oerlemans AJM, Tromp M, Kullberg BJ, ten Oever J, Schouten JA, Hulscher ME. Quality of outpatient parenteral antimicrobial therapy (OPAT) care from the patient’s perspective: a qualitative study. BMJ Open. 2018;8: e024564. https://doi.org/10.1136/bmjopen-2018-024564 .
Wong KK, Fraser TG, Shrestha NK, Fatica C, Deshpande A. Low incidence of Clostridium difficile infection (CDI) in patients treated with outpatient parenteral antimicrobial therapy (OPAT). Infect Control Hosp Epidemiol. 2015;36:110–2. https://doi.org/10.1017/ice.2014.6 .
MacKenzie M, Rae N, Nathwani D. Outcomes from global adult outpatient parenteral antimicrobial therapy programmes: a review of the last decade. Int J Antimicrob Agents. 2014;43:7–16. https://doi.org/10.1016/j.ijantimicag.2013.09.006 .
Staples JA, Ho M, Ferris D, Hayek J, Liu G, Tran KC, Sutherland JM. Outpatient Versus Inpatient Intravenous Antimicrobial Therapy: A Population-Based Observational Cohort Study of Adverse Events and Costs. Clin Infect Dis. 2022;75:1921–9. https://doi.org/10.1093/cid/ciac298 .
Board N, Brennan N, Caplan GA. A randomised controlled trial of the costs of hospital as compared with hospital in the home for acute medical patients. Aust N Z J Public Health. 2000;24:305–11. https://doi.org/10.1111/j.1467-842x.2000.tb01573.x .
Corwin P, Toop L, McGeoch G, Than M, Wynn-Thomas S, Wells JE, et al. Randomised controlled trial of intravenous antibiotic treatment for cellulitis at home compared with hospital. BMJ. 2005;330:129. https://doi.org/10.1136/bmj.38309.447975.EB .
Chapman ALN, Seaton RA, Cooper MA, Hedderwick S, Goodall V, Reed C, et al. Good practice recommendations for outpatient parenteral antimicrobial therapy (OPAT) in adults in the UK: a consensus statement. J Antimicrob Chemother. 2012;67:1053–62. https://doi.org/10.1093/jac/dks003 .
Hatcher J, Costelloe C, Cele R, Viljanen A, Samarasinghe D, Satta G, et al. Factors associated with successful completion of outpatient parenteral antibiotic therapy (OPAT): A 10-year review from a large West London service. Int J Antimicrob Agents. 2019;54:207–14. https://doi.org/10.1016/j.ijantimicag.2019.04.008 .
Rieg S, Küpper MF. Infectious diseases consultations can make the difference: a brief review and a plea for more infectious diseases specialists in Germany. Infection. 2016;44:159–66. https://doi.org/10.1007/s15010-016-0883-1 .
Schmidt-Hellerau K, Baade N, Günther M, Scholten N, Lindemann CH, Leisse C, et al. Outpatient parenteral antimicrobial therapy (OPAT) in Germany: insights and clinical outcomes from the K-APAT cohort study. Infection. 2024. https://doi.org/10.1007/s15010-024-02199-9 .
Scholten N, Leisse C, Brandes V, Oberröhrmann C, Ihle P, Peter S, et al. Outpatient parenteral antimicrobial therapy in Germany: a prospective cohort study protocol. BMJ Open. 2022;12:e061417. https://doi.org/10.1136/bmjopen-2022-061417 .
Cresswell JW. A concise introduction to mixed methods research. 2nd ed. Thousand Oaks, CA: SAGE Publications; 2022.
Google Scholar
Ansari AA. Outpatient Parenteral Antimicrobial Therapy (OPAT) in the Kingdom of Bahrain: Efficacy. Patient Satisfaction and Cost Effectiveness TOIDJ. 2013;7:90–5. https://doi.org/10.2174/1874279301307010090 .
Baecker H, Gessmann J, Hanusrichter Y, Zahn PK, Schildhauer TA, Frieler S. Die ambulante i. v. Antibiotikatherapie mittels PICC Line in der Behandlung von chronischen periprothetischen Infektionen. [Outpatient Parenteral Antibiotic Therapy (OPAT) with Peripherally Inserted Central Catheter in Patients with Periprosthetic Joint Infection]. Z Orthop Unfall. 2019;157:510–4. https://doi.org/10.1055/a-0830-4776 .
Esposito S, Noviello S, Leone S, Tice A, Seibold G, Nathwani D, Scaglione F. Outpatient parenteral antibiotic therapy (OPAT) in different countries: a comparison. Int J Antimicrob Agents. 2004;24:473–8. https://doi.org/10.1016/j.ijantimicag.2004.06.004 .
Saillen L, Arensdorff L, Moulin E, Voumard R, Cochet C, Boillat-Blanco N, et al. Patient satisfaction in an outpatient parenteral antimicrobial therapy (OPAT) unit practising predominantly self-administration of antibiotics with elastomeric pumps. Eur J Clin Microbiol Infect Dis. 2017;36:1387–92. https://doi.org/10.1007/s10096-017-2944-5 .
Townsend J, Keller S, Tibuakuu M, Thakker S, Webster B, Siegel M, et al. Outpatient parenteral therapy for complicated Staphylococcus aureus infections: a snapshot of processes and outcomes in the real world. Open Forum Infect Dis. 2018;5:ofy274. https://doi.org/10.1093/ofid/ofy274 .
Twiddy M, Czoski Murray CJ, Mason SJ, Meads D, Wright JM, Mitchell ED, Minton J. A qualitative study of patients’ feedback about Outpatient Parenteral Antimicrobial Therapy (OPAT) services in Northern England: implications for service improvement. BMJ Open. 2018;8:e019099. https://doi.org/10.1136/bmjopen-2017-019099
Gardiol C, de Vallière S. Ambulante parenterale Antibiotikatherapie: Aktuelle Empfehlungen für die parenterale Behandlung von Infektionen. Swiss Medical Forum - Schweizerisches Medizin-Forum. 2016;16:314–8.
Lehmann C, Leisse C, Lindemann C, Scholten N, Oberröhrmann C, Ihle P, et al. Ergebnisbericht: Ambulante parenterale Antibiotikatherapie in der Kölner Metropolregion (K-APAT). 2023. https://innovationsfonds.g-ba.de/downloads/beschluss-dokumente/436/2023-08-16_K-APAT_Ergebnisbericht.pdf . Accessed 26 Mar 2024.
Kuckartz U. Qualitative Inhaltsanalyse: Methoden, Praxis, Computerunterstützung. 4th ed. Weinheim: Beltz Verlagsgruppe; 2018.
Quintens C, Steffens E, Jacobs K, Schuermans A, van Eldere J, Lagrou K, et al. Efficacy and safety of a Belgian tertiary care outpatient parenteral antimicrobial therapy (OPAT) program. Infection. 2020;48:357–66. https://doi.org/10.1007/s15010-020-01398-4 .
Gonçalves-Bradley DC, Lannin NA, Clemson L, Cameron ID, Shepperd S. Discharge planning from hospital. Cochrane Database Syst Rev. 2022;2:CD000313.
PubMed Google Scholar
Mäkelä P, Stott D, Godfrey M, Ellis G, Schiff R, Shepperd S. The work of older people and their informal caregivers in managing an acute health event in a hospital at home or hospital inpatient setting. Age Ageing. 2020;49:856–64. https://doi.org/10.1093/ageing/afaa085 .
Chambers ST, Basevi A, Gallagher K, Carswell-Moyna A, Isenman H, Pithie A, et al. Outpatient parenteral antimicrobial therapy (OPAT) in Christchurch: 18 years on. N Z Med J. 2019;132:21–32.
Hase R, Yokoyama Y, Suzuki H, Uno S, Mikawa T, Suzuki D, et al. Review of the first comprehensive outpatient parenteral antimicrobial therapy program in a tertiary care hospital in Japan. Int J Infect Dis. 2020;95:210–5. https://doi.org/10.1016/j.ijid.2020.03.033 .
Kwok CS, Whittaker JJ, Malbon C, White B, Snape J, Lloyd V, et al. Outpatient parenteral antimicrobial therapy (OPAT) service is associated with inpatient-bed cost savings. Br J Cardiol. 2021;28:38. https://doi.org/10.5837/bjc.2021.038 .
Al Shareef HJ, Al Harbi A, Alatawi Y, Aljabri A, Al-Ghanmi MA, Alzahrani MS, et al. Evaluate the Effectiveness of Outpatient Parenteral Antimicrobial Therapy (OPAT) Program in Saudi Arabia: A Retrospective Study. Antibiotics (Basel). 2022. https://doi.org/10.3390/antibiotics11040441 .
Schoonenboom J, Johnson RB. How to Construct a Mixed Methods Research Design. Kolner Z Soz Sozpsychol. 2017;69:107–31. https://doi.org/10.1007/s11577-017-0454-1 .
Bundesministerium für Justiz. Sozialgesetzbuch (SGB) Fünftes Buch (V) - Gesetzliche Krankenversicherung - § 39 Krankenhausbehandlung; 1988. https://www.gesetze-im-internet.de/sgb_5/__39.html . Accessed 26 Mar 2024.
Chapman ALN, Patel S, Horner C, Gilchrist M, Seaton RA. Outpatient parenteral antimicrobial therapy: updated recommendations from the UK. J Antimicrob Chemother. 2019;74:3125–7. https://doi.org/10.1093/jac/dkz343 .
Download references
Acknowledgements
We would like to thank all patients who participated in our study. We would also like to thank all of the staff at the study centres and the pharmacy service providers who cared for the patients together with the study physicians.
Open Access funding enabled and organized by Projekt DEAL. This work was supported by the German Federal Joined Committee (grant number 01VSF18036).
Author information
Authors and affiliations.
Chair of General Practice II and Patient-Centredness in Primary Care, Institute of General Practice and Primary Care, Faculty of Health, Witten/Herdecke University, Witten, Germany
Sophie Peter
University of Cologne, Faculty of Medicine and University Hospital Cologne, Institute of Medical Sociology, Health Services Research and Rehabilitation Science, Chair of Health Services Research, Cologne, Germany
Sophie Peter, Charlotte Oberröhrmann & Nadine Scholten
University of Cologne, Faculty of Human Sciences and Faculty of Medicine and University Hospital Cologne, Institute of Medical Sociology, Health Services Research and Rehabilitation Science Cologne, Cologne, Germany
Holger Pfaff
Center for Health Services Research Cologne, Cologne, Germany
Department I of Internal Medicine, Medical Faculty, University Hospital Cologne, University of Cologne, Cologne, Germany
Clara Lehmann, Kirsten Schmidt-Hellerau, Vanessa Brandes & Charlotte Leisse
Center for Molecular Medicine Cologne (CMMC), University of Cologne, Cologne, Germany
Clara Lehmann
German Center for Infection Research (DZIF), Bonn-Cologne, Germany
Department II of Internal Medicine and Center for Molecular Medicine Cologne (CMMC),, University of Cologne, Faculty of Medicine and University Hospital Cologne, Cologne, Germany
Christoph Heinrich Lindemann
PMV forschungsgruppe, Faculty of Medicine and University Hospital Cologne, Cologne, Germany
Peter Ihle & Jutta Küpper-Nybelen
Institute of Medical Statistics and Computational Biology (IMSB), Faculty of Medicine and University Hospital Cologne, University of Cologne, Cologne, Germany
Anna Hagemeier
You can also search for this author in PubMed Google Scholar
Contributions
ClL led the K-APAT study. NS, CO and SP designed the questionnaires and the interview guide, and have mainly carried out and evaluated the data collection. SP wrote the first draft of the manuscript. AH, ChL, ClL, CO, HP, JKN, KSH, NS, PI and VB substantively revised the work. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Sophie Peter .

Ethics declarations
Ethics approval and consent to participate.
The study has been approved by the Institutional Review Board of the University of Cologne, Germany (19-1284-1). Participants signed a written consent form to participate in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Peter, S., Oberröhrmann, C., Pfaff, H. et al. Exploring patients’ perspectives: a mixed methods study on Outpatient Parenteral Antimicrobial Therapy (OPAT) experiences. BMC Health Serv Res 24 , 544 (2024). https://doi.org/10.1186/s12913-024-11017-9
Download citation
Received : 20 February 2024
Accepted : 19 April 2024
Published : 29 April 2024
DOI : https://doi.org/10.1186/s12913-024-11017-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Patient Reported Outcome Measures
- Patient satisfaction
- Intravenous therapy
- Bacterial/viral infections
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Open access
- Published: 23 April 2024
Characteristics, outcomes, facilitators and barriers for psychosocial interventions on inpatient mental health dementia wards: a systematic review
- Naomi Thompson 1 , 2 ,
- Ming-Hung Hsu 1 , 2 ,
- Helen Odell-Miller 1 , 2 ,
- Benjamin R. Underwood 3 , 4 , 5 &
- Emma Wolverson 6 , 7
BMC Geriatrics volume 24 , Article number: 364 ( 2024 ) Cite this article
218 Accesses
4 Altmetric
Metrics details
The National Institute for Health and Care Excellence guidelines state that psychosocial interventions should be the first line of treatment for people with dementia who are experiencing distress behaviours, such as agitation and depression. However, little is known about the characteristics and outcomes of psychosocial interventions or the facilitators and barriers to implementation on inpatient mental health dementia wards which provide care for people with dementia who are often experiencing high levels of distress.
A systematic search was conducted on MEDLINE, CINAHL, PsycINFO, Psychology and Behavioural Sciences Collection, and Scopus in May 2023, following PRISMA guidelines. Reference and citation searches were conducted on included articles. Peer-reviewed literature of any study design, relating to psychosocial interventions in inpatient mental health dementia wards, was included. One author reviewed all articles, with a third of results reviewed independently by a second author. Data were extracted to a bespoke form and synthesised using a narrative review. The quality of included studies was appraised using the Mixed Methods Appraisal Tool.
Sixteen studies were included in the synthesis, which together included a total of 538 people with dementia. Study methods and quality varied. Psychosocial interventions delivered on wards included music therapy (five studies), multisensory interventions (four studies), multicomponent interventions (two studies), technology-based interventions (two studies), massage interventions (two studies) and physical exercise (one study). Reduction in distress and improvement in wellbeing was demonstrated inconsistently across studies. Delivering interventions in a caring and individualised way responding to patient need facilitated implementation. Lack of staff time and understanding of interventions, as well as high levels of staff turnover, were barriers to implementation.
This review highlights a striking lack of research and therefore evidence base for the use of psychosocial interventions to reduce distress in this vulnerable population, despite current healthcare guidelines. More research is needed to understand which psychosocial interventions can reduce distress and improve wellbeing on inpatient mental health dementia wards, and how interventions should be delivered, to establish clinical and cost effectiveness and minimise staff burden.
Peer Review reports
The already high prevalence of dementia and the significant predicted increase in those diagnosed with the condition in the coming decades has been widely documented [ 1 ]. Behavioural and psychological symptoms of dementia, which can include agitation, anxiety, depression, sleep disturbances, hallucinations, apathy, and disinhibition, are experienced by 80% of people with dementia in the UK [ 2 ]. Throughout this paper we refer to these as distress or distress behaviours, using preferred language by people with dementia reflecting that distress can be caused by symptoms of dementia and/or be an expression of unmet needs [ 3 ].
Inpatient mental health dementia wards, also known as psychiatric wards, provide care for people with dementia experiencing acute levels of distress that is putting their safety or the safety of others at risk [ 4 , 5 ]. The aim of the mental health admission is to assess and treat the crisis, including distress behaviours. In the UK, people are often detained using the provisions of the Mental Health Act 2007 meaning they can be treated without their consent, and admission often follows a breakdown of care in the home or care home, which can be traumatic for the person with dementia and their family caregiver(s) [ 6 , 7 ]. Caring for this population is complex as many have multiple long term conditions, and may need palliative care as they come to end of life [ 5 , 8 ]. A recent systematic review of the characteristics and outcomes of patients on these wards internationally highlights that little is known about current standards of practice and how best to deliver care in this setting [ 5 ].
The National Institute for Health and Care Excellence (NICE), who provide evidence-based recommendations for care in the UK, emphasise that psychosocial interventions, also described as nonpharmacological interventions, should be the first line of treatment for distress behaviours in dementia care [ 9 ]. NICE defines psychosocial interventions as interventions that require specific competencies for delivery, are supported by relevant training and supervision, and provide an enhanced level of intervention [ 10 ].
Increasingly such interventions are manualised and their effectiveness to reduce distress and support wellbeing for people with dementia in residential care settings has been tested [ 11 , 12 , 13 ]. However, there are still significant gaps in dementia care research and practice [ 14 ]. In particular, little is known about what psychosocial interventions have been delivered in inpatient mental health dementia care, and whether these were helpful. This is concerning as these wards provide specialist care for those who cannot be safely cared for in residential care, and pharmacological interventions, such as antipsychotic medication, are frequently used to manage distress with concomitant increase in risk of falls, strokes and death [ 4 , 15 ]. Further understanding of the current research on inpatient mental health dementia wards, including which psychosocial interventions have been delivered and how, positive and negative patient outcomes, and the facilitators and barriers to implementation, is needed to inform future research and practice.
To understand the current literature on this topic, a systematic review of psychosocial interventions in inpatient mental health dementia care was conducted. Based on expert-by-experience and stakeholder feedback, the review focussed on interventions that aim to reduce distress or improve wellbeing for people with dementia, as this is the primary focus of the admission. The following review questions were established:
What are the characteristics of psychosocial interventions designed to improve wellbeing and reduce distress for patients within inpatient mental health dementia wards?
What are the positive and negative outcomes for patients receiving these interventions?
What are the facilitators and barriers to successful implementation?
This systematic review follows the PRISMA reporting guidelines, and is registered on PROSPERO (CRD42023429983) [ 16 ].
Search strategy
A systematic search of the databases MEDLINE, CINAHL, PsycINFO, and Psychology and Behavioural Sciences Collection was conducted on the EBSCOhost platform, with an additional search on Scopus. Searches were piloted and performed in May 2023. The search strategy was developed with a librarian experienced in systematic reviews and conducted by NT. Reference lists of included studies were examined, and backward and forward citation searches conducted on Google Scholar.
Search terms were: (old* OR elder* OR geriatric* OR senior*) AND ((Psychiatr* OR psychogeriatric* OR “mental health”) N2 (inpatient* OR ward* OR unit* OR acute)) AND (dementia OR alzheimer* OR “cognitive impairment” OR “memory loss”) AND (psychosocial OR psychological OR psychotherapy OR mental health intervention OR nonpharmacological OR person-centred).
Search results were exported to an online software, Rayyan, for screening [ 17 ]. All titles and abstracts were screened by NT, with one third of results independently reviewed by EW. Where there was uncertainty, the full text was retrieved. Screening of the full texts was conducted by NT, with one third independently reviewed by EW. All reasons for exclusion were recorded. At both stages of screening, discrepancies were resolved between the two authors following discussion. Where additional information was required to inform inclusion decisions, authors were contacted via email.
Quality assessment of all included articles was conducted by NT using the Mixed Methods Appraisal Tool (MMAT), with one third conducted independently by EW [ 18 ]. This tool is not designed to give a score or inform inclusion and exclusion decisions, but provides a framework for assessing qualitative, quantitative and mixed methods studies. One article included authors of this current review (NT, HOM, and BRU) and so was assessed by EW to minimise bias. In case of uncertainty or discrepancies, decisions were discussed between NT and EW to reach consensus without the need to involve a third reviewer.
Inclusion and exclusion criteria
Inclusion and exclusion criteria were developed and outlined using an adapted PICOS framework (see Supplementary File 1 for justification for the criteria):
Population: Intervention actively involves patients with dementia, with a diagnosis from a diagnostic criteria or from a clinician. Studies where results for patients with a formal diagnosis cannot be separated from those with other cognitive impairments or other mental health diagnoses were not included.
Intervention: Psychosocial intervention, using the NICE definition: requires specific competencies for delivery, is supported by relevant training and supervision, and provides an enhanced level of intervention [ 10 ]. An additional definition for psychosocial interventions was helpful in clarifying inclusion, in particular for aspects relating to the aims of the intervention [ 19 ].
Context: Mental health or psychiatric ward providing specialist inpatient care for people with dementia in any country. Studies where results for inpatients and community patients cannot be separated were not included.
Outcome: Outcomes related to reduced distress or improved wellbeing for the person with dementia. Outcomes must be measured using a standardised questionnaire, or where qualitative data or researcher-designed tool is used, the measurement tool must be published and clearly described to enable quality assessment.
Study type: Presenting novel findings of any design, conducted internationally, published in a peer-reviewed journal in English. No restrictions for date of publication were given.
Data extraction and synthesis
Data were extracted to a bespoke data extraction form by NT, checked by EW, recording: author(s); date; country; setting; study design; study participants (include dementia stage and type); aims; intervention (dosage, frequency, duration, mode of delivery); interventionist (training); measurement tools (frequency of use); main findings (positive and negative outcomes); and facilitators and barriers to implementation (who reported these). Due to anticipated heterogeneity of interventions, a narrative synthesis was conducted using the tabulation to synthesise data in relation to the stated research questions, following the guidance of Popay et al. [ 20 ]. Facilitators and barriers to implementation were coded using inductive coding, and grouped into themes using thematic analysis [ 21 ]. Based on a previous scoping of the literature, interventions were grouped by type of intervention. Where there were two or more studies looking at a similar intervention these were combined to create a new category. Where studies reported outcomes not relating to people with dementia, for example for staff or family members, data were not extracted as this is outside the scope of the review questions.
The online searches retrieved 1221 articles. After removal of 355 duplicates, 866 titles and abstracts were screened. Of these, 835 articles were excluded, with full texts retrieved for 31 articles. Eight articles met the inclusion criteria (see Figure 1 for exclusion reasons). An additional eight articles were included from searching reference lists and citation searches of included articles. A total of 16 articles, involving 16 separate studies, are included in this review.
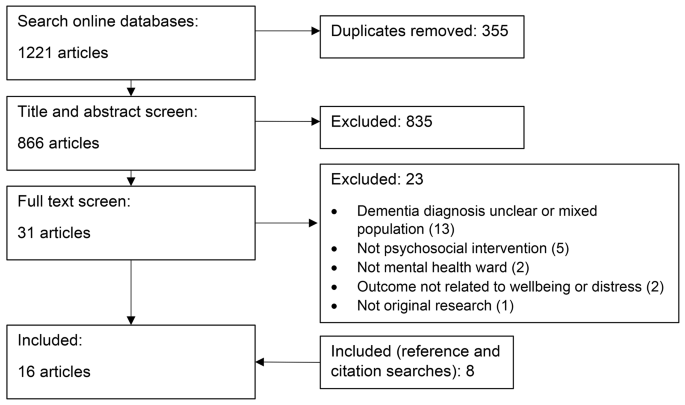
PRISMA diagram of study selection procedure
Study characteristics
Study characteristics are displayed in Table 1 . Half of the studies were conducted in the United Kingdom (5 studies) and the United States of America (3 studies), while two took place in Canada and Japan, and one in Finland, Switzerland and Germany respectively. It was not possible to clarify where one study was conducted [ 22 ]. Articles were published between 1998 and 2023. Methods used included randomised controlled trials [ 23 , 24 , 25 , 26 ], non-randomised trials [ 27 , 28 , 29 ], quantitative descriptive methods [ 22 , 30 , 31 , 32 ], mixed methods [ 33 , 34 ], and qualitative studies [ 35 , 36 , 37 ]. Outcomes were measured using standardised quantitative tools [ 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 ], non-standardised quantitative tools [ 22 , 32 , 33 ], biophysiological measures such as pulse and saliva samples [ 23 , 27 , 29 , 33 ], qualitative data collection [ 33 , 34 , 35 , 36 , 37 ], and routinely collected ward data [ 24 , 26 , 28 , 30 , 34 ].
The majority of studies investigated a psychosocial intervention on one inpatient mental health ward, while one looked at two wards [ 34 ], and another included three wards [ 26 ]. There was a combined total of 538 participants across studies, ranging from four to 175 participants. For details of participant characteristics, see Table 1 .
Quality Appraisal
Results from the MMAT showed the varying quality of the included studies, with an average (both mean and mode) of four out of seven criteria met across all studies, ranging from one to seven (l Supplementary File 2). The two screening questions applied to all studies were not consistently met, with two studies not clearly stating the research questions [ 30 , 36 ], and four not clearly demonstrating they collected appropriate data to answer research questions [ 22 , 30 , 35 , 36 ]. However, due to the small number of studies meeting inclusion criteria, these are included in the synthesis.
Intervention characteristics
The types of interventions delivered included music therapy (five studies [ 25 , 29 , 34 , 36 , 37 ]), multisensory interventions (four studies [ 24 , 30 , 31 , 33 ]), multicomponent interventions (two studies [ 22 , 28 ]), technology-based interventions, such as using applications or watching videos on tablets, (two studies [ 32 , 35 ]), massage interventions (two studies [ 23 , 27 ]), and physical exercise (one study [ 26 ]),.
Stated aims of the interventions were wide ranging, with the majority (15 studies) citing multiple aims. The most common aims related to reducing distress behaviours (also referred to as immediate, responsive or negative behaviours) [ 29 , 31 , 33 , 34 , 35 , 36 ], reducing agitation [ 23 , 24 , 30 , 32 ], reducing neuropsychiatric or behavioural and psychological symptoms of dementia [ 25 , 26 , 27 , 28 ], and improving activities of daily living and functional abilities [ 22 , 24 , 27 , 28 ]. Other aims included the feasibility and acceptability of the intervention in relation to the population [ 32 ] and the environment [ 25 , 35 ], improving mood and wellbeing [ 31 , 36 , 37 ], quality of life [ 22 ], quality of care [ 35 ], social interaction and engagement [ 22 , 35 , 36 , 37 ], and cognition [ 27 , 29 ], as well as reducing apathy [ 24 ], use of psychotropic medication [ 26 , 28 ], and stress (including biomarkers for stress) [ 23 , 27 , 29 ].
Intervention delivery was led by ward staff in eight studies (including nurses, care assistants and volunteers) [ 22 , 23 , 27 , 28 , 30 , 32 , 33 , 35 ], four of which specified that training was provided [ 23 , 27 , 28 , 33 ]. Training included ad hoc delivery to individuals as required, and group training ranging from two hours to 5.5 days. In five studies the intervention was delivered by a music therapist [ 25 , 29 , 34 , 36 , 37 ], with all but one specifying that the therapist was accredited with the relevant healthcare board [ 29 ], and three of which stated that ward staff supported in the sessions [ 29 , 36 , 37 ]. An occupational therapist delivered the intervention in one study, although training was not stated [ 31 ]. The interventionist was not specified in two studies [ 24 , 26 ].
Most studies delivered the intervention on an individual basis [ 23 , 24 , 25 , 27 , 30 , 31 , 32 , 33 , 35 ], while six interventions were delivered on a group basis [ 22 , 26 , 29 , 34 , 36 , 37 ]. One multicomponent intervention study included both group and individual sessions [ 28 ].
Intervention frequency ranged from weekly [ 22 , 34 , 36 , 37 ], to twice a week [ 23 , 25 , 29 ], and more than twice a week [ 26 , 27 , 28 , 31 ], with three interventions conducted as needed [ 30 , 32 , 33 ]. The dosage (i.e. length of each session) was reported by 13 studies, with five lasting up to 30 min [ 23 , 24 , 27 , 30 , 31 ], six between 31and 60 min [ 25 , 28 , 29 , 34 , 36 , 37 ], and two over 60 min [ 22 , 26 ]. The duration of the intervention period was reported by 11 studies with the majority running for up to four weeks [ 23 , 25 , 26 , 31 ], or five to ten weeks [ 22 , 27 , 29 , 37 ], and others lasting four months [ 36 ], one year [ 34 ], and two years [ 28 ].
