Clinical Presentation: Case History # 1 Ms. C is a 35 year old white female. She came to Neurology Clinic for evaluation of her long-term neurologic complaints. The patient relates that for many years she had noticed some significant changes in neurologic functions, particularly heat intolerance precipitating a stumbling gait and a tendency to fall. Her visual acuity also seemed to change periodically during several years. Two months ago the patient was working very hard and was under a lot of stress. She got sick with a flu and her neurologic condition worsened. At that time, she could not hold objects in her hands, had significant tremors and severe exhaustion. She also had several bad falls. Since that time she had noticed arthralgia on the right and subsequently on the left side of her body. Then, the patient abruptly developed a right hemisensory deficit after several days of work. The MRI scan was performed at that time and revealed a multifocal white matter disease - areas of increased T2 signal in both cerebral hemispheres. Spinal tap was also done which revealed the presence of oligoclonal bands in CSF. Visual evoked response testing was abnormal with slowed conduction in optic nerves. (Q.1) (Q. 2) (Q.3) Today, the patient has multiple problems related to her disease: she remains weak and numb on the right side; she has impaired urinary bladder function which requires multiple voids in the mornings, and nocturia times 3. She became incontinent and now has to wear a pad during the day. (Q.4) She also has persistent balance problems with some sensation of spinning, and she is extremely fatigued. REVIEW OF SYSTEMS is also significant for a number of problems related to her suspected MS. The patient has a tendency to aspirate liquids and also solids. (Q.5) (Q.6) She complains of tinnitus which is continuous and associated with hearing loss, more prominent on the left. She has decreased finger dexterity and weakness of the hands bilaterally. She also complains of impaired short-term memory and irritability. FAMILY HISTORY is significant for high blood pressure, cancer and heart disease in the immediate family. PERSONAL HISTORY is significant for mumps and chicken pox as a child, and anemia and allergies with hives later in life. She also had a tubal ligation. NEUROLOGIC EXAMINATION: Cranial Nerve II - disks are sharp and of normal color. Funduscopic examination is normal. Cranial Nerves III, IV, VI - no extraocular motor palsy or difficulties with smooth pursuit or saccades are seen. Remainder of the cranial nerve exam is normal except for decreased hearing on the left, and numbness in the right face, which extends down into the entire right side. The Weber test reveals greater conductance to the right. Rinne's test reveals air greater than bone bilaterally. (Q.7) The palate elevates well. Swallow appears to be intact. Tongue movements are slowed, but tongue power appears to be intact. Motor examination reveals relatively normal strength in the upper extremities throughout. However, rapid alternating movements are decreased in both upper extremities and the patient has dysdiadochokinesia in the left hand. (Q.8) Mild paraparesis is noted in both legs without severe spasticity. Deep tendon reflexes are +2 and symmetrical in the arms, +3 at the ankles and at the knees. Bilateral extensor toe sign are present. Sensory exam reveals paresthesia on the right to touch and decreased pin sensation on the right diffusely. The patient has mild vibratory sense loss in the distal lower extremities. Romberg's is negative. (Q.9) Tandem gait is mildly unstable. Ambulation index is 7.0 seconds for 25 feet. (The patient takes 7.0 seconds to walk 25 feet.) Diagnosis: Multiple Sclerosis with laboratory support. © John W.Rose, M.D., Maria Houtchens, MSIII, Sharon G. Lynch, M.D.
- Campus Directory
- Current Students
- Faculty & Staff


Multiple Sclerosis Case Study
Janet has experienced periodic episodes of tingling in her extremities, dizziness, and even episodes of blindness. After 12 years, doctors have finally given her a diagnosis. Follow Janet through her journey and find out why her disease is so difficult to diagnose.
Module 3: Multiple Sclerosis

Janet, age 22, was preparing for her 6-week postpartum checkup...
MS - Page 1
Three years later, at 34, Janet awoke to a prickly tingling feeling...
MS - Page 2
The neurologist made a diagnosis of multiple sclerosis based on the MRI...
MS - Page 3
Case Summary
Summary of the Case
MS - Summary

Answers to Case Questions
MS - Answers

Professionals
Health Professionals Introduced in Case
MS - Professionals
Additional Links
Optional Links to Explore Further
Cognitive Changes and Multiple Sclerosis
Overview of cognitive changes and ms.
- Learn and remember information
- Process incoming information
- Organize, plan, problem-solve and make decisions
- Focus, maintain and shift attention
- Act on information and communicate it to others
- Relate visual information to the space around you (accurately perceiving your environment)
- Perform calculations
Relationship Between MS and Cognition
- Can happen with any disease course but are more common in progressive MS.
- Are usually mild and generally progress slowly but can become more challenging over time.
- Are unrelated to the degree of physical disability. You may have significant physical limitations with no cognitive issues or you may have significant cognitive limitations with no physical limitations.
- Can lead you to leave the workforce early.
- Can affect self-esteem, interfere with communication and impact relationships.
- Are more likely to occur during an exacerbation.
Early Recognition of MS Cognitive Challenges
Cognitive health self-assessment, talk to your doctor.
Comprehensive Evaluation of Cognitive Functioning
National ms society recommendations for managing cognitive symptoms.
- Early screening to set a baseline and annual reassessment of cognitive health to identify potential problems
- Comprehensive evaluation, including a mood evaluation, for any adult or child who tests positive for dysfunction in the initial screening or demonstrates a significant cognitive decline (depression and anxiety can impact cognitive functioning)
- Comprehensive evaluation for any individual who is applying for disability insurance due to cognitive impairment
- Education for people with MS and their family members
- Interventions to improve cognitive functioning and participation in everyday activities
- Open access
- Published: 10 April 2024
“So at least now I know how to deal with things myself, what I can do if it gets really bad again”—experiences with a long-term cross-sectoral advocacy care and case management for severe multiple sclerosis: a qualitative study
- Anne Müller ORCID: orcid.org/0000-0002-2456-2492 1 ,
- Fabian Hebben ORCID: orcid.org/0009-0003-6401-3433 1 ,
- Kim Dillen 1 ,
- Veronika Dunkl 1 ,
- Yasemin Goereci 2 ,
- Raymond Voltz 1 , 3 , 4 ,
- Peter Löcherbach 5 ,
- Clemens Warnke ORCID: orcid.org/0000-0002-3510-9255 2 &
- Heidrun Golla ORCID: orcid.org/0000-0002-4403-630X 1
on behalf of the COCOS-MS trial group represented by Martin Hellmich
BMC Health Services Research volume 24 , Article number: 453 ( 2024 ) Cite this article
199 Accesses
Metrics details
Persons with severe Multiple Sclerosis (PwsMS) face complex needs and daily limitations that make it challenging to receive optimal care. The implementation and coordination of health care, social services, and support in financial affairs can be particularly time consuming and burdensome for both PwsMS and caregivers. Care and case management (CCM) helps ensure optimal individual care as well as care at a higher-level. The goal of the current qualitative study was to determine the experiences of PwsMS, caregivers and health care specialists (HCSs) with the CCM.
In the current qualitative sub study, as part of a larger trial, in-depth semi-structured interviews with PwsMS, caregivers and HCSs who had been in contact with the CCM were conducted between 02/2022 and 01/2023. Data was transcribed, pseudonymized, tested for saturation and analyzed using structuring content analysis according to Kuckartz. Sociodemographic and interview characteristics were analyzed descriptively.
Thirteen PwsMS, 12 caregivers and 10 HCSs completed interviews. Main categories of CCM functions were derived deductively: (1) gatekeeper function, (2) broker function, (3) advocacy function, (4) outlook on CCM in standard care. Subcategories were then derived inductively from the interview material. 852 segments were coded. Participants appreciated the CCM as a continuous and objective contact person, a person of trust (92 codes), a competent source of information and advice (on MS) (68 codes) and comprehensive cross-insurance support (128 codes), relieving and supporting PwsMS, their caregivers and HCSs (67 codes).
Conclusions
Through the cross-sectoral continuous support in health-related, social, financial and everyday bureaucratic matters, the CCM provides comprehensive and overriding support and relief for PwsMS, caregivers and HCSs. This intervention bears the potential to be fine-tuned and applied to similar complex patient groups.
Trial registration
The study was approved by the Ethics Committee of the University of Cologne (#20–1436), registered at the German Register for Clinical Studies (DRKS00022771) and in accordance with the Declaration of Helsinki.
Peer Review reports
Introduction
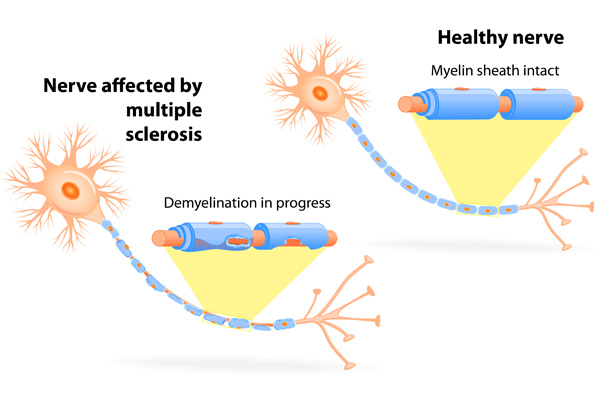
Multiple sclerosis (MS) is the most frequent and incurable chronic inflammatory and degenerative disease of the central nervous system (CNS). Illness awareness and the number of specialized MS clinics have increased since the 1990s, paralleled by the increased availability of disease-modifying therapies [ 1 ]. There are attempts in the literature for the definition of severe MS [ 2 , 3 ]. These include a high EDSS (Expanded disability Status Scale [ 4 ]) of ≥ 6, which we took into account in our study. There are also other factors to consider, such as a highly active disease course with complex therapies that are associated with side effects. These persons are (still) less disabled, but may feel overwhelmed with regard to therapy, side effects and risk monitoring of therapies [ 5 , 6 ].
Persons with severe MS (PwsMS) develop individual disease trajectories marked by a spectrum of heterogeneous symptoms, functional limitations, and uncertainties [ 7 , 8 ] manifesting individually and unpredictably [ 9 ]. This variability can lead to irreversible physical and mental impairment culminating in complex needs and daily challenges, particularly for those with progressive and severe MS [ 5 , 10 , 11 ]. Such challenges span the spectrum from reorganizing biographical continuity and organizing care and everyday live, to monitoring disease-specific therapies and integrating palliative and hospice care [ 5 , 10 ]. Moreover, severe MS exerts a profound of social and economic impact [ 9 , 12 , 13 , 14 ]. PwsMS and their caregivers (defined in this manuscript as relatives or closely related individuals directly involved in patients’ care) often find themselves grappling with overwhelming challenges. The process of organizing and coordinating optimal care becomes demanding, as they contend with the perceived unmanageability of searching for, implementing and coordinating health care and social services [ 5 , 15 , 16 , 17 ].
Case management (CM) proved to have a positive effect on patients with neurological disorders and/or patients with palliative care needs [ 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 ]. However, a focus on severe MS has been missed so far Case managers primarily function as: (1) gatekeeper involving the allocation of necessary and available resources to a case, ensuring the equitable distribution of resources; as (2) broker assisting clients in pursuing their interests, requiring negotiation to provide individualized assistance that aligns as closely as possible with individual needs and (3) advocate working to enhance clients’ individual autonomy, to advocate for essential care offers, and to identify gaps in care [ 25 , 26 , 27 , 28 , 29 ].
Difficulties in understanding, acting, and making decisions regarding health care-related aspects (health literacy) poses a significant challenge for 54% of the German population [ 30 ]. Additionally acting on a superordinate level as an overarching link, a care and case management (CCM) tries to reduce disintegration in the social and health care system [ 31 , 32 ]. Our hypothesis is that a CCM allows PwsMS and their caregivers to regain time and resources outside of disease management and to facilitate the recovery and establishment of biographical continuity that might be disrupted due to severe MS [ 33 , 34 ].
Health care specialists (HCSs) often perceive their work with numerous time and economic constraints, especially when treating complex and severely ill individuals like PwsMS and often have concerns about being blamed by patients when expectations could not be met [ 35 , 36 ]. Our hypothesis is that the CCM will help to reduce time constraints and free up resources for specialized tasks.
To the best of our knowledge there is no long-term cross-sectoral and outreaching authority or service dedicated to assisting in the organization and coordination of the complex care concerns of PwsMS within the framework of standard care addressing needs in health, social, financial, every day and bureaucratic aspects. While some studies have attempted to design and test care programs for persons with MS (PwMS), severely affected individuals were often not included [ 37 , 38 , 39 ]. They often remain overlooked by existing health and social care structures [ 5 , 9 , 15 ].
The COCOS-MS trial developed and applied a long-term cross-sectoral CCM intervention consisting of weekly telephone contacts and monthly re-assessments with PwsMS and caregivers, aiming to provide optimal care. Their problems, resources and (unmet) needs were assessed holistically including physical health, mental health, self-sufficiency and social situation and participation. Based on assessed (unmet) needs, individual care plans with individual actions and goals were developed and constantly adapted during the CCM intervention. Contacts with HCSs were established to ensure optimal care. The CCM intervention was structured through and documented in a CCM manual designed for the trial [ 40 , 41 ].
Our aim was to find out how PwsMS, caregivers and HCSs experienced the cross-sectoral long-term, outreaching patient advocacy CCM.
This study is part of a larger phase II, randomized, controlled clinical trial “Communication, Coordination and Security for people with severe Multiple Sclerosis (COCOS-MS)” [ 41 ]. This explorative clinical trial, employing a mixed-method design, incorporates a qualitative study component with PwsMS, caregivers and HCSs to enrich the findings of the quantitative data. This manuscript focuses on the qualitative data collected between February 2022 and January 2023, following the Consolidated Criteria for Reporting Qualitative Research (COREQ) guidelines [ 42 ].
Research team
Three trained authors AM, KD and FH (AM, female, research associate, M.A. degree in Rehabilitation Sciences; KD, female, researcher, Dr. rer. medic.; FH, male, research assistant, B.Sc. degree in Health Care Management), who had no prior relationship with patients, caregivers or HCSs conducted qualitative interviews. A research team, consisting of clinical experts and health services researchers, discussed the development of the interview guides and the finalized category system.
Theoretical framework
Interview data was analyzed with the structuring content analysis according to Kuckartz. This method enables a deductive structuring of interview material, as well as the integration of new aspects found in the interview material through the inductive addition of categories in an iterative analysis process [ 43 ].
Sociodemographic and interview characteristics were analyzed descriptively (mean, median, range, SD). PwsMS, caregivers and HCSs were contacted by the authors AM, KD or FH via telephone or e-mail after providing full written informed consent. Participants had the option to choose between online interviews conducted via the GoToMeeting 10.19.0® Software or face-to-face. Peasgood et al. (2023) found no significant differences in understanding questions, engagement or concentration between face-to-face and online interviews [ 44 , 45 ]. Digital assessments were familiar to participants due to pandemic-related adjustments within the trial.
Out of 14 PwsMS and 14 caregivers who were approached to participate in interviews, three declined to complete interviews, resulting in 13 PwsMS (5 male, 8 female) and 12 caregiver (7 male, 5 female) interviews, respectively (see Fig. 1 ). Thirty-one HCSs were contacted of whom ten (2 male, 8 female) agreed to be interviewed (see Fig. 2 ).
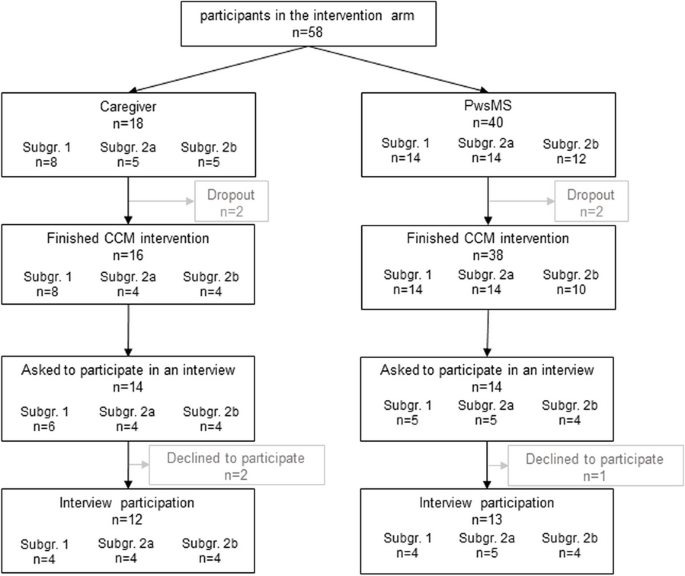
Flowchart of PwsMS and caregiver participation in the intervention group of the COCOS-MS trial. Patients could participate with and without a respective caregiver taking part in the trial. Therefore, number of caregivers does not correspond to patients. For detailed inclusion criteria see also Table 1 in Golla et al. [ 41 ]
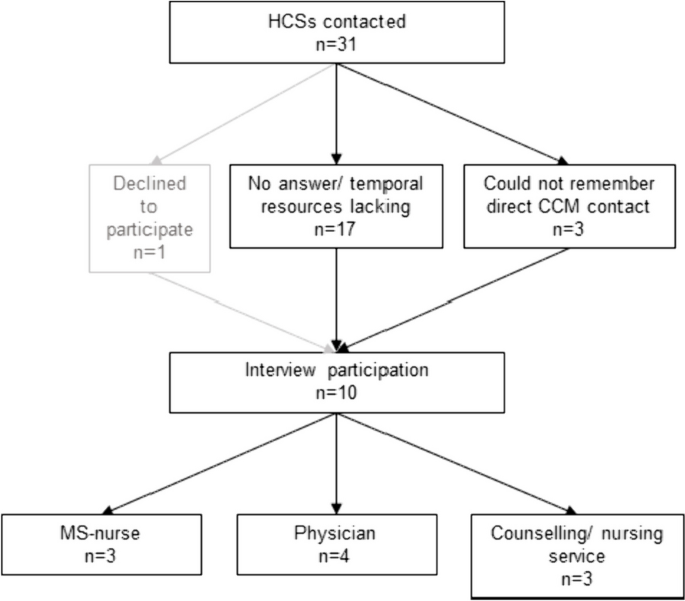
Flowchart of HCSs interview participation
Setting and data collection
Interviews were carried out where participants preferred, e.g. at home, workplace, online, and no third person being present. In total, we conducted 35 interviews whereof 7 interviews face-to-face (3 PwsMS, 3 caregivers, 1 HCS).
