Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals

Type 2 diabetes articles from across Nature Portfolio
Type 2 diabetes mellitus, the most frequent subtype of diabetes, is a disease characterized by high levels of blood glucose (hyperglycaemia). It arises from a resistance to and relative deficiency of the pancreatic β-cell hormone insulin.

Metformin induces a Lac-Phe gut–brain signalling axis
The mechanism by which metformin affects food intake remains controversial. Now, two studies link metformin treatment with the induction of the appetite-suppressing metabolite N -lactoyl-phenylalanine, which is produced by the intestine.
- Tara TeSlaa
Latest Research and Reviews
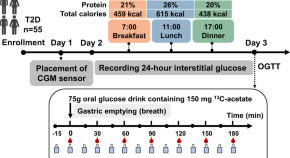
Gastric emptying of a glucose drink is predictive of the glycaemic response to oral glucose and mixed meals, but unrelated to antecedent glycaemic control, in type 2 diabetes
- Chunjie Xiang
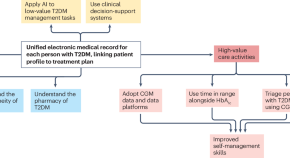
Continuous glucose monitoring for the routine care of type 2 diabetes mellitus
Continuous glucose monitoring (CGM) is an effective tool in the management of diabetes mellitus. This Perspective discusses the potential benefits of widespread adoption of CGM in people with type 2 diabetes mellitus at different stages of disease progression and treatment intensification.
- Ramzi A. Ajjan
- Tadej Battelino
- Samuel Seidu

Comparative impact of Roux-en-Y gastric bypass, sleeve gastrectomy or diet alone on beta-cell function in insulin-treated type 2 diabetes patients
- Matthias Lannoo
- Caroline Simoens
- Bart Van der Schueren
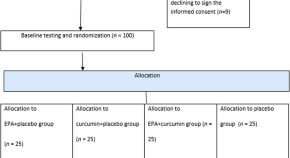
The effect of curcumin and high-content eicosapentaenoic acid supplementations in type 2 diabetes mellitus patients: a double-blinded randomized clinical trial
- Kimia Motlagh Asghari
- Parviz Saleh
- Maryam Hashemian
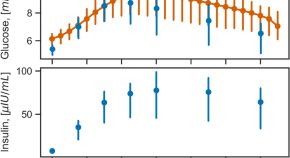
Leveraging continuous glucose monitoring for personalized modeling of insulin-regulated glucose metabolism
- Balázs Erdős
- Shauna D. O’Donovan
- Ilja C. W. Arts
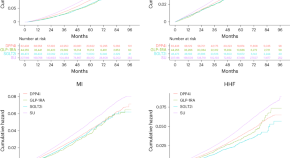
Effectiveness of glucose-lowering medications on cardiovascular outcomes in patients with type 2 diabetes at moderate cardiovascular risk
In a retrospective cohort study examining the comparative effectiveness of diabetes drugs in adults at moderate risk for cardiovascular disease, GLP-1 receptor agonists and SGLT2 inhibitors reduced the risk of cardiovascular events compared to DPP4 inhibitors, whereas sulfonylureas increased the risk.
- Rozalina G. McCoy
- Jeph Herrin
- Eric C. Polley
News and Comment
Metformin acts through appetite-suppressing metabolite: Lac-Phe
- Shimona Starling
Slowly progressive insulin-dependent diabetes mellitus in type 1 diabetes endotype 2
- Tetsuro Kobayashi
- Takashi Kadowaki
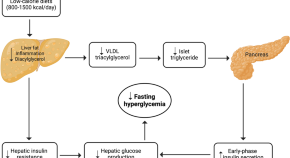
Low-calorie diets for people with isolated impaired fasting glucose
Thirunavukkarasu et al. discuss how standard lifestyle interventions prove ineffective in preventing type 2 diabetes in individuals with isolated impaired fasting glucose, a highly prevalent prediabetes phenotype globally. They propose low-calorie diets as a promising strategy for diabetes prevention in this high-risk population.
- Sathish Thirunavukkarasu
- Jonathan E. Shaw
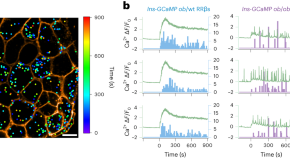
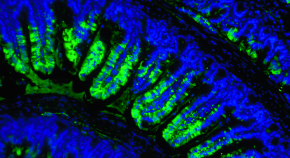
Functionally heterogeneous β cells regulate biphasic insulin secretion
Here, we reveal functional heterogeneity among β cells and discover that readily releasable β cells (RRβs) are a subpopulation that disproportionally contributes to biphasic glucose-stimulated insulin secretion. We further show that the dysfunction of RRβs has a crucial role in the progression of diabetes.

A second step towards precision medicine in diabetes
Dwibedi et al. carry out a randomized controlled trial to evaluate whether subgroups of patients with diabetes could receive the greatest metabolic benefit from novel anti-diabetic drugs.
- Xiantong Zou
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
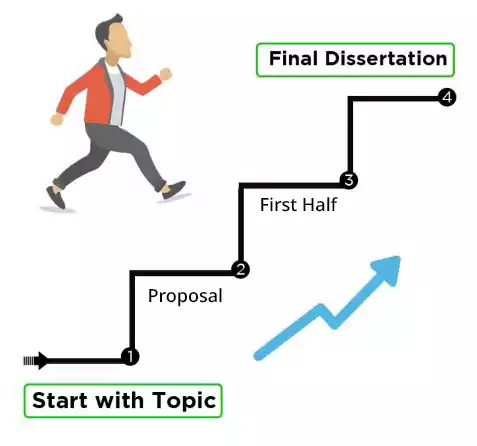
- How it works
Useful Links
How much will your dissertation cost?
Have an expert academic write your dissertation paper!
Dissertation Services
Get unlimited topic ideas and a dissertation plan for just £45.00
Order topics and plan
Get 1 free topic in your area of study with aim and justification
Yes I want the free topic
45 of the Best Diabetes Dissertation Topics
Published by Owen Ingram at January 2nd, 2023 , Revised On August 16, 2023
The prevalence of diabetes among the world’s population has been increasing steadily over the last few decades, thanks to the growing consumption of fast food and an increasingly comfortable lifestyle. With the field of diabetes evolving rapidly, it is essential to base your dissertation on a trending diabetes dissertation topic that fills a gap in research.
Finding a perfect research topic is one of the most challenging aspects of dissertation writing in any discipline . Several resources are available to students on the internet to help them conduct research and brainstorm to develop their topic selection, but this can take a significant amount of time. So, we decided to provide a list of well-researched, unique and intriguing diabetes research topics and ideas to help you get started.
Other Subject Links:
- Evidence-based Practice Nursing Dissertation Topics
- Child Health Nursing Dissertation Topics
- Adult Nursing Dissertation Topics
- Critical Care Nursing Dissertation Topics
- Palliative Care Nursing Dissertation Topics
- Mental Health Nursing Dissertation Topics
- Nursing Dissertation Topics
- Coronavirus (COVID-19) Nursing Dissertation Topics
List of Diabetes Dissertation Topics
- Why do people recently diagnosed with diabetes have such difficulty accepting reality and controlling their health?
- What are the reactions of children who have recently been diagnosed with diabetes? What can be done to improve their grasp of how to treat the disease?
- In long-term research, people getting intensive therapy for the condition had a worse quality of life. What role should health professionals have in mitigating this effect?
- Why do so many individuals experience severe depression the months after their diagnosis despite displaying no other signs of deteriorating health?
- Discuss some of the advantages of a low-carbohydrate, high-fat diet for people with diabetes
- Discuss the notion of diabetes in paediatrics and why it is necessary to do this research regularly.
- Explain the current threat and difficulty of childhood obesity and diabetes, stressing some areas where parents are failing in their position as guardians to avoid the situation
- Explain some of the difficulties that persons with diabetes have, particularly when obtaining the necessary information and medical treatment
- Explain some of the most frequent problems that people with diabetes face, as well as how they affect the prevalence of the disease. Put out steps that can be implemented to help the problem.
- Discuss the diabetes problem among Asian American teens
- Even though it is a worldwide disease, particular ethnic groups are more likely to be diagnosed as a function of nutrition and culture. What can be done to improve their health literacy?
- Explain how self-management may be beneficial in coping with diabetes, particularly for people unable to get prompt treatment for their illness
- Discuss the possibility of better management for those with diabetes who are hospitalized
- What current therapies have had the most influence on reducing the number of short-term problems in patients’ bodies?
- How have various types of steroids altered the way the body responds in people with hypoglycemia more frequently than usual?
- What effects do type 1, and type 2 diabetes have on the kidneys? How do the most widely used monitoring approaches influence this?
- Is it true that people from specific ethnic groups are more likely to acquire heart disease or eye illness due to their diabetes diagnosis?
- How has the new a1c test helped to reduce the detrimental consequences of diabetes on the body by detecting the condition early?
- Explain the difficulty of uncontrolled diabetes and how it can eventually harm the kidneys and the heart
- Discuss how the diabetic genetic strain may be handed down from generation to generation
- What difficulties do diabetic people have while attempting to check their glucose levels and keep a balanced food plan?
- How have some individuals with type 1 or type 2 diabetes managed to live better lives than others with the disease?
- Is it true that eating too much sugar causes diabetes, cavities, acne, hyperactivity, and weight gain?
- What effect does insulin treatment have on type 2 diabetes?
- How does diabetes contribute to depression?
- What impact does snap participation have on diabetes rates?
- Why has the number of persons who perform blood glucose self-tests decreased? Could other variables, such as social or environmental, have contributed to this decrease?
- Why do patients in the United States struggle to obtain the treatment they require to monitor and maintain appropriate glucose levels? Is this due to increased healthcare costs?
- Nutrition is critical to a healthy lifestyle, yet many diabetic patients are unaware of what they should consume. Discuss
- Why have injuries and diabetes been designated as national health priorities?
- What factors contribute to the growing prevalence of type ii diabetes in adolescents?
- Does socioeconomic status influence the prevalence of diabetes?
- Alzheimer’s disease and type 2 diabetes: a critical assessment of the shared pathological traits
- What are the effects and consequences of diabetes on peripheral blood vessels?
- What is the link between genetic predisposition, obesity, and type 2 diabetes development?
- Diabetes modifies the activation and repression of pro- and anti-inflammatory signalling pathways in the vascular system.
- Understanding autoimmune diabetes through the tri-molecular complex prism
- Does economic status influence the regional variation of diabetes caused by malnutrition?
- What evidence is there for using traditional Chinese medicine and natural products to treat depression in people who also have diabetes?
- Why was the qualitative method used to evaluate diabetes programs?
- Investigate the most common symptoms of undiagnosed diabetes
- How can artificial intelligence help diabetes patients?
- What effect does the palaeolithic diet have on type 2 diabetes?
- What are the most common diabetes causes and treatments?
- What causes diabetes mellitus, and how does it affect the United Kingdom?
Hire an Expert Writer
Orders completed by our expert writers are
- Formally drafted in an academic style
- Free Amendments and 100% Plagiarism Free – or your money back!
- 100% Confidential and Timely Delivery!
- Free anti-plagiarism report
- Appreciated by thousands of clients. Check client reviews
You can contact our 24/7 customer service for a bespoke list of customized diabetes dissertation topics , proposals, or essays written by our experienced writers . Each of our professionals is accredited and well-trained to provide excellent content on a wide range of topics. Getting a good grade on your dissertation course is our priority, and we make sure that happens. Find out more here .
Free Dissertation Topic
Phone Number
Academic Level Select Academic Level Undergraduate Graduate PHD
Academic Subject
Area of Research
Frequently Asked Questions
How to find diabetes dissertation topics.
To find diabetes dissertation topics:
- Study recent research in diabetes.
- Focus on emerging trends.
- Explore prevention, treatment, tech, etc.
- Consider cultural or demographic aspects.
- Consult experts or professors.
- Select a niche that resonates with you.
You May Also Like
Can’t find a topic for your radiology dissertation? Pick from our top radiology research topics to prepare your dissertation or radiology publication.
Choosing the right Asset Management dissertation topic can be a nightmare for many students. The topic of your dissertation determines how well it ranks. This is due to the fact that your topics are the first thing your readers will notice about your article.
Need interesting and manageable tourism and hospitality dissertation topics? Here are the trending tourism and hospitality dissertation titles so you can choose the most suitable one.
USEFUL LINKS
LEARNING RESOURCES

COMPANY DETAILS

- How It Works
Changing our Future Through Research
The ADA is committed to innovation and breakthrough research that will improve the lives of all people living with diabetes.

ADA Research: Science. Progress. Hope.
ADA research provides critical funding for diabetes research. With 100% of donations directed to research, our goal is to ensure adequate financial resources to support innovative scientific discovery that will translate to life-changing treatments and eventual cures.
of our funded researchers remain dedicated to careers in diabetes science
publications per grant, cited an average of 28 times, proving expertise and credibility
Every $1 the ADA invests in diabetes research leads to $12.47 in additional research funding
ADA Research Impact
Explore some of the latest innovations and discoveries and see how the ADA continues to advance science, leverage investments and retain scientists.

Research Funds at Work
Imagine what 290 scientists, each working on a unique project at 117 institutions across the U.S. can do. Learn about the research we fund to move the diabetes fight forward.

Helping People Thrive
Uncover inspiring patient stories and find out how our research is transforming lives.

Discover programs on research, career development, training, and more.
Learn more about the current opportunities for 2024 research funding.
Pathway to Stop Diabetes ®
A bold initiative dedicated to bringing 100 brilliant scientists to diabetes research.
Explore Research Projects
As part of our mission, ADA’s Research Programs invest in projects that have the potential to prevent the development of diabetes and help people living with diabetes.

Type 1 Diabetes Research
Project topics span technology, islet transplantation, immunology, improving transition to self-management, and more.

Type 2 Diabetes Research
Project topics include support for potential new treatments, a better understating of genetic factors, addressing disparities, and more.

Prediabetes/Insulin Resistance Research
Projects include understanding the role of exercise, novel therapies, and more.

Gestational Diabetes Research
Projects focus on advancing the prevention of gestational diabetes and to properly diagnose and treat it when it occurs.

Research on Obesity
Projects include studying the biology of appetite regulation and metabolism, identification of new treatment targets, and trials exploring interventions for weight loss.
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Entire Site
- Research & Funding
- Health Information
- About NIDDK
- Research Programs & Contacts
Clinical Research in Type 2 Diabetes
Studies in humans aimed at the prevention, treatment, and diagnosis of Type 2 Diabetes and the mechanistic aspects of its etiology.
The Clinical Research in Type 2 Diabetes (T2D) program supports human studies across the lifespan aimed at understanding, preventing and treating T2D. This program includes clinical trials that test pharmacologic, behavioral, surgical or practice-level approaches to the treatment and/or prevention of T2D, including promoting the preservation of beta cell function. Studies may also advance the development of new surrogate markers for use in clinical trials. Studies can be designed to understand the pathophysiology of T2D, including the role of gestational diabetes and metabolic imprinting on the development of T2D, as well as factors influencing the response to treatment. The program also encompasses epidemiologic studies that improve our understanding of the natural history and pathogenesis of T2D, and the development of diagnostic criteria to distinguish type 1 and type 2 diabetes, especially in the pediatric population. The program also supports research to understand and test approaches to accelerate the translation of efficacious interventions into real-world practice and adoption; and to address health equity by reducing health disparities in the incidence and/or clinical outcomes of T2D.
NIDDK Program Staff
- Shavon Artis Dickerson, Dr.P.H., M.P.H. Health Equity and Implementation Science
- Henry B. Burch, M.D. Clinical studies utilizing existing digital health technology for the prevention and treatment of type 2 diabetes, clinical and basic science studies involving non-neoplastic disorders of the thyroid, clinical studies involving medical and novel dietary treatment of type 2 diabetes.
- Maureen Monaghan Center, Ph.D., CDCES Health Psychology, Behavioral Science, Clinical Management of Diabetes
- Jean M. Lawrence, Sc.D., M.P.H., M.S.S.A. Type 2 diabetes risk and prevention after gestational diabetes; Studies of adults with diabetes/pre-diabetes using secondary data and observational designs, and natural experiments
- Hanyu Liang, M.D., Ph.D. Hepatic Metabolism; Insulin Resistance; Type 2 Diabetes; Obesity; Bariatric Surgery
- Barbara Linder, M.D., Ph.D. Type 2 diabetes in children and youth; human studies of metabolic imprinting
- Saul Malozowski, M.D., Ph.D., M.B.A. Neuroendocrinology of hypothalamic-pituitary axis, neuropeptide signaling and receptors; hormonal regulation of bone and mineral metabolism; HIV/AIDS-associated metabolic and endocrine dysfunction
- Pamela L. Thornton, Ph.D. Health Equity and Translational Research; Centers for Diabetes Translation Research (P30) Program
- Theresa Teslovich Woo, Ph.D. Human behavior, developmental cognitive neuroscience, and brain-based mechanisms involved in obesity and diabetes
Recent Funding Opportunities
Rare diseases clinical research consortia (rdcrc) for the rare diseases clinical research network (rdcrn) (u54 clinical trial optional), discovery of early type 1 diabetes disease processes in the human pancreas [hirn consortium on beta cell death and survival (cbds)] (u01 clinical trial not allowed), adaptation of diabetes control technologies for older adults with t1d (r01 clinical trial optional), diabetes research centers (p30 clinical trial optional), notice of special interest (nosi): supporting the exploration of cloud in nih-supported research, related links.
View related clinical trials from ClinicalTrials.gov.
Study sections conduct initial peer review of applications in a designated scientific area. Visit the NIH’s Center for Scientific Review website to search for study sections.
Research Resources
NIDDK makes publicly supported resources, data sets, and studies available to researchers to accelerate the rate and lower the cost of new discoveries.
- Ancillary Studies to Major Ongoing Clinical Studies to extend our knowledge of the diseases being studied by the parent study investigators under a defined protocol or to study diseases and conditions not within the original scope of the parent study but within the mission of the NIDDK.
- NIDDK Central Repository for access to clinical resources including data and biospecimens from NIDDK-funded studies.
- NIDDK Information Network (dkNET) for simultaneous search of digital resources, including multiple datasets and biomedical resources relevant to the mission of the NIDDK.
Additional Research Programs
Research training.
NIDDK supports the training and career development of medical and graduate students, postdoctoral fellows, and physician scientists through institutional and individual grants.
Diversity Programs
The NIDDK offers and participates in a variety of opportunities for trainees and researchers from communities underrepresented in the biomedical research enterprise. These opportunities include travel and scholarship awards, research supplements, small clinical grants, high school and undergraduate programs, and a network of minority health research investigators.
Small Business
Small business programs.
NIDDK participates in the Small Business Innovation Research (SBIR) and Small Business Technology Transfer (STTR) programs. These programs support innovative research conducted by small businesses that has the potential for commercialization.
Human Subjects Research
NIDDK provides funding for pivotal clinical research, from preliminary clinical feasibility to large multi-center studies.
Translational Research
NIDDK provides funding opportunities and resources to encourage translation of basic discoveries into novel therapeutics.
Meetings & Workshops

Supports researchers with tools to enhance scientific rigor, reproducibility, and transparency, and provides a big data knowledge base for genomic and pathway hypothesis generation.

Providing education and training for the next generation of biomedical and behavioral scientist

Stay informed about the latest events, or connect through social media.