Intervention outcomes
Music therapy intervention outcomes.
A reduction in agitation and distress behaviours, and increase in positive moods and behaviours, was reported in four of the five music therapy interventions on days when the intervention was delivered [ 29 , 34 , 36 , 37 ], one of which also reporting a reduction in biomarkers for stress [ 29 ]. Two of these studies found that a minority of participants displayed increased frustration or agitation during group music therapy sessions [ 36 , 37 ]. One study suggested that this could be a response from the participant to being drawn out of passivity [ 36 ], and another that the open nature of the group enabled participants to leave if they chose to [ 37 ]. However, one study reported no reduction in agitation or distress behaviours when music therapy was compared to an active control, though the groups were not comparable at baseline and it was not clear whether participants had adhered to the assigned intervention [ 25 ].
Multisensory intervention outcomes
All of the multisensory interventions reported short term positive outcomes relating to reduction in agitation and distress behaviours and increases in positive moods and interactive behaviours during sessions [ 24 , 30 , 31 , 33 ], with one study reporting this lasted up to one hour post intervention [ 30 ]. Additional reported outcomes were improved independence in activities of daily living [ 24 ], and reduction in apathy [ 24 ]. No change was reported for aggressive behaviours [ 30 ], wellbeing [ 31 ], heart rate [ 33 ], and prescribed medication [ 24 ].
Multicomponent, massage, technology-based and physical exercise intervention outcomes
Outcomes for massage interventions were inconclusive. Two studies reported a reduction in biomarkers for stress following massage [ 23 , 27 ], with one study, which accounted for confounding factors in the analysis, reaching statistical significance [ 27 ]. One study found no change in cognition but a significant reduction in aggression [ 27 ], while one found no difference in agitation [ 23 ], although authors suggest this could be because scores for agitation were low at baseline, and quality assessment showed that reported outcome data were not complete.
For multicomponent interventions, reported outcomes were conflicting. One study reported short term development of group cohesion, reduction in anxiety and changes in social interactions following weekly movement and sensory stimulation groups [ 22 ]. However, another found no significant differences between the intervention group, receiving group and individual music and physical exercise, and a control group of previous patient cohorts receiving standard care, although data suggested a reduction in anxiety and worsening of sleep and nighttime behaviour [ 28 ]. This study was a randomised controlled trial with a large number of participants, but it was not clear whether the intervention was administered as intended and confounding factors were not accounted for in the design and analysis.
Reported findings for technology-based interventions suggest positive changes in mood and reduction in anxiety, agitation and resistance to care [ 32 , 35 ]. However, one intervention using simulated presence through recorded videos of family members, found that videos with too many people could cause a negative response [ 35 ].
Finally, a study of a physical exercise intervention found a significant reduction in agitation, lability and verbal aggression in the intervention group, but no reduction in physical aggression or prescribed medication [ 26 ]. This study also reported that participants did not adhere to the assigned intervention.
Facilitators and barriers to implementation
All except one [ 31 ] of the included studies reported facilitators and/or barriers to implementation of the psychosocial intervention in the ward setting. Most were reported by the researchers, but some were reflections from staff, with one [ 37 ] also including feedback from family members. Inductive coding of reported facilitators and barriers led to the emergence of three themes: factors relating to the interventionist, factors relating to the intervention, and factors relating to the ward environment.
Factors relating to the interventionist
Researchers, staff and family members reported that staff support and understanding of the intervention, and delivering it with a caring approach enabling patients to express themselves and interact as they were able in the moment, facilitated implementation [ 22 , 32 , 34 , 35 , 37 ]. Researchers reported that the provision of supervision supported understanding [ 32 ], and family members and staff stated that observing the positive effects of the intervention with opportunities for positive interactions with patients were additional facilitators [ 37 ]. One study reported that nurse initiation of the intervention without referral to more senior staff members for approval supported implementation [ 30 ]. Barriers to implementation support these findings, with five studies, two of which reported staff feedback, stating that lack of understanding, scepticism of the intervention, and resistance to having close relationships with patients, were barriers to implementation and effectiveness [ 23 , 27 , 34 , 35 , 37 ]. This included staff reported fears about using equipment incorrectly or causing negative effects [ 33 ].
Factors relating to the intervention
Seven studies, two reporting staff responses, stated that the ability to individualise the intervention to patient preference, ability and the patient’s culture facilitated implementation [ 22 , 24 , 29 , 30 , 32 , 34 , 37 ]. In addition, researchers and staff in four studies reported that utilising nonverbal methods of communication, such as touch and music, enabled emotional expression, increased engagement and attention, and helped deepen the relationship between participants [ 27 , 29 , 34 , 37 ]. Other facilitating elements reported by researchers were safe, easy and accessible delivery [ 35 ], and gradually increasing the length of the intervention [ 24 ], while staff reported using good quality video and audio materials as supporting factors [ 35 ]. Factors reported by researchers as barriers to implementation of interventions were overstimulation for the person with dementia [ 35 ], and not being tailored to the cognitive abilities of the individual, such as concentration, with one study reporting that this was particularly evident towards the beginning of the hospital stay [ 28 , 35 ]. Additionally, how interventions were introduced to the wards could be a barrier to implementation including a lack of clear plans for implementation in the design [ 33 ], and introducing multiple interventions simultaneously [ 28 ].
Factors relating to the ward environment
Elements relating to the ward environment were cited as both facilitators and barriers to implementation. Enabling factors reported by staff and researchers were the ability to create a calm space on the ward [ 22 , 35 ], regular intervention delivery, which may enable a trusting relationship to be established between patient and interventionist [ 23 , 26 , 27 , 29 ], and timing the intervention around patients’ needs and ward routines [ 23 , 26 , 27 ]. Inhibiting factors reported by researchers were rigid timing of intervention delivery to fit around ward routines [ 23 ], a clinical focus on behaviour rather than mood on the ward [ 36 ], lack of staff time to support and deliver interventions [ 28 , 37 ], high levels of staff turnover, and not having regular access to an appropriate space [ 33 ]. In addition, one study suggested that patients being in late stages of dementia could be a barrier to engaging in interventions [ 25 ]. However, in this study, treatment groups were not comparable at baseline and the intervention did not appear to be individualised to the patient [ 25 ].
This review provides a systematic, narrative analysis of psychosocial interventions reported on inpatient mental health dementia wards, the outcomes for patients, staff and families, and the factors influencing implementation. The 16 included studies were small and of varying quality, but suggest that psychosocial interventions may help reduce distress experienced by people with dementia on these wards. The lack of good quality research is particularly striking given that NICE guidelines call for psychosocial interventions as the first line of treatment for people with dementia experiencing distress, and these wards provide care for those experiencing the highest levels of distress in our communities [ 4 , 9 ]. There is therefore a critical need for more research in this area, as reported in previous systematic reviews [ 5 ].
The research included in this review was of varying methodological quality and mostly in early stages of research development, with small samples and using single sites. This is reflected in the results of the MMAT with studies not consistently stating the research questions or demonstrating data collected were appropriate to answer research questions. This limits the comparability of results between studies, and the generalisability of findings to other settings. In addition, justification for the chosen intervention, the way it was delivered, and the theory for how and why it is expected to reduce distress and improve wellbeing, was poorly reported.
Overall findings suggest that psychosocial interventions, in particular music therapy and multisensory interventions, may be helpful in reducing distress and potentially improving wellbeing, although findings were not consistent. This is supported by a reduction in stress biomarkers in some included studies, suggesting interventions could have a biophysiological impact on people with dementia which enables a reduction in distress [ 23 , 27 , 29 ]. However, the need for careful intervention design and delivery were highlighted by reported negative outcomes including worsening sleep behaviour and overstimulation [ 28 , 35 ]. The potential challenges of implementing psychosocial interventions in this ward environment were shown. In particular, most interventions relied on staff for delivery, but lack of staff time and understanding of the intervention, and high levels of staff turnover, were barriers to implementation.
Findings from this review suggest that psychosocial interventions should be mainly nonverbal, person-centred, culturally sensitive, and delivered flexibly by a trained and skilled interventionist who is able to respond and regulate arousal in the moment. They should also minimise reliance on staff to deliver them and provide adequate training for staff to understand the potential benefits of the intervention. This has implications for policy, with psychosocial interventions reviewed against these criteria to increase their usefulness and helpfulness in reducing distress for people with dementia on mental health wards. In particular, policies should support training for staff to deliver specific psychosocial interventions, with accompanying funding for this post above the current staffing on wards, and the inclusion of mandatory training on interventions for all staff. Additionally, policies should include the development of standards for dementia friendly ward environments to ensure that psychosocial interventions can be implemented, including having private spaces available to deliver individual and small group interventions.
However, included studies do not provide evidence for which interventions should be delivered, how and when to deliver them, the support needed for implementation, and how this links with the wider care plan and support for the individual. There was also a lack of evidence for the involvement and impact for family members, with only one [ 37 ] study mentioning their involvement. Future research should consult current guidelines on developing and evaluating complex interventions, such as those from the Medical Research Council [ 38 ]. Involving people with lived experience, such as staff, family members and patients, in the design of interventions and studies will be crucial to supporting feasibility of delivery and helpfulness [ 39 , 40 ]. Once these factors are identified, multi-site, randomised and masked studies are needed to establish clinical and cost effectiveness. Outcomes should include the effectiveness of interventions to reduce distress, with definitions and outcome measures agreed with staff, patients and family members; the cost-effectiveness of the intervention; the impact on staff time, care delivery and the ward environment; the impact on patient, staff and family member wellbeing; the impact on patient length of stay, including communication with the discharge destination; and the impact on use of as-needed (pro re nata) and prescribed medication.
Limitations of this review include the use of a second reviewer for only one third of the titles and abstracts and full text articles during the screening process meaning it is possible that articles were wrongly excluded during screening. Only articles written in English were included due to resource limitations, and articles not published in peer-review journals were excluded, potentially missing ward-based evaluations and audits. Additionally, the varied language used to describe inpatient mental health wards internationally further complicated the screening process. Studies specifying they took place on hospital wards and focused on distress behaviours in dementia were included, and any uncertainties were discussed with the team. Due to the small number of studies expected to meet the criteria a time limit was not used so some studies may not reflect current practice.
Further research is required to increase our understanding of whether specific psychosocial interventions can help reduce distress and improve wellbeing for people with dementia on inpatient mental health dementia wards, and how these should be delivered. This can enable the development of cost-effective toolkits and protocols for psychosocial interventions that are feasible to deliver with limited resource and have been shown to reduce distress and improve wellbeing on inpatient mental health dementia wards.
Data availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Abbreviations
Emma Wolverson
Mixed Methods Appraisal Tool
National Institute for Health and Care Excellence
Naomi Thompson
Participant, Intervention, Control, Outcome, Study Type
7. References
Wittenberg R, Hu B, Barraza-Araiza LF, Rehill A. Projections of Older People with Dementia and Costs of Dementia Care in the United Kingdom, 2019–2040. CPEC Working Paper 5. 2019;(November):1–79.
Alzheimer’s Society. Counting the cost - Caring for people with dementia on hospital wards [Internet]. Alzheimer’s Society. 2009. http://wpp01.msss.gouv.qc.ca/appl/K30/K30Redirection.asp?doc=p&id=2748
Dementia Australia. Dementia language guidelines [Internet]. 2021 [cited 2022 Nov 1]. https://www.dementia.org.au/sites/default/files/resources/dementia-language-guidelines.pdf
Edmans BG, Wolverson E, Dunning R, Slann M, Russell G, Crowther G et al. Inpatient psychiatric care for patients with dementia at four sites in the United Kingdom 1|. Int J Geriatr Psychiatry. 2021;1–4.
Wolverson E, Dunning R, Crowther G, Russell G, Underwood BR. The characteristics and outcomes of people with dementia in Inpatient Mental Health Care: a review. Clinical Gerontologist. Routledge; 2022.
Wolverson EL, Dening KH, Dunning R, Crowther G, Russell G, Underwood BR. Family experiences of inpatient mental health care for people with dementia. Front Psychiatry. 2023;14(1093894).
Mental health act 2007 [Internet]. 2007. https://www.legislation.gov.uk/ukpga/2007/12/data.pdf
Wolverson E, Appleyard S, Stirland S, Gower Z. The palliative care symptoms of people with dementia on admission to a mental health ward. Int J Geriatr Psychiatry [Internet]. 2023;38(9). https://onlinelibrary.wiley.com/doi/ https://doi.org/10.1002/gps.5995
National Institute for Health and Care Excellence. Dementia. Quality standard 184. 2019;(June 2019):39. https://www.nice.org.uk/guidance/qs184/resources/dementia-pdf-75545721373381
National Institute for Health and Care Excellence. Drug use disorders in adults: Quality standard [Internet]. 2012. www.nice.org.uk/guidance/qs23
Livingston G, Kelly L, Lewis-Holmes E, Baio G, Morris S, Patel N, et al. Non-pharmacological interventions for agitation in dementia: systematic review of randomised controlled trials. Br J Psychiatry. 2014;205(6):436–42.
Article PubMed Google Scholar
Backhouse T, Dudzinski E, Killett A, Mioshi E. Strategies and interventions to reduce or manage refusals in personal care in dementia: A systematic review. Int J Nurs Stud [Internet]. 2020;109. https://www.scopus.com/inward/record.uri?eid=2-s2.0-85086383101&doi=10.1016/j.ijnurstu.2020.103640&partnerID=40&md5=095e6a623aad23cfa4c58e8ce677c5a5
Legere LE, McNeill S, Schindel Martin L, Acorn M, An D. Nonpharmacological approaches for behavioural and psychological symptoms of dementia in older adults: a systematic review of reviews. Journal of Clinical Nursing. Volume 27. Blackwell Publishing Ltd; 2018. pp. e1360–76.
World Health Organisation. A blueprint for dementia research. 2022.
Nørgaard A, Jensen-Dahm C, Wimberley T, Svendsen JH, Ishtiak-Ahmed K, Laursen TM et al. Effect of antipsychotics on mortality risk in patients with dementia with and without comorbidities. J Am Geriatr Soc. 2022;(November):1–11.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Volume 372. The BMJ: BMJ Publishing Group; 2021.
Google Scholar
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210.
Article PubMed PubMed Central Google Scholar
Nha HONGQ, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M et al. MIXED METHODS APPRAISAL TOOL (MMAT) VERSION 2018 User guide [Internet]. http://mixedmethodsappraisaltoolpublic.pbworks.com/
Moniz-Cook E, Vernooij-Dassen M, Woods B, Orrell M. Psychosocial interventions in dementia care research: the INTERDEM manifesto. 15, Aging and Mental Health. 2011. p. 283–90.
Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rogers M et al. Guidance on the conduct of narrative synthesis in systematic reviews. 2006.
Braun V, Clarke V. Thematic analysis: a practical guide. London: SAGE Publications Ltd; 2021. pp. 0–376.
Arno S, Frank DI. A Group for Wandering Institutionalized clients with primary degenerative dementia. Perspect Psychiatr Care. 1994;30(3):13–6.
Article CAS PubMed Google Scholar
Schaub C, Von Gunten A, Morin D, Wild P, Gomez P, Popp J. The effects of Hand Massage on stress and agitation among people with dementia in a hospital setting: a pilot study. Appl Psychophysiol Biofeedback. 2018;43(4):319–32.
Staal JA, Sacks A, Matheis R, Collier L, Calia T, Hanif H et al. The effects of snoezelen (multi-sensory behavior therapy) and psychiatric care on agitation, apathy, and activities of daily living in dementia patients on a short term geriatric psychiatric inpatient unit. Int J Psychiatry Med [Internet]. 2007;37(4):357–70. https://www.scopus.com/inward/record.uri?eid=2-s2.0-41549119352&doi=10.2190/PM.37.4.a&partnerID=40&md5=4ae9d5d898dd2721b6b4f6c6d0916e63
Thornley J, Hirjee H, Vasudev A. Music therapy in patients with dementia and behavioral disturbance on an inpatient psychiatry unit: Results from a pilot randomized controlled study. Int Psychogeriatr [Internet]. 2016;28(5):869–71. https://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2015-52624-001&site=ehost-live
Fleiner T, Dauth H, Gersie M, Zijlstra W, Haussermann P. Structured physical exercise improves neuropsychiatric symptoms in acute dementia care: a hospital-based RCT. Alzheimers Res Ther. 2017;9(1).
Suzuki M, Tatsumi A, Otsuka T, Kikuchi K, Mizuta A, Makino K, et al. Physical and psychological effects of 6-week tactile massage on elderly patients with severe dementia. Am J Alzheimers Dis Other Demen. 2010;25(8):680–6.
Pitkanen A, Alanen HM, Kampman O, Suontaka-Jamalainen K, Leinonen E. Implementing physical exercise and music interventions for patients suffering from dementia on an acute psychogeriatric inpatient ward. Nord J Psychiatry. 2019;73(7):401–8.
Suzuki M, Kanamori M, Watanabe M, Nagasawa S, Kojima E, Ooshiro H et al. Behavioral and endocrinological evaluation of music therapy for elderly patients with dementia. Nurs Health Sci [Internet]. 2004;6(1):11–8. https://onlinelibrary.wiley.com/doi/ https://doi.org/10.1111/j.1442-2018.2003.00168.x
Mitchell AM, Chiappetta L, Boucek L, Cain M, Patterson G, Owens K et al. Nonpharmacological Therapeutic Techniques to Decrease Agitation in Geriatric Psychiatric Patients With Dementia. J Gerontol Nurs [Internet]. 2015;41(2):53–9. https://journals.healio.com/doi/ https://doi.org/10.3928/00989134-20141014-02
Spaull D, Leach C, Frampton I. An evaluation of the effects of sensory stimulation with people who have dementia. Behavioural and Cognitive Psychotherapy [Internet]. 1998;26(1):77–86. https://www.scopus.com/inward/record.uri?eid=2-s2.0-0031935448&doi=10.1017/S1352465898000083&partnerID=40&md5=d29ff263af9ace0d82c3ac9fcaf84b6d
Vahia IV, Kamat R, Vang C, Posada C, Ross L, Oreck S et al. Use of Tablet Devices in the Management of Agitation Among Inpatients with Dementia: An Open-Label Study. American Journal of Geriatric Psychiatry [Internet]. 2017;25(8):860–4. https://www.scopus.com/inward/record.uri?eid=2-s2.0-84998710184&doi=10.1016/j.jagp.2016.07.011&partnerID=40&md5=25ae5b356021ba34cca3ffd75898a14f
Hope KW. The effects of multisensory environments on older people with dementia. J Psychiatr Ment Health Nurs. 1998;5(5):377–85.
Thompson N, Iyemere K, Underwood BR, Odell-Miller H. Investigating the impact of music therapy on two in-patient psychiatric wards for people living with dementia: retrospective observational study. BJPsych Open [Internet]. 2023;9(2):e42. https://www.cambridge.org/core/product/identifier/S2056472423000200/type/journal_article
Hung L, Au-Yeung A, Helmer C, Ip A, Elijah L, Wilkins-Ho M, et al. Feasibility and acceptability of an iPad intervention to support dementia care in the hospital setting. Contemp Nurse. 2018;54(4–5):350–61.
Gold K. But does it do any good? Measuring the impact of music therapy on people with advanced dementia: (innovative practice). DEMENTIA-INTERNATIONAL J SOCIAL Res Pract. 2014;13(2):258–64.
Melhuish R. Group Music Therapy on a Dementia Assessment Ward: An Approach to Evaluation. British Journal of Music Therapy [Internet]. 2013;27(1):16–31. http://journals.sagepub.com/doi/10.1177/135945751302700103
Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM et al. A new framework for developing and evaluating complex interventions: Update of Medical Research Council guidance. Vol. 374, The BMJ. 2021.
NHS England. Patient and Public Participation Policy. 2017;1–16. https://www.england.nhs.uk/wp-content/uploads/2017/04/ppp-policy.pdf
Care D, of H. and S. Working in partnership with people and communities. NHS Engl Statutory Guidance. 2022.
Download references
Acknowledgements
We would like to acknowledge Jolene Cushion, subject librarian at Anglia Ruskin University, for their advice in designing the search strategy.
Funding for the Doctoral Scholarship for NT was provided by Anglia Ruskin University. BRU’s post is part-funded by a donation from Gnodde Goldman Sachs. This research was supported by the National Institute for Health and Care Research (NIHR) Cambridge Biomedical Research Centre (grant BRC-1215-20014). The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Author information
Authors and affiliations.
Cambridge Institute for Music Therapy Research, Anglia Ruskin University, Cambridge, UK
Naomi Thompson, Ming-Hung Hsu & Helen Odell-Miller
Arts Therapies Services, Cambridgeshire and Peterborough NHS Foundation Trust, Fulbourn Hospital, Fulbourn, UK
Department of Psychiatry, University of Cambridge, Cambridge, UK
Benjamin R. Underwood
Cambridgeshire and Peterborough NHS Foundation Trust, Fulbourn Hospital, Fulbourn, UK
Faculty of Science and Engineering, Anglia Ruskin University, Cambridge, UK
Dementia UK, London, UK
Faculty of Health Sciences, University of Hull, Hull, UK
You can also search for this author in PubMed Google Scholar
Contributions
All authors designed the study. NT designed the search strategy. NT and EW collected and synthesised the data. NT analysed data and drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Naomi Thompson .
Ethics declarations
Ethics approval and consent to participate.
Not Applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Thompson, N., Hsu, MH., Odell-Miller, H. et al. Characteristics, outcomes, facilitators and barriers for psychosocial interventions on inpatient mental health dementia wards: a systematic review. BMC Geriatr 24 , 364 (2024). https://doi.org/10.1186/s12877-024-04965-8
Download citation
Received : 15 November 2023
Accepted : 11 April 2024
Published : 23 April 2024
DOI : https://doi.org/10.1186/s12877-024-04965-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Psychosocial interventions
- Inpatient dementia care
- Mental health
- Systematic review
BMC Geriatrics
ISSN: 1471-2318
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 18 April 2024
The design of an Obstetric Telephone Triage Guideline (OTTG): a mixed method study
- Farzaneh Rashidi ORCID: orcid.org/0000-0001-7497-4180 1 ,
- Masoumeh Simbar ORCID: orcid.org/0000-0003-2843-3150 2 ,
- Saeed Safari ORCID: orcid.org/0000-0002-7407-1739 3 &
- Zahra Kiani ORCID: orcid.org/0000-0002-4548-7305 4
BMC Women's Health volume 24 , Article number: 246 ( 2024 ) Cite this article
192 Accesses
Metrics details
Clarifying the dimensions and characteristics of obstetric telephone triage is important in improving the quality of services in the health system because researchers can evaluate the effectiveness of treatment, care and diagnostic measures in the form of obstetric telephone triage by developing a guideline. Therefore, this study aimed to design an Obstetric Telephone Triage Guideline (OTTG) using a mixed-method study.
The present study was carried out using an exploratory sequential mixed method study in two qualitative and quantitative phases. An inductive-deductive approach was also used to determine the concept of obstetric telephone triage. In this respect, a qualitative study and a literature review were used in the inductive and deductive stages, respectively. Moreover, the validity of the developed guideline was confirmed based on experts’ opinions and results of the AGREE II tool.
The guideline included the items for evaluating the severity of obstetric symptoms at five levels including “critical”, “urgent”, “less urgent”, “no urgent”, and “recommendations”. The validity of the guideline was approved at 96%, 95%, 97%, 95%, 93%, and 100% for six dimensions of AGREE II including scope and purpose, stakeholder involvement, the rigor of development, clarity of presentation, applicability, and editorial independence, respectively.
The OTTG is a clinically comprehensive, easy-to-use, practical, and valid tool. This guideline is a standardized tool for evaluating the severity of symptoms and determining the urgency for obstetrics triage services. By using this integrated and uniform guideline, personal biases can be avoided, leading to improved performance and ensuring that patients are not overlooked. Additionally, the use of OTTG promotes independent decision-making and reduces errors in triage decision-making.
Peer Review reports
Introduction
Hospitals receive 20 to 30 phone calls from pregnant women per day. During these calls, healthcare providers use their obstetric knowledge and experiences to determine the severity of the problem and the urgency of a physical consultation with an obstetrician [ 1 , 2 , 3 ]. Obstetric triage services are usually provided physically (face-to-face), however, in many Western societies, women typically make an initial phone call to inquire about the need for counseling or a visit to the emergency room [ 4 , 5 , 6 , 7 , 8 , 9 ]. Telephone triage is a service delivery system that is currently not performed uniformly due to the lack of specific instructions [ 1 , 2 , 3 ].
While most existing guidelines for obstetric triage are based on physical triage. However, telephone triage has many positive aspects such as efficacy and uniformity. However, there are some challenges due to the lack of clinical perspective during the telephone call and the lack of specific diagnostic information [ 10 ].
Obstetric physical triage is an independent and efficient unit [ 11 , 12 ] with versatile dimensions such as parturient admission, evaluation of fetal well-being, as well as acute obstetric and gynecological emergencies [ 13 ]. The use of triage is important throughout the pregnancy and labor stages. Triage ensures appropriate care based on the clinical priorities of the patient and the effective use of resources [ 14 , 15 ]. However, some problems of obstetric triage include patient dissatisfaction and prolonged waiting times [ 16 , 17 , 18 ]. Prolonged waiting time results in leaving patients without examination, delayed delivery of necessary care and treatment, patient dissatisfaction, and increased mortality and morbidity [ 19 , 20 ]. On the other hand, reducing the waiting time decreases the duration of hospital stay, lowers the treatment cost, and saves hospital resources [ 21 ].
Studies show that triage standardization favorably affects its efficiency and safety [ 17 ]. The telephone is a 24-hour means of communication between patients and health care providers [ 22 ], and the importance of the telephone answering system has been specified [ 23 ].
Some of the advantages of telephone triage include increased access to services, reduced waiting time to receive services, avoidance of unnecessary referrals, and long and expensive trips [ 24 , 25 ].
Understanding the correct telephone triage approach by obstetric triage personnel is extremely important since improper communication leads to untimely acceptance of pregnant women and incorrect decisions [ 26 ].
The results of a review study showed that there is no agreement on the existence of a standard system in the field of obstetric triage [ 17 ]. Bailey et al. (2018) conducted a review study to investigate obstetric telephone triage. The results showed that more research is needed to examine midwives’ perceptions of their role in obstetric telephone triage, reviewing obstetric telephone triage processes and tools [ 27 ]. Engeltjes et al. (2020) conducted a Delphi study in the Netherlands to design obstetric telephone triage guidelines. The telephone obstetric triage guidelines were designed based on the physical obstetric triage system ROTS with five prioritization categories, which 91.9% of professional users declared complete, good, and user-friendly [ 28 ]. Limited studies have focused on the design and psychometrics of obstetric telephone triage guidelines [ 27 ], whereas the design of obstetric telephone triage guidelines can strengthen obstetric performance [ 29 ].
Given the importance of clarifying the dimensions and characteristics of obstetric telephone triage in improving the quality of services in the health system, researchers can evaluate the effectiveness of treatment care and diagnostic measures in the form of obstetric telephone triage by using this guideline. In addition, different health service providers and managers can use the results of these assessments to improve the quality of obstetric telephone triage. With this background in mind, the present study aimed to develop an obstetric telephone triage guideline.
This was an exploratory sequential mixed method study in two qualitative and quantitative phases to develop and validity assessments of the guideline an inductive-deductive approach was performed to explain the concept of obstetric telephone triage. In this respect, a qualitative study and a literature review were carried out to extract the codes and convert them to the items of the OTTG. After item generation and developing the first draft of OTTG, its validity was assessed by the experts using Appraisal of Guidelines for Research and Evaluation II (AGREE II). Figure 1 shows the procedure of the study for OTTG development and validation.
