Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic

RELATED TOPICS
INTRODUCTION
This topic will provide an overview of major issues related to breech presentation, including choosing the best route for delivery. Techniques for breech delivery, with a focus on the technique for vaginal breech delivery, are discussed separately. (See "Delivery of the singleton fetus in breech presentation" .)
TYPES OF BREECH PRESENTATION
● Frank breech – Both hips are flexed and both knees are extended so that the feet are adjacent to the head ( figure 1 ); accounts for 50 to 70 percent of breech fetuses at term.
● Complete breech – Both hips and both knees are flexed ( figure 2 ); accounts for 5 to 10 percent of breech fetuses at term.
Disclaimer » Advertising
- HealthyChildren.org
- Facebook Icon
- Twitter Icon
- LinkedIn Icon
Report recommends changes in screening for developmental dysplasia of the hip :
However, most of the guidance remains unchanged from a 2000 clinical practice guideline.
Evaluation and Referral for Developmental Dysplasia of the Hip in Infants , from the AAP Section on Orthopaedics, is available at http://dx.doi.org/10.1542/peds.2016-3107 and will be published in the December issue of Pediatrics .
Latest guidance

- If parents choose to swaddle their infants, encourage hip-healthy swaddling that allows freedom of hip motion and avoids forced position of hip extension and adduction (see http://bit.ly/2fh8gZ8 ).
- Risk factors for which the pediatrician may wish to consider an imaging study in the child with a normal screening physical examination are:
- breech position in the third trimester — both males and females;
- family history of DDH;
- history of improper swaddling; and
- history of abnormal hip physical examination in the neonatal period, which subsequently normalizes.
Periodic hip examination crucial
The report reinforces the earlier advice to carefully perform and document the periodic hip examination until the child is walking. This exam should include the Ortolani test (see resources), hip abduction, gluteal or major thigh crease asymmetry (low specificity) and leg length inequality (Galeazzi sign). The importance of the periodic exam cannot be overemphasized because other than female gender, most children with DDH do not have risk factors. In other words, risk factors are poor indicators of DDH, and all children need to undergo periodic hip examination until they begin walking.
The report confirmed that no screening method completely eliminates the risk of late presentation of DDH.
Use of imaging
When an imaging study is indicated, whether by risk factors or by suspicious physical examination, it is best to defer diagnostic hip ultrasound until age 6 weeks (adjust for prematurity) or plain anteroposterior pelvis radiograph at ages 4-6 months. Ultrasonography may be done earlier in guiding treatment of an Ortolani-positive hip. Initial diagnostic ultrasound usually is deferred until after age 6 weeks because of the high rate of false positives or immature hips, which spontaneously resolve most often by age 6 weeks.
In using imaging for assessment of babies with one or more risk factors but negative physical exam, there is no proven benefit to ultrasound at 6 weeks vs. radiograph at 4-6 months; the report recommends choosing based on local conditions and availability of experienced, trained pediatric hip sonographers.
Regarding breech position in the third trimester as a risk factor, the term breech is used broadly: It doesn’t matter if the child is delivered breech, turns or is turned.
When considering family history as a risk factor, the term again is used broadly without specificity. Clinicians may include early (age younger than 40 years) hip replacement for dysplasia in a close relative.
Finally, there is sensitivity to the medicolegal concerns of AAP members. This report provides only guidance; there is no DDH screening method that completely eliminates late presenting DDH or mild degrees of dysplasia. When in doubt, it’s best to make a referral and listen carefully to any parental concerns.
Drs. Shaw and Segal are lead authors of the clinical report and members of the AAP Section on Orthopaedics Executive Committee.
- A link to a video showing how to perform the Barlow and Ortolani maneuvers is on the AAP Section on Orthopaedics website.
- International Hip Dysplasia Institute
Advertising Disclaimer »
Email alerts
1. 4 million children lose Medicaid, CHIP insurance after public health emergency protections end
2. Autism diagnosis in primary care promotes equity, benefits families
3. Long hours, guilt, more compassion: Pediatrician moms share stresses, rewards
April issue digital edition

Subscribe to AAP News
Column collections
Topic collections
Affiliations
Advertising.
- Submit a story
- American Academy of Pediatrics
- Online ISSN 1556-3332
- Print ISSN 1073-0397
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Key Points |
Abnormal fetal lie or presentation may occur due to fetal size, fetal anomalies, uterine structural abnormalities, multiple gestation, or other factors. Diagnosis is by examination or ultrasonography. Management is with physical maneuvers to reposition the fetus, operative vaginal delivery , or cesarean delivery .
Terms that describe the fetus in relation to the uterus, cervix, and maternal pelvis are
Fetal presentation: Fetal part that overlies the maternal pelvic inlet; vertex (cephalic), face, brow, breech, shoulder, funic (umbilical cord), or compound (more than one part, eg, shoulder and hand)
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse
Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position.
Abnormal fetal lie, presentation, or position may occur with
Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal congenital anomalies
Uterine structural abnormalities (eg, fibroids, synechiae)
Multiple gestation
Several common types of abnormal lie or presentation are discussed here.

Transverse lie
Fetal position is transverse, with the fetal long axis oblique or perpendicular rather than parallel to the maternal long axis. Transverse lie is often accompanied by shoulder presentation, which requires cesarean delivery.
Breech presentation
There are several types of breech presentation.
Frank breech: The fetal hips are flexed, and the knees extended (pike position).
Complete breech: The fetus seems to be sitting with hips and knees flexed.
Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
Types of breech presentations
Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows. The head, which is the part with the largest diameter, can then be trapped during delivery.
Additionally, the trapped fetal head can compress the umbilical cord if the fetal umbilicus is visible at the introitus, particularly in primiparas whose pelvic tissues have not been dilated by previous deliveries. Umbilical cord compression may cause fetal hypoxemia.

Predisposing factors for breech presentation include
Preterm labor
Uterine abnormalities
Fetal anomalies
If delivery is vaginal, breech presentation may increase risk of
Umbilical cord prolapse
Birth trauma
Perinatal death

Face or brow presentation
In face presentation, the head is hyperextended, and position is designated by the position of the chin (mentum). When the chin is posterior, the head is less likely to rotate and less likely to deliver vaginally, necessitating cesarean delivery.
Brow presentation usually converts spontaneously to vertex or face presentation.
Occiput posterior position
The most common abnormal position is occiput posterior.
The fetal neck is usually somewhat deflexed; thus, a larger diameter of the head must pass through the pelvis.
Progress may arrest in the second phase of labor. Operative vaginal delivery or cesarean delivery is often required.
Position and Presentation of the Fetus
If a fetus is in the occiput posterior position, operative vaginal delivery or cesarean delivery is often required.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord.
For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.

- Pregnancy Classes

Breech Births
In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby’s buttocks, feet, or both are positioned to come out first during birth. This happens in 3–4% of full-term births.
What are the different types of breech birth presentations?
- Complete breech: Here, the buttocks are pointing downward with the legs folded at the knees and feet near the buttocks.
- Frank breech: In this position, the baby’s buttocks are aimed at the birth canal with its legs sticking straight up in front of his or her body and the feet near the head.
- Footling breech: In this position, one or both of the baby’s feet point downward and will deliver before the rest of the body.
What causes a breech presentation?
The causes of breech presentations are not fully understood. However, the data show that breech birth is more common when:
- You have been pregnant before
- In pregnancies of multiples
- When there is a history of premature delivery
- When the uterus has too much or too little amniotic fluid
- When there is an abnormally shaped uterus or a uterus with abnormal growths, such as fibroids
- The placenta covers all or part of the opening of the uterus placenta previa
How is a breech presentation diagnosed?
A few weeks prior to the due date, the health care provider will place her hands on the mother’s lower abdomen to locate the baby’s head, back, and buttocks. If it appears that the baby might be in a breech position, they can use ultrasound or pelvic exam to confirm the position. Special x-rays can also be used to determine the baby’s position and the size of the pelvis to determine if a vaginal delivery of a breech baby can be safely attempted.
Can a breech presentation mean something is wrong?
Even though most breech babies are born healthy, there is a slightly elevated risk for certain problems. Birth defects are slightly more common in breech babies and the defect might be the reason that the baby failed to move into the right position prior to delivery.
Can a breech presentation be changed?
It is preferable to try to turn a breech baby between the 32nd and 37th weeks of pregnancy . The methods of turning a baby will vary and the success rate for each method can also vary. It is best to discuss the options with the health care provider to see which method she recommends.
Medical Techniques
External Cephalic Version (EVC) is a non-surgical technique to move the baby in the uterus. In this procedure, a medication is given to help relax the uterus. There might also be the use of an ultrasound to determine the position of the baby, the location of the placenta and the amount of amniotic fluid in the uterus.
Gentle pushing on the lower abdomen can turn the baby into the head-down position. Throughout the external version the baby’s heartbeat will be closely monitored so that if a problem develops, the health care provider will immediately stop the procedure. ECV usually is done near a delivery room so if a problem occurs, a cesarean delivery can be performed quickly. The external version has a high success rate and can be considered if you have had a previous cesarean delivery.
ECV will not be tried if:
- You are carrying more than one fetus
- There are concerns about the health of the fetus
- You have certain abnormalities of the reproductive system
- The placenta is in the wrong place
- The placenta has come away from the wall of the uterus ( placental abruption )
Complications of EVC include:
- Prelabor rupture of membranes
- Changes in the fetus’s heart rate
- Placental abruption
- Preterm labor
Vaginal delivery versus cesarean for breech birth?
Most health care providers do not believe in attempting a vaginal delivery for a breech position. However, some will delay making a final decision until the woman is in labor. The following conditions are considered necessary in order to attempt a vaginal birth:
- The baby is full-term and in the frank breech presentation
- The baby does not show signs of distress while its heart rate is closely monitored.
- The process of labor is smooth and steady with the cervix widening as the baby descends.
- The health care provider estimates that the baby is not too big or the mother’s pelvis too narrow for the baby to pass safely through the birth canal.
- Anesthesia is available and a cesarean delivery possible on short notice
What are the risks and complications of a vaginal delivery?
In a breech birth, the baby’s head is the last part of its body to emerge making it more difficult to ease it through the birth canal. Sometimes forceps are used to guide the baby’s head out of the birth canal. Another potential problem is cord prolapse . In this situation the umbilical cord is squeezed as the baby moves toward the birth canal, thus slowing the baby’s supply of oxygen and blood. In a vaginal breech delivery, electronic fetal monitoring will be used to monitor the baby’s heartbeat throughout the course of labor. Cesarean delivery may be an option if signs develop that the baby may be in distress.
When is a cesarean delivery used with a breech presentation?
Most health care providers recommend a cesarean delivery for all babies in a breech position, especially babies that are premature. Since premature babies are small and more fragile, and because the head of a premature baby is relatively larger in proportion to its body, the baby is unlikely to stretch the cervix as much as a full-term baby. This means that there might be less room for the head to emerge.
Want to Know More?
- Creating Your Birth Plan
- Labor & Birth Terms to Know
- Cesarean Birth After Care
Compiled using information from the following sources:
- ACOG: If Your Baby is Breech
- William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 24.
- Danforth’s Obstetrics and Gynecology Ninth Ed. Scott, James R., et al, Ch. 21.
BLOG CATEGORIES
- Can I get pregnant if… ? 3
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Breastfeeding 29
- Changes In Your Body 5
- Cord Blood 4
- Genetic Disorders & Birth Defects 17
- Health & Nutrition 2
- Is it Safe While Pregnant 54
- Labor and Birth 65
- Multiple Births 10
- Planning and Preparing 24
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Pregnancy Health and Wellness 149
- Pregnancy Products & Tests 8
- Pregnancy Supplements & Medications 14
- The First Year 41
- Week by Week Newsletter 40
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Paternity Tests 2
- Pregnancy Symptoms 5
- Prenatal Testing 16
- The Bumpy Truth Blog 7
- Uncategorized 4
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Women's Health 34
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
Share this post:
Similar post.

