Essay on Addiction for Students and Children
500 words essay on addiction.
As we all know that excess of anything can be very dangerous, the same way, addiction of any kind can hamper the life quality of an individual. The phrase states that addiction is a family disease as one person uses and the whole family suffers. The above statement stands true in all its essence as the addict does not merely suffer but the people around him suffer greatly too. However, that does not mean they can’t be helped. Addiction is curable and we must not give up on the person who is addicted, rather help them out for a better life.


Cost of Addiction
Addiction comes at a great cost and we need to be able to recognize its harmful consequences to not let ourselves or anyone become an addict. Firstly, addiction has major health hazards. Intake of anything is bad for our body , and it does not matter what type of addiction it is, it will always impact the mental and physical health of a person.
For instance, if you are addicted to drugs or food, you will get various diseases and illnesses. Similarly, if you are addicted to video games, your mental health will also suffer along with physical health.
Moreover, people who are addicts usually face monetary issues. As they use that thing in excess, they spend loads of money on it. People become obsessed with spending all their fortunes on that one thing to satisfy their addiction. Thus, all these addictions of drugs , alcohol , gambling, and more drain the finances of a person and they usually end up in debt or even worse.
Furthermore, the personal and professional relationships of addicts suffer the most. They end up doing things or making decisions that do not work in their favor. This constraint the relationships of people and they drift apart.
Moreover, it also hampers their studies or work life. When you are spending all your money and time on your addiction, naturally your concentration levels in other things will drop. However, all this is not impossible to beat. There are many ways through which one can beat their addiction.
Get the huge list of more than 500 Essay Topics and Ideas
Beat Your Addiction
It is best to work towards beating your addiction rather than getting beat by it. One can try many ways to do so. Firstly, recognize and identify that you have an addiction problem. That is the first step to getting cured. You need to take some time and understand the symptoms in order to treat them. Motivate yourself to do better.
After that, understand that the journey will be long but worthwhile. Identify the triggers in your life and try to stay away from them as far as possible. There is no shame in asking for professional help. Always remember that professionals can always help you get better. Enroll yourself in rehabilitation programs and try to make the most out of them.
Most importantly, do not be hesitant in talking to your loved ones. Approach them and talk it out as they care most about you. They will surely help you get on the right path and help you in beating addiction for better health and life.
Q.1 What are the consequences of addiction?
A.1 Addiction has very severe consequences. Some of them are health hazards, monetary issues, relationship problems, adverse problems on studies and work of a person. It seriously hampers the quality of life of a person.
Q.2 How can one get rid of addiction?
A.2 A little help can go a long way. One can get rid of addiction by enrolling in rehabilitation programs and opening up about their struggle. Try to take professional help and talk with your close ones to become better.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Neuropsychopharmacology
- v.46(10); 2021 Sep
Addiction as a brain disease revised: why it still matters, and the need for consilience
Markus heilig.
1 Center for Social and Affective Neuroscience, Department of Biomedical and Clinical Sciences, Linköping University, Linköping, Sweden
James MacKillop
2 Peter Boris Centre for Addictions Research, McMaster University and St. Joseph’s Healthcare Hamilton, Hamilton, ON Canada
3 Homewood Research Institute, Guelph, ON Canada
Diana Martinez
4 New York State Psychiatric Institute and Columbia University Irving Medical Center, New York, NY USA
Jürgen Rehm
5 Institute for Mental Health Policy Research & Campbell Family Mental Health Research Institute, Centre for Addiction and Mental Health (CAMH), Toronto, ON Canada
6 Dalla Lana School of Public Health and Department of Psychiatry, University of Toronto (UofT), Toronto, ON Canada
7 Klinische Psychologie & Psychotherapie, Technische Universität Dresden, Dresden, Germany
8 Department of International Health Projects, Institute for Leadership and Health Management, I.M. Sechenov First Moscow State Medical University, Moscow, Russia
Lorenzo Leggio
9 Clinical Psychoneuroendocrinology and Neuropsychopharmacology Section, Translational Addiction Medicine Branch, National Institute on Drug Abuse Intramural Research Program and National Institute on Alcohol Abuse and Alcoholism Division of Intramural Clinical and Biological Research, National Institutes of Health, Baltimore and Bethesda, MD USA
Louk J. M. J. Vanderschuren
10 Department of Population Health Sciences, Unit Animals in Science and Society, Faculty of Veterinary Medicine, Utrecht University, Utrecht, the Netherlands
The view that substance addiction is a brain disease, although widely accepted in the neuroscience community, has become subject to acerbic criticism in recent years. These criticisms state that the brain disease view is deterministic, fails to account for heterogeneity in remission and recovery, places too much emphasis on a compulsive dimension of addiction, and that a specific neural signature of addiction has not been identified. We acknowledge that some of these criticisms have merit, but assert that the foundational premise that addiction has a neurobiological basis is fundamentally sound. We also emphasize that denying that addiction is a brain disease is a harmful standpoint since it contributes to reducing access to healthcare and treatment, the consequences of which are catastrophic. Here, we therefore address these criticisms, and in doing so provide a contemporary update of the brain disease view of addiction. We provide arguments to support this view, discuss why apparently spontaneous remission does not negate it, and how seemingly compulsive behaviors can co-exist with the sensitivity to alternative reinforcement in addiction. Most importantly, we argue that the brain is the biological substrate from which both addiction and the capacity for behavior change arise, arguing for an intensified neuroscientific study of recovery. More broadly, we propose that these disagreements reveal the need for multidisciplinary research that integrates neuroscientific, behavioral, clinical, and sociocultural perspectives.
Introduction
Close to a quarter of a century ago, then director of the US National Institute on Drug Abuse Alan Leshner famously asserted that “addiction is a brain disease”, articulated a set of implications of this position, and outlined an agenda for realizing its promise [ 1 ]. The paper, now cited almost 2000 times, put forward a position that has been highly influential in guiding the efforts of researchers, and resource allocation by funding agencies. A subsequent 2000 paper by McLellan et al. [ 2 ] examined whether data justify distinguishing addiction from other conditions for which a disease label is rarely questioned, such as diabetes, hypertension or asthma. It concluded that neither genetic risk, the role of personal choices, nor the influence of environmental factors differentiated addiction in a manner that would warrant viewing it differently; neither did relapse rates, nor compliance with treatment. The authors outlined an agenda closely related to that put forward by Leshner, but with a more clinical focus. Their conclusion was that addiction should be insured, treated, and evaluated like other diseases. This paper, too, has been exceptionally influential by academic standards, as witnessed by its ~3000 citations to date. What may be less appreciated among scientists is that its impact in the real world of addiction treatment has remained more limited, with large numbers of patients still not receiving evidence-based treatments.
In recent years, the conceptualization of addiction as a brain disease has come under increasing criticism. When first put forward, the brain disease view was mainly an attempt to articulate an effective response to prevailing nonscientific, moralizing, and stigmatizing attitudes to addiction. According to these attitudes, addiction was simply the result of a person’s moral failing or weakness of character, rather than a “real” disease [ 3 ]. These attitudes created barriers for people with substance use problems to access evidence-based treatments, both those available at the time, such as opioid agonist maintenance, cognitive behavioral therapy-based relapse prevention, community reinforcement or contingency management, and those that could result from research. To promote patient access to treatments, scientists needed to argue that there is a biological basis beneath the challenging behaviors of individuals suffering from addiction. This argument was particularly targeted to the public, policymakers and health care professionals, many of whom held that since addiction was a misery people brought upon themselves, it fell beyond the scope of medicine, and was neither amenable to treatment, nor warranted the use of taxpayer money.
Present-day criticism directed at the conceptualization of addiction as a brain disease is of a very different nature. It originates from within the scientific community itself, and asserts that this conceptualization is neither supported by data, nor helpful for people with substance use problems [ 4 – 8 ]. Addressing these critiques requires a very different perspective, and is the objective of our paper. We readily acknowledge that in some cases, recent critiques of the notion of addiction as a brain disease as postulated originally have merit, and that those critiques require the postulates to be re-assessed and refined. In other cases, we believe the arguments have less validity, but still provide an opportunity to update the position of addiction as a brain disease. Our overarching concern is that questionable arguments against the notion of addiction as a brain disease may harm patients, by impeding access to care, and slowing development of novel treatments.
A premise of our argument is that any useful conceptualization of addiction requires an understanding both of the brains involved, and of environmental factors that interact with those brains [ 9 ]. These environmental factors critically include availability of drugs, but also of healthy alternative rewards and opportunities. As we will show, stating that brain mechanisms are critical for understanding and treating addiction in no way negates the role of psychological, social and socioeconomic processes as both causes and consequences of substance use. To reflect this complex nature of addiction, we have assembled a team with expertise that spans from molecular neuroscience, through animal models of addiction, human brain imaging, clinical addiction medicine, to epidemiology. What brings us together is a passionate commitment to improving the lives of people with substance use problems through science and science-based treatments, with empirical evidence as the guiding principle.
To achieve this goal, we first discuss the nature of the disease concept itself, and why we believe it is important for the science and treatment of addiction. This is followed by a discussion of the main points raised when the notion of addiction as a brain disease has come under criticism. Key among those are claims that spontaneous remission rates are high; that a specific brain pathology is lacking; and that people suffering from addiction, rather than behaving “compulsively”, in fact show a preserved ability to make informed and advantageous choices. In the process of discussing these issues, we also address the common criticism that viewing addiction as a brain disease is a fully deterministic theory of addiction. For our argument, we use the term “addiction” as originally used by Leshner [ 1 ]; in Box 1 , we map out and discuss how this construct may relate to the current diagnostic categories, such as Substance Use Disorder (SUD) and its different levels of severity (Fig. 1) .

