Essay on Smoking
500 words essay on smoking.
One of the most common problems we are facing in today’s world which is killing people is smoking. A lot of people pick up this habit because of stress , personal issues and more. In fact, some even begin showing it off. When someone smokes a cigarette, they not only hurt themselves but everyone around them. It has many ill-effects on the human body which we will go through in the essay on smoking.


Ill-Effects of Smoking
Tobacco can have a disastrous impact on our health. Nonetheless, people consume it daily for a long period of time till it’s too late. Nearly one billion people in the whole world smoke. It is a shocking figure as that 1 billion puts millions of people at risk along with themselves.
Cigarettes have a major impact on the lungs. Around a third of all cancer cases happen due to smoking. For instance, it can affect breathing and causes shortness of breath and coughing. Further, it also increases the risk of respiratory tract infection which ultimately reduces the quality of life.
In addition to these serious health consequences, smoking impacts the well-being of a person as well. It alters the sense of smell and taste. Further, it also reduces the ability to perform physical exercises.
It also hampers your physical appearances like giving yellow teeth and aged skin. You also get a greater risk of depression or anxiety . Smoking also affects our relationship with our family, friends and colleagues.
Most importantly, it is also an expensive habit. In other words, it entails heavy financial costs. Even though some people don’t have money to get by, they waste it on cigarettes because of their addiction.
How to Quit Smoking?
There are many ways through which one can quit smoking. The first one is preparing for the day when you will quit. It is not easy to quit a habit abruptly, so set a date to give yourself time to prepare mentally.
Further, you can also use NRTs for your nicotine dependence. They can reduce your craving and withdrawal symptoms. NRTs like skin patches, chewing gums, lozenges, nasal spray and inhalers can help greatly.
Moreover, you can also consider non-nicotine medications. They require a prescription so it is essential to talk to your doctor to get access to it. Most importantly, seek behavioural support. To tackle your dependence on nicotine, it is essential to get counselling services, self-materials or more to get through this phase.
One can also try alternative therapies if they want to try them. There is no harm in trying as long as you are determined to quit smoking. For instance, filters, smoking deterrents, e-cigarettes, acupuncture, cold laser therapy, yoga and more can work for some people.
Always remember that you cannot quit smoking instantly as it will be bad for you as well. Try cutting down on it and then slowly and steadily give it up altogether.
Get the huge list of more than 500 Essay Topics and Ideas
Conclusion of the Essay on Smoking
Thus, if anyone is a slave to cigarettes, it is essential for them to understand that it is never too late to stop smoking. With the help and a good action plan, anyone can quit it for good. Moreover, the benefits will be evident within a few days of quitting.
FAQ of Essay on Smoking
Question 1: What are the effects of smoking?
Answer 1: Smoking has major effects like cancer, heart disease, stroke, lung diseases, diabetes, and more. It also increases the risk for tuberculosis, certain eye diseases, and problems with the immune system .
Question 2: Why should we avoid smoking?
Answer 2: We must avoid smoking as it can lengthen your life expectancy. Moreover, by not smoking, you decrease your risk of disease which includes lung cancer, throat cancer, heart disease, high blood pressure, and more.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App

Health Effects of Cigarette Smoking
Smoking and death, smoking and increased health risks, smoking and cardiovascular disease, smoking and respiratory disease, smoking and cancer, smoking and other health risks, quitting and reduced risks.
Cigarette smoking harms nearly every organ of the body, causes many diseases, and reduces the health of smokers in general. 1,2
Quitting smoking lowers your risk for smoking-related diseases and can add years to your life. 1,2
Cigarette smoking is the leading cause of preventable death in the United States. 1
- Cigarette smoking causes more than 480,000 deaths each year in the United States. This is nearly one in five deaths. 1,2,3
- Human immunodeficiency virus (HIV)
- Illegal drug use
- Alcohol use
- Motor vehicle injuries
- Firearm-related incidents
- More than 10 times as many U.S. citizens have died prematurely from cigarette smoking than have died in all the wars fought by the United States. 1
- Smoking causes about 90% (or 9 out of 10) of all lung cancer deaths. 1,2 More women die from lung cancer each year than from breast cancer. 5
- Smoking causes about 80% (or 8 out of 10) of all deaths from chronic obstructive pulmonary disease (COPD). 1
- Cigarette smoking increases risk for death from all causes in men and women. 1
- The risk of dying from cigarette smoking has increased over the last 50 years in the U.S. 1
Smokers are more likely than nonsmokers to develop heart disease, stroke, and lung cancer. 1
- For coronary heart disease by 2 to 4 times 1,6
- For stroke by 2 to 4 times 1
- Of men developing lung cancer by 25 times 1
- Of women developing lung cancer by 25.7 times 1
- Smoking causes diminished overall health, increased absenteeism from work, and increased health care utilization and cost. 1
Smokers are at greater risk for diseases that affect the heart and blood vessels (cardiovascular disease). 1,2
- Smoking causes stroke and coronary heart disease, which are among the leading causes of death in the United States. 1,3
- Even people who smoke fewer than five cigarettes a day can have early signs of cardiovascular disease. 1
- Smoking damages blood vessels and can make them thicken and grow narrower. This makes your heart beat faster and your blood pressure go up. Clots can also form. 1,2
- A clot blocks the blood flow to part of your brain;
- A blood vessel in or around your brain bursts. 1,2
- Blockages caused by smoking can also reduce blood flow to your legs and skin. 1,2
Smoking can cause lung disease by damaging your airways and the small air sacs (alveoli) found in your lungs. 1,2
- Lung diseases caused by smoking include COPD, which includes emphysema and chronic bronchitis. 1,2
- Cigarette smoking causes most cases of lung cancer. 1,2
- If you have asthma, tobacco smoke can trigger an attack or make an attack worse. 1,2
- Smokers are 12 to 13 times more likely to die from COPD than nonsmokers. 1
Smoking can cause cancer almost anywhere in your body: 1,2
- Blood (acute myeloid leukemia)
- Colon and rectum (colorectal)
- Kidney and ureter
- Oropharynx (includes parts of the throat, tongue, soft palate, and the tonsils)
- Trachea, bronchus, and lung
Smoking also increases the risk of dying from cancer and other diseases in cancer patients and survivors. 1
If nobody smoked, one of every three cancer deaths in the United States would not happen. 1,2
Smoking harms nearly every organ of the body and affects a person’s overall health. 1,2
- Preterm (early) delivery
- Stillbirth (death of the baby before birth)
- Low birth weight
- Sudden infant death syndrome (known as SIDS or crib death)
- Ectopic pregnancy
- Orofacial clefts in infants
- Smoking can also affect men’s sperm, which can reduce fertility and also increase risks for birth defects and miscarriage. 2
- Women past childbearing years who smoke have weaker bones than women who never smoked. They are also at greater risk for broken bones.
- Smoking affects the health of your teeth and gums and can cause tooth loss. 1
- Smoking can increase your risk for cataracts (clouding of the eye’s lens that makes it hard for you to see). It can also cause age-related macular degeneration (AMD). AMD is damage to a small spot near the center of the retina, the part of the eye needed for central vision. 1
- Smoking is a cause of type 2 diabetes mellitus and can make it harder to control. The risk of developing diabetes is 30–40% higher for active smokers than nonsmokers. 1,2
- Smoking causes general adverse effects on the body, including inflammation and decreased immune function. 1
- Smoking is a cause of rheumatoid arthritis. 1
- Quitting smoking is one of the most important actions people can take to improve their health. This is true regardless of their age or how long they have been smoking. Visit the Benefits of Quitting page for more information about how quitting smoking can improve your health.
- U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General . Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2014 [accessed 2017 Apr 20].
- U.S. Department of Health and Human Services. How Tobacco Smoke Causes Disease: What It Means to You . Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2010 [accessed 2017 Apr 20].
- Centers for Disease Control and Prevention. QuickStats: Number of Deaths from 10 Leading Causes—National Vital Statistics System, United States, 2010 . Morbidity and Mortality Weekly Report 2013:62(08);155. [accessed 2017 Apr 20].
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual Causes of Death in the United States . JAMA: Journal of the American Medical Association 2004;291(10):1238–45 [cited 2017 Apr 20].
- U.S. Department of Health and Human Services. Women and Smoking: A Report of the Surgeon General . Rockville (MD): U.S. Department of Health and Human Services, Public Health Service, Office of the Surgeon General, 2001 [accessed 2017 Apr 20].
- U.S. Department of Health and Human Services. Reducing the Health Consequences of Smoking: 25 Years of Progress. A Report of the Surgeon General . Rockville (MD): U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 1989 [accessed 2017 Apr 20].
To receive email updates about Smoking & Tobacco Use, enter your email address:
- Tips From Former Smokers ®
- Division of Cancer Prevention and Control
- Lung Cancer
- National Comprehensive Cancer Control Program
- Division of Reproductive Health

Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Smoking: Causes and Effects Essay
Among numerous bad habits of modern society smoking seems to be of the greatest importance. Not only does it affect the person who smokes, but also those who are around him. Many people argue about the appropriate definition of smoking, whether it is a disease or just a bad habit. Considering the peculiarities of a habit and of a disease, smoking can be considered as a habit rather than a disease. Among signifiers of a bad habit, it should be pointed out that a bad habit can be controlled by willpower, it can be prevented, and it can be cured (Gilman and Zun 33). Smoking can be fought against with the help of all the points mentioned above. Thus, it is a bad habit which can be easily refused if an individual possessing it has a strong decision to quit. Moreover, it can be cured in many different ways, and it can be prevented by education and other social norms.
Considering the first element, which one of the most important out of the three, willpower is a key to get rid of such a bad habit as smoking, which is very difficult to give up. If a person has a strong determination to quit smoking, he will have to endure considerably a short period of time of physical discomfort. One of the most important part of quitting, is that that is doesn’t require medical help, that is to say, a person is not likely to suffer a procedure that is risky to health and life. In comparison to alcoholism or drug addiction, where medical help is essential to save life of a person who needs a certain amount of an alcohol or drug substance in has blood to survive, the lack of nicotine in blood produces just a physical discomfort that is not dangerous for health and can be handled with the help of willpower. Regarding the second aspect of a bad habit, prevention, smoking can be prevented in early childhood with the help of proper education and social norms (Brinkman et al 689). Many people start smoking when they are teenagers just to prove they are adults in companies. If the society was able to produce a negative impression of this bad habit, so that it doesn’t seem to be sign of being an adult, it would be easier to prevent many children from smoking (Albaum et al 11).
The last aspect of a bad habit is a cure for it. Smoking can be cured in many different ways. There are many different techniques, starting from a nicotine plaster and ending with special clinics and communities helping people to get rid of this problem. If a person wants to quit, he or she has various options to help him or her to solve this problem. To conclude, smoking is a bad habit that can be easily quitted. Although there is an addiction to smoking, the lack of nicotine is not dangerous to the life of a smoker and can be handled without medical intervention. The most important aspect of this bad habit, which actually makes a habit, is that it can be quitted with the help of willpower. Moreover, it can be prevented with alteration of attitude towards smoking and it can be cured in many different ways (Albaum et al 23).
Despite widespread public awareness of the multiple health risks associated with smoking, one out of every four girls under age 18 is a smoker and more than 25 million American women smoke. Whereas the last two decades have seen an overall decrease in smoking prevalence, the rate of smoking has declined much more slowly among women than among men. If current trends continue, smoking rates of women will overtake those of men by the year 2000. Smoking rates are highest, approaching 30%, among women of reproductive age (18–44 years). Rates of smoking are particularly high among young White women with a high school education or less and low income. Cessation rates are lower among African American women (30% have quit) compared to White women (43% have quit). Minority and young women who have low rates of self-initiated cessation are also underrepresented in formal smoking cessation programs (Gilman and Zun 87). A greater proportion of women than men are pre-contemplators, that is, not considering quitting smoking within 6 months and have lower self-confidence that they could quit if they were to try. The debate continues regarding whether or not women are less likely to be successful at quitting when they try than men, with some evidence suggesting that women are more likely than men to relapse and others indicating no gender differences). Regardless, rates of relapse are very high, both among self-quitters and those who participate in formal cessation programs (Albaum et al 24).
Interventions specifically designed for smokers have attempted to address the role of weight concerns as an inhibitor to cessation and long-term maintenance. A randomized trial tested nicotine gum or a behavioral weight control program each alone, or in combination as adjuncts to an intensive group cessation intervention for weight concerned women smokers. The intervention integrated accepted cognitive and behavioral coping strategies for quitting smoking, changing eating behaviors, and developing a walking program.
Works Cited
Albaum, G., Baker, K.G., Hozier, G.C., Rogers, R.D. Smoking Behavior, Information Sources, and Consumption Values of Teenagers: Implications for Public Policy and Other Intervention Failures. Journal of Consumer Affairs , 36 (1), 2002: 5-55.
Brinkman, M.C., Callahan, P.J., Gordon, S.M., Kenny, D.V., Wallace, L.A. Volatile Organic Compounds as Breath Biomarkers for Active and Passive Smoking. Environmental Health Perspectives, 110 (7), 2002, p. 689.
Gilman Sander L. and Xhou Zun. Smoke: A GlobalHistory of Smoking. Reaktion Books; illustrated edition edition, 2004.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2021, November 29). Smoking: Causes and Effects. https://ivypanda.com/essays/smoking-causes-and-effects/
"Smoking: Causes and Effects." IvyPanda , 29 Nov. 2021, ivypanda.com/essays/smoking-causes-and-effects/.
IvyPanda . (2021) 'Smoking: Causes and Effects'. 29 November.
IvyPanda . 2021. "Smoking: Causes and Effects." November 29, 2021. https://ivypanda.com/essays/smoking-causes-and-effects/.
1. IvyPanda . "Smoking: Causes and Effects." November 29, 2021. https://ivypanda.com/essays/smoking-causes-and-effects/.
Bibliography
IvyPanda . "Smoking: Causes and Effects." November 29, 2021. https://ivypanda.com/essays/smoking-causes-and-effects/.
- Free Will and Willpower: Is Consciousness Necessary?
- Francois Marie Arouet (Voltaire)
- Smoking Cessation for Ages 15-30
- Quitting Smoking: Strategies and Consequences
- Importance of Quitting Smoking
- Phineas Taylor Barnum - Biography Study
- Smoking Cessation Project Implementation
- Lifestyle Management While Quitting Smoking
- Is Alex in Burgess' "A Clockwork Orange" Cured?
- Advocating for Smoking Cessation: Health Professional Role
- The Relationship Between the High Rate of Urbanization in Africa and AIDS Spread
- California’s Growing Healthcare Crisis: An Existing Reality
- Environmental Health Problems and Health Inequity
- Public Health: Pertussis Cases in Wisconsin
- The Need for Health Care Reform in the USA
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

The hazards of smoking and the benefits of cessation: A critical summation of the epidemiological evidence in high-income countries
Prabhat jha.
Centre for Global Health Research, Dalla Lana School of Public Health and Unity Health, Toronto, University of Toronto, Ontario, Canada
In high-income countries, the biggest cause of premature death, defined as death before 70 years, is smoking of manufactured cigarettes. Smoking-related disease was responsible for about 41 million deaths in the United States, United Kingdom and Canada, cumulatively, from 1960 to 2020. Every million cigarettes smoked leads to one death in the US and Canada, but slightly more than one death in the UK. The 21 st century hazards reveal that smokers who start smoking early in adult life and do not quit lose a decade of life expectancy versus non-smokers. Cessation, particularly before age 40 years, yields large reductions in mortality risk. Up to two-thirds of deaths among smokers are avoidable at non-smoking death rates, and former smokers have about only a quarter of the excess risk of death compared to current smokers. The gap between scientific and popular understanding of smoking hazards is surprisingly large.
I summarize the causative role of smoking for the most common causes of death among adults in high-income countries, drawing on data from Canada, the United States (US) and the United Kingdom (UK). The main objective of this analysis is to review the hazards of smoking and the benefits of cessation. I do so by examining the cause, nature and extent of tobacco-related diseases in high-income countries between 1960 and 2020. The review has seven main conclusions.
First, in much of Europe and North America, the biggest cause of premature death, defined as death before 70 years, is smoking of manufactured cigarettes. Smoking as an important cause of many diseases in many populations has been recognized widely in the scientific literature for the last five decades. However, three surprising features of health hazards of smoking have been established reliably only since about 2012. The first feature is that risk of developing disease among smokers is big. The second feature is that for smokers to develop these big risks, they need to start smoking early in adult life and to continue smoking. If smokers don’t start early in life, their risks are substantially smaller. Third, if smokers stop smoking before they develop some serious disease, then their risks are substantially reduced.
However, most smokers whom start early in adult life and who continue to smoke are eventually killed by their tobacco use. This is because in every year during middle age (defined here as ages 30–69 years), the death rates among smokers are about three-fold higher than that of similar non-smokers (considering differences between smokers and non-smokers in heavy alcohol use, obesity patterns or different educational or economic status). So two-thirds of the mortality among smokers would not be happening if they had the non-smoker death rates. Most of this excess risk arises from diseases that are caused by smoking. This includes disease such as lung cancer, emphysema, heart attack, stroke, cancer of the upper aerodigestive areas, bladder cancer and various other conditions. Thus this excess risk of disease and death is a cause and effect relationship.
Second, despite substantial declines in the proportion of adults who smoke in most high-income countries, cigarette smoking remains a common exposure in many countries. There were approximately 34 million smokers in the US, 7 million in the UK and 5 million in Canada in 2017 and the number of cigarettes sold in recent years has remained mostly unchanged for the past decade in Canada, while it has declined in the US and the UK. In recent years, electronic cigarettes appear to have accelerated the decline in smoking among younger adults. E-cigarettes are far less hazardous than cigarettes, but do carry some risks, most notably the risk of addiction to nicotine among youths.
Third, a proper understanding of the hazards of smoking requires due consideration of the lag of decades between onset of smoking and the development of disease(s). For both individuals and populations to experience increases in the risk of death, prolonged smoking from early adulthood without cessation is required. The increases in the risk of death can be gauged reliably by studying trends in national lung cancer mortality of different generations. The age-specific health hazards can also be documented in large prospective studies, which monitor groups of smokers and non-smokers for the development of disease(s) over time. Conservatively, smoking-related disease was responsible for about 41 million deaths in the US, UK and Canada, cumulatively, from 1960 to 2020. Every million cigarettes smoked causes approximately one death in the US and Canada, but about 1.3 deaths in the UK.
Fourth, the hazards of smoking are much bigger than was documented just two decades ago. Differences in death rates among smokers and non-smokers imply that smokers lose on average at least a decade of life. About half of all smoking-attributable deaths occur in middle age. The specific conditions caused by smoking include vascular, respiratory and neoplastic (cancer) disease (which account for approximately 75% of all causes of death in most high-income countries). Smoking is increasingly linked to conditions such as diabetes, rheumatoid arthritis, age-related macular degeneration of the eye, orofacial clefts and ectopic pregnancy. Indeed, the list of smoking-attributable diseases continues to expand with additional studies and monitoring. Hence, total mortality differences between otherwise similar smokers and non-smokers are a robust yet simple way to estimate the effects of smoking.
Fifth, cessation is effective in reducing the increased risks of developing smoking-related disease. Smokers who successfully quit before age 40 avoid nearly all increased mortality risks of continued smoking. Smoking cessation yields specific benefits of reducing fatal and non-fatal vascular, respiratory and neoplastic disease. Former smokers have about only a quarter of the excess risk of death than do current smokers. Studying cessation provides further evidence about the causal nature of smoking and disease development.
Sixth, the biological evidence about particular carcinogens and other toxins found in manufactured cigarettes and the possible mechanisms that trigger heart attacks and strokes are consistent with the epidemiological evidence. Genetics is an important factor in disease susceptibility but does not negate the substantial importance of smoking in explaining the marked changes in cause-specific mortality and total mortality attributable to smoking over the last few decades.
Finally, there continues to be gross underestimation of the health hazards of smoking by the public, non-experts and even some experts. The large health risks inherent in smoking are often wrongly equated with the far smaller risks of other health exposures. For example, smoking remains far more hazardous to the individual adult in high-income countries versus moderate obesity, heavy alcohol use and other factors. Most adults surveyed in the US remained surprisingly unaware of the high levels of disease risk that occur today from smoking.
Introduction
Tobacco use is well established as a major cause of death worldwide, accounting for about five to six million deaths per year worldwide ( Jha and Peto, 2014 ). On current smoking patterns, about one billion deaths may occur from smoking during the 21 st century, in contrast to ‘only’ 100 million deaths in the 20 th century ( Peto et al., 1994 ). Already about 100 million tobacco deaths have occurred this century and there will be another 250 million tobacco deaths before 2050. The vast majority of the deaths before 2050 will occur among current smokers. Hence, the major public health priority is to increase the proportions of adults who quit smoking as well as to reduce the uptake of smoking by young adults and children.
In order for individuals to properly understand their risks of smoking, an understanding of the risks of smoking and benefits of cessation is required. This in turn requires a detailed understanding of the cause, nature, and extent of tobacco-related disease, including an understanding of the evolution of cigarette smoking in populations. Relationships between smoking and disease depend on changes in consumption patterns of smokers and ingredients of commonly manufactured cigarettes. This review is intended to inform governments, researchers, health care providers and individuals about the contemporary hazards of smoking. To do so, I outline the contemporary evidence that defines the causal relationship between smoking and the development of major causes of premature death. I focus mostly on evidence relevant from the US, UK and Canada, as typical of most high-income countries.
As most of the evidence regarding the relationship between smoking and disease has been on mortality, I focus on mortality by cause. Mortality has less misclassification than non-fatal outcomes, such as a first or recurrent non-fatal heart attack ( Jha, 2014 ; Menon et al., 2019 ). However, I assess to some extent the evidence on the development of new diseases in previously non-diseased (or healthy) populations (or incidence).
This review is in eight sections. This first section covers key sources of data and methods. Section two reviews the current number of smokers in the US, UK and Canada. It also looks at historical trends in smoking, specifically trends from 1920 to 2010, with an emphasis on trends over the last five decades. It describes changes in the manufactured cigarette which have influenced the addictive properties of cigarettes, and thus, the risks of disease development. A brief review of electronic cigarettes follows.
Section three focuses on smoking as a cause of disease. It reviews, briefly, the history of studies linking smoking to disease, with particular attention to the importance of prolonged smoking to the development of disease. Because lung cancer is a highly-studied disease, this section draws upon national rates of lung cancer mortality and prospective studies of individuals who were smokers or non-smokers and who were observed for the development of the disease. This section also provides estimates of total mortality from smoking from 1960 to 2020 in the three countries (totalling about 41 million deaths), including the relationship of number of cigarettes smoked with mortality.
Section four reviews the epidemiological evidence that relates smoking to both total mortality and cause-specific death rates from the most established conditions linked to smoking. It provides estimates of the avoidable proportion of deaths had the smokers had death rates of comparable non-smokers. Section five outlines the recent evidence on the reduction in total mortality and cause-specific mortality from smoking cessation. Cessation is a powerful way to establish the causal relationships between smoking, total mortality and specific diseases. This section also quantifies the reduction in excess risk among former smokers compared to continued smoking.
Section six briefly summarizes the biological evidence regarding the link between nicotine addiction and smoking, and between smoking and disease. It outlines how biological data can help dispel some commonly held myths about the ‘genetic basis’ of smoking-attributable disease. This summary reemphasizes the central point that reliable quantification of smoking hazards is best done at the level of populations, using epidemiological studies to determine both health risks in individual humans and death rates in populations. Section seven reviews and contrasts the commonly perceived risks of alcohol use and pollution or environmental exposures that influence human health to epidemiological findings on hazards of smoking. Section eight discusses implications for future research and provides a brief conclusion.
This review focuses on the consequences of smoking, and not on the causes of smoking (including the key biological, social, economic and marketing influences that lead to variable rates of smoking initiation and cessation across different populations). However, I do examine the engineering of addictive nicotine to the modern manufactured cigarette, which plays a central role in explaining smoking patterns. For a careful review of the causes of smoking, I refer the reader to various US Surgeon General Reports (USSGR), most notably those of 1989 and 2014 ( U.S. Department of Health and Human Services, 1989 ; U.S. Department of Health and Human Services, 2014 ). Similarly, the emphasis is on high-income countries and not low and middle-income countries, where the evolution of the tobacco epidemic is not yet mature, and which has much lower rates of cessation ( Jha and Peto, 2014 ). The issues related to disease patterns in low and middle-income countries are also quite distinct ( Jha and Peto, 2014 ; International Agency for Research on Cancer (IARC), 2004 ; Jha et al., 2008 ; Liu et al., 1998 ). The review of the consequences of smoking does not include second-hand smoking. Rigorous assessments on the relationship of second-hand smoking to cancer and other diseases have been completed by the International Agency for Research on Cancer ( IARC Working Group on the Evaluation of Carcinogenic Risk to Humans, 2004 ; International Agency for Research on Cancer (IARC), 2012 ), and the US Surgeon General (USSGR; U.S. Department of Health and Human Services, 2004 ; U.S. Department of Health and Human Services, 2014 ). Finally, this does not focus on control of smoking, including the most important role of higher exicse taxes to raise cigarette prices, for which there are several reviews and WHO reports ( Jha and Chaloupka, 1999 ; Jha et al., 2015 ; World Health Organization, 2017 ; Jha and Peto, 2014 ).
Sources of evidence
The main sources of evidence in this report are the published literature, which is accessible publicly through the PubMed portal ( https://www.ncbi.nlm.nih.gov/pubmed/ ); scholarly summations done by key technical agencies such as the US Surgeon General, International Agency for Research on Cancer (IARC), WHO, the US Institute of Medicine, and other independent technical groups; and my own epidemiological research. Like most academic researchers, I did not have access to the scientific research conducted by tobacco industries, much of which remains closed to the public.
The office of the US Surgeon General periodically assembles global evidence on the hazards of smoking ( https://www.surgeongeneral.gov/library/reports/ ). The most important of these compiled evidences was the 1989 report covering the 25 years of progress after 1964 (when the first US Surgeon General’s report on smoking was published) and the 2014 report covering 50 years of progress ( U.S. Department of Health and Human Services, 1989 ; U.S. Department of Health and Human Services, 2014 ). IARC publishes similarly comprehensive reviews of known carcinogens in humans and has examined tobacco in these reviews over various years ( http://monographs.iarc.fr/ ), with the most notable being the 2004 report ( IARC Working Group on the Evaluation of Carcinogenic Risk to Humans, 2004 ). Finally, in 1981, an influential report for the US Congress Office of Technology Assessment concluded that tobacco smoking was the leading cause of cancer deaths in the US, accounting for more avoidable deaths than the sum of several pollutants or other environmental exposures ( Doll and Peto, 1981 ).
The authors of these aforementioned reviews have followed reasonably strict rules to assess evidence. These rules require that in considering the result of any particular study, reviewers are to examine if bias, confounding or misclassification of exposure or outcome could explain the observed results. Only those studies that examines such biases, and ensure that such biases do not account for the observed relationship of smoking and disease are included into any quantitative synthesis of the evidence. Many of the sources of data in this report are from the US and the UK, where there have been more studies over longer durations done than in Canada or other high-income countries. There are, of course, some differences between American,Canadian, and UK citizens and populations, in terms of disease distribution, access to health-care and other factors, as well as in the ingredient formulation of the most common cigarettes smoked. However, these differences are quite small compared to the similarity of mortality rates from specific causes, such as particular cancers, vascular and respiratory diseases ( World Health Organization, 2016 ).
The three countries have similar rates of exposure to smoking (beginning in early adulthood), among a substantial proportion of adults. The differences in disease risks between smokers and non-smokers due to prolonged smoking are very large for many diseases. Hence, differences in disease patterns or smoking product do little to alter the main conclusions about the degree to which smoking is a causative factor for the development of the diseases common in most high-income countries, including those outside Canada, the US and the UK.
A central consideration of this epidemiological evidence is the delay between the onset of smoking in adolescence or early adult life and the development of disease in middle-age, implying a lag between initial exposure and eventual effect. This delay between the onset of smoking and its potential eventual consequences is a major source of confusion among the public, non-experts, and even some experts, about the causal relationship between smoking and specific diseases. Hence, I pay detailed attention to describing the full risks where they are already documented and point out populations (such as women) and diseases for which such risks are still not fully documented.
Smoking trends in the US, UK and Canada
Despite substantial declines in smoking, a large proportion of Americans, Canadians and UK citizens continue to smoke. Largely attributable to the addictive nature of cigarettes, the declines in smoking prevalence have not been matched by declines in the number of cigarettes smoked daily by continuing smokers.
Current smoking prevalence
In the US in 2017, an estimated 34.3 million adults aged 18 and older or 14.0% of US adults smoke cigarettes ( Centers for Disease Control and Prevention, 2018 ). The smoking prevalence is higher among men than women (15.8% vs 12.2%). In the same year, 7.4 million adults in the UK smoked, or 15.1% of adults (17.0% of men and 13.3% of women) ( Office for National Statistics, 2018a ). In Canada, about 5 million Canadians smoked (16.2% of those aged 12 and older; 19.1% of men and 13.4% of women [ Statistics Canada, 2019 ]). The majority of the current smokers (meaning those those who report themselves as non-daily or daily smokers) smoke daily. Other types of tobacco use are less common than cigarettes, with cigars and cigarillos smoking reported by 4% of Americans and 3% of Canadians ( Centers for Disease Control and Prevention, 2018 ; Reid et al., 2017 ).
Current trends in smoking prevalence reflect a combination of those that smoke daily or occasionally, former smokers and people who never started smoking. The prevalence of smoking is also affected by changes in the denominators of all people, including immigration, which tends to lower smoking prevalence ( Newbold and Neligan, 2012 ). I examine historical trends in smoking by sex. This is significant as women’s smoking has increased substantially the over the last few decades.
Historical smoking trends and changes in prevalence in the last four decades
Prior to 1900, most tobacco consumed was in the form of chewed tobacco, snuff, pipes and cigars. Some of the first reports of smoked tobacco came from Spain, where beggars in the 16 th century collected discarded cigar butts, shredded them and rolled them in scraps of paper for smoking. These ‘poor man’s cigars’ were known as cigarillos (which translates, from Spanish, to ‘little cigars’). Late in the 18th century, cigarillos acquired respectability. Their use spread throughout Europe, aided by their popularity among troops in the Napoleonic Wars. The French named them cigarettes. British tastes switched to cigarettes filled with unmixed Virginia tobacco, while the US market preferred blended tobacco ( Encyclopaedia Britannica, 2018 ).
Prior to the early 20th century, cigarettes were made by hand, either by the smoker or in factories. The factory process consisted of hand-rolling on a table, pasting and hand-packaging. In 1880, American James A. Bonsack was granted a US patent for a cigarette machine. Automated machines could produce 120,000 cigarettes in ten hours (approximately 200 per minute). This machine revolutionized the industry and supported a substantial expansion of the major cigarette companies in the US, as well as exports to the UK and European countries. By 1920, there was a marked increase in the use of cigarettes in much of Europe and North America and accelerated further during World War II (WWII), when cigarettes were part of soldier rations. This dissemination contributed to a major expansion in cigarette smoking during the first-half of the 20th century, displacing pipe smoking, chewed tobacco, snuff, cigars and other types of tobacco product ( Encyclopaedia Britannica, 2018 ; Thun et al., 2002 ).
Figure 1 provides the per capita cigarette consumption in the US, Canada, and the UK from 1920 to 2010, based on a global compilation of sales data that includes tobacco industry sources ( Forey et al., 2016 ). Sales data provide a useful indicator of overall consumption trends over prolonged periods. These data are obviously crude and subject to various reporting errors, such as illegal or undocumented sales, which in recent years has paralleled the increase in smuggling; given the tobacco industry’s active role in smuggling their own products ( Merriman, 2012 ). Furthermore, sales data do not capture changes in the length of manufactured cigarettes, the amount of tobacco within various lengths, and mostly do not capture gender-specific smoking patterns, including the notable time lag between increased male smoking and female smoking in the three countries. Importantly, peak consumption among American males, as reported from prevalence surveys, was the year 1963, when overall US cigarette sales also peaked. In contrast, in the UK and in Canada, peak sales occurred around 1975 to 1980.

Note. Data from Forey et al. (2016) , International smoking statistics.
Figure 2 shows trends in overall smoking prevalence in both sexes over the last five decades in the three countries, during which better-quality surveys of smoking prevalence in the adult population became available. These surveys document the steady decline in smoking prevalence that began around the same time as the publishing of the 1962 Royal College Report in the UK and the 1964 Surgeon General’s report in the US, both which provided expert opinion linking smoking to lung cancer ( Royal College of Physicians, 1962 ; U.S. Department of Health, Education, and Welfare, 1964 ).

