- Case report
- Open access
- Published: 11 July 2020

Obsessive compulsive disorder in very young children – a case series from a specialized outpatient clinic
- Veronika Brezinka ORCID: orcid.org/0000-0003-2192-3093 1 ,
- Veronika Mailänder 1 &
- Susanne Walitza 1
BMC Psychiatry volume 20 , Article number: 366 ( 2020 ) Cite this article
23k Accesses
5 Citations
1 Altmetric
Metrics details
Paediatric obsessive-compulsive disorder (OCD) is a chronic condition often associated with severe disruptions of family functioning, impairment of peer relationships and academic performance. Mean age of onset of juvenile OCD is 10.3 years; however, reports on young children with OCD show that the disorder can manifest itself at an earlier age. Both an earlier age of onset and a longer duration of illness have been associated with increased persistence of OCD. There seems to be difficulty for health professionals to recognize and diagnose OCD in young children appropriately, which in turn may prolong the interval between help seeking and receiving an adequate diagnosis and treatment. The objective of this study is to enhance knowledge about the clinical presentation, diagnosis and possible treatment of OCD in very young children.
Case presentation
We describe a prospective 6 month follow-up of five cases of OCD in very young children (between 4 and 5 years old). At the moment of first presentation, all children were so severely impaired that attendance of compulsory Kindergarten was uncertain. Parents were deeply involved in accommodating their child’s rituals. Because of the children’s young age, medication was not indicated. Therefore, a minimal CBT intervention for parents was offered, mainly focusing on reducing family accommodation. Parents were asked to bring video tapes of critical situations that were watched together. They were coached to reduce family accommodation for OCD, while enhancing praise and reward for adequate behaviors of the child. CY-BOCS scores at the beginning and after 3 months show an impressive decline in OCD severity that remained stable after 6 months. At 3 months follow-up, all children were able to attend Kindergarten daily, and at 6 months follow-up, every child was admitted to the next level / class.
Conclusions
Disseminating knowledge about the clinical presentation, diagnosis and treatment of early OCD may shorten the long delay between first OCD symptoms and disease-specific treatment that is reported as main predictor for persistent OCD.
Peer Review reports
Paediatric obsessive compulsive disorder [ 1 ] is a chronic condition with lifetime prevalence estimates ranging from 0.25 [ 2 ] to 2–3% [ 3 ]. OCD is often associated with severe disruptions of family functioning [ 4 ] and impairment of peer relationships as well as academic performance [ 5 ]. Mean age of onset of early onset OCD is 10.3 years, with a range from 7.5 to 12.5 years [ 6 ] or at an average of 11 years [ 7 ]. However, OCD can manifest itself also at a very early age - in a sample of 58 children, mean age of onset was 4.95 years [ 8 ], and in a study from Turkey, OCD is described in children as young as two and a half years [ 9 ]. According to different epidemiological surveys the prevalence of subclinical OC syndromes was estimated between 7 and 25%, and already very common at the age of 11 years [ 10 ].
Understanding the phenomenology of OCD in young children is important because both an earlier age of onset and a longer duration of illness have been associated with increased persistence of OCD [ 11 , 12 , 13 ]. One of the main predictors for persistent OCD is duration of illness at assessment, which underlines that early recognition and treatment of the disorder are crucial to prevent chronicity [ 10 , 14 , 15 ]. OCD in very young children can be so severe that it has to be treated in an inpatient-clinic [ 16 ]. This might be prevented if the disorder were diagnosed and treated earlier.
In order to disseminate knowledge about early childhood OCD, detailed descriptions of its phenomenology are necessary to enable clinicians to recognize and assess the disorder in time. Yet, studies on this young population are scarce and differ in the definition of what is described as ‘very young’. For example, 292 treatment seeking youth with OCD were divided into a younger group (3–9 years old) and an older group (10–18 years old) [ 17 ]. While overall OCD severity did not differ between groups, younger children exhibited poorer insight, increased incidence of hoarding compulsions, and higher rates of separation anxiety and social fears than older youth. It is not clear how many very young children (between 3 and 5 years old) were included in this study. Skriner et al. [ 18 ] investigated characteristics of 127 young children (from 5 to 8) enrolled in a pilot sample of the POTS Jr. Study. These young children revealed moderate to severe OCD symptoms, high levels of impairment and significant comorbidity, providing further evidence that symptom severity in young children with OCD is similar to that observed in older samples. To our knowledge, the only European studies describing OCD in very young children on a detailed, phenotypic level are a single-case study of a 4 year old girl [ 16 ] and a report from Turkey on 25 children under 6 years with OCD [ 9 ]. Subjects were fifteen boys and ten girls between 2 and 5 years old. Mean age of onset of OCD symptoms was 3 years, with some OCD symptoms appearing as early as 18 months of age. All subjects had at least one comorbid disorder; the most frequent comorbidity was an anxiety disorder, and boys exhibited more comorbid diagnoses than girls. In 68% of the subjects, at least one parent received a lifetime OCD diagnosis. The study reports no further information on follow-up or treatment of these young patients.
In comparison to other mental disorders, duration of untreated illness in obsessive compulsive disorder is one of the longest [ 19 ]. One reason may be that obsessive-compulsive symptoms in young children are mistaken as a normal developmental phase [ 20 ]. Parents as well as professionals not experienced with OCD may tend to ‘watch and wait’ instead of asking for referral to a specialist, thus contributing to the long delay between symptom onset and assessment / treatment [ 10 ]. This might ameliorate if health professionals become more familiar with the clinical presentation, diagnosis and treatment of the disorder in the very young. The purpose of this study is to provide a detailed description of the clinical presentation, diagnosis and treatment of OCD in five very young children.
We describe a prospective 6 month follow-up of five cases of OCD in very young children (between 4 and 5 years old) who were referred to the OCD Outpatient Treatment Unit of a Psychiatric University Hospital. Three patients were directly referred by their parents, one by the paediatrician and one by another specialist. Parents and child were offered a first session within 1 week of referral. An experienced clinician (V.B.) globally assessed comorbidity, intelligence and functioning, and a CY-BOCS was administered with the parents.
Instruments
To assess OCD severity in youth, the Children Yale-Brown Obsessive Compulsive Scale CY-BOCS [ 21 ] is regarded as the gold standard, with excellent inter-rater and test-retest reliability as well as construct validity [ 21 , 22 ]. The CY-BOCS has been validated in very young children by obtaining information from the parent. As in the clinical interview Y-BOCS for adults, severity of obsessions and compulsions are assessed separately. If both obsessions and compulsions are reported, a score of 16 is regarded as the cut-off for clinically meaningful OCD. If only compulsions are reported, Lewin et al. [ 23 ] suggest a cut-off score of 8. In their CY-BOCS classification, a score between 5 and 13 corresponds to mild symptoms / little functional impairment or a Clinical Global Impression Severity (CGI-S) of 2. A score between 14 and 24 corresponds to moderate symptoms / functioning with effort or a CGI-S of 3. Generally, it is recommended to obtain information from both child and parents. However, in case of the very young patients presented here, CY-BOCS scores were exclusively obtained from the parents. The parents of all five children reported not being familiar with any obsessions their child might have. In accordance with previous recommendations [ 23 ], a cut-off point of 8 for clinically meaningful OCD was used.
Patient vignettes
Patient 1 is a 4 year old girl, a single child living with both parents. She had never been separated an entire day from her mother. At the nursery, she suffered from separation anxiety for months. Parents reported that the girl had insisted on rituals already at the age of two. In the evening, she ‚had‘ to take her toys into bed and had got up several times crying because she ‚had to‘ pick up more toys. In the morning, only she ‚had the right‘ to open the apartment door. When dressing in the morning, she ‚had‘ to be ready before the parents. Only she was allowed to flush the toilet, even if it concerned toilet use of the parents. Moreover, only she ‘had the right’ to switch on the light, and this had to be with ten fingers at the same time. If she did not succeed, she got extremely upset and pressed the light button again and again until she was satisfied. The girl was not able to throw away garbage and kept packaging waste in a separate box. In the evening, she had to tidy her room for a long time until everything was ‚right‘. Whenever her routine was changed, she protested by crying, shouting and yelling at her parents. Moreover, she insisted on repeating routines if there had been a ‚mistake‘. In order to avoid conflict, both parents adapted their behavior to their daughter’s desires. In the first assessment with the parents, her score on the CY-BOCS was 15, implying clinically meaningful OCD. Psychiatric family history revealed that the mother had suffered from severe separation anxiety as a child and the father from severe night mares. Both parents described themselves as healthy adults.
Patient 2 is a four and a half year old boy, the younger of two brothers. He was reported to have been very oppositional since the age of two. Since the age of three, he insisted on a specific ritual when flushing the toilet – he had to pronounce several distinct sentences and then to run away quickly. Some months later he developed a complicated fare-well ritual and insisted on every family member using exactly the sentences he wanted to hear. If one of these words changed, he started to shout and threw himself on the floor. After a short time, he insisted on unknown people like the cashier at the supermarket to use the same words when saying good-bye.Moreover, he insisted that objects and meals had to be put back to the same place as before in case they had been moved. When walking outside, he had to count his steps and had to start this over and over again. In the morning, he determined where his mother had to stand and how her face had to look when saying good-bye. In order to avoid conflict, parents and brother had deeply accommodated their behavior to his whims. On the CY-BOCS, patient 2 reached a score of 15, which is equivalent to clinically meaningful OCD. Neither his father nor his mother reported any psychiatric disorder in past or present.
Patient 3 is a 4 year old boy referred because of possible OCD. Since the age of three, he had insisted on things going his way. When this was not the case, he threw a temper tantrum and demanded that time should be turned back. If, for example, he had cut a piece of bread from the loaf and was not satisfied with its form, he insisted that the piece should be ‘glued’ to the loaf again. Since he entered Kindergarten at the age of four, his behavior became more severe. If he was not satisfied with a certain routine like, for example, dressing in the morning, he demanded that the entire family had to undress and go to bed again, that objects had to lie at the same place as before or that the clock had to be turned back. In order to avoid conflict, the parents had repeatedly consented to his wishes. His behavior was judged as problematic at Kindergarten, because he demanded certain situations to be repeated or ‚played back‘. When the teacher refused to do that, the boy once run away furiously. On the CY-BOCS, patient 3 reached a score of 15. The mother described herself as being rather anxious (but not in treatment), the father himself as not suffering from any psychiatric symptoms. However, his mother had suffered from such severe OCD when he was a child that she had undergone inpatient treatment several times. This was also the reason why the parents had asked for referral to a specialist for the symptoms of their son.
Patient 4 is a 5 year old girl, the eldest of three siblings. Since the age of two, she was only able to wear certain clothes. For months, she refused to wear any shoes besides Espadrilles; she was unable to wear jeans and could only wear one certain pair of leggings. Wearing warm or thicker garments was extremely difficult, leading to numerous conflicts with her mother in winter. Socks had to have the same height, stockings had to be thin, and slips slack. When dressing in the morning, she regularly got angry and despaired and engaged in severe conflicts with her mother; dressing took a long time, whereas she had to be in Kindergarten on time. Her compulsions with clothes seemed to influence her social behavior as well; she had been watching other children at the playground for 40 min and did not participate because her winter coat did not ‚feel right‘. She started to join peers only when she was allowed to pull the coat off. She also had to dry herself excessively after peeing and was reported to be perfectionist in drawing, cleaning or tidying. Her CY-BOCS score was 15, equivalent to clinically meaningful OCD. Both parents described themselves as not suffering from any psychiatric problem in past or present. However, the grandmother on the mother’s side was reported to have had similar compulsions when she was a child.
Patient 5 was a four and a half year old girl referred because of early OCD. She had one elder brother and lived with both parents. At the age of 1 year, patient 5 was diagnosed with a benign brain tumor (astrocytoma). The tumor had been removed for 90% by surgery; the remaining tumor was treated with chemotherapy. The first chemotherapy at the age of 3 years was reasonably well tolerated. Shortly thereafter, the girl developed just-right-compulsions concerning her shoes. When the second chemotherapy (with a different drug) was started at the age of four, compulsions increased so dramatically that she was referred to our outpatient clinic by the treating oncologist. She insisted on her shoes being closed very tightly, her socks and underwear being put on according to a certain ritual, and her belt being closed so tightly that her father had to punch an additional hole. She refused to wear slack or new clothes and was not able to leave the toilet after peeing because ‘something might still come’; she used large amounts of toilet paper and complained that she wasn’t dry yet. She also insisted on straightening the blanket of her bed many times. She was described by her mother as extremely stressed, impatient and irritable; she woke up every night and insisted to go to the toilet, from where she would come back only after intense cleaning rituals. In the morning, she frequently threw a severe temper tantrum, including hitting and scratching the mother, staying naked in the bathroom and refusing to get dressed because clothes were not fitting ‚just right‘or were not tight enough. Shortly after the start of the second chemotherapy, the girl had entered Kindergarten which was in a different language than the family language. Moreover, her mother had just taken up a new job and had to make a trip of several days during the first month. Although the mother gave up her job after the dramatic increase in OCD severity, the girl’s symptoms did not change. As an association between chemotherapy and the increase in OCD symptoms could not be excluded, the treating oncologist decided to stop chemotherapy 2 weeks after patient 5 was presented with OCD at our department. At the moment of presentation, she arrived at Kindergarten too late daily, after long scenes of crying and shouting, or refused to go altogether. She reached a score of 20 on the CY-BOCS, the highest score of the five children presented here. Her father described himself as free of any psychiatric symptoms in past or present. Her mother had been extremely socially anxious as a child.
None of the siblings of the children described above was reported to show any psychiatric symptoms in past or present (Table 1 ).
The five cases described above show a broad range of OCD symptomatology in young children. Besides Just-Right compulsions concerning clothes, compulsive behavior on the toilet was reported such as having to pee frequently, having to dry oneself over and over again as well as rituals concerning flushing. Other symptoms were pronouncing certain words or phrases compulsively, insisting on a ‘perfect’ action and claiming that time or situations must be played back like a video or DVD if the action or situation were not ‘perfect enough’. The patients described here have in common that parents were already much involved in the process of family accommodation. For example, the parents of patient 3 had consented several times to undress and go to bed again in order to ‘play back’ certain situations; they had also consented turning back the clock in the house. The parents of patient 2 had accommodated his complicated fare-well ritual, thus having to rush to work in the morning themselves. However, all parents were smart enough not just to indulge their child’s behavior, but to seek professional advice.
Treatment recommendations
Practice Parameters and guidelines for the assessment and treatment of OCD in older children and adolescents recommend cognitive behavior therapy (CBT) as first line treatment for mild to moderate cases, and medication in addition to CBT for moderate to severe OCD [ 24 , 25 ]. However, there is a lack of treatment studies including young children with OCD [ 26 ]. A case series with seven children between the age of 3 and 8 years diagnosed with OCD describes an intervention adapted to this young age group. Treatment emphasized reducing family accommodation and anxiety-enhancing parenting behaviors while enhancing problem solving skills of the parents [ 27 ]. A much larger randomized clinical trial for 127 young children (5 to 8 years of age) with OCD showed family-based CBT superior to a relaxation protocol for this age group [ 14 ]. Despite these advances in treatment for early childhood OCD, availability of CBT for paediatric OCD in the community is scarce due to workforce limitations and regional limitations in paediatric OCD expertise [ 28 ]. This is certainly not only true for the US, but for most European countries as well.
When discussing treatment of OCD in young children, the topic of family accommodation is of utmost importance. Family accommodation, also referred to as a ‘hallmark of early childhood OCD’ [ 15 ] means that parents of children with OCD tend to accommodate and even participate in rituals of the affected child. In order to avoid temper tantrums and aggressive behavior of the child, parents often adapt daily routines by engaging in child rituals or facilitating OCD by allowing extra time, purchasing special products or adapting family rules and organisation to OCD [ 29 , 30 , 31 ]. Although driven by empathy for and compassion with the child, family accommodation is reported to be detrimental because it further reinforces OCD symptoms and avoidance behavior, thus enhancing stress and anxiety [ 4 , 32 ].
Parent-oriented CBT intervention
At the moment of first presentation, the five children were so severely impaired by their OCD that attendance of (compulsory) Kindergarten was uncertain. All parents reported being utterly worried and stressed by their child’s symptoms and the associated conflicts in the family. However, no single family wanted an in-patient treatment of their child, and because of the children’s young age, medication was not indicated. Some families lived far away from our clinic and / or had to take care of young siblings.
Therefore, a CBT-intervention was offered to the parents, mainly focusing on reducing family accommodation. This approach is in line with current treatment recommendations to aggressively target family accommodation in children with OCD [ 15 ]. Parents and child were seen together in a first session. The following sessions were done with the parents only, who were encouraged to bring video tapes of critical situations. The scenes were watched together and parents were coached to reduce family accommodation for OCD, while enhancing praise and reward for adequate behaviors of the child. Parents were also encouraged to use ignoring and time-out for problematic behaviors. As some families lived far away and had to take care of young siblings as well, telephone sessions were offered as an alternative whenever parents felt the need for it. Moreover, parents were prompted to facilitate developmental tasks of their child such as attending Kindergarten regularly, or building friendships with peers. The minimal number of treatment sessions was four and the maximal number ten, with a median of six sessions.
