Advertisement

How to define CSF overdrainage: a systematic literature review
- Review Article - Neurosurgery General
- Published: 14 January 2023
- Volume 165 , pages 429–441, ( 2023 )
Cite this article

- Sarah Hornshoej Pedersen ORCID: orcid.org/0000-0002-3436-6081 1 ,
- Tobias Hannibal Prein 2 ,
- Ahmed Ammar 3 ,
- André Grotenhuis 4 ,
- Mark G. Hamilton 5 ,
- Torben Skovbo Hansen 6 ,
- Uwe Kehler 7 ,
- Harold Rekate 8 ,
- Ulrich-Wilhelm Thomale 9 &
- Marianne Juhler 1 , 6
915 Accesses
2 Citations
2 Altmetric
Explore all metrics
Overdrainage (OD) is one of the most frequent complications related to drainage of the cerebrospinal fluid (CSF). It is mostly associated with valve-bearing shunt systems but should probably be considered as a risk factor in any type of CSF diversion procedure. There is extreme variation in the reported incidence of OD due to the lack of consensus on defining criteria and an unclear perception of the pathophysiology. Hence, OD is probably underreported and underestimated. The objective of this paper was to establish a definition of OD, based on a systematic review of the literature.
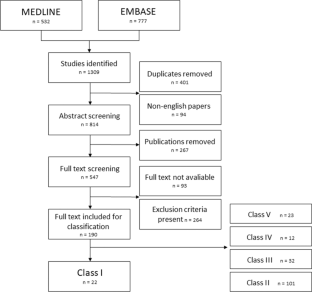
A systematic search was conducted in MEDLNE and EMBASE. Studies providing a definition or a description of diagnostic findings related to OD in ventriculoperitoneal shunt treated hydrocephalus were included. Non-English titles, abstracts and manuscripts were excluded. Extracted descriptions were graded into five groups (class I-V studies) based on how precise the terminology used to describe OD was. Class I studies were included for further analysis and characteristics of OD were extracted. The quality of included descriptions was assessed by a clinical expert panel.
A total of 1309 studies were screened, 190 were graded into groups, and 22, which provided specific definitions or descriptions of OD, were graded as class I studies. We extracted 32 different characteristics consistent with OD (e.g., clinical symptoms, radiological signs, and syndromes).
There was an overall agreement that CSF overdrainage following implantation of a ventriculoperitoneal shunt in a mixed pediatric and adult population is characterized as a persistent condition with clinically manifestations as postural dependent headache, nausea, and vomiting and/or radiological signs of slim ventricles and/or subdural collections.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Contemporary management of aneurysmal subarachnoid haemorrhage. An update for the intensivist

Non-invasive biomarkers for spontaneous intracranial hypotension (SIH) through phase-contrast MRI