Note. Data from National Center for Health Statistics, 2008 , 1965–2012 National Health Interview Survey (NHIS); Office for National Statistics, 2018, Adult Smoking habits in Great Britain ; and Reid et al., 2017 , Tobacco Use in Canada: Patterns and Trends, 2017 Edition .
In most high-income countries, there has been a notable reduction in heavy smoking (over 20 cigarettes/day). For example, in the UK, in 1974, 26% of men and 13% of women were heavy smokers compared to 5% of men and 3% of women in 2012.
The average number of cigarettes smoked per day by men and women has decreased across all age groups, consistent with the declines of per capita consumption as shown in Figure 2 ( Action on Smoking and Health, 2016 ). Nevertheless, significant amounts of smoking defined as at least half a pack (ten cigarettes) a day persists in many populations.
From 2000 to 2015, smoking prevalence fell steadily by well over a third in the US, UK and Canada ( Table 1 ). By contrast, the reduction in smoking amount among daily smokers has been more modest, at about one-fifth.
* Daily and non-daily smokers.
Note. Data from National Centre for Health Statistics, NHIS; Office of National Statistics, Adult Smoking habits in Great Britain ; Statistics Canada and Reid et al., 2017 , Tobacco Use in Canada: Patterns and Trends, 2017 Edition –Defined as having smoked in the past 30 days and having smoked 100 cigarettes in a lifetime. Adult ages are 15+ in Canada and the UK and 18+ in the US.
The main conclusion remains that in these three countries, about one in six to one in seven of adults, were smokers in 2017. In absolute terms, this represents about 45 million cigarette smokers in the three countries.
Changes in the manufactured cigarette
Here I will outline three documented strategies used by the tobacco industry to increase uptake and maintain behaviour of smoking (construction, tar content, and use of filters). The tobacco industry conducts much of the scientific research on nicotine, addiction and the role of advertising and promotion to start and maintain tobacco addiction. Little of this research is available publicly.
Thun et al. (2002) point out that the change in the manufacturing process in the US starting about 1930 for cigarettes resulted in increased exposure to surfaces within the respiratory tract. Snuff and other smokeless tobacco, much of which was commonly used before 1900, exposed the local areas of the lip and the oral cavity, as well as extracts absorbed in saliva, and hence caused mostly oral cancers. The smoke from cigars, pipes and traditional roll-your-own cigarettes was traditionally strongly alkaline, which discouraged deep inhalation. Early cigarettes released an un-ionized form of nicotine that could be absorbed by the linking of the mouth and upper airway. Improvements in cultivation and processing lowered the acid content of cigarettes and made them easier to inhale. These improvements also allowed for the release of ionized nicotine, which could be absorbed by the lower parts of the lung (including the tracheal and large bronchi). Thus, changes to the manufactured cigarette shifted the location of cancers from the upper airways to those of the trachea, bronchus and lung.
Reported levels of tar content in manufactured cigarettes have dropped substantially over time. However, a large UK study showed that even low-tar cigarettes sharply increased rates of myocardial infraction. Especially among smokers in their Thirties, Fourties or Fiftees much of the excess risks of continued smoking are avoided by cessation, and less so by changing from one type of cigarette to another ( Parish et al., 1995 ).
Most, but not all, reviews of changes in tar content in US cigarettes have concluded that while there might be some reductions in lung cancer from smoking lower-tar cigarettes, the overall risks of disease are not greatly diminished ( Thun and Burns, 2001 ). The Institute of Medicine ( Bondurant et al., 2001 ), and the National Institutes of Health, National Cancer Institute, 1996 , have examined evidence that low-tar-yield cigarettes reduce disease risk and concluded, “ there have been many efforts in the past to develop less harmful cigarettes, none of which has proved to be successful.” The UK Royal College of Physicians (2000) reached similar conclusions. The National Cancer Institute review concluded: “ Epidemiological and other scientific evidence, including patterns of mortality from smoking caused diseases, does not indicate a benefit to public health from changes in cigarette design and manufacturing over the last 50 years .” Lower-tar cigarettes do appear to result in lower lung cancer deaths. However, there might well be compensatory smoking among smokers who smoke these lower-tar cigarettes, in which the smoke inhalation tends to be more forceful, pulling the smoke deeper into the lungs ( Thun and Burns, 2001 ).
Filters have been in place in most cigarettes for the last four decades. The purpose of the filter is to reduce the amount of tar, smoke, and fine particles inhaled from combustible tobacco, as well as to reduce tobacco flakes from entering the mouth. Many filters are perforated with small holes that intend to dilute the inhaled smoke with external air. When machines are used to test these cigarettes, the findings tend to assign the content of these cigarettes as low-tar or low-nicotine. However, smokers cover these ventilation holes with their lips or fingers. There is also evidence that smokers inhale filtered cigarettes more deeply. The combination of these factors means that these so-called ‘safer’ cigarettes are, in fact, no safer than others ( Kozlowski et al., 1998 ).
In conclusion, smoking is best understood largely as a manifestation of nicotine addiction. The design of the Western, manufactured cigarette likely considers the optimization of initiation and addiction maintenance ( U.S. Department of Health and Human Services, 1990 ). Additional social cues, achieved by mass-marketing, and policies that enable smoking in social setting, such as bars and restaurants, might well enforce the addictive properties of smoking, increasing uptake rates and making cessation less common ( U.S. Department of Health and Human Services, 2010a ; U.S. Department of Health and Human Services, 2020 ).
Recent emergence of e-cigarettes
Alternative nicotine delivery systems include lower-risk nicotine and tobacco products like nicotine replacement therapy pharmaceuticals, low-nitrosamine smokeless tobacco products, and most notably electronic -cigarettes (also referred to as ‘vaping’ products). E-cigarettes were introduced around 2010 but have become particularly popular since about 2015, as they mimic the look and feel of conventional cigarettes (unlike nicotine chewing gum or patches). They are hand-held, generate a smoke-like vapour and hence recreate sensations similar to smoking the smoke from conventional cigarettes. E-cigarettes can be used with or without nicotine. Much of the recent attention in the US has been on the ‘JUUL’ (which has high doses of nicotine) and in Japan on the ‘iQOS’ product (which heats tobacco to generate a nicotine vapour but does not burn it) ( Foundation for a Smoke-Free World, 2018 ; U.S. Department of Health and Human Services, 2016 ). There has notable increase in e-cigarette use in many high-income countries, particularly among youth ( Thatcher, 2015 ). A full review of e-cigarettes is beyond the scope of this review, but Warner (2019) provides useful suggestions for regulation based on the limited evidence base.
E-cigarettes have lower levels of possible carcinogens and toxins than conventional cigarettes, such as 450-fold and 120-fold lower levels of acetaldehyde and toluene, respectively ( Goniewicz et al., 2014 ). E-cigarettes are not completely risk free, as they contain nicotine which has short-term cardiac and other effects. The recent reports of lung-injury among e-cigarette users appears to mostly arise from tampering with products to add marijuana and other agents, and not from the nicotine or flavoring of most e-cigarettes ( Blount et al., 2020 ). Moreover, in contrast to cigarettes, long-term studies of e-cigarettes use to determine the mortality risks among users and quitters have not yet been completed. Nonetheless, there is general consensus that e-cigarettes are considerably safer than cigarettes. The National Academies of Sciences, Engineering, and Medicine, 2018 report noted “ conclusive evidence that completely substituting e-cigarettes for combustible tobacco cigarettes reduces users’ exposure to numerous toxicants and carcinogens present in combustible tobacco cigarettes” and “ substantial evidence that completely switching from regular use of combustible tobacco cigarettes to e-cigarettes results in reduced short-term adverse health outcomes in several organ systems.”
The use e-cigarettes increased most sharply in the US and Japan from about 2015 onwards, and has led to a major major debate if e-cigarettes act as a ‘gateway’, to encourage youth to smoke cigarettes who would not otherwise take up smoking. There have been competing, limited and generally, short-term studies, and these have methodical challenges in determining if the kids who take up e-cigarettes are the ones who might have smoked cigarettes anyway. Moreover, limitations about the sample size, use of many types of vaping products (including some without nicotine), and duration of follow up that limit definitive conclusions ( Warner, 2019 ).
However, a few key features of the trends in use of e-cigarettes by youth are already clear. First, even prior to widespread use of e-cigarettes, prevalence and initiation rates of cigarette smoking were falling in youth in the US, UK and Canada. E-cigarette use seems to have accelerated declines in cigarette smoking, particularly for the age group cohorts most likely to use e-cigarettes. For example, from 2010 to 2017, in the US and the UK overall cigarette prevalence fell by an absolute 5% (from 19.3% to 14.0% in the US and 20.1% to 15.1% in UK). At ages 18–24 years, prevalence in the US by 10% (from 20.1% to 10.4%) and in the UK it fell by 8% (from 25.5% to 17.8%) ( Office for National Statistics, 2018b ; Centers for Disease Control and Prevention, 2019 ).
Across the three countries, most e-cigarette experimentation does not appear to turn into regular use. In the Canadian and UK studies, the youngest age groups appear to have a greater proportion of e-cigarette among never smokers than at older ages, perhaps reflecting a shift to vaping alone. Among adolescents, most of the uptake of e-cigarettes has been among current or past cigarette smokers. In the US, among high school students (15–18 years), only 0.3% were frequent e-cigarette users (20 or more days of past 30), and 4.6% used any in the past 30 days. As compared to never smokers, cigarette smokers were much more likely to vape daily (16.9% v 0.2%), or frequently (21.8% v 0.3%) ( Levy et al., 2019 ) In the UK, among 11–18 year old vapers, only 0.8% were among never smokers, versus 40.3% of smokers and 12.2% of former smokers ( Action on Smoking and Health, 2019 ). Finally, in Canada, 83% of vapers were current (60%) or former smokers (23%) with only 16% of vapers among never smokers (but more in age group 15–19 years; Environics Research, 2019 ).
There is little evidence to justify the claim that e-cigarettes leads to increases in cigarette smoking by youth in the US ( Warner, 2019 ), or the UK ( Bauld et al., 2017 ). Notably, the reported patterns show that daily e-cigarettes use (typically over the last 30 days) remains generally lower than for cigarettes ( Levy et al., 2019 ) suggesting that while youth might be experimenting, e-cigarette is not fully displacing cigarette use. Moreover, in the US, it appears that even if increased e-cigarette use by never-smoking adolescents raises their risk of trying smoking, that effect is more than offset by the longer secular trends of falling cigarette smoking ( Warner, 2019 ).
The major increase in vaping in youth has not occurred in the UK, perhaps because regulations cap maximal nicotine content at <20 mg/ml (which are the European Union caps for cigarettes). By contrast, the current Canadian limits are 65 mg/ml and the JUUL product in the US is widely sold at 59 mg/ml. Moreover, the UK has taken mostly a harm reduction strategy toward e-cigarettes, including regulations on marketing and promotion. The US and some Canadian provinces, such as Ontario, have little regulation, and substantial social media campaigns try to increase uptake by young adults ( U.S. Department of Health and Human Services, 2020 ; Cummings and Hammond, 2020 ). Finally, there are differences across the three countries in marketing efforts, regulations, and in the effects of peer-influences in US high schools.
The most important motivator for adults in several high-income counties to use e-cigarettes has been to decrease the amount smoked or to quit ( Riahi et al., 2019 ). A Cochrane Collaboration review concluded that based on three randomized trials, that e-cigarettes containing nicotine did help smokers stop smoking in the long term compared with placebo e-cigarettes ( Hartmann-Boyce et al., 2016 ). A more recent randomized trial in the UK found that e-cigarettes achieved about twice the cessation rates at one year than did users of nicotine patches (which are well established to aid cessation; Hajek et al., 2019 ). Finally, the population-level impact of e-cigarettes on adult cessation in the US and UK suggests that their introduction has accelerated adult cessation rates somewhat ( Zhu et al., 2017 ; Beard et al., 2016 ).
In conclusion, far more epidemiological evidence is needed to settle the ongoing heated debates about e-cigarettes. The most important question is to better understand the extent to which e-cigarettes might help the very large numbers of current smokers in the world to quit, given the overwhelming evidence on the benefits of quitting cigarettes.
Smoking as a cause of disease
History of studies linking smoking to disease.
Lung cancer was a rare disease in most high-income countries in the 19 th and early 20 th centuries. By the early 20 th century, most deaths were registered and certified by doctors, and these routine mortality statistics showed a very large increase in lung cancer mortality, particularly among urban men. Several cancer registries also showed a major increase in new-lung cancer cases in men in the early 20 th century, for example some 15-fold increases in the UK. The reasons for this marked increase in lung cancer were believed to be from better detection and diagnosis or from car exhaust (as men were more exposed than women were). However, researchers also noted a large simultaneous increase in male smoking.
By the 1930s, preliminary investigation of the parallel rise in cigarette consumption and lung cancer adopted ‘case-control’ epidemiology. Two studies published in German language in 1939 and 1943 used a ‘case-control’ methodology that examined the smoking histories of adults with lung cancer in contrast to cancer-free controls ( Müller, 1940 ; Schairer and Schöniger, 1944 ). Both studies showed that most lung cancer cases smoked cigarettes. These studies were noticed within Germany ( Bachinger et al., 2008 ), but were not widely cited in the English-language scientific literature until much later, due in part to WWII. Curiously, a US mathematician, Raymond Pearl used a different method-analysis of the insurance records of 7,000 US adults from the early 1930s to report significant (perhaps implausibly large given that smoking prevalence peaked after this time period) reductions in survival among smokers ( Pearl, 1938 ; Figure 3 ).

While cited by some in the medical literature, Pearl’s finding was also largely ignored. This was, in part, because the ideas of causation in epidemiology were not well-defined, and most people dismissed these findings as chance correlations.
Major breakthroughs came with several near-simultaneous epidemiological studies published around 1950, that also used the case-control methodology, including by Ernst Wynder and Evarts Graham in the US and Richard Doll and Bradford Hill in the UK ( Wynder and Graham, 1950 ; Doll and Hill, 1950 ). The Doll and Hill paper showed that cigarette smoking was far more commonly reported among patients with lung cancer than those with other diseases or those free of disease. The obvious criticism made of these studies was that of ‘recall bias;’ meaning that those with lung cancer were more likely to remember a history of smoking than those without. However, the marked differences in the prevalence of smoking between lung cancer cases and controls were far beyond that which could be expected simply from differing memories. Moreover, Doll and Hill showed that the prevalence of smoking among a subset of men who were suspected of lung cancer but were subsequently shown to have other ailments, were very similar to the control men.
Doubts persisted in the popular press and among medical establishments, due, in part, to the fact that about 80% of UK doctors themselves smoked during the 1950s. Around 1955, further epidemiological studies confirmed the striking role of smoking in development of lung cancer using a series of prospective ‘cohort’ studies, conducted to eliminate the possibility of diseased individuals remembering their smoking history more accurately than healthy individuals. Doll and Hill recruited about 40,000 doctors in the UK. This cohort was reasonably homogenous in race, social status and other factors, had strong medical record-keeping and completed questions promptly. Doll and Hill followed groups of doctors who smoked and groups who did not. Both of these groups were otherwise similar in terms of alcohol use and exposure to air pollution. The results of the study were unequivocal: smokers of 35 or more cigarettes per day had 40 times the risk of dying from lung cancer than non-smokers ( Doll and Hill, 1964 ). Eventually, smoking prevalence fell to about 5% among the UK doctors ( Doll et al., 2005 ). Presumably, the doctors realized that smoking was not only killing their patients but also them.
In the US, Hammond and Horn (1954) published the results of a cohort study of 180,000 men that concluded that smoking was ‘beyond a reasonable doubt’ a cause of lung cancer. By 1959, Hammond and Horn also established a much larger study of 1 million US adult men and women. The results of this study showed markedly increased risk for men, but importantly, not for women, as the majority of the women had not smoked since early adolescence ( Hammond, 1966 ). The lack of finding an association of smoking with lung cancer in women was used by the tobacco industry to argue against a causative role of smoking for disease ( U.S. Department of Health, Education, and Welfare, 1964 ).
Two landmark government reports summarized the cumulative evidence. The 1962 Royal College of Physicians in the UK documented strong association between smoking and lung cancer, other lung diseases, heart disease and gastrointestinal problems ( Royal College of Physicians, 1962 ). The 1964 US Surgeon General, Luther Terry, released the Surgeon General's Advisory Committee on Smoking and Health ( U.S. Department of Health, Education, and Welfare, 1964 ). This was one of the first ‘exhaustive’ reports, covering more than 7,000 articles relating to smoking and disease in the biomedical literature. It concluded that cigarette smoking was a cause of lung cancer and laryngeal cancer and chronic bronchitis in men and a probable cause of lung cancer in women.
Subsequent to these two reports, there have been periodic systematic assemblies of global evidence on the hazards of smoking as noted above.
Importance of prolonged smoking to disease risks
The mid-century evidence on the disease risks attributable to smoking was not taken seriously, even in the countries where it was generated. This was in part because of the potentially misleading delay of several decades between cause and full effect. Increased mortality from smoking requires early uptake and continued smoking. Hence, there was a delay of up to 50 years from when the young men in any particular country took up smoking (followed by the young women taking up smoking, a decade or two later) and the time when these studies could document the main hazards in middle ages for various diseases (most notably lung and other cancers, and emphysema). However, there is a shorter latency between smoking and vascular diseases ( Jha and Peto, 2014 ).
In the US, cigarette consumption averaged 1, 4 and 10 per-day, in 1910, 1930 and 1950, respectively, after which it stabilized and subsequently fell ( Forey et al., 2016 ; Peto and Lopez, 2001 ). Peak lung cancer death rates did not however occur until after 1990 in US men and about 2005 in US women ( Figure 4 ). Indeed, measurement of the full effects of prolonged smoking from adolescence to middle-age may require 100 years to observe at the population level ( Thun et al., 2013 ). For example, the full effects of prolonged male smoking (without cessation) were reliably documented only in 2005, among UK doctors born between 1900 and 1930, who were tracked and followed for mortality until the last re-survey in 2001. The UK doctors born between 1900 and 1930 represented those with the highest prevalence of smoking as adults and those who smoked from early adult life. In other words, these doctors represented ‘peak exposure’ measured at the population level ( Doll et al., 2005 ).

Adapted from American Cancer Society (2013) .
Smokers who start smoking may not feel any of the major ill effects until years or decades later, making the link of smoking to disease counter-intuitive. This underestimation of smoking-related health risks in adolescence is particularly relevant to the increased risk of developing cancers from smoking in early-adult life. For example, the risk of developing lung cancer is far higher in individuals who begin smoking at age 15 and smoke one pack of cigarettes a day until they turn 45, than those who start at age 30 years and smoke two packs a day until age 45 years ( Peto, 1986 ). In both instances, the total amount smoked is equal, but early and prolonged smoking markedly increases the risk of lung, and likely, other cancers. (Clinicians often determine their patients’ ‘pack years’ of smoking, but this fails to distinguish those at markedly higher risk because they started early).
The two major sources of evidence on prolonged exposure are national lung cancer mortality data or prospective studies that follow smokers and non-smokers for the development of disease. Lung cancer trends are useful in high-income countries, including Canada, which have had high completeness of death certification and reasonably reliable certification of the causes of death by physicians. Death certification and causes of death are more reliable in middle-age (ages 30–69 years) as compared to older ages (age 70 or older). This various reasons for the difference in reliability have been reviewed earlier ( Doll and Peto, 1981 ; Jha, 2014 ).
The age-specific patterns of lung cancer deaths provide a very useful way to examine the relevance of age-specific smoking. Lung cancer is nearly entirely caused by smoking in high-income countries (exposure to indoor air pollution from solid fuel use does account for a substantial proportion of lung cancer, particularly in women, in China [ Liu et al., 1998 ]), though such exposure has been uncommon in high-income countries for most of the last century). Moreover, careful reviews of lung cancer rates in mostly non-smoking populations (such as women in Asia), and in prospective studies has shown that rates of lung cancer among non-smokers are substantially lower than among smokers and have changed little over the last few decades ( Thun et al., 2008 ).
Closer examination of national lung cancer mortality trends at specific and reasonably narrow ages provides insight on the importance of prolonged and early smoking to subsequent mortality risks. Lung cancer trends can then be related to age-specific different levels and patterns of smoking recorded for different generations. Consider the trends in lung cancer in three age groups separated by two decades (representing roughly one generation): 35 to 39, 55 to 59 and 75 to 79 years. Figure 5 shows that among 35 to 39 year-old and 55 to 59 year-old men, the peak lung cancer death rates occurred around 1970 and 1990 in the US and in Canada, respectively. These men, who died in 1970 and 1990, were born, on average, in 1933 (= 1970–37 and = 1990–57). This means that the typical age of uptake of smoking for these men would have been in the decade after WWII. This represents the period during which a substantial increase occurred in per capita cigarette consumption in both countries ( Figure 2 ). For men aged 75–79, the peak lung cancer deaths in the US and Canada occurred in 1990 and thus correspond to a mean birth year of around 1913. This generation of men in both countries had particularly heavy exposure to high-tar cigarettes and likely smoked in different subtle fashion, in terms of puffing, inhalation, and other features than subsequent generations.

A more consistent pattern emerges when examining death rates and smoking patterns in the UK. Here, the lung cancer death rates had peaked about two decades earlier among UK men aged 35 to 39, 55 to 59 and 75 to 79 years, representing a mean year of birth of 1903. This also corresponds to the observation that the peak increase in male smoking occurred between WWI and WWII in the UK but during and after WWII in the US and Canada. These data also support the stronger likelihood that most of the cigarettes smoked and the manner of their smoking were more similar over time in the UK than they were in the US ( Doll and Peto, 1981 ).
As a further comparison, men in Sweden never took up smoking at levels observed in other Western countries. This lack of increase in smoking has been attributed mostly to the widespread use of ‘snus’, which provides rapid nicotine stimulus to the brain with similar rapidity as cigarettes, in Sweden ( Ramström et al., 2016 ).
In Swedish men aged 55 to 59 years, the peak lung cancer death rates in Sweden were only a quarter of that seen in UK men. Moreover, the mean age of birth of the men in the three age comparison groups was approximately 1938; meaning Swedish men who took up smoking during so the 1960s.
Similarly, the lung cancer death rates in women peaked at these age groups about two decades later than that of men (and indeed have plateaued in older women aged 75–79 only recently). These findings also correspond to the period in which women typically born around WWII began to smoke heavily in the 1960s.
The robustness of such analyses is of course affected by differences in death certification and coding of lung cancer ( Doll and Peto, 1981 ). In all three countries, lung cancer is a reasonably distinct diagnosis, particularly before older ages (about 70 or 80 years of age), and nearly 100% of deaths from about 1950 onward were medically certified. The trends in the death rates from lung cancer in various age groups from 1960 to 2010 have been reasonably similar in the US and Canada, which is expected given the similarities in the causes of death ( World Health Organization, 2016 ), smoking patterns ( Figure 1 ), and the procedures for certifying both death and lung cancer in the two countries. Note, however that the US peak rates at ages 35 to 39 years in men, are about double that of Canadian men, though similar at ages 55 to 59 years and 75 to 79 years. This may be due in part to smaller numbers of lung cancer deaths in the smaller Canadian population, or, may reflect subtle differences in the type of smoking or undocumented differences in the types of common cigarettes smoked between the two countries ( Fischer et al., 1990a ; Fischer et al., 1990b ). The cohorts of men and women born after 1950 have mostly smoked lower-tar cigarettes than the men who began to smoke either between the two World Wars or just after WWII.
Earlier careful review of US lung cancer death rates in prospective studies of US veterans finds that lung cancer risks are particularly elevated among those who began to smoke significant amounts from early adulthood ( Doll and Peto, 1981 ). The age-specific relationship of smoking to lung cancer is likely similar for selected other cancers, particularly upper aerodigestive cancers, though this relationship likely differs for other diseases made more common by smoking. Prolonged smoking and early initiation appear to be a particularly relevant risk factor for emphysema and chronic lung diseases. Vascular disease is more responsive to short-term effects given the role of smoking in causing vascular spasm and in the shorter time period for development of atherosclerotic plaques, which cause heart attacks and strokes.
The peak mortality effect of smoking among men occurred in most high-income countries in the last quarter of the 20 th century. The full effects of persistent smoking on premature mortality in women can be assessed only in the first quarter of the 21 st century. In the US, the lung cancer death rate among women who never smoked has been low and approximately constant for many decades, while the lung cancer rate among women who smoke has been increasing steeply. The US female lung cancer death rate ratio (current-smoker versus never-smoker), has increased greatly over the last half-century ( Figure 6 ). In the 1960s, it was 3-fold; in the 1980 s, 13-fold and in the 2000 s, 26-fold (similar to the death rate ratio among men in the US [ Thun et al., 2013 ] or among men or women in the UK [ Pirie et al., 2013 ]).

Adapted from U.S. Department of Health and Human Services (2014) .
This is because US women aged about 60 years who were smokers in the 2000s had smoked since early adult life, whereas women who were smokers in the 1960s had not. Similar relationships are seen for chronic lung-disease. The key implication is, of course, that the hazards among men and women from various diseases are now comparable among women and men who start early in life and do not quit smoking.
Quantifying mortality from smoking in the US, UK and Canada from 1960 to 2020
Peto et al. (1992) developed a method that provides indirect estimates of tobacco-attributable mortality across countries which have reasonably high coverage and quality of routine death certification, including most high-income countries. This is based on the observation that most lung cancer deaths occur among smokers, and that non-smoker lung cancer rates are comparably low across most high-income countries and have been mostly unchanged over the last few decades ( Thun et al., 2008 ). Lung cancer is then used as an indicator not only of the extent to which smoking causes lung cancer, but also to what extent if that particular population is affected by smoking exposure. This involves indexing the absolute lung cancer deaths (subtracting the low rates among non-smokers) to the relative risks from the large US prospective studies (effectively very similar to the USSGR relative risks shown in Appendix 1—table 1 ). This allows a reasonable estimate of the extent to which cancers other than lung, respiratory disease, ischemic heart disease, stroke and other causes of death are caused by smoking.
Use of lung cancer as an index of smoking is a crude method but is reliable over time, and useful in settings that meet these conditions such as by social strata ( Jha et al., 2006 ) and including men in north Mexico, but not in South Mexico ( Reynales-Shigematsu et al., 2018 ). The Peto estimates (updated to 2015; Peto et al., 2018 ) provide totals for 1955 to 2015 and I interpolated the annual results using the trends per decade. I did backward calculations to 1950 using the same annual rate of change as documented between 1955 and 1965.
These reveal that cummulatively from 1960 to 2020, there were about 29.5 million, 9.3 million and 2.6 million deaths from smoking in the US, the UK and Canada, respectively ( Table 2 ) or a total of 41.3 million adult deaths. Over 60% of these deaths occured in males, and these collectively represented about 22% of all adult deaths in these three countries. Of these deaths, about 40% were between ages 35-69 years, comprising about 16 million deaths, with an average loss of life of about 20-25 years. The remainder of the deaths occured after the age of 70 years.
* 1960-2020 * 1960–2020 totals by taking totals for 1965, 1975, 1986, 1995, 2005 and 2015 totals multiplied by 10. Note. Author’s calculations based on Peto et al. (2018) .
Cumulatively, from 1960 to 2020, smoking killed about 29.5 million Americans, 9.3 million UK residents, and 2.6 million Canadians, or a total of 41.3 million adults ( Table 2 ).
Globally, there were about 6 trillion cigarettes consumed worldwide, of which about a third are consumed in China alone. Global consumption has increased from about 5 trillion cigarettes in 1990 ( Jha and Peto, 2014 ). For the US, UK and Canada I obtained cigarette sales data from global smoking sales statistics ( Forey et al., 2016 ). Under tobacco reporting regulations by the federal government of Canada, tobacco manufacturers and importers must give Health Canada annual reports that include sales data manufacturing information and product information. These data are publicly available on an aggregated industry basis. As such, the reporting of sales of tobacco in Canada over time is more reliable versus that of other countries. I lagged the ratio of deaths to cigarette smoke by 20 years to take into account the delay between the uptake of smoking and the development of disease as I have discussed above.
During this same period, cigarettes sold in the US, UK and Canada were about 32.6 trillion, 7.0 trillion and 3.2 trillion, respectively. Using the 20 year lag between smoking and disease development as a reference point, the relationship of total cigarette sales in Canada and in the US suggests approximately every 1.0 to 1.2 million cigarettes smoked yielded one death ( Figure 7 ). This estimate is consistent with another published in 2014 using global sales ( Jha and Peto, 2014 ). However, for the UK, the relationship shows that every million cigarettes smoked yielded 1.3 deaths. This might reflect the composition of cigarettes, and the use of higher-tar cigarettes in the UK with the peak of smoking occurring prior to WWII.

Note. Author’s calculations.
In 2014, cigarettes sales in billions in the US, UK and Canada were 263, 51 and 30, respectively, each of which in absolute terms is a substantial decline from the peak annual sales. Nonetheless, the absolute sales have remained steady since about 2005 in Canada, but with continuing declines in the US and UK. An increase in sales in Canada from 1993 to 1995 was in response to a well-funded tobacco industry effort to smuggle its own products and to force a reduction in the tax rate ( World Bank, 2019 ). The effects of the smuggled cigarettes, both in direction consumption but also in reducing prices of legal cigarette (which raised consumption) were approximately 30 to 40 billion excess cigarettes over a decade. Hence, eventually, about 30,000-40,000 Canadians will be killed from this excess consumption ( Jha et al., 2020 ).
These sales do not, of course, adjust for population size and growth. However, that is deliberate. If the goal is to quantify the extent to which cigarette sales translate into future deaths, then the absolute sales totals and absolute death totals is a relevant statistic.
Smoking risks for total mortality and for specific conditions
Key messages for the individual smokers.
The main messages for smokers, based on the contemporary epidemiological evidence are three-fold ( Box 1 ).
Three main implications for individuals who become cigarette smokers in adolescence or early adult life.
- Continued smoking eventually kills at least half of men and women who smoke. Among persistent cigarette smokers, whether men or women, the overall relative risk of death throughout middle-age and well into old age is at least twofold higher than otherwise similar never-smokers. Among smokers of a given age, more than half of those who die in the near-future would not have done so at never-smoker death rates.
- On average, smokers lose at least one decade of life. This average combines a zero loss for those not killed by tobacco with the loss of much more than one decade for those who are killed by it.
- Some of those killed in middle-age might have died anyway, but others might have lived on for another 10, 20, 30, or more years.
- On average, those killed in middle age lose about 20–25 years of never-smoker life expectancy.
- Those who stop smoking before age 40 avoid more than 90% of the excess risk among those who continue to smoke. Those who stop smoking before age 30 avoid nearly all of the smokers’ excess risk.
- Those who have smoked cigarettes since early adult life but stop at 30, 40, 50, or 60 years of age, gain, respectively, about 10, 9, 6, and 4 years of life expectancy, compared with those who continue smoking.
Source: Author’s calculations from various citations.
Here, I elaborate on the first two of these messages. A following section on cessation provides greater details of the benefits of cessation.
First, the risk is big. Large epidemiological studies in the UK ( Doll et al., 2005 ; Pirie et al., 2013 ), US ( Jha et al., 2013 ; Thun et al., 2013 ), Japan ( Sakata et al., 2012 ), and India ( Jha et al., 2008 ; Jha et al., 2015 ) have examined the eventual effects on mortality in populations where many began to smoke cigarettes seriously in early adult life and did not quit smoking ( Figure 8 ). Among persistent men or women cigarette smokers, the overall relative risk of death throughout middle age and well into old age is about two to three-fold higher than otherwise similar people who never begin smoking. Among smokers of a given age, more than half of those who die in the near future would not have done so at the rate of people who never smoked.

Adapted from Jha and Peto (2014) , p. 62.
This increased risk is now seen among women who began smoking early in adult life and did not quit, chiefly those women born around WWII. The loss of a full decade of life is seen, surprisingly, among male cigarette smokers in India, despite the later age of uptake and generally fewer cigarettes smoked ( Jha et al., 2008 ). These findings further suggest that 3-fold higher death rates among persisting smokers represents that of a fully-mature smoking epidemic, given the fact that the late 20 th century risk among women also reached 3-fold of that versus non-smokers, as observed for men two decades earlier.
Secondly, many of those killed are of middle age. On average, those killed at ages 35–69 years lose 23 years of life in the US, UK or Canada ( Peto et al., 2018 ). This continued difference in risk throughout middle age and into old age leads to an overall reduction in survival by an average of one decade ( Figure 8 ). The decade of lost life expectancy for typical smokers combines a zero-loss for some of the smokers who are not killed by smoking and about a 20 to 25 year loss for those smokers who are killed by smoking.
Although there has been a decrease in the amount of smoking in recent years in US, UK and Canada as noted in Table 1 the contemporary epidemiological evidence finds that smoking as little as five cigarettes a day is substantially hazardous ( Pirie et al., 2013 ). Despite the reduction in smoking amount, smoking will continue to be a major cause of excess mortality among the significant minority of adults that remain smokers.
Similarly, careful reviews ( Doll and Peto, 1981 ), and recent use of indirect-based methods that rely on lung cancer mortality to estimate smoking-attributable deaths ( Peto et al., 1994 ), find that the age-standardized rates of cancers not attributable to smoking are falling in Canada (and in nearly all high-income countries). This is contrary to popular misperceptions about an ‘epidemic’ of cancer.
The 21 st century evidence suggests that there is an eventual risk of about three-fold mortality rate versus that of non-smokers, corresponding to about two-thirds of smokers being killed eventually by their addiction. Hence, the effect on total mortality is an appropriate starting point to quantify smoking hazards in high-income countries, which is supported by the specific evidence on particular diseases.
Key diseases attributable to smoking
The evidence for the range of diseases caused by smoking has expanded considerably since the early studies focusing mostly on lung cancer. Importantly, the leading causes of death that are due to smoking are also the major diseases that, even in non-smokers, constitute the leading causes of death in US, UK and Canada. In each country, vascular, neoplastic, and respiratory disease collectively accounted for about 75% of all current adult deaths from all causes ( World Health Organization, 2016 ).
Given the strong evidence that at every age, smokers have about a two to three-fold higher death rates versus otherwise similar non-smokers, the key issue here is to analyse if the specific conditions that contribute to higher overall excess risk of death is, in fact, due to smoking. This in turn requires scrutiny of all the scientific evidence linking smoking with particular disease and careful analysis of ‘negative’ studies that do not find an association between smoking and disease or, indeed, find that smokers have lower rates of disease than non-smokers. To avoid ‘publication bias,’ where positive results linking smoking and disease are published, but negative studies that do not support this link remain unpublished, researchers have outlined methods of comprehensive searches of all available scientific literature, and statistical methods to ascertain the likely extent of negative studies sitting on the shelf, impacting final conclusions ( IARC Working Group on the Evaluation of Carcinogenic Risk to Humans, 2004 ; U.S. Department of Health and Human Services, 1989 ). Of course, the publication bias would almost certainly go in the other direction for most internal tobacco-industry studies, many of which remain outside searchable scientific arenas.
The US Surgeon General and the IARC have periodically assembled expert groups for such systematic reviews. These expert groups use slightly different criteria to assess the strength of the evidence. The USSGR definitions use three levels: ‘sufficient evidence’ in terms of the risk of a particular disease to smoking (or, less commonly, a protective effect of smoking), suggestive evidence, or insufficient evidence. Figure 9 shows the adult anatomic sites and cancer sites of which the 2014 USSGR linked to smoking. The bolded text represents those conditions, which are newly deemed to have ‘sufficient’ links to smoking.

The list of tobacco-attributable conditions is expanding over time, as highlighted in the 2014 USSGR. This suggests that overall mortality is a robust and valid metric to estimate tobacco-attributable risk (particularly, that since there are very few diseases reduced by smoking, a focus on total mortality is not misleading). Note further that for most conditions there is a strong correlation between death and disability ( Menon et al., 2019 ), with only a few exceptions, such as loss of teeth or rheumatoid arthritis, conditions that cause far more disability than mortality. The use of mortality totals is likely to also reflect also on disability totals.
Avoidable proportion of major diseases at non-smoking death rates
The 2014 USSGR published for relevant age groups and for men and women, the relative risks (RR) for various conditions, after adjusting for differences in age, alcohol use, obesity, education or some related measure of social status. This full table is attached as Appendix 1—table 1 .
The main sources of the USSGR estimates include the second US prospective cancer study, which surveyed one million Americans, the CPS II study, and the results from five pooled studies of more contemporary cohorts, represent the most recent period (2000–2010). These include the National Institutes of Health–American Association of Retired Persons Diet and Health Study ( Schatzkin et al., 2001 ), the American Cancer Society CPS II Nutrition Cohort (a subset of the original CPS II mortality study [ Calle et al., 2002 ]), the Women's Health Initiative ( Paskett et al., 2007 ), the Nurses' Health Study ( Holmes et al., 2007 ) and the Health Professionals Follow-up Study ( Kenfield et al., 2011 ). These represent US results, but similar results have been reported in Canada with smaller sample sizes ( Manuel et al., 2012 ). Similarly, among women and men the nationally representative US National Health Interview Study reported similar relative risks for lung cancer, vascular and respiratory disease ( Jha et al., 2013 ), as did the Million Women Study in the UK among women ( Pirie et al., 2013 ). Finally, the prospective study among Japanese Atomic survivors also reported similar relative risks ( Sakata et al., 2012 ). For the most part, the smoker: non-smoker relative risks were unaffected by adjustments for other risk factors in most of the studies, even though smokers tend to drink alcohol more commonly, and have lower education levels.
Table 3 provides the avoidable proportion of deaths for each major disease. This is calculated by (RR-1)/RR with the RRs derived from the USSGR report of 2014. This analysis shows that among smokers, over 90% of deaths from lung cancer at various ages or chronic obstructive deaths at ages 65 or older would have been avoided at non-smoking death rates, reflecting the very high relative risks of smoking for these conditions. About half to four-fifths of coronary heart disease deaths among smokers would have been avoided; the proportion avoidable was even larger in younger adults. Approximately a third to half of stroke deaths among smokers would have been avoided. Overall, up to two-thirds of all deaths among smokers would have been avoided at non-smoking death rates.
Notes: Author calculations. The avoidable proportion for each condition and sex is calculated as (RR c -1)/RR c , where RR c refers to the smoker: non-smoker relative risks (RR) for current smoking in the U.S. Department of Health and Human Services (2014) (Appendix 1).
The avoidable proportion should be taken as conservative, as the relative risks in the USSGR report may be underestimates. The prospective studies had enrolled smokers and non-smokers before they developed disease, and smoking status was collected only at this baseline. Some of those who reporting smoking at baseline would have quit subsequently, as there have been, in recent years, increases in cessation by older adults. This cessation would reduce their risk of death, bringing them closer to the observed mortality rates of non-smokers. Had they not quit, the observed differences in relative risks between smokers and non-smokers would most likely have been larger.
Understanding the contemporary risks: specific conditions
Cancers, vascular and respiratory disease.
Cancers : The USSGR ( U.S. Department of Health and Human Services, 2014 ). and IARC Reports ( IARC Working Group on the Evaluation of Carcinogenic Risk to Humans, 2004 ) have previously concluded that there are sufficiently strong associations to define tobacco use as a cause of several cancers including lung, tongue, lip, larynx, oropharynx, bladder, kidney, oesophagus, stomach, pancreas, cervix and liver.
The 2014 USSGR also found that existing strong evidence for smoking as a cause of squamous cell lung cancer in men is strongly enforced by recent evidence of these links in women, who typically begin smoking later in life. Moreover, among smokers, the risk of developing adenocarcinoma of the lung has risen since the 1960s. This increased risk is likely the result of changes in the design and composition of cigarettes, which might include use of ventilated filters (leading to deeper inhalation of tobacco smoke), and perhaps changes in nitrosamines levels since the 1950s. There is sufficient evidence for a causal relationship between smoking and hepatocellular cancer. The report noted a suggestive relationship of smoking to adenomatous polyps and colorectal cancer. Smoking was found not to be a cause of new prostate cancers, though it is important to note that smokers do have high risks of death if diagnosed with prostate cancer, as well as a greater chance of more advanced and poorly differentiated cancers.
Cardiovascular disease , including coronary artery disease, stroke, aortic aneurysm, and peripheral artery disease, is the leading cause of death in most countries worldwide. Hence, while the relative risks of smoking for specific vascular diseases are smaller than that for cancers and respiratory disease, vascular mortality dominates the absolute burdens of tobacco-attributable diseases in many countries.
The chief finding from the 2014 USSGR Report and the more contemporary cohort studies is that the smoker: non-smoker mortality risks for ischemic heart disease have become more extreme over time. This is due in part to rapid improvements in the treatment of vascular disease that have contributed to rapidly falling background rates among non-smokers. By contrast, smokers are not receiving the full benefit of technologies that benefit non-smokers ( Jha et al., 2013 ).
The relative risks for non-fatal heart attack are greater than those for fatal heart attack ( Table 4 ). This would suggest, for example, that the true population burden of smoking-attributable ischemic heart disease for the number of hospital admissions is much larger than that derived from mortality studies. Moreover, the relative risks are greater at younger ages, so that at ages 30–39, about 80% of the heart attacks in UK men can be attributed to smoking ( Parish et al., 1995 ). Naturally, the absolute rates are greater at older ages.
Note. Author’s calculations based on an earlier review ( Jha et al., 2010 ).
For respiratory disease , including emphysema and chronic bronchitis, there have also been substantial increases in mortality among smokers in the last two to three decades, with the smoker: non-smoker hazards becoming particularly extreme among women ( Thun et al., 2013 ). The 2014 USSGR also identified that smoking as a cause of tuberculosis death and recurrent tuberculosis, but stated that evidence was not sufficient to evaluate if smoking causes infection. While tuberculosis deaths and infection are uncommon in Canada, they remain a major cause of death in low and middle-income countries ( Bates et al., 2007 ; Gajalakshmi et al., 2003 ). Smoking compromises the immune system, which leads to increased risk of pulmonary infection, as well as loss of voice.
Other outcomes
The 2014 USSGR added newer conditions that were not listed as being causally related to smoking in the 2004 USSGR. Maternal smoking in early pregnancy is a cause of orofacial clefts and might be linked to clubfoot, gastric and vascular malformations. Maternal smoking might be linked to behavioural disorders and attention deficit in children. Smoking is a cause of ectopic pregnancy, and of erectile dysfunction in men. Rheumatoid arthritis, congenital effects and colorectal cancer are possibly attributable to smoking.
Diseases not attributable to smoking or protected by smoking
Some conditions are not sufficiently proven to be caused by smoking, or are (less commony) reduced by smoking. These include Alzheimer’s disease, breast cancer, inflammatory bowel disease and uterine cancer. A popular myth is that smoking protects against dementia and Alzheimer’s disease. However, the UK doctor’s prospective study ( Doll et al., 2005 ) noted that dementia risks were unaffected by smoking history. A systematic review of about 50 epidemiological studies found that smoking modestly raised the risk for Alzheimer’s but had no effect on the development of dementia ( Peters et al., 2008 ). The 2014 USSGR noted that there is some evidence that smoking reduces the risk of endometrial cancer in women. Among the inflammatory bowel diseases cases, smoking might reduce ulcerative colitis but raise the risks of Crohn’s disease. Finally, the 2014 USSGR found that there was no definitive evidence that smoking causes breast cancer.
The presence of some diseases not attributable to smoking strengthens the argument about the causal nature of the link between smoking and specific diseases. The strength of association of various conditions to smoking also varies, as defined by the relative risk of death between otherwise similar smokers and non-smokers. For example, there is a strong and consistent relationship of tobacco smoking to lung and many upper digestive cancers. By contrast, the relationship between smoking and colorectal cancer is weaker. However, the excess risk for almost all of these conditions is likely causal. Thus, the strength of the association is less relevant for public health action than is the list of the most common conditions in the population that accrue the largest absolute number of deaths.
Reductions in total and in cause-specific mortality from smoking cessation
In contrast to the long delay between smoking onset and the development of disease, the main effects of widespread cessation are seen much more rapidly. Worldwide, cessation is the only practicable way to avoid a substantial proportion of tobacco deaths before 2050 ( Jha and Chaloupka, 1999 ), as a substantial reduction in uptake by adolescents will have its main effect on mortality rates after 2050.
Cessation trends in US, UK and Canada
The prevalence of former smoking in middle-age is a useful measure of the success of tobacco control. Currently in Canada, the US and the UK, there are as many former as current smokers between the ages of 45 to 64 years ( Figure 10 ) The short-term relapse rates among smokers considering cessation is very high. However, among those who persist in cessation, few re-start smoking.