The research team developed a topic guide which was meticulously discussed with research and clinical staff to enhance credibility. It included relevant aspects for the evaluation of the CCM (see Tables 1 and 2 , for detailed topic guides see Supplementary Material ). Patient and caregiver characteristics (covering age, sex, marital status, living situation, EDSS (patients only), subgroup) were collected during the first assessment of the COCOS-MS trial and HCSs characteristics (age, sex, profession) as well as interview information (length and setting) were collected during the interviews. The interview guides developed for this study addressed consistent aspects both for PwsMS and caregivers (see Supplementary Material ):
For HCSs it contained the following guides:
Probing questions were asked to get more specific and in-depth information. Interviews were carried out once and recorded using a recording device or the recording function of the GoToMeeting 10.19.0® Software. Data were pseudonymized (including sensitive information, such as personal names, dates of birth, or addresses), audio files were safely stored in a data protection folder. The interview duration ranged from 11 to 56 min (mean: 23.9 min, SD: 11.1 min). Interviews were continued until we found that data saturation was reached. Audio recordings were transcribed verbatim by an external source and not returned to participants.
Data analysis
Two coders (AM, FH) coded the interviews. Initially, the first author (AM) thoroughly reviewed the transcripts to gain a sense of the interview material. Using the topic guide and literature, she deductively developed a category system based on the primary functions of CM [ 25 , 26 , 27 , 28 , 29 ]. Three interviews were coded repeatedly for piloting, and inductive subcategories were added when new themes emerged in the interview material. This category system proved suitable for the interview material. The second coder (FH) familiarized himself with the interview material and category system. Both coders (AM, FH) independently coded all interviews, engaging in discussions and adjusting codes iteratively. The finalized category system was discussed and consolidated in a research workshop and within the COCOS-MS trial group and finally we reached an intercoder agreement of 90% between the two coders AM and FH, computed by the MAXQDA Standard 2022® software.
We analyzed sociodemographic and interview characteristics using IBM SPSS Statistics 27® and Excel 2016®. Transcripts were managed and analyzed using MAXQDA Standard 2022®.
Participants were provided with oral and written information about the trial and gave written informed consent. Ethical approvals were obtained from the Ethics Committee of the University of Cologne (#20–1436). The trial is registered in the German Register for Clinical Studies (DRKS) (DRKS00022771) and is conducted under the Declaration of Helsinki.
Characteristics of participants and interviews
PwsMS participating in an interview were mainly German (84.6%), had a mean EDSS of 6.8 (range: 6–8) and MS for 13.5 years (median: 14; SD: 8.1). For detailed characteristics see Table 3 .
Most of the interviewed caregivers (9 caregivers) were the partners of the PwsMS with whom they lived in the same household. For further details see Table 3 .
HCSs involved in the study comprised various professions, including MS-nurse (3), neurologist (2), general physician with further training in palliative care (1), physician with further training in palliative care and pain therapist (1), housing counselling service (1), outpatient nursing service manager (1), participation counselling service (1).
Structuring qualitative content analysis
The experiences of PwsMS, caregivers and HCSs were a priori deductively assigned to four main categories: (1) gatekeeper function, (2) broker function, (3) advocacy function [ 25 , 26 , 27 , 28 , 29 ] and (4) Outlook on CCM in standard care, whereas the subcategories were developed inductively (see Fig. 3 ).
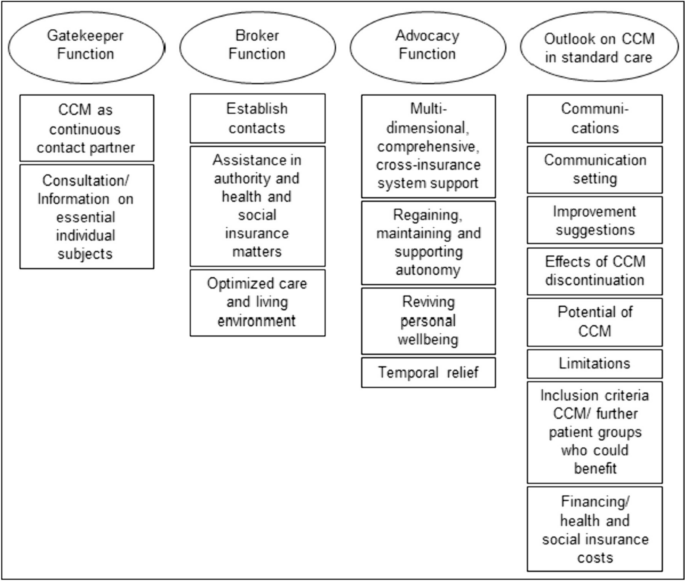
Category system including main and subcategories of the qualitative thematic content analysis
The most extensive category, housing the highest number of codes and subcodes, was the “ Outlook on CCM in standard care ” (281 codes). Following this, the category “ Advocacy Function ” contained 261 codes. The “ Broker Function ” (150 codes) and the “ Gatekeeper Function ” (160 codes) constituted two smaller categories. The majority of codes was identified in the caregivers’ interviews, followed by those of PwsMS (see Table 4 ). Illustrative quotes for each category and subcategory can be found in Table 5 .
Persons with severe multiple sclerosis
In the gatekeeper function (59 codes), PwsMS particularly valued the CCM as a continuous contact person . They appreciated the CCM as a person of trust who was reliably accessible throughout the intervention period. This aspect, with 41 codes, held significant importance for PwsMS.
Within the broker function (44 codes), establishing contact was most important for PwsMS (22 codes). This involved the CCM as successfully connecting PwsMS and caregivers with physicians and therapists, as well as coordinating and arranging medical appointments, which were highly valued. Assistance in authority and health and social insurance matters (10 codes) was another subcategory, where the CCM encompassed support in communication with health insurance companies, such as improving the level of care, assisting with retirement pension applications, and facilitating rehabilitation program applications. Optimized care (12 codes) resulted in improved living conditions and the provision of assistive devices through the CCM intervention.
The advocacy function (103 codes) emerged as the most critical aspect for PwsMS, representing the core of the category system. PwsMS experienced multidimensional, comprehensive, cross-insurance system support from the CCM. This category, with 43 statements, was the largest within all subcategories. PwsMS described the CCM as addressing their concerns, providing help, and assisting with the challenges posed by the illness in everyday life. The second-largest subcategory, regaining, maintaining and supporting autonomy (25 codes), highlighted the CCM’s role in supporting self-sufficiency and independence. Reviving personal wellbeing (17 codes) involved PwsMSs’ needs of regaining positive feelings, improved quality of life, and a sense of support and acceptance, which could be improved by the CCM. Temporal relief (18 codes) was reported, with the CCM intervention taking over or reducing tasks.
Within the outlook on CCM in standard care (84 codes), eight subcategories were identified. Communications was described as friendly and open (9 codes), with the setting of communication (29 codes) including the frequency of contacts deemed appropriate by the interviewed PwsMS, who preferred face-to-face contact over virtual or telephone interactions. Improvement suggestions for CCM (10 codes) predominantly revolved around the desire for the continuation of the CCM beyond the trial, expressing intense satisfaction with the CCM contact person and program. PwsMS rarely wished for better cooperation with the CCM. With respect to limitations (7 codes), PwsMS distinguished between individual limitations (e.g. when not feeling ready for using a wheelchair) and overriding structural limitations (e.g. unsuccessful search for an accessible apartment despite CCM support). Some PwsMS mentioned needing the CCM earlier in the course of the disease and believed it would beneficial for anyone with a chronic illness (6 codes).
In the gatekeeper function (75 codes), caregivers highly valued the CCM as a continuous contact partner (33 codes). More frequently than among the PwsMS interviewed, caregivers valued the CCM as a source of consultation/ information on essential individual subjects (42 codes). The need for basic information about the illness, its potential course, treatment and therapy options, possible supportive equipment, and basic medical advice/ information could be met by the CCM.
Within the broker function (63 codes), caregivers primarily experienced the subcategory establish contacts (24 codes). They found the CCM as helpful in establishing and managing contact with physicians, therapists and especially with health insurance companies. In the subcategory assistance in authority and health and social insurance matters (22 codes), caregivers highlighted similar aspects as the PwsMS interviewed. However, there was a particular emphasis on assistance with patients' retirement matters. Caregivers also valued the optimization of patients’ care and living environment (17 codes) in various life areas during the CCM intervention, including improved access to assistive devices, home modification, and involvement of a household support and/ or nursing services.
The advocacy function, with 115 codes, was by far the broadest category . The subcategory multidimensional, comprehensive, cross-insurance system support represented the largest subcategory of caregivers, with 70 statements. In summary, caregivers felt supported by the CCM in all domains of life. Regaining, maintaining and supporting autonomy (11 codes) and reviving personal wellbeing (8 codes) in the form of an improved quality of life played a role not only for patients but also for caregivers, albeit to a lower extend. Caregivers experienced temporal relief (26 codes) as the CCM undertook a wide range of organizational tasks, freeing up more needed resources for their own interests.
For the Outlook on CCM in standard care , caregivers provided various suggestions (81 codes). Similar to PwsMS, caregivers felt that setting (home based face-to-face, telephone, virtual) and frequency of contact were appropriate (10 codes, communication setting ) and communications (7 codes) were recognized as open and friendly. However, to avoid conflicts between caregiver and PwsMS, caregivers preferred meeting the CCM separately from the PwsMS in the future. Some caregivers wished the CCM to specify all services it might offer at the beginning, while others emphasized not wanting this. Like PwsMS, caregivers criticized the CCM intervention being (trial-related) limited to one year, regardless of whether further support was needed or processes being incomplete (13 codes, improvement suggestions ). After the CCM intervention time had expired, the continuous contact person and assistance were missed and new problems had arisen and had to be managed with their own resources again (9 codes, effects of CCM discontinuation ), which was perceived as an exhausting or unsolvable endeavor. Caregivers identified analogous limitations (8 codes), both individual and structural. However, the largest subcategory, was the experienced potential of CCM (27 codes), reflected in extremely high satisfaction with the CCM intervention. Like PwsMS, caregivers regarded severe chronically ill persons in general as target groups for a CCM (7 codes) and would implement it even earlier, starting from the time of diagnosis. They considered a CCM to be particularly helpful for patients without caregivers or for caregivers with limited (time) resources, as it was true for most caregivers.
Health care specialists
In the gatekeeper function (26 codes) HCSs particularly valued the CCM as a continuous contact partner (18 codes). They primarily described their valuable collaboration with the CCM, emphasizing professional exchange between the CCM and HCSs.
Within the broker function (43 codes), the CCM was seen as a connecting link between patients and HCSs, frequently establishing contacts (18 codes). This not only improved optimal care on an individual patient level (case management) but also at a higher, superordinate care level (care management). HCSs appreciated the optimized care and living environment (18 codes) for PwsMS, including improved medical and therapeutic access and the introduction of new assistive devices. The CCM was also recognized as providing assistance in authority and health and social matters (7 codes) for PwsMS and their caregivers.
In the advocacy function (43 codes), HCSs primarily reported temporal relief through CCM intervention (23 codes). They experienced this relief, especially as the CCM provided multidimensional, comprehensive, and cross-insurance system support (15 codes) for PwsMS and their caregivers. Through this support, HCSs felt relieved from time intensive responsibilities that may not fall within their area of expertise, freeing up more time resources for their actual professional tasks.
The largest category within the HCSs interviews was the outlook on CCM in standard care (116 codes). In the largest subcategory, HCSs made suggestions for further patient groups who could benefit (38 codes) from a CCM. Chronic neurological diseases like neurodegenerative diseases (e.g. amyotrophic lateral sclerosis), typical and atypical Parkinson syndromes were mentioned. HCSs considered the enrollment of the CCM directly after the diagnosis of these complex chronic diseases. Additionally, chronic progressive diseases in general or oncological diseases, which may also run chronically, were regarded worthwhile for this approach. HCSs also provided suggestions regarding improvement (21 codes). They wished e.g. for information or contact when patients were enrolled to the CCM, regular updates, exchange and collaborative effort. On the other hand, HCSs reported, that their suggestions for improvement would hardly be feasible due to their limited time resources. Similar to patients and caregivers, HCSs experienced structural limits (13 codes), which a CCM could not exceed due to overriding structural limitations (e.g. insufficient supply of (household) aids, lack of outreach services like psychotherapists, and long processing times on health and pension insurers' side). HCSs were also asked about their opinions on financial resources (14 codes) of a CCM in standard care. All interviewed HCSs agreed that CCM would initially cause more costs for health and social insurers, but they were convinced of cost savings in the long run. HCSs particularly perceived the potential of the CCM (20 codes) through the feedback of PwsMS, highlighting the trustful relationship enabling individualized help for PwsMS and their caregivers.
Persons with severe multiple sclerosis and their caregivers
The long-term cross-sectoral CCM intervention implemented in the COCOS-MS trial addressed significant unmet needs of PwsMS and their caregivers which previous research revealed as burdensome and hardly or even not possible to improve without assistance [ 5 , 6 , 9 , 10 , 33 , 35 , 46 ]. Notably, the CCM service met the need for a reliable, continuous contact partner, guiding patients through the complexities of regulations, authorities and the insurance system. Both, PwsMS and their caregivers highly valued the professional, objective perspective provided by the CCM, recognizing it as a source of relief, support and improved care in line with previous studies [ 37 , 47 ]. Caregivers emphasized the CCM’s competence in offering concrete assistance and information on caregiving and the fundamentals of MS, including bureaucratic, authority and insurances matters. On the other hand, PwsMS particularly appreciated the CCMs external reflective and advisory function, along with empathic social support tailored to their individual concerns. Above all, the continuous partnership of trust, available irrespective of the care sector, was a key aspect that both PwsMS and their caregivers highlighted. This consistent support was identified as one of the main components in the care of PwsMS in previous studies [ 5 , 33 , 35 ].
As the health literacy is inadequate or problematic for 54% of the German population and disintegration in the health and social care system is high [ 30 , 31 , 32 ], the CCM approach serves to enhance health literacy and reduce disintegration of PwsMS and their caregivers by providing cross-insurance navigational guidance in the German health and social insurance sector on a superordinate level. Simultaneously PwsMS and caregivers experienced relief and gained more (time) resources for all areas of life outside of the disease and its management, including own interests and establishing biographical continuity. This empowerment enables patients to find a sense of purpose beyond their illness, regain autonomy, and enhance social participation, reducing the feeling of being a burden to those closest to them. Such feelings are often experienced as burdensome and shameful by PwsMS [ 6 , 48 , 49 , 50 ]. Finding a sense of purpose beyond the illness also contributes to caregivers perceiving their loved ones not primarily as patient but as individuals outside of the disease, reinforcing valuable relationships such as partners, siblings, or children, strengthening emotional bonds. These factors are also highly relevant and well-documented in a suicide-preventive context, as the suicide rate is higher in persons diagnosed with neurological disorders [ 19 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 ] and the feeling of being a burden to others, loss of autonomy, and perceived loss of dignity are significant factors in patients with severe chronic neurological diseases for suicide [ 50 , 57 ].
The temporal relief experienced by the CCM was particularly significant for HCSs and did not only improve the satisfaction of HCSs but also removed unfulfilled expectations and concerns about being blamed by patients when expectations could not be met, which previous studied elaborated [ 35 , 36 ]. Moreover, the CCM alleviated the burden on HCSs by addressing patients’ concerns, allowing them to focus on their own medical responsibilities. This aspect probably reduced the dissatisfaction that arises when HCSs are expected to address issues beyond their medical expertise, such as assistive devices, health and social insurance, and the organization and coordination of supplementary therapies, appointments, and contacts [ 35 , 36 , 61 ]. Consequently, the CCM reduced difficulties of HCSs treating persons with neurological or chronical illnesses, which previous research identified as problematic.
HCSs perceive their work as increasingly condensed with numerous time and economic constraints, especially when treating complex and severely ill individuals like PwsMS [ 36 ]. This constraint was mentioned by HCSs in the interviews and was one of the main reasons why they were hesitant to participate in interviews and may also be an explanation for a shorter interview duration than initially planned in the interview guides. The CCM’s overarching navigational competence in the health and social insurance system was particularly valued by HCSs. The complex and often small-scale specialties in the health and social care system are not easily manageable or well-known even for HCSs, and dealing with them can exceed their skills and time capacities [ 61 ]. The CCM played a crucial role in keeping (temporal) resources available for what HCSs are professionally trained and qualified to work on. However, there remains a challenge in finding solutions to the dilemma faced by HCSs regarding their wish to be informed about CCM procedures and linked with each other, while also managing the strain of additional requests and contact with the CCM due to limited (time) resources [ 62 ]. Hudon et al. (2023) suggest that optimizing time resources and improving exchange could involve meetings, information sharing via fax, e-mail, secure online platforms, or, prospectively, within the electronic patient record (EPR). The implementation of an EPR has shown promise in improving the quality of health care and time resources, when properly implemented [ 63 , 64 ]. The challenge lies ineffective information exchange between HCSs and CCM for optimal patient care. The prospect of time saving in the long run and at best for a financial incentive, e.g., when anchoring in the Social Security Code, will help best to win over the HCSs.If this crucial factor can be resolved, there is a chance that HCSs will thoroughly accept the CCM as an important pillar, benefiting not only PwsMS but also other complex patient groups, especially those with long-term neurological or complex oncological conditions that might run chronically.
Care and case management and implications for the health care system
The results of our study suggest that the cross-sectoral long-term advocacy CCM in the COCOS-MS trial, with continuous personal contacts at short intervals and constant reevaluation of needs, problems, resources and goals, is highly valued by PwsMS, caregivers, and HCSs. The trial addresses several key aspects that may have been overlooked in previous studies which have shown great potential for the integration of case management [ 17 , 47 , 62 , 65 , 66 ]. However, they often excluded the overriding care management, missed those patient groups with special severity and complexity who might struggle to reach social and health care structures independently or the interventions were not intended for long-term [ 22 , 37 ]. Our results indicate that the CCM intervention had a positive impact on PwsMS and caregivers as HCSs experienced them with benefits such as increased invigoration, reduced demands, and enhanced self-confidence. However, there was a notable loss experienced by PwsMS and caregivers after the completion of the CCM intervention, even if they had stabilized during the intervention period. The experiences of optimized social and health care for the addressed population, both at an individual and superordinate care level, support the integration of this service into standard care. Beyond the quantitatively measurable outcomes and economic considerations reported elsewhere [ 16 , 20 , 21 ], our results emphasize the importance of regaining control, self-efficacy, self-worth, dignity, autonomy, and social participation. These aspects are highlighted as preventive measures in suicidal contexts, which is particularly relevant for individuals with severe and complex illnesses [ 19 , 50 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 ]. Our findings further emphasize the societal responsibilities to offer individuals with severe and complex illnesses the opportunity to regain control and meaningful aspects of life, irrespective of purely economic considerations. This underscores the need for a comprehensive evaluation that not only takes into account quantitative measures but also the qualitative aspects of well-being and quality of life when making recommendations of a CCM in standard care.