Intracranial pressure: current perspectives on physiology and monitoring
Becker DP, Nulsen FE (1968) Control of hydrocephalus by valve-regulated venous shunt: avoidance of complications in prolonged shunt maintenance. J Neurosurg 28(3):215–226
Article CAS PubMed Google Scholar
Beni-Adani L, Siomin V, Segev Y, Beni S, Constantini S (2000) Increasing chronic subdural hematoma after endoscopic III ventriculostomy. Child’s Nerv Syst 16(7):402–405
Article CAS Google Scholar
Chan SM, Chodakiewitz YG, Maya MM, Schievink WI, Moser FG (2019) Intracranial hypotension and cerebrospinal fluid leak. Neuroimaging Clin N Am 29(2):213–226
Article PubMed Google Scholar
Chari A, Dasgupta D, Smedley A, Craven C, Dyson E, Matloob S, Thompson S, Thorne L, Toma AK, Watkins L (2017) Intraparenchymal intracranial pressure monitoring for hydrocephalus and cerebrospinal fluid disorders. Acta Neurochir (Wien) 159(10):1967–1978
Decq P, Barat J-L, Duplessis E, Leguerinel C, Gendrault P, Keravel Y (1995) Shunt failure in adult hydrocephalus: flow-controlled shunt versus differential pressure shunts—a cooperative study in 289 patients. Surg Neurol 43(4):333–339
Desai VR, Sadrameli SS, Jenson AV, Asante SK, Daniels B, Trask TW, Britz G (2020) Ventriculoperitoneal shunt complications in an adult population: a comparison of various shunt designs to prevent overdrainage. Surg Neurol Int 11:269
Article PubMed PubMed Central Google Scholar
Di Rocco C (1994) Is the slit ventricle syndrome always a slit ventricle syndrome? Child’s Nerv Syst 10(1):49–58
Article Google Scholar
Diesner N, Freimann F, Clajus C, Kallenberg K, Rohde V, Stockhammer F (2016) Female gender predisposes for cerebrospinal fluid overdrainage in ventriculoperitoneal shunting. Acta Neurochir (Wien) 158(7):1273–1278
Feletti A, D’Avella D, Wikkelsø C et al (2019) Ventriculoperitoneal shunt complications in the European idiopathic normal pressure hydrocephalus multicenter study. Oper Neurosurg 17(1):97–102
Fouyas IP, Casey ATH, Thompson D, Harkness WF, Hayward RD (1996) Use of intracranial pressure monitoring in the management of childhood hydrocephalus and shunt-related problems. Neurosurgery 38(4):726–732
Freimann FB, Sprung C (2012) Shunting with gravitational valves - Can adjustments end the era of revisions for overdrainage-related events? J Neurosurg 117(6):1197–1204
Hall BJ, Gillespie CS, Hennigan D, Bagga V, Mallucci C, Pettorini B (2021) Efficacy and safety of the Miethke programmable differential pressure valve (proGAV®2.0): a single-centre retrospective analysis. Child’s Nerv Syst 37(8):2605–2612
Henderson D, Budu A, Zaki H, Sinha S, de Lacy P, McMullan J, Ushewokunze S (2020) A comparison between flow-regulated and adjustable valves used in hydrocephalus during infancy. Child’s Nerv Syst 36(9):2013–2019
Hung AL, Vivas-Buitrago T, Adam A, Lu J, Robison J, Elder BD, Goodwin CR, Jusué-Torres I, Rigamonti D (2017) Ventriculoatrial versus ventriculoperitoneal shunt complications in idiopathic normal pressure hydrocephalus. Clin Neurol Neurosurg 157(February):1–6
Hung C-W, Lin W-C, Chang W-N et al (2018) Risk factors and outcomes of cerebrospinal fluid overdrainage in HIV-negative patients with cryptococcal meningitis after the ventriculoperitoneal shunting procedure. J Microbiol Immunol Infect 51(4):545–551
Iglesias S, Ros B, Martín Á et al (2017) Factors related to shunt survival in paediatric hydrocephalus. Could failure be avoided? Neurocirugia 28(4):159–166
Kajimoto Y, Ohita T, Miyake H, Matsukawa M, Ogawa D, Nagao K, Kuroiwa T (2000) Posture-related changes in the pressure environment of the ventriculoperitoneal shunt system. J Neurosurg 93:614–617
Kestle JRW (2003) Pediatric hydrocephalus: current management. Neurol Clin 21(4):883–895
Khan QU, Wharen RE, Grewal SS, Thomas CS, Deen HG, Reimer R, Van Gerpen JA, Crook JE, Graff-Radford NR (2013) Overdrainage shunt complications in idiopathic normal-pressure hydrocephalus and lumbar puncture opening pressure. J Neurosurg 119(6):1498–1502
Kiefer M, Eymann R, Meier U (2002) Five years experience with gravitational shunts in chronic hydrocephalus of adults. Acta Neurochir (Wien) 144(8):755–767
Kimura T, Schulz M, Shimoji K, Miyajima M, Arai H, Thomale U-W (2016) In vitro performance of the fixed and adjustable gravity-assisted unit with and without motion-evidence of motion-induced flow. Acta Neurochir (Wien) 158(10):2011–2018
Kondageski C, Thompson D, Reynolds M, Hayward RD (2007) Experience with the Strata valve in the management of shunt overdrainage. J Neurosurg 106(2 SUPPL.):95–102
PubMed Google Scholar
Kraemer MR, Sandoval-Garcia C, Bragg T, Iskandar BJ (2017) Shunt-dependent hydrocephalus: management style among members of the American Society of Pediatric Neurosurgeons. J Neurosurg Pediatr 20(3):216–224
Krahulik D, Vaverka M, Hrabalek L, Hampl M, Halaj M, Jablonsky J, Langova K (2020) Ventriculoperitoneal shunt in treating of idiopathic normal pressure hydrocephalus—single-center study. Acta Neurochir (Wien) 162(1):1–7
Lee W-C, Seo D-H, Choe I-S, Park S-C, Ha Y-S, Lee KC (2010) A comparative result of ventriculoperitoneal shunt, focusing mainly on gravity-assisted valve and programmable valve. J Korean Neurosurg Soc 48(3):251–258
Lemcke J, Meier U, Müller C et al (2013) Safety and efficacy of gravitational shunt valves in patients with idiopathic normal pressure hydrocephalus: a pragmatic, randomised, open label, multicentre trial (SVASONA). J Neurol Neurosurg Psychiatry 84(8):850–857
Meier U, Kiefer M, Sprung C (2002) The Miethke Dual-Switch Valve in patients with normal pressure hydrocephalus. Neurosurg Q 12(2):114–121
Meier U, Kiefer M, Sprung C (2004) Evaluation of the Miethke dual- switch valve in patients with normal pressure hydrocephalus. Surg Neurol 61(2):118–119
Meier U, Stengel D, Müller C et al (2013) Predictors of subsequent overdrainage and clinical outcomes after ventriculoperitoneal shunting for idiopathic normal pressure hydrocephalus. Neurosurgery 73(6):1054–1060
Mokri B, Atkinson JL, Piepgras DG (2000) Absent headache despite CSF volume depletion (intracranial hypotension). Neurology 55(11):1722–1724
Naftel RP, Argo JL, Shannon CN et al (2011) Laparoscopic versus open insertion of the peritoneal catheter in ventriculoperitoneal shunt placement: Review of 810 consecutive cases. J Neurosurg 115(1):151–158
Norager NH, Olsen MH, Pedersen SH, Riedel CS, Czosnyka M, Juhler M (2021) Reference values for intracranial pressure and lumbar cerebrospinal fluid pressure: a systematic review. Fluids Barriers CNS 18(1):1–10
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan—a web and mobile app for systematic reviews. Syst Rev 5(1):210
Panagopoulos D, Karydakis P, Themistocleous M (2021) Slit ventricle syndrome: historical considerations, diagnosis, pathophysiology, and treatment review. Brain Circ 7(3):167
Panagopoulos D, Stranjalis G, Gavra M, Boviatsis E, Korfias S (2022) Shunt over-drainage, slit ventricle syndrome, programmable valves and anti-siphon devices. A narrative review of a multifactorial and intractable problem. J Integr Neurosci 21(3):84
Pedersen SH, Lilja-Cyron A, Andresen M, Juhler M (2018) The relationship between intracranial pressure and age—chasing age-related reference values. World Neurosurg 110:e119–e123
Pudenz RH, Foltz EL (1991) Hydrocephalus: overdrainage by ventricular shunts. A review and recommendations. Surg Neurol 35(3):200–212
Qvarlander S, Sundstrom N, Malm J, Eklund A (2013) Postural effects on intracranial pressure: modeling and clinical evaluation. J Appl Physiol 115(10):1474–1480
Rekate HL (1993) Classification of slit-ventricle syndromes using intracranial pressure monitoring. Pediatr Neurosurg 19(1):15–20
Rekate HL (2004) The slit ventricle syndrome: advances based on technology and understanding. Pediatr Neurosurg 40(6):259–263
Ros B, Iglesias S, Martín Á, Carrasco A, Ibáñez G, Arráez MA (2018) Shunt overdrainage syndrome: review of the literature. Neurosurg Rev 41(4):969–981
Ros B, Iglesias S, Linares J, Cerro L, Casado J, Arráez MA (2021) Shunt overdrainage: reappraisal of the syndrome and proposal for an integrative model. J Clin Med. https://doi.org/10.3390/jcm10163620
Sainz LV, Hockel K, Schuhmann MU (2018) Chronic overdrainage syndrome: pathophysiological insights based on ICP analysis: a case-based review. Child’s Nerv Syst 34(3):401–408
Saukkonen AL, Serlo W, von Wendt L (1988) Electroencephalographic findings and epilepsy in the slit ventricle syndrome of shunt-treated hydrocephalic children. Childs Nerv Syst 4(6):344–347
Serlo W, Heikkinen E, Saukkonen AL, von Wendt L (1985) Classification and management of the slit ventricle syndrome. Child’s Nerv Syst 1(4):194–199
Sklar FH, Nagy L, Robertson BD (2012) The use of abdominal binders to treat over-shunting headaches. J Neurosurg Pediatr 9(6):615–620
Tan K, Meiri A, Mowrey WB, Abbott R, Goodrich JT, Sandler AL, Suri AK, Lipton ML, Wagshul ME (2018) Diffusion tensor imaging and ventricle volume quantification in patients with chronic shunt-treated hydrocephalus: a matched case-control study. J Neurosurg 129(6):1611–1622
Toma AK, Tarnaris A, Kitchen ND, Watkins LD (2010) Investigating shunt function using continuous intracranial pressure monitoring in adults: single center experience - clinical article. J Neurosurg 113(6):1326–1330
Trinh VT, Duckworth EAM (2013) Revision to an adjustable non-siphon control valve in low pressure hydrocephalus: Therapeutic siphoning and a new perspective on NPH. Clin Neurol Neurosurg 115(2):175–178
Tschan CA, Antes S, Huthmann A et al (2014) Overcoming CSF overdrainage with the adjustable gravitational valve proSA. Acta Neurochir (Wien) 156(4):767–776
Weinzweig J, Bartlett SP, Chen JC, Losee J, Sutton L, Duhaime A-C, Whitaker LA (2008) Cranial vault expansion in the management of postshunt craniosynostosis and slit ventricle syndrome. Plast Reconstr Surg 122(4):1171–1180
Download references
Author information
Authors and affiliations.
Department of Neurosurgery, Copenhagen University Hospital, Copenhagen, Denmark
Sarah Hornshoej Pedersen & Marianne Juhler
Centre for Orthopaedic Research and Innovation, Slagelse Hospital, Slagelse, Denmark
Tobias Hannibal Prein
Department of Neurosurgery, King Fahd University Hospital, Al Khobar, Saudi Arabia
Ahmed Ammar
Medical Centre, Radboud University, Nijmegen, The Netherlands
André Grotenhuis
Department of Clinical Neurosciences, Division of Neurosurgery, University of Calgary, Calgary, Canada
Mark G. Hamilton
Department of Neurosurgery, Aarhus University Hospital, Aarhus, Denmark
Torben Skovbo Hansen & Marianne Juhler
Department of Neurosurgery, Asklepios Klinik Altona, Hamburg, Germany
The Donald and Barbara Zucker Hofstra Northwell School of Medicine, Hempstead, New York, USA
Harold Rekate
Department of Neurosurgery, Charité-Universitätsmedizin Berlin, Berlin, Germany
Ulrich-Wilhelm Thomale
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Sarah Hornshoej Pedersen .
Ethics declarations
Ethics approval.
The manuscript does not contain clinical patient data; thus, an ethical approval was not necessary to conduct the study.
Consent to participate
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neurosurgery general
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (DOCX 32 KB)
Supplementary file2 (docx 19 kb), supplementary file3 (docx 19 kb), supplementary file4 (docx 43 kb), rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Pedersen, S.H., Prein, T.H., Ammar, A. et al. How to define CSF overdrainage: a systematic literature review. Acta Neurochir 165 , 429–441 (2023). https://doi.org/10.1007/s00701-022-05469-3
Download citation
Received : 27 October 2022
Accepted : 20 December 2022
Published : 14 January 2023
Issue Date : February 2023
DOI : https://doi.org/10.1007/s00701-022-05469-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Overdrainage
- Hyperdrainage
- Excessive CSF drainage
- Overshunting
- CSF shunting
- VP shunting
- Find a journal
- Publish with us
- Track your research