Note. Data from National Center for Health Statistics, 2017, NHIS , Office for National Statistics, 2017, Adult Smoking habits in Great Britain ; Statistics Canada, 2016, Canadian Community Health Survey.
There is a large gap in high-income countries between the intent to quit smoking and actual success rates. This is mostly a consequence of the strongly addictive nature of cigarettes. Two-thirds of smokers wish to quit, while only about half of that actually try, while far fewer succeed ( U.S. Department of Health and Human Services, 2020 ). In 2015, nearly two-thirds (65.8%) of Canadian smokers were seriously considering quitting in the next six months. Of those, about half (48.2%) were considering quitting within the next thirty days, which was equivalent to 31.1% of all current smokers. Between 1999 and 2015, the percentage of Canadian smokers seriously considering quitting in the next six months appears to have increased slightly ( Reid et al., 2017 ). In 2015, over half (52.3%) of Canadian smokers and recent quitters reported having made at least one attempt at successful cessation in the past year, while more than one-third had made multiple attempts. From 1999 to 2015, the percentage of smokers and recent quitters who had attempted to quit in the past 12 months appears to have remained fairly stable, at around half ( Reid et al., 2017 ). The US and the UK reports similar patterns of attempted cessation ( Babb, 2017 ; Office for National Statistics, 2018b ).
Reduction in overall mortality from cessation
Smokers who stop smoking before age 40 (preferably well before age 40), avoid more than 90% of the excess risk for overall mortality among those who continue to smoke. Those who stop before age 30 avoid 97% of the risk of death. Those who have smoked cigarettes since early adult life but stop at 30, 40, or 50 years of age gain, respectively, about 10, 9, and 6 years of life expectancy, compared to those who continue smoking ( Jha et al., 2013 ; Pirie et al., 2013 ).
The reductions in smoking risk for all deaths and for lung cancer mortality among women in the UK are shown in Figure 11 . Very similar results were seen in the US for these same age groups among men and women ( Jha et al., 2013 ). The smoker/non-smoker risks quickly converge for vascular disease, for some cancers other than lung, though less quickly for lung cancers, with intermediate convergence for respiratory disease. The overall persisting hazard for death from any cause is reduced but not eliminated. For those who smoke until age 40 years and then stop, the remaining excess risk of about 20% (relative risk, 1.2, hence 120% risk less 100% baseline risk = 20% excess risk) is substantial and implies that about one in six of these former smokers who dies before the age of 80 years would not have died if their death rates had been the same as otherwise similar non-smokers. However, this 20% excess has to be compared to an excess risk of 200% if they continued to smoke (RR = 3, hence 300% risk less 100% baseline risk = 200% excess risk). Similarly, for lung cancer, quitters by age 40 retain a substantial excess risk of 230%, but this is dwarfed by the 2000% excess risk from continued smoking. In both cases, the relative reduction in excess risk among former versus current smokers exceeds 90%.

Adapted from Pirie et al. (2013) , p. 138.
Similar results on reductions in lung cancer risk in former smokers are seen in other settings. The excess lung cancer mortality avoided in men who stopped smoking by age 40 was 91% in Germany and 80% in Italy ( Crispo et al., 2004 ). In countries such as Canada, the UK, US or Poland, where high mortality rates from smoking were followed by widespread cessation, mortality from smoking has greatly decreased, for example by 25% per decade in Canada ( Peto et al., 2018 ; Jha, 2009 ).
Earlier reviews note that the relationships of excess-risk for overall mortality with halving smoking amount reduces mortality risk far less than cessation ( U.S. Department of Health and Human Services, 2014 ). This would imply that the mean reduction in daily amount smoked in the three countries from 1999 to 2013 (about three cigarettes fewer, per day, per smoker; Table 1 ) has had only a minimal impact on the risk of death. Cessation remains far more important than reduced smoking amount.
Reduction in specific diseases from cessation
The US Surgeon General has issued a series of reports on the health benefits of smoking cessation starting in 1990 ( U.S. Department of Health and Human Services, 1990 ). Those conclusions were updated in subsequent reports in 2001, 2004, 2006, 2010, 2014 and 2020. A brief summary of the effects of cessation on cardiovascular disease, cancers and respiratory disease follows.
Cardiovascular disease: In patients with existing heart disease who smoke, cessation significantly reduces all-cause mortality, deaths due to cardiac causes, sudden death and the risk of both new and recurrent cardiac events. The reduction in risk of recurrence or death is estimated to be about 30–45%. Smoking cessation benefits people at any age, but the benefits are greater at younger ages compared with older ages ( Parish et al., 1995 ). The risk of coronary heart disease falls rapidly after cessation and then declines more slowly. The excess risk falls by about half after five years of cessation and then gradually approaches the risk of people who have never smoked. Smoking cessation also reduces inflammatory markers and hypercoagulability, rapidly improves the levels of high-density lipoprotein cholesterol (which protects against heart attack), and may lead to improved endothelial function. Smoking cessation reduces the development and progression of markers of subclinical atherosclerosis, with larger reductions shown in cases where the cessation period has been substantial.
In patients with existing stroke, smoking cessation reduces risk of stroke morbidity and mortality. The evidence is strongest for subarachnoid haemorrhage and less consistent for intracerebral haemorrhage. After some years of smoking cessation, the risk of stroke approaches that of those who never smoked.
Respiratory disease: Smoking cessation reduces asthma symptoms, improves treatment outcomes and asthma-specific quality of life scores among persons with asthma, and improves peak expiratory flow among persons with asthma who smoke. However, it is not sufficiently clear if smoking cessation among smokers lowers the risk of developing asthma. Indeed, the extreme smoker: non-smoker risks for respiratory disease, particularly for emphysema, match that of lung cancer ( Thun et al., 2013 ). The benefits of cessation, once disease has begun, may have less impact on lung cancer and emphysema than on some other cancers and cardiovascular disease.
Cancers : Smoking cessation reduces risk of cancers of the lung, larynx, oral cavity and pharynx, oesophagus, pancreas, bladder, stomach, colon, rectum, liver, cervix and kidney, and acute myeloid leukemia.
Estimates of the reduction in excess risk among former smokers
The USSGR 2014 published also a summation of the relative risks for former smokers, based on the prospective studies noted above. A comparison of excess risk, meaning RR-1 (the risk among non-smokers) for both former smokers and current smokers is informative. Based on the RRs in the USSGR report, I calculate the relative reduction in excess risk for various specific conditions ( Table 5 ).
Notes: Author calculations. The reduction in excess risk for each condition and sex is calculated as (1- [RR f -1)/ [RR c -1]), where RR f and RR c refer to the smoker: non-smoker relative risks (RR) for former and current smoking, respectively in the U.S. Department of Health and Human Services, 2014 (Appendix 1).
This analyses shows that, depending on age and sex (and age of cessation, which is not considered in the USSGR 2014 estimates), that versus current smokers, former smokers have about at least a three-quarters reduction in mortality from lung cancer, stroke and coronary heart disease. Reductions in excess mortality risk from chronic obstructive pulmonary disease are also about three quarters for men, but notably smaller in women. Overall, former smokers have only about a quarter of the excess risk of overall mortality versus continued smokers.
The true gain of life-years from the time of cessation could be somewhat greater than implied from Table 5 . Some deaths may well reflect deaths among smokers who quit because they became ill. Large scale, well-designed epidemiological studies consider this possible ‘reverse causality’ by, for example, excluding the first few years of follow-up data ( Banks et al., 2015 ; Jha et al., 2013 ; Pirie et al., 2013 ; Thun et al., 2013 ). The reductions in risks are of course strongly dependent on the age at smoking, and the calculation of RR among former smokers is likely not a robust as those for current smokers, as these prospective studies had slightly different definitions of former smoking and due to various adjustments to take into account reverse causality.
Biological evidence of smoking hazards
Thus far, I have focused on the epidemiological evidence of the causal links of smoking to specific diseases and to overall mortality. Here, I turn briefly to the biological evidence. A common criticism of the epidemiological studies is that the exact ‘mechanism’ that causes smoking to induce lung cancer has not yet been identified. This is mostly irrelevant. As Thun et al. (2002) point out, the epidemiological evidence of association is so strong between smoking and various diseases, that further biological evidence on mechanisms is not required to establish causality. Moreover, as smoking causes a wide range of diseases, it is likely different biological mechanisms apply (for example, there may be different mechanisms at the cellular level in cancers than in cardiovascular diseases).
Doll and Peto (1981) illustrate that human population trends have distinct advantages in studying smoking as an exposure. In Canada, the US and the UK, there have been substantial earlier increases and more recent decreases in smoking-attributable mortality and from specific conditions from about 1970. During that time period, the genetic susceptibility of the relevant populations has not likely changed; say, towards reduced expression of the genetic factors that predict lung cancer or genetic factors that decrease addictiveness to nicotine. Increases and the more recent decreases in smoking account for most of the dramatic changes in smoking-attributable diseases in recent decades; genetics has likely played only a minor or no role in explaining the marked changes in tobacco-attributable mortality in recent decades.
Biologic evidence on nicotine addiction
The nicotine in cigarettes is the central ingredient that leads to initiation and sustained smoking. Prior to about the mid-1980s, the common understanding was that tobacco use did not qualify as a drug addiction ( Koop, 2003 ). The UK’s Medical Research Council and the US Surgeon General’s Office began to review their evidence using the logic that tobacco prevention and addiction treatment required a better understanding of the addictive properties of nicotine and cigarettes as an effective and toxic delivery system. The findings of the 1988 US Surgeon General’s report suggest that cigarettes and other forms of tobacco (such as chewed tobacco) are addicting and that nicotine is the major agent responsible for this addiction ( U.S. Department of Health and Human Services, 1988 ). These findings have been supported by many subsequent studies and reports. In 2000, the British Royal College of Physicians concluded: “ Nicotine is an addictive drug, and the primary purpose of smoking tobacco is to deliver a dose of nicotine rapidly to receptors in the brain…Tobacco smoke inhalation is the most highly-optimized vehicle for nicotine administration…” ( Royal College of Physicians of London, 2000 ). In most aspects of dependence, nicotine is on par with other powerfully addictive drugs, such as heroin and cocaine.
The epidemiological evidence on smoking trends and consequences is now supported by better understanding of the neurobiological mechanisms of nicotine reinforcement and dependence. Though there are over 4,000chemicals found in cigarette smoke, there is little doubt that nicotine is the major component responsible for tobacco addiction.
Nicotine is a psychoactive drug that appears to trigger a cascade of neurobiological events in the brain and throughout the body which can, in turn, act in concert to reinforce tobacco use and affect subsequent behaviour ( Markou and Henningfield, 2003 ). Much of the psychoactive effects of nicotine can be attributed to its rapid delivery to the brain. Absorption of cigarette smoke is accelerated and complete, with delivery of nicotine to the brain almost 10–16 seconds faster than by intravenous injection ( Jarvis, 2004 ). Moreover, each subsequent exposure to cigarette smoke leads to the establishment and strengthening of tolerance to the adverse effects of nicotine, physiological dependence and the biologically rewarding effects of nicotine. This cascade of effects can lead to increased self-administration and progression of the dependence process. It is not known if all nicotine-induced changes in brain function, such as tripling of the levels of certain brain neurotransmitters in some brain regions ( Perry and Chalkley, 1982 ), and alterations of brain nicotine reinforcement systems ( Laviolette and van der Kooy, 2004 ; Mansvelder et al., 2002 ), are fully reversed after nicotine abstinence. It is plausible that persisting brain alterations may confer a continuing need for nicotine in some individuals ( Henningfield and Slade, 1998 ). While all adults are susceptible to the biological effects of nicotine, it also appears plausible that early onset of use is associated with a higher risk of developing dependence. Jarvis notes that, “ in experimental models, if nicotine’s neurobiological effects are blocked pharmacologically, or if nicotine is removed from cigarette smoke, then smoking eventually ceases” . The neurobiological effects of nicotine differ greatly from that of other licit and illicit substances. For example, for most alcohol drinkers, there is not a comparable neurobiological dependence on repeat ‘hits’ (ingestions), as there is with nicotine ( Jarvis, 2004 ).
Biological evidence for smoking and cancer
Proctor (2012) reviews the history of the early biological evidence that linked smoking to cancer, which I summarize. Early studies in the 1930s and early 1940s in Argentina and in Germany (published mostly in Spanish and German) examined the application of ‘tobacco juice’ to the skin and other organs in laboratory animals and showed that painting the tar of cigarette smoke on the shaved backs of mice generated tumours in the mice. The cigarette industry ridiculed these findings and funded alternatives to counter these discoveries. Next, pathologists established that smoking interfered with the small hair-like structures (cilia) in the lungs that were responsible for clearing contaminants in the lungs ( Hilding, 1956 ). Investigations on cancer-causing chemicals in cigarette smoke such as polycyclic aromatic hydrocarbons and later benzopyrene were also underway around this time. The cigarette industry’s own research similarly identified such ingredients in their products. By the end of the 1950s, cigarette manufacturers had characterized several dozen carcinogens in cigarette smoke, including arsenic, chromium, nickel and a wide variety of polycyclic aromatic hydrocarbons.
To date, over 7,000 chemicals have been identified in cigarette smoke, including acetone (solvent and paint stripper), ammonia (powerful and poisonous gas), arsenic (potent ant poison), benzene (poisonous toxin), butane (flammable chemical in lighter fluid), cadmium (employed in batteries), carbon monoxide (poisonous gas in auto exhaust), formaldehyde (preservative for dead bodies), hydrogen cyanide (deadly ingredient in rat poison), methanol (jet engine and rocket fuel), polonium-210 (radioactive element) and toluene (poisonous industrial solvent) ( IARC Working Group on the Evaluation of Carcinogenic Risk to Humans, 2004 ; U.S. Department of Health and Human Services, 1989 ; U.S. Department of Health and Human Services, 2014 ). Many of these have been classified independently as carcinogens by the rigorous IARC review process ( IARC Working Group on the Evaluation of Carcinogenic Risk to Humans, 2004 ).
More recent evidence has identified the role of tobacco smoking in triggering or enabling possible mechanisms of cancer, most notably somatic mutations (meaning genetic alternations that are passed on during cell replications). Smoking also appears to alter DNA methylation, one of the main forms of epigenetic modification (meaning smoking can change how genes express into proteins, without changing the DNA itself) ( Vucic et al., 2014 ). A recent review of the somatic mutations and DNA methylation in cancers of types for which tobacco smoking confers an elevated risk, found that smoking caused multiple mutations, most notably the misreplication of DNA by tobacco carcinogens, or indirect activation of DNA editing ( Alexandrov et al., 2016 ). Finally, the p53 protein is responsible for a wide range of factors that suppress cancerous growth. Smoking-related malignancies have a high genome-wide burden of mutations, including in gene encoding for p53 ( Gibbons et al., 2014 ).
By contrast, one paper suggested that ‘bad luck,’ that is random errors in DNA replication, were responsible for variation in cancer risk among 25 different types of cancer ( Tomasetti and Vogelstein, 2015 ). This paper observed a strong correlation between the number of lifetime stem cell divisions in an organ and the lifetime organ-specific cancer risk in the US. The authors concluded that luck, far more than ‘environmental or genetic susceptibility,’ accounted for these cancers. As Blot and Tarone (2015) review, this is a misleading analysis to determine cancer causation. Any particular cancer usually requires multiple genetic changes ( Peto, 2016 ). Both random errors and those due to genetic susceptibility or damage from environmental causes, such as smoking, increase with the total number of stem cell divisions. Hence, both types of mutations would contribute to the observed positive correlation between stem cell divisions and lifetime cancer risk. Blot and Taroneconclude, “…the mutation rates and the totals of lifetime stem cell divisions at various organs or tissues are not likely to differ widely among different human populations, and thus even if most mutations in the majority of cancers are the result of random replication errors, the large geographic variation in cancer rates observed in most organs suggests that the percentage of cancers arising entirely by such random errors is relatively low” ( Blot and Tarone, 2015 ).
Biological evidence for smoking and vascular disease and diabetes
The US Surgeon General provides detailed reviews of possible mechanisms that link smoking to vascular disease. The 2004 Surgeon General’s report provided a detailed overview of mechanisms linking smoking with cardiovascular diseases development. The report concluded that smoking (1) promotes harm to the linings of the cardiac arteries; (2) produces a substantial shift in blood based factors, clotting, and inflammation, all of which can contribute to sudden heart attack; (3) diminishes the ability of the blood to carry oxygen; (4) increases physiologic demands of the heart; and (5) causes irregular heartbeats (arrhythmias and spasm) ( U.S. Department of Health and Human Services, 1990 ; U.S. Department of Health and Human Services, 2004 ; U.S. Department of Health and Human Services, 2014 ). Through these mechanisms, smoking results in substantial adverse alterations in the haemostatic balance of the cardiovascular system, which explains the relationships between smoking and subclinical and clinical manifestations of atherosclerosis.
The USSGR 2010 report reviewed in detail the mechanisms through which cigarette smoking causes coronary heart disease ( U.S. Department of Health and Human Services, 2010b ), concluding that smoking produces insulin resistance that could, in tandem with chronic inflammation, accelerate the development of damage to the arteries supplying the heart and kidney, and other organs. The 2014 USSGR expanded on the research related to mechanisms through which smoking affects cardiovascular function, focusing on how smoking affects coronary artery narrowing, blood clotting and inflammation ( U.S. Department of Health and Human Services, 2014 ). Csordas and Bernhard (2013) thoroughly reviewed the biology of these effects of smoking and found similar conclusions. A recent examination in rat models noted that nicotine alone increases the body’s stress response, raising blood glucose levels, and thus diabetes ( Duncan et al., 2019 ). This finding might help explain the higher prevalence of diabetes among cigarette smokers. It would also suggest similar effects on diabetes from prolonged use of nicotine in e-cigarettes.
Most of these mechanisms take less time from exposure to disease than is the case with cancer. Hence, these findings may help to explain why smoking cessation induces much faster reversibility of heart disease risk than it does for common cancers. These findings also help to explain why the relative risks for heart attack are much greater in younger than in older smokers ( Table 4 ).
Scientific and popular understanding of smoking risks
Despite about 40,000 studies since about 1950 on the relationship between smoking and disease, there continues to be widespread ignorance about the hazards of smoking by the public, non-experts and even some experts. For example, adults do not know that smoking is a cause of stroke based on numerous surveys, particularly in low-income countries or among less educated adults in high-income countries ( Jha and Chaloupka, 1999 ; Jha and Chaloupka, 2000 ). What is surprising however, is the extent to which even informed professionals can be unaware of the hazards of smoking.
This confusion about smoking hazards in part reflects definitions of causality. Consider lung cancer, which is among the most widely-studied of the tobacco-attributable diseases. Despite the common myth, smoking is not the only cause of lung cancer. Smoking is a cause of about 90% of lung cancer deaths in high-income countries. However lung cancer occurs (albeit rarely) in non-smokers. These rare occurrences may be related to factors such as radon exposure, though it is useful to note the rate of lung cancer among non-smokers has changed little over time ( Thun et al., 2008 ). Hence, smoking is not a necessary cause of disease. Some smokers do not die a premature death from their smoking, and not every smoker will develop lung cancer (or heart disease or other tobacco-attributable conditions). Hence, smoking is not a sufficient cause of disease. With that said, smoking is an important cause of lung cancer and other diseases. In epidemiological terms, when we state that smoking is an important cause of lung cancer, we are stating that, among people of the same age, smokers have a (statistically significant) increased probability of developing lung cancer in the near future than do otherwise similar non-smokers. Similarly, smoking is an important cause of vascular and respiratory disease and other diseases ( U.S. Department of Health and Human Services, 1989 ).
Once causality is established for a particular condition, it is important to then consider the implications for public health. Here, we have to understand the relevant concept of the combination of two risks, together, as a cause of disease. For example, asbestos was used widely among shipyards in the UK that were built during WWI and WWII, prior to awareness of the hazards of asbestos on lung cancer and respiratory disease. Similar Canadian workers faced lower risks in part as the type of asbestos exposure was less carcinogenic than in the UK ( Peto, 1985 ). Thus, large numbers of male UK shipyard workers were exposed to asbestos dust during each working day for many years. In these men, lung cancer developed at about ten times the rate of its development in otherwise similar men not exposed to asbestos dust ( Barlow et al., 2017 ). Among these male shipyard workers, many smoked, and smoking made new lung cancer ten times more likely. Thus, shipyard workers who smoked and were exposed to asbestos dust were, by age 60 years, 100 times as likely to get lung cancer as men who had never smoked and who had not been exposed to asbestos dust ( Markowitz et al., 2013 ).
If around 1950, we took 100 smokers who were exposed to asbestos and died of lung cancer, 90 of those 100 lung cancer deaths would not have happened if the individual had not smoked. Similarly, 90 of those 100 lung cancer deaths would not have happened if the individual had not been exposed to the particular types of asbestos dust. Thus, smoking and asbestos are each a cause of 90 of these 100 lung cancer deaths. The attributed fractions obviously add up to over 100%. Naturally, it follows that avoidance of both smoking and asbestos exposure would not avoid much more than the 90 deaths that each caused. Moreover, using the same analogy as above for asbestos, the fractions caused by genetic factors and caused by environmental factors are not mutually exclusive ( Doll and Peto, 1981 ). A specific disease has both genetic and environmental causes.
In addition to misunderstanding of causality, two additional aspects of the divergence between the scientific evidence and popular understanding: underestimation of smoking hazards and confusion with other risks.
Underestimation of the hazards of smoking
Widespread underestimation of the hazards of smoking arises from the long delay between uptake of smoking and the development of most diseases, as discussed earlier. Smoking is so common that many people appear to believe that something so widely used cannot be harmful. Finally, as smoking does not kill each of its users, there is always the reference to individual anecdote: many people will personally know a relative or family friend who smoked to age 85 and died peacefully in his sleep. Of course, the many mothers and fathers who died early in adult life and smoked usually do not appear often in these anecdotes.
Consider two examples of the misunderstanding of the hazards of smoking and the benefits of cessation. The first is excerpted from the notable journal The Economist , which is read widely by government officials and academics around the world:
“The public-health rhetoric often implies that smoking must be daft, because it is deadly. In fact, most smokers (two-thirds or more) do not die of smoking-related disease. They gamble and win. Moreover, the years lost to smoking come from the end of life, when people are most likely to die of something else anyway. [Then US President] Bill Clinton's mother, who died of cancer at the age of 70 after smoking two packs a day for most of her life, might, as Mr. Clinton notes, have extended her life by not smoking; but she might also have extended it by eating better or exercising more, and in any case she could never have been sure.” ( The Economist, 1998 ).
The second is by Nobel-Prize winning economist Angus Deaton, who, in his 2013 book, The Great Escape , wrote:
“Although smokers are ten to twenty times more likely to die of lung cancer than non-smokers, the vast majority of smokers do not die of the disease; the Memorial Sloan-Kettering Cancer center has an online calculator that estimates the risks. For example, a 50 year old man who has smoked a pack a day for thirty years has a one percent chance of developing lung cancer if he quits now and a two percent chance if he does not.” ( Deaton, 2013 , p. 135).
The epidemiological evidence does not support either assertion. Firstly, smoking kills at least half of all those who smoke continuously and the years of life lost are substantial in middle-age. Moreover, The Economist quote confuses the fact that ‘eating better’ and ‘exercising more’ do little to offset the harmful effects of smoking. The confusion of big and small risks is a common mistake in media reporting of scientific research, as I take up further in the next section.
Angus Deaton substantially underestimates the actual risks of death from lung cancer. Among US men aged 50 who continue to smoke, close to 16–20%, not 2%, will be killed by lung cancer. Quitting smoking by age 50 reduces the risk of death from lung cancer by about two-thirds, not by one-half ( Jha, 2009 ; Peto et al., 2000 ; U.S. Department of Health and Human Services, 2014 ; Pirie et al., 2013 ; Figure 11 ). Reassuringly, The Economist has changed its stance on tobacco completely, and now argues for much higher excise taxation and other approaches to reduce tobacco deaths ( The Economist, 2017 ).
It is therefore unsurprising to note that among US adults surveyed randomly ( Oklahoma Tobacco Research Center, 2017 ), there was widespread lack of awareness of the levels of risk conferred by smoking. While 82% of the adults in the US survey knew that smoking caused heart disease, emphysema, leukemia and various cancers, only 41% knew that smoking kills on average 1,200 Americans every day. Only 37% knew that more people die from smoking then from murder, AIDS, suicide drugs, car crashes and alcohol combined. Similarly, 90% of the respondents stated that smoking is highly addictive and that nicotine is the addictive drug in tobacco. High proportions of this population believed that it was not easy to quit smoking. However less than 65% of respondents knew that cigarette companies intentionally designed cigarettes with enough nicotine to create and sustain addiction. Just over 60% knew that nicotine affects the brain, making cessation quite difficult for most. This survey also noted low levels of awareness regarding the fact that low-tar and light cigarettes are as equally harmful as regular cigarettes ( U.S. Department of Health and Human Services, 2014 ). More recently, the perception of risk of e-cigarettes as being as harmful as cigarettes has become common, and mostly likely a consequence of the considerable media attention focused on youth gateways to smoking or to addiction ( McNeill et al., 2020 ).
Confusion of the large hazards of smoking with the smaller hazards of most other exposures
Let’s consider one of the statements made by the British American Tobacco, a global multi-national cigarette manufacturing, in response to requests made by the US Congress in 2003 ( Waxman, 2003 ) about their belief of the causal role of cigarette smoking:
“…that causes of lung cancer, chronic obstructive pulmonary disease, and cardiovascular diseases are complex, and the mechanism of causation, as well as the possible role of any cigarette smoke constituent in causation, have not been scientifically established” ( Waxman, 2003 ).
Over the last decade, many tobacco companies have admitted that smoking causes disease, but most continue to fudge their belief in causality. Indeed many politicians have made similar arguments that minize the hazards of smoking. For argument’s sake, let’s extend the tobacco industry concerns about causality to a widely held suggestion that other ‘complex’ factors are responsible for smoking harms at the population level or in particular individuals. These other factors, based on common sense, should be closely associated with being a smoker. These might include lack of exercise, poor nutrition, alcohol drinking, peer pressure to smoke, low social status, psychology influences, and stress. Additional factors that might also be more common in smokers could include poor in-utero environment, poorer access to medical treatment, food choices, and the emerging area of science on the gut microbiome environment ( Finlay and the Microbiome, 2020 ).
A noted UK geneticist, Sir Ronald Fisher, attacked the Doll and Hill studies of the early 1950s, suggesting that the case-control study design could not establish causality, instead hypothesizing that there was an underlying gene that resulted both in smoking and in lung cancer. Fisher was later reported to have received funding from the tobacco industry and eventually recanted some of his criticisms of Doll and Hill ( Christopher, 2016 ).
Careful epidemiological studies have been able to examine many, but certainly not all of the first list of factors that by common sense occur in smokers. These find, for the most part, that ‘adjustment’ for such differences between smokers and non-smokers makes little difference to the observed smoker: non-smoker relative risks. What then of unmeasured variables or as yet unknown variables, as these are, by definition, bound to exist in any study? It would be expected that even undetermined factors should, for the most part, also correlate with known factors. Thus a mystery factor, either behavioural, environmental or genetic, that I will call ‘Zulu’ likely correlates closely with poor nutrition, lack of exercise as well as to smoking. It follows that, were Zulu the main true explanation for the observed smoker: non-smoker risks, adjustment for a closely correlated surrogate like lack of exercise would reduce the observed smoking relative risks. Most careful studies find, in fact, little diminution of smoker: non-smoker risks with such adjustment. This suggests that ‘residual confounding’ with unknown or unexplained risk factors does not explain most of the large observed risks for smoking. It also suggests that smoking acts independently of the other factors, even though they may be correlated.
Indeed, adjustment for smoking explains many of these other factors. Consider low social status, which is well described as a risk factor for many diseases. The UK Million Women’s study examined the social differences in hospitalization or death from ischemic heart disease. Heart disease death or hospitalization was strongly associated with lower levels of education or greater (neighborhood) deprivation, with clear dose-responses. However, smoking, alcohol consumption, physical inactivity and body mass index accounted for most of the risk factors, and of these four factors, smoking accounted for the biggest share ( Floud et al., 2016 ; Jha et al., 2019 ).
Any particular disease can have in fact two (or more) causes. Therefore, obesity and smoking may both contribute to heart disease and avoidance of either might have prevented a particular heart attack. However, from a population health perspective, what is useful is to understand the comparative risks for each and to what extent are these risks avoidable.
I now review some of these major identified ‘other factors’ beginning first with obesity (presumed to be both ‘physiological’ and ‘based on lifestyle choices’ in tobacco industry parlance), then turning to alcohol, and finally genetics and environment. I selected these factors as the WHO has identified these as major risk factors for adult health ( World Health Organization, 2016 ) and because clinicians and the public often turn to genetic differences to explain disease occurrence. Moreover, smoking and drinking, and to a lesser extent obesity are strongly correlated in healthy as well as in diseased individuals ( Thun et al., 1997 ).
Comparison with obesity
Smoking risks are substantially greater than those of obesity for adults in high-income countries. Obesity (at its most extreme called severe obesity) is defined as excess body fat, and measured by body-mass index (BMI; or weight divided by height squared). Higher BMI causes a loss of premature life ( Finucane et al., 2011 ). The loss of a decade of life requires a BMI of around 43, which is well above the averages seen in any country including the most obese populations of the US. More moderate levels of obesity, meaning of BMI of around 32, contibute to an average of three years of life loss. Hence, at the population level, a 2 kg per meter extra BMI if overweight or a 10% higher smoking prevalence both reduce life expectancy by one year ( Figure 12 ; Peto et al., 2010 ).