Three of the five children (patients 3, 4 and 5) were raised in a different language at home than the one spoken at Kindergarten. This can be interpreted as an additional stressor for the child, possibly enhancing OCD symptoms. Instead of expecting their child to learn the foreign language mainly by ‚trial and error‘, parents were encouraged to speak this language at home themselves, to praise their child for progress in language skills and to facilitate playdates with children native in the foreign language.
Three and six months after intake, assessment of OCD-severity by means of the CY-BOCS was repeated. Table 2 shows an impressive decline in OCD-severity after 3 months that remained stable after 6 months. At 3 months follow-up, all children were able to attend Kindergarten daily, and at 6 months follow-up, every child was admitted to the next level of Kindergarten or, in the case of patient 4, to school.
We report on five children of 4 and 5 years with very early onset OCD who were presented at a University Department of Child and Adolescent Psychiatry. These children are ‚early starters‘with regard to OCD. As underlined in a recent consensus statement [ 10 ], delayed initiation of treatment is seen as an important aspect of the overall burden of OCD (see also [ 19 ]). In our small sample, a CBT-based parent-oriented intervention targeting mainly family accommodation led to a significant decline in CY-BOCS scores after 3 months that was maintained at 6 months. At 3 months, all children were able to attend Kindergarten daily, and at 6 months, every child was admitted to the next grade. This can be seen as an encouraging result, as it allowed the children to continue their developmental milestones without disruptions, like staying at home for a long period or following an inpatient treatment that would have demanded high expenses and probably led to separation problems at this young age. Moreover, the reduction on CY-BOCS scores was reached without medication. The number of sessions of the CBT-based intervention with the parents varied between four and ten sessions, depending on the need of the family. Families stayed in touch with the therapist during the 6 month period and knew they could get an appointment quickly when needed.
A possible objection to these results might be the question of differential diagnosis. Couldn’t the problematic behaviors described merely be classified as benign childhood rituals that would change automatically with time? As described in the patient vignettes, the five children were so severely impaired by their OCD that attendance of Kindergarten – a developmental milestone – was uncertain. Moreover, parents were extremely worried and stressed by their child’s symptoms and associated family conflicts. In our view, it would have been a professional mistake to judge these symptoms as benign rituals not worthy of diagnosis or disorder-specific treatment. One possible, but rare and debated cause of OCD are streptococcal infections, often referred to as PANS [ 33 ]. However, in none of the cases parents reported an abrupt and sudden onset of OCD symptoms after an infection. Instead, symptoms seem to have developed gradually over a period of several months or even years. In the case of patient 5 with the astrocytoma, first just-right compulsions appeared at the age of three (after the first chemotherapy), and were followed by more severe compulsions at the age of four, when – within a period of 6 weeks – a new chemotherapy was started, the mother took up a new job and the patient entered Kindergarten. Diagnosing the severe compulsions of patient 5 as, for example, adjustment disorder due to her medical condition would not have delivered a disorder-specific treatment encouraging parents to reduce their accommodation. This might have led to even more family accommodation and to more severe OCD symptoms in the young girl. Last but not least, a possible objection might be that the behaviors described were stereotypies. However, stereotypies are defined as repetitive or ritualistic movements, postures or utterances and are often associated with an autism spectrum disorder or intellectual disability. The careful intake with the children revealed no indication for any of these disorders.
Data reported here have several limitations. The children did not undergo intelligence testing; their reactions and behavior during the first session, as well as their acceptance and graduation at Kindergarten were assumed as sufficient to judge them as average intelligent. Comorbidities were assessed according to clinical impression and parents’ reports. The CBT treatment was based on our clinical expertise as a specialized OCD outpatient clinic. It included parent-oriented CBT elements, but did not have a fixed protocol and was adjusted individually to the needs of every family. Last but not least, no control group of young patients without an intervention was included.
Conclusions and clinical implications
We described a prospective 6 month follow-up of five cases of OCD in very young children. At the moment of first presentation, all children were so severely impaired that attendance of Kindergarten was uncertain. Parents were deeply involved in accommodating their child’s rituals. Because of the children’s young age, medication was not indicated. Therefore, a minimal CBT intervention for parents was offered, mainly focusing on reducing family accommodation. CY-BOCS scores at the beginning and after 3 months show an impressive decline in OCD severity that remained stable after 6 months. At 3 months follow-up, all children were able to attend Kindergarten daily, and at 6 months follow-up, every child had been admitted to the next grade. OCD is known to be a chronic condition. Therefore, in spite of treatment success, relapse might occur. However, as our treatment approach mainly targeted family accommodation, parents will hopefully react with less accommodation, should a new episode of OCD occur. Moreover, parents stay in touch with the outpatient clinic and can call when needed.
The clinical implications of our findings are that clinicians should not hesitate to think of OCD in a young child when obsessive-compulsive symptoms are reported. The assessment of the disorder should include the CY-BOCS, which has been validated in very young children by obtaining information from the parent. If CY-BOCS scores are clinically meaningful (for young children, a score above 8), a parent-based treatment targeting family accommodation should be offered.
By disseminating knowledge about the clinical presentation, assessment and treatment of early childhood OCD, it should be possible to shorten the long delay between first symptoms of OCD and disease-specific treatment that is reported as main predictor for persistent OCD. Early recognition and treatment of OCD are crucial to prevent chronicity [ 14 , 15 ]. As children and adolescents with OCD have a heightened risk for clinically significant psychiatric and psychosocial problems as adults, intervening early offers an important opportunity to prevent the development of long-standing problem behaviors [ 10 , 19 ].
Availability of data and materials
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Abbreviations
Obsessive compulsive behavior
Child Yale-Brown Obsessive Compulsive Scale
Cognitive Behavior Therapy
Pediatric OCD Treatment Study PT. Cognitive-behavior therapy, sertraline, and their combination for children and adolescents with obsessive-compulsive disorder. The Pediatric OCD Treatment Study (POTS) randomized controlled trial. JAMA. 2004;292(16):1969–76.
Article Google Scholar
Heyman I, Fombonne E, Simmons H, Ford T, Meltzer H, Goodman R. Prevalence of obsessive-compulsive disorder in the British nationwide survey of child mental health. Int Rev Psychiatry. 2003;15:178–84.
Article CAS PubMed Google Scholar
Zohar AH. The epidemiology of obsessive-compulsive disorder in children and adolescents. Child & Adolescent Psychiatric Clinics of North America. 1999;8:445–60.
Article CAS Google Scholar
Renshaw KD, Steketee GS, Chambless DL. Involving family members in the treatment of OCD. Cogn Behav Ther. 2005;34(3):164–75.
Article PubMed Google Scholar
Barrett P, Farrell L, Dadds M, Boulter N. Cognitive-behavioral family treatment of childhood obsessive-compulsive disorder: long-term follow-up and predictors of outcome. J Am Acad Child Adolesc Psychiatry. 2005;44(10):1005–14.
Geller DA. Obsessive-compulsive and spectrum disorders in children and adolescents. Psychiatr Clin N Am. 2006;29:353–70.
Taylor S. Early versus late onset obsessive-compulsive disorder: evidence for distinct subtypes. Clin Psychol Review. 2011;31:1083–100.
Garcia A, Freeman J, Himle M, Berman N, Ogata AK, Ng J, et al. Phenomenology of early childhood onset obsessive compulsive disorder. J Psychopathol Behav Assess. 2009;31:104–11.
Article PubMed PubMed Central Google Scholar
Coskun M, Zoroglu S, Ozturk M. Phenomenology, psychiatric comorbidity and family history in referred preschool children with obsessive-compulsive disorder. Child Adolesc Psychiatry Ment Health. 2012;6(1):36.
Fineberg NA, Dell'Osso B, Albert U, Maina G, Geller DA, Carmi L, et al. Early intervention for obsessive compulsive disorder: an expert consensus statement. Eur Neuropsychopharmacol. 2019. https://doi.org/10.1016/j.euroneuro.2019.02.002 .
Micali N, Heyman I, Perez M, Hilton K, Nakatani E, Turner C, et al. Long-term outcomes of obsessive-compulsive disorder: follow-up of 142 children and adolescents. Br J Psychiatry. 2010;197:128–34.
Zellmann H, Jans T, Irblich B, Hemminger U, Reinecker H, Sauer C, et al. Children and adolescents with obsessive-compulsive disorders. Zeitschrift für Kinder- und Jugendpsychiatrie und Psychotherapie. 2009;37(3):173–82.
Stewart SE, Geller DA, Jenike M, Pauls D, Shaw D, Mullin B, et al. Long-term outcome of pediatric obsessive-compulsive disorder: a meta-analysis and qualitative review of the literature. Acta Psychiatr Scand. 2004;110(1):4–13.
Freeman J, Sapyta JJ, Garcia A, Compton S, Khanna M, Flessner C, et al. Family-based Treatment of early childhood obsessive-compulsive disorder: the Pediatric obsessive-compulsive disorder Treatment Study for young children (POTS Jr) - a randomized clinical trial. JAMA Psychiatry. 2014;71(6):689–98.
Lewin AB, Park JM, Jones AM, Crawford EA, De Nadai AS, Menzel J, et al. Family-based exposure and response prevention therapy for preschool-aged children with obsessive-compulsive disorder: a pilot randomized controlled trial. Behav Res Ther. 2014;56:30–8.
Renner T, Walitza S. Schwere frühkindliche Zwangsstörung - Kasuistik eines 4-jährigen Mädchens. Zeitschrift für Kinder- und Jugendpsychiatrie und Psychotherapie. 2006;34:287–93.
Selles RR, Storch EA, Lewin AB. Variations in symptom prevalence and clinical correlates in younger versus older youth with obsessive–compulsive disorder. Child Psychiatry Hum Dev. 2014;45:666–74.
Skriner LC, Freeman J, Garcia A, Benito K, Sapyta J, Franklin M. Characteristics of young children with obsessive–compulsive disorder: baseline features from the POTS Jr. Sample Child Psychiatry and Human Development. 2016;47:83–93.
Walitza S, van Ameringen M, Geller D. Early detection and intervention for obsessive-compulsive disorder in childhood and adolescence. Lancet Child Adolesc Health. 2019. https://doi.org/10.1016/S2352-4642(19)30376-1 .
Nakatani E, Krebs G, Micali N, Turner C, Heyman I, Mataix-Cols D. Children with very early onset obsessive-compulsive disorder: clinical features and treatment outcome. J Child Psychol Psychiatry. 2011;52(12):1261–8.
Scahill L, Riddle MA, McSwiggin-Hardin M. Children's Yale-Brown obsessive-compulsive scale: reliability and validity. J Am Acad Child Adolesc Psychiatry. 1997;36:844–52.
Freeman J, Flessner C, Garcia A. The Children’s Yale-Brown obsessive compulsive scale: reliability and validity for use among 5 to 8 year olds with obsessive-compulsive disorder. J Abnorm Child Psychol. 2011;39:877–83.
Lewin AB, Piacentini J, De Nadai AS, Jones AM, Peris TS, Geffken GR, et al. Defining clinical severity in pediatric obsessive-compulsive disorder. Psychol Assess. 2014;26(2):679–84.
AACAP. Practice parameter for the assessment and Treatment of children and adolescents with obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry. 2012;51(1):98–113.
NICE. Treatment options for children and young people with obsessive-compulsive disorder or body dysmorphic disorder. In: Excellence NIfHaC, 2019.
Google Scholar
Freeman J, Choate-Summers ML, Moore PS, Garcia AM, Sapyta JJ, Leonard HL, et al. Cognitive behavioral Treatment for young children with obsessive-compulsive disorder. Biol Psychiatry. 2007;61(3):337–43.
Ginsburg GS, Burstein M, Becker KD, Drake KL. Treatment of obsessive compulsive disorder in young children: an intervention model and case series. Child Family Behav Ther. 2011;33(2):97–122.
Comer JS, Furr JM, Kerns CE, Miguel E, Coxe S, Elkins RM, et al. Internet-delivered, family-based treatment for early-onset OCD: a pilot randomized trial. J Consult Clin Psychol. 2017;85(2):178–86.
Storch EA, Geffken GR, Merlo LJ, Jacob ML, Murphy TK, Goodman WK, et al. Family accommodation in Pediatric obsessive-compulsive disorder. J Clin Child Adolesc Psychol. 2007;36(2):207–16.
Brezinka V. Zwangsstörungen bei Kindern. Die Rolle der Angehörigen. Schweizer Zeitschrift für Psychiatrie & Neurologie. 2015;15(4):4–6.
Lebowitz ER. Treatment of extreme family accommodation in a youth with obsessive-compulsive disorder. In: Storch EA, Lewin AB, editors. Clinical handbook of obsessive-compulsive and related disorders. New York: Springer; 2016. p. 321–35.
Chapter Google Scholar
Lebowitz ER. Parent-based treatment for childhood and adolescent OCD. J Obsessive-Compulsive Related Dis. 2013;2(4):425–31.
Chang K, Frankovich J, Cooperstock M, Cunningham M, Latimer ME, Murphy TK, et al. Clinical evaluation of youth with Pediatric acute onset neuropsychiatric syndrome (PANS). Recommendations from the 2013 PANS consensus conference. J Child Adolesc Psychopharmacol. 2015;25:3–13.
Download references
Acknowledgements
Not applicable.
no funding was obtained for this study.
Author information
Authors and affiliations.
Department of Child and Adolescent Psychiatry and Psychotherapy, University Hospital of Psychiatry Zurich, University of Zurich, Neumünsterallee 3, 8032, Zurich, Switzerland
Veronika Brezinka, Veronika Mailänder & Susanne Walitza
You can also search for this author in PubMed Google Scholar
Contributions
V.B. conducted the diagnostic and therapeutic sessions and wrote the manuscript. V.M. was responsible for medical supervision and revised the manuscript. S.W. supervised the OCD treatment and research overall, applied for ethics approval and revised the manuscript. All authors have read and approved the manuscript.
Corresponding author
Correspondence to Veronika Brezinka .
Ethics declarations
Ethics approval and consent to participate.
the study was approved by the Kantonale Ethikkommission Zürich, July 22nd, 2019.
Consent for publication
Written informed consent was obtained from the parents for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Competing interests
V.B. and V.M. declare that they have no competing interests. S.W. has received royalties from Thieme, Hogrefe, Kohlhammer, Springer, Beltz in the last 5 years. Her work was supported in the last 5 years by the Swiss National Science Foundation (SNF), diff. EU FP7s, HSM Hochspezialisierte Medizin of the Kanton Zurich, Switzerland, Bfarm Germany, ZInEP, Hartmann Müller Stiftung, Olga Mayenfisch, Gertrud Thalmann, Vontobel-, Unisciencia and Erika Schwarz Fonds. Outside professional activities and interests are declared under the link of the University of Zurich www.uzh.ch/prof/ssl-dir/interessenbindungen/client/web/
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Brezinka, V., Mailänder, V. & Walitza, S. Obsessive compulsive disorder in very young children – a case series from a specialized outpatient clinic. BMC Psychiatry 20 , 366 (2020). https://doi.org/10.1186/s12888-020-02780-0
Download citation
Received : 02 March 2020
Accepted : 05 July 2020
Published : 11 July 2020
DOI : https://doi.org/10.1186/s12888-020-02780-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Obsessive compulsive disorder
- Early childhood
- Family accommodation
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
CLINICAL CASE STUDY article
A clinical case study of the use of ecological momentary assessment in obsessive compulsive disorder.

- Brain, Behaviour and Mental Health Research Group, School of Psychology and Speech Pathology, Curtin University, Perth, WA, Australia
Accurate assessment of obsessions and compulsions is a crucial step in treatment planning for Obsessive-Compulsive Disorder (OCD). In this clinical case study, we sought to determine if the use of Ecological Momentary Assessment (EMA) could provide additional symptom information beyond that captured during standard assessment of OCD. We studied three adults diagnosed with OCD and compared the number and types of obsessions and compulsions captured using the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS) compared to EMA. Following completion of the Y-BOCS interview, participants then recorded their OCD symptoms into a digital voice recorder across a 12-h period in reply to randomly sent mobile phone SMS prompts. The EMA approach yielded a lower number of symptoms of obsessions and compulsions than the Y-BOCS but produced additional types of obsessions and compulsions not previously identified by the Y-BOCS. We conclude that the EMA-OCD procedure may represent a worthy addition to the suite of assessment tools used when working with clients who have OCD. Further research with larger samples is required to strengthen this conclusion.
Introduction
Obsessive-Compulsive Disorder (OCD) is a disabling anxiety disorder characterized by upsetting, unwanted cognitions (obsessions) and intense and time consuming recurrent compulsions ( American Psychiatric Association, 2000 ). The idiosyncratic nature of the symptoms of OCD ( Whittal et al., 2010 ) represents a challenge to completing accurate and comprehensive assessments, which if not achieved, can have a deleterious effect on the provision of effective treatment for the disorder ( Kim et al., 1989 ; Taylor, 1995 ; Steketee and Barlow, 2002 ; Deacon and Abramowitz, 2005 ).