The study by J. Y. Joo and Huber (2019) highlighted that CM interventions aligned with the standards of the Case Management Society of America varied in duration, ranging from 1 month to 15.9 years, and implemented in community- or hospital-based settings. However, they noted a limitation in understanding how CM processes unfold [ 67 ]. In contrast, our trial addressed this criticism by providing transparent explanations of the CCM process, which also extends to a superordinate care management [ 40 , 41 ]. Our CCM manual [ 40 ] outlines a standardized and structured procedure for measuring and reevaluating individual resources, problems, and unmet needs on predefined dimensions. It also identifies goals and actions at reducing unmet needs and improving the individual resources of PwsMS and caregivers. Importantly, the CCM manual demonstrates that the CCM process can be structured and standardized, while accounting for the unique aspects of each individual’s serious illness, disease courses, complex needs, available resources, and environmental conditions. Furthermore, the adaptability of the CCM manual to other complex chronically ill patient groups suggests the potential for a standardized approach in various health care settings. This standardized procedure allows for consistency in assessing and addressing the individual needs of patients, ensuring that the CCM process remains flexible while maintaining a structured and goal-oriented framework.
The discussion about the disintegration in the social and health care system and the increasing specialization dates back to 2009 [ 31 , 32 ]. Three strategies were identified to address this issue: (a) “driver-minimizing” [Treiberminimierende], (b) “effect-modifying” [Effektmodifizierende] and (c) “disintegration-impact-minimizing” [Desintegrationsfolgenminimierende] strategies. “Driver-minimizing strategies” involve comprehensive and radical changes within the existing health and social care system, requiring political and social pursuit. “Disintegration-impact-minimizing strategies” are strategies like quality management or tele-monitoring, which are limited in scope and effectiveness. “Effect-modifying strategies”, to which CCM belongs, acknowledges the segmentation within the system but aims to overcome it through cooperative, communicative, and integrative measures. CCM, being an “effect-modifying strategy”, operates the “integrated segmentation model” [Integrierte Segmentierung] rather than the “general contractor model” [Generalunternehmer-Modell] or “total service provider model” [Gesamtdienstleister-Modell] [ 31 , 32 ]. In this model, the advantage lies in providing an overarching and coordinating service to link different HCSs and services cross-sectorally. The superordinate care management aspect of the CCM plays a crucial role in identifying gaps in care, which is essential for future development strategies within the health and social care system. It aims to find or develop (regional) alternatives to ensure optimal care [ 17 , 23 , 24 , 68 , 69 ], using regional services of existing health and social care structures. Therefore, superordinate care management within the CCM process is decisive for reducing disintegration in the system.
Strengths and limitations
The qualitative study results of the explorative COCOS-MS clinical trial, which employed an integrated mixed-method design, provide valuable insights into the individual experiences of three leading stakeholders: PwsMS, caregivers and HCSs with a long-term cross-sectoral CCM. In addition to in-depth interviews, patient and caregiver reported outcome measurements were utilized and will be reported elsewhere. The qualitative study’s strengths include the inclusion of patients who, due to the severity of their condition (e.g. EDSS mean: 6.8, range: 6–8, highly active MS), age (mean: 53.9 years, range: 36–73 years) family constellations, are often underrepresented in research studies and often get lost in existing social and health care structures. The study population is specific to the wider district region of Cologne, but the broad inclusion criteria make it representative of severe MS in Germany. The methodological approach of a deductive and inductive structuring content analysis made it possible to include new findings into an existing theoretical framework.
However, the study acknowledges some limitations. While efforts were made to include more HCSs, time constraints on their side limited the number of interviews conducted and might have biased the results. Some professions are underrepresented in the interviews. Complex symptoms (e.g. fatigue, ability to concentrate), medical or therapeutic appointments and organization of the everyday live may have been reasons for the patients’ and caregivers’ interviews lasting shorter than initially planned.
The provision of functions of a CCM, might have pre-structured the answers of the participants.
At current, there is no support system for PwsMS, their caregivers and HCSs that addresses their complex and unmet needs comprehensively and continuously. There are rare qualitative insights of the three important stakeholders: PwsMS, caregivers and HCSs in one analysis about a supporting service like a CCM. In response to this gap, we developed and implemented a long-term cross-sectoral advocacy CCM and analyzed it qualitatively. PwsMS, their caregivers and HCSs expressed positive experiences, perceiving the CCM as a source of relief and support that improved care across various aspects of life. For patients, the CCM intervention resulted in enhanced autonomy, reviving of personal wellbeing and new established contacts with HCSs. Caregivers reported a reduced organizational burden and felt better informed, and HCSs experienced primarily temporal relief, allowing them to concentrate on their core professional responsibilities. At a higher level of care, the study suggests that the CCM contributed to a reduction in disintegration within the social and health care system.
The feedback from participants is seen as valuable for adapting the CCM intervention and the CCM manual for follow-up studies, involving further complex patient groups such as neurological long-term diseases apart from MS and tailoring the duration of the intervention depending on the complexity of evolving demands.
Availability of data and materials
Generated and/or analyzed datasets of participants are available from the corresponding author on reasonable request to protect participants. Preliminary partial results have been presented as a poster during the EAPC World Congress in June 2023 and the abstract has been published in the corresponding abstract booklet [ 70 ].
Abbreviations
Amyotrophic lateral sclerosis
- Care and case management
Case management
Central nervous system
Communication, Coordination and security for people with multiple sclerosis
Consolidated criteria for reporting qualitative research
German register for clinical studies
Extended disability status scale
Electronic patient record
Quality of life
Multiple sclerosis
Koch-Henriksen N, Magyari M. Apparent changes in the epidemiology and severity of multiple sclerosis. Nat Rev Neurol. 2021;17:676–88. https://doi.org/10.1038/s41582-021-00556-y .
Article PubMed Google Scholar
Ellenberger D, Flachenecker P, Fneish F, Frahm N, Hellwig K, Paul F, et al. Aggressive multiple sclerosis: a matter of measurement and timing. Brain. 2020;143:e97. https://doi.org/10.1093/brain/awaa306 .
Article PubMed PubMed Central Google Scholar
Edmonds P, Vivat B, Burman R, Silber E, Higginson IJ. Loss and change: experiences of people severely affected by multiple sclerosis. Palliat Med. 2007;21:101–7. https://doi.org/10.1177/0269216307076333 .
Kurtzke JF. Rating neurologic impairment in multiple rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology. 1983;33(11):1444–52.
Article CAS PubMed Google Scholar
Galushko M, Golla H, Strupp J, Karbach U, Kaiser C, Ernstmann N, et al. Unmet needs of patients feeling severely affected by multiple sclerosis in Germany: a qualitative study. J Palliat Med. 2014;17:274–81. https://doi.org/10.1089/jpm.2013.0497 .
Borreani C, Bianchi E, Pietrolongo E, Rossi I, Cilia S, Giuntoli M, et al. Unmet needs of people with severe multiple sclerosis and their carers: qualitative findings for a home-based intervention. PLoS One. 2014:e109679. https://doi.org/10.1371/journal.pone.0109679 .
Yamout BI, Alroughani R. Multiple Sclerosis. Semin Neurol. 2018;38:212–25. https://doi.org/10.1055/s-0038-1649502 .
Nissen N, Lemche J, Reestorff CM, Schmidt M, Skjerbæk AG, Skovgaard L, et al. The lived experience of uncertainty in everyday life with MS. Disabil Rehabil. 2022;44:5957–63. https://doi.org/10.1080/09638288.2021.1955302 .
Strupp J, Hartwig A, Golla H, Galushko M, Pfaff H, Voltz R. Feeling severely affected by multiple sclerosis: what does this mean? Palliat Med. 2012;26:1001–10. https://doi.org/10.1177/0269216311425420 .
Strupp J, Voltz R, Golla H. Opening locked doors: Integrating a palliative care approach into the management of patients with severe multiple sclerosis. Mult Scler J. 2016;22:13–8.
Article CAS Google Scholar
Kraft AK, Berger K. Kernaspekte einer bedarfsgerechten Versorgung von Patienten mit Multipler Sklerose : Inanspruchnahme ambulanter Leistungen und „shared decision making“ [Core aspects of a needs-conform care of patients with multiple sclerosis : Utilization of outpatient services and shared decision making]. Nervenarzt. 2020;91:503–10. https://doi.org/10.1007/s00115-020-00906-z .
Doshi A, Chataway J. Multiple sclerosis, a treatable disease. Clin Med (Lond). 2017;17:530–6. https://doi.org/10.7861/clinmedicine.17-6-530 .
Kobelt G, Thompson A, Berg J, Gannedahl M, Eriksson J. New insights into the burden and costs of multiple sclerosis in Europe. Mult Scler. 2017;23:1123–36. https://doi.org/10.1177/1352458517694432 .
Conradsson D, Ytterberg C, Engelkes C, Johansson S, Gottberg K. Activity limitations and participation restrictions in people with multiple sclerosis: a detailed 10-year perspective. Disabil Rehabil. 2021;43:406–13. https://doi.org/10.1080/09638288.2019.1626919 .
Sorensen PS, Giovannoni G, Montalban X, Thalheim C, Zaratin P, Comi G. The Multiple Sclerosis Care Unit. Mult Scler J. 2019;5:627–36.
Article Google Scholar
Tan H, Yu J, Tabby D, Devries A, Singer J. Clinical and economic impact of a specialty care management program among patients with multiple sclerosis: a cohort study. Mult Scler. 2010;16:956–63. https://doi.org/10.1177/1352458510373487 .
Article CAS PubMed PubMed Central Google Scholar
Oeseburg B, Wynia K, Middel B, Reijneveld SA. Effects of case management for frail older people or those with chronic illness: a systematic review. Nurs Res. 2009;58:201–10.
Aiken LS, Butner J, Lockhart CA, Volk-Craft BE, Hamilton G, Williams FG. Outcome evaluation of a randomized trial of the PhoenixCare intervention: program of case management and coordinated care for the seriously chronically ill. J Palliat Med. 2006;9:111–26. https://doi.org/10.1089/jpm.2006.9.111 .
Kuhn U, Düsterdiek A, Galushko M, Dose C, Montag T, Ostgathe C, Voltz R. Identifying patients suitable for palliative care—a descriptive analysis of enquiries using a Case Management Process Model approach. BMC Res Notes. 2012;5:611. https://doi.org/10.1186/1756-0500-5-611 .
Leary A, Quinn D, Bowen A. Impact of proactive case management by multiple sclerosis specialist nurses on use of unscheduled care and emergency presentation in multiple sclerosis: a case study. Int J MS Care. 2015;17:159–63. https://doi.org/10.7224/1537-2073.2014-011 .
Strupp J, Dose C, Kuhn U, Galushko M, Duesterdiek A, Ernstmann N, et al. Analysing the impact of a case management model on the specialised palliative care multi-professional team. Support Care Cancer. 2018;26:673–9. https://doi.org/10.1007/s00520-017-3893-3 .
Wynia K, Annema C, Nissen H, de Keyser J, Middel B. Design of a Randomised Controlled Trial (RCT) on the effectiveness of a Dutch patient advocacy case management intervention among severely disabled Multiple Sclerosis patients. BMC Health Serv Res. 2010;10:142. https://doi.org/10.1186/1472-6963-10-142 .
Ewers M, Schaeffer D, editors. Case Management in Theorie und Praxis. Bern: Huber; 2005.
Google Scholar
Neuffer M. Case Management: Soziale Arbeit mit Einzelnen und Familien. 5th ed. Weinheim, Basel: Beltz Juventa; 2013.
Case Management Society of America. The standards of practice for case management. 2022.
Deutsche Gesellschaft für Care und Case Management e.V., editor. Case Management Leitlinien: Rahmenempfehlung, Standards und ethische Grundlagen. 2nd ed. Heidelberg: Medhochzwei; 2020.
Monzer M. Case Management Grundlagen. 2nd ed. Heidelberg: Medhochzwei; 2018.
Wissert M. Grundfunktionen und fachliche Standards des Unterstützungsmanagements. Z Gerontol Geriat. 1998;31(5):331–7.
Wissert M. Tools und Werkzeuge beim Case Management: Die Hilfeplanung. Case Manag. 2007;1:35–7.
Schaeffer D, Berens E-M, Vogt D. Health literacy in the German population. Dtsch Arztebl Int. 2017;114:53–60. https://doi.org/10.3238/arztebl.2017.0053 .
Pfaff H, Schulte H. Der onkologische Patient der Zukunft. Onkologe. 2012;18:127–33. https://doi.org/10.1007/s00761-011-2201-y .
Pfaff H, Kowalski C, Ommen O. Modelle zur Analyse von Integration und Koordination im Versorgungssystem. In: Ameldung, Sydow, Windeler, editor. Vernetzung im Gesundheitswesen: Wettbewerb und Kooperation. Stuttgart: Kohlhammer Verlag; 2009. p. 75–90.
Golla H, Mammeas S, Galushko M, Pfaff H, Voltz R. Unmet needs of caregivers of severely affected multiple sclerosis patients: A qualitative study. Palliat Support Care. 2015;13(6):1685–93.
Golla H, Galushko M, Pfaff H, Voltz R. Multiple sclerosis and palliative care - perceptions of severely affected multiple sclerosis patients and their health professionals: a qualitative study. BMC Palliat Care. 2014;13:11. https://doi.org/10.1186/1472-684x-13-11 .
Golla H, Galushko M, Pfaff H, Voltz R. Unmet needs of severely affected multiple sclerosis patients: the health professionals’ view. Palliat Med. 2012;26:139–51. https://doi.org/10.1177/0269216311401465 .
Methley AM, Chew-Graham CA, Cheraghi-Sohi S, Campbell SM. A qualitative study of patient and professional perspectives of healthcare services for multiple sclerosis: implications for service development and policy. Health Soc Care Community. 2017;25:848–57. https://doi.org/10.1111/hsc.12369 .
Kalb R, Costello K, Guiod L. Case management services to meet the complex needs of patients with multiple sclerosis in the community—the successes and challenges of a unique program from the national multiple sclerosis society. US Neurology. 2019;15:27–31.
Krüger K, Fricke LM, Dilger E-M, Thiele A, Schaubert K, Hoekstra D, et al. How is and how should healthcare for people with multiple sclerosis in Germany be designed?-The rationale and protocol for the mixed-methods study Multiple Sclerosis-Patient-Oriented Care in Lower Saxony (MS-PoV). PLoS One. 2021;16:e0259855. https://doi.org/10.1371/journal.pone.0259855 .
Ivancevic S, Weegen L, Korff L, Jahn R, Walendzik A, Mostardt S, et al. Effektivität und Kosteneffektivät von Versorgungsmanagement-Programmen bei Multipler Sklerose in Deutschland – Eine Übersichtsarbeit. Akt Neurol. 2015;42:503–8. https://doi.org/10.1055/s-0035-1564111 .
Müller A, Dillen K, Dojan T, Ungeheuer S, Goereci Y, Dunkl V, et al. Development of a long-term cross-sectoral case and care management manual for patients with severe multiple sclerosis and their caregivers. Prof Case Manag. 2023;28:183–93. https://doi.org/10.1097/NCM.0000000000000608 .
Golla H, Dillen K, Hellmich M, Dojan T, Ungeheuer S, Schmalz P, et al. Communication, Coordination, and Security for People with Multiple Sclerosis (COCOS-MS): a randomised phase II clinical trial protocol. BMJ Open. 2022;12:e049300. https://doi.org/10.1136/bmjopen-2021-049300 .
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–57. https://doi.org/10.1093/intqhc/mzm042 .
Kuckartz U. Qualitative Inhaltsanalyse: Methoden, Praxis, Computerunterstützung. 4th ed. Weinheim: Beltz Juventa; 2018.
Akyirem S, Ekpor E, Aidoo-Frimpong GA, Salifu Y, Nelson LE. Online interviews for qualitative health research in Africa: a scoping review. Int Health. 2023. https://doi.org/10.1093/inthealth/ihad010 .
Peasgood T, Bourke M, Devlin N, Rowen D, Yang Y, Dalziel K. Randomised comparison of online interviews versus face-to-face interviews to value health states. Soc Sci Med. 2023;323:115818. https://doi.org/10.1016/j.socscimed.2023.115818 .
Giordano A, Cimino V, Campanella A, Morone G, Fusco A, Farinotti M, et al. Low quality of life and psychological wellbeing contrast with moderate perceived burden in carers of people with severe multiple sclerosis. J Neurol Sci. 2016;366:139–45. https://doi.org/10.1016/j.jns.2016.05.016 .
Joo JY, Liu MF. Experiences of case management with chronic illnesses: a qualitative systematic review. Int Nurs Rev. 2018;65(1):102–1113.
Freeman J, Gorst T, Gunn H, Robens S. “A non-person to the rest of the world”: experiences of social isolation amongst severely impaired people with multiple sclerosis. Disabil Rehabil. 2020;42:2295–303. https://doi.org/10.1080/09638288.2018.1557267 .
National Institute for Health and Care Excellence. Multiple sclerosis: Management of multiple sclerosis in primary and secondary care. 2014.
Erdmann A, Spoden C, Hirschberg I, Neitzke G. The wish to die and hastening death in amyotrophic lateral sclerosis: A scoping review. BMJ Support Palliat Care. 2021;11:271–87. https://doi.org/10.1136/bmjspcare-2020-002640 .
Erlangsen A, Stenager E, Conwell Y, Andersen PK, Hawton K, Benros ME, et al. Association between neurological disorders and death by suicide in Denmark. JAMA. 2020;323:444–54. https://doi.org/10.1001/jama.2019.21834 .
Kalb R, Feinstein A, Rohrig A, Sankary L, Willis A. Depression and suicidality in multiple sclerosis: red flags, management strategies, and ethical considerations. Curr Neurol Neurosci Rep. 2019;19:77. https://doi.org/10.1007/s11910-019-0992-1 .