Risky (hazardous) substance use refers to quantity/frequency indicators of consumption; SUD refers to individuals who meet criteria for a DSM-5 diagnosis (mild, moderate, or severe); and addiction refers to individuals who exhibit persistent difficulties with self-regulation of drug consumption. Among high-risk individuals, a subgroup will meet criteria for SUD and, among those who have an SUD, a further subgroup would be considered to be addicted to the drug. However, the boundary for addiction is intentionally blurred to reflect that the dividing line for defining addiction within the category of SUD remains an open empirical question.
Box 1 What’s in a name? Differentiating hazardous use, substance use disorder, and addiction
Although our principal focus is on the brain disease model of addiction, the definition of addiction itself is a source of ambiguity. Here, we provide a perspective on the major forms of terminology in the field.
Hazardous Substance Use
Hazardous (risky) substance use refers to quantitative levels of consumption that increase an individual’s risk for adverse health consequences. In practice, this pertains to alcohol use [ 110 , 111 ]. Clinically, alcohol consumption that exceeds guidelines for moderate drinking has been used to prompt brief interventions or referral for specialist care [ 112 ]. More recently, a reduction in these quantitative levels has been validated as treatment endpoints [ 113 ].
Substance Use Disorder
SUD refers to the DSM-5 diagnosis category that encompasses significant impairment or distress resulting from specific categories of psychoactive drug use. The diagnosis of SUD is operationalized as 2 or more of 11 symptoms over the past year. As a result, the diagnosis is heterogenous, with more than 1100 symptom permutations possible. The diagnosis in DSM-5 is the result of combining two diagnoses from the DSM-IV, abuse and dependence, which proved to be less valid than a single dimensional approach [ 114 ]. Critically, SUD includes three levels of severity: mild (2–3 symptoms), moderate (4–5 symptoms), and severe (6+ symptoms). The International Classification of Diseases (ICD) system retains two diagnoses, harmful use (lower severity) and substance dependence (higher severity).
Addiction is a natural language concept, etymologically meaning enslavement, with the contemporary meaning traceable to the Middle and Late Roman Republic periods [ 115 ]. As a scientific construct, drug addiction can be defined as a state in which an individual exhibits an inability to self-regulate consumption of a substance, although it does not have an operational definition. Regarding clinical diagnosis, as it is typically used in scientific and clinical parlance, addiction is not synonymous with the simple presence of SUD. Nowhere in DSM-5 is it articulated that the diagnostic threshold (or any specific number/type of symptoms) should be interpreted as reflecting addiction, which inherently connotes a high degree of severity. Indeed, concerns were raised about setting the diagnostic standard too low because of the issue of potentially conflating a low-severity SUD with addiction [ 116 ]. In scientific and clinical usage, addiction typically refers to individuals at a moderate or high severity of SUD. This is consistent with the fact that moderate-to-severe SUD has the closest correspondence with the more severe diagnosis in ICD [ 117 – 119 ]. Nonetheless, akin to the undefined overlap between hazardous use and SUD, the field has not identified the exact thresholds of SUD symptoms above which addiction would be definitively present.
Integration
The ambiguous relationships among these terms contribute to misunderstandings and disagreements. Figure 1 provides a simple working model of how these terms overlap. Fundamentally, we consider that these terms represent successive dimensions of severity, clinical “nesting dolls”. Not all individuals consuming substances at hazardous levels have an SUD, but a subgroup do. Not all individuals with a SUD are addicted to the drug in question, but a subgroup are. At the severe end of the spectrum, these domains converge (heavy consumption, numerous symptoms, the unambiguous presence of addiction), but at low severity, the overlap is more modest. The exact mapping of addiction onto SUD is an open empirical question, warranting systematic study among scientists, clinicians, and patients with lived experience. No less important will be future research situating our definition of SUD using more objective indicators (e.g., [ 55 , 120 ]), brain-based and otherwise, and more precisely in relation to clinical needs [ 121 ]. Finally, such work should ultimately be codified in both the DSM and ICD systems to demarcate clearly where the attribution of addiction belongs within the clinical nosology, and to foster greater clarity and specificity in scientific discourse.
What is a disease?
In his classic 1960 book “The Disease Concept of Alcoholism”, Jellinek noted that in the alcohol field, the debate over the disease concept was plagued by too many definitions of “alcoholism” and too few definitions of “disease” [ 10 ]. He suggested that the addiction field needed to follow the rest of medicine in moving away from viewing disease as an “entity”, i.e., something that has “its own independent existence, apart from other things” [ 11 ]. To modern medicine, he pointed out, a disease is simply a label that is agreed upon to describe a cluster of substantial, deteriorating changes in the structure or function of the human body, and the accompanying deterioration in biopsychosocial functioning. Thus, he concluded that alcoholism can simply be defined as changes in structure or function of the body due to drinking that cause disability or death. A disease label is useful to identify groups of people with commonly co-occurring constellations of problems—syndromes—that significantly impair function, and that lead to clinically significant distress, harm, or both. This convention allows a systematic study of the condition, and of whether group members benefit from a specific intervention.
It is not trivial to delineate the exact category of harmful substance use for which a label such as addiction is warranted (See Box 1 ). Challenges to diagnostic categorization are not unique to addiction, however. Throughout clinical medicine, diagnostic cut-offs are set by consensus, commonly based on an evolving understanding of thresholds above which people tend to benefit from available interventions. Because assessing benefits in large patient groups over time is difficult, diagnostic thresholds are always subject to debate and adjustments. It can be debated whether diagnostic thresholds “merely” capture the extreme of a single underlying population, or actually identify a subpopulation that is at some level distinct. Resolving this issue remains challenging in addiction, but once again, this is not different from other areas of medicine [see e.g., [ 12 ] for type 2 diabetes]. Longitudinal studies that track patient trajectories over time may have a better ability to identify subpopulations than cross-sectional assessments [ 13 ].
By this pragmatic, clinical understanding of the disease concept, it is difficult to argue that “addiction” is unjustified as a disease label. Among people who use drugs or alcohol, some progress to using with a quantity and frequency that results in impaired function and often death, making substance use a major cause of global disease burden [ 14 ]. In these people, use occurs with a pattern that in milder forms may be challenging to capture by current diagnostic criteria (See Box 1 ), but is readily recognized by patients, their families and treatment providers when it reaches a severity that is clinically significant [see [ 15 ] for a classical discussion]. In some cases, such as opioid addiction, those who receive the diagnosis stand to obtain some of the greatest benefits from medical treatments in all of clinical medicine [ 16 , 17 ]. Although effect sizes of available treatments are more modest in nicotine [ 18 ] and alcohol addiction [ 19 ], the evidence supporting their efficacy is also indisputable. A view of addiction as a disease is justified, because it is beneficial: a failure to diagnose addiction drastically increases the risk of a failure to treat it [ 20 ].
Of course, establishing a diagnosis is not a requirement for interventions to be meaningful. People with hazardous or harmful substance use who have not (yet) developed addiction should also be identified, and interventions should be initiated to address their substance-related risks. This is particularly relevant for alcohol, where even in the absence of addiction, use is frequently associated with risks or harm to self, e.g., through cardiovascular disease, liver disease or cancer, and to others, e.g., through accidents or violence [ 21 ]. Interventions to reduce hazardous or harmful substance use in people who have not developed addiction are in fact particularly appealing. In these individuals, limited interventions are able to achieve robust and meaningful benefits [ 22 ], presumably because patterns of misuse have not yet become entrenched.
Thus, as originally pointed out by McLellan and colleagues, most of the criticisms of addiction as a disease could equally be applied to other medical conditions [ 2 ]. This type of criticism could also be applied to other psychiatric disorders, and that has indeed been the case historically [ 23 , 24 ]. Today, there is broad consensus that those criticisms were misguided. Few, if any healthcare professionals continue to maintain that schizophrenia, rather than being a disease, is a normal response to societal conditions. Why, then, do people continue to question if addiction is a disease, but not whether schizophrenia, major depressive disorder or post-traumatic stress disorder are diseases? This is particularly troubling given the decades of data showing high co-morbidity of addiction with these conditions [ 25 , 26 ]. We argue that it comes down to stigma. Dysregulated substance use continues to be perceived as a self-inflicted condition characterized by a lack of willpower, thus falling outside the scope of medicine and into that of morality [ 3 ].
Chronic and relapsing, developmentally-limited, or spontaneously remitting?
Much of the critique targeted at the conceptualization of addiction as a brain disease focuses on its original assertion that addiction is a chronic and relapsing condition. Epidemiological data are cited in support of the notion that large proportions of individuals achieve remission [ 27 ], frequently without any formal treatment [ 28 , 29 ] and in some cases resuming low risk substance use [ 30 ]. For instance, based on data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) study [ 27 ], it has been pointed out that a significant proportion of people with an addictive disorder quit each year, and that most afflicted individuals ultimately remit. These spontaneous remission rates are argued to invalidate the concept of a chronic, relapsing disease [ 4 ].
Interpreting these and similar data is complicated by several methodological and conceptual issues. First, people may appear to remit spontaneously because they actually do, but also because of limited test–retest reliability of the diagnosis [ 31 ]. For instance, using a validated diagnostic interview and trained interviewers, the Collaborative Studies on Genetics of Alcoholism examined the likelihood that an individual diagnosed with a lifetime history of substance dependence would retain this classification after 5 years. This is obviously a diagnosis that, once met, by definition cannot truly remit. Lifetime alcohol dependence was indeed stable in individuals recruited from addiction treatment units, ~90% for women, and 95% for men. In contrast, in a community-based sample similar to that used in the NESARC [ 27 ], stability was only ~30% and 65% for women and men, respectively. The most important characteristic that determined diagnostic stability was severity. Diagnosis was stable in severe, treatment-seeking cases, but not in general population cases of alcohol dependence.
These data suggest that commonly used diagnostic criteria alone are simply over-inclusive for a reliable, clinically meaningful diagnosis of addiction. They do identify a core group of treatment seeking individuals with a reliable diagnosis, but, if applied to nonclinical populations, also flag as “cases” a considerable halo of individuals for whom the diagnostic categorization is unreliable. Any meaningful discussion of remission rates needs to take this into account, and specify which of these two populations that is being discussed. Unfortunately, the DSM-5 has not made this task easier. With only 2 out of 11 symptoms being sufficient for a diagnosis of SUD, it captures under a single diagnostic label individuals in a “mild” category, whose diagnosis is likely to have very low test–retest reliability, and who are unlikely to exhibit a chronic relapsing course, together with people at the severe end of the spectrum, whose diagnosis is reliable, many of whom do show a chronic relapsing course.
The NESARC data nevertheless show that close to 10% of people in the general population who are diagnosed with alcohol addiction (here equated with DSM-IV “dependence” used in the NESARC study) never remitted throughout their participation in the survey. The base life-time prevalence of alcohol dependence in NESARC was 12.5% [ 32 ]. Thus, the data cited against the concept of addiction as a chronic relapsing disease in fact indicate that over 1% of the US population develops an alcohol-related condition that is associated with high morbidity and mortality, and whose chronic and/or relapsing nature cannot be disputed, since it does not remit.
Secondly, the analysis of NESARC data [ 4 , 27 ] omits opioid addiction, which, together with alcohol and tobacco, is the largest addiction-related public health problem in the US [ 33 ]. This is probably the addictive condition where an analysis of cumulative evidence most strikingly supports the notion of a chronic disorder with frequent relapses in a large proportion of people affected [ 34 ]. Of course, a large number of people with opioid addiction are unable to express the chronic, relapsing course of their disease, because over the long term, their mortality rate is about 15 times greater than that of the general population [ 35 ]. However, even among those who remain alive, the prevalence of stable abstinence from opioid use after 10–30 years of observation is <30%. Remission may not always require abstinence, for instance in the case of alcohol addiction, but is a reasonable proxy for remission with opioids, where return to controlled use is rare. Embedded in these data is a message of literally vital importance: when opioid addiction is diagnosed and treated as a chronic relapsing disease, outcomes are markedly improved, and retention in treatment is associated with a greater likelihood of abstinence.
The fact that significant numbers of individuals exhibit a chronic relapsing course does not negate that even larger numbers of individuals with SUD according to current diagnostic criteria do not. For instance, in many countries, the highest prevalence of substance use problems is found among young adults, aged 18–25 [ 36 ], and a majority of these ‘age out’ of excessive substance use [ 37 ]. It is also well documented that many individuals with SUD achieve longstanding remission, in many cases without any formal treatment (see e.g., [ 27 , 30 , 38 ]).
Collectively, the data show that the course of SUD, as defined by current diagnostic criteria, is highly heterogeneous. Accordingly, we do not maintain that a chronic relapsing course is a defining feature of SUD. When present in a patient, however, such as course is of clinical significance, because it identifies a need for long-term disease management [ 2 ], rather than expectations of a recovery that may not be within the individual’s reach [ 39 ]. From a conceptual standpoint, however, a chronic relapsing course is neither necessary nor implied in a view that addiction is a brain disease. This view also does not mean that it is irreversible and hopeless. Human neuroscience documents restoration of functioning after abstinence [ 40 , 41 ] and reveals predictors of clinical success [ 42 ]. If anything, this evidence suggests a need to increase efforts devoted to neuroscientific research on addiction recovery [ 40 , 43 ].
Lessons from genetics
For alcohol addiction, meta-analysis of twin and adoption studies has estimated heritability at ~50%, while estimates for opioid addiction are even higher [ 44 , 45 ]. Genetic risk factors are to a large extent shared across substances [ 46 ]. It has been argued that a genetic contribution cannot support a disease view of a behavior, because most behavioral traits, including religious and political inclinations, have a genetic contribution [ 4 ]. This statement, while correct in pointing out broad heritability of behavioral traits, misses a fundamental point. Genetic architecture is much like organ structure. The fact that normal anatomy shapes healthy organ function does not negate that an altered structure can contribute to pathophysiology of disease. The structure of the genetic landscape is no different. Critics further state that a “genetic predisposition is not a recipe for compulsion”, but no neuroscientist or geneticist would claim that genetic risk is “a recipe for compulsion”. Genetic risk is probabilistic, not deterministic. However, as we will see below, in the case of addiction, it contributes to large, consistent probability shifts towards maladaptive behavior.
In dismissing the relevance of genetic risk for addiction, Hall writes that “a large number of alleles are involved in the genetic susceptibility to addiction and individually these alleles might very weakly predict a risk of addiction”. He goes on to conclude that “generally, genetic prediction of the risk of disease (even with whole-genome sequencing data) is unlikely to be informative for most people who have a so-called average risk of developing an addiction disorder” [ 7 ]. This reflects a fundamental misunderstanding of polygenic risk. It is true that a large number of risk alleles are involved, and that the explanatory power of currently available polygenic risk scores for addictive disorders lags behind those for e.g., schizophrenia or major depression [ 47 , 48 ]. The only implication of this, however, is that low average effect sizes of risk alleles in addiction necessitate larger study samples to construct polygenic scores that account for a large proportion of the known heritability.
However, a heritability of addiction of ~50% indicates that DNA sequence variation accounts for 50% of the risk for this condition. Once whole genome sequencing is readily available, it is likely that it will be possible to identify most of that DNA variation. For clinical purposes, those polygenic scores will of course not replace an understanding of the intricate web of biological and social factors that promote or prevent expression of addiction in an individual case; rather, they will add to it [ 49 ]. Meanwhile, however, genome-wide association studies in addiction have already provided important information. For instance, they have established that the genetic underpinnings of alcohol addiction only partially overlap with those for alcohol consumption, underscoring the genetic distinction between pathological and nonpathological drinking behaviors [ 50 ].
It thus seems that, rather than negating a rationale for a disease view of addiction, the important implication of the polygenic nature of addiction risk is a very different one. Genome-wide association studies of complex traits have largely confirmed the century old “infinitisemal model” in which Fisher reconciled Mendelian and polygenic traits [ 51 ]. A key implication of this model is that genetic susceptibility for a complex, polygenic trait is continuously distributed in the population. This may seem antithetical to a view of addiction as a distinct disease category, but the contradiction is only apparent, and one that has long been familiar to quantitative genetics. Viewing addiction susceptibility as a polygenic quantitative trait, and addiction as a disease category is entirely in line with Falconer’s theorem, according to which, in a given set of environmental conditions, a certain level of genetic susceptibility will determine a threshold above which disease will arise.
A brain disease? Then show me the brain lesion!
The notion of addiction as a brain disease is commonly criticized with the argument that a specific pathognomonic brain lesion has not been identified. Indeed, brain imaging findings in addiction (perhaps with the exception of extensive neurotoxic gray matter loss in advanced alcohol addiction) are nowhere near the level of specificity and sensitivity required of clinical diagnostic tests. However, this criticism neglects the fact that neuroimaging is not used to diagnose many neurologic and psychiatric disorders, including epilepsy, ALS, migraine, Huntington’s disease, bipolar disorder, or schizophrenia. Even among conditions where signs of disease can be detected using brain imaging, such as Alzheimer’s and Parkinson’s disease, a scan is best used in conjunction with clinical acumen when making the diagnosis. Thus, the requirement that addiction be detectable with a brain scan in order to be classified as a disease does not recognize the role of neuroimaging in the clinic.
For the foreseeable future, the main objective of imaging in addiction research is not to diagnose addiction, but rather to improve our understanding of mechanisms that underlie it. The hope is that mechanistic insights will help bring forward new treatments, by identifying candidate targets for them, by pointing to treatment-responsive biomarkers, or both [ 52 ]. Developing innovative treatments is essential to address unmet treatment needs, in particular in stimulant and cannabis addiction, where no approved medications are currently available. Although the task to develop novel treatments is challenging, promising candidates await evaluation [ 53 ]. A particular opportunity for imaging-based research is related to the complex and heterogeneous nature of addictive disorders. Imaging-based biomarkers hold the promise of allowing this complexity to be deconstructed into specific functional domains, as proposed by the RDoC initiative [ 54 ] and its application to addiction [ 55 , 56 ]. This can ultimately guide the development of personalized medicine strategies to addiction treatment.
Countless imaging studies have reported differences in brain structure and function between people with addictive disorders and those without them. Meta-analyses of structural data show that alcohol addiction is associated with gray matter losses in the prefrontal cortex, dorsal striatum, insula, and posterior cingulate cortex [ 57 ], and similar results have been obtained in stimulant-addicted individuals [ 58 ]. Meta-analysis of functional imaging studies has demonstrated common alterations in dorsal striatal, and frontal circuits engaged in reward and salience processing, habit formation, and executive control, across different substances and task-paradigms [ 59 ]. Molecular imaging studies have shown that large and fast increases in dopamine are associated with the reinforcing effects of drugs of abuse, but that after chronic drug use and during withdrawal, brain dopamine function is markedly decreased and that these decreases are associated with dysfunction of prefrontal regions [ 60 ]. Collectively, these findings have given rise to a widely held view of addiction as a disorder of fronto-striatal circuitry that mediates top-down regulation of behavior [ 61 ].
Critics reply that none of the brain imaging findings are sufficiently specific to distinguish between addiction and its absence, and that they are typically obtained in cross-sectional studies that can at best establish correlative rather than causal links. In this, they are largely right, and an updated version of a conceptualization of addiction as a brain disease needs to acknowledge this. Many of the structural brain findings reported are not specific for addiction, but rather shared across psychiatric disorders [ 62 ]. Also, for now, the most sophisticated tools of human brain imaging remain crude in face of complex neural circuit function. Importantly however, a vast literature from animal studies also documents functional changes in fronto-striatal circuits, as well their limbic and midbrain inputs, associated with addictive behaviors [ 63 – 68 ]. These are circuits akin to those identified by neuroimaging studies in humans, implicated in positive and negative emotions, learning processes and executive functions, altered function of which is thought to underlie addiction. These animal studies, by virtue of their cellular and molecular level resolution, and their ability to establish causality under experimental control, are therefore an important complement to human neuroimaging work.
Nevertheless, factors that seem remote from the activity of brain circuits, such as policies, substance availability and cost, as well as socioeconomic factors, also are critically important determinants of substance use. In this complex landscape, is the brain really a defensible focal point for research and treatment? The answer is “yes”. As powerfully articulated by Francis Crick [ 69 ], “You, your joys and your sorrows, your memories and your ambitions, your sense of personal identity and free will, are in fact no more than the behavior of a vast assembly of nerve cells and their associated molecules”. Social and interpersonal factors are critically important in addiction, but they can only exert their influences by impacting neural processes. They must be encoded as sensory data, represented together with memories of the past and predictions about the future, and combined with representations of interoceptive and other influences to provide inputs to the valuation machinery of the brain. Collectively, these inputs drive action selection and execution of behavior—say, to drink or not to drink, and then, within an episode, to stop drinking or keep drinking. Stating that the pathophysiology of addiction is largely about the brain does not ignore the role of other influences. It is just the opposite: it is attempting to understand how those important influences contribute to drug seeking and taking in the context of the brain, and vice versa.
But if the criticism is one of emphasis rather than of principle—i.e., too much brain, too little social and environmental factors – then neuroscientists need to acknowledge that they are in part guilty as charged. Brain-centric accounts of addiction have for a long time failed to pay enough attention to the inputs that social factors provide to neural processing behind drug seeking and taking [ 9 ]. This landscape is, however, rapidly changing. For instance, using animal models, scientists are finding that lack of social play early in life increases the motivation to take addictive substances in adulthood [ 70 ]. Others find that the opportunity to interact with a fellow rat is protective against addiction-like behaviors [ 71 ]. In humans, a relationship has been found between perceived social support, socioeconomic status, and the availability of dopamine D2 receptors [ 72 , 73 ], a biological marker of addiction vulnerability. Those findings in turn provided translation of data from nonhuman primates, which showed that D2 receptor availability can be altered by changes in social hierarchy, and that these changes are associated with the motivation to obtain cocaine [ 74 ].
Epidemiologically, it is well established that social determinants of health, including major racial and ethnic disparities, play a significant role in the risk for addiction [ 75 , 76 ]. Contemporary neuroscience is illuminating how those factors penetrate the brain [ 77 ] and, in some cases, reveals pathways of resilience [ 78 ] and how evidence-based prevention can interrupt those adverse consequences [ 79 , 80 ]. In other words, from our perspective, viewing addiction as a brain disease in no way negates the importance of social determinants of health or societal inequalities as critical influences. In fact, as shown by the studies correlating dopamine receptors with social experience, imaging is capable of capturing the impact of the social environment on brain function. This provides a platform for understanding how those influences become embedded in the biology of the brain, which provides a biological roadmap for prevention and intervention.
We therefore argue that a contemporary view of addiction as a brain disease does not deny the influence of social, environmental, developmental, or socioeconomic processes, but rather proposes that the brain is the underlying material substrate upon which those factors impinge and from which the responses originate. Because of this, neurobiology is a critical level of analysis for understanding addiction, although certainly not the only one. It is recognized throughout modern medicine that a host of biological and non-biological factors give rise to disease; understanding the biological pathophysiology is critical for understanding etiology and informing treatment.
Is a view of addiction as a brain disease deterministic?
A common criticism of the notion that addiction is a brain disease is that it is reductionist and in the end therefore deterministic [ 81 , 82 ]. This is a fundamental misrepresentation. As indicated above, viewing addiction as a brain disease simply states that neurobiology is an undeniable component of addiction. A reason for deterministic interpretations may be that modern neuroscience emphasizes an understanding of proximal causality within research designs (e.g., whether an observed link between biological processes is mediated by a specific mechanism). That does not in any way reflect a superordinate assumption that neuroscience will achieve global causality. On the contrary, since we realize that addiction involves interactions between biology, environment and society, ultimate (complete) prediction of behavior based on an understanding of neural processes alone is neither expected, nor a goal.
A fairer representation of a contemporary neuroscience view is that it believes insights from neurobiology allow useful probabilistic models to be developed of the inherently stochastic processes involved in behavior [see [ 83 ] for an elegant recent example]. Changes in brain function and structure in addiction exert a powerful probabilistic influence over a person’s behavior, but one that is highly multifactorial, variable, and thus stochastic. Philosophically, this is best understood as being aligned with indeterminism, a perspective that has a deep history in philosophy and psychology [ 84 ]. In modern neuroscience, it refers to the position that the dynamic complexity of the brain, given the probabilistic threshold-gated nature of its biology (e.g., action potential depolarization, ion channel gating), means that behavior cannot be definitively predicted in any individual instance [ 85 , 86 ].
Driven by compulsion, or free to choose?
A major criticism of the brain disease view of addiction, and one that is related to the issue of determinism vs indeterminism, centers around the term “compulsivity” [ 6 , 87 – 90 ] and the different meanings it is given. Prominent addiction theories state that addiction is characterized by a transition from controlled to “compulsive” drug seeking and taking [ 91 – 95 ], but allocate somewhat different meanings to “compulsivity”. By some accounts, compulsive substance use is habitual and insensitive to its outcomes [ 92 , 94 , 96 ]. Others refer to compulsive use as a result of increasing incentive value of drug associated cues [ 97 ], while others view it as driven by a recruitment of systems that encode negative affective states [ 95 , 98 ].
The prototype for compulsive behavior is provided by obsessive-compulsive disorder (OCD), where compulsion refers to repeatedly and stereotypically carrying out actions that in themselves may be meaningful, but lose their purpose and become harmful when performed in excess, such as persistent handwashing until skin injuries result. Crucially, this happens despite a conscious desire to do otherwise. Attempts to resist these compulsions result in increasing and ultimately intractable anxiety [ 99 ]. This is in important ways different from the meaning of compulsivity as commonly used in addiction theories. In the addiction field, compulsive drug use typically refers to inflexible, drug-centered behavior in which substance use is insensitive to adverse consequences [ 100 ]. Although this phenomenon is not necessarily present in every patient, it reflects important symptoms of clinical addiction, and is captured by several DSM-5 criteria for SUD [ 101 ]. Examples are needle-sharing despite knowledge of a risk to contract HIV or Hepatitis C, drinking despite a knowledge of having liver cirrhosis, but also the neglect of social and professional activities that previously were more important than substance use. While these behaviors do show similarities with the compulsions of OCD, there are also important differences. For example, “compulsive” substance use is not necessarily accompanied by a conscious desire to withhold the behavior, nor is addictive behavior consistently impervious to change.
Critics question the existence of compulsivity in addiction altogether [ 5 – 7 , 89 ], typically using a literal interpretation, i.e., that a person who uses alcohol or drugs simply can not do otherwise. Were that the intended meaning in theories of addiction—which it is not—it would clearly be invalidated by observations of preserved sensitivity of behavior to contingencies in addiction. Indeed, substance use is influenced both by the availability of alternative reinforcers, and the state of the organism. The roots of this insight date back to 1940, when Spragg found that chimpanzees would normally choose a banana over morphine. However, when physically dependent and in a state of withdrawal, their choice preference would reverse [ 102 ]. The critical role of alternative reinforcers was elegantly brought into modern neuroscience by Ahmed et al., who showed that rats extensively trained to self-administer cocaine would readily forego the drug if offered a sweet solution as an alternative [ 103 ]. This was later also found to be the case for heroin [ 103 ], methamphetamine [ 104 ] and alcohol [ 105 ]. Early residential laboratory studies on alcohol use disorder indeed revealed orderly operant control over alcohol consumption [ 106 ]. Furthermore, efficacy of treatment approaches such as contingency management, which provides systematic incentives for abstinence [ 107 ], supports the notion that behavioral choices in patients with addictions remain sensitive to reward contingencies.
Evidence that a capacity for choosing advantageously is preserved in addiction provides a valid argument against a narrow concept of “compulsivity” as rigid, immutable behavior that applies to all patients. It does not, however, provide an argument against addiction as a brain disease. If not from the brain, from where do the healthy and unhealthy choices people make originate? The critical question is whether addictive behaviors—for the most part—result from healthy brains responding normally to externally determined contingencies; or rather from a pathology of brain circuits that, through probabilistic shifts, promotes the likelihood of maladaptive choices even when reward contingencies are within a normal range. To resolve this question, it is critical to understand that the ability to choose advantageously is not an all-or-nothing phenomenon, but rather is about probabilities and their shifts, multiple faculties within human cognition, and their interaction. Yes, it is clear that most people whom we would consider to suffer from addiction remain able to choose advantageously much, if not most, of the time. However, it is also clear that the probability of them choosing to their own disadvantage, even when more salutary options are available and sometimes at the expense of losing their life, is systematically and quantifiably increased. There is a freedom of choice, yet there is a shift of prevailing choices that nevertheless can kill.
Synthesized, the notion of addiction as a disease of choice and addiction as a brain disease can be understood as two sides of the same coin. Both of these perspectives are informative, and they are complementary. Viewed this way, addiction is a brain disease in which a person’s choice faculties become profoundly compromised. To articulate it more specifically, embedded in and principally executed by the central nervous system, addiction can be understood as a disorder of choice preferences, preferences that overvalue immediate reinforcement (both positive and negative), preferences for drug-reinforcement in spite of costs, and preferences that are unstable ( “I’ll never drink like that again;” “this will be my last cigarette” ), prone to reversals in the form of lapses and relapse. From a contemporary neuroscience perspective, pre-existing vulnerabilities and persistent drug use lead to a vicious circle of substantive disruptions in the brain that impair and undermine choice capacities for adaptive behavior, but do not annihilate them. Evidence of generally intact decision making does not fundamentally contradict addiction as a brain disease.
Conclusions
The present paper is a response to the increasing number of criticisms of the view that addiction is a chronic relapsing brain disease. In many cases, we show that those criticisms target tenets that are neither needed nor held by a contemporary version of this view. Common themes are that viewing addiction as a brain disease is criticized for being both too narrow (addiction is only a brain disease; no other perspectives or factors are important) or too far reaching (it purports to discover the final causes of addiction). With regard to disease course, we propose that viewing addiction as a chronic relapsing disease is appropriate for some populations, and much less so for others, simply necessitating better ways of delineating the populations being discussed. We argue that when considering addiction as a disease, the lens of neurobiology is valuable to use. It is not the only lens, and it does not have supremacy over other scientific approaches. We agree that critiques of neuroscience are warranted [ 108 ] and that critical thinking is essential to avoid deterministic language and scientific overreach.
Beyond making the case for a view of addiction as a brain disease, perhaps the more important question is when a specific level of analysis is most useful. For understanding the biology of addiction and designing biological interventions, a neurobiological view is almost certainly the most appropriate level of analysis, in particular when informed by an understanding of the behavioral manifestations. In contrast, for understanding the psychology of addiction and designing psychological interventions, behavioral science is the natural realm, but one that can often benefit from an understanding of the underlying neurobiology. For designing policies, such as taxation and regulation of access, economics and public administration provide the most pertinent perspectives, but these also benefit from biological and behavioral science insights.
Finally, we argue that progress would come from integration of these scientific perspectives and traditions. E.O. Wilson has argued more broadly for greater consilience [ 109 ], unity of knowledge, in science. We believe that addiction is among the areas where consilience is most needed. A plurality of disciplines brings important and trenchant insights to bear on this condition; it is the exclusive remit of no single perspective or field. Addiction inherently and necessarily requires multidisciplinary examination. Moreover, those who suffer from addiction will benefit most from the application of the full armamentarium of scientific perspectives.
Funding and disclosures
Supported by the Swedish Research Council grants 2013-07434, 2019-01138 (MH); Netherlands Organisation for Health Research and Development (ZonMw) under project number 912.14.093 (LJMJV); NIDA and NIAAA intramural research programs (LL; the content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health); the Peter Boris Chair in Addictions Research, Homewood Research Institute, and the National Institute on Alcohol Abuse and Alcoholism grants AA025911, AA024930, AA025849, AA027679 (JM; the content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health).
MH has received consulting fees, research support or other compensation from Indivior, Camurus, BrainsWay, Aelis Farma, and Janssen Pharmaceuticals. JM is a Principal and Senior Scientist at BEAM Diagnostics, Inc. DM, JR, LL, and LJMJV declare no conflict of interest.
Acknowledgements
The authors want to acknowledge comments by Drs. David Epstein, Kenneth Kendler and Naomi Wray.
Author contributions
All authors jointly drafted the paper.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 181, NO. 4 CURRENT ISSUE pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Substance Use Disorders and Addiction: Mechanisms, Trends, and Treatment Implications
- Ned H. Kalin , M.D.
Search for more papers by this author
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health ( 1 ) suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol. When considering other substances, the report estimated that 4.4 million individuals had a marijuana use disorder and that 2 million people suffered from an opiate use disorder. It is well known that stress is associated with an increase in the use of alcohol and other substances, and this is particularly relevant today in relation to the chronic uncertainty and distress associated with the COVID-19 pandemic along with the traumatic effects of racism and social injustice. In part related to stress, substance use disorders are highly comorbid with other psychiatric illnesses: 9.2 million adults were estimated to have a 1-year prevalence of both a mental illness and at least one substance use disorder. Although they may not necessarily meet criteria for a substance use disorder, it is well known that psychiatric patients have increased usage of alcohol, cigarettes, and other illicit substances. As an example, the survey estimated that over the preceding month, 37.2% of individuals with serious mental illnesses were cigarette smokers, compared with 16.3% of individuals without mental illnesses. Substance use frequently accompanies suicide and suicide attempts, and substance use disorders are associated with a long-term increased risk of suicide.
Addiction is the key process that underlies substance use disorders, and research using animal models and humans has revealed important insights into the neural circuits and molecules that mediate addiction. More specifically, research has shed light onto mechanisms underlying the critical components of addiction and relapse: reinforcement and reward, tolerance, withdrawal, negative affect, craving, and stress sensitization. In addition, clinical research has been instrumental in developing an evidence base for the use of pharmacological agents in the treatment of substance use disorders, which, in combination with psychosocial approaches, can provide effective treatments. However, despite the existence of therapeutic tools, relapse is common, and substance use disorders remain grossly undertreated. For example, whether at an inpatient hospital treatment facility or at a drug or alcohol rehabilitation program, it was estimated that only 11% of individuals needing treatment for substance use received appropriate care in 2018. Additionally, it is worth emphasizing that current practice frequently does not effectively integrate dual diagnosis treatment approaches, which is important because psychiatric and substance use disorders are highly comorbid. The barriers to receiving treatment are numerous and directly interact with existing health care inequities. It is imperative that as a field we overcome the obstacles to treatment, including the lack of resources at the individual level, a dearth of trained providers and appropriate treatment facilities, racial biases, and the marked stigmatization that is focused on individuals with addictions.
This issue of the Journal is focused on understanding factors contributing to substance use disorders and their comorbidity with psychiatric disorders, the effects of prenatal alcohol use on preadolescents, and brain mechanisms that are associated with addiction and relapse. An important theme that emerges from this issue is the necessity for understanding maladaptive substance use and its treatment in relation to health care inequities. This highlights the imperative to focus resources and treatment efforts on underprivileged and marginalized populations. The centerpiece of this issue is an overview on addiction written by Dr. George Koob, the director of the National Institute on Alcohol Abuse and Alcoholism (NIAAA), and coauthors Drs. Patricia Powell (NIAAA deputy director) and Aaron White ( 2 ). This outstanding article will serve as a foundational knowledge base for those interested in understanding the complex factors that mediate drug addiction. Of particular interest to the practice of psychiatry is the emphasis on the negative affect state “hyperkatifeia” as a major driver of addictive behavior and relapse. This places the dysphoria and psychological distress that are associated with prolonged withdrawal at the heart of treatment and underscores the importance of treating not only maladaptive drug-related behaviors but also the prolonged dysphoria and negative affect associated with addiction. It also speaks to why it is crucial to concurrently treat psychiatric comorbidities that commonly accompany substance use disorders.
Insights Into Mechanisms Related to Cocaine Addiction Using a Novel Imaging Method for Dopamine Neurons
Cassidy et al. ( 3 ) introduce a relatively new imaging technique that allows for an estimation of dopamine integrity and function in the substantia nigra, the site of origin of dopamine neurons that project to the striatum. Capitalizing on the high levels of neuromelanin that are found in substantia nigra dopamine neurons and the interaction between neuromelanin and intracellular iron, this MRI technique, termed neuromelanin-sensitive MRI (NM-MRI), shows promise in studying the involvement of substantia nigra dopamine neurons in neurodegenerative diseases and psychiatric illnesses. The authors used this technique to assess dopamine function in active cocaine users with the aim of exploring the hypothesis that cocaine use disorder is associated with blunted presynaptic striatal dopamine function that would be reflected in decreased “integrity” of the substantia nigra dopamine system. Surprisingly, NM-MRI revealed evidence for increased dopamine in the substantia nigra of individuals using cocaine. The authors suggest that this finding, in conjunction with prior work suggesting a blunted dopamine response, points to the possibility that cocaine use is associated with an altered intracellular distribution of dopamine. Specifically, the idea is that dopamine is shifted from being concentrated in releasable, functional vesicles at the synapse to a nonreleasable cytosolic pool. In addition to providing an intriguing alternative hypothesis underlying the cocaine-related alterations observed in substantia nigra dopamine function, this article highlights an innovative imaging method that can be used in further investigations involving the role of substantia nigra dopamine systems in neuropsychiatric disorders. Dr. Charles Bradberry, chief of the Preclinical Pharmacology Section at the National Institute on Drug Abuse, contributes an editorial that further explains the use of NM-MRI and discusses the theoretical implications of these unexpected findings in relation to cocaine use ( 4 ).
Treatment Implications of Understanding Brain Function During Early Abstinence in Patients With Alcohol Use Disorder
Developing a better understanding of the neural processes that are associated with substance use disorders is critical for conceptualizing improved treatment approaches. Blaine et al. ( 5 ) present neuroimaging data collected during early abstinence in patients with alcohol use disorder and link these data to relapses occurring during treatment. Of note, the findings from this study dovetail with the neural circuit schema Koob et al. provide in this issue’s overview on addiction ( 2 ). The first study in the Blaine et al. article uses 44 patients and 43 control subjects to demonstrate that patients with alcohol use disorder have a blunted neural response to the presentation of stress- and alcohol-related cues. This blunting was observed mainly in the ventromedial prefrontal cortex, a key prefrontal regulatory region, as well as in subcortical regions associated with reward processing, specifically the ventral striatum. Importantly, this finding was replicated in a second study in which 69 patients were studied in relation to their length of abstinence prior to treatment and treatment outcomes. The results demonstrated that individuals with the shortest abstinence times had greater alterations in neural responses to stress and alcohol cues. The authors also found that an individual’s length of abstinence prior to treatment, independent of the number of days of abstinence, was a predictor of relapse and that the magnitude of an individual’s neural alterations predicted the amount of heavy drinking occurring early in treatment. Although relapse is an all too common outcome in patients with substance use disorders, this study highlights an approach that has the potential to refine and develop new treatments that are based on addiction- and abstinence-related brain changes. In her thoughtful editorial, Dr. Edith Sullivan from Stanford University comments on the details of the study, the value of studying patients during early abstinence, and the implications of these findings for new treatment development ( 6 ).
Relatively Low Amounts of Alcohol Intake During Pregnancy Are Associated With Subtle Neurodevelopmental Effects in Preadolescent Offspring
Excessive substance use not only affects the user and their immediate family but also has transgenerational effects that can be mediated in utero. Lees et al. ( 7 ) present data suggesting that even the consumption of relatively low amounts of alcohol by expectant mothers can affect brain development, cognition, and emotion in their offspring. The researchers used data from the Adolescent Brain Cognitive Development Study, a large national community-based study, which allowed them to assess brain structure and function as well as behavioral, cognitive, and psychological outcomes in 9,719 preadolescents. The mothers of 2,518 of the subjects in this study reported some alcohol use during pregnancy, albeit at relatively low levels (0 to 80 drinks throughout pregnancy). Interestingly, and opposite of that expected in relation to data from individuals with fetal alcohol spectrum disorders, increases in brain volume and surface area were found in offspring of mothers who consumed the relatively low amounts of alcohol. Notably, any prenatal alcohol exposure was associated with small but significant increases in psychological problems that included increases in separation anxiety disorder and oppositional defiant disorder. Additionally, a dose-response effect was found for internalizing psychopathology, somatic complaints, and attentional deficits. While subtle, these findings point to neurodevelopmental alterations that may be mediated by even small amounts of prenatal alcohol consumption. Drs. Clare McCormack and Catherine Monk from Columbia University contribute an editorial that provides an in-depth assessment of these findings in relation to other studies, including those assessing severe deficits in individuals with fetal alcohol syndrome ( 8 ). McCormack and Monk emphasize that the behavioral and psychological effects reported in the Lees et al. article would not be clinically meaningful. However, it is feasible that the influences of these low amounts of alcohol could interact with other predisposing factors that might lead to more substantial negative outcomes.
Increased Comorbidity Between Substance Use and Psychiatric Disorders in Sexual Identity Minorities
There is no question that victims of societal marginalization experience disproportionate adversity and stress. Evans-Polce et al. ( 9 ) focus on this concern in relation to individuals who identify as sexual minorities by comparing their incidence of comorbid substance use and psychiatric disorders with that of individuals who identify as heterosexual. By using 2012−2013 data from 36,309 participants in the National Epidemiologic Study on Alcohol and Related Conditions–III, the authors examine the incidence of comorbid alcohol and tobacco use disorders with anxiety, mood disorders, and posttraumatic stress disorder (PTSD). The findings demonstrate increased incidences of substance use and psychiatric disorders in individuals who identified as bisexual or as gay or lesbian compared with those who identified as heterosexual. For example, a fourfold increase in the prevalence of PTSD was found in bisexual individuals compared with heterosexual individuals. In addition, the authors found an increased prevalence of substance use and psychiatric comorbidities in individuals who identified as bisexual and as gay or lesbian compared with individuals who identified as heterosexual. This was most prominent in women who identified as bisexual. For example, of the bisexual women who had an alcohol use disorder, 60.5% also had a psychiatric comorbidity, compared with 44.6% of heterosexual women. Additionally, the amount of reported sexual orientation discrimination and number of lifetime stressful events were associated with a greater likelihood of having comorbid substance use and psychiatric disorders. These findings are important but not surprising, as sexual minority individuals have a history of increased early-life trauma and throughout their lives may experience the painful and unwarranted consequences of bias and denigration. Nonetheless, these findings underscore the strong negative societal impacts experienced by minority groups and should sensitize providers to the additional needs of these individuals.
Trends in Nicotine Use and Dependence From 2001–2002 to 2012–2013
Although considerable efforts over earlier years have curbed the use of tobacco and nicotine, the use of these substances continues to be a significant public health problem. As noted above, individuals with psychiatric disorders are particularly vulnerable. Grant et al. ( 10 ) use data from the National Epidemiologic Survey on Alcohol and Related Conditions collected from a very large cohort to characterize trends in nicotine use and dependence over time. Results from their analysis support the so-called hardening hypothesis, which posits that although intervention-related reductions in nicotine use may have occurred over time, the impact of these interventions is less potent in individuals with more severe addictive behavior (i.e., nicotine dependence). When adjusted for sociodemographic factors, the results demonstrated a small but significant increase in nicotine use from 2001–2002 to 2012–2013. However, a much greater increase in nicotine dependence (46.1% to 52%) was observed over this time frame in individuals who had used nicotine during the preceding 12 months. The increases in nicotine use and dependence were associated with factors related to socioeconomic status, such as lower income and lower educational attainment. The authors interpret these findings as evidence for the hardening hypothesis, suggesting that despite the impression that nicotine use has plateaued, there is a growing number of highly dependent nicotine users who would benefit from nicotine dependence intervention programs. Dr. Kathleen Brady, from the Medical University of South Carolina, provides an editorial ( 11 ) that reviews the consequences of tobacco use and the history of the public measures that were initially taken to combat its use. Importantly, her editorial emphasizes the need to address health care inequity issues that affect individuals of lower socioeconomic status by devoting resources to develop and deploy effective smoking cessation interventions for at-risk and underresourced populations.
Conclusions
Maladaptive substance use and substance use disorders are highly prevalent and are among the most significant public health problems. Substance use is commonly comorbid with psychiatric disorders, and treatment efforts need to concurrently address both. The papers in this issue highlight new findings that are directly relevant to understanding, treating, and developing policies to better serve those afflicted with addictions. While treatments exist, the need for more effective treatments is clear, especially those focused on decreasing relapse rates. The negative affective state, hyperkatifeia, that accompanies longer-term abstinence is an important treatment target that should be emphasized in current practice as well as in new treatment development. In addition to developing a better understanding of the neurobiology of addictions and abstinence, it is necessary to ensure that there is equitable access to currently available treatments and treatment programs. Additional resources must be allocated to this cause. This depends on the recognition that health care inequities and societal barriers are major contributors to the continued high prevalence of substance use disorders, the individual suffering they inflict, and the huge toll that they incur at a societal level.
Disclosures of Editors’ financial relationships appear in the April 2020 issue of the Journal .
1 US Department of Health and Human Services: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality: National Survey on Drug Use and Health 2018. Rockville, Md, SAMHSA, 2019 ( https://www.samhsa.gov/data/nsduh/reports-detailed-tables-2018-NSDUH ) Google Scholar
2 Koob GF, Powell P, White A : Addiction as a coping response: hyperkatifeia, deaths of despair, and COVID-19 . Am J Psychiatry 2020 ; 177:1031–1037 Link , Google Scholar
3 Cassidy CM, Carpenter KM, Konova AB, et al. : Evidence for dopamine abnormalities in the substantia nigra in cocaine addiction revealed by neuromelanin-sensitive MRI . Am J Psychiatry 2020 ; 177:1038–1047 Link , Google Scholar
4 Bradberry CW : Neuromelanin MRI: dark substance shines a light on dopamine dysfunction and cocaine use (editorial). Am J Psychiatry 2020 ; 177:1019–1021 Abstract , Google Scholar
5 Blaine SK, Wemm S, Fogelman N, et al. : Association of prefrontal-striatal functional pathology with alcohol abstinence days at treatment initiation and heavy drinking after treatment initiation . Am J Psychiatry 2020 ; 177:1048–1059 Abstract , Google Scholar
6 Sullivan EV : Why timing matters in alcohol use disorder recovery (editorial). Am J Psychiatry 2020 ; 177:1022–1024 Abstract , Google Scholar
7 Lees B, Mewton L, Jacobus J, et al. : Association of prenatal alcohol exposure with psychological, behavioral, and neurodevelopmental outcomes in children from the Adolescent Brain Cognitive Development Study . Am J Psychiatry 2020 ; 177:1060–1072 Link , Google Scholar
8 McCormack C, Monk C : Considering prenatal alcohol exposure in a developmental origins of health and disease framework (editorial). Am J Psychiatry 2020 ; 177:1025–1028 Abstract , Google Scholar
9 Evans-Polce RJ, Kcomt L, Veliz PT, et al. : Alcohol, tobacco, and comorbid psychiatric disorders and associations with sexual identity and stress-related correlates . Am J Psychiatry 2020 ; 177:1073–1081 Abstract , Google Scholar
10 Grant BF, Shmulewitz D, Compton WM : Nicotine use and DSM-IV nicotine dependence in the United States, 2001–2002 and 2012–2013 . Am J Psychiatry 2020 ; 177:1082–1090 Link , Google Scholar
11 Brady KT : Social determinants of health and smoking cessation: a challenge (editorial). Am J Psychiatry 2020 ; 177:1029–1030 Abstract , Google Scholar
- Cited by None
- Substance-Related and Addictive Disorders
- Addiction Psychiatry
- Transgender (LGBT) Issues

Essay on Addiction
Students are often asked to write an essay on Addiction in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Addiction
Understanding addiction.
Addiction is a strong desire to do something repeatedly, even if it’s harmful. It’s like a brain disease. People can get addicted to different things like drugs, alcohol, or even activities like gambling.
Why People Get Addicted
People can get addicted for many reasons. Some may feel good when they do something, so they repeat it. Others may want to escape from problems or stress. Sometimes, it’s because of peer pressure or trying to fit in.
Effects of Addiction
Addiction can harm a person’s health. It can lead to diseases, mental problems, and even death. It can also ruin relationships and cause problems at work or school.
Overcoming Addiction
Overcoming addiction is hard, but possible. It needs strong willpower and often help from doctors or therapists. Support from family and friends is also important. Remember, it’s okay to ask for help.
Preventing Addiction
To avoid addiction, we should learn about its dangers. It’s also important to make good friends and have healthy habits. Always remember, it’s okay to say no if something doesn’t feel right.
250 Words Essay on Addiction
What is addiction.
Addiction is when a person can’t stop doing something, even if it’s harmful. It can be about drugs, alcohol, games, or even food. The person knows it’s bad but can’t stop. It’s like a strong pull that keeps them going back.
How Does it Start?
Addiction often starts with trying something new. This could be a friend offering a cigarette, or playing a new video game. At first, it seems fun and exciting. But over time, the person starts needing it more and more. It becomes a need, not just a want.
The Impact of Addiction
Addiction can hurt a person in many ways. It can make them sick, or cause problems at school or work. It can also hurt their relationships with family and friends. They may lie or steal to keep doing what they’re addicted to. This can lead to feelings of guilt and shame.
Fighting Addiction
Fighting addiction is hard, but not impossible. It starts with admitting there’s a problem. Then, the person needs help from professionals like doctors or counselors. They can give advice, medicine, or therapy to help the person quit. Support from family and friends is also important.
Remember, it’s okay to ask for help. Everyone struggles with something at some point. With the right help and support, anyone can overcome addiction.
Addiction is a serious problem that can harm a person’s health, work, and relationships. But with help and support, it can be overcome. It’s important to understand addiction so we can help others or ourselves if needed.
500 Words Essay on Addiction
Addiction is a serious issue that affects many people around the world. It is a state where a person cannot stop using a substance or engaging in a behavior, even if it is harmful. The person becomes dependent on the substance or the activity to feel good or normal.
Types of Addiction
Addiction can be of two types: substance addiction and behavioral addiction. Substance addiction involves drugs, alcohol, nicotine, or other substances. Behavioral addiction involves activities like gambling, eating, or using the internet.
Causes of Addiction
There is no single reason why someone becomes addicted. It can be due to a mix of genetic, environmental, and psychological factors. Some people may be more prone to addiction because of their genes. Others may turn to addictive substances or behaviors to cope with stress or emotional issues.
Addiction has a negative impact on a person’s health, relationships, and daily life. It can lead to physical health problems like heart disease or mental health issues like depression. Addiction can also strain relationships with family and friends and make it hard for the person to perform well at school or work.
Overcoming addiction is not easy, but it is possible with the right help and support. This can include professional treatment like therapy or medication, as well as support from loved ones. It is important for the person to learn healthy ways to cope with stress and other triggers that may lead to addictive behavior.
Prevention is key in the fight against addiction. This can involve teaching young people about the dangers of substance use and addictive behaviors. It also means creating supportive environments where people can talk about their struggles and seek help if they need it.
In conclusion, addiction is a complex issue that requires understanding, support, and prevention efforts. It is important for everyone to be aware of the signs of addiction and to seek help if they or someone they know is struggling. Remember, overcoming addiction is possible with the right help and support.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on Actual Self
- Essay on Things To Argue
- Essay on Things That Matter
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Search Menu
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Urban Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Papyrology
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Acquisition
- Language Evolution
- Language Reference
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Religion
- Music and Media
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Science
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Lifestyle, Home, and Garden
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Clinical Neuroscience
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Strategy
- Business Ethics
- Business History
- Business and Government
- Business and Technology
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic Systems
- Economic History
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Behaviour
- Political Economy
- Political Institutions
- Political Theory
- Politics and Law
- Public Administration
- Public Policy
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Developmental and Physical Disabilities Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