Note: 2 kg/m 2 extra BMI (if overweight) or 10% smoking prevalence shortens life by ~1 year. Adapted from Peto et al. (2010) , p. 856.
These individual risks also translate to the overall life expectancy gaps at the population level. About 15% of American smoke cigarettes, and smoking accounts, on average, for 10 years of life lost. Thus, smoking is reducing American life expectancy by about 1.5 years of life (i.e. 15% X 10 years). The mean BMI in the US is 28 and about 30% of the American population is modestly obese. If modest obesity accounts for 3 years of life lost, then obesity is reducing American life expectancy by 0.9 years (i.e. 30% X 3 years). Hence, smoking causes more lost life than does obesity in the US. Moreover, the main mechanisms for increased mortality from higher BMI from vascular disease are due to hypertension, ‘bad’ lipids and development of diabetes. Most of these factors driven by higher BMI are very treatable even without reducing weight ( Yusuf et al., 2004 ; Yusuf et al., 2020 ). By contrast, the only plausible way to reduce smoking risks is by quitting ( Jha et al., 2013 ).
Comparison with alcohol
Heavy alcohol use increases the death rate from some conditions (most notably, road traffic and other injuries, suicide, poisoning, liver cirrhosis, certain cancers and perhaps haemorrhagic stroke) ( Thun et al., 1997 ); and recent studies have documented hazards from drinking for ischemic stroke and no protective effect for ischemic heart disease ( Millwood et al., 2019 ). Thus, the overall survival of otherwise comparable drinkers and non-drinkers in Canada, the US and the UK are similar (the slightly greater survival in drinkers shown in earlier studies is mostly likely due to ‘reverse causality’ whereby sicker people give up drinking). This balance of risks is distinct from the extreme binge-drinking patterns of vodka among Russian men, in whom loss of life from such binge-drinking exceeds that of smoking ( Zaridze et al., 2009 ; Zaridze et al., 2014 ). However, the hazards of smoking are observed in both drinkers and non-drinkers ( Table 6 ).
Adapted from Alcohol consumption and mortality among middle-aged and elderly US adults , by Thun et al. (1997) , New England Journal of Medicine, 337 (24), p. 1712.
Even epidemiologists often underestimate the extreme hazards of tobacco. Consider the following comparisons. Firstly, among 1,000 male smokers aged 20, at least 500 (and perhaps up to 670), will die from smoking throughout their lifetimes. Of these, at least 250 will die from smoking in middle-age (meaning before 70 years). By contrast, only 20 would die from road accidents or violence and 30 from all alcohol-related conditions ( Jha and Chaloupka, 2000 ).
Comparison with genetics
To return to the idea of causation; a common statement made by people (including doctors) is that ‘genetics was responsible’ for a particular person’s heart attack or lung cancer, even though they may have also smoked. At the population level, both genetics and smoking could for example, play roles in causing either disease. The population-based evidence should also guide the magnitude of the risk. For example, no single genetic factor has been identified that explains a significant proportion of heart attacks, although the combination of all tested factors suggest just over a quarter of heritability of heart disease ( McPherson and Tybjaerg-Hansen, 2016 ).
However, smoking alone accounts for at least a quarter of the deaths from heart attack in the US ( U.S. Department of Health and Human Services, 2014 ). Moreover, the largest identified single genetic factor (the relative risk from a specific lipid factor (lipoprotein (a), Loci SLC22A3-LPAL2-LPA SNP, rs2048327 ) carries a relative risk of 1.4, which is comparable to smoking 3–4 cigarettes a day. Similarly, a range of genetic factors has recently been suggested to modestly predict lung cancer risk in smokers and non-smokers ( Timofeeva et al., 2012 ). These genetic factors do not negate the importance of smoking in explaining lung cancer risks.
Comparison to environmental pollutants and other exposures
Doll and Peto (1981) conducted an exhaustive review of the possible causes of cancer in the US in the late 1970s. Their focus was on the widely held belief that ‘pollutants’ in the environment were a major cause of cancer. They documented the available epidemiological evidence on the environmental exposures most commonly believed to be linked to cancer, such as pesticides, food additives, industrial products, ultraviolet light, and pollution. (They did not specifically study ambient air pollution). They concluded that tobacco smoking accounted for more of the proportions of cancer deaths than did a reasonable summation of all of the known risk factors, including nearly every known pollutant. Table 7 shows their summary results.
Adapted from The causes of cancer: Quantitative estimates of avoidable risks of cancer in the United States today , Doll and Peto (1981) , Journal of the National Cancer Institute, 66 (6), p. 1192–1308.
Doll and Peto also pointed out that, excluding smoking-attributable cancers, there was no ‘epidemic’ of cancer, as was commonly believed at that time. In fact cancer death rates except those attributable to smoking were falling modestly. Finally, they pointed out that smoking causes more death from causes other than cancer than it does from cancer itself.
Future research directions and conclusions
In this review, I have considered the cause, nature and extent of tobacco related diseases in high-income countries between 1960 and 2020. I have drawn on existing epidemiological evidence, with careful re-interpretation of risks in individuals and rates among populations. It follows naturally to ask what additional epidemiological or biological evidence is needed on the consequences of smoking in high-income countries. A full treatise on research priorities is beyond the scope of this review, but a few priorities should be considered. First, the rapidly changing prevalence of smoking, including increases in cigarette cessation require ongoing studies to document the benefits of quitting, particularly on various diseases and at different ages ( U.S. Department of Health and Human Services, 2020 ). Second, the emergence of e-cigarettes demands further documentation of the long-term risks (and possible benefits) of their use among adults and by adolescents. The current state of evidence is mostly insufficient for conclusions on the net effects of e-cigarettes on population health. Third, research to better understand how risks are perceived and internalized by individuals and governments is needed to ensure that epidemiological studies on the consequences of smoking are incorporated into decision-making.
Based on the existing epidemiological and biological evidence, I provide four overall conclusions.
Firstly, in much of North America and Western Europe, the biggest cause of premature death, defined as death before 70 years, is the smoking of manufactured cigarettes. Smoking as an important cause of many diseases in many populations has been recognized widely in the scientific literature for the last five decades. However, three surprising features of health hazards of smoking have been established reliably only in the last decade. The first feature is that risk of developing disease among smokers is big. The second feature is that for smokers to develop these big risks, they need to start smoking early in adult life and to continue smoking. If smokers don’t start early in life, their risks are substantially smaller. Third, if smokers stop smoking before they develop some serious disease, then their risks are substantially reduced. However, most smokers whom start early in adult life and who continue to smoke are eventually killed by their tobacco use. This is because in every year during middle age, the death rates among smokers are about three-fold higher than that of similar non-smokers (taking into account differences between smokers and non-smokers in heavy alcohol use, obesity patterns or different social status). So up to two-thirds of the mortality among smokers would not be happening if they had the non-smoker death rates. Most of this excess risk arises from diseases that are caused by smoking. This includes disease such as lung cancer, emphysema, heart attack, stroke, cancer of the upper aerodigestive areas, bladder cancer and various other conditions. Thus this excess risk is a cause and effect relationship.
Secondly, from 1960 to 2020, smoking has likely killed 29.5 million Americans, 9.3 million UK residents, and 2.6 million Canadians, or a total of 41.3 million adults. This constitutes a crude ratio of one death per million cigarettes smoked in the US and Canada, but slightly more than one death per million cigarettes smoked in the UK.
Third, cessation, particularly before age 40 avoids nearly all the excess risk of continued smoking. Cessation at any age is effective, restoring substantial years of like lost versus continued smoking.
Finally, there continues to be widespread, serious underestimation of the hazards of smoking by the public, non-experts and even some experts.
Acknowledgements
The author thanks Richard Peto for guidance on an earlier version of the manuscript. The author also thanks Varsha Malhotra and Om Prakash Malhotra for editorial assistance, Daphne Wu and Benjamin Wong for graphics support, and Vedika Jha and Shivani Shah for assistance on references.
Appendix 1—table 1.
Source: USSGR Report, 2014. Analyses of Cancer Prevention Study II (CPS-II) and updated analyses of the pooled contemporary cohort population described in Thun et al. (2013) provided to the Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. See Table 12.3 of the USSGR Report for important details on each condition.
Appendix 1—table 2.
Note. Author’s calculations. Tobacco sales to deaths are shown in the column entitled ‘Deaths from smoking at all ages’. For particular years, some data were missing. In this case, I interpolated these data or did forward projections based on earlier years. These more uncertain numbers are shown in italics.
Funding Statement
The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Contributor Information
Eduardo Franco, McGill University, Canada.
Funding Information
This paper was supported by the following grants:
- Canadian Institutes of Health Research FDN154277 to Prabhat Jha.
- National Institutes of Health R01TW0599101 to Prabhat Jha.
Additional information
Reviewing Editor at eLife.
- Action on Smoking and Health . Smoking Statistics: Who Smokes and How Much. London, UK: Action on Smoking and Health; 2016. [ Google Scholar ]
- Action on Smoking and Health . Use of E-Cigarettes Among Young People in Great Britain. London, UK: Action on Smoking and Health; 2019. [ Google Scholar ]
- Alexandrov LB, Ju YS, Haase K, Van Loo P, Martincorena I, Nik-Zainal S, Totoki Y, Fujimoto A, Nakagawa H, Shibata T, Campbell PJ, Vineis P, Phillips DH, Stratton MR. Mutational signatures associated with tobacco smoking in human Cancer. Science. 2016; 354 :618–622. doi: 10.1126/science.aag0299. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- American Cancer Society . Cancer Facts & Figures. US: American Cancer Society; 2013. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2013.html [ Google Scholar ]
- Babb S. Quitting smoking among adults—United States, 2000–2015. MMW: Morbidity and Mortality Weekly Report. 2017; 65 :1457–1464. doi: 10.15585/mmwr.mm6552a1. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bachinger E, McKee M, Gilmore A. Tobacco policies in nazi Germany: not as simple as it seems. Public Health. 2008; 122 :497–505. doi: 10.1016/j.puhe.2007.08.005. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Banks E, Joshy G, Weber MF, Liu B, Grenfell R, Egger S, Paige E, Lopez AD, Sitas F, Beral V. Tobacco smoking and all-cause mortality in a large australian cohort study: findings from a mature epidemic with current low smoking prevalence. BMC Medicine. 2015; 13 :38. doi: 10.1186/s12916-015-0281-z. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Barlow CA, Sahmel J, Paustenbach DJ, Henshaw JL. History of knowledge and evolution of occupational health and regulatory aspects of asbestos exposure science: 1900-1975. Critical Reviews in Toxicology. 2017; 47 :286–316. doi: 10.1080/10408444.2016.1258391. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bates MN, Khalakdina A, Pai M, Chang L, Lessa F, Smith KR. Risk of tuberculosis from exposure to tobacco smoke: a systematic review and meta-analysis. Archives of Internal Medicine. 2007; 167 :335–342. doi: 10.1001/archinte.167.4.335. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bauld L, MacKintosh AM, Eastwood B, Ford A, Moore G, Dockrell M, Arnott D, Cheeseman H, McNeill A. Young people's Use of E-Cigarettes across the United Kingdom: Findings from Five Surveys 2015-2017. International Journal of Environmental Research and Public Health. 2017; 14 :e973. doi: 10.3390/ijerph14090973. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Beard E, West R, Michie S, Brown J. Association between electronic cigarette use and changes in quit attempts, success of quit attempts, use of smoking cessation pharmacotherapy, and use of stop smoking services in England: time series analysis of population trends. BMJ. 2016; 354 :i4645. doi: 10.1136/bmj.i4645. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Blot WJ, Tarone RE. Doll and Peto's quantitative estimates of cancer risks: holding generally true for 35 years. JNCI Journal of the National Cancer Institute. 2015; 107 :djv044. doi: 10.1093/jnci/djv044. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Blount BC, Karwowski MP, Shields PG, Morel-Espinosa M, Valentin-Blasini L, Gardner M, Braselton M, Brosius CR, Caron KT, Chambers D, Corstvet J, Cowan E, De Jesús VR, Espinosa P, Fernandez C, Holder C, Kuklenyik Z, Kusovschi JD, Newman C, Reis GB, Rees J, Reese C, Silva L, Seyler T, Song MA, Sosnoff C, Spitzer CR, Tevis D, Wang L, Watson C, Wewers MD, Xia B, Heitkemper DT, Ghinai I, Layden J, Briss P, King BA, Delaney LJ, Jones CM, Baldwin GT, Patel A, Meaney-Delman D, Rose D, Krishnasamy V, Barr JR, Thomas J, Pirkle JL, Lung Injury Response Laboratory Working Group Vitamin E acetate in Bronchoalveolar-Lavage fluid associated with EVALI. New England Journal of Medicine. 2020; 382 :697–705. doi: 10.1056/NEJMoa1916433. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bondurant S, Wallace R, Shetty P, Stratton K. Clearing the Smoke: Assessing the Science Base for Tobacco Harm Reduction. Washington, DC, US: National Academies Press; 2001. [ PubMed ] [ Google Scholar ]
- Calle EE, Rodriguez C, Jacobs EJ, Almon ML, Chao A, McCullough ML, Feigelson HS, Thun MJ. The american Cancer society Cancer prevention study II nutrition cohort: rationale, study design, and baseline characteristics. Cancer. 2002; 94 :2490–2501. doi: 10.1002/cncr.101970. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Centers for Disease Control and Prevention Cigarette smoking among U.S. adults lowest ever recorded: 14% in 2017. 2018. [February 12, 2020]. https://www.cdc.gov/media/releases/2018/p1108-cigarette-smoking-adults.html
- Centers for Disease Control and Prevention Current cigarette smoking among adults in the united states. 2019. [February 12, 2020]. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm
- Christopher B. Why the father of modern statistics didn’t believe smoking caused cancer. 2016. [February 12, 2020]. https://priceonomics.com/why-the-father-of-modern-statistics-didnt-believe/
- Crispo A, Brennan P, Jöckel KH, Schaffrath-Rosario A, Wichmann HE, Nyberg F, Simonato L, Merletti F, Forastiere F, Boffetta P, Darby S. The cumulative risk of lung Cancer among current, ex- and never-smokers in european men. British Journal of Cancer. 2004; 91 :1280–1286. doi: 10.1038/sj.bjc.6602078. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Csordas A, Bernhard D. The biology behind the atherothrombotic effects of cigarette smoke. Nature Reviews Cardiology. 2013; 10 :219–230. doi: 10.1038/nrcardio.2013.8. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cummings KM, Hammond D. E-cigarettes: striking the right balance. The Lancet Public Health. 2020; 1 :pii: S2468-2667(20)30004-9. doi: 10.1016/S2468-2667(20)30004-9. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Deaton A. The Great Escape: Health, Wealth, and the Origins of Inequality. Princeton: Princeton University Press; 2013. [ Google Scholar ]
- Doll R, Peto R, Boreham J, Sutherland I. Mortality from Cancer in relation to smoking: 50 years observations on british doctors. British Journal of Cancer. 2005; 92 :426–429. doi: 10.1038/sj.bjc.6602359. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Doll R, Hill AB. Smoking and carcinoma of the lung. BMJ. 1950; 2 :739–748. doi: 10.1136/bmj.2.4682.739. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Doll R, Hill AB. Mortality in relation to smoking: ten years' OBSERVATIONS of british doctors. BMJ. 1964; 1 :1399–1410. doi: 10.1136/bmj.1.5395.1399. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Doll R, Peto R. The causes of Cancer: quantitative estimates of avoidable risks of Cancer in the united states today. JNCI: Journal of the National Cancer Institute. 1981; 66 :1192–1308. doi: 10.1093/jnci/66.6.1192. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Duncan A, Heyer MP, Ishikawa M, Caligiuri SPB, Liu XA, Chen Z, Micioni Di Bonaventura MV, Elayouby KS, Ables JL, Howe WM, Bali P, Fillinger C, Williams M, O'Connor RM, Wang Z, Lu Q, Kamenecka TM, Ma'ayan A, O'Neill HC, Ibanez-Tallon I, Geurts AM, Kenny PJ. Habenular TCF7L2 links nicotine addiction to diabetes. Nature. 2019; 574 :372–377. doi: 10.1038/s41586-019-1653-x. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Encyclopaedia Britannica Cigarillo. 2018. [February 12, 2020]. https://www.britannica.com/topic/cigarillo
- Environics Research Vapers panel survey to measure attitudes and behaviours regarding vaping products. 2019. [February 12, 2020]. http://epe.lac-bac.gc.ca/100/200/301/pwgsc-tpsgc/por-ef/health/2019/083-18-e/report.pdf
- Finlay BB, the Microbiome Are noncommunicable diseases communicable? Science. 2020; 367 :250–251. doi: 10.1126/science.aaz3834. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, Singh GM, Gutierrez HR, Lu Y, Bahalim AN, Farzadfar F, Riley LM, Ezzati M. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. The Lancet. 2011; 377 :557–567. doi: 10.1016/S0140-6736(10)62037-5. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fischer S, Spiegelhalder B, Eisenbarth J, Preussmann R. Investigations on the origin of tobacco-specific nitrosamines n mainstream smoke of cigarettes. Carcinogenesis. 1990a; 11 :723–730. doi: 10.1093/carcin/11.5.723. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fischer S, Castonguay A, Kaiserman M, Spiegelhalder B, Preussmann R. Tobacco-specific nitrosamines in canadian cigarettes. Journal of Cancer Research and Clinical Oncology. 1990b; 116 :563–568. doi: 10.1007/BF01637075. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Floud S, Balkwill A, Moser K, Reeves GK, Green J, Beral V, Cairns BJ. The role of health-related behavioural factors in accounting for inequalities in coronary heart disease risk by education and area deprivation: prospective study of 1.2 million UK women. BMC Medicine. 2016; 14 :145. doi: 10.1186/s12916-016-0687-2. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Forey B, Hamling J, Hamling J, Thornton A, Lee P. International smoking statistics web edition. 2016. [February 12, 2020]. http://www.pnlee.co.uk/iss3.htm
- Foundation for a Smoke-Free World Global trends in nicotine. 2018. [February 12, 2020]. https://www.smokefreeworld.org/sites/default/files/fsfw-report-trends-in-nicotine-1005201811.pdf
- Gajalakshmi V, Peto R, Kanaka TS, Jha P. Smoking and mortality from tuberculosis and other diseases in India: retrospective study of 43000 adult male deaths and 35000 controls. The Lancet. 2003; 362 :507–515. doi: 10.1016/S0140-6736(03)14109-8. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gibbons DL, Byers LA, Kurie JM. Smoking, p53 mutation, and lung Cancer. Molecular Cancer Research. 2014; 12 :3–13. doi: 10.1158/1541-7786.MCR-13-0539. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Goniewicz ML, Knysak J, Gawron M, Kosmider L, Sobczak A, Kurek J, Prokopowicz A, Jablonska-Czapla M, Rosik-Dulewska C, Havel C, Jacob P, Benowitz N. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tobacco Control. 2014; 23 :133–139. doi: 10.1136/tobaccocontrol-2012-050859. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hajek P, Phillips-Waller A, Przulj D, Pesola F, Myers Smith K, Bisal N, Li J, Parrott S, Sasieni P, Dawkins L, Ross L, Goniewicz M, Wu Q, McRobbie HJ. A randomized trial of E-Cigarettes versus Nicotine-Replacement therapy. New England Journal of Medicine. 2019; 380 :629–637. doi: 10.1056/NEJMoa1808779. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hammond EC. Smoking in relation to the death rates of one million men and women. In: Haenszel W, editor. Epidemiological Study of Cancer and Other Chronic Diseases. Washington, DC: U.S. Department of Health, Education and Welfare, Public Health Service; 1966. pp. 127–204. [ Google Scholar ]
- Hammond EC, Horn D. The relationship between human smoking habits and death rates: a follow-up study of 187,766 men. Journal of the American Medical Association. 1954; 155 :1316–1328. doi: 10.1001/jama.1954.03690330020006. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hartmann-Boyce J, McRobbie H, Bullen C, Begh R, Stead LF, Hajek P, Cochrane Tobacco Addiction Group Electronic cigarettes for smoking cessation. Cochrane Database of Systematic Reviews. 2016; 11 :CD010216. doi: 10.1002/14651858.CD010216.pub3. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Henningfield JE, Slade J. Tobacco-dependence medications: public health and regulatory issues. Food and Drug Law Journal. 1998; 53 :75–114. [ PubMed ] [ Google Scholar ]
- Hilding AC. Ciliary streaming through the larynx and distribution of laryngeal epithelium. The Laryngoscope. 1956; 66 :1362–1363. doi: 10.1288/00005537-195610000-00015. [ CrossRef ] [ Google Scholar ]
- Holmes MD, Murin S, Chen WY, Kroenke CH, Spiegelman D, Colditz GA. Smoking and survival after breast Cancer diagnosis. International Journal of Cancer. 2007; 120 :2672–2677. doi: 10.1002/ijc.22575. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- IARC Working Group on the Evaluation of Carcinogenic Risk to Humans . Tobacco Smoke and Involuntary Smoking. Vol. 83. Lyon, France: International Agency for Research on Cancer; 2004. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- International Agency for Research on Cancer (IARC) IARC Monographs on the Evaluation of Carcinogenic Risks to Humans: Tobacco Smoke and Involuntary Smoking. Lyon, France: International Agency for Research on Cancer; 2004. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- International Agency for Research on Cancer (IARC) Personal Habits and Indoor Combustions. Vol. 100. International Agency for Research on Cancer; 2012. [ Google Scholar ]
- Jarvis MJ. ABC of smoking cessation: why people smoke. British Medical Journal. 2004; 328 :277–279. doi: 10.1136/bmj.328.7434.277. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jha P, Peto R, Zatonski W, Boreham J, Jarvis MJ, Lopez AD. Social inequalities in male mortality, and in male mortality from smoking: indirect estimation from national death rates in England and Wales, Poland, and north america. The Lancet. 2006; 368 :367–370. doi: 10.1016/S0140-6736(06)68975-7. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jha P, Jacob B, Gajalakshmi V, Gupta PC, Dhingra N, Kumar R, Sinha DN, Dikshit RP, Parida DK, Kamadod R, Boreham J, Peto R, RGI-CGHR Investigators A nationally representative case-control study of smoking and death in India. New England Journal of Medicine. 2008; 358 :1137–1147. doi: 10.1056/NEJMsa0707719. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jha P. Avoidable global Cancer deaths and total deaths from smoking. Nature Reviews Cancer. 2009; 9 :655–664. doi: 10.1038/nrc2703. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jha P, Mony P, Moore JA, Zatonski W. Avoidance of worldwide vascular deaths and total deaths from smoking. In: Yusuf S, Cairns J. A, Camm A. J, editors. Evidence-Based Cardiology. Oxford, UK: John Wiley & Sons, Ltd; 2010. pp. 111–124. [ CrossRef ] [ Google Scholar ]
- Jha P, Ramasundarahettige C, Landsman V, Rostron B, Thun M, Anderson RN, McAfee T, Peto R. 21st-century hazards of smoking and benefits of cessation in the united states. New England Journal of Medicine. 2013; 368 :341–350. doi: 10.1056/NEJMsa1211128. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jha P. Reliable direct measurement of causes of death in low- and middle-income countries. BMC Medicine. 2014; 12 :19. doi: 10.1186/1741-7015-12-19. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jha P, MacLennan M, Chaloupka FJ, Yurekli A, Ramasundarahettige C, Palipudi K, Zatonksi W, Asma S, Gupta PC. Global hazards of tobacco and the benefits of smoking cessation and tobacco taxes. In: Gelband H, Jha P, Sankaranarayanan R, Horton S, editors. Disease Control Priorities. Vol. 3. Washington, DC: Cancer World Bank; 2015. [ PubMed ] [ Google Scholar ]
- Jha P, Gelband H, Irving H, Mishra S. Reducing Social Inequalities in Cancer: Evidence and Priorities for Research. IARC, Social Inequalities and Cancer; 2019. Tobacco Taxation, Tobacco-Related Diseases and Poverty in Low- and Middle-Income Countries. [ Google Scholar ]
- Jha P, Hill C, Wu DCN, Peto R. Cigarette prices, smuggling, and deaths in France and Canada. The Lancet. 2020; 395 :27–28. doi: 10.1016/S0140-6736(19)31291-7. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jha P, Chaloupka FJ. Curbing the Epidemic: Governments and the Economics of Tobacco Control. Washington, DC: World Bank; 1999. [ Google Scholar ]
- Jha P, Chaloupka FJ. Tobacco Control in Developing Countries. Oxford, UK: Oxford University Press; 2000. [ CrossRef ] [ Google Scholar ]
- Jha P, Peto R. Global effects of smoking, of quitting, and of taxing tobacco. New England Journal of Medicine. 2014; 370 :60–68. doi: 10.1056/NEJMra1308383. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kenfield SA, Stampfer MJ, Giovannucci E, Chan JM. Physical activity and survival after prostate Cancer diagnosis in the health professionals follow-up study. Journal of Clinical Oncology. 2011; 29 :726–732. doi: 10.1200/JCO.2010.31.5226. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Koop CE. Tobacco addiction: accomplishments and challenges in science, health, and policy. Nicotine & Tobacco Research. 2003; 5 :613–619. doi: 10.1080/1462220031000158726. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kozlowski LT, Mehta NY, Sweeney CT, Schwartz SS, Vogler GP, Jarvis MJ, West RJ. Filter ventilation and nicotine content of tobacco in cigarettes from Canada, the united kingdom, and the united states. Tobacco Control. 1998; 7 :369–375. doi: 10.1136/tc.7.4.369. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Laviolette SR, van der Kooy D. The neurobiology of nicotine addiction: bridging the gap from molecules to behaviour. Nature Reviews Neuroscience. 2004; 5 :55–65. doi: 10.1038/nrn1298. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Levy DT, Warner KE, Cummings KM, Hammond D, Kuo C, Fong GT, Thrasher JF, Goniewicz ML, Borland R. Examining the relationship of vaping to smoking initiation among US youth and young adults: a reality check. Tobacco Control. 2019; 28 :629–635. doi: 10.1136/tobaccocontrol-2018-054446. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Liu BQ, Peto R, Chen ZM, Boreham J, Wu YP, Li JY, Campbell TC, Chen JS. Emerging tobacco hazards in China: 1. retrospective proportional mortality study of one million deaths. BMJ. 1998; 317 :1411–1422. doi: 10.1136/bmj.317.7170.1411. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mansvelder HD, Keath JR, McGehee DS. Synaptic mechanisms underlie nicotine-induced excitability of brain reward Areas. Neuron. 2002; 33 :905–919. doi: 10.1016/S0896-6273(02)00625-6. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Manuel DG, Perez R, Bennett C, Rosella L, Taljaard M, Roberts M, Sanderson R, Tuna M, Tanuseputro P, Manson H. Seven More Years: The Impact of Smoking, Alcohol, Diet, Physical Activity and Stress on Health and Life Expectancy in Ontario. Toronto, Canada: Institute for Clinical Evaluative Sciences; 2012. [ Google Scholar ]
- Markou A, Henningfield JE. Background paper on the neurobiology of nicotine addiction. Paper Presented at the Disease Control Priorities Project Nicotine Addiction Workshop; Mumbai. 2003. [ Google Scholar ]
- Markowitz SB, Levin SM, Miller A, Morabia A. Asbestos, asbestosis, smoking, and lung cancer. New findings from the North American insulator cohort. American Journal of Respiratory and Critical Care Medicine. 2013; 188 :90–96. doi: 10.1164/rccm.201302-0257OC. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McNeill A, Brose LS, Calder R, Bauld L, Robson D. Vaping in England: An Evidence Update Including Mental Health and Pregnancy, March 2020: A Report Commissioned by Public Health England. London: Public Health England; 2020. [ Google Scholar ]
- McPherson R, Tybjaerg-Hansen A. Genetics of coronary artery disease. Circulation Research. 2016; 118 :564–578. doi: 10.1161/CIRCRESAHA.115.306566. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Menon GR, Singh L, Sharma P, Yadav P, Sharma S, Kalaskar S, Singh H, Adinarayanan S, Joshua V, Kulothungan V, Yadav J, Watson LK, Fadel SA, Suraweera W, Rao MVV, Dhaliwal RS, Begum R, Sati P, Jamison DT, Jha P. National burden estimates of healthy life lost in India, 2017: an analysis using direct mortality data and indirect disability data. The Lancet Global Health. 2019; 7 :e1675–e1684. doi: 10.1016/S2214-109X(19)30451-6. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Merriman D. Understand, Measure and Combat Tobacco Smuggling. Washington, DC: World Bank Economics of Tobacco Toolkit; 2012. [ Google Scholar ]
- Millwood IY, Walters RG, Mei XW, Guo Y, Yang L, Bian Z, Bennett DA, Chen Y, Dong C, Hu R, Zhou G, Yu B, Jia W, Parish S, Clarke R, Davey Smith G, Collins R, Holmes MV, Li L, Peto R, Chen Z. Conventional and genetic evidence on alcohol and vascular disease aetiology: a prospective study of 500000 men and women in China. The Lancet. 2019; 393 :1831–1842. doi: 10.1016/S0140-6736(18)31772-0. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Müller FH. Tabakmißbrauch und lungencarcinom. Zeitschrift Für Krebsforschung. 1940; 49 :57–85. doi: 10.1007/BF01633114. [ CrossRef ] [ Google Scholar ]
- National Academies of Sciences, Engineering, and Medicine . In: Public Health Consequences of E-Cigarettes. Eaton DL, Kwan LY, Stratton K, editors. Washington, DC: National Academies Press; 2018. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- National Center for Health Statistics . 2007 National Health Interview Survey (NHIS): Public Use Data release:NHIS Survey Description. Hyattsville, MD: Department of Health and Human Services, Centers for DiseaseControl and Prevention, National Center for Health Statistics; 2008. [ Google Scholar ]
- National Institutes of Health, National Cancer Institute . The FTC Cigarette Test Method for Determining Tar, Nicotine, and Carbon Monoxide Yields of U.S. Cigarettes: Report of the NCI Expert Committee. Bethesda, US: US Department of Health and Human Services, Public Health Service, National Institutes of Health; 1996. [ Google Scholar ]
- Newbold KB, Neligan D. Disaggregating Canadian immigrant smoking behaviour by country of birth. Social Science & Medicine. 2012; 75 :997–1005. doi: 10.1016/j.socscimed.2012.05.008. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Office for National Statistics . Adult Smoking Habits in Great Britain. London, UK: Office for National Statistics; 2018a. [ Google Scholar ]
- Office for National Statistics Adult smoking habits in the UK: 2017. 2018b. [February 12, 2020]. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandlifeexpectancies/bulletins/adultsmokinghabitsingreatbritain/2017
- Oklahoma Tobacco Research Center . Oklahoma Tobacco Research Centre Research Study: Court-Ordered Corrections of Tobacco Industry Racketeering. Oklahoma: Oklahoma Tobacco Research Center; 2017. [ Google Scholar ]
- Parish S, Collins R, Peto R, Youngman L, Barton J, Jayne K, Clarke R, Appleby P, Lyon V, Cederholm-Williams S, Marshall J, Sleight P. Cigarette smoking, tar yields, and non-fatal myocardial infarction: 14000 cases and 32000 controls in the United Kingdom. BMJ. 1995; 311 :471–477. doi: 10.1136/bmj.311.7003.471. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Paskett ED, Reeves KW, Rohan TE, Allison MA, Williams CD, Messina CR, Whitlock E, Sato A, Hunt JR. Association between cigarette smoking and colorectal Cancer in the women's Health Initiative. JNCI Journal of the National Cancer Institute. 2007; 99 :1729–1735. doi: 10.1093/jnci/djm176. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pearl R. Tobacco smoking and longevity. Science. 1938; 87 :216–217. doi: 10.1126/science.87.2253.216. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Perry M, Chalkley R. Histone acetylation increases the solubility of chromatin and occurs sequentially over most of the chromatin. A novel model for the biological role of histone acetylation. The Journal of Biological Chemistry. 1982; 257 :7336–7347. [ PubMed ] [ Google Scholar ]
- Peters R, Poulter R, Warner J, Beckett N, Burch L, Bulpitt C. Smoking, dementia and cognitive decline in the elderly, a systematic review. BMC Geriatrics. 2008; 8 :36. doi: 10.1186/1471-2318-8-36. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Peto J. Problems in dose response and risk assessment: The example of asbestos. In: Castellani A, editor. Epidemiology and Quantitation of Environmental Risk in Humans From Radiation and Other Agents. Vol. 96. Boston, MA: Springer; 1985. pp. 175–185. [ CrossRef ] [ Google Scholar ]
- Peto R. Influence of dose and duration of smoking on lung Cancer rates. IARC Scientific Publications. 1986; 74 :23–33. [ PubMed ] [ Google Scholar ]
- Peto R, Boreham J, Lopez AD, Thun M, Heath C. Mortality from tobacco in developed countries: indirect estimation from national vital statistics. The Lancet. 1992; 339 :1268–1278. doi: 10.1016/0140-6736(92)91600-D. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Peto R, Lopez AD, Boreham J, Thun M, Heath CJ. Mortality From Smoking in Developed Countries 1950-2000. Indirect Estimates From National Vital Statistics. Oxford, UK: Oxford University Press; 1994. [ Google Scholar ]
- Peto R, Darby S, Deo H, Silcocks P, Whitley E, Doll R. Smoking, smoking cessation, and lung Cancer in the UK since 1950: combination of national statistics with two case-control studies. BMJ. 2000; 321 :323–329. doi: 10.1136/bmj.321.7257.323. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Peto R, Whitlock G, Jha P. Effects of obesity and smoking on US life expectancy. The New England Journal of Medicine. 2010; 362 :855–856. doi: 10.1056/NEJMc1000079. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Peto R. Epidemiology, multistage models, and short-term mutagenicity tests. International Journal of Epidemiology. 2016; 45 :621–637. doi: 10.1093/ije/dyv199. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Peto R, Lopez AD, Pan H, Boreham J, Thun M. Mortality from smoking in developed countries, 1950-2020: trends in smoking-attributed mortality and total mortality. 2018. [February 12, 2020]. https://gas.ctsu.ox.ac.uk/tobacco/SMK_ALL_PAGES.pdf
- Peto R, Lopez AD. Future worldwide health effects of current smoking patterns. In: Koop E. C, Pearson C. E, Schwarz M. R, editors. Jossey-Bass. New York: Critical issues in global health; 2001. [ Google Scholar ]
- Pirie K, Peto R, Reeves GK, Green J, Beral V, Million Women Study Collaborators The 21st century hazards of smoking and benefits of stopping. Lancet. 2013; 381 :133–141. doi: 10.1016/S0140-6736(12)61720-6. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Proctor RN. The history of the discovery of the cigarette–lung cancer link: evidentiary traditions, corporate denial, global toll: Table 1. Tobacco Control. 2012; 21 :87–91. doi: 10.1136/tobaccocontrol-2011-050338. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ramström L, Borland R, Wikmans T. Patterns of smoking and snus use in Sweden: implications for public health. International Journal of Environmental Research and Public Health. 2016; 13 :1110. doi: 10.3390/ijerph13111110. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Reid JL, Hammond D, Rynard VL, Madill CL, Burkhalter R. Tobacco Use in Canada: Patterns and Trends, 2017 Edition. Waterloo, Ontario, Canada: Propel Centre for Population Health Impact, University of Waterloo; 2017. [ Google Scholar ]
- Reynales-Shigematsu LM, Guerrero-López CM, Hernández Ávila M, Irving H, Jha P. Divergence and convergence in cause-specific premature adult mortality in Mexico and US mexican hispanics from 1995 to 2015: analyses of 4.9 million individual deaths. International Journal of Epidemiology. 2018; 47 :97–106. doi: 10.1093/ije/dyx185. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Riahi F, Rajkumar S, Yach D. Tobacco smoking and nicotine delivery alternatives: patterns of product use and perceptions in 13 countries. F1000Research. 2019; 8 :80. doi: 10.12688/f1000research.17635.2. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Royal College of Physicians . Smoking and Health: A Report of the Royal College of Physicians on Smoking in Relation to Cancer of the Lung and Other Diseases. London, UK: Pitman Medical Publishing; 1962. [ Google Scholar ]
- Royal College of Physicians of London . Nicotine Addiction in Britain: A Report of the Tobacco Advisory Group of the Royal College of Physicians. London, UK: Royal College of Physicians of London; 2000. [ Google Scholar ]
- Sakata R, McGale P, Grant EJ, Ozasa K, Peto R, Darby SC. Impact of smoking on mortality and life expectancy in Japanese smokers: a prospective cohort study. BMJ. 2012; 345 :e7093. doi: 10.1136/bmj.e7093. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schairer E, Schöniger E. Lungenkrebs und tabakverbrauch. Zeitschrift Für Krebsforschung. 1944; 54 :261–269. doi: 10.1007/BF01628727. [ CrossRef ] [ Google Scholar ]
- Schatzkin A, Subar AF, Thompson FE, Harlan LC, Tangrea J, Hollenbeck AR, Hurwitz PE, Coyle L, Schussler N, Michaud DS, Freedman LS, Brown CC, Midthune D, Kipnis V. Design and serendipity in establishing a large cohort with wide dietary intake distributions. American Journal of Epidemiology. 2001; 154 :1119–1125. doi: 10.1093/aje/154.12.1119. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Statistics Canada Table 13-10-0096-10, smokers, by age group. 2019. [February 12, 2020]. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310009610
- Thatcher A. E-cigarettes more popular than tobacco among youth. Canadian Medical Association Journal. 2015; 187 :E184. doi: 10.1503/cmaj.109-5010. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- The Economist Tobacco and tolerance: blowing smoke. The Economist. 1998. [December 20, 1998]. https://www.economist.com/leaders/2000/07/20/blowing-smoke
- The Economist How to cut smoking in poor countries. The Economist. 2017. [June 1, 2017]. https://www.economist.com/leaders/2017/06/01/how-to-cut-smoking-in-poor-countries
- Thun MJ, Peto R, Lopez AD, Monaco JH, Henley SJ, Heath CW, Doll R. Alcohol consumption and mortality among middle-aged and elderly U.S. adults. New England Journal of Medicine. 1997; 337 :1705–1714. doi: 10.1056/NEJM199712113372401. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Thun MJ, Henley SJ, Calle EE. Tobacco use and Cancer: an epidemiologic perspective for geneticists. Oncogene. 2002; 21 :7307–7325. doi: 10.1038/sj.onc.1205807. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Thun MJ, Hannan LM, Adams-Campbell LL, Boffetta P, Buring JE, Feskanich D, Flanders WD, Jee SH, Katanoda K, Kolonel LN, Lee IM, Marugame T, Palmer JR, Riboli E, Sobue T, Avila-Tang E, Wilkens LR, Samet JM. Lung Cancer occurrence in never-smokers: an analysis of 13 cohorts and 22 Cancer registry studies. PLOS Medicine. 2008; 5 :e185. doi: 10.1371/journal.pmed.0050185. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Thun MJ, Carter BD, Feskanich D, Freedman ND, Prentice R, Lopez AD, Hartge P, Gapstur SM. 50-year trends in smoking-related mortality in the united states. New England Journal of Medicine. 2013; 368 :351–364. doi: 10.1056/NEJMsa1211127. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Thun MJ, Burns DM. Health impact of “Reduced yield” cigarettes: A critical assessment of the epidemiological evidence. Tobacco Control. 2001; 10 :i4–i11. doi: 10.1136/tc.10.suppl_1.i4. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Timofeeva MN, Hung RJ, Rafnar T, Christiani DC, Field JK, Bickeböller H, Risch A, McKay JD, Wang Y, Dai J, Gaborieau V, McLaughlin J, Brenner D, Narod SA, Caporaso NE, Albanes D, Thun M, Eisen T, Wichmann HE, Rosenberger A, Han Y, Chen W, Zhu D, Spitz M, Wu X, Pande M, Zhao Y, Zaridze D, Szeszenia-Dabrowska N, Lissowska J, Rudnai P, Fabianova E, Mates D, Bencko V, Foretova L, Janout V, Krokan HE, Gabrielsen ME, Skorpen F, Vatten L, Njølstad I, Chen C, Goodman G, Lathrop M, Benhamou S, Vooder T, Välk K, Nelis M, Metspalu A, Raji O, Chen Y, Gosney J, Liloglou T, Muley T, Dienemann H, Thorleifsson G, Shen H, Stefansson K, Brennan P, Amos CI, Houlston R, Landi MT, Transdisciplinary Research in Cancer of the Lung (TRICL) Research Team Influence of common genetic variation on lung Cancer risk: meta-analysis of 14 900 cases and 29 485 controls. Human Molecular Genetics. 2012; 21 :4980–4995. doi: 10.1093/hmg/dds334. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tomasetti C, Vogelstein B. Variation in cancer risk among tissues can be explained by the number of stem cell divisions. Science. 2015; 347 :78–81. doi: 10.1126/science.1260825. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- U.S. Department of Health and Human Services . The Health Consequences of Smoking: Nicotine Addiction: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1988. [ Google Scholar ]
- U.S. Department of Health and Human Services . Reducing the Health Consequences of Smoking: 25 Years of Progress. a Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1989. [ Google Scholar ]
- U.S. Department of Health and Human Services . The Health Benefits of Smoking Cessation: A Report of the Surgeon General. Rockville, MD: Department of Health and Human Services, Centers for Disease Control, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1990. [ Google Scholar ]
- U.S. Department of Health and Human Services . The Health Consequences of Smoking: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2004. [ Google Scholar ]
- U.S. Department of Health and Human Services . Ending the Tobacco Epidemic: A Tobacco Control Strategic Action Plan for the U.S. Department of Health and Human Services. Washington, DC: Office of the Assistant Secretary for Health; 2010a. [ Google Scholar ]
- U.S. Department of Health and Human Services . How Tobacco Smoke Causes Disease—The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2010b. [ Google Scholar ]
- U.S. Department of Health and Human Services . Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [ Google Scholar ]
- U.S. Department of Health and Human Services . E-Cigarette Use Among Youth and Young Adults; a Report of the Surgeon General. Atlanta, US: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2016. [ Google Scholar ]
- U.S. Department of Health and Human Services . Smoking Cessation: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service, Office of the Surgeon General; 2020. [ Google Scholar ]
- U.S. Department of Health, Education, and Welfare . Smoking and Health: Report of the Advisory Committee to the Surgeon General. Washington, DC: U.S. Department of Health, Education, and Welfare, Public Health Service; 1964. [ Google Scholar ]
- Vucic EA, Chari R, Thu KL, Wilson IM, Cotton AM, Kennett JY, Zhang M, Lonergan KM, Steiling K, Brown CJ, McWilliams A, Ohtani K, Lenburg ME, Sin DD, Spira A, Macaulay CE, Lam S, Lam WL. DNA methylation is globally disrupted and associated with expression changes in chronic obstructive pulmonary disease small airways. American Journal of Respiratory Cell and Molecular Biology. 2014; 50 :912–922. doi: 10.1165/rcmb.2013-0304OC. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Warner KE. How to Think-Not Feel-about tobacco harm reduction. Nicotine & Tobacco Research. 2019; 21 :1299–1309. doi: 10.1093/ntr/nty084. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Waxman HA. Tobacco industry statements in the US department of justice lawsuit. Tobacco Control. 2003; 12 :94–101. doi: 10.1136/tc.12.1.94. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- World Bank . Confronting Illicit Tobacco Trade: A Global Review of Country Experiences (English). WBG Global Tobacco Control Program. Washington, US: World Bank Group; 2019. [ Google Scholar ]
- World Health Organization . Summary Tables of Mortality Estimates by Cause, Age and Sex, by Country, 2000–2015. Geneva: World Health Organization; 2016. [ Google Scholar ]
- World Health Organization . WHO Report on the Global Tobacco Epidemic 2017: Monitoring Tobacco Use and Prevention Policies. Geneva: World Health Organization; 2017. [ Google Scholar ]
- Wynder EL, Graham EA. Tobacco smoking as a possible etiologic factor in Bronchiogenic Carcinoma; a study of 684 proved cases. Journal of the American Medical Association. 1950; 143 :329–336. doi: 10.1001/jama.1950.02910390001001. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yusuf S, Hawken S, Ôunpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. The Lancet. 2004; 364 :937–952. doi: 10.1016/S0140-6736(04)17018-9. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yusuf S, Joseph P, Rangarajan S, Islam S, Mente A, Hystad P, Brauer M, Kutty VR, Gupta R, Wielgosz A, AlHabib KF, Dans A, Lopez-Jaramillo P, Avezum A, Lanas F, Oguz A, Kruger IM, Diaz R, Yusoff K, Mony P, Chifamba J, Yeates K, Kelishadi R, Yusufali A, Khatib R, Rahman O, Zatonska K, Iqbal R, Wei L, Bo H, Rosengren A, Kaur M, Mohan V, Lear SA, Teo KK, Leong D, O'Donnell M, McKee M, Dagenais G. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. The Lancet. 2020; 395 :795–808. doi: 10.1016/S0140-6736(19)32008-2. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zaridze D, Brennan P, Boreham J, Boroda A, Karpov R, Lazarev A, Konobeevskaya I, Igitov V, Terechova T, Boffetta P, Peto R. Alcohol and cause-specific mortality in Russia: a retrospective case–control study of 48557 adult deaths. The Lancet. 2009; 373 :2201–2214. doi: 10.1016/S0140-6736(09)61034-5. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zaridze D, Lewington S, Boroda A, Scélo G, Karpov R, Lazarev A, Konobeevskaya I, Igitov V, Terechova T, Boffetta P, Sherliker P, Kong X, Whitlock G, Boreham J, Brennan P, Peto R. Alcohol and mortality in Russia: prospective observational study of 151000 adults. The Lancet. 2014; 383 :1465–1473. doi: 10.1016/S0140-6736(13)62247-3. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zhu SH, Zhuang YL, Wong S, Cummins SE, Tedeschi GJ. E-cigarette use and associated changes in population smoking cessation: evidence from US current population surveys. BMJ. 2017; 358 :j3262. doi: 10.1136/bmj.j3262. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Persuasive Essay Guide
Persuasive Essay About Smoking
Persuasive Essay About Smoking - Making a Powerful Argument with Examples