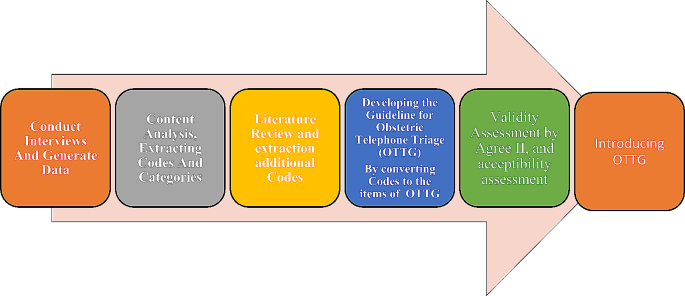
The procedure of the study to develop and validation of Obstetric Telephone Triage Guideline (OTTG)
The details for the procedure of the study are as follows:
Qualitative phase
This qualitative study with a content analysis approach was performed as the first part of a multi-stage large study [ 30 , 31 , 32 ].
The participants with maximum diversity and different educational levels, fields, and specialties related to obstetric triage were interviewed. The mean call volume was 400 calls per month.
The obstetric triage personnel were recruited from medical educational hospitals with obstetric and telephone triage services, specifically from Shahid Beheshti University of Medical Sciences in Tehran-Iran.
The inclusion criteria for obstetric triage personnel were: the ability to express experiences, and willingness to participate in the study, having at least 6 months of work experience in the obstetric department, and being familiar with telephone triage. The exclusion criteria included: refusing to continue the interview.
The participants were recruited using the purposive sampling method that continued until data saturation. The semi-structured individual interviews were performed to explain the participants’ perceptions and work experiences about telephone triage. The interviews were conducted by the first author of the research, and recorded and immediately transcribed verbatim. Following receiving permission to do the research in the setting, the objectives were explained to the participants of the study before the interviews.
Afterward, informed consent was obtained from all participants and they were ensured of the confidentiality of the information. Moreover, participation in the study was voluntary. The participants were asked to add anything left about the subject at the end of the interviews. Ultimately, the researcher referred to the possibility of future interviews in addition to appreciating the cooperation of the participants. Data analysis was conducted using Granheim and Lundman’s method, which was performed simultaneously with data collection [ 33 ]. The interviews were transcribed immediately after each interview and completed on the same day. The average, duration of the interviews was 28.52 min (with a duration between 20 and 49 min). Based on the participants’ viewpoints, the most significant factors influencing obstetric telephone triage were categorized into two main categories: common complaints (27 codes) and communication (8 codes). The initial guideline framework, number of levels, and criteria for evaluating maternal and fetal health were developed based on the findings of a qualitative study.
In the deductive approach and using a literature review, a comprehensive search was conducted on databases such as Scopus, PubMed, Embase, ProQuest, Web of Science, Cochrane, Science Direct, and Google Scholar, using keywords such as pregnancy, obstetric, triage guideline, system, index, tool, questionnaire, scale, telephone, midwifery, and maternity. A total of 26 articles were included in the study, and items related to obstetric telephone triage not existing in the pool of items obtained from the qualitative stage were added to the main items.
Quantitative phase (validity assessment)
The AGREE II tool was used to assess the internal validity of the guideline. The primary draft of the guideline was sent via email to 10 experts in questionnaire development, emergency medicine, reproductive health, obstetrics, and telephone triage (different from the participants in the qualitative phase) for their feedback on the decision-making process for the risk classification based on maternal and fetal criteria and symptoms, the severity of the emergency, patient arrival time at the hospital.
AGREE II encompasses 23 key criteria in six domains scope and purpose (criteria 1–3), stakeholder involvement (criteria 4–7), rigor of development (criteria 8–14), clarity of presentation (criteria 15–17), applicability (criteria 18–21), and editorial independence (criteria 22 and 23) [ 27 ].
The score of each domain was calculated by adding the score given to the criteria and after total score calculation, it was standardized by converting to a 0-100 score range based on the following formula: X-Min Score / Max-Min Score) × 100. The guideline remained in the study in case of earning a score above 60% in each area [ 34 ].
To assess the acceptability of the guideline, it was sent again to the same 10 experts via email who rated the final guideline in terms of feasibility and applicability (extremely high = 4, high = 3, low = 2, and very low = 1), being scientific (completely agree = 4 to completely disagree = 1), and importance (completely agree = 4 to completely disagree = 1). Finally, data analysis was performed, and validity was confirmed with 70% consensus about the acceptable utility of the guideline [ 35 ].
The participants were 21 obstetric triage personnel and the key informants, including emergency medicine specialists, clients, gynecologists, and reproductive health specialists. The average work experience of obstetric triage personnel was 13.6 years (work experience of 3 to 28 years).
Based on the results of the qualitative phase, 124 primary codes and 35 integrated codes were extracted through the semi-structured interviews.
According to the participants’ opinion, the most significant factors influencing the use of obstetric telephone triage services were in two main categories: common complaints (27 codes) and communication (8 codes).
The common complaints category includes items such as abdominal pain, hemorrhage, hypertension, postpartum concerns, membrane rupture, suspicion of labor onset, illness/other, and decreased fetal movements. The communication category includes items such as last menstrual period, age, gestational age, number of pregnancies and parity, and obstetric and medical history. These items were included in the obstetric telephone triage guidelines. The extracted items from the qualitative interviews are listed in Table 1 .
Ten items were also extracted from the review of the searched articles. In the deductive approach, otherwise, the items related to obstetric telephone triage, which were not identified in the qualitative phase, were then added to the main items. These additional items include headache with aura, headache without aura [ 36 ], severe and continuous pain after 24 weeks of gestation [ 28 ], lack of fetal movements before 20 weeks [ 28 ], lack of fetal movements between 20 and 24 weeks, pain and gestational age between 24 and 37 weeks [ 28 ], confirmed uterine pregnancy by ultrasound or unconfirmed pregnancy by ultrasound between 5 and 16 weeks [ 37 ] and mild vaginal bleeding [ 38 , 39 ], dyspnea lasting less than 24 h and mild diarrhea before 16 weeks [ 28 , 40 ].
Finally, the items extracted from the qualitative study (using an inductive approach) were integrated with the items extracted from the literature review (using a deductive approach) results and initial draft of the obstetric telephone triage guideline was created.
Figure 2 the components of obstetric telephone triage guidelines.

The components of obstetric telephone triage guideline
The guideline was then reviewed by experts, who prioritized the recommendations into five levels: critical, urgent, less urgent, no urgent, and recommendation. The critical level included life-saving measures for both the mother and fetus, while the other levels consisted of hospital referral within one hour, four hours, and 24 h, as well as the need for a consultation (Fig. 3 ).
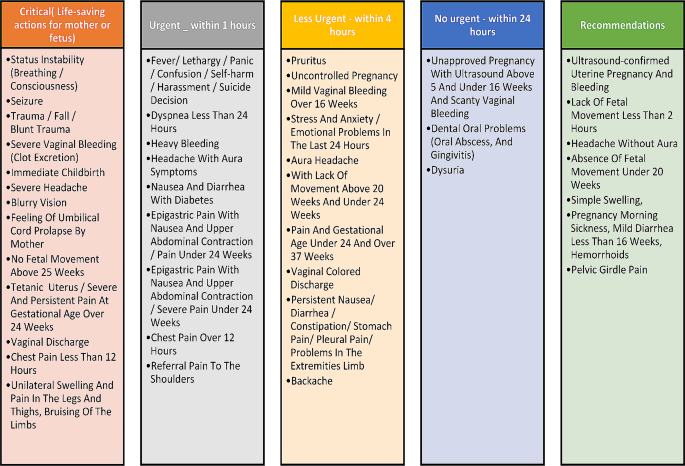
Levels of priority based on the obstetric telephone triage guideline
The obstetric telephone triage guidelines included multiple levels and evaluation criteria for both the mother and fetus and were once again provided to experts for validation.
Table 2 shows the validity and quality of the developed guideline based on the AGREE II tool (Table 2 ). According to the experts’s opinion, the score obtained in all domains of the AGREE II tool was above 60%, so the designed guideline has a content validity.
The final validation of the guideline was carried out based on the opinions of experts in terms of applicability (93%), scientific (90%), and importance (100%).
Discussion and recommendations
The present study introduces an understandable, applicable, and valid guideline for obstetric telephone triage. This guideline is the first obstetric telephone triage guideline designed in Iran, which is based on the modified Emergency Severity Index (ESI) obstetric triage [ 41 ]. This guideline helps to perform obstetric telephone triage based on cause, the severity of symptoms, and treatment for pregnant women in 5 levels including Critical (life-saving measures for mother or fetus), Urgent (visit the hospital within an hour), Less Urgent (Refer to the hospital within four hours), No urgent (refer to the hospital within twenty-four hours) and Recommendations (need to consult) [ 41 ]. In a study conducted in the United States of America to develop a telephone triage of candidiasis diagnosis, Hoffstetter et al. (2012) showed that it is difficult to diagnose candidiasis using symptoms and self-report through telephone triage as well as telephone treatment in symptomatic women. However, a telephone symptom guide for the diagnosis of candidiasis increased the accuracy of treatment by telephone triage [ 42 ]. While obstetric telephone triage guidelines are intended to guide triage personnel, they should not reduce their decision-making ability or professional responsibility and should be consistent with the patient’s professional insights and preferences.
Based on a survey, providing friendly advice in telephone triage leads to mothers’ reassurance and prevention of premature delivery for childbirth [ 43 ]. In a study, Huibers et al. reported that the majority of calls responded to by triage personnel were non-urgent [ 44 ]. In a study, pregnant women often make several calls for pregnancy and childbirth counseling. Triage personnel often provide different responses that are not documented, which leads to safety problems for the caller. Therefore, it is important to develop an evidence-based process for telephone triage [ 45 ]. In a study by Wahlberg et al., triage personnel reported callers’ anger, loud voice, and disrespectful behavior. In addition, they barely listened to the triage personnel’s guidance and were ultimately dissatisfied with the call. An inaccurate understanding of the situation or exaggeration of the event disrupts triage personnel’s judgment and causes loss of information [ 46 ]. Obstetric telephone triage is a complex multifaceted process affected by different internal and external factors [ 27 ]. Having a unified national guideline on telephone triage can reduce weaknesses in management and planning.
The results of the present study showed the validity of 93%, 90%, and 100%, respecting the guideline’s applicability, scientific, and importance, respectively. In a study by Engeltjes et al., an obstetric telephone triage guideline was designed based on the Rotterdam Obstetric Triage System (ROTS) in the Netherlands. The guideline included the examination of emergency obstetric symptoms at five levels. Their results showed that 91.9% of the experts considered the tool to be complete, accurate, and user-friendly, and 98.4% of them expressed that the tool was ready to be used [ 28 ]. The results of the studies showed that the validity of The Maternal Fetal Triage Index (MFTI), the Perinatal Emergency Team Response Assessment (PETRA), and the Swiss Emergency Triage Scale (SETS), all three obstetric triage systems, were 72.9%, 80%, and 78.4%, respectively [ 6 , 8 , 47 ].
The validation was performed using different methods for triage guidelines. The results showed that external validity is one of the most valid methods [ 15 ]. In maternal care, developing valid obstetric triage guidelines is critical [ 48 , 49 ], and that also requires training packages [ 50 ]. There is limited evidence on the implementation and evaluation of such a system [ 51 ]. A successful triage unit follows a consistent policy. All instructions should be for the management of all clients for various reasons. If providers fail to follow the guidelines or standards, difficulties in fulfilling responsibilities and risks for clients may occur [ 52 ]. The guidelines allow all triage personnel to quickly evaluate and provide services to clients. Coordinated use of protocols, guidelines, and team training are effective ways to improve the quality of the services. In all cases, the use of guidelines and timely evaluation enables team action and coordination to ensure appropriate results [ 53 ].
One of the major limitations of the present study was the lack of access to obstetric telephone triage guidelines of different countries with various healthcare systems in the world. Another limitation of the present study was the lack of consideration of the patient’s voice and cultural factors.
In this study, we examined various dimensions of obstetric telephone triage. Our findings indicate that the obstetric telephone triage guideline is clinically comprehensive, easy to understand, practical, and valid. This guideline serves as a standardized tool for evaluating the severity of symptoms and determining the urgency of obstetric care for triage personnel. By following this integrated and uniform guideline, personal biases can be avoided, leading to improved performance and ensuring that patients are not overlooked. Additionally, the use of an integrated obstetric telephone triage guideline promotes independent decision-making and reduces errors in triage decision-making.
Data availability
The data that support the findings of this study are available from Masoumeh Simbar but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Shahid Beheshti University of Medical Sciences.
Abbreviations
Appraisal of Guidelines Research and Evaluation
The Rotterdam Obstetric Triage System
Obstetric Telephone Triage Guideline
The Maternal Fetal Triage Index
Perinatal Emergency Team Response Assessment
Swiss Emergency Triage Scale
Poeran J, Borsboom GJ, de Graaf JP, Birnie E, Steegers EA, Mackenbach JP, et al. Does centralisation of acute obstetric care reduce intrapartum and first-week mortality? An empirical study of over 1 million births in the Netherlands. Health Policy. 2014;117(1):28–38.
Article PubMed Google Scholar
Wiegers TA, de Borst J. Organisation of emergency transfer in maternity care in the Netherlands. Midwifery. 2013;29(8):973–80.
Bailey CM, Newton JM, Hall HG. Telephone triage in midwifery practice: a cross-sectional survey. Int J Nurs Stud. 2019;91:110–8.
Gratton RJ, Bazaracai N, Cameron I, Watts N, Brayman C, Hancock G, et al. Acuity Assessment in Obstetrical Triage. J Obstet Gynecol Can. 2016;38(2):125–33.
Article Google Scholar
Smithson DS, Twohey R, Rice T, Watts N, Fernandes CM, Gratton RJ. Implementing an obstetric triage acuity scale: interrater reliability and patient flow analysis. Am J Obstet Gynecol. 2013;209(4):287–93.
Veit-Rubin N, Brossard P, Gayet‐Ageron A, Montandon CY, Simon J, Irion O, et al. Validation of an emergency triage scale for obstetrics and gynaecology: a prospective study. BJOG: Int J Obstet Gynecol. 2017;124(12):1867–73.
Article CAS Google Scholar
Kenyon S, Hewison A, Dann S-A, Easterbrook J, Hamilton-Giachritsis C, Beckmann A, et al. The design and implementation of an obstetric triage system for unscheduled pregnancy related attendances: a mixed methods evaluation. BMC Pregnancy Childbirth. 2017;17:1–10.
Ruhl C, Scheich B, Onokpise B, Bingham D. Interrater reliability testing of the maternal fetal triage index. J Obstetric Gynecologic Neonatal Nurs. 2015;44(6):710–6.
Ruhl C, Scheich B, Onokpise B, Bingham D. Content validity testing of the maternal fetal triage index. J Obstetric Gynecologic Neonatal Nurs. 2015;44(6):701–9.
Engeltjes B, Wouters E, Rijke R, Scheele F. Obstetric telephone triage. Risk management and healthcare policy. 2020:2497 – 506.
Matteson KA, Weitzen SH, Lafontaine D, Phipps MG. Accessing care: use of a specialized women’s emergency care facility for nonemergent problems. J Women’s Health. 2008;17(2):269–77.
Panicker S, Chitra T. Is obstetric triage necessary? Int J Reprod Contracept Obstet Gynecol. 2014;3(1):44–8.
Angelini DJ, Stevens E, MacDonald A, Wiener S, Wieczorek B. Obstetric triage: models and trends in resident education by midwives. J Midwifery Women’s Health. 2009;54(4):294–300.
Cooke MW, Jinks S. Does the Manchester triage system detect the critically ill? Emerg Med J. 1999;16(3):179–81.
Speake D, Teece S, Mackway-Jones K. Detecting high-risk patients with chest pain. Emerg Nurse (through 2013). 2003;11(5):19.
Angelini DJ. Obstetric triage and advanced practice nursing. J Perinat Neonatal Nurs. 2000;13(4):1–12.
Article CAS PubMed Google Scholar
Fakari FR, Simbar M. Obstetric triage scales; a narrative review. Archives Acad Emerg Med. 2019;7(1).
Zocco J, Williams MJ, Longobucco DB, Bernstein B. A systems analysis of obstetric triage. J Perinat Neonatal Nurs. 2007;21(4):315–22.
Johnson M, Myers S, Wineholt J, Pollack M, Kusmiesz AL. Patients who leave the emergency department without being seen. J Emerg Nurs. 2009;35(2):105–8.
Monzon J, Friedman SM, Clarke C, Arenovich T. Patients who leave the emergency department without being seen by a physician: a control-matched study. Can J Emerg Med. 2005;7(2):107–13.
Asefzadeh S. Patient flow analysis in a children’s clinic. Int J Qual Health Care. 1997;9(2):143–7.
Manning NA, Magann EF, Rhoads SJ, Ivey TL, Williams DJ. Role of telephone triage in obstetrics. Obstet Gynecol Surv. 2012;67(12):810–6.
Hildebrandt DE, Westfall JM, Smith PC. After-hours telephone triage affects patient safety. J Fam Pract. 2003;52(3):222–6.
PubMed Google Scholar
Car J, Sheikh A. Telephone consultations. BMJ. 2003;326(7396):966–9.
Article PubMed PubMed Central Google Scholar
Kennedy S. Telephone triage in maternity care: senior sister midwife Susan Kennedy in charge of the maternity triage department at Stirling Royal Infirmary at NHS Forth Valley details the wide and positive benefits that telephone triage has brought to both midwives and clients. Midwives Magazine. 2007;10(10):478–81.
Google Scholar
Huibers L, Smits M, Renaud V, Giesen P, Wensing M. Safety of telephone triage in out-of-hours care: a systematic review. Scand J Prim Health Care. 2011;29(4):198–209.
Bailey CM, Newton JM, Hall HG. Telephone triage and midwifery: a scoping review. Women Birth. 2018;31(5):414–21.
Engeltjes B, Wouters E, Rijke R, Scheele F. Obstetric telephone triage. Risk Manage Healthc Policy. 2020;13:2497.
Bailey C. Midwifery telephone triage: a mixed methods study. Monash University; 2020.
Rashidi Fakari F, Simbar M. Explaining challenges of obstetric triage structure: a qualitative study. Nurs Open. 2020;7(4):1074–80.
Rashidi-Fakari F, Simbar M, Safari S, Zadeh-Modares S, Alavi-Majd H. The quality of the maternity triage process: a qualitative study. Adv J Emerg Med. 2020;4(1).
Fakari FR, Simbar M. Satisfaction Assessment Tool for Obstetrics Triage (SATOT): Development and Psychometric Properties. 2020.
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–12.
Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, et al. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010;182(18):E839–42.
Polit DF, Beck CT. Essentials of nursing research: appraising evidence for nursing practice. Lippincott Williams & Wilkins; 2009.
DeVore NE. Telephone triage: a challenge for practicing midwives. J Nurse-Midwifery. 1999;44(5):471–9.
Lindroos L, Korsoski R, Öhman MO, Elden H, Karlsson O, Sengpiel V. Improving assessment of acute obstetric patients–introducing a Swedish obstetric triage system. BMC Health Serv Res. 2021;21:1–10.
Smulian JC, Reeve AD, Donoghue EA, Knuppel RA, McCann TO, Ananth CV. After-hours telephone calls to obstetrician-gynecologists. Obstet Gynecol. 2000;96(3):459–64.
CAS PubMed Google Scholar
Paisley KS, Wallace R, DuRant PG. The development of an obstetric triage acuity tool. MCN: Am J Maternal/Child Nurs. 2011;36(5):290–6.
Birmingham Women’s and Children’s NHS Foundation Trust UoB. Birmingham Symptom Specific Obtetric Triage System (BSOTS):. 2017.
Yazdimoghaddam H, Sadrzadeh SM, Karimi FZ. The obstetric and gynecological service providers’ and recipients’ perception and experience of the quality of obstetric triage services during the COVID-19 pandemic in Iran. BMC Pregnancy Childbirth. 2023;23(1):1–12.
Hoffstetter S, Barr S, LeFevre C, Gavard JA. Telephone triage: diagnosis of candidiasis based upon self-reported vulvovaginal symptoms. J Lower Genit Tract Dis. 2012;16(3):251–5.
Weavers A, Nash K. Setting up a triage telephone line for women in early labour. Br J Midwifery. 2012;20(5):333–8.
Huibers L, Keizer E, Giesen P, Grol R, Wensing M. Nurse telephone triage: good quality associated with appropriate decisions. Fam Pract. 2012;29(5):547–52.
Parsons M. Answering the call: evaluation of the Obstetric Telephone Triage Process. J Obstetric Gynecologic Neonatal Nurs. 2012;41:S114–5.
Wahlberg AC, Cedersund E, Wredling R. Telephone nurses’ experience of problems with telephone advice in Sweden. J Clin Nurs. 2003;12(1):37–45.
Balki M, Hoppe D, Monks D, Sharples L, Cooke ME, Tsen L, et al. The PETRA (Perinatal Emergency Team Response Assessment) scale: a high-fidelity simulation validation study. J Obstet Gynecol Can. 2017;39(7):523–33. e12.
Gerdtz MF, Collins M, Chu M, Grant A, Tchernomoroff R, Pollard C, et al. Optimizing triage consistency in Australian emergency departments: the emergency Triage Education Kit. Emerg Med Australasia. 2008;20(3):250–9.
Considine J, LeVasseur SA, Charles A. Development of physiological discriminators for the Australasian Triage Scale. Accid Emerg Nurs. 2002;10(4):221–34.
Gerdtz MF, Chu M, Collins M, Considine J, Crellin D, Sands N, et al. Factors influencing consistency of triage using the Australasian Triage Scale: implications for guideline development. Emerg Med Australasia. 2009;21(4):277–85.
Perry H, Lindley C, Northover E, Connor J, Parasuraman R. A Novel System of Maternity Triage in the Obstetric Assessment Unit. Archives Disease Childhood-Fetal Neonatal Ed. 2014;99(Suppl 1):A31–A.
Angelini D, Howard E. Obstetric triage: a systematic review of the past fifteen years: 1998–2013. MCN: Am J Maternal/Child Nurs. 2014;39(5):284–97.
Lyons A. Managing unexpected births in the emergency department. Emerg Nurse. 2010;18(5).
Download references
Acknowledgements
The authors thankfully acknowledge the midwifery and Reproductive Health Research Center of Shahid Beheshti University of Medical Sciences for support of the grant. We are greatly thankful for participating women.
No funding or sponsoring organization was involved in the carrying out of this work.
Author information
Authors and affiliations.
Midwifery and Reproductive Health Research Center, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Farzaneh Rashidi
Midwifery and Reproductive Health Research Center, Department of Midwifery and Reproductive Health, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Masoumeh Simbar
Department of Emergency Medicine, Shohadaye Tajrish Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Saeed Safari
Zahra Kiani
You can also search for this author in PubMed Google Scholar
Contributions
FR and MS conceived of the study, interpreted the results, and co-wrote the manuscript. SS, ZK, MS and FR collected the data, helped with data interpretation, and co-wrote the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Correspondence to Masoumeh Simbar .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethics approval and consent to participate
This article is the result of a postdoctoral project approved by the Midwifery and Reproductive Health Research Center of Shahid Beheshti University of Medical Sciences with the ethical code IR.SBMU.PHARMACY.REC.1400.213. All methods were carried out according to relevant guidelines and regulations. Informed consent was obtained from all subjects.
Consent for publication
“Not applicable” in this section.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Rashidi, F., Simbar, M., Safari, S. et al. The design of an Obstetric Telephone Triage Guideline (OTTG): a mixed method study. BMC Women's Health 24 , 246 (2024). https://doi.org/10.1186/s12905-024-03076-1
Download citation
Received : 25 April 2023
Accepted : 04 April 2024
Published : 18 April 2024
DOI : https://doi.org/10.1186/s12905-024-03076-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Obstetric triage
- Clinical guidelines
BMC Women's Health
ISSN: 1472-6874
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 29 April 2024
Development and psychometric evaluation of "Caring Ability of Mother with Preterm Infant Scale" (CAMPIS): a sequential exploratory mixed-method study
- Saleheh Tajalli ORCID: orcid.org/0000-0002-2045-6430 1 ,
- Abbas Ebadi ORCID: orcid.org/0000-0002-2911-7005 2 ,
- Soroor Parvizy ORCID: orcid.org/0000-0002-9361-9923 3 , 4 &
- Carole Kenner ORCID: orcid.org/0000-0002-1573-5240 5
BMC Nursing volume 23 , Article number: 297 ( 2024 ) Cite this article
Metrics details
Caring ability is one of the most important indicators regarding care outcomes. A valid and reliable scale for the evaluation of caring ability in mothers with preterm infants is lacking.
The present study was conducted with the aim of designing and psychometric evaluation of the tool for assessing caring ability in mothers with preterm infants.
A mixed-method exploratory design was conducted from 2021 to 2023. First the concept of caring ability of mothers with preterm infants was clarified using literature review and comparative content analysis, and a pool of items was created. Then, in the quantitative study, the psychometric properties of the scale were evaluated using validity and reliability tests. A maximum likelihood extraction with promax rotation was performed on 401 mothers with the mean age of 31.67 ± 6.14 years to assess the construct validity.
Initial caring ability of mother with preterm infant scale (CAMPIS) was developed with 64 items by findings of the literature review, comparative content analysis, and other related questionnaire items, on a 5-point Likert scale to be psychometrically evaluated. Face, content, and construct validity, as well as reliability, were measured to evaluate the psychometric properties of CAMPIS. So, the initial survey yielded 201 valid responses. The three components: 'cognitive ability'; knowledge and skills abilities'; and 'psychological ability'; explained 47.44% of the total observed variance for CAMPIS with 21 items. A subsequent survey garnered 200 valid responses. The confirmatory factor analysis results indicated: χ2/df = 1.972, comparative fit index (CFI) = 0.933, and incremental fit index (IFI) = 0.933. These results demonstrate good structural, convergent, discriminant validity and reliability. OMEGA, average inter-item correlation (AIC), intraclass correlation coefficients (ICC) for the entire scale were at 0.900, 0.27 and 0.91 respectively.
Based on the results of the psychometric evaluation of CAMPIS, it was found that the concept of caring ability in the Iranian mothers with preterm infants is a multi-dimensional concept, which mainly focuses on cognitive ability, technical ability, and psychological ability. The designed scale has acceptable validity and reliability characteristics that can be used in future studies to assess this concept in the mothers of preterm infants.
Peer Review reports
Introduction
In recent years, the technology advancements in the field of caring for mothers during pregnancy and delivery, and their infants resulted in increased survival of preterm infants [ 1 ]. According to the assessment of the world health organization (WHO), the prevalence of preterm birth globally is 10.6% [ 2 ].
Preterm birth is often an unexpected event for women [ 3 ], and hospitalization in the NICU is considered unavoidable [ 4 ]. The birth of a preterm infant and hospital stay in the NICU is very stressful for parents. The source of this stress includes the medical condition and parental separation from their infant. Mother-infant separation often results in the feelings of anxiety, fear, depression thus potentially decreasing the mother’s sensitivity to infant cues, which in turn, may delay infant development [ 5 ]. Many mothers experience acute stress disorder, which can last from 3 days to 1 month. It can be associated with symptoms such as troublesome memories, frequent and annoying restlessness and sadness, as well as post-traumatic stress [ 6 ].