Episiotomy: Advantages & Complications

Retained Placenta

What is Dilation in Pregnancy?
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
- A 28-year-old G1P0 woman at 37 weeks of gestation presents to her obstetrician for a prenatal care appointment. She describes feeling some soreness under her ribs in the past few weeks and feels her baby kicking in her lower abdomen. An ultrasound is performed and is seen in the image. The obstetrician describes management approaches, including an external cephalic version before labor.
- flexion of the hips and knees
- some deflexion of one hip and knee
- flexion of both hips with extension of both knees
- 3-4% of all deliveries
- 22-25% of births before 28 weeks of gestation
- 7-15% of births at 32 weeks of gestation
- 3-4% of births at term
- prematurity
- uterine malformations
- uterine fibroids
- polyhydramnios
- placenta previa
- multiple gestations
- subcostal discomfort (due to fetal head in the uterine fundus)
- feeling of kicking in the lower abdomen
- presence of soft mass (buttocks) and absence of hard fetal skull on transabdominal examination of the lower uterine segment
- when cervix is dilated
- detection of breech presentation prior to 37 weeks does not warrant intervention
- fetal head in the uterine fundus
- buttocks in the lower uterine segment
- extension angle > 90 degrees
- at 37 weeks gestation or later
- perform trial of vaginal delivery if the version is successful
- may be planned for breech presentation, without a trial of external cephalic version
- may be performed if trial of vaginal delivery is unsuccessful after external cephalic labor
- ↑ up to 4-fold with breech presetnation
- associated with malformations, prematurity, and intrauterine fetal demise
- 17% of preterm breech deliveries
- 9% of term breech deliveries
- abnormalities include CNS malformations, neck masses, and aneuploidy
- - Breech Presentation
Please Login to add comment
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
- Identification of breech presentation
Evidence review L
NICE Guideline, No. 201
National Guideline Alliance (UK) .
- Copyright and Permissions
Review question
What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation?
Introduction
Breech presentation in late pregnancy may result in prolonged or obstructed labour for the woman. There are interventions that can correct or assist breech presentation which are important for the woman’s and the baby’s health. This review aims to determine the most effective way of identifying a breech presentation in late pregnancy.
Summary of the protocol
Please see Table 1 for a summary of the Population, Intervention, Comparison and Outcome (PICO) characteristics of this review.
Summary of the protocol (PICO table).
For further details see the review protocol in appendix A .
Methods and process
This evidence review was developed using the methods and process described in Developing NICE guidelines: the manual 2014 . Methods specific to this review question are described in the review protocol in appendix A .
Declarations of interest were recorded according to NICE’s conflicts of interest policy .
Clinical evidence
Included studies.
One single centre randomised controlled trial (RCT) was included in this review ( McKenna 2003 ). The study was carried out in Northern Ireland, UK. The study compared ultrasound examination at 30-32 and 36-37 weeks with maternal abdomen palpation during the same gestation period. The intervention group in the study had the ultrasound scans in addition to the abdomen palpation, while the control group had only the abdomen palpation. Clinical management options reported in the study based on the ultrasound scan or the abdomen palpation include referral for full biophysical assessment which included umbilical artery Doppler ultrasound, early antenatal review, admission to antenatal ward, and induction of labour.
The included study is summarised in Table 2 .
See the literature search strategy in appendix B and study selection flow chart in appendix C .
Excluded studies
Studies not included in this review are listed, and reasons for their exclusion are provided in appendix K .
Summary of clinical studies included in the evidence review
Summaries of the studies that were included in this review are presented in Table 2 .
Summary of included studies.
See the full evidence tables in appendix D . No meta-analysis was conducted (and so there are no forest plots in appendix E ).
Quality assessment of clinical outcomes included in the evidence review
See the evidence profiles in appendix F .
Economic evidence
One study, a cost utility analysis was included ( Wastlund 2019 ).
See the literature search strategy in appendix B and economic study selection flow chart in appendix G .
Studies not included in this review with reasons for their exclusions are provided in appendix K .
Summary of studies included in the economic evidence review
For full details of the economic evidence, see the economic evidence tables in appendix H and economic evidence profiles in appendix I .
Wastlund (2019) assessed the cost effectiveness of universal ultrasound scanning for breech presentation at 36 weeks’ gestational age in nulliparous woman (N=3879). The comparator was selective ultrasound scanning which was reported as current practice. In this instance, fetal presentation was assessed by palpation of the abdomen by a midwife, obstetrician or general practitioner. The sensitivity of this method ranges between 57%-70% whereas ultrasound scanning is detected with 100% sensitivity and 100% specificity. Women in the selective ultrasound scan arm only received an ultrasound scan after detection of a breech presentation by abdominal palpation. Where a breech was detected, a woman was offered external cephalic version (ECV). The structure of the model undertook a decision tree, with end states being the mode of birth; either vaginal, elective or emergency caesarean section. Long term health outcomes were modelled based on the mortality risk associated with each mode of birth. Average lifetime quality-adjusted life years (QALYs) were estimated from Euroqol general UK population values.
Only the probabilistic results (n=100000 simulations) were reported which showed that on average, universal ultrasound resulted in an absolute decrease in breech deliveries by 0.39% compared with selective ultrasound scanning. The expected cost per person with breech presentation of universal ultrasound was £2957 (95% Credibility Interval [CrI]: £2922 to £2991), compared to £2,949 (95%CrI: £2915 to £2984) from selective ultrasound. The expected QALYs per person was 24.27615 in the universal ultrasound cohort and 24.27582 in the selective ultrasound cohort. The incremental cost effectiveness ratio (ICER) from the probabilistic analysis was £23611 (95%CrI: £8184 to £44851).
A series of one-way sensitivity analysis were conducted which showed that the most important cost parameter was the unit cost of a universal ultrasound scan. This parameter is particularly noteworthy as the study costed this scan at a much lower value than the ‘standard antenatal ultrasound’ scan in NHS reference costs on the basis that such a scan can be performed by a midwife during a routine antenatal care visit in primary care. According to the NICE guideline manual economic evaluation checklist this model was assessed as being directly applicable with potentially severe limitations. The limitations were mostly attributable to the limitations of the clinical inputs.
Economic model
No economic modelling was undertaken for this review because the committee agreed that other topics were higher priorities for economic evaluation.
Evidence statements
Clinical evidence statements, comparison 1. routine ultrasound scan versus selective ultrasound scan, critical outcomes, unexpected breech presentation in labour.
No evidence was identified to inform this outcome.
Mode of birth
- Moderate quality evidence from 1 RCT (N=1993) showed that there is no clinically important difference between routine ultrasound scan at 36-37 weeks and selective ultrasound scan on the number of women who had elective caesarean section: RR 1.22 (95% CI 0.91 to 1.63).
- Moderate quality evidence from 1 RCT (N=1993) showed that there is no clinically important difference between routine ultrasound scan at 36-37 weeks and selective ultrasound scan on number of women who had emergency caesarean section: RR 1.20 (95% CI 0.90 to 1.60).
- High quality evidence from 1 RCT (N=1993) showed that there is no clinically important difference between routine ultrasound scan at 36-37 weeks and selective ultrasound scan on number of women who had vaginal birth: RR 0.95 (95% CI 0.89 to 1.01).
Important outcomes
Maternal anxiety, women’s experience and satisfaction of care, gestational age at birth.
- High quality evidence from 1 RCT (N=1993) showed that there is no clinically important difference between routine ultrasound scan at 36-37 weeks and selective ultrasound scan on the number of babies’ born between 39-42 gestational weeks: RR 0.98 (95% CI 0.94 to 1.02).
Admission to neonatal unit
- Low quality evidence from 1 RCT (N=1993) showed that there is no clinically important difference between routine ultrasound scan at 36-37 weeks and selective ultrasound scan on the number of babies admitted into the neonatal unit: RR 0.83 (95% CI 0.51 to 1.35).
Economic evidence statements
One directly applicable cost-utility analysis from the UK with potentially serious limitations compared universal ultrasound scanning for breech presentation at 36 weeks’ gestational age with selective ultrasound scanning, stated as current practice. Universal ultrasound scanning was found to be borderline cost effective; the incremental cost-effectiveness ratio was £23611 per QALY gained. The cost of the scan was seen to be a key driver in the cost effectiveness result.
The committee’s discussion of the evidence
Interpreting the evidence, the outcomes that matter most.
Unexpected breech presentation in labour and mode of birth were prioritised as critical outcomes by the committee. This reflects the different options available to women with a known breech presentation in pregnancy and the different choices that women make. There are some women and/or clinicians who may feel uncomfortable with the risks of aiming for vaginal breech birth, and for these women and/or clinicians avoiding an unexpected breech presentation in labour would be the preferred option.
As existing evidence suggests that aiming for vaginal breech birth carries greater risk to the fetus than planned caesarean birth, it is important to consider whether earlier detection of the breech presentation would reduce the risk of these outcomes.
The committee agreed that maternal anxiety and women’s experience and satisfaction of care were important outcomes to consider as the introduction of an additional routine scan during pregnancy could have a treatment burden for women. Gestational age at birth and admission to neonatal unit were also chosen as important outcomes as the committee wanted to find out whether earlier detection of breech presentation would have an impact on whether the baby was born preterm, and as a consequence admitted to the neonatal unit. These outcomes were agreed to be important rather than critical as they are indirect outcomes of earlier detection of breech presentation.
The quality of the evidence
The quality of the evidence ranged from low to high. Most of the evidence was rated high or moderate, with only 1 outcome rated as low. The quality of the evidence was downgraded due to imprecision around the effect estimates for emergency caesarean section, elective caesarean section and admissions to neonatal unit.
No evidence was identified for the following outcomes: unexpected breech presentation in labour, maternal anxiety, women’s experiences and satisfaction of care.
The committee had hoped to find evidence that would inform whether early identification of breech presentation had an impact on preterm births, and although the review reported evidence for gestational age as birth, the available evidence was for births 39-42 weeks of gestation.
Benefits and harms
The available evidence compared routine ultrasound scanning with selective ultrasound scanning, and found no clinically important differences for mode of birth, gestational age at birth, or admissions to the neonatal unit. However, the committee discussed that it was important to note that the study did not focus on identifying breech presentation. The committee discussed the differences between the intervention in the study, which was an ultrasound scan to assess placental maturity, liquor volume, and fetal weight, to an ultrasound scan used to detect breech presentation. Whilst the ultrasound scan in the study has the ability to determine breech presentation, there are additional and costlier training required for the assessment of the other criteria. As such, it is important to separate the interventions. The committee also highlighted that the study did not look at whether an identification of breech presentation had an impact on the outcomes which were selected for this review.
In light of this, the committee felt that they were unable to reach a conclusion as to whether routine scanning to identify breech presentation, was associated with any benefits or harms. The committee agreed that while this review suggests routine ultrasound scanning to be no more effective than selective scanning, it does not definitively establish equivalence. Therefore, the committee agreed to recommend a continuation of the current practice with selective scanning and make a research recommendation to compare the clinical and cost effectiveness of routine ultrasound scanning versus selective ultrasound scanning from 36 weeks to identify fetal breech presentation.
Cost effectiveness and resource use
The committee acknowledged that there was included economic evidence on the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation.
The 1 included study suggested that offering a routine scan for breech is borderline cost effective. A key driver of cost effectiveness was the cost of the scan, which was substantially lower in the economic model than the figure quoted in NHS reference costs for routine ultrasound scanning. The committee noted that a scan for breech presentation only is a simpler technique and uses a cheaper machine. The committee agreed that the other costing assumptions presented in the study seemed appropriate.
However, the committee expressed concerns about the cohort study which underpinned the economic analysis which had a high risk of bias. The committee noted that a number of assumptions in the model which were key drivers of cost effectiveness, including the palpation diagnosis rates and prevalence of breech position, were from this 1 cohort study. This increased the uncertainty around the cost effectiveness of the routine scan. The committee also noted that, whilst the cost of the scan was fairly inexpensive, the resource impact would be substantial if a routine scan for breech presentation was offered to all pregnant women.
Overall, the committee felt that the clinical and cost effectiveness evidence presented was not strong enough to recommend offering a routine ultrasound scan given the potential for a significant resource impact. The recommendation to offer abdominal palpation to all pregnant women, and to offer an ultrasound scan where breech is suspected reflects current practice and so no substantial resource impact is anticipated.
McKenna 2003
Wastlund 2019
Appendix A. Review protocols
Review protocol for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 244K)
Appendix B. Literature search strategies
Literature search strategies for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 370K)
Appendix C. Clinical evidence study selection
Clinical study selection for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 117K)
Appendix D. Clinical evidence tables
Clinical evidence tables for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 213K)
Appendix E. Forest plots
Forest plots for review question: what is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation.
This section includes forest plots only for outcomes that are meta-analysed. Outcomes from single studies are not presented here, but the quality assessment for these outcomes is provided in the GRADE profiles in appendix F .
Appendix F. GRADE tables
GRADE tables for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 196K)
Appendix G. Economic evidence study selection
Economic evidence study selection for review question: what is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation.
A single economic search was undertaken for all topics included in the scope of this guideline. One economic study was identified which was applicable to this review question. See supplementary material 2 for details.
Appendix H. Economic evidence tables
Economic evidence tables for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 143K)
Appendix I. Economic evidence profiles
Economic evidence profiles for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 129K)
Appendix J. Economic analysis
Economic evidence analysis for review question: what is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation.
No economic analysis was conducted for this review question.
Appendix K. Excluded studies
Excluded clinical and economic studies for review question: what is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation, clinical studies, table 8 excluded studies and reasons for their exclusion.
View in own window
Economic studies
A single economic search was undertaken for all topics included in the scope of this guideline. No economic studies were identified which were applicable to this review question. See supplementary material 2 for details.
Appendix L. Research recommendations
Research recommendations for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 164K)
Evidence reviews underpinning recommendations 1.2.36 to 1.2.37
These evidence reviews were developed by the National Guideline Alliance, which is a part of the Royal College of Obstetricians and Gynaecologists
Disclaimer : The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or service users. The recommendations in this guideline are not mandatory and the guideline does not override the responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or their carer or guardian.
Local commissioners and/or providers have a responsibility to enable the guideline to be applied when individual health professionals and their patients or service users wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Nothing in this guideline should be interpreted in a way that would be inconsistent with compliance with those duties.
NICE guidelines cover health and care in England. Decisions on how they apply in other UK countries are made by ministers in the Welsh Government , Scottish Government , and Northern Ireland Executive . All NICE guidance is subject to regular review and may be updated or withdrawn.
- Cite this Page National Guideline Alliance (UK). Identification of breech presentation: Antenatal care: Evidence review L. London: National Institute for Health and Care Excellence (NICE); 2021 Aug. (NICE Guideline, No. 201.)
- PDF version of this title (518K)
In this Page
Other titles in this collection.
- NICE Evidence Reviews Collection
Related NICE guidance and evidence
- NICE Guideline 201: Antenatal care
Supplemental NICE documents
- Supplement 1: Methods (PDF)
- Supplement 2: Health economics (PDF)
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Management of breech presentation: Antenatal care: Evidence review M [ 2021] Review Management of breech presentation: Antenatal care: Evidence review M National Guideline Alliance (UK). 2021 Aug
- Vaginal delivery of breech presentation. [J Obstet Gynaecol Can. 2009] Vaginal delivery of breech presentation. Kotaska A, Menticoglou S, Gagnon R, MATERNAL FETAL MEDICINE COMMITTEE. J Obstet Gynaecol Can. 2009 Jun; 31(6):557-566.
- [The effect of the woman's age on the course of pregnancy and labor in breech presentation]. [Akush Ginekol (Sofiia). 1996] [The effect of the woman's age on the course of pregnancy and labor in breech presentation]. Dimitrov A, Borisov S, Nalbanski B, Kovacheva M, Chintolova G, Dzherov L. Akush Ginekol (Sofiia). 1996; 35(1-2):7-9.
- Review Cephalic version by moxibustion for breech presentation. [Cochrane Database Syst Rev. 2005] Review Cephalic version by moxibustion for breech presentation. Coyle ME, Smith CA, Peat B. Cochrane Database Syst Rev. 2005 Apr 18; (2):CD003928. Epub 2005 Apr 18.
- Review Hands and knees posture in late pregnancy or labour for fetal malposition (lateral or posterior). [Cochrane Database Syst Rev. 2005] Review Hands and knees posture in late pregnancy or labour for fetal malposition (lateral or posterior). Hofmeyr GJ, Kulier R. Cochrane Database Syst Rev. 2005 Apr 18; (2):CD001063. Epub 2005 Apr 18.
Recent Activity
- Identification of breech presentation Identification of breech presentation
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Search Please fill out this field.
- Newsletters
- Sweepstakes
- Labor & Delivery