People also read
A Comprehensive Guide to Writing an Effective Persuasive Essay
200+ Persuasive Essay Topics to Help You Out
Learn How to Create a Persuasive Essay Outline
30+ Free Persuasive Essay Examples To Get You Started
Read Excellent Examples of Persuasive Essay About Gun Control
How to Write a Persuasive Essay About Covid19 | Examples & Tips
Crafting a Convincing Persuasive Essay About Abortion
Learn to Write Persuasive Essay About Business With Examples and Tips
Check Out 12 Persuasive Essay About Online Education Examples
Are you wondering how to write your next persuasive essay about smoking?
Smoking has been one of the most controversial topics in our society for years. It is associated with many health risks and can be seen as a danger to both individuals and communities.
Writing an effective persuasive essay about smoking can help sway public opinion. It can also encourage people to make healthier choices and stop smoking.
But where do you begin?
In this blog, we’ll provide some examples to get you started. So read on to get inspired!
- 1. What You Need To Know About Persuasive Essay
- 2. Persuasive Essay Examples About Smoking
- 3. Argumentative Essay About Smoking Examples
- 4. Tips for Writing a Persuasive Essay About Smoking
What You Need To Know About Persuasive Essay
A persuasive essay is a type of writing that aims to convince its readers to take a certain stance or action. It often uses logical arguments and evidence to back up its argument in order to persuade readers.
It also utilizes rhetorical techniques such as ethos, pathos, and logos to make the argument more convincing. In other words, persuasive essays use facts and evidence as well as emotion to make their points.
A persuasive essay about smoking would use these techniques to convince its readers about any point about smoking. Check out an example below:
Simple persuasive essay about smoking
Tough Essay Due? Hire Tough Writers!
Persuasive Essay Examples About Smoking
Smoking is one of the leading causes of preventable death in the world. It leads to adverse health effects, including lung cancer, heart disease, and damage to the respiratory tract. However, the number of people who smoke cigarettes has been on the rise globally.
A lot has been written on topics related to the effects of smoking. Reading essays about it can help you get an idea of what makes a good persuasive essay.
Here are some sample persuasive essays about smoking that you can use as inspiration for your own writing:
Persuasive speech on smoking outline
Persuasive essay about smoking should be banned
Persuasive essay about smoking pdf
Persuasive essay about smoking cannot relieve stress
Persuasive essay about smoking in public places
Speech about smoking is dangerous
Persuasive Essay About Smoking Introduction
Persuasive Essay About Stop Smoking
Short Persuasive Essay About Smoking
Stop Smoking Persuasive Speech
Check out some more persuasive essay examples on various other topics.
Argumentative Essay About Smoking Examples
An argumentative essay is a type of essay that uses facts and logical arguments to back up a point. It is similar to a persuasive essay but differs in that it utilizes more evidence than emotion.
If you’re looking to write an argumentative essay about smoking, here are some examples to get you started on the arguments of why you should not smoke.
Argumentative essay about smoking pdf
Argumentative essay about smoking in public places
Argumentative essay about smoking introduction
Check out the video below to find useful arguments against smoking:
Tips for Writing a Persuasive Essay About Smoking
You have read some examples of persuasive and argumentative essays about smoking. Now here are some tips that will help you craft a powerful essay on this topic.
Choose a Specific Angle
Select a particular perspective on the issue that you can use to form your argument. When talking about smoking, you can focus on any aspect such as the health risks, economic costs, or environmental impact.
Think about how you want to approach the topic. For instance, you could write about why smoking should be banned.
Check out the list of persuasive essay topics to help you while you are thinking of an angle to choose!
Research the Facts
Before writing your essay, make sure to research the facts about smoking. This will give you reliable information to use in your arguments and evidence for why people should avoid smoking.
You can find and use credible data and information from reputable sources such as government websites, health organizations, and scientific studies.
For instance, you should gather facts about health issues and negative effects of tobacco if arguing against smoking. Moreover, you should use and cite sources carefully.
Paper Due? Why Suffer? That's our Job!
Make an Outline
The next step is to create an outline for your essay. This will help you organize your thoughts and make sure that all the points in your essay flow together logically.
Your outline should include the introduction, body paragraphs, and conclusion. This will help ensure that your essay has a clear structure and argument.
Use Persuasive Language
When writing your essay, make sure to use persuasive language such as “it is necessary” or “people must be aware”. This will help you convey your message more effectively and emphasize the importance of your point.
Also, don’t forget to use rhetorical devices such as ethos, pathos, and logos to make your arguments more convincing. That is, you should incorporate emotion, personal experience, and logic into your arguments.
Introduce Opposing Arguments
Another important tip when writing a persuasive essay on smoking is to introduce opposing arguments. It will show that you are aware of the counterarguments and can provide evidence to refute them. This will help you strengthen your argument.
By doing this, your essay will come off as more balanced and objective, making it more convincing.
Finish Strong
Finally, make sure to finish your essay with a powerful conclusion. This will help you leave a lasting impression on your readers and reinforce the main points of your argument. You can end by summarizing the key points or giving some advice to the reader.
A powerful conclusion could either include food for thought or a call to action. So be sure to use persuasive language and make your conclusion strong.
To conclude,
By following these tips, you can write an effective and persuasive essay on smoking. Remember to research the facts, make an outline, and use persuasive language.
However, don't stress if you need expert help to write your essay! We're the best essay writing service for you!
Our persuasive essay writing service is fast, affordable, and trustworthy.
Try it out today!

Write Essay Within 60 Seconds!

Caleb S. has been providing writing services for over five years and has a Masters degree from Oxford University. He is an expert in his craft and takes great pride in helping students achieve their academic goals. Caleb is a dedicated professional who always puts his clients first.

Paper Due? Why Suffer? That’s our Job!
Keep reading


Essay on Harmful Effects of Smoking
Students are often asked to write an essay on Harmful Effects of Smoking in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Harmful Effects of Smoking
Introduction.
Smoking is a dangerous habit that poses significant health risks. It’s not only harmful to smokers, but also to those around them.
Health Risks
Smoking can cause lung cancer, heart disease, and stroke. It damages nearly every organ in the body, leading to premature death.
Secondhand Smoke
Non-smokers exposed to secondhand smoke face similar health risks. They can develop respiratory problems and increased risk of heart disease.
Impact on Environment
Cigarette butts litter the environment and release toxic chemicals into the soil and water, harming wildlife.
Smoking is harmful for everyone. It’s important to stay away from this deadly habit.
250 Words Essay on Harmful Effects of Smoking
Smoking is a widespread habit, yet it is one of the most detrimental practices to human health. Despite the awareness campaigns and statutory warnings, many continue to smoke, oblivious of the damaging effects it has on their health and wellbeing.
Physical Health Risks
Primarily, smoking causes numerous fatal diseases. It is the leading cause of lung cancer, accounting for about 85% of all cases. It also significantly increases the risk of heart diseases and stroke. The harmful chemicals in cigarettes damage blood vessels, leading to atherosclerosis, which can result in heart attack or stroke.
Impact on Respiratory System
Moreover, smoking adversely affects the respiratory system. It leads to chronic bronchitis, emphysema, and other lung diseases. The smoke and toxins inhaled damage the airways and alveoli, the tiny air sacs in the lungs, causing chronic obstructive pulmonary disease (COPD).
Effect on Mental Health
Smoking also influences mental health. Nicotine addiction can lead to increased stress, anxiety, and depression. The temporary relief from stress that smoking provides is often mistaken for a stress reliever, while it is actually exacerbating the problem.
In conclusion, smoking is a harmful habit that poses significant threats to physical and mental health. The myriad diseases it causes, coupled with its addictive nature, make it a dangerous lifestyle choice. It is imperative to raise awareness about these harmful effects and encourage cessation to safeguard public health.
500 Words Essay on Harmful Effects of Smoking
Smoking is a prevalent habit, often started out of curiosity, peer pressure, or stress management. However, its harmful effects are well-documented, impacting nearly every organ in the human body. Despite the widespread knowledge of its adverse effects, smoking continues to be a significant public health concern.
The Impact on Physical Health
One of the most severe consequences of smoking is its impact on physical health. Smokers are at a higher risk of developing a plethora of diseases, including lung cancer, heart disease, stroke, and chronic obstructive pulmonary disease (COPD). These conditions are often fatal, leading to premature death. The toxins in cigarette smoke damage the lining of the lungs, making smokers more susceptible to infections like pneumonia.
Detrimental Effects on Mental Health
Smoking doesn’t just harm the physical body; it also has a profound effect on mental health. Nicotine, the addictive substance in tobacco, alters the brain chemistry, leading to dependence. This dependence can exacerbate mental health conditions such as anxiety and depression. Furthermore, the stress of addiction and the struggle to quit smoking can also take a toll on mental well-being.
Smoking and Second-hand Smoke
The harmful effects of smoking are not confined to the smoker alone. Second-hand smoke, also known as passive smoking, is a significant concern. Non-smokers exposed to second-hand smoke inhale the same dangerous chemicals as smokers. This exposure increases their risk of developing heart disease, lung cancer, and other respiratory conditions.
Societal Impact
Smoking also has societal implications. The economic burden of smoking is substantial, with healthcare costs for smoking-related illnesses reaching astronomical levels. Additionally, the loss of productivity due to illness or premature death contributes to economic strain.
In conclusion, the harmful effects of smoking are far-reaching, affecting not only the smoker but also those around them and society at large. The physical and mental health implications, coupled with the economic burden, make it a significant public health issue. Despite the addictive nature of smoking, quitting is possible with the right support and resources, leading to improved health outcomes and quality of life. Understanding the full scope of smoking’s harmful effects is crucial in motivating smokers to quit and preventing non-smokers from starting.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on Effects of Smoking
- Essay on Dangers of Smoking
- Essay on Cyclone
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Undergraduate
- High School
- Architecture
- American History
- Asian History
- Antique Literature
- American Literature
- Asian Literature
- Classic English Literature
- World Literature
- Creative Writing
- Linguistics
- Criminal Justice
- Legal Issues
- Anthropology
- Archaeology
- Political Science
- World Affairs
- African-American Studies
- East European Studies
- Latin-American Studies
- Native-American Studies
- West European Studies
- Family and Consumer Science
- Social Issues
- Women and Gender Studies
- Social Work
- Natural Sciences
- Pharmacology
- Earth science
- Agriculture
- Agricultural Studies
- Computer Science
- IT Management
- Mathematics
- Investments
- Engineering and Technology
- Engineering
- Aeronautics
- Medicine and Health
- Alternative Medicine
- Communications and Media
- Advertising
- Communication Strategies
- Public Relations
- Educational Theories
- Teacher's Career
- Chicago/Turabian
- Company Analysis
- Education Theories
- Shakespeare
- Canadian Studies
- Food Safety
- Relation of Global Warming and Extreme Weather Condition
- Movie Review
- Admission Essay
- Annotated Bibliography
- Application Essay
- Article Critique
- Article Review
- Article Writing
- Book Review
- Business Plan
- Business Proposal
- Capstone Project
- Cover Letter
- Creative Essay
- Dissertation
- Dissertation - Abstract
- Dissertation - Conclusion
- Dissertation - Discussion
- Dissertation - Hypothesis
- Dissertation - Introduction
- Dissertation - Literature
- Dissertation - Methodology
- Dissertation - Results
- GCSE Coursework
- Grant Proposal
- Marketing Plan
- Multiple Choice Quiz
- Personal Statement
- Power Point Presentation
- Power Point Presentation With Speaker Notes
- Questionnaire
- Reaction Paper
- Research Paper
Research Proposal
- SWOT analysis
- Thesis Paper
- Online Quiz
- Literature Review
- Movie Analysis
- Statistics problem
- Math Problem
- All papers examples
- How It Works
- Money Back Policy
- Terms of Use
- Privacy Policy
- We Are Hiring
Cause and Effects of Smoking Cigarettes, Essay Example
Pages: 3
Words: 914
Hire a Writer for Custom Essay
Use 10% Off Discount: "custom10" in 1 Click 👇
You are free to use it as an inspiration or a source for your own work.
Smoking cigarettes has historically been a leisurely and highly popular social activity that a litany of people turn to as a way to assuage daily stress, lose weight, and feel socially accepted in a constantly evolving social world. Tobacco, the main ingredient in cigarettes, has high levels of nicotine, which is a highly addictive ingredient that makes it hard for people to quit smoking if nicotine is ingested on a quotidian basis (Woolbright, 1994, p. 337). According to the CDC (2014), cigarette smoking causes over 480,000 deaths annually in the United States alone, which translates into one out of every five people extirpating due to the ingestion of tobacco. A preventable cause of death, cigarette smoking kills more persons than accidents caused due motor vehicle accidents, alcohol consumption, illegal drug use, deaths involving firearms, and the HIV/AIDS virus altogether (Center For Disease Control and Prevention, 2014). Women who smoke tobacco disproportionately suffer from even more health problems as it directly harms not only their reproductive health but also their mortality and morbidity rates of their progeny or future children (American Lung Association, n.d.). People should not smoke because it not only spawns negative health effects but also because it is not economically useful. If people stopped smoking, many lives would be both indirectly and directly saved from premature and preventative deaths as a result.
Doctors and other medical experts pinpoint the various health hazards caused by smoking, especially to the statistics pertaining to the nexus between smoking cigarettes and premature death, in order to convince people to quit smoking. In the past five decades, the risk of premature death in both female and male smokers has profoundly increased (Centers for Disease Control and Prevention, 2014). According to the CDC (2014), smoking cigarettes causes a handful of diseases because it adversely impacts almost all bodily organs and detracts from the general health of enthusiastic smokers. The risk of developing coronary heart disease (COPD), various cardiovascular maladies, and stroke–the leading cause of death in the United States alone–increases two to four times as much due to the damage it spawns to blood vessels because tobacco narrows and thickens them. These ramifications cause rapid heartbeat, which results in higher blood pressure levels which renders smokers vulnerable to blood clots. If blood clots prevent blood from reaching the heart, people put themselves at risk for heart attack due to the fact that the heart does not get enough oxygen and thus kills the heart muscle. In addition, blood clots can also cause a stroke because they can hinder blood flow to the brain. Shockingly, quitting smoking even after just one year drastically enhances an individual’s risk of incurring poor cardiovascular health. Moreover, smoking is directly connected to various respiratory diseases due to the fact that it harms both airways and alveoli, or the minute air vacs, that are in the lungs. Chronic Obstructive Pulmonary Disease (COPD), emphysema, and bronchitis are common forms of lung disease that chronic smokers often develop. In addition, medical experts correlate cigarette smoking with a litany of cancers, which have been pinpointed as the primary cause of lung cancer in individuals who smoke for a protracted period of time. Smoking cigarettes can also spawn various other types of cancer, including cancer in the stomach, liver, kidneys, bladders, pancreas, and oropharynx. Smoking not only puts smokers at risk for these often fatal types of cancer but also to those around smokes as a result of second-hand smoking. Second-hand smoke, according to the CDC (2014), causes an estimated 34,000 deaths per year in non-smokers because they too develop various cardiovascular diseases while an estimated 8,000 persons prematurely dying as a result of stroke (CDC, 2014). They also are put at risk for developing lung cancer by approximately thirty percent, and their risk for heart attack is also amplified. Physicians estimate that if nobody smoked cigarettes around the world, an estimated one out of every three deaths caused by cancer would not manifest (1).
More poignantly, smoking cigarettes negatively impacts women’s reproductive health, and children who are exposed to cigarette smoke suffer from often fatal effects. Many studies have analyzed and outlined the negative ramifications of maternal smoking on both the mother and the baby and/or infant ( Hofhuis, de Jongste, & Merkus, 2003 & Woolbright, 1994). Many states require documentation on birth certificates of maternal tobacco consumption (Woolbright, 1994). Despite the Surgeon General’s stern warning that maternal smoking has been linked to fetal injury, premature birth, and/or low birth rate, 15-37% of pregnant women still smoke cigarettes while pregnant (Hofhuis, de Jongste, & Merkus, 2003). Mothers who smoke also frequently participate in other high-risk behaviors that also negatively impacts the health of their progeny. Additionally, factors including marital and socio-economic status in addition education level affect the outcome of pregnancies due to increased vulnerability to cigarette smoking (Woolbright, 1994, p. 330). Low birth weight is the main impact of maternal smoking, although the existing literature pinpoints infant death and premature birth as major ramifications of it as well. Infant exposure to tobacco after they are born puts him or her at risk of premature death if they develop respiratory diseases in addition to Sudden Infant Death Syndrome (Woolbright, 1994). Hofhuis, de Jongste, and Merkus (2003) assessed how smoking cigarettes during pregnancy in addition to passive smoking thereafter affects both the mortality and morbidity rates in children. Statistics show that other obstetric complications directly linked to smoking, including spontaneous abortions, premature rupture of membranes, ectopic pregnancies, and complications related to the placenta. Smoking also stunts the lung growth that fetuses need in utero, which results in the child suffering from weakened lungs after birth while also exponentially increases the child’s chance of suffering from asthma and a vast array of other crippling respiratory diseases. In addition, it stunts brain development and detracts from the child’s mental acuity.
Health Effects of Cigarette Smoking. (2014, February 6). Centers for Disease Control and Prevention . Retrieved November 21, 2015 from http://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_ cig_smoking/
American Lung Association. (n.d.). Women and tobacco use. American Lung Association . Retrieved November 21, 2015 from http://www.lung.org/stop- smoking/about-smoking/facts- figures/women-and-tobacco-use.html
Ault, R. W., Jr., R. E., Jackson, J. D., Saba, R. S., & Saurman, D. S. (1991). Smoking and Absenteeism. Applied Economics , 23 , 743-754.
Hodgson TA. Cigarette Smoking and Lifetime Medical Expenditures. Millbank Q 1992, 70, 81-125.
Hofhuis, W., de Jongste, J. C., & Merkus, P. J. (2003). Adverse Health Effects of Prenatal and Postnatal Tobacco Smoke Exposure on Children. Arch Dis Child , 88 , 1086-1090.
Woolbright, L. A. (1994). The effects of maternal smoking on infant health. Population Research and Policy Review , 13 (3), 327-339.
Stuck with your Essay?
Get in touch with one of our experts for instant help!
Are ADHD Medications Overprescribed in Children? Research Proposal Example
The Vow, Essay Example
Time is precious
don’t waste it!
Plagiarism-free guarantee
Privacy guarantee
Secure checkout
Money back guarantee

Related Essay Samples & Examples
Voting as a civic responsibility, essay example.
Pages: 1
Words: 287
Utilitarianism and Its Applications, Essay Example
Words: 356
The Age-Related Changes of the Older Person, Essay Example
Pages: 2
Words: 448
The Problems ESOL Teachers Face, Essay Example
Pages: 8
Words: 2293
Should English Be the Primary Language? Essay Example
Pages: 4
Words: 999

The Term “Social Construction of Reality”, Essay Example
Words: 371
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 17 April 2024
- Correction 18 April 2024
Smoking bans are coming: what does the evidence say?
- Carissa Wong
You can also search for this author in PubMed Google Scholar
Smoking rates have declined globally over the past few decades. Credit: Debbie Bragg/Everynight Images via Alamy
Nations worldwide are aiming to introduce some of the tightest restrictions ever on smoking and vaping, especially among young people.
On 16 April, UK lawmakers backed one of the world’s most ambitious plans — to create by 2040 a ‘smoke-free’ generation of people who will never be able to legally buy tobacco. The proposal is now a step closer to becoming law. The UK, Australian and French governments are also clamping down on vaping with e-cigarettes. These countries’ bold policies are currently in the minority, say researchers, but such measures would almost certainly prevent diseases, as well as save lives and billions of dollars in health-care costs.

Smoking scars the immune system for years after quitting
The UK plan would probably “be the most impactful public-health policy ever introduced”, says health-policy researcher Duncan Gillespie at the University of Sheffield, UK. The Conservative government’s Prime Minister Rishi Sunak initiated the proposal. The government hopes that the smoking restrictions, alongside offering health benefits for individuals, will reduce toxic chemicals leaching from used vapes into the environment.
Smoke-free generations
The health harms of smoking tobacco have been established for decades — it substantially raises the risk of diseases including cancer, heart disease and diabetes. Increased awareness of these health risks has led to a global decline in the deadly habit in the past few decades (see ‘Smoke clearing’).
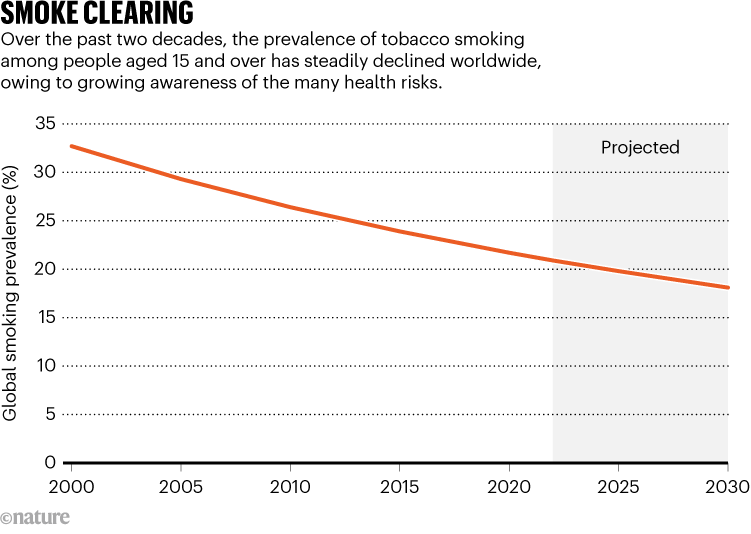
Source: WHO
Any drop in smoking rates saves money and reduces the burden on health-care systems, says Alison Commar, who studies tobacco policy at the World Health Organization (WHO) in Geneva, Switzerland. The WHO estimates that tobacco use costs the world US$1.4 trillion every year in health expenditures and lost productivity. “Every tobacco-related illness is adding to the burden on the health system unnecessarily,” says Commar.
The UK proposal, announced last October, would ban the sale of tobacco to any person born in or after 2009. That would prevent anyone who turns 15 or younger this year from ever buying cigarettes legally in the country. From 2027, the minimum legal age to purchase tobacco products would increase from 18 years old by one year each year — meaning that the threshold in 2028, for instance, would be 20. This strategy, the government hopes, will by 2040 create a smoke-free generation. The UK move follows similar legislation announced in 2021 by New Zealand. The nation reversed its intended ban because tobacco sales were needed to help pay for tax cuts, but the government said last month that it will seek to ban disposable vapes.
Modelling smokers
The UK government’s policies are backed by a modelling study published in December that predicts how the proposal would affect smoking rates and people over time. Its ‘pessimistic’ model predicts that the policy could reduce the smoking rate among people aged 14–30 from 13% in 2023 to around 8% in 2030. By 2040, just 5% of this age group would smoke. In the baseline scenario, 8% of 14- to 30-year-olds would smoke. In the ‘optimistic’ scenario, only 0.4% of that age group would start smoking by 2040 (see ‘Ban plan’). That model suggests that, by 2075, the policy would save tens of thousands of lives and £11 billion ($13.7 billion) in health-care costs by preventing smoking-related diseases.
These projections are based on solid evidence and are of high quality, says tobacco researcher Allen Gallagher at the University of Bath, UK.
Still, no country has ever introduced a policy that raises the minimum tobacco-purchasing age in this way — only time will tell what the effects will be, says Commar.
Vaping bans
Nations are also targeting vaping, a trend that began around 2010 and has surged among younger people. Many people have perceived it as a potentially healthier alternative to smoking — for which there is substantial evidence. But whether vaping itself harms health has long been controversial, and the evidence is uncertain.
“The results are not super clear, but certainly hint towards vaping causing damage to the lungs and other organs,” says Carolyn Baglole, who studies lung disease at the McGill University Health Centre in Montreal, Canada.
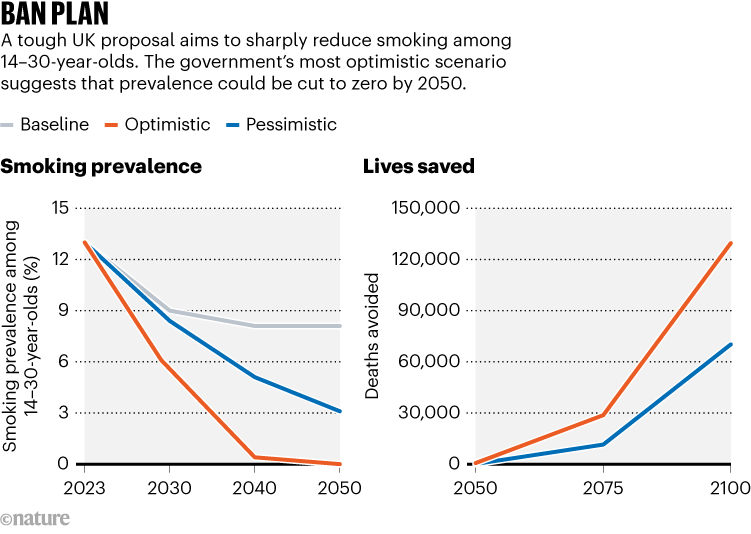
Source: UK government
Vapes are made of a box filled with liquid that usually contains nicotine, a heating element that turns the liquid into aerosols and a mouthpiece to inhale the aerosol ‘vape’ clouds, which are often fruity or dessert-flavoured. Although vapes lack tobacco and most of the toxic chemicals in cigarettes, the nicotine is still harmful. Nicotine can raise blood pressure, increase the risk of heart and lung disease and disrupt brain development in children and adolescents. In turn, this can lead to impairments in attention, memory and learning.
The UK plan includes banning disposable vapes, restricting vape flavours that appeal to young users and limiting how vapes are advertised. Most young people in Great Britain use disposable vapes rather than rechargeable ones than can be refilled with liquid, according to a survey by the public-health charity Action on Smoking and Health, based in London. Rechargeable vapes would remain legal.
Global policies
The French government also wants to ban disposable vapes this year, and in December its parliament unanimously backed the proposal. And in 2021, Australia restricted e-cigarette sales to smokers who have a prescription for using vapes to quit smoking. “There is a good consensus that vaping is likely to pose only a small fraction of risks of smoking over the long term,” says psychologist Peter Hajek at Queen Mary University of London, who led a study 1 that suggested vaping safely helped pregnant women to stop smoking.
But illegal vaping is still surging among people under the legal age of 18 in Australia, according to research by the Australian Institute of Health and Welfare. That’s led the government to tighten rules on vape products. “This policy push should see the upswing in youth vaping contained and reversed,” says epidemiologist Tony Blakely at the University of Melbourne in Australia.
The flavoured liquid in vapes also contains solvents such as propylene glycol and glycerin. Agencies including the US and European Union drug regulators have approved these chemicals for oral consumption. But animal studies suggest that inhaling them could cause damage and inflammation, raising the risk of lung and heart disease 2 . “The issue is we don’t know much about what happens when you heat these products and aerosolize them for inhalation,” says Baglole.
One thing researchers know is that the heating element in e-cigarettes can release heavy metals into the inhaled aerosols. These particles have been linked to a raised risk of heart and respiratory disease, she says.
Ultimately, scientists seem to be overwhelmingly in favour of tough restrictions on smoking and vaping. Research is needed to establish the long-term health impacts of such policies, says Baglole. “Hopefully, different types of studies, different models, in addition to human participants, will start to paint a more complete picture,” she says.
doi: https://doi.org/10.1038/d41586-024-00472-3
Updates & Corrections
Correction 18 April 2024 : The graphic ‘Smoking prevalence’ wrongly coloured the chart lines for the optimistic and pessimistic scenarios. This has been corrected.
Pesola, F. et al. Addiction 119 , 875–884 (2024).
Article PubMed Google Scholar
Traboulsi, H. et al. Int. J. Mol. Sci. 21 , 3495 (2020).
Download references
Reprints and permissions
Related Articles

- Public health

We must protect the global plastics treaty from corporate interference
World View 17 APR 24

UN plastics treaty: don’t let lobbyists drown out researchers
Editorial 17 APR 24

Canadian science gets biggest boost to PhD and postdoc pay in 20 years
News 17 APR 24

What toilets can reveal about COVID, cancer and other health threats
News Feature 17 APR 24
It’s time to talk about the hidden human cost of the green transition
Correspondence 16 APR 24