Feinstein A, Pavisian B. Multiple sclerosis and suicide. Mult Scler. 2017;23:923–7. https://doi.org/10.1177/1352458517702553 .
Marrie RA, Salter A, Tyry T, Cutter GR, Cofield S, Fox RJ. High hypothetical interest in physician-assisted death in multiple sclerosis. Neurology. 2017;88:1528–34. https://doi.org/10.1212/WNL.0000000000003831 .
Gauthier S, Mausbach J, Reisch T, Bartsch C. Suicide tourism: a pilot study on the Swiss phenomenon. J Med Ethics. 2015;41:611–7. https://doi.org/10.1136/medethics-2014-102091 .
Fischer S, Huber CA, Imhof L, MahrerImhof R, Furter M, Ziegler SJ, Bosshard G. Suicide assisted by two Swiss right-to-die organisations. J Med Ethics. 2008;34:810–4. https://doi.org/10.1136/jme.2007.023887 .
Strupp J, Ehmann C, Galushko M, Bücken R, Perrar KM, Hamacher S, et al. Risk factors for suicidal ideation in patients feeling severely affected by multiple sclerosis. J Palliat Med. 2016;19:523–8. https://doi.org/10.1089/jpm.2015.0418 .
Spence RA, Blanke CD, Keating TJ, Taylor LP. Responding to patient requests for hastened death: physician aid in dying and the clinical oncologist. J Oncol Pract. 2017;13:693–9. https://doi.org/10.1200/JOP.2016.019299 .
Monforte-Royo C, Villavicencio-Chávez C, Tomás-Sábado J, Balaguer A. The wish to hasten death: a review of clinical studies. Psychooncology. 2011;20:795–804. https://doi.org/10.1002/pon.1839 .
Blanke C, LeBlanc M, Hershman D, Ellis L, Meyskens F. Characterizing 18 years of the death with dignity act in Oregon. JAMA Oncol. 2017;3:1403–6. https://doi.org/10.1001/jamaoncol.2017.0243 .
Methley A, Campbell S, Cheraghi-Sohi S, Chew-Graham C. Meeting the mental health needs of people with multiple sclerosis: a qualitative study of patients and professionals. Disabil Rehab. 2017;39(11):1097-105. https://doi.org/10.1080/09638288.2016.1180547 .
Hudon C, Bisson M, Chouinard M-C, Delahunty-Pike A, Lambert M, Howse D, et al. Implementation analysis of a case management intervention for people with complex care needs in primary care: a multiple case study across Canada. BMC Health Serv Res. 2023;23:377. https://doi.org/10.1186/s12913-023-09379-7 .
Beckmann M, Dittmer K, Jaschke J, Karbach U, Köberlein-Neu J, Nocon M, et al. Electronic patient record and its effects on social aspects of interprofessional collaboration and clinical workflows in hospitals (eCoCo): a mixed methods study protocol. BMC Health Serv Res. 2021;21:377. https://doi.org/10.1186/s12913-021-06377-5 .
Campanella P, Lovato E, Marone C, Fallacara L, Mancuso A, Ricciardi W, Specchia ML. The impact of electronic health records on healthcare quality: a systematic review and meta-analysis. Eur J Public Health. 2016;26:60–4. https://doi.org/10.1093/eurpub/ckv122 .
García-Hernández M, González de León B, Barreto-Cruz S, Vázquez-Díaz JR. Multicomponent, high-intensity, and patient-centered care intervention for complex patients in transitional care: SPICA program. Front Med (Lausanne). 2022;9:1033689. https://doi.org/10.3389/fmed.2022.1033689 .
Meisinger C, Stollenwerk B, Kirchberger I, Seidl H, Wende R, Kuch B, Holle R. Effects of a nurse-based case management compared to usual care among aged patients with myocardial infarction: results from the randomized controlled KORINNA study. BMC Geriatr. 2013. https://doi.org/10.1186/1471-2318-13-115 .
Joo JY, Huber DL. Case management effectiveness on health care utilization outcomes: a systematic review of reviews. West J Nurs Res. 2019;41:111–33. https://doi.org/10.1177/0193945918762135 .
Stergiopoulos V, Gozdzik A, Misir V, Skosireva A, Connelly J, Sarang A, et al. Effectiveness of housing first with intensive case management in an ethnically diverse sample of homeless adults with mental illness: a randomized controlled trial. PLoS One. 2015;10:e0130281. https://doi.org/10.1371/journal.pone.0130281 .
Löcherbach P, Wendt R, editors. Care und Case Management: Transprofessionelle Versorgungsstrukturen und Netzwerke. 1st ed. Stuttgart: Kohlhammer; 2020.
EAPC2023 Abstract Book. Palliat Med. 2023;37:1–302. https://doi.org/10.1177/02692163231172891 .
Download references
Acknowledgements
We would like to thank all the patients, caregivers and health care specialists who volunteered their time to participate in an interview and the trial, Carola Janßen for transcribing the interviews, Fiona Brown for translating the illustrative quotes and Beatrix Münzberg, Kerstin Weiß and Monika Höveler for data collection in the quantitative study part.
COCOS-MS Trial Group
Anne Müller 1 , Fabian Hebben 1 , Kim Dillen 1 , Veronika Dunkl 1 , Yasemin Goereci 2 , Raymond Voltz 1,3,4 , Peter Löcherbach 5 , Clemens Warnke 2 , Heidrun Golla 1 , Dirk Müller 6 , Dorthe Hobus 1 , Eckhard Bonmann 7 , Franziska Schwartzkopff 8 , Gereon Nelles 9 , Gundula Palmbach 8 , Herbert Temmes 10 , Isabel Franke 1 , Judith Haas 10 , Julia Strupp 1 , Kathrin Gerbershagen 7 , Laura Becker-Peters 8 , Lothar Burghaus 11 , Martin Hellmich 12 , Martin Paus 8 , Solveig Ungeheuer 1 , Sophia Kochs 1 , Stephanie Stock 6 , Thomas Joist 13 , Volker Limmroth 14
1 Department of Palliative Medicine, Faculty of Medicine and University Hospital, University of Cologne, Cologne, Germany
2 Department of Neurology, Faculty of Medicine and University Hospital, University of Cologne, Cologne, Germany
3 Center for Integrated Oncology Aachen Bonn Cologne Düsseldorf (CIO ABCD), University of Cologne, Cologne, Germany
4 Center for Health Services Research (ZVFK), University of Cologne, Cologne, Germany
5 German Society of Care and Case Management e.V. (DGCC), Münster, Germany
6 Institute for Health Economics and Clinical Epidemiology (IGKE), Faculty of Medicine and University Hospital, University of Cologne, Cologne, Germany
7 Department of Neurology, Klinikum Köln, Cologne, Germany
8 Clinical Trials Centre Cologne (CTCC), Faculty of Medicine and University Hospital, University of Cologne, Cologne, Germany
9 NeuroMed Campus, MedCampus Hohenlind, Cologne, Germany
10 German Multiple Sclerosis Society Federal Association (DMSG), Hannover, Germany
11 Department of Neurology, Heilig Geist-Krankenhaus Köln, Cologne, Germany
12 Institute of Medical Statistics and Computational Biology (IMSB), Faculty of Medicine and University Hospital, University of Cologne, Cologne, Germany
13 Academic Teaching Practice, University of Cologne, Cologne, Germany
14 Department of Neurology, Klinikum Köln-Merheim, Cologne, Germany
Open Access funding enabled and organized by Projekt DEAL. This work was supported by the Innovation Funds of the Federal Joint Committee (G-BA), grant number: 01VSF19029.
Author information
Authors and affiliations.
Department of Palliative Medicine, Faculty of Medicine and University Hospital, University of Cologne, Cologne, Germany
Anne Müller, Fabian Hebben, Kim Dillen, Veronika Dunkl, Raymond Voltz & Heidrun Golla
Department of Neurology, Faculty of Medicine and University Hospital, University of Cologne, Cologne, Germany
Yasemin Goereci & Clemens Warnke
Center for Integrated Oncology Aachen Bonn Cologne Düsseldorf (CIO ABCD), University of Cologne, Cologne, Germany
Raymond Voltz
Center for Health Services Research, University of Cologne, Cologne, Germany
German Society of Care and Case Management E.V. (DGCC), Münster, Germany
Peter Löcherbach
You can also search for this author in PubMed Google Scholar
- Anne Müller
- , Fabian Hebben
- , Kim Dillen
- , Veronika Dunkl
- , Yasemin Goereci
- , Raymond Voltz
- , Peter Löcherbach
- , Clemens Warnke
- , Heidrun Golla
- , Dirk Müller
- , Dorthe Hobus
- , Eckhard Bonmann
- , Franziska Schwartzkopff
- , Gereon Nelles
- , Gundula Palmbach
- , Herbert Temmes
- , Isabel Franke
- , Judith Haas
- , Julia Strupp
- , Kathrin Gerbershagen
- , Laura Becker-Peters
- , Lothar Burghaus
- , Martin Hellmich
- , Martin Paus
- , Solveig Ungeheuer
- , Sophia Kochs
- , Stephanie Stock
- , Thomas Joist
- & Volker Limmroth
Contributions
HG, KD, CW designed the trial. HG, KD obtained ethical approvals. HG, KD developed the interview guidelines with help of the CCM (SU). AM was responsible for collecting qualitative data, developing the code system, coding, analysis of the data and writing the first draft of the manuscript, thoroughly revised and partly rewritten by HG. FH supported in collecting qualitative data, coding and analysis of the interviews. KD supported in collecting qualitative data. AM, FH, KD, VD, YG, RV, PL, CW, HG discussed and con-solidated the finalized category system. AM, FH, KD, VD, YG, RV, PL, CW, HG read and commented on the manuscript and agreed to the final version.
Authors’ information
Not applicable.
Corresponding author
Correspondence to Anne Müller .
Ethics declarations
Ethics approval and consent to participate.
Participants were provided with oral and written information about the trial and provided written informed consent. Ethical approval was obtained from the Ethics Committee of the University of Cologne (#20–1436). The trial is registered in the German Register for Clinical Studies (DRKS) (DRKS00022771) and is conducted under the Declaration of Helsinki.
Consent for publication
Competing interests.
Clemens Warnke has received institutional support from Novartis, Alexion, Sanofi Genzyme, Janssen, Biogen, Merck and Roche. The other authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Müller, A., Hebben, F., Dillen, K. et al. “So at least now I know how to deal with things myself, what I can do if it gets really bad again”—experiences with a long-term cross-sectoral advocacy care and case management for severe multiple sclerosis: a qualitative study. BMC Health Serv Res 24 , 453 (2024). https://doi.org/10.1186/s12913-024-10851-1
Download citation
Received : 23 November 2023
Accepted : 11 March 2024
Published : 10 April 2024
DOI : https://doi.org/10.1186/s12913-024-10851-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cross-sectoral
- Qualitative research
- Health care specialist
- Severe multiple sclerosis
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Signs of multiple sclerosis show up in blood years before symptoms
Scientists clear a potential path toward earlier treatment for a disease that affects nearly 1,000,000 people in the united states.
In a discovery that could hasten treatment for patients with multiple sclerosis (MS), UC San Francisco scientists have discovered a harbinger in the blood of some people who later went on to develop the disease.
In about 1 in 10 cases of MS, the body begins producing a distinctive set of antibodies against its own proteins years before symptoms emerge. These autoantibodies appear to bind to both human cells and common pathogens, possibly explaining the immune attacks on the brain and spinal cord that are the hallmark of MS.
The findings were published in Nature Medicine on April 19.
MS can lead to a devastating loss of motor control, although new treatments can slow the progress of the disease and, for example, preserve a patient's ability to walk. The scientists hope the autoantibodies they have discovered will one day be detected with a simple blood test, giving patients a head start on receiving treatment.
"Over the last few decades, there's been a move in the field to treat MS earlier and more aggressively with newer, more potent therapies," said UCSF neurologist Michael Wilson, MD, a senior author of the paper. "A diagnostic result like this makes such early intervention more likely, giving patients hope for a better life."
Linking infections with autoimmune disease
Autoimmune diseases like MS are believed to result, in part, from rare immune reactions to common infections.
In 2014, Wilson joined forces with Joe DeRisi, PhD, president of the Chan Zuckerberg Biohub SF and a senior author of the paper, to develop better tools for unmasking the culprits behind autoimmune disease. They took a technique in which viruses are engineered to display bits of proteins like flags on their surface, called phage display immunoprecipitation sequencing (PhIP-Seq), and further optimized it to screen human blood for autoantibodies.
PhIP-Seq detects autoantibodies against more than 10,000 human proteins, enough to investigate nearly any autoimmune disease. In 2019, they successfully used it to discover a rare autoimmune disease that seemed to arise from testicular cancer.
MS affects more than 900,000 people in the US. Its early symptoms, like dizziness, spasms, and fatigue, can resemble other conditions, and diagnosis requires careful analysis of brain MRI scans.
The phage display system, the scientists reasoned, could reveal the autoantibodies behind the immune attacks of MS and create new opportunities to understand and treat the disease.
The project was spearheaded by first co-authors Colin Zamecnik, PhD, a postdoctoral researcher in DeRisi's and Wilson's labs; and Gavin Sowa, MD, MS, former UCSF medical student and now internal medicine resident at Northwestern University.
They partnered with Mitch Wallin, MD, MPH, from the University of Maryland and a senior author of the paper, to search for autoantibodies in the blood of people with MS. These samples were obtained from the U.S. Department of Defense Serum Repository, which stores blood taken from armed service members when they apply to join the military.
The group analyzed blood from 250 MS patients collected after their diagnosis, plus samples taken five or more years earlier when they joined the military. The researchers also looked at comparable blood samples from 250 healthy veterans.
Between the large number of subjects and the before-and-after timing of the samples, it was "a phenomenal cohort of individuals to look at to see how this kind of autoimmunity develops over the course of clinical onset of this disease," said Zamecnik.
A consistent signature of MS
Using a mere one-thousandth of a milliliter of blood from each time point, the scientists thought they would see a jump in autoantibodies as the first symptoms of MS appeared.
Instead, they found that 10% of the MS patients had a striking abundance of autoantibodies years before their diagnosis.
The dozen or so autoantibodies all stuck to a chemical pattern that resembled one found in common viruses, including Epstein-Barr Virus (EBV), which infects more than 85% of all people, yet has been flagged in previous studies as a contributing cause for MS.
Years before diagnosis, this subset of MS patients had other signs of an immune war in the brain. Ahmed Abdelhak, MD, co-author of the paper and a postdoctoral researcher in the UCSF laboratory of Ari Green, MD, found that patients with these autoantibodies had elevated levels of neurofilament light (Nfl), a protein that gets released as neurons break down.
Perhaps, the researchers speculated, the immune system was mistaking friendly human proteins for some viral foe, leading to a lifetime of MS.
"When we analyze healthy people using our technology, everybody looks unique, with their own fingerprint of immunological experience, like a snowflake," DeRisi said. "It's when the immunological signature of a person looks like someone else, and they stop looking like snowflakes that we begin to suspect something is wrong, and that's what we found in these MS patients."
A test to speed patients toward the right therapies
To confirm their findings, the team analyzed blood samples from patients in the UCSF ORIGINS study. These patients all had neurological symptoms and many, but not all, went on to be diagnosed with MS.
Once again, 10% of the patients in the ORIGINS study who were diagnosed with MS had the same autoantibody pattern. The pattern was 100% predictive of an MS diagnosis. Across both the Department of Defense group and the ORIGINS group, every patient with this autoantibody pattern had MS.
"Diagnosis is not always straightforward for MS, because we haven't had disease specific biomarkers," Wilson said. "We're excited to have anything that can give more diagnostic certainty earlier on, to have a concrete discussion about whether to start treatment for each patient."
Many questions remain about MS, ranging from what's instigating the immune response in some MS patients to how the disease develops in the other 90% of patients. But the researchers believe they now have a definitive sign that MS is brewing.
"Imagine if we could diagnose MS before some patients reach the clinic," said Stephen Hauser, MD, director of the UCSF Weill Institute for Neurosciences and a senior author of the paper. "It enhances our chances of moving from suppression to cure."
- Immune System
- Today's Healthcare
- Diseases and Conditions
- Alzheimer's
- Multiple Sclerosis
- Brain-Computer Interfaces
- Disorders and Syndromes
- Multiple sclerosis
- Drug discovery
- Excitotoxicity and cell damage
- Pharmaceutical company
- Atherosclerosis
- Salmonella infection
- Cerebral contusion
- Alzheimer's disease
Story Source:
Materials provided by University of California - San Francisco . Original written by Levi Gadye. Note: Content may be edited for style and length.
Journal Reference :
- Colin R. Zamecnik, Gavin M. Sowa, Ahmed Abdelhak, Ravi Dandekar, Rebecca D. Bair, Kristen J. Wade, Christopher M. Bartley, Kerry Kizer, Danillo G. Augusto, Asritha Tubati, Refujia Gomez, Camille Fouassier, Chloe Gerungan, Colette M. Caspar, Jessica Alexander, Anne E. Wapniarski, Rita P. Loudermilk, Erica L. Eggers, Kelsey C. Zorn, Kirtana Ananth, Nora Jabassini, Sabrina A. Mann, Nicholas R. Ragan, Adam Santaniello, Roland G. Henry, Sergio E. Baranzini, Scott S. Zamvil, Joseph J. Sabatino, Riley M. Bove, Chu-Yueh Guo, Jeffrey M. Gelfand, Richard Cuneo, H.-Christian von Büdingen, Jorge R. Oksenberg, Bruce A. C. Cree, Jill A. Hollenbach, Ari J. Green, Stephen L. Hauser, Mitchell T. Wallin, Joseph L. DeRisi, Michael R. Wilson. An autoantibody signature predictive for multiple sclerosis . Nature Medicine , 2024; DOI: 10.1038/s41591-024-02938-3
Cite This Page :

Explore More
- Advance in Heart Regenerative Therapy
- Bioluminescence in Animals 540 Million Years Ago
- Profound Link Between Diet and Brain Health
- Loneliness Runs Deep Among Parents
- Food in Sight? The Liver Is Ready!
- Acid Reflux Drugs and Risk of Migraine
- Do Cells Have a Hidden Communication System?
- Mice Given Mouse-Rat Brains Can Smell Again
- How Do Birds Flock? New Aerodynamics
- Cancer: Epigenetic Origin Without DNA Mutation
Trending Topics
Strange & offbeat.