What Causes Breech Presentation?
Learn more about the types, causes, and risks of breech presentation, along with how breech babies are typically delivered.
What Is Breech Presentation?
Types of breech presentation, what causes a breech baby, can you turn a breech baby, how are breech babies delivered.
FatCamera/Getty Images
Toward the end of pregnancy, your baby will start to get into position for delivery, with their head pointed down toward the vagina. This is otherwise known as vertex presentation. However, some babies turn inside the womb so that their feet or buttocks are poised to be delivered first, which is commonly referred to as breech presentation, or a breech baby.
As you near the end of your pregnancy journey, an OB-GYN or health care provider will check your baby's positioning. You might find yourself wondering: What causes breech presentation? Are there risks involved? And how are breech babies delivered? We turned to experts and research to answer some of the most common questions surrounding breech presentation, along with what causes this positioning in the first place.
During your pregnancy, your baby constantly moves around the uterus. Indeed, most babies do somersaults up until the 36th week of pregnancy , when they pick their final position in the womb, says Laura Riley , MD, an OB-GYN in New York City. Approximately 3-4% of babies end up “upside-down” in breech presentation, with their feet or buttocks near the cervix.
Breech presentation is typically diagnosed during a visit to an OB-GYN, midwife, or health care provider. Your physician can feel the position of your baby's head through your abdominal wall—or they can conduct a vaginal exam if your cervix is open. A suspected breech presentation should ultimately be confirmed via an ultrasound, after which you and your provider would have a discussion about delivery options, potential issues, and risks.
There are three types of breech babies: frank, footling, and complete. Learn about the differences between these breech presentations.
Frank Breech
With frank breech presentation, your baby’s bottom faces the cervix and their legs are straight up. This is the most common type of breech presentation.
Footling Breech
Like its name suggests, a footling breech is when one (single footling) or both (double footling) of the baby's feet are in the birth canal, where they’re positioned to be delivered first .
Complete Breech
In a complete breech presentation, baby’s bottom faces the cervix. Their legs are bent at the knees, and their feet are near their bottom. A complete breech is the least common type of breech presentation.
Other Types of Mal Presentations
The baby can also be in a transverse position, meaning that they're sideways in the uterus. Another type is called oblique presentation, which means they're pointing toward one of the pregnant person’s hips.
Typically, your baby's positioning is determined by the fetus itself and the shape of your uterus. Because you can't can’t control either of these factors, breech presentation typically isn’t considered preventable. And while the cause often isn't known, there are certain risk factors that may increase your risk of a breech baby, including the following:
- The fetus may have abnormalities involving the muscular or central nervous system
- The uterus may have abnormal growths or fibroids
- There might be insufficient amniotic fluid in the uterus (too much or too little)
- This isn’t your first pregnancy
- You have a history of premature delivery
- You have placenta previa (the placenta partially or fully covers the cervix)
- You’re pregnant with multiples
- You’ve had a previous breech baby
In some cases, your health care provider may attempt to help turn a baby in breech presentation through a procedure known as external cephalic version (ECV). This is when a health care professional applies gentle pressure on your lower abdomen to try and coax your baby into a head-down position. During the entire procedure, the fetus's health will be monitored, and an ECV is often performed near a delivery room, in the event of any potential issues or complications.
However, it's important to note that ECVs aren't for everyone. If you're carrying multiples, there's health concerns about you or the baby, or you've experienced certain complications with your placenta or based on placental location, a health care provider will not attempt an ECV.
The majority of breech babies are born through C-sections . These are usually scheduled between 38 and 39 weeks of pregnancy, before labor can begin naturally. However, with a health care provider experienced in delivering breech babies vaginally, a natural delivery might be a safe option for some people. In fact, a 2017 study showed similar complication and success rates with vaginal and C-section deliveries of breech babies.
That said, there are certain known risks and complications that can arise with an attempt to deliver a breech baby vaginally, many of which relate to problems with the umbilical cord. If you and your medical team decide on a vaginal delivery, your baby will be monitored closely for any potential signs of distress.
Ultimately, it's important to know that most breech babies are born healthy. Your provider will consider your specific medical condition and the position of your baby to determine which type of delivery will be the safest option for a healthy and successful birth.
ACOG. If Your Baby Is Breech .
American Pregnancy Association. Breech Presentation .
Gray CJ, Shanahan MM. Breech Presentation . [Updated 2022 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
Mount Sinai. Breech Babies .
Takeda J, Ishikawa G, Takeda S. Clinical Tips of Cesarean Section in Case of Breech, Transverse Presentation, and Incarcerated Uterus . Surg J (N Y). 2020 Mar 18;6(Suppl 2):S81-S91. doi: 10.1055/s-0040-1702985. PMID: 32760790; PMCID: PMC7396468.
Shanahan MM, Gray CJ. External Cephalic Version . [Updated 2022 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
Fonseca A, Silva R, Rato I, Neves AR, Peixoto C, Ferraz Z, Ramalho I, Carocha A, Félix N, Valdoleiros S, Galvão A, Gonçalves D, Curado J, Palma MJ, Antunes IL, Clode N, Graça LM. Breech Presentation: Vaginal Versus Cesarean Delivery, Which Intervention Leads to the Best Outcomes? Acta Med Port. 2017 Jun 30;30(6):479-484. doi: 10.20344/amp.7920. Epub 2017 Jun 30. PMID: 28898615.
Related Articles
Ultrasound Examination for Infants Born Breech by Elective Cesarean Section With a Normal Hip Exam for Instability
Affiliation.
- 1 Department of Orthopedics, Penn State College of Medicine, Hershey, PA.
- PMID: 26491915
- DOI: 10.1097/BPO.0000000000000668
Introduction: Because of the risk of developmental dysplasia of the hip in infants born breech-despite a normal physical exam-the American Academy of Pediatrics (AAP) guidelines recommend ultrasound (US) hip imaging at 6 weeks of age for breech females and optional imaging for breech males. The purpose of this study is to report US results and follow-up of infants born breech with a normal physical exam.
Methods: The electronic medical record for children born at 1 hospital from 2008 to 2011 was reviewed. Data were analyzed for sex, birth weight, breech position, birth order, ethnicity, US and x-ray results, follow-up, and cost.
Results: A total of 237 infants were born breech with a normal physical examination, all delivered by cesarean section. Of the infants, 55% were male and 45% female. About 151 breech infants (64%) with a normal Barlow and Ortolani exam had a precautionary hip US as recommended by the AAP performed at an average of 7 weeks of age. Eighty-six breech infants (35%) did not have an US and were followed clinically. Of the 151 infants that had an US, 140 (93%) were read as normal. None had a dislocated hip. Two patients had a normal physical exam but laxity on US. These 2 patients were the only infants treated in a Pavlik harness. A pediatric orthopaedic surgeon followed those with subtle US findings and no laxity until normal.
Conclusions: The decision by the AAP to recommend US screening at 6 weeks of age for infants with a normal physical exam but breech position was based on an extensive literature review and expert opinion. Not all pediatricians are following the AAP guidelines. The decision to perform an US should be done on a case-by-case basis by the examining physician. A more practical, cost-effective strategy would be to skip the US if the physical exam is normal and simply obtain an AP pelvis x-ray at 4 months.
Level of evidence: Level III-this is a case-control study investigating the outcomes of infants on data drawn from the electronic medical record.
- Breech Presentation / surgery*
- Case-Control Studies
- Cesarean Section / methods
- Hip Dislocation, Congenital / diagnosis*
- Joint Instability / diagnosis*
- Physical Examination / methods
- Risk Assessment / methods
- Ultrasonography / methods*

Variation in fetal presentation
- Report problem with article
- View revision history
Citation, DOI, disclosures and article data
At the time the article was created The Radswiki had no recorded disclosures.
At the time the article was last revised Yuranga Weerakkody had no financial relationships to ineligible companies to disclose.
- Delivery presentations
- Variation in delivary presentation
- Abnormal fetal presentations
There can be many variations in the fetal presentation which is determined by which part of the fetus is projecting towards the internal cervical os . This includes:
cephalic presentation : fetal head presenting towards the internal cervical os, considered normal and occurs in the vast majority of births (~97%); this can have many variations which include
left occipito-anterior (LOA)
left occipito-posterior (LOP)
left occipito-transverse (LOT)
right occipito-anterior (ROA)
right occipito-posterior (ROP)
right occipito-transverse (ROT)
straight occipito-anterior
straight occipito-posterior
breech presentation : fetal rump presenting towards the internal cervical os, this has three main types
frank breech presentation (50-70% of all breech presentation): hips flexed, knees extended (pike position)
complete breech presentation (5-10%): hips flexed, knees flexed (cannonball position)
footling presentation or incomplete (10-30%): one or both hips extended, foot presenting
other, e.g one leg flexed and one leg extended
shoulder presentation
cord presentation : umbilical cord presenting towards the internal cervical os
- 1. Fox AJ, Chapman MG. Longitudinal ultrasound assessment of fetal presentation: a review of 1010 consecutive cases. Aust N Z J Obstet Gynaecol. 2006;46 (4): 341-4. doi:10.1111/j.1479-828X.2006.00603.x - Pubmed citation
- 2. Merz E, Bahlmann F. Ultrasound in obstetrics and gynecology. Thieme Medical Publishers. (2005) ISBN:1588901475. Read it at Google Books - Find it at Amazon
Incoming Links
- Obstetric curriculum
- Cord presentation
- Polyhydramnios
- Footling presentation
- Normal obstetrics scan (third trimester singleton)
Promoted articles (advertising)
ADVERTISEMENT: Supporters see fewer/no ads
By Section:
- Artificial Intelligence
- Classifications
- Imaging Technology
- Interventional Radiology
- Radiography
- Central Nervous System
- Gastrointestinal
- Gynaecology
- Haematology
- Head & Neck
- Hepatobiliary
- Interventional
- Musculoskeletal
- Paediatrics
- Not Applicable
Radiopaedia.org
- Feature Sponsor
- Expert advisers

Loading metrics
Open Access
Peer-reviewed
Research Article
Impact of point-of-care ultrasound and routine third trimester ultrasound on undiagnosed breech presentation and perinatal outcomes: An observational multicentre cohort study
Contributed equally to this work with: Samantha Knights, Smriti Prasad
Roles Data curation
Affiliation Department of Obstetrics and Gynaecology, Norfolk and Norwich University Hospitals NHS Foundation Trust, Norwich, United Kingdom
Roles Conceptualization, Data curation, Writing – original draft, Writing – review & editing
Affiliation Fetal Medicine Unit, St George’s University Hospitals NHS Foundation Trust, London, United Kingdom
Roles Conceptualization, Formal analysis, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing
Affiliations Department of Statistics, Middle East Technical University, Faculty of Arts and Sciences, Ankara, Turkey, Department of Obstetrics and Gynaecology, Koc University, School of Medicine, Istanbul, Turkey
Roles Conceptualization
Roles Conceptualization, Writing – review & editing
Roles Conceptualization, Methodology, Supervision, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliations Fetal Medicine Unit, St George’s University Hospitals NHS Foundation Trust, London, United Kingdom, Vascular Biology Research Centre, Molecular and Clinical Sciences Research Institute, St George’s University of London, London, United Kingdom, Fetal Medicine Unit, Liverpool Women’s Hospital, Liverpool, United Kingdom
- Samantha Knights,
- Smriti Prasad,
- Erkan Kalafat,
- Anahita Dadali,
- Pam Sizer,
- Francoise Harlow,
- Asma Khalil