Springer Medizin

14.01.2023 | Review Article - Neurosurgery General
How to define CSF overdrainage: a systematic literature review
verfasst von: Sarah Hornshoej Pedersen, Tobias Hannibal Prein, Ahmed Ammar, André Grotenhuis, Mark G. Hamilton, Torben Skovbo Hansen, Uwe Kehler, Harold Rekate, Ulrich-Wilhelm Thomale, Marianne Juhler
Erschienen in: Acta Neurochirurgica | Ausgabe 2/2023
Bitte loggen Sie sich ein, um Zugang zu diesem Inhalt zu erhalten
Weitere artikel der ausgabe 2/2023, correction to: the aspect hydrocephalus system: a non‑hierarchical descriptive system for clinical use.
Original Article - Spine - Other
Recovery ratios and minimum clinically important difference for clinical outcomes in workers’ compensation recipients undergoing MIS-TLIF versus ALIF
Original Article - Brain Trauma
Optic nerve sheath diameter as a quantitative parameter associated with the outcome in patients with traumatic brain injury undergoing hematoma removal
Original Article - Vascular Neurosurgery - Aneurysm
Comprehensive morphomechanical analysis of brain aneurysms
Letter to the editor - Brain trauma
Prevalence of post-traumatic hydrocephalus in moderate to severe head injury
Letter to the Editor (by Invitation) - Brain trauma
Reply to the comments by Paolo Missori, Sergio Paolini, and Antonio Currà regarding our publication in Acta Neurochirurgica July 2022, titled Incidence of surgically treated post-traumatic hydrocephalus 6 months following head injury in patients undergoing acute head computed tomography
Leitlinien kompakt für die Neurologie
Mit medbee Pocketcards sicher entscheiden.
Seit 2022 gehört die medbee GmbH zum Springer Medizin Verlag
Neu im Fachgebiet Neurologie
Niedriger diastolischer Blutdruck erhöht Risiko für schwere kardiovaskuläre Komplikationen
Wenn unter einer medikamentösen Hochdrucktherapie der diastolische Blutdruck in den Keller geht, steigt das Risiko für schwere kardiovaskuläre Ereignisse: Darauf deutet eine Sekundäranalyse der SPRINT-Studie hin.
Frühe Alzheimertherapie lohnt sich
Ist die Tau-Last noch gering, scheint der Vorteil von Lecanemab besonders groß zu sein. Und beginnen Erkrankte verzögert mit der Behandlung, erreichen sie nicht mehr die kognitive Leistung wie bei einem früheren Start. Darauf deuten neue Analysen der Phase-3-Studie Clarity AD.
Viel Bewegung in der Parkinsonforschung
Neue arznei- und zellbasierte Ansätze, Frühdiagnose mit Bewegungssensoren, Rückenmarkstimulation gegen Gehblockaden – in der Parkinsonforschung tut sich einiges. Auf dem Deutschen Parkinsonkongress ging es auch viel um technische Innovationen.
Demenzkranke durch Antipsychotika vielfach gefährdet
Wenn Demenzkranke aufgrund von Symptomen wie Agitation oder Aggressivität mit Antipsychotika behandelt werden, sind damit offenbar noch mehr Risiken verbunden als bislang angenommen.

Update Neurologie
Bestellen Sie unseren Fach-Newsletter und bleiben Sie gut informiert.
- Facharzt-Training
- Zeitschriften
- Springer Medizin Podcast – der Talk für Gesundheitsprofis
- Info & Hilfe
- Anästhesiologie
- Allgemeinmedizin
- Arbeitsmedizin
- Augenheilkunde
- Dermatologie
- Gynäkologie und Geburtshilfe
- Innere Medizin
- Kardiologie
- Onkologie und Hämatologie
- Orthopädie und Unfallchirurgie
- Psychiatrie
- Rechtsmedizin
- Zahnmedizin
- Klimawandel und Gesundheit
- Neues aus dem Markt
- Praxis und Beruf
- Seltene Erkrankungen
- GOÄ & EBM
- Kasuistiken
- Algorithmen & Infografiken
- Blickdiagnosen
- Arthropedia
- Kongressberichterstattung
- Medizin für Apothekerinnen und Apotheker
- Für Ärztinnen und Ärzte in Weiterbildung
- Für Medizinstudierende
The truth and coherence behind the concept of overdrainage of cerebrospinal fluid in hydrocephalic patients
- Original Paper
- Published: 15 January 2014
- Volume 30 , pages 599–606, ( 2014 )
Cite this article