The feeling of loss is a source of suffering and grief for the mothers of preterm infants. In the initial days following birth, the primary focus of parents is often on the infant's chances for survival. However, as time passes, this preoccupation can evolve into a potential cause of grief, anxiety, and feelings of culpability (related to an incomplete pregnancy)[ 6 ]. Therefore, in some cases, the mothers cannot focus on their preterm infants. Becoming a mother requires reorganizing and changing one’s personal identity. Mothers must change their identity from being a daughter and a wife in the generation to which they belong to being a mother for the next generation. They start this process from the pregnancy period, initially fantasizing about motherhood [ 7 ]. However, at the end of the pregnancy period, with the birth of a preterm infant, this process stops. In fact, preterm birth is a sudden stop in the process of mother's self-representation [ 8 ]. Consequently, the experience of transitioning into motherhood for women who give birth prematurely may differ from that of others. This is due to the fact that the psychological readiness and preparation required for assuming the role of a mother comes to an abrupt halt upon the premature birth of their infant. As a result, these women are forced to quickly adapt to their new circumstances [ 9 ].
Review of literature shows caring ability concept have three dimensions: cognitive, knowledge and patience [ 10 ]. Published caring ability scales evaluate ability of take care in informal caregiver of patient with cancer named ‘caring ability of family caregivers of patients with cancer scale (CAFCPCS)’ [ 11 ] or professional care giver named ‘The caring ability inventory’[ 10 ]. Also, published tools, focused on others aspects of take caring ability. So family empowerment tool named ‘Family Empowerment Scale’ [ 12 ], asses the empowerment of family members of patients with chronic disease as an outcome of taking care empowerment. The parent Engagement tool is another scale named ‘parent risk evaluation and engagement model and instrument (PREEMI)’ that evaluates parent risk evaluation and engagement of mothers with preterm infants [ 13 ]. The discharge preparedness scales were ‘perceived readiness for discharge after birth scale (PRDBS) and ‘Parent discharge readiness’ [ 14 ], that evaluate readiness for discharge. These evaluate postpartum mother’s perceptions of readiness for discharge from the hospital that was adapted from a scale measuring adult and elderly postsurgical patients’ perceptions of their readiness for discharge. Also assert for readiness is different from the ability to continue taking care after discharge. The scales 'Perceived maternal parenting self‐efficacy (PMP S‐E)' and 'Self‐efficacy in infant care scale' [ 15 , 16 ] were developed to assess the caregiver's belief in their ability to effectively care for their child, with a specific emphasis on self-confidence. These scales aim to provide a means of measuring the caregiver's expectations regarding the outcomes of their caregiving efforts. Although our previous study show a mother with optimal caring ability has sufficient cognitive ability, technical ability, and psychological ability [ 17 ]. This is a clear gap in the designed scale that could be overcome by a new scale that focuses take caring ability of mother with preterm infants. To sum up, there is no scale developed for the caring ability of mothers with preterm infants; therefore, the purpose of this study is to examine the real-life experiences of mothers with preterm infants and other professional and family. Caregivers, who have directly experienced taking care of preterm infants in order to then, design and perform the psychometric evaluation of a tool to assess the caring ability of mothers with preterm infants.
The purpose of this study was to develop a preterm caring ability scale and to examine its psychodynamic properties in mother of preterm infants with gestational age less than 32 weeks.
This study utilized a mixed-method exploratory design to develop and psychometric evaluate the caring ability of mother with preterm infant scale (CAMPIS) from July 2021 to October 2023. The research involved both mothers and professionals caring for preterm infants. The research consisted of two main phases: first, a qualitative study was conducted to generate the scale items, followed by a quantitative approach to evaluate the psychometric properties of the scale.
First step: qualitative study and item generation
The purpose of this step was to explain the concept of caring ability in the mothers of preterm infants, and to create a set of items to design the target scale. This step involved the identification of concepts through literature review published from 1995 to 2020 [ 17 ] .
In the second step, 18 semi-structured individual interviews of 60–80 min were organized to understand better the caring ability of mother with preterm infant concept. The face-to-face semi-structured interviews were conducted in a serene setting, either in the hospital room or the participants' home, as per their request and preference. The interviews involved mothers, grandmothers, and fathers, and were carried out without the presence of any other individuals. Due to the coronavirus social distance limitation, the interviews with the physicians and the nurses were conducted online and also recorded via Skyroom software.
We decided to finish the interview, when we interviewed the 18 participants, the information he/she provided is similar to those provided by the former ten participants (data saturation). Totally, 11 mothers, 2 fathers, 2 grandmothers of preterm infants, 1 neonatal nurse, and 2 neonatologists working in these wards participated in the present study. The participants were residents in the NICU in 5 hospitals in Tehran, Iran, representing a range of ages, genders, and caring role. The interview process started with a general question such as "Would you please explain mothers’ ability to take care of a preterm infant?", "In which situations do you feel she are more capable?", and "Which factors decreased her ability?" Then, based on the participant’s responses, the interviews continued with exploratory questions such as "Could you please explain more? or “Could you give an example in this regard?".
All participants were interviewed individually and each interview lasted between 60 and 80 min. The texts of the interviews were analyzed using the using Lindgern et al. [ 18 ] approach by MAXQDA software version 10. Qualitative interview resulted in initial items generation.
Second step: quantitative study and CAMPIS psychometric properties evaluation
Face validity.
Face validity was evaluated through qualitative and quantitative approaches. In the qualitative approach, the scale was sent to 10 mothers of preterm infants, they were asked to evaluate the scale in terms of difficulty, relevance, and ambiguity. The participants assessed the items based on their own judgment, ensuring that they were able to understand them. In order to further evaluate the suitability of the items, five additional mothers were included in the quantitative approach. These mothers were asked to rate the items on a 5-point Likert scale, ranging from completely suitable to not suitable at all. The impact score was calculated through the following equation: impact score = frequency (%) × appropriateness. A score above 1.5 was considered acceptable [ 19 ].
Content validity
The content validity of CAMPIS was evaluated through quantitative and qualitative approaches. In the qualitative approach, the scale was distributed among 22 neonatal nursing specialists, neonatal subspecialists, and scale development specialists to evaluate the items in terms of grammar and wording, item allocation, and scaling.
Then the content validity of the scale was modified by measuring content validity ratio (CVR) and content validity index (CVI) to ensure that the scale measures the intended construct in two separate stages. So, the 26 specialists, as highly knowledgeable about the mother of preterm infant or scale development, were asked to evaluate the items regarding necessity and relevancy. In CVR, 12 specialists evaluated the necessity of CAMPIS on a 3-point Likert scale (1 = not necessary, 2 = useful but not necessary, and 3 = necessary). CVR was calculated through the following formula: [ne – (N/2)]/(N/2), where “ne” is the number of the experts who rate the items as “essential”, and N is the total number of the items. The result was interpreted using Lawshe's content validity ratio [ 20 ].
Following the implementation of the required modifications based on the feedback provided by experts, the effectiveness of CAMPIS was further evaluated by 14 additional specialists in terms of the CVI. This evaluation was conducted using a four-point Likert scale, where a score of 1 indicated irrelevance, 2 denoted relative relevance, 3 represented relevance, and 4 signified complete relevance. The I-CVI, Kappa statistic, and S-CVI/Ave were computed to assess the content validity index at both the item-level and scale-level. A Kappa value exceeding 0.75 was deemed indicative of excellent agreement [ 19 ].
Item analysis
Before construct validity of the structure, the items were analyzed to identify the possible problems. At this step, 48 mothers of preterm infants, with the mean age of 31.88 ± 5.9 years, were selected through convenience sampling and enrolled. They were asked to identify that there were problems such as inappropriate reverse questions. Also they were asked to completed the hardcopy of CAMPIS and item-total correlations was evaluated for some items. A correlation coefficient lower than 0.32 or above 0.9 was considered as the criteria for removing the items [ 19 ].
Participants
The sample included the mothers of the preterm infants with a gestational age < 34 weeks. The criteria for entering the study consisted of the infant’s having been hospitalized in the NICU for more than two weeks, the infant’s not suffering from any major congenital anomalies, giving consent to participate in the study, and being able to use social networks such as WhatsApp. Based on the rule of thumb, that is, which considers 200 participants as an appropriate sample size [ 19 ], 401 mothers were considered for two phases at this step: 201 for the exploratory factor analysis (EFA) assessment, and 200 for the confirmatory factor analysis (CFA).
The participants were selected using convenience sampling through being in the hospital on the day of discharge, membership in the social groups related to following up mothers with preterm infants discharged from the NICU, and recommendations. In this step, data was collected online. For this purpose, an online questionnaire was created through the Porsline form, and its URL link ( https://survey.porsline.ir/s/d8uW4Jp ) was sent to the participants through the Telegram or WhatsApp social network applications (as the most common social networks among Iranian users).
The questionnaire used in this step included two parts. The first part was related to the infant's demographic characteristics, such as the infant's gender, and gestational age, and the mother's demographic characteristics, such as the mother's age, the infant's age, the mother's education, mothers' parity, assisted reproductive methods, the type of delivery, and previous experience in caring for infants. The second part included initial CAMPIS, with 38 items, for measuring the concept of the caring ability of mothers with preterm infants, on a five-point Likert scale (1 = never to 5 = always).
Construct validity
The construct validity of this scale was evaluated using EFA and CFA by SPSS 26 (SPSS Inc., Chicago, IL, USA). According to normal distribution of variables (skewness of ± 3, kurtosis of ± 7 and Mardia's coefficient less than 20) EFA was evaluated through Maximum likelihood factor analysis using Promax rotation. In addition, Kaiser–Meyer–Olkin (KMO) and Bartlett tests were used to estimate the adequacy and the appropriateness of the sample. KMO values higher than 0.9 were interpreted as excellent [ 19 ]. In order to extract the factors according to Thompson and Daniel recommendation [ 21 ] multivariate approach was used to identify the number of factors to extract in the EFA.
Then the factors were analyzed using the method of maximum likelihood analysis, which is one of the most common methods of data reduction. At first, 5 factors had an eigenvalue greater than 1, but considering that 3 factors explained an eigenvalue greater than 1.5 and a variance greater than 5%.
To extract the factor structure, exploratory graph analysis was used. The actual values of the matrix were compared with the randomly generated matrix. The number of the components which have a higher variance in comparison with the components obtained from random data, after successive repetitions, is considered as the correct number of factors for extraction [ 22 ]. A factor loading of approximately 0.3 was considered to determine the presence of an item in a latent factor, and the items with communalities < 0.2 were excluded from EFA. The factor loading was estimated using the following formula: CV = 5.152 ÷ √ (n—2), where CV is the number of the extractable factors, and N is the sample size.
In the next step, the factor structure determined by EFA was evaluated by CFA. For this purpose, CFA was evaluated using Maximum likelihood factor analysis and the most common goodness-of-fit indices using SPSS/AMOS 26 software [ 22 ].
To discuss the fitness of the model on CFA, we can consider the various criteria for model fit indices. It has been suggested that Root Mean Square Error of Approximation (RMSEA) values less than 0.05 are good, and values between 0.05 and 0.08 are acceptable [ 23 ]. Therefore, the RMSEA value of 0.059 in this sample indicates an acceptable fit. The goodness of fit index (GFI) value of this sample, 0.88, is below 0.9, but the GFI is known depending on the sample size [ 24 ]. The frequency interference index (RFI) value, 0.085, is close to 0.9, which shows a relatively good fit [ 25 ]. The other fit indices, comparative fit index (CFI), incremental fit index (IFI), and Tucker-Lewis index (TLI), should be over 0.9 and parsimonious normed fit index (PNFI) should be over 0.5 for a good fit [ 25 ].
Reliability
The reliability was evaluated using internal consistency, stability, and absolute reliability approaches with SPSS 26. The internal consistency was evaluated using, McDonald's omega (Ω), and average inter-item correlation (AIC). The McDonald Omega of 0.7 or above, and the AIC of 0.2 to 0.4 were considered as acceptable criteria to evaluate the internal consistency. The consistency of CAMPIS was evaluated through calculating intraclass correlation coefficients (ICC) using a two-way random effects model [ 19 ]. The retest method with a time interval of 72 h (the day before discharge and 72 h after discharge) was used in 48 mothers with preterm infants. An ICC value > 0.8 is considered as the acceptable value for stability. In addition, the absolute reliability was evaluated using the standard error of measurement with the formula Standard Error of Measurement (SEM) = SD √ (1- ICC).
Finally, the responsiveness was evaluated using minimum detectable change (MDC) with the formula MDC = SEM × Z × √ 2, and minimal important change (MIC) with the following formula: MIC = SD × 0.5. If the MIC is smaller than the MDC, the scale is responsive. Besides, the interpretability was evaluated through calculating the MDC and testing the hypothesis [ 22 ].
Ethical consideration
The present study was extracted from the nursing Ph.D. thesis fund by Nursing Care Research Center (NCRC), School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran. All ethical considerations of the study were approved by the ethics committee at the University of Medical Sciences (IR. IUMS. REC.1398.1407).
In qualitative step a total of 43 articles were selected in the study after reviewing 23291 extracted articles. We explored attribute of take caring ability concept. Findings showed a mother with optimal caring ability has sufficient knowledge, high skills, a sense of sufficient self-efficacy [ 17 ]. This step resulted in 69 initial items generation.
Using the findings of the literature review, comparative content analysis, and other related questionnaire items, the research teammates designed the initial items to measure the caring ability of mothers with preterm infants. An example of item generation has been presented in Table 1 . Then all the initial items (n: 104) were reviewed, and the generation of items was completed. In the selection of items, the focus was mainly on the features of the concept. The items of the pool were examined during joint meetings with the research team, and the items that were not in line with the purpose of this study were omitted according to experts’ opinions. First, repetitive descriptive items were deleted. For example, “I have access to healthcare providers and whenever I have questions, I can ask them” and “A healthcare provider answers my questions regarding the care of my child all day long 7 days a week.” This step resulted in 71 items. In the next step, the items with similar descriptions items were combined. For example, “I simply understand my child's needs.” and “When my child severely cries, I can figure out what my child wants.”
Therefore, at this step, CAMPIS was developed with 64 items, descriptions about behaviors and attitudes, on a 5-point Likert scale (always, most of the time, sometimes, rarely, never) to be psychometrically evaluated. Face, content, and construct validity, as well as reliability, were measured to evaluate the psychometric properties of CAMPIS.
In quantitative study and CAMPIS psychometric properties evaluation phase the impact score evaluation of face validity step, score of all items were above 1.5, and was considered appropriate. According to degree of mothers’ judgement all items of CAMPIS were appropriate to assessment of take caring ability. Therefore, no item was deleted.
During the process of content validity, some items were modified according to panelist feedbacks. While evaluating content validity, in the qualitative approach, 8 items were merged into one item based on the suggestion of the expert panel. Regarding number of participants for CVR were 12, the minimum acceptable CVR score was 0.56. In this step, the CVRs of 7 items were less than 0.56 and removed. In the CVI assessment, the I-CVI for all the items was in the range of 0.83–1, the modified Kappa was in the range of 0.84–1, and the total S-CVI/Ave and S-CVI/UA were 0.93 and 0.40 respectively. In content validity step according to the results, the Kappa values of 8 items were lower than 0.75, so they were removed. Therefore, 23 items were eliminated and the total number of CAMPIS was reduced from 64 to 41 items in content validity evaluation step.
In the item analysis step, the item-total correlation for 3 items was 0.32 or less, therefore were removed. The final CAMPIS with 38 items entered the factor analysis step.
In construct validity step, totally 401 mothers with a gestational age of 34 weeks or less participated in the present study. Their infants did not have any major surgical problems/anomalies, and had been hospitalized in the NICU for more than two weeks. The mean age of the mothers was 31.77 ± 6.02 years, with the minimum age of 16 and the maximum of 53 years. Out of 401 mothers, 204 (50.87%) had other children. All of them were married and lived with their spouses. The details of the socio-demographic characteristics of the participants have been shown in Table 2 .
In the construct validity phase, based on the results, the sample’s KMO and Bartlett's values were sufficient and appropriate, 0.897 and 1758.593, respectively ( P ≤ 0.001). In this step, 17 items were removed as their shared values were less than 0.2 and their factor loadings were less than 0.3. After Promax rotation, 3 factors (totally 21 items) were extracted: cognitive ability (9 items), technical ability (7 items), and psychological ability (5 items). These factors respectively explained 30.59, 9.62, and 7.28% of the total variance (47.44%) of the concept of the caring ability of mothers with preterm infants. The details of the factor analysis result have been presented in Table 3 .
Based on CFA indices, this sample has an acceptable fit to the 3 factors model and all of these indices in our study are excellent. The results of model fit indices have been given in Table 4 .
Prior to modeling modification, the goodness of fit measures for the CFA-generated 3-factor model indicated that the model fit but not optimally. To improve the factor structure model, we identified the following item content redundancies: Item 24 (If I see signs of an feeding difficulties, I know what to do) is related to Item 23 (I can recognize the signs and symptoms of shortness of breath and cyanosis), and item 8 (Given that my baby was born preterm, I am aware of the differences in growth and development with other babies.) is related to item 7 (I have enough information about my baby being preterm and its complications.).
Also, item 18 (I'm afraid my baby might be harmed.) is related to item 17 (I do not sleep well because I am worried about my baby's health.) Given the similarities of conceptual meaning, these correlated error terms indicated that these variables may share specific variances.
As shown in Fig. 1 , the aforementioned changes improved the goodness of fit of the model. This indicated the model of the caring ability of mothers with preterm infants fits the data (Fig. 1 ).
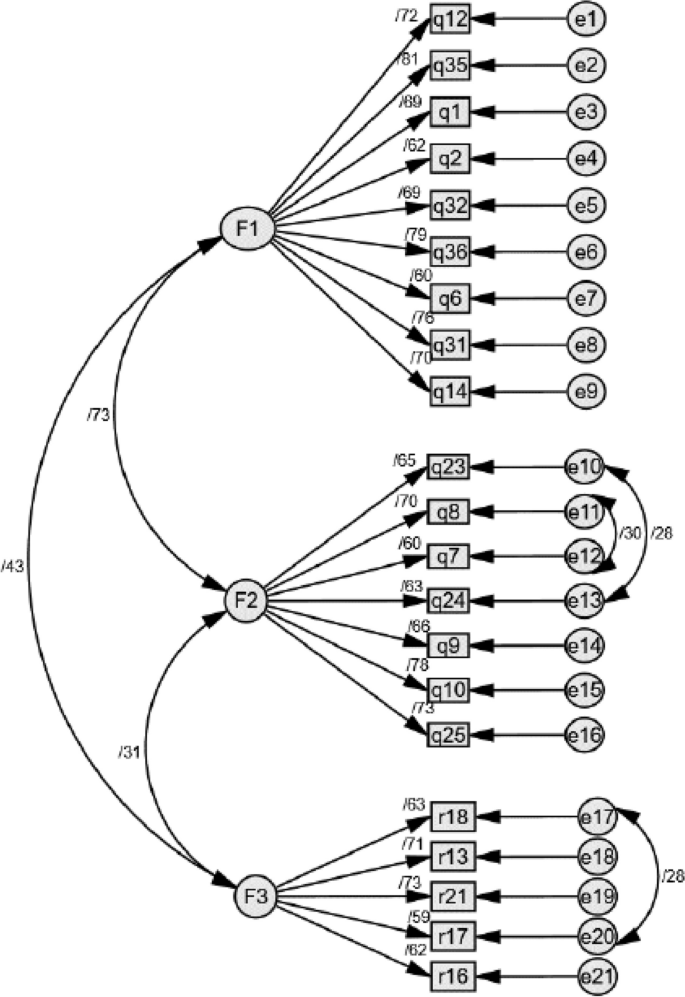
The results of CFA showed that a three-factor model of the care ability of the mothers with preterm infants indicated that the model fitted well. F1: Cognitive Ability; F2: Knowledge and Skills Abilities; F3: Psychological Ability
The retest method with a time interval of 72 h (the day before discharge and 72 h after discharge) was used in 48 mothers with preterm infants. An ICC value > 0.8 is considered as the acceptable value for stability. In addition, the absolute reliability was evaluated using the standard error of measurement with the formula Standard Error of Measurement (SEM) = SD √ (1- ICC). The details of the responsiveness are reported in Fig. 1 .
The results of McDonald Omega coefficient (ω = 0.90), and AIC (0.27) for the 3 factors were excellent. Based on the result, the ICC was 0.91 in the confidence interval of 0.84%-0.95%, which shows that the tool has acceptable measurement stability over time. Based on the SEM results, the absolute reliability was 3.18. This value shows that the scale scores of an individual vary ± 3.18 in repeated tests (Table 5 ). Based on the results, MDC = 8.78, MDC% = 11.79 and MIC = 0.50, this scale is responsive and interpretable.
The study’s results demonstrated that the concept of caring ability in mothers with preterm infants has three dimensions: cognitive ability, knowledge and skills abilities, and psychological ability. Therefore, CAMPIS is a valid and reliable scale to assess this concept in mothers with preterm infants. This scale includes 21 items, and three factors, cognitive, knowledge and skills, and psychological abilities, which explained 47.44% of the total variance of this concept. The CAMPIS model obtained through EFA was confirmed using CFA.
CAMPIS has three factors: "cognitive ability ", "knowledge and skills abilities" and "psychological ability". The first factor extracted from the scale was "cognitive ability". This factor includes 9 items regarding perception skills, cognitive skills, decision-making skills, movement skills, and attitude, which were extracted with the highest variance (30.59%). Cognitive abilities are the skills that a person needs to do anything from the simplest to the most complex, including perception skills, decision-making skills, movement skills, language skills, and social skills [ 26 ]. Cognitive abilities are the link between behavior and the brain structure, which include a wide range of abilities including planning, paying attention, problem solving, performing tasks simultaneously, and cognitive flexibility [ 27 ]. In this scale, cognitive ability was defined as the ability of a mother with a preterm baby to use skills which help her process information, think, reason, and solve problems faster and more efficiently. By developing cognitive skills, a person can go through the process of reasoning, decision making, and taking action. In this way, she can make sure that she can perceive the new situation, and perform her role effectively. The findings of a study conducted in 2004 showed that the mother’s possessing the desired attitudinal-cognitive ability had a significant impact on the infant’s health [ 28 ].
The second factor extracted from the scale was "technical ability". This factor includes 7 items regarding care knowledge and skills, as well as the ability to apply them; it was extracted with an acceptable variance (9.62%). In the science of care, knowledge is defined as the caregiver's awareness of the care recipient’s needs, strengths, and weaknesses as a unique member [ 10 ]. Moreover, in a study conducted by Galvin et al. in 2017, which was conducted with the aim of investigating the analytical features of the concept of readiness for discharge from the hospital, having sufficient knowledge and skills was mentioned as one of the characteristics of readiness for discharge [ 29 ]. In this scale, knowledge-skill ability is defined as that the mother’s awareness of the tasks that she must know how to perform in order to provide effective, efficient, and reliable care for her infant. The mothers of preterm infants often have poor knowledge regarding infant care after discharge [ 30 ], while the main factor which shows the mother's ability to provide care for the infant is having sufficient knowledge and skills. The mother should know what, how, why, and when to provide care for her infant [ 30 ].
The lived experience of the parents with preterm infants showed that in most cases, they are not prepared for the infant’s birth. The birth of a preterm infant puts them in a special situation which requires new care skills [ 31 ]. The parents need to acquire these skills that are a prelude to the discharge and transfer of the infant to home [ 32 ]. Providing quality care for complex disorders requires specialized caregiving knowledge and skills. When there is a deficiency in these areas, negative psychological impact on the parents and their relationship with their infant can ensue [ 33 ]. Studies have shown that having sufficient preparation for discharge and transitional care can help the families of preterm infants with a successful transition from the hospital to the family, reducing the rehospitalization rates [ 34 ]. To this end, health care professionals should provide the parents with useful information regarding illness management, strengthen their relationships with the hospital staff, encourage sharing experiences and emotions, and perform home visits [ 35 ]. The empowerment method should be appropriate to the caregiver's conditions. It should predict the caregiver's psychological condition as well as his/her emotional and behavioral responses. It should be used to train and support the caregiver in decision-making and managing the caregiving situation, considering his/her experiences, social status, cultural level, and beliefs [ 36 ].
The third factor extracted from the scale was "psychological ability". This factor includes 5 items regarding the psychological characteristics of the mothers taking care of preterm infants, with an acceptable variance (7.28%). An individual who is aware of his/her abilities and need for self-dependence, to manage care after discharge, has good psychological ability [ 29 ]. It is necessary to achieve psychological ability for an individual to deal with post-discharge challenges and have control over the situation [ 37 ]. In the present study, the mother's psychological ability is defined as her possessing the psychological characteristics and mental makeup to feel ready to continue care provision after discharge from the NICU, and to be able to fulfill her caring role successfully. During a traumatic event such as an infant's hospitalization in the NICU, the mothers try to improve their psychological ability [ 38 ].
The most mothers of preterm infants are not psychologically prepared for delivery and motherhood [ 39 ]. Preterm birth is considered a sudden and unpredictable event, which is accompanied by a feeling of shock and helplessness. The mothers of preterm infants often describe these conditions using terms such as falling to the bottom of a deep well, and being stuck in a whirlwind and storm happening around them; they admit they do not have enough control over what is happening, and lack the ability to take care of their infants [ 40 ]. Hospitalization in the NICU and mother-infant separation cause a feeling of inadequacy in the mother [ 41 ], which can subsequently affect her psychological ability. This maybe cause using different methods to deal with it. Using ineffective coping methods regarding changes in lifestyle and playing one’s role impacts on mother's caretaking tasks. If the use of ineffective coping methods is not recognized at the right time, and if appropriate measures are not taken, then the nursing diagnosis of coping disability disorder will be imminent [ 42 ]. Improved mental health and sufficient psychological ability are an important prerequisite for behavior change, which acts as a link between awareness and action. It can have a moderating role in empowering individuals, leading to positive thoughts, greater self-esteem and goals, more positive emotions and desirable behaviors [ 43 ]. Therefore, it is very important to measure the psychological ability of the mother in order for her to acquire the ability to provide quality care for the preterm infant.
Being aware of the caring ability of their mothers, as the main care givers, and designing an intervention to improve their caring ability can prevent negative side effects and help to improve the quality of care. The present study was conducted with the aim of designing and psychometric evaluation of the tool for assessing caring ability in mothers with preterm infants. Since one of the main goals of psychometric evaluation and factor analysis is to maximizing the explained variance by the model, in this research, the variance was 47.44%. Among the scales designed to measure caring ability, regardless of factor analysis extraction method, only one scale, the caring ability scale of the caregivers of cancer patients (67.7%), explains variance more than CAMPIS does [ 11 ].
In addition, this CAMPIS had very good internal consistency based on the results of Cronbach's alpha, AIC, and McDonald omega. It should be noted that one of the advantages of this scale is having strong stability based on the ICC value. Another advantage of this study was the assessment of measurement error, responsiveness, and interpretation of the CAMPIS. The results showed that the CAMPIS has the minimum amount of SEM, responsiveness, and interpretability. SEM shows the accuracy of the measurement for each individual, and it is important that this value be small. Responsiveness refers to the ability of a scale to reflect changes in an individual's position over a period. Finally, interpretability refers to the scale's ability to show the significance of changes. These characteristics are an important and necessary part of consensus-based standards for the selection of health measurement tools, which have not been reported in the previous studies on the psychometric characteristics of caring ability.
CAMPIS measures the caring ability of the mother of a preterm infant in the three factors namely ‘Cognitive Ability’ (items: 1–9), ‘knowledge and skills abilities' (items: 10–16), and ‘Psychological Ability’ (items: 17–21). The answer to the items is based on a five-point Likert scale (always (5), most of the time (4), sometimes (3), rarely (2), never (1)). Scoring of items 17,18,19,20 and 21 is reverse so (always (1), most of the time (2), sometimes (3), rarely (4), never (5)). To have an overall score: Sum cognitive ability + sum knowledge and skills abilities + sum psychological ability = Total score. The best way is to calculate the average score for every scale, and compare the results with the average score. In our studies we set the average score for cognitive ability from 9–45, knowledge and skills abilities 7–35, psychological ability 5–25, and overall score 21–105 (Additional file 1 : Appendix A). CAMPIS, is a useful scale for professional caregivers and researchers, thanks to its brief items, good variance, reliability, as well as exclusively belonging to this group.