- Alumni & Friends
Current Students
- Faculty & Staff
- Parents & Family
Prospective Students
My unc charlotte, campus events.
- About UNC Charlotte
- Campus Life
- Graduate Admissions
Faculty and Staff
- Human Resources
- Auxiliary Services
- Inside UNC Charlotte
- Academic Affairs
- Financial Aid
- Student Health Center
Alumni and Friends
- Alumni Association
- Advancement
- Make a Gift
- News and Features
Groundbreaking study reveals potential diagnostic marker for Multiple sclerosis years before symptom onset

A new study published today in Nature Medicine unveils a significant breakthrough in the understanding and early detection of multiple sclerosis (MS). Researchers have identified a unique autoantibody signature present in approximately 10% of patients with MS years before the onset of clinical symptoms.
Danillo Augusto , Ph.D., an assistant professor in biology at UNC Charlotte and a co-author of the study, stated, "This study sheds light on the preclinical phase of MS and provides a promising avenue for early detection and intervention. Identifying patients at high risk of developing MS before symptom onset could revolutionize patient care and treatment strategies."
Autoantibodies are basically antibodies that are supposed to fight off invaders but end up turning against one’s own body, causing problems like autoimmune diseases. Utilizing the U.S. Department of Defense Serum Repository, a cohort encompassing more than 10 million individuals, researchers conducted whole-proteome autoantibody profiling on hundreds of MS patients’ samples collected before and after symptom onset. They discovered a distinct cluster of patients exhibiting an autoantibody signature targeting a common recognizable pattern. Notably, these patients showed antibody reactivity years before developing any MS symptoms and had elevated levels of serum neurofilament light (sNfL), indicating early neuroaxonal injury.
Further validation of this autoantibody signature was conducted on samples from a separate MS cohort, confirming its high specificity for patients diagnosed with MS. This finding marks a significant milestone in MS research, potentially paving the way for the development of antigen-specific biomarkers for high-risk individuals with clinically or radiologically isolated neuroinflammatory syndromes.
The study, led by Michael Wilson, M.D., a professor of neurology at the University of California, San Francisco, offers hope for improved early diagnosis and intervention in MS, potentially leading to better patient outcomes. Further research is underway to elucidate the underlying immunological mechanisms and explore additional diagnostic and therapeutic implications.
Inside UNC Charlotte is produced and maintained by the Office of University Communications. Faculty and staff members can submit news or story/video ideas for consideration via the online form or email [email protected] .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Surgery and risk for multiple sclerosis: a systematic review and meta-analysis of case–control studies
Carole lunny.
1 Centre for Nursing and Health Studies, Faculty of Health Disciplines, Athabasca University, 1 University Drive Athabasca, Alberta, T9S 3A3, Canada
Jennifer A Knopp-Sihota
Shawn n fraser.
Although the precise etiology of multiple sclerosis is largely unknown, there is some speculation that a prior history of surgery may be associated with the subsequent risk for developing the disease. Therefore, we aimed to examine surgery as a risk factor for the diagnosis of multiple sclerosis.
We searched for observational studies that evaluated the risk for developing multiple sclerosis after surgery that occurred in childhood (≤ 20 years of age) or “premorbid” (> 20 years of age). We specifically included surgeries classified as: tonsillectomy, appendectomy, adenoidectomy, or “surgery”. We performed a systematic review and meta-analyses and calculated odds ratios (OR) and their 95% confidence intervals (CIs) using a random effects model.
We identified 33 case–control studies, involving 27,373 multiple sclerosis cases and 211,756 controls. There was a statistically significant association between tonsillectomy (OR = 1.32, 95% CI 1.08-1.61; 12 studies, I 2 = 44%) and appendectomy (OR = 1.16, 95% CI 1.01-1.34; 7 studies, I 2 = 0%) in individual’s ≤ 20 years of age and the subsequent risk for developing multiple sclerosis. There was no statistically significant association between risk for multiple sclerosis and tonsillectomy occurring after age 20 (OR = 1.20, 95% CI 0.94-1.53; 9 studies, I 2 = 32%), in those with appendectomy at > 20 years (OR = 1.26, 95% CI 0.92-1.72; 5 studies, I 2 = 46%), and in those with adenoidectomy at ≤ 20 years of age (OR = 1.06, 95% CI 0.68-1.68; 3 studies, I 2 = 35%). The combined OR of 15 studies (N = 2,380) looking at “surgery” before multiple sclerosis diagnosis was not statistically significant (OR = 1.19, 95% CI 0.83-1.70; I 2 = 71%).
Conclusions
We found a small but statistically significant and clinically important increased risk for developing multiple sclerosis, in those with tonsillectomy and appendectomy at ≤ 20 years of age. There was no convincing evidence to support the association of other surgeries and the risk for multiple sclerosis. Well-designed prospective etiological studies, pertaining to the risk for developing multiple sclerosis, ought to be conducted and should include the examination of various surgeries as risk factors.
Multiple sclerosis (MS) is a complex immune-mediated inflammatory disease of the central nervous system affecting an estimated 2 million people worldwide [ 1 ]. MS, one of the most common non-traumatic neurological disorders in younger adults, affects more females (than males) with a population prevalence of approximately 0.1% in North America [ 1 ]. The epidemiological and clinical importance of MS lies in the significant disability and morbidity attributed to the disease. Not only is the condition relatively common, it is costly with an estimated economic burden exceeding $6 billion annually in the United States alone [ 2 ].
Description of the condition
The first symptoms or signs of MS, diagnosed by a physician, are referred to as the clinical onset of the disease. As there are limited (and consistent) clinical, laboratory, and imaging findings in MS, diagnostic classifications are generally reduced to “definite MS” and “possible MS”. Several established diagnostic standards have been used over the years to assist physicians in the diagnosis of MS; these include criterion such as the Poser criteria [ 3 ] and most recently the McDonald criteria [ 4 ].
Although the precise etiology of MS is largely unknown, epidemiological studies point at an important role in both genetic and environmental factors that seem to act synergistically increasing an individual’s risk of developing the disease. Specifically, risks such as genetic factors (the presence of HLA-DRB1*15 alleles), infectious causes including Epstein-Barr virus (EBV), vitamin D insufficiency, exposure to cigarette smoke, and a more northern geographic residence (latitude) have all been well documented in the literature [ 5 - 9 ]. There is some speculation that other factors, including a history of tonsillectomy, appendectomy, or other surgery may also be associated with the risk of developing MS [ 10 ].
Relevance of systematic review and meta-analysis
Although there have been studies examining prior surgery as a risk factor for MS, these studies have generally been smaller-scale observational studies of varied methodological quality in which a wide range of both positive and negative results have been reported. Therefore, we conducted a formal Cochrane style systematic review and meta-analysis of observational studies to examine the association between tonsillectomy, appendectomy, adenoidectomy, and other “surgery” and the risk of developing MS. We are not aware of another similar published meta-analysis on this topic; therefore, a systematic review (SR) including meta-analysis is timely.
We followed the procedures for conducting systematic reviews and meta-analysis as outlined by the Cochrane Collaboration [ 11 ] and the reporting guidelines of the Meta-Analysis of Observational Studies in Epidemiology (MOOSE) [ 12 ].
Search strategy
Studies were identified by several methods. First, we searched for completed reviews in the Database of Abstracts of Reviews of Effects (DARE), Evidence for Policy and Practice Information (EPPI) Centre, the HealthEvidence.ca website, and the Cochrane Database of Systematic Reviews (CDSR). We searched for individual studies in the MEDLINE, EMBASE, SCIRUS, Web of Science, PubMed, and the LILACS (Latin American and Caribbean Computer Library Center) databases. The Google Web search engine ( http://www.google.com ) and Google Scholar ( http://www.scholar.google.com ) were used to locate articles that may not have been included in the above databases. Grey literature was searched using ‘OpenSIGLE’, ‘NTIS’, ‘Health Management Information’, ‘British National Bibliography for Report Literature’, Proquest Dissertations and Theses - Full Text, Dissertation Abstracts, CINHAL, and CyberTesis.
We used the following text words and Medical Subject Headings: (a) multiple sclerosis OR demyelinating disease , and (b) s urgery; surgical intervention; operations; medical history; hospitalisation; tonsillectomy; anaesthetic; appendectomy; adenoidectomy; risk factor; etiologic factor; severe; minor; association; causation; case–control; cohort. In addition, reference lists of all relevant articles were examined for further pertinent studies; and conference proceedings were sought from various web sites and organizations. Forward citation searches of included studies and relevant literature reviews were also done. Primary authors and experts in the field were contacted to identify additional published, unpublished, or 'in-progress' studies. The search was not limited by publication date, language, or publication status. All databases were last accessed in August 2012.
Inclusion criteria
We planned to include a broad range of observational studies: cohort, case–control, and cross sectional designs. As there were few primary studies, we also planned to include retrospective studies utilizing secondary data from healthcare databases. To be eligible for inclusion, studies needed to include patients with physician diagnosed MS (preferably by using diagnostic criteria for a definite diagnosis of MS) and report original data. Studies were excluded if there was no control group.
The primary outcome of interest was the development of MS following a past history of tonsillectomy, appendectomy, adenoidectomy, or other surgery. If the authors did not specify the type of surgery, we included these studies and classified them as “other surgery”. Surgeries were defined according to their classification in each individual study. Further, due to the estimated mean latency period and the critical age at puberty, these categories and sub-categories were divided by age at the time of surgery: (1) age ≤ 20 years, and (2) > 20 years.
Data collection and analysis
Selection of studies.
One of the study investigators (CL) performed the initial search of all databases to identify potentially relevant citations. Where it was not possible to accept or reject the study, the full text of the citation was obtained for further evaluation. Following the screening of titles and abstracts, the full texts of potential articles were retrieved (and translated into English where required) and assessed independently by two of the study investigators (CL, JKS). If any differences in opinion occurred, they were resolved by consensus with a third reviewer.
Data extraction and management
Data were independently extracted by one unmasked reviewer (CL) using a standardized electronic data collection form and were then checked by a second reviewer (JKS) for accuracy. When raw data were not provided, the data were extracted from figures; where necessary, we attempted to seek additional information from first or corresponding authors of the included studies via electronic mail. The following information was obtained for each study (where possible): source, eligibility, methods, participant demographics, MS diagnostic information, confounding variables adjusted for, outcome exposures, and results.
Quality assessment: Risk of bias in included studies
After identification of articles meeting the inclusion criteria, two review authors (CL, JKS) independently assessed the methodological quality of studies according to the criteria of the Newcastle-Ottawa Quality Assessment Scale (NOS) as recommended by the Cochrane Collaboration for assessing the quality of non-randomized studies [ 13 ]. The NOS is based on a cumulative score in each of three broad categories: selection of study groups, comparability of their cases and controls, and their ascertainment of the outcome / exposure on cases and controls. If a study fulfils the criteria for an item, a score of 1 point is allocated, with the exception of comparability which can score up to 2 points, resulting in a maximum score of 9. Similar to other reviews, we considered studies that received a score of ≥ 6 on the NOS criteria to be of high quality. We specifically classified studies as high risk of bias (1–3 points), medium risk of bias (4–5 points), or low risk of bias (6–9 points). In the case of disagreement between reviewers, differences were to be resolved by discussion until consensus was achieved.
Dealing with missing data
As missing data (statistics) were evident in many of the included studies, we attempted to contact 13 separate investigators at least twice. Six authors replied, and two provided the requested data; therefore, available data were extracted from published reports, and missing data were imputed. For those studies reporting “no significance”, with no additional statistical data, we assumed an odds ratio (OR) of 1.0 and estimated the confidence intervals (CIs) based on the number of reported MS cases [ 14 ]. Sensitivity analyses were performed to check the effect of imputation.
Assessment of heterogeneity and reporting bias
Heterogeneity between studies was examined visually using the I 2 statistic. Deeks and colleagues (for the Cochrane Collaboration) [ 15 ] suggest the following as a rough guide for interpreting the I 2 statistic:
•0% to 40%: might not be important;
•30% to 60%: may represent moderate heterogeneity;
•50% to 90%: may represent substantial heterogeneity;
•75% to 100%: considerable heterogeneity.
Possible sources of heterogeneity were assessed by sensitivity analyses and described qualitatively in Table 1 (Characteristics of included studies).
Characteristics of included studies
1 Odds ratio for combined surgeries using a random effects model.
2 Reported as not statistically significant, no data provided.
* Indicates statistically significant results.
A = Allison & Miller criteria, Append = appendectomy, Adenoid = adenoidectomy, B = Bauer criteria, CI = confidence interval, Dx = diagnosis, LAT = latitude, Mc = McAlpine criteria, M = McDonald criteria, MS = multiple sclerosis, NOS = Newcastle-Ottawa Scale, N = neurologist diagnosed, NS = not significant, OR = odds ratio, P = Poser criteria, Pre : Premorbid, age not specified other than surgery occurring before MS diagnosis, Tonsil = tonsillectomy, Y = years.
Stratified meta-regression, based on sub-groups including 10 or more studies, was performed to further examine heterogeneity. A priori , we planned to explore the following population-level continuous variables (geographic latitude, female-to-male MS case ratio, mean age of MS onset), and study-level dichotomous variables (language [English vs. non-English]), publication type [published vs. unpublished], number of covariates adjusted for [≤ 2 vs. > 2], total sample size [≤ 100 vs. > 100], and sample size of MS cases [≤ 100 vs. > 100]. Odds ratios (β) and 95% CIs were calculated using the study level log OR and the standard error (SE) of the estimate by constructing univariate random effects (RE) meta-regression models in STATA 12 using the megareg command. A plot of ORs was done against NOS scores to determine if there was a linear relationship between the methodological quality of the studies and their results [ 16 ]. We planned to explore publication bias and other potential reporting biases, in those pooled comparisons with 10 or more studies, using funnel plots. We used the graphical approach described by Peters et al. for assessing dichotomous outcomes with effects measured as odds ratios [ 17 ].
Effect measurement and data synthesis
Meta-analyses were performed using the Cochrane Collaboration software program Review Manager (Rev Man) Version 5.1 [ 18 ]. To estimate the strength of association between surgery exposure variables and risk for MS diagnosis, data were pooled using the inverse variance (IV) approach to calculate the OR and 95% CIs and statistical significance was set at p < 0.05. When interpreting results of the forest plots for dichotomous data, the area to the right side of the forest plot graph (> 1) favoured the control group. Studies were weighted based on sample size and the number of events.
Meta-analyses methods were selected based on study heterogeneity and the number of studies included in the analyses. When the I 2 statistic was greater than 75%, we considered it substantial heterogeneity and pooled the study results using a RE model [ 19 ].
Subgroup analysis and investigation of heterogeneity
A priori , we planned to explore and address possible clinical heterogeneity as well as to investigate the magnitude and precision of effects by performing sub-group analyses based on type of surgery (tonsillectomy, appendectomy, adenoidectomy, other surgery), and age at time of surgery (≤ 20 years of age and those > 20 years of age). Sub-group analyses were also performed on reported association (number of covariates), female to male sex ratio, NOS score, latitude, and age at MS onset.
Sensitivity analysis
We performed sensitivity analyses by examining the results of the meta-analysis under different assumptions and checked for robustness of the observed findings. A priori , the following sensitivity analyses were planned:
1. By limiting included studies in the analyses to those with the highest methodological quality, do the results change?
2. For studies in which the OR was reported as “not significant” and therefore had to be imputed, do the results of the pooled analysis change if these are excluded from the results?
After excluding duplicate studies, we identified 100 individual studies, of which 75 were potentially relevant. Of these, despite our best attempts to contact primary or corresponding authors, eight studies could not be located [ 20 - 27 ]; therefore, 67 potentially relevant full text articles were retrieved for closer examination. Of the retrieved articles, 34 were excluded for the following reasons: 18 did not examine surgery as a risk factor [ 28 - 45 ]; six did not have a control group [ 46 - 51 ]; five were review articles [ 52 - 56 ]; four were not specific to MS [ 57 - 60 ]; and one had insufficient data, and we were unable to locate study authors [ 61 ]. A total of 33 studies were identified which met the inclusion criteria for the systematic review [ 62 - 94 ]. One additional cohort study was found but was not included due to heterogeneity in study design and exposure [ 95 ]. Figure 1 outlines the study selection process.

Flow diagram of study selection.
All of the included studies were case–control studies and were published between 1953 and 2011. Seventeen individual studies reported tonsillectomy data [ 62 , 64 , 67 - 69 , 71 , 73 , 75 , 76 , 78 ],[ 79 , 82 , 84 , 87 , 88 , 92 , 93 ], 11 reported appendectomy data [ 62 , 64 , 68 , 73 , 75 , 78 , 82 , 84 ],[ 85 , 87 , 89 ], three reported adenoidectomy data [ 64 , 82 , 93 ], and 18 reported on other surgeries [ 63 , 65 , 66 , 70 , 72 - 74 , 77 , 80 , 81 ],[ 83 , 85 , 86 , 88 , 90 , 91 , 93 , 94 ]. The majority of the studies (17 studies) were published in European countries [ 64 , 67 , 69 - 71 , 73 , 75 , 78 , 82 , 83 ],[ 85 , 87 , 89 , 92 - 94 ], followed by nine in North America [ 63 , 68 , 72 , 77 , 80 , 81 , 84 , 88 ],[ 90 ], four published in the Middle East [ 62 , 65 , 91 , 93 ], and lastly one each from India [ 66 ], Brazil [ 74 ], and Cuba [ 86 ].
Exposure risks for MS were reported as ORs in most of the studies while others simply reported whether the exposure risk for MS was “significant” or “not significant” [ 65 , 80 , 81 , 85 , 88 ]. The ORs ranged from 0.46 to 5.0 depending on the type of surgery reported. Eight independent studies reported statistically significant results for specific exposures [ 75 , 78 , 85 , 87 , 90 - 92 , 94 ], while the remaining 25 did not. See characteristics of included studies in Table 1 .
Quality assessment
Included studies were classified according to the NOS with seven studies considered high risk of bias [ 66 , 69 , 71 , 73 , 75 , 77 , 79 ]; 16 studies had a medium risk of bias [ 63 , 65 , 67 , 70 , 72 , 74 , 78 , 81 ],[ 83 - 86 , 88 , 90 , 91 , 94 ]; and nine studies had a low risk of bias [ 62 , 64 , 68 , 80 , 82 , 87 , 89 , 92 ],[ 93 ]. One study could not be assessed due to lack of included data [ 76 ].