- < Previous chapter
- Next chapter >

50 What is Addiction?
Walter Sinnott-Armstrong is Chauncey Stillman Professor in the Department of Philosophy and Kenan Institute for Ethics at Duke University. He is Co-Director of the MacArthur Law and Neuroscience Project and co-investigator at Oxford’s Wellcome Centre for Neuroethics. His current research focuses on moral psychology and neuroscience.
Hanna Pickard, Oxford Centre for Neuroethics, Faculty of Philosophy, University of Oxford, Oxford, UK
- Published: 05 September 2013
- Cite Icon Cite
- Permissions Icon Permissions
Variation in addiction suggests that a good definition will be précising: it should serve a purpose. The authors canvass the various purposes served by a definition of addiction in psychiatric, social, legal, economic, interpersonal and scientific contexts. They argue that addiction is a strong and habitual want that significantly reduces control and leads to significant harm. What counts as significant varies relative to purpose and context. The authors offer a basic account of the nature of control and how and why it can be reduced. The chapter explores the nature of harm and why it is part of the definition. And it concludes by suggesting that progress in understanding addiction depends on bearing in mind the various purposes and contexts of enquiry, together with the common-sense but often neglected point that both control and harm come in degrees.
Clinicians debate whether addiction is a disease ( Heyman 2009 ; Hyman 2005 ; Leshner 1997 ; Pickard and Pearce, in press ). Philosophers and lawyers argue about whether addicts are morally or legally responsible ( Sinnott-Armstrong, in press ). Scientists disagree about which drug users to include in experimental studies of addiction. People wonder whether their friends or they themselves are addicted—and what that means. None of these issues can be settled until we determine what addiction is. That is the task of this chapter.
The Challenge
It is not easy to define addiction. One problem is that addiction takes many forms. There is wide variation in who is addicted, what they are addicted to, and the precise form, health effects, and motivation for the addiction.
Paradigmatic addictive substances are illegal drugs, including heroin, cocaine, morphine, barbiturates, and amphetamines. People can also become addicted to legal drugs, including alcohol, nicotine, caffeine, and prescribed medications, such as benzodiazepines and hypnotics (including Z drugs, as they are commonly known). In addition, popular culture and expert opinion increasingly count forms of behavior as addictions: for instance, gambling, sex, work, food, shopping, and Internet surfing or gaming (cf. Ross 2008 ). Propensity and rate of drug use leading to addiction varies across population group and kind of substance. Substances also differ with respect to health risks: from lung cancer and sclerosis of the liver, to malnutrition and risk of mental illness. The existence and nature of withdrawal symptoms also vary across kind of substance and, no doubt, individual addict. Physical withdrawal from heroin is comparable to a bad flu. In contrast, cocaine withdrawal is more like depression, with loss of energy and interest. Alcohol withdrawal is the most severe, with risk of hallucinations, delirium tremens, and death.
There is also variation in who gets addicted. Addiction occurs across levels of socioeconomic status (SES), intelligence (IQ), and education. Still, rates of addiction are positively correlated with low SES, low IQ, adolescence and early adulthood, childhood abuse, stress, psychiatric disorders (in particular, personality disorders), and religion (unsurprisingly, Mormons don’t get addicted as often as others).
In addition, the motivation for drug use varies. Müller and Schumann (2011) identify the following eight goals of non-addictive consumption: (1) improved social interaction, (2) facilitated sexual behavior, (3) improved cognitive performance, (4) coping with stress, (5) alleviating psychiatric symptoms, (6) novel perceptual and sensory experiences, (7) hedonia or euphoria, and (8) improved physical and sexual appearance. Many of these motivations may survive once consumption becomes addiction ( Pickard 2011 ). Further, once addicted, people may use drugs to maintain normal functioning and avoid withdrawal, as when former heroin addicts take up methadone maintenance.
Such variation issues a challenge to define addiction. A definition needs to specify what is common and peculiar to all these cases that make them count as cases of addiction. We need a definition to know what addiction is.
Definitions
Just as there are various kinds of addiction, so too there are various kinds of definition. When a definition is required, especially in philosophy or science, we need to establish the kind needed (Sinnott-Armstrong and Fogelin 2009).
Dictionary definitions report common usage. However, common usage can be very loose and vague, so dictionary definitions are often useless or misleading in philosophy and science. Stipulative definitions are likely to be more precise, but, because they are stipulative, they too may be useless or misleading. When we ask what addiction is, we need a definition that is neither a dictionary definition nor a stipulative definition. Instead, we need what is called a precising (or sometimes theoretical) definition.
A precising definition picks out a relatively precise class of conditions that lies within the limits of common usage (and so is not arbitrarily stipulative) but does not reflect all the vagueness of common usage (and so is not a dictionary definition). The goal of precising definitions is to be useful, either theoretically or practically. This pragmatic element in precising definitions might seem unusual, but it is not. The purpose of the standard definition of water as H 2 O is to simplify theories of chemical bonding. For this reason, the definition is neutral with respect to the exact isotopes of hydrogen and oxygen, for isotopes are not relevant to chemical bonding. Similarly, precising definitions of death may be chosen partly for their usefulness in medicine, or, alternatively, moral theories. Precising definitions cannot stray too far from common usage if they are not to mislead. Nor should they conflict with our best scientific or theoretical understanding of the subject matter if they are to be accurate. But they are judged in large part by their usefulness, relative to a particular purpose.
The question we must therefore ask is: Which purposes should a precising definition of addiction serve? The answer is: several. Clinicians need to decide whom to treat. They need a definition of addiction that is relevant to that aim. Health insurance companies need to decide for whom they are willing to pay for treatment. The goals of insurers are, of course, not always consonant with the goals of treatment. Law courts need to decide whether a defendant is criminally responsible and so should be held straightforwardly accountable before the law and potentially imprisoned, or whether they should be remanded to a treatment program. These courts will have different purposes than clinicians or insurers. Scientists who study addiction want a definition that allows them to collect data in ways that enable precise scientific generalizations and theories. Finally, individuals need to decide how to think and feel about friends and family members who abuse drugs. Personal relationships can be affected significantly according to whether or not a person is seen as addicted. The definitions resulting from these various purposes can inform one another. They can also potentially, at least to some degree, conflict. But the purposes are all legitimate in their particular context.
As a result, there may be multiple definitions of addiction, each appropriate to different purposes and contexts. Or, if there is a single definition, it will need to include a variable term like “significant” that gets filled in differently in different contexts. (That is the kind of definition that we will propose here.) Either way, it is important to keep this pragmatic issue in mind in assessing various proposed definitions of addiction.
The Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR; American Psychiatric Association 2000 ) defines substance dependence (which is synonymous with addiction) thus:
A maladaptive pattern of substance use, leading to clinically significant impairment or distress, as manifested by three (or more) of the following, occurring at any time within the same 12-month period: (1) tolerance (2) withdrawal (3) using more than was intended (4) persistent desire or unsuccessful efforts to control use (5) a great deal of time spent obtaining, using, or recovering (6) reduction in other important activities because of use (7) continued use despite knowledge of its causing a persistent or recurrent physical or psychological problem.
This definition was formulated by a committee of leading experts for use by practicing psychiatrists and clinicians.
This definition is useful for at least one clinical purpose. If a prospective patient has three or more of these symptoms, along with “clinically significant impairment or distress,” that could be a reasonable basis for treating the individual for addiction. It could also justify inclusion of addiction as a condition that we expect health insurers to cover and public health providers, such as the UK National Health Service, to treat. After all, people with three or more of these symptoms, leading to clinically significant impairment or distress, need help, which psychiatrists and clinicians may be in a position to provide.
The difficulty is that the polythetic nature of this definition means that very different patterns of substance use and attendant problems will all count as addiction. This limits this definition’s capacity to fulfill another core clinical purpose of diagnosis, namely, to establish prognosis and indicate treatment course. For instance, compare (a) a drug user who develops tolerance and withdrawal, who spends a great deal of time obtaining drugs and correspondingly reduces other important activities, and whose anxiety about ensuring a regular supply of drugs reaches clinically significant proportions, but who has no other symptoms—no overuse, no unsuccessful efforts to stop, no clear recognition of the connection between use and anxiety; with (b) a drug user who routinely uses more than intended, makes unsuccessful efforts to control use, and continues use despite knowledge of its causing persistent and recurrent physical and psychological problems which together lead to clinically significant impairment and distress, but who has no other symptoms—no increased tolerance, withdrawal, or reduction in other activities, and little time spent obtaining, using, or recovering.
From a clinical perspective, both patients should be treated. But appropriate treatment is symptom dependent. In the first case, treatment (depending on the drug of abuse) is likely to require medically supervised gradual reduction in use and management of withdrawal symptoms, medication and/or cognitive behavioral therapy for anxiety, and life skills coaching for developing replacement activities. In contrast, the treatment for the second case is unlikely to require medical supervision, as opposed to any number of therapeutic interventions designed to improve control, develop strategies for relapse prevention, increase self-esteem and self-worth, and identify and address any underlying reasons for use as well as the attendant physical and psychological problems. In short, because of the polythetic nature of the diagnostic criteria, the DSM-IV-TR does not offer a unified set of diagnostic criteria for addiction. This limits its capacity to establish prognosis and indicate treatment course. Of course, clinicians take case histories, and in that context they can tailor treatment to individual needs. Nonetheless, this disunity suggests that the definition could in principle be improved in order to better serve clinical practice.
It also means that the DSM-IV-TR definition of substance dependence cannot adequately serve scientists who study the neural bases or psychological mechanisms of addiction, or philosophers who are interested in whether addicts are appropriately held responsible for their drug-connected and drug-consequent behavior. There is likely to be too much variety among individual addicts diagnosed with substance dependence according to the DSM-IV-TR for science to discern a unified set of neural bases and psychological mechanisms, or for philosophers to construct any unified, general principles for responsibility ascriptions to addicts. For the purposes of scientists and philosophers, then, we also need a different definition.
Philosophical definitions of addiction tend to be pithy. Foddy and Savulescu define it thus: “An addiction is a strong appetite” (2010, p. 35). Of course, we now need to know what an appetite is. They define an appetite as: “a disposition that generates desires that are urgent, oriented toward some rewarding behavior, periodically recurring, often in predictable circumstances, sated temporarily by their fulfillment, and generally provide pleasure” ( Foddy and Savulescu 2010 , p. 35). So much for pithiness. Note that this definition does not restrict addiction to substances: arguably, as mentioned earlier, the appetite could be for gambling, sex, work, food, shopping, or the Internet (cf. Foddy 2011 ).
From a scientific or philosophical point of view, this definition does have some advantage over that in DSM-IV-TR. It enables scientists to seek the neural bases and psychological mechanisms for such strong appetites, and philosophers to ask whether people are responsible for what they do as a result of such strong appetites.
Nonetheless, Foddy and Savulescu’s definition is too narrow. To see why, it is useful to import the distinction between liking and wanting as developed by the theory of incentive sensitization ( Robinson and Berridge 1993 ). We engage in some activities because we get pleasure or reward from them. In short, we like them. For example, many people like watching comedies, or eating ice-cream, or physical thrills. But we also engage in some activities because we are motivated to do them regardless of whether we expect to get any pleasure or reward from them. In short, we may want to do them, but not because we like to do them. These motivations may be various, but, in the case of addiction, the theory is that addictive wants are triggered by drug-related cues that have become associated through sustained, heavy use with consumption: they are perhaps not unlike the desires of a salt-deprived rat for salty water. The salty water does not taste good even to the rat: the rat does not like the water. But it nonetheless wants the water very much ( Robinson and Berridge 1993 ).
Foddy and Savulescu’s definition of appetite seem to combine liking with wanting. They mention “rewarding behavior” and “pleasure,” so liking seems essential to addiction on their account. But then their phrase “a disposition that generates desires that are urgent” sounds more like the wants of a salt-deprived rat. Hence, they seem to require that addicts both (strongly) like and (strongly) want to use drugs.
This double requirement is a problem, because some extreme addicts report no longer liking the drugs that they nonetheless want. Perhaps that is why Foddy and Savulescu add “generally” before “provide pleasure” in their definition, since people in general do get pleasure from drugs. However, Foddy and Savulescu’s definition is also too broad, because it fails to distinguish addiction from heavy use based on strong desire. One of us has a disposition that generates urgent desires to play golf, and those desires periodically recur in predictable circumstances: when the sun shines. The desired activity generally provides pleasure: playing golf is rewarding. And the desire can be sated temporarily: playing eighteen holes usually does it. According to Foddy and Savulescu’s definition, this desire counts as a strong appetite to play golf and hence as an addiction to golf. However, although golf might be as good a candidate as any for a behavioral addiction, if there is any, this case is not an addiction to golf. The author in question has no difficulty quitting, when it rains or even when it shines (if there is a good reason not to play golf), and playing golf does not cause significant personal harm or risk of harm (unlike skiing). In these ways, the author’s relationship to golf is substantially different from a heroin addict’s relationship to his needle (for discussion of that relationship, see Pates and McBride 2005 ).
Thus, Foddy and Savulescu’s definition hides important differences and does not capture the core of our common understanding of addiction, for it allows far too much to count. Foddy and Savulescu might be happy to include regular golfers as addicts, but a precising definition needs to distinguish a strong appetite for golf leading to “heavy golf use” from heroin addiction in order to capture common usage, let alone prove theoretically useful to scientists and philosophers.
What is the difference between heavy use and addiction? A natural answer is: control. The importance of control in understanding addiction is reflected in three of the diagnostic criteria of the DSM-IV-TR definition given earlier: (3) using more than was intended, (4) persistent desire or unsuccessful efforts to control use, and (7) continued use despite knowledge of resulting persistent or recurrent physical or psychological problems. It is equally present in common understanding and testimony. To take one famous example, Burroughs (1959 , xxxix) says that “dope fiends” are “not in a position to act in any other way” and “cannot act other than they do.” Indeed, the reason why the strong appetite for golf described earlier seems not to count as addiction is that the author can stop playing or can play less.
What exactly does it mean to say that addicts cannot stop taking drugs? At one end of the spectrum of possible interpretations lies the “cannot” of hard determinism. Hard determinists often claim that nobody can act in any way other than they do. Here “cannot” means something like: holding fixed the laws of nature and past history, only one future course of events can obtain.
This use of “cannot” does not violate any semantic rules, but it does not shed any light on addiction. It cannot distinguish addicts from non-addicts, since addicts are no more or less determined than anyone else. So, whatever it means to say that addicts lack the ability to stop taking drugs, it cannot mean that their behavior is determined by the laws of nature and past history.
At the opposite end of the spectrum, the term “cannot” is also used in statements like this: “I cannot go out tonight, because I have to work.” This use of “cannot” does not deny that one has the physical and psychological ability to go out. All it denies is that one has good enough reason. The point is that it would be irrational or at least irresponsible to go out, given the greater importance of work. No doubt, some addicts might claim that they cannot quit using drugs because it would be irrational or irresponsible for them to quit (perhaps because their gang will kill them or their family if they stop using drugs). However, that is not what addicts normally mean when they claim to lack the ability to stop. They do not seem to mean that they have the physical and psychological ability but lack good enough reason to quit (but see Pickard 2011 , 2012 for a dissenting view).
Then what does it mean to say that addicts lack the ability to stop or that they cannot stop taking drugs? Burroughs exaggerates when he claims that he cannot act “in any other way,” but there is a grain of truth beneath his exaggeration. The truth is that his physical and psychological ability to control his use is reduced: he lacks the degree of control that we normally expect people to have over their behavior.
So, what is control? Two accounts are common. One focuses on wants and claims that an agent has control over a type of action if and only if:
If they want overall to perform that type of action, then usually they do it; and
If they want overall not to perform that type of action, then usually they don’t do it.
On this account, golfers have control over playing golf if and only if they usually play golf when they want overall to play golf and usually do not play golf when they want overall not to play golf. The qualification “usually” is necessary because they might fail to play golf when they want to because the only golf course is closed or their car breaks down or they miss their starting time. Occasional lapses do not prove lack of control. Similarly, the qualification “overall” is necessary because desires can conflict. If a golfer decides not to play, even though he has some desire to play, because he has a stronger desire to go swimming, then the golfer still has control over whether he golfs or swims. First-order desires (to golf) can also conflict with second-order desires (not to desire to golf). Such conflict and ambivalence can produce significant uncertainty, confusion, oscillation, and, hence, unclarity about what an agent in fact wants overall or how they or we could ever come to know what they want overall. ( Holton and Schute (2007) offer a similar account of control that is based on overall judgments rather than wants.)
Such want-based accounts of control contrast with reasons-responsiveness accounts (cf. Duggan and Gert 1979 ; Fischer and Ravizza, 1998 ). On this kind of account, an agent has control over a type of action if and only if:
If they have a strong overall reason to perform that type of action, then usually they do it; and
If they have a strong overall reason not to perform that type of action, then usually they don’t do it.
On this account, golfers have control over playing golf if and only if they usually play golf when they have strong overall reason to play golf and usually do not play golf when they have strong overall reason not to play golf.
These accounts might seem very close, especially to internalists who assume that all reasons are based on desires ( Williams 1979/1981 ). However, these accounts come apart in various cases that are relevant to addiction. First, if agents have no reason to fulfill some desires, then those agents can act on their desires without being responsive to reasons. For example, some heavy users claim that they want drugs in the sense of having a strong desire even though they no longer like them or get any pleasure from them (and also would not suffer withdrawal if they quit). If so, these users might have control over their drug use on the want-based account because they take drugs when they want to and cease when they want not to. However, such users would lack control on reasons-responsiveness accounts if they continue to use drugs because of their strong wants even when they know that they have little or no reason to use drugs and strong reason not to use drugs.
These accounts of control also come apart in another kind of situation: Imagine that a desire to take drugs causes a user to think only about drugs and then forget about or not notice conflicting considerations, such as detrimental effects on self or loved ones. This user would want not to take drugs if he paid attention to the reasons not to take drugs, but his desires for drugs prevent him from becoming aware of those conflicting considerations (at least at the time when he takes drugs), so he does not actually want not to take drugs. Then it can be true that he takes drugs when he wants and does not take drugs when he wants not to take drugs, so he has control on the want-based account. Nonetheless, he lacks control on the reasons-responsiveness account, because he does not respond to the reasons that he never notices or becomes aware of. (It still might be true that he would respond to reasons that he did notice, so he would have control on a third account that adds “they know” before “they have” in (1′) and (2′).)
It is not completely clear which of these accounts of control is most appropriate for a definition of addiction. Here we will usually talk in terms of what the agent wants overall, because it is a less philosophically technical and controversial notion than reasons, and one can have control over irrational or less-than-perfectly rational behavior. Nonetheless, fans of reasons-responsiveness may recast our discussion into their favored terms, if they want.
With this rough account of control in place, we can now see how various factors can remove or reduce control. Consider an analogy. Suppose that one wants overall (or has and recognizes a strong reason) to lift a heavy weight off the floor for a substantial period of time. If so, how could one fail to lift the weight for that time? Putting aside extreme situations, such as death, external restraint, or changes in the laws of nature, a number of more ordinary factors can affect one’s agency. Most obviously, one might not be strong enough to lift that much weight, either because the weight is too heavy or because one is weakened by disease. In addition, one might get tired of holding up the weight. Or one’s attention might lapse or, alternatively, one’s attention may become fixed on the relief that would come from putting the weight down. Or one might not try hard enough or exert enough willpower, possibly because of some conflicting desire that persists despite one’s overall desire to hold up the weight or because one’s self-conception is decidedly not as a weight-lifter. These factors correspond to the kinds of factors that reduce control over drug use (for further discussion of some of these factors, see Pickard 2012 ; Pickard and Pearce, in press ).
First, the desire to use drugs can become strong and habitual. Immoderate long-term drug use can affect neural mechanisms. Many drugs directly increase levels of synaptic dopamine, which, over time, may affect normal processes of associationist learning related to survival and the pursuit of rewards (for a review, see Hyman 2005 ). Once drug-related pathways are thus established, cues associated with the drug use cause addicts to be motivated to pursue the reward of drugs to an unusually strong extent. Moreover, there is increasing evidence that as drug use escalates, control devolves from the prefrontal cortex to the striatum, in line with a shift from action-outcome to stimulus-response learning (for a review, see Everitt and Robbins 2005 ). Drug use becomes increasingly habitual: more wanted than liked, more automatic than deliberately chosen. Acting against strong and habitual desire requires willpower: an active attempt to resist the pull of the drug (cf. Levy 2010 ).
Second, it takes effort and resolve to keep exercising willpower. Exercising willpower depletes its strength in the short term but can increase it in the long term, much like a muscle ( Muraven and Baumeister 2000 ). The longer willpower is exercised, the more depleted resources may become. So, the need for addicts to persevere in resisting the desire to use drugs, especially in the face of strong associations and cues, may weaken their willpower, potentially to depletion. This is one reason why many clinical interventions require addicts to remove themselves from their habitual environment, or at least identify and as much as possible steer clear of drug-related triggers.
Third, attention and cognition affect the capacity for long-term control. In addition to affecting strength of desire and habit, drug associations and cues may cause intrusive, incessant, obsessional drug-related thinking. This in turn may make it very difficult for addicts to recall and attend to non-drug-related desires and values or to the positive consequences of abstinence and the negative consequences of use. This may produce a “judgment-shift” whereby, faced with immediate temptation, prior resolutions are abandoned on the ground that they do not express present desires and values. Addicts overestimate the benefits of using drugs (including the pleasure or relief they will get) and the costs of not using (including the likelihood and intensity of cravings and withdrawal pains); and underestimate the harms of using (including health effects) and the benefits of not using (including the value of other activities as well as friends). They also seem to discount the future in extreme ways: hyperbolically ( Ainslie 2001 ). And some addicts fail to take in or use information about fictive losses—losses in what they would have gained if they had acted differently—that is relevant to rational choice (see Chiu et al. 2008 on smokers).
Fourth, an addict who resolves to stop using drugs will still experience some motivational conflict with the appetite that constitutes their addiction. Even if they want overall to stop using, the desire for drugs does not thereby disappear. This is why techniques such as motivational interviewing can be clinically helpful to motivate some addicts to change: the aim is to explore and resolve ambivalence, highlighting the positive consequences of abstinence and the negative consequences of use.
Moreover, abstinence for many addicts requires undergoing withdrawal symptoms, which may be physically unpleasant, or even life threatening in certain cases if they do not seek medical advice and management. In addition, for many addicts, drug use may provide relief from life’s various miseries, especially strong negative emotions and other psychopathological symptoms (for discussion, see Pickard 2012 ; Pickard and Pearce, in press ). Until alternative methods of coping have been learned or the underlying distress alleviated, the psychological cost of abstinence is high. There can also be positive consequences associated with addiction, such as the possibility of status, role, and community within an established drug culture and network, and the corresponding construction of a positive self-conception. Many addicts have lost family and friends due to their addiction, so they might have few social and employment opportunities outside of the drug culture and community. The costs of forsaking drugs is then potentially very high, unless and until alternative, comparable goods within a non-drug-using culture and community are on offer.
These factors, in combination, show how or why control can be reduced in addiction. Desires for drugs can be strong and habitual. Willpower can get depleted. Drug-related associations and cues can affect cognition and attention. Drug use may serve psychological, social, and economic functions that produce motivational conflicts and oscillations. For all these reasons, even if heavy users want overall (and recognize strong reasons) to abstain, they still might not usually abstain, and then their control is understandably diminished.
We can now add control to the definition of addiction: Addiction is a strong and habitual want that significantly reduces control. To say that the strong and habitual want causes the reduction in control is not to say that it is the sole cause. As detailed earlier, multiple factors, in combination, often contribute to diminished control. It is important to remember that the strong and habitual want is usually only part of what causes the reduction in control.
Notice that this definition applies equally to the majority of addicts who are ambivalent and, at least on occasion, try unsuccessfully to control their use, and also to those “willing addicts” who endorse their addiction and never try to control their use ( Frankfurt 1971 ). What makes “willing addicts” willing is that they want overall to use drugs; so they do what they want overall to do when they use. Nonetheless, if ex hypothesis they became “unwilling” and no longer wanted to use (or if they came to recognize strong overall reasons not to use), then they would still use at least usually. This is what makes “willing addicts” addicts.
Notice also that control comes in degrees, depending on the range of situations in which the agent acts in accordance with wants or reasons. Thus, control can be reduced without being extinguished completely. For addiction, the reduction or loss must be significant. This notion of significance cannot be captured in a purely descriptive statistical way. Any measure of standard deviation from the mean level of control in the general population could only be arbitrarily selected as defining significance. Instead of being purely mathematical, the notion of significance at stake is pragmatic. This should not be surprising given the essential pragmatic function of precising definitions (discussed earlier). Within legal contexts, both criminal and civil, degree of control is relevant to legal responsibility; in psychiatric contexts, degree of control is relevant to decisions about diagnosis and treatment; in family and friendship, degree of control may be relevant to the possibility of sustaining relationships despite harm perpetrated toward self and others. More generally, we suggest that it is appropriate to count heavy drug use as a case of addiction if the degree of control falls below the degree of control that captures what is at stake in making a judgment about addiction in that context. Hence the definition of addiction as a strong and habitual want that significantly reduces control must be understood as a precising definition. It is to be judged in large part by its usefulness, relative to a particular purpose, in yielding a verdict on what counts as addiction and who is an addict. No doubt, the verdict may shift from context to context, according to what is at stake. Nonetheless, the general principle on which these various verdicts are based is consistent across contexts: the question in each case is whether the reduction in control is significant in the context.
This definition of addiction still might seem to lack an essential element. Desire and loss of control are, after all, also often associated with romantic love. Head over heels in love, one can become single-minded, obsessed, and devoted at the expense of many other goods.
Nonetheless, love differs in at least one crucial way from drugs and behaviors that many count as addictions. Only in extreme and unusual circumstances is love genuinely dangerous. Addictions, in contrast, typically cause serious harm to self. This is reflected in the DSM-IV-TR definition, which requires distress or impairment for addiction. In other words, it is only when a condition normally causes harm that it counts as an addiction.
Is the reference to harm essential? A critic might object that some addictions can be harmless. For instance, consider the following cases. Sue has a strong desire for alcohol and would find it extremely difficult to stop or even reduce her drinking if she tried. Nonetheless, her drinking does not seem to affect her life adversely. She works for a company where her colleagues go out for several drinks every day after work. Drinking with them improves Sue’s social and professional life in various ways. If she didn’t drink with these colleagues, she would not be as professionally successful. Or consider Joe, who is a gambler. He, too, would struggle to stop or reduce the frequency and time spent gambling, so he lacks control over whether or not he gambles. Nonetheless, he successfully controls which games he plays and which bets he places. He plays games of skill, like poker, rather than games of pure chance, like slot machines. Joe is very good at gambling. He plays games that he can win, and he wins a lot. He ends up richer and happier than he would be if he did not gamble so much. Moreover, he probably would not gamble so much were he not addicted to gambling.
How should we diagnose Sue and Joe? There are three possibilities. One possibility is that Sue and Joe are not addicts because they are not harmed by their behavior. A second possibility is that Sue and Joe are addicts, but, because they are not harmed by their behavior, that shows that addictions are not all harmful. A third possibility is that Sue and Joe are addicts who are harmed by their conditions, despite their happiness and successes in business and gambling.
According to this third possibility, what distinguishes successful addicts, like Sue and Joe, from their counterparts, who are equally successful but not addicted to alcohol or gambling, is simply that Sue’s and Joe’s control is significantly reduced. Such diminution of control can arguably count as harmful in itself. One reason is that, in nearby possible worlds with only minor differences in circumstances, Sue’s and Joe’s behavior causes them substantial harm. If Sue’s company is bought by teetotalers, then her inability to control her drinking could cost her her job. If Joe fell in love with a woman who disliked gambling, his inability to control his gambling could cost him his happiness. Diminished control thus brings a substantial risk of further harm if it avoids harm only in a very narrow environmental niche. This risk of harm can itself arguably count as a harm. If it is, then Sue and Joe do not present counterexamples to the claims that addictions cause harm.
On this third view, it is not necessary to add any clause about harm to the definition of addiction, because the loss of control will already ensure risk of harm at a minimum. Nonetheless, to be explicit, we will expand our precising definition to say that an addiction is a strong and habitual want that significantly reduces control and leads to significant harm. As before, to say that the want and reduction in control cause harm is not to say that they are the sole causes. Many factors typically contribute to the harms of addiction.
In this definition, harm includes death, pain, distress, and dysfunction, as well as substantial risk of these within a normal environment. Like control, harm comes in degrees, and disagreement may occur as to when the degree of harm or degree of risk of harm counts as significant. Some cases will be clear, as when drug use results in death. Other cases will be unclear, as when Sue’s and Joe’s reduced control creates or constitutes risk of unhappiness. In unclear cases, verdicts may depend on context and purpose. For instance, Joe’s risk of harm may not be significant enough for psychiatric treatment to be compulsorily imposed as opposed to made available should he choose it, but it may be significant enough to the woman he counterfactually loves to cause her not to love him in return.
Many definitions leave scope for disagreement as to how and when they apply to individual cases. This caveat is especially true of precising definitions in general and of our precising definition of addiction in particular. Nonetheless, this definition can still provide a consistent principle for determining what counts as addiction across different contexts and cases.
One final advantage of this definition is that it does not apply to normal romantic love, which does not lead to significant harm. It thus captures the intuitions expressed in common usage of the term, which distinguishes addictions from other extreme forms of behavior in part on the basis of harm. Note that, interestingly, it might apply to the kind of love that sometimes ties an abused woman to her abusive partner. But this kind of love—if love indeed it is, as opposed to fear or coercion—is arguably pathological. In contrast to normal romantic love, it is not obviously wrong to see such love as a form of addiction. In this case, perhaps the exception proves the rule.
Addiction is a strong and habitual want that significantly reduces control and leads to significant harm. Control and harm come in degrees. Addicts have some control over their choices and actions, but they do not have full or normal control; and hence they have less control than non-addicts (including non-addicted drug users).
This point about degrees of control and harm might seem obvious and innocuous, but it undermines many traditional debates. There is a long-standing debate about whether or not addiction is a form of compulsion (see, e.g., Charland 2002 ; Foddy and Savulescu 2006 ; Leshner 1997 ; Levy 2010 ; Pickard 2012 ; Pickard and Pearce, in press ). Those who deny that addiction is a form of compulsion and claim that addicts have control seem to require a lot for compulsion and only a little for control. Those who claim that addiction is a form of compulsion and claim that addicts lack control seem to require a lot for control and a little for compulsion. One way to resolve this debate is to recognize that it may be fruitless: the debate is arguably about whether this particular glass is half-full or half-empty, when obviously it is both. The point about control and harm coming in degrees allows us to move forward: addiction is a form of compulsion to the degree that an addict lacks control.
Another long-standing debate is over whether addiction is objective or subjective. This debate can also be resolved by recognizing that, even if degrees of control and harm exist independently of our purposes, our purposes can still determine where we should draw a line between significant and insignificant harms and losses of control and, hence, between addicts and non-addicts. Compare vision. Optometrists can determine whether a person’s eyesight is 20–20, 20–30, 20–40, or 20–400; as well as whether a person is colorblind, nearsighted or far-sighted, or has less than usual night vision. Still, optometry by itself cannot define when visual acuity is sufficient to get a license to drive a car or a bus, to pilot a plane, to get disability benefits, or to serve in the military or the police. The lines between adequate and inadequate vision are drawn at different places for different practical purposes, depending on the likelihood and harms of different kinds of mistakes in different circumstances.
The same goes for lines between addicts and non-addicts. As we have emphasized, clinicians, insurers, courts of law, friends and family, and scientists have various purposes. Courts may draw the line relatively high in order to count fewer people as addicts and thereby hold more people responsible for crimes. Insurers also may wish to count as few as possible as addicts, so that they will have to pay for as few claims as possible. Private citizens, in contrast, might draw the line relatively low in order to count more of their friends as addicts so that they can find more ways of maintaining good relations and offering care and support when relationships flounder due to drug use. Clinicians may draw the line in the middle, with regard to who is most likely to benefit from treatment. And scientists might draw the line between addicts and non-addicts so as to discover the highest correlations with neural or psychological mechanisms or genetic or environmental factors.
This variation in where the line between addicts and non-addicts should be drawn may be confusing if the rationale behind it is not explicit. But there is nothing illegitimate about drawing the line at different places for different purposes (compare again visual acuity). We simply need to be explicit about what we are doing and avoid the temptation to ask and answer overly simplistic questions about whether or not a person is really an addict. Instead, we must ask about the degree of diminished control and harm they suffer and about whether or not, given the particular context and what is at stake, we are justified in counting a person an addict. Such questions are often very difficult to answer, especially in contexts where time is limited and practical consequences are real. Nonetheless, good practice in all contexts where questions of addiction arise—from the courts to the clinic, from the personal to the laboratory—demands that we recognize that control and harm come in degrees and that judgments about where to draw the line between addicts and non-addicts can be made only relative to particular contexts and purposes.
Ainslie, G. ( 2001 ). Breakdown of Will . New York, NY: Cambridge University Press.
Google Scholar
Google Preview
American Psychiatric Association. ( 2000 ). Diagnostic and Statistical Manual of Mental Disorders , Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association.
Burroughs, W. S. ( 1959 ). Naked Lunch . New York, NY: Grove Weidenfeld.
Charland, L. ( 2002 ). Cynthia’s dilemma: consenting to heroin prescription. American Journal of Bioethics , 2(2), 37–47.
Chiu, P. H. , Lohrenz, T. M. , and Montague, P. R. ( 2008 ). Smokers’ brains compute, but ignore, a fictive error signal in a sequential investment task. Nature Neuroscience , 11(4), 514–20.
Duggan, T. and Gert, B. ( 1979 ). Free will as the ability to will. Nous , 13, 197–217.
Everitt, B. J. and Robbins, T. M. W. ( 2005 ). Neural systems of reinforcement for drug addiction: from actions to habits to compulsion. Nature Neuroscience , 8, 1481–9.
Fischer, J. M. and Ravizza, M. ( 1998 ). Responsibility and Control: A Theory of Moral Responsibility . Cambridge: Cambridge.
Foddy, B. ( 2011 ). Addicted to food, hungry for drugs. Neuroethics , 4(2), 79–89.
Foddy, B. and Savulescu, J. ( 2006 ). Addiction and autonomy: can addicted people consent to the prescription of their drug of addiction? Bioethics , 20(1), 1–15.
Foddy, B. and Savulescu, J. ( 2010 ). Relating addiction to disease, disability, autonomy, and the good life. Philosophy, Psychiatry, & Psychology , 17(1), 35–42.
Frankfurt, H. ( 1971 ). Freedom of the will and the concept of a person. Journal of Philosophy , 68, 5–20.
Gert, B. ( 2005 ). Morality: Its Nature and Justification . New York, NY: Oxford University Press.
Heyman, G. ( 2009 ). Addiction: A Disorder of Choice . Cambridge, MA: Harvard University Press.
Holton, R. and Schute, S. ( 2007 ). Self-control in the modern provocation defence. Oxford Journal of Legal Studies , 27(1), 49–73.
Hyman, S. ( 2005 ). Addiction: A disease of learning and memory. American Journal of Psychiatry , 162, 1414–22.
Leshner, A. I. ( 1997 ). Addiction is a brain disease, and it matters. Science , 278(5335), 45–7.
Levy, N. ( 2010 ). Addiction and compulsion. In T. O’Connor and C. Sandis (Eds), A Companion to the Philosophy of Action , pp. 267–73. Oxford: Blackwell.
Müller, C. and Schumann, G. ( 2011 ). Drugs as instruments—a new framework for nonaddictive psychoactive drug use. Behavioral and Brain Sciences , 34(6), 293–310.
Muraven, M. and Baumeister, R. F. ( 2000 ). Self-regulation and depletion of limited resources: Does self-control resemble a muscle? Psychological Bulletin , 126, 247–59.
Pates, R. , McBride, A. , and Arnold, K. (Eds) ( 2005 ). Injecting Illicit Drugs . Oxford: Blackwell.
Pickard, H. ( 2011 ). The instrumental rationality of addiction. Behavioral and Brain Sciences , 34(6), 320–1.
Pickard, H. ( 2012 ). The purpose in chronic addiction. American Journal of Bioethics Neuroscience , 3(2), 40–9.
Pickard, H. and Pearce, S. ( in press ). Addiction in context: Philosophical lessons from a personality disorder clinic. In N. Levy (Ed.), Addiction and Self-Control . New York, NY: Oxford University Press.
Robinson, T. E. and Berridge, K. C. ( 1993 ). The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Research , 18(3), 247–91.
Ross, D. , Sharp, C. , Vuchinich, R. E. , and Spurrett, D. ( 2008 ). Midbrain Mutiny: The Picoeconomics and Neuroeconomics of Disordered Gambling . Cambridge, MA: MIT Press.
Sinnott-Armstrong, W. ( in press ). Are addicts responsible? In N. Levy (Ed.), Addiction and Self-Control . New York, NY: Oxford University Press.
Sinnott-Armstrong, W. and Fogelin, R. ( 2010 ). Understanding Arguments: An Introduction to Informal Logic , Eighth Edition. Belmont, CA: Wadsworth.
Williams, B. (1979). Internal and external reasons. (Reprinted in Williams, B. ( 1981 ). Moral Luck , pp. 101–113. Cambridge: Cambridge University Press.)
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Home — Essay Samples — Nursing & Health — Drug Addiction — Drug Addiction: Choice or Disease?
Drug Addiction: Choice Or Disease?
- Categories: Drug Addiction Drugs
About this sample

Words: 677 |
Published: Sep 16, 2023
Words: 677 | Page: 1 | 4 min read
Table of contents
The choice argument, the disease model, psychological and sociological factors, a holistic perspective.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr. Karlyna PhD
Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
4 pages / 1976 words
4 pages / 1634 words
3 pages / 1587 words
4 pages / 1991 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Drug Addiction
Drug addiction has been a significant issue worldwide for many decades, impacting not only individuals addicted to illegal substances but also the society surrounding them. This essay aims to explore the influence of drug [...]
Millions of individuals are affected by the devastating consequences of substance abuse, making it a significant public health concern worldwide. As societies strive to address this issue, innovations in technology have emerged [...]
The issue of substance abuse presents a pervasive and multifaceted challenge, impacting individuals, families, and communities globally. Its consequences extend far beyond individual suffering, posing significant threats to [...]
Drug addiction is a complex and chronic disease characterized by compulsive drug seeking, continued use despite harmful consequences, and long-lasting changes in the brain. As a college student, I never thought I would find [...]
The film Requiem for a Dream (dir. Darren Aronofsky, 2000) depicts four individuals and their increasing addiction to substances. This psychological drama narrates parallel encounters linked by the relationship among the lonely. [...]
Drugabuse.gov. (2023). Commonly Abused Drugs Charts. National Institute on Drug Abuse. National Institute on Drug Abuse. (2022). Understanding Drug Use and Addiction DrugFacts. Retrieved from Press.

Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
- Find a meeting
- How to start a meeting
- Information about NA
- Is NA for me?
- Resources for professionals
- What happens at an NA Meeting
- Conference Reports
- Miscellaneous Reports
- NAWS Annual Reports
- NAWS News and emails
- Reaching Out
- The NA Way Magazine
- Subscribe to our Periodicals
- Zonal, Regional, and Area Events
- Annual Events
- NAWS Web Meetings
- World Convention
- World Service Conference
- World Service Participation Request Form
- Virtual Meetings
- ASL Resources
- Contribute to NA World Services
- Group/Reg Updates
- Service Committee Updates
- Issue Discussions
- Local Service Resources
- NAWS Webinars
- Projects & Surveys
- Public Relations
- Service Material Area
- Serving at the World Level
- NA Literature in Digital Formats
- Main Entrance to all NAWS Web Stores
- Order online from NAWS US Web Store
- Order online from NAWS Canada Web Store
- Order Online from NAWS Europe Web Store
- Product Catalog & Order Forms
- Privacy Policy
What is addiction?
News for the public.
Contains links to items of interest to the general public and professionals about the Fellowship of Narcotics Anonymous
PSA about Narcotics Anonymous
Information About NA
Resources for Professionals
Am I an Addict?
Welcome to NA
Please contact the webmaster if you have any comments, are not able to find something that you are looking for, or have any questions about the web site.

- Undergraduate
- High School
- Architecture
- American History
- Asian History
- Antique Literature
- American Literature
- Asian Literature
- Classic English Literature
- World Literature
- Creative Writing
- Linguistics
- Criminal Justice
- Legal Issues
- Anthropology
- Archaeology
- Political Science
- World Affairs
- African-American Studies
- East European Studies
- Latin-American Studies
- Native-American Studies
- West European Studies
- Family and Consumer Science
- Social Issues
- Women and Gender Studies
- Social Work
- Natural Sciences
- Pharmacology
- Earth science
- Agriculture
- Agricultural Studies
- Computer Science
- IT Management
- Mathematics
- Investments
- Engineering and Technology
- Engineering
- Aeronautics
- Medicine and Health
- Alternative Medicine
- Communications and Media
- Advertising
- Communication Strategies
- Public Relations
- Educational Theories
- Teacher's Career
- Chicago/Turabian
- Company Analysis
- Education Theories
- Shakespeare
- Canadian Studies
- Food Safety
- Relation of Global Warming and Extreme Weather Condition
- Movie Review
- Admission Essay
- Annotated Bibliography
- Application Essay
- Article Critique
- Article Review
- Article Writing
- Book Review
- Business Plan
- Business Proposal
- Capstone Project
- Cover Letter
- Creative Essay
- Dissertation
- Dissertation - Abstract
- Dissertation - Conclusion
- Dissertation - Discussion
- Dissertation - Hypothesis
- Dissertation - Introduction
- Dissertation - Literature
- Dissertation - Methodology
- Dissertation - Results
- GCSE Coursework
- Grant Proposal
- Marketing Plan
- Multiple Choice Quiz
- Personal Statement
- Power Point Presentation
- Power Point Presentation With Speaker Notes
- Questionnaire
- Reaction Paper
- Research Paper
- Research Proposal
- SWOT analysis
- Thesis Paper
- Online Quiz
- Literature Review
- Movie Analysis
- Statistics problem
- Math Problem
- All papers examples
- How It Works
- Money Back Policy
- Terms of Use
- Privacy Policy
- We Are Hiring
What Is Addiction? Essay Example
Pages: 3
Words: 853
Hire a Writer for Custom Essay
Use 10% Off Discount: "custom10" in 1 Click 👇
You are free to use it as an inspiration or a source for your own work.
Introduction
There are many instances where people can get addicted as it is said too much of a particular thing is poisonous. Although many people think that addiction only occurs when one abuses drugs. Even so, addictions occur in several forms from drugs, friends, lovers, and even certain pleasurable activities. This paper delves into the concept of addiction and the way social media has influenced people into addiction.
What Is Addiction?
Although there is a misconception about what addiction is, it is evident that it is a state that happens when one cannot do without a particular substance or activity. This condition arises from continued intake of that substance or activity mainly because it is considered pleasurable by the user. The usage of this particular substance or activity results into compulsiveness and begins to interfere with the life of the user. The usual activities of the user begin to be affected as the user begins to enjoy the addicting component more than he enjoys his or her usual activities. The most shocking factor is that the addicted person does not realize that he or she is addicted because they deem the behavior normal. Additionally, the problems from this individual begin by affecting him or her then it begins affecting the relations.
Addiction can be described in diverse ways depending on the substance that has caused the addiction. First, addiction can be said to be physical arising from the fact that the body adapts to a certain substance biologically. In this case, the effect of the substance on the body reduces mainly because the body has established a tolerance for it. The body begins to feel that the substance is part of its system because of continued use. This gives rise to withdrawal symptoms, which is common with people with addictions. For instance, a person addicted to cocaine will feel attracted to have a sniff not because he or she wants to but because of these withdrawal symptoms.
Even so, addiction occurs mainly because of emotional stress, which is usually brought about by the stressful events in an individual’s life. In this regard, the second form of addiction is psychological as the addiction starts in the brain. Individuals use drugs, bet or even do shopping impulsively mainly because of psychological reasons. This definition implies that drugs do not have to play a role in addiction. This is the reason individuals change from one addictive activity to another. Psychological addiction does not necessarily arise from stressful events. They also occur from enjoyable situations the way drug addiction occurs. Indeed, one takes part in an enjoyable activity continuously until a time when they cannot do without the activity. These activities include shopping and even surfing the internet.
Addiction to Social Media
The advancement of the internet to include social sites where people meet, talk, and play games has brought a new dimension into the concept of addiction. Although most people spend most of their time on computers and the internet mainly because of their work, others remain glued on it because of socialization. Online games and relationships mean that many people frequent the internet in order to get these services. The frequency of surfing the internet increases as the user continues using the sites. Moreover, the attachment with the services provided by the sites and the new friendships created over these sites makes the user prone to frequenting the internet. Recent studies show that several youths surf the internet several times a day to check on messages from their friends, play online games, and chat with their online friends. All these activities take most of these people’s time.
There are several social sites created in the internet with Facebook leading these sites. Facebook has grown to become a social phenomenon where all the people can meet and create friendships even with people unknown to them. The site has done away with the social rules of creating friendships where people have to meet before becoming friends. Moreover, the site allows the people to interact freely and without fear mainly because there is no physical interaction.
The fact that Facebook has more than four hundred million users states how the internet social sites have taken over from physical socialization. All these users are active with more than fifty percent being active each day. This shows how the sites have taken over the time of individuals making it the most visited site on the internet after Google.
The fact that all the users in these social sites have more friends than in the real world shows how the media has taken over the lives of individuals. Additionally, the fact that people have turned their emotional needs into the internet shows how the sites have become a means of satisfying one’s emotional needs.
In summary, the social media has changed the perceptions of people from relying on physical social solutions to relying on the internet. Currently, a large percentage of internet users utilize the social sites for socialization and enjoyment. These people spend most of their time in these sites with most people not able to stay a day without being on social media. This shows how the sites are addictive.
Stuck with your Essay?
Get in touch with one of our experts for instant help!
How Has the Internet Affected Education? Essay Example
Advances in Technology and Changes in Society, Essay Example
Time is precious
don’t waste it!
Plagiarism-free guarantee
Privacy guarantee
Secure checkout
Money back guarantee

Related Essay Samples & Examples
Voting as a civic responsibility, essay example.
Pages: 1
Words: 287
Utilitarianism and Its Applications, Essay Example
Words: 356
The Age-Related Changes of the Older Person, Essay Example
Pages: 2
Words: 448
The Problems ESOL Teachers Face, Essay Example
Pages: 8
Words: 2293
Should English Be the Primary Language? Essay Example
Pages: 4
Words: 999
The Term “Social Construction of Reality”, Essay Example
Words: 371
Module 9: Substance-Related and Addictive Disorders
Perspectives on addiction, learning objectives.
- Describe and discuss the various psychological explanations for addiction
There are a number of genetic and environmental risk factors for explaining drug or alcohol abuse that vary across the population. Genetic and environmental risk factors each account for roughly half of an individual’s risk for developing an addiction; the contribution from epigenetic risk factors to the total risk is unknown. Even in individuals with a relatively low genetic risk, exposure to sufficiently high doses of an addictive drug for a long period of time (e.g., weeks to months) can result in an addiction.
This video explains how substance abuse disorders may develop.
You can view the transcript for “The development of substance use – Why do people use legal and illegal substances? | Khan Academy” here (opens in new window) .
Genetic and Biological Approaches to Addiction
Epidemiological studies estimate that genetic factors account for 40–60% of the risk factors for alcoholism. Similar rates of heritability for other types of drug addiction have been indicated by other studies. Overall, the data implicating specific genes in the development of drug addiction is mixed for most genes. One reason for this may be that the case is due to a focus of current research on common variants. Many addiction studies focus on common variants with an allele frequency of greater than 5% in the general population; however, when associated with the disease, these only confer a small amount of additional risk with an odds ratio of 1.1%–1.3%.
Genome-wide association studies (GWAS) are used to examine genetic associations with dependence, addiction, and drug use. These studies employ an unbiased approach to finding genetic associations with specific phenotypes and give equal weight to all regions of DNA, including those with no ostensible relationship to drug metabolism or response. These studies rarely identify genes from proteins previously described via animal-knockout models and candidate-gene analysis. Instead, large percentages of genes involved in processes such as cell adhesion are commonly identified.
Cross addiction is when one already has a predisposed addiction and then starts to become addicted to something different. If one family member has a history of addiction, the chances of a relative or close family developing those same habits are much higher than one who has not been introduced to addiction at a young age. In a recent study done by the National Institute on Drug Abuse, from 2002 to 2017, overdose deaths have almost tripled amongst male and females. In 2017, 72,306 overdose deaths happened in the United States that were reported.
Epigenetic Factors
Epigenetic genes and their products (e.g., proteins) are the key components through which environmental influences can affect the genes of an individual; they also serve as the mechanism responsible for transgenerational epigenetic inheritance, a phenomenon in which environmental influences on the genes of a parent can affect the associated traits and behavioral phenotypes of their offspring (e.g., behavioral responses to environmental stimuli). In addiction, epigenetic mechanisms play a central role in the pathophysiology of the disease; it has been noted that some of the alterations to the epigenome that arise through chronic exposure to addictive stimuli during an addiction can be transmitted across generations, in turn affecting the behavior of one’s children (e.g., the child’s behavioral responses to addictive drugs and natural rewards).

Figure 1. Reasons for addiction may be influenced by a myriad of factors, including genetic and biological, social, environmental, and personal reasons.
The general classes of epigenetic alterations that have been implicated in transgenerational epigenetic inheritance include DNA mythylation, histone modifcations, and downregulation or upregulation of microRNAs. With respect to addiction, more research is needed to determine the specific heritable epigenetic alterations that arise from various forms of addiction in humans and the corresponding behavioral phenotypes from these epigenetic alterations that occur in human offspring. More generally, the heritable behavioral phenotypes that are derived from addiction-induced epigenetic alterations and transmitted from parent to offspring may serve to either increase or decrease the offspring’s risk of developing an addiction.
Psychodynamic Approaches
The psychodynamic approach emphasizes systematic study of the psychological forces that underlie human behavior, feelings, and emotions and how they might relate to early experience. It is especially interested in the dynamic relations between conscious motivation and unconscious motivation. The psychodynamic approach may explain addiction associated with unconscious factors from the past that could create something similar to a trauma response of negative coping by substances. The negative coping by partaking in drugs and alcohol could turn into addiction easily if the unconscious factors are not resolved based on the approach.
According to Edward Khantzian’s self-medication hypothesis (SMH), a person may choose to medicate by using a drug as an “ego solvent,” which acts on parts of the self that are cut off from consciousness by defense mechanisms. [1] According to Khantzian, drug-dependent individuals generally experience more psychiatric distress than nondrug-dependent individuals, and the development of drug dependence involves the gradual incorporation of the drug effects and the need to sustain these effects into the defensive structure-building activity of the ego itself. The addict’s choice of drug is a result of the interaction between the psychopharmacologic properties of the drug and the affective states from which the addict was seeking relief. The drug’s effects substitute for defective or non-existent ego mechanisms of defense. The addict’s drug of choice, therefore, is not random.
Khantzian revisited the self-medication hypothesis (SMH), suggesting there is more evidence that psychiatric symptoms, rather than personality styles, lie at the heart of drug use disorders. Khantzian specified that the two crucial aspects of the self-medication hypothesis (SMH) were that (1) drugs of abuse produce a relief from psychological suffering and (2) the individual’s preference for a particular drug is based on its psychopharmacological properties. The individual’s drug of choice is determined through experimentation, whereby the interaction of the main effects of the drug, the individual’s inner psychological turmoil, and underlying personality traits identify the drug that produces the desired effects.
While Khantzian takes a psychodynamic approach to self-medication, David Duncan proposed a self-medication model that focuses on behavioral factors. Duncan described the nature of positive reinforcement (e.g., the “high feeling” or approval from peers), negative reinforcement (e.g. reduction of negative affect), and avoidance of withdrawal symptoms, all of which are seen in those who develop problematic drug use, but are not all found in all recreational drug users. While earlier behavioral formulations of drug dependence using operant conditioning maintained that positive and negative reinforcement were necessary for drug dependence, Duncan maintained that drug dependence was not maintained by positive reinforcement, but rather by negative reinforcement. Duncan applied a public health model to drug dependence, where the agent (the drug of choice) infects the host (the drug user) through a vector (e.g., peers), while the environment supports the disease process through stressors and lack of support. A crucial determinant of whether a drug user develops drug abuse is the presence or absence of negative reinforcement, which is experienced by problematic users, but not by recreational users. According to Duncan, drug dependence is an avoidance behavior, where an individual finds a drug that produces a temporary escape from a problem, and taking the drug is reinforced as an operant behavior.
Personality theories of addiction are psychological models that associate personality traits or modes of thinking (i.e., affective states) with an individual’s proclivity for developing an addiction. Models of addiction risk that have been proposed in psychology literature include an affect dysregulation model of positive and negative psychological effects, the reinforcement sensitivity theory model of impulsiveness and behavioral inhibition, and an impulsivity model of reward sensitization and impulsiveness.
Research has consistently shown strong associations between affective disorders and substance use disorders. Specifically, people with mood disorders are at increased risk of substance use disorders. Affect and addiction can be related in a variety of ways as they play a crucial role in influencing motivated behaviors. For instance, affect facilitates action, directs attention, prepares the individual for a physical response, and guides behavior to meet particular needs. Moreover, affect is implicated in a range of concepts relevant to addiction: positive reinforcement, behavior motivation, regulation of cognition and mood, and reasoning and decision making. Emotion-motivated reasoning has been shown to influence addictive behaviors via selecting outcomes that minimize negative affective states while maximizing positive affective states.
Cognitive Approaches
Cognitive control, and particularly inhibitory control over behavior, is impaired in addiction. Executive functions (collectively referred to as executive function and cognitive control) are a set of cognitive processes that are necessary for the cognitive control of behavior: selecting and successfully monitoring behaviors that facilitate the attainment of chosen goals. Executive functions include basic cognitive processes such as attentional control, cognitive inhibition, inhibitory control, working memory, and cognitive flexibility. Higher-order executive functions require the simultaneous use of multiple basic executive functions and include planning and fluid intelligence (e.g., reasoning and problem-solving).
Expectancy theory proposes that an individual will behave or act in a certain way because they are motivated to select a specific behavior over others due to what they expect the result of that selected behavior will be. In essence, the motivation of the behavior selection is determined by the desirability of the outcome. However, at the core of the theory is the cognitive process of how an individual processes the different motivational elements. As related to addiction, expectancy theory explains how there may be a motivation to experience the “high” of the substance and the euphoric state that the drug brings to the body. Also, this euphoric state may motivate individuals in the future to take the substance again and again, and hence exacerbating the addiction process. Expectancy theory may also explain how some view drug use as “cool,” or that what they perceive as the benefits of drug use outweigh the consequences.
Behavioral Approaches
Behaviorists explain drug use and addiction by emphasizing the way that these behaviors are learned or habitualized. According to social learning theory, which holds that behaviors are learned through imitating and observing others, someone might be peer pressured into trying drugs for the first time. Operant conditioning, which emphasizes repeating behaviors that result in a reward, may explain why an individual would seek out a “high” or the reduction in stress they may get from using a drug. Eventually, this could lead to an increased desire to obtain or use the drug.
As mentioned above, the self-medication hypothesis argues that specific psychiatric withdrawal symptoms, which increase during abstinence, may be the main driver of persistent drug use because of negative reinforcement. Positive reinforcement theories, by contrast, argue that the excessively rewarding effects of drugs drive persistent drug use independently of the withdrawal syndrome. The challenge for positive reinforcement theories is to explain why drug use persists when addicts claim the drug has lost its value. To solve this contradiction, there are several theories like those that emphasize the classical conditioning of behaviors, where an addicted person has learned to associate certain behaviors and drug use, so that they become dependent on the drug. [2]
Environmental Factors
Environmental risk factors for addiction are the experiences of an individual during their lifetime that interact with the individual’s genetic composition to increase or decrease their vulnerability to addiction. A number of different environmental factors have been implicated as risk factors for addiction, including various psychosocial stressors. The National Institute on Drug Abuse (NIDA) cites lack of parental supervision, the prevalence of peer substance use, drug availability, and poverty as risk factors for substance use among children and adolescents. The brain disease model of addiction posits that an individual’s exposure to an addictive drug is the most significant environmental risk factor for addiction. However, many researchers, including neuroscientists, indicate that the brain disease model presents a misleading, incomplete, and potentially detrimental explanation of addiction.
Adverse childhood experiences (ACEs) are various forms of maltreatment and household dysfunction experienced in childhood. A study of 900 court cases involving children who experienced abuse found that a vast amount of them went on to suffer from some form of addiction in their adolescence or adult life. This pathway towards addiction, which is opened through stressful experiences during childhood, can be avoided by a change in environmental factors throughout an individual’s life and opportunities of professional help. If one has friends or peers who engage in drug use favorably, the chances of them developing an addiction increases. Family conflict and home management may also lead to alcohol or other drug use.
Adolescence represents a period of unique vulnerability for developing an addiction. In adolescence, the incentive-rewards systems in the brain mature well before the cognitive control center. Therefore, adolescents are increasingly likely to act on their impulses and engage in risky, potentially addicting behavior before considering the consequences. Not only are adolescents more likely to initiate and maintain drug use, but once addicted they are more resistant to treatment and more liable to relapse.
Statistics have shown that those who start to drink alcohol at a younger age are more likely to become dependent later on. About 33% of the population tasted their first alcohol between the ages of 15 and 17, while 18% experienced it prior to this. As for alcohol abuse or dependence, the numbers start off high with those who first drank before they were 12 and then drop off after that. For example, 16% of alcoholics began drinking prior to turning 12 years old, while only 9% first touched alcohol between 15 and 17. This percentage is even lower, at 2.6%, for those who first started the habit after they were 21.
Most individuals are exposed to and use addictive drugs for the first time during their teenage years. In the United States, there were just over 2.8 million new users of illicit drugs in 2013 (~7,800 new users per day); among them, 54.1% were under 18 years of age. In 2011, there were approximately 20.6 million people in the United States over the age of 12 with an addiction. Over 90% of those with an addiction began drinking, smoking, or using illicit drugs before the age of 18.
Comorbid Disorders
Individuals with comorbid (i.e., co-occurring) mental health disorders such as depression, anxiety, attention-deficit/hyperactivity disorder (ADHD) or post-traumatic stress disorder are more likely to develop substance use disorders. The NIDA cites early aggressive behavior as a risk factor for substance use. A study by the National Bureau of Economic Research found that there is a “definite connection between mental illness and the use of addictive substances” and a majority of mental health patients participate in the use of these substances: 38% alcohol, 44% cocaine, and 40% cigarettes.
Sociocultural Factors
Due to cultural variations, the proportion of individuals who develop a drug or behavioral addiction within a specified time period (i.e., the prevalence) varies over time, by country, and across national population demographics (e.g., by age group, socioeconomic status (SES), etc.)
Internationally, the United States and Eastern Europe contain the countries with the highest substance abuse disorder occurrence (5%-6%). Africa, Asia, and the Middle East contain countries with the lowest worldwide occurrence (1%-2%). Across the globe, those that tended to have a higher prevalence of substance dependence were in their twenties, unemployed, and male. The National Survey on Drug Use and Health (NSDUH) reports on substance dependence/abuse rates in various population demographics across the United States. When surveying populations based on race and ethnicity in those ages 12 and older, it was observed that American Indian/Alaskan Natives were among the highest rates and Asians were among the lowest rates in comparison to other racial/ethnic groups.
When surveying populations based on gender in those ages 12 and older, it was observed that males had a higher substance dependence rate than females. However, the difference in the rates are not apparent until after age 17. Drug and Alcohol Dependence reports that older adults abuse drugs including alcohol at a rate of 15–20%. It’s estimated that 52 million Americans beyond 12 years old have abused a substance.
Alcohol dependence or abuse rates were shown to have no correspondence with any person’s education level when populations were surveyed in varying degrees of education from ages 26 and older. However, when it came to illicit drug use, there was a correlation in which those that graduated from college had the lowest rates. Furthermore, dependence rates were greater in unemployed populations ages 18 and older and in metropolitan-residing populations ages 12 and older.
The National Opinion Research Center at the University of Chicago reported an analysis on disparities within admissions for substance abuse treatment in the Appalachian region, which comprises 13 states and 410 counties in the eastern part of the United States. While their findings for most demographic categories were similar to the national findings by NSDUH, they had different results for racial/ethnic groups that varied by sub-regions. Overall, Whites were the demographic with the largest admission rate (83%), while Alaskan Native, American Indian, Pacific Islander, and Asian populations had the lowest admissions (1.8%).
Alcohol and Drug Abuse Around the World
In Asia, the prevalence of alcohol dependence is not as high as is seen in other regions. Many Asians (30% to 50% of people of Chinese, Japanese, and Korean ancestry) have at least one ALDH2*2 allele, which may cause alcohol flush reaction, or a sensitivity to alcohol that causes flushes or blotches on the body after alcoholic consumption. In Europe in 2015, the estimated prevalence among the adult population was 18.4% for heavy episodic alcohol use (in the past 30 days); 15.2% for daily tobacco smoking; and 3.8, 0.77, 0.37 and 0.35% in 2017 for cannabis, amphetamine, opioid, and cocaine use, respectively. The mortality rates for alcohol and illicit drugs were highest in Eastern Europe.

Figure 2 . Alcohol consumption throughout the world. Hannah Ritchie (2018) – “Alcohol Consumption”. Published online at OurWorldInData.org. Retrieved from: ‘https://ourworldindata.org/alcohol-consumption’ [Online Resource]

Figure 3 . Alcohol use disorder around the world is estimated to affect around 1.4% of the population. For most countries, the rate of prevalence is around 1 or 2%, but some countries, such as Russia, Greenland, and Brazil, have higher prevalence rates. Hannah Ritchie (2019) – “Drug Use”. Published online at OurWorldInData.org. Retrieved from: ‘https://ourworldindata.org/drug-use’ [Online Resource]
The realities of opioid use and abuse in Latin America may be deceptive if observations are limited to epidemiological findings. In the United Nations Office on Drugs and Crime report, although South America produced 3% of the world’s morphine and heroin and 0.01% of its opium, the prevalence of use is uneven. According to the Inter-American Commission on Drug Abuse Control, consumption of heroin is low in most Latin American countries, although Colombia is the area’s largest opium producer. Mexico, because of its border with the United States, has the highest incidence of use.