Accurately assessing the full range of symptoms of OCD requires reliable and psychometrically sound diagnostic instruments and measures ( Taylor, 1995 , 1998 ; Rees, 2009 ) alongside the standard clinical interview. Although the most commonly used psychometric instrument for assessing OCD, the Yale-Brown Obsessive Compulsive Scale (Y-BOCS) ( Goodman et al., 1989a , b ), has acceptable reliability and convergent validity, it has been criticized by Taylor (1995) for weak discriminant validity. Taylor also highlighted that it remains susceptible to administration variance, relies on client memory recall, and is time consuming to administer. As with all measures completed retrospectively, selective memory biases affect the type of information reported by clients about their symptoms ( Clark, 1988 ; Stone and Shiffman, 2002 ; Stone et al., 2004 ). Glass and Arnkoff (1997 , p. 912) have summarized several disadvantages of structured inventories; first, they contain prototypical statements which may fail to capture the idiosyncratic nature of the client's actual thoughts; second, they can be affected by post-hoc reappraisals of what clients feel, as the data is subject to memory recall biases; and finally they may fail to adequately capture the client's internal dialog due to the limitations of the best fit question structure.
Discrepancies have been reported between data collected in the client's natural environment ( in situ ) and those based on the client's later recall ( de Beurs et al., 1992 ; Marks and Hemsley, 1999 ; Stone et al., 2004) . Such discrepancies may be further affected by factors such as the complexity and diversity of obsessions and compulsions, not to mention the ego-dystonic nature of many OCD clients' obsessional thoughts. It seems likely that clients with distressing ego-dystonic obsessions, for example, those involving sexual, aggressive, and/or religious themes may experience a heightened level of discomfort in reporting their obsessions in a face to face assessment with a clinician, thus reducing their willingness to accurately report ( Taylor, 1995 ; Newth and Rachman, 2001 ; Grant et al., 2006 ; Rees, 2009 ). This may contribute to an underreporting of these obsessions, and hence an inaccurate understanding and a restriction of the clinician's ability to adequately treat the client ( Grant et al., 2006 ; Rachman, 2007 ).
Exposure and response prevention, cognitive therapy, and pharmacological interventions have been shown to be effective in the treatment of OCD ( Abramowitz, 1997 , 2001 ; Foa and Franklin, 2001 ; Steketee and Barlow, 2002 ; Fisher and Wells, 2008 ; Chosak et al., 2009 ). Self-monitoring is a useful therapeutic technique that provides essential information to assist in the development of exposure hierarchies and behavioral experiments used in cognitive therapy ( Tolin, 2009 ). Clients typically observe and record their experiences of target behaviors, including triggers, environmental events surrounding those experiences, and their response to those experiences ( Cormier and Nurius, 2003 ). Such self-monitoring can be used to both assist assessment and/or as an intervention. Cormier and Nurius (2003) explained that the mere act of observing and monitoring one's own behavior and experiences can produce change. As people observe themselves and collect data about what they observe, their behavior may be influenced.
A form of self-monitoring and alternative to the typical clinic-based assessment of OCD is the use of sampling from the client's real-world experiences, a procedure known as Ecological Momentary Assessment (EMA) ( Schwartz and Stone, 1998 ; Stone and Shiffman, 1994 , 2002 ). EMA does not rely on measurements using memory recall within the clinical setting, but rather allows for collection of information about the client's experiences in their natural setting, potentially improving the assessment's ecological validity ( Stone and Shiffman, 2002 ). In situ sampling techniques have been successfully used in psychology, psychiatry, and occupational therapy (for a more detailed account see research by Morgan et al., 1990 ; de Beurs et al., 1992 ; Kamarack et al., 1998 ; Litt et al., 1998 ; Kimhy et al., 2006 ; Gloster et al., 2008 ; Putnam and McSweeney, 2008 ; Trull et al., 2008 ). Generally it is agreed that EMA offers broader assessment within the client's natural environment, as it includes random time sampling of the client's experience, recording of events associated with the client's experience, and self-reports regarding the client's behaviors and physiological experiences ( Stone and Shiffman, 2002 ). Because this assessment method accesses information about the client's situation, the difficulties of memory distortions like recall bias are reduced ( Schwartz and Stone, 1998 ; Stone and Shiffman, 2002 ).
Given that accurate assessment of obsessions and compulsions is a critical aspect of treatment planning and that reliance on self-report and clinician interview has some known limitations, the purpose of this study was to investigate the utility of EMA as a potential adjunct to the conventional assessment of OCD. Specifically, we sought to compare the amount and type of information regarding obsessions and compulsions collected via EMA vs. standard assessment using the gold-standard symptom interview for OCD. As this is a pilot clinical case study, we offer the following tentative hypothesis: (1) EMA will yield additional types of obsessions and compulsions not captured by the Y-BOCS.
Participants and Setting
Participants were recruited through clients presenting to the OCD clinic at Curtin University. They were assessed using the Structured Clinical Interview for DSM-IV (SCID-IV) ( First et al., 1997 ). Inclusion in the study was based on receiving a primary diagnosis of OCD, and a Y-BOCS ( Goodman et al., 1989a , b ) score of more than 16, placing their OCD symptom severity within the clinical range ( Steketee and Barlow, 2002 ). Participants were excluded if they presented with current suicidal ideation, psychotic disorders, apparent organic causes of anxiety, were severely depressed, or if they had an intellectual disability. One potential participant was excluded post evaluation despite meeting the inclusion criteria, as she did not own a mobile phone, and reported having “blackouts” throughout the day. The three participants all had OCD symptoms in the “severe” range according to the YBOCS. In order to ensure that participants remain anonymous, pseudonyms have been used.
Participant A
Mary was a 28-year-old female who lived with her husband and small dog. She reported that for approximately 1 year she had been experiencing distressing intrusive thoughts in relation to harming her loved ones, herself, or her dog; for example, by stabbing, electrocution, or breaking the dog's neck. Mary said that she also had reoccurring thoughts and images that her husband or other family members might die. She reported engaging in some rituals, for example straightening pillows and rearranging tea-towels; but mostly reported using “safety nets” in response to her unwanted cognitions; for example ensuring that she was not alone (to prevent self-harm); avoidance and removal of feared object; extensive reassurance seeking from family members. According to the Y-BOCS measure, Mary scored a subtotal of 14 for Obsessions and a subtotal of 18 for Compulsions, giving an overall total of 32, classifying her symptoms as “severe” ( Steketee and Barlow, 2002 ).
Mary reported that her OCD first occurred after her grandmother passed away about 6 years ago. She explained they had a very close relationship, she said she found it “unbearably distressing” to visit her while she was dying. Mary reported that on one occasion whilst in a coma, her grandmother sat up and gasped, which she found extremely frightening and still remembers it in vivid detail. She reported that she experienced thoughts that her grandmother was in pain and was going “into the unknown, to a scary place.” Mary reported feeling afraid of death and that if someone “even closer” to her died she “would not be able to cope” and that she would “lose control completely.” She stated that her biggest fear was that her husband, mother or father might die. Mary reported that she has been on various anti-depressants for about 10 years. She stated that recently her psychiatrist prescribed Solian (an antipsychotic) which she tried, and found was very effective at blocking out the intrusive thoughts. However, she ceased taking the medication due to nausea.
Participant B
John was a 5-year-old man who lived with his wife and adult son. He reported a long history of distressing intrusive thoughts, and compulsive behaviors. They are summarized in three ways. First, those that relate to religious obsessions, specifically the occult and satanic experiences/fear of being “possessed.” He reported responding to these unwanted cognitions by either washing his hands to cleanse himself; using more than six pieces of toilet paper to wipe after defecating to prevent the devil entering him via his anus; or looking for the number “555,” which represents “God. This is good.” John reported that failing to act in these ways would risk causing harm to his wife and son. Second, those that relate to checking compulsions, specifically when driving, and also checking that doors are locked—which he reported doing 4–12 times per night. He reported that if he thought he heard a “bump” when driving he would have to turn back to check he had not run anyone over, or would seek reassurance from his son or wife if they were passengers in the car with him. He stated that he feared that harm would come to his wife and son if he didn't perform these checks. Third, John said that he arranged shoes so that they were “lined up” and that the clothes in the cupboard were in the “right order.” He also reported the need to compulsively clean his son's bedroom, and that he wouldn't feel “right” until he had done so. According to the Y-BOCS measure, John scored a subtotal of 13 for Obsessions and a subtotal of 15 for Compulsions, giving an overall total of 28, classifying his symptoms as “severe” ( Steketee and Barlow, 2002 ).
John reported that his symptoms have been present for at least the last 29 years. He reported that his OCD first occurred after he had a “break-down” and tried to commit suicide by stabbing himself in the stomach before he turned 25 years of age. In the years leading up to this, John reported two poignant experiences which appear relevant to the development of his symptoms; he reported being involved in the euthanizing of two dogs whilst working as a Ranger's assistant; and that when he was young, he and his girlfriend at the time had a pregnancy termination. John reported feeling that these were “blasphemous” acts, and posed the question “Is God punishing me?” John reported that he had been on several different anti-depressants for about 19 years, with varying degrees of success and side-effects. He reported that he had seen a psychiatrist every 6 weeks for “many years” and finds being able to talk helpful.
Participant C
Paul was a 35-year-old man, who reported distressing intrusive thoughts and images in relation to harm coming to others as a consequence of him not checking that he had done what he is “supposed to do.” For example, he was concerned that someone at work would be harmed if he forgot to adequately cover shifts on the roster (something he is responsible for); or when a client of the service he coordinates was recently given a stereo, Paul reported that he feared that harm would come to the client if he didn't correctly check it to see if it was faulty, something he felt responsible to do.
Paul reported that only his partner knew of his difficulties. He stated that he did not allow his anxiety to interfere too much with his occupational functioning; however he did report that the main reason he does not practice in his profession is because of his OCD. According to the Y-BOCS measure, Paul scored a subtotal of 12 for Obsessions and a subtotal of 13 for Compulsions, giving an overall total of 25, classifying his symptoms as “severe” ( Steketee and Barlow, 2002 ).
Paul reported that his intrusive thoughts have “always been there.” He explained that one of the first clear memories he has of them, was when he was seven years old and he saw the film the “The Omen.” He reported remembering checking his head for the numbers “666.” Additionally, he reported remembering that he was concerned for his mother's safety. He reported that he had never taken medication for his OCD. He stated that he saw two therapists when he lived in the UK at an OCD center in London approximately 18 months ago. Paul said that he did not gain much from the first therapist, but believes that second therapist assisted him to look at his cognitions as “just thoughts.”
Materials and Methods
All screening of participants, interviewing and assessment, as well as administration of the study, was conducted by the first author, who was a provisionally registered psychologist undergoing postgraduate training at the time of the research, and was supervised by the second author, an experienced OCD clinician and academic. Potential participants were recruited from the Curtin OCD clinic. They were screened via telephone to ascertain their suitability for the study. A face-to-face assessment session using the Structured Clinical Interview for DSM-IV (SCID-IV; First et al., 1997 ) was conducted to determine a primary OCD diagnosis, followed by the administration of the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS) interview and checklist ( Goodman et al., 1989b ) to identify the participants' obsessions and compulsions and their symptom severity. The Y-BOCS is the most widely used scale for OCD symptoms assessment and is considered by researchers to be the “gold standard” measure for symptom severity ( Deacon and Abramowitz, 2005 ; Himle and Franklin, 2009 ). It consists of two parts; a checklist of prelisted types of obsessions, usually endorsed by the clinician based on disclosures made by the client; and the severity scale which requires the client to rate the severity of their experience by answering the questions based on their recall. Goodman et al. (1989) note that the Y-BOCS has shown adequate interrater agreement, internal consistency, and validity.
Suitable participants then attended a second session where they signed consent forms and were given instructions about the study procedure. During the data collection using the Ecological Momentary Assessment data (EMA-OCD), participants used an Olympus WS-110 digital voice recorder to record their experiences throughout a 12 h period. Participants used their existing mobile phones to receive prompts via the mobile phone Short Message Service (SMS) to record their responses to the research questions. All three participants were then provided with an envelope containing the Olympus WS-100 digital voice recorder, a spare battery, and the participant prompt questions (see Table 1 ).
Table 1. Prompt questions .
Participants were asked to turn their mobile phones on during the data collection day by 10 am, ready to receive their SMS prompts. The researcher manually sent SMS prompts to the participants at random intervals; at least every 2 h (across 1 day, from 10 am to 10 pm), for a minimum of 10 data entries in keeping with research using EMA procedures (see, Stone and Shiffman, 2002 ); asking them to complete their responses to all four questions as details on the EMA-OCD Participant Questions Sheet. Participants were instructed not to respond to the SMS prompts if driving, and were asked to respond as quickly as possible to the prompts. Data was then downloaded from the voice recorder to the researcher's computer, and transcribed. During this process all identifying details were removed. During the debrief session open-ended questions were used to gather as much information as possible regarding the participant's experiences of the study, and suggestions for improvements. During the data collection day the researcher completed a journal to record his observations and reflections related to the use of the EMA. At the completion of the EMD-OCD data collection, each of the participants was provided with a debrief session (Mary by phone, and John and Paul, face to face). The debrief session focused on their experiences of the research and use of the digital voice recorder; and provided the opportunity for them to discuss anything else that arose they wished to tell the researcher. As stated above, the data was downloaded and transcribed by the first author. The Y-BOCS obsession and compulsion categories were used as a framework to compare the data generated from the EMA-OCD procedure. After the complete de-identified data set was tabled, it was provided to a second person who was an expert in OCD for verification of categories. In the case of any discrepancies agreement was reached via consensus.
Number of reported symptoms
Table 2 provides a summary of the frequency and type of symptoms recorded during both the face-to-face session, which will be referred to as the Y-BOCS data and the EMA-OCD phase for the study, which will be referred to as the EMA–OCD data. As can be seen when comparing the data contained in the two columns, there are variations between the Y-BOCS data and the EMA-OCD data. All three participants reported more categories of both obsessions and compulsions in the Y-BOCS data, compared to that reported in the EMA-OCD data.
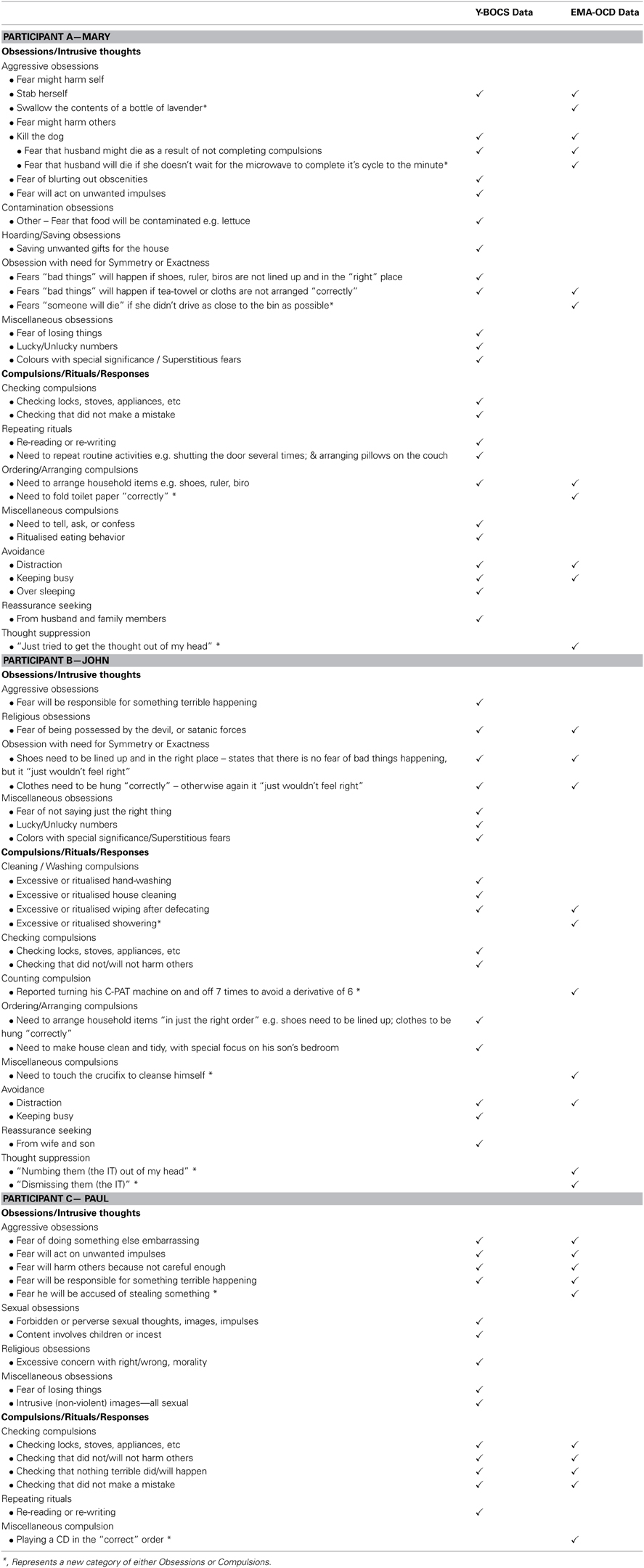
Table 2. Summary by participant of Y-BOCS data and EMA-OCD data .