Learn about current projects and view funding opportunities sponsored by the NIH Common Fund .
Registration is required at eRA Commons and grants.gov and can take 4 weeks.
357 Diabetes Essay Topics & Examples
When you write about the science behind nutrition, heart diseases, and alternative medicine, checking titles for diabetes research papers can be quite beneficial. Below, our experts have gathered original ideas and examples for the task.
🏆 Best Diabetes Essay Examples & Topics
⭐ most interesting diabetes research paper topics, ✅ simple & easy diabetes essay topics, 🎓 good research topics about diabetes, 💡 interesting topics to write about diabetes, 👍 good essay topics on diabetes, ❓ diabetes research question examples.
- Type 2 Diabetes The two major types of diabetes are type 1 diabetes and type 2 diabetes. Doctor: The first step in the treatment of type 2 diabetes is consumption of healthy diet.
- Living With a Chronic Disease: Diabetes and Asthma This paper will look at the main effects of chronic diseases in the lifestyle of the individuals and analyze the causes and the preventive measures of diabetes as a chronic disease.
- Diabetes Mellitus: Symptoms, Types, Effects Insulin is the hormone that controls the levels of glucose in the blood, and when the pancreas releases it, immediately the high levels are controlled, like after a meal.
- Type 2 Diabetes as a Public Health Issue In recent years, a steady increase in the incidence and prevalence of diabetes is observed in almost all countries of the world.
- Leadership in Diabetes Management Nurses can collaborate and apply evidence-based strategies to empower their diabetic patients. The involvement of all key stakeholders is also necessary.
- Health Promotion: Diabetes Mellitus and Comorbidities This offers a unique challenge in the management of diabetes and other chronic diseases; the fragmented healthcare system that is geared towards management of short-term medical emergencies often is not well prepared for the patient […]
- Relation Between Diabetes And Nutrition Any efforts to lessen and eliminate the risk of developing diabetes must involve the dietary habit of limiting the consumption of carbohydrates, sugar, and fats. According to Belfort-DeAguiar and Dongju, the three factors of obesity, […]
- Diabetes Management: Case Study Type 1 and Type 2 diabetes contrast based on their definitions, the causes, and the management of the conditions. Since the CDC promotes the avoidance of saturated fat and the increase of fiber intake for […]
- Diabetes Mellitus Management in the Elderly Diabetes mellitus is a health complication involving an increase in the concentration in the concentration of blood sugar either due to a failure by cells to effectively respond to the production of insulin in the […]
- The Aboriginal Diabetes Initiative in Canada The ADI’s goal in the CDS was to raise type 2 diabetes awareness and lower the incidence of associated consequences among Aboriginal people.
- Diabetes and Its Economic Effect on Healthcare For many years, there has been an active increase in the number of cases of diabetes of all types among the global population, which further aggravates the situation.
- Diabetes Issues: Insulin Price and Unaffordability According to the forecast of researchers from Stanford University, the number of people with type 2 diabetes who need insulin-containing drugs in the world will increase by about 79 million people by 2030, which will […]
- The Minority Diabetes Initiative Act’s Analysis The bill provides the right to the Department of Health and Human Services to generate grants to public and nonprofit private health care institutions with the aim of providing treatment for diabetes in minority communities.
- Diabetes Self-Management: Evidence-Based Nursing The article by Seley and Weinger, improving diabetes self management attempts to address the possible barriers to patient education and the role of the nurse in assisting the patient to manage diabetes.
- Diabetes Mellitus Type 2: Pathophysiology and Treatment The primary etiologies linked to the patient’s T2DM condition include morbid obesity and family history. The genetic factors implicated in T2DM pathogenesis relate to a family history of the disease.
- Type II Diabetes Susceptibility and Socioeconomic Status As the focus is made on the correlation between socioeconomic status and susceptibility to type II diabetes, primary search requests were the following: socioeconomic status, causes of type II diabetes, socioeconomic status and diabetes mellitus, […]
- Gestational Diabetes in a 38-Year-Old Woman The concept map, created to meet B.’s needs, considers her educational requirements and cultural and racial hurdles to recognize her risk factors and interventions to increase her adherence to the recommended course of treatment.B.said in […]
- Type 2 Diabetes Mellitus and Its Implications You call an ambulance and she is taken in to the ED. Background: Jean is still very active and works on the farm 3 days a week.
- Development of Comprehensive Inpatient and Outpatient Programs for Diabetes Overcoming the fiscal and resource utilization issues in the development of a comprehensive diabetes program is essential for the improvement of health and the reduction of treatment costs.
- Healthcare Cost Depending on Chronic Disease Management of Diabetes and Hypertension A sufficient level of process optimization and the presence of a professional treating staff in the necessary number will be able to help improve the indicators.
- Improving Glycemic Control in Black Patients with Type 2 Diabetes Information in them is critical for answering the question and supporting them with the data that might help to acquire an enhanced understanding of the issue under research. Finally, answering the PICOT question, it is […]
- Shared Decision-Making That Affects the Management of Diabetes The article by Peek et al.is a qualitative study investigating the phenomenon of shared decision-making that affects the management of diabetes. The researchers demonstrate the racial disparity that can arise in the choice of approaches […]
- Managing Obesity as a Strategy for Addressing Type 2 Diabetes When a patient, as in the case of Amanda, requires a quick solution to the existing problem, it is necessary to effectively evaluate all options in the shortest possible time.
- Tests and Screenings: Diabetes and Chronic Kidney Disease The test is offered to patients regardless of gender, while the age category is usually above 45 years. CDC1 recommends doing the test regardless of gender and is conducted once or twice to check the […]
- Obesity Management for the Treatment of Type 2 Diabetes American Diabetes Association states that for overweight and obese individuals with type 2 diabetes who are ready to lose weight, a 5% weight reduction diet, physical exercise, and behavioral counseling should be provided.
- COVID-19 and Diabetes Mellitus Lim et al, in their article, “COVID-19 and diabetes mellitus: from pathophysiology to clinical management”, explored how COVID-19 can worsen the symptoms of diabetes mellitus.
- The Importance of Physical Exercise in Diabetes II Patients The various activities help to improve blood sugar levels, reduce cardiovascular cases and promote the overall immunity of the patient. Subsequently, the aerobic part will help to promote muscle development and strengthen the bones.
- Diabetes Education Workflow Process Mapping DSN also introduces the patient to the roles of specialists involved in managing the condition, describes the patient’s actions, and offers the necessary educational materials.
- Diabetes: Treatment Complications and Adjustments One of the doctor’s main priorities is to check the compatibility of a patient’s medications. The prescriptions of other doctors need to be thoroughly checked and, if necessary, replaced with more appropriate medication.
- The Type 2 Diabetes Mellitus PICOT (Evidence-Based) Project Blood glucose levels, A1C, weight, and stress management are the parameters to indicate the adequacy of physical exercise in managing T2DM.
- Chronic Disease Cost Calculator (Diabetes) This paper aims at a thorough, detailed, and exhaustive explanation of such a chronic disease as diabetes in terms of the prevalence and cost of treatment in the United States and Maryland.
- Diabetes Mellitus Epidemiology Statistics This study entails a standard established observation order from the established starting time to an endpoint, in this case, the onset of disease, death, or the study’s end. It is crucial to state this value […]
- Epidemiology: Type II Diabetes in Hispanic Americans The prevalence of type II diabetes in Hispanic Americans is well-established, and the search for inexpensive prevention methods is in the limelight.
- Diabetes: Risk Factors and Effects Trends in improved medical care and the development of technology and medicine are certainly contributing to the reduction of the problem. All of the above indicates the seriousness of the problem of diabetes and insufficient […]
- Barriers to Engagement in Collaborative Care Treatment of Uncontrolled Diabetes The primary role of physicians, nurses, and other healthcare team members is to provide patients with medical treatment and coordinate that care while also working to keep costs down and expand access.
- Hereditary Diabetes Prevention With Lifestyle Modification Yeast infections between the fingers and toes, beneath the breast, and in or around the genital organs are the common symptoms of type 2 diabetes.
- Health Equity Regarding Type 2 Diabetes According to Tajkarimi, the number of research reports focusing on T2D’s prevalence and characteristics in underserved minorities in the U. Adapting the program’s toolkits to rural Americans’ eating and self-management habits could also be instrumental […]
- Diabetes Mellitus: Treatment Methods Moreover, according to the multiple findings conducted by Park et al, Billeter et al, and Tsilingiris et al, bariatric surgeries have a positive rate of sending diabetes into remission.
- Diagnosing Patient with Insulin-Dependent Diabetes The possible outcomes of the issues that can be achieved are discussing the violations with the patient’s family and convincing them to follow the medical regulations; convincing the girl’s family to leave her at the […]
- Human Service for Diabetes in Late Adulthood The mission of the Georgia Diabetic Foot Care Program is to make a positive difference in the health of persons living with diabetes.
- Diabetes: Symptoms and Risk Factors In terms of the problem, according to estimates, 415 million individuals worldwide had diabetes mellitus in 2015, and it is expected to rise to 642 million by the year 2040.
- Diabetes: Types and Management Diabetes is one of the most prevalent diseases in the United States caused when the body fails to optimally metabolize food into energy.
- Type 2 Diabetes’ Impact on Australian Society Consequently, the most significant impact of the disease is the increased number of deaths among the population which puts their lives in jeopardy. Further, other opportunistic diseases are on the rise lowering the quality of […]
- Epidemiology of Diabetes and Forecasted Trends The authors note that urbanization and the rapid development of economies of different countries are the main causes of diabetes. The authors warn that current diabetes strategies are not effective since the rate of the […]
- Communicating the Issue of Diabetes The example with a CGM sensor is meant to show that doctors should focus on educating people with diabetes on how to manage their condition and what to do in extreme situations.
- Obesity and Diabetes Mellitus Type 2 The goal is to define the features of patient information to provide data on the general course of the illness and its manifestations following the criteria of age, sex, BMI, and experimental data.
- The Prevention of Diabetes and Its Consequences on the Population At the same time, these findings can also be included in educational programs for people living with diabetes to warn them of the risks of fractures and prevent them.
- Uncontrolled Type 2 Diabetes and Depression Treatment The data synthesis demonstrates that carefully chosen depression and anxiety treatment is likely to result in better A1C outcomes for the patient on the condition that the treatment is regular and convenient for the patients.
- Type 2 Diabetes: Prevention and Education Schillinger et al.came to the same conclusion; thus, their findings on the study of the Bigger Picture campaign effectiveness among youth of color are necessary to explore diabetes prevention.
- A Diabetes Quantitative Article Analysis The article “Correlates of accelerometer-assessed physical activity and sedentary time among adults with type 2 diabetes” by Mathe et al.refers to the global issue of the prevention of diabetes and its complications.
- A Type 2 Diabetes Quantitative Article Critique Therefore, the main issue is the prevention of type 2 diabetes and its consequences, and this paper will examine one of the scientific studies that will be used for its exploration.
- The Diabetes Prevention Articles by Ford and Mathe The main goal of the researchers was to measure the baseline MVPA of participants and increase their activity to the recommended 150 minutes per week through their participation in the Diabetes Community Lifestyle Improvement Program.
- Type 2 Diabetes in Hispanic Americans The HP2020 objectives and the “who, where, and when” of the problem highlight the significance of developing new, focused, culturally sensitive T2D prevention programs for Hispanic Americans.
- Diabetes Mellitus as Problem in US Healthcare Simultaneously, insurance companies are interested in decreasing the incidence of diabetes to reduce the costs of testing, treatment, and provision of medicines.
- Diabetes Prevention as a Change Project All of these queries are relevant and demonstrate the importance of including people at high risk of acquiring diabetes in the intervention.
- Evidence Synthesis Assignment: Prevention of Diabetes and Its Complications The purpose of this research is to analyze and synthesize evidence of good quality from three quantitative research and three non-research sources to present the problem of diabetes and justify the intervention to address it.
- Diabetes Mellitus: Causes and Health Challenges Second, the nature of this problem is a clear indication of other medical concerns in this country, such as poor health objectives and strategies and absence of resources.
- Diabetes in Adults in Oxfordshire On a national level, Diabetes Research and Wellness Foundation aims to prevent the spread of the decease through research of the causes and effective treatment of diabetes 2 type.
- Diabetes Mellitus (DM) Disorder Case Study Analysis Thus, informing the patient about the importance of regular medication intake, physical activity, and adherence to diet in maintaining diabetes can solve the problem.
- Diabetes Mellitus in Young Adults Thus, programs for young adults should predominantly focus on the features of the transition from adolescence to adulthood. As a consequence, educational programs on diabetes improve the physical and psychological health of young adults.
- A Healthcare Issue of Diabetes Mellitus Diabetes mellitus is seen as a primary healthcare issue that affects populations across the globe and necessitates the combination of a healthy lifestyle and medication to improve the quality of life of people who suffer […]
- Control of LDL Cholesterol Levels in Patients, Gestational Diabetes Mellitus In addition, some patients with hypercholesterolemia may have statin intolerance, which reduces adherence to therapy, limits treatment efficacy, and increases the risk of CVD.
- Exploring Glucose Tolerance and Gestational Diabetes Mellitus In the case of a glucose tolerance test for the purpose of diagnosing GDM type, the interpretation of the test results is carried out according to the norms for the overall population.
- Type 2 Diabetes Health Issue and Exercise This approach will motivate the patient to engage in exercise and achieve better results while reducing the risk of diabetes-related complications.
- Diabetes Interventions in Children The study aims to answer the PICOT Question: In children with obesity, how does the use of m-Health applications for controlling their dieting choices compare to the supervision of their parents affect children’s understanding of […]
- Diabetes Tracker Device and Its Advantages The proposed diabetes tracker is a device that combines the functionality of an electronic BGL tester and a personal assistant to help patients stick to their diet plan.
- Disease Management for Diabetes Mellitus The selection of the appropriate philosophical and theoretical basis for the lesson is essential as it allows for the use of an evidence-based method for learning about a particular disease.
- Latino People and Type 2 Diabetes The primary aim of the study is to determine the facilitators and barriers to investigating the decision-making process in the Latin population and their values associated with type 2 diabetes.
- Diabetes Self-Management Education and Support Program The choice of this topic and question is based on the fact that despite the high prevalence of diabetes among adolescents in the United States, the use of DSMES among DM patients is relatively low, […]
- Diabetes Mellitus Care Coordination The aim is to establish what medical technologies, care coordination and community resources, and standards of nursing practice contribute to the quality of care and safety of patients with diabetes.
- Healthy Lifestyle Interventions in Comorbid Asthma and Diabetes In most research, the weight loss in cases of comorbid asthma and obesity is reached through a combination of dietary interventions and physical exercise programs.
- Case Study of Patient with DKA and Diabetes Mellitus It is manifested by a sharp increase in glucose levels and the concentration of ketone bodies in the blood, their appearance in the urine, regardless of the degree of violation of the patient’s consciousness.
- PDSA in Diabetes Prevention The second step in the “Do” phase would be to isolate a few members of the community who are affected by diabetes voluntarily.
- Diabetes: Statistics, Disparities, Therapies The inability to produce adequate insulin or the body’s resistance to the hormone is the primary cause of diabetes. Diabetes is a serious health condition in the U.S.and the world.
- Type 2 Diabetes Prescriptions and Interventions The disadvantage is the difficulty of obtaining a universal model due to the complexity of many factors that can affect the implementation of recommendations: from the variety of demographic data to the patient’s medical history.
- Health Education for Female African Americans With Diabetes In order to address and inform the public about the challenges, nurses are required to intervene by educating the population on the issues to enhance their understanding of the risks associated with the conditions they […]
- Diabetes Risk Assessment and Prevention It is one of the factors predisposing patients suffering from diabetes to various cardiovascular diseases. With diabetes, it is important to learn how to determine the presence of carbohydrates in foods.
- Diabetes Mellitus: Preventive Measures In addition to addressing the medical specialists who will be of service in disease prevention, it will emphasize the intervention programs required to help control the spread of the illness.
- “The Diabetes Online Community” by Litchman et al. The researchers applied the method of telephone interviews to determine the results and effectiveness of the program. The study described the value of DOC in providing support and knowledge to older diabetes patients.
- Mobile App for Improved Self-Management of Type 2 Diabetes The central focus of the study was to assess the effectiveness of the BlueStar app in controlling glucose levels among the participants.
- Type 2 Diabetes in Minorities from Cultural Perspective The purpose of this paper is to examine the ethical and cultural perspectives on the issue of T2DM in minorities. Level 2: What are the ethical obstacles to treating T2DM in ethnic and cultural minorities?
- Ethics of Type 2 Diabetes Prevalence in Minorities The purpose of this article analysis is to dwell on scholarly evidence that raises the question of ethical and cultural aspects of T2DM prevalence in minorities.
- Type 2 Diabetes in Minorities: Research Questions The Level 2 research questions are: What are the pathophysiological implications of T2DM in minorities? What are the statistical implications of T2DM in minorities?
- Improving Adherence to Diabetes Treatment in Primary Care Settings Additionally, the patients from the intervention group will receive a detailed explanation of the negative consequences of low adherence to diabetes treatment.
- An Advocacy Tool for Diabetes Care in the US To ensure the implementation and consideration of my plea, I sent a copy of the letter to the government officials so it could reach the president.
- Diabetes and Allergies: A Statistical Check The current dataset allowed us to test the OR for the relationship between family history of diabetes and the presence of diabetes in a particular patient: all variables were dichotomous and discrete and could take […]
- Type 2 Diabetes in Adolescents According to a National Diabetes Statistics Report released by the Centers for Disease Control and Prevention, the estimated prevalence of the disease was 25 cases per 10,000 adolescents in 2017. A proper understanding of T2D […]
- Analysis of Diabetes and Its Huge Effects In the US, diabetes is costly to treat and has caused much physical, emotional and mental harm to the people and the families of those who have been affected by the disease.
- Nursing: Self-Management of Type II Diabetes Sandra Fernandes and Shobha Naidu’s journal illustrates the authors’ understanding of a significant topic in the nursing profession.”Promoting Participation in self-care management among patients with diabetes mellitus” article exposes readers to Peplau’s theory to understand […]
- The Impact of Vegan and Vegetarian Diets on Diabetes Vegetarian diets are popular for a variety of reasons; according to the National Health Interview Survey in the United States, about 2% of the population reported following a vegetarian dietary pattern for health reasons in […]
- “Diabetes Prevention in U.S. Hispanic Adults” by McCurley et al. This information allows for supposing that face-to-face interventions can be suitable to my practicum project that considers measures to improve access to care among African Americans with heart failure diseases. Finally, it is possible to […]
- Diabetes Disease of the First and Second Types It is a decrease in the biological response of cells to one or more effects of insulin at its average concentration in the blood. During the first type of diabetes, insulin Degludec is required together […]
- The Trend of the Higher Prevalence of Diabetes According to the CDC, while new cases of diabetes have steadily decreased over the decades, the prevalence of the disease among people aged below twenty has not.
- Person-Centered Strategy of Diabetes and Dementia Care The population of focus for this study will be Afro-American women aged between sixty and ninety who have diabetes of the second type and dementia or are likely to develop dementia in the future.
- Video Consultations Between Patients and Clinicians in Diabetes, Cancer, and Heart Failure Services For example, during one of my interactions with the patient, I was asked whether the hospital had the policy to avoid face-to-face interaction during the pandemic with the help of video examinations.
- Diets to Prevent Heart Disease, Cancer, and Diabetes In order to prevent heart disease, cancer, and diabetes, people are required to adhere to strict routines, including in terms of diet. Additionally, people wanting to prevent heart disease, cancer, and diabetes also need to […]
- The Centers for Diabetes’ Risks Assessment In general, the business case for the Centers for Diabetes appears to be positive since the project is closely aligned with the needs of the community and the targets set by the Affordable Care Act.
- Intervention Methods for Type 2 Diabetes Mellitus An individual should maintain a regulated glycemic control using the tenets of self-management to reduce the possibility of complications related to diabetes.
- Diabetes Mellitus as Leading Cause of Disability The researchers used data from the Centers for Disease Control and Prevention, where more than 12% of older people in the US live with the condition.
- Depression in Diabetes Patients The presence of depression concomitant to diabetes mellitus prevents the adaptation of the patient and negatively affects the course of the underlying disease.
- The Relationship Between Diabetes and COVID-19 After completing the research and analyzing the articles, it is possible to suggest a best practice that may be helpful and effective in defining the relationship between diabetes and COVID-19 and providing a way to […]
- Pre-diabetes and Urinary Incontinence Most recent reports indicate that a physiotherapy procedure gives a positive result in up to 80% of patients with stage I or SUI and mixed form and 50% of patients with stage II SUI.
- Type 1 Diabetes: Recommendations for Alternative Drug Treatments Then, they have to assess the existing levels of literacy and numeracy a patient has. Tailoring educational initiatives to a person’s unique ethnic and cultural background is the basis of cultural competence in patient education.
- Type 2 Diabetes: A Pharmacologic Update Diabetes presents one of the most common diagnoses in causes of ED visits among adults and one of the leading causes of death in the United States.
- Type 2 Diabetes and Its Treatment The main difference in type 2 diabetes is the insensitivity of the body’s cells to the action of the hormone insulin and their insulin resistance.
- Diabetes: Vulnerability, Resilience, and Care In nursing care, resilience is a critical concept that shows the possibility of a person to continue functioning and meeting objectives despite the existing challenges.
- Diabetes Prevention in the United States The analysis of these policies and the other strategies provides the opportunity to understand what role they might play in the improvement of human health. NDPP policy, on the other hand, emphasizes the role of […]
- Teaching Experience: Diabetes Prevention The primary objective of the seminar is to reduce the annual number of diabetes cases and familiarize the audience with the very first signs of this disease.
- Summary of Type 2 Diabetes: A Pharmacologic Update The authors first emphasize that T2D is one of the most widespread diseases in the United States and the seventh leading cause of death.
- Insulin Effects in a Diabetes Person I will use this source to support my research because the perception of diabetes patients on insulin therapy is essential for understanding the impact they cause on the person.
- Diabetes and Medical Intervention In the research conducted by Moin et al, the authors attempted to define the scope of efficiency of such a tool as an online diabetes prevention program in the prevention of diabetes among obese/overweight population […]
- Diabetes Mellitus Type 2 and a Healthy Lifestyle Relationship The advantage of this study over the first is that the method uses a medical approach to determining the level of fasting glucose, while the dependences in the study of Ugandans were found using a […]
- Diabetes: Epidemiological Analysis I would like to pose the following question: how can epidemiology principles be applied to these statistics for further improvements of policies that aim to reduce the impact of diabetes on the U.S.population? The limited […]
- Pathogenesis and Prevention of Diabetes Mellitus and Hypertension The hormone is produced by the cells of the islets of Langerhans found in the pancreas. It is attributed to the variation in the lifestyle of these individuals in these two geographical zones.
- Parental Intervention on Self-Management of an Adolescent With Diabetes Diabetes development and exposure are strongly tied to lifestyle, and the increasing incidents rate emphasizes the severity of the population’s health problem.
- Addressing the Needs of Hispanic Patients With Diabetes Similarly, in the program at hand, the needs of Hispanic patients with diabetes will be considered through the prism of the key specifics of the community, as well as the cultural background of the patients.
- Diabetes: Epidemiologic Study Design For instance, the range of their parents’ involvement in the self-management practices can be a crucial factor in treatment and control.
- What to Know About Diabetes? Type 1 diabetes is caused by autoimmune reaction that prevent realization of insulin in a body. Estimated 5-10% of people who have diabetes have type 1.
- Diabetes in Saudi Arabia It is expected that should this underlying factor be discovered, whether it is cultural, societal, or genetic in nature, this should help policymakers within Saudi Arabia create new governmental initiatives to address the problem of […]
- “Medical Nutrition Therapy: A Key to Diabetes Management and Prevention” Article Analysis In the process of MNT application, the dietitian keeps a record of the changes in the main components of food and other components of the blood such as blood sugars to determine the trend to […]
- Nutrition and Physical Activity for Children With a Diabetes When a child understands that the family supports him or her, this is a great way to bring enthusiasm in dealing with the disease.
- Global and Societal Implications of the Diabetes Epidemic The main aim of the authors of this article seems to be alerting the reader on the consequences of diabetes to the society and to the whole world.
- Diabetes and Hypertension Avoiding Recommendations Thus, the promotion of a healthy lifestyle should entail the encouragement of the population to cease smoking and monitor for cholesterol levels.
- Pregnant Women With Type I Diabetes: COVID-19 Disease Management The grounded theory was selected for the given topic, and there are benefits and drawbacks of utilizing it to study the experiences of pregnant women with type I diabetes and COVID-19.
- Current Recommendations for the Glycemic Control in Diabetes Management of blood glucose is one of the critical issues in the care of people with diabetes. Therefore, the interval of the A1C testing should also depend on the condition of the patient, the physician’s […]
- Diabetes Mellitus: Types, Causes, Presentation, Treatment, and Examination Diabetes mellitus is a chronic endocrinologic disease, which is characterized by increased blood glucose concentration.
- Diabetes Problem at Country Walk Community: Intervention and Evaluation This presentation develops a community health nursing intervention and evaluation tool for the diabetes problem affecting Country Walk community.
- Communication Challenges Between Nurses and Patients With Type 2 Diabetes According to Pung and Goh, one of the limitations of communication in a multicultural environment is the language barrier that manifests itself in the direct interaction of nurses with patients and in the engagement work […]
- Diabetes Type 2 from Management Viewpoint Demonstrate the effects of type 2 diabetes and provide background information on the disease; Discuss the management plans of diabetes centers and critically analyze the frameworks implemented in the hospitals; Examine the existing methodology models […]
- Nursing Plan for the Patient with Diabetes Type 2, HTN, and CAD The health of the population is the most valuable achievement of society, so the preservation and strengthening of it is an essential task in which everyone should participate without exception.
- Diagnosis and Classification of Diabetes Mellitus Diabetes is a serious public health concern that introduces a group of metabolic disorders caused by changes in the sugar blood level.
- Diabetes Mellitus Type II: A Case of a Female Adult Patient In this presentation, we are going to develop a care plan for a 47-year-old woman with a 3-year-old history of Diabetes Mellitus Type 2 (also known as Type II DM).
- Diabetes Insipidus: Disease Process With Implications for Healthcare Professionals This presentation will consider the topic of Diabetes Insipidus (DI) with a focus on its etiology and progress.
- The Nature of Type 1 Diabetes Mellitus Type 1 diabetes mellitus is a chronic autoimmune disease that has an active genetic component, which is identified by increased blood glucose levels, also known as hyperglycemia.
- A Study of Juvenile Type 1 Diabetes in the Northwest of England The total number of children under seventeen years living with type 1 diabetes in North West England by 2009 was 2,630.
- Imperial Diabetes Center Field Study The purpose is to examine the leadership’s practices used to maintain and improve the quality and safety standards of the facility and, using the observations and scholarly research, offer recommendations for improvement.
- Diabetes Risk Assessment After completing the questionnaire, I learned that my risk for the development of diabetes is above average. Modern risk assessment tools allow identifying the current state of health and possibilities of developing the disease.
- The Role of Telenursing in the Management of Diabetes Type 1 Telemedicine is the solution that could potentially increase the coverage and improve the situation for many t1DM patients in the world.
- Health Issues of Heart Failure and Pediatric Diabetes As for the population, which is intended to participate in the research, I am convinced that there is the need to specify the patients who should be examined and monitored.
- Juvenile Diabetes: Demographics, Statistics and Risk Factors Juvenile diabetes, also referred to as Type 2 diabetes or insulin-dependent diabetes, describes a health condition associated with the pancreas’s limited insulin production. The condition is characterized by the destruction of the cells that make […]
- Diabetes Mellitus: Pathophysiologic Processes The main function of insulin produced by cells within the pancreas in response to food intake is to lower blood sugar levels by the facilitation of glucose uptake in the cells of the liver, fat, […]
- Type 2 Diabetes Management in Gulf Countries One such study is the systematic review on the quality of type 2 diabetes management in the countries of the cooperation council for the Arab states of the Gulf, prepared by Alhyas, McKay, Balasanthiran, and […]
- Patient with Ataxia and Diabetes Mellitus Therefore, the therapist prioritizes using the cushion to the client and persuades the patient to accept the product by discussing the merits of the infinity cushion with a low profile in enabling the customer to […]
- Diabetes Evidence-Based Project: Disseminating Results In this presentation, the involvement of mentors and collaboration with administration and other stakeholders are the preferred steps, and the idea to use social networking and web pages has to be removed.
- The Problem of Diabetes Among African Americans Taking into consideration the results of the research and the information found in the articles, the problem of diabetes among African Americans has to be identified and discussed at different levels.
- Childhood Obesity, Diabetes and Heart Problems Based on the data given in the introduction it can be seen that childhood obesity is a real problem within the country and as such it is believed that through proper education children will be […]
- Hypertension and Antihypertensive Therapy and Type 2 Diabetes Mellitus In particular, Acebutolol impairs the functions of epinephrine and norepinephrine, which are neurotransmitters that mediate the functioning of the heart and the sympathetic nervous system.
- Adult-Onset Type 2 Diabetes: Patient’s Profile Any immediate care as well as post-discharge treatment should be explained in the best manner possible that is accessible and understandable to the patient.
- Diabetes: Diagnosis and Treatment The disease is characterized by the pancreas almost not producing its own insulin, which leads to an increase in glucose levels in the blood.
- How to Manage Type 2 Diabetes The article is significant to the current research problem as the researchers concluded that the assessment of metabolic processes in diabetic patients was imperative for adjusting in the management of the condition.
- Type 2 Diabetes Analysis Thus, type 2 diabetes has medical costs, or the difficulties of coping up with the illness, economic ones, which are the financial costs of managing it, and the organizational ones for the healthcare systems.
- Clinical Trial of Diabetes Mellitus On the other hand, type II diabetes mellitus is caused by the failure of the liver and muscle cells to recognize the insulin produced by the pancreatic cells.
- Diabetes: Diagnosis and Related Prevention & Treatment Measures The information presented on the articles offers an insight in the diagnosis of diabetes among various groups of persons and the related preventive and treatment measures. The study identified 3666 cases of initial stages of […]
- Reinforcing Nutrition in Schools to Reduce Diabetes and Childhood Obesity For example, the 2010 report says that the rates of childhood obesity have peaked greatly compared to the previous decades: “Obesity has doubled in Maryland over the past 20 years, and nearly one-third of youth […]
- The Connection Between Diabetes and Consuming Red Meat In light of reporting the findings of this research, the Times Healthland gave a detailed report on the various aspects of this research.
- Synthesizing the Data From Relative Risk Factors of Type 2 Diabetes Speaking of such demographic factors as race, the white population suffers from it in the majority of cases, unlike the rest of the races, the remaining 0.
- Using Exenatide as Treatment of Type 2 Diabetes Mellitus in Adults Kendal et al.analyzed the effects of exenatide as an adjunct to a combination of metformin and sulfonylurea against the combination of the same drugs without the adjunct.
- Enhancing Health Literacy for People With Type 2 Diabetes Two professionals, Andrew Long, a professor in the school of heath care in the University of Leeds, and Tina Gambling, senior lecturer in the school of health care studies from the University of Cardiff, conducted […]
- The Scientific Method of Understanding if Coffee Can Impact Diabetes The hypothesis of the experiment ought to be straightforward and understandable. The control group and the experiment group for the test are then identified.
- Gestational Diabetes Mellitus: Review This is because of the current patterns that show an increase in the prevalence of diabetes in offspring born to mothers with GDM.
- Health Service Management of Diabetes
- Necrotizing Fasciitis: Pathophysiology, Role of Diabetes
- The Benefits of Sharing Knowledge About Diabetes With Physicians
- Gestational Diabetes Mellitus – NSW, Australia
- Health and Wellness: Stress, Diabetes and Tobacco Related Problems
- 52-Year-Old Female Patient With Type II Diabetes
- Healthy People Project: Personal Review About Diabetes
- Nursing Diagnosis: Type 1 Diabetes & Hypertension
- Nursing Care For the Patient With Diabetes
- Nursing Care Development Plan for Diabetes and Hypertension
- Coronary Heart Disease Aggravated by Type 2 Diabetes and Age
- Diabetes as the Scourge of the 21st Century: Locating the Solution
- Psychosocial Implications of Diabetes Management
- Gestational Diabetes in a Pregnant Woman
- Diabetes Mellitus: Prominent Metabolic Disorder
- Holistic Approach to Man’s Health: Diabetes Prevention
- Holistic Image in Prevention of Diabetes
- Educational Strategies for Diabetes to Patients
- Diabetes and Obesity in the United Arab Emirates
- Epidemiological Problem: Diabetes in Illinois
- Diabetes as a Chronic Condition
- Managing Diabetes Through Genetic Engineering
- Diabetes, Functions of Insulin, and Preventive Practices
- Treating of Diabetes in Adults
- Counseling and Education Session in Type II Diabetes
- Diabetes II: Reduction in the Incidence
- Community Health Advocacy Project: Diabetes Among Hispanics
- Community Health Advocacy Project: Hispanics With Diabetes
- Hispanics Are More Susceptible to Diabetes That Non-Hispanics
- Rates Diabetes Between Hispanics Males and Females
- Diabetes Mellitus and HFSON Conceptual Framework
- Prince Georges County Community Health Concern: Diabetes
- Fats and Proteins in Relation to Type 2 Diabetes
- Alcohol Interaction With Medication: Type 2 Diabetes
- Diabetes Management and Evidence-Based Practice
- Critical Analysis of Policy for Type 2 Diabetes Mellitus in Australia
- The Treatment and Management of Diabetes
- Obesity and Diabetes: The Enemies Within
- Impact of Diabetes on the United Arab Emirates’ Economy
- Childhood Obesity and Type 2 Diabetes
- Health Nursing and Managing Diabetes
- Diabetes Management: How Lifestyle, Daily Routine Affect Blood Sugar
- Diabetes Management: Diagnostics and Treatment
- Diabetes Mellitus Type 2: The Family Genetic History
- Diabetes Type II: Hormonal Mechanism and Intracellular Effects of Insulin
- Social, Behavioral, and Psychosocial Causes of Diseases: Type 2 Diabetes
- Supportive Intervention in the Control of Diabetes Mellitus
- Enhancing Foot Care Practices in Patients With Diabetes
- Community Health Promotion: The Fight Against Diabetes in a Community Setting
- Diabetes in Australia and Saudi Arabia
- Diabetes: The Advantages and Disadvantages of Point of Care Testing
- Diabetes Mellitus Type 2 or Non-Insulin-Dependent Diabetes Mellitus
- Qualitative Research in Diabetes Management in Elderly Patient
- Diabetes Prevention Measures in the Republic of the Marshall Islands
- Impact of Diabetes on Healthcare
- Gestational Diabetes: American Diabetes Association Publishers
- Gestational Diabetes: Child Bearing Experience
- Diabetes Mellitus Effects on Periodontal Disease
- Diabetes Type II Disease in the Community
- The Relationship of Type 2 Diabetes and Depression
- Glycemic Control in Individuals With Type 2 Diabetes
- The Diagnosis of Diabetes in Older Adults and Adolescents
- Physical Activity in Managing Type-2 Diabetes
- High Risk of Developing Type 1 and Type 2 Diabetes Mellitus
- Children With Type 1 Diabetes in Clinical Practice
- Type 2 Diabetes Treatment Analysis
- Type 2 Diabetes Mellitus: Revealing the Diagnosis
- The Type 2 Diabetes Prevention: Lifestyle Choices
- Indigenous and Torres Strait Population and Diabetes
- Interpretation of the Diabetes Interview Transcript
- Type 1 Diabetes: Using Glucose Monitoring in Treatment
- Managing Type 2 Diabetes Patients’ Blood Sugar Prior to and After Surgical Procedures
- Dubai Diabetes… We Care: Leaflet Review
- Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes: Medical Terminology Definition
- Modern Diabetes Treatment Tools
- Diabetes: Encapsulation to Treat a Disease
- Current Dietary for the Treatment of Diabetes
- Diabetes: Discussion of the Disease
- Stranahan on Diabetes Impairs Hippocampal Function
- A Clinical-Based Study of Young Adults Who Have Diabetes
- Panax Ginseng for Diabetes Treatment
- Depression and Diabetes Association in Adults
- Is There Anu Cure For Diabetes?
- Diabetes Type 2 in Children: Causes and Effects
- Type 1 Diabetes Mellitus Case
- Health, Culture, and Identity as Diabetes Treatment Factors
- Diabetes Prevention in Chinese Elderly in Hunan
- “Experiences of Patients With Type 2 Diabetes Starting Insulin Therapy” by Phillips
- Type 2 Diabetes: Nursing Change Project
- Diabetes and Health Promotion Concepts
- Type 2 Diabetes Project Results Dissemination
- Type 2 Diabetes in Geriatric Patients
- Type 2 Diabetes and Geriatric Evidence-Based Care
- Cultural Empowerment. Diabetes in Afro-Americans
- Diabetes Self-Management: Relationships & Expectations
- Diagnosis and Classification of Diabetes Mellitus