Figure 4 . While alcohol abuse is more common in Russia and Eastern Europe, the United States has the highest percentage of the population suffering from drug use disorders. Hannah Ritchie (2019) – “Drug Use”. Published online at OurWorldInData.org. Retrieved from: ‘https://ourworldindata.org/drug-use’ [Online Resource]

Figure 5 . Map showing the share of the population with alcohol or drug use disorders. Hannah Ritchie (2019) – “Drug Use”. Published online at OurWorldInData.org. Retrieved from: ‘https://ourworldindata.org/drug-use’ [Online Resource]
United States

Figure 6. One-third of inpatient hospital costs and 20% of all deaths in the United States every year are the result of untreated addictions and risky substance use.
Based upon representative samples of the U.S. youth population in 2011, the lifetime prevalence of addictions to alcohol and illicit drugs has been estimated to be approximately 8% and 2%-3%, respectively. Based upon representative samples of the U.S. adult population in 2011, the 12-month prevalence of alcohol and illicit drug addictions were estimated at roughly 12% and 2%-3% respectively. The lifetime prevalence of prescription drug addictions is currently around 4.7%.
As of 2016, about 22 million people in the United States need treatment for an addiction to alcohol, nicotine, or other drugs. Only about 10%, or a little over two million, receive any form of treatment, and those that do generally do not receive evidence-based care. One-third of inpatient hospital costs and 20% of all deaths in the United States every year are the result of untreated addictions and risky substance use. In spite of the massive overall economic cost to society, which is greater than the cost of diabetes and all forms of cancer combined, most doctors in the United States lack the training to effectively address drug addiction.
In 2019, opioid addiction was acknowledged as a national crisis in the United States. An article in The Washington Post stated that “America’s largest drug companies flooded the country with pain pills from 2006 through 2012, even when it became apparent that they were fueling addiction and overdoses.
In this video, Dr. Femke Buisman-Pijlman explains how biological, psychological, and social factors interact to either increase or reduce the risk that a person may develop a drug use disorder.
You can view the transcript for “Biopsychosocial Model” here (opens in new window) .
Other Addictions
There are other types of addictions, unrelated to drugs, that elicit similar behaviors and patterns of abuse in individuals. Recall that a mental disorder is characterized by deviance, dysfunction, distress, and danger. Some behaviors may become so addictive that a person’s thinking is dysfunctional, their behaviors are deviant, and that causes obvious distress. One disorder fitting this category in the DSM-5 is gambling disorder . This is classified when an individual has at least four of the following symptoms in a 12-month period:
- Needs to gamble with increasing amounts of money in order to achieve the desired excitement
- Is restless or irritable when attempting to cut down or stop gambling
- Has made repeated unsuccessful efforts to control, cut back, or stop gambling
- Is often preoccupied with gambling (e.g., having persistent thoughts of reliving past gambling experiences, handicapping or planning the next venture, thinking of ways to get money with which to gamble)
- Often gambles when feeling distressed (e.g., helpless, guilty, anxious, depressed)
- After losing money gambling, often returns another day to get even (“chasing” one’s losses)
- Lies to conceal the extent of involvement with gambling
- Has jeopardized or lost a significant relationship, job, education, or career opportunity because of gambling
- Relies on others to provide money to relieve desperate financial situations caused by gambling
Would you consider yourself addicted to any social media platforms or games? Excessive Internet use has not been recognized as a disorder by the World Health Organization, the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), or the International Classification of Diseases (ICD-11), though the diagnosis of gaming disorder has been included in the International Classification of Diseases (ICD-11). Gaming disorder is defined as the problematic, compulsive use of video games that results in significant impairment to an individual’s ability to function in various life domains over a prolonged period of time.
Mental health professionals have debated including compulsive shopping, stealing, excessive sexual behavior, and internet use as possible disorders, though there is controversy about whether or not a repetitive behavior in and of itself should constitute an addiction. There is also disagreement about whether these types of addictions should constitute a separate clinical entity, or whether they are a manifestation of underlying psychiatric disorders. Research has approached the question from a variety of viewpoints, with no universally standardized or agreed definitions, leading to difficulties in developing evidence-based recommendations.
gambling disorder: mental disorder defined by an addiction to gambling
gaming disorder : controversial disorder described in the ICD-11 related to video game addiction
expectancy theory: idea that an individual will behave or act in a certain way because they are motivated to select a specific behavior over others due to what they expect the result of that selected behavior will be
personality theories of addiction: psychological models that associate personality traits or modes of thinking (i.e., affective states) with an individual’s proclivity for developing an addiction
self-medication hypothesis: idea that an individual uses a substance or any exogenous influence to self-administer treatment for physical or psychological ailments
- Khantzian E.J. (1997). "The self-medication hypothesis of drug use disorders: A reconsideration and recent applications". Harvard Review of Psychiatry . 4 (5): 231–244. doi:10.3109/10673229709030550. PMID 9385000. S2CID 39531697. ↵
- Hogarth, L. Addiction is driven by excessive goal-directed drug choice under negative affect: translational critique of habit and compulsion theory. Neuropsychopharmacol. 45, 720–735 (2020). https://doi.org/10.1038/s41386-020-0600-8 ↵
- Modification, adaptation, and original content. Authored by : Bob Hoople for Lumen Learning. Provided by : Lumen Learning. License : CC BY-SA: Attribution-ShareAlike
- Loss of love. Authored by : Tumisu. Located at : https://pixabay.com/illustrations/love-mind-cranium-head-thought-4757313/ . License : Other . License Terms : Pixabay License
- Drug therapist. Authored by : rc-respect. Located at : https://pixabay.com/photos/doctor-drug-therapist-treatment-5634847/ . License : Other . License Terms : Pixabay License
- Alcoholism. Authored by : rebcenter-moscow. Located at : https://pixabay.com/photos/female-alcoholism-woman-girl-2847443/ . License : Other . License Terms : Pixabay License
- Substance dependence. Provided by : Wikipedia. Located at : https://en.wikipedia.org/wiki/Substance_dependence . License : CC BY-SA: Attribution-ShareAlike
- Addiction. Provided by : Wikipedia. Located at : https://en.wikipedia.org/wiki/Addiction . License : CC BY-SA: Attribution-ShareAlike
- Executive functions. Provided by : Wikipedia. Located at : https://en.wikipedia.org/wiki/Executive_functions . License : CC BY-SA: Attribution-ShareAlike
- Psychodynamics. Provided by : Wikipedia. Located at : https://en.wikipedia.org/wiki/Psychodynamics . License : CC BY-SA: Attribution-ShareAlike
- Self-medication hypothesis. Provided by : Wikipedia. Located at : https://en.wikipedia.org/wiki/Self-medication#Self-medication_hypothesis . License : CC BY-SA: Attribution-ShareAlike
- Expectancy theory. Provided by : Wikipedia. Located at : https://en.wikipedia.org/wiki/Expectancy_theory . License : CC BY-SA: Attribution-ShareAlike
- Alcohol Flush Reaction. Provided by : Wikipedia. Located at : https://en.wikipedia.org/wiki/Alcohol_flush_reaction . License : CC BY-SA: Attribution-ShareAlike
- Problem gambling. Provided by : Wikipedia. Located at : https://en.wikipedia.org/wiki/Problem_gambling#:~:text=The%20DSM%2DV%20has%20since,to%20that%20of%20substance%2Dabuse. . License : CC BY-SA: Attribution-ShareAlike
- Internet Addiction Disorder. Provided by : Wikipedia. Located at : https://en.wikipedia.org/wiki/Internet_addiction_disorder . License : CC BY-SA: Attribution-ShareAlike
- Video Game Addiction. Provided by : Wikipedia. Located at : https://en.wikipedia.org/wiki/Video_game_addiction . License : CC BY-SA: Attribution-ShareAlike
- Biopsychosocial Model. Provided by : AddictionXManaging Addiction: A Framework for Successful Treatment. Located at : https://www.youtube.com/watch?v=VqyEEx9e8jg&feature=emb_logo . License : Other . License Terms : Standard YouTube License
- Khan Academy. Provided by : The development of substance use - Why do people use legal and illegal substances? | . Located at : https://www.youtube.com/watch?v=0nKP1FdSzEg&feature=emb_logo . License : Other . License Terms : Standard YouTube License

Is Addiction a Disease?
Reviewed by Psychology Today Staff
Addiction is a condition that has long baffled physicians and philosophers, to say nothing of those struggling with it and those around them. What to make of a set of behaviors that in fact induces changes in brain structure and function, provides short-term relief of distress only to create long-term problems of living and self-management, and is difficult to stop even when there is a strong desire to do so?
Once seen as a moral failure, addiction has more recently been viewed strictly as a medical problem. The push to regard addiction as a disease is well-intentioned—driven by a desire to lessen stigma—but fails to account for the many facets and facts of the condition. Worse, it robs sufferers of the sense that they can overcome the problem with courage, creativity, and some hard work . Rather, there is significant evidence that addiction is a complex cultural, social, and psychological phenomenon, as much as it is a biological phenomenon.
While addiction is very costly to individuals, families, and society at large, it reflects the brain’s remarkable plasticity—its ability to shape and reshape itself, adapt itself, in response to experience and environment—as well as the deep human need for joy and rewards in life and opportunities for accessing them. The fact is that the brain changes that are the hallmark of addiction are set in motion by the behaviors of substance-seeking coalescing into near-automatic habit. The evidence indicates that they can be reversed by changes in behavior and environment.
On This Page
- How does a person's view of addiction influence recovery?
- Why is addiction considered a disease?
- Is addiction a disease of the brain?
- Is addiction a habit?
- Is addiction a choice?
- If addiction isn't a disease, what is it?
- Can drug addiction be cured?
Because addiction is such a complex phenomenon, there are many theories about what addiction is. They are of more than academic interest. It matters how people view addiction because that influences what they are willing to do about it, or even whether they believe they can do anything about it.
Seeing addiction as a disease can make individuals feel hopeless about change and helpless, with no possibility of control over their own behavior. That doesn’t mean it is easy to gain control of the behaviors involved in addiction—but it is possible, and people do it every day. The disease model of addiction also suggests to people that they existing in a fragile state of recovery forever, always in danger of failing. It keeps them focused on the problem more than the solution.
Perhaps most of all, regarding addiction as a disease and not a deeply ingrained habit defies the evidence and obscures the true pathway out— discovering personally rewarding goals and activities that, repeated again and again because they are meaningful, help rewire the brain. People have to discover new goals worthy of pursuit for them. In pursuing them, new habits override old ones.
Addiction is considered a disease largely as a way to remove stigma, guilt, moral blame, and shame from those who use substances or certain behaviors repeatedly to feel intense euphoria and as a way to encourage humane treatment. It is also viewed as a disease in order to facilitate insurance coverage of any treatment.
Unfortunately, at the very same time, it prods people to see themselves as hapless victims of a process beyond their control. Addiction is definitely difficult to understand, because it starts out as a voluntary activity but, for many people, the brain adapts so quickly to that activity it becomes difficult to control. Changes in neural circuitry make the reward extra compelling; it becomes difficult to pay attention to anything else and difficult to stop, even when use creates problems and there is a desire to quit.
The fact that addiction changes the way the brain works lends credibility to the idea of a lifelong disease, even though, according to the National Institute of Drug Abuse, the changes are “persistent”—which is not the same as permanent. But turning addicts into patients keeps them from doing what is essential for recovery— discovering a personal goal deeply, individually meaningful and rewarding enough to satisfy the neural circuitry of desire.
Addiction changes the circuitry of the brain in ways that make it difficult for people to regulate through deliberative efforts the allure of a concentrated chemical rush of reward. Continued use of a drug increasingly dysregulates reward, motivation, and executive control systems. But the brain changes are not a malfunction of biology, which is the defining feature of disease. Rather, the brain changes of addiction reflect the normal plasticity processes of the brain, its every-day capacity to change in response to experience, the basis of all learning. Unlike other organs, the brain is designed to change .
The act of repeatedly using a highly pleasurable experience—drugs, gambling—alters neurons; they adjust their wiring to become increasingly efficient at the experience. They prune away their capacity to respond to other inputs. It is a form of deep learning. As problematic as the consequences can be in someone’s life, the process can, through effort, be reversed. Recovery also relies on neuroplasticity; changing behavior rewires the brain.
Habits are behavioral routines that are repeated so often they get wired into the brain as a matter of efficiency. The brain is always changing and adapting to experience—even now, as you read this. Habits are a kind of mental shortcut, fast-tracking the neural connections involved in an activity so that you don’t need to consciously think out every step. The brain is designed to work that way. Unfortunately, that wired-in efficiency is what makes habits hard to break .
Consuming certain substances or engaging in certain activities is so pleasurable for some people they are driven to repeat the experience. Habits make behaviors near-automatic in response to any elements related to that activity—in other words, hard to control. Recognizing that addiction is a habit in the scientific sense of the word makes clear that recovery is possible with deliberate action to change, which reverses the changes to the brain .
No one chooses to get addicted. The process of addiction is set in motion automatically, by the brain’s response to a behavior repeated often enough because it is reinforced by the very pleasurable—but, alas, short-lasting—reward of dopamine surge. What starts out as a voluntary choice gets quickly encoded in the neural circuity and relegated to automatic processes that leave little room for conscious control.
In addition, the part of the brain focused on goal-pursuit and reward (nucleus accumbens, or ventral striatum) actually changes and gets ever-more sensitive to dopamine, making the cocaine or gambling increasingly attractive and all-consuming—compelling, you could say. And the prefrontal cortex, the area of the brain responsible for rational decision-making, judgment, and control of behavior gets weakened, its connections to other parts of the brain pruned away.
While there is an element of choice in substance use, the neural actions of dopamine tilt the brain to be so interested in the immediate reward that it can’t even contemplate longer-term goals or exert control. That is why those who are addicted repeatedly act against their own best interests, frustrating everyone around them—and themselves.
Neuroscience research supports the idea that addiction is a habit that becomes quickly and deeply entrenched and self-perpetuating , rapidly rewiring the circuitry of the brain because it is aided and abetted by dopamine. Because the surge of dopamine reward is very short-lasting, it drive frequent repetition and habit formation. In many ways, addiction is like a disease: It causes serious problems in functioning. It creates feelings of helplessness, whereby those in the grip of addiction feel like they can’t get better of their own accord. The problem is incredibly persistent. But “disease” might best be seen as a metaphor when it related to addiction. As a habit, addiction can be seen as a form of deep or extreme learning, operating through the brain’s remarkable powers of neuroplasticity, as all learning does.
Most people who meet the clinical criteria for an alcohol or other drug use disorder achieve full recovery, data show. Perhaps the most interesting proof of the curability of addiction came from a natural experiment, when soldiers returned home to America from Vietnam, where heroin use and addiction were widespread , affecting 15 to 35 percent of enlisted men. Heroin use was so common that soldiers were required to be tested for heroin addiction before being allowed to depart Vietnam.
As soldiers left the strange mixture of fear, boredom, combat tensions, and poor living conditions of the battle zone in the early 1970s, the vast majority—95 percent, according to studies—left their addiction behind, despite opportunities to become readdicted. The Vietnam experience highlights the significant role that factors other than human biology and the nature of the addictive agent play in addiction. Environments and opportunities for other experiences matter—they also shape brain pathways of reward. They are critical to helping those recovering from addiction find a new sense of purpose.

Two Matthews (McConaughey and Perry) wrote memoirs about their acting careers. However, only one memoir reflected how multiple sources of meaning can promote happiness.

Substance use disorders and toxic relationships are a potent mix that can be life-threatening. A SUD can be a toxic relationship to oneself.

Some goals are seen as incompatible, while others as competitions for resources. How people view the conflict determines the strategy they think is best for resolving it.

Ibogaine, illegal in the United States, is a "new" but very old treatment approach in curing opioid and other addictions, as well as improving traumatic brain injury.

Travel can be a trigger for mood episodes in individuals living with mental health conditions. Here are 5 strategies for maintaining your wellness while traveling.

When someone dies from taking fentanyl, is it an accidental overdose? An overdose? Or have they been poisoned? Which do you think fits best?

Dating apps are designed to help people find dates and develop long-term relationships. But they are also designed to keep users involved with the app.

The death rate is rising—and it's rising fastest among women and young people. Here's what to know, and how to protect yourself.

Desires and cravings can often trap us in the grip of unhealthy addictions or relationships. Fortunately, there's a surprisingly simple way to rewire your brain and get free.

Medical interventions for addiction have been life-saving, yet we should be wary of the "medicalization" of addiction.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
What is Drug Addiction?
How it works
It’s no secret the abuse of drugs has become a widespread epidemic. Although it seems to be stereotypical for teens, this problem is rising more in the adult population. There really is no set population or genre to label as the specific drug abuser. Many people don’t understand why or how other people become addicted to drugs. They may mistakenly think that those who use drugs lack moral principles or willpower and that they could stop their drug use simply by choosing to.
In reality, drug addiction is a complex disease, and quitting usually takes more than good intentions or a strong will. Drugs change the brain in ways that make quitting hard, even for those who want to. Fortunately, researchers know more now than ever about how drugs affect the brain and have found treatments that can help people recover from drug addiction and lead productive lives. A question most people ask is “what is drug addiction?” Addiction is a chronic disease characterized by drug seeking and use that is compulsive, or difficult to control, despite harmful consequences. The initial decision to take drugs is voluntary for most people, but repeated drug use can lead to brain changes that challenge an addicted person’s self-control and interfere with their ability to resist intense urges to take drugs. These brain changes can be persistent, which is why drug addiction is considered a ‘relapsing’ disease—people in recovery from drug use disorders are at increased risk for returning to drug use even after years of not taking the drug. It’s common for a person to relapse, but relapse doesn’t mean that treatment doesn’t work. As with other chronic health conditions, treatment should be ongoing and should be adjusted based on how the patient responds. Treatment plans need to be reviewed often and modified to fit the patient’s changing needs. Another question that is asked a lot by people is “What happens to a person when a person takes drugs?” Most drugs affect the brain’s ‘reward circuit,’ causing euphoria as well as flooding it with the chemical messenger dopamine. A properly functioning reward system motivates a person to repeat behaviors needed to thrive, such as eating and spending time with loved ones. Surges of dopamine in the reward circuit cause the reinforcement of pleasurable but unhealthy behaviors like taking drugs, leading people to repeat the behavior again and again.
As a person continues to use drugs, the brain adapts by reducing the ability of cells in the reward circuit to respond to it. This reduces the high that the person feels compared to the high they felt when first taking the drug—an effect known as tolerance. They might take more of the drug to try and achieve the same high. These brain adaptations often lead to the person becoming less and less able to derive pleasure from other things they once enjoyed, like food, sex, or social activities. Long-term use also causes changes in other brain chemical systems and circuits as well, affecting functions that include: Learning, Judgment, decision-making,stress, memory, and behavior. Despite being aware of these harmful outcomes, many people who use drugs continue to take them, which is the nature of addiction. As with most other chronic diseases, such as diabetes, asthma, or heart disease, treatment for drug addiction generally isn’t a cure. However, addiction is treatable and can be successfully managed. People who are recovering from an addiction will be at risk for relapse for years and possibly for their whole lives. Research shows that combining addiction treatment medicines with behavioral therapy ensures the best chance of success for most patients. Treatment approaches tailored to each patient’s drug use patterns and any co-occurring medical, mental, and social problems can lead to continued recovery. More good news is that drug use and addiction are preventable. Results from NIDA-funded research have shown that prevention programs involving families, schools, communities, and the media are effective for preventing or reducing drug use and addiction. Although personal events and cultural factors affect drug use trends, when young people view drug use as harmful, they tend to decrease their drug taking. Therefore, education and outreach are key in helping people understand the possible risks of drug use. Teachers, parents, and health care providers have crucial roles in educating young people and preventing drug use and addiction. They have these key roles because of the trust people have in them and by doing so they try to keep teens and adults away from drug abuse to help guide them to live lives where they don’t need to depend on these things on a daily basis to go on with their day. Having to depend on drugs for a daily use gets very costly and tends to have the users do anything to obtain the drug such as stealing money from family members, steal valuable items from the household to sell for money, and lie to get the drug. Neighbors, friends, and coworkers also experience the effects of substance abuse because a person who abuses substances often is unreliable. Friends may be asked to help financially or in other ways. Coworkers may be forced to compensate for decreased productivity or carry a disproportionate share of the workload. As a consequence, they may resent the person abusing substances. People who abuse substances are likely to find themselves increasingly isolated from their families.
A main psychoactive drug that many people have an addiction to is alcohol. Alcohol is a major depressant even though some people don’t feel that it isn’t. Alcohol acts as a disinhibitor, which slows brain activity that controls judgement and inhibitions. Prolonged excessive drinking characterizes alcohol use disorder and can shrink the brain. Adult women have less of a stomach enzyme that digests alcohol and can become addicted to alcohol more quickly than men, they are at risk for lung, brain, and liver damage at lower consumption levels. Along with alcoholism lower doses of alcohol relax the the drinker by slowing sympathetic nervous system activity. While larger doses cause reactions to slow, speech to slur, and skilled performance to deteriorate. If paired with sleep deprivation, alcohol is a potent sedative. When you add these physical effects to lowered inhibitions, the result can be deadly. Alcohol can also be life threatening when heavy drinking follows an earlier period of moderate drinking, which depresses the moderate response. Memory disruption is also affiliated with alcohol. It can disrupt memory formation and heavy drinking can have long term effects on the brain and cognition. Also if a person drinks too much it may lead to that person blacking out, in which drinkers are unable to recall the people they met that night, what they said, or even did while intoxicated. These result partly from the way alcohol suppresses REM sleep, which helps fix the day’s experience into permanent experiences.
Cite this page
What Is Drug Addiction?. (2022, Jun 20). Retrieved from https://papersowl.com/examples/what-is-drug-addiction/
"What Is Drug Addiction?." PapersOwl.com , 20 Jun 2022, https://papersowl.com/examples/what-is-drug-addiction/
PapersOwl.com. (2022). What Is Drug Addiction? . [Online]. Available at: https://papersowl.com/examples/what-is-drug-addiction/ [Accessed: 15 Apr. 2024]
"What Is Drug Addiction?." PapersOwl.com, Jun 20, 2022. Accessed April 15, 2024. https://papersowl.com/examples/what-is-drug-addiction/
"What Is Drug Addiction?," PapersOwl.com , 20-Jun-2022. [Online]. Available: https://papersowl.com/examples/what-is-drug-addiction/. [Accessed: 15-Apr-2024]
PapersOwl.com. (2022). What Is Drug Addiction? . [Online]. Available at: https://papersowl.com/examples/what-is-drug-addiction/ [Accessed: 15-Apr-2024]
Don't let plagiarism ruin your grade
Hire a writer to get a unique paper crafted to your needs.

Our writers will help you fix any mistakes and get an A+!
Please check your inbox.
You can order an original essay written according to your instructions.
Trusted by over 1 million students worldwide
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Open access
- Published: 22 February 2021
Addiction as a brain disease revised: why it still matters, and the need for consilience
- Markus Heilig 1 ,
- James MacKillop ORCID: orcid.org/0000-0003-4118-9500 2 , 3 ,
- Diana Martinez 4 ,
- Jürgen Rehm ORCID: orcid.org/0000-0001-5665-0385 5 , 6 , 7 , 8 ,
- Lorenzo Leggio ORCID: orcid.org/0000-0001-7284-8754 9 &
- Louk J. M. J. Vanderschuren ORCID: orcid.org/0000-0002-5379-0363 10
Neuropsychopharmacology volume 46 , pages 1715–1723 ( 2021 ) Cite this article
85k Accesses
97 Citations
322 Altmetric
Metrics details
The view that substance addiction is a brain disease, although widely accepted in the neuroscience community, has become subject to acerbic criticism in recent years. These criticisms state that the brain disease view is deterministic, fails to account for heterogeneity in remission and recovery, places too much emphasis on a compulsive dimension of addiction, and that a specific neural signature of addiction has not been identified. We acknowledge that some of these criticisms have merit, but assert that the foundational premise that addiction has a neurobiological basis is fundamentally sound. We also emphasize that denying that addiction is a brain disease is a harmful standpoint since it contributes to reducing access to healthcare and treatment, the consequences of which are catastrophic. Here, we therefore address these criticisms, and in doing so provide a contemporary update of the brain disease view of addiction. We provide arguments to support this view, discuss why apparently spontaneous remission does not negate it, and how seemingly compulsive behaviors can co-exist with the sensitivity to alternative reinforcement in addiction. Most importantly, we argue that the brain is the biological substrate from which both addiction and the capacity for behavior change arise, arguing for an intensified neuroscientific study of recovery. More broadly, we propose that these disagreements reveal the need for multidisciplinary research that integrates neuroscientific, behavioral, clinical, and sociocultural perspectives.
Similar content being viewed by others
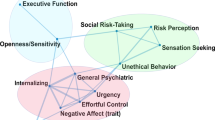
Subtypes in addiction and their neurobehavioral profiles across three functional domains
Gunner Drossel, Leyla R. Brucar, … Anna Zilverstand

Drug addiction: from bench to bedside
Julian Cheron & Alban de Kerchove d’Exaerde