Mary reported experiencing five categories of Y-BOCS Obsessions and six categories of Compulsions in the Y-BOCS data. In the EMA-OCD data she reported experiencing two categories of Y-BOCS Obsessions, and three categories of Y-BOCS Compulsions. John reported experiencing four categories of Y-BOCS Obsessions and five categories of Compulsions in the Y-BOCS data. In the EMA-OCD data he reported experiencing two categories of Y-BOCS Obsessions, and five categories of Y-BOCS Compulsions. Paul reported experiencing four categories of Y-BOCS Obsessions and two categories of Compulsions in the Y-BOCS data. In the EMA-OCD data he reported experiencing one category of Y-BOCS Obsessions, and two categories of Compulsions.
Comparison of content of symptoms
Both Mary and Paul reported previously unidentified Obsessions or intrusive thoughts in the EMA-OCD data, compared to the Y-BOCS data; and all three participants reported previously unidentified compulsions/rituals/responses in the EMA-OCD data. As can be seen in Table 2 , Mary reported two intrusive thoughts in the EMA-OCD data that were not recorded in the Y-BOCS data. Additionally, she reported a previously unreported obsession under the obsession category Obsession with need for Symmetry or Exactness , not reported in the Y-BOCS data. Mary also reported variations on her compulsive behaviors and the presence of thought suppression not identified during the administration of the Y-BOCS. The EMA-OCD data indicated that John substituted one of his compulsions for an alternative anxiety reducing act, which was not recorded in the Y-BOCS data and suggests the identification of a previously unreported compulsion. Additionally, the EMA-OCD data indicated that John engaged in thought suppression to neutralize his intrusive thoughts. Likewise, John's reported compulsive behaviors also varied between data sets. In the EMA-OCD data he reported three previously unreported compulsive behaviors, and like Mary also the presence of thought suppression. In addition to the above, the EMA-OCD data indicated that John substituted one of his rituals for another, when he touched a crucifix instead of performing his usual hand washing ritual to cleanse him-self of the potential satanic possession. This was not something reported in the Y-BOCS data.
This study investigated the utility of EMA as an adjunct assessment approach for OCD. Each of our study hypotheses was supported. As predicted the EMA procedure resulted in the identification of additional types of obsessions and compulsions not captured by the Y-BOCS interview. The finding that the EMA procedure identifies obsession and compulsion symptoms not captured by the Y-BOCS suggests that further studies in this area are warranted. As a pilot case study we cannot generalize from these initial findings but our results indicate that a larger study replicating the procedure used here, is justified. Importantly, the three participants in our study were representative of quite typical OCD clients in that they had severe levels of symptoms and had OCD for a number of years. The EMA procedure we used was found to be satisfactory to all three participants. Feedback from the participants at the de-briefing session included suggestions that this process would be helpful for therapy because it would provide the therapist and client with rich and current material regarding their symptom patterns. From a clinician's point of view, collecting the EMA data is not onerous because the entries are simply short answers collected on 12 occasions and thus is not a time-consuming exercise.
The EMA procedure as used in this study could provide clinicians with a new method by which to gain a current and accurate snap-shot of clients symptoms as they occur in real-time. This information could augment information gained from standard pencil and paper measures but also provide an “active” process which may help to engage clients in the therapeutic process. It seems likely that using a procedure like EMA with OCD clients will assist in understanding their OCD experiences, and thus assist in generating valuable information, supporting accurate assessment, client conceptualization, and ultimately treatment.
Despite these valuable findings, there are limitations of this study. As a pilot study and exploratory in nature, it is only possible to draw limited interpretations from the data provided. However, the preliminary findings of this study support the benefit of conducting further research into this procedure, where it may be possible to draw more empirically valid findings from a larger and more statistically powerful sample. Second, due to the lack of availability of date stamping, participants were asked to record the time they made each recording. Unfortunately this was not routinely provided by all participants, and hence creates an unanswerable question regarding the accuracy of the data recorded. As Stone and Shiffman (2002) discuss, a potential problem relates to participants recording their data based on their recall of what was occurring at the time of the SMS prompt, rather than immediately. Hence introducing possible memory bias, and undermining the premise of the study. Although this is certainly an unwanted variable, based on the EMA-OCD data provided it seems that except for Mary, both John and Paul responded promptly to the SMS messages, or recorded the time if they didn't. Mary on the other hand, reported during the debrief session that she was unable to record the time for the initial targets, but did so for subsequent SMS prompts. It was not possible to ascertain from her data the delay in time between the first SMS prompts and her recordings. In future applications of this procedure, it is recommended that the device used provides automatic date-stamping to address this limitation. Indeed, it may be possible to adapt the EMA methodology for use with smart phones via a dedicated OCD application.
Concluding Remarks
The findings from this study of three patients with severe OCD suggest that the use of EMA provides important additional information regarding obsessions and compulsions and may thus be a useful adjunct to the clinical assessment of OCD.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank the three participants for taking part in this study.
Abramowitz, J. S. (1997). Effectiveness of psychological and pharmacological treatments for obsessive-compulsive disorder: a quantitative review. J. Consul. Clin. Psychol . 65, 44–52. doi: 10.1037/0022-006X.65.1.44
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text
Abramowitz, J. S. (2001). Treatment of scrupulous obsessions and compulsions using exposure and response prevention: a case report. Cogn. Behav. Pract . 8, 79–85. doi: 10.1016/S1077-7229(01)80046-8
CrossRef Full Text
American Psychiatric Association. (2000). Diagnostic and Statistical Manual of Mental Disorders, 4th Edn . Washington, DC: American Psychiatric Association.
Chosak, A., Marques, L., Fama, J., Renaud, S., and Wilhelm, S. (2009). Cognitive therapy for obsessive-compulsive disorder: a case example. Cogn. Behav. Pract . 16, 7–17. doi: 10.1016/j.cbpra.2008.01.005
Clark, D. A. (1988). The validity of measures of cognition: a review of the literature. Cogn. Ther. Res . 12, 1–20. doi: 10.1007/BF01172777
Cormier, S., and Nurius, P. S. (2003). Interviewing and Change Strategies for Helpers: Fundamental Skills and Cognitive Behavioral Interventions . Pacific Grove, CA: Thomson Brooks/Cole.
Deacon, B. J., and Abramowitz, J. S. (2005). The Yale-Brown Obsessive Compulsive Scale: factor analysis, construct validity, and suggestions for refinement. J. Anxiety Disord . 19, 573–585. doi: 10.1016/j.janxdis.2004.04.009
de Beurs, E., Lange, A., and Van Dyck, R. (1992). Self-monitoring of panic attacks and retrospective estimates of panic: discordant findings. Behav. Res. Ther . 30, 411–413. doi: 10.1016/0005-7967(92)90054-K
First, M. B., Spitzer, R. L., Gibbon, M., and Williams, J. B. W. (1997). Structured Clinical Interview for DSM-IV Axis I Disorders Patient Edition (SCID-IP Version 2.0) . New York, NY: Biometrics Research Department, New York State Psychiatric Institute.
Fisher, P. L., and Wells, A. (2008). Metacognitive therapy for obsessive–compulsive disorder: a case series. J. Behav. Ther. Exp. Psychiatry 39, 117–132. doi: 10.1016/j.jbtep.2006.12.001
Foa, E. B., and Franklin, M. E. (2001). “Obsessive-compulsive disorder,” in Clinical Handbook Of Psychological Disorders , ed D. H. Barlow (New York, NY: Guilford Press), 209–263.
Glass, C. R., and Arnkoff, D. B. (1997). Questionnaire methods of cognitive self-statement assessment. J. Consul. Clin. Psychol . 65, 919–927. doi: 10.1037/0022-006X.65.6.911
Gloster, A. T., Richard, D. C. S., Himle, J., Koch, E., Anson, H., Lokers, L., et al. (2008). Accuracy of retrospective memory and covariation estimation in patients with obsessive–compulsive disorder. Behav. Res. Ther . 46, 642–655. doi: 10.1016/j.brat.2008.02.010
Goodman, W. K., Price, L. H., Rasmussen, S. A., Mazure, C., Delgado, P., Heninger, G. R., et al. (1989a). The yale-brown obsessive compulsive scale: ii. validity. Arch Gen. Psychiatry 46, 1012–1016. doi: 10.1001/archpsyc.1989.01810110054008
Goodman, W. K., Price, L. H., Rasmussen, S. A., Mazure, C., Fleischmann, R. L., Hill, C. L., et al. (1989b). The yale-brown obsessive compulsive scale: i. development, use, and reliability. Arch Gen. Psychiatry 46, 1006–1011. doi: 10.1001/archpsyc.1989.01810110048007
Grant, J. E., Pinto, A., Gunnip, M., Mancebo, M. C., Eisen, J. L., and Rasmussen, S. A. (2006). Sexual obsessions and clinical correlates in adults with obsessive-compulsive disorder. Comprehen. Psychiatry 47, 325–329. doi: 10.1016/j.comppsych.2006.01.007
Himle, M. B., and Franklin, M. E. (2009). The more you do it, the easier it gets: exposure and response prevention for OCD. Cogn. Behav. Pract . 16, 29–39. doi: 10.1016/j.cbpra.2008.03.002
Kamarack, T. W., Shiffman, S. M., Smithline, L., Goodie, J. L., Paty, J. A., Gyns, M., et al. (1998). Effects of task strain, social conflict, and emotional activation on ambulatory cardiovascular activity: daily life consequences of recurring stress in a multiethnic adult sample. Health Psychol . 17, 17–29. doi: 10.1037/0278-6133.17.1.17
Kim, J. A., Dysken, M. W., and Katz, R. (1989). Rating scales for obsessive compulsive disorder. Psychiat. Anna . 19, 74–79.
Kimhy, D., Delespaul, P., Corcoran, C., Ahn, H., Yale, S., and Malaspina, D. (2006). Computerized experience sampling method (ESMc): assessing feasibility and validity among individuals with schizophrenia. J. Psychiat. Res . 40, 221–230. doi: 10.1016/j.jpsychires.2005.09.007
Litt, M. D., Cooney, N. L., and Morse, P. (1998). Ecological momentary assessment (EMA) with treated alcoholics: methodological problems and potential solutions. Health Psychol . 17, 48–52. doi: 10.1037/0278-6133.17.1.48
Marks, M., and Hemsley, D. (1999). Retrospective versus prospective self-rating of anxiety symptoms and cognitions. J. Anxiety Disord . 13, 463–472. doi: 10.1016/S0887-6185(99)00015-8
Morgan, J., McSharry, K., and Sireling, L. (1990). Comparison of a system of staff prompting with a programmable electronic diary in a patient with Korsakoff's Syndrome. Int. J. Soc. Psychiatry 36, 225–229. doi: 10.1177/002076409003600308
Newth, S., and Rachman, S. (2001). The concealment of obsessions. Behav. Res. Ther . 39, 457–464. doi: 10.1016/s0005-7967(00)00006-1
Putnam, K. M., and McSweeney, L. B. (2008). Depressive symptoms and baseline prefrontal EEG alpha activity: a study utilizing Ecological Momentary Assessment. Biol. Psychol . 77, 237–240. doi: 10.1016/j.biopsycho.2007.10.010
Rachman, S. (2007). Unwanted intrusive images in obsessive compulsive disorders. J. Behav. Ther. Exp. Psychiatry 38, 402–410. doi: 10.1016/j.jbtep.2007.10.008
Rees, C. S. (2009). Obsessive-Compulsive Disorder: A Practical Guide to Treatment . East Hawthorn, VIC: IP Communications.
Schwartz, J. E., and Stone, A. A. (1998). Strategies for analyzing ecological momentary assessment data. Health Psychol . 17, 6–16. doi: 10.1037/0278-6133.17.1.6
Steketee, G., and Barlow, D. H. (2002). “Obsessive-compulsive disorder,” in Anxiety and its Disorders: The Nature and Treatment of Anxiety and Panic, 2nd Edn . ed D. H. Barlow (New York, NY: Guilford Press), 516–550.
Stone, A., and Shiffman, S. (2002). Capturing momentary, self-report data: a proposal for reporting guidelines. Ann. Behav. Med . 24, 236–243. doi: 10.1207/s15324796abm2403_09
Stone, A. A., Broderick, J. E., Shiffman, S. S., and Schwartz, J. E. (2004). Understanding recall of weekly pain from a momentary assessment perspective: absolute agreement, between- and within-person consistency, and judged change in weekly pain. Pain , 107, 61–69. doi: 10.1016/j.pain.2003.09.020
Stone, A. A., and Shiffman, S. (1994). Ecological momentary assessment (EMA) in behavorial medicine. Ann. Behav. Med . 16, 199–202.
Taylor, S. (1995). Assessment of obsessions and compulsions: reliability, validity, and sensitivity to treatment effects. Clin. Psychol. Rev . 15, 261–296. doi: 10.1016/0272-7358(95)00015-h
Taylor, S. (1998). “Assessment of obsessive-compulsive disorder,” in Obsessive-Compulsive Disorder: Theory, Research, and Treatment , eds R. P. Swinson, M. M. Antony, S. Rachman, and M. A. Richter (New York, NY: Guildford Press), 229–258.
Tolin, D. F. (2009). Alphabet Soup: ERP, CT, and ACT for OCD. Cogn. Behav. Pract . 16, 40–48. doi: 10.1016/j.cbpra.2008.07.001
Trull, T. J., Solhan, M. B., Tragesser, S. L., Jahng, S., Wood, P. K., Piasecki, T. M., et al. (2008). Affective instability: measuring a core feature of borderline personality disorder with ecological momentary assessment. J. Abnorm. Psychol . 117, 647–661. doi: 10.1037/a0012532
Whittal, M. L., Robichaud, M., and Woody, S. R. (2010). Cognitive treatment of obsessions: enhancing dissemination with video components. Cogn. Behav. Pract . 17, 1–8. doi: 10.1016/j.cbpra.2009.07.001
Keywords: obsessive-compulsive disorder (OCD), ecological momentary assessment, ecological momentary assessment data, anxiety disorders, assessment
Citation: Tilley PJM and Rees CS (2014) A clinical case study of the use of ecological momentary assessment in obsessive compulsive disorder. Front. Psychol . 5 :339. doi: 10.3389/fpsyg.2014.00339
Received: 10 March 2014; Accepted: 01 April 2014; Published online: 17 April 2014.
Reviewed by:
Copyright © 2014 Tilley and Rees. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Clare S. Rees, Brain, Behaviour and Mental Health Research Group, School of Psychology and Speech Pathology, Curtin University, Perth, WA, Australia e-mail: [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Mental Health Academy

- Case Studies
- Communication Skills
- Counselling Microskills
- Counselling Process
- Children & Families
- Ethical Issues
- Sexuality & Gender Issues
- Neuropsychology
- Practice Management
- Relationship Counselling
- Social Support
- Therapies & Approaches
- Workplace Issues
- Anxiety & Depression
- Personality Disorders
- Self-Harming & Suicide
- Effectiveness Skills
- Stress & Burnout
- Diploma of Counselling
- Diploma of Financial Counselling
- Diploma of Community Services (Case Management)
- Diploma of Youth Work
- Bachelor of Counselling
- Bachelor of Human Services
- Master of Counselling
Case Study: Obsessive-Compulsive Disorder
In a previous article we reviewed a range of treatments that are used to help clients suffering from obsessive-compulsive disorder (OCD). In this edition we showcase the case study of Darcy [fictional name], who worked with a psychologist to address the symptoms and history of her OCD.
Marian, a psychologist who specialised in anxiety disorders, closed the file and put it into the filing cabinet with a smile on her face. This time she had the satisfaction of filing it into the “Work Completed” files, for she had just today celebrated the final session with a very long-term client: Darcy Dawson. They’d come through a lot together, Darcy and Marian, during the twelve years of Darcy’s treatment for Obsessive-Compulsive Disorder, and they had had a particularly strong therapeutic alliance.
Marian reflected on the symptoms and history which had brought Darcy into her practice.
Obsessions at age nine
Now 37, Darcy reckoned that she had begun having obsessions around age nine, soon after her beloved grandma had died. Already grieving the loss of the person she was closest to in life, Darcy experienced further alienation – and resultant anxiety — when her father relocated the family from the small town in Victoria where they lived to Melbourne. Adjusting to big-city life wasn’t easy for someone as anxious as Darcy, and she soon found that she was obsessing. She had fears of being hit by a speeding car if she stepped off the kerb. She feared that the new friends she began to develop in Melbourne would be kidnapped by bad people. And she was terrified that, if she didn’t do an elaborate prayer routine at night, all manner of terrible things would befall her family.
The prayer routine, relatively simple at first, grew to gigantic proportions, containing many rules and restrictions. Darcy believed that she had to repeat each family member’s full name 15 times, say a sentence that asked for each person to be kept safe, promise God that she would improve herself, clap her hands 20 times for each person, kneel down and get up 5 times, and then put her hands into a prayer position while bowing. She “had” to do this routine at least 10 times each night, and if she made a mistake anywhere along the way, she had to start totally over again from the beginning, or else something bad would happen to her parents or little brother. Once she went flying to her mother’s side in the kitchen, tears streaming down her face, because she couldn’t get her “prayers” right. Darcy was certain that she was a huge disappointment to God and everybody.