- Stephanie Cheok 1 ,
- Jason Chen 1 &
- Jorge Lazareff 1
819 Accesses
16 Citations
Explore all metrics
Introduction
Overdrainage, siphoning, and slit-ventricle syndrome are well-documented complications of shunting in hydrocephalic patients. Despite the prevalence of these conditions, their mechanisms are still not fully understood. In this paper, the authors trace the concept of overdrainage and the related phenomena of siphoning and slit-ventricle syndrome.
To provide a historical overview of overdrainage and to reignite discussion of a topic that has been settled.
Methods and results
A medical literature search and review were performed via Google Scholar. Of 565 publications, 3 primary papers were identified and a timeline was developed demonstrating the convergence of the aforementioned concepts. From the primary papers, 25 relevant publications were selected and further analyzed searching for hypothesis, evidence, and conclusions.
Overdrainage, siphoning, and slit-ventricle syndrome are associated concepts that have converged into a pathophysiological theory where siphoning of CSF leads to overdrainage, which is then hypothesized to cause slit-ventricle syndrome in a small subset of patients. Our data suggests that while there have been numerous reports regarding overdrainage and its consequences, the evidence is not as robust as currently presumed and this subject requires prospective exploration.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

How to define CSF overdrainage: a systematic literature review

Shunt overdrainage syndrome: review of the literature

Cerebrospinal fluid shunt malfunctions: A reflective review
Aguiar PH, Shu ES, Freitas AB, Leme RJ, Miura FK, Marino R Jr (2000) Causes and treatment of intracranial haemorrhage complicating shunting for paediatric hydrocephalus. Childs Nerv Sys 16:218–221
Article CAS Google Scholar
Andersson H (1966) Craniosynostosis as a complication after operation for hydrocephalus. Acta Paediatr 55:192–196
Article Google Scholar
Aschoff A, Kremer P, Benesch C, Fruh K, Klank A, Kunze S (1995) Overdrainage and shunt technology. Childs Nerv Sys 11:193–202
Baskin JJ, Manwaring KH, Rekate HL (1998) Ventricular shunt removal: the ultimate treatment of the slit ventricle syndrome. J Neurosurg 88:478–484
Article CAS PubMed Google Scholar
Becker DP, Nulsen FE (1968) Control of hydrocephalus by valve-regulated venous shunt: avoidance of complications in prolonged shunt maintenance. J Neurosurg 28:215–226
Benzel EC, Reeves JD, Kesterson L, Hadden TA (1992) Slit ventricle syndrome in children: clinical presentation and treatment. Acta Neurochir 117:7–14
Bergsneider M, Peacock WJ, Mazziotta JC, Becker DP (1999) Beneficial effect of siphoning in treatment of adult hydrocephalus. Arch Neurol 56:1224
Browd SR, Gottfried ON, Ragel BT, Kestle JR (2006) Failure of cerebrospinal fluid shunts: part II: overdrainage, loculation, and abdominal complications. Pediatr Neurol 34:171–176
Article PubMed Google Scholar
Butler WE, Khan SA (2001) The application of controlled intracranial hypertension in slit ventricle syndrome patients with obstructive hydrocephalus and shunt malfunction. Pediatr Neurosurg 35:305–310
Chrabrerie A, Black P (2002) Ventricular shunts. J Intensive Care Med 17:218–229
Dandy W (1932) Lewis’ practice of surgery. Prior, Hagerstown
Google Scholar
Di Rocco C (1994) Is the slit ventricle syndrome always a slit ventricle syndrome? Childs Nerv Sys 10:49–58
Drake JM, Kestle JR, Milner R et al (1998) Randomized trial of cerebrospinal fluid shunt valve design in pediatric hydrocephalus. Neurosurg 43:294–303
Drake JM, Tenti G, Sivalsganathan S (1994) Computer modeling of siphoning for CSF shunt design evaluation. Pediatr Neurosurg 21:6–15
Drake JM, Kestle J (1996) Rationale and methodology of the multicenter pediatric cerebrospinal fluid shunt design trial. Childs Nerv Sys 12:434–447
El-Shafei IL (1987) Ventriculojugular shunt against the direction of blood flow. Childs Nerv Sys 3:342–349
El-Shafei IL (1985) Ventriculovenous shunt against the direction of blood flow: a new approach for shunting the cerebrospinal fluid to the venous circulation. Childs Nerv Sys 1:200–207
Epstein FJ, Fleischer AS, Hochwald GM, Ransohoff J (1974) Subtemporal craniectomy for recurrent shunt obstruction secondary to small ventricles. J Neurosurg 41:29–31
Epstein F, Lapras C, Wisoff JH (1988) ‘Slit-ventricle syndrome’: etiology and treatment. Pediatr Neurosurg 14:5–10
Faulhauer K, Schmitz P (1978) Overdrainage phenomena in shunt treated hydrocephalus. Acta Neurochir 45:89–101
Forrest DM, Cooper DG (1968) Complications of ventriculo-atrial shunts: a review of 455 cases. J Neurosurg 29:506–512
Fox JL, McCullough DC, Green RC (1973) Effect of cerebrospinal fluid shunts on intracranial pressure and on cerebrospinal fluid dynamics 2. A new technique of pressure measurements: results and concepts 3. A concept of hydrocephalus. J Neurol Neurosurg Psychiatry 36:302–312
Article PubMed Central CAS PubMed Google Scholar
Fried AH, Epstein MH (1994) Childhood hydrocephalus: clinical features, treatment, and the slit-ventricle syndrome. Neurosurg Q 4:51–65
Gruber RW, Roehrig B (2010) Prevention of ventricular catheter obstruction and slit ventricle syndrome by the prophylactic use of the Integra antisiphon device in shunt therapy for pediatric hypertensive hydrocephalus: a 25-year follow-up study: clinical article. J Neurosurg: Pediatr 5:4–16
Hahn YS (1994) Use of the distal double-slit valve system in children with hydrocephalus. Childs Nerv Sys 10:99–103
Holness RO, Hoffman HJ, Hendrick EB (1979) Subtemporal decompression for the slit-ventricle syndrome after shunting in hydrocephalic children. Pediatr Neurosurg 5:137–144
Hoppe-Hirsch E, Sainte-Rose C, Renier D, Hirsch JF (1987) Pericerebral collections after shunting. Childs Nerv Sys 3:97–102
Hyde-Rowan MD, Rekate HL, Nulsen FE (1982) Reexpansion of previously collapsed ventricles: the slit ventricle syndrome. J Neurosurg 56:536–539
Illingworth RD, Logue V, Symon L, Uemura K (1971) The ventriculocaval shunt in the treatment of adult hydrocephalus: results and complications in 101 patients. J Neurosurg 35:681–685
Johnston I, Teo C (2000) Disorders of CSF hydrodynamics. Childs Nerv Sys 16:776–799
Kempe LG, Blaylock R (1977) Ventriculolymphatic shunt. J Neurosurg 47:86–95
Lam CH, Dubuisson D (1990) Treatment of hemispheric collapse and herniation beneath the falx in a case of shunted hydrocephalus. Surg Neurol 33(3):202–205
Lange S (1966) Surgical treatment of progressive hydrocephalus. North-Holland, Amsterdam
Le H, Yamini B, Frim DM (2002) Lumboperitoneal shunting as a treatment for slit ventricle syndrome. Pediatr Neurosurg 36(4):178–182