Lethal dust storms blanket Asia every spring — now AI could help predict them
News 15 APR 24
Postdoctoral Position
We are seeking highly motivated and skilled candidates for postdoctoral fellow positions
Boston, Massachusetts (US)
Boston Children's Hospital (BCH)
Qiushi Chair Professor
Distinguished scholars with notable achievements and extensive international influence.
Hangzhou, Zhejiang, China
Zhejiang University
ZJU 100 Young Professor
Promising young scholars who can independently establish and develop a research direction.
Head of the Thrust of Robotics and Autonomous Systems
Reporting to the Dean of Systems Hub, the Head of ROAS is an executive assuming overall responsibility for the academic, student, human resources...
Guangzhou, Guangdong, China
The Hong Kong University of Science and Technology (Guangzhou)
Head of Biology, Bio-island
Head of Biology to lead the discovery biology group.
BeiGene Ltd.
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
- Tobacco Products
- Public Health Education
- Health Effects of Tobacco Use
The Relative Risks of Tobacco Products
On this page:
- What Is Meant by the “Relative Risks” of Tobacco Products?
- Are E-Cigarettes a Lower-Risk Alternative to Cigarettes?
- What Options Are Available to Adults Who Smoke Cigarettes and Are Looking to Quit?
- Why Is It Important for Adults Who Smoke to Understand the Relative Risks of Tobacco Products?
What Is CTP Doing to Educate Adults Who Smoke About the Relative Risks of Tobacco Products?
Significant progress has been made in reducing cigarette smoking in the United States through comprehensive, population-level strategies. However, more than 30 million U.S. adults still smoke cigarettes, and smoking remains the leading cause of premature disease and death nationwide.
FDA’s Center for Tobacco Products (CTP) is committed to protecting the health of all people in the United States through a comprehensive approach to reduce the burden of tobacco use. This includes timely and evidence-based public health education that complements the agency’s regulatory actions.
In addition to preventing youth initiation and promoting cessation among people who use tobacco products, CTP is working to educate adults who smoke about the relative risks of tobacco products.
What Is Meant by “Relative Risks” of Tobacco Products?
No tobacco product is safe. However, the health risks for different tobacco products exist on a spectrum, which is sometimes referred to as a “continuum of risk.” Combusted, or smoked, tobacco products - such as cigarettes - are the most harmful type of tobacco product. Non-combusted products - such as e-cigarettes and other smokeless tobacco products - generally have lower health risks than cigarettes and other combustible tobacco products.
Before introducing a new tobacco product to the U.S. market, a company must submit a marketing application to the FDA and receive authorization. New tobacco product applications are evaluated by FDA scientists who determine if the application shows the new tobacco product meets the applicable statutory standards. Tobacco products that may be legally marketed in the United States are listed in FDA’s Searchable Tobacco Products Database .
Additionally, to market a tobacco product as a modified risk tobacco product (MRTP), an MRTP application must be submitted to the FDA. An order permitting the sale of an MRTP refers to specific products, not an entire class of tobacco products. An MRTP application generally must demonstrate that the product will significantly reduce harm and the risk of tobacco-related disease to individual tobacco users and benefit the health of the population as a whole.
Are E-Cigarettes a Lower-Risk Alternative to Cigarettes?
While e-cigarettes can generally be a lower-risk alternative for adults who smoke cigarettes, the use of e-cigarettes is not risk-free. These products deliver harmful chemicals and contain nicotine, which is highly addictive. Moreover, given the harmful chemicals found in e-cigarettes, further high-quality research on both short- and long-term health outcomes is needed.
Given that there is no safe tobacco product, youth and adults who do not use tobacco products should not start using e-cigarettes.
For adults who smoke, switching completely from cigarettes to e-cigarettes may reduce exposure to many harmful chemicals present in cigarettes. However, it is important that they switch completely from cigarettes to e-cigarettes to get the full health benefit. Long periods of dual use of cigarettes and e-cigarettes can result in harms to health similar to, or in addition to, the harms from exclusive use of cigarettes.
To date, FDA has authorized 23 e-cigarette products and devices . These products have undergone rigorous scientific review, including toxicologic assessments, and have been found by FDA to meet the statutory public health standard.
What Options Are Available to Adults Who Smoke Cigarettes and Are Looking to Quit?
For adults who currently smoke cigarettes, fully quitting the use of all forms of tobacco products would most benefit their health. Evidence-based, FDA-approved medications - including nicotine replacement therapy (NRT), bupropion, and varenicline - have been proven to be safe and effective. These approved medications, along with behavioral counseling, should be the first line of therapeutic treatment for adults seeking to quit smoking. Behavioral counseling and medication are independently effective and combining them increases the likelihood of cessation.
As part of its efforts to encourage quitting among adults, CTP has developed cessation education materials for a wide range of audiences. CTP also partners with the National Cancer Institute’s smokefree.gov , which provides quitting support to people who use tobacco products.
For adults who smoke who choose to use e-cigarettes, it is important that they switch completely from cigarettes to e-cigarettes to get the full health benefit. Since there is no safe tobacco product, eventual abstinence from all tobacco products should be the end goal.
Why Is It Important for Adults Who Smoke to Understand the Relative Risks of Tobacco Products?
Many people who use tobacco products have misperceptions about nicotine and the risks of various tobacco products. Despite science that shows that e-cigarettes generally have lower levels of harmful ingredients than cigarettes, many adults believe that e-cigarettes are just as harmful or more harmful than cigarettes .
Research has found that some adults who perceive e-cigarettes to be as or more harmful than cigarettes are less likely to switch from cigarette smoking to exclusive e-cigarette use .
The concept of relative risk is complex, and it is important to ensure efforts to educate adults who smoke on this topic are evidence-based and likely to achieve desired outcomes, while also minimizing impact on unintended audiences, including youth.
CTP is continuing to build scientific knowledge through research to inform the development of educational strategies and approaches, including potential messaging. A priority of this research is identifying effective ways to reach intended audiences while minimizing the impact of any potential consequences on unintended audiences.
Studies are planned on messages related to the relative risks of tobacco products that include participation by adults who smoke, as well as research among health care providers in primary care settings who may play a key role in the delivery of potential messaging. For example, on August 2, 2023, the National Institutes of Health, in coordination with FDA, published a Notice of Funding Opportunity for “ Public Health Communication Messaging about the Continuum of Risk for Tobacco Products .”
- Open access
- Published: 15 June 2023
Association of cigarette smoking habits with the risk of prostate cancer: a systematic review and meta-analysis
- Xiangwei Yang 1 na1 ,
- Hong Chen 2 na1 ,
- Shiqiang Zhang 1 ,
- Xianju Chen 1 ,
- Yiyu Sheng 1 &
- Jun Pang 1
BMC Public Health volume 23 , Article number: 1150 ( 2023 ) Cite this article
2046 Accesses
2 Citations
Metrics details
Association of cigarette smoking habits with the risk of prostate cancer is still a matter of debate. This systematic review and meta-analysis aimed to assess the association between cigarette smoking and prostate cancer risk.
We conducted a systematic search on PubMed, Embase, Cochrane Library, and Web of Science without language or time restrictions on June 11, 2022. Literature search and study screening were performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement. Prospective cohort studies that assessed the association between cigarette smoking habits and the risk of prostate cancer were included. Quality assessment was conducted using the Newcastle–Ottawa Scale. We used random-effects models to obtain pooled estimates and the corresponding 95% confidence intervals.
A total of 7296 publications were screened, of which 44 cohort studies were identified for qualitative analysis; 39 articles comprising 3 296 398 participants and 130 924 cases were selected for further meta-analysis. Current smoking had a significantly reduced risk of prostate cancer (RR, 0.74; 95% CI, 0.68–0.80; P < 0.001), especially in studies completed in the prostate-specific antigen screening era. Compared to former smokers, current smokers had a significant lower risk of PCa (RR, 0.70; 95% CI, 0.65–0.75; P < 0.001). Ever smoking showed no association with prostate cancer risk in overall analyses (RR, 0.96; 95% CI, 0.93–1.00; P = 0.074), but an increased risk of prostate cancer in the pre-prostate-specific antigen screening era (RR, 1.05; 95% CI, 1.00–1.10; P = 0.046) and a lower risk of prostate cancer in the prostate-specific antigen screening era (RR, 0.95; 95% CI, 0.91–0.99; P = 0.011) were observed. Former smoking did not show any association with the risk of prostate cancer.
Conclusions
The findings suggest that the lower risk of prostate cancer in smokers can probably be attributed to their poor adherence to cancer screening and the occurrence of deadly smoking-related diseases, and we should take measures to help smokers to be more compliant with early cancer screening and to quit smoking.
Trial registration
This study was registered on PROSPERO (CRD42022326464).
Peer Review reports
Prostate cancer (PCa) is the second most commonly diagnosed cancer and the fifth leading cause of cancer death among males, with an estimated 1.4 million new cases and 375 000 deaths worldwide in 2020, accounting for 7.3% and 3.8% of all cancers diagnosed, respectively [ 1 ]. Various endogenous and exogenous risk factors for PCa have been discussed for decades. Several factors have been identified to be associated with an increased risk of PCa, for instance, family history [ 2 ], elevated hormone levels [ 2 ], black ethnicity [ 2 ], and high alcohol consumption [ 3 ]. Conversely, several factors have been associated with a decreased risk of PCa, such as higher intake of tomatoes [ 4 ], increased coffee consumption [ 5 ] and sexual activity [ 6 ].
Smoking is a well-established risk factor for several cancers, such as lung cancer, head and neck cancer, bladder cancer, and esophageal cancer [ 7 , 8 ]. However, the data on the association between smoking and PCa incidence are conflicting [ 9 , 10 ]. In a meta-analysis of 24 prospective cohort studies [ 11 ], M. Huncharek showed that current smokers had no increased risk of incident PCa, but in data stratified by amount smoked, a significant elevated risk was observed, and former smokers had a higher risk of PCa in comparison with never smokers. Another meta-analysis conducted in 2014 [ 12 ] revealed an inverse association between current smoking and PCa risk, while in studies completed before the prostate-specific antigen (PSA) screening era, ever smoking was positively associated with PCa. In addition, a recent pooled study of five Swedish cohorts [ 13 ] demonstrated that former smokers and current smokers had a lower risk of PCa than never smokers, and smoking intensity was inversely associated with PCa risk, especially in the PSA screening era.
Biological mechanisms underlying smoking and PCa risk have been studied for many years. Burning cigarettes can produce more than 7000 chemicals, and at least 70 carcinogens such as polycyclic aromatic hydrocarbons (PAHs) and cadmium [ 14 ]. Mutations or functional polymorphism in genes involved in PAH metabolism and detoxification may increase the risk of PCa [ 15 ]. The glutathione-S-transferases (GSTs) are a class of enzymes that can detoxify PAHs. The most common subtypes of GSTs in human prostate are GSTP and GSTM, which were reported to be associated with an increased risk of PCa in smokers [ 15 , 16 ]. Cadmium induces prostate carcinogenesis through interaction with the androgen receptor because of its androgen-like activity, and it also enhances androgen-mediated transcriptional activity when in combination with the androgen [ 17 ]. A higher level of androgen was related to increased PCa risk [ 2 , 18 ]. Smoking can increase testosterone concentrations by promoting testosterone secretion from Leydig cells or acting as an aromatase inhibitor [ 19 ]. Mutations in the p53 gene and CYP1A1 gene showed a higher risk of PCa in smokers, suggesting that smoking may have a joint effect on PCa risk when combined with susceptible genotypes [ 20 ]. Increased heme oxygenase 1 (HO-1) messenger RNA expression and upregulated HO-1 protein levels were observed in PCa cell lines DU 145 and PC3 [ 21 ], implying that HO-1 may play a role in the development of PCa for its function in promoting angiogenesis [ 22 ]. Evidence also suggested that prostatic inflammation may be involved in the development and progression of PCa [ 23 ]. Cigarette smoke augments the production of numerous pro-inflammatory cytokines, decreases the levels of anti-inflammatory cytokines, and activates macrophage and dendritic cell activity in many ways [ 24 ].
We performed this systematic review and meta-analysis to investigate the association of cigarette smoking habits with the risk of PCa. We aimed to include a larger sample of studies than previous meta-analyses and collect the latest evidence and the most comprehensive information on the association between cigarette smoking and PCa risk. Our primary objective was to assess the risk of PCa in current smokers, former smokers, and ever smokers. We hypothesized that smokers have a higher risk of PCa compared to non-smokers.
Search strategy
This systematic review and meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [ 25 ]. Two independent investigators (XWY and HC) searched PubMed, Embase, Cochrane Library, and Web of Science for publications from database inception to June 11, 2022. The following search terms were used: ("Prostate cancer") AND ("Cigarette" OR "Smoking" OR "Tobacco") AND ("Risk" OR "Incidence"). No language restrictions were applied. Reference lists of identified articles and relevant reviews were screened for additional studies. Details of the protocol for this systematic review were registered on PROSPERO and can be accessed by CRD42022326464.
Selection criteria
Prospective cohort studies investigating the association between cigarette smoking and PCa risk were included for analysis. The primary outcome was the risk of PCa. Those studies that provided an effect measure (i.e., a relative risk) quantifying the impact of smoking on the risk of PCa were considered for further quantitative synthesis (meta-analysis). The removal of duplicates and assessment of article eligibility were conducted independently by XWY and HC, and any disagreements were resolved by consulting the senior author (JP). Review articles, editorials, meeting abstracts, case‒control studies, cross-sectional studies, and those not on the topic were excluded.
Quality assessment
All included studies were independently assessed by XWY and HC for risk of bias using the Newcastle‒Ottawa Scale for cohort studies [ 26 ]. This scale assesses the selection of the study groups, the comparability of the groups, and the ascertainment of the outcome of interest. Studies with 7–9 scores were considered to be of high quality, those with 5–6 scores were classified as intermediate quality, and those with less than 4 scores were classified as low quality. Disagreements in the quality assessment were resolved by consulting JP.
Data extraction
Data were independently extracted by XWY and HC. All extracted variables were cross-checked to ensure their reliability. We recorded the total number of participants, PCa cases, and the mean or median follow-up time across all included studies. Relative risks (RRs) and the corresponding 95% confidence intervals (CIs) were retrieved or calculated using frequency distributions. Considering the prevalence rate of PCa in the public, we believed that the odds ratio was close to the RR [ 27 , 28 ]. Hazard ratios (HRs) and RRs are different, HRs contain temporal information but RRs do not [ 28 ]. We converted HRs to RRs based on the formula provided by Shor E et al. [ 29 ], and the corresponding 95% CIs were converted using the same method. RRs and 95% CIs of ever smokers were computed by combining the results for former and current smokers when these results were not reported in the original papers. In addition, we recorded the baseline characteristics, methods, adjusted confounding factors, and other important comments to establish comparability. Discrepancies were discussed and resolved by consensus.
Statistical analysis
Three authors (SZQ, XJC and YYS) performed statistical analyses using Stata software, version 16.0 (StataCorp). When both crude and adjusted RRs were provided, we used the most fully adjusted value. We calculated the pooled RRs and 95% CIs and plotted forest plots using random-effects models (DerSimonian‒Laird method) for the association of current smoking, former smoking, and ever smoking with the risk of PCa [ 30 ]. Statistical heterogeneity across the trials was assessed using the I 2 statistic and the Cochran’s Q test. Values of the I 2 statistic of approximately 25%, 50%, and 75% were interpreted as low, moderate, and high heterogeneity, respectively [ 31 ]. In the case of low heterogeneity, a fixed-effects model (Inverse variance method) was applied. We plotted funnel plots and used Egger’s test to examine publication bias. Additionally, a series of sensitivity analyses were performed to assess the robustness of our results. We stratified studies by reference status (never smoker, former smokers), completion year (pre-PSA screening era vs. PSA screening era), world region (North America vs. Europe vs. Asia vs. Australia), and the Newcastle‒Ottawa Scale score (≤ 6 points vs. > 6 points). We considered 1995 as a cutoff year of study completion to distinguish studies before and after the PSA screening era [ 12 ]. All tests were two-tailed, and P < 0.05 was considered statistically significant.
Study population
We identified 7296 citations, and after removing duplicates, 4963 citations remained for screening. After the removal of ineligible citations, we retained 60 articles that we assessed for eligibility by reading the full text; 16 of these were excluded for specific reasons. Finally, 44 studies met our inclusion criteria for qualitative synthesis and meta-analysis (Fig. 1 ). The number of participants and PCa cases from each selected study for systematic review ranged separately from 997 to 844 455 and 54 to 40 821, with a median of 22 677 and 382, respectively. Overall, 39 studies with 3 296 398 participants and 130 924 cases were identified for meta-analysis, and 5 studies with 91 377 participants and 1364 cases were not included in meta-analysis due to lack of information (Additional file 1 ). Articles were published between 1989 and 2022 and were from studies conducted in the following geographic regions: 19 from Europe (4 from the United Kingdom, 4 from Norway, 3 from Sweden, 2 from Finland, 1 from France, 1 from the Netherlands, 1 from Denmark, 1 from Lithuania, 1 from Iceland, and one from 10 European countries), 18 from North America (17 from the United States, 1 from Canada), 5 from Asia (3 from Japan, 1 from South Korea, 1 from Singapore), and 2 from Australia. The median score of quality assessment for all eligible studies was 7, with a range of 6–9 (Additional file 2 ).
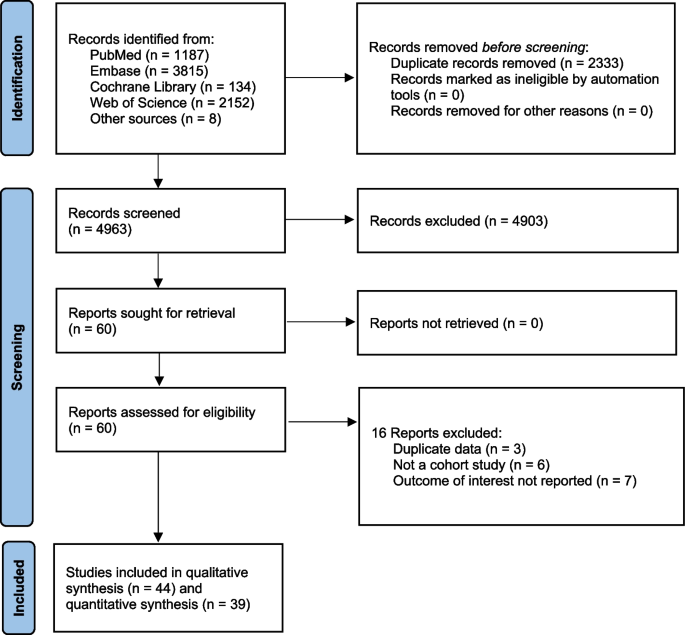
Flow diagram of included studies
Current smoking
In total, 37 studies [ 6 , 13 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 ] reported the risk of current smoking on PCa, among which 6 studies [ 32 , 35 , 41 , 53 , 55 , 63 ] took non-smokers as the reference and the remaining 31 studies [ 6 , 13 , 33 , 34 , 36 , 37 , 38 , 39 , 40 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 54 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 64 , 65 , 66 ] took never smokers as the reference. We defined non-smokers as never smokers plus former smokers. RRs and 95% CIs of current smokers versus non-smokers were calculated using frequency distributions in never smokers and former smokers when the risk estimates were not provided in original studies. Ten studies [ 34 , 36 , 38 , 39 , 42 , 43 , 54 , 58 , 59 , 66 ] did not provide enough data on frequency distribution and were not included in analysis. Twenty-seven studies [ 6 , 13 , 32 , 33 , 35 , 37 , 40 , 41 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 55 , 56 , 57 , 60 , 61 , 62 , 63 , 64 , 65 ] were included to calculate the pooled RR and 95% CI. The results showed that current smoking at baseline was associated with a reduced risk of PCa (RR, 0.74; 95% CI, 0.68–0.80; P < 0.001) (Fig. 2 ). The I 2 statistic and the Cochran’s Q test showed high heterogeneity (I 2 = 90.5%; P < 0.001). Inspection of the funnel plot did not demonstrate publication bias ( P = 0.231; Fig. 3 ).
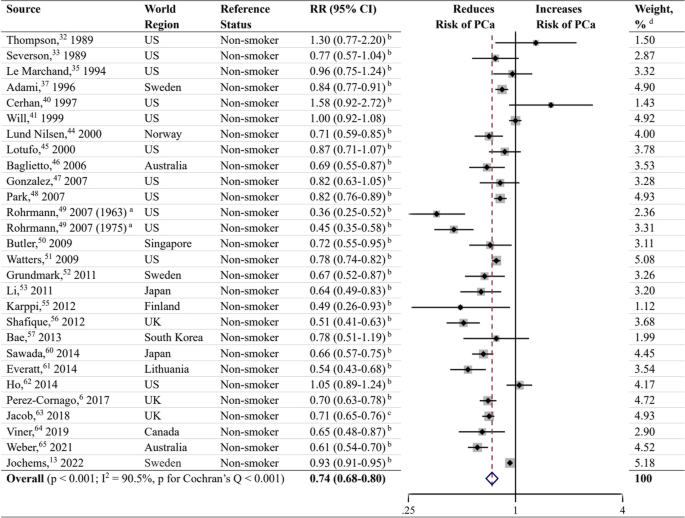
Forest plot for the association between current smoking and prostate cancer. RR, relative risk; CI, confidence interval; PCa, prostate cancer; US, United States; UK, United Kingdom. a Rohrmann et al. [ 49 ] had two sub-populations. b RR and 95% CI were calculated using frequency distributions. c RR and 95% CI were converted from HR and corresponding 95% CI using the formula RR ≈ (1-e HR x ln (1−P0) )/P 0 (P 0 refers to the incidence rate of PCa in the control group). d Weights were from random effects analysis
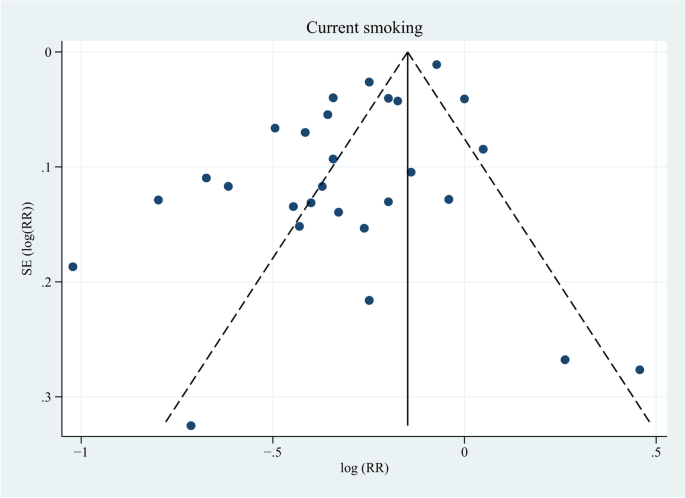
Funnel plot for publication bias in the studies investigating current smoking and prostate cancer risk. SE, standard error. Twenty-eight dots from 27 studies. P = 0.231
When performing sensitivity analyses (Additional file 3 ) stratified by reference status, studies using never smokers as the reference [ 6 , 13 , 33 , 34 , 36 , 37 , 38 , 39 , 40 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 54 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 64 , 65 , 66 ] showed a similar inverse association with PCa risk (RR, 0.90; 95% CI, 0.86–0.95; P < 0.001), with the heterogeneity lower than that of analysis of studies using non-smokers as the reference (I 2 = 66.7%; P < 0.001). Compared to former smokers, current smokers had a significant lower risk of PCa (RR, 0.70; 95% CI, 0.65–0.75; P < 0.001) based on 21 studies [ 6 , 13 , 33 , 37 , 40 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 56 , 57 , 60 , 61 , 62 , 64 , 65 ]. In the pre-PSA screening era, current smoking showed a decreased risk of PCa (RR, 0.79; 95% CI, 0.64–0.98; P = 0.033) compared to non-smokers, while in the PSA screening era, the risk was significantly lower (RR, 0.72; 95% CI, 0.66–0.79; P < 0.001). When stratified by world region, studies conducted in North America, Europe, Asia, and Australia showed a negative association between current smoking and PCa risk. We also performed subgroup analyses in 21 studies with quality scores ≥ 7 [ 6 , 13 , 32 , 33 , 35 , 40 , 44 , 45 , 46 , 49 , 50 , 51 , 52 , 55 , 56 , 57 , 60 , 61 , 62 , 64 , 65 ] and 6 studies with quality scores of 6 [ 37 , 41 , 47 , 48 , 53 , 63 ]. Thereupon, both demonstrated a reduced risk of PCa.
Former smoking
Meta-analysis on former smoking as a risk factor for PCa was performed in 31 studies (Fig. 4 ) [ 6 , 13 , 33 , 34 , 36 , 37 , 38 , 39 , 40 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 54 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 64 , 65 , 66 ], and the results showed no significant association between former smoking and the risk of PCa (RR, 0.98; 95% CI, 0.95–1.02; P = 0.313). The data were heterogeneous according to the I 2 statistic and the Cochran’s Q test (I 2 = 61.5%; P < 0.001). Inspection of the corresponding funnel plot did not show evidence of publication bias ( P = 0.431; Fig. 5 ). Sensitivity analyses stratified by PSA screening era, world region, and quality score also demonstrated no association between former smoking and PCa risk (Additional file 3 ).
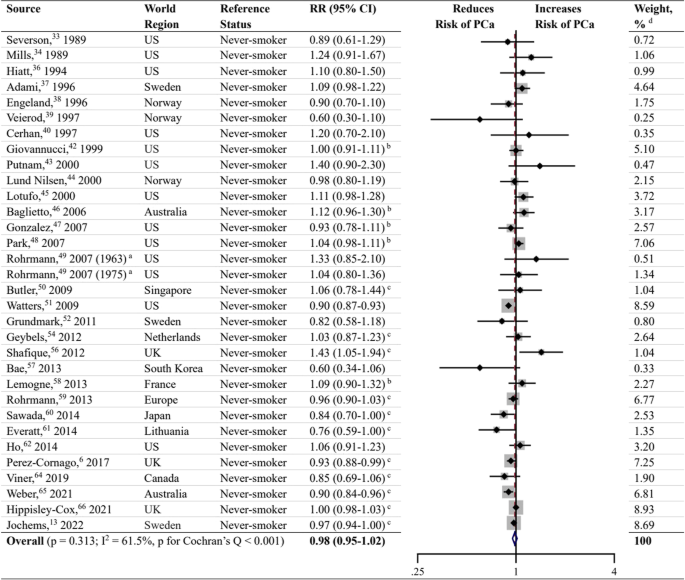
Forest plot for the association between former smoking and prostate cancer. a Rohrmann et al. [ 49 ] had two sub-populations. b RR and 95% CI were calculated using frequency distributions. c RR and 95% CI were converted from HR and corresponding 95% CI using the formula RR ≈ (1-e HR x ln (1−P0) )/P 0 (P 0 refers to the incidence rate of PCa in the control group). d Weights were from random effects analysis
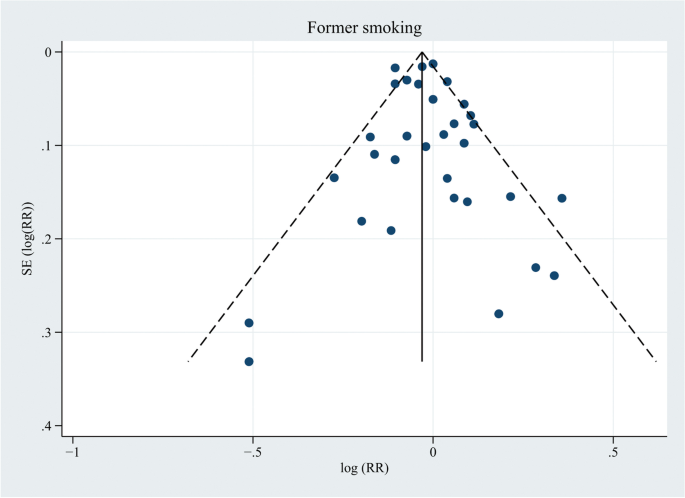
Funnel plot for publication bias in the studies investigating former smoking and prostate cancer risk. Thirty-two dots from 31 studies. P = 0.431
Ever smoking
Thirty-three studies were included in the meta-analysis to assess the association of ever smoking with the risk of PCa (Fig. 6 ) [ 6 , 13 , 33 , 34 , 36 , 37 , 38 , 39 , 40 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 54 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 64 , 65 , 66 , 67 , 68 ]. Two of those studies [ 67 , 68 ] provided RRs and 95% CIs in the original paper, and the risk estimates of the remaining 31 studies [ 6 , 13 , 33 , 34 , 36 , 37 , 38 , 39 , 40 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 54 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 64 , 65 , 66 ] were calculated by combining results for former and current smokers. Thereupon, the pooled RR and 95% CI showed no association with the risk of PCa (RR, 0.96; 95% CI, 0.93–1.00; P = 0.074), with an I 2 value of 67.0% and a negative result of publication bias (( P = 0.672; Fig. 7 ). The association was inverse when analyzing studies completed in the PSA screening era (RR, 0.95; 95% CI, 0.91–0.99; P = 0.011), but in the pre-PSA screening era, ever smokers showed a significantly increased risk of PCa compared to never smokers (RR, 1.05; 95% CI, 1.00–1.10; P = 0.046) (Additional file 3 ). Four studies [ 50 , 57 , 60 , 67 ] from Asia showed a pooled reduced risk of PCa in ever smokers (RR, 0.82; 95% CI, 0.74–0.91; P < 0.001), and studies from North America, Europe, and Australia revealed no association between ever smoking and PCa incidence. In terms of subgroup analyses stratified by quality score, the studies with a quality score ≥ 7 showed a modest negative association with PCa risk (RR, 0.96; 95% CI, 0.92–1.00; P = 0.047), while the studies with a quality score of 6 showed no association.
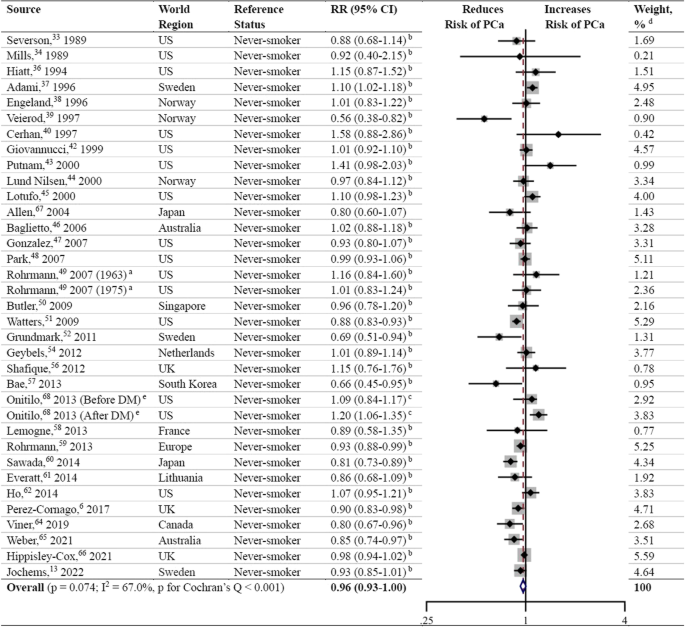
Forest plot for the association between ever smoking and prostate cancer. DM, diabetes mellitus. a Rohrmann et al. [ 49 ] had two sub-populations. b RR and 95% CI were calculated using frequency distributions or risk estimates and 95% CIs in subgroups. c RR and 95% CI were converted from HR and corresponding 95% CI using the formula RR ≈ (1-e HR x ln (1−P0) )/P 0 (P 0 refers to the incidence rate of PCa in the control group). d Weights were from random effects analysis. e Onitilo et al. [ 68 ] had two sub-populations
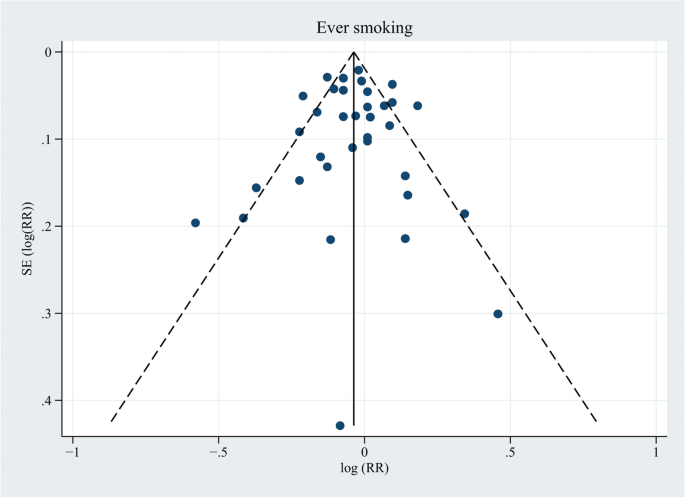
Funnel plot for publication bias in the studies investigating ever smoking and prostate cancer risk. Thirty-five dots from 33 studies. P = 0.672
Studies not included in the meta-analysis
Of these 5 studies (Additional file 1 ) [ 69 , 70 , 71 , 72 , 73 ], 4 studies (involving 211 cases, 524 cases, 127 cases, and 129 cases) [ 69 , 70 , 72 , 73 ] reported no significant association between cigarette smoking and the risk of PCa, 2 of which had a smoking category increment of 10 cigarette per day [ 69 ] or cigarette pack-years per 10 years [ 72 ]. The study conducted by Karlsen et al. [ 73 ] did not differentiate cigarette, cigar, cheroot, and pipe when assessing the risk of PCa in smokers, and as a result, this study could not be included in the meta-analysis. In the study conducted by Chamie et al. [ 71 ], a reduced PCa risk was reported in participants with a smoking history (with 13,144 participants and 363 cases; RR, 0.78; 95% CI, 0.72–0.85; P < 0.001).
In this systematic review and meta-analysis, we found that current smoking was inversely associated with the risk of PCa, especially in the PSA screening era, which was inconsistent with our hypothesis but was consistent with the results of the recent studies [ 12 , 13 ]. In studies using never smokers as the reference, current smoking revealed a similar negative correlation with PCa risk, accompanied by less heterogeneity. Current smokers had a lower risk of PCa compared to former smokers. Former smoking and ever smoking were not associated with PCa risk in the overall analyses. However, when stratified by completion year, ever smoking showed an increased risk of PCa in the pre-PSA screening era and a lower risk of PCa in the PSA screening era. Studies from North America, Europe, Asia, and Australia showed a similar reduced PCa risk in current smokers compared to non-smokers, whereas in ever smokers, only studies conducted in Asia demonstrated a decreased risk of PCa. There are several explanations for these results. Current smoking was believed to be associated with a lower likelihood of PSA testing [ 74 , 75 ], and individuals with a smoking history were less likely to undergo prostate biopsy [ 62 , 76 ]. As a consequence, the detection rate of PCa could be relatively lower among participants in the PSA screening era. The difference in the patterns of the association between ever smoking and PCa risk in Asia and other regions can be attributed to the higher proportion of studies in the PSA screening era in Asia than afterward. Additionally, the differences in race/ethnicity, socioeconomic status, educational attainment, and health literacy may also play important roles in explaining regional distinctions [ 77 , 78 , 79 ]. In a national cross-sectional survey, PSA testing was significantly higher in US-born men and older non-Hispanic White men than in foreign-born men and men from other racial categories [ 77 ]. Another study revealed that White men aged > 50 years were more likely than Black men to undergo PSA testing, and those with lower socioeconomic status were associated with less PSA testing [ 78 ]. The association of education levels with the preference for PSA screening was inconsistent [ 77 , 79 ]. Johnson JA et al. [ 77 ] declared that higher educational levels were associated with higher odds of ever having had a PSA test; however, Pickles K et al. [ 79 ] announced that the preference for PSA screening was stronger in those without tertiary education and with inadequate health literacy. The age of the participants in the selected studies varied widely, and therefore, the willingness to receive PSA screening differs considerably; older people often show poorer adherence to PSA testing guidelines [ 77 ]. On the other hand, the relationship between PSA levels and smoking is still a matter of debate. According to an Italian cross-sectional study [ 80 ], PSA accuracy was reported to be lower in smokers than in nonsmokers and former smokers, suggesting that the need for PSA-based prostate biopsy can be affected to a certain extent by smoking.
Another possible explanation is that smoking is the leading risk factor for death among males [ 81 ]. Smokers may die from smoking attributable diseases including cancers, cardiovascular diseases, and respiratory diseases before their diagnosis of PCa. The majority of cases of lung cancer [ 7 ], head and neck cancer [ 82 ], approximately 50% of bladder cancer cases [ 83 ], and 49% of esophageal squamous cell carcinoma cases [ 84 ] are caused by cigarette smoking. Furthermore, smoking was reported to cause nearly 90% of lung cancer deaths [ 7 ] and showed significant associations with poor survival in patients with head and neck cancer [ 85 ]. Moreover, the detection of asymptomatic PCa can be frequently ignored when focusing on a more aggressive cancer. In addition, smoking increases the risk for stroke and coronary heart disease by 2 to 4 times, and stroke and coronary heart disease are considered to be the leading causes of death in the United States [ 8 ], and most of these deaths are caused by smoking [ 86 ]. Smoking can also cause chronic obstructive pulmonary disease (COPD), increasing 12 to 13-fold risk of dying from COPD than nonsmokers [ 8 ], and nearly 80% of deaths from COPD can be ascribed to smoking [ 86 ].
Our study found an increased risk of PCa among ever smokers in the pre-PSA screening era, indicating that it is necessary to promote smoking cessation as early as possible. Nearly one in five deaths are caused by cigarette smoking in the United States, leading to more than 480 000 deaths each year [ 8 ]. Continued tobacco use has been shown to limit the effectiveness of major cancer treatments, increase the risk of treatment-related complications and the development of secondary cancers, and lower cancer survival rates and the quality of life of patients [ 7 ]. In patients with PCa, smokers at the time of PCa diagnosis are associated with more aggressive characteristics, and the risk of experiencing biochemical recurrence, distant metastasis, cancer-specific mortality, and overall mortality is much higher [ 9 , 10 , 12 , 87 , 88 ]. Nicotine-induced chronic prostatic inflammation [ 23 , 89 ], aberrant CpG methylations of adenomatous polyposis coli and glutathione S-transferase pi are the potential biological mechanisms responsible for these [ 90 ]. Although the effect of smoking cessation on PCa progression remains unclear, the negative impact of smoking has suggested to be maintained as long as 10 years after smoking cessation [ 10 ]. Additionally, active smoking is associated with adverse reproductive health outcomes, type 2 diabetes mellitus, and rheumatoid arthritis, harming nearly every organ of the body and resulting in significant economic costs for smokers, their families, and society [ 7 ].
Much progress has been made in promoting smoking cessation in recent decades. However, it is far from sufficient. In 2018, 13.7% of all adults (34.2 million people) in the United States were reported as current cigarette smokers [ 91 ]. Of them, 55.1% had made an attempt to quit in the past 12 months, but only 7.5% achieved success. Overcoming both physical nicotine dependence and long-standing rewarding behavior is a huge challenge, and most individuals relapse within 3 months after quitting smoking [ 92 ]. Evidence has indicated that the combination of behavioral and pharmacological interventions produces the largest cessation effects [ 7 , 8 , 92 ]. Nevertheless, fewer than one-half of tobacco users were offered cessation treatment according to a survey of oncology providers [ 93 ], and the inability to get patients to quit and patient resistance to treatment are two dominant barriers to cessation intervention. A brief intervention may be more acceptable and sustainable to help smokers quit smoking, according to a randomized clinical trial performed at emergency departments in Hong Kong [ 94 ]. Quitlines are good alternatives to interventions for both patients and clinicians because of their convenience and specialization, and their roles in improving smoking cessation rates have been confirmed [ 95 ]. For smokers with time constraints, internet-based self-help materials such as the website smokefred.gov and newer smartphone applications have also shown benefits in promoting smoking cessation and can serve as good alternatives [ 96 , 97 ].
Strengths and limitations
The key strength of this systematic review is that the study comprised a total of 44 prospective cohort studies, 39 of which were included in the meta-analysis, with the largest number of participants and PCa cases to date. Furthermore, we included all the data on current smoking, former smoking, and ever smoking in the analysis without date and language restrictions, which means that the study provides the latest evidence and the most comprehensive information on the association between cigarette smoking and risk of PCa. We assessed the quality of each selected study using the Newcastle‒Ottawa Scale for cohort studies, and the median score was 7 and the lowest score was 6, suggesting that the quality of the included studies can be guaranteed. Other strengths include applying independent literature search, quality assessment, and data extraction by two investigators; conducting several sensitivity analyses; and using Egger’s test to examine publication bias.There are some limitations of our study. Most of the information on smoking habits was obtained from self-administered questionnaires, and the definitions of current smokers and former smokers were not completely the same between different studies. Some participants may have changed their smoking habits after baseline investigations, but repeated assessment of smoking exposure was absent in primary studies. We calculated RRs and the corresponding 95% CIs using frequency distributions without adjusting confounding factors when risk estimates were not reported. We focused on the impact of cigarette smoking on the risk of PCa; second-hand cigarette smoke and the use of other tobacco products (cigars, smokeless tobacco, e-cigarettes, pipes, etc.) that have showed increased risk of many cancers in numerous studies [ 98 , 99 ] were not discussed. Alcohol consumption showed a significant dose–response relationship with PCa risk in several studies [ 3 , 100 ], and were often used concurrently with cigarette smoking [ 101 ], but we didn’t analyze the effect of concurrent use of cigarette and alcohol on risk of PCa due to lack of information on alcohol consumption in the included studies. High heterogeneity was showed by the I 2 statistics and the Cochran’s Q test, and the difference in adjusted confounding factors may be one of the reasons. We have included multivariate results as much as possible to reduce the bias, and there was no indication of publication bias. Dividing studies into pre-PSA screening era and PSA screening era based on publication year (1995 as the cut-off) may produce bias because many of the cohorts published and categorized into the PSA screening era extended into the pre-PSA screening era. Another limitation is that we failed to calculate the impact of quantitative cigarette consumption on the PCa risk due to a lack of data. However, we have to point out that the meta-regression conducted by Islami et al. [ 12 ] was methodologically wrong as including multiple data points from a single study with the same control group counts the effect of that control group multiple times (i.e., unit-of-analysis error).
To the best of our knowledge, this systematic review and meta-analysis contained the largest sample of prospective cohort studies, the latest evidence and the most comprehensive information on the association between cigarette smoking habits and the risk of PCa. The smokers’ poor adherence to cancer screening and the occurrence of smoking-related aggressive cancers as well as cardiovascular, pulmonary, and several other deadly diseases may explain the negative association. Regional distinctions can be attributed to the difference of participants in age, ethnicity, socioeconomic status, and educational levels. In addition, a correct methodology is important, the choice of different effect models should base on the heterogeneity and characteristics of enrolled studies. However, it is difficult to conclude a positive association between cigarette smoking and PCa risk as we hypothesized due to these affecting factors. We should focus on taking measures to help smokers to be more compliant with early cancer screening and to quit smoking.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Abbreviations
- Prostate cancer
Prostate-specific antigen
Polycyclic aromatic hydrocarbons
Glutathione-S-transferases
Heme oxygenase 1
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Cigarettes per day
Confidence interval
Relative risk
Not reported
United States
Blood pressure
Body mass index
United Kingdom
Diabetes mellitus
Non-significant
Chronic obstructive pulmonary disease
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Article PubMed Google Scholar
Bostwick DG, Burke HB, Djakiew D, Euling S, Ho SM, Landolph J, et al. Human prostate cancer risk factors. Cancer. 2004;101(10 Suppl):2371–490.
Article CAS PubMed Google Scholar
Dickerman BA, Markt SC, Koskenvuo M, Pukkala E, Mucci LA, Kaprio J. Alcohol intake, drinking patterns, and prostate cancer risk and mortality: a 30-year prospective cohort study of Finnish twins. Cancer Causes Control. 2016;27(9):1049–58.
Article PubMed PubMed Central Google Scholar
Rowles JL 3rd, Ranard KM, Applegate CC, Jeon S, An R, Erdman JW Jr. Processed and raw tomato consumption and risk of prostate cancer: a systematic review and dose-response meta-analysis. Prostate Cancer Prostatic Dis. 2018;21(3):319–36.
Chen X, Zhao Y, Tao Z, Wang K. Coffee consumption and risk of prostate cancer: a systematic review and meta-analysis. BMJ Open. 2021;11(2): e038902.
Perez-Cornago A, Key TJ, Allen NE, Fensom GK, Bradbury KE, Martin RM, et al. Prospective investigation of risk factors for prostate cancer in the UK Biobank cohort study. Br J Cancer. 2017;117(10):1562–71.
Karam-Hage M, Cinciripini PM, Gritz ER. Tobacco use and cessation for cancer survivors: an overview for clinicians. CA Cancer J Clin. 2014;64(4):272–90.
U.S. Department of Health and Human Services. Smoking cessation. A report of the surgeon general. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2020. (Accessed 30 Sep 2022).
De Nunzio C, Andriole GL, Thompson IM Jr, Freedland SJ. Smoking and prostate cancer: a systematic review. Eur Urol Focus. 2015;1(1):28–38.
Brookman-May SD, Campi R, Henríquez JDS, Klatte T, Langenhuijsen JF, Brausi M, et al. Latest evidence on the impact of smoking, sports, and sexual activity as modifiable lifestyle risk factors for prostate cancer incidence, recurrence, and progression: a systematic review of the literature by the European Association of Urology Section of Oncological Urology (ESOU). Eur Urol Focus. 2019;5(5):756–87.
Huncharek M, Haddock KS, Reid R, Kupelnick B. Smoking as a risk factor for prostate cancer: a meta-analysis of 24 prospective cohort studies. Am J Public Health. 2010;100(4):693–701.
Islami F, Moreira DM, Boffetta P, Freedland SJ. A systematic review and meta-analysis of tobacco use and prostate cancer mortality and incidence in prospective cohort studies. Eur Urol. 2014;66(6):1054–64.
Jochems SHJ, Fritz J, Häggström C, Järvholm B, Stattin P, Stocks T. Smoking and risk of prostate cancer and prostate cancer death: a pooled study. Eur Urol. 2022;3:S0302-2838(22)01804-8.
Centers for Disease Control and Prevention (US); National Center for Chronic Disease Prevention and Health Promotion (US); Office on Smoking and Health (US). How tobacco smoke causes disease: the biology and behavioral basis for smoking-attributable disease: a report of the surgeon general. Atlanta: Centers for Disease Control and Prevention (US); 2010.
Nock NL, Tang D, Rundle A, Neslund-Dudas C, Savera AT, Bock CH, et al. Associations between smoking, polymorphisms in polycyclic aromatic hydrocarbon (PAH) metabolism and conjugation genes and PAH-DNA adducts in prostate tumors differ by race. Cancer Epidemiol Biomarkers Prev. 2007;16(6):1236–45.
Article CAS PubMed PubMed Central Google Scholar
Mao GE, Morris G, Lu QY, Cao W, Reuter VE, Cordon-Cardo C, et al. Glutathione S-transferase P1 Ile105Val polymorphism, cigarette smoking and prostate cancer. Cancer Detect Prev. 2004;28(5):368–74.
Ye J, Wang S, Barger M, Castranova V, Shi X. Activation of androgen response element by cadmium: a potential mechanism for a carcinogenic effect of cadmium in the prostate. J Environ Pathol Toxicol Oncol. 2000;19(3):275–80.
CAS PubMed Google Scholar
Watts EL, Appleby PN, Perez-Cornago A, Bueno-de-Mesquita HB, Chan JM, Chen C, et al. Low free testosterone and prostate cancer risk: a collaborative analysis of 20 prospective studies. Eur Urol. 2018;74(5):585–94.
Shiels MS, Rohrmann S, Menke A, Selvin E, Crespo CJ, Rifai N, et al. Association of cigarette smoking, alcohol consumption, and physical activity with sex steroid hormone levels in US men. Cancer Causes Control. 2009;20(6):877–86.
Quiñones LA, Irarrázabal CE, Rojas CR, Orellana CE, Acevedo C, Huidobro C, et al. Joint effect among p53, CYP1A1, GSTM1 polymorphism combinations and smoking on prostate cancer risk: an exploratory genotype-environment interaction study. Asian J Androl. 2006;8(3):349–55.
Birrane G, Li H, Yang S, Tachado SD, Seng S. Cigarette smoke induces nuclear translocation of heme oxygenase 1 (HO-1) in prostate cancer cells: nuclear HO-1 promotes vascular endothelial growth factor secretion. Int J Oncol. 2013;42(6):1919–28.
Miyake M, Fujimoto K, Anai S, Ohnishi S, Kuwada M, Nakai Y, et al. Heme oxygenase-1 promotes angiogenesis in urothelial carcinoma of the urinary bladder. Oncol Rep. 2011;25(3):653–60.
De Nunzio C, Kramer G, Marberger M, Montironi R, Nelson W, et al. The controversial relationship between benign prostatic hyperplasia and prostate cancer: the role of inflammation. Eur Urol. 2011;60(1):106–17.
Arnson Y, Shoenfeld Y, Amital H. Effects of tobacco smoke on immunity, inflammation and autoimmunity. J Autoimmun. 2010;34(3):J258–65.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
Lo CK, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 2014;14:45.
Davies HT, Crombie IK, Tavakoli M. When can odds ratios mislead? BMJ. 1998;316(7136):989–91.
Janez S, Maucort-Boulch D. Odds ratio, hazard ratio and relative risk. Adv Methodol Stat. 2016;13(1):59–67.
Google Scholar
Shor E, Roelfs D, Vang ZM. The “Hispanic mortality paradox” revisited: Meta-analysis and meta-regression of life-course differentials in Latin American and Caribbean immigrants’ mortality. Soc Sci Med. 2017;186:20–33.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Thompson MM, Garland C, Barrett-Connor E, Khaw KT, Friedlander NJ, Wingard DL. Heart disease risk factors, diabetes, and prostatic cancer in an adult community. Am J Epidemiol. 1989;129(3):511–7.
Severson RK, Nomura AM, Grove JS, Stemmermann GN. A prospective study of demographics, diet, and prostate cancer among men of Japanese ancestry in Hawaii. Cancer Res. 1989;49(7):1857–60.
Mills PK, Beeson WL, Phillips RL, Fraser GE. Cohort study of diet, lifestyle, and prostate cancer in Adventist men. Cancer. 1989;64(3):598–604.
Le Marchand L, Kolonel LN, Wilkens LR, Myers BC, Hirohata T. Animal fat consumption and prostate cancer: a prospective study in Hawaii. Epidemiology. 1994;5(3):276–82.
Hiatt RA, Armstrong MA, Klatsky AL, Sidney S. Alcohol consumption, smoking, and other risk factors and prostate cancer in a large health plan cohort in California (United States). Cancer Causes Control. 1994;5(1):66–72.
Adami HO, Bergström R, Engholm G, Nyrén O, Wolk A, Ekbom A, et al. A prospective study of smoking and risk of prostate cancer. Int J Cancer. 1996;67(6):764–8.
Engeland A, Andersen A, Haldorsen T, Tretli S. Smoking habits and risk of cancers other than lung cancer: 28 years’ follow-up of 26,000 Norwegian men and women. Cancer Causes Control. 1996;7(5):497–506.
Veierød MB, Laake P, Thelle DS. Dietary fat intake and risk of prostate cancer: a prospective study of 25,708 Norwegian men. Int J Cancer. 1997;73(5):634–8.
Cerhan JR, Torner JC, Lynch CF, Rubenstein LM, Lemke JH, Cohen MB, et al. Association of smoking, body mass, and physical activity with risk of prostate cancer in the Iowa 65+ Rural Health Study (United States). Cancer Causes Control. 1997;8(2):229–38.
Will JC, Vinicor F, Calle EE. Is diabetes mellitus associated with prostate cancer incidence and survival? Epidemiology. 1999;10(3):313–8.
Giovannucci E, Rimm EB, Ascherio A, Colditz GA, Spiegelman D, Stampfer HJ, et al. Smoking and risk of total and fatal prostate cancer in United States health professionals. Cancer Epidemiol Biomarkers Prev. 1999;8(4):277–82.
Putnam SD, Cerhan JR, Parker AS, Bianchi GD, Wallace RB, Cantor KP, et al. Lifestyle and anthropometric risk factors for prostate cancer in a cohort of Iowa men. Ann Epidemiol. 2000;10(6):361–9.
Lund Nilsen TL, Johnsen R, Vatten LJ. Socio-economic and lifestyle factors associated with the risk of prostate cancer. Br J Cancer. 2000;82(7):1358–63.
Lotufo PA, Lee IM, Ajani UA, Hennekens CH, Manson JE. Cigarette smoking and risk of prostate cancer in the physicians’ health study (United States). Int J Cancer. 2000;87(1):141–4.
Baglietto L, Severi G, English DR, Hopper JL, Giles GG. Alcohol consumption and prostate cancer risk: results from the Melbourne collaborative cohort study. Int J Cancer. 2006;119(6):1501–4.
Gonzalez A, Peters U, Lampe JW, White E. Boron intake and prostate cancer risk. Cancer Causes Control. 2007;18(10):1131–40.
Park SY, Murphy SP, Wilkens LR, Henderson BE, Kolonel LN. Fat and meat intake and prostate cancer risk: the multiethnic cohort study. Int J Cancer. 2007;121(6):1339–45.
Rohrmann S, Genkinger JM, Burke A, Helzlsouer KJ, Comstock GW, Alberg AJ, et al. Smoking and risk of fatal prostate cancer in a prospective U.S. study. Urology. 2007;69(4):721–5.
Butler LM, Wang R, Wong AS, Koh WP, Yu MC. Cigarette smoking and risk of prostate cancer among Singapore Chinese. Cancer Causes Control. 2009;20(10):1967–74.
Watters JL, Park Y, Hollenbeck A, Schatzkin A, Albanes D. Cigarette smoking and prostate cancer in a prospective US cohort study. Cancer Epidemiol Biomarkers Prev. 2009;18(9):2427–35.
Grundmark B, Zethelius B, Garmo H, Holmberg L. Serum levels of selenium and smoking habits at age 50 influence long term prostate cancer risk; a 34 year ULSAM follow-up. BMC Cancer. 2011;11:431.
Li Q, Kuriyama S, Kakizaki M, Yan H, Nagai M, Sugawara Y, et al. History of cholelithiasis and the risk of prostate cancer: the Ohsaki Cohort Study. Int J Cancer. 2011;128(1):185–91.
Geybels MS, Verhage BA, van Schooten FJ, van den Brandt PA. Measures of combined antioxidant and pro-oxidant exposures and risk of overall and advanced stage prostate cancer. Ann Epidemiol. 2012;22(11):814–20.
Karppi J, Kurl S, Laukkanen JA, Kauhanen J. Serum β-carotene in relation to risk of prostate cancer: the Kuopio Ischaemic Heart Disease Risk Factor study. Nutr Cancer. 2012;64(3):361–7.
Shafique K, McLoone P, Qureshi K, Leung H, Hart C, Morrison DS. Coffee consumption and prostate cancer risk: further evidence for inverse relationship. Nutr J. 2012;11:42.
Bae JM, Li ZM, Shin MH, Kim DH, Lee MS, Ahn YO. Cigarette smoking and prostate cancer risk: negative results of the Seoul Male Cancer Cohort Study. Asian Pac J Cancer Prev. 2013;14(8):4667–9.
Lemogne C, Consoli SM, Geoffroy-Perez B, Coeuret-Pellicer M, Nabi H, Melchior M, et al. Personality and the risk of cancer: a 16-year follow-up study of the GAZEL cohort. Psychosom Med. 2013;75(3):262–71.
Rohrmann S, Linseisen J, Allen N, Bueno-de-Mesquita HB, Johnsen NF, Tjønneland A, et al. Smoking and the risk of prostate cancer in the European Prospective Investigation into Cancer and Nutrition. Br J Cancer. 2013;108(3):708–14.
Sawada N, Inoue M, Iwasaki M, Sasazuki S, Yamaji T, Shimazu T, et al. Alcohol and smoking and subsequent risk of prostate cancer in Japanese men: the Japan Public Health Center-based prospective study. Int J Cancer. 2014;134(4):971–8.
Everatt R, Kuzmickienė I, Virvičiūtė D, Tamošiūnas A. Cigarette smoking, educational level and total and site-specific cancer: a cohort study in men in Lithuania. Eur J Cancer Prev. 2014;23(6):579–86.
Ho T, Howard L, Vidal A, Gerber L, Moreira D, McKeever M, et al. Smoking and risk of low- and high-grade prostate cancer: results from the REDUCE study. Clin Cancer Res. 2014;20(20):5331–8.
Jacob L, Freyn M, Kalder M, Dinas K, Kostev K. Impact of tobacco smoking on the risk of developing 25 different cancers in the UK: a retrospective study of 422,010 patients followed for up to 30 years. Oncotarget. 2018;9(25):17420–9.
Viner B, Barberio AM, Haig TR, Friedenreich CM, Brenner DR. The individual and combined effects of alcohol consumption and cigarette smoking on site-specific cancer risk in a prospective cohort of 26,607 adults: results from Alberta’s Tomorrow Project. Cancer Causes Control. 2019;30(12):1313–26.
Weber MF, Sarich PEA, Vaneckova P, Wade S, Egger S, Ngo P, et al. Cancer incidence and cancer death in relation to tobacco smoking in a population-based Australian cohort study. Int J Cancer. 2021;149(5):1076–88.
Hippisley-Cox J, Coupland C. Predicting the risk of prostate cancer in asymptomatic men: a cohort study to develop and validate a novel algorithm. Br J Gen Pract. 2021;71(706):e364–71.
Allen NE, Sauvaget C, Roddam AW, Appleby P, Nagano J, Suzuki G, et al. A prospective study of diet and prostate cancer in Japanese men. Cancer Causes Control. 2004;15(9):911–20.
Onitilo AA, Berg RL, Engel JM, Stankowski RV, Glurich I, Williams GM, et al. Prostate cancer risk in pre-diabetic men: a matched cohort study. Clin Med Res. 2013;11(4):201–9.
Thune I, Lund E. Physical activity and the risk of prostate and testicular cancer: a cohort study of 53,000 Norwegian men. Cancer Causes Control. 1994;5(6):549–56.
Tulinius H, Sigfússon N, Sigvaldason H, Bjarnadóttir K, Tryggvadóttir L. Risk factors for malignant diseases: a cohort study on a population of 22,946 Icelanders. Cancer Epidemiol Biomarkers Prev. 1997;6(11):863–73.
Chamie K, DeVere White RW, Lee D, Ok JH, Ellison LM. Agent Orange exposure, Vietnam War veterans, and the risk of prostate cancer. Cancer. 2008;113(9):2464–70.
Laukkanen JA, Pukkala E, Rauramaa R, Makikallio TH, Toriola AT, Kurl S. Cardiorespiratory fitness, lifestyle factors and cancer risk and mortality in Finnish men. Eur J Cancer. 2010;46(2):355–63.
Karlsen RV, Bidstrup PE, Christensen J, Larsen SB, Tjønneland A, Dalton SO, et al. Men with cancer change their health behaviour: a prospective study from the Danish diet, cancer and health study. Br J Cancer. 2012;107(1):201–6.
Rolison JJ, Hanoch Y, Miron-Shatz T. Smokers: at risk for prostate cancer but unlikely to screen. Addict Behav. 2012;37(6):736–8.
Littlejohns TJ, Travis RC, Key TJ, Allen NE. Lifestyle factors and prostate-specific antigen (PSA) testing in UK Biobank: Implications for epidemiological research. Cancer Epidemiol. 2016;45:40–6.
Tangen C, Goodman P, Till C, Schenk J, Lucia M, Thompson I. Biases in recommendations for and acceptance of prostate biopsy significantly affect assessment of prostate cancer risk factors: results from two large randomized clinical trials. J Clin Oncol. 2016;34(36):4338–44.
Johnson JA, Moser RP, Ellison GL, Martin DN. Associations of prostate-specific antigen (PSA) testing in the US population: results from a national cross-sectional survey. J Community Health. 2021;46(2):389–98.
Moses KA, Zhao Z, Bi Y, Acquaye J, Holmes A, Blot WJ, et al. The impact of sociodemographic factors and PSA screening among low-income Black and White men: data from the Southern Community Cohort Study. Prostate Cancer Prostatic Dis. 2017;20(4):424–9.
Pickles K, Scherer LD, Cvejic E, Hersch J, Barratt A, McCaffery KJ. Preferences for more or less health care and association with health literacy of men eligible for prostate-specific antigen screening in Australia. JAMA Netw Open. 2021;4(10): e2128380.
de Nunzio C, Tema G, Trucchi A, Cicione A, Sica A, Lombardo R, et al. Smoking reduces PSA accuracy for detection of prostate cancer: Results from an Italian cross-sectional study. Minerva Urol Nefrol. 2019;71(6):583–9.
GBD 2019 Tobacco Collaborators. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990–2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet. 2021;397(10292):2337-2360.
Sturgis EM, Wei Q, Spitz MR. Descriptive epidemiology and risk factors for head and neck cancer. Semin Oncol. 2004;31(6):726–33.
Burger M, Catto JW, Dalbagni G, Grossman HB, Herr H, Karakiewicz P, et al. Epidemiology and risk factors of urothelial bladder cancer. Eur Urol. 2013;63(2):234–41.
Cook MB, Kamangar F, Whiteman DC, Freedman ND, Gammon MD, Bernstein L, et al. Cigarette smoking and adenocarcinomas of the esophagus and esophagogastric junction: a pooled analysis from the international BEACON consortium. J Natl Cancer Inst. 2010;102(17):1344–53.
Duffy SA, Ronis DL, McLean S, Fowler KE, Gruber SB, Wolf GT, et al. Pretreatment health behaviors predict survival among patients with head and neck squamous cell carcinoma. J Clin Oncol. 2009;27(12):1969–75.
Centers for Disease Control and Prevention (CDC). Smoking-attributable mortality, years of potential life lost, and productivity losses--United States, 2000-2004. MMWR Morb Mortal Wkly Rep. 2008;57(45):1226–8.
Foerster B, Pozo C, Abufaraj M, Mari A, Kimura S, D’Andrea D, et al. Association of smoking status with recurrence, metastasis, and mortality among patients with localized prostate cancer undergoing prostatectomy or radiotherapy: a systematic review and meta-analysis. JAMA Oncol. 2018;4(7):953–61.
Darcey E, Boyle T. Tobacco smoking and survival after a prostate cancer diagnosis: a systematic review and meta-analysis. Cancer Treat Rev. 2018;70:30–40.
Prueitt RL, Wallace TA, Glynn SA, Yi M, Tang W, Luo J, et al. An immune-inflammation gene expression signature in prostate tumors of smokers. Cancer Res. 2016;76(5):1055–65.
Enokida H, Shiina H, Urakami S, Terashima M, Ogishima T, Li LC, et al. Smoking influences aberrant CpG hypermethylation of multiple genes in human prostate carcinoma. Cancer. 2006;106(1):79–86.
Creamer MR, Wang TW, Babb S, Cullen KA, Day H, Willis G, et al. Tobacco product use and cessation indicators among adults - United States, 2018. MMWR Morb Mortal Wkly Rep. 2019;68(45):1013–9.
Rigotti NA, Kruse GR, Livingstone-Banks J, Hartmann-Boyce J. Treatment of tobacco smoking: a review. JAMA. 2022;327(6):566–77.
Warren GW, Marshall JR, Cummings KM, Toll BA, Gritz ER, Hutson A, et al. Addressing tobacco use in patients with cancer: a survey of American Society of Clinical Oncology members. J Oncol Pract. 2013;9(5):258–62.
Li WHC, Ho KY, Wang MP, Cheung DYT, Lam KKW, Xia W, et al. Effectiveness of a brief self-determination theory-based smoking cessation intervention for smokers at Emergency Departments in Hong Kong: a randomized clinical trial. JAMA Intern Med. 2020;180(2):206–14.
Stead LF, Hartmann-Boyce J, Perera R, Lancaster T. Telephone counselling for smoking cessation. Cochrane Database Syst Rev. 2013;(8):CD002850.
Lancaster T, Stead LF. Self-help interventions for smoking cessation. Cochrane Database Syst Rev. 2005;(3):CD001118.
Civljak M, Sheikh A, Stead LF, Car J. Internet-based interventions for smoking cessation. Cochrane Database Syst Rev. 2010;(9):CD007078.
Kim AS, Ko HJ, Kwon JH, Lee JM. Exposure to secondhand smoke and risk of cancer in never smokers: a meta-analysis of epidemiologic studies. Int J Environ Res Public Health. 2018;15(9):1981.
Andreotti G, Freedman ND, Silverman DT, Lerro CC, Koutros S, Hartge P, et al. Tobacco use and cancer risk in the agricultural health study. Cancer Epidemiol Biomarkers Prev. 2017;26(5):769–78.
Zhao J, Stockwell T, Roemer A, Chikritzhs T. Is alcohol consumption a risk factor for prostate cancer? A systematic review and meta-analysis. BMC Cancer. 2016;16(1):845.
Sharma R, Lodhi S, Sahota P, Thakkar MM. Nicotine administration in the wake-promoting basal forebrain attenuates sleep-promoting effects of alcohol. J Neurochem. 2015;135(2):323–31.
Download references
Acknowledgements
Not applicable.
This work was supported by the Sanming Project of Medicine in Shenzhen (grant number: SZSM202011011). The funder had no role in the study design, data collection, analysis and interpretation, or writing of the report.
Author information
Xiangwei Yang and Hong Chen contributed equally to this work.
Authors and Affiliations
Department of Urology, Kidney and Urology Center, Pelvic Floor Disorders Center, The Seventh Affiliated Hospital, Sun Yat-Sen University, No.628 Zhenyuan Road, Shenzhen, 518107, China
Xiangwei Yang, Shiqiang Zhang, Xianju Chen, Yiyu Sheng & Jun Pang
School of Nursing, LKS Faculty of Medicine, University of Hong Kong, Hong Kong, China
You can also search for this author in PubMed Google Scholar
Contributions
XWY, HC and JP conceptualized the study and developed the registered protocol for the review. XWY and HC conducted the literature search, quality assessment, data extraction, and drafted the manuscript. SQZ, XJC and YYS performed statistical analyses. JP revised the manuscript, obtained funding and supervised the project. JP is responsible for the overall content and serves as the guarantor. All authors helped refine the final version of the manuscript and approve with its submission.
Corresponding author
Correspondence to Jun Pang .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
A. Characteristics of the 39 studies included in the meta-analysis. B. Characteristics of the 5 studies not included in the meta-analysis due to lack of information.
Additional file 2.
Results of quality assessment using the Newcastle-Ottawa Scale for cohort studies.
Additional file 3.
Sensitivity analyses of association between smoking status and risk of prostate cancer.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Yang, X., Chen, H., Zhang, S. et al. Association of cigarette smoking habits with the risk of prostate cancer: a systematic review and meta-analysis. BMC Public Health 23 , 1150 (2023). https://doi.org/10.1186/s12889-023-16085-w
Download citation
Received : 21 November 2022
Accepted : 09 June 2023
Published : 15 June 2023
DOI : https://doi.org/10.1186/s12889-023-16085-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cigarette smoking
- Systematic review
- Meta-analysis
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Home — Essay Samples — Nursing & Health — Smoking — The Effects Of Smoking On Health
The Effects of Smoking on Health
- Categories: Smoking Tobacco
About this sample