- Improving Comprehensive Care for Patients With Diabetes
- Diabetes Impact on Cardiovascular and Nervous Systems
- Side Effects of Metformin in Diabetes Treatment
- Type 2 Diabetes and Drug Treatments
- Diabetes Mellitus and Health Determinants
- Nursing Leadership in Diabetes Management
- Diabetes Education for African American Women
- Latent Autoimmune Adult Diabetes
- Obesity: Epidemiology and Health Consequences
- Diabetes in Urban Cities of United States
- Diabetes in Australia: Analysis
- Type 2 Diabetes in the Afro-American Bronx Community
- Type 2 Diabetes From Cultural and Genetic Aspects
- Type 2 Diabetes in Bronx: Evidence-Based Practice
- Type 2 Diabetes in Bronx Project for Social Change
- Cardiovascular Care in Type 2 Diabetes Patients
- Ambition Diabetes and Diet on Macbeths’ Example
- Diabetes as Community Health Issue in the Bronx
- Diabetes Management Plan: Diagnosis and Development
- Diabetes Treatment and Care
- Transition from Pediatric to Adult Diabetes Care
- Diabetes Awareness Program and Strategic Planning
- Diabetes: Disease Control and Investigation
- Diabetes Pain Questionnaire and Patient Feedback
- Perception of Diabetes in the Hispanic Population
- Clinical Studies of Diabetes Mellitus
- Diabetes Mellitus and Problems at Work
- Diabetes in the US: Cost Effectiveness Analysis
- Diabetes Investigation in Space Flight Research
- Diabetes Care Advice by Food and Drug Administration
- Artificial Intelligence for Diabetes: Project Experiences
- Diabetes Patients’ Long-Term Care and Life Quality
- Chronic Care Model for Diabetes Patients in the UAE
- Diabetes Among British Adults and Children
- Endocrine Disorders: Diabetes and Fibromyalgia
- Future Technologies: Diabetes Treatment and Care
- Epidemiology of Type 1 Diabetes
- Diabetes: Treatment Technology and Billing
- Pathophysiology of Mellitus and Insipidus Diabetes
- Cure for Diabetes: The Impossible Takes a Little Longer
- Stem Cell Therapy as a Potential Cure for Diabetes
- Stem Cell Therapy and Diabetes Medical Research
- Obesity and Hypertension in Type 2 Diabetes Patients
- Strongyloides Stercoralis Infection and Type 2 Diabetes
- Socioeconomic Status and Susceptibility to Type II Diabetes
- Diabetes Mellitus: Differential Diagnosis
- Diabetes Disease in the USA Adults
- Education for African Americans With Type 2 Diabetes
- Diabetes Treatment and Funding in Fulton County
- Diabetes Care: Leadership and Strategy Plan
- Diabetes Mellitus’ New Treatment: Principles and Process
- Diet and Nutrition: European Diabetes
- Preventing the Proliferation Diabetes
- Diabetes: Symptoms, Treatment, and Prevention
- Diabetes and Cardiovascular Diseases in Medicine
- Ecological Models to Deal with Diabetes in Medicine
- Different Types of Diabetes Found in Different Countries
- Analysis of Program “Prevent Diabetes Live Life Well”
- The Effect of Physical, Social, and Health Variables on Diabetes
- Micro and Macro-Cosmos in Medicine and Care Models for Prevention of Diabetes
- Why Qualitative Method Was Chosen for Diabetes Program Evaluation
- Humanistic Image of Managing Diabetes
- Diabetes mellitus Education and hemoglobin A1C level
- Obesity, Diabetes and Heart Disease
- Illuminate Diabetes Event Design
- Cause and Diagnosis of Type 2 diabetes
- Patient Voices: Type 2 Diabetes. Podcast Review
- Type I Diabetes: Pathogenesis and Treatment
- Human Body Organ Systems Disorders: Diabetes
- Age Influence on Physical Activity: Exercise and Diabetes
- Hemoglobin A1C Test for Diabetes
- Why Injury and Diabetes Have Been Identified as National Health Priority?
- What Factors Are Involved in the Increasing Prevalence of Type II Diabetes in Adolescents?
- Does the Socioeconomic Position Determine the Incidence of Diabetes?
- What Are the Four Types of Diabetes?
- How Fat and Obesity Cause Diabetes?
- How Exercise Affects Type 2 Diabetes?
- How Does the Treatment With Insulin Affect Type 2 Diabetes?
- How Diabetes Does Cause Depression?
- Does Diabetes Prevention Pay For Itself?
- How Does Snap Participation Affect Rates of Diabetes?
- Does Overeating Sugar Cause Diabetes, Cavities, Acne, Hyperactivity and Make You Fat?
- Why Diabetes Mellitus and How It Affects the United States?
- Does Alcohol Decrease the Risk of Diabetes?
- How Does a Person With Diabetes Feel?
- Does Periodontal Inflammation Affect Type 1 Diabetes in Childhood and Adolescence?
- How Can the Paleolithic Diet Control Type 2 Diabetes?
- How Does Insulin Help Diabetes Be Controlled?
- Does Economic Status Matter for the Regional Variation of Malnutrition-Related Diabetes?
- How Can Artificial Intelligence Technology Be Used to Treat Diabetes?
- What Are the Main Causes and Treatments of Diabetes?
- What Evidence Exists for Treatments Depression With Comorbid Diabetes Using Traditional Chinese Medicine and Natural Products?
- Why Was Qualitative Method Chosen for Diabetes Program Evaluation?
- What Are the Three Types of Diabetes?
- How Does Poverty Affect Diabetes?
- What Is the Leading Cause of Diabetes?
- How Is Diabetes Diagnosed?
- What Are the Main Symptoms of Diabetes?
- How Diabetes Adversely Affects Your Body?
- What Are the Most Common Symptoms of Undiagnosed Diabetes?
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, February 25). 357 Diabetes Essay Topics & Examples. https://ivypanda.com/essays/topic/diabetes-essay-examples/
"357 Diabetes Essay Topics & Examples." IvyPanda , 25 Feb. 2024, ivypanda.com/essays/topic/diabetes-essay-examples/.
IvyPanda . (2024) '357 Diabetes Essay Topics & Examples'. 25 February.
IvyPanda . 2024. "357 Diabetes Essay Topics & Examples." February 25, 2024. https://ivypanda.com/essays/topic/diabetes-essay-examples/.
1. IvyPanda . "357 Diabetes Essay Topics & Examples." February 25, 2024. https://ivypanda.com/essays/topic/diabetes-essay-examples/.
Bibliography
IvyPanda . "357 Diabetes Essay Topics & Examples." February 25, 2024. https://ivypanda.com/essays/topic/diabetes-essay-examples/.
- Disease Questions
- Health Promotion Research Topics
- Metabolism Research Topics
- Healthcare Questions
- Obesity Ideas
- Heart Failure Titles
- Childhood Obesity Research Ideas
- Epigenetics Essay Titles
- Alcohol Abuse Paper Topics
- Pathogenesis Research Ideas
- Therapeutics Research Ideas
- Hypertension Topics
- Osteoarthritis Ideas
- Cardiomyopathy Titles
- Malnutrition Titles
Research Summaries
Keep up with the latest diabetes and diabetes-related studies with these brief overviews. Each summary provides main points, methods, and findings and includes a link to the article.
Diabetes Management and Education
Reaching treatment goals could help people living with type 2 diabetes increase their life expectancy by 3 years or in some cases by as much as 10 years. Read the summary .
Adults who receive diabetes education are more likely to follow recommended preventive care practices that lead to better diabetes management. Read the summary .
In 2017, the total cost of diabetes complications was over $37 billion among Medicare beneficiaries 65 or older with type 2 diabetes. Read the summary .
Kids and teens can get both type 1 and type 2 diabetes. New research shows how diabetes rates in young people may rise by 2060. Read the summary .
New USPSTF and ADA guidelines lower the age for prediabetes and type 2 diabetes screening to 35. This study examined if testing practices aligned with guidelines and which populations were less likely to receive testing. Read the summary .
The SEARCH for Diabetes in Youth study reports trends in young people who are being diagnosed with type 1 and type 2 diabetes. Read the summary .
Recent guidelines recommend newer types of diabetes medications, and most Americans living with type 2 diabetes are eligible. Read the summary .
Chronic Kidney Disease
End-stage kidney disease—kidney failure that requires dialysis or a kidney transplant—can lead to disability and early death, is expensive to treat, and cases are on the rise. Read the summary .
- Reports and Publications
- Research Projects
- US Diabetes Surveillance System
To receive updates about diabetes topics, enter your email address:
- Diabetes Home
- State, Local, and National Partner Diabetes Programs
- National Diabetes Prevention Program
- Native Diabetes Wellness Program
- Chronic Kidney Disease
- Vision Health Initiative
- Heart Disease and Stroke
- Overweight & Obesity
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Introduction
- Conclusions
- Article Information
eFigure. i Count Participant Enrollment and Flow
eTable 1. Baseline Characteristics of TODAY Randomized Clinical Trial and i Count Analysis Cohort
eTable 2. Participant Characteristics for Those Included vs Excluded in Analyses
eTable 3. Participant Characteristics of HbA 1c Change Groups (T1 to T2 Change)
eTable 4. Psychosocial Factors Associated With HbA 1c Level at T1
eTable 5. Psychosocial Factors Associated With HbA 1c Level Change Over Time
eAppendix. Material Needs Insecurities Survey
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Trief PM , Wen H , Burke B, et al. Psychosocial Factors and Glycemic Control in Young Adults With Youth-Onset Type 2 Diabetes. JAMA Netw Open. 2024;7(4):e245620. doi:10.1001/jamanetworkopen.2024.5620
Manage citations:
© 2024
- Permissions
Psychosocial Factors and Glycemic Control in Young Adults With Youth-Onset Type 2 Diabetes
- 1 Department of Psychiatry and Behavioral Sciences, State University of New York Upstate Medical University, Syracuse
- 2 Biostatistics Center, George Washington University, Rockville, Maryland
- 3 Department of Pediatrics-Psychology, Baylor College of Medicine, Houston, Texas
- 4 Department of Medicine, State University of New York Upstate Medical University, Syracuse
Question What psychosocial factors are associated with glycated hemoglobin (HbA 1c ) levels in young adults with youth-onset type 2 diabetes?
Findings In this cohort study of 348 participants, diabetes distress, beliefs that medicines are necessary, and concerns about medicines were associated with higher odds of high HbA 1c (≥8.0%) 1 year later; these beliefs were also associated with an HbA 1c decrease of at least 0.5%. Self-management support and self-efficacy were associated with lower odds of high HbA 1c , whereas diabetes distress was associated with higher HbA 1c level.
Meaning These findings suggest that high HbA 1c is associated with psychosocial factors that may be targets for future interventions to improve glycemic control in young adults with youth-onset type 2 diabetes.
Importance Youth-onset type 2 diabetes is associated with poor glycemic control and early onset of complications. Identification of psychosocial factors associated with poor glycemic control is needed to inform efficacious interventions.
Objective To identify psychosocial factors associated with glycated hemoglobin (HbA 1c ) levels in young adults with youth-onset type 2 diabetes.
Design, Setting, and Participants For the i Count cohort study, HbA 1c levels were measured twice (at baseline [T1] and at 1 year [T2]) during the last years (2017-2019) of the observational phase of the multicenter Treatment Options for Type 2 Diabetes in Adolescents and Youth (TODAY2) study. Participants were young adults who had been diagnosed with type 2 diabetes during childhood or adolescence. Data were analyzed from December 2021 to September 2023.
Main Outcomes and Measures Glycemic control was examined categorically (high [≥8.0%] vs low [<8.0%] HbA 1c ), continuously (HbA 1c level), and over time (change in HbA 1c : decreased ≥0.5%, remained stable, or increased ≥0.5%). Psychosocial measures included beliefs about medicines, depression and anxiety symptoms, diabetes distress, diabetes self-efficacy, self-management support, and unmet material needs. Multivariable logistic and linear regression models evaluated the association of each psychosocial factor with the probability of T2 HbA 1c of 8.0% or greater, T2 HbA 1c level, and change in HbA 1c .
Results Of the 411 TODAY2 participants approached, 381 enrolled in the i Count study, and 348 with T1 and T2 HbA 1c data comprised the analysis group. The 348 participants had a mean (SD) age of 26.1 (2.5) years and a mean (SD) HbA 1c of 9.4% (2.8%). Most participants (229 [65.8%]) were women. In adjusted multivariable regressions, greater beliefs that diabetes medicines are necessary (odds ratio [OR], 1.19 [95% CI, 1.03-1.37]; P = .02), concerns about medicines (OR, 1.20 [95% CI, 1.00-1.45]; P = .049), diabetes distress (OR, 1.08 [95% CI, 1.02-1.15]; P = .006), and high distress (OR, 2.18 [95% CI, 1.15-4.13]; P = .02) increased the odds of high HbA 1c at T2. Greater support (OR, 0.67 [95% CI, 0.46-0.97]; P = .04) and diabetes self-efficacy (OR, 0.91 [95% CI, 0.84-0.99]; P = .02) decreased the odds of high HbA 1c at T2. Diabetes distress was associated with higher HbA 1c level at T2 (coefficient, 0.08 [95% CI, 0.02-0.13]; P = .01). Beliefs that diabetes medicines are necessary (OR, 1.20 [95% CI, 1.03-1.39]; P = .02) and concerns about medicines (OR, 1.22 [95% CI, 1.00-1.47]; P = .048) increased the odds of an HbA 1c decrease of at least 0.5% over 1 year.
Conclusions and Relevance In this cohort study of young adults with youth-onset type 2 diabetes, beliefs about medicines, high diabetes distress, low diabetes self-efficacy, and self-management support were associated with high HbA 1c over time. Future research should assess whether interventions that address these factors result in improved glycemic control in this at-risk group.
Outcomes in type 2 diabetes are heavily determined by self-management behaviors that often affect glycemic control. 1 Several studies seek to identify psychosocial factors associated with glycemic control, commonly defined by hemoglobin A 1c (HbA 1c ) levels. Psychosocial factors studied include depressive symptoms, 2 anxiety symptoms, 3 diabetes distress, 4 social support, 5 self-efficacy, 6 and social determinants of health. 7 Significant factors might serve as targets of behavioral interventions to improve outcomes. However, the evidence of associations between these factors and HbA 1c is mixed; the available studies were mostly cross-sectional, and participants were middle-aged to older adults with adult-onset type 2 diabetes (diagnosed after age 18 years).
There has been a marked increase in the incidence and prevalence of youth-onset type 2 diabetes (diagnosed before age 18 years). 8 Compared with adult-onset diabetes, youth-onset diabetes is associated with poorer health outcomes, including earlier onset and severity of diabetes-related complications. 9 - 11 Developmental, social, and emotional challenges among this cohort make it difficult to generalize from existing research on older adults. The Treatment Options for Type 2 Diabetes in Adolescents and Youth (TODAY) study recruited a large, diverse sample of 699 children and adolescents with youth-onset type 2 diabetes to participate in a randomized clinical trial to evaluate 3 treatment regimens. 12 Following the TODAY intervention study, 572 participants enrolled in the TODAY2 observational follow-up study of a unique cohort (ie, young adults with youth-onset type 2 diabetes). Looking at one psychosocial factor (depression) and HbA 1c , 14.8% of TODAY youth participants reported clinically significant depression symptoms, but symptoms were not associated with HbA 1c . 13 Over the last 6 years of the TODAY2 study when participants moved into adulthood, the percentage of participants with significant depression symptoms increased (from 14.0% to 19.2%) and symptoms were associated with higher HbA 1c , hypertension, and progression of retinopathy. 14
There are gaps in the literature. First, there are no studies of the association of psychosocial factors with HbA 1c in young adults with youth-onset type 2 diabetes; existing data are from middle-aged to older adults with adult-onset type 2 diabetes and may not generalize. Second, previous studies have been cross-sectional, thus longitudinal data are needed. Finally, unstudied psychosocial factors (eg, beliefs about medicines) should be included. To address these gaps, the present study used data from the TODAY2 i Count study (an ancillary study of medication adherence and health care usage among the TODAY2 cohort), including repeated measures of HbA 1c and selected psychosocial factors. The primary i Count results were published previously. 15 - 17 The aim of these preplanned secondary analyses was to identify psychosocial factors associated with HbA 1c over time in this cohort.
The TODAY, TODAY2, and i Count studies were approved by institutional review boards at 15 participating centers. Informed consent (and assent for children and adolescents when applicable) was obtained from all participants. This cohort study followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
For the TODAY study, children and adolescents (aged 10 to <18 years) were recruited at 15 US centers. They had recently (within 2 years) received a type 2 diabetes diagnosis (using 2004 American Diabetes Association criteria 18 ) and had a body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) at or above the 85th percentile, negative islet cell autoantibodies, and fasting C-peptide greater than 0.6 ng/mL (to convert to nmol/L, multiply by 0.331). Participants were randomized to 1 of 3 treatment groups (metformin, metformin plus rosiglitazone, or metformin with lifestyle intervention) and followed for 2 to 6 years (2004-2011) to assess treatment effects on primary (time to treatment failure) and secondary (complications) outcomes. 12 After the TODAY trial, 572 individuals were enrolled in the TODAY2 observational follow-up study (2014-2020); they received care in their communities and underwent annual assessments. Publications from TODAY and TODAY2 are available online. 19
The TODAY2 i Count ancillary study (July 2017 to February 2019) enrolled participants aged 19 to 31 years, with independent data collection and access to TODAY2 assessment data. Participants were recruited by staff at an annual TODAY2 visit and were informed about i Count procedures, detailed in a signed consent document. All other assessments (eg, HbA 1c levels and complications or comorbidities) were performed per TODAY2 protocols. 12 Participants completed psychosocial questionnaires at the i Count enrollment visit (baseline [T1]) and at the subsequent 1-year TODAY2 annual visit (follow-up [T2]). Participants received financial compensation for assessment time.
Data on participant characteristics were obtained using a self-report questionnaire and included the following: age, gender, race and ethnicity, years of education, annual income, employment status, duration of diabetes, and diabetes in the nuclear family. Race and ethnicity were included because it is well established that average glycemic control varies across racial and ethnic groups. These data are reported as Hispanic, non-Hispanic Black (hereinafter, Black), non-Hispanic White (hereinafter, White), or other race or ethnicity (American Indian or Alaska Native or Asian). Participant BMI, HbA 1c (analyzed at the University of Washington Northwest Lipid Research Laboratories in Seattle), and number of comorbidities or complications (ie, hypertension, neuropathy, dyslipidemia, kidney disease, or retinopathy) were assessed per TODAY2 standardized protocol procedures. 12 Outcomes of interest were high HbA 1c (≥8.0%) at T1 and T2, continuous HbA 1c level at T1 and T2, and change in HbA 1c from T1 to T2 (decrease ≥0.5%, −0.5% to 0.5%, or increase ≥0.5%) (to convert to proportion of total hemoglobin, multiply by 0.01).
Eight psychosocial measures were used in this study. Psychological factors were assessed with the Diabetes Self-Efficacy Scale (DSES), the Beliefs About Medicines Questionnaire (BMQ), the Problem Areas in Diabetes Scale–5 (PAID-5), the Diabetes Attitude Scale (DAS), the Patient Health Questionnaire–8 (PHQ-8), and the Generalized Anxiety Disorder Questionnaire–7 (GAD-7). Social factors were assessed with the Chronic Illness Resources Survey (CIRS) and the Material Needs Insecurities Survey (MNIS).
The 8-item DSES (range, 8-80) 20 measures how confident one is in their ability to perform self-care behaviors. Higher scores reflect greater diabetes self-efficacy. The DSES scores were rescaled to align with other measures ranging from 1 to 5 by dividing by 5. Each point on this rescaled measure represents a 5-point change on the original continuous scale.
On the BMQ (range, 5-25), 21 two 5-item scales measure beliefs in the necessity of diabetes medicines (eg, “My medicines protect me from getting worse”) and concerns about diabetes medicines (eg, “I worry about the long-term effects of my medicines”). Two 4-item scales (range, 4-20) measure beliefs that medicines are harmful (eg, “Medicines do more harm than good”) or overused (eg, “Doctors use too many medicines”). Higher scores reflect stronger beliefs. Subscale scores were rescaled to align with other measures ranging from 1 to 5 by dividing by 5. Each point on this rescaled measure represents a 5-point change on the original continuous scale.
The 5-item PAID-5 (range, 0-20) 22 measures diabetes-related emotional distress using a list of common diabetes-related concerns. Respondents indicate the degree to which each concern is a problem, and higher scores reflect greater diabetes distress (continuous). A score of 8 or greater defines distress warranting further assessment (ie, high diabetes distress; categorical).
The 33-item DAS 23 is a continuous scale that measures attitudes toward diabetes. We used 3 DAS subscales (range, 1-5): perceived seriousness of diabetes, its psychosocial impact, and attitudes toward patient autonomy. Higher numbers indicate greater perceived seriousness and impact and a positive attitude toward patient autonomy (ie, the right to decide how hard one works to control blood glucose).
The 8-item PHQ-8 (range, 0-20) 24 measures the presence and severity of depressive symptoms in the prior 2 weeks. Higher scores reflect a greater number of and greater severity of depressive symptoms (continuous). A PHQ-8 score of 10 or greater is a screen for major depressive disorder, which we refer to as moderate to severe depressive symptoms here (categorical).
The 7-item GAD-7 (range, 0-21) 25 measures the presence and severity of anxiety disorder symptoms over the prior 2 weeks. Higher scores reflect a greater number of and greater severity of anxiety symptoms (continuous). A GAD-7 score of 10 or greater is a screen for anxiety disorders, which we refer to as moderate to severe anxiety symptoms here (categorical).
The 22-item CIRS 26 , 27 is a continuous scale (range, 1-5) that measures multilevel self-management support, including support from one’s family or friends, neighborhood, and larger community. The CIRS is a list of available resources that support self-care, and respondents indicate how often they have used each resource over the prior 6 months. Higher scores indicate more support.
The MNIS 28 is composed of validated measures of several material need insecurities or social determinants of health. We used subscales assessing food, housing, and medication insecurities (eAppendix in Supplement 1 ). Participants also completed a health care usage survey that asked, “In the past 12 months, were you covered by a health care plan?” Lack of health care coverage was a fourth insecurity. Respondents indicated whether each need was met due to cost (categorical) over the previous 12 months.
Demographics, clinical parameters, and psychosocial measures are summarized as means (SDs) for continuous variables or as proportions for categorical variables. Multivariable logistic regression models evaluated the independent association of each psychosocial factor with the likelihood of an HbA 1c level of 8.0% or greater at T1 and T2. We chose 8.0% as the cutoff defining high HbA 1c because this was the benchmark for loss of glycemic control in the TODAY study and is clinically meaningful. Multivariable linear regression models assessed associations with HbA 1c level at T1 and T2, a continuous variable. Separate models were fit for each psychosocial factor. All models were adjusted for race and ethnicity, employment status, BMI, number of comorbidities and complications, and diabetes in the nuclear family. Additional covariates were identified from univariate analyses and therefore varied based on the specific analysis. In cross-sectional analyses of T1 HbA 1c groups, age was also a covariate. Analyses of T1 HbA 1c level included age, education, and income as adjustments. In the longitudinal analyses of T2 HbA 1c groups and HbA 1c level, education was included. We also performed analyses comparing 3 groups: those whose HbA 1c decreased 0.5% or more, those whose HbA 1c increased 0.5% or more, and those whose HbA 1c remained stable (ie, change between −0.5% and 0.5%; eTable 3 in Supplement 1 ). In these adjusted analyses, BMI and number of complications were added. Finally, we explored whether changes in psychosocial factors over time were associated with T2 HbA 1c levels. P < .05 (2-sided) was considered statistically significant. All analyses and P values were considered exploratory per TODAY and i Count Study Group analysis plans. Analyses were performed using SAS, version 9.4 (SAS Institute Inc). Data were analyzed from December 2021 to September 2023.
Of the 411 eligible TODAY2 participants approached, 381 consented to participate in the i Count study. Of the 381 enrolled, 348 had HbA 1c measurements at both T1 and T2 and comprised the analysis cohort (eFigure in Supplement 1 ). The analysis group included 229 women (65.8%) and 119 men (34.2%). Their mean (SD) age was 26.1 (2.5) years, and most (269 [77.3%]) were employed or students. A total of 131 participants (37.6%) were Black, 127 (36.5%) were Hispanic, 71 (20.4%) were White, and 19 (5.5%) were of other race or ethnicity. Most i Count participants were from economically disadvantaged populations. A total of 209 (74.6%) reported at least 1 unmet need, 267 (76.7%) had a high school diploma or fewer years of education, and 265 (82.0%) had an annual income less than $35 000 ( Table 1 ). On average, participants had poor glycemic control (mean [SD] HbA 1c , 9.4% [2.8%]), with a mean (SD) of 2.5 (1.4) complications. We compared the analysis cohort with the original TODAY cohort on selected demographic variables and found no statistically significant differences (eTable 1 in Supplement 1 ). We also compared the analysis cohort with participants who were recruited to the i Count study but excluded due to missing T2 HbA 1c levels. Excluded individuals had a slightly shorter diabetes duration (mean [SD], 11.8 [1.6] vs 12.5 [1.5] years; P = .04) and were more likely to be of other race or ethnicity (7 [21.2%] vs 19 [5.5%]; overall P = .007) (eTable 2 in Supplement 1 ).
Participants in the high HbA 1c group were significantly younger than those in the low HbA 1c group (mean [SD], 25.9 [2.5] vs 26.5 [2.4] years; P = .03) and had higher rates of unemployment or disability (61 [77.2%] vs. 18 [22.8%]; P = .008). In addition, participants in the high HbA 1c group were more likely to be racial or ethnic minority individuals: 67.2% of Black participants (n = 88), 74.0% of Hispanic participants (n = 94), and 52.6% of participants (n = 10) of other race or ethnicity had high HbA 1c compared with 49.3% of White participants (n = 35) ( P = .003). The high HbA 1c group had a lower mean (SD) BMI (35.5 [8.0] vs 37.9 [9.3]; P = .02), a greater mean (SD) number of complications (2.8 [1.3] vs 1.9 [1.4]; P < .001), and a higher percentage of participants with a family member with diabetes (145 [71.4%] vs 58 [28.6%]; P = .004) ( Table 1 ).
Group mean (SD) HbA 1c did not change significantly from T1 to T2 (9.3% [2.8%] vs 9.3% [2.7%]; P = .60). In the comparison of participants whose HbA 1c decreased 0.5% or more (108 [31.0%]) vs increased 0.5% or more (129 [37.1%]) or remained stable (111 [31.9%]), the stable group had the highest mean (SD) BMI (38.5 [9.6] vs 35.1 [7.4] vs 35.4 [8.2]; P = .008) and the lowest mean (SD) number of complications (2.2 [1.5] vs 2.7 [1.3] vs 2.6 [1.3]; P = .03) (eTable 3 in Supplement 1 ).
In adjusted logistic regression analyses of psychosocial factors associated with high HbA 1c (≥8.0%) at T1, beliefs about medicines, diabetes distress, and self-management support were associated with high T1 HbA 1c ( Table 2 ). Specifically, every 5-point higher BMQ-necessity beliefs and concerns score increased the odds of high HbA 1c 1.2 and 1.3 times (adjusted odds ratio [OR], 1.23 [95% CI, 1.07-1.43]; P = .004; OR, 1.33 [95% CI, 1.10-1.61]; P = .003). Every 1-point higher PAID-5 diabetes distress score and high diabetes distress increased the odds of high HbA 1c 1.1 and 2.7 times (OR, 1.10 [95% CI, 1.04-1.17]; P = .002; OR, 2.72 [95% CI, 1.37-5.38]; P = .004). Finally, every 1-point higher CIRS self-management support score decreased the odds of high HbA 1c by 40.0% (OR, 0.60 [95% CI, 0.41-0.88]; P = .009).
Adjusted analyses of psychosocial factors associated with high T2 HbA 1c yielded similar findings ( Table 3 ). Every 5-point higher BMQ-necessity beliefs and concerns score increased the odds of high T2 HbA 1c 1.2 times (OR, 1.19 [95% CI, 1.03-1.37]; P = .02; OR, 1.20 [95% CI, 1.00-1.45]; P = .049). Every 1-point higher diabetes distress score and high diabetes distress increased the odds of high T2 HbA 1c (OR, 1.08 [95% CI, 1.02-1.15]; P = .006; OR, 2.18 [95% CI, 1.15-4.13]; P = .02). Every 1-point higher CIRS self-management support score decreased the odds of high T2 HbA 1c by 30.0% (OR, 0.67 [95% CI, 0.46-0.97]; P = .04). Additionally, diabetes self-efficacy emerged as a statistically significant factor. Every 5-point higher DSES score decreased the odds of high T2 HbA 1c by 10.0% (OR, 0.91 [95% CI, 0.84-0.99]; P = .02).
In adjusted linear regression analyses of psychosocial factors associated with T1 HbA 1c level, diabetes distress was a significant factor. For every 1-point higher diabetes distress score, T1 HbA 1c was higher by 0.09 ( P = .01) (eTable 4 in Supplement 1 ).
In adjusted analyses of psychosocial factors associated with T2 HbA 1c , diabetes distress was again significant. For every 1-point higher T1 diabetes distress score, T2 HbA 1c was higher by 0.08 (95% CI, 0.02-0.13; P = .01) ( Table 4 ).
In adjusted logistic regressions, BMQ-necessity beliefs and concerns scores were associated with higher odds of decreased T2 HbA 1c vs stable HbA 1c levels ( Table 5 ). Specifically, every 5-point higher necessity beliefs and concerns score increased the odds of decreased HbA 1c 1.2 times (OR, 1.20 [95% CI, 1.03-1.39]; P = .02; OR, 1.22 [95% CI, 1.00- 1.47]; P = .048).
In adjusted analyses, none of the psychosocial factors were associated with change in HbA 1c level from T1 to T2. Additional details are provided in eTable 5 in Supplement 1 .
From T1 to T2, despite no planned intervention, mean (SD) scores on the DAS seriousness of diabetes subscale increased from T1 to T2 (4.03 [0.53] vs 4.10 [0.56]; P = .007), mean (SD) scores on the BMQ concerns subscale decreased (9.78 [7.18] vs 8.59 [7.08]; P = .004), the percentage of participants with moderate to severe anxiety symptoms increased (20 [5.7%] vs 33 [9.6%]; P = .02), and the percentage of participants with food insecurity decreased (130 [44.2%] vs 98 [34.3%]; P = .01). Other psychosocial factors were stable. Changes in psychosocial factors were not associated with T2 HbA 1c , either categorically or continuously.
In this first (to our knowledge) longitudinal study of the association of psychosocial factors with glycemic control in young adults with youth-onset type 2 diabetes, beliefs about diabetes medicines were associated with HbA 1c over time. Individuals with greater belief that diabetes medicines are necessary and more concerns about diabetes medicines were significantly more likely to have high HbA 1c and to have at least a 0.5% decrease in HbA 1c (without planned intervention) 1 year later. Those with higher diabetes distress were more likely to have high HbA 1c and higher HbA 1c level 1 year later. Finally, those with higher diabetes self-efficacy or self-management support were less likely to have high HbA 1c 1 year later.
Beliefs about medicines have been studied within the Necessity-Concerns Framework to understand factors associated with medication adherence. This framework posits that adherence is affected by beliefs that medicines are necessary balanced against concerns about them. 29 We previously reported that in a longitudinal study of young adults with youth-onset type 2 diabetes, having more concerns about diabetes medicines was associated with higher odds of low adherence to oral medications (ie, taking <80% of pills), greater belief that medicines are overused was associated with higher odds of low adherence to insulin, and harm and overuse beliefs were associated with a lower percentage of insulin adherence. 17 However, we are unaware of any reports relating beliefs about medicines to HbA 1c in this group; therefore, we looked to research with older adults (adult-onset diabetes) for comparison. In one cross-sectional report of older adults with type 2 diabetes, necessity and concern beliefs about medicines were not associated with HbA 1c , although they were associated with medication underuse. 30 Noting the lack of publications that examine the relationships between these beliefs and HbA 1c , our data provide compelling evidence of associations over time.
We found that lower diabetes self-efficacy was associated with high HbA 1c over time. Because of a lack of data relevant to this association from a comparable cohort, we looked to studies of those with adult-onset type 2 diabetes. A previously published meta-analysis of cross-sectional studies examined biobehavioral predictors of glycemic control in older adults. 6 The investigators reported no association between self-efficacy and HbA 1c , although self-efficacy was the most consistent predictor of adherence behaviors and was strongly related to dietary adherence, a consistent predictor of HbA 1c . 6 In contrast, our longitudinal data in young adults with youth-onset type 2 diabetes support an association between self-efficacy and HbA 1c levels over time.
Looking at diabetes distress among individuals with youth-onset type 2 diabetes, high diabetes distress was associated with higher HbA 1c levels in the TODAY2 cohort in cross-sectional analyses. 31 There is a robust literature reporting cross-sectional associations between diabetes distress and HbA 1c among individuals with adult-onset type 2 diabetes, 32 but there are few longitudinal studies. A prospective study (mean age, 57.8 years) reported cross-sectional associations between distress and HbA 1c but no associations in longitudinal analyses (9-month and 18-month follow-up). 33 In contrast, our data support an association between distress and HbA 1c over time in this cohort. Our longitudinal finding that self-management support was associated with better glycemic control is also consistent with the extant literature on persons with adult-onset diabetes. 26
We also assessed whether anxiety and depressive symptoms were associated with HbA 1c because cross-sectional studies of individuals with adult-onset type 2 diabetes often report associations between these factors and HbA 1c , although the results are inconsistent. 2 , 34 , 35 In the longitudinal study cited earlier, 33 no association between depression and HbA 1c was found at 9-month and 18-month follow-up. Similarly, we found no associations.
Our finding that unmet material needs (ie, social determinants of health) were not associated with HbA 1c is in contrast with the adult-onset diabetes literature, in which unmet needs have been linked to negative diabetes-related outcomes. 36 However, most i Count participants were from economically disadvantaged populations; as noted earlier, 209 (74.6%) reported at least 1 unmet need, 267 (76.7%) had a high school diploma or fewer years of education, and 265 (82.0%) had an annual income less than $35 000. The relatively low number of participants with no material need insecurities or financial stress likely limited our ability to find statistically significant differences based on unmet needs.
Young adults with type 2 diabetes experience many of the developmental challenges faced by peers with type 1 diabetes, such as changes in support networks, responsibilities, and health care systems. 37 The few cross-sectional studies assessing the association of psychosocial factors with HbA 1c in young adults with type 1 diabetes reported that depression, 38 diabetes distress, 39 anxiety disorders, 40 social support, 41 and health care coverage insecurity 42 were associated with HbA 1c . However, because the management of type 1 diabetes frequently involves technologies (eg, insulin pumps and continuous glucose monitoring) that pose unique challenges, it is important to study the 2 groups separately and in longitudinal studies.
Unlike most prior studies, these analyses were longitudinal and examined HbA 1c levels categorically (high vs low; decreased vs stable vs increased) and continuously (percentages). Notably, participants were members of the diverse and unique TODAY2 cohort, now young adults with youth-onset type 2 diabetes.
However, the study also has limitations. Participants recruited to the TODAY study may have differed from the general population with youth-onset type 2 diabetes in measured variables, including psychosocial factors. They had regular contact with TODAY staff over many years; individuals without that education and support might have higher HbA 1c levels. The small percentage of participants with symptoms of moderate to severe depression (9.6%) or anxiety (5.8%) and the high percentage with material needs may have limited power to find associations. Other unmeasured psychosocial factors (eg, health literacy) likely relate to HbA 1c . Additional factors that can contribute to high HbA 1c (eg, health care practitioner–related clinical inertia 43 or prescribing bias 44 ) were not considered. Results may not generalize to countries with different health care systems.
The overarching aim of i Count was to identify targets for interventions to improve HbA 1c . Beliefs about medicines may be targets, supporting beliefs that medicines are necessary to treat diabetes and addressing unvoiced concerns about them.
Diabetes self-efficacy is another potential target. There are many studies of behavior change programs that improve self-efficacy, including family-based, 45 peer-supported, 46 and lay-led 47 interventions. However, self-efficacy is commonly a secondary, not primary, focus. Our data suggest that interventions that focus on enhancing self-efficacy as the primary outcome may be beneficial and may lead to other innovative approaches. Also, interventions could address high levels of diabetes distress and provide needed support for self-management. These data can inform future interventions; however, because this was not an intervention trial, we do not know whether addressing beliefs about medicines, ameliorating diabetes distress, enhancing self-efficacy, or promoting self-management support will lead to better glycemic control among individuals with youth-onset type 2 diabetes. Future research is needed to answer these questions.
In this cohort study of young adults with youth-onset type 2 diabetes, psychosocial factors including beliefs about medicines, diabetes distress, diabetes self-efficacy, and self-management support were associated with HbA 1c levels over time. These data extend the Necessity-Concerns Framework of beliefs about medicines and medication adherence to glycemic control outcomes. Our results suggest that these potentially modifiable psychosocial factors may affect glycemic control, and thus the development of complications in this highly vulnerable group, but intervention trials are needed.
Accepted for Publication: February 12, 2024.
Published: April 8, 2024. doi:10.1001/jamanetworkopen.2024.5620
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2024 Trief PM et al. JAMA Network Open .
Corresponding Author: Paula M. Trief, PhD, Department of Psychiatry and Behavioral Sciences, State University of New York Upstate Medical University, 750 E Adams St, Syracuse, NY 13210 ( [email protected] ).
Author Contributions: Dr Trief had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Trief, Uschner, Anderson, Weinstock.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Trief, Wen, Bulger, Weinstock.
Critical review of the manuscript for important intellectual content: Trief, Wen, Burke, Uschner, Anderson, Liu, Weinstock.
Statistical analysis: Trief, Wen, Burke, Uschner, Liu.
Obtained funding: Trief, Anderson.
Administrative, technical, or material support: Trief, Burke, Uschner, Anderson, Bulger, Weinstock.
Supervision: Uschner, Anderson, Weinstock.
Conflict of Interest Disclosures: Dr Trief reported receiving grants from the National Institutes of Health during the conduct of the study. Dr Weinstock reported receiving grants (paid to State University of New York Upstate Medical University) from Eli Lilly, Insulet, Tandem, Amgen, Diasome, MannKind Corporation, and Novo Nordisk outside the submitted work. Dr Weinstock also reported receiving discounted devices from DexCom for clinical research outside the submitted work. No other disclosures were reported.
Funding/Support: This work was completed with funding through grants R01-DK110456, U01-DK61212, U01-DK61230, U01-DK61239, U01-DK61242, and U01-DK61254 from the National Institute of Diabetes and Digestive and Kidney Diseases.
Role of the Funder/Sponsor: The funder approved of the design and conduct of the study. The funder played no role in the collection, management, analysis, and interpretation of the data; in the preparation, review or approval of the manuscript; or in the decision to submit the manuscript for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Meeting Presentation: This work was presented at the American Diabetes Association Annual Scientific Sessions; June 23, 2023; Orlando, Florida.
Data Sharing Statement: See Supplement 2 .
Additional Contributions: We acknowledge and thank the TODAY (Treatment Options for Type 2 Diabetes in Adolescents and Youth) Study Group, including the leadership, site principal investigators, study coordinators, and George Washington University Coordinating Center staff, for their ongoing support and expertise; the educational support of the New York Regional Center for Diabetes Translation Research (which is funded by grant DK111022 from the National Institute of Diabetes and Digestive and Kidney Diseases); and the TODAY2 study participants for their commitment.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Embracing complexity: making sense of diet, nutrition, obesity and type 2 diabetes
- Open access
- Published: 14 February 2023
- Volume 66 , pages 786–799, ( 2023 )
Cite this article
You have full access to this open access article
- Nita G. Forouhi 1
13k Accesses
7 Citations
57 Altmetric
Explore all metrics
Nutrition therapy has been emphasised for decades for people with type 2 diabetes, and the vital importance of diet and nutrition is now also recognised for type 2 diabetes prevention. However, the complexity of diet and mixed messages on what is unhealthy, healthy or optimal have led to confusion among people with diabetes and their physicians as well as the general public. What should people eat for the prevention, management and remission of type 2 diabetes? Recently, progress has been made in research evidence that has advanced our understanding in several areas of past uncertainty. This article examines some of these issues, focusing on the role of diet in weight management and in the prevention and management of type 2 diabetes. It considers nutritional strategies including low-energy, low-fat and low-carbohydrate diets, discusses inter-relationships between nutrients, foods and dietary patterns, and examines aspects of quantity and quality together with new developments, challenges and future directions.
Graphical abstract
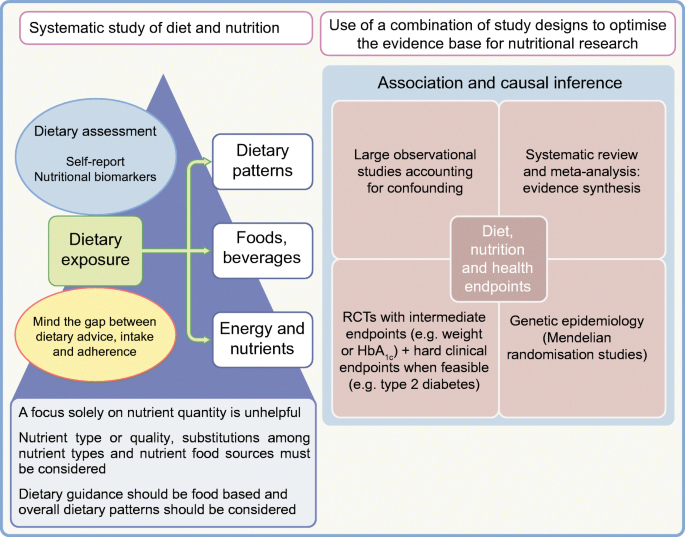
Similar content being viewed by others