Major O, Fedorcsák I, Sipos L et al (1994) Slit-ventricle syndrome in shunt operated children. Acta Neurochir 127(1–2):69–72
McNab GH (1959) The Spitz-Holter valve. J Neurol Neurosurg Psychiatry 22:82
Oi S, Matsumoto S (1987) Infantile hydrocephalus and the slit ventricle syndrome in early infancy. Childs Nerv Sys 3(3):145–150
Portnoy HD, Schulte RR, Fox JL, Croissant PD, Tripp L (1973) Anti-siphon and reversible occlusion valves for shunting in hydrocephalus and preventing post-shunt subdural hematomas. J Neurosurg 38(6):729–738
Pudenz RH, Foltz EL (1991) Hydrocephalus: overdrainage by ventricular shunts. A review and recommendations. Surg Neurol 35(3):200–212
Reinprecht A, Dietrich W, Bertalanffy A, Czech T (1997) The Medos Hakim programmable valve in the treatment of pediatric hydrocephalus. Childs Nerv Sys 13(11–12):588–593
Rekate HL (1993) Classification of slit-ventricle syndromes using intracranial pressure monitoring. Pediatr Neurosurg 19(1):15–20
Rekate HL (2004) The slit ventricle syndrome: advances based on technology and understanding. Pediatr Neurosurg 40(6):259–263
Sainte-Rose C, Hooven MD, Hirsch JF (1987) A new approach in the treatment of hydrocephalus. J Neurosurg 66(2):213–226
Serlo W, Heikkinen E, Saukkonen AL, Wendt LV (1985) Classification and management of the slit ventricle syndrome. Childs Nerv Sys 1(4):194–199
Sood S, Barrett RJ, Powell T, Ham SD (2005) The role of lumbar shunts in the management of slit ventricles: does the slit-ventricle syndrome exist? J Neurosurg: Pediatr 103(2):119–123
Sotelo J, Rubalcava MA, Gomez-Llata S (1995) A new shunt for hydrocephalus that relies on CSF production rather than on ventricular pressure: initial clinical experiences. Surg Neurol 43(4):324–332
Sotelo J (2012) The hydrokinetic parameters of shunts for hydrocephalus might be inadequate. Surg Neurol Int 3:40
Article PubMed Central PubMed Google Scholar
Stein SC, Guo W (2008) Have we made progress in preventing shunt failure? A critical analysis. J Neurosurg Pediatr 1(1):40–47
Strenger L (1963) Complications of ventriculovenous shunts. J Neurosurg 20(3):219–224
Virella AA, Galarza M, Masterman-Smith M, Lemus R, Lazareff JA (2002) Distal slit valve and clinically relevant CSF overdrainage in children with hydrocephalus. Childs Nerv Sys 18(1–2):15–18
Yamada H, Tajima M, Nagaya M (1975) Effect of respiratory movement on cerebrospinal fluid dynamics in hydrocephalic infants with shunts. J Neurosurg 42(2):194–200
Download references
Author information
Authors and affiliations.
Department of Neurosurgery, UCLA David Geffen School of Medicine, 10833 Le Conte Avenue, 13-154 CHS, Los Angeles, CA, 90095, USA
Stephanie Cheok, Jason Chen & Jorge Lazareff
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Jorge Lazareff .
Rights and permissions
Reprints and permissions
About this article
Cheok, S., Chen, J. & Lazareff, J. The truth and coherence behind the concept of overdrainage of cerebrospinal fluid in hydrocephalic patients. Childs Nerv Syst 30 , 599–606 (2014). https://doi.org/10.1007/s00381-013-2327-x
Download citation
Received : 08 October 2013
Accepted : 11 November 2013
Published : 15 January 2014
Issue Date : April 2014
DOI : https://doi.org/10.1007/s00381-013-2327-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Overdrainage
- Hydrocephalus
- Slit-ventricle syndrome
- Find a journal
- Publish with us
- Track your research
How to define CSF overdrainage: a systematic literature review
Affiliations.
- 1 Department of Neurosurgery, Copenhagen University Hospital, Copenhagen, Denmark. [email protected].
- 2 Centre for Orthopaedic Research and Innovation, Slagelse Hospital, Slagelse, Denmark.
- 3 Department of Neurosurgery, King Fahd University Hospital, Al Khobar, Saudi Arabia.
- 4 Medical Centre, Radboud University, Nijmegen, The Netherlands.
- 5 Department of Clinical Neurosciences, Division of Neurosurgery, University of Calgary, Calgary, Canada.
- 6 Department of Neurosurgery, Aarhus University Hospital, Aarhus, Denmark.
- 7 Department of Neurosurgery, Asklepios Klinik Altona, Hamburg, Germany.
- 8 The Donald and Barbara Zucker Hofstra Northwell School of Medicine, Hempstead, New York, USA.
- 9 Department of Neurosurgery, Charité-Universitätsmedizin Berlin, Berlin, Germany.
- 10 Department of Neurosurgery, Copenhagen University Hospital, Copenhagen, Denmark.
- PMID: 36639536
- DOI: 10.1007/s00701-022-05469-3
Purpose: Overdrainage (OD) is one of the most frequent complications related to drainage of the cerebrospinal fluid (CSF). It is mostly associated with valve-bearing shunt systems but should probably be considered as a risk factor in any type of CSF diversion procedure. There is extreme variation in the reported incidence of OD due to the lack of consensus on defining criteria and an unclear perception of the pathophysiology. Hence, OD is probably underreported and underestimated. The objective of this paper was to establish a definition of OD, based on a systematic review of the literature.
Methods: A systematic search was conducted in MEDLNE and EMBASE. Studies providing a definition or a description of diagnostic findings related to OD in ventriculoperitoneal shunt treated hydrocephalus were included. Non-English titles, abstracts and manuscripts were excluded. Extracted descriptions were graded into five groups (class I-V studies) based on how precise the terminology used to describe OD was. Class I studies were included for further analysis and characteristics of OD were extracted. The quality of included descriptions was assessed by a clinical expert panel.
Results: A total of 1309 studies were screened, 190 were graded into groups, and 22, which provided specific definitions or descriptions of OD, were graded as class I studies. We extracted 32 different characteristics consistent with OD (e.g., clinical symptoms, radiological signs, and syndromes).
Conclusion: There was an overall agreement that CSF overdrainage following implantation of a ventriculoperitoneal shunt in a mixed pediatric and adult population is characterized as a persistent condition with clinically manifestations as postural dependent headache, nausea, and vomiting and/or radiological signs of slim ventricles and/or subdural collections.
Keywords: CSF shunting; Excessive CSF drainage; Hyperdrainage; Overdrainage; Overshunting; VP shunting.
© 2023. The Author(s), under exclusive licence to Springer-Verlag GmbH Austria, part of Springer Nature.
Publication types
- Systematic Review
- Cerebrospinal Fluid Shunts* / adverse effects
- Cerebrospinal Fluid Shunts* / methods
- Hydrocephalus* / complications
- Radiography
- Risk Factors
- Ventriculoperitoneal Shunt / adverse effects
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.12(9); 2020 Sep