The findings of this study demonstrated that CAMPIS is a reliable and valid scale with 21 items, which includes the 3 dimensions of attitudinal-cognitive ability, knowledge-skill ability, and psychological ability for measuring the concept of tenacity in family caregivers. Although the exclusiveness of CAMPIS to evaluate the caring ability of mothers with preterm infants is one of the points of strengths in this study, but considering that the samples were selected from the population of Iranian mothers with preterm infants with a gestational age of 34 weeks or less. It should be used with caution in mothers with preterm infants with a gestational age over 34 weeks. Therefore, one of the important limitations was the concern about the generalizability of the findings.
Limitations and strength
In the construct validity step, data collection was done online. Although the use of online questionnaires, especially during the period of social restrictions due to COVID-19 pandemic, has many advantages, such as the possibility of eliminating the missing data, speeding up the data collection process, and the possibility of collecting data from other provinces and counties. There are also some limitations like self-selection bias, and the lack of interaction with the participants. Furthermore, some qualified mothers were excluded from the study due to illiteracy, the lack of internet access, and the inability to use the phone/laptop to access social networks.
During the item generation step, we considered the different directions of items, but during data reduction, opposite directions were removed. Finally, all items of each factor of CAMPIS have oriented in the same direction, and it is imaginable to create a possibility for response tendency.
One of the problems of self-report scales is that they are subject to the respondent's interpretation of the items, which may not be what the scale designer has intended. In order to reduce this potential problem, continuous testing and modification of the scale has been done. Since ability is a personal matter, the participants were asked not to reveal their names, cities, and the name of the hospitals where their infants were hospitalized. This study has points of strength. One of them is the evaluation of SEM, ICC, responsiveness, and interpretability as important and required items of the COSMIN checklist, which had not been reported previously regarding caring ability scales, but were evaluated in this study.
Availability of data and materials
The original contributions presented in the study are included in the article. Request access to other supplementary material can be directed to the first or corresponding author.
Abbreviations
Caring Ability of Mother with Preterm Infant Scale
Exploratory factor analysis
Confirmatory factor analysis
Neonatal Intensive Care Unit
World Health Organization
Content validity ratio
Content validity index
Item-level content validity index,
Scale-level content validity index average
Kaiser–Meyer–Olkin
Average Inter-Item Correlation
Intraclass correlation coefficients
Minimum Detectable Change Analysis
Minimal Important Change
Comparative Fit Index
Incremental Fit Index
Frequency Interference Index
Parsimonious Normed Fit Index
Tucker-Lewis Index
Goodness of Fit Index
Root Mean Square Error of Approximation
Confidence Interval
Standard Error of Measurement
Cao Y, Jiang S, Sun J, Hei M, Wang L, Zhang H, et al. Assessment of neonatal intensive care unit practices, morbidity, and mortality among very preterm infants in China. JAMA Network Open. 2021;4(8):e2118904-e.
Article Google Scholar
Chawanpaiboon S, Vogel JP, Moller A-B, Lumbiganon P, Petzold M, Hogan D, et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob Health. 2019;7(1):e37–46.
Article PubMed Google Scholar
Lasiuk GC, Comeau T, Newburn-Cook C. Unexpected: an interpretive description of parental traumas’ associated with preterm birth. BMC Pregnancy Childbirth. 2013;13(1):1–10.
Google Scholar
Howson C, Merialdi M, Lawn J, Requejo J, Say L. March of dimes white paper on preterm birth: the global and regional toll. March of dimes foundation. 2009:13.
Gerstein ED, Njoroge WF, Paul RA, Smyser CD, Rogers CE. Maternal depression and stress in the neonatal intensive care unit: associations with mother− child interactions at age 5 years. J Am Acad Child Adolesc Psychiatry. 2019;58(3):350-8. e2.
Article PubMed PubMed Central Google Scholar
Fowler N, Vo PT, Sisk CL, Klump KL. Stress as a potential moderator of ovarian hormone influences on binge eating in women. F1000Research. 2019;8.
Stern DN, Bruschweiler-Stern N. The birth of a mother: How the motherhood experience changes you forever: Basic Books; 1998.
Slade A, Cohen LJ, Sadler LS, Miller M. The psychology and psychopathology of pregnancy. Handbook of Infant Mental Health. 2009;3:22–39.
Spinelli M, Frigerio A, Montali L, Fasolo M, Spada MS, Mangili G. ‘I still have difficulties feeling like a mother’: the transition to motherhood of preterm infants mothers. Psychol Health. 2016;31(2):184–204.
Nkongho NO. The caring ability inventory. Measure Nurs Outcomes. 2003;3:184–98.
Nemati S, Rassouli M, Ilkhani M, Baghestani AR, Nemati M. Development and validation of ‘caring ability of family caregivers of patients with cancer scale (CAFCPCS).’ Scand J Caring Sci. 2020;34(4):899–908.
Koren PE, DeChillo N, Friesen BJ. Measuring empowerment in families whose children have emotional disabilities: a brief questionnaire. Rehabil Psychol. 1992;37(4):305.
Samra HA, McGrath JM, Fischer S, Schumacher B, Dutcher J, Hansen J. The NICU parent risk evaluation and engagement model and instrument (PREEMI) for neonates in intensive care units. J Obstet Gynecol Neonatal Nurs. 2015;44(1):114–26.
Smith V, Young S, Pursley D, McCormick M, Zupancic J. Are families prepared for discharge from the NICU? J Perinatol. 2009;29(9):623–9.
Article CAS PubMed Google Scholar
Barnes CR, Adamson-Macedo EN. Perceived maternal parenting self-efficacy (PMP S-E) tool: development and validation with mothers of hospitalized preterm neonates. J Adv Nurs. 2007;60(5):550–60.
Prasopkittikun T, Tilokskulchai F, Sinsuksai N, Sitthimongkol Y. Self-efficacy in infant care scale: development and psychometric testing. Nurs Health Sci. 2006;8(1):44–50.
Tajalli S, Ebadi A, Parvizy S, Kenner C. Maternal caring ability with the preterm infant: a Rogerian concept analysis. Nurs Forum. 2022;57(5):920–31.
Lindgren B-M, Lundman B, Graneheim UH. Abstraction and interpretation during the qualitative content analysis process. Int J Nurs Stud. 2020;108:103632.
Sharif Nia H, Zareiyan A, Ebadi A. Test Development Process in Health Sciences; Designing and Psychometric properties. Tehran: Jame-e-negar; 2022.
Lawshe CH. A quantitative approach to content validity. Pers Psychol. 1975;28(4):563–75.
Thompson B, Daniel LG. Factor analytic evidence for the construct validity of scores: A historical overview and some guidelines. Thousand Oaks: Sage Publications Sage CA; 1996. p. 197–208.
Pahlevan Sharif S, Sharif NH. Factor analysis and structural equation modeling with SPSS and AMOS. Tehran: Jame-e-Negar; 2020.
Fabrigar L, Wegener Dt, MacCullum R. Strahan, e. J. Evaluating the use of factor analysis in psychological research. Psychological Methods. 1999;4:272-99.
Mulaik SA, James LR, Van Alstine J, Bennett N, Lind S, Stilwell CD. Evaluation of goodness-of-fit indices for structural equation models. Psychol Bull. 1989;105(3):430.
Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107(2):238.
Benjamin DJ, Brown SA, Shapiro JM. Who is ‘behavioral’? Cognitive ability and anomalous preferences. J Eur Econ Assoc. 2013;11(6):1231–55.
Ones DS, Dilchert S, Viswesvaran C, Salgado JF. Cognitive abilities: Taylor & Francis Group; 2010. 255–75 p.
Rubalcava LN, Teruel GM. The role of maternal cognitive ability on child health. Econ Hum Biol. 2004;2(3):439–55.
Galvin EC, Wills T, Coffey A. Readiness for hospital discharge: a concept analysis. J Adv Nurs. 2017;73(11):2547–57.
Hochreiter D, Kuruvilla D, Grossman M, Silberg J, Rodriguez A, Lary L, et al. Improving guidance and maternal knowledge retention after well-newborn unit discharge. Hosp Pediatr. 2022;12(2):148–56.
Amorim M, Alves E, Kelly-Irving M, Silva S. Needs of parents of very preterm infants in Neonatal Intensive Care Units: a mixed methods study. Intensive Crit Care Nurs. 2019;54:88–95.
Jing L, Bethancourt C-N, McDonagh T. Assessing infant and maternal readiness for newborn discharge. Curr Opin Pediatr. 2017;29(5):598–605.
Hellesø R, Eines J, Fagermoen MS. The significance of informal caregivers in information management from the perspective of heart failure patients. J Clin Nurs. 2012;21(3–4):495–503.
Boykova M, Kenner C. Transition from hospital to home for parents of preterm infants. J Perinat Neonatal Nurs. 2012;26(1):81–7.
Lundqvist P, Weis J, Sivberg B. Parents’ journey caring for a preterm infant until discharge from hospital-based neonatal home care—A challenging process to cope with. J Clin Nurs. 2019;28(15–16):2966–78.
Hamilton DL. Personality attributes associated with extreme response style. Psychol Bull. 1968;69(3):192.
Carroll Á, Dowling M. Discharge planning: communication, education and patient participation. Br J Nurs. 2007;16(14):882–6.
Aftyka A, Rozalska-Walaszek I, Rosa W, Rybojad B, Karakuła-Juchnowicz H. Post-traumatic growth in parents after infants’ neonatal intensive care unit hospitalisation. J Clin Nurs. 2017;26(5–6):727–34.
Rossman B, Greene MM, Meier PP. The role of peer support in the development of maternal identity for “NICU moms”. J Obstet Gynecol Neonatal Nurs. 2015;44(1):3–16.
O’Donovan A, Nixon E. “Weathering the storm:” Mothers’ and fathers’ experiences of parenting a preterm infant. Infant Ment Health J. 2019;40(4):573–87.
Kestler-Peleg M, Lavenda O, Stenger V, Bendett H, Alhalel-Lederman S, Maayan-Metzger A, et al. Maternal self-efficacy mediates the association between spousal support and stress among mothers of NICU hospitalized preterm babies. Early Human Dev. 2020;146:105077.
Ackley BJ, Ladwig GB, Makic MBF, Martinez-Kratz M, Zanotti M. Nursing Diagnosis Handbook, Revised Reprint with 2021–2023 NANDA-I® Updates-E-Book: Elsevier Health Sciences; 2021.
Karademas EC. Self-efficacy, social support and well-being: The mediating role of optimism. Personality Individ Differ. 2006;40(6):1281–90.
Download references
Acknowledgements
This article extracted from Ph.D. thesis of the first author, which was financially supported by the Nursing and Midwifery Care Research Center in ……… University of Medical Sciences (NCRC-1407). The authors would like to extend their sincere thanks to mothers, healthcare providers and other participants who shared their experiences with us.
Clinical trial registration
Not applicable.
Preprint disclosure
Saleheh Tajalli, Abbas Ebadi and Carole Kenner have no funding to disclose. Soroor Parvizy is supported by a grant from the vice chancellor of research from Nursing and Midwifery Care Research Center in Iran University of Medical Sciences under Grant number [1398–12-27–1407] CRediT.
Author information
Authors and affiliations.
School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran
Saleheh Tajalli
Behavioral Sciences Research Center, Life Style Institute, Nursing Faculty, Baqiyatallah University of Medical Sciences, Tehran, Iran
Abbas Ebadi
Nursing and Midwifery Care Research Center, Pediatric Nursing Department, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran
Soroor Parvizy
Center for Educational Research in Medical Sciences (CERMS), Department of Medical Education, School of Medicine, Iran University of Medical Sciences, Tehran, Iran
School of Nursing and Health Sciences, The College of New Jersey, Ewing, NJ, USA
Carole Kenner
You can also search for this author in PubMed Google Scholar
Contributions
S.T: Conceptualization, Investigation, Methodology, Software, Writing—original draft, Writing—review & editing. S.P: Data curation, Formal analysis, Investigation, Methodology, Software, Writing—original draft, Writing—review & editing, Validation, Funding acquisition. A.E: Investigation, Methodology, Project administration, Supervision, Validation, Writing review & editing, Resources. C.K: Writing -review & editing, Resources. All authors contributed to the article and approved the submitted version.
Corresponding authors
Correspondence to Abbas Ebadi or Soroor Parvizy .
Ethics declarations
Ethics approval and consent to participate, consent to participate and publication.
All parents of neonate in the study were informed of the study objectives and signed a written informed consent form.
Consent for publication
Consent to publish was obtained from the study participants.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: appendix a..
The last version of "Caring Ability of Mother with Preterm Infant Scale" (CAMPIS).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Tajalli, S., Ebadi, A., Parvizy, S. et al. Development and psychometric evaluation of "Caring Ability of Mother with Preterm Infant Scale" (CAMPIS): a sequential exploratory mixed-method study. BMC Nurs 23 , 297 (2024). https://doi.org/10.1186/s12912-024-01960-7
Download citation
Received : 24 November 2023
Accepted : 22 April 2024
Published : 29 April 2024
DOI : https://doi.org/10.1186/s12912-024-01960-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Caring ability
- Maternal caregiving
- Preterm infant
- Psychometric
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Open access
- Published: 25 April 2024
A scoping review of academic and grey literature on migrant health research conducted in Scotland
- G. Petrie 1 ,
- K. Angus 2 &
- R. O’Donnell 2
BMC Public Health volume 24 , Article number: 1156 ( 2024 ) Cite this article
248 Accesses
8 Altmetric
Metrics details
Migration to Scotland has increased since 2002 with an increase in European residents and participation in the Asylum dispersal scheme. Scotland has become more ethnically diverse, and 10% of the current population were born abroad. Migration and ethnicity are determinants of health, and information on the health status of migrants to Scotland and their access to and barriers to care facilitates the planning and delivery of equitable health services. This study aimed to scope existing peer-reviewed research and grey literature to identify gaps in evidence regarding the health of migrants in Scotland.
A scoping review on the health of migrants in Scotland was carried out for dates January 2002 to March 2023, inclusive of peer-reviewed journals and grey literature. CINAHL/ Web of Science/SocIndex and Medline databases were systematically searched along with government and third-sector websites. The searches identified 2166 journal articles and 170 grey literature documents for screening. Included articles were categorised according to the World Health Organisation’s 2016 Strategy and Action Plan for Refugee and Migrant Health in the European region. This approach builds on a previously published literature review on Migrant Health in the Republic of Ireland.
Seventy-one peer reviewed journal articles and 29 grey literature documents were included in the review. 66% were carried out from 2013 onwards and the majority focused on asylum seekers or unspecified migrant groups. Most research identified was on the World Health Organisation’s strategic areas of right to health of refugees, social determinants of health and public health planning and strengthening health systems. There were fewer studies on the strategic areas of frameworks for collaborative action, preventing communicable disease, preventing non-communicable disease, health screening and assessment and improving health information and communication.
While research on migrant health in Scotland has increased in recent years significant gaps remain. Future priorities should include studies of undocumented migrants, migrant workers, and additional research is required on the issue of improving health information and communication.
Peer Review reports
The term migrant is defined by the International Organisation for Migration as “ a person who moves away from his or her place of usual residence, whether within a country or across an international border, temporarily or permanently, and for a variety of reasons. The term includes several well-defined legal categories of people, including migrant workers; persons whose particular types of movements are legally-defined, such as smuggled migrants; as well as those whose status are not specifically defined under international law, such as international students.” [ 1 ] Internationally there are an estimated 281 million migrants – 3.6% of the world population, including 26.4 million refugees and 4.1 million asylum seekers – the highest number ever recorded [ 2 ]. The UN Refugee Society defines the term refugee as “ someone who has been forced to flee his or her country because of persecution, war or violence…most likely, they cannot return home or are afraid to do so .” The term asylum-seeker is defined as “someone whose request for sanctuary has yet to be processed.” [ 3 ].
Net-migration to Europe was negative in the 19th century due to higher levels of emigration, however in the mid-20th century immigration began to rise, because of an increase in migrant workers and following conflicts in the Middle East and North Africa [ 4 ]. Current migration drivers include conflicts alongside world-wide economic instability, exacerbated by the Covid-19 pandemic [ 5 ]. Environmental damage due to climate change is expected to inflate the number of asylum seekers entering Europe in future [ 6 ]. The increase in migration to Europe is not a short-term influx but a long-term phenomenon, and European nations must adapt and find solutions to resulting financial, safeguarding and health challenges [ 7 ].
Data on healthcare use by migrants in Europe is variable, which means cross-country comparisons are inadequate [ 8 ]. Many countries do not record migration information within health records and all use disparate criteria to classify migrant status. The lack of comparative data hinders public health surveillance and effective interventions [ 9 ]. Even where information is available, results can be contradictory due to the multifarious migrant population. Migrants have a wide range of origin countries, socio-economic position, age and journeys undertaken which can affect health status [ 10 ].
Migrants initially may have better health than the general population, known as the ‘Healthy Migrant effect’ [ 11 ]. However, health declines with increasing length of residence [ 12 ] and over time to levels comparable with the general population [ 13 ]. Second generation immigrants may have higher mortality than average [ 14 ]. The process of acculturation to the host country, with adoption of unhealthy lifestyle and behaviours, increases the risk for chronic disease [ 15 ]. In addition, inequalities in health of migrants compared to host populations has been confirmed by wide-ranging research [ 16 ].
Host countries may limit healthcare access, with undocumented migrants sometimes only entitled to emergency care [ 17 ]. Even when access is granted, inequitable services can affect quality of care due to language barriers and cultural factors [ 18 ]. Poor working/living conditions and discrimination can exacerbate health inequalities [ 12 ]. Processing facilities for asylum seekers are frequently overpopulated, stressful environments [ 19 ] and threat of deportation, lack of citizenship rights and integration can negatively affect health and access to care [ 20 ]. Undocumented workers are unprotected by health and safety legislation leading to dangerous working conditions and injuries [ 15 ].
A systematic review of migrant health in the European Union (EU) found migrants have worse self-perceived health than the general population [ 21 ]. Research evidence indicates increased prevalence of cardiovascular disease, diabetes, mental health disorders and adverse pregnancy outcomes. Exposure to conflict, harsh travel conditions and suboptimal vaccine programmes can mean higher risk of communicable disease [ 22 ]. Scoping reviews have also been conducted to describe trends within migration health research in the United Kingdom (UK) [ 23 ] and identify gaps for future research agendas in the UK [ 23 ] and in the Republic of Ireland [ 24 ].
Almost three-quarters (73%) of published migration health research in the UK has been conducted in England, focusing primarily on infectious diseases and mental health. There is limited evidence on the social determinants of health, access to and use of healthcare and structural and behavioural factors behaviours that influence migrant health in the UK [ 23 ]. By contrast, a large amount of the migration research conducted in the Republic of Ireland has focused on the social determinants of health, and on health system adaptations, with a paucity of research focusing on improving health information systems [ 24 ].
Migration and Health in Scotland
Immigration to Scotland began to rise in 2003 with the expansion of the EU [ 25 ]. The population in Scotland increased from 5.11 million to 5.47 million between 2005 and 2020 and is predicted to continue rising until 2028 [ 26 ] despite low birth rates, with the increased population resulting from inward migration [ 27 ]. Scotland’s population is becoming more ethnically diverse [ 28 ] and susceptibility to different health conditions varies by ethnic group, which has implications for the planning and provision of health services [ 29 ]. 7% of the current Scottish population are non-UK nationals and 10% were born outside Britain. The commonest countries of origin were Poland, Ireland, Italy, Nigeria and India [ 30 ].
Within Scotland, linking health data to ethnicity is standard in order to monitor and improve health of minority groups [ 31 ]. Ethnic background can differ from country of birth which means migration status cannot be assumed [ 32 ], although health inequalities experienced by migrants often extend to affect all ethnic minority groups [ 33 ]. The Scottish Health and Ethnicity Linkage Study (SHELS) linked census data to health records of 91% of the population which has provided information on mortality and morbidity by ethnic group and country of birth [ 34 ]. SHELS research indicates that the white-Scottish population have a higher mortality rate than other ethnic groups. This may be consequent to the comparatively poor health of the Scottish population relative to other European nations: high mortality rates in the general population may cause a perception that the health of minorities is more advantageous than in reality [ 35 ].
Cezard et al’s [ 13 ] analysis of self-perceived health among people in Scotland found that being born abroad had a positive impact on health status. Health declined with increased length of residence, which may be explained by cultural convergence with the majority population. Allik et al. [ 36 ] compared health inequalities by ethnic background and found that with increasing age, health differences reduced thus people aged over 75 of all ethnicities had similar or worse health status than White-Scottish people. While working-age migrants appear to be healthier than the White Scottish population, it cannot be assumed that in future this would extend to older age groups.
Research has shown deprivation as a cause of heath inequalities among ethnic minority and migrant groups [ 37 ]. The socio-economic status of minority ethnic groups in Scotland is unusual, as most are of similar or higher status than the white-Scottish population [ 38 ]. Therefore, public health interventions targeting deprivation may not address risk-factors for ethnic minorities and migrants [ 36 ]. Further research on determinants of health in migrants can help with planning and design of inclusive policies.
The 2011 census indicated that 50% of immigrants lived in the cities of Edinburgh, Glasgow, and Aberdeen. Glasgow had a greater percentage of non-European immigrants due to participation in the Asylum dispersal programme [ 39 ]. 10% of UK asylum seekers are placed in Glasgow, but records are not kept following approval of asylum claims, therefore the size of the refugee population is unknown [ 40 ]. While immigration is controlled by the British government, in policy areas devolved to the Scottish government, refugees and asylum seekers have more rights than elsewhere in UK, including access to primary healthcare for undocumented migrants [ 40 ]. Despite the mitigating effect of Scottish policies, asylum seekers’ health is worsened by the asylum process and associated poverty, marginalisation, and discrimination [ 40 ]. Health deteriorates with increasing length of time in the asylum system [ 40 ] and asylum seekers and refugees have additional health needs and require enhanced support [ 41 ]. Research on the health needs of asylum seekers in Scotland is required to ensure adequate healthcare.
Aim and objectives
While scoping reviews on migrant health have been carried out in Europe [ 12 ], Ireland [ 24 ] and the UK [ 23 ] none are currently specific to the Scottish context. Given the devolved government of Scotland and demographics described above, a targeted review would help to clarify research priorities, with the aim of improving health and health care within the migrant community in Scotland. This work therefore builds on the published scoping review of migrant health in the Republic of Ireland [ 24 ]. The authors recommend replication of the study in other countries to facilitate cross-country comparison. Our aim was to scope peer-reviewed research and grey literature on migrant health conducted in Scotland and identify any gaps in the evidence. Our objectives were to: [1] understand the extent of the available research by topic area [2] summarise the types of research already conducted, populations studied, topics covered and approaches taken [3], map the existing research conducted in Scotland and [4] identify areas for future research based on any gaps in the evidence identified.
A scoping review was conducted as they can aid detection of evidence gaps [ 42 ] and allow incorporation of grey literature in topics with insufficient published research [ 43 ]. Arksey and O’Malley’s [ 44 ] five stage scoping review framework was used.
Stage 1: identifying the research question
Arskey and O’Malley [ 44 ] suggest maintaining a broad approach to identifying the research question, in order to generate breadth of coverage. On this basis, and in line with the research question identified in the Villarroel et al. [ 24 ] scoping review, our research question was framed as follows: What is the scope, main topics and gaps in evidence in the existing literature on health of international migrants living in Scotland? Arksey and O’Malley [ 44 ] highlight the importance of defining terminology at the outset of scoping reviews. For consistency, we used the broad definition of ‘migrant’ as per Villaroel et al. [ 24 ], from the International Organisation for Migration (IOM) [ 1 ]. References to refugees or asylum seekers followed the United Nations Refugee Agency definitions [ 3 ].
Stage 2: identifying relevant studies
Electronic database searches identified reports alongside a grey literature search, in line with Arskey and O’Malley’s [ 44 ] guidance to search for evidence via different sources. CINAHL, Web of Science, SocIndex and Medline academic databases were selected with input from co-authors. Search terms for the review were based upon those used by Villaroel et al. [ 24 ] with additional relevant terms from Hannigan et al. [ 9 ] The strategy combined three sets of terms for: Migrants (e.g., refugee, migrant, immigrant or newcomer), Scotland and Health. Both free text terms and index terms were used and adapted to the 4 academic databases and searches were run on 10th March 2023 (see Additional File 1 for database search strategies). Thirteen Government, University, and third-sector websites in Scotland were scoped for selection then hand-searched for grey literature (listed in Additional File 1 ).
Stage 3: study selection
Net-migration to Scotland increased in the 2000s [ 27 ] hence a date range of January 2002-March 2023 was used to identify evidence. The search was limited to English only. Inclusion/exclusion criteria for the studies were based on those used by Villaroel et al. [ 24 ] and expanded upon following discussion with co-authors (see Table 1 ). Reports were included if based on primary or secondary research on the health of international migrants in Scotland and used qualitative, quantitative or mixed methods research design. International or UK based reports were only included if Scottish results were documented separately. Reports on the health of ethnic minority groups in Scotland was included if place of birth was recorded. Research on internal (non-international) migrants within Scotland, either moving from one Scottish area to another or from another part of the United Kingdom to Scotland, were excluded.
Stage 4: data charting
All records were saved to RefWorks for screening. Records were first screened at title/abstract stage with 10% independently checked by the co-authors. The remaining reports were single screened using full text by the first author. Data from the included records was extracted and organised in tabular form under the following headings, which were agreed by team members: article type (peer-reviewed article or grey literature), publication date, geographical setting, study/intervention’s target population, funding, primary research focus on migrant health (y/n), study objective, data collection method, study design (qualitative/quantitative/mixed) and main finding. Reports were not critically appraised in this scoping review.
Stage 5: collating, summarising and reporting results
A report (either a peer-reviewed journal article or grey literature report) is used as our unit of analysis. In order to present the range of research identified, reports were grouped by the different headings in our data charting table and the outcomes considered for relevance to our scoping review’s aim. Our Results summarise the recency, focus, study designs and funding sources of the identified research, followed by the geographical settings and whether Scotland was included in international research reports. Reports were grouped by their study population and further sub-divided by publication type and geographical area for summarising. Finally, the WHO’s European strategy and action plan (SAAP) for refugee and migrant health [ 7 ] is a policy framework designed to help governments and other stakeholders monitor and improve migrant health in Europe. There are nine strategic areas in the WHO’s SAAP, which prioritise the most salient issues. In line with Villaroel et al’s [ 24 ] approach and in order to compare scoping review outcomes, these areas were used to categorise the findings of this review. Each report was matched to the most appropriate SAAP:
Establishing a Framework for Collaborative Action.
Advocating for the right to health of refugees.
Addressing the social determinants of health.
Achieving public health preparedness and ensuring an effective response.
Strengthening health systems and their resilience.
Preventing communicable disease.
Preventing and reducing the risks caused by non-communicable disease.
Ensuring ethical and effective health screening and assessment.
Improving health information and communication.
The primary focus (aims and objectives) of each report was used to identify the relevant SAAP area/areas. To improve reliability, results were compared using coding criteria used in Villaroel et al’s study (MacFarlane 2023, personal communication, 31st May). 10% of the reports were checked by one co-author to ensure consistent coding to SAAP categories. Any instances of uncertainty in mapping reports to the relevant SAAP area/areas were discussed and resolved by team members.
This scoping review of the literature on migrant health in Scotland identified 2166 records from academic literature databases, following duplicate removal, and 170 records from website searches (see Fig. 1 ). Following screening, a total of 71 peer-reviewed journal articles and 29 grey literature studies (totalling 100 reports) were included for analysis (Results table and reference list are presented in Additional File 2 ).