Evidence-based European recommendations for the dietary management of diabetes
The Diabetes and Nutrition Study Group (DNSG) of the European Association for the Study of Diabetes (EASD)

Nutrition in Lifestyle Medicine: Overview

Diet: The Balancing Act
Sheel Sharma & Deepika Dhawan
Avoid common mistakes on your manuscript.
Diet, nutrition and type 2 diabetes: what is the evidence?
Diabetes is a metabolic disorder with the potential for multiple adverse health consequences. It is also a public health challenge, with a rising global burden. Estimates indicate that there were approximately 537 million people worldwide with diabetes in 2021, which is projected to rise to 783 million by 2045, with type 2 diabetes constituting the majority (>90%) of this burden [ 1 ]. Diet and nutrition are of indisputable significance in reducing this burden because the development of type 2 diabetes is characterised by obesity and insulin resistance, leading to hyperglycaemia, and both weight and glycaemic control are directly related to food consumption.
Diet and nutrition are thus central as modifiable factors in both the management and the prevention of type 2 diabetes. This is supported by three lines of evidence. First, when adhered to, medical nutrition therapy in those with type 2 diabetes can match or exceed the glycaemic control that can be achieved by glucose-lowering medication in the short term, and can be useful in maintaining control [ 2 ]. Second, the proof of principle was established in the early 2000s that, among people with non-diabetic hyperglycaemia, the onset of type 2 diabetes can be delayed or prevented, with as much as a 58% relative risk reduction, through a supported intensive lifestyle intervention including dietary changes and physical activity [ 3 ]. The real-world impact of lifestyle modification strategies has been demonstrated [ 4 ], outside the highly controlled conditions of clinical trials, and such a strategy has been found to be effective in the UK National Health Service (NHS) [ 5 ]. Third, it has been demonstrated that remission of type 2 diabetes can be achieved through dietary means [ 6 ], resulting in a major shift in scientific understanding of the pathophysiology of type 2 diabetes, from a condition previously thought to be progressive and irreversible to one that can be brought under control to normal functioning.
However, defining the optimal diet for type 2 diabetes is a challenge and dietary strategies used in research have varied between different studies. This is largely because diet is intensely complex, with multiple components and influences on food consumption (Fig. 1 ). Concomitantly, interest in diet, nutrition and health is intense, with a deluge of scientific publications, matched equally by popular media coverage that is saturated with nutrition over-claims and ‘miracle diets’. This is also a field where vested interests are rife [ 7 ]. A search on PubMed (25 November 2022) using the terms ‘diet OR nutrition OR food OR nutrient OR dietary pattern OR diet quality’ and ‘type 2 diabetes OR non-insulin dependent diabetes’ yielded 52,833 hits, with over 3000 articles published each year since 2014; repeating the search using the term ‘obesity’ yielded 165,617 hits. What evidence should we trust?
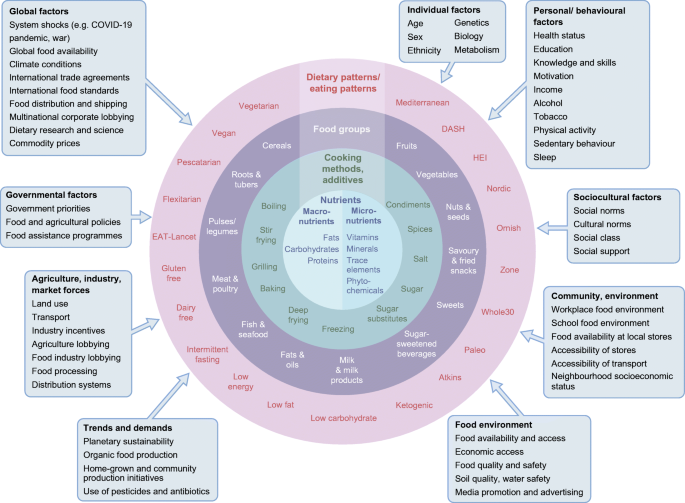
Complexity of diets and multiple influences affecting food intakes. HEI, Healthy Eating Index. Influencing factors (boxes) adapted with permission from Afshin et al [ 83 ] © 2014 John Wiley & Sons. This figure is available as a downloadable slide .
The hierarchy of evidence framework and quality assessment tools have been applied to sift through the vast amount of evidence. Several reviews of the research evidence have been carried out [ 8 , 9 , 10 , 11 , 12 , 13 , 14 ], enabling the incorporation of the best available evidence in dietary guidelines issued by authoritative agencies, including but not limited to the ADA [ 15 ] and Diabetes UK [ 16 ].
In a nutshell, this evidence highlights some key dietary principles. Healthy weight maintenance is critical to both prevent and manage type 2 diabetes; a pattern of food intake that mitigates type 2 diabetes risk includes the habitual consumption of vegetables, fruits, legumes, whole grains and cereal fibre, dairy products such as yoghurt, and nuts, and several overall dietary patterns are effective. In contrast, type 2 diabetes risk is elevated with a pattern of habitual dietary intake that includes processed and unprocessed red meat, refined grains and sugar-sweetened beverages. This evidence provides support that some foods should be emphasised and promoted while the consumption of others should be reduced or avoided, rather than the adage about everything in moderation.
This article does not cover the wide range of topics already discussed in existing reviews and guidelines. It focuses instead on selected hot topics that have been the subject of debate and on new developments in understanding in the field.
Weight management at the core, but how?
Body weight with increased adiposity is mechanistically linked to both the development and the progression of type 2 diabetes, typified by resistance to insulin action (insulin resistance) and an inadequate compensatory insulin secretory response by pancreatic beta cells. The relationship between adiposity, insulin resistance and beta cell function varies between individuals but the benefits of weight loss apply across the different pathophysiologies [ 17 ]. Weight loss is related to improved glycaemic control: the greater the weight loss, the greater the improvement in HbA 1c . A weight loss goal of 5–7% of initial body weight for people with overweight or obesity is recommended for clinical benefit, while weight loss of 15% can be disease modifying with the possibility of remission of type 2 diabetes [ 2 , 18 ].
Of the three options for weight management, bariatric surgery and pharmacotherapy are effective, but dietary strategies offer population-wide benefits without medicalisation. However, the weight loss and weight management diet market is vast and is projected to increase from US$192.2 billion in 2019 to US$295.3 billion by 2027. This promotion of a vast range of dietary products and strategies can be bewildering. An important question is therefore which dietary strategies are effective?
Remission of type 2 diabetes through diet-related weight loss
The proof of principle of the potential for reversibility or remission of type 2 diabetes with weight loss came first from the field of bariatric surgery [ 19 , 20 ]. However, surgery is not suitable for, or acceptable to, all people with type 2 diabetes. Surgery also has the potential for complications, side effects and challenges. One such challenge is the large prevalence of type 2 diabetes, which renders surgery an unrealistic option at the scale required, even if it were financially possible. There is high interest, therefore, in dietary means to achieve diabetes remission.
The nutritional basis for the remission of type 2 diabetes used in the UK-based Diabetes Remission Clinical Trial (DiRECT) was centred on major caloric restriction and weight loss with an associated reduction in hepatic fat and hepatic glucose output and improved beta cell function [ 6 ]. Among people with type 2 diabetes in primary care who were randomised to either a diet very low in energy (very low calorie diet) or usual care, mean body weight fell by 10 kg in the intervention group and 46% remained free of diabetes (i.e. in remission; HbA 1c <48 mmol/mol [<6.5%]) at 1 year and off all glucose-lowering and antihypertensive medications [ 21 ]. The intervention comprised total diet replacement (3452–3569 kJ/day [825–853 kcal/day] liquid formula diet for 12–20 weeks), stepped food reintroduction (2–8 weeks) and then structured support for weight loss maintenance. The greater the weight loss, the greater the likelihood of remission (86% at 1 year for weight loss ≥15kg; 57%, 34% and 7% for weight loss of 10–15 kg, 5–10 kg and <5 kg respectively). In addition, the effects were durable, with 36% of people in sustained remission at 2 years [ 22 ]. Further research is needed to understand the longer term effects of remission on the complications of type 2 diabetes, but current results support the remission of type 2 diabetes as a practical target in primary care.
In an endorsement of this approach, the UK NHS has rolled out a 12 week intervention consisting of a low-energy meal replacement diet for people with type 2 diabetes and a BMI >27 kg/m 2 (or >25 kg/m 2 if from a minority ethnic group in whom risk occurs at a lower BMI) ( https://www.england.nhs.uk/2022/01/nhs-soups-and-shakes-diet-helps-thousands-shed-the-pounds/ ). The goal is to recruit 5000 people from general practice; over 2000 people have already participated, showing the feasibility of this approach.
A focus on nutrients for weight and glycaemic control
Traditionally, dietary guidance has focused on macronutrient composition. Most dietary guidelines recommend intakes of <30–35% of energy from total fat, 45–55% of energy from carbohydrates and the remainder, ~15–20% of energy, from protein, both in the general population and in those with type 2 diabetes. For weight management, low-fat diets were favoured based on the higher energy density of fat, at 38kJ/g (9 kcal/g), compared with that of carbohydrate or protein, at 17kJ/g (4 kcal/g). More recently, low-carbohydrate diets have gained popularity. The optimal macronutrient composition is hotly debated.
Low-fat or low-carbohydrate diets for weight management?
The Look-AHEAD: Action for Health in Diabetes (Look-AHEAD) trial compared an intensive lifestyle intervention with a control condition of support and education in people with type 2 diabetes. The weight loss strategy, comprising energy reduction (5021–7531 kJ/day [1200–1800 kcal/day]) through a low-fat diet, was effective. Greater weight loss was achieved in the intervention group at 1 year, with a net difference in weight of –7.9% (95% CI –8.3% to –7.6%); at year 4, the net difference in weight was –3.9% (95% CI –4.4% to –3.5%) [ 23 ]. Similar low-fat diet approaches have been used in other trials of the primary prevention of type 2 diabetes [ 3 ]. In contrast, in the energy-deficit diet in the type 2 diabetes remission trial (DiRECT), the proportions of macronutrients were inconsequential, with >50% of energy coming from carbohydrates [ 22 ]. A recent umbrella review of the evidence concluded that weight management in type 2 diabetes using hypocaloric diets does not depend on any particular macronutrient profile [ 24 ].
More broadly, among adults with overweight or obesity in the population without consideration of type 2 diabetes, individual studies show differing results favouring one nutrient or another but, when the totality of the evidence is appraised, both low-fat and low-carbohydrate diets of varying protein content are effective for weight loss [ 25 ]. The challenge lies in adherence to the prescribed diets. A systematic review of the effects of low-fat and low-carbohydrate diets on weight loss in RCTs of at least 1 year’s duration and with a similar intervention intensity across groups found that low-fat diets were efficacious compared with usual intake [ 26 ]. But, when low-fat diets were compared with low-carbohydrate diets, there was greater weight loss in the low-carbohydrate diet group. However, the magnitude of the difference in weight loss between low-carbohydrate and low-fat diets was modest at only 1.15 kg, which is statistically significant but may have little clinical meaning. As a limitation, caloric restriction was a component of many of the weight loss interventions included, but not all; for example, some included studies gave dietary advice to eat a low-carbohydrate diet ad libitum [ 26 ]. Future research should seek to address design limitations; however, current research indicates that small effects on weight loss from one macronutrient type or another are unlikely to be of clinical significance. A key challenge is weight maintenance and prevention of weight regain, which is typical following weight loss.
Although overall dietary carbohydrate or fat content has been extensively studied in relation to weight loss and maintenance, protein intake has been less so. Higher protein intake after weight loss has been shown to result in significantly lower weight regain, related to increased satiety and energy efficiency [ 27 ]. For early weight loss maintenance over 6 months, an RCT tested different combinations of protein consumption and glycaemic index (GI) compared with a control diet among those who had lost at least 8% (equivalent to 11 kg) of their initial weight on a 3347 kJ/day (800 kcal/day) diet [ 28 ]. Consuming a low-protein/high GI diet led to subsequent weight regain (mean of 1.7 kg [95% CI 0.5 to 2.9]), while a modest increase in protein content and a modest reduction in GI led to improvements (reductions) in the degree of weight regain over 6 months. Evidence for long-term weight loss maintenance is generally sparse. Observational prospective data from the National Weight Loss Registry indicated that weight loss maintenance over 10 years was related to low-fat-based energy restraint combined with physical activity [ 29 ]. Further research is needed to better understand the dietary strategies and other factors important in weight loss maintenance.
Low-carbohydrate diets for glycaemic control in type 2 diabetes
For glycaemic control in type 2 diabetes, studies from clinical practice or from digital or commercial programmes have promoted low-carbohydrate diets based on significant benefits for HbA 1c , of a mean decrease of 11 mmol/mol (1% unit decrease), together with reductions in glucose-lowering medication use [ 30 , 31 ]. Interpretive challenges include the presence of bias owing to the lack of randomisation, self-selection into groups and unbalanced sample sizes or intensities of interventions in the study arms and lack of a comparator group. However, a number of systematic reviews and meta-analyses of RCTs are available that reduce such limitations [ 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 ].
Evidence from RCTs indicates that lower carbohydrate diets have benefits over higher carbohydrate diets in the short term up to 6 months, but these are not maintained over time [ 34 , 36 ]. In the UK, the Scientific Advisory Committee on Nutrition appraised the available evidence, including 48 individual RCTs from eight systematic reviews. It concluded that lower carbohydrate diets were effective for glycaemic control in type 2 diabetes compared with higher carbohydrate diets, with a greater reduction in HbA 1c (weighted mean difference –4.7 mmol/mol [–0.47%]) in the short term (3–6 months), but this benefit was not maintained at 12 months [ 39 ].
Despite extensive research on low-carbohydrate diets, there are several challenges that limit firm conclusions. First, definitions of what a ‘low-carbohydrate diet’ is range from moderate carbohydrate restriction to very-low-carbohydrate or ketogenic diets (see Text box ‘Definitions of carbohydrate-focused diets’). Across RCTs, prescribed carbohydrate intakes in the lower carbohydrate groups ranged widely, from 14% to 50% of energy intake, and reported carbohydrate intakes were moderate at 26–45% of energy intake in the majority of the primary RCTs [ 39 ]. Second, in the case of isoenergetic diets (maintaining the same overall energy intake), a low-carbohydrate diet is by default higher in fat and vice versa. As many individual studies did not specify isoenergetic study arms, it is difficult to tease out whether the glycaemic change was influenced by differential changes in weight as a result of differing energy intakes. Third, because of differences in or a lack of information in study protocols on adjustment of glucose-lowering medication, it is hard to infer whether criteria for remission of type 2 diabetes were met [ 40 ].
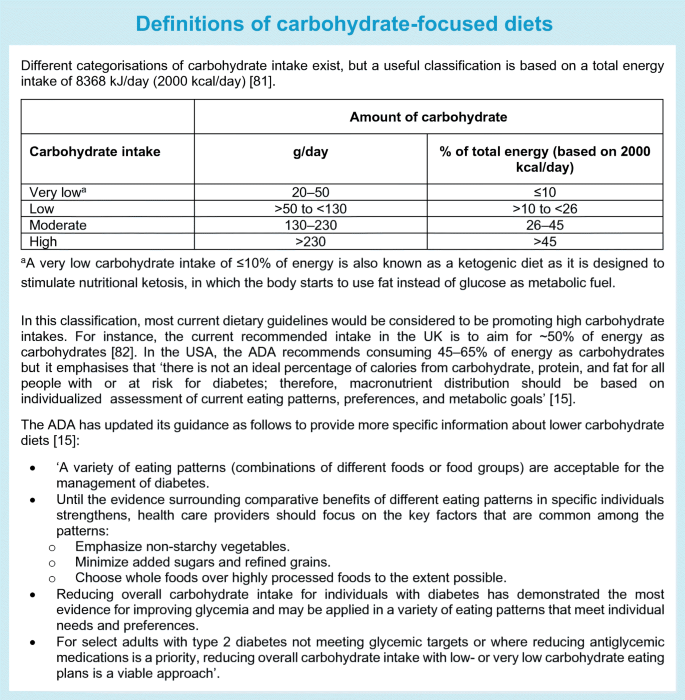
Low-carbohydrate diets seem to be generally safe and well tolerated in the short term; concerns in the longer term relate to the potential atherogenic lipid profile [ 38 , 41 ] or micronutrient deficiency [ 42 ] or their use in people with chronic kidney disease or pregnant women, in whom there is a need for further evaluation. Accumulating evidence from prospective studies with long-term follow-up data indicates that both high and low intakes of carbohydrates may have adverse health impacts on mortality risk, with a U-shaped relationship [ 43 ]. However, such research has been carried out in general populations and needs to be replicated, and further research is needed in those with type 2 diabetes. In the meantime, the ADA dietary guidelines for people with diabetes were updated in 2019, making it explicit that low-carbohydrate diets can be endorsed (see Text box ‘Definitions of carbohydrate-focused diets’).
Nutrition and pathways to obesity and type 2 diabetes
The above focus on energy and macronutrients is rooted in two contesting mechanistic explanations that link dietary intake to obesity and type 2 diabetes. In the energy balance model, energy matters because the law of thermodynamics dictates that when energy intake exceeds energy expenditure weight gain occurs. The link between obesity and the development of type 2 diabetes is strong and, with caloric deficit-induced weight loss, remission of type 2 diabetes is possible. In these scenarios, a calorie is a calorie and excess calories result in adipose tissue accumulation and weight gain.
In contrast, the ‘carbohydrate–insulin model’ proposes that obesity is a cause, not the consequence, of excess caloric intake [ 44 ]. Here, the dysregulation of fat storage and metabolism is the central defect, driven by high-carbohydrate diets that produce spikes of hyperinsulinaemia that promote glucose uptake into tissues, suppress release of fatty acids from adipose tissue and stimulate fat and glycogen storage. Thus, less energy remains available for use by the rest of the body, driving hunger and overeating. In this scenario, not all calories are equal. It has been proposed that energy from refined carbohydrates promote a disturbed hormonal milieu linked with increased hunger, a slower metabolic rate and reduced energy expenditure, leading to adiposity.
The debate between these mechanistic processes continues [ 45 , 46 , 47 ]. However, it is increasingly clear that a focus on energy intake does not account for the impact that diet quality has on long-term weight gain and type 2 diabetes through diverse physiological processes. These include diet-induced thermogenesis, brain reward, appetite, hunger, satiety, digestion, the release and action of hormones, for example insulin, hepatic de novo lipogenesis, interactions with the gut microbiome and energy expenditure [ 48 ]. Moreover, a focus on considering a single macronutrient type has limitations that can lead to unhelpful reductionist messages to avoid a macronutrient without reference to its quality and food sources.
Beyond a focus on nutrient quantity: the relevance of nutrient type, quality and food sources
RCTs of macronutrient manipulation have focused exclusively on quantity. This ignores the fact that health effects will vary substantially by nutrient type or quality. For dietary fats, a vast literature exists on the importance of distinguishing between saturated, polyunsaturated, monounsaturated and trans fats. Health effects also vary by carbohydrate type (starch, sugar or fibre), degree of processing (whole grain vs refined grain), glycaemic response after consumption (GI and load) and food structure (solid or liquid form).
There is substantial evidence from meta-analyses for inverse (beneficial) associations between the consumption of fibre [ 49 ], particularly cereal fibre [ 50 ] and wholegrains [ 11 ], and the incidence of type 2 diabetes. However, evidence is more mixed for the dietary GI, which reflects the differential blood glucose-raising potential of foods with similar carbohydrate content, and a related measure, the glycaemic load (GL), which accounts for the amount of available carbohydrate. For example, the meta-analysis by Reynolds et al found inverse associations between fibre intake and several disease endpoints, including type 2 diabetes and mortality, but associations with GI and GL were non-significant [ 49 ]. Mixed and inconclusive results were also reported in reviews of a link between GI, GL and HbA 1c or fasting glucose [ 15 ]. The OmniCarb RCT compared four diets with varying GI and carbohydrate content in overweight or obese individuals with hypertension or pre-hypertension. This was a crossover feeding study with each diet based on a Dietary Approaches to Stop Hypertension (DASH)-type diet pattern [ 51 ]. Compared with a high GI (65% on the glucose scale), high-carbohydrate (58% energy) diet, a low GI (40% on the glucose scale), low-carbohydrate (40% energy) diet did not significantly improve insulin sensitivity, lipid levels or blood pressure. This type of evidence indicates that GI values have a low utility, but further research contradicts this. Other reviews with a more nuanced approach have reported a positive association between GI or GL and type 2 diabetes [ 52 ]. Similarly, some reviews and individual large cohorts have also reported a positive (adverse) association of high GI or GL with CHD or CVD [ 53 ], as well as a likely benefit of low GI or GL dietary patterns for glycaemic control and cardiometabolic risk factors in people with type 1 diabetes or type 2 diabetes [ 54 ]. A take-home message is that multiple aspects of carbohydrate quality are relevant and should be considered where possible because intakes of fibre, wholegrain and the GI and GL values of foods are likely to be highly correlated and may have confounding effects if not accounted for in diet–disease associations.
A point to note is that, when consumption of one nutrient type is manipulated (to eat less or more of it), this impacts the consumption of other nutrient types—the so-called ‘nutrient substitution’, in which one nutrient substitutes for another within isoenergetic consumption. Moreover, there are both ‘healthy’ and ‘unhealthy’ low-fat or low-carbohydrate diets.
The Diet Intervention Examining The Factors Interacting with Treatment Success (DIETFITS) RCT tested diet quality, comparing ‘healthy’ low-carbohydrate and low-fat regimens [ 55 ]. Both diet groups were instructed to maximise their non-starchy vegetable intake, minimise added sugars, refined flours and trans fats and focus on whole foods. Both diet types were effective, with a mean weight loss of 5.3 kg and 6 kg for the healthy low-fat and healthy low-carbohydrate diets, respectively, at 12 months, but there was no significant between-group difference [ 55 ]. In both diet groups there were also improvements at 12 months in secondary outcomes, including fasting glucose and insulin levels, body fat percentage, waist circumference, blood pressure and lipid profiles, except for LDL-cholesterol level, which was reduced in the low-fat group but increased in the low-carbohydrate group.
A crossover trial compared different levels of carbohydrate restriction and food sources in people with prediabetes or type 2 diabetes over two 12 week periods. Carbohydrates comprised <20% of energy in the very-low-carbohydrate ketogenic diet and <40% in the low-carbohydrate Mediterranean-style diet [ 56 ]. Both diets incorporated non-starchy vegetables and avoided added sugars and refined grains; the ketogenic diet avoided legumes, most fruits (except a few berries in small amounts) and whole grains whereas the Mediterranean-style diet incorporated these foods. Both diets resulted in improvements that were not significantly different. Specifically, mean HbA 1c levels decreased by 9% and 7% in the ketogenic and Mediterranean-style diet groups, respectively, and weight decreased by 8% and 7%, respectively. The ketogenic diet group achieved greater improvements in triglyceride and HDL-cholesterol levels than the Mediterranean-style diet group but had higher LDL-cholesterol levels (percentage change +10% vs –5%, respectively). The diets were ad libitum but participants in both groups reported consuming on average 1046–1255 kJ/day (250–300 kcal/day) less compared with baseline. The ketogenic diet group had a lower fibre intake and consumed lower levels of micronutrients (folate, vitamin C and magnesium). This study was of short duration and longer term research is needed, but its findings do not justify achieving a low-carbohydrate status by avoiding fruits, legumes and whole grains, which are considered part of a healthy diet in other longstanding research.
In sum, the consideration of nutrients in isolation has led to unhelpful polarised debates on whether low-fat or low-carbohydrate diets are superior. Macronutrients are not homogeneous entities: individual nutrients are derived from foods and people eat food in overall dietary patterns.
Beyond nutrients: foods and dietary patterns
Foods are complex mixtures of thousands of components—the food matrix—that have different physicochemical properties and health effects. This is illustrated by the opposite directions of association with the incidence of CHD seen for different foods rich in saturated fats. Consumption of dairy products such as yoghurt and cheese is inversely related to CHD incidence whereas consumption of red and processed meat is positively associated with CHD incidence [ 57 ]. This was corroborated by research showing that people who ate more saturated fats from red meat and butter were more likely to develop CHD than those who ate more saturated fats from cheese, yoghurt and fish [ 58 ]. This highlights the need to consider food sources together with the macronutrients they contain rather than the nutrients in isolation.
A consensus on dietary factors for the prevention of type 2 diabetes has been established from the comprehensive evidence base and incorporated into dietary guidelines. Broadly this suggests the benefits of the consumption of fruit, vegetables, nuts, seeds, wholegrains and yoghurt and the potential harms associated with sugar-sweetened beverages and red and processed meat. For some foods, such as fruit juice, artificially sweetened beverages, lean and fatty fish, milk and eggs, uncertainty remains with regard to their benefits for type 2 diabetes prevention [ 14 ].
Highly processed or ultra-processed foods of both plant and animal origin are increasingly consumed globally and have been related to a number of adverse health impacts. They include foods that have undergone industrial processing and that contain added ingredients such as salt, sugar, fat and artificial preservatives, stabilisers or colours, prolonging shelf life and reducing cost. An RCT compared the ad libitum consumption of ultra-processed foods with consumption of unprocessed foods. A total of 20 participants received all meals, matched for energy and macronutrient content, in a controlled setting for 28 days [ 59 ]. Ultra-processed food consumption led to substantially greater energy intake (+2090 kJ/day [+500 kcal/day] on average over 14 days) and weight gain (+0.9 kg over 14 days vs weight loss of equal magnitude during the 14 days of the unprocessed diet phase). Longer term prospective studies have provided evidence for an association of ultra-processed food consumption with the development of type 2 diabetes [ 60 ].
A number of food-based dietary patterns have a place in the prevention of type 2 diabetes based on observational evidence, including the Mediterranean, DASH and plant-based diets, but only the Mediterranean diet has been investigated in an RCT, both for the prevention and for the management of type 2 diabetes [ 61 ]. For many named popular diets such as the paleo, Atkins, Ornish and Zone diets, there is RCT evidence for short-term weight management but without any meaningful differences between them [ 25 ], while no evidence for their role in the prevention of type 2 diabetes is available.
For dietary patterns, quality matters too. For instance, plant-based diets are generally considered healthy, but not all such diets are alike. In one study, plant-based diets that were high in refined carbohydrates or were ultra-processed were associated positively with the incidence of type 2 diabetes [ 62 ].
Embracing complexity: key messages
Diet is a complex risk exposure.
Diet is non-binary, unlike, for example, tobacco, for which zero is best. Diet is multidimensional and hierarchical in nature. Foods belong within food groups and may be consumed unprocessed (e.g. beef or pork) or processed (e.g. ham or bacon). Foods contain nutrients (e.g. meat fat or protein as macronutrients; haem iron as a micronutrient) or additives and preservatives if processed, and are part of overall dietary patterns (e.g. the Mediterranean diet with relatively low intakes of red meat or a low-carbohydrate diet regimen with relatively high intakes of meat).
The continuum of dietary exposures should be considered, as well as ‘food substitution effects’, because when more or less of one food type is consumed it impacts the consumption of other foods as part of the overall energy intake.
Diet is hard to measure