Cerebellar Hemorrhage and Spinal Fluid Overdrainage With Tonsillar Herniation Following Spine Surgery
Sudhakar kinthala.
1 Anesthesiology, Guthrie Robert Packer Hospital, Sayre, USA
Kuiran Jiao
Abistanand ankam, christopher g paramore.
2 Neurological Surgery, Guthrie Robert Packer Hospital, Sayre, USA
Spinal fluid overdrainage with cerebellar hemorrhage is a rare complication of spinal surgery that can have severe consequences if not detected quickly. We present the case of a 72-year-old Caucasian female who underwent thoracolumbar fixation for flatback syndrome. Intraoperatively, the patient suffered a dural injury that was repaired. In the immediate postoperative period, the patient’s neurological status rapidly deteriorated within an hour and Jackson-Pratt (JP) drain output measured 300 ml of serosanguinous fluid. A stat CT scan revealed cerebellar hemorrhage, pneumocephalus, and tonsillar herniation. The postoperative drain was immediately removed, and a ventriculostomy tube was placed, confirming low intracranial pressure. Postoperatively, the patient was electively ventilated for three days, continued with remote cerebellar hemorrhage (RCH) treatment and precaution, and extubated on the third day as the patient’s neurological function continued to improve. The patient was discharged home nine days after the initial surgery, with a complete recovery. This case indicates that wound drainage in the face of durotomy can induce cerebellar herniation as early as within an hour postoperatively following spine surgery with a dural tear, even after dural repair. This case also suggests that early recognition and appropriate management of RCH is the key to a full recovery. Even in the event of tonsillar herniation and cerebellar hemorrhage, a complete recovery is possible with early recognition and proper management.
Introduction
Tonsillar herniation associated with remote cerebellar hemorrhage (RCH), which develops distant to the site of surgery, is a rare but potentially lethal complication of supratentorial craniotomy or spinal surgery [ 1 ]. Chadduck first described an RCH after a cervical laminectomy with cerebrospinal fluid (CSF) loss in 1981 [ 2 ]. Cevik et al. found that the incidence rate of RCH in more than 2,000 lumbar procedures was 0.08% [ 3 ]. Floman et al. observed an incidence rate of 0.26% for RCH in their study of 210 patients who had CSF loss following lumbar spine surgery [ 4 ]. RCH has a variable timeline of presentation. Konya et al. reviewed the published literature up to 2006 and noted that an RCH was diagnosed between 16 and 120 hours after surgery (47 hours on average) [ 5 , 6 ]. Although RCH was believed to be a delayed complication, a few recent cases of an RCH that presented prior to extubation [ 7 ] or in the immediate postoperative period (first one hour) have been reported [ 8 - 10 ]; however, none of them developed cerebellar herniation in the immediate postoperative period.
To the best of our knowledge, this is the first case where the patient developed cerebellar herniation, associated with RCH and pneumocephalus in the first hour following spine surgery. More importantly, with early recognition and proper management, the patient was able to completely recover from this extreme event.
Case presentation
A 72-year-old Caucasian female, with a body mass index of 29, with a past medical history of hypertension and American Society of Anesthesiology grade (ASA) II, was diagnosed with the flat back syndrome. Following failed medical management, the patient was scheduled for a posterior osteotomy with interbody fusion of the L2-3, L3-4, and L5-S1 vertebra using interbody cages and autograft, posterior lateral fusion at L1-2 utilizing allograft, and posterior segmental fixation from T11- S1 with S2 pelvic instrumentation utilizing neuronavigation. Under the standard ASA monitoring, arterial line placement, and electrophysiological neuromonitoring, the patient received general anesthesia with an endotracheal tube. Induction, intubation, and positioning were uneventful. Anesthesia was maintained with total intravenous anesthesia with remifentanil and propofol to facilitate electrophysiological neuromonitoring of the spine. Intraoperative O arm and neuronavigation were used for instrumentation guidance. The duration of surgery and anesthesia was 6.5 and 7.5 hours, respectively. The total intraoperative fluid input was 5.5 L of crystalloid. The estimated blood loss was 500 mL and urine output was 700 mL. Other than an accidental iatrogenic dural tear at the L3 level, which was repaired with multiple sutures, there were no intraoperative critical events. The patient was extubated in the operating room upon meeting the standard extubation criteria. The extubation was smooth and not associated with any coughing or bucking.
Postoperatively, the patient progressively became unarousable, Glasgow Coma Scale (GCS) 9-10, with labored breathing, requiring bilevel positive airway pressure (BiPAP). The pupils were still reacting to light though sluggish, associated with hypertension and tachycardia. A stat CT scan was ordered to rule out an intracranial process. By the time the CT scan was completed, the patient’s eyes were rolling downward, pupils were dilated with no reaction to light. Meanwhile, the Jackson-Pratt (JP) drain from the surgical site drained out approximately 300 mL of blood-tinged fluid over the past one hour following surgery. The head CT scan revealed the right cerebellar hemorrhage (Figure (Figure1A), 1A ), pneumocephalus, and herniated cerebellar tonsils at the foramen magnum (Figure (Figure1B). 1B ). The JP drain was removed immediately. The patient was intubated and a ventriculostomy was placed, which confirmed low intracranial pressure (ICP). Intraoperatively, the patient was started on a phenylephrine infusion to support her blood pressure; otherwise, there were no intraoperative events.