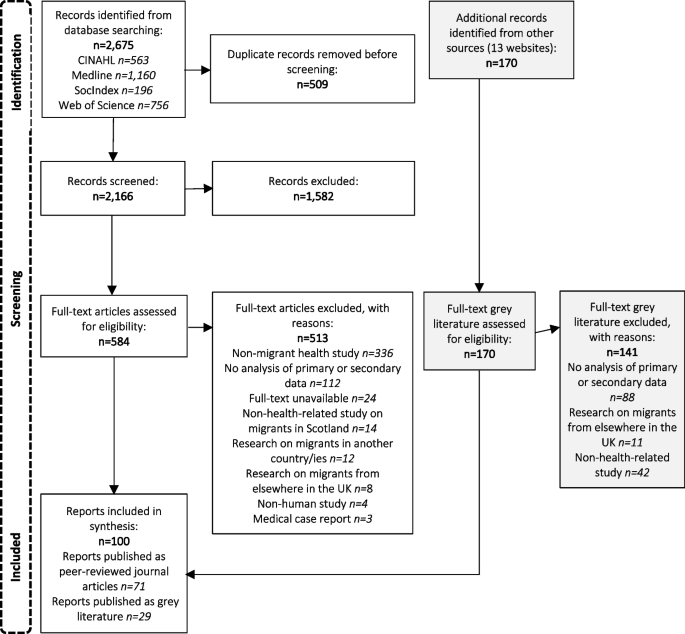
Flow chart illustrating the identification of sources of evidence included in the scoping review
Overall findings
The majority of reports were published between 2013 and 2022. Fifty-eight reports (58%) focused exclusively on migrant health [ 18 , 39 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 ]. 23 centred on health but included other populations in addition to migrants – for example research on ethnic minorities or other vulnerable groups [ 13 , 31 , 35 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 ]. Seventeen reports were included where the sample population were migrants, but the primary topic was not health – for example destitution, integration, and service needs [ 27 , 73 , 74 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 ]. Health data was reported as part of the wider subject matter. One report [ 136 ] looked at the social determinants of breastfeeding including migrant status and one [ 137 ] compared attitudes to aging and family support between countries.
Funding sources were not declared for 35 (35%) of reports. The Scottish Government funded 20 reports (20%) [ 13 , 27 , 32 , 39 , 45 , 46 , 47 , 66 , 77 , 88 , 99 , 100 , 101 , 102 , 113 , 116 , 119 , 121 , 129 , 134 ]. Other common sources of funding included Government funded public bodies ( n = 13) [ 45 , 48 , 49 , 50 , 51 , 52 , 53 , 104 , 107 , 113 , 116 , 131 , 136 ], the Scottish Health Service ( n = 18) (either the National Health Service (NHS) [ 13 , 54 , 56 , 57 , 58 , 59 , 102 , 113 , 116 ], local NHS trusts [ 45 , 60 , 61 , 77 , 102 , 103 , 112 ] or by Public Health Scotland [ 13 , 113 ]) Eleven reports (11%) were funded by Universities. The charity sector financed 15 (15%) reports [ 53 , 63 , 66 , 69 , 70 , 71 , 72 , 73 , 74 , 103 , 111 , 123 , 125 , 132 , 138 ] and the EU and Scottish local authorities funded four reports each [ 45 , 62 , 75 , 76 , 77 , 102 , 125 , 135 ]. Professional bodies financed one report [ 126 ] as did the Japanese government [ 64 ]. No reports received funding from the business sector. The biggest sources of funding for grey literature were Refugee charities (40%) and the Scottish government (30%) (see Fig. 2 ).
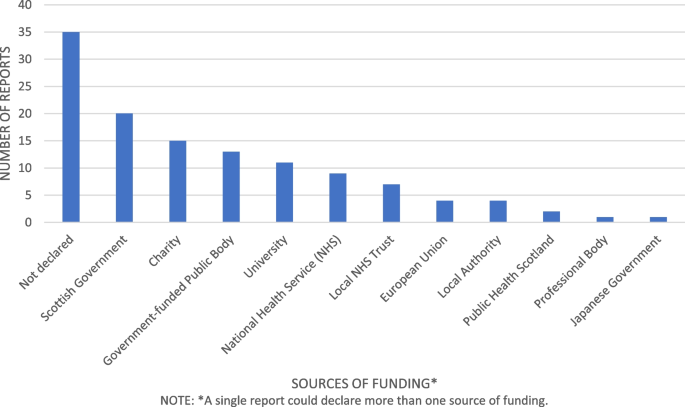
Sources of funding for migrant health research in Scotland
Research methods and data collection
52% of reports used qualitative research methods. Forty-five reports (86%) collected data using 1–1 interviews and 24 (46%) used focus groups. Other methods of data collection included questionnaires (six studies (11%)), workshops (two studies (3.85%)) and observation (two studies (3.85%)). Oral/written evidence, guided play sessions, family case studies and participatory activity sessions were used in one report each.
28% of reports used quantitative research methods, most commonly cross section design (ten studies (36%)) and cohort design (18 studies (64%)). Information was obtained from databases including medical records, Census data and national records in 21 reports (75%). Questionnaires were used in six reports (21%). Other methods including body measurements, food diaries, blood samples, interviews and case reviews were used in 1 report each.
20% of reports used mixed methods. The most common method of data collection was questionnaires in 14 reports (70%), interviews in ten reports (50%), focus groups in seven reports (35%), workshops in three reports (13.6%), and databases in three reports (13.6%). Other methods included literature review in two reports (10%), case note reviews in two reports (10%) and one reports each used mapping and school records.
Geographical areas of study
Ninety-one reports were situated in Scotland, of which 35 (38.5%) covered the whole country and 56 (61.5%) specified a city or area where research was undertaken. Some UK and international reports also specified the area of Scotland. The largest share of research within Scotland overall was in Glasgow with 36 reports, followed by Edinburgh with 16 reports, Lothian with six reports, Aberdeen with five reports and Grampian with three reports. The Northeast, Stirling, Highlands, Inverness, Lanarkshire, Motherwell and Selkirk had one report in each area.
There were seven international reports, three on mortality by country of birth [ 75 , 76 , 78 ], one on cross cultural communication [ 79 ], one on maternity care in Poland and Scotland [ 99 ], one comparing attitudes to aging in China and Scotland [ 137 ] and one on the link between birthweights and integration of migrants [ 64 ]. The remaining two reports were UK based, one on immunisation of Roma and traveller communities [ 117 ] and one on the link between ethnic diversity and mortality [ 104 ]. All the included international and UK reports documented the Scottish data separately within results.
Migrant population
Thirty-one reports included all migrants in the study population. The remaining reports included 30 studies on asylum seekers/refugees, 11 on Polish migrants, ten on Africans, six each on South Asians/Chinese/European, three on Arabs, and two on Roma populations (see Fig. 3 ). Most reports did not specify the country of origin for Asylum seekers and refugees - where country of birth was specified, reports were also included in the appropriate category.
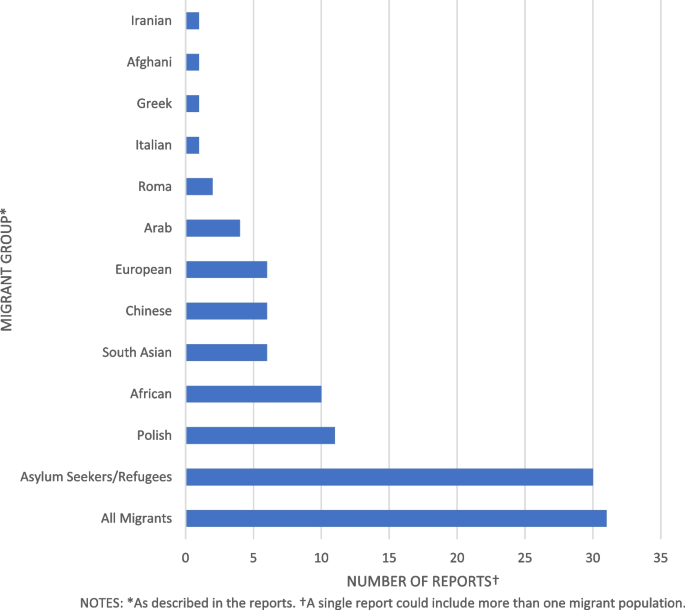
Migrant populations studied in health research in Scotland
Grey literature and peer-reviewed reports differed in population focus. The most common populations of interest in grey literature were asylum seekers/refugees consisting of 18 reports (62%) [ 27 , 47 , 54 , 55 , 59 , 63 , 70 , 71 , 72 , 73 , 74 , 123 , 125 , 127 , 128 , 132 , 134 , 138 ] while for peer-reviewed journals 24 reports (34%) focused on all migrants [ 13 , 35 , 45 , 48 , 64 , 76 , 78 , 79 , 80 , 81 , 104 , 105 , 108 , 109 , 113 , 114 , 115 , 116 , 118 , 120 , 121 , 122 , 136 ].
Migrant study population also differed by local area; Glasgow city, where the majority of research occurred, had 18 reports of 36 (50%) on Asylum seekers/refugees [ 47 , 48 , 52 , 53 , 54 , 55 , 58 , 63 , 70 , 71 , 72 , 82 , 83 , 127 , 128 , 130 , 138 , 139 ] eight reports (22%) on Africans [ 52 , 53 , 84 , 85 , 86 , 87 , 106 , 107 ], seven reports (19%) on all migrants [ 45 , 48 , 80 , 102 , 104 , 105 , 121 ] and two reports (5.5%) on Roma migrants [ 103 , 117 ]. Other populations had one reports each. In Edinburgh five reports of 16 (31%) were on the Polish population [ 56 , 67 , 68 , 89 , 90 ], and two reports (12.5%) on Asylum seekers/refugees [ 60 , 133 ], Chinese [ 62 , 137 ], South Asian [ 46 , 119 ], all migrants [ 105 , 121 ] and Africans [ 87 , 107 ]. The remaining migrant groups had one report each. Other areas of Scotland show no clear pattern with studies in disparate migrant population groups.
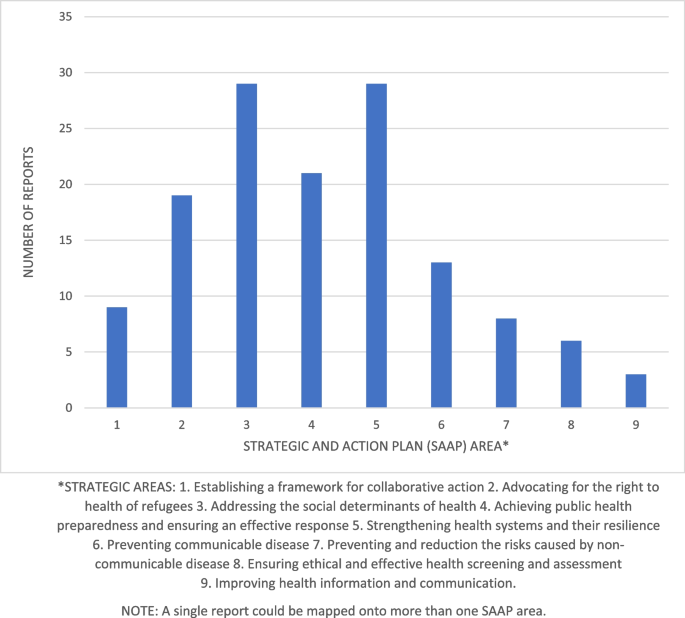
Number of reports per Strategic and Action Plan (SAAP) Area
SAAP Area mapping
1. establishing a framework for collaborative action.
Nine reports had a primary focus on collaborative action and were categorised under SAAP area 1 (see Fig. 4 ) [ 66 , 70 , 72 , 73 , 103 , 125 , 129 , 132 , 134 ]. Four reports (33%) used a mixed methods study design, the remaining five reports (67%) used a qualitative design. One report [ 66 ] focused on the epidemiology of female genital mutilation and a proposed intervention strategy. One report [ 66 ] focused on the epidemiology of female genital mutilation and a proposed intervention strategy. One report [ 103 ] evaluated service provision to the Roma community in Glasgow. The remaining reports focused on refugees and asylum seekers: four [ 73 , 125 , 132 , 134 ] evaluations of refugee integration projects, one [ 70 ] on services available to pregnant women, and one [ 72 ] an assessment of a peer-education service. One report [ 129 ] was a review of service provisions for migrants during the Covid-19 pandemic. All reports in SAAP area 1 were grey literature and three (37.5%) had a primary focus on migrant health while four (50%) focused on integration, one (11%) included data on ethnic minorities and one (11%) on services during the covid-19 pandemic. The majority (seven reports (78%)) were also categorised to another SAAP area most commonly area 2 (five studies (55%)) or area 5 (four studies (44%)).
2. Advocating for the right to health of refugees
Nineteen reports focused on SAAP area 2, advocating for the right to health of refugees (see Fig. 4 ) [ 47 , 52 , 53 , 54 , 55 , 63 , 70 , 71 , 83 , 103 , 123 , 124 , 125 , 127 , 128 , 129 , 134 , 138 , 140 ]. Sixteen reports (84%) had a qualitative study design and the remaining three (16%) reports used mixed methods. Nine reports (47%) focused on the health impact of the asylum system [ 52 , 55 , 71 , 74 , 123 , 127 , 128 , 129 , 138 ], five (26%) on health and access to care [ 47 , 54 , 83 , 103 , 124 ], two (10.5%) on maternity care [ 63 , 70 ], two (10.5%) on integration services [ 125 , 134 ] and one report on mental health in HIV positive migrants [ 53 ]. Nine reports (47%) had a primary focus on migrant health while the remaining 10 (53%) also involved wider social issues. The majority (15 (79%)) of reports were grey literature. All the articles in this group overlapped with another SAAP area. Area 3 is the most common joint category with ten reports (53%) followed by area 5 with seven reports (37%), area 1 shares five reports (26%), while areas 4 and 8 share one report each (5%).
3. Addressing the social determinants of health
Twenty-nine reports were categorised to SAAP area 3 – addressing the social determinants of health (see Fig. 4 ) [ 13 , 27 , 45 , 50 , 52 , 55 , 60 , 62 , 63 , 65 , 68 , 71 , 74 , 80 , 81 , 82 , 91 , 92 , 93 , 102 , 112 , 123 , 124 , 127 , 128 , 136 , 137 , 138 ]. The majority (14 (48%)) used a qualitative study method, eight (28%) used quantitative methodology and the remaining seven reports (24%) used mixed methods. Nineteen reports (65.5%) were peer-reviewed journals [ 13 , 45 , 50 , 52 , 60 , 62 , 63 , 65 , 68 , 80 , 81 , 82 , 91 , 92 , 93 , 104 , 112 , 124 , 136 , 137 ] and ten (34.5%) were grey literature [ 27 , 55 , 63 , 71 , 74 , 102 , 123 , 127 , 128 , 138 ]. Ten reports (34.5%) discussed the effects of the asylum system on health [ 27 , 52 , 63 , 71 , 74 , 123 , 124 , 127 , 128 , 137 ] and one (3.5%) migration and health [ 50 ]. Six reports (21%) focused on culture and ethnicity [ 82 , 92 , 102 , 104 , 112 , 137 ], five reports (17%) discussed economic and environmental determinants of health [ 13 , 45 , 67 , 81 , 93 ] and five reports (17%) the health impact of social activities [ 55 , 60 , 62 , 80 , 91 ]. Of the remaining reports, one [ 65 ] discussed Brexit and mental health of European migrants and one discussed the effect of coping strategies on wellbeing in Polish migrants [ 68 ]. Most reports, 18 (62%) had a primary focus on migrant health [ 45 , 50 , 52 , 55 , 60 , 62 , 63 , 65 , 67 , 68 , 71 , 80 , 81 , 82 , 91 , 92 , 93 , 102 ], six reports (21%) discussed wider social factors in addition to health [ 74 , 123 , 124 , 127 , 128 , 138 ]. Of the remaining reports three (10%) looked at ethnic background and country of birth [ 13 , 112 , 136 ], one [ 27 ] included other vulnerable groups and one [ 137 ] included people living in China and Chinese migrants to Scotland. Thirteen reports were also categorised to one or more additional SAAP area - ten (34%) were also applicable to area 2 [ 52 , 55 , 63 , 71 , 74 , 123 , 124 , 127 , 128 , 138 ], three (10%) to area 5 [ 63 , 82 , 92 ] and one (7%) to area 4 [ 27 ].
4. Achieving public health preparedness and ensuring an effective response
Twenty-one reports were assigned to SAAP area 4 (see Fig. 4 ) [ 27 , 31 , 35 , 39 , 47 , 57 , 64 , 75 , 76 , 77 , 78 , 94 , 104 , 108 , 109 , 111 , 113 , 114 , 116 , 120 , 135 ] of which fourteen (67%) used quantitative research methods, four (19%) mixed methods and three (14%) qualitative methods. Thirteen (62%) reports were peer-reviewed journals [ 35 , 59 , 64 , 75 , 78 , 104 , 108 , 109 , 111 , 113 , 114 , 116 , 120 ] and eight (38%) grey literature [ 27 , 31 , 39 , 47 , 57 , 77 , 94 , 135 ]. Most reports (12 (57%)) focused on morbidity and mortality in migrant populations [ 31 , 35 , 64 , 75 , 76 , 78 , 104 , 108 , 109 , 113 , 114 , 116 ]. Six (29%) investigated health status and healthcare needs in migrant groups in Scotland [ 39 , 47 , 57 , 77 , 94 , 135 ]. Two reports (9.5%) analysed the epidemiology of HIV infections [ 111 , 120 ] and the remaining report focused on the health needs of young people during the covid-19 pandemic [ 27 ]. Nine reports (43%) had a primary focus on migrant health [ 39 , 47 , 55 , 64 , 75 , 76 , 77 , 78 , 94 ] while eight (38%) also analysed data by ethnicity [ 31 , 35 , 104 , 108 , 109 , 113 , 114 , 116 ]. Of the remaining reports, three (14%) included other populations within Scotland [ 27 , 111 , 120 ] and one (5%) included other characteristics in addition to health information [ 135 ]. Ten reports (48%) were also categorised to another SAAP area; one to area 2 [ 47 ], one to area 3 [ 27 ], four to area 5 [ 47 , 57 , 77 , 135 ], two to area 6 [ 111 , 120 ] and two to area 9 [ 31 , 108 ].
5. Strengthening health systems and their resilience
Twenty-nine reports were assigned to SAAP area 5 (see Fig. 4 ) [ 18 , 47 , 48 , 49 , 54 , 57 , 63 , 69 , 70 , 72 , 77 , 79 , 82 , 83 , 92 , 95 , 96 , 97 , 99 , 101 , 103 , 118 , 119 , 126 , 129 , 131 , 133 , 135 , 141 ] of which 23 (79%) used qualitative research methods. Three reports used quantitative methods (10.3%) and the remaining three used mixed methods (10.3%). Twelve reports (41%) examined migrants needs and experiences of health care [ 47 , 49 , 54 , 57 , 58 , 77 , 83 , 95 , 103 , 119 , 129 , 135 ], eight (24%) focused on pregnancy and childcare [ 63 , 70 , 92 , 96 , 97 , 99 , 101 , 118 ] and two (7%) on barriers to healthcare access [ 48 , 131 ]. Two reports (7%) evaluated healthcare programmes [ 72 , 133 ] and two focused on communication in primary care [ 79 ] and maternity services [ 69 ]. The remaining three reports (10%) covered sexual health [ 82 ], health information needs of Syrian refugees [ 126 ] and general practitioner training [ 18 ]. Nineteen (65.5%) were peer reviewed journals [ 18 , 48 , 49 , 58 , 69 , 79 , 82 , 83 , 92 , 95 , 96 , 97 , 99 , 101 , 118 , 119 , 125 , 131 , 133 ] and ten (34.5%) were grey literature [ 47 , 54 , 57 , 63 , 70 , 72 , 77 , 103 , 129 , 135 ]. Twenty-one (72%) had a primary focus on migrant health [ 18 , 47 , 48 , 49 , 54 , 57 , 58 , 63 , 69 , 70 , 72 , 77 , 79 , 82 , 83 , 92 , 95 , 96 , 97 , 99 , 101 ]. Six reports (21%) included research on other characteristics or services [ 103 , 126 , 129 , 131 , 133 , 135 ]. The remaining two reports (7%) included ethnic groups as well as migrants in the data [ 118 , 119 ]. Nineteen reports (65.5%) were also assigned to one or more other category areas: five reports (17%) to area 1 [ 47 , 70 , 72 , 103 , 129 ], five reports (17%) to area 2 [ 54 , 63 , 83 , 103 , 129 ], three reports (10%) to area 3 [ 63 , 82 , 92 ], four reports (14%) to area 4 [ 47 , 57 , 77 , 135 ], one (3.5%) to area 7 [ 119 ] and one (3.5%) to area 9 [ 48 ].
6. Preventing communicable diseases
Fourteen reports were assigned to SAAP area 6 (see Fig. 4 ) [ 56 , 61 , 87 , 88 , 89 , 90 , 105 , 106 , 107 , 111 , 115 , 117 , 120 , 122 ] of which four (31%) used quantitative methods, five (38%) used qualitative methods and five (38%) used mixed methods. Five reports (38.5%) examined immunisation behaviour [ 56 , 61 , 89 , 90 , 117 ], five (38%) on epidemiology and treatment of HIV [ 106 , 107 , 111 , 120 , 122 ]. The remaining four reports (31%) focused on tuberculosis in healthcare workers [ 115 ], malaria [ 105 ] and sexual health services [ 87 , 88 ]. Only one reports was grey literature [ 88 ], the remainder were peer-reviewed journals. Six reports (46%) had a primary focus on migrant health [ 56 , 61 , 87 , 88 , 89 , 90 ] while seven reports (54%) also included other at-risk groups in the analysis. Four reports (31%) were also assigned to another SAAP category, two (15%) to area 4 [ 111 , 120 ] and two (15%) to area 8 [ 88 , 115 ].
7. Preventing and reducing the risks posed by non-communicable diseases
Eight reports were categorised to SAAP area 7 (see Fig. 4 ) [ 46 , 51 , 59 , 84 , 85 , 86 , 98 , 119 ] of which six (75%) used qualitative research methods, one (12.5%) used quantitative methods and one (12.5%) used mixed methods. Only one report (12.5%) was grey literature [ 59 ] the remaining seven reports (87.5%) were peer-reviewed journals [ 48 , 87 , 92 , 126 , 127 , 128 , 140 ]. Three reports (37.5%) focused on health behaviours [ 51 , 85 , 98 ], two (25%) on mental health, two (25%) on diabetes and one (12.5%) on chronic disease. Seven reports(87.5%) had a primary focus on migrant health [ 46 , 51 , 59 , 84 , 85 , 86 , 98 ], with the remaining report (12.5%) including ethnic minority groups [ 119 ]. One report (12.5%) was also assigned to SAAP area number 5 [ 119 ].
8. Ensuring ethical and effective health screening and assessment
There were six reports assigned to category 8 (see Fig. 4 ) [ 53 , 88 , 100 , 110 , 115 , 121 ] of which two (33%) used a quantitative research method, three (50%) used a qualitative method and one used mixed methods. One report (14%) was grey literature [ 88 ] the remaining five reports (83%) were peer reviewed journals [ 53 , 100 , 110 , 115 , 121 ]. Three reports (50%) focused on cancer screening in migrant women [ 21 , 100 , 110 ], one (17%) analysed access to HIV testing among African migrants [ 53 ], one (17%) on T.B in healthcare workers [ 72 ] and one (17%) on sexual health [ 36 ]. Three reports (50%) had a primary focus on migrant health [ 53 , 88 , 100 ] while the remaining three reports (50%) included other at-risk groups in the analysis [ 110 , 115 , 121 ]. There were three reports which overlapped with other SAAP areas: one [ 53 ] (17%) was categorised to area 2 while two [ 88 , 115 ] (33%) were categorised to area 6.
9. Improving health information and communication
Three reports were assigned to SAAP area 9 (see Fig. 4 ) [ 31 , 108 , 130 ]. One of these (33%) used a qualitative approach, one (33%) used a quantitative approach and one (33%) used mixed methods. Two [ 108 , 130 ] (66%) were peer-reviewed journal articles and one [ 31 ] (33%) was grey literature. Two reports (66%) focused on improving migrant demographics and health information using databases [ 31 , 108 ] while one (33%) described an information-needs matrix for refugees and asylum seekers [ 130 ]. Two [ 31 , 108 ] included ethnicities in the data while one [ 130 ] had a primary focus on migrant health. Two reports [ 31 , 108 ] (66%) also applied to SAAP area 4 while one report [ 130 ] (33%) was in SAAP area 9 only.
To our knowledge this is the first scoping review conducted on migrant health in Scotland. A previous rapid literature review [ 94 ] found most research focused on health behaviours, mental health, communicable disease and use of and access to healthcare; however, the review limited migrant definition to those who had immigrated within five years and asylum seekers were not included.
In our review, the majority of reports were published from 2013 onwards, aligning with the expansion in migrant research internationally [ 142 ]. 52% used qualitative research methods, 28% used quantitative methods and 20% used mixed methods. 58% focused on migrant health: the remaining papers included other populations or health as part of a wider remit. Research funding was mostly provided by the Scottish Government, NHS, refugee charities and Universities. No studies received funding from the private sector, although this sector has the potential resource and capacity to play a key role in funding future research to improve migrant health in Scotland. Geographically, most studies took place in Glasgow (36%), nationwide (38.5%) or Edinburgh (16%) – other areas were under-represented including Aberdeen (5%), despite being the city with the largest migrant population [ 30 ]. There was a lack of studies in rural localities. These findings concur with a UK migrant health review by Burns et al. [ 23 ] where research was concentrated in larger cities and data was sparse in rural areas relative to the migrant population.
Half of the research identified that was conducted in Glasgow focused on asylum seekers/refugees. Glasgow was previously the only Scottish city to host asylum seekers [ 143 ] and currently supports the most asylum seekers of any local authority in the UK [ 29 ]. In April 2022, the UK government widened the Asylum dispersal scheme to all local authorities [ 144 ]. Around 70% of Scotland’s refugee support services are based in Glasgow and the South-west [ 145 ]. As reduced access to services may impact the health of asylum seekers, research in Glasgow may not be generalizable to other regions of Scotland.
Almost one-third (30%) of all reports focused on asylum seekers and refugees – an overrepresentation given that only 18% of migrants to the UK are asylum seekers [ 146 ] and as low as 2% of all migrants in Scotland [ 147 ]. Asylum seekers and refugees are at risk of poor health due to trauma, difficult journeys, overcrowded camps, poor nutrition and lack of access to healthcare [ 148 ]. They have worse maternity outcomes and increased rates of mental illness [ 149 ]. Increased research on health of asylum seekers and refugees is necessary due to their additional vulnerabilities [ 142 ]. However, asylum seeker’s country of origin was generally not specified. Asylum seekers have heterogenic backgrounds [ 150 ] and nationality and trauma experience affect health status [ 151 ]. Further research focused on specific nationalities of asylum seekers would enhance understanding of the health needs in this population.
Almost one-third (31%) of studies did not specify a migrant group. This concurs with a Norwegian migrant health study by Laue et al. [ 152 ] where 36% of research did not identify country of birth. Where nationality was identified, Polish, African and South Asian were most prevalent. Poles are the largest migrant group in Scotland, however for the other most common immigrant groups of Irish, Italian and Nigerian [ 30 ] there was an absence of research. No studies took place on Nigerian migrants – nine studies indicated African populations, but country of birth was not specified. Since March 2022, 23,000 Ukrainians have migrated to Scotland [ 153 ], however no studies on Ukrainians were identified currently. Research may be underway which is yet to be published.