Words: 491 |
Published: Mar 1, 2019
Words: 491 | Page: 1 | 3 min read

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr Jacklynne
Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
2 pages / 789 words
6 pages / 2528 words
2 pages / 783 words
6 pages / 2929 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Smoking
Smoking is a prevalent practice in many societies, with approximately 1 billion people engaging in this habit. The act of smoking involves burning substances, such as tobacco or cannabis, and inhaling the resulting smoke into [...]
Good afternoon, ladies and gentlemen. Today, I would like to talk to you about the dangers of smoking and the impact it has on individuals and society as a whole. Smoking is a prevalent habit that has been around for centuries, [...]
Smoking has numerous health effects, both short-term and long-term. Some of the short-term effects include bad breath, yellow teeth, and decreased sense of taste and smell. The long-term effects, however, are much more severe. [...]
Vape has become one of the most popular means of smoking nowadays. People find that vaping is better than smoking cigarettes. Vape has many characteristics those attract people to take it instead of cigarettes. As people are [...]
For years there has been conflicting research whether smoking should be banned or not and it is a significant issue today. Many people have given up smoking while others still continue to smoke. Smoking is the inhalation and [...]
Vaping is not a traditional smoking. Many of us don’t even consider it as a substitute of smoking. That’s why a large chunk of non-smokers get attracted towards vaping because it’s harmless, flavored, aromatic and obviously [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Free Cause and Effect Essay on Smoking
Published by gudwriter on May 30, 2018 May 30, 2018
Causes and effects of smoking is a broad application that requires adequate research and knowledge to write and expound on the subject, thus students who doubt their research skills can opt to purchase a research proposal from a legit service like Gudwriter to help them with the homework.
Elevate Your Writing with Our Free Writing Tools!
Did you know that we provide a free essay and speech generator, plagiarism checker, summarizer, paraphraser, and other writing tools for free?
Smoking Cause and Effect Essay Outline
Introduction .
Thesis: To understand the social and health implications of smoking it is essential to look into some of its causes and effects.
Paragraph 1:
Peer pressure is the most prevalent cause of smoking.
- Most people start smoking through the influence of their friends,
- Smoking begins when most people are young; that is during adolescence and in their early twenties.
- Quitting smoking due to addiction is difficult.
Paragraph 2:
Parenting style determines whether or not one will be a smoker.
- A child whose parents were smokers is highly likely to become a smoker.
- Children take after their parents’ behaviors.
Paragraph 3:
People are duped into believing that smoking relieves stress.
- People engage in smoking as a way of managing stress.
- Smoking does not relieve stress; instead, it increases it.
- The level of stress in smokers is higher compared to non-smokers.
Paragraph 4:
Smoking is the leading cause of lung cancer in the world.
- Smoking causes cancer both in active and passive smokers.
- Smoking also causes anxiety on the victim.
- Smoking damages the lining of one’s lungs thus causing lung cancer.
- Continued smoking leads to permanent damage to lung tissues.
Paragraph 5:
Smoking causes loss of sight.
- Cataracts are the number one cause of blindness in the world.
- Smokers are twice at the risk of developing cataracts than non-smokers.
- AMD is the leading cause of permanent blindness in people aged 65years and above.
- Smokers are three times likely to develop AMD than non-smokers.
Paragraph 6:
Smoking is one of the major causes of type-2 diabetes.
- 40% of smokers are likely to develop type-2 diabetes.
- Diabetic smokers make it hard to control the disease progress and insulin levels thus increasing their chances of dying from the disease.
- Diabetic smokers are also likely to suffer from other health complications linked to diabetes such as heart failure, kidney problems, high blood pressure, retinopathy, and peripheral neuropathy.
Paragraph 7:
Smoking is the number one cause of death in the US among all the causes of preventable deaths.
- 480,000 deaths in the country are caused by cigarette smoking each year.
- This translates to 20% of the total yearly deaths.
Conclusion:
Smoking is a general lifestyle behavior among young people. People engage in the practice as a way of having fun. Peer pressure is one of the leading factors that drive people to smoke. Parenting style also contributes to the chances of one becoming a smoker. Most people underestimate the health risks associated with smoking. Lung cancer, blindness, and type-2 diabetes are some of the few health effects attributed to smoking.
Learn how to write a cause and effect essay that will get you good grades.
Cause and Effect Essay on Smoking
Introduction.
Smoking is considered a lifestyle behavior. Many people engage in the practice without the awareness of the health risks it is associated with. Smoking is one of the most addictive lifestyle behaviors and has life-changing implications. It has been termed as one of the most significant health challenges that health organizations are facing today (Onor et al., 2017). According to reports by World Health Organization, there were more than 1 billion smokers all over the world in 2014. To understand the social and health implications of smoking, it is essential to look into some of its causes and effects.
Peer pressure is the most prevalent cause of smoking. According to research, most smokers start the smoking habit at a tender age. During adolescence and in the early twenties, most people are infatuated with friendships (Ukwayi, Eja & Unwanede, 2012). At this stage in life, friends hold great value and meaning in individuals. It is at this age that most people are either in their final years in high school or just starting off in college. Most young people particularly those at the college and high school levels engage in various dangerous and life-harming activities, one of which is smoking (Ukwayi, Eja & Unwanede, 2012). Often, their intent is not to become smokers but to enjoy the experience of being young and feel a celebrated status over their peers. If one belongs to a group whose members are smokers, then they too will likely start smoking (Ukwayi, Eja & Unwanede, 2012). Later in life, such people try to drop the smoking behavior, but it becomes challenging due to withdrawal effects.
Parenting style is another factor that may determine whether or not one will become a smoker. The manner in which a child is raised contributes significantly to their behavior as adults (Gilman et al., 2009). Most children look up to their parents and will adopt most of the lifestyle behaviors portrayed by the parents (Gilman et al., 2009). There are parents who have the habit of smoking in the presence of their children, a behavior which is utterly irresponsible (Gilman et al., 2009). Children get the idea that smoking is not unhealthy if their parents do it in their presence (Gilman et al., 2009). Once such children grow up, they develop a liking for tobacco smoking without knowing that it is an unhealthy lifestyle behavior.
There is also a misconception that smoking acts as strain reliever. This delusion blinds most people that smoking helps one relieve stress. Many people therefore find themselves engaging in the habit as a stress management strategy (Choi, Ota & Watanuki, 2015). Noteworthy, continued smoking leads to addiction, thereby making it very difficult for one to do away with the habit once they start it. Research has shown that smoking does not relieve stress, instead it increases it (Choi, Ota & Watanuki, 2015). The level of stress in smokers is twice as high as that in non-smokers.
Smoking is the leading cause of lung cancer in the world, according to research. The practice is likely to cause lung cancer both in active and passive smokers. Passive smokers are people who do not smoke but are exposed to cigarette smoke (Onor et al., 2017). According to medics, smoking damages the lining of one’s lungs thus causing lung cancer. When one inhales cigarette smoke, which consists of cancer-causing carcinogens, lung tissues start changing immediately (Onor et al., 2017). If one smokes for a small period then quits, the lung tissues will repair themselves thus reducing the chances of contracting lung cancer (Onor et al., 2017). However, continued smoking leads to permanent damage of the lung tissues to the extent that they become irreparable. These damages accelerate the development of lung cancer.
Smoking also causes loss of sight. According to medical research, cataracts are the number one cause of blindness in the world. Cataract is the blurring of the eyes standard lens. Studies reveal that smokers are twice at the risk of developing cataracts than non-smokers (Kennedy et al., 2017). Age-related Macular Degeneration (AMD) has an impact on the retina, which is the part of the eye that is responsible for the sharp vision that people use while driving and reading. AMD has been termed as the leading cause of permanent blindness in people aged 65years and above (Kennedy et al., 2017). Research shows that smokers are three times likely to develop AMD than non-smokers (Kennedy et al., 2017). However, if one quits smoking at an early stage, the damage caused to the eyes is repairable, but prolonged smoking leads to increased destruction of the eyes that in turn translates to permanent blindness.
Further, smoking is one of the major causes of type-2 diabetes. Research shows that 40% of smokers are likely to develop type-2 diabetes (Onor et al., 2017). Diabetic people who smoke are likely to experience difficulties in managing insulin levels in their bodies even with prescribed medications. Since increased smoking leads to increased chances of developing type-2 diabetes, diabetic smokers make it hard to control the disease’s progress and insulin levels thus increasing their chances of dying from it (Onor et al., 2017). Diabetic smokers are also likely to suffer from other health complications linked to diabetes such as heart failure, kidney problems, high blood pressure, retinopathy, and peripheral neuropathy (Onor et al., 2017). For a diabetic person, quitting smoking can help control insulin levels in the body.
Even more disheartening is the fact that even though preventable, cigarette smoking is the number one cause of death in the US among all the causes of deaths that are preventable. The same applies to the United Kingdom. In the US alone, 480,000 deaths are caused by cigarette smoking each year, translating to 20% of the total yearly deaths ( Marshall , 2016). The total deaths resulting from a combination of the following causes every year is less than the number of deaths caused by cigarette smoking: firearm-related accidents, motor vehicle injuries, alcohol use, illegal drug use, and HIV. This further shows the seriousness of the effects of smoking on human health.
Smoking is a general lifestyle behavior among young and older people alike. People engage in the practice as a way of having fun. Peer pressure is one of the leading factors that drive people to smoke. Parenting style also contributes to the chances of one becoming a smoker. Many people underestimate the health risks associated with smoking. Lung cancer, blindness, and type-2 diabetes are some of the health effects associated with this habit.
Choi, D., Ota, S., & Watanuki, S. (2015). Does cigarette smoking relieve stress? Evidence from the event-related potential (ERP). International Journal of Psychophysiology , 98 (3), 470-476.
Gilman, S. E., Rende, R., Boergers, J., Abrams, D. B., Buka, S. L., Clark, M. A., … & Lloyd-Richardson, E. E. (2009). Parental smoking and adolescent smoking initiation: an intergenerational perspective on tobacco control. Pediatrics , 123 (2), e274-e281.
Kennedy, R. D., Hammond, D., Spafford, M. M., Douglas, O., Brûlé, J., Fong, G. T., & Schultz, A. S. (2016). Educating smokers about the risk of blindness–insights to improve tobacco product health warning labels. Tobacco Induced Diseases , 14 (1), 30.
Marshall, T. (2016). Public opinion, public policy, and smoking: the transformation of American attitudes and cigarette use, 1890–2016 (1st ed.) . Lanham, MD: Rowman & Littlefield.
Onor, I. O., Stirling, D. L., Williams, S. R., Bediako, D., Borghol, A., Harris, M. B., … & Sarpong, D. F. (2017). Clinical effects of cigarette smoking: epidemiologic impact and review of pharmacotherapy options. International Journal of Environmental Research and Public Health , 14 (10), 1147.
Ukwayi, J. K., Eja, O. F., & Unwanede, C. C. (2012). Peer pressure and tobacco smoking among undergraduate students of the University of Calabar, Cross River State. Higher Education Studies , 2 (3), 92.
Smoking Essay 2: The Effects of Smoking on Health and Social Care
A sample smoking essay outline.
Thesis: Smoking is harmful to nearly all body organs and thus quitting has health benefits.
Smoking damages the human heart and interferes with normal blood circulation.
- This increases the risks of such conditions as cerebrovascular disease, peripheral vascular disease, stroke, heart attack, and coronary heart disease.
- The heart is made to work faster and thereby strained.
- The cigarette contents increase the risks of blood clots.
- Smoking leads to furring of the coronary arteries.
Paragraph 2:
Smoking can cause lung disease.
- Chronic obstructive pulmonary disease (COPD) is one of the lung diseases.
- Most cases of lung cancer are caused by smoking.
- An attack can be triggered or made worse by tobacco smoke in asthmatic people.
Smoking can cause serious damages to the mouth and throat.
- It can cause strained teeth, bad breath and gum disease.
- It causes an increased cancer risk in the gullet, voice box, throat, tongue, and lips.
Smoking can make a woman to experience difficulties in becoming pregnant.
- There are higher risks for a pregnant smoker to miscarry.
- They may have their baby born with a cleft palate and/or cleft lip,
- They may give birth before time to a baby with an abnormally low birth weight,
- They may have an ectopic pregnancy.
Quitting smoking reduces the risk of many diseases caused by the habit.
- Reduced chances of dying from illnesses that are smoking-related
- Quitters have substantial life expectancy gains in comparison to those who continue to smoke.
Paragraph 6:
It is only through quitting that one would be free from the problems caused by smoking.
- Set the stage to quit by mentally preparing oneself.
- Control cravings of smoking by using nicotine replacement products.
- Apply SmokEnders’ behavioral changes in completely breaking emotional bonds developed between smokers and cigarettes.
Smoking affects almost every organ of the human body and is thus detrimental to health. It causes fatal diseases such as cancer, heart disease, COPD, and can also damage the mouth and throat. Quitting is highly recommendable.
Smoking Essay Sample
The harmful effects of smoking on health and social care essay.
There are many chemicals contained in tobacco smoke that pose health risks both to smokers and nonsmokers. It can be harmful to even breathe a little tobacco smoke. “Of the more than 7,000 chemicals in tobacco smoke, at least 250 are known to be harmful, including hydrogen cyanide, carbon monoxide, and ammonia” (National Cancer Institute, 2017). At least 69 of these 250 known harmful chemicals in tobacco smoke cause cancer. This explains why cigarette smoking is the leading cause of preventable premature deaths in the United States. Overall, smoking is harmful to nearly all body organs and thus quitting has health benefits.
Smoking damages the human heart and interferes with normal blood circulation. This increases the risks of such conditions as cerebrovascular disease (damage to arteries supplying blood to the brain), peripheral vascular disease (damaged blood vessels), stroke, heart attack, and coronary heart disease. The heart is made to work faster by nicotine and carbon monoxide from the smoke thereby straining it. The cigarette contents also increase the risks of one experiencing blood clots in their circulation system. In addition, smoking leads to furring of the coronary arteries as the lining of the arteries are damaged by other chemicals in the cigarette smoke. As a matter of fact, one faces a double risk of having a heart attack by smoking (NHS, 2018). Their risk of dying from coronary heart disease is also twice that of nonsmokers.
According to CDC (2018), “Smoking can cause lung disease by damaging your airways and the small air sacs (alveoli) found in your lungs.” Chronic obstructive pulmonary disease (COPD) is one of the lung diseases caused by smoking and it includes chronic bronchitis and emphysema. It is also noteworthy that most cases of lung cancer are caused by smoking. An attack can be triggered or made worse by tobacco smoke in people who have asthma. Compared to nonsmokers, the chances of smokers dying from COPD are 12 to 13 times higher. Additionally, smoking causes a cancer that forms in the intestines (rectum or colon) known as colorectal cancer and is the second leading contributor to cancer deaths in the U.S. (American Lung Association, 2018). A smoker has higher risks of developing this type of cancer.
Smoking can also cause serious damages to the mouth and throat. It can cause such unattractive problems as strained teeth, bad breath, and gum disease, as well as damage one’s sense of taste. The most serious damage caused by smoking in the throat and mouth is an increased cancer risk in the gullet (esophagus), voice box, throat, tongue, and lips. This risk increases with an increase in the intake of tobacco contents. “More than 93% of oropharyngeal cancers (cancer in part of the throat) are caused by smoking” (NHS, 2018). This implies that nonsmokers have a greatly reduced risk of developing mouth and throat cancers.
Further, smoking can make a woman to experience difficulties in becoming pregnant. Even if they succeed at conceiving, there are higher risks for a pregnant smoker to miscarry. In addition, they may have their baby born with a cleft palate and/or cleft lip, they may give birth before time to a baby with an abnormally low birth weight, and they may also have an ectopic pregnancy. Moreover, if a woman smokes during or after pregnancy, her infant would have higher risks of dying from Sudden Infant Death Syndrome (SIDS) (National Cancer Institute, 2017). This implies that even after birth, a mother’s consumption of tobacco contents is harmful to the baby because the baby feeds from her breasts. Furthermore, according to CDC (2018), a pregnant smoker may likely experience stillbirth whereby her baby may die before birth.
Quitting smoking reduces the risk of many diseases caused by the habit, including COPD, heart disease, and cancer. Data from the U.S. National Health Interview Survey indicate that if one quits smoking, they have reduced chances of dying from illnesses that are smoking-related as compared to those who continues to smoke. “Smokers who quit before age 40 reduce their chance of dying prematurely from smoking-related diseases by about 90%, and those who quit by age 45-54 reduce their chance of dying prematurely by about two-thirds” (National Cancer Institute, 2017). Generally, quitters have substantial life expectancy gains in comparison to those who continue to smoke. According to the U.S. National Health Interview Survey, quitters aged between 25 and 34 live longer for about ten years, 35 and 44 for about nine years, 45 and 54 for about six years, and 55 and 64 for about four years.
It is therefore only through quitting that one would be free from the problems caused by smoking. In this respect, there can never be specific solutions to specific health problems caused by smoking; rather, the problems may be best addressed through solutions whose target would be to make one quit. One of the solutions, as suggested by Usman and Davidson (2016), would be to set the stage to quit by mentally preparing oneself. One may also quit by controlling cravings of smoking by using nicotine replacement products which should be used based on consultations with a doctor. Another solution may be to apply SmokEnders’ behavioral changes in completely breaking emotional bonds developed between smokers and cigarettes.
Smoking affects almost every organ of the human body and is thus detrimental to health. It causes fatal diseases such as cancer, heart disease, COPD, and can also damage the mouth and throat. It results into premature deaths that could otherwise be prevented. It also affects pregnant women who may experience increased risks of orofacial clefts in infants, ectopic pregnancy, sudden infant death syndrome, low birth weight, stillbirth, and preterm delivery. As such, quitting smoking has several health benefits and generally increases one’s life expectancy. This is so irrespective of the age at which one quits the habit.
American Lung Association. (2018). “10 health effects caused by smoking you didn’t know about”. American Lung Association . Retrieved May 28, 2018 from http://www.lung.org/our-initiatives/tobacco/reports-resources/sotc/by-the-numbers/10-health-effects-caused-by-smoking.html
CDC. (2018). “Health effects of cigarette smoking”. Centers for Disease Control and Prevention . Retrieved May 28, 2018 from https://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/index.htm
National Cancer Institute. (2017). “Harms of cigarette smoking and health benefits of quitting”. National Cancer Institute . Retrieved May 28, 2018 from https://www.cancer.gov/about-cancer/causes-prevention/risk/tobacco/cessation-fact-sheet#q8
NHS. (2018). “How smoking affects your body”. NHS . Retrieved May 28, 2018 from https://www.nhs.uk/smokefree/why-quit/smoking-health-problems
Usman, M. & Davidson, J. (2016). Tips on how to stop smoking . Mendon, MA: Mendon Cottage Books.
More examples of cause and effect essays;
- Environmental Sciences and Causes of Climate Change
- Essay Sample on Causes and Effects of Stress on Students
Special offer! Get 20% discount on your first order. Promo code: SAVE20
Related Posts
Free essays and research papers, artificial intelligence argumentative essay – with outline.
Artificial Intelligence Argumentative Essay Outline In recent years, Artificial Intelligence (AI) has become one of the rapidly developing fields and as its capabilities continue to expand, its potential impact on society has become a topic Read more…
Synthesis Essay Example – With Outline
The goal of a synthesis paper is to show that you can handle in-depth research, dissect complex ideas, and present the arguments. Most college or university students have a hard time writing a synthesis essay, Read more…
Examples of Spatial Order – With Outline
A spatial order is an organizational style that helps in the presentation of ideas or things as is in their locations. Most students struggle to understand the meaning of spatial order in writing and have Read more…