- Published: April 6, 2023
- https://doi.org/10.1371/journal.pmed.1004192
- Peer Review
- Reader Comments
Accurate knowledge of fetal presentation at term is vital for optimal antenatal and intrapartum care. The primary objective was to compare the impact of routine third trimester ultrasound or point-of-care ultrasound (POCUS) with standard antenatal care, on the incidence of overall and proportion of all term breech presentations that were undiagnosed at term, and on the related adverse perinatal outcomes.
Methods and findings
This was a retrospective multicentre cohort study where we included data from St. George’s (SGH) and Norfolk and Norwich University Hospitals (NNUH). Pregnancies were grouped according to whether they received routine third trimester scan (SGH) or POCUS (NNUH). Women with multiple pregnancy, preterm birth prior to 37 weeks, congenital abnormality, and those undergoing planned cesarean section for breech presentation were excluded. Undiagnosed breech presentation was defined as follows: (a) women presenting in labour or with ruptured membranes at term subsequently discovered to have a breech presentation; and (b) women attending for induction of labour at term found to have a breech presentation before induction. The primary outcome was the proportion of all term breech presentations that were undiagnosed. The secondary outcomes included mode of birth, gestational age at birth, birth weight, incidence of emergency cesarean section, and the following neonatal adverse outcomes: Apgar score <7 at 5 minutes, unexpected neonatal unit (NNU) admission, hypoxic ischemic encephalopathy (HIE), and perinatal mortality (including stillbirths and early neonatal deaths). We employed a Bayesian approach using informative priors from a previous similar study; updating their estimates (prior) with our own data (likelihood). The association of undiagnosed breech presentation at birth with adverse perinatal outcomes was analyzed with Bayesian log-binomial regression models. All analyses were conducted using R for Statistical Software (v.4.2.0).
Before and after the implementation of routine third trimester scan or POCUS, there were 16,777 and 7,351 births in SGH and 5,119 and 4,575 in NNUH, respectively. The rate of breech presentation in labour was consistent across all groups (3% to 4%). In the SGH cohort, the percentage of all term breech presentations that were undiagnosed was 14.2% (82/578) before (years 2016 to 2020) and 2.8% (7/251) after (year 2020 to 2021) the implementation of universal screening ( p < 0.001). Similarly, in the NNUH cohort, the percentage of all term breech presentations that were undiagnosed was 16.2% (27/167) before (year 2015) and 3.5% (5/142) after (year 2020 to 2021) the implementation of universal POCUS screening ( p < 0.001). Bayesian regression analysis with informative priors showed that the rate of undiagnosed breech was 71% lower after the implementation of universal ultrasound (RR, 0.29; 95% CrI 0.20, 0.38) with a posterior probability greater than 99.9%. Among the pregnancies with breech presentation, there was also a very high probability (>99.9%) of reduced rate of low Apgar score (<7) at 5 minutes by 77% (RR, 0.23; 95% CrI 0.14, 0.38). There was moderate to high probability (posterior probability: 89.5% and 85.1%, respectively) of a reduction of HIE (RR, 0.32; 95% CrI 0.0.05, 1.77) and extended perinatal mortality rates (RR, 0.21; 95% CrI 0.01, 3.00). Using informative priors, the proportion of all term breech presentations that were undiagnosed was 69% lower after the initiation of universal POCUS (RR, 0.31; 95% CrI 0.21, 0.45) with a posterior probability greater of 99.9%. There was also a very high probability (99.5%) of a reduced rate of low Apgar score (<7) at 5 minutes by 40% (RR, 0.60; 95% CrI 0.39, 0.88). We do not have reliable data on number of facility-based ultrasound scans via the standard antenatal referral pathway or external cephalic versions (ECVs) performed during the study period.
Conclusions
In our study, we observed that both a policy of routine facility-based third trimester ultrasound or POCUS are associated with a reduction in the proportion of term breech presentations that were undiagnosed, with an improvement in neonatal outcomes. The findings from our study support the policy of third trimester ultrasound scan for fetal presentation. Future studies should focus on exploring the cost-effectiveness of POCUS for fetal presentation.
Author summary
Why was this study done.
- Accurate knowledge of fetal presentation is essential for optimal care during pregnancy and birth. Vaginal breech delivery is associated with adverse maternal and perinatal outcomes.
- Abdominal palpation has poor sensitivity (50% to 70%) for determination of fetal presentation.
- The role of a routine third ultrasound assessment of fetal presentation has been reported but the impact on neonatal outcomes is yet to be determined.
- There are limited reports on antenatal use of handheld point-of-care ultrasound (POCUS) for the determination of fetal presentation, but the impact of their systematic use for this purpose is largely unknown.
What did the researchers do and find?
- We analysed 2 cohorts of pregnant women from 2 large teaching hospitals in the United Kingdom where a policy of routine third trimester ultrasound or POCUS has been implemented.
- We studied the impact of routine third trimester ultrasound or POCUS on the percentage of all term breech presentations that were undiagnosed and adverse neonatal outcomes, in pre- and post-screening epochs.
- Due to the rarity of adverse outcomes, we employed Bayesian regression analysis with informative priors. This statistical tool permits updating previous findings with new data to generate new evidence.
- We found that the incidence of all term breech presentations that were undiagnosed reduced drastically in the post-screening epoch following the implementation of either a third trimester ultrasound (decreased from 14.2% to 2.8%) or POCUS (decreased from 16.2% to 3.5%). There was an associated improvement in neonatal outcomes.
What do these findings mean?
- Our findings imply that a policy of either a third trimester ultrasound by sonographers or POCUS by trained midwives was effective in reducing the proportion of all term breech presentations at the time of birth that were undiagnosed and associated neonatal complications.
- Cost-effectiveness of POCUS needs to be explored further for feasibility of implementation on a wider scale for assessment of fetal presentation at term.
Citation: Knights S, Prasad S, Kalafat E, Dadali A, Sizer P, Harlow F, et al. (2023) Impact of point-of-care ultrasound and routine third trimester ultrasound on undiagnosed breech presentation and perinatal outcomes: An observational multicentre cohort study. PLoS Med 20(4): e1004192. https://doi.org/10.1371/journal.pmed.1004192
Received: August 19, 2022; Accepted: February 7, 2023; Published: April 6, 2023
Copyright: © 2023 Knights et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: Data cannot be shared publicly because consent was not obtained from women; permission for sharing data was not sought as part of ethical approval. Data is only available following approval from Research Ethics Committee and Confidentiality Advisory Group. Enquiries and requests should be made to the the Research Governance and Delivery team at St George's University of London ( [email protected] ).
Funding: The author(s) received no specific funding for this work.
Competing interests: I have read the journal’s policy and the authors of this manuscript have the following competing interests: AK is a Vice President of the Royal College of Obstetricians and Gynaecologists. AK is a Trustee (and the Treasurer) of the International Society of Ultrasound in Obstetrics and Gynecology AK has lectured at and consulted in several ultrasound-based projects, webinars and educational events.
Abbreviations: BAME, black, Asian, and minority ethnic; BMI, body mass index; CrI, credible intervals; ECV, external cephalic version; HIE, hypoxic ischemic encephalopathy; HRA, Health Research Authority; HTA, Health Technology Assessment; IMD, index of multiple deprivation; NICE, National Institute for Health and Care Excellence; NIHR, National Institute for Health Research; NNU, neonatal unit; NNUH, Norfolk and Norwich University Hospital; NSC, National Screening Committee; POCUS, point-of-care ultrasound; RR, risk ratio; SGH, St. George’s Hospital
Introduction
The incidence of breech presentation at term is 3% to 4% [ 1 ]. Breech vaginal birth is associated with an increase in both perinatal mortality and morbidity as well as maternal morbidity [ 2 – 7 ]. Correct knowledge of fetal presentation at term is essential for providing optimum antepartum and intrapartum care. Women with breech presentation at term can be effectively counselled about their options—external cephalic version (ECV), planned vaginal birth, or elective cesarean birth—with their inherent risks and perceived benefits [ 1 ]. There is substantial evidence that clinical examination is not accurate enough for determination of fetal presentation, with unacceptably high rates of missed breech/noncephalic presentations at term [ 8 , 9 ].
There are 2 modalities to screen for fetal presentation at term, each with its advantages and disadvantages: routine third trimester ultrasound or point-of-care/portable ultrasound (POCUS). Currently, routine third trimester ultrasound is not recommended by the United Kingdom National Institute for Health and Care Excellence (NICE) in low-risk pregnancies due to insufficient clinical and cost-effectiveness evidence [ 10 , 11 ]. In the UK, the current practice is to perform an early pregnancy risk assessment followed by referral pathways for low-risk and high-risk women. These risks relate to maternal, fetal, and placental pathology but are unrelated to the risk of breech presentation at term. Women deemed to be at high risk are referred for an ultrasound scan at 28 weeks’ gestation for fetal biometry with or without additional follow-up ultrasound scans. Low-risk women are followed up with clinical assessment (serial measurement of symphysio-fundal height) and referred for third trimester ultrasound if fetal growth restriction is suspected or if it is difficult to perform clinical examination, as in women with high body mass index (BMI), multiple pregnancy, or multiple uterine fibroids, or there is clinical suspicion of noncephalic fetal presentation at term [ 12 – 14 ]. Emerging data from observational studies and a systematic review indicate that it is feasible to accurately diagnose fetal presentation at term by third trimester ultrasound, thereby reducing the proportion of all term breech presentations that were undiagnosed at the time of labour and birth [ 15 – 18 ]. The clinical end point of any study of the diagnosis of breech presentation at term would be an improvement in neonatal outcomes, associated with reduction in incidence of undiagnosed breech. Hitherto published literature, however, could not demonstrate a translation of increased antenatal diagnosis of breech presentation into a statistically significant improvement in neonatal outcomes, most likely owing to the rarity of adverse outcomes.
Most of the data on the use of POCUS in antenatal settings are from low-resource settings where there is inadequate access to ultrasound owing to both material and physical constraints; hence, the focus is on task-shifting of obstetric ultrasound from sonographers to primary care providers [ 19 , 20 ]. A recently published review reported improved diagnostic accuracy with POCUS compared to clinical examination only, for high-risk obstetric conditions including fetal malpresentation, albeit studies were heterogeneous and referred to varying standards [ 21 ]. The Society of Obstetricians and Gynaecologists of Canada identifies POCUS as a useful modality for timely determination of fetal presentation [ 22 ]. A retrospective criterion-based audit performed in one of our study hospitals demonstrated that the use of POCUS by midwives in the antenatal ward/labour ward was associated with identification of previously unrecognized breech presentation, thereby preventing inappropriate induction of labour [ 23 ]. A recent validation study of POCUS in obstetric care showed near perfect agreement for assessment of fetal presentation [95.6% agreement, Kappa −0.887, 95% CI (0.78 to 0.99)] when compared to routine ultrasound [ 24 ]. There is, however, scanty literature on the diagnostic accuracy of POCUS in antenatal care settings for assessment of fetal presentation, compared to standard antenatal care, i.e., routine abdominal palpation, with referral for ultrasound when there is clinical suspicion of breech presentation.
In our study, we aimed to compare the impact of routine third trimester ultrasound or POCUS with standard antenatal care, on the incidence of overall and proportion of all term breech presentations that were undiagnosed at term, and on the related adverse perinatal outcomes.
The study included data from St. George’s University Hospital NHS Foundation Trust (SGH) and Norfolk and Norwich University Hospital NHS Foundation Trust (NNUH). For both centres, pregnancies were grouped according to whether they received routine third trimester scan (SGH) or POCUS (NNUH).
Routine third trimester scan cohort
We included a cohort of pregnant women who gave birth between 4 April 2016 and 30 September 2021, at SGH, a large teaching hospital in South West London. The chosen starting point was the date when birth records were first systematically entered into the current electronic database. At SGH, a policy of routine third trimester (at 36 weeks) ultrasound scan by sonographers for all pregnant women has been implemented since January 2020; this includes assessment of fetal biometry, umbilical and middle cerebral artery Doppler, placental localization, amniotic fluid volume, and fetal presentation. Following a diagnosis of breech presentation during the ultrasound scan, women are counselled about their options: ECV, planned cesarean birth, or planned vaginal birth. If women declined ECV or if it was unsuccessful, they were offered elective cesarean delivery from 39 weeks of gestation. The population was divided into 2 study groups: Group 1 (women who were offered and accepted a routine third trimester scan) and Group 2 (women who received standard antenatal care in line with national guidance, without a routine third trimester scan).
POCUS cohort
The POCUS cohort included pregnant women from NNUH where a policy of routine POCUS at the 36-week antenatal visit was fully adopted from November 2020 following stage-wise implementation in 2016. The POCUS is performed by a midwife using Vscan Air (GE Healthcare). NNUH is a large teaching hospital with approximately 6,000 births per year, and approximately 250 midwives working across the hospital and community. We included 2 groups: a historical cohort of women who received routine care—abdominal palpation and referral for selective ultrasound on clinical suspicion of breech presentation (2015) and those who had POCUS at the 36- to 37-week visit (November 2020 to 2021). Through 2016 to November 2020, POCUS was variably used, either on the labour ward or via referral from community midwives, on clinical suspicion of noncephalic presentation, and these women were not included in this study.
Training of midwives for POCUS cohort
The midwives in NNUH underwent a structured 3-month training programme. The workshops consisted of daily handheld scanning sessions with an hour of dedicated lectures. The theoretical lectures were followed by practice on consenting women in the antenatal ward. All the trainee midwives maintained a competency logbook, detailing both successful and unsuccessful cases. Following the initial workshops, “midwife champions” were identified who were deemed competent or held other ultrasound qualifications and were suitable for cascade training. POCUS training was a part of preceptor ship training of newly qualified midwives, while midwives working in nonpermanent roles were supported and advised to work with one of the champions.
The primary outcome was the proportion of all term breech presentations that were undiagnosed. Undiagnosed breech presentation was defined as follows: (a) breech presentation after the onset of labour or rupture of membranes at term; and (b) breech presentation diagnosed immediately before commencing induction of labour. The secondary outcomes included mode of birth, gestational age at birth, birth weight, incidence of emergency cesarean section, and the following neonatal adverse outcomes: Apgar score <7 at 5 minutes, unexpected neonatal unit (NNU) admission, hypoxic ischemic encephalopathy (HIE) 1 to 3, and perinatal mortality (includes stillbirths and early neonatal deaths).
Women with multiple pregnancies, preterm birth <37 weeks, and congenital abnormalities were excluded. Pregnancies undergoing planned cesarean section for breech presentation were excluded from the analysis of the study outcomes, except for the neonatal outcomes. Maternal demographic characteristics, antenatal, intrapartum, and perinatal data were extracted from Euroking E3 maternity information system and Viewpoint database (ViewPoint 5.6.8.428, ViewPoint Bildverarbeitung GmbH, Weßling, Germany). Routinely collected clinical data were collated from electronic health records and were deemed not to require ethics approval or signed patient consent as per the Health Research Authority (HRA) decision tool.
Statistical analysis