Postoperatively, the patient was transported to the intensive care unit for elective ventilation. The patient remained in the supine position postoperatively, and the ventriculostomy tube was clamped off. On the first postoperative day, the patient was still intubated and unarousable. However, she was breathing spontaneously, able to move the right upper and both lower extremities randomly, but her eyes were still rolling downwards. The phenylephrine infusion was stopped. Over the next two days, the patient’s neurological function continued to improve. While maintaining in the supine position for most of the time, the patient’s head was gently raised to 10 degrees for a short period of time every day. On the third day, the patient was awake and alert, following commands, moving all her extremities with good strength, pupils reacted to light briskly, and was extubated on day 3. The patient had a complete neurological recovery and was discharged home on day 9 after the initial surgery. At a follow-up visit one month, the patient was doing well, having an excellent functional and neurological status, with no residual complication.
Overdrainange of spinal fluid associated with tonsillar herniation and cerebellar hemorrhage is a potentially lethal complication of supratentorial craniotomy and spinal surgery [ 11 ], Sturiale et al. reviewed 57 cases of RCH and found that intraoperative dural lesions were described in approximately 93% of patients. Coagulation disorders, hypertension, and placement of postoperative subfascial drainages were the most frequently reported risk factors for the development of RCH [ 1 ]. The most likely mechanism of RCH development is intraoperative or postoperative CSF leakage, resulting in excessive CSF drainage and downward displacement and stretching/occlusion of the cerebellar veins resulting in a hemorrhagic venous infarction [ 11 ]. Even with tight closure of the dural wound, an excessive CSF leak can occur and potentially result in an RCH and tonsillar herniation [ 12 ].
Most of the available literature mentions that RCH develops as a delayed complication of spinal surgery. The clinical presentation ranges from headache, drowsiness, deterioration in consciousness, features of transient cerebellar, and brainstem dysfunction to a large hematoma, causing obstructive hydrocephalus [ 11 , 13 , 14 ]. However, an RCH should be suspected in any patient with a delayed emergence from anesthesia, following spine surgery complicated by a dural tear and CSF leak, unexplained deterioration of consciousness, and postoperative neurological changes [ 13 , 14 ]. If an RCH is suspected, an emergency CT scan should be performed because of potential cerebellar herniation, and any delay could lead to significant neurological damage. If the patient is clinically stable, a myelogram could be performed to diagnose CSF leak, and an epidural blood patch could be placed to prevent further CSF leak [ 12 ].
In our case, despite an intraoperative durotomy that was repaired, the use of a JP drain led to excessive CSF drainage (300 mL within an hour) leak and rapid ICP drop. When a pressure gradient was developed across the foramen magnum, downward displacement of cerebellum eventually caused cerebellar tonsillar herniation and hemorrhage.
The management of cerebellar hematomas depends on the size and speed of development. Small hematomas can be medically managed and followed up with serial imaging to monitor any changes in size. However, large hematomas, which cause a significant mass effect in the posterior fossa or cause signs and symptoms of brainstem compression, may require surgical decompression [ 1 , 2 , 11 ]. In our case, since the patient’s neurological status rapidly deteriorated postoperatively, associated with clinical and radiological signs of cerebellar herniation, we did perform an emergency ventriculostomy. Retrospectively, the emergent ventriculostomy likely added little to the patient’s eventual recovery other than confirmed low ICP.
The prognosis following an RCH is generally good, with more than 50%-75% of cases having either a complete recovery or only mild residual neurological symptoms. However, there is a mortality risk of 10%-15% [ 1 , 12 ]. The prognosis following an RCH depends on the extent of bleeding, the severity of clinical features, and the time taken from diagnosis to intervention. In our case, although the patient developed cerebral herniation, which is the worst complication of spine surgery, since we diagnosed it early, recognized the cause correctly, and took action immediately, there was no delay from diagnosis to intervention. We believe that was the key to a full recovery from this catastrophic event.
Conclusions
Wound drainage in patients following spine surgery should be curtailed in the presence of a dural tear, even if the repair is deemed watertight. If wound drainage is placed intraoperatively, we should bear in mind that RCH and cerebellar herniation can even develop as early as in the first hour postoperatively, particularly with a large output from the JP drain. Therefore, it is very important to closely monitor the patient’s neurological function and JP drain output. Neurological deterioration and delayed emergence from anesthesia following spine surgery should raise suspicion on the possibility of the development of RCH and tonsillar herniation.
Complete recovery is possible, even in the event of cerebellar herniation, which is the worst complication of spine surgery. The key is early recognition and appropriate management of RCH and cerebellar herniation.
Acknowledgments
We thank Dr.Ravi Ananath for reading the scans
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study
Shunt Overdrainage: Reappraisal of the Syndrome and Proposal for an Integrative Model
Citation Count
The Role of Antisiphon Devices in the Prevention of Central Ventricular Catheter Obliteration for Hydrocephalus: A 15-Years Institution’s Experience Retrospective Analysis
Incidental and clinical significance of slit ventricles in fixed pressure valves, how to define csf overdrainage: a systematic literature review, about gladiators and a sacred disease, preterm-related posthemorrhagic hydrocephalus: review of our institutional series with a long-term follow-up, mechanical complications in shunts, the scientific history of hydrocephalus and its treatment., anti-siphon and reversible occlusion valves for shunting in hydrocephalus and preventing post-shunt subdural hematomas, hydrocephalus: overdrainage by ventricular shunts. a review and recommendations, tonsillar herniation: the rule rather than the exception after lumboperitoneal shunting in the pediatric population, related papers (5), shunt overdrainage syndrome: review of the literature., the treatment of hydrocephalus., diagnosis and prognosis in idiopathic normal pressure hydrocephalus, neuroimaging of ventriculoperitoneal shunt complications in children, surgical management of idiopathic normal-pressure hydrocephalus..
Browse by Audience
Update Your Profile Member Spotlights Refer a Member: IASP Champions Join a Special Interest Group (SIG) Find a Chapter Join Now
PAIN PAIN Reports Pain Research Forum Papers of the Week Webinars and Podcasts Events
HEALTH CARE PROVIDER
Online Learning - PERC Webinars & Podcasts Curricula Graduate Opportunities Events
PATIENT & CAREGIVER
RELIEF News Resources for Living with Pain Global Alliance of Partners in Pain Advocacy (GAPPA) Events
Support IASP Sponsor an Event Become a Partner

Papers of the Week
< BACK TO ARCHIVE
DATE PUBLISHED: 2023 Jan 14
JOURNAL: Acta Neurochir (Wien)
PUBMED: http://www.ncbi.nlm.nih.gov/pubmed/36639536?dopt=Abstract
How to define CSF overdrainage: a systematic literature review.
- Google Scholar
Overdrainage (OD) is one of the most frequent complications related to drainage of the cerebrospinal fluid (CSF). It is mostly associated with valve-bearing shunt systems but should probably be considered as a risk factor in any type of CSF diversion procedure. There is extreme variation in the reported incidence of OD due to the lack of consensus on defining criteria and an unclear perception of the pathophysiology. Hence, OD is probably underreported and underestimated. The objective of this paper was to establish a definition of OD, based on a systematic review of the literature.
- Find in topic
INTRODUCTION
Intracranial hypotension most commonly occurs from a persistent CSF leak after lumbar puncture but may also be spontaneous.
This topic will review the treatment and prognosis of spontaneous intracranial hypotension. The pathophysiology, clinical features, and diagnosis of spontaneous intracranial hypotension are discussed separately. (See "Spontaneous intracranial hypotension: Pathophysiology, clinical features, and diagnosis" .)
Post-dural puncture headache is reviewed elsewhere. (See "Post dural puncture headache" .)
INITIAL TREATMENT
To continue reading this article, you must sign in . For more information or to purchase a personal subscription, click below on the option that best describes you:
- Medical Professional
- Resident, Fellow or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
Print Options