Tools such as food frequency questionnaires or 24 h dietary recall instruments are commonly used to assess habitual dietary intakes. Despite efforts towards validating these tools and their ability to produce credible estimates of diet–disease associations, critics have called for them to be abandoned, considering them flawed because of their reliance on memory and cognition and issues of bias and measurement error [ 63 , 64 ]. Suggestions for suitable alternatives are sparse, however. Emerging digital technologies—smartphone apps, cameras for food imaging and wearable devices—hold promise but are not yet of ‘research grade’, with demonstrable validity and reliability [ 65 ]. They are also not free from measurement error, nor gaming, consciously or subconsciously. A promising complementary approach is the use of objective biomarkers of dietary intakes, for instance plasma vitamin C and carotenoids as markers for fruit and vegetable intake, or plasma omega-3 fatty acids as a marker for seafood consumption [ 66 ]. However, these too have sources of random and systematic errors as well as interpretive challenges, that is, the extent to which circulating levels reflect intake compared with metabolism.
No method is perfect, but the use of validated dietary instruments with repeat measures can approximate habitual diet. Moreover, there are benefits in using a combination of methods to harness their complementary strengths and deal with relative weaknesses.
The study design of nutritional research is challenging
The RCT design is considered the gold standard in the hierarchy of evidence-based medicine framework, but for complex behavioural exposures such as diet, unlike for pharmaceuticals, RCTs are more challenging. The bulk of the evidence base for nutrition and health has come from long-term observational prospective cohort studies. Both observational and interventional studies have relative strengths and weaknesses. Observational studies are typically limited by confounding and bias but when rigorously conducted they can yield reliable and valid results, from which causal inference can be made [ 14 ]. Dietary RCTs have several challenges. They have a specific set of limitations including a lack of blinding, lack of an appropriate control group, issues with feasibility and cost and challenges of adherence and attrition. The inability to pinpoint the specific nutritional component(s) is another challenge, such as in some of the above-cited RCTs, which could not separate out the effects of macronutrient type and energy intake. Moreover, dietary trials can vary greatly in quality, and consistency of findings and comparability are limited by the populations and endpoints included, for example healthy or diseased participants, free-living or tightly controlled conditions, and a variety of intermediate endpoints or clinical outcomes. In practice, RCTs also suffer from poor methodology and unreliable findings, as evidenced by an appraisal of nearly 21,000 RCTs [ 67 ].
Causal inference is strengthened when there is consistent evidence from different study designs. Inferring causality from observational evidence is possible by applying the Bradford Hill criteria, and Mendelian randomisation is a tool that can be applied in some situations to evaluate causal relationships [ 68 ].
No design is perfect and the evolution of improvements in all study designs—RCTs and observational studies—must continue. New concepts are emerging, such as ‘ n -of-1’ trials and adaptive trial design, which need robust testing in the nutrition field. There is strong concordance in findings from prospective observational studies and RCTs and the two study designs should complement each other [ 7 ]. The best evidence base is that which evaluates all the relevant diverse types of evidence.
Uncertainty remains for some dietary factors
Consensus on the potential benefits and harms of many foods and dietary patterns has been established. However, for some dietary factors controversy remains, for example in the case of non-nutritive or artificial sweeteners such as aspartame, saccharin and sucralose. These sugar substitutes can help decrease daily energy and carbohydrate intakes but whether they are helpful for obesity and type 2 diabetes in the long term is debated [ 69 ]. The use of such sweeteners is predicted to rise in line with the public health policy on sugar reduction, which in the UK includes a soft drinks industry levy applied to soft drinks containing high amounts of added sugar; manufacturers have responded to this with reformulations using sugar substitutes. To resolve this uncertainty, future research will ideally use a combination of research designs including well-conducted short-term RCTs and long-term prospective studies and employ nutritional biomarkers of artificial sweeteners.
Noise and confusion are commonplace in the nutritional field
Everyone is interested in food. From news media to social media, books and blogs, information and misinformation on nutritional topics is everywhere. Conflicts of interest cannot always be avoided. Trusted resources are needed, including high-quality research evidence, improved dietary guidelines [ 70 ] and greater involvement of academic institutions and health agencies.
There are many influences on what we eat beyond individual lifestyle choice (Fig. 1 )
There is a gap between dietary advice and dietary intakes. Consider the public health message to eat five portions a day of fruit and vegetables. Despite strong health promotion efforts, ~12% of the population aged over 15 years in Europe meet this goal [ 71 ]. In a global context, compliance with eating five portions a day of fruit and vegetables is affected disproportionately by income, such that achieving this goal costs an estimated 52%, 18%, 16% and 2% of household income in low-, low- to middle-, middle- to upper- and high-income countries, respectively [ 72 ]. Further, sobering current examples of wider determinants of food choice include the effects of Brexit, the COVID-19 pandemic and the Russian invasion of Ukraine on availability, access and food security.
To improve and maintain dietary adherence, there is a need to operate both at the individual level and in the policy space across the entire food system (see Text box ‘Strategies to promote dietary adherence to healthy eating’). Education, dietary guidelines and strategies that enable people to make healthy food choices are necessary but not yet universally available.
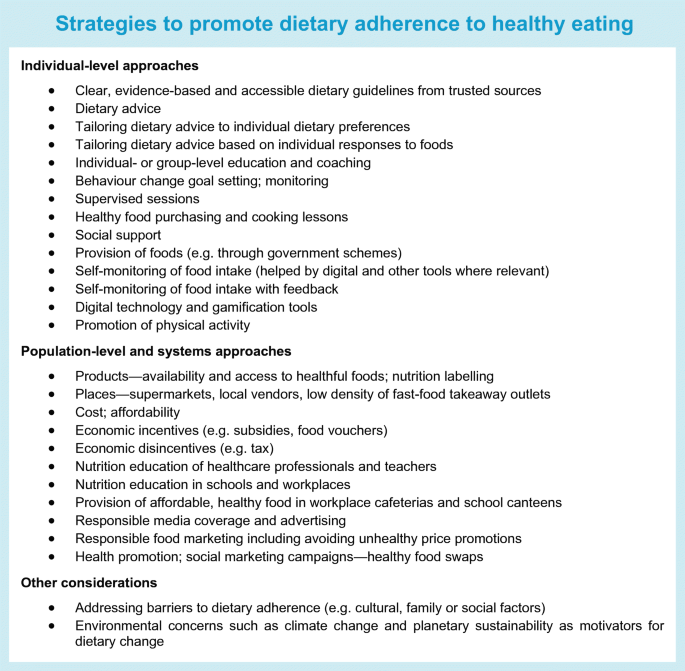
Interest has recently risen in ‘food is medicine’ interventions in healthcare systems, such that a healthy diet can be prescribed in a manner equivalent to the prescription of medication, particularly for those with food insecurity. Such interventions include food prescriptions or the provision of medically tailored groceries or meals, which in those with diabetes can achieve improvements in diet quality and in HbA 1c of a comparable magnitude to those seen with glucose-lowering medication [ 73 ]. Pilot data in people with uncontrolled type 2 diabetes and food insecurity are impressive, with substantial reductions in HbA 1c in those enrolled to receive fresh food on prescription [ 74 ]. Similarly, a meta-analysis of healthy food prescription programmes reported that an increase in consumption of fruit and vegetables by a mean of 0.8 daily servings was associated with significant reductions in BMI and HbA 1c [ 75 ]. Although there were methodological limitations, these studies highlight the potential effectiveness of such dietary interventions and the case for investment in further research.
There are exciting new developments on the horizon
This is illustrated by two examples. First, greater understanding of the relationships between eating and circadian biology is emerging to shed light on so-called chrononutrition [ 76 ]. In addition to considerations of quantity and quality appraised above, chrononutrition considers the impact of the timing of food intake on metabolic health. As an example, the benefits of intermittent fasting and time-restricted feeding are becoming apparent for weight loss [ 77 ] and health more broadly [ 78 ], but research specifically targeted at type 2 diabetes is needed. Second, to improve on current dietary guidance, which is based on population averages, promising research on ‘precision nutrition’ aims to combine information from personal, biological, social and environmental factors to target individuals or population subgroups sharing similar characteristics [ 79 ]. Although still in its infancy, the use of technologies that enable information from genetics, metabolomics, proteomics and the gut microbiome to be integrated with clinical and biochemical data together with machine learning has the potential to enable the development of personalised nutrition interventions [ 80 ].
Conclusions
Diet and nutrition play a central role in both the prevention and the management of type 2 diabetes but the complexity of diet and some key controversies have posed challenges in the field. The latest research evidence has advanced our understanding of the importance of shifting away from the decades-long focus on the quantity of isolated nutrients to nutrient quality, nutrient food sources and overall dietary patterns. New advances in research hold promise for helping to resolve current ongoing uncertainties, and exciting future directions are anticipated (see Text box ‘Future directions: food for thought’).
Abbreviations
Dietary Approaches to Stop Hypertension
Glycaemic index
Glycaemic load
National Health Service
Sun H, Saeedi P, Karuranga S et al (2022) IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract 183:109119. https://doi.org/10.1016/j.diabres.2021.109119
Article PubMed Google Scholar
Franz MJ, MacLeod J, Evert A et al (2017) Academy of nutrition and dietetics nutrition practice guideline for type 1 and type 2 diabetes in adults: systematic review of evidence for medical nutrition therapy effectiveness and recommendations for integration into the nutrition care process. J Acad Nutr Diet 117:1659–1679. https://doi.org/10.1016/j.jand.2017.03.022
Tuomilehto J, Lindstrom J, Eriksson JG et al (2001) Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 344:1343–1350. https://doi.org/10.1056/NEJM200105033441801
Article CAS PubMed Google Scholar
Galaviz KI, Weber MB, Straus A, Haw JS, Narayan KMV, Ali MK (2018) Global diabetes prevention interventions: a systematic review and network meta-analysis of the real-world impact on incidence, weight, and glucose. Diabetes Care 41:1526–1534. https://doi.org/10.2337/dc17-2222
Article PubMed PubMed Central Google Scholar
Valabhji J, Barron E, Bradley D et al (2020) Early outcomes from the english national health service diabetes prevention programme. Diabetes Care 43:152–160. https://doi.org/10.2337/dc19-1425
Taylor R, Ramachandran A, Yancy WS Jr, Forouhi NG (2021) Nutritional basis of type 2 diabetes remission. BMJ 374:n1449. https://doi.org/10.1136/bmj.n1449
Mozaffarian D, Forouhi NG (2018) Dietary guidelines and health-is nutrition science up to the task? Bmj 360:k822. https://doi.org/10.1136/bmj.k822
Forouhi NG, Misra A, Mohan V, Taylor R, Yancy W (2018) Dietary and nutritional approaches for prevention and management of type 2 diabetes. BMJ 361:k2234. https://doi.org/10.1136/bmj.k2234
Mozaffarian D (2016) Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: a comprehensive review. Circulation 133:187–225. https://doi.org/10.1161/CIRCULATIONAHA.115.018585
Article CAS PubMed PubMed Central Google Scholar
Ley SH, Hamdy O, Mohan V, Hu FB (2014) Prevention and management of type 2 diabetes: dietary components and nutritional strategies. Lancet 383:1999–2007. https://doi.org/10.1016/S0140-6736(14)60613-9
Schwingshackl L, Hoffmann G, Lampousi AM et al (2017) Food groups and risk of type 2 diabetes mellitus: a systematic review and meta-analysis of prospective studies. Eur J Epidemiol 32:363–375. https://doi.org/10.1007/s10654-017-0246-y
Micha R, Shulkin ML, Penalvo JL et al (2017) Etiologic effects and optimal intakes of foods and nutrients for risk of cardiovascular diseases and diabetes: Systematic reviews and meta-analyses from the Nutrition and Chronic Diseases Expert Group (NutriCoDE). PLoS One 12:e0175149. https://doi.org/10.1371/journal.pone.0175149
Neuenschwander M, Ballon A, Weber KS et al (2019) Role of diet in type 2 diabetes incidence: umbrella review of meta-analyses of prospective observational studies. BMJ 366:l2368. https://doi.org/10.1136/bmj.l2368
Miller V, Micha R, Choi E, Karageorgou D, Webb P, Mozaffarian D (2022) Evaluation of the quality of evidence of the association of foods and nutrients with cardiovascular disease and diabetes: a systematic review. JAMA Netw Open 5:e2146705. https://doi.org/10.1001/jamanetworkopen.2021.46705
Evert AB, Dennison M, Gardner CD et al (2019) Nutrition therapy for adults with diabetes or prediabetes: a consensus report. Diabetes Care 42:731–754. https://doi.org/10.2337/dci19-0014
Diabetes UK (2018) Evidence-based nutrition guidelines for the prevention and management of diabetes. Available from https://diabetes-resources-production.s3.eu-west-1.amazonaws.com/resources-s3/2018-03/1373_Nutrition%20guidelines_0.pdf . Accessed 25 Nov 2022.
Lingvay I, Sumithran P, Cohen RV, le Roux CW (2022) Obesity management as a primary treatment goal for type 2 diabetes: time to reframe the conversation. Lancet 399:394–405. https://doi.org/10.1016/S0140-6736(21)01919-X
American Diabetes Association Professional Practice Committee, Draznin B, Aroda VR et al (2022) 8. Obesity and Weight Management for the Prevention and Treatment of Type 2 Diabetes: Standards of Medical Care in Diabetes-2022. Diabetes Care 45:S113–S124. https://doi.org/10.2337/dc22-S008
Article Google Scholar
Sjöström L, Lindroos A-K, Peltonen M et al (2004) Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med 351:2683–2693. https://doi.org/10.1056/NEJMoa035622
Panunzi S, Carlsson L, De Gaetano A et al (2016) Determinants of diabetes remission and glycemic control after bariatric surgery. Diabetes Care 39:166–174. https://doi.org/10.2337/dc15-0575
Lean ME, Leslie WS, Barnes AC et al (2018) Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. Lancet 391:541–551. https://doi.org/10.1016/S0140-6736(17)33102-1
Lean MEJ, Leslie WS, Barnes AC et al (2019) Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet Diabetes Endocrinol 7:344–355. https://doi.org/10.1016/S2213-8587(19)30068-3
Gregg EW, Chen H, Wagenknecht LE et al (2012) Association of an intensive lifestyle intervention with remission of type 2 diabetes. JAMA 308:2489–2496. https://doi.org/10.1001/jama.2012.67929
Churuangsuk C, Hall J, Reynolds A, Griffin SJ, Combet E, Lean MEJ (2022) Diets for weight management in adults with type 2 diabetes: an umbrella review of published meta-analyses and systematic review of trials of diets for diabetes remission. Diabetologia 65:14–36. https://doi.org/10.1007/s00125-021-05577-2
Ge L, Sadeghirad B, Ball GDC et al (2020) Comparison of dietary macronutrient patterns of 14 popular named dietary programmes for weight and cardiovascular risk factor reduction in adults: systematic review and network meta-analysis of randomised trials. BMJ 369:m696. https://doi.org/10.1136/bmj.m696
Tobias DK, Chen M, Manson JE, Ludwig DS, Willett W, Hu FB (2015) Effect of low-fat diet interventions versus other diet interventions on long-term weight change in adults: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 3:968–979. https://doi.org/10.1016/S2213-8587(15)00367-8
Westerterp-Plantenga MS, Lejeune MPGM, Nijs I, van Ooijen M, Kovacs EMR (2003) High protein intake sustains weight maintenance after body weight loss in humans. Int J Obes 28:57–64. https://doi.org/10.1038/sj.ijo.0802461
Article CAS Google Scholar
Larsen TM, Dalskov S-M, van Baak M et al (2010) Diets with high or low protein content and glycemic index for weight-loss maintenance. N Engl J Med 363:2102–2113. https://doi.org/10.1056/NEJMoa1007137
Thomas JG, Bond DS, Phelan S, Hill JO, Wing RR (2014) Weight-loss maintenance for 10 years in the national weight control registry. Am J Prev Med 46:17–23. https://doi.org/10.1016/j.amepre.2013.08.019
Athinarayanan SJ, Adams RN, Hallberg SJ et al (2019) Long-term effects of a novel continuous remote care intervention including nutritional ketosis for the management of type 2 diabetes: a 2-year non-randomized clinical trial. Front Endocrinol (Lausanne) 10:348. https://doi.org/10.3389/fendo.2019.00348
Saslow LR, Summers C, Aikens JE, Unwin DJ (2018) Outcomes of a digitally delivered low-carbohydrate type 2 diabetes self-management program: 1-year results of a single-arm longitudinal study. JMIR Diabetes 3:e12. https://doi.org/10.2196/diabetes.9333
Huntriss R, Campbell M, Bedwell C (2018) The interpretation and effect of a low-carbohydrate diet in the management of type 2 diabetes: a systematic review and meta-analysis of randomised controlled trials. Eur J Clin Nutr 72:311–325. https://doi.org/10.1038/s41430-017-0019-4
Korsmo-Haugen HK, Brurberg KG, Mann J, Aas AM (2019) Carbohydrate quantity in the dietary management of type 2 diabetes: a systematic review and meta-analysis. Diabetes Obes Metab 21:15–27. https://doi.org/10.1111/dom.13499
Sainsbury E, Kizirian NV, Partridge SR, Gill T, Colagiuri S, Gibson AA (2018) Effect of dietary carbohydrate restriction on glycemic control in adults with diabetes: a systematic review and meta-analysis. Diabetes Res Clin Pract 139:239–252. https://doi.org/10.1016/j.diabres.2018.02.026
van Zuuren EJ, Fedorowicz Z, Kuijpers T, Pijl H (2018) Effects of low-carbohydrate- compared with low-fat-diet interventions on metabolic control in people with type 2 diabetes: a systematic review including GRADE assessments. Am J Clin Nutr 108:300–331. https://doi.org/10.1093/ajcn/nqy096
Snorgaard O, Poulsen GM, Andersen HK, Astrup A (2017) Systematic review and meta-analysis of dietary carbohydrate restriction in patients with type 2 diabetes. BMJ Open Diabetes Res Care 5:e000354. https://doi.org/10.1136/bmjdrc-2016-000354
McArdle PD, Greenfield SM, Rilstone SK, Narendran P, Haque MS, Gill PS (2019) Carbohydrate restriction for glycaemic control in Type 2 diabetes: a systematic review and meta-analysis. Diabet Med 36:335–348. https://doi.org/10.1111/dme.13862
Goldenberg JZ, Day A, Brinkworth GD et al (2021) Efficacy and safety of low and very low carbohydrate diets for type 2 diabetes remission: systematic review and meta-analysis of published and unpublished randomized trial data. BMJ 372:m4743. https://doi.org/10.1136/bmj.m4743
Scientific Advisory Committee on Nutrition (2021) Lower carbohydrate diets for adults with type 2 diabetes. Available from https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1014673/SACN_report_on_lower_carbohydrate_diets_for_type_2_diabetes.pdf . Accessed 25 Nov 2022
Riddle MC, Cefalu WT, Evans PH et al (2021) Consensus report: definition and interpretation of remission in type 2 diabetes. Diabetes Care 44:2438–2444. https://doi.org/10.2337/dci21-0034
Nordmann AJ, Nordmann A, Briel M et al (2006) Effects of low-carbohydrate vs low-fat diets on weight loss and cardiovascular risk factors: a meta-analysis of randomized controlled trials. Arch Intern Med 166:285–293. https://doi.org/10.1001/archinte.166.3.285
Churuangsuk C, Griffiths D, Lean MEJ, Combet E (2019) Impacts of carbohydrate-restricted diets on micronutrient intakes and status: a systematic review. Obes Rev 20:1132–1147. https://doi.org/10.1111/obr.12857
Seidelmann SB, Claggett B, Cheng S et al (2018) Dietary carbohydrate intake and mortality: a prospective cohort study and meta-analysis. Lancet Public Health 3:e419–e428. https://doi.org/10.1016/S2468-2667(18)30135-X
Ludwig DS, Ebbeling CB (2018) The carbohydrate-insulin model of obesity: beyond “Calories In, Calories Out”. JAMA Intern Med 178:1098–1103. https://doi.org/10.1001/jamainternmed.2018.2933
Ludwig DS, Aronne LJ, Astrup A et al (2021) The carbohydrate-insulin model: a physiological perspective on the obesity pandemic. Am J Clin Nutr 114:1873–1885. https://doi.org/10.1093/ajcn/nqab270
Hall KD, Farooqi IS, Friedman JM et al (2022) The energy balance model of obesity: beyond calories in, calories out. Am J Clin Nutr 115:1243–1254. https://doi.org/10.1093/ajcn/nqac031
Ludwig DS, Apovian CM, Aronne LJ et al (2022) Competing paradigms of obesity pathogenesis: energy balance versus carbohydrate-insulin models. Eur J Clin Nutr 76:1209–1221. https://doi.org/10.1038/s41430-022-01179-2
Mozaffarian D (2017) Foods, obesity, and diabetes-are all calories created equal? Nutr Rev 75:19–31. https://doi.org/10.1093/nutrit/nuw024
Reynolds A, Mann J, Cummings J, Winter N, Mete E, Te Morenga L (2019) Carbohydrate quality and human health: a series of systematic reviews and meta-analyses. Lancet 393:434–445. https://doi.org/10.1016/S0140-6736(18)31809-9
Kuijsten A, Aune D, Schulze MB et al (2015) Dietary fibre and incidence of type 2 diabetes in eight European countries: the EPIC-InterAct Study and a meta-analysis of prospective studies. Diabetologia 58:1394–1408. https://doi.org/10.1007/s00125-015-3585-9
Sacks FM, Carey VJ, Anderson CA et al (2014) Effects of high vs low glycemic index of dietary carbohydrate on cardiovascular disease risk factors and insulin sensitivity: the OmniCarb randomized clinical trial. JAMA 312:2531–2541. https://doi.org/10.1001/jama.2014.16658
Livesey G, Livesey H (2019) Coronary heart disease and dietary carbohydrate, glycemic index, and glycemic load: dose-response meta-analyses of prospective cohort studies. Mayo Clin Proc Innov Qual Outcomes 3:52–69. https://doi.org/10.1016/j.mayocpiqo.2018.12.007
Jenkins DJA, Dehghan M, Mente A et al (2021) Glycemic index, glycemic load, and cardiovascular disease and mortality. N Engl J Med 384:1312–1322. https://doi.org/10.1056/NEJMoa2007123
Chiavaroli L, Lee D, Ahmed A et al (2021) Effect of low glycaemic index or load dietary patterns on glycaemic control and cardiometabolic risk factors in diabetes: systematic review and meta-analysis of randomised controlled trials. Bmj 374:n1651. https://doi.org/10.1136/bmj.n1651
Gardner CD, Trepanowski JF, Del Gobbo LC et al (2018) Effect of low-fat vs low-carbohydrate diet on 12-month weight loss in overweight adults and the association with genotype pattern or insulin secretion: the DIETFITS randomized clinical trial. Jama 319:667–679. https://doi.org/10.1001/jama.2018.0245
Gardner CD, Landry MJ, Perelman D et al (2022) Effect of a ketogenic diet versus mediterranean diet on HbA1c in individuals with prediabetes and type 2 diabetes mellitus: the interventional keto-med randomized crossover trial. Am J Clin Nutr 116:640–652. https://doi.org/10.1093/ajcn/nqac154
Key TJ, Appleby PN, Bradbury KE et al (2019) Consumption of meat, fish, dairy products, and eggs and risk of ischemic heart disease. Circulation 139:2835–2845. https://doi.org/10.1161/CIRCULATIONAHA.118.038813
Steur M, Johnson L, Sharp SJ et al (2021) Dietary fatty acids, macronutrient substitutions, food sources and incidence of coronary heart disease: findings from the EPIC-CVD case-cohort study across nine european countries. J Am Heart Assoc 10:e019814. https://doi.org/10.1161/JAHA.120.019814
Hall KD, Ayuketah A, Brychta R et al (2019) Ultra-processed diets cause excess calorie intake and weight gain: an inpatient randomized controlled trial of ad libitum food intake. Cell Metab 30:67–77 e63. https://doi.org/10.1016/j.cmet.2019.05.008
Delpino FM, Figueiredo LM, Bielemann RM et al (2021) Ultra-processed food and risk of type 2 diabetes: a systematic review and meta-analysis of longitudinal studies. Int J Epidemiol 51:1120–1141. https://doi.org/10.1093/ije/dyab247
Schulze MB, Martinez-Gonzalez MA, Fung TT, Lichtenstein AH, Forouhi NG (2018) Food based dietary patterns and chronic disease prevention. BMJ 361:k2396. https://doi.org/10.1136/bmj.k2396
Satija A, Bhupathiraju SN, Rimm EB et al (2016) Plant-based dietary patterns and incidence of type 2 diabetes in US men and women: results from three prospective cohort studies. PLoS Med 13:e1002039. https://doi.org/10.1371/journal.pmed.1002039
Archer E, Marlow ML, Lavie CJ (2018) Controversy and debate: memory-based methods paper 1: the fatal flaws of food frequency questionnaires and other memory-based dietary assessment methods. J Clin Epidemiol 104:113–124. https://doi.org/10.1016/j.jclinepi.2018.08.003
Archer E, Lavie CJ, Hill JO (2018) The failure to measure dietary intake engendered a fictional discourse on diet-disease relations. Front Nutr 5:105. https://doi.org/10.3389/fnut.2018.00105
Eldridge A, Piernas C, Illner A-K et al (2019) Evaluation of new technology-based tools for dietary intake assessment—an ILSI europe dietary intake and exposure task force evaluation. Nutrients 11:55. https://doi.org/10.3390/nu11010055
Zheng JS, Sharp SJ, Imamura F et al (2020) Association of plasma biomarkers of fruit and vegetable intake with incident type 2 diabetes: EPIC-InterAct case-cohort study in eight European countries. BMJ 370:m2194. https://doi.org/10.1136/bmj.m2194
Dechartres A, Trinquart L, Atal I et al (2017) Evolution of poor reporting and inadequate methods over time in 20 920 randomised controlled trials included in Cochrane reviews: research on research study. Bmj 357:j2490. https://doi.org/10.1136/bmj.j2490
Lawlor DA, Harbord RM, Sterne JA, Timpson N, Davey SG (2008) Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Stat Med 27:1133–1163. https://doi.org/10.1002/sim.3034
Lohner S, Kuellenberg de Gaudry D, Toews I, Ferenci T, Meerpohl JJ (2020) Non-nutritive sweeteners for diabetes mellitus. Cochrane Database Syst Rev 5:CD012885. https://doi.org/10.1002/14651858.CD012885.pub2
Bero LA, Norris SL, Lawrence MA (2019) Making nutrition guidelines fit for purpose. Bmj 365:l1579. https://doi.org/10.1136/bmj.l1579
Eurostat (2022) How much fruit and vegetables do you eat daily? Available from https://ec.europa.eu/eurostat/web/products-eurostat-news/-/ddn-20220104-1 . Accessed 25 Nov 2022
Miller V, Yusuf S, Chow CK et al (2016) Availability, affordability, and consumption of fruits and vegetables in 18 countries across income levels: findings from the Prospective Urban Rural Epidemiology (PURE) study. Lancet Global Health 4:e695–e703. https://doi.org/10.1016/S2214-109X(16)30186-3
Sherifali D, Nerenberg K, Pullenayegum E, Cheng JE, Gerstein HC (2010) The effect of oral antidiabetic agents on A1C levels: a systematic review and meta-analysis. Diabetes Care 33:1859–1864. https://doi.org/10.2337/dc09-1727
Hess A, Passaretti M, Coolbaugh S (2019) Fresh food farmacy. Am J Health Promotion 33:830–832. https://doi.org/10.1177/0890117119845711d
Bhat S, Coyle DH, Trieu K et al (2021) Healthy food prescription programs and their impact on dietary behavior and cardiometabolic risk factors: a systematic review and meta-analysis. Adv Nutr (Bethesda, Md) 12:1944–1956. https://doi.org/10.1093/advances/nmab039
Hawley JA, Sassone-Corsi P, Zierath JR (2020) Chrono-nutrition for the prevention and treatment of obesity and type 2 diabetes: from mice to men. Diabetologia 63:2253–2259. https://doi.org/10.1007/s00125-020-05238-w
Welton S, Minty R, O'Driscoll T et al (2020) Intermittent fasting and weight loss: systematic review. Can Fam Physician 66:117–125
PubMed PubMed Central Google Scholar
de Cabo R, Mattson MP (2019) Effects of intermittent fasting on health, aging, and disease. N Engl J Med 381:2541–2551. https://doi.org/10.1056/NEJMra1905136
Merino J (2022) Precision nutrition in diabetes: when population-based dietary advice gets personal. Diabetologia 65:1839–1848. https://doi.org/10.1007/s00125-022-05721-6
National Institutes of Health (2022) NIH awards $170 million for precision nutrition study 2022. Available from https://www.nih.gov/news-events/news-releases/nih-awards-170-million-precision-nutrition-study . Accessed 25 Nov 2022
Feinman RD, Pogozelski WK, Astrup A et al (2015) Dietary carbohydrate restriction as the first approach in diabetes management: critical review and evidence base. Nutrition 31:1–13. https://doi.org/10.1016/j.nut.2014.06.011
Scientific Advisory Committee on Nutrition (2015) Carbohydrates and health. TSO, London. Available from https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/445503/SACN_Carbohydrates_and_Health.pdf . Accessed 6 Feb 2023
Afshin A, Micha R, Khatibzadeh S et al (2014) Dietary policies to reduce non-communicable diseases. In: Brown GW, Yamey G, Wamala S (eds) The handbook of global health policy, 1st edn. Wiley, Chichester, UK, pp 175–193
Chapter Google Scholar
Download references
Acknowledgements
I acknowledge D. Bhagtani’s help with Fig. 1 (MRC Epidemiology Unit, University of Cambridge School of Clinical Medicine).
Author’s relationships and activities
NGF was a member of the Joint Scientific Advisory Committee on Nutrition/NHS England/Diabetes UK Working Group, which was initiated to review the evidence on lower carbohydrate diets compared with current government advice for adults with type 2 diabetes. The views expressed are her own and not those of the Group.
Contribution statement
The author was the sole contributor to this article.
NGF is supported by the Medical Research Council Epidemiology Unit (MC_UU_00006/3) and the NIHR Biomedical Research Centre Cambridge: Nutrition, Diet, and Lifestyle Research Theme (IS-BRC-1215-20014). She is an NIHR Senior Investigator. The views expressed are those of the author and not necessarily those of the NIHR or the Department of Health and Social Care.
Author information
Authors and affiliations.
MRC Epidemiology Unit, University of Cambridge School of Clinical Medicine, Institute of Metabolic Science, Cambridge Biomedical Campus, Cambridge, UK
Nita G. Forouhi
You can also search for this author in PubMed Google Scholar