Exposure results
The meta-analysis included data from all 33 studies with 27,373 MS cases and 211,756 controls; there were twice as many females than males included in the studies and the mean age of MS diagnosis was 31 years. See Table 2 for pooled surgery exposure results.
Odds ratios for pooled surgery exposures using a random effects model
* Indicates statistically significant results at p < 0.05.
CI = confidence interval , MS = multiple sclerosis, OR = odds ratio .
Tonsillectomy
Of the 17 separate studies reporting on tonsillectomy, 12 examined tonsillectomy at age ≤ 20 and 9 examined tonsillectomy at age > 20, or simply “premorbid”. Pooled analyses displayed statistical heterogeneity hence the estimates were based on the RE model.
The 12 studies examining tonsillectomy at age ≤ 20 included 4,414 MS cases and 4,422 controls. The pooled RE model revealed moderate heterogeneity in the sample (I 2 = 44%; p = 0.05) and a statistically significant relationship between tonsillectomy and MS onset (OR = 1.32; 95% CI, 1.08-1.61; p = 0.006). To further explore heterogeneity, we conducted a sensitivity analysis based on study quality (removing those studies with a NOS score < 6). Although removing the six studies with a NOS score of < 6 provided a more homogenous sample (I 2 = 12%; p = 0.34) the difference was not significant as the direction and magnitude of the effect did not change (OR = 1.29; 95% CI, 1.08-1.53; p = 0.005); therefore, we included all 12 studies in the final analysis. Sensitivity analysis based on removing the one study where the OR was imputed did not change the significance nor magnitude of the effect (OR = 1.27; 95% CI, 1.02-1.58; p = 0.03); therefore, we included all 12 studies in the final analysis. Forest plot results for tonsillectomy exposure occurring at ≤ 20 years of age are presented in Figure 2 .

Forest plot for tonsillectomy exposure occurring at ≤ 20 years of age. Forest plot of 12 included studies reporting tonsillectomy in those ≤ 20 years of age in cases with multiple sclerosis and controls. Horizontal lines , 95% CIs of each study; squares , odds ratios of each individual study (the size represents the weight that the study was given in the meta-analysis); diamond , the pooled summary estimate; solid vertical line , null value. OR > one favoured the control group.
The nine studies examining tonsillectomy in patients’ > 20 years or “premorbid” included 1,801 MS cases and 1,618 controls. The RE model revealed a homogeneous sample (I 2 = 32%; p = 0.16) with no statistical difference between the groups (OR = 1.20; 95% CI, 0.94-1.53; p = 0.15). When four studies with a NOS score of < 6 were excluded, the pooled results became more homogeneous (I 2 = 0%; p = 0.88) but the magnitude and the significance of the results did not change (OR = 1.04; 95% CI, 0.78-1.37; p = 0.85). All nine studies reported exact OR data thus, sensitivity analysis, based on the imputation of data, was not required and all nine studies were included in the final analysis.
Appendectomy
Eleven separate studies examined appendectomy; nine examined appendectomy in those ≤ 20 years and five examined appendectomy at age > 20, or “premorbid”. Pooled analyses displayed statistical heterogeneity, for that reason the estimates were based on the RE model.
The nine studies examining appendectomy in those ≤ 20 years included 21,574 MS cases and 205,480 controls. Moderate heterogeneity (I 2 = 48%; p = 0.05) of the RE pooled results was demonstrated with no statistical relationship between appendectomy in those ≤ 20 and MS onset (OR = 1.16; 95% CI, 0.87-1.53; p = 0.31).We further conducted sensitivity analysis based on study quality. Although removing the five studies with a NOS score of < 6 provided a more homogenous sample (I 2 = 13%; p = 0.33) the difference was not significant as the magnitude and precision of the effect did not change (OR = 1.21; 95% CI, 0.87-1.69; p = 0.27). Sensitivity analysis based on removing two studies where the ORs were imputed reduced the heterogeneity (I 2 = 0%; p = 0.54) and changed the significance of the result (OR = 1.16; 95% CI, 1.01-1.34; p = 0.04) thus, we used the reduced, statistically significant model in the final analysis.
The five studies examining appendectomy occurring in those patients > 20 years or “premorbid” included 21,360 MS cases and 205,021 controls. The RE model revealed a moderately homogeneous sample (I 2 = 46%; p = 0.11) with no statistical difference between groups (OR = 1.26; 95% CI, 0.92-1.72; p = 0.15). When studies with a NOS score of < 6 were excluded, the results did not change. All five studies reported exact OR data, consequently, sensitivity analysis based on the imputation of ORs was not required and all five studies were included in the final analysis.
Adenoidectomy
Three studies, involving 458 MS cases and 636 controls, reported on adenoidectomy in patient’s ≤ 20 years. The RE model revealed a homogeneous sample (I 2 = 35%; p = 0.21) with no statistical difference between groups (OR = 1.06; 95% CI, 0.68-1.68; p = 0.79). All three studies were of high quality and all reported exact OR data, as a result, sensitivity analyses were not required.
Eighteen discrete studies examined “other surgery”; four examined surgery occurring in those ≤ 20 years and 15 examined surgery in patients > 20, or “premorbid”. Pooled analyses displayed statistical heterogeneity thus the estimates were based on the RE model.
The four studies reporting on other surgery occurring in subject’s ≤ 20 years included 485 MS cases and 1,202 controls. The RE model revealed a homogeneous sample (I 2 = 19%; p = 0.30) with no statistical difference between groups (OR = 0.95; 95% CI, 0.70-1.31; p = 0.77). Sensitivity analysis, based on study quality, was not done as all but one of the four studies had a NOS score of < 6. Further sensitivity analysis, excluding those studies that did not report a specific OR, did not significantly change the results (OR = 1.01; 95% CI, 0.28-3.57; p = 0.99).
The 15 studies examining other surgery in patients > 20, or “premorbid” included 1,099 MS cases and 1,371 controls. Significant heterogeneity (I 2 = 71%; p < 0.0001) of the RE pooled results was demonstrated; regardless, there were no statistical differences between groups (OR = 1.19; 95% CI, 0.83-1.70; p = 0.35). Sensitivity analysis, based on study quality, was not done as all but two of the 15 included studies had a NOS score of < 6. Further sensitivity analysis, excluding those studies that did not report a specific OR, did not significantly change the results (OR = 1.32; 95% CI, 0.92-1.91; p = 0.14).
Examining bias
To visually assess for heterogeneity, we plotted the ORs of high quality versus low quality studies. The plot showed no distinct linear relationship between methodological quality of studies (NOS score) and ORs, with no obvious clustering, indicating a low risk of bias.
For the tonsillectomy exposure (≤ 20 years), the test for publication bias was not statistically significant ( p = 0.94), with a symmetrical funnel plot indicating a low risk for publication bias [ 96 ]. For the surgery premorbid exposure, the test for publication bias was also not statistically significant ( p = 0.62); although, the plot was more asymmetrical indicating the potential for publication bias. Given the small number of studies included in the other exposures (< 10 studies), the interpretation of funnel plots must be undertaken with caution and are therefore not included here.
Meta-regression
Results from the meta- regression are presented in Table 3 . Meta-regression was performed on the subgroups including at least 10 studies, namely tonsillectomy at age ≤ 20 and premorbid “surgery”. None of the variables entered into the regression analysis, for the surgery premorbid exposure, reached statistical significance therefore not significantly influencing the effect sizes. For the tonsillectomy at age ≤ 20, only one of the variables, the number of covariates adjusted for (≤ 2 vs. > 2), reached statistical significance (β = 1.64; 95% CI, 1.02-2.62). That is, the effect size or risk for MS diagnosis increased as the number of covariates that were adjusted for (in the individual included studies) increased. This further indicates limited residual heterogeneity after controlling for the influence of latitude, female to male sex ratio, mean age of MS onset, NOS score, language, publication status, and sample size. Although not a statistically significant finding ( p = 0.45), the tonsillectomy exposure, in those ≤ 20 years, increased as the female to male ratio increased.
Sensitivity analyses and stratified meta-regression for assessing heterogeneity among case–control studies looking at the exposures tonsillectomy in childhood and “surgery” premorbid 1
1 All analyses weighted by sample size.
2 OR (95 % CI) were calculated using the random effects model in RevMan.
3 β (95 % CI) were calculated using the study level log OR and the SE of the estimate (calculated in RevMan) by univariate random effects meta-regression in STATA 12 using the megareg command.
4 All studies were published – analysis not warranted.
5 Number of potentially confounding variables adjusted for in individual studies.
CI = confidence interval , MS = multiple sclerosis , NOS = Newcastle-Ottawa Scale, OR = odds ratio, Pub = Publication, SE = Standard error.
Overall, the evidence presented in this review supports a relationship between tonsillectomy and appendectomy in childhood and the subsequent risk of MS. More specifically, those with tonsillectomy or appendectomy at ≤ 20 years of age were approximately 30% more likely to be diagnosed with MS in comparison to similar patients who did not have a tonsillectomy or appendectomy at ≤ 20 years of age. The findings of this review do not support an association between tonsillectomy or appendectomy occurring in those > 20 years, adenoidectomy, and “other surgery” occurring at any age and the subsequent risk for the onset of MS. Although we did not find an association between these variables and risk for MS, it is important to note that due to the multi-factorial and heterogeneous nature of MS, surgery may indeed pose a slight risk for certain individuals.
Several theories linking tonsillectomy to MS risk have been postulated over the years. Meurman and Wising [ 39 ] proposed tonsillectecomy as a possible risk factor for MS in that an upper respiratory tract infection may trigger MS or that a locally deficient immune system may facilitate the invasion of an etiologically relevant, infectious agents. Tonsillectomy may leave sufficient lymphoid tissue adjacent to the central nervous system to instigate the exaggerated immune response seen in MS [ 39 , 69 , 87 ]. Poskanzer (1965) was particulary interested in examining tonsillectomy and MS risk at it predisposes to the development of neurological complications in poliomyelitis, another infection that is much more widespread than is suggested by its neurological manifestations [ 87 , 97 - 99 ].
Of particular interest is the association between recurrent tonsillitis and EBV infection and reactivation [ 100 ]. A recent meta-analysis of case–control and cohort studies found a statistically significant combined relative risk (RR) for MS in those with a past history of infectious mononucleosis (RR = 2.17; 95% CI, 1.97-2.39) [ 101 ]. Furthermore, others have found statistically significant elevated levels of antibody to some common infectious agents, other than EBV, in children and adults with MS compared to controls [ 92 , 102 - 104 ]. Krone and collegues [ 104 ] postulate that these findings reflect a dysregulation of immune function as a consequence of the development of the disease. They assert that immune dysregulation in MS is likely to be an early event preceding the onset of MS disease by many years or even decades [ 14 , 105 , 106 ]. It is likely that the elevated antibody concentrations do not directly cause MS but rather reflect a shift in patterns of immune reactivity away from protection towards enhancement of the risk of disease. These authors suggest that studies on MS-associated infectious agents could lead to the identification of specific antigenic determinants involved in the generation and maintenance of immune dysregulation.
There seems to be similarities between MS and appendicitis, which often results in appendectomy. More recently, scientists have recognized the role of the appendix as part of the body’s immune system, as it contains white blood cells and acts as a reservoir for “good” bacteria for the gut [ 107 ]. The role of the appendix is to contain “good bacteria”; when bacteria in the intestines die or are purged from dysentery or cholera, the “good bacteria” are replaced from the stores in the appendix. As a result, appendicitis (inflammation of the appendix) may indicate inadequate immunological function [ 84 , 89 , 108 ]; thereby providing an association of both EBV and appendicitis (resulting in appendectomy) with MS [ 109 - 111 ]. Immunological reaction relevant to appendicitis may indicate MS risk as activation of peripheral blood mononuclear cells, including those causing inflammatory destruction of myelin, which occurs in lymphoid tissue [ 89 , 108 ]. Appendicitis is a marker of immune characteristics influencing immune-mediated disease risk, as it has a direct role in the development of ulcerative colitis [ 89 , 112 , 113 ]. Further, CD8+ T-cell deficiency is a feature of both ulcerative colitis and MS [ 114 ].
There seems to be other possible similarities between MS and appendicitis. First, appendicitis and MS are autoimmune diseases. Both appendicitis and MS are diseases associated with industrialized countries but not developing countries [ 115 , 116 ]. MS is a disease largely prevalent in Europe, North America, Australia, and New Zealand, but is rare among Asians and Africans [ 116 ]. Lastly, several epidemiological and experimental studies support the hygiene hypothesis in both appendicitis [ 115 , 117 ] and MS [ 109 , 118 ], which postulates that immunopathology may be an unanticipated consequence of advances in sanitation and public health [ 109 , 118 , 119 ].
Quality of the evidence
One of the main challenges of the review related to the varying definitions of “surgery” in the included studies. Some studies included only tonsillectomy or appendectomy, and some included all surgeries. More importantly, the number of surgeries in individual patients (prior to MS onset) would have been a significant variable to assess; however, none of the included studies reported this as a potential risk factor. Another potential limitation pertained to the fact that, with the exception of a single study [ 89 ], the majority of studies reporting on appendectomy did not indicate the reason for surgery; therefore, we had to assume that appendectomy was as a result of appendicitis (infection / inflammation). It must be emphasized that characterizing appendectomy, by underlying diagnosis, may be important when assessing true MS risk.
Ideally, in case–control studies, cases should be representative of the entire population and be identified by independent MS diagnostic criteria. Controls should be randomly selected within the community of the residing representative MS cases. Only nine case–control studies examined in this review selected controls from the community [ 64 , 65 , 67 , 79 , 80 , 82 , 88 , 90 ],[ 93 ]. To further control for bias, control subjects should have no prior history of disease, representing healthy individuals of the same socio-economic class.
Age at disease onset is very important in MS etiologic studies and ought to have been used as a matching variable to potentially control for bias. The age at disease diagnosis is used to allow researchers a timeframe to assess for potential exposure to associated agents. Ideally, case–control matching ought to be done for universal variables such as age, sex, and age at MS diagnosis. Other matching variables to be considered in MS studies include residence and place of birth. Interviewer blinding, another means of controlling for bias, was done by only one study [ 94 ].
Potential bias in the review process
The two review authors who assessed the methodological quality were not blinded for authors, journal, or institution. The potential bias caused by the non-blinded quality assessment was expected to be low as neither review author had a conflict of interest. Specifically, the review authors did not have any (financial or other) interest in positive or negative results. Furthermore, we searched the grey literature extensively for eligible studies, presented the search strategy and the inclusion criteria list, and all of the final results of the assessment, so that readers can make their own determinations of the results and our conclusions.
There is a possibility of publication bias or study selection bias in this meta-analysis. For example, by missing unpublished negative studies we may be over-estimating the association between prior surgery and the risk for developing MS. However, a comprehensive search of the published literature for potentially relevant studies was conducted, using a systematic strategy to avoid bias. This was followed by attempts to contact corresponding and first authors, as we recognize that unpublished or negative studies may exist.
This result of this meta-analysis suggests a statistically significant and clinically important increased risk for developing MS in those with tonsillectomy and appendectomy at ≤ 20 years of age. Despite this significant finding, this in no way suggests or demonstrates causality, in that epidemiological studies can only provide etiological clues at best. More rigorous prospective studies, with high statistical power, are needed to prove an effect. Future prospective studies, that take into consideration the long latency period between the age of putative biological onset and clinical onset of MS, are needed in order to definitively rule out any links between tonsillectomy (or other surgeries) and MS.
Competing interests
The authors have no financial, personal, or any other kind of competing interests with this paper.
Authors’ contributions
Study concept and design: CL, JAK-S, and SF; acquisition and preparation of data: CL; analysis and interpretation of the data: CL, JAK-S, and SF; risk of bias assessment: CL and JAK-S; first draft of the manuscript: CL. All authors critically reviewed the manuscript and approved the final version of the manuscript to be published.
Pre-publication history
The pre-publication history for this paper can be accessed here:
http://www.biomedcentral.com/1471-2377/13/41/prepub
Authors’ note
We would be grateful if readers would send us reprints of any published or unpublished studies on multiple sclerosis and surgeries that have not been included in this paper, as well as any additional data missed from the included studies.
This study was supported by the Academic Research Fund of Athabasca University.