Descriptive variables were compared with Wilcoxon-signed rank test, t test, or chi-squared test, where appropriate. An adequately powered analysis is not practically feasible due to rarity of adverse outcomes following breech delivery. Therefore, we employed a Bayesian approach using informative priors from a previous similar study; updating their estimates (prior) with our own data (likelihood) [ 18 ]. The association of undiagnosed breech presentation at birth with adverse perinatal outcomes was analyzed with Bayesian log-binomial regression models and reported as RR (risk ratios) with credible intervals (CrI). Informative priors ( N ~ μ, σ ) for population mean were derived from Salim and colleagues and a weakly informative prior (Student t , df = 3) for model intercept. Prior parameters were estimated by using the log-risk ratios and log-confidence intervals from Salim and colleagues, and in case an effect could not be estimated in the original study due to a no-event situation, we added a single event to the corresponding group and reestimated the risk ratios. Two Markov chains were run for 1,500 iterations after an initial 500 burn-in period. Posterior probabilities were calculated using the probability density function of normal distribution. A sensitivity analysis using flat priors (noninformative) was also undertaken to investigate the weight of informative prior on the posterior density. Number needed to treat for important outcomes was calculated using current population numbers without incorporating external data. Convergence was checked with trace plots. All analyses were conducted using R for Statistical Software (v.4.2.0) using “brms” and “its.analysis” packages [ 25 , 26 ]. This study is reported as per the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline ( S1 STROBE Checklist).
Study cohorts
In the SGH cohort, there were 24,128 singleton pregnancies during the eligibility period, of which 16,777 births were before the introduction of universal third trimester ultrasound scan and 7,351 after. Baseline characteristics of included pregnancies are presented in Table 1 . Women who gave birth before universal ultrasound scan were significantly younger (33.2 versus 35.7 years, p < 0.001), had similar BMI (25.6 versus 25.7 kg/m 2 , p = 0.194) and multiparity rate (49.6% [8,316/16,777] versus 49.2% [3,617/7,351], p = 0.612) compared to those who gave birth after. There was a slight drop in the proportion of births that were in women from black, Asian, and minority ethnic (BAME) background (39.3% [6,588/16,777] versus 37.9% [2,785/7,351], p = 0.044). The index of multiple deprivation (IMD) quintiles were similar between the 2 epochs ( p > 0.05 for all quintiles; Table 1 ), as was the total number of breech presentations at the time of birth (3.4% [578/16,777] versus 3.4% [251/7,351], p = 0.953), including all diagnosed and undiagnosed cases. A comparison of the baseline characteristics, as well as the gestational age at delivery in weeks and mode of birth of pregnancies with breech presentation at birth in the study epochs before and after the introduction of universal 36-week ultrasound scan is shown in Table 2 . Pregnancies with breech presentation at term were significantly more likely to be delivered by elective cesarean section (76.9% [193/251] versus 60.7% [351/278], p < 0.001) after compared to before the implementation of the universal 36-week ultrasound scan. Emergency cesarean section was lower (17.1% [43/251] versus 30.8% [178/578], p < 0.001) after compared to before the implementation of the universal 36-week ultrasound scan. A similar trend was noted for vaginal breech delivery ( Table 2 ). The gestational age at birth was 39.1 weeks in both groups with a mean difference of 1 day. Although the difference was statistically significant, it would be deemed clinically inconsequential.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pmed.1004192.t001
https://doi.org/10.1371/journal.pmed.1004192.t002
The percentage of all term breech presentations that were undiagnosed was 14.2% (82/578) before and 2.8% (7/251) after the implementation of universal screening ( p < 0.001) ( Table 3 ). The rate of elective cesarean delivery was higher during the universal scan epoch (13.0% [959/7,351] versus 12.0% [2,019/16,777], p = 0.029), while the emergency cesarean rate was lower (12.9% [2,169/16,777] versus 11.5% [845/7,351], p = 0.029) compared to the previous epoch. The total number of vaginal breech births reduced from 29 per 10,000 births to 20 per 10,000 births, but this difference did not reach statistical significance ( p = 0.276). A regression discontinuity (interrupted time series) analysis showed significant variation in the number of undiagnosed breech presentations between 2 epochs (before and after universal ultrasound, p < 0.001) ( Fig 1 ).
Dotted line represents the fitted regression curve with splines.
https://doi.org/10.1371/journal.pmed.1004192.g001
https://doi.org/10.1371/journal.pmed.1004192.t003
In the NNUH cohort, there were 9,694 singleton births during the eligibility period, of which 5,119 births were before the initiation of POCUS screening and 4,575 births after the complete implementation of POCUS. Women who gave birth before POCUS were significantly older (34.6 versus 31.6 years, p < 0.001) and had a lower BMI (25.6 versus 26.5 kg/m 2 , p < 0.001) than those who gave birth after. The percentage of all term breech presentations that were undiagnosed was 16.2% (27/167) before and 3.5% (5/142) after the implementation of universal POCUS screening ( p < 0.001) ( Table 4 ).
https://doi.org/10.1371/journal.pmed.1004192.t004
Perinatal outcomes
We analysed the SGH cohort using Bayesian regression analysis with both flat (noninformative) and informative priors (Using data from Salim and colleagues) [ 18 ]. Regression with informative priors showed the percentage of all term breech presentations that were undiagnosed was 71% lower after the implementation of universal ultrasound (RR, 0.29; 95% CrI 0.20, 0.38) with a posterior probability greater than 99.9% ( Table 3 ). Among the pregnancies with breech presentation, there was also a very high probability (>99.9%) of reduced rate of low Apgar score (<7) at 5 minutes by 77% (RR, 0.23; 95% CrI 0.14, 0.38). There was moderate to high probability (posterior probability: 89.5% and 85.1%, respectively) of a reduction of HIE (RR, 0.32; 95% CrI 0.05, 1.77) and extended perinatal mortality rates (RR, 0.21; 95% CrI 0.01, 3.00). Analysis using flat priors (noninformative) also showed that the percentage of all term breech presentations that were undiagnosed was 74% lower (RR, 0.26; 95% CrI 0.10, 0.59) with very high posterior probability of 99.8%. The reduction in low Apgar scores was also observed in flat prior analysis that corresponded to a 65% reduction (RR, 0.35; 95% CrI 0.06, 1.42) with a moderate to high probability (89.8%). The number needed to scan to prevent one case of undiagnosed breech presentation was 255 (95% CI: 192 to 376).
We analysed the NNUH cohort using the same methods. Using informative priors, the proportion of all term breech presentations that were undiagnosed was 69% lower after the initiation of universal POCUS (RR, 0.31; 95% CrI 0.21, 0.45) with a posterior probability greater of 99.9% ( Table 4 ). There was also a very high probability (99.5%) of a reduced rate of low Apgar score (<7) at 5 minutes by 40% (RR, 0.60; 95% CrI 0.39, 0.88). Flat prior analysis also showed that undiagnosed breech presentation was lower by 80% (RR, 0.20; 95% CrI: 0.07, 0.51) with very high posterior probability of 99.9%. No inference could be made for HIE or extended perinatal mortality as there were no events in either period.
In our study, use of a policy of either routine third trimester scan or routine third trimester POCUS was associated with a significant reduction in the proportion of all breech presentations that were undiagnosed at term, when compared to standard antenatal care. Short-term adverse perinatal outcomes, including NNU admission and low Apgar scores, were significantly lower for the pregnancies with diagnosed breech presentation at term following a policy for screening by either routine third trimester scan or POCUS. Previous studies were unable to study perinatal outcomes due to their small numbers.
Our cohorts are derived from real-world data from 2 large teaching hospitals in the UK. Much of the previously reported literature on use of third trimester ultrasound for diagnosis of breech presentation is from research settings with a dedicated breech clinic and available expertise and skills for manoeuvres like ECV and vaginal breech births. Conclusions from research settings may not be generalizable to clinical settings and may be prone to bias. Furthermore, our study is the first to compare the impact of POCUS with routine antenatal care for diagnosis of fetal presentation. Routine ultrasound scan is effective at reducing the proportion of all term breech presentations that were undiagnosed, but the clinical impact of this change is hard to assess owing to the rarity of adverse outcomes [ 18 ]. We employed a Bayesian approach using both informative priors from similar studies and flat priors as a sensitivity analysis that allowed us to estimate the effect of universal ultrasound in probabilistic terms without depending on P values.
There are some limitations to our study. Firstly, we did not have reliable data on ECV for both our cohorts. The universal scan might have implications, not just for babies that were breech at birth (e.g., ECV could be performed, which could lead to not being breech and therefore not being included in the outcomes, or some other benefit, or indeed, theoretically, harm). Salim and colleagues included all babies diagnosed as breech. The method employed by Salim and colleagues also has drawbacks as it did not include those undiagnosed before the universal scan. Nevertheless, it is unlikely to have had a substantial impact on our results given the low acceptance and variable success rates. This is reflected in the almost identical incidence of overall (undiagnosed and diagnosed) breech presentation before and after screening. Salim and colleagues also reported no difference in the rates of overall breech presentations despite systematic use of ECV with acceptance rates of as high as 80% [ 18 ]. Secondly, the number of adverse neonatal outcomes such as extended perinatal mortality and HIE were not sufficient to estimate an effect in the NNUH cohort. Finally, the maternity records at NNUH were uploaded on electronic database only from April 2015. Therefore, reliable data on demographic parameters like BMI, ethnicity, and IMD were not available for the first quarter of 2015. These factors, however, are unlikely to influence the results.
Our findings of a reduction in the proportion of all term breech presentations that were undiagnosed at term after implementation of routine third trimester scan resonates with those of Salim and colleagues, who reported a reduction from 22.3% to 4.7% following the introduction of universal third trimester scan, compared to standard antenatal care [ 18 ]. Yet there are no published data from the UK on the impact of routine POCUS on the reduction of the percentage of all term breech presentations that were undiagnosed at term. Observational studies from Kenya [ 19 ], Uganda [ 27 ], and Guatemala [ 28 ] have reported that midwives who underwent focused basic obstetric ultrasound training for 3 to 8 weeks were able to identify fetal presentation with high sensitivity and specificity. The proportion of all term breech presentations that were undiagnosed at term, however, could not be eliminated in both cohorts, with 7 and 5 such cases in the routine third trimester scan and POCUS cohorts, respectively. Most of these cases were a consequence of spontaneous version to breech from cephalic presentation in multiparous women. Salim and colleagues also described spontaneous version to breech in multiparous women (76% of cases of undiagnosed breech) in their cohort. Wastlund and colleagues reported in their prospective cohort of 3,879 women that a policy of universal third trimester scan virtually eliminated undiagnosed breech presentations in labour [ 16 ]. It should, however, be noted that their cohort comprised of nulliparous women only in a strict research setting.
We also noted a significant improvement in short-term neonatal outcomes including low Apgar scores at 5 minutes and NNU admission. Salim and colleague demonstrated a nonsignificant improvement in short-term neonatal outcomes [ 18 ]. Although we were unable to demonstrate an effect on outcomes such as HIE and neonatal mortality, observational data from low-resource settings report a reduction in neonatal mortality when women were referred in a timely manner for fetal malpresentation [ 29 ].
Accurate knowledge of fetal presentation at term is crucial for optimal antenatal and intrapartum care. Both routine third trimester scan by a sonographer/clinician or use of POCUS by trained midwives can achieve this objective. Although evidence suggests that a planned breech vaginal birth may be offered after careful case selection and counselling, a large proportion of maternity units in the UK and worldwide lack skilled providers for vaginal breech births. Antenatal identification of breech presentation would allow healthcare providers to offer unbiased information such that pregnant women feel empowered to make an informed decision and have a positive birth experience. A meeting of the UK National Screening Committee (NSC) in March 2021 acknowledged that ultrasound for fetal presentation appears promising; however, the committee recommended that further work on screening for fetal presentation could not be commissioned at that time. The NSC agreed to add screening for fetal presentation to the recommendations list for reconsideration in 3 years’ time if significant evidence evolves in the interim [ 30 ]. Our findings add to that evidence base. A cost-effectiveness analysis study conducted in the UK showed that universal third trimester ultrasound would “virtually eliminate” the proportion of all term breech presentations that were undiagnosed and would be cost-effective if fetal presentation could be assessed at £19.80 pounds per woman or less [ 16 ]. A National Institute for Health Research (NIHR) Health Technology Assessment (HTA) review has suggested that handheld portable ultrasound can readily close this gap as a low-cost device that antenatal care providers like midwives could use for fetal presentation with minimal training [ 31 ]. The major obstacles to routine third trimester scan policy include the costs incurred, whereas a policy of using POCUS in community clinics and the labour ward by healthcare providers, after a short period of training, appears to be as effective as a policy of routine third trimester formal departmental ultrasound. Implementation of POCUS in the community for fetal presentation would also curtail indirect costs by reduction in referrals for facility-based ultrasound based on clinical suspicion, apart from also instilling a sense of empowerment among the care providers and satisfaction among pregnant women. The policy of POCUS was acceptable to pregnant women in our cohort who wanted to avoid nonessential hospital visits during the COVID-19 pandemic. A potential pitfall of the portable ultrasound cited when used in low-resource settings was dependence on internet coverage, which is unlikely to be a deterrent in the UK. Nonetheless, regular audits, ongoing training, and quality improvement measures should be in place to support community healthcare providers to ensure safe practice.
Our data suggest that a policy of either third trimester ultrasound or POCUS by healthcare providers could be effective in reducing the proportion of all term breech presentations that were undiagnosed at birth with an associated improvement in neonatal outcomes.
Supporting information
S1 strobe checklist. strobe checklist..
https://doi.org/10.1371/journal.pmed.1004192.s001
- 1. Management of Breech Presentation (Green-top Guideline No. 20b) [Internet]. Royal College of Obstetricians & Gynaecologists. [cited 2022 May 1]. Available from: https://www.rcog.org.uk/en/guidelines-research-services/guidelines/gtg20b/
- View Article
- PubMed/NCBI
- Google Scholar
- 10. Universal ultrasound in late pregnancy did not reduce serious harms to babies [Internet]. NIHR Evidence. [cited 2022 May 1]. Available from: https://evidence.nihr.ac.uk/alert/universal-ultrasound-in-late-pregnancy-did-not-reduce-serious-harms-to-babies/
- 11. National Guideline Alliance (UK). Identification of breech presentation: Antenatal care: Evidence review L [Internet]. London: National Institute for Health and Care Excellence (NICE); 2021 [cited 2022 May 1]. (NICE Evidence Reviews Collection). Available from: http://www.ncbi.nlm.nih.gov/books/NBK573936/
- 12. Overview | Antenatal care | Guidance | NICE [Internet]. NICE; [cited 2022 May 1]. Available from: https://www.nice.org.uk/guidance/ng201
- 13. Small-for-Gestational-Age Fetus, Investigation and Management (Green-top Guideline No. 31) [Internet]. Royal College of Obstetricians & Gynaecologists. [cited 2022 May 1]. Available from: https://www.rcog.org.uk/en/guidelines-research-services/guidelines/gtg31/
- 14. Perinatal Institute: Programme [Internet]. [cited 2022 May 1]. Available from: https://www.perinatal.org.uk/GAP/programme
- 23. British Journal of Midwifery—Detection of breech presentation: Abdominal palpation and hand-held scanning by midwives [Internet]. Br J Midwifery. [cited 2022 May 1]. Available from: https://www.britishjournalofmidwifery.com/articles/detection-of-breech-presentation-abdominal-palpation-and-hand-held-scanning-by-midwives/
- 26. English P The its.analysis R Package–Modelling Short Time Series Data (June 6, 2019). Available from: https://ssrn.com/abstract=3398189 . https://doi.org/10.2139/ssrn.3398189
- 30. UK NSC minutes March 2021 [Internet]. GOV.UK. [cited 2022 Jul 10]. Available from: https://www.gov.uk/government/publications/uk-nsc-meeting-march-2021/uk-nsc-minutes-march-2021
- 31. 21/582 Point of care ultrasound for breech presentation at term commissioning brief [Internet]. [cited 2022 May 1]. Available from: https://www.nihr.ac.uk/documents/21582-point-of-care-ultrasound-for-breech-presentation-at-term-commissioning-brief/29207
Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.
Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.

Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.

Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.

If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.

- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
- Case report
- Open access
- Published: 26 April 2024
An unusual case of severe asphyxia with the fetal position unexpectedly inverted in a malformed uterus: a case report
- Jiro Abe ORCID: orcid.org/0000-0002-3977-2679 1 , 2 , 3 ,
- Takashi Nasu 1 ,
- Ayumu Noro 1 &
- Junko Tsubaki 1
Journal of Medical Case Reports volume 18 , Article number: 209 ( 2024 ) Cite this article
75 Accesses
1 Altmetric
Metrics details
We present a severe neonatal consequence due to the unexpected and crucial inversion of the fetal position after sudden termination of tocolysis during early labor of a woman with congenital uterine anomaly. It has been reported that congenital uterine anomalies latently affect the fetal position. The clinical pitfalls in childbirth with uterine anomalies are discussed here on the basis of clinical evidence.
Case presentation
At a perinatal medical center in Japan, a 29-year-old Japanese mother who had a history of bicornuate uterus, received tocolysis to prolong her pregnancy for 5 days during the late preterm period after preterm-premature rupture of the membrane. She gave birth to a 2304 g male neonate of the gestational age of 35 weeks and 5 days with severe asphyxia by means of crash cesarean section for fetal sustained bradycardia after sudden termination of tocolysis. We found the fetal position to reverse from cephalic to breech position during early labor. He ended up having severe cerebral palsy after brain cooling against hypoxic-ischemic encephalopathy for 3 days. The mechanism of inversion from cephalic to breech position without amnionic fluid remains unclear, although women with a known diagnosis of a uterine anomaly have higher risk of adverse outcomes such as malpresentation.
Conclusions
When considering the clinical course of this case on the basis of the medical reports, we suspected that uterine anomalies and changes in intrauterine pressure could cause fetal malpresentation and adverse neonatal outcomes.
Peer Review reports
Uterine abnormalities may be overlooked in women with successful reproductive outcomes, but one study estimated that, even in women with normal pregnancy outcomes, the incidence of congenital uterine anomalies is approximately 3%. The likelihood of fetal malpresentation at the time of delivery is notably increased by the presence of uterine anomalies [ 1 ]. A case is presented where a mother with bicornuate uterus received tocolytic treatment with β-stimulants after surpassing 35 weeks of gestation. Following the discontinuation of tocolysis associated with the onset of labor, the fetus experienced distress and malpresentation, ultimately resulting in severe cerebral palsy in the child. There are no existing case reports that show a change in fetal presentation during labor with uterine anomalies resulting in fetal asphyxia.
A 29-year-old Japanese mother who had a history of bicornuate uterus gave birth to a 2304 g male neonate of the gestational age of 35 weeks and 5 days with severe asphyxia. She was a primigravida without health issues, and her pregnancy course, including changes in maternal body mass index (BMI) and gestational weight gain, was smooth. She was admitted to our hospital to receive tocolysis treatments using ritodrine hydrochloride because of preterm premature rupture of membrane at 35 weeks’ gestation, receiving antibiotics, no antenatal corticosteroids, and no magnesium sulfate. The ultrasound examinations revealed overall fetal growth, reduced amniotic fluid, and a fetal vertex position. A total of 3 hours before the birth, the administration of the tocolytic agent, by ritodrine hydrochloride using the maximum dose of 200 µg per minute, was terminated to promote vaginal delivery, and she was transferred to a delivery room. Non-reassuring patterns repetitively emerged at 1 hour prior to the birth, which were only confirmed by cardiotocography without an ultrasound examination performed at that time (Fig. 1 A). General fetal resuscitation such as maternal oxygen administration and intravenous infusion of a liter of non-glucose crystalloid without acute tocolysis was used as part of the obstetric management of labor, while preparing for cesarean delivery for fetal distress. Quick pelvic examinations ensured the fetus’s cephalic position while observing the mother in preparation for an emergency cesarean operation, although the fetal position during delivery was not confirmed by ultrasound. Half an hour before the birth, fetal bradycardia was sustained while the pelvic examination indicated that the fetal head was unexpectedly floating (Fig. 1 A). A crash cesarean section was performed, where he was found to be in a breech presentation. We found quite little amniotic fluid without the evidence of meconium-stained amniotic fluid or cord coiling. The pathological findings of the placenta and umbilical cord proved only mild chorioamnionitis without any evidence of delivery injury or anomaly afterward.
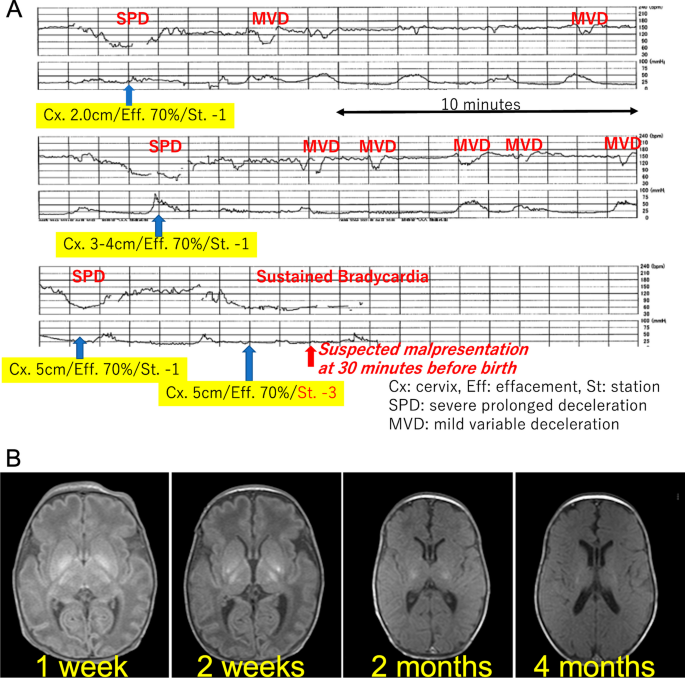
(A) Cardiotocography immediately before birth. Non-reassuring patterns repetitively emerged 1 hour prior to birth. Pelvic examinations revealed a fixed cephalic position. At half an hour, fetal bradycardia was sustained while the pelvic examination indicated that the fetal head was unexpectedly floating. (B) Sequential brain magnetic resonance imaging (MRI). According to sequential brain MRI findings, his lesions post hypoxic-ischemic encephalopathy (HIE) were mainly located in the basal ganglia and the brain stem
After delivery he presented with bradycardia and deep cyanosis without breathing, muscle movements, and reflections. Because his asphyxia turned out to be refractory to routine resuscitation, he was intubated after 1 minute. His skin color rapidly became pink, and the heart rate returned to a normal range without the recovery of muscle movements and reflex actions. He received an appearance, pulse, grimace, activity, and respiration (APGAR) score of 1 at 1 minute and 3 at 5 minutes; the arterial cord blood sample was not available, because of technical difficulty in sampling umbilical cord blood. He needed special care that included mechanical ventilation and correction of mixed acidosis (pH 6.85, pvCO2 77 mmHg, HCO 3 − 12.6 mmol/l at 15 minutes after birth), and then he was given phenobarbital. At 1.5 hours after birth, he was transferred to another tertiary care hospital where he received therapeutic hypothermia for hypoxic-ischemic encephalopathy; the Sarnat grade was moderate, and the Thompson score was calculated as 16 points [ 2 ]. He was a late preterm and low-birth-weight newborn with no congenital anomalies or other problems that would be predictive of neonatal asphyxia through newborn screening especially focusing on the brain, heart, or metabolism. We could not find clinical and pathological evidence of his severe asphyxia in the end. Chromosomal testing was not conducted. He ended up having severe cerebral palsy after brain cooling for 3 days. His sequential brain MRI findings supported the severity of the encephalopathy that mainly affected the basal ganglia and brain stem (Fig. 1 B). He is now 9 months of age and remains in bed with special healthcare requirements that include tube feeding, while presenting with dystonia with severe mental developmental retardation.
Discussion and conclusions
The mother had some delivery risks as follows: a uterine anomaly, absent amniotic fluid after preterm-premature rupture of membrane, and threatened late-preterm labor. The placental blood flow in mothers with congenital uterine anomalies is reduced, and there is a predicted decrease in the reserve capacity for blood supply to the fetus, particularly during delivery. When a mother has congenital uterine anomalies, there is a 5-fold increased risk of preterm birth and a 20-fold increased risk of placental abruption [ 3 ]. This case is believed to be caused by circulatory insufficiency between the mother and fetus, with the influence of congenital uterine anomaly likely playing a background role. Increased intrauterine pressure might have occurred by abrupt termination of tocolysis with the lack of amniotic fluid, which would make the fetal status worse, although there was no evidence of excessively rapid uterine contractions in the tocography (Fig. 1 A).
Uterine anomalies are known to significantly elevate the chances of fetal malpresentation during delivery. According to the meta-analysis by Chan, the likelihood of fetal malpresentation was found to be higher in cases of arcuate uterus, unification defects, and canalization defects, with the odds being 2.53 [95% confidence interval (CI) 1.54–4.18; p < 0.001], 3.87 (95% CI 2.42–6.18; p < 0.001), and 6.24 (95% CI 4.05–9.62; p < 0.001) times, respectively [ 4 ]. Furthermore, a retrospective study by Hua and colleagues, which encompassed all types of uterine anomalies (including uterine septum, unicornuate uterus, bicornuate uterus, and uterine didelphys), revealed that women with these anomalies were 8.6 times more likely to experience breech presentation of the fetus compared with women with standard uterine anatomy (95% CI 6.2–12.0; p < 0.01) [ 5 ]. Additionally, a comprehensive retrospective cross-sectional study, examining a total of 109,736 singleton infants (both preterm and full-term), of which 4535 were breech at birth, determined that women with any form of uterine malformation had an almost 10-fold increase in the likelihood of breech fetal presentation (odds ratio, 9.47; 95% CI 6.77–13.25) [ 6 ]. Possible causes are thought to be changes in intrauterine and external pressure, for example, the effects of uterine malformations, the sudden discontinuation of uterine contraction inhibiting drugs, and the transfer from the delivery table to the bed. The unexpected inversion of the fetal position with very little amniotic fluid during early labor would have led to the poor consequence, causing the umbilical cord to twist and consequently leading to the interruption of placental blood flow.
It may have been unavoidable, but we can suggest two preventive plans for this case. One plan would be ongoing expectant management with or without tocolysis. The issue of whether to suppress or allow progressive labor to proceed during the late-preterm period remains controversial [ 7 ]. If waiting for labor while inhibiting uterine contractions, it is necessary to carefully monitor changes in intrauterine pressure when stopping tocolytic agents. The other one would be planned earlier delivery including elective cesarean operation. Bicornuate uterus has been reported to be a risk factor for unsuccessful vaginal delivery [ 8 ]. A major meta-analysis discovered that the likelihood of undergoing a primary cesarean delivery was 2.6 times higher for women with congenital uterine anomalies (adjusted odds ratio [aOR], 2.6; 95% CI 1.7–4.0; p < 0.01) [ 5 ]. Additionally, a retrospective cohort study over a decade at a French university hospital assessed women known to have uterine malformations, focusing on the baby’s presentation and the method of delivery. In this group, women with uterine abnormalities showed a significantly increased incidence of breech presentations (36.51% as opposed to 4.52%; p < 0.01) and cesarean deliveries (55.26% compared with 18.70%; p < 0.01), in contrast to women with normally formed uteri [ 9 ].
Women with congenital uterine anomalies face significantly higher risks of preterm birth, placental abruption, fetal malpresentation, and breech presentation. Several studies highlight the increased odds of complications such as fetal malpresentation and breech births, indicating a need for careful monitoring and possibly alternative delivery plans, including elective cesarean operations. Our report concludes with suggestions for managing such high-risk cases, emphasizing the importance of careful monitoring or possibly opting for an earlier planned delivery to mitigate risks.
Availability of data and materials
The approval from the parent allowed us to use the patient’s data and report this case with data anonymization.
Simón C, Martinez L, Pardo F, et al . Müllerian defects in women with normal reproductive outcome. Fertil Steril. 1991;56:1192–3.
Article PubMed Google Scholar
Chansarn P, Torgalkar R, Wilson D, Fan CPS, Widjaja E, Whyte H, Tam WYE, Lee KS. Correlation of Thompson and modified Sarnat scores in neonatal hypoxic ischemic encephalopathy. J Perinatol. 2021;41:1522–3.
Vaz SA, Dotters-Katz SK, Kuller JA. Diagnosis and management of congenital uterine anomalies in pregnancy. Obstet Gynecol Surv. 2017;72:194–201.
Chan YY, Jayaprakasan K, Tan A, et al . Reproductive outcomes in women with congenital uterine anomalies: a systematic review. Ultrasound Obstet Gynecol. 2011;38:371–82.
Article CAS PubMed Google Scholar
Hua M, Odibo AO, Longman RE, et al . Congenital uterine anomalies and adverse pregnancy outcomes. Am J Obstet Gynecol. 2011;205:558e1–5.
Article Google Scholar
Cui H, Chen Y, Li Q, et al . Cesarean rate and risk factors for singleton breech presentation in China. J Reprod Med. 2016;61:270–4.
PubMed Google Scholar
Kugelman A, Colin AA. Late preterm infants: near term but still in a critical developmental time period. Pediatrics. 2013;132:741–51.
Mastrolia SA, Baumfeld Y, Hershkovitz R, Loverro G, Naro ED, Yohai D, Schwarzman P, Weintraub AY. Bicornuate uterus is an independent risk factor for cervical OS insufficiency: a retrospective population based cohort study. Matern Fetal Neonatal Med. 2017;30:2705–10.
Guinard E, Subtil D, Deruelle P. Congenital müllerian anomalies and delivery: analysis of 304 cases between 2000 and 2010 at the university hospital of Lille [in French]. Gynecol Obstet Fertil. 2014;42:471–6.
Download references
Acknowledgements
We appreciate clinical support from Asuka Takahata, Tetsuo Onda, Naho Fuseya.
We all declare no financial support or relationships that may pose a conflict of interest by disclosing any financial arrangements we have with a company whose product figures prominently in the submitted manuscript or with a company making a competing product, or any conflict relating to technology or methodology.
Author information
Authors and affiliations.
Department of Pediatrics, JCHO Hokkaido Hospital, 3-18, Nakanoshima 1 Jyou 8 Tyoume, Sapporo, Japan
Jiro Abe, Takashi Nasu, Ayumu Noro & Junko Tsubaki
Department of Pediatrics, Graduate School of Medicine, Hokkaido University, Kita-15, Nishi 7, Kita-Ku, Sapporo, 060-8638, Japan
Mitochondrial Redox Biology, Medical Research Council Mitochondrial Biology Unit and Department of Medicine, University of Cambridge, The Keith Peters Building, Cambridge Biomedical Campus Hills Road, Cambridge, CB2 0XY, UK
You can also search for this author in PubMed Google Scholar
Contributions
Jiro Abe designed and prepared the manuscript; Takashi Nasu, Ayumu Noro, and Junko Tsubaki provided technical support and conceptual advice. All of the authors read and approved the final version of the manuscript.
Corresponding author
Correspondence to Jiro Abe .
Ethics declarations
Ethics approval and consent to participate.
We strictly followed the rules for publication by the research ethics committee in Hokkaido University Hospital, which permitted us to participate.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
We have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Abe, J., Nasu, T., Noro, A. et al. An unusual case of severe asphyxia with the fetal position unexpectedly inverted in a malformed uterus: a case report. J Med Case Reports 18 , 209 (2024). https://doi.org/10.1186/s13256-024-04524-0
Download citation
Received : 01 February 2022
Accepted : 25 March 2024
Published : 26 April 2024
DOI : https://doi.org/10.1186/s13256-024-04524-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Inverted fetal position
- Neonatal asphyxia
- Hypoxic-ischemic encephalopathy
- Late preterm
- Uterine anomalies
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Correlations and discrepancies between cardiac ultrasound, clinical diagnosis and the autopsy findings in early deceased patients with suspected cardiovascular emergencies
- Original Paper
- Published: 23 April 2024
Cite this article