Just like Granddad
Marian had asked Darcy if her parents were similar at all, and Darcy couldn’t think of many ways in which they were. Then she remembered something. “Ah,” she said, “my parents aren’t having these awful thoughts like me, but I remember my mum often telling me, ‘You’re just like your grandfather.’” Darcy’s grandfather had died when she was only five, so she didn’t have strong recollections of him, but there were two images that she always remembered about him: Grandfather standing by the kitchen sink in their farmhouse, washing his hands – always washing his hands. And if they decided to take a walk around the farm, he would take a seeming eternity to check that all the windows and doors were locked, even though they were on good terms with everyone within a ten-mile radius!
Obsessions and compulsions worsen through Uni
Marian had felt huge compassion for Darcy as she outlined the course that the disorder had taken. While the intrusive thoughts waxed during high-stress times and waned when Darcy felt relatively stable, there was nevertheless a general broadening of the obsessions – and resultant compulsion to do certain repetitive acts – throughout Darcy’s growing-up years. In high school, for instance, Darcy began to have an aversion to looking at any woman with a scoop-neck top on, going so far as to grab a glass and pretend to be holding it high up near her lips (as if to drink) if she had to talk to someone dressed in any but the most conservative top. In that way, she felt, she would be blocked from seeing what she should not see and thus sinning. Short skirts were also a problem, as Darcy feared that she was looking at people in inappropriate ways, and was offensive.
If anyone at a party crossed their legs while she was looking at them, Darcy assumed that they had done that because they were offended by her having glanced at them; she feared that they would think she was looking at their crotch area. She prayed constantly for forgiveness, but ended up ceasing hugs to family and friends because she felt like a hypocrite. Of course, not feeling that she could/should touch anyone made for huge social problems, and dating anyone became impossible: a huge punishment for a friendly extravert like Darcy. She petitioned God relentlessly, asking to be a better, less sinful person. It did not seem to help.
When Darcy began University, the experience was defined by a series of irrational obsessions. She would worry incessantly about having written something offensive on an email or an assignment. Walking around campus, she would pick up rubbish: papers that she had never seen before; she would worry that she might have written something on one of them. She feared that she would accidentally hurt one of her fellow students by something that she might do or say. By this time Darcy was repeating certain phrases over and over again to ward off disaster. She was amazed that she was getting through school at all (she often made straight A’s), because her rampant perfectionism caused her to take at least twice as long as other students to complete assignments, and she still wasn’t happy then. The anxiety and depression were overwhelming Darcy to the point where she recognised that she could barely function and something needed to change.
The Uni psychologist says, “You’re fine”
Marian shook her head in amazement as she recalled how Darcy’s first attempts to find out what was wrong with her had been fruitless; all the health professionals had completely missed the OCD! Upon first coming to Marian, Darcy had recounted how getting along to the University psychologist in her senior year was a “non-event”. He had asked a few questions, chatted to her about her schoolwork, told her she was basically fine, and then told her to go see a psychiatrist, who merely prescribed a sleeping pill. Darcy had taken this, as instructed, because the intrusive thoughts in her mind often did keep her from sleeping, but when she was awake she still had the thoughts and the horrible compulsion to perform the anxiety-alleviating acts: routines which now occupied several hours each day. Moreover, Darcy’s parents still didn’t believe that anything was wrong with her; they even found it funny that she was “quirky” like her grandfather.
Age 25: Treatment begins
Darcy was to graduate and spend another three years being held prisoner by her out-of-control mind before a chance meeting of her mother with a specialist in OCD at a conference. The specialist didn’t live in Melbourne, but – by incredible coincidence – he had a highly recommended colleague who did: Marian. Marian recalled with some fondness how Darcy had sat in her office during the first session, shedding tears of joy at being truly “seen”: both as a person and in her disorder. When Marian had issued the magical words, “Obsessive-Compulsive Disorder”, Darcy had been surprised – after all, her sense of OCD was people who continually washed their hands – but she also felt like she had just been given the key to her prison. Her treatment began soon after.
Marian worked intensively with Darcy at first, and then steadily. She helped Darcy get onto an even keel emotionally first by raising her serotonin levels (which had been quite low). Marian then began the laborious process of helping Darcy to change her habits of thinking: the assumptions that she made, the irrationalities that controlled her behaviour, and the intrusive obsessions that seemed to take over her life. Marian helped Darcy to see the importance of an exercise regimen, a good diet, and a stillness practice. Darcy joined an online support group, and Marian and Darcy enlisted the help of Darcy’s family and a few close friends. Partway through the therapy, Darcy was even able to come off the medications: a goal she had long sought, because she had married a “wonderful” man and they wanted to start a family.
At 37, Darcy is a happy and fulfilled person, with a solid marriage and an eight-year-old daughter. She believes that she worries about her “like a normal mother”, rather than in the obsessional way she used to pray in order to protect her family from imagined harm. She still petitions God, as she is active in her church, but now the petitions are free of the superstitious routines she used to perform, and she is quick to be thankful for her many blessings.
Unwanted thoughts still come to her, but now she has tools to focus elsewhere, and when the intrusive thoughts come, Darcy knows how to keep them from causing her to repeat irrational acts in a compulsive way. She knows that she will probably always be managing her disorder, as there is no cure for OCD. But the difference now is that she controls it, rather than having it control her. As far as Darcy is concerned, Marian gave her back her life.
Marian smiled again as she recalled Darcy’s journey and her original fear of being a “disappointment to God and everyone”. Indeed, Marian felt blessed to have had Darcy as a client.
This article is an extract of the upcoming Mental Health Academy “OCD and OCPD Case Studies” CPD course. Click here for a full list of currently available MHA continuing professional development courses.
Subscribe to our newsletter

You’ll regularly receive powerful strategies for personal development, tips to improve the growth of your counselling practice, the latest industry news, and much more.
Keyword search

AIPC specialises in providing high quality counselling and community services courses, with a particular focus on highly supported external education. AIPC is the largest provider of counselling courses in the Australia, with over 27 years specialist experience.
Learn more: www.aipc.net.au

Recent Posts
- Men and Emotions: From Repression to Expression
- Men, Emotions and Alexithymia
- The Fine Art of Compassion
- The Benefits of Intentional Daydreaming
- Solution-focused Techniques in Counselling
Recommended Websites
- Australian Counselling Association
- Life Coaching Institute
Case Report: Obsessive compulsive disorder in posterior cerebellar infarction - illustrating clinical and functional connectivity modulation using MRI-informed transcranial magnetic stimulation
Urvakhsh Meherwan Mehta Roles: Conceptualization, Data Curation, Formal Analysis, Funding Acquisition, Investigation, Methodology, Writing – Original Draft Preparation, Writing – Review & Editing Darshan Shadakshari Roles: Data Curation, Investigation, Resources, Writing – Review & Editing Pulaparambil Vani Roles: Data Curation, Investigation, Methodology, Supervision, Writing – Review & Editing Shalini S Naik Roles: Methodology, Project Administration, Writing – Review & Editing V Kiran Raj Roles: Data Curation, Formal Analysis, Visualization, Writing – Review & Editing Reddy Rani Vangimalla Roles: Data Curation, Formal Analysis, Visualization, Writing – Review & Editing YC Janardhan Reddy Roles: Supervision, Writing – Review & Editing Jaya Sreevalsan-Nair Roles: Formal Analysis, Investigation, Visualization, Writing – Review & Editing Rose Dawn Bharath Roles: Conceptualization, Formal Analysis, Investigation, Methodology, Supervision, Visualization, Writing – Review & Editing
This article is included in the Wellcome Trust/DBT India Alliance gateway.
Obsessive Compulsive Disorder, Cerebellar cognitive affective syndrome, Neuromodulation, Functional brain connectivity, Cerebellar infarct, Theta burst stimulation
Revised Amendments from Version 1
The new version provides more clinical details about the patient, in response to the review comments raised. These include details and justifications for past treatment, iTBS treatment details, rationale for performing an MRI scan and follow-up information beyond the earlier reported period of three months.
See the authors' detailed response to the review by Shubhmohan Singh See the authors' detailed response to the review by Peter Enticott
Introduction
Cortico-striato-thalamocortical circuitry dysfunction is central to an integrated neuroscience formulation of obsessive-compulsive disorder (OCD) 1 , 2 . However, more recent large-scale brain connectivity analyses implicate the role of the cerebello-thalamocortical networks also 3 . Here, we report a case of OCD secondary to a cerebellar lesion. We test the mediating role of the cerebellum in the manifestation of OCD by manipulating the frontal-cerebellar network using MRI-informed transcranial magnetic stimulation (TMS).
Case report
A 21-year-old male, an undergraduate student from rural south India, presented to our emergency with suicidal thoughts. History revealed three years of academic decline, pathological slowness in routine activities (e.g., bathing, eating, dressing up, and using the toilet), repetitive ‘just-right’ behaviors (e.g., wiping his mouth after eating, clearing his throat, pulling down his shirt, mixing his food in the plate and walking back and forth until ‘feeling satisfied’). As a result, he spent up to three hours completing a meal or his toilet routines. Before presentation to us, he had received trials with two separate courses of electroconvulsive therapy (ECT) – six bitemporal ECTs at first, followed by nine bifrontal) spaced about two months apart. ECT was prescribed because of a further deterioration in his condition over the prior 18-months, with reduced oral intake, weight loss, grossly diminished speech output, and passing urine in bed (as he would remain in bed secondary to his obsessive ambitendency, as disclosed later). His oral intake and speech output improved with both ECT treatments, only to gradually worsen over the next few weeks. Given the potential catatonic phenomena (withdrawn behaviour and mutism) in the background of ongoing academic decline, slowness and stereotypies, he was also treated with oral olanzapine 20mg for eight weeks and risperidone 6mg for six weeks with minimal change in his slowness and repetitive behaviors. He did not receive any antidepressant medications. Psychotherapy was also not considered given the limited feasibility due to the severe withdrawal and near mutism. We could not elicit any contributory clinical history of prodromal or mood symptoms from adolescence when we evaluated his past psychiatric and medical history. Two months after the last ECT treatment, he presented to our emergency services with suicidal thoughts. He was admitted, and mental status examination revealed aggressive (urges to harm himself by jumping in front of a moving vehicle or touching electric outlets) and sexual obsessions with mental compulsions and passing urine in bed (as he could not go to the toilet in time due to obsessive ambitendency). The Yale-Brown Obsessive-Compulsive Scale (YBOCS) severity score was 29 4 . He had good insight into obsessions, but not the ‘just right’ repetitive behaviors; it was, therefore, challenging to engage him in psychotherapy. We treated him with escitalopram 40mg and brief psychoeducation before being discharged. After three months, his obsessions had resolved, but pathological slowness, ‘just right’ phenomena, and passing urine in bed had worsened (YBOCS score 31).
We then obtained a plain and contrast brain MRI, to rule out an organic aetiology given the atypical nature of symptoms (apparent urinary incontinence) and the poor treatment response. The MRI revealed a wedge-shaped lesion in the right posterior cerebellum, suggestive of a chronic infarct in the posterior inferior cerebellar artery territory ( Figure-1A ). MR-angiogram revealed no focal narrowing of intracranial and extracranial vessels. Electroencephalography, cerebrospinal fluid analysis, autoimmune and vasculitis investigations were unremarkable. Echocardiogram was normal and the sickling test for sickle cell anemia was also negative. We specifically inquired about history of loss of consciousness, seizures or motor incoordination, but these were absent. His neurological examination with a detailed focus on cerebellar signs was unremarkable. The International Cooperative Ataxia Rating Scale (ICARS) score was zero. The Cerebellar Cognitive Affective Syndrome (CCAS) scale revealed >3 failed tests – in domains of attention, category switching, response inhibition, verbal fluency, and visuospatial drawing, suggestive of definite CCAS 5 .
Cerebellar lesion detection ( A & B ), its functional connectivity map ( C ) and MRI-guided transcranial magnetic stimulation delivery ( D ). Average blood oxygen level-dependent (BOLD) signal time-series were extracted from voxels within a binarized lesion-mask that overlapped with the right crus II ( 1A & 1B ). This was used as the model predictor in a general linear model to determine the brain regions that temporally correlated with the lesion-mask using FSL-FEAT 11 . The resultant seed-to-voxel connectivity map (z-thresholded at 4) was used to identify the best connectivity of the seed with voxels in the pre-supplementary motor area (pre-SMA; MNI x=3; y=13; z=58; 1C ). Six-hundred pulses were delivered as triplet bursts at theta frequency and 90% of the resting motor threshold (50 Hz; 2s on; 8s off) using a MagPro X100 (MagVenture, Denmark) device under MR-guided neuronavigation using the Brainsight stereotaxic system (Rogue Research, Montreal, Canada) with a figure-of-eight coil held with the handle in line with the sagittal plane, pointing toward the occiput to stimulate the pre-SMA site ( 1D ).
MRI-informed neuromodulation
Owing to inadequate treatment response and the possibility of OCD secondary to the cerebellar lesion, we discussed with the patient about MRI-informed repetitive transcranial magnetic stimulation (rTMS) and obtained his consent. The presence of a lesion involving a node (cerebellum) within the cerebello-thalamo-cortical circuit – a key pathway for error monitoring 6 and inhibitory control 7 – cognitive processes typically impacted in OCD prompted us to utilize a personalized-medicine approach to treatment. We acquired a resting-state functional-MRI echoplanar sequence (8m 20s; 250-volumes) in duplicate – before, and one-month after rTMS treatment on a 3-Tesla scanner (Skyra, Siemens), using a 20-channel coil with the following parameters: TR/TE/FA= 2000ms/30ms/78; voxel=3mm isotropic; FOV=192*192.
Image processing was performed using the FMRIB Software Library (FSL version-5.0.10) 8 . Figure 1 describes how we obtained a seed-to-voxel connectivity map to identify the best connectivity of the cerebellar lesion-seed with voxels in the pre-supplementary motor area (pre-SMA; MNI x=3; y=13; z=58) – a commonly used site for neuromodulation in OCD 9 . This area demonstrates connections with the non-motor (ventral dentate nucleus) parts of the posterolateral cerebellum 10 and contributes to error processing and inhibitory control along with the cerebellum 7 .
We augmented escitalopram with rTMS, administered as intermittent theta-burst stimulation (iTBS) to the pre-SMA coordinates ( Figure-1D ). Six-hundred pulses were delivered as triplet bursts at theta frequency and 90% of the resting motor threshold (50 Hz; 2s on; 8s off) using a MagPro X100 (MagVenture, Farum, Denmark) device under MR-guided neuronavigation using the BrainSight stereotaxic system (Rogue Research, Montreal, Canada) with a figure-of-eight (MagVenture MCF-B-70) coil held with the handle in line with the sagittal plane, pointing toward the occiput to stimulate the pre-SMA site. We hypothesized that iTBS 12 to the pre-SMA could adaptively engage the cerebellum lesion, with which it shares neuronal oscillation frequencies, and hence improve the disabling symptoms. He received 27 iTBS sessions, once daily over the next month. Following ten sessions, he began to show a reduction in his repetitive behaviors, and by the 15 th session, he acknowledged that his behaviors were irrational. The YBOCS severity score had reduced to 24 (~22.5% improvement), which remained the same, even at the end of 27 sessions of iTBS treatment. There was no change in the CCAS and ICARS scores. The clinical benefits remained unchanged until three months of follow-up. Subsequently, we observed a gradual reversal to pre-TMS symptom severity. Maintenance TMS was suggested but was not feasible due to logistic reasons and therefore he was initiated on oral fluoxetine that was gradually increased to 80mg/day, with which we observed minimal change in symptoms over the next four months.
Post-neuromodulation functional connectivity visualization
The pre- and post-rTMS scans 13 were parcellated into 48-cortical, 15-subcortical, and 28-cerebellar regions as per the Harvard-Oxford 14 and the Cerebellum MNI-FLIRT atlases 15 . Average BOLD-signal time-series from each of these nodes, obtained after processing within FSL version-5.0.10, were then concatenated to obtain a Pearson’s correlation matrix between 91 nodes, separately for the pre- and post-TMS studies.
We analyzed the two 91 × 91 matrices using the Rank-two ellipse (R2E) seriation technique for node clustering 16 ( Figure 2 ). This technique reorders the nodes by moving the ones with a higher correlation closer to the diagonal. Thus, blocks along the diagonal of the matrix visualization show possible functional coactivating clusters.
Rank-two ellipse seriation-based visualization of correlation matrix before ( A ) and after ( B ) rTMS treatment. The dotted-black boxes denote the cerebellar network and other connected networks, where the green boxes show the inter-network overlap. Thus, we see that the overlapped region in ( 2A ) has now transitioned to three different overlapped areas in ( 2B ), which shows the increase in the overlap between modular networks after treatment. Cerebellar nodes are denoted in black, cortical nodes in blue and subcortical nodes in green. The lesion node (right crus II) and the region of neuro-stimulation are given in red; R2E= Rank-two ellipse.