- Compston A, Coles A. Multiple sclerosis. Lancet. 2002; 359 (9313):1221–1231. doi: 10.1016/S0140-6736(02)08220-X. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Whetten-Goldstein K, Sloan FA, Goldstein LB, Kulas ED. A comprehensive assessment of the cost of multiple sclerosis in the United States. Mult Scler. 1998; 4 (5):419–425. [ PubMed ] [ Google Scholar ]
- Poser CM, Paty DW, Scheinberg L, McDonald WI, Davis FA, Ebers GC, Johnson KP, Sibley WA, Silberberg DH, Tourtellotte WW. New diagnostic criteria for multiple sclerosis: guidelines for research protocols. Ann Neurol. 1983; 13 (3):227–231. doi: 10.1002/ana.410130302. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McDonald WI, Compston A, Edan G, Goodkin D, Hartung HP, Lublin FD, McFarland HF, Paty DW, Polman CH, Reingold SC, Sandberg-Wollheim M, Sibley W, Thompson A, van den Noort S, Weinshenker BY, Wolinsky JS. Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the diagnosis of multiple sclerosis. Ann Neurol. 2001; 50 (1):121–127. doi: 10.1002/ana.1032. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Banwell B, Bar-Or A, Arnold DL, Sadovnick D, Narayanan S, McGowan M, O'Mahony J, Magalhaes S, Hanwell H, Vieth R, Tellier R, Vincent T, Disanto G, Ebers G, Wambera K, Connolly MB, Yager J, Mah JK, Booth F, Sebire G, Callen D, Meaney B, Dilenge M-E, Lortie A, Pohl D, Doja A, Venketaswaran S, Levin S, MacDonald EA, Meek D. et al. Clinical, environmental, and genetic determinants of multiple sclerosis in children with acute demyelination: a prospective national cohort study. Lancet Neurol. 2011; 10 (5):436–445. doi: 10.1016/S1474-4422(11)70045-X. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Handel AE, Handunnetthi L, Giovannoni G, Ebers GC, Ramagopalan SV. Genetic and environmental factors and the distribution of multiple sclerosis in Europe. Eur J Neurol. 2010; 17 (9):1210–1214. doi: 10.1111/j.1468-1331.2010.03003.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tselis A. Epstein–Barr virus cause of multiple sclerosis. Curr Opin Rheumatol. 2012; 24 (4):424–428. doi: 10.1097/BOR.0b013e3283542cf8. 410.1097/BOR.1090b1013e3283542cf3283548. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Disanto G, Morahan J, Ramagopalan S. Multiple sclerosis: risk factors and their interactions. CNS Neurol Disord Drug Targets. 2012; 11 (5):545–555. doi: 10.2174/187152712801661266. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Simpson S Jr, Blizzard L, Otahal P, Van der Mei I, Taylor B. Latitude is significantly associated with the prevalence of multiple sclerosis: a meta-analysis. J Neurol Neurosurg Psychiatry. 2011; 82 (10):1132–1141. doi: 10.1136/jnnp.2011.240432. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ascherio A, Munger KL. Environmental risk factors for multiple sclerosis. Part I: the role of infection. Ann Neurol. 2007; 61 (4):288–299. doi: 10.1002/ana.21117. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Higgins J, Green S, editor. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 [updated September 2009] 2009. [ Google Scholar ]
- Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000; 283 (15):2008–2012. doi: 10.1001/jama.283.15.2008. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. [ http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm ] [ PubMed ]
- Thacker EL, Mirzaei F, Ascherio A. Infectious mononucleosis and risk for multiple sclerosis: a meta-analysis. Ann Neurol. 2006; 59 (3):499–503. doi: 10.1002/ana.20820. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Deeks JJ, Higgins JPT, Altman DG. In: Cochrane Handbook for Systematic Reviews of Interventions Version 510 (updated March 2011) The Cochrane Collaboration, Higgins J, Green S, editor. 2011. Chapter 9: Analysing data and undertaking meta-analysis. [ Google Scholar ]
- Ernst E, Pittler MH. Re-analysis of previous meta-analysis of clinical trials of homeopathy. J Clin Epidemiol. 2000; 53 (11):1188. doi: 10.1016/S0895-4356(99)00226-7. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Comparison of two methods to detect publication bias in meta-analysis. JAMA. 2006; 295 (6):676–680. doi: 10.1001/jama.295.6.676. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Review Manager (RevMan) [Computer program] 51. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; 2011. [ Google Scholar ]
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, Guyatt GH. In: Cochrane Handbook for Systematic Reviews of Interventions Version 501. The Cochrane Collaboration, Higgins J, Green S, editor. 2008. Chapter 12: Interpreting results and drawing conclusions. [ Google Scholar ]
- Becker H, Chochon F, de Toffol B, Defebvre L, Leger JM, Pierrot-Deseilligny C, Sellal F. [Report of the 55th meeting of the American Academy of Neurology. Honolulu, March 29-April 6, 2003] Rev Neurol (Paris) 2003; 159 (4):470–486. [ PubMed ] [ Google Scholar ]
- De Portugal AJ, Fereres JS. [Considerations on the relationship of injury and multiple sclerosis] Med Clin (Barc) 1965; 44 (4):252–255. [ PubMed ] [ Google Scholar ]
- Goncharova ZA, Baliazin VA. [Risk factors of multiple sclerosis development in the population of the Rostov region] Zh Nevrol Psikhiatr Im S S Korsakova. 2009; 109 (7 Suppl 2):10–15. [ PubMed ] [ Google Scholar ]
- Kurtzke JF, Hyllested K. Multiple sclerosis in the Faroe Islands and the lack of protection by exposure in infancy. Neuroepidemiology. 1992; 11 (2):90–99. doi: 10.1159/000110917. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Levine NS, Atkins A, McKeel DW Jr, Peck SD, Pruitt BA Jr. Spinal cord injury following electrical accidents: case reports. J Trauma. 1975; 15 (5):459–463. doi: 10.1097/00005373-197505000-00015. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Popescu D, Popescu VG. [Risk factors in multiple sclerosis: epidemiological studies in the Arges region] Rev Med Interna Neurol Psihiatr Neurochir Dermatovenerol Neurol Psihiatr Neurochir. 1981; 26 (1):23–31. [ PubMed ] [ Google Scholar ]
- Beziehungen W. Zwischen erkrankkungen ins Kindesalter und multiple-sklerose-erkrankung. Schweiz Arch Neurol Neurchir Psychiatr. 1970; 106 (2):311–317. [ PubMed ] [ Google Scholar ]
- Delilović-Vranić J, Tiric-Campara M, Subasic N. Newly discovered MS cases. 12th Congress of the European Federation of Neurological Societies. 2008 Annual Meeting. 2008. August 23–26.
- Beltran I, Molto-Jorda JM, Diaz-Marin C, Martin R, Matias-Guiu J. [Analytical epidemiological study of multiple sclerosis in Alcoi] Rev Neurol. 1998; 26 (149):67–69. [ PubMed ] [ Google Scholar ]
- Benedikz J, Magnusson H, Guthmundsson G. Multiple sclerosis in Iceland, with observations on the alleged epidemic in the Faroe Islands. Ann Neurol. 1994; 36 (Suppl 2):S175–179. [ PubMed ] [ Google Scholar ]
- Boiko A, Deomina T, Favorova O, Gusev E, Sudomoina M, Turetskaya R. Epidemiology of multiple sclerosis in Russia and other countries of the former Soviet Union: investigations of environmental and genetic factors. Acta Neurol Scand Suppl. 1995; 161 :71–76. [ PubMed ] [ Google Scholar ]
- Di Legge S, Piattella MC, Pozzilli C, Pantano P, Caramia F, Pestalozza IF, Paolillo A, Lenzi GL. Longitudinal evaluation of depression and anxiety in patients with clinically isolated syndrome at high risk of developing early multiple sclerosis. Mult Scler. 2003; 9 (3):302–306. doi: 10.1191/1352458503ms921oa. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Frutos Alegria MT, Beltran-Blasco I, Quilez-Iborra C, Molto-Jorda J, Diaz-Marin C, Matias-Guiu J. [The epidemiology of multiples sclerosis in Alcoi. Analytical data] Rev Neurol. 2002; 34 (9):813–816. [ PubMed ] [ Google Scholar ]
- Gusev EI, Boiko AN, Demina TL, Sudomoina MA, Alekseev AP, Boldyreva MN, Trofimov D, Favorova OO. [The risk factors for the development of multiple sclerosis in the Moscow population. II. The combination of exogenous and hereditary factors] Zh Nevrol Psikhiatr Im S S Korsakova. 1999; 99 (6):47–52. [ PubMed ] [ Google Scholar ]
- Gusev EI, Boiko AN, Smirnova NF, Demina TL. [Risk factors of multiple sclerosis in Moscow population. I. Exogenous risk factors] Zh Nevrol Psikhiatr Im S S Korsakova. 1999; 99 (5):32–40. [ PubMed ] [ Google Scholar ]
- Gusev EI, Zavalishin IA, Boiko AN, Khoroshilova NL, Iakovlev AP. [Epidemiological characteristics of multiple sclerosis in Russia] Zh Nevrol Psikhiatr Im S S Korsakova. 2002; Suppl :3–6. [ PubMed ] [ Google Scholar ]
- Kahana E, Zilber N, Abramson JH, Biton V, Leibowitz Y, Abramsky O. Multiple sclerosis: genetic versus environmental aetiology: epidemiology in Israel updated. J Neurol. 1994; 241 (5):341–346. doi: 10.1007/BF00868444. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Karnaukh VN. [Epidemiology of multiple sclerosis in Amur region] Zh Nevrol Psikhiatr Im S S Korsakova. 2009; 109 (8):59–62. [ PubMed ] [ Google Scholar ]
- Li J, Johansen C, Bronnum-Hansen H, Stenager E, Koch-Henriksen N, Olsen J. The risk of multiple sclerosis in bereaved parents: a nationwide cohort study in Denmark. Neurology. 2004; 62 (5):726–729. doi: 10.1212/01.WNL.0000113766.21896.B1. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Meurman L, Wising P. [Multiple sclerosis, tonsillectomy, and herpes zoster varicellosus] Lakartidningen. 1966; 63 (14):1318–1319. [ PubMed ] [ Google Scholar ]
- Poser CM. The multiple sclerosis trait and the development of multiple sclerosis: genetic vulnerability and environmental effect. Clin Neurol Neurosurg. 2006; 108 (3):227–233. doi: 10.1016/j.clineuro.2005.11.019. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Souberbielle BE, Martin-Mondiere C, O'Brien ME, Carydakis C, Cesaro P, Degos JD. A case–control epidemiological study of MS in the Paris area with particular reference to past disease history and profession. Acta Neurol Scand. 1990; 82 (5):303–310. [ PubMed ] [ Google Scholar ]
- Spitzer C, Bouchain M, Winkler LY, Wingenfeld K, Gold SM, Grabe HJ, Barnow S, Otte C, Heesen C. Childhood trauma in multiple sclerosis: a case–control study. Psychosom Med. 2012; 74 (3):312–318. doi: 10.1097/PSY.0b013e31824c2013. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Warren S, Cockerill R, Warren KG. Risk factors by onset age in multiple sclerosis. Neuroepidemiology. 1991; 10 (1):9–17. doi: 10.1159/000110241. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Weilbach FX, Hartung HP. [Physical trauma and multiple sclerosis] Nervenarzt. 1997; 68 (12):940–944. doi: 10.1007/s001150050220. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bangsi D, Ghadirian P, Ducic S, Morisset R, Ciccocioppo S, McMullen E, Krewski D. Dental amalgam and multiple sclerosis: a case–control study in Montreal, Canada. Int J Epidemiol. 1998; 27 (4):667–671. doi: 10.1093/ije/27.4.667. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Adams DK, Sutherland JM, Fletcher WB. Early clinical manifestations of disseminated sclerosis. BMJ. 1950; 2 (4676):431–436. doi: 10.1136/bmj.2.4676.431. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hollander E. Trauma, multiple sclerosis, delayed sleep phase disorder, subjective experiences, and duration of illness in GAD. CNS Spectr. 2008; 13 (5):361–362. [ PubMed ] [ Google Scholar ]
- Horton AM Jr, Siegel E. Comparison of multiple sclerosis and head trauma patients: a neuropsychological pilot study. Int J Neurosci. 1990; 53 (2–4):213–215. [ PubMed ] [ Google Scholar ]
- Mutlu N. Multiple sclerosis in Turkey; etiologic and symptomatologic study of four hundred ten cases. AMA Arch Neurol Psychiatry. 1954; 71 (4):511–516. doi: 10.1001/archneurpsyc.1954.02320400107011. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Selcen D, Anlar B, Renda Y. Multiple sclerosis in childhood: report of 16 cases. Eur Neurol. 1996; 36 (2):79–84. doi: 10.1159/000117213. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stazio A, Paddison RM, Kurland LT. Multiple sclerosis in New Orleans, Louisiana, and Winnipeg, Manitoba, Canada: follow-up of a previous survey in New Orleans, and comparison between the patient populations in the two communities. J Chronic Dis. 1967; 20 (5):311–332. doi: 10.1016/0021-9681(67)90059-8. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kranz JM, Kurland LT, Schuman LM, Layton D. Multiple sclerosis in Olmsted and Mower counties, Minnesota. Neuroepidemiology. 1983; 2 (3–4):106–118. [ Google Scholar ]
- Lauer K. Environmental associations with the risk of multiple sclerosis: the contribution of ecological studies. Acta Neurol Scand Suppl. 1995; 161 :77–88. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lauer K, Firnhaber W. Prognostic criteria in an epidemiological group of patients with multiple sclerosis: an exploratory study. J Neurol. 1992; 239 (2):93–97. doi: 10.1007/BF00862981. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mellor A. Case–control study to collect medical and epidemiological data and blood samples for research into the causes of multiple sclerosis and selected demyelinating diseases. Waltham, MA: Accelerated Cure Project for MS; 2006. pp. 1–18. [ Google Scholar ]
- Visscher BR, Clark VA, Detels R, Malmgren RM, Valdiviezo NL, Dudley JP. Two populations with multiple sclerosis. Clinical and demographic characteristics. J Neurol. 1981; 225 (4):237–249. doi: 10.1007/BF00313296. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Alonso A, Hernan MA, Ascherio A. Allergy, family history of autoimmune diseases, and the risk of multiple sclerosis. Acta Neurol Scand. 2008; 117 (1):15–20. [ PubMed ] [ Google Scholar ]
- Antonovsky A, Leibowitz U, Medalie JM, Smith HA, Halpern L, Alter M. Reappraisal of possible etiologic factors in multiple sclerosis. Am J Public Health Nations Health. 1968; 58 (5):836–848. doi: 10.2105/AJPH.58.5.836. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brain R, Wilkinson M. The association of cervical spondylosis and disseminated sclerosis. Brain. 1957; 80 (4):456–478. doi: 10.1093/brain/80.4.456. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Conradi S, Malzahn U, Schroter F, Paul F, Quill S, Spruth E, Harms L, Then Bergh F, Ditzenbach A, Georgi T, Heuschmann P, Rosche B. Environmental factors in early childhood are associated with multiple sclerosis: a case–control study. BMC Neurol. 2011; 11 :123. doi: 10.1186/1471-2377-11-123. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- The Coordinating Center and the Neurological Centers of the Cooperative Group. Cooperative Italian study on multiple sclerosis and risk factors: a case–control study. Ital J Neurol Sci. 1987; Suppl 6 :17–20. [ PubMed ] [ Google Scholar ]
- Alonso A, Cook SD, Maghzi AH, Divani AA. A case–control study of risk factors for multiple sclerosis in Iran. Mult Scler. 2011; 17 (5):550–555. doi: 10.1177/1352458510397685. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Alter M, Speer J. Clinical evaluation of possible etiologic factors in multiple sclerosis. Neurology. 1968; 18 (2):109–116. doi: 10.1212/WNL.18.2.109. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Andersen E, Isager H, Hyllested K. Risk factors in multiple sclerosis: tuberculin reactivity, age at measles infection, tonsillectomy and appendectomy. Acta Neurol Scand. 1981; 63 (2):131–135. [ PubMed ] [ Google Scholar ]
- Antonovsky A, Leibowitz U, Smith HA, Medalie JM, Balogh M, Kats R, Halpern L, Alter M. Epidemiologic study of multiple sclerosis in Israel. An overall review of methods and findings. Arch Neurol. 1965; 13 :183–193. doi: 10.1001/archneur.1965.00470020073010. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bansil S, Singhal BS, Ahuja GK, Riise T, Ladiwala U, Behari M, Cook SD. Multiple sclerosis in India: a case–control study of environmental exposures. Acta Neurol Scand. 1997; 95 (2):90–95. doi: 10.1111/j.1600-0404.1997.tb00075.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Berr C, Puel J, Clanet M, Ruidavets JB, Mas JL, Alperovitch A. Risk factors in multiple sclerosis: a population-based case–control study in Hautes-Pyrenees, France. Acta Neurol Scand. 1989; 80 (1):46–50. doi: 10.1111/j.1600-0404.1989.tb03841.x. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bobowick AR, Kurtzke JF, Brody JA, Hrubec Z, Gillespie M. Twin study of multiple sclerosis: an epidemiologic inquiry. Neurology. 1978; 28 (10):978–987. doi: 10.1212/WNL.28.10.978. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Broadley SA, Deans J, Chataway SJ, Sawcer SJ, Compston DA. Multiple sclerosis and tonsillectomy: no evidence for an influence on the development of disease or clinical phenotype. Mult Scler. 2000; 6 (2):121–123. [ PubMed ] [ Google Scholar ]
- Casetta I, Granieri E, Malagu S, Tola MR, Paolino E, Caniatti LM, Govoni V, Monetti VC, Fainardi E. Environmental risk factors and multiple sclerosis: a community-based, case–control study in the province of Ferrara, Italy. Neuroepidemiology. 1994; 13 (3):120–128. doi: 10.1159/000110369. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cendrowski W, Wender M, Dominik W, Flejsierowicz Z, Owsianowski M, Popiel M. Epidemiological study of multiple sclerosis in western Poland. Eur Neurol. 1969; 2 (2):90–108. doi: 10.1159/000113777. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Currier RD, Eldridge R. Possible risk factors in multiple sclerosis as found in a national twin study. Arch Neurol. 1982; 39 (3):140–144. doi: 10.1001/archneur.1982.00510150010003. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Currier RD, Martin EA, Woosley PC. Prior events in multiple sclerosis. Neurology. 1974; 24 (8):748–754. doi: 10.1212/WNL.24.8.748. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- da Silva KR, Alvarenga RM, Fernandez YFO, Alvarenga H, Thuler LC. Potential risk factors for multiple sclerosis in Rio de Janeiro: a case–control study. Arq Neuropsiquiatr. 2009; 67 (2A):229–234. [ PubMed ] [ Google Scholar ]
- De Gennaro RE, Ragazzi M, Caniatti E, Cesnik P, Fazio V, Simioni V, Govoni I, Casetta E, Granieri E. Environmental risk factors in multiple sclerosis. Different exposure in 3 genetically distinct populations with analytical approach. Padova, Palazzo della Fiera: XL Congresso Società Italiana di Neurologia; 2009. [ Google Scholar ]
- Dokuchaeva NN, Boiko AN. [Clinical and epidemiological study of multiple sclerosis in Volgograd city] Zh Nevrol Psikhiatr Im S S Korsakova. 2006; Spec No 3 :4–10. [ PubMed ] [ Google Scholar ]
- Dolan R. Epidemiological Review of the Cluster of Multiple Sclerosis within East Boston and Winthrop, MA: Possible Roles of Childhood Nutrition and Xenobiotics Exposure as Causative Factors for the Disease. http://www.areco.org/ms.pdf; 2003.