The neurobiology of drug addiction: cross-species insights into the dysfunction and recovery of the prefrontal cortex
Ahmet O. Ceceli, Charles W. Bradberry & Rita Z. Goldstein
Introduction
Close to a quarter of a century ago, then director of the US National Institute on Drug Abuse Alan Leshner famously asserted that “addiction is a brain disease”, articulated a set of implications of this position, and outlined an agenda for realizing its promise [ 1 ]. The paper, now cited almost 2000 times, put forward a position that has been highly influential in guiding the efforts of researchers, and resource allocation by funding agencies. A subsequent 2000 paper by McLellan et al. [ 2 ] examined whether data justify distinguishing addiction from other conditions for which a disease label is rarely questioned, such as diabetes, hypertension or asthma. It concluded that neither genetic risk, the role of personal choices, nor the influence of environmental factors differentiated addiction in a manner that would warrant viewing it differently; neither did relapse rates, nor compliance with treatment. The authors outlined an agenda closely related to that put forward by Leshner, but with a more clinical focus. Their conclusion was that addiction should be insured, treated, and evaluated like other diseases. This paper, too, has been exceptionally influential by academic standards, as witnessed by its ~3000 citations to date. What may be less appreciated among scientists is that its impact in the real world of addiction treatment has remained more limited, with large numbers of patients still not receiving evidence-based treatments.
In recent years, the conceptualization of addiction as a brain disease has come under increasing criticism. When first put forward, the brain disease view was mainly an attempt to articulate an effective response to prevailing nonscientific, moralizing, and stigmatizing attitudes to addiction. According to these attitudes, addiction was simply the result of a person’s moral failing or weakness of character, rather than a “real” disease [ 3 ]. These attitudes created barriers for people with substance use problems to access evidence-based treatments, both those available at the time, such as opioid agonist maintenance, cognitive behavioral therapy-based relapse prevention, community reinforcement or contingency management, and those that could result from research. To promote patient access to treatments, scientists needed to argue that there is a biological basis beneath the challenging behaviors of individuals suffering from addiction. This argument was particularly targeted to the public, policymakers and health care professionals, many of whom held that since addiction was a misery people brought upon themselves, it fell beyond the scope of medicine, and was neither amenable to treatment, nor warranted the use of taxpayer money.
Present-day criticism directed at the conceptualization of addiction as a brain disease is of a very different nature. It originates from within the scientific community itself, and asserts that this conceptualization is neither supported by data, nor helpful for people with substance use problems [ 4 , 5 , 6 , 7 , 8 ]. Addressing these critiques requires a very different perspective, and is the objective of our paper. We readily acknowledge that in some cases, recent critiques of the notion of addiction as a brain disease as postulated originally have merit, and that those critiques require the postulates to be re-assessed and refined. In other cases, we believe the arguments have less validity, but still provide an opportunity to update the position of addiction as a brain disease. Our overarching concern is that questionable arguments against the notion of addiction as a brain disease may harm patients, by impeding access to care, and slowing development of novel treatments.
A premise of our argument is that any useful conceptualization of addiction requires an understanding both of the brains involved, and of environmental factors that interact with those brains [ 9 ]. These environmental factors critically include availability of drugs, but also of healthy alternative rewards and opportunities. As we will show, stating that brain mechanisms are critical for understanding and treating addiction in no way negates the role of psychological, social and socioeconomic processes as both causes and consequences of substance use. To reflect this complex nature of addiction, we have assembled a team with expertise that spans from molecular neuroscience, through animal models of addiction, human brain imaging, clinical addiction medicine, to epidemiology. What brings us together is a passionate commitment to improving the lives of people with substance use problems through science and science-based treatments, with empirical evidence as the guiding principle.
To achieve this goal, we first discuss the nature of the disease concept itself, and why we believe it is important for the science and treatment of addiction. This is followed by a discussion of the main points raised when the notion of addiction as a brain disease has come under criticism. Key among those are claims that spontaneous remission rates are high; that a specific brain pathology is lacking; and that people suffering from addiction, rather than behaving “compulsively”, in fact show a preserved ability to make informed and advantageous choices. In the process of discussing these issues, we also address the common criticism that viewing addiction as a brain disease is a fully deterministic theory of addiction. For our argument, we use the term “addiction” as originally used by Leshner [ 1 ]; in Box 1 , we map out and discuss how this construct may relate to the current diagnostic categories, such as Substance Use Disorder (SUD) and its different levels of severity (Fig. 1) .
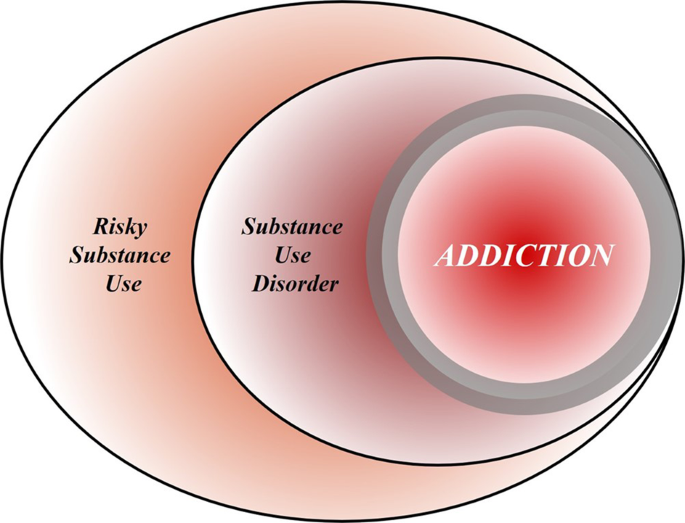
Risky (hazardous) substance use refers to quantity/frequency indicators of consumption; SUD refers to individuals who meet criteria for a DSM-5 diagnosis (mild, moderate, or severe); and addiction refers to individuals who exhibit persistent difficulties with self-regulation of drug consumption. Among high-risk individuals, a subgroup will meet criteria for SUD and, among those who have an SUD, a further subgroup would be considered to be addicted to the drug. However, the boundary for addiction is intentionally blurred to reflect that the dividing line for defining addiction within the category of SUD remains an open empirical question.
Box 1 What’s in a name? Differentiating hazardous use, substance use disorder, and addiction
Although our principal focus is on the brain disease model of addiction, the definition of addiction itself is a source of ambiguity. Here, we provide a perspective on the major forms of terminology in the field.
Hazardous Substance Use
Hazardous (risky) substance use refers to quantitative levels of consumption that increase an individual’s risk for adverse health consequences. In practice, this pertains to alcohol use [ 110 , 111 ]. Clinically, alcohol consumption that exceeds guidelines for moderate drinking has been used to prompt brief interventions or referral for specialist care [ 112 ]. More recently, a reduction in these quantitative levels has been validated as treatment endpoints [ 113 ].
Substance Use Disorder
SUD refers to the DSM-5 diagnosis category that encompasses significant impairment or distress resulting from specific categories of psychoactive drug use. The diagnosis of SUD is operationalized as 2 or more of 11 symptoms over the past year. As a result, the diagnosis is heterogenous, with more than 1100 symptom permutations possible. The diagnosis in DSM-5 is the result of combining two diagnoses from the DSM-IV, abuse and dependence, which proved to be less valid than a single dimensional approach [ 114 ]. Critically, SUD includes three levels of severity: mild (2–3 symptoms), moderate (4–5 symptoms), and severe (6+ symptoms). The International Classification of Diseases (ICD) system retains two diagnoses, harmful use (lower severity) and substance dependence (higher severity).
Addiction is a natural language concept, etymologically meaning enslavement, with the contemporary meaning traceable to the Middle and Late Roman Republic periods [ 115 ]. As a scientific construct, drug addiction can be defined as a state in which an individual exhibits an inability to self-regulate consumption of a substance, although it does not have an operational definition. Regarding clinical diagnosis, as it is typically used in scientific and clinical parlance, addiction is not synonymous with the simple presence of SUD. Nowhere in DSM-5 is it articulated that the diagnostic threshold (or any specific number/type of symptoms) should be interpreted as reflecting addiction, which inherently connotes a high degree of severity. Indeed, concerns were raised about setting the diagnostic standard too low because of the issue of potentially conflating a low-severity SUD with addiction [ 116 ]. In scientific and clinical usage, addiction typically refers to individuals at a moderate or high severity of SUD. This is consistent with the fact that moderate-to-severe SUD has the closest correspondence with the more severe diagnosis in ICD [ 117 , 118 , 119 ]. Nonetheless, akin to the undefined overlap between hazardous use and SUD, the field has not identified the exact thresholds of SUD symptoms above which addiction would be definitively present.
Integration
The ambiguous relationships among these terms contribute to misunderstandings and disagreements. Figure 1 provides a simple working model of how these terms overlap. Fundamentally, we consider that these terms represent successive dimensions of severity, clinical “nesting dolls”. Not all individuals consuming substances at hazardous levels have an SUD, but a subgroup do. Not all individuals with a SUD are addicted to the drug in question, but a subgroup are. At the severe end of the spectrum, these domains converge (heavy consumption, numerous symptoms, the unambiguous presence of addiction), but at low severity, the overlap is more modest. The exact mapping of addiction onto SUD is an open empirical question, warranting systematic study among scientists, clinicians, and patients with lived experience. No less important will be future research situating our definition of SUD using more objective indicators (e.g., [ 55 , 120 ]), brain-based and otherwise, and more precisely in relation to clinical needs [ 121 ]. Finally, such work should ultimately be codified in both the DSM and ICD systems to demarcate clearly where the attribution of addiction belongs within the clinical nosology, and to foster greater clarity and specificity in scientific discourse.
What is a disease?
In his classic 1960 book “The Disease Concept of Alcoholism”, Jellinek noted that in the alcohol field, the debate over the disease concept was plagued by too many definitions of “alcoholism” and too few definitions of “disease” [ 10 ]. He suggested that the addiction field needed to follow the rest of medicine in moving away from viewing disease as an “entity”, i.e., something that has “its own independent existence, apart from other things” [ 11 ]. To modern medicine, he pointed out, a disease is simply a label that is agreed upon to describe a cluster of substantial, deteriorating changes in the structure or function of the human body, and the accompanying deterioration in biopsychosocial functioning. Thus, he concluded that alcoholism can simply be defined as changes in structure or function of the body due to drinking that cause disability or death. A disease label is useful to identify groups of people with commonly co-occurring constellations of problems—syndromes—that significantly impair function, and that lead to clinically significant distress, harm, or both. This convention allows a systematic study of the condition, and of whether group members benefit from a specific intervention.
It is not trivial to delineate the exact category of harmful substance use for which a label such as addiction is warranted (See Box 1 ). Challenges to diagnostic categorization are not unique to addiction, however. Throughout clinical medicine, diagnostic cut-offs are set by consensus, commonly based on an evolving understanding of thresholds above which people tend to benefit from available interventions. Because assessing benefits in large patient groups over time is difficult, diagnostic thresholds are always subject to debate and adjustments. It can be debated whether diagnostic thresholds “merely” capture the extreme of a single underlying population, or actually identify a subpopulation that is at some level distinct. Resolving this issue remains challenging in addiction, but once again, this is not different from other areas of medicine [see e.g., [ 12 ] for type 2 diabetes]. Longitudinal studies that track patient trajectories over time may have a better ability to identify subpopulations than cross-sectional assessments [ 13 ].
By this pragmatic, clinical understanding of the disease concept, it is difficult to argue that “addiction” is unjustified as a disease label. Among people who use drugs or alcohol, some progress to using with a quantity and frequency that results in impaired function and often death, making substance use a major cause of global disease burden [ 14 ]. In these people, use occurs with a pattern that in milder forms may be challenging to capture by current diagnostic criteria (See Box 1 ), but is readily recognized by patients, their families and treatment providers when it reaches a severity that is clinically significant [see [ 15 ] for a classical discussion]. In some cases, such as opioid addiction, those who receive the diagnosis stand to obtain some of the greatest benefits from medical treatments in all of clinical medicine [ 16 , 17 ]. Although effect sizes of available treatments are more modest in nicotine [ 18 ] and alcohol addiction [ 19 ], the evidence supporting their efficacy is also indisputable. A view of addiction as a disease is justified, because it is beneficial: a failure to diagnose addiction drastically increases the risk of a failure to treat it [ 20 ].
Of course, establishing a diagnosis is not a requirement for interventions to be meaningful. People with hazardous or harmful substance use who have not (yet) developed addiction should also be identified, and interventions should be initiated to address their substance-related risks. This is particularly relevant for alcohol, where even in the absence of addiction, use is frequently associated with risks or harm to self, e.g., through cardiovascular disease, liver disease or cancer, and to others, e.g., through accidents or violence [ 21 ]. Interventions to reduce hazardous or harmful substance use in people who have not developed addiction are in fact particularly appealing. In these individuals, limited interventions are able to achieve robust and meaningful benefits [ 22 ], presumably because patterns of misuse have not yet become entrenched.
Thus, as originally pointed out by McLellan and colleagues, most of the criticisms of addiction as a disease could equally be applied to other medical conditions [ 2 ]. This type of criticism could also be applied to other psychiatric disorders, and that has indeed been the case historically [ 23 , 24 ]. Today, there is broad consensus that those criticisms were misguided. Few, if any healthcare professionals continue to maintain that schizophrenia, rather than being a disease, is a normal response to societal conditions. Why, then, do people continue to question if addiction is a disease, but not whether schizophrenia, major depressive disorder or post-traumatic stress disorder are diseases? This is particularly troubling given the decades of data showing high co-morbidity of addiction with these conditions [ 25 , 26 ]. We argue that it comes down to stigma. Dysregulated substance use continues to be perceived as a self-inflicted condition characterized by a lack of willpower, thus falling outside the scope of medicine and into that of morality [ 3 ].
Chronic and relapsing, developmentally-limited, or spontaneously remitting?
Much of the critique targeted at the conceptualization of addiction as a brain disease focuses on its original assertion that addiction is a chronic and relapsing condition. Epidemiological data are cited in support of the notion that large proportions of individuals achieve remission [ 27 ], frequently without any formal treatment [ 28 , 29 ] and in some cases resuming low risk substance use [ 30 ]. For instance, based on data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) study [ 27 ], it has been pointed out that a significant proportion of people with an addictive disorder quit each year, and that most afflicted individuals ultimately remit. These spontaneous remission rates are argued to invalidate the concept of a chronic, relapsing disease [ 4 ].
Interpreting these and similar data is complicated by several methodological and conceptual issues. First, people may appear to remit spontaneously because they actually do, but also because of limited test–retest reliability of the diagnosis [ 31 ]. For instance, using a validated diagnostic interview and trained interviewers, the Collaborative Studies on Genetics of Alcoholism examined the likelihood that an individual diagnosed with a lifetime history of substance dependence would retain this classification after 5 years. This is obviously a diagnosis that, once met, by definition cannot truly remit. Lifetime alcohol dependence was indeed stable in individuals recruited from addiction treatment units, ~90% for women, and 95% for men. In contrast, in a community-based sample similar to that used in the NESARC [ 27 ], stability was only ~30% and 65% for women and men, respectively. The most important characteristic that determined diagnostic stability was severity. Diagnosis was stable in severe, treatment-seeking cases, but not in general population cases of alcohol dependence.
These data suggest that commonly used diagnostic criteria alone are simply over-inclusive for a reliable, clinically meaningful diagnosis of addiction. They do identify a core group of treatment seeking individuals with a reliable diagnosis, but, if applied to nonclinical populations, also flag as “cases” a considerable halo of individuals for whom the diagnostic categorization is unreliable. Any meaningful discussion of remission rates needs to take this into account, and specify which of these two populations that is being discussed. Unfortunately, the DSM-5 has not made this task easier. With only 2 out of 11 symptoms being sufficient for a diagnosis of SUD, it captures under a single diagnostic label individuals in a “mild” category, whose diagnosis is likely to have very low test–retest reliability, and who are unlikely to exhibit a chronic relapsing course, together with people at the severe end of the spectrum, whose diagnosis is reliable, many of whom do show a chronic relapsing course.
The NESARC data nevertheless show that close to 10% of people in the general population who are diagnosed with alcohol addiction (here equated with DSM-IV “dependence” used in the NESARC study) never remitted throughout their participation in the survey. The base life-time prevalence of alcohol dependence in NESARC was 12.5% [ 32 ]. Thus, the data cited against the concept of addiction as a chronic relapsing disease in fact indicate that over 1% of the US population develops an alcohol-related condition that is associated with high morbidity and mortality, and whose chronic and/or relapsing nature cannot be disputed, since it does not remit.
Secondly, the analysis of NESARC data [ 4 , 27 ] omits opioid addiction, which, together with alcohol and tobacco, is the largest addiction-related public health problem in the US [ 33 ]. This is probably the addictive condition where an analysis of cumulative evidence most strikingly supports the notion of a chronic disorder with frequent relapses in a large proportion of people affected [ 34 ]. Of course, a large number of people with opioid addiction are unable to express the chronic, relapsing course of their disease, because over the long term, their mortality rate is about 15 times greater than that of the general population [ 35 ]. However, even among those who remain alive, the prevalence of stable abstinence from opioid use after 10–30 years of observation is <30%. Remission may not always require abstinence, for instance in the case of alcohol addiction, but is a reasonable proxy for remission with opioids, where return to controlled use is rare. Embedded in these data is a message of literally vital importance: when opioid addiction is diagnosed and treated as a chronic relapsing disease, outcomes are markedly improved, and retention in treatment is associated with a greater likelihood of abstinence.
The fact that significant numbers of individuals exhibit a chronic relapsing course does not negate that even larger numbers of individuals with SUD according to current diagnostic criteria do not. For instance, in many countries, the highest prevalence of substance use problems is found among young adults, aged 18–25 [ 36 ], and a majority of these ‘age out’ of excessive substance use [ 37 ]. It is also well documented that many individuals with SUD achieve longstanding remission, in many cases without any formal treatment (see e.g., [ 27 , 30 , 38 ]).
Collectively, the data show that the course of SUD, as defined by current diagnostic criteria, is highly heterogeneous. Accordingly, we do not maintain that a chronic relapsing course is a defining feature of SUD. When present in a patient, however, such as course is of clinical significance, because it identifies a need for long-term disease management [ 2 ], rather than expectations of a recovery that may not be within the individual’s reach [ 39 ]. From a conceptual standpoint, however, a chronic relapsing course is neither necessary nor implied in a view that addiction is a brain disease. This view also does not mean that it is irreversible and hopeless. Human neuroscience documents restoration of functioning after abstinence [ 40 , 41 ] and reveals predictors of clinical success [ 42 ]. If anything, this evidence suggests a need to increase efforts devoted to neuroscientific research on addiction recovery [ 40 , 43 ].
Lessons from genetics
For alcohol addiction, meta-analysis of twin and adoption studies has estimated heritability at ~50%, while estimates for opioid addiction are even higher [ 44 , 45 ]. Genetic risk factors are to a large extent shared across substances [ 46 ]. It has been argued that a genetic contribution cannot support a disease view of a behavior, because most behavioral traits, including religious and political inclinations, have a genetic contribution [ 4 ]. This statement, while correct in pointing out broad heritability of behavioral traits, misses a fundamental point. Genetic architecture is much like organ structure. The fact that normal anatomy shapes healthy organ function does not negate that an altered structure can contribute to pathophysiology of disease. The structure of the genetic landscape is no different. Critics further state that a “genetic predisposition is not a recipe for compulsion”, but no neuroscientist or geneticist would claim that genetic risk is “a recipe for compulsion”. Genetic risk is probabilistic, not deterministic. However, as we will see below, in the case of addiction, it contributes to large, consistent probability shifts towards maladaptive behavior.
In dismissing the relevance of genetic risk for addiction, Hall writes that “a large number of alleles are involved in the genetic susceptibility to addiction and individually these alleles might very weakly predict a risk of addiction”. He goes on to conclude that “generally, genetic prediction of the risk of disease (even with whole-genome sequencing data) is unlikely to be informative for most people who have a so-called average risk of developing an addiction disorder” [ 7 ]. This reflects a fundamental misunderstanding of polygenic risk. It is true that a large number of risk alleles are involved, and that the explanatory power of currently available polygenic risk scores for addictive disorders lags behind those for e.g., schizophrenia or major depression [ 47 , 48 ]. The only implication of this, however, is that low average effect sizes of risk alleles in addiction necessitate larger study samples to construct polygenic scores that account for a large proportion of the known heritability.
However, a heritability of addiction of ~50% indicates that DNA sequence variation accounts for 50% of the risk for this condition. Once whole genome sequencing is readily available, it is likely that it will be possible to identify most of that DNA variation. For clinical purposes, those polygenic scores will of course not replace an understanding of the intricate web of biological and social factors that promote or prevent expression of addiction in an individual case; rather, they will add to it [ 49 ]. Meanwhile, however, genome-wide association studies in addiction have already provided important information. For instance, they have established that the genetic underpinnings of alcohol addiction only partially overlap with those for alcohol consumption, underscoring the genetic distinction between pathological and nonpathological drinking behaviors [ 50 ].
It thus seems that, rather than negating a rationale for a disease view of addiction, the important implication of the polygenic nature of addiction risk is a very different one. Genome-wide association studies of complex traits have largely confirmed the century old “infinitisemal model” in which Fisher reconciled Mendelian and polygenic traits [ 51 ]. A key implication of this model is that genetic susceptibility for a complex, polygenic trait is continuously distributed in the population. This may seem antithetical to a view of addiction as a distinct disease category, but the contradiction is only apparent, and one that has long been familiar to quantitative genetics. Viewing addiction susceptibility as a polygenic quantitative trait, and addiction as a disease category is entirely in line with Falconer’s theorem, according to which, in a given set of environmental conditions, a certain level of genetic susceptibility will determine a threshold above which disease will arise.
A brain disease? Then show me the brain lesion!
The notion of addiction as a brain disease is commonly criticized with the argument that a specific pathognomonic brain lesion has not been identified. Indeed, brain imaging findings in addiction (perhaps with the exception of extensive neurotoxic gray matter loss in advanced alcohol addiction) are nowhere near the level of specificity and sensitivity required of clinical diagnostic tests. However, this criticism neglects the fact that neuroimaging is not used to diagnose many neurologic and psychiatric disorders, including epilepsy, ALS, migraine, Huntington’s disease, bipolar disorder, or schizophrenia. Even among conditions where signs of disease can be detected using brain imaging, such as Alzheimer’s and Parkinson’s disease, a scan is best used in conjunction with clinical acumen when making the diagnosis. Thus, the requirement that addiction be detectable with a brain scan in order to be classified as a disease does not recognize the role of neuroimaging in the clinic.
For the foreseeable future, the main objective of imaging in addiction research is not to diagnose addiction, but rather to improve our understanding of mechanisms that underlie it. The hope is that mechanistic insights will help bring forward new treatments, by identifying candidate targets for them, by pointing to treatment-responsive biomarkers, or both [ 52 ]. Developing innovative treatments is essential to address unmet treatment needs, in particular in stimulant and cannabis addiction, where no approved medications are currently available. Although the task to develop novel treatments is challenging, promising candidates await evaluation [ 53 ]. A particular opportunity for imaging-based research is related to the complex and heterogeneous nature of addictive disorders. Imaging-based biomarkers hold the promise of allowing this complexity to be deconstructed into specific functional domains, as proposed by the RDoC initiative [ 54 ] and its application to addiction [ 55 , 56 ]. This can ultimately guide the development of personalized medicine strategies to addiction treatment.
Countless imaging studies have reported differences in brain structure and function between people with addictive disorders and those without them. Meta-analyses of structural data show that alcohol addiction is associated with gray matter losses in the prefrontal cortex, dorsal striatum, insula, and posterior cingulate cortex [ 57 ], and similar results have been obtained in stimulant-addicted individuals [ 58 ]. Meta-analysis of functional imaging studies has demonstrated common alterations in dorsal striatal, and frontal circuits engaged in reward and salience processing, habit formation, and executive control, across different substances and task-paradigms [ 59 ]. Molecular imaging studies have shown that large and fast increases in dopamine are associated with the reinforcing effects of drugs of abuse, but that after chronic drug use and during withdrawal, brain dopamine function is markedly decreased and that these decreases are associated with dysfunction of prefrontal regions [ 60 ]. Collectively, these findings have given rise to a widely held view of addiction as a disorder of fronto-striatal circuitry that mediates top-down regulation of behavior [ 61 ].
Critics reply that none of the brain imaging findings are sufficiently specific to distinguish between addiction and its absence, and that they are typically obtained in cross-sectional studies that can at best establish correlative rather than causal links. In this, they are largely right, and an updated version of a conceptualization of addiction as a brain disease needs to acknowledge this. Many of the structural brain findings reported are not specific for addiction, but rather shared across psychiatric disorders [ 62 ]. Also, for now, the most sophisticated tools of human brain imaging remain crude in face of complex neural circuit function. Importantly however, a vast literature from animal studies also documents functional changes in fronto-striatal circuits, as well their limbic and midbrain inputs, associated with addictive behaviors [ 63 , 64 , 65 , 66 , 67 , 68 ]. These are circuits akin to those identified by neuroimaging studies in humans, implicated in positive and negative emotions, learning processes and executive functions, altered function of which is thought to underlie addiction. These animal studies, by virtue of their cellular and molecular level resolution, and their ability to establish causality under experimental control, are therefore an important complement to human neuroimaging work.
Nevertheless, factors that seem remote from the activity of brain circuits, such as policies, substance availability and cost, as well as socioeconomic factors, also are critically important determinants of substance use. In this complex landscape, is the brain really a defensible focal point for research and treatment? The answer is “yes”. As powerfully articulated by Francis Crick [ 69 ], “You, your joys and your sorrows, your memories and your ambitions, your sense of personal identity and free will, are in fact no more than the behavior of a vast assembly of nerve cells and their associated molecules”. Social and interpersonal factors are critically important in addiction, but they can only exert their influences by impacting neural processes. They must be encoded as sensory data, represented together with memories of the past and predictions about the future, and combined with representations of interoceptive and other influences to provide inputs to the valuation machinery of the brain. Collectively, these inputs drive action selection and execution of behavior—say, to drink or not to drink, and then, within an episode, to stop drinking or keep drinking. Stating that the pathophysiology of addiction is largely about the brain does not ignore the role of other influences. It is just the opposite: it is attempting to understand how those important influences contribute to drug seeking and taking in the context of the brain, and vice versa.
But if the criticism is one of emphasis rather than of principle—i.e., too much brain, too little social and environmental factors – then neuroscientists need to acknowledge that they are in part guilty as charged. Brain-centric accounts of addiction have for a long time failed to pay enough attention to the inputs that social factors provide to neural processing behind drug seeking and taking [ 9 ]. This landscape is, however, rapidly changing. For instance, using animal models, scientists are finding that lack of social play early in life increases the motivation to take addictive substances in adulthood [ 70 ]. Others find that the opportunity to interact with a fellow rat is protective against addiction-like behaviors [ 71 ]. In humans, a relationship has been found between perceived social support, socioeconomic status, and the availability of dopamine D2 receptors [ 72 , 73 ], a biological marker of addiction vulnerability. Those findings in turn provided translation of data from nonhuman primates, which showed that D2 receptor availability can be altered by changes in social hierarchy, and that these changes are associated with the motivation to obtain cocaine [ 74 ].
Epidemiologically, it is well established that social determinants of health, including major racial and ethnic disparities, play a significant role in the risk for addiction [ 75 , 76 ]. Contemporary neuroscience is illuminating how those factors penetrate the brain [ 77 ] and, in some cases, reveals pathways of resilience [ 78 ] and how evidence-based prevention can interrupt those adverse consequences [ 79 , 80 ]. In other words, from our perspective, viewing addiction as a brain disease in no way negates the importance of social determinants of health or societal inequalities as critical influences. In fact, as shown by the studies correlating dopamine receptors with social experience, imaging is capable of capturing the impact of the social environment on brain function. This provides a platform for understanding how those influences become embedded in the biology of the brain, which provides a biological roadmap for prevention and intervention.
We therefore argue that a contemporary view of addiction as a brain disease does not deny the influence of social, environmental, developmental, or socioeconomic processes, but rather proposes that the brain is the underlying material substrate upon which those factors impinge and from which the responses originate. Because of this, neurobiology is a critical level of analysis for understanding addiction, although certainly not the only one. It is recognized throughout modern medicine that a host of biological and non-biological factors give rise to disease; understanding the biological pathophysiology is critical for understanding etiology and informing treatment.
Is a view of addiction as a brain disease deterministic?
A common criticism of the notion that addiction is a brain disease is that it is reductionist and in the end therefore deterministic [ 81 , 82 ]. This is a fundamental misrepresentation. As indicated above, viewing addiction as a brain disease simply states that neurobiology is an undeniable component of addiction. A reason for deterministic interpretations may be that modern neuroscience emphasizes an understanding of proximal causality within research designs (e.g., whether an observed link between biological processes is mediated by a specific mechanism). That does not in any way reflect a superordinate assumption that neuroscience will achieve global causality. On the contrary, since we realize that addiction involves interactions between biology, environment and society, ultimate (complete) prediction of behavior based on an understanding of neural processes alone is neither expected, nor a goal.
A fairer representation of a contemporary neuroscience view is that it believes insights from neurobiology allow useful probabilistic models to be developed of the inherently stochastic processes involved in behavior [see [ 83 ] for an elegant recent example]. Changes in brain function and structure in addiction exert a powerful probabilistic influence over a person’s behavior, but one that is highly multifactorial, variable, and thus stochastic. Philosophically, this is best understood as being aligned with indeterminism, a perspective that has a deep history in philosophy and psychology [ 84 ]. In modern neuroscience, it refers to the position that the dynamic complexity of the brain, given the probabilistic threshold-gated nature of its biology (e.g., action potential depolarization, ion channel gating), means that behavior cannot be definitively predicted in any individual instance [ 85 , 86 ].
Driven by compulsion, or free to choose?
A major criticism of the brain disease view of addiction, and one that is related to the issue of determinism vs indeterminism, centers around the term “compulsivity” [ 6 , 87 , 88 , 89 , 90 ] and the different meanings it is given. Prominent addiction theories state that addiction is characterized by a transition from controlled to “compulsive” drug seeking and taking [ 91 , 92 , 93 , 94 , 95 ], but allocate somewhat different meanings to “compulsivity”. By some accounts, compulsive substance use is habitual and insensitive to its outcomes [ 92 , 94 , 96 ]. Others refer to compulsive use as a result of increasing incentive value of drug associated cues [ 97 ], while others view it as driven by a recruitment of systems that encode negative affective states [ 95 , 98 ].
The prototype for compulsive behavior is provided by obsessive-compulsive disorder (OCD), where compulsion refers to repeatedly and stereotypically carrying out actions that in themselves may be meaningful, but lose their purpose and become harmful when performed in excess, such as persistent handwashing until skin injuries result. Crucially, this happens despite a conscious desire to do otherwise. Attempts to resist these compulsions result in increasing and ultimately intractable anxiety [ 99 ]. This is in important ways different from the meaning of compulsivity as commonly used in addiction theories. In the addiction field, compulsive drug use typically refers to inflexible, drug-centered behavior in which substance use is insensitive to adverse consequences [ 100 ]. Although this phenomenon is not necessarily present in every patient, it reflects important symptoms of clinical addiction, and is captured by several DSM-5 criteria for SUD [ 101 ]. Examples are needle-sharing despite knowledge of a risk to contract HIV or Hepatitis C, drinking despite a knowledge of having liver cirrhosis, but also the neglect of social and professional activities that previously were more important than substance use. While these behaviors do show similarities with the compulsions of OCD, there are also important differences. For example, “compulsive” substance use is not necessarily accompanied by a conscious desire to withhold the behavior, nor is addictive behavior consistently impervious to change.
Critics question the existence of compulsivity in addiction altogether [ 5 , 6 , 7 , 89 ], typically using a literal interpretation, i.e., that a person who uses alcohol or drugs simply can not do otherwise. Were that the intended meaning in theories of addiction—which it is not—it would clearly be invalidated by observations of preserved sensitivity of behavior to contingencies in addiction. Indeed, substance use is influenced both by the availability of alternative reinforcers, and the state of the organism. The roots of this insight date back to 1940, when Spragg found that chimpanzees would normally choose a banana over morphine. However, when physically dependent and in a state of withdrawal, their choice preference would reverse [ 102 ]. The critical role of alternative reinforcers was elegantly brought into modern neuroscience by Ahmed et al., who showed that rats extensively trained to self-administer cocaine would readily forego the drug if offered a sweet solution as an alternative [ 103 ]. This was later also found to be the case for heroin [ 103 ], methamphetamine [ 104 ] and alcohol [ 105 ]. Early residential laboratory studies on alcohol use disorder indeed revealed orderly operant control over alcohol consumption [ 106 ]. Furthermore, efficacy of treatment approaches such as contingency management, which provides systematic incentives for abstinence [ 107 ], supports the notion that behavioral choices in patients with addictions remain sensitive to reward contingencies.
Evidence that a capacity for choosing advantageously is preserved in addiction provides a valid argument against a narrow concept of “compulsivity” as rigid, immutable behavior that applies to all patients. It does not, however, provide an argument against addiction as a brain disease. If not from the brain, from where do the healthy and unhealthy choices people make originate? The critical question is whether addictive behaviors—for the most part—result from healthy brains responding normally to externally determined contingencies; or rather from a pathology of brain circuits that, through probabilistic shifts, promotes the likelihood of maladaptive choices even when reward contingencies are within a normal range. To resolve this question, it is critical to understand that the ability to choose advantageously is not an all-or-nothing phenomenon, but rather is about probabilities and their shifts, multiple faculties within human cognition, and their interaction. Yes, it is clear that most people whom we would consider to suffer from addiction remain able to choose advantageously much, if not most, of the time. However, it is also clear that the probability of them choosing to their own disadvantage, even when more salutary options are available and sometimes at the expense of losing their life, is systematically and quantifiably increased. There is a freedom of choice, yet there is a shift of prevailing choices that nevertheless can kill.
Synthesized, the notion of addiction as a disease of choice and addiction as a brain disease can be understood as two sides of the same coin. Both of these perspectives are informative, and they are complementary. Viewed this way, addiction is a brain disease in which a person’s choice faculties become profoundly compromised. To articulate it more specifically, embedded in and principally executed by the central nervous system, addiction can be understood as a disorder of choice preferences, preferences that overvalue immediate reinforcement (both positive and negative), preferences for drug-reinforcement in spite of costs, and preferences that are unstable ( “I’ll never drink like that again;” “this will be my last cigarette” ), prone to reversals in the form of lapses and relapse. From a contemporary neuroscience perspective, pre-existing vulnerabilities and persistent drug use lead to a vicious circle of substantive disruptions in the brain that impair and undermine choice capacities for adaptive behavior, but do not annihilate them. Evidence of generally intact decision making does not fundamentally contradict addiction as a brain disease.
Conclusions
The present paper is a response to the increasing number of criticisms of the view that addiction is a chronic relapsing brain disease. In many cases, we show that those criticisms target tenets that are neither needed nor held by a contemporary version of this view. Common themes are that viewing addiction as a brain disease is criticized for being both too narrow (addiction is only a brain disease; no other perspectives or factors are important) or too far reaching (it purports to discover the final causes of addiction). With regard to disease course, we propose that viewing addiction as a chronic relapsing disease is appropriate for some populations, and much less so for others, simply necessitating better ways of delineating the populations being discussed. We argue that when considering addiction as a disease, the lens of neurobiology is valuable to use. It is not the only lens, and it does not have supremacy over other scientific approaches. We agree that critiques of neuroscience are warranted [ 108 ] and that critical thinking is essential to avoid deterministic language and scientific overreach.
Beyond making the case for a view of addiction as a brain disease, perhaps the more important question is when a specific level of analysis is most useful. For understanding the biology of addiction and designing biological interventions, a neurobiological view is almost certainly the most appropriate level of analysis, in particular when informed by an understanding of the behavioral manifestations. In contrast, for understanding the psychology of addiction and designing psychological interventions, behavioral science is the natural realm, but one that can often benefit from an understanding of the underlying neurobiology. For designing policies, such as taxation and regulation of access, economics and public administration provide the most pertinent perspectives, but these also benefit from biological and behavioral science insights.
Finally, we argue that progress would come from integration of these scientific perspectives and traditions. E.O. Wilson has argued more broadly for greater consilience [ 109 ], unity of knowledge, in science. We believe that addiction is among the areas where consilience is most needed. A plurality of disciplines brings important and trenchant insights to bear on this condition; it is the exclusive remit of no single perspective or field. Addiction inherently and necessarily requires multidisciplinary examination. Moreover, those who suffer from addiction will benefit most from the application of the full armamentarium of scientific perspectives.
Funding and disclosures
Supported by the Swedish Research Council grants 2013-07434, 2019-01138 (MH); Netherlands Organisation for Health Research and Development (ZonMw) under project number 912.14.093 (LJMJV); NIDA and NIAAA intramural research programs (LL; the content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health); the Peter Boris Chair in Addictions Research, Homewood Research Institute, and the National Institute on Alcohol Abuse and Alcoholism grants AA025911, AA024930, AA025849, AA027679 (JM; the content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health).
MH has received consulting fees, research support or other compensation from Indivior, Camurus, BrainsWay, Aelis Farma, and Janssen Pharmaceuticals. JM is a Principal and Senior Scientist at BEAM Diagnostics, Inc. DM, JR, LL, and LJMJV declare no conflict of interest.
Leshner AI. Addiction is a brain disease, and it matters. Science. 1997;278:45–7.
Article CAS PubMed Google Scholar
McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–95.
Schomerus G, Lucht M, Holzinger A, Matschinger H, Carta MG, Angermeyer MC. The stigma of alcohol dependence compared with other mental disorders: a review of population studies. Alcohol Alcohol. 2011;46:105–12.
Heyman GM. Addiction and choice: theory and new data. Front Psychiatry. 2013;4:31.
Article PubMed PubMed Central Google Scholar
Heather N, Best D, Kawalek A, Field M, Lewis M, Rotgers F, et al. Challenging the brain disease model of addiction: European launch of the addiction theory network. Addict Res Theory. 2018;26:249–55.
Article Google Scholar
Pickard H, Ahmed SH, Foddy B. Alternative models of addiction. Front Psychiatr.y 2015;6:20.
Google Scholar
Hall W, Carter A, Forlini C. The brain disease model of addiction: is it supported by the evidence and has it delivered on its promises? Lancet Psychiatr. 2015;2:105–10.
Hart CL. Viewing addiction as a brain disease promotes social injustice. Nat Hum Behav. 2017;1:0055.
Heilig M, Epstein DH, Nader MA, Shaham Y. Time to connect: bringing social context into addiction neuroscience. Nat Rev Neurosc.i 2016;17:592–9.
Article CAS Google Scholar
Jellinek EM. The disease concept of alcoholism. Hillhouse Press on behalf of the Christopher J. Smithers Foundation: New Haven, CT; 1960.
Stevenson A. Oxford dictionary of English. 3 ed. New York, NY: Oxford University Press; 2010.
Fan J, May SJ, Zhou Y, Barrett-Connor E. Bimodality of 2-h plasma glucose distributions in whites: the Rancho Bernardo study. Diabetes Care 2005;28:1451–6.
King AC, Vena A, Hasin D, De Wit D, O’Connor CJ, Cao D. Subjective responses to alcohol in the development and maintenance of alcohol use disorder (AUD). Am J Psychiatry. 2021. https://doi.org/10.1176/appi.ajp.2020.20030247 .
GBD. 2016 Alcohol and Drug Use Collaborators. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry. 2018;5:987–1012.
Edwards G, Gross MM. Alcohol dependence: provisional description of a clinical syndrome. Br Med J. 1976;1:1058–61.
Article CAS PubMed PubMed Central Google Scholar
Epstein DH, Heilig M, Shaham Y. Science-based actions can help address the opioid crisis. Trends Pharm Sci. 2018;39:911–16.
Amato L, Davoli M, Perucci CA, Ferri M, Faggiano F, Mattick RP. An overview of systematic reviews of the effectiveness of opiate maintenance therapies: available evidence to inform clinical practice and research. J Subst Abus Treat. 2005;28:321–9.
Cahill K, Stevens S, Perera R, Lancaster T. Pharmacological interventions for smoking cessation: an overview and network meta-analysis. Cochrane Datab System Rev. 2013;5:CD009329.
Jonas DE, Amick HR, Feltner C, Bobashev G, Thomas K, Wines R, et al. Pharmacotherapy for adults with alcohol use disorders in outpatient settings a systematic review and meta-analysis. JAMA. 2014;311:1889–900.
Article PubMed CAS Google Scholar
Mark TL, Kranzler HR, Song X. Understanding US addiction physicians’ low rate of naltrexone prescription. Drug Alcohol Depend. 2003;71:219–28.
Article PubMed Google Scholar
Nutt DJ, King LA, Phillips LD. Drug harms in the UK: a multicriteria decision analysis. Lancet. 2010;376:1558–65.
Wilk AI, Jensen NM, Havighurst TC. Meta-analysis of randomized control trials addressing brief interventions in heavy alcohol drinkers. J Gen Intern Med. 1997;12:274–83.
Laing RD. The divided self; a study of sanity and madness. London: Tavistock Publications; 1960.
Foucault M, Khalfa J. History of madness. New York: Routledge; 2006.
Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL. et al.Comorbidity of mental disorders with alcohol and other drug abuse. Results Epidemiologic Catchment Area (ECA) study.JAMA. 1990;264:2511–8.
Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–16.
Lopez-Quintero C, Hasin DS, de Los Cobos JP, Pines A, Wang S, Grant BF, et al. Probability and predictors of remission from life-time nicotine, alcohol, cannabis or cocaine dependence: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Addiction. 2011;106:657–69.
Humphreys K. Addiction treatment professionals are not the gatekeepers of recovery. Subst Use Misuse. 2015;50:1024–7.
Cohen E, Feinn R, Arias A, Kranzler HR. Alcohol treatment utilization: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2007;86:214–21.
Sobell LC, Cunningham JA, Sobell MB. Recovery from alcohol problems with and without treatment: prevalence in two population surveys. Am J Public Health. 1996;86:966–72.
Culverhouse R, Bucholz KK, Crowe RR, Hesselbrock V, Nurnberger JI Jr, Porjesz B, et al. Long-term stability of alcohol and other substance dependence diagnoses and habitual smoking: an evaluation after 5 years. Arch Gen Psychiatry. 2005;62:753–60.
Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830–42.
Skolnick P. The opioid epidemic: crisis and solutions. Annu Rev Pharm Toxicol. 2018;58:143–59.
Hser YI, Evans E, Grella C, Ling W, Anglin D. Long-term course of opioid addiction. Harv Rev Psychiatry. 2015;23:76–89.
Mathers BM, Degenhardt L, Bucello C, Lemon J, Wiessing L, Hickman M. Mortality among people who inject drugs: a systematic review and meta-analysis. Bull World Health Organ. 2013;91:102–23.
Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, et al. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72:757–66.
Article PubMed PubMed Central CAS Google Scholar
Lee MR, Sher KJ. “Maturing Out” of binge and problem drinking. Alcohol Res: Curr Rev. 2018;39:31–42.
Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ. Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction. 2005;100:281–92.
Berridge V. The rise, fall, and revival of recovery in drug policy. Lancet. 2012;379:22–23.
Parvaz MA, Moeller SJ, d’Oleire Uquillas F, Pflumm A, Maloney T, Alia-Klein N, et al. Prefrontal gray matter volume recovery in treatment-seeking cocaine-addicted individuals: a longitudinal study. Addict Biol. 2017;22:1391–401.
Korponay C, Kosson DS, Decety J, Kiehl KA, Koenigs M. Brain volume correlates with duration of abstinence from substance abuse in a region-specific and substance-specific manner. Biol Psychiatry Cogn Neurosci Neuroimaging. 2017;2:626–35.
PubMed PubMed Central Google Scholar
Janes AC, Datko M, Roy A, Barton B, Druker S, Neal C, et al. Quitting starts in the brain: a randomized controlled trial of app-based mindfulness shows decreases in neural responses to smoking cues that predict reductions in smoking. Neuropsychopharmacology. 2019;44:1631–38.
Humphreys K, Bickel WK. Toward a neuroscience of long-term recovery from addiction. JAMA Psychiatry. 2018;75:875–76.
Verhulst B, Neale MC, Kendler KS. The heritability of alcohol use disorders: a meta-analysis of twin and adoption studies. Psychol Med. 2015;45:1061–72.
Goldman D, Oroszi G, Ducci F. The genetics of addictions: uncovering the genes. Nat Rev Genet. 2005;6:521–32.
Kendler KS, Jacobson KC, Prescott CA, Neale MC. Specificity of genetic and environmental risk factors for use and abuse/dependence of cannabis, cocaine, hallucinogens, sedatives, stimulants, and opiates in male twins. AJ Psychiatry. 2003;160:687–95.
Schizophrenia Working Group of the Psychiatric Genomics C. Biological insights from 108 schizophrenia-associated genetic loci. Nature. 2014;511:421–7.
Wray NR, Ripke S, Mattheisen M, Trzaskowski M, Byrne EM, Abdellaoui A, et al. Genome-wide association analyses identify 44 risk variants and refine the genetic architecture of major depression. Nat Genet. 2018;50:668–81.
Wray NR, Lin T, Austin J, McGrath JJ, Hickie IB, Murray GK, et al. From basic science to clinical application of polygenic risk scores: a primer. JAMA Psychiatry. 2021;78:101–9.
Walters RK, Polimanti R, Johnson EC, McClintick JN, Adams MJ, Adkins AE, et al. Transancestral GWAS of alcohol dependence reveals common genetic underpinnings with psychiatric disorders. Nat Neurosci. 2018;21:1656–69.
Visscher PM, Wray NR. Concepts and misconceptions about the polygenic additive model applied to disease. Hum Hered. 2015;80:165–70.
Heilig M, Leggio L. What the alcohol doctor ordered from the neuroscientist: theragnostic biomarkers for personalized treatments. Prog Brain Res. 2016;224:401–18.
Rasmussen K, White DA, Acri JB. NIDA’s medication development priorities in response to the Opioid Crisis: ten most wanted. Neuropsychopharmacology. 2019;44:657–59.
Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. AJ Psychiatry. 2010;167:748–51.
Kwako LE, Schwandt ML, Ramchandani VA, Diazgranados N, Koob GF, Volkow ND, et al. Neurofunctional domains derived from deep behavioral phenotyping in alcohol use disorder. AJ Psychiatry. 2019;176:744–53.
Kwako LE, Bickel WK, Goldman D. Addiction biomarkers: dimensional approaches to understanding addiction. Trends Mol Med. 2018;24:121–28.
Xiao P, Dai Z, Zhong J, Zhu Y, Shi H, Pan P. Regional gray matter deficits in alcohol dependence: a meta-analysis of voxel-based morphometry studies. Drug Alcohol Depend. 2015;153:22–8.
Ersche KD, Williams GB, Robbins TW, Bullmore ET. Meta-analysis of structural brain abnormalities associated with stimulant drug dependence and neuroimaging of addiction vulnerability and resilience. Curr Opin Neurobiol. 2013;23:615–24.
Klugah-Brown B, Di X, Zweerings J, Mathiak K, Becker B, Biswal B. Common and separable neural alterations in substance use disorders: a coordinate-based meta-analyses of functional neuroimaging studies in humans. Hum Brain Mapp. 2020;41:4459–77.
Volkow ND, Fowler JS, Wang GJ. The addicted human brain: insights from imaging studies. J Clin Investig. 2003;111:1444–51.
Goldstein RZ, Volkow ND. Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications. Nat Rev Neurosci. 2011;12:652–69.
Goodkind M, Eickhoff SB, Oathes DJ, Jiang Y, Chang A, Jones-Hagata LB, et al. Identification of a common neurobiological substrate for mental illness. JAMA Psychiatry. 2015;72:305–15.
Scofield MD, Heinsbroek JA, Gipson CD, Kupchik YM, Spencer S, Smith AC, et al. The nucleus accumbens: mechanisms of addiction across drug classes reflect the importance of glutamate homeostasis. Pharm Rev. 2016;68:816–71.
Korpi ER, den Hollander B, Farooq U, Vashchinkina E, Rajkumar R, Nutt DJ, et al. Mechanisms of action and persistent neuroplasticity by drugs of abuse. Pharm Rev. 2015;67:872–1004.
Luscher C, Malenka RC. Drug-evoked synaptic plasticity in addiction: from molecular changes to circuit remodeling. Neuron. 2011;69:650–63.
Everitt BJ. Neural and psychological mechanisms underlying compulsive drug seeking habits and drug memories–indications for novel treatments of addiction. Eur J Neurosci. 2014;40:2163–82.
Lesscher HM, Vanderschuren LJ. Compulsive drug use and its neural substrates. Rev Neurosci. 2012;23:731–45.
Cruz FC, Koya E, Guez-Barber DH, Bossert JM, Lupica CR, Shaham Y, et al. New technologies for examining the role of neuronal ensembles in drug addiction and fear. Nat Rev Neurosci. 2013;14:743–54.
Crick F. The astonishing hypothesis: the scientific search for the soul. Scribner; Maxwell Macmillan International: New York, NY; 1994.
Vanderschuren LJ, Achterberg EJ, Trezza V. The neurobiology of social play and its rewarding value in rats. Neurosci Biobehav Rev. 2016;70:86–105.