Please enable JavaScript or use a Browser that supports JavaScript
- Advanced Search
- Browse by Analyte
- Browse by Pre-analytical Factor
- Search SOPs
- SOP Compendiums
- Suggest a New Paper
- Submit an SOP
- Curator Home
- Back Office
Platelet activation and blood extracellular vesicles: The influence of venepuncture and short blood storage.
Author(s): Marić I, Žiberna K, Kolenc A, Maličev E
Publication: Blood Cells Mol Dis , 2024, Vol. 106 , Page 102842
PubMed ID: 38492545 PubMed Review Paper? No
Purpose of Paper
This paper investigated the effects of volunteer characteristics (age, gender, smoking status, and fasting status), needle gauge (16- versus 21-gauge), and delayed plasma separation (up to 4 h at room temperature) on platelet activation and extracellular vesicle (EV) endpoints by comparing the percentage of activated platelets relative to total platelets (CD62p+/CD61+) and the concentration, size, and surface marker mean fluorescent intensity (MFI) among EVs isolated from the platelet-depleted plasma (PDP) of twenty healthy volunteers.
Conclusion of Paper
Plasma from the men (17 male volunteers) had a significantly higher concentration of EVs and the EVs had higher MFI for HLA-DRDQDP than observed in plasma/EVs from women (3 female volunteers);volunteer age, gender, smoking status (18 non-smokers, 2 smokers), and fasting status (17 non-fasting, 3 fasting) did not affect EV concentration, size, or surface marker expression or platelet activation, although the disproportionate sample sizes among experimental groups was not considered as a potentially confounding factor by the authors. EV concentration was lower when blood was collected using a 16-gauge rather than a 21-gauge needle, but EV concentration, platelet activation, and EV surface markers were comparable between needle gauges. Platelet activation increased with the duration of room temperature storage before plasma separation, whereas the concentration, size, and MFI of surface markers of EVs in plasma were not affected.
Study Purpose
This study investigated the effects of volunteer characteristics (age, gender, smoking status, and fasting status), needle gauge (16- versus 21-), and delayed plasma separation (up to 4 h at room temperature) on platelet activation and EV endpoints by comparing the percentage of activated platelets relative to total platelets (CD62p+/CD61+) and the concentration, size, and surface marker MFI among EVs isolated from the plasma of twenty healthy volunteers. Unless otherwise specified, blood was collected using a 21-gauge needle from the cubital vein of 17 healthy men (24-62 years of age) and three healthy women (24-62 years of age); donors included 18 non-smokers and 2 smokers; 17 non-fasting and 3 fasting individuals. Blood was collected into EDTA Monovette tubes and was mixed by inverting the tube six times before separation of platelet-rich plasma (PRP) by centrifugation at 120 x g for 7 min. PDP was isolated from PRP by two centrifugations at 2500 x g for 15 min at room temperature and stored at -80°C until analysis. Platelet activation was measured by the ratio of activated (CD62p+) to total (CD61+) platelets by flow cytometry. EVs were isolated from PDP by centrifugation at 10,000 × g for 20 min at 4°C, mixing the resultant supernatant with sucrose and phosphate-buffered saline (PBS), and ultracentrifugation at 100,000 × g for 135 min at 4°C. EVs were resuspended in PBS and stored at -80°C. Evs were assayed by nanoparticle tracking and flow cytometry for 37 surface markers, of which 30 were detected. For needle gauge comparisons, blood was collected from 10 men using a 21-gauge needle followed by a collection of a subsequent sample using a 16-gauge needle. For delayed processing comparisons, blood from seven men and three women was mixed by inverting the tubes six times and storing the pool sample at room temperature for 0, 1, 2, 3, or 4 h before separation of platelet rich plasma. Correlation coefficients were not included for most correlation analyses.
Summary of Findings:
Plasma from the seventeen male donors had a significantly higher concentration of EVs than plasma from the three female donors (5.19 versus 2.62, P=0.42), but EV concentration was not affected by volunteer age, smoking status (18 non-smokers, 2 smokers), or fasting status (17 non-fasting, 3 fasting)). EV size was correlated with EV concentration (P<0.001), but was not affected by volunteer gender, age, smoking status, or fasting status. Platelet activation was highly variable between volunteers (CV 68%), but was not affected by volunteer gender, age, smoking status, or fasting status. Platelet activation was also not correlated with EV concentration or size. Except for a higher mean fluorescent intensity (MFI) of HLA-DRDQDP in EVs from men in comparison to those from women (33.4 vs. 15.1, P=0.019), there were no effects of volunteer gender, age, smoking status, or fasting status on the MFI of the thirty EV surface markers investigated, but variability was high (CV 49-364%). EV concentration was lower when blood was collected using a 16-gauge rather than 21-gauge needle (3.07 versus 4.62, P=0.02), but EV concentration, platelet activation, and EV surface markers were comparable between specimens collected with different needle gauges. Platelet activation increased with the duration of room temperature storage prior to plasma separation (P=0.01), but the duration of blood storage did not affect the concentration, size, or MFI of surface markers of EVs in plasma. EV concentration was negatively correlated with the MFI of some markers, including CD49e (P=0.036), CD40 (P 0.044), CD41b (P=0.025), CD62p (P=0.037), CD146 (P=0.030), and CD31 (P = 0.024). EV size was modestly correlated with the MFI of CD62p (P=0.001, R2=0.491) and CD40 (P=0.001, R2=0.473).
Please enable JavaScript or use a Browser that supports JavaScript for more on this study.
Biospecimens
- Bodily Fluid - Plasma
- Bodily Fluid - Blood
Preservative Types
Pre-analytical factors:, you recently viewed , news and announcements.
- April 24, 2024: Biobanking for Precision Medicine Seminar
- Most Popular SOPs in March 2024
- New SOPs Available
- U.S. Department of Health and Human Services
- National Institutes of Health
- National Cancer Institute
- Share full article
Advertisement
Supported by
Guest Essay
We Don’t See What Climate Change Is Doing to Us

By R. Jisung Park
Dr. Park is an environmental and labor economist and assistant professor at the University of Pennsylvania and the author of “Slow Burn: The Hidden Costs of a Warming World.”
Many of us realize climate change is a threat to our well-being. But what we have not yet grasped is that the devastation wreaked by climate change comes not just from headline-grabbing catastrophes but also from the subtler accumulation of innumerable slow and unequal burns that are already underway — the nearly invisible costs that may not raise the same alarm but that, in their pervasiveness and inequality, may be much more harmful than commonly realized. Recognizing these hidden costs will be essential as we prepare ourselves for the warming that we have ahead of us.
Responsibility for mitigating climate change on the local level lies in part with public institutions not only in encouraging emissions reductions but also in facilitating adaptation. Public discourse around climate change too often misses the central role that local institutions play in this latter function, how much of the realized pain locally depends on not simply the physical phenomena of climate change per se but also how they interact with human systems — economic, educational, legal and political.
Let’s start with heat, which is killing more people than most other natural disasters combined. Research shows that record-breaking heat waves are only part of the story. Instead, it may be the far more numerous unremarkably hot days that cause the bulk of societal destruction, including through their complex and often unnoticed effects on human health and productivity. In the United States, even moderately elevated temperatures — days in the 80s or 90s Fahrenheit — are responsible for just as many excess deaths as the record triple-digit heat waves, if not more, according to my calculations based on a recent analysis of Medicare records.
In some highly exposed and physically demanding industries, like mining, a day in the 90s can increase injury risk by over 65 percent relative to a day in the 60s. While some of these incidents involve clear cases of heat illness, my colleagues and I have found that a vast majority appear to come from ostensibly unrelated accidents, like construction workers falling off ladders and manufacturing workers mishandling hazardous machinery. In California, our research shows, heat might have routinely caused 20,000 workplace injuries per year, only a tiny fraction of which were officially recorded as heat-related.
A growing body of literature links temperature to cognitive performance and decision making. Research shows that hotter days lead to more mistakes, including among professional athletes ; more local crime ; and more violence in prisons , according to working papers. They also correspond with more use of profanity on social media , suggesting that even an incrementally hotter world is likely to be a nontrivially more irritable, error-prone and conflictual one.
Children are not immune. In research using over four million student test scores from New York City, I found that, from 1999 to 2011, students who took their high school Regents exams on a 90-degree day were 10 percent less likely to pass their subjects relative to a day in the 60s. In other research, my colleagues Joshua Goodman, Michael Hurwitz and Jonathan Smith and I found that across the country, hotter school years led to slower gains on standardized exams like the Preliminary SAT exams. It may not seem a huge effect, on average: roughly 1 percent of learning lost per one-degree-hotter school year temperatures. Probably hardly noticeable in any given year. But because these learning effects are cumulative, they may have significant consequences.
And that’s just heat. Researchers are bringing to light the more subtle yet cumulatively damaging effects of increased wildfires and other natural disasters. The hidden consequences of wildfire smoke may cut even deeper than the more visible death and destruction caused by the flames. Tallying the downstream economic and health costs of smoke exposure, researchers have estimated in a not-yet-published paper that increased wildfire smoke due to climate change may cause more than 20,000 additional deaths per year nationwide by 2050. Very few of these will be officially categorized as having been caused by wildfires, because they will have been the result of the cumulative influence of worsened air quality and weakened health over the course of many weeks and months. Research now suggests that wildfire smoke can adversely affect fetal health , student learning and workers’ earnings as well.
Since even noncatastrophic climate change may be more subtly damaging and inequality amplifying than we used to think, local interventions are essential to help us prepare for the warming that is to come.
At present, our social and economic systems are not well prepared to adjust to the accumulating damage wreaked by climate change, even though much of what determines whether climate change hurts us depends on the choices we make as individuals and as a society. Whether a hot day leads to mild discomfort or widespread mortality comes down to human decisions — individual decisions such as whether to install and operate air-conditioning and collective decisions around the pricing and availability of insurance, the allocation of hospital beds or the procedures and norms governing how and when people work.
Recent research indicates that how temperature affects human health depends greatly on the adaptations that happen to be at play locally. For instance, a day above 85 degrees in the coldest U.S. ZIP codes has nearly 10 times the effect on elderly mortality relative to in the warmest ZIP codes. In other words, a string of such days in a place like Seattle will lead to a much higher increase in the mortality rate than in a place like Houston, even though both places have similar income levels. In rural India , institutional factors like access to banking may affect how many lives are ultimately lost because of heat; heat can reduce crop yields, leaving subsistence farmers dependent on financing sources to keep them afloat.
In our research of heat and learning , we found that the adverse effects of a one-degree-hotter school year are two to three times as large for Black and Hispanic students, who are less likely to have working air-conditioning at school or at home even within a given city, and are virtually nonexistent in schools and neighborhoods with high levels of home and school air-conditioning. We estimate that hotter temperatures may already be responsible for 5 percent of racial academic achievement gaps. Without remedial investments, climate change is likely to widen these gaps. With a shift in focus to these subtler social costs, we can devise and carry out more effective strategies. But right now, adaptation efforts remain highly fragmented and are often focused on more visibly salient climate hazards, like storm surges .
And, of course, an empirically nuanced understanding of climate damages makes it even clearer that reducing emissions aggressively makes cost-benefit sense not only because we want to insure against total ecological breakdown (cue “extinction rebellion” and “tipping points”) but also because the economic costs of even noncatastrophic warming may be considerable. Recent Environmental Protection Agency estimates that incorporate just some of these cumulative impacts suggest that a single ton of carbon dioxide sets in motion $190 worth of future social costs, which means that technologies that can reduce such emissions at a lower per-ton cost are most likely worth pursuing.
Climate change is a complex phenomenon whose ultimate costs will depend not only on how quickly we transition away from fossil fuels but also on how well we adapt our social and economic systems to the warming we have in store. A proactive stance toward adaptation and resilience may be useful from the standpoint of safeguarding one’s own physical and financial security, whether as a homeowner or the head of a Fortune 500 company. It may be vital for ensuring that the ladders of economic opportunity are not deteriorating for those attempting to climb its lower rungs.
R. Jisung Park is an environmental and labor economist and assistant professor at the University of Pennsylvania and the author of “Slow Burn: The Hidden Costs of a Warming World.”
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .
The Huge Risks From AI In an Election Year
On the eve of New Hampshire’s primary election, a flood of robocalls exhorted Democratic voters to sit out a write-in campaign supporting President Joe Biden during the state’s presidential primary. An AI-generated voice on the line matched the uncanny cadence and signature catchphrase— (“malarkey!”)—characteristic to Biden. From that call to fake creations envisioning a cascade of calamities under Biden’s watch to AI deepfakes of a Slovakian candidate for country leader pondering vote rigging and raising beer prices, AI is making its mark on elections worldwide. Against this backdrop, governments and several tech companies are taking some steps to mitigate risks—European lawmakers just approved a watershed law, and as recently as February tech companies signed a pledge at the Munich Security Conference. But much more needs to be done to protect American democracy.
In Munich, companies including OpenAI, Apple, Meta, Microsoft, TikTok, Google, X, and others announced a compact to undertake measures to protect elections as America and other countries go to the polls in 2024. The companies pledged to help audiences track the origin of AI-generated and authentic content, to try to detect deceptive AI media in elections, and to deploy “reasonable precautions” to curb risks from AI-fueled election trickery. While not unwelcome, the success of the compact will depend on how its commitments are executed. They were couched in slippery language—“proportionate responses,” “where appropriate and technically feasible,” “attempting to,” and so on—that give latitude to companies to do very little if they so choose. While some are taking further steps, of course, the urgency of the situation demands stronger and more universal action.
This year is the first national American election since AI developments will allow fraudsters to produce phony but close-to-perfect pictures, video, or audio of candidates and officials doing or saying almost anything with minimal time, little to no cost, and on a widespread basis. And the technology underlying generative AI chatbots lets hoaxers spoof election websites or spawn pretend news sites in a matter of seconds and on a mammoth scale. It also gives bad actors— foreign and domestic—the ability to conduct supercharged, hard-to-track interactive influence campaigns.
As generative AI is integrated into common search engines and voters converse with chatbots, people seeking basic information about elections have at times been met with misinformation, pure bunkum, or links to fringe websites. A recent study by AI Democracy Projects and Proof News indicated that popular AI tools—including Google’s Gemini, OpenAI’s GPT-4, and Meta’s Llama 2— “ performed poorly on accuracy ” when fed certain election questions. The more traditional, non-generative AI could fuel mass challenges to thousands of voters’ eligibility, risking wrongful purges from voter rolls and burdening election offices. As election officials consider using new AI tools in their day-to-day tasks, the lack of meaningful regulation risks putting some voting access in harm’s way even as AI unlocks time-saving opportunities for short-staffed offices.
Before the Munich conference the world’s premier generative AI operation, OpenAI, had recently announced a slate of company policies designed to curtail election harms as America votes in 2024. These include forbidding users from building custom AI chatbots that impersonate candidates, barring users from deploying OpenAI tools to spread falsehoods about when and how to vote, and encrypting images with digital codes that will help observers figure out whether OpenAI’s Dall-E made an image that is multiplying in the wild.
But these actions—while more robust than those of some other major AI companies to date—fall short in important ways and underscore the limitations of what we may see in future months as OpenAI and other tech giants make gestures towards honoring the commitments made in Munich. First: the company’s public-facing policies do not call out several core false narratives and depictions that have haunted prior election cycles and are likely to be resurrected in new guises this year. For example, they do not expressly name fakeries that supposedly show election officials interfering with the vote count, fabrications of unreliable or impaired voting machines, or baseless claims that widespread voter fraud has occurred. (According to Brennan Center tracking , these rank among the most common false narratives promoted by election deniers in the 2022 midterm elections.) While OpenAI policies addressing misleading others and intentional deception arguably cover some, or all, such content, specifically naming these categories as being barred from creation and spread would give more clarity to users and protection to voters. Since election procedures— and the occasional fast-resolved Election Day glitch—vary from county to county, the company should have conduits for the sharing of information between local election officials and OpenAI staff in the months leading up to the election.
Perhaps most importantly, the tech wunderkind needs to do more to curb the risks of working with third party developers—that is, the companies that license OpenAI’s technology and integrate its models into their own services and products . For instance, if a user enters basic election questions into a third-party search engine that cannibalizes OpenAI models, the answers can be rife with errors, outdated facts, and other blunders. (WIRED reporting on Microsoft Copilot last December revealed several issues at that time with the search engine—which uses OpenAI technology— though some of those problems may have since been addressed.) To better protect voters this election season, the company must create and enforce stricter requirements for its partnerships with developers that integrate OpenAI models into search engines—or any digital platform where voters may go to seek information on the ABCs of voting and elections. While the accord signed in Munich was targeted to intentionally deceptive content, voters can also be harmed by AI “hallucinations”—fabrications spit out by systems’ algorithms—or other hiccups that AI creators and service providers have failed to prevent.
But, OpenAI can’t go it alone. Other tech titans must release their own election policies for generative AI tools, unmasking any behind-the-scenes tinkering and opening internal practices to public scrutiny and knowledge. As a first step, more major tech companies—including Apple, ByteDance, Samsung, and X—should sign onto the Coalition for Content Provenance and Authenticity ’s open standard for embedding content with digital markers that help prove that it is AI-generated or authentic as it travels through the online ether. (While Apple and X committed to consider attaching similar signals to their content in Munich, a consistent standard would improve detection and coordination across the board.) The markers, meanwhile, should be made more difficult to remove. And social media companies must act swiftly to address deepfakes and bot accounts that mimic human activity, as well as instituting meaningful account verification processes for election officials and bonafide news organizations to help voters find accurate information in feeds flush with misinformation, impersonators, and accounts masquerading as real news.
One company’s—or a handful of companies’ —steps to address election harms, while important, are not enough in a landscape awash with unsecured, open-source AI models where systems’ underlying code and the mathematical instructions that make them tick are publicly available, downloadable, and manipulatable. Companies as prominent as Meta and Stability AI have released unsecured AI systems, and other players have rapidly churned out many more. Anyone who wishes to interfere in elections today has a suite of AI technology to choose from to bolster their efforts, and multiple ways to deploy it. That means that governments at all levels must also take urgent action to protect voters.
Congress, agencies, and states have a plethora of options at hand to blunt AI’s risks ahead of the 2024 election. Congress and states should regulate deepfakes—particularly those spread by campaigns, political action committees, and paid influencers—by requiring disclaimers on deceptive and digitally manipulated images, video, and audio clips that could suppress votes, or that misrepresent candidates’ and election officials’ words and actions. Lawmakers should also require campaigns and political action committees to clearly label a subset of content produced by the technology underlying generative AI chatbots, particularly where politicos deploy the technology to engage in continuous conversations with voters or to deceptively impersonate humans to influence elections. Policymakers should protect voters against frivolous challenges to their voting eligibility by setting constraints on the evidence that may be used to substantiate a challenge — including evidence unearthed or created through AI.
Federal agencies should act quickly to publish guidance for certifying the authenticity and provenance of government content—as envisioned by the executive order on AI issued by the administration last year—and state and local election officials should apply similar practices to their official content. Longer term, federal and state governments should also create guidance and benchmarks that help election officials evaluate AI systems before purchasing them, checking for reliability, accuracy, biases, and transparency.
These steps are all pivotal to dealing with challenges that arise specifically from AI technology. But the election risks that AI amplifies—disinformation, vote suppression, election security hazards, and so on—long predate the advent of the generative-AI boom. To fully protect voting and elections, lawmakers must also pass reforms like the Freedom to Vote Act—a set of wide-ranging provisions that stalled in the U.S. Senate. It also means updating political ad disclosure requirements for the 21 st century. And it means maintaining an expansive vision for democracy that is impervious to age-old and persistent efforts to subvert it.
More Must-Reads From TIME
- The 100 Most Influential People of 2024
- The Revolution of Yulia Navalnaya
- 6 Compliments That Land Every Time
- What's the Deal With the Bitcoin Halving?
- If You're Dating Right Now , You're Brave: Column
- The AI That Could Heal a Divided Internet
- Fallout Is a Brilliant Model for the Future of Video Game Adaptations
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at [email protected]

IMAGES
VIDEO
COMMENTS
Once in your blood, chemicals from cigarette smoke travel throughout your body. This damages your: Bones. Nicotine decreases the absorption of calcium and the production of bone-forming cells, causing you to have thinner, brittler bones. Eyes. The chemicals in cigarettes plus a lack of oxygen damage your eyes.
Introduction. Tobacco use, including smoking, has become a universally recognized issue that endangers the health of the population of our entire planet through both active and second-hand smoking. Pro-tobacco arguments are next to non-existent, while its harm is well-documented and proven through past and contemporary studies (Jha et al., 2013).
Background and objectives: Despite reductions in prevalence in recent years, tobacco smoking remains one of the main preventable causes of ill-health and premature death worldwide.This paper reviews the extent and nature of harms caused by smoking, the benefits of stopping, patterns of smoking, psychological, pharmacological and social factors that contribute to uptake and maintenance of ...
500 Words Essay On Smoking. One of the most common problems we are facing in today's world which is killing people is smoking. A lot of people pick up this habit because of stress, personal issues and more. In fact, some even begin showing it off. When someone smokes a cigarette, they not only hurt themselves but everyone around them.
Smokers are at greater risk for diseases that affect the heart and blood vessels (cardiovascular disease). 1,2 Smoking causes stroke and coronary heart disease, which are among the leading causes of death in the United States. 1,3 Even people who smoke fewer than five cigarettes a day can have early signs of cardiovascular disease. 1 Smoking damages blood vessels and can make them thicken and ...
Smoking can result in stroke and heart attacks since it hinders blood flow, interrupting oxygen to various parts of the body, such as feet and hands. Introduction of cigarettes with low tar does not reduce these effects since smokers often prefer deeper puffs and hold the smoke in lungs for a long period.
Smoking can affect a person's health in many other ways as well, harming nearly every organ in the body. Here are a few examples of other ways smoking tobacco can affect your health: Increased risk of gum disease and tooth loss. Lowered immune system function. Increased risk of type 2 diabetes.
Smoking: Causes and Effects Essay. Exclusively available on IvyPanda. Among numerous bad habits of modern society smoking seems to be of the greatest importance. Not only does it affect the person who smokes, but also those who are around him. Many people argue about the appropriate definition of smoking, whether it is a disease or just a bad ...
We identified three outcomes with a 4-star association with smoking: COPD (72% increase in risk based on the BPRF, 0.54 ROS), lower respiratory tract infection (54%, 0.43) and pancreatic cancer ...
Smoking, a widespread habit with serious health implications, is a topic of concern that merits significant attention. Despite the known dangers, millions globally continue to smoke, affecting not only their health but also those in their vicinity. This essay delves into the effects of smoking, focusing on health, environmental, and social impacts.
Smoking Essay Smoking is a widespread habit that involves inhaling smoke from the burning of tobacco. It is a highly addictive habit that has numerous negative effects on the body, including lung cancer, heart disease, and respiratory issues. Writing an essay on smoking can be a challenging task, but it is an important topic to discuss.
Smoking has adverse health effects on the entire lung—affecting every aspect of lung structure and function—including impairing lung defenses against infection and causing the sustained lung injury that leads to chronic obstructive pulmonary disease (COPD). In fact, among the postulated causes of COPD are acute respiratory infections, for which smokers are at an increased risk. This ...
The reductions in smoking risk for all deaths and for lung cancer mortality among women in the UK are shown in Figure 11. Very similar results were seen in the US for these same age groups among men and women (Jha et al., 2013). The smoker/non-smoker risks quickly converge for vascular disease, for some cancers other than lung, though less ...
Persuasive Essay Examples About Smoking. Smoking is one of the leading causes of preventable death in the world. It leads to adverse health effects, including lung cancer, heart disease, and damage to the respiratory tract. However, the number of people who smoke cigarettes has been on the rise globally. A lot has been written on topics related ...
The Hazards of Smoking: Effects, Bans, and Prevention Essay. Smoking has numerous health effects, both short-term and long-term. Some of the short-term effects include bad breath, yellow teeth, and decreased sense of taste and smell. The long-term effects, however, are much more severe.
The dangers of smoking cigarettes have been well-documented, yet millions of people continue to engage in this harmful habit. The debate over the impact of smoking on public health is ongoing, with some arguing for stricter regulations and others advocating for personal freedom. In this essay, we will explore the various arguments surrounding smoking cigarettes and ultimately make the case for ...
500 Words Essay on Harmful Effects of Smoking Introduction. Smoking is a prevalent habit, often started out of curiosity, peer pressure, or stress management. However, its harmful effects are well-documented, impacting nearly every organ in the human body. Despite the widespread knowledge of its adverse effects, smoking continues to be a ...
Smoking cigarettes can also spawn various other types of cancer, including cancer in the stomach, liver, kidneys, bladders, pancreas, and oropharynx. Smoking not only puts smokers at risk for these often fatal types of cancer but also to those around smokes as a result of second-hand smoking. Second-hand smoke, according to the CDC (2014 ...
Its 'pessimistic' model predicts that the policy could reduce the smoking rate among people aged 14-30 from 13% in 2023 to around 8% in 2030. By 2040, just 5% of this age group would smoke ...
Smoking has a number of negative physiological, social, and psychological impacts that can seriously affect a person's life.This is just a smoking essay introduction. Reading the essay on smoking will discuss the various negative effects of smoking as well as preventative measures. Read and download this smoking in public places essay pdf here.
Essay on Smoking Risks. One of the most popular habits in today's society is smoking. Yet each year, cigarette smoking kills more Americans than AIDS, alcohol, car accidents, homicides, suicides, illegal drugs and fires combined. Smoking is an extremely bad pastime, practiced for centuries, for an individual's health and those surrounding ...
Long periods of dual use of cigarettes and e-cigarettes can result in harms to health similar to, or in addition to, the harms from exclusive use of cigarettes. To date, FDA has authorized 23 e ...
The health risks of smoking to include Lung disease. According to smokinglungs.com, lung cancer is the number one cause of cancer deaths in men and women, while 90% of lung cancer is preventable. There are 2,000 cancer causing materials in a single cigarette. Second hand smoke can cause lung disease but is not as prevalent as smoking straight ...
Background Association of cigarette smoking habits with the risk of prostate cancer is still a matter of debate. This systematic review and meta-analysis aimed to assess the association between cigarette smoking and prostate cancer risk. Methods We conducted a systematic search on PubMed, Embase, Cochrane Library, and Web of Science without language or time restrictions on June 11, 2022 ...
The Hazards of Smoking: Effects, Bans, and Prevention Essay. Smoking has numerous health effects, both short-term and long-term. Some of the short-term effects include bad breath, yellow teeth, and decreased sense of taste and smell. The long-term effects, however, are much more severe.
Smoking Essay Sample The Harmful Effects of Smoking on Health and Social Care Essay Introduction. There are many chemicals contained in tobacco smoke that pose health risks both to smokers and nonsmokers. It can be harmful to even breathe a little tobacco smoke. "Of the more than 7,000 chemicals in tobacco smoke, at least 250 are known to be ...
Studies. Study Purpose. This study investigated the effects of volunteer characteristics (age, gender, smoking status, and fasting status), needle gauge (16- versus 21-), and delayed plasma separation (up to 4 h at room temperature) on platelet activation and EV endpoints by comparing the percentage of activated platelets relative to total platelets (CD62p+/CD61+) and the concentration, size ...
Tallying the downstream economic and health costs of smoke exposure, researchers have estimated in a not-yet-published paper that increased wildfire smoke due to climate change may cause more than ...
The Pfizer and Moderna COVID-19 vaccines can cause myocarditis, but do not appear to cause infertility, Guillain-Barré syndrome, Bell's palsy, thrombosis with thrombocytopenia syndrome (TTS) or heart attack, according to a new National Academies of Sciences, Engineering, and Medicine report examining whether COVID-19 vaccines can cause certain harms.
But the election risks that AI amplifies—disinformation, vote suppression, election security hazards, and so on—long predate the advent of the generative-AI boom. To fully protect voting and ...