- Gronning M, Riise T, Kvale G, Albrektsen G, Midgard R, Nyland H. Infections in childhood and adolescence in multiple sclerosis. A case–control study. Neuroepidemiology. 1993; 12 (2):61–69. doi: 10.1159/000110302. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gusev E, Boiko A, Lauer K, Riise T, Deomina T. Environmental risk factors in MS: a case–control study in Moscow. Acta Neurol Scand. 1996; 94 (6):386–394. [ PubMed ] [ Google Scholar ]
- Hopkins RS, Indian RW, Pinnow E, Conomy J. Multiple sclerosis in Galion, Ohio: prevalence and results of a case–control study. Neuroepidemiology. 1991; 10 (4):192–199. doi: 10.1159/000110269. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Koch MJ, Reed D, Stern R, Brody JA. Multiple sclerosis. A cluster in a small Northwestern United States community. JAMA. 1974; 228 (12):1555–1557. doi: 10.1001/jama.1974.03230370037020. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Koch-Henriksen N. An epidemiological study of multiple sclerosis. Familial aggregation social determinants, and exogenic factors. Acta Neurol Scand Suppl. 1989; 124 :1–123. [ PubMed ] [ Google Scholar ]
- Kurtzke JF, Hyllested K, Arbuckle JD, Bronnum-Hansen H, Wallin MT, Heltberg A, Jacobsen H, Olsen A, Eriksen LS. Multiple sclerosis in the Faroe Islands. Results of a case control questionnaire with multiple controls. Acta Neurol Scand. 1997; 96 (3):149–157. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lamoureux G, Giard N, Jolicoeur R, Toughlian V, Desrosiers M. Immunological features in multiple sclerosis. BMJ. 1976; 1 (6003):183–186. doi: 10.1136/bmj.1.6003.183. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lauer K, Firnhaber W. In: Multiple Sclerosis in Europe: An Epidemiological Update. edn. Firnhaber W, Lauer K, editor. Darmstadt: LTV Press; 1994. Descriptive and analytical epidemiological data on multiple sclerosis from a long-term study in southern Hesse, Germany; pp. 147–158. [ Google Scholar ]
- Martinez Sobrepera HJ, Cabrera Gomez JA, Tuero Iglesias A. [Exogenous factors in the aetiology of multiple sclerosis in Cuba. A study of cases and controls] Rev Neurol. 2001; 33 (10):931–937. [ PubMed ] [ Google Scholar ]
- Poskanzer DC. Tonsillectomy and multiple sclerosis. Lancet. 1965; 2 (7425):1264–1266. [ PubMed ] [ Google Scholar ]
- Poskanzer DC, Sheridan JL, Prenney LB, Walker AM. Multiple sclerosis in the Orkney and Shetland Islands. II: the search for an exogenous aetiology. J Epidemiol Comm Health. 1980; 34 (4):240–252. doi: 10.1136/jech.34.4.240. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Roshanisefat H, Bahmanyar S, Hillert J, Olsson T, Montgomery SM. Appendicectomy and multiple sclerosis risk. Eur J Neurol. 2011; 18 (4):667–669. doi: 10.1111/j.1468-1331.2010.03147.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Westlund KB, Kurland LT. Studies on multiple sclerosis in Winnepeg, Manitoba, and New Orleans, Louisiana. I. Prevalence; comparison between the patient groups in Winnipeg and New Orleans. Am J Hyg. 1953; 57 (3):380–396. [ PubMed ] [ Google Scholar ]
- YosefiPour G, Rasekhi A. Multiple sclerosis: a risk factor analysis in Iran. Arch Iran Med. 2002; 5 (3):191–193. [ Google Scholar ]
- Zaadstra BM, Chorus AM, van Buuren S, Kalsbeek H, van Noort JM. Selective association of multiple sclerosis with infectious mononucleosis. Mult Scler. 2008; 14 (3):307–313. doi: 10.1177/1352458507084265. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zilber N, Kahana E. Risk factors for multiple sclerosis: a case–control study in Israel. Acta Neurol Scand. 1996; 94 (6):395–403. doi: 10.1111/j.1600-0404.1996.tb00051.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zorzon M, Zivadinov R, Nasuelli D, Dolfini P, Bosco A, Bratina A, Tommasi MA, Locatelli L, Cazzato G. Risk factors of multiple sclerosis: a case–control study. Neurological Sciences. 2003; 24 (4):242–247. doi: 10.1007/s10072-003-0147-6. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Siva A, Radhakrishnan K, Kurland LT, O'Brien PC, Swanson JW, Rodriguez M. Trauma and multiple sclerosis: a population-based cohort study from Olmsted County, Minnesota. Neurology. 1993; 43 (10):1878–1882. doi: 10.1212/WNL.43.10.1878. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sterne JAC, Egger M, Moher D. In: Cochrane Handbook for Systematic Reviews of Interventions Version 510 (updated March 2011) Higgins JPT, Green S, editor. The Cochrane Collaboration; 2011. Chapter 10: Addressing reporting biases. [ Google Scholar ]
- Paffenbarger RS Jr. The effect of prior tonsillectomy on incidence and clinical type of acute poliomyelitis. Am J Hyg. 1957; 66 (2):131–150. [ PubMed ] [ Google Scholar ]
- Paffenbarger RS Jr, Wilson VO. Previous tonsillectomy and current pregnancy as they affect risk of poliomyelitis attack. Ann N Y Acad Sci. 1955; 61 (4):856–868. doi: 10.1111/j.1749-6632.1955.tb42543.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Siegel M, Greenberg M, Magee MC. Tonsillectomy and poliomyelitis. II. Frequency of bulbar paralysis, 1944–1949. J Pediatr. 1951; 38 (5):548–558. doi: 10.1016/S0022-3476(51)80296-8. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yamanaka N, Kataura A. Viral infections associated with recurrent tonsillitis. Acta Otolaryngol Suppl. 1984; 416 :30–37. [ PubMed ] [ Google Scholar ]
- Lucas RM, Hughes AM, Lay M-LJ, Ponsonby A-L, Dwyer DE, Taylor BV, Pender MP. Epstein–Barr virus and multiple sclerosis. J Neurol Neurosurg Psychiatry. 2011; 82 (10):1142–1148. doi: 10.1136/jnnp-2011-300174. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bagos PG, Nikolopoulos G, Ioannidis A. Chlamydia pneumoniae infection and the risk of multiple sclerosis: a meta-analysis. Mult Scler. 2006; 12 (4):397–411. doi: 10.1191/1352458506ms1291oa. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cook SD, Rohowsky-Kochan C, Bansil S, Dowling PC. Evidence for multiple sclerosis as an infectious disease. Acta Neurol Scand Suppl. 1995; 161 :34–42. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Krone B, Oeffner F, Grange JM. Is the risk of multiple sclerosis related to the 'biography' of the immune system? J Neurol. 2009; 256 (7):1052–1060. doi: 10.1007/s00415-009-5068-8. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jilek S, Schluep M, Meylan P, Vingerhoets F, Guignard L, Monney A, Kleeberg J, Le Goff G, Pantaleo G, Du Pasquier RA. Strong EBV-specific CD8+ T-cell response in patients with early multiple sclerosis. Brain. 2008; 131 (Pt 7):1712–1721. [ PubMed ] [ Google Scholar ]
- Levin LI, Munger KL, Rubertone MV, Peck CA, Lennette ET, Spiegelman D, Ascherio A. Temporal relationship between elevation of epstein-barr virus antibody titers and initial onset of neurological symptoms in multiple sclerosis. JAMA. 2005; 293 (20):2496–2500. doi: 10.1001/jama.293.20.2496. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Randal Bollinger R, Barbas AS, Bush EL, Lin SS, Parker W. Biofilms in the large bowel suggest an apparent function of the human vermiform appendix. J Theor Biol. 2007; 249 (4):826–831. doi: 10.1016/j.jtbi.2007.08.032. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Franciotta D, Salvetti M, Lolli F, Serafini B, Aloisi F. B cells and multiple sclerosis. Lancet Neurol. 2008; 7 (9):852–858. doi: 10.1016/S1474-4422(08)70192-3. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Correale J, Farez MF. The impact of environmental infections (parasites) on MS activity. Mult Scler. 2011; 17 (10):1162–1169. doi: 10.1177/1352458511418027. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Norgaard M, Nielsen RB, Jacobsen JB, Gradus JL, Stenager E, Koch-Henriksen N, Lash TL, Sorensen HT. Use of penicillin and other antibiotics and risk of multiple sclerosis: a population-based case–control study. Am J Epidemiol. 2011; 174 (8):945–948. doi: 10.1093/aje/kwr201. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Alder AC, Fomby TB, Woodward WA, Haley RW, Sarosi G, Livingston EH. Association of viral infection and appendicitis. Arch Surg. 2010; 145 (1):63–71. doi: 10.1001/archsurg.2009.250. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bernstein CN, Wajda A, Blanchard JF. The clustering of other chronic inflammatory diseases in inflammatory bowel disease: a population-based study. Gastroenterol. 2005; 129 (3):827–836. doi: 10.1053/j.gastro.2005.06.021. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Matsushita M, Takakuwa H, Matsubayashi Y, Nishio A, Ikehara S, Okazaki K. Appendix is a priming site in the development of ulcerative colitis. World J Gastroenterol. 2005; 11 (31):4869–4874. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pender MP. CD8+ T-cell deficiency, Epstein-Barr virus infection, vitamin D deficiency, and steps to autoimmunity: a unifying hypothesis. Autoimmune Dis. 2012; 2012 :189096. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Laurin M, Everett ML, Parker W. The cecal appendix: one more immune component with a function disturbed by post-industrial culture. Anat Rec (Hoboken) 2011; 294 (4):567–579. doi: 10.1002/ar.21357. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rosati G. The prevalence of multiple sclerosis in the world: an update. Neurol Sci. 2001; 22 (2):117–139. doi: 10.1007/s100720170011. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Livingston EH, Fomby TB, Woodward WA, Haley RW. Epidemiological similarities between appendicitis and diverticulitis suggesting a common underlying pathogenesis. Arch Surg. 2011; 146 (3):308–314. doi: 10.1001/archsurg.2011.2. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fleming JO, Carrithers MD. Diagnosis and management of multiple sclerosis: a handful of patience. Neurol. 2010; 74 (11):876–877. doi: 10.1212/WNL.0b013e3181d561c8. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Krone B, Pohl D, Rostasy K, Kahler E, Brunner E, Oeffner F, Grange JM, Gartner J, Hanefeld F. Common infectious agents in multiple sclerosis: a case–control study in children. Mult Scler. 2008; 14 (1):136–139. doi: 10.1177/1352458507082069. [ PubMed ] [ CrossRef ] [ Google Scholar ]
We've detected unusual activity from your computer network
To continue, please click the box below to let us know you're not a robot.
Why did this happen?
Please make sure your browser supports JavaScript and cookies and that you are not blocking them from loading. For more information you can review our Terms of Service and Cookie Policy .
For inquiries related to this message please contact our support team and provide the reference ID below.

COMMENTS
Case Study 44 Multiple Sclerosis. Identify four risk factors in this patient that consistent with multiple sclerosis The patient being of Northern European Descent (Belgian) and 2). the region she resides in of the Northen Atlantic (Wisconin) 3) Sex- Female (Ratio now 3:1, female to male occurrence) 4) Caucasian (Incidence 2x as high in Caucasian Americans, and Asians).
What is the pathophysiology of MS? -demyelination of nerve fibers in the white matter of the brain, spinal cord, and cranial nerves. What is this demyelination process caused by? the invasion of CD4+ and CD8+, T-lymphocytes and macrophages. -demyelination is ultimately caused by activated macrophages.
Case Study 44 MS; 1. Identify four risk factors in this patient that are consistent with multiple sclerosis. The patient being of northern european descent, the region she resides in the north of the atlantic ocean, sex: female, caucasion. 2 probably precipitated this most recent attack of multiple sclerosis? Pt developed a viral infection. 3.
Bilateral internuclear ophthalmoplegia is pathognomonic of MS. The diagnosis of MS is based on the clinical features of the attacks including the history and examination findings. The guiding principle of the diagnosis is that of dissemination in time (DIT) and dissemination in space (DIS). There is no single diagnostic laboratory test for MS.
The PROs, related to domains that most care to multiple sclerosis patients (case study) defined by the PROMOPROMS initiative (manual ability, bladder functions, motor, cognitive, psychosocial fatigue, anxiety, and depression, quality of life), are currently used to measure disease progression and the efficacy of treatments (drugs and/or ...
Case Study 44 - Multiple Sclerosis Patient Case Study.pdf. Solutions Available. American Career College, Ontario. LVN 191104-3. Case study neuro #6 (3).docx. Solutions Available. University of Wisconsin, Milwaukee. NURSING 672. NURS 6531 Midterm Exam 2020 , Walden University.docx. Walden University.
View Case Study 44 - Multiple Sclerosis Patient Case Study.pdf from LVN 191104-3 at American Career College, Ontario. Case Study 44: Multiple Sclerosis - Patient Case Study Gabrielle
Clinical Presentation: Case History # 1. Ms. C is a 35 year old white female. She came to Neurology Clinic for evaluation of her long-term neurologic complaints. The patient relates that for many years she had noticed some significant changes in neurologic functions, particularly heat intolerance precipitating a stumbling gait and a tendency to ...
Case Study Multiple Sclerosis. 8 terms. gavinjacob99. Case Study #3: Multiple Sclerosis. 22 terms. Images. justintryan Teacher. Multiple Sclerosis Case Study (Davidsons) ... Case 44 Multiple Sclerosis. 82 terms. kristina_scherrer. Other sets by this creator. Brainstem 1. 15 terms. moni1306. Cranial Nerves. 79 terms. moni1306. Meningoccal ...
Multiple sclerosis (MS) is the most common disabling neurologic disease in people ages 18 to 60, second overall only to trauma. This prevalence is more than matched by the complexity of the disease, which is compounded by the dearth of definitive evidence to guide clinical decision making and leaves physicians to rely on their judgment and anecdotal experience.
Chapter 44 - Palliative Care in Multiple Sclerosis Navigating Chronic Disease Can Be a Difficult Pill to Swallow at a Young Age from Section 6 - Demyelinating Diseases and Autoimmune Neurology
The mean age of onset is from 28 to 31 years. The age of onset varies among the clinical subtypes (phenotypes). RRMS has an earlier onset, averaging between 25 and 29 years, with SPMS presenting at a mean age between 40 and 49 years of age. The estimated male to female ratio is 1.4-2.3 to 1.
Frexalimab Promising for Relapsing Multiple Sclerosis US FDA Declines to Approve Viatris's Injection for Multiple Sclerosis 3090D553-9492-4563-8681-AD288FA52ACE
Case Study: Adult with Multiple Sclerosis. STANDARDIZED LIFE SKETCH. 18. Setting of Encounter: NP Office. SP: Seated in wheelchair in exam room fully clothed The Mother SP is sitting in waiting room. EXAMINER WASHES HANDS ON ENTERING EXAMINING ROOM. 19.
Multiple Sclerosis Program, Department of Neurology, University of Texas Southwestern Medical Center, 5323 Harry Hines Boulevard, Dallas, TX 75390-9036, USA. Multiple sclerosis (MS) is the most common disabling neurologic disease in people ages 18 to 60, second overall only to trauma. This prevalence is more than matched by the complexity of ...
Multiple Sclerosis (MS) is a chronic, inflammatory, demyelinating disease of CNS that afects cerebral cortex and grey matter including basal ganglia and Cerebellar cortex [1]. MS prevails in a total of 2.8 million people worldwide according to a study conducted in 2020 with an estimation of one person being diagnosed with MS every five minutes [2].
Multiple Sclerosis Case Study. Janet has experienced periodic episodes of tingling in her extremities, dizziness, and even episodes of blindness. After 12 years, doctors have finally given her a diagnosis. Follow Janet through her journey and find out why her disease is so difficult to diagnose.
Stanford Center for Continuing Medical Education, Multiple Sclerosis: Case Studies on the Importance of Early Diagnosis and Optimal Treatment, 12/20/2022 12:00:00 AM - 12/19/2025 11:59:00 PM, Internet Enduring Material sponsored by Stanford University School of Medicine. Presented by the Stanford University School of Medicine Department of Neurology and Center for Continuing Medical Education ...
balance issues secondary to a medical diagnosis such as multiple sclerosis (MS). The purpose of this retrospective case study is to describe the outcomes of using neuromuscular re-education as well as lower extremity muscle strengthening in a 44-year-old female patient with a LAS and a medical diagnosis of MS.
Functional Assessment of Multiple Sclerosis (FAMS) N=45 44.1 years 71.1%: Increase in general score FAMS from T1 to T2 (p<0.001) and from T2 to T3 (p=1). ... In a study by Case et al, 112 the experimental group attended 10 1-hour weekly sessions of healing light guided imagery. They found a greater increase in QoL in this group than with 10 ...
©️ 2024 The National Multiple Sclerosis Society is a tax exempt 501(c)3 nonprofit organization. Its Identification Number (EIN) is 13-5661935. The National Multiple Sclerosis Society is proud to be a source of information on multiple sclerosis related topics.
This study is part of a larger phase II, randomized, controlled clinical trial "Communication, Coordination and Security for people with severe Multiple Sclerosis (COCOS-MS)" [].This explorative clinical trial, employing a mixed-method design, incorporates a qualitative study component with PwsMS, caregivers and HCSs to enrich the findings of the quantitative data.
June 28, 2023 — A study of more than 22,000 people with multiple sclerosis (MS) has for the first time identified a genetic variant associated with faster progression of the disease, an ...
A new study published today in Nature Medicine unveils a significant breakthrough in the understanding and early detection of multiple sclerosis (MS). Researchers have identified a unique autoantibody signature present in approximately 10% of patients with MS years before the onset of clinical symptoms.
Results. We identified 33 case-control studies, involving 27,373 multiple sclerosis cases and 211,756 controls. There was a statistically significant association between tonsillectomy (OR = 1.32, 95% CI 1.08-1.61; 12 studies, I 2 = 44%) and appendectomy (OR = 1.16, 95% CI 1.01-1.34; 7 studies, I 2 = 0%) in individual's ≤ 20 years of age and the subsequent risk for developing multiple ...
Multiple sclerosis (MS) arises from a complex interplay between host genetic factors and environmental components, with the gut microbiota emerging as a key area of investigation. In the current study, we used ion torrent sequencing to delve into the bacteriome (bacterial microbiota) and mycobiome (fungal microbiota) of people with MS (pwMS), and compared them to healthy controls (HC).
EMEA +44 20 7330 7500. Asia Pacific +65 6212 1000. ... This Multiple Sclerosis Discovery Could Be a Breakthrough. ... let alone intervene or study it in its earliest stages, before damage has been ...
Background: With the purpose of exploring the development of new quality productive forces in Guangdong, the present study hypothesized that reducing energy and carbon inputs was beneficial for increasing Guangdong's multi-cropping agricultural energy output and economic returns. Methods: The energy use efficiency of crop production and the corresponding carbon input and agricultural benefit ...