Venniro M, Zhang M, Caprioli D, Hoots JK, Golden SA, Heins C, et al. Volitional social interaction prevents drug addiction in rat models. Nat Neurosci. 2018;21:1520–29.
Martinez D, Orlowska D, Narendran R, Slifstein M, Liu F, Kumar D, et al. Dopamine type 2/3 receptor availability in the striatum and social status in human volunteers. Biol Psychiatry. 2010;67:275–8.
Wiers CE, Shokri-Kojori E, Cabrera E, Cunningham S, Wong C, Tomasi D, et al. Socioeconomic status is associated with striatal dopamine D2/D3 receptors in healthy volunteers but not in cocaine abusers. Neurosci Lett. 2016;617:27–31.
Morgan D, Grant KA, Gage HD, Mach RH, Kaplan JR, Prioleau O, et al. Social dominance in monkeys: dopamine D2 receptors and cocaine self-administration. Nat Neurosci. 2002;5:169–74.
Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017;2:e356–e66.
Gilbert PA, Zemore SE. Discrimination and drinking: a systematic review of the evidence. Soc Sci Med 2016;161:178–94.
Oshri A, Gray JC, Owens MM, Liu S, Duprey EB, Sweet LH, et al. Adverse childhood experiences and amygdalar reduction: high-resolution segmentation reveals associations with subnuclei and psychiatric outcomes. Child Maltreat. 2019;24:400–10.
Holmes CJ, Barton AW, MacKillop J, Galván A, Owens MM, McCormick MJ, et al. Parenting and salience network connectivity among African Americans: a protective pathway for health-risk behaviors. Biol Psychiatry. 2018;84:365–71.
Brody GH, Gray JC, Yu T, Barton AW, Beach SR, Galván A, et al. Protective prevention effects on the association of poverty with brain development. JAMA Pediatr. 2017;171:46–52.
Hanson JL, Gillmore AD, Yu T, Holmes CJ, Hallowell ES, Barton AW, et al. A family focused intervention influences hippocampal-prefrontal connectivity through gains in self-regulation. Child Dev. 2019;90:1389–401.
Borsboom D, Cramer A, Kalis A. Brain disorders? Not really… why network structures block reductionism in psychopathology research. Behav Brain Sci. 2018;42:1–54.
Field M, Heather N, Wiers RW. Indeed, not really a brain disorder: Implications for reductionist accounts of addiction. Behav Brain Sci. 2019;42:e9.
Pascoli V, Hiver A, Van Zessen R, Loureiro M, Achargui R, Harada M, et al. Stochastic synaptic plasticity underlying compulsion in a model of addiction. Nature. 2018;564:366–71.
James W. The dilemma of determinism. Whitefish, MT: Kessinger Publishing; 2005.
Gessell B. Indeterminism in the brain. Biol Philos. 2017;32:1205–23.
Jedlicka P. Revisiting the quantum brain hypothesis: toward quantum (neuro)biology? Front Mol Neurosci. 2017;10:366.
Heyman GM. Addiction: a disorder of choice. Cambridge, MA: Harvard University Press; 2010.
Heather NQ. Is addiction a brain disease or a moral failing? A: Neither. Neuroethics. 2017;10:115–24.
Ahmed SH, Lenoir M, Guillem K. Neurobiology of addiction versus drug use driven by lack of choice. Curr Opin Neurobiol. 2013;23:581–7.
Hogarth L, Lam-Cassettari C, Pacitti H, Currah T, Mahlberg J, Hartley L, et al. Intact goal-directed control in treatment-seeking drug users indexed by outcome-devaluation and Pavlovian to instrumental transfer: critique of habit theory. Eur J Neurosci. 2019;50:2513–25.
Mathis V, Kenny PJ. From controlled to compulsive drug-taking: the role of the habenula in addiction. Neurosci Biobehav Rev. 2019;106:102–11.
Luscher C, Robbins TW, Everitt BJ. The transition to compulsion in addiction. Nat Rev Neurosci. 2020;21:247–63.
Robinson TE, Berridge KC. Addiction. Annu Rev Psychol. 2003;54:25–53.
Everitt BJ, Robbins TW. Neural systems of reinforcement for drug addiction: from actions to habits to compulsion. Nat Neurosci. 2005;8:1481–89.
Koob GF, Volkow ND. Neurocircuitry of addiction. Neuropsychopharmacology. 2010;35:217–38.
Tiffany ST. A cognitive model of drug urges and drug-use behavior: role of automatic and nonautomatic processes. Psychol Rev. 1990;97:147–68.
Robinson TE, Berridge KC. The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Res Rev. 1993;18:247–91.
Koob GF, Le Moal M. Plasticity of reward neurocircuitry and the ‘dark side’ of drug addiction. Nat Neurosci. 2005;8:1442–4.
Stein DJ, Costa DLC, Lochner C, Miguel EC, Reddy YCJ, Shavitt RG, et al. Obsessive-compulsive disorder. Nat Rev Dis Prim. 2019;5:52.
Vanderschuren LJ, Everitt BJ. Drug seeking becomes compulsive after prolonged cocaine self-administration. Science 2004;305:1017–9.
American_Psychiatric_Association. Diagnostic and statistical manual of mental disorders: DSM-5™. 5th ed. Arlington, VA, US: American Psychiatric Publishing, Inc; 2013.
Book Google Scholar
Spragg SDS. Morphine addiction in chimpanzees. Comp Psychol Monogr. 1940;15:132–32.
Lenoir M, Cantin L, Vanhille N, Serre F, Ahmed SH. Extended heroin access increases heroin choices over a potent nondrug alternative. Neuropsychopharmacology. 2013;38:1209–20.
Caprioli D, Venniro M, Zeric T, Li X, Adhikary S, Madangopal R, et al. Effect of the novel positive allosteric modulator of metabotropic glutamate receptor 2 AZD8529 on incubation of methamphetamine craving after prolonged voluntary abstinence in a rat model. Biol Psychiatry. 2015;78:463–73.
Augier E, Barbier E, Dulman RS, Licheri V, Augier G, Domi E, et al. A molecular mechanism for choosing alcohol over an alternative reward. Science. 2018;360:1321–26.
Bigelow GE. An operant behavioral perspective on alcohol abuse and dependence. In: Heather N, Peters TJ, Stockwell T, editors. International handbook of alcohol dependence and problems. John Wiley & Sons Ltd; 2001. p. 299–315.
Higgins ST, Heil SH, Lussier JP. Clinical implications of reinforcement as a determinant of substance use disorders. Annu Rev Psychol. 2004;55:431–61.
Satel S, Lilienfeld SO. Brainwashed: the seductive appeal of mindless neuroscience. New York, NY: Basic Books; 2015.
Wilson EO. Consilience: the unity of knowledge. New York, NY: Vintage Books; 1999.
Saunders JB, Degenhardt L, Reed GM, Poznyak V. Alcohol use disorders in ICD-11: past, present, and future. Alcohol Clin Exp Res 2019;43:1617–31.
Organization. WH. ICD-11 for mortality and morbidity statistics. 2018. https://icd.who.int/browse11/l-m/en . Accessed 21 Oct 2020.
Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, brief intervention, and referral to treatment (SBIRT): toward a public health approach to the management of substance abuse. Subst Abus. 2007;28:7–30.
Witkiewitz K, Hallgren KA, Kranzler HR, Mann KF, Hasin DS, Falk DE, et al. Clinical validation of reduced alcohol consumption after treatment for alcohol dependence using the World Health Organization risk drinking levels. Alcohol Clin Exp Res 2017;41:179–86.
Hasin DS, O’Brien CP, Auriacombe M, Borges G, Bucholz K, Budney A, et al. DSM-5 criteria for substance use disorders: recommendations and rationale. AJ Psychiatry. 2013;170:834–51.
Rosenthal RJ, Faris SB. The etymology and early history of ‘addiction’. Addict Res Theory. 2019;27:437–49.
Martin CS, Steinley DL, Verges A, Sher KJ. The proposed 2/11 symptom algorithm for DSM-5 substance-use disorders is too lenient. Psychol Med. 2011;41:2008–10.
Degenhardt L, Bharat C, Bruno R, Glantz MD, Sampson NA, Lago L, et al. Concordance between the diagnostic guidelines for alcohol and cannabis use disorders in the draft ICD-11 and other classification systems: analysis of data from the WHO’s World Mental Health Surveys. Addiction. 2019;114:534–52.
PubMed Google Scholar
Lago L, Bruno R, Degenhardt L. Concordance of ICD-11 and DSM-5 definitions of alcohol and cannabis use disorders: a population survey. Lancet Psychiatry. 2016;3:673–84.
Lundin A, Hallgren M, Forsman M, Forsell Y. Comparison of DSM-5 classifications of alcohol use disorders with those of DSM-IV, DSM-III-R, and ICD-10 in a general population sample in Sweden. J Stud Alcohol Drugs. 2015;76:773–80.
Kwako LE, Momenan R, Litten RZ, Koob GF, Goldman D. Addictions neuroclinical assessment: a neuroscience-based framework for addictive disorders. Biol Psychiatry. 2016;80:179–89.
Rehm J, Heilig M, Gual A. ICD-11 for alcohol use disorders: not a convincing answer to the challenges. Alcohol Clin Exp Res. 2019;43:2296–300.
Download references
Acknowledgements
The authors want to acknowledge comments by Drs. David Epstein, Kenneth Kendler and Naomi Wray.
Author information
Authors and affiliations.
Center for Social and Affective Neuroscience, Department of Biomedical and Clinical Sciences, Linköping University, Linköping, Sweden
Markus Heilig
Peter Boris Centre for Addictions Research, McMaster University and St. Joseph’s Healthcare Hamilton, Hamilton, ON, Canada
- James MacKillop
Homewood Research Institute, Guelph, ON, Canada
New York State Psychiatric Institute and Columbia University Irving Medical Center, New York, NY, USA
Diana Martinez
Institute for Mental Health Policy Research & Campbell Family Mental Health Research Institute, Centre for Addiction and Mental Health (CAMH), Toronto, ON, Canada
Jürgen Rehm
Dalla Lana School of Public Health and Department of Psychiatry, University of Toronto (UofT), Toronto, ON, Canada
Klinische Psychologie & Psychotherapie, Technische Universität Dresden, Dresden, Germany
Department of International Health Projects, Institute for Leadership and Health Management, I.M. Sechenov First Moscow State Medical University, Moscow, Russia
Clinical Psychoneuroendocrinology and Neuropsychopharmacology Section, Translational Addiction Medicine Branch, National Institute on Drug Abuse Intramural Research Program and National Institute on Alcohol Abuse and Alcoholism Division of Intramural Clinical and Biological Research, National Institutes of Health, Baltimore and Bethesda, MD, USA
Lorenzo Leggio
Department of Population Health Sciences, Unit Animals in Science and Society, Faculty of Veterinary Medicine, Utrecht University, Utrecht, the Netherlands
Louk J. M. J. Vanderschuren
You can also search for this author in PubMed Google Scholar
Contributions
All authors jointly drafted the paper.
Corresponding author
Correspondence to Markus Heilig .
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Heilig, M., MacKillop, J., Martinez, D. et al. Addiction as a brain disease revised: why it still matters, and the need for consilience. Neuropsychopharmacol. 46 , 1715–1723 (2021). https://doi.org/10.1038/s41386-020-00950-y
Download citation
Received : 10 November 2020
Revised : 11 December 2020
Accepted : 14 December 2020
Published : 22 February 2021
Issue Date : September 2021
DOI : https://doi.org/10.1038/s41386-020-00950-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Persistent impacts of smoking on resting-state eeg in male chronic smokers and past-smokers with 20 years of abstinence.
- Yoonji Jeon
- Dongil Chung
Scientific Reports (2023)
A contextualized reinforcer pathology approach to addiction
- Samuel F. Acuff
- James G. Murphy
Nature Reviews Psychology (2023)
Functional genomic mechanisms of opioid action and opioid use disorder: a systematic review of animal models and human studies
- Camille Falconnier
- Alba Caparros-Roissard
- Pierre-Eric Lutz
Molecular Psychiatry (2023)
A neuromarker for drug and food craving distinguishes drug users from non-users
- Leonie Koban
- Tor D. Wager
Nature Neuroscience (2023)
Does a Survivorship Model of Opioid Use Disorder Improve Public Stigma or Policy Support? A General Population Randomized Experiment
- Jarratt D. Pytell
- Geetanjali Chander
- Emma E. McGinty
Journal of General Internal Medicine (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
239 Addiction Essay Topic Ideas & Examples
🏆 best addiction topic ideas & essay examples, 👍 good essay topics on addiction, 📌 simple & easy addiction essay titles, 💡 most interesting addiction topics to write about, 📑 good research topics about addiction, ✍️ addiction essay topics for college.
- Addiction to Online Gaming: A Review of Literature The present paper is an overview of scholarly sources on online gaming addiction and the analysis of narrative inquiry as the most suitable qualitative research method to use for the investigation of this problem.
- Smartphone Addiction Problem Statement Uncontrolled use of smartphone requires users to review the need to respond to smartphone alerts, deactivate the alerts, and consult their colleagues rather than the phone because such actions can reduce anxiety. Smartphone addiction is […] We will write a custom essay specifically for you by our professional experts 808 writers online Learn More
- Problems of Internet Addiction Disorder Another possible cause of a reduction in the brain capabilities is the kind of the materials that one is exposed to on the Internet.
- Problems of Pornography Addiction This paper provides you with a deep insight into the issues related to pornography including the factors leading to wide spread of this, the various perspective and attitudes towards the matter, and lastly, discuss its […]
- The Concept of Addiction The recent developments in psychology, as well as intensive studies in the concept of addiction, has drawn considerable debates and concerns on the issue of relationships between the legal system and addiction.
- Phone Addiction Among Adolescents The ethical principle that the paper will base on is the principle of nonmaleficence, which aims to weigh the benefits versus the harms of phone addiction. However, it is ethical to be addicted to smartphone […]
- Jim Carroll’s Drug Addiction in the Movie “The Basketball Diaries” by Leonardo Dicaprio After the bursting of Jim and apprehending of his friends, using drugs red handed by the couch, disintegration starts taking place in the group and most of the boys lose their essence for being thrown […]
- Symbolic Interactionism on Drug Addiction Genetic factors in addiction include the number of receptors in the brain that influence the perception of drugs and other substances.
- Online Gambling Addiction Gambling is an addiction as one becomes dependent on the activity; he cannot do without it, it becomes a necessity to him. Online gambling is more of an addiction than a game to the players.
- Amy Winehouse: Addiction Case Study The singer’s relationships with her dad and husband serve as the representation of the abuse she had to face as a pop-star.
- Facebook Addiction in the Modern Society As a result of these occurrences, it has been proposed that Facebook is addictive since people appear to be hooked to the site and cannot keep away from it even considering the negative consequences.
- The Qualitative and Quantitative Research Strategies: Drug Addiction This is why another purpose of this paper is to evaluate what kind of research strategy is more effective and better in regards to the topic of drug addiction.
- Social Media Addiction in Society The person takes the substance, or in case of social media, keeps checking and updating online status or website on and on.
- Deviant Behavior: Drug Addiction Drug addiction as a form of deviant behavior is seen as a loss of a person’s former moral and spiritual values, which leads to intellectual degradation and a reduced desire to function as a member […]
- Device Addiction: Consequences and Solutions One of the essential traits of smartphone addiction is tolerance which is defined as “a gradual increase in the mobile phone use to obtain the same level of satisfaction”.
- Effects of Internet Addiction on Family Relationships Among Teenagers In the modern society, cyber bullying refers to the instances where the individual uses the internet to interfere with the rights and freedoms of others.
- “A Star Is Born”: Addiction Analysis From the BPS+ Perspective Most importantly, the movie points to the presence of a much more significant factor that pushes Jack toward the abuse of alcohol and the use of drugs.
- The Theme of Addiction in Tennessee Williams’ Plays Apart from that, one can mention that addiction is depicted as a force that ruins the family of the characters. This is one of the points that should be distinguished.
- On Internet Addiction in Swift’s Satirical Style In the modern world, it is difficult to find any person who is unfamiliar with the Internet. People began to abuse the Internet and live a virtual life, forgetting the real world.
- Internet Addiction Among College Students It is definitely advisable that the schedule include at least a few hours to login to Facebook because at the end of the day the aim is not to put the person in total isolation.
- Drug Addiction and Its Effects The main cause of drug addiction is, obviously, the use of drugs but there are specific predictors making some people engage in drug abuse. Another sign of addiction is the need to use drugs in […]
- Women’s Addiction in All Its Manifestations Analysis In the Substance Addiction category, women usually indulge in Food, Alcohol, and Drugs in that order of priority; however, addiction of women to alcohol and drugs is more prevalent in Western countries {albeit to a […]
- Online Gaming Addiction Intervention HC’s philosophical stand is to stop the addiction, meaning that he is motivated and hopes that the obsession will end. The addiction process started at a very young age of 7 years, back when HC […]
- College Students: Internet Addiction The authors also note that the use and access of the internet have increased in the past decades. Additionally, the authors argue that conflicts between parents and young individuals are likely to result in internet […]
- The Effect of Internet Addiction on Students’ Emotional and Academic Performance The participants will be told the goals and objectives of the study, and their experience of Internet addiction will be clarified.
- Addiction: Is It a Disease or Moral Failing? According to the journal article of clinical and research news, a disease can be defined as a complicated relationship existing between the environment of an individual and the general genetic makeup that combines together resulting […]
- The Intervention of Positive Coping and Drug Addiction The intervention in question is based on the three domains that are referred to as “the pleasant life”, “the engaged life” and “the meaningful life”.
- Internet Addiction in Modern Society Good internet connectivity coupled with the fact that the cost of using the internet is very cheap make people to spent countless hours in the internet.
- Video Games Addiction: Is It Real? Addiction is associated with the need of substance while in some cases a behaviour which someone finds hard to move on without it, where the unavailability to a way out leads to abnormality.
- The Role Play in Drug Addiction Treatment Moreover, the client believes that everyone in the law field uses coke, including his father, and this is the culture of the sphere.
- Impact of Digital Drug and Electronic Addiction on UAE Youth Therefore, the primary purpose of this dissertation is to determine the impact of digital drugs and the electronic addiction they cause on the youth of the UAE to highlight the existing problem in society.
- Alcoholic Anonymous Organization Fighting Addiction By accepting the problem and causes, a participant can try to resolve. In the program, participants have to admit their past wrongs and errors to a group and receive support to change.
- Likecoholic: Social Media Addiction Modern scholars have started likening the addiction to the use of social media to smoking, stating that companies such as Facebook must be regulated “exactly the same way you regulated the cigarette industry,” in which […]
- Social Work and Addiction in Family Settings The patient experiences urges to use drugs regardless of the apparent negative consequences of this practice. Therapists and clients consider this stage to be the most difficult.
- Comparison of Theories of Addiction: The Biological Model and the Genetic Model Genetic and biological models aim at disclosing the essence of addiction as something natural and irreversible and the methods which are supported by neurobiology and physiology and become more appropriate for using and controlling human […]
- Online Gaming Addiction Analysis For example, in World of Warcraft, there are 10 million players around the world who pay about $15 a month to blitz around the world of Azeroth.
- Mental Health Care in Cannabis Addiction Case Based on the experience of studying the stories of juvenile delinquents, Bowlby revealed the influence of early separation from the mother and the experiences of loss and separation associated with it on the violation of […]
- Addiction Assessment Tool Evaluation The purpose of the present paper is to conduct a review of the 10-item yes/no Drug Abuse Screening Test to evaluate its benefits and limitations.
- Alcohol Addiction and Psychological Assistance Smith is a supporter of the Democratic Party like most people in her family and among her friends and colleagues. Smith was asked what goals she wanted to achieve in the course of her treatment.
- Social Cognitive Theory Against Addiction All the sources are closely related to the problem of alcohol addiction and, therefore, are included in the research. The study aimed to investigate the effect of the social cognitive theory implementation on people willing […]
- Theories of Substance Addiction The risk is confounded when these factors occur in combination; thus, the more the risk factors, the higher the probability that the use of substances can result into addiction.
- Addiction of Whitney Houston This paper looks at the causes of addiction, hindrances to recovery, and the causes of relapse or successful recovery using the life of Whitney Houston as a model.
- Mobile Addiction and Anxiety: The Relationship Analysis The purpose of the study is to establish the nature of the relationship that exists between mobile addiction and anxiety among students.
- Psychodrama in Treating Trauma and Addiction In all cases, it is problematic for the individual to reconcile with the anxiety they feel and to cope with the problems with trust.
- Society’s Obligation to Help People With Addiction The first and foremost point is that the group approach shifts treatment to the natural environment and reconnects addiction therapy to a more comprehensive and long-lasting recovery process.
- Men and Porn Addiction Discussion Watching porn trains men to differentiate reality from acting, implying that it does not alter men’s perception of women in real life.
- Impaired Nurses: Prescription Drug Addiction Work with drugs and psychotropic substances in medical organizations is constantly in the field of view of law enforcement agencies for the control of drug trafficking and health authorities.
- Psilocybin as a Smoking Addiction Remedy Additionally, the biotech company hopes to seek approval from FDA for psilocybin-based therapy treatment as a cigarette smoking addiction long-term remedy.
- Advocacy Programs to Address Disparities in Mental Health and Addiction Management Due to the absence of coverage offered by state Medicaid programs, the problem with the community’s overall health likely resides in a population segment that is unable to receive care, especially individuals with mental health […]
- The History of ADHD Treatment: Drug Addiction Disorders Therefore, the gathered data would be classified by year, treatment type, and gender to better comprehend the statistical distribution of the prevalence of drug addiction.
- Teen Vaping: The New Wave of Nicotine Addiction It might have a significant effect if state officials asked the region’s health authority to ban all flavored vape goods in reaction to this issue to safeguard the youth’s well-being.
- The Epidemic of Opioid Addiction in the US Although the author presents facts about kratom benefits, the article still lacks scientific evidence, likely due to insufficient research in this area, so it may not convince the reader that this herb should be legal.
- Opioid Addiction and Pharmacological Treatment LAAM has several merits over the use of methadone, particularly regarding its use of three doses per week, which can reduce the potential of contracting HIV/AIDS, improve the relationship between the patients and the clinicians, […]
- Misconceptions About Addiction In addition, addicts are not always drug abusers, as addiction is a treatable disorder, and people seeking help can recover and become productive.
- Smartphone Addiction in the United States With the advent of phones that have the function of many other gadgets, people began to move away from the real world into the virtual one. This paper examines the essence of the issue of […]
- The Truth About Food Addiction in Society One of the most important tasks is understanding the reality of food addiction. The first line of food addiction prevention is the decision people have to make.
- The Opium Addiction Treatment Above all, the main problem is the reluctance of pharmaceutical companies to find a common approach and method of facing opium addiction since the first thing to think about is profits, just like any other […]
- Discussion: Social Media Addiction Social media use impacts the nerves in the brain and can cause psychological and physical addiction. The brain gets used to the rewards from such channels, and it becomes automatic for the person to use […]
- Opioid Addiction in Adults: A Group Counselling Plan A group leader ensures that the group is led in a healthy discussion and that the group’s objectives are achieved. When this culture is properly outlined, and members are aware of their targets, the group’s […]
- Tackling Drug: Addiction Among Youth Drug addiction is a serious problem, and while it spreads to less marginalized parts of society, this problem affects more people.
- The Nature of Addiction The purpose of this critical writing is to understand why people begin to want to get rid of the shackles of addictive behavior.
- Tobacco Addictions Among Teenagers This makes it urgent to fight all forms of tobacco and nicotine use in order to preserve the health of adolescents.
- Program to Tackle Drug Addiction Among Youth The core area of emphasis will be training the students on different ways to avoid the temptations of using drugs in order to lower the rate of addiction.
- Parental Role in Adolescents’ Phone Addiction In other words, the connection between the guardian and the teenagers is critical and should be maintained to allow children experience the love of their parents.
- A Manifesto on the Phone Addiction Issue It seems to be common knowledge that being too attached to one’s phone is bad for mental and physical health, and the dangers may be greater for the younger generation.
- Discussion of Tobacco Addiction in Miami The problem analyzed in the presentation is related to the increased risk of tobacco use among adults associated with nicotine dependence.
- Lysergic Acid Diethylamide (LCD): Addiction, Treatment, and Prevention The problems are not only depicted in the area of concentration but also in the suburbs that are out of the stereotypical view of intoxication of the drug.
- Drug and Alcohol Addiction: Abby’s Case The amounts of money Abby spends weekly on fulfilling her addictive desires and her long history of drug usage imply that she has an addiction problem.
- Drug Addiction in Teenagers: Smoking and Other Lifestyles In the first part of this assignment, the health problem of drug addiction was considered among teens and the most vulnerable group was established.
- Instagram Addiction and Impact on Self-Esteem The effect of social media use is reported to have a mixed effect on the user. First, social media addiction may have a varying effect on self-esteem depending on the type of use.
- Comprehensive Addiction and Recovery Act The policy authorizes the secretary to award grants to states with a higher rate of substances and drugs as this indicates the state of mental health.
- How Alvin Ailey’s Dances Help With Drug Addiction Ailey is the founder of the famous theater in New York and is known for popularizing modern dance and mixing it with ballet, jazz and elements of African culture.
- Molecular Dynamics Modeling: Treating Addiction The resulting mechanism of the three sites provides the separation of antagonists from the agonists and explains the selectivity of the subtypes.
- Drug Addiction Treatment for a Pregnant Woman The drug has affected various aspects of her life, causing her to lose her job and making her turn to crime to afford the drugs.
- You Are What You Eat: How Does Food Become an Addiction One of the most important problems that arouse the interest of researchers is the influence of advertising on the formation of models of food behavior and, above all, its involvement in the formation of food […]
- Instagram Addiction and Self-Esteem in Kuwaiti High School Students Besides, the study will explore the impact of social media and reveal the possible ways to resolve the social media addiction issues affecting the youth.
- Instagram Addiction and Self-Esteem in High School Students To test the relationship between social media Instagram addiction and self-esteem in American high school students, a descriptive survey where students will be enrolled in an online, blinded survey will apply.
- Tobacco as a Chemical Addiction Chemical addiction is a global disease of the mind, soul, and body. It is necessary to remove the mechanism of a disease-dependent state of origin and engage all the spheres of human life to overcome […]
- Drug Addiction: Overview of the Main Principles and Recovery Plan On the one hand, the term’ drug addiction is specifically defined by NIDA as “characterized by intense and, at times, uncontrollable drug craving, along with compulsive drug seeking and use that persist even in the […]
- How Opioid Addiction Affects the United States Addicted people have a constant desire to increase the dose, which is a severe medical and social problem. The crisis has acquired enormous proportions and become a brake on the economy and a threat to […]
- Drug and Alcohol Addiction in Atlantic City The prevalent part of the population of Atlantic City consists of African-Americans and Caucasians. Because of this, alcohol and drugs are very popular among residents, which may pose a community health issue and is applicable […]
- The Role of Mitochondria in Cocaine Addiction In many instances, the drug users tend to sniff it, and the powder gets through the nasal materials to the bloodstream.
- Why Addiction Develops and How a Person Can Overcome It The interview process was good; I called the interviewee at a scheduled time and asked her the questions from the list.
- Preventing Childhood Exposure to Addiction-Forming Factors The implementation of the method relied on the use of advanced questionnaire that provided the researchers with sufficient data to reflect and address the children’s inclination toward any form of addiction. Evidently, the role of […]
- History and Social Side of Drug Addiction Heroin and fentanyl are the most dangerous drugs created on the basis of papaver somniferum due to produced effects and the outcomes for the body.
- Drug and Substance Addiction Standardization has to be used to ensure that patients’ experiences and different clinical services are the same, regardless of the process.
- My Personal Beliefs About People With Addictions Therefore, in my opinion, the main reason people get addicted is related to the desire to forget about the problems of this reality and feel differently.
- Biopsychological and Spiritual Models in Addiction Studies More specifically, it is the “simplification” of the real-world conditions provides an opportunity to neglect different factors to provide a qualitative conclusion concerning the object of learning.
- Economic Inequality During COVID-19: Correlation With Depression and Addiction Thus, during the pandemic, people with lower incomes experienced depression and increased their addictive behaviors to cope with the stress of COVID-19.
- Opioid Use and Addiction in Afghanistan and Iraq Veterans My chosen topic integrates the welfare of veterans of recent wars, such as conflicts in Iraq and Afghanistan, the prescription of opioids for trauma, general mental well-being, and adaptation to civilian and even academic life.
- Tobacco Addiction: Causes and Effects However, it has also been proven that, in general, smoking has causal roots in human genetics, with different percentages of the message affecting, respectively, the start of smoking, the duration of the experience, and the […]
- Drug Addiction and Problems Related to It It is one of the main sources of dopamine, and other pleasure hormones, which are essential for a person to feel joy in their life.
- Chemical Dependency and Crisis of Addiction The scope of the damaging effects of alcohol abuse on the well-being of the person is astounding. Based on the WHO’s data, socio-cultural determinants of health are the issues that are linked to culture and […]
- Social Facet of Substance Addiction Even though the determination of the hazardous society is important for analyzing the social facet of drug addiction, it is crucial to fundamentally understand the society’s influential factors of engaging a person in drug addiction.
- Alcohol Addiction: Biological & Social Perspective At the same time, the UK is one of the most drinking countries, as the average number of liters of alcohol per person there was 11. In addition, taking acetaldehyde dehydrogenase inhibitors allows to break […]
- Drug and Alcohol Addiction Crisis Among Adults in Baltimore While a lot of the violence in Baltimore is related to the drug trade, the drugs themselves killed at least 180 more people than homicides in the city as of 2019.
- Addiction in Sexton’s, Marshall’s, Flynn’s Poems The poems The Addict by Anne Sexton, Habitual by Nate Marshall, and Philip Seymour Hoffman by Nick Flynn, address the issue from the psychological perspective as an inner struggle within a person.
- John S. McCain Opioid Addiction Prevention Act’s Analysis Anderson, the President and Chief Executive Officer of the National Association of Chain Drug Stores, backed the legislation enactment believing in its potential to reduce opioid abuse and addiction.
- Alcohol Addiction and the Role of a Community New Horizons Group of Alcoholics Anonymous is a local fellowship to support men and women with alcoholic problems in Miami Springs.
- Analysis of the Addiction’s Aspects Addiction in the modern world is one of the phenomena that occur in the vast majority of people. However, if the goal is not achieved, there will be a sharp decline in this hormone, and […]
- Workout and Addiction: Review As a result of personal factors and the presence of eating or image disorders, an individual can be unable to stop exercising even when it is detrimental to their life.
- Counseling of a Client With Heroin Addiction Although he has a son, he does not maintain any relationship with him, and his son does not try to communicate with Dante. First, the client did not address this aspect and was unwilling to […]
- Drug Addiction and Drug Legalization Rosenthal views drug addiction as slavery and the idea for drug legalization is revolting because most of the victims of addiction are adolescents and children. Without honesty and responsibility, legalization of drugs is just a […]
- The Issue of Opioid Abuse and Addiction in Treatment The project will primarily focus on the issue of opioid abuse and addiction to treat and minimize the effects of pain through the given pharmacological method of pain management.
- Fundamental Determination of Substance Abuse and Addiction and Their Difference Due to the difference in regularity and intensity of drug absorption, substance abuse and addiction can be correctly separated from another so that there is a concrete measure that identifies an abuse and an addiction […]
- Alcohol Addiction Among Women Women are a population of interest because of the increased mortality rates from alcohol-related health complications and the effect of this substance on childbearing. Similarly, to the previous organization, Alcove is a recovery facility that […]
- Drug Addiction Treatment Approaches In this way, some state that the objectives and aims of treatment should be to entirely drug-free the drug addict and that treatment should include drug-free techniques of achieving this aim.
- Drug Addiction From Pharmacological Perspective In the history of human society, drug addiction is almost always spoken of as a crime. Understanding drug effects allow criminologists and sociologists to recognize the relationship between drug addiction and crime.
- Drug Addiction Problem Among Homeless People There is a need to fill the data gap regarding the issues of magnitude, location, period, severity, and changeability of the SUD in the Skid Row community.
- Nuances of Alcohol Using Addiction Despite the traced co-occurrence of criminal activities and alcohol consumption, people argue that there are many positive aspects of drinking moderately, such as relaxation that is useful in many social environments. Goode argues that “for […]
- Systemic Interventions Overview: Cocaine Addiction She shared her recovery story in the Portrait of Addiction, and though she was successful on her way to a normal life, a systemic intervention approach would make it much easier and more comfortable for […]
- Substance Addiction Challenges for American Indians In the case presented by Paul et al, the distinctions between male and female addicts can be seen in the cultural features and traits of the American Indian population.
- Loneliness and Social Networking Addiction in Students The hypothesis of the study was as follows: the higher the level of loneliness, the higher the likelihood of social networking addiction; conversely, the lower the level of loneliness, the lower the likelihood of social […]
- Warm Hand-off for Overdose Survivors to Addiction Treatment The first responders facilitate the identification of survivors needing emergency health care systems House Bill 424 of the General Assembly of Pennsylvania, known as the Warm Hand-Off to Treatment Act, provides a comprehensive initiative that […]
- Reasons of Alcohol Addiction in Teenagers Given the clinical diagnoses, the wide-spread nature of the problem, and the severe consequences impacting the life and health of millions of people, the in-depth investigation of the causes of the disorder is of critical […]
- The John Muir Health Facility’s Addiction Medicine Recovery Services The aim of this evaluation plan is to establish the effectiveness of the program in addressing patients’ behavioral and attitudinal issues affecting their commitment to sobriety.
- Criticism of Injecting Rooms – Drug Addiction Supporters of injecting rooms claim that injecting rooms are beneficial to the society and that the ones which are in existence have saved many lives especially from the dangers of drug overdosing.
- Drug Addiction: Importance of Policy Change Drug addiction and abuse are the issues that have to be discussed and analyzed from different aspects to make sure that the policy change and offered practices can work effectively to reduce the number of […]
- The Drug Addiction and Clonidine As soon as it gets to the brain, it reacts by binding on the a2 receptors, a process that leads to a reduction in the levels of presynaptic calcium.
- How Serotonin Affects the Brain and Addictions The purpose of this paper is to discuss the effects that serotonin has in the brain and how it interacts with other chemicals in the body Serotonin is an indoleamine chemical secreted by the brain […]
- Impacts of Internet on Children Health and Addiction Among the worst hit are children, who find themselves addicted to it given that they are in the process of development. To help nurture children’s behavior, parents should educate them on the safety and risks […]
- Searching the Web for Research Evidence: Drug Addiction Among School Aged Children Defining the topic in the form of a question or statement and separating the question into specific logical components or concepts is the principal strategy to search the CINAHL database.
- Caffeine Addiction and Negative Effects The thesis of this paper is that scientists need to reclassify caffeine as a potentially addictive stimulant drug. In addition to the potential to cause addictive behavior, caffeine can have an adverse effect on the […]
- The Case of Katie’s Addiction Katie became one of the unfortunate people who had to deal with chronic pain, which led her to develop an addiction to the medication which was supposed to benefit her and relieve the car accident’s […]
- Valium and Heroin Addiction: Compare and Contrast The purpose of this paper is to contrast and compare Valium and heroin from a point of view of addiction and withdrawal.
- Mental Health Nursing of Cocaine Addiction The 1983 Mental Health Act is an Act of the Parliament of the United Kingdom that applies to the residents of England and Wales.
- Refraining From Diet Coke: Substance Use Addiction Speaking of my plans on the use of diet coke, I would like to emphasize that I do not plan to drink it.
- Addiction in the Elderly: Structured Critical Review Therefore, it is in the interest of national and global communities to prioritize the needs of the elderly and investigate the particularities of their addiction to substances.
- DSM-5 and Introduction of Behavioral Addictions The combination of substance abuse and behavioral addiction is another point that is widely debated to be recognized in the DSM-5.
- Symptoms of Addiction: Case Analysis Second, the inability to fall asleep without alcohol or a sleeping pill is a definite sign of addiction. Third, the client initially takes large doses of alcohol, which is a sign of increased tolerance.
- Team of Professionals: Addiction Case Analysis Second, the client needs to undergo a thorough medical assessment to understand if he presents the signs of comorbidities. Considering that the client may find it difficult to organize and keep track of all appointments, […]
- Anxiety Among Us: How and Why, Drug Addiction As the effects of the drug are not long-lasting, people who take phenobarbital tend to use the medicine more often than it is allowed in the drug prescription.
- Addiction Treatment: Challenges in Case Management Settings Case management has a vital role in addiction treatment as it helps to adopt a holistic approach and empower the client. According to the US Department of Health and Human Services (HHS, 2004), “substance abusers have better treatment outcomes if their other problems are addressed concurrently” (pp.1-2). Case management aims at planning and coordinating health […]
- Adolescent Substance Abuse, Addiction, and Dependence And while overall statistics show a decrease in the number of unique and persistent cases of substance abuse in Western countries in general and in the US in particular, this problem is still extremely urgent.
- Food Addiction and Obesity in Children and Teens Many turn to comfort eating to cope with this stress, to the point where it takes on the characteristics of an addiction. Overeating and obesity can also become a vicious cycle: children would eat to […]
- Shopping Addiction: Personal Experiences She realized that she had wasted most of her life and she was heading to destruction. She began thinking of taking a positive turn in her life; although she knew it would not be easy […]
- Drug Abuse and Addiction Holimon has succeeded in reviving some of her family relations, and she is still putting a lot of effort to get ahead in this area to the fullest extent possible.
- Facebook Addiction Problem Overview This paper is an in-depth analysis of the risks that Facebook poses to children and the steps that parents should take to ensure that their children do not become victims of Facebook use.
- Facebook: The Latest Addiction Most delegates had laptops in the room connected to the internet and my surprise a good number of them were misusing the privileges of the internet provided by the UN by accessing Facebook and other […]
- Psychoactive Substances and Addiction Substances that could easily lead to addiction are the elements that directly motivate the dopaminergic system such as marijuana, cocaine, nicotine, and heroin.
- The Development of Phobias and Addictions On the other hand, addictions are the behavioral pattern that is characterized by either psychological or physical reliance on substances abuse which is known to have negative impacts on the health and the life of […]
- Addictions and Emotions in Biopsychology The impulse sent to the brain in response to the stimuli is sent to two different parts of the brain: cortex and thalamus.
- The Addiction From Cocaine Main Aspects The impact of the cocaine on the human brain can be explained by the chemical dopamine and its variations in the brain of the drug addict, as well as by three main areas of the […]
- Drug Addiction Treatment: Variety of the Methods Basing on the importance of the learning process in the development of drug addiction practice, CBT makes use of the learning process, firstly, in helping the patients to recognize the conditions which stimulate them to […]
- Online Video Games Addiction The changes are far-reaching: the definition of online video game; the nature of the information ‘commons’ for the citizen; the right of privacy in communicated expressions; the regulation of information infrastructures; the definition of information […]
- The Problem of Gambling in the Modern Society as the Type of Addiction Old people and adolescents, rich and poor, all of them may become the prisoners of this addiction and the only way out may be the treatment, serious psychological treatment, as gambling addiction is the disease […]
- Behavioral Change: Drugs and Addiction The reasons for such usage could vary according to the substance used and to the life rhythm of the addicted person.
- Computer Addiction: Side Effects and Possible Solutions Since that time humanity started to speak of different signs of “computer addiction” the term stands to emphasize the seriousness of the problem and implies the possibility of drastic consequences that computer mania might have.
- Caffeine Addiction as a Mental Disorder And it is a rather pragmatic question stipulated by the professionals need to debate about, but not by the addiction nature itself.
- Drug Addiction: A General View of New Concepts Users who are weak-minded or peer adulating, tend to imitate others and use the drug not because they really want to, but in order to appear ‘cool’ and ‘one of the group.’ This is a […]
- Antidepressant Addiction and Abuse Depressed addicts need to have a proper examination of their addictive behavior to be able to abstain from processes and substances for altering moods fully.
- Sexual Addiction, Compulsivity, or Problematic Behavior Sex, in general, is most common among the male, they are the ones who can have many ladies just to have sex with them, and they will never think of sex as being sacred or […]
- Alcohol Addiction Issue in USA In order to do well in the group of Alcoholics Anonymous, it is better if the individual is talkative and open to conversations, as the main way of psychological therapy is telling stories about their […]
- The Reality TV Shows Addiction: Cause-Effect The viewers feel like the actors are just in the same scenario as them and every development is a success to both the actor and his viewer.
- Advanced Addiction Psychology Contemporary Perspectives The aptest critique of the test is provided by the discussion that Cox has provided when they suggest that the test should be considered along with the connectionist model.
- Opium Addiction: Cause and Effect The traffic of opium became unlawful only at the beginning of the 20th century when the scientists discovered the real properties of this drug and found out that it causes addiction.
- Methamphetamine and Cocaine Addiction Treatment In fact, by doing so, people subconsciously try to prove that aggressiveness, anxiety, and panic attacks are not implications of drug dependence but the states they medicate with the help of methamphetamine.
- Addictions Assessment Process The first four stages are designed to assist in making the correct diagnosis and determining the level of care to ensure further rehabilitation of the client. The psychiatrist attended to the PTSD and mental issues […]
- Addiction Assessment Tools Terrance is to use two assessment tools: the Drug Abuse Screening Test and the Alcohol Use Disorders Identification Test. In short, Terrance is recommended to use these two tools for a quick and low-cost assessment […]
- Alcohol Addiction: Opting for a Correct Referral Method The psychological content of codependency is evidence of the uniqueness of health disorders and personal functioning of a family member as compared with alcohol-related disorders.
- Relevant Therapy Approaches: Probationers With Alcohol Addiction
- How Does Addiction Affect Families
- Hallucinogens: Addiction and Treatment
- Clinical and Addictions Assessment Tools
- Models of Addiction and the Assessment Process
- Ethical Codes and Principles in Addictions: Implications of Labeling
- Ethical Codes and Principles in Addictions Assessment
- Food Addiction: How to Overcome It?
- Addiction as Moral Defect From Cultural Perspective
- Heroin Addiction and Its Biological Aspect
- The Crisis of Opiate Addiction
- Drug Addiction in Australia and Management Methods
- Addiction in Adolescences: Factors and Treatments
- Alcohol Addiction as a Learned Behavior
- Drug Addiction Diagnostics and Therapy Prescription
- The Psychology of Addiction and Addictive Behaviors
- Conditioning in Phobias and Addictions
- Connecticut Community for Addiction Recovery
- Drug and Alcohol Addiction: Athletes and Student Leaders
- Addiction Counseling and Certification in Arizona
- The Opioid Crisis: Preventing Addiction
- Addictions in Cultural Groups: Study Challenges
- Addiction Recovery and Its Ethical Risks
- Substance Addiction Treatment in Students
- Heroin Addiction Educational and Preventive Program
- Stop Heroin Addiction: Service Delivery Program
- Opioids Addiction in the United States
- Primary Care Providers Treating Opiate Addiction
- Addiction History and Concepts
- Nicotine Addiction Research and Assessment
- Addictions: Treatment and Prevention
- Addiction Prevention Programs in Miami-Dade County
- Addiction Occurrence and Reduction in Adolescence
- Addictions in Free Markets
- Video Game Addiction and Maslow’s Hierarchy of Needs
- Second Life Games Addiction and Its Reasons
- Drug Addiction Issues in The Corner Miniseries
- Alcohol Addiction and Its Societal Influence
- Disease Harm Reduction Addiction Treatment Model
- Addiction’s Etiology: Models and Theories
- Addiction: Methods and Approaches
- Gambling and Addiction’s Effects on Neuroplasticity
- Martyrdom as Addiction to Offset the Injustice
- Caffeine: Carriers, Addiction and Diseases
- Cognitive Therapy for Anxiety and Addiction Withdrawal
- Gender Identity and Addiction Treatment
- Drug Addiction History in Urban Areas Since the 1970s
- Social Issues: Alcoholism as a Mode of Addiction
- Breaking the Chains of Cocaine Addiction
- Addiction Counseling and Psychosocial Crisis in Elderly
- Gambling Addiction Research Approaches
- “Breaking the Chains of Cocaine: Black Male Addiction and Recovery” Book
- Adolescent Risk: Substance and Addiction
- Methamphetamine Addiction and Prevention
- Biblical Word Study: Counseling and Addiction Categories
- Drug Addictions Counseling: Assessment and Diagnosing
- Attachment Dimensions and Adolescence Drug Addiction in Relation to School Counseling
- Case Management: Drug Addiction
- Peculiarities of the Addiction Treatments
- Link Between Environment and Addiction
- Theories of Addiction: General Counseling Methods
- Addiction to an Experience
- The Role of Spirituality in Overcoming Addictions
- Problem of Hydrocodone Addiction in US
- Literature Review and Research Methodology Draft: Effects of Internet Addiction on Family Relationships Among Teenagers
- Definition of Alcohol Misuse (Alcohol Abuse and Addiction) in Youth Population Age 18-29
- Computer Addiction in Modern Society
- Pharmaceutical Drug Addiction Among African American Male Adolescents
- Addiction of Digital Media in Society
- “Cocaine: Abuse and Addiction” by National Institute on Drug Abuse
- Understanding Drug & Alcohol Addiction
- Substance Abuse, Addiction and Dependency Among Adolescents
- Is Drug (Legal or Illegal) Addiction and or Abuse Individual Responsibility or Societies Responsibility?
- Analyzing Love and Love Addiction in Relationships
- Addiction Severity Index
- Fast Food, Quick Problem Emergence, Rapid Addiction and Slow Recovery Process
- Sex Addiction as a Psychological Disorder
- Where Does the Path to Smoking Addiction Start?
- Problems of Everyday Addictions in Society
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, March 2). 239 Addiction Essay Topic Ideas & Examples. https://ivypanda.com/essays/topic/addiction-essay-topics/
"239 Addiction Essay Topic Ideas & Examples." IvyPanda , 2 Mar. 2024, ivypanda.com/essays/topic/addiction-essay-topics/.
IvyPanda . (2024) '239 Addiction Essay Topic Ideas & Examples'. 2 March.
IvyPanda . 2024. "239 Addiction Essay Topic Ideas & Examples." March 2, 2024. https://ivypanda.com/essays/topic/addiction-essay-topics/.
1. IvyPanda . "239 Addiction Essay Topic Ideas & Examples." March 2, 2024. https://ivypanda.com/essays/topic/addiction-essay-topics/.
Bibliography
IvyPanda . "239 Addiction Essay Topic Ideas & Examples." March 2, 2024. https://ivypanda.com/essays/topic/addiction-essay-topics/.
- Alcohol Essay Titles
- Abnormal Psychology Paper Topics
- Drug Abuse Research Topics
- Smoking Research Topics
- Alcohol Abuse Paper Topics
- Cognitive Behavioral Therapy Topics
- Gambling Essay Titles
- Drugs Titles
- Eating Disorders Questions
- Alcoholism Essay Titles
- Developmental Psychology Essay Ideas
- Epigenetics Essay Titles
- Mental Disorder Essay Topics
- Neuropsychology Topics
- Criminal Behavior Essay Topics
NY, LI need more overdose prevention centers
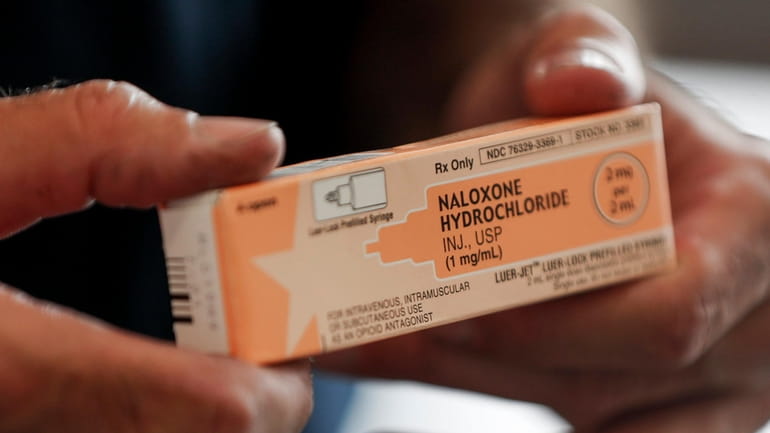
Naloxone, a lifesaving medication that reverses opioid overdoses, is carried at all overdose prevention centers. Credit: AP/Keith Srakocic
Every 90 minutes, a New Yorker dies from a preventable drug overdose. Long Island, too, has been ravaged; Nassau and Suffolk counties have two of the 10 highest overdose death rates in New York State. Drug overdoses have become the leading cause of death for New Yorkers under 50, with mortality rates skyrocketing over the past decade — from 8 to 30 deaths per 100,000 people. As the crisis escalates, we must turn to proven solutions: overdose prevention centers, or OPCs.
In the U.S., the first two legally sanctioned OPCs opened in 2021 in East Harlem and Washington Heights, under the nonprofit OnPoint. They reversed 1,300 overdoses in their first year. Three years later, these two centers remain the only OPCs in New York. None have been proposed on Long Island despite the need.
Overdose prevention centers provide a safe space for people struggling with addiction. They can use drugs in a supervised and hygienic environment, access health and social services, find supportive community, and make progress toward recovery. We understand there is often significant community resistance to these centers, but decades of research on OPCs in more than 50 countries has affirmed their efficacy — not only do they reduce overdose deaths, they also reduce disease transmission, public drug use, syringe litter, and drug-related crime, while expanding access to treatment. Naloxone, a lifesaving medication that reverses opioid overdoses and is carried at all OPCs, keeps participants safe and gives them another chance to enter treatment. Not a single person has died at a center, numerous studies have found.
Overdoses consistently rank in the top 15 causes for emergency room admissions. As medical students, we’ve witnessed firsthand the inadequacies of our emergency medical infrastructure in addressing substance use disorders. Our ERs are flooded. We’ve seen patients waiting up to eight hours — and the same patients returning to the ER weeks later because they were discharged to the same conditions that led to their initial overdose with no follow-up care. OPCs provide more comprehensive support and reduce ER strain; OPCs have been shown to reduce ambulance calls for overdoses by up to 67%.
This guest essay reflects the views of Aidan Pillard and Mia Pattillo, medical students at the Icahn School of Medicine at Mount Sinai and Weill Cornell Medical College in Manhattan.
Our experiences volunteering at OnPoint’s OPCs have shown us a compelling vision of what effective support for those battling addiction should involve. People find respite from the streets to shower, wash their clothes, eat a snack, and use their drugs in a safe environment. OPCs serve as gateways to physical and behavioral health services, social services, and job opportunities. The trust between staff and participants catalyzes transformations; some participants begin addiction treatment and others staff the center themselves.
From our Editorial Board, get inside the local, city and state political scenes.
By clicking Sign up, you agree to our privacy policy .
Some critics argue that OPCs increase crime and nuisance conditions in surrounding neighborhoods. But data from the two existing OPCs paints a different picture: Rates of theft, low-level drug enforcement, and police narcotics activity have all decreased. Moreover, staff engage actively with the community and solicit feedback from neighbors.
Another misconception is that OPCs condone drug use. This argument echoes past objections to harm reduction measures, such as syringe service programs introduced amid the HIV/AIDS epidemic or condom distribution on college campuses — both of which are now highly successful and widely adopted. Providing safe spaces for drug use does not serve to promote it; instead, it minimizes risk.
OPCs treat clients with dignity, save lives, and advance public health and safety. New York must expand OPCs on Long Island and elsewhere and lead the country in combating the overdose crisis.
This guest essay reflects the views of Aidan Pillard and Mia Pattillo, medical students at the Icahn School of Medicine at Mount Sinai and Weill Cornell Medical College in Manhattan.