IMAGES
VIDEO
COMMENTS
Purpose Overdrainage (OD) is one of the most frequent complications related to drainage of the cerebrospinal fluid (CSF). It is mostly associated with valve-bearing shunt systems but should probably be considered as a risk factor in any type of CSF diversion procedure. There is extreme variation in the reported incidence of OD due to the lack of consensus on defining criteria and an unclear ...
Overdrainage (OD) is a recognized complication due to. excessive therapeutic drainag e of the cerebrospinal fluid. (CSF). The term "overdrainage" was firs t introduced in the. literature in ...
(CSF). The term "overdrainage" was rst introduced in the literature in 1968 [] and has gained increasing attention 1 since the 1990s [, 537]. OD is one of the most frequent complications related to CSF drainage [50]. It should be considered a risk factor in any type of CSF diversion procedure but is mostly associated with valve-bearing shunt
The objective of this paper was to establish a definition of OD, based on a systematic review of the literature. Methods A systematic search was conducted in MEDLNE and EMBASE. Studies providing a definition or a description of diagnostic findings related to OD in ventriculoperitoneal shunt treated hydrocephalus were included.
Overdrainage (OD) is a recognized complication due to excessive therapeutic drainage of the cerebrospinal fluid (CSF). The term "overdrainage" was first introduced in the literature in 1968 [ 1 ] and has gained increasing attention since the 1990s …
A systematic and organized literature review to identify inaugural and fundamental papers on overdrainage following CSF shunting was performed online using Google Scholar. We searched the keywords representative of the three main concepts: overdrainage, siphoning, and slit-ventricle syndrome.
PURPOSE Overdrainage (OD) is one of the most frequent complications related to drainage of the cerebrospinal fluid (CSF). It is mostly associated with valve-bearing shunt systems but should probably be.
Cerebrospinal-fluid (CSF) drainage is recommended by current guidelines for spinal protection during open and endovascular repairs of thoracic and thoraco-abdominal aortic aneurysms. In the published literature, great variability exists in the rate of CSF-related complications and morbidity. Herein, we perform a systematic review and meta-analysis on the incidence of CSF drainage-related ...
Abstract. Article abstract CSF volume depletions, whether from leak or shunt overdrainage, typically cause low CSF opening pressures, orthostatic headaches, and diffuse pachymeningeal gadolinium enhancement on MRI. The authors report three patients—two with overdraining CSF shunts and one with proven CSF leak—with the typical pachymeningeal ...
Abstract. Purpose: Overdrainage (OD) is one of the most frequent complications related to drainage of the cerebrospinal fluid (CSF). It is mostly associated with valve-bearing shunt systems but should probably be considered as a risk factor in any type of CSF diversion procedure. There is extreme variation in the reported incidence of OD due to ...
This systematic review and meta-analysis assessed the outcome after CSF shunting for IIH by analyzing the published literature on the topic over a period of approximately 21 years. Although these are largely retrospective observational studies with some heterogeneity, a total of 372 patients from 15 studies were available for analysis.
37 38 A recent systematic review by Wong et al identified 46 studies comprising a total of 4,936 patients, aiming to determine the appropriate role of CSFD in TEVAR. The overall incidence of SCI was reported to be 3.89%, and the pooled rate of SCI for patients who received prophylactic CSFD was 3.2% compared with 3.47% in patients who did not ...
In this review, all the main facets related with shunt overdrainage are commented on. Shunt overdrainage in patients with hydrocephalus still represents a challenge for neurosurgeons, in part due to the lack of agreement or uniformity concerning the entity. Important problems exist relating to the real incidence of the entity, its definition, classification, and the pathophysiological theories ...
How to define CSF overdrainage: a systematic literature review. S. H. Pedersen Tobias ... There was an overall agreement that CSF overdrainage following implantation of a ventriculoperitoneal shunt in a mixed pediatric and adult population is characterized as a persistent condition with clinically manifestations as postural dependent headache ...
Floman et al. observed an incidence rate of 0.26% for RCH in their study of 210 patients who had CSF loss following lumbar spine surgery . RCH has a variable timeline of presentation. Konya et al. reviewed the published literature up to 2006 and noted that an RCH was diagnosed between 16 and 120 hours after surgery (47 hours on average) [5,6].
The objective of this paper was to establish a definition of OD, based on a systematic review of the literature. A systematic search was conducted in MEDLNE and EMBASE. Studies providing a definition or a description of diagnostic findings related to OD in ventriculoperitoneal shunt treated hydrocephalus were included.
Overdrainage (OD) is one of the most frequent complications related to drainage of the cerebrospinal fluid (CSF). It is mostly associated with valve-bearing shunt systems but should probably be considered as a risk factor in any type of CSF diversion procedure. There is extreme variation in the reported incidence of OD due to the lack of ...
Method details Overview. A Systematic Literature Review (SLR) is a research methodology to collect, identify, and critically analyze the available research studies (e.g., articles, conference proceedings, books, dissertations) through a systematic procedure [12].An SLR updates the reader with current literature about a subject [6].The goal is to review critical points of current knowledge on a ...
This systematic review is the first to provide position-dependent reference values for intracranial pressure and lumbar cerebrospinal fluid pressure and highlights the need for further research on the matter. Background Although widely used in the evaluation of the diseased, normal intracranial pressure and lumbar cerebrospinal fluid pressure remain sparsely documented. Intracranial pressure ...
Overdrainage (OD) is one of the most frequent complications related to drainage of the cerebrospinal fluid (CSF). It is mostly associated with valve-bearing shunt systems but should probably be considered as a risk factor in any type of CSF diversion procedure. There is extreme variation in the reported incidence of OD due to the lack of consensus on defining criteria and an unclear perception ...
Literature reviews establish the foundation of academic inquires. However, in the planning field, we lack rigorous systematic reviews. In this article, through a systematic search on the methodology of literature review, we categorize a typology of literature reviews, discuss steps in conducting a systematic literature review, and provide suggestions on how to enhance rigor in literature ...
An integrative model based on determination of pathophysiological mechanisms and predisposing factors behind each individual case is proposed and active prophylaxis and management are proposed according to this model. Although shunt overdrainage is a well-known complication in hydrocephalus management, the problem has been underestimated. Current literature suggests that the topic requires ...
The production, absorption, and flow of cerebrospinal fluid (CSF) play key roles in the dynamics of intracranial pressure. Alterations in CSF pressure can lead to neurologic symptoms, the most common being headache. Most often, the headaches associated with low CSF pressure are orthostatic and occur after lumbar puncture, but similar headaches ...