We observed (a) extended connectivity of the cerebellar network after iTBS treatment as evidenced through its diminished modularity – the larger cerebellar cluster/block had an increased overlap with both anterior and posterior brain networks as observed along the diagonal in ( Figure 2B ), and (b) formation of better-defined sub-clusters within the larger cerebellar cluster indicating improved within-network modularity of distinct functional cerebellar networks [e.g., vestibular (lobules IX and X) and cognitive-limbic (crus I/II and vermis)].
Conclusions
We illustrate a case of OCD possibly secondary to a posterior cerebellar infarct, supporting the role of the cerebellum in the pathophysiology of OCD 3 . That OCD was perhaps secondary to the posterior cerebellar lesion is supported by several lines of evidence. Firstly, there seemed to be a possible temporal correlation between the duration of OCD and the chronic nature of the cerebellar lesion. Despite the challenges in inferring a precise temporal relationship based on clinical history, the signal changes with free diffusion and atrophy indicated that the infarct was indeed chronic, supporting the symptom onset at about three years before presentation. Previous studies have indeed reported OCD in posterior cerebellar lesions 17 – 19 . Secondly, the clinical phenotype was somewhat atypical, characterized by severe ambitendency, precipitating urinary incontinence, and poor insight into compulsions along with comorbid CCAS. Thirdly, our patient was resistant to an anti-obsessional medication but improved partially with neuromodulation of the related circuit. The MRI-informed iTBS engaged the lesion-area by targeting its more superficial connections in the frontal lobe. The changes in clinical observations paralleled the changes in cerebellar functional connectivity – enhanced within-cerebellum modularity and expanded cerebellum to whole-brain connectivity.
This report adds to the growing evidence-base for the involvement of the posterior cerebellum in the pathogenesis of OCD. Drawing conclusions from a single case study and the absence of a placebo treatment will prevent any confirmatory causal inferences from being made. The opportunity to examine network-changes that parallel therapeutic response in an individual with lesion-triggered psychiatric manifestations not only helps mapping symptoms to brain networks at an individual level 13 but also takes us a step further to refine methods to deliver more effective personalized-medicine in the years to come.
Data availability
Underlying data.
Harvard Dataverse: PICA OCD Raw fMRI files NII format. https://doi.org/10.7910/DVN/X12BZD 20 .
This project contains the following underlying data:
- postTMS_fmri.nii (raw post TMS fMRI file)
- preTMS_fmri.nii (Raw pre TMS fMRI file)
Reporting guidelines
Harvard Dataverse: PICA OCD case report CARE guidelines for case reports: 13-item checklist. https://doi.org/10.7910/DVN/2XKSXL 21 .
Data are available under the terms of the Creative Commons Zero "No rights reserved" data waiver (CC0 1.0 Public domain dedication).
Written informed consent for publication of their clinical details and clinical images was obtained from the patient.
Acknowledgments
We thank our patient and his parents for permitting us to collate this data for publication.
- 1. Dougherty DD, Brennan BP, Stewart SE, et al. : Neuroscientifically Informed Formulation and Treatment Planning for Patients With Obsessive-Compulsive Disorder: A Review. JAMA Psychiatry. 2018; 75 (10): 1081–1087. PubMed Abstract | Publisher Full Text
- 2. Rotge JY, Guehl D, Dilharreguy B, et al. : Meta-Analysis of Brain Volume Changes in Obsessive-Compulsive Disorder. Biol Psychiatry. 2009; 65 (1): 75–83. PubMed Abstract | Publisher Full Text
- 3. Sha Z, Edmiston EK, Versace A, et al. : Functional Disruption of Cerebello-thalamo-cortical Networks in Obsessive-Compulsive Disorder. Biol Psychiatry Cogn Neurosci Neuroimaging. 2020; 5 (4): 438–447. PubMed Abstract | Publisher Full Text | Free Full Text
- 4. Goodman WK, Price LH, Rasmussen SA, et al. : The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry. 1989; 46 (11): 1006–1011. PubMed Abstract | Publisher Full Text
- 5. Argyropoulos GPD, van Dun K, Adamaszek M, et al. : The Cerebellar Cognitive Affective/Schmahmann Syndrome: a Task Force Paper. Cerebellum. 2020; 19 (1): 102–125. PubMed Abstract | Publisher Full Text | Free Full Text
- 6. Ide JS, Li CR: A cerebellar thalamic cortical circuit for error-related cognitive control. NeuroImage. 2011; 54 (1): 455–464. PubMed Abstract | Publisher Full Text | Free Full Text
- 7. Norman LJ, Taylor SF, Liu Y, et al. : Error Processing and Inhibitory Control in Obsessive-Compulsive Disorder: A Meta-analysis Using Statistical Parametric Maps. Biol Psychiatry. 2019; 85 (9): 713–725. PubMed Abstract | Publisher Full Text | Free Full Text
- 8. Woolrich MW, Jbabdi S, Patenaude B, et al. : Bayesian analysis of neuroimaging data in FSL. NeuroImage. 2009; 45 (1 Suppl): S173–186. PubMed Abstract | Publisher Full Text
- 9. Gomes PVO, Brasil-Neto JP, Allam N, et al. : A randomized, double-blind trial of repetitive transcranial magnetic stimulation in obsessive-compulsive disorder with three-month follow-up. J Neuropsychiatry Clin Neurosci. 2012; 24 (4): 437–443. PubMed Abstract | Publisher Full Text
- 10. Akkal D, Dum RP, Strick PL: Supplementary Motor Area and Presupplementary Motor Area: Targets of Basal Ganglia and Cerebellar Output. J Neurosci. 2007; 27 (40): 10659–10673. PubMed Abstract | Publisher Full Text | Free Full Text
- 11. Woolrich MW, Ripley BD, Brady M, et al. : Temporal Autocorrelation in Univariate Linear Modeling of FMRI Data. NeuroImage. 2001; 14 (6): 1370–1386. PubMed Abstract | Publisher Full Text
- 12. Huang YZ, Edwards MJ, Rounis E, et al. : Theta burst stimulation of the human motor cortex. Neuron. 2005; 45 (2): 201–206. PubMed Abstract | Publisher Full Text
- 13. Fox MD: Mapping Symptoms to Brain Networks with the Human Connectome. N Engl J Med. 2018; 379 (23): 2237–2245. PubMed Abstract | Publisher Full Text
- 14. Frazier JA, Chiu S, Breeze JL, et al. : Structural brain magnetic resonance imaging of limbic and thalamic volumes in pediatric bipolar disorder. Am J Psychiatry. 2005; 162 (7): 1256–1265. PubMed Abstract | Publisher Full Text
- 15. Diedrichsen J, Balsters JH, Flavell J, et al. : A probabilistic MR atlas of the human cerebellum. NeuroImage. 2009; 46 (1): 39–46. PubMed Abstract | Publisher Full Text
- 16. Chen CH: Generalized Association Plots: Information Visualization via Iteratively Generated Correlation Matrices. Stat Sin. 2002; 12 (1): 7–29. Reference Source
- 17. Schmahmann JD, Sherman JC: The cerebellar cognitive affective syndrome. Brain J Neurol. 1998; 121 (Pt 4): 561–579. PubMed Abstract | Publisher Full Text
- 18. Schmahmann JD, Weilburg JB, Sherman JC: The neuropsychiatry of the cerebellum - insights from the clinic. Cerebellum. 2007; 6 (3): 254–267. PubMed Abstract | Publisher Full Text
- 19. Wolff JEA, Hüttermann U, Askins MA: Quantifying health status outcomes in pediatric medulloblastoma patients. Anticancer Res. 2007; 27 (1B): 523–529. PubMed Abstract
- 20. Mehta U: PICA OCD Raw fMRI files NII format. Harvard Dataverse, V1. 2020. http://www.doi.org/10.7910/DVN/X12BZD
- 21. Mehta U: PICA OCD case report CARE guidelines for case reports: 13 item checklist. Harvard Dataverse, V1. 2020. http://www.doi.org/10.7910/DVN/2XKSXL
Comments on this article Comments (0)
Open peer review.
Competing Interests: No competing interests were disclosed.
Reviewer Expertise: Cognitive neuroscience
- Respond or Comment
- COMMENT ON THIS REPORT
Is the background of the case’s history and progression described in sufficient detail?
Are enough details provided of any physical examination and diagnostic tests, treatment given and outcomes?
Is sufficient discussion included of the importance of the findings and their relevance to future understanding of disease processes, diagnosis or treatment?
Is the case presented with sufficient detail to be useful for other practitioners?
- This is a very interesting case report, even without the intervention component (which itself is a fascinating approach to neuromodulation). I particularly appreciated the approach to regional (SMA)
- This is a very interesting case report, even without the intervention component (which itself is a fascinating approach to neuromodulation). I particularly appreciated the approach to regional (SMA) targeting, which involved resting state fMRI to detect functional connectivity with the affected cerebellar region. The report itself is very clear and well-written.
- ECT appears to have been provided in the context of a depressive episode, but were other (e.g., psychotherapy, pharmacotherapy) treatments initially trialled? It would be useful to present any clinical history from adolescence, although this may not be feasible.
- Please describe the reason for conducting MRI; why was this not undertaken earlier?
- Was iTBS the “standard” course (i.e., 600 pulses, trains comprising 3 pulses at 50 Hz, repeated for 2 seconds at 5 Hz, followed by an 8-second ITI)? How was intensity determined (e.g., 70%RMT, 80%AMT)? Specify the stimulator, coil type, and neuronavigation method.
- Given that the duration of both the cerebellar lesion and OCD symptoms seems quite unclear, it is somewhat difficult to suggest a temporal relationship (as stated in the Conclusion).
- Was the patient followed-up over a longer-term period? I would be interested to know if these improvements are lasting (i.e., longer than 3 months), although again this might not be possible.
Reviewer Expertise: Neuromodulation, psychiatry
- Author Response 11 Sep 2020 Urvakhsh Mehta , Department of Psychiatry, National Institute of Mental Health and Neurosciences, India, Bangalore, 560029, India 11 Sep 2020 Author Response We thank this reviewer for the time taken to provide constructive feedback and the encouraging comments on this report. Competing Interests: None We thank this reviewer for the time taken to provide constructive feedback and the encouraging comments on this report. We thank this reviewer for the time taken to provide constructive feedback and the encouraging comments on this report. Competing Interests: None Close Report a concern Reply -->
Reviewer Status
Alongside their report, reviewers assign a status to the article:
Reviewer Reports
- Shubhmohan Singh , Postgraduate Institute of Medical Education and Research, Chandigarh, India
- Peter Enticott , Deakin University, Geelong, Australia
Comments on this article
All Comments (0)
Competing Interests Policy
Provide sufficient details of any financial or non-financial competing interests to enable users to assess whether your comments might lead a reasonable person to question your impartiality. Consider the following examples, but note that this is not an exhaustive list:
- Within the past 4 years, you have held joint grants, published or collaborated with any of the authors of the selected paper.
- You have a close personal relationship (e.g. parent, spouse, sibling, or domestic partner) with any of the authors.
- You are a close professional associate of any of the authors (e.g. scientific mentor, recent student).
- You work at the same institute as any of the authors.
- You hope/expect to benefit (e.g. favour or employment) as a result of your submission.
- You are an Editor for the journal in which the article is published.
- You expect to receive, or in the past 4 years have received, any of the following from any commercial organisation that may gain financially from your submission: a salary, fees, funding, reimbursements.
- You expect to receive, or in the past 4 years have received, shared grant support or other funding with any of the authors.
- You hold, or are currently applying for, any patents or significant stocks/shares relating to the subject matter of the paper you are commenting on.
Stay Updated
Sign up for content alerts and receive a weekly or monthly email with all newly published articles
Register with Wellcome Open Research
Already registered? Sign in
Not now, thanks
Are you a Wellcome-funded researcher?
If you are a previous or current Wellcome grant holder, sign up for information about developments, publishing and publications from Wellcome Open Research.
We'll keep you updated on any major new updates to Wellcome Open Research
The email address should be the one you originally registered with F1000.
You registered with F1000 via Google, so we cannot reset your password.
To sign in, please click here .
If you still need help with your Google account password, please click here .
You registered with F1000 via Facebook, so we cannot reset your password.
If you still need help with your Facebook account password, please click here .
If your email address is registered with us, we will email you instructions to reset your password.
If you think you should have received this email but it has not arrived, please check your spam filters and/or contact for further assistance.

Patient Case Study
Case study: ronald, a 59 year-old male with obsessive compulsive disorder, by addressing the microbiome issues, vitamin levels and supporting depressive symptoms, ocd symptoms can be more effectively addressed., initial presentation.
Ronald was a 59-year-old male with a long history of debilitating obsessive-compulsive disorder (OCD). He would obsess about cleanliness and often washed his hands 20, 30 or more times throughout the day. He also had problems getting to work, returning to check that the front door of his home was locked multiple times. The symptoms were destroying his self esteem, damaging his relationships and left him feeling irritable, exhausted and hopeless.
While numerous medications and counseling strategies had been explored, the symptoms were virtually non-responsive to standard treatments. The medications also led to intolerable side effects, flattening his affect and reducing his energy levels. Due to numerous treatment failures, he had been referred to our clinic for a more integrative treatment approach.
Initial Relevant labs
- Numerous elevated markers indicating dysbiosis
- HPHPA was elevated indicating the presence of Clostridium in the gut
- Kryptopyrrole levels were within normal limits
- 25-hydroxy vitamin D was low at 13 ng/ml
Initial Treatment
- Vitamin D, 5000 iu
- Probiotic and herbal antimicrobial to target Clostridium and decrease HPHPA
- High EPA Omega-3 fish oil, two grams daily
- Lithium Orotate, 5 mg daily
- Rhodiola, 1 cap twice daily
Explanation
Vitamin D is necessary for serotonin production in the brain ( DeLuca 2013 ). Evidence is also suggestive that levels may be lower in patients with OCD, and that symptoms may be worse in those patients with more significant vitamin D deficiencies ( di Michele 2018 , Soyak 2022 ).
While the data on omega-3 fatty acid supplementation for treatment of OCD is insufficient to draw direct conclusions, due to Ronald’s many overlapping depressive symptoms, a high EPA-containing fish oil was included in the initial treatment. As a treatment, EPA has been shown to provide benefits for reducing depressive symptoms ( Kelaiditis 2023 ).
HPHPA or 3-(3-hydroxyphenyl)-3-hydroxypropionic acid is a metabolite from clostridia bacteria that can indicate overgrowth of clostridia species in the gastrointestinal tract. The metabolite appears to be neurotoxic, interfering with neurotransmitter function in the brain, contributing to schizophrenia, autism and other forms of mental illness ( Shaw 2010 ). When present, the simplest initial treatment is high-dose probiotics, herbal antimicrobials or both. In Ronald’s case, due to the duration of his symptoms, a combination of probiotics and herbal antimicrobials were prescribed.
Low-dose lithium has also been proposed as a potential support for OCD that targets numerous underlying mechanisms, including inflammation, oxidative stress and dysregulated glutamate neurotransmitter signaling ( Vallée 2021 ). In addition, low-dose lithium can be helpful for irritability, a symptom which Ronald initially also struggled to control.
Rhodiola rosea or rhodiola, is an herb from arctic regions around the world with a long history of use to improve stress resiliency. In the mental health literature, rhodiola has been shown to be helpful for treating depression and anxiety disorders ( Sarris 2018 ).
Follow-up Presentation
At the two month follow-up, Ronald started to notice some improvements in his compulsions. While he still had them, at times it was easier to overcome the desire to follow through. He was encouraged by the progress, especially since previous standard treatments were of very little help for his symptoms. Based on his progress, follow-up testing was ordered.
Follow-up Testing
- HPHPA levels were within normal limits
- Some dysbiosis markers were still elevated suggesting yeast overgrowth
Follow-up Treatment
- Stop herbal antimicrobial
- Add Saccharomyces boulardii
- Reduce overall sugar intake
Explanation for Follow-up Treatment
The herbal antimicrobial and probiotic had been effective for clearing the clostridia bacteria in the gut as evidenced by the reduced HPHPA levels. Due to indications of potential yeast from the organic acids test, Saccharomyces boulardii , a yeast-based probiotic was added. As Ronald liked to indulge in sweets, reducing sugar consumption was also recommended to discourage yeast overgrowth.
Additional Follow-up
At the six-month mark, Ronald’s symptoms had continued to improve. While the compulsions were not gone, they were more manageable and not as disruptive to his daily routine. He was doing better at work and his family life had noticeably improved. Ronald’s mood had also stabilized as his own outlook about the future had become more positive with treatment.
Case Summary
OCD can be a challenging condition to treat, as symptoms are often recalcitrant to standard medication-based treatments. By assessing for and treating the underlying factors that disrupt normal brain function, OCD symptoms can be more effectively addressed. For Ronald, disruption in the normal gut flora by both clostridia species and yeast were likely disrupting normal neurotransmitter function and increasing inflammation throughout the body. By addressing the gut flora issues, low vitamin D levels and supporting his depressive symptoms with additional treatments, Ronald’s symptoms improved and his ability to function in daily life was restored.
Want to learn nutritional and functional medicine interventions like these to help your patients? Enroll in our comprehensive Fellowship for mental health providers! Book a private phone call with our faculty to learn more today.