- Ivan Stankovic ORCID: orcid.org/0000-0001-5825-5821 1 , 2 ,
- Aleksandra Zivanic 1 ,
- Ivona Vranic 1 &
- Aleksandar N. Neskovic 1 , 2
23 Accesses
5 Altmetric
Explore all metrics
Cardiac ultrasound (CUS), either focused cardiac ultrasound (FoCUS) or emergency echocardiography, is frequently used in cardiovascular (CV) emergencies. We assessed correlations and discrepancies between CUS, clinical diagnosis and the autopsy findings in early deceased patients with suspected CV emergencies. We retrospectively analysed clinical and autopsy data of 131 consecutive patients who died within 24 h of hospital admission. The type of CUS and its findings were analysed in relation to the clinical and autopsy diagnoses. CUS was performed in 58% of patients - FoCUS in 83%, emergency echocardiography in 12%, and both types of CUS in 5% of cases. CUS was performed more frequently in patients without a history of CV disease (64 vs. 40%, p = 0.08) and when the time between admission and death was longer (6 vs. 2 h, p = 0.021). In 7% of patients, CUS was inconclusive. In 10% of patients, the ante-mortem cause of death could not be determined, while discrepancies between the clinical and post-mortem diagnosis were found in 26% of cases. In the multivariate logistic regression model, only conclusive CUS [odds ratio (OR) 2.76, 95% confidence interval (CI) 1.30–7.39, p = 0.044] and chest pain at presentation (OR 30.19, 95%CI 5.65 -161.22, p < 0.001) were independently associated with congruent clinical and autopsy diagnosis. In a tertiary university hospital, FoCUS was used more frequently than emergency echocardiography in critically ill patients with suspected cardiac emergencies. Chest pain at presentation and a conclusive CUS were associated with concordant clinical and autopsy diagnoses.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
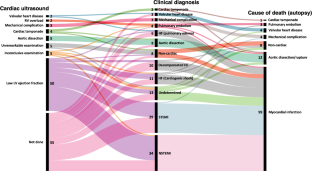
Similar content being viewed by others
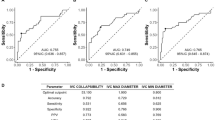
Results of the implementation of a double-check protocol with point-of-care ultrasound for acute heart failure in the emergency department
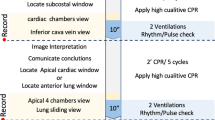
Point-of-care ultrasound in cardiorespiratory arrest (POCUS-CA): narrative review article