Corresponding author
Correspondence to Nita G. Forouhi .
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Figure slide.
(PPTX 232 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Forouhi, N.G. Embracing complexity: making sense of diet, nutrition, obesity and type 2 diabetes. Diabetologia 66 , 786–799 (2023). https://doi.org/10.1007/s00125-023-05873-z
Download citation
Received : 27 July 2022
Accepted : 13 December 2022
Published : 14 February 2023
Issue Date : May 2023
DOI : https://doi.org/10.1007/s00125-023-05873-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Epidemiology
- Study design
- Type 2 diabetes
- Find a journal
- Publish with us
- Track your research
Wait! Try this Special Offer
Subscribe now and save 15%, wait – try this special offer.

Plus 2 free gifts

- Facebook . opens in new tab
- Twitter . opens in new tab
- LinkedIn . opens in new tab
- Open Athens/Shibboleth
- Activate Print Subscription
- Create Account
- Renew subscription

Stay Informed, with Concise, Evidence-Based Information

Renew today to continue your uninterrupted access to NEJM Journal Watch.
Stay Informed
Subscribe Or Renew

Sign into your account
Forgot Password? Login via Athens or your Institution
Already a print subscriber? Activate your online access.
- SUMMARY AND COMMENT |
April 6, 2024
Semaglutide Improves Outcomes in Patients with Obesity, HFpEF, and Type 2 Diabetes
Karol E. Watson, MD, PhD, FACC , reviewing Kosiborod MN et al. N Engl J Med 2024 Apr 6
In a randomized, controlled trial, semaglutide resulted in greater weight loss, improved symptoms, and fewer serious adverse events compared with placebo.
Obesity and type 2 diabetes are common comorbidities in patients with heart failure with preserved ejection fraction (HFpEF). Currently, there are no FDA-approved therapies that specifically treat all three conditions at the same time; however, semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist, has the potential to do so.
In an industry-funded trial ( NCT04916470 ), investigators randomized 616 adults with HFpEF (left ventricular ejection fraction ≥45%), body-mass index >30, and type 2 diabetes to receive semaglutide (2.4 mg) or matching placebo once weekly for 52 weeks. They assessed dual primary endpoints of change in heart failure symptoms via Kansas City Cardiomyopathy Questionnaire clinical summary score (KCCQ-CSS; range, 0–100, with higher score indicating fewer symptoms) and change in body weight.
The mean change in the KCCQ-CSS was +13.7 points with semaglutide and +6.4 points with placebo, indicating improved symptoms with semaglutide. The mean change in body weight was −9.8% with semaglutide and −3.4% with placebo. Confirmatory secondary end points also favored semaglutide, including 6-minute walk distance, a composite end point (including death, heart failure events, and differences in KCCQ-CSS and 6-minute walk distance), and C-reactive protein level. Serious adverse events occurred in 18% of patients in the semaglutide group and 29% in the placebo group.
Semaglutide once again shows clinical benefit. Prior research has shown improved outcomes in patients with diabetes and high cardiovascular risk, in patients with overweight or obesity and high cardiovascular risk, and in patients with HFpEF and obesity but no diabetes. Now, this research shows efficacy in patients with HFpEF, obesity, and type 2 diabetes. The many benefits of semaglutide make me very likely to recommend this therapy in appropriate patients for improving symptoms and reducing cardiovascular risk.
Kosiborod MN et al. Semaglutide in patients with obesity-related heart failure with preserved ejection fraction and type 2 diabetes. N Engl J Med 2024 Apr 6; [e-pub]. ( https://doi.org/10.1056/NEJMoa2313917 )
Facebook | Twitter | LinkedIn | Email | Copy URL
- Disclosures
Disclosures for Karol E. Watson, MD, PhD, FACC, at time of publication
Topics nutrition/obesity, latest in general medicine.
- Apr 4, 2024
Why Do Some People Develop Obesity Despite High Levels of Physical Activity?
Thomas L. Schwenk, MD
Can Routine Chest X-Ray Predict Risk for Adverse Cardiac Events?
Daniel D. Dressler, MD, MSc, MHM, FACP
Inpatient Delirium Is Associated with Future Dementia
Bruce Soloway, MD
- Apr 2, 2024
Long-Term Efficacy and Safety of Renal Denervation for Blood Pressure Reduction
Karol e. watson, md, phd, facc, long-term follow-up confirms that delaying drainage of infected necrotizing pancreatitis is safe.
Patricia Kritek, MD
- Apr 1, 2024
Observations from ID and Beyond: Think Again Before Sending Your Patient Home on Intravenous Vancomycin

Editor-in-Chief
NEJM Journal Watch Cardiology
- Frontiers in Physiology
- Clinical and Translational Physiology
- Research Topics
Type 2 Diabetes Management: A Focus on Metabolic Defects
Total Downloads
Total Views and Downloads
About this Research Topic
Type 2 diabetes is on its rise and has become a widespread epidemic in recent years. It is one of the leading causes of cardiovascular disease, blindness, end stage renal failure, and nontraumatic lower limb amputations, leading to subsequently growing social and clinical burden globally. As a result, an ...
Keywords : Diabetes, metabolic defects, β-cell function, dietary intervention, physical exercise
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, recent articles, submission deadlines.
Submission closed.
Participating Journals
Total views.
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
April 8, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
Heavy alcohol use may increase type 2 diabetes risk in middle-aged adults
by American Physiological Society

Heavy alcohol use may increase middle-aged adults' risk of developing Type 2 diabetes, according to research to be presented this week at the American Physiology Summit in Long Beach, California. The Summit is the flagship annual meeting of the American Physiological Society (APS).
Heavy alcohol use is defined by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) as five or more drinks per day or 15 or more drinks per week for men and, for women, more than four drinks per day or eight or more drinks per week.
Heavy alcohol use can diminish liver and pancreas function. Reduced function of these organs, in turn, can affect the control of glucose (blood sugar) in the body. In regard to heavy drinking , research suggests young adults do not typically experience severe impairment of fasting glucose levels and insulin resistance. However, as the U.S. population ages, the number of people who develop Type 2 diabetes is increasing. The association between alcohol use and diabetes in older adults is not clear.
Researchers from the University of Texas at Arlington's Cardiovascular Laboratory of Health studied two groups of middle-aged adults between the ages of 50 and 64. One group of volunteers ("heavy drinkers") was at risk for developing alcohol use disorder , as defined by the U.S. Alcohol Use Disorders Identification Test—a questionnaire that asks about drinking frequency and volume—and a dried blood spot phosphatidyl ethanol (PEth) test.
A PEth test measures levels of a biomarker that forms in the blood after consuming alcohol. The PEth biomarker can be detected in the blood up to four weeks after drinking alcohol. A PEth score of 20 nanograms per milliliter (ng/mL) or higher indicates alcohol consumption that exceeds NIAAA recommendations. The second group of volunteers was labeled "nonheavy drinkers," with PEth scores under 20 ng/mL.
The research team analyzed additional blood samples from both volunteer groups. The heavy drinkers had higher fasting glucose levels , which "suggest[s] that heavy alcohol use may have negative effects on glucose regulation in aged populations," the researchers wrote.
Although there were no significant differences in kidney or liver function between the two groups, "alcohol drinking that exceeds the recommended limits causes organ damage throughout the body and increases not only the risk of potentially developing Type 2 diabetes but also other diseases," said Chueh-Lung "Laura" Hwang, Ph.D., PT, senior author of the study.
"Our team recommends not drinking every day. If [people] do drink alcohol, make sure for men, [it's] no more than four drinks on any single day … and for women, no more than three drinks on any single day."
Explore further
Feedback to editors