DeLuca GC, Kimball SM, Kolasinski J, Ramagopalan SV, Ebers GC. Review: the role of vitamin D in nervous system health and disease. Neuropathol Appl Neurobiol . 2013;39(5):458-484. doi:10.1111/nan.12020
Kelaiditis CF, Gibson EL, Dyall SC. Effects of long-chain omega-3 polyunsaturated fatty acids on reducing anxiety and/or depression in adults; A systematic review and meta-analysis of randomised controlled trials. Prostaglandins Leukot Essent Fatty Acids . 2023;192:102572. doi:10.1016/j.plefa.2023.102572
di Michele F. Vitamin D supplementation in obsessive-compulsive disorder. Psychiatry Res . 2018;270:1174. doi:10.1016/j.psychres.2018.06.059
Sarris J. Herbal medicines in the treatment of psychiatric disorders: 10-year updated review. Phytother Res . 2018;32(7):1147-1162. doi:10.1002/ptr.6055
Soyak HM, Karakükcü Ç. Investıgation of vitamin D levels in obsessive-compulsive disorder. Indian J Psychiatry . 2022;64(4):349-353. doi:10.4103/indianjpsychiatry.indianjpsychiatry_26_22
Shaw W. Increased urinary excretion of a 3-(3-hydroxyphenyl)-3-hydroxypropionic acid (HPHPA), an abnormal phenylalanine metabolite of Clostridia spp. in the gastrointestinal tract, in urine samples from patients with autism and schizophrenia. Nutr Neurosci . 2010;13(3):135-143. doi:10.1179/147683010X12611460763968
Vallée A, Vallée JN, Lecarpentier Y. Lithium: a potential therapeutic strategy in obsessive-compulsive disorder by targeting the canonical WNT/β pathway. Transl Psychiatry . 2021;11(1):204. Published 2021 Apr 7. doi:10.1038/s41398-021-01329-3

Home About Faculty Affiliate Program Contact
Courses Conferences Webinars Integrative Psychiatry Fellowship
Articles Books Low-Dose Lithium Provider Directory
The information on this site is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. The views and opinions expressed by those on this website are entirely their own. James Greenblatt, MD, assumes no responsibility whatsoever for the content of any such views or opinions, or for any information provided by any such individual.
By accessing or utilizing www.PsychiatryRedefined.org in any way, any user thereof releases James Greenblatt, MD (including Comprehensive Psychiatric Resources, Inc. d/b/a Psychiatry Redefined™, his principals, employees, agents and assigns) from and against any and all liability of any kind whatsoever, and indemnifies James Greenblatt, MD, against any and all claims of any kind.
Privacy Policy & Course Policies | Terms & Conditions
© 2024 Psychiatry Redefined. Psychiatry Redefined™. All Rights Reserved.
- What is Functional Psychiatry?
- New? Start Here
- Affiliate Program
- Schedule & Curriculum
- Certification
- Discovery Calls
- Testimonials
- Scholarships
- Discovery Calls & Webinars
- Child & Adolescent Mental Health Training
- Depression Intensive
- Depression & Mood Disorders Training
- View All Courses
- CME Courses
- Course Subscriptions
- Dr. Carson Course Bundle
- New! Photobiomodulation (PBM)
- Anorexia Nervosa
- Anxiety & OCD
- Endocannabinoids, CBD & Women’s Health
- Medication Side Effects
- Suicide Prevention
- Upcoming Webinars
- Webinar Library
- Psychiatry Reimagined 2024 Conference
- Lithium Orotate
- Nutritional Psychiatry for Anorexia
- Nutritional Psychiatry for BPD
- Supplement Protocols for Clinicians
- FMMH 2023 Annual Conference
- Low-Dose Lithium
- Binge-Eating & Food Addiction
- Child & Adolescent Psychiatry
- Functional Medicine for Psychiatry
- Ketogenic Diets
- Genetic Testing
- NE Conference on ADHD
- Well Woman Conference
- Enews Issues
- FinallyFocused.org
- Supplements
- Provider Directory
- Enewsletter
- JamesGreenblattMD.com
- Course Log-In
Privacy Overview
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Indian J Psychiatry
- v.61(Suppl 1); 2019 Jan
Exposure and response prevention for obsessive-compulsive disorder: A review and new directions
Dianne m. hezel.
1 Anxiety Disorders Clinic, New York State Psychiatric Institute, Columbia University, New York, NY, USA
2 Department of Psychiatry, Columbia University, New York, NY, USA
H. Blair Simpson
Obsessive-compulsive disorder (OCD) is characterized by distressing thoughts and repetitive behaviors that are interfering, time-consuming, and difficult to control. Although OCD was once thought to be untreatable, the last few decades have seen great success in reducing symptoms with exposure and response prevention (ERP), which is now considered to be the first-line psychotherapy for the disorder. Despite these significant therapeutic advances, there remain a number of challenges in treating OCD. In this review, we will describe the theoretical underpinnings and elements of ERP, examine the evidence for its effectiveness, and discuss new directions for enhancing it as a therapy for OCD.
INTRODUCTION
Considered one of the most debilitating psychiatric illnesses,[ 1 , 2 ] obsessive-compulsive disorder (OCD) is characterized by distressing thoughts and repetitive behaviors that are interfering, time-consuming, and difficult to control.[ 3 ] Historically, OCD was thought to be untreatable, as people with the disorder did not respond that well to traditional psychodynamic psychotherapy, medication, or available behavioral interventions such as systematic desensitization or aversion therapy.[ 4 ] The first significant nonpharmacological advance in treatment occurred after Meyer[ 5 ] reported that patients’ OCD symptoms improved when they were exposed to feared stimuli while, crucially, refraining from performing compulsions. Subsequent studies indicated that this method of exposure and response prevention (ERP) was effective in both a hospital and outpatient setting and that a majority of patients experienced significant improvement which was maintained for many up to two years post-treatment.[ 6 , 7 , 8 ] Since then, ERP has become the first-line psychotherapeutic treatment for OCD and will, therefore, be the focus of the current paper. In this review, we will describe the theoretical underpinnings and elements of ERP, examine the evidence for its effectiveness, and discuss new directions for enhancing it as a therapy for OCD.
ELEMENTS OF EXPOSURE AND RESPONSE PREVENTION
Mowrer's[ 9 ] two-factor theory of fear and avoidance provided an influential framework for understanding the etiology of OCD that inspired the development of behavioral treatments for the disorder, including ERP. Specifically, Mowrer asserted that individuals experience anticipatory anxiety in the presence of environmental stimuli that are associated with painful or aversive experiences through classical conditioning. Subsequent avoidance of the feared stimuli serves to alleviate people's anxiety, which in turn reinforces the avoidant behavior through operant conditioning. Similarly, individuals with OCD experience anxiety-provoking obsessions that are triggered by various situations and subsequently perform compulsions or engage in avoidance behaviors to decrease the anxiety associated with these thoughts. Paradoxically, these ritual and avoidance behaviors reinforce individuals’ fear and strengthen both obsessions and compulsions. ERP aims to break this cycle of symptoms by eliminating rituals and avoidance, thereby teaching patients how to tolerate distress without engaging in counterproductive behaviors and providing “corrective information” that challenges people's existing fear response.[ 4 ]
ERP can be conducted at varying levels of intensity, including outpatient, partial hospitalization, and residential treatment settings, depending on the severity of the patients’ symptoms. Irrespective of the symptom severity, however, ERP typically shares certain elements across settings.[ 4 ] First, there is an assessment and treatment planning phase during which the clinician provides psychoeducation about OCD and its treatment and collects information about the patient's symptoms. The patient and clinician work together to identify external (situations, objects, people, etc.) and internal (thoughts and physiological reactions) stimuli that trigger the person's obsessive thoughts and subsequent distress. Importantly, they also catalog the specific content of the person's obsessions and compulsions, discuss the functional relationship between the two, and identify the feared outcome if the rituals are not performed. For example, one patient might repeatedly wash his hands to disinfect them, thereby preventing a feared outcome of contracting an illness and dying. Another patient, however, might wash her hands because she is disgusted by the physical sensation of having residue on her hands and will, therefore, keep washing them until they “feel right.” The patient and clinician then work collaboratively to rank different situations in order from least to most distressing (as measured by subjective units of distress or SUDs), which results in a fear hierarchy.
Over the subsequent treatment sessions, the clinician coaches the patient as he or she repeatedly confronts the situations on his or her fear hierarchy while refraining from engaging in compulsions. For example, a man who has a fear of contracting an illness from unclean surfaces might hold his hands on various bathroom surfaces for a prolonged period of time, but not wash his hands afterward. The patients may also engage in imaginal exposures during which they envision their feared outcome triggered by their obsessive thoughts (e.g., pushing someone into oncoming traffic and then being sent to prison). By practicing both in vivo and imaginal exposures, the patients learn that the consequences they fear do not occur, as well as how to tolerate distress and uncertainty without engaging in compulsions.[ 4 ] Following each in-session exposure, the therapist and patient engage in post-exposure processing to review the patient's experience and how his or her expectations were violated and what he or she learned. The patients are also asked to practice exposures on their own for homework and to attempt to eliminate all rituals in their day-to-day life. As patients habituate to various scenarios, they then gradually work their way up the fear hierarchy to confront increasingly distressing situations. Typically, a course of ERP will conclude with relapse prevention planning.
Since ERP was recognized as a viable treatment for OCD, a large body of literature has supported its efficacy. Early studies demonstrated its superiority in reducing patients’ OCD symptoms relative to relaxation therapy, anxiety management, or a wait-list condition.[ 10 , 11 , 12 , 13 , 14 ] Subsequent reports have similarly pointed to its effectiveness across multiple countries, treatment settings, and intensity.[ 11 , 12 , 13 , 14 , 15 ] Indeed, a meta-analysis by Eddy et al .[ 16 ] indicated that approximately two-thirds of patients who received ERP experienced improvement in symptoms, and approximately one-third of patients were considered to be recovered. Moreover, although the majority of patients treated with cognitive-behavioral therapy (without ERP specifically) or cognitive therapy also experienced a reduction in symptoms post-treatment, ERP outperformed the other treatments. Specifically, there was a slightly stronger effect size for ERP, and it resulted in lower OCD severity scores post-treatment relative to the other two modalities.[ 17 ]
Importantly, research indicates that the treatment is effective not only with highly controlled study samples of OCD that are not necessarily representative of the general clinical population but also with less restricted samples with comorbidities and complicated treatment histories and that are concurrently taking medication.[ 11 , 18 ] That patients in a representative outpatient treatment setting experienced significant symptom improvement after a course of ERP speaks to the treatment's generalizability. A review by Storch et al .[ 15 ] provides further support for the treatment's utility in a variety of settings (e.g., home vs. office), delivered in different intensities (e.g., weekly vs. intensive treatment), and with pediatric and adolescent populations. Moreover, ERP has also been shown to lead not only to symptom reduction but also to a decrease in sleep disturbances and improved quality of life more generally.[ 15 , 19 , 20 ]
Treatment studies have also examined the efficacy of ERP relative to and in combination with medication. A review of four studies indicated that medication neither enhanced nor impeded treatment with ERP.[ 21 ] That is, individuals taking a combination of medication and ERP had similar outcomes to individuals in ERP alone but improved more than individuals on medication alone. In a subsequent study examining the combined effects of ERP with selective serotonin reuptake inhibitors (the pharmacological frontline treatment for OCD), Foa et al .[ 22 ] randomized OCD participants into one of four treatment conditions as follows: ERP only, clomipramine only, ERP plus clomipramine, and placebo. At the end of 12 weeks, participants treated with ERP or a combination of ERP plus medication showed a greater decrease in symptoms relative to those treated with clomipramine alone [ Figure 1 , left panel]. Moreover, those in the ERP plus medication condition did not differ in post-treatment symptom severity from those treated with ERP alone, indicating that medication did not bolster the efficacy of ERP.[ 7 ]

Effectiveness of exposure and response prevention versus other treatments. SRI – Serotonin reuptake inhibitor; ERP – Exposure and response prevention; SMT – Stress management therapy; RIS – Risperidone; symptom severity was assessed with the Yale–Brown Obsessive-Compulsive Scale (Y-BOCS); error bars – Standard error
More recent studies have similarly tested the effectiveness of ERP as an augmentation approach for individuals who benefit from serotonin reuptake inhibitors (SRIs) but continue to suffer from clinically significant OCD symptoms. Simpson et al .[ 23 ] found that patients on a stable dose of SRIs experienced greater symptom reduction after additional treatment with 17 weeks of ERP compared to those who received augmentation with stress management training [ Figure 1 , center panel]. A similar pattern of findings emerged when comparing augmentation with ERP to that with risperidone. Specifically, individuals taking SRIs had lower OCD severity scores immediately[ 24 ] and 6 months[ 25 ] following additional treatment with ERP than those who had additional treatment with risperidone or placebo [ Figure 1 , right panel]. The OCD severity of groups who received risperidone or placebo did not significantly differ from one another post-treatment.
Although the current guidelines recommend ERP as the first-line treatment for OCD, only about half of the patients who receive it will reach complete symptom remission.[ 26 ] There are a number of factors that are associated with poor response, including lack of adherence to treatment, poor insight, comorbid depression, and OCD severity (for a review of treatment-resistance Middleton, Wheaton, Kayser, & Simpson (2019)[ 27 ]). Approximately 20–30% of patients drop out of ERP prematurely,[ 11 ] perhaps unsurprising given the challenging and time-consuming nature of the treatment. Moreover, there is variation in the extent to which patients adhere to treatment recommendations even if they do complete a full course of ERP. One study found that low adherence to completing exposures assigned between ERP sessions predicted higher symptom severity post-treatment.[ 28 ] Similarly, clinicians are susceptible to making errors in how they deliver the treatment to patients, which likewise inhibits its effectiveness.[ 29 ] Given the strong association of adherence to treatment outcome, future interventions that increase patient and therapist fidelity to ERP would be worthwhile.
Research investigating the relationship between outcomes and other factors such as insight and depression and symptom severity has yielded mixed results. Whereas some studies indicate that individuals with poor insight have a lower response to ERP than do those with good or fair insight, other studies fail to find an association between the two.[ 27 ] Discrepant findings may be due to a restricted range of insight in OCD study samples. That is, people with very low insight may be less likely to seek treatment for symptoms than do those with better insight.
Similarly, some studies have found that people suffering from severe symptoms and those with comorbid depression have worse treatment outcomes than people with no or mild depression and those with less severe OCD. However, a meta-analysis by Olatunji et al .[ 30 ] reported no differences in treatment outcome effect sizes for a range of moderators, including depression and symptom severity. One explanation for these inconsistent findings is that these factors may impact treatment adherence rather than outcomes more directly. For example, individuals with poor insight (e.g., a man who believes that his feared outcomes are realistic or that his rituals will prevent negative events) may be less likely to adhere to treatment and engage in exposures than someone who recognizes her fears and behaviors as excessive and unrealistic.
MECHANISMS OF CHANGE
Researchers have proposed different theories of how ERP works or its mechanism of action. Early cognitive models of OCD proposed that people develop the disorder when they misinterpret the significance of normal, intrusive thoughts that the majority of individuals will experience at some point in their lives.[ 31 , 32 ] Dysfunctional thoughts such as an inflated sense of responsibility for preventing harm to oneself and others, overestimation of threat, intolerance of uncertainty, a need for perfectionism, and over-importance of and need to control thoughts have also been identified as potential etiological and maintaining factors for OCD, as they cause people to interpret their intrusive thoughts as significant and potentially dangerous.[ 33 ] According to this perspective then, ERP works by disconfirming people's distorted beliefs through exposures. For example, if a woman overestimates the likelihood of danger, then repeated exposures to feared situations in which she tests this belief would presumably lead to less-biased thinking, thereby resulting in decreased OCD symptoms. Since its inception, the cognitive theory of OCD has received empirical support,[ 34 ] including from studies showing that decrements in dysfunctional thinking mediate symptom improvement post-treatment.[ 35 ] However, other studies have found that OCD severity predicts changes in dysfunctional thinking, thus calling into question the causal direction of change.[ 36 ] Specifically, Olatunji et al .[ 37 ] found that changes in OCD symptoms preceded altered beliefs about inflated responsibility rather than the other way around.
A behavioral perspective asserts that ERP works by breaking the conditioned response between obsessions and compulsions.[ 5 ] According to this model, compulsions temporarily alleviate people's anxiety that obsessive thoughts trigger. The decrease in distress strengthens the rituals and conditions people to continue using them when confronted with subsequent intrusive thoughts. On the other hand, when individuals confront triggering situations while simultaneously refraining from engaging in rituals, their distress decreases naturally in the absence of their feared outcome. With repeated exposure, the fear response is eventually extinguished and OCD symptoms subside.
According to emotion processing theory, fear and other emotions are stored in memory structures that contain information about stimuli that elicit the emotional response, as well as the response itself.[ 7 ] This theory states that exposure therapy provides information that is contradictory to the existing fear structure when patients’ dreaded outcomes do not occur. Consequently, individuals form new, more realistic memory structures that do not include a pathological fear response. Repeated practice confronting distressing situations strengthens the activation of this competing structure, thereby weakening the occurrence of the fear response.