Cardiac Ultrasound in Acute Coronary Syndromes
Data availability.
The data underlying this article will be shared on reasonable request to the corresponding author.
Neskovic AN, Hagendorff A, Lancellotti P, Guarracino F, Varga A, Cosyns B et al (2013) European Association of Cardiovascular Imaging. Emergency echocardiography: the European Association of Cardiovascular Imaging recommendations. Eur Heart J Cardiovasc Imaging 14(1):1–11. https://doi.org/10.1093/ehjci/jes193
Article PubMed Google Scholar
Neskovic AN, Skinner H, Price S, Via G, De Hert S, Stankovic I et al (2018) Focus cardiac ultrasound core curriculum and core syllabus of the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 19(5):475–481. https://doi.org/10.1093/ehjci/jey006
Truhlář A, Deakin CD, Soar J, Khalifa GE, Alfonzo A, Bierens JJ et al (2015) Cardiac arrest in special circumstances section collaborators. European Resuscitation Council Guidelines for Resuscitation 2015: Sect. 4. Cardiac arrest in special circumstances. Resuscitation 95:148–201. https://doi.org/10.1016/j.resuscitation.2015.07.017
Panchal AR, Bartos JA, Cabañas JG, Donnino MW, Drennan IR, Hirsch KG, Adult Basic and Advanced Life Support Writing Group et al (2020) Part 3: adult basic and advanced life support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 142(16suppl2):S366–S468. https://doi.org/10.1161/CIR.0000000000000916
Soliman-Aboumarie H, Breithardt OA, Gargani L, Trambaiolo P, Neskovic AN (2022) How-to: focus cardiac ultrasound in acute settings. Eur Heart J Cardiovasc Imaging 23(2):150–153
Cardim N, Dalen H, Voigt JU, Ionescu A, Price S, Neskovic AN et al (2019) The use of handheld ultrasound devices: a position statement of the European Association of Cardiovascular Imaging (2018 update). Eur Heart J Cardiovasc Imaging 20(3):245–252. https://doi.org/10.1093/ehjci/jey145
Spencer KT, Flachskampf FA (2019) Focused Cardiac Ultrasonography. JACC Cardiovasc Imaging. ;12(7 Pt 1):1243–1253. https://doi.org/10.1016/j.jcmg.2018.12.036 . PMID: 31272607
Kongkatong M, Ottenhoff J, Thom C, Han D (2023) Focused Ultrasonography in Cardiac arrest. Emerg Med Clin North Am 41(3):633–675. https://doi.org/10.1016/j.emc.2023.03.012
Casado-López I, Tung-Chen Y, Torres-Arrese M, Luordo-Tedesco D, Mata-Martínez A, Casas-Rojo JM et al (2022) Usefulness of Multi-organ Point-of-care Ultrasound as a complement to the decision-making process in Internal Medicine. J Clin Med 11(8):2256. https://doi.org/10.3390/jcm11082256
Article PubMed PubMed Central Google Scholar
Shen-Wagner J, Deutchman M (2020) Point-of-care Ultrasound: a practical guide for primary care. Fam Pract Manag 27(6):33–40 PMID: 33169960
PubMed Google Scholar
Basso C, Stone JR (2022) Autopsy in the era of advanced cardiovascular imaging. Eur Heart J 43(26):2461–2468
Goldman L, Sayson R, Robbins S, Cohn LH, Bettmann M, Weisberg M (1983) The value of the autopsy in three medical eras. N Engl J Med 308(17):1000–1005. https://doi.org/10.1056/NEJM198304283081704
Article CAS PubMed Google Scholar
Miller CR, Johnston RD, Blake BH, Aronson JF (2023 Jul) The role of autopsy in Quality Assurance: pilot study of a method for prospective reporting of diagnostic errors discovered at autopsy. Am J Forensic Med Pathol 4. https://doi.org/10.1097/PAF.0000000000000857 Epub ahead of print. PMID: 37417529. [in press]
Panizo-Alcañiz J, Frutos-Vivar F, Thille AW, Peñuelas Ó, Aguilar-Rivilla E, Muriel A et al (2020) Diagnostic accuracy of portable chest radiograph in mechanically ventilated patients when compared with autopsy findings. J Crit Care 60:6–9. https://doi.org/10.1016/j.jcrc.2020.06.015
Liu D, Gan R, Zhang W, Wang W, Saiyin H, Zeng W et al (2018) Autopsy interrogation of emergency medicine dispute cases: how often are clinical diagnoses incorrect? J Clin Pathol 71(1):67–71. https://doi.org/10.1136/jclinpath-2017-204484
Rusu S, Lavis P, Domingues Salgado V, Van Craynest MP, Creteur J, Salmon I et al (2021) Comparison of antemortem clinical diagnosis and post-mortem findings in intensive care unit patients. Virchows Arch 479(2):385–392. https://doi.org/10.1007/s00428-020-03016-y
Giugni FR, Salvadori FA, Smeili LAA, Marcílio I, Perondi B, Mauad T et al (2022) Discrepancies between clinical and autopsy diagnoses in Rapid Response Team-assisted patients: what are we missing? J Patient Saf 18(7):653–658. https://doi.org/10.1097/PTS.0000000000000962
Driessen RGH, Latten BGH, Bergmans DCJJ, Hulsewe RPMG, Holtkamp JWM, van der Horst ICC et al (2021) Clinical diagnoses vs. autopsy findings in early deceased septic patients in the intensive care: a retrospective cohort study. Virchows Arch 478(6):1173–1178. https://doi.org/10.1007/s00428-020-02984-5
Singh H, Giardina TD, Meyer AN, Forjuoh SN, Reis MD, Thomas EJ (2013) Types and origins of diagnostic errors in primary care settings. JAMA Intern Med 173(6):418–425. https://doi.org/10.1001/jamainternmed.2013.2777
Kurz SD, Sido V, Herbst H, Ulm B, Salkic E, Ruschinski TM et al (2021) Discrepancies between clinical diagnosis and hospital autopsy: A comparative retrospective analysis of 1,112 cases. PLoS One. ;16(8):e0255490. https://doi.org/10.1371/journal.pone.0255490 . PMID
Issa VS, Dinardi LFL, Pereira TV, de Almeida LKR, Barbosa TS, Benvenutti LA et al (2017) Diagnostic discrepancies in clinical practice: an autopsy study in patients with heart failure. Med (Baltim) 96(4):e5978. https://doi.org/10.1097/MD.0000000000005978
Article Google Scholar
Tejerina E, Esteban A, Fernández-Segoviano P, María Rodríguez-Barbero J, Gordo F, Frutos-Vivar F et al (2012) Clinical diagnoses and autopsy findings: discrepancies in critically ill patients. Crit Care Med 40(3):842–846. https://doi.org/10.1097/CCM.0b013e318236f64f
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA et al (2019) Fourth Universal Definition of Myocardial Infarction (2018). Eur Heart J 40(3):237–269. https://doi.org/10.1093/eurheartj/ehy462 . Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction
Jangaard N, Sarkisian L, Saaby L, Mikkelsen S, Lassen AM, Marcussen N et al (2017) Incidence, frequency, and clinical characteristics of type 3 myocardial infarction in clinical practice. Am J Med 130(7):862e. 9-862.e14
Michaud K, Basso C, d’Amati G, Giordano C, Kholová I, Preston SD et al (2020) Association for European Cardiovascular Pathology (AECVP). Diagnosis of myocardial infarction at autopsy: AECVP reappraisal in the light of the current clinical classification. Virchows Arch 476(2):179–194. https://doi.org/10.1007/s00428-019-02662-1
Huis In ‘t Veld MA, Allison MG, Bostick DS, Fisher KR, Goloubeva OG, Witting MD, et al. Ultrasound use during cardiopulmonary resuscitation is associated with delays in chest compressions. Resuscitation. (2017) ;119:95–98. https://doi.org/10.1016/j.resuscitation.2017.07.021
Clattenburg EJ, Wroe P, Brown S, Gardner K, Losonczy L, Singh A et al (2018) Point-of-care ultrasound use in patients with cardiac arrest is associated prolonged cardiopulmonary resuscitation pauses: a prospective cohort study. Resuscitation 122:65–68. https://doi.org/10.1016/j.resuscitation.2017.11.056
Breitkreutz R, Price S, Steiger HV, Seeger FH, Ilper H, Ackermann H, Emergency Ultrasound Working Group of the Johann Wolfgang Goethe-University Hospital et al (2010) Frankfurt am main. Focused echocardiographic evaluation in life support and peri-resuscitation of emergency patients: a prospective trial. Resuscitation 81(11):1527–1533. https://doi.org/10.1016/j.resuscitation.2010.07.013
Reynolds JC, Issa MS, Nicholson C, Drennan T, Berg IR, O’Neil KM, Advanced Life Support Task Force of the International Liaison Committee on Resuscitation (2020) Prognostication with point-of-care echocardiography during cardiac arrest: a systematic review. Resuscitation 152:56–68. https://doi.org/10.1016/j.resuscitation.2020.05.004
Zöllner K, Sellmann T, Wetzchewald D, Schwager H, Cleff C, Thal SC et al (2021) U SO CARE-The impact of Cardiac Ultrasound during Cardiopulmonary Resuscitation: a prospective Randomized Simulator-based trial. J Clin Med 10(22):5218. https://doi.org/10.3390/jcm10225218
Download references
Acknowledgements
The authors would like to thank all medical professionals involved in the care of patients in the Emergency room and Coronary Care Unit of Clinical Hospital Centre Zemun, Belgrade, Serbia, as well as the forensic pathologists and technicians who performed the autopsies at the Institute of Forensic Medicine, Belgrade, Serbia.
Not applicable.
Author information
Authors and affiliations.
Department of Cardiology, Clinical Hospital Centre Zemun, Vukova 9, Belgrade, 11080, Serbia
Ivan Stankovic, Aleksandra Zivanic, Ivona Vranic & Aleksandar N. Neskovic
Faculty of Medicine, University of Belgrade, Belgrade, Serbia
Ivan Stankovic & Aleksandar N. Neskovic
You can also search for this author in PubMed Google Scholar
Contributions
All listed authors contributed to the manuscript, in the following manner: - conception and design or analysis and interpretation of data, or both (IS, AZ, IV, ANN) - drafting of the manuscript or revising it critically for important intellectual content (IS, AZ, IV, ANN)- final approval of the manuscript submitted (IS, AZ, IV, ANN).
Corresponding author
Correspondence to Ivan Stankovic .
Ethics declarations
Competing interests.
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Stankovic, I., Zivanic, A., Vranic, I. et al. Correlations and discrepancies between cardiac ultrasound, clinical diagnosis and the autopsy findings in early deceased patients with suspected cardiovascular emergencies. Int J Cardiovasc Imaging (2024). https://doi.org/10.1007/s10554-024-03107-w
Download citation
Received : 08 August 2023
Accepted : 03 April 2024
Published : 23 April 2024
DOI : https://doi.org/10.1007/s10554-024-03107-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cardiac ultrasound
- Echocardiography
- Find a journal
- Publish with us
- Track your research
Jul 12, 2014
941 likes | 3.14k Views
Moscow. Moscow. Moscow, the capital of Russia, is one of ancient Russian cities. It was founded by Prince Yuri Dolgoruki in 1147 . The city stands on the Moskva River. Moscow is the country's political, economic, religious, financial, educational and transportation centre. .
Share Presentation
- prezented ru
- supreme court
- kremlin wall
- dmitri donskoito peter
- tourist destinations

Moscow - City Map PowerPoint Template
City map of Moscow with administrative districts and numerous design examples
Instant Download:
- 100% Editable Powerpoint Slides / Graphics
- Outstanding Customer Support
- SSL Secure Payment
- Made in Germany
- Information
- Template (4:3)
High quality city map "Moscow" for PowerPoint
This detailed citymap of "Moscow" you can present in Microsoft PowerPoint. The vector graphic enables you to easily edit and scale your map as much as you need to. Change the colour and edit the separate districts. The map comes in different design-variations.
Infographics Bundle
Flat design – presentation people bundle, change management bundle, 150 strategy & management models, agile management bundle, gearwheel bundle, project charter, growth mindset, project canvas, artificial intelligence, gdpr: data protection powerpoint template, digital transformation, corporate services.
We’ll optimize your existing PowerPoint presentation and create slides in your corporate design.
New PowerPoint Templates
We are continually bringing you new PowerPoint templates on current business topics and in modern designs.

IMAGES
VIDEO
COMMENTS
Breech presentation may be the most important single risk factor, ... With the support of perinatal network pediatricians, ultrasound screening was offered to all girls and to boys presenting with risk factors or abnormalities on clinical examination at one month old. All reports indicate a prevalence of 90% for girls, 70% with no risk factors.
The main types of breech presentation are: Frank breech - Both hips are flexed and both knees are extended so that the feet are adjacent to the head ( figure 1 ); accounts for 50 to 70 percent of breech fetuses at term. Complete breech - Both hips and both knees are flexed ( figure 2 ); accounts for 5 to 10 percent of breech fetuses at term.
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. ... On ultrasound, the fetal lie and presenting part should be visualized and documented. If breech presentation is ...
The report confirmed that no screening method completely eliminates the risk of late presentation of DDH. Use of imaging When an imaging study is indicated, whether by risk factors or by suspicious physical examination, it is best to defer diagnostic hip ultrasound until age 6 weeks (adjust for prematurity) or plain anteroposterior pelvis ...
.hipexam (≥32 wks GA h/o breech presentation): "Breech presentation at delivery or at time of a third trimester antenatal ultrasound is a risk for Developmental Dysplasia of the Hip (DDH). As per AAP recommendations, it is suggested for pediatricians to perform serial surveillance physical exams and obtain a screening hip ultrasound at 46
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord. For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks. ...
This is called a vertex presentation. A breech presentation occurs when the baby's buttocks, feet, or both are positioned to come out first during birth. This happens in 3-4% of full-term births. ... If it appears that the baby might be in a breech position, they can use ultrasound or pelvic exam to confirm the position.
The incidence of breech presentation at term is around 3%-4% [1-3], and fewer than 10% of foetuses who are breech at term revert spontaneously to a vertex presentation . Although breech presentation is easy to detect through ultrasound screening, many women go into labour with an undetected breech presentation . The majority of these women ...
Management of Breech Presentation. This is the fourth edition of this guideline originally published in 1999 and revised in 2001 and 2006 under the same title. ... and the fetal weight should be estimated using ultrasound, and the woman counselled as with planned vaginal breech birth.
Breech Presentation. A 28-year-old G1P0 woman at 37 weeks of gestation presents to her obstetrician for a prenatal care appointment. She describes feeling some soreness under her ribs in the past few weeks and feels her baby kicking in her lower abdomen. An ultrasound is performed and is seen in the image.
Only the probabilistic results (n=100000 simulations) were reported which showed that on average, universal ultrasound resulted in an absolute decrease in breech deliveries by 0.39% compared with selective ultrasound scanning. The expected cost per person with breech presentation of universal ultrasound was £2957 (95% Credibility Interval [CrI ...
A suspected breech presentation should ultimately be confirmed via an ultrasound, after which you and your provider would have a discussion about delivery options, potential issues, and risks ...
Introduction: Because of the risk of developmental dysplasia of the hip in infants born breech-despite a normal physical exam-the American Academy of Pediatrics (AAP) guidelines recommend ultrasound (US) hip imaging at 6 weeks of age for breech females and optional imaging for breech males. The purpose of this study is to report US results and follow-up of infants born breech with a normal ...
breech presentation: fetal rump presenting towards the internal cervical os, this has three main types. frank breech presentation (50-70% of all breech presentation): hips flexed, knees extended (pike position) complete breech presentation (5-10%): hips flexed, knees flexed (cannonball position) footling presentation or incomplete (10-30%): one ...
A breech baby, or breech birth, is when your baby's feet or buttocks are positioned to come out of your vagina first. Your baby's head is up closest to your chest and its bottom is closest to your vagina. Most babies will naturally move so their head is positioned to come out of the vagina first during birth. Breech is common in early ...
Following a diagnosis of breech presentation during the ultrasound scan, women are counselled about their options: ECV, planned cesarean birth, or planned vaginal birth. If women declined ECV or if it was unsuccessful, they were offered elective cesarean delivery from 39 weeks of gestation. The population was divided into 2 study groups: Group ...
Breech Presentation Frank breech means the buttocks are presenting and the legs are up along the fetal chest. The fetal feet are next to the fetal face. This is the safest arrangement for breech delivery. Footling breech means either one foot ("Single Footling") or both feet ("Double Footling") is presenting. This is also known as an incomplete breech.
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
Additionally, a comprehensive retrospective cross-sectional study, examining a total of 109,736 singleton infants (both preterm and full-term), of which 4535 were breech at birth, determined that women with any form of uterine malformation had an almost 10-fold increase in the likelihood of breech fetal presentation (odds ratio, 9.47; 95% CI 6. ...
Cardiac ultrasound (CUS), either focused cardiac ultrasound (FoCUS) or emergency echocardiography, is frequently used in cardiovascular (CV) emergencies. We assessed correlations and discrepancies between CUS, clinical diagnosis and the autopsy findings in early deceased patients with suspected CV emergencies. We retrospectively analysed clinical and autopsy data of 131 consecutive patients ...
Jul 12, 2014. 941 likes | 3.15k Views. Moscow. Moscow. Moscow, the capital of Russia, is one of ancient Russian cities. It was founded by Prince Yuri Dolgoruki in 1147 . The city stands on the Moskva River. Moscow is the country's political, economic, religious, financial, educational and transportation centre. . Download Presentation.
RESEARCH 4 MIBC MOSCOW-C ITY JUNE 2016 Russian companies Foreign companies 28% 72% *Legal/ Consulting **Technology/ Media/ Telecommunication ***Fast moving consumer goods
Firebird SQL Case Study Medical Analytical System for Moscow City Hospital #31 About us Moscow City Hospital #31 is a modern, 620 bed medical institution providing emergency
Moscow - City Map PowerPoint Template. (M4010) City map of Moscow with administrative districts and numerous design examples. Add to cart. $19.00*. Add to wish list. Quantity of slides. : 20.