Only one study explored the impact of Brexit on European migrants’ health despite 56% of migrants to Scotland being EU nationals [ 30 ]. Again, research may be taking place currently, which is yet to be published. No studies involved undocumented migrants despite this populations’ high rates of poor physical/mental health exacerbated by poor housing and working conditions [ 154 ]. An estimated 7.2–9.5% of the workforce in the UK are migrant workers who have higher risks of poor working conditions and injury [ 155 ]. Scotland depends on a migrant workforce for some industries such as agriculture [ 156 ] but only two research papers specified migrant workers.
Most research papers related to the right to health of refugees (SAAP 2), social determinants of health (SAAP 3), public health planning (SAAP 4) and strengthening health systems (SAAP 5). Areas with less research were frameworks for collaborative action (SAAP 1), preventing communicable disease (SAAP 6), preventing non-communicable disease (SAAP 7) and health screening and assessment (SAAP 8). Only three studies related to improving health information and communication (SAAP 9). Lebano et al. [ 12 ] conducted a literature review of migrant health in Europe and found data collection unreliable and disorganised. There is a lack of data on the numbers and types of migrants entering Scotland and research tends not to differentiate between ethnic minorities and migrants [ 94 ]. As poor-quality information hinders surveillance and planning of services SAAP area 9 is an important consideration for increased research.
Villarroel et al. [ 24 ] also found more research in SAAP areas 3 to 5 and less in areas 6 to 9. However, their study returned no results in category 1, collaborative action, or 2, the right to health of refugees, while this study assigned 9% of articles to category 1 and 19% to category 2. Most articles in our study relating to categories 1 and 2 were grey literature, which was excluded from the original Irish scoping review. This highlights a potential difference in the focus of peer-reviewed articles compared to government/refugee charity commissioned reports. Collaborative action and the right to health of refugees and asylum seekers are entwined in Scotland due to the complex policy environment; the social determinants of health such as housing, education, welfare rights and social integration are influenced by a variety of UK and Scottish statutory bodies as well as third sector organisations [ 157 ]. Despite this complexity, organisations work well together [ 158 ]. Further academic research in this area would enhance joint working practices and networks.
A scoping review in the UK [ 23 ] found similar quantities of research corresponding to SAAP areas 3, 2 and 9. However in Scotland areas 1, 5 and 8 were a combined 44% of included papers compared with 27.8% of results on health systems and structures in Burns et al’s [ 23 ] study. Almost half of the articles in SAAP areas 1,5 and 8 were grey literature, which was not included in Burns et al’s [ 23 ] review. Conversely, Burns et al. [ 23 ] found 81.9% of research in the UK related to epidemiology, equivalent to SAAP categories 4,6 and 7. In a Norwegian scoping review of migrant health [ 152 ] 65% of research was related to epidemiological data on health and disease. Only 42% of the research in this current study related to epidemiological data; the quantity of evidence was reduced by excluding combined research from the UK. As Scotland has higher mortality and morbidity than elsewhere in the UK [ 29 ] it is important to undertake further epidemiological research limited to Scotland.
Strengths and weaknesses
Strengths of this review include the use of the WHO’s SAAP categories [ 7 ] to classify data, in accordance with the Villarroel et al’s [ 24 ] study: this means results are linked to policy on migrant health and facilitates comparability to the Irish study results. Additionally results include data on migrant groups, locality, and funding of included papers; these highlight potential omissions for future research consideration. Results include diverse research methods and published and grey literature giving a wide overview of available evidence, reported using the Preferred Reporting Items for Systematic reviews and Meta-Analyses for Scoping Reviews (PRISMA-ScR) checklist (see Additional File 3 ) [ 159 ].
Limitations included the lack of an open-access protocol and search limitations of English language and selected databases. This means some relevant reports may be omitted. Due to time and resource limitations no quality appraisal was planned for included reports. Whilst we did not synthesise the findings for each topic area and migrant group, future systematic reviews could be undertaken to address this limitation and build on this work.
Conclusions
Immigration and ethnic diversity in Scotland have increased since 2002 which is reflected in the expansion of migrant health research. This review highlights evidence gaps including a lack of research in rural areas, undocumented migrants and migrant workers. There is a tendency to cluster asylum seekers together rather than differentiate between national groups. Within the SAAP areas there is less evidence relating to collaborative action, preventing communicable disease, preventing non-communicable disease and health screening and assessment. Further research is required on improving health information and communication for migrant populations in Scotland – a significant omission given the importance of accurate information for health service planning.
Availability of data and materials
All data analysed during this review comes from the papers listed in Additional file 2 .
Abbreviations
European Union
Human Immunodeficiency Virus
National Health Service
Strategy and Action Plan
The Scottish Health and Ethnicity Linkage Study
United Kingdom
World Health Organisation
International Organisation for Migration (IOM). IOM Definition of Migrant. 2024. Available from: https://www.iom.int/about-migration .Cited 2024 Feb 8.
International Organisation for Migration United Nations. World Migration Report. 2022. Available from: available: https://worldmigrationreport.iom.int/wmr-2022-interactive/ .
The United Nations Refugee Angency. Refugee facts: What is a refugee? 2024. Available from: https://www.unrefugees.org/refugee-facts/what-is-a-refugee/ . Cited 2024 Feb 8.
Migration Data Portal. Migration data in Europe. 2023. Available from: https://www.migrationdataportal.org/regional-data-overview/europe#past-and-present-trends . Cited 2023 Aug 22.
International Centre for Migration Policy Development. Migration Outlook 2022 Twelve migration issues to look out for in 2022 Origins, key events and priorities for Europe. 2022. Available from: https://www.icmpd.org/file/download/56783/file/ICMPD%2520Migration%2520Outlook%25202022.pdf .
European Parliament. Exploring migration causes: why people migrate. 2023. Available from: https://www.europarl.europa.eu/news/en/headlines/world/20200624STO81906/exploring-migration-causes-why-people-migrate .
World Health Organisation. Strategic plan: Strategy and Action Plan for Refugee and Migrant Health in the WHO European Region 2016–2022. 2016. Available from: https://www.who.int/publications/i/item/strategic-plan-strategy-and-action-plan-for-refugee-and-migrant-health-in-the-who-european-region-2016-2022 .
Graetz V, Rechel B, Groot W, Norredam M, Pavlova M. Utilization of health care services by migrants in Europe—a systematic literature review. Br Med Bull. 2017;121(1):5–18. Available from: https://www.academic.oup.com/bmb/article-lookup/doi/10.1093/bmb/ldw057 .
Article CAS PubMed Google Scholar
Hannigan A, O'Donnell P, O'Keeffe M, MacFarlane A. How do Variations in Definitions of “Migrant” and their Application Influence the Access of Migrants to Health Care Services? Copenhagen: WHO Regional Office for Europe; 2016. (Health Evidence Network Synthesis Report, No. 46.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK391032/ .
Rechel B, Mladovsky P, Ingleby D, Mackenbach JP, McKee M. Migration and health in an increasingly diverse Europe. Lancet. 2013;381(9873):1235–45. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0140673612620868 .
Article PubMed Google Scholar
Giannoni M, Franzini L, Masiero G. Migrant integration policies and health inequalities in Europe. BMC Public Health. 2016;16(1):463. Available from: http://www.bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-016-3095-9 .
Article PubMed PubMed Central Google Scholar
Lebano A, Hamed S, Bradby H, Gil-Salmerón A, Durá-Ferrandis E, Garcés-Ferrer J, et al. Migrants’ and refugees’ health status and healthcare in Europe: a scoping literature review. BMC Public Health. 2020;20(1):1039. Available from: https://www.bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-020-08749-8 .
Cézard G, Finney N, Kulu H, Marshall A. Ethnic differences in self-assessed health in Scotland: The role of socio-economic status and migrant generation. Popul Space Place. 2022;28(3):e2403. Available from: https://onlinelibrary.wiley.com/doi/10.1002/psp.2403 .
Article Google Scholar
Anson J. The migrant mortality advantage: a 70 month follow-up of the brussels population. Eur J Popul. 2004;20(3):191–218.
World Health Organisation. Health of refugees and migrants. WHO European Region. 2018. Available from: https://www.who.int/publications/i/item/health-of-refugees-and-migrants---who-european-region-(2018) .
Mladovsky P. A framework for analysing migrant health policies in Europe. Health Policy (New York). 2009;93(1):55–63. Available from: https://www.linkinghub.elsevier.com/retrieve/pii/S0168851009001444 .
De Vito E, de Waure C, Specchia ML, Parente P, Azzolini E, Frisicale EM, et al. Are undocumented migrants’ entitlements and barriers to healthcare a public health challenge for the European Union? Public Health Rev. 2016;37(1):13. Available from: http://publichealthreviews.biomedcentral.com/articles/10.1186/s40985-016-0026-3 .
Katikireddi SV, Bhopal R, Quickfall JA. GPs need training and funding in caring for refugees and asylum seekers. BMJ. 2004;328(7442):770.1. Available from: https://www.bmj.com/lookup/doi/10.1136/bmj.328.7442.770 .
Carballo M, Hargreaves S, Gudumac I, Maclean EC. Evolving migrant crisis in Europe: implications for health systems. Lancet Glob Heal. 2017;5(3):e252-253. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2214109X17300402 .
Juárez SP, Honkaniemi H, Dunlavy AC, Aldridge RW, Barreto ML, Katikireddi SV et al. Effects of non-health-targeted policies on migrant health: a systematic review and meta-analysis. Lancet Glob Heal. 2019;7(4):e420–35. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2214109X18305606 .
Nielsen SS, Krasnik A. Poorer self-perceived health among migrants and ethnic minorities versus the majority population in Europe: a systematic review. Int J Public Health. 2010;55(5):357–71. Available from: ( http://link.springer.com/10.1007/s00038-010-0145-4 ).
World Health Organsation. World report on the health of refugees and migrants. 2022. Available from: https://www.who.int/publications/i/item/9789240054462 .
Burns R, Zhang CX, Patel P, Eley I, Campos-Matos I, Aldridge RW. Migration health research in the United Kingdom: a scoping review. J Migr Heal. 2021;4:100061. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2666623521000283 .
Villarroel N, Hannigan A, Severoni S, Puthoopparambil S, MacFarlane A. Migrant health research in the Republic of Ireland: a scoping review. BMC Public Health. 2019;19(1):324. Available from: ( https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-019-6651-2 ).
Scottish Government. Demographic Change in Scotland. 2010. Available from: https://www.gov.scot/binaries/content/documents/govscot/publications/research-and-analysis/2010/11/demographic-change-scotland/documents/0108163-pdf/0108163-pdf/govscot%3Adocument/0108163.pdf .
National Records of Scotland. Projected Population of Scotland (Interim) 2020-based. 2022. Available from: https://www.nrscotland.gov.uk/files/statistics/population-projections/2020-based/pop-proj-2020-scot-nat-pub.pdf .
Scottish Government. Coronavirus (COVID-19) - experiences of vulnerable children, young people, and parents: research. 2021. Available from: https://www.gov.scot/publications/experiences-vulnerable-children-young-people-parents-during-covid-19-pandemic/ .
Scotland’s Census. Scotland’s Census: Ethnicity. 2011. Available from: https://www.scotlandscensus.gov.uk/census-results/at-a-glance/ethnicity/#:~:text=Scotland’spopulationwas96.0%25 .
Walsh D. The changing ethnic profiles of Glasgow and Scotland, and the implications for population health. 2017. Available from: https://www.gcph.co.uk/assets/0000/6255/The_changing_ethnic_profiles_of_Glasgow_and_Scotland.pdf .
National Records of Scotland. Migration Statistics Quarterly Summary for Scotland. 2021. Available from: https://www.nrscotland.gov.uk/files/statistics/migration/quarterly-summary/miration-statistics-quarterly-summary-february-2021.pdf .
The Scottish Ethnicity and Health Research Strategy Working Group. Health in our Multi-ethnic Scotland Future Research Priorities. 2009. Available from: https://www.healthscotland.scot/media/1842/health-in-our-multi-ethnic-scotland-full-report.pdf .
The Scottish Public Health Observatory. Ethnic minorities: defining ethnicity and race. 2023. Available from: https://www.scotpho.org.uk/population-groups/ethnic-minorities/defining-ethnicity-and-race/ . Cited 2023 Aug 22.
Krasnik A, Bhopal RS, Gruer L, Kumanyika SK. Advancing a unified, global effort to address health disadvantages associated with migration, ethnicity and race. Eur J Public Health. 2018;28(suppl_1). Available from: https://academic.oup.com/eurpub/article/doi/10.1093/eurpub/cky046/4956664 .
Bhopal R, Fischbacher C, Povey C, Chalmers J, Mueller G, Steiner M, et al. Cohort profile: scottish health and ethnicity linkage study of 4.65 million people exploring ethnic variations in disease in Scotland. Int J Epidemiol. 2011;40(5):1168–75. Available from: https://academic.oup.com/ije/article-lookup/doi/10.1093/ije/dyq118 .
Bhopal RS, Gruer L, Cezard G, Douglas A, Steiner MFC, Millard A, et al. Mortality, ethnicity, and country of birth on a national scale, 2001–2013: a retrospective cohort (Scottish Health and Ethnicity Linkage Study). Basu S, editor. Plos Med. 2018;15(3):e1002515. https://doi.org/10.1371/journal.pmed.1002515 . Basu S, editor.
Allik M, Brown D, Dundas R, Leyland AH. Differences in ill health and in socioeconomic inequalities in health by ethnic groups: a cross-sectional study using 2011 Scottish census. Ethn Health. 2022;27(1):190–208. https://doi.org/10.1080/13557858.2019.1643009 ( https://www.tandfonline.com/doi/full/ ).
Watkinson RE, Sutton M, Turner AJ. Ethnic inequalities in health-related quality of life among older adults in England: secondary analysis of a national cross-sectional survey. Lancet Public Hea. 2021;6(3):e145-154.
Fischbacher CM, Cezard G, Bhopal RS, Pearce J, Bansal N. Measures of socioeconomic position are not consistently associated with ethnic differences in cardiovascular disease in Scotland: methods from the Scottish Health and Ethnicity Linkage Study (SHELS). Int J Epidemiol. 2014;43(1):129–39. Available from: https://academic.oup.com/ije/article-lookup/doi/10.1093/ije/dyt237 .
Scottish Government. Characteristics of Recent and Established EEA and non-EEA migrants in Scotland: Analysis of the 2011 Census. 2015. Available from: https://www.gov.scot/publications/characteristics-recent-established-eea-non-eea-migrants-scotland-analysis-2011-census/ .
House of Lords Library. Refugees and asylum-seekers: UK policy. 2022. https://lordslibrary.parliament.uk/refugees-and-asylum-seekers-uk-policy/ .
British Medical Association. Refugee and asylum seeker patient health toolkit. Unique health challenges for refugees and asylum seekers. 2022. Available from: https://www.bma.org.uk/advice-and-support/ethics/refugees-overseas-visitors-and-vulnerable-migrants/refugee-and-asylum-seeker-patient-health-toolkit/unique-health-challenges-for-refugees-and-asylum-seekers .
Khalil H, Peters M, Godfrey CM, McInerney P, Soares CB, Parker D. An evidence-based approach to scoping reviews. Worldviews Evidence-Based Nurs. 2016;13(2):118–23. Available from: https://doi.org/10.1111/wvn.12144 .
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69. Available from: ( http://implementationscience.biomedcentral.com/articles/10.1186/1748-5908-5-69 ).
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.Available from: http://www.tandfonline.com/doi/abs/10.1080/1364557032000119616 ).
Kearns A, Whitley E, Egan M, Tabbner C, Tannahill C. Healthy migrants in an unhealthy city? The Effects of time on the health of migrants living in deprived areas of glasgow. J Int Migr Integr. 2017;18(3):675–98. Available from: http://link.springer.com/10.1007/s12134-016-0497-6 .
PubMed Google Scholar
Porqueddu T. Herbal medicines for diabetes control among Indian and Pakistani migrants with diabetes. Anthropol Med. 2017;24(1):17–31. Available from: https://www.tandfonline.com/doi/full/10.1080/13648470.2016.1249338 .
Roshan N. Supporting new communities: a qualitative study of health needs among asylum seekers and refugee communities in North Glasgow final report. 2005. Available from: https://www.stor.scot.nhs.uk/handle/11289/579930 .
Piacentini T, O’Donnell C, Phipps A, Jackson I, Stack N. Moving beyond the ‘language problem’: developing an understanding of the intersections of health, language and immigration status in interpreter-mediated health encounters. Lang Intercult Commun. 2019;19(3):256–71. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1353829214001233 .
Sime D. ‘I think that Polish doctors are better’: Newly arrived migrant children and their parents׳ experiences and views of health services in Scotland. Health Place. 2014;30:86–93. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1353829214001233 .
Steven K, Munoz S, Migrants, Matter. Report of a Peer Researched Project on EU Migrant Health in the Highlands of Scotland. University of the Highlands and Islands. 2016. Available from: https://www.spiritadvocacy.org.uk/assets/Birchwood-Highland-HUG-Migrants-Matter-study-2015-2016.pdf .
Anderson AS, Bush H, Lean M, Bradby H, Williams R, Lea E. Evolution of atherogenic diets in South Asian and Italian women after migration to a higher risk region. J Hum Nutr Diet. 2005;18(1):33–43. Available from: ( https://onlinelibrary.wiley.com/doi/10.1111/j.1365-277X.2004.00584.x ).
Isaacs A, Burns N, Macdonald S, O’Donnell CA. ‘I don’t think there’s anything I can do which can keep me healthy’: how the UK immigration and asylum system shapes the health and wellbeing of refugees and asylum seekers in Scotland. Crit Public Health. 2022;32(3):422–32. Available from: https://www.tandfonline.com/doi/full/10.1080/09581596.2020.1853058 .
Palattiyil G, Sidhva D. Caught in a web of multiple jeopardy: post-traumatic stress disorder and HIV-positive asylum seekers in Scotland. Clin Soc Work J. 2015;43(4):362–74. Available from: http://link.springer.com/10.1007/s10615-015-0542-5 ).
Abdulkadir J, Azzudin A, Buick A, Curtice L, Dzingisai M, Easton D, et al. What do you mean, I have a right to health? Participatory action research on health and human rights. 2016. Available from: https://strathprints.strath.ac.uk/58209/1/Abdulkadir_etal_IPPI_2016_What_do_you_mean_I_have_a_right_to_health.pdf .
Strang A, Quinn N. Integration or isolation? Mapping social connections and well-being amongst refugees in Glasgow. 2014. Available from: https://eresearch.qmu.ac.uk/bitstream/handle/20.500.12289/4139/eResearch%25204139.pdf?sequence=1&isAllowed=y .
Gorman DR, Bielecki K, Larson HJ, Willocks LJ, Craig J, Pollock KG. Comparing vaccination hesitancy in polish migrant parents who accept or refuse nasal flu vaccination for their children. Vaccine. 2020;38(13):2795–9. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0264410X20302255 .
Love J, Vertigans S, Domaszk E, Zdeb K, Love A, Sutton P. Health & ethnicity in Aberdeenshire: a study of Polish in-migrants; a report for the Scottish Health Council. 2007. Available from: https://rgu-repository.worktribe.com/output/247667 .
O’Donnell CA, Higgins M, Chauhan R, Mullen K. Asylum seekers’ expectations of and trust in general practice: a qualitative study. Br J Gen Pract. 2008;58(557):e1-11. Available from: https://bjgp.org/lookup/doi/10.3399/bjgp08X376104 .
Quinn N, Shirjeel S, Siebelt L, Donnelly R, Pietka E. An evaluation of the sanctuary community conversation programme to address mental health stigma with asylum seekers and refugees in Glasgow. 2011. Available from: https://www.healthscotland.com/uploads/documents/5584-SanctuaryCommunityConversationEvaluation.pdf .
Ager A. Community contact and mental health amongst socially isolated refugees in Edinburgh. J Refug Stud. 2002;15(1):71–80. Available from: https://academic.oup.com/jrs/article-lookup/doi/10.1093/jrs/15.1.71 .
Sim JA, Ulanika AA, Katikireddi SV, Gorman D. Out of two bad choices, I took the slightly better one’: Vaccination dilemmas for Scottish and Polish migrant women during the H1N1 influenza pandemic. Public Health. 2011;125(8):505–11. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0033350611001697 .
Zhao S, Patuano A. International Chinese Students in the UK: association between use of green spaces and lower stress levels. Sustainability. 2021;4(1):89. Available from: https://www.mdpi.com/2071-1050/14/1/89 .
Da Lomba S, Murray N. Women and Children First? Refused asylum seekers’ access to and experiences of maternity care in Glasgow. 2014. Available from: https://strathprints.strath.ac.uk/58655/1/Lomba_Murray_SRC_2014_Women_and_Children_First_Refused_Asylum_Seekers_Access_to_and_Experiences.pdf .
Sørbye IK, Vangen S, Juarez SP, Bolumar F, Morisaki N, Gissler M, et al. Birthweight of babies born to migrant mothers - What role do integration policies play? SSM - Popul Heal. 2019;9:100503. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2352827319301971 .
Teodorowski P, Woods R, Czarnecka M, Kennedy C. Brexit, acculturative stress and mental health among EU citizens in Scotland. Popul Space Place. 2021;27(6). Available from: https://onlinelibrary.wiley.com/doi/10.1002/psp.2436 .
Baillot H, Murray N, Connelly E, Howard N. Tackling Female Genital Mutilation in Scotland: A Scottish model of intervention. 2014. Available from: https://www.celcis.org/application/files/8116/2185/5421/Tackling_Female_Genital_Mutilation_-_A_Scottish_Model_of_Intervention.pdf .
Weishaar HB. Consequences of international migration: a qualitative study on stress among Polish migrant workers in Scotland. Public Health. 2008;122(11):1250–6. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0033350608000942 .
Weishaar HB. You have to be flexible—coping among polish migrant workers in Scotland. Health Place. 2010;16(5):820–7. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1353829210000432 .
Crowther S, Lau A. Migrant polish women overcoming communication challenges in scottish maternity services: a qualitative descriptive study. Midwifery. 2019;72:30–8. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0266613819300361 .
Fassetta G, Da Lomba S, Quinn N. A healthy start? Experiences of pregnant refugee and asylum seeking women in Scotland. 2016. Available from: https://www.redcross.org.uk/-/media/documents/about-us/research-publications/refugee-support/a-healthy-start-report.pdf .
Positive Action in Housing. 12 months since the Park Inn Tragedy in Glasgow, one in three hotel asylum seekers say their mental health has deteriorated. 2021. Available from: https://www.paih.org/one-in-three-glasgow-asylum-seekers-suffering-depression-and-anxiety .
Strang A. Refugee Peer Education for Health and Well-being. Evaluation Report. 2015. Available from: https://www.scottishrefugeecouncil.org.uk/wp-content/uploads/2019/10/Peer-Education-Evaluation-Report.pdf .
Strang A, Marsden R, Mignard E. The Holistic Integration Service: Learning and Evaluation Year 1. 2014. Available from: https://www.scottishrefugeecouncil.org.uk/wp-content/uploads/2019/10/Holistic-Integration-Service-year-1-evaluation-report.pdf .
British Red Cross. How will we survive? Steps to preventing destitution in the asylum system. 2021. Available from: https://www.redcross.org.uk/-/media/documents/about-us/how-will-we-survive-preventing-destitution-in-the-asylum-system.pdf .
Bhopal RS, Rafnsson SB, Agyemang C, Fagot-Campagna A, Giampaoli S, Hammar N, et al. Mortality from circulatory diseases by specific country of birth across six European countries: test of concept. Eur J Public Health. 2012;22(3):353–9. Available from: https://academic.oup.com/eurpub/article-lookup/doi/10.1093/eurpub/ckr062 .
Rafnsson SB, Bhopal RS, Agyemang C, Fagot-Campagna A, Harding S, Hammar N, et al. Sizable variations in circulatory disease mortality by region and country of birth in six European countries. Eur J Public Health. 2013;23(4):594–605. Available from: https://academic.oup.com/eurpub/article-lookup/doi/10.1093/eurpub/ckt023 ).
de Lima P, Masud Chaudhry M, Whelton R, Arshad R. A study of migrant workers in Grampian. 2007. Available from: . http://www.communitiesscotland.gov.uk/stellent/groups/public/%0Adocuments/webpages/pubcs_019731.pdff .
Ikram UZ, Mackenbach JP, Harding S, Rey G, Bhopal RS, Regidor E, et al. All-cause and cause-specific mortality of different migrant populations in Europe. Eur J Epidemiol. 2016;31(7):655–65. Available from: http://link.springer.com/10.1007/s10654-015-0083-9 .
de Brún T, De-Brún MO, van Weel-Baumgarten E, van Weel C, Dowrick C, Lionis C, et al. Guidelines and training initiatives that support communication in cross-cultural primary-care settings: appraising their implementability using Normalization Process Theory. Fam Pract. 2015;cmv022. Available from: https://academic.oup.com/fampra/article-lookup/doi/10.1093/fampra/cmv022 .
García-Medrano S, Panhofer H. Improving migrant well-being: spontaneous movement as a way to increase the creativity, spontaneity and welfare of migrants in Glasgow. Body Mov Danc Psychother. 2020;15(3):189–203. Available from: https://www.tandfonline.com/doi/full/10.1080/17432979.2020.1767208 .
Jamil NA, Gray SR, Fraser WD, Fielding S, Macdonald HM. The relationship between vitamin D status and muscle strength in young healthy adults from sunny climate countries currently living in the northeast of Scotland. Osteoporos Int. 2017;28(4):1433–43. Available from: http://link.springer.com/10.1007/s00198-016-3901-3 .
Kaneoka M, Spence W. The cultural context of sexual and reproductive health support: an exploration of sexual and reproductive health literacy among female Asylum Seekers and Refugees in Glasgow. Int J Migr Heal Soc Care. 2019;16(1):46–64. Available from: https://www.emerald.com/insight/content/doi/10.1108/IJMHSC-01-2019-0002/full/html .
O’Donnell CA, Higgins M, Chauhan R, Mullen K. They think we’re OK and we know we’re not. A qualitative study of asylum seekers’ access, knowledge and views to health care in the UK. BMC Health Serv Res. 2007;7(1):75. Available from: https://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-7-75 .
Cooper M, Harding S, Mullen K, O’Donnell C. ‘A chronic disease is a disease which keeps coming back … it is like the flu’: chronic disease risk perception and explanatory models among French- and Swahili-speaking African migrants. Ethn Health. 2012;17(6):597–613. Available from: http://www.tandfonline.com/doi/abs/10.1080/13557858.2012.740003 .
Ezika EA. An exploration of smoking behavior of african male immigrants living in glasgow. Tob Use Insights. 2014;7:TUI .S13262. Available from: http://journals.sagepub.com/doi/10.4137/TUI.S13262 .
Karadzhov D, White R. Between the whispers of the devil and the revelation of the word : christian clergy’s mental health literacy and pastoral support for BME congregants. J Spiritual Ment Heal. 2020;22(2):147–72. Available from: https://www.tandfonline.com/doi/full/10.1080/19349637.2018.1537755 ).
Yakubu BD, Simkhada P, van Teijlingen E, Eboh W. Sexual health information and uptake of sexual health services by African women in Scotland: a pilot study. Int J Heal Promot Educ. 2010;48(3):79–84. Available from: http://www.tandfonline.com/doi/abs/10.1080/14635240.2010.10708186 .
Goff J, Kay K, Lima M, Shallangwa S, We All Have A. Different Consciousness About It: Exploring the Sexual Health Needs of People From African Communities in Scotland. 2021. Available from: https://www.waverleycare.org/wp-content/uploads/2023/05/We_All_Have_Different_Consciousness_About_It_Report.pdf .