More recently, researchers have proposed that inhibitory learning is central to extinction through exposure therapy.[ 38 , 39 ] Specifically, this theory purports that the initial conditioned association between the stimulus and the unconditioned fear response does not disappear, but rather that a new association is learned that competes with the former response. Craske et al . explain that “…after extinction, the [conditioned stimulus] possesses two meanings; its original excitatory meaning (conditioned stimulus–unconditioned stimulus) as well as an additional inhibitory meaning (conditioned stimulus–no unconditioned stimulus)” (p. 11-12).[ 38 ] Therefore, the newly formed association inhibits the memory of the original excitatory response with repeated practice, but does not prevent it from being reactivated at some point in the future, thus underscoring the importance of continued exposure to once-feared stimuli.
In recent years, there has been an increasing interest in the neural mechanisms underlying the etiology and treatment of psychiatric disorders, including OCD. For example, using a neurobiological framework, Gillan and Robbins[ 40 ] propose that compulsions are the result of excessive habit formation and that obsessions develop when the sufferer makes inferences about his or her behavior (e.g., “I check the knobs on the stove so I must be afraid of accidentally starting a fire”). Therefore, when refraining from engaging in compulsions during ERP, the patients are learning to break the habitual ritualistic behavior, which, in turn, reduces obsessions. A number of studies examining neural mechanisms of change have identified differences in the brain from pre- to post-treatment with psychotherapy.[ 41 , 42 , 43 ] However, researchers have yet to identify how these changes are directly related to processes that then lead to clinical improvement.[ 44 ]
NEW DIRECTIONS
Despite the success of ERP in treating OCD, there is room for improvement. As noted above, many people drop out of treatment prematurely and a substantial number of those who do complete a course of ERP do not achieve a clinically significant reduction of symptoms. Some especially notable challenges in treating OCD include addressing people's limited access to evidence-based treatments, finding novel ways to improve upon ERP to increase its efficacy, and integrating biological and psychological frameworks to fine-tune treatment.
Access to care
There are numerous barriers to treatment, including high costs of care, stigma surrounding mental health issues, and lack of access to clinicians who are trained in evidence-based practices.[ 45 , 46 , 47 ] One solution to improve access to care is the development of an internet-based ERP program that individuals can use to guide themselves through treatment with the support of a therapist through e-mail, phone, or the online treatment platform.[ 48 , 49 ] Results from studies implementing these internet programs are promising; they have demonstrated not only the feasibility, but also the efficacy, of delivering ERP online. Specifically, individuals who completed these online programs experienced a clinically significant decrease in OCD symptoms[ 47 , 49 , 50 ] which were maintained at follow-up.[ 49 , 51 ] Given the growing ubiquity of internet access and cellular phones, continuing to develop programs that increase the dissemination of ERP is worthwhile.
Enhancing exposure and response prevention
Technological advances have been used not only to disseminate ERP but also in an attempt to improve its effects. Najmi and Amir (2010) recruited individuals with subclinical OCD contamination concerns to complete attention bias modification (ABM) before a subsequent behavioral approach task. In the attention task, half of the participants were placed in an active condition, in which they were trained to shift their attention away from “threatening” words (i.e., related to contamination), whereas the other half in the nonactive condition did not receive such training. The authors found that relative to those in the nonactive condition, individuals in the active ABM group were less avoidant of contaminated objects during a subsequent behavioral approach task. It is possible, then, that reducing attention to threat may diminish avoidance behaviors, thus making people more willing to engage in exposures.[ 52 ] However, a subsequent study using a clinical population found that ABM alone did not reduce OCD symptoms, thus suggesting that it may be more effective in addition to ERP rather than in place of it.[ 53 ]
Virtual reality is similarly being studied as a way to enhance exposure therapy for a number of disorders, including post-traumatic stress disorder and anxiety disorders.[ 54 , 55 ] Although it has not been tested extensively with OCD patients, a preliminary study demonstrated its effectiveness in triggering and measuring anxiety in people through a virtual reality platform.[ 56 ] Virtual reality may be especially effective in designing exposures to situations or stimuli that are impossible to reproduce in vivo and are otherwise left to imaginal exposures.
Craske et al .[ 39 ] have proposed a number of ways to enhance extinction learning based on the aforementioned inhibitory learning perspective. This orientation emphasizes that the overarching goal of exposure should be distress tolerance rather than fear reduction. Accordingly, the authors outline ideas for how to translate this approach into clinical practice with exposure therapy, such as maximizing the extent to which people's expectancies of feared outcomes are violated, pairing a previously extinguished cue with a new conditioned stimulus, removing safety signals, and practicing exposures in multiple contexts (e.g., with different people, settings, times of day, etc.[ 39 ]). By homing in on processes thought to underlie mechanisms of change, it may be possible to maximize the benefits of extinction learning, thus leading to greater improvement in psychopathological symptoms.
Finally, some studies have investigated the advantage of enhancing ERP with medication implicated in facilitated extinction learning. Specifically, research demonstrated that, relative to those given a placebo pill, patients taking d-cycloserine before engaging in exposure therapy experienced a faster rate of symptom improvement in the first few weeks of receiving ERP.[ 57 ] However, there were no group differences in symptom improvement by the end of treatment, suggesting that the drug's utility lies primarily in speeding up treatment response.[ 58 ]
Integrating biological and psychological approaches
Investigations on the biological underpinnings of OCD have identified genetic factors and abnormalities in neurocircuitry that are associated with the disorder.[ 59 ] However, very little research has bridged the gap between biological and psychological approaches in psychopathology, and consequently, there is a dearth of information regarding how information about genetics or neurobiology might meaningfully improve our treatment of psychiatric disorders. Notable exceptions are recent studies that have identified gene variants of brain-derived neurotrophic factor (BDNF) and fatty acid amide hydrolase (FAAH) that mediate outcome to psychotherapeutic treatment. The BDNF gene codes for a protein that promotes neuron development and growth and helps to regulate the neurophysiological response to stress, making it especially relevant to better understanding mood and anxiety disorders.[ 60 ] A series of studies have reported that variants of the BDNF gene are associated with improved treatment outcomes with medication for schizophrenia,[ 61 ] with dialectical behavior therapy for borderline personality disorder,[ 62 ] and, most recently, with cognitive behavioral therapy (CBT) for children with anxiety disorders.[ 63 ]
FAAH, on the other hand, is a gene in the endocannabinoid system, which plays an important role in regulating anxiety and facilitating fear extinction, which is central to ERP as noted above.[ 60 ] Dincheva et al .[ 64 ] found an association between a variant of FAAH and accelerated fear extinction in late stages of an extinction learning task as well as reduced levels of anxiety. This finding suggests that it may be possible to identify individuals who are more responsive to treatments that entail extinction learning. However, a more recent study in children with anxiety disorders found only minimal evidence of a correlation between gene variants in the endocannabinoid system and response to CBT.[ 60 ] The authors assert that though further research on the endocannabinoid system specifically and on “therapygenetics” (p. 153) more generally is worthwhile, we are unlikely to identify single gene variants that predict response to psychological treatments.
Finally, several surgical and noninvasive neurological interventions are available to patients who have not had success with psychotherapy or medication. Neuromodulating methods such as transcranial direct-current stimulation (tDCS) and transcranial magnetic stimulation (TMS), as well as surgical procedures such as deep brain stimulation, work to decrease symptoms by targeting underlying neurocircuitry implicated in the pathophysiology of OCD.[ 65 , 66 , 67 , 68 ] Few studies have examined the effect of augmenting therapy with these methods and fewer still specifically for the treatment of OCD. However, there are encouraging reports that indicate some benefit of combining tDCS with CBT for treatment-resistant depression,[ 69 ] suggesting it might likewise be useful as an augmentation for the treatment of other disorders. Moreover, a recent study demonstrated that combining DBS with CBT (which included ERP) resulted in a reduction of OCD symptoms in a treatment-refractory sample.[ 70 ] Indeed, DBS has been shown to enhance fear extinction,[ 71 , 72 ] thus highlighting its potential usefulness when paired with a treatment such as ERP. Finally, in their meta-analysis, Berlim et al .[ 73 ] found that repetitive TMS was an effective augmentation for medication when treating refractory OCD. None of the studies included in the meta-analysis examined TMS in combination with ERP; hence, whether or not they would be beneficial when used together merits further study.
Morphometric studies have revealed that the thickness[ 74 ] and volume[ 75 ] of different brain regions in individuals with OCD are correlated with treatment outcomes with exposure therapy. What remains to be seen, however, is if variation in neurocircuitry, such as genetic variants, can ultimately predict differential response to treatment and whether brain imaging findings at baseline can be usefully applied to individual patients. Since OCD is caused by a complex interaction among genetic, neurocircuitry, environmental, and developmental factors, it is essential that researchers continue to integrate psychological and biological approaches to more effectively treat this debilitating disease.
ALTERNATIVES TO EXPOSURE AND RESPONSE PREVENTION
Although ERP has been identified as a (nonpharmacological) gold standard treatment for OCD, other psychotherapeutic treatments have been developed and their efficacy empirically supported (see Manjula and Sudhir review in this issue for more details).
Two that have been found to be effective in treating OCD include cognitive therapy and acceptance and commitment therapy (ACT). Despite the fact that ERP, cognitive therapy, and ACT are considered distinct treatments grounded in different theoretical perspectives, they share common elements that perhaps make them more similar than they seem on the surface.[ 76 ] Moreover, though some data support their efficacy as standalone treatments for OCD,[ 77 , 78 ] some argue that integrating components of cognitive therapy (Rector, in press) or ACT into ERP may have added benefits.[ 79 ] Future research in this area is needed.
ERP is a highly efficacious treatment for many people who suffer from OCD. Although there are a number of explanations for its mechanism of action, it is still unclear exactly how it works or why some people respond to it whereas others do not.[ 44 ] Although up to half of people will achieve minimal symptoms after acute treatment with ERP as either a monotherapy[ 22 ] or in combination with medication,[ 23 , 24 ] many who undergo the therapy will remain symptomatic and some will not benefit at all. These shortcomings underscore the need to continue to improve upon ERP by enhancing it with new methods, incorporating genetic and neurobiological approaches, and developing alternative treatments.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
- Study Guides
- Homework Questions
%22Unstuck%22 Case Report

IMAGES
VIDEO
COMMENTS
Case Study Details. John is a 56-year-old man who presents to you for treatment. His symptoms started slowly; he tells you that he was always described as an anxious person and remembers being worried about a lot of things throughout his life. For instance, he reported he was very afraid he'd contract HIV by touching doorknobs, even though he ...
Obsessive-compulsive disorder (OCD) is a clinically heterogeneous disorder with many possible subtypes.[] The lifetime prevalence of OCD is around 2-3%.[] Evidence points to a bimodal distribution of the age of onset, with studies of juvenile OCD finding a mean age at onset of around 10 years, and adult OCD studies finding a mean age at onset of 21 years.[2,3] Treatment is often delayed in ...
Paediatric obsessive-compulsive disorder (OCD) is a chronic condition often associated with severe disruptions of family functioning, impairment of peer relationships and academic performance. ... phenotypic level are a single-case study of a 4 year old girl and a report from Turkey on 25 children under 6 years with OCD . Subjects were fifteen ...
Obsessive-compulsive disorder (OCD) is a mental disorder where people feel the. need to check things repeatedly, perform certain routines repeatedly (called "rituals"), or have. certain thoughts repeatedly (called "obsessions"). Obsessive compulsive disorder (OCD) is a. debilitating neuropsychiatric disorder with a lifetime prevalence of 2 to ...
A Case Study of Obsessive-Compulsive Disorder: Some Diagnostic Consideratio ns. Obsessive-Compulsive Disorder (OCD) was considered a rare disorderprior to 1984 when the initial resultsfrom theEpidemiologicCatchment Areasururydemonstrated a substantial prevalence of the disorder (1). Thus there ma)'be mmrypatients today whoentered treatment ...
Obsessive-compulsive disorder (OCD) is a highly prevalent and chronic condition that is associated with substantial global disability. OCD is the key example of the 'obsessive-compulsive and related disorders', a group of conditions which are now classified together in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, and the International Classification of ...
Obsessive-compulsive disorder (OCD) is a chronic, distressing and substantially impairing neuropsychiatric disorder, characterized by obsessions or compulsions. The current case describes a 44-year-old adult female diagnosed with OCD. The patient had an incomplete response to several SSRIs alone during her past treatment, and led a poor-quality ...
The client Hope provides a good example of a very positive outcome from sustained, multifaceted psychotherapy with a 30-year-old woman presenting with obsessive compulsive disorder (OCD), fear of flying, panic disorder without agoraphobia, nightmare disorder, and a childhood history of separation anxiety disorder. Based on ratings at the beginning of therapy and end of therapy on a structured ...
Introduction. Obsessive-Compulsive Disorder (OCD) is a disabling anxiety disorder characterized by upsetting, unwanted cognitions (obsessions) and intense and time consuming recurrent compulsions (American Psychiatric Association, 2000).The idiosyncratic nature of the symptoms of OCD (Whittal et al., 2010) represents a challenge to completing accurate and comprehensive assessments, which if ...
Case Study: Obsessive-Compulsive Disorder. June 7, 2013. In a previous article we reviewed a range of treatments that are used to help clients suffering from obsessive-compulsive disorder (OCD). In this edition we showcase the case study of Darcy [fictional name], who worked with a psychologist to address the symptoms and history of her OCD.
Background: The pandemic caused by the sars-cov2 coronavirus can be considered the biggest international public health crisis. Outbreaks of emerging diseases can trigger fear reactions. Strict adherence to the strategies can cause harmful consequences, particularly for people with pathology on the spectrum of obsessive-compulsive disorder. Case presentation: We describe the clinical case of a ...
We describe a case of OCD that was successfully treated with eight sessions of ACT, with the results being maintained over a one-month follow-up period. Postintervention tests revealed a significant decrease in obsessive-compulsive symptoms and an associated increase in psychological flexibility. This case study highlights the possible ...
OCD is associated with a reduced quality of life and is often co-morbid with anxiety and mood (affective) disorders, namely depressive disorder and is associated with sig-nificant impairment in functioning. The WHO ranked OCD within the top ten disabling disorders is associated with dysfunction and decreased quality of life [3,5].
Abstract. Over the past three decades, obsessive-compulsive disorder (OCD) has moved from an almost untreatable, life-long psychiatric disorder to a highly manageable one. This is a very welcome change to the 1%-3% of children and adults with this disorder as, thanks to advances in both pharmacological and psychological therapies, prognosis for ...
This case study illustrates the use of cognitive-behavioral therapy (CBT) for a 10-year-old girl with obsessive-compulsive disorder (OCD). Exposure and response prevention (ERP) is a form of CBT that involves facing feared triggers over an extended period of time without any rituals.
Cortico-striato-thalamocortical circuitry dysfunction is central to an integrated neuroscience formulation of obsessive-compulsive disorder (OCD) 1, 2. However, more recent large-scale brain connectivity analyses implicate the role of the cerebello-thalamocortical networks also 3. Here, we report a case of OCD secondary to a cerebellar lesion.
We present here a case study of a complex 14 years old girl, with adolescence onset dysthymia, anorexia nervosa and obsessive-compulsive disorder and its management issues. Discover the world's ...
Patient Case Study Obsessive Compulsive Disorder (Ronald) Case Study: Ronald, a 59 Year-Old Male with Obsessive Compulsive Disorder ... Vallée A, Vallée JN, Lecarpentier Y. Lithium: a potential therapeutic strategy in obsessive-compulsive disorder by targeting the canonical WNT/β pathway. Transl Psychiatry. 2021;11(1):204. Published 2021 Apr ...
Obsessive-compulsive disorder, integrative model, case study . Abstract: Taking a Chinese college student with obsessive-compulsive disorder as the object, this paper analyzes and explains the occurrence, development and maintenance mechanism of the obsessive-compulsive symptoms from three theoretical models of
Abstract. A patient's own account of her obsessive-compulsive disorder is presented. She describes her distressing experiences, the impact of the disturbance on her and her family's life and her subsequent improvement using the technique of exposure and response prevention. The treatments available are discussed and the benefits of self ...
The present study presents the case of psychosis. The subject of the disorder was Mr. S (Initial instead of real name), 26 years old young man. Mr. S was having sign and symptoms of aggressive ...
The case presented involves an unhappy 24-year-old man who appears to meet diagnostic criteria for a diagnosis of obsessive-compulsive personality disorder. Note that the therapist spends as much ...
Virtual reality is similarly being studied as a way to enhance exposure therapy for a number of disorders, including post-traumatic stress disorder and anxiety disorders.[54,55] Although it has not been tested extensively with OCD patients, a preliminary study demonstrated its effectiveness in triggering and measuring anxiety in people through ...
Priscilla Grima "Unstuck" Case Report PSYC 3406 02/29/2024 The short film, "Unstuck," intimately captures the lives of children dealing with obsessive-compulsive disorder (OCD), showcasing the profound impact on their daily existence and relationships. Vanessa, Holden, Ariel, Shariff, Sarah, and Jake represent the varied experiences within the spectrum of OCD, where obsessions and compulsions ...