IMAGES
VIDEO
COMMENTS
500 Words Essay on Addiction. As we all know that excess of anything can be very dangerous, the same way, addiction of any kind can hamper the life quality of an individual. The phrase states that addiction is a family disease as one person uses and the whole family suffers. The above statement stands true in all its essence as the addict does ...
Addiction is an illness that requires, for most, professional help and that once you are an addict you are always an addict. Addiction is everywhere, from celebrity tabloids, to television, and possibly to a family member or close friend. There is alcoholism, drug abuse, and gambling. 2651 Words. 11 Pages.
Drug addiction is a chronic disease characterized by drug seeking and use that is compulsive, or difficult to control, despite harmful consequences. Brain changes that occur over time with drug use challenge an addicted person's self-control and interfere with their ability to resist intense urges to take drugs.
Addiction is a chronic (lifelong) condition that involves compulsive seeking and taking of a substance or performing of an activity despite negative or harmful consequences. Addiction can significantly impact your health, relationships and overall quality of life. It's crucial to seek help as soon as you develop signs of addiction.
Introduction. Close to a quarter of a century ago, then director of the US National Institute on Drug Abuse Alan Leshner famously asserted that "addiction is a brain disease", articulated a set of implications of this position, and outlined an agenda for realizing its promise [].The paper, now cited almost 2000 times, put forward a position that has been highly influential in guiding the ...
the hallmark of addiction. Brain imaging studies of people with addiction show physical changes in areas of the brain that are critical to judgment, decision making, learning and memory, and behavior control.7Scientists believe that these changes alter the way the brain works and may help explain the compulsive and destructive behaviors of ...
Addiction is the key process that underlies substance use disorders, and research using animal models and humans has revealed important insights into the neural circuits and molecules that mediate addiction. ... The papers in this issue highlight new findings that are directly relevant to understanding, treating, and developing policies to ...
500 Words Essay on Addiction Understanding Addiction. Addiction is a serious issue that affects many people around the world. It is a state where a person cannot stop using a substance or engaging in a behavior, even if it is harmful. The person becomes dependent on the substance or the activity to feel good or normal. Types of Addiction
There are many theories about the causes of addiction, the use and abuse of legal and illegal psychoactive substances. Biology, psychology, and social and cultural elements all play a role in the ...
The authors canvass the various purposes served by a definition of addiction in psychiatric, social, legal, economic, interpersonal and scientific contexts. They argue that addiction is a strong and habitual want that significantly reduces control and leads to significant harm. What counts as significant varies relative to purpose and context.
1: the quality or state of being addicted 2: compulsive need for and use of a habit-forming substance (as heroin, nicotine, or alcohol) characterized by tolerance and by well-defined physiological symptoms upon withdrawal; broadly: persistent compulsive use of a substance known by the user to be harmful. (14)
Drug addiction is a complex and contentious issue that has sparked debates for decades. At the heart of this debate is the question of whether drug addiction should be viewed as a choice made by individuals or as a disease that requires medical treatment. This essay will explore the multifaceted nature of drug addiction, examining both the ...
The essay is intended to stimulate members' thinking discussion about the nature of addiction. As members awaken spiritually and share with one another, the answers get woven into the fabric of the fellowship's conventional wisdom.
Even so, addiction occurs mainly because of emotional stress, which is usually brought about by the stressful events in an individual's life. In this regard, the second form of addiction is psychological as the addiction starts in the brain. Individuals use drugs, bet or even do shopping impulsively mainly because of psychological reasons.
Models of addiction risk that have been proposed in psychology literature include an affect dysregulation model of positive and negative psychological effects, the reinforcement sensitivity theory model of impulsiveness and behavioral inhibition, and an impulsivity model of reward sensitization and impulsiveness.
Essay on Addiction: Addiction is an illness- be it a drug, habit, or a person, that changes the way our brain thinks, functions, and processes information. Addiction leads to compulsive behaviour that provides temporary pleasure but holds long-term harmful effects on an addict's life.
Addiction is a condition that has long baffled physicians and philosophers, to say nothing of those struggling with it and those around them. What to make of a set of behaviors that in fact ...
Essay Example: It's no secret the abuse of drugs has become a widespread epidemic. Although it seems to be stereotypical for teens, this problem is rising more in the adult population. ... Addiction is a chronic disease characterized by drug seeking and use that is compulsive, or difficult to control, despite harmful consequences. The initial ...
The view that substance addiction is a brain disease, although widely accepted in the neuroscience community, has become subject to acerbic criticism in recent years. These criticisms state that ...
To begin with, studies have found that inherited genes are responsible for a considerably large part of the probability that someone will become addicted to any kind of substance or behavior. Addiction is strongly influenced by genetic factors in the later stages of addiction, such as problem use and dependence of an addictive substance.
Opioid Use and Addiction in Afghanistan and Iraq Veterans. My chosen topic integrates the welfare of veterans of recent wars, such as conflicts in Iraq and Afghanistan, the prescription of opioids for trauma, general mental well-being, and adaptation to civilian and even academic life.
Drug overdoses have become the leading cause of death for New Yorkers under 50, with mortality rates skyrocketing over the past decade — from 8 to 30 deaths per 100,000 people. As the crisis ...