Bielecki K, Craig J, Willocks LJ, Pollock KG, Gorman DR. Impact of an influenza information pamphlet on vaccination uptake among Polish pupils in Edinburgh, Scotland and the role of social media in parental decision making. BMC Public Health. 2020;20(1):1381. Available from: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-020-09481-z .
Article CAS PubMed PubMed Central Google Scholar
Gorman DR, Bielecki K, Willocks LJ, Pollock KG. A qualitative study of vaccination behaviour amongst female Polish migrants in Edinburgh, Scotland. Vaccine. 2019;37(20):2741–7. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0264410X19304220 .
Bak-Klimek A, Karatzias T, Elliott L, MacLean R. The determinants of well-being among polish economic immigrants. Testing the sustainable happiness model in migrant population. J Happiness Stud. 2018;19(6):1565–88. Available from: http://link.springer.com/10.1007/s10902-017-9877-7 .
Cheung NF. The cultural and social meanings of childbearing for Chinese and Scottish women in Scotland. Midwifery. 2002;18(4):279–95. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0266613802903281 .
Papadaki A, Scott J. The impact on eating habits of temporary translocation from a Mediterranean to a Northern European environment. Eur J Clin Nutr. 2002;56(5):455–61. Available from: https://www.nature.com/articles/1601337 .
McCann A, Mackie P. Improving the Health of Migrants to Scotland: An update for Scottish Directors of Public Health. 2016. Available from: https://www.scotphn.net/wp-content/uploads/2016/04/2016_03_23-Migrant-Health-Report-FINAL-1.pdf .
Ahmed A, Cameron S, Dickson C, Mountain K. Arabic-speaking students’ primary care experiences in Scotland. Community Pract J Community Pract Heal Visit Assoc. 2010;83(2):23–6.
Google Scholar
Bray J, Gorman D, Dundas K, Sim J. Obstetric care of New European migrants in Scotland: an audit of antenatal care, obstetric outcomes and communication. Scott Med J. 2010;55(3):26–31. Available from: ( http://journals.sagepub.com/doi/10.1258/rsmsmj.55.3.26 .
Cheung NF. Choice and control as experienced by Chinese and Scottish childbearing women in Scotland. Midwifery. 2002;18(3):200–13. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0266613802903153 .
Spence W, Zhu L. Perceptions of smoking cessation among Glasgow’s Chinese community. Tob Prev Cessat. 2017;3(October). Available from: http://www.journalssystem.com/tpc/Perceptions-of-smoking-cessation-among-Glasgow-s-Chinese-community,77942,0,2.html .
Gorman DR, Katikireddi SV, Morris C, Chalmers JWT, Sim J, Szamotulska K, et al. Ethnic variation in maternity care: a comparison of Polish and Scottish women delivering in Scotland 2004–2009. Public Health. 2014;128(3):262–7. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0033350613003910 .
Gorman DR, Porteous LA. Influences on Polish migrants’ breast screening uptake in Lothian, Scotland. Public Health. 2018;158:86–92. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0033350617304018 .
Hogg R, de Kok B, Netto G, Hanley J, Haycock-Stuart E. Supporting Pakistani and Chinese families with young children: perspectives of mothers and health visitors. Child Care Health Dev. 2015;41(3):416–23. Available from: https://onlinelibrary.wiley.com/doi/10.1111/cch.12154 .
Kearns A, Whitley E. Health, Wellbeing and Social Inclusion of Migrants in North Glasgow. 2010. Available from: https://www.gowellonline.com/assets/0000/0521/Health_Wellbeing_and_Social_Inclusion_of_Migrants_in_North_Glasgow.pdf .
Poole L, Adamson K. Report on the Situation of the Roma Community in Govanhill, Glasgow. 2008. Available from: https://www.bemis.org.uk/resources/gt/scotland/reportonthesituationoftheromacommunityingovanhill,Glasgow.pdf .
Schofield L, Walsh D, Feng Z, Buchanan D, Dibben C, Fischbacher C, et al. Does ethnic diversity explain intra-UK variation in mortality? A longitudinal cohort study. BMJ Open. 2019;9(3):e024563. Available from: https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2018-024563 .
Unger HW, McCallum AD, Ukachukwu V, McGoldrick C, Perrow K, Latin G, et al. Imported malaria in Scotland – an overview of surveillance, reporting and trends. Travel Med Infect Dis. 2011;9(6):289–97. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1477893911001074 .
Young I, Flowers P, McDaid LM. Barriers to uptake and use of pre-exposure prophylaxis (PrEP) among communities most affected by HIV in the UK: findings from a qualitative study in Scotland. BMJ Open. 2014;4(11):e005717. Available from: https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2014-005717 .
Young I, Flowers P, McDaid LM. Key factors in the acceptability of treatment as prevention (TasP) in Scotland: a qualitative study with communities affected by HIV. Sex Transm Infect. 2015;91(4):269–74. Available from: https://sti.bmj.com/lookup/doi/10.1136/sextrans-2014-051711 .
Bhopal R, Cm FI, Teiner SM, Halmers CJ, Ovey PC, Amieson J. Ethnicity and health in Scotland: Can we fill the information gap ? A demonstration project focusing on coronary heart disease and linkage of census and health records. Ethics. 2005. Available from: http://www.cphs.mvm.ed.ac.uk/docs/Retrocodingfinalreport.pdf .
Cezard GI, Bhopal RS, Ward HJT, Bansal N, Bhala N. Ethnic variations in upper gastrointestinal hospitalizations and deaths: the Scottish Health and Ethnicity Linkage Study. Eur J Public Health. 2016;26(2):254–60. Available from: https://academic.oup.com/eurpub/article-lookup/doi/10.1093/eurpub/ckv182 .
Christie-de Jong F, Kotzur M, Amiri R, Ling J, Mooney JD, Robb KA. Qualitative evaluation of a codesigned faith-based intervention for muslim women in Scotland to encourage uptake of breast, colorectal and cervical cancer screening. BMJ Open. 2022;12(5):e058739. Available from: https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2021-058739 .
Cree VE, Sidhva D. Children and HIV in Scotland: findings from a cross-sector needs assessment of children and young people infected and affected by HIV in Scotland. Br J Soc Work. 2011;41(8):1586–603. Available from: https://academic.oup.com/bjsw/article-lookup/doi/10.1093/bjsw/bcr036 .
Gallimore A, Irshad T, Cooper M, Cameron S. Influence of culture, religion and experience on the decision of Pakistani women in Lothian, Scotland to use postnatal contraception: a qualitative study. BMJ Sex Reprod Heal. 2021;47(1):43–8. Available from: https://jfprhc.bmj.com/lookup/doi/10.1136/bmjsrh-2019-200497 .
Gruer LD, Cézard GI, Wallace LA, Hutchinson SJ, Douglas AF, Buchanan D, et al. Complex differences in infection rates between ethnic groups in Scotland: a retrospective, national census-linked cohort study of 1.65 million cases. J Public Health (Bangkok). 2022;44(1):60–9. Available from: https://academic.oup.com/jpubhealth/article/44/1/60/6106111 .
Article CAS Google Scholar
Bhala N, Cézard G, Ward HJT, Bansal N, Bhopal R. Ethnic variations in liver- and alcohol-related disease hospitalisations and mortality: the Scottish health and ethnicity linkage study. Alcohol Alcohol. 2016;51(5):593–601. Available from: https://academic.oup.com/alcalc/article-lookup/doi/10.1093/alcalc/agw018 .
Pollock KG, McDonald E, Smith-Palmer A, Johnston F, Ahmed S. Tuberculosis in healthcare workers, Scotland. Scott Med J. 2017;62(3):101–3. Available from: http://journals.sagepub.com/doi/10.1177/0036933017727963 .
Gruer LD, Millard AD, Williams LJ, Bhopal RS, Katikireddi SV, Cézard GI, et al. Differences in all-cause hospitalisation by ethnic group: a data linkage cohort study of 4.62 million people in Scotland, 2001–2013. Public Health. 2018;161:5–11. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0033350618301501 .
Jackson C, Bedford H, Cheater FM, Condon L, Emslie C, Ireland L, et al. Needles, Jabs and Jags: a qualitative exploration of barriers and facilitators to child and adult immunisation uptake among Gypsies, Travellers and Roma. BMC Public Health. 2017;17(1):254. Available from: http://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-017-4178-y .
John JR, Curry G, Cunningham-Burley S. Exploring ethnic minority women’s experiences of maternity care during the SARS-CoV-2 pandemic: a qualitative study. BMJ Open. 2021;11(9):e050666. Available from: https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2021-050666 .
Lawton J, Ahmad N, Hanna L, Douglas M, Hallowell N. Diabetes service provision: a qualitative study of the experiences and views of Pakistani and Indian patients with Type 2 diabetes. Diabet Med. 2006;23(9):1003–7. Available from: https://onlinelibrary.wiley.com/doi/10.1111/j.1464-5491.2006.01922.x .
Livingston MR, Shaw LE, Codere G, Goldberg DJ. Human immunodeficiency virus acquired heterosexually abroad: expert panel assessment of the indigenous/nonindigenous to the united kingdom status of cases. J Travel Med. 2006;12(1):19–25. Available from: https://academic.oup.com/jtm/article-lookup/doi/10.2310/7060.2005.00005 .
Nelson M, Patton A, Robb K, Weller D, Sheikh A, Ragupathy K, et al. Experiences of cervical screening participation and non-participation in women from minority ethnic populations in Scotland. Heal Expect. 2021;24(4):1459–72. Available from: https://onlinelibrary.wiley.com/doi/10.1111/hex.13287 .
Noble G, Okpo E, Tonna I, Fielding S. Factors associated with late HIV diagnosis in North-East Scotland: a six-year retrospective study. Public Health. 2016;139:36–43. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0033350616301020 .
Gillespie M. Trapped: Destitution and Asylum in Scotland. 2012. Available from: http://www.rst.org.uk/wp-content/uploads/2012/11/Trapped-destitution-and-asylum-summary-final-compressed-pictures.pdf .
Hopkins P, Hill M. The needs and strengths of unaccompanied asylum-seeking children and young people in Scotland. Child Fam Soc Work. 2010;15(4):399–408. Available from: https://onlinelibrary.wiley.com/doi/10.1111/j.1365-2206.2010.00687.x .
Marsden R, Harris C. “We started life again”: Integration experiences of refugee families reuniting in Glasgow. 2015. Available from: https://www.refworld.org/docid/560cde294.html .
Martzoukou K, Burnett S. Exploring the everyday life information needs and the socio-cultural adaptation barriers of Syrian refugees in Scotland. J Doc. 2018;74(5):1104–32. Available from: https://www.emerald.com/insight/content/doi/10.1108/JD-10-2017-0142/full/html .
McKenna R. From pillar to post: Destitution among people refused asylum in Scotland. 2019; Available from: https://www.rst.org.uk/wp-content/uploads/2019/03/From-Pillar-to-Post-Feb-2019.pdf .
Independent Commission of Inquiry. Failings in the provision of care to New Scots during the Covid pandemic: Part 2. 2022. Available from: https://static1.squarespace.com/static/62af1289a666c80e00b17253/t/636b9190408f81778746eaa7/1667994032702/AIS+Phase+2+Report+Full.pdf .
Trevena P, Gawlewicz A, Wright S. Addressing the needs of Scotland’s migrant and minority ethnic populations under Covid-19: lessons for the future. 2022. Available from: https://migrantessentialworkers.com/wp-content/uploads/2022/11/SC-Migrant-C19-Innovations.pdf .
Oduntan O, Ruthven I. The information needs matrix: a navigational guide for refugee integration. Inf Process Manag. 2019;56(3):791–808. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0306457318306939 .
Sime D, Fox R, Migrant C. Social capital and access to services post-migration: transitions, negotiations and complex agencies. Child Soc. 2015;29(6):524–34. Available from: https://onlinelibrary.wiley.com/doi/10.1111/chso.12092 .
Strang A, Baillot H, Mignard E. Insights into integration pathways. New Scots and the Holistic Integration Service. A report drawing on year two of the Holistic Integration Service. 2015. Available from: https://scottishrefugeecouncil.org.uk/wp-content/uploads/2019/10/Holistic-Integration-Service-Year-2-report.pdf .
Weir KEA, Wilson SJ, Gorman DR. The Syrian vulnerable person resettlement programme: evaluation of Edinburgh’s reception arrangements. J Public Health (Bangkok). 2018;40(3):451–60. Available from: https://academic.oup.com/jpubhealth/article/40/3/451/4600209 .
Hammond CN. Scots 2- Engagement analysis of the New Scot Refugee Integration Strategy 2018–2022. 2018. Available from: https://www.gov.scot/binaries/content/documents/govscot/publications/research-and-analysis/2018/06/news-scots-2-engagement-analysis-new-scots-refugee-integration-strategy/documents/00537019-pdf/00537019-pdf/govscot%3Adocument/00537019.pdf .
Blake Stevenson. A8 Nationals in Glasgow. 2007. Available from: http://crosshillandgovanhill.org.uk/grindocs/A8NationalsinGlasgow.pdf .
Ajetunmobi O, Whyte B, Chalmers J, Fleming M, Stockton D, Wood R. Informing the ‘early years’ agenda in Scotland: understanding infant feeding patterns using linked datasets. J Epidemiol Community Health. 2014;68(1):83–92. Available from: https://jech.bmj.com/lookup/doi/10.1136/jech-2013-202718 .
Laidlaw K, Wang D, Coelho C, Power M. Attitudes to ageing and expectations for filial piety across Chinese and British cultures: a pilot exploratory evaluation. Aging Ment Health. 2010;14(3):283–92. Available from: http://www.tandfonline.com/doi/abs/10.1080/13607860903483060 .
Marsden R, Aldegheri E, Khan A, Lowe M, Strang A, Salinas E, et al. “What’s going on?” A study into destitution and poverty faced by asylum seekers and refugees in Scotland. 2005. Available from: http://www.rst.org.uk/wp-content/uploads/2012/11/Whats_going_on_A_study.pdf .
Quinn N. Participatory action research with asylum seekers and refugees experiencing stigma and discrimination: the experience from Scotland. Disabil Soc. 2014;29(1):58–70. Available from: http://www.tandfonline.com/doi/abs/10.1080/09687599.2013.769863 .
British Red Cross, Refugee Survival Trust. How will we survive? Steps to preventing destitution in the asylum system. 2021. Available from: https://mcusercontent.com/c17c136fc126588cb51e5471d/files/a35dd0e1-d785-f962-6a41-01e928493775/DASS_Research_Report_2021.pdf .
O’Donnell R, Angus K, McCulloch P, Amos A, Greaves L, Semple S. Fathers’ views and experiences of creating a smoke-free home: a scoping review. Int J Environ Res Public Health. 2019;16(24):5164. Available from: https://www.mdpi.com/1660-4601/16/24/5164 .
Sweileh WM, Wickramage K, Pottie K, Hui C, Roberts B, Sawalha AF, et al. Bibliometric analysis of global migration health research in peer-reviewed literature (2000–2016). BMC Public Health. 2018;18(1):777. Available from: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-018-5689-x .
Wren K. Supporting asylum seekers and refugees in glasgow: the role of multi-agency networks. J Refug Stud. 2007;20(3):391–413. Available from: https://academic.oup.com/jrs/article-lookup/doi/10.1093/jrs/fem006 .
UK Government Home Office. A Fairer Asylum Accommodation System. 2022. Available from: https://www.emcouncils.gov.uk/write/Migration/Asylum_Dispersal_Factsheet_PDF.pdf .
Scottish Refugee Council. Scotland’s Welcome: an analysis of community support for refugee integration. 2020. Available from https://scottishrefugeecouncil.org.uk/wp-content/uploads/2021/01/Community-support-analysis-2020.pdf .
Sturge G, UK Parliament House of Commons Library Asylum statistics Research Briefing. 2023. Available from: https://commonslibrary.parliament.uk/research-briefings/sn01403/#:~:text=IntheyearendingJune,ofimmigrantstotheUK .
The Migration Observatory. Where do migrants live in the UK? The Migration Observatory at the University of Oxford. 2022. Available from: https://migrationobservatory.ox.ac.uk/resources/briefings/where-do-migrants-live-in-the-uk .
Pavli A, Maltezou H. Health problems of newly arrived migrants and refugees in Europe. J Travel Med. 2017;24(4). Available from: http://academic.oup.com/jtm/article/doi/10.1093/jtm/tax016/3095987/Health-problems-of-newly-arrived-migrants-and .
Humphris R, Bradby H. Health Status of Refugees and Asylum Seekers in Europe. In: Oxford Research Encyclopedia of Global Public Health. Oxford University Press; 2017. Available from: https://oxfordre.com/publichealth/view/10.1093/acrefore/9780190632366.001.0001/acrefore-9780190632366-e-8 .
Bradby H, Humphris R, Newall D, Phillimore J. Public Health Aspects of Migrant Health: A Review of the Evidence on Health Status for Refugees and Asylum Seekers in the European Region. (Health Evidence Network Synthesis Report, No. 44.) ANNEX 2, DEFINITIONS OF REFUGEES, ASYLUM SEEKERS AND MIGRANTS IN THE LITERATURE. Copenhagen: Eerat; 2015. Available from: https://www.ncbi.nlm.nih.gov/books/NBK379415/ .
Gerritsen AAM, Bramsen I, Devillé W, van Willigen LHM, Hovens JE, van der Ploeg HM. Physical and mental health of Afghan, Iranian and Somali asylum seekers and refugees living in the Netherlands. Soc Psychiatry Psychiatr Epidemiol. 2006;41(1):18–26. Available from: http://link.springer.com/10.1007/s00127-005-0003-5 .
Laue J, Diaz E, Eriksen L, Risør T. Migration health research in Norway: a scoping review. Scand J Public Health. 2023;51(3):381–90. Available from: http://journals.sagepub.com/doi/10.1177/14034948211032494 .
Scottish Refugee Council. Ukraine response one year on. 2023. Available from: https://scottishrefugeecouncil.org.uk/ukraine-response-one-year-on/ . Cited 2023 Aug 26.
Woodward A, Howard N, Wolffers I. Health and access to care for undocumented migrants living in the European Union: a scoping review. Health Policy Plan. 2014;29(7):818–30. Available from: https://academic.oup.com/heapol/article-lookup/doi/10.1093/heapol/czt061 .
Simon J, Kiss N, Laszewska A, Mayer S. Public health aspects of migrant health: a review of the evidence on health status for labour migrants in the European Region. Health Evidence Network Synthesis Report 43. 2015. Available from: http://www.epgencms.europarl.europa.eu/cmsdata/upload/114f16b6-1667-44ab-802b-a5a83dd50af0/WHO-HEN-Report-A5-1-Labour-FINAL_EN.pdf .
Scottish Government. Seasonal migrant workers in Scottish agriculture: research report. 2023. Available from: https://www.gov.scot/publications/seasonal-migrant-workers-scottish-agriculture/pages/10/ .
Scottish Government. New Scots: refugee integration strategy 2018–2022. 2018. Available from: https://www.gov.scot/publications/new-scots-refugee-integration-strategy-2018-2022/pages/11/ .
Oliva A, Palavra V, Caloun J. Refugees in Scotland: understanding the policy domain. 2016. Available from: https://www.academia.edu/34097718/REFUGEES_IN_SCOTLAND_UNDERSTANDING_THE_POLICY_DOMAIN .
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. Available from: https://www.acpjournals.org/doi/10.7326/M18-0850 .
Download references
Acknowledgements
Thank-you to Professor Anne MacFarlane and PHD student Anne Cronin, of the University of Limerick, Ireland for sharing the coding guidelines currently used in an update to Villarroel et. al’s 2019 study on Migrant Health in the Republic of Ireland.
No funding was received for this work, which was undertaken as G. Petrie’s Master of Public Health dissertation module at the University of Stirling.
Author information
Authors and affiliations.
Caledonia House, NHS Greater Glasgow and Clyde, Glasgow, Scotland, UK
Institute for Social Marketing and Health, Faculty of Health Sciences and Sport, University of Stirling, Stirling, FK9 4LA, Scotland, UK
K. Angus & R. O’Donnell
You can also search for this author in PubMed Google Scholar
Contributions
KA, RO and GP finalised the study design collectively. GP conducted the searches, analysis and write up, with support from KA and RO. All three authors read and approved the manuscript prior to submission.
Corresponding author
Correspondence to R. O’Donnell .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Petrie, G., Angus, K. & O’Donnell, R. A scoping review of academic and grey literature on migrant health research conducted in Scotland. BMC Public Health 24 , 1156 (2024). https://doi.org/10.1186/s12889-024-18628-1
Download citation
Received : 04 September 2023
Accepted : 16 April 2024
Published : 25 April 2024
DOI : https://doi.org/10.1186/s12889-024-18628-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Asylum seekers
- Scoping review
- Research funding
- Immigration
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]

COMMENTS
Mixed methods literature reviews (MMLRs) are distinct in that they summarize and integrate findings from qualitative, quantitative, and mixed methods studies via qualitative and/or quantitative methods. ... systematic literature review, evidence base. Subject. Research Methods in Psychology Psychology. Series. Oxford Library of Psychology ...
Objective: The objective of this paper is to outline the updated methodological approach for conducting a JBI mixed methods systematic review with a focus on data synthesis; specifically, methods related to how data are combined and the overall integration of the quantitative and qualitative evidence. Introduction: Mixed methods systematic reviews provide a more complete basis for complex ...
A mixed-methods systematic review applies the principles of mixed-methods research to the review process, that is, studies from different research traditions (but focused on the same topic) are combined to generate evidence to guide decision-making. Thus, a mixed-methods review designed to provide guidance to clinical decision makers on the ...
Abstract. Researchers conducting a mixed methods research synthesis (MMRS) carry out a literature review by systematically collecting, evaluating, and synthesizing qualitative, quantitative, and ...
Mixed methods research combines elements of quantitative research and qualitative research in order to answer your research question. Mixed methods can help you gain a more complete picture than a standalone quantitative or qualitative study, as it integrates benefits of both methods. Mixed methods research is often used in the behavioral ...
Mixed methods research can be viewed as an approach which draws upon the strengths and perspectives of each method, ... Methods. This literature review has used systematic principles (Cochrane, 2009, Khan, 2001) to search for mixed methods studies within healthcare research. The first search was conducted in September 2009 in the data bases ...
Mixed Methods Reviews are best designed for: Multidisciplinary topics or topics with a body of literature that includes quantitative, qualitative, and mixed methods studies. To determine not only the effects of interventions but also their appropriateness. To identify research gaps. To provide an explanation for possible heterogeneity between ...
Combining methods in social scientific research has recently gained momentum through a research strand called Mixed Methods Research (MMR). This approach, which explicitly aims to offer a framework for combining methods, has rapidly spread through the social and behavioural sciences, and this article offers an analysis of the approach from a field theoretical perspective. After a brief outline ...
Mixed methods reviews. As one reason for the growth in qualitative synthesis is what they can add to quantitative reviews, it is not surprising that there is also growing interest in mixed methods reviews. This reflects similar developments in primary research in mixing methods to examine the relationship between theory and empirical data which ...
First Edition. This practical guide provides step-by-step instruction for conducting a mixed methods research synthesis (MMRS) that integrates both qualitative and quantitative evidence. The book progresses through a systematic, comprehensive approach to conducting an MMRS literature review to analyze and summarize the empirical evidence ...
Mixed studies review/mixed methods review: Refers to any combination of methods where one significant component is a literature review (usually systematic). Within a review context, it refers to a combination of review approaches, for example, combining quantitative with qualitative research or outcome with process studies.
These authors argue that mixed methods research has a number of unique features with respect to monomethod research and, as such, should be appraised according to its own set of quality criteria. Based on a systematic search of the literature, this review (1) examines the features and trends of the literature on the quality of mixed methods ...
The relevance of mixed-methods in health research. The overall goal of the mixed-methods research design is to provide a better and deeper understanding, by providing a fuller picture that can enhance description and understanding of the phenomena [].Mixed-methods research has become popular because it uses quantitative and qualitative data in one single study which provides stronger inference ...
Mixed Methods Reviews are best designed for: Multidisciplinary topics or topics with a body of literature that includes quantitative, qualitative, and mixed methods studies. To determine not only the effects of interventions but also their appropriateness. To identify research gaps. To provide an explanation for possible heterogeneity between ...
Demystifying Mixed Methods Research Design: A Review of the Literature Gail D. Caruth* Amberton University, Garland, Texas USA Article history Received: 31.05.2013 Received in revised form: 08.07.2013 Accepted: 09.07..2013 Mixed methods research evolved in response to the observed limitations of both quantitative and qualitative designs and is a
Abstract. The existing literature mapping the state of mixed methods research in tourism does not provide in-depth information concerning the number and type of mixed methods studies published in tourism, or the paradigmatic beliefs informing the mix of quantitative and qualitative studies in the same project.
As mentioned previously, there are a number of existing guidelines for literature reviews. Depending on the methodology needed to achieve the purpose of the review, all types can be helpful and appropriate to reach a specific goal (for examples, please see Table 1).These approaches can be qualitative, quantitative, or have a mixed design depending on the phase of the review.
Authors of the studies sampled for this literature review did not always label their studies as mixed methods, which is consistent with the noted variability in terminologies used across the landscape of mixed methods research studies (Creswell & Plano Clark, 2011). Therefore, mixed method research studies were first identified by reviewing the ...
Further describes confirmation and complementarity as two purposes of mixed research method. The paper identifies multiple advantages of mixed research method over using one method in a study. Finally it was identified six key research designs that described in mixed research method literature.
Research Methodology: A quantitative to the qualitative sequential mixed method was used to get research data. The respondents and participants to the study were tourism operators, media ...
This systematic literature review provides information on the use of mixed methods research in human factors and ergonomics (HFE) research in health care. Using the PRISMA methodology, we searched four databases (PubMed, PsycInfo, Web of Science, and Engineering Village) for studies that met the following inclusion criteria: (1) field study in ...
definition refers to mixed methods research as a type of. research that would involve mixing a single study; a mixed. method p rogram would involve mixing within a program of. research and the ...
Mixed methods research. Known as the third methodological movement, mixed methods research can be defined as empirical research that "combines elements of qualitative and quantitative research approaches (e.g., use of qualitative and quantitative viewpoints, data collection, analysis, inference techniques) for the broad purpose of breadth and depth of understanding and corroboration ...
Results Twenty-three studies were included (1999 to 2020), with a mix of qualitative (n=14), quantitative (n=6) and mixed-methods (n=3) studies. Participant numbers ranged from 9 to 604 people (median 21) and included people with intellectual disability, health professionals, carers and support people, and others working with people with intellectual disability.
The study has been approved by the Institutional Review Board of the University of Cologne, Germany (19-1284-1). ... The questionnaires were developed based on the current literature [2, 11, ... A concise introduction to mixed methods research. 2nd ed. Thousand Oaks, CA: SAGE Publications; 2022. Google Scholar
Data were extracted to a bespoke form and synthesised using a narrative review. The quality of included studies was appraised using the Mixed Methods Appraisal Tool. Sixteen studies were included in the synthesis, which together included a total of 538 people with dementia. Study methods and quality varied.
The present study was carried out using an exploratory sequential mixed method study in two qualitative and quantitative phases. An inductive-deductive approach was also used to determine the concept of obstetric telephone triage. In this respect, a qualitative study and a literature review were used in the inductive and deductive stages ...
A mixed-method exploratory design was conducted from 2021 to 2023. First the concept of caring ability of mothers with preterm infants was clarified using literature review and comparative content analysis, and a pool of items was created.
In our review, the majority of reports were published from 2013 onwards, aligning with the expansion in migrant research internationally . 52% used qualitative research methods, 28% used quantitative methods and 20% used mixed methods. 58% focused on migrant health: the remaining papers included other populations or health as part of a wider ...
A review of the literature revealed that it has been gaining acceptance among researchers, researchers have begun using mixed methods research, it has the potential to offer more robust research ...