Low cardiorespiratory fitness in youth associated with decreased work ability throughout adulthood, finds 45-year study
29 minutes ago

Long COVID leaves telltale traces in the blood, finds new study

Preventive percutaneous coronary intervention for high-risk coronary plaques found to reduce cardiac events

Heart-on-a-chip model used to glean insights into COVID-19-induced heart inflammation

Biomedical engineers use AI to build new tool for studying and diagnosing heart function

Everyday social interactions predict language development in infants

Research shows pregnancy accelerates biological aging in a healthy, young adult population
2 hours ago

Researchers uncover underlying mechanism driving membranous nephropathy, a chronic kidney disease in children

Researchers find more action is needed to prevent arthritis after knee reconstruction surgery

Coronary sinus reducer relieves angina, but how it works remains unclear
3 hours ago
Related Stories

Binge drinking boosts heart risks, especially for women
Mar 28, 2024
Simple blood test identifies critically ill patients who misuse alcohol, study finds
Nov 9, 2017

Blood test that measures alcohol use may predict risk for bleeding strokes
Jun 16, 2020

Greater enjoyment, not greater tolerance, may motivate heavy drinking among high-risk drinkers
Aug 14, 2023

Heavy drinking and HIV don't mix
Aug 22, 2019

Objective blood alcohol measures confirm the limitations of questionnaires, offer increased clinical opportunities
Dec 15, 2022
Recommended for you

Electronic sock detects unhealthy walking style linked to cardiovascular and diabetic complications
7 hours ago

A deep dive into the genetics of alcohol consumption
Apr 5, 2024

Vaping additives harm a vital membrane in the lungs, researchers find
Apr 4, 2024

Team moves forward in developing a vaccine for the 'zombie drug' xylazine
Apr 3, 2024

In people with opioid use disorder, telemedicine for HCV was more than twice as successful as off-site referral

Study suggests lung cancer does not decrease in line with reduced smoking
Apr 2, 2024
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
Few newly diagnosed type 2 diabetics succeed in losing weight -- weight gain linked to much higher risk of complications
A register-based study from Finland identified three distinct BMI trajectory groups among patients with newly diagnosed type 2 diabetes. In a four-year follow-up, most patients followed a stable trajectory without much weight change. Only 10% of patients lost weight, whereas 3% gained weight. Mean BMI exceeded the threshold of obesity in all groups at baseline. Weight loss is a central treatment goal in type 2 diabetes, but the study shows that few patients succeed in it.
The study was carried out by researchers at the University of Eastern Finland, and the results were published in Clinical Epidemiology.
Patients belonging to each trajectory group were followed up for another eight years for diabetes complications. During the follow-up, 13% of all patients developed microvascular complications, 21% developed macrovascular complications and 20% of patients deceased. The risk of microvascular complications was 2.9 times higher and the risk of macrovascular complications 2.5 times higher among patients with an increasing BMI compared to those with a stable BMI. Micro- and macrovascular complications of diabetes can include, for example, retinopathy, nephropathy and neuropathy, as well as cardiovascular diseases.
"These results underscore the significance of continuous BMI monitoring and weight management in patients with type 2 diabetes. Tailored treatments and support with lifestyle changes are crucial for efficiently preventing weight gain and reducing the risk of diabetes complications," says Doctoral Researcher Zhiting Wang of the University of Eastern Finland.
The study was carried out in North Karelia, Finland, using electronic health records from both primary and specialised health care. The study included a total of 889 adults with newly diagnosed type 2 diabetes in 2011 or 2012. The participants were grouped based on individual BMI trajectories from the diagnosis until 2014. Risks for microvascular complications, macrovascular complications, any diabetes complications and all-cause mortality from 2015 to 2022 across BMI trajectory groups were estimated.
- Diet and Weight Loss
- Wounds and Healing
- Diseases and Conditions
- Patient Education and Counseling
- Today's Healthcare
- Diabetes mellitus type 1
- Hyperthyroidism
- Anti-obesity drug
- Weight Watchers
- Diabetes mellitus type 2
- Body mass index
Story Source:
Materials provided by University of Eastern Finland . Note: Content may be edited for style and length.
Journal Reference :
- Zhiting Wang, Piia Lavikainen, Katja Wikström, Tiina Laatikainen. Trajectories of Body Mass Index and Risk for Diabetes Complications and All-Cause Mortality in Finnish Type 2 Diabetes Patients . Clinical Epidemiology , 2024; Volume 16: 203 DOI: 10.2147/CLEP.S450455
Cite This Page :
Explore More
- Climate Change Threatens Antarctic Meteorites
- Precise Measurement of Our Expanding Universe
- Little Research On 'Polycrisis' Humanity Faces
- Prebiotic Molecular Kitchen
- A Neurodegenerative Disease Triggered by Virus
- Drug Development Made Easier
- RNA That Doesn't Age
- 'Rainbow' Detected On an Exoplanet
- Spears and Throwing Sticks 300,000 Years Old
- High Carbon Impact of Tourism at Yellowstone
Trending Topics
Strange & offbeat.
- Acute Coronary Syndromes
- Cardiac Surgery
- Heart Failure
- Heart Health
- Heart Rhythm
- Hypertension
- Interventional Cardiology
- Mitral Valve
- Pharmaceutics
- Structural Heart Disease
- Tricuspid Valve
- Vascular & Endovascular
- Chest Pain Guidelines
- Compensation
- Education & Training
- Patient Care
- Policy & Regulations
- Professional Associations
- Cardiac Imaging
- Informatics
- Nuclear Cardiology
- Remote Monitoring
- Experience Stories
- Webinars & Videos
Search form

Semaglutide, the first weight loss drug approved by the U.S. Food and Drug Administration to reduce the risk of major adverse cardiovascular events, is associated with significant reductions in heart failure symptoms among obese patients with heart failure with preserved ejection fraction (HFpEF) and type 2 diabetes. That’s according to new research presented at ACC.24 , the annual meeting of the American College of Cardiology , and simultaneously published in the New England Journal of Medicine .[1]
Mikhail Kosiborod, MD , a cardiologist with Saint Luke’s Mid America Heart Institute in Kansas City, presented the data Saturday, April 6, during the first day of ACC.24. Kosiborod and his team explored data from 616 obese patients with symptomatic HFpEF. Patients were randomized to receive treatment with once-weekly semaglutide 2.4 mg—sold by Novo Nordisk under the brand name Wegovy—or a placebo for 52 weeks.
The mean change in quality of life, as determined by Kansas City Cardiomyopathy Questionnaire (KCCQ) clinical summary scores, was 13.7 points for the semaglutide group and 6.4 points for the placebo group. The mean change in body weight was -9.8% for the semaglutide group and -3.4% for the placebo group. Serious adverse events, meanwhile, were reported in 17.7% of semaglutide patients and 28.8% of placebo patients. Those events resulted in 1.9% of semaglutide patients and 3.6% of placebo patients discontinuing treatment before the end of 52 weeks.

“Obesity forms a ‘common soil’ that can lead to the development of heart failure with preserved ejection fraction and type 2 diabetes, and patients living with both conditions suffer from an especially high symptom burden but have few available treatment options,” Kosiborod said in a statement. “Today’s results, especially when combined with those from the STEP-HFpEF trial , open a new chapter of targeting obesity as a new and effective treatment strategy in patients with obesity-related HFpEF, both with and without diabetes.”
Click here to read the full analysis in the New England Journal of Medicine .
Medicare covering semaglutide for some patients
Back in March , the U.S. Centers for Medicare and Medicaid Services (CMS) announced that Medicare would cover semaglutide/Wegovy if prescribed for its cardiac benefits. Medicare prescription drug plans had not previously covered medications designed to help patients lose weight.
Related Content:
Medicare will now cover weight loss drug semaglutide if taken for heart benefits, are glp-1 agonists safe fda finds no evidence popular weight loss medications cause suicidal thoughts or actions, weight loss drug semaglutide linked to multiple benefits for heart failure patients, weight loss drug semaglutide reduces risk of adverse cardiovascular events by 20% among overweight, obese patients.
1. Mikhail N. Kosiborod, MD, Mark C. Petrie, MD, Barry A. Borlaug, MD, et al. Semaglutide in Patients with Obesity-Related Heart Failure and Type 2 Diabetes. NEJM. April 6, 2024.

Michael has more than 16 years of experience as a professional writer and editor. He has written at length about cardiology, radiology, artificial intelligence and other key healthcare topics.
Related Content
Around the web.
Eleven medical societies have signed on to a consensus statement aimed at standardizing imaging for suspected cardiovascular infections.
Kate Hanneman, MD, explains why many vendors and hospitals want to lower radiology's impact on the environment. "Taking steps to reduce the carbon footprint in healthcare isn’t just an opportunity," she said. "It’s also a responsibility."
Philips introduced a new CT system at ECR aimed at the rapidly growing cardiac CT market, incorporating numerous AI features to optimize workflow and image quality.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Major Advances and Discoveries in Diabetes - 2019 in Review
Juleen r. zierath.
1 Section of Integrative Physiology, Department of Molecular Medicine and Surgery, Karolinska Institutet, Biomedicum, Solnavägen 9, 171 65 Stockholm, SE Sweden
2 Integrative Physiology, Department of Physiology and Pharmacology, Karolinska Institutet, Stockholm, Sweden
3 The Novo Nordisk Foundation Center for Basic Metabolic Research, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark
This review is based on a recent invited lecture at the American Diabetes Association’s 79th annual Scientific Sessions entitled “Major Advances and Discoveries in Diabetes - The Year in Review.”
Recent Findings
Here I provide a written account of my presentation entitled “Major Discoveries in Diabetes over the Past Year.” I highlight several recent advances in basic science that are relevant for the diabetes field, with insight into how the key takeaways impact basic science. I also speculate on how these breakthroughs challenge the field to move the basic science “discovery” into the clinic, as well as offering a perspective on unanswered questions in relation to these advances.
The review should in no way be taken as an endorsement of the highlighted work or a denunciation of any work not selected. Rather, it is a personal reflection that provides a glimpse into what is on the horizon in this rapidly evolving and exciting field!
Introduction
Last February, I received an email from the American Diabetes Association’s (ADA) Scientific Sessions Planning Committee inviting me to participate as a speaker at the 79th annual meeting. I have always enjoyed attending the ADA Scientific Sessions, having done so each year since enrolling in my doctoral studies at Karolinska Institutet. In fact, my first scientific presentation in the diabetes field was communicated as a poster at the 50th annual meeting in 1990. Throughout my career, my interests have been focused on the pathophysiology of type 2 diabetes. In particular, on the role of epigenetic modifications in the development insulin resistance, as well the interaction between circadian rhythms and the metabolic response to exercise. The overarching goal of this research is to identify and validate molecules, pathways and ultimately new treatments that confer the benefits of exercise to improve insulin sensitivity, and attenuate the loss of skeletal muscle function with aging and type 2 diabetes. Needless to say, I was taken aback when I read the title of the proposed session - “Major Advances and Discoveries in Diabetes - The Year in Review.” This was a new concept that the program committee was exploring and they invited me and Dr. Daniel J. Drucker to be their test drivers. The session was divided into two parts to highlight “ Major Breakthroughs ” in the Clinic and at the Bench. Dr. Drucker was asked to speak about clinical developments, and I was tasked with covering advances in basic science. The session was designed to facilitate discussions between clinicians and basic scientists, with the hope of enlightening basic scientists on the latest clinical advancements and clinicians on where the field is headed in terms of bench research.
With this review, I will provide a written account of my presentation entitled “ Major Discoveries in Diabetes over the Past Year. ” I will highlight a few recent advances in basic science and give my perspective on unanswered questions and unmet needs in relationship to these advances from published literature over the last 12–18 months. Before commencing, I wish to share a few words about the process I took to select the different “ Major Breakthroughs. ” Each year, thousands of articles are written on different aspects of diabetes research and care. My initial reaction when I accepted this task was that I would never be able to go through all of this literature in the few months I had to prepare. Even if I had unlimited time to review all of the papers published over this period, any short-list would simply be my own view. Certainly another person facing the same challenge may come up with a completely different list. Diabetes is a huge field and I did not want the session to be limited to my views on this broad topic. I felt for this topic to be of interest to a wider audience, diverse views from people at different career stages and scientific interests needed to be taken into account. Consequently, I sought input from my research group and other colleagues in the field by asking “ What do you think is the major breakthrough in the field this year ”?
In the early spring, I met with my team to discuss several dozen papers highlighting potential “ Major Breakthroughs ” in diabetes research. We interrogated this literature by asking: 1) What was the question raised? 2) What did they find? 3) How does this impact basic science? 4) What was the key takeaway from the study? 5) What were the limitations? 6) What are the challenges to move the “discovery” into the clinic? In the end, we pruned the list to 19 papers. I will briefly review these papers by taking these questions into account. A caveat with shortlisting a few select papers is that I likely have missed one of your favorite discoveries or advances. Thus, I apologize in advance for any omissions. Importantly, the fact that I have selected one paper over another is by no means an endorsement of the highlighted work or a denunciation of any work not selected.
Many Subgroups of Type 2 Diabetes
For decades, diabetes has been classified into two forms, based on the presence (type 1 diabetes) or the absence (type 2 diabetes) of autoantibodies against pancreatic islet β-cell antigens and age at diagnosis. Nevertheless, diabetes is a highly heterogeneous disorder and consequently current classifications are not sufficient for disease stratification and outcome prediction. Indeed, this is exemplified by the identification of a third subgroup of diabetes termed “latent autoimmune diabetes in adults” that is diagnosed by the presence of glutamic acid decarboxylase antibodies. Refining diabetes classification based on biomarkers and deep phenotyping may bring clinicians closer to personalized medicine and better assessment of the risk of complications at diagnosis.
To assess whether type 2 diabetes is a uniform disease and if the response to intervention can be predicted based biomarkers, Leif Groop and colleagues [ 1 ] performed a “data-driven” cluster analysis in patients with newly diagnosed diabetes from the Swedish All New Diabetics in Scania cohort. Clusters were based on six variables including glutamate decarboxylase antibodies, age at diagnosis, body mass index (BMI), glycated hemoglobin (HbA1c), and homeostatic model assessment 2 estimates of β-cell function and insulin resistance, and were related to prospective data from patient records on the development of complications and prescription of medication. The study was replicated in three independent cohorts. The authors identified five novel subgroups of adult-onset diabetes and their association with clinical outcomes including severe autoimmune diabetes (SAID); severe insulin-deficient diabetes (SIDD); severe insulin-resistant diabetes (SIRD); mild obesity-related diabetes (MOD); and mild age-related diabetes (MARD). The authors propose that the combined information from the six variables, which are central to the development of diabetes, offers a superior metric for sub-classification of type 2 diabetes versus the conventional assessment of glucose levels. They conclude that implementation of this new substratification may eventually help to tailor and target early treatment to patients, thereby representing a first step towards precision medicine in diabetes. In addition to the obvious clinical advances from this study directed towards improving the care of people living with diabetes, these findings also impact basic science. Each subgroup might differ from a genetic or epigenetic perspective, and thus understanding the biology associated with each subtype may uncover novel molecular mechanisms controlling glucose homeostasis and complications arising from diabetes. Nevertheless, this study has some limitations in that only a few markers were identified and this approach may not necessarily reveal all of the subgroups of type 2 diabetes. Other limitations include that these phenotypic variables may change throughout the disease course, such that they can only be applied at the time the clusters were derived here, i.e. soon after disease onset; and that one thing is to derive clusters from a large body of data and quite another to be able to place an individual categorically within a cluster, given the quantitative distribution of these variables in people. However, the clustering approach has direct clinical relevance and can be readily applied to existing cohorts, moving the field one step closer to personalized medicine. In addition, the stratification offers insight into the progression of disease over time and insight into risk for complications including chronic kidney disease and retinopathy. Clinicians may also use these markers to stratify patients to assess outcomes to different therapeutic interventions.
Studying Obesity to Learn More about Thinness
Obesity is a chronic lifelong condition that results from the interaction between heritable factors with environmental influences. Excess fat accumulation due to an imbalance between energy intake and expenditure causes obesity. The increasing prevalence of obesity is recognized as a major risk for a variety of diseases including type 2 diabetes, cardiovascular disease, cancer, and musculoskeletal disorders. Given that obesity is a driving force behind the diabetes epidemic, better adherence to exercise and diet regimes, as well as safe, effective and durable weight loss therapies are needed. To this end, I. Sadaf Farooqi and colleagues [ 2 ] studied the melanocortin 4 receptor (MC4R), a brain-expressed G protein coupled receptor (GPCR) involved in weight regulation. The authors were interested in gaining a more refined understanding of MC4R signaling and its impact on clinical phenotypes. Such knowledge could inform the design of drugs targeting this pathway to treat common obesity and its complications. Earlier studies report a frameshift mutation in MC4R that reduces Gαs-mediated cyclic adenosine monophosphate accumulation is associated with dominantly inherited obesity in humans [ 3 , 4 ]. Here, the authors characterized 61 MC4R variants identified in 0.5 million people from the UK Biobank and examined the associations of these variants with BMI and obesity-related cardiometabolic diseases. They found that gain-of-function variants in the MC4R gene were associated with lower BMI and lower odds of obesity, type 2 diabetes, and coronary artery disease. These variants exhibited a signaling bias for the recruitment of β-arrestin, rather than canonical Gαs-mediated cAMP production. One limitation of the study is that the functional characterization of this obesity protective variant was performed in cell culture models. Thus, the authors provide indirect evidence for a genetic association between the variant and the clinical features of the carriers. To move this discovery into the clinic, additional functional validation using in vivo models would be required to confirm the protective effects of this variant on energy homeostasis and the development of cardiometabolic impairments. Pharmacological studies are also warranted, with exploratory efforts directed towards the development of preferential agonists rather than broad spectrum agonists with a bias towards β-arrestin signaling for weight loss and for the treatment of obesity-associated metabolic disease. Overall, the authors provide insight into molecular mechanisms underpinning genetic associations with the development and protection against obesity and cardiometabolic diseases.
New Insight into Insulin Signaling
The canonical signal transduction pathways controlling glucose metabolism involve insulin binding to the insulin receptor α-subunit, followed by autophosphorylation of the β-subunit, leading to activation of down-stream signaling events. Insulin-receptor substrates are regulatory docking proteins that associate with the insulin receptor and play a central role in the selection and differentiation of the insulin signal towards further metabolic or mitogenic events. Two papers that gained particular attention this year dealt with novel aspects of the insulin signaling cascade [ 5 , 6 ]. The insulin receptor is a cell-surface receptor, however, John G. Flanagan and colleagues [ 5 ] asked whether there is a non-canonical pathway, whereby the insulin receptor play a role within the nucleus and exerts long-term effects of insulin including transcriptional regulation. They provide evidence that the insulin receptor translocates to the nuclei and interacts with transcriptional machinery at promoters, thereby identifying a novel non-canonical pathway regulating target genes highly enriched for insulin-related functions including lipid metabolism and protein synthesis and diseases including diabetes, neurodegeneration, and cancer. This finding may have relevance for type 2 diabetes, given that insulin receptor binding was impaired in an insulin-resistant disease model. However, the mechanism was mainly elucidated in HepG2 cells and ob / ob mice. Thus, further evidence from clinical material from people with diabetes studied under physiological conditions is required before fully understanding the impact of this pathway in the pathophysiology of insulin resistance in humans. Moreover, the importance of this pathway for gene regulation versus the canonical signaling pathway for metabolic regulation needs to be elucidated. Insulin receptor translocation to the nuclei is however a new pathway to enhance our understanding of insulin signaling and insulin resistance.
Mutations in the insulin receptor cause severe forms of insulin resistance [ 7 ]. Keeping with the theme of insulin receptor signaling, Nicolas Rohner and colleagues [ 6 ] used a rather unconventional model to study diabetes-associated pathologies, namely the cave-dwelling fish species A. mexicanus (cavefish). They found that these particular cavefish had higher fasting blood glucose levels and insulin resistant features that were attributed to a mutation in the insulin receptor that decreased insulin binding. The hyperglycemic insulin receptor mutant cavefish, paradoxically were otherwise healthy and had a normal life span. The cavefish may have acquired compensatory mechanisms to circumvent the typical deleterious effects associated with insulin resistance and hyperglycemia. In this case, reduced insulin signaling may be beneficial in a nutrient-limited environment. Despite the fact that this study was conducted in cavefish, there may be some translation to humans. The mutation identified in the insulin receptor of these cavefish is implicated in at least two known cases of the Rabson-Mendenhall syndrome, a form of severe insulin resistance in humans. A deeper analysis of these mutant cavefish might uncover an underlying evolutionary force responsible for the striking metabolic adaptations. Identification of the putative mechanisms allowing the mutant cavefish to thrive despite severe insulin resistance and hyperglycemia could be relevant for the treatment of hyperglycemia-related complications in people with diabetes.
Breakthroughs in Islet Cell Biology
Autoimmune destruction of insulin-producing pancreatic β cells, resulting in persistent hyperglycemia, underlies the pathogenesis of type 1 diabetes. Preserving and restoring functional β-cell mass is therefore a fundamental objective of diabetes therapy. However, adult human β cells have limited regeneration potential, therefore the possibility of reprogramming other cell types into glucose-responsive, insulin-secreting β-like cells is being actively pursued. Pancreatic α cells represent a potential source of β-like cells due to their developmental similarities and their location in the pancreatic islet. Moreover, a marked decrease in α cells in mice does not affect normal glucose metabolism. Pedro L. Herrera and colleagues interrogated mechanisms regulating islet cell plasticity [ 8 , 9 ]. They determined the cellular mechanisms regulating the expression of insulin in glucagon + α cells with a focus on the “brake” signals [ 8 ]. They found that paracrine repressive signals originating from β and δ cells maintain the α-cell identity, with a constant repressive influence of somatostatin and insulin. Local signals drive the conversion of α-cells, such that inhibition of proximal β and δ cells leads to a substantial increase in insulin + α-cell numbers. Finally, they report that α-cell conversion is only partially improved by dual inhibition of insulin and somatostatin signals, which suggests that α-cell conversion is synergistically influenced by multiple signals. These findings provide mechanistic insights into how the cell identity–differentiation equilibrium is established and advice the notion that differentiated cells maintain some “plasticity potential”. One key takeaway from this study is the finding that spontaneous insulin production in α cells is not simply due to uncontrolled stress-induced insulin gene dysregulation, but is dynamically regulated, representing a physiological compensatory response to cope with insulin insufficiency. A limitation of the work is the lack of long-term, detailed metabolic studies, and a focus primarily on rodent cells. To move this discovery into the clinic, additional studies using human cells, as well a thorough characterization of the signals that promote insulin production in α cells are warranted.
In a complementary study using islets from donors with and without diabetes they addressed the notion of “cell-identity switches”, a process in which terminally differentiated cells are converted into different cell types when stressed [ 9 ]. They found that α cells and polypeptide-producing γ cells, obtained from pancreatic islet cells from deceased human donors with and without diabetes, can be lineage traced and reprogrammed by the transcription factors PDX1 and MAFA to produce and secrete insulin in a glucose-responsive manner. The modified α cells triggered a weaker immune response when co-cultured with T cells from people with type 1 diabetes, and thus might be less likely to be destroyed than native β cells as they retain the α-cell identity. When transplanted into diabetic mice, the converted human α cells ameliorated diabetes and produced insulin for several months. These findings advance basic science in that they may lead to the identification of a gene signature to confer glucose-stimulated insulin secretion to non-β cells, possibly through small-molecule screening. This study provides conceptual evidence for islet plasticity of human cells and confirms that cell identity and maturity are flexible states. To move this “discovery” into the clinic, further work is required to elucidate pharmacological or gene therapy approaches to stimulate cell interconversion within the patient’s own pancreas, but without causing adverse effects on other cell types.
In addition to the cell reprogramming strategies highlighted above, other groups are working to restore insulin-producing β cells by immunomodulation approaches to suppress the autoimmune attack characteristic of type 1 diabetes. This is a clinically relevant approach since type 1 diabetes is characterized by pancreatic islet infiltration by autoreactive immune cells and a nearly complete loss of β cells. Using several genetically modified mouse models of severe diabetes, Rohit N. Kulkarni and colleagues [ 10 ] report that enhancing β-cell proliferation before an immune attack provides protection against the development of type 1 diabetes by preserving the immunological self-tolerance of islets through the induction of regulatory T cells. This study advances the notion that increased β-cell proliferation early in life, before immune cell invasion, prevents the progression of type 1 diabetes. While the translational significance of the findings in mouse models to human type 1 diabetes needs to be determined, the findings suggest that parental history of diabetes, or alterations secondary to obesity, type 2 diabetes, or the sex of the parent, may affect β-cell proliferation in offspring and the identity of β cells to influence the onset of type 1 diabetes in the offspring. Moving forward, future studies to determine the factors that impact the identity of β cells and trigger type 1 diabetes in the offspring are required.
The Gut Microbiome and Metabolism
The gut microbiome has co-evolved with its host and influences health and disease throughout the lifespan. Interactions between the gut microbiota, diet, and the host have been associated with metabolic diseases including obesity, diabetes, and cardiovascular disease. Nevertheless this link is often correlative, with only a few studies investigating whether specific microbiota or microbiota-dependent metabolites can directly affect metabolic homeostasis. Microbiota-dependent metabolites in systemic circulation may influence peripheral organs and modify insulin sensitivity. Fredrik Bäckhed and colleagues [ 11 ] performed a metabolomics screen of plasma from patients with type 2 diabetes and severe obesity, and BMI-matched subjects without diabetes to identify circulating amino acid-derived metabolites. They found the concentration of imidazole propionate, a microbially produced amino acid-derived metabolite, was higher in portal and peripheral blood from the obese people with type 2 diabetes. They also reported that daily injection of imidazole propionate into germ-free mice impairs glucose tolerance and insulin signaling, suggesting imidazole propionate directly affects glucose metabolism. Using a variety of cell models, they also report that imidazole propionate inhibits insulin receptor substrate signaling through mTORC1. The key finding is the identification of imidazole propionate, a microbiota-dependent metabolite, which is coupled to the development of insulin resistance. Nevertheless, there are some caveats as this metabolite is unlikely to cause all forms of type 2 diabetes. The authors measured imidazole propionate levels in obese people with or without type 2 diabetes and a different profile may emerge for moderately overweight or normal weight people with insulin resistance or type 2 diabetes. Given that dietary factors influence the gut microbiome, clarification of the interplay between diets, bacteria and the gut environment would also be important to understand, as different macro or micro nutrients may influence the metabolomics profile in people with type 2 diabetes or obesity. Finally, to move this “discovery” into the clinic, further insight into the identity of the molecular mechanism and signaling pathways induced by imidazole propionate or other microbiota-dependent metabolites may reveal pharmacological targets to treat metabolic diseases.
Endothelial-to-Adipocyte Extracellular Vesicle Cross-Talk
An area of fertile research is the identification of systemic factors that integrate the individual organ response with the entire body. Many researchers have been focused on identifying secreted proteins (“ tissue-kines” ) that are produced and released by various organs that exert autocrine, paracrine and/or endocrine effects on tissue-specific or whole body glucose or energy homeostasis. Philipp E. Scherer and colleagues [ 12 ] have discovered the existence of extracellular vesicle-mediated signal transduction between cell types within adipose tissue. This unexpected finding was made when the team generated an adipocyte-specific caveolin 1 knockout mouse. Caveolin 1 is a membrane-bound structural and signaling protein that is highly abundant in adipocytes and endothelial cells. Although they were successful in ablating the caveolin 1 gene from adipocytes, unexpectedly, the protein remained abundant in the cells. They found that endothelial cells in close proximity to the adipocytes delivered caveolin 1 protein in extracellular vesicle to the cells. They uncovered a network of extracellular vesicle-mediated exchange of cellular material exists in adipose tissue, whereby this exchange can replace protein levels of caveolin 1 in adipocytes despite gene disruption. This extracellular vesicle trafficking process is regulated by the systemic metabolic state and requires communication between endothelial cells in order to package the extracellular cargo into vesicles for release into the adipose tissue. The study uncovers new insight into the complex signaling mechanisms that exist among various cell types including adipocytes and vascular cells, which may also affect distal organs. The transfer of cargo packaged in these extracellular vesicles is not a passive process, but rather a physiologically regulated event, participating in the tissue response to changes in the systemic nutrient state induced by fasting/refeeding paradigms or obesity. The study has implications for the interpretation of tissue-specific knockout models and importance of single cell sequencing. While the clinical relevance may not be immediately obvious, the findings may advance the development of tissue-specific drug delivery systems by targeting endogenous extracellular vesicles or engineering biosynthetic vesicles to treat diabetes.
New Insight into an Old Drug - Metformin
Metformin is one of the most widely prescribed drugs to treat type 2 diabetes [ 13 ]. The drug was first used to treat diabetes over 60 years ago and is currently recommended in many clinical guidelines on the management of type 2 diabetes as the first-line oral glucose-lowering agent. Metformin mainly works by inhibiting hepatic glucose production, and enhancing insulin sensitivity. Nevertheless, the precise mode of action for the glucose lowering effects of metformin remain somewhat elusive and several mechanisms have been evoked including inhibition of mitochondrial respiration, elevation of 5′-adenosine monophosphate (AMP) levels, and activation of AMP-kinase. Kei Sakamoto and colleagues [ 14 ] revisit this question and ask whether metformin targets the AMP-inhibited enzyme fructose-1,6-bisphosphatase-1 (FBP1) to lower hepatic glucose production. They found that metformin induces a mild energy stress in liver, thereby increasing the AMP concentration, which allosterically inhibits the AMP-inhibited enzyme FBP1, to lower hepatic glucose production. Using molecular approaches, they identified a point mutation in FBP1 that rendered it insensitive to AMP. Thereafter, they studied “knock-in” mice harboring the mutant form of FBP1 and found they are insensitive to metformin. The authors discovered that FBP1, a rate-controlling enzyme in gluconeogenesis, functions as a major contributor to the therapeutic action of metformin. These results are clinically relevant and suggest that FBP1 could be a key target for the treatment of type 2 diabetes, either directly using targeted inhibition, or indirectly as a consequence of inducing energy stress.
Timing Matters - Aligning the Circadian Clock with Environmental Cues, with Implications for Chronomedicine to Treat Metabolic Diseases
The next set of “Major Discoveries” are focused on recent advances in circadian biology, including mechanism of action, impact on cellular and whole-body metabolism, and alignment of the circadian clock with diet and exercise paradigms. Circadian rhythms are controlled by central and peripheral molecular clocks that anticipate day/night cycles to optimize numerous physiological and behavioral responses over a ~24 h cycle. Perturbed circadian rhythms are associated with metabolic dysfunction, obesity, and type 2 diabetes [ 15 ]. Over the past years, there has been a surge in interest in understanding how an alignment between the molecular circadian clocks and hormone action or environmental cues (diet, exercise, and sleep) can affect metabolism.
Insight from Structural Biology or Melatonin Receptors
Melatonin is a hormone that is involved in synchronizing circadian rhythms and regulating the sleep–wake cycle. One new advance in receptor biology, by Vadim Cherezov and colleagues [ 16 ] deals specifically with the structural biology of the melatonin receptors MT1 and MT2, two GPCRs involved in the regulation of circadian rhythm and sleep patterns. These receptors are candidates for drug development efforts to treat insomnia, circadian rhythm and mood disorders, cancer, and type 2 diabetes. The authors used mutated and stabilized MT2 to determine structural differences to MT1, as well as altered melatonin dissociation kinetics. The authors reveal insight into the molecular understanding of melatonin receptor subtype selectivity and ligand access modes, which may be important for the design of selective melatonin tool compounds and therapeutic agents that will help to dissect the melatonin system. Single-nucleotide polymorphisms associated with type 2 diabetes mapped onto MT2 structure clustered at residues near the ligand binding pocket, and receptor surface. This implies that single-nucleotide polymorphisms associated with altered melatonin sensing may be involved in the pathogenesis of type 2 diabetes, but this finding requires additional confirmation and physiological validation. The potential long-term outcome from this work may be the development of therapies targeted towards melatonin receptors for the treatment of type 2 diabetes and metabolic disease. Nevertheless, the realization of this goal may be decades away.
Insulin Resets the Clock
Circadian rhythms are generated by an auto-regulatory transcriptional-translational feedback loop composed of positive regulators (CLOCK/BMAL1) and repressors (CRY1/2 and PER1/2) that control a large fraction of protein coding genes in mammalian cells. The central clock located in the suprachiasmatic nuclei of the hypothalamus is mainly entrained by light, while peripheral clocks respond to external cues including temperature, feeding/fasting cycles, exercise and hormones. Recent work by John S. O’Neill and colleagues [ 17 ] tested whether insulin and insulin-like growth factor 1 (IGF1), two hormones important for the control of growth and metabolism, provide signals to the molecular clock machinery in conjunction with meals. In a series of elegant work, they report that insulin and IGF1 reset circadian clocks by inducing the PER protein. The effect of insulin and IGF1 on PER protein synthesis is not restricted to any particular tissue, and facilitates circadian entrainment of gene expression, thereby providing a mechanism by which feeding cues synchronize biological clocks throughout the body. The insulin/IGF-1 induction of PER protein requires mTOR activation, increased phosphoinositide signaling and microRNA downregulation. Whether these findings have physiological relevance is still an unresolved question since the level of insulin (600 nM) that was used for many of the experiments is lethal in humans. Moreover, there is an interplay between insulin and a variety of hormones and peptides that contribute to food entrainment, and thus the effect of other nutritional cues has yet to be unraveled. Nevertheless, this work has clinical relevance since disturbing the temporal relationship between light cures and hormonal cues may be a key physiological driver underlying the association between disturbances in circadian rhythms (shift-work, jet lag) and ill health. Management of light exposure and meal timing may prevent the adverse physiological consequences of circadian disturbances on metabolic health.
Timing of Dietary Cues
Over-nutrition/obesity has been associated with disturbed circadian rhythms and altered expression of genes controlling metabolism. Obesity may drive a vicious cycle to further impact global transcriptional and epigenomic circadian rhythms. Nevertheless, the underlying mechanism by which nutritional/dietary cues impact circadian rhythms are not well understood. Mitchell A. Lazar and co-workers, [ 18 ] studied high-fat diet-induced obese mice and reported that obesity remodeled circadian enhancers in liver, triggering synchronous high-amplitude circadian rhythms of opposing lipid pathways namely fatty acid synthesis and oxidation. The obesity-enhanced circadian transcription of lipid genes in liver required genes involved in lipogenesis (SREBP) and fatty acid oxidation (PPARα). Of interest, pharmacological lipid lowering drug therapy was more effective in the obese mice when treatment was timed at the peak expression of the nuclear receptor and fatty acid oxidation gene PPARα. The key takeaway from this study is that at least in mice, over-nutrition intensifies circadian rhythms of the non-core clock factors SREBP and PPARα in liver, such that pharmacological lipid lowering drugs are more effective when PPARα is highest. If similar results are observed in obese humans, this work may have clinical relevance. For example, it may be possible to take circadian rhythms into consideration when prescribing PPARα agonists as lipid lowering therapy to achieve optimal effects on fat oxidation and energy homeostasis. The application of “ chronomedicine ” by aligning circadian rhythms with medicine/drugs or diet/exercise/sleep regimes to manage diabetes may be a clinical reality in the future.
In keeping with the theme chronomedicine , Satchidananda Panda and his team have been studying the interaction between eating and timing [ 19 ]. Remarkably, they have reported that obese mice maintained on a feeding schedule in which food availability is restricted to a defined period of 8–12 h (so called time-restricted feeding ), have sustained rhythmic expression of circadian clock components and many key metabolic regulators. Strikingly, time-restricted feeding ameliorates obesity-associated metabolic disorders compared to mice fed an isocaloric diet ad libitum [ 20 ]. In this latest work, they studied high-fat fed obese whole-body Cry1;Cry2 and liver-specific Bmal1 and Rev-erbα/β knockout mice subjected to time-restricted feeding or ad libitum diets and reported that feeding-fasting rhythms are sufficient to alleviate key metabolic diseases, including obesity and metabolic syndrome, independently of the circadian clock. Time-restricted feeding restored rhythms in feeding-fasting, metabolic and nutrient-sensing pathways and prevented fatty liver, dyslipidemia and glucose intolerance and activated cellular homeostasis maintenance pathways in clock mutant mice. This finding was unexpected given the importance of the core clock machinery in controlling gene expression. A key takeaway as from this study is that the circadian clock maintains metabolic homeostasis by sustaining daily rhythms in feeding-fasting and by maintaining balance between nutrient and cellular stress responses. The benefits of time-restricted feeding regimes in the long-term have not been assess, nor have studies been confirmed in older mice. Consequently, the durability of this dietary regime to sustain the improvements in metabolic homeostasis is unknown. In translating these findings into the clinic, it may be important to determine whether humans with circadian rhythm defects, (jet lag, shift-workers), who may be predisposed to aberrant eating patterns, as well as people with metabolic disease, can voluntarily impose a strict time-restricted eating regime to prevent or reverse metabolic diseases. The type of diet and calorie content are also other important considerations for maintaining metabolic health. For example, Bente Kiens and coworkers [ 21 ] reported saturated or polyunsaturated fat-rich diets induce extensive metabolic adaptations that maintain peripheral insulin sensitivity, lower circulating lipids, and decrease hepatic de novo lipogenesis and gluconeogenesis, enabling disposition of dietary fat without metabolic complications in humans and mice, irrespective of fatty acid type, provided caloric intake is balanced. This was an unexpected finding, but reinforces the importance of calorie balance rather than degree of fat in the diet. Thus, at least in healthy slightly overweight men, as long as calorie balance is maintained, fat-rich diets appear to be well-tolerated.
Timing of Exercise
Time of day may be important to achieve the most robust effects of exercise training on metabolic homeostasis. Acute exercise increases glucose uptake, promotes mitochondrial biogenesis, and enhances insulin sensitivity [ 22 ], consequently regular physical exercise is recommended for the treatment and prevention of chronic conditions/diseases including obesity and diabetes [ 23 ]. Nevertheless, the most effective time of day to achieve beneficial effects on blood glucose control in people with type 2 diabetes remains unknown. In a recent study men with type 2 diabetes underwent a randomized crossover trial of two weeks morning versus afternoon high intensity interval exercise training [ 24 ]. Afternoon high intensity interval training (4 PM) was more efficacious than morning interval training (8 AM) at improving blood glucose control as assessed in the men with type 2 diabetes by continuous glucose monitors. Strikingly, morning exercise training had an acute, deleterious effect, increasing blood glucose levels, which may be related to an exaggerated counter-regulatory hormonal responses in men with type 2 diabetes after maximal dynamic exercise [ 25 ]. While the study supports the long-standing view that exercise is a critical adjunct in the management of type 2 diabetes, it highlights the importance of optimizing the timing of exercise sessions to improve glycemic control in people with type 2 diabetes. The effect of exercise training on blood glucose control at various times of day may also differ in response to exercise intensity or modality, as well as age, sex, and metabolic status (metabolically healthy, type 1 diabetes, type 2 diabetes, obesity, gestational diabetes) of the participant. Integrating regular exercise training into a daily routine, with workouts at a consistent time of day, may help to ensure that daily activity goals are met. Thus, for most people, the best time to exercise is when you can do it.
Exercise-Responsive Systemic Factors that Control Metabolism
Exercise perturbs whole body homeostasis and ultimately every cell and organ in the body needs to adapt to the increased mechanical, metabolic, and thermoregulatory demands associated with the increased work load [ 26 ]. Exercise-responsive factors can be released from a variety of peripheral organs during work and recovery to communicate information about the status of the different tissues to maintain whole body glucose and energy homeostasis [ 27 ]. In searching for novel adipose tissue derived exercise-responsive secreted factors Laurie J. Goodyear and colleagues [ 28 ] asked whether transforming growth factor-β2 (TGF-β2) contributes to the exercise-induced improvements in metabolic homeostasis. TGF-β2 regulates embryonic development and is an immune suppressor. They found that endurance exercise training increased TGF-β2 mRNA in subcutaneous white adipose tissue from healthy young men and mice. They report TGF-β2 is an exercise-induced “adipokine” that increases with training and promotes glucose and fatty acid metabolism, presumably by normalizing inflammation. Treatment of mice for 12 days with recombinant TGF-β2 reversed the deleterious effects of high-fat diet on glucose and lipid metabolism. While the mechanism remains elusive, exercise-induced elevations in lactate appear to act as a trigger to modulate TGF-β2 expression. To move this discovery into the clinic, additional mechanistic studies are warranted, particularly in regard to the mode of action and whether any side-effects develop from TGF-β2 treatment on inflammation. Dosing will also be a factor to titer out- given that levels during exercise are transient, and levels during a protein-based therapy may be sustained. Nevertheless, the findings uncover novel molecular connections between adipose tissue and skeletal muscle in the context of exercise physiology.
Interleukin-6 (IL-6) is another exercise-responsive “ tissue-kine ” implicated in metabolic regulation [ 29 , 30 ]. IL-6 is released from skeletal muscle during exercise and stimulates lipolysis. Two recent studies further biologically validate IL-6 at the level of adipose tissue as treatment for obesity [ 30 ] and at the level of the gut for the control of gastric emptying [ 29 ]. To determine the role of IL-6 on exercise-induced reductions in visceral adiposity in Krogh-Madsen and colleagues [ 30 ] performed a randomized placebo-controlled trial whereby abdominally obese adults were treated with tocilizumab (IL-6 receptor antibody) or placebo during a 12-week intervention with either bicycle exercise or no exercise. Strikingly, they found treatment with an IL-6 receptor agonist prevented the exercise-induced loss of visceral fat, indicating IL-6 is required for the training-induced reductions in adiposity. Conversely, the cardiorespiratory improvements following exercise training were IL-6-independent. In addition to the effects of IL-6 on weight loss, Helga Ellingsgaard and colleagues [ 29 ] report an acute increase in IL-6 improves glycemic in healthy and type 2 diabetic men by inhibiting gastric motility in a GLP-1-dependent manner. Treatment with the IL-6 receptor agonist also enhance gastric emptying after acute exercise in healthy men. Collectively, these two studies provide clues regarding possible therapeutic targets for treatment of obesity and insulin resistance, implicating exercise-induced IL-6 may be required to achieve weight loss and improve glucose homeostasis. The results also raise a potential concern for increased adiposity or gastric emptying in patients prescribed IL-6 receptor agonists for the treatment of some forms of arthritis. Patients receiving this type of therapy may have difficulty in preventing weight gain or promoting weight loss with exercise, or may have issues related to the mechanisms controlling neurohumoral signals that regulate gastric emptying.
Concluding Remarks
This is an exciting time of great discovery and advances in the field of diabetology and endocrinology as many researchers are striving to move basic discoveries towards the clinic. The need for continued support of basic research is stronger than ever given the complexity associated with diabetes and obesity, the increasing number of individuals suffering with these diseases, and the long journey from discovery to treatment. If there are no discoveries emanating from basic biology, there will be no advances to translate into the clinic. Hopefully, some of the discoveries highlighted in this review will move into the clinic. Several of the “breakthroughs” discussed, particularly those related to diet and exercise, are already being practiced in the clinic and are important for the prevention of metabolic diseases and the promotion of healthy living. In closing, I have provided just a glimpse of what is on the horizon in this rapidly evolving and exciting field! The task has been daunting, but for every breakthrough highlighted, there are surely hundreds more to come! I hope you have enjoyed the year in review.
J.R.Z is supported by grants from the Novo Nordisk Foundation (NNF14OC0011493, NNF14OC0009941), Swedish Diabetes Foundation (DIA2018-357), Swedish Research Council (2015–00165), and the Strategic Research Program in Diabetes at Karolinska Institutet (2009–1068).
Funding Information
Open access funding provided by Karolinska Institute.
Compliance with Ethical Standards
Juleen R. Zierath declares that she has no conflict of interest.
This article does not contain any studies with human or animal subjects performed by the author.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance

These 3 Eating Habits Could Increase Your Risk for Diabetes, According to New Research
T o help lower your chances of developing type 2 diabetes, check out these simple food swaps and tips on eating for healthy blood sugar levels.
It's no secret that a nutritious, balanced diet is a critical component of your overall health. What you eat affects everything from your mood to your energy and sleep patterns . If your eating pattern is lacking the nutrients your body needs to thrive, it can lead to numerous chronic health problems including heart disease, obesity, type 2 diabetes and the list goes on. Luckily for us, a new study aimed to take the guess work out of what dietary factors impact your diabetes risk the most. Read on for the details, plus how to put their findings into practice in your own life.
What This Diabetes Study Found
A new meta-analysis, published on April 17, 2023 in the journal Nature Medicine , found that unbalanced eating patterns (what the authors broadly referred to as "poor diet") contributed to over 14.1 million cases of type 2 diabetes worldwide in 2018. This study used the United Nations' Global Dietary Database (GDD) to assess the dietary habits in 184 countries with data from 1990 to 2018 to help illuminate the specifics.
Out of the 11 dietary factors examined, three played the largest role in increasing type 2 diabetes risk: insufficient intake of whole grains, excesses of refined rice and wheat and the overconsumption of processed meat.
There are a few reasons why these specific foods were associated with a higher diabetes risk and chronic elevated blood sugar levels. Whole grains are packed with fiber, vitamins and minerals which help slow down the absorption of food and help keep blood sugar and energy levels more consistent for a longer period of time.
Refined grains like the rice and wheat are typically found in more highly-processed foods and lack much fiber, so they are burned more quickly and can lead to a blood sugar spike and subsequent crash. When the body regularly experiences blood sugar spikes and crashes, it can lead to insulin resistance and increase the risk for type 2 diabetes. Research has also found that processed meat is typically high in saturated fat, cholesterol and sodium, all of which can contribute to type 2 diabetes risk.
The good news is that there are several simple dietary changes that can help lower your chances of developing this health condition.
Healthy Food Swaps to Help Lower Your Risk
First, to incorporate more whole grains into your meals, try swapping in a whole grain food in place of something that you're already eating. For example, try to choose whole-wheat bread instead of white bread or whole-wheat pasta instead of regular pasta the next time you're at the store. Many grocers offer a variety of whole-wheat versions of products like wraps, bread rolls and even pizza doughs that make it easier to up your intake.
Additionally, try to reduce your intake of refined grains by swapping in higher-fiber foods like brown rice, quinoa, cauliflower rice, barley or oats. This doesn't mean you should never enjoy foods like white rice or other more refined grains if you enjoy them, but just be mindful about adding another source of fiber to your plate.
Lastly, you can replace processed red meats with these convenient protein options . Foods like canned beans, fish (fresh, frozen or canned), eggs, cheese, peas and lentils are all rich in protein, quick to prepare and packed with nutrition.
The Bottom Line
When it comes to chronic health conditions, there are certain factors that are beyond your control such as age, genetics and environment. However, your lifestyle habits—including your diet—are more modifiable and can have a big impact on your risk for diseases like diabetes. Small changes to your eating pattern can add up over time and may go a long way in protecting your health. And eating more whole grains and limiting intake of processed meats and refined grains is a great place to start.
Up Next: Why You Might Be Tested For Type 2 Diabetes at Your Next Physical, Even if You Don't Have Family History


IMAGES
VIDEO
COMMENTS
Type 2 diabetes mellitus, the most frequent subtype of diabetes, is a disease characterized by high levels of blood glucose (hyperglycaemia). It arises from a resistance to and relative deficiency ...
About 20% of the UK population are living with, or are at risk of, type 2 diabetes, with estimated annual National Health Service treatment costs of £8·8 billion.1 This rising tide identifies an urgent need to reduce uncertainties around the causes, prevention, and treatment of type 2 diabetes. A patient-centred approach is a cornerstone of high-quality diabetes care and is mirrored in ...
Introduction. Insulin resistance and β-cell dysfunction are the 2 major hallmarks of type 2 diabetes mellitus (T2DM) that appear as the result of disturbed homeostasis [].Failure of β-cells (∼80% of their β-cell function) and insulin resistance in muscles and the liver is a vicious triumvirate responsible for the core physiological defects.
The chronic complications of type 2 diabetes are a major cause of mortality and disability worldwide [ 1, 2 ]. Clinical research is the main way to gain knowledge about long-term diabetic complications and reduce the burden of diabetes. This allows for designing effective programs for screening and follow-up and fine-targeted therapeutic ...
I. Introduction. Diabetes mellitus, a metabolic disease defined by elevated fasting blood glucose levels due to insufficient insulin production, has reached epidemic proportions worldwide (World Health Organization, 2020).Type 1 and type 2 diabetes (T1D and T2D, respectively) make up the majority of diabetes cases with T1D characterized by autoimmune destruction of the insulin-producing ...
The ADA is committed to continuing progress in the fight against type 2 diabetes by funding research, including support for potential new treatments, a better understating of genetic factors, addressing disparities, and more. For specific examples of projects currently funded by the ADA, see below. Greg J. Morton, PhD.
Diabetes Self-Management: Potential Risks and Resilience Factors. Roberta Lamptey. Michael Harris. 376 views. An innovative journal that advances our understanding of diabetes and its treatment in clinical settings and the community. It explores therapies, nutrition, complications and self-management, ulti...
July 05, 2023. Editorial: New trends in type 2 diabetes diagnosis and management in primary care. Aleksandra Klisic. and. I-Shiang Tzeng. Type 2 diabetes mellitus (T2DM) is a global health concern (1-3), with rising prevalence especially in middle and low income countries (4). In order to raise awareness and to timely diagnose this metabolic ...
Building on the success of New Trends in Type 2 Diabetes Diagnosis and Management in Primary Care, we are pleased to relaunch Volume II of this Research Topic.Type 2 diabetes mellitus (T2DM) accounts for around 95% of all cases of diabetes and results from the body's ineffective use of insulin. With the prevalence of T2DM rising, particularly in low and middle income countries, it is ...
45 of the Best Diabetes Dissertation Topics. Published by Owen Ingram at January 2nd, 2023 , Revised On August 16, 2023. The prevalence of diabetes among the world's population has been increasing steadily over the last few decades, thanks to the growing consumption of fast food and an increasingly comfortable lifestyle.
Amelioration of Both Central and Peripheral Neuropathy in Mouse Models of Type 1 and Type 2 Diabetes by the Neurogenic Molecule NSI-189. Diabetes, 68(11), 2143-2154. Read more. ADA-funded researcher studying link between ageing and type 2 diabetes. One of the most important risk factors for developing type 2 diabetes is age.
Type 2 Diabetes Research Project topics include support for potential new treatments, a better understating of genetic factors, addressing disparities, and more. See Project Examples Prediabetes/Insulin Resistance Research Projects include understanding the role of exercise, novel therapies, and more. ...
St. Petersburg, Fla. - September 12, 2023 - Scientists at Johns Hopkins All Children's Hospital, along with an international team of researchers, are shedding new light on the causes of Type 2 diabetes. The new research, published in the journal Nature Communications, offers a potential strategy for developing new therapies that could restore dysfunctional pancreatic beta-cells or ...
The Clinical Research in Type 2 Diabetes (T2D) program supports human studies across the lifespan aimed at understanding, preventing and treating T2D. This program includes clinical trials that test pharmacologic, behavioral, surgical or practice-level approaches to the treatment and/or prevention of T2D, including promoting the preservation of ...
357 Diabetes Essay Topics & Examples. Updated: Feb 25th, 2024. 26 min. When you write about the science behind nutrition, heart diseases, and alternative medicine, checking titles for diabetes research papers can be quite beneficial. Below, our experts have gathered original ideas and examples for the task. We will write.
Two authors independently identified the research topics as six topics, including drug therapy, complication, comorbidity, related treatment, risk factors, and others. ... The third study was a meta-analysis of weight and type 2 diabetes after bariatric surgery, which was published in the American Journal of Medicine and cited 1540 times .
An Additional 12 Million US Adults Become Eligible for Diabetes Screening. New USPSTF and ADA guidelines lower the age for prediabetes and type 2 diabetes screening to 35. This study examined if testing practices aligned with guidelines and which populations were less likely to receive testing. Read the summary.
Key Points. Question What psychosocial factors are associated with glycated hemoglobin (HbA 1c) levels in young adults with youth-onset type 2 diabetes?. Findings In this cohort study of 348 participants, diabetes distress, beliefs that medicines are necessary, and concerns about medicines were associated with higher odds of high HbA 1c (≥8.0%) 1 year later; these beliefs were also ...
Nutrition therapy has been emphasised for decades for people with type 2 diabetes, and the vital importance of diet and nutrition is now also recognised for type 2 diabetes prevention. ... This article does not cover the wide range of topics already discussed in existing reviews and guidelines. ... and further research is needed in those with ...
Empagliflozin improves cardiovascular outcomes in patients with heart failure, patients with type 2 diabetes who are at high cardiovascular risk, and patients with chronic kidney disease. The safet...
Obesity and type 2 diabetes are common comorbidities in patients with heart failure with preserved ejection fraction (HFpEF). Currently, there are no FDA-approved therapies that specifically treat all three conditions at the same time; however, semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist, has the potential to do so.
In this Research Topic, we aim to promote the latest research in physiology that focuses on the metabolic defects underlying the onset of type 2 diabetes or its complications, with direct or indirect connections to the clinical applications and/or practice. We also plan to advance our knowledge about the effectiveness of lifestyle modifications ...
Provided by American Physiological Society. Heavy alcohol use may increase middle-aged adults' risk of developing Type 2 diabetes, according to research to be presented this week at the American ...
The study included a total of 889 adults with newly diagnosed type 2 diabetes in 2011 or 2012. The participants were grouped based on individual BMI trajectories from the diagnosis until 2014.
Semaglutide, the first weight loss drug approved by the U.S. Food and Drug Administration to reduce the risk of major adverse cardiovascular events, is associated with significant reductions in heart failure symptoms among obese patients with heart failure with preserved ejection fraction (HFpEF) and type 2 diabetes. That's according to new research presented at ACC.24, the annual meeting of ...
With this review, I will provide a written account of my presentation entitled " Major Discoveries in Diabetes over the Past Year. " I will highlight a few recent advances in basic science and give my perspective on unanswered questions and unmet needs in relationship to these advances from published literature over the last 12-18 months.
The ARISE-HF trial enrolled 691 patients (median age 67 years), of whom half were women, at 62 sites around the world. Patients had had Type 2 diabetes for an average of 14 years.
When the body regularly experiences blood sugar spikes and crashes, it can lead to insulin resistance and increase the risk for type 2 diabetes. Research has also found that processed meat is ...